User login
How are your otoscopy skills?
If the name Michael E. Pichichero, MD, is unfamiliar, you haven’t been reading some of the best articles on this website . Dr. Pichichero, an infectious disease specialist at the Research Institute at the Rochester General Hospital in New York, reports in his most recent ID Consult column on new research presented at the June 2019 meeting of the International Society for Otitis Media, including topics such as transtympanic antibiotic delivery, biofilms, probiotics, and biomarkers.
Dr. Pichichero described work he and his colleagues have been doing on the impact of overdiagnosis of acute otitis media (AOM). They found when “validated otoscopists” evaluated children, half as many reached the diagnostic threshold of being labeled “otitis prone” as when community-based pediatricians performed the exams.
Looking around at the colleagues with whom you share patients, do you find that some of them diagnose AOM much more frequently than does the coverage group average? How often do you see a child a day or two after he has been diagnosed with AOM by a colleague and find that the child’s tympanic membranes are transparent and mobile? Do you or your practice group keep track of each provider’s diagnostic tendencies? If these data exists, is there a mechanism for addressing apparent outliers? I suspect that the answer to those last two questions is a firm “No.”
I don’t have the stomach this morning to open those two cans of worms. But certainly Dr. Pichichero’s findings suggest that these are issues that need to be addressed. How the process should proceed in a nonthreatening way is a story for another day. But I’m not sure that involving your community ear, nose, and throat (ENT) specialist as a resource is the best answer. The scenarios in which pediatricians and ENTs perform otoscopies couldn’t be more different. In the pediatrician’s office, the child is generally sick, feverish, and possibly in pain. In the ENT’s office, the acute process has probably passed and the assessment may lean more heavily on history. The child is more likely to accept the exam without resistance, and the findings are not those of AOM but of a chronic process. The fact that Dr. Pichichero has been able to find and train “validated otoscopists” suggests that improving the quality of otoscopy among the physicians in communities like yours and mine is achievable.
How are your otoscopy skills? Do feel comfortable that you can do a good exam and accurately diagnose AOM? When did you acquire that comfort level? Probably not in medical school. More likely as a house officer when you were guided by a more senior house officer who may nor not been a master otoscopist. How would you rate your training? Or were you self-taught? Do you insufflate? Are you a skilled cerumen extractor? Or do you give up after one attempt? Be honest. How is your equipment? Are the bulbs and batteries fresh? Do you find yourself frustrated by an otoscope that is tethered to the wall charger by a cord that ensnarls you, the parent, and the patient? Have you complained to the practice administrators that your otoscopes are inadequate?
These are not minor issues. It is clear that overdiagnosis of AOM happens. It may occur even more often than Dr. Pichichero suggests, but I doubt it is less. Overdiagnosis can result in overtreatment with antibiotics, and the cascade of consequences both for the patient, the community, and the environment. Overdiagnosis can be the first step on the path to unnecessary surgery. It is incumbent on all of us to make sure that our otoscopy skills and those of our colleagues are sharp, that our equipment is well maintained and that we remain abreast of the latest developments in the diagnosis and treatment of AOM.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
If the name Michael E. Pichichero, MD, is unfamiliar, you haven’t been reading some of the best articles on this website . Dr. Pichichero, an infectious disease specialist at the Research Institute at the Rochester General Hospital in New York, reports in his most recent ID Consult column on new research presented at the June 2019 meeting of the International Society for Otitis Media, including topics such as transtympanic antibiotic delivery, biofilms, probiotics, and biomarkers.
Dr. Pichichero described work he and his colleagues have been doing on the impact of overdiagnosis of acute otitis media (AOM). They found when “validated otoscopists” evaluated children, half as many reached the diagnostic threshold of being labeled “otitis prone” as when community-based pediatricians performed the exams.
Looking around at the colleagues with whom you share patients, do you find that some of them diagnose AOM much more frequently than does the coverage group average? How often do you see a child a day or two after he has been diagnosed with AOM by a colleague and find that the child’s tympanic membranes are transparent and mobile? Do you or your practice group keep track of each provider’s diagnostic tendencies? If these data exists, is there a mechanism for addressing apparent outliers? I suspect that the answer to those last two questions is a firm “No.”
I don’t have the stomach this morning to open those two cans of worms. But certainly Dr. Pichichero’s findings suggest that these are issues that need to be addressed. How the process should proceed in a nonthreatening way is a story for another day. But I’m not sure that involving your community ear, nose, and throat (ENT) specialist as a resource is the best answer. The scenarios in which pediatricians and ENTs perform otoscopies couldn’t be more different. In the pediatrician’s office, the child is generally sick, feverish, and possibly in pain. In the ENT’s office, the acute process has probably passed and the assessment may lean more heavily on history. The child is more likely to accept the exam without resistance, and the findings are not those of AOM but of a chronic process. The fact that Dr. Pichichero has been able to find and train “validated otoscopists” suggests that improving the quality of otoscopy among the physicians in communities like yours and mine is achievable.
How are your otoscopy skills? Do feel comfortable that you can do a good exam and accurately diagnose AOM? When did you acquire that comfort level? Probably not in medical school. More likely as a house officer when you were guided by a more senior house officer who may nor not been a master otoscopist. How would you rate your training? Or were you self-taught? Do you insufflate? Are you a skilled cerumen extractor? Or do you give up after one attempt? Be honest. How is your equipment? Are the bulbs and batteries fresh? Do you find yourself frustrated by an otoscope that is tethered to the wall charger by a cord that ensnarls you, the parent, and the patient? Have you complained to the practice administrators that your otoscopes are inadequate?
These are not minor issues. It is clear that overdiagnosis of AOM happens. It may occur even more often than Dr. Pichichero suggests, but I doubt it is less. Overdiagnosis can result in overtreatment with antibiotics, and the cascade of consequences both for the patient, the community, and the environment. Overdiagnosis can be the first step on the path to unnecessary surgery. It is incumbent on all of us to make sure that our otoscopy skills and those of our colleagues are sharp, that our equipment is well maintained and that we remain abreast of the latest developments in the diagnosis and treatment of AOM.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
If the name Michael E. Pichichero, MD, is unfamiliar, you haven’t been reading some of the best articles on this website . Dr. Pichichero, an infectious disease specialist at the Research Institute at the Rochester General Hospital in New York, reports in his most recent ID Consult column on new research presented at the June 2019 meeting of the International Society for Otitis Media, including topics such as transtympanic antibiotic delivery, biofilms, probiotics, and biomarkers.
Dr. Pichichero described work he and his colleagues have been doing on the impact of overdiagnosis of acute otitis media (AOM). They found when “validated otoscopists” evaluated children, half as many reached the diagnostic threshold of being labeled “otitis prone” as when community-based pediatricians performed the exams.
Looking around at the colleagues with whom you share patients, do you find that some of them diagnose AOM much more frequently than does the coverage group average? How often do you see a child a day or two after he has been diagnosed with AOM by a colleague and find that the child’s tympanic membranes are transparent and mobile? Do you or your practice group keep track of each provider’s diagnostic tendencies? If these data exists, is there a mechanism for addressing apparent outliers? I suspect that the answer to those last two questions is a firm “No.”
I don’t have the stomach this morning to open those two cans of worms. But certainly Dr. Pichichero’s findings suggest that these are issues that need to be addressed. How the process should proceed in a nonthreatening way is a story for another day. But I’m not sure that involving your community ear, nose, and throat (ENT) specialist as a resource is the best answer. The scenarios in which pediatricians and ENTs perform otoscopies couldn’t be more different. In the pediatrician’s office, the child is generally sick, feverish, and possibly in pain. In the ENT’s office, the acute process has probably passed and the assessment may lean more heavily on history. The child is more likely to accept the exam without resistance, and the findings are not those of AOM but of a chronic process. The fact that Dr. Pichichero has been able to find and train “validated otoscopists” suggests that improving the quality of otoscopy among the physicians in communities like yours and mine is achievable.
How are your otoscopy skills? Do feel comfortable that you can do a good exam and accurately diagnose AOM? When did you acquire that comfort level? Probably not in medical school. More likely as a house officer when you were guided by a more senior house officer who may nor not been a master otoscopist. How would you rate your training? Or were you self-taught? Do you insufflate? Are you a skilled cerumen extractor? Or do you give up after one attempt? Be honest. How is your equipment? Are the bulbs and batteries fresh? Do you find yourself frustrated by an otoscope that is tethered to the wall charger by a cord that ensnarls you, the parent, and the patient? Have you complained to the practice administrators that your otoscopes are inadequate?
These are not minor issues. It is clear that overdiagnosis of AOM happens. It may occur even more often than Dr. Pichichero suggests, but I doubt it is less. Overdiagnosis can result in overtreatment with antibiotics, and the cascade of consequences both for the patient, the community, and the environment. Overdiagnosis can be the first step on the path to unnecessary surgery. It is incumbent on all of us to make sure that our otoscopy skills and those of our colleagues are sharp, that our equipment is well maintained and that we remain abreast of the latest developments in the diagnosis and treatment of AOM.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Living small
I’m sitting on the porch looking out at our little harbor, listening to the murmurings of the family of renters who have just moved into the cottage next door. We are on the cusp of the tourist season that draws millions of visitors – more than 36 million in 2017 – to a state that has less than a million and a half year-round residents during the other 9 months. Why do the “people from away” come?
The water is too cold for swimming most of the summer in Maine. But we have forested mountains, rocky shores, and we’re small. When I chat with the visitors sharing our stony little beach, they often ask if I live here and tell me how lucky I am because they envy the quiet, the friendly people, the lack of traffic, and the sense of community that they feel here in Vacationland.
My being here in Maine wasn’t a stroke of luck. It was a conscious decision that my wife and I made when I finished my training. The lucky part was meeting my wife who was born here. Through her I learned what Maine was about. I had grown up in a small town of 5,000 (although it was the suburb of a city of millions) and went to a small college in rural New Hampshire with an enrollment of a little more than 3,000. I turned down residencies in pediatric radiology and dermatology because I knew that to have a sustainable patient base we would have needed to live in a major metropolitan center.
I was accustomed to the benefits of living small. In the 1970s, the local economy in mid-coast Maine was shaky, the biggest employer had not yet secured the large military contracts it needed to thrive. But we decided it was a risk worth taking, and we have never regretted for a second living and practicing in a town of less than 20,000.
With this history as a backdrop, you can understand why I am a bit puzzled and disappointed by the results of a 2019 survey final-year medical residents recently published by the medical search and consulting firm Merritt Hawkins. Although the sample size is small (391 respondents out of 20,000 email surveys), the responses probably are a reasonable reflection of the opinions of the entire population of final-year residents. More than 80% of the respondents said that they would most like to practice in a community with a population of more than 100,000, and 65% would prefer a population base of more than 250,000. This would automatically rule out Maine, where our largest city has less than 80,000 people.
I can easily understand why physicians finishing their residency would avoid practice opportunities in remote, thinly populated regions in which they might find themselves as the only, or one of only two physicians serving a medically needy, economically depressed population spread out over a wide geographic area. That kind of challenge has some appeal for the saintly few, or the dreamy-eyed idealists. But in my experience, those work environments require so much energy that most physicians last only a few years because being on call is so taxing.
However, I know of several right here in Maine. What is driving young physicians to seek larger communities? It may be that because teaching hospitals are usually in more densely populated communities, many residents lack sufficient exposure to role models who are practicing in smaller settings. Compounding this dearth of role models is the unfortunate and often inaccurate image in which local doctors are cast as bumbling and clueless. I was fortunate because where I did my first 2 years of training, the local pediatricians played an active role and were very visible role models of how one can enjoy practice in a smaller community.
I guess I can’t ignore the obvious that a larger population base may be able guarantee an income that could sound appealing to the more than 50% of residents who will complete their training with a sizable debt.
However, I fear that too many residents nearing the end of their training believe that the “quality of life” that they claim to be seeking can’t be found in a small community practice. They would do well to speak to a few of us who have enjoyed and prospered by living small.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
I’m sitting on the porch looking out at our little harbor, listening to the murmurings of the family of renters who have just moved into the cottage next door. We are on the cusp of the tourist season that draws millions of visitors – more than 36 million in 2017 – to a state that has less than a million and a half year-round residents during the other 9 months. Why do the “people from away” come?
The water is too cold for swimming most of the summer in Maine. But we have forested mountains, rocky shores, and we’re small. When I chat with the visitors sharing our stony little beach, they often ask if I live here and tell me how lucky I am because they envy the quiet, the friendly people, the lack of traffic, and the sense of community that they feel here in Vacationland.
My being here in Maine wasn’t a stroke of luck. It was a conscious decision that my wife and I made when I finished my training. The lucky part was meeting my wife who was born here. Through her I learned what Maine was about. I had grown up in a small town of 5,000 (although it was the suburb of a city of millions) and went to a small college in rural New Hampshire with an enrollment of a little more than 3,000. I turned down residencies in pediatric radiology and dermatology because I knew that to have a sustainable patient base we would have needed to live in a major metropolitan center.
I was accustomed to the benefits of living small. In the 1970s, the local economy in mid-coast Maine was shaky, the biggest employer had not yet secured the large military contracts it needed to thrive. But we decided it was a risk worth taking, and we have never regretted for a second living and practicing in a town of less than 20,000.
With this history as a backdrop, you can understand why I am a bit puzzled and disappointed by the results of a 2019 survey final-year medical residents recently published by the medical search and consulting firm Merritt Hawkins. Although the sample size is small (391 respondents out of 20,000 email surveys), the responses probably are a reasonable reflection of the opinions of the entire population of final-year residents. More than 80% of the respondents said that they would most like to practice in a community with a population of more than 100,000, and 65% would prefer a population base of more than 250,000. This would automatically rule out Maine, where our largest city has less than 80,000 people.
I can easily understand why physicians finishing their residency would avoid practice opportunities in remote, thinly populated regions in which they might find themselves as the only, or one of only two physicians serving a medically needy, economically depressed population spread out over a wide geographic area. That kind of challenge has some appeal for the saintly few, or the dreamy-eyed idealists. But in my experience, those work environments require so much energy that most physicians last only a few years because being on call is so taxing.
