User login
Caring for the aging transgender patient
The elderly transgender population is rapidly expanding and remains significantly overlooked. Although emerging evidence provides some guidance for medical and surgical treatment for transgender youth, there is still a paucity of research directed at the management of gender-diverse elders.
To a large extent, the challenges that transgender elders face are no different from those experienced by the general elder population. Irrespective of gender identity, patients begin to undergo cognitive and physical changes, encounter difficulties with activities of daily living, suffer the loss of social networks and friends, and face end-of-life issues.1 Attributes that contribute to successful aging in the general population include good health, social engagement and support, and having a positive outlook on life.1 Yet, stigma surrounding gender identity and sexual orientation continues to negatively affect elder transgender people.
Many members of the LGBTQIA+ population have higher rates of obesity, sedentary lifestyle, smoking, cardiovascular disease, substance abuse, depression, suicide, and intimate partner violence than the general same-age cohort.2 Compared with lesbian, gay, and bisexual elders of age-matched cohorts, transgender elders have significantly poorer overall physical health, disability, depressive symptoms, and perceived stress.2
Rates of sexually transmitted infections are also rising in the aging general population and increased by 30% between 2014 and 2017.2 There have been no current studies examining these rates in the LGBTQIA+ population. As providers interact more frequently with these patients, it’s not only essential to screen for conditions such as diabetes, lipid disorders, and sexually transmitted infections, but also to evaluate current gender-affirming hormone therapy (GAHT) regimens and order appropriate screening tests.
Hormonal therapy for transfeminine patients should be continued as patients age. One of the biggest concerns providers have in continuing hormone therapy is the development of cardiovascular disease (CVD) and increasing thromboembolic risk, both of which tend to occur naturally as patients age. Overall, studies on the prevalence of CVD or stroke in gender-diverse individuals indicate an elevated risk independent of GAHT.3 While the overall rates of thromboembolic events are low in transfeminine populations, estrogen therapy does confer an increased risk. However, most transgender women who have experienced cardiac events or stroke were over the age of 50, had one or more CVD risk factors, or were using synthetic estrogens.3
How these studies affect screening is unclear. Current guidelines recommend using tailored risk-based calculators, which take into consideration the patient’s sex assigned at birth, hormone regimen, length of hormone usage, and additional modifiable risk factors, such as diabetes, obesity, and smoking.3 For transfeminine patients who want to continue GAHT but either develop a venous thromboembolism on estrogen or have increased risk for VTE, providers should consider transitioning them to a transdermal application. Patients who stay on GAHT should be counseled accordingly on the heightened risk of VTE recurrence. It is not unreasonable to consider life-long anticoagulation for patients who remain on estrogen therapy after a VTE.4
While exogenous estrogen exposure is one risk factor for the development of breast cancer in cisgender females, the role of GAHT in breast cancer in transgender women is ambiguous. Therefore, breast screening guidelines should follow current recommendations for cisgender female patients with some caveats. The provider must also take into consideration current estrogen dosage, the age at which hormones were initiated, and whether a patient has undergone an augmentation mammaplasty.3
Both estrogen and testosterone play an important role in bone formation and health. Patients who undergo either medical or surgical interventions that alter sex hormone production, such as GAHT, orchiectomy, or androgen blockade, may be at elevated risk for osteoporosis. Providers should take a thorough medical history to determine patients who may be at risk for osteoporosis and treat them accordingly. Overall, GAHT has a positive effect on bone mineral density. Conversely, gonadectomy, particularly if a patient is not taking GAHT, can decrease bone density. Generally, transgender women, like cisgender women, should undergo DEXA scans starting at the age of 65, with earlier screening considered if they have undergone an orchiectomy and are not currently taking GAHT.3
There is no evidence that GAHT or surgery increases the rate of prostate cancer. Providers should note that the prostate is not removed at the time of gender-affirming surgery and that malignancy or benign prostatic hypertrophy can still occur. The U.S. Preventive Services Task Force recommends that clinicians have a discussion with cisgender men between the ages of 55 and 69 about the risks and benefits of prostate-specific antigen (PSA) screening.5 For cisgender men aged 70 and older, the USPSTF recommends against PSA-based screening.5 If digital examination of the prostate is warranted for transfeminine patients, the examination is performed through the neovaginal canal.
Caring for elderly transgender patients is complex. Even though evidence guiding the management of elderly transgender patients is improving, there are still not enough definitive long-term data on this dynamic demographic. Like clinical approaches with hormonal or surgical treatments, caring for transgender elders is also multidisciplinary. Providers should be prepared to work with social workers, geriatric care physicians, endocrinologists, surgeons, and other relevant specialists to assist with potential knowledge gaps. The goals for the aging transgender population are the same as those for cisgender patients – preventing preventable diseases and reducing overall mortality so our patients can enjoy their golden years.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa. Contact her at [email protected].
References
1. Carroll L. Psychiatr Clin N Am. 2017;40:127-40.
2. Selix NW et al. Clinical care of the aging LGBT population. J Nurse Pract. 2020;16(7):349-54.
3. World Professional Association for Transgender Health. Standards of care for the health of transgender and gender diverse people. 2022;8th version.
4. Shatzel JJ et al. Am J Hematol. 2017;92(2):204-8.
5. Wolf-Gould CS and Wolf-Gould CH. Primary and preventative care for transgender patients. In: Ferrando CA, ed. Comprehensive Care of the Transgender Patient. Philadelphia: Elsevier, 2020, p. 114-30.
The elderly transgender population is rapidly expanding and remains significantly overlooked. Although emerging evidence provides some guidance for medical and surgical treatment for transgender youth, there is still a paucity of research directed at the management of gender-diverse elders.
To a large extent, the challenges that transgender elders face are no different from those experienced by the general elder population. Irrespective of gender identity, patients begin to undergo cognitive and physical changes, encounter difficulties with activities of daily living, suffer the loss of social networks and friends, and face end-of-life issues.1 Attributes that contribute to successful aging in the general population include good health, social engagement and support, and having a positive outlook on life.1 Yet, stigma surrounding gender identity and sexual orientation continues to negatively affect elder transgender people.
Many members of the LGBTQIA+ population have higher rates of obesity, sedentary lifestyle, smoking, cardiovascular disease, substance abuse, depression, suicide, and intimate partner violence than the general same-age cohort.2 Compared with lesbian, gay, and bisexual elders of age-matched cohorts, transgender elders have significantly poorer overall physical health, disability, depressive symptoms, and perceived stress.2
Rates of sexually transmitted infections are also rising in the aging general population and increased by 30% between 2014 and 2017.2 There have been no current studies examining these rates in the LGBTQIA+ population. As providers interact more frequently with these patients, it’s not only essential to screen for conditions such as diabetes, lipid disorders, and sexually transmitted infections, but also to evaluate current gender-affirming hormone therapy (GAHT) regimens and order appropriate screening tests.
Hormonal therapy for transfeminine patients should be continued as patients age. One of the biggest concerns providers have in continuing hormone therapy is the development of cardiovascular disease (CVD) and increasing thromboembolic risk, both of which tend to occur naturally as patients age. Overall, studies on the prevalence of CVD or stroke in gender-diverse individuals indicate an elevated risk independent of GAHT.3 While the overall rates of thromboembolic events are low in transfeminine populations, estrogen therapy does confer an increased risk. However, most transgender women who have experienced cardiac events or stroke were over the age of 50, had one or more CVD risk factors, or were using synthetic estrogens.3
How these studies affect screening is unclear. Current guidelines recommend using tailored risk-based calculators, which take into consideration the patient’s sex assigned at birth, hormone regimen, length of hormone usage, and additional modifiable risk factors, such as diabetes, obesity, and smoking.3 For transfeminine patients who want to continue GAHT but either develop a venous thromboembolism on estrogen or have increased risk for VTE, providers should consider transitioning them to a transdermal application. Patients who stay on GAHT should be counseled accordingly on the heightened risk of VTE recurrence. It is not unreasonable to consider life-long anticoagulation for patients who remain on estrogen therapy after a VTE.4
While exogenous estrogen exposure is one risk factor for the development of breast cancer in cisgender females, the role of GAHT in breast cancer in transgender women is ambiguous. Therefore, breast screening guidelines should follow current recommendations for cisgender female patients with some caveats. The provider must also take into consideration current estrogen dosage, the age at which hormones were initiated, and whether a patient has undergone an augmentation mammaplasty.3
Both estrogen and testosterone play an important role in bone formation and health. Patients who undergo either medical or surgical interventions that alter sex hormone production, such as GAHT, orchiectomy, or androgen blockade, may be at elevated risk for osteoporosis. Providers should take a thorough medical history to determine patients who may be at risk for osteoporosis and treat them accordingly. Overall, GAHT has a positive effect on bone mineral density. Conversely, gonadectomy, particularly if a patient is not taking GAHT, can decrease bone density. Generally, transgender women, like cisgender women, should undergo DEXA scans starting at the age of 65, with earlier screening considered if they have undergone an orchiectomy and are not currently taking GAHT.3
There is no evidence that GAHT or surgery increases the rate of prostate cancer. Providers should note that the prostate is not removed at the time of gender-affirming surgery and that malignancy or benign prostatic hypertrophy can still occur. The U.S. Preventive Services Task Force recommends that clinicians have a discussion with cisgender men between the ages of 55 and 69 about the risks and benefits of prostate-specific antigen (PSA) screening.5 For cisgender men aged 70 and older, the USPSTF recommends against PSA-based screening.5 If digital examination of the prostate is warranted for transfeminine patients, the examination is performed through the neovaginal canal.
Caring for elderly transgender patients is complex. Even though evidence guiding the management of elderly transgender patients is improving, there are still not enough definitive long-term data on this dynamic demographic. Like clinical approaches with hormonal or surgical treatments, caring for transgender elders is also multidisciplinary. Providers should be prepared to work with social workers, geriatric care physicians, endocrinologists, surgeons, and other relevant specialists to assist with potential knowledge gaps. The goals for the aging transgender population are the same as those for cisgender patients – preventing preventable diseases and reducing overall mortality so our patients can enjoy their golden years.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa. Contact her at [email protected].
References
1. Carroll L. Psychiatr Clin N Am. 2017;40:127-40.
2. Selix NW et al. Clinical care of the aging LGBT population. J Nurse Pract. 2020;16(7):349-54.
3. World Professional Association for Transgender Health. Standards of care for the health of transgender and gender diverse people. 2022;8th version.
4. Shatzel JJ et al. Am J Hematol. 2017;92(2):204-8.
5. Wolf-Gould CS and Wolf-Gould CH. Primary and preventative care for transgender patients. In: Ferrando CA, ed. Comprehensive Care of the Transgender Patient. Philadelphia: Elsevier, 2020, p. 114-30.
The elderly transgender population is rapidly expanding and remains significantly overlooked. Although emerging evidence provides some guidance for medical and surgical treatment for transgender youth, there is still a paucity of research directed at the management of gender-diverse elders.
To a large extent, the challenges that transgender elders face are no different from those experienced by the general elder population. Irrespective of gender identity, patients begin to undergo cognitive and physical changes, encounter difficulties with activities of daily living, suffer the loss of social networks and friends, and face end-of-life issues.1 Attributes that contribute to successful aging in the general population include good health, social engagement and support, and having a positive outlook on life.1 Yet, stigma surrounding gender identity and sexual orientation continues to negatively affect elder transgender people.
Many members of the LGBTQIA+ population have higher rates of obesity, sedentary lifestyle, smoking, cardiovascular disease, substance abuse, depression, suicide, and intimate partner violence than the general same-age cohort.2 Compared with lesbian, gay, and bisexual elders of age-matched cohorts, transgender elders have significantly poorer overall physical health, disability, depressive symptoms, and perceived stress.2
Rates of sexually transmitted infections are also rising in the aging general population and increased by 30% between 2014 and 2017.2 There have been no current studies examining these rates in the LGBTQIA+ population. As providers interact more frequently with these patients, it’s not only essential to screen for conditions such as diabetes, lipid disorders, and sexually transmitted infections, but also to evaluate current gender-affirming hormone therapy (GAHT) regimens and order appropriate screening tests.
Hormonal therapy for transfeminine patients should be continued as patients age. One of the biggest concerns providers have in continuing hormone therapy is the development of cardiovascular disease (CVD) and increasing thromboembolic risk, both of which tend to occur naturally as patients age. Overall, studies on the prevalence of CVD or stroke in gender-diverse individuals indicate an elevated risk independent of GAHT.3 While the overall rates of thromboembolic events are low in transfeminine populations, estrogen therapy does confer an increased risk. However, most transgender women who have experienced cardiac events or stroke were over the age of 50, had one or more CVD risk factors, or were using synthetic estrogens.3
How these studies affect screening is unclear. Current guidelines recommend using tailored risk-based calculators, which take into consideration the patient’s sex assigned at birth, hormone regimen, length of hormone usage, and additional modifiable risk factors, such as diabetes, obesity, and smoking.3 For transfeminine patients who want to continue GAHT but either develop a venous thromboembolism on estrogen or have increased risk for VTE, providers should consider transitioning them to a transdermal application. Patients who stay on GAHT should be counseled accordingly on the heightened risk of VTE recurrence. It is not unreasonable to consider life-long anticoagulation for patients who remain on estrogen therapy after a VTE.4
While exogenous estrogen exposure is one risk factor for the development of breast cancer in cisgender females, the role of GAHT in breast cancer in transgender women is ambiguous. Therefore, breast screening guidelines should follow current recommendations for cisgender female patients with some caveats. The provider must also take into consideration current estrogen dosage, the age at which hormones were initiated, and whether a patient has undergone an augmentation mammaplasty.3
Both estrogen and testosterone play an important role in bone formation and health. Patients who undergo either medical or surgical interventions that alter sex hormone production, such as GAHT, orchiectomy, or androgen blockade, may be at elevated risk for osteoporosis. Providers should take a thorough medical history to determine patients who may be at risk for osteoporosis and treat them accordingly. Overall, GAHT has a positive effect on bone mineral density. Conversely, gonadectomy, particularly if a patient is not taking GAHT, can decrease bone density. Generally, transgender women, like cisgender women, should undergo DEXA scans starting at the age of 65, with earlier screening considered if they have undergone an orchiectomy and are not currently taking GAHT.3
There is no evidence that GAHT or surgery increases the rate of prostate cancer. Providers should note that the prostate is not removed at the time of gender-affirming surgery and that malignancy or benign prostatic hypertrophy can still occur. The U.S. Preventive Services Task Force recommends that clinicians have a discussion with cisgender men between the ages of 55 and 69 about the risks and benefits of prostate-specific antigen (PSA) screening.5 For cisgender men aged 70 and older, the USPSTF recommends against PSA-based screening.5 If digital examination of the prostate is warranted for transfeminine patients, the examination is performed through the neovaginal canal.
Caring for elderly transgender patients is complex. Even though evidence guiding the management of elderly transgender patients is improving, there are still not enough definitive long-term data on this dynamic demographic. Like clinical approaches with hormonal or surgical treatments, caring for transgender elders is also multidisciplinary. Providers should be prepared to work with social workers, geriatric care physicians, endocrinologists, surgeons, and other relevant specialists to assist with potential knowledge gaps. The goals for the aging transgender population are the same as those for cisgender patients – preventing preventable diseases and reducing overall mortality so our patients can enjoy their golden years.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa. Contact her at [email protected].
References
1. Carroll L. Psychiatr Clin N Am. 2017;40:127-40.
2. Selix NW et al. Clinical care of the aging LGBT population. J Nurse Pract. 2020;16(7):349-54.
3. World Professional Association for Transgender Health. Standards of care for the health of transgender and gender diverse people. 2022;8th version.
4. Shatzel JJ et al. Am J Hematol. 2017;92(2):204-8.
5. Wolf-Gould CS and Wolf-Gould CH. Primary and preventative care for transgender patients. In: Ferrando CA, ed. Comprehensive Care of the Transgender Patient. Philadelphia: Elsevier, 2020, p. 114-30.
Global Initiative for Chronic Obstructive Lung Disease guidelines 2022: Management and treatment
In the United States and around the globe, chronic obstructive pulmonary disease (COPD) remains one of the leading causes of death. In addition to new diagnostic guidelines, the Global Initiative for Chronic Obstructive Lung Disease 2022 Report, or GOLD report, sets forth recommendations for management and treatment.
According to the GOLD report, initial management of COPD should aim at reducing exposure to risk factors such as smoking or other chemical exposures. In addition to medications, stable COPD patients should be evaluated for inhaler technique, adherence to prescribed therapies, smoking status, and continued exposure to other risk factors. Also, physical activity should be advised and pulmonary rehabilitation should be considered. Spirometry should be performed annually.
