User login
Medication pricing: So this is how it works
This is the second part in a series on medication pricing.
In my last column, I looked at the tremendous variation in prices among pharmacies for two psychotropic medications, aripiprazole and modafinil. The cash price variation could be as much as 45 times more from one pharmacy to the next, which I found to be both outrageous and incomprehensible.
To learn more about pharmaceutical pricing, I contacted Doug Hirsch, the cofounder of GoodRx, a firm based in Santa Monica, Calif., that offers deep discounts on some medications. The company sends discount cards to physicians’ offices – call me if you need some, I have many boxes of GoodRx cards – and has a website (www.GoodRx.com) and an app. It advertises that it is about transparency, and if you’ve ever tried the company’s site or app, the service it offers is remarkable and simple to use.
I approached Mr. Hirsch with two simple questions. The company offers “up to 90% discount” on the cash price of medications through its app, website, or discount card – all of which can be gotten for free. I wanted to know 1) Who pays for this difference in the medication cost, and 2) How does the company, with 95 employees, make any money? Mr. Hirsch was gracious enough (and patient enough!) to spend the next hour walking me through the steps of medication pricing. It was a lively conversation, so let me share with you what I have learned.
Medications are made by a pharmaceutical company or, for generics, there may be many manufacturers. The medications are sent to a pharmaceutical distributor, such as McKesson, and it, in turn, sells and delivers the products to pharmacy chains, as well as to smaller, independent pharmacies. The pharmacies pay an acquisition cost for medications then set a price for these medications that are considerably – or even astronomically – higher than the acquisition price. This is the cash retail price, or in medicine, what is called the Usual & Customary (U&C) cost of the medication. The price may be neither usual, customary, nor reasonable, and it’s not the price the pharmacy expects to recoup on sales.
Every major insurance company contracts with a pharmacy benefits manager (for example, Caremark, Express Scripts, and Optum) to negotiate the cost of medications with each major pharmacy chain. Physicians are familiar with PBMs, who intercede by requiring preauthorization procedures for certain medications or by instituting stepwise, fail-first, requirements before they will allow pharmacy benefits toward the purchase of medications. When the PBMs negotiate with the pharmacies, they will negotiate for a discount off the pharmacy’s U&C charge for medication, perhaps a discount as much as 75% or 80%. Mr. Hirsch noted, “The discount is not negotiated on a per-medication basis but as an across-the-board average, so for one medication, the insurance price may be 2% discount from the U&C cost, and on another medicine it may be 95%. There is a dramatic variation, more than you’d ever expect.”
GoodRx gathers prices from many places, including partnerships with a number of PBMs. In addition to providing discounted prices for insured customers, the PBMs also include in their negotiations a slightly less-discounted price for cash-paying patients who present with a GoodRx card or coupon. You might be surprised to learn that discounted prices can often be less than the typical patient copay. For patients with a high deductible, for medications that are not covered at all, or for times when the copay is higher than the cost of the medication, it will often be less expensive for patients to use a GoodRx discount instead of their insurance. And whether patients uses either their insurance or a GoodRx discount, part of the cost of the prescription includes an administrative fee that goes to the PBM. When GoodRx cards are used, the PBM pays GoodRx part of that fee. I hope you are still with me, because this is the part of the conversation where I started telling Mr. Hirsch that I was getting a headache.
I went back to the enormous cost discrepancy that I had discovered a couple of years ago with Provigil (modafinil). Thirty pills cost just under $35 at Costco, while all other pharmacies were charging close to $1,000. Mr. Hirsch explained, “From what I’ve been told, Costco bases their prices on their acquisition costs and then raises them a certain percent. It’s one way to provide a fair price, but that doesn’t mean they always have the lowest price. They are also the only major pharmacy that lists their drug prices on their website.”
I wanted to know what was in it for the PBMs. Why would Express Scripts be motivated to negotiate a discount in price for cash-paying customers outside of the insurance networks, and how did partnering with GoodRx benefit them? The answer, in part, lies with the fact that the website and app allow patients to comparison shop and go to pharmacies with lower prices. If patients use their insurance, the insurance company is paying less; if they don’t use their insurance because they learned the cash cost is less, then the cost burden has shifted from the insurance company entirely to the patient.
What’s in it for the pharmacies? Why would they be willing to accept less money from a patient bearing a discount card? Mr. Hirsch explained, “Pharmacies want to honor their contracts with PBMs, and the U&C prices are set high to enable negotiation so that they still make some profit. Most people couldn’t afford to pay the high U&C, but they can’t lower them for individual cash-pay customers because that would violate their agreements with PBMs, and Medicare and Medicaid, which is a felony. With the GoodRx price, they still make a profit, and people in drugstores buy other items as well.
GoodRx has 95 employees, and I was still left wondering how they generate income. Mr. Hirsch pinned it down to three sources: the portion of the administration fees the PBMs pay GoodRx, a small amount of advertising, and finally, GoodRx provides technology for the PBMs and charges for this service.
“We started asking how we could gather prices in this bizarre marketplace and address the pricing inefficiencies,” Mr. Hirsch said, “and now I get emails every day expressing gratitude.”
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
This is the second part in a series on medication pricing.
In my last column, I looked at the tremendous variation in prices among pharmacies for two psychotropic medications, aripiprazole and modafinil. The cash price variation could be as much as 45 times more from one pharmacy to the next, which I found to be both outrageous and incomprehensible.
To learn more about pharmaceutical pricing, I contacted Doug Hirsch, the cofounder of GoodRx, a firm based in Santa Monica, Calif., that offers deep discounts on some medications. The company sends discount cards to physicians’ offices – call me if you need some, I have many boxes of GoodRx cards – and has a website (www.GoodRx.com) and an app. It advertises that it is about transparency, and if you’ve ever tried the company’s site or app, the service it offers is remarkable and simple to use.
I approached Mr. Hirsch with two simple questions. The company offers “up to 90% discount” on the cash price of medications through its app, website, or discount card – all of which can be gotten for free. I wanted to know 1) Who pays for this difference in the medication cost, and 2) How does the company, with 95 employees, make any money? Mr. Hirsch was gracious enough (and patient enough!) to spend the next hour walking me through the steps of medication pricing. It was a lively conversation, so let me share with you what I have learned.
Medications are made by a pharmaceutical company or, for generics, there may be many manufacturers. The medications are sent to a pharmaceutical distributor, such as McKesson, and it, in turn, sells and delivers the products to pharmacy chains, as well as to smaller, independent pharmacies. The pharmacies pay an acquisition cost for medications then set a price for these medications that are considerably – or even astronomically – higher than the acquisition price. This is the cash retail price, or in medicine, what is called the Usual & Customary (U&C) cost of the medication. The price may be neither usual, customary, nor reasonable, and it’s not the price the pharmacy expects to recoup on sales.
Every major insurance company contracts with a pharmacy benefits manager (for example, Caremark, Express Scripts, and Optum) to negotiate the cost of medications with each major pharmacy chain. Physicians are familiar with PBMs, who intercede by requiring preauthorization procedures for certain medications or by instituting stepwise, fail-first, requirements before they will allow pharmacy benefits toward the purchase of medications. When the PBMs negotiate with the pharmacies, they will negotiate for a discount off the pharmacy’s U&C charge for medication, perhaps a discount as much as 75% or 80%. Mr. Hirsch noted, “The discount is not negotiated on a per-medication basis but as an across-the-board average, so for one medication, the insurance price may be 2% discount from the U&C cost, and on another medicine it may be 95%. There is a dramatic variation, more than you’d ever expect.”
GoodRx gathers prices from many places, including partnerships with a number of PBMs. In addition to providing discounted prices for insured customers, the PBMs also include in their negotiations a slightly less-discounted price for cash-paying patients who present with a GoodRx card or coupon. You might be surprised to learn that discounted prices can often be less than the typical patient copay. For patients with a high deductible, for medications that are not covered at all, or for times when the copay is higher than the cost of the medication, it will often be less expensive for patients to use a GoodRx discount instead of their insurance. And whether patients uses either their insurance or a GoodRx discount, part of the cost of the prescription includes an administrative fee that goes to the PBM. When GoodRx cards are used, the PBM pays GoodRx part of that fee. I hope you are still with me, because this is the part of the conversation where I started telling Mr. Hirsch that I was getting a headache.
I went back to the enormous cost discrepancy that I had discovered a couple of years ago with Provigil (modafinil). Thirty pills cost just under $35 at Costco, while all other pharmacies were charging close to $1,000. Mr. Hirsch explained, “From what I’ve been told, Costco bases their prices on their acquisition costs and then raises them a certain percent. It’s one way to provide a fair price, but that doesn’t mean they always have the lowest price. They are also the only major pharmacy that lists their drug prices on their website.”
I wanted to know what was in it for the PBMs. Why would Express Scripts be motivated to negotiate a discount in price for cash-paying customers outside of the insurance networks, and how did partnering with GoodRx benefit them? The answer, in part, lies with the fact that the website and app allow patients to comparison shop and go to pharmacies with lower prices. If patients use their insurance, the insurance company is paying less; if they don’t use their insurance because they learned the cash cost is less, then the cost burden has shifted from the insurance company entirely to the patient.
What’s in it for the pharmacies? Why would they be willing to accept less money from a patient bearing a discount card? Mr. Hirsch explained, “Pharmacies want to honor their contracts with PBMs, and the U&C prices are set high to enable negotiation so that they still make some profit. Most people couldn’t afford to pay the high U&C, but they can’t lower them for individual cash-pay customers because that would violate their agreements with PBMs, and Medicare and Medicaid, which is a felony. With the GoodRx price, they still make a profit, and people in drugstores buy other items as well.
GoodRx has 95 employees, and I was still left wondering how they generate income. Mr. Hirsch pinned it down to three sources: the portion of the administration fees the PBMs pay GoodRx, a small amount of advertising, and finally, GoodRx provides technology for the PBMs and charges for this service.
“We started asking how we could gather prices in this bizarre marketplace and address the pricing inefficiencies,” Mr. Hirsch said, “and now I get emails every day expressing gratitude.”
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
This is the second part in a series on medication pricing.
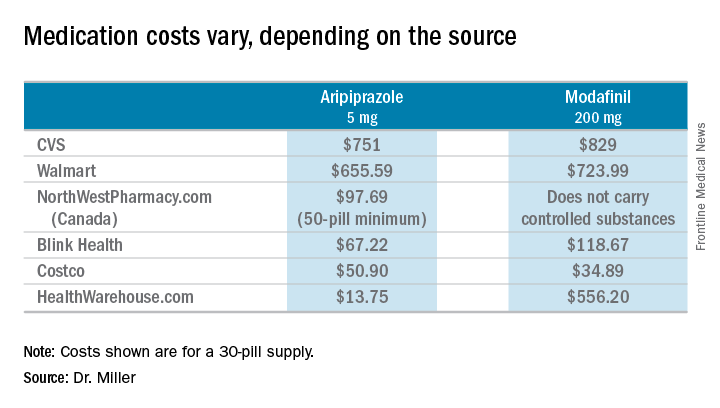
In my last column, I looked at the tremendous variation in prices among pharmacies for two psychotropic medications, aripiprazole and modafinil. The cash price variation could be as much as 45 times more from one pharmacy to the next, which I found to be both outrageous and incomprehensible.
To learn more about pharmaceutical pricing, I contacted Doug Hirsch, the cofounder of GoodRx, a firm based in Santa Monica, Calif., that offers deep discounts on some medications. The company sends discount cards to physicians’ offices – call me if you need some, I have many boxes of GoodRx cards – and has a website (www.GoodRx.com) and an app. It advertises that it is about transparency, and if you’ve ever tried the company’s site or app, the service it offers is remarkable and simple to use.
I approached Mr. Hirsch with two simple questions. The company offers “up to 90% discount” on the cash price of medications through its app, website, or discount card – all of which can be gotten for free. I wanted to know 1) Who pays for this difference in the medication cost, and 2) How does the company, with 95 employees, make any money? Mr. Hirsch was gracious enough (and patient enough!) to spend the next hour walking me through the steps of medication pricing. It was a lively conversation, so let me share with you what I have learned.
Medications are made by a pharmaceutical company or, for generics, there may be many manufacturers. The medications are sent to a pharmaceutical distributor, such as McKesson, and it, in turn, sells and delivers the products to pharmacy chains, as well as to smaller, independent pharmacies. The pharmacies pay an acquisition cost for medications then set a price for these medications that are considerably – or even astronomically – higher than the acquisition price. This is the cash retail price, or in medicine, what is called the Usual & Customary (U&C) cost of the medication. The price may be neither usual, customary, nor reasonable, and it’s not the price the pharmacy expects to recoup on sales.
Every major insurance company contracts with a pharmacy benefits manager (for example, Caremark, Express Scripts, and Optum) to negotiate the cost of medications with each major pharmacy chain. Physicians are familiar with PBMs, who intercede by requiring preauthorization procedures for certain medications or by instituting stepwise, fail-first, requirements before they will allow pharmacy benefits toward the purchase of medications. When the PBMs negotiate with the pharmacies, they will negotiate for a discount off the pharmacy’s U&C charge for medication, perhaps a discount as much as 75% or 80%. Mr. Hirsch noted, “The discount is not negotiated on a per-medication basis but as an across-the-board average, so for one medication, the insurance price may be 2% discount from the U&C cost, and on another medicine it may be 95%. There is a dramatic variation, more than you’d ever expect.”
GoodRx gathers prices from many places, including partnerships with a number of PBMs. In addition to providing discounted prices for insured customers, the PBMs also include in their negotiations a slightly less-discounted price for cash-paying patients who present with a GoodRx card or coupon. You might be surprised to learn that discounted prices can often be less than the typical patient copay. For patients with a high deductible, for medications that are not covered at all, or for times when the copay is higher than the cost of the medication, it will often be less expensive for patients to use a GoodRx discount instead of their insurance. And whether patients uses either their insurance or a GoodRx discount, part of the cost of the prescription includes an administrative fee that goes to the PBM. When GoodRx cards are used, the PBM pays GoodRx part of that fee. I hope you are still with me, because this is the part of the conversation where I started telling Mr. Hirsch that I was getting a headache.
I went back to the enormous cost discrepancy that I had discovered a couple of years ago with Provigil (modafinil). Thirty pills cost just under $35 at Costco, while all other pharmacies were charging close to $1,000. Mr. Hirsch explained, “From what I’ve been told, Costco bases their prices on their acquisition costs and then raises them a certain percent. It’s one way to provide a fair price, but that doesn’t mean they always have the lowest price. They are also the only major pharmacy that lists their drug prices on their website.”
I wanted to know what was in it for the PBMs. Why would Express Scripts be motivated to negotiate a discount in price for cash-paying customers outside of the insurance networks, and how did partnering with GoodRx benefit them? The answer, in part, lies with the fact that the website and app allow patients to comparison shop and go to pharmacies with lower prices. If patients use their insurance, the insurance company is paying less; if they don’t use their insurance because they learned the cash cost is less, then the cost burden has shifted from the insurance company entirely to the patient.
What’s in it for the pharmacies? Why would they be willing to accept less money from a patient bearing a discount card? Mr. Hirsch explained, “Pharmacies want to honor their contracts with PBMs, and the U&C prices are set high to enable negotiation so that they still make some profit. Most people couldn’t afford to pay the high U&C, but they can’t lower them for individual cash-pay customers because that would violate their agreements with PBMs, and Medicare and Medicaid, which is a felony. With the GoodRx price, they still make a profit, and people in drugstores buy other items as well.
GoodRx has 95 employees, and I was still left wondering how they generate income. Mr. Hirsch pinned it down to three sources: the portion of the administration fees the PBMs pay GoodRx, a small amount of advertising, and finally, GoodRx provides technology for the PBMs and charges for this service.
“We started asking how we could gather prices in this bizarre marketplace and address the pricing inefficiencies,” Mr. Hirsch said, “and now I get emails every day expressing gratitude.”
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
The toxic zeitgeist of hyper-partisanship: A psychiatric perspective
It is always judicious to avoid discussing religious or political issues because inevitably someone will be offended. As a lifetime member of the American Psychiatric Association, I adhere to its "Goldwater Rule," which proscribes the gratuitous diagnosis of any president absent of a formal face-to-face psychiatric evaluation. But it is perfectly permissible to express a psychiatric opinion about the contemporary national political scene.
Frankly, the status of the political arena has become ugly. This should not be surprising, given that at its core, politics is an unquenchable thirst for power, and Machiavelli is its anointed godfather. The current political zeitgeist of the country is becoming downright grotesque and spiteful. Although fierce political rivalry is widely accepted as a tradition to achieve the national goals promulgated by each party, what we are witnessing today is a veritable blood sport fueled by “hyper-partisanship,” where drawing blood, not promoting the public good, has become an undisguised intent.
The intensity of hyper-partisanship has engulfed the collective national psyche and is bordering on the “religification” of politics. What used to be reasonable political views have been transformed into irrefutable articles of faith that do not lend themselves to rational debate or productive compromise. The metastasis of social media into our daily lives over the past decade is catalyzing the venomous crossfire across the political divide that used to be passionate and civil, but recently has degenerated into a raucous cacophony of hateful speech. Thoughtful debate of issues that promote the public good is becoming scarce. Instead of effectively defending the validity of their arguments, extremists focus on spewing accusations and ad hominem insults. It is worrisome that both fringe groups tenaciously uphold fixed and extreme political positions, the tenets of which can never be challenged.
Psychiatrically, those extreme ideological positions appear to be consistent with Jasper’s criteria for a delusion (a belief with an unparalleled degree of subjective feeling of certainty that cannot be influenced by experience or arguments) or McHugh’s definition of an overvalued idea, which resembles an egosyntonic obsession that is relished, amplified, and defended. Given that extremism is not just a “folie à deux” shared by 2 individuals but by many individuals, it may qualify as a “folie en masse.”
Having a political orientation is perfectly normal, a healthy evidence of absence of indolent apathy. However, the unconstrained fervor of political extremism can be as psychologically unhealthy as lethargic passivity. A significant segment of the population may see some merit on both sides of the gaping political chasm, but they are appalled by the intransigence of political extremism, which has become an impediment to the constructive compromise that is vital for progress in politics and in all human interactions.
Beliefs are a transcendent human trait. Homo sapiens represent the only animal species endowed by evolution with a large prefrontal cortex that enables each of its members to harbor a belief system. It prompts me to propose that Descartes’ famous dictum “I think, therefore I am” be revised to “I believe, therefore I am human.” But while many beliefs are reasonable and anchored in reality, irrational beliefs are odd and ambiguous, ranging from superstitions and overvalued ideas to conspiracy theories and cults, which I wrote about a decade ago.1 In fact, epidemiologic research studies have confirmed a high prevalence of subthreshold and pre-psychotic beliefs in the general population.2-5 Thus, radical political partisanship falls on the extreme end of that continuum.
The zeitgeist generated by extreme partisanship is intellectually stunting and emotionally numbing. Psychiatrists may wonder what consequences the intense anger and antipathy and scarcity of compromise between the opposing parties will have for the country’s citizens. Although psychiatrists cannot repair the dysfunctional political fragmentation at the national level, we can help patients who may be negatively affected by the conflicts permeating the national scene when we read or watch the daily news.
Just as it is disturbing for children to watch their parents undermine each other by arguing ferociously and hurling insults, so it is for a populace aghast at how frenzied and intolerant their leaders and their extremist followers have become, failing to work together for the common good and adversely impacting the mental health zeitgeist.
1. Nasrallah HA. Irrational beliefs: a ubiquitous human trait. Current Psychiatry. 2007;6(2):15-16.
2. Kelleher I, Wigman JT, Harley M, et al. Psychotic experiences in the population: association with functioning and mental distress. Schizophr Res. 2015;165(1):9-14.
3. Landin-Romero R, McKenna PJ, Romaguera A, et al. Examining the continuum of psychosis: frequency and characteristics of psychotic-like symptoms in relatives and non-relatives of patients with schizophrenia. Schizophr Res. 2016;178(1-3):6-11.
4. Hanssen M, Bak M, Bijl R, et al. The incidence and outcome of subclinical psychotic experiences in the general population. Br J Clin Psychol. 2005;44(pt 2):181-191.
5. Nelson B, Fusar-Poli P, Yung AR. Can we detect psychotic-like experiences in the general population? Curr Pharm Des. 2012;18(4):376-385.
It is always judicious to avoid discussing religious or political issues because inevitably someone will be offended. As a lifetime member of the American Psychiatric Association, I adhere to its "Goldwater Rule," which proscribes the gratuitous diagnosis of any president absent of a formal face-to-face psychiatric evaluation. But it is perfectly permissible to express a psychiatric opinion about the contemporary national political scene.
