User login
From the Editors: The Clinical Congress: Something for everyone
In this issue of ACS Surgery News, you will see articles highlighting the program of the ACS Clinical Congress that took place in Washington, D.C., in mid-October.
This year’s theme, “The Best Surgical Education, All in One Place,” could not be more apt to represent the ACS Clinical Congress. And yet, the Clinical Congress is much, much more than an educational exercise for those who are able to attend. No matter what your age, whether it was your first time attending or, like me, your 41st, there is something at this meeting for everyone. Although the focus is on education, and the meeting does have a dizzying array of educational options, it is also an opportunity to see old friends and make new ones, connect with people with whom you share problems, work with colleagues to devise strategies to solve challenges, put faces with names you’ve only read about, participate in service and governance of our profession, and be inspired by the thoughtful leaders of our profession.
As the years pass by
I remember vividly my earliest ACS Clinical Congress, as a surgical resident at University of California, San Francisco, in October, 1975. It was 3 months into my research year and therefore I was able to attend the congress, which was in San Francisco that year. As one of the few women physicians in attendance at that meeting, I was in strange territory. I watched the opening ceremony with surgical leaders standing on stage, and I thought how homogeneous the group appeared: undeniably brilliant and accomplished, but all white-haired, white, and male. Fast-forward 41 years, and the surgical leaders who appeared on that stage at this year’s meeting were every bit as brilliant and accomplished, but the leaders are now younger and more diverse than in years past. The diversity in the college was evident as I walked the halls of the convention center where Fellows, residents, and guest physicians paused in their rushed transit from Hall D to Ballroom C to converse with an old or new friend.
The program itself has also become far more varied over the years. There is a continued emphasis on basic and clinical research in the scientific forum and scientific sessions. Postgraduate courses still impart new knowledge and skills, and state-of-the-art clinical practice is still taught in panel sessions. But the program now includes numerous nonclinical topics that are of crucial importance to present and future surgeons, such as ethics, end-of-life care, practice management, burnout, deciphering CMS regulations, and global health and humanitarian surgical outreach, to mention only a few. The named lectures continue to feature outstanding speakers who are often inspiring, and even sometimes provocative, and they are well worth attending. I would not want to have missed Past-President Carlos Pellegrini’s profoundly thoughtful John J. Conley Ethics and Philosophy Lecture on “TRUST: The Keystone of the Patient Physician Relationship,” for example.
Even the topics at the scientific forum have expanded over the years. In addition to the traditional basic science and clinical topics, five separate sessions this year on surgical education and on quality, safety, and outcomes attest to the increasing significance of these areas, unheard of when I was a resident. The important topics of ethics, geriatric surgery and palliative care, and global surgery/humanitarian outreach have gained sufficient interest that they now warrant their own sessions. There is something on the program to satisfy everyone’s interests. The forum presentations also provide us aging surgeons a chance to see the impressive contributions that our surgical progeny are making to the future of our profession. That, in itself, is encouraging and comforting.
Serving the profession
Many surgeons attend the congress in part to participate in committees of the ACS or other surgical organizations that meet during the congress to conserve time away from their “real jobs” as surgeons. These meetings offer attendees a chance to “give back” as well as to develop leadership in their profession. Participation in these committees can lead eventually to service on the Board of Governors or Regents, which offer opportunities to help shape the future of our organization and profession.
Profound positive changes in our profession have occurred through the leadership of the college. And some of these initiatives are reflected in the standing committees such as the Women in Surgery Committee, the Committee on Diversity Issues, and the Committee on Health Care Disparities, to name only three. Long-standing groups such as the Committee on Trauma (COT) have evolved greatly through the years and have raised the quality of trauma care and education in trauma across the United States and also globally.
Social and networking opportunities
The educational opportunities are unparalleled at the Clinical Congress, but the opportunities to connect with fellow surgeons is a close second. The chance to meet old friends from residency, recruit new partners for one’s practice, or be introduced to someone whom you have only known through postings on the ACS Communities are all invaluable aspects of the week. An email or telephone conversation is no substitute for these enriching face-to-face activities. And there is no substitute for this unique opportunity to create and extend your network of friends, colleagues, and allies. The Clinical Congress is often the beginning of relationships and professional connections that can last a lifetime.
Perhaps my enjoyment of the ACS Clinical Congress stems in part from how familiar it is after all these years and the comfort of being a member of this amazing organization. But my enthusiasm also comes from seeing how increasingly important and relevant the college has become to all of us – student, resident, Fellow, or guest. For surgeons, there is no substitute for the American College of Surgeons and there is indeed something for everyone at the Clinical Congress.
Dr. Deveney is professor of surgery and vice chair of education in the department of surgery, Oregon Health & Science University, Portland. She is the Coeditor of ACS Surgery News.
In this issue of ACS Surgery News, you will see articles highlighting the program of the ACS Clinical Congress that took place in Washington, D.C., in mid-October.
This year’s theme, “The Best Surgical Education, All in One Place,” could not be more apt to represent the ACS Clinical Congress. And yet, the Clinical Congress is much, much more than an educational exercise for those who are able to attend. No matter what your age, whether it was your first time attending or, like me, your 41st, there is something at this meeting for everyone. Although the focus is on education, and the meeting does have a dizzying array of educational options, it is also an opportunity to see old friends and make new ones, connect with people with whom you share problems, work with colleagues to devise strategies to solve challenges, put faces with names you’ve only read about, participate in service and governance of our profession, and be inspired by the thoughtful leaders of our profession.
As the years pass by
I remember vividly my earliest ACS Clinical Congress, as a surgical resident at University of California, San Francisco, in October, 1975. It was 3 months into my research year and therefore I was able to attend the congress, which was in San Francisco that year. As one of the few women physicians in attendance at that meeting, I was in strange territory. I watched the opening ceremony with surgical leaders standing on stage, and I thought how homogeneous the group appeared: undeniably brilliant and accomplished, but all white-haired, white, and male. Fast-forward 41 years, and the surgical leaders who appeared on that stage at this year’s meeting were every bit as brilliant and accomplished, but the leaders are now younger and more diverse than in years past. The diversity in the college was evident as I walked the halls of the convention center where Fellows, residents, and guest physicians paused in their rushed transit from Hall D to Ballroom C to converse with an old or new friend.
The program itself has also become far more varied over the years. There is a continued emphasis on basic and clinical research in the scientific forum and scientific sessions. Postgraduate courses still impart new knowledge and skills, and state-of-the-art clinical practice is still taught in panel sessions. But the program now includes numerous nonclinical topics that are of crucial importance to present and future surgeons, such as ethics, end-of-life care, practice management, burnout, deciphering CMS regulations, and global health and humanitarian surgical outreach, to mention only a few. The named lectures continue to feature outstanding speakers who are often inspiring, and even sometimes provocative, and they are well worth attending. I would not want to have missed Past-President Carlos Pellegrini’s profoundly thoughtful John J. Conley Ethics and Philosophy Lecture on “TRUST: The Keystone of the Patient Physician Relationship,” for example.
Even the topics at the scientific forum have expanded over the years. In addition to the traditional basic science and clinical topics, five separate sessions this year on surgical education and on quality, safety, and outcomes attest to the increasing significance of these areas, unheard of when I was a resident. The important topics of ethics, geriatric surgery and palliative care, and global surgery/humanitarian outreach have gained sufficient interest that they now warrant their own sessions. There is something on the program to satisfy everyone’s interests. The forum presentations also provide us aging surgeons a chance to see the impressive contributions that our surgical progeny are making to the future of our profession. That, in itself, is encouraging and comforting.
Serving the profession
Many surgeons attend the congress in part to participate in committees of the ACS or other surgical organizations that meet during the congress to conserve time away from their “real jobs” as surgeons. These meetings offer attendees a chance to “give back” as well as to develop leadership in their profession. Participation in these committees can lead eventually to service on the Board of Governors or Regents, which offer opportunities to help shape the future of our organization and profession.
Profound positive changes in our profession have occurred through the leadership of the college. And some of these initiatives are reflected in the standing committees such as the Women in Surgery Committee, the Committee on Diversity Issues, and the Committee on Health Care Disparities, to name only three. Long-standing groups such as the Committee on Trauma (COT) have evolved greatly through the years and have raised the quality of trauma care and education in trauma across the United States and also globally.
Social and networking opportunities
The educational opportunities are unparalleled at the Clinical Congress, but the opportunities to connect with fellow surgeons is a close second. The chance to meet old friends from residency, recruit new partners for one’s practice, or be introduced to someone whom you have only known through postings on the ACS Communities are all invaluable aspects of the week. An email or telephone conversation is no substitute for these enriching face-to-face activities. And there is no substitute for this unique opportunity to create and extend your network of friends, colleagues, and allies. The Clinical Congress is often the beginning of relationships and professional connections that can last a lifetime.
Perhaps my enjoyment of the ACS Clinical Congress stems in part from how familiar it is after all these years and the comfort of being a member of this amazing organization. But my enthusiasm also comes from seeing how increasingly important and relevant the college has become to all of us – student, resident, Fellow, or guest. For surgeons, there is no substitute for the American College of Surgeons and there is indeed something for everyone at the Clinical Congress.
Dr. Deveney is professor of surgery and vice chair of education in the department of surgery, Oregon Health & Science University, Portland. She is the Coeditor of ACS Surgery News.
In this issue of ACS Surgery News, you will see articles highlighting the program of the ACS Clinical Congress that took place in Washington, D.C., in mid-October.
This year’s theme, “The Best Surgical Education, All in One Place,” could not be more apt to represent the ACS Clinical Congress. And yet, the Clinical Congress is much, much more than an educational exercise for those who are able to attend. No matter what your age, whether it was your first time attending or, like me, your 41st, there is something at this meeting for everyone. Although the focus is on education, and the meeting does have a dizzying array of educational options, it is also an opportunity to see old friends and make new ones, connect with people with whom you share problems, work with colleagues to devise strategies to solve challenges, put faces with names you’ve only read about, participate in service and governance of our profession, and be inspired by the thoughtful leaders of our profession.
As the years pass by
I remember vividly my earliest ACS Clinical Congress, as a surgical resident at University of California, San Francisco, in October, 1975. It was 3 months into my research year and therefore I was able to attend the congress, which was in San Francisco that year. As one of the few women physicians in attendance at that meeting, I was in strange territory. I watched the opening ceremony with surgical leaders standing on stage, and I thought how homogeneous the group appeared: undeniably brilliant and accomplished, but all white-haired, white, and male. Fast-forward 41 years, and the surgical leaders who appeared on that stage at this year’s meeting were every bit as brilliant and accomplished, but the leaders are now younger and more diverse than in years past. The diversity in the college was evident as I walked the halls of the convention center where Fellows, residents, and guest physicians paused in their rushed transit from Hall D to Ballroom C to converse with an old or new friend.
The program itself has also become far more varied over the years. There is a continued emphasis on basic and clinical research in the scientific forum and scientific sessions. Postgraduate courses still impart new knowledge and skills, and state-of-the-art clinical practice is still taught in panel sessions. But the program now includes numerous nonclinical topics that are of crucial importance to present and future surgeons, such as ethics, end-of-life care, practice management, burnout, deciphering CMS regulations, and global health and humanitarian surgical outreach, to mention only a few. The named lectures continue to feature outstanding speakers who are often inspiring, and even sometimes provocative, and they are well worth attending. I would not want to have missed Past-President Carlos Pellegrini’s profoundly thoughtful John J. Conley Ethics and Philosophy Lecture on “TRUST: The Keystone of the Patient Physician Relationship,” for example.
Even the topics at the scientific forum have expanded over the years. In addition to the traditional basic science and clinical topics, five separate sessions this year on surgical education and on quality, safety, and outcomes attest to the increasing significance of these areas, unheard of when I was a resident. The important topics of ethics, geriatric surgery and palliative care, and global surgery/humanitarian outreach have gained sufficient interest that they now warrant their own sessions. There is something on the program to satisfy everyone’s interests. The forum presentations also provide us aging surgeons a chance to see the impressive contributions that our surgical progeny are making to the future of our profession. That, in itself, is encouraging and comforting.
Serving the profession
Many surgeons attend the congress in part to participate in committees of the ACS or other surgical organizations that meet during the congress to conserve time away from their “real jobs” as surgeons. These meetings offer attendees a chance to “give back” as well as to develop leadership in their profession. Participation in these committees can lead eventually to service on the Board of Governors or Regents, which offer opportunities to help shape the future of our organization and profession.
Profound positive changes in our profession have occurred through the leadership of the college. And some of these initiatives are reflected in the standing committees such as the Women in Surgery Committee, the Committee on Diversity Issues, and the Committee on Health Care Disparities, to name only three. Long-standing groups such as the Committee on Trauma (COT) have evolved greatly through the years and have raised the quality of trauma care and education in trauma across the United States and also globally.
Social and networking opportunities
The educational opportunities are unparalleled at the Clinical Congress, but the opportunities to connect with fellow surgeons is a close second. The chance to meet old friends from residency, recruit new partners for one’s practice, or be introduced to someone whom you have only known through postings on the ACS Communities are all invaluable aspects of the week. An email or telephone conversation is no substitute for these enriching face-to-face activities. And there is no substitute for this unique opportunity to create and extend your network of friends, colleagues, and allies. The Clinical Congress is often the beginning of relationships and professional connections that can last a lifetime.
Perhaps my enjoyment of the ACS Clinical Congress stems in part from how familiar it is after all these years and the comfort of being a member of this amazing organization. But my enthusiasm also comes from seeing how increasingly important and relevant the college has become to all of us – student, resident, Fellow, or guest. For surgeons, there is no substitute for the American College of Surgeons and there is indeed something for everyone at the Clinical Congress.
Dr. Deveney is professor of surgery and vice chair of education in the department of surgery, Oregon Health & Science University, Portland. She is the Coeditor of ACS Surgery News.
SVS (Specialty of Vascular Surgery): Why, How, and When
The November 2016 issue of Annals of Vascular Surgery was devoted entirely to the history of the American Board of Vascular Surgery (ABVS) and the unsuccessful attempt to establish an independent specialty of Vascular Surgery. The manuscript is methodically detailed by founders of the ABVS, James Stanley, MD, and Frank Veith, MD, and supplemented by commentaries from past board members as well as thought leaders in vascular surgery. In an attempt to maintain neutrality, readers are also provided with many of the documents that were either supportive or contrary to the development of the ABVS. Most senior vascular surgeons will recall the intense discussion and sometimes acrimonious arguments that accompanied the progress of the Board and its failed attempt to be recognized by the American Board of Medical Specialties (ABMS).
Younger vascular surgeons may not realize that the ABVS was ever established. Some may not even realize that, until relatively recently, vascular surgeons were not able to claim board certification even if they had completed a fellowship. Accordingly, as an historical document detailing an important aspect of the evolution of our specialty, this edition of Annals of Vascular surgery is a must read.
Cogent arguments both for and against an independent specialty were made by the leaders of our specialty at the time that the ABVS was being developed. Unfortunately, this did not lead to a uniform policy but rather long-standing, rancorous, and bitter divisions that in all probability prevented the ABVS from being recognized by the ABMS. Despite this failure, the debate around this issue elevated the stature of vascular surgery when the American Board of Surgery conceded that vascular surgeons could now claim “Board certification in vascular surgery” without having to be trained in general surgery. However, all important modifications to the current design of vascular residency and fellowship programs still need to be decided by the American Board of Surgery and its associated Residency Review Committee for Surgery (RRC-S). Further, many hospital administrators subordinate vascular surgery by insisting that vascular surgeons' interests be controlled by general or cardiothoracic surgeons.
Most notably, this issue of Annals reignites fundamental questions that are at the heart of our existence as vascular surgeons. For example, has vascular surgery matured sufficiently to be considered a distinct specialty equivalent to other surgical specialties such as orthopedics, colorectal, urology, and otolaryngology surgery? If so, why did this not occur earlier? Does it warrant becoming independent from the American Board of Surgery such that only vascular surgeons will be in control of training programs, graduate education, and the practice of vascular surgery at universities, hospitals, and community practices? More significantly, why should these institutions, health agencies and the lay public care that there is a separate independent specialty – vascular surgery? The answer to these questions becomes apparent by an analysis of four historic elements that have changed since the ABVS was being formulated.
First, and perhaps most importantly, the argument for an ABVS occurred when vascular surgery had just entered the endovascular revolution. How difficult it must have been for those early vascular surgeons to realize that within a few years perhaps upward of 70%-80% of all procedures would not be performed in a standard operating room but rather an angiography suite, cath lab, or hybrid room? Could they envisage an era where abdominal aneurysms were treated not only without a laparotomy scar but even without a groin incision? That carotid endarterectomy may be replaced by a stent or that varicose veins would be abolished by an outpatient laser procedure? Without such foresight, general surgeons and even those early vascular surgeons had to believe that vascular surgery, as then practiced, required general surgery training.
A second historical reality that impacted the progress of the ABVS was the fragmentation of the governance of vascular surgeons on both a local and national level. Locally, university surgeons, assuming that vascular surgery was an intrinsic part of general surgery, may have been concerned that their leadership roles would be diminished if they were relegated to division heads rather than department chairs. Nationally, there existed three bodies representing vascular surgeons, each with its own leadership and motivations. These were the Society for Vascular Surgery (SVS), the North American chapter of the International Society for Cardiovascular Surgery (NA-ISCVS) which later changed its name to the American Association for Vascular Surgery (AAVS) and the Society for Clinical Vascular Surgery (SCVS).