These guidelines offer very practical advice but often are difficult to implement in clinical practice. Everyone knows smoking is harmful and quitting provides huge health benefits, not only regarding COPD. However, nicotine is very addictive, and most smokers cannot just quit. Many need smoking cessation aids and counseling. Additionally, some smokers just don’t want to quit. Regarding workplace exposures, it often is not easy for someone just to change their job. Many are afraid to speak because they are afraid of losing their jobs. Everyone, not just patients with COPD, can benefit from increased physical activity, and all doctors know how difficult it is to motivate patients to do this.
The decision to initiate medications should be based on an individual patient’s symptoms and risk of exacerbations. In general, long-acting bronchodilators, including long-acting beta agonists (LABA) and long-acting muscarinic antagonists (LAMA), are preferred except when immediate relief of dyspnea is needed, and then short-acting bronchodilators should be used. Either a single long-acting or dual long-acting bronchodilator can be initiated. If a patient continues to have dyspnea on a single long-acting bronchodilator, treatment should be switched to a dual therapy.
In general, inhaled corticosteroids (ICS) are not recommended for stable COPD patients. If a patient has exacerbations despite appropriate treatment with LABAs, an ICS may be added to the LABA, the GOLD guidelines say. Oral corticosteroids are not recommended for long-term use. PDE4 inhibitors should be considered in patents with severe to very severe airflow obstruction, chronic bronchitis, and exacerbations. Macrolide antibiotics, especially azithromycin, can be considered in acute exacerbations. There is no evidence to support the use of antitussives and mucolytics are advised in only certain patients. Inhaled bronchodilators are advised over oral ones and theophylline is recommended when long-acting bronchodilators are unavailable or unaffordable.
In clinical practice, I see many patients treated based on symptomatology with spirometry testing not being done. This may help control many symptoms, but unless my patient has an accurate diagnosis, I won’t know if my patient is receiving the correct treatment.
It is important to keep in mind that COPD is a progressive disease and without appropriate treatment and monitoring, it will just get worse, and this is most likely to be irreversible.
Medications and treatment goals for patients with COPD
Patients with alpha-1 antitrypsin deficiency may benefit from the addition of alpha-1 antitrypsin augmentation therapy, the new guidelines say. In patients with severe disease experiencing dyspnea, oral and parental opioids can be considered. Medications that are used to treat primary pulmonary hypertension are not advised to treat pulmonary hypertension secondary to COPD.
The treatment goals of COPD should be to decrease severity of symptoms, reduce the occurrence of exacerbations, and improve exercise tolerance. Peripheral eosinophil counts can be used to guide the use of ICS to prevent exacerbations. However, the best predictor of exacerbations is previous exacerbations. Frequent exacerbations are defined as two or more annually. Additionally, deteriorating airflow is correlated with increased risk of exacerbations, hospitalizations, and death. Forced expiratory volume in 1 second (FEV1) alone lacks precision to predict exacerbations or death.
Vaccines and pulmonary rehabilitation recommended
The Centers for Disease Control and Prevention and World Health Organization recommend several vaccines for stable patients with COPD. Influenza vaccine was shown to reduce serious complications in COPD patients. Pneumococcal vaccines (PCV13 and PPSV23) reduced the likelihood of COPD exacerbations. The COVID-19 vaccine also has been effective at reducing hospitalizations, in particular ICU admissions, and death in patients with COPD. The CDC also recommends TdaP and Zoster vaccines.
An acute exacerbation of COPD occurs when a patient experiences worsening of respiratory symptoms that requires additional treatment, according to the updated GOLD guidelines. They are usually associated with increased airway inflammation, mucous productions, and trapping of gases. They are often triggered by viral infections, but bacterial and environment factors play a role as well. Less commonly, fungi such as Aspergillus can be observed as well. COPD exacerbations contribute to overall progression of the disease.
In patients with hypoxemia, supplemental oxygen should be titrated to a target O2 saturation of 88%-92%. It is important to follow blood gases to be sure adequate oxygenation is taking place while at the same time avoiding carbon dioxide retention and/or worsening acidosis. In patients with severe exacerbations whose dyspnea does not respond to initial emergency therapy, ICU admission is warranted. Other factors indicating the need for ICU admission include mental status changes, persistent or worsening hypoxemia, severe or worsening respiratory acidosis, the need for mechanical ventilation, and hemodynamic instability. Following an acute exacerbation, steps to prevent further exacerbations should be initiated.
Systemic glucocorticoids are indicated during acute exacerbations. They have been shown to hasten recovery time and improve functioning of the lungs as well as oxygenation. It is recommended to give prednisone 40 mg per day for 5 days. Antibiotics should be used in exacerbations if patients have dyspnea, sputum production, and purulence of the sputum or require mechanical ventilation. The choice of which antibiotic to use should be based on local bacterial resistance.
Pulmonary rehabilitation is an important component of COPD management. It incorporates exercise, education, and self-management aimed to change behavior and improve conditioning. The benefits of rehab have been shown to be considerable. The optimal length is 6-8 weeks. Palliative and end-of-life care are also very important factors to consider when treating COPD patients, according to the GOLD guidelines.
COPD is a very common disease and cause of mortality seen by family physicians. The GOLD report is an extensive document providing very clear guidelines and evidence to support these guidelines in every level of the treatment of COPD patients. As primary care doctors, we are often the first to treat patients with COPD and it is important to know the latest guidelines.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, N.J. You can contact her at [email protected].
In the United States and around the globe, chronic obstructive pulmonary disease (COPD) remains one of the leading causes of death. In addition to new diagnostic guidelines, the Global Initiative for Chronic Obstructive Lung Disease 2022 Report, or GOLD report, sets forth recommendations for management and treatment.
According to the GOLD report, initial management of COPD should aim at reducing exposure to risk factors such as smoking or other chemical exposures. In addition to medications, stable COPD patients should be evaluated for inhaler technique, adherence to prescribed therapies, smoking status, and continued exposure to other risk factors. Also, physical activity should be advised and pulmonary rehabilitation should be considered. Spirometry should be performed annually.
These guidelines offer very practical advice but often are difficult to implement in clinical practice. Everyone knows smoking is harmful and quitting provides huge health benefits, not only regarding COPD. However, nicotine is very addictive, and most smokers cannot just quit. Many need smoking cessation aids and counseling. Additionally, some smokers just don’t want to quit. Regarding workplace exposures, it often is not easy for someone just to change their job. Many are afraid to speak because they are afraid of losing their jobs. Everyone, not just patients with COPD, can benefit from increased physical activity, and all doctors know how difficult it is to motivate patients to do this.
The decision to initiate medications should be based on an individual patient’s symptoms and risk of exacerbations. In general, long-acting bronchodilators, including long-acting beta agonists (LABA) and long-acting muscarinic antagonists (LAMA), are preferred except when immediate relief of dyspnea is needed, and then short-acting bronchodilators should be used. Either a single long-acting or dual long-acting bronchodilator can be initiated. If a patient continues to have dyspnea on a single long-acting bronchodilator, treatment should be switched to a dual therapy.
In general, inhaled corticosteroids (ICS) are not recommended for stable COPD patients. If a patient has exacerbations despite appropriate treatment with LABAs, an ICS may be added to the LABA, the GOLD guidelines say. Oral corticosteroids are not recommended for long-term use. PDE4 inhibitors should be considered in patents with severe to very severe airflow obstruction, chronic bronchitis, and exacerbations. Macrolide antibiotics, especially azithromycin, can be considered in acute exacerbations. There is no evidence to support the use of antitussives and mucolytics are advised in only certain patients. Inhaled bronchodilators are advised over oral ones and theophylline is recommended when long-acting bronchodilators are unavailable or unaffordable.
In clinical practice, I see many patients treated based on symptomatology with spirometry testing not being done. This may help control many symptoms, but unless my patient has an accurate diagnosis, I won’t know if my patient is receiving the correct treatment.
It is important to keep in mind that COPD is a progressive disease and without appropriate treatment and monitoring, it will just get worse, and this is most likely to be irreversible.
Medications and treatment goals for patients with COPD
Patients with alpha-1 antitrypsin deficiency may benefit from the addition of alpha-1 antitrypsin augmentation therapy, the new guidelines say. In patients with severe disease experiencing dyspnea, oral and parental opioids can be considered. Medications that are used to treat primary pulmonary hypertension are not advised to treat pulmonary hypertension secondary to COPD.
The treatment goals of COPD should be to decrease severity of symptoms, reduce the occurrence of exacerbations, and improve exercise tolerance. Peripheral eosinophil counts can be used to guide the use of ICS to prevent exacerbations. However, the best predictor of exacerbations is previous exacerbations. Frequent exacerbations are defined as two or more annually. Additionally, deteriorating airflow is correlated with increased risk of exacerbations, hospitalizations, and death. Forced expiratory volume in 1 second (FEV1) alone lacks precision to predict exacerbations or death.
Vaccines and pulmonary rehabilitation recommended
The Centers for Disease Control and Prevention and World Health Organization recommend several vaccines for stable patients with COPD. Influenza vaccine was shown to reduce serious complications in COPD patients. Pneumococcal vaccines (PCV13 and PPSV23) reduced the likelihood of COPD exacerbations. The COVID-19 vaccine also has been effective at reducing hospitalizations, in particular ICU admissions, and death in patients with COPD. The CDC also recommends TdaP and Zoster vaccines.
An acute exacerbation of COPD occurs when a patient experiences worsening of respiratory symptoms that requires additional treatment, according to the updated GOLD guidelines. They are usually associated with increased airway inflammation, mucous productions, and trapping of gases. They are often triggered by viral infections, but bacterial and environment factors play a role as well. Less commonly, fungi such as Aspergillus can be observed as well. COPD exacerbations contribute to overall progression of the disease.
In patients with hypoxemia, supplemental oxygen should be titrated to a target O2 saturation of 88%-92%. It is important to follow blood gases to be sure adequate oxygenation is taking place while at the same time avoiding carbon dioxide retention and/or worsening acidosis. In patients with severe exacerbations whose dyspnea does not respond to initial emergency therapy, ICU admission is warranted. Other factors indicating the need for ICU admission include mental status changes, persistent or worsening hypoxemia, severe or worsening respiratory acidosis, the need for mechanical ventilation, and hemodynamic instability. Following an acute exacerbation, steps to prevent further exacerbations should be initiated.
Systemic glucocorticoids are indicated during acute exacerbations. They have been shown to hasten recovery time and improve functioning of the lungs as well as oxygenation. It is recommended to give prednisone 40 mg per day for 5 days. Antibiotics should be used in exacerbations if patients have dyspnea, sputum production, and purulence of the sputum or require mechanical ventilation. The choice of which antibiotic to use should be based on local bacterial resistance.
Pulmonary rehabilitation is an important component of COPD management. It incorporates exercise, education, and self-management aimed to change behavior and improve conditioning. The benefits of rehab have been shown to be considerable. The optimal length is 6-8 weeks. Palliative and end-of-life care are also very important factors to consider when treating COPD patients, according to the GOLD guidelines.
COPD is a very common disease and cause of mortality seen by family physicians. The GOLD report is an extensive document providing very clear guidelines and evidence to support these guidelines in every level of the treatment of COPD patients. As primary care doctors, we are often the first to treat patients with COPD and it is important to know the latest guidelines.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, N.J. You can contact her at [email protected].
In the United States and around the globe, chronic obstructive pulmonary disease (COPD) remains one of the leading causes of death. In addition to new diagnostic guidelines, the Global Initiative for Chronic Obstructive Lung Disease 2022 Report, or GOLD report, sets forth recommendations for management and treatment.
According to the GOLD report, initial management of COPD should aim at reducing exposure to risk factors such as smoking or other chemical exposures. In addition to medications, stable COPD patients should be evaluated for inhaler technique, adherence to prescribed therapies, smoking status, and continued exposure to other risk factors. Also, physical activity should be advised and pulmonary rehabilitation should be considered. Spirometry should be performed annually.
These guidelines offer very practical advice but often are difficult to implement in clinical practice. Everyone knows smoking is harmful and quitting provides huge health benefits, not only regarding COPD. However, nicotine is very addictive, and most smokers cannot just quit. Many need smoking cessation aids and counseling. Additionally, some smokers just don’t want to quit. Regarding workplace exposures, it often is not easy for someone just to change their job. Many are afraid to speak because they are afraid of losing their jobs. Everyone, not just patients with COPD, can benefit from increased physical activity, and all doctors know how difficult it is to motivate patients to do this.
The decision to initiate medications should be based on an individual patient’s symptoms and risk of exacerbations. In general, long-acting bronchodilators, including long-acting beta agonists (LABA) and long-acting muscarinic antagonists (LAMA), are preferred except when immediate relief of dyspnea is needed, and then short-acting bronchodilators should be used. Either a single long-acting or dual long-acting bronchodilator can be initiated. If a patient continues to have dyspnea on a single long-acting bronchodilator, treatment should be switched to a dual therapy.
In general, inhaled corticosteroids (ICS) are not recommended for stable COPD patients. If a patient has exacerbations despite appropriate treatment with LABAs, an ICS may be added to the LABA, the GOLD guidelines say. Oral corticosteroids are not recommended for long-term use. PDE4 inhibitors should be considered in patents with severe to very severe airflow obstruction, chronic bronchitis, and exacerbations. Macrolide antibiotics, especially azithromycin, can be considered in acute exacerbations. There is no evidence to support the use of antitussives and mucolytics are advised in only certain patients. Inhaled bronchodilators are advised over oral ones and theophylline is recommended when long-acting bronchodilators are unavailable or unaffordable.
In clinical practice, I see many patients treated based on symptomatology with spirometry testing not being done. This may help control many symptoms, but unless my patient has an accurate diagnosis, I won’t know if my patient is receiving the correct treatment.
It is important to keep in mind that COPD is a progressive disease and without appropriate treatment and monitoring, it will just get worse, and this is most likely to be irreversible.
Medications and treatment goals for patients with COPD
Patients with alpha-1 antitrypsin deficiency may benefit from the addition of alpha-1 antitrypsin augmentation therapy, the new guidelines say. In patients with severe disease experiencing dyspnea, oral and parental opioids can be considered. Medications that are used to treat primary pulmonary hypertension are not advised to treat pulmonary hypertension secondary to COPD.
The treatment goals of COPD should be to decrease severity of symptoms, reduce the occurrence of exacerbations, and improve exercise tolerance. Peripheral eosinophil counts can be used to guide the use of ICS to prevent exacerbations. However, the best predictor of exacerbations is previous exacerbations. Frequent exacerbations are defined as two or more annually. Additionally, deteriorating airflow is correlated with increased risk of exacerbations, hospitalizations, and death. Forced expiratory volume in 1 second (FEV1) alone lacks precision to predict exacerbations or death.
Vaccines and pulmonary rehabilitation recommended
The Centers for Disease Control and Prevention and World Health Organization recommend several vaccines for stable patients with COPD. Influenza vaccine was shown to reduce serious complications in COPD patients. Pneumococcal vaccines (PCV13 and PPSV23) reduced the likelihood of COPD exacerbations. The COVID-19 vaccine also has been effective at reducing hospitalizations, in particular ICU admissions, and death in patients with COPD. The CDC also recommends TdaP and Zoster vaccines.
An acute exacerbation of COPD occurs when a patient experiences worsening of respiratory symptoms that requires additional treatment, according to the updated GOLD guidelines. They are usually associated with increased airway inflammation, mucous productions, and trapping of gases. They are often triggered by viral infections, but bacterial and environment factors play a role as well. Less commonly, fungi such as Aspergillus can be observed as well. COPD exacerbations contribute to overall progression of the disease.
In patients with hypoxemia, supplemental oxygen should be titrated to a target O2 saturation of 88%-92%. It is important to follow blood gases to be sure adequate oxygenation is taking place while at the same time avoiding carbon dioxide retention and/or worsening acidosis. In patients with severe exacerbations whose dyspnea does not respond to initial emergency therapy, ICU admission is warranted. Other factors indicating the need for ICU admission include mental status changes, persistent or worsening hypoxemia, severe or worsening respiratory acidosis, the need for mechanical ventilation, and hemodynamic instability. Following an acute exacerbation, steps to prevent further exacerbations should be initiated.
Systemic glucocorticoids are indicated during acute exacerbations. They have been shown to hasten recovery time and improve functioning of the lungs as well as oxygenation. It is recommended to give prednisone 40 mg per day for 5 days. Antibiotics should be used in exacerbations if patients have dyspnea, sputum production, and purulence of the sputum or require mechanical ventilation. The choice of which antibiotic to use should be based on local bacterial resistance.
Pulmonary rehabilitation is an important component of COPD management. It incorporates exercise, education, and self-management aimed to change behavior and improve conditioning. The benefits of rehab have been shown to be considerable. The optimal length is 6-8 weeks. Palliative and end-of-life care are also very important factors to consider when treating COPD patients, according to the GOLD guidelines.