Frankly, the status of the political arena has become ugly. This should not be surprising, given that at its core, politics is an unquenchable thirst for power, and Machiavelli is its anointed godfather. The current political zeitgeist of the country is becoming downright grotesque and spiteful. Although fierce political rivalry is widely accepted as a tradition to achieve the national goals promulgated by each party, what we are witnessing today is a veritable blood sport fueled by “hyper-partisanship,” where drawing blood, not promoting the public good, has become an undisguised intent.
The intensity of hyper-partisanship has engulfed the collective national psyche and is bordering on the “religification” of politics. What used to be reasonable political views have been transformed into irrefutable articles of faith that do not lend themselves to rational debate or productive compromise. The metastasis of social media into our daily lives over the past decade is catalyzing the venomous crossfire across the political divide that used to be passionate and civil, but recently has degenerated into a raucous cacophony of hateful speech. Thoughtful debate of issues that promote the public good is becoming scarce. Instead of effectively defending the validity of their arguments, extremists focus on spewing accusations and ad hominem insults. It is worrisome that both fringe groups tenaciously uphold fixed and extreme political positions, the tenets of which can never be challenged.
Psychiatrically, those extreme ideological positions appear to be consistent with Jasper’s criteria for a delusion (a belief with an unparalleled degree of subjective feeling of certainty that cannot be influenced by experience or arguments) or McHugh’s definition of an overvalued idea, which resembles an egosyntonic obsession that is relished, amplified, and defended. Given that extremism is not just a “folie à deux” shared by 2 individuals but by many individuals, it may qualify as a “folie en masse.”
Having a political orientation is perfectly normal, a healthy evidence of absence of indolent apathy. However, the unconstrained fervor of political extremism can be as psychologically unhealthy as lethargic passivity. A significant segment of the population may see some merit on both sides of the gaping political chasm, but they are appalled by the intransigence of political extremism, which has become an impediment to the constructive compromise that is vital for progress in politics and in all human interactions.
Beliefs are a transcendent human trait. Homo sapiens represent the only animal species endowed by evolution with a large prefrontal cortex that enables each of its members to harbor a belief system. It prompts me to propose that Descartes’ famous dictum “I think, therefore I am” be revised to “I believe, therefore I am human.” But while many beliefs are reasonable and anchored in reality, irrational beliefs are odd and ambiguous, ranging from superstitions and overvalued ideas to conspiracy theories and cults, which I wrote about a decade ago.1 In fact, epidemiologic research studies have confirmed a high prevalence of subthreshold and pre-psychotic beliefs in the general population.2-5 Thus, radical political partisanship falls on the extreme end of that continuum.
The zeitgeist generated by extreme partisanship is intellectually stunting and emotionally numbing. Psychiatrists may wonder what consequences the intense anger and antipathy and scarcity of compromise between the opposing parties will have for the country’s citizens. Although psychiatrists cannot repair the dysfunctional political fragmentation at the national level, we can help patients who may be negatively affected by the conflicts permeating the national scene when we read or watch the daily news.
Just as it is disturbing for children to watch their parents undermine each other by arguing ferociously and hurling insults, so it is for a populace aghast at how frenzied and intolerant their leaders and their extremist followers have become, failing to work together for the common good and adversely impacting the mental health zeitgeist.
It is always judicious to avoid discussing religious or political issues because inevitably someone will be offended. As a lifetime member of the American Psychiatric Association, I adhere to its "Goldwater Rule," which proscribes the gratuitous diagnosis of any president absent of a formal face-to-face psychiatric evaluation. But it is perfectly permissible to express a psychiatric opinion about the contemporary national political scene.
Frankly, the status of the political arena has become ugly. This should not be surprising, given that at its core, politics is an unquenchable thirst for power, and Machiavelli is its anointed godfather. The current political zeitgeist of the country is becoming downright grotesque and spiteful. Although fierce political rivalry is widely accepted as a tradition to achieve the national goals promulgated by each party, what we are witnessing today is a veritable blood sport fueled by “hyper-partisanship,” where drawing blood, not promoting the public good, has become an undisguised intent.
The intensity of hyper-partisanship has engulfed the collective national psyche and is bordering on the “religification” of politics. What used to be reasonable political views have been transformed into irrefutable articles of faith that do not lend themselves to rational debate or productive compromise. The metastasis of social media into our daily lives over the past decade is catalyzing the venomous crossfire across the political divide that used to be passionate and civil, but recently has degenerated into a raucous cacophony of hateful speech. Thoughtful debate of issues that promote the public good is becoming scarce. Instead of effectively defending the validity of their arguments, extremists focus on spewing accusations and ad hominem insults. It is worrisome that both fringe groups tenaciously uphold fixed and extreme political positions, the tenets of which can never be challenged.
Psychiatrically, those extreme ideological positions appear to be consistent with Jasper’s criteria for a delusion (a belief with an unparalleled degree of subjective feeling of certainty that cannot be influenced by experience or arguments) or McHugh’s definition of an overvalued idea, which resembles an egosyntonic obsession that is relished, amplified, and defended. Given that extremism is not just a “folie à deux” shared by 2 individuals but by many individuals, it may qualify as a “folie en masse.”
Having a political orientation is perfectly normal, a healthy evidence of absence of indolent apathy. However, the unconstrained fervor of political extremism can be as psychologically unhealthy as lethargic passivity. A significant segment of the population may see some merit on both sides of the gaping political chasm, but they are appalled by the intransigence of political extremism, which has become an impediment to the constructive compromise that is vital for progress in politics and in all human interactions.
Beliefs are a transcendent human trait. Homo sapiens represent the only animal species endowed by evolution with a large prefrontal cortex that enables each of its members to harbor a belief system. It prompts me to propose that Descartes’ famous dictum “I think, therefore I am” be revised to “I believe, therefore I am human.” But while many beliefs are reasonable and anchored in reality, irrational beliefs are odd and ambiguous, ranging from superstitions and overvalued ideas to conspiracy theories and cults, which I wrote about a decade ago.1 In fact, epidemiologic research studies have confirmed a high prevalence of subthreshold and pre-psychotic beliefs in the general population.2-5 Thus, radical political partisanship falls on the extreme end of that continuum.
The zeitgeist generated by extreme partisanship is intellectually stunting and emotionally numbing. Psychiatrists may wonder what consequences the intense anger and antipathy and scarcity of compromise between the opposing parties will have for the country’s citizens. Although psychiatrists cannot repair the dysfunctional political fragmentation at the national level, we can help patients who may be negatively affected by the conflicts permeating the national scene when we read or watch the daily news.
Just as it is disturbing for children to watch their parents undermine each other by arguing ferociously and hurling insults, so it is for a populace aghast at how frenzied and intolerant their leaders and their extremist followers have become, failing to work together for the common good and adversely impacting the mental health zeitgeist.
1. Nasrallah HA. Irrational beliefs: a ubiquitous human trait. Current Psychiatry. 2007;6(2):15-16.
2. Kelleher I, Wigman JT, Harley M, et al. Psychotic experiences in the population: association with functioning and mental distress. Schizophr Res. 2015;165(1):9-14.
3. Landin-Romero R, McKenna PJ, Romaguera A, et al. Examining the continuum of psychosis: frequency and characteristics of psychotic-like symptoms in relatives and non-relatives of patients with schizophrenia. Schizophr Res. 2016;178(1-3):6-11.
4. Hanssen M, Bak M, Bijl R, et al. The incidence and outcome of subclinical psychotic experiences in the general population. Br J Clin Psychol. 2005;44(pt 2):181-191.
5. Nelson B, Fusar-Poli P, Yung AR. Can we detect psychotic-like experiences in the general population? Curr Pharm Des. 2012;18(4):376-385.
1. Nasrallah HA. Irrational beliefs: a ubiquitous human trait. Current Psychiatry. 2007;6(2):15-16.
2. Kelleher I, Wigman JT, Harley M, et al. Psychotic experiences in the population: association with functioning and mental distress. Schizophr Res. 2015;165(1):9-14.
3. Landin-Romero R, McKenna PJ, Romaguera A, et al. Examining the continuum of psychosis: frequency and characteristics of psychotic-like symptoms in relatives and non-relatives of patients with schizophrenia. Schizophr Res. 2016;178(1-3):6-11.
4. Hanssen M, Bak M, Bijl R, et al. The incidence and outcome of subclinical psychotic experiences in the general population. Br J Clin Psychol. 2005;44(pt 2):181-191.
5. Nelson B, Fusar-Poli P, Yung AR. Can we detect psychotic-like experiences in the general population? Curr Pharm Des. 2012;18(4):376-385.
You paid how much for that medicine?
This is the first article in a series on the cost of medications.
While it’s not news that some pharmaceuticals are exorbitantly expensive and therefore unavailable to our patients, I have learned that there are ways around the obstacle of cost for at least some medications. I want to tell you what I’ve learned about the high cost of two medications: aripiprazole, the generic of Abilify, and modafinil, the generic of Provigil, but the lessons learned may apply to other psychotropics – and Smokey Robinson and the Miracles said it best in a line from their 1960 hit song, “You’d better shop around.”
Over the past few years, the price of aripiprazole has come down considerably, or so I believed. A patient recently complained that his copay after insurance for a 1-month supply of 2-mg tablets was hundreds of dollars, and he showed me a bill where the cost before insurance was more than $2,000! Another patient, also someone with commercial insurance, said he couldn’t afford aripiprazole and asked me to phone in a prescription to healthwarehouse.com. The medication was mailed to him for about $35 a month. Finally, a third patient with Medicare used an online service called Blink Health. He explained that he paid for the medicine online with a credit card – about $80, far less than the price quoted by the pharmacy. He was then given some type of code to present to the pharmacist, who then supplied the medications. In this case, the same pills, the same pharmacy, at a fraction of the cost. With that, I called several pharmacies and asked about the price of generic Abilify, 5 mg, 30 tablets.
I also wrote a column about the tremendous difficulty I had trying to get preauthorization for modafinil, in “Preauthorization of medications: Who oversees the placement of the hoops?” In that case, I spent weeks trying to get approval for the medication, and in the end, it was not approved, and the patient was not able to get it. Soon after, I learned on a Psychiatry Network Facebook discussion that generic Provigil is not expensive at all! Once again, I fired up my phone and called around. Those prices and those I found for Abilify are listed in the chart.
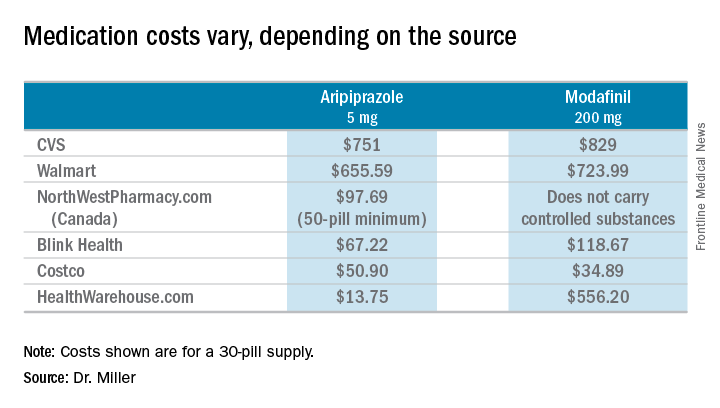
So these are cash prices; they do not take into account the cost with insurance. My patients have educated me after they could not afford the insurance copays. I wondered about my own coverage, and signed on to my pharmacy benefits manager account to look up the cost of both Abilify and Provigil. I’m sorry to say that I can’t report back: With my health insurance, Empire Blue Cross and Express Scripts, both medications require Coverage Review. It was also noted that Abilify requires Step treatment; I must first fail other medications. Should I ever need either of these medications, you’ll know where to find me: in line at the Costco pharmacy. I’ll be the one dancing to Smokey Robinson and the Miracles. https://www.youtube.com/watch?v=AQGXa3FiXKM
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
This is the first article in a series on the cost of medications.
While it’s not news that some pharmaceuticals are exorbitantly expensive and therefore unavailable to our patients, I have learned that there are ways around the obstacle of cost for at least some medications. I want to tell you what I’ve learned about the high cost of two medications: aripiprazole, the generic of Abilify, and modafinil, the generic of Provigil, but the lessons learned may apply to other psychotropics – and Smokey Robinson and the Miracles said it best in a line from their 1960 hit song, “You’d better shop around.”
Over the past few years, the price of aripiprazole has come down considerably, or so I believed. A patient recently complained that his copay after insurance for a 1-month supply of 2-mg tablets was hundreds of dollars, and he showed me a bill where the cost before insurance was more than $2,000! Another patient, also someone with commercial insurance, said he couldn’t afford aripiprazole and asked me to phone in a prescription to healthwarehouse.com. The medication was mailed to him for about $35 a month. Finally, a third patient with Medicare used an online service called Blink Health. He explained that he paid for the medicine online with a credit card – about $80, far less than the price quoted by the pharmacy. He was then given some type of code to present to the pharmacist, who then supplied the medications. In this case, the same pills, the same pharmacy, at a fraction of the cost. With that, I called several pharmacies and asked about the price of generic Abilify, 5 mg, 30 tablets.
I also wrote a column about the tremendous difficulty I had trying to get preauthorization for modafinil, in “Preauthorization of medications: Who oversees the placement of the hoops?” In that case, I spent weeks trying to get approval for the medication, and in the end, it was not approved, and the patient was not able to get it. Soon after, I learned on a Psychiatry Network Facebook discussion that generic Provigil is not expensive at all! Once again, I fired up my phone and called around. Those prices and those I found for Abilify are listed in the chart.
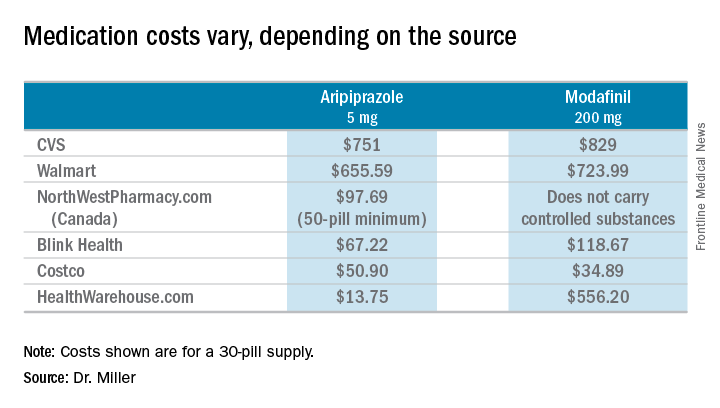
So these are cash prices; they do not take into account the cost with insurance. My patients have educated me after they could not afford the insurance copays. I wondered about my own coverage, and signed on to my pharmacy benefits manager account to look up the cost of both Abilify and Provigil. I’m sorry to say that I can’t report back: With my health insurance, Empire Blue Cross and Express Scripts, both medications require Coverage Review. It was also noted that Abilify requires Step treatment; I must first fail other medications. Should I ever need either of these medications, you’ll know where to find me: in line at the Costco pharmacy. I’ll be the one dancing to Smokey Robinson and the Miracles. https://www.youtube.com/watch?v=AQGXa3FiXKM
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
This is the first article in a series on the cost of medications.
While it’s not news that some pharmaceuticals are exorbitantly expensive and therefore unavailable to our patients, I have learned that there are ways around the obstacle of cost for at least some medications. I want to tell you what I’ve learned about the high cost of two medications: aripiprazole, the generic of Abilify, and modafinil, the generic of Provigil, but the lessons learned may apply to other psychotropics – and Smokey Robinson and the Miracles said it best in a line from their 1960 hit song, “You’d better shop around.”
Over the past few years, the price of aripiprazole has come down considerably, or so I believed. A patient recently complained that his copay after insurance for a 1-month supply of 2-mg tablets was hundreds of dollars, and he showed me a bill where the cost before insurance was more than $2,000! Another patient, also someone with commercial insurance, said he couldn’t afford aripiprazole and asked me to phone in a prescription to healthwarehouse.com. The medication was mailed to him for about $35 a month. Finally, a third patient with Medicare used an online service called Blink Health. He explained that he paid for the medicine online with a credit card – about $80, far less than the price quoted by the pharmacy. He was then given some type of code to present to the pharmacist, who then supplied the medications. In this case, the same pills, the same pharmacy, at a fraction of the cost. With that, I called several pharmacies and asked about the price of generic Abilify, 5 mg, 30 tablets.
I also wrote a column about the tremendous difficulty I had trying to get preauthorization for modafinil, in “Preauthorization of medications: Who oversees the placement of the hoops?” In that case, I spent weeks trying to get approval for the medication, and in the end, it was not approved, and the patient was not able to get it. Soon after, I learned on a Psychiatry Network Facebook discussion that generic Provigil is not expensive at all! Once again, I fired up my phone and called around. Those prices and those I found for Abilify are listed in the chart.
So these are cash prices; they do not take into account the cost with insurance. My patients have educated me after they could not afford the insurance copays. I wondered about my own coverage, and signed on to my pharmacy benefits manager account to look up the cost of both Abilify and Provigil. I’m sorry to say that I can’t report back: With my health insurance, Empire Blue Cross and Express Scripts, both medications require Coverage Review. It was also noted that Abilify requires Step treatment; I must first fail other medications. Should I ever need either of these medications, you’ll know where to find me: in line at the Costco pharmacy. I’ll be the one dancing to Smokey Robinson and the Miracles. https://www.youtube.com/watch?v=AQGXa3FiXKM
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
Approach to the asymptomatic adnexal mass: When to operate, refer, or observe
Adnexal masses are common findings in women. While the decision to operate on symptomatic adnexal masses is straightforward, the decision-making process for asymptomatic masses is more complicated. Here we address how to approach an asymptomatic adnexal mass, including how to decide when to operate, when to refer, or how to monitor.
It is important to minimize the number of surgeries for benign, asymptomatic adnexal masses because complications are reported in 2%-15% of surgeries for adnexal masses and these can range from minimal to devastating.1 In addition, unnecessary surgery is associated with a burden of cost to the health care system. Therefore, there is a paradigm shift in the management of asymptomatic adnexal masses trending toward surveillance of any masses that are likely to be benign. What becomes critical in this approach is the ability to accurately classify these masses preoperatively.
Determining the malignant potential of a mass
Guidance is provided by the ACOG Practice Bulletin Number 174, which was published in 2016: “Evaluation and Management of Adnexal Masses.”2 These guidelines remind clinicians that:
- Most adnexal masses are benign, even in postmenopausal patients.
- The recommended imaging modality is quality transvaginal ultrasonography with an ultrasonographer accredited through the American Registry of Diagnostic Medical Sonographers.
- Simple cysts up to 10 cm can be monitored using repeat imaging every 6 months without surgical intervention, even in postmenopausal patients. In prospective studies, no cases of malignancy were diagnosed over 6 years of surveillance and most resolved. Those that persist are likely to be serous cystadenomas.
- Many benign lesions such as endometriomas and cystic teratomas have characteristic radiologic features. Surgery for these lesions is warranted for large size, symptoms, or growth in size.
- Ultrasound characteristics of malignant masses include:
1. Cyst size greater than 10 cm
2. Papillary or solid components
3. Septations
4. Internal blood flow on color Doppler.
An alternative approach that has been proposed is an ultrasound scoring system devised by International Ovarian Tumor Analysis Group. The scoring system uses 10 ultrasound findings that are characteristic of malignant and benign and is designed to characterize masses as either benign or malignant.3 This approach is able to correctly classify 77% of masses. The remaining masses with features that do not fit the “simple rules” are considered potentially malignant and should be referred to an oncology specialist for further decision making.
Decision to operate
After referral to gynecologic oncologists, surgery is not always inevitable, particularly for women with indeterminate masses. The gynecologic oncologist uses a decision-making process that factors in the underlying surgical risks for that patient with the likelihood of malignancy based on the features of the mass. The threshold to operate is higher in women with underlying major comorbidities, such as morbid obesity, complex prior surgical history, or cardiopulmonary disease. Healthier surgical candidates are more likely to be considered for a surgery, even if the suspicion for malignancy is lower. However, low surgical risk does not equate to no surgical risk. Therefore, even in apparently “good” surgical candidates, the suspicion for underlying malignancy needs to be reasonably high in order to justify the cost and risk of surgery in an asymptomatic patient. Sometimes it is patient anxiety and a desire to avoid repeated surveillance that prompts a decision to operate.
How to monitor
The role of surveillance and monitoring is to establish a natural history of the lesion or to allow it to reveal itself to be stable or regressive. Surveillance with serial sonography has shown that most asymptomatic adnexal masses with low risk features will resolve over time. Lack of resolution in the setting of stable findings is not a worrisome feature and is not suggestive of malignancy. The mere persistence of an otherwise benign-appearing lesion is not a reason to intervene with surgery.
Unfortunately, there is no clear guidance on the surveillance intervals. Some experts recommend an initial repeat scan in 3 months. If at that point the morphologic features and size are stable or decreasing, ultrasounds can be repeated at annual intervals for 5 years. In one study, masses that became malignant demonstrated growth by 7 months. Other experts recommend limiting the period of surveillance of cystic lesions to 1 year and lesions with solid components to 2 years.