The SVS at the time was predominantly an academic association with its primary goal being the annual meeting. The SCVS was a casual community of predominantly private practice surgeons. The AAVS was the most representative but it did not have the infrastructure to be a dominant force. Further, there also existed the Association of Program Directors in Vascular Surgery (APDVS). This division was compounded by the formation of the ABVS. Despite three polls of vascular surgeons, the majority of which supported an independent specialty, the divided leadership of these various organizations refused to abide by the voice of their respective memberships. The destructive internecine arguments that developed are detailed in the Annals manuscript, and this disunion of the vascular community and its leadership clearly hampered a collective identity.
Thirdly, the members of the ABVS argued that an independent specialty was necessary in order to train vascular surgeons in the evolving field of endovascular procedures. However, many established leaders balked at this proposal and resisted incorporating such training into their programs. Their refusal to assist in the education of endo-competent vascular surgeons and the development of an independent specialty allowed cardiologists and interventional radiologists to infiltrate the field. Now, the argument for an independent specialty of vascular surgery is not so much with general surgeons but rather with Cardiologists and interventional radiologists.
Fourth, the ABS at the time still considered itself an authoritative Board protective of an all-encompassing General surgery. Its leaders feared that separation of vascular surgery would lead to a stampede with other subspecialties such as pediatric and hand surgery clamoring for independence.
It is not surprising that there was little chance that the ABVS would succeed. However, much can be learned from this historical review that predicts a new initiative in today’s healthcare environment will likely be successful and benefit not only vascular surgeons but also their patients.
In this modern era the practice of vascular surgery involves multiple disciplines and various forms of therapy. As I have frequently claimed, vascular surgeons “operate, medicate, and dilate”. When so much of what vascular surgeons do is beyond the realm of open surgery, wouldn’t most agree that vascular surgery should not be controlled by a governing body, the ABS, whose primary motivation remains operative therapy?
On the other hand, the current ABS recognizes all its subspecialties are similarly morphing away from general surgery and so the ABS is evolving into a Federation of quasi-independent boards. Accordingly, it is likely to be less resistant to a fully independent vascular specialty board existing under its umbrella organization.
Concomitantly, heads of divisions of vascular surgery in universities as well as community practice hospitals can no longer rely on the largesse of chairpersons of general or cardiothoracic surgery since most will not have clinical vascular experience. Accordingly, these vascular surgeons must have complete autonomy with titles and positions elevated to chairs of a department rather than a division.
Vascular surgeons should also acknowledge that they can no longer claim total control of vascular patients. Vascular internists, cardiologists, interventional radiologists and even interventional nephrologists are all involved. An attempt to block further inroads will alienate these other specialties who in turn will attempt to deny us independent specialty designation. We need to work in conjunction, while remaining the only specialty that can offer all forms of therapy. By providing quality care vascular surgeons will gain the respect of government, insurance agencies and our patients and thus support for our independent status.
Although our small specialty of probably no more than 3000 active vascular surgeons is still represented by many differing societies, the SVS has now become the de facto union of vascular surgeons. It has the ability to bring together all factions and it has the finances, the manpower and the organizational structure to represent all vascular surgeons on the national and international level. As such it is already recognized by governmental and commercial agencies as the authoritative voice of vascular surgeons. The SVS, which has built a strong relationship with the APDVS, is also in a strong position to support and facilitate the undergraduate and postgraduate training of vascular surgeons and strengthen all aspects of an independent specialty of vascular surgery. Although there may still be disagreements about whether vascular surgery should be an independent specialty, the SVS should be the organization that serves as “convener” and ultimately implements the decision of the majority of vascular surgeons. It may be appropriate that the SVS Executive Committee authorizes one more survey of its membership to determine whether we continue to seek independent specialty designation and to approve it as a binding membership referendum.
The plusses and minuses should be carefully defined and much thought given to how the questions in the opinion poll are defined. Whatever the results, they should stand, and be implemented.
Finally, as a practicing vascular surgeon and not necessarily in my role as medical editor of the Vascular Specialist I would like to thank Dr. Timothy M. Sullivan and the Annals of Vascular Surgery for publication of this review and Drs. Stanley and Veith for providing us with the gift of historical perspective. Now our goal should not be to repeat history, but rather to learn from our past experiences. I am sure most will commend Drs. Stanley and Veith and all the other vascular surgeons who dedicated so much of their time in the pursuit of an independent vascular specialty.
However, we should not demonize those that held a contrary view, for most were a product of their times. As recent Nobel Laureate Bob Dylan has written, “The times they are a’changing,” and they are changing in our favor. ■
The November 2016 issue of Annals of Vascular Surgery was devoted entirely to the history of the American Board of Vascular Surgery (ABVS) and the unsuccessful attempt to establish an independent specialty of Vascular Surgery. The manuscript is methodically detailed by founders of the ABVS, James Stanley, MD, and Frank Veith, MD, and supplemented by commentaries from past board members as well as thought leaders in vascular surgery. In an attempt to maintain neutrality, readers are also provided with many of the documents that were either supportive or contrary to the development of the ABVS. Most senior vascular surgeons will recall the intense discussion and sometimes acrimonious arguments that accompanied the progress of the Board and its failed attempt to be recognized by the American Board of Medical Specialties (ABMS).
Younger vascular surgeons may not realize that the ABVS was ever established. Some may not even realize that, until relatively recently, vascular surgeons were not able to claim board certification even if they had completed a fellowship. Accordingly, as an historical document detailing an important aspect of the evolution of our specialty, this edition of Annals of Vascular surgery is a must read.
Cogent arguments both for and against an independent specialty were made by the leaders of our specialty at the time that the ABVS was being developed. Unfortunately, this did not lead to a uniform policy but rather long-standing, rancorous, and bitter divisions that in all probability prevented the ABVS from being recognized by the ABMS. Despite this failure, the debate around this issue elevated the stature of vascular surgery when the American Board of Surgery conceded that vascular surgeons could now claim “Board certification in vascular surgery” without having to be trained in general surgery. However, all important modifications to the current design of vascular residency and fellowship programs still need to be decided by the American Board of Surgery and its associated Residency Review Committee for Surgery (RRC-S). Further, many hospital administrators subordinate vascular surgery by insisting that vascular surgeons' interests be controlled by general or cardiothoracic surgeons.
Most notably, this issue of Annals reignites fundamental questions that are at the heart of our existence as vascular surgeons. For example, has vascular surgery matured sufficiently to be considered a distinct specialty equivalent to other surgical specialties such as orthopedics, colorectal, urology, and otolaryngology surgery? If so, why did this not occur earlier? Does it warrant becoming independent from the American Board of Surgery such that only vascular surgeons will be in control of training programs, graduate education, and the practice of vascular surgery at universities, hospitals, and community practices? More significantly, why should these institutions, health agencies and the lay public care that there is a separate independent specialty – vascular surgery? The answer to these questions becomes apparent by an analysis of four historic elements that have changed since the ABVS was being formulated.
First, and perhaps most importantly, the argument for an ABVS occurred when vascular surgery had just entered the endovascular revolution. How difficult it must have been for those early vascular surgeons to realize that within a few years perhaps upward of 70%-80% of all procedures would not be performed in a standard operating room but rather an angiography suite, cath lab, or hybrid room? Could they envisage an era where abdominal aneurysms were treated not only without a laparotomy scar but even without a groin incision? That carotid endarterectomy may be replaced by a stent or that varicose veins would be abolished by an outpatient laser procedure? Without such foresight, general surgeons and even those early vascular surgeons had to believe that vascular surgery, as then practiced, required general surgery training.
A second historical reality that impacted the progress of the ABVS was the fragmentation of the governance of vascular surgeons on both a local and national level. Locally, university surgeons, assuming that vascular surgery was an intrinsic part of general surgery, may have been concerned that their leadership roles would be diminished if they were relegated to division heads rather than department chairs. Nationally, there existed three bodies representing vascular surgeons, each with its own leadership and motivations. These were the Society for Vascular Surgery (SVS), the North American chapter of the International Society for Cardiovascular Surgery (NA-ISCVS) which later changed its name to the American Association for Vascular Surgery (AAVS) and the Society for Clinical Vascular Surgery (SCVS).
The SVS at the time was predominantly an academic association with its primary goal being the annual meeting. The SCVS was a casual community of predominantly private practice surgeons. The AAVS was the most representative but it did not have the infrastructure to be a dominant force. Further, there also existed the Association of Program Directors in Vascular Surgery (APDVS). This division was compounded by the formation of the ABVS. Despite three polls of vascular surgeons, the majority of which supported an independent specialty, the divided leadership of these various organizations refused to abide by the voice of their respective memberships. The destructive internecine arguments that developed are detailed in the Annals manuscript, and this disunion of the vascular community and its leadership clearly hampered a collective identity.
Thirdly, the members of the ABVS argued that an independent specialty was necessary in order to train vascular surgeons in the evolving field of endovascular procedures. However, many established leaders balked at this proposal and resisted incorporating such training into their programs. Their refusal to assist in the education of endo-competent vascular surgeons and the development of an independent specialty allowed cardiologists and interventional radiologists to infiltrate the field. Now, the argument for an independent specialty of vascular surgery is not so much with general surgeons but rather with Cardiologists and interventional radiologists.
Fourth, the ABS at the time still considered itself an authoritative Board protective of an all-encompassing General surgery. Its leaders feared that separation of vascular surgery would lead to a stampede with other subspecialties such as pediatric and hand surgery clamoring for independence.
It is not surprising that there was little chance that the ABVS would succeed. However, much can be learned from this historical review that predicts a new initiative in today’s healthcare environment will likely be successful and benefit not only vascular surgeons but also their patients.
In this modern era the practice of vascular surgery involves multiple disciplines and various forms of therapy. As I have frequently claimed, vascular surgeons “operate, medicate, and dilate”. When so much of what vascular surgeons do is beyond the realm of open surgery, wouldn’t most agree that vascular surgery should not be controlled by a governing body, the ABS, whose primary motivation remains operative therapy?
On the other hand, the current ABS recognizes all its subspecialties are similarly morphing away from general surgery and so the ABS is evolving into a Federation of quasi-independent boards. Accordingly, it is likely to be less resistant to a fully independent vascular specialty board existing under its umbrella organization.
Concomitantly, heads of divisions of vascular surgery in universities as well as community practice hospitals can no longer rely on the largesse of chairpersons of general or cardiothoracic surgery since most will not have clinical vascular experience. Accordingly, these vascular surgeons must have complete autonomy with titles and positions elevated to chairs of a department rather than a division.
Vascular surgeons should also acknowledge that they can no longer claim total control of vascular patients. Vascular internists, cardiologists, interventional radiologists and even interventional nephrologists are all involved. An attempt to block further inroads will alienate these other specialties who in turn will attempt to deny us independent specialty designation. We need to work in conjunction, while remaining the only specialty that can offer all forms of therapy. By providing quality care vascular surgeons will gain the respect of government, insurance agencies and our patients and thus support for our independent status.
Although our small specialty of probably no more than 3000 active vascular surgeons is still represented by many differing societies, the SVS has now become the de facto union of vascular surgeons. It has the ability to bring together all factions and it has the finances, the manpower and the organizational structure to represent all vascular surgeons on the national and international level. As such it is already recognized by governmental and commercial agencies as the authoritative voice of vascular surgeons. The SVS, which has built a strong relationship with the APDVS, is also in a strong position to support and facilitate the undergraduate and postgraduate training of vascular surgeons and strengthen all aspects of an independent specialty of vascular surgery. Although there may still be disagreements about whether vascular surgery should be an independent specialty, the SVS should be the organization that serves as “convener” and ultimately implements the decision of the majority of vascular surgeons. It may be appropriate that the SVS Executive Committee authorizes one more survey of its membership to determine whether we continue to seek independent specialty designation and to approve it as a binding membership referendum.
The plusses and minuses should be carefully defined and much thought given to how the questions in the opinion poll are defined. Whatever the results, they should stand, and be implemented.
Finally, as a practicing vascular surgeon and not necessarily in my role as medical editor of the Vascular Specialist I would like to thank Dr. Timothy M. Sullivan and the Annals of Vascular Surgery for publication of this review and Drs. Stanley and Veith for providing us with the gift of historical perspective. Now our goal should not be to repeat history, but rather to learn from our past experiences. I am sure most will commend Drs. Stanley and Veith and all the other vascular surgeons who dedicated so much of their time in the pursuit of an independent vascular specialty.
However, we should not demonize those that held a contrary view, for most were a product of their times. As recent Nobel Laureate Bob Dylan has written, “The times they are a’changing,” and they are changing in our favor. ■
The November 2016 issue of Annals of Vascular Surgery was devoted entirely to the history of the American Board of Vascular Surgery (ABVS) and the unsuccessful attempt to establish an independent specialty of Vascular Surgery. The manuscript is methodically detailed by founders of the ABVS, James Stanley, MD, and Frank Veith, MD, and supplemented by commentaries from past board members as well as thought leaders in vascular surgery. In an attempt to maintain neutrality, readers are also provided with many of the documents that were either supportive or contrary to the development of the ABVS. Most senior vascular surgeons will recall the intense discussion and sometimes acrimonious arguments that accompanied the progress of the Board and its failed attempt to be recognized by the American Board of Medical Specialties (ABMS).
Younger vascular surgeons may not realize that the ABVS was ever established. Some may not even realize that, until relatively recently, vascular surgeons were not able to claim board certification even if they had completed a fellowship. Accordingly, as an historical document detailing an important aspect of the evolution of our specialty, this edition of Annals of Vascular surgery is a must read.
Cogent arguments both for and against an independent specialty were made by the leaders of our specialty at the time that the ABVS was being developed. Unfortunately, this did not lead to a uniform policy but rather long-standing, rancorous, and bitter divisions that in all probability prevented the ABVS from being recognized by the ABMS. Despite this failure, the debate around this issue elevated the stature of vascular surgery when the American Board of Surgery conceded that vascular surgeons could now claim “Board certification in vascular surgery” without having to be trained in general surgery. However, all important modifications to the current design of vascular residency and fellowship programs still need to be decided by the American Board of Surgery and its associated Residency Review Committee for Surgery (RRC-S). Further, many hospital administrators subordinate vascular surgery by insisting that vascular surgeons' interests be controlled by general or cardiothoracic surgeons.
Most notably, this issue of Annals reignites fundamental questions that are at the heart of our existence as vascular surgeons. For example, has vascular surgery matured sufficiently to be considered a distinct specialty equivalent to other surgical specialties such as orthopedics, colorectal, urology, and otolaryngology surgery? If so, why did this not occur earlier? Does it warrant becoming independent from the American Board of Surgery such that only vascular surgeons will be in control of training programs, graduate education, and the practice of vascular surgery at universities, hospitals, and community practices? More significantly, why should these institutions, health agencies and the lay public care that there is a separate independent specialty – vascular surgery? The answer to these questions becomes apparent by an analysis of four historic elements that have changed since the ABVS was being formulated.
First, and perhaps most importantly, the argument for an ABVS occurred when vascular surgery had just entered the endovascular revolution. How difficult it must have been for those early vascular surgeons to realize that within a few years perhaps upward of 70%-80% of all procedures would not be performed in a standard operating room but rather an angiography suite, cath lab, or hybrid room? Could they envisage an era where abdominal aneurysms were treated not only without a laparotomy scar but even without a groin incision? That carotid endarterectomy may be replaced by a stent or that varicose veins would be abolished by an outpatient laser procedure? Without such foresight, general surgeons and even those early vascular surgeons had to believe that vascular surgery, as then practiced, required general surgery training.
A second historical reality that impacted the progress of the ABVS was the fragmentation of the governance of vascular surgeons on both a local and national level. Locally, university surgeons, assuming that vascular surgery was an intrinsic part of general surgery, may have been concerned that their leadership roles would be diminished if they were relegated to division heads rather than department chairs. Nationally, there existed three bodies representing vascular surgeons, each with its own leadership and motivations. These were the Society for Vascular Surgery (SVS), the North American chapter of the International Society for Cardiovascular Surgery (NA-ISCVS) which later changed its name to the American Association for Vascular Surgery (AAVS) and the Society for Clinical Vascular Surgery (SCVS).
The SVS at the time was predominantly an academic association with its primary goal being the annual meeting. The SCVS was a casual community of predominantly private practice surgeons. The AAVS was the most representative but it did not have the infrastructure to be a dominant force. Further, there also existed the Association of Program Directors in Vascular Surgery (APDVS). This division was compounded by the formation of the ABVS. Despite three polls of vascular surgeons, the majority of which supported an independent specialty, the divided leadership of these various organizations refused to abide by the voice of their respective memberships. The destructive internecine arguments that developed are detailed in the Annals manuscript, and this disunion of the vascular community and its leadership clearly hampered a collective identity.
Thirdly, the members of the ABVS argued that an independent specialty was necessary in order to train vascular surgeons in the evolving field of endovascular procedures. However, many established leaders balked at this proposal and resisted incorporating such training into their programs. Their refusal to assist in the education of endo-competent vascular surgeons and the development of an independent specialty allowed cardiologists and interventional radiologists to infiltrate the field. Now, the argument for an independent specialty of vascular surgery is not so much with general surgeons but rather with Cardiologists and interventional radiologists.
Fourth, the ABS at the time still considered itself an authoritative Board protective of an all-encompassing General surgery. Its leaders feared that separation of vascular surgery would lead to a stampede with other subspecialties such as pediatric and hand surgery clamoring for independence.
