User login
Prescribing is the culmination of extensive medical training and psychologists don’t qualify
Practicing medicine without a license is a crime, but it seems to have become a hollow law. Politicians are now cynically legalizing it by granting prescribing privileges to individuals with no prior foundation of medical training. Perhaps it is because of serious ignorance of the difference between psychiatry and psychology or MD and PhD degrees. Or perhaps it is a quid pro quo to generous donors to their re-election campaigns who seek a convenient shortcut to the 28,000 hours it takes to become a psychiatrist in 8 years of medical school and psychiatric residency—and that comes after 4 years of college.
I recently consulted an attorney to discuss some legal documents. When he asked me what my line of work is, I then asked him if he knew the difference between a psychiatrist and a psychologist. He hesitated before admitting in an embarrassed tone that he did not really know and thought that they were all “shrinks” and very similar. I then informed him that both go through undergraduate college education, albeit taking very different courses, with pre-med scientific emphasis for future psychiatric physicians and predominately psychology emphasis for future psychologists.
However, psychiatrists then attend medical school for 4 years and rotate on multiple hospital-based medical specialties, such as internal medicine, surgery, pediatrics, obstetrics and gynecology, family medicine, neurology, pathology, psychiatry, ophthalmology, dermatology, anesthesia, radiology, otolaryngology, etc.
Psychologists, on the other hand, take additional advanced psychology courses in graduate school and write a dissertation that requires quite a bit of library time. After getting a MD, future psychiatrists spend 4 years in extensive training in residency programs across inpatient wards and outpatient clinics, assessing the physical and mental health of seriously sick patients with emphasis on both pharmacological and psychotherapeutic treatments for serious psychiatric disorders in patients, the majority of whom have comorbid medical conditions as well. Psychologists, on the other hand, spend 1 year of internship after getting their PhD or PsyD degree, essentially focused on developing counseling and psychotherapy skills. By the time they complete their training, psychologists and psychiatrists have disparate skills: heavily medical and pharmacological skills in psychiatrists and strong psychotherapeutic skills in psychologists.
After this long explanation, I asked the attorney what he thought about psychologists seeking prescription privileges. He was astounded that psychologists would attempt to expand this scope of practice through state legislations rather than going through medical training like all physicians. “That would be like practicing medicine without a license, which is a felony,” he said. He wryly added that his fellow malpractice and litigation lawyers will be the big winners while poorly treated patients will be the biggest losers. Being an avid runner, he also added that such a short-cut to prescribe without the requisite years of medial training reminded him of Rosie Ruiz, who snuck into the Boston marathon a couple of miles before the finish line and “won” the race, before she was caught and discredited.1
Psychology is a respected mental health discipline with strong psychotherapy training and orientation. For decades, psychologists have vigorously criticized the medical model of mental disorders that psychiatric physicians employ to diagnose and treat brain disorders that disrupt thinking, emotions, mood, cognition, and behavior. However, about 25 years ago, a small group of militant psychologists brazenly decided to lobby state legislatures to give them the right to prescribe psychotropics, although they have no formal medical training. Psychiatric physicians, represented by the American Psychiatric Association (APA), strongly opposed this initiative and regarded it as reckless disregard of the obvious need for extensive medical training to be able to prescribe drugs that affect every organ in the body, not only the brain. Psychiatric medications are associated with serious risks of morbidity and mortality.2 The ability to safely prescribe any medication represents the tip of a huge iceberg of 8 years of rigorous medical school education and specialty training. Yet, one of the early proponents of prescription privileges for psychologists, Patrick De Leon, sarcastically likened the ability to prescribe drugs to learning how to operate a desktop computer!
Not all psychologists agreed with the political campaign to lobby state legislatures to pass a law authorizing prescriptive privileges for psychologists.3-6 In fact, most academic psychologists oppose it.7 Most of the early supporters had a PsyD degree from professional schools of psychology, not a PhD degree in psychology, which is obtained from a university department of psychology. The National Alliance on Mental Illness is opposed to psychologists prescribing medications.8 Psychiatrists are outraged by this hazardous “solution” to the shortage of psychiatrists and point to the many potential dangers to patients. Some suggested that this is a quick way to enhance psychologists’ income and to generate more revenue for their professional journals and meetings with lucrative pharmaceutical ads and exhibit booths.
The campaign is ongoing, as Idaho became the fifth state to adopt such an ill-conceived “solution” to increasing access to mental health care, despite valiant effort by the APA to lobby against such laws. Although New Mexico (2002), Louisiana (2004), Illinois (2014), and Iowa (2016) have passed prescriptive authority for psychologists before Idaho, the APA has defeated such measures in numerous other states. But the painful truth is that this has been a lengthy political chess game in which psychologists have been gradually gaining ground and “capturing more pieces.”
Here is a brief, common sense rationale as to the need for full medical training necessary before safely and accurately prescribing medications, most of which are synthetic molecules, which are essentially foreign substances, with both benefits and risks detailed in the FDA-approved label of each drug that reaches the medical marketplace.
First: Making an accurate clinical diagnosis. If a patient presents with depression, the clinician must rule out other possible causes before diagnosing it as primary major depressive disorder for which an antidepressant can be prescribed. The panoply of secondary depressions, which are not treated with antidepressants, includes a variety of recreational drug-induced mood changes and dysphoria and depression induced by numerous prescription drugs (such as antihypertensives, hormonal contraceptives, steroids, interferon, proton pump inhibitors, H2 blockers, malaria drugs, etc.).
After drug-induced depression is ruled out, the clinician must rule out the possibility that an underlying medical condition might be causing the depression, which includes disorders such as hypothyroidism and other endocrinopathies, anemia, stroke, heart disease, hyperkalemia, lupus and other autoimmune disorders, cancer, Parkinsonism, etc. Therefore, a targeted exploration of past and current medical history, accompanied by a battery of lab tests (complete blood count, electrolytes, liver and kidney function tests, metabolic profile, thyroid-stimulating hormone, etc.) must be done to systematically arrive at the correct diagnosis. Only then can the proper treatment plan be determined, which may or may not include prescribing an antidepressant.
Conclusion: Medical training and psychiatric residency are required for an accurate diagnosis of a mental disorder. Even physicians with no psychiatric training might not have the full repertoire of knowledge needed to systematically rule out secondary depression.
Second: Drug selection. Psychiatric drugs can have various iatrogenic effects. Thus, the selection of an appropriate prescription medication from the available array of drugs approved for a given psychiatric indication must be safe and consistent with the patient’s medical history and must not potentially exacerbate ≥1 comorbid medical conditions.
Conclusion: Medical training and psychiatric residency are required.
Third: Knowledge of metabolic pathways of each psychiatric medication to be prescribed as well as the metabolic pathway of all other medications (psychiatric and non-psychiatric) the patient receives is essential to avoid adverse drug–drug interactions. This includes the hepatic enzymes (cytochromes), which often are responsible for metabolizing all the psychiatric and non-psychiatric drugs a patient is receiving. Knowledge of inhibitors and inducers of various cytochrome enzymes is vital for selecting a medication that does not cause a pharmacokinetic adverse reaction that can produce serious adverse effects (even death, such as with QTc prolongation) or can cause loss of efficacy of ≥1 medications that the patient is receiving, in addition to the antidepressant. Also, in addition to evaluating hepatic pathways, knowledge of renal excretion of the drug to be selected and the status of the patient’s kidney function or impairment must be evaluated.
Conclusion: Medical training is required.
Fourth: Laboratory ordering and monitoring. Ordering laboratory data during follow-up of a patient receiving a psychotropic drug is necessary to monitor serum concentrations and ensure a therapeutic range, or to check for serious adverse effects on various organ systems that could be affected by many psychiatric drugs (CNS, cardiovascular, gastrointestinal, sexual, endocrine, pulmonary, hepatic, renal, dermatologic, ophthalmologic, etc.).
Conclusion: Medical training is required.
Fifth: General medical treatment. Many patients might require combination drug therapy because of inadequate response to monotherapy. Clinicians must know what is rational and evidence-based polypharmacy and what is irrational, dangerous, or absurd polypharmacy.9 When possible, parsimonious pharmacotherapy should be employed to minimize the number of medications prescribed.10 A patient could experience severe drug–drug reactions that could lead to cardiopulmonary crises. The clinician must be able to examine, intervene, and manage the patient’s medical distress until help arrives.
Conclusion: Medical training is required.
Sixth: Pregnancy. Knowledge about the pharmacotherapeutic aspects of pregnant women with mental illness is critical. Full knowledge about what can or should not be prescribed during pregnancy (ie, avoiding teratogenic agents) is vital for physicians treating women with psychiatric illness who become pregnant.
Conclusion: Medical training is required.
Although I am against prescriptive privileges for psychologists, I want to emphasize how much I appreciate and respect what psychologists do for patients with mental illness. Their psychotherapy skills often are honed beyond those of psychiatrists who, by necessity, focus on medical diagnosis and pharmacotherapeutic management. Combination of pharmacotherapy and psychotherapy has been demonstrated to be superior to medications alone. In the 25 years since psychologists have been eagerly pursuing prescriptive privileges, neuroscience research has revealed the neurobiologic effects of psychotherapy. Many studies have shown that evidence-based psychotherapy can induce the same structural and functional brain changes as medications11,12 and can influence biomarkers that accompany psychiatric disorders just as medications do.13
Psychologists should reconsider the many potential hazards of prescription drugs compared with the relative safety and efficacy of psychotherapy. They should focus on their qualifications and main strength, which is psychotherapy, and collaborate with psychiatrists and nurse practitioners on a biopsychosocial approach to mental illness. They also should realize how physically ill most psychiatric patients are and the complex medical management they need for their myriad comorbidities.
Just as I began this editorial with an anecdote, I will end with an illustrative one as well. As an academic professor for the past 3 decades who has trained and supervised numerous psychiatric residents, I once closely supervised a former PhD psychologist who decided to become a psychiatrist by going to medical school, followed by a 4-year psychiatric residency. I asked her to compare her experience and functioning as a psychologist with her current work as a fourth-year psychiatric resident. Her response was enlightening: She said the 2 professions are vastly different in their knowledge base and in terms of how they conceptualize mental illness from a psychological vs medical model. As for prescribing medications, she added that even after 8 years of extensive medical training as a physician and a psychiatrist, she feels there is still much to learn about psychopharmacology to ensure not only efficacy but also safety, because a majority of psychiatric patients have ≥1 coexisting medical conditions and substance use as well. Based on her own experience as a psychologist who became a psychiatric physician, she was completely opposed to prescriptive privileges for psychologists unless they go to medical school and become eligible to prescribe safely.
