User login
Pediatric HM Literature Review
Clinical question: What is the relationship between duration of intravenous (IV) antibiotic therapy and treatment failure in infants <6 months of age hospitalized with urinary tract infections (UTIs)?
Background: There is an inadequate evidence base to drive decisions regarding duration of IV antibiotic therapy in young infants hospitalized with UTIs. Documented variability exists in length of stay (LOS) and resource utilization for these infants, which might be a direct result of practice variation with respect to IV therapy.
Study design: Retrospective cohort study.
Setting: Twenty-four freestanding children’s hospitals.
Synopsis: The Pediatric Health Information System (PHIS) administrative database was used to identify healthy infants <6 months of age admitted with a primary or secondary diagnosis of UTI or pyelonephritis from 1999 to 2004 to participating hospitals. Duration of IV therapy was defined as a dichotomous variable with three days (short course: three days) selected because it was the median length of therapy. Treatment failure was defined as readmission within 30 days.
More than 12,300 records were analyzed. Male gender, neonatal status, black race, Hispanic ethnicity, nonprivate insurance, severity of illness, known bacteremia, known genitourinary tract disorders, and specific hospital were independently associated with increased likelihood of long-course (four days) therapy.
Unadjusted analysis initially revealed that long-course therapy was significantly associated with a higher rate of treatment failure. After multivariate (to include propensity scores) adjustment, a significant association between treatment duration and failure was no longer identified. Treatment failure association with known genitourinary abnormalities and higher severity of illness remained.
A significant limitation of this study is the potential for multivariate analysis to fail to mitigate a bias toward sicker patients receiving longer duration of antibiotic therapy and, thus, having a higher likelihood of treatment failure. In addition, the greater question of when IV antibiotics (and hospital admission) are indicated in this population was not addressed by the study design.
Nonetheless, the data likely support a limited utility to long-course IV antibiotic therapy in this population. The study also adds to the evolving picture of considerable and widespread variation in physician practice.
Bottom line: Short-course IV therapy for infants with UTIs does not increase risk of treatment failure.
Citation: Brady PW, Conway PH, Goudie A. Length of intravenous antibiotic therapy and treatment failure in infants with urinary tract infections. Pediatrics. 2010;126(2):196-203.
Reviewed by Pediatric Editor Mark Shen, MD, medical director of hospital medicine at Dell Children’s Medical Center, Austin, Texas.
Clinical question: What is the relationship between duration of intravenous (IV) antibiotic therapy and treatment failure in infants <6 months of age hospitalized with urinary tract infections (UTIs)?
Background: There is an inadequate evidence base to drive decisions regarding duration of IV antibiotic therapy in young infants hospitalized with UTIs. Documented variability exists in length of stay (LOS) and resource utilization for these infants, which might be a direct result of practice variation with respect to IV therapy.
Study design: Retrospective cohort study.
Setting: Twenty-four freestanding children’s hospitals.
Synopsis: The Pediatric Health Information System (PHIS) administrative database was used to identify healthy infants <6 months of age admitted with a primary or secondary diagnosis of UTI or pyelonephritis from 1999 to 2004 to participating hospitals. Duration of IV therapy was defined as a dichotomous variable with three days (short course: three days) selected because it was the median length of therapy. Treatment failure was defined as readmission within 30 days.
More than 12,300 records were analyzed. Male gender, neonatal status, black race, Hispanic ethnicity, nonprivate insurance, severity of illness, known bacteremia, known genitourinary tract disorders, and specific hospital were independently associated with increased likelihood of long-course (four days) therapy.
Unadjusted analysis initially revealed that long-course therapy was significantly associated with a higher rate of treatment failure. After multivariate (to include propensity scores) adjustment, a significant association between treatment duration and failure was no longer identified. Treatment failure association with known genitourinary abnormalities and higher severity of illness remained.
A significant limitation of this study is the potential for multivariate analysis to fail to mitigate a bias toward sicker patients receiving longer duration of antibiotic therapy and, thus, having a higher likelihood of treatment failure. In addition, the greater question of when IV antibiotics (and hospital admission) are indicated in this population was not addressed by the study design.
Nonetheless, the data likely support a limited utility to long-course IV antibiotic therapy in this population. The study also adds to the evolving picture of considerable and widespread variation in physician practice.
Bottom line: Short-course IV therapy for infants with UTIs does not increase risk of treatment failure.
Citation: Brady PW, Conway PH, Goudie A. Length of intravenous antibiotic therapy and treatment failure in infants with urinary tract infections. Pediatrics. 2010;126(2):196-203.
Reviewed by Pediatric Editor Mark Shen, MD, medical director of hospital medicine at Dell Children’s Medical Center, Austin, Texas.
Clinical question: What is the relationship between duration of intravenous (IV) antibiotic therapy and treatment failure in infants <6 months of age hospitalized with urinary tract infections (UTIs)?
Background: There is an inadequate evidence base to drive decisions regarding duration of IV antibiotic therapy in young infants hospitalized with UTIs. Documented variability exists in length of stay (LOS) and resource utilization for these infants, which might be a direct result of practice variation with respect to IV therapy.
Study design: Retrospective cohort study.
Setting: Twenty-four freestanding children’s hospitals.
Synopsis: The Pediatric Health Information System (PHIS) administrative database was used to identify healthy infants <6 months of age admitted with a primary or secondary diagnosis of UTI or pyelonephritis from 1999 to 2004 to participating hospitals. Duration of IV therapy was defined as a dichotomous variable with three days (short course: three days) selected because it was the median length of therapy. Treatment failure was defined as readmission within 30 days.
More than 12,300 records were analyzed. Male gender, neonatal status, black race, Hispanic ethnicity, nonprivate insurance, severity of illness, known bacteremia, known genitourinary tract disorders, and specific hospital were independently associated with increased likelihood of long-course (four days) therapy.
Unadjusted analysis initially revealed that long-course therapy was significantly associated with a higher rate of treatment failure. After multivariate (to include propensity scores) adjustment, a significant association between treatment duration and failure was no longer identified. Treatment failure association with known genitourinary abnormalities and higher severity of illness remained.
A significant limitation of this study is the potential for multivariate analysis to fail to mitigate a bias toward sicker patients receiving longer duration of antibiotic therapy and, thus, having a higher likelihood of treatment failure. In addition, the greater question of when IV antibiotics (and hospital admission) are indicated in this population was not addressed by the study design.
Nonetheless, the data likely support a limited utility to long-course IV antibiotic therapy in this population. The study also adds to the evolving picture of considerable and widespread variation in physician practice.
Bottom line: Short-course IV therapy for infants with UTIs does not increase risk of treatment failure.
Citation: Brady PW, Conway PH, Goudie A. Length of intravenous antibiotic therapy and treatment failure in infants with urinary tract infections. Pediatrics. 2010;126(2):196-203.
Reviewed by Pediatric Editor Mark Shen, MD, medical director of hospital medicine at Dell Children’s Medical Center, Austin, Texas.
Sound Advice
Recent media reports about the dangers surrounding unused prescription medications, including abuse by teens and medications finding their way into the water supply, have prompted an increase in inquiries to healthcare providers about disposing of unused medication. These issues are complicated when controlled substances are involved.
Often, providers are unsure how to respond to patient questions about medication disposal. For example, what would you do if a patient requests an alternative medication because of an unwanted side effect and brings the originally prescribed medication back to you? What if the family of a recently expired patient brings unused medication to you and asks you to donate it to other patients? What if you have a colleague who performs mission work; could you accept and donate unused medication for use in another country?
Unfortunately, the Controlled Substances Act (CSA) does not provide a readily available mechanism to accomplish efficient, secure, and environmentally sound methods to collect and use or dispose of unwanted controlled substances. This article explains the rules physicians must adhere to and guidelines for “taking back” controlled substances.
The Legislation
Enacted in 1970, the CSA combined all existing federal drug laws into a single statute. It created five “schedules” in which certain drugs are classified. These “scheduled” drugs are commonly referred to as controlled substances. A drug’s classification depends on its potential for abuse and its currently accepted medical use in the U.S. Additionally, provisions of international treaties impact classification.
Under the classification system, Schedule I drugs have a high potential for abuse and have no currently accepted medical use in treatment in the U.S. In contrast, Schedule V drugs have a low potential for abuse and do have a currently accepted medical use in treatment in the U.S.
The CSA governs the manufacture, import, export, possession, use, and distribution of controlled substances. In doing so, the CSA established a system to register those authorized to handle controlled substances. Manufacturers, dispensers, distributors, and individual practitioners who prescribe controlled substances must be registered with the Drug Enforcement Administration (DEA).
The CSA requires registrants to keep certain records for at least two years related to their handling of controlled substances. For example, physician registrants must keep records of controlled substances in Schedules II, III, IV, and V that are dispensed via methods other than prescribing or administering (e.g., industry samples). Inventories of controlled substances are required. Most notably, physicians generally are not required to keep records of prescribed medications; however, records must be kept if drugs are dispensed or administered. Moreover, there are heightened recordkeeping responsibilities for providers who prescribe, dispense, or administer for maintenance or detoxification.
Controlled Substance “Takeback”
The system of registration established by the CSA prohibits a DEA registrant from acquiring controlled substances from nonregistered entities and, in turn, bars an end-user from distributing pharmaceutical controlled substances to a DEA registrant. In other words, physicians cannot receive controlled substances from anyone who does not also have a registration. Thus, physicians may not “take back” prescribed medications from patients or their family members. Similarly, except in cases of a drug being recalled or a dispensing error, patients are not allowed to return controlled medications to a pharmacy.
Information on how a patient or family member should properly dispose of medication is commonly misunderstood. DEA regulations provide a process for nonregistrants to dispose of unused medication; however, it is cumbersome and meant to be used only when dealing with large quantities of controlled substances (e.g., large quantities of abandoned drugs). In such cases, the DEA special agent in charge (SAC) may instruct on disposal, which may include transfer of the substance to a DEA registrant, delivery to a DEA agent or office, destruction in the presence of an agent of the administration or other authorized person, or by other means. The person must submit a letter to the local SAC, which includes:
- Name and address of the person;
- Name and quantity of each controlled substance to be disposed of;
- Explanation of how the applicant obtained the controlled substance, if known; and
- Name, address, and registration number, if known, of the person who possessed the controlled substances prior to the applicant.
Federal legislation also provides a way for the DEA to grant approval to law-enforcement agencies to operate “takeback” programs. The regulation states that “any person in possession of a controlled substance and desiring to dispose of such substance may request assistance from the SAC in the area in which the person is located.” The regulation allows the SAC to authorize and specify the means of disposal to assure that the controlled substances do not become available to unauthorized persons.
State and local government agencies and community associations might hold takeback programs only if law enforcement makes the request, takes custody of the controlled substances, and is responsible for the disposal.
The U.S. Office of National Drug Control Policy has published guidelines for medication disposal. These guidelines advise flushing medications only if the prescription label or accompanying patient information specifically states to do so. Instead of flushing, the guidelines recommend that medications be disposed of through a takeback program or by:
- Taking the prescription drugs out of their original containers;
- Mixing the drugs with an undesirable substance, such as cat litter or used coffee grounds;
- Placing the mixture into a disposable container with a lid, such as an empty margarine tub, or into a sealable bag;
- Concealing or removing personal information, including Rx number, on the empty containers by covering it with black permanent marker or duct tape, or by scratching it off; and
- Placing the sealed container with the mixture, and the empty drug containers, in the trash.
Unused Medication Donation
The rising cost of prescription medication leaves many questioning whether there is a need for a safe method to allow unused medication to be donated to others. At least 10 states have passed laws allowing or encouraging the donation of unused pharmaceutical drugs. Many of these programs involve healthcare facilities, nursing homes, or pharmacies. The CSA and current DEA regulations, however, prohibit patients from delivering or distributing controlled substances to a DEA registrant, even if it is for the purpose of a donation. Moreover, the Food and Drug Administration (FDA) does not permit redistribution of medications, except under limited circumstances.
Consequently, state law may be inconsistent with federal law for donation and reuse of controlled substances.
Conclusion
Physicians who fail to comply with CSA handling requirements are subject to criminal charges, discipline against their DEA registration, and discipline against their license to practice medicine. Consequently, physicians should use caution whenever handling unused medication.
The application of various aspects of the CSA and implementing rules is situation-specific. Moreover, the DEA may issue additional regulations. Accordingly, if you have a question about a specific situation, consult an attorney, or contact your local DEA field division office and ask for the diversion duty agent. TH
Patrick O’Rourke works in the Office of University Counsel, Department of Litigation, University of Colorado Denver.
Recent media reports about the dangers surrounding unused prescription medications, including abuse by teens and medications finding their way into the water supply, have prompted an increase in inquiries to healthcare providers about disposing of unused medication. These issues are complicated when controlled substances are involved.
Often, providers are unsure how to respond to patient questions about medication disposal. For example, what would you do if a patient requests an alternative medication because of an unwanted side effect and brings the originally prescribed medication back to you? What if the family of a recently expired patient brings unused medication to you and asks you to donate it to other patients? What if you have a colleague who performs mission work; could you accept and donate unused medication for use in another country?
Unfortunately, the Controlled Substances Act (CSA) does not provide a readily available mechanism to accomplish efficient, secure, and environmentally sound methods to collect and use or dispose of unwanted controlled substances. This article explains the rules physicians must adhere to and guidelines for “taking back” controlled substances.
The Legislation
Enacted in 1970, the CSA combined all existing federal drug laws into a single statute. It created five “schedules” in which certain drugs are classified. These “scheduled” drugs are commonly referred to as controlled substances. A drug’s classification depends on its potential for abuse and its currently accepted medical use in the U.S. Additionally, provisions of international treaties impact classification.
Under the classification system, Schedule I drugs have a high potential for abuse and have no currently accepted medical use in treatment in the U.S. In contrast, Schedule V drugs have a low potential for abuse and do have a currently accepted medical use in treatment in the U.S.
The CSA governs the manufacture, import, export, possession, use, and distribution of controlled substances. In doing so, the CSA established a system to register those authorized to handle controlled substances. Manufacturers, dispensers, distributors, and individual practitioners who prescribe controlled substances must be registered with the Drug Enforcement Administration (DEA).
The CSA requires registrants to keep certain records for at least two years related to their handling of controlled substances. For example, physician registrants must keep records of controlled substances in Schedules II, III, IV, and V that are dispensed via methods other than prescribing or administering (e.g., industry samples). Inventories of controlled substances are required. Most notably, physicians generally are not required to keep records of prescribed medications; however, records must be kept if drugs are dispensed or administered. Moreover, there are heightened recordkeeping responsibilities for providers who prescribe, dispense, or administer for maintenance or detoxification.
Controlled Substance “Takeback”
The system of registration established by the CSA prohibits a DEA registrant from acquiring controlled substances from nonregistered entities and, in turn, bars an end-user from distributing pharmaceutical controlled substances to a DEA registrant. In other words, physicians cannot receive controlled substances from anyone who does not also have a registration. Thus, physicians may not “take back” prescribed medications from patients or their family members. Similarly, except in cases of a drug being recalled or a dispensing error, patients are not allowed to return controlled medications to a pharmacy.
Information on how a patient or family member should properly dispose of medication is commonly misunderstood. DEA regulations provide a process for nonregistrants to dispose of unused medication; however, it is cumbersome and meant to be used only when dealing with large quantities of controlled substances (e.g., large quantities of abandoned drugs). In such cases, the DEA special agent in charge (SAC) may instruct on disposal, which may include transfer of the substance to a DEA registrant, delivery to a DEA agent or office, destruction in the presence of an agent of the administration or other authorized person, or by other means. The person must submit a letter to the local SAC, which includes:
- Name and address of the person;
- Name and quantity of each controlled substance to be disposed of;
- Explanation of how the applicant obtained the controlled substance, if known; and
- Name, address, and registration number, if known, of the person who possessed the controlled substances prior to the applicant.
Federal legislation also provides a way for the DEA to grant approval to law-enforcement agencies to operate “takeback” programs. The regulation states that “any person in possession of a controlled substance and desiring to dispose of such substance may request assistance from the SAC in the area in which the person is located.” The regulation allows the SAC to authorize and specify the means of disposal to assure that the controlled substances do not become available to unauthorized persons.
State and local government agencies and community associations might hold takeback programs only if law enforcement makes the request, takes custody of the controlled substances, and is responsible for the disposal.
The U.S. Office of National Drug Control Policy has published guidelines for medication disposal. These guidelines advise flushing medications only if the prescription label or accompanying patient information specifically states to do so. Instead of flushing, the guidelines recommend that medications be disposed of through a takeback program or by:
- Taking the prescription drugs out of their original containers;
- Mixing the drugs with an undesirable substance, such as cat litter or used coffee grounds;
- Placing the mixture into a disposable container with a lid, such as an empty margarine tub, or into a sealable bag;
- Concealing or removing personal information, including Rx number, on the empty containers by covering it with black permanent marker or duct tape, or by scratching it off; and
- Placing the sealed container with the mixture, and the empty drug containers, in the trash.
Unused Medication Donation
The rising cost of prescription medication leaves many questioning whether there is a need for a safe method to allow unused medication to be donated to others. At least 10 states have passed laws allowing or encouraging the donation of unused pharmaceutical drugs. Many of these programs involve healthcare facilities, nursing homes, or pharmacies. The CSA and current DEA regulations, however, prohibit patients from delivering or distributing controlled substances to a DEA registrant, even if it is for the purpose of a donation. Moreover, the Food and Drug Administration (FDA) does not permit redistribution of medications, except under limited circumstances.
Consequently, state law may be inconsistent with federal law for donation and reuse of controlled substances.
Conclusion
Physicians who fail to comply with CSA handling requirements are subject to criminal charges, discipline against their DEA registration, and discipline against their license to practice medicine. Consequently, physicians should use caution whenever handling unused medication.
The application of various aspects of the CSA and implementing rules is situation-specific. Moreover, the DEA may issue additional regulations. Accordingly, if you have a question about a specific situation, consult an attorney, or contact your local DEA field division office and ask for the diversion duty agent. TH
Patrick O’Rourke works in the Office of University Counsel, Department of Litigation, University of Colorado Denver.
Recent media reports about the dangers surrounding unused prescription medications, including abuse by teens and medications finding their way into the water supply, have prompted an increase in inquiries to healthcare providers about disposing of unused medication. These issues are complicated when controlled substances are involved.
Often, providers are unsure how to respond to patient questions about medication disposal. For example, what would you do if a patient requests an alternative medication because of an unwanted side effect and brings the originally prescribed medication back to you? What if the family of a recently expired patient brings unused medication to you and asks you to donate it to other patients? What if you have a colleague who performs mission work; could you accept and donate unused medication for use in another country?
Unfortunately, the Controlled Substances Act (CSA) does not provide a readily available mechanism to accomplish efficient, secure, and environmentally sound methods to collect and use or dispose of unwanted controlled substances. This article explains the rules physicians must adhere to and guidelines for “taking back” controlled substances.
The Legislation
Enacted in 1970, the CSA combined all existing federal drug laws into a single statute. It created five “schedules” in which certain drugs are classified. These “scheduled” drugs are commonly referred to as controlled substances. A drug’s classification depends on its potential for abuse and its currently accepted medical use in the U.S. Additionally, provisions of international treaties impact classification.
Under the classification system, Schedule I drugs have a high potential for abuse and have no currently accepted medical use in treatment in the U.S. In contrast, Schedule V drugs have a low potential for abuse and do have a currently accepted medical use in treatment in the U.S.
The CSA governs the manufacture, import, export, possession, use, and distribution of controlled substances. In doing so, the CSA established a system to register those authorized to handle controlled substances. Manufacturers, dispensers, distributors, and individual practitioners who prescribe controlled substances must be registered with the Drug Enforcement Administration (DEA).
The CSA requires registrants to keep certain records for at least two years related to their handling of controlled substances. For example, physician registrants must keep records of controlled substances in Schedules II, III, IV, and V that are dispensed via methods other than prescribing or administering (e.g., industry samples). Inventories of controlled substances are required. Most notably, physicians generally are not required to keep records of prescribed medications; however, records must be kept if drugs are dispensed or administered. Moreover, there are heightened recordkeeping responsibilities for providers who prescribe, dispense, or administer for maintenance or detoxification.
Controlled Substance “Takeback”
The system of registration established by the CSA prohibits a DEA registrant from acquiring controlled substances from nonregistered entities and, in turn, bars an end-user from distributing pharmaceutical controlled substances to a DEA registrant. In other words, physicians cannot receive controlled substances from anyone who does not also have a registration. Thus, physicians may not “take back” prescribed medications from patients or their family members. Similarly, except in cases of a drug being recalled or a dispensing error, patients are not allowed to return controlled medications to a pharmacy.
Information on how a patient or family member should properly dispose of medication is commonly misunderstood. DEA regulations provide a process for nonregistrants to dispose of unused medication; however, it is cumbersome and meant to be used only when dealing with large quantities of controlled substances (e.g., large quantities of abandoned drugs). In such cases, the DEA special agent in charge (SAC) may instruct on disposal, which may include transfer of the substance to a DEA registrant, delivery to a DEA agent or office, destruction in the presence of an agent of the administration or other authorized person, or by other means. The person must submit a letter to the local SAC, which includes:
- Name and address of the person;
- Name and quantity of each controlled substance to be disposed of;
- Explanation of how the applicant obtained the controlled substance, if known; and
- Name, address, and registration number, if known, of the person who possessed the controlled substances prior to the applicant.
Federal legislation also provides a way for the DEA to grant approval to law-enforcement agencies to operate “takeback” programs. The regulation states that “any person in possession of a controlled substance and desiring to dispose of such substance may request assistance from the SAC in the area in which the person is located.” The regulation allows the SAC to authorize and specify the means of disposal to assure that the controlled substances do not become available to unauthorized persons.
State and local government agencies and community associations might hold takeback programs only if law enforcement makes the request, takes custody of the controlled substances, and is responsible for the disposal.
The U.S. Office of National Drug Control Policy has published guidelines for medication disposal. These guidelines advise flushing medications only if the prescription label or accompanying patient information specifically states to do so. Instead of flushing, the guidelines recommend that medications be disposed of through a takeback program or by:
- Taking the prescription drugs out of their original containers;
- Mixing the drugs with an undesirable substance, such as cat litter or used coffee grounds;
- Placing the mixture into a disposable container with a lid, such as an empty margarine tub, or into a sealable bag;
- Concealing or removing personal information, including Rx number, on the empty containers by covering it with black permanent marker or duct tape, or by scratching it off; and
- Placing the sealed container with the mixture, and the empty drug containers, in the trash.
Unused Medication Donation
The rising cost of prescription medication leaves many questioning whether there is a need for a safe method to allow unused medication to be donated to others. At least 10 states have passed laws allowing or encouraging the donation of unused pharmaceutical drugs. Many of these programs involve healthcare facilities, nursing homes, or pharmacies. The CSA and current DEA regulations, however, prohibit patients from delivering or distributing controlled substances to a DEA registrant, even if it is for the purpose of a donation. Moreover, the Food and Drug Administration (FDA) does not permit redistribution of medications, except under limited circumstances.
Consequently, state law may be inconsistent with federal law for donation and reuse of controlled substances.
Conclusion
Physicians who fail to comply with CSA handling requirements are subject to criminal charges, discipline against their DEA registration, and discipline against their license to practice medicine. Consequently, physicians should use caution whenever handling unused medication.
The application of various aspects of the CSA and implementing rules is situation-specific. Moreover, the DEA may issue additional regulations. Accordingly, if you have a question about a specific situation, consult an attorney, or contact your local DEA field division office and ask for the diversion duty agent. TH
Patrick O’Rourke works in the Office of University Counsel, Department of Litigation, University of Colorado Denver.
Malpractice Chronicle
Reprinted with permission from Medical Malpractice Verdicts, Settlements and Experts, Lewis Laska, Editor, (800) 298-6288.