It is not surprising that there was little chance that the ABVS would succeed. However, much can be learned from this historical review that predicts a new initiative in today’s healthcare environment will likely be successful and benefit not only vascular surgeons but also their patients.
In this modern era the practice of vascular surgery involves multiple disciplines and various forms of therapy. As I have frequently claimed, vascular surgeons “operate, medicate, and dilate”. When so much of what vascular surgeons do is beyond the realm of open surgery, wouldn’t most agree that vascular surgery should not be controlled by a governing body, the ABS, whose primary motivation remains operative therapy?
On the other hand, the current ABS recognizes all its subspecialties are similarly morphing away from general surgery and so the ABS is evolving into a Federation of quasi-independent boards. Accordingly, it is likely to be less resistant to a fully independent vascular specialty board existing under its umbrella organization.
Concomitantly, heads of divisions of vascular surgery in universities as well as community practice hospitals can no longer rely on the largesse of chairpersons of general or cardiothoracic surgery since most will not have clinical vascular experience. Accordingly, these vascular surgeons must have complete autonomy with titles and positions elevated to chairs of a department rather than a division.
Vascular surgeons should also acknowledge that they can no longer claim total control of vascular patients. Vascular internists, cardiologists, interventional radiologists and even interventional nephrologists are all involved. An attempt to block further inroads will alienate these other specialties who in turn will attempt to deny us independent specialty designation. We need to work in conjunction, while remaining the only specialty that can offer all forms of therapy. By providing quality care vascular surgeons will gain the respect of government, insurance agencies and our patients and thus support for our independent status.
Although our small specialty of probably no more than 3000 active vascular surgeons is still represented by many differing societies, the SVS has now become the de facto union of vascular surgeons. It has the ability to bring together all factions and it has the finances, the manpower and the organizational structure to represent all vascular surgeons on the national and international level. As such it is already recognized by governmental and commercial agencies as the authoritative voice of vascular surgeons. The SVS, which has built a strong relationship with the APDVS, is also in a strong position to support and facilitate the undergraduate and postgraduate training of vascular surgeons and strengthen all aspects of an independent specialty of vascular surgery. Although there may still be disagreements about whether vascular surgery should be an independent specialty, the SVS should be the organization that serves as “convener” and ultimately implements the decision of the majority of vascular surgeons. It may be appropriate that the SVS Executive Committee authorizes one more survey of its membership to determine whether we continue to seek independent specialty designation and to approve it as a binding membership referendum.
The plusses and minuses should be carefully defined and much thought given to how the questions in the opinion poll are defined. Whatever the results, they should stand, and be implemented.
Finally, as a practicing vascular surgeon and not necessarily in my role as medical editor of the Vascular Specialist I would like to thank Dr. Timothy M. Sullivan and the Annals of Vascular Surgery for publication of this review and Drs. Stanley and Veith for providing us with the gift of historical perspective. Now our goal should not be to repeat history, but rather to learn from our past experiences. I am sure most will commend Drs. Stanley and Veith and all the other vascular surgeons who dedicated so much of their time in the pursuit of an independent vascular specialty.
However, we should not demonize those that held a contrary view, for most were a product of their times. As recent Nobel Laureate Bob Dylan has written, “The times they are a’changing,” and they are changing in our favor. ■
Hiding in clear sight: Complications of immunosuppressive therapies
In this issue of the Journal, Ota et al provide a clinical image and vignette of a woman with emphysematous cystitis and a psoas abscess. Genitourinary infections with Escherichia coli are well known to occasionally produce gas—especially, it seems, in people with diabetes. But I thought it valuable to publish these images to provide a reminder of this infectious complication, as well as to highlight the cloaking effect of pharmacologic immunosuppression.
The patient they describe was receiving corticosteroids for brain metastases and was thus likely receiving a high dose. She had experienced abdominal pain for 3 days before seeking medical attention, but the infectious process undoubtedly predated that. Despite receiving appropriate antibiotics for more than 3 weeks, she harbored an expanding psoas abscess that was heralded by fever after the antibiotics were discontinued. This scenario is of little surprise in an ill 69-year-old diabetic woman with metastatic cancer who was receiving high-dose corticosteroids. We have all been taught about and likely have witnessed the devastating effect of delayed diagnosis of abdominal infections in patients on high-dose steroids.
With the current explosion of new targeted therapies for systemic and organ-specific inflammatory diseases, it is hard to keep up with their names, not to mention their mechanisms of action and potential complications. Much attention has been given, highlighted by the requisite warnings in direct-to-consumer advertising, to the reactivation of tuberculosis, the occurrence of fungal infections, and the risk of malignancy in patients taking many of these drugs. The risk of cancer seems to have been overstated, at least for the anti-tumor necrosis factor (anti-TNF) agents, but there is no question that some new biologics carry a real risk of reactivating latent tuberculosis and even some viral infections. But I have seen a more common problem, one that is inadequately emphasized: the delayed diagnosis of deep-tissue infection due to a blunting of the signs of inflammation that would normally accompany the infection.
Anti-TNF therapies (eg, infliximab, etanercept, adalimumab) are being increasingly prescribed for the gamut of systemic and organ-specific inflammatory diseases, from sarcoidosis and rheumatoid arthritis to uveitis. I have no doubt that these agents suppress the inflammatory response in ways that can delay diagnosis. I have seen it happen in patients with diverticular abscess, bacterial pneumonia, epidural abscess, and bacterial septic arthritis, and I believe it is a more concerning clinical issue than any actual increase in the number of opportunistic infections.
The anti-interleukin 6 biologic agent tocilizumab, like the anti-TNF agents, not only blunts the inflammatory response and masks infection, but also seems to contribute to an increased occurrence of lower intestinal perforation.1 This is potentially important, as it seems likely that indications for this agent will be expanded to diseases other than rheumatoid arthritis.
Equal concern is likely warranted at the present time in patients receiving newer drugs such as Janus kinase (JAK) inhibitors and blockers of the interleukin 17 and 23 pathways, at least until more “real-life” patient experience is accumulated. Not all anti-inflammatory and immunosuppressive drugs have this dramatic blunting effect on findings of infection-associated inflammation (methotrexate seems not to), but we need to be wary and should perform extra-fastidious physical examinations followed by imaging studies when our patients complain of any localizing symptoms that are not readily and completely explained.
At the end of a tumultuous and divisive year, we at the Journal send to you, our readers, our heartfelt wishes for personal tranquility and for a universally peaceful and harmonious 2017.
- Strangfeld A, Richter A, Siegmund B, et al. Risk for lower intestinal perforations in patients with rheumatoid arthritis treated with tocilizumab in comparison to treatment with other biologic or conventional synthetic DMARDs. Ann Rheum Dis 2016 Jul 12. pii: annrheumdis-2016-209773. doi: 10.1136/annrheumdis-2016-209773. [Epub ahead of print]
In this issue of the Journal, Ota et al provide a clinical image and vignette of a woman with emphysematous cystitis and a psoas abscess. Genitourinary infections with Escherichia coli are well known to occasionally produce gas—especially, it seems, in people with diabetes. But I thought it valuable to publish these images to provide a reminder of this infectious complication, as well as to highlight the cloaking effect of pharmacologic immunosuppression.
The patient they describe was receiving corticosteroids for brain metastases and was thus likely receiving a high dose. She had experienced abdominal pain for 3 days before seeking medical attention, but the infectious process undoubtedly predated that. Despite receiving appropriate antibiotics for more than 3 weeks, she harbored an expanding psoas abscess that was heralded by fever after the antibiotics were discontinued. This scenario is of little surprise in an ill 69-year-old diabetic woman with metastatic cancer who was receiving high-dose corticosteroids. We have all been taught about and likely have witnessed the devastating effect of delayed diagnosis of abdominal infections in patients on high-dose steroids.
With the current explosion of new targeted therapies for systemic and organ-specific inflammatory diseases, it is hard to keep up with their names, not to mention their mechanisms of action and potential complications. Much attention has been given, highlighted by the requisite warnings in direct-to-consumer advertising, to the reactivation of tuberculosis, the occurrence of fungal infections, and the risk of malignancy in patients taking many of these drugs. The risk of cancer seems to have been overstated, at least for the anti-tumor necrosis factor (anti-TNF) agents, but there is no question that some new biologics carry a real risk of reactivating latent tuberculosis and even some viral infections. But I have seen a more common problem, one that is inadequately emphasized: the delayed diagnosis of deep-tissue infection due to a blunting of the signs of inflammation that would normally accompany the infection.
Anti-TNF therapies (eg, infliximab, etanercept, adalimumab) are being increasingly prescribed for the gamut of systemic and organ-specific inflammatory diseases, from sarcoidosis and rheumatoid arthritis to uveitis. I have no doubt that these agents suppress the inflammatory response in ways that can delay diagnosis. I have seen it happen in patients with diverticular abscess, bacterial pneumonia, epidural abscess, and bacterial septic arthritis, and I believe it is a more concerning clinical issue than any actual increase in the number of opportunistic infections.
The anti-interleukin 6 biologic agent tocilizumab, like the anti-TNF agents, not only blunts the inflammatory response and masks infection, but also seems to contribute to an increased occurrence of lower intestinal perforation.1 This is potentially important, as it seems likely that indications for this agent will be expanded to diseases other than rheumatoid arthritis.
Equal concern is likely warranted at the present time in patients receiving newer drugs such as Janus kinase (JAK) inhibitors and blockers of the interleukin 17 and 23 pathways, at least until more “real-life” patient experience is accumulated. Not all anti-inflammatory and immunosuppressive drugs have this dramatic blunting effect on findings of infection-associated inflammation (methotrexate seems not to), but we need to be wary and should perform extra-fastidious physical examinations followed by imaging studies when our patients complain of any localizing symptoms that are not readily and completely explained.
At the end of a tumultuous and divisive year, we at the Journal send to you, our readers, our heartfelt wishes for personal tranquility and for a universally peaceful and harmonious 2017.
In this issue of the Journal, Ota et al provide a clinical image and vignette of a woman with emphysematous cystitis and a psoas abscess. Genitourinary infections with Escherichia coli are well known to occasionally produce gas—especially, it seems, in people with diabetes. But I thought it valuable to publish these images to provide a reminder of this infectious complication, as well as to highlight the cloaking effect of pharmacologic immunosuppression.
The patient they describe was receiving corticosteroids for brain metastases and was thus likely receiving a high dose. She had experienced abdominal pain for 3 days before seeking medical attention, but the infectious process undoubtedly predated that. Despite receiving appropriate antibiotics for more than 3 weeks, she harbored an expanding psoas abscess that was heralded by fever after the antibiotics were discontinued. This scenario is of little surprise in an ill 69-year-old diabetic woman with metastatic cancer who was receiving high-dose corticosteroids. We have all been taught about and likely have witnessed the devastating effect of delayed diagnosis of abdominal infections in patients on high-dose steroids.
With the current explosion of new targeted therapies for systemic and organ-specific inflammatory diseases, it is hard to keep up with their names, not to mention their mechanisms of action and potential complications. Much attention has been given, highlighted by the requisite warnings in direct-to-consumer advertising, to the reactivation of tuberculosis, the occurrence of fungal infections, and the risk of malignancy in patients taking many of these drugs. The risk of cancer seems to have been overstated, at least for the anti-tumor necrosis factor (anti-TNF) agents, but there is no question that some new biologics carry a real risk of reactivating latent tuberculosis and even some viral infections. But I have seen a more common problem, one that is inadequately emphasized: the delayed diagnosis of deep-tissue infection due to a blunting of the signs of inflammation that would normally accompany the infection.
Anti-TNF therapies (eg, infliximab, etanercept, adalimumab) are being increasingly prescribed for the gamut of systemic and organ-specific inflammatory diseases, from sarcoidosis and rheumatoid arthritis to uveitis. I have no doubt that these agents suppress the inflammatory response in ways that can delay diagnosis. I have seen it happen in patients with diverticular abscess, bacterial pneumonia, epidural abscess, and bacterial septic arthritis, and I believe it is a more concerning clinical issue than any actual increase in the number of opportunistic infections.
The anti-interleukin 6 biologic agent tocilizumab, like the anti-TNF agents, not only blunts the inflammatory response and masks infection, but also seems to contribute to an increased occurrence of lower intestinal perforation.1 This is potentially important, as it seems likely that indications for this agent will be expanded to diseases other than rheumatoid arthritis.
Equal concern is likely warranted at the present time in patients receiving newer drugs such as Janus kinase (JAK) inhibitors and blockers of the interleukin 17 and 23 pathways, at least until more “real-life” patient experience is accumulated. Not all anti-inflammatory and immunosuppressive drugs have this dramatic blunting effect on findings of infection-associated inflammation (methotrexate seems not to), but we need to be wary and should perform extra-fastidious physical examinations followed by imaging studies when our patients complain of any localizing symptoms that are not readily and completely explained.
At the end of a tumultuous and divisive year, we at the Journal send to you, our readers, our heartfelt wishes for personal tranquility and for a universally peaceful and harmonious 2017.
- Strangfeld A, Richter A, Siegmund B, et al. Risk for lower intestinal perforations in patients with rheumatoid arthritis treated with tocilizumab in comparison to treatment with other biologic or conventional synthetic DMARDs. Ann Rheum Dis 2016 Jul 12. pii: annrheumdis-2016-209773. doi: 10.1136/annrheumdis-2016-209773. [Epub ahead of print]
- Strangfeld A, Richter A, Siegmund B, et al. Risk for lower intestinal perforations in patients with rheumatoid arthritis treated with tocilizumab in comparison to treatment with other biologic or conventional synthetic DMARDs. Ann Rheum Dis 2016 Jul 12. pii: annrheumdis-2016-209773. doi: 10.1136/annrheumdis-2016-209773. [Epub ahead of print]
Are you neuroprotecting your patients? 10 Adjunctive therapies to consider
Are you ‘neuroprotecting’ your patients?
Fortunately, many studies have demonstrated that in addition to controlling clinical symptoms, antidepressants, mood stabilizers, and atypical antipsychotics all have neuroprotective effects, including stimulating neurogenesis, preventing apoptosis, and increasing neurotrophins. However, more needs to be done to protect the brain’s gray and white matter and to prevent negative neuroplasticity and disconnectivity of brain circuits that often are documented in patients with psychotic and mood disorders.
There are, in fact, many off-label supplements with strong neuroprotective effects that psychiatrists can use as an adjunct to standard evidence-based pharmacotherapy. These agents generally are safe and well tolerated and often are sold over the counter, but are not covered by insurance. However, considering the disability that often is associated with schizophrenia, treatment-resistant depression, or psychotic mania, it is reasonable to consider using these agents, many of which are supported by studies published in peer-reviewed journals. However, because they are widely available and not proprietary and large, expensive registration trials such as the ones conducted by the pharmaceutical industry are not done, none is likely to receive FDA approval. Therefore, it is up to psychiatrists and nurse practitioners to use them judiciously in patients at risk for neurotoxicity.
Here are 10 agents with neuroprotective effects supported by published data that can be considered as add-on to the standard treatments in an effort to mitigate neurotoxicity and protect the brain from the destructive processes that accompany acute episodes of psychosis, mania, and depression.
Omega-3 fatty acids have been shown in several studies to help reduce psychopathology of psychosis, mania, or depression when used as an adjunctive agent.1 It appears to be more effective in the early stages of psychiatric disorders than in the chronic phase. It has anti-inflammatory, anti-oxidant, and anti-apoptotic effects; activates cell-signaling pathways; and prevents synaptic loss as well as neuronal and glial death.2
N-acetylcysteine (NAC) is a powerful antioxidant that increases glutathione, which is produced in the mitochondria. Schizophrenia is associated with mitochondrial dysfunction with low levels of glutathione, which puts the brain at risk for neurodegeneration caused by high levels of free radicals produced during psychosis. Adding NAC to antipsychotics during acute psychotic episodes—especially the first episode—can significantly reduce the neurotoxic effects of reactive oxygen and nitrogen species, also known as free radicals.3 In studies of traumatic brain injury in rats, NAC reduced brain edema, neuroinflammation, blood–brain barrier permeability, and apoptosis.4
Minocycline. This antibiotic has been studied extensively as an adjunctive treatment in schizophrenia and has proven to have several neuroprotective effects including anti-inflammatory, anti-oxidant, and anti-apoptotic, and reduces glutamate excitotoxicity.5 Several studies have documented its usefulness in acute psychotic episodes.
Vitamin D. Because of its vital role in neurodevelopment (neuronal differentiation, axonal connectivity), vitamin D deficiency has been associated with several psychiatric disorders including autism, schizophrenia, depression, and Alzheimer’s disease.6 Measure serum levels of vitamin D in patients with psychotic and mood disorders and implement supplementation if it is low—and it often is in these patients.
Nicotine is neuroprotective against glutamate excitotoxicity and it also inhibits apoptosis.7 However, it should never be administered via cigarettes, which are loaded with hundreds of toxic substances! It can be administered via patches or nicotine gum, which are usually used to help in smoking cessation. Nicotine also also can have a pro-cognitive effect.
Melatonin. Many people associate melatonin with sleep. However, it has multiple neuroprotective effects by being an antioxidant, protecting mitochondrial integrity, and modulating the immune system, as well as attenuating microglial activation, which triggers neuroinflammation and oxidative stress. It also protects against cellular senescence, which is due to inflammation and reactive oxygen species. Furthermore, melatonin is useful in ameliorating the metabolic syndrome, which is associated with neurotoxic effects on brain tissue caused by the pro-inflammatory effects of peri-omental fat in obesity.8 Adjunctive melatonin could be helpful in patients with schizophrenia or depression who suffer from metabolic syndrome.