This former resident is now a successful academic psychiatrist who continues to hone her psychopharmacology skills. State legislators should listen to professionals like her before they pass a law giving prescriptive authority to psychologists without having to go through the rigors of 28,000 hours of training in the 8 years of medical school and psychiatric residency. Legislators should also understand that like psychologists, social work counselors have hardly any medical training, yet they have never sought prescriptive privileges. That’s clearly rational and wise.
1. Rosie Ruiz tries to steal the Boston marathon. Runner’s World. http://www.runnersworld.com/running-times-info/rosie-ruiz-tries-to-steal-the-boston-marathon. Published July 1, 1980. Accessed May 15, 2017.
2. Nelson, JC, Spyker DA. Morbidity and mortality associated with medications used in the treatment of depression: an analysis of cases reported to U.S. Poison Control Centers, 2000-2014. Am J Psychiatry. 2017;174(5):438-450.
3. Robiner WN, Bearman DL, Berman M, et al. Prescriptive authority for psychologists: despite deficits in education and knowledge? J Clin Psychol Med Settings. 2003;10(3):211-221.
4. Robiner WN, Bearman DL, Berman M, et al. Prescriptive authority for psychologists: a looming health hazard? Clinical Psychology Science and Practice. 2002;9(3):231-248.
5. Kingsbury SJ. Some effects of prescribing privileges. Am Psychol. 1992;47(3):426-427.
6. Pollitt B. Fools gold: psychologists using disingenuous reasoning to mislead legislatures into granting psychologists prescriptive authority. Am J Law Med. 2003;29:489-524.
7. DeNelsky GY. The case against prescription privileges for psychologists. Am Psychol. 1996;51(3):207-212.
8. Walker K. An ethical dilemma: clinical psychologists prescribing psychotropic medications. Issues Ment Health Nurs. 2002;23(1):17-29.
9. Nasrallah HA. Polypharmacy subtypes: the necessary, the reasonable, the ridiculous and the hazardous. Current Psychiatry. 2011;10(4):10-12.
10. Nasrallah HA. Parsimonious pharmacotherapy. Current Psychiatry. 2011;10(5):12-16.
11. Shou H, Yang Z, Satterthwaite TD, et al. Cognitive behavioral therapy increases amygdala connectivity with the cognitive control network in both MDD and PTSD. Neuroimage Clin. 2017;14:464-470.
12. Månsson KN, Salami A, Frick A, et al. Neuroplasticity in response to cognitive behavior therapy for social anxiety disorder. Transl Psychiatry. 2015;5:e727.
13. Redei EE, Andrus BM, Kwasny MJ, et al. Blood transcriptomic biomarkers in adult primary care patients with major depressive disorder undergoing cognitive behavioral therapy. Transl Psychiatry. 2014;4:e442.
Practicing medicine without a license is a crime, but it seems to have become a hollow law. Politicians are now cynically legalizing it by granting prescribing privileges to individuals with no prior foundation of medical training. Perhaps it is because of serious ignorance of the difference between psychiatry and psychology or MD and PhD degrees. Or perhaps it is a quid pro quo to generous donors to their re-election campaigns who seek a convenient shortcut to the 28,000 hours it takes to become a psychiatrist in 8 years of medical school and psychiatric residency—and that comes after 4 years of college.
I recently consulted an attorney to discuss some legal documents. When he asked me what my line of work is, I then asked him if he knew the difference between a psychiatrist and a psychologist. He hesitated before admitting in an embarrassed tone that he did not really know and thought that they were all “shrinks” and very similar. I then informed him that both go through undergraduate college education, albeit taking very different courses, with pre-med scientific emphasis for future psychiatric physicians and predominately psychology emphasis for future psychologists.
However, psychiatrists then attend medical school for 4 years and rotate on multiple hospital-based medical specialties, such as internal medicine, surgery, pediatrics, obstetrics and gynecology, family medicine, neurology, pathology, psychiatry, ophthalmology, dermatology, anesthesia, radiology, otolaryngology, etc.
Psychologists, on the other hand, take additional advanced psychology courses in graduate school and write a dissertation that requires quite a bit of library time. After getting a MD, future psychiatrists spend 4 years in extensive training in residency programs across inpatient wards and outpatient clinics, assessing the physical and mental health of seriously sick patients with emphasis on both pharmacological and psychotherapeutic treatments for serious psychiatric disorders in patients, the majority of whom have comorbid medical conditions as well. Psychologists, on the other hand, spend 1 year of internship after getting their PhD or PsyD degree, essentially focused on developing counseling and psychotherapy skills. By the time they complete their training, psychologists and psychiatrists have disparate skills: heavily medical and pharmacological skills in psychiatrists and strong psychotherapeutic skills in psychologists.
After this long explanation, I asked the attorney what he thought about psychologists seeking prescription privileges. He was astounded that psychologists would attempt to expand this scope of practice through state legislations rather than going through medical training like all physicians. “That would be like practicing medicine without a license, which is a felony,” he said. He wryly added that his fellow malpractice and litigation lawyers will be the big winners while poorly treated patients will be the biggest losers. Being an avid runner, he also added that such a short-cut to prescribe without the requisite years of medial training reminded him of Rosie Ruiz, who snuck into the Boston marathon a couple of miles before the finish line and “won” the race, before she was caught and discredited.1
Psychology is a respected mental health discipline with strong psychotherapy training and orientation. For decades, psychologists have vigorously criticized the medical model of mental disorders that psychiatric physicians employ to diagnose and treat brain disorders that disrupt thinking, emotions, mood, cognition, and behavior. However, about 25 years ago, a small group of militant psychologists brazenly decided to lobby state legislatures to give them the right to prescribe psychotropics, although they have no formal medical training. Psychiatric physicians, represented by the American Psychiatric Association (APA), strongly opposed this initiative and regarded it as reckless disregard of the obvious need for extensive medical training to be able to prescribe drugs that affect every organ in the body, not only the brain. Psychiatric medications are associated with serious risks of morbidity and mortality.2 The ability to safely prescribe any medication represents the tip of a huge iceberg of 8 years of rigorous medical school education and specialty training. Yet, one of the early proponents of prescription privileges for psychologists, Patrick De Leon, sarcastically likened the ability to prescribe drugs to learning how to operate a desktop computer!
Not all psychologists agreed with the political campaign to lobby state legislatures to pass a law authorizing prescriptive privileges for psychologists.3-6 In fact, most academic psychologists oppose it.7 Most of the early supporters had a PsyD degree from professional schools of psychology, not a PhD degree in psychology, which is obtained from a university department of psychology. The National Alliance on Mental Illness is opposed to psychologists prescribing medications.8 Psychiatrists are outraged by this hazardous “solution” to the shortage of psychiatrists and point to the many potential dangers to patients. Some suggested that this is a quick way to enhance psychologists’ income and to generate more revenue for their professional journals and meetings with lucrative pharmaceutical ads and exhibit booths.
The campaign is ongoing, as Idaho became the fifth state to adopt such an ill-conceived “solution” to increasing access to mental health care, despite valiant effort by the APA to lobby against such laws. Although New Mexico (2002), Louisiana (2004), Illinois (2014), and Iowa (2016) have passed prescriptive authority for psychologists before Idaho, the APA has defeated such measures in numerous other states. But the painful truth is that this has been a lengthy political chess game in which psychologists have been gradually gaining ground and “capturing more pieces.”
Here is a brief, common sense rationale as to the need for full medical training necessary before safely and accurately prescribing medications, most of which are synthetic molecules, which are essentially foreign substances, with both benefits and risks detailed in the FDA-approved label of each drug that reaches the medical marketplace.
First: Making an accurate clinical diagnosis. If a patient presents with depression, the clinician must rule out other possible causes before diagnosing it as primary major depressive disorder for which an antidepressant can be prescribed. The panoply of secondary depressions, which are not treated with antidepressants, includes a variety of recreational drug-induced mood changes and dysphoria and depression induced by numerous prescription drugs (such as antihypertensives, hormonal contraceptives, steroids, interferon, proton pump inhibitors, H2 blockers, malaria drugs, etc.).
After drug-induced depression is ruled out, the clinician must rule out the possibility that an underlying medical condition might be causing the depression, which includes disorders such as hypothyroidism and other endocrinopathies, anemia, stroke, heart disease, hyperkalemia, lupus and other autoimmune disorders, cancer, Parkinsonism, etc. Therefore, a targeted exploration of past and current medical history, accompanied by a battery of lab tests (complete blood count, electrolytes, liver and kidney function tests, metabolic profile, thyroid-stimulating hormone, etc.) must be done to systematically arrive at the correct diagnosis. Only then can the proper treatment plan be determined, which may or may not include prescribing an antidepressant.
Conclusion: Medical training and psychiatric residency are required for an accurate diagnosis of a mental disorder. Even physicians with no psychiatric training might not have the full repertoire of knowledge needed to systematically rule out secondary depression.
Second: Drug selection. Psychiatric drugs can have various iatrogenic effects. Thus, the selection of an appropriate prescription medication from the available array of drugs approved for a given psychiatric indication must be safe and consistent with the patient’s medical history and must not potentially exacerbate ≥1 comorbid medical conditions.
Conclusion: Medical training and psychiatric residency are required.
Third: Knowledge of metabolic pathways of each psychiatric medication to be prescribed as well as the metabolic pathway of all other medications (psychiatric and non-psychiatric) the patient receives is essential to avoid adverse drug–drug interactions. This includes the hepatic enzymes (cytochromes), which often are responsible for metabolizing all the psychiatric and non-psychiatric drugs a patient is receiving. Knowledge of inhibitors and inducers of various cytochrome enzymes is vital for selecting a medication that does not cause a pharmacokinetic adverse reaction that can produce serious adverse effects (even death, such as with QTc prolongation) or can cause loss of efficacy of ≥1 medications that the patient is receiving, in addition to the antidepressant. Also, in addition to evaluating hepatic pathways, knowledge of renal excretion of the drug to be selected and the status of the patient’s kidney function or impairment must be evaluated.