However, I know of several right here in Maine. What is driving young physicians to seek larger communities? It may be that because teaching hospitals are usually in more densely populated communities, many residents lack sufficient exposure to role models who are practicing in smaller settings. Compounding this dearth of role models is the unfortunate and often inaccurate image in which local doctors are cast as bumbling and clueless. I was fortunate because where I did my first 2 years of training, the local pediatricians played an active role and were very visible role models of how one can enjoy practice in a smaller community.
I guess I can’t ignore the obvious that a larger population base may be able guarantee an income that could sound appealing to the more than 50% of residents who will complete their training with a sizable debt.
However, I fear that too many residents nearing the end of their training believe that the “quality of life” that they claim to be seeking can’t be found in a small community practice. They would do well to speak to a few of us who have enjoyed and prospered by living small.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
I’m sitting on the porch looking out at our little harbor, listening to the murmurings of the family of renters who have just moved into the cottage next door. We are on the cusp of the tourist season that draws millions of visitors – more than 36 million in 2017 – to a state that has less than a million and a half year-round residents during the other 9 months. Why do the “people from away” come?
The water is too cold for swimming most of the summer in Maine. But we have forested mountains, rocky shores, and we’re small. When I chat with the visitors sharing our stony little beach, they often ask if I live here and tell me how lucky I am because they envy the quiet, the friendly people, the lack of traffic, and the sense of community that they feel here in Vacationland.
My being here in Maine wasn’t a stroke of luck. It was a conscious decision that my wife and I made when I finished my training. The lucky part was meeting my wife who was born here. Through her I learned what Maine was about. I had grown up in a small town of 5,000 (although it was the suburb of a city of millions) and went to a small college in rural New Hampshire with an enrollment of a little more than 3,000. I turned down residencies in pediatric radiology and dermatology because I knew that to have a sustainable patient base we would have needed to live in a major metropolitan center.
I was accustomed to the benefits of living small. In the 1970s, the local economy in mid-coast Maine was shaky, the biggest employer had not yet secured the large military contracts it needed to thrive. But we decided it was a risk worth taking, and we have never regretted for a second living and practicing in a town of less than 20,000.
With this history as a backdrop, you can understand why I am a bit puzzled and disappointed by the results of a 2019 survey final-year medical residents recently published by the medical search and consulting firm Merritt Hawkins. Although the sample size is small (391 respondents out of 20,000 email surveys), the responses probably are a reasonable reflection of the opinions of the entire population of final-year residents. More than 80% of the respondents said that they would most like to practice in a community with a population of more than 100,000, and 65% would prefer a population base of more than 250,000. This would automatically rule out Maine, where our largest city has less than 80,000 people.
I can easily understand why physicians finishing their residency would avoid practice opportunities in remote, thinly populated regions in which they might find themselves as the only, or one of only two physicians serving a medically needy, economically depressed population spread out over a wide geographic area. That kind of challenge has some appeal for the saintly few, or the dreamy-eyed idealists. But in my experience, those work environments require so much energy that most physicians last only a few years because being on call is so taxing.
However, I know of several right here in Maine. What is driving young physicians to seek larger communities? It may be that because teaching hospitals are usually in more densely populated communities, many residents lack sufficient exposure to role models who are practicing in smaller settings. Compounding this dearth of role models is the unfortunate and often inaccurate image in which local doctors are cast as bumbling and clueless. I was fortunate because where I did my first 2 years of training, the local pediatricians played an active role and were very visible role models of how one can enjoy practice in a smaller community.
I guess I can’t ignore the obvious that a larger population base may be able guarantee an income that could sound appealing to the more than 50% of residents who will complete their training with a sizable debt.
However, I fear that too many residents nearing the end of their training believe that the “quality of life” that they claim to be seeking can’t be found in a small community practice. They would do well to speak to a few of us who have enjoyed and prospered by living small.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Potential improvements in convenience, tolerability of hematologic treatment
In this edition of “How I will treat my next patient,” I highlight two recent presentations regarding potential improvements in the convenience and tolerability of treatment for two hematologic malignancies: multiple myeloma and chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL).
SC-Dara in myeloma
At the 2019 annual meeting of the American Society of Clinical Oncology, Maria-Victoria Mateos, MD, PhD, and colleagues, reported the results of COLUMBA, a phase 3 evaluation in 522 patients with multiple myeloma who were randomized to subcutaneous daratumumab (SC-Dara) or standard intravenous infusions of daratumumab (IV-Dara). A previous phase 1b study (Blood. 2017;130:838) had suggested comparable efficacy from the more convenient SC regime. Whereas conventional infusions of IV-Dara (16 mg/kg) take several hours, the SC formulation (1,800 mg–flat dose) is delivered in minutes. In COLUMBA, patients were randomized between SC- and IV-Dara weekly (cycles 1-2), then every 2 weeks (cycles 3-6), then every 4 weeks until disease progression.
Among the IV-Dara patients, the median duration of the first infusion was 421 minutes in cycle 1, 255 minutes in cycle 2, and 205 minutes in subsequent cycles – compatible with standard practice in the United States. As reported, at a median follow-up of 7.46 months, the efficacy (overall response rate, complete response rate, stringent-complete response rate, very good-partial response rate, progression-free survival, and 6-month overall survival) and safety profile were non-inferior for SC-Dara. SC-Dara patients also reported higher satisfaction with therapy.
What this means in practice
It is always a good idea to await publication of the manuscript because there may be study details and statistical nuances that make SC-Dara appear better than it will prove to be. For example, patient characteristics were slightly different between the two arms. Peer review of the final manuscript could be important in placing these results in context.
However, for treatments that demand frequent office visits over many months, reducing treatment burden for patients has value. Based on COLUMBA, it appears likely that SC-Dara will be a major convenience for patients, without obvious drawbacks in efficacy or toxicity. Meanwhile, flat dosing will be a time-saver for physicians, nursing, and pharmacy staff. If the price of the SC formulation is not exorbitant, I would expect a “win-win” that will support converting from IV- to SC-Dara as standard practice.
Acalabrutinib in CLL/SLL
Preclinical studies have shown acalabrutinib (Acala) to be more selective for Bruton’s tyrosine kinase (BTK) than the first-in-class agent ibrutinib, with less off-target kinase inhibition. As reported at the 2019 annual congress of the European Hematology Association by Paolo Ghia, MD, PhD, and colleagues in the phase 3 ASCEND trial, 310 patients with previously treated CLL were randomized between oral Acala twice daily and treatment of physician’s choice (TPC) – either idelalisib plus rituximab (maximum of seven infusions) or bendamustine plus rituximab (maximum of six cycles).
Progression-free survival was the primary endpoint. At a median of 16.1 months, progression-free survival had not been reached for Acala, in comparison with 16.5 months for TPC. Significant benefit of Acala was observed in all prognostic subsets.
Although there was no difference in overall survival at a median follow-up of about 16 months, 85% of Acala patients had a response lasting at least 12 months, compared with 60% of TPC patients. Adverse events of any grade occurred in 94% of patients treated with Acala, with 45% being grade 3-4 toxicities and six treatment-related deaths.
What this means in practice
The vast majority of CLL/SLL patients will relapse after primary therapy and will require further treatment, so the progression-free survival improvement associated with Acala in ASCEND is eye-catching. However, there are important considerations that demand closer scrutiny.
With oral agents administered until progression or unacceptable toxicity, low-grade toxicities can influence patient adherence, quality of life, and potentially the need for dose reduction or treatment interruptions. Regimens of finite duration and easy adherence monitoring may be, on balance, preferred by patients and providers – especially if the oral agent can be given in later-line with comparable overall survival.
With ibrutinib (Blood. 2017;129:2612-5), Paul M. Barr, MD, and colleagues demonstrated that higher dose intensity was associated with improved progression-free survival and that holds were associated with worsened progression-free survival. Acala’s promise of high efficacy and lower off-target toxicity will be solidified if the large (more than 500 patients) phase 3 ACE-CL-006 study (Acala vs. ibrutinib) demonstrates its relative benefit from efficacy, toxicity, and adherence perspectives, in comparison with a standard therapy that similarly demands adherence until disease progression or unacceptable toxicity.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers and in expanding access to clinical trials to medically underserved populations.
In this edition of “How I will treat my next patient,” I highlight two recent presentations regarding potential improvements in the convenience and tolerability of treatment for two hematologic malignancies: multiple myeloma and chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL).
SC-Dara in myeloma
At the 2019 annual meeting of the American Society of Clinical Oncology, Maria-Victoria Mateos, MD, PhD, and colleagues, reported the results of COLUMBA, a phase 3 evaluation in 522 patients with multiple myeloma who were randomized to subcutaneous daratumumab (SC-Dara) or standard intravenous infusions of daratumumab (IV-Dara). A previous phase 1b study (Blood. 2017;130:838) had suggested comparable efficacy from the more convenient SC regime. Whereas conventional infusions of IV-Dara (16 mg/kg) take several hours, the SC formulation (1,800 mg–flat dose) is delivered in minutes. In COLUMBA, patients were randomized between SC- and IV-Dara weekly (cycles 1-2), then every 2 weeks (cycles 3-6), then every 4 weeks until disease progression.
Among the IV-Dara patients, the median duration of the first infusion was 421 minutes in cycle 1, 255 minutes in cycle 2, and 205 minutes in subsequent cycles – compatible with standard practice in the United States. As reported, at a median follow-up of 7.46 months, the efficacy (overall response rate, complete response rate, stringent-complete response rate, very good-partial response rate, progression-free survival, and 6-month overall survival) and safety profile were non-inferior for SC-Dara. SC-Dara patients also reported higher satisfaction with therapy.
What this means in practice
It is always a good idea to await publication of the manuscript because there may be study details and statistical nuances that make SC-Dara appear better than it will prove to be. For example, patient characteristics were slightly different between the two arms. Peer review of the final manuscript could be important in placing these results in context.
However, for treatments that demand frequent office visits over many months, reducing treatment burden for patients has value. Based on COLUMBA, it appears likely that SC-Dara will be a major convenience for patients, without obvious drawbacks in efficacy or toxicity. Meanwhile, flat dosing will be a time-saver for physicians, nursing, and pharmacy staff. If the price of the SC formulation is not exorbitant, I would expect a “win-win” that will support converting from IV- to SC-Dara as standard practice.
Acalabrutinib in CLL/SLL
Preclinical studies have shown acalabrutinib (Acala) to be more selective for Bruton’s tyrosine kinase (BTK) than the first-in-class agent ibrutinib, with less off-target kinase inhibition. As reported at the 2019 annual congress of the European Hematology Association by Paolo Ghia, MD, PhD, and colleagues in the phase 3 ASCEND trial, 310 patients with previously treated CLL were randomized between oral Acala twice daily and treatment of physician’s choice (TPC) – either idelalisib plus rituximab (maximum of seven infusions) or bendamustine plus rituximab (maximum of six cycles).
Progression-free survival was the primary endpoint. At a median of 16.1 months, progression-free survival had not been reached for Acala, in comparison with 16.5 months for TPC. Significant benefit of Acala was observed in all prognostic subsets.
Although there was no difference in overall survival at a median follow-up of about 16 months, 85% of Acala patients had a response lasting at least 12 months, compared with 60% of TPC patients. Adverse events of any grade occurred in 94% of patients treated with Acala, with 45% being grade 3-4 toxicities and six treatment-related deaths.
What this means in practice
The vast majority of CLL/SLL patients will relapse after primary therapy and will require further treatment, so the progression-free survival improvement associated with Acala in ASCEND is eye-catching. However, there are important considerations that demand closer scrutiny.
With oral agents administered until progression or unacceptable toxicity, low-grade toxicities can influence patient adherence, quality of life, and potentially the need for dose reduction or treatment interruptions. Regimens of finite duration and easy adherence monitoring may be, on balance, preferred by patients and providers – especially if the oral agent can be given in later-line with comparable overall survival.
With ibrutinib (Blood. 2017;129:2612-5), Paul M. Barr, MD, and colleagues demonstrated that higher dose intensity was associated with improved progression-free survival and that holds were associated with worsened progression-free survival. Acala’s promise of high efficacy and lower off-target toxicity will be solidified if the large (more than 500 patients) phase 3 ACE-CL-006 study (Acala vs. ibrutinib) demonstrates its relative benefit from efficacy, toxicity, and adherence perspectives, in comparison with a standard therapy that similarly demands adherence until disease progression or unacceptable toxicity.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers and in expanding access to clinical trials to medically underserved populations.
In this edition of “How I will treat my next patient,” I highlight two recent presentations regarding potential improvements in the convenience and tolerability of treatment for two hematologic malignancies: multiple myeloma and chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL).
SC-Dara in myeloma
At the 2019 annual meeting of the American Society of Clinical Oncology, Maria-Victoria Mateos, MD, PhD, and colleagues, reported the results of COLUMBA, a phase 3 evaluation in 522 patients with multiple myeloma who were randomized to subcutaneous daratumumab (SC-Dara) or standard intravenous infusions of daratumumab (IV-Dara). A previous phase 1b study (Blood. 2017;130:838) had suggested comparable efficacy from the more convenient SC regime. Whereas conventional infusions of IV-Dara (16 mg/kg) take several hours, the SC formulation (1,800 mg–flat dose) is delivered in minutes. In COLUMBA, patients were randomized between SC- and IV-Dara weekly (cycles 1-2), then every 2 weeks (cycles 3-6), then every 4 weeks until disease progression.
Among the IV-Dara patients, the median duration of the first infusion was 421 minutes in cycle 1, 255 minutes in cycle 2, and 205 minutes in subsequent cycles – compatible with standard practice in the United States. As reported, at a median follow-up of 7.46 months, the efficacy (overall response rate, complete response rate, stringent-complete response rate, very good-partial response rate, progression-free survival, and 6-month overall survival) and safety profile were non-inferior for SC-Dara. SC-Dara patients also reported higher satisfaction with therapy.
What this means in practice
It is always a good idea to await publication of the manuscript because there may be study details and statistical nuances that make SC-Dara appear better than it will prove to be. For example, patient characteristics were slightly different between the two arms. Peer review of the final manuscript could be important in placing these results in context.
