User login
Violent behavior in autism spectrum disorder: Is it a fact, or fiction?
When Kanner first described autism,1 the disorder was believed to be an uncommon condition, occurring in 4 of every 10,000 children. Over the past few years, however, the rate of autism has increased substantially. Autism is now regarded as a childhood-onset spectrum disordera characterized by persistent deficits in social communication, with a restricted pattern of interests and activities, occurring in approximately 1% of children.3
In DSM-IV-TR, Asperger’s disorder (AD), first described as “autistic psychopathy,”4 is categorized as a subtype of ASD in which the patient, without a history of language delay or mental retardation, has autistic social deficits that do not meet full criteria for autism.
DSM-5 eliminated AD as an independent category, including it instead as part of ASD.5 The label “high-functioning autism” is sometimes used to refer to persons with autism who have normal intelligence (usually defined as full-scale IQ >70), whereas those who have severe intellectual and communication disability are referred to as “low-functioning.” I use “high-functioning autism” and “Asperger’s disorder” interchangeably.
Violent crime and ASD/AD
Reports in the past 2 decades have described violent behavior in persons with ASD/AD. Because of the sensational and unusual nature of these criminal incidents, there is a perception by the public that persons with these disorders, especially those with AD, are predisposed to violent behavior. (Incidents allegedly committed by persons with ASD include the 2007 Virginia Tech campus shooting and the 2012 Newtown, Connecticut, school massacre.6)
Yet neither the original descriptions by Kanner (of autism) and Asperger, nor follow-up studies based on the initial samples studied, showed an increased prevalence of violent crime among persons with ASD/AD.7
In this article, I examine the evidence behind the claim that people who have ASD/AD are predisposed to criminal violence. At the conclusion, you should, as a physician without special training in autism, have a better understanding of when to suspect ASD/AD in an adult who is involved in criminal behavior.
When should you suspect ASD/AD in an adult?
Although autism is a childhood-onset disorder, its symptoms persist across the life
span. If the diagnosis is missed in childhood, which is likely to happen if the person has normal intelligence and relatively good verbal skills, he (she) might come to medical attention for the first time as an adult.
Because most psychiatrists who treat adults do not receive adequate training in the assessment of childhood psychiatric disorders, ASD/AD might be misdiagnosed as schizophrenia or another psychotic disorder. What clues help identify underlying ASD/AD when a patient is referred to you for psychiatric evaluation after allegedly committing a violent crime?
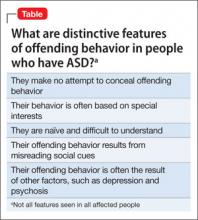
Clue #1. He makes no attempt to deny or conceal the act. The behavior appears to be part of ritualistic behavior or excessive interest (Table).
Often, the alleged crime occurs when the patient’s excessive interests “get out of control,” perhaps because of an external event. For example, a teenager with AD who is fixated on video games might stumble upon pornographic web sites and begin making obscene telephone calls. Particular attention should be paid to a history of rigid, restricted interests beginning in early childhood.
These restricted interests change over time and correlate with intelligence level: The higher the level of intelligence, the more sophisticated the level of fixation. Examples of fixations include computers, technology, and scientific experiments and pursuits. Repeated acts of arson have been reported to be part of an autistic person’s fixation with starting fires.8
Clue #2. He appears to lack sound and prudent judgment despite normal intelligence.
Although most patients with ASD score in the intellectually disabled or mentally retarded range, at least one-third have an IQ in the normal range.9 Examine school records and reports from other agencies when evaluating a patient. Pay attention to a history of difficulty relating to peers at an early age, combined with evidence of rigid, restricted fixations and interests.
It is important to obtain a reliable history going back to early childhood, and not rely just on the patient’s mental status; presenting symptoms might mask underlying traits of ASD, especially in higher-functioning adults. (I once cared for a young man with ASD who had been fired a few days after landing his first job selling used cars because he was “sexually harassing” his colleagues. When questioned, he said that he was only trying to be “friendly” and “practicing his social skills.”)
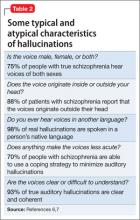
Clue #3. He has been given a diagnosis of schizophrenia without a clear history of hallucinations or delusions.
Differentiating chronic schizophrenia and autism in adults is not always easy, especially in those who have an intellectual disability. In patients whose cognitive and verbal skills are relatively well preserved (such as AD), the presence of intense, focused interests, a pedantic manner of speaking, and abnormalities of nonverbal communication can help clarify the diagnosis. In particular, a recorded history of “childhood schizophrenia” or “obsessive-compulsive behavior” going back to preschool years should alert you to possible ASD.
Scales and screens. Apart from obtaining an accurate developmental history from a variety of sources, you can use rating scales and screening instruments, such as the Social and Communication Questionnaire10—although their utility is limited in adults. It is important not to risk overdiagnosis on the basis of these instruments alone: The gold standard of diagnosis remains clinical. The critical point is that the combination of core symptoms of social communication deficits and restricted interests is more important than the presence of a single symptom. A touch of oddity does not mean that one has ASD/AD.
Is the prevalence of violent crime increased in ASD/AD?
It is important to distinguish violent crime from aggressive behavior. The latter, which can be verbal or nonverbal, is not always intentional or malevolent. In some persons who have an intellectual disability, a desire to communicate might lead to inappropriate touching or pushing. This distinction is particularly relevant to psychiatrists because many people who have ASD have an intellectual disability.
Violent crime is more deliberate, serious, and planned. It involves force or threat of force. According to the Federal Bureau of Investigation Uniform Crime Reporting Program, violent crime comprises four offenses: murder and non-negligent manslaughter, forcible rape, robbery, and aggravated assault.11
Earlier descriptions of ASD/AD did not mention criminal violence as an important feature of these disorders. However, reports began to emerge about two decades ago suggesting that people who have ASD—particularly AD—are prone to violent crime. Some of the patients described in Wing’s original series12 of AD showed violent tendencies, ranging from sudden outbursts of violence to injury to others because of fixation on hobbies such as chemistry experimentation.
Reports such as these were based on isolated case reports or select samples, such as residents of maximum-security hospitals. Scragg and Shah, for example, surveyed the male population of Broadmoor Hospital, a high-security facility in the United Kingdom, and found that the prevalence of AD was higher than expected in the general population.13
Recent reports have not been able to confirm that violent crime is increased in persons with ASD, however:
- In a clinical sample of 313 Danish adults with ASD (age 25 to 59) drawn from the Danish Register of Criminality, Mouridsen and colleagues found that persons with ASD had a lower rate of criminal conviction than matched controls (9%, compared with 18%).14
- In a small community study, Woodbury-Smith and colleagues examined the prevalence rates and types of offending behavior in persons with ASD. Based on official records, only two (18%) had a history of criminal conviction.15
The role of psychiatric comorbidity
Psychiatric disorders are common in persons who have ASD. In one study, 70% of a sample of 114 children with ASD (age 10 to 14) had a psychiatric disorder, based on a parent interview.16 Although people with mental illness are not inherently criminal or violent, having an additional psychiatric disorder independently increases the risk of offending behavior.17 For example, the association of attention-deficit/hyperactivity disorder with criminality is well established.16 Some patients with severe depression and psychotic disorders, including schizophrenia, also are at increased risk of committing a violent act.
To examine the contribution of mental health factors to the commission of crime by persons with ASD, Newman and Ghaziuddin18 used online databases to identify relevant articles, which were then cross-referenced with keyword searches for “violence,” “crime,” “murder,” “assault,” “rape,” and “sex offenses.” Thirty-seven cases were identified in the 17 publications that met inclusion criteria. Out of these, 30% had a definite psychiatric disorder and 54% had a probable psychiatric disorder at the time they committed the crime.18
Any patient with ASD/AD who is evaluated for criminal behavior should be screened for a comorbid psychiatric disorder. In adolescents, stressors such as bullying in school and problems surrounding dating might contribute to offending behavior.
What are management options in the face of violence?
Managing ASD/AD when an offending behavior has occurred first requires a correct diagnosis.19 Professionals working in the criminal justice system have little awareness of the variants of ASD; a defendant with an intellectual disability and a characteristic facial appearance (for example, someone with Down syndrome) can be easily identified, but a high-functioning person who has mild autistic features often is missed. This is more likely to occur in adults because the symptoms of ASD, including the type and severity of isolated interests, change over time.
Here is how I recommend that you proceed:
Step #1. Confirm the ASD diagnosis based on developmental history and the presence of persistent social and communication deficits plus restricted interests.
Step #2. Screen for comorbid psychiatric and medical disorders, including depression, psychosis, and seizure disorder.
Step #3. Treat any disorders you identify with a combination of medication and behavioral intervention.
Step #4. Carefully examine the circumstances surrounding the offending behavior. Involve forensic services on a case-by-case basis, depending on the type and seriousness of the offending behavior (see Related Resources for information on the role of forensic services). When the crime does not involve serious violence, lengthy incarceration might be unnecessary. Because psychopathy and ASD/AD are not mutually exclusive, persons who commit a heinous crime, such as rape or murder, should be dealt with in accordance with the law.
Need for greater awareness of the complexion of ASD
Patients who have ASD/AD form a heterogeneous group in which the levels of cognitive and communication skills are variable. Those who are low-functioning and who have severe behavioral and adaptive deficits occasionally commit aggressive acts against their caregivers.
Most patients with ASD/AD are neither violent nor criminal. Those who are at the higher end of the spectrum, with relatively preserved communication and intellectual skills, occasionally indulge in criminal behavior—behavior that is nonviolent and results from their inability to read social cues or excessive preoccupations.
Most reports that link criminal violence with ASD are based on isolated case reports or on biased samples that use unreliable diagnostic criteria. In higher-functioning persons with ASD, violent crime is almost always precipitated by a comorbid psychiatric disorder, such as severe depression and psychosis.
In short: There is a need to increase our awareness of the special challenges faced by persons with ASD/AD in the criminal justice system.
aGiven the term pervasive developmental disorders (PDD) in the DSM-IV-TR, the spectrum includes autistic disorder, Asperger’s disorder, and pervasive developmental disorder not otherwise specified.2
Bottom Line
Most people who have an autism spectrum disorder (ASD) do not commit violent crime. When violent crime occurs at the hands of a person with ASD, it is almost always precipitated by a comorbid psychiatric disorder, such as severe depression or psychosis. Treating a person with ASD who has committed a violent crime is multimodal, including forensic services when necessary.
Related Resources
- Autism Speaks. No link between autism and violence. www.autismspeaks.org/science/science-news/no-link-between-autism-and-violence.
- Haskins BG, Silva JA. Asperger’s disorder and criminal behavior: Forensic-psychiatric considerations. J Am Acad Psychiatry Law. 2006;34(3):374-384.
- Newman SS, Ghaziuddin M. Violent crime and Asperger syndrome: the role of psychiatric comorbidity. J Autism Dev Disord. 2008;38:1848-1852.
- Wing L. Asperger’s syndrome: a clinical account. Psychol Med. 1981;11(1):115-129.
Disclosure
Dr. Ghaziuddin reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kanner L. Autistic disturbances of affective contact. Nerv Child. 1943;2:217-250.
2. Diagnostic and statistical manual of mental disorders, 4th ed. Washington, DC: American Psychiatric Association; 2000.
3. Autism and Developmental Disabilities Monitoring Network Surveillance Year 2008 Principal Investigators. Prevalence of autism spectrum disorders--Autism and Developmental Disabilities Monitoring Network, 14 sites, United States, 2008. MMWR Surveill Summ. 2012;61(3):1-19.
4. Asperger H. Die autistichen psychopathen im kindesalter. Arch Psychiatr Nervenkr. 1944;117:76-136.
5. Happe F. Criteria, categories, and continua: autism and related disorders in DSM-5. J Am Acad Child and Adolesc Psychiatry. 2011;50:540-542.
6. Walkup JT, Rubin DH. Social withdrawal and violence. N Engl J Med. 2013;368:399-401.
7. Hippler K, Vidding E, Klicpera C, et al. Brief report: no increase in criminal convictions in Asperger’s original cohort. J Autism Dev Disord. 2010;40:774-780.
8. Siponmaa L, Kristiansson M, Jonson C, et al. Juvenile and young adult mentally disordered offenders: the role of child neuropsychiatric disorders. J Am Acad Psychiatry Law. 2001;29(4):420-426.
9. Matson JL, Shoemaker M. Intellectual disability and its relationship to autism spectrum disorders. Res Dev Disabil. 2009;30(6):1107-1114.
10. Rutter M, Bailey A, Lord C. Social communication questionnaire. Los Angeles, CA: Western Psychological Services; 2003.
11. US Department of Justice. Violent crime. http://www2.fbi.gov/ucr/cius2009/offenses/violent_crime. Published September, 2010. Accessed April 26, 2013.
12. Wing L. Asperger’s syndrome: a clinical account. Psychol Med. 1981;11(1):115-129.
13. Scragg P, Shah A. The prevalence of Asperger’s syndrome in a secure hospital. Br J Psychiatry. 1994;165:67-72.
14. Mouridsen SE, Rich B, Isager T, et al. Pervasive developmental disorders and criminal behaviour: a case control study. Int J Offender Ther Comp Criminol. 2008; 52(2):196-205.
15. Woodbury-Smith MR, Clare ICH, Holland AJ, et al. High functioning autistic spectrum disorders, offending and other law-breaking: findings from a community sample. J Forens Psychiatry Psychol. 2006;17(1):108-120.
16. Simonoff E, Pickles A, Charman T, et al. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):
921-929.
17. Ghaziuddin M. Mental health aspects of autism and Asperger syndrome. London, United Kingdom: Jessica Kingsley Press; 2005.
18. Newman SS, Ghaziuddin M. Violent crime and Asperger syndrome: the role of psychiatric comorbidity. J Autism Dev Disord. 2008;38:1848-1852.
19. Wing L. Asperger’s syndrome: management requires diagnosis. The Journal of Forensic Psychiatry. 1997;8(2):253-257.
When Kanner first described autism,1 the disorder was believed to be an uncommon condition, occurring in 4 of every 10,000 children. Over the past few years, however, the rate of autism has increased substantially. Autism is now regarded as a childhood-onset spectrum disordera characterized by persistent deficits in social communication, with a restricted pattern of interests and activities, occurring in approximately 1% of children.3
In DSM-IV-TR, Asperger’s disorder (AD), first described as “autistic psychopathy,”4 is categorized as a subtype of ASD in which the patient, without a history of language delay or mental retardation, has autistic social deficits that do not meet full criteria for autism.
DSM-5 eliminated AD as an independent category, including it instead as part of ASD.5 The label “high-functioning autism” is sometimes used to refer to persons with autism who have normal intelligence (usually defined as full-scale IQ >70), whereas those who have severe intellectual and communication disability are referred to as “low-functioning.” I use “high-functioning autism” and “Asperger’s disorder” interchangeably.
Violent crime and ASD/AD
Reports in the past 2 decades have described violent behavior in persons with ASD/AD. Because of the sensational and unusual nature of these criminal incidents, there is a perception by the public that persons with these disorders, especially those with AD, are predisposed to violent behavior. (Incidents allegedly committed by persons with ASD include the 2007 Virginia Tech campus shooting and the 2012 Newtown, Connecticut, school massacre.6)
Yet neither the original descriptions by Kanner (of autism) and Asperger, nor follow-up studies based on the initial samples studied, showed an increased prevalence of violent crime among persons with ASD/AD.7
In this article, I examine the evidence behind the claim that people who have ASD/AD are predisposed to criminal violence. At the conclusion, you should, as a physician without special training in autism, have a better understanding of when to suspect ASD/AD in an adult who is involved in criminal behavior.
When should you suspect ASD/AD in an adult?
Although autism is a childhood-onset disorder, its symptoms persist across the life
span. If the diagnosis is missed in childhood, which is likely to happen if the person has normal intelligence and relatively good verbal skills, he (she) might come to medical attention for the first time as an adult.
Because most psychiatrists who treat adults do not receive adequate training in the assessment of childhood psychiatric disorders, ASD/AD might be misdiagnosed as schizophrenia or another psychotic disorder. What clues help identify underlying ASD/AD when a patient is referred to you for psychiatric evaluation after allegedly committing a violent crime?
Clue #1. He makes no attempt to deny or conceal the act. The behavior appears to be part of ritualistic behavior or excessive interest (Table).
Often, the alleged crime occurs when the patient’s excessive interests “get out of control,” perhaps because of an external event. For example, a teenager with AD who is fixated on video games might stumble upon pornographic web sites and begin making obscene telephone calls. Particular attention should be paid to a history of rigid, restricted interests beginning in early childhood.
These restricted interests change over time and correlate with intelligence level: The higher the level of intelligence, the more sophisticated the level of fixation. Examples of fixations include computers, technology, and scientific experiments and pursuits. Repeated acts of arson have been reported to be part of an autistic person’s fixation with starting fires.8
Clue #2. He appears to lack sound and prudent judgment despite normal intelligence.
Although most patients with ASD score in the intellectually disabled or mentally retarded range, at least one-third have an IQ in the normal range.9 Examine school records and reports from other agencies when evaluating a patient. Pay attention to a history of difficulty relating to peers at an early age, combined with evidence of rigid, restricted fixations and interests.
It is important to obtain a reliable history going back to early childhood, and not rely just on the patient’s mental status; presenting symptoms might mask underlying traits of ASD, especially in higher-functioning adults. (I once cared for a young man with ASD who had been fired a few days after landing his first job selling used cars because he was “sexually harassing” his colleagues. When questioned, he said that he was only trying to be “friendly” and “practicing his social skills.”)
Clue #3. He has been given a diagnosis of schizophrenia without a clear history of hallucinations or delusions.
Differentiating chronic schizophrenia and autism in adults is not always easy, especially in those who have an intellectual disability. In patients whose cognitive and verbal skills are relatively well preserved (such as AD), the presence of intense, focused interests, a pedantic manner of speaking, and abnormalities of nonverbal communication can help clarify the diagnosis. In particular, a recorded history of “childhood schizophrenia” or “obsessive-compulsive behavior” going back to preschool years should alert you to possible ASD.
Scales and screens. Apart from obtaining an accurate developmental history from a variety of sources, you can use rating scales and screening instruments, such as the Social and Communication Questionnaire10—although their utility is limited in adults. It is important not to risk overdiagnosis on the basis of these instruments alone: The gold standard of diagnosis remains clinical. The critical point is that the combination of core symptoms of social communication deficits and restricted interests is more important than the presence of a single symptom. A touch of oddity does not mean that one has ASD/AD.
Is the prevalence of violent crime increased in ASD/AD?
It is important to distinguish violent crime from aggressive behavior. The latter, which can be verbal or nonverbal, is not always intentional or malevolent. In some persons who have an intellectual disability, a desire to communicate might lead to inappropriate touching or pushing. This distinction is particularly relevant to psychiatrists because many people who have ASD have an intellectual disability.
Violent crime is more deliberate, serious, and planned. It involves force or threat of force. According to the Federal Bureau of Investigation Uniform Crime Reporting Program, violent crime comprises four offenses: murder and non-negligent manslaughter, forcible rape, robbery, and aggravated assault.11
Earlier descriptions of ASD/AD did not mention criminal violence as an important feature of these disorders. However, reports began to emerge about two decades ago suggesting that people who have ASD—particularly AD—are prone to violent crime. Some of the patients described in Wing’s original series12 of AD showed violent tendencies, ranging from sudden outbursts of violence to injury to others because of fixation on hobbies such as chemistry experimentation.
Reports such as these were based on isolated case reports or select samples, such as residents of maximum-security hospitals. Scragg and Shah, for example, surveyed the male population of Broadmoor Hospital, a high-security facility in the United Kingdom, and found that the prevalence of AD was higher than expected in the general population.13
Recent reports have not been able to confirm that violent crime is increased in persons with ASD, however:
- In a clinical sample of 313 Danish adults with ASD (age 25 to 59) drawn from the Danish Register of Criminality, Mouridsen and colleagues found that persons with ASD had a lower rate of criminal conviction than matched controls (9%, compared with 18%).14
- In a small community study, Woodbury-Smith and colleagues examined the prevalence rates and types of offending behavior in persons with ASD. Based on official records, only two (18%) had a history of criminal conviction.15
The role of psychiatric comorbidity
Psychiatric disorders are common in persons who have ASD. In one study, 70% of a sample of 114 children with ASD (age 10 to 14) had a psychiatric disorder, based on a parent interview.16 Although people with mental illness are not inherently criminal or violent, having an additional psychiatric disorder independently increases the risk of offending behavior.17 For example, the association of attention-deficit/hyperactivity disorder with criminality is well established.16 Some patients with severe depression and psychotic disorders, including schizophrenia, also are at increased risk of committing a violent act.
To examine the contribution of mental health factors to the commission of crime by persons with ASD, Newman and Ghaziuddin18 used online databases to identify relevant articles, which were then cross-referenced with keyword searches for “violence,” “crime,” “murder,” “assault,” “rape,” and “sex offenses.” Thirty-seven cases were identified in the 17 publications that met inclusion criteria. Out of these, 30% had a definite psychiatric disorder and 54% had a probable psychiatric disorder at the time they committed the crime.18
Any patient with ASD/AD who is evaluated for criminal behavior should be screened for a comorbid psychiatric disorder. In adolescents, stressors such as bullying in school and problems surrounding dating might contribute to offending behavior.
What are management options in the face of violence?
Managing ASD/AD when an offending behavior has occurred first requires a correct diagnosis.19 Professionals working in the criminal justice system have little awareness of the variants of ASD; a defendant with an intellectual disability and a characteristic facial appearance (for example, someone with Down syndrome) can be easily identified, but a high-functioning person who has mild autistic features often is missed. This is more likely to occur in adults because the symptoms of ASD, including the type and severity of isolated interests, change over time.
Here is how I recommend that you proceed:
Step #1. Confirm the ASD diagnosis based on developmental history and the presence of persistent social and communication deficits plus restricted interests.
Step #2. Screen for comorbid psychiatric and medical disorders, including depression, psychosis, and seizure disorder.
Step #3. Treat any disorders you identify with a combination of medication and behavioral intervention.
Step #4. Carefully examine the circumstances surrounding the offending behavior. Involve forensic services on a case-by-case basis, depending on the type and seriousness of the offending behavior (see Related Resources for information on the role of forensic services). When the crime does not involve serious violence, lengthy incarceration might be unnecessary. Because psychopathy and ASD/AD are not mutually exclusive, persons who commit a heinous crime, such as rape or murder, should be dealt with in accordance with the law.
Need for greater awareness of the complexion of ASD
Patients who have ASD/AD form a heterogeneous group in which the levels of cognitive and communication skills are variable. Those who are low-functioning and who have severe behavioral and adaptive deficits occasionally commit aggressive acts against their caregivers.
Most patients with ASD/AD are neither violent nor criminal. Those who are at the higher end of the spectrum, with relatively preserved communication and intellectual skills, occasionally indulge in criminal behavior—behavior that is nonviolent and results from their inability to read social cues or excessive preoccupations.
Most reports that link criminal violence with ASD are based on isolated case reports or on biased samples that use unreliable diagnostic criteria. In higher-functioning persons with ASD, violent crime is almost always precipitated by a comorbid psychiatric disorder, such as severe depression and psychosis.
In short: There is a need to increase our awareness of the special challenges faced by persons with ASD/AD in the criminal justice system.
aGiven the term pervasive developmental disorders (PDD) in the DSM-IV-TR, the spectrum includes autistic disorder, Asperger’s disorder, and pervasive developmental disorder not otherwise specified.2
Bottom Line
Most people who have an autism spectrum disorder (ASD) do not commit violent crime. When violent crime occurs at the hands of a person with ASD, it is almost always precipitated by a comorbid psychiatric disorder, such as severe depression or psychosis. Treating a person with ASD who has committed a violent crime is multimodal, including forensic services when necessary.
Related Resources
- Autism Speaks. No link between autism and violence. www.autismspeaks.org/science/science-news/no-link-between-autism-and-violence.
- Haskins BG, Silva JA. Asperger’s disorder and criminal behavior: Forensic-psychiatric considerations. J Am Acad Psychiatry Law. 2006;34(3):374-384.
- Newman SS, Ghaziuddin M. Violent crime and Asperger syndrome: the role of psychiatric comorbidity. J Autism Dev Disord. 2008;38:1848-1852.
- Wing L. Asperger’s syndrome: a clinical account. Psychol Med. 1981;11(1):115-129.
Disclosure
Dr. Ghaziuddin reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
When Kanner first described autism,1 the disorder was believed to be an uncommon condition, occurring in 4 of every 10,000 children. Over the past few years, however, the rate of autism has increased substantially. Autism is now regarded as a childhood-onset spectrum disordera characterized by persistent deficits in social communication, with a restricted pattern of interests and activities, occurring in approximately 1% of children.3
In DSM-IV-TR, Asperger’s disorder (AD), first described as “autistic psychopathy,”4 is categorized as a subtype of ASD in which the patient, without a history of language delay or mental retardation, has autistic social deficits that do not meet full criteria for autism.
DSM-5 eliminated AD as an independent category, including it instead as part of ASD.5 The label “high-functioning autism” is sometimes used to refer to persons with autism who have normal intelligence (usually defined as full-scale IQ >70), whereas those who have severe intellectual and communication disability are referred to as “low-functioning.” I use “high-functioning autism” and “Asperger’s disorder” interchangeably.
Violent crime and ASD/AD
Reports in the past 2 decades have described violent behavior in persons with ASD/AD. Because of the sensational and unusual nature of these criminal incidents, there is a perception by the public that persons with these disorders, especially those with AD, are predisposed to violent behavior. (Incidents allegedly committed by persons with ASD include the 2007 Virginia Tech campus shooting and the 2012 Newtown, Connecticut, school massacre.6)
Yet neither the original descriptions by Kanner (of autism) and Asperger, nor follow-up studies based on the initial samples studied, showed an increased prevalence of violent crime among persons with ASD/AD.7
In this article, I examine the evidence behind the claim that people who have ASD/AD are predisposed to criminal violence. At the conclusion, you should, as a physician without special training in autism, have a better understanding of when to suspect ASD/AD in an adult who is involved in criminal behavior.
When should you suspect ASD/AD in an adult?
Although autism is a childhood-onset disorder, its symptoms persist across the life
span. If the diagnosis is missed in childhood, which is likely to happen if the person has normal intelligence and relatively good verbal skills, he (she) might come to medical attention for the first time as an adult.
Because most psychiatrists who treat adults do not receive adequate training in the assessment of childhood psychiatric disorders, ASD/AD might be misdiagnosed as schizophrenia or another psychotic disorder. What clues help identify underlying ASD/AD when a patient is referred to you for psychiatric evaluation after allegedly committing a violent crime?
Clue #1. He makes no attempt to deny or conceal the act. The behavior appears to be part of ritualistic behavior or excessive interest (Table).
Often, the alleged crime occurs when the patient’s excessive interests “get out of control,” perhaps because of an external event. For example, a teenager with AD who is fixated on video games might stumble upon pornographic web sites and begin making obscene telephone calls. Particular attention should be paid to a history of rigid, restricted interests beginning in early childhood.
These restricted interests change over time and correlate with intelligence level: The higher the level of intelligence, the more sophisticated the level of fixation. Examples of fixations include computers, technology, and scientific experiments and pursuits. Repeated acts of arson have been reported to be part of an autistic person’s fixation with starting fires.8
Clue #2. He appears to lack sound and prudent judgment despite normal intelligence.
Although most patients with ASD score in the intellectually disabled or mentally retarded range, at least one-third have an IQ in the normal range.9 Examine school records and reports from other agencies when evaluating a patient. Pay attention to a history of difficulty relating to peers at an early age, combined with evidence of rigid, restricted fixations and interests.
It is important to obtain a reliable history going back to early childhood, and not rely just on the patient’s mental status; presenting symptoms might mask underlying traits of ASD, especially in higher-functioning adults. (I once cared for a young man with ASD who had been fired a few days after landing his first job selling used cars because he was “sexually harassing” his colleagues. When questioned, he said that he was only trying to be “friendly” and “practicing his social skills.”)
Clue #3. He has been given a diagnosis of schizophrenia without a clear history of hallucinations or delusions.
Differentiating chronic schizophrenia and autism in adults is not always easy, especially in those who have an intellectual disability. In patients whose cognitive and verbal skills are relatively well preserved (such as AD), the presence of intense, focused interests, a pedantic manner of speaking, and abnormalities of nonverbal communication can help clarify the diagnosis. In particular, a recorded history of “childhood schizophrenia” or “obsessive-compulsive behavior” going back to preschool years should alert you to possible ASD.
Scales and screens. Apart from obtaining an accurate developmental history from a variety of sources, you can use rating scales and screening instruments, such as the Social and Communication Questionnaire10—although their utility is limited in adults. It is important not to risk overdiagnosis on the basis of these instruments alone: The gold standard of diagnosis remains clinical. The critical point is that the combination of core symptoms of social communication deficits and restricted interests is more important than the presence of a single symptom. A touch of oddity does not mean that one has ASD/AD.
Is the prevalence of violent crime increased in ASD/AD?
It is important to distinguish violent crime from aggressive behavior. The latter, which can be verbal or nonverbal, is not always intentional or malevolent. In some persons who have an intellectual disability, a desire to communicate might lead to inappropriate touching or pushing. This distinction is particularly relevant to psychiatrists because many people who have ASD have an intellectual disability.
Violent crime is more deliberate, serious, and planned. It involves force or threat of force. According to the Federal Bureau of Investigation Uniform Crime Reporting Program, violent crime comprises four offenses: murder and non-negligent manslaughter, forcible rape, robbery, and aggravated assault.11
Earlier descriptions of ASD/AD did not mention criminal violence as an important feature of these disorders. However, reports began to emerge about two decades ago suggesting that people who have ASD—particularly AD—are prone to violent crime. Some of the patients described in Wing’s original series12 of AD showed violent tendencies, ranging from sudden outbursts of violence to injury to others because of fixation on hobbies such as chemistry experimentation.
Reports such as these were based on isolated case reports or select samples, such as residents of maximum-security hospitals. Scragg and Shah, for example, surveyed the male population of Broadmoor Hospital, a high-security facility in the United Kingdom, and found that the prevalence of AD was higher than expected in the general population.13
Recent reports have not been able to confirm that violent crime is increased in persons with ASD, however:
- In a clinical sample of 313 Danish adults with ASD (age 25 to 59) drawn from the Danish Register of Criminality, Mouridsen and colleagues found that persons with ASD had a lower rate of criminal conviction than matched controls (9%, compared with 18%).14
- In a small community study, Woodbury-Smith and colleagues examined the prevalence rates and types of offending behavior in persons with ASD. Based on official records, only two (18%) had a history of criminal conviction.15
The role of psychiatric comorbidity
Psychiatric disorders are common in persons who have ASD. In one study, 70% of a sample of 114 children with ASD (age 10 to 14) had a psychiatric disorder, based on a parent interview.16 Although people with mental illness are not inherently criminal or violent, having an additional psychiatric disorder independently increases the risk of offending behavior.17 For example, the association of attention-deficit/hyperactivity disorder with criminality is well established.16 Some patients with severe depression and psychotic disorders, including schizophrenia, also are at increased risk of committing a violent act.
To examine the contribution of mental health factors to the commission of crime by persons with ASD, Newman and Ghaziuddin18 used online databases to identify relevant articles, which were then cross-referenced with keyword searches for “violence,” “crime,” “murder,” “assault,” “rape,” and “sex offenses.” Thirty-seven cases were identified in the 17 publications that met inclusion criteria. Out of these, 30% had a definite psychiatric disorder and 54% had a probable psychiatric disorder at the time they committed the crime.18
Any patient with ASD/AD who is evaluated for criminal behavior should be screened for a comorbid psychiatric disorder. In adolescents, stressors such as bullying in school and problems surrounding dating might contribute to offending behavior.
What are management options in the face of violence?
Managing ASD/AD when an offending behavior has occurred first requires a correct diagnosis.19 Professionals working in the criminal justice system have little awareness of the variants of ASD; a defendant with an intellectual disability and a characteristic facial appearance (for example, someone with Down syndrome) can be easily identified, but a high-functioning person who has mild autistic features often is missed. This is more likely to occur in adults because the symptoms of ASD, including the type and severity of isolated interests, change over time.
Here is how I recommend that you proceed:
Step #1. Confirm the ASD diagnosis based on developmental history and the presence of persistent social and communication deficits plus restricted interests.
Step #2. Screen for comorbid psychiatric and medical disorders, including depression, psychosis, and seizure disorder.
Step #3. Treat any disorders you identify with a combination of medication and behavioral intervention.
Step #4. Carefully examine the circumstances surrounding the offending behavior. Involve forensic services on a case-by-case basis, depending on the type and seriousness of the offending behavior (see Related Resources for information on the role of forensic services). When the crime does not involve serious violence, lengthy incarceration might be unnecessary. Because psychopathy and ASD/AD are not mutually exclusive, persons who commit a heinous crime, such as rape or murder, should be dealt with in accordance with the law.
Need for greater awareness of the complexion of ASD
Patients who have ASD/AD form a heterogeneous group in which the levels of cognitive and communication skills are variable. Those who are low-functioning and who have severe behavioral and adaptive deficits occasionally commit aggressive acts against their caregivers.
Most patients with ASD/AD are neither violent nor criminal. Those who are at the higher end of the spectrum, with relatively preserved communication and intellectual skills, occasionally indulge in criminal behavior—behavior that is nonviolent and results from their inability to read social cues or excessive preoccupations.
Most reports that link criminal violence with ASD are based on isolated case reports or on biased samples that use unreliable diagnostic criteria. In higher-functioning persons with ASD, violent crime is almost always precipitated by a comorbid psychiatric disorder, such as severe depression and psychosis.
In short: There is a need to increase our awareness of the special challenges faced by persons with ASD/AD in the criminal justice system.
aGiven the term pervasive developmental disorders (PDD) in the DSM-IV-TR, the spectrum includes autistic disorder, Asperger’s disorder, and pervasive developmental disorder not otherwise specified.2
Bottom Line
Most people who have an autism spectrum disorder (ASD) do not commit violent crime. When violent crime occurs at the hands of a person with ASD, it is almost always precipitated by a comorbid psychiatric disorder, such as severe depression or psychosis. Treating a person with ASD who has committed a violent crime is multimodal, including forensic services when necessary.
Related Resources
- Autism Speaks. No link between autism and violence. www.autismspeaks.org/science/science-news/no-link-between-autism-and-violence.
- Haskins BG, Silva JA. Asperger’s disorder and criminal behavior: Forensic-psychiatric considerations. J Am Acad Psychiatry Law. 2006;34(3):374-384.
- Newman SS, Ghaziuddin M. Violent crime and Asperger syndrome: the role of psychiatric comorbidity. J Autism Dev Disord. 2008;38:1848-1852.
- Wing L. Asperger’s syndrome: a clinical account. Psychol Med. 1981;11(1):115-129.
Disclosure
Dr. Ghaziuddin reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kanner L. Autistic disturbances of affective contact. Nerv Child. 1943;2:217-250.
2. Diagnostic and statistical manual of mental disorders, 4th ed. Washington, DC: American Psychiatric Association; 2000.
3. Autism and Developmental Disabilities Monitoring Network Surveillance Year 2008 Principal Investigators. Prevalence of autism spectrum disorders--Autism and Developmental Disabilities Monitoring Network, 14 sites, United States, 2008. MMWR Surveill Summ. 2012;61(3):1-19.
4. Asperger H. Die autistichen psychopathen im kindesalter. Arch Psychiatr Nervenkr. 1944;117:76-136.
5. Happe F. Criteria, categories, and continua: autism and related disorders in DSM-5. J Am Acad Child and Adolesc Psychiatry. 2011;50:540-542.
6. Walkup JT, Rubin DH. Social withdrawal and violence. N Engl J Med. 2013;368:399-401.
7. Hippler K, Vidding E, Klicpera C, et al. Brief report: no increase in criminal convictions in Asperger’s original cohort. J Autism Dev Disord. 2010;40:774-780.
8. Siponmaa L, Kristiansson M, Jonson C, et al. Juvenile and young adult mentally disordered offenders: the role of child neuropsychiatric disorders. J Am Acad Psychiatry Law. 2001;29(4):420-426.
9. Matson JL, Shoemaker M. Intellectual disability and its relationship to autism spectrum disorders. Res Dev Disabil. 2009;30(6):1107-1114.
10. Rutter M, Bailey A, Lord C. Social communication questionnaire. Los Angeles, CA: Western Psychological Services; 2003.
11. US Department of Justice. Violent crime. http://www2.fbi.gov/ucr/cius2009/offenses/violent_crime. Published September, 2010. Accessed April 26, 2013.
12. Wing L. Asperger’s syndrome: a clinical account. Psychol Med. 1981;11(1):115-129.
13. Scragg P, Shah A. The prevalence of Asperger’s syndrome in a secure hospital. Br J Psychiatry. 1994;165:67-72.
14. Mouridsen SE, Rich B, Isager T, et al. Pervasive developmental disorders and criminal behaviour: a case control study. Int J Offender Ther Comp Criminol. 2008; 52(2):196-205.
15. Woodbury-Smith MR, Clare ICH, Holland AJ, et al. High functioning autistic spectrum disorders, offending and other law-breaking: findings from a community sample. J Forens Psychiatry Psychol. 2006;17(1):108-120.
16. Simonoff E, Pickles A, Charman T, et al. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):
921-929.
17. Ghaziuddin M. Mental health aspects of autism and Asperger syndrome. London, United Kingdom: Jessica Kingsley Press; 2005.
18. Newman SS, Ghaziuddin M. Violent crime and Asperger syndrome: the role of psychiatric comorbidity. J Autism Dev Disord. 2008;38:1848-1852.
19. Wing L. Asperger’s syndrome: management requires diagnosis. The Journal of Forensic Psychiatry. 1997;8(2):253-257.
1. Kanner L. Autistic disturbances of affective contact. Nerv Child. 1943;2:217-250.
2. Diagnostic and statistical manual of mental disorders, 4th ed. Washington, DC: American Psychiatric Association; 2000.
3. Autism and Developmental Disabilities Monitoring Network Surveillance Year 2008 Principal Investigators. Prevalence of autism spectrum disorders--Autism and Developmental Disabilities Monitoring Network, 14 sites, United States, 2008. MMWR Surveill Summ. 2012;61(3):1-19.
4. Asperger H. Die autistichen psychopathen im kindesalter. Arch Psychiatr Nervenkr. 1944;117:76-136.
5. Happe F. Criteria, categories, and continua: autism and related disorders in DSM-5. J Am Acad Child and Adolesc Psychiatry. 2011;50:540-542.
6. Walkup JT, Rubin DH. Social withdrawal and violence. N Engl J Med. 2013;368:399-401.
7. Hippler K, Vidding E, Klicpera C, et al. Brief report: no increase in criminal convictions in Asperger’s original cohort. J Autism Dev Disord. 2010;40:774-780.
8. Siponmaa L, Kristiansson M, Jonson C, et al. Juvenile and young adult mentally disordered offenders: the role of child neuropsychiatric disorders. J Am Acad Psychiatry Law. 2001;29(4):420-426.
9. Matson JL, Shoemaker M. Intellectual disability and its relationship to autism spectrum disorders. Res Dev Disabil. 2009;30(6):1107-1114.
10. Rutter M, Bailey A, Lord C. Social communication questionnaire. Los Angeles, CA: Western Psychological Services; 2003.
11. US Department of Justice. Violent crime. http://www2.fbi.gov/ucr/cius2009/offenses/violent_crime. Published September, 2010. Accessed April 26, 2013.
12. Wing L. Asperger’s syndrome: a clinical account. Psychol Med. 1981;11(1):115-129.
13. Scragg P, Shah A. The prevalence of Asperger’s syndrome in a secure hospital. Br J Psychiatry. 1994;165:67-72.
14. Mouridsen SE, Rich B, Isager T, et al. Pervasive developmental disorders and criminal behaviour: a case control study. Int J Offender Ther Comp Criminol. 2008; 52(2):196-205.
15. Woodbury-Smith MR, Clare ICH, Holland AJ, et al. High functioning autistic spectrum disorders, offending and other law-breaking: findings from a community sample. J Forens Psychiatry Psychol. 2006;17(1):108-120.
16. Simonoff E, Pickles A, Charman T, et al. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):
921-929.
17. Ghaziuddin M. Mental health aspects of autism and Asperger syndrome. London, United Kingdom: Jessica Kingsley Press; 2005.
18. Newman SS, Ghaziuddin M. Violent crime and Asperger syndrome: the role of psychiatric comorbidity. J Autism Dev Disord. 2008;38:1848-1852.
19. Wing L. Asperger’s syndrome: management requires diagnosis. The Journal of Forensic Psychiatry. 1997;8(2):253-257.
Problematic pruritus: Seeking a cure for psychogenic itch
Psychogenic itch—an excessive impulse to scratch, gouge, or pick at skin in the absence of dermatologic cause—is common among psychiatric inpatients, but can be challenging to assess and manage in outpatients. Patients with psychogenic itch predominantly are female, with average age of onset between 30 and 45 years.1 Psychiatric disorders associated with psychogenic itch include depression, obsessive-compulsive disorder, anxiety, somatoform disorders, mania, psychosis, and substance abuse.2 Body dysmorphic disorder, trichotillomania, kleptomania, and borderline personality disorder may be comorbid in patients with psychogenic itch.3
Characteristics of psychogenic itch
Consider psychogenic itch in patients who have recurring physical symptoms and demand examination despite repeated negative results. Other indicators include psychological factors—loss of a loved one, unemployment, relocation, etc.—that may be associated with onset, severity, elicitation, or maintenance of the itching; impairments in the patient’s social or professional life; and marked preoccupation with itching or the state of her (his) skin. Characteristically, itching can be provoked by emotional triggers, most notably during stages of excitement, and also by mechanical or chemical stimuli.
Skin changes associated with psychogenic itch often are found on areas accessible to the patient’s hand: face, arms, legs, abdomen, thighs, upper back, and shoulders. These changes can be seen in varying stages, from discrete superficial excoriations, erosions, and ulcers to thick, darkened nodules and colorless atrophic scars. Patients often complain of burning. In some cases, a patient uses a tool or instrument to autoaggressively manipulate his (her) skin in response to tingling or stabbing sensations. Artificial lesions or eczemas brought on by self-
manipulation can occur. Stress, life changes, or inhibited rage may be evoking the burning sensation and subsequent complaints.
Interventions to consider
After you have ruled out other causes of pruritus and made a diagnosis of psychogenic itch, educate your patient about the multifactorial etiology. Explain possible associations between skin disorders and unconscious reaction patterns, and the role of emotional and cognitive stimuli.
Moisturizing the skin can help the dryness associated with repetitive scratching. Consider prescribing an antihistamine, moisturizer, topical steroid, antibiotic, or
occlusive dressing.
Some pharmacological properties of antidepressants that are not related to their antidepressant activity—eg, the histamine-1 blocking effect of tricyclic antidepressants—are beneficial for treating psychogenic itch.4 Sedating antihistamines (hydroxyzine) and antidepressants (doxepin) may help break cycles of itching and depression or itching and scratching.4 Tricyclic antidepressants also are recommended for treating burning, stabbing, or tingling sensations.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Yosipovitch G, Samuel LS. Neuropathic and psychogenic itch. Dermatol Ther. 2008;21(1):32-41.
2. Krishnan A, Koo J. Psyche, opioids, and itch: therapeutic consequences. Dermatol Ther. 2005;18(4):314-322.
3. Arnold LM, Auchenbach MB, McElroy SL. Psychogenic excoriation. Clinical features, proposed diagnostic criteria, epidemiology and approaches to treatment. CNS Drugs. 2001;15(5):351-359.
4. Gupta MA, Guptat AK. The use of antidepressant drugs in dermatology. J Eur Acad Dermatol Venereol. 2001;15(6):512-518.
Psychogenic itch—an excessive impulse to scratch, gouge, or pick at skin in the absence of dermatologic cause—is common among psychiatric inpatients, but can be challenging to assess and manage in outpatients. Patients with psychogenic itch predominantly are female, with average age of onset between 30 and 45 years.1 Psychiatric disorders associated with psychogenic itch include depression, obsessive-compulsive disorder, anxiety, somatoform disorders, mania, psychosis, and substance abuse.2 Body dysmorphic disorder, trichotillomania, kleptomania, and borderline personality disorder may be comorbid in patients with psychogenic itch.3
Characteristics of psychogenic itch
Consider psychogenic itch in patients who have recurring physical symptoms and demand examination despite repeated negative results. Other indicators include psychological factors—loss of a loved one, unemployment, relocation, etc.—that may be associated with onset, severity, elicitation, or maintenance of the itching; impairments in the patient’s social or professional life; and marked preoccupation with itching or the state of her (his) skin. Characteristically, itching can be provoked by emotional triggers, most notably during stages of excitement, and also by mechanical or chemical stimuli.
Skin changes associated with psychogenic itch often are found on areas accessible to the patient’s hand: face, arms, legs, abdomen, thighs, upper back, and shoulders. These changes can be seen in varying stages, from discrete superficial excoriations, erosions, and ulcers to thick, darkened nodules and colorless atrophic scars. Patients often complain of burning. In some cases, a patient uses a tool or instrument to autoaggressively manipulate his (her) skin in response to tingling or stabbing sensations. Artificial lesions or eczemas brought on by self-
manipulation can occur. Stress, life changes, or inhibited rage may be evoking the burning sensation and subsequent complaints.
Interventions to consider
After you have ruled out other causes of pruritus and made a diagnosis of psychogenic itch, educate your patient about the multifactorial etiology. Explain possible associations between skin disorders and unconscious reaction patterns, and the role of emotional and cognitive stimuli.
Moisturizing the skin can help the dryness associated with repetitive scratching. Consider prescribing an antihistamine, moisturizer, topical steroid, antibiotic, or
occlusive dressing.
Some pharmacological properties of antidepressants that are not related to their antidepressant activity—eg, the histamine-1 blocking effect of tricyclic antidepressants—are beneficial for treating psychogenic itch.4 Sedating antihistamines (hydroxyzine) and antidepressants (doxepin) may help break cycles of itching and depression or itching and scratching.4 Tricyclic antidepressants also are recommended for treating burning, stabbing, or tingling sensations.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Psychogenic itch—an excessive impulse to scratch, gouge, or pick at skin in the absence of dermatologic cause—is common among psychiatric inpatients, but can be challenging to assess and manage in outpatients. Patients with psychogenic itch predominantly are female, with average age of onset between 30 and 45 years.1 Psychiatric disorders associated with psychogenic itch include depression, obsessive-compulsive disorder, anxiety, somatoform disorders, mania, psychosis, and substance abuse.2 Body dysmorphic disorder, trichotillomania, kleptomania, and borderline personality disorder may be comorbid in patients with psychogenic itch.3
Characteristics of psychogenic itch
Consider psychogenic itch in patients who have recurring physical symptoms and demand examination despite repeated negative results. Other indicators include psychological factors—loss of a loved one, unemployment, relocation, etc.—that may be associated with onset, severity, elicitation, or maintenance of the itching; impairments in the patient’s social or professional life; and marked preoccupation with itching or the state of her (his) skin. Characteristically, itching can be provoked by emotional triggers, most notably during stages of excitement, and also by mechanical or chemical stimuli.
