User login
Alcohol-Associated Liver Disease’s Changing Demographics
, accounting for approximately 5% of all disease and injury. In the United States, the prevalence of ALD has increased since 2014, and the trajectory accelerated during the COVID-19 pandemic.
ALD encompasses a spectrum of diseases that includes steatosis, fibrosis, cirrhosis, and hepatocellular carcinoma, as well as related complications. Although earlier stages of ALD may be asymptomatic, hepatologists and gastroenterologists rarely see patients at this point.
“Unfortunately, patients with ALD more often present in late stages of disease (decompensated cirrhosis) as compared with other chronic liver diseases, such as metabolic dysfunction-associated steatotic liver disease or hepatitis C,” Doug A. Simonetto, MD, associate professor of medicine and director of the Gastroenterology and Hepatology Fellowship Program at the Mayo Clinic, Rochester, Minnesota, told this news organization.
Recent data have identified three demographic groups experiencing higher rates of ALD relative to previous periods and who may therefore require special attention. Understanding what makes these groups increasingly susceptible to ALD may allow for improved screening, earlier diagnosis, and potentially the prevention of its most dire consequences.
As Women Consume More Alcohol, ALD Follows
Historically, men have had higher rates of alcohol use, heavy drinking, and alcohol disorders than women. But this gender gap has begun to narrow.
Men born in the early 1900s were 2.2 times more likely to drink alcohol and 3.6 times more likely to experience alcohol-related harms than women, according to a 2016 meta-analysis. By the end of the 1990s, however, women’s drinking had begun to catch up. Men still led in these categories, but only by 1.1 and 1.3 times, respectively.
Rates of binge drinking (defined as at least five drinks in men or at least four drinks in women in an approximately 2-hour period) are also converging between the sexes. The authors of a longitudinal analysis hypothesized that an uptick in young women reporting drinking for social reasons — from 53% in 1987 to 87% in 2020 — was a possible cause.
Greater alcohol consumption among women has translated into higher rates of ALD. Analyzing data from the Global Burden of Disease Study 2019, which looked at hundreds of diseases across 204 countries and territories, researchers reported that the worldwide prevalence of ALD among young women (15-49 years) rose within the past decade. Those in the 20- to 24-year-old age group had the most significant increases in ALD prevalence rates.
Recent US statistics highlight the relative imbalance in ALD’s impact on women, according to George F. Koob, PhD, director of the National Institute on Alcohol Abuse and Alcoholism (NIAAA).
“The age-adjusted death rate from alcohol-associated liver cirrhosis increased by 47% between 2000 and 2019, with larger increases for females than for males (83.5% compared to 33%),” Dr. Koob told this news organization. “Larger increases for women are consistent with a general increase in alcohol use among adult women and larger increases in alcohol-related emergency department visits, hospitalizations, and deaths.”
Physiologically, women have a higher risk than men of developing ALD and more severe disease, even at lower levels of alcohol exposure. According to a 2021 review, several proposed mechanisms might play a role, including differences in alcohol metabolism and first-pass metabolism, hormones, and endotoxin and Kupffer cell activation.
Crucially, women are less likely than men to receive in-person therapy or approved medications for alcohol use disorder, according to a 2019 analysis of over 66,000 privately insured adult patients.
Certain Ethnic, Racial Minorities Have Higher Rates of ALD
In the United States, rates of ALD and associated complications are higher among certain minority groups, most prominently Hispanic and Native American individuals.
A 2021 analysis of three large US databases found that Hispanic ethnicity was associated with a 17% increased risk for acute-on-chronic liver failure in patients with ALD-related admissions.
Data also show that Hispanic and White patients have a higher proportion of alcoholic hepatitis than African American patients. And for Hispanic patients admitted for alcoholic hepatitis, they incur significantly more total hospital costs despite having similar mortality rates as White patients.
ALD-related mortality appears higher within certain subgroups of Hispanic patient populations. NIAAA surveillance reports track deaths resulting from cirrhosis in the White, Black, and Hispanic populations. From 2000 to 2019, these statistics show that although death rates from cirrhosis decreased for Hispanic White men, they increased for Hispanic White women, Dr. Koob said.
The latest data show that Native American populations are experiencing ALD at relatively higher rates than other racial/ethnic groups as well. An analysis of nearly 200,000 cirrhosis-related hospitalizations found that ALD, including alcoholic hepatitis, was the most common etiology in American Indian/Alaska Native patients. A separate analysis of the National Inpatient Sample database revealed that discharges resulting from ALD were disproportionately higher among Native American women.
As with Hispanic populations, ALD-associated mortality rates are also higher in Native American populations. The death rate from ALD increased for all racial and ethnic groups by 23.4% from 2019 to 2020, but the biggest increase occurred in the American Indian or Alaska Native populations (34.3% increase, from 20.1 to 27 per 100,000 people). Additionally, over the first two decades of the 21st century, mortality rates resulting from cirrhosis were highest among the American Indian and Alaska Native populations, according to a recently published systematic analysis of US health disparities across five racial/ethnic groups.
Discrepancies in these and other minority groups may be due partly to genetic mechanisms, such as the relatively higher frequency of the PNPLA3 G/G polymorphism, a known risk factor for the development of advanced ALD, among those with Native American ancestry. A host of complex socioeconomic factors, such as income discrepancies and access to care, likely contribute too.
Evidence suggests that alcohol screening interventions are not applied equally across various racial and ethnic groups, Dr. Koob noted.
“For instance, Subbaraman and colleagues reported that, compared to non-Hispanic White patients, those who identify as Hispanic, Black, or other race or ethnicity were less likely to be screened for alcohol use during visits to healthcare providers. This was particularly true for those with a high school education or less,” he told this news organization. “However, other studies have not found such disparities.”
ALD Rates High in Young Adults, but the Tide May Be Changing
Globally, the prevalence of ALD has increased among both adolescents and young adults since the beginning of the 21st century. The global incidence of alcohol-associated hepatitis in recent years has been greatest among those aged 15-44 years.
In the United States, the increasing rate of ALD-related hospitalizations is primarily driven by the rise in cases of alcoholic hepatitis and acute-on-chronic liver failure among those aged 35 years and younger.
ALD is now the most common indication for liver transplant in those younger than 40 years of age, having increased fourfold between 2003 and 2018.
From 2009 to 2016, people aged 25-34 years experienced the highest average annual increase in cirrhosis-related mortality (10.5%), a trend the authors noted was “driven entirely by alcohol-related liver disease.”
Younger adults may be more susceptible to ALD due to the way they drink.
In a 2021 analysis of the National Health and Nutrition Examination Survey database, the weighted prevalence of harmful alcohol use was 29.3% in those younger than 35 years, compared with 16.9% in those aged 35-64 years. Higher blood alcohol levels resulting from binge drinking may make patients more susceptible to bacterial translocation and liver fibrosis and can increase the likelihood of cirrhosis in those with an underlying metabolic syndrome.
Yet, Dr. Koob said, thinking of “young adults” as one cohort may be misguided because he’s found very different attitudes toward alcohol within that population. Cross-sectional survey data obtained from more than 180,000 young adults indicated that alcohol abstinence increased between 2002 and 2018. Young adults report various reasons for not drinking, ranging from lack of interest to financial and situational barriers (eg, not wanting to interfere with school or work).
“The tide is coming in and out at the same time,” he said. “Younger people under the age of 25 are drinking less each year, are increasingly interested in things like Dry January, and more than half view moderate levels of consumption as unhealthy. People who are 26 years and older are drinking more, are not as interested in cutting back or taking breaks, and are less likely to consider 1 or 2 drinks per day as potentially unhealthy.”
Dr. Koob would like to believe the positive trends around alcohol in the under-25 set prove not only resilient, but someday, dominant.
“We have seen historic increases in alcohol consumption in the last few years — the largest increases in more than 50 years. But we are hopeful that, as the younger cohorts age, we will see lower levels of drinking by adults in mid-life and beyond.”
A version of this article first appeared on Medscape.com.
, accounting for approximately 5% of all disease and injury. In the United States, the prevalence of ALD has increased since 2014, and the trajectory accelerated during the COVID-19 pandemic.
ALD encompasses a spectrum of diseases that includes steatosis, fibrosis, cirrhosis, and hepatocellular carcinoma, as well as related complications. Although earlier stages of ALD may be asymptomatic, hepatologists and gastroenterologists rarely see patients at this point.
“Unfortunately, patients with ALD more often present in late stages of disease (decompensated cirrhosis) as compared with other chronic liver diseases, such as metabolic dysfunction-associated steatotic liver disease or hepatitis C,” Doug A. Simonetto, MD, associate professor of medicine and director of the Gastroenterology and Hepatology Fellowship Program at the Mayo Clinic, Rochester, Minnesota, told this news organization.
Recent data have identified three demographic groups experiencing higher rates of ALD relative to previous periods and who may therefore require special attention. Understanding what makes these groups increasingly susceptible to ALD may allow for improved screening, earlier diagnosis, and potentially the prevention of its most dire consequences.
As Women Consume More Alcohol, ALD Follows
Historically, men have had higher rates of alcohol use, heavy drinking, and alcohol disorders than women. But this gender gap has begun to narrow.
Men born in the early 1900s were 2.2 times more likely to drink alcohol and 3.6 times more likely to experience alcohol-related harms than women, according to a 2016 meta-analysis. By the end of the 1990s, however, women’s drinking had begun to catch up. Men still led in these categories, but only by 1.1 and 1.3 times, respectively.
Rates of binge drinking (defined as at least five drinks in men or at least four drinks in women in an approximately 2-hour period) are also converging between the sexes. The authors of a longitudinal analysis hypothesized that an uptick in young women reporting drinking for social reasons — from 53% in 1987 to 87% in 2020 — was a possible cause.
Greater alcohol consumption among women has translated into higher rates of ALD. Analyzing data from the Global Burden of Disease Study 2019, which looked at hundreds of diseases across 204 countries and territories, researchers reported that the worldwide prevalence of ALD among young women (15-49 years) rose within the past decade. Those in the 20- to 24-year-old age group had the most significant increases in ALD prevalence rates.
Recent US statistics highlight the relative imbalance in ALD’s impact on women, according to George F. Koob, PhD, director of the National Institute on Alcohol Abuse and Alcoholism (NIAAA).
“The age-adjusted death rate from alcohol-associated liver cirrhosis increased by 47% between 2000 and 2019, with larger increases for females than for males (83.5% compared to 33%),” Dr. Koob told this news organization. “Larger increases for women are consistent with a general increase in alcohol use among adult women and larger increases in alcohol-related emergency department visits, hospitalizations, and deaths.”
Physiologically, women have a higher risk than men of developing ALD and more severe disease, even at lower levels of alcohol exposure. According to a 2021 review, several proposed mechanisms might play a role, including differences in alcohol metabolism and first-pass metabolism, hormones, and endotoxin and Kupffer cell activation.
Crucially, women are less likely than men to receive in-person therapy or approved medications for alcohol use disorder, according to a 2019 analysis of over 66,000 privately insured adult patients.
Certain Ethnic, Racial Minorities Have Higher Rates of ALD
In the United States, rates of ALD and associated complications are higher among certain minority groups, most prominently Hispanic and Native American individuals.
A 2021 analysis of three large US databases found that Hispanic ethnicity was associated with a 17% increased risk for acute-on-chronic liver failure in patients with ALD-related admissions.
Data also show that Hispanic and White patients have a higher proportion of alcoholic hepatitis than African American patients. And for Hispanic patients admitted for alcoholic hepatitis, they incur significantly more total hospital costs despite having similar mortality rates as White patients.
ALD-related mortality appears higher within certain subgroups of Hispanic patient populations. NIAAA surveillance reports track deaths resulting from cirrhosis in the White, Black, and Hispanic populations. From 2000 to 2019, these statistics show that although death rates from cirrhosis decreased for Hispanic White men, they increased for Hispanic White women, Dr. Koob said.
The latest data show that Native American populations are experiencing ALD at relatively higher rates than other racial/ethnic groups as well. An analysis of nearly 200,000 cirrhosis-related hospitalizations found that ALD, including alcoholic hepatitis, was the most common etiology in American Indian/Alaska Native patients. A separate analysis of the National Inpatient Sample database revealed that discharges resulting from ALD were disproportionately higher among Native American women.
As with Hispanic populations, ALD-associated mortality rates are also higher in Native American populations. The death rate from ALD increased for all racial and ethnic groups by 23.4% from 2019 to 2020, but the biggest increase occurred in the American Indian or Alaska Native populations (34.3% increase, from 20.1 to 27 per 100,000 people). Additionally, over the first two decades of the 21st century, mortality rates resulting from cirrhosis were highest among the American Indian and Alaska Native populations, according to a recently published systematic analysis of US health disparities across five racial/ethnic groups.