However, for treatments that demand frequent office visits over many months, reducing treatment burden for patients has value. Based on COLUMBA, it appears likely that SC-Dara will be a major convenience for patients, without obvious drawbacks in efficacy or toxicity. Meanwhile, flat dosing will be a time-saver for physicians, nursing, and pharmacy staff. If the price of the SC formulation is not exorbitant, I would expect a “win-win” that will support converting from IV- to SC-Dara as standard practice.
Acalabrutinib in CLL/SLL
Preclinical studies have shown acalabrutinib (Acala) to be more selective for Bruton’s tyrosine kinase (BTK) than the first-in-class agent ibrutinib, with less off-target kinase inhibition. As reported at the 2019 annual congress of the European Hematology Association by Paolo Ghia, MD, PhD, and colleagues in the phase 3 ASCEND trial, 310 patients with previously treated CLL were randomized between oral Acala twice daily and treatment of physician’s choice (TPC) – either idelalisib plus rituximab (maximum of seven infusions) or bendamustine plus rituximab (maximum of six cycles).
Progression-free survival was the primary endpoint. At a median of 16.1 months, progression-free survival had not been reached for Acala, in comparison with 16.5 months for TPC. Significant benefit of Acala was observed in all prognostic subsets.
Although there was no difference in overall survival at a median follow-up of about 16 months, 85% of Acala patients had a response lasting at least 12 months, compared with 60% of TPC patients. Adverse events of any grade occurred in 94% of patients treated with Acala, with 45% being grade 3-4 toxicities and six treatment-related deaths.
What this means in practice
The vast majority of CLL/SLL patients will relapse after primary therapy and will require further treatment, so the progression-free survival improvement associated with Acala in ASCEND is eye-catching. However, there are important considerations that demand closer scrutiny.
With oral agents administered until progression or unacceptable toxicity, low-grade toxicities can influence patient adherence, quality of life, and potentially the need for dose reduction or treatment interruptions. Regimens of finite duration and easy adherence monitoring may be, on balance, preferred by patients and providers – especially if the oral agent can be given in later-line with comparable overall survival.
With ibrutinib (Blood. 2017;129:2612-5), Paul M. Barr, MD, and colleagues demonstrated that higher dose intensity was associated with improved progression-free survival and that holds were associated with worsened progression-free survival. Acala’s promise of high efficacy and lower off-target toxicity will be solidified if the large (more than 500 patients) phase 3 ACE-CL-006 study (Acala vs. ibrutinib) demonstrates its relative benefit from efficacy, toxicity, and adherence perspectives, in comparison with a standard therapy that similarly demands adherence until disease progression or unacceptable toxicity.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers and in expanding access to clinical trials to medically underserved populations.
When’s the right time to use dementia as a diagnosis?
Is dementia a diagnosis?
I use it myself, although I find that some neurologists consider this blasphemy.
The problem is that there aren’t many terms to cover cognitive disorders beyond mild cognitive impairment (MCI). Phrases like “cortical degeneration” and “frontotemporal disorder” are difficult for families and patients. They aren’t medically trained and want something easy to write down.
“Alzheimer’s,” or – as one patient’s family member says, “the A-word” – is often more accurate, but has stigma attached to it that many don’t want, especially at a first visit. It also immediately conjures up feared images of nursing homes, wheelchairs, and bed-bound people.
So I use a diagnosis of dementia with many families, at least initially. Since, with occasional exceptions, we tend to perform a work-up of all cognitive disorders the same way, I don’t have a problem with using a more generic blanket term. As I sometimes try to simplify things, I’ll say, “It’s like squares and rectangles. Alzheimer’s disease is a dementia, but not all dementias are Alzheimer’s disease.”
I don’t do this to avoid confrontation, be dishonest, mislead patients and families, or avoid telling the truth. I still make it very clear that this is a progressive neurologic illness that will cause worsening cognitive problems over time. But many times families aren’t ready for “the A-word” early on, or there’s a concern the patient will harm themselves while they still have that capacity. Sometimes, it’s better to use a different phrase.
It may all be semantics, but on a personal level, a word can make a huge difference.
So I say dementia. In spite of some editorials I’ve seen saying we should retire the phrase, I argue that in many circumstances it’s still valid and useful.
It may not be a final, or even specific, diagnosis, but it is often the best and most socially acceptable one at the beginning of the doctor-patient-family relationship. When you’re trying to build rapport with them, that’s equally critical when you know what’s to come down the road.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Is dementia a diagnosis?
I use it myself, although I find that some neurologists consider this blasphemy.
The problem is that there aren’t many terms to cover cognitive disorders beyond mild cognitive impairment (MCI). Phrases like “cortical degeneration” and “frontotemporal disorder” are difficult for families and patients. They aren’t medically trained and want something easy to write down.
“Alzheimer’s,” or – as one patient’s family member says, “the A-word” – is often more accurate, but has stigma attached to it that many don’t want, especially at a first visit. It also immediately conjures up feared images of nursing homes, wheelchairs, and bed-bound people.
So I use a diagnosis of dementia with many families, at least initially. Since, with occasional exceptions, we tend to perform a work-up of all cognitive disorders the same way, I don’t have a problem with using a more generic blanket term. As I sometimes try to simplify things, I’ll say, “It’s like squares and rectangles. Alzheimer’s disease is a dementia, but not all dementias are Alzheimer’s disease.”
I don’t do this to avoid confrontation, be dishonest, mislead patients and families, or avoid telling the truth. I still make it very clear that this is a progressive neurologic illness that will cause worsening cognitive problems over time. But many times families aren’t ready for “the A-word” early on, or there’s a concern the patient will harm themselves while they still have that capacity. Sometimes, it’s better to use a different phrase.
It may all be semantics, but on a personal level, a word can make a huge difference.
So I say dementia. In spite of some editorials I’ve seen saying we should retire the phrase, I argue that in many circumstances it’s still valid and useful.
It may not be a final, or even specific, diagnosis, but it is often the best and most socially acceptable one at the beginning of the doctor-patient-family relationship. When you’re trying to build rapport with them, that’s equally critical when you know what’s to come down the road.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Is dementia a diagnosis?
I use it myself, although I find that some neurologists consider this blasphemy.
The problem is that there aren’t many terms to cover cognitive disorders beyond mild cognitive impairment (MCI). Phrases like “cortical degeneration” and “frontotemporal disorder” are difficult for families and patients. They aren’t medically trained and want something easy to write down.
“Alzheimer’s,” or – as one patient’s family member says, “the A-word” – is often more accurate, but has stigma attached to it that many don’t want, especially at a first visit. It also immediately conjures up feared images of nursing homes, wheelchairs, and bed-bound people.
So I use a diagnosis of dementia with many families, at least initially. Since, with occasional exceptions, we tend to perform a work-up of all cognitive disorders the same way, I don’t have a problem with using a more generic blanket term. As I sometimes try to simplify things, I’ll say, “It’s like squares and rectangles. Alzheimer’s disease is a dementia, but not all dementias are Alzheimer’s disease.”
I don’t do this to avoid confrontation, be dishonest, mislead patients and families, or avoid telling the truth. I still make it very clear that this is a progressive neurologic illness that will cause worsening cognitive problems over time. But many times families aren’t ready for “the A-word” early on, or there’s a concern the patient will harm themselves while they still have that capacity. Sometimes, it’s better to use a different phrase.
It may all be semantics, but on a personal level, a word can make a huge difference.
So I say dementia. In spite of some editorials I’ve seen saying we should retire the phrase, I argue that in many circumstances it’s still valid and useful.
It may not be a final, or even specific, diagnosis, but it is often the best and most socially acceptable one at the beginning of the doctor-patient-family relationship. When you’re trying to build rapport with them, that’s equally critical when you know what’s to come down the road.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The pool is closed!
At a recent Recreation Commission meeting here in Brunswick, the first agenda item under new business was “Coffin Pond Pool Closing.” As I and my fellow commissioners listened, we were told that for the first time in the last 3 decades the town’s only public swimming area would not be opening. While in the past there have been delayed openings and temporary closings due to water conditions, this year the pool would not open, period. The cause of the pool’s closure was the Parks and Recreation Department’s failure to fill even a skeleton crew of lifeguards.
We learned that the situation here in Brunswick was not unique and most other communities around the state and even around the country were struggling to find lifeguards. The shortage of trained staff has been nationwide for several years, and many beaches and pools particularly in the Northeast and Middle Atlantic states were being forced to close or shorten hours of operation (“During the Pool Season Even Lifeguard Numbers are Taking a Dive,” by Leoneda Inge, July 28, 2015, NPR’s All Thing Considered).
You might think that here on the coast we would have ample places for children to swim, but in Brunswick our shore is rocky and often inaccessible. At the few sandy beaches, the water temperature is too cold for all but the hardy souls until late August. Lower-income families will be particularly affected by the loss of the pool.
When I was growing up, lifeguarding was a plum job that was highly coveted. While it did not pay as well as working construction, the perks of a pleasant atmosphere, the chance to swim every day, and the opportunity to work outside with children prompted me at age 16 to sell my lawn mower and bequeath my lucrative landscaping customers to a couple of preteens. Looking back, my 4 years of lifeguarding were probably a major influence when it came time to choose a specialty.
However, a perfect storm of socioeconomic factors has combined to create a climate in which being a lifeguard has lost its appeal as a summertime job. First, there is record low unemployment nationwide. Young people looking for work have their pick, and while wages still remain low, they can be choosy when it comes to hours and benefits. Lifeguarding does require a skill set and several hoops of certification to be navigated. I don’t recall having to pay much of anything to become certified. But I understand that the process now costs hundreds of dollars of upfront investment with no guarantee of passing the test.
In May, the American Academy of Pediatrics published a policy paper titled “Prevention of Drowning” (Pediatrics. 2019 May 1. doi: 10.1542/peds.2019-0850) in which the authors offer the troubling statistics on the toll that water-related accidents take on the children of this country annually. They go on to provide a broad list of actions that parents, communities, and pediatricians can take to prevent drownings. Under the category of Community Interventions and Advocacy Opportunities, recommendation No. 4 is “Pediatricians should work with community partners to provide access to programs that develop water-competency swim skills for all children.”
Obviously, these programs can’t happen without an adequate supply of lifeguards.
Unfortunately, the AAP’s statement fails to acknowledge or directly address the lifeguard shortage that has been going on for several years. While an adequate supply of lifeguards is probably not as important as increasing parental attentiveness and mandating pool fences in the overall scheme of drowning prevention, it is an issue that demands action both by the academy and those of us practicing in communities both large and small.
For my part, I am going to work here in Brunswick to see that we can offer lifeguards pay that is more than competitive and then develop an in-house training program to ensure a continuing supply for the future. If we are committed to encouraging our patients to be active, swimming is one of the best activities we should promote and support.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
At a recent Recreation Commission meeting here in Brunswick, the first agenda item under new business was “Coffin Pond Pool Closing.” As I and my fellow commissioners listened, we were told that for the first time in the last 3 decades the town’s only public swimming area would not be opening. While in the past there have been delayed openings and temporary closings due to water conditions, this year the pool would not open, period. The cause of the pool’s closure was the Parks and Recreation Department’s failure to fill even a skeleton crew of lifeguards.
We learned that the situation here in Brunswick was not unique and most other communities around the state and even around the country were struggling to find lifeguards. The shortage of trained staff has been nationwide for several years, and many beaches and pools particularly in the Northeast and Middle Atlantic states were being forced to close or shorten hours of operation (“During the Pool Season Even Lifeguard Numbers are Taking a Dive,” by Leoneda Inge, July 28, 2015, NPR’s All Thing Considered).
You might think that here on the coast we would have ample places for children to swim, but in Brunswick our shore is rocky and often inaccessible. At the few sandy beaches, the water temperature is too cold for all but the hardy souls until late August. Lower-income families will be particularly affected by the loss of the pool.
When I was growing up, lifeguarding was a plum job that was highly coveted. While it did not pay as well as working construction, the perks of a pleasant atmosphere, the chance to swim every day, and the opportunity to work outside with children prompted me at age 16 to sell my lawn mower and bequeath my lucrative landscaping customers to a couple of preteens. Looking back, my 4 years of lifeguarding were probably a major influence when it came time to choose a specialty.
However, a perfect storm of socioeconomic factors has combined to create a climate in which being a lifeguard has lost its appeal as a summertime job. First, there is record low unemployment nationwide. Young people looking for work have their pick, and while wages still remain low, they can be choosy when it comes to hours and benefits. Lifeguarding does require a skill set and several hoops of certification to be navigated. I don’t recall having to pay much of anything to become certified. But I understand that the process now costs hundreds of dollars of upfront investment with no guarantee of passing the test.
In May, the American Academy of Pediatrics published a policy paper titled “Prevention of Drowning” (Pediatrics. 2019 May 1. doi: 10.1542/peds.2019-0850) in which the authors offer the troubling statistics on the toll that water-related accidents take on the children of this country annually. They go on to provide a broad list of actions that parents, communities, and pediatricians can take to prevent drownings. Under the category of Community Interventions and Advocacy Opportunities, recommendation No. 4 is “Pediatricians should work with community partners to provide access to programs that develop water-competency swim skills for all children.”
Obviously, these programs can’t happen without an adequate supply of lifeguards.
Unfortunately, the AAP’s statement fails to acknowledge or directly address the lifeguard shortage that has been going on for several years. While an adequate supply of lifeguards is probably not as important as increasing parental attentiveness and mandating pool fences in the overall scheme of drowning prevention, it is an issue that demands action both by the academy and those of us practicing in communities both large and small.
For my part, I am going to work here in Brunswick to see that we can offer lifeguards pay that is more than competitive and then develop an in-house training program to ensure a continuing supply for the future. If we are committed to encouraging our patients to be active, swimming is one of the best activities we should promote and support.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
At a recent Recreation Commission meeting here in Brunswick, the first agenda item under new business was “Coffin Pond Pool Closing.” As I and my fellow commissioners listened, we were told that for the first time in the last 3 decades the town’s only public swimming area would not be opening. While in the past there have been delayed openings and temporary closings due to water conditions, this year the pool would not open, period. The cause of the pool’s closure was the Parks and Recreation Department’s failure to fill even a skeleton crew of lifeguards.