Conclusion: Medical training is required.
Fourth: Laboratory ordering and monitoring. Ordering laboratory data during follow-up of a patient receiving a psychotropic drug is necessary to monitor serum concentrations and ensure a therapeutic range, or to check for serious adverse effects on various organ systems that could be affected by many psychiatric drugs (CNS, cardiovascular, gastrointestinal, sexual, endocrine, pulmonary, hepatic, renal, dermatologic, ophthalmologic, etc.).
Conclusion: Medical training is required.
Fifth: General medical treatment. Many patients might require combination drug therapy because of inadequate response to monotherapy. Clinicians must know what is rational and evidence-based polypharmacy and what is irrational, dangerous, or absurd polypharmacy.9 When possible, parsimonious pharmacotherapy should be employed to minimize the number of medications prescribed.10 A patient could experience severe drug–drug reactions that could lead to cardiopulmonary crises. The clinician must be able to examine, intervene, and manage the patient’s medical distress until help arrives.
Conclusion: Medical training is required.
Sixth: Pregnancy. Knowledge about the pharmacotherapeutic aspects of pregnant women with mental illness is critical. Full knowledge about what can or should not be prescribed during pregnancy (ie, avoiding teratogenic agents) is vital for physicians treating women with psychiatric illness who become pregnant.
Conclusion: Medical training is required.
Although I am against prescriptive privileges for psychologists, I want to emphasize how much I appreciate and respect what psychologists do for patients with mental illness. Their psychotherapy skills often are honed beyond those of psychiatrists who, by necessity, focus on medical diagnosis and pharmacotherapeutic management. Combination of pharmacotherapy and psychotherapy has been demonstrated to be superior to medications alone. In the 25 years since psychologists have been eagerly pursuing prescriptive privileges, neuroscience research has revealed the neurobiologic effects of psychotherapy. Many studies have shown that evidence-based psychotherapy can induce the same structural and functional brain changes as medications11,12 and can influence biomarkers that accompany psychiatric disorders just as medications do.13
Psychologists should reconsider the many potential hazards of prescription drugs compared with the relative safety and efficacy of psychotherapy. They should focus on their qualifications and main strength, which is psychotherapy, and collaborate with psychiatrists and nurse practitioners on a biopsychosocial approach to mental illness. They also should realize how physically ill most psychiatric patients are and the complex medical management they need for their myriad comorbidities.
Just as I began this editorial with an anecdote, I will end with an illustrative one as well. As an academic professor for the past 3 decades who has trained and supervised numerous psychiatric residents, I once closely supervised a former PhD psychologist who decided to become a psychiatrist by going to medical school, followed by a 4-year psychiatric residency. I asked her to compare her experience and functioning as a psychologist with her current work as a fourth-year psychiatric resident. Her response was enlightening: She said the 2 professions are vastly different in their knowledge base and in terms of how they conceptualize mental illness from a psychological vs medical model. As for prescribing medications, she added that even after 8 years of extensive medical training as a physician and a psychiatrist, she feels there is still much to learn about psychopharmacology to ensure not only efficacy but also safety, because a majority of psychiatric patients have ≥1 coexisting medical conditions and substance use as well. Based on her own experience as a psychologist who became a psychiatric physician, she was completely opposed to prescriptive privileges for psychologists unless they go to medical school and become eligible to prescribe safely.
This former resident is now a successful academic psychiatrist who continues to hone her psychopharmacology skills. State legislators should listen to professionals like her before they pass a law giving prescriptive authority to psychologists without having to go through the rigors of 28,000 hours of training in the 8 years of medical school and psychiatric residency. Legislators should also understand that like psychologists, social work counselors have hardly any medical training, yet they have never sought prescriptive privileges. That’s clearly rational and wise.
Practicing medicine without a license is a crime, but it seems to have become a hollow law. Politicians are now cynically legalizing it by granting prescribing privileges to individuals with no prior foundation of medical training. Perhaps it is because of serious ignorance of the difference between psychiatry and psychology or MD and PhD degrees. Or perhaps it is a quid pro quo to generous donors to their re-election campaigns who seek a convenient shortcut to the 28,000 hours it takes to become a psychiatrist in 8 years of medical school and psychiatric residency—and that comes after 4 years of college.
I recently consulted an attorney to discuss some legal documents. When he asked me what my line of work is, I then asked him if he knew the difference between a psychiatrist and a psychologist. He hesitated before admitting in an embarrassed tone that he did not really know and thought that they were all “shrinks” and very similar. I then informed him that both go through undergraduate college education, albeit taking very different courses, with pre-med scientific emphasis for future psychiatric physicians and predominately psychology emphasis for future psychologists.
However, psychiatrists then attend medical school for 4 years and rotate on multiple hospital-based medical specialties, such as internal medicine, surgery, pediatrics, obstetrics and gynecology, family medicine, neurology, pathology, psychiatry, ophthalmology, dermatology, anesthesia, radiology, otolaryngology, etc.
Psychologists, on the other hand, take additional advanced psychology courses in graduate school and write a dissertation that requires quite a bit of library time. After getting a MD, future psychiatrists spend 4 years in extensive training in residency programs across inpatient wards and outpatient clinics, assessing the physical and mental health of seriously sick patients with emphasis on both pharmacological and psychotherapeutic treatments for serious psychiatric disorders in patients, the majority of whom have comorbid medical conditions as well. Psychologists, on the other hand, spend 1 year of internship after getting their PhD or PsyD degree, essentially focused on developing counseling and psychotherapy skills. By the time they complete their training, psychologists and psychiatrists have disparate skills: heavily medical and pharmacological skills in psychiatrists and strong psychotherapeutic skills in psychologists.
After this long explanation, I asked the attorney what he thought about psychologists seeking prescription privileges. He was astounded that psychologists would attempt to expand this scope of practice through state legislations rather than going through medical training like all physicians. “That would be like practicing medicine without a license, which is a felony,” he said. He wryly added that his fellow malpractice and litigation lawyers will be the big winners while poorly treated patients will be the biggest losers. Being an avid runner, he also added that such a short-cut to prescribe without the requisite years of medial training reminded him of Rosie Ruiz, who snuck into the Boston marathon a couple of miles before the finish line and “won” the race, before she was caught and discredited.1
Psychology is a respected mental health discipline with strong psychotherapy training and orientation. For decades, psychologists have vigorously criticized the medical model of mental disorders that psychiatric physicians employ to diagnose and treat brain disorders that disrupt thinking, emotions, mood, cognition, and behavior. However, about 25 years ago, a small group of militant psychologists brazenly decided to lobby state legislatures to give them the right to prescribe psychotropics, although they have no formal medical training. Psychiatric physicians, represented by the American Psychiatric Association (APA), strongly opposed this initiative and regarded it as reckless disregard of the obvious need for extensive medical training to be able to prescribe drugs that affect every organ in the body, not only the brain. Psychiatric medications are associated with serious risks of morbidity and mortality.2 The ability to safely prescribe any medication represents the tip of a huge iceberg of 8 years of rigorous medical school education and specialty training. Yet, one of the early proponents of prescription privileges for psychologists, Patrick De Leon, sarcastically likened the ability to prescribe drugs to learning how to operate a desktop computer!
Not all psychologists agreed with the political campaign to lobby state legislatures to pass a law authorizing prescriptive privileges for psychologists.3-6 In fact, most academic psychologists oppose it.7 Most of the early supporters had a PsyD degree from professional schools of psychology, not a PhD degree in psychology, which is obtained from a university department of psychology. The National Alliance on Mental Illness is opposed to psychologists prescribing medications.8 Psychiatrists are outraged by this hazardous “solution” to the shortage of psychiatrists and point to the many potential dangers to patients. Some suggested that this is a quick way to enhance psychologists’ income and to generate more revenue for their professional journals and meetings with lucrative pharmaceutical ads and exhibit booths.
The campaign is ongoing, as Idaho became the fifth state to adopt such an ill-conceived “solution” to increasing access to mental health care, despite valiant effort by the APA to lobby against such laws. Although New Mexico (2002), Louisiana (2004), Illinois (2014), and Iowa (2016) have passed prescriptive authority for psychologists before Idaho, the APA has defeated such measures in numerous other states. But the painful truth is that this has been a lengthy political chess game in which psychologists have been gradually gaining ground and “capturing more pieces.”
Here is a brief, common sense rationale as to the need for full medical training necessary before safely and accurately prescribing medications, most of which are synthetic molecules, which are essentially foreign substances, with both benefits and risks detailed in the FDA-approved label of each drug that reaches the medical marketplace.
First: Making an accurate clinical diagnosis. If a patient presents with depression, the clinician must rule out other possible causes before diagnosing it as primary major depressive disorder for which an antidepressant can be prescribed. The panoply of secondary depressions, which are not treated with antidepressants, includes a variety of recreational drug-induced mood changes and dysphoria and depression induced by numerous prescription drugs (such as antihypertensives, hormonal contraceptives, steroids, interferon, proton pump inhibitors, H2 blockers, malaria drugs, etc.).
After drug-induced depression is ruled out, the clinician must rule out the possibility that an underlying medical condition might be causing the depression, which includes disorders such as hypothyroidism and other endocrinopathies, anemia, stroke, heart disease, hyperkalemia, lupus and other autoimmune disorders, cancer, Parkinsonism, etc. Therefore, a targeted exploration of past and current medical history, accompanied by a battery of lab tests (complete blood count, electrolytes, liver and kidney function tests, metabolic profile, thyroid-stimulating hormone, etc.) must be done to systematically arrive at the correct diagnosis. Only then can the proper treatment plan be determined, which may or may not include prescribing an antidepressant.
Conclusion: Medical training and psychiatric residency are required for an accurate diagnosis of a mental disorder. Even physicians with no psychiatric training might not have the full repertoire of knowledge needed to systematically rule out secondary depression.
Second: Drug selection. Psychiatric drugs can have various iatrogenic effects. Thus, the selection of an appropriate prescription medication from the available array of drugs approved for a given psychiatric indication must be safe and consistent with the patient’s medical history and must not potentially exacerbate ≥1 comorbid medical conditions.
Conclusion: Medical training and psychiatric residency are required.