Discrepancies in these and other minority groups may be due partly to genetic mechanisms, such as the relatively higher frequency of the PNPLA3 G/G polymorphism, a known risk factor for the development of advanced ALD, among those with Native American ancestry. A host of complex socioeconomic factors, such as income discrepancies and access to care, likely contribute too.
Evidence suggests that alcohol screening interventions are not applied equally across various racial and ethnic groups, Dr. Koob noted.
“For instance, Subbaraman and colleagues reported that, compared to non-Hispanic White patients, those who identify as Hispanic, Black, or other race or ethnicity were less likely to be screened for alcohol use during visits to healthcare providers. This was particularly true for those with a high school education or less,” he told this news organization. “However, other studies have not found such disparities.”
ALD Rates High in Young Adults, but the Tide May Be Changing
Globally, the prevalence of ALD has increased among both adolescents and young adults since the beginning of the 21st century. The global incidence of alcohol-associated hepatitis in recent years has been greatest among those aged 15-44 years.
In the United States, the increasing rate of ALD-related hospitalizations is primarily driven by the rise in cases of alcoholic hepatitis and acute-on-chronic liver failure among those aged 35 years and younger.
ALD is now the most common indication for liver transplant in those younger than 40 years of age, having increased fourfold between 2003 and 2018.
From 2009 to 2016, people aged 25-34 years experienced the highest average annual increase in cirrhosis-related mortality (10.5%), a trend the authors noted was “driven entirely by alcohol-related liver disease.”
Younger adults may be more susceptible to ALD due to the way they drink.
In a 2021 analysis of the National Health and Nutrition Examination Survey database, the weighted prevalence of harmful alcohol use was 29.3% in those younger than 35 years, compared with 16.9% in those aged 35-64 years. Higher blood alcohol levels resulting from binge drinking may make patients more susceptible to bacterial translocation and liver fibrosis and can increase the likelihood of cirrhosis in those with an underlying metabolic syndrome.
Yet, Dr. Koob said, thinking of “young adults” as one cohort may be misguided because he’s found very different attitudes toward alcohol within that population. Cross-sectional survey data obtained from more than 180,000 young adults indicated that alcohol abstinence increased between 2002 and 2018. Young adults report various reasons for not drinking, ranging from lack of interest to financial and situational barriers (eg, not wanting to interfere with school or work).
“The tide is coming in and out at the same time,” he said. “Younger people under the age of 25 are drinking less each year, are increasingly interested in things like Dry January, and more than half view moderate levels of consumption as unhealthy. People who are 26 years and older are drinking more, are not as interested in cutting back or taking breaks, and are less likely to consider 1 or 2 drinks per day as potentially unhealthy.”
Dr. Koob would like to believe the positive trends around alcohol in the under-25 set prove not only resilient, but someday, dominant.
“We have seen historic increases in alcohol consumption in the last few years — the largest increases in more than 50 years. But we are hopeful that, as the younger cohorts age, we will see lower levels of drinking by adults in mid-life and beyond.”
A version of this article first appeared on Medscape.com.
, accounting for approximately 5% of all disease and injury. In the United States, the prevalence of ALD has increased since 2014, and the trajectory accelerated during the COVID-19 pandemic.
ALD encompasses a spectrum of diseases that includes steatosis, fibrosis, cirrhosis, and hepatocellular carcinoma, as well as related complications. Although earlier stages of ALD may be asymptomatic, hepatologists and gastroenterologists rarely see patients at this point.
“Unfortunately, patients with ALD more often present in late stages of disease (decompensated cirrhosis) as compared with other chronic liver diseases, such as metabolic dysfunction-associated steatotic liver disease or hepatitis C,” Doug A. Simonetto, MD, associate professor of medicine and director of the Gastroenterology and Hepatology Fellowship Program at the Mayo Clinic, Rochester, Minnesota, told this news organization.
Recent data have identified three demographic groups experiencing higher rates of ALD relative to previous periods and who may therefore require special attention. Understanding what makes these groups increasingly susceptible to ALD may allow for improved screening, earlier diagnosis, and potentially the prevention of its most dire consequences.
As Women Consume More Alcohol, ALD Follows
Historically, men have had higher rates of alcohol use, heavy drinking, and alcohol disorders than women. But this gender gap has begun to narrow.
Men born in the early 1900s were 2.2 times more likely to drink alcohol and 3.6 times more likely to experience alcohol-related harms than women, according to a 2016 meta-analysis. By the end of the 1990s, however, women’s drinking had begun to catch up. Men still led in these categories, but only by 1.1 and 1.3 times, respectively.
Rates of binge drinking (defined as at least five drinks in men or at least four drinks in women in an approximately 2-hour period) are also converging between the sexes. The authors of a longitudinal analysis hypothesized that an uptick in young women reporting drinking for social reasons — from 53% in 1987 to 87% in 2020 — was a possible cause.
Greater alcohol consumption among women has translated into higher rates of ALD. Analyzing data from the Global Burden of Disease Study 2019, which looked at hundreds of diseases across 204 countries and territories, researchers reported that the worldwide prevalence of ALD among young women (15-49 years) rose within the past decade. Those in the 20- to 24-year-old age group had the most significant increases in ALD prevalence rates.
Recent US statistics highlight the relative imbalance in ALD’s impact on women, according to George F. Koob, PhD, director of the National Institute on Alcohol Abuse and Alcoholism (NIAAA).
“The age-adjusted death rate from alcohol-associated liver cirrhosis increased by 47% between 2000 and 2019, with larger increases for females than for males (83.5% compared to 33%),” Dr. Koob told this news organization. “Larger increases for women are consistent with a general increase in alcohol use among adult women and larger increases in alcohol-related emergency department visits, hospitalizations, and deaths.”
Physiologically, women have a higher risk than men of developing ALD and more severe disease, even at lower levels of alcohol exposure. According to a 2021 review, several proposed mechanisms might play a role, including differences in alcohol metabolism and first-pass metabolism, hormones, and endotoxin and Kupffer cell activation.
Crucially, women are less likely than men to receive in-person therapy or approved medications for alcohol use disorder, according to a 2019 analysis of over 66,000 privately insured adult patients.
Certain Ethnic, Racial Minorities Have Higher Rates of ALD
In the United States, rates of ALD and associated complications are higher among certain minority groups, most prominently Hispanic and Native American individuals.
A 2021 analysis of three large US databases found that Hispanic ethnicity was associated with a 17% increased risk for acute-on-chronic liver failure in patients with ALD-related admissions.
Data also show that Hispanic and White patients have a higher proportion of alcoholic hepatitis than African American patients. And for Hispanic patients admitted for alcoholic hepatitis, they incur significantly more total hospital costs despite having similar mortality rates as White patients.
ALD-related mortality appears higher within certain subgroups of Hispanic patient populations. NIAAA surveillance reports track deaths resulting from cirrhosis in the White, Black, and Hispanic populations. From 2000 to 2019, these statistics show that although death rates from cirrhosis decreased for Hispanic White men, they increased for Hispanic White women, Dr. Koob said.
The latest data show that Native American populations are experiencing ALD at relatively higher rates than other racial/ethnic groups as well. An analysis of nearly 200,000 cirrhosis-related hospitalizations found that ALD, including alcoholic hepatitis, was the most common etiology in American Indian/Alaska Native patients. A separate analysis of the National Inpatient Sample database revealed that discharges resulting from ALD were disproportionately higher among Native American women.
As with Hispanic populations, ALD-associated mortality rates are also higher in Native American populations. The death rate from ALD increased for all racial and ethnic groups by 23.4% from 2019 to 2020, but the biggest increase occurred in the American Indian or Alaska Native populations (34.3% increase, from 20.1 to 27 per 100,000 people). Additionally, over the first two decades of the 21st century, mortality rates resulting from cirrhosis were highest among the American Indian and Alaska Native populations, according to a recently published systematic analysis of US health disparities across five racial/ethnic groups.
Discrepancies in these and other minority groups may be due partly to genetic mechanisms, such as the relatively higher frequency of the PNPLA3 G/G polymorphism, a known risk factor for the development of advanced ALD, among those with Native American ancestry. A host of complex socioeconomic factors, such as income discrepancies and access to care, likely contribute too.
Evidence suggests that alcohol screening interventions are not applied equally across various racial and ethnic groups, Dr. Koob noted.
“For instance, Subbaraman and colleagues reported that, compared to non-Hispanic White patients, those who identify as Hispanic, Black, or other race or ethnicity were less likely to be screened for alcohol use during visits to healthcare providers. This was particularly true for those with a high school education or less,” he told this news organization. “However, other studies have not found such disparities.”
ALD Rates High in Young Adults, but the Tide May Be Changing
Globally, the prevalence of ALD has increased among both adolescents and young adults since the beginning of the 21st century. The global incidence of alcohol-associated hepatitis in recent years has been greatest among those aged 15-44 years.
In the United States, the increasing rate of ALD-related hospitalizations is primarily driven by the rise in cases of alcoholic hepatitis and acute-on-chronic liver failure among those aged 35 years and younger.
ALD is now the most common indication for liver transplant in those younger than 40 years of age, having increased fourfold between 2003 and 2018.
From 2009 to 2016, people aged 25-34 years experienced the highest average annual increase in cirrhosis-related mortality (10.5%), a trend the authors noted was “driven entirely by alcohol-related liver disease.”
Younger adults may be more susceptible to ALD due to the way they drink.
In a 2021 analysis of the National Health and Nutrition Examination Survey database, the weighted prevalence of harmful alcohol use was 29.3% in those younger than 35 years, compared with 16.9% in those aged 35-64 years. Higher blood alcohol levels resulting from binge drinking may make patients more susceptible to bacterial translocation and liver fibrosis and can increase the likelihood of cirrhosis in those with an underlying metabolic syndrome.
Yet, Dr. Koob said, thinking of “young adults” as one cohort may be misguided because he’s found very different attitudes toward alcohol within that population. Cross-sectional survey data obtained from more than 180,000 young adults indicated that alcohol abstinence increased between 2002 and 2018. Young adults report various reasons for not drinking, ranging from lack of interest to financial and situational barriers (eg, not wanting to interfere with school or work).
“The tide is coming in and out at the same time,” he said. “Younger people under the age of 25 are drinking less each year, are increasingly interested in things like Dry January, and more than half view moderate levels of consumption as unhealthy. People who are 26 years and older are drinking more, are not as interested in cutting back or taking breaks, and are less likely to consider 1 or 2 drinks per day as potentially unhealthy.”
Dr. Koob would like to believe the positive trends around alcohol in the under-25 set prove not only resilient, but someday, dominant.
“We have seen historic increases in alcohol consumption in the last few years — the largest increases in more than 50 years. But we are hopeful that, as the younger cohorts age, we will see lower levels of drinking by adults in mid-life and beyond.”
A version of this article first appeared on Medscape.com.
Hand Sanitizers and Alcohol Abuse: A Dangerous Cocktail
Since the COVID-19 pandemic, alcoholic hand sanitizers have become widely accessible nationwide. They can pose a problem, especially for emergency departments, when alcohol-dependent patients start drinking them. One example that demonstrates the challenge of diagnosing alcohol abuse is the medical history of a young man, as reported by Mahmoud El Hussein, MD, and colleagues from Hôpital Lariboisière in Paris, France.
Presentation and History
A 26-year-old man presented with severe abdominal pain at the emergency department. Upon arrival, he was hemodynamically stable but nervous and verbally aggressive at times. The patient reported no relevant preexisting conditions and was not taking any medications.
Findings
Upon initial physical examination, the patient had a soft, diffusely tender abdomen; tachycardia; and notably poor hygiene. The patient was afebrile. An ECG confirmed the tachycardia but showed no signs of ischemia. Blood work, except for slightly elevated liver values, did not reveal any abnormalities, particularly ruling out bleeding or kidney disease.
A urease rapid test to rule out kidney stones also showed no pathologic findings. In consultation with the surgical department, a CT scan of the abdomen was performed to rule out organ perforation, volvulus, or mesenteric ischemia. Only signs of fatty liver were found.
A Neighbor’s Tip
During all examinations, the patient’s abdomen was repeatedly palpated to promptly detect signs of an acute abdomen. However, there was never any defense tension at any point.
Intravenous analgesics and proton pump inhibitors (ie, paracetamol, phloroglucin, and pantoprazole) did not relieve the patient’s symptoms. Morphine was administered intravenously for sedation.