COPD is a very common disease and cause of mortality seen by family physicians. The GOLD report is an extensive document providing very clear guidelines and evidence to support these guidelines in every level of the treatment of COPD patients. As primary care doctors, we are often the first to treat patients with COPD and it is important to know the latest guidelines.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, N.J. You can contact her at [email protected].
Germline genetic testing: Why it matters and where we are failing
Historically, the role of genetic testing has been to identify familial cancer syndromes and initiate cascade testing. If a germline pathogenic variant is found in an individual, cascade testing involves genetic counseling and testing of blood relatives, starting with those closest in relation to the proband, to identify other family members at high hereditary cancer risk. Once testing identifies those family members at higher cancer risk, these individuals can be referred for risk-reducing procedures. They can undergo screening tests starting at an earlier age and/or increased frequency to help prevent invasive cancer or diagnose it at an earlier stage.
Genetic testing can also inform prognosis. While women with a BRCA1 or BRCA2 mutation are at higher risk of developing ovarian cancer compared with the baseline population, the presence of a germline BRCA mutation has been shown to confer improved survival compared with no BRCA mutation (BRCA wild type). However, more recent data have shown that when long-term survival was analyzed, the prognostic benefit seen in patients with a germline BRCA mutation was lost. The initial survival advantage seen in this population may be related to increased sensitivity to treatment. There appears to be improved response to platinum therapy, which is the standard of care for upfront treatment, in germline BRCA mutation carriers.
Most recently, genetic testing has been used to guide treatment decisions in gynecologic cancers. In 2014, the first poly ADP-ribose polymerase (PARP) inhibitor, olaparib, received Food and Drug Administration approval for the treatment of recurrent ovarian cancer in the presence of a germline BRCA mutation. Now there are multiple PARP inhibitors that have FDA approval for ovarian cancer treatment, some as frontline treatment.
Previous data indicate that 13%-18% of women with ovarian cancer have a germline BRCA mutation that places them at increased risk of hereditary ovarian cancer.1 Current guidelines from the American Society of Clinical Oncology, the U.S. Preventive Services Task Force, the National Comprehensive Cancer Network, the Society of Gynecologic Oncology (SGO), and the American College of Obstetricians and Gynecologists recommend universal genetic counseling and testing for patients diagnosed with epithelial ovarian cancer. Despite these guidelines, rates of referral for genetic counseling and completion of genetic testing are low.
There has been improvement for both referrals and testing since the publication of the 2014 SGO clinical practice statement on genetic testing for ovarian cancer patients, which recommended that all women, even those without any significant family history, should receive genetic counseling and be offered genetic testing.2 When including only studies that collected data after the publication of the 2014 SGO clinical practice statement on genetic testing, a recent systematic review found that 64% of patients were referred for genetic counseling and 63% underwent testing.3
Clinical interventions to target genetic evaluation appear to improve uptake of both counseling and testing. These interventions include using telemedicine to deliver genetic counseling services, mainstreaming (counseling and testing are provided in an oncology clinic by nongenetics specialists), having a genetic counselor within the clinic, and performing reflex testing. With limited numbers of genetic counselors (and even further limited numbers of cancer-specific genetic counselors),4 referral for genetic counseling before testing is often challenging and may not be feasible. There is continued need for strategies to help overcome the barrier to accessing genetic counseling.
While the data are limited, there appear to be significant disparities in rates of genetic testing. Genetic counseling and testing were completed by White (43% and 40%) patients more frequently than by either Black (24% and 26%) or Asian (23% and 14%) patients.4 Uninsured patients were about half as likely (23% vs. 47%) to complete genetic testing as were those with private insurance.4
Genetic testing is an important tool to help identify individuals and families at risk of having hereditary cancer syndromes. This identification allows us to prevent many cancers and identify others while still early stage, significantly decreasing the health care and financial burden on our society and improving outcomes for patients. While we have seen improvement in rates of referral for genetic counseling and testing, we are still falling short. Given the shortage of genetic counselors, it is imperative that we find solutions to ensure continued and improved access to genetic testing for our patients.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Norquist BM et al. JAMA Oncol. 2016;2(4):482-90.
2. SGO Clinical Practice Statement. 2014 Oct 1.
3. Lin J et al. Gynecol Oncol. 2021;162(2):506-16.
4. American Society of Clinical Oncology. J Oncol Pract. 2016 Apr;12(4):339-83.
Historically, the role of genetic testing has been to identify familial cancer syndromes and initiate cascade testing. If a germline pathogenic variant is found in an individual, cascade testing involves genetic counseling and testing of blood relatives, starting with those closest in relation to the proband, to identify other family members at high hereditary cancer risk. Once testing identifies those family members at higher cancer risk, these individuals can be referred for risk-reducing procedures. They can undergo screening tests starting at an earlier age and/or increased frequency to help prevent invasive cancer or diagnose it at an earlier stage.
Genetic testing can also inform prognosis. While women with a BRCA1 or BRCA2 mutation are at higher risk of developing ovarian cancer compared with the baseline population, the presence of a germline BRCA mutation has been shown to confer improved survival compared with no BRCA mutation (BRCA wild type). However, more recent data have shown that when long-term survival was analyzed, the prognostic benefit seen in patients with a germline BRCA mutation was lost. The initial survival advantage seen in this population may be related to increased sensitivity to treatment. There appears to be improved response to platinum therapy, which is the standard of care for upfront treatment, in germline BRCA mutation carriers.
Most recently, genetic testing has been used to guide treatment decisions in gynecologic cancers. In 2014, the first poly ADP-ribose polymerase (PARP) inhibitor, olaparib, received Food and Drug Administration approval for the treatment of recurrent ovarian cancer in the presence of a germline BRCA mutation. Now there are multiple PARP inhibitors that have FDA approval for ovarian cancer treatment, some as frontline treatment.
Previous data indicate that 13%-18% of women with ovarian cancer have a germline BRCA mutation that places them at increased risk of hereditary ovarian cancer.1 Current guidelines from the American Society of Clinical Oncology, the U.S. Preventive Services Task Force, the National Comprehensive Cancer Network, the Society of Gynecologic Oncology (SGO), and the American College of Obstetricians and Gynecologists recommend universal genetic counseling and testing for patients diagnosed with epithelial ovarian cancer. Despite these guidelines, rates of referral for genetic counseling and completion of genetic testing are low.
There has been improvement for both referrals and testing since the publication of the 2014 SGO clinical practice statement on genetic testing for ovarian cancer patients, which recommended that all women, even those without any significant family history, should receive genetic counseling and be offered genetic testing.2 When including only studies that collected data after the publication of the 2014 SGO clinical practice statement on genetic testing, a recent systematic review found that 64% of patients were referred for genetic counseling and 63% underwent testing.3
Clinical interventions to target genetic evaluation appear to improve uptake of both counseling and testing. These interventions include using telemedicine to deliver genetic counseling services, mainstreaming (counseling and testing are provided in an oncology clinic by nongenetics specialists), having a genetic counselor within the clinic, and performing reflex testing. With limited numbers of genetic counselors (and even further limited numbers of cancer-specific genetic counselors),4 referral for genetic counseling before testing is often challenging and may not be feasible. There is continued need for strategies to help overcome the barrier to accessing genetic counseling.
While the data are limited, there appear to be significant disparities in rates of genetic testing. Genetic counseling and testing were completed by White (43% and 40%) patients more frequently than by either Black (24% and 26%) or Asian (23% and 14%) patients.4 Uninsured patients were about half as likely (23% vs. 47%) to complete genetic testing as were those with private insurance.4
Genetic testing is an important tool to help identify individuals and families at risk of having hereditary cancer syndromes. This identification allows us to prevent many cancers and identify others while still early stage, significantly decreasing the health care and financial burden on our society and improving outcomes for patients. While we have seen improvement in rates of referral for genetic counseling and testing, we are still falling short. Given the shortage of genetic counselors, it is imperative that we find solutions to ensure continued and improved access to genetic testing for our patients.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Norquist BM et al. JAMA Oncol. 2016;2(4):482-90.
2. SGO Clinical Practice Statement. 2014 Oct 1.
3. Lin J et al. Gynecol Oncol. 2021;162(2):506-16.
4. American Society of Clinical Oncology. J Oncol Pract. 2016 Apr;12(4):339-83.
Historically, the role of genetic testing has been to identify familial cancer syndromes and initiate cascade testing. If a germline pathogenic variant is found in an individual, cascade testing involves genetic counseling and testing of blood relatives, starting with those closest in relation to the proband, to identify other family members at high hereditary cancer risk. Once testing identifies those family members at higher cancer risk, these individuals can be referred for risk-reducing procedures. They can undergo screening tests starting at an earlier age and/or increased frequency to help prevent invasive cancer or diagnose it at an earlier stage.
Genetic testing can also inform prognosis. While women with a BRCA1 or BRCA2 mutation are at higher risk of developing ovarian cancer compared with the baseline population, the presence of a germline BRCA mutation has been shown to confer improved survival compared with no BRCA mutation (BRCA wild type). However, more recent data have shown that when long-term survival was analyzed, the prognostic benefit seen in patients with a germline BRCA mutation was lost. The initial survival advantage seen in this population may be related to increased sensitivity to treatment. There appears to be improved response to platinum therapy, which is the standard of care for upfront treatment, in germline BRCA mutation carriers.
Most recently, genetic testing has been used to guide treatment decisions in gynecologic cancers. In 2014, the first poly ADP-ribose polymerase (PARP) inhibitor, olaparib, received Food and Drug Administration approval for the treatment of recurrent ovarian cancer in the presence of a germline BRCA mutation. Now there are multiple PARP inhibitors that have FDA approval for ovarian cancer treatment, some as frontline treatment.
Previous data indicate that 13%-18% of women with ovarian cancer have a germline BRCA mutation that places them at increased risk of hereditary ovarian cancer.1 Current guidelines from the American Society of Clinical Oncology, the U.S. Preventive Services Task Force, the National Comprehensive Cancer Network, the Society of Gynecologic Oncology (SGO), and the American College of Obstetricians and Gynecologists recommend universal genetic counseling and testing for patients diagnosed with epithelial ovarian cancer. Despite these guidelines, rates of referral for genetic counseling and completion of genetic testing are low.
There has been improvement for both referrals and testing since the publication of the 2014 SGO clinical practice statement on genetic testing for ovarian cancer patients, which recommended that all women, even those without any significant family history, should receive genetic counseling and be offered genetic testing.2 When including only studies that collected data after the publication of the 2014 SGO clinical practice statement on genetic testing, a recent systematic review found that 64% of patients were referred for genetic counseling and 63% underwent testing.3
Clinical interventions to target genetic evaluation appear to improve uptake of both counseling and testing. These interventions include using telemedicine to deliver genetic counseling services, mainstreaming (counseling and testing are provided in an oncology clinic by nongenetics specialists), having a genetic counselor within the clinic, and performing reflex testing. With limited numbers of genetic counselors (and even further limited numbers of cancer-specific genetic counselors),4 referral for genetic counseling before testing is often challenging and may not be feasible. There is continued need for strategies to help overcome the barrier to accessing genetic counseling.
While the data are limited, there appear to be significant disparities in rates of genetic testing. Genetic counseling and testing were completed by White (43% and 40%) patients more frequently than by either Black (24% and 26%) or Asian (23% and 14%) patients.4 Uninsured patients were about half as likely (23% vs. 47%) to complete genetic testing as were those with private insurance.4
Genetic testing is an important tool to help identify individuals and families at risk of having hereditary cancer syndromes. This identification allows us to prevent many cancers and identify others while still early stage, significantly decreasing the health care and financial burden on our society and improving outcomes for patients. While we have seen improvement in rates of referral for genetic counseling and testing, we are still falling short. Given the shortage of genetic counselors, it is imperative that we find solutions to ensure continued and improved access to genetic testing for our patients.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Norquist BM et al. JAMA Oncol. 2016;2(4):482-90.
2. SGO Clinical Practice Statement. 2014 Oct 1.
3. Lin J et al. Gynecol Oncol. 2021;162(2):506-16.
4. American Society of Clinical Oncology. J Oncol Pract. 2016 Apr;12(4):339-83.
Rules for performing research with children
The road to hell is paved with good intentions – especially true in clinical research. A Food and Drug Administration press release notes, “Historically, children were not included in clinical trials because of a misperception that excluding them from research was in fact protecting them. This resulted in many FDA-approved, licensed, cleared, or authorized drugs, biological products, and medical devices lacking pediatric-specific labeling information.” In an effort to improve on this situation, the FDA published in September 2022 a proposed new draft guidance on performing research with children that is open for public comment for 3 months.
There is a long history of government attempts to promote research and development for the benefit of society. Sometimes government succeeds and sometimes not. For instance, when the U.S. federal government funded scientific research in the 1960s, it sought to increase the common good by promulgating those discoveries. The government insisted that all federally funded research be in the public domain. The funding produced a spectacular number of technological advancements that have enriched society. However, a decade later, the government concluded that too many good research ideas were never developed into beneficial products because without the ability to patent the results, the costs and risks of product development were not profitable for industry. By the late 1970s, new laws were enacted to enable universities and their faculty to patent the results of government-funded research and share in any wealth created.
Pharmaceutical research in the 1970s and 1980s was mostly performed on men in order to reduce the risk of giving treatments of unknown safety to pregnant women. The unintended consequence was that the new drugs frequently were less effective for women. This was particularly true for cardiac medications for which lifestyle risk factors differed between the sexes.
Similarly, children were often excluded from research because of the unknown risks of new drugs on growing bodies and brains. Children were also seen as a vulnerable population for whom informed consent was problematic. The result of these well-intentioned restrictions was the creation of new products that did not have pediatric dosing recommendations, pediatric safety assessments, or approval for pediatric indications. To remediate these deficiencies, in 1997 and 2007 the FDA offered a 6-month extension on patent protection as motivation for companies to develop those pediatric recommendations. Alas, those laws were primarily used to extend the profitability of blockbuster products rather than truly benefit children.
Over the past 4 decades, pediatric ethicists proposed and refined rules to govern research on children. The Common Rule used by institutional review boards (IRBs) to protect human research subjects was expanded with guidelines covering children. The new draft guidance is the latest iteration of this effort. Nothing in the 14 pages of draft regulation appears revolutionary to me. The ideas are tweaks, based on theory and experience, of principles agreed upon 30 years ago. Finding the optimal social moral contract involves some empirical assessment of praxis and effectiveness.
I am loathe to summarize this new document, which itself is a summary of a vast body of literature, that supports the Code of Federal Regulations Title 21 Part 50 and 45 CFR Part 46. The draft document is well organized and I recommend it as an excellent primer for the area of pediatric research ethics if the subject is new to you. I also recommend it as required reading for anyone serving on an IRB.
IRBs usually review and approve any research on people. Generally, the selection of people for research should be done equitably. However, children should not be enrolled unless it is necessary to answer an important question relevant to children. For the past 2 decades, there has been an emphasis on obtaining the assent of the child as well as informed consent by the parents.
An important determination is whether the research is likely to help that particular child or whether it is aimed at advancing general knowledge. If there is no prospect of direct benefit, research is still permissible but more restricted for safety and comfort reasons. Next is determining whether the research carries only minimal risk or a minor increase over minimal risk. The draft defines and provides anchor examples of these situations. For instance, oral placebos and single blood draws are typically minimal risk. Multiple injections and blood draws over a year fall into the second category. One MRI is minimal risk but a minor increase in risk if it involves sedation or contrast.
I strongly support the ideals expressed in these guidelines. They represent the best blend of intentions and practical experience. They will become the law of the land. In ethics, there is merit in striving to do things properly, orderly, and enforceably.
The cynic in me sees two weaknesses in the stated approach. First, the volume of harm to children occurring during organized clinical research is extremely small. The greater harms come from off-label use, nonsystematic research, and the ignorance resulting from a lack of research. Second, my observation in all endeavors of morality is, “Raise the bar high enough and people walk under it.”
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
The road to hell is paved with good intentions – especially true in clinical research. A Food and Drug Administration press release notes, “Historically, children were not included in clinical trials because of a misperception that excluding them from research was in fact protecting them. This resulted in many FDA-approved, licensed, cleared, or authorized drugs, biological products, and medical devices lacking pediatric-specific labeling information.” In an effort to improve on this situation, the FDA published in September 2022 a proposed new draft guidance on performing research with children that is open for public comment for 3 months.
There is a long history of government attempts to promote research and development for the benefit of society. Sometimes government succeeds and sometimes not. For instance, when the U.S. federal government funded scientific research in the 1960s, it sought to increase the common good by promulgating those discoveries. The government insisted that all federally funded research be in the public domain. The funding produced a spectacular number of technological advancements that have enriched society. However, a decade later, the government concluded that too many good research ideas were never developed into beneficial products because without the ability to patent the results, the costs and risks of product development were not profitable for industry. By the late 1970s, new laws were enacted to enable universities and their faculty to patent the results of government-funded research and share in any wealth created.