Conclusions
Many asymptomatic adnexal masses discovered on imaging can be monitored with serial sonography. Lesions with more worrisome morphology that’s suggestive of malignancy should prompt referral to a gynecologic oncologist. Surgery on benign masses can be avoided. Outcome data is needed to advise the optimal timing intervals and the limit of follow-up serial ultrasonography. A caveat of this watch-and-see approach is having to allay the patient’s fears of the malignant potential of the mass. This requires conversations with the patient informing them that the stability of the mass will be shown over time and that surgery can be safely avoided.
References
1. Glanc P et al. J Ultrasound Med. 2017;36:849-63.
2. American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins – Gynecology. Obstet Gynecol. 2016 Nov;128(5):e210-26.
3. Timmerman D et al. Ultrasound Obstet Gynecol. 2008 Jun;31(6):681-90.
Dr. Jackson-Moore is an associate professor in gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Rossi is an assistant professor in the division of gynecologic oncology at UNC. They reported having no relevant financial disclosures.
Adnexal masses are common findings in women. While the decision to operate on symptomatic adnexal masses is straightforward, the decision-making process for asymptomatic masses is more complicated. Here we address how to approach an asymptomatic adnexal mass, including how to decide when to operate, when to refer, or how to monitor.
It is important to minimize the number of surgeries for benign, asymptomatic adnexal masses because complications are reported in 2%-15% of surgeries for adnexal masses and these can range from minimal to devastating.1 In addition, unnecessary surgery is associated with a burden of cost to the health care system. Therefore, there is a paradigm shift in the management of asymptomatic adnexal masses trending toward surveillance of any masses that are likely to be benign. What becomes critical in this approach is the ability to accurately classify these masses preoperatively.
Determining the malignant potential of a mass
Guidance is provided by the ACOG Practice Bulletin Number 174, which was published in 2016: “Evaluation and Management of Adnexal Masses.”2 These guidelines remind clinicians that:
- Most adnexal masses are benign, even in postmenopausal patients.
- The recommended imaging modality is quality transvaginal ultrasonography with an ultrasonographer accredited through the American Registry of Diagnostic Medical Sonographers.
- Simple cysts up to 10 cm can be monitored using repeat imaging every 6 months without surgical intervention, even in postmenopausal patients. In prospective studies, no cases of malignancy were diagnosed over 6 years of surveillance and most resolved. Those that persist are likely to be serous cystadenomas.
- Many benign lesions such as endometriomas and cystic teratomas have characteristic radiologic features. Surgery for these lesions is warranted for large size, symptoms, or growth in size.
- Ultrasound characteristics of malignant masses include:
1. Cyst size greater than 10 cm
2. Papillary or solid components
3. Septations
4. Internal blood flow on color Doppler.
An alternative approach that has been proposed is an ultrasound scoring system devised by International Ovarian Tumor Analysis Group. The scoring system uses 10 ultrasound findings that are characteristic of malignant and benign and is designed to characterize masses as either benign or malignant.3 This approach is able to correctly classify 77% of masses. The remaining masses with features that do not fit the “simple rules” are considered potentially malignant and should be referred to an oncology specialist for further decision making.
Decision to operate
After referral to gynecologic oncologists, surgery is not always inevitable, particularly for women with indeterminate masses. The gynecologic oncologist uses a decision-making process that factors in the underlying surgical risks for that patient with the likelihood of malignancy based on the features of the mass. The threshold to operate is higher in women with underlying major comorbidities, such as morbid obesity, complex prior surgical history, or cardiopulmonary disease. Healthier surgical candidates are more likely to be considered for a surgery, even if the suspicion for malignancy is lower. However, low surgical risk does not equate to no surgical risk. Therefore, even in apparently “good” surgical candidates, the suspicion for underlying malignancy needs to be reasonably high in order to justify the cost and risk of surgery in an asymptomatic patient. Sometimes it is patient anxiety and a desire to avoid repeated surveillance that prompts a decision to operate.
How to monitor
The role of surveillance and monitoring is to establish a natural history of the lesion or to allow it to reveal itself to be stable or regressive. Surveillance with serial sonography has shown that most asymptomatic adnexal masses with low risk features will resolve over time. Lack of resolution in the setting of stable findings is not a worrisome feature and is not suggestive of malignancy. The mere persistence of an otherwise benign-appearing lesion is not a reason to intervene with surgery.
Unfortunately, there is no clear guidance on the surveillance intervals. Some experts recommend an initial repeat scan in 3 months. If at that point the morphologic features and size are stable or decreasing, ultrasounds can be repeated at annual intervals for 5 years. In one study, masses that became malignant demonstrated growth by 7 months. Other experts recommend limiting the period of surveillance of cystic lesions to 1 year and lesions with solid components to 2 years.
Conclusions
Many asymptomatic adnexal masses discovered on imaging can be monitored with serial sonography. Lesions with more worrisome morphology that’s suggestive of malignancy should prompt referral to a gynecologic oncologist. Surgery on benign masses can be avoided. Outcome data is needed to advise the optimal timing intervals and the limit of follow-up serial ultrasonography. A caveat of this watch-and-see approach is having to allay the patient’s fears of the malignant potential of the mass. This requires conversations with the patient informing them that the stability of the mass will be shown over time and that surgery can be safely avoided.
References
1. Glanc P et al. J Ultrasound Med. 2017;36:849-63.
2. American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins – Gynecology. Obstet Gynecol. 2016 Nov;128(5):e210-26.
3. Timmerman D et al. Ultrasound Obstet Gynecol. 2008 Jun;31(6):681-90.
Dr. Jackson-Moore is an associate professor in gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Rossi is an assistant professor in the division of gynecologic oncology at UNC. They reported having no relevant financial disclosures.
Adnexal masses are common findings in women. While the decision to operate on symptomatic adnexal masses is straightforward, the decision-making process for asymptomatic masses is more complicated. Here we address how to approach an asymptomatic adnexal mass, including how to decide when to operate, when to refer, or how to monitor.
It is important to minimize the number of surgeries for benign, asymptomatic adnexal masses because complications are reported in 2%-15% of surgeries for adnexal masses and these can range from minimal to devastating.1 In addition, unnecessary surgery is associated with a burden of cost to the health care system. Therefore, there is a paradigm shift in the management of asymptomatic adnexal masses trending toward surveillance of any masses that are likely to be benign. What becomes critical in this approach is the ability to accurately classify these masses preoperatively.
Determining the malignant potential of a mass
Guidance is provided by the ACOG Practice Bulletin Number 174, which was published in 2016: “Evaluation and Management of Adnexal Masses.”2 These guidelines remind clinicians that:
- Most adnexal masses are benign, even in postmenopausal patients.
- The recommended imaging modality is quality transvaginal ultrasonography with an ultrasonographer accredited through the American Registry of Diagnostic Medical Sonographers.
- Simple cysts up to 10 cm can be monitored using repeat imaging every 6 months without surgical intervention, even in postmenopausal patients. In prospective studies, no cases of malignancy were diagnosed over 6 years of surveillance and most resolved. Those that persist are likely to be serous cystadenomas.
- Many benign lesions such as endometriomas and cystic teratomas have characteristic radiologic features. Surgery for these lesions is warranted for large size, symptoms, or growth in size.
- Ultrasound characteristics of malignant masses include:
1. Cyst size greater than 10 cm
2. Papillary or solid components
3. Septations
4. Internal blood flow on color Doppler.
An alternative approach that has been proposed is an ultrasound scoring system devised by International Ovarian Tumor Analysis Group. The scoring system uses 10 ultrasound findings that are characteristic of malignant and benign and is designed to characterize masses as either benign or malignant.3 This approach is able to correctly classify 77% of masses. The remaining masses with features that do not fit the “simple rules” are considered potentially malignant and should be referred to an oncology specialist for further decision making.
Decision to operate
After referral to gynecologic oncologists, surgery is not always inevitable, particularly for women with indeterminate masses. The gynecologic oncologist uses a decision-making process that factors in the underlying surgical risks for that patient with the likelihood of malignancy based on the features of the mass. The threshold to operate is higher in women with underlying major comorbidities, such as morbid obesity, complex prior surgical history, or cardiopulmonary disease. Healthier surgical candidates are more likely to be considered for a surgery, even if the suspicion for malignancy is lower. However, low surgical risk does not equate to no surgical risk. Therefore, even in apparently “good” surgical candidates, the suspicion for underlying malignancy needs to be reasonably high in order to justify the cost and risk of surgery in an asymptomatic patient. Sometimes it is patient anxiety and a desire to avoid repeated surveillance that prompts a decision to operate.
How to monitor
The role of surveillance and monitoring is to establish a natural history of the lesion or to allow it to reveal itself to be stable or regressive. Surveillance with serial sonography has shown that most asymptomatic adnexal masses with low risk features will resolve over time. Lack of resolution in the setting of stable findings is not a worrisome feature and is not suggestive of malignancy. The mere persistence of an otherwise benign-appearing lesion is not a reason to intervene with surgery.
Unfortunately, there is no clear guidance on the surveillance intervals. Some experts recommend an initial repeat scan in 3 months. If at that point the morphologic features and size are stable or decreasing, ultrasounds can be repeated at annual intervals for 5 years. In one study, masses that became malignant demonstrated growth by 7 months. Other experts recommend limiting the period of surveillance of cystic lesions to 1 year and lesions with solid components to 2 years.
Conclusions
Many asymptomatic adnexal masses discovered on imaging can be monitored with serial sonography. Lesions with more worrisome morphology that’s suggestive of malignancy should prompt referral to a gynecologic oncologist. Surgery on benign masses can be avoided. Outcome data is needed to advise the optimal timing intervals and the limit of follow-up serial ultrasonography. A caveat of this watch-and-see approach is having to allay the patient’s fears of the malignant potential of the mass. This requires conversations with the patient informing them that the stability of the mass will be shown over time and that surgery can be safely avoided.
References
1. Glanc P et al. J Ultrasound Med. 2017;36:849-63.
2. American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins – Gynecology. Obstet Gynecol. 2016 Nov;128(5):e210-26.
3. Timmerman D et al. Ultrasound Obstet Gynecol. 2008 Jun;31(6):681-90.
Dr. Jackson-Moore is an associate professor in gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Rossi is an assistant professor in the division of gynecologic oncology at UNC. They reported having no relevant financial disclosures.
Influenza vaccination of pregnant women needs surveillance
Seasonal influenza vaccine is specifically recommended for women who are or who might become pregnant in the flu season. This special population is targeted for vaccination because pregnant women are at increased risks of serious complications if infected with influenza virus. Despite this recommendation, recent evidence indicates that still fewer than 50% of women in the United States are vaccinated during pregnancy (MMWR Morb Mortal Wkly Rep. 2016 Dec 9;65[48]:1370-3).
Potential reasons for this lack of uptake are concerns about safety of the vaccine for mothers and fetuses (Vaccine. 2012 Dec 17;31[1]:213-8). This has highlighted the need for systematic safety surveillance for influenza vaccination with each subsequent seasonal formulation. To that end, season-specific studies of birth and infant outcomes since the 2009 season have been conducted; findings have been generally reassuring (Vaccine. 2016 Aug 17;34[37]:4443-9; Vaccine. 2016 Aug 17;34[37]:4450-9).
The authors found a doubling of risk for spontaneous abortion within that 28-day exposure window, but no association if the vaccination took place outside that period. This was in contrast to null findings for a similar analysis that the same group had conducted for vaccination in the 2005-2006 and 2006-2007 seasons. Of further interest, the authors noted even higher risks among women who had also been vaccinated for influenza in the previous season (adjusted odds ratio, 7.7; 95% confidence interval, 2.2-27.3). The highest odds ratios were among women who had been vaccinated in the 2010-2011 season and had also been vaccinated with monovalent pandemic H1N1 vaccine in the 2009-2010 season (aOR, 32.5; 95% CI, 2.9-359.0).
The VSD findings raise interesting questions about the biologic plausibility of strain-specific risks for spontaneous abortion, and risks of receiving a second vaccine containing the same strain in a subsequent season. However, this study should be interpreted with caution. With respect to the overall finding of a doubling of risk for spontaneous abortion, this is inconsistent with previous studies. A systematic review of 19 observational studies, 14 of which included exposure to the 2009 monovalent pandemic H1N1 strain, noted hazard ratios or odds ratios for spontaneous abortion ranging from 0.45 to 1.23 and 95% confidence intervals that crossed or were below the null (Vaccine. 2015 Apr 27;33[18]:2108-17). More recently, the Vaccines and Medications in Pregnancy Surveillance System investigators evaluated spontaneous abortion in pregnancies exposed to influenza vaccine over four seasons from 2010 to 2014 and found an overall hazard ratio of 1.09 (95% CI, 0.49-2.40).
However, there are a number of limitations that must be considered. Many previous studies, including the VSD analysis, could have had misclassification of exposure, especially in recent years when vaccines are often received in nontraditional settings. The VSD study findings could have been influenced by unmeasured confounding. For example, there could be differential vaccine uptake in women with comorbidities that are also associated with spontaneous abortion, such as subfertility and psychiatric disorders.
In summary, at present the data viewed as a whole do not support a change to the current recommendation that pregnant women be vaccinated for influenza regardless of trimester. However, these data do call for continued surveillance for the safety of each seasonal formulation of influenza vaccine, and for further exploration of the association between repeat vaccination and spontaneous abortion in other datasets.
Dr. Chambers is professor of pediatrics and director of clinical research at Rady Children’s Hospital and associate director of the Clinical and Translational Research Institute at the University of California, San Diego. She is also director of MotherToBaby California, a past president of the Organization of Teratology Information Specialists, and past president of the Teratology Society. She has no direct conflicts of interest to disclose, but has received grant funding to study influenza vaccine from the Biomedical Advanced Research and Development Authority (BARDA) in the Department of Health and Human Services, and from Seqirus Corporation.
Seasonal influenza vaccine is specifically recommended for women who are or who might become pregnant in the flu season. This special population is targeted for vaccination because pregnant women are at increased risks of serious complications if infected with influenza virus. Despite this recommendation, recent evidence indicates that still fewer than 50% of women in the United States are vaccinated during pregnancy (MMWR Morb Mortal Wkly Rep. 2016 Dec 9;65[48]:1370-3).
Potential reasons for this lack of uptake are concerns about safety of the vaccine for mothers and fetuses (Vaccine. 2012 Dec 17;31[1]:213-8). This has highlighted the need for systematic safety surveillance for influenza vaccination with each subsequent seasonal formulation. To that end, season-specific studies of birth and infant outcomes since the 2009 season have been conducted; findings have been generally reassuring (Vaccine. 2016 Aug 17;34[37]:4443-9; Vaccine. 2016 Aug 17;34[37]:4450-9).
The authors found a doubling of risk for spontaneous abortion within that 28-day exposure window, but no association if the vaccination took place outside that period. This was in contrast to null findings for a similar analysis that the same group had conducted for vaccination in the 2005-2006 and 2006-2007 seasons. Of further interest, the authors noted even higher risks among women who had also been vaccinated for influenza in the previous season (adjusted odds ratio, 7.7; 95% confidence interval, 2.2-27.3). The highest odds ratios were among women who had been vaccinated in the 2010-2011 season and had also been vaccinated with monovalent pandemic H1N1 vaccine in the 2009-2010 season (aOR, 32.5; 95% CI, 2.9-359.0).
The VSD findings raise interesting questions about the biologic plausibility of strain-specific risks for spontaneous abortion, and risks of receiving a second vaccine containing the same strain in a subsequent season. However, this study should be interpreted with caution. With respect to the overall finding of a doubling of risk for spontaneous abortion, this is inconsistent with previous studies. A systematic review of 19 observational studies, 14 of which included exposure to the 2009 monovalent pandemic H1N1 strain, noted hazard ratios or odds ratios for spontaneous abortion ranging from 0.45 to 1.23 and 95% confidence intervals that crossed or were below the null (Vaccine. 2015 Apr 27;33[18]:2108-17). More recently, the Vaccines and Medications in Pregnancy Surveillance System investigators evaluated spontaneous abortion in pregnancies exposed to influenza vaccine over four seasons from 2010 to 2014 and found an overall hazard ratio of 1.09 (95% CI, 0.49-2.40).
However, there are a number of limitations that must be considered. Many previous studies, including the VSD analysis, could have had misclassification of exposure, especially in recent years when vaccines are often received in nontraditional settings. The VSD study findings could have been influenced by unmeasured confounding. For example, there could be differential vaccine uptake in women with comorbidities that are also associated with spontaneous abortion, such as subfertility and psychiatric disorders.
In summary, at present the data viewed as a whole do not support a change to the current recommendation that pregnant women be vaccinated for influenza regardless of trimester. However, these data do call for continued surveillance for the safety of each seasonal formulation of influenza vaccine, and for further exploration of the association between repeat vaccination and spontaneous abortion in other datasets.
Dr. Chambers is professor of pediatrics and director of clinical research at Rady Children’s Hospital and associate director of the Clinical and Translational Research Institute at the University of California, San Diego. She is also director of MotherToBaby California, a past president of the Organization of Teratology Information Specialists, and past president of the Teratology Society. She has no direct conflicts of interest to disclose, but has received grant funding to study influenza vaccine from the Biomedical Advanced Research and Development Authority (BARDA) in the Department of Health and Human Services, and from Seqirus Corporation.
Seasonal influenza vaccine is specifically recommended for women who are or who might become pregnant in the flu season. This special population is targeted for vaccination because pregnant women are at increased risks of serious complications if infected with influenza virus. Despite this recommendation, recent evidence indicates that still fewer than 50% of women in the United States are vaccinated during pregnancy (MMWR Morb Mortal Wkly Rep. 2016 Dec 9;65[48]:1370-3).
Potential reasons for this lack of uptake are concerns about safety of the vaccine for mothers and fetuses (Vaccine. 2012 Dec 17;31[1]:213-8). This has highlighted the need for systematic safety surveillance for influenza vaccination with each subsequent seasonal formulation. To that end, season-specific studies of birth and infant outcomes since the 2009 season have been conducted; findings have been generally reassuring (Vaccine. 2016 Aug 17;34[37]:4443-9; Vaccine. 2016 Aug 17;34[37]:4450-9).
The authors found a doubling of risk for spontaneous abortion within that 28-day exposure window, but no association if the vaccination took place outside that period. This was in contrast to null findings for a similar analysis that the same group had conducted for vaccination in the 2005-2006 and 2006-2007 seasons. Of further interest, the authors noted even higher risks among women who had also been vaccinated for influenza in the previous season (adjusted odds ratio, 7.7; 95% confidence interval, 2.2-27.3). The highest odds ratios were among women who had been vaccinated in the 2010-2011 season and had also been vaccinated with monovalent pandemic H1N1 vaccine in the 2009-2010 season (aOR, 32.5; 95% CI, 2.9-359.0).
The VSD findings raise interesting questions about the biologic plausibility of strain-specific risks for spontaneous abortion, and risks of receiving a second vaccine containing the same strain in a subsequent season. However, this study should be interpreted with caution. With respect to the overall finding of a doubling of risk for spontaneous abortion, this is inconsistent with previous studies. A systematic review of 19 observational studies, 14 of which included exposure to the 2009 monovalent pandemic H1N1 strain, noted hazard ratios or odds ratios for spontaneous abortion ranging from 0.45 to 1.23 and 95% confidence intervals that crossed or were below the null (Vaccine. 2015 Apr 27;33[18]:2108-17). More recently, the Vaccines and Medications in Pregnancy Surveillance System investigators evaluated spontaneous abortion in pregnancies exposed to influenza vaccine over four seasons from 2010 to 2014 and found an overall hazard ratio of 1.09 (95% CI, 0.49-2.40).
However, there are a number of limitations that must be considered. Many previous studies, including the VSD analysis, could have had misclassification of exposure, especially in recent years when vaccines are often received in nontraditional settings. The VSD study findings could have been influenced by unmeasured confounding. For example, there could be differential vaccine uptake in women with comorbidities that are also associated with spontaneous abortion, such as subfertility and psychiatric disorders.
In summary, at present the data viewed as a whole do not support a change to the current recommendation that pregnant women be vaccinated for influenza regardless of trimester. However, these data do call for continued surveillance for the safety of each seasonal formulation of influenza vaccine, and for further exploration of the association between repeat vaccination and spontaneous abortion in other datasets.
Dr. Chambers is professor of pediatrics and director of clinical research at Rady Children’s Hospital and associate director of the Clinical and Translational Research Institute at the University of California, San Diego. She is also director of MotherToBaby California, a past president of the Organization of Teratology Information Specialists, and past president of the Teratology Society. She has no direct conflicts of interest to disclose, but has received grant funding to study influenza vaccine from the Biomedical Advanced Research and Development Authority (BARDA) in the Department of Health and Human Services, and from Seqirus Corporation.