Only after a frustrating diagnostic process did a neighbor of the patient inform a nurse that he suspected the patient of stealing and consuming hand sanitizer. With the patient’s consent, a blood alcohol test was performed, revealing a blood alcohol concentration of 0.2% (2 g/L). A urine test, also conducted with the patient’s consent, tested positive for tetrahydrocannabinol. Additional tests showed the following results:
- Venous pH: 7.29 (normal, 7.32-7.38)
- Anion gap (mEq/L): 14 (normal, 3-9)
- Ketone bodies (mmol/L): 0.2 (normal, < 0.6)
- Calculated serum osmolality (mOsm/kg): 292 (normal, 285-295)
- Measured serum osmolality (mOsm/kg): 320 (normal, 285-295)
- Osmolality gap (mOsm/kg): 2 (normal, < 10)
The patient was informed of the test results and confessed to feigning abdominal pain. He was dependent on alcohol and experiencing withdrawal symptoms. The patient had stolen seven 475-mL bottles of hand sanitizer and consumed one and a half in the past 4-6 hours. According to the authors, the sanitizer consisted of 80% ethanol, 1.45% glycerol, and 0.13% hydrogen peroxide.
Discussion
In Germany, alcohol consumption results in approximately €57 billion in direct economic costs annually, according to data from the Federal Ministry of Health. In 2021, about 7.9 million people aged 18-64 years consumed alcohol in a risky manner (approximately 9.6% of the German population). About 9 million people (approximately 11%) were classified as alcoholics.
Therefore, staff in emergency departments, where potential abusers encounter a wide range of potential abuse items, should exercise caution.
Although hand sanitizers are mainly composed of ethanol, they may also contain isopropanol, methanol, or acetone. Methanol poisoning can cause abdominal pain, visual disturbances, central nervous system damage, and death. Other alcohols such as ethylene glycol, commonly found in antifreeze, can distort blood values (lactate) and complicate a correct diagnosis.
Physicians working in emergency departments should proceed with caution when suspecting alcohol abuse. Questioning the patient’s environment and determining additional laboratory parameters (such as osmolality gap in the case report) can help unmask substance abuse if it is in doubt.
This story was translated from Univadis Germany, which is part of the Medscape professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Since the COVID-19 pandemic, alcoholic hand sanitizers have become widely accessible nationwide. They can pose a problem, especially for emergency departments, when alcohol-dependent patients start drinking them. One example that demonstrates the challenge of diagnosing alcohol abuse is the medical history of a young man, as reported by Mahmoud El Hussein, MD, and colleagues from Hôpital Lariboisière in Paris, France.
Presentation and History
A 26-year-old man presented with severe abdominal pain at the emergency department. Upon arrival, he was hemodynamically stable but nervous and verbally aggressive at times. The patient reported no relevant preexisting conditions and was not taking any medications.
Findings
Upon initial physical examination, the patient had a soft, diffusely tender abdomen; tachycardia; and notably poor hygiene. The patient was afebrile. An ECG confirmed the tachycardia but showed no signs of ischemia. Blood work, except for slightly elevated liver values, did not reveal any abnormalities, particularly ruling out bleeding or kidney disease.
A urease rapid test to rule out kidney stones also showed no pathologic findings. In consultation with the surgical department, a CT scan of the abdomen was performed to rule out organ perforation, volvulus, or mesenteric ischemia. Only signs of fatty liver were found.
A Neighbor’s Tip
During all examinations, the patient’s abdomen was repeatedly palpated to promptly detect signs of an acute abdomen. However, there was never any defense tension at any point.
Intravenous analgesics and proton pump inhibitors (ie, paracetamol, phloroglucin, and pantoprazole) did not relieve the patient’s symptoms. Morphine was administered intravenously for sedation.
Only after a frustrating diagnostic process did a neighbor of the patient inform a nurse that he suspected the patient of stealing and consuming hand sanitizer. With the patient’s consent, a blood alcohol test was performed, revealing a blood alcohol concentration of 0.2% (2 g/L). A urine test, also conducted with the patient’s consent, tested positive for tetrahydrocannabinol. Additional tests showed the following results:
- Venous pH: 7.29 (normal, 7.32-7.38)
- Anion gap (mEq/L): 14 (normal, 3-9)
- Ketone bodies (mmol/L): 0.2 (normal, < 0.6)
- Calculated serum osmolality (mOsm/kg): 292 (normal, 285-295)
- Measured serum osmolality (mOsm/kg): 320 (normal, 285-295)
- Osmolality gap (mOsm/kg): 2 (normal, < 10)
The patient was informed of the test results and confessed to feigning abdominal pain. He was dependent on alcohol and experiencing withdrawal symptoms. The patient had stolen seven 475-mL bottles of hand sanitizer and consumed one and a half in the past 4-6 hours. According to the authors, the sanitizer consisted of 80% ethanol, 1.45% glycerol, and 0.13% hydrogen peroxide.
Discussion
In Germany, alcohol consumption results in approximately €57 billion in direct economic costs annually, according to data from the Federal Ministry of Health. In 2021, about 7.9 million people aged 18-64 years consumed alcohol in a risky manner (approximately 9.6% of the German population). About 9 million people (approximately 11%) were classified as alcoholics.
Therefore, staff in emergency departments, where potential abusers encounter a wide range of potential abuse items, should exercise caution.
Although hand sanitizers are mainly composed of ethanol, they may also contain isopropanol, methanol, or acetone. Methanol poisoning can cause abdominal pain, visual disturbances, central nervous system damage, and death. Other alcohols such as ethylene glycol, commonly found in antifreeze, can distort blood values (lactate) and complicate a correct diagnosis.
Physicians working in emergency departments should proceed with caution when suspecting alcohol abuse. Questioning the patient’s environment and determining additional laboratory parameters (such as osmolality gap in the case report) can help unmask substance abuse if it is in doubt.
This story was translated from Univadis Germany, which is part of the Medscape professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Since the COVID-19 pandemic, alcoholic hand sanitizers have become widely accessible nationwide. They can pose a problem, especially for emergency departments, when alcohol-dependent patients start drinking them. One example that demonstrates the challenge of diagnosing alcohol abuse is the medical history of a young man, as reported by Mahmoud El Hussein, MD, and colleagues from Hôpital Lariboisière in Paris, France.
Presentation and History
A 26-year-old man presented with severe abdominal pain at the emergency department. Upon arrival, he was hemodynamically stable but nervous and verbally aggressive at times. The patient reported no relevant preexisting conditions and was not taking any medications.
Findings
Upon initial physical examination, the patient had a soft, diffusely tender abdomen; tachycardia; and notably poor hygiene. The patient was afebrile. An ECG confirmed the tachycardia but showed no signs of ischemia. Blood work, except for slightly elevated liver values, did not reveal any abnormalities, particularly ruling out bleeding or kidney disease.
A urease rapid test to rule out kidney stones also showed no pathologic findings. In consultation with the surgical department, a CT scan of the abdomen was performed to rule out organ perforation, volvulus, or mesenteric ischemia. Only signs of fatty liver were found.
A Neighbor’s Tip
During all examinations, the patient’s abdomen was repeatedly palpated to promptly detect signs of an acute abdomen. However, there was never any defense tension at any point.
Intravenous analgesics and proton pump inhibitors (ie, paracetamol, phloroglucin, and pantoprazole) did not relieve the patient’s symptoms. Morphine was administered intravenously for sedation.
Only after a frustrating diagnostic process did a neighbor of the patient inform a nurse that he suspected the patient of stealing and consuming hand sanitizer. With the patient’s consent, a blood alcohol test was performed, revealing a blood alcohol concentration of 0.2% (2 g/L). A urine test, also conducted with the patient’s consent, tested positive for tetrahydrocannabinol. Additional tests showed the following results:
- Venous pH: 7.29 (normal, 7.32-7.38)
- Anion gap (mEq/L): 14 (normal, 3-9)
- Ketone bodies (mmol/L): 0.2 (normal, < 0.6)
- Calculated serum osmolality (mOsm/kg): 292 (normal, 285-295)
- Measured serum osmolality (mOsm/kg): 320 (normal, 285-295)
- Osmolality gap (mOsm/kg): 2 (normal, < 10)
The patient was informed of the test results and confessed to feigning abdominal pain. He was dependent on alcohol and experiencing withdrawal symptoms. The patient had stolen seven 475-mL bottles of hand sanitizer and consumed one and a half in the past 4-6 hours. According to the authors, the sanitizer consisted of 80% ethanol, 1.45% glycerol, and 0.13% hydrogen peroxide.
Discussion
In Germany, alcohol consumption results in approximately €57 billion in direct economic costs annually, according to data from the Federal Ministry of Health. In 2021, about 7.9 million people aged 18-64 years consumed alcohol in a risky manner (approximately 9.6% of the German population). About 9 million people (approximately 11%) were classified as alcoholics.
Therefore, staff in emergency departments, where potential abusers encounter a wide range of potential abuse items, should exercise caution.
Although hand sanitizers are mainly composed of ethanol, they may also contain isopropanol, methanol, or acetone. Methanol poisoning can cause abdominal pain, visual disturbances, central nervous system damage, and death. Other alcohols such as ethylene glycol, commonly found in antifreeze, can distort blood values (lactate) and complicate a correct diagnosis.
Physicians working in emergency departments should proceed with caution when suspecting alcohol abuse. Questioning the patient’s environment and determining additional laboratory parameters (such as osmolality gap in the case report) can help unmask substance abuse if it is in doubt.
This story was translated from Univadis Germany, which is part of the Medscape professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
It’s Never Too Late to Convince Patients to Quit Smoking
An estimated 450,000 US deaths are expected this year from conditions attributed to cigarette smoking. Although the percentage of adults who smoke declined from 21% in 2005 to 11% in 2022, the annual death toll has been stable since 2005 and isn’t expected to decline until 2030, owing to an aging population of current and former smokers.
In 2022, based on a national survey, two thirds of the 28.8 million US adult smokers wanted to quit, and more than half tried quitting on their own or with the help of clinicians, but less than 9% succeeded in kicking the habit. The health benefits of quitting, summarized in a patient education handout from the American Cancer Society, include a lower risk for cancer, diabetes, and cardiovascular disease. Furthermore, the handout states, “quitting smoking can add as much as 10 years to your life, compared to if you continued to smoke.”
For my patients older than age 50 who are lifelong smokers, the qualifier “as much as” can be a sticking point. Although most recognize that continuing to smoke exposes them to greater health risks and are willing to undergo lung cancer screening and receive pneumococcal vaccines, a kind of fatalism frequently sets in. I’ve heard more times than I can recall some version of the declaration, “It’s too late for quitting to make much difference for me.” Many smokers think that once they reach middle age, gains in life expectancy will be too small to be worth the intense effort and multiple failed attempts that are typically required to quit permanently. Until recently, there were few data I could call on to persuade them they were wrong.
In February 2024, Dr. Eo Rin Cho and colleagues pooled data from four national cohort studies (United States, United Kingdom, Norway, and Canada) to calculate mortality differences among current, former, and never smokers aged 20-79 years. Compared with never smokers, lifelong smokers died an average of 12-13 years earlier. However, quitting before age 50 nearly eliminated the excess mortality associated with smoking, and in the 50- to 59-year-old age group, cessation eventually reduced excess mortality by 92%-95%. Better yet, more than half of the benefits occurred within the first 3 years after cessation.
At first glance, these estimates may seem too good to be true. A few months later, though, a different research group, using data from a large cancer prevention study and 2018 US population census and mortality rates, largely confirmed their findings. Dr. Thuy Le and colleagues found that quitting at age 35, 45, 55, 65, or 75 years resulted in average life gains of 8, 5.6, 3.5, 1.7, and 0.7 years, respectively, relative to continuing to smoke. Because no patient is average, the analysis also presented some helpful probabilities. For example, a smoker who quits at age 65 has about a 1 in 4 chance of gaining at least 1 full year of life and a 1 in 6 chance of gaining at least 4 years. In other words, from a life expectancy perspective alone, it’s almost never too late to quit smoking.
Dr. Lin is a family physician and Associate Director, Family Medicine Residency Program, Lancaster General Hospital, Lancaster, Pennsylvania. He blogs at Common Sense Family Doctor. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An estimated 450,000 US deaths are expected this year from conditions attributed to cigarette smoking. Although the percentage of adults who smoke declined from 21% in 2005 to 11% in 2022, the annual death toll has been stable since 2005 and isn’t expected to decline until 2030, owing to an aging population of current and former smokers.
In 2022, based on a national survey, two thirds of the 28.8 million US adult smokers wanted to quit, and more than half tried quitting on their own or with the help of clinicians, but less than 9% succeeded in kicking the habit. The health benefits of quitting, summarized in a patient education handout from the American Cancer Society, include a lower risk for cancer, diabetes, and cardiovascular disease. Furthermore, the handout states, “quitting smoking can add as much as 10 years to your life, compared to if you continued to smoke.”