Signs and Symptoms of Preeclampsia Repeatedly Overlooked
During her second pregnancy, a 23-year-old Michigan woman received prenatal care from Dr. L., beginning in April 2004. Her due date was December 2004.
In late November, the woman presented to a hospital emergency department (ED) with chest pain, cough, and shortness of breath. She was admitted with noted high blood pressure and tachycardia. During her hospitalization, the patient was examined by an emergency physician, who discharged her with a diagnosis of bronchitis and dyspnea.
Two days later, the patient returned to Dr. L. for a scheduled prenatal visit, at which time she still had high blood pressure. She was instructed to go to a second hospital; there, she was seen by a PA, who noted edema in her extremities. Attempts to draw blood for arterial blood gas analysis were unsuccessful, and crackles were noted throughout the woman’s lungs. An obstetrician/gynecologist, Dr. D., was contacted regarding worsening preeclampsia with pulmonary edema. It was decided to perform a cesarean delivery.
The woman became unresponsive on the way to surgery. After delivery, she experienced cardiopulmonary arrest and sustained an anoxic brain injury. She was declared brain dead and died after life support was withdrawn.
Upon autopsy, the cause of death was determined to be anoxic encephalopathy due to respiratory arrest caused by preeclampsia. The plaintiff claimed that Dr. L. failed to provide proper prenatal care and failed to recognize the signs and symptoms of preeclampsia, which the plaintiff alleged were evident in October. The plaintiff also claimed that the emergency physician at the first hospital failed to recognize the signs and symptoms of preeclampsia and failed to contact a specialist and to hospitalize the decedent immediately for monitoring and treatment.
As for the PA and Dr. D., the plaintiff claimed that they negligently administered a bolus of IV fluids when the decedent showed signs of preeclampsia, failed to administer proper dosages of furosemide, and failed to admit the decedent in a timely fashion.
The defendants all denied any negligence.
According to a published report, a $1.5 million settlement was reached.
No Action Taken on Abnormal Blood Cultures
Headache, fever, chills, vomiting, and wide-ranging muscle pain prompted an Indiana woman, age 44, to present to a hospital ED. She was examined by the defendant emergency physician, Dr. M., who ordered tests and made a diagnosis of influenza.
He ordered acetaminophen and prescription-strength ibuprofen and discharged the woman to home with instructions to consume copious amounts of fluid. Two days later, the laboratory staff contacted the ED by phone to report that the patient’s blood culture results were abnormal, indicating a possible bacterial infection. No one on the ED staff acted on this information.
Shortly before midnight the following evening, the patient returned to the ED complaining of similar symptoms. Based on the results of additional testing, acute renal failure and shock secondary to necrotizing soft tissue were diagnosed. The patient was transferred to another hospital, where she underwent extensive treatment, including several surgeries to remove infected tissue. The woman died, however, as a result of multiple organ failure and septic shock secondary to group A streptococcal infection.
The plaintiff alleged negligence by Dr. M. for his failure to investigate the possibility that the patient had a bacterial infection. The plaintiff also alleged negligence on the part of the ED personnel for their failure to act on the notification from the lab. The defendants denied any negligence.
According to a published report, a defense verdict was returned.
Claim Heart Spasm, Not MI, After Treadmill Stress Test
A California man, age 51, saw his primary care physician and internist, Dr. C., and reported a 20-minute-long episode of chest pain in bed that morning. He also said he had had chest pain two mornings earlier, also in bed, that lasted longer than an hour. The patient had cardiac risk factors of obesity, hypertension, a history of smoking, and a strong family history of dyslipidemia and heart disease.
Dr. C. performed an ECG, with results interpreted as normal. He then prescribed a treadmill stress test, which was administered four days later by a cardiologist, Dr. W. The patient was able to complete the test, with his heart rate measured as high as 160 beats/min. Dr. W. interpreted the stress test as normal. The man did not complain of chest pain during the test. His blood pressure, which was expected to rise during the test, remained flat.
About 30 minutes after leaving the treadmill lab, the patient was found in full cardiac arrest at his desk at work. Paramedics were called, but he could not be resuscitated.
An autopsy revealed evidence of MI on the posterior portion of the heart, which corresponded with the complaints of chest pain about a week earlier. The decedent had 75% narrowing of the left anterior descending coronary artery, 75% narrowing of the right circumflex artery, and 30% narrowing of the right coronary artery. No thrombus or plaque rupture was identified. The cause of death was determined to be MI secondary to fatal arrhythmia, associated with coronary artery disease.
The plaintiffs claimed that Dr. C. should have included unstable angina in the differential diagnosis and should have assumed that the decedent had had a heart attack until proven otherwise. The plaintiffs claimed that the ECG taken in Dr. C.’s office was subtly abnormal and that the decedent should have been sent to a hospital immediately; there, they argued, blood would have been drawn and abnormal troponin levels detected. The plaintiffs claimed that the decedent would have then been sent to the catheterization lab for treatment—most likely, stenting.
The plaintiffs further claimed that Dr. W. took an inadequate history and that a treadmill test should not have been performed. The plaintiffs claimed that a myocardial perfusion test or nuclear imaging should have been performed. Further, the plaintiffs maintained that the ECG portion of the treadmill test had subtle abnormalities that Dr. W. overlooked, and that Dr. W. failed to appreciate the abnormality in the decedent’s blood pressure remaining flat during the test.
Dr. C. claimed that the decedent’s claims of chest pain at night suggested that the pain was not cardiac in origin. Dr. C. also claimed that he had acted reasonably in performing and interpreting the ECG. Dr. W. claimed that a treadmill stress test was appropriate for the decedent and that test results were normal.
The defendants both argued that the cause of death was not coronary artery disease, but coronary spasm. They maintained that there was only 50% narrowing in the coronary arteries and that the absence of thrombus or plaque rupture was inconsistent with a classic cardiac death resulting from coronary artery occlusion.
According to a published account, a defense verdict was returned for Dr. W. The jury was undecided in the case against Dr. C.
Obstetrician “Forgets” to Perform Tubal Ligation
A young woman in California became pregnant with her fourth child, although she was using birth control. During her prenatal care, she and her husband told the defendant obstetrician that they did not want, nor could they afford, any more children. They requested a bilateral tubal ligation at the time of a cesarean delivery, which was scheduled for a week before the projected due date.
The woman went into labor two days before the scheduled surgery. The prenatal records could not be found and the obstetrician’s office was closed. He delivered the baby by cesarean section but did not perform the tubal ligation. The mother was in the hospital for three days and was seen by the defendant for a six-week postpartum visit, but she claimed he never told her that he had not performed the tubal ligation. The mother did not take precautions to prevent pregnancy and subsequently conceived her fifth child. The plaintiffs did not opt to abort.
The plaintiffs alleged negligence and wrongful birth, contending that they were never told the tubal ligation had not been performed until after the fifth child was conceived.
The defendant claimed he told the mother at her six-week visit that the tubal ligation had not been performed and advised her to use birth control until she recovered from the cesarean delivery, when she could then undergo a tubal ligation. The obstetrician acknowledged that he had forgotten to perform the tubal ligation but insisted that there was no negligence involved.
According to a published account, a defense verdict was returned.
Reprinted with permission from Medical Malpractice Verdicts, Settlements and Experts, Lewis Laska, Editor, (800) 298-6288.
Signs and Symptoms of Preeclampsia Repeatedly Overlooked
During her second pregnancy, a 23-year-old Michigan woman received prenatal care from Dr. L., beginning in April 2004. Her due date was December 2004.
In late November, the woman presented to a hospital emergency department (ED) with chest pain, cough, and shortness of breath. She was admitted with noted high blood pressure and tachycardia. During her hospitalization, the patient was examined by an emergency physician, who discharged her with a diagnosis of bronchitis and dyspnea.
Two days later, the patient returned to Dr. L. for a scheduled prenatal visit, at which time she still had high blood pressure. She was instructed to go to a second hospital; there, she was seen by a PA, who noted edema in her extremities. Attempts to draw blood for arterial blood gas analysis were unsuccessful, and crackles were noted throughout the woman’s lungs. An obstetrician/gynecologist, Dr. D., was contacted regarding worsening preeclampsia with pulmonary edema. It was decided to perform a cesarean delivery.
The woman became unresponsive on the way to surgery. After delivery, she experienced cardiopulmonary arrest and sustained an anoxic brain injury. She was declared brain dead and died after life support was withdrawn.
Upon autopsy, the cause of death was determined to be anoxic encephalopathy due to respiratory arrest caused by preeclampsia. The plaintiff claimed that Dr. L. failed to provide proper prenatal care and failed to recognize the signs and symptoms of preeclampsia, which the plaintiff alleged were evident in October. The plaintiff also claimed that the emergency physician at the first hospital failed to recognize the signs and symptoms of preeclampsia and failed to contact a specialist and to hospitalize the decedent immediately for monitoring and treatment.
As for the PA and Dr. D., the plaintiff claimed that they negligently administered a bolus of IV fluids when the decedent showed signs of preeclampsia, failed to administer proper dosages of furosemide, and failed to admit the decedent in a timely fashion.
The defendants all denied any negligence.
According to a published report, a $1.5 million settlement was reached.
No Action Taken on Abnormal Blood Cultures
Headache, fever, chills, vomiting, and wide-ranging muscle pain prompted an Indiana woman, age 44, to present to a hospital ED. She was examined by the defendant emergency physician, Dr. M., who ordered tests and made a diagnosis of influenza.
He ordered acetaminophen and prescription-strength ibuprofen and discharged the woman to home with instructions to consume copious amounts of fluid. Two days later, the laboratory staff contacted the ED by phone to report that the patient’s blood culture results were abnormal, indicating a possible bacterial infection. No one on the ED staff acted on this information.
Shortly before midnight the following evening, the patient returned to the ED complaining of similar symptoms. Based on the results of additional testing, acute renal failure and shock secondary to necrotizing soft tissue were diagnosed. The patient was transferred to another hospital, where she underwent extensive treatment, including several surgeries to remove infected tissue. The woman died, however, as a result of multiple organ failure and septic shock secondary to group A streptococcal infection.
The plaintiff alleged negligence by Dr. M. for his failure to investigate the possibility that the patient had a bacterial infection. The plaintiff also alleged negligence on the part of the ED personnel for their failure to act on the notification from the lab. The defendants denied any negligence.
According to a published report, a defense verdict was returned.
Claim Heart Spasm, Not MI, After Treadmill Stress Test
A California man, age 51, saw his primary care physician and internist, Dr. C., and reported a 20-minute-long episode of chest pain in bed that morning. He also said he had had chest pain two mornings earlier, also in bed, that lasted longer than an hour. The patient had cardiac risk factors of obesity, hypertension, a history of smoking, and a strong family history of dyslipidemia and heart disease.
Dr. C. performed an ECG, with results interpreted as normal. He then prescribed a treadmill stress test, which was administered four days later by a cardiologist, Dr. W. The patient was able to complete the test, with his heart rate measured as high as 160 beats/min. Dr. W. interpreted the stress test as normal. The man did not complain of chest pain during the test. His blood pressure, which was expected to rise during the test, remained flat.
About 30 minutes after leaving the treadmill lab, the patient was found in full cardiac arrest at his desk at work. Paramedics were called, but he could not be resuscitated.
An autopsy revealed evidence of MI on the posterior portion of the heart, which corresponded with the complaints of chest pain about a week earlier. The decedent had 75% narrowing of the left anterior descending coronary artery, 75% narrowing of the right circumflex artery, and 30% narrowing of the right coronary artery. No thrombus or plaque rupture was identified. The cause of death was determined to be MI secondary to fatal arrhythmia, associated with coronary artery disease.
The plaintiffs claimed that Dr. C. should have included unstable angina in the differential diagnosis and should have assumed that the decedent had had a heart attack until proven otherwise. The plaintiffs claimed that the ECG taken in Dr. C.’s office was subtly abnormal and that the decedent should have been sent to a hospital immediately; there, they argued, blood would have been drawn and abnormal troponin levels detected. The plaintiffs claimed that the decedent would have then been sent to the catheterization lab for treatment—most likely, stenting.
The plaintiffs further claimed that Dr. W. took an inadequate history and that a treadmill test should not have been performed. The plaintiffs claimed that a myocardial perfusion test or nuclear imaging should have been performed. Further, the plaintiffs maintained that the ECG portion of the treadmill test had subtle abnormalities that Dr. W. overlooked, and that Dr. W. failed to appreciate the abnormality in the decedent’s blood pressure remaining flat during the test.
Dr. C. claimed that the decedent’s claims of chest pain at night suggested that the pain was not cardiac in origin. Dr. C. also claimed that he had acted reasonably in performing and interpreting the ECG. Dr. W. claimed that a treadmill stress test was appropriate for the decedent and that test results were normal.
The defendants both argued that the cause of death was not coronary artery disease, but coronary spasm. They maintained that there was only 50% narrowing in the coronary arteries and that the absence of thrombus or plaque rupture was inconsistent with a classic cardiac death resulting from coronary artery occlusion.
According to a published account, a defense verdict was returned for Dr. W. The jury was undecided in the case against Dr. C.
Obstetrician “Forgets” to Perform Tubal Ligation
A young woman in California became pregnant with her fourth child, although she was using birth control. During her prenatal care, she and her husband told the defendant obstetrician that they did not want, nor could they afford, any more children. They requested a bilateral tubal ligation at the time of a cesarean delivery, which was scheduled for a week before the projected due date.
The woman went into labor two days before the scheduled surgery. The prenatal records could not be found and the obstetrician’s office was closed. He delivered the baby by cesarean section but did not perform the tubal ligation. The mother was in the hospital for three days and was seen by the defendant for a six-week postpartum visit, but she claimed he never told her that he had not performed the tubal ligation. The mother did not take precautions to prevent pregnancy and subsequently conceived her fifth child. The plaintiffs did not opt to abort.
The plaintiffs alleged negligence and wrongful birth, contending that they were never told the tubal ligation had not been performed until after the fifth child was conceived.
The defendant claimed he told the mother at her six-week visit that the tubal ligation had not been performed and advised her to use birth control until she recovered from the cesarean delivery, when she could then undergo a tubal ligation. The obstetrician acknowledged that he had forgotten to perform the tubal ligation but insisted that there was no negligence involved.
According to a published account, a defense verdict was returned.
Reprinted with permission from Medical Malpractice Verdicts, Settlements and Experts, Lewis Laska, Editor, (800) 298-6288.
Signs and Symptoms of Preeclampsia Repeatedly Overlooked
During her second pregnancy, a 23-year-old Michigan woman received prenatal care from Dr. L., beginning in April 2004. Her due date was December 2004.
In late November, the woman presented to a hospital emergency department (ED) with chest pain, cough, and shortness of breath. She was admitted with noted high blood pressure and tachycardia. During her hospitalization, the patient was examined by an emergency physician, who discharged her with a diagnosis of bronchitis and dyspnea.
Two days later, the patient returned to Dr. L. for a scheduled prenatal visit, at which time she still had high blood pressure. She was instructed to go to a second hospital; there, she was seen by a PA, who noted edema in her extremities. Attempts to draw blood for arterial blood gas analysis were unsuccessful, and crackles were noted throughout the woman’s lungs. An obstetrician/gynecologist, Dr. D., was contacted regarding worsening preeclampsia with pulmonary edema. It was decided to perform a cesarean delivery.
The woman became unresponsive on the way to surgery. After delivery, she experienced cardiopulmonary arrest and sustained an anoxic brain injury. She was declared brain dead and died after life support was withdrawn.
Upon autopsy, the cause of death was determined to be anoxic encephalopathy due to respiratory arrest caused by preeclampsia. The plaintiff claimed that Dr. L. failed to provide proper prenatal care and failed to recognize the signs and symptoms of preeclampsia, which the plaintiff alleged were evident in October. The plaintiff also claimed that the emergency physician at the first hospital failed to recognize the signs and symptoms of preeclampsia and failed to contact a specialist and to hospitalize the decedent immediately for monitoring and treatment.
As for the PA and Dr. D., the plaintiff claimed that they negligently administered a bolus of IV fluids when the decedent showed signs of preeclampsia, failed to administer proper dosages of furosemide, and failed to admit the decedent in a timely fashion.
The defendants all denied any negligence.
According to a published report, a $1.5 million settlement was reached.
No Action Taken on Abnormal Blood Cultures
Headache, fever, chills, vomiting, and wide-ranging muscle pain prompted an Indiana woman, age 44, to present to a hospital ED. She was examined by the defendant emergency physician, Dr. M., who ordered tests and made a diagnosis of influenza.
He ordered acetaminophen and prescription-strength ibuprofen and discharged the woman to home with instructions to consume copious amounts of fluid. Two days later, the laboratory staff contacted the ED by phone to report that the patient’s blood culture results were abnormal, indicating a possible bacterial infection. No one on the ED staff acted on this information.
Shortly before midnight the following evening, the patient returned to the ED complaining of similar symptoms. Based on the results of additional testing, acute renal failure and shock secondary to necrotizing soft tissue were diagnosed. The patient was transferred to another hospital, where she underwent extensive treatment, including several surgeries to remove infected tissue. The woman died, however, as a result of multiple organ failure and septic shock secondary to group A streptococcal infection.
The plaintiff alleged negligence by Dr. M. for his failure to investigate the possibility that the patient had a bacterial infection. The plaintiff also alleged negligence on the part of the ED personnel for their failure to act on the notification from the lab. The defendants denied any negligence.
According to a published report, a defense verdict was returned.
Claim Heart Spasm, Not MI, After Treadmill Stress Test
A California man, age 51, saw his primary care physician and internist, Dr. C., and reported a 20-minute-long episode of chest pain in bed that morning. He also said he had had chest pain two mornings earlier, also in bed, that lasted longer than an hour. The patient had cardiac risk factors of obesity, hypertension, a history of smoking, and a strong family history of dyslipidemia and heart disease.
Dr. C. performed an ECG, with results interpreted as normal. He then prescribed a treadmill stress test, which was administered four days later by a cardiologist, Dr. W. The patient was able to complete the test, with his heart rate measured as high as 160 beats/min. Dr. W. interpreted the stress test as normal. The man did not complain of chest pain during the test. His blood pressure, which was expected to rise during the test, remained flat.
About 30 minutes after leaving the treadmill lab, the patient was found in full cardiac arrest at his desk at work. Paramedics were called, but he could not be resuscitated.
An autopsy revealed evidence of MI on the posterior portion of the heart, which corresponded with the complaints of chest pain about a week earlier. The decedent had 75% narrowing of the left anterior descending coronary artery, 75% narrowing of the right circumflex artery, and 30% narrowing of the right coronary artery. No thrombus or plaque rupture was identified. The cause of death was determined to be MI secondary to fatal arrhythmia, associated with coronary artery disease.
The plaintiffs claimed that Dr. C. should have included unstable angina in the differential diagnosis and should have assumed that the decedent had had a heart attack until proven otherwise. The plaintiffs claimed that the ECG taken in Dr. C.’s office was subtly abnormal and that the decedent should have been sent to a hospital immediately; there, they argued, blood would have been drawn and abnormal troponin levels detected. The plaintiffs claimed that the decedent would have then been sent to the catheterization lab for treatment—most likely, stenting.
The plaintiffs further claimed that Dr. W. took an inadequate history and that a treadmill test should not have been performed. The plaintiffs claimed that a myocardial perfusion test or nuclear imaging should have been performed. Further, the plaintiffs maintained that the ECG portion of the treadmill test had subtle abnormalities that Dr. W. overlooked, and that Dr. W. failed to appreciate the abnormality in the decedent’s blood pressure remaining flat during the test.
Dr. C. claimed that the decedent’s claims of chest pain at night suggested that the pain was not cardiac in origin. Dr. C. also claimed that he had acted reasonably in performing and interpreting the ECG. Dr. W. claimed that a treadmill stress test was appropriate for the decedent and that test results were normal.
The defendants both argued that the cause of death was not coronary artery disease, but coronary spasm. They maintained that there was only 50% narrowing in the coronary arteries and that the absence of thrombus or plaque rupture was inconsistent with a classic cardiac death resulting from coronary artery occlusion.
According to a published account, a defense verdict was returned for Dr. W. The jury was undecided in the case against Dr. C.
Obstetrician “Forgets” to Perform Tubal Ligation
A young woman in California became pregnant with her fourth child, although she was using birth control. During her prenatal care, she and her husband told the defendant obstetrician that they did not want, nor could they afford, any more children. They requested a bilateral tubal ligation at the time of a cesarean delivery, which was scheduled for a week before the projected due date.
The woman went into labor two days before the scheduled surgery. The prenatal records could not be found and the obstetrician’s office was closed. He delivered the baby by cesarean section but did not perform the tubal ligation. The mother was in the hospital for three days and was seen by the defendant for a six-week postpartum visit, but she claimed he never told her that he had not performed the tubal ligation. The mother did not take precautions to prevent pregnancy and subsequently conceived her fifth child. The plaintiffs did not opt to abort.
The plaintiffs alleged negligence and wrongful birth, contending that they were never told the tubal ligation had not been performed until after the fifth child was conceived.
The defendant claimed he told the mother at her six-week visit that the tubal ligation had not been performed and advised her to use birth control until she recovered from the cesarean delivery, when she could then undergo a tubal ligation. The obstetrician acknowledged that he had forgotten to perform the tubal ligation but insisted that there was no negligence involved.
According to a published account, a defense verdict was returned.
Lethal liver injury blamed on birth trauma...and more

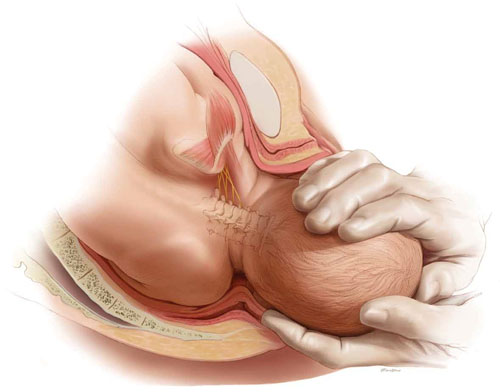
BECAUSE OF PREMATURE CONTRACTIONS and bleeding, a woman underwent cesarean delivery by her ObGyns. When Dr. A reached in to extract the fetus, it floated away. Dr. B then attempted delivery while Dr. A applied fundal pressure. Photographs of the baby taken by the father 2 minutes after birth showed severe bruising over the liver area. Sonography performed shortly after birth revealed a liver laceration. Surgery to repair the liver was unsuccessful. The infant died.
ESTATE’S CLAIM The trauma from improper fundal pressure and improper manipulation when extracting the infant through an inadequately sized incision caused the liver to rupture. A vertical incision should have been made initially, instead of a transverse incision, because of the small size of the fetus and uterus. When the fetus could not be extracted, a reverse “T” incision should have been made so the fetus could be extracted without trauma.
PHYSICIANS’ DEFENSE The mother had a preexisting disorder that caused bleeding before delivery; the liver laceration occurred hours before delivery.
VERDICT A $1,461,507 Maryland verdict was returned, including $461,507 to the infant’s estate, and $500,000 to each parent.
Perforated colon after hysteroscopy
A 44-YEAR-OLD WOMAN UNDERWENT hysteroscopic surgery to remove polyps and a fibroid tumor. During the procedure, the ObGyn used a hysteroscopic resection loop. Two days later, the patient developed peritonitis. A perforation was detected, requiring resection of part of the colon and a temporary colostomy.
PATIENT’S CLAIM The injury occurred when the ObGyn pushed the resection loop of the hysteroscope through the uterus, burning a hole in the uterus and the colon. The ObGyn should have performed a more extensive check to ensure that no perforation had occurred.
PHYSICIAN’S DEFENSE Perforation was a delayed thermal effect that did not occur until 2 days after the procedure. There was no negligence.
VERDICT A $1.55 million New York verdict was returned.
Did retractors cause neuropathy?