Skin changes associated with psychogenic itch often are found on areas accessible to the patient’s hand: face, arms, legs, abdomen, thighs, upper back, and shoulders. These changes can be seen in varying stages, from discrete superficial excoriations, erosions, and ulcers to thick, darkened nodules and colorless atrophic scars. Patients often complain of burning. In some cases, a patient uses a tool or instrument to autoaggressively manipulate his (her) skin in response to tingling or stabbing sensations. Artificial lesions or eczemas brought on by self-
manipulation can occur. Stress, life changes, or inhibited rage may be evoking the burning sensation and subsequent complaints.
Interventions to consider
After you have ruled out other causes of pruritus and made a diagnosis of psychogenic itch, educate your patient about the multifactorial etiology. Explain possible associations between skin disorders and unconscious reaction patterns, and the role of emotional and cognitive stimuli.
Moisturizing the skin can help the dryness associated with repetitive scratching. Consider prescribing an antihistamine, moisturizer, topical steroid, antibiotic, or
occlusive dressing.
Some pharmacological properties of antidepressants that are not related to their antidepressant activity—eg, the histamine-1 blocking effect of tricyclic antidepressants—are beneficial for treating psychogenic itch.4 Sedating antihistamines (hydroxyzine) and antidepressants (doxepin) may help break cycles of itching and depression or itching and scratching.4 Tricyclic antidepressants also are recommended for treating burning, stabbing, or tingling sensations.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Yosipovitch G, Samuel LS. Neuropathic and psychogenic itch. Dermatol Ther. 2008;21(1):32-41.
2. Krishnan A, Koo J. Psyche, opioids, and itch: therapeutic consequences. Dermatol Ther. 2005;18(4):314-322.
3. Arnold LM, Auchenbach MB, McElroy SL. Psychogenic excoriation. Clinical features, proposed diagnostic criteria, epidemiology and approaches to treatment. CNS Drugs. 2001;15(5):351-359.
4. Gupta MA, Guptat AK. The use of antidepressant drugs in dermatology. J Eur Acad Dermatol Venereol. 2001;15(6):512-518.
1. Yosipovitch G, Samuel LS. Neuropathic and psychogenic itch. Dermatol Ther. 2008;21(1):32-41.
2. Krishnan A, Koo J. Psyche, opioids, and itch: therapeutic consequences. Dermatol Ther. 2005;18(4):314-322.
3. Arnold LM, Auchenbach MB, McElroy SL. Psychogenic excoriation. Clinical features, proposed diagnostic criteria, epidemiology and approaches to treatment. CNS Drugs. 2001;15(5):351-359.
4. Gupta MA, Guptat AK. The use of antidepressant drugs in dermatology. J Eur Acad Dermatol Venereol. 2001;15(6):512-518.
Are robotic surgery complications underreported?
Although US hospitals have been quick to embrace surgical robot technology over the past decade, a “slapdash” system of reporting complications paints an unclear picture of its safety, according to Johns Hopkins researchers.
The Johns Hopkins team, led by Martin A. Makary, MD, MPH, found that, among the 1 million or so robotic surgeries performed since 2000, only 245 complications—including 71 deaths—were reported to the US Food and Drug Administration (FDA).1 When an adverse event or device malfunction occurs, hospitals are required to report these incidents to the manufacturer, which in turn is required to report them to the FDA—but this reporting doesn’t always happen.
“The number reported is very low for any complex technology used over a million times,” says Dr. Makary, associate professor of surgery at the Johns Hopkins University School of Medicine. “Doctors and patients can’t properly evaluate safety when we have a haphazard system of collecting data that is not independent and not transparent. There may be some complications specific to the use of this device, but we can only learn about them if we accurately track outcomes.”
The use of the robot in surgery has skyrocketed. Between 2007 and 2011, for example, the number of procedures involving the robot increased by more than 400% in the United States and more than 300% internationally. At the end of 2011, there were 1,400 surgical robots installed in US hospitals, up from 800 just 4 years earlier.
Some incidents went unreported until the news media highlighted them
Dr. Makary and colleagues found several incidents reported in the national news media that were not reported to the FDA until after the stories appeared in the press, even though the incidents took place long before the media exposure. Dr. Makary says it’s likely that many other incidents go unreported, never to be captured by research like his or by the FDA.
“We need innovation in medicine and, in this country, we are tremendously good at introducing new technologies,” he says. “But we have to evaluate new technology properly so we don’t over-adopt—or under-adopt—important advances that could benefit patients.”
How the study was conducted
Makary and colleagues reviewed the FDA adverse events database from January 1, 2000, to August 1, 2012. They also searched legal judgments and adverse events using LexisNexis to scan news media, and PACER to scan court records. The cases then were cross-referenced to see if they matched. The investigators found that eight cases were not appropriately reported to the FDA, five of which were never reported and two of which were reported only after a story about them appeared in the press.
Complication rate was highest for hysterectomy
When investigators reviewed complications that were reported, the procedures most commonly associated with death were:
- gynecologic (22 of the 71 deaths)
- urologic (15 deaths)
- cardiothoracic (12 deaths).
The cause of death was most often excessive bleeding. In cases where patients survived, hysterectomy by far had the most complications (43% of injuries).
A call for standardized reporting
Dr. Makary contends that standardized reporting is needed for all adverse events related to robotic devices. One rare complication that occurs, he says, is that a surgeon can accidentally cut the aorta because the surgeon cannot feel its firmness. For reporting purposes, however, it’s unclear whether such an event is surgeon error or device-related error. The FDA currently collects only device-related errors.
Dr. Makary argues that errors such as inadvertent cutting of the aorta, although preventable with proper technique, should be tracked as device-related errors because they are more common with robotic surgery than with conventional surgery. Without better reporting standards, he says, these complications are less likely to be reported to the FDA at all. And if they go unreported, they cannot contribute to the understanding or identification of safety problems.
He suggests one solution: use of a database like the one maintained by the American College of Surgeons, in which independent nurses identify and track adverse events and complications of traditional operations.
Good information on robotic surgery is needed not only for research, but also to ensure that patients are fully informed about potential risks. Right now, Dr. Makary says, it’s too easy for a surgeon to claim that there are no additional risks related to robotic surgery because the evidence is nowhere to be found.
“Decisions should not be made based on the information in the FDA database,” he says. “We need to be able to give patients answers to their questions about safety and how much risk is associated with the robot. We have all suspected the answer has not been zero. We still don’t really know what the true answer is.”
We want to hear from you! Tell us what you think.
Although US hospitals have been quick to embrace surgical robot technology over the past decade, a “slapdash” system of reporting complications paints an unclear picture of its safety, according to Johns Hopkins researchers.
The Johns Hopkins team, led by Martin A. Makary, MD, MPH, found that, among the 1 million or so robotic surgeries performed since 2000, only 245 complications—including 71 deaths—were reported to the US Food and Drug Administration (FDA).1 When an adverse event or device malfunction occurs, hospitals are required to report these incidents to the manufacturer, which in turn is required to report them to the FDA—but this reporting doesn’t always happen.
“The number reported is very low for any complex technology used over a million times,” says Dr. Makary, associate professor of surgery at the Johns Hopkins University School of Medicine. “Doctors and patients can’t properly evaluate safety when we have a haphazard system of collecting data that is not independent and not transparent. There may be some complications specific to the use of this device, but we can only learn about them if we accurately track outcomes.”
The use of the robot in surgery has skyrocketed. Between 2007 and 2011, for example, the number of procedures involving the robot increased by more than 400% in the United States and more than 300% internationally. At the end of 2011, there were 1,400 surgical robots installed in US hospitals, up from 800 just 4 years earlier.
Some incidents went unreported until the news media highlighted them
Dr. Makary and colleagues found several incidents reported in the national news media that were not reported to the FDA until after the stories appeared in the press, even though the incidents took place long before the media exposure. Dr. Makary says it’s likely that many other incidents go unreported, never to be captured by research like his or by the FDA.
“We need innovation in medicine and, in this country, we are tremendously good at introducing new technologies,” he says. “But we have to evaluate new technology properly so we don’t over-adopt—or under-adopt—important advances that could benefit patients.”
How the study was conducted
Makary and colleagues reviewed the FDA adverse events database from January 1, 2000, to August 1, 2012. They also searched legal judgments and adverse events using LexisNexis to scan news media, and PACER to scan court records. The cases then were cross-referenced to see if they matched. The investigators found that eight cases were not appropriately reported to the FDA, five of which were never reported and two of which were reported only after a story about them appeared in the press.
Complication rate was highest for hysterectomy
When investigators reviewed complications that were reported, the procedures most commonly associated with death were:
- gynecologic (22 of the 71 deaths)
- urologic (15 deaths)
- cardiothoracic (12 deaths).
The cause of death was most often excessive bleeding. In cases where patients survived, hysterectomy by far had the most complications (43% of injuries).
A call for standardized reporting
Dr. Makary contends that standardized reporting is needed for all adverse events related to robotic devices. One rare complication that occurs, he says, is that a surgeon can accidentally cut the aorta because the surgeon cannot feel its firmness. For reporting purposes, however, it’s unclear whether such an event is surgeon error or device-related error. The FDA currently collects only device-related errors.
Dr. Makary argues that errors such as inadvertent cutting of the aorta, although preventable with proper technique, should be tracked as device-related errors because they are more common with robotic surgery than with conventional surgery. Without better reporting standards, he says, these complications are less likely to be reported to the FDA at all. And if they go unreported, they cannot contribute to the understanding or identification of safety problems.
He suggests one solution: use of a database like the one maintained by the American College of Surgeons, in which independent nurses identify and track adverse events and complications of traditional operations.
Good information on robotic surgery is needed not only for research, but also to ensure that patients are fully informed about potential risks. Right now, Dr. Makary says, it’s too easy for a surgeon to claim that there are no additional risks related to robotic surgery because the evidence is nowhere to be found.
“Decisions should not be made based on the information in the FDA database,” he says. “We need to be able to give patients answers to their questions about safety and how much risk is associated with the robot. We have all suspected the answer has not been zero. We still don’t really know what the true answer is.”
We want to hear from you! Tell us what you think.
Although US hospitals have been quick to embrace surgical robot technology over the past decade, a “slapdash” system of reporting complications paints an unclear picture of its safety, according to Johns Hopkins researchers.
The Johns Hopkins team, led by Martin A. Makary, MD, MPH, found that, among the 1 million or so robotic surgeries performed since 2000, only 245 complications—including 71 deaths—were reported to the US Food and Drug Administration (FDA).1 When an adverse event or device malfunction occurs, hospitals are required to report these incidents to the manufacturer, which in turn is required to report them to the FDA—but this reporting doesn’t always happen.
“The number reported is very low for any complex technology used over a million times,” says Dr. Makary, associate professor of surgery at the Johns Hopkins University School of Medicine. “Doctors and patients can’t properly evaluate safety when we have a haphazard system of collecting data that is not independent and not transparent. There may be some complications specific to the use of this device, but we can only learn about them if we accurately track outcomes.”
The use of the robot in surgery has skyrocketed. Between 2007 and 2011, for example, the number of procedures involving the robot increased by more than 400% in the United States and more than 300% internationally. At the end of 2011, there were 1,400 surgical robots installed in US hospitals, up from 800 just 4 years earlier.
Some incidents went unreported until the news media highlighted them
Dr. Makary and colleagues found several incidents reported in the national news media that were not reported to the FDA until after the stories appeared in the press, even though the incidents took place long before the media exposure. Dr. Makary says it’s likely that many other incidents go unreported, never to be captured by research like his or by the FDA.
“We need innovation in medicine and, in this country, we are tremendously good at introducing new technologies,” he says. “But we have to evaluate new technology properly so we don’t over-adopt—or under-adopt—important advances that could benefit patients.”
How the study was conducted
Makary and colleagues reviewed the FDA adverse events database from January 1, 2000, to August 1, 2012. They also searched legal judgments and adverse events using LexisNexis to scan news media, and PACER to scan court records. The cases then were cross-referenced to see if they matched. The investigators found that eight cases were not appropriately reported to the FDA, five of which were never reported and two of which were reported only after a story about them appeared in the press.
Complication rate was highest for hysterectomy
When investigators reviewed complications that were reported, the procedures most commonly associated with death were:
- gynecologic (22 of the 71 deaths)
- urologic (15 deaths)
- cardiothoracic (12 deaths).
The cause of death was most often excessive bleeding. In cases where patients survived, hysterectomy by far had the most complications (43% of injuries).
A call for standardized reporting
Dr. Makary contends that standardized reporting is needed for all adverse events related to robotic devices. One rare complication that occurs, he says, is that a surgeon can accidentally cut the aorta because the surgeon cannot feel its firmness. For reporting purposes, however, it’s unclear whether such an event is surgeon error or device-related error. The FDA currently collects only device-related errors.
Dr. Makary argues that errors such as inadvertent cutting of the aorta, although preventable with proper technique, should be tracked as device-related errors because they are more common with robotic surgery than with conventional surgery. Without better reporting standards, he says, these complications are less likely to be reported to the FDA at all. And if they go unreported, they cannot contribute to the understanding or identification of safety problems.
He suggests one solution: use of a database like the one maintained by the American College of Surgeons, in which independent nurses identify and track adverse events and complications of traditional operations.
Good information on robotic surgery is needed not only for research, but also to ensure that patients are fully informed about potential risks. Right now, Dr. Makary says, it’s too easy for a surgeon to claim that there are no additional risks related to robotic surgery because the evidence is nowhere to be found.
“Decisions should not be made based on the information in the FDA database,” he says. “We need to be able to give patients answers to their questions about safety and how much risk is associated with the robot. We have all suspected the answer has not been zero. We still don’t really know what the true answer is.”
We want to hear from you! Tell us what you think.
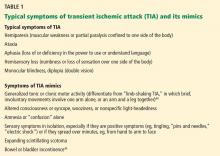
“I just saw Big Bird. He was 100 feet tall!” Malingering in the emergency room
The economic downturn in the United States has prompted numerous state and county budget cuts, in turn forcing many patients to receive their mental health care in the emergency room (ER). Most patients evaluated in the ER for mental health-related reasons have a legitimate psychiatric crisis—but that isn’t always the case. And as the number of people seeking care in the ER has increased, it appears that so too has the number of those who feign symptoms for secondary gain—that is, who are malingering.
This article highlights several red flags for malingered behavior; emphasizes typical (compared with atypical) symptoms of psychosis; and provides an overview of four instruments that you can use to help assess for malingering in the ED.
A difficult diagnosis
No single factor is indicative of malingering, and no objective tests exist to diagnose malingering definitively. Rather, the tests we discuss provide additional information that can help formulate a clinical impression.
According to DSM-5, malingering is “…the intentional production of false or grossly exaggerated physical or psychological symptoms, motivated by external incentives…”1 Despite a relatively straightforward definition, the diagnosis is difficult to make because it is a diagnosis of exclusion.
Even with sufficient evidence, many clinicians are reluctant to diagnose malingering because they fear retaliation and diagnostic uncertainty. Psychiatrists also might be reluctant to diagnose malingering because the negative connotation that the label carries risks stigmatizing a patient who might, in fact, be suffering. This is true especially when there is suspicion of partial malingering, the conscious exaggeration of existing symptoms.
Despite physicians’ reluctance to diagnose malingering, it is a real problem, especially in the ER. Research suggests that as many as 13% of patients in the ER feign illness, and that their secondary gain most often includes food, shelter, prescription drugs, financial gain, and avoidance of jail, work, or family responsibilities.2
CASE REPORT ‘The voices are telling me to kill myself’
Mr. K, a 36-year-old white man, walks into the ER on a late December day. He tells the triage nurse that he suicidal; she escorts him to the psychiatric pod of the ER. Nursing staff provide line-of-sight care, monitor his vital signs, and draw blood for testing.
Within hours, Mr. K is deemed “medically cleared” and ready for assessment by the psychiatric social worker.
Interview and assessment. During the interview with the social worker, Mr. K reports that he has been depressed, adamantly maintaining that he is suicidal, with a plan to “walk in traffic” or “eat the end of a gun.” The social worker places him on a 72-hour involuntary psychiatric hold. ER physicians order psychiatric consultation.
Mr. K is well-known to the psychiatrist on call, from prior ER visits and psychiatric hospital admissions. In fact, two days earlier, he put a psychiatric nurse in a headlock while being escorted from the psychiatric inpatient unit under protest.
On assessment by the psychiatrist, Mr. K continues to endorse feeling suicidal; he adds: “If I don’t get some help, I’m gonna kill somebody else!”
Without prompting, the patient states that “the voices are telling me to kill myself.” He says that those voices have been relentless since he left the hospital two days earlier. According to Mr. K, nothing he did helped quiet the voices, although previous prescriptions for quetiapine have been helpful.
Mr. K says that he is unable to recall the clinic or name of his prior psychiatrist. He claims that he was hospitalized four months ago, (despite the psychiatrist’s knowledge that he had been discharged two days ago) and estimates that his psychotic symptoms began one year ago. He explains that he is homeless and does not have social support. He is unable to provide a telephone number or a name to contact family for collateral information.
Mental status exam. The mental status examination reveals a tall, thin, disheveled man who has poor dentition. He is now calm and cooperative despite his reported level of distress. His speech is unremarkable and his eye contact is appropriate. His thought process is linear, organized, and coherent.
Mr. K does not endorse additional symptoms, but is quick to agree with the psychiatrist’s follow-up questions about hallucinations: “Yeah! I’ve been seeing all kinds of crazy stuff.” When prompted for details, he says, “I just saw Big Bird… He was 100 feet tall!”
Lab testing. Mr. K’s blood work is remarkable for positive urine toxicology for amphetamines.
Nursing notes indicate that Mr. K slept overnight and ate 100% of the food on his dinner and breakfast trays.
Red flags flying
Mr. K’s case highlights several red flags that should raise suspicion of malingering (Table 1)3,4:
- A conditional statement by which a patient threatens to harm himself or others, contingent upon a demand—for example, “If I don’t get A, I’ll do B.”
- An overly dramatic presentation, in which the patient is quick to endorse
distressing symptoms. Consider Mr. K: He was quick to report that he saw Big Bird, and that this Sesame Street character “was 100 feet tall.” Patients who have been experiencing true psychotic symptoms might be reluctant to speak of their distressing symptoms, especially if they have not experienced such symptoms in the past (the first psychotic break). Mr. K, however, volunteered and called attention to particularly dramatic psychotic symptoms. - A subjective report of distress that is inconsistent with the objective presentation. Mr. K’s report of depression—a diagnosis that typically includes insomnia and poor appetite—was inconsistent with his behavior: He slept and he ate all of his meals.
Atypical (vs typical) psychosis
Malingering can occur in various arenas and take many different forms. In forensic settings, such as prison, malingered conditions more often present as posttraumatic stress disorder or cognitive impairment.5 In non-forensic settings, such as the ER, the most commonly malingered conditions include suicidality and psychosis.
To detect malingered psychosis, one must first understand how true psychotic symptoms manifest. The following discussion describes and compares typical and atypical symptoms of psychosis; examples are given in Table 2.6,7No single atypical psychotic symptom is indicative of malingering. Rather, a collection of atypical symptoms, when considered in clinical context, should raise suspicion of malingering and prompt you to seek additional collateral information or perform appropriate testing for malingering.
Hallucinations
Typically, hallucinations take three forms: auditory, visual, and tactile. In primary psychiatric conditions, auditory hallucinations are the most common of those three.
Tactile hallucinations can be present during episodes of substance intoxication or withdrawal (eg, so-called coke bugs).
Auditory hallucinations. Patients who malinger psychosis are often unaware of the nuances of hallucinations. For example, they might report the atypical symptom of continuous voices; in fact, most patients who have schizophrenia hear voices intermittently. Keep in mind, too, that 75% of patients who have schizophrenia hear male and female voices, and that 70% have some type of coping strategy to minimize their internal stimuli (eg, listening to music).6,7
Visual hallucinations are most often associated with neurologic disease, but also occur often in primary psychotic disorders, such as schizophrenia.
Patients who malinger psychotic symptoms often are open to suggestion, and are quick to endorse visual hallucinations. When asked to describe their hallucinations, however, they often respond without details (“I don’t know”). Other times, they overcompensate with wild exaggeration of atypical visions—recall Mr. K’s description of a towering Big Bird. Asked if the visions are in black and white, they might eagerly agree. Research suggests, however, that patients who have schizophrenia more often experience life-sized hallucinations of vivid scenes with family members, religious figures, or animals.8 Furthermore, genuine visual hallucinations typically are in color.
Putting malingering in the differential
Regardless of the number of atypical symptoms a patient exhibits, malingering will be missed if you do not include it in the differential diagnosis. This fact was made evident in a 1973 study.9
In that study, Rosenhan and seven of his colleagues—a psychology graduate student, three psychologists, a pediatrician, a psychiatrist, a painter, and a housewife—presented to various ERs and intake units, and, as they had been instructed, endorsed vague auditory hallucinations of “empty,” “hollow,” or “thud” sounds—but nothing more. All were admitted to psychiatric hospitals. Once admitted, they refrained (again, as instructed) from endorsing or exhibiting any psychotic symptoms.
Despite the vague nature of the reported auditory hallucinations and how rapidly symptoms resolved on admission, seven of these pseudo-patients were given a diagnosis of schizophrenia, and one was given a diagnosis of manic-depressive psychosis. Duration of admission ranged from 7 to 52 days (average, 19 days). None of the study participants were suspected of feigning symptoms.
It’s fortunate that, since then, mental health professionals have developed more structured techniques of assessment to detect malingering in inpatient and triage settings.
Testing to identify and assess malingering
The ER is a fast-paced environment, in which treatment teams are challenged to make rapid clinical assessments. With the overwhelming number of patients seeking mental health care in the ER, however, overall wait times are increasing; in some regions, it is common to write, then to rewrite, involuntary psychiatric holds for patients awaiting transfer to a psychiatric hospital. This extended duration presents an opportunity to serially evaluate patients suspected of malingering.
Even in environments that allow for a more comprehensive evaluation (eg, jail or inpatient psychiatric wards), few psychometric tests have been validated to detect malingering. The most validated tests include the Structured Interview of Reported Symptoms (SIRS), distributed now as the Structured Interview of Reported Symptoms, 2nd edition (SIRS-2), and the Minnesota Multiphasic Personality Inventory Revised (MMPI-2). These tests typically require ≥30 minutes to administer and generally are not feasible in the fast-paced ER.
Despite the high prevalence of malingered behaviors in the ER, no single test has been validated in such a setting. Furthermore, there is no test designed to specifically assess for malingered suicidality or homicidality. The results of one test do not, in isolation, represent a comprehensive neuropsychological examination; rather, those results provide additional data to formulate a clinical impression. The instruments discussed below are administered and scored in a defined, objective manner.
When evaluating a patient whom you suspect of malingering, gathering collateral information—from family members, friends, nurses, social workers, emergency medicine physicians, and others—becomes important. You might discover pertinent information in ambulance and police reports and a review of the patient’s prior ER visits.
During the initial interview, ask open-ended questions; do not lead the patient by listing clusters of symptoms associated with a particular diagnosis. Because it is often difficult for a patient to malinger symptoms for a prolonged period, serial observations of a patient’s behavior and interview responses over time can provide additional information to make a clinical diagnosis of malingering.4
What testing is feasible in the ER?
Miller Forensic Assessment of Symptoms Test. The M-FAST measures rare symptom combinations, excessive reporting, and atypical symptoms of psychosis, using the same principles as the SIRS-2.
The 25-item screen begins by advising the examinee that he (she) will be asked questions about his psychological symptoms and that the questions that follow might or might not apply to his specific symptoms.
After that brief introduction, the examinee is asked if he hears ringing in his ears. Based on his response, the examiner reads one of two responses—both of which suggest the false notion that patients with true mental illness will suffer from ringing in their ears.
The examinee is then asked a series of Yes or No questions. Some pertain to legitimate symptoms a person with a psychotic illness might suffer (such as, “Do voices tell you to do things? Yes or No?”). Conversely, other questions screen for improbable symptoms that are atypical of patients who have a true psychotic disorder (such as “On many days I feel so bad that I can’t even remember my full name: Yes or No?”).
The exam concludes with a question about a ringing in the examinee’s ear. Affirmative responses are tallied; a score of ≥6 in a clinical setting is 83% specific and 93% sensitive for malingering.10
Visual Memory Test. Rey’s 15-Item Visual Memory Test capitalizes on the false belief that intellectual deficits, in addition to psychotic symptoms, make a claim of mental illness more believable.
In this simple test, the provider tells the examinee, “I am going to show you a card with 15 things on it that I want you to remember. When I take the card away, I want you to write down as many of the 15 things as you can remember.”3 The examinee is shown 15 common symbols (eg, 1, 2, 3; A, B, C; I, II, III, a, b, c; and the geometrics ●, ■, ▲).
At 5 seconds, the examinee is prompted, “Be sure to remember all of them.” After 10 seconds, the stimulus is removed, and the examinee is asked to recreate the figure.
Normative data indicate that even a patient who has a severe traumatic brain injury is able to recreate at least eight of the symbols. Although controversial, research indicates that a score of <9 symbols is predictive of malingering with 40% sensitivity and 100% specificity.11
Critics argued that confounding variables (IQ, memory disorder, age) might skew the quantitative score. For that reason, the same group developed the Rey’s II Test, which includes a supplementary qualitative scoring system that emphasizes embellishment errors (eg, the wrong symbol) and ordering errors (eg, wrong row). The Rey’s II Test proved to be more sensitive (accurate classification of malingers): A cut-off score of ≥2 qualitative errors is predictive of malingering with 86% sensitivity and 100% specificity.12
Coin-in-the-Hand Test. Perhaps the simplest test to administer is the Coin-in-the-Hand, designed to seem—superficially—to be a challenging memory test.
The patient must guess in which hand the examiner is holding a coin. The patient is shown the coin for two seconds, and then asked to close his eyes and count back from 10. The patient then points to one of the two clenched hands.
This task is repeated 10 times; each time, the provider gives verbal feedback about the accuracy or inaccuracy of that attempt. Studies indicate that a patient who has a severe traumatic brain injury is able to score 85% correct. A score <85%, however, suggests feigning of symptoms (sensitivity, 92.5%; specificity 87.5%).13 Hanley and co-workers demonstrated that people who are simulating cognitive impairment had a mean accurate response of 4.1, whereas people who had true amnesia had a mean accurate response of 9.65.14
Persons who feign psychosis or mood symptoms often inaccurately believe that people with mental illness also have cognitive impairment. Both Rey’s test and the Coin-in-the-Hand Test capitalize on this misconception.
Mini-Mental State Examination. Research also has shown that the Folstein Mini-Mental State Examination (MMSE) can screen for malingered cognitive impairment. Powell compared 40 mental health clinicians who were instructed to feign psychosis and 40 patients with schizophrenia. Using the MMSE, the researchers found that the malingers more often gave approximate answers.15 Moreover, Myers argued that, when compared with Rey’s Test, the MMSE is superior for assessing malingered cognitive impairment because it has a higher positive predictive value (67%, compared with 43% for Rey’s Test) and a higher negative predictive value (93% and 89%).16
What can you do for these patients after diagnosis?
Malingering is not considered a psychiatric diagnosis; there are no indicated therapies with which to manage it—only guidelines. When you suspect a patient of malingering, you should avoid accusing him (her) of faking symptoms. Rather, when feasible, gently confront the person and provide the opportunity for him to explain his current behaviors. For example, you might say: “I’ve treated many patients with the symptoms that you’re reporting, but the details you provide are different, and don’t ring completely true. Is there anything else that could explain this?”17
Regardless of a patient’s challenging behaviors, it is important to remember that people who feign illness—whether partial malingering or pure malingering—often do need help. The assistance they require, however, might be best obtained from a housing agency, a chemical dependency program, or another social service—not from the ER. Identifying malingered behaviors saves time and money and shifts limited resources to people who have a legitimate mental health condition.
Last, despite an empathetic approach, some malingering patients continue to feign symptoms—as Mr. K did.
CASE CONTINUED
Although the psychiatrist on call considered forsaking the police to escort Mr. K out of the ER, he eventually agreed to leave the hospital on his own, stating, “My death is going to be on your hands.”
Eight days later, Mr. K visited the ER at a different hospital, endorsing chronic pain and demanding narcotics.
Bottom Line
As the number of people seeking care in the emergency room (ER) has increased, so has the number of those who feign symptoms for secondary gain. No single factor is indicative of malingering, and no objective tests exist to diagnose it definitively. Furthermore, there are no indicated therapies with which to manage malingering—only guidelines. Keep in mind that people who feign illness, whether partial or pure malingering, often do need help—although not the services of an ER.
Related Resources
- Miller Forensic Assessment of Symptoms Test (M-FAST). Psychological Assessment Resources, Inc. www4.parinc.com (enter “M-FAST” in search field).
- Duffy S. Malingering psychological symptoms: An empirical review. Illinois State University, Department of Psychology. http://psychology.illinoisstate.edu/cc/Comps/Duffy%20-%20Malingering.pdf. Accessed September 10, 2013.
Drug Brand Names
Quetiapine • Seroquel
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Featured Audio
M. Cait Brady, MD, shares strategies for assessing malingering. Dr. Brady is a Third-Year Resident in General Psychiatry, University of California, Davis Medical Center - Sacramento, Sacramento, California.
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Yates BD, Nordquist CR, Schultz-Ross RA. Feigned psychiatric symptoms in the emergency room. Psychiatr Serv. 1996;47(9):998-1000.
3. Reccoppa L. Mentally ill or malingering? 3 clues cast doubt. Current Psychiatry. 2009;8(12):110.
4. Resnick PJ, Knoll J. Faking it: how to detect malingered psychosis. Current Psychiatry. 2005;4(11):12-25.
5. Gunn J, Taylor P. Forensic psychiatry: clinical, legal and ethical issues. Oxford, United Kingdom: Butterworth-Heinemann; 1998.
6. Farhall J, Greenwood K, Jackson H. Coping with hallucinated voices in schizophrenia: a review of self-initiated and therapeutic interventions. Clin Psychol Rev. 2007;27(4):476-493.
7. Goodwin DW, Anderson P, Rosenthal R. Clinical significance of hallucinations in psychiatric disorders: a study of 116 hallucinatory patients. Arch Gen Psychiatry. 1971;24:76-80.
8. Small IJ, Small JG, Andersen JM. Clinical characteristics of hallucinations of schizophrenia. Dis Nerv Syst. 1966;27(5):349-353.
9. Rosenhan DL. On being sane in insane places. Science. 1973;179(70):250-258.
10. Miller HA. M-FAST interview booklet. Lutz, FL: Psychological Assessment Resources; 2001.
11. Hom J, Denney RL. Detection of response bias in forensic neuropsychology. Binghamton, NY: Haworth Medical Press; 2002.
12. Whitney KA, Hook JN, Steiner AR, et al. Is the Rey 15-Item Memory Test II (Rey II) a valid symptom validity test?: comparison with the TOMM. Appl Neuropsychol. 2008;15(4):287-292.
13. Kelly PJ, Baker GA, van den Broek MD, et al. The detection of malingering in memory performance: the sensitivity and specificity of four measures in a UK population. Br J Clin Psychol. 2005;44(3):333-341.
14. Hanley JR, Backer G, Ledson S. Detecting the faking of amnesia: a comparison of the effectiveness of three different techniques for distinguishing simulators from patients with amnesia. J Clin Exp Neuropsychol. 1999;21(1):59-69.
15. Rogers R. Clinical assessment of malingering and deception, 3rd ed. New York, NY: The Gilford Press; 2008:54.
16. Myers W, Hall R, Tolou-Shams M. Prevalence and assessment of malingering in homicide defendants using the mini-mental state examination and the Rey 15-Item Memory Test. Homicide Stud. 2013;17(3):314-328.
17. Resnick PJ. In session with Phillip J. Resnick, MD: malingering of psychiatric symptoms. Prim Psychiatry. 2006;13(6):35-38.
The economic downturn in the United States has prompted numerous state and county budget cuts, in turn forcing many patients to receive their mental health care in the emergency room (ER). Most patients evaluated in the ER for mental health-related reasons have a legitimate psychiatric crisis—but that isn’t always the case. And as the number of people seeking care in the ER has increased, it appears that so too has the number of those who feign symptoms for secondary gain—that is, who are malingering.
This article highlights several red flags for malingered behavior; emphasizes typical (compared with atypical) symptoms of psychosis; and provides an overview of four instruments that you can use to help assess for malingering in the ED.
A difficult diagnosis
No single factor is indicative of malingering, and no objective tests exist to diagnose malingering definitively. Rather, the tests we discuss provide additional information that can help formulate a clinical impression.
According to DSM-5, malingering is “…the intentional production of false or grossly exaggerated physical or psychological symptoms, motivated by external incentives…”1 Despite a relatively straightforward definition, the diagnosis is difficult to make because it is a diagnosis of exclusion.
Even with sufficient evidence, many clinicians are reluctant to diagnose malingering because they fear retaliation and diagnostic uncertainty. Psychiatrists also might be reluctant to diagnose malingering because the negative connotation that the label carries risks stigmatizing a patient who might, in fact, be suffering. This is true especially when there is suspicion of partial malingering, the conscious exaggeration of existing symptoms.
Despite physicians’ reluctance to diagnose malingering, it is a real problem, especially in the ER. Research suggests that as many as 13% of patients in the ER feign illness, and that their secondary gain most often includes food, shelter, prescription drugs, financial gain, and avoidance of jail, work, or family responsibilities.2
CASE REPORT ‘The voices are telling me to kill myself’
Mr. K, a 36-year-old white man, walks into the ER on a late December day. He tells the triage nurse that he suicidal; she escorts him to the psychiatric pod of the ER. Nursing staff provide line-of-sight care, monitor his vital signs, and draw blood for testing.
Within hours, Mr. K is deemed “medically cleared” and ready for assessment by the psychiatric social worker.
Interview and assessment. During the interview with the social worker, Mr. K reports that he has been depressed, adamantly maintaining that he is suicidal, with a plan to “walk in traffic” or “eat the end of a gun.” The social worker places him on a 72-hour involuntary psychiatric hold. ER physicians order psychiatric consultation.
Mr. K is well-known to the psychiatrist on call, from prior ER visits and psychiatric hospital admissions. In fact, two days earlier, he put a psychiatric nurse in a headlock while being escorted from the psychiatric inpatient unit under protest.
On assessment by the psychiatrist, Mr. K continues to endorse feeling suicidal; he adds: “If I don’t get some help, I’m gonna kill somebody else!”
Without prompting, the patient states that “the voices are telling me to kill myself.” He says that those voices have been relentless since he left the hospital two days earlier. According to Mr. K, nothing he did helped quiet the voices, although previous prescriptions for quetiapine have been helpful.
Mr. K says that he is unable to recall the clinic or name of his prior psychiatrist. He claims that he was hospitalized four months ago, (despite the psychiatrist’s knowledge that he had been discharged two days ago) and estimates that his psychotic symptoms began one year ago. He explains that he is homeless and does not have social support. He is unable to provide a telephone number or a name to contact family for collateral information.
Mental status exam. The mental status examination reveals a tall, thin, disheveled man who has poor dentition. He is now calm and cooperative despite his reported level of distress. His speech is unremarkable and his eye contact is appropriate. His thought process is linear, organized, and coherent.
Mr. K does not endorse additional symptoms, but is quick to agree with the psychiatrist’s follow-up questions about hallucinations: “Yeah! I’ve been seeing all kinds of crazy stuff.” When prompted for details, he says, “I just saw Big Bird… He was 100 feet tall!”
Lab testing. Mr. K’s blood work is remarkable for positive urine toxicology for amphetamines.
Nursing notes indicate that Mr. K slept overnight and ate 100% of the food on his dinner and breakfast trays.
Red flags flying
Mr. K’s case highlights several red flags that should raise suspicion of malingering (Table 1)3,4:
- A conditional statement by which a patient threatens to harm himself or others, contingent upon a demand—for example, “If I don’t get A, I’ll do B.”
- An overly dramatic presentation, in which the patient is quick to endorse
distressing symptoms. Consider Mr. K: He was quick to report that he saw Big Bird, and that this Sesame Street character “was 100 feet tall.” Patients who have been experiencing true psychotic symptoms might be reluctant to speak of their distressing symptoms, especially if they have not experienced such symptoms in the past (the first psychotic break). Mr. K, however, volunteered and called attention to particularly dramatic psychotic symptoms. - A subjective report of distress that is inconsistent with the objective presentation. Mr. K’s report of depression—a diagnosis that typically includes insomnia and poor appetite—was inconsistent with his behavior: He slept and he ate all of his meals.
Atypical (vs typical) psychosis
Malingering can occur in various arenas and take many different forms. In forensic settings, such as prison, malingered conditions more often present as posttraumatic stress disorder or cognitive impairment.5 In non-forensic settings, such as the ER, the most commonly malingered conditions include suicidality and psychosis.
To detect malingered psychosis, one must first understand how true psychotic symptoms manifest. The following discussion describes and compares typical and atypical symptoms of psychosis; examples are given in Table 2.6,7No single atypical psychotic symptom is indicative of malingering. Rather, a collection of atypical symptoms, when considered in clinical context, should raise suspicion of malingering and prompt you to seek additional collateral information or perform appropriate testing for malingering.
Hallucinations
Typically, hallucinations take three forms: auditory, visual, and tactile. In primary psychiatric conditions, auditory hallucinations are the most common of those three.
Tactile hallucinations can be present during episodes of substance intoxication or withdrawal (eg, so-called coke bugs).
Auditory hallucinations. Patients who malinger psychosis are often unaware of the nuances of hallucinations. For example, they might report the atypical symptom of continuous voices; in fact, most patients who have schizophrenia hear voices intermittently. Keep in mind, too, that 75% of patients who have schizophrenia hear male and female voices, and that 70% have some type of coping strategy to minimize their internal stimuli (eg, listening to music).6,7
Visual hallucinations are most often associated with neurologic disease, but also occur often in primary psychotic disorders, such as schizophrenia.
Patients who malinger psychotic symptoms often are open to suggestion, and are quick to endorse visual hallucinations. When asked to describe their hallucinations, however, they often respond without details (“I don’t know”). Other times, they overcompensate with wild exaggeration of atypical visions—recall Mr. K’s description of a towering Big Bird. Asked if the visions are in black and white, they might eagerly agree. Research suggests, however, that patients who have schizophrenia more often experience life-sized hallucinations of vivid scenes with family members, religious figures, or animals.8 Furthermore, genuine visual hallucinations typically are in color.
Putting malingering in the differential
Regardless of the number of atypical symptoms a patient exhibits, malingering will be missed if you do not include it in the differential diagnosis. This fact was made evident in a 1973 study.9
In that study, Rosenhan and seven of his colleagues—a psychology graduate student, three psychologists, a pediatrician, a psychiatrist, a painter, and a housewife—presented to various ERs and intake units, and, as they had been instructed, endorsed vague auditory hallucinations of “empty,” “hollow,” or “thud” sounds—but nothing more. All were admitted to psychiatric hospitals. Once admitted, they refrained (again, as instructed) from endorsing or exhibiting any psychotic symptoms.
Despite the vague nature of the reported auditory hallucinations and how rapidly symptoms resolved on admission, seven of these pseudo-patients were given a diagnosis of schizophrenia, and one was given a diagnosis of manic-depressive psychosis. Duration of admission ranged from 7 to 52 days (average, 19 days). None of the study participants were suspected of feigning symptoms.
It’s fortunate that, since then, mental health professionals have developed more structured techniques of assessment to detect malingering in inpatient and triage settings.
Testing to identify and assess malingering
The ER is a fast-paced environment, in which treatment teams are challenged to make rapid clinical assessments. With the overwhelming number of patients seeking mental health care in the ER, however, overall wait times are increasing; in some regions, it is common to write, then to rewrite, involuntary psychiatric holds for patients awaiting transfer to a psychiatric hospital. This extended duration presents an opportunity to serially evaluate patients suspected of malingering.
Even in environments that allow for a more comprehensive evaluation (eg, jail or inpatient psychiatric wards), few psychometric tests have been validated to detect malingering. The most validated tests include the Structured Interview of Reported Symptoms (SIRS), distributed now as the Structured Interview of Reported Symptoms, 2nd edition (SIRS-2), and the Minnesota Multiphasic Personality Inventory Revised (MMPI-2). These tests typically require ≥30 minutes to administer and generally are not feasible in the fast-paced ER.
Despite the high prevalence of malingered behaviors in the ER, no single test has been validated in such a setting. Furthermore, there is no test designed to specifically assess for malingered suicidality or homicidality. The results of one test do not, in isolation, represent a comprehensive neuropsychological examination; rather, those results provide additional data to formulate a clinical impression. The instruments discussed below are administered and scored in a defined, objective manner.
When evaluating a patient whom you suspect of malingering, gathering collateral information—from family members, friends, nurses, social workers, emergency medicine physicians, and others—becomes important. You might discover pertinent information in ambulance and police reports and a review of the patient’s prior ER visits.
During the initial interview, ask open-ended questions; do not lead the patient by listing clusters of symptoms associated with a particular diagnosis. Because it is often difficult for a patient to malinger symptoms for a prolonged period, serial observations of a patient’s behavior and interview responses over time can provide additional information to make a clinical diagnosis of malingering.4
What testing is feasible in the ER?
Miller Forensic Assessment of Symptoms Test. The M-FAST measures rare symptom combinations, excessive reporting, and atypical symptoms of psychosis, using the same principles as the SIRS-2.
The 25-item screen begins by advising the examinee that he (she) will be asked questions about his psychological symptoms and that the questions that follow might or might not apply to his specific symptoms.
After that brief introduction, the examinee is asked if he hears ringing in his ears. Based on his response, the examiner reads one of two responses—both of which suggest the false notion that patients with true mental illness will suffer from ringing in their ears.
The examinee is then asked a series of Yes or No questions. Some pertain to legitimate symptoms a person with a psychotic illness might suffer (such as, “Do voices tell you to do things? Yes or No?”). Conversely, other questions screen for improbable symptoms that are atypical of patients who have a true psychotic disorder (such as “On many days I feel so bad that I can’t even remember my full name: Yes or No?”).
The exam concludes with a question about a ringing in the examinee’s ear. Affirmative responses are tallied; a score of ≥6 in a clinical setting is 83% specific and 93% sensitive for malingering.10
Visual Memory Test. Rey’s 15-Item Visual Memory Test capitalizes on the false belief that intellectual deficits, in addition to psychotic symptoms, make a claim of mental illness more believable.
In this simple test, the provider tells the examinee, “I am going to show you a card with 15 things on it that I want you to remember. When I take the card away, I want you to write down as many of the 15 things as you can remember.”3 The examinee is shown 15 common symbols (eg, 1, 2, 3; A, B, C; I, II, III, a, b, c; and the geometrics ●, ■, ▲).
At 5 seconds, the examinee is prompted, “Be sure to remember all of them.” After 10 seconds, the stimulus is removed, and the examinee is asked to recreate the figure.
Normative data indicate that even a patient who has a severe traumatic brain injury is able to recreate at least eight of the symbols. Although controversial, research indicates that a score of <9 symbols is predictive of malingering with 40% sensitivity and 100% specificity.11
Critics argued that confounding variables (IQ, memory disorder, age) might skew the quantitative score. For that reason, the same group developed the Rey’s II Test, which includes a supplementary qualitative scoring system that emphasizes embellishment errors (eg, the wrong symbol) and ordering errors (eg, wrong row). The Rey’s II Test proved to be more sensitive (accurate classification of malingers): A cut-off score of ≥2 qualitative errors is predictive of malingering with 86% sensitivity and 100% specificity.12
Coin-in-the-Hand Test. Perhaps the simplest test to administer is the Coin-in-the-Hand, designed to seem—superficially—to be a challenging memory test.
The patient must guess in which hand the examiner is holding a coin. The patient is shown the coin for two seconds, and then asked to close his eyes and count back from 10. The patient then points to one of the two clenched hands.
This task is repeated 10 times; each time, the provider gives verbal feedback about the accuracy or inaccuracy of that attempt. Studies indicate that a patient who has a severe traumatic brain injury is able to score 85% correct. A score <85%, however, suggests feigning of symptoms (sensitivity, 92.5%; specificity 87.5%).13 Hanley and co-workers demonstrated that people who are simulating cognitive impairment had a mean accurate response of 4.1, whereas people who had true amnesia had a mean accurate response of 9.65.14
Persons who feign psychosis or mood symptoms often inaccurately believe that people with mental illness also have cognitive impairment. Both Rey’s test and the Coin-in-the-Hand Test capitalize on this misconception.
Mini-Mental State Examination. Research also has shown that the Folstein Mini-Mental State Examination (MMSE) can screen for malingered cognitive impairment. Powell compared 40 mental health clinicians who were instructed to feign psychosis and 40 patients with schizophrenia. Using the MMSE, the researchers found that the malingers more often gave approximate answers.15 Moreover, Myers argued that, when compared with Rey’s Test, the MMSE is superior for assessing malingered cognitive impairment because it has a higher positive predictive value (67%, compared with 43% for Rey’s Test) and a higher negative predictive value (93% and 89%).16
What can you do for these patients after diagnosis?
Malingering is not considered a psychiatric diagnosis; there are no indicated therapies with which to manage it—only guidelines. When you suspect a patient of malingering, you should avoid accusing him (her) of faking symptoms. Rather, when feasible, gently confront the person and provide the opportunity for him to explain his current behaviors. For example, you might say: “I’ve treated many patients with the symptoms that you’re reporting, but the details you provide are different, and don’t ring completely true. Is there anything else that could explain this?”17
Regardless of a patient’s challenging behaviors, it is important to remember that people who feign illness—whether partial malingering or pure malingering—often do need help. The assistance they require, however, might be best obtained from a housing agency, a chemical dependency program, or another social service—not from the ER. Identifying malingered behaviors saves time and money and shifts limited resources to people who have a legitimate mental health condition.
Last, despite an empathetic approach, some malingering patients continue to feign symptoms—as Mr. K did.
CASE CONTINUED
Although the psychiatrist on call considered forsaking the police to escort Mr. K out of the ER, he eventually agreed to leave the hospital on his own, stating, “My death is going to be on your hands.”
Eight days later, Mr. K visited the ER at a different hospital, endorsing chronic pain and demanding narcotics.
Bottom Line
As the number of people seeking care in the emergency room (ER) has increased, so has the number of those who feign symptoms for secondary gain. No single factor is indicative of malingering, and no objective tests exist to diagnose it definitively. Furthermore, there are no indicated therapies with which to manage malingering—only guidelines. Keep in mind that people who feign illness, whether partial or pure malingering, often do need help—although not the services of an ER.