Families are essential partners in treating substance use disorders
Addiction used to be considered a moral failing, and the family was blamed for keeping the relative with addictions sick, through behaviors labeled “codependency” and “enabling.” The opioid epidemic can take credit for putting a serious dent in these destructive and stigmatizing notions. When psychiatrists actively include families as educated treatment partners, fatalities are less likely, and the havoc created by addiction on families is mitigated.
Genes and addiction
What causes addiction? Statistics show that Native Americans fare the worst of all minority groups, with death by opiates in whites and Native Americans double or triple the rates of African Americans and Latinos. Reasons put forward for Native American deaths are their vulnerability related to systemic racism, intergenerational trauma, and lack of access to health care. These “reasons” are well known to contribute to poor overall health status of impoverished communities.
Among impoverished white communities, the Monongahela Valley of Pennsylvania has been studied by Katherine McLean, PhD, as an example of postindustrial decay (Int J Drug Policy. 2016;[29]:19-26). Once a global center of steel production, the exodus of jobs, residents, and businesses since the early 1980s is thought to contribute to the high numbers of opioid deaths. A qualitative study of the people with addiction in the deteriorating mill city of McKeesport, Pa., characterized a risk environment hidden behind closed doors, and populated by unprepared, ambivalent overdose “assistants.” These people are “co-drug” users who themselves are reluctant to step forward because of fear of getting in trouble. The participants described the hopelessness and lack of opportunity as driving the use of heroin, with many stating that jobs and community reinvestment are needed to reduce fatalities. This certainly resonates with the Native American experience.
People with the AA variant of OXTR also have been shown to have less secure adult attachment and more social anxiety (World J Biol Psychiatry. 2016;17[1]:76-83). Comparing people with OXTR variants, the AA genotype was associated with a perceived negative social environment and significantly increased PTSD symptoms, whereas the GG genotype was protective.
However, for many decades, psychological theories about the defects of individuals and their moral failing have prevailed. In the family, aspersions have been cast on the family’s deficits in terms of setting limits and their enabling behaviors, mostly focusing on wives and mothers. The social mantra has been that since not all people get addicted, the strong resist and the weak succumb. Psychiatry has focused on providing psychotherapy to correct the personal deficits of the weak and addicted and, from a family perspective, on correcting negative personality traits in the caregivers, classified as codependency.
Roots of codependency
The concept of codependency began as a grassroots idea in the 1960s to describe family members, usually wives or mothers, who were deemed excessive in their caring for their husband or son with addiction. The term was used to describe women who had an overresponsibility for relationships, rather than a responsibility to self. Support groups for codependency, such as Co-Dependents Anonymous, Al-Anon/Alateen, Nar-Anon, and Adult Children of Alcoholics, based on the 12-step program model of Alcoholics Anonymous, were established. Codependents were negatively labeled as rescuers, supporters, and confidantes of their family member with substance use disorder. These helpers were described as dependent on the other person’s poor functioning to satisfy their own emotional needs.
In these early descriptions, there was a lack of discussion about possible deeper family dynamics: Inequality in financial independence of each partner, the desire for family stability focusing on the welfare of children, the real possibility that disrupting a relationship might result in violence if the woman was more assertive. Women were blamed for trying to love their spouse out of the addiction. One aspect of codependency is self-sacrifice, which used to be considered an important trait of the good wife but became a negative trait in the 1960s. Recovery from codependence was considered achieved when the wife or mother expressed healthy self-assertiveness. Some scholars did state, however, that they believed that codependency was not a negative trait, but rather a healthy personality trait taken to excess. In most studies, women with high codependency ratings have tended to be unemployed and with lower educations. Their behavior had been considered worthy of a DSM inclusion as a personality disorder, but luckily, this was thwarted.
A family is forced to make some accounting when an individual develops a substance use disorder. If the family tries to maintain equilibrium and keeps things as stable as possible for the sake of maintaining the family unit or the stability of the lives of the children, accommodation will be required. Accommodation minimizes the impact of the addiction: the sober spouse stepping up to complete the roles of the ill relative and in all ways reducing the impact of dysfunction on the family. If you swap out the illness and consider the ill family member as having cancer or respiratory distress, then you reframe the spouse’s “codependence” as the behavior of a caring spouse.
This long preamble is intended to illustrate how little family dynamics have to do with the etiology of addiction. Addiction is a chronic neurobiological disease, and like all diseases, individuals, and couples and families have the option of learning to cope well. We, as psychiatrists, must move away from blaming people (usually women who have less-than-optimal coping skills) and consider how best to engage partners and families in optimal programs.*
Families can benefit from specialist treatment and thus contribute to the recovery process. One example is a telepsychiatry program that aimed to improve family coping skills to cope with relatives who have substance use disorders. The Tele-intervention Model and Monitoring of Families of Drug Users is based on motivational interviewing and stages of change. Families were randomized into the intervention group (n = 163) or the usual treatment (n = 162). After 6 months of follow-up, the family members of the telepsychiatry group were twice as likely to modify their behavior (odds ratio; 2.08; 95% confidence interval, 1.18-3.65) (J Sub Use Misuse. 2017 Jan 28;52[2]:164-74). This model was organized so that each of nine calls had a specific goal to stimulate the family members in their process of change.
Family change and engagement also can occur through Alanon (Subst Use Misuse. 2015; 50[1]:62-71) and the use of the Arise program of Judith Landau, MD, (Landau J et al. Am J Drug Alcohol Abuse. 2000;26[3]:379-98).
In summary, the family can be engaged in treatment and can develop family coping skills to support their relative with this chronic neurobiological disease.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose.
*Updated on January 12, 2018.
Addiction used to be considered a moral failing, and the family was blamed for keeping the relative with addictions sick, through behaviors labeled “codependency” and “enabling.” The opioid epidemic can take credit for putting a serious dent in these destructive and stigmatizing notions. When psychiatrists actively include families as educated treatment partners, fatalities are less likely, and the havoc created by addiction on families is mitigated.
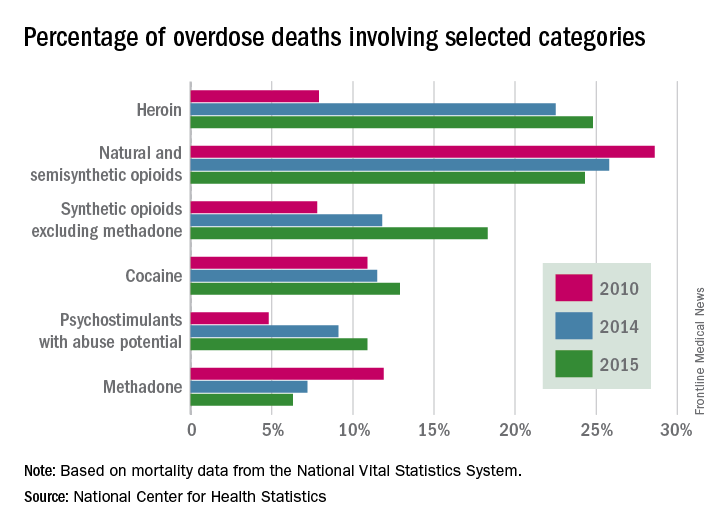
Genes and addiction
What causes addiction? Statistics show that Native Americans fare the worst of all minority groups, with death by opiates in whites and Native Americans double or triple the rates of African Americans and Latinos. Reasons put forward for Native American deaths are their vulnerability related to systemic racism, intergenerational trauma, and lack of access to health care. These “reasons” are well known to contribute to poor overall health status of impoverished communities.
Among impoverished white communities, the Monongahela Valley of Pennsylvania has been studied by Katherine McLean, PhD, as an example of postindustrial decay (Int J Drug Policy. 2016;[29]:19-26). Once a global center of steel production, the exodus of jobs, residents, and businesses since the early 1980s is thought to contribute to the high numbers of opioid deaths. A qualitative study of the people with addiction in the deteriorating mill city of McKeesport, Pa., characterized a risk environment hidden behind closed doors, and populated by unprepared, ambivalent overdose “assistants.” These people are “co-drug” users who themselves are reluctant to step forward because of fear of getting in trouble. The participants described the hopelessness and lack of opportunity as driving the use of heroin, with many stating that jobs and community reinvestment are needed to reduce fatalities. This certainly resonates with the Native American experience.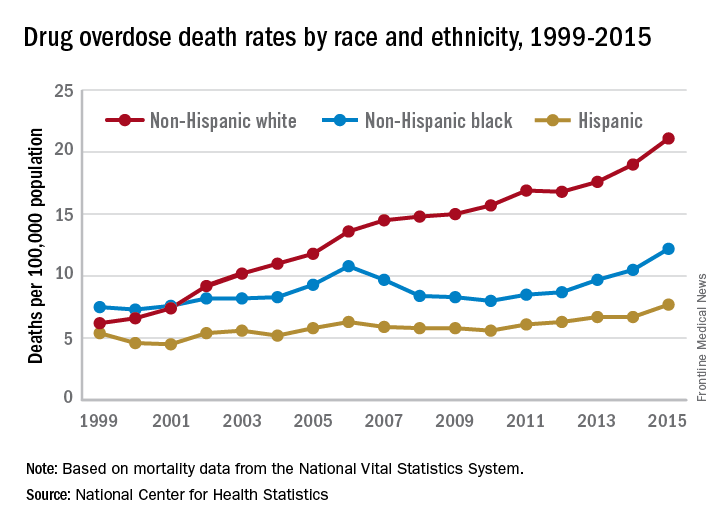
People with the AA variant of OXTR also have been shown to have less secure adult attachment and more social anxiety (World J Biol Psychiatry. 2016;17[1]:76-83). Comparing people with OXTR variants, the AA genotype was associated with a perceived negative social environment and significantly increased PTSD symptoms, whereas the GG genotype was protective.
However, for many decades, psychological theories about the defects of individuals and their moral failing have prevailed. In the family, aspersions have been cast on the family’s deficits in terms of setting limits and their enabling behaviors, mostly focusing on wives and mothers. The social mantra has been that since not all people get addicted, the strong resist and the weak succumb. Psychiatry has focused on providing psychotherapy to correct the personal deficits of the weak and addicted and, from a family perspective, on correcting negative personality traits in the caregivers, classified as codependency.
Roots of codependency
The concept of codependency began as a grassroots idea in the 1960s to describe family members, usually wives or mothers, who were deemed excessive in their caring for their husband or son with addiction. The term was used to describe women who had an overresponsibility for relationships, rather than a responsibility to self. Support groups for codependency, such as Co-Dependents Anonymous, Al-Anon/Alateen, Nar-Anon, and Adult Children of Alcoholics, based on the 12-step program model of Alcoholics Anonymous, were established. Codependents were negatively labeled as rescuers, supporters, and confidantes of their family member with substance use disorder. These helpers were described as dependent on the other person’s poor functioning to satisfy their own emotional needs.
In these early descriptions, there was a lack of discussion about possible deeper family dynamics: Inequality in financial independence of each partner, the desire for family stability focusing on the welfare of children, the real possibility that disrupting a relationship might result in violence if the woman was more assertive. Women were blamed for trying to love their spouse out of the addiction. One aspect of codependency is self-sacrifice, which used to be considered an important trait of the good wife but became a negative trait in the 1960s. Recovery from codependence was considered achieved when the wife or mother expressed healthy self-assertiveness. Some scholars did state, however, that they believed that codependency was not a negative trait, but rather a healthy personality trait taken to excess. In most studies, women with high codependency ratings have tended to be unemployed and with lower educations. Their behavior had been considered worthy of a DSM inclusion as a personality disorder, but luckily, this was thwarted.
A family is forced to make some accounting when an individual develops a substance use disorder. If the family tries to maintain equilibrium and keeps things as stable as possible for the sake of maintaining the family unit or the stability of the lives of the children, accommodation will be required. Accommodation minimizes the impact of the addiction: the sober spouse stepping up to complete the roles of the ill relative and in all ways reducing the impact of dysfunction on the family. If you swap out the illness and consider the ill family member as having cancer or respiratory distress, then you reframe the spouse’s “codependence” as the behavior of a caring spouse.
This long preamble is intended to illustrate how little family dynamics have to do with the etiology of addiction. Addiction is a chronic neurobiological disease, and like all diseases, individuals, and couples and families have the option of learning to cope well. We, as psychiatrists, must move away from blaming people (usually women who have less-than-optimal coping skills) and consider how best to engage partners and families in optimal programs.*
Families can benefit from specialist treatment and thus contribute to the recovery process. One example is a telepsychiatry program that aimed to improve family coping skills to cope with relatives who have substance use disorders. The Tele-intervention Model and Monitoring of Families of Drug Users is based on motivational interviewing and stages of change. Families were randomized into the intervention group (n = 163) or the usual treatment (n = 162). After 6 months of follow-up, the family members of the telepsychiatry group were twice as likely to modify their behavior (odds ratio; 2.08; 95% confidence interval, 1.18-3.65) (J Sub Use Misuse. 2017 Jan 28;52[2]:164-74). This model was organized so that each of nine calls had a specific goal to stimulate the family members in their process of change.
Family change and engagement also can occur through Alanon (Subst Use Misuse. 2015; 50[1]:62-71) and the use of the Arise program of Judith Landau, MD, (Landau J et al. Am J Drug Alcohol Abuse. 2000;26[3]:379-98).
In summary, the family can be engaged in treatment and can develop family coping skills to support their relative with this chronic neurobiological disease.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose.
*Updated on January 12, 2018.
Addiction used to be considered a moral failing, and the family was blamed for keeping the relative with addictions sick, through behaviors labeled “codependency” and “enabling.” The opioid epidemic can take credit for putting a serious dent in these destructive and stigmatizing notions. When psychiatrists actively include families as educated treatment partners, fatalities are less likely, and the havoc created by addiction on families is mitigated.
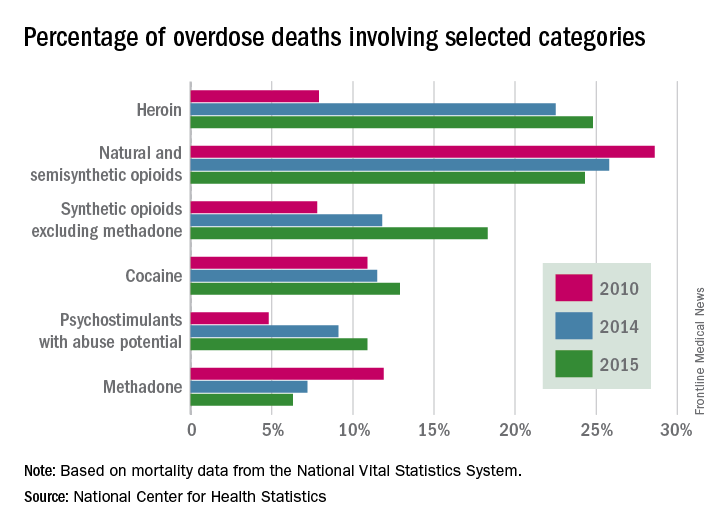
Genes and addiction
What causes addiction? Statistics show that Native Americans fare the worst of all minority groups, with death by opiates in whites and Native Americans double or triple the rates of African Americans and Latinos. Reasons put forward for Native American deaths are their vulnerability related to systemic racism, intergenerational trauma, and lack of access to health care. These “reasons” are well known to contribute to poor overall health status of impoverished communities.
Among impoverished white communities, the Monongahela Valley of Pennsylvania has been studied by Katherine McLean, PhD, as an example of postindustrial decay (Int J Drug Policy. 2016;[29]:19-26). Once a global center of steel production, the exodus of jobs, residents, and businesses since the early 1980s is thought to contribute to the high numbers of opioid deaths. A qualitative study of the people with addiction in the deteriorating mill city of McKeesport, Pa., characterized a risk environment hidden behind closed doors, and populated by unprepared, ambivalent overdose “assistants.” These people are “co-drug” users who themselves are reluctant to step forward because of fear of getting in trouble. The participants described the hopelessness and lack of opportunity as driving the use of heroin, with many stating that jobs and community reinvestment are needed to reduce fatalities. This certainly resonates with the Native American experience.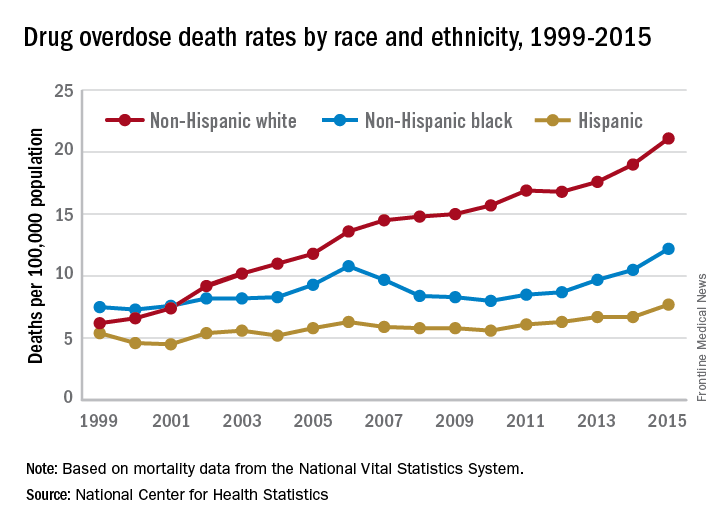
People with the AA variant of OXTR also have been shown to have less secure adult attachment and more social anxiety (World J Biol Psychiatry. 2016;17[1]:76-83). Comparing people with OXTR variants, the AA genotype was associated with a perceived negative social environment and significantly increased PTSD symptoms, whereas the GG genotype was protective.
However, for many decades, psychological theories about the defects of individuals and their moral failing have prevailed. In the family, aspersions have been cast on the family’s deficits in terms of setting limits and their enabling behaviors, mostly focusing on wives and mothers. The social mantra has been that since not all people get addicted, the strong resist and the weak succumb. Psychiatry has focused on providing psychotherapy to correct the personal deficits of the weak and addicted and, from a family perspective, on correcting negative personality traits in the caregivers, classified as codependency.
Roots of codependency
The concept of codependency began as a grassroots idea in the 1960s to describe family members, usually wives or mothers, who were deemed excessive in their caring for their husband or son with addiction. The term was used to describe women who had an overresponsibility for relationships, rather than a responsibility to self. Support groups for codependency, such as Co-Dependents Anonymous, Al-Anon/Alateen, Nar-Anon, and Adult Children of Alcoholics, based on the 12-step program model of Alcoholics Anonymous, were established. Codependents were negatively labeled as rescuers, supporters, and confidantes of their family member with substance use disorder. These helpers were described as dependent on the other person’s poor functioning to satisfy their own emotional needs.
In these early descriptions, there was a lack of discussion about possible deeper family dynamics: Inequality in financial independence of each partner, the desire for family stability focusing on the welfare of children, the real possibility that disrupting a relationship might result in violence if the woman was more assertive. Women were blamed for trying to love their spouse out of the addiction. One aspect of codependency is self-sacrifice, which used to be considered an important trait of the good wife but became a negative trait in the 1960s. Recovery from codependence was considered achieved when the wife or mother expressed healthy self-assertiveness. Some scholars did state, however, that they believed that codependency was not a negative trait, but rather a healthy personality trait taken to excess. In most studies, women with high codependency ratings have tended to be unemployed and with lower educations. Their behavior had been considered worthy of a DSM inclusion as a personality disorder, but luckily, this was thwarted.
A family is forced to make some accounting when an individual develops a substance use disorder. If the family tries to maintain equilibrium and keeps things as stable as possible for the sake of maintaining the family unit or the stability of the lives of the children, accommodation will be required. Accommodation minimizes the impact of the addiction: the sober spouse stepping up to complete the roles of the ill relative and in all ways reducing the impact of dysfunction on the family. If you swap out the illness and consider the ill family member as having cancer or respiratory distress, then you reframe the spouse’s “codependence” as the behavior of a caring spouse.
This long preamble is intended to illustrate how little family dynamics have to do with the etiology of addiction. Addiction is a chronic neurobiological disease, and like all diseases, individuals, and couples and families have the option of learning to cope well. We, as psychiatrists, must move away from blaming people (usually women who have less-than-optimal coping skills) and consider how best to engage partners and families in optimal programs.*
Families can benefit from specialist treatment and thus contribute to the recovery process. One example is a telepsychiatry program that aimed to improve family coping skills to cope with relatives who have substance use disorders. The Tele-intervention Model and Monitoring of Families of Drug Users is based on motivational interviewing and stages of change. Families were randomized into the intervention group (n = 163) or the usual treatment (n = 162). After 6 months of follow-up, the family members of the telepsychiatry group were twice as likely to modify their behavior (odds ratio; 2.08; 95% confidence interval, 1.18-3.65) (J Sub Use Misuse. 2017 Jan 28;52[2]:164-74). This model was organized so that each of nine calls had a specific goal to stimulate the family members in their process of change.