Pharmaceutical research in the 1970s and 1980s was mostly performed on men in order to reduce the risk of giving treatments of unknown safety to pregnant women. The unintended consequence was that the new drugs frequently were less effective for women. This was particularly true for cardiac medications for which lifestyle risk factors differed between the sexes.
Similarly, children were often excluded from research because of the unknown risks of new drugs on growing bodies and brains. Children were also seen as a vulnerable population for whom informed consent was problematic. The result of these well-intentioned restrictions was the creation of new products that did not have pediatric dosing recommendations, pediatric safety assessments, or approval for pediatric indications. To remediate these deficiencies, in 1997 and 2007 the FDA offered a 6-month extension on patent protection as motivation for companies to develop those pediatric recommendations. Alas, those laws were primarily used to extend the profitability of blockbuster products rather than truly benefit children.
Over the past 4 decades, pediatric ethicists proposed and refined rules to govern research on children. The Common Rule used by institutional review boards (IRBs) to protect human research subjects was expanded with guidelines covering children. The new draft guidance is the latest iteration of this effort. Nothing in the 14 pages of draft regulation appears revolutionary to me. The ideas are tweaks, based on theory and experience, of principles agreed upon 30 years ago. Finding the optimal social moral contract involves some empirical assessment of praxis and effectiveness.
I am loathe to summarize this new document, which itself is a summary of a vast body of literature, that supports the Code of Federal Regulations Title 21 Part 50 and 45 CFR Part 46. The draft document is well organized and I recommend it as an excellent primer for the area of pediatric research ethics if the subject is new to you. I also recommend it as required reading for anyone serving on an IRB.
IRBs usually review and approve any research on people. Generally, the selection of people for research should be done equitably. However, children should not be enrolled unless it is necessary to answer an important question relevant to children. For the past 2 decades, there has been an emphasis on obtaining the assent of the child as well as informed consent by the parents.
An important determination is whether the research is likely to help that particular child or whether it is aimed at advancing general knowledge. If there is no prospect of direct benefit, research is still permissible but more restricted for safety and comfort reasons. Next is determining whether the research carries only minimal risk or a minor increase over minimal risk. The draft defines and provides anchor examples of these situations. For instance, oral placebos and single blood draws are typically minimal risk. Multiple injections and blood draws over a year fall into the second category. One MRI is minimal risk but a minor increase in risk if it involves sedation or contrast.
I strongly support the ideals expressed in these guidelines. They represent the best blend of intentions and practical experience. They will become the law of the land. In ethics, there is merit in striving to do things properly, orderly, and enforceably.
The cynic in me sees two weaknesses in the stated approach. First, the volume of harm to children occurring during organized clinical research is extremely small. The greater harms come from off-label use, nonsystematic research, and the ignorance resulting from a lack of research. Second, my observation in all endeavors of morality is, “Raise the bar high enough and people walk under it.”
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
The road to hell is paved with good intentions – especially true in clinical research. A Food and Drug Administration press release notes, “Historically, children were not included in clinical trials because of a misperception that excluding them from research was in fact protecting them. This resulted in many FDA-approved, licensed, cleared, or authorized drugs, biological products, and medical devices lacking pediatric-specific labeling information.” In an effort to improve on this situation, the FDA published in September 2022 a proposed new draft guidance on performing research with children that is open for public comment for 3 months.
There is a long history of government attempts to promote research and development for the benefit of society. Sometimes government succeeds and sometimes not. For instance, when the U.S. federal government funded scientific research in the 1960s, it sought to increase the common good by promulgating those discoveries. The government insisted that all federally funded research be in the public domain. The funding produced a spectacular number of technological advancements that have enriched society. However, a decade later, the government concluded that too many good research ideas were never developed into beneficial products because without the ability to patent the results, the costs and risks of product development were not profitable for industry. By the late 1970s, new laws were enacted to enable universities and their faculty to patent the results of government-funded research and share in any wealth created.
Pharmaceutical research in the 1970s and 1980s was mostly performed on men in order to reduce the risk of giving treatments of unknown safety to pregnant women. The unintended consequence was that the new drugs frequently were less effective for women. This was particularly true for cardiac medications for which lifestyle risk factors differed between the sexes.
Similarly, children were often excluded from research because of the unknown risks of new drugs on growing bodies and brains. Children were also seen as a vulnerable population for whom informed consent was problematic. The result of these well-intentioned restrictions was the creation of new products that did not have pediatric dosing recommendations, pediatric safety assessments, or approval for pediatric indications. To remediate these deficiencies, in 1997 and 2007 the FDA offered a 6-month extension on patent protection as motivation for companies to develop those pediatric recommendations. Alas, those laws were primarily used to extend the profitability of blockbuster products rather than truly benefit children.
Over the past 4 decades, pediatric ethicists proposed and refined rules to govern research on children. The Common Rule used by institutional review boards (IRBs) to protect human research subjects was expanded with guidelines covering children. The new draft guidance is the latest iteration of this effort. Nothing in the 14 pages of draft regulation appears revolutionary to me. The ideas are tweaks, based on theory and experience, of principles agreed upon 30 years ago. Finding the optimal social moral contract involves some empirical assessment of praxis and effectiveness.
I am loathe to summarize this new document, which itself is a summary of a vast body of literature, that supports the Code of Federal Regulations Title 21 Part 50 and 45 CFR Part 46. The draft document is well organized and I recommend it as an excellent primer for the area of pediatric research ethics if the subject is new to you. I also recommend it as required reading for anyone serving on an IRB.
IRBs usually review and approve any research on people. Generally, the selection of people for research should be done equitably. However, children should not be enrolled unless it is necessary to answer an important question relevant to children. For the past 2 decades, there has been an emphasis on obtaining the assent of the child as well as informed consent by the parents.
An important determination is whether the research is likely to help that particular child or whether it is aimed at advancing general knowledge. If there is no prospect of direct benefit, research is still permissible but more restricted for safety and comfort reasons. Next is determining whether the research carries only minimal risk or a minor increase over minimal risk. The draft defines and provides anchor examples of these situations. For instance, oral placebos and single blood draws are typically minimal risk. Multiple injections and blood draws over a year fall into the second category. One MRI is minimal risk but a minor increase in risk if it involves sedation or contrast.
I strongly support the ideals expressed in these guidelines. They represent the best blend of intentions and practical experience. They will become the law of the land. In ethics, there is merit in striving to do things properly, orderly, and enforceably.
The cynic in me sees two weaknesses in the stated approach. First, the volume of harm to children occurring during organized clinical research is extremely small. The greater harms come from off-label use, nonsystematic research, and the ignorance resulting from a lack of research. Second, my observation in all endeavors of morality is, “Raise the bar high enough and people walk under it.”
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
Why the 5-day isolation period for COVID makes no sense
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
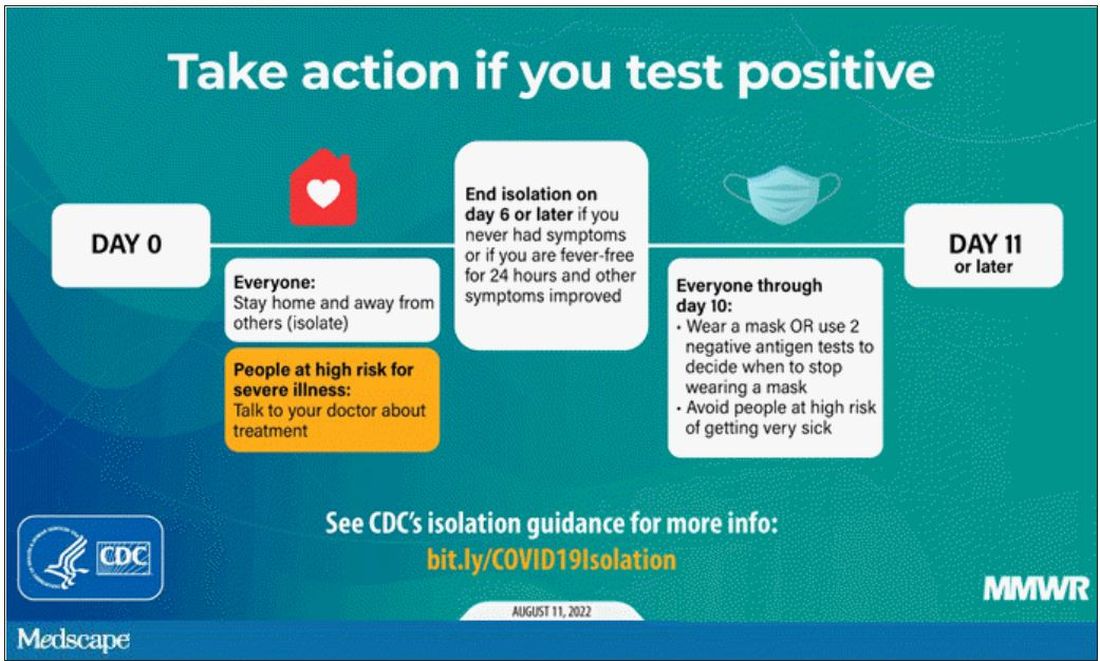
One of the more baffling decisions the CDC made during this pandemic was when they reduced the duration of isolation after a positive COVID test from 10 days to 5 days and did not require a negative antigen test to end isolation.
Multiple studies had suggested, after all, that positive antigen tests, while not perfect, were a decent proxy for infectivity. And if the purpose of isolation is to keep other community members safe, why not use a readily available test to know when it might be safe to go out in public again?
Also, 5 days just wasn’t that much time. Many individuals are symptomatic long after that point. Many people test positive long after that point. What exactly is the point of the 5-day isolation period?
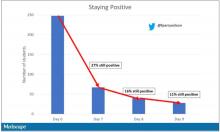
We got some hard numbers this week to show just how good (or bad) an arbitrary-seeming 5-day isolation period is, thanks to this study from JAMA Network Open, which gives us a low-end estimate for the proportion of people who remain positive on antigen tests, which is to say infectious, after an isolation period.
This study estimates the low end of postisolation infectivity because of the study population: student athletes at an NCAA Division I school, which may or may not be Stanford. These athletes tested positive for COVID after having at least one dose of vaccine from January to May 2022. School protocol was to put the students in isolation for 7 days, at which time they could “test out” with a negative antigen test.
Put simply, these were healthy people. They were young. They were athletes. They were vaccinated. If anyone is going to have a brief, easy COVID course, it would be them. And they are doing at least a week of isolation, not 5 days.
So – isolation for 7 days. Antigen testing on day 7. How many still tested positive? Of 248 individuals tested, 67 (27%) tested positive. One in four.
More than half of those positive on day 7 tested positive on day 8, and more than half of those tested positive again on day 9. By day 10, they were released from isolation without further testing.
So, right there .
There were some predictors of prolonged positivity.
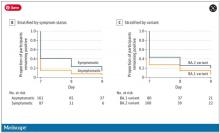
Symptomatic athletes were much more likely to test positive than asymptomatic athletes.
And the particular variant seemed to matter as well. In this time period, BA.1 and BA.2 were dominant, and it was pretty clear that BA.2 persisted longer than BA.1.
This brings me back to my original question: What is the point of the 5-day isolation period? On the basis of this study, you could imagine a guideline based on symptoms: Stay home until you feel better. You could imagine a guideline based on testing: Stay home until you test negative. A guideline based on time alone just doesn’t comport with the data. The benefit of policies based on symptoms or testing are obvious; some people would be out of isolation even before 5 days. But the downside, of course, is that some people would be stuck in isolation for much longer.
Maybe we should just say it. At this point, you could even imagine there being no recommendation at all – no isolation period. Like, you just stay home if you feel like you should stay home. I’m not entirely sure that such a policy would necessarily result in a greater number of infectious people out in the community.
In any case, as the arbitrariness of this particular 5-day isolation policy becomes more clear, the policy itself may be living on borrowed time.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com. He disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
One of the more baffling decisions the CDC made during this pandemic was when they reduced the duration of isolation after a positive COVID test from 10 days to 5 days and did not require a negative antigen test to end isolation.
Multiple studies had suggested, after all, that positive antigen tests, while not perfect, were a decent proxy for infectivity. And if the purpose of isolation is to keep other community members safe, why not use a readily available test to know when it might be safe to go out in public again?
Also, 5 days just wasn’t that much time. Many individuals are symptomatic long after that point. Many people test positive long after that point. What exactly is the point of the 5-day isolation period?
We got some hard numbers this week to show just how good (or bad) an arbitrary-seeming 5-day isolation period is, thanks to this study from JAMA Network Open, which gives us a low-end estimate for the proportion of people who remain positive on antigen tests, which is to say infectious, after an isolation period.
This study estimates the low end of postisolation infectivity because of the study population: student athletes at an NCAA Division I school, which may or may not be Stanford. These athletes tested positive for COVID after having at least one dose of vaccine from January to May 2022. School protocol was to put the students in isolation for 7 days, at which time they could “test out” with a negative antigen test.
Put simply, these were healthy people. They were young. They were athletes. They were vaccinated. If anyone is going to have a brief, easy COVID course, it would be them. And they are doing at least a week of isolation, not 5 days.
So – isolation for 7 days. Antigen testing on day 7. How many still tested positive? Of 248 individuals tested, 67 (27%) tested positive. One in four.
More than half of those positive on day 7 tested positive on day 8, and more than half of those tested positive again on day 9. By day 10, they were released from isolation without further testing.
So, right there .
There were some predictors of prolonged positivity.
Symptomatic athletes were much more likely to test positive than asymptomatic athletes.
And the particular variant seemed to matter as well. In this time period, BA.1 and BA.2 were dominant, and it was pretty clear that BA.2 persisted longer than BA.1.
This brings me back to my original question: What is the point of the 5-day isolation period? On the basis of this study, you could imagine a guideline based on symptoms: Stay home until you feel better. You could imagine a guideline based on testing: Stay home until you test negative. A guideline based on time alone just doesn’t comport with the data. The benefit of policies based on symptoms or testing are obvious; some people would be out of isolation even before 5 days. But the downside, of course, is that some people would be stuck in isolation for much longer.
Maybe we should just say it. At this point, you could even imagine there being no recommendation at all – no isolation period. Like, you just stay home if you feel like you should stay home. I’m not entirely sure that such a policy would necessarily result in a greater number of infectious people out in the community.
In any case, as the arbitrariness of this particular 5-day isolation policy becomes more clear, the policy itself may be living on borrowed time.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com. He disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
One of the more baffling decisions the CDC made during this pandemic was when they reduced the duration of isolation after a positive COVID test from 10 days to 5 days and did not require a negative antigen test to end isolation.
Multiple studies had suggested, after all, that positive antigen tests, while not perfect, were a decent proxy for infectivity. And if the purpose of isolation is to keep other community members safe, why not use a readily available test to know when it might be safe to go out in public again?
Also, 5 days just wasn’t that much time. Many individuals are symptomatic long after that point. Many people test positive long after that point. What exactly is the point of the 5-day isolation period?
We got some hard numbers this week to show just how good (or bad) an arbitrary-seeming 5-day isolation period is, thanks to this study from JAMA Network Open, which gives us a low-end estimate for the proportion of people who remain positive on antigen tests, which is to say infectious, after an isolation period.
This study estimates the low end of postisolation infectivity because of the study population: student athletes at an NCAA Division I school, which may or may not be Stanford. These athletes tested positive for COVID after having at least one dose of vaccine from January to May 2022. School protocol was to put the students in isolation for 7 days, at which time they could “test out” with a negative antigen test.
Put simply, these were healthy people. They were young. They were athletes. They were vaccinated. If anyone is going to have a brief, easy COVID course, it would be them. And they are doing at least a week of isolation, not 5 days.
So – isolation for 7 days. Antigen testing on day 7. How many still tested positive? Of 248 individuals tested, 67 (27%) tested positive. One in four.
More than half of those positive on day 7 tested positive on day 8, and more than half of those tested positive again on day 9. By day 10, they were released from isolation without further testing.
So, right there .
There were some predictors of prolonged positivity.
Symptomatic athletes were much more likely to test positive than asymptomatic athletes.
And the particular variant seemed to matter as well. In this time period, BA.1 and BA.2 were dominant, and it was pretty clear that BA.2 persisted longer than BA.1.
This brings me back to my original question: What is the point of the 5-day isolation period? On the basis of this study, you could imagine a guideline based on symptoms: Stay home until you feel better. You could imagine a guideline based on testing: Stay home until you test negative. A guideline based on time alone just doesn’t comport with the data. The benefit of policies based on symptoms or testing are obvious; some people would be out of isolation even before 5 days. But the downside, of course, is that some people would be stuck in isolation for much longer.
Maybe we should just say it. At this point, you could even imagine there being no recommendation at all – no isolation period. Like, you just stay home if you feel like you should stay home. I’m not entirely sure that such a policy would necessarily result in a greater number of infectious people out in the community.