Related Resources
- Miller Forensic Assessment of Symptoms Test (M-FAST). Psychological Assessment Resources, Inc. www4.parinc.com (enter “M-FAST” in search field).
- Duffy S. Malingering psychological symptoms: An empirical review. Illinois State University, Department of Psychology. http://psychology.illinoisstate.edu/cc/Comps/Duffy%20-%20Malingering.pdf. Accessed September 10, 2013.
Drug Brand Names
Quetiapine • Seroquel
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Featured Audio
M. Cait Brady, MD, shares strategies for assessing malingering. Dr. Brady is a Third-Year Resident in General Psychiatry, University of California, Davis Medical Center - Sacramento, Sacramento, California.
The economic downturn in the United States has prompted numerous state and county budget cuts, in turn forcing many patients to receive their mental health care in the emergency room (ER). Most patients evaluated in the ER for mental health-related reasons have a legitimate psychiatric crisis—but that isn’t always the case. And as the number of people seeking care in the ER has increased, it appears that so too has the number of those who feign symptoms for secondary gain—that is, who are malingering.
This article highlights several red flags for malingered behavior; emphasizes typical (compared with atypical) symptoms of psychosis; and provides an overview of four instruments that you can use to help assess for malingering in the ED.
A difficult diagnosis
No single factor is indicative of malingering, and no objective tests exist to diagnose malingering definitively. Rather, the tests we discuss provide additional information that can help formulate a clinical impression.
According to DSM-5, malingering is “…the intentional production of false or grossly exaggerated physical or psychological symptoms, motivated by external incentives…”1 Despite a relatively straightforward definition, the diagnosis is difficult to make because it is a diagnosis of exclusion.
Even with sufficient evidence, many clinicians are reluctant to diagnose malingering because they fear retaliation and diagnostic uncertainty. Psychiatrists also might be reluctant to diagnose malingering because the negative connotation that the label carries risks stigmatizing a patient who might, in fact, be suffering. This is true especially when there is suspicion of partial malingering, the conscious exaggeration of existing symptoms.
Despite physicians’ reluctance to diagnose malingering, it is a real problem, especially in the ER. Research suggests that as many as 13% of patients in the ER feign illness, and that their secondary gain most often includes food, shelter, prescription drugs, financial gain, and avoidance of jail, work, or family responsibilities.2
CASE REPORT ‘The voices are telling me to kill myself’
Mr. K, a 36-year-old white man, walks into the ER on a late December day. He tells the triage nurse that he suicidal; she escorts him to the psychiatric pod of the ER. Nursing staff provide line-of-sight care, monitor his vital signs, and draw blood for testing.
Within hours, Mr. K is deemed “medically cleared” and ready for assessment by the psychiatric social worker.
Interview and assessment. During the interview with the social worker, Mr. K reports that he has been depressed, adamantly maintaining that he is suicidal, with a plan to “walk in traffic” or “eat the end of a gun.” The social worker places him on a 72-hour involuntary psychiatric hold. ER physicians order psychiatric consultation.
Mr. K is well-known to the psychiatrist on call, from prior ER visits and psychiatric hospital admissions. In fact, two days earlier, he put a psychiatric nurse in a headlock while being escorted from the psychiatric inpatient unit under protest.
On assessment by the psychiatrist, Mr. K continues to endorse feeling suicidal; he adds: “If I don’t get some help, I’m gonna kill somebody else!”
Without prompting, the patient states that “the voices are telling me to kill myself.” He says that those voices have been relentless since he left the hospital two days earlier. According to Mr. K, nothing he did helped quiet the voices, although previous prescriptions for quetiapine have been helpful.
Mr. K says that he is unable to recall the clinic or name of his prior psychiatrist. He claims that he was hospitalized four months ago, (despite the psychiatrist’s knowledge that he had been discharged two days ago) and estimates that his psychotic symptoms began one year ago. He explains that he is homeless and does not have social support. He is unable to provide a telephone number or a name to contact family for collateral information.
Mental status exam. The mental status examination reveals a tall, thin, disheveled man who has poor dentition. He is now calm and cooperative despite his reported level of distress. His speech is unremarkable and his eye contact is appropriate. His thought process is linear, organized, and coherent.
Mr. K does not endorse additional symptoms, but is quick to agree with the psychiatrist’s follow-up questions about hallucinations: “Yeah! I’ve been seeing all kinds of crazy stuff.” When prompted for details, he says, “I just saw Big Bird… He was 100 feet tall!”
Lab testing. Mr. K’s blood work is remarkable for positive urine toxicology for amphetamines.
Nursing notes indicate that Mr. K slept overnight and ate 100% of the food on his dinner and breakfast trays.
Red flags flying
Mr. K’s case highlights several red flags that should raise suspicion of malingering (Table 1)3,4:
- A conditional statement by which a patient threatens to harm himself or others, contingent upon a demand—for example, “If I don’t get A, I’ll do B.”
- An overly dramatic presentation, in which the patient is quick to endorse
distressing symptoms. Consider Mr. K: He was quick to report that he saw Big Bird, and that this Sesame Street character “was 100 feet tall.” Patients who have been experiencing true psychotic symptoms might be reluctant to speak of their distressing symptoms, especially if they have not experienced such symptoms in the past (the first psychotic break). Mr. K, however, volunteered and called attention to particularly dramatic psychotic symptoms. - A subjective report of distress that is inconsistent with the objective presentation. Mr. K’s report of depression—a diagnosis that typically includes insomnia and poor appetite—was inconsistent with his behavior: He slept and he ate all of his meals.
Atypical (vs typical) psychosis
Malingering can occur in various arenas and take many different forms. In forensic settings, such as prison, malingered conditions more often present as posttraumatic stress disorder or cognitive impairment.5 In non-forensic settings, such as the ER, the most commonly malingered conditions include suicidality and psychosis.
To detect malingered psychosis, one must first understand how true psychotic symptoms manifest. The following discussion describes and compares typical and atypical symptoms of psychosis; examples are given in Table 2.6,7No single atypical psychotic symptom is indicative of malingering. Rather, a collection of atypical symptoms, when considered in clinical context, should raise suspicion of malingering and prompt you to seek additional collateral information or perform appropriate testing for malingering.
Hallucinations
Typically, hallucinations take three forms: auditory, visual, and tactile. In primary psychiatric conditions, auditory hallucinations are the most common of those three.
Tactile hallucinations can be present during episodes of substance intoxication or withdrawal (eg, so-called coke bugs).
Auditory hallucinations. Patients who malinger psychosis are often unaware of the nuances of hallucinations. For example, they might report the atypical symptom of continuous voices; in fact, most patients who have schizophrenia hear voices intermittently. Keep in mind, too, that 75% of patients who have schizophrenia hear male and female voices, and that 70% have some type of coping strategy to minimize their internal stimuli (eg, listening to music).6,7
Visual hallucinations are most often associated with neurologic disease, but also occur often in primary psychotic disorders, such as schizophrenia.
Patients who malinger psychotic symptoms often are open to suggestion, and are quick to endorse visual hallucinations. When asked to describe their hallucinations, however, they often respond without details (“I don’t know”). Other times, they overcompensate with wild exaggeration of atypical visions—recall Mr. K’s description of a towering Big Bird. Asked if the visions are in black and white, they might eagerly agree. Research suggests, however, that patients who have schizophrenia more often experience life-sized hallucinations of vivid scenes with family members, religious figures, or animals.8 Furthermore, genuine visual hallucinations typically are in color.
Putting malingering in the differential
Regardless of the number of atypical symptoms a patient exhibits, malingering will be missed if you do not include it in the differential diagnosis. This fact was made evident in a 1973 study.9
In that study, Rosenhan and seven of his colleagues—a psychology graduate student, three psychologists, a pediatrician, a psychiatrist, a painter, and a housewife—presented to various ERs and intake units, and, as they had been instructed, endorsed vague auditory hallucinations of “empty,” “hollow,” or “thud” sounds—but nothing more. All were admitted to psychiatric hospitals. Once admitted, they refrained (again, as instructed) from endorsing or exhibiting any psychotic symptoms.
Despite the vague nature of the reported auditory hallucinations and how rapidly symptoms resolved on admission, seven of these pseudo-patients were given a diagnosis of schizophrenia, and one was given a diagnosis of manic-depressive psychosis. Duration of admission ranged from 7 to 52 days (average, 19 days). None of the study participants were suspected of feigning symptoms.
It’s fortunate that, since then, mental health professionals have developed more structured techniques of assessment to detect malingering in inpatient and triage settings.
Testing to identify and assess malingering
The ER is a fast-paced environment, in which treatment teams are challenged to make rapid clinical assessments. With the overwhelming number of patients seeking mental health care in the ER, however, overall wait times are increasing; in some regions, it is common to write, then to rewrite, involuntary psychiatric holds for patients awaiting transfer to a psychiatric hospital. This extended duration presents an opportunity to serially evaluate patients suspected of malingering.
Even in environments that allow for a more comprehensive evaluation (eg, jail or inpatient psychiatric wards), few psychometric tests have been validated to detect malingering. The most validated tests include the Structured Interview of Reported Symptoms (SIRS), distributed now as the Structured Interview of Reported Symptoms, 2nd edition (SIRS-2), and the Minnesota Multiphasic Personality Inventory Revised (MMPI-2). These tests typically require ≥30 minutes to administer and generally are not feasible in the fast-paced ER.
Despite the high prevalence of malingered behaviors in the ER, no single test has been validated in such a setting. Furthermore, there is no test designed to specifically assess for malingered suicidality or homicidality. The results of one test do not, in isolation, represent a comprehensive neuropsychological examination; rather, those results provide additional data to formulate a clinical impression. The instruments discussed below are administered and scored in a defined, objective manner.
When evaluating a patient whom you suspect of malingering, gathering collateral information—from family members, friends, nurses, social workers, emergency medicine physicians, and others—becomes important. You might discover pertinent information in ambulance and police reports and a review of the patient’s prior ER visits.
During the initial interview, ask open-ended questions; do not lead the patient by listing clusters of symptoms associated with a particular diagnosis. Because it is often difficult for a patient to malinger symptoms for a prolonged period, serial observations of a patient’s behavior and interview responses over time can provide additional information to make a clinical diagnosis of malingering.4
What testing is feasible in the ER?
Miller Forensic Assessment of Symptoms Test. The M-FAST measures rare symptom combinations, excessive reporting, and atypical symptoms of psychosis, using the same principles as the SIRS-2.
The 25-item screen begins by advising the examinee that he (she) will be asked questions about his psychological symptoms and that the questions that follow might or might not apply to his specific symptoms.
After that brief introduction, the examinee is asked if he hears ringing in his ears. Based on his response, the examiner reads one of two responses—both of which suggest the false notion that patients with true mental illness will suffer from ringing in their ears.
The examinee is then asked a series of Yes or No questions. Some pertain to legitimate symptoms a person with a psychotic illness might suffer (such as, “Do voices tell you to do things? Yes or No?”). Conversely, other questions screen for improbable symptoms that are atypical of patients who have a true psychotic disorder (such as “On many days I feel so bad that I can’t even remember my full name: Yes or No?”).
The exam concludes with a question about a ringing in the examinee’s ear. Affirmative responses are tallied; a score of ≥6 in a clinical setting is 83% specific and 93% sensitive for malingering.10
Visual Memory Test. Rey’s 15-Item Visual Memory Test capitalizes on the false belief that intellectual deficits, in addition to psychotic symptoms, make a claim of mental illness more believable.
In this simple test, the provider tells the examinee, “I am going to show you a card with 15 things on it that I want you to remember. When I take the card away, I want you to write down as many of the 15 things as you can remember.”3 The examinee is shown 15 common symbols (eg, 1, 2, 3; A, B, C; I, II, III, a, b, c; and the geometrics ●, ■, ▲).
At 5 seconds, the examinee is prompted, “Be sure to remember all of them.” After 10 seconds, the stimulus is removed, and the examinee is asked to recreate the figure.
Normative data indicate that even a patient who has a severe traumatic brain injury is able to recreate at least eight of the symbols. Although controversial, research indicates that a score of <9 symbols is predictive of malingering with 40% sensitivity and 100% specificity.11
Critics argued that confounding variables (IQ, memory disorder, age) might skew the quantitative score. For that reason, the same group developed the Rey’s II Test, which includes a supplementary qualitative scoring system that emphasizes embellishment errors (eg, the wrong symbol) and ordering errors (eg, wrong row). The Rey’s II Test proved to be more sensitive (accurate classification of malingers): A cut-off score of ≥2 qualitative errors is predictive of malingering with 86% sensitivity and 100% specificity.12
Coin-in-the-Hand Test. Perhaps the simplest test to administer is the Coin-in-the-Hand, designed to seem—superficially—to be a challenging memory test.
The patient must guess in which hand the examiner is holding a coin. The patient is shown the coin for two seconds, and then asked to close his eyes and count back from 10. The patient then points to one of the two clenched hands.
This task is repeated 10 times; each time, the provider gives verbal feedback about the accuracy or inaccuracy of that attempt. Studies indicate that a patient who has a severe traumatic brain injury is able to score 85% correct. A score <85%, however, suggests feigning of symptoms (sensitivity, 92.5%; specificity 87.5%).13 Hanley and co-workers demonstrated that people who are simulating cognitive impairment had a mean accurate response of 4.1, whereas people who had true amnesia had a mean accurate response of 9.65.14
Persons who feign psychosis or mood symptoms often inaccurately believe that people with mental illness also have cognitive impairment. Both Rey’s test and the Coin-in-the-Hand Test capitalize on this misconception.
Mini-Mental State Examination. Research also has shown that the Folstein Mini-Mental State Examination (MMSE) can screen for malingered cognitive impairment. Powell compared 40 mental health clinicians who were instructed to feign psychosis and 40 patients with schizophrenia. Using the MMSE, the researchers found that the malingers more often gave approximate answers.15 Moreover, Myers argued that, when compared with Rey’s Test, the MMSE is superior for assessing malingered cognitive impairment because it has a higher positive predictive value (67%, compared with 43% for Rey’s Test) and a higher negative predictive value (93% and 89%).16
What can you do for these patients after diagnosis?
Malingering is not considered a psychiatric diagnosis; there are no indicated therapies with which to manage it—only guidelines. When you suspect a patient of malingering, you should avoid accusing him (her) of faking symptoms. Rather, when feasible, gently confront the person and provide the opportunity for him to explain his current behaviors. For example, you might say: “I’ve treated many patients with the symptoms that you’re reporting, but the details you provide are different, and don’t ring completely true. Is there anything else that could explain this?”17
Regardless of a patient’s challenging behaviors, it is important to remember that people who feign illness—whether partial malingering or pure malingering—often do need help. The assistance they require, however, might be best obtained from a housing agency, a chemical dependency program, or another social service—not from the ER. Identifying malingered behaviors saves time and money and shifts limited resources to people who have a legitimate mental health condition.
Last, despite an empathetic approach, some malingering patients continue to feign symptoms—as Mr. K did.
CASE CONTINUED
Although the psychiatrist on call considered forsaking the police to escort Mr. K out of the ER, he eventually agreed to leave the hospital on his own, stating, “My death is going to be on your hands.”
Eight days later, Mr. K visited the ER at a different hospital, endorsing chronic pain and demanding narcotics.
Bottom Line
As the number of people seeking care in the emergency room (ER) has increased, so has the number of those who feign symptoms for secondary gain. No single factor is indicative of malingering, and no objective tests exist to diagnose it definitively. Furthermore, there are no indicated therapies with which to manage malingering—only guidelines. Keep in mind that people who feign illness, whether partial or pure malingering, often do need help—although not the services of an ER.
Related Resources
- Miller Forensic Assessment of Symptoms Test (M-FAST). Psychological Assessment Resources, Inc. www4.parinc.com (enter “M-FAST” in search field).
- Duffy S. Malingering psychological symptoms: An empirical review. Illinois State University, Department of Psychology. http://psychology.illinoisstate.edu/cc/Comps/Duffy%20-%20Malingering.pdf. Accessed September 10, 2013.
Drug Brand Names
Quetiapine • Seroquel
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Featured Audio
M. Cait Brady, MD, shares strategies for assessing malingering. Dr. Brady is a Third-Year Resident in General Psychiatry, University of California, Davis Medical Center - Sacramento, Sacramento, California.
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Yates BD, Nordquist CR, Schultz-Ross RA. Feigned psychiatric symptoms in the emergency room. Psychiatr Serv. 1996;47(9):998-1000.
3. Reccoppa L. Mentally ill or malingering? 3 clues cast doubt. Current Psychiatry. 2009;8(12):110.
4. Resnick PJ, Knoll J. Faking it: how to detect malingered psychosis. Current Psychiatry. 2005;4(11):12-25.
5. Gunn J, Taylor P. Forensic psychiatry: clinical, legal and ethical issues. Oxford, United Kingdom: Butterworth-Heinemann; 1998.
6. Farhall J, Greenwood K, Jackson H. Coping with hallucinated voices in schizophrenia: a review of self-initiated and therapeutic interventions. Clin Psychol Rev. 2007;27(4):476-493.
7. Goodwin DW, Anderson P, Rosenthal R. Clinical significance of hallucinations in psychiatric disorders: a study of 116 hallucinatory patients. Arch Gen Psychiatry. 1971;24:76-80.
8. Small IJ, Small JG, Andersen JM. Clinical characteristics of hallucinations of schizophrenia. Dis Nerv Syst. 1966;27(5):349-353.
9. Rosenhan DL. On being sane in insane places. Science. 1973;179(70):250-258.
10. Miller HA. M-FAST interview booklet. Lutz, FL: Psychological Assessment Resources; 2001.
11. Hom J, Denney RL. Detection of response bias in forensic neuropsychology. Binghamton, NY: Haworth Medical Press; 2002.
12. Whitney KA, Hook JN, Steiner AR, et al. Is the Rey 15-Item Memory Test II (Rey II) a valid symptom validity test?: comparison with the TOMM. Appl Neuropsychol. 2008;15(4):287-292.
13. Kelly PJ, Baker GA, van den Broek MD, et al. The detection of malingering in memory performance: the sensitivity and specificity of four measures in a UK population. Br J Clin Psychol. 2005;44(3):333-341.
14. Hanley JR, Backer G, Ledson S. Detecting the faking of amnesia: a comparison of the effectiveness of three different techniques for distinguishing simulators from patients with amnesia. J Clin Exp Neuropsychol. 1999;21(1):59-69.
15. Rogers R. Clinical assessment of malingering and deception, 3rd ed. New York, NY: The Gilford Press; 2008:54.
16. Myers W, Hall R, Tolou-Shams M. Prevalence and assessment of malingering in homicide defendants using the mini-mental state examination and the Rey 15-Item Memory Test. Homicide Stud. 2013;17(3):314-328.
17. Resnick PJ. In session with Phillip J. Resnick, MD: malingering of psychiatric symptoms. Prim Psychiatry. 2006;13(6):35-38.
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Yates BD, Nordquist CR, Schultz-Ross RA. Feigned psychiatric symptoms in the emergency room. Psychiatr Serv. 1996;47(9):998-1000.
3. Reccoppa L. Mentally ill or malingering? 3 clues cast doubt. Current Psychiatry. 2009;8(12):110.
4. Resnick PJ, Knoll J. Faking it: how to detect malingered psychosis. Current Psychiatry. 2005;4(11):12-25.
5. Gunn J, Taylor P. Forensic psychiatry: clinical, legal and ethical issues. Oxford, United Kingdom: Butterworth-Heinemann; 1998.
6. Farhall J, Greenwood K, Jackson H. Coping with hallucinated voices in schizophrenia: a review of self-initiated and therapeutic interventions. Clin Psychol Rev. 2007;27(4):476-493.
7. Goodwin DW, Anderson P, Rosenthal R. Clinical significance of hallucinations in psychiatric disorders: a study of 116 hallucinatory patients. Arch Gen Psychiatry. 1971;24:76-80.
8. Small IJ, Small JG, Andersen JM. Clinical characteristics of hallucinations of schizophrenia. Dis Nerv Syst. 1966;27(5):349-353.
9. Rosenhan DL. On being sane in insane places. Science. 1973;179(70):250-258.
10. Miller HA. M-FAST interview booklet. Lutz, FL: Psychological Assessment Resources; 2001.
11. Hom J, Denney RL. Detection of response bias in forensic neuropsychology. Binghamton, NY: Haworth Medical Press; 2002.
12. Whitney KA, Hook JN, Steiner AR, et al. Is the Rey 15-Item Memory Test II (Rey II) a valid symptom validity test?: comparison with the TOMM. Appl Neuropsychol. 2008;15(4):287-292.
13. Kelly PJ, Baker GA, van den Broek MD, et al. The detection of malingering in memory performance: the sensitivity and specificity of four measures in a UK population. Br J Clin Psychol. 2005;44(3):333-341.
14. Hanley JR, Backer G, Ledson S. Detecting the faking of amnesia: a comparison of the effectiveness of three different techniques for distinguishing simulators from patients with amnesia. J Clin Exp Neuropsychol. 1999;21(1):59-69.
15. Rogers R. Clinical assessment of malingering and deception, 3rd ed. New York, NY: The Gilford Press; 2008:54.
16. Myers W, Hall R, Tolou-Shams M. Prevalence and assessment of malingering in homicide defendants using the mini-mental state examination and the Rey 15-Item Memory Test. Homicide Stud. 2013;17(3):314-328.
17. Resnick PJ. In session with Phillip J. Resnick, MD: malingering of psychiatric symptoms. Prim Psychiatry. 2006;13(6):35-38.
An app to help your patient lose weight
HAVE YOU SEEN THESE OTHER APP REVIEWS BY DR. GUNTER?
An app to help your patient with chronic pelvic pain (February 2013)
Sprout Pregnancy Essentials: An app to help your patient track her pregnancy (September 2012)
An app to help your patient remember to take her OC (July 2012)
The increasing use of smartphones among women presents an opportunity to address health issues, such as obesity.
Forty-four percent of US women own a smartphone, according to the latest data.1 Ownership is highest among younger women, with more than 60% of women between the ages of 18 and 34 owning one of these devices.1
One of the features that makes a smartphone, well, smart is the ability to run apps (short for software “applications”). Apps started out as ways to enhance access to email or calendars, but the market has ex-ploded—both demand and supply—so that there are now apps for essentially anything you might ever need. Apple’s app store, the largest, boasts more than 500,000 apps, and more than 25 billion apps had been downloaded by March 2012.2 Medical app developers are keen to capitalize on our ever-increasing “app”-etite.
Medical apps can be divided into two categories: those that can help the patient and those that can help the provider. This series will review what I call prescription apps—in other words, apps that you might consider recommending to your patient to enhance her medical care.
Apps are not new to your patients
Many of your patients are already looking at medical apps and want to hear your opinion. I know that my smartphone users are uniformly interested in hearing my recommendations, and it is not uncommon that the free apps I recommend are downloaded before my patient leaves the office.
If you are not an app user yourself, there are two basic things that you should know. First, some apps are free and others are not, although that is not necessarily a measure of quality or utility. Second, apps must be written for the particular device, so it is important to know whether the app you are recommending is supported by your patient’s smartphone. As of February 2012, the most common devices are the Android (20% of cell phone users), iPhone (19%), and Blackberry (6%).1 Some apps can also be used on tablets (e.g., iPad, Galaxy) and e-book readers (e.g., Nook, Kindle). Use of these devices is also increasing; currently, 29% of Americans own either a tablet or an e-book reader.3

When the clinical need is weight loss
Lose It! is a weight-management app that tracks calories, exercise, and weight. Considering that more than 30% of US women are obese, working toward a healthy weight is a common office discussion and any additional tool is wel-come.4 Journaling, or recording every single thing that is eaten, is a key component of successful dieting. Smartphone users tend to have their phones with them wherever they are, so an app is an ideal tool for the journaling commitment needed for weight loss.
Lose It! is free and works on the following platforms:
- Android
- iPhone
- iPad
- Nook Color
- Nook Tablet.
Advantages include ease of use
The patient need only enter her current weight and height (measure your patient during the visit to ensure that she gets started with accurate numbers), the weight she hopes to attain (you can discuss this as well), and how many pounds she hopes to lose each week, and the app calculates the recommended calorie intake to achieve this goal. The app comes preloaded with thousands of foods, and it enables barcode scanning to upload the food and nutritional content with just a click of the phone’s camera.
The database can be expanded by adding unlisted foods and even recipes. Synchronizing the phone with Loseit.com allows for emailed summaries and reminders when the patient forgets to log a meal. There is also a wide repository of exercises to choose from when logging an activity.
A couple of cons
There is no Lose It! app for the Blackberry—and no plans to write one.
Another disadvantage is the extremely basic exercise journaling (no weekly or review function), and exercise calories are automatically added into the user’s daily allotment—not every dieter wants their calories set up this way.
This is the app I used to journal my 50-lb weight loss (and 6 months of maintenance). I think that testimonial speaks for itself.
In the next installment: an app that reminds your patient to take her birth control pills.
- Why (and how) you should encourage your patients' search for health information on the Web (December 2011)
- Does the risk of unplanned pregnancy outweight the risk of VTE from hormonal contraception? (Guest Editorial, October 2012)
- To blog or not to blog? What's the answer for you and your practice? (August 2011)
- For better or, maybe worse, patients are judging your care online (March 2011)
- Twitter 101 for ObGyns: Pearls, pitfalls, and potential (September 2010)
We want to hear from you! Tell us what you think.
1. Pew Internet & American Life Project. Nearly half of American adults are Smartphone owners. http://pewinternet.org/Reports/2012/Smartphone-Update-2012/Findings.aspx. Accessed April 9, 2012.
2. Apple app store downloads top 25 billion [press release]. http://www.apple.com/pr/library/2012/03/05Apples-App-Store-Downloads-Top-25-Billion.html. Accessed April 9, 2012 .
3. Pew Internet & American Life Project. Tablet and e-book reader ownership nearly doubled over the holiday gift-giving period. http://libraries.pewinternet.org/2012/01/23/tablet-and-e-book-reader-ownership-nearly-double-over-the-holiday-gift-giving-period/. Accessed April 9, 2012.
4. National Center for Health Statistics. Obesity in the United States, 2009–2010. NCHS Data Brief No. 82; January 2012.
HAVE YOU SEEN THESE OTHER APP REVIEWS BY DR. GUNTER?
An app to help your patient with chronic pelvic pain (February 2013)
Sprout Pregnancy Essentials: An app to help your patient track her pregnancy (September 2012)
An app to help your patient remember to take her OC (July 2012)
The increasing use of smartphones among women presents an opportunity to address health issues, such as obesity.
Forty-four percent of US women own a smartphone, according to the latest data.1 Ownership is highest among younger women, with more than 60% of women between the ages of 18 and 34 owning one of these devices.1
One of the features that makes a smartphone, well, smart is the ability to run apps (short for software “applications”). Apps started out as ways to enhance access to email or calendars, but the market has ex-ploded—both demand and supply—so that there are now apps for essentially anything you might ever need. Apple’s app store, the largest, boasts more than 500,000 apps, and more than 25 billion apps had been downloaded by March 2012.2 Medical app developers are keen to capitalize on our ever-increasing “app”-etite.
Medical apps can be divided into two categories: those that can help the patient and those that can help the provider. This series will review what I call prescription apps—in other words, apps that you might consider recommending to your patient to enhance her medical care.
Apps are not new to your patients
Many of your patients are already looking at medical apps and want to hear your opinion. I know that my smartphone users are uniformly interested in hearing my recommendations, and it is not uncommon that the free apps I recommend are downloaded before my patient leaves the office.
If you are not an app user yourself, there are two basic things that you should know. First, some apps are free and others are not, although that is not necessarily a measure of quality or utility. Second, apps must be written for the particular device, so it is important to know whether the app you are recommending is supported by your patient’s smartphone. As of February 2012, the most common devices are the Android (20% of cell phone users), iPhone (19%), and Blackberry (6%).1 Some apps can also be used on tablets (e.g., iPad, Galaxy) and e-book readers (e.g., Nook, Kindle). Use of these devices is also increasing; currently, 29% of Americans own either a tablet or an e-book reader.3

When the clinical need is weight loss
Lose It! is a weight-management app that tracks calories, exercise, and weight. Considering that more than 30% of US women are obese, working toward a healthy weight is a common office discussion and any additional tool is wel-come.4 Journaling, or recording every single thing that is eaten, is a key component of successful dieting. Smartphone users tend to have their phones with them wherever they are, so an app is an ideal tool for the journaling commitment needed for weight loss.
Lose It! is free and works on the following platforms:
- Android
- iPhone
- iPad
- Nook Color
- Nook Tablet.
Advantages include ease of use
The patient need only enter her current weight and height (measure your patient during the visit to ensure that she gets started with accurate numbers), the weight she hopes to attain (you can discuss this as well), and how many pounds she hopes to lose each week, and the app calculates the recommended calorie intake to achieve this goal. The app comes preloaded with thousands of foods, and it enables barcode scanning to upload the food and nutritional content with just a click of the phone’s camera.
The database can be expanded by adding unlisted foods and even recipes. Synchronizing the phone with Loseit.com allows for emailed summaries and reminders when the patient forgets to log a meal. There is also a wide repository of exercises to choose from when logging an activity.
A couple of cons
There is no Lose It! app for the Blackberry—and no plans to write one.
Another disadvantage is the extremely basic exercise journaling (no weekly or review function), and exercise calories are automatically added into the user’s daily allotment—not every dieter wants their calories set up this way.
This is the app I used to journal my 50-lb weight loss (and 6 months of maintenance). I think that testimonial speaks for itself.
In the next installment: an app that reminds your patient to take her birth control pills.
- Why (and how) you should encourage your patients' search for health information on the Web (December 2011)
- Does the risk of unplanned pregnancy outweight the risk of VTE from hormonal contraception? (Guest Editorial, October 2012)
- To blog or not to blog? What's the answer for you and your practice? (August 2011)
- For better or, maybe worse, patients are judging your care online (March 2011)
- Twitter 101 for ObGyns: Pearls, pitfalls, and potential (September 2010)
We want to hear from you! Tell us what you think.
HAVE YOU SEEN THESE OTHER APP REVIEWS BY DR. GUNTER?
An app to help your patient with chronic pelvic pain (February 2013)
Sprout Pregnancy Essentials: An app to help your patient track her pregnancy (September 2012)
An app to help your patient remember to take her OC (July 2012)
The increasing use of smartphones among women presents an opportunity to address health issues, such as obesity.
Forty-four percent of US women own a smartphone, according to the latest data.1 Ownership is highest among younger women, with more than 60% of women between the ages of 18 and 34 owning one of these devices.1
One of the features that makes a smartphone, well, smart is the ability to run apps (short for software “applications”). Apps started out as ways to enhance access to email or calendars, but the market has ex-ploded—both demand and supply—so that there are now apps for essentially anything you might ever need. Apple’s app store, the largest, boasts more than 500,000 apps, and more than 25 billion apps had been downloaded by March 2012.2 Medical app developers are keen to capitalize on our ever-increasing “app”-etite.
Medical apps can be divided into two categories: those that can help the patient and those that can help the provider. This series will review what I call prescription apps—in other words, apps that you might consider recommending to your patient to enhance her medical care.
Apps are not new to your patients
Many of your patients are already looking at medical apps and want to hear your opinion. I know that my smartphone users are uniformly interested in hearing my recommendations, and it is not uncommon that the free apps I recommend are downloaded before my patient leaves the office.
If you are not an app user yourself, there are two basic things that you should know. First, some apps are free and others are not, although that is not necessarily a measure of quality or utility. Second, apps must be written for the particular device, so it is important to know whether the app you are recommending is supported by your patient’s smartphone. As of February 2012, the most common devices are the Android (20% of cell phone users), iPhone (19%), and Blackberry (6%).1 Some apps can also be used on tablets (e.g., iPad, Galaxy) and e-book readers (e.g., Nook, Kindle). Use of these devices is also increasing; currently, 29% of Americans own either a tablet or an e-book reader.3

When the clinical need is weight loss
Lose It! is a weight-management app that tracks calories, exercise, and weight. Considering that more than 30% of US women are obese, working toward a healthy weight is a common office discussion and any additional tool is wel-come.4 Journaling, or recording every single thing that is eaten, is a key component of successful dieting. Smartphone users tend to have their phones with them wherever they are, so an app is an ideal tool for the journaling commitment needed for weight loss.
Lose It! is free and works on the following platforms:
- Android
- iPhone
- iPad
- Nook Color
- Nook Tablet.
Advantages include ease of use
The patient need only enter her current weight and height (measure your patient during the visit to ensure that she gets started with accurate numbers), the weight she hopes to attain (you can discuss this as well), and how many pounds she hopes to lose each week, and the app calculates the recommended calorie intake to achieve this goal. The app comes preloaded with thousands of foods, and it enables barcode scanning to upload the food and nutritional content with just a click of the phone’s camera.
The database can be expanded by adding unlisted foods and even recipes. Synchronizing the phone with Loseit.com allows for emailed summaries and reminders when the patient forgets to log a meal. There is also a wide repository of exercises to choose from when logging an activity.
A couple of cons
There is no Lose It! app for the Blackberry—and no plans to write one.
Another disadvantage is the extremely basic exercise journaling (no weekly or review function), and exercise calories are automatically added into the user’s daily allotment—not every dieter wants their calories set up this way.
This is the app I used to journal my 50-lb weight loss (and 6 months of maintenance). I think that testimonial speaks for itself.
In the next installment: an app that reminds your patient to take her birth control pills.
- Why (and how) you should encourage your patients' search for health information on the Web (December 2011)
- Does the risk of unplanned pregnancy outweight the risk of VTE from hormonal contraception? (Guest Editorial, October 2012)
- To blog or not to blog? What's the answer for you and your practice? (August 2011)
- For better or, maybe worse, patients are judging your care online (March 2011)
- Twitter 101 for ObGyns: Pearls, pitfalls, and potential (September 2010)
We want to hear from you! Tell us what you think.
1. Pew Internet & American Life Project. Nearly half of American adults are Smartphone owners. http://pewinternet.org/Reports/2012/Smartphone-Update-2012/Findings.aspx. Accessed April 9, 2012.
2. Apple app store downloads top 25 billion [press release]. http://www.apple.com/pr/library/2012/03/05Apples-App-Store-Downloads-Top-25-Billion.html. Accessed April 9, 2012 .
3. Pew Internet & American Life Project. Tablet and e-book reader ownership nearly doubled over the holiday gift-giving period. http://libraries.pewinternet.org/2012/01/23/tablet-and-e-book-reader-ownership-nearly-double-over-the-holiday-gift-giving-period/. Accessed April 9, 2012.
4. National Center for Health Statistics. Obesity in the United States, 2009–2010. NCHS Data Brief No. 82; January 2012.
1. Pew Internet & American Life Project. Nearly half of American adults are Smartphone owners. http://pewinternet.org/Reports/2012/Smartphone-Update-2012/Findings.aspx. Accessed April 9, 2012.
2. Apple app store downloads top 25 billion [press release]. http://www.apple.com/pr/library/2012/03/05Apples-App-Store-Downloads-Top-25-Billion.html. Accessed April 9, 2012 .
3. Pew Internet & American Life Project. Tablet and e-book reader ownership nearly doubled over the holiday gift-giving period. http://libraries.pewinternet.org/2012/01/23/tablet-and-e-book-reader-ownership-nearly-double-over-the-holiday-gift-giving-period/. Accessed April 9, 2012.
4. National Center for Health Statistics. Obesity in the United States, 2009–2010. NCHS Data Brief No. 82; January 2012.
Minimizing cancer’s impact on bone with denosumab: current and future perspectives
Bone metastasis is a serious complication of advanced cancer. It is most commonly observed in patients with metastatic breast and prostate cancers, but also occurs in most other metastatic solid cancers. Without treatment, patients may experience complications including intractable bone pain, hypercalcemia, fracture, spinal cord compression and/or a requirement for surgical or radiotherapeutic intervention. In 2010, denosumab, a fully human monoclonal antibody that inhibits RANK ligand (RANKL) and subsequent osteoclast-mediated bone destruction, was approved by the Food and Drug Administration for the prevention of skeletal-related events (SREs) in patients with bone metastases from solid tumors. This article reviews the role of denosumab in preventing SREs due to bone metastases, treating bone loss due to hormone-ablative cancer therapies, and describes denosumab’s safety profile and potential future indications under investigation.
Click on the PDF icon at the top of this introduction to read the full article.
Bone metastasis is a serious complication of advanced cancer. It is most commonly observed in patients with metastatic breast and prostate cancers, but also occurs in most other metastatic solid cancers. Without treatment, patients may experience complications including intractable bone pain, hypercalcemia, fracture, spinal cord compression and/or a requirement for surgical or radiotherapeutic intervention. In 2010, denosumab, a fully human monoclonal antibody that inhibits RANK ligand (RANKL) and subsequent osteoclast-mediated bone destruction, was approved by the Food and Drug Administration for the prevention of skeletal-related events (SREs) in patients with bone metastases from solid tumors. This article reviews the role of denosumab in preventing SREs due to bone metastases, treating bone loss due to hormone-ablative cancer therapies, and describes denosumab’s safety profile and potential future indications under investigation.
Click on the PDF icon at the top of this introduction to read the full article.
Bone metastasis is a serious complication of advanced cancer. It is most commonly observed in patients with metastatic breast and prostate cancers, but also occurs in most other metastatic solid cancers. Without treatment, patients may experience complications including intractable bone pain, hypercalcemia, fracture, spinal cord compression and/or a requirement for surgical or radiotherapeutic intervention. In 2010, denosumab, a fully human monoclonal antibody that inhibits RANK ligand (RANKL) and subsequent osteoclast-mediated bone destruction, was approved by the Food and Drug Administration for the prevention of skeletal-related events (SREs) in patients with bone metastases from solid tumors. This article reviews the role of denosumab in preventing SREs due to bone metastases, treating bone loss due to hormone-ablative cancer therapies, and describes denosumab’s safety profile and potential future indications under investigation.
Click on the PDF icon at the top of this introduction to read the full article.
Diagnosis and Management of Immunoglobulin Light Chain Amyloidosis
The term amyloidosis refers to a fascinating group of disorders that share a common pathogenesis of extracellular deposition of amyloid material. Fundamentally, it is a disorder of the secondary structure of select proteins whereby the amyloidogenic proteins are misfolded into a β-pleated sheet configuration, resulting in the formation of insoluble extracellular amyloid fibrils. The amyloid fibrils appear as amorphous eosinophilic material when hematoxylin and eosin–stained tissue is examined under light microscope. Electron microscopy reveals remarkable similarity between the amyloid fibrils derived from different precursor proteins in that they range from 7.5 to 10 nm in diameter. This ultrastructural similarity is the underlying basis for the characteristic red-green birefringence with Congo red staining observed under polarized microscopy, the pathological hallmark of the disease.
To read the full article in PDF:
The term amyloidosis refers to a fascinating group of disorders that share a common pathogenesis of extracellular deposition of amyloid material. Fundamentally, it is a disorder of the secondary structure of select proteins whereby the amyloidogenic proteins are misfolded into a β-pleated sheet configuration, resulting in the formation of insoluble extracellular amyloid fibrils. The amyloid fibrils appear as amorphous eosinophilic material when hematoxylin and eosin–stained tissue is examined under light microscope. Electron microscopy reveals remarkable similarity between the amyloid fibrils derived from different precursor proteins in that they range from 7.5 to 10 nm in diameter. This ultrastructural similarity is the underlying basis for the characteristic red-green birefringence with Congo red staining observed under polarized microscopy, the pathological hallmark of the disease.
To read the full article in PDF:
The term amyloidosis refers to a fascinating group of disorders that share a common pathogenesis of extracellular deposition of amyloid material. Fundamentally, it is a disorder of the secondary structure of select proteins whereby the amyloidogenic proteins are misfolded into a β-pleated sheet configuration, resulting in the formation of insoluble extracellular amyloid fibrils. The amyloid fibrils appear as amorphous eosinophilic material when hematoxylin and eosin–stained tissue is examined under light microscope. Electron microscopy reveals remarkable similarity between the amyloid fibrils derived from different precursor proteins in that they range from 7.5 to 10 nm in diameter. This ultrastructural similarity is the underlying basis for the characteristic red-green birefringence with Congo red staining observed under polarized microscopy, the pathological hallmark of the disease.
To read the full article in PDF:
Biomarkers in the emergency workup of chest pain: Uses, limitations, and future
Each year in the United States, more than 8 million people come to the emergency department with chest pain, but only a minority are eventually diagnosed with a heart attack.1
Confronted with signs and symptoms that could represent an acute coronary syndrome, clinicians need to know whether the patient has a benign condition and can safely be sent home or is in urgent need of hospitalization—and they need to do so in a safe, timely, and cost-effective manner.2,3
Testing for biomarkers of cardiac injury, especially troponins I and T, is an accepted part of the assessment of chest pain. However, the interpretation of these cardiac biomarkers is complicated by the fact they can be elevated from noncoronary causes of chest pain such as pulmonary embolism or renal impairment, and thus should be considered only as part of the patient’s total clinical picture. This uncertainty can result in longer hospital stays and increased testing.
Thus, researchers are searching for new biomarkers that could allow for more rapid and accurate diagnosis and estimation of prognosis.
In this article we will examine the advantages and limitations of measuring cardiac biomarkers. We then discuss the emerging data on new biomarkers, including the very promising high-sensitivity troponin assays, cystatin C, and other markers, and the potential for biomarkers to be used instead of or in combination with stress testing in the evaluation of patients who have no initial evidence of ischemia.
SCENARIO 1: ELEVATED TROPONIN AND ST-SEGMENT ELEVATION
A 46-year-old woman presents to the emergency department with chest pain that started 2 hours earlier. Electrocardiography (ECG) initially shows sinus tachycardia with ST-segment depression and negative T waves in lead aVL. Her cardiac biomarker values (troponin I and creatine kinase MB) are normal. Repeated troponin I measurements show elevations of 250 ng/L, whereas her creatine kinase MB level is within the optimal range. Coronary angiography is unremarkable. Echocardiography shows right ventricular pressure overload in the pulmonary artery and the right ventricle. How should this patient be further evaluated?
SCENARIO 2: ELEVATED TROPONIN AND LEFT VENTRICULAR HYPERTROPHY
A 47-year-old man is admitted with worsening dyspnea and chest pain that worsens with coughing and inspiration. He has a history of end-stage renal disease secondary to poorly controlled hypertension and is being treated with hemodialysis, which he missed for the past 4 weeks while failing to take his hypertension medication. His blood pressure is 270/130 mm Hg. Chest auscultation reveals signs of pulmonary edema—ie, crackles at the end of inspiration. His troponin T level is 394 ng/L. ECG indicates left ventricular hypertrophy. How should this patient be further evaluated?
TROPONIN IS SPECIFIC FOR INJURY, BUT NOT FOR INFARCTION
American College of Cardiology and American Heart Association (ACC/AHA) guidelines4 recommend that clinicians ask themselves two questions: what is the likelihood that the patient is truly having an acute coronary syndrome secondary to coronary artery disease, and what is the likelihood of an adverse clinical outcome? Clues come from the initial measurements of biomarkers of cardiac injury, history, physical examination, and ECG (Table 1),5 and subsequent care is based on the estimated degree of risk.
Troponin revolutionized the diagnosis and risk stratification of chest pain. The ACC/AHA guidelines call for measuring biomarkers—preferably troponin—in all patients who present with chest discomfort consistent with an acute coronary syndrome.4,6
Cardiac troponins I and T have been the biomarkers of choice for detecting myocardial injury,4,6 since elevated concentrations are highly sensitive and tissue-specific.7 Moreover, they identify patients at short-term and long-term risk of cardiac events.4,8
The introduction of troponin testing led to a substantial increase in the rate of diagnosis of myocardial infarction (MI), with an increase in cardiac care unit admissions of more than 20%.9,10 This was partly because troponin is released into the blood with even minute myocardial damage, so that some patients who previously would have been diagnosed with unstable angina are now found to have non-ST-segment-elevation MI.10 However, the increase in admissions may also represent an increase in misdiagnoses, with many clinicians equating an elevated troponin level with acute MI.11
Although an elevated troponin level is 100% specific for myocardial injury, it is not synonymous with MI.12 Myocardial injury can be caused by a cardiac condition such as tachyarrhythmia, cardiac trauma, congestive heart failure, ventricular hypertrophy, myocarditis, or pericarditis, or by a noncardiac condition such as sepsis, respiratory failure, pulmonary embolism, pulmonary hypertension, cancer chemotherapy, or renal insufficiency.4,13 Therefore, to avoid a misdiagnosis of MI, the troponin level must be considered in the clinical context.
In fact, Alcalai et al11 noted that almost half of patients with elevated troponin did not really have an acute coronary syndrome. More importantly, in-hospital and long-term survival rates were significantly better for patients with an acute coronary syndrome than for those without, illustrating the importance of identifying and treating the true disease instead of mislabeling the problem as MI.
Bayesian theory predicts that patients with chest pain who have elevated troponin are less likely to truly have an acute coronary syndrome if the rest of their clinical presentation indicates a low probability for heart disease.14 Indeed, when McDonald et al15 used a risk-scoring index based on sex, a history of heart failure or coronary artery disease, the ECG, and use of aspirin, the positive predictive value of an abnormal troponin level was 83% at a risk score of 4 or greater, 63% at a score of 3, 52% at a score of 2, 32% at a score of 1, and 29% at a score of 0.
Thus, cardiac biomarkers are not a substitute for traditional clinical assessment, but rather should be used “in conjunction with the clinical history, physical examination, and interpretation of the ECG.”6 Consequently, diagnostic protocols that incorporate pretest clinical features to identify low-risk patients have a higher negative predictive value.
This was illustrated in a study by Than et al16 that aimed to prospectively validate the safety of an accelerated diagnostic protocol to assess chest pain suggestive of an acute coronary syndrome. The protocol included a structured pretest probability scoring method (ie, the Thrombolysis in Myocardial Infarction [TIMI] score), ECG, and a point-of-care biomarker panel of troponin, creatine kinase MB, and myoglobin. The protocol had a negative predictive value of 99.1%, whereas the use of biomarkers alone had a value of 96.1%.
HISTORY AND PHYSICAL EXAMINATION PROVIDE KEY INFORMATION
In a review, Heidenreich et al8 noted certain demographic characteristics associated with worse outcomes—ie, older age and male sex; a history of medical conditions such as diabetes, MI, and hypertension; and heart failure on presentation.