AFTER CERVICAL CANCER was diagnosed, a 37-year-old woman was referred to a gynecologic oncologist. He performed a modified radical hysterectomy with pelvic node dissection and lymphadenectomy. A Pfannenstiel incision was used, and the procedure involved removal of the uterus, cervix, upper quarter of the vagina, pelvic lymph nodes, and surrounding tissue. Surgery lasted longer than 5 hours.
The next day, the patient reported pain, burning, tingling, and numbness in her left thigh, which was eventually diagnosed as lateral femoral cutaneous neuropathy. This condition did not resolve.
PATIENT’S CLAIM The surgeon failed to reposition retractors with sufficient frequency. He allowed the retractor blades to press on the psoas muscles, thus injuring the lateral femoral cutaneous nerve.
PHYSICIAN’S DEFENSE The retractors were used properly; they were periodically shifted to gain better exposure to the surgical area. The surgeon also used his hands to determine that the retractors were properly positioned.
VERDICT An Illinois defense verdict was returned.
“I would have terminated my pregnancy if…”
A PREGNANT WOMAN UNDERWENT a blood test that indicated that the fetus had an elevated risk of being born with Down syndrome. The child was born 7 months later with Down syndrome.
PATIENT’S CLAIM She was not told of the increased risk that her child would have Down syndrome. If she had been informed, she would have terminated the pregnancy.
PHYSICIAN’S DEFENSE According to the physician’s records, the mother was told the blood test results many times. Amniocentesis was recommended, but the mother had declined.
VERDICT A Maryland defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
We want to hear from you! Tell us what you think.

BECAUSE OF PREMATURE CONTRACTIONS and bleeding, a woman underwent cesarean delivery by her ObGyns. When Dr. A reached in to extract the fetus, it floated away. Dr. B then attempted delivery while Dr. A applied fundal pressure. Photographs of the baby taken by the father 2 minutes after birth showed severe bruising over the liver area. Sonography performed shortly after birth revealed a liver laceration. Surgery to repair the liver was unsuccessful. The infant died.
ESTATE’S CLAIM The trauma from improper fundal pressure and improper manipulation when extracting the infant through an inadequately sized incision caused the liver to rupture. A vertical incision should have been made initially, instead of a transverse incision, because of the small size of the fetus and uterus. When the fetus could not be extracted, a reverse “T” incision should have been made so the fetus could be extracted without trauma.
PHYSICIANS’ DEFENSE The mother had a preexisting disorder that caused bleeding before delivery; the liver laceration occurred hours before delivery.
VERDICT A $1,461,507 Maryland verdict was returned, including $461,507 to the infant’s estate, and $500,000 to each parent.
Perforated colon after hysteroscopy
A 44-YEAR-OLD WOMAN UNDERWENT hysteroscopic surgery to remove polyps and a fibroid tumor. During the procedure, the ObGyn used a hysteroscopic resection loop. Two days later, the patient developed peritonitis. A perforation was detected, requiring resection of part of the colon and a temporary colostomy.
PATIENT’S CLAIM The injury occurred when the ObGyn pushed the resection loop of the hysteroscope through the uterus, burning a hole in the uterus and the colon. The ObGyn should have performed a more extensive check to ensure that no perforation had occurred.
PHYSICIAN’S DEFENSE Perforation was a delayed thermal effect that did not occur until 2 days after the procedure. There was no negligence.
VERDICT A $1.55 million New York verdict was returned.
Did retractors cause neuropathy?
AFTER CERVICAL CANCER was diagnosed, a 37-year-old woman was referred to a gynecologic oncologist. He performed a modified radical hysterectomy with pelvic node dissection and lymphadenectomy. A Pfannenstiel incision was used, and the procedure involved removal of the uterus, cervix, upper quarter of the vagina, pelvic lymph nodes, and surrounding tissue. Surgery lasted longer than 5 hours.
The next day, the patient reported pain, burning, tingling, and numbness in her left thigh, which was eventually diagnosed as lateral femoral cutaneous neuropathy. This condition did not resolve.
PATIENT’S CLAIM The surgeon failed to reposition retractors with sufficient frequency. He allowed the retractor blades to press on the psoas muscles, thus injuring the lateral femoral cutaneous nerve.
PHYSICIAN’S DEFENSE The retractors were used properly; they were periodically shifted to gain better exposure to the surgical area. The surgeon also used his hands to determine that the retractors were properly positioned.
VERDICT An Illinois defense verdict was returned.
“I would have terminated my pregnancy if…”
A PREGNANT WOMAN UNDERWENT a blood test that indicated that the fetus had an elevated risk of being born with Down syndrome. The child was born 7 months later with Down syndrome.
PATIENT’S CLAIM She was not told of the increased risk that her child would have Down syndrome. If she had been informed, she would have terminated the pregnancy.
PHYSICIAN’S DEFENSE According to the physician’s records, the mother was told the blood test results many times. Amniocentesis was recommended, but the mother had declined.
VERDICT A Maryland defense verdict was returned.

BECAUSE OF PREMATURE CONTRACTIONS and bleeding, a woman underwent cesarean delivery by her ObGyns. When Dr. A reached in to extract the fetus, it floated away. Dr. B then attempted delivery while Dr. A applied fundal pressure. Photographs of the baby taken by the father 2 minutes after birth showed severe bruising over the liver area. Sonography performed shortly after birth revealed a liver laceration. Surgery to repair the liver was unsuccessful. The infant died.
ESTATE’S CLAIM The trauma from improper fundal pressure and improper manipulation when extracting the infant through an inadequately sized incision caused the liver to rupture. A vertical incision should have been made initially, instead of a transverse incision, because of the small size of the fetus and uterus. When the fetus could not be extracted, a reverse “T” incision should have been made so the fetus could be extracted without trauma.
PHYSICIANS’ DEFENSE The mother had a preexisting disorder that caused bleeding before delivery; the liver laceration occurred hours before delivery.
VERDICT A $1,461,507 Maryland verdict was returned, including $461,507 to the infant’s estate, and $500,000 to each parent.
Perforated colon after hysteroscopy
A 44-YEAR-OLD WOMAN UNDERWENT hysteroscopic surgery to remove polyps and a fibroid tumor. During the procedure, the ObGyn used a hysteroscopic resection loop. Two days later, the patient developed peritonitis. A perforation was detected, requiring resection of part of the colon and a temporary colostomy.
PATIENT’S CLAIM The injury occurred when the ObGyn pushed the resection loop of the hysteroscope through the uterus, burning a hole in the uterus and the colon. The ObGyn should have performed a more extensive check to ensure that no perforation had occurred.
PHYSICIAN’S DEFENSE Perforation was a delayed thermal effect that did not occur until 2 days after the procedure. There was no negligence.
VERDICT A $1.55 million New York verdict was returned.
Did retractors cause neuropathy?
AFTER CERVICAL CANCER was diagnosed, a 37-year-old woman was referred to a gynecologic oncologist. He performed a modified radical hysterectomy with pelvic node dissection and lymphadenectomy. A Pfannenstiel incision was used, and the procedure involved removal of the uterus, cervix, upper quarter of the vagina, pelvic lymph nodes, and surrounding tissue. Surgery lasted longer than 5 hours.
The next day, the patient reported pain, burning, tingling, and numbness in her left thigh, which was eventually diagnosed as lateral femoral cutaneous neuropathy. This condition did not resolve.
PATIENT’S CLAIM The surgeon failed to reposition retractors with sufficient frequency. He allowed the retractor blades to press on the psoas muscles, thus injuring the lateral femoral cutaneous nerve.
PHYSICIAN’S DEFENSE The retractors were used properly; they were periodically shifted to gain better exposure to the surgical area. The surgeon also used his hands to determine that the retractors were properly positioned.
VERDICT An Illinois defense verdict was returned.
“I would have terminated my pregnancy if…”
A PREGNANT WOMAN UNDERWENT a blood test that indicated that the fetus had an elevated risk of being born with Down syndrome. The child was born 7 months later with Down syndrome.
PATIENT’S CLAIM She was not told of the increased risk that her child would have Down syndrome. If she had been informed, she would have terminated the pregnancy.
PHYSICIAN’S DEFENSE According to the physician’s records, the mother was told the blood test results many times. Amniocentesis was recommended, but the mother had declined.
VERDICT A Maryland defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
We want to hear from you! Tell us what you think.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
We want to hear from you! Tell us what you think.
Sound strategies to avoid malpractice hazards on labor and delivery
CASE: Is TOLAC feasible?
Your patient is a 33-year-old gravida 3, para 2002, with a previous cesarean delivery who was admitted to labor and delivery with premature ruptured membranes at term. She is not contracting. Fetal status is reassuring.
Her obstetric history is of one normal, spontaneous delivery followed by one cesarean delivery, both occurring at term.
She wants to know if she can safely undergo a trial of labor, or if she must have a repeat cesarean delivery. How should you counsel her?
At the start of any discussion about how to reduce your risk of being sued for malpractice because of your work as an obstetrician, in particular during labor and delivery, two distinct, underlying avenues of concern need to be addressed. Before moving on to discuss strategy, then, let’s consider what they are and how they arise: Allegation (perception). You are at risk of an allegation of malpractice (or of a perception of malpractice) because of an unexpected event or outcome for mother or baby. Allegation and perception can arise apart from any specific clinical action you undertook, or did not undertake. An example? Counseling about options for care that falls short of full understanding by the patient.
Allegation and perception are the subjects of this first installment of our two-part article on strategies for avoiding claims of malpractice in L & D that begin with the first prenatal visit.
Causation. Your actions—what you do in the course of providing prenatal care and delivering a baby—put you at risk of a charge of malpractice when you have provided medical care that 1) is inconsistent with current medical practice and thus 2) harmed the mother or newborn.
For a medical malpractice case to go forward, it must meet a well-defined paradigm that teases apart components of causation, beginning with your duty to the patient (TABLE 1).
TABLE 1 Signposts in the medical malpractice paradigm
| When the clinical issue at hand is … | … Then the legal term is … |
|---|---|
| A health-care professional’s obligation to provide care | “Duty” |
| A deviation in the care that was provided | “Standard of care” |
| An allegation that a breach in the standard of care resulted in injury | “Proximate cause” |
| An assertion or finding that an injury is “compensable” | “Damages” |
| Source: Yale New Haven Medical Center, 1997.5 | |
Allegation of malpractice arises from a range of sources, as we’ll discuss, but it is causation that reflects the actual, hands-on practice of medicine. We’ll examine strategies for avoiding charges of causation in the second part of this article.
(For now, we’ll just note that a recent excellent review of intrapartum interventions and their basis in evidence1 offers a model for evaluating a number of widely utilized practices in obstetrics. The goal, of course, is to minimize bad outcomes that follow from causation. Regrettably, that evidence-based approach is a limited one, because of a paucity of adequately controlled studies about OB practice.)
CASE: Continued
You consider your patient’s comment that she would like to avoid a repeat cesarean delivery, and advise her that she may safely attempt vaginal birth.
When spontaneous labor does not occur in 6 hours, oxytocin is administered. She dilates to 9 cm and begins to push spontaneously.
The fetal heart rate then drops to 70/min; fetal station, which had been +2, is now -1. A Stat cesarean delivery is performed. Uterine rupture with partial fetal expulsion is found. Apgar scores are 1, 3, and 5 at 1, 5, and 10 minutes.
Your patient requires a hysterectomy to control bleeding.
Some broad considerations for the physician arising from this CASE
- The counseling that you provide to a patient should be nondirective; it should include your opinion, however, about the best option available to her. Insert yourself into this hypothetical case, for discussion’s sake: Did you provide that important opinion to her?
- You must make certain that she clearly understands the risks and benefits of a procedure or other action, and the available alternatives. Did you undertake a check of her comprehension, given the anxiety and confusion of the moment?
- When an adverse outcome ensues—however unlikely it was to occur—it is necessary for you to review the circumstances with the patient as soon as clinically possible. Did you “debrief” and counsel her before and after the hysterectomy?
No more “perfect outcomes”: Our role changed, so did our risk
From the moment an OB patient enters triage, until her arrival home with her infant, this crucial period of her life is colored by concern, curiosity, myth, and fear.
Every woman anticipates the birth of a healthy infant. In an earlier era, the patient and her family relied on the sage advice of their physician to ensure this outcome. To an extent, physicians themselves reinforced this reliance, embracing the notion that they were, in fact, able to provide such a perfect outcome.
With advances that have been made in reproductive medicine, pregnancy has become more readily available to women with increasingly advanced disease; this has made labor and delivery more challenging to them and to their physicians. Realistically, our role as physicians is now better expressed as providing advice to help a woman achieve the best possible outcome, recognizing her individual clinical circumstances, instead of ensuring a perfect outcome.
Every woman anticipates the birth of a healthy baby. But the role of the OB is better expressed as helping her achieve the best possible outcome, not a perfect outcome. ABOVE: Shoulder dystocia is one of the most treacherous and frightening—and litigated—complications of childbirth, yet it is, for the most part, unpredictable and unpreventable in the course of even routine delivery.
Key concept #1
COMMUNICATION
Communication is central to patients’ comprehension about the care that you provide to them. But to enter a genuine dialogue with a patient under your care, and with her family, can challenge your communication skills.
First, you need written and verbal skills. Second, you need to know how to read visual cues.
Third, the messages that you deliver to the patient are influenced by:
- your style of communication
- your cultural background
- the setting in which you’re providing care (office, hospital).
Where are such skills developed? For one, biopsychosocial models that are employed in medical student education and resident training aid the physician in developing appropriate communication skills.
But training alone cannot overcome the fact that communication is a double-sided activity: Patients bring many of their own variables to a dialogue. How patients understand and interact with you—and with other providers and the health-care system—is not, therefore, directly or strictly within your sphere of influence.
Yet your sensitivity to a patient’s issues can go a long way toward ameliorating her misconceptions and prejudices. Here are several suggestions, developed by others, to optimize patients’ understanding of their care2,3:
- Apply what’s known as flip default. Assume the patient does not understand the information that you’re providing. Ask her to repeat your instructions back to you (as is done with a verbal order in the hospital).
- Manage face-to-face time effectively. Don’t attempt to teach a patient everything about her care at once. Focus on the critical aspects of her case and on providing understanding; use a strategy of sequential learning.
- Reduce the “overwhelm” factor. Periodically, stop and ask the patient if she has questions. Don’t wait until the end of the appointment to do this.
- Eliminate jargon. When you notify a patient about the results of testing, for example, clarify what the results say about her health and mean for her care. Do so in plain language.
- Recognize her preconceptions. Discuss any psychosocial issues head on with the patient. Use an interpreter or a social worker, or counselors from other fields, as appropriate.
Remember: All health-care personnel need to understand the importance of making the patient comfortable in the often foreign, and sometimes sterile, milieu of the medical office and hospital.
Key concept #2
TRUST
Trust between patient and clinician is, we believe, the most basic necessity for ameliorating allegations of malpractice—secondary only, perhaps, to your knowledge of medicine.
Trust can be enhanced by interactions that demonstrate to both parties the advisability of working together to resolve a problem. Any aspect of the physician-patient interaction that is potentially adversarial does not serve the interests of either.
We encourage you to construct a communication bridge, so to speak, with your patient. Begin by:
- introducing yourself to her and explaining your role in her care
- making appropriate eye contact with her
- maintaining a positive attitude
- dressing appropriately
- making her feel that she is your No. 1 priority.
There is more.
Recognize the duality of respect
- Ask the patient how she wishes to be addressed
- Ask about her belief system
- Explain the specifics of her care without arrogance.
Engender trust
- Be honest with her
- Be on her side
- Take time with her
- Allow her the right that she has to select from the options or to refuse treatment
- Disclose to the patient your status as a student or resident, if that is your rank.
Recognize the benefits of partnership
Forging a partnership with the patient:
- improves the accuracy of information
- eases ongoing communication
- facilitates informed consent
- provides an opportunity for you to educate her.
TABLE 2 When building trust, both patient and physician
are charged with responsibilities
| In regard to … | The patient’s responsibility is to … | The physician’s responsibility is to … |
|---|---|---|
| Gathering an honest and complete medical history | Know and report | Question completely |
| Being adherent to prescribed care | Follow through | Make reasonable demands |
| Making decisions about care | Ask questions and actively participate in choices Make realistic requests | Be knowledgeable about available alternatives Individualize options |
Key concept #3
SHARED RESPONSIBILITY
Patient and physician both have responsibilities that are important to achieving an optimal outcome; so does the hospital (TABLE 2 and TABLE 3). Both patient and physician should practice full disclosure throughout the course of care; this will benefit both of you.4 Here are a few select examples.
TABLE 3 Relative degrees of responsibility for a good outcome
vary across interested parties, but none are exempt
| Area of emphasis | Hospital’s responsibility | Physician’s responsibility | Patient’s responsibility |
|---|---|---|---|
| Creating a positive environment for care | 3+ | 2+ | 1+ |
| Providing clear communication | 3+ | 3+ | 3+ |
| Obtaining informed consent | 3+ | 3+ | 3+ |
| Making reasonable requests | 1+ | 1+ | 3+ |
| Compliance | 3+ | 3+ | 3+ |
| Key to the relative scale: 1+: at the least, minimally responsible; 2+: at the least, somewhat responsible; 3+, responsible to the greatest degree. | |||
The importance of the intake form
At the outset of OB care, in most practices, the patient provides the initial detailed medical history by completing a form in the waiting room. In reviewing and completing this survey with her during the appointment, pay particular attention to those questions for which the response has been left blank.
Patients need to understand that key recommendations about their care, and a proper analysis of their concerns, are based on the information that they provide on this survey. In our practices, we find that patients answer most of these early questions without difficulty—even inquiries of a personal nature, such as the number of prior pregnancies, or drug, alcohol, and smoking habits—as long as they understand why it’s in their best interests for you to have this information. If they leave a question blank and you do not follow up verbally, you may have lost invaluable information that can affect the outcome of her pregnancy.
What should you do when, occasionally, a patient refuses to answer one of your questions? We recommend that you record her refusal on the form itself, where the note remains part of the record.
Keep in mind that all necessary and useful information about a patient may not be available, or may not be appropriate to consider, at the initial prenatal visit. In that case, you have an ongoing opportunity—at subsequent visits during the pregnancy—to develop her full medical profile and algorithm.
The necessity of adherence
It almost goes without saying: To provide the care that our patients need, we sometimes require the unpleasant of them—to undergo evaluations, or testing, or to take medications that may be inconvenient or costly.
After you explain the specific course of care to a patient—whether you’re ordering a test or writing a prescription—your follow-up must include notation in the record of adherence. The fact is that both of you share responsibility for having her understand the importance of adherence to your instructions and the consequences of limited adherence or nonadherence.
Recall one of the lessons from the case that introduced this article: For the patient to make an informed decision about her care, the clinician must have thorough knowledge of 1) the risks and benefits of whatever intervention is being proposed in the particular clinical scenario and 2) the available alternatives. It is key that you communicate your risk-benefit assessment accurately to the patient.
Follow-up
Sometimes, new medical problems arise during subsequent prenatal visits. Follow-up appointments also provide an opportunity for you to expand your attention to problems identified earlier. Regardless of what the patient reported about her history and current health at the initial prenatal visit, listen for her to bring new issues to light for resolution later in the pregnancy that will have an impact on L & D. Again, it goes without saying but needs to be said: The OB clinician needs to have whatever skills are necessary to 1) fully evaluate the progress of a pregnancy and 2) make recommendations for care in light of changes in the status of mother and fetus along the way.
TABLE 4 Examples of the cardinal rule of “Be specific”
when you document care
| Instead of noting … | … Use alternative wording |
|---|---|
| “Mild vaginal bleeding” | “Vaginal bleeding requiring two pads an hour” |
| “Gentle traction” | “The shoulders were rotated before assisting the patient’s expulsive efforts” |
| “Patient refuses…” [or “declines…”] | “Patient voiced the nature of the problem and the alternatives that i have explained to her” |
| “Expedited cesarean section” | “The time from decision to incision was 35 minutes” |
Basic principles of documentation
The medical record is the best witness to interactions between a physician and a patient. In the record, we’re required to write a “5-C” description of events—namely, one that is:
- correct
- comprehensive
- conscientious
- clear
- contemporaneous.
Avoid medical jargon in the record. Be careful not to use vague terminology or descriptions, such as “mild vaginal bleeding,” “gentle traction,” or “patient refuses and accepts the consequences.” Specificity is the key to accuracy with respect to documentation (TABLE 4).
Editor’s note: Part 2 of this article will appear in the January 2011 issue of OBG Management. The authors’ analysis of L & D malpractice claims moves to a discussion of causation—by way of 4 troubling cases.
You’ll find a rich, useful archive of expert analysis of your professional liability and malpractice risk, at www.obgmanagement.com
• 10 keys to defending (or, better, keeping clear of) a shoulder dystocia suit
Andrew K. Worek, Esq (March 2008)
• After a patient’s unexpected death, First Aid for the emotionally wounded
Ronald A. Chez, MD, and Wayne Fortin, MS (April 2010)
• Afraid of getting sued? A plaintiff attorney offers counsel (but no sympathy)
Janelle Yates, Senior Editor, with Lewis Laska, JD, PhD (October 2009)
• Can a change in practice patterns reduce the number of OB malpractice claims?
Jason K. Baxter, MD, MSCP, and Louis Weinstein, MD (April 2009)
• Strategies for breaking bad news to patients
Barry Bub, MD (September 2008)
• Stuff of nightmares: Criminal prosecution for malpractice
Gary Steinman, MD, PhD (August 2008)
• Deposition Dos and Don’ts: How to answer 8 tricky questions
James L. Knoll, IV, MD, and Phillip J. Resnick, MD (May 2008)
• Playing high-stakes poker: Do you fight—or settle—that malpractice lawsuit?
Jeffrey Segal, MD (April 2008)
We want to hear from you! Tell us what you think.
1. Berghella V, Baxter JK, Chauhan SP. Evidence-based labor and delivery management. Am J Obstet Gynecol. 2008;199(5):445-454.
2. Paasche-Orlow MK, Riekert KA, Bilderback A, et al. Tailored education may reduce health literacy disparities in asthma self-management. Am J Respir Crit Care Med. 2005;172:980-986.
3. Huvane K. Health literacy: reading is just the beginning. Focus on multicultural healthcare. 2007;3(4):16-19.
4. Giordano K. Legal Principles. In: O’Grady JP, Gimovsky ML, Bayer-Zwirello L, Giordano K, eds. Operative Obstetrics. 2nd ed. New York: Cambridge University Press; 2008.
5. The Four Elements of Medical Malpractice Yale New Haven Medical Center: Issues in Risk Management. 1997.
CASE: Is TOLAC feasible?
Your patient is a 33-year-old gravida 3, para 2002, with a previous cesarean delivery who was admitted to labor and delivery with premature ruptured membranes at term. She is not contracting. Fetal status is reassuring.
Her obstetric history is of one normal, spontaneous delivery followed by one cesarean delivery, both occurring at term.
She wants to know if she can safely undergo a trial of labor, or if she must have a repeat cesarean delivery. How should you counsel her?
At the start of any discussion about how to reduce your risk of being sued for malpractice because of your work as an obstetrician, in particular during labor and delivery, two distinct, underlying avenues of concern need to be addressed. Before moving on to discuss strategy, then, let’s consider what they are and how they arise: Allegation (perception). You are at risk of an allegation of malpractice (or of a perception of malpractice) because of an unexpected event or outcome for mother or baby. Allegation and perception can arise apart from any specific clinical action you undertook, or did not undertake. An example? Counseling about options for care that falls short of full understanding by the patient.
Allegation and perception are the subjects of this first installment of our two-part article on strategies for avoiding claims of malpractice in L & D that begin with the first prenatal visit.
Causation. Your actions—what you do in the course of providing prenatal care and delivering a baby—put you at risk of a charge of malpractice when you have provided medical care that 1) is inconsistent with current medical practice and thus 2) harmed the mother or newborn.
For a medical malpractice case to go forward, it must meet a well-defined paradigm that teases apart components of causation, beginning with your duty to the patient (TABLE 1).