Family change and engagement also can occur through Alanon (Subst Use Misuse. 2015; 50[1]:62-71) and the use of the Arise program of Judith Landau, MD, (Landau J et al. Am J Drug Alcohol Abuse. 2000;26[3]:379-98).
In summary, the family can be engaged in treatment and can develop family coping skills to support their relative with this chronic neurobiological disease.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose.
*Updated on January 12, 2018.
Massachusetts and the opioid crisis: Can involuntary holds work?
My son played on a neighborhood little league team for several years. I have such sweet memories of little boys in baseball uniforms lined up on the bench singing cheers while they waited their turns to go to bat. The two devoted dads who worked together coaching the team were a gentle presence in the background of my family’s life every spring for years. One might hope that the love and attention those fathers invested in their sons and their teammates might confer some special protection from life’s tragedies, but the opioid epidemic spares no hostages, and last year, one of those singing little boys from so many years ago – the son of one of the coaches – died of a drug overdose.
President Trump has punted on how to stop the epidemic, one he finally deemed a national public health emergency in October, with no clear addition of federal resources. States have varied in their responses, and Massachusetts, in particular, has been aggressive with new legislation and funding. The laws in Massachusetts allow for involuntary rehab for substance abusers if a family member petitions the court under the state’s decades-old section 35. The irony is that much of this “involuntary” treatment is voluntary: People will ask family members to apply for them as a way of getting into treatment and as a way of bypassing the cost. Section 35 admissions are funded by the state, not by the individual or by health insurance.
As a Boston Globe article (“Mass. governor aims to expand battle against opioid addiction,” Nov. 15, 2017) explains, “Two years ago, Baker stirred controversy with a proposal to hold addicted patients for 72 hours against their will in emergency departments. That idea was rejected by the Legislature. The new bill takes a different approach to the 72-hour hold, enabling doctors to transfer patients with addiction to a treatment facility, much as they would with a person deemed a danger because of mental illness.”
The issues with involuntary care are complicated and nuanced in psychiatric disorders, and perhaps even more so with substance abuse. The time frame of 72 hours for mental health conditions allows for assessment and sometimes for the start of treatment. In some states, a hearing must be held for continued involuntary detention; in other states, a decision must be made as to whether further inpatient care will be pursued, and the actual hearing takes place days to weeks later, depending on the state. For the purposes of allowing someone to clear from an opioid intoxication, then persuading them to engage in voluntary substance abuse treatment, it seems that 72 hours could be the exact wrong time period.
Ideally, a patient would be placed in a comfortable inpatient unit, begun on medication-assisted withdrawal, and offered a high quality of care for those 72 hours so that continuing with treatment might be a palatable option. But would that actually happen? Does Massachusetts have the means and facilities for all its overdose patients? Massachusetts has, in fact, been aggressive with funding. Since 2015, the state has added 1,100 new treatment beds. The efforts to fund and offer novel treatments are commendable. My concern remains that without adequate treatment or a positive experience – a difficult target in the best of circumstances for a patient who is 72 hours into opioid withdrawal – patients would leave only to resume their substance abuse. In a disastrous scenario, patients who have overdosed and fear being detained might not call for help, and the death rate could actually rise.
John A. Renner Jr., MD, is the past president of the American Academy of Addiction Psychiatry and coeditor of Office-Based Buprenorphine Treatment of Opioid Use Disorder (American Psychiatric Association Publishing, 2018). Dr. Renner, who is a professor at Boston University, said, “I would like to see some evidence and research to be sure there were not unintended harms before we go this route.”
Eric C. Strain, MD, director of the Johns Hopkins Center for Substance Abuse Treatment and Research, Baltimore, noted: “Simply holding someone for 3 days, especially against their will, doesn’t make a lot of sense. They are certainly not going to be all better either from a physiological or psychological standpoint. It might, however, be possible to get a person who was not interested in treatment engaged in treatment, and that would be a success.”
Despite the increased numbers of beds and aggressive, thoughtful interventions, Massachusetts still had 1,450 overdose deaths in the first 9 months of 2017, a decrease of only 10% from the year before, according to the Globe article. For the sake of the former Little League players in Maryland, and all the other victims of this lethal nationwide epidemic, it is imperative that any untested treatments be the source of new research. If these measures are implemented, it is essential that Massachusetts follow the people who are the beneficiaries of interventions and create the data that allow other states to either follow suit if these efforts are successful, or allocate resources to other treatments if they are not.
Dr. Miller is coauthor with Annette Hanson, MD, of Committed: The Battle Over Involuntary Psychiatry Care (Baltimore: Johns Hopkins University Press, 2016).
My son played on a neighborhood little league team for several years. I have such sweet memories of little boys in baseball uniforms lined up on the bench singing cheers while they waited their turns to go to bat. The two devoted dads who worked together coaching the team were a gentle presence in the background of my family’s life every spring for years. One might hope that the love and attention those fathers invested in their sons and their teammates might confer some special protection from life’s tragedies, but the opioid epidemic spares no hostages, and last year, one of those singing little boys from so many years ago – the son of one of the coaches – died of a drug overdose.
President Trump has punted on how to stop the epidemic, one he finally deemed a national public health emergency in October, with no clear addition of federal resources. States have varied in their responses, and Massachusetts, in particular, has been aggressive with new legislation and funding. The laws in Massachusetts allow for involuntary rehab for substance abusers if a family member petitions the court under the state’s decades-old section 35. The irony is that much of this “involuntary” treatment is voluntary: People will ask family members to apply for them as a way of getting into treatment and as a way of bypassing the cost. Section 35 admissions are funded by the state, not by the individual or by health insurance.
As a Boston Globe article (“Mass. governor aims to expand battle against opioid addiction,” Nov. 15, 2017) explains, “Two years ago, Baker stirred controversy with a proposal to hold addicted patients for 72 hours against their will in emergency departments. That idea was rejected by the Legislature. The new bill takes a different approach to the 72-hour hold, enabling doctors to transfer patients with addiction to a treatment facility, much as they would with a person deemed a danger because of mental illness.”
The issues with involuntary care are complicated and nuanced in psychiatric disorders, and perhaps even more so with substance abuse. The time frame of 72 hours for mental health conditions allows for assessment and sometimes for the start of treatment. In some states, a hearing must be held for continued involuntary detention; in other states, a decision must be made as to whether further inpatient care will be pursued, and the actual hearing takes place days to weeks later, depending on the state. For the purposes of allowing someone to clear from an opioid intoxication, then persuading them to engage in voluntary substance abuse treatment, it seems that 72 hours could be the exact wrong time period.
Ideally, a patient would be placed in a comfortable inpatient unit, begun on medication-assisted withdrawal, and offered a high quality of care for those 72 hours so that continuing with treatment might be a palatable option. But would that actually happen? Does Massachusetts have the means and facilities for all its overdose patients? Massachusetts has, in fact, been aggressive with funding. Since 2015, the state has added 1,100 new treatment beds. The efforts to fund and offer novel treatments are commendable. My concern remains that without adequate treatment or a positive experience – a difficult target in the best of circumstances for a patient who is 72 hours into opioid withdrawal – patients would leave only to resume their substance abuse. In a disastrous scenario, patients who have overdosed and fear being detained might not call for help, and the death rate could actually rise.
John A. Renner Jr., MD, is the past president of the American Academy of Addiction Psychiatry and coeditor of Office-Based Buprenorphine Treatment of Opioid Use Disorder (American Psychiatric Association Publishing, 2018). Dr. Renner, who is a professor at Boston University, said, “I would like to see some evidence and research to be sure there were not unintended harms before we go this route.”
Eric C. Strain, MD, director of the Johns Hopkins Center for Substance Abuse Treatment and Research, Baltimore, noted: “Simply holding someone for 3 days, especially against their will, doesn’t make a lot of sense. They are certainly not going to be all better either from a physiological or psychological standpoint. It might, however, be possible to get a person who was not interested in treatment engaged in treatment, and that would be a success.”
Despite the increased numbers of beds and aggressive, thoughtful interventions, Massachusetts still had 1,450 overdose deaths in the first 9 months of 2017, a decrease of only 10% from the year before, according to the Globe article. For the sake of the former Little League players in Maryland, and all the other victims of this lethal nationwide epidemic, it is imperative that any untested treatments be the source of new research. If these measures are implemented, it is essential that Massachusetts follow the people who are the beneficiaries of interventions and create the data that allow other states to either follow suit if these efforts are successful, or allocate resources to other treatments if they are not.
Dr. Miller is coauthor with Annette Hanson, MD, of Committed: The Battle Over Involuntary Psychiatry Care (Baltimore: Johns Hopkins University Press, 2016).
My son played on a neighborhood little league team for several years. I have such sweet memories of little boys in baseball uniforms lined up on the bench singing cheers while they waited their turns to go to bat. The two devoted dads who worked together coaching the team were a gentle presence in the background of my family’s life every spring for years. One might hope that the love and attention those fathers invested in their sons and their teammates might confer some special protection from life’s tragedies, but the opioid epidemic spares no hostages, and last year, one of those singing little boys from so many years ago – the son of one of the coaches – died of a drug overdose.
President Trump has punted on how to stop the epidemic, one he finally deemed a national public health emergency in October, with no clear addition of federal resources. States have varied in their responses, and Massachusetts, in particular, has been aggressive with new legislation and funding. The laws in Massachusetts allow for involuntary rehab for substance abusers if a family member petitions the court under the state’s decades-old section 35. The irony is that much of this “involuntary” treatment is voluntary: People will ask family members to apply for them as a way of getting into treatment and as a way of bypassing the cost. Section 35 admissions are funded by the state, not by the individual or by health insurance.
As a Boston Globe article (“Mass. governor aims to expand battle against opioid addiction,” Nov. 15, 2017) explains, “Two years ago, Baker stirred controversy with a proposal to hold addicted patients for 72 hours against their will in emergency departments. That idea was rejected by the Legislature. The new bill takes a different approach to the 72-hour hold, enabling doctors to transfer patients with addiction to a treatment facility, much as they would with a person deemed a danger because of mental illness.”
The issues with involuntary care are complicated and nuanced in psychiatric disorders, and perhaps even more so with substance abuse. The time frame of 72 hours for mental health conditions allows for assessment and sometimes for the start of treatment. In some states, a hearing must be held for continued involuntary detention; in other states, a decision must be made as to whether further inpatient care will be pursued, and the actual hearing takes place days to weeks later, depending on the state. For the purposes of allowing someone to clear from an opioid intoxication, then persuading them to engage in voluntary substance abuse treatment, it seems that 72 hours could be the exact wrong time period.
Ideally, a patient would be placed in a comfortable inpatient unit, begun on medication-assisted withdrawal, and offered a high quality of care for those 72 hours so that continuing with treatment might be a palatable option. But would that actually happen? Does Massachusetts have the means and facilities for all its overdose patients? Massachusetts has, in fact, been aggressive with funding. Since 2015, the state has added 1,100 new treatment beds. The efforts to fund and offer novel treatments are commendable. My concern remains that without adequate treatment or a positive experience – a difficult target in the best of circumstances for a patient who is 72 hours into opioid withdrawal – patients would leave only to resume their substance abuse. In a disastrous scenario, patients who have overdosed and fear being detained might not call for help, and the death rate could actually rise.
John A. Renner Jr., MD, is the past president of the American Academy of Addiction Psychiatry and coeditor of Office-Based Buprenorphine Treatment of Opioid Use Disorder (American Psychiatric Association Publishing, 2018). Dr. Renner, who is a professor at Boston University, said, “I would like to see some evidence and research to be sure there were not unintended harms before we go this route.”
Eric C. Strain, MD, director of the Johns Hopkins Center for Substance Abuse Treatment and Research, Baltimore, noted: “Simply holding someone for 3 days, especially against their will, doesn’t make a lot of sense. They are certainly not going to be all better either from a physiological or psychological standpoint. It might, however, be possible to get a person who was not interested in treatment engaged in treatment, and that would be a success.”
Despite the increased numbers of beds and aggressive, thoughtful interventions, Massachusetts still had 1,450 overdose deaths in the first 9 months of 2017, a decrease of only 10% from the year before, according to the Globe article. For the sake of the former Little League players in Maryland, and all the other victims of this lethal nationwide epidemic, it is imperative that any untested treatments be the source of new research. If these measures are implemented, it is essential that Massachusetts follow the people who are the beneficiaries of interventions and create the data that allow other states to either follow suit if these efforts are successful, or allocate resources to other treatments if they are not.
Dr. Miller is coauthor with Annette Hanson, MD, of Committed: The Battle Over Involuntary Psychiatry Care (Baltimore: Johns Hopkins University Press, 2016).
The puzzling relationship between cholesterol and psychopathology
Cholesterol generally is regarded as a cardiovascular risk factor when elevated. However, numerous studies suggest that cholesterol levels—both high and low—may be associated with various psychiatric brai
The relationship between cholesterol and mental illness is fascinating, complex, and perplexing. Whether elevated or reduced, cholesterol’s effects can be deleterious or salutary, but the literature is riddled with conflicting reports. Physicians should measure their patients’ serum cholesterol levels not only to assess cardiovascular risk, but because cholesterol can be associated with certain neuropsychiatric disorders or may predict the lack of response to psychopharmacotherapy.2
The fact that lowering total cholesterol levels in people with hypercholesterolemia reduces the risk of coronary heart disease is indisputable. Large-scale cardiology clinical trials have shown a significant reduction in mortality from heart disease or stroke with cholesterol-lowering drugs (statins). However, the same trials found an uptick in “unnatural deaths,” mostly suicide or homicide.3 Those findings triggered numerous intriguing reports of the association between cholesterol levels and psychopathology.
Consider the following:
- Low cholesterol levels have been associated with depression, antisocial personality disorder, borderline personality disorder, and dissociative disorder.4
- High cholesterol levels have been associated with schizophrenia, obsessive-compulsive disorder, panic disorder, generalized anxiety disorder, and posttraumatic stress disorder.4
- Some studies suggest that high cholesterol levels are associated with better mental health, mental processing speed, social skills, responsibility, self-control, and self-awareness.5
- In the Clinical Antipsychotic Trials of Intervention Effectiveness schizophrenia study, better cognitive scores were found in patients with higher fasting cholesterol and triglyceride levels (H.A.N., unpublished data, 2017).
The brain is only 2% of body weight, but it contains 25% of the body’s cholesterol.6 Cholesterol is important for brain function and neurotransmission because neuroactive steroids (NASs) are synthesized from cholesterol and they modulate brain processes and interact with γ-aminobutyric acid, N-methyl-
Interestingly, both extremes in cholesterol levels represent a high risk for premature mortality.10 Hypercholesterolemia leads to early death from coronary artery disease. Studies that evaluated statins to lower cholesterol found increased mortality from suicide, accidents, and violence.11 Even without statin treatment, among persons with naturally low cholesterol, there is a significant increase in mortality from non-medical causes.12 However, some studies did not find an association between hypocholesterolemia and suicide.13,14
There also is some evidence that elevated cholesterol may play a role in dementia.15 Reducing cholesterol with statins decreases beta-amyloid in mice, while the opposite occurs with elevated cholesterol.2 Another possible mechanism by which high cholesterol worsens dementia is that neurodegeneration in Alzheimer’s disease (AD) breaks down neuronal cell membranes, which releases the neurotoxic metabolite of cholesterol (24-hydroxycholesterol), which leads to further neurodegeneration.16 Statins may decrease the production of 24-hydroxycholesterol in AD patients and slow down neurodegeneration.16
A large study of 4,444 consecutive patients in Taiwan found that those with low total cholesterol (<160 mg/dL) had higher scores of anxiety, phobia, psychoticism, and aggressive hostility.17 In the same study, women with low high-density lipoprotein cholesterol (<35 mg/dL) had significantly higher scores for depression, phobia, anxiety, interpersonal sensitivity, somatization, and aggressive hostility.17
Not surprisingly, low cholesterol has been proposed as a biomarker for mood dysregulation, depression, and suicidality,18 as well as a predictor of the depression severity and increased suicide risk.19 Clinical recovery in depression may be accompanied by a significant increase of total cholesterol20 but, interestingly, a decrease in cholesterol levels after treatment of mania. High cholesterol was reported to predict poorer response to selective serotonin reuptake inhibitors, and total cholesterol levels >200 mg/dL were associated with lack of response to fluoxetine and nortriptyline.2 Interestingly, clozapine, which elevates lipids, exerts a strong anti-suicide effect in schizophrenia and schizoaffective disorder, but that may not be the main reason for its efficacy in preventing suicide in patients with psychosis.
Cholesterol is an important lipid for brain function. At lower levels, it appears to be associated with depression, suicide, violence, anxiety, schizophrenia, and severe personality disorders (including antisocial personality disorder and borderline personality disorder). However, at high levels, it may improve cognition in schizophrenia and ameliorate the pace of AD and neurodegeneration. Psychiatrists should monitor patients for hypercholesterolemia and hypocholesterolemia, both of which are common among psychiatric patients. High levels may be genetic or the result of weight gain, hypercortisolemia, diabetes, or immune or inflammatory processes. Similarly, low levels may be genetic or secondary to statin therapy.
The bottom line: As psychiatric physicians, we should protect both the hearts and brains of our patients.
1. Hallahan B, Garland MR. Essential fatty acids and mental health. British J Psychiatry. 2005;186(4):275-277.
2. Papakostas GI, Ongür D, Iosifescu DV, et al. Cholesterol in mood and anxiety disorders: review of the literature and new hypotheses. Eur Neuropsychopharmacol. 2004;14(2):135-142.
3. Muldoon MF, Manuck SB, Matthews KA, et al. Lowering cholesterol concentrations and mortality: a quantitative review of primary prevention trials. BMJ. 1990;301(647):309-314.
4. Jakovljevic
5. Rogers PJ. A healthy body, a healthy mind: long-term impact of diet on mood and cognitive function. Pro Nutr Soc. 2001;60(1):135-143.
6. Björkhem I. Crossing the barrier: oxysterols as cholesterol transporters and metabolic modulators in the brain. J Intern Med. 2006;260(6):493-508.
7. Tuem KB, Atey TM. Neuroactive steroids: receptor interactions and responses. Front Neurol. 2017;8:442.
8. Borroni MV, Vallés AS, Barrantes FJ. The lipid habitats of neurotransmitter receptors in the brain. Biochim Biophys Acta. 2016;1858(1):2662-2670.
9. Pfrieger FW. Cholesterol homeostasis and function in neurons of the central nervous system. Cell Mol Life Sci. 2003;60(6):1158-1171.
10. Graham I, Atar D, Borch-Johnsen K, et al; European Society of Cardiology (ESC); European Association for Cardiovascular Prevention and Rehabilitation (EACPR); Council on Cardiovascular Nursing; European Association for Study of Diabetes (EASD); International Diabetes Federation Europe (IDF-Europe); European Stroke Initiative (EUSI); Society of Behavioural Medicine (ISBM); European Society of Hypertension (ESH); WONCA Europe (European Society of General Practice/Family Medicine); European Heart Network (EHN); European Atherosclerosis Society (EAS). European guidelines on cardiovascular disease prevention in clinical practice: full text. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of none societies and by invited experts). Eur J Cardiovasc Prev Rehabil. 2007;14(suppl 2):S1-S113.
11. Almeida-Montes LG, Valles-Sanchez V, Moreno-Aguilar J, et al. Relation of serum cholesterol, lipid, serotonin and tryptophan levels to severity of depression and to suicide attempts. J Psychiatry Neurosci. 2000;25(4):371-377.
12. Ryman A. Cholesterol, violent death, and mental disorder. BMJ. 1994;309(69525):421-422.
13. Wardle J. Cholesterol and psychological well-being. J Psychosom Res. 1995;39(5):549-562.
14. Irribarren C, Reed DM, Chen R, et al. Low serum cholesterol and mortality. Which is the cause and which is the effect? Circulation. 1995;92(9):2396-2403.
15. Stampfer MJ. Cardiovascular disease and Alzheimer’s disease: common links. J Intern Med. 2006;260(3):211-223.
16. Raffai RL, Weisgraber KH. Cholesterol: from heart attacks to Alzheimer’s disease. J Lipid Res. 2003;44(8):1423-1430.
17. Chen CC, Lu FH, Wu JS, et al. Correlation between serum lipid concentrations and psychological distress. Psychiatry Res. 2003;102(2):153-162.
18. Mössmer R, Mikova O, Koutsilieri E, et al. Consensus paper of the WFSBP Task Force on Biological Markers: biological markers in depression. World J Biol Psychiatry. 2007;8(3):141-174.
19. Papakostas GI, Petersen T, Sonawalla SB, et al. Serum cholesterol in treatment-resistant depression. Neuropsychobiology. 2003;47(3):146-151.
20. Gabriel A. Changes in plasma cholesterol in mood disorder patients: does treatment make a difference? J Affect Disord. 2007;99(1-3):273-278.