We learned that the situation here in Brunswick was not unique and most other communities around the state and even around the country were struggling to find lifeguards. The shortage of trained staff has been nationwide for several years, and many beaches and pools particularly in the Northeast and Middle Atlantic states were being forced to close or shorten hours of operation (“During the Pool Season Even Lifeguard Numbers are Taking a Dive,” by Leoneda Inge, July 28, 2015, NPR’s All Thing Considered).
You might think that here on the coast we would have ample places for children to swim, but in Brunswick our shore is rocky and often inaccessible. At the few sandy beaches, the water temperature is too cold for all but the hardy souls until late August. Lower-income families will be particularly affected by the loss of the pool.
When I was growing up, lifeguarding was a plum job that was highly coveted. While it did not pay as well as working construction, the perks of a pleasant atmosphere, the chance to swim every day, and the opportunity to work outside with children prompted me at age 16 to sell my lawn mower and bequeath my lucrative landscaping customers to a couple of preteens. Looking back, my 4 years of lifeguarding were probably a major influence when it came time to choose a specialty.
However, a perfect storm of socioeconomic factors has combined to create a climate in which being a lifeguard has lost its appeal as a summertime job. First, there is record low unemployment nationwide. Young people looking for work have their pick, and while wages still remain low, they can be choosy when it comes to hours and benefits. Lifeguarding does require a skill set and several hoops of certification to be navigated. I don’t recall having to pay much of anything to become certified. But I understand that the process now costs hundreds of dollars of upfront investment with no guarantee of passing the test.
In May, the American Academy of Pediatrics published a policy paper titled “Prevention of Drowning” (Pediatrics. 2019 May 1. doi: 10.1542/peds.2019-0850) in which the authors offer the troubling statistics on the toll that water-related accidents take on the children of this country annually. They go on to provide a broad list of actions that parents, communities, and pediatricians can take to prevent drownings. Under the category of Community Interventions and Advocacy Opportunities, recommendation No. 4 is “Pediatricians should work with community partners to provide access to programs that develop water-competency swim skills for all children.”
Obviously, these programs can’t happen without an adequate supply of lifeguards.
Unfortunately, the AAP’s statement fails to acknowledge or directly address the lifeguard shortage that has been going on for several years. While an adequate supply of lifeguards is probably not as important as increasing parental attentiveness and mandating pool fences in the overall scheme of drowning prevention, it is an issue that demands action both by the academy and those of us practicing in communities both large and small.
For my part, I am going to work here in Brunswick to see that we can offer lifeguards pay that is more than competitive and then develop an in-house training program to ensure a continuing supply for the future. If we are committed to encouraging our patients to be active, swimming is one of the best activities we should promote and support.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
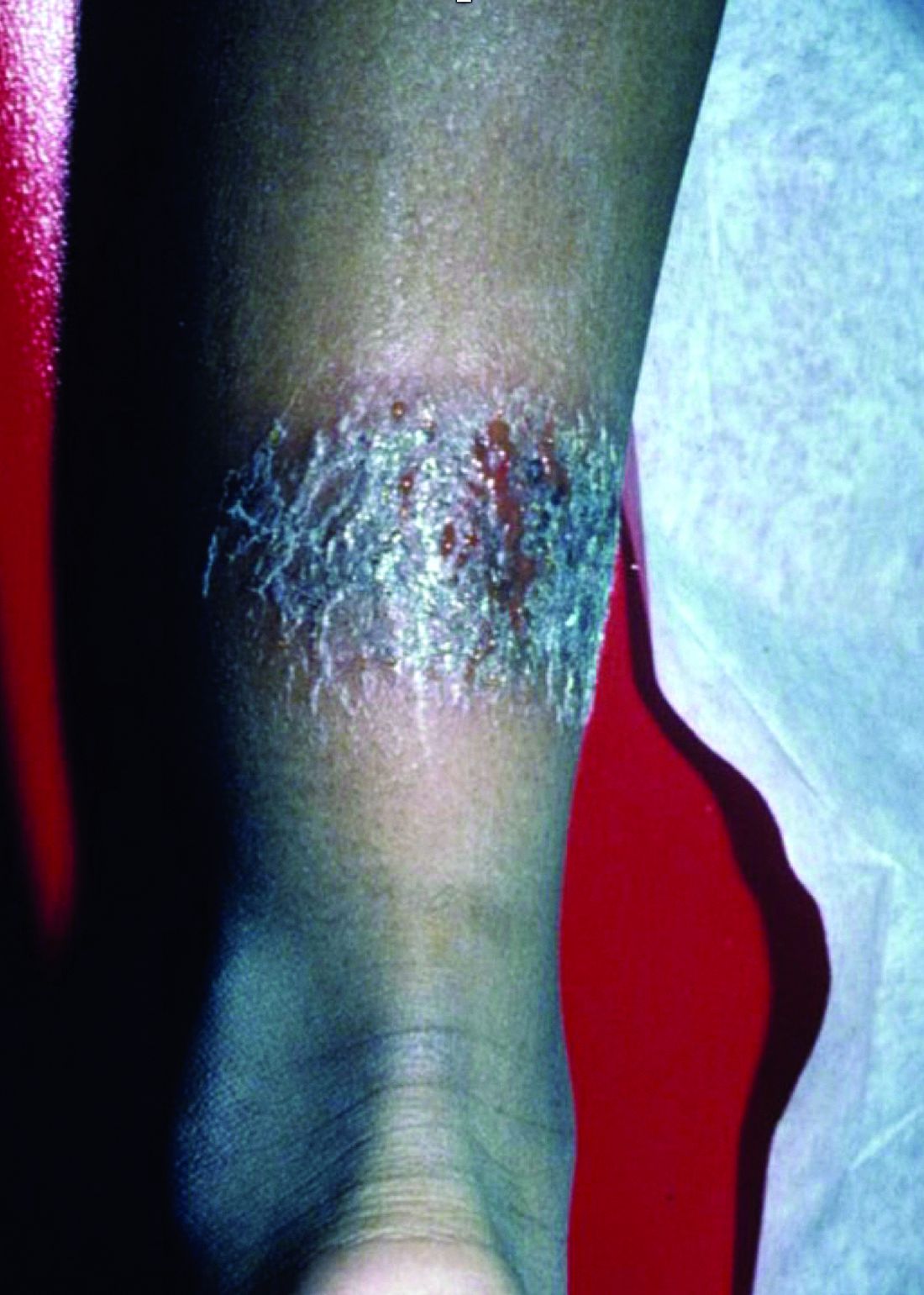
A 3-year-old is brought to the clinic for evaluation of a localized, scaling inflamed lesion on the left leg
Nummular dermatitis, or nummular eczema, is an inflammatory skin condition that is considered to be a distinctive form of idiopathic eczema, while the term also is used to describe lesional morphology associated with other conditions.
The term nummular derives from the Latin word for “coin,” as lesions are commonly annular plaques. Lesions of nummular dermatitis can be single or multiple. The typical distribution involves the extremities and, although less common, it can affect the trunk as well.
Nummular dermatitis may be associated with atopic dermatitis, or it can be an isolated condition.1 While the pathogenesis is uncertain, instigating factors include xerotic skin, insect bites, or scratches or scrapes.1Staphylococcus infection or colonization, contact allergies to metals such as nickel and less commonly mercury, sensitivity to formaldehyde or medicines such as neomycin, and sensitization to an environmental aeroallergen (such as Candida albicans, dust mites) are considered risk factors.2
The diagnosis of nummular dermatitis is clinical. Laboratory testing and/or biopsy generally are not necessary, although a bacterial culture can be considered in patients with exudative and/or crusted lesions to rule out impetigo as a primary process of secondary infection. In some cases, patch testing for allergic contact dermatitis may be useful.
The differential diagnosis of nummular dermatitis includes tinea corporis (ringworm), atopic dermatitis, allergic contact dermatitis, impetigo, and psoriasis. Tinea corporis usually presents as annular lesions with a distinct peripheral scaling, rather than the diffuse induration of nummular dermatitis. Potassium hydroxide preparation or fungal culture can identify tinea species. Nummular dermatitis may be seen in patients with atopic dermatitis, who should have typical history, morphology, and course consistent with standard diagnostic criteria. Allergic contact dermatitis can present with regional, localized eczematous plaques in areas exposed to contact allergens. Patterns of lesions in areas of contact and worsening with repeat exposures can be clues to this diagnosis. Impetigo can present with honey-colored crusted lesions and/or superficial erosions, or purulent pyoderma. Lesions can be single or multiple and generally appear less inflammatory than nummular dermatitis. Psoriasis lesions may be annular, are more common on extensor surfaces, and usually have more prominent overlying pinkish, silvery white or micaceous scale.
Management of nummular dermatitis requires strong anti-inflammatory medications, usually mid-potency or higher topical corticosteroids, along with moisturizers and limiting exposure to skin irritants. “Wet wraps,” with application of topical corticosteroids to wet skin with occlusive wet dressings can enhance response. Transition from higher strength topical corticosteroids to lower strength agents used intermittently can help achieve remission or cure. Management practices include less frequent bathing with lukewarm water, using hypoallergenic cleansers and detergents, and applying moisturizers frequently. If plaques do recur, they tend to do so in the same location and in some patients resolution may result in hyper or hypopigmentation. Refractory disease may be managed with intralesional steroid injections, or systemic medications such as methotrexate.3
Dr. Tracy is a research fellow in pediatric dermatology at Rady Children’s Hospital–San Diego and the University of California, San Diego. Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children’s Hospital–San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. Neither Dr. Tracy nor Dr. Eichenfield have any relevant financial disclosures. Email them at [email protected].
References
1. Pediatr Dermatol. 2012 Sep-Oct;29(5):580-3.
2. American Academy of Dermatology. Nummular Dermatitis Overview
3. Pediatr Dermatol. 2018 Sep;35(5):611-5.
Nummular dermatitis, or nummular eczema, is an inflammatory skin condition that is considered to be a distinctive form of idiopathic eczema, while the term also is used to describe lesional morphology associated with other conditions.
The term nummular derives from the Latin word for “coin,” as lesions are commonly annular plaques. Lesions of nummular dermatitis can be single or multiple. The typical distribution involves the extremities and, although less common, it can affect the trunk as well.
Nummular dermatitis may be associated with atopic dermatitis, or it can be an isolated condition.1 While the pathogenesis is uncertain, instigating factors include xerotic skin, insect bites, or scratches or scrapes.1Staphylococcus infection or colonization, contact allergies to metals such as nickel and less commonly mercury, sensitivity to formaldehyde or medicines such as neomycin, and sensitization to an environmental aeroallergen (such as Candida albicans, dust mites) are considered risk factors.2
The diagnosis of nummular dermatitis is clinical. Laboratory testing and/or biopsy generally are not necessary, although a bacterial culture can be considered in patients with exudative and/or crusted lesions to rule out impetigo as a primary process of secondary infection. In some cases, patch testing for allergic contact dermatitis may be useful.
The differential diagnosis of nummular dermatitis includes tinea corporis (ringworm), atopic dermatitis, allergic contact dermatitis, impetigo, and psoriasis. Tinea corporis usually presents as annular lesions with a distinct peripheral scaling, rather than the diffuse induration of nummular dermatitis. Potassium hydroxide preparation or fungal culture can identify tinea species. Nummular dermatitis may be seen in patients with atopic dermatitis, who should have typical history, morphology, and course consistent with standard diagnostic criteria. Allergic contact dermatitis can present with regional, localized eczematous plaques in areas exposed to contact allergens. Patterns of lesions in areas of contact and worsening with repeat exposures can be clues to this diagnosis. Impetigo can present with honey-colored crusted lesions and/or superficial erosions, or purulent pyoderma. Lesions can be single or multiple and generally appear less inflammatory than nummular dermatitis. Psoriasis lesions may be annular, are more common on extensor surfaces, and usually have more prominent overlying pinkish, silvery white or micaceous scale.
Management of nummular dermatitis requires strong anti-inflammatory medications, usually mid-potency or higher topical corticosteroids, along with moisturizers and limiting exposure to skin irritants. “Wet wraps,” with application of topical corticosteroids to wet skin with occlusive wet dressings can enhance response. Transition from higher strength topical corticosteroids to lower strength agents used intermittently can help achieve remission or cure. Management practices include less frequent bathing with lukewarm water, using hypoallergenic cleansers and detergents, and applying moisturizers frequently. If plaques do recur, they tend to do so in the same location and in some patients resolution may result in hyper or hypopigmentation. Refractory disease may be managed with intralesional steroid injections, or systemic medications such as methotrexate.3
Dr. Tracy is a research fellow in pediatric dermatology at Rady Children’s Hospital–San Diego and the University of California, San Diego. Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children’s Hospital–San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. Neither Dr. Tracy nor Dr. Eichenfield have any relevant financial disclosures. Email them at [email protected].
References
1. Pediatr Dermatol. 2012 Sep-Oct;29(5):580-3.
2. American Academy of Dermatology. Nummular Dermatitis Overview
3. Pediatr Dermatol. 2018 Sep;35(5):611-5.
Nummular dermatitis, or nummular eczema, is an inflammatory skin condition that is considered to be a distinctive form of idiopathic eczema, while the term also is used to describe lesional morphology associated with other conditions.
The term nummular derives from the Latin word for “coin,” as lesions are commonly annular plaques. Lesions of nummular dermatitis can be single or multiple. The typical distribution involves the extremities and, although less common, it can affect the trunk as well.
Nummular dermatitis may be associated with atopic dermatitis, or it can be an isolated condition.1 While the pathogenesis is uncertain, instigating factors include xerotic skin, insect bites, or scratches or scrapes.1Staphylococcus infection or colonization, contact allergies to metals such as nickel and less commonly mercury, sensitivity to formaldehyde or medicines such as neomycin, and sensitization to an environmental aeroallergen (such as Candida albicans, dust mites) are considered risk factors.2
The diagnosis of nummular dermatitis is clinical. Laboratory testing and/or biopsy generally are not necessary, although a bacterial culture can be considered in patients with exudative and/or crusted lesions to rule out impetigo as a primary process of secondary infection. In some cases, patch testing for allergic contact dermatitis may be useful.
