User login
The Hospitalist only
CMS modifies the inpatient admission order requirement, or did it?
Ensure inpatient admission orders are completed and signed
When the Centers for Medicare & Medicaid Services make a significant change to the inpatient hospital rules, hospitalists are among the first to feel the effects.
You probably remember that, starting in October 2013, when a resident, nurse practitioner (NP), or physician assistant (PA) entered an inpatient admission order on your behalf, you were told to cosign that order before discharge or the hospital would forfeit payment for the entire stay. This policy was put in place by an annual piece of governmental policy known as the Inpatient Prospective Payment System (IPPS) Final Rule – the same one, in fact, that established the Two Midnight Rule.
The CMS felt that the decision to admit a Medicare beneficiary to inpatient care is such a significant event that it was appropriate to require the attending physician to complete a series of certification requirements to justify every inpatient stay. If not completed and finalized prior to discharge, the CMS would not pay for the stay. After 15 months of enforcing that policy, the CMS backed off on most of the certification requirements for most stays. However, the requirement for an authenticated inpatient order prior to discharge was kept in place for all stays. (“Authenticated” is CMS-speak for signed, or, in the case of inpatient orders initially placed by a resident/NP/PA without admitting privileges, cosigned, by a practitioner with admitting privileges.)
In the spring of 2018, the CMS proposed a change to “revise the admission order documentation requirements by removing the requirement that written inpatient admission orders are a specific requirement for Medicare Part A [inpatient hospital] payment.” The CMS also stated that it did not intend for Medicare auditors to deny hospital inpatient claims based solely on a deficiency in the inpatient order, such as a missing order or one signed after discharge, which the CMS found out was happening.
The description sounded great. In comments to the CMS, many providers assumed that they, too, would be provided similar discretion if they discovered the order defect. Are inpatient orders now optional? What rate of inpatient order technical deficiencies is acceptable to still submit inpatient claims for payment? Can 2-day observation stays where medical necessity for hospital care was present, but no inpatient order given, be billed as an inpatient now?
But these providers had not read the fine print. Consider that the annual IPPS Final Rule has a length of about 2,000 pages. Of those, only about 30 pages represent changes to a group of policies known as the Code of Federal Regulations (CFR). The CFR carries the weight of law (as long as it does not contradict law). When you appeal a Medicare denial to a judge, she will ask what portion of the CFR supports your viewpoint. The other 1,970 pages can be thought of as supporting analysis and reasoning to justify the 30 pages of changes. What changes were actually made to the CFR?
Consider the following two sentences.
- “For purposes of payment under Medicare Part A, an individual is considered an inpatient of a hospital, including a critical access hospital, if formally admitted as an inpatient pursuant to an order for inpatient admission by a physician or other qualified practitioner.”
- “This physician order must be present in the medical record and be supported by the physician admission and progress notes, in order for the hospital to be paid for hospital inpatient services under Medicare Part A.”
These are the first two sentences of 42 CFR 412.3(a), the regulation that defines the inpatient order requirement. On Oct. 1, 2018, the second sentence was removed, but the first sentence still remains. That’s the only change for this section. Does removal of the second sentence absolve providers of the requirement to document inpatient admission orders? Does it absolve providers of the requirement to cosign a resident’s admission order prior to discharge? The Medicare Benefit Policy Manual (MBPM) Chapter 1, Section 10(B) still reads “if the order is not properly documented in the medical record prior to discharge, the hospital should not submit a claim for Part A payment.”
Understanding what changed and what did not change in the CFR is key to understanding why, in this year’s IPPS Final Rule, the CMS repeatedly responded to providers that an inpatient order is still a requirement for a Part A stay and that none of the MBPM guidance regarding the inpatient order, such as the excerpt above, is changing.
At this point, we can only be reasonably certain that if a claim a hospital submits for Part A payment happens to get audited and found to have only one deficiency which is related to the inpatient order, per this guidance it probably won’t get denied. That is very different from saying the attending physician no longer has to provide a signed (or cosigned) inpatient admission order prior to discharge, or at all.
Providers actually did ask the CMS if a hospital could still submit a claim the hospital knows has a missing or incomplete inpatient admission order at the time of discharge. The CMS responded that Medicare contractors have the discretion in extremely rare circumstances to approve cases where an order to admit may be missing or defective, and yet the intent, decision, and recommendation of the ordering practitioner to admit as inpatient can be clearly derived from the medical record. However, note that the discretion belongs to the Medicare contractor, not the provider.
The American College of Physician Advisors (ACPA) asked the CMS the following question about the inpatient order policy change during the 2019 IPPS Final Rule Open Door Forum held on Sept. 11, 2018: “Can providers thus submit a claim, that the provider believes meets all other requirements for Part A payment, in the rare circumstance of an inpatient order deficiency, such as an inpatient order that was cosigned shortly after discharge?”
The CMS declined to answer the question on the call, asking us to submit the question to the Open Door Forum electronic mailbox. If the inpatient order was truly no longer being required for the CMS to pay for inpatient hospital stays, the answer would have been an easy “yes,” but it was not. Subsequently, the CMS responded in writing to the ACPA that “the responsibilities of providers regarding inpatient admission orders is unchanged.” In other words, Medicare auditors have been given discretion to overlook an inpatient order flaw, but providers have not.
At this time, our recommendation is to continue your processes to ensure that the inpatient admission order is completed and signed (or cosigned) prior to discharge by the attending physician for every Medicare patient. This will not only help make sure that the decision to make a hospitalized Medicare beneficiary an inpatient remains with the attending physician, but it will also reduce the risk of nonpayment.
Dr. Hu is executive director of physician advisor services of University of North Carolina Health Care System in Chapel Hill, N.C., and president of the ACPA. Dr. Locke is senior physician advisor at Johns Hopkins Hospital in Baltimore, and president-elect of the ACPA.
Ensure inpatient admission orders are completed and signed
Ensure inpatient admission orders are completed and signed
When the Centers for Medicare & Medicaid Services make a significant change to the inpatient hospital rules, hospitalists are among the first to feel the effects.
You probably remember that, starting in October 2013, when a resident, nurse practitioner (NP), or physician assistant (PA) entered an inpatient admission order on your behalf, you were told to cosign that order before discharge or the hospital would forfeit payment for the entire stay. This policy was put in place by an annual piece of governmental policy known as the Inpatient Prospective Payment System (IPPS) Final Rule – the same one, in fact, that established the Two Midnight Rule.
The CMS felt that the decision to admit a Medicare beneficiary to inpatient care is such a significant event that it was appropriate to require the attending physician to complete a series of certification requirements to justify every inpatient stay. If not completed and finalized prior to discharge, the CMS would not pay for the stay. After 15 months of enforcing that policy, the CMS backed off on most of the certification requirements for most stays. However, the requirement for an authenticated inpatient order prior to discharge was kept in place for all stays. (“Authenticated” is CMS-speak for signed, or, in the case of inpatient orders initially placed by a resident/NP/PA without admitting privileges, cosigned, by a practitioner with admitting privileges.)
In the spring of 2018, the CMS proposed a change to “revise the admission order documentation requirements by removing the requirement that written inpatient admission orders are a specific requirement for Medicare Part A [inpatient hospital] payment.” The CMS also stated that it did not intend for Medicare auditors to deny hospital inpatient claims based solely on a deficiency in the inpatient order, such as a missing order or one signed after discharge, which the CMS found out was happening.
The description sounded great. In comments to the CMS, many providers assumed that they, too, would be provided similar discretion if they discovered the order defect. Are inpatient orders now optional? What rate of inpatient order technical deficiencies is acceptable to still submit inpatient claims for payment? Can 2-day observation stays where medical necessity for hospital care was present, but no inpatient order given, be billed as an inpatient now?
But these providers had not read the fine print. Consider that the annual IPPS Final Rule has a length of about 2,000 pages. Of those, only about 30 pages represent changes to a group of policies known as the Code of Federal Regulations (CFR). The CFR carries the weight of law (as long as it does not contradict law). When you appeal a Medicare denial to a judge, she will ask what portion of the CFR supports your viewpoint. The other 1,970 pages can be thought of as supporting analysis and reasoning to justify the 30 pages of changes. What changes were actually made to the CFR?
Consider the following two sentences.
- “For purposes of payment under Medicare Part A, an individual is considered an inpatient of a hospital, including a critical access hospital, if formally admitted as an inpatient pursuant to an order for inpatient admission by a physician or other qualified practitioner.”
- “This physician order must be present in the medical record and be supported by the physician admission and progress notes, in order for the hospital to be paid for hospital inpatient services under Medicare Part A.”
These are the first two sentences of 42 CFR 412.3(a), the regulation that defines the inpatient order requirement. On Oct. 1, 2018, the second sentence was removed, but the first sentence still remains. That’s the only change for this section. Does removal of the second sentence absolve providers of the requirement to document inpatient admission orders? Does it absolve providers of the requirement to cosign a resident’s admission order prior to discharge? The Medicare Benefit Policy Manual (MBPM) Chapter 1, Section 10(B) still reads “if the order is not properly documented in the medical record prior to discharge, the hospital should not submit a claim for Part A payment.”
Understanding what changed and what did not change in the CFR is key to understanding why, in this year’s IPPS Final Rule, the CMS repeatedly responded to providers that an inpatient order is still a requirement for a Part A stay and that none of the MBPM guidance regarding the inpatient order, such as the excerpt above, is changing.
At this point, we can only be reasonably certain that if a claim a hospital submits for Part A payment happens to get audited and found to have only one deficiency which is related to the inpatient order, per this guidance it probably won’t get denied. That is very different from saying the attending physician no longer has to provide a signed (or cosigned) inpatient admission order prior to discharge, or at all.
Providers actually did ask the CMS if a hospital could still submit a claim the hospital knows has a missing or incomplete inpatient admission order at the time of discharge. The CMS responded that Medicare contractors have the discretion in extremely rare circumstances to approve cases where an order to admit may be missing or defective, and yet the intent, decision, and recommendation of the ordering practitioner to admit as inpatient can be clearly derived from the medical record. However, note that the discretion belongs to the Medicare contractor, not the provider.
The American College of Physician Advisors (ACPA) asked the CMS the following question about the inpatient order policy change during the 2019 IPPS Final Rule Open Door Forum held on Sept. 11, 2018: “Can providers thus submit a claim, that the provider believes meets all other requirements for Part A payment, in the rare circumstance of an inpatient order deficiency, such as an inpatient order that was cosigned shortly after discharge?”
The CMS declined to answer the question on the call, asking us to submit the question to the Open Door Forum electronic mailbox. If the inpatient order was truly no longer being required for the CMS to pay for inpatient hospital stays, the answer would have been an easy “yes,” but it was not. Subsequently, the CMS responded in writing to the ACPA that “the responsibilities of providers regarding inpatient admission orders is unchanged.” In other words, Medicare auditors have been given discretion to overlook an inpatient order flaw, but providers have not.
At this time, our recommendation is to continue your processes to ensure that the inpatient admission order is completed and signed (or cosigned) prior to discharge by the attending physician for every Medicare patient. This will not only help make sure that the decision to make a hospitalized Medicare beneficiary an inpatient remains with the attending physician, but it will also reduce the risk of nonpayment.
Dr. Hu is executive director of physician advisor services of University of North Carolina Health Care System in Chapel Hill, N.C., and president of the ACPA. Dr. Locke is senior physician advisor at Johns Hopkins Hospital in Baltimore, and president-elect of the ACPA.
When the Centers for Medicare & Medicaid Services make a significant change to the inpatient hospital rules, hospitalists are among the first to feel the effects.
You probably remember that, starting in October 2013, when a resident, nurse practitioner (NP), or physician assistant (PA) entered an inpatient admission order on your behalf, you were told to cosign that order before discharge or the hospital would forfeit payment for the entire stay. This policy was put in place by an annual piece of governmental policy known as the Inpatient Prospective Payment System (IPPS) Final Rule – the same one, in fact, that established the Two Midnight Rule.
The CMS felt that the decision to admit a Medicare beneficiary to inpatient care is such a significant event that it was appropriate to require the attending physician to complete a series of certification requirements to justify every inpatient stay. If not completed and finalized prior to discharge, the CMS would not pay for the stay. After 15 months of enforcing that policy, the CMS backed off on most of the certification requirements for most stays. However, the requirement for an authenticated inpatient order prior to discharge was kept in place for all stays. (“Authenticated” is CMS-speak for signed, or, in the case of inpatient orders initially placed by a resident/NP/PA without admitting privileges, cosigned, by a practitioner with admitting privileges.)
In the spring of 2018, the CMS proposed a change to “revise the admission order documentation requirements by removing the requirement that written inpatient admission orders are a specific requirement for Medicare Part A [inpatient hospital] payment.” The CMS also stated that it did not intend for Medicare auditors to deny hospital inpatient claims based solely on a deficiency in the inpatient order, such as a missing order or one signed after discharge, which the CMS found out was happening.
The description sounded great. In comments to the CMS, many providers assumed that they, too, would be provided similar discretion if they discovered the order defect. Are inpatient orders now optional? What rate of inpatient order technical deficiencies is acceptable to still submit inpatient claims for payment? Can 2-day observation stays where medical necessity for hospital care was present, but no inpatient order given, be billed as an inpatient now?
But these providers had not read the fine print. Consider that the annual IPPS Final Rule has a length of about 2,000 pages. Of those, only about 30 pages represent changes to a group of policies known as the Code of Federal Regulations (CFR). The CFR carries the weight of law (as long as it does not contradict law). When you appeal a Medicare denial to a judge, she will ask what portion of the CFR supports your viewpoint. The other 1,970 pages can be thought of as supporting analysis and reasoning to justify the 30 pages of changes. What changes were actually made to the CFR?
Consider the following two sentences.
- “For purposes of payment under Medicare Part A, an individual is considered an inpatient of a hospital, including a critical access hospital, if formally admitted as an inpatient pursuant to an order for inpatient admission by a physician or other qualified practitioner.”
- “This physician order must be present in the medical record and be supported by the physician admission and progress notes, in order for the hospital to be paid for hospital inpatient services under Medicare Part A.”
These are the first two sentences of 42 CFR 412.3(a), the regulation that defines the inpatient order requirement. On Oct. 1, 2018, the second sentence was removed, but the first sentence still remains. That’s the only change for this section. Does removal of the second sentence absolve providers of the requirement to document inpatient admission orders? Does it absolve providers of the requirement to cosign a resident’s admission order prior to discharge? The Medicare Benefit Policy Manual (MBPM) Chapter 1, Section 10(B) still reads “if the order is not properly documented in the medical record prior to discharge, the hospital should not submit a claim for Part A payment.”
Understanding what changed and what did not change in the CFR is key to understanding why, in this year’s IPPS Final Rule, the CMS repeatedly responded to providers that an inpatient order is still a requirement for a Part A stay and that none of the MBPM guidance regarding the inpatient order, such as the excerpt above, is changing.
At this point, we can only be reasonably certain that if a claim a hospital submits for Part A payment happens to get audited and found to have only one deficiency which is related to the inpatient order, per this guidance it probably won’t get denied. That is very different from saying the attending physician no longer has to provide a signed (or cosigned) inpatient admission order prior to discharge, or at all.
Providers actually did ask the CMS if a hospital could still submit a claim the hospital knows has a missing or incomplete inpatient admission order at the time of discharge. The CMS responded that Medicare contractors have the discretion in extremely rare circumstances to approve cases where an order to admit may be missing or defective, and yet the intent, decision, and recommendation of the ordering practitioner to admit as inpatient can be clearly derived from the medical record. However, note that the discretion belongs to the Medicare contractor, not the provider.
The American College of Physician Advisors (ACPA) asked the CMS the following question about the inpatient order policy change during the 2019 IPPS Final Rule Open Door Forum held on Sept. 11, 2018: “Can providers thus submit a claim, that the provider believes meets all other requirements for Part A payment, in the rare circumstance of an inpatient order deficiency, such as an inpatient order that was cosigned shortly after discharge?”
The CMS declined to answer the question on the call, asking us to submit the question to the Open Door Forum electronic mailbox. If the inpatient order was truly no longer being required for the CMS to pay for inpatient hospital stays, the answer would have been an easy “yes,” but it was not. Subsequently, the CMS responded in writing to the ACPA that “the responsibilities of providers regarding inpatient admission orders is unchanged.” In other words, Medicare auditors have been given discretion to overlook an inpatient order flaw, but providers have not.
At this time, our recommendation is to continue your processes to ensure that the inpatient admission order is completed and signed (or cosigned) prior to discharge by the attending physician for every Medicare patient. This will not only help make sure that the decision to make a hospitalized Medicare beneficiary an inpatient remains with the attending physician, but it will also reduce the risk of nonpayment.
Dr. Hu is executive director of physician advisor services of University of North Carolina Health Care System in Chapel Hill, N.C., and president of the ACPA. Dr. Locke is senior physician advisor at Johns Hopkins Hospital in Baltimore, and president-elect of the ACPA.
Hospitalist groups explore use of medical scribes
Can scribes reduce doctors’ job stress?
Physician stress and burnout remain major concerns for the U.S. health care system, with frustrations over the electronic health record (EHR) driving much of the dissatisfaction experienced by hospitalists and other physicians in the hospital.1 Underlying the EHR conundrum is a deeper question: Is entering clinical data on a computer the best use of a doctor’s time and professional skills? Or could a portion of that clerical function be delegated to nonphysicians?
Trained medical scribes, charting specialists who input EHR data for physicians on rounds, have been offered as a solution to potentially affect job stress for physicians and shorten their work days. But while scribes have been used and tested by different hospitalist groups around the country, the concept has not taken off in hospital medicine the way it has in certain other settings, such as emergency departments.
“The demand for scribes doesn’t seem to have materialized in a big way for hospital medicine,” said John Nelson, MD, MHM, a hospitalist and consultant in Bellevue, Wash., and a cofounder of the Society of Hospital Medicine. “I’m not convinced that scribes have had a big impact on hospitalist burnout.” It’s difficult to share scribes between doctors on a shift, and it’s a problem if the scribe and doctor get physically separated in the hospital. There’s also the question of who should pay the scribe’s salary, Dr. Nelson said.
Frustrations with the EHR can be a major factor in the experience of physician burnout, but Dr. Nelson said hospitalists can get proficient more quickly because they’re using the same computer system all day. “The bigger problem is that other doctors like surgeons don’t learn how to use the EHR and dump their routine tasks involving the EHR on the hospitalist, which means more work that is less satisfying.”
Could pairing a scribe with a hospitalist improve efficiency and decrease costs relative to the expense of employing the scribe? Are there specific settings, applications, and caseloads in hospital medicine where it makes more sense to use a scribe to support and assist doctors while they’re meeting with patients, with the doctor reviewing and editing the scribe’s work for accuracy? Could the scribe even help with physician staffing shortages by making doctors more productive?
TeamHealth, a national physician services company based in Knoxville, Tenn., has used scribes in emergency departments for years but had concluded that they made less sense for its hospitalist groups after a failure to document significant net increases in productivity, according to a 2015 report in The Hospitalist.2 Michael Corvini, MD, FACP, FACEP, TeamHealth’s new regional medical director for acute care services, said he brought extensive positive experience with scribes to his new job and is quite excited about their potential for hospital medicine. “When I came to TeamHealth in July, I began to suggest that there was unrealized potential for scribes,” he said.
Dr. Corvini noted that a potential benefit of scribes for patients is that their presence may allow for more face time with the doctor. Providers, relieved of worrying about completing the chart in its entirety would be more able to focus on the patient and critical thinking. There are even benefits for scribes themselves. Often scribes are medical students, and those who are interested in pursuing a future in the health professions gain invaluable experience in the workings of medicine. “They are making a real contribution to patient care. They are a member of the health care team,” he said.
Dr. Corvini sees two primary areas in which scribes can contribute to hospital medicine. The first is shadowing the physician who is admitting patients during a high-volume admissions shift. Regular tasks like capturing the patient’s medication list and populating the History and Physical document lend themselves well to data entry by scribes, in contrast to completing more routine daily progress notes, which does not.
“They can also be helpful when there is a major transition from paper charting to the EHR or from one EHR system to another, when there is a lot of stress on the physician and risk for lost billing revenue,” Dr. Corvini said. “If scribes are trained in a particular EHR, they could help teach the physician how to use it.” TeamHealth is now in the process of running a trial of scribes at one of its sites, and the organization plans to measure productivity, provider satisfaction, and HCAHPS patient satisfaction scores.
A workaround – or a problem solver?
In a 2015 Viewpoint article in JAMA,3 George Gellert, MD, MPH, MPA, former chief medical information officer for the CHRISTUS Santa Rosa health system in San Antonio, Texas, and his coauthors labeled the use of scribes as a “workaround” that could curtail efforts to make EHRs more functionally operational because their use allows physicians to be satisfied with inferior EHR products.