A careful assessment of chest pain and associated symptoms helps narrow the differential diagnosis. Features that increase the likelihood of a cardiac origin of chest pain are:
- Chest pain at the time of presentation (likelihood ratio [LR] = 2.0)
- Radiation of the pain to the right shoulder (LR = 2.9), the left arm (LR = 2.3), or both arms (LR = 7.1)
- Nausea or vomiting (LR = 1.9)
- Diaphoresis (LR = 2.0).17
The physical examination can detect highrisk features such as new murmurs, hypotension, diaphoresis, pulmonary edema, and rales. It is more specific than sensitive and is useful in identifying low-risk patients by targeting potential noncardiac causes of the patient’s symptoms.18
The efficacy of clinical assessment was studied in 2,271 patients with chest pain presenting to the emergency department.19 In this cohort, a low-risk group with a 30-day major cardiovascular event rate (death, MI, stroke, or revascularization) of 2.5% could be identified through the use of the US Agency for Health Care Policy and Research criteria.
Electrocardiography
ECG provides important diagnostic and prognostic information and independently predicts death or MI, even after adjustment for cardiac biomarker measurements,20,21 making it pivotal in the evaluation.4 The key features on ECG that increase the probability of MI are:
- New ST-segment elevation (LR 5.7–53.9)
- New Q waves (LR 5.3–24.8).17
One study20 found that while the troponin T level was a powerful independent marker in patients presenting with MI, its value for risk stratification was enhanced when it was combined with a standard measure such as ECG.20 While more than 90% of patients with STsegment elevation had an adverse outcome, only 31.7% of those patients had an elevated troponin T level.
No component is sufficient by itself
Thus, in spite of the proliferation of cardiac diagnostic tests, the initial bedside assessment of chest pain remains paramount. In fact, in patients presenting to the emergency department with chest pain, low risk (ie, those with a < 5% probability of MI) may be identified by presenting symptoms, medical history, and ECG alone.19
Furthermore, although clinical assessment, ECG, and cardiac biomarker testing each provide incremental benefit in assessing chest pain, no component is sufficient by itself. Sanchis et al22 found that even in patients with a normal troponin I level, the risk remained high in the case of ST-segment depression, and that even without signs of ischemia, the probability of cardiac events was 16% when the chest pain score was 11 points or higher.22 Consequently, a normal troponin level, ECG, or any other predictor alone would not ensure a good prognosis.
BIOMARKERS INSTEAD OF STRESS TESTING?
The ACC/AHA guidelines for the diagnosis of patients with unstable angina and non-STsegment elevation MI say that stable patients at low risk with no evidence of ischemia on initial assessment can be admitted to a chest pain unit for observation with serial cardiac biomarkers and ECG.4 At the end of the observation period, those who have reassuring results on ECG and normal cardiac biomarker measurements undergo functional cardiac testing or stress testing, or both.4
Exercise treadmill testing is a cornerstone of confirmatory testing in an accelerated diagnostic protocol because it is readily available, safe, and easy to do.18 A low-risk result was shown to have a high negative predictive value,23,24 so that the likelihood of an acute coronary syndrome is low enough for safe discharge.
However, the overall process is not ideal since it is time-consuming, generates additional costs, and can have false-positive results in patients who are otherwise deemed not to be at high risk. While some studies provided an optimistic view about discharging low-risk patients with negative biomarkers without stress testing,7,25 others have discouraged omitting exercise treadmill testing from protocols.22,26
Others have proposed combining a biomarker with an imaging study such as coronary computed tomographic (CT) angiography.27 Normal findings on this study have been shown to have a negative predictive value of up to 100% for ruling out an acute coronary syndrome and the occurrence of major adverse cardiovascular events in the long term.28,29 Furthermore, it allows more-inclusive assessments of chest pain and can exclude other life-threatening causes such as pulmonary embolism and aortic dissection (referred to as the “triple rule-out”).30
However, 25% to 50% of patients presenting to the emergency department with chest pain may not be candidates for CT angiography because of obesity, contrast allergy, intolerance to beta-blockade, arrhythmia, renal insufficiency, or a history of coronary artery disease.18 Moreover, it may be more efficient and less costly to discharge some patients without coronary CT angiography31 with the help of novel biomarkers without routine additional testing. This may spare patients the additional radiation exposure from CT angiography or nuclear imaging.27,32
New biomarkers may, it is hoped, better distinguish patients at low risk from those at high risk without resorting to stress testing. Several of these markers are moving toward mainstream clinical use. For a biomarker to be prognostically equivalent to stress testing, it must be able to tell us if the likelihood of an acute coronary syndrome is low enough for safe discharge—ie, it must have a significantly high negative predictive value. Also, it must be an independent predictor of adverse outcomes, particularly in patients deemed at low risk by initial low troponin measurements. Biomarkers that have shown promise in this regard include high-sensitivity troponin, brain-type natriuretic peptide (BNP), cystatin C, and ischemia-modified albumin.
HIGH-SENSITIVITY CARDIAC TROPONIN ASSAYS
Although we speak of “high-sensitivity troponin,” these new assays detect the same molecule as do traditional troponin assays. The difference is that high-sensitivity assays can detect and measure troponin at concentrations much lower than the traditional assays can. In fact, high-sensitivity troponin assays can detect and measure troponin at very low levels in almost all healthy people.
Studies have shown that the high-sensitivity assays have better analytical accuracy and sensitivity than older assays.12
Aldous et al33 reported that, in patients who presented to the emergency department within 4 hours of the onset of chest pain, an elevation in troponin T on a high-sensitivity assay had a positive predictive value of 53.8% and a negative predictive value of 98.3%.
Weber et al34 found the diagnostic value of the high-sensitivity troponin T assay to be superior to that of a contemporary troponin T assay (area under the receiver-operating-characteristics curve [AUC] of 0.949 vs 0.929). Even when the contemporary troponin T assay was negative, the high-sensitivity assay provided strong diagnostic information (AUC 0.81). Furthermore, the high-sensitivity assay provided superior independent prognostic power for death within 6 months.
Hochholzer et al35 reported a prognostic accuracy for death significantly higher (AUC 0.79) than that of contemporary troponin T (AUC 0.69). A concentration of high-sensitivity troponin T above 14 ng/L improved the prediction of death (hazard ratio 2.60) but not of subsequent acute MI in patients with acute chest pain. Therefore, a negative high-sensitivity troponin T assay identifies patients with a good prognosis and who may be discharged without further testing if their clinical presentation and ECG are also reassuring.
Keller et al36 compared the diagnostic performance of the high-sensitivity cardiac troponin I assay against 11 other biomarkers, including a contemporary cardiac troponin I assay. The contemporary troponin I and the high-sensitivity troponin I assays performed best. The high-sensitivity troponin I assay at admission had a sensitivity of 82.3% and a negative predictive value of 94.7% for ruling out acute MI, whereas the contemporary troponin I assay had a sensitivity of 79.4% and a negative predictive value of 94.0%.
Using levels obtained at 3 hours after admission, the sensitivity was 98.2% and the negative predictive value was 99.4% for both troponin I assays. Combining the 99th percentile cutoff at admission with the serial change in troponin concentration within 3 hours, the positive predictive value for ruling in acute MI for high-sensitivity cardiac troponin I increased from 75.1% at admission to 95.8% after 3 hours; for the contemporary assay, it increased from 80.9% at admission to 96.1%.36
The authors concluded that performing either of the cardiac troponin I assays 3 hours after admission may help in ruling out MI early on, with a negative predictive value greater than 99%. Moreover, the relative change in concentration within the 3 hours after admission, combined with the 99th percentile diagnostic cutoff value on admission, improves specificity, allowing acute MI to be accurately ruled in.36
Of note, though studies have confirmed that a measurement at 3 hours identifies most cases of MI early, they have not used the recommended maximal sensitivity interval for troponin measurements (6 hours or more).6
A proposed algorithm for diagnosing acute MI with a high-sensitivity assay
While high-sensitivity troponin T assays can improve the early diagnosis of acute MI, how best to use them is yet to be defined. They still lack specificity for acute coronary syndromes, with positive predictive values as low as 50%.37
Reichlin et al38 developed and validated an algorithm for rapidly ruling out or ruling in acute MI using a high-sensitivity cardiac troponin T assay, incorporating baseline values and absolute changes within the first hour. Using a baseline threshold of 12 ng/L or less and an absolute change of 3 ng/L or less, they found a sensitivity and negative predictive value of 100%, making these good criteria for ruling out acute MI.
Using a baseline threshold of 60 ng/L or greater and a change from baseline to 1 hour of at least 15 ng/L, the specificity was 97% and the positive predictive value was 84%, making these good criteria for ruling in acute MI.
Patients whose values were in between were classified as being in an “observationalzone group,” in which the prevalence of acute MI was 8%. The cumulative 30-day survival rate was 99.8% in patients in whom the test ruled out MI, 98.6% in the observational-zone patients, and 95.3% in patients in whom the test ruled in MI.38 Using this simple algorithm allowed a safe rule-out as well as an accurate rule-in of acute MI within 1 hour in 77% of unselected patients with acute chest pain; thus, it may obviate the need for prolonged monitoring and serial measurements in three out of four patients.”
Newby39 stated that such an algorithmic approach must be validated in a prospective study that assesses not only sensitivity, negative predictive value, specificity, and positive predictive value, but also the implications for clinical outcomes and the cost of widespread implementation.
In the meantime, clinicians must keep in mind that patient populations in clinical practice are less selected, the prevalence of MI may broadly vary, and confounding comorbidities such as heart failure and renal insufficiency are more common. Studies are also needed to verify whether other factors such as age, sex, and time from symptom onset should be considered.
BRAIN-TYPE NATRIURETIC PEPTIDE
BNP is a 32-amino-acid natriuretic peptide that is released from myocytes. The amount released depends on wall stress brought on by heart failure, ischemic heart disease, or other conditions.
In a study of the diagnostic utility of BNP in the workup of acute chest pain, Haaf et al40 found that BNP levels at presentation were significantly higher in patients with acute MI than in patients with other diagnoses. However, the diagnostic accuracy of BNP was lower than that of cardiac troponin T at presentation, though its independent predictive value for all-cause mortality was more accurate than that of troponin T.
Elevation of the BNP 41 or the N-terminal pro-BNP 42,43 level was shown to also provide unique prognostic information in patients with suspected and confirmed acute coronary syndrome and was associated with higher rates of short-term and long-term mortality. Therefore, BNP appears useful for the prognosis but not the diagnosis of acute coronary syndromes.
CYSTATIN C
The protein cystatin C, widely used as a biomarker for kidney disease, has more recently been touted as a prognostic marker in acute coronary syndromes.
Jernberg et al44 reported that, in patients with a suspected or confirmed acute coronary syndrome, a single measurement of cystatin C significantly improved the early stratification of risk.44 Specifically, the cystatin C level was independently associated with mortality risk but not with the risk of subsequent MI.
In another study,45 the cystatin C concentration independently predicted the risk of cardiovascular death or MI in non-ST-segment elevation acute coronary syndrome. However, the additive predictive value of cystatin C in these patients was found to be small when clinical risk factors and biomarkers of MI were used in the prediction model. Therefore, cystatin C may predict global risk but does not appear to be useful in diagnosing MI.
ISCHEMIA-MODIFIED ALBUMIN
A major limitation of troponin is that it cannot detect reversible myocardial ischemia in the absence of cardiac necrosis, making stress testing necessary to unmask potential reversible ischemia.
Ischemia-modified albumin has been proposed as a means of detecting cardiac ischemia even if necrosis is absent. It is a product of the N-terminus alteration of albumin caused by myocardial ischemia, which reduces the ability of cobalt to bind to albumin and can be detected with the albumin cobalt binding test. This marker might have a high negative predictive value, ruling out acute coronary syndromes in conditions of low pretest probability with negative necrosis markers and ECG.13,46
Although ischemia-modified albumin does show promise, doubt remains as to its validity as a biomarker, as its mechanism of generation is not known. Some have suggested that it is in fact a marker of oxidative stress.47
PANELS OF MARKERS
The individual biomarkers we have discussed here have advantages and limitations in the emergency workup of chest pain. The concept of using a multimarker panel has been raised as a way of amplifying the positive attributes of individual biomarkers and compensating for their shortcomings.
Sabatine et al48 tested this approach in patients with acute coronary syndromes who were at high risk of an adverse outcome. When patients were categorized at presentation on the basis of the number of elevated biomarkers such as cardiac troponin I, C-reactive protein, and BNP, the risk of death nearly doubled with each additional biomarker that was elevated.
The relationship was similar for the end points of MI, heart failure, and the composite at 30 days and 10 months. In a cohort of 1,635 patients, the number of elevated biomarkers remained a predictor of the composite end point after adjustment for known clinical predictors. The risk of death, MI, or heart failure by 6 months was 2.1 times higher in patients with one elevated biomarker, 3.1 times higher in those with two, and 3.7 times higher in those with three.
The authors concluded that a multimarker strategy that categorizes patients on the basis of the number of elevated biomarkers at presentation allows risk-stratification of short- and long-term cardiac events.
Tello-Montoliu et al49 tested this idea in patients with non-ST-segment elevation acute coronary syndromes using a panel consisting of cardiac troponin T, C-reactive protein, N-terminal pro-BNP, and fibrin D-dimer. The risk of a major event (death, new acute coronary syndrome, revascularization, or heart failure) at 6 months was associated with abnormal biomarker levels, especially with the presence of three positive biomarkers, even after adjustment for clinical characteristics and ECG findings.
van der Zee et al43 showed that a positive biomarker panel consisting of C-reactive protein and N-terminal pro-BNP identified patients with chest pain and a normal or nondiagnostic ECG who have a high long-term risk of cardiovascular death.
Glaser et al50 evaluated the combination of cardiac troponin I, BNP, homocysteine, C-reactive protein, placental growth factor, myeloperoxidase, choline, soluble CD40 ligand, ischemia-modified albumin, and lipoprotein-associated phospholipase A2 in patients with a suspected acute coronary syndrome. The combination of BNP, placental growth factor, and estimated glomerular filtration rate was the most accurate predictor of major adverse cardiovascular events compared with any other biomarker or clinical factor. With appropriate cutoff values, the negative predictive value for a major adverse cardiovascular event at 1 year was as high as 99.1%.
This study highlighted the importance of combining biomarkers, showing that with a negative predictive value of 97% for 30-day events, the combination of placental growth factor, BNP, and cardiac troponin I may help surmount the delay from symptom onset to cardiac troponin increase, thus permitting a more timely diagnosis and safe discharge within 12 hours.
Comment. These studies raise the promise that panels of biomarkers can be used in patients deemed to be at low risk after clinical assessment and troponin evaluation to enable them to be safely discharged early and to obviate the need for stress testing.
If we assume that unstable cardiac disease requiring hospitalization accounts for 35% of patients with chest pain, a hypothetical panel of biomarkers with a sensitivity and specificity of 95% for adverse cardiac outcomes would have a positive predictive value of 91% and a negative predictive value of 97%. The negative likelihood ratio of this hypothetical biomarker panel would be 0.05, while the positive likelihood ratio would be 19. This performance level means that in patients with a pretest probability less than 50%, the posttest probability can be reduced to below 10%, so that such patients can be safely discharged without further hospital evaluation.
Conversely, a positive test result in patients with pretest probability of 30% or greater raises the posttest probability to nearly 90%, meaning that such patients should be considered for aggressive intervention without the need for stress testing.
RETURN TO OUR SCENARIOS
Chest pain remains a nonspecific complaint, and the interpretation of biomarkers to find the cause presents clinicians with challenges, as illustrated by the cases introduced at the beginning of this article.
The cardiac troponin I elevation in scenario 1 led to an initial diagnosis of unstable angina. However, coronary angiography showed lesion-free coronary arteries, thus excluding ischemic heart disease. When other diseases that could cause elevated cardiac troponin I were considered and investigated with further diagnostic tests such as D-dimer, pulmonary embolism became the new working diagnosis, and this was confirmed by CT angiography.
Similarly, given the laboratory values for the patient in scenario 2, the condition could have been mistaken for an acute coronary syndrome. However, the absence of evidence on ECG to support this diagnosis would indicate an erroneously elevated biomarker secondary to his background of chronic renal insufficiency.
- Pitts SR, Niska RW, Xu J, Burt CW. National hospital ambulatory medical care survey: 2006 emergency department summary. Natl Health Stat Report 2008;1–38.
- Vucic R, Knezevic S, Lazic Z, et al. Elevation of troponin values in differential diagnosis of chest pain in view of pulmonary thromboembolism. Vojnosanit Pregl 2012; 69:913–916.
- Croitoru M, Taegtmeyer H. Spurious rises in troponin T in end-stage renal disease. Lancet 1995; 346:974.
- Anderson JL, Adams CD, Antman EM, et al; 2011 Writing Group Members; ACCF/AHA Task Force Members. 2011 ACCF/AHA focused update incorporated into the ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2011; 123:e426–e579.
- Unstable angina: diagnosis and management. Guideline overview. Agency for Health Care Policy and Research. J Natl Med Assoc 1994; 86:649,710–712.
- Morrow DA, Cannon CP, Jesse RL, et al; National Academy of Clinical Biochemistry. National Academy of Clinical Biochemistry Laboratory Medicine Practice Guidelines: clinical characteristics and utilization of biochemical markers in acute coronary syndromes. Circulation 2007; 115:e356–e375.
- Hamm CW, Goldmann BU, Heeschen C, Kreymann G, Berger J, Meinertz T. Emergency room triage of patients with acute chest pain by means of rapid testing for cardiac troponin T or troponin I. N Engl J Med 1997; 337:1648–1653.
- Heidenreich PA, Go A, Melsop KA, et al. Prediction of risk for patients with unstable angina. Evid Rep Technol Assess (Summ) 2000; August:1–3.
- Kontos MC, Fritz LM, Anderson FP, Tatum JL, Ornato JP, Jesse RL. Impact of the troponin standard on the prevalence of acute myocardial infarction. Am Heart J 2003; 146:446–452.
- Amit G, Gilutz H, Cafri C, Wolak A, Ilia R, Zahger D. What have the new definition of acute myocardial infarction and the introduction of troponin measurement done to the coronary care unit? Impacts on admission rate, length of stay, case mix and mortality. Cardiology 2004; 102:171–176.
- Alcalai R, Planer D, Culhaoglu A, Osman A, Pollak A, Lotan C. Acute coronary syndrome vs nonspecific troponin elevation: clinical predictors and survival analysis. Arch Intern Med 2007; 167:276–281.
- Thygesen K, Mair J, Katus H, et al. Study Group on Biomarkers in Cardiology of the ESC Working Group on Acute Cardiac Care. Recommendations for the use of cardiac troponin measurement in acute cardiac care. Eur Heart J 2010; 31:2197–2204.
- Jaffe AS, Babuin L, Apple FS. Biomarkers in acute cardiac disease: the present and the future. J Am Coll Cardiol 2006; 48:1–11.
- Jaeschke R, Guyatt GH, Sackett DL. Users’ guides to the medical literature. III. How to use an article about a diagnostic test. B. What are the results and will they help me in caring for my patients? The Evidence-Based Medicine Working Group. JAMA 1994; 271:703–707.
- McDonald MA, Holroyd B, Comeau A, Hervas-Malo M, Welsh RC. Clinical risk scoring beyond initial troponin values: results from a large, prospective, unselected acute chest pain population. Can J Cardiol 2007; 23:287–292.
- Than M, Cullen L, Reid CM, et al. A 2-h diagnostic protocol to assess patients with chest pain symptoms in the Asia-Pacific region (ASPECT): a prospective observational validation study. Lancet 2011; 377:1077–1084.
- Panju AA, Hemmelgarn BR, Guyatt GH, Simel DL. The rational clinical examination. Is this patient having a myocardial infarction? JAMA 1998; 280:1256–1263.
- Amsterdam EA, Kirk JD, Bluemke DA, et al; American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee of the Council on Clinical Cardiology, Council on Cardiovascular Nursing, and Interdisciplinary Council on Quality of Care and Outcomes Research. Testing of low-risk patients presenting to the emergency department with chest pain: a scientific statement from the American Heart Association. Circulation 2010; 122:1756–1776.
- Farkouh ME, Aneja A, Reeder GS, et al. Clinical risk stratification in the emergency department predicts long-term cardiovascular outcomes in a population-based cohort presenting with acute chest pain: primary results of the Olmsted county chest pain study. Medicine (Baltimore) 2009; 88:307–313.
- Ohman EM, Armstrong PW, Christenson RH, et al. Cardiac troponin T levels for risk stratification in acute myocardial ischemia. GUSTO IIA Investigators. N Engl J Med 1996; 335:1333–1341.
- Antman EM, Tanasijevic MJ, Thompson B, et al. Cardiac-specific troponin I levels to predict the risk of mortality in patients with acute coronary syndromes. N Engl J Med 1996; 335:1342–1349.
- Sanchis J, Bodí V, Llácer A, et al. Predictors of short-term outcome in acute chest pain without ST-segment elevation. Int J Cardiol 2003; 92:193–199.
- Gomez MA, Anderson JL, Karagounis LA, Muhlestein JB, Mooers FB. An emergency department-based protocol for rapidly ruling out myocardial ischemia reduces hospital time and expense: results of a randomized study (ROMIO). J Am Coll Cardiol 1996; 28:25–33.
- Diercks DB, Gibler WB, Liu T, Sayre MR, Storrow AB. Identification of patients at risk by graded exercise testing in an emergency department chest pain center. Am J Cardiol 2000; 86:289–292.
- Rahman F, Mitra B, Cameron PA, Coleridge J. Stress testing before discharge is not required for patients with low and intermediate risk of acute coronary syndrome after emergency department short stay assessment. Emerg Med Australas 2010; 22:449–456.
- Kontos MC, Anderson FP, Alimard R, Ornato JP, Tatum JL, Jesse RL. Ability of troponin I to predict cardiac events in patients admitted from the emergency department. J Am Coll Cardiol 2000; 36:1818–1823.
- Hoffmann U, Truong QA, Schoenfeld DA, et al; ROMICAT-II Investigators. Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med 2012; 367:299–308.
- Hoffmann U, Bamberg F, Chae CU, et al. Coronary computed tomography angiography for early triage of patients with acute chest pain: the ROMICAT (Rule Out Myocardial Infarction using Computer Assisted Tomography) trial. J Am Coll Cardiol 2009; 53:1642–1650.
- Goldstein JA, Chinnaiyan KM, Abidov A, et al; CT-STAT Investigators. The CT-STAT (Coronary Computed Tomographic Angiography for Systematic Triage of Acute Chest Pain Patients to Treatment) trial. J Am Coll Cardiol 2011; 58:1414–1422.
- White CS, Kuo D, Kelemen M, et al. Chest pain evaluation in the emergency department: can MDCT provide a comprehensive evaluation? AJR Am J Roentgenol 2005; 185:533–540.
- Redberg RF. Coronary CT angiography for acute chest pain. N Engl J Med 2012; 367:375–376.
- Shreibati JB, Baker LC, Hlatky MA. Association of coronary CT angiography or stress testing with subsequent utilization and spending among Medicare beneficiaries. JAMA 2011; 306:2128–2136.
- Aldous S, Pemberton C, Richards AM, Troughton R, Than M. High-sensitivity troponin T for early rule-out of myocardial infarction in recent onset chest pain. Emerg Med J 2012; 29:805–810.
- Weber M, Bazzino O, Navarro Estrada JL, et al. Improved diagnostic and prognostic performance of a new high-sensitive troponin T assay in patients with acute coronary syndrome. Am Heart J 2011; 162:81–88.
- Hochholzer W, Reichlin T, Twerenbold R, et al. Incremental value of high-sensitivity cardiac troponin T for risk prediction in patients with suspected acute myocardial infarction. Clin Chem 2011; 57:1318–1326.
- Keller T, Zeller T, Ojeda F, et al. Serial changes in highly sensitive troponin I assay and early diagnosis of myocardial infarction. JAMA 2011; 306:2684–2693.
- Reichlin T, Hochholzer W, Bassetti S, et al. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med 2009; 361:858–867.
- Reichlin T, Schindler C, Drexler B, et al. One-hour rule-out and rule-in of acute myocardial infarction using high-sensitivity cardiac troponin T. Arch Intern Med 2012; 172:1211–1218.
- Newby LK. Myocardial infarction rule-out in the emergency department: are high-sensitivity troponins the answer?: Comment on “One-hour rule-out and rule-in of acute myocardial infarction using high-sensitivity cardiac troponin T”. Arch Intern Med 2012; 172:1218–1219.
- Haaf P, Reichlin T, Corson N, et al. B-type natriuretic peptide in the early diagnosis and risk stratification of acute chest pain. Am J Med 2011; 124:444–445.
- Sun T, Wang L, Zhang Y. Prognostic value of B-type natriuretic peptide in patients with acute coronary syndromes. Arch Med Res 2006; 37:502–505.
- Galvani M, Ottani F, Oltrona L, et al; Italian Working Group on Atherosclerosis, Thrombosis, and Vascular Biology and the Associazione Nazionale Medici Cardiologi Ospedalieri (ANMCO). N-terminal pro-brain natriuretic peptide on admission has prognostic value across the whole spectrum of acute coronary syndromes. Circulation 2004; 110:128–134.
- van der Zee PM, Cornel JH, Bholasingh R, Fischer JC, van Straalen JP, De Winter RJ. N-terminal pro B-type natriuretic peptide identifies patients with chest pain at high long-term cardiovascular risk. Am J Med 2011; 124:961–969.
- Jernberg T, Lindahl B, James S, Larsson A, Hansson LO, Wallentin L. Cystatin C: a novel predictor of outcome in suspected or confirmed non-ST-elevation acute coronary syndrome. Circulation 2004; 110:2342–2348.
- Akerblom Å, Wallentin L, Siegbahn A, et al. Cystatin C and estimated glomerular filtration rate as predictors for adverse outcome in patients with ST-elevation and non-ST-elevation acute coronary syndromes: results from the Platelet Inhibition and Patient Outcomes study. Clin Chem 2012; 58:190–199.
- Anwaruddin S, Januzzi JL, Baggish AL, Lewandrowski EL, Lewandrowski KB. Ischemia-modified albumin improves the usefulness of standard cardiac biomarkers for the diagnosis of myocardial ischemia in the emergency department setting. Am J Clin Pathol 2005; 123:140–145.
- Senes M, Kazan N, Coskun O, Zengi O, Inan L, Yücel D. Oxidative and nitrosative stress in acute ischaemic stroke. Ann Clin Biochem 2007; 44:43–47.
- Sabatine MS, Morrow DA, de Lemos JA, et al. Multimarker approach to risk stratification in non-ST elevation acute coronary syndromes: simultaneous assessment of troponin I, C-reactive protein, and B-type natriuretic peptide. Circulation 2002; 105:1760–1763.
- Tello-Montoliu A, Marín F, Roldán V, et al. A multimarker risk stratification approach to non-ST elevation acute coronary syndrome: implications of troponin T, CRP, NT pro-BNP and fibrin D-dimer levels. J Intern Med 2007; 262:651–658.
- Glaser R, Peacock WF, Wu AH, Muller R, Möckel M, Apple FS. Placental growth factor and B-type natriuretic peptide as independent predictors of risk from a multibiomarker panel in suspected acute coronary syndrome (Acute Risk and Related Outcomes Assessed With Cardiac Biomarkers [ARROW]) study. Am J Cardiol 2011; 107:821–826.
Each year in the United States, more than 8 million people come to the emergency department with chest pain, but only a minority are eventually diagnosed with a heart attack.1
Confronted with signs and symptoms that could represent an acute coronary syndrome, clinicians need to know whether the patient has a benign condition and can safely be sent home or is in urgent need of hospitalization—and they need to do so in a safe, timely, and cost-effective manner.2,3
Testing for biomarkers of cardiac injury, especially troponins I and T, is an accepted part of the assessment of chest pain. However, the interpretation of these cardiac biomarkers is complicated by the fact they can be elevated from noncoronary causes of chest pain such as pulmonary embolism or renal impairment, and thus should be considered only as part of the patient’s total clinical picture. This uncertainty can result in longer hospital stays and increased testing.
Thus, researchers are searching for new biomarkers that could allow for more rapid and accurate diagnosis and estimation of prognosis.
In this article we will examine the advantages and limitations of measuring cardiac biomarkers. We then discuss the emerging data on new biomarkers, including the very promising high-sensitivity troponin assays, cystatin C, and other markers, and the potential for biomarkers to be used instead of or in combination with stress testing in the evaluation of patients who have no initial evidence of ischemia.
SCENARIO 1: ELEVATED TROPONIN AND ST-SEGMENT ELEVATION
A 46-year-old woman presents to the emergency department with chest pain that started 2 hours earlier. Electrocardiography (ECG) initially shows sinus tachycardia with ST-segment depression and negative T waves in lead aVL. Her cardiac biomarker values (troponin I and creatine kinase MB) are normal. Repeated troponin I measurements show elevations of 250 ng/L, whereas her creatine kinase MB level is within the optimal range. Coronary angiography is unremarkable. Echocardiography shows right ventricular pressure overload in the pulmonary artery and the right ventricle. How should this patient be further evaluated?
SCENARIO 2: ELEVATED TROPONIN AND LEFT VENTRICULAR HYPERTROPHY
A 47-year-old man is admitted with worsening dyspnea and chest pain that worsens with coughing and inspiration. He has a history of end-stage renal disease secondary to poorly controlled hypertension and is being treated with hemodialysis, which he missed for the past 4 weeks while failing to take his hypertension medication. His blood pressure is 270/130 mm Hg. Chest auscultation reveals signs of pulmonary edema—ie, crackles at the end of inspiration. His troponin T level is 394 ng/L. ECG indicates left ventricular hypertrophy. How should this patient be further evaluated?
TROPONIN IS SPECIFIC FOR INJURY, BUT NOT FOR INFARCTION
American College of Cardiology and American Heart Association (ACC/AHA) guidelines4 recommend that clinicians ask themselves two questions: what is the likelihood that the patient is truly having an acute coronary syndrome secondary to coronary artery disease, and what is the likelihood of an adverse clinical outcome? Clues come from the initial measurements of biomarkers of cardiac injury, history, physical examination, and ECG (Table 1),5 and subsequent care is based on the estimated degree of risk.
Troponin revolutionized the diagnosis and risk stratification of chest pain. The ACC/AHA guidelines call for measuring biomarkers—preferably troponin—in all patients who present with chest discomfort consistent with an acute coronary syndrome.4,6
Cardiac troponins I and T have been the biomarkers of choice for detecting myocardial injury,4,6 since elevated concentrations are highly sensitive and tissue-specific.7 Moreover, they identify patients at short-term and long-term risk of cardiac events.4,8
The introduction of troponin testing led to a substantial increase in the rate of diagnosis of myocardial infarction (MI), with an increase in cardiac care unit admissions of more than 20%.9,10 This was partly because troponin is released into the blood with even minute myocardial damage, so that some patients who previously would have been diagnosed with unstable angina are now found to have non-ST-segment-elevation MI.10 However, the increase in admissions may also represent an increase in misdiagnoses, with many clinicians equating an elevated troponin level with acute MI.11
Although an elevated troponin level is 100% specific for myocardial injury, it is not synonymous with MI.12 Myocardial injury can be caused by a cardiac condition such as tachyarrhythmia, cardiac trauma, congestive heart failure, ventricular hypertrophy, myocarditis, or pericarditis, or by a noncardiac condition such as sepsis, respiratory failure, pulmonary embolism, pulmonary hypertension, cancer chemotherapy, or renal insufficiency.4,13 Therefore, to avoid a misdiagnosis of MI, the troponin level must be considered in the clinical context.
In fact, Alcalai et al11 noted that almost half of patients with elevated troponin did not really have an acute coronary syndrome. More importantly, in-hospital and long-term survival rates were significantly better for patients with an acute coronary syndrome than for those without, illustrating the importance of identifying and treating the true disease instead of mislabeling the problem as MI.
Bayesian theory predicts that patients with chest pain who have elevated troponin are less likely to truly have an acute coronary syndrome if the rest of their clinical presentation indicates a low probability for heart disease.14 Indeed, when McDonald et al15 used a risk-scoring index based on sex, a history of heart failure or coronary artery disease, the ECG, and use of aspirin, the positive predictive value of an abnormal troponin level was 83% at a risk score of 4 or greater, 63% at a score of 3, 52% at a score of 2, 32% at a score of 1, and 29% at a score of 0.
Thus, cardiac biomarkers are not a substitute for traditional clinical assessment, but rather should be used “in conjunction with the clinical history, physical examination, and interpretation of the ECG.”6 Consequently, diagnostic protocols that incorporate pretest clinical features to identify low-risk patients have a higher negative predictive value.
This was illustrated in a study by Than et al16 that aimed to prospectively validate the safety of an accelerated diagnostic protocol to assess chest pain suggestive of an acute coronary syndrome. The protocol included a structured pretest probability scoring method (ie, the Thrombolysis in Myocardial Infarction [TIMI] score), ECG, and a point-of-care biomarker panel of troponin, creatine kinase MB, and myoglobin. The protocol had a negative predictive value of 99.1%, whereas the use of biomarkers alone had a value of 96.1%.
HISTORY AND PHYSICAL EXAMINATION PROVIDE KEY INFORMATION
In a review, Heidenreich et al8 noted certain demographic characteristics associated with worse outcomes—ie, older age and male sex; a history of medical conditions such as diabetes, MI, and hypertension; and heart failure on presentation.
A careful assessment of chest pain and associated symptoms helps narrow the differential diagnosis. Features that increase the likelihood of a cardiac origin of chest pain are:
- Chest pain at the time of presentation (likelihood ratio [LR] = 2.0)
- Radiation of the pain to the right shoulder (LR = 2.9), the left arm (LR = 2.3), or both arms (LR = 7.1)
- Nausea or vomiting (LR = 1.9)
- Diaphoresis (LR = 2.0).17
The physical examination can detect highrisk features such as new murmurs, hypotension, diaphoresis, pulmonary edema, and rales. It is more specific than sensitive and is useful in identifying low-risk patients by targeting potential noncardiac causes of the patient’s symptoms.18
The efficacy of clinical assessment was studied in 2,271 patients with chest pain presenting to the emergency department.19 In this cohort, a low-risk group with a 30-day major cardiovascular event rate (death, MI, stroke, or revascularization) of 2.5% could be identified through the use of the US Agency for Health Care Policy and Research criteria.
Electrocardiography
ECG provides important diagnostic and prognostic information and independently predicts death or MI, even after adjustment for cardiac biomarker measurements,20,21 making it pivotal in the evaluation.4 The key features on ECG that increase the probability of MI are:
- New ST-segment elevation (LR 5.7–53.9)
- New Q waves (LR 5.3–24.8).17
One study20 found that while the troponin T level was a powerful independent marker in patients presenting with MI, its value for risk stratification was enhanced when it was combined with a standard measure such as ECG.20 While more than 90% of patients with STsegment elevation had an adverse outcome, only 31.7% of those patients had an elevated troponin T level.
No component is sufficient by itself
Thus, in spite of the proliferation of cardiac diagnostic tests, the initial bedside assessment of chest pain remains paramount. In fact, in patients presenting to the emergency department with chest pain, low risk (ie, those with a < 5% probability of MI) may be identified by presenting symptoms, medical history, and ECG alone.19
Furthermore, although clinical assessment, ECG, and cardiac biomarker testing each provide incremental benefit in assessing chest pain, no component is sufficient by itself. Sanchis et al22 found that even in patients with a normal troponin I level, the risk remained high in the case of ST-segment depression, and that even without signs of ischemia, the probability of cardiac events was 16% when the chest pain score was 11 points or higher.22 Consequently, a normal troponin level, ECG, or any other predictor alone would not ensure a good prognosis.
BIOMARKERS INSTEAD OF STRESS TESTING?
The ACC/AHA guidelines for the diagnosis of patients with unstable angina and non-STsegment elevation MI say that stable patients at low risk with no evidence of ischemia on initial assessment can be admitted to a chest pain unit for observation with serial cardiac biomarkers and ECG.4 At the end of the observation period, those who have reassuring results on ECG and normal cardiac biomarker measurements undergo functional cardiac testing or stress testing, or both.4
Exercise treadmill testing is a cornerstone of confirmatory testing in an accelerated diagnostic protocol because it is readily available, safe, and easy to do.18 A low-risk result was shown to have a high negative predictive value,23,24 so that the likelihood of an acute coronary syndrome is low enough for safe discharge.
However, the overall process is not ideal since it is time-consuming, generates additional costs, and can have false-positive results in patients who are otherwise deemed not to be at high risk. While some studies provided an optimistic view about discharging low-risk patients with negative biomarkers without stress testing,7,25 others have discouraged omitting exercise treadmill testing from protocols.22,26
Others have proposed combining a biomarker with an imaging study such as coronary computed tomographic (CT) angiography.27 Normal findings on this study have been shown to have a negative predictive value of up to 100% for ruling out an acute coronary syndrome and the occurrence of major adverse cardiovascular events in the long term.28,29 Furthermore, it allows more-inclusive assessments of chest pain and can exclude other life-threatening causes such as pulmonary embolism and aortic dissection (referred to as the “triple rule-out”).30
However, 25% to 50% of patients presenting to the emergency department with chest pain may not be candidates for CT angiography because of obesity, contrast allergy, intolerance to beta-blockade, arrhythmia, renal insufficiency, or a history of coronary artery disease.18 Moreover, it may be more efficient and less costly to discharge some patients without coronary CT angiography31 with the help of novel biomarkers without routine additional testing. This may spare patients the additional radiation exposure from CT angiography or nuclear imaging.27,32
New biomarkers may, it is hoped, better distinguish patients at low risk from those at high risk without resorting to stress testing. Several of these markers are moving toward mainstream clinical use. For a biomarker to be prognostically equivalent to stress testing, it must be able to tell us if the likelihood of an acute coronary syndrome is low enough for safe discharge—ie, it must have a significantly high negative predictive value. Also, it must be an independent predictor of adverse outcomes, particularly in patients deemed at low risk by initial low troponin measurements. Biomarkers that have shown promise in this regard include high-sensitivity troponin, brain-type natriuretic peptide (BNP), cystatin C, and ischemia-modified albumin.
HIGH-SENSITIVITY CARDIAC TROPONIN ASSAYS
Although we speak of “high-sensitivity troponin,” these new assays detect the same molecule as do traditional troponin assays. The difference is that high-sensitivity assays can detect and measure troponin at concentrations much lower than the traditional assays can. In fact, high-sensitivity troponin assays can detect and measure troponin at very low levels in almost all healthy people.
Studies have shown that the high-sensitivity assays have better analytical accuracy and sensitivity than older assays.12
Aldous et al33 reported that, in patients who presented to the emergency department within 4 hours of the onset of chest pain, an elevation in troponin T on a high-sensitivity assay had a positive predictive value of 53.8% and a negative predictive value of 98.3%.
Weber et al34 found the diagnostic value of the high-sensitivity troponin T assay to be superior to that of a contemporary troponin T assay (area under the receiver-operating-characteristics curve [AUC] of 0.949 vs 0.929). Even when the contemporary troponin T assay was negative, the high-sensitivity assay provided strong diagnostic information (AUC 0.81). Furthermore, the high-sensitivity assay provided superior independent prognostic power for death within 6 months.
Hochholzer et al35 reported a prognostic accuracy for death significantly higher (AUC 0.79) than that of contemporary troponin T (AUC 0.69). A concentration of high-sensitivity troponin T above 14 ng/L improved the prediction of death (hazard ratio 2.60) but not of subsequent acute MI in patients with acute chest pain. Therefore, a negative high-sensitivity troponin T assay identifies patients with a good prognosis and who may be discharged without further testing if their clinical presentation and ECG are also reassuring.
Keller et al36 compared the diagnostic performance of the high-sensitivity cardiac troponin I assay against 11 other biomarkers, including a contemporary cardiac troponin I assay. The contemporary troponin I and the high-sensitivity troponin I assays performed best. The high-sensitivity troponin I assay at admission had a sensitivity of 82.3% and a negative predictive value of 94.7% for ruling out acute MI, whereas the contemporary troponin I assay had a sensitivity of 79.4% and a negative predictive value of 94.0%.
Using levels obtained at 3 hours after admission, the sensitivity was 98.2% and the negative predictive value was 99.4% for both troponin I assays. Combining the 99th percentile cutoff at admission with the serial change in troponin concentration within 3 hours, the positive predictive value for ruling in acute MI for high-sensitivity cardiac troponin I increased from 75.1% at admission to 95.8% after 3 hours; for the contemporary assay, it increased from 80.9% at admission to 96.1%.36
The authors concluded that performing either of the cardiac troponin I assays 3 hours after admission may help in ruling out MI early on, with a negative predictive value greater than 99%. Moreover, the relative change in concentration within the 3 hours after admission, combined with the 99th percentile diagnostic cutoff value on admission, improves specificity, allowing acute MI to be accurately ruled in.36
Of note, though studies have confirmed that a measurement at 3 hours identifies most cases of MI early, they have not used the recommended maximal sensitivity interval for troponin measurements (6 hours or more).6
A proposed algorithm for diagnosing acute MI with a high-sensitivity assay
While high-sensitivity troponin T assays can improve the early diagnosis of acute MI, how best to use them is yet to be defined. They still lack specificity for acute coronary syndromes, with positive predictive values as low as 50%.37
Reichlin et al38 developed and validated an algorithm for rapidly ruling out or ruling in acute MI using a high-sensitivity cardiac troponin T assay, incorporating baseline values and absolute changes within the first hour. Using a baseline threshold of 12 ng/L or less and an absolute change of 3 ng/L or less, they found a sensitivity and negative predictive value of 100%, making these good criteria for ruling out acute MI.
Using a baseline threshold of 60 ng/L or greater and a change from baseline to 1 hour of at least 15 ng/L, the specificity was 97% and the positive predictive value was 84%, making these good criteria for ruling in acute MI.
Patients whose values were in between were classified as being in an “observationalzone group,” in which the prevalence of acute MI was 8%. The cumulative 30-day survival rate was 99.8% in patients in whom the test ruled out MI, 98.6% in the observational-zone patients, and 95.3% in patients in whom the test ruled in MI.38 Using this simple algorithm allowed a safe rule-out as well as an accurate rule-in of acute MI within 1 hour in 77% of unselected patients with acute chest pain; thus, it may obviate the need for prolonged monitoring and serial measurements in three out of four patients.”
Newby39 stated that such an algorithmic approach must be validated in a prospective study that assesses not only sensitivity, negative predictive value, specificity, and positive predictive value, but also the implications for clinical outcomes and the cost of widespread implementation.
In the meantime, clinicians must keep in mind that patient populations in clinical practice are less selected, the prevalence of MI may broadly vary, and confounding comorbidities such as heart failure and renal insufficiency are more common. Studies are also needed to verify whether other factors such as age, sex, and time from symptom onset should be considered.
BRAIN-TYPE NATRIURETIC PEPTIDE
BNP is a 32-amino-acid natriuretic peptide that is released from myocytes. The amount released depends on wall stress brought on by heart failure, ischemic heart disease, or other conditions.
In a study of the diagnostic utility of BNP in the workup of acute chest pain, Haaf et al40 found that BNP levels at presentation were significantly higher in patients with acute MI than in patients with other diagnoses. However, the diagnostic accuracy of BNP was lower than that of cardiac troponin T at presentation, though its independent predictive value for all-cause mortality was more accurate than that of troponin T.
Elevation of the BNP 41 or the N-terminal pro-BNP 42,43 level was shown to also provide unique prognostic information in patients with suspected and confirmed acute coronary syndrome and was associated with higher rates of short-term and long-term mortality. Therefore, BNP appears useful for the prognosis but not the diagnosis of acute coronary syndromes.
CYSTATIN C
The protein cystatin C, widely used as a biomarker for kidney disease, has more recently been touted as a prognostic marker in acute coronary syndromes.
Jernberg et al44 reported that, in patients with a suspected or confirmed acute coronary syndrome, a single measurement of cystatin C significantly improved the early stratification of risk.44 Specifically, the cystatin C level was independently associated with mortality risk but not with the risk of subsequent MI.
In another study,45 the cystatin C concentration independently predicted the risk of cardiovascular death or MI in non-ST-segment elevation acute coronary syndrome. However, the additive predictive value of cystatin C in these patients was found to be small when clinical risk factors and biomarkers of MI were used in the prediction model. Therefore, cystatin C may predict global risk but does not appear to be useful in diagnosing MI.
ISCHEMIA-MODIFIED ALBUMIN
A major limitation of troponin is that it cannot detect reversible myocardial ischemia in the absence of cardiac necrosis, making stress testing necessary to unmask potential reversible ischemia.
Ischemia-modified albumin has been proposed as a means of detecting cardiac ischemia even if necrosis is absent. It is a product of the N-terminus alteration of albumin caused by myocardial ischemia, which reduces the ability of cobalt to bind to albumin and can be detected with the albumin cobalt binding test. This marker might have a high negative predictive value, ruling out acute coronary syndromes in conditions of low pretest probability with negative necrosis markers and ECG.13,46
Although ischemia-modified albumin does show promise, doubt remains as to its validity as a biomarker, as its mechanism of generation is not known. Some have suggested that it is in fact a marker of oxidative stress.47
PANELS OF MARKERS
The individual biomarkers we have discussed here have advantages and limitations in the emergency workup of chest pain. The concept of using a multimarker panel has been raised as a way of amplifying the positive attributes of individual biomarkers and compensating for their shortcomings.
Sabatine et al48 tested this approach in patients with acute coronary syndromes who were at high risk of an adverse outcome. When patients were categorized at presentation on the basis of the number of elevated biomarkers such as cardiac troponin I, C-reactive protein, and BNP, the risk of death nearly doubled with each additional biomarker that was elevated.
The relationship was similar for the end points of MI, heart failure, and the composite at 30 days and 10 months. In a cohort of 1,635 patients, the number of elevated biomarkers remained a predictor of the composite end point after adjustment for known clinical predictors. The risk of death, MI, or heart failure by 6 months was 2.1 times higher in patients with one elevated biomarker, 3.1 times higher in those with two, and 3.7 times higher in those with three.
The authors concluded that a multimarker strategy that categorizes patients on the basis of the number of elevated biomarkers at presentation allows risk-stratification of short- and long-term cardiac events.
Tello-Montoliu et al49 tested this idea in patients with non-ST-segment elevation acute coronary syndromes using a panel consisting of cardiac troponin T, C-reactive protein, N-terminal pro-BNP, and fibrin D-dimer. The risk of a major event (death, new acute coronary syndrome, revascularization, or heart failure) at 6 months was associated with abnormal biomarker levels, especially with the presence of three positive biomarkers, even after adjustment for clinical characteristics and ECG findings.
van der Zee et al43 showed that a positive biomarker panel consisting of C-reactive protein and N-terminal pro-BNP identified patients with chest pain and a normal or nondiagnostic ECG who have a high long-term risk of cardiovascular death.
Glaser et al50 evaluated the combination of cardiac troponin I, BNP, homocysteine, C-reactive protein, placental growth factor, myeloperoxidase, choline, soluble CD40 ligand, ischemia-modified albumin, and lipoprotein-associated phospholipase A2 in patients with a suspected acute coronary syndrome. The combination of BNP, placental growth factor, and estimated glomerular filtration rate was the most accurate predictor of major adverse cardiovascular events compared with any other biomarker or clinical factor. With appropriate cutoff values, the negative predictive value for a major adverse cardiovascular event at 1 year was as high as 99.1%.