TABLE 1 Signposts in the medical malpractice paradigm
| When the clinical issue at hand is … | … Then the legal term is … |
|---|---|
| A health-care professional’s obligation to provide care | “Duty” |
| A deviation in the care that was provided | “Standard of care” |
| An allegation that a breach in the standard of care resulted in injury | “Proximate cause” |
| An assertion or finding that an injury is “compensable” | “Damages” |
| Source: Yale New Haven Medical Center, 1997.5 | |
Allegation of malpractice arises from a range of sources, as we’ll discuss, but it is causation that reflects the actual, hands-on practice of medicine. We’ll examine strategies for avoiding charges of causation in the second part of this article.
(For now, we’ll just note that a recent excellent review of intrapartum interventions and their basis in evidence1 offers a model for evaluating a number of widely utilized practices in obstetrics. The goal, of course, is to minimize bad outcomes that follow from causation. Regrettably, that evidence-based approach is a limited one, because of a paucity of adequately controlled studies about OB practice.)
CASE: Continued
You consider your patient’s comment that she would like to avoid a repeat cesarean delivery, and advise her that she may safely attempt vaginal birth.
When spontaneous labor does not occur in 6 hours, oxytocin is administered. She dilates to 9 cm and begins to push spontaneously.
The fetal heart rate then drops to 70/min; fetal station, which had been +2, is now -1. A Stat cesarean delivery is performed. Uterine rupture with partial fetal expulsion is found. Apgar scores are 1, 3, and 5 at 1, 5, and 10 minutes.
Your patient requires a hysterectomy to control bleeding.
Some broad considerations for the physician arising from this CASE
- The counseling that you provide to a patient should be nondirective; it should include your opinion, however, about the best option available to her. Insert yourself into this hypothetical case, for discussion’s sake: Did you provide that important opinion to her?
- You must make certain that she clearly understands the risks and benefits of a procedure or other action, and the available alternatives. Did you undertake a check of her comprehension, given the anxiety and confusion of the moment?
- When an adverse outcome ensues—however unlikely it was to occur—it is necessary for you to review the circumstances with the patient as soon as clinically possible. Did you “debrief” and counsel her before and after the hysterectomy?
No more “perfect outcomes”: Our role changed, so did our risk
From the moment an OB patient enters triage, until her arrival home with her infant, this crucial period of her life is colored by concern, curiosity, myth, and fear.
Every woman anticipates the birth of a healthy infant. In an earlier era, the patient and her family relied on the sage advice of their physician to ensure this outcome. To an extent, physicians themselves reinforced this reliance, embracing the notion that they were, in fact, able to provide such a perfect outcome.
With advances that have been made in reproductive medicine, pregnancy has become more readily available to women with increasingly advanced disease; this has made labor and delivery more challenging to them and to their physicians. Realistically, our role as physicians is now better expressed as providing advice to help a woman achieve the best possible outcome, recognizing her individual clinical circumstances, instead of ensuring a perfect outcome.
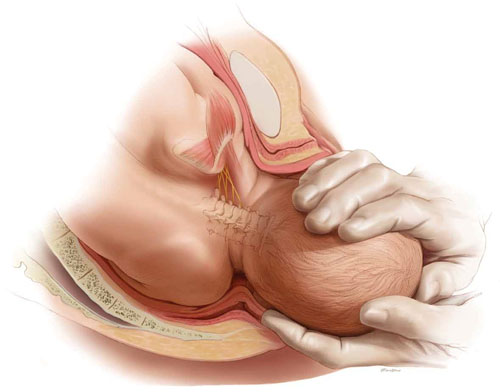
Every woman anticipates the birth of a healthy baby. But the role of the OB is better expressed as helping her achieve the best possible outcome, not a perfect outcome. ABOVE: Shoulder dystocia is one of the most treacherous and frightening—and litigated—complications of childbirth, yet it is, for the most part, unpredictable and unpreventable in the course of even routine delivery.
Key concept #1
COMMUNICATION
Communication is central to patients’ comprehension about the care that you provide to them. But to enter a genuine dialogue with a patient under your care, and with her family, can challenge your communication skills.
First, you need written and verbal skills. Second, you need to know how to read visual cues.
Third, the messages that you deliver to the patient are influenced by:
- your style of communication
- your cultural background
- the setting in which you’re providing care (office, hospital).
Where are such skills developed? For one, biopsychosocial models that are employed in medical student education and resident training aid the physician in developing appropriate communication skills.
But training alone cannot overcome the fact that communication is a double-sided activity: Patients bring many of their own variables to a dialogue. How patients understand and interact with you—and with other providers and the health-care system—is not, therefore, directly or strictly within your sphere of influence.
Yet your sensitivity to a patient’s issues can go a long way toward ameliorating her misconceptions and prejudices. Here are several suggestions, developed by others, to optimize patients’ understanding of their care2,3:
- Apply what’s known as flip default. Assume the patient does not understand the information that you’re providing. Ask her to repeat your instructions back to you (as is done with a verbal order in the hospital).
- Manage face-to-face time effectively. Don’t attempt to teach a patient everything about her care at once. Focus on the critical aspects of her case and on providing understanding; use a strategy of sequential learning.
- Reduce the “overwhelm” factor. Periodically, stop and ask the patient if she has questions. Don’t wait until the end of the appointment to do this.
- Eliminate jargon. When you notify a patient about the results of testing, for example, clarify what the results say about her health and mean for her care. Do so in plain language.
- Recognize her preconceptions. Discuss any psychosocial issues head on with the patient. Use an interpreter or a social worker, or counselors from other fields, as appropriate.
Remember: All health-care personnel need to understand the importance of making the patient comfortable in the often foreign, and sometimes sterile, milieu of the medical office and hospital.
Key concept #2
TRUST
Trust between patient and clinician is, we believe, the most basic necessity for ameliorating allegations of malpractice—secondary only, perhaps, to your knowledge of medicine.
Trust can be enhanced by interactions that demonstrate to both parties the advisability of working together to resolve a problem. Any aspect of the physician-patient interaction that is potentially adversarial does not serve the interests of either.
We encourage you to construct a communication bridge, so to speak, with your patient. Begin by:
- introducing yourself to her and explaining your role in her care
- making appropriate eye contact with her
- maintaining a positive attitude
- dressing appropriately
- making her feel that she is your No. 1 priority.
There is more.
Recognize the duality of respect
- Ask the patient how she wishes to be addressed
- Ask about her belief system
- Explain the specifics of her care without arrogance.
Engender trust
- Be honest with her
- Be on her side
- Take time with her
- Allow her the right that she has to select from the options or to refuse treatment
- Disclose to the patient your status as a student or resident, if that is your rank.
Recognize the benefits of partnership
Forging a partnership with the patient:
- improves the accuracy of information
- eases ongoing communication
- facilitates informed consent
- provides an opportunity for you to educate her.
TABLE 2 When building trust, both patient and physician
are charged with responsibilities
| In regard to … | The patient’s responsibility is to … | The physician’s responsibility is to … |
|---|---|---|
| Gathering an honest and complete medical history | Know and report | Question completely |
| Being adherent to prescribed care | Follow through | Make reasonable demands |
| Making decisions about care | Ask questions and actively participate in choices Make realistic requests | Be knowledgeable about available alternatives Individualize options |
Key concept #3
SHARED RESPONSIBILITY
Patient and physician both have responsibilities that are important to achieving an optimal outcome; so does the hospital (TABLE 2 and TABLE 3). Both patient and physician should practice full disclosure throughout the course of care; this will benefit both of you.4 Here are a few select examples.
TABLE 3 Relative degrees of responsibility for a good outcome
vary across interested parties, but none are exempt
| Area of emphasis | Hospital’s responsibility | Physician’s responsibility | Patient’s responsibility |
|---|---|---|---|
| Creating a positive environment for care | 3+ | 2+ | 1+ |
| Providing clear communication | 3+ | 3+ | 3+ |
| Obtaining informed consent | 3+ | 3+ | 3+ |
| Making reasonable requests | 1+ | 1+ | 3+ |
| Compliance | 3+ | 3+ | 3+ |
| Key to the relative scale: 1+: at the least, minimally responsible; 2+: at the least, somewhat responsible; 3+, responsible to the greatest degree. | |||
The importance of the intake form
At the outset of OB care, in most practices, the patient provides the initial detailed medical history by completing a form in the waiting room. In reviewing and completing this survey with her during the appointment, pay particular attention to those questions for which the response has been left blank.
Patients need to understand that key recommendations about their care, and a proper analysis of their concerns, are based on the information that they provide on this survey. In our practices, we find that patients answer most of these early questions without difficulty—even inquiries of a personal nature, such as the number of prior pregnancies, or drug, alcohol, and smoking habits—as long as they understand why it’s in their best interests for you to have this information. If they leave a question blank and you do not follow up verbally, you may have lost invaluable information that can affect the outcome of her pregnancy.
What should you do when, occasionally, a patient refuses to answer one of your questions? We recommend that you record her refusal on the form itself, where the note remains part of the record.
Keep in mind that all necessary and useful information about a patient may not be available, or may not be appropriate to consider, at the initial prenatal visit. In that case, you have an ongoing opportunity—at subsequent visits during the pregnancy—to develop her full medical profile and algorithm.
The necessity of adherence
It almost goes without saying: To provide the care that our patients need, we sometimes require the unpleasant of them—to undergo evaluations, or testing, or to take medications that may be inconvenient or costly.
After you explain the specific course of care to a patient—whether you’re ordering a test or writing a prescription—your follow-up must include notation in the record of adherence. The fact is that both of you share responsibility for having her understand the importance of adherence to your instructions and the consequences of limited adherence or nonadherence.
Recall one of the lessons from the case that introduced this article: For the patient to make an informed decision about her care, the clinician must have thorough knowledge of 1) the risks and benefits of whatever intervention is being proposed in the particular clinical scenario and 2) the available alternatives. It is key that you communicate your risk-benefit assessment accurately to the patient.
Follow-up
Sometimes, new medical problems arise during subsequent prenatal visits. Follow-up appointments also provide an opportunity for you to expand your attention to problems identified earlier. Regardless of what the patient reported about her history and current health at the initial prenatal visit, listen for her to bring new issues to light for resolution later in the pregnancy that will have an impact on L & D. Again, it goes without saying but needs to be said: The OB clinician needs to have whatever skills are necessary to 1) fully evaluate the progress of a pregnancy and 2) make recommendations for care in light of changes in the status of mother and fetus along the way.
TABLE 4 Examples of the cardinal rule of “Be specific”
when you document care
| Instead of noting … | … Use alternative wording |
|---|---|
| “Mild vaginal bleeding” | “Vaginal bleeding requiring two pads an hour” |
| “Gentle traction” | “The shoulders were rotated before assisting the patient’s expulsive efforts” |
| “Patient refuses…” [or “declines…”] | “Patient voiced the nature of the problem and the alternatives that i have explained to her” |
| “Expedited cesarean section” | “The time from decision to incision was 35 minutes” |
Basic principles of documentation
The medical record is the best witness to interactions between a physician and a patient. In the record, we’re required to write a “5-C” description of events—namely, one that is:
- correct
- comprehensive
- conscientious
- clear
- contemporaneous.
Avoid medical jargon in the record. Be careful not to use vague terminology or descriptions, such as “mild vaginal bleeding,” “gentle traction,” or “patient refuses and accepts the consequences.” Specificity is the key to accuracy with respect to documentation (TABLE 4).
Editor’s note: Part 2 of this article will appear in the January 2011 issue of OBG Management. The authors’ analysis of L & D malpractice claims moves to a discussion of causation—by way of 4 troubling cases.
You’ll find a rich, useful archive of expert analysis of your professional liability and malpractice risk, at www.obgmanagement.com
• 10 keys to defending (or, better, keeping clear of) a shoulder dystocia suit
Andrew K. Worek, Esq (March 2008)
• After a patient’s unexpected death, First Aid for the emotionally wounded
Ronald A. Chez, MD, and Wayne Fortin, MS (April 2010)
• Afraid of getting sued? A plaintiff attorney offers counsel (but no sympathy)
Janelle Yates, Senior Editor, with Lewis Laska, JD, PhD (October 2009)
• Can a change in practice patterns reduce the number of OB malpractice claims?
Jason K. Baxter, MD, MSCP, and Louis Weinstein, MD (April 2009)
• Strategies for breaking bad news to patients
Barry Bub, MD (September 2008)
• Stuff of nightmares: Criminal prosecution for malpractice
Gary Steinman, MD, PhD (August 2008)
• Deposition Dos and Don’ts: How to answer 8 tricky questions
James L. Knoll, IV, MD, and Phillip J. Resnick, MD (May 2008)
• Playing high-stakes poker: Do you fight—or settle—that malpractice lawsuit?
Jeffrey Segal, MD (April 2008)
We want to hear from you! Tell us what you think.
CASE: Is TOLAC feasible?
Your patient is a 33-year-old gravida 3, para 2002, with a previous cesarean delivery who was admitted to labor and delivery with premature ruptured membranes at term. She is not contracting. Fetal status is reassuring.
Her obstetric history is of one normal, spontaneous delivery followed by one cesarean delivery, both occurring at term.
She wants to know if she can safely undergo a trial of labor, or if she must have a repeat cesarean delivery. How should you counsel her?
At the start of any discussion about how to reduce your risk of being sued for malpractice because of your work as an obstetrician, in particular during labor and delivery, two distinct, underlying avenues of concern need to be addressed. Before moving on to discuss strategy, then, let’s consider what they are and how they arise: Allegation (perception). You are at risk of an allegation of malpractice (or of a perception of malpractice) because of an unexpected event or outcome for mother or baby. Allegation and perception can arise apart from any specific clinical action you undertook, or did not undertake. An example? Counseling about options for care that falls short of full understanding by the patient.
Allegation and perception are the subjects of this first installment of our two-part article on strategies for avoiding claims of malpractice in L & D that begin with the first prenatal visit.
Causation. Your actions—what you do in the course of providing prenatal care and delivering a baby—put you at risk of a charge of malpractice when you have provided medical care that 1) is inconsistent with current medical practice and thus 2) harmed the mother or newborn.
For a medical malpractice case to go forward, it must meet a well-defined paradigm that teases apart components of causation, beginning with your duty to the patient (TABLE 1).
TABLE 1 Signposts in the medical malpractice paradigm
| When the clinical issue at hand is … | … Then the legal term is … |
|---|---|
| A health-care professional’s obligation to provide care | “Duty” |
| A deviation in the care that was provided | “Standard of care” |
| An allegation that a breach in the standard of care resulted in injury | “Proximate cause” |
| An assertion or finding that an injury is “compensable” | “Damages” |
| Source: Yale New Haven Medical Center, 1997.5 | |
Allegation of malpractice arises from a range of sources, as we’ll discuss, but it is causation that reflects the actual, hands-on practice of medicine. We’ll examine strategies for avoiding charges of causation in the second part of this article.
(For now, we’ll just note that a recent excellent review of intrapartum interventions and their basis in evidence1 offers a model for evaluating a number of widely utilized practices in obstetrics. The goal, of course, is to minimize bad outcomes that follow from causation. Regrettably, that evidence-based approach is a limited one, because of a paucity of adequately controlled studies about OB practice.)
CASE: Continued
You consider your patient’s comment that she would like to avoid a repeat cesarean delivery, and advise her that she may safely attempt vaginal birth.
When spontaneous labor does not occur in 6 hours, oxytocin is administered. She dilates to 9 cm and begins to push spontaneously.
The fetal heart rate then drops to 70/min; fetal station, which had been +2, is now -1. A Stat cesarean delivery is performed. Uterine rupture with partial fetal expulsion is found. Apgar scores are 1, 3, and 5 at 1, 5, and 10 minutes.
Your patient requires a hysterectomy to control bleeding.
Some broad considerations for the physician arising from this CASE
- The counseling that you provide to a patient should be nondirective; it should include your opinion, however, about the best option available to her. Insert yourself into this hypothetical case, for discussion’s sake: Did you provide that important opinion to her?
- You must make certain that she clearly understands the risks and benefits of a procedure or other action, and the available alternatives. Did you undertake a check of her comprehension, given the anxiety and confusion of the moment?
- When an adverse outcome ensues—however unlikely it was to occur—it is necessary for you to review the circumstances with the patient as soon as clinically possible. Did you “debrief” and counsel her before and after the hysterectomy?
No more “perfect outcomes”: Our role changed, so did our risk
From the moment an OB patient enters triage, until her arrival home with her infant, this crucial period of her life is colored by concern, curiosity, myth, and fear.
Every woman anticipates the birth of a healthy infant. In an earlier era, the patient and her family relied on the sage advice of their physician to ensure this outcome. To an extent, physicians themselves reinforced this reliance, embracing the notion that they were, in fact, able to provide such a perfect outcome.
With advances that have been made in reproductive medicine, pregnancy has become more readily available to women with increasingly advanced disease; this has made labor and delivery more challenging to them and to their physicians. Realistically, our role as physicians is now better expressed as providing advice to help a woman achieve the best possible outcome, recognizing her individual clinical circumstances, instead of ensuring a perfect outcome.
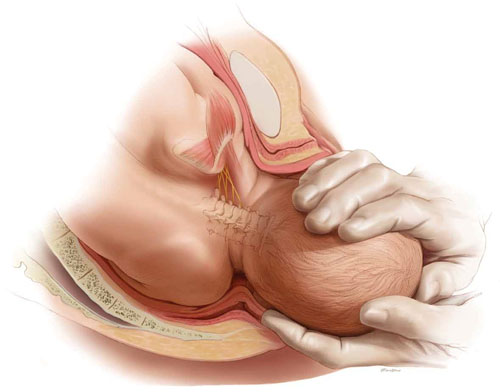
Every woman anticipates the birth of a healthy baby. But the role of the OB is better expressed as helping her achieve the best possible outcome, not a perfect outcome. ABOVE: Shoulder dystocia is one of the most treacherous and frightening—and litigated—complications of childbirth, yet it is, for the most part, unpredictable and unpreventable in the course of even routine delivery.
Key concept #1
COMMUNICATION
Communication is central to patients’ comprehension about the care that you provide to them. But to enter a genuine dialogue with a patient under your care, and with her family, can challenge your communication skills.
First, you need written and verbal skills. Second, you need to know how to read visual cues.
Third, the messages that you deliver to the patient are influenced by:
- your style of communication
- your cultural background
- the setting in which you’re providing care (office, hospital).
Where are such skills developed? For one, biopsychosocial models that are employed in medical student education and resident training aid the physician in developing appropriate communication skills.
But training alone cannot overcome the fact that communication is a double-sided activity: Patients bring many of their own variables to a dialogue. How patients understand and interact with you—and with other providers and the health-care system—is not, therefore, directly or strictly within your sphere of influence.
Yet your sensitivity to a patient’s issues can go a long way toward ameliorating her misconceptions and prejudices. Here are several suggestions, developed by others, to optimize patients’ understanding of their care2,3:
- Apply what’s known as flip default. Assume the patient does not understand the information that you’re providing. Ask her to repeat your instructions back to you (as is done with a verbal order in the hospital).
- Manage face-to-face time effectively. Don’t attempt to teach a patient everything about her care at once. Focus on the critical aspects of her case and on providing understanding; use a strategy of sequential learning.
- Reduce the “overwhelm” factor. Periodically, stop and ask the patient if she has questions. Don’t wait until the end of the appointment to do this.
- Eliminate jargon. When you notify a patient about the results of testing, for example, clarify what the results say about her health and mean for her care. Do so in plain language.
- Recognize her preconceptions. Discuss any psychosocial issues head on with the patient. Use an interpreter or a social worker, or counselors from other fields, as appropriate.
Remember: All health-care personnel need to understand the importance of making the patient comfortable in the often foreign, and sometimes sterile, milieu of the medical office and hospital.
Key concept #2
TRUST
Trust between patient and clinician is, we believe, the most basic necessity for ameliorating allegations of malpractice—secondary only, perhaps, to your knowledge of medicine.
Trust can be enhanced by interactions that demonstrate to both parties the advisability of working together to resolve a problem. Any aspect of the physician-patient interaction that is potentially adversarial does not serve the interests of either.
We encourage you to construct a communication bridge, so to speak, with your patient. Begin by:
- introducing yourself to her and explaining your role in her care
- making appropriate eye contact with her
- maintaining a positive attitude
- dressing appropriately
- making her feel that she is your No. 1 priority.
There is more.
Recognize the duality of respect
- Ask the patient how she wishes to be addressed
- Ask about her belief system
- Explain the specifics of her care without arrogance.
Engender trust
- Be honest with her
- Be on her side
- Take time with her
- Allow her the right that she has to select from the options or to refuse treatment
- Disclose to the patient your status as a student or resident, if that is your rank.
Recognize the benefits of partnership
Forging a partnership with the patient:
- improves the accuracy of information
- eases ongoing communication
- facilitates informed consent
- provides an opportunity for you to educate her.
TABLE 2 When building trust, both patient and physician
are charged with responsibilities
| In regard to … | The patient’s responsibility is to … | The physician’s responsibility is to … |
|---|---|---|
| Gathering an honest and complete medical history | Know and report | Question completely |
| Being adherent to prescribed care | Follow through | Make reasonable demands |
| Making decisions about care | Ask questions and actively participate in choices Make realistic requests | Be knowledgeable about available alternatives Individualize options |
Key concept #3
SHARED RESPONSIBILITY
Patient and physician both have responsibilities that are important to achieving an optimal outcome; so does the hospital (TABLE 2 and TABLE 3). Both patient and physician should practice full disclosure throughout the course of care; this will benefit both of you.4 Here are a few select examples.
TABLE 3 Relative degrees of responsibility for a good outcome
vary across interested parties, but none are exempt
| Area of emphasis | Hospital’s responsibility | Physician’s responsibility | Patient’s responsibility |
|---|---|---|---|
| Creating a positive environment for care | 3+ | 2+ | 1+ |
| Providing clear communication | 3+ | 3+ | 3+ |
| Obtaining informed consent | 3+ | 3+ | 3+ |
| Making reasonable requests | 1+ | 1+ | 3+ |
| Compliance | 3+ | 3+ | 3+ |
| Key to the relative scale: 1+: at the least, minimally responsible; 2+: at the least, somewhat responsible; 3+, responsible to the greatest degree. | |||
The importance of the intake form
At the outset of OB care, in most practices, the patient provides the initial detailed medical history by completing a form in the waiting room. In reviewing and completing this survey with her during the appointment, pay particular attention to those questions for which the response has been left blank.
Patients need to understand that key recommendations about their care, and a proper analysis of their concerns, are based on the information that they provide on this survey. In our practices, we find that patients answer most of these early questions without difficulty—even inquiries of a personal nature, such as the number of prior pregnancies, or drug, alcohol, and smoking habits—as long as they understand why it’s in their best interests for you to have this information. If they leave a question blank and you do not follow up verbally, you may have lost invaluable information that can affect the outcome of her pregnancy.
What should you do when, occasionally, a patient refuses to answer one of your questions? We recommend that you record her refusal on the form itself, where the note remains part of the record.
Keep in mind that all necessary and useful information about a patient may not be available, or may not be appropriate to consider, at the initial prenatal visit. In that case, you have an ongoing opportunity—at subsequent visits during the pregnancy—to develop her full medical profile and algorithm.
The necessity of adherence
It almost goes without saying: To provide the care that our patients need, we sometimes require the unpleasant of them—to undergo evaluations, or testing, or to take medications that may be inconvenient or costly.
After you explain the specific course of care to a patient—whether you’re ordering a test or writing a prescription—your follow-up must include notation in the record of adherence. The fact is that both of you share responsibility for having her understand the importance of adherence to your instructions and the consequences of limited adherence or nonadherence.
Recall one of the lessons from the case that introduced this article: For the patient to make an informed decision about her care, the clinician must have thorough knowledge of 1) the risks and benefits of whatever intervention is being proposed in the particular clinical scenario and 2) the available alternatives. It is key that you communicate your risk-benefit assessment accurately to the patient.