In an interview, Dr. Gellert stated that he hasn’t changed his views about the negative consequences of scribes on EHR improvement. “The work of clinicians in using and advancing EHR technology is presently the only method we have for massively distributing and ensuring the use of evidence-based medicine,” he said. “That in turn is a critical strategy for reducing high rates of medical errors through a variety of decision-support applications.”
For better or worse, EHRs are an essential part of the solution to the epidemic of preventable, medical error–caused patient deaths, Dr. Gellert said. He also believes that substantial progress has already been made in advancing EHR usability, as reflected in the most recent product releases by leading EHR companies. However, considerable evolution is still needed in both usability and optimization of clinical decision support.
“With respect to your readers, my recommendation is to not use medical scribes, or else delimit their use to only where absolutely required. Instead, develop systematic processes to regularly capture specific physician concerns with the EHR being used, and transmit that critical information to their EHR vendor with a clear expectation that the manufacturer will address the issue in the near term, or at least in their next major product iteration or generation,” Dr. Gellert said.
By contrast, at the Management of the Hospitalized Patient conference in San Francisco in October 2015, Christine Sinsky, MD, FACP, vice president for professional satisfaction at the American Medical Association, identified documentation assistance as a helpful intervention for physician stress and burnout.4 In a recent email, Dr. Sinsky called documentation assistance “the most powerful intervention to give patients the time, attention, and care they need from their physicians. The data entry and data retrieval work of health care has grown over the last decade. Sharing this work with nonphysicians allows society to get the most value for its investment in physicians’ training.”
Dr. Sinsky calls documentation assistance – such as that provided by medical scribes – “a logical and strategic delegation of work according to ability for greater value,” not a workaround. She said it makes patient care safer by allowing physicians to focus on medical decision making and relationship building – rather than record keeping.
Experience from the front lines
Eric Edwards, MD, FAAP, FHM, of the division of hospital medicine at the University of North Carolina’s Hillsborough Hospital campus, recently presented a poster on his group’s experience with medical scribes at a meeting of the North Carolina Triangle Chapter of SHM. Their research concluded that scribes can be successfully incorporated into an inpatient hospital medicine practice and thus increase provider satisfaction and decrease the time clinicians spend charting.
“We were able to get the support of the hospital administration to pilot the use of scribes 3 days per week, which we’ve now done for almost a year,” Dr. Edwards said. Scribes are employed through a local company, MedScribes, and they work alongside admitting hospitalists during their 10-hour shifts. The hospitalists have been overwhelmingly positive about their experience, he said. “We established that it saves the physician 15 minutes per patient encounter by helping with documentation.”
It’s important that the scribe gets to know an individual provider’s personal preferences, Dr. Edwards said. Some hospitalists create their own charting templates. There’s also a need to train the clinician in how to use the medical scribe. For example, physicians are instructed to call out physical findings during their exam, which simultaneously informs the patient while allowing the scribe to document the exam.
“We are working on getting more formal data about the scribe experience,” he added. “But we have found that our providers love it, and it improves their efficiency and productivity. The danger is if the physician becomes too reliant on the scribe and fails to exercise due diligence in reviewing the scribe’s notes to ensure that all relevant information is in the chart and irrelevant information is not. We need to make sure we are carefully reviewing and signing off on the scribe’s notes,” he explained.
“I think we’re years away from improving the EHR to the point that would allow us to call it doctor friendly,” Dr. Edwards said. “For now, the scribe is a great way to alleviate some of the physician’s burden. But for hospitalist groups to use scribes successfully, it can’t be done haphazardly. We are lucky to have an experienced local scribe company to partner with. They provide systematic training and orientation. It’s also important that scribes are trained in the specific EHR that they will be using.”
Christine Lum Lung, MD, SFHM, CEO and medical director of Northern Colorado Hospitalists, a hospital medicine group at the University of Colorado’s North Campus hospitals in Fort Collins, has been studying the use of scribes since 2014. “We had a gap in bringing on new doctors fast enough for our group’s needs, so I looked into the return on investment from scribes and pitched it to our group,” she said. “It’s difficult to say what has been the actual impact on caseload, but we all think it has reduced physician workdays by an hour or greater.”
The 32-member hospitalist group, which covers two facilities, has a designated director of scribes who periodically surveys the hospitalists’ satisfaction with the scribes. “Now we all embrace the use of scribes. Satisfaction is high, and quality of life has improved,” Dr. Lum Lung said. “It’s hard to quantify, but we feel like it helps with burnout for us to be able to leave work earlier, and it alleviates some of the other stresses in our workday.”
She said scribes are important to the medical team not just with managing the EHR but also with other burdens such as documenting compliance with code status, VTEs, and other quality requirements, and to help with other regulatory issues. Scribes can look up lab values and radiology reports. When there are downtimes, they can prepare discharge plans.
Typically, there are five scribes on duty for 18 hours a day at each hospital, Dr. Lum Lung said. But only those doctors primarily doing admissions are assured of having a scribe to round with them. “Most doctors in the group would say the greatest efficiency of scribes is with admitting,” she said. The company that provides scribes to the UC hospitals, ScribeAmerica, handles administration, training, and human resource issues, and the scribe team has a designated Lead Scribe and Quality Scribe at their facility.
Studying the benefits
Andrew Friedson, PhD, a health care economist at the University of Colorado in Denver, recently conducted a 9-month randomized experiment in three hospital emergency rooms in the Denver area to determine the effects of scribes on measures of emergency physician productivity.5 He found that scribes reduced patient wait times in the emergency department by about 13 minutes per patient, while greatly decreasing the amount of time physicians spent after a shift completing their charting, which thus lowered overtime costs for ED physicians.
“This is one of the first times medical scribes have been studied with a randomized, controlled trial,” Dr. Friedson said. “I tracked the amount of overtime, patient waiting, and charge capture for each encounter. These were hospitals where the emergency doctors weren’t allowed to go home until their charting was done.” He discovered that there was a large drop in the time between when patients arrived at the ED and when a decision was made regarding whether to admit them. Additionally, charge capture increased significantly, and physicians had more time to perform medical procedures. Dr. Friedson believes that his findings hold implications for other settings and medical groups, including hospital medicine. To the extent that scribes free up hospitalists to perform tasks other than charting, they should provide an efficiency benefit.
So why hasn’t the medical scribe caught on in a bigger way for hospitalists, compared with ED physicians? For Dr. Corvini, the ED is an obvious, high-pressure, high-volume setting where the cost of the scribe can be easily recouped. “That doesn’t exist in such an obvious fashion in hospital medicine, except where high-volume admissions are concentrated in a single physician’s caseload,” he said. Not all hospitalist groups will fit that model. Some may divide admissions between hospitalists on a shift, and others may not be large enough to experience significant caseload pressures.
“EDs are obviously time pressured, and once scribes demonstrate the ability to produce documentation in a high-quality fashion, they are quickly accepted. In hospital medicine, the time pressures are different – not necessarily less, but different,” Dr. Corvini said. There are also differences in physician responsibilities between the ED and hospital medicine, as well as in physicians’ willingness to let go of documentation responsibilities. “My prediction, if the scribe test is rolled out successfully in TeamHealth, with measurable benefits, it will be adopted in other settings where it fits.”
References
1. Shanafelt TD et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016 Jul;91(7):836-48.
2. Collins TR. Use of medical scribes spurs debate about costs, difficulties of electronic health records. The Hospitalist; 2015 Oct.
3. Gellert GA et al. The rise of the medical scribe industry: Implications for the advancement of electronic health records. JAMA; 2015;313(13):1315-6.
4. Beresford L. Electronic Health Records Key Driver of Physician Burnout. The Hospitalist; 2015 Dec.
5. Friedson AI. Medical scribes as an input in healthcare production: Evidence from a randomized experiment. Am J Health Econ. 2017 Oct 2. doi: /10.1162/ajhe_a_00103.
Can scribes reduce doctors’ job stress?
Can scribes reduce doctors’ job stress?
Physician stress and burnout remain major concerns for the U.S. health care system, with frustrations over the electronic health record (EHR) driving much of the dissatisfaction experienced by hospitalists and other physicians in the hospital.1 Underlying the EHR conundrum is a deeper question: Is entering clinical data on a computer the best use of a doctor’s time and professional skills? Or could a portion of that clerical function be delegated to nonphysicians?
Trained medical scribes, charting specialists who input EHR data for physicians on rounds, have been offered as a solution to potentially affect job stress for physicians and shorten their work days. But while scribes have been used and tested by different hospitalist groups around the country, the concept has not taken off in hospital medicine the way it has in certain other settings, such as emergency departments.
“The demand for scribes doesn’t seem to have materialized in a big way for hospital medicine,” said John Nelson, MD, MHM, a hospitalist and consultant in Bellevue, Wash., and a cofounder of the Society of Hospital Medicine. “I’m not convinced that scribes have had a big impact on hospitalist burnout.” It’s difficult to share scribes between doctors on a shift, and it’s a problem if the scribe and doctor get physically separated in the hospital. There’s also the question of who should pay the scribe’s salary, Dr. Nelson said.
Frustrations with the EHR can be a major factor in the experience of physician burnout, but Dr. Nelson said hospitalists can get proficient more quickly because they’re using the same computer system all day. “The bigger problem is that other doctors like surgeons don’t learn how to use the EHR and dump their routine tasks involving the EHR on the hospitalist, which means more work that is less satisfying.”
Could pairing a scribe with a hospitalist improve efficiency and decrease costs relative to the expense of employing the scribe? Are there specific settings, applications, and caseloads in hospital medicine where it makes more sense to use a scribe to support and assist doctors while they’re meeting with patients, with the doctor reviewing and editing the scribe’s work for accuracy? Could the scribe even help with physician staffing shortages by making doctors more productive?
TeamHealth, a national physician services company based in Knoxville, Tenn., has used scribes in emergency departments for years but had concluded that they made less sense for its hospitalist groups after a failure to document significant net increases in productivity, according to a 2015 report in The Hospitalist.2 Michael Corvini, MD, FACP, FACEP, TeamHealth’s new regional medical director for acute care services, said he brought extensive positive experience with scribes to his new job and is quite excited about their potential for hospital medicine. “When I came to TeamHealth in July, I began to suggest that there was unrealized potential for scribes,” he said.
Dr. Corvini noted that a potential benefit of scribes for patients is that their presence may allow for more face time with the doctor. Providers, relieved of worrying about completing the chart in its entirety would be more able to focus on the patient and critical thinking. There are even benefits for scribes themselves. Often scribes are medical students, and those who are interested in pursuing a future in the health professions gain invaluable experience in the workings of medicine. “They are making a real contribution to patient care. They are a member of the health care team,” he said.
Dr. Corvini sees two primary areas in which scribes can contribute to hospital medicine. The first is shadowing the physician who is admitting patients during a high-volume admissions shift. Regular tasks like capturing the patient’s medication list and populating the History and Physical document lend themselves well to data entry by scribes, in contrast to completing more routine daily progress notes, which does not.
“They can also be helpful when there is a major transition from paper charting to the EHR or from one EHR system to another, when there is a lot of stress on the physician and risk for lost billing revenue,” Dr. Corvini said. “If scribes are trained in a particular EHR, they could help teach the physician how to use it.” TeamHealth is now in the process of running a trial of scribes at one of its sites, and the organization plans to measure productivity, provider satisfaction, and HCAHPS patient satisfaction scores.
A workaround – or a problem solver?
In a 2015 Viewpoint article in JAMA,3 George Gellert, MD, MPH, MPA, former chief medical information officer for the CHRISTUS Santa Rosa health system in San Antonio, Texas, and his coauthors labeled the use of scribes as a “workaround” that could curtail efforts to make EHRs more functionally operational because their use allows physicians to be satisfied with inferior EHR products.
In an interview, Dr. Gellert stated that he hasn’t changed his views about the negative consequences of scribes on EHR improvement. “The work of clinicians in using and advancing EHR technology is presently the only method we have for massively distributing and ensuring the use of evidence-based medicine,” he said. “That in turn is a critical strategy for reducing high rates of medical errors through a variety of decision-support applications.”
For better or worse, EHRs are an essential part of the solution to the epidemic of preventable, medical error–caused patient deaths, Dr. Gellert said. He also believes that substantial progress has already been made in advancing EHR usability, as reflected in the most recent product releases by leading EHR companies. However, considerable evolution is still needed in both usability and optimization of clinical decision support.
“With respect to your readers, my recommendation is to not use medical scribes, or else delimit their use to only where absolutely required. Instead, develop systematic processes to regularly capture specific physician concerns with the EHR being used, and transmit that critical information to their EHR vendor with a clear expectation that the manufacturer will address the issue in the near term, or at least in their next major product iteration or generation,” Dr. Gellert said.
By contrast, at the Management of the Hospitalized Patient conference in San Francisco in October 2015, Christine Sinsky, MD, FACP, vice president for professional satisfaction at the American Medical Association, identified documentation assistance as a helpful intervention for physician stress and burnout.4 In a recent email, Dr. Sinsky called documentation assistance “the most powerful intervention to give patients the time, attention, and care they need from their physicians. The data entry and data retrieval work of health care has grown over the last decade. Sharing this work with nonphysicians allows society to get the most value for its investment in physicians’ training.”
Dr. Sinsky calls documentation assistance – such as that provided by medical scribes – “a logical and strategic delegation of work according to ability for greater value,” not a workaround. She said it makes patient care safer by allowing physicians to focus on medical decision making and relationship building – rather than record keeping.
Experience from the front lines
Eric Edwards, MD, FAAP, FHM, of the division of hospital medicine at the University of North Carolina’s Hillsborough Hospital campus, recently presented a poster on his group’s experience with medical scribes at a meeting of the North Carolina Triangle Chapter of SHM. Their research concluded that scribes can be successfully incorporated into an inpatient hospital medicine practice and thus increase provider satisfaction and decrease the time clinicians spend charting.
“We were able to get the support of the hospital administration to pilot the use of scribes 3 days per week, which we’ve now done for almost a year,” Dr. Edwards said. Scribes are employed through a local company, MedScribes, and they work alongside admitting hospitalists during their 10-hour shifts. The hospitalists have been overwhelmingly positive about their experience, he said. “We established that it saves the physician 15 minutes per patient encounter by helping with documentation.”
It’s important that the scribe gets to know an individual provider’s personal preferences, Dr. Edwards said. Some hospitalists create their own charting templates. There’s also a need to train the clinician in how to use the medical scribe. For example, physicians are instructed to call out physical findings during their exam, which simultaneously informs the patient while allowing the scribe to document the exam.
“We are working on getting more formal data about the scribe experience,” he added. “But we have found that our providers love it, and it improves their efficiency and productivity. The danger is if the physician becomes too reliant on the scribe and fails to exercise due diligence in reviewing the scribe’s notes to ensure that all relevant information is in the chart and irrelevant information is not. We need to make sure we are carefully reviewing and signing off on the scribe’s notes,” he explained.
“I think we’re years away from improving the EHR to the point that would allow us to call it doctor friendly,” Dr. Edwards said. “For now, the scribe is a great way to alleviate some of the physician’s burden. But for hospitalist groups to use scribes successfully, it can’t be done haphazardly. We are lucky to have an experienced local scribe company to partner with. They provide systematic training and orientation. It’s also important that scribes are trained in the specific EHR that they will be using.”
Christine Lum Lung, MD, SFHM, CEO and medical director of Northern Colorado Hospitalists, a hospital medicine group at the University of Colorado’s North Campus hospitals in Fort Collins, has been studying the use of scribes since 2014. “We had a gap in bringing on new doctors fast enough for our group’s needs, so I looked into the return on investment from scribes and pitched it to our group,” she said. “It’s difficult to say what has been the actual impact on caseload, but we all think it has reduced physician workdays by an hour or greater.”
The 32-member hospitalist group, which covers two facilities, has a designated director of scribes who periodically surveys the hospitalists’ satisfaction with the scribes. “Now we all embrace the use of scribes. Satisfaction is high, and quality of life has improved,” Dr. Lum Lung said. “It’s hard to quantify, but we feel like it helps with burnout for us to be able to leave work earlier, and it alleviates some of the other stresses in our workday.”
She said scribes are important to the medical team not just with managing the EHR but also with other burdens such as documenting compliance with code status, VTEs, and other quality requirements, and to help with other regulatory issues. Scribes can look up lab values and radiology reports. When there are downtimes, they can prepare discharge plans.
Typically, there are five scribes on duty for 18 hours a day at each hospital, Dr. Lum Lung said. But only those doctors primarily doing admissions are assured of having a scribe to round with them. “Most doctors in the group would say the greatest efficiency of scribes is with admitting,” she said. The company that provides scribes to the UC hospitals, ScribeAmerica, handles administration, training, and human resource issues, and the scribe team has a designated Lead Scribe and Quality Scribe at their facility.
Studying the benefits
Andrew Friedson, PhD, a health care economist at the University of Colorado in Denver, recently conducted a 9-month randomized experiment in three hospital emergency rooms in the Denver area to determine the effects of scribes on measures of emergency physician productivity.5 He found that scribes reduced patient wait times in the emergency department by about 13 minutes per patient, while greatly decreasing the amount of time physicians spent after a shift completing their charting, which thus lowered overtime costs for ED physicians.
“This is one of the first times medical scribes have been studied with a randomized, controlled trial,” Dr. Friedson said. “I tracked the amount of overtime, patient waiting, and charge capture for each encounter. These were hospitals where the emergency doctors weren’t allowed to go home until their charting was done.” He discovered that there was a large drop in the time between when patients arrived at the ED and when a decision was made regarding whether to admit them. Additionally, charge capture increased significantly, and physicians had more time to perform medical procedures. Dr. Friedson believes that his findings hold implications for other settings and medical groups, including hospital medicine. To the extent that scribes free up hospitalists to perform tasks other than charting, they should provide an efficiency benefit.
So why hasn’t the medical scribe caught on in a bigger way for hospitalists, compared with ED physicians? For Dr. Corvini, the ED is an obvious, high-pressure, high-volume setting where the cost of the scribe can be easily recouped. “That doesn’t exist in such an obvious fashion in hospital medicine, except where high-volume admissions are concentrated in a single physician’s caseload,” he said. Not all hospitalist groups will fit that model. Some may divide admissions between hospitalists on a shift, and others may not be large enough to experience significant caseload pressures.
“EDs are obviously time pressured, and once scribes demonstrate the ability to produce documentation in a high-quality fashion, they are quickly accepted. In hospital medicine, the time pressures are different – not necessarily less, but different,” Dr. Corvini said. There are also differences in physician responsibilities between the ED and hospital medicine, as well as in physicians’ willingness to let go of documentation responsibilities. “My prediction, if the scribe test is rolled out successfully in TeamHealth, with measurable benefits, it will be adopted in other settings where it fits.”
References
1. Shanafelt TD et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016 Jul;91(7):836-48.
2. Collins TR. Use of medical scribes spurs debate about costs, difficulties of electronic health records. The Hospitalist; 2015 Oct.
3. Gellert GA et al. The rise of the medical scribe industry: Implications for the advancement of electronic health records. JAMA; 2015;313(13):1315-6.
4. Beresford L. Electronic Health Records Key Driver of Physician Burnout. The Hospitalist; 2015 Dec.
5. Friedson AI. Medical scribes as an input in healthcare production: Evidence from a randomized experiment. Am J Health Econ. 2017 Oct 2. doi: /10.1162/ajhe_a_00103.
Physician stress and burnout remain major concerns for the U.S. health care system, with frustrations over the electronic health record (EHR) driving much of the dissatisfaction experienced by hospitalists and other physicians in the hospital.1 Underlying the EHR conundrum is a deeper question: Is entering clinical data on a computer the best use of a doctor’s time and professional skills? Or could a portion of that clerical function be delegated to nonphysicians?
Trained medical scribes, charting specialists who input EHR data for physicians on rounds, have been offered as a solution to potentially affect job stress for physicians and shorten their work days. But while scribes have been used and tested by different hospitalist groups around the country, the concept has not taken off in hospital medicine the way it has in certain other settings, such as emergency departments.
“The demand for scribes doesn’t seem to have materialized in a big way for hospital medicine,” said John Nelson, MD, MHM, a hospitalist and consultant in Bellevue, Wash., and a cofounder of the Society of Hospital Medicine. “I’m not convinced that scribes have had a big impact on hospitalist burnout.” It’s difficult to share scribes between doctors on a shift, and it’s a problem if the scribe and doctor get physically separated in the hospital. There’s also the question of who should pay the scribe’s salary, Dr. Nelson said.
Frustrations with the EHR can be a major factor in the experience of physician burnout, but Dr. Nelson said hospitalists can get proficient more quickly because they’re using the same computer system all day. “The bigger problem is that other doctors like surgeons don’t learn how to use the EHR and dump their routine tasks involving the EHR on the hospitalist, which means more work that is less satisfying.”