The differential diagnosis of nummular dermatitis includes tinea corporis (ringworm), atopic dermatitis, allergic contact dermatitis, impetigo, and psoriasis. Tinea corporis usually presents as annular lesions with a distinct peripheral scaling, rather than the diffuse induration of nummular dermatitis. Potassium hydroxide preparation or fungal culture can identify tinea species. Nummular dermatitis may be seen in patients with atopic dermatitis, who should have typical history, morphology, and course consistent with standard diagnostic criteria. Allergic contact dermatitis can present with regional, localized eczematous plaques in areas exposed to contact allergens. Patterns of lesions in areas of contact and worsening with repeat exposures can be clues to this diagnosis. Impetigo can present with honey-colored crusted lesions and/or superficial erosions, or purulent pyoderma. Lesions can be single or multiple and generally appear less inflammatory than nummular dermatitis. Psoriasis lesions may be annular, are more common on extensor surfaces, and usually have more prominent overlying pinkish, silvery white or micaceous scale.
Management of nummular dermatitis requires strong anti-inflammatory medications, usually mid-potency or higher topical corticosteroids, along with moisturizers and limiting exposure to skin irritants. “Wet wraps,” with application of topical corticosteroids to wet skin with occlusive wet dressings can enhance response. Transition from higher strength topical corticosteroids to lower strength agents used intermittently can help achieve remission or cure. Management practices include less frequent bathing with lukewarm water, using hypoallergenic cleansers and detergents, and applying moisturizers frequently. If plaques do recur, they tend to do so in the same location and in some patients resolution may result in hyper or hypopigmentation. Refractory disease may be managed with intralesional steroid injections, or systemic medications such as methotrexate.3
Dr. Tracy is a research fellow in pediatric dermatology at Rady Children’s Hospital–San Diego and the University of California, San Diego. Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children’s Hospital–San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. Neither Dr. Tracy nor Dr. Eichenfield have any relevant financial disclosures. Email them at [email protected].
References
1. Pediatr Dermatol. 2012 Sep-Oct;29(5):580-3.
2. American Academy of Dermatology. Nummular Dermatitis Overview
3. Pediatr Dermatol. 2018 Sep;35(5):611-5.
On physical exam, he is noted to have a localized eczematous plaque with erythema and edema. Also, he is noted to have diffuse, fine xerosis of the bilateral lower extremities. His skin is otherwise nonremarkable.
Mothers, migraine, colic ... and sleep
In a recent article on this website, Jake Remaly reports on a study suggesting that maternal migraine is associated with infant colic. In a presentation at the annual meeting of the American Headache Society, Amy Gelfand, MD, a neurologist at the University of California, San Francisco, reported the results of a national survey of more than 1,400 parents (827 mothers, 592 fathers) collected via social media. She and her colleagues found that mothers with migraine were more likely to have an infant with colic, with an odds ratio of 1.7 that increased to 2.5 for mothers with more frequent migraine. Fathers with migraine were no more likely to have an infant with colic.
In a video clip included in the article, Dr. Gelfand discusses the possibilities that she and her group considered as they attempted to explain the study’s findings. Are there such things as “migraine genes?” If so, the failure to discover a paternal association might suggest that these would be mitochondrial genes. The researchers wondered if a substance in breast milk was acting as trigger, but they found that the association between colic and migraine was unrelated to whether the baby was fed by breast or bottle.
In full disclosure, I was not one of the investigators. Neither my wife nor I have migraine, and although our children cried as infants, they wouldn’t have qualified as having colic. However, I spent more than 40 years immersed in more than 300,000 patient encounters and can claim membership in the International Brother/Sisterhood of Anecdotal Observers. And, as such will offer up my explanation for Dr. Gelfand’s findings.
It is clear to me that most, if not all, children with migraine have their headaches when they are sleep deprived. While my sample size is smaller, I believe the same association also is true for many of the adults I know who have migraine. At least in children, restorative sleep ends the migraine much as it does for an epileptic seizure.
Traditionally, colic has been thought to be somehow related to a gastrointestinal phenomenon by many extended family members and some physicians. However, in my experience, it is usually a symptom of sleep deprivation compounded by the failure of those around the children to realize the obvious and take appropriate action. Of course, some babies are reacting to sore tummies, but my guess is that most are having headaches. We may never know. Dr. Gelfand also shares my observation that colicky crying is more likely to occur “at the end of the day,” a time when we are tired and are less tolerant of overstimulation.
However, the presentation varies depending on the age of the patients. Remember, infants can’t talk. It already has been shown that adults with migraine often were more likely to have been colicky infants. (Dr. Gelfand mentions this as well.) These unfortunate individuals probably have inherited a vulnerability to sleep deprivation that manifests itself as a headache. I hope to live long enough to be around when someone discovers the wrinkle in the genome that creates this vulnerability.
So, why did the researchers fail to find an association between fathers and colic? The answer is simple. We fathers are beginning to take on a larger role in parenting of infants and like to complain about how difficult it is. However, it is mothers who still have the lioness’ share of the work. They lose the most sleep and are starting off parenthood with 9 months of less than optimal sleep followed by who knows how many hours of energy-sapping labor. It’s surprising they all don’t have migraines.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
In a recent article on this website, Jake Remaly reports on a study suggesting that maternal migraine is associated with infant colic. In a presentation at the annual meeting of the American Headache Society, Amy Gelfand, MD, a neurologist at the University of California, San Francisco, reported the results of a national survey of more than 1,400 parents (827 mothers, 592 fathers) collected via social media. She and her colleagues found that mothers with migraine were more likely to have an infant with colic, with an odds ratio of 1.7 that increased to 2.5 for mothers with more frequent migraine. Fathers with migraine were no more likely to have an infant with colic.
In a video clip included in the article, Dr. Gelfand discusses the possibilities that she and her group considered as they attempted to explain the study’s findings. Are there such things as “migraine genes?” If so, the failure to discover a paternal association might suggest that these would be mitochondrial genes. The researchers wondered if a substance in breast milk was acting as trigger, but they found that the association between colic and migraine was unrelated to whether the baby was fed by breast or bottle.
In full disclosure, I was not one of the investigators. Neither my wife nor I have migraine, and although our children cried as infants, they wouldn’t have qualified as having colic. However, I spent more than 40 years immersed in more than 300,000 patient encounters and can claim membership in the International Brother/Sisterhood of Anecdotal Observers. And, as such will offer up my explanation for Dr. Gelfand’s findings.
It is clear to me that most, if not all, children with migraine have their headaches when they are sleep deprived. While my sample size is smaller, I believe the same association also is true for many of the adults I know who have migraine. At least in children, restorative sleep ends the migraine much as it does for an epileptic seizure.
Traditionally, colic has been thought to be somehow related to a gastrointestinal phenomenon by many extended family members and some physicians. However, in my experience, it is usually a symptom of sleep deprivation compounded by the failure of those around the children to realize the obvious and take appropriate action. Of course, some babies are reacting to sore tummies, but my guess is that most are having headaches. We may never know. Dr. Gelfand also shares my observation that colicky crying is more likely to occur “at the end of the day,” a time when we are tired and are less tolerant of overstimulation.
However, the presentation varies depending on the age of the patients. Remember, infants can’t talk. It already has been shown that adults with migraine often were more likely to have been colicky infants. (Dr. Gelfand mentions this as well.) These unfortunate individuals probably have inherited a vulnerability to sleep deprivation that manifests itself as a headache. I hope to live long enough to be around when someone discovers the wrinkle in the genome that creates this vulnerability.
So, why did the researchers fail to find an association between fathers and colic? The answer is simple. We fathers are beginning to take on a larger role in parenting of infants and like to complain about how difficult it is. However, it is mothers who still have the lioness’ share of the work. They lose the most sleep and are starting off parenthood with 9 months of less than optimal sleep followed by who knows how many hours of energy-sapping labor. It’s surprising they all don’t have migraines.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
In a recent article on this website, Jake Remaly reports on a study suggesting that maternal migraine is associated with infant colic. In a presentation at the annual meeting of the American Headache Society, Amy Gelfand, MD, a neurologist at the University of California, San Francisco, reported the results of a national survey of more than 1,400 parents (827 mothers, 592 fathers) collected via social media. She and her colleagues found that mothers with migraine were more likely to have an infant with colic, with an odds ratio of 1.7 that increased to 2.5 for mothers with more frequent migraine. Fathers with migraine were no more likely to have an infant with colic.
In a video clip included in the article, Dr. Gelfand discusses the possibilities that she and her group considered as they attempted to explain the study’s findings. Are there such things as “migraine genes?” If so, the failure to discover a paternal association might suggest that these would be mitochondrial genes. The researchers wondered if a substance in breast milk was acting as trigger, but they found that the association between colic and migraine was unrelated to whether the baby was fed by breast or bottle.
In full disclosure, I was not one of the investigators. Neither my wife nor I have migraine, and although our children cried as infants, they wouldn’t have qualified as having colic. However, I spent more than 40 years immersed in more than 300,000 patient encounters and can claim membership in the International Brother/Sisterhood of Anecdotal Observers. And, as such will offer up my explanation for Dr. Gelfand’s findings.
It is clear to me that most, if not all, children with migraine have their headaches when they are sleep deprived. While my sample size is smaller, I believe the same association also is true for many of the adults I know who have migraine. At least in children, restorative sleep ends the migraine much as it does for an epileptic seizure.
Traditionally, colic has been thought to be somehow related to a gastrointestinal phenomenon by many extended family members and some physicians. However, in my experience, it is usually a symptom of sleep deprivation compounded by the failure of those around the children to realize the obvious and take appropriate action. Of course, some babies are reacting to sore tummies, but my guess is that most are having headaches. We may never know. Dr. Gelfand also shares my observation that colicky crying is more likely to occur “at the end of the day,” a time when we are tired and are less tolerant of overstimulation.
However, the presentation varies depending on the age of the patients. Remember, infants can’t talk. It already has been shown that adults with migraine often were more likely to have been colicky infants. (Dr. Gelfand mentions this as well.) These unfortunate individuals probably have inherited a vulnerability to sleep deprivation that manifests itself as a headache. I hope to live long enough to be around when someone discovers the wrinkle in the genome that creates this vulnerability.
So, why did the researchers fail to find an association between fathers and colic? The answer is simple. We fathers are beginning to take on a larger role in parenting of infants and like to complain about how difficult it is. However, it is mothers who still have the lioness’ share of the work. They lose the most sleep and are starting off parenthood with 9 months of less than optimal sleep followed by who knows how many hours of energy-sapping labor. It’s surprising they all don’t have migraines.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Sensitive gray matters in treating teen depression
Carla is an otherwise-healthy 14-year-old female followed by her pediatrician for symptoms of depression and anxiety that have worsened over the past 8 months. Anhedonia, irritability, poor concentration, fatigue, hypersomnolence, and significant weight gain have increasingly led to further dysphoria, social isolation, and obsessive rumination, all of which now contribute to more dysfunction in both her home and school life. Based on Carla’s apprehension over “taking pills,” she was referred for outpatient therapy 5 months ago but because of difficulty maintaining weekly appointments, she stopped attending after 6 weeks, citing difficulty aligning with her therapist.
Carla was seen in an urgent, unscheduled follow-up appointment 2 months prior to address increased thoughts of wishing to be dead. She had neither a plan nor a desire to act on these ideations. During an interview, she was distant with poor eye contact, and her affect was notably blunted. Her mother, who had accompanied her in the waiting room, expressed frustration to the nurse about discovering that Carla was using cannabis, that she often appeared aloof and unmotivated to do much of anything but “sit in her room and play on her phone for hours on end.” She compared Carla with her ex-husband, who had similar mood swings that often led to erratic and violent outbursts towards Carla and her mother, behaviors that ultimately led them to leave him when Carla was 6 years old.
After a discussion over the risks and benefits of various treatment options, Carla was started on low-dose fluoxetine with a plan to titrate the medication after 2 weeks. A referral for outpatient substance use treatment also was initiated. Carla’s mother telephoned 10 days later in an update that things have drastically improved in Carla’s mood and activity. The following week her mother called back again with concerns that Carla is no longer sleeping, appears restless, impulsive, and disinhibited.
Discussion
Carla’s initial presentation is common to primary care settings. Based on her earliest reported symptoms, she would qualify for a diagnosis of major depression. Decisions regarding initial treatment for children and adolescents must take into account the severity of symptoms, risks, autonomy of the patient and family, as well as available evidence. Her response to outpatient therapy is not an anomaly. With an ever-increasing demand on mental health services, the availability of consistent, quality outpatient therapy for this population is not always easy to secure.1,2 Combining targeted therapy with pharmacologic interventions for major depression appear to have the most effective outcomes.3
Carla’s progression also illustrates the challenges and potential pitfalls of attempting to understand and address her symptoms according to a single nosology. Depression is a like a fever. It can be caused by a myriad of factors and, left to linger, may lead to further residual complications. Focusing attention to her symptoms also may lead to a differential including adjustment problems, social anxiety, effects of trauma, surreptitious substance use, or even bipolar depression.
To begin with, a clear delineation of Carla’s historic symptoms and any possible medical contributions to her presentation are necessary to investigate. Specific inquiries into past episodes of activation including hyperarousal, impulsivity, restlessness, and insomnia should be elucidated prior to consideration of medication selection.4 Considering Carla’s age and the known association between antidepressant-induced manic conversion among children aged 10-14 years,5 any pharmacologic intervention will benefit from the maxim “start low and go slow.” Her symptoms of activation arise within the setting of titration of an antidepressant. This may raise considerations to her specific metabolism and physiological concentrations of the medication as well as cumulative day exposure.