Cholesterol generally is regarded as a cardiovascular risk factor when elevated. However, numerous studies suggest that cholesterol levels—both high and low—may be associated with various psychiatric brai
The relationship between cholesterol and mental illness is fascinating, complex, and perplexing. Whether elevated or reduced, cholesterol’s effects can be deleterious or salutary, but the literature is riddled with conflicting reports. Physicians should measure their patients’ serum cholesterol levels not only to assess cardiovascular risk, but because cholesterol can be associated with certain neuropsychiatric disorders or may predict the lack of response to psychopharmacotherapy.2
The fact that lowering total cholesterol levels in people with hypercholesterolemia reduces the risk of coronary heart disease is indisputable. Large-scale cardiology clinical trials have shown a significant reduction in mortality from heart disease or stroke with cholesterol-lowering drugs (statins). However, the same trials found an uptick in “unnatural deaths,” mostly suicide or homicide.3 Those findings triggered numerous intriguing reports of the association between cholesterol levels and psychopathology.
Consider the following:
- Low cholesterol levels have been associated with depression, antisocial personality disorder, borderline personality disorder, and dissociative disorder.4
- High cholesterol levels have been associated with schizophrenia, obsessive-compulsive disorder, panic disorder, generalized anxiety disorder, and posttraumatic stress disorder.4
- Some studies suggest that high cholesterol levels are associated with better mental health, mental processing speed, social skills, responsibility, self-control, and self-awareness.5
- In the Clinical Antipsychotic Trials of Intervention Effectiveness schizophrenia study, better cognitive scores were found in patients with higher fasting cholesterol and triglyceride levels (H.A.N., unpublished data, 2017).
The brain is only 2% of body weight, but it contains 25% of the body’s cholesterol.6 Cholesterol is important for brain function and neurotransmission because neuroactive steroids (NASs) are synthesized from cholesterol and they modulate brain processes and interact with γ-aminobutyric acid, N-methyl-
Interestingly, both extremes in cholesterol levels represent a high risk for premature mortality.10 Hypercholesterolemia leads to early death from coronary artery disease. Studies that evaluated statins to lower cholesterol found increased mortality from suicide, accidents, and violence.11 Even without statin treatment, among persons with naturally low cholesterol, there is a significant increase in mortality from non-medical causes.12 However, some studies did not find an association between hypocholesterolemia and suicide.13,14
There also is some evidence that elevated cholesterol may play a role in dementia.15 Reducing cholesterol with statins decreases beta-amyloid in mice, while the opposite occurs with elevated cholesterol.2 Another possible mechanism by which high cholesterol worsens dementia is that neurodegeneration in Alzheimer’s disease (AD) breaks down neuronal cell membranes, which releases the neurotoxic metabolite of cholesterol (24-hydroxycholesterol), which leads to further neurodegeneration.16 Statins may decrease the production of 24-hydroxycholesterol in AD patients and slow down neurodegeneration.16
A large study of 4,444 consecutive patients in Taiwan found that those with low total cholesterol (<160 mg/dL) had higher scores of anxiety, phobia, psychoticism, and aggressive hostility.17 In the same study, women with low high-density lipoprotein cholesterol (<35 mg/dL) had significantly higher scores for depression, phobia, anxiety, interpersonal sensitivity, somatization, and aggressive hostility.17
Not surprisingly, low cholesterol has been proposed as a biomarker for mood dysregulation, depression, and suicidality,18 as well as a predictor of the depression severity and increased suicide risk.19 Clinical recovery in depression may be accompanied by a significant increase of total cholesterol20 but, interestingly, a decrease in cholesterol levels after treatment of mania. High cholesterol was reported to predict poorer response to selective serotonin reuptake inhibitors, and total cholesterol levels >200 mg/dL were associated with lack of response to fluoxetine and nortriptyline.2 Interestingly, clozapine, which elevates lipids, exerts a strong anti-suicide effect in schizophrenia and schizoaffective disorder, but that may not be the main reason for its efficacy in preventing suicide in patients with psychosis.
Cholesterol is an important lipid for brain function. At lower levels, it appears to be associated with depression, suicide, violence, anxiety, schizophrenia, and severe personality disorders (including antisocial personality disorder and borderline personality disorder). However, at high levels, it may improve cognition in schizophrenia and ameliorate the pace of AD and neurodegeneration. Psychiatrists should monitor patients for hypercholesterolemia and hypocholesterolemia, both of which are common among psychiatric patients. High levels may be genetic or the result of weight gain, hypercortisolemia, diabetes, or immune or inflammatory processes. Similarly, low levels may be genetic or secondary to statin therapy.
The bottom line: As psychiatric physicians, we should protect both the hearts and brains of our patients.
Cholesterol generally is regarded as a cardiovascular risk factor when elevated. However, numerous studies suggest that cholesterol levels—both high and low—may be associated with various psychiatric brai
The relationship between cholesterol and mental illness is fascinating, complex, and perplexing. Whether elevated or reduced, cholesterol’s effects can be deleterious or salutary, but the literature is riddled with conflicting reports. Physicians should measure their patients’ serum cholesterol levels not only to assess cardiovascular risk, but because cholesterol can be associated with certain neuropsychiatric disorders or may predict the lack of response to psychopharmacotherapy.2
The fact that lowering total cholesterol levels in people with hypercholesterolemia reduces the risk of coronary heart disease is indisputable. Large-scale cardiology clinical trials have shown a significant reduction in mortality from heart disease or stroke with cholesterol-lowering drugs (statins). However, the same trials found an uptick in “unnatural deaths,” mostly suicide or homicide.3 Those findings triggered numerous intriguing reports of the association between cholesterol levels and psychopathology.
Consider the following:
- Low cholesterol levels have been associated with depression, antisocial personality disorder, borderline personality disorder, and dissociative disorder.4
- High cholesterol levels have been associated with schizophrenia, obsessive-compulsive disorder, panic disorder, generalized anxiety disorder, and posttraumatic stress disorder.4
- Some studies suggest that high cholesterol levels are associated with better mental health, mental processing speed, social skills, responsibility, self-control, and self-awareness.5
- In the Clinical Antipsychotic Trials of Intervention Effectiveness schizophrenia study, better cognitive scores were found in patients with higher fasting cholesterol and triglyceride levels (H.A.N., unpublished data, 2017).
The brain is only 2% of body weight, but it contains 25% of the body’s cholesterol.6 Cholesterol is important for brain function and neurotransmission because neuroactive steroids (NASs) are synthesized from cholesterol and they modulate brain processes and interact with γ-aminobutyric acid, N-methyl-
Interestingly, both extremes in cholesterol levels represent a high risk for premature mortality.10 Hypercholesterolemia leads to early death from coronary artery disease. Studies that evaluated statins to lower cholesterol found increased mortality from suicide, accidents, and violence.11 Even without statin treatment, among persons with naturally low cholesterol, there is a significant increase in mortality from non-medical causes.12 However, some studies did not find an association between hypocholesterolemia and suicide.13,14
There also is some evidence that elevated cholesterol may play a role in dementia.15 Reducing cholesterol with statins decreases beta-amyloid in mice, while the opposite occurs with elevated cholesterol.2 Another possible mechanism by which high cholesterol worsens dementia is that neurodegeneration in Alzheimer’s disease (AD) breaks down neuronal cell membranes, which releases the neurotoxic metabolite of cholesterol (24-hydroxycholesterol), which leads to further neurodegeneration.16 Statins may decrease the production of 24-hydroxycholesterol in AD patients and slow down neurodegeneration.16
A large study of 4,444 consecutive patients in Taiwan found that those with low total cholesterol (<160 mg/dL) had higher scores of anxiety, phobia, psychoticism, and aggressive hostility.17 In the same study, women with low high-density lipoprotein cholesterol (<35 mg/dL) had significantly higher scores for depression, phobia, anxiety, interpersonal sensitivity, somatization, and aggressive hostility.17
Not surprisingly, low cholesterol has been proposed as a biomarker for mood dysregulation, depression, and suicidality,18 as well as a predictor of the depression severity and increased suicide risk.19 Clinical recovery in depression may be accompanied by a significant increase of total cholesterol20 but, interestingly, a decrease in cholesterol levels after treatment of mania. High cholesterol was reported to predict poorer response to selective serotonin reuptake inhibitors, and total cholesterol levels >200 mg/dL were associated with lack of response to fluoxetine and nortriptyline.2 Interestingly, clozapine, which elevates lipids, exerts a strong anti-suicide effect in schizophrenia and schizoaffective disorder, but that may not be the main reason for its efficacy in preventing suicide in patients with psychosis.
Cholesterol is an important lipid for brain function. At lower levels, it appears to be associated with depression, suicide, violence, anxiety, schizophrenia, and severe personality disorders (including antisocial personality disorder and borderline personality disorder). However, at high levels, it may improve cognition in schizophrenia and ameliorate the pace of AD and neurodegeneration. Psychiatrists should monitor patients for hypercholesterolemia and hypocholesterolemia, both of which are common among psychiatric patients. High levels may be genetic or the result of weight gain, hypercortisolemia, diabetes, or immune or inflammatory processes. Similarly, low levels may be genetic or secondary to statin therapy.
The bottom line: As psychiatric physicians, we should protect both the hearts and brains of our patients.
1. Hallahan B, Garland MR. Essential fatty acids and mental health. British J Psychiatry. 2005;186(4):275-277.
2. Papakostas GI, Ongür D, Iosifescu DV, et al. Cholesterol in mood and anxiety disorders: review of the literature and new hypotheses. Eur Neuropsychopharmacol. 2004;14(2):135-142.
3. Muldoon MF, Manuck SB, Matthews KA, et al. Lowering cholesterol concentrations and mortality: a quantitative review of primary prevention trials. BMJ. 1990;301(647):309-314.
4. Jakovljevic
5. Rogers PJ. A healthy body, a healthy mind: long-term impact of diet on mood and cognitive function. Pro Nutr Soc. 2001;60(1):135-143.
6. Björkhem I. Crossing the barrier: oxysterols as cholesterol transporters and metabolic modulators in the brain. J Intern Med. 2006;260(6):493-508.
7. Tuem KB, Atey TM. Neuroactive steroids: receptor interactions and responses. Front Neurol. 2017;8:442.
8. Borroni MV, Vallés AS, Barrantes FJ. The lipid habitats of neurotransmitter receptors in the brain. Biochim Biophys Acta. 2016;1858(1):2662-2670.
9. Pfrieger FW. Cholesterol homeostasis and function in neurons of the central nervous system. Cell Mol Life Sci. 2003;60(6):1158-1171.
10. Graham I, Atar D, Borch-Johnsen K, et al; European Society of Cardiology (ESC); European Association for Cardiovascular Prevention and Rehabilitation (EACPR); Council on Cardiovascular Nursing; European Association for Study of Diabetes (EASD); International Diabetes Federation Europe (IDF-Europe); European Stroke Initiative (EUSI); Society of Behavioural Medicine (ISBM); European Society of Hypertension (ESH); WONCA Europe (European Society of General Practice/Family Medicine); European Heart Network (EHN); European Atherosclerosis Society (EAS). European guidelines on cardiovascular disease prevention in clinical practice: full text. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of none societies and by invited experts). Eur J Cardiovasc Prev Rehabil. 2007;14(suppl 2):S1-S113.
11. Almeida-Montes LG, Valles-Sanchez V, Moreno-Aguilar J, et al. Relation of serum cholesterol, lipid, serotonin and tryptophan levels to severity of depression and to suicide attempts. J Psychiatry Neurosci. 2000;25(4):371-377.
12. Ryman A. Cholesterol, violent death, and mental disorder. BMJ. 1994;309(69525):421-422.
13. Wardle J. Cholesterol and psychological well-being. J Psychosom Res. 1995;39(5):549-562.
14. Irribarren C, Reed DM, Chen R, et al. Low serum cholesterol and mortality. Which is the cause and which is the effect? Circulation. 1995;92(9):2396-2403.
15. Stampfer MJ. Cardiovascular disease and Alzheimer’s disease: common links. J Intern Med. 2006;260(3):211-223.
16. Raffai RL, Weisgraber KH. Cholesterol: from heart attacks to Alzheimer’s disease. J Lipid Res. 2003;44(8):1423-1430.
17. Chen CC, Lu FH, Wu JS, et al. Correlation between serum lipid concentrations and psychological distress. Psychiatry Res. 2003;102(2):153-162.
18. Mössmer R, Mikova O, Koutsilieri E, et al. Consensus paper of the WFSBP Task Force on Biological Markers: biological markers in depression. World J Biol Psychiatry. 2007;8(3):141-174.
19. Papakostas GI, Petersen T, Sonawalla SB, et al. Serum cholesterol in treatment-resistant depression. Neuropsychobiology. 2003;47(3):146-151.
20. Gabriel A. Changes in plasma cholesterol in mood disorder patients: does treatment make a difference? J Affect Disord. 2007;99(1-3):273-278.
1. Hallahan B, Garland MR. Essential fatty acids and mental health. British J Psychiatry. 2005;186(4):275-277.
2. Papakostas GI, Ongür D, Iosifescu DV, et al. Cholesterol in mood and anxiety disorders: review of the literature and new hypotheses. Eur Neuropsychopharmacol. 2004;14(2):135-142.
3. Muldoon MF, Manuck SB, Matthews KA, et al. Lowering cholesterol concentrations and mortality: a quantitative review of primary prevention trials. BMJ. 1990;301(647):309-314.
4. Jakovljevic
5. Rogers PJ. A healthy body, a healthy mind: long-term impact of diet on mood and cognitive function. Pro Nutr Soc. 2001;60(1):135-143.
6. Björkhem I. Crossing the barrier: oxysterols as cholesterol transporters and metabolic modulators in the brain. J Intern Med. 2006;260(6):493-508.
7. Tuem KB, Atey TM. Neuroactive steroids: receptor interactions and responses. Front Neurol. 2017;8:442.
8. Borroni MV, Vallés AS, Barrantes FJ. The lipid habitats of neurotransmitter receptors in the brain. Biochim Biophys Acta. 2016;1858(1):2662-2670.
9. Pfrieger FW. Cholesterol homeostasis and function in neurons of the central nervous system. Cell Mol Life Sci. 2003;60(6):1158-1171.
10. Graham I, Atar D, Borch-Johnsen K, et al; European Society of Cardiology (ESC); European Association for Cardiovascular Prevention and Rehabilitation (EACPR); Council on Cardiovascular Nursing; European Association for Study of Diabetes (EASD); International Diabetes Federation Europe (IDF-Europe); European Stroke Initiative (EUSI); Society of Behavioural Medicine (ISBM); European Society of Hypertension (ESH); WONCA Europe (European Society of General Practice/Family Medicine); European Heart Network (EHN); European Atherosclerosis Society (EAS). European guidelines on cardiovascular disease prevention in clinical practice: full text. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of none societies and by invited experts). Eur J Cardiovasc Prev Rehabil. 2007;14(suppl 2):S1-S113.
11. Almeida-Montes LG, Valles-Sanchez V, Moreno-Aguilar J, et al. Relation of serum cholesterol, lipid, serotonin and tryptophan levels to severity of depression and to suicide attempts. J Psychiatry Neurosci. 2000;25(4):371-377.
12. Ryman A. Cholesterol, violent death, and mental disorder. BMJ. 1994;309(69525):421-422.
13. Wardle J. Cholesterol and psychological well-being. J Psychosom Res. 1995;39(5):549-562.
14. Irribarren C, Reed DM, Chen R, et al. Low serum cholesterol and mortality. Which is the cause and which is the effect? Circulation. 1995;92(9):2396-2403.
15. Stampfer MJ. Cardiovascular disease and Alzheimer’s disease: common links. J Intern Med. 2006;260(3):211-223.
16. Raffai RL, Weisgraber KH. Cholesterol: from heart attacks to Alzheimer’s disease. J Lipid Res. 2003;44(8):1423-1430.
17. Chen CC, Lu FH, Wu JS, et al. Correlation between serum lipid concentrations and psychological distress. Psychiatry Res. 2003;102(2):153-162.
18. Mössmer R, Mikova O, Koutsilieri E, et al. Consensus paper of the WFSBP Task Force on Biological Markers: biological markers in depression. World J Biol Psychiatry. 2007;8(3):141-174.
19. Papakostas GI, Petersen T, Sonawalla SB, et al. Serum cholesterol in treatment-resistant depression. Neuropsychobiology. 2003;47(3):146-151.
20. Gabriel A. Changes in plasma cholesterol in mood disorder patients: does treatment make a difference? J Affect Disord. 2007;99(1-3):273-278.
Career Choices: State hospital psychiatry
Editor’s note: Career Choices is a new feature of Residents’ Voices. It features a psychiatry resident/fellow interviewing a psychiatrist about why he (she) has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths. Future installments will feature interviews with psychiatrists who have focused their careers on consultation-liaison psychiatry, academic psychiatry, rural psychiatry, and other career paths.
In this first Career Choices, Cornel Stanciu, MD, talked with Samantha Gnanasegaram, MD, a state hospital psychiatrist at New Hampshire Hospital, where she treats severe and chronic mental illness and testifies in various court proceedings.
Dr. Stanciu: What made you choose to become a state hospital psychiatrist?
Dr. Gnanasegaram: When I started thinking about career options after residency, I knew I wanted to start my career in a facility where I could be challenged, remain up-to-date with the most current evidence-based literature, and have the support and mentorship of seasoned psychiatrists in the field. The opportunity to work under the auspices of a great academic institution with the “bread and butter” of psychiatry reminds me every day why I chose the field in the first place. The often chronic and sometimes refractory cases I encounter daily are extremely thought-provoking, and they motivate me to think and pursue more complex management options. [This setting] also enables me to work closely as [part of] an interdisciplinary team with nursing, social work, and recreational and occupational therapy in ensuring these individuals get the best care and aftercare plans.
We often forget that psychosis often takes weeks to respond [to treatment]. Unfortunately, often in private hospitals, the longer stays that are necessary for patient care are not always possible, leading to premature psychotropic changes and discharge. In this setting, I am able to practice medicine based on what is best for the patient from an evidence-based standpoint. Additionally, being in the state system also allows me to learn first-hand and work closely with the legal system in this state and to testify in various settings to ensure my patients get the best possible care.
Dr. Stanciu: How did your career path prepare you to become a state hospital psychiatrist?
Dr. Gnanasegaram: During my residency, I had exposure to the affiliated state psychiatric hospital and spent some time on various units, each geared toward different patient populations. I also became very familiar with a wide range of psychotropics, ranging from first-line to second- and third-tier medications, as well as off-label. The ECT exposure as well as Crisis Prevention Institute training in how to deal with violent and aggressive individuals certainly added extra layers to my proficiency.
Dr. Stanciu: How would you describe a physician who is well-suited for such a setting?
Dr. Gnanasegaram: This setting is great for someone who likes to be challenged and stay current with literature. Furthermore, this is a great setting for those who are comfortable with the use of medications such as [clozapine] and long-acting injectables, and procedures such as ECT. Additionally, an ideal candidate is someone who understands the chronicity and complexity of mental illness, and has the patience to follow the course and does not rush to make drastic changes or panics at the first sign of a patient taking a step back.
A good candidate also should be comfortable with medical comorbidities, because severe mental illness often leads to poor self-care, diabetes, hypertension, etc., and should be able to work effectively in a team setting and interact with other specialties. State hospital physicians need to be cognizant of outpatient resources available to prevent decompensation in the community and not only focus on acute stabilization. Additionally, this is a great setting for those who enjoy working in an interdisciplinary team and learning from the expertise of different members of a treatment team.
Dr. Stanciu: What challenges and surprises did you encounter when you first began to practice in this setting?
Dr. Gnanasegaram: When I started, the biggest challenge was learning about the differences in practice and legislature in a different state, because all states vary in their involuntary commitment laws, process, and ability to institute forced medications. Learning this as well as how they apply to my practice occurred quicker than I anticipated. As I started practicing, I became more proficient in being able to incorporate the resources I have available.
Dr. Stanciu: What are the disadvantages compared with other branches of psychiatry?
Dr. Gnanasegaram: This is a subjective question. Some physicians may desire a rapid turnaround of patients, which is not always the case in state psychiatric hospitals. Even at discharge, some patients may have low-functioning baselines, requiring guardianship and/or placement in a more supervised setting to ensure they receive the care they need. It is also important to realize these are primarily not voluntary patients, but rather patients committed here involuntarily for treatment due to impaired insight and judgment. At times, the acuity can be high, but the potential for violence is mitigated through comprehensive risk assessments, staff training, and prevention strategies to help ensure patient and staff safety.
Dr. Stanciu: What advice do you have for early career psychiatrists and trainees who are contemplating a state hospital career?