Erythropoietin is a hormone produced by the kidneys to promote the formation of red blood cells. It is a potent neuroprotective cytokine that promotes neuronal survival via anti-apoptotic effects. It protects against glutamate and nitrous oxide toxicity9 and haloperidol-induced neuronal death.10 It is clinically used (since FDA approval in 1989) in severe anemia due to chronic kidney disease or chemotherapy, as well as in inflammatory bowel disease. It does have some “black-box” warnings so its use should be limited.
Cox-2 inhibitors. This is a well-known class of anti-inflammatory drugs, which are FDA-approved for pain and inflammation. Studies of adjunctive use of cox-2 inhibitors in acute psychosis show that these drugs accentuate the efficacy of antipsychotic medications.11 The reason is that acute psychosis is associated with neuro-inflammation, which leads to neurotoxicity.
Lithium. Dosages to treat mania are usually 900 to 1500 mg/d. However, in minute (homeopathic) dosages as low as 1 mg/d, lithium has been shown to prevent progression of amnestic mild cognitive impairment to full dementia.12 This interesting observation suggests that lithium not only induces neurogenesis and increases gray matter volume,13 but may be neuroprotective against amyloid neurotoxicity. The effects of very low doses of lithium in depression and schizophrenia have not been studied yet.
Caffeine. Yes, the good old brew people seek all day is neuroprotective and prevents mood and memory dysfunction caused by stress.14 Caffeine should be avoided in patients with anxiety disorders, but it may be helpful for the brains of patients with mood or psychotic disorders. Caffeine reverses synaptic dysfunction in the circuits of the hippocampus caused by chronic unpredictable stress (quite common among our psychiatric patients).
The above interventions may be helpful for some patients but not others. Practitioners should consider using 1 or more of those adjunctive neuroprotective agents in patients who are at risk for neurodegenerative changes secondary to recurrences of acute and severe psychosis or mood episodes. Although clinicians cannot monitor brain structural integrity, they can assess the rate of symptomatic improvement and degree of functional restoration in their patients. Until a cure is found, these little steps—taken cautiously and judiciously—could help alleviate our patients’ suffering and the risk of neurotoxicity associated with their serious psychiatric disorder.
1. Chen AT, Chibnall JT, Nasrallah HA. A meta-analysis of placebo-controlled trials of omega-3 fatty acid augmentation in schizophrenia: possible stage-specific effects. Ann Clin Psychiatry. 2015;27(4):289-296.
2. Calon F, Cole G. Neuroprotective action of omega-3 polyunsaturated fatty acids against neurodegenerative diseases: evidence from animal studies. Prostaglandins Leukot Essent Fatty Acids. 2007;7(5-6):287-293.
3. Chen AT, Chibnall JT, Nasrallah HA. Placebo-controlled augmentation trials of the antioxidant NAC in schizophrenia: a review. Ann Clin Psychiatry. 2016;28(3):190-196.
4. Chen G, Shi J, Hu Z, et al. Inhibitory effect on cerebral inflammatory response following traumatic brain injury in rats: a potential neuroprotective mechanism of N-acetylcysteine. Mediators Inflamm. 2008;2008:716458. doi: 10.1155/2008/716458
5. Dean OM, Data-Franco J, Giorlando F, et al. Minocycline: therapeutic potential in psychiatry. CNS Drugs. 2012;26(5):391-401.
6. Eyles DW, Burne TH, McGrath JJ. Vitamin D, effects on brain development, adult brain function and the links between low levels of vitamin D and neuropsychiatric disease. Front Neuroendocrinol. 2013;34(1):47-64.
7. Akaike A, Tkada-Takatori Y, Kume T, et al. Mechanisms of neuroprotective effects of nicotine and acetylcholinesterase inhibitors: role of alpha4 and alpha7 receptors in neuroprotection. J Mol Neurosci. 2010;40(1-2):211-216.
8. Cardinali DP, Hardeland R. Inflammaging, metabolic syndrome and melatonin: a call for treatment studies [published online May 11, 2016]. Neuroendocrinology. doi:10.1159/000446543.
9. Yamasaki M, Mishima HK, Yamashita H, et al. Neuroprotective effects of erythropoietin on glutamate and nitric oxide toxicity in primary cultured retinal ganglion cells. Brain Res. 2005;1050(1-2):15-26.
10. Pilllai A, Dhandapani KM, Pillai BA, et al. Erythropoietin prevents haloperidol treatment-induced neuronal apoptosis through regulation of BDNF. Neuropsychopharmacology. 2008;33(8):1942-1951.
11. Müller N, Myint AM, Weidinger E, et al. Anti-inflammatory treatment in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2013;42:146-153.
12. Forlenza OV, Diniz BS, Radanovic M, et al. Disease-modifying properties of long-term lithium treatment for amnestic mild cognitive impairment: randomised controlled trial. Br J Psychiatry. 2011;198(5):351-356.
13. Dong BT, Tu GJ, Han YX, et al. Lithium enhanced cell proliferation and differentiation of mesenchymal stem cells to neural cells in rat spinal cord. Int J Clin Exp Pathol. 2015;8(3):2473-2483.
14. Kaster MP, Machado NJ, Silva HB, et al. Caffeine acts through neuronal adenosine A24 receptors to prevent mood and memory dysfunction triggered by chronic stress. Proc Natl Acad Sci U S A. 2015;112(25):7833-7838.
Are you ‘neuroprotecting’ your patients?
Fortunately, many studies have demonstrated that in addition to controlling clinical symptoms, antidepressants, mood stabilizers, and atypical antipsychotics all have neuroprotective effects, including stimulating neurogenesis, preventing apoptosis, and increasing neurotrophins. However, more needs to be done to protect the brain’s gray and white matter and to prevent negative neuroplasticity and disconnectivity of brain circuits that often are documented in patients with psychotic and mood disorders.
There are, in fact, many off-label supplements with strong neuroprotective effects that psychiatrists can use as an adjunct to standard evidence-based pharmacotherapy. These agents generally are safe and well tolerated and often are sold over the counter, but are not covered by insurance. However, considering the disability that often is associated with schizophrenia, treatment-resistant depression, or psychotic mania, it is reasonable to consider using these agents, many of which are supported by studies published in peer-reviewed journals. However, because they are widely available and not proprietary and large, expensive registration trials such as the ones conducted by the pharmaceutical industry are not done, none is likely to receive FDA approval. Therefore, it is up to psychiatrists and nurse practitioners to use them judiciously in patients at risk for neurotoxicity.
Here are 10 agents with neuroprotective effects supported by published data that can be considered as add-on to the standard treatments in an effort to mitigate neurotoxicity and protect the brain from the destructive processes that accompany acute episodes of psychosis, mania, and depression.
Omega-3 fatty acids have been shown in several studies to help reduce psychopathology of psychosis, mania, or depression when used as an adjunctive agent.1 It appears to be more effective in the early stages of psychiatric disorders than in the chronic phase. It has anti-inflammatory, anti-oxidant, and anti-apoptotic effects; activates cell-signaling pathways; and prevents synaptic loss as well as neuronal and glial death.2
N-acetylcysteine (NAC) is a powerful antioxidant that increases glutathione, which is produced in the mitochondria. Schizophrenia is associated with mitochondrial dysfunction with low levels of glutathione, which puts the brain at risk for neurodegeneration caused by high levels of free radicals produced during psychosis. Adding NAC to antipsychotics during acute psychotic episodes—especially the first episode—can significantly reduce the neurotoxic effects of reactive oxygen and nitrogen species, also known as free radicals.3 In studies of traumatic brain injury in rats, NAC reduced brain edema, neuroinflammation, blood–brain barrier permeability, and apoptosis.4
Minocycline. This antibiotic has been studied extensively as an adjunctive treatment in schizophrenia and has proven to have several neuroprotective effects including anti-inflammatory, anti-oxidant, and anti-apoptotic, and reduces glutamate excitotoxicity.5 Several studies have documented its usefulness in acute psychotic episodes.
Vitamin D. Because of its vital role in neurodevelopment (neuronal differentiation, axonal connectivity), vitamin D deficiency has been associated with several psychiatric disorders including autism, schizophrenia, depression, and Alzheimer’s disease.6 Measure serum levels of vitamin D in patients with psychotic and mood disorders and implement supplementation if it is low—and it often is in these patients.
Nicotine is neuroprotective against glutamate excitotoxicity and it also inhibits apoptosis.7 However, it should never be administered via cigarettes, which are loaded with hundreds of toxic substances! It can be administered via patches or nicotine gum, which are usually used to help in smoking cessation. Nicotine also also can have a pro-cognitive effect.
Melatonin. Many people associate melatonin with sleep. However, it has multiple neuroprotective effects by being an antioxidant, protecting mitochondrial integrity, and modulating the immune system, as well as attenuating microglial activation, which triggers neuroinflammation and oxidative stress. It also protects against cellular senescence, which is due to inflammation and reactive oxygen species. Furthermore, melatonin is useful in ameliorating the metabolic syndrome, which is associated with neurotoxic effects on brain tissue caused by the pro-inflammatory effects of peri-omental fat in obesity.8 Adjunctive melatonin could be helpful in patients with schizophrenia or depression who suffer from metabolic syndrome.
Erythropoietin is a hormone produced by the kidneys to promote the formation of red blood cells. It is a potent neuroprotective cytokine that promotes neuronal survival via anti-apoptotic effects. It protects against glutamate and nitrous oxide toxicity9 and haloperidol-induced neuronal death.10 It is clinically used (since FDA approval in 1989) in severe anemia due to chronic kidney disease or chemotherapy, as well as in inflammatory bowel disease. It does have some “black-box” warnings so its use should be limited.
Cox-2 inhibitors. This is a well-known class of anti-inflammatory drugs, which are FDA-approved for pain and inflammation. Studies of adjunctive use of cox-2 inhibitors in acute psychosis show that these drugs accentuate the efficacy of antipsychotic medications.11 The reason is that acute psychosis is associated with neuro-inflammation, which leads to neurotoxicity.
Lithium. Dosages to treat mania are usually 900 to 1500 mg/d. However, in minute (homeopathic) dosages as low as 1 mg/d, lithium has been shown to prevent progression of amnestic mild cognitive impairment to full dementia.12 This interesting observation suggests that lithium not only induces neurogenesis and increases gray matter volume,13 but may be neuroprotective against amyloid neurotoxicity. The effects of very low doses of lithium in depression and schizophrenia have not been studied yet.
Caffeine. Yes, the good old brew people seek all day is neuroprotective and prevents mood and memory dysfunction caused by stress.14 Caffeine should be avoided in patients with anxiety disorders, but it may be helpful for the brains of patients with mood or psychotic disorders. Caffeine reverses synaptic dysfunction in the circuits of the hippocampus caused by chronic unpredictable stress (quite common among our psychiatric patients).
The above interventions may be helpful for some patients but not others. Practitioners should consider using 1 or more of those adjunctive neuroprotective agents in patients who are at risk for neurodegenerative changes secondary to recurrences of acute and severe psychosis or mood episodes. Although clinicians cannot monitor brain structural integrity, they can assess the rate of symptomatic improvement and degree of functional restoration in their patients. Until a cure is found, these little steps—taken cautiously and judiciously—could help alleviate our patients’ suffering and the risk of neurotoxicity associated with their serious psychiatric disorder.
Are you ‘neuroprotecting’ your patients?
Fortunately, many studies have demonstrated that in addition to controlling clinical symptoms, antidepressants, mood stabilizers, and atypical antipsychotics all have neuroprotective effects, including stimulating neurogenesis, preventing apoptosis, and increasing neurotrophins. However, more needs to be done to protect the brain’s gray and white matter and to prevent negative neuroplasticity and disconnectivity of brain circuits that often are documented in patients with psychotic and mood disorders.
There are, in fact, many off-label supplements with strong neuroprotective effects that psychiatrists can use as an adjunct to standard evidence-based pharmacotherapy. These agents generally are safe and well tolerated and often are sold over the counter, but are not covered by insurance. However, considering the disability that often is associated with schizophrenia, treatment-resistant depression, or psychotic mania, it is reasonable to consider using these agents, many of which are supported by studies published in peer-reviewed journals. However, because they are widely available and not proprietary and large, expensive registration trials such as the ones conducted by the pharmaceutical industry are not done, none is likely to receive FDA approval. Therefore, it is up to psychiatrists and nurse practitioners to use them judiciously in patients at risk for neurotoxicity.
Here are 10 agents with neuroprotective effects supported by published data that can be considered as add-on to the standard treatments in an effort to mitigate neurotoxicity and protect the brain from the destructive processes that accompany acute episodes of psychosis, mania, and depression.
Omega-3 fatty acids have been shown in several studies to help reduce psychopathology of psychosis, mania, or depression when used as an adjunctive agent.1 It appears to be more effective in the early stages of psychiatric disorders than in the chronic phase. It has anti-inflammatory, anti-oxidant, and anti-apoptotic effects; activates cell-signaling pathways; and prevents synaptic loss as well as neuronal and glial death.2
N-acetylcysteine (NAC) is a powerful antioxidant that increases glutathione, which is produced in the mitochondria. Schizophrenia is associated with mitochondrial dysfunction with low levels of glutathione, which puts the brain at risk for neurodegeneration caused by high levels of free radicals produced during psychosis. Adding NAC to antipsychotics during acute psychotic episodes—especially the first episode—can significantly reduce the neurotoxic effects of reactive oxygen and nitrogen species, also known as free radicals.3 In studies of traumatic brain injury in rats, NAC reduced brain edema, neuroinflammation, blood–brain barrier permeability, and apoptosis.4
Minocycline. This antibiotic has been studied extensively as an adjunctive treatment in schizophrenia and has proven to have several neuroprotective effects including anti-inflammatory, anti-oxidant, and anti-apoptotic, and reduces glutamate excitotoxicity.5 Several studies have documented its usefulness in acute psychotic episodes.
Vitamin D. Because of its vital role in neurodevelopment (neuronal differentiation, axonal connectivity), vitamin D deficiency has been associated with several psychiatric disorders including autism, schizophrenia, depression, and Alzheimer’s disease.6 Measure serum levels of vitamin D in patients with psychotic and mood disorders and implement supplementation if it is low—and it often is in these patients.
Nicotine is neuroprotective against glutamate excitotoxicity and it also inhibits apoptosis.7 However, it should never be administered via cigarettes, which are loaded with hundreds of toxic substances! It can be administered via patches or nicotine gum, which are usually used to help in smoking cessation. Nicotine also also can have a pro-cognitive effect.
Melatonin. Many people associate melatonin with sleep. However, it has multiple neuroprotective effects by being an antioxidant, protecting mitochondrial integrity, and modulating the immune system, as well as attenuating microglial activation, which triggers neuroinflammation and oxidative stress. It also protects against cellular senescence, which is due to inflammation and reactive oxygen species. Furthermore, melatonin is useful in ameliorating the metabolic syndrome, which is associated with neurotoxic effects on brain tissue caused by the pro-inflammatory effects of peri-omental fat in obesity.8 Adjunctive melatonin could be helpful in patients with schizophrenia or depression who suffer from metabolic syndrome.
Erythropoietin is a hormone produced by the kidneys to promote the formation of red blood cells. It is a potent neuroprotective cytokine that promotes neuronal survival via anti-apoptotic effects. It protects against glutamate and nitrous oxide toxicity9 and haloperidol-induced neuronal death.10 It is clinically used (since FDA approval in 1989) in severe anemia due to chronic kidney disease or chemotherapy, as well as in inflammatory bowel disease. It does have some “black-box” warnings so its use should be limited.
Cox-2 inhibitors. This is a well-known class of anti-inflammatory drugs, which are FDA-approved for pain and inflammation. Studies of adjunctive use of cox-2 inhibitors in acute psychosis show that these drugs accentuate the efficacy of antipsychotic medications.11 The reason is that acute psychosis is associated with neuro-inflammation, which leads to neurotoxicity.
Lithium. Dosages to treat mania are usually 900 to 1500 mg/d. However, in minute (homeopathic) dosages as low as 1 mg/d, lithium has been shown to prevent progression of amnestic mild cognitive impairment to full dementia.12 This interesting observation suggests that lithium not only induces neurogenesis and increases gray matter volume,13 but may be neuroprotective against amyloid neurotoxicity. The effects of very low doses of lithium in depression and schizophrenia have not been studied yet.
Caffeine. Yes, the good old brew people seek all day is neuroprotective and prevents mood and memory dysfunction caused by stress.14 Caffeine should be avoided in patients with anxiety disorders, but it may be helpful for the brains of patients with mood or psychotic disorders. Caffeine reverses synaptic dysfunction in the circuits of the hippocampus caused by chronic unpredictable stress (quite common among our psychiatric patients).
The above interventions may be helpful for some patients but not others. Practitioners should consider using 1 or more of those adjunctive neuroprotective agents in patients who are at risk for neurodegenerative changes secondary to recurrences of acute and severe psychosis or mood episodes. Although clinicians cannot monitor brain structural integrity, they can assess the rate of symptomatic improvement and degree of functional restoration in their patients. Until a cure is found, these little steps—taken cautiously and judiciously—could help alleviate our patients’ suffering and the risk of neurotoxicity associated with their serious psychiatric disorder.