Follow-up
Sometimes, new medical problems arise during subsequent prenatal visits. Follow-up appointments also provide an opportunity for you to expand your attention to problems identified earlier. Regardless of what the patient reported about her history and current health at the initial prenatal visit, listen for her to bring new issues to light for resolution later in the pregnancy that will have an impact on L & D. Again, it goes without saying but needs to be said: The OB clinician needs to have whatever skills are necessary to 1) fully evaluate the progress of a pregnancy and 2) make recommendations for care in light of changes in the status of mother and fetus along the way.
TABLE 4 Examples of the cardinal rule of “Be specific”
when you document care
| Instead of noting … | … Use alternative wording |
|---|---|
| “Mild vaginal bleeding” | “Vaginal bleeding requiring two pads an hour” |
| “Gentle traction” | “The shoulders were rotated before assisting the patient’s expulsive efforts” |
| “Patient refuses…” [or “declines…”] | “Patient voiced the nature of the problem and the alternatives that i have explained to her” |
| “Expedited cesarean section” | “The time from decision to incision was 35 minutes” |
Basic principles of documentation
The medical record is the best witness to interactions between a physician and a patient. In the record, we’re required to write a “5-C” description of events—namely, one that is:
- correct
- comprehensive
- conscientious
- clear
- contemporaneous.
Avoid medical jargon in the record. Be careful not to use vague terminology or descriptions, such as “mild vaginal bleeding,” “gentle traction,” or “patient refuses and accepts the consequences.” Specificity is the key to accuracy with respect to documentation (TABLE 4).
Editor’s note: Part 2 of this article will appear in the January 2011 issue of OBG Management. The authors’ analysis of L & D malpractice claims moves to a discussion of causation—by way of 4 troubling cases.
You’ll find a rich, useful archive of expert analysis of your professional liability and malpractice risk, at www.obgmanagement.com
• 10 keys to defending (or, better, keeping clear of) a shoulder dystocia suit
Andrew K. Worek, Esq (March 2008)
• After a patient’s unexpected death, First Aid for the emotionally wounded
Ronald A. Chez, MD, and Wayne Fortin, MS (April 2010)
• Afraid of getting sued? A plaintiff attorney offers counsel (but no sympathy)
Janelle Yates, Senior Editor, with Lewis Laska, JD, PhD (October 2009)
• Can a change in practice patterns reduce the number of OB malpractice claims?
Jason K. Baxter, MD, MSCP, and Louis Weinstein, MD (April 2009)
• Strategies for breaking bad news to patients
Barry Bub, MD (September 2008)
• Stuff of nightmares: Criminal prosecution for malpractice
Gary Steinman, MD, PhD (August 2008)
• Deposition Dos and Don’ts: How to answer 8 tricky questions
James L. Knoll, IV, MD, and Phillip J. Resnick, MD (May 2008)
• Playing high-stakes poker: Do you fight—or settle—that malpractice lawsuit?
Jeffrey Segal, MD (April 2008)
We want to hear from you! Tell us what you think.
1. Berghella V, Baxter JK, Chauhan SP. Evidence-based labor and delivery management. Am J Obstet Gynecol. 2008;199(5):445-454.
2. Paasche-Orlow MK, Riekert KA, Bilderback A, et al. Tailored education may reduce health literacy disparities in asthma self-management. Am J Respir Crit Care Med. 2005;172:980-986.
3. Huvane K. Health literacy: reading is just the beginning. Focus on multicultural healthcare. 2007;3(4):16-19.
4. Giordano K. Legal Principles. In: O’Grady JP, Gimovsky ML, Bayer-Zwirello L, Giordano K, eds. Operative Obstetrics. 2nd ed. New York: Cambridge University Press; 2008.
5. The Four Elements of Medical Malpractice Yale New Haven Medical Center: Issues in Risk Management. 1997.
1. Berghella V, Baxter JK, Chauhan SP. Evidence-based labor and delivery management. Am J Obstet Gynecol. 2008;199(5):445-454.
2. Paasche-Orlow MK, Riekert KA, Bilderback A, et al. Tailored education may reduce health literacy disparities in asthma self-management. Am J Respir Crit Care Med. 2005;172:980-986.
3. Huvane K. Health literacy: reading is just the beginning. Focus on multicultural healthcare. 2007;3(4):16-19.
4. Giordano K. Legal Principles. In: O’Grady JP, Gimovsky ML, Bayer-Zwirello L, Giordano K, eds. Operative Obstetrics. 2nd ed. New York: Cambridge University Press; 2008.
5. The Four Elements of Medical Malpractice Yale New Haven Medical Center: Issues in Risk Management. 1997.
‘Firing’ a patient: May a psychiatrist unilaterally terminate care?
Dear Dr. Mossman:
One of my patients, Ms. A, keeps calling in to refill her prescription, but will not come in for an appointment; she needs the medication, but I really shouldn’t keep prescribing it without seeing her. Another patient, Mr. B, has an open chart, but he stopped seeing me last year after I treated him for an acute depressive episode. May I “fire” these patients? If so, what should I do?—Submitted by “Dr. C”
All physicians occasionally encounter patients whom we’d like to stop treating, but because we feel devoted to those we treat, the idea of “firing” a patient makes us uncomfortable. Sometimes, however, ending a treatment relationship is the right choice for the doctor and patient.1
To know why, how, and when you may terminate your professional relationship with a patient, you need to:
- understand the legal and ethical status of a doctor-patient relationship
- know the proper way to end treatment relationships
- decide whether ending your care of the patient is the right medical and ethical choice.
After exploring these points, we’ll return to the cases of Ms. A and Mr. B and consider what Dr. C might do.
- Submit your malpractice-related questions to Dr. Mossman at [email protected].
- Include your name, address, and practice location. If your question is chosen for publication, your name can be withheld by request.
Doctor-patient relationships
Legal and medical authorities characterize the treatment relationship as an implicit contract that imposes certain obligations on the doctor and the patient.2,3 Doctors are compelled to conduct themselves in accordance with the prevailing “standard of care.” Patients’ obligations include being honest and cooperating with care once they have agreed to a treatment plan (Table 1).3
Patients may stop seeing their doctors at any time, but a physician usually must continue to provide all necessary medical attention until either the treatment episode has concluded or both parties agree to end the doctor-patient relationship.2 If a physician wishes to withdraw from a case before the need for services has ended, the physician must either make arrangements for another competent physician to assume care or give the patient ample notice and opportunity to obtain treatment elsewhere.2 If a doctor fails to do this and harm to the patient results, the doctor is guilty of “abandonment,” legally defined as termination of the physician-patient relationship “at an unreasonable time or without affording the patient the opportunity to procure an equally qualified replacement.”2 Physician abandonment can lead to malpractice liability,4 complaints to state licensing authorities,5 and ethical condemnation.6
Table 1
A patient’s responsibilities
| Being truthful |
| Providing a complete medical history |
| Cooperating with agreed-upon treatment and keeping appointments |
| Meeting financial obligations for medical care |
| Health-enhancing behavior |
| Not participating in fraudulent health care |
| Source: Reference 3 |
Terminating without abandoning
Doctors commonly terminate care of their patients when they decide to move or close their practices. Accusations of abandonment may arise if such career decisions are executed improperly, but these matters are not as emotionally troubling for physicians as a decision to “fire” a patient because of the patient’s behavior. Common, legitimate reasons a doctor may consider unilateral termination appear in Table 2.7,8
Certain circumstances are not valid grounds for terminating a doctor-patient relationship. You cannot ethically decline to treat a patient whose problem lies within your areas of clinical competence solely because the patient is seropositive for human immunodeficiency virus,9 nor because of a patient’s race, religion, or other reasons that would constitute illegal discrimination.3 Doctors who practice in rural areas must be especially cautious about terminating care because their patients may have limited access to alternate care sources.10
Meeting with or verbally informing a patient of a termination may be reasonable in some cases, but appropriate unilateral termination of a patient usually requires providing written notification to the patient or person responsible for the patient’s care. Attorneys who specialize in risk management advise doctors to seek legal consultation when preparing a termination-of-care letter and to send it by certified mail. The letter should conform to any applicable rules or regulations where you practice. Typically, required content includes:
- notification that the physician-patient relationship is terminated
- a statement of willingness to provide emergency treatment and access to services for up to 30 days from the mailing date to allow the patient to arrange care from another provider
- an offer to transfer records to the new provider upon receiving the patient’s signed authorization to do so.11
More discussion of the possible contents of termination letters appears in Table 3.7,12-14
Table 2
Common reasons to consider terminating a patient’s care
| Failing to pay bills |
| Repeatedly cancelling or missing appointments |
| Repeatedly failing to follow the agreed-upon treatment plan |
| Overly demanding, rude, disruptive, threatening, or violent behavior toward staff or other patients |
| Patient is very dissatisfied with care |
| Needing specialized services that the physician cannot provide |
| Filing a complaint or legal action against the physician |
| Dishonesty that compromises safety or legality of treatment |
| Physician feels treatment is ineffective |
| Conflict of interest (eg, physician’s religious beliefs preclude providing certain treatments that might be indicated) |
| Developing and acting upon an inappropriate personal interest in the physician |
| Inappropriate response by physician to feelings about the patient (eg, physician feels tempted to act upon an attraction) |
| Source: References 7,8 |
Table 3
Potential elements of termination letters
| Element | Comment | |
|---|---|---|
| Reason for termination | Giving a reason is not required. If an explanation seems necessary, offer a general statement (eg, ‘I have determined it would be best…’) | |
| Adequate time to seek care elsewhere | Typically, at least 30 days. Courts have described appropriate time frames in general terms, such as ‘ample,’ ‘sufficient,’ or ‘reasonable’ | |
| Interim care provisions | Offer interim care for urgent problems until the time limit stated above | |
| Continued care provisions |
| |
| Medical record copies | Offer to provide a summary of treatment or copy of the record to a new provider. Consider enclosing a ‘release of information’ authorization to be returned to the office with the patient’s signature | |
| Sending the letter | Regular and certified mail (return receipt requested). Place a copy of this letter in the patient’s medical record, along with the original certified mail receipt and, if received, the original return receipt | |
| Source: References 7,12-14 | ||
Deciding to ‘fire‘ a patient
Physicians in all specialties encounter patients whose actions generate intensely negative feelings—resentment, anger, even hate.15 But “firing” a patient should be a rare circumstance that’s not undertaken lightly. Many different circumstances can make it reasonable for a physician to consider terminating a patient’s care, so it’s difficult to provide general advice about when firing a patient really is the right thing to do. But 1 “prescription” seems clear: consult a respected colleague first. According to psychiatrist Robert Michels, “Any physician who is thinking of firing a patient should first speak to a colleague… This is an enormous decision and, while it might even be right at times, the physician is probably having a countertransference reaction to his patient and should really understand that before taking action.”1
Having an anonymous consultation with a colleague offers several potential benefits, such as:
- If you’re thinking about firing a patient, you’re probably very upset. A colleague who isn’t emotionally involved can help you assess the matter more dispassionately.
- You may be feeling guilty about disliking the patient. A colleague’s empathy (“Of course you’re angry!”) can help you avoid disowning your feelings, which may make it easier to figure out how to use those feelings to help the patient.15,16
- A colleague may think of solutions that you haven’t considered, which might help you feel less frustrated about how treatment is going.
- A colleague may help you see ways that you’re actually helping the patient, despite feeling that your work is futile.
- If a thoughtful colleague confirms your view that terminating care is appropriate, you’ll feel better about the decision. If you document the anonymous consultation in the patient’s chart, you’ll create a record of your reasonableness and prudence—which will be helpful if you have to defend your action in court.12
Revisiting the case patients
With these thoughts in mind, we return to Dr. C’s clinical dilemmas.
Ms. A. In retrospect, Dr. C might wish he had been clearer with Ms. A about how often she would need to see him for medication monitoring. At this point, however, Dr. C still has options besides firing Ms. A:
- Dr. C can call Ms. A to ask how she’s doing and to explain his medical responsibility to see and reassess her if he is to continue prescribing her medication. He can then follow up with a letter summarizing the conversation.
- Dr. C might ask whether some problem is preventing Ms. A from making an appointment. If, for example, Ms. A has lost her job and health insurance coverage for office visits, Dr. C might suggest options (such as seeing Ms. A once at no charge) or help Ms. A find other ways to obtain follow-up care.
Mr. B. Concerning Mr. B, we wonder, “Why not just leave the chart open?” As is the case with care provided by other specialists—including internists, obstetricians, or dermatologists—psychiatric treatment may occur in discrete episodes over many years. Patients regard a previous care provider as “their doctor” for decades after a treatment episode, and it’s comforting and valuable for former patients to know they can see their “shrink” again if they need to.
Related Resource
- Henderson SM. Advice on abandonment. Oklahoma Board of Medical Licensure and Supervision. www.okmedicalboard.org/download/19980401MD.htm.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Friedman RA. Should a doctor fire a patient? Sometimes it is good medicine. New York Times. September 27, 2005;sect F:1.
2. Dietz LH, Jacobs A, Leming TL, et al. Physicians, surgeons, and other healers, §§130, 216-218. In: American jurisprudence. Vol 61. 2nd ed. New York, NY: Thomson Reuters; 2010.
3. American Medical Association. Code of ethics. Opinions 9.12, 10.02, and 10.015. Available at: http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics.shtml. Accessed October 18, 2010.
4. Lowery v Miller, 157 Wis 2d 503, 460 NW2d 446 (Wis App 1990).
5. Crausman RS. Board of medical licensure and discipline. Available at: http://www.health.ri.gov/hsr/bmld. Accessed October 27, 2010.
6. Pellegrino ED. Nonabandonment: an old obligation revisited. Ann Intern Med. 1995;122:377-378.
7. Harris SM. Take care when firing a patient. American Medical News. Available at: http://www.ama-assn.org/amednews/2008/02/04/bica0204.htm. Accessed October 18, 2010.
8. Gabbard GO. Long-term psychodynamic psychotherapy: a basic text. Arlington, VA: American Psychiatric Publishing, Inc.; 2004.
9. Bragdon v Abbott, 524 U.S. 624 (1998).
10. Henderson SM. Advice on abandonment. Oklahoma Board of Medical Licensure and Supervision. Available at: http://www.okmedicalboard.org/download/19980401MD.htm. Accessed October 18, 2010.
11. Ohio Admin Code Ch, 4731-27(A)(1).
12. Appelbaum PS, Gutheil T. Clinical handbook of psychiatry and the law. 4th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2006.
13. Appelbaum PS. Law & psychiatry: can a psychiatrist be held responsible when a patient commits murder? Psychiatr Serv. 2002;53:27-29.
14. Tan MW, McDonough WJ. Risk management in psychiatry. Psychiatr Clin North Am. 1990;13:135-147.
15. Groves JE. Taking care of the hateful patient. N Engl J Med. 1978;298:883-887.
16. Strous RD, Ulman AM, Kotler M. The hateful patient revisited: relevance for 21st century medicine. Eur J Intern Med. 2006;17:387-393.
Dear Dr. Mossman:
One of my patients, Ms. A, keeps calling in to refill her prescription, but will not come in for an appointment; she needs the medication, but I really shouldn’t keep prescribing it without seeing her. Another patient, Mr. B, has an open chart, but he stopped seeing me last year after I treated him for an acute depressive episode. May I “fire” these patients? If so, what should I do?—Submitted by “Dr. C”
All physicians occasionally encounter patients whom we’d like to stop treating, but because we feel devoted to those we treat, the idea of “firing” a patient makes us uncomfortable. Sometimes, however, ending a treatment relationship is the right choice for the doctor and patient.1
To know why, how, and when you may terminate your professional relationship with a patient, you need to:
- understand the legal and ethical status of a doctor-patient relationship
- know the proper way to end treatment relationships
- decide whether ending your care of the patient is the right medical and ethical choice.
After exploring these points, we’ll return to the cases of Ms. A and Mr. B and consider what Dr. C might do.
- Submit your malpractice-related questions to Dr. Mossman at [email protected].
- Include your name, address, and practice location. If your question is chosen for publication, your name can be withheld by request.
Doctor-patient relationships
Legal and medical authorities characterize the treatment relationship as an implicit contract that imposes certain obligations on the doctor and the patient.2,3 Doctors are compelled to conduct themselves in accordance with the prevailing “standard of care.” Patients’ obligations include being honest and cooperating with care once they have agreed to a treatment plan (Table 1).3
Patients may stop seeing their doctors at any time, but a physician usually must continue to provide all necessary medical attention until either the treatment episode has concluded or both parties agree to end the doctor-patient relationship.2 If a physician wishes to withdraw from a case before the need for services has ended, the physician must either make arrangements for another competent physician to assume care or give the patient ample notice and opportunity to obtain treatment elsewhere.2 If a doctor fails to do this and harm to the patient results, the doctor is guilty of “abandonment,” legally defined as termination of the physician-patient relationship “at an unreasonable time or without affording the patient the opportunity to procure an equally qualified replacement.”2 Physician abandonment can lead to malpractice liability,4 complaints to state licensing authorities,5 and ethical condemnation.6
Table 1
A patient’s responsibilities
| Being truthful |
| Providing a complete medical history |
| Cooperating with agreed-upon treatment and keeping appointments |
| Meeting financial obligations for medical care |
| Health-enhancing behavior |
| Not participating in fraudulent health care |
| Source: Reference 3 |
Terminating without abandoning
Doctors commonly terminate care of their patients when they decide to move or close their practices. Accusations of abandonment may arise if such career decisions are executed improperly, but these matters are not as emotionally troubling for physicians as a decision to “fire” a patient because of the patient’s behavior. Common, legitimate reasons a doctor may consider unilateral termination appear in Table 2.7,8
Certain circumstances are not valid grounds for terminating a doctor-patient relationship. You cannot ethically decline to treat a patient whose problem lies within your areas of clinical competence solely because the patient is seropositive for human immunodeficiency virus,9 nor because of a patient’s race, religion, or other reasons that would constitute illegal discrimination.3 Doctors who practice in rural areas must be especially cautious about terminating care because their patients may have limited access to alternate care sources.10
Meeting with or verbally informing a patient of a termination may be reasonable in some cases, but appropriate unilateral termination of a patient usually requires providing written notification to the patient or person responsible for the patient’s care. Attorneys who specialize in risk management advise doctors to seek legal consultation when preparing a termination-of-care letter and to send it by certified mail. The letter should conform to any applicable rules or regulations where you practice. Typically, required content includes:
- notification that the physician-patient relationship is terminated
- a statement of willingness to provide emergency treatment and access to services for up to 30 days from the mailing date to allow the patient to arrange care from another provider
- an offer to transfer records to the new provider upon receiving the patient’s signed authorization to do so.11
More discussion of the possible contents of termination letters appears in Table 3.7,12-14
Table 2
Common reasons to consider terminating a patient’s care
| Failing to pay bills |
| Repeatedly cancelling or missing appointments |
| Repeatedly failing to follow the agreed-upon treatment plan |
| Overly demanding, rude, disruptive, threatening, or violent behavior toward staff or other patients |
| Patient is very dissatisfied with care |
| Needing specialized services that the physician cannot provide |
| Filing a complaint or legal action against the physician |
| Dishonesty that compromises safety or legality of treatment |
| Physician feels treatment is ineffective |
| Conflict of interest (eg, physician’s religious beliefs preclude providing certain treatments that might be indicated) |
| Developing and acting upon an inappropriate personal interest in the physician |
| Inappropriate response by physician to feelings about the patient (eg, physician feels tempted to act upon an attraction) |
| Source: References 7,8 |
Table 3
Potential elements of termination letters
| Element | Comment | |
|---|---|---|
| Reason for termination | Giving a reason is not required. If an explanation seems necessary, offer a general statement (eg, ‘I have determined it would be best…’) | |
| Adequate time to seek care elsewhere | Typically, at least 30 days. Courts have described appropriate time frames in general terms, such as ‘ample,’ ‘sufficient,’ or ‘reasonable’ | |
| Interim care provisions | Offer interim care for urgent problems until the time limit stated above | |
| Continued care provisions |
| |
| Medical record copies | Offer to provide a summary of treatment or copy of the record to a new provider. Consider enclosing a ‘release of information’ authorization to be returned to the office with the patient’s signature | |
| Sending the letter | Regular and certified mail (return receipt requested). Place a copy of this letter in the patient’s medical record, along with the original certified mail receipt and, if received, the original return receipt | |
| Source: References 7,12-14 | ||
Deciding to ‘fire‘ a patient
Physicians in all specialties encounter patients whose actions generate intensely negative feelings—resentment, anger, even hate.15 But “firing” a patient should be a rare circumstance that’s not undertaken lightly. Many different circumstances can make it reasonable for a physician to consider terminating a patient’s care, so it’s difficult to provide general advice about when firing a patient really is the right thing to do. But 1 “prescription” seems clear: consult a respected colleague first. According to psychiatrist Robert Michels, “Any physician who is thinking of firing a patient should first speak to a colleague… This is an enormous decision and, while it might even be right at times, the physician is probably having a countertransference reaction to his patient and should really understand that before taking action.”1
Having an anonymous consultation with a colleague offers several potential benefits, such as:
- If you’re thinking about firing a patient, you’re probably very upset. A colleague who isn’t emotionally involved can help you assess the matter more dispassionately.
- You may be feeling guilty about disliking the patient. A colleague’s empathy (“Of course you’re angry!”) can help you avoid disowning your feelings, which may make it easier to figure out how to use those feelings to help the patient.15,16
- A colleague may think of solutions that you haven’t considered, which might help you feel less frustrated about how treatment is going.
- A colleague may help you see ways that you’re actually helping the patient, despite feeling that your work is futile.
- If a thoughtful colleague confirms your view that terminating care is appropriate, you’ll feel better about the decision. If you document the anonymous consultation in the patient’s chart, you’ll create a record of your reasonableness and prudence—which will be helpful if you have to defend your action in court.12
Revisiting the case patients
With these thoughts in mind, we return to Dr. C’s clinical dilemmas.
Ms. A. In retrospect, Dr. C might wish he had been clearer with Ms. A about how often she would need to see him for medication monitoring. At this point, however, Dr. C still has options besides firing Ms. A:
- Dr. C can call Ms. A to ask how she’s doing and to explain his medical responsibility to see and reassess her if he is to continue prescribing her medication. He can then follow up with a letter summarizing the conversation.
- Dr. C might ask whether some problem is preventing Ms. A from making an appointment. If, for example, Ms. A has lost her job and health insurance coverage for office visits, Dr. C might suggest options (such as seeing Ms. A once at no charge) or help Ms. A find other ways to obtain follow-up care.
Mr. B. Concerning Mr. B, we wonder, “Why not just leave the chart open?” As is the case with care provided by other specialists—including internists, obstetricians, or dermatologists—psychiatric treatment may occur in discrete episodes over many years. Patients regard a previous care provider as “their doctor” for decades after a treatment episode, and it’s comforting and valuable for former patients to know they can see their “shrink” again if they need to.
Related Resource
- Henderson SM. Advice on abandonment. Oklahoma Board of Medical Licensure and Supervision. www.okmedicalboard.org/download/19980401MD.htm.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dear Dr. Mossman:
One of my patients, Ms. A, keeps calling in to refill her prescription, but will not come in for an appointment; she needs the medication, but I really shouldn’t keep prescribing it without seeing her. Another patient, Mr. B, has an open chart, but he stopped seeing me last year after I treated him for an acute depressive episode. May I “fire” these patients? If so, what should I do?—Submitted by “Dr. C”
All physicians occasionally encounter patients whom we’d like to stop treating, but because we feel devoted to those we treat, the idea of “firing” a patient makes us uncomfortable. Sometimes, however, ending a treatment relationship is the right choice for the doctor and patient.1
To know why, how, and when you may terminate your professional relationship with a patient, you need to:
- understand the legal and ethical status of a doctor-patient relationship
- know the proper way to end treatment relationships
- decide whether ending your care of the patient is the right medical and ethical choice.