Could pairing a scribe with a hospitalist improve efficiency and decrease costs relative to the expense of employing the scribe? Are there specific settings, applications, and caseloads in hospital medicine where it makes more sense to use a scribe to support and assist doctors while they’re meeting with patients, with the doctor reviewing and editing the scribe’s work for accuracy? Could the scribe even help with physician staffing shortages by making doctors more productive?
TeamHealth, a national physician services company based in Knoxville, Tenn., has used scribes in emergency departments for years but had concluded that they made less sense for its hospitalist groups after a failure to document significant net increases in productivity, according to a 2015 report in The Hospitalist.2 Michael Corvini, MD, FACP, FACEP, TeamHealth’s new regional medical director for acute care services, said he brought extensive positive experience with scribes to his new job and is quite excited about their potential for hospital medicine. “When I came to TeamHealth in July, I began to suggest that there was unrealized potential for scribes,” he said.
Dr. Corvini noted that a potential benefit of scribes for patients is that their presence may allow for more face time with the doctor. Providers, relieved of worrying about completing the chart in its entirety would be more able to focus on the patient and critical thinking. There are even benefits for scribes themselves. Often scribes are medical students, and those who are interested in pursuing a future in the health professions gain invaluable experience in the workings of medicine. “They are making a real contribution to patient care. They are a member of the health care team,” he said.
Dr. Corvini sees two primary areas in which scribes can contribute to hospital medicine. The first is shadowing the physician who is admitting patients during a high-volume admissions shift. Regular tasks like capturing the patient’s medication list and populating the History and Physical document lend themselves well to data entry by scribes, in contrast to completing more routine daily progress notes, which does not.
“They can also be helpful when there is a major transition from paper charting to the EHR or from one EHR system to another, when there is a lot of stress on the physician and risk for lost billing revenue,” Dr. Corvini said. “If scribes are trained in a particular EHR, they could help teach the physician how to use it.” TeamHealth is now in the process of running a trial of scribes at one of its sites, and the organization plans to measure productivity, provider satisfaction, and HCAHPS patient satisfaction scores.
A workaround – or a problem solver?
In a 2015 Viewpoint article in JAMA,3 George Gellert, MD, MPH, MPA, former chief medical information officer for the CHRISTUS Santa Rosa health system in San Antonio, Texas, and his coauthors labeled the use of scribes as a “workaround” that could curtail efforts to make EHRs more functionally operational because their use allows physicians to be satisfied with inferior EHR products.
In an interview, Dr. Gellert stated that he hasn’t changed his views about the negative consequences of scribes on EHR improvement. “The work of clinicians in using and advancing EHR technology is presently the only method we have for massively distributing and ensuring the use of evidence-based medicine,” he said. “That in turn is a critical strategy for reducing high rates of medical errors through a variety of decision-support applications.”
For better or worse, EHRs are an essential part of the solution to the epidemic of preventable, medical error–caused patient deaths, Dr. Gellert said. He also believes that substantial progress has already been made in advancing EHR usability, as reflected in the most recent product releases by leading EHR companies. However, considerable evolution is still needed in both usability and optimization of clinical decision support.
“With respect to your readers, my recommendation is to not use medical scribes, or else delimit their use to only where absolutely required. Instead, develop systematic processes to regularly capture specific physician concerns with the EHR being used, and transmit that critical information to their EHR vendor with a clear expectation that the manufacturer will address the issue in the near term, or at least in their next major product iteration or generation,” Dr. Gellert said.
By contrast, at the Management of the Hospitalized Patient conference in San Francisco in October 2015, Christine Sinsky, MD, FACP, vice president for professional satisfaction at the American Medical Association, identified documentation assistance as a helpful intervention for physician stress and burnout.4 In a recent email, Dr. Sinsky called documentation assistance “the most powerful intervention to give patients the time, attention, and care they need from their physicians. The data entry and data retrieval work of health care has grown over the last decade. Sharing this work with nonphysicians allows society to get the most value for its investment in physicians’ training.”
Dr. Sinsky calls documentation assistance – such as that provided by medical scribes – “a logical and strategic delegation of work according to ability for greater value,” not a workaround. She said it makes patient care safer by allowing physicians to focus on medical decision making and relationship building – rather than record keeping.
Experience from the front lines
Eric Edwards, MD, FAAP, FHM, of the division of hospital medicine at the University of North Carolina’s Hillsborough Hospital campus, recently presented a poster on his group’s experience with medical scribes at a meeting of the North Carolina Triangle Chapter of SHM. Their research concluded that scribes can be successfully incorporated into an inpatient hospital medicine practice and thus increase provider satisfaction and decrease the time clinicians spend charting.
“We were able to get the support of the hospital administration to pilot the use of scribes 3 days per week, which we’ve now done for almost a year,” Dr. Edwards said. Scribes are employed through a local company, MedScribes, and they work alongside admitting hospitalists during their 10-hour shifts. The hospitalists have been overwhelmingly positive about their experience, he said. “We established that it saves the physician 15 minutes per patient encounter by helping with documentation.”
It’s important that the scribe gets to know an individual provider’s personal preferences, Dr. Edwards said. Some hospitalists create their own charting templates. There’s also a need to train the clinician in how to use the medical scribe. For example, physicians are instructed to call out physical findings during their exam, which simultaneously informs the patient while allowing the scribe to document the exam.
“We are working on getting more formal data about the scribe experience,” he added. “But we have found that our providers love it, and it improves their efficiency and productivity. The danger is if the physician becomes too reliant on the scribe and fails to exercise due diligence in reviewing the scribe’s notes to ensure that all relevant information is in the chart and irrelevant information is not. We need to make sure we are carefully reviewing and signing off on the scribe’s notes,” he explained.
“I think we’re years away from improving the EHR to the point that would allow us to call it doctor friendly,” Dr. Edwards said. “For now, the scribe is a great way to alleviate some of the physician’s burden. But for hospitalist groups to use scribes successfully, it can’t be done haphazardly. We are lucky to have an experienced local scribe company to partner with. They provide systematic training and orientation. It’s also important that scribes are trained in the specific EHR that they will be using.”
Christine Lum Lung, MD, SFHM, CEO and medical director of Northern Colorado Hospitalists, a hospital medicine group at the University of Colorado’s North Campus hospitals in Fort Collins, has been studying the use of scribes since 2014. “We had a gap in bringing on new doctors fast enough for our group’s needs, so I looked into the return on investment from scribes and pitched it to our group,” she said. “It’s difficult to say what has been the actual impact on caseload, but we all think it has reduced physician workdays by an hour or greater.”
The 32-member hospitalist group, which covers two facilities, has a designated director of scribes who periodically surveys the hospitalists’ satisfaction with the scribes. “Now we all embrace the use of scribes. Satisfaction is high, and quality of life has improved,” Dr. Lum Lung said. “It’s hard to quantify, but we feel like it helps with burnout for us to be able to leave work earlier, and it alleviates some of the other stresses in our workday.”
She said scribes are important to the medical team not just with managing the EHR but also with other burdens such as documenting compliance with code status, VTEs, and other quality requirements, and to help with other regulatory issues. Scribes can look up lab values and radiology reports. When there are downtimes, they can prepare discharge plans.
Typically, there are five scribes on duty for 18 hours a day at each hospital, Dr. Lum Lung said. But only those doctors primarily doing admissions are assured of having a scribe to round with them. “Most doctors in the group would say the greatest efficiency of scribes is with admitting,” she said. The company that provides scribes to the UC hospitals, ScribeAmerica, handles administration, training, and human resource issues, and the scribe team has a designated Lead Scribe and Quality Scribe at their facility.
Studying the benefits
Andrew Friedson, PhD, a health care economist at the University of Colorado in Denver, recently conducted a 9-month randomized experiment in three hospital emergency rooms in the Denver area to determine the effects of scribes on measures of emergency physician productivity.5 He found that scribes reduced patient wait times in the emergency department by about 13 minutes per patient, while greatly decreasing the amount of time physicians spent after a shift completing their charting, which thus lowered overtime costs for ED physicians.
“This is one of the first times medical scribes have been studied with a randomized, controlled trial,” Dr. Friedson said. “I tracked the amount of overtime, patient waiting, and charge capture for each encounter. These were hospitals where the emergency doctors weren’t allowed to go home until their charting was done.” He discovered that there was a large drop in the time between when patients arrived at the ED and when a decision was made regarding whether to admit them. Additionally, charge capture increased significantly, and physicians had more time to perform medical procedures. Dr. Friedson believes that his findings hold implications for other settings and medical groups, including hospital medicine. To the extent that scribes free up hospitalists to perform tasks other than charting, they should provide an efficiency benefit.
So why hasn’t the medical scribe caught on in a bigger way for hospitalists, compared with ED physicians? For Dr. Corvini, the ED is an obvious, high-pressure, high-volume setting where the cost of the scribe can be easily recouped. “That doesn’t exist in such an obvious fashion in hospital medicine, except where high-volume admissions are concentrated in a single physician’s caseload,” he said. Not all hospitalist groups will fit that model. Some may divide admissions between hospitalists on a shift, and others may not be large enough to experience significant caseload pressures.
“EDs are obviously time pressured, and once scribes demonstrate the ability to produce documentation in a high-quality fashion, they are quickly accepted. In hospital medicine, the time pressures are different – not necessarily less, but different,” Dr. Corvini said. There are also differences in physician responsibilities between the ED and hospital medicine, as well as in physicians’ willingness to let go of documentation responsibilities. “My prediction, if the scribe test is rolled out successfully in TeamHealth, with measurable benefits, it will be adopted in other settings where it fits.”
References
1. Shanafelt TD et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016 Jul;91(7):836-48.
2. Collins TR. Use of medical scribes spurs debate about costs, difficulties of electronic health records. The Hospitalist; 2015 Oct.
3. Gellert GA et al. The rise of the medical scribe industry: Implications for the advancement of electronic health records. JAMA; 2015;313(13):1315-6.
4. Beresford L. Electronic Health Records Key Driver of Physician Burnout. The Hospitalist; 2015 Dec.
5. Friedson AI. Medical scribes as an input in healthcare production: Evidence from a randomized experiment. Am J Health Econ. 2017 Oct 2. doi: /10.1162/ajhe_a_00103.
Guideline authors inconsistently disclose conflicts
Financial conflicts are often underreported by authors of clinical practice guidelines (CPGs) in several specialties including oncology, rheumatology, and gastroenterology, according to a pair of research letters published in JAMA Internal Medicine. The Institute of Medicine recommends that guideline authors include no more than 50% individuals with financial conflicts.
In one research letter, Rishad Khan, BSc, of the University of Toronto in Ontario and his colleagues reviewed data on undeclared financial conflicts of interest among authors of guidelines related to high-revenue medications.
The researchers identified CPGs via the National Guideline Clearinghouse and selected 18 CPGs for 10 high-revenue medications published between 2013 and 2017. Financial conflicts of interest were based on the Centers for Medicare & Medicaid Services Open Payments.
Of the 160 authors involved in the various guidelines, 79 (49.4%) disclosed a payment in the CPG or supplemental materials, and 50 (31.3%) disclosed payments from companies marketing 1 of the 10 high-revenue medications in the related guidelines.
Another 41 authors (25.6%) received but did not disclose payments from companies marketing 1 of the 10 high-revenue medications in CPGs.
Overall, 91 authors (56.9%) were found to have financial conflicts of interest that involved 1 of the 10 high-revenue medications, and “the median value of undeclared payments from companies marketing 1 of the 10 high-revenue medications recommended in the CPGs was $522 (interquartile range, $0-$40,444) from two companies,” the researchers said.
The study findings were limited by several factors including “potential inaccuracies in CMS-OP reporting, which are rarely corrected, and lack of generalizability outside the United States” and by the limited time frame for data collection, which may have led to underestimation of conflicts for the guidelines, the researchers noted. In addition, “we did not have access to guideline voting records and thus did not know when conflicted panel members recommended against a medication or recused themselves from voting,” they said.
Mr. Khan disclosed research funding from AbbVie and Ferring Pharmaceuticals.
In a second research letter, half of the authors of gastroenterology guidelines received payments from industry, wrote Tyler Combs, BS, of Oklahoma State University, Tulsa, and his colleagues. Previous studies have reviewed the financial conflicts of interest in specialties including oncology, dermatology, and otolaryngology, but financial conflicts of interest among authors of gastroenterology guidelines have not been examined, the researchers said.
Mr. Combs and his colleagues identified 15 CPGs published by the American College of Gastroenterology between 2014 and 2016. They identified 83 authors, with an average of 4 authors for each guideline. Overall, 53% of the authors received industry payments, according to based on data from the 2014 to 2016 Centers for Medicare and Medicaid Services Open Payments database (OPD).
However, OPD information was not always consistent with information published with the guidelines, the researchers noted. They found that 16 (19%) of the 83 authors both disclosed financial conflicts of interests in the CPGs and had received payments according to OPD or had disclosed no financial conflicts of interest and had received no payments according to OPD. In addition, 49 (34%) of 146 cumulative financial conflicts of interest disclosed in the CPGs and 148 relationships identified on OPD were both disclosed as financial conflicts of interest and evidenced by OPD payment records. In this review, the median total payment was $1,000, with an interquartile range from $0 to $39,938.
The study findings were limited by a relatively short 12-month time frame, the researchers noted. However, “our finding that FCOI [financial conflicts of interest] disclosure only corroborates with OPD payment records between 19% and 34% of the time also suggests that guidance from the ACG [American College of Gastroenterology] may be needed to improve FCOI disclosure efforts in future iterations of gastroenterology CPGs,” they said.
The researchers had no financial conflicts to disclose.
SOURCE: Combs T et al. JAMA Intern Med. 2018 Oct 29. doi: 10.1001/jamainternmed.2018.4730. Khan R et al. JAMA Intern Med. 2018 Oct 29. doi: 10.1001/jamainternmed.2018.5106.
None of the guidelines included in either study was fully compliant with National Academy of Medicine standards, which include written disclosure, appointing committee chairs or cochairs with no conflicts of interest, and keeping committee members with conflicts to a minority of the committee membership, wrote Colette DeJong, MD, and Robert Steinbrook, MD, in an accompanying editorial. In the study by Khan et al., “Notably, 14 of the 18 panels had chairs with industry payments, and 10 had a majority of members with payments,” they wrote.
However, the federal government has so far shown no interest in supporting a fully independent entity to develop clinical practice guidelines, as occurs in the United Kingdom via the National Institute for Health and Care Excellence. “Preparation of guidelines by an independent public body with assured funding and independence could be an effective approach, not only for eliminating issues related to financial conflicts of interest but also for assuring the use of rigorous methodologies and avoiding the wasteful duplication of efforts by multiple committees,” they wrote.
Financial conflicts in clinical practice guidelines persist in the United States in part because many professional societies have financial conflicts with industry, the editorialists wrote.
“Robust, objective, and unbiased clinical practice guidelines support improvements in patient care; the best interests of patients are the paramount consideration,” they emphasized (JAMA Intern Med. 2018 Oct 29. doi: 10.1001/jamainternmed.2018.4974).
Dr. DeJong is affiliated with the University of California, San Francisco; Dr. Steinbrook is Editor at Large for JAMA Internal Medicine. They had no financial conflicts to disclose.
None of the guidelines included in either study was fully compliant with National Academy of Medicine standards, which include written disclosure, appointing committee chairs or cochairs with no conflicts of interest, and keeping committee members with conflicts to a minority of the committee membership, wrote Colette DeJong, MD, and Robert Steinbrook, MD, in an accompanying editorial. In the study by Khan et al., “Notably, 14 of the 18 panels had chairs with industry payments, and 10 had a majority of members with payments,” they wrote.
However, the federal government has so far shown no interest in supporting a fully independent entity to develop clinical practice guidelines, as occurs in the United Kingdom via the National Institute for Health and Care Excellence. “Preparation of guidelines by an independent public body with assured funding and independence could be an effective approach, not only for eliminating issues related to financial conflicts of interest but also for assuring the use of rigorous methodologies and avoiding the wasteful duplication of efforts by multiple committees,” they wrote.
Financial conflicts in clinical practice guidelines persist in the United States in part because many professional societies have financial conflicts with industry, the editorialists wrote.
“Robust, objective, and unbiased clinical practice guidelines support improvements in patient care; the best interests of patients are the paramount consideration,” they emphasized (JAMA Intern Med. 2018 Oct 29. doi: 10.1001/jamainternmed.2018.4974).
Dr. DeJong is affiliated with the University of California, San Francisco; Dr. Steinbrook is Editor at Large for JAMA Internal Medicine. They had no financial conflicts to disclose.
None of the guidelines included in either study was fully compliant with National Academy of Medicine standards, which include written disclosure, appointing committee chairs or cochairs with no conflicts of interest, and keeping committee members with conflicts to a minority of the committee membership, wrote Colette DeJong, MD, and Robert Steinbrook, MD, in an accompanying editorial. In the study by Khan et al., “Notably, 14 of the 18 panels had chairs with industry payments, and 10 had a majority of members with payments,” they wrote.
However, the federal government has so far shown no interest in supporting a fully independent entity to develop clinical practice guidelines, as occurs in the United Kingdom via the National Institute for Health and Care Excellence. “Preparation of guidelines by an independent public body with assured funding and independence could be an effective approach, not only for eliminating issues related to financial conflicts of interest but also for assuring the use of rigorous methodologies and avoiding the wasteful duplication of efforts by multiple committees,” they wrote.
Financial conflicts in clinical practice guidelines persist in the United States in part because many professional societies have financial conflicts with industry, the editorialists wrote.
“Robust, objective, and unbiased clinical practice guidelines support improvements in patient care; the best interests of patients are the paramount consideration,” they emphasized (JAMA Intern Med. 2018 Oct 29. doi: 10.1001/jamainternmed.2018.4974).
Dr. DeJong is affiliated with the University of California, San Francisco; Dr. Steinbrook is Editor at Large for JAMA Internal Medicine. They had no financial conflicts to disclose.
Financial conflicts are often underreported by authors of clinical practice guidelines (CPGs) in several specialties including oncology, rheumatology, and gastroenterology, according to a pair of research letters published in JAMA Internal Medicine. The Institute of Medicine recommends that guideline authors include no more than 50% individuals with financial conflicts.
In one research letter, Rishad Khan, BSc, of the University of Toronto in Ontario and his colleagues reviewed data on undeclared financial conflicts of interest among authors of guidelines related to high-revenue medications.
The researchers identified CPGs via the National Guideline Clearinghouse and selected 18 CPGs for 10 high-revenue medications published between 2013 and 2017. Financial conflicts of interest were based on the Centers for Medicare & Medicaid Services Open Payments.
Of the 160 authors involved in the various guidelines, 79 (49.4%) disclosed a payment in the CPG or supplemental materials, and 50 (31.3%) disclosed payments from companies marketing 1 of the 10 high-revenue medications in the related guidelines.
Another 41 authors (25.6%) received but did not disclose payments from companies marketing 1 of the 10 high-revenue medications in CPGs.
Overall, 91 authors (56.9%) were found to have financial conflicts of interest that involved 1 of the 10 high-revenue medications, and “the median value of undeclared payments from companies marketing 1 of the 10 high-revenue medications recommended in the CPGs was $522 (interquartile range, $0-$40,444) from two companies,” the researchers said.
The study findings were limited by several factors including “potential inaccuracies in CMS-OP reporting, which are rarely corrected, and lack of generalizability outside the United States” and by the limited time frame for data collection, which may have led to underestimation of conflicts for the guidelines, the researchers noted. In addition, “we did not have access to guideline voting records and thus did not know when conflicted panel members recommended against a medication or recused themselves from voting,” they said.
Mr. Khan disclosed research funding from AbbVie and Ferring Pharmaceuticals.
In a second research letter, half of the authors of gastroenterology guidelines received payments from industry, wrote Tyler Combs, BS, of Oklahoma State University, Tulsa, and his colleagues. Previous studies have reviewed the financial conflicts of interest in specialties including oncology, dermatology, and otolaryngology, but financial conflicts of interest among authors of gastroenterology guidelines have not been examined, the researchers said.
Mr. Combs and his colleagues identified 15 CPGs published by the American College of Gastroenterology between 2014 and 2016. They identified 83 authors, with an average of 4 authors for each guideline. Overall, 53% of the authors received industry payments, according to based on data from the 2014 to 2016 Centers for Medicare and Medicaid Services Open Payments database (OPD).
However, OPD information was not always consistent with information published with the guidelines, the researchers noted. They found that 16 (19%) of the 83 authors both disclosed financial conflicts of interests in the CPGs and had received payments according to OPD or had disclosed no financial conflicts of interest and had received no payments according to OPD. In addition, 49 (34%) of 146 cumulative financial conflicts of interest disclosed in the CPGs and 148 relationships identified on OPD were both disclosed as financial conflicts of interest and evidenced by OPD payment records. In this review, the median total payment was $1,000, with an interquartile range from $0 to $39,938.