1. Chen AT, Chibnall JT, Nasrallah HA. A meta-analysis of placebo-controlled trials of omega-3 fatty acid augmentation in schizophrenia: possible stage-specific effects. Ann Clin Psychiatry. 2015;27(4):289-296.
2. Calon F, Cole G. Neuroprotective action of omega-3 polyunsaturated fatty acids against neurodegenerative diseases: evidence from animal studies. Prostaglandins Leukot Essent Fatty Acids. 2007;7(5-6):287-293.
3. Chen AT, Chibnall JT, Nasrallah HA. Placebo-controlled augmentation trials of the antioxidant NAC in schizophrenia: a review. Ann Clin Psychiatry. 2016;28(3):190-196.
4. Chen G, Shi J, Hu Z, et al. Inhibitory effect on cerebral inflammatory response following traumatic brain injury in rats: a potential neuroprotective mechanism of N-acetylcysteine. Mediators Inflamm. 2008;2008:716458. doi: 10.1155/2008/716458
5. Dean OM, Data-Franco J, Giorlando F, et al. Minocycline: therapeutic potential in psychiatry. CNS Drugs. 2012;26(5):391-401.
6. Eyles DW, Burne TH, McGrath JJ. Vitamin D, effects on brain development, adult brain function and the links between low levels of vitamin D and neuropsychiatric disease. Front Neuroendocrinol. 2013;34(1):47-64.
7. Akaike A, Tkada-Takatori Y, Kume T, et al. Mechanisms of neuroprotective effects of nicotine and acetylcholinesterase inhibitors: role of alpha4 and alpha7 receptors in neuroprotection. J Mol Neurosci. 2010;40(1-2):211-216.
8. Cardinali DP, Hardeland R. Inflammaging, metabolic syndrome and melatonin: a call for treatment studies [published online May 11, 2016]. Neuroendocrinology. doi:10.1159/000446543.
9. Yamasaki M, Mishima HK, Yamashita H, et al. Neuroprotective effects of erythropoietin on glutamate and nitric oxide toxicity in primary cultured retinal ganglion cells. Brain Res. 2005;1050(1-2):15-26.
10. Pilllai A, Dhandapani KM, Pillai BA, et al. Erythropoietin prevents haloperidol treatment-induced neuronal apoptosis through regulation of BDNF. Neuropsychopharmacology. 2008;33(8):1942-1951.
11. Müller N, Myint AM, Weidinger E, et al. Anti-inflammatory treatment in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2013;42:146-153.
12. Forlenza OV, Diniz BS, Radanovic M, et al. Disease-modifying properties of long-term lithium treatment for amnestic mild cognitive impairment: randomised controlled trial. Br J Psychiatry. 2011;198(5):351-356.
13. Dong BT, Tu GJ, Han YX, et al. Lithium enhanced cell proliferation and differentiation of mesenchymal stem cells to neural cells in rat spinal cord. Int J Clin Exp Pathol. 2015;8(3):2473-2483.
14. Kaster MP, Machado NJ, Silva HB, et al. Caffeine acts through neuronal adenosine A24 receptors to prevent mood and memory dysfunction triggered by chronic stress. Proc Natl Acad Sci U S A. 2015;112(25):7833-7838.
1. Chen AT, Chibnall JT, Nasrallah HA. A meta-analysis of placebo-controlled trials of omega-3 fatty acid augmentation in schizophrenia: possible stage-specific effects. Ann Clin Psychiatry. 2015;27(4):289-296.
2. Calon F, Cole G. Neuroprotective action of omega-3 polyunsaturated fatty acids against neurodegenerative diseases: evidence from animal studies. Prostaglandins Leukot Essent Fatty Acids. 2007;7(5-6):287-293.
3. Chen AT, Chibnall JT, Nasrallah HA. Placebo-controlled augmentation trials of the antioxidant NAC in schizophrenia: a review. Ann Clin Psychiatry. 2016;28(3):190-196.
4. Chen G, Shi J, Hu Z, et al. Inhibitory effect on cerebral inflammatory response following traumatic brain injury in rats: a potential neuroprotective mechanism of N-acetylcysteine. Mediators Inflamm. 2008;2008:716458. doi: 10.1155/2008/716458
5. Dean OM, Data-Franco J, Giorlando F, et al. Minocycline: therapeutic potential in psychiatry. CNS Drugs. 2012;26(5):391-401.
6. Eyles DW, Burne TH, McGrath JJ. Vitamin D, effects on brain development, adult brain function and the links between low levels of vitamin D and neuropsychiatric disease. Front Neuroendocrinol. 2013;34(1):47-64.
7. Akaike A, Tkada-Takatori Y, Kume T, et al. Mechanisms of neuroprotective effects of nicotine and acetylcholinesterase inhibitors: role of alpha4 and alpha7 receptors in neuroprotection. J Mol Neurosci. 2010;40(1-2):211-216.
8. Cardinali DP, Hardeland R. Inflammaging, metabolic syndrome and melatonin: a call for treatment studies [published online May 11, 2016]. Neuroendocrinology. doi:10.1159/000446543.
9. Yamasaki M, Mishima HK, Yamashita H, et al. Neuroprotective effects of erythropoietin on glutamate and nitric oxide toxicity in primary cultured retinal ganglion cells. Brain Res. 2005;1050(1-2):15-26.
10. Pilllai A, Dhandapani KM, Pillai BA, et al. Erythropoietin prevents haloperidol treatment-induced neuronal apoptosis through regulation of BDNF. Neuropsychopharmacology. 2008;33(8):1942-1951.
11. Müller N, Myint AM, Weidinger E, et al. Anti-inflammatory treatment in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2013;42:146-153.
12. Forlenza OV, Diniz BS, Radanovic M, et al. Disease-modifying properties of long-term lithium treatment for amnestic mild cognitive impairment: randomised controlled trial. Br J Psychiatry. 2011;198(5):351-356.
13. Dong BT, Tu GJ, Han YX, et al. Lithium enhanced cell proliferation and differentiation of mesenchymal stem cells to neural cells in rat spinal cord. Int J Clin Exp Pathol. 2015;8(3):2473-2483.
14. Kaster MP, Machado NJ, Silva HB, et al. Caffeine acts through neuronal adenosine A24 receptors to prevent mood and memory dysfunction triggered by chronic stress. Proc Natl Acad Sci U S A. 2015;112(25):7833-7838.
Management of wound complications following obstetric anal sphincter injury (OASIS)
During vaginal delivery spontaneous perineal trauma and extension of episiotomy incisions are common. A severe perineal laceration that extends into or through the anal sphincter complex is referred to as an obstetric anal sphincter injury (OASIS) and requires meticulous repair. Following the repair of an OASIS, serious wound complications, including dehiscence and infection, may occur. In Europe the reported rate of OASIS varies widely among countries, with a rate of 0.1% in Romania, possibly due to underreporting, and 4.9% in Iceland.1 In the United States the rates of 3rd- and 4th-degree lacerations were reported to be 3.3% and 1.1%, respectively.2
Risk factors for OASIS include forceps delivery (odds ratio [OR], 5.50), vacuum-assisted delivery (OR, 3.98), and midline episiotomy (OR, 3.82).3 Additional risk factors for severe perineal injury at vaginal delivery include nulliparity (adjusted odds ratio [aOR], 2.58), delivery from a persistent occiput posterior position (aOR, 2.24), and above-average newborn birth weight (aOR, 1.28).4
In a meta-analysis of randomized trials, the researchers reported that restrictive use of episiotomy reduced the risk of severe perineal trauma (relative risk [RR], 0.67) but increased the risk of anterior perineal trauma (RR, 1.84).5 The American College of Obstetricians and Gynecologists (ACOG) recommends that episiotomy should not be a routine practice and is best restricted to use in a limited number of cases where fetal and maternal benefit is likely.6 In addition, ACOG recommends that if episiotomy is indicated, a mediolateral incision is favored over a midline incision. In my practice I perform only mediolateral episiotomy incisions. However, mediolateral episiotomy may be associated with an increased risk of postpartum perineal pain and dyspareunia.7 Use of warm compresses applied to the perineum during the second stage of labor may reduce the risk of 3rd- and 4th-degree lacerations.8 Techniques to ensure that the fetal head and shoulders are birthed in a slow and controlled fashion may decrease the risk of OASIS.9 See the TABLE, “Four maneuvers to control and slow the birth of the fetal head.”10–14
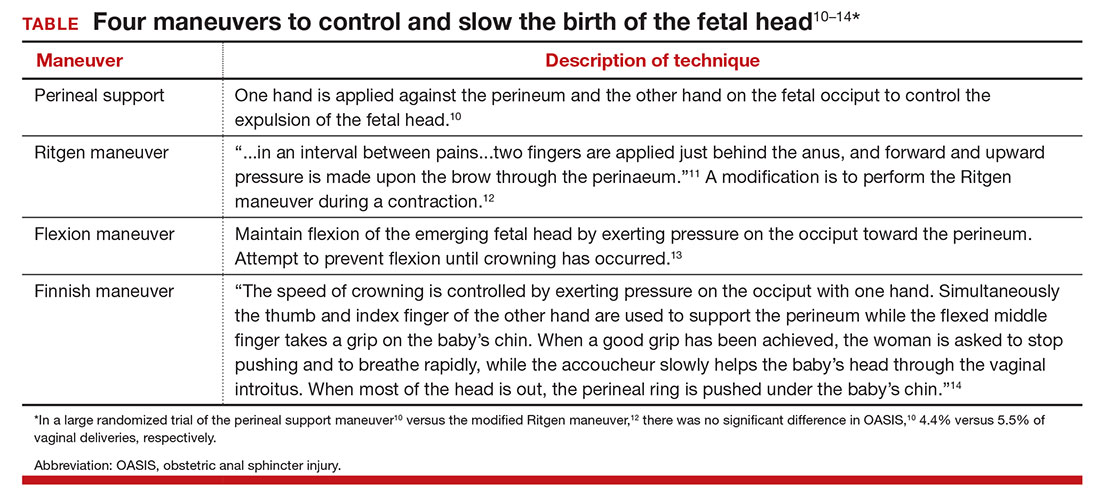
Related article:
Stop performing median episiotomy!
Wound complications following the repair of a 3rd- or 4th-degree laceration are reported to occur in approximately 5% to 10% of cases.15 The most common wound complications are dehiscence, infection, abscess formation, pain, sexual dysfunction, and anal incontinence. Minor wound complications, including superficial epithelial separation, can be managed expectantly. However, major wound complications need intensive treatment.
In one study of 21 women who had a major wound complication following the repair of a 4th-degree laceration, 53% had dehiscence plus infection, 33% had dehiscence alone, and 14% had infection alone.16 Major wound complications present at a mean of 5 days after delivery, with a wide range from 1 to 17 days following delivery.17 In a study of 144 cases of wound breakdown following a perineal laceration repair, the major risk factors for wound breakdown were episiotomy (aOR, 11.1), smoking (aOR, 6.4), midwife repair of laceration (aOR, 4.7), use of chromic suture (aOR, 3.9), and operative vaginal delivery (aOR, 3.4).18 In one study of 66 women with a wound complication following the repair of a 3rd- or 4th-degree laceration, clinical risk factors for a wound complication were cigarette smoking (OR, 4.04), 4th-degree laceration (OR, 1.89), and operative vaginal delivery (OR, 1.76).19 The use of intrapartum antibiotics appears to be protective (OR, 0.29) against wound complications following a major perineal laceration.19
Approach to the patient with a dehisced and infected perineal wound
Historically, wound dehiscence following surgical repair of a perineal injury was managed by allowing the wound to slowly close. This approach adversely impacts the quality of life of the affected woman because it may take weeks for the wound to heal. One small randomized trial17 and multiple case series20–24 report that an active multistep management algorithm permits early closure of the majority of these wounds, thereby accelerating the patient’s full recovery. Delayed primary (within 72 hours postpartum) or early secondary reconstruction (within 14 days of delivery) has been demonstrated to be safe with acceptable long-term functional out-comes.25 The modern approach to the treatment of a patient with an infected wound dehiscence following a severe perineal injury involves 3 steps.
Related article:
It’s time to restrict the use of episiotomy
Step 1. Restore tissue to health
The dehisced wound is cultured and, if infection is present, treatment is initiated with intravenous antibiotics appropriate for an infection with colorectal flora. One antibiotic option includes a cephalosporin (cefotetan 2 g IV every 6 hours) plus metronidazole (500 mg IV every 8 hours).
In the operating room, the wound should be thoroughly assessed, cleansed, and debrided. This step includes irrigation of the wound with a warm fluid, mechanical debridement, and sharp dissection of necrotic tissue. If the wound is infected, removal of stitches that are visible in the open wound is recommended.
Often more than one session of debridement may be needed to obtain wound edges that are free from exudate and show granulation at the wound margins. Between debridement sessions, wet-to-dry dressings are utilized. Two to 10 days of wound care may be needed before an attempt is made to close the wound. The wound is suitable for repair when there is no infected tissue and granulation tissue is present. Some surgeons prefer a mechanical bowel preparation regimen just before surgically closing the open wound. This may prevent early bowel movements and provide for tissue healing after surgery.26 The same preparations recommended for colonoscopy can be considered prior to surgical repair.
Step 2. Surgically close the wound
The wound is surgically closed in the operating room. If in Step 1 the assessment of the wound shows major trauma, assistance from a urogynecologist may be warranted. Surgical management of a perineal wound dehiscence requires a clear understanding of perineal anatomy and the structures contained between the vagina and the anorectum.
Six key structures may be involved in perineal injury: the anorectal mucosa, internal anal sphincter, external anal sphincter, vaginal wall and perineal skin, bulbocavernosus muscle, and transverse perineal muscles. It is important to definitively identify the individual structures that need to be repaired. Careful dissection is then carried out to mobilize these structures for repair. Additional debridement may be necessary to remove excess granulation tissue.
Anorectal mucosa repair. With repair of a 4th-degree perineal wound dehiscence, the apex of the defect in the anorectal mucosa is identified. The defect is repaired beginning at the apex using closely spaced interrupted sutures or a running suture of 3-0 or 4-0 polyglactin 910. Adequate tissue bites that will resist tearing should be taken. If interrupted sutures are used, tying the knots within the anorectal canal prevents them from being located within the healing wound.
Internal anal sphincter repair. After the anorectal mucosa is closed, attention is turned to reapproximation of the internal anal sphincter. The ends of a torn internal anal sphincter are often located lateral to the anorectal mucosa and appear as shiny gray-white fibrous tissue. The surgeon’s gloved index finger can be placed within the anorectal canal to aid in identification of the internal anal sphincter, as it tends to have a rubbery feel. Additionally, while the surgeon’s gloved index finger is in the anorectal canal, the surgeon’s gloved thumb can be used to retract the anorectal mucosa slightly medial and inferior so that adequate bites of the internal anal sphincter can be taken on each side.
Alternatively, Allis clamps canbe placed on the ends of the retracted internal anal sphincter to facilitate repair. Suture selection for repair of the internal anal sphincter can include 3-0 polyglactin 910 or 3-0 monofilament, delayed-absorbable suture such as polydioxanone sulfate (PDS). Some surgeons prefer delayed-absorbable suture (PDS) for this layer given the internal anal sphincter is constantly contracting and relaxing as it samples stool.26 This layer also can be closed with either interrupted sutures or a running suture.
External anal sphincter repair. After the anorectal mucosa and internal anal sphincter defects are reapproximated, attention is turned to the external anal sphincter. Like the internal anal sphincter, the ends of the external anal sphincter are often retracted laterally and must be definitively identified and mobilized in order to ensure an adequate tension-free repair. It is important to include the fascial sheath in the repair of the external anal sphincter.27 Allis clamps can be used to grasp the ends of the torn muscle after they are identified.
We recommend 0 or 2-0 PDS for repair of the external sphincter. Repair can be performed using either an end-to-end or overlapping technique. An end-to-end repair traditionally involves reapproximating the ends of the torn muscle and its overlying fascial sheath using interrupted sutures placed at four quadrants (12:00, 3:00, 6:00, 9:00).
In contrast, in an overlapping repair, the ends of the muscle are brought together with mattress sutures. Suture is passed top down through the medial aspect of the more superior muscle flap and top down through the inferior muscle flap more laterally. The same suture is then passed bottom up through the inferior muscle flap more laterally and finally bottom up through the medial aspect of the more superior muscle flap. Two to four mattress sutures are usually placed. After all sutures are placed, they are tied securely.
An overlapping repair results in a greater amount of tissue contact between the two torn muscle ends. However, adequate mobility of the external anal sphincter is necessary to perform this type of repair.
Vaginal wall and perineal body repair. After the anal sphincters have been repaired, the vaginal wall and remainder of the perineal body are reconstructed using the same techniques involved in a 2nd-degree laceration repair. Care must be taken to retrieve and reapproximate the torn ends of the bulbocavernosus muscles, which are also often retracted laterally and superiorly. After the bulbocavernosus and transverse perineal muscles are brought together in the midline, the posterior vaginal wall should be perpendicular to the perineum.