This study highlighted the importance of combining biomarkers, showing that with a negative predictive value of 97% for 30-day events, the combination of placental growth factor, BNP, and cardiac troponin I may help surmount the delay from symptom onset to cardiac troponin increase, thus permitting a more timely diagnosis and safe discharge within 12 hours.
Comment. These studies raise the promise that panels of biomarkers can be used in patients deemed to be at low risk after clinical assessment and troponin evaluation to enable them to be safely discharged early and to obviate the need for stress testing.
If we assume that unstable cardiac disease requiring hospitalization accounts for 35% of patients with chest pain, a hypothetical panel of biomarkers with a sensitivity and specificity of 95% for adverse cardiac outcomes would have a positive predictive value of 91% and a negative predictive value of 97%. The negative likelihood ratio of this hypothetical biomarker panel would be 0.05, while the positive likelihood ratio would be 19. This performance level means that in patients with a pretest probability less than 50%, the posttest probability can be reduced to below 10%, so that such patients can be safely discharged without further hospital evaluation.
Conversely, a positive test result in patients with pretest probability of 30% or greater raises the posttest probability to nearly 90%, meaning that such patients should be considered for aggressive intervention without the need for stress testing.
RETURN TO OUR SCENARIOS
Chest pain remains a nonspecific complaint, and the interpretation of biomarkers to find the cause presents clinicians with challenges, as illustrated by the cases introduced at the beginning of this article.
The cardiac troponin I elevation in scenario 1 led to an initial diagnosis of unstable angina. However, coronary angiography showed lesion-free coronary arteries, thus excluding ischemic heart disease. When other diseases that could cause elevated cardiac troponin I were considered and investigated with further diagnostic tests such as D-dimer, pulmonary embolism became the new working diagnosis, and this was confirmed by CT angiography.
Similarly, given the laboratory values for the patient in scenario 2, the condition could have been mistaken for an acute coronary syndrome. However, the absence of evidence on ECG to support this diagnosis would indicate an erroneously elevated biomarker secondary to his background of chronic renal insufficiency.
Each year in the United States, more than 8 million people come to the emergency department with chest pain, but only a minority are eventually diagnosed with a heart attack.1
Confronted with signs and symptoms that could represent an acute coronary syndrome, clinicians need to know whether the patient has a benign condition and can safely be sent home or is in urgent need of hospitalization—and they need to do so in a safe, timely, and cost-effective manner.2,3
Testing for biomarkers of cardiac injury, especially troponins I and T, is an accepted part of the assessment of chest pain. However, the interpretation of these cardiac biomarkers is complicated by the fact they can be elevated from noncoronary causes of chest pain such as pulmonary embolism or renal impairment, and thus should be considered only as part of the patient’s total clinical picture. This uncertainty can result in longer hospital stays and increased testing.
Thus, researchers are searching for new biomarkers that could allow for more rapid and accurate diagnosis and estimation of prognosis.
In this article we will examine the advantages and limitations of measuring cardiac biomarkers. We then discuss the emerging data on new biomarkers, including the very promising high-sensitivity troponin assays, cystatin C, and other markers, and the potential for biomarkers to be used instead of or in combination with stress testing in the evaluation of patients who have no initial evidence of ischemia.
SCENARIO 1: ELEVATED TROPONIN AND ST-SEGMENT ELEVATION
A 46-year-old woman presents to the emergency department with chest pain that started 2 hours earlier. Electrocardiography (ECG) initially shows sinus tachycardia with ST-segment depression and negative T waves in lead aVL. Her cardiac biomarker values (troponin I and creatine kinase MB) are normal. Repeated troponin I measurements show elevations of 250 ng/L, whereas her creatine kinase MB level is within the optimal range. Coronary angiography is unremarkable. Echocardiography shows right ventricular pressure overload in the pulmonary artery and the right ventricle. How should this patient be further evaluated?
SCENARIO 2: ELEVATED TROPONIN AND LEFT VENTRICULAR HYPERTROPHY
A 47-year-old man is admitted with worsening dyspnea and chest pain that worsens with coughing and inspiration. He has a history of end-stage renal disease secondary to poorly controlled hypertension and is being treated with hemodialysis, which he missed for the past 4 weeks while failing to take his hypertension medication. His blood pressure is 270/130 mm Hg. Chest auscultation reveals signs of pulmonary edema—ie, crackles at the end of inspiration. His troponin T level is 394 ng/L. ECG indicates left ventricular hypertrophy. How should this patient be further evaluated?
TROPONIN IS SPECIFIC FOR INJURY, BUT NOT FOR INFARCTION
American College of Cardiology and American Heart Association (ACC/AHA) guidelines4 recommend that clinicians ask themselves two questions: what is the likelihood that the patient is truly having an acute coronary syndrome secondary to coronary artery disease, and what is the likelihood of an adverse clinical outcome? Clues come from the initial measurements of biomarkers of cardiac injury, history, physical examination, and ECG (Table 1),5 and subsequent care is based on the estimated degree of risk.
Troponin revolutionized the diagnosis and risk stratification of chest pain. The ACC/AHA guidelines call for measuring biomarkers—preferably troponin—in all patients who present with chest discomfort consistent with an acute coronary syndrome.4,6
Cardiac troponins I and T have been the biomarkers of choice for detecting myocardial injury,4,6 since elevated concentrations are highly sensitive and tissue-specific.7 Moreover, they identify patients at short-term and long-term risk of cardiac events.4,8
The introduction of troponin testing led to a substantial increase in the rate of diagnosis of myocardial infarction (MI), with an increase in cardiac care unit admissions of more than 20%.9,10 This was partly because troponin is released into the blood with even minute myocardial damage, so that some patients who previously would have been diagnosed with unstable angina are now found to have non-ST-segment-elevation MI.10 However, the increase in admissions may also represent an increase in misdiagnoses, with many clinicians equating an elevated troponin level with acute MI.11
Although an elevated troponin level is 100% specific for myocardial injury, it is not synonymous with MI.12 Myocardial injury can be caused by a cardiac condition such as tachyarrhythmia, cardiac trauma, congestive heart failure, ventricular hypertrophy, myocarditis, or pericarditis, or by a noncardiac condition such as sepsis, respiratory failure, pulmonary embolism, pulmonary hypertension, cancer chemotherapy, or renal insufficiency.4,13 Therefore, to avoid a misdiagnosis of MI, the troponin level must be considered in the clinical context.
In fact, Alcalai et al11 noted that almost half of patients with elevated troponin did not really have an acute coronary syndrome. More importantly, in-hospital and long-term survival rates were significantly better for patients with an acute coronary syndrome than for those without, illustrating the importance of identifying and treating the true disease instead of mislabeling the problem as MI.
Bayesian theory predicts that patients with chest pain who have elevated troponin are less likely to truly have an acute coronary syndrome if the rest of their clinical presentation indicates a low probability for heart disease.14 Indeed, when McDonald et al15 used a risk-scoring index based on sex, a history of heart failure or coronary artery disease, the ECG, and use of aspirin, the positive predictive value of an abnormal troponin level was 83% at a risk score of 4 or greater, 63% at a score of 3, 52% at a score of 2, 32% at a score of 1, and 29% at a score of 0.
Thus, cardiac biomarkers are not a substitute for traditional clinical assessment, but rather should be used “in conjunction with the clinical history, physical examination, and interpretation of the ECG.”6 Consequently, diagnostic protocols that incorporate pretest clinical features to identify low-risk patients have a higher negative predictive value.
This was illustrated in a study by Than et al16 that aimed to prospectively validate the safety of an accelerated diagnostic protocol to assess chest pain suggestive of an acute coronary syndrome. The protocol included a structured pretest probability scoring method (ie, the Thrombolysis in Myocardial Infarction [TIMI] score), ECG, and a point-of-care biomarker panel of troponin, creatine kinase MB, and myoglobin. The protocol had a negative predictive value of 99.1%, whereas the use of biomarkers alone had a value of 96.1%.
HISTORY AND PHYSICAL EXAMINATION PROVIDE KEY INFORMATION
In a review, Heidenreich et al8 noted certain demographic characteristics associated with worse outcomes—ie, older age and male sex; a history of medical conditions such as diabetes, MI, and hypertension; and heart failure on presentation.
A careful assessment of chest pain and associated symptoms helps narrow the differential diagnosis. Features that increase the likelihood of a cardiac origin of chest pain are:
- Chest pain at the time of presentation (likelihood ratio [LR] = 2.0)
- Radiation of the pain to the right shoulder (LR = 2.9), the left arm (LR = 2.3), or both arms (LR = 7.1)
- Nausea or vomiting (LR = 1.9)
- Diaphoresis (LR = 2.0).17
The physical examination can detect highrisk features such as new murmurs, hypotension, diaphoresis, pulmonary edema, and rales. It is more specific than sensitive and is useful in identifying low-risk patients by targeting potential noncardiac causes of the patient’s symptoms.18
The efficacy of clinical assessment was studied in 2,271 patients with chest pain presenting to the emergency department.19 In this cohort, a low-risk group with a 30-day major cardiovascular event rate (death, MI, stroke, or revascularization) of 2.5% could be identified through the use of the US Agency for Health Care Policy and Research criteria.
Electrocardiography
ECG provides important diagnostic and prognostic information and independently predicts death or MI, even after adjustment for cardiac biomarker measurements,20,21 making it pivotal in the evaluation.4 The key features on ECG that increase the probability of MI are:
- New ST-segment elevation (LR 5.7–53.9)
- New Q waves (LR 5.3–24.8).17
One study20 found that while the troponin T level was a powerful independent marker in patients presenting with MI, its value for risk stratification was enhanced when it was combined with a standard measure such as ECG.20 While more than 90% of patients with STsegment elevation had an adverse outcome, only 31.7% of those patients had an elevated troponin T level.
No component is sufficient by itself
Thus, in spite of the proliferation of cardiac diagnostic tests, the initial bedside assessment of chest pain remains paramount. In fact, in patients presenting to the emergency department with chest pain, low risk (ie, those with a < 5% probability of MI) may be identified by presenting symptoms, medical history, and ECG alone.19
Furthermore, although clinical assessment, ECG, and cardiac biomarker testing each provide incremental benefit in assessing chest pain, no component is sufficient by itself. Sanchis et al22 found that even in patients with a normal troponin I level, the risk remained high in the case of ST-segment depression, and that even without signs of ischemia, the probability of cardiac events was 16% when the chest pain score was 11 points or higher.22 Consequently, a normal troponin level, ECG, or any other predictor alone would not ensure a good prognosis.
BIOMARKERS INSTEAD OF STRESS TESTING?
The ACC/AHA guidelines for the diagnosis of patients with unstable angina and non-STsegment elevation MI say that stable patients at low risk with no evidence of ischemia on initial assessment can be admitted to a chest pain unit for observation with serial cardiac biomarkers and ECG.4 At the end of the observation period, those who have reassuring results on ECG and normal cardiac biomarker measurements undergo functional cardiac testing or stress testing, or both.4
Exercise treadmill testing is a cornerstone of confirmatory testing in an accelerated diagnostic protocol because it is readily available, safe, and easy to do.18 A low-risk result was shown to have a high negative predictive value,23,24 so that the likelihood of an acute coronary syndrome is low enough for safe discharge.
However, the overall process is not ideal since it is time-consuming, generates additional costs, and can have false-positive results in patients who are otherwise deemed not to be at high risk. While some studies provided an optimistic view about discharging low-risk patients with negative biomarkers without stress testing,7,25 others have discouraged omitting exercise treadmill testing from protocols.22,26
Others have proposed combining a biomarker with an imaging study such as coronary computed tomographic (CT) angiography.27 Normal findings on this study have been shown to have a negative predictive value of up to 100% for ruling out an acute coronary syndrome and the occurrence of major adverse cardiovascular events in the long term.28,29 Furthermore, it allows more-inclusive assessments of chest pain and can exclude other life-threatening causes such as pulmonary embolism and aortic dissection (referred to as the “triple rule-out”).30
However, 25% to 50% of patients presenting to the emergency department with chest pain may not be candidates for CT angiography because of obesity, contrast allergy, intolerance to beta-blockade, arrhythmia, renal insufficiency, or a history of coronary artery disease.18 Moreover, it may be more efficient and less costly to discharge some patients without coronary CT angiography31 with the help of novel biomarkers without routine additional testing. This may spare patients the additional radiation exposure from CT angiography or nuclear imaging.27,32
New biomarkers may, it is hoped, better distinguish patients at low risk from those at high risk without resorting to stress testing. Several of these markers are moving toward mainstream clinical use. For a biomarker to be prognostically equivalent to stress testing, it must be able to tell us if the likelihood of an acute coronary syndrome is low enough for safe discharge—ie, it must have a significantly high negative predictive value. Also, it must be an independent predictor of adverse outcomes, particularly in patients deemed at low risk by initial low troponin measurements. Biomarkers that have shown promise in this regard include high-sensitivity troponin, brain-type natriuretic peptide (BNP), cystatin C, and ischemia-modified albumin.
HIGH-SENSITIVITY CARDIAC TROPONIN ASSAYS
Although we speak of “high-sensitivity troponin,” these new assays detect the same molecule as do traditional troponin assays. The difference is that high-sensitivity assays can detect and measure troponin at concentrations much lower than the traditional assays can. In fact, high-sensitivity troponin assays can detect and measure troponin at very low levels in almost all healthy people.
Studies have shown that the high-sensitivity assays have better analytical accuracy and sensitivity than older assays.12
Aldous et al33 reported that, in patients who presented to the emergency department within 4 hours of the onset of chest pain, an elevation in troponin T on a high-sensitivity assay had a positive predictive value of 53.8% and a negative predictive value of 98.3%.
Weber et al34 found the diagnostic value of the high-sensitivity troponin T assay to be superior to that of a contemporary troponin T assay (area under the receiver-operating-characteristics curve [AUC] of 0.949 vs 0.929). Even when the contemporary troponin T assay was negative, the high-sensitivity assay provided strong diagnostic information (AUC 0.81). Furthermore, the high-sensitivity assay provided superior independent prognostic power for death within 6 months.
Hochholzer et al35 reported a prognostic accuracy for death significantly higher (AUC 0.79) than that of contemporary troponin T (AUC 0.69). A concentration of high-sensitivity troponin T above 14 ng/L improved the prediction of death (hazard ratio 2.60) but not of subsequent acute MI in patients with acute chest pain. Therefore, a negative high-sensitivity troponin T assay identifies patients with a good prognosis and who may be discharged without further testing if their clinical presentation and ECG are also reassuring.
Keller et al36 compared the diagnostic performance of the high-sensitivity cardiac troponin I assay against 11 other biomarkers, including a contemporary cardiac troponin I assay. The contemporary troponin I and the high-sensitivity troponin I assays performed best. The high-sensitivity troponin I assay at admission had a sensitivity of 82.3% and a negative predictive value of 94.7% for ruling out acute MI, whereas the contemporary troponin I assay had a sensitivity of 79.4% and a negative predictive value of 94.0%.
Using levels obtained at 3 hours after admission, the sensitivity was 98.2% and the negative predictive value was 99.4% for both troponin I assays. Combining the 99th percentile cutoff at admission with the serial change in troponin concentration within 3 hours, the positive predictive value for ruling in acute MI for high-sensitivity cardiac troponin I increased from 75.1% at admission to 95.8% after 3 hours; for the contemporary assay, it increased from 80.9% at admission to 96.1%.36
The authors concluded that performing either of the cardiac troponin I assays 3 hours after admission may help in ruling out MI early on, with a negative predictive value greater than 99%. Moreover, the relative change in concentration within the 3 hours after admission, combined with the 99th percentile diagnostic cutoff value on admission, improves specificity, allowing acute MI to be accurately ruled in.36
Of note, though studies have confirmed that a measurement at 3 hours identifies most cases of MI early, they have not used the recommended maximal sensitivity interval for troponin measurements (6 hours or more).6
A proposed algorithm for diagnosing acute MI with a high-sensitivity assay
While high-sensitivity troponin T assays can improve the early diagnosis of acute MI, how best to use them is yet to be defined. They still lack specificity for acute coronary syndromes, with positive predictive values as low as 50%.37
Reichlin et al38 developed and validated an algorithm for rapidly ruling out or ruling in acute MI using a high-sensitivity cardiac troponin T assay, incorporating baseline values and absolute changes within the first hour. Using a baseline threshold of 12 ng/L or less and an absolute change of 3 ng/L or less, they found a sensitivity and negative predictive value of 100%, making these good criteria for ruling out acute MI.
Using a baseline threshold of 60 ng/L or greater and a change from baseline to 1 hour of at least 15 ng/L, the specificity was 97% and the positive predictive value was 84%, making these good criteria for ruling in acute MI.
Patients whose values were in between were classified as being in an “observationalzone group,” in which the prevalence of acute MI was 8%. The cumulative 30-day survival rate was 99.8% in patients in whom the test ruled out MI, 98.6% in the observational-zone patients, and 95.3% in patients in whom the test ruled in MI.38 Using this simple algorithm allowed a safe rule-out as well as an accurate rule-in of acute MI within 1 hour in 77% of unselected patients with acute chest pain; thus, it may obviate the need for prolonged monitoring and serial measurements in three out of four patients.”
Newby39 stated that such an algorithmic approach must be validated in a prospective study that assesses not only sensitivity, negative predictive value, specificity, and positive predictive value, but also the implications for clinical outcomes and the cost of widespread implementation.
In the meantime, clinicians must keep in mind that patient populations in clinical practice are less selected, the prevalence of MI may broadly vary, and confounding comorbidities such as heart failure and renal insufficiency are more common. Studies are also needed to verify whether other factors such as age, sex, and time from symptom onset should be considered.
BRAIN-TYPE NATRIURETIC PEPTIDE
BNP is a 32-amino-acid natriuretic peptide that is released from myocytes. The amount released depends on wall stress brought on by heart failure, ischemic heart disease, or other conditions.
In a study of the diagnostic utility of BNP in the workup of acute chest pain, Haaf et al40 found that BNP levels at presentation were significantly higher in patients with acute MI than in patients with other diagnoses. However, the diagnostic accuracy of BNP was lower than that of cardiac troponin T at presentation, though its independent predictive value for all-cause mortality was more accurate than that of troponin T.
Elevation of the BNP 41 or the N-terminal pro-BNP 42,43 level was shown to also provide unique prognostic information in patients with suspected and confirmed acute coronary syndrome and was associated with higher rates of short-term and long-term mortality. Therefore, BNP appears useful for the prognosis but not the diagnosis of acute coronary syndromes.
CYSTATIN C
The protein cystatin C, widely used as a biomarker for kidney disease, has more recently been touted as a prognostic marker in acute coronary syndromes.
Jernberg et al44 reported that, in patients with a suspected or confirmed acute coronary syndrome, a single measurement of cystatin C significantly improved the early stratification of risk.44 Specifically, the cystatin C level was independently associated with mortality risk but not with the risk of subsequent MI.
In another study,45 the cystatin C concentration independently predicted the risk of cardiovascular death or MI in non-ST-segment elevation acute coronary syndrome. However, the additive predictive value of cystatin C in these patients was found to be small when clinical risk factors and biomarkers of MI were used in the prediction model. Therefore, cystatin C may predict global risk but does not appear to be useful in diagnosing MI.
ISCHEMIA-MODIFIED ALBUMIN
A major limitation of troponin is that it cannot detect reversible myocardial ischemia in the absence of cardiac necrosis, making stress testing necessary to unmask potential reversible ischemia.
Ischemia-modified albumin has been proposed as a means of detecting cardiac ischemia even if necrosis is absent. It is a product of the N-terminus alteration of albumin caused by myocardial ischemia, which reduces the ability of cobalt to bind to albumin and can be detected with the albumin cobalt binding test. This marker might have a high negative predictive value, ruling out acute coronary syndromes in conditions of low pretest probability with negative necrosis markers and ECG.13,46
Although ischemia-modified albumin does show promise, doubt remains as to its validity as a biomarker, as its mechanism of generation is not known. Some have suggested that it is in fact a marker of oxidative stress.47
PANELS OF MARKERS
The individual biomarkers we have discussed here have advantages and limitations in the emergency workup of chest pain. The concept of using a multimarker panel has been raised as a way of amplifying the positive attributes of individual biomarkers and compensating for their shortcomings.
Sabatine et al48 tested this approach in patients with acute coronary syndromes who were at high risk of an adverse outcome. When patients were categorized at presentation on the basis of the number of elevated biomarkers such as cardiac troponin I, C-reactive protein, and BNP, the risk of death nearly doubled with each additional biomarker that was elevated.
The relationship was similar for the end points of MI, heart failure, and the composite at 30 days and 10 months. In a cohort of 1,635 patients, the number of elevated biomarkers remained a predictor of the composite end point after adjustment for known clinical predictors. The risk of death, MI, or heart failure by 6 months was 2.1 times higher in patients with one elevated biomarker, 3.1 times higher in those with two, and 3.7 times higher in those with three.
The authors concluded that a multimarker strategy that categorizes patients on the basis of the number of elevated biomarkers at presentation allows risk-stratification of short- and long-term cardiac events.
Tello-Montoliu et al49 tested this idea in patients with non-ST-segment elevation acute coronary syndromes using a panel consisting of cardiac troponin T, C-reactive protein, N-terminal pro-BNP, and fibrin D-dimer. The risk of a major event (death, new acute coronary syndrome, revascularization, or heart failure) at 6 months was associated with abnormal biomarker levels, especially with the presence of three positive biomarkers, even after adjustment for clinical characteristics and ECG findings.
van der Zee et al43 showed that a positive biomarker panel consisting of C-reactive protein and N-terminal pro-BNP identified patients with chest pain and a normal or nondiagnostic ECG who have a high long-term risk of cardiovascular death.
Glaser et al50 evaluated the combination of cardiac troponin I, BNP, homocysteine, C-reactive protein, placental growth factor, myeloperoxidase, choline, soluble CD40 ligand, ischemia-modified albumin, and lipoprotein-associated phospholipase A2 in patients with a suspected acute coronary syndrome. The combination of BNP, placental growth factor, and estimated glomerular filtration rate was the most accurate predictor of major adverse cardiovascular events compared with any other biomarker or clinical factor. With appropriate cutoff values, the negative predictive value for a major adverse cardiovascular event at 1 year was as high as 99.1%.
This study highlighted the importance of combining biomarkers, showing that with a negative predictive value of 97% for 30-day events, the combination of placental growth factor, BNP, and cardiac troponin I may help surmount the delay from symptom onset to cardiac troponin increase, thus permitting a more timely diagnosis and safe discharge within 12 hours.
Comment. These studies raise the promise that panels of biomarkers can be used in patients deemed to be at low risk after clinical assessment and troponin evaluation to enable them to be safely discharged early and to obviate the need for stress testing.
If we assume that unstable cardiac disease requiring hospitalization accounts for 35% of patients with chest pain, a hypothetical panel of biomarkers with a sensitivity and specificity of 95% for adverse cardiac outcomes would have a positive predictive value of 91% and a negative predictive value of 97%. The negative likelihood ratio of this hypothetical biomarker panel would be 0.05, while the positive likelihood ratio would be 19. This performance level means that in patients with a pretest probability less than 50%, the posttest probability can be reduced to below 10%, so that such patients can be safely discharged without further hospital evaluation.
Conversely, a positive test result in patients with pretest probability of 30% or greater raises the posttest probability to nearly 90%, meaning that such patients should be considered for aggressive intervention without the need for stress testing.
RETURN TO OUR SCENARIOS
Chest pain remains a nonspecific complaint, and the interpretation of biomarkers to find the cause presents clinicians with challenges, as illustrated by the cases introduced at the beginning of this article.
The cardiac troponin I elevation in scenario 1 led to an initial diagnosis of unstable angina. However, coronary angiography showed lesion-free coronary arteries, thus excluding ischemic heart disease. When other diseases that could cause elevated cardiac troponin I were considered and investigated with further diagnostic tests such as D-dimer, pulmonary embolism became the new working diagnosis, and this was confirmed by CT angiography.
Similarly, given the laboratory values for the patient in scenario 2, the condition could have been mistaken for an acute coronary syndrome. However, the absence of evidence on ECG to support this diagnosis would indicate an erroneously elevated biomarker secondary to his background of chronic renal insufficiency.
- Pitts SR, Niska RW, Xu J, Burt CW. National hospital ambulatory medical care survey: 2006 emergency department summary. Natl Health Stat Report 2008;1–38.
- Vucic R, Knezevic S, Lazic Z, et al. Elevation of troponin values in differential diagnosis of chest pain in view of pulmonary thromboembolism. Vojnosanit Pregl 2012; 69:913–916.
- Croitoru M, Taegtmeyer H. Spurious rises in troponin T in end-stage renal disease. Lancet 1995; 346:974.
- Anderson JL, Adams CD, Antman EM, et al; 2011 Writing Group Members; ACCF/AHA Task Force Members. 2011 ACCF/AHA focused update incorporated into the ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2011; 123:e426–e579.
- Unstable angina: diagnosis and management. Guideline overview. Agency for Health Care Policy and Research. J Natl Med Assoc 1994; 86:649,710–712.
- Morrow DA, Cannon CP, Jesse RL, et al; National Academy of Clinical Biochemistry. National Academy of Clinical Biochemistry Laboratory Medicine Practice Guidelines: clinical characteristics and utilization of biochemical markers in acute coronary syndromes. Circulation 2007; 115:e356–e375.
- Hamm CW, Goldmann BU, Heeschen C, Kreymann G, Berger J, Meinertz T. Emergency room triage of patients with acute chest pain by means of rapid testing for cardiac troponin T or troponin I. N Engl J Med 1997; 337:1648–1653.
- Heidenreich PA, Go A, Melsop KA, et al. Prediction of risk for patients with unstable angina. Evid Rep Technol Assess (Summ) 2000; August:1–3.
- Kontos MC, Fritz LM, Anderson FP, Tatum JL, Ornato JP, Jesse RL. Impact of the troponin standard on the prevalence of acute myocardial infarction. Am Heart J 2003; 146:446–452.
- Amit G, Gilutz H, Cafri C, Wolak A, Ilia R, Zahger D. What have the new definition of acute myocardial infarction and the introduction of troponin measurement done to the coronary care unit? Impacts on admission rate, length of stay, case mix and mortality. Cardiology 2004; 102:171–176.
- Alcalai R, Planer D, Culhaoglu A, Osman A, Pollak A, Lotan C. Acute coronary syndrome vs nonspecific troponin elevation: clinical predictors and survival analysis. Arch Intern Med 2007; 167:276–281.
- Thygesen K, Mair J, Katus H, et al. Study Group on Biomarkers in Cardiology of the ESC Working Group on Acute Cardiac Care. Recommendations for the use of cardiac troponin measurement in acute cardiac care. Eur Heart J 2010; 31:2197–2204.
- Jaffe AS, Babuin L, Apple FS. Biomarkers in acute cardiac disease: the present and the future. J Am Coll Cardiol 2006; 48:1–11.
- Jaeschke R, Guyatt GH, Sackett DL. Users’ guides to the medical literature. III. How to use an article about a diagnostic test. B. What are the results and will they help me in caring for my patients? The Evidence-Based Medicine Working Group. JAMA 1994; 271:703–707.
- McDonald MA, Holroyd B, Comeau A, Hervas-Malo M, Welsh RC. Clinical risk scoring beyond initial troponin values: results from a large, prospective, unselected acute chest pain population. Can J Cardiol 2007; 23:287–292.
- Than M, Cullen L, Reid CM, et al. A 2-h diagnostic protocol to assess patients with chest pain symptoms in the Asia-Pacific region (ASPECT): a prospective observational validation study. Lancet 2011; 377:1077–1084.
- Panju AA, Hemmelgarn BR, Guyatt GH, Simel DL. The rational clinical examination. Is this patient having a myocardial infarction? JAMA 1998; 280:1256–1263.
- Amsterdam EA, Kirk JD, Bluemke DA, et al; American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee of the Council on Clinical Cardiology, Council on Cardiovascular Nursing, and Interdisciplinary Council on Quality of Care and Outcomes Research. Testing of low-risk patients presenting to the emergency department with chest pain: a scientific statement from the American Heart Association. Circulation 2010; 122:1756–1776.
- Farkouh ME, Aneja A, Reeder GS, et al. Clinical risk stratification in the emergency department predicts long-term cardiovascular outcomes in a population-based cohort presenting with acute chest pain: primary results of the Olmsted county chest pain study. Medicine (Baltimore) 2009; 88:307–313.
- Ohman EM, Armstrong PW, Christenson RH, et al. Cardiac troponin T levels for risk stratification in acute myocardial ischemia. GUSTO IIA Investigators. N Engl J Med 1996; 335:1333–1341.
- Antman EM, Tanasijevic MJ, Thompson B, et al. Cardiac-specific troponin I levels to predict the risk of mortality in patients with acute coronary syndromes. N Engl J Med 1996; 335:1342–1349.
- Sanchis J, Bodí V, Llácer A, et al. Predictors of short-term outcome in acute chest pain without ST-segment elevation. Int J Cardiol 2003; 92:193–199.
- Gomez MA, Anderson JL, Karagounis LA, Muhlestein JB, Mooers FB. An emergency department-based protocol for rapidly ruling out myocardial ischemia reduces hospital time and expense: results of a randomized study (ROMIO). J Am Coll Cardiol 1996; 28:25–33.
- Diercks DB, Gibler WB, Liu T, Sayre MR, Storrow AB. Identification of patients at risk by graded exercise testing in an emergency department chest pain center. Am J Cardiol 2000; 86:289–292.
- Rahman F, Mitra B, Cameron PA, Coleridge J. Stress testing before discharge is not required for patients with low and intermediate risk of acute coronary syndrome after emergency department short stay assessment. Emerg Med Australas 2010; 22:449–456.
- Kontos MC, Anderson FP, Alimard R, Ornato JP, Tatum JL, Jesse RL. Ability of troponin I to predict cardiac events in patients admitted from the emergency department. J Am Coll Cardiol 2000; 36:1818–1823.
- Hoffmann U, Truong QA, Schoenfeld DA, et al; ROMICAT-II Investigators. Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med 2012; 367:299–308.
- Hoffmann U, Bamberg F, Chae CU, et al. Coronary computed tomography angiography for early triage of patients with acute chest pain: the ROMICAT (Rule Out Myocardial Infarction using Computer Assisted Tomography) trial. J Am Coll Cardiol 2009; 53:1642–1650.
- Goldstein JA, Chinnaiyan KM, Abidov A, et al; CT-STAT Investigators. The CT-STAT (Coronary Computed Tomographic Angiography for Systematic Triage of Acute Chest Pain Patients to Treatment) trial. J Am Coll Cardiol 2011; 58:1414–1422.
- White CS, Kuo D, Kelemen M, et al. Chest pain evaluation in the emergency department: can MDCT provide a comprehensive evaluation? AJR Am J Roentgenol 2005; 185:533–540.
- Redberg RF. Coronary CT angiography for acute chest pain. N Engl J Med 2012; 367:375–376.
- Shreibati JB, Baker LC, Hlatky MA. Association of coronary CT angiography or stress testing with subsequent utilization and spending among Medicare beneficiaries. JAMA 2011; 306:2128–2136.
- Aldous S, Pemberton C, Richards AM, Troughton R, Than M. High-sensitivity troponin T for early rule-out of myocardial infarction in recent onset chest pain. Emerg Med J 2012; 29:805–810.
- Weber M, Bazzino O, Navarro Estrada JL, et al. Improved diagnostic and prognostic performance of a new high-sensitive troponin T assay in patients with acute coronary syndrome. Am Heart J 2011; 162:81–88.
- Hochholzer W, Reichlin T, Twerenbold R, et al. Incremental value of high-sensitivity cardiac troponin T for risk prediction in patients with suspected acute myocardial infarction. Clin Chem 2011; 57:1318–1326.
- Keller T, Zeller T, Ojeda F, et al. Serial changes in highly sensitive troponin I assay and early diagnosis of myocardial infarction. JAMA 2011; 306:2684–2693.
- Reichlin T, Hochholzer W, Bassetti S, et al. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med 2009; 361:858–867.
- Reichlin T, Schindler C, Drexler B, et al. One-hour rule-out and rule-in of acute myocardial infarction using high-sensitivity cardiac troponin T. Arch Intern Med 2012; 172:1211–1218.
- Newby LK. Myocardial infarction rule-out in the emergency department: are high-sensitivity troponins the answer?: Comment on “One-hour rule-out and rule-in of acute myocardial infarction using high-sensitivity cardiac troponin T”. Arch Intern Med 2012; 172:1218–1219.
- Haaf P, Reichlin T, Corson N, et al. B-type natriuretic peptide in the early diagnosis and risk stratification of acute chest pain. Am J Med 2011; 124:444–445.
- Sun T, Wang L, Zhang Y. Prognostic value of B-type natriuretic peptide in patients with acute coronary syndromes. Arch Med Res 2006; 37:502–505.
- Galvani M, Ottani F, Oltrona L, et al; Italian Working Group on Atherosclerosis, Thrombosis, and Vascular Biology and the Associazione Nazionale Medici Cardiologi Ospedalieri (ANMCO). N-terminal pro-brain natriuretic peptide on admission has prognostic value across the whole spectrum of acute coronary syndromes. Circulation 2004; 110:128–134.
- van der Zee PM, Cornel JH, Bholasingh R, Fischer JC, van Straalen JP, De Winter RJ. N-terminal pro B-type natriuretic peptide identifies patients with chest pain at high long-term cardiovascular risk. Am J Med 2011; 124:961–969.
- Jernberg T, Lindahl B, James S, Larsson A, Hansson LO, Wallentin L. Cystatin C: a novel predictor of outcome in suspected or confirmed non-ST-elevation acute coronary syndrome. Circulation 2004; 110:2342–2348.
- Akerblom Å, Wallentin L, Siegbahn A, et al. Cystatin C and estimated glomerular filtration rate as predictors for adverse outcome in patients with ST-elevation and non-ST-elevation acute coronary syndromes: results from the Platelet Inhibition and Patient Outcomes study. Clin Chem 2012; 58:190–199.
- Anwaruddin S, Januzzi JL, Baggish AL, Lewandrowski EL, Lewandrowski KB. Ischemia-modified albumin improves the usefulness of standard cardiac biomarkers for the diagnosis of myocardial ischemia in the emergency department setting. Am J Clin Pathol 2005; 123:140–145.
- Senes M, Kazan N, Coskun O, Zengi O, Inan L, Yücel D. Oxidative and nitrosative stress in acute ischaemic stroke. Ann Clin Biochem 2007; 44:43–47.
- Sabatine MS, Morrow DA, de Lemos JA, et al. Multimarker approach to risk stratification in non-ST elevation acute coronary syndromes: simultaneous assessment of troponin I, C-reactive protein, and B-type natriuretic peptide. Circulation 2002; 105:1760–1763.
- Tello-Montoliu A, Marín F, Roldán V, et al. A multimarker risk stratification approach to non-ST elevation acute coronary syndrome: implications of troponin T, CRP, NT pro-BNP and fibrin D-dimer levels. J Intern Med 2007; 262:651–658.
- Glaser R, Peacock WF, Wu AH, Muller R, Möckel M, Apple FS. Placental growth factor and B-type natriuretic peptide as independent predictors of risk from a multibiomarker panel in suspected acute coronary syndrome (Acute Risk and Related Outcomes Assessed With Cardiac Biomarkers [ARROW]) study. Am J Cardiol 2011; 107:821–826.
- Pitts SR, Niska RW, Xu J, Burt CW. National hospital ambulatory medical care survey: 2006 emergency department summary. Natl Health Stat Report 2008;1–38.
- Vucic R, Knezevic S, Lazic Z, et al. Elevation of troponin values in differential diagnosis of chest pain in view of pulmonary thromboembolism. Vojnosanit Pregl 2012; 69:913–916.
- Croitoru M, Taegtmeyer H. Spurious rises in troponin T in end-stage renal disease. Lancet 1995; 346:974.
- Anderson JL, Adams CD, Antman EM, et al; 2011 Writing Group Members; ACCF/AHA Task Force Members. 2011 ACCF/AHA focused update incorporated into the ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2011; 123:e426–e579.
- Unstable angina: diagnosis and management. Guideline overview. Agency for Health Care Policy and Research. J Natl Med Assoc 1994; 86:649,710–712.
- Morrow DA, Cannon CP, Jesse RL, et al; National Academy of Clinical Biochemistry. National Academy of Clinical Biochemistry Laboratory Medicine Practice Guidelines: clinical characteristics and utilization of biochemical markers in acute coronary syndromes. Circulation 2007; 115:e356–e375.
- Hamm CW, Goldmann BU, Heeschen C, Kreymann G, Berger J, Meinertz T. Emergency room triage of patients with acute chest pain by means of rapid testing for cardiac troponin T or troponin I. N Engl J Med 1997; 337:1648–1653.
- Heidenreich PA, Go A, Melsop KA, et al. Prediction of risk for patients with unstable angina. Evid Rep Technol Assess (Summ) 2000; August:1–3.
- Kontos MC, Fritz LM, Anderson FP, Tatum JL, Ornato JP, Jesse RL. Impact of the troponin standard on the prevalence of acute myocardial infarction. Am Heart J 2003; 146:446–452.
- Amit G, Gilutz H, Cafri C, Wolak A, Ilia R, Zahger D. What have the new definition of acute myocardial infarction and the introduction of troponin measurement done to the coronary care unit? Impacts on admission rate, length of stay, case mix and mortality. Cardiology 2004; 102:171–176.
- Alcalai R, Planer D, Culhaoglu A, Osman A, Pollak A, Lotan C. Acute coronary syndrome vs nonspecific troponin elevation: clinical predictors and survival analysis. Arch Intern Med 2007; 167:276–281.
- Thygesen K, Mair J, Katus H, et al. Study Group on Biomarkers in Cardiology of the ESC Working Group on Acute Cardiac Care. Recommendations for the use of cardiac troponin measurement in acute cardiac care. Eur Heart J 2010; 31:2197–2204.
- Jaffe AS, Babuin L, Apple FS. Biomarkers in acute cardiac disease: the present and the future. J Am Coll Cardiol 2006; 48:1–11.
- Jaeschke R, Guyatt GH, Sackett DL. Users’ guides to the medical literature. III. How to use an article about a diagnostic test. B. What are the results and will they help me in caring for my patients? The Evidence-Based Medicine Working Group. JAMA 1994; 271:703–707.
- McDonald MA, Holroyd B, Comeau A, Hervas-Malo M, Welsh RC. Clinical risk scoring beyond initial troponin values: results from a large, prospective, unselected acute chest pain population. Can J Cardiol 2007; 23:287–292.
- Than M, Cullen L, Reid CM, et al. A 2-h diagnostic protocol to assess patients with chest pain symptoms in the Asia-Pacific region (ASPECT): a prospective observational validation study. Lancet 2011; 377:1077–1084.
- Panju AA, Hemmelgarn BR, Guyatt GH, Simel DL. The rational clinical examination. Is this patient having a myocardial infarction? JAMA 1998; 280:1256–1263.
- Amsterdam EA, Kirk JD, Bluemke DA, et al; American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee of the Council on Clinical Cardiology, Council on Cardiovascular Nursing, and Interdisciplinary Council on Quality of Care and Outcomes Research. Testing of low-risk patients presenting to the emergency department with chest pain: a scientific statement from the American Heart Association. Circulation 2010; 122:1756–1776.
- Farkouh ME, Aneja A, Reeder GS, et al. Clinical risk stratification in the emergency department predicts long-term cardiovascular outcomes in a population-based cohort presenting with acute chest pain: primary results of the Olmsted county chest pain study. Medicine (Baltimore) 2009; 88:307–313.
- Ohman EM, Armstrong PW, Christenson RH, et al. Cardiac troponin T levels for risk stratification in acute myocardial ischemia. GUSTO IIA Investigators. N Engl J Med 1996; 335:1333–1341.
- Antman EM, Tanasijevic MJ, Thompson B, et al. Cardiac-specific troponin I levels to predict the risk of mortality in patients with acute coronary syndromes. N Engl J Med 1996; 335:1342–1349.
- Sanchis J, Bodí V, Llácer A, et al. Predictors of short-term outcome in acute chest pain without ST-segment elevation. Int J Cardiol 2003; 92:193–199.
- Gomez MA, Anderson JL, Karagounis LA, Muhlestein JB, Mooers FB. An emergency department-based protocol for rapidly ruling out myocardial ischemia reduces hospital time and expense: results of a randomized study (ROMIO). J Am Coll Cardiol 1996; 28:25–33.
- Diercks DB, Gibler WB, Liu T, Sayre MR, Storrow AB. Identification of patients at risk by graded exercise testing in an emergency department chest pain center. Am J Cardiol 2000; 86:289–292.
- Rahman F, Mitra B, Cameron PA, Coleridge J. Stress testing before discharge is not required for patients with low and intermediate risk of acute coronary syndrome after emergency department short stay assessment. Emerg Med Australas 2010; 22:449–456.
- Kontos MC, Anderson FP, Alimard R, Ornato JP, Tatum JL, Jesse RL. Ability of troponin I to predict cardiac events in patients admitted from the emergency department. J Am Coll Cardiol 2000; 36:1818–1823.
- Hoffmann U, Truong QA, Schoenfeld DA, et al; ROMICAT-II Investigators. Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med 2012; 367:299–308.
- Hoffmann U, Bamberg F, Chae CU, et al. Coronary computed tomography angiography for early triage of patients with acute chest pain: the ROMICAT (Rule Out Myocardial Infarction using Computer Assisted Tomography) trial. J Am Coll Cardiol 2009; 53:1642–1650.
- Goldstein JA, Chinnaiyan KM, Abidov A, et al; CT-STAT Investigators. The CT-STAT (Coronary Computed Tomographic Angiography for Systematic Triage of Acute Chest Pain Patients to Treatment) trial. J Am Coll Cardiol 2011; 58:1414–1422.
- White CS, Kuo D, Kelemen M, et al. Chest pain evaluation in the emergency department: can MDCT provide a comprehensive evaluation? AJR Am J Roentgenol 2005; 185:533–540.
- Redberg RF. Coronary CT angiography for acute chest pain. N Engl J Med 2012; 367:375–376.
- Shreibati JB, Baker LC, Hlatky MA. Association of coronary CT angiography or stress testing with subsequent utilization and spending among Medicare beneficiaries. JAMA 2011; 306:2128–2136.
- Aldous S, Pemberton C, Richards AM, Troughton R, Than M. High-sensitivity troponin T for early rule-out of myocardial infarction in recent onset chest pain. Emerg Med J 2012; 29:805–810.
- Weber M, Bazzino O, Navarro Estrada JL, et al. Improved diagnostic and prognostic performance of a new high-sensitive troponin T assay in patients with acute coronary syndrome. Am Heart J 2011; 162:81–88.
- Hochholzer W, Reichlin T, Twerenbold R, et al. Incremental value of high-sensitivity cardiac troponin T for risk prediction in patients with suspected acute myocardial infarction. Clin Chem 2011; 57:1318–1326.
- Keller T, Zeller T, Ojeda F, et al. Serial changes in highly sensitive troponin I assay and early diagnosis of myocardial infarction. JAMA 2011; 306:2684–2693.
- Reichlin T, Hochholzer W, Bassetti S, et al. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med 2009; 361:858–867.
- Reichlin T, Schindler C, Drexler B, et al. One-hour rule-out and rule-in of acute myocardial infarction using high-sensitivity cardiac troponin T. Arch Intern Med 2012; 172:1211–1218.
- Newby LK. Myocardial infarction rule-out in the emergency department: are high-sensitivity troponins the answer?: Comment on “One-hour rule-out and rule-in of acute myocardial infarction using high-sensitivity cardiac troponin T”. Arch Intern Med 2012; 172:1218–1219.
- Haaf P, Reichlin T, Corson N, et al. B-type natriuretic peptide in the early diagnosis and risk stratification of acute chest pain. Am J Med 2011; 124:444–445.
- Sun T, Wang L, Zhang Y. Prognostic value of B-type natriuretic peptide in patients with acute coronary syndromes. Arch Med Res 2006; 37:502–505.
- Galvani M, Ottani F, Oltrona L, et al; Italian Working Group on Atherosclerosis, Thrombosis, and Vascular Biology and the Associazione Nazionale Medici Cardiologi Ospedalieri (ANMCO). N-terminal pro-brain natriuretic peptide on admission has prognostic value across the whole spectrum of acute coronary syndromes. Circulation 2004; 110:128–134.
- van der Zee PM, Cornel JH, Bholasingh R, Fischer JC, van Straalen JP, De Winter RJ. N-terminal pro B-type natriuretic peptide identifies patients with chest pain at high long-term cardiovascular risk. Am J Med 2011; 124:961–969.
- Jernberg T, Lindahl B, James S, Larsson A, Hansson LO, Wallentin L. Cystatin C: a novel predictor of outcome in suspected or confirmed non-ST-elevation acute coronary syndrome. Circulation 2004; 110:2342–2348.
- Akerblom Å, Wallentin L, Siegbahn A, et al. Cystatin C and estimated glomerular filtration rate as predictors for adverse outcome in patients with ST-elevation and non-ST-elevation acute coronary syndromes: results from the Platelet Inhibition and Patient Outcomes study. Clin Chem 2012; 58:190–199.
- Anwaruddin S, Januzzi JL, Baggish AL, Lewandrowski EL, Lewandrowski KB. Ischemia-modified albumin improves the usefulness of standard cardiac biomarkers for the diagnosis of myocardial ischemia in the emergency department setting. Am J Clin Pathol 2005; 123:140–145.
- Senes M, Kazan N, Coskun O, Zengi O, Inan L, Yücel D. Oxidative and nitrosative stress in acute ischaemic stroke. Ann Clin Biochem 2007; 44:43–47.
- Sabatine MS, Morrow DA, de Lemos JA, et al. Multimarker approach to risk stratification in non-ST elevation acute coronary syndromes: simultaneous assessment of troponin I, C-reactive protein, and B-type natriuretic peptide. Circulation 2002; 105:1760–1763.
- Tello-Montoliu A, Marín F, Roldán V, et al. A multimarker risk stratification approach to non-ST elevation acute coronary syndrome: implications of troponin T, CRP, NT pro-BNP and fibrin D-dimer levels. J Intern Med 2007; 262:651–658.
- Glaser R, Peacock WF, Wu AH, Muller R, Möckel M, Apple FS. Placental growth factor and B-type natriuretic peptide as independent predictors of risk from a multibiomarker panel in suspected acute coronary syndrome (Acute Risk and Related Outcomes Assessed With Cardiac Biomarkers [ARROW]) study. Am J Cardiol 2011; 107:821–826.
KEY POINTS
- Biomarkers of cardiac necrosis, particularly troponins I and T, can aid in risk assessment, but one must pay close attention to the underlying clinical context.
- Stable patients at low risk with no evidence of ischemia on initial assessment can be admitted to a chest pain unit for observation with serial biomarker testing and ECG.