In any case, as the arbitrariness of this particular 5-day isolation policy becomes more clear, the policy itself may be living on borrowed time.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com. He disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
How to remain apolitical with patients
It is assumed that psychiatrists in general, but particularly in academia, are progressive liberals. There is evidence to support this idea, with a survey finding that more than three-quarters of U.S. psychiatrists are registered Democrats.1
Other corroborating factors to our field’s progressive tendency include the publication of pseudo-political books like “The Dangerous Case of Donald Trump: 27 Psychiatrists and Mental Health Experts Assess a President” – without a well-known equivalent on the other side.
Additionally, psychiatry has in the recent past, rightfully spent significant effort examining the disproportional trauma faced by patients with underprivileged backgrounds, which is often seen as a political position. The American Psychiatric Association has itself taken a stance on the national debate about abortion to warn against the psychiatric consequences of the Dobbs v. Jackson Supreme Court decision despite the clear political statement it makes.
We understand a likely rationale for psychiatry’s liberal tendency. Most psychiatrists support political objectives that provide resources for the treatment of the severely mentally ill. In general, the psychosocial consequences of mental illness place a downward economic pressure on our patients that leads to poverty and its associated traumas that then tend to feedback to worsen the severity of the illness itself. It is thus natural for psychiatry to promote political causes such as progressivism that focus on the needs of economically and socially struggling communities. If one posits a natural role for psychiatry in promoting the interests of patients, then it is a short leap to psychiatry promoting the political causes of the underprivileged, often in the form of endorsing the Democratic party.
As a result, a proportion of patients come into psychiatric treatment with expectations that their providers will negatively judge them and possibly punish their conservative beliefs or Republican political affiliation. Herein lies a question – “Is psychiatry willing to make 46.9% of Americans uncomfortable?” How should psychiatry address the 46.9% of Americans who voted Republican during the 2020 presidential election? In our desire to support the disadvantaged, how political are we willing to get and at what cost? While we cannot speak for the field as a whole, it is our concern that a vast percentage of Americans feel alienated from talking to us, which is particularly problematic in a field based on mutual trust and understanding.
This problem may be particularly palpable to us, as we are psychiatrists in a large metropolitan area of California who often treat specialty populations like veterans and law enforcement. In one study, law enforcement officers were found to be twice as likely to be Republicans as civilians.2 Michael McHale, the president of the National Association of Police Organizations, spoke at the 2020 Republican Party’s national convention as documented in an article titled “Union leader tells Republican convention why cops back Trump.”3 Similarly, about 60% of veterans identify as Republicans.4
Within the first few sessions, when patients are most vulnerable and sensitive to the perception of being judged, we commonly get asked questions to test our political beliefs. Some patients will display clothing that suggests a political affiliation; those wardrobe arrangements are, at times, an attempt at testing our knowledge of their in-group. While a bright-red cap with a reminder to keep the United States “great” in capital letters may be an overt invitation to address the topic, other patients may have a small symbol of a rattlesnake to test our ability to recognize the “Don’t Tread on Me” Gadsden flag.
Alternatively, other patients will ask our opinion, or bring up news topics, to share their concerns and/or examine our response and reactions. We remember, in particular, a patient who subtly asked if they needed to be vaccinated to attend therapy visits in person as a leading statement into their conservative political beliefs. It is a reminder that many patients fear how we will judge them or where we will draw the line – “Is there something I, the patient, can say that will make him dislike me?”
While the concept of making all patients comfortable may feel abstract or trivial to some, the consequences can be very real. We remember a patient with severe depression and occasional suicidality, who required many months of treatment for him to reveal that he owned a gun. His conservative beliefs made him very resistant to discuss gun ownership with someone who is presumably liberal and has the power to restrict such ownership. However, after a frank discussion that our concerns about his gun were not constitutional or political but medical, the patient agreed to relinquish his gun, at least temporarily, a likely more important intervention than many in psychiatry.
The ramifications are also wider than most imagine. In California, a particularly liberal state, many consistently and reliably liberal patients have some conservative beliefs. Those beliefs are often closeted: a Democratic mother who doesn’t think her 3-year-old daughter should wear a mask in school; a Democratic woman who questioned the veracity of Amber Heard during the Johnny Depp defamation trial and feels guilty about her prior dedication to the #MeToo movement.
Patients may feel torn about those beliefs and may be apprehensive to discuss them despite a nagging need to express or examine them in a place without judgment.
that we attempted to highlight in this article. In particular, a vast proportion of Americans may feel alienated from treatment or may refuse to divulge clinically relevant information, and a large number of patients may enter psychiatric treatment with concerns that they will be judged.
Psychiatry is founded on the honest exchange of thoughts and feelings between patients and providers without the fear of harsh judgment and intellectual retaliation. Psychiatrists would be wise to consider those factors and their repercussions when choosing to take political positions and setting a frame of care with their patients.
Dr. Lehman is a professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He has no conflicts of interest. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest.
References
1. Sanger-Katz M. Your surgeon is probably a Republican, your psychiatrist probably a Democrat. New York Times. 2016 Oct 6.
2. Ba B et al. Who are the police? Descriptive representation in the coercive arm of government. 2022 Mar 21.
3. Rainey J. Union leader tells Republican convention why cops back Trump. Los Angeles Times. 2020 Aug 26.
4. Igielnik R et al. Trump draws stronger support from veterans than from the public on leadership of U.S. military. Pew Research Center. 2019 July 10.
It is assumed that psychiatrists in general, but particularly in academia, are progressive liberals. There is evidence to support this idea, with a survey finding that more than three-quarters of U.S. psychiatrists are registered Democrats.1
Other corroborating factors to our field’s progressive tendency include the publication of pseudo-political books like “The Dangerous Case of Donald Trump: 27 Psychiatrists and Mental Health Experts Assess a President” – without a well-known equivalent on the other side.
Additionally, psychiatry has in the recent past, rightfully spent significant effort examining the disproportional trauma faced by patients with underprivileged backgrounds, which is often seen as a political position. The American Psychiatric Association has itself taken a stance on the national debate about abortion to warn against the psychiatric consequences of the Dobbs v. Jackson Supreme Court decision despite the clear political statement it makes.
We understand a likely rationale for psychiatry’s liberal tendency. Most psychiatrists support political objectives that provide resources for the treatment of the severely mentally ill. In general, the psychosocial consequences of mental illness place a downward economic pressure on our patients that leads to poverty and its associated traumas that then tend to feedback to worsen the severity of the illness itself. It is thus natural for psychiatry to promote political causes such as progressivism that focus on the needs of economically and socially struggling communities. If one posits a natural role for psychiatry in promoting the interests of patients, then it is a short leap to psychiatry promoting the political causes of the underprivileged, often in the form of endorsing the Democratic party.
As a result, a proportion of patients come into psychiatric treatment with expectations that their providers will negatively judge them and possibly punish their conservative beliefs or Republican political affiliation. Herein lies a question – “Is psychiatry willing to make 46.9% of Americans uncomfortable?” How should psychiatry address the 46.9% of Americans who voted Republican during the 2020 presidential election? In our desire to support the disadvantaged, how political are we willing to get and at what cost? While we cannot speak for the field as a whole, it is our concern that a vast percentage of Americans feel alienated from talking to us, which is particularly problematic in a field based on mutual trust and understanding.
This problem may be particularly palpable to us, as we are psychiatrists in a large metropolitan area of California who often treat specialty populations like veterans and law enforcement. In one study, law enforcement officers were found to be twice as likely to be Republicans as civilians.2 Michael McHale, the president of the National Association of Police Organizations, spoke at the 2020 Republican Party’s national convention as documented in an article titled “Union leader tells Republican convention why cops back Trump.”3 Similarly, about 60% of veterans identify as Republicans.4
Within the first few sessions, when patients are most vulnerable and sensitive to the perception of being judged, we commonly get asked questions to test our political beliefs. Some patients will display clothing that suggests a political affiliation; those wardrobe arrangements are, at times, an attempt at testing our knowledge of their in-group. While a bright-red cap with a reminder to keep the United States “great” in capital letters may be an overt invitation to address the topic, other patients may have a small symbol of a rattlesnake to test our ability to recognize the “Don’t Tread on Me” Gadsden flag.
Alternatively, other patients will ask our opinion, or bring up news topics, to share their concerns and/or examine our response and reactions. We remember, in particular, a patient who subtly asked if they needed to be vaccinated to attend therapy visits in person as a leading statement into their conservative political beliefs. It is a reminder that many patients fear how we will judge them or where we will draw the line – “Is there something I, the patient, can say that will make him dislike me?”
While the concept of making all patients comfortable may feel abstract or trivial to some, the consequences can be very real. We remember a patient with severe depression and occasional suicidality, who required many months of treatment for him to reveal that he owned a gun. His conservative beliefs made him very resistant to discuss gun ownership with someone who is presumably liberal and has the power to restrict such ownership. However, after a frank discussion that our concerns about his gun were not constitutional or political but medical, the patient agreed to relinquish his gun, at least temporarily, a likely more important intervention than many in psychiatry.
The ramifications are also wider than most imagine. In California, a particularly liberal state, many consistently and reliably liberal patients have some conservative beliefs. Those beliefs are often closeted: a Democratic mother who doesn’t think her 3-year-old daughter should wear a mask in school; a Democratic woman who questioned the veracity of Amber Heard during the Johnny Depp defamation trial and feels guilty about her prior dedication to the #MeToo movement.
Patients may feel torn about those beliefs and may be apprehensive to discuss them despite a nagging need to express or examine them in a place without judgment.
that we attempted to highlight in this article. In particular, a vast proportion of Americans may feel alienated from treatment or may refuse to divulge clinically relevant information, and a large number of patients may enter psychiatric treatment with concerns that they will be judged.
Psychiatry is founded on the honest exchange of thoughts and feelings between patients and providers without the fear of harsh judgment and intellectual retaliation. Psychiatrists would be wise to consider those factors and their repercussions when choosing to take political positions and setting a frame of care with their patients.
Dr. Lehman is a professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He has no conflicts of interest. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest.
References
1. Sanger-Katz M. Your surgeon is probably a Republican, your psychiatrist probably a Democrat. New York Times. 2016 Oct 6.
2. Ba B et al. Who are the police? Descriptive representation in the coercive arm of government. 2022 Mar 21.
3. Rainey J. Union leader tells Republican convention why cops back Trump. Los Angeles Times. 2020 Aug 26.
4. Igielnik R et al. Trump draws stronger support from veterans than from the public on leadership of U.S. military. Pew Research Center. 2019 July 10.
It is assumed that psychiatrists in general, but particularly in academia, are progressive liberals. There is evidence to support this idea, with a survey finding that more than three-quarters of U.S. psychiatrists are registered Democrats.1
Other corroborating factors to our field’s progressive tendency include the publication of pseudo-political books like “The Dangerous Case of Donald Trump: 27 Psychiatrists and Mental Health Experts Assess a President” – without a well-known equivalent on the other side.
Additionally, psychiatry has in the recent past, rightfully spent significant effort examining the disproportional trauma faced by patients with underprivileged backgrounds, which is often seen as a political position. The American Psychiatric Association has itself taken a stance on the national debate about abortion to warn against the psychiatric consequences of the Dobbs v. Jackson Supreme Court decision despite the clear political statement it makes.
We understand a likely rationale for psychiatry’s liberal tendency. Most psychiatrists support political objectives that provide resources for the treatment of the severely mentally ill. In general, the psychosocial consequences of mental illness place a downward economic pressure on our patients that leads to poverty and its associated traumas that then tend to feedback to worsen the severity of the illness itself. It is thus natural for psychiatry to promote political causes such as progressivism that focus on the needs of economically and socially struggling communities. If one posits a natural role for psychiatry in promoting the interests of patients, then it is a short leap to psychiatry promoting the political causes of the underprivileged, often in the form of endorsing the Democratic party.
As a result, a proportion of patients come into psychiatric treatment with expectations that their providers will negatively judge them and possibly punish their conservative beliefs or Republican political affiliation. Herein lies a question – “Is psychiatry willing to make 46.9% of Americans uncomfortable?” How should psychiatry address the 46.9% of Americans who voted Republican during the 2020 presidential election? In our desire to support the disadvantaged, how political are we willing to get and at what cost? While we cannot speak for the field as a whole, it is our concern that a vast percentage of Americans feel alienated from talking to us, which is particularly problematic in a field based on mutual trust and understanding.
This problem may be particularly palpable to us, as we are psychiatrists in a large metropolitan area of California who often treat specialty populations like veterans and law enforcement. In one study, law enforcement officers were found to be twice as likely to be Republicans as civilians.2 Michael McHale, the president of the National Association of Police Organizations, spoke at the 2020 Republican Party’s national convention as documented in an article titled “Union leader tells Republican convention why cops back Trump.”3 Similarly, about 60% of veterans identify as Republicans.4
Within the first few sessions, when patients are most vulnerable and sensitive to the perception of being judged, we commonly get asked questions to test our political beliefs. Some patients will display clothing that suggests a political affiliation; those wardrobe arrangements are, at times, an attempt at testing our knowledge of their in-group. While a bright-red cap with a reminder to keep the United States “great” in capital letters may be an overt invitation to address the topic, other patients may have a small symbol of a rattlesnake to test our ability to recognize the “Don’t Tread on Me” Gadsden flag.
Alternatively, other patients will ask our opinion, or bring up news topics, to share their concerns and/or examine our response and reactions. We remember, in particular, a patient who subtly asked if they needed to be vaccinated to attend therapy visits in person as a leading statement into their conservative political beliefs. It is a reminder that many patients fear how we will judge them or where we will draw the line – “Is there something I, the patient, can say that will make him dislike me?”
While the concept of making all patients comfortable may feel abstract or trivial to some, the consequences can be very real. We remember a patient with severe depression and occasional suicidality, who required many months of treatment for him to reveal that he owned a gun. His conservative beliefs made him very resistant to discuss gun ownership with someone who is presumably liberal and has the power to restrict such ownership. However, after a frank discussion that our concerns about his gun were not constitutional or political but medical, the patient agreed to relinquish his gun, at least temporarily, a likely more important intervention than many in psychiatry.
The ramifications are also wider than most imagine. In California, a particularly liberal state, many consistently and reliably liberal patients have some conservative beliefs. Those beliefs are often closeted: a Democratic mother who doesn’t think her 3-year-old daughter should wear a mask in school; a Democratic woman who questioned the veracity of Amber Heard during the Johnny Depp defamation trial and feels guilty about her prior dedication to the #MeToo movement.
Patients may feel torn about those beliefs and may be apprehensive to discuss them despite a nagging need to express or examine them in a place without judgment.
that we attempted to highlight in this article. In particular, a vast proportion of Americans may feel alienated from treatment or may refuse to divulge clinically relevant information, and a large number of patients may enter psychiatric treatment with concerns that they will be judged.
Psychiatry is founded on the honest exchange of thoughts and feelings between patients and providers without the fear of harsh judgment and intellectual retaliation. Psychiatrists would be wise to consider those factors and their repercussions when choosing to take political positions and setting a frame of care with their patients.
Dr. Lehman is a professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He has no conflicts of interest. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest.
References
1. Sanger-Katz M. Your surgeon is probably a Republican, your psychiatrist probably a Democrat. New York Times. 2016 Oct 6.
2. Ba B et al. Who are the police? Descriptive representation in the coercive arm of government. 2022 Mar 21.
3. Rainey J. Union leader tells Republican convention why cops back Trump. Los Angeles Times. 2020 Aug 26.
4. Igielnik R et al. Trump draws stronger support from veterans than from the public on leadership of U.S. military. Pew Research Center. 2019 July 10.
An infant with a tender bump on her ear
A biopsy of the lesion was performed that showed a well-defined nodulocystic tumor composed of nests of basaloid cells that are undergoing trichilemmal keratinization. Shadow cells are seen as well as small areas of calcification. There is also a histiocytic infiltrate with multinucleated giant cells. The histologic diagnosis is of a pilomatrixoma.
Pilomatrixoma, also known as calcifying epithelioma of Malherbe, was first described in 1880, as a tumor of sebaceous gland origin. Later, in 1961, Robert Forbis Jr, MD, and Elson B. Helwig, MD, coined the term pilomatrixoma to describe the hair follicle matrix as the source of the tumor. Pilomatrixomas are commonly seen in the pediatric population, usually in children between 8 and 13 years of age. Our patient is one of the youngest described. The lesions are commonly seen on the face and neck in about 70% of the cases followed by the upper extremities, back, and legs. Clinically, the lesions appear as a firm dermal papule or nodule, which moves freely and may have associated erythema on the skin surface or a blueish gray hue on the underlying skin.