After exploring these points, we’ll return to the cases of Ms. A and Mr. B and consider what Dr. C might do.
- Submit your malpractice-related questions to Dr. Mossman at [email protected].
- Include your name, address, and practice location. If your question is chosen for publication, your name can be withheld by request.
Doctor-patient relationships
Legal and medical authorities characterize the treatment relationship as an implicit contract that imposes certain obligations on the doctor and the patient.2,3 Doctors are compelled to conduct themselves in accordance with the prevailing “standard of care.” Patients’ obligations include being honest and cooperating with care once they have agreed to a treatment plan (Table 1).3
Patients may stop seeing their doctors at any time, but a physician usually must continue to provide all necessary medical attention until either the treatment episode has concluded or both parties agree to end the doctor-patient relationship.2 If a physician wishes to withdraw from a case before the need for services has ended, the physician must either make arrangements for another competent physician to assume care or give the patient ample notice and opportunity to obtain treatment elsewhere.2 If a doctor fails to do this and harm to the patient results, the doctor is guilty of “abandonment,” legally defined as termination of the physician-patient relationship “at an unreasonable time or without affording the patient the opportunity to procure an equally qualified replacement.”2 Physician abandonment can lead to malpractice liability,4 complaints to state licensing authorities,5 and ethical condemnation.6
Table 1
A patient’s responsibilities
| Being truthful |
| Providing a complete medical history |
| Cooperating with agreed-upon treatment and keeping appointments |
| Meeting financial obligations for medical care |
| Health-enhancing behavior |
| Not participating in fraudulent health care |
| Source: Reference 3 |
Terminating without abandoning
Doctors commonly terminate care of their patients when they decide to move or close their practices. Accusations of abandonment may arise if such career decisions are executed improperly, but these matters are not as emotionally troubling for physicians as a decision to “fire” a patient because of the patient’s behavior. Common, legitimate reasons a doctor may consider unilateral termination appear in Table 2.7,8
Certain circumstances are not valid grounds for terminating a doctor-patient relationship. You cannot ethically decline to treat a patient whose problem lies within your areas of clinical competence solely because the patient is seropositive for human immunodeficiency virus,9 nor because of a patient’s race, religion, or other reasons that would constitute illegal discrimination.3 Doctors who practice in rural areas must be especially cautious about terminating care because their patients may have limited access to alternate care sources.10
Meeting with or verbally informing a patient of a termination may be reasonable in some cases, but appropriate unilateral termination of a patient usually requires providing written notification to the patient or person responsible for the patient’s care. Attorneys who specialize in risk management advise doctors to seek legal consultation when preparing a termination-of-care letter and to send it by certified mail. The letter should conform to any applicable rules or regulations where you practice. Typically, required content includes:
- notification that the physician-patient relationship is terminated
- a statement of willingness to provide emergency treatment and access to services for up to 30 days from the mailing date to allow the patient to arrange care from another provider
- an offer to transfer records to the new provider upon receiving the patient’s signed authorization to do so.11
More discussion of the possible contents of termination letters appears in Table 3.7,12-14
Table 2
Common reasons to consider terminating a patient’s care
| Failing to pay bills |
| Repeatedly cancelling or missing appointments |
| Repeatedly failing to follow the agreed-upon treatment plan |
| Overly demanding, rude, disruptive, threatening, or violent behavior toward staff or other patients |
| Patient is very dissatisfied with care |
| Needing specialized services that the physician cannot provide |
| Filing a complaint or legal action against the physician |
| Dishonesty that compromises safety or legality of treatment |
| Physician feels treatment is ineffective |
| Conflict of interest (eg, physician’s religious beliefs preclude providing certain treatments that might be indicated) |
| Developing and acting upon an inappropriate personal interest in the physician |
| Inappropriate response by physician to feelings about the patient (eg, physician feels tempted to act upon an attraction) |
| Source: References 7,8 |
Table 3
Potential elements of termination letters
| Element | Comment | |
|---|---|---|
| Reason for termination | Giving a reason is not required. If an explanation seems necessary, offer a general statement (eg, ‘I have determined it would be best…’) | |
| Adequate time to seek care elsewhere | Typically, at least 30 days. Courts have described appropriate time frames in general terms, such as ‘ample,’ ‘sufficient,’ or ‘reasonable’ | |
| Interim care provisions | Offer interim care for urgent problems until the time limit stated above | |
| Continued care provisions |
| |
| Medical record copies | Offer to provide a summary of treatment or copy of the record to a new provider. Consider enclosing a ‘release of information’ authorization to be returned to the office with the patient’s signature | |
| Sending the letter | Regular and certified mail (return receipt requested). Place a copy of this letter in the patient’s medical record, along with the original certified mail receipt and, if received, the original return receipt | |
| Source: References 7,12-14 | ||
Deciding to ‘fire‘ a patient
Physicians in all specialties encounter patients whose actions generate intensely negative feelings—resentment, anger, even hate.15 But “firing” a patient should be a rare circumstance that’s not undertaken lightly. Many different circumstances can make it reasonable for a physician to consider terminating a patient’s care, so it’s difficult to provide general advice about when firing a patient really is the right thing to do. But 1 “prescription” seems clear: consult a respected colleague first. According to psychiatrist Robert Michels, “Any physician who is thinking of firing a patient should first speak to a colleague… This is an enormous decision and, while it might even be right at times, the physician is probably having a countertransference reaction to his patient and should really understand that before taking action.”1
Having an anonymous consultation with a colleague offers several potential benefits, such as:
- If you’re thinking about firing a patient, you’re probably very upset. A colleague who isn’t emotionally involved can help you assess the matter more dispassionately.
- You may be feeling guilty about disliking the patient. A colleague’s empathy (“Of course you’re angry!”) can help you avoid disowning your feelings, which may make it easier to figure out how to use those feelings to help the patient.15,16
- A colleague may think of solutions that you haven’t considered, which might help you feel less frustrated about how treatment is going.
- A colleague may help you see ways that you’re actually helping the patient, despite feeling that your work is futile.
- If a thoughtful colleague confirms your view that terminating care is appropriate, you’ll feel better about the decision. If you document the anonymous consultation in the patient’s chart, you’ll create a record of your reasonableness and prudence—which will be helpful if you have to defend your action in court.12
Revisiting the case patients
With these thoughts in mind, we return to Dr. C’s clinical dilemmas.
Ms. A. In retrospect, Dr. C might wish he had been clearer with Ms. A about how often she would need to see him for medication monitoring. At this point, however, Dr. C still has options besides firing Ms. A:
- Dr. C can call Ms. A to ask how she’s doing and to explain his medical responsibility to see and reassess her if he is to continue prescribing her medication. He can then follow up with a letter summarizing the conversation.
- Dr. C might ask whether some problem is preventing Ms. A from making an appointment. If, for example, Ms. A has lost her job and health insurance coverage for office visits, Dr. C might suggest options (such as seeing Ms. A once at no charge) or help Ms. A find other ways to obtain follow-up care.
Mr. B. Concerning Mr. B, we wonder, “Why not just leave the chart open?” As is the case with care provided by other specialists—including internists, obstetricians, or dermatologists—psychiatric treatment may occur in discrete episodes over many years. Patients regard a previous care provider as “their doctor” for decades after a treatment episode, and it’s comforting and valuable for former patients to know they can see their “shrink” again if they need to.
Related Resource
- Henderson SM. Advice on abandonment. Oklahoma Board of Medical Licensure and Supervision. www.okmedicalboard.org/download/19980401MD.htm.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Friedman RA. Should a doctor fire a patient? Sometimes it is good medicine. New York Times. September 27, 2005;sect F:1.
2. Dietz LH, Jacobs A, Leming TL, et al. Physicians, surgeons, and other healers, §§130, 216-218. In: American jurisprudence. Vol 61. 2nd ed. New York, NY: Thomson Reuters; 2010.
3. American Medical Association. Code of ethics. Opinions 9.12, 10.02, and 10.015. Available at: http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics.shtml. Accessed October 18, 2010.
4. Lowery v Miller, 157 Wis 2d 503, 460 NW2d 446 (Wis App 1990).
5. Crausman RS. Board of medical licensure and discipline. Available at: http://www.health.ri.gov/hsr/bmld. Accessed October 27, 2010.
6. Pellegrino ED. Nonabandonment: an old obligation revisited. Ann Intern Med. 1995;122:377-378.
7. Harris SM. Take care when firing a patient. American Medical News. Available at: http://www.ama-assn.org/amednews/2008/02/04/bica0204.htm. Accessed October 18, 2010.
8. Gabbard GO. Long-term psychodynamic psychotherapy: a basic text. Arlington, VA: American Psychiatric Publishing, Inc.; 2004.
9. Bragdon v Abbott, 524 U.S. 624 (1998).
10. Henderson SM. Advice on abandonment. Oklahoma Board of Medical Licensure and Supervision. Available at: http://www.okmedicalboard.org/download/19980401MD.htm. Accessed October 18, 2010.
11. Ohio Admin Code Ch, 4731-27(A)(1).
12. Appelbaum PS, Gutheil T. Clinical handbook of psychiatry and the law. 4th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2006.
13. Appelbaum PS. Law & psychiatry: can a psychiatrist be held responsible when a patient commits murder? Psychiatr Serv. 2002;53:27-29.
14. Tan MW, McDonough WJ. Risk management in psychiatry. Psychiatr Clin North Am. 1990;13:135-147.
15. Groves JE. Taking care of the hateful patient. N Engl J Med. 1978;298:883-887.
16. Strous RD, Ulman AM, Kotler M. The hateful patient revisited: relevance for 21st century medicine. Eur J Intern Med. 2006;17:387-393.
1. Friedman RA. Should a doctor fire a patient? Sometimes it is good medicine. New York Times. September 27, 2005;sect F:1.
2. Dietz LH, Jacobs A, Leming TL, et al. Physicians, surgeons, and other healers, §§130, 216-218. In: American jurisprudence. Vol 61. 2nd ed. New York, NY: Thomson Reuters; 2010.
3. American Medical Association. Code of ethics. Opinions 9.12, 10.02, and 10.015. Available at: http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics.shtml. Accessed October 18, 2010.
4. Lowery v Miller, 157 Wis 2d 503, 460 NW2d 446 (Wis App 1990).
5. Crausman RS. Board of medical licensure and discipline. Available at: http://www.health.ri.gov/hsr/bmld. Accessed October 27, 2010.
6. Pellegrino ED. Nonabandonment: an old obligation revisited. Ann Intern Med. 1995;122:377-378.
7. Harris SM. Take care when firing a patient. American Medical News. Available at: http://www.ama-assn.org/amednews/2008/02/04/bica0204.htm. Accessed October 18, 2010.
8. Gabbard GO. Long-term psychodynamic psychotherapy: a basic text. Arlington, VA: American Psychiatric Publishing, Inc.; 2004.
9. Bragdon v Abbott, 524 U.S. 624 (1998).
10. Henderson SM. Advice on abandonment. Oklahoma Board of Medical Licensure and Supervision. Available at: http://www.okmedicalboard.org/download/19980401MD.htm. Accessed October 18, 2010.
11. Ohio Admin Code Ch, 4731-27(A)(1).
12. Appelbaum PS, Gutheil T. Clinical handbook of psychiatry and the law. 4th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2006.
13. Appelbaum PS. Law & psychiatry: can a psychiatrist be held responsible when a patient commits murder? Psychiatr Serv. 2002;53:27-29.
14. Tan MW, McDonough WJ. Risk management in psychiatry. Psychiatr Clin North Am. 1990;13:135-147.
15. Groves JE. Taking care of the hateful patient. N Engl J Med. 1978;298:883-887.
16. Strous RD, Ulman AM, Kotler M. The hateful patient revisited: relevance for 21st century medicine. Eur J Intern Med. 2006;17:387-393.
BCBS of North Carolina’s refund to customers due to changes in health reform legislation
Bryn Nelson in the October issue of The Hospitalist (see “A Taxing Future for HM?,” p. 16) incorrectly states that Blue Cross Blue Shield of North Carolina’s refund to customers was a result of an overcharge. In point of fact, the refund is a result of a one-time opportunity due to the changes brought about by the health reform law. The new rating and grandfathering rules in the Patient Protection and Affordable Care Act create a one-time circumstance enabling these refunds.
The funds come from active life reserves, which are portions of the premium set aside in the early years of a policy to pay future claims and keep rates stable as customers’ medical expenses rise during the life of the policy. However, policies purchased or substantially modified after March 23, 2010, will end in 2014 under the new healthcare reform law, which is when the new products under health reform will be introduced. Therefore, the reserves held for these products will cover a much shorter period of time, allowing for these funds to be released.
Lew Borman,
media relations,
Blue Cross Blue Shield of North Carolina
Bryn Nelson in the October issue of The Hospitalist (see “A Taxing Future for HM?,” p. 16) incorrectly states that Blue Cross Blue Shield of North Carolina’s refund to customers was a result of an overcharge. In point of fact, the refund is a result of a one-time opportunity due to the changes brought about by the health reform law. The new rating and grandfathering rules in the Patient Protection and Affordable Care Act create a one-time circumstance enabling these refunds.
The funds come from active life reserves, which are portions of the premium set aside in the early years of a policy to pay future claims and keep rates stable as customers’ medical expenses rise during the life of the policy. However, policies purchased or substantially modified after March 23, 2010, will end in 2014 under the new healthcare reform law, which is when the new products under health reform will be introduced. Therefore, the reserves held for these products will cover a much shorter period of time, allowing for these funds to be released.
Lew Borman,
media relations,
Blue Cross Blue Shield of North Carolina
Bryn Nelson in the October issue of The Hospitalist (see “A Taxing Future for HM?,” p. 16) incorrectly states that Blue Cross Blue Shield of North Carolina’s refund to customers was a result of an overcharge. In point of fact, the refund is a result of a one-time opportunity due to the changes brought about by the health reform law. The new rating and grandfathering rules in the Patient Protection and Affordable Care Act create a one-time circumstance enabling these refunds.
The funds come from active life reserves, which are portions of the premium set aside in the early years of a policy to pay future claims and keep rates stable as customers’ medical expenses rise during the life of the policy. However, policies purchased or substantially modified after March 23, 2010, will end in 2014 under the new healthcare reform law, which is when the new products under health reform will be introduced. Therefore, the reserves held for these products will cover a much shorter period of time, allowing for these funds to be released.
Lew Borman,
media relations,
Blue Cross Blue Shield of North Carolina
A Taxing Future for HM?
When Congress returns for a likely lame-duck session after the midterm elections, the biggest battle might be fought over whether to extend the 2001 and 2003 tax cuts to everyone or only to those earning less than $200,000 annually ($250,000 for families). And depending on the makeup of the 112th Congress, which will be seated in January, Republicans might try to make good on a campaign pledge to repeal all or most of the healthcare reform legislation.
The expected flashpoints are being teased endlessly with media sound bites featuring phrases that most of us love to hate: higher taxes, spiraling medical bills, soaring insurance premiums. Insurance companies already are blaming a spike in premiums on the healthcare legislation, claiming that new provisions and mandates are forcing them to further hike their rates.
Closer to home, the high-profile frays could put hospitalists in the awkward position of supporting political positions that sock them in the wallet. After all, doctors are workers and healthcare consumers, too. So what impact could higher taxes and higher insurance premiums really have? Let’s start with health insurance.
Insurance Cost Increases
Signed into law in March, the Affordable Care Act includes tax credits for small businesses to help defray the costs of health insurance coverage. But in 2013, it also raises the threshold for medical expense deductions for most taxpayers, to 10% from 7.5% of adjusted gross income. In other words, families can claim tax deductions only after having spent 10% or more of their adjusted gross income on medical bills. For families with hefty medical bills, that 2.5% difference could translate into a significant shortfall.
CMS was able to negotiate with insurers to achieve a slight drop in Medicare Advantage premiums, but many individual states have had less luck in preventing rate increases from private insurers who blame their higher premiums on new mandates. The Wall Street Journal has documented rate increases of 18% in states like Wisconsin and North Carolina—about 9% of which insurance company officials pinned on the new law.1 Such increases are hardly inevitable, however. The Obama administration’s White House blog, for instance, has cited the example of North Carolina Blue Cross and Blue Shield, which announced Sept. 20 that it will provide $156 million in refunds to more than 215,000 customers after state regulators found an overcharge that should be reversed due to new rules in the reform law.2 WellPoint will similarly refund $20 million to its health insurance customers in Colorado.2
The requested premium increases and identified overcharges have contributed to plenty of finger-pointing among insurers, state regulators, and the Obama administration, which has assailed insurers for using the law as a convenient excuse to raise rates. Highlighting the unease of many consumers, however, is the verdict that the proposed increases—if approved—would hit small businesses and individuals hardest.
According to the State of Hospital Medicine: 2010 Report Based on 2009 Data, released in September by SHM and the Medical Group Management Association, participating hospitalist groups have a median of 10 physician full-time equivalents. Roughly 25% of respondents are in physician-owned groups, while 14% are in a management services organization (MSO) or physician practice management company (PPMC). Smaller HM groups wouldn’t be alone in feeling the pinch, but they might need to consider some serious comparison-shopping to avoid costly premium increases.
Cherilyn Murer, president and CEO of Joliet, Ill.-based Murer Consultants Inc., has worked with healthcare systems and providers in 42 states, but even her company has not been immune to having to contend with rising premiums. “Our managing partner just renegotiated our health benefits [premiums] that were supposed to have gone up 30% by our previous carrier,” Murer says. “Through protracted negotiations and diligence, he was able to find a plan that did not increase our costs, and retained pretty much the same benefits.”
For at least the next three to five years, Murer says, niche firms will need to be diligent about shopping around and managing their expenses in a volatile insurance marketplace. Healthcare reform, she says, is certainly not a panacea for reining in costs, but “just the beginning.”
Concerns over healthcare costs, in fact, could be among the factors driving what Robert Zipper, MD, FHM, regional chief medical officer for Tacoma, Wash.-based Sound Physicians, sees as continuing consolidation among hospitalist groups. “By that, I mean that either groups are swallowed up by the hospital in which they work or they become part of a regional or national company,” he says. Sound Physicians, with about 400 hospitalists in seven states, offers health insurance policies that don’t vary by state, easing its negotiations.
Eyes on the Bottom Line
What about the dreaded “T” word? Dr. Zipper says he hasn’t heard that many concerns about the potential tax increase just yet. “I think it’s not an issue to hospitalists in a broad sense yet,” he says, “but if you look at the salary trajectory and where things have been over the past 10 years, it’s pretty easy to predict that it will be an issue for single-income [households] where the hospitalist is the sole breadwinner.”
The 2010 State of Hospital Medicine report, which surveyed 4,211 nonacademic hospitalists from 443 groups, found a median annual income of $215,000. Calculating trends from past income surveys is difficult due to very different respondent populations, but many hospitalists are clearly near or above the $200,000 threshold for individuals and near the $250,000 threshold for families already, even before considering spousal income. The survey, for example, found median salaries of about $235,700 in the 13 states that make up the Southern region.
Even if higher-earning hospitalists are subjected to a higher tax rate next year—if the current rates expire, a climb of 4.6 percentage points, to 39.6% from 35%—not all of them are necessarily opposed to it. Political polling on the issue isn’t broken down by specific professions, but a number of blogs have pointed to a Quinnipiac University poll conducted back in March that suggested nearly two-thirds of upper-income Americans were prepared to sacrifice some of their take-home pay to help reduce the deficit. In that poll (www.quinnipiac.edu/x1295.xml?ReleaseID=1438), some 64% of respondents earning more than $250,000 agreed that raising income taxes on themselves and other households making more than $250,000 should be a main part of any government approach to the deficit.
If taxes and insurance premiums are more immediate concerns, some HM observers are eyeing longer trends that could impact the pre-tax pay of the profession. Most hospitalists still earn far less than their specialist counterparts, of course, but increasing demand for hospitalist services has helped fuel a rise in median salaries. Last year, some observers predicted that after an impressive run, annual pay would plateau or even fall, given the current economic uncertainty, tightening profit margins, and assessment that many hospitals run HM programs at a loss.3 And in the current RVU-driven system, the “What have you done for me lately?” mentality can indeed make it difficult for hospitalists to demonstrate a solid return on the investment.
The State of Hospital Medicine report suggests that respondent HM groups have been subsidized by an average of $111,486 per physician FTE (median is $98,253), with the highest numbers in hospital-owned practices. But many experts see a window of a few years in which new healthcare delivery and payment experiments will be trotted out, whether modeled on a bundled system, accountable-care organization (ACO), or other vehicle. Under these models, payment incentives to physicians—and to hospitalists especially—could be fundamentally restructured to better reflect their true contributions as the emphasis on quality and efficiency increases.
Within the next three years, Murer says, hospitalists need to continue to infiltrate inpatient medical services, demonstrate their worth, and show the cost efficiencies that arise from their profession. “I think they’ve got a window of three years to really decide how much of that [inpatient physician] market they will retain,” she says.
Despite the current volatility, both Murer and Dr. Zipper agree that hospitalists are well positioned to take advantage of the coming changes in the healthcare delivery system. But to seize the opportunity, hospitalists must clearly demonstrate the necessity of their services in the emerging models of care and claim an early seat at the table where decisions will be made about how the pot of money is dispersed. Doing so could help resolve one of the most important financial considerations of all: job security. TH
Bryn Nelson is a freelance medical writer based in Seattle.
References
- Adamy J. Health insurers plan hikes. Wall Street Journal website. Available at: http://online.wsj.com/article/SB10001424052748703720004575478200948908976.html. Accessed Sept. 21, 2010.
- Cutter S. Look you in the eye. The White House website. Available at: www.whitehouse.gov/blog/2010/09/23/look-you-eye. Accessed Sept. 27, 2010.
- How will the economy affect hospitalist salaries? MedPage Today website. Available at: www.kevinmd .com/blog/2009/03/how-will-economy-affect-hospitalist-2.html. Accessed Sept. 27, 2010.
When Congress returns for a likely lame-duck session after the midterm elections, the biggest battle might be fought over whether to extend the 2001 and 2003 tax cuts to everyone or only to those earning less than $200,000 annually ($250,000 for families). And depending on the makeup of the 112th Congress, which will be seated in January, Republicans might try to make good on a campaign pledge to repeal all or most of the healthcare reform legislation.
The expected flashpoints are being teased endlessly with media sound bites featuring phrases that most of us love to hate: higher taxes, spiraling medical bills, soaring insurance premiums. Insurance companies already are blaming a spike in premiums on the healthcare legislation, claiming that new provisions and mandates are forcing them to further hike their rates.
Closer to home, the high-profile frays could put hospitalists in the awkward position of supporting political positions that sock them in the wallet. After all, doctors are workers and healthcare consumers, too. So what impact could higher taxes and higher insurance premiums really have? Let’s start with health insurance.
Insurance Cost Increases
Signed into law in March, the Affordable Care Act includes tax credits for small businesses to help defray the costs of health insurance coverage. But in 2013, it also raises the threshold for medical expense deductions for most taxpayers, to 10% from 7.5% of adjusted gross income. In other words, families can claim tax deductions only after having spent 10% or more of their adjusted gross income on medical bills. For families with hefty medical bills, that 2.5% difference could translate into a significant shortfall.
CMS was able to negotiate with insurers to achieve a slight drop in Medicare Advantage premiums, but many individual states have had less luck in preventing rate increases from private insurers who blame their higher premiums on new mandates. The Wall Street Journal has documented rate increases of 18% in states like Wisconsin and North Carolina—about 9% of which insurance company officials pinned on the new law.1 Such increases are hardly inevitable, however. The Obama administration’s White House blog, for instance, has cited the example of North Carolina Blue Cross and Blue Shield, which announced Sept. 20 that it will provide $156 million in refunds to more than 215,000 customers after state regulators found an overcharge that should be reversed due to new rules in the reform law.2 WellPoint will similarly refund $20 million to its health insurance customers in Colorado.2
The requested premium increases and identified overcharges have contributed to plenty of finger-pointing among insurers, state regulators, and the Obama administration, which has assailed insurers for using the law as a convenient excuse to raise rates. Highlighting the unease of many consumers, however, is the verdict that the proposed increases—if approved—would hit small businesses and individuals hardest.