The study findings were limited by a relatively short 12-month time frame, the researchers noted. However, “our finding that FCOI [financial conflicts of interest] disclosure only corroborates with OPD payment records between 19% and 34% of the time also suggests that guidance from the ACG [American College of Gastroenterology] may be needed to improve FCOI disclosure efforts in future iterations of gastroenterology CPGs,” they said.
The researchers had no financial conflicts to disclose.
SOURCE: Combs T et al. JAMA Intern Med. 2018 Oct 29. doi: 10.1001/jamainternmed.2018.4730. Khan R et al. JAMA Intern Med. 2018 Oct 29. doi: 10.1001/jamainternmed.2018.5106.
Financial conflicts are often underreported by authors of clinical practice guidelines (CPGs) in several specialties including oncology, rheumatology, and gastroenterology, according to a pair of research letters published in JAMA Internal Medicine. The Institute of Medicine recommends that guideline authors include no more than 50% individuals with financial conflicts.
In one research letter, Rishad Khan, BSc, of the University of Toronto in Ontario and his colleagues reviewed data on undeclared financial conflicts of interest among authors of guidelines related to high-revenue medications.
The researchers identified CPGs via the National Guideline Clearinghouse and selected 18 CPGs for 10 high-revenue medications published between 2013 and 2017. Financial conflicts of interest were based on the Centers for Medicare & Medicaid Services Open Payments.
Of the 160 authors involved in the various guidelines, 79 (49.4%) disclosed a payment in the CPG or supplemental materials, and 50 (31.3%) disclosed payments from companies marketing 1 of the 10 high-revenue medications in the related guidelines.
Another 41 authors (25.6%) received but did not disclose payments from companies marketing 1 of the 10 high-revenue medications in CPGs.
Overall, 91 authors (56.9%) were found to have financial conflicts of interest that involved 1 of the 10 high-revenue medications, and “the median value of undeclared payments from companies marketing 1 of the 10 high-revenue medications recommended in the CPGs was $522 (interquartile range, $0-$40,444) from two companies,” the researchers said.
The study findings were limited by several factors including “potential inaccuracies in CMS-OP reporting, which are rarely corrected, and lack of generalizability outside the United States” and by the limited time frame for data collection, which may have led to underestimation of conflicts for the guidelines, the researchers noted. In addition, “we did not have access to guideline voting records and thus did not know when conflicted panel members recommended against a medication or recused themselves from voting,” they said.
Mr. Khan disclosed research funding from AbbVie and Ferring Pharmaceuticals.
In a second research letter, half of the authors of gastroenterology guidelines received payments from industry, wrote Tyler Combs, BS, of Oklahoma State University, Tulsa, and his colleagues. Previous studies have reviewed the financial conflicts of interest in specialties including oncology, dermatology, and otolaryngology, but financial conflicts of interest among authors of gastroenterology guidelines have not been examined, the researchers said.
Mr. Combs and his colleagues identified 15 CPGs published by the American College of Gastroenterology between 2014 and 2016. They identified 83 authors, with an average of 4 authors for each guideline. Overall, 53% of the authors received industry payments, according to based on data from the 2014 to 2016 Centers for Medicare and Medicaid Services Open Payments database (OPD).
However, OPD information was not always consistent with information published with the guidelines, the researchers noted. They found that 16 (19%) of the 83 authors both disclosed financial conflicts of interests in the CPGs and had received payments according to OPD or had disclosed no financial conflicts of interest and had received no payments according to OPD. In addition, 49 (34%) of 146 cumulative financial conflicts of interest disclosed in the CPGs and 148 relationships identified on OPD were both disclosed as financial conflicts of interest and evidenced by OPD payment records. In this review, the median total payment was $1,000, with an interquartile range from $0 to $39,938.
The study findings were limited by a relatively short 12-month time frame, the researchers noted. However, “our finding that FCOI [financial conflicts of interest] disclosure only corroborates with OPD payment records between 19% and 34% of the time also suggests that guidance from the ACG [American College of Gastroenterology] may be needed to improve FCOI disclosure efforts in future iterations of gastroenterology CPGs,” they said.
The researchers had no financial conflicts to disclose.
SOURCE: Combs T et al. JAMA Intern Med. 2018 Oct 29. doi: 10.1001/jamainternmed.2018.4730. Khan R et al. JAMA Intern Med. 2018 Oct 29. doi: 10.1001/jamainternmed.2018.5106.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Financial conflicts of interest in the development of clinical guidelines persist in the United States.
Major finding: Approximately half of the committee members of guidelines in both studies had financial relationships; many were undisclosed and involved substantial payments.
Study details: The data come from two research letters, including 15 gastroenterology guidelines and 18 guidelines from multiple specialties.
Disclosures: Mr. Khan disclosed research funding from AbbVie and Ferring Pharmaceuticals. Mr. Combs had no financial conflicts to disclose.
Source: Combs T et al. JAMA Intern Med. 2018 Oct 29. doi: 10.1001/jamainternmed.2018.4730. Khan R et al. JAMA Intern Med. 2018 Oct 29. doi: 10.1001/jamainternmed.2018.5106.
Healthy, ethical environments can alleviate ‘moral distress’ in clinicians
SAN ANTONIO – Understanding the experience of “moral distress” in critical care is essential because of its potential negative effects on health care providers and the need to prevent or address those effects, according to Marian Altman, PhD, RN, a clinical practice specialist from the American Association of Critical Care Nurses.
Dr. Altman spoke about moral distress as part of a panel discussion at the annual meeting of the American College of Chest Physicians on how to handle nonbeneficial treatment requests from families, including the legal and ethical obligations of care providers when a patient is receiving life-sustaining treatment.
“The key point about moral distress is that these are personal constraints, and so the choices of what is best for a patient often conflicts with what is best for the organization,” Dr. Altman told CHEST 2018 attendees. “It could conflict with what’s best for the care providers, the family, or even other patients, and so it’s that personal experience of moral compromise that often originates in this broader practice of our routine.”
While it does not necessarily occur frequently, moral distress is intense when it does occur.
“It really threatens the identity and the integrity of those who experience it because they truly believe they are seriously compromised with this deep personal effect,” Dr. Altman said.
Dr. Altman credited Andrew Jameton, a bioethicist who authored a seminal book on ethical issues in nursing in 1984, with defining exactly what moral distress is: “painful feelings and/or the psychological disequilibrium that occurs when a person is conscious of the morally appropriate action a situation requires but cannot carry out that action because of the institutionalized obstacles, such as lack of time, lack of supervisory support, exercise of medical power, and institutional policy or legal limits.” Or, in plainer terms, “Moral distress occurs when one knows the ethically correct action to take but feels powerless to take that action,” as Elizabeth G. Epstein, PhD, RN, and Sarah Delgado, MSN, RN, wrote in the Online Journal of Issues in Nursing.
To understand moral distress, it’s important to know what it’s not, too, Dr. Altman said. It’s not the daily stress of work or compassion fatigue or even burnout, though it can lead to burnout.
“Burnout is the state of physical, emotional, and mental fatigue and exhaustion caused by long-term involvement in situations that are emotionally demanding,” Dr. Altman said. “Burnout has been linked with moral distress, but they are two very different things.”
It’s also not a disagreement among colleagues or “an excuse to avoid a challenging situation.” In fact, the No. 1 cause of moral distress, in study after study, Dr. Altman said, is providing medical care, particularly medically futile care.
“Providing really unnecessary treatments and providing end-of-life care can lead to it as well as complex patients and challenging situations,” Dr. Altman said. Other causes include inadequate staffing, incompetent providers, poor communication, and advanced technology used to sustain life.
Though people often associate moral distress with intensive care, it can occur “wherever care is provided” and can “affect all members of the health care team,” Dr. Altman said. Though the early research into moral distress focused on critical care nurses, the field has since exploded, across all medical disciplines and in countries around the world.
That research has revealed how intensely moral distress can impact the psychological, biological, and social health of people. Physical symptoms that can result from moral distress include diarrhea, headache, heart palpitations, neck pain, muscle aches, and vomiting. The emotions it rouses include frustration, fear, anger, anxiety, and, especially, powerlessness and guilt.
Moral distress can lead to burnout and dissatisfaction in individuals and, subsequently, reduced retention and productivity within institutions. Health care providers who experience moral distress may leave their position, their unit, or the profession altogether.
“That can have a huge impact in a time when we need many more health care providers to care for this exploding population,” Dr. Altman said. It can also negatively influence the patient-provider relationship, potentially affecting the quantity and safety of care delivered, she explained.
But there are ways to address moral distress, she said.
“We’re not going to eradicate it because we will never eradicate critical care or end-of-life care, and those are the causes that lead to moral distress,” Dr. Altman said. “But what we can do, and what the research is now focusing on, is concentrate on improving our work environment, and help people recognize that they’re experiencing moral distress before it gets to burnout … or mitigating moral distress when it occurs.”
Those improvements include fostering both a positive ethical environment, with ethics education, an ethics committee, and on-site ethics experts, and a healthy work environment with collaboration and skillful communication.
Research has shown that “a higher ethical work environment is correlated with a decrease in moral distress frequency,” Dr. Altman said. And structured communication processes should focus on the goals of care, she said. More formal programs may include moral distress workshops, a moral distress consult service, an ethics consult service, and distress debriefings, during which a facilitator leads providers in a structured, collaborative discussion about a distressing event that has occurred.
SAN ANTONIO – Understanding the experience of “moral distress” in critical care is essential because of its potential negative effects on health care providers and the need to prevent or address those effects, according to Marian Altman, PhD, RN, a clinical practice specialist from the American Association of Critical Care Nurses.
Dr. Altman spoke about moral distress as part of a panel discussion at the annual meeting of the American College of Chest Physicians on how to handle nonbeneficial treatment requests from families, including the legal and ethical obligations of care providers when a patient is receiving life-sustaining treatment.
“The key point about moral distress is that these are personal constraints, and so the choices of what is best for a patient often conflicts with what is best for the organization,” Dr. Altman told CHEST 2018 attendees. “It could conflict with what’s best for the care providers, the family, or even other patients, and so it’s that personal experience of moral compromise that often originates in this broader practice of our routine.”
While it does not necessarily occur frequently, moral distress is intense when it does occur.
“It really threatens the identity and the integrity of those who experience it because they truly believe they are seriously compromised with this deep personal effect,” Dr. Altman said.
Dr. Altman credited Andrew Jameton, a bioethicist who authored a seminal book on ethical issues in nursing in 1984, with defining exactly what moral distress is: “painful feelings and/or the psychological disequilibrium that occurs when a person is conscious of the morally appropriate action a situation requires but cannot carry out that action because of the institutionalized obstacles, such as lack of time, lack of supervisory support, exercise of medical power, and institutional policy or legal limits.” Or, in plainer terms, “Moral distress occurs when one knows the ethically correct action to take but feels powerless to take that action,” as Elizabeth G. Epstein, PhD, RN, and Sarah Delgado, MSN, RN, wrote in the Online Journal of Issues in Nursing.
To understand moral distress, it’s important to know what it’s not, too, Dr. Altman said. It’s not the daily stress of work or compassion fatigue or even burnout, though it can lead to burnout.
“Burnout is the state of physical, emotional, and mental fatigue and exhaustion caused by long-term involvement in situations that are emotionally demanding,” Dr. Altman said. “Burnout has been linked with moral distress, but they are two very different things.”
It’s also not a disagreement among colleagues or “an excuse to avoid a challenging situation.” In fact, the No. 1 cause of moral distress, in study after study, Dr. Altman said, is providing medical care, particularly medically futile care.
“Providing really unnecessary treatments and providing end-of-life care can lead to it as well as complex patients and challenging situations,” Dr. Altman said. Other causes include inadequate staffing, incompetent providers, poor communication, and advanced technology used to sustain life.
Though people often associate moral distress with intensive care, it can occur “wherever care is provided” and can “affect all members of the health care team,” Dr. Altman said. Though the early research into moral distress focused on critical care nurses, the field has since exploded, across all medical disciplines and in countries around the world.
That research has revealed how intensely moral distress can impact the psychological, biological, and social health of people. Physical symptoms that can result from moral distress include diarrhea, headache, heart palpitations, neck pain, muscle aches, and vomiting. The emotions it rouses include frustration, fear, anger, anxiety, and, especially, powerlessness and guilt.
Moral distress can lead to burnout and dissatisfaction in individuals and, subsequently, reduced retention and productivity within institutions. Health care providers who experience moral distress may leave their position, their unit, or the profession altogether.
“That can have a huge impact in a time when we need many more health care providers to care for this exploding population,” Dr. Altman said. It can also negatively influence the patient-provider relationship, potentially affecting the quantity and safety of care delivered, she explained.
But there are ways to address moral distress, she said.
“We’re not going to eradicate it because we will never eradicate critical care or end-of-life care, and those are the causes that lead to moral distress,” Dr. Altman said. “But what we can do, and what the research is now focusing on, is concentrate on improving our work environment, and help people recognize that they’re experiencing moral distress before it gets to burnout … or mitigating moral distress when it occurs.”
Those improvements include fostering both a positive ethical environment, with ethics education, an ethics committee, and on-site ethics experts, and a healthy work environment with collaboration and skillful communication.
Research has shown that “a higher ethical work environment is correlated with a decrease in moral distress frequency,” Dr. Altman said. And structured communication processes should focus on the goals of care, she said. More formal programs may include moral distress workshops, a moral distress consult service, an ethics consult service, and distress debriefings, during which a facilitator leads providers in a structured, collaborative discussion about a distressing event that has occurred.
SAN ANTONIO – Understanding the experience of “moral distress” in critical care is essential because of its potential negative effects on health care providers and the need to prevent or address those effects, according to Marian Altman, PhD, RN, a clinical practice specialist from the American Association of Critical Care Nurses.
Dr. Altman spoke about moral distress as part of a panel discussion at the annual meeting of the American College of Chest Physicians on how to handle nonbeneficial treatment requests from families, including the legal and ethical obligations of care providers when a patient is receiving life-sustaining treatment.
“The key point about moral distress is that these are personal constraints, and so the choices of what is best for a patient often conflicts with what is best for the organization,” Dr. Altman told CHEST 2018 attendees. “It could conflict with what’s best for the care providers, the family, or even other patients, and so it’s that personal experience of moral compromise that often originates in this broader practice of our routine.”
While it does not necessarily occur frequently, moral distress is intense when it does occur.
“It really threatens the identity and the integrity of those who experience it because they truly believe they are seriously compromised with this deep personal effect,” Dr. Altman said.
Dr. Altman credited Andrew Jameton, a bioethicist who authored a seminal book on ethical issues in nursing in 1984, with defining exactly what moral distress is: “painful feelings and/or the psychological disequilibrium that occurs when a person is conscious of the morally appropriate action a situation requires but cannot carry out that action because of the institutionalized obstacles, such as lack of time, lack of supervisory support, exercise of medical power, and institutional policy or legal limits.” Or, in plainer terms, “Moral distress occurs when one knows the ethically correct action to take but feels powerless to take that action,” as Elizabeth G. Epstein, PhD, RN, and Sarah Delgado, MSN, RN, wrote in the Online Journal of Issues in Nursing.
To understand moral distress, it’s important to know what it’s not, too, Dr. Altman said. It’s not the daily stress of work or compassion fatigue or even burnout, though it can lead to burnout.
“Burnout is the state of physical, emotional, and mental fatigue and exhaustion caused by long-term involvement in situations that are emotionally demanding,” Dr. Altman said. “Burnout has been linked with moral distress, but they are two very different things.”
It’s also not a disagreement among colleagues or “an excuse to avoid a challenging situation.” In fact, the No. 1 cause of moral distress, in study after study, Dr. Altman said, is providing medical care, particularly medically futile care.
“Providing really unnecessary treatments and providing end-of-life care can lead to it as well as complex patients and challenging situations,” Dr. Altman said. Other causes include inadequate staffing, incompetent providers, poor communication, and advanced technology used to sustain life.
Though people often associate moral distress with intensive care, it can occur “wherever care is provided” and can “affect all members of the health care team,” Dr. Altman said. Though the early research into moral distress focused on critical care nurses, the field has since exploded, across all medical disciplines and in countries around the world.
That research has revealed how intensely moral distress can impact the psychological, biological, and social health of people. Physical symptoms that can result from moral distress include diarrhea, headache, heart palpitations, neck pain, muscle aches, and vomiting. The emotions it rouses include frustration, fear, anger, anxiety, and, especially, powerlessness and guilt.
Moral distress can lead to burnout and dissatisfaction in individuals and, subsequently, reduced retention and productivity within institutions. Health care providers who experience moral distress may leave their position, their unit, or the profession altogether.
“That can have a huge impact in a time when we need many more health care providers to care for this exploding population,” Dr. Altman said. It can also negatively influence the patient-provider relationship, potentially affecting the quantity and safety of care delivered, she explained.
But there are ways to address moral distress, she said.
“We’re not going to eradicate it because we will never eradicate critical care or end-of-life care, and those are the causes that lead to moral distress,” Dr. Altman said. “But what we can do, and what the research is now focusing on, is concentrate on improving our work environment, and help people recognize that they’re experiencing moral distress before it gets to burnout … or mitigating moral distress when it occurs.”
Those improvements include fostering both a positive ethical environment, with ethics education, an ethics committee, and on-site ethics experts, and a healthy work environment with collaboration and skillful communication.
Research has shown that “a higher ethical work environment is correlated with a decrease in moral distress frequency,” Dr. Altman said. And structured communication processes should focus on the goals of care, she said. More formal programs may include moral distress workshops, a moral distress consult service, an ethics consult service, and distress debriefings, during which a facilitator leads providers in a structured, collaborative discussion about a distressing event that has occurred.
REPORTING FROM CHEST 2018
Helping alleviate hospitalist burnout
Focus on systemic factors
For hospitalists, burnout is a widespread and ongoing problem. In 2011, a Mayo Clinic study found that 45% of U.S. physicians had at least one symptom of professional burnout; by 2014, that number had risen to 54%.
“Burnout among physicians has been shown to be linked to quality of care, impacting medical errors, mortality ratios in hospitalized patients, and lower patient satisfaction,” said Ingrid T. Katz, MD, MHS, assistant professor of medicine at Harvard Medical School, Boston, and coauthor of a recent column on the subject published in the New England Journal of Medicine.
Widespread burnout is caused by systemic factors, not individual failures. “These systemic factors range from excessive clerical burden to ‘work beyond work,’ where people end up taking work home at night and are often found interfacing with the EHR well after their normal work day,” Dr. Katz said. “Many also express their disdain for the model of practice that no longer values autonomy, which was seen as inherent in the profession prior to the current model of care.”
Moving towards a better framework would require an inherent trust in physicians, limiting unnecessary intrusions into a physician’s practice that do not impact medical care. “It would remove the burden of excessive documentation and allow for physicians to get reinspired by the practice of medicine, an inherently altruistic profession,” Dr. Katz said.
Changes might include eliminating excessive clerical demands and improving EHRs to allow physicians to return to the bedside. Workloads would be geared towards quality in care and not focused on improving the bottom line of a health care system. One health system Dr. Katz wrote about instituted a team-based model; under this system medical assistants gather data and reconcile medications, allowing physicians to focus on performing physical exams and making medical decisions.
“Burnout will diminish when physicians are empowered to be part of the solution and hospital systems make changes that recognize the totality of the challenges that physicians face,” Dr. Katz said, adding that hospitalists are in a unique position to promote such changes on a systemic level. “Leadership needs to be willing to inform and engage their physicians, monitor well-being of physicians as closely as they monitor quality in care, and implement changes when needed.”
Reference
1. Katz IT et al. Beyond Burnout – Redesigning Care to Restore Meaning and Sanity for Physicians. N Engl J Med. 2018 Jan 25. doi: 10.1056/NEJMp1716845.
Focus on systemic factors
Focus on systemic factors
For hospitalists, burnout is a widespread and ongoing problem. In 2011, a Mayo Clinic study found that 45% of U.S. physicians had at least one symptom of professional burnout; by 2014, that number had risen to 54%.
“Burnout among physicians has been shown to be linked to quality of care, impacting medical errors, mortality ratios in hospitalized patients, and lower patient satisfaction,” said Ingrid T. Katz, MD, MHS, assistant professor of medicine at Harvard Medical School, Boston, and coauthor of a recent column on the subject published in the New England Journal of Medicine.
Widespread burnout is caused by systemic factors, not individual failures. “These systemic factors range from excessive clerical burden to ‘work beyond work,’ where people end up taking work home at night and are often found interfacing with the EHR well after their normal work day,” Dr. Katz said. “Many also express their disdain for the model of practice that no longer values autonomy, which was seen as inherent in the profession prior to the current model of care.”
Moving towards a better framework would require an inherent trust in physicians, limiting unnecessary intrusions into a physician’s practice that do not impact medical care. “It would remove the burden of excessive documentation and allow for physicians to get reinspired by the practice of medicine, an inherently altruistic profession,” Dr. Katz said.