Most pilomatrixomas that have been studied have shown a mutation in Exon 3 of the beta-catenin gene (CTNNB1). The beta-catenin molecule is a subunit of the cadherin protein, which is part of an important pathway in the terminal hair follicle differentiation. Beta-catenin also plays an important role in the Wnt pathway, which regulates cell fate as well as early embryonic patterning. Beta-catenin is responsible for forming adhesion junctions among cells. There have also been immunohistochemical studies that have shown a BCL2 proto-oncogene overexpression to pilomatrixoma.
There are several genetic syndromes that have been associated with the presence of pilomatrixomas: Turner syndrome (XO chromosome abnormality associated with short stature and cardiac defects), Gardner syndrome (polyposis coli and colon and rectal cancer), myotonic dystrophy, Rubinstein-Taybi syndrome (characterized by broad thumbs and toes, short stature, distinctive facial features, and varying degrees of intellectual disability), and trisomy 9. On physical examination our patient didn’t present with any of the typical features or history that could suggest any of these syndromes. A close follow-up and evaluation by a geneticist was recommended because after the initial visit she developed a second lesion on the forehead.
The differential diagnosis for this lesion includes other cysts that may occur on the ear such as epidermal inclusion cyst or dermoid cysts, though these lesions do not tend to be as firm as pilomatrixomas are, which can help with the diagnosis. Dermoid cysts are made of dermal and epidermal components. They are usually present at birth and are commonly seen on the scalp and the periorbital face.
Keloids are rubbery nodules of scar tissue that can form on sites of trauma, and although the lesion occurred after she had her ears pierced, the consistency and rapid growth of the lesion as well as the pathological description made this benign fibrous growth less likely.
When pilomatrixomas are inflamed they can be confused with vascular growths: in this particular case, a hemangioma or another vascular tumor such as a tufted angioma or kaposiform hemangioendothelioma. An ultrasound of the lesion could have helped in the differential diagnosis of the lesion.
Pilomatrixomas can grow significantly and in some cases get inflamed or infected. Surgical management of pilomatrixomas is often required because the lesions do not regress spontaneously.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
Forbis R Jr and Helwig EB. Arch Dermatol 1961;83:606-18.
Schwarz Y et al. Int J Pediatr Otorhinolaryngol. 2016 Jun;85:148-53.
A biopsy of the lesion was performed that showed a well-defined nodulocystic tumor composed of nests of basaloid cells that are undergoing trichilemmal keratinization. Shadow cells are seen as well as small areas of calcification. There is also a histiocytic infiltrate with multinucleated giant cells. The histologic diagnosis is of a pilomatrixoma.
Pilomatrixoma, also known as calcifying epithelioma of Malherbe, was first described in 1880, as a tumor of sebaceous gland origin. Later, in 1961, Robert Forbis Jr, MD, and Elson B. Helwig, MD, coined the term pilomatrixoma to describe the hair follicle matrix as the source of the tumor. Pilomatrixomas are commonly seen in the pediatric population, usually in children between 8 and 13 years of age. Our patient is one of the youngest described. The lesions are commonly seen on the face and neck in about 70% of the cases followed by the upper extremities, back, and legs. Clinically, the lesions appear as a firm dermal papule or nodule, which moves freely and may have associated erythema on the skin surface or a blueish gray hue on the underlying skin.
Most pilomatrixomas that have been studied have shown a mutation in Exon 3 of the beta-catenin gene (CTNNB1). The beta-catenin molecule is a subunit of the cadherin protein, which is part of an important pathway in the terminal hair follicle differentiation. Beta-catenin also plays an important role in the Wnt pathway, which regulates cell fate as well as early embryonic patterning. Beta-catenin is responsible for forming adhesion junctions among cells. There have also been immunohistochemical studies that have shown a BCL2 proto-oncogene overexpression to pilomatrixoma.
There are several genetic syndromes that have been associated with the presence of pilomatrixomas: Turner syndrome (XO chromosome abnormality associated with short stature and cardiac defects), Gardner syndrome (polyposis coli and colon and rectal cancer), myotonic dystrophy, Rubinstein-Taybi syndrome (characterized by broad thumbs and toes, short stature, distinctive facial features, and varying degrees of intellectual disability), and trisomy 9. On physical examination our patient didn’t present with any of the typical features or history that could suggest any of these syndromes. A close follow-up and evaluation by a geneticist was recommended because after the initial visit she developed a second lesion on the forehead.
The differential diagnosis for this lesion includes other cysts that may occur on the ear such as epidermal inclusion cyst or dermoid cysts, though these lesions do not tend to be as firm as pilomatrixomas are, which can help with the diagnosis. Dermoid cysts are made of dermal and epidermal components. They are usually present at birth and are commonly seen on the scalp and the periorbital face.
Keloids are rubbery nodules of scar tissue that can form on sites of trauma, and although the lesion occurred after she had her ears pierced, the consistency and rapid growth of the lesion as well as the pathological description made this benign fibrous growth less likely.
When pilomatrixomas are inflamed they can be confused with vascular growths: in this particular case, a hemangioma or another vascular tumor such as a tufted angioma or kaposiform hemangioendothelioma. An ultrasound of the lesion could have helped in the differential diagnosis of the lesion.
Pilomatrixomas can grow significantly and in some cases get inflamed or infected. Surgical management of pilomatrixomas is often required because the lesions do not regress spontaneously.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
Forbis R Jr and Helwig EB. Arch Dermatol 1961;83:606-18.
Schwarz Y et al. Int J Pediatr Otorhinolaryngol. 2016 Jun;85:148-53.
A biopsy of the lesion was performed that showed a well-defined nodulocystic tumor composed of nests of basaloid cells that are undergoing trichilemmal keratinization. Shadow cells are seen as well as small areas of calcification. There is also a histiocytic infiltrate with multinucleated giant cells. The histologic diagnosis is of a pilomatrixoma.
Pilomatrixoma, also known as calcifying epithelioma of Malherbe, was first described in 1880, as a tumor of sebaceous gland origin. Later, in 1961, Robert Forbis Jr, MD, and Elson B. Helwig, MD, coined the term pilomatrixoma to describe the hair follicle matrix as the source of the tumor. Pilomatrixomas are commonly seen in the pediatric population, usually in children between 8 and 13 years of age. Our patient is one of the youngest described. The lesions are commonly seen on the face and neck in about 70% of the cases followed by the upper extremities, back, and legs. Clinically, the lesions appear as a firm dermal papule or nodule, which moves freely and may have associated erythema on the skin surface or a blueish gray hue on the underlying skin.
Most pilomatrixomas that have been studied have shown a mutation in Exon 3 of the beta-catenin gene (CTNNB1). The beta-catenin molecule is a subunit of the cadherin protein, which is part of an important pathway in the terminal hair follicle differentiation. Beta-catenin also plays an important role in the Wnt pathway, which regulates cell fate as well as early embryonic patterning. Beta-catenin is responsible for forming adhesion junctions among cells. There have also been immunohistochemical studies that have shown a BCL2 proto-oncogene overexpression to pilomatrixoma.
There are several genetic syndromes that have been associated with the presence of pilomatrixomas: Turner syndrome (XO chromosome abnormality associated with short stature and cardiac defects), Gardner syndrome (polyposis coli and colon and rectal cancer), myotonic dystrophy, Rubinstein-Taybi syndrome (characterized by broad thumbs and toes, short stature, distinctive facial features, and varying degrees of intellectual disability), and trisomy 9. On physical examination our patient didn’t present with any of the typical features or history that could suggest any of these syndromes. A close follow-up and evaluation by a geneticist was recommended because after the initial visit she developed a second lesion on the forehead.
The differential diagnosis for this lesion includes other cysts that may occur on the ear such as epidermal inclusion cyst or dermoid cysts, though these lesions do not tend to be as firm as pilomatrixomas are, which can help with the diagnosis. Dermoid cysts are made of dermal and epidermal components. They are usually present at birth and are commonly seen on the scalp and the periorbital face.
Keloids are rubbery nodules of scar tissue that can form on sites of trauma, and although the lesion occurred after she had her ears pierced, the consistency and rapid growth of the lesion as well as the pathological description made this benign fibrous growth less likely.
When pilomatrixomas are inflamed they can be confused with vascular growths: in this particular case, a hemangioma or another vascular tumor such as a tufted angioma or kaposiform hemangioendothelioma. An ultrasound of the lesion could have helped in the differential diagnosis of the lesion.
Pilomatrixomas can grow significantly and in some cases get inflamed or infected. Surgical management of pilomatrixomas is often required because the lesions do not regress spontaneously.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
Forbis R Jr and Helwig EB. Arch Dermatol 1961;83:606-18.
Schwarz Y et al. Int J Pediatr Otorhinolaryngol. 2016 Jun;85:148-53.
A 4-month-old female was referred to our clinic for evaluation of a bump on the right ear. The lesion was first noted at 2 months of age as a little pimple. She was evaluated by her pediatrician and was treated with topical and oral antibiotics without resolution of the lesion. The bump continued to grow and seemed tender to palpation, so she was referred to dermatology for evaluation.
She was born via normal vaginal delivery at 40 weeks. Her mother has no medical conditions and the pregnancy was uneventful. She has been growing and developing well. She takes vitamin D and is currently breast fed.
There have been no other family members with similar lesions. She had her ears pierced at a month of age without any complications.
On skin examination she has a firm red nodule on the right ear that appears slightly tender to touch. She has no other skin lesions of concern. She has normal muscle tone and there are no other abnormalities noted on the physical exam. She has no hepatomegaly, splenomegaly, or lymphadenopathy.
Since when does providing pediatric care require courage?
I have been noticing “jokes” lately about doctors. Magazine cartoons depict doctors as conveying a bad prognosis in abrupt, indirect, vague ways. I remember, from medical school, the joke about pediatricians being doctors for patients “from the waist up” – wimps about tough topics such as sexuality. As an inherently shy person, I have appreciated the structure of the contractual relationship with families that both gives me permission and requires me to be direct about topics that would not be socially acceptable to discuss in other relationships.
Examples include our asking about bowel movements, genital symptoms, marital conflict, past abortions, food insecurity, adherence to medication, history of trauma or discrimination, substance use, illegal conduct, and suicidal ideation, among others. By bringing up these topics nonjudgmentally and with skill, we are demonstrating openness and making it safe for the patient/parent to ask questions about their own concerns.
Since these may be topics for which we lack knowledge or have very little power to help, it is far easier to not bring them up. Yet failing to have the courage to elicit sensitive information may delay the correct diagnosis, result in inappropriate tests or treatments, or miss factors critical in either the cause or solution for the patient’s problems.
Historically, being a physician has conveyed a promise of confidentiality and always trying to do what is best for the patient. The fact that we had to swear an oath to do so may also indicate that these things are not easy to do.
Yes, we need a lot of knowledge to know what is truly in the patient’s best interest. But we need to take personal risks to do it as well. There have been times when a parent has shouted “That is none of your business” at me or stormed out. Although only one patient has ever connected when striking out at me, other clinicians have not been as lucky (or had such small patients); some have even been killed.
For those of us in private practice, upsetting a patient with our well-intentioned words may mean losing them from our income stream or having them post negative comments online, which may affect our reputation in the community. Patients may not return for needed follow-up if a conversation was too uncomfortable for them. Current political divisions make this even trickier.
These days anxiety about getting behind in seeing the next patient may be a covert reason for avoiding difficult conversations as tears or anger take extra time. Certainly, fears of these outcomes can make us hold back from talking about important but potentially upsetting topics.
Of course, courage does not just mean being direct with questions, stating your observations, or giving advice. Courage requires thoughtfulness about possible adverse outcomes and their effect on others. It is not just “stupid bravery,” to proceed even when sensing danger. Courage is thus best paired with skill. It is:
- Setting up potentially difficult discussions with privacy (from the child or parent), seating, and enough time to listen.
- Normalizing questions by saying “I ask all my patients about ...” so patients do not feel singled out.
- Asking the patient or family first what they think is going on and how their own culture might regard the issue.
- Using simple language and arranging a translator when needed.
- Not just stating facts but checking “to be sure I explained well enough” rather than setting a patient up to appear ignorant for not understanding.
- Offering to contact the patient or other family member/support soon to review what you said and answer more questions.
- Offering a second opinion option.
- Promising to get more information when you do not know.
- Always leaving room for hope and sharing in that hope with them.
And it is crucial to have a way to keep notes about past trauma or difficult topics for a patient so neither you nor subsequent clinicians unnecessarily ask about sensitive topics.
Courage includes facing difficult situations without undue delay. Making that call about an abnormal test result right away, even when you are tired and upset, takes courage. Each time you overcome your own reluctance it takes moral strength but tends to make future courageous acts easier. Speaking up to a specialist on rounds when you think he or she is incorrect takes courage to serve the patient’s best interest. Being willing to try a new workflow in your office takes the courage to risk looking awkward or being judged by your team, but can be essential to progress. Asking for help or an opinion, sometimes from a medical assistant or student, can take courage but may reduce status barriers and improve relationships. Standing up for your values when they are not popular may take courage in some organizations. It takes courage to admit a mistake, even when your mistake may not otherwise be noticed.
How can we grow in courage? T. Berry Brazelton, MD, was a model of courage for me during my training – able and willing to tell about a child’s delays or ask about a parent’s well-being with empathy and by giving hope. Dr. Brazelton, pediatrician, developer of the Neonatal Behavioral Assessment Scale, professor at Harvard Medical School and founder of its Child Development Unit, was a world-renowned educator about the development of children and founder of the Touchpoints program. Our goal should be to promise to partner with the family in dealing with the problem, no matter how difficult or tender. I hope you had role models who not only said what to do but also demonstrated it with patients.
We had the privilege of hearing stories of difficult situations from hundreds of pediatricians in group sessions over the years in the Collaborative Office Rounds program. What group members often said that they valued most from these sessions was hearing examples of words they might say in these cases, either modeled by the coleaders or suggested by their pediatrician peers. Opportunities to share the tough times with trusted empathic peers is an important resource rarer and thus even more worth securing for yourself.
Being courageous may not be natural part of your personality but Aristotle said, “We become what we repeatedly do.” Even if you do not consider yourself so now, with practice you can become courageous and reap its benefits for your patients and yourself.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
I have been noticing “jokes” lately about doctors. Magazine cartoons depict doctors as conveying a bad prognosis in abrupt, indirect, vague ways. I remember, from medical school, the joke about pediatricians being doctors for patients “from the waist up” – wimps about tough topics such as sexuality. As an inherently shy person, I have appreciated the structure of the contractual relationship with families that both gives me permission and requires me to be direct about topics that would not be socially acceptable to discuss in other relationships.
Examples include our asking about bowel movements, genital symptoms, marital conflict, past abortions, food insecurity, adherence to medication, history of trauma or discrimination, substance use, illegal conduct, and suicidal ideation, among others. By bringing up these topics nonjudgmentally and with skill, we are demonstrating openness and making it safe for the patient/parent to ask questions about their own concerns.
Since these may be topics for which we lack knowledge or have very little power to help, it is far easier to not bring them up. Yet failing to have the courage to elicit sensitive information may delay the correct diagnosis, result in inappropriate tests or treatments, or miss factors critical in either the cause or solution for the patient’s problems.
Historically, being a physician has conveyed a promise of confidentiality and always trying to do what is best for the patient. The fact that we had to swear an oath to do so may also indicate that these things are not easy to do.
Yes, we need a lot of knowledge to know what is truly in the patient’s best interest. But we need to take personal risks to do it as well. There have been times when a parent has shouted “That is none of your business” at me or stormed out. Although only one patient has ever connected when striking out at me, other clinicians have not been as lucky (or had such small patients); some have even been killed.
For those of us in private practice, upsetting a patient with our well-intentioned words may mean losing them from our income stream or having them post negative comments online, which may affect our reputation in the community. Patients may not return for needed follow-up if a conversation was too uncomfortable for them. Current political divisions make this even trickier.
These days anxiety about getting behind in seeing the next patient may be a covert reason for avoiding difficult conversations as tears or anger take extra time. Certainly, fears of these outcomes can make us hold back from talking about important but potentially upsetting topics.
Of course, courage does not just mean being direct with questions, stating your observations, or giving advice. Courage requires thoughtfulness about possible adverse outcomes and their effect on others. It is not just “stupid bravery,” to proceed even when sensing danger. Courage is thus best paired with skill. It is:
- Setting up potentially difficult discussions with privacy (from the child or parent), seating, and enough time to listen.
- Normalizing questions by saying “I ask all my patients about ...” so patients do not feel singled out.
- Asking the patient or family first what they think is going on and how their own culture might regard the issue.
- Using simple language and arranging a translator when needed.
- Not just stating facts but checking “to be sure I explained well enough” rather than setting a patient up to appear ignorant for not understanding.
- Offering to contact the patient or other family member/support soon to review what you said and answer more questions.
- Offering a second opinion option.
- Promising to get more information when you do not know.
- Always leaving room for hope and sharing in that hope with them.
And it is crucial to have a way to keep notes about past trauma or difficult topics for a patient so neither you nor subsequent clinicians unnecessarily ask about sensitive topics.