For my patients older than age 50 who are lifelong smokers, the qualifier “as much as” can be a sticking point. Although most recognize that continuing to smoke exposes them to greater health risks and are willing to undergo lung cancer screening and receive pneumococcal vaccines, a kind of fatalism frequently sets in. I’ve heard more times than I can recall some version of the declaration, “It’s too late for quitting to make much difference for me.” Many smokers think that once they reach middle age, gains in life expectancy will be too small to be worth the intense effort and multiple failed attempts that are typically required to quit permanently. Until recently, there were few data I could call on to persuade them they were wrong.
In February 2024, Dr. Eo Rin Cho and colleagues pooled data from four national cohort studies (United States, United Kingdom, Norway, and Canada) to calculate mortality differences among current, former, and never smokers aged 20-79 years. Compared with never smokers, lifelong smokers died an average of 12-13 years earlier. However, quitting before age 50 nearly eliminated the excess mortality associated with smoking, and in the 50- to 59-year-old age group, cessation eventually reduced excess mortality by 92%-95%. Better yet, more than half of the benefits occurred within the first 3 years after cessation.
At first glance, these estimates may seem too good to be true. A few months later, though, a different research group, using data from a large cancer prevention study and 2018 US population census and mortality rates, largely confirmed their findings. Dr. Thuy Le and colleagues found that quitting at age 35, 45, 55, 65, or 75 years resulted in average life gains of 8, 5.6, 3.5, 1.7, and 0.7 years, respectively, relative to continuing to smoke. Because no patient is average, the analysis also presented some helpful probabilities. For example, a smoker who quits at age 65 has about a 1 in 4 chance of gaining at least 1 full year of life and a 1 in 6 chance of gaining at least 4 years. In other words, from a life expectancy perspective alone, it’s almost never too late to quit smoking.
Dr. Lin is a family physician and Associate Director, Family Medicine Residency Program, Lancaster General Hospital, Lancaster, Pennsylvania. He blogs at Common Sense Family Doctor. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An estimated 450,000 US deaths are expected this year from conditions attributed to cigarette smoking. Although the percentage of adults who smoke declined from 21% in 2005 to 11% in 2022, the annual death toll has been stable since 2005 and isn’t expected to decline until 2030, owing to an aging population of current and former smokers.
In 2022, based on a national survey, two thirds of the 28.8 million US adult smokers wanted to quit, and more than half tried quitting on their own or with the help of clinicians, but less than 9% succeeded in kicking the habit. The health benefits of quitting, summarized in a patient education handout from the American Cancer Society, include a lower risk for cancer, diabetes, and cardiovascular disease. Furthermore, the handout states, “quitting smoking can add as much as 10 years to your life, compared to if you continued to smoke.”
For my patients older than age 50 who are lifelong smokers, the qualifier “as much as” can be a sticking point. Although most recognize that continuing to smoke exposes them to greater health risks and are willing to undergo lung cancer screening and receive pneumococcal vaccines, a kind of fatalism frequently sets in. I’ve heard more times than I can recall some version of the declaration, “It’s too late for quitting to make much difference for me.” Many smokers think that once they reach middle age, gains in life expectancy will be too small to be worth the intense effort and multiple failed attempts that are typically required to quit permanently. Until recently, there were few data I could call on to persuade them they were wrong.
In February 2024, Dr. Eo Rin Cho and colleagues pooled data from four national cohort studies (United States, United Kingdom, Norway, and Canada) to calculate mortality differences among current, former, and never smokers aged 20-79 years. Compared with never smokers, lifelong smokers died an average of 12-13 years earlier. However, quitting before age 50 nearly eliminated the excess mortality associated with smoking, and in the 50- to 59-year-old age group, cessation eventually reduced excess mortality by 92%-95%. Better yet, more than half of the benefits occurred within the first 3 years after cessation.
At first glance, these estimates may seem too good to be true. A few months later, though, a different research group, using data from a large cancer prevention study and 2018 US population census and mortality rates, largely confirmed their findings. Dr. Thuy Le and colleagues found that quitting at age 35, 45, 55, 65, or 75 years resulted in average life gains of 8, 5.6, 3.5, 1.7, and 0.7 years, respectively, relative to continuing to smoke. Because no patient is average, the analysis also presented some helpful probabilities. For example, a smoker who quits at age 65 has about a 1 in 4 chance of gaining at least 1 full year of life and a 1 in 6 chance of gaining at least 4 years. In other words, from a life expectancy perspective alone, it’s almost never too late to quit smoking.
Dr. Lin is a family physician and Associate Director, Family Medicine Residency Program, Lancaster General Hospital, Lancaster, Pennsylvania. He blogs at Common Sense Family Doctor. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Regularly Drinking Alcohol After Age 60 Linked to Early Death
That’s according to the findings of a new, large study that was published in JAMA Network Openand build upon numerous other recent studies concluding that any amount of alcohol consumption is linked to significant health risks. That’s a change from decades of public health messaging suggesting that moderate alcohol intake (one or two drinks per day) wasn’t dangerous. Recently, experts have uncovered flaws in how researchers came to those earlier conclusions.
In this latest study, researchers in Spain analyzed health data for more than 135,000 people, all of whom were at least 60 years old, lived in the United Kingdom, and provided their health information to the UK Biobank database. The average age of people at the start of the analysis period was 64.
The researchers compared 12 years of health outcomes for occasional drinkers with those who averaged drinking at least some alcohol on a daily basis. The greatest health risks were seen between occasional drinkers and those whom the researchers labeled “high risk.” Occasional drinkers had less than about two drinks per week. The high-risk group included men who averaged nearly three drinks per day or more, and women who averaged about a drink and a half per day or more. The analysis showed that, compared with occasional drinking, high-risk drinking was linked to a 33% increased risk of early death, a 39% increased risk of dying from cancer, and a 21% increased risk of dying from problems with the heart and blood vessels.
More moderate drinking habits were also linked to an increased risk of early death and dying from cancer, and even just averaging about one drink or less daily was associated with an 11% higher risk of dying from cancer. Low and moderate drinkers were most at risk if they also had health problems or experienced socioeconomic factors like living in less affluent neighborhoods.
The findings also suggested the potential that mostly drinking wine, or drinking mostly with meals, may be lower risk, but the researchers called for further study on those topics since “it may mostly reflect the effect of healthier lifestyles, slower alcohol absorption, or nonalcoholic components of beverages.”
A recent Gallup poll showed that overall, Americans’ attitudes toward the health impacts of alcohol are changing, with 65% of young adults (ages 18-34) saying that drinking can have negative health effects. But just 39% of adults age 55 or older agreed that drinking is bad for a person’s health. The gap in perspectives between younger and older adults about drinking is the largest on record, Gallup reported.
The study investigators reported no conflicts of interest.
A version of this article first appeared on WebMD.com.
That’s according to the findings of a new, large study that was published in JAMA Network Openand build upon numerous other recent studies concluding that any amount of alcohol consumption is linked to significant health risks. That’s a change from decades of public health messaging suggesting that moderate alcohol intake (one or two drinks per day) wasn’t dangerous. Recently, experts have uncovered flaws in how researchers came to those earlier conclusions.
In this latest study, researchers in Spain analyzed health data for more than 135,000 people, all of whom were at least 60 years old, lived in the United Kingdom, and provided their health information to the UK Biobank database. The average age of people at the start of the analysis period was 64.
The researchers compared 12 years of health outcomes for occasional drinkers with those who averaged drinking at least some alcohol on a daily basis. The greatest health risks were seen between occasional drinkers and those whom the researchers labeled “high risk.” Occasional drinkers had less than about two drinks per week. The high-risk group included men who averaged nearly three drinks per day or more, and women who averaged about a drink and a half per day or more. The analysis showed that, compared with occasional drinking, high-risk drinking was linked to a 33% increased risk of early death, a 39% increased risk of dying from cancer, and a 21% increased risk of dying from problems with the heart and blood vessels.
More moderate drinking habits were also linked to an increased risk of early death and dying from cancer, and even just averaging about one drink or less daily was associated with an 11% higher risk of dying from cancer. Low and moderate drinkers were most at risk if they also had health problems or experienced socioeconomic factors like living in less affluent neighborhoods.
The findings also suggested the potential that mostly drinking wine, or drinking mostly with meals, may be lower risk, but the researchers called for further study on those topics since “it may mostly reflect the effect of healthier lifestyles, slower alcohol absorption, or nonalcoholic components of beverages.”
A recent Gallup poll showed that overall, Americans’ attitudes toward the health impacts of alcohol are changing, with 65% of young adults (ages 18-34) saying that drinking can have negative health effects. But just 39% of adults age 55 or older agreed that drinking is bad for a person’s health. The gap in perspectives between younger and older adults about drinking is the largest on record, Gallup reported.
The study investigators reported no conflicts of interest.
A version of this article first appeared on WebMD.com.
That’s according to the findings of a new, large study that was published in JAMA Network Openand build upon numerous other recent studies concluding that any amount of alcohol consumption is linked to significant health risks. That’s a change from decades of public health messaging suggesting that moderate alcohol intake (one or two drinks per day) wasn’t dangerous. Recently, experts have uncovered flaws in how researchers came to those earlier conclusions.
In this latest study, researchers in Spain analyzed health data for more than 135,000 people, all of whom were at least 60 years old, lived in the United Kingdom, and provided their health information to the UK Biobank database. The average age of people at the start of the analysis period was 64.
The researchers compared 12 years of health outcomes for occasional drinkers with those who averaged drinking at least some alcohol on a daily basis. The greatest health risks were seen between occasional drinkers and those whom the researchers labeled “high risk.” Occasional drinkers had less than about two drinks per week. The high-risk group included men who averaged nearly three drinks per day or more, and women who averaged about a drink and a half per day or more. The analysis showed that, compared with occasional drinking, high-risk drinking was linked to a 33% increased risk of early death, a 39% increased risk of dying from cancer, and a 21% increased risk of dying from problems with the heart and blood vessels.
More moderate drinking habits were also linked to an increased risk of early death and dying from cancer, and even just averaging about one drink or less daily was associated with an 11% higher risk of dying from cancer. Low and moderate drinkers were most at risk if they also had health problems or experienced socioeconomic factors like living in less affluent neighborhoods.
The findings also suggested the potential that mostly drinking wine, or drinking mostly with meals, may be lower risk, but the researchers called for further study on those topics since “it may mostly reflect the effect of healthier lifestyles, slower alcohol absorption, or nonalcoholic components of beverages.”
A recent Gallup poll showed that overall, Americans’ attitudes toward the health impacts of alcohol are changing, with 65% of young adults (ages 18-34) saying that drinking can have negative health effects. But just 39% of adults age 55 or older agreed that drinking is bad for a person’s health. The gap in perspectives between younger and older adults about drinking is the largest on record, Gallup reported.
The study investigators reported no conflicts of interest.
A version of this article first appeared on WebMD.com.
FROM JAMA NETWORK OPEN
One in Ten Chronic Pain Patients May Develop Opioid Use Disorder
TOPLINE:
Nearly 10% of patients with chronic pain treated with opioids develop opioid use disorder, whereas 30% show signs and symptoms of dependence, highlighting the need for monitoring and alternative pain management strategies.
METHODOLOGY:
- Researchers conducted a systematic review and meta-analysis using MEDLINE, Embase, and PsycINFO databases from inception to January 27, 2021.
- The studies analyzed were predominantly from the United States (n = 115) as well as high-income countries such as the United Kingdom (n = 5), France (n = 3), Spain (n = 4), Germany (n = 4), and Australia (n = 2).
- A total of 148 studies from various settings with over 4.3 million participants were included, focusing on patients aged ≥ 12 years with chronic non-cancer pain of ≥ 3 months duration, treated with opioid analgesics.
- Problematic opioid use was categorized into four categories: dependence and opioid use disorder, signs and symptoms of dependence and opioid use disorder, aberrant behavior, and at risk for dependence and opioid use disorder.
TAKEAWAY:
- The pooled prevalence of dependence and opioid use disorder was 9.3% (95% CI, 5.7%-14.8%), with significant heterogeneity across studies.
- Signs and symptoms of dependence were observed in 29.6% (95% CI, 22.1%-38.3%) of patients, indicating a high prevalence of problematic opioid use.
- Aberrant behavior was reported in 22% (95% CI, 17.4%-27.3%) of patients, highlighting the need for careful monitoring and intervention.
- The prevalence of patients at risk of developing dependence was 12.4% (95% CI, 4.3%-30.7%), suggesting the importance of early identification and prevention strategies.