- Highly sensitive troponin assays can improve the early diagnosis of acute myocardial infarction, but how best to use them is not yet defined.
- Biomarkers, used alone or in combination, have the potential to complement or replace stress testing, permitting more timely, accurate, and cost-effective diagnosis and earlier discharge of patients at low risk.
- Newer markers such as brain-type natriuretic peptide, cystatin C, and ischemia-modified albumin have shown promise but need to be thoroughly evaluated.
Transient ischemic attack: Omen and opportunity
A transient ischemic attack (TIA), like an episode of unstable angina, is an ominous portent of future morbidity and death even though, by definition, the event leaves no residual neurologic deficit.
But there is a positive side. When a patient presents with a TIA, the physician has the rare opportunity to reduce the risk of a disabling outcome—in this case, stroke. Therefore, patients deserve a rapid and thorough evaluation and appropriate stroke-preventive treatment.
MANY ‘TIAs’ ARE ACTUALLY STROKES
TIA has traditionally been described as a sudden focal neurologic deficit that lasts less than 24 hours, is presumed to be of vascular origin, and is confined to an area of the brain, spinal cord, or eye perfused by a specific artery. This symptom-based definition was based on the arbitrary and inaccurate assumption that brief symptoms would not be associated with damage to brain parenchyma.
The definition has since been updated and made more rational based on new concepts of brain ischemia informed by imaging, especially diffusion-weighted magnetic resonance imaging (MRI).1 One-third of episodes characterized as a TIA according to the classic definition would be considered an infarction on the basis of diffusion-weighted MRI.2 The new tissue-based definition characterizes TIA as a brief episode of neurologic dysfunction caused by focal ischemia of the brain, spinal cord, or retina, with clinical symptoms lasting less than 24 hours and without evidence of acute infarction.3
AN OPPORTUNITY TO INTERVENE
Most TIAs resolve in less than 30 minutes. The US National Institute of Neurological Disorders and Stroke trial of tissue plasminogen activator found that if symptoms of cerebral ischemia had not resolved by 1 hour or had not rapidly improved within 3 hours, complete resolution was rare (only 2% at 24 hours).4 Hence, physicians evaluating and treating patients with TIAs should treat these episodes with the urgency they deserve.
Moreover, half of the strokes that follow TIAs occur within 48 hours.5 A rapid and thorough evaluation and the initiation of secondary preventive treatments have been shown to reduce the early occurrence of stroke by up to 80%.6 Hence, the correct diagnosis of TIA gives the clinician the best opportunity to prevent stroke and its personal, social, and sometimes fatal consequences.
STROKES OUTNUMBER TIAs, BUT TIAs ARE UNDERREPORTED
According to 2012 statistics, nearly 795,000 strokes occur in the United States each year, 610,000 of which are first attacks and 185,000 are recurrences. Every 40 seconds, someone in the United States has a stroke.7
In comparison, the incidence of TIA in the United States is estimated at 200,000 to 500,000 per year, though the true number is difficult to know because of underreporting.8,9 About half of patients who experience a TIA fail to report it to their health care provider—a lost opportunity for intervention and stroke prevention.10,11
A meta-analysis showed that the risk of stroke after TIA was 9.9% at 2 days, 13.4% at 30 days, and 17.3% at 90 days.12
Interestingly, the risk of stroke after TIA exceeds the risk of recurrent stroke after a first stroke. This was shown in a study that found that patients who had made a substantial recovery within 24 hours (ie, patients with a TIA) were more likely to suffer neurologic deterioration in the next 3 months than were those who did not have significant early improvement.13
RISK FACTORS FOR TIA ARE THE SAME AS FOR STROKE
The risk of cerebrovascular disease increases with age and is higher in men14 and in blacks and Hispanics.15
The risk factors and clinical presentation do not differ between TIA and stroke, so the evaluation and treatment should not differ either. These two events represent a continuum of the same disease entity.
Some risk factors for TIA are modifiable, others are not.
Nonmodifiable risk factors
Nonmodifiable risk factors for TIA include older age, male sex, African American race, low birth weight, Hispanic ethnicity, and family history. If the patient has nonmodifiable risk factors, we should try all the harder to correct the modifiable ones.
Older age. The risk of ischemic stroke and intracranial hemorrhage doubles with each decade after age 55 in both sexes.16
Sex. Men have a significantly higher incidence of TIA than women,11 whereas the opposite is true for stroke: women have a higher lifetime risk of stroke than men.17
African Americans have an incidence of stroke (all types) 38% higher than that of whites,18 and an incidence of TIA (inpatient and out-of-hospital) 40% higher than the overall age- and sex-adjusted rate in the white population.11
Low birth weight. The odds of stroke are more than twice as high in people who weighed less than 2,500 g at birth compared with those who weighed 4,000 g or more, probably because of a correlation between low birth weight and hypertension.19
A family history of stroke increases the risk of stroke by nearly 30%, the association being stronger with large-vessel and smallvessel stroke than with cardioembolic stroke.20
Modifiable risk factors
Modifiable risk factors include cigarette smoking, hypertension, diabetes, lipid abnormalities, atrial fibrillation, carotid stenosis, and dietary and hormonal factors. Detecting these factors, which often coexist, is the first step in trying to modify them and reduce the patient’s risk.
Cigarette smoking approximately doubles the risk of ischemic stroke.21–23
Hypertension has a relationship with stroke risk that is strong, continuous, graded, consistent, and significant.24
Diabetes increases stroke risk nearly six times.25
Lipid abnormalities. Most studies have found an association between lipid levels (total cholesterol and low-density lipoprotein cholesterol) and the risk of death from ischemic stroke,26–28 and an inverse relationship between high-density lipoprotein cholesterol levels and stroke risk.29
Atrial fibrillation increases the risk of ischemic stroke up to fivefold, even in the absence of cardiac valvular disease. The mechanism is embolism of stasis-induced thrombi that form in the left atrial appendage.30
Carotid stenosis. Asymptomatic carotid atherosclerotic stenotic lesions in the extracranial internal carotid artery or carotid bulb are associated with a higher risk of stroke.24,31
Lifestyle factors. Diets that lower blood pressure have been found to decrease stroke risk.24 Exercise in men and women reduces the risk of stroke or death by 25% to 30% compared with inactive people.32 Weight reduction has been found to lower blood pressure and reduce stroke risk.24
Other potentially modifiable risk factors include migraine with aura, metabolic syndrome, excess alcohol consumption (and, paradoxically, complete abstinence from alcohol), drug abuse, sleep-disordered breathing, hyperhomocysteinemia, high lipoprotein (a) levels, hypercoagulability, infection with organisms such as Chlamydia pneumoniae, cytomegalovirus, and Helicobacter pylori, and acute infections such as respiratory and urinary infections.26
Conditions in certain demographic groups
Patients in certain demographic groups present with rarer conditions associated with stroke and TIA.
Sickle cell disease. Eleven percent of patients with sickle cell disease have clinical strokes, and a substantial number have “silent” infarcts identified on neuroimaging.33,34
Postmenopausal hormone replacement therapy with any product containing conjugated equine estrogen carries a risk of cerebrovascular events,35 and the higher the dose, the higher the risk.36 Also, oral contraceptives may be harmful in women who have additional risk factors such as cigarette smoking, prior thromboembolic events, or migraine with aura.37,38
THREE CAUSES OF STROKE AND TIA
Stroke and TIA should not be considered diagnoses in themselves, but rather the end point of many other diseases. The diagnosis lies in identifying the mechanism of the cerebrovascular event. The three main mechanisms are thrombosis, embolism, and decreased perfusion.
Thrombosis is caused by obstruction of blood flow within one or more blood vessels, the most common cause being atherosclerosis. Large-artery atherosclerosis, such as in the carotid bifurcation or extracranial internal carotid, causes TIAs that occur over a period of weeks or months with a variety of presentations in that vascular territory, from years of gradual accumulation of atherosclerotic plaque.39
In patients with small-artery or penetrating artery disease, hypertension is the primary risk factor and the pathology, specific to small arterioles, is lipohyalinosis rather than atherosclerosis. These patients may present with a stuttering clinical course, and episodes are more stereotypical.
Less common obstructive vascular pathologies include fibromuscular dysplasia, arteritides, and dissection.
Embolism can occur from a proximal source such as the heart or from proximal vessels such as the aorta, carotid, or vertebral arteries. The embolic particle may form on heart valves or lesions within the heart (eg, clot, tumor), or in the venous circulation and paradoxically cross over to the arterial side through an intracardiac or transpulmonary shunt. Embolism may also be due to a hypercoagulable state.40 Embolic stroke is suspected when multiple vascular territories within the brain are clinically or radiographically affected.
Decreased systemic perfusion caused by severe heart failure or systemic hypotension can cause ischemia to the brain diffusely and bilaterally, limiting the ability of the blood-stream to wash out microemboli, especially in the border zones (also known as “watershed areas”), thus leading to ischemia or infarction.41 Decreased perfusion can also be local, due to a fixed vessel stenosis.
Using another classification system, a study in Rochester, MN, found the following incident rates of stroke subtypes, adjusted for age and sex, per 100,000 population42:
- Large-vessel cervical or intracranial atherosclerosis with more than 50% stenosis—27
- Cardioembolism—40
- Lacunar, small-vessel disease—25
- Uncertain cause—52
- Other identifiable cause—4.
THREE CLINICAL FEATURES SUGGEST TIA
TIAs can be hard to distinguish from nonischemic neurologic events in the acute setting such as an emergency room. Up to 60% of patients suspected of having a TIA actually have a nonischemic cause of their symptoms.43
Three clinical features suggest a TIA during the emergency room evaluation:
- Rapid onset of symptoms—“like lightning” or “in seconds,” in contrast to migraine and seizures, which develop over minutes
- No history of similar episodes in the past
- Absence of nonspecific symptoms—eg, stomach upset or tightness in the chest.
CLINICAL DIAGNOSIS
Because most TIA symptoms and signs have already resolved by the time of evaluation, the diagnosis depends on a careful history with special attention to the pace of onset and resolution, the duration and nature of the symptoms, circumstances at the time of symptom onset, previous similar episodes, associated features, vascular risk factors, and family history (Table 1).44,45
A detailed neurologic examination is imperative and should include fundoscopy. A cardiovascular assessment should include cardiac rhythm, bruits in the neck, orbits, and groin, peripheral pulses, and electrocardiography.
Do neurologists do a better job at diagnosing TIA and stroke?
Primary care physicians, internists, and emergency department physicians are often the ones to carry out the clinical assessment of possible TIA.
Determining if transient neurologic symptoms are caused by ischemia can be a challenge. When in doubt, referral to a neurologist with subspecialty training in cerebrovascular disease should be considered.
But do neurologists really do a better job? A recent study sought to compare the accuracy of diagnosis of TIA made by general practitioners, emergency physicians, and neurologists. The nonneurologists considered “confusion” and “unexplained fall” suggestive of TIA and “lower facial palsy” and “monocular blindness” less suggestive of TIA—whereas the opposite is true. This shows that nonneurologists often label minor strokes and several nonvascular transient neurologic disturbances as TIAs, and up to half of patients could be mislabeled as a result.46
Differences in diagnosing cerebrovascular events between emergency room physicians and attending neurologists have been tested,47 with an accuracy of diagnosis as low as 38% by emergency department physicians in one study.48 However, other studies did not show such a trend.49,50
A study at a university-based teaching hospital found the sensitivity of emergency room physician diagnosis to be 98.6% with a positive predictive value of 94.8%,49 showing that at a large teaching hospital with a comprehensive stroke intervention program, emergency physicians could identify patients with stroke, particularly hemorrhagic stroke, very accurately.
Improving the diagnosis of stroke and TIA
Routine use of imaging and involvement of a neurologist increase the sensitivity and accuracy of diagnosis. Education and written guidelines for acute stroke treatment both in the emergency department and in out-of-hospital settings seem to dramatically improve the rates of diagnostic accuracy and appropriate treatment.50
Emergency medical service personnel use two screening tools in the field to identify TIA and stroke symptoms:
- The Cincinnati Prehospital Stroke Scale, a three-item scale based on three signs: facial droop, arm drift, and slurring of speech51
- The Los Angeles Prehospital Stroke Screen, which uses screening questions and asymmetry in the face, hand grip strength, and arm drift.52
Knowing that the patient is having a minor stroke or TIA is important. Urgent treatment of these conditions decreases the risk of stroke in the next 90 days, which was 10.5% in one study.5 Urgent assessment and early intervention could reduce this risk of subsequent stroke down to 2%.6
ASSESSING RISK OF STROKE AFTER TIA
There is a practical need for prediction of stroke during the first few days after the event. The ABCD and ABCD2 scores were developed to stratify the short-term risk of stroke in patients with recent TIA.
The ABCD score
The ABCD score53 was derived to allow primary care physicians and other physicians to identify which patients with a suspected diagnosis of TIA should be referred for emergency assessment, to allow secondary-care physicians to determine which patients with probable or definite TIA need emergency investigation and treatment, to allow public education about the need for medical attention after a TIA, and to identify people at high risk.
The ABCD2 score
The ABCD2 score predicts the short-term risk of stroke following a TIA.54 Points are assigned as follows:
- Age > 60 years: 1 point
- Blood pressure (systolic) > 140 mm Hg or diastolic blood pressure > 90 mm Hg: 1 point
- Clinical factors: unilateral weakness with or without speech impairment: 2 points (1 point for speech impairment without weakness)
- Duration of symptoms > 60 minutes: 2 points (1 point for 10–59 minutes)
- Diabetes: 1 point.
Thus, the possible total ranges from 0 to 7 points. Higher scores indicate a greater risk of stroke at 2, 7, 30, and 90 days:
- Total score 0, 1, 2, or 3: 2-day stroke risk 1.0% (low risk)
- Total score 4 or 5: 2-day stroke risk 4.1% (moderate risk)
- Total score 6 or 7: 2-day stroke risk 8.1% (high risk).
WHO SHOULD BE HOSPITALIZED?
It has been suggested that the ABCD2 score can help in triaging patients to hospital admission or outpatient care, though no randomized trial has actually evaluated the utility of the ABCD2 score in this way.3
A study of consecutive TIA patients admitted over 12 months55 found that patients with an ABCD2 score of 3 or less had the same chance of requiring hospitalization (based on positive diffusion-weighted MRI studies, risk factor identification, and treatment initiation) as those with a score of 4 to 7. Hence, admitting TIA patients on the basis of the ABCD2 score alone requires further study. However, such decisions, though informed by clinical data, depend heavily on societal input (eg, from insurance companies, national health protocols) and may be outside the purview of clinical investigation.
The benefits of hospitalization include the ability to rapidly carry out tests such as cardiac monitoring for atrial fibrillation; to detect atherosclerosis, aortic arch atheroma, and paradoxical emboli; and to quickly start secondary prevention treatments and education about the importance of adhering to them. Early endarterectomy in the case of carotid stenosis can be offered. Additionally, if stroke symptoms recur, thrombolytic drug therapy can be started quickly.
Nguyen-Huynh et al56 analyzed the cost utility of 24-hour hospitalization for patients diagnosed with a recent TIA who were candidates for tissue plasminogen activator if a stroke occurred. They found hospitalization to be borderline cost-effective on the whole, with definite cost-effectiveness found in patients with higher stroke risk.
If patients come to medical attention several days after the TIA, then assessing risk with the ABCD2 score may no longer be reliable.57
INVESTIGATIONS
Parenchymal neuroimaging
Computed tomography (CT) without contrast is the most widely used neuroimaging test in the acute setting, since it is widely available, fast, and relatively low-cost. It will not show any abnormality in TIA or early ischemic stroke. However, it is helpful as a screening tool to rule out intracranial lesions such as hemorrhage or tumor. It may also show evidence of established infarction, which would indicate that the ischemia probably had been present for at least 6 to 12 hours.
MRI is clearly superior to noncontrast CT for detecting small areas of ischemia in patients with TIA, and it should be used unless the patient has a contraindication to it. Roughly one-third of TIA patients have lesions detectable on diffusion-weighted imaging, which helps to confirm that the episode was caused by cerebral ischemia, but nearly half of the diffusion MRI changes may be fully reversible.58 Evidence of prior stroke, leukoaraiosis, or white matter disease on fluid-attenuated inversion recovery and T2 sequences and microhemorrhages (on gradient echo sequences) help to determine a mechanistic diagnosis.
Subcategorizing TIA patients on the basis of the findings on diffusion-weighted MRI and the ABCD2 score is prognostically helpful.59 It can help to determine which patients need hospitalization and aggressive treatment, and in the case of identified diffusion-weighted MRI-positive stroke, it helps to localize and elucidate the mechanism of stroke. Hence, MRI is the preferred neuroimaging study for evaluating patients with TIA.3
Vascular imaging
Establishing the status of both intracranial and extracranial vessels is important for understanding the etiology, estimating the risk of future ischemic events, and formulating a treatment plan—eg, carotid endarterectomy in cases of significant stenosis (70% to 99%), which reduces the risk of ipsilateral stroke.60 Imaging studies include CT angiography, magnetic resonance angiography, extracranial and transcranial ultrasonography, and conventional catheter-based angiography.
CT angiography has higher spatial resolution, but vessels may be obscured by calcification associated with atherosclerotic plaque. It has the advantage of wide availability, low cost, short scanning time, and excellent patient tolerability.
Magnetic resonance angiography with gadolinium enhancement offers good quality imaging from the great vessels in the chest to the medium-sized vessels distal to the circle of Willis.
The contrast agents used in MRI and CT can have negative consequences in patients with renal disease. MRI contrast has been associated with nephrogenic fibrosing dermopathy, 61 and CT contrast can cause contrast-induced nephropathy.62
Carotid ultrasonography and transcranial Doppler ultrasonography are noninvasive and are not associated with significant adverse events. They can be used safely in patients with renal dysfunction, and they provide physiologic information that cannot be obtained with MRI and CT, which are static imaging techniques. Detecting microemboli on transcranial Doppler is an independent predictor of recurrent ischemic events.63,64
Catheter-based angiography is occasionally needed in confusing or more complicated cases, but it is invasive and occasionally is associated with iatrogenic stroke and other vascular complications.
Cardiac and aortic imaging
Echocardiography is used to detect lesions that can be sources of embolism such as regional wall-motion abnormalities, cardiac thrombus or mass, endocarditis, aortic arch atheroma, and patent foramen ovale. In patients with cryptogenic TIA or stroke, those with patent foramen ovale alone were found to have a lower risk of recurrent stroke than those who had both atrial septal aneurysm and patent foramen ovale.65
Transesophageal echocardiography is more sensitive than transthoracic echocardiography for detecting cardioembolic lesions, especially patent foramen ovale.66 In patients with cerebral ischemia and normal transthoracic findings, cardiac sources of embolism may be detected in about 40% of patients with transesophageal echocardiography.67
Cardiac rhythm monitoring
Electrocardiography and prolonged telemetry are recommended in patients with cryptogenic TIA to detect cardiac ischemia and paroxysmal atrial fibrillation. In one study, Holter monitoring detected atrial fibrillation in 6% of patients hospitalized with ischemic stroke or TIA.68 In another study, atrial fibrillation was detected after a median of 21 days of outpatient cardiac monitoring in 23% of patients.69
The optimal duration of outpatient telemetry has not yet been established, but studies have found significant increases in detection of paroxysms of atrial fibrillation with monitoring for 7 or longer.70
Laboratory tests in the acute setting
These include lipid profile, hemoglobin A1c, and cardiac enzymes. The advantages of hospitalization are early detection of these modifiable risk factors and early initiation of treatment.
Tests for rarer disorders
Tests for rarer disorders are sometimes indicated in unusual cases, such as ischemic symptoms occurring in young patients without other common risk factors. This includes testing for prothrombotic states, toxicology, blood cultures, inflammatory markers, hemoglobin electrophoresis, and lumbar puncture. The benefit of routine testing for thrombophilic disorders in cerebrovascular disease remains uncertain, with no clear association demonstrated with arterial stroke, but testing is more relevant in the case of venous (and paradoxical) thromboembolism.71
TREAT THE UNDERLYING DISORDER
Treatment depends on the mechanism that is thought to be responsible for the ischemic event. Vascular risk factors are important to identify and modify for all stroke subtypes.
Illustrating the importance of treating TIA and minor stroke, one study72 found that for antiplatelet therapy (aspirin, dipyridamole, or aspirin plus dipyridamole), the number needed to treat for 2 years was around 18.
Anticoagulation for cardioembolism
Atrial fibrillation, especially following a cerebrovascular ischemic event, should be treated with long-term anticoagulation with warfarin (Coumadin), dabigatran (Pradaxa), rivaroxaban (Xarelto), or apixaban (Eliquis).73 If the patient cannot tolerate anticoagulation, aspirin is recommended, and if he or she cannot tolerate aspirin, clopidogrel (Plavix) is recommended.
Antiplatelet therapy for large-vessel atherosclerosis and small-vessel disease
In the acute phase, aspirin 81 mg to 325 mg orally can be given. If the patient is allergic to aspirin, a loading dose of clopidogrel 300 mg and then 75 mg daily may be given.
A pilot study of loading with aspirin 325 mg or clopidogrel 375 mg in acute ischemic stroke and TIA patients showed that these treatments were safe when given within 36 hours and decreased the risk of neurologic deterioration.74 The patient should continue on aspirin 81 mg or clopidogrel 75 mg, as suggested by the Fast Assessment of Stroke and Transient Ischaemic Attack to Prevent Early Recurrence (FASTER) trial.75 In the long term, an antiplatelet drug such as aspirin or clopidogrel or the combination of aspirin and extended-release dipyridamole is reasonable.76
Cilostazol (Pletal) is not inferior and is possibly superior to aspirin in preventing noncardioembolic ischemic stroke. It is used off-label for secondary prevention of stroke of noncardioembolic origin.77
Statins
In the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial, high-dose atorvastatin (Lipitor)—80 mg daily—was found to reduce the risk of subsequent stroke and other cardiovascular events in patients with recent stroke irrespective of low-density lipoprotein cholesterol (LDL-C) level, but there was a small increase in the risk of hemorrhagic stroke.78
In patients with hyperlipidemia, current recommendations suggest a target LDL-C level lower than 100 mg/dL in patients with atherosclerotic stroke or TIA, and lower than 70 mg/dL in those with concomitant diabetes.79
Antihypertensive therapy
In the acute period, ie, the first 24 hours after symptoms, guidelines have advocated allowing high blood pressure to remain high (“permissive hypertension”) unless the systolic pressure is greater than 200 mm Hg or the diastolic pressure is greater than 120 mm Hg or the patient is receiving thrombolytic therapy.80 However, this has recently been challenged by findings in randomized trials.81 Permissive hypertension and avoidance of dehydration with intravenous normal saline may improve cerebral perfusion, which is especially important in patients with high-grade intracranial or extracranial stenosis. Within the parameters outlined above, we recommend against aggressively treating high blood pressure in the acute phase.
In the long term, antihypertensive therapy reduces the risk of recurrent stroke or TIA.82 The goal is to keep blood pressure lower than 140/90 mm Hg, or lower than 130/80 mm Hg in patients with diabetes. A study of patients with ischemic noncardioembolic stroke showed a higher risk of recurrent stroke if the systolic blood pressure was lower than 120 or higher than 140 mm Hg.83
Some classes of antihypertensive medication may be more beneficial than others. There is some evidence that angiotensin-converting enzyme (ACE) inhibitors alone or in combination with a diuretic or an angiotensin receptor blocker are superior to other regimens, possibly because of neuroprotective mechanisms.84 A recent meta-analysis found angiotensin receptor blockers to be more effective than either ACE inhibitors or beta-blockers in stroke prevention; however, calcium channel blockers were superior to renin-angiotensin system blockers (ACE inhibitors and angiotensin receptor blockers).85
Lifestyle modifications
Smoking cessation and cardiovascular exercise for more than 10 minutes more than 3 times per week is strongly recommended.
For patients with diabetes, the goal is to keep the fasting blood glucose level lower than 126 mg/dL.
Moderate alcohol intake has been shown to decrease stroke risk compared with excessive intake or none at all.86
Carotid endarterectomy
Carotid endarterectomy has been recommended within 2 weeks of cerebral or retinal TIA in those cases attributable to high-grade internal carotid artery stenosis in patients who have low surgical risk.87 This risk can be estimated on the basis of patient factors, surgeon factors, and hospital volume. The specific recommendations are as follows:
- 70% to 99% carotid stenosis: carotid endarterectomy recommended
- 50% to 69% carotid stenosis: carotid endarterectomy recommended in select patients with a perioperative complication rate < 6%
- < 50% carotid stenosis: carotid endarterectomy not routinely recommended.
Carotid artery angioplasty and stenting with distal embolic protection device
Data from the Carotid Revascularization Endarterectomy Versus Stenting Trial (CREST) and European stenting trials indicate that in patients over age 70, carotid endarterectomy appears to be superior to carotid artery stenting, whereas in younger patients the periprocedural risks of stroke and death are similar. Hence, carotid artery stenting performed by an interventionist with a low complication rate is a reasonable alternative to carotid endarterectomy.88,89
- Albers GW, Caplan LR, Easton JD, et al; TIA Working Group. Transient ischemic attack—proposal for a new definition. N Engl J Med 2002; 347:1713–1716.
- Ovbiagele B, Kidwell CS, Saver JL. Epidemiological impact in the United States of a tissue-based definition of transient ischemic attack. Stroke 2003; 34:919–924.
- Easton JD, Saver JL, Albers GW, et al; American Heart Association. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke 2009; 40:2276–2293.
- Marler JR, Tilley BC, Lu M, et al. Early stroke treatment associated with better outcome: the NINDS rt-PA stroke study. Neurology 2000; 55:1649–1655.
- Johnston SC, Gress DR, Browner WS, Sidney S. Short-term prognosis after emergency department diagnosis of TIA. JAMA 2000; 284:2901–2906.
- Rothwell PM, Giles MF, Chandratheva A, et al; Early use of Existing Preventive Strategies for Stroke (EXPRESS) study. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet 2007; 370:1432–1442.
- Roger VL, Go AS, Lloyd-Jones DM, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation 2012; 125:e2–e220.
- Johnston SC. Clinical practice. Transient ischemic attack. N Engl J Med 2002; 347:1687–1692.
- Johnston SC, Fayad PB, Gorelick PB, et al. Prevalence and knowledge of transient ischemic attack among US adults. Neurology 2003; 60:1429–1434.
- Eliasziw M, Kennedy J, Hill MD, Buchan AM, Barnett HJ; North American Symptomatic Carotid Endarterectomy Trial Group. Early risk of stroke after a transient ischemic attack in patients with internal carotid artery disease. CMAJ 2004; 170:1105–1109.
- Kleindorfer D, Panagos P, Pancioli A, et al. Incidence and short-term prognosis of transient ischemic attack in a population-based study. Stroke 2005; 36:720–723.
- Wu CM, McLaughlin K, Lorenzetti DL, Hill MD, Manns BJ, Ghali WA. Early risk of stroke after transient ischemic attack: a systematic review and meta-analysis. Arch Intern Med 2007; 167:2417–2422.
- Johnston SC, Leira EC, Hansen MD, Adams HP. Early recovery after cerebral ischemia risk of subsequent neurological deterioration. Ann Neurol 2003; 54:439–444.
- Bots ML, van der Wilk EC, Koudstaal PJ, Hofman A, Grobbee DE. Transient neurological attacks in the general population. Prevalence, risk factors, and clinical relevance. Stroke 1997; 28:768–773.
- White H, Boden-Albala B, Wang C, et al. Ischemic stroke subtype incidence among whites, blacks, and Hispanics: the Northern Manhattan Study. Circulation 2005; 111:1327–1331.
- Brown RD, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO. Stroke incidence, prevalence, and survival: secular trends in Rochester, Minnesota, through 1989. Stroke 1996; 27:373–380.
- Seshadri S, Beiser A, Kelly-Hayes M, et al. The lifetime risk of stroke: estimates from the Framingham Study. Stroke 2006; 37:345–350.
- Rosamond WD, Folsom AR, Chambless LE, et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerosis Risk in Communities (ARIC) cohort. Stroke 1999; 30:736–743.
- Lackland DT, Egan BM, Ferguson PL. Low birth weight as a risk factor for hypertension. J Clin Hypertens (Greenwich) 2003; 5:133–136.
- Flossmann E, Schulz UG, Rothwell PM. Systematic review of methods and results of studies of the genetic epidemiology of ischemic stroke. Stroke 2004; 35:212–227.
- Rodriguez BL, D’Agostino R, Abbott RD, et al. Risk of hospitalized stroke in men enrolled in the Honolulu Heart Program and the Framingham Study: a comparison of incidence and risk factor effects. Stroke 2002; 33:230–236.
- Manolio TA, Kronmal RA, Burke GL, O’Leary DH, Price TR. Short-term predictors of incident stroke in older adults. The Cardiovascular Health Study. Stroke 1996; 27:1479–1486.
- Wolf PA, D’Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: a risk profile from the Framingham Study. Stroke 1991; 22:312–318.
- Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289:2560–2572.
- Allen TW. Guide to clinical preventive services. Report of the US Preventive Services Task Force. J Am Osteopath Assoc 1991; 91:281–289.
- Goldstein LB, Bushnell CD, Adams RJ, et al; American Heart Association Stroke Council. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011; 42:517–584.
- Iso H, Jacobs DR, Wentworth D, Neaton JD, Cohen JD. Serum cholesterol levels and six-year mortality from stroke in 350,977 men screened for the multiple risk factor intervention trial. N Engl J Med 1989; 320:904–910.
- Zhang X, Patel A, Horibe H, et al; Asia Pacific Cohort Studies Collaboration. Cholesterol, coronary heart disease, and stroke in the Asia Pacific region. Int J Epidemiol 2003; 32:563–572.
- Sanossian N, Saver JL, Navab M, Ovbiagele B. High-density lipoprotein cholesterol: an emerging target for stroke treatment. Stroke 2007; 38:1104–1109.
- Kannel WB, Benjamin EJ. Status of the epidemiology of atrial fibrillation. Med Clin North Am 2008; 92:17–40.
- Inzitari D, Eliasziw M, Gates P, et al. The causes and risk of stroke in patients with asymptomatic internal-carotid-artery stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 2000; 342:1693–1700.
- Physical Activity Guidelines Advisory Committee report, 2008. To the Secretary of Health and Human Services. Part A: executive summary. Nutr Rev 2009; 67:114–120.
- Armstrong FD, Thompson RJ, Wang W, et al. Cognitive functioning and brain magnetic resonance imaging in children with sickle cell disease. Neuropsychology Committee of the Cooperative Study of Sickle Cell Disease. Pediatrics 1996; 97:864–870.
- Ohene-Frempong K, Weiner SJ, Sleeper LA, et al. Cerebrovascular accidents in sickle cell disease: rates and risk factors. Blood 1998; 91:288–294.
- Mosca L, Banka CL, Benjamin EJ, et al; Expert Panel/Writing Group; American Heart Association; American Academy of Family Physicians; American College of Obstetricians and Gynecologists; American College of Cardiology Foundation; Society of Thoracic Surgeons; American Medical Women's Association; Centers for Disease Control and Prevention; Office of Research on Women's Health; Association of Black Cardiologists; American College of Physicians; World Heart Federation; National Heart, Lung, and Blood Institute; American College of Nurse Practitioners. Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation 2007; 115:1481–1501.
- Lidegaard Ø, Løkkegaard E, Jensen A, Skovlund CW, Keiding N. Thrombotic stroke and myocardial infarction with hormonal contraception. N Engl J Med 2012; 366:2257–2266.
- Chan WS, Ray J, Wai EK, et al. Risk of stroke in women exposed to low-dose oral contraceptives: a critical evaluation of the evidence. Arch Intern Med 2004; 164:741–747.
- Bousser MG, Conard J, Kittner S, et al. Recommendations on the risk of ischaemic stroke associated with use of combined oral contraceptives and hormone replacement therapy in women with migraine. The International Headache Society Task Force on Combined Oral Contraceptives & Hormone Replacement Therapy. Cephalalgia 2000; 20:155–156.
- Mohr JP, Caplan LR, Melski JW, et al. The Harvard Cooperative Stroke Registry: a prospective registry. Neurology 1978; 28:754–762.
- Caplan LR. Brain embolism, revisited. Neurology 1993; 43:1281–1287.
- Caplan LR, Hennerici M. Impaired clearance of emboli (washout) is an important link between hypoperfusion, embolism, and ischemic stroke. Arch Neurol 1998; 55:1475–1482.
- Petty GW, Brown RD, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO. Ischemic stroke subtypes: a population-based study of incidence and risk factors. Stroke 1999; 30:2513–2516.
- Prabhakaran S, Silver AJ, Warrior L, McClenathan B, Lee VH. Misdiagnosis of transient ischemic attacks in the emergency room. Cerebrovasc Dis 2008; 26:630–635.
- Baquis GD, Pessin MS, Scott RM. Limb shaking—a carotid TIA. Stroke 1985; 16:444–448.
- Luengo-Fernandez R, Gray AM, Rothwell PM. Effect of urgent treatment for transient ischaemic attack and minor stroke on disability and hospital costs (EXPRESS study): a prospective population-based sequential comparison. Lancet Neurol 2009; 8:235–243.
- Ferro JM, Falcão I, Rodrigues G, et al. Diagnosis of transient ischemic attack by the nonneurologist. A validation study. Stroke 1996; 27:2225–2229.
- Norris JW, Hachinski VC. Misdiagnosis of stroke. Lancet 1982; 1:328–331.
- Ferro JM, Pinto AN, Falcão I, et al. Diagnosis of stroke by the nonneurologist. A validation study. Stroke 1998; 29:1106–1109.
- Kothari RU, Brott T, Broderick JP, Hamilton CA. Emergency physicians. Accuracy in the diagnosis of stroke. Stroke 1995; 26:2238–2241.
- Artto V, Putaala J, Strbian D, et al; Helsinki Stroke Thrombolysis Registry Group. Stroke mimics and intravenous thrombolysis. Ann Emerg Med 2012; 59:27–32.
- Kothari RU, Pancioli A, Liu T, Brott T, Broderick J. Cincinnati Prehospital Stroke Scale: reproducibility and validity. Ann Emerg Med 1999; 33:373–378.
- Kidwell CS, Starkman S, Eckstein M, Weems K, Saver JL. Identifying stroke in the field. Prospective validation of the Los Angeles prehospital stroke screen (LAPSS). Stroke 2000; 31:71–76.
- Rothwell PM, Giles MF, Flossmann E, et al. A simple score (ABCD) to identify individuals at high early risk of stroke after transient ischaemic attack. Lancet 2005; 366:29–36.
- Johnston SC, Rothwell PM, Nguyen-Huynh MN, et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet 2007; 369:283–292.
- Lou M, Safdar A, Edlow JA, et al. Can ABCD score predict the need for in-hospital intervention in patients with transient ischemic attacks? Int J Emerg Med 2010; 3:75–80.
- Nguyen-Huynh MN, Johnston SC. Is hospitalization after TIA cost-effective on the basis of treatment with tPA? Neurology 2005; 65:1799–1801.
- Calvet D, Lamy C, Touzé E, Oppenheim C, Meder JF, Mas JL. Management and outcome of patients with transient ischemic attack admitted to a stroke unit. Cerebrovasc Dis 2007; 24:80–85.
- Kidwell CS, Alger JR, Di Salle F, et al. Diffusion MRI in patients with transient ischemic attacks. Stroke 1999; 30:1174–1180.
- Giles MF, Albers GW, Amarenco P, et al. Early stroke risk and ABCD2 score performance in tissue- vs time-defined TIA: a multicenter study. Neurology 2011; 77:1222–1228.
- Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet 1998; 351:1379–1387.
- Thomsen HS. Nephrogenic systemic fibrosis: history and epidemiology. Radiol Clin North Am 2009; 47:827–831.
- Barrett BJ, Parfrey PS. Clinical practice. Preventing nephropathy induced by contrast medium. N Engl J Med 2006; 354:379–386.
- Valton L, Larrue V, le Traon AP, Massabuau P, Géraud G. Microembolic signals and risk of early recurrence in patients with stroke or transient ischemic attack. Stroke 1998; 29:2125–2128.
- Gao S, Wong KS, Hansberg T, Lam WW, Droste DW, Ringelstein EB. Microembolic signal predicts recurrent cerebral ischemic events in acute stroke patients with middle cerebral artery stenosis. Stroke 2004; 35:2832–2836.
- Mas JL, Zuber M. Recurrent cerebrovascular events in patients with patent foramen ovale, atrial septal aneurysm, or both and cryptogenic stroke or transient ischemic attack. French Study Group on Patent Foramen Ovale and Atrial Septal Aneurysm. Am Heart J 1995; 130:1083–1088.
- Di Tullio M, Sacco RL, Venketasubramanian N, Sherman D, Mohr JP, Homma S. Comparison of diagnostic techniques for the detection of a patent foramen ovale in stroke patients. Stroke 1993; 24:1020–1024.
- de Bruijn SF, Agema WR, Lammers GJ, et al. Transesophageal echocardiography is superior to transthoracic echocardiography in management of patients of any age with transient ischemic attack or stroke. Stroke 2006; 37:2531–2534.
- Lazzaro MA, Krishnan K, Prabhakaran S. Detection of atrial fibrillation with concurrent Holter monitoring and continuous cardiac telemetry following ischemic stroke and transient ischemic attack. J Stroke Cerebrovasc Dis 2012; 21:89–93.
- Tayal AH, Tian M, Kelly KM, et al. Atrial fibrillation detected by mobile cardiac outpatient telemetry in cryptogenic TIA or stroke. Neurology 2008; 71:1696–1701.
- Seet RC, Friedman PA, Rabinstein AA. Prolonged rhythm monitoring for the detection of occult paroxysmal atrial fibrillation in ischemic stroke of unknown cause. Circulation 2011; 124:477–486.
- Morris JG, Singh S, Fisher M. Testing for inherited thrombophilias in arterial stroke: can it cause more harm than good? Stroke 2010; 41:2985–2990.
- Diener HC, Cunha L, Forbes C, Sivenius J, Smets P, Lowenthal A. European Stroke Prevention Study. 2. Dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci 1996; 143:1–13.
- Connolly SJ, Ezekowitz MD, Yusuf S, et al; RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009; 361:1139–1151.
- Meyer DM, Albright KC, Allison TA, Grotta JC. LOAD: a pilot study of the safety of loading of aspirin and clopidogrel in acute ischemic stroke and transient ischemic attack. J Stroke Cerebrovasc Dis 2008; 17:26–29.
- Kennedy J, Hill MD, Ryckborst KJ, Eliasziw M, Demchuk AM, Buchan AM; FASTER Investigators. Fast Assessment of Stroke and Transient Ischaemic Attack to Prevent Early Recurrence (FASTER): a randomised controlled pilot trial. Lancet Neurol 2007; 6:961–969.
- Sacco RL, Diener HC, Yusuf S, et al; PRoFESS Study Group. Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke. N Engl J Med 2008; 359:1238–1251.
- Shinohara Y, Katayama Y, Uchiyama S, et al; CSPS 2 group. Cilostazol for prevention of secondary stroke (CSPS 2): an aspirin-controlled, double-blind, randomised non-inferiority trial. Lancet Neurol 2010; 9:959–968.
- Amarenco P, Bogousslavsky J, Callahan A, et al; Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Investigators. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med 2006; 355:549–559.
- Furie KL, Kasner SE, Adams RJ, et al; American Heart Association Stroke Council, Council on Cardiovascular Nursing, Council on Clinical Cardiology, and Interdisciplinary Council on Quality of Care and Outcomes Research. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011; 42:227–276.
- Koenig MA, Geocadin RG, de Grouchy M, et al. Safety of induced hypertension therapy in patients with acute ischemic stroke. Neurocrit Care 2006; 4:3–7.
- Elijovich F, Laffer CL. Acute stroke: lower blood pressure looks better and better. Hypertension 2010; 56:808–810.
- Lawes CM, Bennett DA, Feigin VL, Rodgers A. Blood pressure and stroke: an overview of published reviews. Stroke 2004; 35:1024.
- Ovbiagele B, Diener HC, Yusuf S, et al; PROFESS Investigators. Level of systolic blood pressure within the normal range and risk of recurrent stroke. JAMA 2011; 306:2137–2144.
- Chrysant SG. The pathophysiologic role of the brain renin-angiotensin system in stroke protection: clinical implications. J Clin Hypertens (Greenwich) 2007; 9:454–459.
- Verdecchia P, Gentile G, Angeli F, Reboldi G. Beyond blood pressure: evidence for cardiovascular, cerebrovascular, and renal protective effects of renin-angiotensin system blockers. Ther Adv Cardiovasc Dis 2012; 6:81–91.
- Elkind MS, Sciacca R, Boden-Albala B, Rundek T, Paik MC, Sacco RL. Moderate alcohol consumption reduces risk of ischemic stroke: the Northern Manhattan Study. Stroke 2006; 37:13–19.
- Rothwell PM, Eliasziw M, Gutnikov SA, Warlow CP, Barnett HJ; Carotid Endarterectomy Trialists Collaboration. Endarterectomy for symptomatic carotid stenosis in relation to clinical subgroups and timing of surgery. Lancet 2004; 363:915–924.
- Brott TG, Hobson RW, Howard G, et al; CREST Investigators. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med 2010; 363:11–23.
- Carotid Stenting Trialists’ Collaboration; Bonati LH, Dobson J, Algra A, et al. Short-term outcome after stenting versus endarterectomy for symptomatic carotid stenosis: a preplanned meta-analysis of individual patient data. Lancet 2010; 376:1062–1073.
A transient ischemic attack (TIA), like an episode of unstable angina, is an ominous portent of future morbidity and death even though, by definition, the event leaves no residual neurologic deficit.
But there is a positive side. When a patient presents with a TIA, the physician has the rare opportunity to reduce the risk of a disabling outcome—in this case, stroke. Therefore, patients deserve a rapid and thorough evaluation and appropriate stroke-preventive treatment.
MANY ‘TIAs’ ARE ACTUALLY STROKES
TIA has traditionally been described as a sudden focal neurologic deficit that lasts less than 24 hours, is presumed to be of vascular origin, and is confined to an area of the brain, spinal cord, or eye perfused by a specific artery. This symptom-based definition was based on the arbitrary and inaccurate assumption that brief symptoms would not be associated with damage to brain parenchyma.
The definition has since been updated and made more rational based on new concepts of brain ischemia informed by imaging, especially diffusion-weighted magnetic resonance imaging (MRI).1 One-third of episodes characterized as a TIA according to the classic definition would be considered an infarction on the basis of diffusion-weighted MRI.2 The new tissue-based definition characterizes TIA as a brief episode of neurologic dysfunction caused by focal ischemia of the brain, spinal cord, or retina, with clinical symptoms lasting less than 24 hours and without evidence of acute infarction.3
AN OPPORTUNITY TO INTERVENE
Most TIAs resolve in less than 30 minutes. The US National Institute of Neurological Disorders and Stroke trial of tissue plasminogen activator found that if symptoms of cerebral ischemia had not resolved by 1 hour or had not rapidly improved within 3 hours, complete resolution was rare (only 2% at 24 hours).4 Hence, physicians evaluating and treating patients with TIAs should treat these episodes with the urgency they deserve.
Moreover, half of the strokes that follow TIAs occur within 48 hours.5 A rapid and thorough evaluation and the initiation of secondary preventive treatments have been shown to reduce the early occurrence of stroke by up to 80%.6 Hence, the correct diagnosis of TIA gives the clinician the best opportunity to prevent stroke and its personal, social, and sometimes fatal consequences.
STROKES OUTNUMBER TIAs, BUT TIAs ARE UNDERREPORTED
According to 2012 statistics, nearly 795,000 strokes occur in the United States each year, 610,000 of which are first attacks and 185,000 are recurrences. Every 40 seconds, someone in the United States has a stroke.7
In comparison, the incidence of TIA in the United States is estimated at 200,000 to 500,000 per year, though the true number is difficult to know because of underreporting.8,9 About half of patients who experience a TIA fail to report it to their health care provider—a lost opportunity for intervention and stroke prevention.10,11
A meta-analysis showed that the risk of stroke after TIA was 9.9% at 2 days, 13.4% at 30 days, and 17.3% at 90 days.12
Interestingly, the risk of stroke after TIA exceeds the risk of recurrent stroke after a first stroke. This was shown in a study that found that patients who had made a substantial recovery within 24 hours (ie, patients with a TIA) were more likely to suffer neurologic deterioration in the next 3 months than were those who did not have significant early improvement.13
RISK FACTORS FOR TIA ARE THE SAME AS FOR STROKE
The risk of cerebrovascular disease increases with age and is higher in men14 and in blacks and Hispanics.15
The risk factors and clinical presentation do not differ between TIA and stroke, so the evaluation and treatment should not differ either. These two events represent a continuum of the same disease entity.
Some risk factors for TIA are modifiable, others are not.
Nonmodifiable risk factors
Nonmodifiable risk factors for TIA include older age, male sex, African American race, low birth weight, Hispanic ethnicity, and family history. If the patient has nonmodifiable risk factors, we should try all the harder to correct the modifiable ones.
Older age. The risk of ischemic stroke and intracranial hemorrhage doubles with each decade after age 55 in both sexes.16
Sex. Men have a significantly higher incidence of TIA than women,11 whereas the opposite is true for stroke: women have a higher lifetime risk of stroke than men.17
African Americans have an incidence of stroke (all types) 38% higher than that of whites,18 and an incidence of TIA (inpatient and out-of-hospital) 40% higher than the overall age- and sex-adjusted rate in the white population.11
Low birth weight. The odds of stroke are more than twice as high in people who weighed less than 2,500 g at birth compared with those who weighed 4,000 g or more, probably because of a correlation between low birth weight and hypertension.19
A family history of stroke increases the risk of stroke by nearly 30%, the association being stronger with large-vessel and smallvessel stroke than with cardioembolic stroke.20
Modifiable risk factors
Modifiable risk factors include cigarette smoking, hypertension, diabetes, lipid abnormalities, atrial fibrillation, carotid stenosis, and dietary and hormonal factors. Detecting these factors, which often coexist, is the first step in trying to modify them and reduce the patient’s risk.