An alternative to surgical closure of a 2nd-degree dehiscence is the use of vacuum-assisted wound closure. Disadvantages of this approach include difficulty in maintaining a vacuum seal in the perineal region and the risk of wound contamination with feces. In one case report, 3 weeks of vacuum-assisted wound closure resulted in healing of a 10-cm wound dehiscence that occurred 5 days following a forceps-assisted vaginal delivery with a mediolateral episiotomy.28
Step 3. Ensure complete healing of the wound
Superb postoperative wound care helps to ensure a quick return to full recovery. Wound care should include regularly scheduled sitz baths (at least 3 times daily) followed by drying the perineum. It is preferable to provide a liquid diet that avoids frequent bowel movements in the initial 3 postoperative days. Stool softeners and fiber supplementation are recommended when a full diet is resumed. Some surgeons have found mineral oil (1 to 2 tablespoons daily) effective in producing soft stools that are easy to pass.26 Ensuring soft stool consistency is important to help prevent repair breakdown that may occur with passage of hard stools, fecal impaction, and/or straining during defecation.
We recommend follow-up 1 to 2 weeks after surgery to assess wound healing. No vaginal intercourseis permitted until complete healing is achieved.
Use a surgical checklist
All obstetricians and midwives strive to reduce the risk of OASIS at vaginal birth. When OASIS occurs, it is often useful to use a surgical checklist to ensure the execution of all steps in the management of the repair and recovery process.29 It is heartbreaking to see an OASIS repair breakdown in the week following a vaginal delivery. But by following the 3 steps outlined here, the secondary repair is likely to be successful and will quickly return most patients to full health.
Related article:
Develop and use a checklist for 3rd- and 4th-degree perineal lacerations

The authors report no financial relationships relevant to this article.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Blondel B, Alexander S, Bjarnadottir RI, et al; Euro-Peristat Scientific Committee. Variations in rates of severe perineal tears and episiotomies in 20 European countries: a study based on routine national data in Euro-Perstat Project. Acta Obstet Gynecol Scand. 2016;95(7):746–754.
- Friedman AM, Ananth CV, Predergast E, D’Alton ME, Wright JD. Evaluation of third-degree and fourth-degree laceration rates as quality indicators. Obstet Gynecol. 2015;125(4):927–937.
- Pergialiotis V, Vlachos D, Protopapas A, Pappa K, Vlachos G. Risk factors for severe perineal lacerations during childbirth. Int J Gynecol Obstet. 2014;125(1):6–14.
- Schmitz T, Alberti C, Andriss B, Moutafoff C, Oury JF, Sibony O. Identification of women at high risk for severe perineal lacerations. Eur J Obstet Gynecol Reprod Biol. 2014;182:11–15.
- Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database Syst Rev. 2009;(1):CD000081.
- ACOG Committee on Practice Bulletins—Obstetrics. Practice bulletin no. 165: Prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol. 2016;128(1):e1–e15.
- Sartore A, De Seta F, Maso G, Pregazzi R, Grimaldi E, Guaschino S. The effects of mediolateral episiotomy on pelvic floor function after vaginal delivery. Obstet Gynecol. 2004;103(4):669–673.
- Aasheim V, Nilsen AB, Lukasse M, Reinar LM. Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database Syst Rev. 2011;(12):CD006672.
- Harvey MA, Pierce M, Alter JE, et al; Society of Obstetricians and Gynaecologists of Canada. Obstetrical anal sphincter injuries (OASIS): prevention, recognition and repair. J Obstet Gynaecol Can. 2015;37(12):1131–1148.
- Jonsson ER, Elfaghi I, Rydhstrom H, Herbst A. Modified Ritgen’s maneuver for anal sphincter injury at delivery: a randomized controlled trial. Obstet Gynecol. 2008;112(2 pt 1):212–217.
- Williams JW. Obstetrics: A Text-book for the Use of Students and Practitioners. New York, NY: D Appleton and Co; 1903:288.
- Cunningham FG. The Ritgen maneuver: another sacred cow questioned. Obstet Gynecol. 2008;112(2 pt 1):210–211.
- Myrfield K, Brook C, Creedy D. Reducing perineal trauma: implications of flexion and extension of the fetal head during birth. Midwifery. 1997;13:197–201.
- Ostergaard Poulsen M, Lund Madsen M, Skriver-Moller AC, Overgaard C. Does the Finnish intervention prevent obstetrical anal sphincter injuries? A systematic review of the literature. BMJ Open. 2015;5:e008346.
- Kamel A, Khaled M. Episiotomy and obstetric perineal wound dehiscence: beyond soreness. J Obstet Gynaecol. 2014;34(3):215–217.
- Goldaber KG, Wendel PJ, McIntire DD, Wendel GD Jr. Postpartum perineal morbidity after fourth-degree perineal repair. Am J Obstet Gynecol. 1993;168(2):489–493.
- Monberg J, Hammen S. Ruptured episiotomia resutured primarily. Acta Obstet Gynecol Scand. 1987;66(2):163–164.
- Jallad K, Steele SE, Barber MD. Breakdown of perineal laceration repair after vaginal delivery: a case-control study. Female Pelvic Med Reconstr Surg. 2016;22(4):276–279.
- Stock L, Basham E, Gossett DR, Lewicky-Gaupp C. Factors associated with wound complications in women with obstetric anal sphincter injuries (OASIS). Am J Obstet Gynecol. 2013;208(4):327.e1–e8.
- Hauth JC, Gilstrap LC 3rd, Ward SC, Hankins GD. Early repair of an external sphincter ani muscle and rectal mucosal dehiscence. Obstet Gynecol. 1986;67(6):806–809.
- Hankins GD, Hauth JC, Gilstrap LC 3rd, Hammond TL, Yeomans ER, Snyder RR. Early repair of episiotomy dehiscence. Obstet Gynecol. 1990;75(1):48–51.
- Ramin SM, Ramus RM, Little BB, Gilstrap LC 3rd. Early repair of episiotomy dehiscence associated with infection. Am J Obstet Gynecol. 1992;167(4 pt 1):1104–1107.
- Arona AJ, Al-Marayati L, Grimes DA, Ballard CA. Early secondary repair of third- and fourth-degree perineal lacerations after outpatient wound preparation. Obstet Gynecol. 1995;86(2):294–296.
- Uygur D, Yesildaglar N, Kis S, Sipahi T. Early repair of episiotomy dehiscence. Aust N Z J Obstet Gynaecol. 2004;44(3):244–246.
- Soerensen MM, Bek KM, Buntzen S, Hojberg KE, Laurberg S. Long-term outcome of delayed primary or early secondary reconstruction of the anal sphincter after obstetrical injury. Dis Colon Rectum. 2008;51(3):312–317.
- Delancey JOL, Berger MB. Surgical approaches to postobstetrical perineal body defects (rectovaginal fistula and chronic third and fourth-degree lacerations). Clin Obstet Gynecol. 2010;53(1):134–144.
- Leeman L, Spearman M, Rogers R. Repair of obstetric perineal lacerations. Am Fam Physician. 2003;68(8):1585–1590.
- Aviki EM, Batalden RP, del Carmen MG, Berkowitz LR. Vacuum-assisted closure for episiotomy dehiscence. Obstet Gynecol. 2015;126(3):530–533.
- Barbieri RL. Develop and use a checklist for 3rd- and 4th-degree perineal lacerations. OBG Manag. 2013;25(8):8–12.
During vaginal delivery spontaneous perineal trauma and extension of episiotomy incisions are common. A severe perineal laceration that extends into or through the anal sphincter complex is referred to as an obstetric anal sphincter injury (OASIS) and requires meticulous repair. Following the repair of an OASIS, serious wound complications, including dehiscence and infection, may occur. In Europe the reported rate of OASIS varies widely among countries, with a rate of 0.1% in Romania, possibly due to underreporting, and 4.9% in Iceland.1 In the United States the rates of 3rd- and 4th-degree lacerations were reported to be 3.3% and 1.1%, respectively.2
Risk factors for OASIS include forceps delivery (odds ratio [OR], 5.50), vacuum-assisted delivery (OR, 3.98), and midline episiotomy (OR, 3.82).3 Additional risk factors for severe perineal injury at vaginal delivery include nulliparity (adjusted odds ratio [aOR], 2.58), delivery from a persistent occiput posterior position (aOR, 2.24), and above-average newborn birth weight (aOR, 1.28).4
In a meta-analysis of randomized trials, the researchers reported that restrictive use of episiotomy reduced the risk of severe perineal trauma (relative risk [RR], 0.67) but increased the risk of anterior perineal trauma (RR, 1.84).5 The American College of Obstetricians and Gynecologists (ACOG) recommends that episiotomy should not be a routine practice and is best restricted to use in a limited number of cases where fetal and maternal benefit is likely.6 In addition, ACOG recommends that if episiotomy is indicated, a mediolateral incision is favored over a midline incision. In my practice I perform only mediolateral episiotomy incisions. However, mediolateral episiotomy may be associated with an increased risk of postpartum perineal pain and dyspareunia.7 Use of warm compresses applied to the perineum during the second stage of labor may reduce the risk of 3rd- and 4th-degree lacerations.8 Techniques to ensure that the fetal head and shoulders are birthed in a slow and controlled fashion may decrease the risk of OASIS.9 See the TABLE, “Four maneuvers to control and slow the birth of the fetal head.”10–14
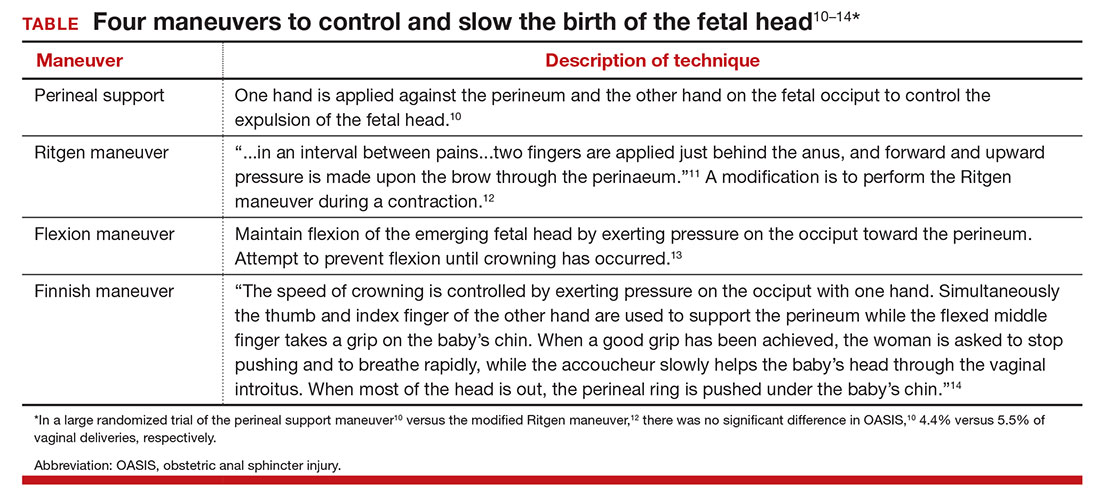
Related article:
Stop performing median episiotomy!
Wound complications following the repair of a 3rd- or 4th-degree laceration are reported to occur in approximately 5% to 10% of cases.15 The most common wound complications are dehiscence, infection, abscess formation, pain, sexual dysfunction, and anal incontinence. Minor wound complications, including superficial epithelial separation, can be managed expectantly. However, major wound complications need intensive treatment.
In one study of 21 women who had a major wound complication following the repair of a 4th-degree laceration, 53% had dehiscence plus infection, 33% had dehiscence alone, and 14% had infection alone.16 Major wound complications present at a mean of 5 days after delivery, with a wide range from 1 to 17 days following delivery.17 In a study of 144 cases of wound breakdown following a perineal laceration repair, the major risk factors for wound breakdown were episiotomy (aOR, 11.1), smoking (aOR, 6.4), midwife repair of laceration (aOR, 4.7), use of chromic suture (aOR, 3.9), and operative vaginal delivery (aOR, 3.4).18 In one study of 66 women with a wound complication following the repair of a 3rd- or 4th-degree laceration, clinical risk factors for a wound complication were cigarette smoking (OR, 4.04), 4th-degree laceration (OR, 1.89), and operative vaginal delivery (OR, 1.76).19 The use of intrapartum antibiotics appears to be protective (OR, 0.29) against wound complications following a major perineal laceration.19
Approach to the patient with a dehisced and infected perineal wound
Historically, wound dehiscence following surgical repair of a perineal injury was managed by allowing the wound to slowly close. This approach adversely impacts the quality of life of the affected woman because it may take weeks for the wound to heal. One small randomized trial17 and multiple case series20–24 report that an active multistep management algorithm permits early closure of the majority of these wounds, thereby accelerating the patient’s full recovery. Delayed primary (within 72 hours postpartum) or early secondary reconstruction (within 14 days of delivery) has been demonstrated to be safe with acceptable long-term functional out-comes.25 The modern approach to the treatment of a patient with an infected wound dehiscence following a severe perineal injury involves 3 steps.
Related article:
It’s time to restrict the use of episiotomy
Step 1. Restore tissue to health
The dehisced wound is cultured and, if infection is present, treatment is initiated with intravenous antibiotics appropriate for an infection with colorectal flora. One antibiotic option includes a cephalosporin (cefotetan 2 g IV every 6 hours) plus metronidazole (500 mg IV every 8 hours).
In the operating room, the wound should be thoroughly assessed, cleansed, and debrided. This step includes irrigation of the wound with a warm fluid, mechanical debridement, and sharp dissection of necrotic tissue. If the wound is infected, removal of stitches that are visible in the open wound is recommended.
Often more than one session of debridement may be needed to obtain wound edges that are free from exudate and show granulation at the wound margins. Between debridement sessions, wet-to-dry dressings are utilized. Two to 10 days of wound care may be needed before an attempt is made to close the wound. The wound is suitable for repair when there is no infected tissue and granulation tissue is present. Some surgeons prefer a mechanical bowel preparation regimen just before surgically closing the open wound. This may prevent early bowel movements and provide for tissue healing after surgery.26 The same preparations recommended for colonoscopy can be considered prior to surgical repair.
Step 2. Surgically close the wound
The wound is surgically closed in the operating room. If in Step 1 the assessment of the wound shows major trauma, assistance from a urogynecologist may be warranted. Surgical management of a perineal wound dehiscence requires a clear understanding of perineal anatomy and the structures contained between the vagina and the anorectum.
Six key structures may be involved in perineal injury: the anorectal mucosa, internal anal sphincter, external anal sphincter, vaginal wall and perineal skin, bulbocavernosus muscle, and transverse perineal muscles. It is important to definitively identify the individual structures that need to be repaired. Careful dissection is then carried out to mobilize these structures for repair. Additional debridement may be necessary to remove excess granulation tissue.
Anorectal mucosa repair. With repair of a 4th-degree perineal wound dehiscence, the apex of the defect in the anorectal mucosa is identified. The defect is repaired beginning at the apex using closely spaced interrupted sutures or a running suture of 3-0 or 4-0 polyglactin 910. Adequate tissue bites that will resist tearing should be taken. If interrupted sutures are used, tying the knots within the anorectal canal prevents them from being located within the healing wound.
Internal anal sphincter repair. After the anorectal mucosa is closed, attention is turned to reapproximation of the internal anal sphincter. The ends of a torn internal anal sphincter are often located lateral to the anorectal mucosa and appear as shiny gray-white fibrous tissue. The surgeon’s gloved index finger can be placed within the anorectal canal to aid in identification of the internal anal sphincter, as it tends to have a rubbery feel. Additionally, while the surgeon’s gloved index finger is in the anorectal canal, the surgeon’s gloved thumb can be used to retract the anorectal mucosa slightly medial and inferior so that adequate bites of the internal anal sphincter can be taken on each side.
Alternatively, Allis clamps canbe placed on the ends of the retracted internal anal sphincter to facilitate repair. Suture selection for repair of the internal anal sphincter can include 3-0 polyglactin 910 or 3-0 monofilament, delayed-absorbable suture such as polydioxanone sulfate (PDS). Some surgeons prefer delayed-absorbable suture (PDS) for this layer given the internal anal sphincter is constantly contracting and relaxing as it samples stool.26 This layer also can be closed with either interrupted sutures or a running suture.
External anal sphincter repair. After the anorectal mucosa and internal anal sphincter defects are reapproximated, attention is turned to the external anal sphincter. Like the internal anal sphincter, the ends of the external anal sphincter are often retracted laterally and must be definitively identified and mobilized in order to ensure an adequate tension-free repair. It is important to include the fascial sheath in the repair of the external anal sphincter.27 Allis clamps can be used to grasp the ends of the torn muscle after they are identified.
We recommend 0 or 2-0 PDS for repair of the external sphincter. Repair can be performed using either an end-to-end or overlapping technique. An end-to-end repair traditionally involves reapproximating the ends of the torn muscle and its overlying fascial sheath using interrupted sutures placed at four quadrants (12:00, 3:00, 6:00, 9:00).
In contrast, in an overlapping repair, the ends of the muscle are brought together with mattress sutures. Suture is passed top down through the medial aspect of the more superior muscle flap and top down through the inferior muscle flap more laterally. The same suture is then passed bottom up through the inferior muscle flap more laterally and finally bottom up through the medial aspect of the more superior muscle flap. Two to four mattress sutures are usually placed. After all sutures are placed, they are tied securely.
An overlapping repair results in a greater amount of tissue contact between the two torn muscle ends. However, adequate mobility of the external anal sphincter is necessary to perform this type of repair.
Vaginal wall and perineal body repair. After the anal sphincters have been repaired, the vaginal wall and remainder of the perineal body are reconstructed using the same techniques involved in a 2nd-degree laceration repair. Care must be taken to retrieve and reapproximate the torn ends of the bulbocavernosus muscles, which are also often retracted laterally and superiorly. After the bulbocavernosus and transverse perineal muscles are brought together in the midline, the posterior vaginal wall should be perpendicular to the perineum.