Complementary to Carla’s own history is that of family members. Often obtaining a reliable family psychiatric history is an exercise fraught with bias, vagueness, and generalizations.6 However, given the known heritability of bipolar disorders and the implications for treating depression in such individuals, compared with unipolar depressive symptoms, clarifying the nature of family illness may elucidate potential susceptibilities previously unconsidered.7 In this case, descriptions of Carla’s father’s behavior raise concerns for underlying bipolar disorder, as do the accounts of traumatic stress exposure and their compounded preponderance for increased suicide risk.8
Unfortunately, Carla’s current environmental cues and maladaptive behaviors may be perpetuating her symptoms and possibly placing her on a trajectory for further illness. Exploration of her relationship with her caregivers regarding the interpretation of her symptoms, and need for treatment should be undertaken so as to expand supportive roles. Education regarding cannabis use among adolescents and age-specific risks for later depression, anxiety, and suicide is warranted in a climate when accessibility is on the rise.9 Whether or not cannabis use itself leads to amotivation is the subject of current debate.10 A growing body of evidence is clearly illustrating that Carla’s sedentary behaviors and perceived loneliness likely exacerbate her mental well-being. Such patterns indicate the need for environmental intervention to change such cycles.
Finally, Carla’s progression through treatment speak to the need for open and honest discussions regarding realistic benefits as well potential risks. Progressive symptoms of depression left untreated can be life-threatening themselves, just as effects of activation as described in the vignette above can easily and quickly progress into situations that pose safety concerns. Amidst such periods of intervention, close communication and follow up with patients and their supports ameliorate potential adverse events and lead to better outcomes.
Outcome
Carla’s mother was advised to discontinue the medication, closely monitor Carla’s behavior and sleep, and schedule an emergent follow-up appointment for the next day. A safety plan indicating circumstances in which Carla would require closer medical supervision for safety was reviewed with her mother. Carla was later initiated on lamotrigine and restarted interpersonal therapy.
References
1. N Engl J Med. 2015 May 21;372(21):2029-38.
2. J Pediatr. 2010 Nov;157(5):848-51.
3. Arch Gen Psychiatry. 2007 Oct;64(10):1132-43.
4. Curr Probl Pediatr Adolesc Health Care. 2018 Feb;48(2):50-62.
5. Arch Pediatr Adolesc Med. 2004 Aug;158(8):773-80.
6. Can J Psychiatry. 1993 Nov;38(9):590-4.
7. Appl Clin Genet. 2014 Feb 12;7:33-42.
8. J Am Acad Child Adolesc Psychiatry. 2017 Dec;56(12):1073-1080.
9. JAMA Psychiatry. 2019;76(4):426-34.
10. Subst Use Misuse. 2018 Jun 7;53(7):1158-69.
Carla is an otherwise-healthy 14-year-old female followed by her pediatrician for symptoms of depression and anxiety that have worsened over the past 8 months. Anhedonia, irritability, poor concentration, fatigue, hypersomnolence, and significant weight gain have increasingly led to further dysphoria, social isolation, and obsessive rumination, all of which now contribute to more dysfunction in both her home and school life. Based on Carla’s apprehension over “taking pills,” she was referred for outpatient therapy 5 months ago but because of difficulty maintaining weekly appointments, she stopped attending after 6 weeks, citing difficulty aligning with her therapist.
Carla was seen in an urgent, unscheduled follow-up appointment 2 months prior to address increased thoughts of wishing to be dead. She had neither a plan nor a desire to act on these ideations. During an interview, she was distant with poor eye contact, and her affect was notably blunted. Her mother, who had accompanied her in the waiting room, expressed frustration to the nurse about discovering that Carla was using cannabis, that she often appeared aloof and unmotivated to do much of anything but “sit in her room and play on her phone for hours on end.” She compared Carla with her ex-husband, who had similar mood swings that often led to erratic and violent outbursts towards Carla and her mother, behaviors that ultimately led them to leave him when Carla was 6 years old.
After a discussion over the risks and benefits of various treatment options, Carla was started on low-dose fluoxetine with a plan to titrate the medication after 2 weeks. A referral for outpatient substance use treatment also was initiated. Carla’s mother telephoned 10 days later in an update that things have drastically improved in Carla’s mood and activity. The following week her mother called back again with concerns that Carla is no longer sleeping, appears restless, impulsive, and disinhibited.
Discussion
Carla’s initial presentation is common to primary care settings. Based on her earliest reported symptoms, she would qualify for a diagnosis of major depression. Decisions regarding initial treatment for children and adolescents must take into account the severity of symptoms, risks, autonomy of the patient and family, as well as available evidence. Her response to outpatient therapy is not an anomaly. With an ever-increasing demand on mental health services, the availability of consistent, quality outpatient therapy for this population is not always easy to secure.1,2 Combining targeted therapy with pharmacologic interventions for major depression appear to have the most effective outcomes.3
Carla’s progression also illustrates the challenges and potential pitfalls of attempting to understand and address her symptoms according to a single nosology. Depression is a like a fever. It can be caused by a myriad of factors and, left to linger, may lead to further residual complications. Focusing attention to her symptoms also may lead to a differential including adjustment problems, social anxiety, effects of trauma, surreptitious substance use, or even bipolar depression.
To begin with, a clear delineation of Carla’s historic symptoms and any possible medical contributions to her presentation are necessary to investigate. Specific inquiries into past episodes of activation including hyperarousal, impulsivity, restlessness, and insomnia should be elucidated prior to consideration of medication selection.4 Considering Carla’s age and the known association between antidepressant-induced manic conversion among children aged 10-14 years,5 any pharmacologic intervention will benefit from the maxim “start low and go slow.” Her symptoms of activation arise within the setting of titration of an antidepressant. This may raise considerations to her specific metabolism and physiological concentrations of the medication as well as cumulative day exposure.
Complementary to Carla’s own history is that of family members. Often obtaining a reliable family psychiatric history is an exercise fraught with bias, vagueness, and generalizations.6 However, given the known heritability of bipolar disorders and the implications for treating depression in such individuals, compared with unipolar depressive symptoms, clarifying the nature of family illness may elucidate potential susceptibilities previously unconsidered.7 In this case, descriptions of Carla’s father’s behavior raise concerns for underlying bipolar disorder, as do the accounts of traumatic stress exposure and their compounded preponderance for increased suicide risk.8
Unfortunately, Carla’s current environmental cues and maladaptive behaviors may be perpetuating her symptoms and possibly placing her on a trajectory for further illness. Exploration of her relationship with her caregivers regarding the interpretation of her symptoms, and need for treatment should be undertaken so as to expand supportive roles. Education regarding cannabis use among adolescents and age-specific risks for later depression, anxiety, and suicide is warranted in a climate when accessibility is on the rise.9 Whether or not cannabis use itself leads to amotivation is the subject of current debate.10 A growing body of evidence is clearly illustrating that Carla’s sedentary behaviors and perceived loneliness likely exacerbate her mental well-being. Such patterns indicate the need for environmental intervention to change such cycles.
Finally, Carla’s progression through treatment speak to the need for open and honest discussions regarding realistic benefits as well potential risks. Progressive symptoms of depression left untreated can be life-threatening themselves, just as effects of activation as described in the vignette above can easily and quickly progress into situations that pose safety concerns. Amidst such periods of intervention, close communication and follow up with patients and their supports ameliorate potential adverse events and lead to better outcomes.
Outcome
Carla’s mother was advised to discontinue the medication, closely monitor Carla’s behavior and sleep, and schedule an emergent follow-up appointment for the next day. A safety plan indicating circumstances in which Carla would require closer medical supervision for safety was reviewed with her mother. Carla was later initiated on lamotrigine and restarted interpersonal therapy.
References
1. N Engl J Med. 2015 May 21;372(21):2029-38.
2. J Pediatr. 2010 Nov;157(5):848-51.
3. Arch Gen Psychiatry. 2007 Oct;64(10):1132-43.
4. Curr Probl Pediatr Adolesc Health Care. 2018 Feb;48(2):50-62.
5. Arch Pediatr Adolesc Med. 2004 Aug;158(8):773-80.
6. Can J Psychiatry. 1993 Nov;38(9):590-4.
7. Appl Clin Genet. 2014 Feb 12;7:33-42.
8. J Am Acad Child Adolesc Psychiatry. 2017 Dec;56(12):1073-1080.
9. JAMA Psychiatry. 2019;76(4):426-34.
10. Subst Use Misuse. 2018 Jun 7;53(7):1158-69.
Carla is an otherwise-healthy 14-year-old female followed by her pediatrician for symptoms of depression and anxiety that have worsened over the past 8 months. Anhedonia, irritability, poor concentration, fatigue, hypersomnolence, and significant weight gain have increasingly led to further dysphoria, social isolation, and obsessive rumination, all of which now contribute to more dysfunction in both her home and school life. Based on Carla’s apprehension over “taking pills,” she was referred for outpatient therapy 5 months ago but because of difficulty maintaining weekly appointments, she stopped attending after 6 weeks, citing difficulty aligning with her therapist.
Carla was seen in an urgent, unscheduled follow-up appointment 2 months prior to address increased thoughts of wishing to be dead. She had neither a plan nor a desire to act on these ideations. During an interview, she was distant with poor eye contact, and her affect was notably blunted. Her mother, who had accompanied her in the waiting room, expressed frustration to the nurse about discovering that Carla was using cannabis, that she often appeared aloof and unmotivated to do much of anything but “sit in her room and play on her phone for hours on end.” She compared Carla with her ex-husband, who had similar mood swings that often led to erratic and violent outbursts towards Carla and her mother, behaviors that ultimately led them to leave him when Carla was 6 years old.
After a discussion over the risks and benefits of various treatment options, Carla was started on low-dose fluoxetine with a plan to titrate the medication after 2 weeks. A referral for outpatient substance use treatment also was initiated. Carla’s mother telephoned 10 days later in an update that things have drastically improved in Carla’s mood and activity. The following week her mother called back again with concerns that Carla is no longer sleeping, appears restless, impulsive, and disinhibited.
Discussion
Carla’s initial presentation is common to primary care settings. Based on her earliest reported symptoms, she would qualify for a diagnosis of major depression. Decisions regarding initial treatment for children and adolescents must take into account the severity of symptoms, risks, autonomy of the patient and family, as well as available evidence. Her response to outpatient therapy is not an anomaly. With an ever-increasing demand on mental health services, the availability of consistent, quality outpatient therapy for this population is not always easy to secure.1,2 Combining targeted therapy with pharmacologic interventions for major depression appear to have the most effective outcomes.3
Carla’s progression also illustrates the challenges and potential pitfalls of attempting to understand and address her symptoms according to a single nosology. Depression is a like a fever. It can be caused by a myriad of factors and, left to linger, may lead to further residual complications. Focusing attention to her symptoms also may lead to a differential including adjustment problems, social anxiety, effects of trauma, surreptitious substance use, or even bipolar depression.
To begin with, a clear delineation of Carla’s historic symptoms and any possible medical contributions to her presentation are necessary to investigate. Specific inquiries into past episodes of activation including hyperarousal, impulsivity, restlessness, and insomnia should be elucidated prior to consideration of medication selection.4 Considering Carla’s age and the known association between antidepressant-induced manic conversion among children aged 10-14 years,5 any pharmacologic intervention will benefit from the maxim “start low and go slow.” Her symptoms of activation arise within the setting of titration of an antidepressant. This may raise considerations to her specific metabolism and physiological concentrations of the medication as well as cumulative day exposure.
Complementary to Carla’s own history is that of family members. Often obtaining a reliable family psychiatric history is an exercise fraught with bias, vagueness, and generalizations.6 However, given the known heritability of bipolar disorders and the implications for treating depression in such individuals, compared with unipolar depressive symptoms, clarifying the nature of family illness may elucidate potential susceptibilities previously unconsidered.7 In this case, descriptions of Carla’s father’s behavior raise concerns for underlying bipolar disorder, as do the accounts of traumatic stress exposure and their compounded preponderance for increased suicide risk.8
Unfortunately, Carla’s current environmental cues and maladaptive behaviors may be perpetuating her symptoms and possibly placing her on a trajectory for further illness. Exploration of her relationship with her caregivers regarding the interpretation of her symptoms, and need for treatment should be undertaken so as to expand supportive roles. Education regarding cannabis use among adolescents and age-specific risks for later depression, anxiety, and suicide is warranted in a climate when accessibility is on the rise.9 Whether or not cannabis use itself leads to amotivation is the subject of current debate.10 A growing body of evidence is clearly illustrating that Carla’s sedentary behaviors and perceived loneliness likely exacerbate her mental well-being. Such patterns indicate the need for environmental intervention to change such cycles.
Finally, Carla’s progression through treatment speak to the need for open and honest discussions regarding realistic benefits as well potential risks. Progressive symptoms of depression left untreated can be life-threatening themselves, just as effects of activation as described in the vignette above can easily and quickly progress into situations that pose safety concerns. Amidst such periods of intervention, close communication and follow up with patients and their supports ameliorate potential adverse events and lead to better outcomes.
Outcome
Carla’s mother was advised to discontinue the medication, closely monitor Carla’s behavior and sleep, and schedule an emergent follow-up appointment for the next day. A safety plan indicating circumstances in which Carla would require closer medical supervision for safety was reviewed with her mother. Carla was later initiated on lamotrigine and restarted interpersonal therapy.
References
1. N Engl J Med. 2015 May 21;372(21):2029-38.
2. J Pediatr. 2010 Nov;157(5):848-51.
3. Arch Gen Psychiatry. 2007 Oct;64(10):1132-43.
4. Curr Probl Pediatr Adolesc Health Care. 2018 Feb;48(2):50-62.
5. Arch Pediatr Adolesc Med. 2004 Aug;158(8):773-80.
6. Can J Psychiatry. 1993 Nov;38(9):590-4.
7. Appl Clin Genet. 2014 Feb 12;7:33-42.
8. J Am Acad Child Adolesc Psychiatry. 2017 Dec;56(12):1073-1080.
9. JAMA Psychiatry. 2019;76(4):426-34.
10. Subst Use Misuse. 2018 Jun 7;53(7):1158-69.
Discovery of peer review and patient safety reports
Question: A patient died unexpectedly during hospitalization for a diabetic foot infection. The autopsy revealed the presence of a large saddle pulmonary embolus. The hospital’s peer review committee met to determine if care was suboptimal and whether prophylactic anticoagulation should have been used. When the attending doctor was subsequently sued for malpractice, the plaintiff’s attorney sought to subpoena all of the medical records, including the minutes of the peer review committee. Given this hypothetical scenario, which of the following can occur?