According to the State of Hospital Medicine: 2010 Report Based on 2009 Data, released in September by SHM and the Medical Group Management Association, participating hospitalist groups have a median of 10 physician full-time equivalents. Roughly 25% of respondents are in physician-owned groups, while 14% are in a management services organization (MSO) or physician practice management company (PPMC). Smaller HM groups wouldn’t be alone in feeling the pinch, but they might need to consider some serious comparison-shopping to avoid costly premium increases.
Cherilyn Murer, president and CEO of Joliet, Ill.-based Murer Consultants Inc., has worked with healthcare systems and providers in 42 states, but even her company has not been immune to having to contend with rising premiums. “Our managing partner just renegotiated our health benefits [premiums] that were supposed to have gone up 30% by our previous carrier,” Murer says. “Through protracted negotiations and diligence, he was able to find a plan that did not increase our costs, and retained pretty much the same benefits.”
For at least the next three to five years, Murer says, niche firms will need to be diligent about shopping around and managing their expenses in a volatile insurance marketplace. Healthcare reform, she says, is certainly not a panacea for reining in costs, but “just the beginning.”
Concerns over healthcare costs, in fact, could be among the factors driving what Robert Zipper, MD, FHM, regional chief medical officer for Tacoma, Wash.-based Sound Physicians, sees as continuing consolidation among hospitalist groups. “By that, I mean that either groups are swallowed up by the hospital in which they work or they become part of a regional or national company,” he says. Sound Physicians, with about 400 hospitalists in seven states, offers health insurance policies that don’t vary by state, easing its negotiations.
Eyes on the Bottom Line
What about the dreaded “T” word? Dr. Zipper says he hasn’t heard that many concerns about the potential tax increase just yet. “I think it’s not an issue to hospitalists in a broad sense yet,” he says, “but if you look at the salary trajectory and where things have been over the past 10 years, it’s pretty easy to predict that it will be an issue for single-income [households] where the hospitalist is the sole breadwinner.”
The 2010 State of Hospital Medicine report, which surveyed 4,211 nonacademic hospitalists from 443 groups, found a median annual income of $215,000. Calculating trends from past income surveys is difficult due to very different respondent populations, but many hospitalists are clearly near or above the $200,000 threshold for individuals and near the $250,000 threshold for families already, even before considering spousal income. The survey, for example, found median salaries of about $235,700 in the 13 states that make up the Southern region.
Even if higher-earning hospitalists are subjected to a higher tax rate next year—if the current rates expire, a climb of 4.6 percentage points, to 39.6% from 35%—not all of them are necessarily opposed to it. Political polling on the issue isn’t broken down by specific professions, but a number of blogs have pointed to a Quinnipiac University poll conducted back in March that suggested nearly two-thirds of upper-income Americans were prepared to sacrifice some of their take-home pay to help reduce the deficit. In that poll (www.quinnipiac.edu/x1295.xml?ReleaseID=1438), some 64% of respondents earning more than $250,000 agreed that raising income taxes on themselves and other households making more than $250,000 should be a main part of any government approach to the deficit.
If taxes and insurance premiums are more immediate concerns, some HM observers are eyeing longer trends that could impact the pre-tax pay of the profession. Most hospitalists still earn far less than their specialist counterparts, of course, but increasing demand for hospitalist services has helped fuel a rise in median salaries. Last year, some observers predicted that after an impressive run, annual pay would plateau or even fall, given the current economic uncertainty, tightening profit margins, and assessment that many hospitals run HM programs at a loss.3 And in the current RVU-driven system, the “What have you done for me lately?” mentality can indeed make it difficult for hospitalists to demonstrate a solid return on the investment.
The State of Hospital Medicine report suggests that respondent HM groups have been subsidized by an average of $111,486 per physician FTE (median is $98,253), with the highest numbers in hospital-owned practices. But many experts see a window of a few years in which new healthcare delivery and payment experiments will be trotted out, whether modeled on a bundled system, accountable-care organization (ACO), or other vehicle. Under these models, payment incentives to physicians—and to hospitalists especially—could be fundamentally restructured to better reflect their true contributions as the emphasis on quality and efficiency increases.
Within the next three years, Murer says, hospitalists need to continue to infiltrate inpatient medical services, demonstrate their worth, and show the cost efficiencies that arise from their profession. “I think they’ve got a window of three years to really decide how much of that [inpatient physician] market they will retain,” she says.
Despite the current volatility, both Murer and Dr. Zipper agree that hospitalists are well positioned to take advantage of the coming changes in the healthcare delivery system. But to seize the opportunity, hospitalists must clearly demonstrate the necessity of their services in the emerging models of care and claim an early seat at the table where decisions will be made about how the pot of money is dispersed. Doing so could help resolve one of the most important financial considerations of all: job security. TH
Bryn Nelson is a freelance medical writer based in Seattle.
References
- Adamy J. Health insurers plan hikes. Wall Street Journal website. Available at: http://online.wsj.com/article/SB10001424052748703720004575478200948908976.html. Accessed Sept. 21, 2010.
- Cutter S. Look you in the eye. The White House website. Available at: www.whitehouse.gov/blog/2010/09/23/look-you-eye. Accessed Sept. 27, 2010.
- How will the economy affect hospitalist salaries? MedPage Today website. Available at: www.kevinmd .com/blog/2009/03/how-will-economy-affect-hospitalist-2.html. Accessed Sept. 27, 2010.
When Congress returns for a likely lame-duck session after the midterm elections, the biggest battle might be fought over whether to extend the 2001 and 2003 tax cuts to everyone or only to those earning less than $200,000 annually ($250,000 for families). And depending on the makeup of the 112th Congress, which will be seated in January, Republicans might try to make good on a campaign pledge to repeal all or most of the healthcare reform legislation.
The expected flashpoints are being teased endlessly with media sound bites featuring phrases that most of us love to hate: higher taxes, spiraling medical bills, soaring insurance premiums. Insurance companies already are blaming a spike in premiums on the healthcare legislation, claiming that new provisions and mandates are forcing them to further hike their rates.
Closer to home, the high-profile frays could put hospitalists in the awkward position of supporting political positions that sock them in the wallet. After all, doctors are workers and healthcare consumers, too. So what impact could higher taxes and higher insurance premiums really have? Let’s start with health insurance.
Insurance Cost Increases
Signed into law in March, the Affordable Care Act includes tax credits for small businesses to help defray the costs of health insurance coverage. But in 2013, it also raises the threshold for medical expense deductions for most taxpayers, to 10% from 7.5% of adjusted gross income. In other words, families can claim tax deductions only after having spent 10% or more of their adjusted gross income on medical bills. For families with hefty medical bills, that 2.5% difference could translate into a significant shortfall.
CMS was able to negotiate with insurers to achieve a slight drop in Medicare Advantage premiums, but many individual states have had less luck in preventing rate increases from private insurers who blame their higher premiums on new mandates. The Wall Street Journal has documented rate increases of 18% in states like Wisconsin and North Carolina—about 9% of which insurance company officials pinned on the new law.1 Such increases are hardly inevitable, however. The Obama administration’s White House blog, for instance, has cited the example of North Carolina Blue Cross and Blue Shield, which announced Sept. 20 that it will provide $156 million in refunds to more than 215,000 customers after state regulators found an overcharge that should be reversed due to new rules in the reform law.2 WellPoint will similarly refund $20 million to its health insurance customers in Colorado.2
The requested premium increases and identified overcharges have contributed to plenty of finger-pointing among insurers, state regulators, and the Obama administration, which has assailed insurers for using the law as a convenient excuse to raise rates. Highlighting the unease of many consumers, however, is the verdict that the proposed increases—if approved—would hit small businesses and individuals hardest.
According to the State of Hospital Medicine: 2010 Report Based on 2009 Data, released in September by SHM and the Medical Group Management Association, participating hospitalist groups have a median of 10 physician full-time equivalents. Roughly 25% of respondents are in physician-owned groups, while 14% are in a management services organization (MSO) or physician practice management company (PPMC). Smaller HM groups wouldn’t be alone in feeling the pinch, but they might need to consider some serious comparison-shopping to avoid costly premium increases.
Cherilyn Murer, president and CEO of Joliet, Ill.-based Murer Consultants Inc., has worked with healthcare systems and providers in 42 states, but even her company has not been immune to having to contend with rising premiums. “Our managing partner just renegotiated our health benefits [premiums] that were supposed to have gone up 30% by our previous carrier,” Murer says. “Through protracted negotiations and diligence, he was able to find a plan that did not increase our costs, and retained pretty much the same benefits.”
For at least the next three to five years, Murer says, niche firms will need to be diligent about shopping around and managing their expenses in a volatile insurance marketplace. Healthcare reform, she says, is certainly not a panacea for reining in costs, but “just the beginning.”
Concerns over healthcare costs, in fact, could be among the factors driving what Robert Zipper, MD, FHM, regional chief medical officer for Tacoma, Wash.-based Sound Physicians, sees as continuing consolidation among hospitalist groups. “By that, I mean that either groups are swallowed up by the hospital in which they work or they become part of a regional or national company,” he says. Sound Physicians, with about 400 hospitalists in seven states, offers health insurance policies that don’t vary by state, easing its negotiations.
Eyes on the Bottom Line
What about the dreaded “T” word? Dr. Zipper says he hasn’t heard that many concerns about the potential tax increase just yet. “I think it’s not an issue to hospitalists in a broad sense yet,” he says, “but if you look at the salary trajectory and where things have been over the past 10 years, it’s pretty easy to predict that it will be an issue for single-income [households] where the hospitalist is the sole breadwinner.”
The 2010 State of Hospital Medicine report, which surveyed 4,211 nonacademic hospitalists from 443 groups, found a median annual income of $215,000. Calculating trends from past income surveys is difficult due to very different respondent populations, but many hospitalists are clearly near or above the $200,000 threshold for individuals and near the $250,000 threshold for families already, even before considering spousal income. The survey, for example, found median salaries of about $235,700 in the 13 states that make up the Southern region.
Even if higher-earning hospitalists are subjected to a higher tax rate next year—if the current rates expire, a climb of 4.6 percentage points, to 39.6% from 35%—not all of them are necessarily opposed to it. Political polling on the issue isn’t broken down by specific professions, but a number of blogs have pointed to a Quinnipiac University poll conducted back in March that suggested nearly two-thirds of upper-income Americans were prepared to sacrifice some of their take-home pay to help reduce the deficit. In that poll (www.quinnipiac.edu/x1295.xml?ReleaseID=1438), some 64% of respondents earning more than $250,000 agreed that raising income taxes on themselves and other households making more than $250,000 should be a main part of any government approach to the deficit.
If taxes and insurance premiums are more immediate concerns, some HM observers are eyeing longer trends that could impact the pre-tax pay of the profession. Most hospitalists still earn far less than their specialist counterparts, of course, but increasing demand for hospitalist services has helped fuel a rise in median salaries. Last year, some observers predicted that after an impressive run, annual pay would plateau or even fall, given the current economic uncertainty, tightening profit margins, and assessment that many hospitals run HM programs at a loss.3 And in the current RVU-driven system, the “What have you done for me lately?” mentality can indeed make it difficult for hospitalists to demonstrate a solid return on the investment.
The State of Hospital Medicine report suggests that respondent HM groups have been subsidized by an average of $111,486 per physician FTE (median is $98,253), with the highest numbers in hospital-owned practices. But many experts see a window of a few years in which new healthcare delivery and payment experiments will be trotted out, whether modeled on a bundled system, accountable-care organization (ACO), or other vehicle. Under these models, payment incentives to physicians—and to hospitalists especially—could be fundamentally restructured to better reflect their true contributions as the emphasis on quality and efficiency increases.
Within the next three years, Murer says, hospitalists need to continue to infiltrate inpatient medical services, demonstrate their worth, and show the cost efficiencies that arise from their profession. “I think they’ve got a window of three years to really decide how much of that [inpatient physician] market they will retain,” she says.
Despite the current volatility, both Murer and Dr. Zipper agree that hospitalists are well positioned to take advantage of the coming changes in the healthcare delivery system. But to seize the opportunity, hospitalists must clearly demonstrate the necessity of their services in the emerging models of care and claim an early seat at the table where decisions will be made about how the pot of money is dispersed. Doing so could help resolve one of the most important financial considerations of all: job security. TH
Bryn Nelson is a freelance medical writer based in Seattle.
References
- Adamy J. Health insurers plan hikes. Wall Street Journal website. Available at: http://online.wsj.com/article/SB10001424052748703720004575478200948908976.html. Accessed Sept. 21, 2010.
- Cutter S. Look you in the eye. The White House website. Available at: www.whitehouse.gov/blog/2010/09/23/look-you-eye. Accessed Sept. 27, 2010.
- How will the economy affect hospitalist salaries? MedPage Today website. Available at: www.kevinmd .com/blog/2009/03/how-will-economy-affect-hospitalist-2.html. Accessed Sept. 27, 2010.
Concurrent Care
Let’s examine a documentation case for hospitalists providing daily care: A 65-year-old male patient is admitted with a left hip fracture. The patient also has hypertension and Type 2 diabetes, which might complicate his care. The orthopedic surgeon manages the patient’s perioperative course for the fracture while the hospitalist provides daily post-op care for hypertension and diabetes.
A common scenario is the hospitalist will provide concurrent care, along with a varying number of specialists, depending on the complexity of the patient’s presenting problems and existing comorbidities. Payors define concurrent care as more than one physician providing care to the same patient on the same date, or during the same hospitalization. Payors often consider two key principles before reimbursing concurrent care:
- Does the patient’s condition warrant more than one physician? and
- Are the services provided by each physician reasonable and necessary?1
When more than one medical condition exists and each physician actively treats the condition related to their expertise, each physician can demonstrate medical necessity. As in the above example, the orthopedic surgeon cares for the patient’s fracture while the hospitalist oversees diabetes and hypertension management. Claim submission follows the same logic. Report each subsequent hospital care code (99231-99233) with the corresponding diagnosis each physician primarily manages (i.e., orthopedic surgeon: 9923x with 820.8; hospitalist: 9923x with 250.00, 401.1).
When each physician assigns a different primary diagnosis code to the visit code, each is more likely to receive payment. Because each of these physicians are in different specialties and different provider groups, most payors do not require modifier 25 (separately identifiable E/M service on the same day as a procedure or other service) appended to the visit code. However, some managed-care payors require each physician to append modifier 25 to the concurrent E/M visit code (i.e., 99232-25) despite claim submission under different tax identification numbers.
Unfortunately, the physicians might not realize this until a claim rejection has been issued. Furthermore, payors might want to see the proof before rendering payment. In other words, they pay the first claim received and deny any subsequent claim in order to confirm medical necessity of the concurrent visit. Appeal denied such claims rejections with supporting documentation that distinguishes each physician visit, if possible. This assists the payors in understanding each physician’s contribution to care.
Reasons for Denial
Concurrent care services are more easily distinguished when separate diagnoses are reported with each service. Conversely, payors are likely to deny services that are hard to differentiate. Furthermore, payors frequently deny concurrent care services for the following reasons:
- Services exceed normal frequency or duration for a given condition without documented circumstances requiring additional care; or
- Services by one physician duplicate or overlap those of another provider without recognizable distinction.2
For example, a hospitalist might be involved in the post-op care of patients with fractures and no other identifiable chronic or acute conditions or complications. In these cases, the hospitalist’s continued involvement might constitute a facility policy (e.g., quality of care, risk reduction, etc.) rather than active clinical management. Claim submission could erroneously occur with each physician reporting 9923x for 820.8. Payors deny medically unnecessary services, or request refunds for inappropriate payments.
Hospitalists might attempt to negotiate other terms with the facility to account for the unpaid time and effort directed toward these types of cases.
Group Practice
Physicians in the same group practice with the same specialty designation must report, and are paid, as a single physician. Multiple visits to the same patient can occur on the same day by members of the same group (e.g., hospitalist A evaluates the patient in the morning, and hospitalist B reviews test results and the resulting course of treatment in the afternoon). However, only one subsequent hospital care service can be reported for the day.
The hospitalists should select the visit level representative of the combined services and submit one appropriately determined code (e.g., 99233), thereby capturing the medically necessary efforts of each physician. To complicate matters, the hospitalists must determine which name to report on the claim: the physician who provided the first encounter, or the physician who provided the most extensive or best-documented encounter.
Tracking productivity for these cases proves challenging. Some practices develop an internal accounting system and credit each physician for their medically necessary efforts (a labor-intensive task for administrators and physicians). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Medicare Benefit Policy Manual: Concurrent Care. Chapter 15, Section 30.E. CMS website. Available at: www.cms.gov/manuals/Downloads/bp102c15.pdf. Accessed July 9, 2010.
- Medicare Claims Processing Manual: Physicians in Group Practice. Chapter 12, Section 30.6.5. CMS website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed July 9, 2010.
- Pohlig, C. Daily care conundrums. The Hospitalist website. Available at: www.the-hospitalist.org/details/article/188735/Daily_Care_Conundrums_.html. Accessed July 9, 2010.
- Medicare Claims Processing Manual: Hospital Visits Same Day But by Different Physicians. Chapter 12, Section 30.6.9.C. CMS website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed July 9, 2010.
- Abraham M, Beebe M, Dalton J, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2010:15.
Let’s examine a documentation case for hospitalists providing daily care: A 65-year-old male patient is admitted with a left hip fracture. The patient also has hypertension and Type 2 diabetes, which might complicate his care. The orthopedic surgeon manages the patient’s perioperative course for the fracture while the hospitalist provides daily post-op care for hypertension and diabetes.
A common scenario is the hospitalist will provide concurrent care, along with a varying number of specialists, depending on the complexity of the patient’s presenting problems and existing comorbidities. Payors define concurrent care as more than one physician providing care to the same patient on the same date, or during the same hospitalization. Payors often consider two key principles before reimbursing concurrent care:
- Does the patient’s condition warrant more than one physician? and
- Are the services provided by each physician reasonable and necessary?1
When more than one medical condition exists and each physician actively treats the condition related to their expertise, each physician can demonstrate medical necessity. As in the above example, the orthopedic surgeon cares for the patient’s fracture while the hospitalist oversees diabetes and hypertension management. Claim submission follows the same logic. Report each subsequent hospital care code (99231-99233) with the corresponding diagnosis each physician primarily manages (i.e., orthopedic surgeon: 9923x with 820.8; hospitalist: 9923x with 250.00, 401.1).
When each physician assigns a different primary diagnosis code to the visit code, each is more likely to receive payment. Because each of these physicians are in different specialties and different provider groups, most payors do not require modifier 25 (separately identifiable E/M service on the same day as a procedure or other service) appended to the visit code. However, some managed-care payors require each physician to append modifier 25 to the concurrent E/M visit code (i.e., 99232-25) despite claim submission under different tax identification numbers.
Unfortunately, the physicians might not realize this until a claim rejection has been issued. Furthermore, payors might want to see the proof before rendering payment. In other words, they pay the first claim received and deny any subsequent claim in order to confirm medical necessity of the concurrent visit. Appeal denied such claims rejections with supporting documentation that distinguishes each physician visit, if possible. This assists the payors in understanding each physician’s contribution to care.
Reasons for Denial
Concurrent care services are more easily distinguished when separate diagnoses are reported with each service. Conversely, payors are likely to deny services that are hard to differentiate. Furthermore, payors frequently deny concurrent care services for the following reasons:
- Services exceed normal frequency or duration for a given condition without documented circumstances requiring additional care; or
- Services by one physician duplicate or overlap those of another provider without recognizable distinction.2
For example, a hospitalist might be involved in the post-op care of patients with fractures and no other identifiable chronic or acute conditions or complications. In these cases, the hospitalist’s continued involvement might constitute a facility policy (e.g., quality of care, risk reduction, etc.) rather than active clinical management. Claim submission could erroneously occur with each physician reporting 9923x for 820.8. Payors deny medically unnecessary services, or request refunds for inappropriate payments.
Hospitalists might attempt to negotiate other terms with the facility to account for the unpaid time and effort directed toward these types of cases.
Group Practice
Physicians in the same group practice with the same specialty designation must report, and are paid, as a single physician. Multiple visits to the same patient can occur on the same day by members of the same group (e.g., hospitalist A evaluates the patient in the morning, and hospitalist B reviews test results and the resulting course of treatment in the afternoon). However, only one subsequent hospital care service can be reported for the day.
The hospitalists should select the visit level representative of the combined services and submit one appropriately determined code (e.g., 99233), thereby capturing the medically necessary efforts of each physician. To complicate matters, the hospitalists must determine which name to report on the claim: the physician who provided the first encounter, or the physician who provided the most extensive or best-documented encounter.
Tracking productivity for these cases proves challenging. Some practices develop an internal accounting system and credit each physician for their medically necessary efforts (a labor-intensive task for administrators and physicians). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Medicare Benefit Policy Manual: Concurrent Care. Chapter 15, Section 30.E. CMS website. Available at: www.cms.gov/manuals/Downloads/bp102c15.pdf. Accessed July 9, 2010.
- Medicare Claims Processing Manual: Physicians in Group Practice. Chapter 12, Section 30.6.5. CMS website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed July 9, 2010.
- Pohlig, C. Daily care conundrums. The Hospitalist website. Available at: www.the-hospitalist.org/details/article/188735/Daily_Care_Conundrums_.html. Accessed July 9, 2010.
- Medicare Claims Processing Manual: Hospital Visits Same Day But by Different Physicians. Chapter 12, Section 30.6.9.C. CMS website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed July 9, 2010.
- Abraham M, Beebe M, Dalton J, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2010:15.
Let’s examine a documentation case for hospitalists providing daily care: A 65-year-old male patient is admitted with a left hip fracture. The patient also has hypertension and Type 2 diabetes, which might complicate his care. The orthopedic surgeon manages the patient’s perioperative course for the fracture while the hospitalist provides daily post-op care for hypertension and diabetes.
A common scenario is the hospitalist will provide concurrent care, along with a varying number of specialists, depending on the complexity of the patient’s presenting problems and existing comorbidities. Payors define concurrent care as more than one physician providing care to the same patient on the same date, or during the same hospitalization. Payors often consider two key principles before reimbursing concurrent care:
- Does the patient’s condition warrant more than one physician? and
- Are the services provided by each physician reasonable and necessary?1
When more than one medical condition exists and each physician actively treats the condition related to their expertise, each physician can demonstrate medical necessity. As in the above example, the orthopedic surgeon cares for the patient’s fracture while the hospitalist oversees diabetes and hypertension management. Claim submission follows the same logic. Report each subsequent hospital care code (99231-99233) with the corresponding diagnosis each physician primarily manages (i.e., orthopedic surgeon: 9923x with 820.8; hospitalist: 9923x with 250.00, 401.1).
When each physician assigns a different primary diagnosis code to the visit code, each is more likely to receive payment. Because each of these physicians are in different specialties and different provider groups, most payors do not require modifier 25 (separately identifiable E/M service on the same day as a procedure or other service) appended to the visit code. However, some managed-care payors require each physician to append modifier 25 to the concurrent E/M visit code (i.e., 99232-25) despite claim submission under different tax identification numbers.
Unfortunately, the physicians might not realize this until a claim rejection has been issued. Furthermore, payors might want to see the proof before rendering payment. In other words, they pay the first claim received and deny any subsequent claim in order to confirm medical necessity of the concurrent visit. Appeal denied such claims rejections with supporting documentation that distinguishes each physician visit, if possible. This assists the payors in understanding each physician’s contribution to care.