Dr. Gnanasegaram: I would recommend seeking exposure to working in a state psychiatric hospital early in your training so you can see the daily routine and protocol. It would help to obtain mentorship from a state hospital psychiatrist in the state where you intend to work. Ask as many questions as needed and seek their insight into the challenges and benefits of working there. During training, it’s important to familiarize yourself with managing difficult and refractory cases, and don’t shy away from challenging patients. The next step would be to apply for a position of interest to interview and learn more about the facility and the staff that you will be working with.
Dr. Stanciu: How important is the academic affiliation?
Dr. Gnanasegaram: Very important. Especially during the early phase of your career, it is important to have at your fingertips senior mentors and to be involved in the conferences and CME activities offered. This ensures good quality measures in patient care. The academic affiliation helps keep you up-to-date with advancements and maintains an atmosphere that fosters ongoing learning and the best possible care for your patients. Working with trainees at various levels, such as medical students, residents, and fellows, allows you to maintain an evidence-based practice approach as well as share your knowledge and experience with those in training. Being in this academic setting, you also have the opportunity for involvement in research activities and publications.
Editor’s note: Career Choices is a new feature of Residents’ Voices. It features a psychiatry resident/fellow interviewing a psychiatrist about why he (she) has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths. Future installments will feature interviews with psychiatrists who have focused their careers on consultation-liaison psychiatry, academic psychiatry, rural psychiatry, and other career paths.
In this first Career Choices, Cornel Stanciu, MD, talked with Samantha Gnanasegaram, MD, a state hospital psychiatrist at New Hampshire Hospital, where she treats severe and chronic mental illness and testifies in various court proceedings.
Dr. Stanciu: What made you choose to become a state hospital psychiatrist?
Dr. Gnanasegaram: When I started thinking about career options after residency, I knew I wanted to start my career in a facility where I could be challenged, remain up-to-date with the most current evidence-based literature, and have the support and mentorship of seasoned psychiatrists in the field. The opportunity to work under the auspices of a great academic institution with the “bread and butter” of psychiatry reminds me every day why I chose the field in the first place. The often chronic and sometimes refractory cases I encounter daily are extremely thought-provoking, and they motivate me to think and pursue more complex management options. [This setting] also enables me to work closely as [part of] an interdisciplinary team with nursing, social work, and recreational and occupational therapy in ensuring these individuals get the best care and aftercare plans.
We often forget that psychosis often takes weeks to respond [to treatment]. Unfortunately, often in private hospitals, the longer stays that are necessary for patient care are not always possible, leading to premature psychotropic changes and discharge. In this setting, I am able to practice medicine based on what is best for the patient from an evidence-based standpoint. Additionally, being in the state system also allows me to learn first-hand and work closely with the legal system in this state and to testify in various settings to ensure my patients get the best possible care.
Dr. Stanciu: How did your career path prepare you to become a state hospital psychiatrist?
Dr. Gnanasegaram: During my residency, I had exposure to the affiliated state psychiatric hospital and spent some time on various units, each geared toward different patient populations. I also became very familiar with a wide range of psychotropics, ranging from first-line to second- and third-tier medications, as well as off-label. The ECT exposure as well as Crisis Prevention Institute training in how to deal with violent and aggressive individuals certainly added extra layers to my proficiency.
Dr. Stanciu: How would you describe a physician who is well-suited for such a setting?
Dr. Gnanasegaram: This setting is great for someone who likes to be challenged and stay current with literature. Furthermore, this is a great setting for those who are comfortable with the use of medications such as [clozapine] and long-acting injectables, and procedures such as ECT. Additionally, an ideal candidate is someone who understands the chronicity and complexity of mental illness, and has the patience to follow the course and does not rush to make drastic changes or panics at the first sign of a patient taking a step back.
A good candidate also should be comfortable with medical comorbidities, because severe mental illness often leads to poor self-care, diabetes, hypertension, etc., and should be able to work effectively in a team setting and interact with other specialties. State hospital physicians need to be cognizant of outpatient resources available to prevent decompensation in the community and not only focus on acute stabilization. Additionally, this is a great setting for those who enjoy working in an interdisciplinary team and learning from the expertise of different members of a treatment team.
Dr. Stanciu: What challenges and surprises did you encounter when you first began to practice in this setting?
Dr. Gnanasegaram: When I started, the biggest challenge was learning about the differences in practice and legislature in a different state, because all states vary in their involuntary commitment laws, process, and ability to institute forced medications. Learning this as well as how they apply to my practice occurred quicker than I anticipated. As I started practicing, I became more proficient in being able to incorporate the resources I have available.
Dr. Stanciu: What are the disadvantages compared with other branches of psychiatry?
Dr. Gnanasegaram: This is a subjective question. Some physicians may desire a rapid turnaround of patients, which is not always the case in state psychiatric hospitals. Even at discharge, some patients may have low-functioning baselines, requiring guardianship and/or placement in a more supervised setting to ensure they receive the care they need. It is also important to realize these are primarily not voluntary patients, but rather patients committed here involuntarily for treatment due to impaired insight and judgment. At times, the acuity can be high, but the potential for violence is mitigated through comprehensive risk assessments, staff training, and prevention strategies to help ensure patient and staff safety.
Dr. Stanciu: What advice do you have for early career psychiatrists and trainees who are contemplating a state hospital career?
Dr. Gnanasegaram: I would recommend seeking exposure to working in a state psychiatric hospital early in your training so you can see the daily routine and protocol. It would help to obtain mentorship from a state hospital psychiatrist in the state where you intend to work. Ask as many questions as needed and seek their insight into the challenges and benefits of working there. During training, it’s important to familiarize yourself with managing difficult and refractory cases, and don’t shy away from challenging patients. The next step would be to apply for a position of interest to interview and learn more about the facility and the staff that you will be working with.
Dr. Stanciu: How important is the academic affiliation?
Dr. Gnanasegaram: Very important. Especially during the early phase of your career, it is important to have at your fingertips senior mentors and to be involved in the conferences and CME activities offered. This ensures good quality measures in patient care. The academic affiliation helps keep you up-to-date with advancements and maintains an atmosphere that fosters ongoing learning and the best possible care for your patients. Working with trainees at various levels, such as medical students, residents, and fellows, allows you to maintain an evidence-based practice approach as well as share your knowledge and experience with those in training. Being in this academic setting, you also have the opportunity for involvement in research activities and publications.
Editor’s note: Career Choices is a new feature of Residents’ Voices. It features a psychiatry resident/fellow interviewing a psychiatrist about why he (she) has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths. Future installments will feature interviews with psychiatrists who have focused their careers on consultation-liaison psychiatry, academic psychiatry, rural psychiatry, and other career paths.
In this first Career Choices, Cornel Stanciu, MD, talked with Samantha Gnanasegaram, MD, a state hospital psychiatrist at New Hampshire Hospital, where she treats severe and chronic mental illness and testifies in various court proceedings.
Dr. Stanciu: What made you choose to become a state hospital psychiatrist?
Dr. Gnanasegaram: When I started thinking about career options after residency, I knew I wanted to start my career in a facility where I could be challenged, remain up-to-date with the most current evidence-based literature, and have the support and mentorship of seasoned psychiatrists in the field. The opportunity to work under the auspices of a great academic institution with the “bread and butter” of psychiatry reminds me every day why I chose the field in the first place. The often chronic and sometimes refractory cases I encounter daily are extremely thought-provoking, and they motivate me to think and pursue more complex management options. [This setting] also enables me to work closely as [part of] an interdisciplinary team with nursing, social work, and recreational and occupational therapy in ensuring these individuals get the best care and aftercare plans.
We often forget that psychosis often takes weeks to respond [to treatment]. Unfortunately, often in private hospitals, the longer stays that are necessary for patient care are not always possible, leading to premature psychotropic changes and discharge. In this setting, I am able to practice medicine based on what is best for the patient from an evidence-based standpoint. Additionally, being in the state system also allows me to learn first-hand and work closely with the legal system in this state and to testify in various settings to ensure my patients get the best possible care.
Dr. Stanciu: How did your career path prepare you to become a state hospital psychiatrist?
Dr. Gnanasegaram: During my residency, I had exposure to the affiliated state psychiatric hospital and spent some time on various units, each geared toward different patient populations. I also became very familiar with a wide range of psychotropics, ranging from first-line to second- and third-tier medications, as well as off-label. The ECT exposure as well as Crisis Prevention Institute training in how to deal with violent and aggressive individuals certainly added extra layers to my proficiency.
Dr. Stanciu: How would you describe a physician who is well-suited for such a setting?
Dr. Gnanasegaram: This setting is great for someone who likes to be challenged and stay current with literature. Furthermore, this is a great setting for those who are comfortable with the use of medications such as [clozapine] and long-acting injectables, and procedures such as ECT. Additionally, an ideal candidate is someone who understands the chronicity and complexity of mental illness, and has the patience to follow the course and does not rush to make drastic changes or panics at the first sign of a patient taking a step back.
A good candidate also should be comfortable with medical comorbidities, because severe mental illness often leads to poor self-care, diabetes, hypertension, etc., and should be able to work effectively in a team setting and interact with other specialties. State hospital physicians need to be cognizant of outpatient resources available to prevent decompensation in the community and not only focus on acute stabilization. Additionally, this is a great setting for those who enjoy working in an interdisciplinary team and learning from the expertise of different members of a treatment team.
Dr. Stanciu: What challenges and surprises did you encounter when you first began to practice in this setting?
Dr. Gnanasegaram: When I started, the biggest challenge was learning about the differences in practice and legislature in a different state, because all states vary in their involuntary commitment laws, process, and ability to institute forced medications. Learning this as well as how they apply to my practice occurred quicker than I anticipated. As I started practicing, I became more proficient in being able to incorporate the resources I have available.
Dr. Stanciu: What are the disadvantages compared with other branches of psychiatry?
Dr. Gnanasegaram: This is a subjective question. Some physicians may desire a rapid turnaround of patients, which is not always the case in state psychiatric hospitals. Even at discharge, some patients may have low-functioning baselines, requiring guardianship and/or placement in a more supervised setting to ensure they receive the care they need. It is also important to realize these are primarily not voluntary patients, but rather patients committed here involuntarily for treatment due to impaired insight and judgment. At times, the acuity can be high, but the potential for violence is mitigated through comprehensive risk assessments, staff training, and prevention strategies to help ensure patient and staff safety.
Dr. Stanciu: What advice do you have for early career psychiatrists and trainees who are contemplating a state hospital career?
Dr. Gnanasegaram: I would recommend seeking exposure to working in a state psychiatric hospital early in your training so you can see the daily routine and protocol. It would help to obtain mentorship from a state hospital psychiatrist in the state where you intend to work. Ask as many questions as needed and seek their insight into the challenges and benefits of working there. During training, it’s important to familiarize yourself with managing difficult and refractory cases, and don’t shy away from challenging patients. The next step would be to apply for a position of interest to interview and learn more about the facility and the staff that you will be working with.
Dr. Stanciu: How important is the academic affiliation?
Dr. Gnanasegaram: Very important. Especially during the early phase of your career, it is important to have at your fingertips senior mentors and to be involved in the conferences and CME activities offered. This ensures good quality measures in patient care. The academic affiliation helps keep you up-to-date with advancements and maintains an atmosphere that fosters ongoing learning and the best possible care for your patients. Working with trainees at various levels, such as medical students, residents, and fellows, allows you to maintain an evidence-based practice approach as well as share your knowledge and experience with those in training. Being in this academic setting, you also have the opportunity for involvement in research activities and publications.
The role of psychiatric APRNs
In Dr. Mary Moller’s Guest Editorial “Advancing the role of advanced practice psychiatric nurses in today’s psychiatric workforce” (
Dr. Moller cited a source from the Federal Trade Commission1 that encourages the autonomous practice of APRNs to increase competition. This again implies the false equivalency between physicians and APRNs. Competition implies that the players are providing the same service. If, as nurse practitioners argue, they practice “nursing,” then they are not practicing “medicine.” Physicians and APRNs do not have the same background. Although both are charged with the care of patients, nursing is not medicine, nor should it be. Both are important and needed, but nursing was never designed to be an autonomous practice. According to the American Association of Colleges of Nursing, “Nursing and medicine are distinct health disciplines that prepare clinicians to assume different roles and meet different practice expectations.”2 In fact, the curriculum and requirements to become an APRN vary depending on the program, and some programs do not even require a BSN.3 There are online programs available for earning an APRN degree. Additionally, APRNs are only required to have 500 to 700 total hours of patient care,4 compared with the >10,000 hours physicians have once they have finished a 3-year residency, which when combined with their education amounts to >20,000 hours.5 This doesn’t account for those who have longer residencies or fellowships to further specialize in their area of training.
Dr. Moller’s main argument is that there is a dire shortage of psychiatrists and that the only way to meet this need for more providers is to make APRNs autonomous. However, no data indicate that autonomous practice of mid-level providers leads to an influx of these providers in rural areas, where the need would be greatest. Although current data on this are quite sparse, some studies indicate that the majority practice in urban areas, even in states with independent practice authority.6,7 Dr. Moller cites a source that only reviewed home zip codes of psychiatric APRNs but did not include zip codes of employment.8 Only 13% of psychiatric APRNs live in rural areas across the United States. Therefore, it is a false assertion to state that these APRNs are found primarily in rural and less populated urban areas. It is also false to imply and assume that these APRNs practice in the rural areas.
In 2017, there were 43,157 registered physician applications, with 35,969 active applications for 31,757 residency positions in the United States, and at least 11,400 medical school graduates were unmatched.9 Imagine how much more we could serve our patients by matching these graduates, whose training far surpasses that of a mid-level provider. The Resident Physician Shortage Reduction Act of 2017 aims to address this problem by increasing Medicare-funded graduate medical education (GME) residency programs in the United States.10 We can make a difference by contacting our members of Congress to encourage them to support this bill. In addition, the AMA is advocating to save funding for GME and provides an easy-to-use Web site (https://savegme.org/take-action) to contact your legislators directly to show your support for GME.
Nurse practitioners have tremendous value when their role is a part of a team; however, they should not practice without supervision, and physicians who supervise them absolutely should be providing adequate supervision. I applaud the APA and the AMA for standing up for the practice of medicine and for our patients. I hope that they continue to do so, and I encourage them to increase their efforts.
Laura Kendall, MD
Assistant Professor of Clinical Psychiatry
Department of Psychiatry and Behavioral Sciences
Keck School of Medicine
University of Southern California
Los Angeles, California
References
1. Koslov T; Office of Policy Planning. The doctor (or nurse practitioner) will see you now: competition and the regulation of advanced practice nurses. Federal Trade Commission. https://www.ftc.gov/news-events/blogs/competition-matters/2014/03/doctor-or-nurse-practitioner-will-see-you-now. Published March 7, 2014. Accessed July 26, 2017.
2. American Association of Colleges of Nursing. DNP talking points. http://www.aacnnursing.org/DNP/about/talking-points. Updated July, 2014. Accessed August 12, 2017.
3. Keyes L. MSN without a BSN? MastersInNursing.com. https://www.mastersinnursing.com/msn-without-a-bsn. Accessed August 12, 2017.
4. Iglehart JK. Expanding the role of advanced nurse practitioners—risks and rewards. New Engl J Med. 2013;368(20):1935-1941.
5. Primary Care Coalition. Issue brief: collaboration between physicians and nurses works. Compare the education gaps between primary care physicians and nurse practitioners. http://www.tafp.org/Media/Default/Downloads/advocacy/scope-education.pdf. Published November 1, 2010. Accessed October 11, 2017.
6. American Medical Association. Issue brief: independent nursing practice. https://www.ama-assn.org/system/files/media-browser/premium/arc/ama-issue-brief-independent-nursing-practice.pdf. Updated 2017.
7. Tabor J, Jennings N, Kohler L, et al. The supply of physician assistants, nurse practitioners, and certified nurse midwives in Arizona. University of Arizona. http://azahec.uahs.arizona.edu/sites/default/files/u9/supply_of_pa_np_cnm.pdf. Accessed October 11, 2017.
8. Hanrahan NP, Hartley D. Employment of advanced-practice psychiatric nurses to stem rural mental health workforce shortages. Psychiatr Serv. 2008;59(1):109-111.
9. 2017 NRMP Main Residency Match the largest match on record [press release]. Washington, DC: National Resident Matching Program; March 17, 2017. http://www.nrmp.org/press-release-2017-nrmp-main-residency-match-the-largest-match-on-record. Accessed October 11, 2017.
10. Resident Physician Shortage Reduction Act of 2017, HR 2267, 115th Cong, 1st session (2017).
The author responds
I would like to thank Dr. Kendall for her passionate letter about my editorial and provide the following response. I neither asserted the equivalency of doctors and nurses or that APRNs can do what MDs do. Rather, APRNs are educated to provide highly qualified, specialty-specific advanced practice nursing, according to the tightly regulated scope of practice defined by individual states. As stated in my editorial, psychiatric mental health (PMH) APRNs engage in the practice of advanced practice PMH nursing. Is there overlap with medicine, social work, and psychology? Of course, but we are not criticized by social workers and psychologists when we engage in various psychotherapeutic approaches; rather, we are collegial and refer to each other. Why are we criticized by physicians when we prescribe from our tightly regulated legend drugs or conduct a psychiatric intake and develop a differential diagnosis and formulation that may save a life in the absence of an available psychiatrist? I would offer that PMH-APRNs are proud of their vast history of collegial relationships with psychiatrists, and that in states where turf is not an issue, there is remarkable respect and mutual referrals based on the ultimate need of finding the most appropriate care for a patient and/or family struggling to live with a psychiatric disorder.
Currently, 26 states have legislated independent practice for APRNs. This legislation was passed after decades of compiling data on the safety and efficacy of patient care outcomes in those states, and then was submitted as testimony to the legislature. State legislature decisions often are influenced by the fact that malpractice claims are decreased in areas where APRNs are independent and increased when APRNs are associated with MDs. A 2009 study1 found that between 1991 and 2007—the first 17 years that the National Practitioner Data Bank was in operation—payments were made on behalf of 37% of physicians but only 3.1% of physician assistants (PAs) and 1.5% of nurse practitioners. The study concluded: “There were no observations or trends to suggest that PAs and APNs increase liability. If anything, they may decrease the rate of reporting malpractice and adverse events.”1
To respond to Dr. Kendall’s comment, “nursing was never designed to be an autonomous practice,” nursing at the entry level of registration was originally conceived by Florence Nightingale as an autonomous profession working side-by-side with physicians, each performing different yet complementary aspects of patient care, each answering to a different hierarchy. Her work in the Crimean War attests to the positive effects of nursing on saving soldiers’ lives, which was heretofore unknown due to all the measures she initiated and meticulously documented. This autonomy, however, was gradually usurped in the private sector. Comparing RNs with MDs is like comparing apples with oranges. We would need to compare all MDs with the 3.4 million registered nurses in the United States, and that is not what my editorial addressed.
For >50 years, master’s prepared advanced practice nurses in psychiatry have been independent in their ability to have private practices, initially focusing on the provision of individual, group, and family psychotherapy. Psychiatrists did not object to this because it opened services they were unable to provide. As psychopharmacologic treatments for psychiatric disorders emerged, APRNs who had the minimum of a master’s degree and substantial psychopharmacology education, which was mandated and regulated by states, were gradually allowed to prescribe starting in the late 1970s. Most typically, these practices were in collaboration with or under supervision of an MD, but as data and outcomes were collected, legislatures began to drop this requirement.
Regarding hours, we could compare the >2,000 classroom and clinical hours and years of clinical experience accumulated by PMH-APRNs in their undergraduate and graduate psychiatric nursing curricula with the 60-hour Psychiatric Medicine course taken in the second semester of the first year of medical school.2 For many physicians, this often is the only psychiatric education they receive when going into primary care. When we consider that 70% of psychiatric care is now provided in a primary care setting, we all should be concerned and be attempting to recruit highly qualified PMH-APRNs to assist in the development and delivery of integrated primary care.
Regarding APRNs working in rural areas, Hanrahan and Hartley3 found that psychiatric APRNs were more likely than psychiatrists to live in rural areas. I contend that the issue is not the zip code of the psychiatric APRN, but rather the need to fix the problem of providers not being drawn to practice in rural and underserved populations due to salary.
Promoting autonomy for PMH-APRNs in all states is not the only way to solve the provider supply shortage, but it is a reasonable way. Unfortunately, there will be a shortage of psychiatric providers no matter what we do. Those of us who are dedicated to providing care to this vulnerable population should be finding ways to maximize our efforts and efficiencies to lessen the critical shortage. Anything less only adds to the problem and sends a negative message to the public. If we psychiatric providers cannot be supportive of each discipline practicing to the full scope and authority of their hard-earned licenses, then we are saying that we are more interested in protecting turf than providing desperately needed care.
Mary D. Moller, DNP, ARNP, PMHCNS-BC, CPRP, FAAN
Associate Professor and Coordinator PMH-DNP ProgramPacific Lutheran University School of Nursing
Director of Psychiatric Services
Northwest Integrated Health
Tacoma, Washington
References
1. Hooker RS, Nicholson JG, Le T. Does the employment of physician assistants and nurse practitioners increase liability? Journal of Medical Licensure and Discipline. 2009;95(2): 6-16.