An alternative to surgical closure of a 2nd-degree dehiscence is the use of vacuum-assisted wound closure. Disadvantages of this approach include difficulty in maintaining a vacuum seal in the perineal region and the risk of wound contamination with feces. In one case report, 3 weeks of vacuum-assisted wound closure resulted in healing of a 10-cm wound dehiscence that occurred 5 days following a forceps-assisted vaginal delivery with a mediolateral episiotomy.28
Step 3. Ensure complete healing of the wound
Superb postoperative wound care helps to ensure a quick return to full recovery. Wound care should include regularly scheduled sitz baths (at least 3 times daily) followed by drying the perineum. It is preferable to provide a liquid diet that avoids frequent bowel movements in the initial 3 postoperative days. Stool softeners and fiber supplementation are recommended when a full diet is resumed. Some surgeons have found mineral oil (1 to 2 tablespoons daily) effective in producing soft stools that are easy to pass.26 Ensuring soft stool consistency is important to help prevent repair breakdown that may occur with passage of hard stools, fecal impaction, and/or straining during defecation.
We recommend follow-up 1 to 2 weeks after surgery to assess wound healing. No vaginal intercourseis permitted until complete healing is achieved.
Use a surgical checklist
All obstetricians and midwives strive to reduce the risk of OASIS at vaginal birth. When OASIS occurs, it is often useful to use a surgical checklist to ensure the execution of all steps in the management of the repair and recovery process.29 It is heartbreaking to see an OASIS repair breakdown in the week following a vaginal delivery. But by following the 3 steps outlined here, the secondary repair is likely to be successful and will quickly return most patients to full health.
Related article:
Develop and use a checklist for 3rd- and 4th-degree perineal lacerations

The authors report no financial relationships relevant to this article.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
During vaginal delivery spontaneous perineal trauma and extension of episiotomy incisions are common. A severe perineal laceration that extends into or through the anal sphincter complex is referred to as an obstetric anal sphincter injury (OASIS) and requires meticulous repair. Following the repair of an OASIS, serious wound complications, including dehiscence and infection, may occur. In Europe the reported rate of OASIS varies widely among countries, with a rate of 0.1% in Romania, possibly due to underreporting, and 4.9% in Iceland.1 In the United States the rates of 3rd- and 4th-degree lacerations were reported to be 3.3% and 1.1%, respectively.2
Risk factors for OASIS include forceps delivery (odds ratio [OR], 5.50), vacuum-assisted delivery (OR, 3.98), and midline episiotomy (OR, 3.82).3 Additional risk factors for severe perineal injury at vaginal delivery include nulliparity (adjusted odds ratio [aOR], 2.58), delivery from a persistent occiput posterior position (aOR, 2.24), and above-average newborn birth weight (aOR, 1.28).4
In a meta-analysis of randomized trials, the researchers reported that restrictive use of episiotomy reduced the risk of severe perineal trauma (relative risk [RR], 0.67) but increased the risk of anterior perineal trauma (RR, 1.84).5 The American College of Obstetricians and Gynecologists (ACOG) recommends that episiotomy should not be a routine practice and is best restricted to use in a limited number of cases where fetal and maternal benefit is likely.6 In addition, ACOG recommends that if episiotomy is indicated, a mediolateral incision is favored over a midline incision. In my practice I perform only mediolateral episiotomy incisions. However, mediolateral episiotomy may be associated with an increased risk of postpartum perineal pain and dyspareunia.7 Use of warm compresses applied to the perineum during the second stage of labor may reduce the risk of 3rd- and 4th-degree lacerations.8 Techniques to ensure that the fetal head and shoulders are birthed in a slow and controlled fashion may decrease the risk of OASIS.9 See the TABLE, “Four maneuvers to control and slow the birth of the fetal head.”10–14
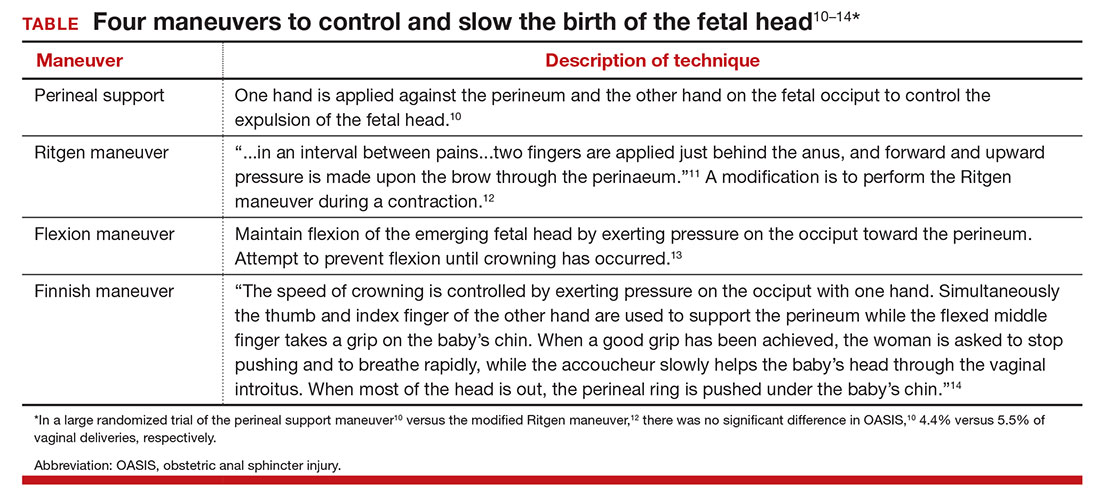
Related article:
Stop performing median episiotomy!
Wound complications following the repair of a 3rd- or 4th-degree laceration are reported to occur in approximately 5% to 10% of cases.15 The most common wound complications are dehiscence, infection, abscess formation, pain, sexual dysfunction, and anal incontinence. Minor wound complications, including superficial epithelial separation, can be managed expectantly. However, major wound complications need intensive treatment.
In one study of 21 women who had a major wound complication following the repair of a 4th-degree laceration, 53% had dehiscence plus infection, 33% had dehiscence alone, and 14% had infection alone.16 Major wound complications present at a mean of 5 days after delivery, with a wide range from 1 to 17 days following delivery.17 In a study of 144 cases of wound breakdown following a perineal laceration repair, the major risk factors for wound breakdown were episiotomy (aOR, 11.1), smoking (aOR, 6.4), midwife repair of laceration (aOR, 4.7), use of chromic suture (aOR, 3.9), and operative vaginal delivery (aOR, 3.4).18 In one study of 66 women with a wound complication following the repair of a 3rd- or 4th-degree laceration, clinical risk factors for a wound complication were cigarette smoking (OR, 4.04), 4th-degree laceration (OR, 1.89), and operative vaginal delivery (OR, 1.76).19 The use of intrapartum antibiotics appears to be protective (OR, 0.29) against wound complications following a major perineal laceration.19
Approach to the patient with a dehisced and infected perineal wound
Historically, wound dehiscence following surgical repair of a perineal injury was managed by allowing the wound to slowly close. This approach adversely impacts the quality of life of the affected woman because it may take weeks for the wound to heal. One small randomized trial17 and multiple case series20–24 report that an active multistep management algorithm permits early closure of the majority of these wounds, thereby accelerating the patient’s full recovery. Delayed primary (within 72 hours postpartum) or early secondary reconstruction (within 14 days of delivery) has been demonstrated to be safe with acceptable long-term functional out-comes.25 The modern approach to the treatment of a patient with an infected wound dehiscence following a severe perineal injury involves 3 steps.
Related article:
It’s time to restrict the use of episiotomy
Step 1. Restore tissue to health
The dehisced wound is cultured and, if infection is present, treatment is initiated with intravenous antibiotics appropriate for an infection with colorectal flora. One antibiotic option includes a cephalosporin (cefotetan 2 g IV every 6 hours) plus metronidazole (500 mg IV every 8 hours).
In the operating room, the wound should be thoroughly assessed, cleansed, and debrided. This step includes irrigation of the wound with a warm fluid, mechanical debridement, and sharp dissection of necrotic tissue. If the wound is infected, removal of stitches that are visible in the open wound is recommended.
Often more than one session of debridement may be needed to obtain wound edges that are free from exudate and show granulation at the wound margins. Between debridement sessions, wet-to-dry dressings are utilized. Two to 10 days of wound care may be needed before an attempt is made to close the wound. The wound is suitable for repair when there is no infected tissue and granulation tissue is present. Some surgeons prefer a mechanical bowel preparation regimen just before surgically closing the open wound. This may prevent early bowel movements and provide for tissue healing after surgery.26 The same preparations recommended for colonoscopy can be considered prior to surgical repair.
Step 2. Surgically close the wound
The wound is surgically closed in the operating room. If in Step 1 the assessment of the wound shows major trauma, assistance from a urogynecologist may be warranted. Surgical management of a perineal wound dehiscence requires a clear understanding of perineal anatomy and the structures contained between the vagina and the anorectum.
Six key structures may be involved in perineal injury: the anorectal mucosa, internal anal sphincter, external anal sphincter, vaginal wall and perineal skin, bulbocavernosus muscle, and transverse perineal muscles. It is important to definitively identify the individual structures that need to be repaired. Careful dissection is then carried out to mobilize these structures for repair. Additional debridement may be necessary to remove excess granulation tissue.
Anorectal mucosa repair. With repair of a 4th-degree perineal wound dehiscence, the apex of the defect in the anorectal mucosa is identified. The defect is repaired beginning at the apex using closely spaced interrupted sutures or a running suture of 3-0 or 4-0 polyglactin 910. Adequate tissue bites that will resist tearing should be taken. If interrupted sutures are used, tying the knots within the anorectal canal prevents them from being located within the healing wound.
Internal anal sphincter repair. After the anorectal mucosa is closed, attention is turned to reapproximation of the internal anal sphincter. The ends of a torn internal anal sphincter are often located lateral to the anorectal mucosa and appear as shiny gray-white fibrous tissue. The surgeon’s gloved index finger can be placed within the anorectal canal to aid in identification of the internal anal sphincter, as it tends to have a rubbery feel. Additionally, while the surgeon’s gloved index finger is in the anorectal canal, the surgeon’s gloved thumb can be used to retract the anorectal mucosa slightly medial and inferior so that adequate bites of the internal anal sphincter can be taken on each side.
Alternatively, Allis clamps canbe placed on the ends of the retracted internal anal sphincter to facilitate repair. Suture selection for repair of the internal anal sphincter can include 3-0 polyglactin 910 or 3-0 monofilament, delayed-absorbable suture such as polydioxanone sulfate (PDS). Some surgeons prefer delayed-absorbable suture (PDS) for this layer given the internal anal sphincter is constantly contracting and relaxing as it samples stool.26 This layer also can be closed with either interrupted sutures or a running suture.
External anal sphincter repair. After the anorectal mucosa and internal anal sphincter defects are reapproximated, attention is turned to the external anal sphincter. Like the internal anal sphincter, the ends of the external anal sphincter are often retracted laterally and must be definitively identified and mobilized in order to ensure an adequate tension-free repair. It is important to include the fascial sheath in the repair of the external anal sphincter.27 Allis clamps can be used to grasp the ends of the torn muscle after they are identified.
We recommend 0 or 2-0 PDS for repair of the external sphincter. Repair can be performed using either an end-to-end or overlapping technique. An end-to-end repair traditionally involves reapproximating the ends of the torn muscle and its overlying fascial sheath using interrupted sutures placed at four quadrants (12:00, 3:00, 6:00, 9:00).
In contrast, in an overlapping repair, the ends of the muscle are brought together with mattress sutures. Suture is passed top down through the medial aspect of the more superior muscle flap and top down through the inferior muscle flap more laterally. The same suture is then passed bottom up through the inferior muscle flap more laterally and finally bottom up through the medial aspect of the more superior muscle flap. Two to four mattress sutures are usually placed. After all sutures are placed, they are tied securely.
An overlapping repair results in a greater amount of tissue contact between the two torn muscle ends. However, adequate mobility of the external anal sphincter is necessary to perform this type of repair.
Vaginal wall and perineal body repair. After the anal sphincters have been repaired, the vaginal wall and remainder of the perineal body are reconstructed using the same techniques involved in a 2nd-degree laceration repair. Care must be taken to retrieve and reapproximate the torn ends of the bulbocavernosus muscles, which are also often retracted laterally and superiorly. After the bulbocavernosus and transverse perineal muscles are brought together in the midline, the posterior vaginal wall should be perpendicular to the perineum.
An alternative to surgical closure of a 2nd-degree dehiscence is the use of vacuum-assisted wound closure. Disadvantages of this approach include difficulty in maintaining a vacuum seal in the perineal region and the risk of wound contamination with feces. In one case report, 3 weeks of vacuum-assisted wound closure resulted in healing of a 10-cm wound dehiscence that occurred 5 days following a forceps-assisted vaginal delivery with a mediolateral episiotomy.28
Step 3. Ensure complete healing of the wound
Superb postoperative wound care helps to ensure a quick return to full recovery. Wound care should include regularly scheduled sitz baths (at least 3 times daily) followed by drying the perineum. It is preferable to provide a liquid diet that avoids frequent bowel movements in the initial 3 postoperative days. Stool softeners and fiber supplementation are recommended when a full diet is resumed. Some surgeons have found mineral oil (1 to 2 tablespoons daily) effective in producing soft stools that are easy to pass.26 Ensuring soft stool consistency is important to help prevent repair breakdown that may occur with passage of hard stools, fecal impaction, and/or straining during defecation.
We recommend follow-up 1 to 2 weeks after surgery to assess wound healing. No vaginal intercourseis permitted until complete healing is achieved.
Use a surgical checklist
All obstetricians and midwives strive to reduce the risk of OASIS at vaginal birth. When OASIS occurs, it is often useful to use a surgical checklist to ensure the execution of all steps in the management of the repair and recovery process.29 It is heartbreaking to see an OASIS repair breakdown in the week following a vaginal delivery. But by following the 3 steps outlined here, the secondary repair is likely to be successful and will quickly return most patients to full health.
Related article:
Develop and use a checklist for 3rd- and 4th-degree perineal lacerations

The authors report no financial relationships relevant to this article.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Blondel B, Alexander S, Bjarnadottir RI, et al; Euro-Peristat Scientific Committee. Variations in rates of severe perineal tears and episiotomies in 20 European countries: a study based on routine national data in Euro-Perstat Project. Acta Obstet Gynecol Scand. 2016;95(7):746–754.
- Friedman AM, Ananth CV, Predergast E, D’Alton ME, Wright JD. Evaluation of third-degree and fourth-degree laceration rates as quality indicators. Obstet Gynecol. 2015;125(4):927–937.
- Pergialiotis V, Vlachos D, Protopapas A, Pappa K, Vlachos G. Risk factors for severe perineal lacerations during childbirth. Int J Gynecol Obstet. 2014;125(1):6–14.
- Schmitz T, Alberti C, Andriss B, Moutafoff C, Oury JF, Sibony O. Identification of women at high risk for severe perineal lacerations. Eur J Obstet Gynecol Reprod Biol. 2014;182:11–15.
- Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database Syst Rev. 2009;(1):CD000081.
- ACOG Committee on Practice Bulletins—Obstetrics. Practice bulletin no. 165: Prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol. 2016;128(1):e1–e15.
- Sartore A, De Seta F, Maso G, Pregazzi R, Grimaldi E, Guaschino S. The effects of mediolateral episiotomy on pelvic floor function after vaginal delivery. Obstet Gynecol. 2004;103(4):669–673.
- Aasheim V, Nilsen AB, Lukasse M, Reinar LM. Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database Syst Rev. 2011;(12):CD006672.
- Harvey MA, Pierce M, Alter JE, et al; Society of Obstetricians and Gynaecologists of Canada. Obstetrical anal sphincter injuries (OASIS): prevention, recognition and repair. J Obstet Gynaecol Can. 2015;37(12):1131–1148.
- Jonsson ER, Elfaghi I, Rydhstrom H, Herbst A. Modified Ritgen’s maneuver for anal sphincter injury at delivery: a randomized controlled trial. Obstet Gynecol. 2008;112(2 pt 1):212–217.
- Williams JW. Obstetrics: A Text-book for the Use of Students and Practitioners. New York, NY: D Appleton and Co; 1903:288.
- Cunningham FG. The Ritgen maneuver: another sacred cow questioned. Obstet Gynecol. 2008;112(2 pt 1):210–211.
- Myrfield K, Brook C, Creedy D. Reducing perineal trauma: implications of flexion and extension of the fetal head during birth. Midwifery. 1997;13:197–201.
- Ostergaard Poulsen M, Lund Madsen M, Skriver-Moller AC, Overgaard C. Does the Finnish intervention prevent obstetrical anal sphincter injuries? A systematic review of the literature. BMJ Open. 2015;5:e008346.
- Kamel A, Khaled M. Episiotomy and obstetric perineal wound dehiscence: beyond soreness. J Obstet Gynaecol. 2014;34(3):215–217.
- Goldaber KG, Wendel PJ, McIntire DD, Wendel GD Jr. Postpartum perineal morbidity after fourth-degree perineal repair. Am J Obstet Gynecol. 1993;168(2):489–493.