IN PRACTICE:
“Clinicians and policymakers need a more accurate estimate of the prevalence of problematic opioid use in pain patients so that they can gauge the true extent of the problem, change prescribing guidance if necessary, and develop and implement effective interventions to manage the problem,” Kyla H. Thomas, PhD, the lead author, noted in a press release. Knowing the size of the problem is a necessary step to managing it, she added.
SOURCE:
The study was led by Dr. Thomas, Population Health Sciences, Bristol Medical School, University of Bristol in England. It was published online, in Addiction.
LIMITATIONS:
The study’s high heterogeneity across included studies suggests caution in interpreting the findings. The reliance on self-reported data and varying definitions of problematic opioid use may affect the accuracy of prevalence estimates. Most studies were conducted in high-income countries, limiting the generalizability to other settings.
DISCLOSURES:
The study was funded by the National Institute for Health and Care Research (NIHR). Dr. Thomas reported receiving financial support from the NIHR for this study.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Nearly 10% of patients with chronic pain treated with opioids develop opioid use disorder, whereas 30% show signs and symptoms of dependence, highlighting the need for monitoring and alternative pain management strategies.
METHODOLOGY:
- Researchers conducted a systematic review and meta-analysis using MEDLINE, Embase, and PsycINFO databases from inception to January 27, 2021.
- The studies analyzed were predominantly from the United States (n = 115) as well as high-income countries such as the United Kingdom (n = 5), France (n = 3), Spain (n = 4), Germany (n = 4), and Australia (n = 2).
- A total of 148 studies from various settings with over 4.3 million participants were included, focusing on patients aged ≥ 12 years with chronic non-cancer pain of ≥ 3 months duration, treated with opioid analgesics.
- Problematic opioid use was categorized into four categories: dependence and opioid use disorder, signs and symptoms of dependence and opioid use disorder, aberrant behavior, and at risk for dependence and opioid use disorder.
TAKEAWAY:
- The pooled prevalence of dependence and opioid use disorder was 9.3% (95% CI, 5.7%-14.8%), with significant heterogeneity across studies.
- Signs and symptoms of dependence were observed in 29.6% (95% CI, 22.1%-38.3%) of patients, indicating a high prevalence of problematic opioid use.
- Aberrant behavior was reported in 22% (95% CI, 17.4%-27.3%) of patients, highlighting the need for careful monitoring and intervention.
- The prevalence of patients at risk of developing dependence was 12.4% (95% CI, 4.3%-30.7%), suggesting the importance of early identification and prevention strategies.
IN PRACTICE:
“Clinicians and policymakers need a more accurate estimate of the prevalence of problematic opioid use in pain patients so that they can gauge the true extent of the problem, change prescribing guidance if necessary, and develop and implement effective interventions to manage the problem,” Kyla H. Thomas, PhD, the lead author, noted in a press release. Knowing the size of the problem is a necessary step to managing it, she added.
SOURCE:
The study was led by Dr. Thomas, Population Health Sciences, Bristol Medical School, University of Bristol in England. It was published online, in Addiction.
LIMITATIONS:
The study’s high heterogeneity across included studies suggests caution in interpreting the findings. The reliance on self-reported data and varying definitions of problematic opioid use may affect the accuracy of prevalence estimates. Most studies were conducted in high-income countries, limiting the generalizability to other settings.
DISCLOSURES:
The study was funded by the National Institute for Health and Care Research (NIHR). Dr. Thomas reported receiving financial support from the NIHR for this study.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Nearly 10% of patients with chronic pain treated with opioids develop opioid use disorder, whereas 30% show signs and symptoms of dependence, highlighting the need for monitoring and alternative pain management strategies.
METHODOLOGY:
- Researchers conducted a systematic review and meta-analysis using MEDLINE, Embase, and PsycINFO databases from inception to January 27, 2021.
- The studies analyzed were predominantly from the United States (n = 115) as well as high-income countries such as the United Kingdom (n = 5), France (n = 3), Spain (n = 4), Germany (n = 4), and Australia (n = 2).
- A total of 148 studies from various settings with over 4.3 million participants were included, focusing on patients aged ≥ 12 years with chronic non-cancer pain of ≥ 3 months duration, treated with opioid analgesics.
- Problematic opioid use was categorized into four categories: dependence and opioid use disorder, signs and symptoms of dependence and opioid use disorder, aberrant behavior, and at risk for dependence and opioid use disorder.
TAKEAWAY:
- The pooled prevalence of dependence and opioid use disorder was 9.3% (95% CI, 5.7%-14.8%), with significant heterogeneity across studies.
- Signs and symptoms of dependence were observed in 29.6% (95% CI, 22.1%-38.3%) of patients, indicating a high prevalence of problematic opioid use.
- Aberrant behavior was reported in 22% (95% CI, 17.4%-27.3%) of patients, highlighting the need for careful monitoring and intervention.
- The prevalence of patients at risk of developing dependence was 12.4% (95% CI, 4.3%-30.7%), suggesting the importance of early identification and prevention strategies.
IN PRACTICE:
“Clinicians and policymakers need a more accurate estimate of the prevalence of problematic opioid use in pain patients so that they can gauge the true extent of the problem, change prescribing guidance if necessary, and develop and implement effective interventions to manage the problem,” Kyla H. Thomas, PhD, the lead author, noted in a press release. Knowing the size of the problem is a necessary step to managing it, she added.
SOURCE:
The study was led by Dr. Thomas, Population Health Sciences, Bristol Medical School, University of Bristol in England. It was published online, in Addiction.
LIMITATIONS:
The study’s high heterogeneity across included studies suggests caution in interpreting the findings. The reliance on self-reported data and varying definitions of problematic opioid use may affect the accuracy of prevalence estimates. Most studies were conducted in high-income countries, limiting the generalizability to other settings.
DISCLOSURES:
The study was funded by the National Institute for Health and Care Research (NIHR). Dr. Thomas reported receiving financial support from the NIHR for this study.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Federal Health Care Data Trends 2024
Federal Health Care Data Trends is a special supplement to Federal Practitioner, showcasing the latest research in health care for veterans and active-duty military members via compelling infographics. Click below to view highlights from the issue:
Federal Health Care Data Trends is a special supplement to Federal Practitioner, showcasing the latest research in health care for veterans and active-duty military members via compelling infographics. Click below to view highlights from the issue:
Federal Health Care Data Trends is a special supplement to Federal Practitioner, showcasing the latest research in health care for veterans and active-duty military members via compelling infographics. Click below to view highlights from the issue:
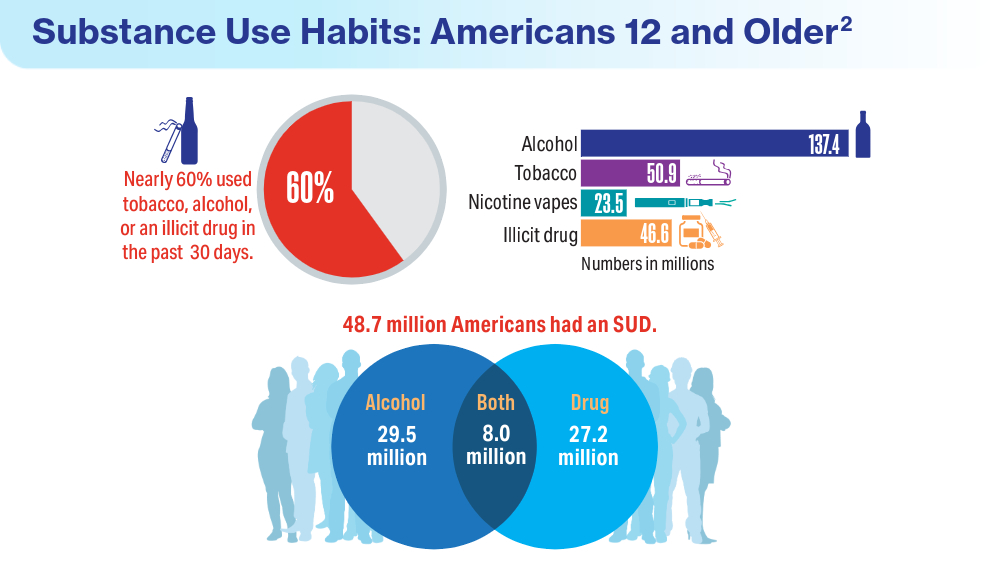
Data Trends 2024: Substance Use Disorder
- Teeters JB, Lancaster CL, Brown DG, Back SE. Substance use disorders in military veterans: prevalence and treatment challenges. Subst Abuse Rehabil. 2017;8:69-77. doi:10.2147/sar.s116720
- Substance Abuse and Mental Health Services Administration. Results from the 2022 National Survey on Drug Use and Health: a companion infographic. SAMHSA publication no. PEP23-07-01-007. November 13, 2023. Accessed March 25, 2024. https://www.samhsa.gov/data/sites/default/files/reports/rpt42730/2022-nsduh-infographic-report.pdf
- Substance Abuse and Mental Health Services Administration. 2022 National Survey on Drug Use and Health: Among the Veteran Population Aged 18 or Older. Accessed March 25, 2024. https://www.samhsa.gov/data/sites/default/files/reports/rpt44472/2022-nsduh-pop-slides-veterans.pdf
- Cypel YS, DePhilippis D, Davey VJ. Substance use in U.S. Vietnam War era veterans and nonveterans: results from the Vietnam Era Health Retrospective Observational Study. Subst Use Misuse. 2023;58(7):858-870. doi:10.1080/10826084.2023.2188427
- Otufowora A, Liu Y, Okusanya A, Ogidan A, Okusanya A, Cottler LB. The effect of veteran status and chronic pain on past 30-day sedative use among community-dwelling adult males. J Am Board Fam Med. 2024;37(1):118-128. doi:10.3122/jabfm.2023.230226R2
- Teeters JB, Lancaster CL, Brown DG, Back SE. Substance use disorders in military veterans: prevalence and treatment challenges. Subst Abuse Rehabil. 2017;8:69-77. doi:10.2147/sar.s116720
- Substance Abuse and Mental Health Services Administration. Results from the 2022 National Survey on Drug Use and Health: a companion infographic. SAMHSA publication no. PEP23-07-01-007. November 13, 2023. Accessed March 25, 2024. https://www.samhsa.gov/data/sites/default/files/reports/rpt42730/2022-nsduh-infographic-report.pdf
- Substance Abuse and Mental Health Services Administration. 2022 National Survey on Drug Use and Health: Among the Veteran Population Aged 18 or Older. Accessed March 25, 2024. https://www.samhsa.gov/data/sites/default/files/reports/rpt44472/2022-nsduh-pop-slides-veterans.pdf
- Cypel YS, DePhilippis D, Davey VJ. Substance use in U.S. Vietnam War era veterans and nonveterans: results from the Vietnam Era Health Retrospective Observational Study. Subst Use Misuse. 2023;58(7):858-870. doi:10.1080/10826084.2023.2188427
- Otufowora A, Liu Y, Okusanya A, Ogidan A, Okusanya A, Cottler LB. The effect of veteran status and chronic pain on past 30-day sedative use among community-dwelling adult males. J Am Board Fam Med. 2024;37(1):118-128. doi:10.3122/jabfm.2023.230226R2
- Teeters JB, Lancaster CL, Brown DG, Back SE. Substance use disorders in military veterans: prevalence and treatment challenges. Subst Abuse Rehabil. 2017;8:69-77. doi:10.2147/sar.s116720
- Substance Abuse and Mental Health Services Administration. Results from the 2022 National Survey on Drug Use and Health: a companion infographic. SAMHSA publication no. PEP23-07-01-007. November 13, 2023. Accessed March 25, 2024. https://www.samhsa.gov/data/sites/default/files/reports/rpt42730/2022-nsduh-infographic-report.pdf
- Substance Abuse and Mental Health Services Administration. 2022 National Survey on Drug Use and Health: Among the Veteran Population Aged 18 or Older. Accessed March 25, 2024. https://www.samhsa.gov/data/sites/default/files/reports/rpt44472/2022-nsduh-pop-slides-veterans.pdf
- Cypel YS, DePhilippis D, Davey VJ. Substance use in U.S. Vietnam War era veterans and nonveterans: results from the Vietnam Era Health Retrospective Observational Study. Subst Use Misuse. 2023;58(7):858-870. doi:10.1080/10826084.2023.2188427
- Otufowora A, Liu Y, Okusanya A, Ogidan A, Okusanya A, Cottler LB. The effect of veteran status and chronic pain on past 30-day sedative use among community-dwelling adult males. J Am Board Fam Med. 2024;37(1):118-128. doi:10.3122/jabfm.2023.230226R2
Is Buprenorphine/Naloxone Safer Than Buprenorphine Alone During Pregnancy?