Cigarette smoking approximately doubles the risk of ischemic stroke.21–23
Hypertension has a relationship with stroke risk that is strong, continuous, graded, consistent, and significant.24
Diabetes increases stroke risk nearly six times.25
Lipid abnormalities. Most studies have found an association between lipid levels (total cholesterol and low-density lipoprotein cholesterol) and the risk of death from ischemic stroke,26–28 and an inverse relationship between high-density lipoprotein cholesterol levels and stroke risk.29
Atrial fibrillation increases the risk of ischemic stroke up to fivefold, even in the absence of cardiac valvular disease. The mechanism is embolism of stasis-induced thrombi that form in the left atrial appendage.30
Carotid stenosis. Asymptomatic carotid atherosclerotic stenotic lesions in the extracranial internal carotid artery or carotid bulb are associated with a higher risk of stroke.24,31
Lifestyle factors. Diets that lower blood pressure have been found to decrease stroke risk.24 Exercise in men and women reduces the risk of stroke or death by 25% to 30% compared with inactive people.32 Weight reduction has been found to lower blood pressure and reduce stroke risk.24
Other potentially modifiable risk factors include migraine with aura, metabolic syndrome, excess alcohol consumption (and, paradoxically, complete abstinence from alcohol), drug abuse, sleep-disordered breathing, hyperhomocysteinemia, high lipoprotein (a) levels, hypercoagulability, infection with organisms such as Chlamydia pneumoniae, cytomegalovirus, and Helicobacter pylori, and acute infections such as respiratory and urinary infections.26
Conditions in certain demographic groups
Patients in certain demographic groups present with rarer conditions associated with stroke and TIA.
Sickle cell disease. Eleven percent of patients with sickle cell disease have clinical strokes, and a substantial number have “silent” infarcts identified on neuroimaging.33,34
Postmenopausal hormone replacement therapy with any product containing conjugated equine estrogen carries a risk of cerebrovascular events,35 and the higher the dose, the higher the risk.36 Also, oral contraceptives may be harmful in women who have additional risk factors such as cigarette smoking, prior thromboembolic events, or migraine with aura.37,38
THREE CAUSES OF STROKE AND TIA
Stroke and TIA should not be considered diagnoses in themselves, but rather the end point of many other diseases. The diagnosis lies in identifying the mechanism of the cerebrovascular event. The three main mechanisms are thrombosis, embolism, and decreased perfusion.
Thrombosis is caused by obstruction of blood flow within one or more blood vessels, the most common cause being atherosclerosis. Large-artery atherosclerosis, such as in the carotid bifurcation or extracranial internal carotid, causes TIAs that occur over a period of weeks or months with a variety of presentations in that vascular territory, from years of gradual accumulation of atherosclerotic plaque.39
In patients with small-artery or penetrating artery disease, hypertension is the primary risk factor and the pathology, specific to small arterioles, is lipohyalinosis rather than atherosclerosis. These patients may present with a stuttering clinical course, and episodes are more stereotypical.
Less common obstructive vascular pathologies include fibromuscular dysplasia, arteritides, and dissection.
Embolism can occur from a proximal source such as the heart or from proximal vessels such as the aorta, carotid, or vertebral arteries. The embolic particle may form on heart valves or lesions within the heart (eg, clot, tumor), or in the venous circulation and paradoxically cross over to the arterial side through an intracardiac or transpulmonary shunt. Embolism may also be due to a hypercoagulable state.40 Embolic stroke is suspected when multiple vascular territories within the brain are clinically or radiographically affected.
Decreased systemic perfusion caused by severe heart failure or systemic hypotension can cause ischemia to the brain diffusely and bilaterally, limiting the ability of the blood-stream to wash out microemboli, especially in the border zones (also known as “watershed areas”), thus leading to ischemia or infarction.41 Decreased perfusion can also be local, due to a fixed vessel stenosis.
Using another classification system, a study in Rochester, MN, found the following incident rates of stroke subtypes, adjusted for age and sex, per 100,000 population42:
- Large-vessel cervical or intracranial atherosclerosis with more than 50% stenosis—27
- Cardioembolism—40
- Lacunar, small-vessel disease—25
- Uncertain cause—52
- Other identifiable cause—4.
THREE CLINICAL FEATURES SUGGEST TIA
TIAs can be hard to distinguish from nonischemic neurologic events in the acute setting such as an emergency room. Up to 60% of patients suspected of having a TIA actually have a nonischemic cause of their symptoms.43
Three clinical features suggest a TIA during the emergency room evaluation:
- Rapid onset of symptoms—“like lightning” or “in seconds,” in contrast to migraine and seizures, which develop over minutes
- No history of similar episodes in the past
- Absence of nonspecific symptoms—eg, stomach upset or tightness in the chest.
CLINICAL DIAGNOSIS
Because most TIA symptoms and signs have already resolved by the time of evaluation, the diagnosis depends on a careful history with special attention to the pace of onset and resolution, the duration and nature of the symptoms, circumstances at the time of symptom onset, previous similar episodes, associated features, vascular risk factors, and family history (Table 1).44,45
A detailed neurologic examination is imperative and should include fundoscopy. A cardiovascular assessment should include cardiac rhythm, bruits in the neck, orbits, and groin, peripheral pulses, and electrocardiography.
Do neurologists do a better job at diagnosing TIA and stroke?
Primary care physicians, internists, and emergency department physicians are often the ones to carry out the clinical assessment of possible TIA.
Determining if transient neurologic symptoms are caused by ischemia can be a challenge. When in doubt, referral to a neurologist with subspecialty training in cerebrovascular disease should be considered.
But do neurologists really do a better job? A recent study sought to compare the accuracy of diagnosis of TIA made by general practitioners, emergency physicians, and neurologists. The nonneurologists considered “confusion” and “unexplained fall” suggestive of TIA and “lower facial palsy” and “monocular blindness” less suggestive of TIA—whereas the opposite is true. This shows that nonneurologists often label minor strokes and several nonvascular transient neurologic disturbances as TIAs, and up to half of patients could be mislabeled as a result.46
Differences in diagnosing cerebrovascular events between emergency room physicians and attending neurologists have been tested,47 with an accuracy of diagnosis as low as 38% by emergency department physicians in one study.48 However, other studies did not show such a trend.49,50
A study at a university-based teaching hospital found the sensitivity of emergency room physician diagnosis to be 98.6% with a positive predictive value of 94.8%,49 showing that at a large teaching hospital with a comprehensive stroke intervention program, emergency physicians could identify patients with stroke, particularly hemorrhagic stroke, very accurately.
Improving the diagnosis of stroke and TIA
Routine use of imaging and involvement of a neurologist increase the sensitivity and accuracy of diagnosis. Education and written guidelines for acute stroke treatment both in the emergency department and in out-of-hospital settings seem to dramatically improve the rates of diagnostic accuracy and appropriate treatment.50
Emergency medical service personnel use two screening tools in the field to identify TIA and stroke symptoms:
- The Cincinnati Prehospital Stroke Scale, a three-item scale based on three signs: facial droop, arm drift, and slurring of speech51
- The Los Angeles Prehospital Stroke Screen, which uses screening questions and asymmetry in the face, hand grip strength, and arm drift.52
Knowing that the patient is having a minor stroke or TIA is important. Urgent treatment of these conditions decreases the risk of stroke in the next 90 days, which was 10.5% in one study.5 Urgent assessment and early intervention could reduce this risk of subsequent stroke down to 2%.6
ASSESSING RISK OF STROKE AFTER TIA
There is a practical need for prediction of stroke during the first few days after the event. The ABCD and ABCD2 scores were developed to stratify the short-term risk of stroke in patients with recent TIA.
The ABCD score
The ABCD score53 was derived to allow primary care physicians and other physicians to identify which patients with a suspected diagnosis of TIA should be referred for emergency assessment, to allow secondary-care physicians to determine which patients with probable or definite TIA need emergency investigation and treatment, to allow public education about the need for medical attention after a TIA, and to identify people at high risk.
The ABCD2 score
The ABCD2 score predicts the short-term risk of stroke following a TIA.54 Points are assigned as follows:
- Age > 60 years: 1 point
- Blood pressure (systolic) > 140 mm Hg or diastolic blood pressure > 90 mm Hg: 1 point
- Clinical factors: unilateral weakness with or without speech impairment: 2 points (1 point for speech impairment without weakness)
- Duration of symptoms > 60 minutes: 2 points (1 point for 10–59 minutes)
- Diabetes: 1 point.
Thus, the possible total ranges from 0 to 7 points. Higher scores indicate a greater risk of stroke at 2, 7, 30, and 90 days:
- Total score 0, 1, 2, or 3: 2-day stroke risk 1.0% (low risk)
- Total score 4 or 5: 2-day stroke risk 4.1% (moderate risk)
- Total score 6 or 7: 2-day stroke risk 8.1% (high risk).
WHO SHOULD BE HOSPITALIZED?
It has been suggested that the ABCD2 score can help in triaging patients to hospital admission or outpatient care, though no randomized trial has actually evaluated the utility of the ABCD2 score in this way.3
A study of consecutive TIA patients admitted over 12 months55 found that patients with an ABCD2 score of 3 or less had the same chance of requiring hospitalization (based on positive diffusion-weighted MRI studies, risk factor identification, and treatment initiation) as those with a score of 4 to 7. Hence, admitting TIA patients on the basis of the ABCD2 score alone requires further study. However, such decisions, though informed by clinical data, depend heavily on societal input (eg, from insurance companies, national health protocols) and may be outside the purview of clinical investigation.
The benefits of hospitalization include the ability to rapidly carry out tests such as cardiac monitoring for atrial fibrillation; to detect atherosclerosis, aortic arch atheroma, and paradoxical emboli; and to quickly start secondary prevention treatments and education about the importance of adhering to them. Early endarterectomy in the case of carotid stenosis can be offered. Additionally, if stroke symptoms recur, thrombolytic drug therapy can be started quickly.
Nguyen-Huynh et al56 analyzed the cost utility of 24-hour hospitalization for patients diagnosed with a recent TIA who were candidates for tissue plasminogen activator if a stroke occurred. They found hospitalization to be borderline cost-effective on the whole, with definite cost-effectiveness found in patients with higher stroke risk.
If patients come to medical attention several days after the TIA, then assessing risk with the ABCD2 score may no longer be reliable.57
INVESTIGATIONS
Parenchymal neuroimaging
Computed tomography (CT) without contrast is the most widely used neuroimaging test in the acute setting, since it is widely available, fast, and relatively low-cost. It will not show any abnormality in TIA or early ischemic stroke. However, it is helpful as a screening tool to rule out intracranial lesions such as hemorrhage or tumor. It may also show evidence of established infarction, which would indicate that the ischemia probably had been present for at least 6 to 12 hours.
MRI is clearly superior to noncontrast CT for detecting small areas of ischemia in patients with TIA, and it should be used unless the patient has a contraindication to it. Roughly one-third of TIA patients have lesions detectable on diffusion-weighted imaging, which helps to confirm that the episode was caused by cerebral ischemia, but nearly half of the diffusion MRI changes may be fully reversible.58 Evidence of prior stroke, leukoaraiosis, or white matter disease on fluid-attenuated inversion recovery and T2 sequences and microhemorrhages (on gradient echo sequences) help to determine a mechanistic diagnosis.
Subcategorizing TIA patients on the basis of the findings on diffusion-weighted MRI and the ABCD2 score is prognostically helpful.59 It can help to determine which patients need hospitalization and aggressive treatment, and in the case of identified diffusion-weighted MRI-positive stroke, it helps to localize and elucidate the mechanism of stroke. Hence, MRI is the preferred neuroimaging study for evaluating patients with TIA.3
Vascular imaging
Establishing the status of both intracranial and extracranial vessels is important for understanding the etiology, estimating the risk of future ischemic events, and formulating a treatment plan—eg, carotid endarterectomy in cases of significant stenosis (70% to 99%), which reduces the risk of ipsilateral stroke.60 Imaging studies include CT angiography, magnetic resonance angiography, extracranial and transcranial ultrasonography, and conventional catheter-based angiography.
CT angiography has higher spatial resolution, but vessels may be obscured by calcification associated with atherosclerotic plaque. It has the advantage of wide availability, low cost, short scanning time, and excellent patient tolerability.
Magnetic resonance angiography with gadolinium enhancement offers good quality imaging from the great vessels in the chest to the medium-sized vessels distal to the circle of Willis.
The contrast agents used in MRI and CT can have negative consequences in patients with renal disease. MRI contrast has been associated with nephrogenic fibrosing dermopathy, 61 and CT contrast can cause contrast-induced nephropathy.62
Carotid ultrasonography and transcranial Doppler ultrasonography are noninvasive and are not associated with significant adverse events. They can be used safely in patients with renal dysfunction, and they provide physiologic information that cannot be obtained with MRI and CT, which are static imaging techniques. Detecting microemboli on transcranial Doppler is an independent predictor of recurrent ischemic events.63,64
Catheter-based angiography is occasionally needed in confusing or more complicated cases, but it is invasive and occasionally is associated with iatrogenic stroke and other vascular complications.
Cardiac and aortic imaging
Echocardiography is used to detect lesions that can be sources of embolism such as regional wall-motion abnormalities, cardiac thrombus or mass, endocarditis, aortic arch atheroma, and patent foramen ovale. In patients with cryptogenic TIA or stroke, those with patent foramen ovale alone were found to have a lower risk of recurrent stroke than those who had both atrial septal aneurysm and patent foramen ovale.65
Transesophageal echocardiography is more sensitive than transthoracic echocardiography for detecting cardioembolic lesions, especially patent foramen ovale.66 In patients with cerebral ischemia and normal transthoracic findings, cardiac sources of embolism may be detected in about 40% of patients with transesophageal echocardiography.67
Cardiac rhythm monitoring
Electrocardiography and prolonged telemetry are recommended in patients with cryptogenic TIA to detect cardiac ischemia and paroxysmal atrial fibrillation. In one study, Holter monitoring detected atrial fibrillation in 6% of patients hospitalized with ischemic stroke or TIA.68 In another study, atrial fibrillation was detected after a median of 21 days of outpatient cardiac monitoring in 23% of patients.69
The optimal duration of outpatient telemetry has not yet been established, but studies have found significant increases in detection of paroxysms of atrial fibrillation with monitoring for 7 or longer.70
Laboratory tests in the acute setting
These include lipid profile, hemoglobin A1c, and cardiac enzymes. The advantages of hospitalization are early detection of these modifiable risk factors and early initiation of treatment.
Tests for rarer disorders
Tests for rarer disorders are sometimes indicated in unusual cases, such as ischemic symptoms occurring in young patients without other common risk factors. This includes testing for prothrombotic states, toxicology, blood cultures, inflammatory markers, hemoglobin electrophoresis, and lumbar puncture. The benefit of routine testing for thrombophilic disorders in cerebrovascular disease remains uncertain, with no clear association demonstrated with arterial stroke, but testing is more relevant in the case of venous (and paradoxical) thromboembolism.71
TREAT THE UNDERLYING DISORDER
Treatment depends on the mechanism that is thought to be responsible for the ischemic event. Vascular risk factors are important to identify and modify for all stroke subtypes.
Illustrating the importance of treating TIA and minor stroke, one study72 found that for antiplatelet therapy (aspirin, dipyridamole, or aspirin plus dipyridamole), the number needed to treat for 2 years was around 18.
Anticoagulation for cardioembolism
Atrial fibrillation, especially following a cerebrovascular ischemic event, should be treated with long-term anticoagulation with warfarin (Coumadin), dabigatran (Pradaxa), rivaroxaban (Xarelto), or apixaban (Eliquis).73 If the patient cannot tolerate anticoagulation, aspirin is recommended, and if he or she cannot tolerate aspirin, clopidogrel (Plavix) is recommended.
Antiplatelet therapy for large-vessel atherosclerosis and small-vessel disease
In the acute phase, aspirin 81 mg to 325 mg orally can be given. If the patient is allergic to aspirin, a loading dose of clopidogrel 300 mg and then 75 mg daily may be given.
A pilot study of loading with aspirin 325 mg or clopidogrel 375 mg in acute ischemic stroke and TIA patients showed that these treatments were safe when given within 36 hours and decreased the risk of neurologic deterioration.74 The patient should continue on aspirin 81 mg or clopidogrel 75 mg, as suggested by the Fast Assessment of Stroke and Transient Ischaemic Attack to Prevent Early Recurrence (FASTER) trial.75 In the long term, an antiplatelet drug such as aspirin or clopidogrel or the combination of aspirin and extended-release dipyridamole is reasonable.76
Cilostazol (Pletal) is not inferior and is possibly superior to aspirin in preventing noncardioembolic ischemic stroke. It is used off-label for secondary prevention of stroke of noncardioembolic origin.77
Statins
In the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial, high-dose atorvastatin (Lipitor)—80 mg daily—was found to reduce the risk of subsequent stroke and other cardiovascular events in patients with recent stroke irrespective of low-density lipoprotein cholesterol (LDL-C) level, but there was a small increase in the risk of hemorrhagic stroke.78
In patients with hyperlipidemia, current recommendations suggest a target LDL-C level lower than 100 mg/dL in patients with atherosclerotic stroke or TIA, and lower than 70 mg/dL in those with concomitant diabetes.79
Antihypertensive therapy
In the acute period, ie, the first 24 hours after symptoms, guidelines have advocated allowing high blood pressure to remain high (“permissive hypertension”) unless the systolic pressure is greater than 200 mm Hg or the diastolic pressure is greater than 120 mm Hg or the patient is receiving thrombolytic therapy.80 However, this has recently been challenged by findings in randomized trials.81 Permissive hypertension and avoidance of dehydration with intravenous normal saline may improve cerebral perfusion, which is especially important in patients with high-grade intracranial or extracranial stenosis. Within the parameters outlined above, we recommend against aggressively treating high blood pressure in the acute phase.
In the long term, antihypertensive therapy reduces the risk of recurrent stroke or TIA.82 The goal is to keep blood pressure lower than 140/90 mm Hg, or lower than 130/80 mm Hg in patients with diabetes. A study of patients with ischemic noncardioembolic stroke showed a higher risk of recurrent stroke if the systolic blood pressure was lower than 120 or higher than 140 mm Hg.83
Some classes of antihypertensive medication may be more beneficial than others. There is some evidence that angiotensin-converting enzyme (ACE) inhibitors alone or in combination with a diuretic or an angiotensin receptor blocker are superior to other regimens, possibly because of neuroprotective mechanisms.84 A recent meta-analysis found angiotensin receptor blockers to be more effective than either ACE inhibitors or beta-blockers in stroke prevention; however, calcium channel blockers were superior to renin-angiotensin system blockers (ACE inhibitors and angiotensin receptor blockers).85
Lifestyle modifications
Smoking cessation and cardiovascular exercise for more than 10 minutes more than 3 times per week is strongly recommended.
For patients with diabetes, the goal is to keep the fasting blood glucose level lower than 126 mg/dL.
Moderate alcohol intake has been shown to decrease stroke risk compared with excessive intake or none at all.86
Carotid endarterectomy
Carotid endarterectomy has been recommended within 2 weeks of cerebral or retinal TIA in those cases attributable to high-grade internal carotid artery stenosis in patients who have low surgical risk.87 This risk can be estimated on the basis of patient factors, surgeon factors, and hospital volume. The specific recommendations are as follows:
- 70% to 99% carotid stenosis: carotid endarterectomy recommended
- 50% to 69% carotid stenosis: carotid endarterectomy recommended in select patients with a perioperative complication rate < 6%
- < 50% carotid stenosis: carotid endarterectomy not routinely recommended.
Carotid artery angioplasty and stenting with distal embolic protection device
Data from the Carotid Revascularization Endarterectomy Versus Stenting Trial (CREST) and European stenting trials indicate that in patients over age 70, carotid endarterectomy appears to be superior to carotid artery stenting, whereas in younger patients the periprocedural risks of stroke and death are similar. Hence, carotid artery stenting performed by an interventionist with a low complication rate is a reasonable alternative to carotid endarterectomy.88,89
A transient ischemic attack (TIA), like an episode of unstable angina, is an ominous portent of future morbidity and death even though, by definition, the event leaves no residual neurologic deficit.
But there is a positive side. When a patient presents with a TIA, the physician has the rare opportunity to reduce the risk of a disabling outcome—in this case, stroke. Therefore, patients deserve a rapid and thorough evaluation and appropriate stroke-preventive treatment.
MANY ‘TIAs’ ARE ACTUALLY STROKES
TIA has traditionally been described as a sudden focal neurologic deficit that lasts less than 24 hours, is presumed to be of vascular origin, and is confined to an area of the brain, spinal cord, or eye perfused by a specific artery. This symptom-based definition was based on the arbitrary and inaccurate assumption that brief symptoms would not be associated with damage to brain parenchyma.
The definition has since been updated and made more rational based on new concepts of brain ischemia informed by imaging, especially diffusion-weighted magnetic resonance imaging (MRI).1 One-third of episodes characterized as a TIA according to the classic definition would be considered an infarction on the basis of diffusion-weighted MRI.2 The new tissue-based definition characterizes TIA as a brief episode of neurologic dysfunction caused by focal ischemia of the brain, spinal cord, or retina, with clinical symptoms lasting less than 24 hours and without evidence of acute infarction.3
AN OPPORTUNITY TO INTERVENE
Most TIAs resolve in less than 30 minutes. The US National Institute of Neurological Disorders and Stroke trial of tissue plasminogen activator found that if symptoms of cerebral ischemia had not resolved by 1 hour or had not rapidly improved within 3 hours, complete resolution was rare (only 2% at 24 hours).4 Hence, physicians evaluating and treating patients with TIAs should treat these episodes with the urgency they deserve.
Moreover, half of the strokes that follow TIAs occur within 48 hours.5 A rapid and thorough evaluation and the initiation of secondary preventive treatments have been shown to reduce the early occurrence of stroke by up to 80%.6 Hence, the correct diagnosis of TIA gives the clinician the best opportunity to prevent stroke and its personal, social, and sometimes fatal consequences.
STROKES OUTNUMBER TIAs, BUT TIAs ARE UNDERREPORTED
According to 2012 statistics, nearly 795,000 strokes occur in the United States each year, 610,000 of which are first attacks and 185,000 are recurrences. Every 40 seconds, someone in the United States has a stroke.7
In comparison, the incidence of TIA in the United States is estimated at 200,000 to 500,000 per year, though the true number is difficult to know because of underreporting.8,9 About half of patients who experience a TIA fail to report it to their health care provider—a lost opportunity for intervention and stroke prevention.10,11
A meta-analysis showed that the risk of stroke after TIA was 9.9% at 2 days, 13.4% at 30 days, and 17.3% at 90 days.12
Interestingly, the risk of stroke after TIA exceeds the risk of recurrent stroke after a first stroke. This was shown in a study that found that patients who had made a substantial recovery within 24 hours (ie, patients with a TIA) were more likely to suffer neurologic deterioration in the next 3 months than were those who did not have significant early improvement.13
RISK FACTORS FOR TIA ARE THE SAME AS FOR STROKE
The risk of cerebrovascular disease increases with age and is higher in men14 and in blacks and Hispanics.15
The risk factors and clinical presentation do not differ between TIA and stroke, so the evaluation and treatment should not differ either. These two events represent a continuum of the same disease entity.
Some risk factors for TIA are modifiable, others are not.
Nonmodifiable risk factors
Nonmodifiable risk factors for TIA include older age, male sex, African American race, low birth weight, Hispanic ethnicity, and family history. If the patient has nonmodifiable risk factors, we should try all the harder to correct the modifiable ones.
Older age. The risk of ischemic stroke and intracranial hemorrhage doubles with each decade after age 55 in both sexes.16
Sex. Men have a significantly higher incidence of TIA than women,11 whereas the opposite is true for stroke: women have a higher lifetime risk of stroke than men.17
African Americans have an incidence of stroke (all types) 38% higher than that of whites,18 and an incidence of TIA (inpatient and out-of-hospital) 40% higher than the overall age- and sex-adjusted rate in the white population.11
Low birth weight. The odds of stroke are more than twice as high in people who weighed less than 2,500 g at birth compared with those who weighed 4,000 g or more, probably because of a correlation between low birth weight and hypertension.19
A family history of stroke increases the risk of stroke by nearly 30%, the association being stronger with large-vessel and smallvessel stroke than with cardioembolic stroke.20
Modifiable risk factors
Modifiable risk factors include cigarette smoking, hypertension, diabetes, lipid abnormalities, atrial fibrillation, carotid stenosis, and dietary and hormonal factors. Detecting these factors, which often coexist, is the first step in trying to modify them and reduce the patient’s risk.
Cigarette smoking approximately doubles the risk of ischemic stroke.21–23
Hypertension has a relationship with stroke risk that is strong, continuous, graded, consistent, and significant.24
Diabetes increases stroke risk nearly six times.25
Lipid abnormalities. Most studies have found an association between lipid levels (total cholesterol and low-density lipoprotein cholesterol) and the risk of death from ischemic stroke,26–28 and an inverse relationship between high-density lipoprotein cholesterol levels and stroke risk.29
Atrial fibrillation increases the risk of ischemic stroke up to fivefold, even in the absence of cardiac valvular disease. The mechanism is embolism of stasis-induced thrombi that form in the left atrial appendage.30
Carotid stenosis. Asymptomatic carotid atherosclerotic stenotic lesions in the extracranial internal carotid artery or carotid bulb are associated with a higher risk of stroke.24,31
Lifestyle factors. Diets that lower blood pressure have been found to decrease stroke risk.24 Exercise in men and women reduces the risk of stroke or death by 25% to 30% compared with inactive people.32 Weight reduction has been found to lower blood pressure and reduce stroke risk.24
Other potentially modifiable risk factors include migraine with aura, metabolic syndrome, excess alcohol consumption (and, paradoxically, complete abstinence from alcohol), drug abuse, sleep-disordered breathing, hyperhomocysteinemia, high lipoprotein (a) levels, hypercoagulability, infection with organisms such as Chlamydia pneumoniae, cytomegalovirus, and Helicobacter pylori, and acute infections such as respiratory and urinary infections.26
Conditions in certain demographic groups
Patients in certain demographic groups present with rarer conditions associated with stroke and TIA.
Sickle cell disease. Eleven percent of patients with sickle cell disease have clinical strokes, and a substantial number have “silent” infarcts identified on neuroimaging.33,34
Postmenopausal hormone replacement therapy with any product containing conjugated equine estrogen carries a risk of cerebrovascular events,35 and the higher the dose, the higher the risk.36 Also, oral contraceptives may be harmful in women who have additional risk factors such as cigarette smoking, prior thromboembolic events, or migraine with aura.37,38
THREE CAUSES OF STROKE AND TIA
Stroke and TIA should not be considered diagnoses in themselves, but rather the end point of many other diseases. The diagnosis lies in identifying the mechanism of the cerebrovascular event. The three main mechanisms are thrombosis, embolism, and decreased perfusion.
Thrombosis is caused by obstruction of blood flow within one or more blood vessels, the most common cause being atherosclerosis. Large-artery atherosclerosis, such as in the carotid bifurcation or extracranial internal carotid, causes TIAs that occur over a period of weeks or months with a variety of presentations in that vascular territory, from years of gradual accumulation of atherosclerotic plaque.39
In patients with small-artery or penetrating artery disease, hypertension is the primary risk factor and the pathology, specific to small arterioles, is lipohyalinosis rather than atherosclerosis. These patients may present with a stuttering clinical course, and episodes are more stereotypical.
Less common obstructive vascular pathologies include fibromuscular dysplasia, arteritides, and dissection.
Embolism can occur from a proximal source such as the heart or from proximal vessels such as the aorta, carotid, or vertebral arteries. The embolic particle may form on heart valves or lesions within the heart (eg, clot, tumor), or in the venous circulation and paradoxically cross over to the arterial side through an intracardiac or transpulmonary shunt. Embolism may also be due to a hypercoagulable state.40 Embolic stroke is suspected when multiple vascular territories within the brain are clinically or radiographically affected.
Decreased systemic perfusion caused by severe heart failure or systemic hypotension can cause ischemia to the brain diffusely and bilaterally, limiting the ability of the blood-stream to wash out microemboli, especially in the border zones (also known as “watershed areas”), thus leading to ischemia or infarction.41 Decreased perfusion can also be local, due to a fixed vessel stenosis.
Using another classification system, a study in Rochester, MN, found the following incident rates of stroke subtypes, adjusted for age and sex, per 100,000 population42:
- Large-vessel cervical or intracranial atherosclerosis with more than 50% stenosis—27
- Cardioembolism—40
- Lacunar, small-vessel disease—25
- Uncertain cause—52
- Other identifiable cause—4.
THREE CLINICAL FEATURES SUGGEST TIA
TIAs can be hard to distinguish from nonischemic neurologic events in the acute setting such as an emergency room. Up to 60% of patients suspected of having a TIA actually have a nonischemic cause of their symptoms.43
Three clinical features suggest a TIA during the emergency room evaluation:
- Rapid onset of symptoms—“like lightning” or “in seconds,” in contrast to migraine and seizures, which develop over minutes
- No history of similar episodes in the past
- Absence of nonspecific symptoms—eg, stomach upset or tightness in the chest.
CLINICAL DIAGNOSIS
Because most TIA symptoms and signs have already resolved by the time of evaluation, the diagnosis depends on a careful history with special attention to the pace of onset and resolution, the duration and nature of the symptoms, circumstances at the time of symptom onset, previous similar episodes, associated features, vascular risk factors, and family history (Table 1).44,45
A detailed neurologic examination is imperative and should include fundoscopy. A cardiovascular assessment should include cardiac rhythm, bruits in the neck, orbits, and groin, peripheral pulses, and electrocardiography.
Do neurologists do a better job at diagnosing TIA and stroke?
Primary care physicians, internists, and emergency department physicians are often the ones to carry out the clinical assessment of possible TIA.
Determining if transient neurologic symptoms are caused by ischemia can be a challenge. When in doubt, referral to a neurologist with subspecialty training in cerebrovascular disease should be considered.
But do neurologists really do a better job? A recent study sought to compare the accuracy of diagnosis of TIA made by general practitioners, emergency physicians, and neurologists. The nonneurologists considered “confusion” and “unexplained fall” suggestive of TIA and “lower facial palsy” and “monocular blindness” less suggestive of TIA—whereas the opposite is true. This shows that nonneurologists often label minor strokes and several nonvascular transient neurologic disturbances as TIAs, and up to half of patients could be mislabeled as a result.46
Differences in diagnosing cerebrovascular events between emergency room physicians and attending neurologists have been tested,47 with an accuracy of diagnosis as low as 38% by emergency department physicians in one study.48 However, other studies did not show such a trend.49,50
A study at a university-based teaching hospital found the sensitivity of emergency room physician diagnosis to be 98.6% with a positive predictive value of 94.8%,49 showing that at a large teaching hospital with a comprehensive stroke intervention program, emergency physicians could identify patients with stroke, particularly hemorrhagic stroke, very accurately.
Improving the diagnosis of stroke and TIA
Routine use of imaging and involvement of a neurologist increase the sensitivity and accuracy of diagnosis. Education and written guidelines for acute stroke treatment both in the emergency department and in out-of-hospital settings seem to dramatically improve the rates of diagnostic accuracy and appropriate treatment.50
Emergency medical service personnel use two screening tools in the field to identify TIA and stroke symptoms:
- The Cincinnati Prehospital Stroke Scale, a three-item scale based on three signs: facial droop, arm drift, and slurring of speech51
- The Los Angeles Prehospital Stroke Screen, which uses screening questions and asymmetry in the face, hand grip strength, and arm drift.52
Knowing that the patient is having a minor stroke or TIA is important. Urgent treatment of these conditions decreases the risk of stroke in the next 90 days, which was 10.5% in one study.5 Urgent assessment and early intervention could reduce this risk of subsequent stroke down to 2%.6
ASSESSING RISK OF STROKE AFTER TIA
There is a practical need for prediction of stroke during the first few days after the event. The ABCD and ABCD2 scores were developed to stratify the short-term risk of stroke in patients with recent TIA.
The ABCD score
The ABCD score53 was derived to allow primary care physicians and other physicians to identify which patients with a suspected diagnosis of TIA should be referred for emergency assessment, to allow secondary-care physicians to determine which patients with probable or definite TIA need emergency investigation and treatment, to allow public education about the need for medical attention after a TIA, and to identify people at high risk.
The ABCD2 score
The ABCD2 score predicts the short-term risk of stroke following a TIA.54 Points are assigned as follows:
- Age > 60 years: 1 point
- Blood pressure (systolic) > 140 mm Hg or diastolic blood pressure > 90 mm Hg: 1 point
- Clinical factors: unilateral weakness with or without speech impairment: 2 points (1 point for speech impairment without weakness)
- Duration of symptoms > 60 minutes: 2 points (1 point for 10–59 minutes)
- Diabetes: 1 point.
Thus, the possible total ranges from 0 to 7 points. Higher scores indicate a greater risk of stroke at 2, 7, 30, and 90 days:
- Total score 0, 1, 2, or 3: 2-day stroke risk 1.0% (low risk)
- Total score 4 or 5: 2-day stroke risk 4.1% (moderate risk)
- Total score 6 or 7: 2-day stroke risk 8.1% (high risk).
WHO SHOULD BE HOSPITALIZED?
It has been suggested that the ABCD2 score can help in triaging patients to hospital admission or outpatient care, though no randomized trial has actually evaluated the utility of the ABCD2 score in this way.3
A study of consecutive TIA patients admitted over 12 months55 found that patients with an ABCD2 score of 3 or less had the same chance of requiring hospitalization (based on positive diffusion-weighted MRI studies, risk factor identification, and treatment initiation) as those with a score of 4 to 7. Hence, admitting TIA patients on the basis of the ABCD2 score alone requires further study. However, such decisions, though informed by clinical data, depend heavily on societal input (eg, from insurance companies, national health protocols) and may be outside the purview of clinical investigation.
The benefits of hospitalization include the ability to rapidly carry out tests such as cardiac monitoring for atrial fibrillation; to detect atherosclerosis, aortic arch atheroma, and paradoxical emboli; and to quickly start secondary prevention treatments and education about the importance of adhering to them. Early endarterectomy in the case of carotid stenosis can be offered. Additionally, if stroke symptoms recur, thrombolytic drug therapy can be started quickly.
Nguyen-Huynh et al56 analyzed the cost utility of 24-hour hospitalization for patients diagnosed with a recent TIA who were candidates for tissue plasminogen activator if a stroke occurred. They found hospitalization to be borderline cost-effective on the whole, with definite cost-effectiveness found in patients with higher stroke risk.
If patients come to medical attention several days after the TIA, then assessing risk with the ABCD2 score may no longer be reliable.57
INVESTIGATIONS
Parenchymal neuroimaging
Computed tomography (CT) without contrast is the most widely used neuroimaging test in the acute setting, since it is widely available, fast, and relatively low-cost. It will not show any abnormality in TIA or early ischemic stroke. However, it is helpful as a screening tool to rule out intracranial lesions such as hemorrhage or tumor. It may also show evidence of established infarction, which would indicate that the ischemia probably had been present for at least 6 to 12 hours.
MRI is clearly superior to noncontrast CT for detecting small areas of ischemia in patients with TIA, and it should be used unless the patient has a contraindication to it. Roughly one-third of TIA patients have lesions detectable on diffusion-weighted imaging, which helps to confirm that the episode was caused by cerebral ischemia, but nearly half of the diffusion MRI changes may be fully reversible.58 Evidence of prior stroke, leukoaraiosis, or white matter disease on fluid-attenuated inversion recovery and T2 sequences and microhemorrhages (on gradient echo sequences) help to determine a mechanistic diagnosis.
Subcategorizing TIA patients on the basis of the findings on diffusion-weighted MRI and the ABCD2 score is prognostically helpful.59 It can help to determine which patients need hospitalization and aggressive treatment, and in the case of identified diffusion-weighted MRI-positive stroke, it helps to localize and elucidate the mechanism of stroke. Hence, MRI is the preferred neuroimaging study for evaluating patients with TIA.3
Vascular imaging
Establishing the status of both intracranial and extracranial vessels is important for understanding the etiology, estimating the risk of future ischemic events, and formulating a treatment plan—eg, carotid endarterectomy in cases of significant stenosis (70% to 99%), which reduces the risk of ipsilateral stroke.60 Imaging studies include CT angiography, magnetic resonance angiography, extracranial and transcranial ultrasonography, and conventional catheter-based angiography.
CT angiography has higher spatial resolution, but vessels may be obscured by calcification associated with atherosclerotic plaque. It has the advantage of wide availability, low cost, short scanning time, and excellent patient tolerability.
Magnetic resonance angiography with gadolinium enhancement offers good quality imaging from the great vessels in the chest to the medium-sized vessels distal to the circle of Willis.
The contrast agents used in MRI and CT can have negative consequences in patients with renal disease. MRI contrast has been associated with nephrogenic fibrosing dermopathy, 61 and CT contrast can cause contrast-induced nephropathy.62
Carotid ultrasonography and transcranial Doppler ultrasonography are noninvasive and are not associated with significant adverse events. They can be used safely in patients with renal dysfunction, and they provide physiologic information that cannot be obtained with MRI and CT, which are static imaging techniques. Detecting microemboli on transcranial Doppler is an independent predictor of recurrent ischemic events.63,64
Catheter-based angiography is occasionally needed in confusing or more complicated cases, but it is invasive and occasionally is associated with iatrogenic stroke and other vascular complications.
Cardiac and aortic imaging
Echocardiography is used to detect lesions that can be sources of embolism such as regional wall-motion abnormalities, cardiac thrombus or mass, endocarditis, aortic arch atheroma, and patent foramen ovale. In patients with cryptogenic TIA or stroke, those with patent foramen ovale alone were found to have a lower risk of recurrent stroke than those who had both atrial septal aneurysm and patent foramen ovale.65
Transesophageal echocardiography is more sensitive than transthoracic echocardiography for detecting cardioembolic lesions, especially patent foramen ovale.66 In patients with cerebral ischemia and normal transthoracic findings, cardiac sources of embolism may be detected in about 40% of patients with transesophageal echocardiography.67
Cardiac rhythm monitoring
Electrocardiography and prolonged telemetry are recommended in patients with cryptogenic TIA to detect cardiac ischemia and paroxysmal atrial fibrillation. In one study, Holter monitoring detected atrial fibrillation in 6% of patients hospitalized with ischemic stroke or TIA.68 In another study, atrial fibrillation was detected after a median of 21 days of outpatient cardiac monitoring in 23% of patients.69
The optimal duration of outpatient telemetry has not yet been established, but studies have found significant increases in detection of paroxysms of atrial fibrillation with monitoring for 7 or longer.70
Laboratory tests in the acute setting
These include lipid profile, hemoglobin A1c, and cardiac enzymes. The advantages of hospitalization are early detection of these modifiable risk factors and early initiation of treatment.
Tests for rarer disorders
Tests for rarer disorders are sometimes indicated in unusual cases, such as ischemic symptoms occurring in young patients without other common risk factors. This includes testing for prothrombotic states, toxicology, blood cultures, inflammatory markers, hemoglobin electrophoresis, and lumbar puncture. The benefit of routine testing for thrombophilic disorders in cerebrovascular disease remains uncertain, with no clear association demonstrated with arterial stroke, but testing is more relevant in the case of venous (and paradoxical) thromboembolism.71
TREAT THE UNDERLYING DISORDER
Treatment depends on the mechanism that is thought to be responsible for the ischemic event. Vascular risk factors are important to identify and modify for all stroke subtypes.
Illustrating the importance of treating TIA and minor stroke, one study72 found that for antiplatelet therapy (aspirin, dipyridamole, or aspirin plus dipyridamole), the number needed to treat for 2 years was around 18.
Anticoagulation for cardioembolism
Atrial fibrillation, especially following a cerebrovascular ischemic event, should be treated with long-term anticoagulation with warfarin (Coumadin), dabigatran (Pradaxa), rivaroxaban (Xarelto), or apixaban (Eliquis).73 If the patient cannot tolerate anticoagulation, aspirin is recommended, and if he or she cannot tolerate aspirin, clopidogrel (Plavix) is recommended.
Antiplatelet therapy for large-vessel atherosclerosis and small-vessel disease
In the acute phase, aspirin 81 mg to 325 mg orally can be given. If the patient is allergic to aspirin, a loading dose of clopidogrel 300 mg and then 75 mg daily may be given.
A pilot study of loading with aspirin 325 mg or clopidogrel 375 mg in acute ischemic stroke and TIA patients showed that these treatments were safe when given within 36 hours and decreased the risk of neurologic deterioration.74 The patient should continue on aspirin 81 mg or clopidogrel 75 mg, as suggested by the Fast Assessment of Stroke and Transient Ischaemic Attack to Prevent Early Recurrence (FASTER) trial.75 In the long term, an antiplatelet drug such as aspirin or clopidogrel or the combination of aspirin and extended-release dipyridamole is reasonable.76
Cilostazol (Pletal) is not inferior and is possibly superior to aspirin in preventing noncardioembolic ischemic stroke. It is used off-label for secondary prevention of stroke of noncardioembolic origin.77
Statins
In the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial, high-dose atorvastatin (Lipitor)—80 mg daily—was found to reduce the risk of subsequent stroke and other cardiovascular events in patients with recent stroke irrespective of low-density lipoprotein cholesterol (LDL-C) level, but there was a small increase in the risk of hemorrhagic stroke.78
In patients with hyperlipidemia, current recommendations suggest a target LDL-C level lower than 100 mg/dL in patients with atherosclerotic stroke or TIA, and lower than 70 mg/dL in those with concomitant diabetes.79
Antihypertensive therapy
In the acute period, ie, the first 24 hours after symptoms, guidelines have advocated allowing high blood pressure to remain high (“permissive hypertension”) unless the systolic pressure is greater than 200 mm Hg or the diastolic pressure is greater than 120 mm Hg or the patient is receiving thrombolytic therapy.80 However, this has recently been challenged by findings in randomized trials.81 Permissive hypertension and avoidance of dehydration with intravenous normal saline may improve cerebral perfusion, which is especially important in patients with high-grade intracranial or extracranial stenosis. Within the parameters outlined above, we recommend against aggressively treating high blood pressure in the acute phase.
In the long term, antihypertensive therapy reduces the risk of recurrent stroke or TIA.82 The goal is to keep blood pressure lower than 140/90 mm Hg, or lower than 130/80 mm Hg in patients with diabetes. A study of patients with ischemic noncardioembolic stroke showed a higher risk of recurrent stroke if the systolic blood pressure was lower than 120 or higher than 140 mm Hg.83
Some classes of antihypertensive medication may be more beneficial than others. There is some evidence that angiotensin-converting enzyme (ACE) inhibitors alone or in combination with a diuretic or an angiotensin receptor blocker are superior to other regimens, possibly because of neuroprotective mechanisms.84 A recent meta-analysis found angiotensin receptor blockers to be more effective than either ACE inhibitors or beta-blockers in stroke prevention; however, calcium channel blockers were superior to renin-angiotensin system blockers (ACE inhibitors and angiotensin receptor blockers).85
Lifestyle modifications
Smoking cessation and cardiovascular exercise for more than 10 minutes more than 3 times per week is strongly recommended.
For patients with diabetes, the goal is to keep the fasting blood glucose level lower than 126 mg/dL.
Moderate alcohol intake has been shown to decrease stroke risk compared with excessive intake or none at all.86
Carotid endarterectomy
Carotid endarterectomy has been recommended within 2 weeks of cerebral or retinal TIA in those cases attributable to high-grade internal carotid artery stenosis in patients who have low surgical risk.87 This risk can be estimated on the basis of patient factors, surgeon factors, and hospital volume. The specific recommendations are as follows:
- 70% to 99% carotid stenosis: carotid endarterectomy recommended
- 50% to 69% carotid stenosis: carotid endarterectomy recommended in select patients with a perioperative complication rate < 6%
- < 50% carotid stenosis: carotid endarterectomy not routinely recommended.
Carotid artery angioplasty and stenting with distal embolic protection device
Data from the Carotid Revascularization Endarterectomy Versus Stenting Trial (CREST) and European stenting trials indicate that in patients over age 70, carotid endarterectomy appears to be superior to carotid artery stenting, whereas in younger patients the periprocedural risks of stroke and death are similar. Hence, carotid artery stenting performed by an interventionist with a low complication rate is a reasonable alternative to carotid endarterectomy.88,89
- Albers GW, Caplan LR, Easton JD, et al; TIA Working Group. Transient ischemic attack—proposal for a new definition. N Engl J Med 2002; 347:1713–1716.
- Ovbiagele B, Kidwell CS, Saver JL. Epidemiological impact in the United States of a tissue-based definition of transient ischemic attack. Stroke 2003; 34:919–924.
- Easton JD, Saver JL, Albers GW, et al; American Heart Association. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke 2009; 40:2276–2293.
- Marler JR, Tilley BC, Lu M, et al. Early stroke treatment associated with better outcome: the NINDS rt-PA stroke study. Neurology 2000; 55:1649–1655.
- Johnston SC, Gress DR, Browner WS, Sidney S. Short-term prognosis after emergency department diagnosis of TIA. JAMA 2000; 284:2901–2906.
- Rothwell PM, Giles MF, Chandratheva A, et al; Early use of Existing Preventive Strategies for Stroke (EXPRESS) study. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet 2007; 370:1432–1442.
- Roger VL, Go AS, Lloyd-Jones DM, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation 2012; 125:e2–e220.
- Johnston SC. Clinical practice. Transient ischemic attack. N Engl J Med 2002; 347:1687–1692.
- Johnston SC, Fayad PB, Gorelick PB, et al. Prevalence and knowledge of transient ischemic attack among US adults. Neurology 2003; 60:1429–1434.
- Eliasziw M, Kennedy J, Hill MD, Buchan AM, Barnett HJ; North American Symptomatic Carotid Endarterectomy Trial Group. Early risk of stroke after a transient ischemic attack in patients with internal carotid artery disease. CMAJ 2004; 170:1105–1109.
- Kleindorfer D, Panagos P, Pancioli A, et al. Incidence and short-term prognosis of transient ischemic attack in a population-based study. Stroke 2005; 36:720–723.
- Wu CM, McLaughlin K, Lorenzetti DL, Hill MD, Manns BJ, Ghali WA. Early risk of stroke after transient ischemic attack: a systematic review and meta-analysis. Arch Intern Med 2007; 167:2417–2422.
- Johnston SC, Leira EC, Hansen MD, Adams HP. Early recovery after cerebral ischemia risk of subsequent neurological deterioration. Ann Neurol 2003; 54:439–444.
- Bots ML, van der Wilk EC, Koudstaal PJ, Hofman A, Grobbee DE. Transient neurological attacks in the general population. Prevalence, risk factors, and clinical relevance. Stroke 1997; 28:768–773.
- White H, Boden-Albala B, Wang C, et al. Ischemic stroke subtype incidence among whites, blacks, and Hispanics: the Northern Manhattan Study. Circulation 2005; 111:1327–1331.
- Brown RD, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO. Stroke incidence, prevalence, and survival: secular trends in Rochester, Minnesota, through 1989. Stroke 1996; 27:373–380.
- Seshadri S, Beiser A, Kelly-Hayes M, et al. The lifetime risk of stroke: estimates from the Framingham Study. Stroke 2006; 37:345–350.
- Rosamond WD, Folsom AR, Chambless LE, et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerosis Risk in Communities (ARIC) cohort. Stroke 1999; 30:736–743.
- Lackland DT, Egan BM, Ferguson PL. Low birth weight as a risk factor for hypertension. J Clin Hypertens (Greenwich) 2003; 5:133–136.