Third: Knowledge of metabolic pathways of each psychiatric medication to be prescribed as well as the metabolic pathway of all other medications (psychiatric and non-psychiatric) the patient receives is essential to avoid adverse drug–drug interactions. This includes the hepatic enzymes (cytochromes), which often are responsible for metabolizing all the psychiatric and non-psychiatric drugs a patient is receiving. Knowledge of inhibitors and inducers of various cytochrome enzymes is vital for selecting a medication that does not cause a pharmacokinetic adverse reaction that can produce serious adverse effects (even death, such as with QTc prolongation) or can cause loss of efficacy of ≥1 medications that the patient is receiving, in addition to the antidepressant. Also, in addition to evaluating hepatic pathways, knowledge of renal excretion of the drug to be selected and the status of the patient’s kidney function or impairment must be evaluated.
Conclusion: Medical training is required.
Fourth: Laboratory ordering and monitoring. Ordering laboratory data during follow-up of a patient receiving a psychotropic drug is necessary to monitor serum concentrations and ensure a therapeutic range, or to check for serious adverse effects on various organ systems that could be affected by many psychiatric drugs (CNS, cardiovascular, gastrointestinal, sexual, endocrine, pulmonary, hepatic, renal, dermatologic, ophthalmologic, etc.).
Conclusion: Medical training is required.
Fifth: General medical treatment. Many patients might require combination drug therapy because of inadequate response to monotherapy. Clinicians must know what is rational and evidence-based polypharmacy and what is irrational, dangerous, or absurd polypharmacy.9 When possible, parsimonious pharmacotherapy should be employed to minimize the number of medications prescribed.10 A patient could experience severe drug–drug reactions that could lead to cardiopulmonary crises. The clinician must be able to examine, intervene, and manage the patient’s medical distress until help arrives.
Conclusion: Medical training is required.
Sixth: Pregnancy. Knowledge about the pharmacotherapeutic aspects of pregnant women with mental illness is critical. Full knowledge about what can or should not be prescribed during pregnancy (ie, avoiding teratogenic agents) is vital for physicians treating women with psychiatric illness who become pregnant.
Conclusion: Medical training is required.
Although I am against prescriptive privileges for psychologists, I want to emphasize how much I appreciate and respect what psychologists do for patients with mental illness. Their psychotherapy skills often are honed beyond those of psychiatrists who, by necessity, focus on medical diagnosis and pharmacotherapeutic management. Combination of pharmacotherapy and psychotherapy has been demonstrated to be superior to medications alone. In the 25 years since psychologists have been eagerly pursuing prescriptive privileges, neuroscience research has revealed the neurobiologic effects of psychotherapy. Many studies have shown that evidence-based psychotherapy can induce the same structural and functional brain changes as medications11,12 and can influence biomarkers that accompany psychiatric disorders just as medications do.13
Psychologists should reconsider the many potential hazards of prescription drugs compared with the relative safety and efficacy of psychotherapy. They should focus on their qualifications and main strength, which is psychotherapy, and collaborate with psychiatrists and nurse practitioners on a biopsychosocial approach to mental illness. They also should realize how physically ill most psychiatric patients are and the complex medical management they need for their myriad comorbidities.
Just as I began this editorial with an anecdote, I will end with an illustrative one as well. As an academic professor for the past 3 decades who has trained and supervised numerous psychiatric residents, I once closely supervised a former PhD psychologist who decided to become a psychiatrist by going to medical school, followed by a 4-year psychiatric residency. I asked her to compare her experience and functioning as a psychologist with her current work as a fourth-year psychiatric resident. Her response was enlightening: She said the 2 professions are vastly different in their knowledge base and in terms of how they conceptualize mental illness from a psychological vs medical model. As for prescribing medications, she added that even after 8 years of extensive medical training as a physician and a psychiatrist, she feels there is still much to learn about psychopharmacology to ensure not only efficacy but also safety, because a majority of psychiatric patients have ≥1 coexisting medical conditions and substance use as well. Based on her own experience as a psychologist who became a psychiatric physician, she was completely opposed to prescriptive privileges for psychologists unless they go to medical school and become eligible to prescribe safely.
This former resident is now a successful academic psychiatrist who continues to hone her psychopharmacology skills. State legislators should listen to professionals like her before they pass a law giving prescriptive authority to psychologists without having to go through the rigors of 28,000 hours of training in the 8 years of medical school and psychiatric residency. Legislators should also understand that like psychologists, social work counselors have hardly any medical training, yet they have never sought prescriptive privileges. That’s clearly rational and wise.
1. Rosie Ruiz tries to steal the Boston marathon. Runner’s World. http://www.runnersworld.com/running-times-info/rosie-ruiz-tries-to-steal-the-boston-marathon. Published July 1, 1980. Accessed May 15, 2017.
2. Nelson, JC, Spyker DA. Morbidity and mortality associated with medications used in the treatment of depression: an analysis of cases reported to U.S. Poison Control Centers, 2000-2014. Am J Psychiatry. 2017;174(5):438-450.
3. Robiner WN, Bearman DL, Berman M, et al. Prescriptive authority for psychologists: despite deficits in education and knowledge? J Clin Psychol Med Settings. 2003;10(3):211-221.
4. Robiner WN, Bearman DL, Berman M, et al. Prescriptive authority for psychologists: a looming health hazard? Clinical Psychology Science and Practice. 2002;9(3):231-248.
5. Kingsbury SJ. Some effects of prescribing privileges. Am Psychol. 1992;47(3):426-427.
6. Pollitt B. Fools gold: psychologists using disingenuous reasoning to mislead legislatures into granting psychologists prescriptive authority. Am J Law Med. 2003;29:489-524.
7. DeNelsky GY. The case against prescription privileges for psychologists. Am Psychol. 1996;51(3):207-212.
8. Walker K. An ethical dilemma: clinical psychologists prescribing psychotropic medications. Issues Ment Health Nurs. 2002;23(1):17-29.
9. Nasrallah HA. Polypharmacy subtypes: the necessary, the reasonable, the ridiculous and the hazardous. Current Psychiatry. 2011;10(4):10-12.
10. Nasrallah HA. Parsimonious pharmacotherapy. Current Psychiatry. 2011;10(5):12-16.
11. Shou H, Yang Z, Satterthwaite TD, et al. Cognitive behavioral therapy increases amygdala connectivity with the cognitive control network in both MDD and PTSD. Neuroimage Clin. 2017;14:464-470.
12. Månsson KN, Salami A, Frick A, et al. Neuroplasticity in response to cognitive behavior therapy for social anxiety disorder. Transl Psychiatry. 2015;5:e727.
13. Redei EE, Andrus BM, Kwasny MJ, et al. Blood transcriptomic biomarkers in adult primary care patients with major depressive disorder undergoing cognitive behavioral therapy. Transl Psychiatry. 2014;4:e442.
1. Rosie Ruiz tries to steal the Boston marathon. Runner’s World. http://www.runnersworld.com/running-times-info/rosie-ruiz-tries-to-steal-the-boston-marathon. Published July 1, 1980. Accessed May 15, 2017.
2. Nelson, JC, Spyker DA. Morbidity and mortality associated with medications used in the treatment of depression: an analysis of cases reported to U.S. Poison Control Centers, 2000-2014. Am J Psychiatry. 2017;174(5):438-450.
3. Robiner WN, Bearman DL, Berman M, et al. Prescriptive authority for psychologists: despite deficits in education and knowledge? J Clin Psychol Med Settings. 2003;10(3):211-221.
4. Robiner WN, Bearman DL, Berman M, et al. Prescriptive authority for psychologists: a looming health hazard? Clinical Psychology Science and Practice. 2002;9(3):231-248.
5. Kingsbury SJ. Some effects of prescribing privileges. Am Psychol. 1992;47(3):426-427.
6. Pollitt B. Fools gold: psychologists using disingenuous reasoning to mislead legislatures into granting psychologists prescriptive authority. Am J Law Med. 2003;29:489-524.
7. DeNelsky GY. The case against prescription privileges for psychologists. Am Psychol. 1996;51(3):207-212.
8. Walker K. An ethical dilemma: clinical psychologists prescribing psychotropic medications. Issues Ment Health Nurs. 2002;23(1):17-29.
9. Nasrallah HA. Polypharmacy subtypes: the necessary, the reasonable, the ridiculous and the hazardous. Current Psychiatry. 2011;10(4):10-12.
10. Nasrallah HA. Parsimonious pharmacotherapy. Current Psychiatry. 2011;10(5):12-16.
11. Shou H, Yang Z, Satterthwaite TD, et al. Cognitive behavioral therapy increases amygdala connectivity with the cognitive control network in both MDD and PTSD. Neuroimage Clin. 2017;14:464-470.
12. Månsson KN, Salami A, Frick A, et al. Neuroplasticity in response to cognitive behavior therapy for social anxiety disorder. Transl Psychiatry. 2015;5:e727.
13. Redei EE, Andrus BM, Kwasny MJ, et al. Blood transcriptomic biomarkers in adult primary care patients with major depressive disorder undergoing cognitive behavioral therapy. Transl Psychiatry. 2014;4:e442.
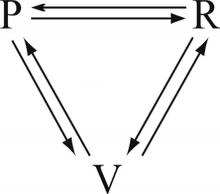
Leadership hacks: The drama triangle
There are plenty of leadership books, seminars, podcasts, and websites available for the aspiring physician leader. However, not all of them are pertinent to the health care environment. As chairman of a large academic department, I have sifted through some of these resources and have found a few that have been particularly helpful to me. One of the more useful is the drama triangle.
Here’s an example: Pat, the administrator, just sent Sam an email stating that, starting today, all computers will be automatically turned off at 5 p.m. and cannot be restarted until 8 a.m. the next day. The reasons are many but unimportant to Sam because they pale in comparison to the inconvenience this places on Sam’s ability to finish work in the evening. No one asked about this change or even gave advance warning.
Anger builds in Sam, especially toward Pat. Something has to be done about this! That something becomes a petition to Kelly, a supervisor/manager/director/chairman with authority. Sam recounts the surprise of the order, details the inefficiencies created, expresses indignation at not being consulted first, lists the personal failings of Pat, and demands an immediate resolution to the problem. Kelly wants to help Sam and approaches Pat to reverse the order. Kelly feels good about helping Sam, and Sam feels great about going to Kelly. Pat doesn’t feel good at all.