Changes might include eliminating excessive clerical demands and improving EHRs to allow physicians to return to the bedside. Workloads would be geared towards quality in care and not focused on improving the bottom line of a health care system. One health system Dr. Katz wrote about instituted a team-based model; under this system medical assistants gather data and reconcile medications, allowing physicians to focus on performing physical exams and making medical decisions.
“Burnout will diminish when physicians are empowered to be part of the solution and hospital systems make changes that recognize the totality of the challenges that physicians face,” Dr. Katz said, adding that hospitalists are in a unique position to promote such changes on a systemic level. “Leadership needs to be willing to inform and engage their physicians, monitor well-being of physicians as closely as they monitor quality in care, and implement changes when needed.”
Reference
1. Katz IT et al. Beyond Burnout – Redesigning Care to Restore Meaning and Sanity for Physicians. N Engl J Med. 2018 Jan 25. doi: 10.1056/NEJMp1716845.
For hospitalists, burnout is a widespread and ongoing problem. In 2011, a Mayo Clinic study found that 45% of U.S. physicians had at least one symptom of professional burnout; by 2014, that number had risen to 54%.
“Burnout among physicians has been shown to be linked to quality of care, impacting medical errors, mortality ratios in hospitalized patients, and lower patient satisfaction,” said Ingrid T. Katz, MD, MHS, assistant professor of medicine at Harvard Medical School, Boston, and coauthor of a recent column on the subject published in the New England Journal of Medicine.
Widespread burnout is caused by systemic factors, not individual failures. “These systemic factors range from excessive clerical burden to ‘work beyond work,’ where people end up taking work home at night and are often found interfacing with the EHR well after their normal work day,” Dr. Katz said. “Many also express their disdain for the model of practice that no longer values autonomy, which was seen as inherent in the profession prior to the current model of care.”
Moving towards a better framework would require an inherent trust in physicians, limiting unnecessary intrusions into a physician’s practice that do not impact medical care. “It would remove the burden of excessive documentation and allow for physicians to get reinspired by the practice of medicine, an inherently altruistic profession,” Dr. Katz said.
Changes might include eliminating excessive clerical demands and improving EHRs to allow physicians to return to the bedside. Workloads would be geared towards quality in care and not focused on improving the bottom line of a health care system. One health system Dr. Katz wrote about instituted a team-based model; under this system medical assistants gather data and reconcile medications, allowing physicians to focus on performing physical exams and making medical decisions.
“Burnout will diminish when physicians are empowered to be part of the solution and hospital systems make changes that recognize the totality of the challenges that physicians face,” Dr. Katz said, adding that hospitalists are in a unique position to promote such changes on a systemic level. “Leadership needs to be willing to inform and engage their physicians, monitor well-being of physicians as closely as they monitor quality in care, and implement changes when needed.”
Reference
1. Katz IT et al. Beyond Burnout – Redesigning Care to Restore Meaning and Sanity for Physicians. N Engl J Med. 2018 Jan 25. doi: 10.1056/NEJMp1716845.
Study: Problems persist with APMs
Physicians continue to support advanced alternative payment models despite the fact that operational issues have not improved over the last 4 years and new ones have cropped up, according to a follow-up survey conducted by the RAND Corporation for the American Medical Association.
“All the things we heard in 2014 were still present in 2018. Both the challenges that practices had experienced back in 2014 having to do with data timeliness, data completeness and accuracy, payment model execution, all those challenges persisted,” Mark W. Friedberg, MD, senior physician policy researcher at RAND, said in an interview.
RAND surveyed 31 practices of varying practice size and specialty across six geographic regions, some of which participated in the 2014 survey. Supplemental information was provided by interviews with 32 market observers, 8 health plan leaders, 10 hospital and hospital system leaders, 10 state and local medical society leaders, and 4 chapter leaders with MGMA (formerly the Medical Group Management Association).
“We had thought we would hear that the problem had gotten a little bit better since there has been some investment in trying to tamp down the wide range of measures that are involved in these alternative payment models,” Dr. Friedberg said. “We did not see any evidence of that having any effect on the practices that participated in this study this time around.”
Indeed, concerns reported in 2014 were again reported in 2018, along with a new set of concerns, including the perceived pace of change in alternative payment models (APMs), the complexity of APMs, and physician concerns over two-sided risk models.
“Practices, especially those that participated both times, said in 2014 we had these challenges [of rapid changes in APM models] and since then, things have just gotten a lot faster,” he said, noting that doctors are complaining of models that are going through changes, sometimes without much warning. “They are changing quite rapidly from year to year. If you look at the MACRA QPP [Quality Payment Program] for example, that model changes every year to some extent and those things are hard for them to keep up with.”
Running hand in hand with the change is the complexity of the changes, a result of expanding performance measures and uncertainty with thresholds for penalties and rewards and in some ways has had little impact on improving care.
Dr. Friedberg noted that some practices are hiring people to examine APMs to devise strategic ways to choose and report data for maximum return.
“In a practice, for example, if their quality of care was already very good, what these folks ended up doing was help them choose measures and work the attribution algorithms in a strategic way to either guarantee a bonus or minimize the risk of incurring a penalty,” he said.
He also noted that practices appear to becoming more risk averse.
“We heard a lot more of the following thing, which is that if [practices] were in a two-sided risk model, several of them reported trying and succeeding in some cases offloading the downside risk to partners,” Dr. Friedberg reported. “And what this resulted in was that the practice, even though from the payer’s perspective they are in a two-sided model, the practice was actually in a one-sided model with a partner who is taking all of the downside risk and a portion of the upside risk, leaving a small upside risk proposition that remained for the practice.”
He said the range of partners that were absorbing the downside risk included hospitals, device manufacturers, consulting companies, or private equity firms.
Despite the concerns surrounding APMs, Dr. Friedberg said that “we did not hear practices broadly saying that they just weren’t interested in alternative payment models. In general, practices still remained pretty enthusiastic about these alternative payment models in theory. If they could be made simpler, if the pace of change weren’t quite so fast, that they would have a chance to really do some important care improvements in alternative payment models.”
He noted some of the surveyed practices were able to make investments in care as a direct result of participating in APMs, such as in behavioral health capabilities in primary care, for example, leading to quality of care improvements.
However, these issues could reveal a future unwillingness to participate in APMs, especially two-sided risk models, something at least the Centers for Medicare & Medicaid Services are pushing for as a stated goal of the QPP is to get practices to participate in APMs and take on more risk.
The growing aversion to taking on downside risk could lead practices to simply stay in fee for service and simply take the payment penalty because it is a fixed amount that can be planned for, as opposed to the fluctuations of bonuses and penalties that comes with a rapidly changing APM environment, Dr. Friedberg said.
Going forward, the report makes a number of recommendations to help create an environment that would potentially make APMs more successful, including simplifying the models; creating stable, predictable, and moderately paced pathways to APM participation; making data available in a more timely fashion; minimizing downside risk or helping practices better manage it; and designing APMs that will encourage clinical changes to help improve the effectiveness of care delivered.
Physicians continue to support advanced alternative payment models despite the fact that operational issues have not improved over the last 4 years and new ones have cropped up, according to a follow-up survey conducted by the RAND Corporation for the American Medical Association.
“All the things we heard in 2014 were still present in 2018. Both the challenges that practices had experienced back in 2014 having to do with data timeliness, data completeness and accuracy, payment model execution, all those challenges persisted,” Mark W. Friedberg, MD, senior physician policy researcher at RAND, said in an interview.
RAND surveyed 31 practices of varying practice size and specialty across six geographic regions, some of which participated in the 2014 survey. Supplemental information was provided by interviews with 32 market observers, 8 health plan leaders, 10 hospital and hospital system leaders, 10 state and local medical society leaders, and 4 chapter leaders with MGMA (formerly the Medical Group Management Association).
“We had thought we would hear that the problem had gotten a little bit better since there has been some investment in trying to tamp down the wide range of measures that are involved in these alternative payment models,” Dr. Friedberg said. “We did not see any evidence of that having any effect on the practices that participated in this study this time around.”
Indeed, concerns reported in 2014 were again reported in 2018, along with a new set of concerns, including the perceived pace of change in alternative payment models (APMs), the complexity of APMs, and physician concerns over two-sided risk models.
“Practices, especially those that participated both times, said in 2014 we had these challenges [of rapid changes in APM models] and since then, things have just gotten a lot faster,” he said, noting that doctors are complaining of models that are going through changes, sometimes without much warning. “They are changing quite rapidly from year to year. If you look at the MACRA QPP [Quality Payment Program] for example, that model changes every year to some extent and those things are hard for them to keep up with.”
Running hand in hand with the change is the complexity of the changes, a result of expanding performance measures and uncertainty with thresholds for penalties and rewards and in some ways has had little impact on improving care.
Dr. Friedberg noted that some practices are hiring people to examine APMs to devise strategic ways to choose and report data for maximum return.
“In a practice, for example, if their quality of care was already very good, what these folks ended up doing was help them choose measures and work the attribution algorithms in a strategic way to either guarantee a bonus or minimize the risk of incurring a penalty,” he said.
He also noted that practices appear to becoming more risk averse.
“We heard a lot more of the following thing, which is that if [practices] were in a two-sided risk model, several of them reported trying and succeeding in some cases offloading the downside risk to partners,” Dr. Friedberg reported. “And what this resulted in was that the practice, even though from the payer’s perspective they are in a two-sided model, the practice was actually in a one-sided model with a partner who is taking all of the downside risk and a portion of the upside risk, leaving a small upside risk proposition that remained for the practice.”
He said the range of partners that were absorbing the downside risk included hospitals, device manufacturers, consulting companies, or private equity firms.
Despite the concerns surrounding APMs, Dr. Friedberg said that “we did not hear practices broadly saying that they just weren’t interested in alternative payment models. In general, practices still remained pretty enthusiastic about these alternative payment models in theory. If they could be made simpler, if the pace of change weren’t quite so fast, that they would have a chance to really do some important care improvements in alternative payment models.”
He noted some of the surveyed practices were able to make investments in care as a direct result of participating in APMs, such as in behavioral health capabilities in primary care, for example, leading to quality of care improvements.
However, these issues could reveal a future unwillingness to participate in APMs, especially two-sided risk models, something at least the Centers for Medicare & Medicaid Services are pushing for as a stated goal of the QPP is to get practices to participate in APMs and take on more risk.
The growing aversion to taking on downside risk could lead practices to simply stay in fee for service and simply take the payment penalty because it is a fixed amount that can be planned for, as opposed to the fluctuations of bonuses and penalties that comes with a rapidly changing APM environment, Dr. Friedberg said.
Going forward, the report makes a number of recommendations to help create an environment that would potentially make APMs more successful, including simplifying the models; creating stable, predictable, and moderately paced pathways to APM participation; making data available in a more timely fashion; minimizing downside risk or helping practices better manage it; and designing APMs that will encourage clinical changes to help improve the effectiveness of care delivered.
Physicians continue to support advanced alternative payment models despite the fact that operational issues have not improved over the last 4 years and new ones have cropped up, according to a follow-up survey conducted by the RAND Corporation for the American Medical Association.
“All the things we heard in 2014 were still present in 2018. Both the challenges that practices had experienced back in 2014 having to do with data timeliness, data completeness and accuracy, payment model execution, all those challenges persisted,” Mark W. Friedberg, MD, senior physician policy researcher at RAND, said in an interview.
RAND surveyed 31 practices of varying practice size and specialty across six geographic regions, some of which participated in the 2014 survey. Supplemental information was provided by interviews with 32 market observers, 8 health plan leaders, 10 hospital and hospital system leaders, 10 state and local medical society leaders, and 4 chapter leaders with MGMA (formerly the Medical Group Management Association).
“We had thought we would hear that the problem had gotten a little bit better since there has been some investment in trying to tamp down the wide range of measures that are involved in these alternative payment models,” Dr. Friedberg said. “We did not see any evidence of that having any effect on the practices that participated in this study this time around.”
Indeed, concerns reported in 2014 were again reported in 2018, along with a new set of concerns, including the perceived pace of change in alternative payment models (APMs), the complexity of APMs, and physician concerns over two-sided risk models.
“Practices, especially those that participated both times, said in 2014 we had these challenges [of rapid changes in APM models] and since then, things have just gotten a lot faster,” he said, noting that doctors are complaining of models that are going through changes, sometimes without much warning. “They are changing quite rapidly from year to year. If you look at the MACRA QPP [Quality Payment Program] for example, that model changes every year to some extent and those things are hard for them to keep up with.”
Running hand in hand with the change is the complexity of the changes, a result of expanding performance measures and uncertainty with thresholds for penalties and rewards and in some ways has had little impact on improving care.
Dr. Friedberg noted that some practices are hiring people to examine APMs to devise strategic ways to choose and report data for maximum return.
“In a practice, for example, if their quality of care was already very good, what these folks ended up doing was help them choose measures and work the attribution algorithms in a strategic way to either guarantee a bonus or minimize the risk of incurring a penalty,” he said.
He also noted that practices appear to becoming more risk averse.
“We heard a lot more of the following thing, which is that if [practices] were in a two-sided risk model, several of them reported trying and succeeding in some cases offloading the downside risk to partners,” Dr. Friedberg reported. “And what this resulted in was that the practice, even though from the payer’s perspective they are in a two-sided model, the practice was actually in a one-sided model with a partner who is taking all of the downside risk and a portion of the upside risk, leaving a small upside risk proposition that remained for the practice.”
He said the range of partners that were absorbing the downside risk included hospitals, device manufacturers, consulting companies, or private equity firms.
Despite the concerns surrounding APMs, Dr. Friedberg said that “we did not hear practices broadly saying that they just weren’t interested in alternative payment models. In general, practices still remained pretty enthusiastic about these alternative payment models in theory. If they could be made simpler, if the pace of change weren’t quite so fast, that they would have a chance to really do some important care improvements in alternative payment models.”
He noted some of the surveyed practices were able to make investments in care as a direct result of participating in APMs, such as in behavioral health capabilities in primary care, for example, leading to quality of care improvements.
However, these issues could reveal a future unwillingness to participate in APMs, especially two-sided risk models, something at least the Centers for Medicare & Medicaid Services are pushing for as a stated goal of the QPP is to get practices to participate in APMs and take on more risk.
The growing aversion to taking on downside risk could lead practices to simply stay in fee for service and simply take the payment penalty because it is a fixed amount that can be planned for, as opposed to the fluctuations of bonuses and penalties that comes with a rapidly changing APM environment, Dr. Friedberg said.
Going forward, the report makes a number of recommendations to help create an environment that would potentially make APMs more successful, including simplifying the models; creating stable, predictable, and moderately paced pathways to APM participation; making data available in a more timely fashion; minimizing downside risk or helping practices better manage it; and designing APMs that will encourage clinical changes to help improve the effectiveness of care delivered.
“You have a pending query”
Specificity is essential in documentation and coding
Throughout medical training, you learn to write complete and detailed notes to communicate with other physicians. As a student and resident, you are praised when you succinctly analyze and address all patient problems while justifying your orders for the day. But notes do not exist just to document patient care; they are the template by which our actual quality of care is judged and our patients’ severity of illness is captured.
Like it or not, ICD-10 coding, documentation, denials, calls, and emails from administrators are integral parts of a hospitalist’s day-to-day job. Why? The specificity and comprehensiveness of diagnoses affect such metrics as hospital length of stay, mortality, and Case Mix Index documentation.
Good documentation can lead to better severity of illness (SOI) and risk of mortality (ROM) scores, better patient safety indicator (PSI) scores, better Healthgrades scores, better University Hospital Consortium (UHC) scores, and decreased Recovery Audit Contractor (RAC) denials as well as appropriate reimbursement. Good documentation can even lead to improved patient care and better perceived treatment outcomes.
It is no surprise that many hospital administrators invest time and money in staff to support the proper usage of language in your notes. Of course, sometimes these well-meaning “queries” can throw you into emotional turmoil as you try to understand what was not clear in your excellent note about your patient’s heart failure exacerbation. In this article, we will try to help you take your specificity and comprehensiveness of diagnoses to the next level.
Basics of billing
Physicians do not need to become coders but it is helpful to have some understanding of what happens behind the scenes. Not everyone realizes that physician billing is completely different from hospital billing. Physician billing pertains to the care provided by the clinician, whereas hospital billing pertains to the overall care the patient received.
Below is an example of a case of pneumonia, (see Table 1) which shows the importance of specificity. Just by specifying ‘Aspiration’ for the type of pneumonia, we increased the SOI and the expected ROM appropriately. Also see a change in relative weight (RW): Each diagnosis-related group (DRG) is assigned a relative weight = estimated use of resources, and payment per case is based on estimated resource consumption = relative weight x “blended rate for each hospital.”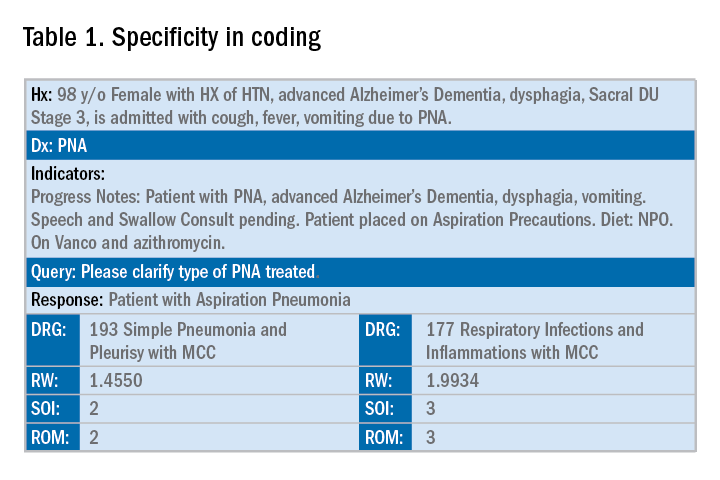
In addition to specificity, it is important to include all secondary diagnosis (know as cc/MCC – complication or comorbidity or a major complication or comorbidity – in the coding world). Table 2 is an example of using the correct terms and documenting secondary diagnosis. By documenting the type and severity of malnutrition we again increase the expected risk of mortality and the severity of illness.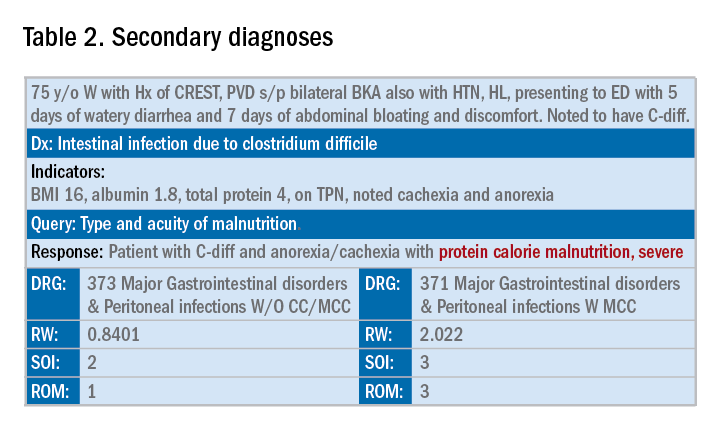
Physicians often do a lot more than what we record in the chart. Learning to document accurately to show the true clinical picture is an important skill set. Here are some tips to help understand and even avoid calls for better documentation.
- Use the terms “probable,” “possible,” “suspected,” or “likely” in documenting uncertain diagnoses (i.e., conditions for which physicians find clinical evidence that leads to a suspicion but not a definitive diagnosis). If conditions are ruled out or confirmed, clearly state so. If it remains uncertain, remember to carry this “possible” or “probable” diagnosis all the way through to the discharge summary or final progress note.
- Use linking of diagnoses when appropriate. For example, if the patient’s neuropathy, nephropathy, and retinopathy are related to their uncontrolled insulin dependent diabetes, state “uncontrolled insulin-dependent DMII with A1c of 11 complicated with nephropathy, neuropathy, and retinopathy.” The coders cannot link these diagnoses, and when you link them, you show a higher complexity of your patient. Remember to link the diagnoses only when they are truly related – this is where your medical knowledge and expertise come into play.
- Use the highest specificity of evidence that supports your medical decision making. You don’t need to be too verbose, all you need is evidence supporting your medical decision making and treatment plan. Think of it as demonstrating the logic of your diagnosis to another physician.
- Use Acuity (acute, chronic, acute on chronic, mild, moderate, severe, etc.) per diagnosis. For example, if you say heart failure exacerbation, it makes perfect sense to your medical colleagues, but in the coding world, it means nothing. Specify if it is acute, or acute on chronic, heart failure.
- Use status of each diagnosis. Is the condition improving, worsening, or resolved? Status does not have to be mentioned in all progress notes. Try to include this descriptor in the discharge summary and the day of the event.