- Flossmann E, Schulz UG, Rothwell PM. Systematic review of methods and results of studies of the genetic epidemiology of ischemic stroke. Stroke 2004; 35:212–227.
- Rodriguez BL, D’Agostino R, Abbott RD, et al. Risk of hospitalized stroke in men enrolled in the Honolulu Heart Program and the Framingham Study: a comparison of incidence and risk factor effects. Stroke 2002; 33:230–236.
- Manolio TA, Kronmal RA, Burke GL, O’Leary DH, Price TR. Short-term predictors of incident stroke in older adults. The Cardiovascular Health Study. Stroke 1996; 27:1479–1486.
- Wolf PA, D’Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: a risk profile from the Framingham Study. Stroke 1991; 22:312–318.
- Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289:2560–2572.
- Allen TW. Guide to clinical preventive services. Report of the US Preventive Services Task Force. J Am Osteopath Assoc 1991; 91:281–289.
- Goldstein LB, Bushnell CD, Adams RJ, et al; American Heart Association Stroke Council. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011; 42:517–584.
- Iso H, Jacobs DR, Wentworth D, Neaton JD, Cohen JD. Serum cholesterol levels and six-year mortality from stroke in 350,977 men screened for the multiple risk factor intervention trial. N Engl J Med 1989; 320:904–910.
- Zhang X, Patel A, Horibe H, et al; Asia Pacific Cohort Studies Collaboration. Cholesterol, coronary heart disease, and stroke in the Asia Pacific region. Int J Epidemiol 2003; 32:563–572.
- Sanossian N, Saver JL, Navab M, Ovbiagele B. High-density lipoprotein cholesterol: an emerging target for stroke treatment. Stroke 2007; 38:1104–1109.
- Kannel WB, Benjamin EJ. Status of the epidemiology of atrial fibrillation. Med Clin North Am 2008; 92:17–40.
- Inzitari D, Eliasziw M, Gates P, et al. The causes and risk of stroke in patients with asymptomatic internal-carotid-artery stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 2000; 342:1693–1700.
- Physical Activity Guidelines Advisory Committee report, 2008. To the Secretary of Health and Human Services. Part A: executive summary. Nutr Rev 2009; 67:114–120.
- Armstrong FD, Thompson RJ, Wang W, et al. Cognitive functioning and brain magnetic resonance imaging in children with sickle cell disease. Neuropsychology Committee of the Cooperative Study of Sickle Cell Disease. Pediatrics 1996; 97:864–870.
- Ohene-Frempong K, Weiner SJ, Sleeper LA, et al. Cerebrovascular accidents in sickle cell disease: rates and risk factors. Blood 1998; 91:288–294.
- Mosca L, Banka CL, Benjamin EJ, et al; Expert Panel/Writing Group; American Heart Association; American Academy of Family Physicians; American College of Obstetricians and Gynecologists; American College of Cardiology Foundation; Society of Thoracic Surgeons; American Medical Women's Association; Centers for Disease Control and Prevention; Office of Research on Women's Health; Association of Black Cardiologists; American College of Physicians; World Heart Federation; National Heart, Lung, and Blood Institute; American College of Nurse Practitioners. Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation 2007; 115:1481–1501.
- Lidegaard Ø, Løkkegaard E, Jensen A, Skovlund CW, Keiding N. Thrombotic stroke and myocardial infarction with hormonal contraception. N Engl J Med 2012; 366:2257–2266.
- Chan WS, Ray J, Wai EK, et al. Risk of stroke in women exposed to low-dose oral contraceptives: a critical evaluation of the evidence. Arch Intern Med 2004; 164:741–747.
- Bousser MG, Conard J, Kittner S, et al. Recommendations on the risk of ischaemic stroke associated with use of combined oral contraceptives and hormone replacement therapy in women with migraine. The International Headache Society Task Force on Combined Oral Contraceptives & Hormone Replacement Therapy. Cephalalgia 2000; 20:155–156.
- Mohr JP, Caplan LR, Melski JW, et al. The Harvard Cooperative Stroke Registry: a prospective registry. Neurology 1978; 28:754–762.
- Caplan LR. Brain embolism, revisited. Neurology 1993; 43:1281–1287.
- Caplan LR, Hennerici M. Impaired clearance of emboli (washout) is an important link between hypoperfusion, embolism, and ischemic stroke. Arch Neurol 1998; 55:1475–1482.
- Petty GW, Brown RD, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO. Ischemic stroke subtypes: a population-based study of incidence and risk factors. Stroke 1999; 30:2513–2516.
- Prabhakaran S, Silver AJ, Warrior L, McClenathan B, Lee VH. Misdiagnosis of transient ischemic attacks in the emergency room. Cerebrovasc Dis 2008; 26:630–635.
- Baquis GD, Pessin MS, Scott RM. Limb shaking—a carotid TIA. Stroke 1985; 16:444–448.
- Luengo-Fernandez R, Gray AM, Rothwell PM. Effect of urgent treatment for transient ischaemic attack and minor stroke on disability and hospital costs (EXPRESS study): a prospective population-based sequential comparison. Lancet Neurol 2009; 8:235–243.
- Ferro JM, Falcão I, Rodrigues G, et al. Diagnosis of transient ischemic attack by the nonneurologist. A validation study. Stroke 1996; 27:2225–2229.
- Norris JW, Hachinski VC. Misdiagnosis of stroke. Lancet 1982; 1:328–331.
- Ferro JM, Pinto AN, Falcão I, et al. Diagnosis of stroke by the nonneurologist. A validation study. Stroke 1998; 29:1106–1109.
- Kothari RU, Brott T, Broderick JP, Hamilton CA. Emergency physicians. Accuracy in the diagnosis of stroke. Stroke 1995; 26:2238–2241.
- Artto V, Putaala J, Strbian D, et al; Helsinki Stroke Thrombolysis Registry Group. Stroke mimics and intravenous thrombolysis. Ann Emerg Med 2012; 59:27–32.
- Kothari RU, Pancioli A, Liu T, Brott T, Broderick J. Cincinnati Prehospital Stroke Scale: reproducibility and validity. Ann Emerg Med 1999; 33:373–378.
- Kidwell CS, Starkman S, Eckstein M, Weems K, Saver JL. Identifying stroke in the field. Prospective validation of the Los Angeles prehospital stroke screen (LAPSS). Stroke 2000; 31:71–76.
- Rothwell PM, Giles MF, Flossmann E, et al. A simple score (ABCD) to identify individuals at high early risk of stroke after transient ischaemic attack. Lancet 2005; 366:29–36.
- Johnston SC, Rothwell PM, Nguyen-Huynh MN, et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet 2007; 369:283–292.
- Lou M, Safdar A, Edlow JA, et al. Can ABCD score predict the need for in-hospital intervention in patients with transient ischemic attacks? Int J Emerg Med 2010; 3:75–80.
- Nguyen-Huynh MN, Johnston SC. Is hospitalization after TIA cost-effective on the basis of treatment with tPA? Neurology 2005; 65:1799–1801.
- Calvet D, Lamy C, Touzé E, Oppenheim C, Meder JF, Mas JL. Management and outcome of patients with transient ischemic attack admitted to a stroke unit. Cerebrovasc Dis 2007; 24:80–85.
- Kidwell CS, Alger JR, Di Salle F, et al. Diffusion MRI in patients with transient ischemic attacks. Stroke 1999; 30:1174–1180.
- Giles MF, Albers GW, Amarenco P, et al. Early stroke risk and ABCD2 score performance in tissue- vs time-defined TIA: a multicenter study. Neurology 2011; 77:1222–1228.
- Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet 1998; 351:1379–1387.
- Thomsen HS. Nephrogenic systemic fibrosis: history and epidemiology. Radiol Clin North Am 2009; 47:827–831.
- Barrett BJ, Parfrey PS. Clinical practice. Preventing nephropathy induced by contrast medium. N Engl J Med 2006; 354:379–386.
- Valton L, Larrue V, le Traon AP, Massabuau P, Géraud G. Microembolic signals and risk of early recurrence in patients with stroke or transient ischemic attack. Stroke 1998; 29:2125–2128.
- Gao S, Wong KS, Hansberg T, Lam WW, Droste DW, Ringelstein EB. Microembolic signal predicts recurrent cerebral ischemic events in acute stroke patients with middle cerebral artery stenosis. Stroke 2004; 35:2832–2836.
- Mas JL, Zuber M. Recurrent cerebrovascular events in patients with patent foramen ovale, atrial septal aneurysm, or both and cryptogenic stroke or transient ischemic attack. French Study Group on Patent Foramen Ovale and Atrial Septal Aneurysm. Am Heart J 1995; 130:1083–1088.
- Di Tullio M, Sacco RL, Venketasubramanian N, Sherman D, Mohr JP, Homma S. Comparison of diagnostic techniques for the detection of a patent foramen ovale in stroke patients. Stroke 1993; 24:1020–1024.
- de Bruijn SF, Agema WR, Lammers GJ, et al. Transesophageal echocardiography is superior to transthoracic echocardiography in management of patients of any age with transient ischemic attack or stroke. Stroke 2006; 37:2531–2534.
- Lazzaro MA, Krishnan K, Prabhakaran S. Detection of atrial fibrillation with concurrent Holter monitoring and continuous cardiac telemetry following ischemic stroke and transient ischemic attack. J Stroke Cerebrovasc Dis 2012; 21:89–93.
- Tayal AH, Tian M, Kelly KM, et al. Atrial fibrillation detected by mobile cardiac outpatient telemetry in cryptogenic TIA or stroke. Neurology 2008; 71:1696–1701.
- Seet RC, Friedman PA, Rabinstein AA. Prolonged rhythm monitoring for the detection of occult paroxysmal atrial fibrillation in ischemic stroke of unknown cause. Circulation 2011; 124:477–486.
- Morris JG, Singh S, Fisher M. Testing for inherited thrombophilias in arterial stroke: can it cause more harm than good? Stroke 2010; 41:2985–2990.
- Diener HC, Cunha L, Forbes C, Sivenius J, Smets P, Lowenthal A. European Stroke Prevention Study. 2. Dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci 1996; 143:1–13.
- Connolly SJ, Ezekowitz MD, Yusuf S, et al; RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009; 361:1139–1151.
- Meyer DM, Albright KC, Allison TA, Grotta JC. LOAD: a pilot study of the safety of loading of aspirin and clopidogrel in acute ischemic stroke and transient ischemic attack. J Stroke Cerebrovasc Dis 2008; 17:26–29.
- Kennedy J, Hill MD, Ryckborst KJ, Eliasziw M, Demchuk AM, Buchan AM; FASTER Investigators. Fast Assessment of Stroke and Transient Ischaemic Attack to Prevent Early Recurrence (FASTER): a randomised controlled pilot trial. Lancet Neurol 2007; 6:961–969.
- Sacco RL, Diener HC, Yusuf S, et al; PRoFESS Study Group. Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke. N Engl J Med 2008; 359:1238–1251.
- Shinohara Y, Katayama Y, Uchiyama S, et al; CSPS 2 group. Cilostazol for prevention of secondary stroke (CSPS 2): an aspirin-controlled, double-blind, randomised non-inferiority trial. Lancet Neurol 2010; 9:959–968.
- Amarenco P, Bogousslavsky J, Callahan A, et al; Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Investigators. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med 2006; 355:549–559.
- Furie KL, Kasner SE, Adams RJ, et al; American Heart Association Stroke Council, Council on Cardiovascular Nursing, Council on Clinical Cardiology, and Interdisciplinary Council on Quality of Care and Outcomes Research. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011; 42:227–276.
- Koenig MA, Geocadin RG, de Grouchy M, et al. Safety of induced hypertension therapy in patients with acute ischemic stroke. Neurocrit Care 2006; 4:3–7.
- Elijovich F, Laffer CL. Acute stroke: lower blood pressure looks better and better. Hypertension 2010; 56:808–810.
- Lawes CM, Bennett DA, Feigin VL, Rodgers A. Blood pressure and stroke: an overview of published reviews. Stroke 2004; 35:1024.
- Ovbiagele B, Diener HC, Yusuf S, et al; PROFESS Investigators. Level of systolic blood pressure within the normal range and risk of recurrent stroke. JAMA 2011; 306:2137–2144.
- Chrysant SG. The pathophysiologic role of the brain renin-angiotensin system in stroke protection: clinical implications. J Clin Hypertens (Greenwich) 2007; 9:454–459.
- Verdecchia P, Gentile G, Angeli F, Reboldi G. Beyond blood pressure: evidence for cardiovascular, cerebrovascular, and renal protective effects of renin-angiotensin system blockers. Ther Adv Cardiovasc Dis 2012; 6:81–91.
- Elkind MS, Sciacca R, Boden-Albala B, Rundek T, Paik MC, Sacco RL. Moderate alcohol consumption reduces risk of ischemic stroke: the Northern Manhattan Study. Stroke 2006; 37:13–19.
- Rothwell PM, Eliasziw M, Gutnikov SA, Warlow CP, Barnett HJ; Carotid Endarterectomy Trialists Collaboration. Endarterectomy for symptomatic carotid stenosis in relation to clinical subgroups and timing of surgery. Lancet 2004; 363:915–924.
- Brott TG, Hobson RW, Howard G, et al; CREST Investigators. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med 2010; 363:11–23.
- Carotid Stenting Trialists’ Collaboration; Bonati LH, Dobson J, Algra A, et al. Short-term outcome after stenting versus endarterectomy for symptomatic carotid stenosis: a preplanned meta-analysis of individual patient data. Lancet 2010; 376:1062–1073.
- Albers GW, Caplan LR, Easton JD, et al; TIA Working Group. Transient ischemic attack—proposal for a new definition. N Engl J Med 2002; 347:1713–1716.
- Ovbiagele B, Kidwell CS, Saver JL. Epidemiological impact in the United States of a tissue-based definition of transient ischemic attack. Stroke 2003; 34:919–924.
- Easton JD, Saver JL, Albers GW, et al; American Heart Association. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke 2009; 40:2276–2293.
- Marler JR, Tilley BC, Lu M, et al. Early stroke treatment associated with better outcome: the NINDS rt-PA stroke study. Neurology 2000; 55:1649–1655.
- Johnston SC, Gress DR, Browner WS, Sidney S. Short-term prognosis after emergency department diagnosis of TIA. JAMA 2000; 284:2901–2906.
- Rothwell PM, Giles MF, Chandratheva A, et al; Early use of Existing Preventive Strategies for Stroke (EXPRESS) study. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet 2007; 370:1432–1442.
- Roger VL, Go AS, Lloyd-Jones DM, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation 2012; 125:e2–e220.
- Johnston SC. Clinical practice. Transient ischemic attack. N Engl J Med 2002; 347:1687–1692.
- Johnston SC, Fayad PB, Gorelick PB, et al. Prevalence and knowledge of transient ischemic attack among US adults. Neurology 2003; 60:1429–1434.
- Eliasziw M, Kennedy J, Hill MD, Buchan AM, Barnett HJ; North American Symptomatic Carotid Endarterectomy Trial Group. Early risk of stroke after a transient ischemic attack in patients with internal carotid artery disease. CMAJ 2004; 170:1105–1109.
- Kleindorfer D, Panagos P, Pancioli A, et al. Incidence and short-term prognosis of transient ischemic attack in a population-based study. Stroke 2005; 36:720–723.
- Wu CM, McLaughlin K, Lorenzetti DL, Hill MD, Manns BJ, Ghali WA. Early risk of stroke after transient ischemic attack: a systematic review and meta-analysis. Arch Intern Med 2007; 167:2417–2422.
- Johnston SC, Leira EC, Hansen MD, Adams HP. Early recovery after cerebral ischemia risk of subsequent neurological deterioration. Ann Neurol 2003; 54:439–444.
- Bots ML, van der Wilk EC, Koudstaal PJ, Hofman A, Grobbee DE. Transient neurological attacks in the general population. Prevalence, risk factors, and clinical relevance. Stroke 1997; 28:768–773.
- White H, Boden-Albala B, Wang C, et al. Ischemic stroke subtype incidence among whites, blacks, and Hispanics: the Northern Manhattan Study. Circulation 2005; 111:1327–1331.
- Brown RD, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO. Stroke incidence, prevalence, and survival: secular trends in Rochester, Minnesota, through 1989. Stroke 1996; 27:373–380.
- Seshadri S, Beiser A, Kelly-Hayes M, et al. The lifetime risk of stroke: estimates from the Framingham Study. Stroke 2006; 37:345–350.
- Rosamond WD, Folsom AR, Chambless LE, et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerosis Risk in Communities (ARIC) cohort. Stroke 1999; 30:736–743.
- Lackland DT, Egan BM, Ferguson PL. Low birth weight as a risk factor for hypertension. J Clin Hypertens (Greenwich) 2003; 5:133–136.
- Flossmann E, Schulz UG, Rothwell PM. Systematic review of methods and results of studies of the genetic epidemiology of ischemic stroke. Stroke 2004; 35:212–227.
- Rodriguez BL, D’Agostino R, Abbott RD, et al. Risk of hospitalized stroke in men enrolled in the Honolulu Heart Program and the Framingham Study: a comparison of incidence and risk factor effects. Stroke 2002; 33:230–236.
- Manolio TA, Kronmal RA, Burke GL, O’Leary DH, Price TR. Short-term predictors of incident stroke in older adults. The Cardiovascular Health Study. Stroke 1996; 27:1479–1486.
- Wolf PA, D’Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: a risk profile from the Framingham Study. Stroke 1991; 22:312–318.
- Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289:2560–2572.
- Allen TW. Guide to clinical preventive services. Report of the US Preventive Services Task Force. J Am Osteopath Assoc 1991; 91:281–289.
- Goldstein LB, Bushnell CD, Adams RJ, et al; American Heart Association Stroke Council. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011; 42:517–584.
- Iso H, Jacobs DR, Wentworth D, Neaton JD, Cohen JD. Serum cholesterol levels and six-year mortality from stroke in 350,977 men screened for the multiple risk factor intervention trial. N Engl J Med 1989; 320:904–910.
- Zhang X, Patel A, Horibe H, et al; Asia Pacific Cohort Studies Collaboration. Cholesterol, coronary heart disease, and stroke in the Asia Pacific region. Int J Epidemiol 2003; 32:563–572.
- Sanossian N, Saver JL, Navab M, Ovbiagele B. High-density lipoprotein cholesterol: an emerging target for stroke treatment. Stroke 2007; 38:1104–1109.
- Kannel WB, Benjamin EJ. Status of the epidemiology of atrial fibrillation. Med Clin North Am 2008; 92:17–40.
- Inzitari D, Eliasziw M, Gates P, et al. The causes and risk of stroke in patients with asymptomatic internal-carotid-artery stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 2000; 342:1693–1700.
- Physical Activity Guidelines Advisory Committee report, 2008. To the Secretary of Health and Human Services. Part A: executive summary. Nutr Rev 2009; 67:114–120.
- Armstrong FD, Thompson RJ, Wang W, et al. Cognitive functioning and brain magnetic resonance imaging in children with sickle cell disease. Neuropsychology Committee of the Cooperative Study of Sickle Cell Disease. Pediatrics 1996; 97:864–870.
- Ohene-Frempong K, Weiner SJ, Sleeper LA, et al. Cerebrovascular accidents in sickle cell disease: rates and risk factors. Blood 1998; 91:288–294.
- Mosca L, Banka CL, Benjamin EJ, et al; Expert Panel/Writing Group; American Heart Association; American Academy of Family Physicians; American College of Obstetricians and Gynecologists; American College of Cardiology Foundation; Society of Thoracic Surgeons; American Medical Women's Association; Centers for Disease Control and Prevention; Office of Research on Women's Health; Association of Black Cardiologists; American College of Physicians; World Heart Federation; National Heart, Lung, and Blood Institute; American College of Nurse Practitioners. Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation 2007; 115:1481–1501.
- Lidegaard Ø, Løkkegaard E, Jensen A, Skovlund CW, Keiding N. Thrombotic stroke and myocardial infarction with hormonal contraception. N Engl J Med 2012; 366:2257–2266.
- Chan WS, Ray J, Wai EK, et al. Risk of stroke in women exposed to low-dose oral contraceptives: a critical evaluation of the evidence. Arch Intern Med 2004; 164:741–747.
- Bousser MG, Conard J, Kittner S, et al. Recommendations on the risk of ischaemic stroke associated with use of combined oral contraceptives and hormone replacement therapy in women with migraine. The International Headache Society Task Force on Combined Oral Contraceptives & Hormone Replacement Therapy. Cephalalgia 2000; 20:155–156.
- Mohr JP, Caplan LR, Melski JW, et al. The Harvard Cooperative Stroke Registry: a prospective registry. Neurology 1978; 28:754–762.
- Caplan LR. Brain embolism, revisited. Neurology 1993; 43:1281–1287.
- Caplan LR, Hennerici M. Impaired clearance of emboli (washout) is an important link between hypoperfusion, embolism, and ischemic stroke. Arch Neurol 1998; 55:1475–1482.
- Petty GW, Brown RD, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO. Ischemic stroke subtypes: a population-based study of incidence and risk factors. Stroke 1999; 30:2513–2516.
- Prabhakaran S, Silver AJ, Warrior L, McClenathan B, Lee VH. Misdiagnosis of transient ischemic attacks in the emergency room. Cerebrovasc Dis 2008; 26:630–635.
- Baquis GD, Pessin MS, Scott RM. Limb shaking—a carotid TIA. Stroke 1985; 16:444–448.
- Luengo-Fernandez R, Gray AM, Rothwell PM. Effect of urgent treatment for transient ischaemic attack and minor stroke on disability and hospital costs (EXPRESS study): a prospective population-based sequential comparison. Lancet Neurol 2009; 8:235–243.
- Ferro JM, Falcão I, Rodrigues G, et al. Diagnosis of transient ischemic attack by the nonneurologist. A validation study. Stroke 1996; 27:2225–2229.
- Norris JW, Hachinski VC. Misdiagnosis of stroke. Lancet 1982; 1:328–331.
- Ferro JM, Pinto AN, Falcão I, et al. Diagnosis of stroke by the nonneurologist. A validation study. Stroke 1998; 29:1106–1109.
- Kothari RU, Brott T, Broderick JP, Hamilton CA. Emergency physicians. Accuracy in the diagnosis of stroke. Stroke 1995; 26:2238–2241.
- Artto V, Putaala J, Strbian D, et al; Helsinki Stroke Thrombolysis Registry Group. Stroke mimics and intravenous thrombolysis. Ann Emerg Med 2012; 59:27–32.
- Kothari RU, Pancioli A, Liu T, Brott T, Broderick J. Cincinnati Prehospital Stroke Scale: reproducibility and validity. Ann Emerg Med 1999; 33:373–378.
- Kidwell CS, Starkman S, Eckstein M, Weems K, Saver JL. Identifying stroke in the field. Prospective validation of the Los Angeles prehospital stroke screen (LAPSS). Stroke 2000; 31:71–76.
- Rothwell PM, Giles MF, Flossmann E, et al. A simple score (ABCD) to identify individuals at high early risk of stroke after transient ischaemic attack. Lancet 2005; 366:29–36.
- Johnston SC, Rothwell PM, Nguyen-Huynh MN, et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet 2007; 369:283–292.
- Lou M, Safdar A, Edlow JA, et al. Can ABCD score predict the need for in-hospital intervention in patients with transient ischemic attacks? Int J Emerg Med 2010; 3:75–80.
- Nguyen-Huynh MN, Johnston SC. Is hospitalization after TIA cost-effective on the basis of treatment with tPA? Neurology 2005; 65:1799–1801.
- Calvet D, Lamy C, Touzé E, Oppenheim C, Meder JF, Mas JL. Management and outcome of patients with transient ischemic attack admitted to a stroke unit. Cerebrovasc Dis 2007; 24:80–85.
- Kidwell CS, Alger JR, Di Salle F, et al. Diffusion MRI in patients with transient ischemic attacks. Stroke 1999; 30:1174–1180.
- Giles MF, Albers GW, Amarenco P, et al. Early stroke risk and ABCD2 score performance in tissue- vs time-defined TIA: a multicenter study. Neurology 2011; 77:1222–1228.
- Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet 1998; 351:1379–1387.
- Thomsen HS. Nephrogenic systemic fibrosis: history and epidemiology. Radiol Clin North Am 2009; 47:827–831.
- Barrett BJ, Parfrey PS. Clinical practice. Preventing nephropathy induced by contrast medium. N Engl J Med 2006; 354:379–386.
- Valton L, Larrue V, le Traon AP, Massabuau P, Géraud G. Microembolic signals and risk of early recurrence in patients with stroke or transient ischemic attack. Stroke 1998; 29:2125–2128.
- Gao S, Wong KS, Hansberg T, Lam WW, Droste DW, Ringelstein EB. Microembolic signal predicts recurrent cerebral ischemic events in acute stroke patients with middle cerebral artery stenosis. Stroke 2004; 35:2832–2836.
- Mas JL, Zuber M. Recurrent cerebrovascular events in patients with patent foramen ovale, atrial septal aneurysm, or both and cryptogenic stroke or transient ischemic attack. French Study Group on Patent Foramen Ovale and Atrial Septal Aneurysm. Am Heart J 1995; 130:1083–1088.
- Di Tullio M, Sacco RL, Venketasubramanian N, Sherman D, Mohr JP, Homma S. Comparison of diagnostic techniques for the detection of a patent foramen ovale in stroke patients. Stroke 1993; 24:1020–1024.
- de Bruijn SF, Agema WR, Lammers GJ, et al. Transesophageal echocardiography is superior to transthoracic echocardiography in management of patients of any age with transient ischemic attack or stroke. Stroke 2006; 37:2531–2534.
- Lazzaro MA, Krishnan K, Prabhakaran S. Detection of atrial fibrillation with concurrent Holter monitoring and continuous cardiac telemetry following ischemic stroke and transient ischemic attack. J Stroke Cerebrovasc Dis 2012; 21:89–93.
- Tayal AH, Tian M, Kelly KM, et al. Atrial fibrillation detected by mobile cardiac outpatient telemetry in cryptogenic TIA or stroke. Neurology 2008; 71:1696–1701.
- Seet RC, Friedman PA, Rabinstein AA. Prolonged rhythm monitoring for the detection of occult paroxysmal atrial fibrillation in ischemic stroke of unknown cause. Circulation 2011; 124:477–486.
- Morris JG, Singh S, Fisher M. Testing for inherited thrombophilias in arterial stroke: can it cause more harm than good? Stroke 2010; 41:2985–2990.
- Diener HC, Cunha L, Forbes C, Sivenius J, Smets P, Lowenthal A. European Stroke Prevention Study. 2. Dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci 1996; 143:1–13.
- Connolly SJ, Ezekowitz MD, Yusuf S, et al; RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009; 361:1139–1151.
- Meyer DM, Albright KC, Allison TA, Grotta JC. LOAD: a pilot study of the safety of loading of aspirin and clopidogrel in acute ischemic stroke and transient ischemic attack. J Stroke Cerebrovasc Dis 2008; 17:26–29.
- Kennedy J, Hill MD, Ryckborst KJ, Eliasziw M, Demchuk AM, Buchan AM; FASTER Investigators. Fast Assessment of Stroke and Transient Ischaemic Attack to Prevent Early Recurrence (FASTER): a randomised controlled pilot trial. Lancet Neurol 2007; 6:961–969.
- Sacco RL, Diener HC, Yusuf S, et al; PRoFESS Study Group. Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke. N Engl J Med 2008; 359:1238–1251.
- Shinohara Y, Katayama Y, Uchiyama S, et al; CSPS 2 group. Cilostazol for prevention of secondary stroke (CSPS 2): an aspirin-controlled, double-blind, randomised non-inferiority trial. Lancet Neurol 2010; 9:959–968.
- Amarenco P, Bogousslavsky J, Callahan A, et al; Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Investigators. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med 2006; 355:549–559.
- Furie KL, Kasner SE, Adams RJ, et al; American Heart Association Stroke Council, Council on Cardiovascular Nursing, Council on Clinical Cardiology, and Interdisciplinary Council on Quality of Care and Outcomes Research. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011; 42:227–276.
- Koenig MA, Geocadin RG, de Grouchy M, et al. Safety of induced hypertension therapy in patients with acute ischemic stroke. Neurocrit Care 2006; 4:3–7.
- Elijovich F, Laffer CL. Acute stroke: lower blood pressure looks better and better. Hypertension 2010; 56:808–810.
- Lawes CM, Bennett DA, Feigin VL, Rodgers A. Blood pressure and stroke: an overview of published reviews. Stroke 2004; 35:1024.
- Ovbiagele B, Diener HC, Yusuf S, et al; PROFESS Investigators. Level of systolic blood pressure within the normal range and risk of recurrent stroke. JAMA 2011; 306:2137–2144.
- Chrysant SG. The pathophysiologic role of the brain renin-angiotensin system in stroke protection: clinical implications. J Clin Hypertens (Greenwich) 2007; 9:454–459.
- Verdecchia P, Gentile G, Angeli F, Reboldi G. Beyond blood pressure: evidence for cardiovascular, cerebrovascular, and renal protective effects of renin-angiotensin system blockers. Ther Adv Cardiovasc Dis 2012; 6:81–91.
- Elkind MS, Sciacca R, Boden-Albala B, Rundek T, Paik MC, Sacco RL. Moderate alcohol consumption reduces risk of ischemic stroke: the Northern Manhattan Study. Stroke 2006; 37:13–19.
- Rothwell PM, Eliasziw M, Gutnikov SA, Warlow CP, Barnett HJ; Carotid Endarterectomy Trialists Collaboration. Endarterectomy for symptomatic carotid stenosis in relation to clinical subgroups and timing of surgery. Lancet 2004; 363:915–924.
- Brott TG, Hobson RW, Howard G, et al; CREST Investigators. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med 2010; 363:11–23.
- Carotid Stenting Trialists’ Collaboration; Bonati LH, Dobson J, Algra A, et al. Short-term outcome after stenting versus endarterectomy for symptomatic carotid stenosis: a preplanned meta-analysis of individual patient data. Lancet 2010; 376:1062–1073.
KEY POINTS
- Modifiable risk factors for stroke and TIA include cigarette smoking, hypertension, diabetes, lipid abnormalities, atrial fibrillation, carotid stenosis, and dietary and hormonal factors.
- The three major mechanisms of stroke and TIA are thrombosis, embolism, and decreased systemic perfusion.
- Typical symptoms of TIA include hemiparesis, hemisensory loss, aphasia, vision loss, ataxia, and diplopia. Three clinical features that suggest TIA are rapid onset of symptoms, no history of similar episodes in the past, and the absence of nonspecific symptoms.
- In suspected TIA, magnetic resonance imaging is clearly superior to noncontrast computed tomography (CT) for detecting small areas of ischemia; this test should be used unless contraindicated.
- Imaging studies of the blood vessels include CT angiography, magnetic resonance angiography, conventional angiography, and extracranial and transcranial ultrasonography.
Ill-advised genetic counseling: $1M verdict
A mother had given birth to two children with thalamic abnormalities that resulted in seizures, developmental delays, and death. Before getting pregnant again, the parents sought genetic counseling and were told that identifying the specific defective gene would be impossible. The geneticist advised them that a child conceived with a donor egg and father’s sperm would have essentially the same risk as the general population. The parents asked in writing if it would be safer to
use both donor egg and donor sperm; the geneticist responded that the difference in risk was negligible.
The mother gave birth in June 2007 to a child conceived with a donated egg and the father’s sperm. After the child began to show the same symptoms as the others, an MRI of the child’s brain revealed a thalamic abnormality, and testing revealed Alpers syndrome caused by POLG gene mutations. The third child died in September 2008.
PARENTS’ CLAIM The chances of having a child with Alpers syndrome are
about 1:200,000 in the general population; if one parent is a known carrier, the chance is 1:1,000. If the parents had known this risk, they would have used donor egg and donor sperm to conceive or adopted. They were not told about Alpers syndrome and its relationship to the POLG gene until after their third child was born. The geneticist was negligent in failing to provide this information.
PHYSICIAN’S DEFENSE The parents received appropriate and accurate genetic counseling.
VERDICT A $1 million Florida verdict was returned.
What caused a delay in breast cancer diagnosis?
A 39-year-old woman underwent mammography in October 2004. After recommending a spotcompression film of a left-breast lesion, and then ultrasonography, the radiologist concluded that the lesion was benign, and suggested a 1-year follow-up. Reports were sent to the patient and her primary care physician.
In August 2006, when mammography was suspicious for breast cancer, a biopsy diagnosed infiltrating ductal carcinoma of the left breast. After undergoing a mastectomy, radiation therapy, and chemotherapy, the patient was cancer-free at the time of the trial.
patient’s CLAIM The radiologist failed to properly interpret the 2004 mammography.
physician’s DEFENSE The radiologist’s interpretations of the 2004 tests were correct. The patient failed to follow up in 1 year, as recommended, and this delayed the cancer diagnosis. The patient’s survival indicated that she had been cured of her breast cancer.
VERDICT A confidential settlement was reached with the hospital before the trial. An Illinois defense verdict was returned for the radiologist.
Heparin overdose for preemie
At 27 weeks' gestation, a woman went to a clinic with preeclampsia. After she was stabilized, the baby was born by emergency cesarean delivery.
At birth, the baby was thrombocytopenic (platelet count, 37,000/mL) with a heart rate of 60 bpm. The child’s cord blood pH was 7.27, indicating no significant hypoxia. At 1 minute of life, the child’s heart rate had not improved. After trying three times to place an endotracheal tube, chest compressions were begun at 10 minutes of life. An umbilical vein catheter (UVC) was placed at 22 minutes. Heparin was used to flush the UVC. After 40 minutes, the baby’s pH was 6.88, indicating severe acidosis. The infant was transferred to another hospital 3 hours after birth.
Head ultrasonography at 5 days of life revealed hemorrhagic and ischemic changes in the baby’s brain. The child suffered massive brain damage, is ventilator-dependent, and has a G-tube for feeding. She cannot sit up, walk, or speak, and will require specialized care for life.
Parent's claim Emergency resuscitation was not performed at birth: the low heart rate and thrombocytopenia were not treated; the UVC was not immediately placed. Twice, adult doses of heparin were used instead of normal saline to flush the UVC; heparin caused bleeding in the baby’s brain.
Defendant's Defense The case was settled during trial.
Verdict A $3 million Maryland settlement was reached.
Uterine rupture: $130M verdict
After a woman's first child was born by cesarean delivery, vaginal birth after cesarean (VBAC) was planned for her second pregnancy. When a nurse recognized a ruptured uterus, the ObGyn ordered a cesarean delivery. The newborn suffered severe brain damage, with seizures. She has cerebral palsy with near-normal intelligence, but cannot talk or walk and continues to have seizures.
Parents' claim The baby’s injuries occurred due to a failure to respond to fetal distress. When the intrauterine pressure catheter (IUPC) stopped working for 27 minutes, the nurse did not notify the ObGyn or apply an external monitor. Fetal heart decelerations occurred, including a prolonged deceleration for 3 minutes; the nurse did not notify the ObGyn, reposition the mother, provide oxygen and extra fluids, or discontinue oxytocin. A cesarean delivery should have occurred 30 to 60 minutes earlier.
Defendants' defense The fetal heart rates were what typically occur during the second stage of labor. The hospital’s accepted practices were followed. When the IUPC failed, the nurse measured contractions by hand and analyzed the fetal heartbeat from audible sounds; therefore, it was not necessary to notify the ObGyn. The physician was promptly called when uterine rupture was suspected. Uterine rupture and placental abruption caused the child’s injury. Uterine rupture cannot be predicted or prevented and is a known complication of VBAC.
Verdict After the parents declined an $8 million settlement, the matter was tried to a defense verdict. That decision was overturned on appeal, and, at a second trial, a $130 million New York verdict was returned against the hospital that employed the ObGyn and nurse.
Uterus, small bowel injured during D&C
A 65-year-old woman underwent dilation and curettage (D&C) to screen for uterine cancer performed by an ObGyn and a general surgeon. Her uterus and small intestine were perforated during the procedure, and a second operation was required to repair the damage.
Patient's claim Both physicians were negligent in performing D&C.
Physician's defense The ObGyn denied negligence and countered that the injuries are known complications of the procedure.
Verdict The surgeon settled for a confidential amount before trial. A New Jersey defense verdict was returned for the ObGyn.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
A mother had given birth to two children with thalamic abnormalities that resulted in seizures, developmental delays, and death. Before getting pregnant again, the parents sought genetic counseling and were told that identifying the specific defective gene would be impossible. The geneticist advised them that a child conceived with a donor egg and father’s sperm would have essentially the same risk as the general population. The parents asked in writing if it would be safer to
use both donor egg and donor sperm; the geneticist responded that the difference in risk was negligible.
The mother gave birth in June 2007 to a child conceived with a donated egg and the father’s sperm. After the child began to show the same symptoms as the others, an MRI of the child’s brain revealed a thalamic abnormality, and testing revealed Alpers syndrome caused by POLG gene mutations. The third child died in September 2008.
PARENTS’ CLAIM The chances of having a child with Alpers syndrome are
about 1:200,000 in the general population; if one parent is a known carrier, the chance is 1:1,000. If the parents had known this risk, they would have used donor egg and donor sperm to conceive or adopted. They were not told about Alpers syndrome and its relationship to the POLG gene until after their third child was born. The geneticist was negligent in failing to provide this information.
PHYSICIAN’S DEFENSE The parents received appropriate and accurate genetic counseling.
VERDICT A $1 million Florida verdict was returned.
What caused a delay in breast cancer diagnosis?
A 39-year-old woman underwent mammography in October 2004. After recommending a spotcompression film of a left-breast lesion, and then ultrasonography, the radiologist concluded that the lesion was benign, and suggested a 1-year follow-up. Reports were sent to the patient and her primary care physician.
In August 2006, when mammography was suspicious for breast cancer, a biopsy diagnosed infiltrating ductal carcinoma of the left breast. After undergoing a mastectomy, radiation therapy, and chemotherapy, the patient was cancer-free at the time of the trial.
patient’s CLAIM The radiologist failed to properly interpret the 2004 mammography.
physician’s DEFENSE The radiologist’s interpretations of the 2004 tests were correct. The patient failed to follow up in 1 year, as recommended, and this delayed the cancer diagnosis. The patient’s survival indicated that she had been cured of her breast cancer.
VERDICT A confidential settlement was reached with the hospital before the trial. An Illinois defense verdict was returned for the radiologist.
Heparin overdose for preemie
At 27 weeks' gestation, a woman went to a clinic with preeclampsia. After she was stabilized, the baby was born by emergency cesarean delivery.
At birth, the baby was thrombocytopenic (platelet count, 37,000/mL) with a heart rate of 60 bpm. The child’s cord blood pH was 7.27, indicating no significant hypoxia. At 1 minute of life, the child’s heart rate had not improved. After trying three times to place an endotracheal tube, chest compressions were begun at 10 minutes of life. An umbilical vein catheter (UVC) was placed at 22 minutes. Heparin was used to flush the UVC. After 40 minutes, the baby’s pH was 6.88, indicating severe acidosis. The infant was transferred to another hospital 3 hours after birth.
Head ultrasonography at 5 days of life revealed hemorrhagic and ischemic changes in the baby’s brain. The child suffered massive brain damage, is ventilator-dependent, and has a G-tube for feeding. She cannot sit up, walk, or speak, and will require specialized care for life.
Parent's claim Emergency resuscitation was not performed at birth: the low heart rate and thrombocytopenia were not treated; the UVC was not immediately placed. Twice, adult doses of heparin were used instead of normal saline to flush the UVC; heparin caused bleeding in the baby’s brain.
Defendant's Defense The case was settled during trial.
Verdict A $3 million Maryland settlement was reached.
Uterine rupture: $130M verdict
After a woman's first child was born by cesarean delivery, vaginal birth after cesarean (VBAC) was planned for her second pregnancy. When a nurse recognized a ruptured uterus, the ObGyn ordered a cesarean delivery. The newborn suffered severe brain damage, with seizures. She has cerebral palsy with near-normal intelligence, but cannot talk or walk and continues to have seizures.
Parents' claim The baby’s injuries occurred due to a failure to respond to fetal distress. When the intrauterine pressure catheter (IUPC) stopped working for 27 minutes, the nurse did not notify the ObGyn or apply an external monitor. Fetal heart decelerations occurred, including a prolonged deceleration for 3 minutes; the nurse did not notify the ObGyn, reposition the mother, provide oxygen and extra fluids, or discontinue oxytocin. A cesarean delivery should have occurred 30 to 60 minutes earlier.
Defendants' defense The fetal heart rates were what typically occur during the second stage of labor. The hospital’s accepted practices were followed. When the IUPC failed, the nurse measured contractions by hand and analyzed the fetal heartbeat from audible sounds; therefore, it was not necessary to notify the ObGyn. The physician was promptly called when uterine rupture was suspected. Uterine rupture and placental abruption caused the child’s injury. Uterine rupture cannot be predicted or prevented and is a known complication of VBAC.
Verdict After the parents declined an $8 million settlement, the matter was tried to a defense verdict. That decision was overturned on appeal, and, at a second trial, a $130 million New York verdict was returned against the hospital that employed the ObGyn and nurse.
Uterus, small bowel injured during D&C
A 65-year-old woman underwent dilation and curettage (D&C) to screen for uterine cancer performed by an ObGyn and a general surgeon. Her uterus and small intestine were perforated during the procedure, and a second operation was required to repair the damage.
Patient's claim Both physicians were negligent in performing D&C.
Physician's defense The ObGyn denied negligence and countered that the injuries are known complications of the procedure.
Verdict The surgeon settled for a confidential amount before trial. A New Jersey defense verdict was returned for the ObGyn.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
A mother had given birth to two children with thalamic abnormalities that resulted in seizures, developmental delays, and death. Before getting pregnant again, the parents sought genetic counseling and were told that identifying the specific defective gene would be impossible. The geneticist advised them that a child conceived with a donor egg and father’s sperm would have essentially the same risk as the general population. The parents asked in writing if it would be safer to
use both donor egg and donor sperm; the geneticist responded that the difference in risk was negligible.
The mother gave birth in June 2007 to a child conceived with a donated egg and the father’s sperm. After the child began to show the same symptoms as the others, an MRI of the child’s brain revealed a thalamic abnormality, and testing revealed Alpers syndrome caused by POLG gene mutations. The third child died in September 2008.
PARENTS’ CLAIM The chances of having a child with Alpers syndrome are
about 1:200,000 in the general population; if one parent is a known carrier, the chance is 1:1,000. If the parents had known this risk, they would have used donor egg and donor sperm to conceive or adopted. They were not told about Alpers syndrome and its relationship to the POLG gene until after their third child was born. The geneticist was negligent in failing to provide this information.
PHYSICIAN’S DEFENSE The parents received appropriate and accurate genetic counseling.
VERDICT A $1 million Florida verdict was returned.
What caused a delay in breast cancer diagnosis?
A 39-year-old woman underwent mammography in October 2004. After recommending a spotcompression film of a left-breast lesion, and then ultrasonography, the radiologist concluded that the lesion was benign, and suggested a 1-year follow-up. Reports were sent to the patient and her primary care physician.
In August 2006, when mammography was suspicious for breast cancer, a biopsy diagnosed infiltrating ductal carcinoma of the left breast. After undergoing a mastectomy, radiation therapy, and chemotherapy, the patient was cancer-free at the time of the trial.
patient’s CLAIM The radiologist failed to properly interpret the 2004 mammography.
physician’s DEFENSE The radiologist’s interpretations of the 2004 tests were correct. The patient failed to follow up in 1 year, as recommended, and this delayed the cancer diagnosis. The patient’s survival indicated that she had been cured of her breast cancer.
VERDICT A confidential settlement was reached with the hospital before the trial. An Illinois defense verdict was returned for the radiologist.
Heparin overdose for preemie
At 27 weeks' gestation, a woman went to a clinic with preeclampsia. After she was stabilized, the baby was born by emergency cesarean delivery.
At birth, the baby was thrombocytopenic (platelet count, 37,000/mL) with a heart rate of 60 bpm. The child’s cord blood pH was 7.27, indicating no significant hypoxia. At 1 minute of life, the child’s heart rate had not improved. After trying three times to place an endotracheal tube, chest compressions were begun at 10 minutes of life. An umbilical vein catheter (UVC) was placed at 22 minutes. Heparin was used to flush the UVC. After 40 minutes, the baby’s pH was 6.88, indicating severe acidosis. The infant was transferred to another hospital 3 hours after birth.
Head ultrasonography at 5 days of life revealed hemorrhagic and ischemic changes in the baby’s brain. The child suffered massive brain damage, is ventilator-dependent, and has a G-tube for feeding. She cannot sit up, walk, or speak, and will require specialized care for life.
Parent's claim Emergency resuscitation was not performed at birth: the low heart rate and thrombocytopenia were not treated; the UVC was not immediately placed. Twice, adult doses of heparin were used instead of normal saline to flush the UVC; heparin caused bleeding in the baby’s brain.
Defendant's Defense The case was settled during trial.
Verdict A $3 million Maryland settlement was reached.
Uterine rupture: $130M verdict
After a woman's first child was born by cesarean delivery, vaginal birth after cesarean (VBAC) was planned for her second pregnancy. When a nurse recognized a ruptured uterus, the ObGyn ordered a cesarean delivery. The newborn suffered severe brain damage, with seizures. She has cerebral palsy with near-normal intelligence, but cannot talk or walk and continues to have seizures.
Parents' claim The baby’s injuries occurred due to a failure to respond to fetal distress. When the intrauterine pressure catheter (IUPC) stopped working for 27 minutes, the nurse did not notify the ObGyn or apply an external monitor. Fetal heart decelerations occurred, including a prolonged deceleration for 3 minutes; the nurse did not notify the ObGyn, reposition the mother, provide oxygen and extra fluids, or discontinue oxytocin. A cesarean delivery should have occurred 30 to 60 minutes earlier.
Defendants' defense The fetal heart rates were what typically occur during the second stage of labor. The hospital’s accepted practices were followed. When the IUPC failed, the nurse measured contractions by hand and analyzed the fetal heartbeat from audible sounds; therefore, it was not necessary to notify the ObGyn. The physician was promptly called when uterine rupture was suspected. Uterine rupture and placental abruption caused the child’s injury. Uterine rupture cannot be predicted or prevented and is a known complication of VBAC.
Verdict After the parents declined an $8 million settlement, the matter was tried to a defense verdict. That decision was overturned on appeal, and, at a second trial, a $130 million New York verdict was returned against the hospital that employed the ObGyn and nurse.
Uterus, small bowel injured during D&C
A 65-year-old woman underwent dilation and curettage (D&C) to screen for uterine cancer performed by an ObGyn and a general surgeon. Her uterus and small intestine were perforated during the procedure, and a second operation was required to repair the damage.
Patient's claim Both physicians were negligent in performing D&C.
Physician's defense The ObGyn denied negligence and countered that the injuries are known complications of the procedure.
Verdict The surgeon settled for a confidential amount before trial. A New Jersey defense verdict was returned for the ObGyn.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.