A. “Discovery” is the legal term given to the process during the pretrial phase for amassing relevant documents and other information.
B. A subpoena duces tecum, which is a court order for the production of relevant documents and one that should normally be obeyed, may be issued.
C. The hospital declines to hand over certain types of hospital records, such as peer review minutes, which in this case are statutorily protected from discovery.
D. The plaintiff attorney goes to the judge for an order to compel production and may or may not be successful.
E. All are correct.
Answer: E. Physicians and other participants regularly meet, under strict confidential conditions, to discuss adverse events that occur in their institution. Such records are protected from “discovery,” which is a pretrial procedure for collecting evidence in preparation for trial. The rationale for keeping these records beyond the reach of the discovery process is to encourage participants to engage in candid and free-rein analysis of adverse medical events so as to avoid future mishaps. If the content and nature of these discussions were freely available to parties in litigation, there would be a natural reluctance to express one’s viewpoints in a forthright manner.
Any given state’s statute on discovery requires careful reading because it could differ from another state’s directive – with important legal consequences. As an example, Hawaii’s statute1 contains several inclusions and exclusions and reads in part: “... the information and data protected shall include proceedings and records of a peer review committee, hospital quality assurance committee, or health care review organization that include recordings, transcripts, minutes, and summaries of meetings, conversations, notes, materials, or reports created for, by, or at the direction of a peer review committee, quality assurance committee, or a health care review organization when related to a medical error reporting system. ... Information and data protected from discovery shall not include incident reports, occurrence reports, statements, or similar reports that state facts concerning a specific situation and shall not include records made in the regular course of business by a hospital ... including patient medical records. Original sources of information ... shall not be construed as being immune from discovery ... merely because they were reviewed ... or were in fact submitted to, a health care review organization.”
Predictably, plaintiff attorneys in a medical malpractice lawsuit will attempt to discover information regarding adverse events, hoping to learn about potential errors and judgment lapses, and thus gain an advantage over the defendant doctor and/or hospital. Several recent court cases highlight the contentious nature regarding whether a particular hospital report is to be deemed discoverable. Organized medicine, led by the American Medical Association, has mounted a vigorous response in arguing against the release of peer review and patient safety documents.
The AMA2 recently weighed in on the case of Daley v. Teruel and Ingalls Memorial Hospital. In 2013, a renal failure patient died in an Illinois hospital from injuries that arose from prolonged hypoglycemia. She had received insulin, but when her blood glucose dropped to 16 mg/dl, the treatment team was not alerted and she was later found unresponsive with irreversible brain damage. The issue was whether incident reports from the case that were submitted to a certified PSO (patient safety organization) could be discovered. The Federal Patient Safety and Quality Improvement Act (PSQIA) had created PSOs to aggregate data from multiple sources to reduce adverse events and errors and improve medication safety.
An Illinois lower court ruled that, as part of the discovery process, the hospital had to turn over the report. However, the Illinois Appellate Court ruled in favor of the hospital, holding that the PSQIA protects the report because it is a “patient safety work product.”3 The AMA amicus brief had emphasized that Congress created a safeguarded patient safety process under the PSQIA to encourage hospitals to submit patient safety outcomes without fear of increased liability risk and that “these voluntarily created materials should be used for their intended purpose, not as a roadmap for litigation.”
New Jersey has also ruled against the discovery of a hospital’s self-critical report of a patient’s care, prepared in accordance with New Jersey’s Patient Safety Act.4 The plaintiff alleged that, when she reported to the emergency room at Chilton Medical Center complaining of persistent abdominal pain, fever, body aches, weakness, and a phlegmatic cough, she was incorrectly diagnosed as having pneumonia. In fact, she had appendicitis and a pelvic abscess. The New Jersey Supreme Court affirmed the panel’s order shielding the redacted document from discovery, but it reversed the judgment to the extent it ended the defendants’ discovery obligation with respect to this dispute, requiring instead that the lower court address, through current discovery rules, the proper balancing of interests between requesting and responding parties.
In a recent Michigan case,5 the trial court had earlier ruled that peer review documents at issue were in fact discoverable. Like similar statutes elsewhere, Michigan’s peer review privileges serve to encourage participation to improve on patient morbidity and mortality. The case centered on a court order compelling a Michigan hospital to release a physician’s credentialing file in a medical liability lawsuit on the narrow basis that the nondiscoverability privilege applied only to peer review deliberations and was inapplicable in the case. The trial judge had opined that, if all materials viewed by peer review committees were deemed undiscoverable, a hospital could never be held accountable for any negligent act within the purview of the committee. In its amicus brief in support of the hospital, the AMA argued that Michigan’s peer review privilege has historically spanned the bounds of the actual peer review process, and it countered that hospitals can be held liable – and are regularly held liable – without opening up these documents and that plaintiffs can use the same discovery mechanisms generally available to plaintiffs in other lawsuits.6 The case is currently under appeal.
In contrast, at least two state supreme courts have ruled to limit protections from discovery. The Florida Supreme Court has held that the federal law was intended to improve overall health care rather than to act as a shield to providers. In a case of alleged malpractice with severe neurological injuries, the court took a restrictive interpretation of the PSQIA as it relates to Florida’s risk-management and discovery laws, holding that patient safety work and related reports, when required by state law, do not come under the definition of patient safety work product and were therefore discoverable.7
The Pennsylvania Supreme Court has likewise ruled that documents generated by a hospital’s outside contractor are not protected from discovery under the state’s Peer Review Protection Act. It agreed with a lower-court ruling that Monongahela Valley Hospital could not claim privilege for a performance file on an emergency department physician employed by the hospital’s contractor University of Pittsburgh Medical Center Emergency Medicine.8 The case alleged that the plaintiff’s chest and back pain was misdiagnosed as reflux disease when in fact it was a myocardial infarct.
Dr. Tan is professor of medicine and former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. Hawaii Revised Statutes §624-25.5 (2012).
2. AMA fights to protect patient-safety work from legal discovery. AMA Morning Rounds. 2018 Aug 1.
3. Daley v. Teruel and Ingalls Memorial Hospital, 2018 Ill. App. LEXIS 440 (Ill. App. Ct. 2018).
4. Brugaletta v. Garcia, 190 A.3d 419 (NJ. 2018).
5. Dwyer v. Ascension Crittenton Hospital. Michigan Supreme Court SC: 158668, 919 N.W.2d 407 (Mi. 2018).
6. Appellate court case puts peer-review protections in danger. AMA Morning Rounds. 2019 Mar 29.
7. Charles v. Southern Baptist Hospital of Florida, Inc., 2017 Fla. LEXIS 231 (Fla. Jan. 31, 2017).
8. Reginelli v. Boggs, 2018 Pa. LEXIS 1503 (Pa. 2018).
Question: A patient died unexpectedly during hospitalization for a diabetic foot infection. The autopsy revealed the presence of a large saddle pulmonary embolus. The hospital’s peer review committee met to determine if care was suboptimal and whether prophylactic anticoagulation should have been used. When the attending doctor was subsequently sued for malpractice, the plaintiff’s attorney sought to subpoena all of the medical records, including the minutes of the peer review committee. Given this hypothetical scenario, which of the following can occur?
A. “Discovery” is the legal term given to the process during the pretrial phase for amassing relevant documents and other information.
B. A subpoena duces tecum, which is a court order for the production of relevant documents and one that should normally be obeyed, may be issued.
C. The hospital declines to hand over certain types of hospital records, such as peer review minutes, which in this case are statutorily protected from discovery.
D. The plaintiff attorney goes to the judge for an order to compel production and may or may not be successful.
E. All are correct.
Answer: E. Physicians and other participants regularly meet, under strict confidential conditions, to discuss adverse events that occur in their institution. Such records are protected from “discovery,” which is a pretrial procedure for collecting evidence in preparation for trial. The rationale for keeping these records beyond the reach of the discovery process is to encourage participants to engage in candid and free-rein analysis of adverse medical events so as to avoid future mishaps. If the content and nature of these discussions were freely available to parties in litigation, there would be a natural reluctance to express one’s viewpoints in a forthright manner.
Any given state’s statute on discovery requires careful reading because it could differ from another state’s directive – with important legal consequences. As an example, Hawaii’s statute1 contains several inclusions and exclusions and reads in part: “... the information and data protected shall include proceedings and records of a peer review committee, hospital quality assurance committee, or health care review organization that include recordings, transcripts, minutes, and summaries of meetings, conversations, notes, materials, or reports created for, by, or at the direction of a peer review committee, quality assurance committee, or a health care review organization when related to a medical error reporting system. ... Information and data protected from discovery shall not include incident reports, occurrence reports, statements, or similar reports that state facts concerning a specific situation and shall not include records made in the regular course of business by a hospital ... including patient medical records. Original sources of information ... shall not be construed as being immune from discovery ... merely because they were reviewed ... or were in fact submitted to, a health care review organization.”
Predictably, plaintiff attorneys in a medical malpractice lawsuit will attempt to discover information regarding adverse events, hoping to learn about potential errors and judgment lapses, and thus gain an advantage over the defendant doctor and/or hospital. Several recent court cases highlight the contentious nature regarding whether a particular hospital report is to be deemed discoverable. Organized medicine, led by the American Medical Association, has mounted a vigorous response in arguing against the release of peer review and patient safety documents.
The AMA2 recently weighed in on the case of Daley v. Teruel and Ingalls Memorial Hospital. In 2013, a renal failure patient died in an Illinois hospital from injuries that arose from prolonged hypoglycemia. She had received insulin, but when her blood glucose dropped to 16 mg/dl, the treatment team was not alerted and she was later found unresponsive with irreversible brain damage. The issue was whether incident reports from the case that were submitted to a certified PSO (patient safety organization) could be discovered. The Federal Patient Safety and Quality Improvement Act (PSQIA) had created PSOs to aggregate data from multiple sources to reduce adverse events and errors and improve medication safety.
An Illinois lower court ruled that, as part of the discovery process, the hospital had to turn over the report. However, the Illinois Appellate Court ruled in favor of the hospital, holding that the PSQIA protects the report because it is a “patient safety work product.”3 The AMA amicus brief had emphasized that Congress created a safeguarded patient safety process under the PSQIA to encourage hospitals to submit patient safety outcomes without fear of increased liability risk and that “these voluntarily created materials should be used for their intended purpose, not as a roadmap for litigation.”
New Jersey has also ruled against the discovery of a hospital’s self-critical report of a patient’s care, prepared in accordance with New Jersey’s Patient Safety Act.4 The plaintiff alleged that, when she reported to the emergency room at Chilton Medical Center complaining of persistent abdominal pain, fever, body aches, weakness, and a phlegmatic cough, she was incorrectly diagnosed as having pneumonia. In fact, she had appendicitis and a pelvic abscess. The New Jersey Supreme Court affirmed the panel’s order shielding the redacted document from discovery, but it reversed the judgment to the extent it ended the defendants’ discovery obligation with respect to this dispute, requiring instead that the lower court address, through current discovery rules, the proper balancing of interests between requesting and responding parties.
In a recent Michigan case,5 the trial court had earlier ruled that peer review documents at issue were in fact discoverable. Like similar statutes elsewhere, Michigan’s peer review privileges serve to encourage participation to improve on patient morbidity and mortality. The case centered on a court order compelling a Michigan hospital to release a physician’s credentialing file in a medical liability lawsuit on the narrow basis that the nondiscoverability privilege applied only to peer review deliberations and was inapplicable in the case. The trial judge had opined that, if all materials viewed by peer review committees were deemed undiscoverable, a hospital could never be held accountable for any negligent act within the purview of the committee. In its amicus brief in support of the hospital, the AMA argued that Michigan’s peer review privilege has historically spanned the bounds of the actual peer review process, and it countered that hospitals can be held liable – and are regularly held liable – without opening up these documents and that plaintiffs can use the same discovery mechanisms generally available to plaintiffs in other lawsuits.6 The case is currently under appeal.
In contrast, at least two state supreme courts have ruled to limit protections from discovery. The Florida Supreme Court has held that the federal law was intended to improve overall health care rather than to act as a shield to providers. In a case of alleged malpractice with severe neurological injuries, the court took a restrictive interpretation of the PSQIA as it relates to Florida’s risk-management and discovery laws, holding that patient safety work and related reports, when required by state law, do not come under the definition of patient safety work product and were therefore discoverable.7
The Pennsylvania Supreme Court has likewise ruled that documents generated by a hospital’s outside contractor are not protected from discovery under the state’s Peer Review Protection Act. It agreed with a lower-court ruling that Monongahela Valley Hospital could not claim privilege for a performance file on an emergency department physician employed by the hospital’s contractor University of Pittsburgh Medical Center Emergency Medicine.8 The case alleged that the plaintiff’s chest and back pain was misdiagnosed as reflux disease when in fact it was a myocardial infarct.
Dr. Tan is professor of medicine and former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. Hawaii Revised Statutes §624-25.5 (2012).
2. AMA fights to protect patient-safety work from legal discovery. AMA Morning Rounds. 2018 Aug 1.
3. Daley v. Teruel and Ingalls Memorial Hospital, 2018 Ill. App. LEXIS 440 (Ill. App. Ct. 2018).
4. Brugaletta v. Garcia, 190 A.3d 419 (NJ. 2018).
5. Dwyer v. Ascension Crittenton Hospital. Michigan Supreme Court SC: 158668, 919 N.W.2d 407 (Mi. 2018).
6. Appellate court case puts peer-review protections in danger. AMA Morning Rounds. 2019 Mar 29.
7. Charles v. Southern Baptist Hospital of Florida, Inc., 2017 Fla. LEXIS 231 (Fla. Jan. 31, 2017).
8. Reginelli v. Boggs, 2018 Pa. LEXIS 1503 (Pa. 2018).
Question: A patient died unexpectedly during hospitalization for a diabetic foot infection. The autopsy revealed the presence of a large saddle pulmonary embolus. The hospital’s peer review committee met to determine if care was suboptimal and whether prophylactic anticoagulation should have been used. When the attending doctor was subsequently sued for malpractice, the plaintiff’s attorney sought to subpoena all of the medical records, including the minutes of the peer review committee. Given this hypothetical scenario, which of the following can occur?