TOPLINE:
Buprenorphine combined with naloxone during pregnancy is associated with lower risks for neonatal abstinence syndrome and neonatal intensive care unit admission than buprenorphine alone. The study also found no significant differences in major congenital malformations between the two treatments.
METHODOLOGY:
- Researchers conducted a population-based cohort study using healthcare utilization data of people who were insured by Medicaid between 2000 and 2018.
- A total of 8695 pregnant individuals were included, with 3369 exposed to buprenorphine/naloxone and 5326 exposed to buprenorphine alone during the first trimester.
- Outcome measures included major congenital malformations, low birth weight, neonatal abstinence syndrome, neonatal intensive care unit admission, preterm birth, respiratory symptoms, small for gestational age, cesarean delivery, and maternal morbidity.
- The study excluded pregnancies with chromosomal anomalies, first-trimester exposure to known teratogens, or methadone use during baseline or the first trimester.
TAKEAWAY:
- According to the authors, buprenorphine/naloxone exposure during pregnancy was associated with a lower risk for neonatal abstinence syndrome (weighted risk ratio [RR], 0.77; 95% CI, 0.70-0.84) than buprenorphine alone.
- The researchers found a modestly lower risk for neonatal intensive care unit admission (weighted RR, 0.91; 95% CI, 0.85-0.98) and small risk for gestational age (weighted RR, 0.86; 95% CI, 0.75-0.98) in the buprenorphine/naloxone group.
- No significant differences were observed between the two groups in major congenital malformations, low birth weight, preterm birth, respiratory symptoms, or cesarean delivery.
IN PRACTICE:
“For the outcomes assessed, compared with buprenorphine alone, buprenorphine combined with naloxone during pregnancy appears to be a safe treatment option. This supports the view that both formulations are reasonable options for treatment of OUD in pregnancy, affirming flexibility in collaborative treatment decision-making,” the study authors wrote.
SOURCE:
The study was led by Loreen Straub, MD, MS, of the Division of Pharmacoepidemiology and Pharmacoeconomics at Brigham and Women’s Hospital and Harvard Medical School in Boston. It was published online in JAMA.
LIMITATIONS:
Some potential confounders, such as alcohol use and cigarette smoking, may not have been recorded in claims data. The findings for many of the neonatal and maternal outcomes suggest that confounding by unmeasured factors is an unlikely explanation for the associations observed. Individuals identified as exposed based on filled prescriptions might not have used the medication. The study used outcome algorithms with relatively high positive predictive values to minimize outcome misclassification. The cohort was restricted to live births to enable linkage to infants and to assess neonatal outcomes.
DISCLOSURES:
Various authors reported receiving grants and personal fees from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institute on Drug Abuse, Roche, Moderna, Takeda, and Janssen Global, among others.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Buprenorphine combined with naloxone during pregnancy is associated with lower risks for neonatal abstinence syndrome and neonatal intensive care unit admission than buprenorphine alone. The study also found no significant differences in major congenital malformations between the two treatments.
METHODOLOGY:
- Researchers conducted a population-based cohort study using healthcare utilization data of people who were insured by Medicaid between 2000 and 2018.
- A total of 8695 pregnant individuals were included, with 3369 exposed to buprenorphine/naloxone and 5326 exposed to buprenorphine alone during the first trimester.
- Outcome measures included major congenital malformations, low birth weight, neonatal abstinence syndrome, neonatal intensive care unit admission, preterm birth, respiratory symptoms, small for gestational age, cesarean delivery, and maternal morbidity.
- The study excluded pregnancies with chromosomal anomalies, first-trimester exposure to known teratogens, or methadone use during baseline or the first trimester.
TAKEAWAY:
- According to the authors, buprenorphine/naloxone exposure during pregnancy was associated with a lower risk for neonatal abstinence syndrome (weighted risk ratio [RR], 0.77; 95% CI, 0.70-0.84) than buprenorphine alone.
- The researchers found a modestly lower risk for neonatal intensive care unit admission (weighted RR, 0.91; 95% CI, 0.85-0.98) and small risk for gestational age (weighted RR, 0.86; 95% CI, 0.75-0.98) in the buprenorphine/naloxone group.
- No significant differences were observed between the two groups in major congenital malformations, low birth weight, preterm birth, respiratory symptoms, or cesarean delivery.
IN PRACTICE:
“For the outcomes assessed, compared with buprenorphine alone, buprenorphine combined with naloxone during pregnancy appears to be a safe treatment option. This supports the view that both formulations are reasonable options for treatment of OUD in pregnancy, affirming flexibility in collaborative treatment decision-making,” the study authors wrote.
SOURCE:
The study was led by Loreen Straub, MD, MS, of the Division of Pharmacoepidemiology and Pharmacoeconomics at Brigham and Women’s Hospital and Harvard Medical School in Boston. It was published online in JAMA.
LIMITATIONS:
Some potential confounders, such as alcohol use and cigarette smoking, may not have been recorded in claims data. The findings for many of the neonatal and maternal outcomes suggest that confounding by unmeasured factors is an unlikely explanation for the associations observed. Individuals identified as exposed based on filled prescriptions might not have used the medication. The study used outcome algorithms with relatively high positive predictive values to minimize outcome misclassification. The cohort was restricted to live births to enable linkage to infants and to assess neonatal outcomes.
DISCLOSURES:
Various authors reported receiving grants and personal fees from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institute on Drug Abuse, Roche, Moderna, Takeda, and Janssen Global, among others.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Buprenorphine combined with naloxone during pregnancy is associated with lower risks for neonatal abstinence syndrome and neonatal intensive care unit admission than buprenorphine alone. The study also found no significant differences in major congenital malformations between the two treatments.
METHODOLOGY:
- Researchers conducted a population-based cohort study using healthcare utilization data of people who were insured by Medicaid between 2000 and 2018.
- A total of 8695 pregnant individuals were included, with 3369 exposed to buprenorphine/naloxone and 5326 exposed to buprenorphine alone during the first trimester.
- Outcome measures included major congenital malformations, low birth weight, neonatal abstinence syndrome, neonatal intensive care unit admission, preterm birth, respiratory symptoms, small for gestational age, cesarean delivery, and maternal morbidity.
- The study excluded pregnancies with chromosomal anomalies, first-trimester exposure to known teratogens, or methadone use during baseline or the first trimester.
TAKEAWAY:
- According to the authors, buprenorphine/naloxone exposure during pregnancy was associated with a lower risk for neonatal abstinence syndrome (weighted risk ratio [RR], 0.77; 95% CI, 0.70-0.84) than buprenorphine alone.
- The researchers found a modestly lower risk for neonatal intensive care unit admission (weighted RR, 0.91; 95% CI, 0.85-0.98) and small risk for gestational age (weighted RR, 0.86; 95% CI, 0.75-0.98) in the buprenorphine/naloxone group.
- No significant differences were observed between the two groups in major congenital malformations, low birth weight, preterm birth, respiratory symptoms, or cesarean delivery.
IN PRACTICE:
“For the outcomes assessed, compared with buprenorphine alone, buprenorphine combined with naloxone during pregnancy appears to be a safe treatment option. This supports the view that both formulations are reasonable options for treatment of OUD in pregnancy, affirming flexibility in collaborative treatment decision-making,” the study authors wrote.
SOURCE:
The study was led by Loreen Straub, MD, MS, of the Division of Pharmacoepidemiology and Pharmacoeconomics at Brigham and Women’s Hospital and Harvard Medical School in Boston. It was published online in JAMA.
LIMITATIONS:
Some potential confounders, such as alcohol use and cigarette smoking, may not have been recorded in claims data. The findings for many of the neonatal and maternal outcomes suggest that confounding by unmeasured factors is an unlikely explanation for the associations observed. Individuals identified as exposed based on filled prescriptions might not have used the medication. The study used outcome algorithms with relatively high positive predictive values to minimize outcome misclassification. The cohort was restricted to live births to enable linkage to infants and to assess neonatal outcomes.
DISCLOSURES:
Various authors reported receiving grants and personal fees from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institute on Drug Abuse, Roche, Moderna, Takeda, and Janssen Global, among others.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Cannabis Overuse Linked to Increased Risk for Head and Neck Cancer
TOPLINE:
The study analyzed data from over four million patients, highlighting the potential carcinogenic effects of the substance.
METHODOLOGY:
- Researchers analyzed data from a globally federated health research network TriNetX, which included over 90 million men and women from 64 health care organizations in the United States.
- More than 4.1 million patients were included in the analysis, including 116,076 individuals diagnosed with cannabis-related disorder and 3.9 million without the disorder. Cannabis-related disorders involve the excessive use of cannabis with associated psychosocial symptoms, such as impaired social and/or occupational functioning.
- Patients with cannabis-related disorder were matched with those without the disorder based on demographic characteristics, alcohol-related disorders, and tobacco use.
- The primary outcome was the diagnosis of head and neck cancer, including subsites such as oral, oropharyngeal, nasopharyngeal, laryngeal, hypopharyngeal, and salivary gland malignancies.
- Propensity score matching and Poisson regression analysis were used to compare the incidence of head and neck cancers between the groups.
TAKEAWAY:
- According to the researchers, patients with a cannabis-related disorder had a higher risk for any head and neck cancer (relative risk [RR], 3.49; 95% CI, 2.78-4.39) than those without the disorder.
- The risk for specific cancers was also higher in the group with cannabis-related disorders, including oral (RR, 2.51; 95% CI, 1.81-3.47) and oropharyngeal malignancies (RR, 4.90; 95% CI, 2.99-8.02).
- The RR for laryngeal cancer was significantly higher in the patients with a cannabis-related disorder (RR, 8.39; 95% CI, 4.72-14.90).
- The findings suggest that cannabis use disorder is associated with an increased risk for head and neck cancers, highlighting the need for further research to understand the mechanisms involved.
IN PRACTICE:
“In this cohort study, cannabis disorder diagnosis was independently associated with greater risk of subsequent development of any [head or neck cancer] as well as cancers in various subsites of the head and neck among US adults. When limited to cases of [such cancers] occurring greater than 1 year after cannabis use disorder diagnosis, many of the associations increased, demonstrating additional strength in the association,” the authors of the study wrote.
“The association of cannabis and head and neck cancer in this study spanned 2 decades during a rapid growth in use. If this association is causative, the burden of [head and neck cancers] attributable to cannabis will continue to increase, and perhaps dramatically,” said the authors of an editorial accompanying the journal article. “Given that cannabis is now a $20 billion industry in the US alone with expanding availability, use, and popularity, this may be “déjà vu, all over again” without appropriate research to understand the potential carcinogenic and salutatory effects of cannabis. Or, in the words of Yogi Berra, “If you don’t know where you are going, you might wind up someplace else.”
SOURCE:
The study was led by Tyler J. Gallagher and Niels C. Kokot, MD, at the Keck School of Medicine of the University of Southern California in Los Angeles. It was published online in JAMA Otolaryngology–Head & Neck Surgery.
LIMITATIONS:
The study had limited information about cohort composition and length of follow-up, which may affect the generalizability of the findings. The lack of direct exposure duration, intensity, and dosage information limits the ability to analyze dose-response relationships. Potential inconsistency of diagnosis and reliance on medical record codes may introduce bias. Cannabis use is likely underreported, which could decrease the relative risks discovered. The study was further limited by the lack of information on dosage and frequency of cannabis use, as well as some controls, including alcohol and tobacco use.
DISCLOSURES:
Gallagher disclosed receiving grants from the Keck School of Medicine of the University of Southern California, Los Angeles. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
The study analyzed data from over four million patients, highlighting the potential carcinogenic effects of the substance.
METHODOLOGY:
- Researchers analyzed data from a globally federated health research network TriNetX, which included over 90 million men and women from 64 health care organizations in the United States.
- More than 4.1 million patients were included in the analysis, including 116,076 individuals diagnosed with cannabis-related disorder and 3.9 million without the disorder. Cannabis-related disorders involve the excessive use of cannabis with associated psychosocial symptoms, such as impaired social and/or occupational functioning.
- Patients with cannabis-related disorder were matched with those without the disorder based on demographic characteristics, alcohol-related disorders, and tobacco use.
- The primary outcome was the diagnosis of head and neck cancer, including subsites such as oral, oropharyngeal, nasopharyngeal, laryngeal, hypopharyngeal, and salivary gland malignancies.
- Propensity score matching and Poisson regression analysis were used to compare the incidence of head and neck cancers between the groups.
TAKEAWAY:
- According to the researchers, patients with a cannabis-related disorder had a higher risk for any head and neck cancer (relative risk [RR], 3.49; 95% CI, 2.78-4.39) than those without the disorder.
- The risk for specific cancers was also higher in the group with cannabis-related disorders, including oral (RR, 2.51; 95% CI, 1.81-3.47) and oropharyngeal malignancies (RR, 4.90; 95% CI, 2.99-8.02).