Courage includes facing difficult situations without undue delay. Making that call about an abnormal test result right away, even when you are tired and upset, takes courage. Each time you overcome your own reluctance it takes moral strength but tends to make future courageous acts easier. Speaking up to a specialist on rounds when you think he or she is incorrect takes courage to serve the patient’s best interest. Being willing to try a new workflow in your office takes the courage to risk looking awkward or being judged by your team, but can be essential to progress. Asking for help or an opinion, sometimes from a medical assistant or student, can take courage but may reduce status barriers and improve relationships. Standing up for your values when they are not popular may take courage in some organizations. It takes courage to admit a mistake, even when your mistake may not otherwise be noticed.
How can we grow in courage? T. Berry Brazelton, MD, was a model of courage for me during my training – able and willing to tell about a child’s delays or ask about a parent’s well-being with empathy and by giving hope. Dr. Brazelton, pediatrician, developer of the Neonatal Behavioral Assessment Scale, professor at Harvard Medical School and founder of its Child Development Unit, was a world-renowned educator about the development of children and founder of the Touchpoints program. Our goal should be to promise to partner with the family in dealing with the problem, no matter how difficult or tender. I hope you had role models who not only said what to do but also demonstrated it with patients.
We had the privilege of hearing stories of difficult situations from hundreds of pediatricians in group sessions over the years in the Collaborative Office Rounds program. What group members often said that they valued most from these sessions was hearing examples of words they might say in these cases, either modeled by the coleaders or suggested by their pediatrician peers. Opportunities to share the tough times with trusted empathic peers is an important resource rarer and thus even more worth securing for yourself.
Being courageous may not be natural part of your personality but Aristotle said, “We become what we repeatedly do.” Even if you do not consider yourself so now, with practice you can become courageous and reap its benefits for your patients and yourself.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
I have been noticing “jokes” lately about doctors. Magazine cartoons depict doctors as conveying a bad prognosis in abrupt, indirect, vague ways. I remember, from medical school, the joke about pediatricians being doctors for patients “from the waist up” – wimps about tough topics such as sexuality. As an inherently shy person, I have appreciated the structure of the contractual relationship with families that both gives me permission and requires me to be direct about topics that would not be socially acceptable to discuss in other relationships.
Examples include our asking about bowel movements, genital symptoms, marital conflict, past abortions, food insecurity, adherence to medication, history of trauma or discrimination, substance use, illegal conduct, and suicidal ideation, among others. By bringing up these topics nonjudgmentally and with skill, we are demonstrating openness and making it safe for the patient/parent to ask questions about their own concerns.
Since these may be topics for which we lack knowledge or have very little power to help, it is far easier to not bring them up. Yet failing to have the courage to elicit sensitive information may delay the correct diagnosis, result in inappropriate tests or treatments, or miss factors critical in either the cause or solution for the patient’s problems.
Historically, being a physician has conveyed a promise of confidentiality and always trying to do what is best for the patient. The fact that we had to swear an oath to do so may also indicate that these things are not easy to do.
Yes, we need a lot of knowledge to know what is truly in the patient’s best interest. But we need to take personal risks to do it as well. There have been times when a parent has shouted “That is none of your business” at me or stormed out. Although only one patient has ever connected when striking out at me, other clinicians have not been as lucky (or had such small patients); some have even been killed.
For those of us in private practice, upsetting a patient with our well-intentioned words may mean losing them from our income stream or having them post negative comments online, which may affect our reputation in the community. Patients may not return for needed follow-up if a conversation was too uncomfortable for them. Current political divisions make this even trickier.
These days anxiety about getting behind in seeing the next patient may be a covert reason for avoiding difficult conversations as tears or anger take extra time. Certainly, fears of these outcomes can make us hold back from talking about important but potentially upsetting topics.
Of course, courage does not just mean being direct with questions, stating your observations, or giving advice. Courage requires thoughtfulness about possible adverse outcomes and their effect on others. It is not just “stupid bravery,” to proceed even when sensing danger. Courage is thus best paired with skill. It is:
- Setting up potentially difficult discussions with privacy (from the child or parent), seating, and enough time to listen.
- Normalizing questions by saying “I ask all my patients about ...” so patients do not feel singled out.
- Asking the patient or family first what they think is going on and how their own culture might regard the issue.
- Using simple language and arranging a translator when needed.
- Not just stating facts but checking “to be sure I explained well enough” rather than setting a patient up to appear ignorant for not understanding.
- Offering to contact the patient or other family member/support soon to review what you said and answer more questions.
- Offering a second opinion option.
- Promising to get more information when you do not know.
- Always leaving room for hope and sharing in that hope with them.
And it is crucial to have a way to keep notes about past trauma or difficult topics for a patient so neither you nor subsequent clinicians unnecessarily ask about sensitive topics.
Courage includes facing difficult situations without undue delay. Making that call about an abnormal test result right away, even when you are tired and upset, takes courage. Each time you overcome your own reluctance it takes moral strength but tends to make future courageous acts easier. Speaking up to a specialist on rounds when you think he or she is incorrect takes courage to serve the patient’s best interest. Being willing to try a new workflow in your office takes the courage to risk looking awkward or being judged by your team, but can be essential to progress. Asking for help or an opinion, sometimes from a medical assistant or student, can take courage but may reduce status barriers and improve relationships. Standing up for your values when they are not popular may take courage in some organizations. It takes courage to admit a mistake, even when your mistake may not otherwise be noticed.
How can we grow in courage? T. Berry Brazelton, MD, was a model of courage for me during my training – able and willing to tell about a child’s delays or ask about a parent’s well-being with empathy and by giving hope. Dr. Brazelton, pediatrician, developer of the Neonatal Behavioral Assessment Scale, professor at Harvard Medical School and founder of its Child Development Unit, was a world-renowned educator about the development of children and founder of the Touchpoints program. Our goal should be to promise to partner with the family in dealing with the problem, no matter how difficult or tender. I hope you had role models who not only said what to do but also demonstrated it with patients.
We had the privilege of hearing stories of difficult situations from hundreds of pediatricians in group sessions over the years in the Collaborative Office Rounds program. What group members often said that they valued most from these sessions was hearing examples of words they might say in these cases, either modeled by the coleaders or suggested by their pediatrician peers. Opportunities to share the tough times with trusted empathic peers is an important resource rarer and thus even more worth securing for yourself.
Being courageous may not be natural part of your personality but Aristotle said, “We become what we repeatedly do.” Even if you do not consider yourself so now, with practice you can become courageous and reap its benefits for your patients and yourself.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
Tourette syndrome: Diagnosis is key for best care
Tourette syndrome, attention-deficit/hyperactivity disorder (ADHD), obsessive-compulsive disorder (OCD), and autism spectrum disorder (ASD) share significant overlap in symptomatology, and it can be challenging at times to distinguish between these conditions. Being able to do so, however, can help guide more targeted interventions and accommodations to optimize a patient’s level of functioning.
Case example
A healthy, bright 6-year-old boy is referred by his family doctor to an academic medical center for a full team evaluation because of suspicion of ASD, after having already been diagnosed with ADHD at the age of 5. His difficulties with inattention, impulsivity, and hyperactivity, as well as his behavioral rigidities and sensory avoidant and sensory seeking behaviors have caused functional impairments for him in his kindergarten classroom. He has been penalized with removal of recess on more than one occasion. A low dose of a stimulant had been tried but resulted in a perceived increase in disruptive behaviors.
The boy, while hyperkinetic and often paying poor attention, is quite capable of high-quality and well-modulated eye contact paired with typical social referencing and reciprocity when actively engaging with the examiner and his parents. He does have a reported history of serial fixated interests and some repetitive behaviors but is also noted to be flexible in his interpersonal style, maintains other varied and typical interests, easily directs affect, utilizes a wide array of fluid gestures paired naturally with verbal communication, and shares enjoyment with smoothly coordinated gaze. He has mild articulation errors but uses pronouns appropriately and has no scripted speech or echolalia, though does engage in some whispered palilalia intermittently.
He is generally quite cooperative and redirectable when focused and has a completely normal physical and neurologic examination. During the visit, the doctor notices the boy making an intermittent honking sound, which parents report as an attention-seeking strategy during times of stress. Further physician-guided information gathering around other repetitive noises and movements elicits a history of engagement in repetitive hand-to-groin movements, some exaggerated blinking, and a number of other waxing and waning subtle motor and phonic tics with onset in preschool. These noises and movements have generally been identified as “fidgeting” and “misbehaving” by well-meaning caregivers in the home and school environments.
Both Tourette syndrome and ASD are more common in males, with stereotyped patterns of movements and behaviors; anxious, obsessive, and compulsive behaviors resulting in behavioral rigidities; sensory sensitivities; and increased rates of hyperkinesis with decreased impulse control which result in increased sensory-seeking behaviors. Diagnostic criteria for Tourette syndrome are met when a child has had multiple motor tics and at least one phonic tic present for at least 1 year, with tic-free intervals lasting no longer than 3 months, and with onset before the age of 18. Typically, tics emerge in late preschool and early grade school, and some children even develop repetitive movements as early as toddlerhood. Tics tend to worsen around the peripubertal era, then often generally improve in the teen years. Tic types, frequency, and severity general fluctuate over time.
Forty percent of children with Tourette syndrome also meet criteria for OCD, with many more having OCD traits, and about 65% of children with Tourette syndrome also meet criteria for ADHD, with many more having ADHD traits. OCD can lead to more rigid and directive social interactions in children as well as obsessive interests, just as ADHD can lead to less socially attuned and less cooperative behaviors, even in children who do not meet criteria for ASD.
For example, a child with OCD in the absence of ASD may still “police” other kids in class and be overly focused on the rules of a game, which may become a social liability. Likewise, a child with ADHD in the absence of ASD may be so distractible that focusing on what other kids are saying and their paired facial expressions is compromised, leading to poor-quality social reciprocity during interactions with peers. Given the remarkable overlap in shared symptoms, it is essential for pediatric providers to consider Tourette syndrome in the differential for any child with repetitive movements and behaviors in addition to ASD and a wide array of other neurodevelopment differences, including global developmental delays and intellectual disabilities. This is of particular importance as the diagnosis of Tourette syndrome can be used to gain access to developmental disability services if the condition has resulted in true adaptive impairments.
It is determined that the boy does in fact meet criteria for ADHD, but also for OCD and Tourette syndrome. Both his Autism Diagnostic Observation Schedule and DSM-5–influenced autism interview are found to be in the nonclinical ranges, given his quality of communication, social engagement, imaginative play, and varied interests. A diagnosis of ASD is not felt to be an appropriate conceptualization of his neurodevelopmental differences. He is started on a low dose of guanfacine, which induces a decline in tics, impulsivity, and hyperkinesis. He is given a 504 plan in school that includes scheduled “tic breaks,” sensory fidgets for use in the classroom, extra movement opportunities as needed, and utilization of a gentle cueing system between him and his teacher for low-key redirection of disruptive behaviors. He is no longer penalized for inattention or tics, and his 504 plan protects him from the use of recess removal as a behavioral modification strategy.
His parents enroll him in the community swim program for extra exercise, focus on decreasing screen time, and give him an earlier bedtime to help decrease his tics and rigidities, while improving his ability to self-regulate. Eventually, a low dose of a newer-generation stimulant is added to his guanfacine, with excellent results and only a mild increase in tolerable tics.
The child in the vignette did well with a 504 plan based on his medical diagnoses, though if related learning difficulties had persisted, eligibility under Other Health Impaired could be used to provide eligibility for an Individualized Education Plan. Alpha-agonists can be helpful for symptom control in those with Tourette syndrome by simultaneously treating tics, hyperkinesis, and impulsivity, while decreasing the risk of tic exacerbation with use of stimulants. Overall, understanding the neurodiversity related to Tourette syndrome can help providers advocate for home and community-based supports to optimize general functioning and quality of life.
Dr. Roth is a developmental and behavioral pediatrician in Eugene, Ore. She has no conflicts of interest.
References
Darrow S et al. J Am Acad Child Adolescent Psych. 2017;56(7):610-7.
AAP Section on Developmental and Behavioral Pediatrics. Developmental and Behavioral Pediatrics. Voigt RG et al, eds. 2018: American Academy of Pediatrics.
Tourette syndrome, attention-deficit/hyperactivity disorder (ADHD), obsessive-compulsive disorder (OCD), and autism spectrum disorder (ASD) share significant overlap in symptomatology, and it can be challenging at times to distinguish between these conditions. Being able to do so, however, can help guide more targeted interventions and accommodations to optimize a patient’s level of functioning.
Case example
A healthy, bright 6-year-old boy is referred by his family doctor to an academic medical center for a full team evaluation because of suspicion of ASD, after having already been diagnosed with ADHD at the age of 5. His difficulties with inattention, impulsivity, and hyperactivity, as well as his behavioral rigidities and sensory avoidant and sensory seeking behaviors have caused functional impairments for him in his kindergarten classroom. He has been penalized with removal of recess on more than one occasion. A low dose of a stimulant had been tried but resulted in a perceived increase in disruptive behaviors.
The boy, while hyperkinetic and often paying poor attention, is quite capable of high-quality and well-modulated eye contact paired with typical social referencing and reciprocity when actively engaging with the examiner and his parents. He does have a reported history of serial fixated interests and some repetitive behaviors but is also noted to be flexible in his interpersonal style, maintains other varied and typical interests, easily directs affect, utilizes a wide array of fluid gestures paired naturally with verbal communication, and shares enjoyment with smoothly coordinated gaze. He has mild articulation errors but uses pronouns appropriately and has no scripted speech or echolalia, though does engage in some whispered palilalia intermittently.
He is generally quite cooperative and redirectable when focused and has a completely normal physical and neurologic examination. During the visit, the doctor notices the boy making an intermittent honking sound, which parents report as an attention-seeking strategy during times of stress. Further physician-guided information gathering around other repetitive noises and movements elicits a history of engagement in repetitive hand-to-groin movements, some exaggerated blinking, and a number of other waxing and waning subtle motor and phonic tics with onset in preschool. These noises and movements have generally been identified as “fidgeting” and “misbehaving” by well-meaning caregivers in the home and school environments.
Both Tourette syndrome and ASD are more common in males, with stereotyped patterns of movements and behaviors; anxious, obsessive, and compulsive behaviors resulting in behavioral rigidities; sensory sensitivities; and increased rates of hyperkinesis with decreased impulse control which result in increased sensory-seeking behaviors. Diagnostic criteria for Tourette syndrome are met when a child has had multiple motor tics and at least one phonic tic present for at least 1 year, with tic-free intervals lasting no longer than 3 months, and with onset before the age of 18. Typically, tics emerge in late preschool and early grade school, and some children even develop repetitive movements as early as toddlerhood. Tics tend to worsen around the peripubertal era, then often generally improve in the teen years. Tic types, frequency, and severity general fluctuate over time.
Forty percent of children with Tourette syndrome also meet criteria for OCD, with many more having OCD traits, and about 65% of children with Tourette syndrome also meet criteria for ADHD, with many more having ADHD traits. OCD can lead to more rigid and directive social interactions in children as well as obsessive interests, just as ADHD can lead to less socially attuned and less cooperative behaviors, even in children who do not meet criteria for ASD.
For example, a child with OCD in the absence of ASD may still “police” other kids in class and be overly focused on the rules of a game, which may become a social liability. Likewise, a child with ADHD in the absence of ASD may be so distractible that focusing on what other kids are saying and their paired facial expressions is compromised, leading to poor-quality social reciprocity during interactions with peers. Given the remarkable overlap in shared symptoms, it is essential for pediatric providers to consider Tourette syndrome in the differential for any child with repetitive movements and behaviors in addition to ASD and a wide array of other neurodevelopment differences, including global developmental delays and intellectual disabilities. This is of particular importance as the diagnosis of Tourette syndrome can be used to gain access to developmental disability services if the condition has resulted in true adaptive impairments.
It is determined that the boy does in fact meet criteria for ADHD, but also for OCD and Tourette syndrome. Both his Autism Diagnostic Observation Schedule and DSM-5–influenced autism interview are found to be in the nonclinical ranges, given his quality of communication, social engagement, imaginative play, and varied interests. A diagnosis of ASD is not felt to be an appropriate conceptualization of his neurodevelopmental differences. He is started on a low dose of guanfacine, which induces a decline in tics, impulsivity, and hyperkinesis. He is given a 504 plan in school that includes scheduled “tic breaks,” sensory fidgets for use in the classroom, extra movement opportunities as needed, and utilization of a gentle cueing system between him and his teacher for low-key redirection of disruptive behaviors. He is no longer penalized for inattention or tics, and his 504 plan protects him from the use of recess removal as a behavioral modification strategy.