Sam started, and Kelly completed, the drama triangle.
Breaking a drama triangle requires uncomfortable work building trust and a more functional relationship between the three players. Ideally, the victim becomes challenged, not threatened. The rescuer becomes a coach, not an enabler. The persecutor raises the bar rather than creating obstacles. With roles redefined, trust is restored. There are many methods and techniques to develop psychological safety and interdependent trust, but the work is the critical first step toward improving the function of a team (Lencioni, P. (2002). The Five Dysfunctions of a Team. Jossey-Bass).
What could Kelly have done to stop a triangle from forming? Sam wanted help, and Kelly’s first instinct is to do just that. However, by completing the triangle with a visit to Pat, Kelly creates more tension between Pat and Sam. To help both Sam and Pat, Kelly has to resist the temptation to rescue Sam from Pat and instead leverage Sam’s trust to begin asking Sam questions that lead Sam toward resolution of Sam’s own problem.
Aware of drama triangles, Kelly asks Sam what the ideal situation would be. Sam replies that all the work would get done by the end of the day. Kelly then asks what the current situation is. According to Pat, the computers turn off at 5, but the work is not done by then. Then, Kelly asks Sam what could be done before 5 that would help get the work done. Sam considers the question and then begins to list some changes to work flow that could allow greater efficiency during the day. Sam also decides to meet with Pat to explain how the two of them can improve communication in the future. Through coaching, Kelly defuses Sam’s anger, avoids a drama triangle, and gets Sam to start considering previously unknown solutions. The model Kelly uses to begin the work of breaking the triangle is sometimes called structural, or dynamic, tension.
Drama triangles compromise trust. The workplace culture can either enable simmering tensions and resentments to persist or it can foster psychological safety that allows for open and honest debate whereby all are heard and validated when change inevitably occurs. Exploring structural tension can build a sense of team and restore trust. A more robust discussion of structural tension will have to wait until my next column. In the meantime, as yourselves, Where do you see drama triangles? What worked to break them? What failed?
For more reading: Emerald, D. (2010). The Power of Ted* (The Empowerment Dynamic). Bainbridge Island, WA: Polaris Publishing.
I invite you to reply to [email protected] to initiate a broader discussion of physician leadership. Responses will be posted to hematologynews.com. Dr. Kalaycio is editor in chief of Hematology News. Dr. Kalaycio chairs the department of hematologic oncology and blood disorders at Cleveland Clinic Taussig Cancer Institute. Contact him at [email protected].
There are plenty of leadership books, seminars, podcasts, and websites available for the aspiring physician leader. However, not all of them are pertinent to the health care environment. As chairman of a large academic department, I have sifted through some of these resources and have found a few that have been particularly helpful to me. One of the more useful is the drama triangle.
Here’s an example: Pat, the administrator, just sent Sam an email stating that, starting today, all computers will be automatically turned off at 5 p.m. and cannot be restarted until 8 a.m. the next day. The reasons are many but unimportant to Sam because they pale in comparison to the inconvenience this places on Sam’s ability to finish work in the evening. No one asked about this change or even gave advance warning.
Anger builds in Sam, especially toward Pat. Something has to be done about this! That something becomes a petition to Kelly, a supervisor/manager/director/chairman with authority. Sam recounts the surprise of the order, details the inefficiencies created, expresses indignation at not being consulted first, lists the personal failings of Pat, and demands an immediate resolution to the problem. Kelly wants to help Sam and approaches Pat to reverse the order. Kelly feels good about helping Sam, and Sam feels great about going to Kelly. Pat doesn’t feel good at all.
Sam started, and Kelly completed, the drama triangle.
Breaking a drama triangle requires uncomfortable work building trust and a more functional relationship between the three players. Ideally, the victim becomes challenged, not threatened. The rescuer becomes a coach, not an enabler. The persecutor raises the bar rather than creating obstacles. With roles redefined, trust is restored. There are many methods and techniques to develop psychological safety and interdependent trust, but the work is the critical first step toward improving the function of a team (Lencioni, P. (2002). The Five Dysfunctions of a Team. Jossey-Bass).
What could Kelly have done to stop a triangle from forming? Sam wanted help, and Kelly’s first instinct is to do just that. However, by completing the triangle with a visit to Pat, Kelly creates more tension between Pat and Sam. To help both Sam and Pat, Kelly has to resist the temptation to rescue Sam from Pat and instead leverage Sam’s trust to begin asking Sam questions that lead Sam toward resolution of Sam’s own problem.
Aware of drama triangles, Kelly asks Sam what the ideal situation would be. Sam replies that all the work would get done by the end of the day. Kelly then asks what the current situation is. According to Pat, the computers turn off at 5, but the work is not done by then. Then, Kelly asks Sam what could be done before 5 that would help get the work done. Sam considers the question and then begins to list some changes to work flow that could allow greater efficiency during the day. Sam also decides to meet with Pat to explain how the two of them can improve communication in the future. Through coaching, Kelly defuses Sam’s anger, avoids a drama triangle, and gets Sam to start considering previously unknown solutions. The model Kelly uses to begin the work of breaking the triangle is sometimes called structural, or dynamic, tension.
Drama triangles compromise trust. The workplace culture can either enable simmering tensions and resentments to persist or it can foster psychological safety that allows for open and honest debate whereby all are heard and validated when change inevitably occurs. Exploring structural tension can build a sense of team and restore trust. A more robust discussion of structural tension will have to wait until my next column. In the meantime, as yourselves, Where do you see drama triangles? What worked to break them? What failed?
For more reading: Emerald, D. (2010). The Power of Ted* (The Empowerment Dynamic). Bainbridge Island, WA: Polaris Publishing.
I invite you to reply to [email protected] to initiate a broader discussion of physician leadership. Responses will be posted to hematologynews.com. Dr. Kalaycio is editor in chief of Hematology News. Dr. Kalaycio chairs the department of hematologic oncology and blood disorders at Cleveland Clinic Taussig Cancer Institute. Contact him at [email protected].
There are plenty of leadership books, seminars, podcasts, and websites available for the aspiring physician leader. However, not all of them are pertinent to the health care environment. As chairman of a large academic department, I have sifted through some of these resources and have found a few that have been particularly helpful to me. One of the more useful is the drama triangle.
Here’s an example: Pat, the administrator, just sent Sam an email stating that, starting today, all computers will be automatically turned off at 5 p.m. and cannot be restarted until 8 a.m. the next day. The reasons are many but unimportant to Sam because they pale in comparison to the inconvenience this places on Sam’s ability to finish work in the evening. No one asked about this change or even gave advance warning.
Anger builds in Sam, especially toward Pat. Something has to be done about this! That something becomes a petition to Kelly, a supervisor/manager/director/chairman with authority. Sam recounts the surprise of the order, details the inefficiencies created, expresses indignation at not being consulted first, lists the personal failings of Pat, and demands an immediate resolution to the problem. Kelly wants to help Sam and approaches Pat to reverse the order. Kelly feels good about helping Sam, and Sam feels great about going to Kelly. Pat doesn’t feel good at all.
Sam started, and Kelly completed, the drama triangle.
Breaking a drama triangle requires uncomfortable work building trust and a more functional relationship between the three players. Ideally, the victim becomes challenged, not threatened. The rescuer becomes a coach, not an enabler. The persecutor raises the bar rather than creating obstacles. With roles redefined, trust is restored. There are many methods and techniques to develop psychological safety and interdependent trust, but the work is the critical first step toward improving the function of a team (Lencioni, P. (2002). The Five Dysfunctions of a Team. Jossey-Bass).
What could Kelly have done to stop a triangle from forming? Sam wanted help, and Kelly’s first instinct is to do just that. However, by completing the triangle with a visit to Pat, Kelly creates more tension between Pat and Sam. To help both Sam and Pat, Kelly has to resist the temptation to rescue Sam from Pat and instead leverage Sam’s trust to begin asking Sam questions that lead Sam toward resolution of Sam’s own problem.
Aware of drama triangles, Kelly asks Sam what the ideal situation would be. Sam replies that all the work would get done by the end of the day. Kelly then asks what the current situation is. According to Pat, the computers turn off at 5, but the work is not done by then. Then, Kelly asks Sam what could be done before 5 that would help get the work done. Sam considers the question and then begins to list some changes to work flow that could allow greater efficiency during the day. Sam also decides to meet with Pat to explain how the two of them can improve communication in the future. Through coaching, Kelly defuses Sam’s anger, avoids a drama triangle, and gets Sam to start considering previously unknown solutions. The model Kelly uses to begin the work of breaking the triangle is sometimes called structural, or dynamic, tension.
Drama triangles compromise trust. The workplace culture can either enable simmering tensions and resentments to persist or it can foster psychological safety that allows for open and honest debate whereby all are heard and validated when change inevitably occurs. Exploring structural tension can build a sense of team and restore trust. A more robust discussion of structural tension will have to wait until my next column. In the meantime, as yourselves, Where do you see drama triangles? What worked to break them? What failed?
For more reading: Emerald, D. (2010). The Power of Ted* (The Empowerment Dynamic). Bainbridge Island, WA: Polaris Publishing.
I invite you to reply to [email protected] to initiate a broader discussion of physician leadership. Responses will be posted to hematologynews.com. Dr. Kalaycio is editor in chief of Hematology News. Dr. Kalaycio chairs the department of hematologic oncology and blood disorders at Cleveland Clinic Taussig Cancer Institute. Contact him at [email protected].
Doing a lot with little – health care in Cuba
Although Cuba lies less than 100 miles from the United States, we Americans tend to know far less about the island nation than about almost any other country in our hemisphere. Only since 2014 has the United States begun to allow its citizens to travel directly to Cuba and has opened official diplomatic relations, although direct trade still remains blocked.
Cuba’s health care system has been touted as providing universal access to primary care services, whose goals are promoting health and preventing disease as well as providing free medical education to a veritable army of health care workers. Less well known are the quality and standards of their surgical services.