- The RR for laryngeal cancer was significantly higher in the patients with a cannabis-related disorder (RR, 8.39; 95% CI, 4.72-14.90).
- The findings suggest that cannabis use disorder is associated with an increased risk for head and neck cancers, highlighting the need for further research to understand the mechanisms involved.
IN PRACTICE:
“In this cohort study, cannabis disorder diagnosis was independently associated with greater risk of subsequent development of any [head or neck cancer] as well as cancers in various subsites of the head and neck among US adults. When limited to cases of [such cancers] occurring greater than 1 year after cannabis use disorder diagnosis, many of the associations increased, demonstrating additional strength in the association,” the authors of the study wrote.
“The association of cannabis and head and neck cancer in this study spanned 2 decades during a rapid growth in use. If this association is causative, the burden of [head and neck cancers] attributable to cannabis will continue to increase, and perhaps dramatically,” said the authors of an editorial accompanying the journal article. “Given that cannabis is now a $20 billion industry in the US alone with expanding availability, use, and popularity, this may be “déjà vu, all over again” without appropriate research to understand the potential carcinogenic and salutatory effects of cannabis. Or, in the words of Yogi Berra, “If you don’t know where you are going, you might wind up someplace else.”
SOURCE:
The study was led by Tyler J. Gallagher and Niels C. Kokot, MD, at the Keck School of Medicine of the University of Southern California in Los Angeles. It was published online in JAMA Otolaryngology–Head & Neck Surgery.
LIMITATIONS:
The study had limited information about cohort composition and length of follow-up, which may affect the generalizability of the findings. The lack of direct exposure duration, intensity, and dosage information limits the ability to analyze dose-response relationships. Potential inconsistency of diagnosis and reliance on medical record codes may introduce bias. Cannabis use is likely underreported, which could decrease the relative risks discovered. The study was further limited by the lack of information on dosage and frequency of cannabis use, as well as some controls, including alcohol and tobacco use.
DISCLOSURES:
Gallagher disclosed receiving grants from the Keck School of Medicine of the University of Southern California, Los Angeles. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
The study analyzed data from over four million patients, highlighting the potential carcinogenic effects of the substance.
METHODOLOGY:
- Researchers analyzed data from a globally federated health research network TriNetX, which included over 90 million men and women from 64 health care organizations in the United States.
- More than 4.1 million patients were included in the analysis, including 116,076 individuals diagnosed with cannabis-related disorder and 3.9 million without the disorder. Cannabis-related disorders involve the excessive use of cannabis with associated psychosocial symptoms, such as impaired social and/or occupational functioning.
- Patients with cannabis-related disorder were matched with those without the disorder based on demographic characteristics, alcohol-related disorders, and tobacco use.
- The primary outcome was the diagnosis of head and neck cancer, including subsites such as oral, oropharyngeal, nasopharyngeal, laryngeal, hypopharyngeal, and salivary gland malignancies.
- Propensity score matching and Poisson regression analysis were used to compare the incidence of head and neck cancers between the groups.
TAKEAWAY:
- According to the researchers, patients with a cannabis-related disorder had a higher risk for any head and neck cancer (relative risk [RR], 3.49; 95% CI, 2.78-4.39) than those without the disorder.
- The risk for specific cancers was also higher in the group with cannabis-related disorders, including oral (RR, 2.51; 95% CI, 1.81-3.47) and oropharyngeal malignancies (RR, 4.90; 95% CI, 2.99-8.02).
- The RR for laryngeal cancer was significantly higher in the patients with a cannabis-related disorder (RR, 8.39; 95% CI, 4.72-14.90).
- The findings suggest that cannabis use disorder is associated with an increased risk for head and neck cancers, highlighting the need for further research to understand the mechanisms involved.
IN PRACTICE:
“In this cohort study, cannabis disorder diagnosis was independently associated with greater risk of subsequent development of any [head or neck cancer] as well as cancers in various subsites of the head and neck among US adults. When limited to cases of [such cancers] occurring greater than 1 year after cannabis use disorder diagnosis, many of the associations increased, demonstrating additional strength in the association,” the authors of the study wrote.
“The association of cannabis and head and neck cancer in this study spanned 2 decades during a rapid growth in use. If this association is causative, the burden of [head and neck cancers] attributable to cannabis will continue to increase, and perhaps dramatically,” said the authors of an editorial accompanying the journal article. “Given that cannabis is now a $20 billion industry in the US alone with expanding availability, use, and popularity, this may be “déjà vu, all over again” without appropriate research to understand the potential carcinogenic and salutatory effects of cannabis. Or, in the words of Yogi Berra, “If you don’t know where you are going, you might wind up someplace else.”
SOURCE:
The study was led by Tyler J. Gallagher and Niels C. Kokot, MD, at the Keck School of Medicine of the University of Southern California in Los Angeles. It was published online in JAMA Otolaryngology–Head & Neck Surgery.
LIMITATIONS:
The study had limited information about cohort composition and length of follow-up, which may affect the generalizability of the findings. The lack of direct exposure duration, intensity, and dosage information limits the ability to analyze dose-response relationships. Potential inconsistency of diagnosis and reliance on medical record codes may introduce bias. Cannabis use is likely underreported, which could decrease the relative risks discovered. The study was further limited by the lack of information on dosage and frequency of cannabis use, as well as some controls, including alcohol and tobacco use.
DISCLOSURES:
Gallagher disclosed receiving grants from the Keck School of Medicine of the University of Southern California, Los Angeles. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Few Smokers Who Want to Quit Seek Healthcare Provider Help
Approximately half of US adult smokers tried to quit in 2022, but fewer than 40% used counseling or medication, and half received assistance or advice about quitting from clinicians, based on a review in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report.
Previous research has shown that clinician intervention and evidence-based treatment increase the odds that smokers can quit successfully, but the extent to which these interventions are applied in practice has not been well studied, the researchers noted.
Although great progress has been made in reducing cigarette smoking in the United States, disparities remain, both in use and in cessation, with an estimated 28.8 million adults reporting cigarette smoking in 2022, lead author Brenna VanFrank, MD, MSPH, said in an interview.
“Cigarette smoking remains the leading preventable cause of death and disease in the United States,” said Dr. VanFrank, Senior Medical Officer, Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion.
In a new review, the researchers examined data from the 2022 National Health Interview Survey. The study population included 27,651 adults aged 18 years and older. Current smoking was defined as currently smoking each day or some days and ever having smoked at least 100 cigarettes. The survey assessed the individuals’ interest in quitting, past-year quit attempts, recent quitting success, receipt of healthcare professional advice about quitting, use of counseling to help quit, and use of medication to help quit.
In 2022, approximately two thirds (67.7%) of the 28.8 million adult smokers in the United States wanted to quit, half (53.3%) tried to quit, but only 8.8% were successful. Of those who reported trying to quit, 38.3% used counseling or medication. Of these, 36.3% used medication, 7.3% used counseling, and 5.3% used both.
Indicators of smoking cessation varied by health characteristics and sociodemographic factors, with the highest prevalence of attempts to quit smoking in the past year among adults aged 18-24 years and the lowest among those aged 45-64 years (74.4% vs 47.5%).
Rates of successful quitting were highest among individuals with higher levels of education and income, and use of smoking cessation treatment was highest among White adults (42.7%), followed by non-Hispanic adults of another race, Black adults, and Hispanic adults (33.6%, 32.6%, and 28.8%, respectively).
Smokers of menthol cigarettes had similarly low success rates for quitting (< 10%), although they were significantly more likely than nonmenthol cigarette smokers to express interest in quitting (72.2% vs 65.4%). Smokers of menthol cigarettes also had significantly lower prevalences than smokers of nonmenthol cigarettes of receiving clinician advance to quit and using treatment strategies (both P < .05).
The study findings were limited by several factors including the use of self-reports, which may be subject to bias, and a lack of data on institutionalized adults or adults in the military, which may limit generalizability of the findings to those populations, the researchers noted.
However, the results suggest that opportunities exist to increase smoking cessation across public health and healthcare sectors by expanding access to and use of services and supports to help smokers quit, they wrote.
Ensuring Support for All Smokers Seeking to Quit
The takeaway for clinical practice remains that quitting smoking “is one of the most important actions people who smoke can take to improve their health,” Dr. VanFrank said in an interview.
“It is important to ensure everyone has an opportunity to quit smoking and has access to proven treatments to help them be successful,” she emphasized. Strategies that include behavioral counseling, cessation medications, and advice and support from healthcare professionals can increase quit success. Given that tobacco dependence is a chronic, relapsing condition driven by addiction to nicotine, quitting successfully often takes multiple tries, and those trying to quit may need long-term support and repeated treatment.
“Health systems changes, such as adoption of treatment protocols and standardized clinical work flows, can systematize clinical treatment delivery, and such changes might also serve to increase treatment access for the 75% of adults who smoke who see a healthcare professional in a given year,” said Dr. VanFrank.
As for additional research, “continued surveillance of tobacco use and cessation-related behaviors will help us monitor progress and identify continued opportunities to eliminate tobacco product use and tobacco-related disparities,” Dr. VanFrank said.
“We know a lot about what works to help people successfully quit smoking and what we can do to support people in making quit attempts,” she said. Including equitable opportunities in all commercial tobacco prevention and control efforts has the potential to reduce tobacco-related health disparities.
Overall smoking prevalence in the United States and the current study shows that most smokers would like to quit, David M. Mannino, MD, a pulmonologist and professor of medicine at the University of Kentucky, Lexington, said in an interview. The lack of success experienced by many smokers seeking to quit emphasizes the highly addictive nature of nicotine products, which cause death and disease when used as directed, added Dr. Mannino, who was not involved in the study.
The results of the review were not surprising, and reflect where tobacco treatment has been for the past 20 years, said Dr. Mannino. The good news is that smoking prevalence has continued to drop in the United States over the past 15 years. However, some bad news is that use of e-cigarettes/vaping is still increasing, especially in younger populations, and new nicotine delivery systems, such as pouches (Zyn) are addicting a new generation.
Always Ask About Smoking
In practice, “clinicians should always ask patients about cigarette smoking, as well as vaping and other nicotine use, advise them to quit, and refer them to tobacco treatment experts,” Dr. Mannino emphasized.
The bottom line is that better treatments are needed for tobacco/nicotine addiction, Dr. Mannino said. “Although we have come a long way, we have a long way to go as millions of smokers in the US and globally would like to quit.”
Tobacco-related disease continues to be the number one cause of morbidly and mortality in the United States, and although many current smokers want to quit, most are not successful, Jamie Garfield, MD, professor of thoracic medicine and surgery at the Lewis Katz School of Medicine at Temple University, Philadelphia, Pennsylvania, said in an interview.
“This review highlights the sheer number of current cigarette smokers who want to quit, how many of them attempted to quit, and how many of those were successful,” said Dr. Garfield, who was not involved in the study. Understanding the characteristics of individuals who are more or less likely to successfully quit smoking can help public health and healthcare sectors to increase smoking cessation by expanding access to and use of services and supports.
“We have to do better to control the sale of tobacco products and make tobacco cessation more accessible to everyone,” Dr. Garfield said. In addition, clinicians need to be consistent in asking patients about tobacco use. “If we don’t ask, we will not know who needs help.” Behavioral counseling helps, as does pharmacotherapy, and the two together are more effective than either alone, she added.
Cessation services need to be tailored to the many demographic groups who use tobacco products, said Dr. Garfield. “Just as marketing campaigns directed to older adults will be different from those directed to young adults, so too must cessation resources. Providers need better options to choose from with regard to cessation resources and behavioral counseling sessions. They need to be aware of what motivates one group of people to smoke and how they can be inspired to quit, including which pharmacotherapies are affordable, available, and will work; the same strategies will not work for all people”
The study was supported by the Centers for Disease Control and Prevention’s National Center for Chronic Disease Prevention and Health Promotion. The researchers had no financial conflicts to disclose. Dr. Mannino disclosed serving as an expert witness for on tobacco use and tobacco-caused disease on behalf of people suing the tobacco and vaping industries. Dr. Garfield had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
Approximately half of US adult smokers tried to quit in 2022, but fewer than 40% used counseling or medication, and half received assistance or advice about quitting from clinicians, based on a review in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report.
Previous research has shown that clinician intervention and evidence-based treatment increase the odds that smokers can quit successfully, but the extent to which these interventions are applied in practice has not been well studied, the researchers noted.
Although great progress has been made in reducing cigarette smoking in the United States, disparities remain, both in use and in cessation, with an estimated 28.8 million adults reporting cigarette smoking in 2022, lead author Brenna VanFrank, MD, MSPH, said in an interview.