His parents enroll him in the community swim program for extra exercise, focus on decreasing screen time, and give him an earlier bedtime to help decrease his tics and rigidities, while improving his ability to self-regulate. Eventually, a low dose of a newer-generation stimulant is added to his guanfacine, with excellent results and only a mild increase in tolerable tics.
The child in the vignette did well with a 504 plan based on his medical diagnoses, though if related learning difficulties had persisted, eligibility under Other Health Impaired could be used to provide eligibility for an Individualized Education Plan. Alpha-agonists can be helpful for symptom control in those with Tourette syndrome by simultaneously treating tics, hyperkinesis, and impulsivity, while decreasing the risk of tic exacerbation with use of stimulants. Overall, understanding the neurodiversity related to Tourette syndrome can help providers advocate for home and community-based supports to optimize general functioning and quality of life.
Dr. Roth is a developmental and behavioral pediatrician in Eugene, Ore. She has no conflicts of interest.
References
Darrow S et al. J Am Acad Child Adolescent Psych. 2017;56(7):610-7.
AAP Section on Developmental and Behavioral Pediatrics. Developmental and Behavioral Pediatrics. Voigt RG et al, eds. 2018: American Academy of Pediatrics.
Tourette syndrome, attention-deficit/hyperactivity disorder (ADHD), obsessive-compulsive disorder (OCD), and autism spectrum disorder (ASD) share significant overlap in symptomatology, and it can be challenging at times to distinguish between these conditions. Being able to do so, however, can help guide more targeted interventions and accommodations to optimize a patient’s level of functioning.
Case example
A healthy, bright 6-year-old boy is referred by his family doctor to an academic medical center for a full team evaluation because of suspicion of ASD, after having already been diagnosed with ADHD at the age of 5. His difficulties with inattention, impulsivity, and hyperactivity, as well as his behavioral rigidities and sensory avoidant and sensory seeking behaviors have caused functional impairments for him in his kindergarten classroom. He has been penalized with removal of recess on more than one occasion. A low dose of a stimulant had been tried but resulted in a perceived increase in disruptive behaviors.
The boy, while hyperkinetic and often paying poor attention, is quite capable of high-quality and well-modulated eye contact paired with typical social referencing and reciprocity when actively engaging with the examiner and his parents. He does have a reported history of serial fixated interests and some repetitive behaviors but is also noted to be flexible in his interpersonal style, maintains other varied and typical interests, easily directs affect, utilizes a wide array of fluid gestures paired naturally with verbal communication, and shares enjoyment with smoothly coordinated gaze. He has mild articulation errors but uses pronouns appropriately and has no scripted speech or echolalia, though does engage in some whispered palilalia intermittently.
He is generally quite cooperative and redirectable when focused and has a completely normal physical and neurologic examination. During the visit, the doctor notices the boy making an intermittent honking sound, which parents report as an attention-seeking strategy during times of stress. Further physician-guided information gathering around other repetitive noises and movements elicits a history of engagement in repetitive hand-to-groin movements, some exaggerated blinking, and a number of other waxing and waning subtle motor and phonic tics with onset in preschool. These noises and movements have generally been identified as “fidgeting” and “misbehaving” by well-meaning caregivers in the home and school environments.
Both Tourette syndrome and ASD are more common in males, with stereotyped patterns of movements and behaviors; anxious, obsessive, and compulsive behaviors resulting in behavioral rigidities; sensory sensitivities; and increased rates of hyperkinesis with decreased impulse control which result in increased sensory-seeking behaviors. Diagnostic criteria for Tourette syndrome are met when a child has had multiple motor tics and at least one phonic tic present for at least 1 year, with tic-free intervals lasting no longer than 3 months, and with onset before the age of 18. Typically, tics emerge in late preschool and early grade school, and some children even develop repetitive movements as early as toddlerhood. Tics tend to worsen around the peripubertal era, then often generally improve in the teen years. Tic types, frequency, and severity general fluctuate over time.
Forty percent of children with Tourette syndrome also meet criteria for OCD, with many more having OCD traits, and about 65% of children with Tourette syndrome also meet criteria for ADHD, with many more having ADHD traits. OCD can lead to more rigid and directive social interactions in children as well as obsessive interests, just as ADHD can lead to less socially attuned and less cooperative behaviors, even in children who do not meet criteria for ASD.
For example, a child with OCD in the absence of ASD may still “police” other kids in class and be overly focused on the rules of a game, which may become a social liability. Likewise, a child with ADHD in the absence of ASD may be so distractible that focusing on what other kids are saying and their paired facial expressions is compromised, leading to poor-quality social reciprocity during interactions with peers. Given the remarkable overlap in shared symptoms, it is essential for pediatric providers to consider Tourette syndrome in the differential for any child with repetitive movements and behaviors in addition to ASD and a wide array of other neurodevelopment differences, including global developmental delays and intellectual disabilities. This is of particular importance as the diagnosis of Tourette syndrome can be used to gain access to developmental disability services if the condition has resulted in true adaptive impairments.
It is determined that the boy does in fact meet criteria for ADHD, but also for OCD and Tourette syndrome. Both his Autism Diagnostic Observation Schedule and DSM-5–influenced autism interview are found to be in the nonclinical ranges, given his quality of communication, social engagement, imaginative play, and varied interests. A diagnosis of ASD is not felt to be an appropriate conceptualization of his neurodevelopmental differences. He is started on a low dose of guanfacine, which induces a decline in tics, impulsivity, and hyperkinesis. He is given a 504 plan in school that includes scheduled “tic breaks,” sensory fidgets for use in the classroom, extra movement opportunities as needed, and utilization of a gentle cueing system between him and his teacher for low-key redirection of disruptive behaviors. He is no longer penalized for inattention or tics, and his 504 plan protects him from the use of recess removal as a behavioral modification strategy.
His parents enroll him in the community swim program for extra exercise, focus on decreasing screen time, and give him an earlier bedtime to help decrease his tics and rigidities, while improving his ability to self-regulate. Eventually, a low dose of a newer-generation stimulant is added to his guanfacine, with excellent results and only a mild increase in tolerable tics.
The child in the vignette did well with a 504 plan based on his medical diagnoses, though if related learning difficulties had persisted, eligibility under Other Health Impaired could be used to provide eligibility for an Individualized Education Plan. Alpha-agonists can be helpful for symptom control in those with Tourette syndrome by simultaneously treating tics, hyperkinesis, and impulsivity, while decreasing the risk of tic exacerbation with use of stimulants. Overall, understanding the neurodiversity related to Tourette syndrome can help providers advocate for home and community-based supports to optimize general functioning and quality of life.
Dr. Roth is a developmental and behavioral pediatrician in Eugene, Ore. She has no conflicts of interest.
References
Darrow S et al. J Am Acad Child Adolescent Psych. 2017;56(7):610-7.
AAP Section on Developmental and Behavioral Pediatrics. Developmental and Behavioral Pediatrics. Voigt RG et al, eds. 2018: American Academy of Pediatrics.
The WPATH guidelines for treatment of adolescents with gender dysphoria have changed
The World Professional Association for Transgender Health (WPATH) is an interdisciplinary professional and educational organization devoted to transgender health. One of their activities is to produce the Standards of Care (SOC) for treatment of individuals with gender dysphoria. According to WPATH, the SOC “articulate a professional consensus about the psychiatric, psychological, medical, and surgical management of gender dysphoria and help professionals understand the parameters within which they may offer assistance to those with these conditions.” Many clinicians around the world use these guidelines to help them care for patients with gender dysphoria and diverse gender expressions.
The most recent SOC, version 8, were released on Sept. 15, 2022, after a 2-year postponement because of the pandemic. These new standards represent the first update to the SOC since version 7, which was released in 2012. Given how recent this update is, this column will attempt to summarize the changes in the new guidelines that affect children and adolescents.
One of the major differences between SOC versions 7 and 8 is that version 8 now includes a chapter specifically dedicated to the care of adolescents. Version 7 lumped children and adolescents together into one chapter. This is an important distinction for SOC 8, as it highlights that care for prepubertal youth is simply social in nature and distinct from that of pubertal adolescents. Social transition includes things such as using an affirmed name/pronouns and changing hair style and clothes. It does not include medications of any kind. Allowing these youth the time and space to explore the natural gender diversity of childhood leads to improved psychological outcomes over time and reduces adversity. Psychological support, where indicated, should be offered to gender-diverse children and their families to explore the persistence, consistence, and insistence of that child’s gender identity.
Once a child reaches puberty, medications may come into play as part of an adolescent’s transition. SOC 7 had established a minimum age of 16 before any partially reversible medications (testosterone, estrogen) were started as part of a patient’s medical transition. Starting with SOC 8, a minimum age has been removed for the initiation of gender-affirming hormone therapy. However, a patient must still have begun their natal puberty before any medication is started. A specific age was removed to acknowledge that maturity in adolescents occurs on a continuum and at different ages. SOC 8 guidelines continue to recommend that the individual’s emotional, cognitive, and psychosocial development be taken into account when determining their ability to provide consent for treatment. These individuals should still undergo a comprehensive assessment, as described below.
Similar to SOC 7, SOC 8 continues to stress the importance of a comprehensive, multidisciplinary evaluation of those adolescents who seek medical therapy as part of their transition. This allows for the exploration of additional coexisting causes of gender dysphoria, such as anxiety, depression, or other mental health conditions. If these exist, then they must be appropriately treated before any gender-affirming medical treatment is initiated. Assessments should be performed by clinicians who have training and expertise with the developmental trajectory of adolescents, as well as with common mental health conditions. These assessments are also critical, as SOC 8 acknowledges a rise in the number of adolescents who may not have had gender-diverse expression in childhood.
SOC 8 and the Endocrine Society Guidelines (see references) provide physicians and other health care professionals with a road map for addressing the needs of transgender and gender-diverse persons. By referencing these guidelines when taking care of these patients, physicians and other health care professionals will know that they are providing the most up-to-date, evidence-based care.
Dr. M. Brett Cooper is an assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
SOC 8: https://www.tandfonline.com/doi/pdf/10.1080/26895269.2022.2100644
SOC 7: https://www.wpath.org/media/cms/Documents/SOC%20v7/SOC%20V7_English2012.pdf?_t=1613669341
Endocrine Society Gender Affirming Care Guidelines: https://academic.oup.com/jcem/article/102/11/3869/4157558?login=false
The World Professional Association for Transgender Health (WPATH) is an interdisciplinary professional and educational organization devoted to transgender health. One of their activities is to produce the Standards of Care (SOC) for treatment of individuals with gender dysphoria. According to WPATH, the SOC “articulate a professional consensus about the psychiatric, psychological, medical, and surgical management of gender dysphoria and help professionals understand the parameters within which they may offer assistance to those with these conditions.” Many clinicians around the world use these guidelines to help them care for patients with gender dysphoria and diverse gender expressions.
The most recent SOC, version 8, were released on Sept. 15, 2022, after a 2-year postponement because of the pandemic. These new standards represent the first update to the SOC since version 7, which was released in 2012. Given how recent this update is, this column will attempt to summarize the changes in the new guidelines that affect children and adolescents.
One of the major differences between SOC versions 7 and 8 is that version 8 now includes a chapter specifically dedicated to the care of adolescents. Version 7 lumped children and adolescents together into one chapter. This is an important distinction for SOC 8, as it highlights that care for prepubertal youth is simply social in nature and distinct from that of pubertal adolescents. Social transition includes things such as using an affirmed name/pronouns and changing hair style and clothes. It does not include medications of any kind. Allowing these youth the time and space to explore the natural gender diversity of childhood leads to improved psychological outcomes over time and reduces adversity. Psychological support, where indicated, should be offered to gender-diverse children and their families to explore the persistence, consistence, and insistence of that child’s gender identity.
Once a child reaches puberty, medications may come into play as part of an adolescent’s transition. SOC 7 had established a minimum age of 16 before any partially reversible medications (testosterone, estrogen) were started as part of a patient’s medical transition. Starting with SOC 8, a minimum age has been removed for the initiation of gender-affirming hormone therapy. However, a patient must still have begun their natal puberty before any medication is started. A specific age was removed to acknowledge that maturity in adolescents occurs on a continuum and at different ages. SOC 8 guidelines continue to recommend that the individual’s emotional, cognitive, and psychosocial development be taken into account when determining their ability to provide consent for treatment. These individuals should still undergo a comprehensive assessment, as described below.
Similar to SOC 7, SOC 8 continues to stress the importance of a comprehensive, multidisciplinary evaluation of those adolescents who seek medical therapy as part of their transition. This allows for the exploration of additional coexisting causes of gender dysphoria, such as anxiety, depression, or other mental health conditions. If these exist, then they must be appropriately treated before any gender-affirming medical treatment is initiated. Assessments should be performed by clinicians who have training and expertise with the developmental trajectory of adolescents, as well as with common mental health conditions. These assessments are also critical, as SOC 8 acknowledges a rise in the number of adolescents who may not have had gender-diverse expression in childhood.
SOC 8 and the Endocrine Society Guidelines (see references) provide physicians and other health care professionals with a road map for addressing the needs of transgender and gender-diverse persons. By referencing these guidelines when taking care of these patients, physicians and other health care professionals will know that they are providing the most up-to-date, evidence-based care.
Dr. M. Brett Cooper is an assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
SOC 8: https://www.tandfonline.com/doi/pdf/10.1080/26895269.2022.2100644
SOC 7: https://www.wpath.org/media/cms/Documents/SOC%20v7/SOC%20V7_English2012.pdf?_t=1613669341
Endocrine Society Gender Affirming Care Guidelines: https://academic.oup.com/jcem/article/102/11/3869/4157558?login=false
The World Professional Association for Transgender Health (WPATH) is an interdisciplinary professional and educational organization devoted to transgender health. One of their activities is to produce the Standards of Care (SOC) for treatment of individuals with gender dysphoria. According to WPATH, the SOC “articulate a professional consensus about the psychiatric, psychological, medical, and surgical management of gender dysphoria and help professionals understand the parameters within which they may offer assistance to those with these conditions.” Many clinicians around the world use these guidelines to help them care for patients with gender dysphoria and diverse gender expressions.
The most recent SOC, version 8, were released on Sept. 15, 2022, after a 2-year postponement because of the pandemic. These new standards represent the first update to the SOC since version 7, which was released in 2012. Given how recent this update is, this column will attempt to summarize the changes in the new guidelines that affect children and adolescents.
One of the major differences between SOC versions 7 and 8 is that version 8 now includes a chapter specifically dedicated to the care of adolescents. Version 7 lumped children and adolescents together into one chapter. This is an important distinction for SOC 8, as it highlights that care for prepubertal youth is simply social in nature and distinct from that of pubertal adolescents. Social transition includes things such as using an affirmed name/pronouns and changing hair style and clothes. It does not include medications of any kind. Allowing these youth the time and space to explore the natural gender diversity of childhood leads to improved psychological outcomes over time and reduces adversity. Psychological support, where indicated, should be offered to gender-diverse children and their families to explore the persistence, consistence, and insistence of that child’s gender identity.
Once a child reaches puberty, medications may come into play as part of an adolescent’s transition. SOC 7 had established a minimum age of 16 before any partially reversible medications (testosterone, estrogen) were started as part of a patient’s medical transition. Starting with SOC 8, a minimum age has been removed for the initiation of gender-affirming hormone therapy. However, a patient must still have begun their natal puberty before any medication is started. A specific age was removed to acknowledge that maturity in adolescents occurs on a continuum and at different ages. SOC 8 guidelines continue to recommend that the individual’s emotional, cognitive, and psychosocial development be taken into account when determining their ability to provide consent for treatment. These individuals should still undergo a comprehensive assessment, as described below.
Similar to SOC 7, SOC 8 continues to stress the importance of a comprehensive, multidisciplinary evaluation of those adolescents who seek medical therapy as part of their transition. This allows for the exploration of additional coexisting causes of gender dysphoria, such as anxiety, depression, or other mental health conditions. If these exist, then they must be appropriately treated before any gender-affirming medical treatment is initiated. Assessments should be performed by clinicians who have training and expertise with the developmental trajectory of adolescents, as well as with common mental health conditions. These assessments are also critical, as SOC 8 acknowledges a rise in the number of adolescents who may not have had gender-diverse expression in childhood.
SOC 8 and the Endocrine Society Guidelines (see references) provide physicians and other health care professionals with a road map for addressing the needs of transgender and gender-diverse persons. By referencing these guidelines when taking care of these patients, physicians and other health care professionals will know that they are providing the most up-to-date, evidence-based care.
Dr. M. Brett Cooper is an assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
SOC 8: https://www.tandfonline.com/doi/pdf/10.1080/26895269.2022.2100644
SOC 7: https://www.wpath.org/media/cms/Documents/SOC%20v7/SOC%20V7_English2012.pdf?_t=1613669341
Endocrine Society Gender Affirming Care Guidelines: https://academic.oup.com/jcem/article/102/11/3869/4157558?login=false