A. “Discovery” is the legal term given to the process during the pretrial phase for amassing relevant documents and other information.
B. A subpoena duces tecum, which is a court order for the production of relevant documents and one that should normally be obeyed, may be issued.
C. The hospital declines to hand over certain types of hospital records, such as peer review minutes, which in this case are statutorily protected from discovery.
D. The plaintiff attorney goes to the judge for an order to compel production and may or may not be successful.
E. All are correct.
Answer: E. Physicians and other participants regularly meet, under strict confidential conditions, to discuss adverse events that occur in their institution. Such records are protected from “discovery,” which is a pretrial procedure for collecting evidence in preparation for trial. The rationale for keeping these records beyond the reach of the discovery process is to encourage participants to engage in candid and free-rein analysis of adverse medical events so as to avoid future mishaps. If the content and nature of these discussions were freely available to parties in litigation, there would be a natural reluctance to express one’s viewpoints in a forthright manner.
Any given state’s statute on discovery requires careful reading because it could differ from another state’s directive – with important legal consequences. As an example, Hawaii’s statute1 contains several inclusions and exclusions and reads in part: “... the information and data protected shall include proceedings and records of a peer review committee, hospital quality assurance committee, or health care review organization that include recordings, transcripts, minutes, and summaries of meetings, conversations, notes, materials, or reports created for, by, or at the direction of a peer review committee, quality assurance committee, or a health care review organization when related to a medical error reporting system. ... Information and data protected from discovery shall not include incident reports, occurrence reports, statements, or similar reports that state facts concerning a specific situation and shall not include records made in the regular course of business by a hospital ... including patient medical records. Original sources of information ... shall not be construed as being immune from discovery ... merely because they were reviewed ... or were in fact submitted to, a health care review organization.”
Predictably, plaintiff attorneys in a medical malpractice lawsuit will attempt to discover information regarding adverse events, hoping to learn about potential errors and judgment lapses, and thus gain an advantage over the defendant doctor and/or hospital. Several recent court cases highlight the contentious nature regarding whether a particular hospital report is to be deemed discoverable. Organized medicine, led by the American Medical Association, has mounted a vigorous response in arguing against the release of peer review and patient safety documents.
The AMA2 recently weighed in on the case of Daley v. Teruel and Ingalls Memorial Hospital. In 2013, a renal failure patient died in an Illinois hospital from injuries that arose from prolonged hypoglycemia. She had received insulin, but when her blood glucose dropped to 16 mg/dl, the treatment team was not alerted and she was later found unresponsive with irreversible brain damage. The issue was whether incident reports from the case that were submitted to a certified PSO (patient safety organization) could be discovered. The Federal Patient Safety and Quality Improvement Act (PSQIA) had created PSOs to aggregate data from multiple sources to reduce adverse events and errors and improve medication safety.
An Illinois lower court ruled that, as part of the discovery process, the hospital had to turn over the report. However, the Illinois Appellate Court ruled in favor of the hospital, holding that the PSQIA protects the report because it is a “patient safety work product.”3 The AMA amicus brief had emphasized that Congress created a safeguarded patient safety process under the PSQIA to encourage hospitals to submit patient safety outcomes without fear of increased liability risk and that “these voluntarily created materials should be used for their intended purpose, not as a roadmap for litigation.”
New Jersey has also ruled against the discovery of a hospital’s self-critical report of a patient’s care, prepared in accordance with New Jersey’s Patient Safety Act.4 The plaintiff alleged that, when she reported to the emergency room at Chilton Medical Center complaining of persistent abdominal pain, fever, body aches, weakness, and a phlegmatic cough, she was incorrectly diagnosed as having pneumonia. In fact, she had appendicitis and a pelvic abscess. The New Jersey Supreme Court affirmed the panel’s order shielding the redacted document from discovery, but it reversed the judgment to the extent it ended the defendants’ discovery obligation with respect to this dispute, requiring instead that the lower court address, through current discovery rules, the proper balancing of interests between requesting and responding parties.
In a recent Michigan case,5 the trial court had earlier ruled that peer review documents at issue were in fact discoverable. Like similar statutes elsewhere, Michigan’s peer review privileges serve to encourage participation to improve on patient morbidity and mortality. The case centered on a court order compelling a Michigan hospital to release a physician’s credentialing file in a medical liability lawsuit on the narrow basis that the nondiscoverability privilege applied only to peer review deliberations and was inapplicable in the case. The trial judge had opined that, if all materials viewed by peer review committees were deemed undiscoverable, a hospital could never be held accountable for any negligent act within the purview of the committee. In its amicus brief in support of the hospital, the AMA argued that Michigan’s peer review privilege has historically spanned the bounds of the actual peer review process, and it countered that hospitals can be held liable – and are regularly held liable – without opening up these documents and that plaintiffs can use the same discovery mechanisms generally available to plaintiffs in other lawsuits.6 The case is currently under appeal.
In contrast, at least two state supreme courts have ruled to limit protections from discovery. The Florida Supreme Court has held that the federal law was intended to improve overall health care rather than to act as a shield to providers. In a case of alleged malpractice with severe neurological injuries, the court took a restrictive interpretation of the PSQIA as it relates to Florida’s risk-management and discovery laws, holding that patient safety work and related reports, when required by state law, do not come under the definition of patient safety work product and were therefore discoverable.7
The Pennsylvania Supreme Court has likewise ruled that documents generated by a hospital’s outside contractor are not protected from discovery under the state’s Peer Review Protection Act. It agreed with a lower-court ruling that Monongahela Valley Hospital could not claim privilege for a performance file on an emergency department physician employed by the hospital’s contractor University of Pittsburgh Medical Center Emergency Medicine.8 The case alleged that the plaintiff’s chest and back pain was misdiagnosed as reflux disease when in fact it was a myocardial infarct.
Dr. Tan is professor of medicine and former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. Hawaii Revised Statutes §624-25.5 (2012).
2. AMA fights to protect patient-safety work from legal discovery. AMA Morning Rounds. 2018 Aug 1.
3. Daley v. Teruel and Ingalls Memorial Hospital, 2018 Ill. App. LEXIS 440 (Ill. App. Ct. 2018).
4. Brugaletta v. Garcia, 190 A.3d 419 (NJ. 2018).
5. Dwyer v. Ascension Crittenton Hospital. Michigan Supreme Court SC: 158668, 919 N.W.2d 407 (Mi. 2018).
6. Appellate court case puts peer-review protections in danger. AMA Morning Rounds. 2019 Mar 29.
7. Charles v. Southern Baptist Hospital of Florida, Inc., 2017 Fla. LEXIS 231 (Fla. Jan. 31, 2017).
8. Reginelli v. Boggs, 2018 Pa. LEXIS 1503 (Pa. 2018).
The expert trap
When you fly as a physician, there’s always a chance you’ll get a free drink. It’s not free, of course. For at least a few minutes, you worked. “Is there a physician onboard? – Ah, just how badly do you want that vodka tonic?
I ring my call button, as I’m sure you do. (It’s worth it to see the flight attendant’s face when I reply: “I’m a dermatologist.”) Last time it was for a 68-year-old man who was vomiting. There was no rash.
I responded along with a pediatrician and an ER nurse – gratitude is an ER nurse at 38,000 feet. The patient had chemotherapy-induced nausea. We three managed to get him well enough to finish the flight. Our ER nurse team member ran the show; she was excellent. She asked all the right questions and helped us all make good decisions. Unlike in clinic, I wasn’t an expert here despite my MD.
Several weeks ago, I saw a patient in the office with severe psoriasis. She stood before me erythrodermic. As I was adjusting her orders, I stepped out of the office to call one of my partners for her opinion. She examined the patient and declared: “I don’t think it’s psoriasis. Despite that biopsy, I think this is chronic eczema.” Brilliant.
In contrast to the former story, I was an expert in my office. And yet, success depended in both instances on my recognizing a cognitive bias: I don’t know everything, and worse, I sometimes don’t realize what I don’t know.
. It’s a common mistake and manifests as overconfidence in our own abilities. For example, what decade did Hawaii join the union? Who is on the 20-dollar bill? Which is the farthest planet? You might be 90% confident of your answers, but most of us are more confident than we ought to be. Chances are you’ll be wrong on one. Recognizing this is hard. And yet, it’s what separates the good from the great clinicians.
Short of having your medical assistant whisper in your ear each day “Memento stultus” (remember you’re stupid), avoiding this bias is difficult. Signs that you might be trapped in an expert mindset are: 1. You believe your patients’ failure to improve is due to lack of adherence to your plan. 2. You cannot recall the last time you tried a new treatment. 3. You never ask others for second opinions. 4. Your colleagues stop asking for your opinion. 5. A flight attendant asks if you would mind returning to your seat rather than help with a medical situation.
If you want to be a better doctor, try working on your sense of self-importance. Remember your limitations and those of medicine. Be methodical in questioning your assumptions. Could you be wrong? Could the data you have be misleading? What are you missing? Ask a colleague to review some of your charts or spend time with you during procedures. Join (or start!) a journal club. Share your difficult cases with others and take note of how their advice differs from your approach.
By recognizing when you might be wrong and humbly stepping aside or taking the time to learn, you might just earn that free drink.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
When you fly as a physician, there’s always a chance you’ll get a free drink. It’s not free, of course. For at least a few minutes, you worked. “Is there a physician onboard? – Ah, just how badly do you want that vodka tonic?
I ring my call button, as I’m sure you do. (It’s worth it to see the flight attendant’s face when I reply: “I’m a dermatologist.”) Last time it was for a 68-year-old man who was vomiting. There was no rash.
I responded along with a pediatrician and an ER nurse – gratitude is an ER nurse at 38,000 feet. The patient had chemotherapy-induced nausea. We three managed to get him well enough to finish the flight. Our ER nurse team member ran the show; she was excellent. She asked all the right questions and helped us all make good decisions. Unlike in clinic, I wasn’t an expert here despite my MD.
Several weeks ago, I saw a patient in the office with severe psoriasis. She stood before me erythrodermic. As I was adjusting her orders, I stepped out of the office to call one of my partners for her opinion. She examined the patient and declared: “I don’t think it’s psoriasis. Despite that biopsy, I think this is chronic eczema.” Brilliant.
In contrast to the former story, I was an expert in my office. And yet, success depended in both instances on my recognizing a cognitive bias: I don’t know everything, and worse, I sometimes don’t realize what I don’t know.
. It’s a common mistake and manifests as overconfidence in our own abilities. For example, what decade did Hawaii join the union? Who is on the 20-dollar bill? Which is the farthest planet? You might be 90% confident of your answers, but most of us are more confident than we ought to be. Chances are you’ll be wrong on one. Recognizing this is hard. And yet, it’s what separates the good from the great clinicians.
Short of having your medical assistant whisper in your ear each day “Memento stultus” (remember you’re stupid), avoiding this bias is difficult. Signs that you might be trapped in an expert mindset are: 1. You believe your patients’ failure to improve is due to lack of adherence to your plan. 2. You cannot recall the last time you tried a new treatment. 3. You never ask others for second opinions. 4. Your colleagues stop asking for your opinion. 5. A flight attendant asks if you would mind returning to your seat rather than help with a medical situation.
If you want to be a better doctor, try working on your sense of self-importance. Remember your limitations and those of medicine. Be methodical in questioning your assumptions. Could you be wrong? Could the data you have be misleading? What are you missing? Ask a colleague to review some of your charts or spend time with you during procedures. Join (or start!) a journal club. Share your difficult cases with others and take note of how their advice differs from your approach.
By recognizing when you might be wrong and humbly stepping aside or taking the time to learn, you might just earn that free drink.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
When you fly as a physician, there’s always a chance you’ll get a free drink. It’s not free, of course. For at least a few minutes, you worked. “Is there a physician onboard? – Ah, just how badly do you want that vodka tonic?
I ring my call button, as I’m sure you do. (It’s worth it to see the flight attendant’s face when I reply: “I’m a dermatologist.”) Last time it was for a 68-year-old man who was vomiting. There was no rash.
I responded along with a pediatrician and an ER nurse – gratitude is an ER nurse at 38,000 feet. The patient had chemotherapy-induced nausea. We three managed to get him well enough to finish the flight. Our ER nurse team member ran the show; she was excellent. She asked all the right questions and helped us all make good decisions. Unlike in clinic, I wasn’t an expert here despite my MD.
Several weeks ago, I saw a patient in the office with severe psoriasis. She stood before me erythrodermic. As I was adjusting her orders, I stepped out of the office to call one of my partners for her opinion. She examined the patient and declared: “I don’t think it’s psoriasis. Despite that biopsy, I think this is chronic eczema.” Brilliant.
In contrast to the former story, I was an expert in my office. And yet, success depended in both instances on my recognizing a cognitive bias: I don’t know everything, and worse, I sometimes don’t realize what I don’t know.
. It’s a common mistake and manifests as overconfidence in our own abilities. For example, what decade did Hawaii join the union? Who is on the 20-dollar bill? Which is the farthest planet? You might be 90% confident of your answers, but most of us are more confident than we ought to be. Chances are you’ll be wrong on one. Recognizing this is hard. And yet, it’s what separates the good from the great clinicians.
Short of having your medical assistant whisper in your ear each day “Memento stultus” (remember you’re stupid), avoiding this bias is difficult. Signs that you might be trapped in an expert mindset are: 1. You believe your patients’ failure to improve is due to lack of adherence to your plan. 2. You cannot recall the last time you tried a new treatment. 3. You never ask others for second opinions. 4. Your colleagues stop asking for your opinion. 5. A flight attendant asks if you would mind returning to your seat rather than help with a medical situation.
If you want to be a better doctor, try working on your sense of self-importance. Remember your limitations and those of medicine. Be methodical in questioning your assumptions. Could you be wrong? Could the data you have be misleading? What are you missing? Ask a colleague to review some of your charts or spend time with you during procedures. Join (or start!) a journal club. Share your difficult cases with others and take note of how their advice differs from your approach.
By recognizing when you might be wrong and humbly stepping aside or taking the time to learn, you might just earn that free drink.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].