“Cigarette smoking remains the leading preventable cause of death and disease in the United States,” said Dr. VanFrank, Senior Medical Officer, Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion.
In a new review, the researchers examined data from the 2022 National Health Interview Survey. The study population included 27,651 adults aged 18 years and older. Current smoking was defined as currently smoking each day or some days and ever having smoked at least 100 cigarettes. The survey assessed the individuals’ interest in quitting, past-year quit attempts, recent quitting success, receipt of healthcare professional advice about quitting, use of counseling to help quit, and use of medication to help quit.
In 2022, approximately two thirds (67.7%) of the 28.8 million adult smokers in the United States wanted to quit, half (53.3%) tried to quit, but only 8.8% were successful. Of those who reported trying to quit, 38.3% used counseling or medication. Of these, 36.3% used medication, 7.3% used counseling, and 5.3% used both.
Indicators of smoking cessation varied by health characteristics and sociodemographic factors, with the highest prevalence of attempts to quit smoking in the past year among adults aged 18-24 years and the lowest among those aged 45-64 years (74.4% vs 47.5%).
Rates of successful quitting were highest among individuals with higher levels of education and income, and use of smoking cessation treatment was highest among White adults (42.7%), followed by non-Hispanic adults of another race, Black adults, and Hispanic adults (33.6%, 32.6%, and 28.8%, respectively).
Smokers of menthol cigarettes had similarly low success rates for quitting (< 10%), although they were significantly more likely than nonmenthol cigarette smokers to express interest in quitting (72.2% vs 65.4%). Smokers of menthol cigarettes also had significantly lower prevalences than smokers of nonmenthol cigarettes of receiving clinician advance to quit and using treatment strategies (both P < .05).
The study findings were limited by several factors including the use of self-reports, which may be subject to bias, and a lack of data on institutionalized adults or adults in the military, which may limit generalizability of the findings to those populations, the researchers noted.
However, the results suggest that opportunities exist to increase smoking cessation across public health and healthcare sectors by expanding access to and use of services and supports to help smokers quit, they wrote.
Ensuring Support for All Smokers Seeking to Quit
The takeaway for clinical practice remains that quitting smoking “is one of the most important actions people who smoke can take to improve their health,” Dr. VanFrank said in an interview.
“It is important to ensure everyone has an opportunity to quit smoking and has access to proven treatments to help them be successful,” she emphasized. Strategies that include behavioral counseling, cessation medications, and advice and support from healthcare professionals can increase quit success. Given that tobacco dependence is a chronic, relapsing condition driven by addiction to nicotine, quitting successfully often takes multiple tries, and those trying to quit may need long-term support and repeated treatment.
“Health systems changes, such as adoption of treatment protocols and standardized clinical work flows, can systematize clinical treatment delivery, and such changes might also serve to increase treatment access for the 75% of adults who smoke who see a healthcare professional in a given year,” said Dr. VanFrank.
As for additional research, “continued surveillance of tobacco use and cessation-related behaviors will help us monitor progress and identify continued opportunities to eliminate tobacco product use and tobacco-related disparities,” Dr. VanFrank said.
“We know a lot about what works to help people successfully quit smoking and what we can do to support people in making quit attempts,” she said. Including equitable opportunities in all commercial tobacco prevention and control efforts has the potential to reduce tobacco-related health disparities.
Overall smoking prevalence in the United States and the current study shows that most smokers would like to quit, David M. Mannino, MD, a pulmonologist and professor of medicine at the University of Kentucky, Lexington, said in an interview. The lack of success experienced by many smokers seeking to quit emphasizes the highly addictive nature of nicotine products, which cause death and disease when used as directed, added Dr. Mannino, who was not involved in the study.
The results of the review were not surprising, and reflect where tobacco treatment has been for the past 20 years, said Dr. Mannino. The good news is that smoking prevalence has continued to drop in the United States over the past 15 years. However, some bad news is that use of e-cigarettes/vaping is still increasing, especially in younger populations, and new nicotine delivery systems, such as pouches (Zyn) are addicting a new generation.
Always Ask About Smoking
In practice, “clinicians should always ask patients about cigarette smoking, as well as vaping and other nicotine use, advise them to quit, and refer them to tobacco treatment experts,” Dr. Mannino emphasized.
The bottom line is that better treatments are needed for tobacco/nicotine addiction, Dr. Mannino said. “Although we have come a long way, we have a long way to go as millions of smokers in the US and globally would like to quit.”
Tobacco-related disease continues to be the number one cause of morbidly and mortality in the United States, and although many current smokers want to quit, most are not successful, Jamie Garfield, MD, professor of thoracic medicine and surgery at the Lewis Katz School of Medicine at Temple University, Philadelphia, Pennsylvania, said in an interview.
“This review highlights the sheer number of current cigarette smokers who want to quit, how many of them attempted to quit, and how many of those were successful,” said Dr. Garfield, who was not involved in the study. Understanding the characteristics of individuals who are more or less likely to successfully quit smoking can help public health and healthcare sectors to increase smoking cessation by expanding access to and use of services and supports.
“We have to do better to control the sale of tobacco products and make tobacco cessation more accessible to everyone,” Dr. Garfield said. In addition, clinicians need to be consistent in asking patients about tobacco use. “If we don’t ask, we will not know who needs help.” Behavioral counseling helps, as does pharmacotherapy, and the two together are more effective than either alone, she added.
Cessation services need to be tailored to the many demographic groups who use tobacco products, said Dr. Garfield. “Just as marketing campaigns directed to older adults will be different from those directed to young adults, so too must cessation resources. Providers need better options to choose from with regard to cessation resources and behavioral counseling sessions. They need to be aware of what motivates one group of people to smoke and how they can be inspired to quit, including which pharmacotherapies are affordable, available, and will work; the same strategies will not work for all people”
The study was supported by the Centers for Disease Control and Prevention’s National Center for Chronic Disease Prevention and Health Promotion. The researchers had no financial conflicts to disclose. Dr. Mannino disclosed serving as an expert witness for on tobacco use and tobacco-caused disease on behalf of people suing the tobacco and vaping industries. Dr. Garfield had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
Approximately half of US adult smokers tried to quit in 2022, but fewer than 40% used counseling or medication, and half received assistance or advice about quitting from clinicians, based on a review in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report.
Previous research has shown that clinician intervention and evidence-based treatment increase the odds that smokers can quit successfully, but the extent to which these interventions are applied in practice has not been well studied, the researchers noted.
Although great progress has been made in reducing cigarette smoking in the United States, disparities remain, both in use and in cessation, with an estimated 28.8 million adults reporting cigarette smoking in 2022, lead author Brenna VanFrank, MD, MSPH, said in an interview.
“Cigarette smoking remains the leading preventable cause of death and disease in the United States,” said Dr. VanFrank, Senior Medical Officer, Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion.
In a new review, the researchers examined data from the 2022 National Health Interview Survey. The study population included 27,651 adults aged 18 years and older. Current smoking was defined as currently smoking each day or some days and ever having smoked at least 100 cigarettes. The survey assessed the individuals’ interest in quitting, past-year quit attempts, recent quitting success, receipt of healthcare professional advice about quitting, use of counseling to help quit, and use of medication to help quit.
In 2022, approximately two thirds (67.7%) of the 28.8 million adult smokers in the United States wanted to quit, half (53.3%) tried to quit, but only 8.8% were successful. Of those who reported trying to quit, 38.3% used counseling or medication. Of these, 36.3% used medication, 7.3% used counseling, and 5.3% used both.
Indicators of smoking cessation varied by health characteristics and sociodemographic factors, with the highest prevalence of attempts to quit smoking in the past year among adults aged 18-24 years and the lowest among those aged 45-64 years (74.4% vs 47.5%).
Rates of successful quitting were highest among individuals with higher levels of education and income, and use of smoking cessation treatment was highest among White adults (42.7%), followed by non-Hispanic adults of another race, Black adults, and Hispanic adults (33.6%, 32.6%, and 28.8%, respectively).
Smokers of menthol cigarettes had similarly low success rates for quitting (< 10%), although they were significantly more likely than nonmenthol cigarette smokers to express interest in quitting (72.2% vs 65.4%). Smokers of menthol cigarettes also had significantly lower prevalences than smokers of nonmenthol cigarettes of receiving clinician advance to quit and using treatment strategies (both P < .05).
The study findings were limited by several factors including the use of self-reports, which may be subject to bias, and a lack of data on institutionalized adults or adults in the military, which may limit generalizability of the findings to those populations, the researchers noted.
However, the results suggest that opportunities exist to increase smoking cessation across public health and healthcare sectors by expanding access to and use of services and supports to help smokers quit, they wrote.
Ensuring Support for All Smokers Seeking to Quit
The takeaway for clinical practice remains that quitting smoking “is one of the most important actions people who smoke can take to improve their health,” Dr. VanFrank said in an interview.
“It is important to ensure everyone has an opportunity to quit smoking and has access to proven treatments to help them be successful,” she emphasized. Strategies that include behavioral counseling, cessation medications, and advice and support from healthcare professionals can increase quit success. Given that tobacco dependence is a chronic, relapsing condition driven by addiction to nicotine, quitting successfully often takes multiple tries, and those trying to quit may need long-term support and repeated treatment.
“Health systems changes, such as adoption of treatment protocols and standardized clinical work flows, can systematize clinical treatment delivery, and such changes might also serve to increase treatment access for the 75% of adults who smoke who see a healthcare professional in a given year,” said Dr. VanFrank.
As for additional research, “continued surveillance of tobacco use and cessation-related behaviors will help us monitor progress and identify continued opportunities to eliminate tobacco product use and tobacco-related disparities,” Dr. VanFrank said.
“We know a lot about what works to help people successfully quit smoking and what we can do to support people in making quit attempts,” she said. Including equitable opportunities in all commercial tobacco prevention and control efforts has the potential to reduce tobacco-related health disparities.
Overall smoking prevalence in the United States and the current study shows that most smokers would like to quit, David M. Mannino, MD, a pulmonologist and professor of medicine at the University of Kentucky, Lexington, said in an interview. The lack of success experienced by many smokers seeking to quit emphasizes the highly addictive nature of nicotine products, which cause death and disease when used as directed, added Dr. Mannino, who was not involved in the study.
The results of the review were not surprising, and reflect where tobacco treatment has been for the past 20 years, said Dr. Mannino. The good news is that smoking prevalence has continued to drop in the United States over the past 15 years. However, some bad news is that use of e-cigarettes/vaping is still increasing, especially in younger populations, and new nicotine delivery systems, such as pouches (Zyn) are addicting a new generation.
Always Ask About Smoking
In practice, “clinicians should always ask patients about cigarette smoking, as well as vaping and other nicotine use, advise them to quit, and refer them to tobacco treatment experts,” Dr. Mannino emphasized.
The bottom line is that better treatments are needed for tobacco/nicotine addiction, Dr. Mannino said. “Although we have come a long way, we have a long way to go as millions of smokers in the US and globally would like to quit.”
Tobacco-related disease continues to be the number one cause of morbidly and mortality in the United States, and although many current smokers want to quit, most are not successful, Jamie Garfield, MD, professor of thoracic medicine and surgery at the Lewis Katz School of Medicine at Temple University, Philadelphia, Pennsylvania, said in an interview.
“This review highlights the sheer number of current cigarette smokers who want to quit, how many of them attempted to quit, and how many of those were successful,” said Dr. Garfield, who was not involved in the study. Understanding the characteristics of individuals who are more or less likely to successfully quit smoking can help public health and healthcare sectors to increase smoking cessation by expanding access to and use of services and supports.
“We have to do better to control the sale of tobacco products and make tobacco cessation more accessible to everyone,” Dr. Garfield said. In addition, clinicians need to be consistent in asking patients about tobacco use. “If we don’t ask, we will not know who needs help.” Behavioral counseling helps, as does pharmacotherapy, and the two together are more effective than either alone, she added.
Cessation services need to be tailored to the many demographic groups who use tobacco products, said Dr. Garfield. “Just as marketing campaigns directed to older adults will be different from those directed to young adults, so too must cessation resources. Providers need better options to choose from with regard to cessation resources and behavioral counseling sessions. They need to be aware of what motivates one group of people to smoke and how they can be inspired to quit, including which pharmacotherapies are affordable, available, and will work; the same strategies will not work for all people”
The study was supported by the Centers for Disease Control and Prevention’s National Center for Chronic Disease Prevention and Health Promotion. The researchers had no financial conflicts to disclose. Dr. Mannino disclosed serving as an expert witness for on tobacco use and tobacco-caused disease on behalf of people suing the tobacco and vaping industries. Dr. Garfield had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
FROM THE MMWR