Reasons for Denial
Concurrent care services are more easily distinguished when separate diagnoses are reported with each service. Conversely, payors are likely to deny services that are hard to differentiate. Furthermore, payors frequently deny concurrent care services for the following reasons:
- Services exceed normal frequency or duration for a given condition without documented circumstances requiring additional care; or
- Services by one physician duplicate or overlap those of another provider without recognizable distinction.2
For example, a hospitalist might be involved in the post-op care of patients with fractures and no other identifiable chronic or acute conditions or complications. In these cases, the hospitalist’s continued involvement might constitute a facility policy (e.g., quality of care, risk reduction, etc.) rather than active clinical management. Claim submission could erroneously occur with each physician reporting 9923x for 820.8. Payors deny medically unnecessary services, or request refunds for inappropriate payments.
Hospitalists might attempt to negotiate other terms with the facility to account for the unpaid time and effort directed toward these types of cases.
Group Practice
Physicians in the same group practice with the same specialty designation must report, and are paid, as a single physician. Multiple visits to the same patient can occur on the same day by members of the same group (e.g., hospitalist A evaluates the patient in the morning, and hospitalist B reviews test results and the resulting course of treatment in the afternoon). However, only one subsequent hospital care service can be reported for the day.
The hospitalists should select the visit level representative of the combined services and submit one appropriately determined code (e.g., 99233), thereby capturing the medically necessary efforts of each physician. To complicate matters, the hospitalists must determine which name to report on the claim: the physician who provided the first encounter, or the physician who provided the most extensive or best-documented encounter.
Tracking productivity for these cases proves challenging. Some practices develop an internal accounting system and credit each physician for their medically necessary efforts (a labor-intensive task for administrators and physicians). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Medicare Benefit Policy Manual: Concurrent Care. Chapter 15, Section 30.E. CMS website. Available at: www.cms.gov/manuals/Downloads/bp102c15.pdf. Accessed July 9, 2010.
- Medicare Claims Processing Manual: Physicians in Group Practice. Chapter 12, Section 30.6.5. CMS website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed July 9, 2010.
- Pohlig, C. Daily care conundrums. The Hospitalist website. Available at: www.the-hospitalist.org/details/article/188735/Daily_Care_Conundrums_.html. Accessed July 9, 2010.
- Medicare Claims Processing Manual: Hospital Visits Same Day But by Different Physicians. Chapter 12, Section 30.6.9.C. CMS website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed July 9, 2010.
- Abraham M, Beebe M, Dalton J, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2010:15.
Malpractice Chronicle
Reprinted with permission from Medical Malpractice Verdicts, Settlements and Experts, Lewis Laska, Editor, (800) 298-6288.
Hemorrhoid or Cancerous Mass?
In May 2000, a 35-year-old woman gave birth to her second child at a Massachusetts hospital. She sustained a second-degree vaginal tear. During repair of the tear, a large hemorrhoid was visualized by the physician, who instructed a nurse-midwife to have the hemorrhoid evaluated, with a possible gastroenterology consult to rule out a mass.
The next day, the patient was examined by another doctor and another nurse-midwife. It was agreed by the clinicians and the patient that she would defer a gastroenterology consult and follow up with her primary care provider in a few weeks. When she saw her primary care physician three weeks after the delivery, her examination was negative for hemorrhoids, and the patient was instructed to call back if she had a recurrence. Since she experienced no recurrence, she did not follow up with the primary care provider. Over the next four years, the woman received medical care from her gynecologist but at no time underwent a rectal examination.
In February 2005, the plaintiff went to her primary care physician with complaints of rectal bleeding during bowel movements. No external hemorrhoids were found, but a rectal mass was present.
The woman was referred for a gastroenterology consult and biopsy, through which an intramucosal adenocarcinoma was identified. Chest CT revealed a nodule in the patient’s right lower lung lobe, which was suspicious for metastasis. Abdominal CT and positron emission tomography showed likely liver metastases. A liver biopsy performed in mid-March 2005 confirmed adenocarcinoma of the liver.
The patient received chemotherapy and chemoradiation. In September 2005, she underwent an abdominal perineal resection, left lateral segmentectomy of the liver, cholecystectomy, and appendectomy. By the time of settlement, she was doing well and was no longer receiving treatment for cancer.
The plaintiff claimed that her primary care provider should have followed up on the initial rectal finding, which would have led to an earlier diagnosis and treatment of her cancer.
The defendant argued that the lesion noted at the time of the delivery was a simple hemorrhoid, which resolved after delivery. The defendant also contended that the absence of any symptoms for nearly five years indicated that the cancer could not have been present in 2000. The defendant further claimed that the cancer found at diagnosis and the hemorrhoid that was originally noted were in different locations.
A $1 million settlement was reached.
Diagnosis, Treatment Delayed by Suspicion of Abuse
A seven-week-old boy was taken to the pediatrician by his parents. They said he had been crying inconsolably all day, with decreased food intake, limited urinary output, and bruising. The pediatrician suspected meningitis and sent them to the emergency department (ED) at a children’s hospital in Georgia. The intake staff and emergency physician, Dr. C., were informed that the pediatrician suspected meningitis.
A blood culture, chest x-ray, and ultrasound were performed. The infant’s white blood cell count was normal, and his condition improved during the ED stay. He was afebrile, and the defendants maintained that he had no symptoms that would indicate meningitis.
Bruising was found on the child’s rib cage and one knee, and an ultrasound indicated that the bruising was due to trauma; thus, a mandatory report was filed with the authorities, and the physician made a diagnosis of abuse. The parents were forced to leave the child at the hospital and were told not to return because the child was in the hospital’s custody. The child was transferred out of the ED and the care of Dr. C.
Subsequently, the blood culture was reported as positive and showed gram-positive cocci. This report was returned about 26 hours after the child’s symptoms had begun at home. The report on the blood culture was relayed to one of the doctors, but no orders were given to evaluate the child. The child was not given antibiotics to treat the meningitis until the following day. The police dropped the report of abuse shortly after the investigation into the allegations began.
The child experienced a severe seizure with catastrophic brain damage, which the plaintiffs attributed to a delay in diagnosis and treatment for meningitis. The child was unable to roll over by age 2 years and would require extensive care and treatment for the remainder of his life.
The defendants claimed that the actions taken were proper and that there was no reason to suspect infection because the child did not have a fever and his condition improved while he was in the ED.
According to a published report, a defense verdict was returned.
Failure to Recognize Adrenal Crisis
A 26-year-old Massachusetts woman had a history of type 2 diabetes and newly diagnosed adrenal insufficiency, for which she was taking hydrocortisone. She presented to an emergency department (ED) complaining of cold symptoms and abdominal pain.
She was evaluated by an emergency physician, who noted moderate pain and tachycardia, a heart rate of 100 beats/min, and tenderness in the woman’s sinuses, neck, and left lower quadrant of the abdomen. Laboratory test results included a positive pregnancy test and an abnormal potassium level. Subsequent cardiac monitoring revealed atrial tachycardia. ECG revealed a rapid heart rate and diffuse, nonspecific abnormalities.
A second physician assumed care of the patient and treated her with potassium chloride, IV fluids of dextrose and sodium chloride, and ondansetron for nausea and vomiting. Neither physician had noted the medications being taken by the patient.
She returned to the ED two days after her initial admission with complaints of vomiting, chest pain, and abdominal pain. Her vital signs were abnormal. A different emergency physician evaluated the patient and noted tachycardia and vitiligo (consistent with adrenal insufficiency). Laboratory study results revealed metabolic abnormalities, and the woman was diagnosed with pregnancy-related nausea and vomiting and poorly controlled diabetes.
Over the following week, five additional physicians examined and/or treated the woman, one of whom was told that she had been taking hydrocortisone but stopped when she learned she was pregnant. The woman’s condition worsened, involving blindness, severe metabolic acidosis, and respiratory arrest. The family agreed to a transfer to a tertiary care facility.
At this time, during conversations between the patient’s family and her physicians, the physicians were made aware that she was taking hydrocortisone for adrenal insufficiency. The physicians immediately began treatment with methylprednisolone. The patient’s neurologic status continued to decline, however, and CT revealed findings consistent with a diffuse anoxic injury. She was placed on comfort measures only, and she died nine days after her original ED admission.
The plaintiffs alleged negligence in the ED staff’s failure to take a thorough medical history. The defendant claimed that the decedent’s symptoms were not consistent with adrenal crisis and that she had not fully disclosed her use of hydrocortisone.
According to a published account, a $3 million settlement was reached.
High-Dose Morphine After DNR Order
At age 79, a woman with chronic obstructive pulmonary disease was admitted to a hospital in Georgia with breathing difficulties. During her hospitalization, the patient experienced respiratory arrest. A code was called and the defendant, the critical care pulmonologist on duty, responded.
Once bag ventilation was implemented, the patient started to breathe and the code was stopped. After the incident, the attending physician, who had also responded to the code, initiated a discussion with the patient’s daughter about the plan of treatment and the patient’s prognosis. At the conclusion of this conversation, the patient’s daughter agreed to a “do-not-resuscitate” order. The attending physician ordered 2 mg morphine as needed to keep the patient comfortable.
Five minutes later, the pulmonologist overrode this order and ordered 20 mg morphine pushed. Shortly after the medication was administered, the patient, who was talking to her daughter and granddaughter, lost consciousness. She died about three hours later without regaining consciousness.
The plaintiff claimed that the decedent’s condition improved during her hospitalization until the night before her arrest, when she was not given her scheduled breathing treatments. The plaintiff also alleged that the defendant pulmonologist was negligent in ordering the 20-mg dose of morphine and that the hospital nurse was negligent in administering such a high dose.
The defendants claimed that no negligence occurred and that the woman would have died sooner than three hours after the morphine was administered, if that indeed was the cause of her death.
According to a published account, a $3 million verdict was returned.
Reprinted with permission from Medical Malpractice Verdicts, Settlements and Experts, Lewis Laska, Editor, (800) 298-6288.
Hemorrhoid or Cancerous Mass?
In May 2000, a 35-year-old woman gave birth to her second child at a Massachusetts hospital. She sustained a second-degree vaginal tear. During repair of the tear, a large hemorrhoid was visualized by the physician, who instructed a nurse-midwife to have the hemorrhoid evaluated, with a possible gastroenterology consult to rule out a mass.
The next day, the patient was examined by another doctor and another nurse-midwife. It was agreed by the clinicians and the patient that she would defer a gastroenterology consult and follow up with her primary care provider in a few weeks. When she saw her primary care physician three weeks after the delivery, her examination was negative for hemorrhoids, and the patient was instructed to call back if she had a recurrence. Since she experienced no recurrence, she did not follow up with the primary care provider. Over the next four years, the woman received medical care from her gynecologist but at no time underwent a rectal examination.
In February 2005, the plaintiff went to her primary care physician with complaints of rectal bleeding during bowel movements. No external hemorrhoids were found, but a rectal mass was present.
The woman was referred for a gastroenterology consult and biopsy, through which an intramucosal adenocarcinoma was identified. Chest CT revealed a nodule in the patient’s right lower lung lobe, which was suspicious for metastasis. Abdominal CT and positron emission tomography showed likely liver metastases. A liver biopsy performed in mid-March 2005 confirmed adenocarcinoma of the liver.
The patient received chemotherapy and chemoradiation. In September 2005, she underwent an abdominal perineal resection, left lateral segmentectomy of the liver, cholecystectomy, and appendectomy. By the time of settlement, she was doing well and was no longer receiving treatment for cancer.
The plaintiff claimed that her primary care provider should have followed up on the initial rectal finding, which would have led to an earlier diagnosis and treatment of her cancer.
The defendant argued that the lesion noted at the time of the delivery was a simple hemorrhoid, which resolved after delivery. The defendant also contended that the absence of any symptoms for nearly five years indicated that the cancer could not have been present in 2000. The defendant further claimed that the cancer found at diagnosis and the hemorrhoid that was originally noted were in different locations.
A $1 million settlement was reached.
Diagnosis, Treatment Delayed by Suspicion of Abuse
A seven-week-old boy was taken to the pediatrician by his parents. They said he had been crying inconsolably all day, with decreased food intake, limited urinary output, and bruising. The pediatrician suspected meningitis and sent them to the emergency department (ED) at a children’s hospital in Georgia. The intake staff and emergency physician, Dr. C., were informed that the pediatrician suspected meningitis.
A blood culture, chest x-ray, and ultrasound were performed. The infant’s white blood cell count was normal, and his condition improved during the ED stay. He was afebrile, and the defendants maintained that he had no symptoms that would indicate meningitis.
Bruising was found on the child’s rib cage and one knee, and an ultrasound indicated that the bruising was due to trauma; thus, a mandatory report was filed with the authorities, and the physician made a diagnosis of abuse. The parents were forced to leave the child at the hospital and were told not to return because the child was in the hospital’s custody. The child was transferred out of the ED and the care of Dr. C.
Subsequently, the blood culture was reported as positive and showed gram-positive cocci. This report was returned about 26 hours after the child’s symptoms had begun at home. The report on the blood culture was relayed to one of the doctors, but no orders were given to evaluate the child. The child was not given antibiotics to treat the meningitis until the following day. The police dropped the report of abuse shortly after the investigation into the allegations began.
The child experienced a severe seizure with catastrophic brain damage, which the plaintiffs attributed to a delay in diagnosis and treatment for meningitis. The child was unable to roll over by age 2 years and would require extensive care and treatment for the remainder of his life.
The defendants claimed that the actions taken were proper and that there was no reason to suspect infection because the child did not have a fever and his condition improved while he was in the ED.
According to a published report, a defense verdict was returned.
Failure to Recognize Adrenal Crisis
A 26-year-old Massachusetts woman had a history of type 2 diabetes and newly diagnosed adrenal insufficiency, for which she was taking hydrocortisone. She presented to an emergency department (ED) complaining of cold symptoms and abdominal pain.
She was evaluated by an emergency physician, who noted moderate pain and tachycardia, a heart rate of 100 beats/min, and tenderness in the woman’s sinuses, neck, and left lower quadrant of the abdomen. Laboratory test results included a positive pregnancy test and an abnormal potassium level. Subsequent cardiac monitoring revealed atrial tachycardia. ECG revealed a rapid heart rate and diffuse, nonspecific abnormalities.
A second physician assumed care of the patient and treated her with potassium chloride, IV fluids of dextrose and sodium chloride, and ondansetron for nausea and vomiting. Neither physician had noted the medications being taken by the patient.
She returned to the ED two days after her initial admission with complaints of vomiting, chest pain, and abdominal pain. Her vital signs were abnormal. A different emergency physician evaluated the patient and noted tachycardia and vitiligo (consistent with adrenal insufficiency). Laboratory study results revealed metabolic abnormalities, and the woman was diagnosed with pregnancy-related nausea and vomiting and poorly controlled diabetes.
Over the following week, five additional physicians examined and/or treated the woman, one of whom was told that she had been taking hydrocortisone but stopped when she learned she was pregnant. The woman’s condition worsened, involving blindness, severe metabolic acidosis, and respiratory arrest. The family agreed to a transfer to a tertiary care facility.
At this time, during conversations between the patient’s family and her physicians, the physicians were made aware that she was taking hydrocortisone for adrenal insufficiency. The physicians immediately began treatment with methylprednisolone. The patient’s neurologic status continued to decline, however, and CT revealed findings consistent with a diffuse anoxic injury. She was placed on comfort measures only, and she died nine days after her original ED admission.
The plaintiffs alleged negligence in the ED staff’s failure to take a thorough medical history. The defendant claimed that the decedent’s symptoms were not consistent with adrenal crisis and that she had not fully disclosed her use of hydrocortisone.
According to a published account, a $3 million settlement was reached.
High-Dose Morphine After DNR Order
At age 79, a woman with chronic obstructive pulmonary disease was admitted to a hospital in Georgia with breathing difficulties. During her hospitalization, the patient experienced respiratory arrest. A code was called and the defendant, the critical care pulmonologist on duty, responded.
Once bag ventilation was implemented, the patient started to breathe and the code was stopped. After the incident, the attending physician, who had also responded to the code, initiated a discussion with the patient’s daughter about the plan of treatment and the patient’s prognosis. At the conclusion of this conversation, the patient’s daughter agreed to a “do-not-resuscitate” order. The attending physician ordered 2 mg morphine as needed to keep the patient comfortable.
Five minutes later, the pulmonologist overrode this order and ordered 20 mg morphine pushed. Shortly after the medication was administered, the patient, who was talking to her daughter and granddaughter, lost consciousness. She died about three hours later without regaining consciousness.
The plaintiff claimed that the decedent’s condition improved during her hospitalization until the night before her arrest, when she was not given her scheduled breathing treatments. The plaintiff also alleged that the defendant pulmonologist was negligent in ordering the 20-mg dose of morphine and that the hospital nurse was negligent in administering such a high dose.
The defendants claimed that no negligence occurred and that the woman would have died sooner than three hours after the morphine was administered, if that indeed was the cause of her death.
According to a published account, a $3 million verdict was returned.
Reprinted with permission from Medical Malpractice Verdicts, Settlements and Experts, Lewis Laska, Editor, (800) 298-6288.
Hemorrhoid or Cancerous Mass?
In May 2000, a 35-year-old woman gave birth to her second child at a Massachusetts hospital. She sustained a second-degree vaginal tear. During repair of the tear, a large hemorrhoid was visualized by the physician, who instructed a nurse-midwife to have the hemorrhoid evaluated, with a possible gastroenterology consult to rule out a mass.
The next day, the patient was examined by another doctor and another nurse-midwife. It was agreed by the clinicians and the patient that she would defer a gastroenterology consult and follow up with her primary care provider in a few weeks. When she saw her primary care physician three weeks after the delivery, her examination was negative for hemorrhoids, and the patient was instructed to call back if she had a recurrence. Since she experienced no recurrence, she did not follow up with the primary care provider. Over the next four years, the woman received medical care from her gynecologist but at no time underwent a rectal examination.
In February 2005, the plaintiff went to her primary care physician with complaints of rectal bleeding during bowel movements. No external hemorrhoids were found, but a rectal mass was present.
The woman was referred for a gastroenterology consult and biopsy, through which an intramucosal adenocarcinoma was identified. Chest CT revealed a nodule in the patient’s right lower lung lobe, which was suspicious for metastasis. Abdominal CT and positron emission tomography showed likely liver metastases. A liver biopsy performed in mid-March 2005 confirmed adenocarcinoma of the liver.
The patient received chemotherapy and chemoradiation. In September 2005, she underwent an abdominal perineal resection, left lateral segmentectomy of the liver, cholecystectomy, and appendectomy. By the time of settlement, she was doing well and was no longer receiving treatment for cancer.
The plaintiff claimed that her primary care provider should have followed up on the initial rectal finding, which would have led to an earlier diagnosis and treatment of her cancer.
The defendant argued that the lesion noted at the time of the delivery was a simple hemorrhoid, which resolved after delivery. The defendant also contended that the absence of any symptoms for nearly five years indicated that the cancer could not have been present in 2000. The defendant further claimed that the cancer found at diagnosis and the hemorrhoid that was originally noted were in different locations.
A $1 million settlement was reached.
Diagnosis, Treatment Delayed by Suspicion of Abuse
A seven-week-old boy was taken to the pediatrician by his parents. They said he had been crying inconsolably all day, with decreased food intake, limited urinary output, and bruising. The pediatrician suspected meningitis and sent them to the emergency department (ED) at a children’s hospital in Georgia. The intake staff and emergency physician, Dr. C., were informed that the pediatrician suspected meningitis.
A blood culture, chest x-ray, and ultrasound were performed. The infant’s white blood cell count was normal, and his condition improved during the ED stay. He was afebrile, and the defendants maintained that he had no symptoms that would indicate meningitis.
Bruising was found on the child’s rib cage and one knee, and an ultrasound indicated that the bruising was due to trauma; thus, a mandatory report was filed with the authorities, and the physician made a diagnosis of abuse. The parents were forced to leave the child at the hospital and were told not to return because the child was in the hospital’s custody. The child was transferred out of the ED and the care of Dr. C.
Subsequently, the blood culture was reported as positive and showed gram-positive cocci. This report was returned about 26 hours after the child’s symptoms had begun at home. The report on the blood culture was relayed to one of the doctors, but no orders were given to evaluate the child. The child was not given antibiotics to treat the meningitis until the following day. The police dropped the report of abuse shortly after the investigation into the allegations began.
The child experienced a severe seizure with catastrophic brain damage, which the plaintiffs attributed to a delay in diagnosis and treatment for meningitis. The child was unable to roll over by age 2 years and would require extensive care and treatment for the remainder of his life.
The defendants claimed that the actions taken were proper and that there was no reason to suspect infection because the child did not have a fever and his condition improved while he was in the ED.
According to a published report, a defense verdict was returned.
Failure to Recognize Adrenal Crisis
A 26-year-old Massachusetts woman had a history of type 2 diabetes and newly diagnosed adrenal insufficiency, for which she was taking hydrocortisone. She presented to an emergency department (ED) complaining of cold symptoms and abdominal pain.
She was evaluated by an emergency physician, who noted moderate pain and tachycardia, a heart rate of 100 beats/min, and tenderness in the woman’s sinuses, neck, and left lower quadrant of the abdomen. Laboratory test results included a positive pregnancy test and an abnormal potassium level. Subsequent cardiac monitoring revealed atrial tachycardia. ECG revealed a rapid heart rate and diffuse, nonspecific abnormalities.
A second physician assumed care of the patient and treated her with potassium chloride, IV fluids of dextrose and sodium chloride, and ondansetron for nausea and vomiting. Neither physician had noted the medications being taken by the patient.
She returned to the ED two days after her initial admission with complaints of vomiting, chest pain, and abdominal pain. Her vital signs were abnormal. A different emergency physician evaluated the patient and noted tachycardia and vitiligo (consistent with adrenal insufficiency). Laboratory study results revealed metabolic abnormalities, and the woman was diagnosed with pregnancy-related nausea and vomiting and poorly controlled diabetes.
Over the following week, five additional physicians examined and/or treated the woman, one of whom was told that she had been taking hydrocortisone but stopped when she learned she was pregnant. The woman’s condition worsened, involving blindness, severe metabolic acidosis, and respiratory arrest. The family agreed to a transfer to a tertiary care facility.
At this time, during conversations between the patient’s family and her physicians, the physicians were made aware that she was taking hydrocortisone for adrenal insufficiency. The physicians immediately began treatment with methylprednisolone. The patient’s neurologic status continued to decline, however, and CT revealed findings consistent with a diffuse anoxic injury. She was placed on comfort measures only, and she died nine days after her original ED admission.
The plaintiffs alleged negligence in the ED staff’s failure to take a thorough medical history. The defendant claimed that the decedent’s symptoms were not consistent with adrenal crisis and that she had not fully disclosed her use of hydrocortisone.
According to a published account, a $3 million settlement was reached.
High-Dose Morphine After DNR Order
At age 79, a woman with chronic obstructive pulmonary disease was admitted to a hospital in Georgia with breathing difficulties. During her hospitalization, the patient experienced respiratory arrest. A code was called and the defendant, the critical care pulmonologist on duty, responded.
Once bag ventilation was implemented, the patient started to breathe and the code was stopped. After the incident, the attending physician, who had also responded to the code, initiated a discussion with the patient’s daughter about the plan of treatment and the patient’s prognosis. At the conclusion of this conversation, the patient’s daughter agreed to a “do-not-resuscitate” order. The attending physician ordered 2 mg morphine as needed to keep the patient comfortable.
Five minutes later, the pulmonologist overrode this order and ordered 20 mg morphine pushed. Shortly after the medication was administered, the patient, who was talking to her daughter and granddaughter, lost consciousness. She died about three hours later without regaining consciousness.
The plaintiff claimed that the decedent’s condition improved during her hospitalization until the night before her arrest, when she was not given her scheduled breathing treatments. The plaintiff also alleged that the defendant pulmonologist was negligent in ordering the 20-mg dose of morphine and that the hospital nurse was negligent in administering such a high dose.
The defendants claimed that no negligence occurred and that the woman would have died sooner than three hours after the morphine was administered, if that indeed was the cause of her death.
According to a published account, a $3 million verdict was returned.