Although the Cuban government is a centralized, one-party state that follows the Marxist-Leninist ideology, every individual with whom we met answered our many questions with apparent candor. Perhaps our easy rapport was based to some degree on our common profession and our shared commitment to patient care. Although they were clearly proud of the quality of their free education and medical care, they were also quick to admit the shortcomings in their system: widespread poverty, shortages of food and advanced pharmaceuticals, and old medical facilities. We were not restricted in any way from moving around Havana or speaking with anyone, although our free time was admittedly limited because our busy schedule was crammed with at least two visits per day with the groups listed above.
We were interested in looking at how primary care was delivered in Cuba. We met with a primary care doctor in her office, which was situated on the ground floor of the apartment complex in which she and her patients lived. We also visited a polyclinic, two blocks from the primary care doctor’s office that serves as the next step up the chain and is the site where medical and surgical specialists come to consult with patients from 40-60 primary care practices clustered around the polyclinic. The walls of the polyclinic have posters that educate the patients about the importance of handwashing and prevention of hypertension and cancer. The polyclinic also has an epidemiologist who monitors such basic preventive services as immunizations and prenatal care, both of which achieve nearly 100% compliance in a society in which acceptance of these services is not optional. Pap smears are performed in the primary care clinics, as is comprehensive medical care.
As interesting and impressive as we found the primary care clinics, it was the visits with the surgeons in their hospitals that intrigued us the most. The surgeons we met were modest and collegial, yet proud of what they had accomplished under challenging resource constraints. The hospitals that we visited were reminiscent of the city and county hospitals in the United States in which many of us on the trip had trained in the 1970s: older facilities that were clean and serviceable, but with older, basic equipment. Nevertheless, C. Julian F. Ruiz Torres, MD, has developed minimally invasive surgery in a hospital dedicated to such technological advances. Although he is 72 years old, he still works tirelessly to obtain the resources to build a state-of-the-art surgical simulation center, now under construction. Basic minimally invasive surgical procedures are available in most hospitals, although advanced procedures are restricted to centers such as Dr. Ruiz Torres’ facility, Centro Nacional De Cirugia De Minimo Acceso, of which he is justifiably proud.
In the short time that we were in Cuba, we obviously could observe only a fraction of their entire system. We were unable to determine how representative the health care workers we met were; those we did meet, however, were committed, hard working, and idealistic. Their rewards are clearly not financial, as they are equally (and poorly) paid, earning the same $70/month, no matter what their “rank” in the system.
Whatever the political realities of life in Cuba may be outside of the medical setting, we connected with our fellow physicians and bonded over our shared passion for patient care. This trip was about meeting them and gaining some understanding of their professional challenges and their efforts to work with what they have. Their system has evolved in the unique cultural, political, and economic circumstances of Cuba, and so of course, such a system could never work here. And yet, it was refreshing and inspiring to see medical professionals dedicated to the ideals of our profession – serving the people by delivering the best care they could for all of their patients. My hat is off to them for accomplishing so much despite their limited resources.
Dr. Deveney is professor of surgery and vice chair of education in the department of surgery, Oregon Health & Science University, Portland. She is the coeditor of ACS Surgery News.
Although Cuba lies less than 100 miles from the United States, we Americans tend to know far less about the island nation than about almost any other country in our hemisphere. Only since 2014 has the United States begun to allow its citizens to travel directly to Cuba and has opened official diplomatic relations, although direct trade still remains blocked.
Cuba’s health care system has been touted as providing universal access to primary care services, whose goals are promoting health and preventing disease as well as providing free medical education to a veritable army of health care workers. Less well known are the quality and standards of their surgical services.
Although the Cuban government is a centralized, one-party state that follows the Marxist-Leninist ideology, every individual with whom we met answered our many questions with apparent candor. Perhaps our easy rapport was based to some degree on our common profession and our shared commitment to patient care. Although they were clearly proud of the quality of their free education and medical care, they were also quick to admit the shortcomings in their system: widespread poverty, shortages of food and advanced pharmaceuticals, and old medical facilities. We were not restricted in any way from moving around Havana or speaking with anyone, although our free time was admittedly limited because our busy schedule was crammed with at least two visits per day with the groups listed above.
We were interested in looking at how primary care was delivered in Cuba. We met with a primary care doctor in her office, which was situated on the ground floor of the apartment complex in which she and her patients lived. We also visited a polyclinic, two blocks from the primary care doctor’s office that serves as the next step up the chain and is the site where medical and surgical specialists come to consult with patients from 40-60 primary care practices clustered around the polyclinic. The walls of the polyclinic have posters that educate the patients about the importance of handwashing and prevention of hypertension and cancer. The polyclinic also has an epidemiologist who monitors such basic preventive services as immunizations and prenatal care, both of which achieve nearly 100% compliance in a society in which acceptance of these services is not optional. Pap smears are performed in the primary care clinics, as is comprehensive medical care.
As interesting and impressive as we found the primary care clinics, it was the visits with the surgeons in their hospitals that intrigued us the most. The surgeons we met were modest and collegial, yet proud of what they had accomplished under challenging resource constraints. The hospitals that we visited were reminiscent of the city and county hospitals in the United States in which many of us on the trip had trained in the 1970s: older facilities that were clean and serviceable, but with older, basic equipment. Nevertheless, C. Julian F. Ruiz Torres, MD, has developed minimally invasive surgery in a hospital dedicated to such technological advances. Although he is 72 years old, he still works tirelessly to obtain the resources to build a state-of-the-art surgical simulation center, now under construction. Basic minimally invasive surgical procedures are available in most hospitals, although advanced procedures are restricted to centers such as Dr. Ruiz Torres’ facility, Centro Nacional De Cirugia De Minimo Acceso, of which he is justifiably proud.
In the short time that we were in Cuba, we obviously could observe only a fraction of their entire system. We were unable to determine how representative the health care workers we met were; those we did meet, however, were committed, hard working, and idealistic. Their rewards are clearly not financial, as they are equally (and poorly) paid, earning the same $70/month, no matter what their “rank” in the system.
Whatever the political realities of life in Cuba may be outside of the medical setting, we connected with our fellow physicians and bonded over our shared passion for patient care. This trip was about meeting them and gaining some understanding of their professional challenges and their efforts to work with what they have. Their system has evolved in the unique cultural, political, and economic circumstances of Cuba, and so of course, such a system could never work here. And yet, it was refreshing and inspiring to see medical professionals dedicated to the ideals of our profession – serving the people by delivering the best care they could for all of their patients. My hat is off to them for accomplishing so much despite their limited resources.
Dr. Deveney is professor of surgery and vice chair of education in the department of surgery, Oregon Health & Science University, Portland. She is the coeditor of ACS Surgery News.
Although Cuba lies less than 100 miles from the United States, we Americans tend to know far less about the island nation than about almost any other country in our hemisphere. Only since 2014 has the United States begun to allow its citizens to travel directly to Cuba and has opened official diplomatic relations, although direct trade still remains blocked.
Cuba’s health care system has been touted as providing universal access to primary care services, whose goals are promoting health and preventing disease as well as providing free medical education to a veritable army of health care workers. Less well known are the quality and standards of their surgical services.
Although the Cuban government is a centralized, one-party state that follows the Marxist-Leninist ideology, every individual with whom we met answered our many questions with apparent candor. Perhaps our easy rapport was based to some degree on our common profession and our shared commitment to patient care. Although they were clearly proud of the quality of their free education and medical care, they were also quick to admit the shortcomings in their system: widespread poverty, shortages of food and advanced pharmaceuticals, and old medical facilities. We were not restricted in any way from moving around Havana or speaking with anyone, although our free time was admittedly limited because our busy schedule was crammed with at least two visits per day with the groups listed above.
We were interested in looking at how primary care was delivered in Cuba. We met with a primary care doctor in her office, which was situated on the ground floor of the apartment complex in which she and her patients lived. We also visited a polyclinic, two blocks from the primary care doctor’s office that serves as the next step up the chain and is the site where medical and surgical specialists come to consult with patients from 40-60 primary care practices clustered around the polyclinic. The walls of the polyclinic have posters that educate the patients about the importance of handwashing and prevention of hypertension and cancer. The polyclinic also has an epidemiologist who monitors such basic preventive services as immunizations and prenatal care, both of which achieve nearly 100% compliance in a society in which acceptance of these services is not optional. Pap smears are performed in the primary care clinics, as is comprehensive medical care.
As interesting and impressive as we found the primary care clinics, it was the visits with the surgeons in their hospitals that intrigued us the most. The surgeons we met were modest and collegial, yet proud of what they had accomplished under challenging resource constraints. The hospitals that we visited were reminiscent of the city and county hospitals in the United States in which many of us on the trip had trained in the 1970s: older facilities that were clean and serviceable, but with older, basic equipment. Nevertheless, C. Julian F. Ruiz Torres, MD, has developed minimally invasive surgery in a hospital dedicated to such technological advances. Although he is 72 years old, he still works tirelessly to obtain the resources to build a state-of-the-art surgical simulation center, now under construction. Basic minimally invasive surgical procedures are available in most hospitals, although advanced procedures are restricted to centers such as Dr. Ruiz Torres’ facility, Centro Nacional De Cirugia De Minimo Acceso, of which he is justifiably proud.
In the short time that we were in Cuba, we obviously could observe only a fraction of their entire system. We were unable to determine how representative the health care workers we met were; those we did meet, however, were committed, hard working, and idealistic. Their rewards are clearly not financial, as they are equally (and poorly) paid, earning the same $70/month, no matter what their “rank” in the system.
Whatever the political realities of life in Cuba may be outside of the medical setting, we connected with our fellow physicians and bonded over our shared passion for patient care. This trip was about meeting them and gaining some understanding of their professional challenges and their efforts to work with what they have. Their system has evolved in the unique cultural, political, and economic circumstances of Cuba, and so of course, such a system could never work here. And yet, it was refreshing and inspiring to see medical professionals dedicated to the ideals of our profession – serving the people by delivering the best care they could for all of their patients. My hat is off to them for accomplishing so much despite their limited resources.
Dr. Deveney is professor of surgery and vice chair of education in the department of surgery, Oregon Health & Science University, Portland. She is the coeditor of ACS Surgery News.
Repeal and replace? How about retain, review, and refine?
A suggestion for Congress: keep what’s working in the Patient Protection and Affordable Care Act (PPACA), adjust what isn’t working – just make the whole thing better and call it what you will.