- Always document the clinical significance of any abnormal laboratory, radiology reports, or pathology finding. Coders cannot use test results as a basis for coding unless a clinician has reviewed, interpreted, and documented the significance of the results in the progress note. Simply copying and pasting a report in the notes is not considered clinical acknowledgment. Shorthand notes like “Na=150, start hydration with 0.45% saline” is not acceptable. The actual diagnosis has to be written (i.e. “hypernatremia”). In addition, coders cannot code from nursing, dietitian, respiratory, and physical therapy notes. For example, if nursing documents that a patient has a pressure ulcer the clinician must still document the diagnosis of pressure ulcer, location, and stage. Although dietitian notes may state a body mass index greater than 40, coders cannot assume that patient is morbidly obese. Physician documentation is needed to support the obesity code assignment.
- Document all conditions that affect the patient’s stay, including complications and chronic conditions for which medications have been ordered. These secondary diagnoses paint the most accurate clinical picture and provide information needed to calculate important data, such as complexity and severity of patient illness and mortality risk. A patient with community-acquired pneumonia without other comorbidities requires fewer resources and has a greater chance of a good outcome than does the same patient with complications, such as acute heart failure.
- Downcoding brings losses, upcoding brings fines. Exaggerating the severity of patient conditions can lead to payer audits, reimbursement take backs, and charges of abuse and fraudulent billing. Never stretch the truth. Make sure you can support every diagnosis in the patient’s chart using clinical criteria.
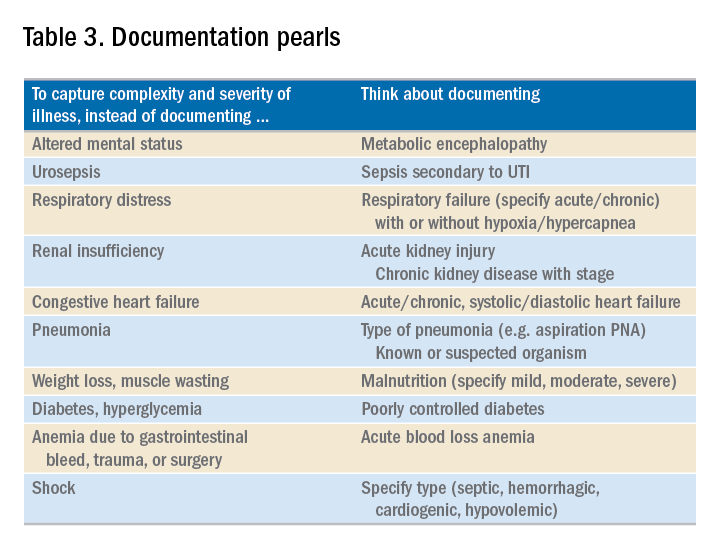
You may be frustrated by the need to choose specific words about diagnoses that seem obvious to you without these descriptors. But accurate documentation can make a huge difference in your hospital’s bottom line and published metrics. Understanding the relative impact of changing your terminology can help you make these changes, until the language becomes second nature. Your hospital administrators will be grateful – and you just might cut down your queries!
Dr. Rajda is medical director of clinical documentation and quality improvement for Mount Sinai Hospital in New York, and medical director for DRG appeals for the Mount Sinai Health System. She serves as assistant professor of medicine at Icahn School of Medicine at Mount Sinai. Dr. Fatemi is an assistant professor at the University of New Mexico, Albuquerque. She is director of documentation, coding, and billing for the division of hospital medicine at UNM. Dr. Reyna is assistant professor in the division of hospital medicine and medical director for clinical documentation and quality improvement at Mount Sinai Medical Center.
Specificity is essential in documentation and coding
Specificity is essential in documentation and coding
Throughout medical training, you learn to write complete and detailed notes to communicate with other physicians. As a student and resident, you are praised when you succinctly analyze and address all patient problems while justifying your orders for the day. But notes do not exist just to document patient care; they are the template by which our actual quality of care is judged and our patients’ severity of illness is captured.
Like it or not, ICD-10 coding, documentation, denials, calls, and emails from administrators are integral parts of a hospitalist’s day-to-day job. Why? The specificity and comprehensiveness of diagnoses affect such metrics as hospital length of stay, mortality, and Case Mix Index documentation.
Good documentation can lead to better severity of illness (SOI) and risk of mortality (ROM) scores, better patient safety indicator (PSI) scores, better Healthgrades scores, better University Hospital Consortium (UHC) scores, and decreased Recovery Audit Contractor (RAC) denials as well as appropriate reimbursement. Good documentation can even lead to improved patient care and better perceived treatment outcomes.
It is no surprise that many hospital administrators invest time and money in staff to support the proper usage of language in your notes. Of course, sometimes these well-meaning “queries” can throw you into emotional turmoil as you try to understand what was not clear in your excellent note about your patient’s heart failure exacerbation. In this article, we will try to help you take your specificity and comprehensiveness of diagnoses to the next level.
Basics of billing
Physicians do not need to become coders but it is helpful to have some understanding of what happens behind the scenes. Not everyone realizes that physician billing is completely different from hospital billing. Physician billing pertains to the care provided by the clinician, whereas hospital billing pertains to the overall care the patient received.
Below is an example of a case of pneumonia, (see Table 1) which shows the importance of specificity. Just by specifying ‘Aspiration’ for the type of pneumonia, we increased the SOI and the expected ROM appropriately. Also see a change in relative weight (RW): Each diagnosis-related group (DRG) is assigned a relative weight = estimated use of resources, and payment per case is based on estimated resource consumption = relative weight x “blended rate for each hospital.”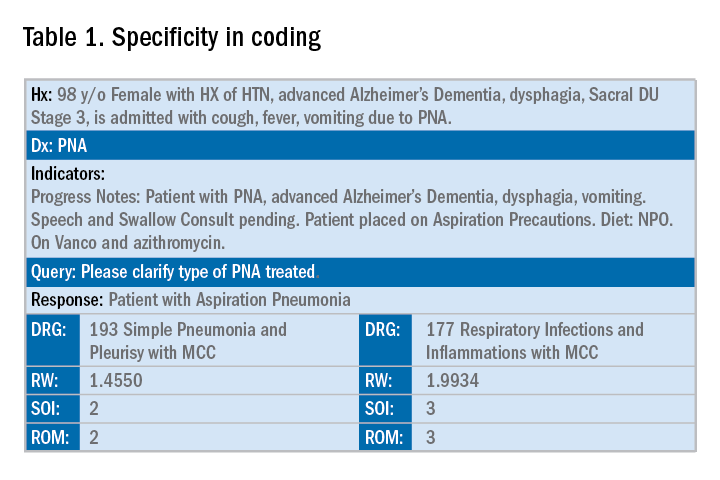
In addition to specificity, it is important to include all secondary diagnosis (know as cc/MCC – complication or comorbidity or a major complication or comorbidity – in the coding world). Table 2 is an example of using the correct terms and documenting secondary diagnosis. By documenting the type and severity of malnutrition we again increase the expected risk of mortality and the severity of illness.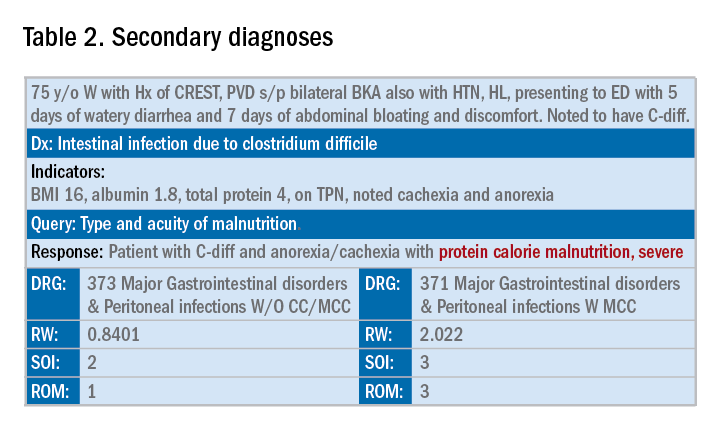
Physicians often do a lot more than what we record in the chart. Learning to document accurately to show the true clinical picture is an important skill set. Here are some tips to help understand and even avoid calls for better documentation.
- Use the terms “probable,” “possible,” “suspected,” or “likely” in documenting uncertain diagnoses (i.e., conditions for which physicians find clinical evidence that leads to a suspicion but not a definitive diagnosis). If conditions are ruled out or confirmed, clearly state so. If it remains uncertain, remember to carry this “possible” or “probable” diagnosis all the way through to the discharge summary or final progress note.
- Use linking of diagnoses when appropriate. For example, if the patient’s neuropathy, nephropathy, and retinopathy are related to their uncontrolled insulin dependent diabetes, state “uncontrolled insulin-dependent DMII with A1c of 11 complicated with nephropathy, neuropathy, and retinopathy.” The coders cannot link these diagnoses, and when you link them, you show a higher complexity of your patient. Remember to link the diagnoses only when they are truly related – this is where your medical knowledge and expertise come into play.
- Use the highest specificity of evidence that supports your medical decision making. You don’t need to be too verbose, all you need is evidence supporting your medical decision making and treatment plan. Think of it as demonstrating the logic of your diagnosis to another physician.
- Use Acuity (acute, chronic, acute on chronic, mild, moderate, severe, etc.) per diagnosis. For example, if you say heart failure exacerbation, it makes perfect sense to your medical colleagues, but in the coding world, it means nothing. Specify if it is acute, or acute on chronic, heart failure.
- Use status of each diagnosis. Is the condition improving, worsening, or resolved? Status does not have to be mentioned in all progress notes. Try to include this descriptor in the discharge summary and the day of the event.
- Always document the clinical significance of any abnormal laboratory, radiology reports, or pathology finding. Coders cannot use test results as a basis for coding unless a clinician has reviewed, interpreted, and documented the significance of the results in the progress note. Simply copying and pasting a report in the notes is not considered clinical acknowledgment. Shorthand notes like “Na=150, start hydration with 0.45% saline” is not acceptable. The actual diagnosis has to be written (i.e. “hypernatremia”). In addition, coders cannot code from nursing, dietitian, respiratory, and physical therapy notes. For example, if nursing documents that a patient has a pressure ulcer the clinician must still document the diagnosis of pressure ulcer, location, and stage. Although dietitian notes may state a body mass index greater than 40, coders cannot assume that patient is morbidly obese. Physician documentation is needed to support the obesity code assignment.
- Document all conditions that affect the patient’s stay, including complications and chronic conditions for which medications have been ordered. These secondary diagnoses paint the most accurate clinical picture and provide information needed to calculate important data, such as complexity and severity of patient illness and mortality risk. A patient with community-acquired pneumonia without other comorbidities requires fewer resources and has a greater chance of a good outcome than does the same patient with complications, such as acute heart failure.
- Downcoding brings losses, upcoding brings fines. Exaggerating the severity of patient conditions can lead to payer audits, reimbursement take backs, and charges of abuse and fraudulent billing. Never stretch the truth. Make sure you can support every diagnosis in the patient’s chart using clinical criteria.
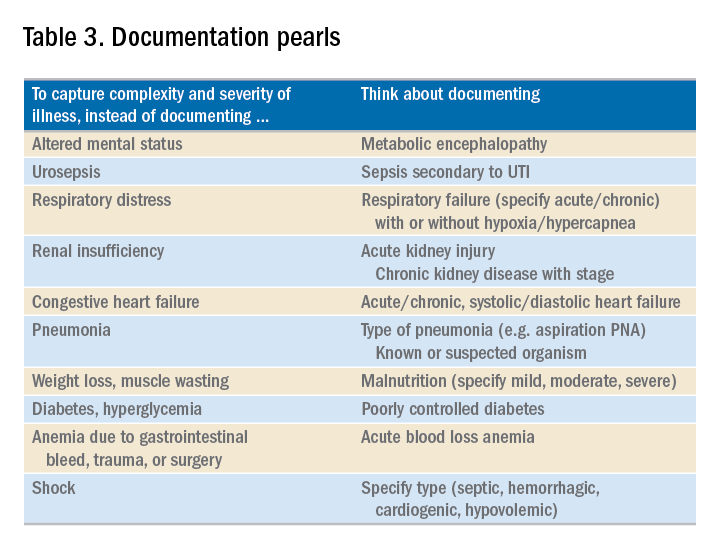
You may be frustrated by the need to choose specific words about diagnoses that seem obvious to you without these descriptors. But accurate documentation can make a huge difference in your hospital’s bottom line and published metrics. Understanding the relative impact of changing your terminology can help you make these changes, until the language becomes second nature. Your hospital administrators will be grateful – and you just might cut down your queries!
Dr. Rajda is medical director of clinical documentation and quality improvement for Mount Sinai Hospital in New York, and medical director for DRG appeals for the Mount Sinai Health System. She serves as assistant professor of medicine at Icahn School of Medicine at Mount Sinai. Dr. Fatemi is an assistant professor at the University of New Mexico, Albuquerque. She is director of documentation, coding, and billing for the division of hospital medicine at UNM. Dr. Reyna is assistant professor in the division of hospital medicine and medical director for clinical documentation and quality improvement at Mount Sinai Medical Center.
Throughout medical training, you learn to write complete and detailed notes to communicate with other physicians. As a student and resident, you are praised when you succinctly analyze and address all patient problems while justifying your orders for the day. But notes do not exist just to document patient care; they are the template by which our actual quality of care is judged and our patients’ severity of illness is captured.
Like it or not, ICD-10 coding, documentation, denials, calls, and emails from administrators are integral parts of a hospitalist’s day-to-day job. Why? The specificity and comprehensiveness of diagnoses affect such metrics as hospital length of stay, mortality, and Case Mix Index documentation.
Good documentation can lead to better severity of illness (SOI) and risk of mortality (ROM) scores, better patient safety indicator (PSI) scores, better Healthgrades scores, better University Hospital Consortium (UHC) scores, and decreased Recovery Audit Contractor (RAC) denials as well as appropriate reimbursement. Good documentation can even lead to improved patient care and better perceived treatment outcomes.
It is no surprise that many hospital administrators invest time and money in staff to support the proper usage of language in your notes. Of course, sometimes these well-meaning “queries” can throw you into emotional turmoil as you try to understand what was not clear in your excellent note about your patient’s heart failure exacerbation. In this article, we will try to help you take your specificity and comprehensiveness of diagnoses to the next level.
Basics of billing
Physicians do not need to become coders but it is helpful to have some understanding of what happens behind the scenes. Not everyone realizes that physician billing is completely different from hospital billing. Physician billing pertains to the care provided by the clinician, whereas hospital billing pertains to the overall care the patient received.
Below is an example of a case of pneumonia, (see Table 1) which shows the importance of specificity. Just by specifying ‘Aspiration’ for the type of pneumonia, we increased the SOI and the expected ROM appropriately. Also see a change in relative weight (RW): Each diagnosis-related group (DRG) is assigned a relative weight = estimated use of resources, and payment per case is based on estimated resource consumption = relative weight x “blended rate for each hospital.”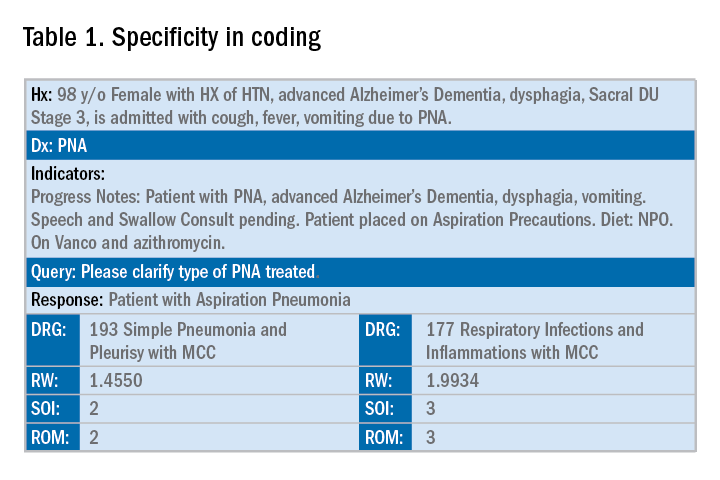
In addition to specificity, it is important to include all secondary diagnosis (know as cc/MCC – complication or comorbidity or a major complication or comorbidity – in the coding world). Table 2 is an example of using the correct terms and documenting secondary diagnosis. By documenting the type and severity of malnutrition we again increase the expected risk of mortality and the severity of illness.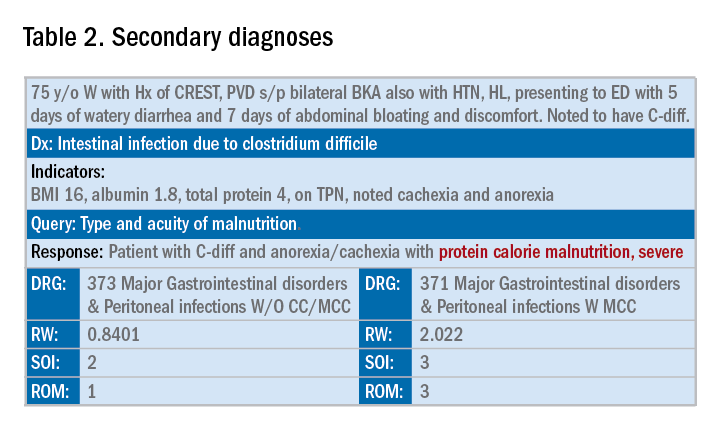
Physicians often do a lot more than what we record in the chart. Learning to document accurately to show the true clinical picture is an important skill set. Here are some tips to help understand and even avoid calls for better documentation.
- Use the terms “probable,” “possible,” “suspected,” or “likely” in documenting uncertain diagnoses (i.e., conditions for which physicians find clinical evidence that leads to a suspicion but not a definitive diagnosis). If conditions are ruled out or confirmed, clearly state so. If it remains uncertain, remember to carry this “possible” or “probable” diagnosis all the way through to the discharge summary or final progress note.
- Use linking of diagnoses when appropriate. For example, if the patient’s neuropathy, nephropathy, and retinopathy are related to their uncontrolled insulin dependent diabetes, state “uncontrolled insulin-dependent DMII with A1c of 11 complicated with nephropathy, neuropathy, and retinopathy.” The coders cannot link these diagnoses, and when you link them, you show a higher complexity of your patient. Remember to link the diagnoses only when they are truly related – this is where your medical knowledge and expertise come into play.
- Use the highest specificity of evidence that supports your medical decision making. You don’t need to be too verbose, all you need is evidence supporting your medical decision making and treatment plan. Think of it as demonstrating the logic of your diagnosis to another physician.
- Use Acuity (acute, chronic, acute on chronic, mild, moderate, severe, etc.) per diagnosis. For example, if you say heart failure exacerbation, it makes perfect sense to your medical colleagues, but in the coding world, it means nothing. Specify if it is acute, or acute on chronic, heart failure.
- Use status of each diagnosis. Is the condition improving, worsening, or resolved? Status does not have to be mentioned in all progress notes. Try to include this descriptor in the discharge summary and the day of the event.
- Always document the clinical significance of any abnormal laboratory, radiology reports, or pathology finding. Coders cannot use test results as a basis for coding unless a clinician has reviewed, interpreted, and documented the significance of the results in the progress note. Simply copying and pasting a report in the notes is not considered clinical acknowledgment. Shorthand notes like “Na=150, start hydration with 0.45% saline” is not acceptable. The actual diagnosis has to be written (i.e. “hypernatremia”). In addition, coders cannot code from nursing, dietitian, respiratory, and physical therapy notes. For example, if nursing documents that a patient has a pressure ulcer the clinician must still document the diagnosis of pressure ulcer, location, and stage. Although dietitian notes may state a body mass index greater than 40, coders cannot assume that patient is morbidly obese. Physician documentation is needed to support the obesity code assignment.
- Document all conditions that affect the patient’s stay, including complications and chronic conditions for which medications have been ordered. These secondary diagnoses paint the most accurate clinical picture and provide information needed to calculate important data, such as complexity and severity of patient illness and mortality risk. A patient with community-acquired pneumonia without other comorbidities requires fewer resources and has a greater chance of a good outcome than does the same patient with complications, such as acute heart failure.
- Downcoding brings losses, upcoding brings fines. Exaggerating the severity of patient conditions can lead to payer audits, reimbursement take backs, and charges of abuse and fraudulent billing. Never stretch the truth. Make sure you can support every diagnosis in the patient’s chart using clinical criteria.