2. Columbia University Medical Center. Medical student education in psychiatry. https://www.columbiapsychiatry.org/education-and-training/medical-student-education-psychiatry. Accessed November 16, 2017.
3. Hanrahan NP, Hartley D. Employment of advanced-practice psychiatric nurses to stem rural mental health workforce shortages. Psychiatr Serv. 2008;59(1):109-111.
In Dr. Mary Moller’s Guest Editorial “Advancing the role of advanced practice psychiatric nurses in today’s psychiatric workforce” (
Dr. Moller cited a source from the Federal Trade Commission1 that encourages the autonomous practice of APRNs to increase competition. This again implies the false equivalency between physicians and APRNs. Competition implies that the players are providing the same service. If, as nurse practitioners argue, they practice “nursing,” then they are not practicing “medicine.” Physicians and APRNs do not have the same background. Although both are charged with the care of patients, nursing is not medicine, nor should it be. Both are important and needed, but nursing was never designed to be an autonomous practice. According to the American Association of Colleges of Nursing, “Nursing and medicine are distinct health disciplines that prepare clinicians to assume different roles and meet different practice expectations.”2 In fact, the curriculum and requirements to become an APRN vary depending on the program, and some programs do not even require a BSN.3 There are online programs available for earning an APRN degree. Additionally, APRNs are only required to have 500 to 700 total hours of patient care,4 compared with the >10,000 hours physicians have once they have finished a 3-year residency, which when combined with their education amounts to >20,000 hours.5 This doesn’t account for those who have longer residencies or fellowships to further specialize in their area of training.
Dr. Moller’s main argument is that there is a dire shortage of psychiatrists and that the only way to meet this need for more providers is to make APRNs autonomous. However, no data indicate that autonomous practice of mid-level providers leads to an influx of these providers in rural areas, where the need would be greatest. Although current data on this are quite sparse, some studies indicate that the majority practice in urban areas, even in states with independent practice authority.6,7 Dr. Moller cites a source that only reviewed home zip codes of psychiatric APRNs but did not include zip codes of employment.8 Only 13% of psychiatric APRNs live in rural areas across the United States. Therefore, it is a false assertion to state that these APRNs are found primarily in rural and less populated urban areas. It is also false to imply and assume that these APRNs practice in the rural areas.
In 2017, there were 43,157 registered physician applications, with 35,969 active applications for 31,757 residency positions in the United States, and at least 11,400 medical school graduates were unmatched.9 Imagine how much more we could serve our patients by matching these graduates, whose training far surpasses that of a mid-level provider. The Resident Physician Shortage Reduction Act of 2017 aims to address this problem by increasing Medicare-funded graduate medical education (GME) residency programs in the United States.10 We can make a difference by contacting our members of Congress to encourage them to support this bill. In addition, the AMA is advocating to save funding for GME and provides an easy-to-use Web site (https://savegme.org/take-action) to contact your legislators directly to show your support for GME.
Nurse practitioners have tremendous value when their role is a part of a team; however, they should not practice without supervision, and physicians who supervise them absolutely should be providing adequate supervision. I applaud the APA and the AMA for standing up for the practice of medicine and for our patients. I hope that they continue to do so, and I encourage them to increase their efforts.
Laura Kendall, MD
Assistant Professor of Clinical Psychiatry
Department of Psychiatry and Behavioral Sciences
Keck School of Medicine
University of Southern California
Los Angeles, California
References
1. Koslov T; Office of Policy Planning. The doctor (or nurse practitioner) will see you now: competition and the regulation of advanced practice nurses. Federal Trade Commission. https://www.ftc.gov/news-events/blogs/competition-matters/2014/03/doctor-or-nurse-practitioner-will-see-you-now. Published March 7, 2014. Accessed July 26, 2017.
2. American Association of Colleges of Nursing. DNP talking points. http://www.aacnnursing.org/DNP/about/talking-points. Updated July, 2014. Accessed August 12, 2017.
3. Keyes L. MSN without a BSN? MastersInNursing.com. https://www.mastersinnursing.com/msn-without-a-bsn. Accessed August 12, 2017.
4. Iglehart JK. Expanding the role of advanced nurse practitioners—risks and rewards. New Engl J Med. 2013;368(20):1935-1941.
5. Primary Care Coalition. Issue brief: collaboration between physicians and nurses works. Compare the education gaps between primary care physicians and nurse practitioners. http://www.tafp.org/Media/Default/Downloads/advocacy/scope-education.pdf. Published November 1, 2010. Accessed October 11, 2017.
6. American Medical Association. Issue brief: independent nursing practice. https://www.ama-assn.org/system/files/media-browser/premium/arc/ama-issue-brief-independent-nursing-practice.pdf. Updated 2017.
7. Tabor J, Jennings N, Kohler L, et al. The supply of physician assistants, nurse practitioners, and certified nurse midwives in Arizona. University of Arizona. http://azahec.uahs.arizona.edu/sites/default/files/u9/supply_of_pa_np_cnm.pdf. Accessed October 11, 2017.
8. Hanrahan NP, Hartley D. Employment of advanced-practice psychiatric nurses to stem rural mental health workforce shortages. Psychiatr Serv. 2008;59(1):109-111.
9. 2017 NRMP Main Residency Match the largest match on record [press release]. Washington, DC: National Resident Matching Program; March 17, 2017. http://www.nrmp.org/press-release-2017-nrmp-main-residency-match-the-largest-match-on-record. Accessed October 11, 2017.
10. Resident Physician Shortage Reduction Act of 2017, HR 2267, 115th Cong, 1st session (2017).
The author responds
I would like to thank Dr. Kendall for her passionate letter about my editorial and provide the following response. I neither asserted the equivalency of doctors and nurses or that APRNs can do what MDs do. Rather, APRNs are educated to provide highly qualified, specialty-specific advanced practice nursing, according to the tightly regulated scope of practice defined by individual states. As stated in my editorial, psychiatric mental health (PMH) APRNs engage in the practice of advanced practice PMH nursing. Is there overlap with medicine, social work, and psychology? Of course, but we are not criticized by social workers and psychologists when we engage in various psychotherapeutic approaches; rather, we are collegial and refer to each other. Why are we criticized by physicians when we prescribe from our tightly regulated legend drugs or conduct a psychiatric intake and develop a differential diagnosis and formulation that may save a life in the absence of an available psychiatrist? I would offer that PMH-APRNs are proud of their vast history of collegial relationships with psychiatrists, and that in states where turf is not an issue, there is remarkable respect and mutual referrals based on the ultimate need of finding the most appropriate care for a patient and/or family struggling to live with a psychiatric disorder.
Currently, 26 states have legislated independent practice for APRNs. This legislation was passed after decades of compiling data on the safety and efficacy of patient care outcomes in those states, and then was submitted as testimony to the legislature. State legislature decisions often are influenced by the fact that malpractice claims are decreased in areas where APRNs are independent and increased when APRNs are associated with MDs. A 2009 study1 found that between 1991 and 2007—the first 17 years that the National Practitioner Data Bank was in operation—payments were made on behalf of 37% of physicians but only 3.1% of physician assistants (PAs) and 1.5% of nurse practitioners. The study concluded: “There were no observations or trends to suggest that PAs and APNs increase liability. If anything, they may decrease the rate of reporting malpractice and adverse events.”1
To respond to Dr. Kendall’s comment, “nursing was never designed to be an autonomous practice,” nursing at the entry level of registration was originally conceived by Florence Nightingale as an autonomous profession working side-by-side with physicians, each performing different yet complementary aspects of patient care, each answering to a different hierarchy. Her work in the Crimean War attests to the positive effects of nursing on saving soldiers’ lives, which was heretofore unknown due to all the measures she initiated and meticulously documented. This autonomy, however, was gradually usurped in the private sector. Comparing RNs with MDs is like comparing apples with oranges. We would need to compare all MDs with the 3.4 million registered nurses in the United States, and that is not what my editorial addressed.
For >50 years, master’s prepared advanced practice nurses in psychiatry have been independent in their ability to have private practices, initially focusing on the provision of individual, group, and family psychotherapy. Psychiatrists did not object to this because it opened services they were unable to provide. As psychopharmacologic treatments for psychiatric disorders emerged, APRNs who had the minimum of a master’s degree and substantial psychopharmacology education, which was mandated and regulated by states, were gradually allowed to prescribe starting in the late 1970s. Most typically, these practices were in collaboration with or under supervision of an MD, but as data and outcomes were collected, legislatures began to drop this requirement.
Regarding hours, we could compare the >2,000 classroom and clinical hours and years of clinical experience accumulated by PMH-APRNs in their undergraduate and graduate psychiatric nursing curricula with the 60-hour Psychiatric Medicine course taken in the second semester of the first year of medical school.2 For many physicians, this often is the only psychiatric education they receive when going into primary care. When we consider that 70% of psychiatric care is now provided in a primary care setting, we all should be concerned and be attempting to recruit highly qualified PMH-APRNs to assist in the development and delivery of integrated primary care.
Regarding APRNs working in rural areas, Hanrahan and Hartley3 found that psychiatric APRNs were more likely than psychiatrists to live in rural areas. I contend that the issue is not the zip code of the psychiatric APRN, but rather the need to fix the problem of providers not being drawn to practice in rural and underserved populations due to salary.
Promoting autonomy for PMH-APRNs in all states is not the only way to solve the provider supply shortage, but it is a reasonable way. Unfortunately, there will be a shortage of psychiatric providers no matter what we do. Those of us who are dedicated to providing care to this vulnerable population should be finding ways to maximize our efforts and efficiencies to lessen the critical shortage. Anything less only adds to the problem and sends a negative message to the public. If we psychiatric providers cannot be supportive of each discipline practicing to the full scope and authority of their hard-earned licenses, then we are saying that we are more interested in protecting turf than providing desperately needed care.
Mary D. Moller, DNP, ARNP, PMHCNS-BC, CPRP, FAAN
Associate Professor and Coordinator PMH-DNP ProgramPacific Lutheran University School of Nursing
Director of Psychiatric Services
Northwest Integrated Health
Tacoma, Washington
References
1. Hooker RS, Nicholson JG, Le T. Does the employment of physician assistants and nurse practitioners increase liability? Journal of Medical Licensure and Discipline. 2009;95(2): 6-16.
2. Columbia University Medical Center. Medical student education in psychiatry. https://www.columbiapsychiatry.org/education-and-training/medical-student-education-psychiatry. Accessed November 16, 2017.
3. Hanrahan NP, Hartley D. Employment of advanced-practice psychiatric nurses to stem rural mental health workforce shortages. Psychiatr Serv. 2008;59(1):109-111.
In Dr. Mary Moller’s Guest Editorial “Advancing the role of advanced practice psychiatric nurses in today’s psychiatric workforce” (
Dr. Moller cited a source from the Federal Trade Commission1 that encourages the autonomous practice of APRNs to increase competition. This again implies the false equivalency between physicians and APRNs. Competition implies that the players are providing the same service. If, as nurse practitioners argue, they practice “nursing,” then they are not practicing “medicine.” Physicians and APRNs do not have the same background. Although both are charged with the care of patients, nursing is not medicine, nor should it be. Both are important and needed, but nursing was never designed to be an autonomous practice. According to the American Association of Colleges of Nursing, “Nursing and medicine are distinct health disciplines that prepare clinicians to assume different roles and meet different practice expectations.”2 In fact, the curriculum and requirements to become an APRN vary depending on the program, and some programs do not even require a BSN.3 There are online programs available for earning an APRN degree. Additionally, APRNs are only required to have 500 to 700 total hours of patient care,4 compared with the >10,000 hours physicians have once they have finished a 3-year residency, which when combined with their education amounts to >20,000 hours.5 This doesn’t account for those who have longer residencies or fellowships to further specialize in their area of training.
Dr. Moller’s main argument is that there is a dire shortage of psychiatrists and that the only way to meet this need for more providers is to make APRNs autonomous. However, no data indicate that autonomous practice of mid-level providers leads to an influx of these providers in rural areas, where the need would be greatest. Although current data on this are quite sparse, some studies indicate that the majority practice in urban areas, even in states with independent practice authority.6,7 Dr. Moller cites a source that only reviewed home zip codes of psychiatric APRNs but did not include zip codes of employment.8 Only 13% of psychiatric APRNs live in rural areas across the United States. Therefore, it is a false assertion to state that these APRNs are found primarily in rural and less populated urban areas. It is also false to imply and assume that these APRNs practice in the rural areas.
In 2017, there were 43,157 registered physician applications, with 35,969 active applications for 31,757 residency positions in the United States, and at least 11,400 medical school graduates were unmatched.9 Imagine how much more we could serve our patients by matching these graduates, whose training far surpasses that of a mid-level provider. The Resident Physician Shortage Reduction Act of 2017 aims to address this problem by increasing Medicare-funded graduate medical education (GME) residency programs in the United States.10 We can make a difference by contacting our members of Congress to encourage them to support this bill. In addition, the AMA is advocating to save funding for GME and provides an easy-to-use Web site (https://savegme.org/take-action) to contact your legislators directly to show your support for GME.
Nurse practitioners have tremendous value when their role is a part of a team; however, they should not practice without supervision, and physicians who supervise them absolutely should be providing adequate supervision. I applaud the APA and the AMA for standing up for the practice of medicine and for our patients. I hope that they continue to do so, and I encourage them to increase their efforts.
Laura Kendall, MD
Assistant Professor of Clinical Psychiatry
Department of Psychiatry and Behavioral Sciences
Keck School of Medicine
University of Southern California
Los Angeles, California
References
1. Koslov T; Office of Policy Planning. The doctor (or nurse practitioner) will see you now: competition and the regulation of advanced practice nurses. Federal Trade Commission. https://www.ftc.gov/news-events/blogs/competition-matters/2014/03/doctor-or-nurse-practitioner-will-see-you-now. Published March 7, 2014. Accessed July 26, 2017.
2. American Association of Colleges of Nursing. DNP talking points. http://www.aacnnursing.org/DNP/about/talking-points. Updated July, 2014. Accessed August 12, 2017.
3. Keyes L. MSN without a BSN? MastersInNursing.com. https://www.mastersinnursing.com/msn-without-a-bsn. Accessed August 12, 2017.
4. Iglehart JK. Expanding the role of advanced nurse practitioners—risks and rewards. New Engl J Med. 2013;368(20):1935-1941.
5. Primary Care Coalition. Issue brief: collaboration between physicians and nurses works. Compare the education gaps between primary care physicians and nurse practitioners. http://www.tafp.org/Media/Default/Downloads/advocacy/scope-education.pdf. Published November 1, 2010. Accessed October 11, 2017.
6. American Medical Association. Issue brief: independent nursing practice. https://www.ama-assn.org/system/files/media-browser/premium/arc/ama-issue-brief-independent-nursing-practice.pdf. Updated 2017.
7. Tabor J, Jennings N, Kohler L, et al. The supply of physician assistants, nurse practitioners, and certified nurse midwives in Arizona. University of Arizona. http://azahec.uahs.arizona.edu/sites/default/files/u9/supply_of_pa_np_cnm.pdf. Accessed October 11, 2017.
8. Hanrahan NP, Hartley D. Employment of advanced-practice psychiatric nurses to stem rural mental health workforce shortages. Psychiatr Serv. 2008;59(1):109-111.
9. 2017 NRMP Main Residency Match the largest match on record [press release]. Washington, DC: National Resident Matching Program; March 17, 2017. http://www.nrmp.org/press-release-2017-nrmp-main-residency-match-the-largest-match-on-record. Accessed October 11, 2017.
10. Resident Physician Shortage Reduction Act of 2017, HR 2267, 115th Cong, 1st session (2017).
The author responds
I would like to thank Dr. Kendall for her passionate letter about my editorial and provide the following response. I neither asserted the equivalency of doctors and nurses or that APRNs can do what MDs do. Rather, APRNs are educated to provide highly qualified, specialty-specific advanced practice nursing, according to the tightly regulated scope of practice defined by individual states. As stated in my editorial, psychiatric mental health (PMH) APRNs engage in the practice of advanced practice PMH nursing. Is there overlap with medicine, social work, and psychology? Of course, but we are not criticized by social workers and psychologists when we engage in various psychotherapeutic approaches; rather, we are collegial and refer to each other. Why are we criticized by physicians when we prescribe from our tightly regulated legend drugs or conduct a psychiatric intake and develop a differential diagnosis and formulation that may save a life in the absence of an available psychiatrist? I would offer that PMH-APRNs are proud of their vast history of collegial relationships with psychiatrists, and that in states where turf is not an issue, there is remarkable respect and mutual referrals based on the ultimate need of finding the most appropriate care for a patient and/or family struggling to live with a psychiatric disorder.
Currently, 26 states have legislated independent practice for APRNs. This legislation was passed after decades of compiling data on the safety and efficacy of patient care outcomes in those states, and then was submitted as testimony to the legislature. State legislature decisions often are influenced by the fact that malpractice claims are decreased in areas where APRNs are independent and increased when APRNs are associated with MDs. A 2009 study1 found that between 1991 and 2007—the first 17 years that the National Practitioner Data Bank was in operation—payments were made on behalf of 37% of physicians but only 3.1% of physician assistants (PAs) and 1.5% of nurse practitioners. The study concluded: “There were no observations or trends to suggest that PAs and APNs increase liability. If anything, they may decrease the rate of reporting malpractice and adverse events.”1
To respond to Dr. Kendall’s comment, “nursing was never designed to be an autonomous practice,” nursing at the entry level of registration was originally conceived by Florence Nightingale as an autonomous profession working side-by-side with physicians, each performing different yet complementary aspects of patient care, each answering to a different hierarchy. Her work in the Crimean War attests to the positive effects of nursing on saving soldiers’ lives, which was heretofore unknown due to all the measures she initiated and meticulously documented. This autonomy, however, was gradually usurped in the private sector. Comparing RNs with MDs is like comparing apples with oranges. We would need to compare all MDs with the 3.4 million registered nurses in the United States, and that is not what my editorial addressed.
For >50 years, master’s prepared advanced practice nurses in psychiatry have been independent in their ability to have private practices, initially focusing on the provision of individual, group, and family psychotherapy. Psychiatrists did not object to this because it opened services they were unable to provide. As psychopharmacologic treatments for psychiatric disorders emerged, APRNs who had the minimum of a master’s degree and substantial psychopharmacology education, which was mandated and regulated by states, were gradually allowed to prescribe starting in the late 1970s. Most typically, these practices were in collaboration with or under supervision of an MD, but as data and outcomes were collected, legislatures began to drop this requirement.
Regarding hours, we could compare the >2,000 classroom and clinical hours and years of clinical experience accumulated by PMH-APRNs in their undergraduate and graduate psychiatric nursing curricula with the 60-hour Psychiatric Medicine course taken in the second semester of the first year of medical school.2 For many physicians, this often is the only psychiatric education they receive when going into primary care. When we consider that 70% of psychiatric care is now provided in a primary care setting, we all should be concerned and be attempting to recruit highly qualified PMH-APRNs to assist in the development and delivery of integrated primary care.
Regarding APRNs working in rural areas, Hanrahan and Hartley3 found that psychiatric APRNs were more likely than psychiatrists to live in rural areas. I contend that the issue is not the zip code of the psychiatric APRN, but rather the need to fix the problem of providers not being drawn to practice in rural and underserved populations due to salary.
Promoting autonomy for PMH-APRNs in all states is not the only way to solve the provider supply shortage, but it is a reasonable way. Unfortunately, there will be a shortage of psychiatric providers no matter what we do. Those of us who are dedicated to providing care to this vulnerable population should be finding ways to maximize our efforts and efficiencies to lessen the critical shortage. Anything less only adds to the problem and sends a negative message to the public. If we psychiatric providers cannot be supportive of each discipline practicing to the full scope and authority of their hard-earned licenses, then we are saying that we are more interested in protecting turf than providing desperately needed care.
Mary D. Moller, DNP, ARNP, PMHCNS-BC, CPRP, FAAN
Associate Professor and Coordinator PMH-DNP ProgramPacific Lutheran University School of Nursing
Director of Psychiatric Services
Northwest Integrated Health
Tacoma, Washington
References
1. Hooker RS, Nicholson JG, Le T. Does the employment of physician assistants and nurse practitioners increase liability? Journal of Medical Licensure and Discipline. 2009;95(2): 6-16.
2. Columbia University Medical Center. Medical student education in psychiatry. https://www.columbiapsychiatry.org/education-and-training/medical-student-education-psychiatry. Accessed November 16, 2017.
3. Hanrahan NP, Hartley D. Employment of advanced-practice psychiatric nurses to stem rural mental health workforce shortages. Psychiatr Serv. 2008;59(1):109-111.