A good thing, but needing work
The PPACA, which is also referred to as Obama care, had a lot in it that any reasonable person would consider good. Let’s take a look. As Dr Valerie Arkoosh wrote in our journal in 2012,2 the law attempted to expand access to health care to the embarrassingly large 30 million or more Americans who were not insured. How would it do this? By expanding Medicaid, enhancing consumer protections in the private health insurance market, requiring large employers to offer insurance or pay a fine, giving tax credits to increase affordability of insurance for small businesses, creating state-based competitive market places, and requiring individuals to purchase health insurance plans (the so-called insurance mandate), thereby creating a pool of large numbers of healthy people who would help defray the costs of those not so fortunate.The law also guaranteed insurability despite any preexisting condition, surely a step in the right direction. Likewise, the need for employers to provide health insurance, the state-based health insurance exchanges, and especially the individual mandate to buy insurance or pay a fine, were all steps in the right direction.
And the law went further – it also addressed preventive care. Medicare and all new insurance plans would have to cover, without copay, co-insurance, or deductible, high-certainty preventive services such as screening for breast, cervical, colorectal, lung, and skin cancers, the annual well-woman visit, breast cancer preventative medications, and many others.3 Medicare recipients would be eligible for one non-copay annual wellness visit to their caregiver. Beyond providing increased access to health care, the PPACA added incentives to caregivers who were coming out of training programs to serve in underserved areas and benefit from a decrease in their med school loans or in their loan repayments.
Finally, and especially important, under the PPACA, our age-old insurance system of fee for service, which tends to incentivize more care, would change to incentivizing high-quality, outcomes-based care , thus replacing “quantity of care” with quality of care. So what’s wrong with the features of the law outlined in the preceding paragraphs? Well, of course, for every 100 ideas, only a few will be implemented and actually pay off. Certainly some of the PPACA could have been better implemented, and perhaps the task now facing Congress, if it could ever abandon its current pitched-camp approach, should be to take the ideas that health care policy scientists have established as being valid and find a way to make them work. Surely that would be best for all players, rather than carping about the repeal-replace approach versus staying with the PPACA.
So my response to the repeal-replace assertion? Retain, review, and refine.
Practitioner-friendly content
Health care calamities notwithstanding, we have a line-up of articles in this issue that uniformly address some of the pressing needs many of us face in our daily practice. Barry and colleagues examined the patterns of care with regard to whole brain radiotherapy technique and delivery at US-based academic centers. Their results show some interesting differences in the way younger and older practitioners deliver that care, with older practitioners placing more importance on tumor histopathology when considering brain irradiation. Speaking of access to care in the context of health reform, how often do our cancer patients use the emergency department? Lash and colleagues looked at the ED-use numbers from two databases in California and found that patients go to the ED at higher rates than previously reported and with notable variability by cancer type. Now we need to examine the reasons for those visits and establish ways to identify predictors of ED use to improve patient quality of care and rein in the higher costs of ED use.
In regard to symptom management, we can never have enough about nausea and vomiting prevention. Schwartzberg and colleagues report on a trial in which they evaluated the clinical benefits of APF530, a subcutaneous formulation of granisetron, compared with ondansetron in patients who had received cisplatin therapy. This longer-acting formulation of granisetron performed very well against a standard of care and might give our patients another option in the clinic for highly emetogenic chemotherapy.
Still on the topic of symptom management, preventing and treating mTOR-inhibitor–associated stomatitis (mIAS) is the subject of a review by Ramchandran and colleagues. The inhibitors have been approved for treatment in renal cell, neuroendocrine, and breast cancers, but of course, many of our newer molecules have some associated toxicity. Based on their literature scan, the authors report that management of mIAS should focus on three major approaches: prevention, early aggressive treatment, and, when needed, more aggressive pain management. Early recognition and diagnosis of mIAS facilitate early intervention to limit potential sequelae of mIAS and minimize the need for mTOR inhibitor dose reduction and interruption.
In a way, stress management could also fall under the symptom management category. I often remember being told during my training that we should always discuss with your patients their level of anxiety and depression. But I think sometimes we are so busy addressing the cancer, its treatment, and treatment side effects, we overlook the fact that the patient is suffering psychologically and might need additional intervention in the form of talk therapy and/or medication. Ramírez-Solá and colleagues describe in our How We Do It section the process of developing and implementing a psychosocial distress management program at their institution in Puerto Rico. The authors also summarize the results of a pilot study to validate the Patient Health Questionnaire (PHQ-9) as a measure to improve the process of emotional distress management in particular.
In recent years, the number of approvals and new indications for therapies for different cancer types has increased significantly. We highlight two such approvals in this issue. One is the PARP inhibitor, rucaparib, which was approved in both the platinum-sensitive and -resistant settings for BRCA1- and BRCA2-mutant patients with ovarian cancer. The other is the new CD38 antibody daratumumab, which was originally approved as a single-agent therapy for relapsed myeloma and which has now received a second approval with demonstrated improvement of progression-free survival when given with the lenalidomide-dexamethasone or bortezomib-dexamethasone combinations.
When it comes to new therapies, immunotherapies are at the cutting edge. Who hasn’t heard of the new checkpoint inhibitor drugs for a range of cancers that have either been approved or are in trial? Until now, we have used these immunotherapies as single agents, but Jane de Lartigue writes of the potential of combining more than one immunotherapy drug and/or combining an immune checkpoint inhibitor with a chemotherapy drug. The key behind this concept is that the more antigenic differentiation and tumor infiltrating lymphocytes in the system, the better the immunotherapy might work.
In the previous issue of the journal, one of our Editors, Thomas Strouse, discussed the issue of physician aid in dying (PAD)4 and asserted he had come to view “active non-participation” in legal PAD as a “toxic form of patient abandonment.” This is, of course, a very challenging and complex topic, and one that we likely have to address on a weekly basis with some of our cancer patients: if palliative care and end-of-life is the goal, how can we most humanely achieve that ethically and legally in concert with our patients’ wishes? Is it right or wrong to aid in some way in the dying process? Dr Alva Weir responds to Dr Strouse’s editorial, taking the view point that physician-assisted suicide is toxic abandonment. Dr Strauss responds, and I encourage you to read this very interesting exchange that highlights the point-counterpoint views of physician involvement in the dying process.
We round off the issue with a bumper crop of Case Reports. They include two that document diagnostic challenges: one in a patient with pulmonary sarcomatoid carcinoma presenting as a necrotizing cavitary lung lesion and another in which atraumatic splenic rupture is the initial presentation of CML. Also included is a report on a case of primary cardiac prosthetic valve-associated lymphoma and another on how a collaborative effort between oncologists and dermatologists contributed to the resolution of palmoplantar exacerbation of psoriasis in a patient who had been treated with nivolumab.
Going digital
I will close by remarking that the Journal of Community and Supportive Oncology, or JCSO, will be going digital only after this print issue. We will continue publishing the same content as a bimonthly digital issue, posting articles directly to our website, and mailing out our regular electronic newsletters. So visit the website, www.jcso-online.com, where you can read the articles as soon as they are posted and also find instructions for downloading the app for the digital edition – it’s quick, easy, and free, in case you were wondering. For a shortcut to the download the app, you can also use http://bit.ly/2nCEPIa.
Finally, if you would like to submit a paper to us for consideration for publication, you can do so by going to www.editorialmanager.com/jso/. We will consider submissions in original research, reviews, How We Do It, case reports, and tumor board summaries – you’ll find all the information you need to submit a paper at the EditorialManager platform. And let’s not forget social media – we’re on Twitter where our handle is @jcs_onc, my personal Twitter handle is @davidhenrymd, so connect with us – follow us, like us, and retweet us.
1. Pear R, Kelly K. Trump concedes health law overhaul is ‘unbelievably complex.’ https://www.nytimes.com/2017/02/27/us/politics/trump-concedes-health-law-overhaul-is-unbelievably-complex.html?_r=0. New York Times. February 27, 2017. Accessed April 4, 2017.
2. Arkoosh VA. The Patient Protection and Affordable Care Act: no rhetoric, just the facts. Commun Oncol. 2012;9(6):206-209.
3. USPSTF A and B Recommendations. US Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/Page/Name/uspstf-a-and-b-recommendations/. January 2017. Accessed April 4, 2017.
4. Strouse T. End-of-life options and the legal pathways to physician aid in dying. J Community Support Oncol. 2017;15(1):1-3.
A suggestion for Congress: keep what’s working in the Patient Protection and Affordable Care Act (PPACA), adjust what isn’t working – just make the whole thing better and call it what you will.
A good thing, but needing work
The PPACA, which is also referred to as Obama care, had a lot in it that any reasonable person would consider good. Let’s take a look. As Dr Valerie Arkoosh wrote in our journal in 2012,2 the law attempted to expand access to health care to the embarrassingly large 30 million or more Americans who were not insured. How would it do this? By expanding Medicaid, enhancing consumer protections in the private health insurance market, requiring large employers to offer insurance or pay a fine, giving tax credits to increase affordability of insurance for small businesses, creating state-based competitive market places, and requiring individuals to purchase health insurance plans (the so-called insurance mandate), thereby creating a pool of large numbers of healthy people who would help defray the costs of those not so fortunate.The law also guaranteed insurability despite any preexisting condition, surely a step in the right direction. Likewise, the need for employers to provide health insurance, the state-based health insurance exchanges, and especially the individual mandate to buy insurance or pay a fine, were all steps in the right direction.
And the law went further – it also addressed preventive care. Medicare and all new insurance plans would have to cover, without copay, co-insurance, or deductible, high-certainty preventive services such as screening for breast, cervical, colorectal, lung, and skin cancers, the annual well-woman visit, breast cancer preventative medications, and many others.3 Medicare recipients would be eligible for one non-copay annual wellness visit to their caregiver. Beyond providing increased access to health care, the PPACA added incentives to caregivers who were coming out of training programs to serve in underserved areas and benefit from a decrease in their med school loans or in their loan repayments.
Finally, and especially important, under the PPACA, our age-old insurance system of fee for service, which tends to incentivize more care, would change to incentivizing high-quality, outcomes-based care , thus replacing “quantity of care” with quality of care. So what’s wrong with the features of the law outlined in the preceding paragraphs? Well, of course, for every 100 ideas, only a few will be implemented and actually pay off. Certainly some of the PPACA could have been better implemented, and perhaps the task now facing Congress, if it could ever abandon its current pitched-camp approach, should be to take the ideas that health care policy scientists have established as being valid and find a way to make them work. Surely that would be best for all players, rather than carping about the repeal-replace approach versus staying with the PPACA.