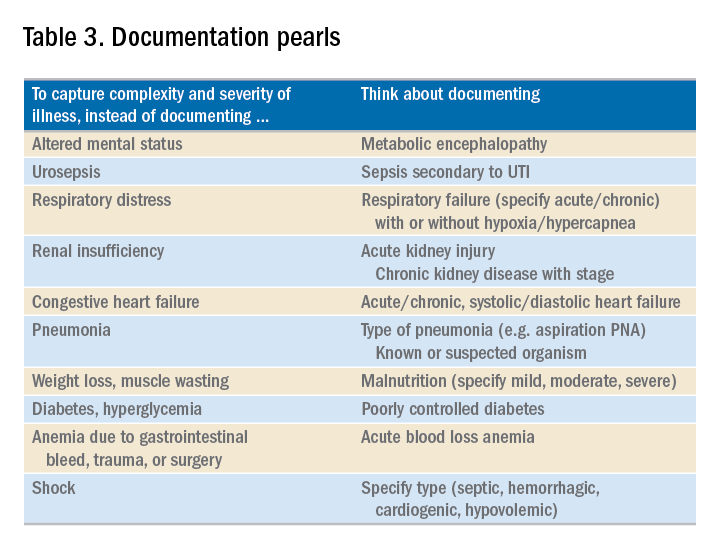
You may be frustrated by the need to choose specific words about diagnoses that seem obvious to you without these descriptors. But accurate documentation can make a huge difference in your hospital’s bottom line and published metrics. Understanding the relative impact of changing your terminology can help you make these changes, until the language becomes second nature. Your hospital administrators will be grateful – and you just might cut down your queries!
Dr. Rajda is medical director of clinical documentation and quality improvement for Mount Sinai Hospital in New York, and medical director for DRG appeals for the Mount Sinai Health System. She serves as assistant professor of medicine at Icahn School of Medicine at Mount Sinai. Dr. Fatemi is an assistant professor at the University of New Mexico, Albuquerque. She is director of documentation, coding, and billing for the division of hospital medicine at UNM. Dr. Reyna is assistant professor in the division of hospital medicine and medical director for clinical documentation and quality improvement at Mount Sinai Medical Center.
Bias in the clinical setting can impact patient care
SAN ANTONIO – Physicians and other health care providers may harbor implicit, or unconscious, biases that contribute to health care disparities, patient communication researcher Stacey Passalacqua, PhD, said here at the annual meeting of the American College of Chest Physicians.
Implicit biases are beliefs or attitudes, for example, about certain social groups, that exist outside of a health care provider’s conscious awareness, said Dr. Passalacqua of the department of communication at the University of Texas, San Antonio. If bias is implicit, it can be difficult self-assess.
among other social, ethnic, and racial groups, Dr. Passalacqua told attendees in workshops at the meeting.
“If a health care provider has negative biases toward a particular patient – maybe they think that these patients doesn’t care that much about their health or that they really have no interest in participating – then obviously that health care provider is far less likely to engage that patient in shared decision making,” she said in a video interview.
Diagnosis and treatment are subject to influence by the bias that physicians have toward certain patient groups, according to Dr. Passalacqua. For example, she said women with heart disease are less likely to be accurately diagnosed.
The bias in the medical setting might be mitigated by the presence of more individuals from the at-risk groups in the health care workforce, she added. In one recent retrospective study, investigators found that after an MI, a woman treated by a male physician was associated with higher mortality, while women and men had similar outcomes when treated by female physicians.
“That is one of the reasons why it is so important to have a diverse workforce, to have health care providers of different ethnicities, of different genders, or different backgrounds, because they are less subject to some of these implicit biases that we know are highly problematic in health care,” she said in the interview.
Dr. Passalacqua had no disclosures related to her presentation.
SAN ANTONIO – Physicians and other health care providers may harbor implicit, or unconscious, biases that contribute to health care disparities, patient communication researcher Stacey Passalacqua, PhD, said here at the annual meeting of the American College of Chest Physicians.
Implicit biases are beliefs or attitudes, for example, about certain social groups, that exist outside of a health care provider’s conscious awareness, said Dr. Passalacqua of the department of communication at the University of Texas, San Antonio. If bias is implicit, it can be difficult self-assess.
among other social, ethnic, and racial groups, Dr. Passalacqua told attendees in workshops at the meeting.
“If a health care provider has negative biases toward a particular patient – maybe they think that these patients doesn’t care that much about their health or that they really have no interest in participating – then obviously that health care provider is far less likely to engage that patient in shared decision making,” she said in a video interview.
Diagnosis and treatment are subject to influence by the bias that physicians have toward certain patient groups, according to Dr. Passalacqua. For example, she said women with heart disease are less likely to be accurately diagnosed.
The bias in the medical setting might be mitigated by the presence of more individuals from the at-risk groups in the health care workforce, she added. In one recent retrospective study, investigators found that after an MI, a woman treated by a male physician was associated with higher mortality, while women and men had similar outcomes when treated by female physicians.
“That is one of the reasons why it is so important to have a diverse workforce, to have health care providers of different ethnicities, of different genders, or different backgrounds, because they are less subject to some of these implicit biases that we know are highly problematic in health care,” she said in the interview.
Dr. Passalacqua had no disclosures related to her presentation.
SAN ANTONIO – Physicians and other health care providers may harbor implicit, or unconscious, biases that contribute to health care disparities, patient communication researcher Stacey Passalacqua, PhD, said here at the annual meeting of the American College of Chest Physicians.
Implicit biases are beliefs or attitudes, for example, about certain social groups, that exist outside of a health care provider’s conscious awareness, said Dr. Passalacqua of the department of communication at the University of Texas, San Antonio. If bias is implicit, it can be difficult self-assess.
among other social, ethnic, and racial groups, Dr. Passalacqua told attendees in workshops at the meeting.
“If a health care provider has negative biases toward a particular patient – maybe they think that these patients doesn’t care that much about their health or that they really have no interest in participating – then obviously that health care provider is far less likely to engage that patient in shared decision making,” she said in a video interview.
Diagnosis and treatment are subject to influence by the bias that physicians have toward certain patient groups, according to Dr. Passalacqua. For example, she said women with heart disease are less likely to be accurately diagnosed.
The bias in the medical setting might be mitigated by the presence of more individuals from the at-risk groups in the health care workforce, she added. In one recent retrospective study, investigators found that after an MI, a woman treated by a male physician was associated with higher mortality, while women and men had similar outcomes when treated by female physicians.
“That is one of the reasons why it is so important to have a diverse workforce, to have health care providers of different ethnicities, of different genders, or different backgrounds, because they are less subject to some of these implicit biases that we know are highly problematic in health care,” she said in the interview.
Dr. Passalacqua had no disclosures related to her presentation.
REPORTING FROM CHEST 2018
The new SoHM report is here, and it’s the best yet!
Survey content more wide-ranging than ever
On behalf of SHM’s Practice Analysis Committee, I’m thrilled to introduce the 2018 State of Hospital Medicine Report (SoHM) and the resumption of this monthly Survey Insights column written by committee members.
It’s a bit like giving birth. A 9-month–long process that started last January with the excitement of launching the survey and encouraging hospital medicine groups (HMGs) to participate. Then the long, drawn-out process of validating and analyzing data, and organizing it into tables and charts, watching our baby grow and take shape before our eyes, with a few small hiccups along the way. Then graphic design and the agonizing process of copy editing – over and over until our eyes crossed – and printing.
Like all expectant parents, by August we were saying, “Enough already; when will this ever end?”
But we finally have a baby, and what proud parents we are! Here are a couple of key things you should know about the 2018 SoHM:
- The total number of HMGs participating in this year’s survey was marginally lower than in 2016 (569 this year vs. 595 in 2016), but the respondent groups are much more diverse. While more than half of respondent HMGs (52%) are employed by hospitals or health systems, multistate management companies employ 25%, and universities or their affiliates employ 12%. More pediatric hospitalist groups (38) and HMGs that serve both adults and children (31) participated this year, compared with 2016, and almost twice as many academic HMGs participated as in the previous survey (96 this year vs. 59 in 2016).
- The survey content is more wide-ranging than ever. As usual, SHM licensed hospitalist compensation and productivity data from the Medical Group Management Association for inclusion in this report, and the SoHM also covers just about every other aspect of hospitalist group structure and operations imaginable. In addition to traditional questions regarding scope of services, staffing and scheduling models, leadership configuration, and financial support, this year’s report includes new information on:
- Hospitalist comanagement roles with surgical and medical subspecialties.
- Information about unfilled positions and how they are covered (including locum tenens use).
- Utilization of dedicated daytime admitters.
- Prevalence of geographic or unit-based assignment models.
- Responsibility for CPT code selection.
- Amount of financial support per wRVU.
The report has retained its colorful, easy-to-read report layout and the user-friendly interface of the digital version. And because we have more diversity this year with regard to HMG employment models, we have been able to reintroduce findings by employment model.
The 2018 SoHM report is now available for purchase at www.hospitalmedicine.org/sohm. I encourage you to obtain the SoHM report for yourself; you’ll almost certainly find more than one interesting and useful tidbit of information. Use the report to assess how your practice compares to your peers, but always keep in mind that surveys don’t tell you what should be – they tell you only what currently is.
New best practices not reflected in survey data are emerging all the time, and the ways others do things won’t always be right for your group’s unique situation and needs. Whether you are partners or employees, you and your colleagues “own” the success of your practice and are the best judges of what is right for you.
Leslie Flores, MHA, SFHM, is a partner with Nelson Flores Hospital Medicine Consultants, and a member of the SHM Practice Analysis Committee.
Survey content more wide-ranging than ever
Survey content more wide-ranging than ever
On behalf of SHM’s Practice Analysis Committee, I’m thrilled to introduce the 2018 State of Hospital Medicine Report (SoHM) and the resumption of this monthly Survey Insights column written by committee members.
It’s a bit like giving birth. A 9-month–long process that started last January with the excitement of launching the survey and encouraging hospital medicine groups (HMGs) to participate. Then the long, drawn-out process of validating and analyzing data, and organizing it into tables and charts, watching our baby grow and take shape before our eyes, with a few small hiccups along the way. Then graphic design and the agonizing process of copy editing – over and over until our eyes crossed – and printing.
Like all expectant parents, by August we were saying, “Enough already; when will this ever end?”
But we finally have a baby, and what proud parents we are! Here are a couple of key things you should know about the 2018 SoHM:
- The total number of HMGs participating in this year’s survey was marginally lower than in 2016 (569 this year vs. 595 in 2016), but the respondent groups are much more diverse. While more than half of respondent HMGs (52%) are employed by hospitals or health systems, multistate management companies employ 25%, and universities or their affiliates employ 12%. More pediatric hospitalist groups (38) and HMGs that serve both adults and children (31) participated this year, compared with 2016, and almost twice as many academic HMGs participated as in the previous survey (96 this year vs. 59 in 2016).
- The survey content is more wide-ranging than ever. As usual, SHM licensed hospitalist compensation and productivity data from the Medical Group Management Association for inclusion in this report, and the SoHM also covers just about every other aspect of hospitalist group structure and operations imaginable. In addition to traditional questions regarding scope of services, staffing and scheduling models, leadership configuration, and financial support, this year’s report includes new information on:
- Hospitalist comanagement roles with surgical and medical subspecialties.
- Information about unfilled positions and how they are covered (including locum tenens use).
- Utilization of dedicated daytime admitters.
- Prevalence of geographic or unit-based assignment models.
- Responsibility for CPT code selection.
- Amount of financial support per wRVU.
The report has retained its colorful, easy-to-read report layout and the user-friendly interface of the digital version. And because we have more diversity this year with regard to HMG employment models, we have been able to reintroduce findings by employment model.
The 2018 SoHM report is now available for purchase at www.hospitalmedicine.org/sohm. I encourage you to obtain the SoHM report for yourself; you’ll almost certainly find more than one interesting and useful tidbit of information. Use the report to assess how your practice compares to your peers, but always keep in mind that surveys don’t tell you what should be – they tell you only what currently is.
New best practices not reflected in survey data are emerging all the time, and the ways others do things won’t always be right for your group’s unique situation and needs. Whether you are partners or employees, you and your colleagues “own” the success of your practice and are the best judges of what is right for you.
Leslie Flores, MHA, SFHM, is a partner with Nelson Flores Hospital Medicine Consultants, and a member of the SHM Practice Analysis Committee.
On behalf of SHM’s Practice Analysis Committee, I’m thrilled to introduce the 2018 State of Hospital Medicine Report (SoHM) and the resumption of this monthly Survey Insights column written by committee members.
It’s a bit like giving birth. A 9-month–long process that started last January with the excitement of launching the survey and encouraging hospital medicine groups (HMGs) to participate. Then the long, drawn-out process of validating and analyzing data, and organizing it into tables and charts, watching our baby grow and take shape before our eyes, with a few small hiccups along the way. Then graphic design and the agonizing process of copy editing – over and over until our eyes crossed – and printing.
Like all expectant parents, by August we were saying, “Enough already; when will this ever end?”
But we finally have a baby, and what proud parents we are! Here are a couple of key things you should know about the 2018 SoHM:
- The total number of HMGs participating in this year’s survey was marginally lower than in 2016 (569 this year vs. 595 in 2016), but the respondent groups are much more diverse. While more than half of respondent HMGs (52%) are employed by hospitals or health systems, multistate management companies employ 25%, and universities or their affiliates employ 12%. More pediatric hospitalist groups (38) and HMGs that serve both adults and children (31) participated this year, compared with 2016, and almost twice as many academic HMGs participated as in the previous survey (96 this year vs. 59 in 2016).
- The survey content is more wide-ranging than ever. As usual, SHM licensed hospitalist compensation and productivity data from the Medical Group Management Association for inclusion in this report, and the SoHM also covers just about every other aspect of hospitalist group structure and operations imaginable. In addition to traditional questions regarding scope of services, staffing and scheduling models, leadership configuration, and financial support, this year’s report includes new information on:
- Hospitalist comanagement roles with surgical and medical subspecialties.
- Information about unfilled positions and how they are covered (including locum tenens use).
- Utilization of dedicated daytime admitters.
- Prevalence of geographic or unit-based assignment models.
- Responsibility for CPT code selection.
- Amount of financial support per wRVU.
The report has retained its colorful, easy-to-read report layout and the user-friendly interface of the digital version. And because we have more diversity this year with regard to HMG employment models, we have been able to reintroduce findings by employment model.
The 2018 SoHM report is now available for purchase at www.hospitalmedicine.org/sohm. I encourage you to obtain the SoHM report for yourself; you’ll almost certainly find more than one interesting and useful tidbit of information. Use the report to assess how your practice compares to your peers, but always keep in mind that surveys don’t tell you what should be – they tell you only what currently is.
New best practices not reflected in survey data are emerging all the time, and the ways others do things won’t always be right for your group’s unique situation and needs. Whether you are partners or employees, you and your colleagues “own” the success of your practice and are the best judges of what is right for you.
Leslie Flores, MHA, SFHM, is a partner with Nelson Flores Hospital Medicine Consultants, and a member of the SHM Practice Analysis Committee.
Telehealth: States broaden options for locations, providers
More states are expanding their telehealth policies to reach patients, and pulling back on rigid in-person requirements.
Several state Medicaid programs now explicitly allow the home to serve as an originating site for telehealth, with 10 states – Delaware, Colorado, Maryland, Michigan, Minnesota, Montana, New York, Texas, Washington, and Wyoming – adding the home as an approved site since 2016.
In addition, 16 jurisdictions now allow schools to serve as originating sites for telehealth, although some have restrictions about when the sites are acceptable, said Mei Kwong, an attorney and executive director for the Center for Connected Health Policy and the author of the center’s Spring 2018 report on telehealth trends.
At the same time, nearly all states have now dropped Medicaid restrictions that limited reimbursable telehealth services to rural or underserved areas. Colorado, Idaho, Nebraska, New Hampshire, Nevada, and Missouri are the most recent states to remove such geographic restrictions.
“[The expanded locations are] extremely helpful in providing greater access for patients to needed services,” Ms. Kwong said in an interview. “For example, a person who has difficulty leaving his or her home for a physical or other reason, they can get care, [or] a child having a rough time in school, can seek out a mental health counselor while at school.”
More telehealth providers
In addition to expanding teleheath sites, states are increasing acceptance for telehealth providers beyond physicians. Most recently, New Jersey enacted a broad telemedicine law that includes doctors, nurses, psychologists, social workers, physician assistants, counselors, respiratory therapists, speech pathologists, and optometrists, among others. The New Jersey law addresses telemedicine practice standards, prescribing, patient consent, privacy, and other requirements for providers.
In addition, more states are carving out telehealth regulations. Since 2016, 11 states have revised or adopted new scope of practice restrictions for counselors providing telemedicine, according to a state telehealth analysis published in July 2018 by law firm Epstein, Becker, Green.
Arkansas, Idaho, Maine, New Jersey, and Rhode Island recently imposed regulations for the practice of telepsychology. In addition, seven states have new or revised scope of practice restrictions for advanced practice registered nurses (APRN) providing telehealth services, while eight states have new licensing requirements specific to telehealth practice by APRNs, according to the Epstein analysis.
A telehealth compact that would allow APRNs to practice nursing via telemedicine across state lines is also in the works. Similar to the physician Interstate Medical Licensure Compact, the APRN Compact would establish an interstate commission and guidelines for uniform licensing requirements and criminal background checks. The compact will become effective when 10 states enact the compact legislation. So far, three states – Wyoming, North Dakota, and Idaho – have enacted the model legislation.
Another telemedicine compact for psychologists is getting ready to launch. In August, Illinois became the seventh state to join the Psychology Interjurisdictional Compact (PSYPACT). The pact requires seven states to enact compact legislation to become effective, however Illinois law does not go into effect until 2020.
The developments highlight the rise in more mid- and lower-level providers practicing telemedicine, said Anjali B. Dooley, an attorney and chief legal and compliance officer for Forefront Telecare, a telehealth platform for behavioral health services. While the increase allows greater care access, the expansion also poses scope of practice challenges, she notes.
“Increasing scope of practice extensions also increases risk if physician extenders are not trained properly in telehealth technology use and protocols,” Ms. Dooley said in an interview. “Providers and provider extenders need to be educated and learned in human factors such as communication, empathy, and etiquette.”
A greater number of nonphysician telemedicine providers is beneficial as long as the providers are adhering to appropriate standards of care and consulting with supervising physicians when necessary, adds Jean R. Sumner, MD, dean of the School of Medicine at Mercer University in Macon, Georgia, and a telemedicine internist.
“The standard should always be equal to an in-person visit,” she said in an interview. “The patient has a right to know who is seeing them, too, to understand [their credentials]. They need to know the person on the telehealth unit is qualified to provide the care.”
Responding to the opioid crisis
The need for increased access to mental health care is a primary driver behind state efforts to expand the pool of telemedicine providers, adds Amy Lerman, an attorney at Epstein, Becker, Green and lead author of her firm’s report.
“The reason it is important for states to continue expanding the scope of health professionals, other than physicians, who can provide behavioral health telemedicine services, is not only to address an overall nationwide shortage of behavioral health providers, but also to expand access to behavioral health services because a wider range of providers are equipped to provide these services,” she said in an interview.
In the same vein, more states are using telehealth to address the opioid crisis, according to both the Epstein report and the Center for Connected Health Policy analysis.
In September, California enacted a law that would allow Medicaid reimbursement for certified substance use disorder counselors who provide treatment via telehealth. In August, Illinois approved a similar law that mandates reimbursement for behavioral and mental health experts who treat Medicaid patients through telehealth technologies.
The laws come after a June 2018 letter from the Centers for Medicare & Medicaid Services that encouraged states to utilize health technology efforts to address the opioid crisis, including through telemedicine and telepsychiatry, said Daniel Kim, an attorney with Epstein, Becker, Green and a coauthor of his firm’s report.
At the same time, a number of states have expanded their controlled substance laws to allow remote prescribing through telehealth for the treatment of psychiatric or substance use disorders. Connecticut’s law, for instance, allows providers to prescribe Schedule I-III controlled substances through telehealth platforms, while banning opioid prescribing. In Indiana, 2017 legislation expanded the types of controlled medications that providers can prescribe through telehealth platforms, primarily drugs used to treat or manage opioid dependence. The states join an increasing number that have enacted laws allowing the remote prescribing of controlled substances, including Delaware, Florida, Indiana, Michigan, New Hampshire, Ohio, and West Virginia.
The new laws will enhance the availability of behavioral health services, while allowing more treatment flexibility and privacy for patients, said Ms. Dooley.
“Treatment in one’s own environment where the addiction takes place is often more effective,” she said. People with addiction disorders “can also receive treatment without having to drive long distances.”
The disappearing in-person requirement
As states define their telehealth policies, they are fading out a once-prevalent requirement – the in-person visit. There is no longer a single state that requires physicians to meet with patients in-person before providing telemedicine services, according to the Epstein report.
States realized that requiring in-person visits before doctors can provide telemedicine creates a barrier to care, said Mr. Kim. A move to eliminate the requirement in Texas influenced other states in phasing out the common regulation. In the widely publicized Teladoc case, the national telemedicine company sued the Texas Medical Board in 2011 over its rule requiring Texas physicians to conduct a face-to-face evaluation before treating a patient via telemedicine. The legal battle continued for years, until Teladoc voluntarily dropped its lawsuit in 2017 after Texas adopted a new law that allowed doctors to treat first-time patients through telemedicine.