- Monberg J, Hammen S. Ruptured episiotomia resutured primarily. Acta Obstet Gynecol Scand. 1987;66(2):163–164.
- Jallad K, Steele SE, Barber MD. Breakdown of perineal laceration repair after vaginal delivery: a case-control study. Female Pelvic Med Reconstr Surg. 2016;22(4):276–279.
- Stock L, Basham E, Gossett DR, Lewicky-Gaupp C. Factors associated with wound complications in women with obstetric anal sphincter injuries (OASIS). Am J Obstet Gynecol. 2013;208(4):327.e1–e8.
- Hauth JC, Gilstrap LC 3rd, Ward SC, Hankins GD. Early repair of an external sphincter ani muscle and rectal mucosal dehiscence. Obstet Gynecol. 1986;67(6):806–809.
- Hankins GD, Hauth JC, Gilstrap LC 3rd, Hammond TL, Yeomans ER, Snyder RR. Early repair of episiotomy dehiscence. Obstet Gynecol. 1990;75(1):48–51.
- Ramin SM, Ramus RM, Little BB, Gilstrap LC 3rd. Early repair of episiotomy dehiscence associated with infection. Am J Obstet Gynecol. 1992;167(4 pt 1):1104–1107.
- Arona AJ, Al-Marayati L, Grimes DA, Ballard CA. Early secondary repair of third- and fourth-degree perineal lacerations after outpatient wound preparation. Obstet Gynecol. 1995;86(2):294–296.
- Uygur D, Yesildaglar N, Kis S, Sipahi T. Early repair of episiotomy dehiscence. Aust N Z J Obstet Gynaecol. 2004;44(3):244–246.
- Soerensen MM, Bek KM, Buntzen S, Hojberg KE, Laurberg S. Long-term outcome of delayed primary or early secondary reconstruction of the anal sphincter after obstetrical injury. Dis Colon Rectum. 2008;51(3):312–317.
- Delancey JOL, Berger MB. Surgical approaches to postobstetrical perineal body defects (rectovaginal fistula and chronic third and fourth-degree lacerations). Clin Obstet Gynecol. 2010;53(1):134–144.
- Leeman L, Spearman M, Rogers R. Repair of obstetric perineal lacerations. Am Fam Physician. 2003;68(8):1585–1590.
- Aviki EM, Batalden RP, del Carmen MG, Berkowitz LR. Vacuum-assisted closure for episiotomy dehiscence. Obstet Gynecol. 2015;126(3):530–533.
- Barbieri RL. Develop and use a checklist for 3rd- and 4th-degree perineal lacerations. OBG Manag. 2013;25(8):8–12.
- Blondel B, Alexander S, Bjarnadottir RI, et al; Euro-Peristat Scientific Committee. Variations in rates of severe perineal tears and episiotomies in 20 European countries: a study based on routine national data in Euro-Perstat Project. Acta Obstet Gynecol Scand. 2016;95(7):746–754.
- Friedman AM, Ananth CV, Predergast E, D’Alton ME, Wright JD. Evaluation of third-degree and fourth-degree laceration rates as quality indicators. Obstet Gynecol. 2015;125(4):927–937.
- Pergialiotis V, Vlachos D, Protopapas A, Pappa K, Vlachos G. Risk factors for severe perineal lacerations during childbirth. Int J Gynecol Obstet. 2014;125(1):6–14.
- Schmitz T, Alberti C, Andriss B, Moutafoff C, Oury JF, Sibony O. Identification of women at high risk for severe perineal lacerations. Eur J Obstet Gynecol Reprod Biol. 2014;182:11–15.
- Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database Syst Rev. 2009;(1):CD000081.
- ACOG Committee on Practice Bulletins—Obstetrics. Practice bulletin no. 165: Prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol. 2016;128(1):e1–e15.
- Sartore A, De Seta F, Maso G, Pregazzi R, Grimaldi E, Guaschino S. The effects of mediolateral episiotomy on pelvic floor function after vaginal delivery. Obstet Gynecol. 2004;103(4):669–673.
- Aasheim V, Nilsen AB, Lukasse M, Reinar LM. Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database Syst Rev. 2011;(12):CD006672.
- Harvey MA, Pierce M, Alter JE, et al; Society of Obstetricians and Gynaecologists of Canada. Obstetrical anal sphincter injuries (OASIS): prevention, recognition and repair. J Obstet Gynaecol Can. 2015;37(12):1131–1148.
- Jonsson ER, Elfaghi I, Rydhstrom H, Herbst A. Modified Ritgen’s maneuver for anal sphincter injury at delivery: a randomized controlled trial. Obstet Gynecol. 2008;112(2 pt 1):212–217.
- Williams JW. Obstetrics: A Text-book for the Use of Students and Practitioners. New York, NY: D Appleton and Co; 1903:288.
- Cunningham FG. The Ritgen maneuver: another sacred cow questioned. Obstet Gynecol. 2008;112(2 pt 1):210–211.
- Myrfield K, Brook C, Creedy D. Reducing perineal trauma: implications of flexion and extension of the fetal head during birth. Midwifery. 1997;13:197–201.
- Ostergaard Poulsen M, Lund Madsen M, Skriver-Moller AC, Overgaard C. Does the Finnish intervention prevent obstetrical anal sphincter injuries? A systematic review of the literature. BMJ Open. 2015;5:e008346.
- Kamel A, Khaled M. Episiotomy and obstetric perineal wound dehiscence: beyond soreness. J Obstet Gynaecol. 2014;34(3):215–217.
- Goldaber KG, Wendel PJ, McIntire DD, Wendel GD Jr. Postpartum perineal morbidity after fourth-degree perineal repair. Am J Obstet Gynecol. 1993;168(2):489–493.
- Monberg J, Hammen S. Ruptured episiotomia resutured primarily. Acta Obstet Gynecol Scand. 1987;66(2):163–164.
- Jallad K, Steele SE, Barber MD. Breakdown of perineal laceration repair after vaginal delivery: a case-control study. Female Pelvic Med Reconstr Surg. 2016;22(4):276–279.
- Stock L, Basham E, Gossett DR, Lewicky-Gaupp C. Factors associated with wound complications in women with obstetric anal sphincter injuries (OASIS). Am J Obstet Gynecol. 2013;208(4):327.e1–e8.
- Hauth JC, Gilstrap LC 3rd, Ward SC, Hankins GD. Early repair of an external sphincter ani muscle and rectal mucosal dehiscence. Obstet Gynecol. 1986;67(6):806–809.
- Hankins GD, Hauth JC, Gilstrap LC 3rd, Hammond TL, Yeomans ER, Snyder RR. Early repair of episiotomy dehiscence. Obstet Gynecol. 1990;75(1):48–51.
- Ramin SM, Ramus RM, Little BB, Gilstrap LC 3rd. Early repair of episiotomy dehiscence associated with infection. Am J Obstet Gynecol. 1992;167(4 pt 1):1104–1107.
- Arona AJ, Al-Marayati L, Grimes DA, Ballard CA. Early secondary repair of third- and fourth-degree perineal lacerations after outpatient wound preparation. Obstet Gynecol. 1995;86(2):294–296.
- Uygur D, Yesildaglar N, Kis S, Sipahi T. Early repair of episiotomy dehiscence. Aust N Z J Obstet Gynaecol. 2004;44(3):244–246.
- Soerensen MM, Bek KM, Buntzen S, Hojberg KE, Laurberg S. Long-term outcome of delayed primary or early secondary reconstruction of the anal sphincter after obstetrical injury. Dis Colon Rectum. 2008;51(3):312–317.
- Delancey JOL, Berger MB. Surgical approaches to postobstetrical perineal body defects (rectovaginal fistula and chronic third and fourth-degree lacerations). Clin Obstet Gynecol. 2010;53(1):134–144.
- Leeman L, Spearman M, Rogers R. Repair of obstetric perineal lacerations. Am Fam Physician. 2003;68(8):1585–1590.
- Aviki EM, Batalden RP, del Carmen MG, Berkowitz LR. Vacuum-assisted closure for episiotomy dehiscence. Obstet Gynecol. 2015;126(3):530–533.
- Barbieri RL. Develop and use a checklist for 3rd- and 4th-degree perineal lacerations. OBG Manag. 2013;25(8):8–12.
Value-based cancer care and the patient perspective
The business of cancer care is in transition. Driven by the Centers for Medicare & Medicaid Services’ (CMS) Oncology Care Model (OCM) program, practices around the country are working to re-engineer the way they provide services, and the way they charge for those services. The implicit goal of all this is to manage (as in reduce) the overall cost of cancer care. A more frequently stated goal is to improve value, typically defined as outcome (numerator) relative to cost (denominator). Alternative payment models are challenged to assess the value of transformational improvement in cancer care.
Click on the PDF icon at the top of this introduction to read the full article.
The business of cancer care is in transition. Driven by the Centers for Medicare & Medicaid Services’ (CMS) Oncology Care Model (OCM) program, practices around the country are working to re-engineer the way they provide services, and the way they charge for those services. The implicit goal of all this is to manage (as in reduce) the overall cost of cancer care. A more frequently stated goal is to improve value, typically defined as outcome (numerator) relative to cost (denominator). Alternative payment models are challenged to assess the value of transformational improvement in cancer care.
Click on the PDF icon at the top of this introduction to read the full article.
The business of cancer care is in transition. Driven by the Centers for Medicare & Medicaid Services’ (CMS) Oncology Care Model (OCM) program, practices around the country are working to re-engineer the way they provide services, and the way they charge for those services. The implicit goal of all this is to manage (as in reduce) the overall cost of cancer care. A more frequently stated goal is to improve value, typically defined as outcome (numerator) relative to cost (denominator). Alternative payment models are challenged to assess the value of transformational improvement in cancer care.
Click on the PDF icon at the top of this introduction to read the full article.
From the Editors: Querencia
In the flood of emails, periodicals, Twitter, Facebook, Doximity, Medscape, and other information that washes over surgeons every day, why should they use their precious time to read ACS Surgery News? That question is foremost in the minds of the editors of this publication as we consider news stories and commentaries for inclusion. Is this an article our readers are going to find informative, pertinent, and stimulating? We want ACS Surgery News to be a querencia: a source of reliable, vetted information that gives surgeons a place of intellectual security along the information highway.
The editors of ACS Surgery News understand surgery from the scrub sink up. While our mission includes keeping our readers informed about these looming thunderstorms, we are also privileged to report progress and innovations that keep coming no matter how the forces of red tape and commerce play against our profession. Bringing news of both challenges and beacons of hope for our profession with commentary and perspective from our colleagues is our objective. For the editors, this is both a mission and a pleasure. Since most of the editors and our Editorial Advisory Board (EAB), like our readers, must focus primarily on our jobs as surgeons, teachers, and researchers, we cannot read every journal or attend every meeting. The role of ACS Surgery News is to find the relevant news of interest and importance to surgeons, wherever it may be found, and to report it succinctly and accurately in a readable form. Before an article appears in ACS Surgery News, it is reviewed by the author of the paper or presentation for accuracy and reviewed by the most appropriate member of the EAB as well as by both Co-Editors for importance and relevance to our surgeon readers. We do not want to shy away from controversial topics, but endeavor to present such topics with balance and sensitivity, just as the ACS itself always attempts to do: to shed light, rather than merely heat, on all subjects that we cover in our pages.
The editors of ACS Surgery News hope that in the months and years to come, this publication can be a querencia for the surgeon: a safe and secure place to engage all the forces that a surgeon must confront to be successful. In these pages we hope you will find knowledge, wisdom, camaraderie, and support for your practice, whatever that may be.
Surgery is a life of great joy and great sorrow, sometimes happening all within the same hour. We hope to be part of the joy and to soften the sorrow by being a publication you look forward to reading and wherein you find those things that contribute to your being a great surgeon and human being.
Dr. Deveney is professor of surgery and vice chair of education in the department of surgery, Oregon Health & Science University, Portland. She is the Co-Editor of ACS Surgery News.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and Co-Editor of ACS Surgery News.
In the flood of emails, periodicals, Twitter, Facebook, Doximity, Medscape, and other information that washes over surgeons every day, why should they use their precious time to read ACS Surgery News? That question is foremost in the minds of the editors of this publication as we consider news stories and commentaries for inclusion. Is this an article our readers are going to find informative, pertinent, and stimulating? We want ACS Surgery News to be a querencia: a source of reliable, vetted information that gives surgeons a place of intellectual security along the information highway.
The editors of ACS Surgery News understand surgery from the scrub sink up. While our mission includes keeping our readers informed about these looming thunderstorms, we are also privileged to report progress and innovations that keep coming no matter how the forces of red tape and commerce play against our profession. Bringing news of both challenges and beacons of hope for our profession with commentary and perspective from our colleagues is our objective. For the editors, this is both a mission and a pleasure. Since most of the editors and our Editorial Advisory Board (EAB), like our readers, must focus primarily on our jobs as surgeons, teachers, and researchers, we cannot read every journal or attend every meeting. The role of ACS Surgery News is to find the relevant news of interest and importance to surgeons, wherever it may be found, and to report it succinctly and accurately in a readable form. Before an article appears in ACS Surgery News, it is reviewed by the author of the paper or presentation for accuracy and reviewed by the most appropriate member of the EAB as well as by both Co-Editors for importance and relevance to our surgeon readers. We do not want to shy away from controversial topics, but endeavor to present such topics with balance and sensitivity, just as the ACS itself always attempts to do: to shed light, rather than merely heat, on all subjects that we cover in our pages.
The editors of ACS Surgery News hope that in the months and years to come, this publication can be a querencia for the surgeon: a safe and secure place to engage all the forces that a surgeon must confront to be successful. In these pages we hope you will find knowledge, wisdom, camaraderie, and support for your practice, whatever that may be.
Surgery is a life of great joy and great sorrow, sometimes happening all within the same hour. We hope to be part of the joy and to soften the sorrow by being a publication you look forward to reading and wherein you find those things that contribute to your being a great surgeon and human being.
Dr. Deveney is professor of surgery and vice chair of education in the department of surgery, Oregon Health & Science University, Portland. She is the Co-Editor of ACS Surgery News.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and Co-Editor of ACS Surgery News.
In the flood of emails, periodicals, Twitter, Facebook, Doximity, Medscape, and other information that washes over surgeons every day, why should they use their precious time to read ACS Surgery News? That question is foremost in the minds of the editors of this publication as we consider news stories and commentaries for inclusion. Is this an article our readers are going to find informative, pertinent, and stimulating? We want ACS Surgery News to be a querencia: a source of reliable, vetted information that gives surgeons a place of intellectual security along the information highway.
The editors of ACS Surgery News understand surgery from the scrub sink up. While our mission includes keeping our readers informed about these looming thunderstorms, we are also privileged to report progress and innovations that keep coming no matter how the forces of red tape and commerce play against our profession. Bringing news of both challenges and beacons of hope for our profession with commentary and perspective from our colleagues is our objective. For the editors, this is both a mission and a pleasure. Since most of the editors and our Editorial Advisory Board (EAB), like our readers, must focus primarily on our jobs as surgeons, teachers, and researchers, we cannot read every journal or attend every meeting. The role of ACS Surgery News is to find the relevant news of interest and importance to surgeons, wherever it may be found, and to report it succinctly and accurately in a readable form. Before an article appears in ACS Surgery News, it is reviewed by the author of the paper or presentation for accuracy and reviewed by the most appropriate member of the EAB as well as by both Co-Editors for importance and relevance to our surgeon readers. We do not want to shy away from controversial topics, but endeavor to present such topics with balance and sensitivity, just as the ACS itself always attempts to do: to shed light, rather than merely heat, on all subjects that we cover in our pages.
The editors of ACS Surgery News hope that in the months and years to come, this publication can be a querencia for the surgeon: a safe and secure place to engage all the forces that a surgeon must confront to be successful. In these pages we hope you will find knowledge, wisdom, camaraderie, and support for your practice, whatever that may be.
Surgery is a life of great joy and great sorrow, sometimes happening all within the same hour. We hope to be part of the joy and to soften the sorrow by being a publication you look forward to reading and wherein you find those things that contribute to your being a great surgeon and human being.
Dr. Deveney is professor of surgery and vice chair of education in the department of surgery, Oregon Health & Science University, Portland. She is the Co-Editor of ACS Surgery News.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and Co-Editor of ACS Surgery News.
Lessons learned from using CDK 4/6 inhibitors to treat metastatic breast cancer
45 new cancer drugs – a significant jump from the average 26 approvals annually from 2006 to 2014. This major shift in the number of approvals is due to many factors, including the intensified efforts by scientists and clinicians to develop new drugs, especially novel immunotherapies, and changes in the FDA’s drug approval process under the leadership of Dr Richard Pazdur.
Click on the PDF icon at the top of this introduction to read the full article.
45 new cancer drugs – a significant jump from the average 26 approvals annually from 2006 to 2014. This major shift in the number of approvals is due to many factors, including the intensified efforts by scientists and clinicians to develop new drugs, especially novel immunotherapies, and changes in the FDA’s drug approval process under the leadership of Dr Richard Pazdur.
Click on the PDF icon at the top of this introduction to read the full article.
45 new cancer drugs – a significant jump from the average 26 approvals annually from 2006 to 2014. This major shift in the number of approvals is due to many factors, including the intensified efforts by scientists and clinicians to develop new drugs, especially novel immunotherapies, and changes in the FDA’s drug approval process under the leadership of Dr Richard Pazdur.
Click on the PDF icon at the top of this introduction to read the full article.