“The medical board [understood] that the in-person requirement wasn’t really a benefit to patients,” Mr. Kim said in an interview. “Once they changed it, a lot of other states have recognized the same and have moved toward getting rid of the requirement.”
In some states, midlevel providers still must see patients face-to-face before providing telehealth care. Arkansas for instance, requires that psychologists, counselors, and APRNs conduct an in-person exam before rendering telehealth. Professional boards in Colorado and Massachusetts recommend a face-to-face visit by midlevel providers as a best practice.
Reimbursement growing, but restrictions remain
Forty-nine states and the District of Columbia reimburse for some form of telehealth, mainly live video services. At least 20 states now pay providers for remote payment monitoring (RPM), according to the Center for Connected Health Policy report. The reimbursement is often restricted, however, to certain clinical conditions and/or rules that limit the type of monitoring device allowed. Colorado, for instance, only reimburses RPM for patients with congestive heart failure, chronic obstructive pulmonary disease, asthma, or diabetes and requires that the patient was hospitalized at least twice in the last 12 months for reasons associated with one of the conditions. Missouri has similar RPM criteria associated with hospitalizations, but allows for a greater number of conditions including pregnancy, stroke, and cancer.
Most states have yet to pay for store-and-forward services, technologies that enable the electronic transfer of photos, prerecorded videos, or documents. Only about 14 states reimburse for such technology, and many policies include limitations. California, for example, only reimburses for store-and-forward services in teledermatology, teledentistry, and teleophthalmology. Connecticut allows for store-and-forward payment between physicians through email. Missouri allows for store-and-forward services in orthopedics, dermatology, optometry, ophthalmology, and in cases of retinopathy, burn and wound care, dental services, and maternal-fetal ultrasounds.
Reimbursement for telehealth is still a challenge for many physicians, Dr. Sumner said. Part of the problem is the wide discrepancy in how telehealth is defined among states, she said. Some states only consider live or interactive two-way technology as telehealth, excluding services such as store-and-forward and RPM. Other states reimburse for certain technology-based services, but they do not consider them telehealth. Maryland’s Medicaid program for example, does not reimburse for store and forward under its telehealth policy. However, store and forward used in dermatology, radiology, and ophthalmology is reimbursed by Maryland under an alternate billing code, though not considered telehealth.
Establishing best practices in telehealth through careful evaluation and research would improve reimbursement, said S. David McSwain, MD, interim chief medical information officer at the Medical University of South Carolina, Charleston, and medical director for telehealth optimization.
“We can use that evidence to reduce the variation in telehealth payment policies across the states,” Dr. McSwain said in an interview. “By leveraging reimbursement models to promote best practices, we can encourage the spread of telehealth services that have the greatest impacts on patients, their families, and the health care system.”
More states are expanding their telehealth policies to reach patients, and pulling back on rigid in-person requirements.
Several state Medicaid programs now explicitly allow the home to serve as an originating site for telehealth, with 10 states – Delaware, Colorado, Maryland, Michigan, Minnesota, Montana, New York, Texas, Washington, and Wyoming – adding the home as an approved site since 2016.
In addition, 16 jurisdictions now allow schools to serve as originating sites for telehealth, although some have restrictions about when the sites are acceptable, said Mei Kwong, an attorney and executive director for the Center for Connected Health Policy and the author of the center’s Spring 2018 report on telehealth trends.
At the same time, nearly all states have now dropped Medicaid restrictions that limited reimbursable telehealth services to rural or underserved areas. Colorado, Idaho, Nebraska, New Hampshire, Nevada, and Missouri are the most recent states to remove such geographic restrictions.
“[The expanded locations are] extremely helpful in providing greater access for patients to needed services,” Ms. Kwong said in an interview. “For example, a person who has difficulty leaving his or her home for a physical or other reason, they can get care, [or] a child having a rough time in school, can seek out a mental health counselor while at school.”
More telehealth providers
In addition to expanding teleheath sites, states are increasing acceptance for telehealth providers beyond physicians. Most recently, New Jersey enacted a broad telemedicine law that includes doctors, nurses, psychologists, social workers, physician assistants, counselors, respiratory therapists, speech pathologists, and optometrists, among others. The New Jersey law addresses telemedicine practice standards, prescribing, patient consent, privacy, and other requirements for providers.
In addition, more states are carving out telehealth regulations. Since 2016, 11 states have revised or adopted new scope of practice restrictions for counselors providing telemedicine, according to a state telehealth analysis published in July 2018 by law firm Epstein, Becker, Green.
Arkansas, Idaho, Maine, New Jersey, and Rhode Island recently imposed regulations for the practice of telepsychology. In addition, seven states have new or revised scope of practice restrictions for advanced practice registered nurses (APRN) providing telehealth services, while eight states have new licensing requirements specific to telehealth practice by APRNs, according to the Epstein analysis.
A telehealth compact that would allow APRNs to practice nursing via telemedicine across state lines is also in the works. Similar to the physician Interstate Medical Licensure Compact, the APRN Compact would establish an interstate commission and guidelines for uniform licensing requirements and criminal background checks. The compact will become effective when 10 states enact the compact legislation. So far, three states – Wyoming, North Dakota, and Idaho – have enacted the model legislation.
Another telemedicine compact for psychologists is getting ready to launch. In August, Illinois became the seventh state to join the Psychology Interjurisdictional Compact (PSYPACT). The pact requires seven states to enact compact legislation to become effective, however Illinois law does not go into effect until 2020.
The developments highlight the rise in more mid- and lower-level providers practicing telemedicine, said Anjali B. Dooley, an attorney and chief legal and compliance officer for Forefront Telecare, a telehealth platform for behavioral health services. While the increase allows greater care access, the expansion also poses scope of practice challenges, she notes.
“Increasing scope of practice extensions also increases risk if physician extenders are not trained properly in telehealth technology use and protocols,” Ms. Dooley said in an interview. “Providers and provider extenders need to be educated and learned in human factors such as communication, empathy, and etiquette.”
A greater number of nonphysician telemedicine providers is beneficial as long as the providers are adhering to appropriate standards of care and consulting with supervising physicians when necessary, adds Jean R. Sumner, MD, dean of the School of Medicine at Mercer University in Macon, Georgia, and a telemedicine internist.
“The standard should always be equal to an in-person visit,” she said in an interview. “The patient has a right to know who is seeing them, too, to understand [their credentials]. They need to know the person on the telehealth unit is qualified to provide the care.”
Responding to the opioid crisis
The need for increased access to mental health care is a primary driver behind state efforts to expand the pool of telemedicine providers, adds Amy Lerman, an attorney at Epstein, Becker, Green and lead author of her firm’s report.
“The reason it is important for states to continue expanding the scope of health professionals, other than physicians, who can provide behavioral health telemedicine services, is not only to address an overall nationwide shortage of behavioral health providers, but also to expand access to behavioral health services because a wider range of providers are equipped to provide these services,” she said in an interview.
In the same vein, more states are using telehealth to address the opioid crisis, according to both the Epstein report and the Center for Connected Health Policy analysis.
In September, California enacted a law that would allow Medicaid reimbursement for certified substance use disorder counselors who provide treatment via telehealth. In August, Illinois approved a similar law that mandates reimbursement for behavioral and mental health experts who treat Medicaid patients through telehealth technologies.
The laws come after a June 2018 letter from the Centers for Medicare & Medicaid Services that encouraged states to utilize health technology efforts to address the opioid crisis, including through telemedicine and telepsychiatry, said Daniel Kim, an attorney with Epstein, Becker, Green and a coauthor of his firm’s report.
At the same time, a number of states have expanded their controlled substance laws to allow remote prescribing through telehealth for the treatment of psychiatric or substance use disorders. Connecticut’s law, for instance, allows providers to prescribe Schedule I-III controlled substances through telehealth platforms, while banning opioid prescribing. In Indiana, 2017 legislation expanded the types of controlled medications that providers can prescribe through telehealth platforms, primarily drugs used to treat or manage opioid dependence. The states join an increasing number that have enacted laws allowing the remote prescribing of controlled substances, including Delaware, Florida, Indiana, Michigan, New Hampshire, Ohio, and West Virginia.
The new laws will enhance the availability of behavioral health services, while allowing more treatment flexibility and privacy for patients, said Ms. Dooley.
“Treatment in one’s own environment where the addiction takes place is often more effective,” she said. People with addiction disorders “can also receive treatment without having to drive long distances.”
The disappearing in-person requirement
As states define their telehealth policies, they are fading out a once-prevalent requirement – the in-person visit. There is no longer a single state that requires physicians to meet with patients in-person before providing telemedicine services, according to the Epstein report.
States realized that requiring in-person visits before doctors can provide telemedicine creates a barrier to care, said Mr. Kim. A move to eliminate the requirement in Texas influenced other states in phasing out the common regulation. In the widely publicized Teladoc case, the national telemedicine company sued the Texas Medical Board in 2011 over its rule requiring Texas physicians to conduct a face-to-face evaluation before treating a patient via telemedicine. The legal battle continued for years, until Teladoc voluntarily dropped its lawsuit in 2017 after Texas adopted a new law that allowed doctors to treat first-time patients through telemedicine.
“The medical board [understood] that the in-person requirement wasn’t really a benefit to patients,” Mr. Kim said in an interview. “Once they changed it, a lot of other states have recognized the same and have moved toward getting rid of the requirement.”
In some states, midlevel providers still must see patients face-to-face before providing telehealth care. Arkansas for instance, requires that psychologists, counselors, and APRNs conduct an in-person exam before rendering telehealth. Professional boards in Colorado and Massachusetts recommend a face-to-face visit by midlevel providers as a best practice.
Reimbursement growing, but restrictions remain
Forty-nine states and the District of Columbia reimburse for some form of telehealth, mainly live video services. At least 20 states now pay providers for remote payment monitoring (RPM), according to the Center for Connected Health Policy report. The reimbursement is often restricted, however, to certain clinical conditions and/or rules that limit the type of monitoring device allowed. Colorado, for instance, only reimburses RPM for patients with congestive heart failure, chronic obstructive pulmonary disease, asthma, or diabetes and requires that the patient was hospitalized at least twice in the last 12 months for reasons associated with one of the conditions. Missouri has similar RPM criteria associated with hospitalizations, but allows for a greater number of conditions including pregnancy, stroke, and cancer.
Most states have yet to pay for store-and-forward services, technologies that enable the electronic transfer of photos, prerecorded videos, or documents. Only about 14 states reimburse for such technology, and many policies include limitations. California, for example, only reimburses for store-and-forward services in teledermatology, teledentistry, and teleophthalmology. Connecticut allows for store-and-forward payment between physicians through email. Missouri allows for store-and-forward services in orthopedics, dermatology, optometry, ophthalmology, and in cases of retinopathy, burn and wound care, dental services, and maternal-fetal ultrasounds.
Reimbursement for telehealth is still a challenge for many physicians, Dr. Sumner said. Part of the problem is the wide discrepancy in how telehealth is defined among states, she said. Some states only consider live or interactive two-way technology as telehealth, excluding services such as store-and-forward and RPM. Other states reimburse for certain technology-based services, but they do not consider them telehealth. Maryland’s Medicaid program for example, does not reimburse for store and forward under its telehealth policy. However, store and forward used in dermatology, radiology, and ophthalmology is reimbursed by Maryland under an alternate billing code, though not considered telehealth.
Establishing best practices in telehealth through careful evaluation and research would improve reimbursement, said S. David McSwain, MD, interim chief medical information officer at the Medical University of South Carolina, Charleston, and medical director for telehealth optimization.
“We can use that evidence to reduce the variation in telehealth payment policies across the states,” Dr. McSwain said in an interview. “By leveraging reimbursement models to promote best practices, we can encourage the spread of telehealth services that have the greatest impacts on patients, their families, and the health care system.”
More states are expanding their telehealth policies to reach patients, and pulling back on rigid in-person requirements.
Several state Medicaid programs now explicitly allow the home to serve as an originating site for telehealth, with 10 states – Delaware, Colorado, Maryland, Michigan, Minnesota, Montana, New York, Texas, Washington, and Wyoming – adding the home as an approved site since 2016.
In addition, 16 jurisdictions now allow schools to serve as originating sites for telehealth, although some have restrictions about when the sites are acceptable, said Mei Kwong, an attorney and executive director for the Center for Connected Health Policy and the author of the center’s Spring 2018 report on telehealth trends.
At the same time, nearly all states have now dropped Medicaid restrictions that limited reimbursable telehealth services to rural or underserved areas. Colorado, Idaho, Nebraska, New Hampshire, Nevada, and Missouri are the most recent states to remove such geographic restrictions.
“[The expanded locations are] extremely helpful in providing greater access for patients to needed services,” Ms. Kwong said in an interview. “For example, a person who has difficulty leaving his or her home for a physical or other reason, they can get care, [or] a child having a rough time in school, can seek out a mental health counselor while at school.”
More telehealth providers
In addition to expanding teleheath sites, states are increasing acceptance for telehealth providers beyond physicians. Most recently, New Jersey enacted a broad telemedicine law that includes doctors, nurses, psychologists, social workers, physician assistants, counselors, respiratory therapists, speech pathologists, and optometrists, among others. The New Jersey law addresses telemedicine practice standards, prescribing, patient consent, privacy, and other requirements for providers.
In addition, more states are carving out telehealth regulations. Since 2016, 11 states have revised or adopted new scope of practice restrictions for counselors providing telemedicine, according to a state telehealth analysis published in July 2018 by law firm Epstein, Becker, Green.
Arkansas, Idaho, Maine, New Jersey, and Rhode Island recently imposed regulations for the practice of telepsychology. In addition, seven states have new or revised scope of practice restrictions for advanced practice registered nurses (APRN) providing telehealth services, while eight states have new licensing requirements specific to telehealth practice by APRNs, according to the Epstein analysis.
A telehealth compact that would allow APRNs to practice nursing via telemedicine across state lines is also in the works. Similar to the physician Interstate Medical Licensure Compact, the APRN Compact would establish an interstate commission and guidelines for uniform licensing requirements and criminal background checks. The compact will become effective when 10 states enact the compact legislation. So far, three states – Wyoming, North Dakota, and Idaho – have enacted the model legislation.
Another telemedicine compact for psychologists is getting ready to launch. In August, Illinois became the seventh state to join the Psychology Interjurisdictional Compact (PSYPACT). The pact requires seven states to enact compact legislation to become effective, however Illinois law does not go into effect until 2020.
The developments highlight the rise in more mid- and lower-level providers practicing telemedicine, said Anjali B. Dooley, an attorney and chief legal and compliance officer for Forefront Telecare, a telehealth platform for behavioral health services. While the increase allows greater care access, the expansion also poses scope of practice challenges, she notes.
“Increasing scope of practice extensions also increases risk if physician extenders are not trained properly in telehealth technology use and protocols,” Ms. Dooley said in an interview. “Providers and provider extenders need to be educated and learned in human factors such as communication, empathy, and etiquette.”
A greater number of nonphysician telemedicine providers is beneficial as long as the providers are adhering to appropriate standards of care and consulting with supervising physicians when necessary, adds Jean R. Sumner, MD, dean of the School of Medicine at Mercer University in Macon, Georgia, and a telemedicine internist.
“The standard should always be equal to an in-person visit,” she said in an interview. “The patient has a right to know who is seeing them, too, to understand [their credentials]. They need to know the person on the telehealth unit is qualified to provide the care.”
Responding to the opioid crisis
The need for increased access to mental health care is a primary driver behind state efforts to expand the pool of telemedicine providers, adds Amy Lerman, an attorney at Epstein, Becker, Green and lead author of her firm’s report.
“The reason it is important for states to continue expanding the scope of health professionals, other than physicians, who can provide behavioral health telemedicine services, is not only to address an overall nationwide shortage of behavioral health providers, but also to expand access to behavioral health services because a wider range of providers are equipped to provide these services,” she said in an interview.
In the same vein, more states are using telehealth to address the opioid crisis, according to both the Epstein report and the Center for Connected Health Policy analysis.
In September, California enacted a law that would allow Medicaid reimbursement for certified substance use disorder counselors who provide treatment via telehealth. In August, Illinois approved a similar law that mandates reimbursement for behavioral and mental health experts who treat Medicaid patients through telehealth technologies.
The laws come after a June 2018 letter from the Centers for Medicare & Medicaid Services that encouraged states to utilize health technology efforts to address the opioid crisis, including through telemedicine and telepsychiatry, said Daniel Kim, an attorney with Epstein, Becker, Green and a coauthor of his firm’s report.
At the same time, a number of states have expanded their controlled substance laws to allow remote prescribing through telehealth for the treatment of psychiatric or substance use disorders. Connecticut’s law, for instance, allows providers to prescribe Schedule I-III controlled substances through telehealth platforms, while banning opioid prescribing. In Indiana, 2017 legislation expanded the types of controlled medications that providers can prescribe through telehealth platforms, primarily drugs used to treat or manage opioid dependence. The states join an increasing number that have enacted laws allowing the remote prescribing of controlled substances, including Delaware, Florida, Indiana, Michigan, New Hampshire, Ohio, and West Virginia.
The new laws will enhance the availability of behavioral health services, while allowing more treatment flexibility and privacy for patients, said Ms. Dooley.
“Treatment in one’s own environment where the addiction takes place is often more effective,” she said. People with addiction disorders “can also receive treatment without having to drive long distances.”
The disappearing in-person requirement
As states define their telehealth policies, they are fading out a once-prevalent requirement – the in-person visit. There is no longer a single state that requires physicians to meet with patients in-person before providing telemedicine services, according to the Epstein report.
States realized that requiring in-person visits before doctors can provide telemedicine creates a barrier to care, said Mr. Kim. A move to eliminate the requirement in Texas influenced other states in phasing out the common regulation. In the widely publicized Teladoc case, the national telemedicine company sued the Texas Medical Board in 2011 over its rule requiring Texas physicians to conduct a face-to-face evaluation before treating a patient via telemedicine. The legal battle continued for years, until Teladoc voluntarily dropped its lawsuit in 2017 after Texas adopted a new law that allowed doctors to treat first-time patients through telemedicine.
“The medical board [understood] that the in-person requirement wasn’t really a benefit to patients,” Mr. Kim said in an interview. “Once they changed it, a lot of other states have recognized the same and have moved toward getting rid of the requirement.”
In some states, midlevel providers still must see patients face-to-face before providing telehealth care. Arkansas for instance, requires that psychologists, counselors, and APRNs conduct an in-person exam before rendering telehealth. Professional boards in Colorado and Massachusetts recommend a face-to-face visit by midlevel providers as a best practice.
Reimbursement growing, but restrictions remain
Forty-nine states and the District of Columbia reimburse for some form of telehealth, mainly live video services. At least 20 states now pay providers for remote payment monitoring (RPM), according to the Center for Connected Health Policy report. The reimbursement is often restricted, however, to certain clinical conditions and/or rules that limit the type of monitoring device allowed. Colorado, for instance, only reimburses RPM for patients with congestive heart failure, chronic obstructive pulmonary disease, asthma, or diabetes and requires that the patient was hospitalized at least twice in the last 12 months for reasons associated with one of the conditions. Missouri has similar RPM criteria associated with hospitalizations, but allows for a greater number of conditions including pregnancy, stroke, and cancer.
Most states have yet to pay for store-and-forward services, technologies that enable the electronic transfer of photos, prerecorded videos, or documents. Only about 14 states reimburse for such technology, and many policies include limitations. California, for example, only reimburses for store-and-forward services in teledermatology, teledentistry, and teleophthalmology. Connecticut allows for store-and-forward payment between physicians through email. Missouri allows for store-and-forward services in orthopedics, dermatology, optometry, ophthalmology, and in cases of retinopathy, burn and wound care, dental services, and maternal-fetal ultrasounds.
Reimbursement for telehealth is still a challenge for many physicians, Dr. Sumner said. Part of the problem is the wide discrepancy in how telehealth is defined among states, she said. Some states only consider live or interactive two-way technology as telehealth, excluding services such as store-and-forward and RPM. Other states reimburse for certain technology-based services, but they do not consider them telehealth. Maryland’s Medicaid program for example, does not reimburse for store and forward under its telehealth policy. However, store and forward used in dermatology, radiology, and ophthalmology is reimbursed by Maryland under an alternate billing code, though not considered telehealth.
Establishing best practices in telehealth through careful evaluation and research would improve reimbursement, said S. David McSwain, MD, interim chief medical information officer at the Medical University of South Carolina, Charleston, and medical director for telehealth optimization.
“We can use that evidence to reduce the variation in telehealth payment policies across the states,” Dr. McSwain said in an interview. “By leveraging reimbursement models to promote best practices, we can encourage the spread of telehealth services that have the greatest impacts on patients, their families, and the health care system.”