So my response to the repeal-replace assertion? Retain, review, and refine.
Practitioner-friendly content
Health care calamities notwithstanding, we have a line-up of articles in this issue that uniformly address some of the pressing needs many of us face in our daily practice. Barry and colleagues examined the patterns of care with regard to whole brain radiotherapy technique and delivery at US-based academic centers. Their results show some interesting differences in the way younger and older practitioners deliver that care, with older practitioners placing more importance on tumor histopathology when considering brain irradiation. Speaking of access to care in the context of health reform, how often do our cancer patients use the emergency department? Lash and colleagues looked at the ED-use numbers from two databases in California and found that patients go to the ED at higher rates than previously reported and with notable variability by cancer type. Now we need to examine the reasons for those visits and establish ways to identify predictors of ED use to improve patient quality of care and rein in the higher costs of ED use.
In regard to symptom management, we can never have enough about nausea and vomiting prevention. Schwartzberg and colleagues report on a trial in which they evaluated the clinical benefits of APF530, a subcutaneous formulation of granisetron, compared with ondansetron in patients who had received cisplatin therapy. This longer-acting formulation of granisetron performed very well against a standard of care and might give our patients another option in the clinic for highly emetogenic chemotherapy.
Still on the topic of symptom management, preventing and treating mTOR-inhibitor–associated stomatitis (mIAS) is the subject of a review by Ramchandran and colleagues. The inhibitors have been approved for treatment in renal cell, neuroendocrine, and breast cancers, but of course, many of our newer molecules have some associated toxicity. Based on their literature scan, the authors report that management of mIAS should focus on three major approaches: prevention, early aggressive treatment, and, when needed, more aggressive pain management. Early recognition and diagnosis of mIAS facilitate early intervention to limit potential sequelae of mIAS and minimize the need for mTOR inhibitor dose reduction and interruption.
In a way, stress management could also fall under the symptom management category. I often remember being told during my training that we should always discuss with your patients their level of anxiety and depression. But I think sometimes we are so busy addressing the cancer, its treatment, and treatment side effects, we overlook the fact that the patient is suffering psychologically and might need additional intervention in the form of talk therapy and/or medication. Ramírez-Solá and colleagues describe in our How We Do It section the process of developing and implementing a psychosocial distress management program at their institution in Puerto Rico. The authors also summarize the results of a pilot study to validate the Patient Health Questionnaire (PHQ-9) as a measure to improve the process of emotional distress management in particular.
In recent years, the number of approvals and new indications for therapies for different cancer types has increased significantly. We highlight two such approvals in this issue. One is the PARP inhibitor, rucaparib, which was approved in both the platinum-sensitive and -resistant settings for BRCA1- and BRCA2-mutant patients with ovarian cancer. The other is the new CD38 antibody daratumumab, which was originally approved as a single-agent therapy for relapsed myeloma and which has now received a second approval with demonstrated improvement of progression-free survival when given with the lenalidomide-dexamethasone or bortezomib-dexamethasone combinations.
When it comes to new therapies, immunotherapies are at the cutting edge. Who hasn’t heard of the new checkpoint inhibitor drugs for a range of cancers that have either been approved or are in trial? Until now, we have used these immunotherapies as single agents, but Jane de Lartigue writes of the potential of combining more than one immunotherapy drug and/or combining an immune checkpoint inhibitor with a chemotherapy drug. The key behind this concept is that the more antigenic differentiation and tumor infiltrating lymphocytes in the system, the better the immunotherapy might work.
In the previous issue of the journal, one of our Editors, Thomas Strouse, discussed the issue of physician aid in dying (PAD)4 and asserted he had come to view “active non-participation” in legal PAD as a “toxic form of patient abandonment.” This is, of course, a very challenging and complex topic, and one that we likely have to address on a weekly basis with some of our cancer patients: if palliative care and end-of-life is the goal, how can we most humanely achieve that ethically and legally in concert with our patients’ wishes? Is it right or wrong to aid in some way in the dying process? Dr Alva Weir responds to Dr Strouse’s editorial, taking the view point that physician-assisted suicide is toxic abandonment. Dr Strauss responds, and I encourage you to read this very interesting exchange that highlights the point-counterpoint views of physician involvement in the dying process.
We round off the issue with a bumper crop of Case Reports. They include two that document diagnostic challenges: one in a patient with pulmonary sarcomatoid carcinoma presenting as a necrotizing cavitary lung lesion and another in which atraumatic splenic rupture is the initial presentation of CML. Also included is a report on a case of primary cardiac prosthetic valve-associated lymphoma and another on how a collaborative effort between oncologists and dermatologists contributed to the resolution of palmoplantar exacerbation of psoriasis in a patient who had been treated with nivolumab.
Going digital
I will close by remarking that the Journal of Community and Supportive Oncology, or JCSO, will be going digital only after this print issue. We will continue publishing the same content as a bimonthly digital issue, posting articles directly to our website, and mailing out our regular electronic newsletters. So visit the website, www.jcso-online.com, where you can read the articles as soon as they are posted and also find instructions for downloading the app for the digital edition – it’s quick, easy, and free, in case you were wondering. For a shortcut to the download the app, you can also use http://bit.ly/2nCEPIa.
Finally, if you would like to submit a paper to us for consideration for publication, you can do so by going to www.editorialmanager.com/jso/. We will consider submissions in original research, reviews, How We Do It, case reports, and tumor board summaries – you’ll find all the information you need to submit a paper at the EditorialManager platform. And let’s not forget social media – we’re on Twitter where our handle is @jcs_onc, my personal Twitter handle is @davidhenrymd, so connect with us – follow us, like us, and retweet us.
A suggestion for Congress: keep what’s working in the Patient Protection and Affordable Care Act (PPACA), adjust what isn’t working – just make the whole thing better and call it what you will.
A good thing, but needing work
The PPACA, which is also referred to as Obama care, had a lot in it that any reasonable person would consider good. Let’s take a look. As Dr Valerie Arkoosh wrote in our journal in 2012,2 the law attempted to expand access to health care to the embarrassingly large 30 million or more Americans who were not insured. How would it do this? By expanding Medicaid, enhancing consumer protections in the private health insurance market, requiring large employers to offer insurance or pay a fine, giving tax credits to increase affordability of insurance for small businesses, creating state-based competitive market places, and requiring individuals to purchase health insurance plans (the so-called insurance mandate), thereby creating a pool of large numbers of healthy people who would help defray the costs of those not so fortunate.The law also guaranteed insurability despite any preexisting condition, surely a step in the right direction. Likewise, the need for employers to provide health insurance, the state-based health insurance exchanges, and especially the individual mandate to buy insurance or pay a fine, were all steps in the right direction.
And the law went further – it also addressed preventive care. Medicare and all new insurance plans would have to cover, without copay, co-insurance, or deductible, high-certainty preventive services such as screening for breast, cervical, colorectal, lung, and skin cancers, the annual well-woman visit, breast cancer preventative medications, and many others.3 Medicare recipients would be eligible for one non-copay annual wellness visit to their caregiver. Beyond providing increased access to health care, the PPACA added incentives to caregivers who were coming out of training programs to serve in underserved areas and benefit from a decrease in their med school loans or in their loan repayments.
Finally, and especially important, under the PPACA, our age-old insurance system of fee for service, which tends to incentivize more care, would change to incentivizing high-quality, outcomes-based care , thus replacing “quantity of care” with quality of care. So what’s wrong with the features of the law outlined in the preceding paragraphs? Well, of course, for every 100 ideas, only a few will be implemented and actually pay off. Certainly some of the PPACA could have been better implemented, and perhaps the task now facing Congress, if it could ever abandon its current pitched-camp approach, should be to take the ideas that health care policy scientists have established as being valid and find a way to make them work. Surely that would be best for all players, rather than carping about the repeal-replace approach versus staying with the PPACA.
So my response to the repeal-replace assertion? Retain, review, and refine.
Practitioner-friendly content
Health care calamities notwithstanding, we have a line-up of articles in this issue that uniformly address some of the pressing needs many of us face in our daily practice. Barry and colleagues examined the patterns of care with regard to whole brain radiotherapy technique and delivery at US-based academic centers. Their results show some interesting differences in the way younger and older practitioners deliver that care, with older practitioners placing more importance on tumor histopathology when considering brain irradiation. Speaking of access to care in the context of health reform, how often do our cancer patients use the emergency department? Lash and colleagues looked at the ED-use numbers from two databases in California and found that patients go to the ED at higher rates than previously reported and with notable variability by cancer type. Now we need to examine the reasons for those visits and establish ways to identify predictors of ED use to improve patient quality of care and rein in the higher costs of ED use.
In regard to symptom management, we can never have enough about nausea and vomiting prevention. Schwartzberg and colleagues report on a trial in which they evaluated the clinical benefits of APF530, a subcutaneous formulation of granisetron, compared with ondansetron in patients who had received cisplatin therapy. This longer-acting formulation of granisetron performed very well against a standard of care and might give our patients another option in the clinic for highly emetogenic chemotherapy.
Still on the topic of symptom management, preventing and treating mTOR-inhibitor–associated stomatitis (mIAS) is the subject of a review by Ramchandran and colleagues. The inhibitors have been approved for treatment in renal cell, neuroendocrine, and breast cancers, but of course, many of our newer molecules have some associated toxicity. Based on their literature scan, the authors report that management of mIAS should focus on three major approaches: prevention, early aggressive treatment, and, when needed, more aggressive pain management. Early recognition and diagnosis of mIAS facilitate early intervention to limit potential sequelae of mIAS and minimize the need for mTOR inhibitor dose reduction and interruption.
In a way, stress management could also fall under the symptom management category. I often remember being told during my training that we should always discuss with your patients their level of anxiety and depression. But I think sometimes we are so busy addressing the cancer, its treatment, and treatment side effects, we overlook the fact that the patient is suffering psychologically and might need additional intervention in the form of talk therapy and/or medication. Ramírez-Solá and colleagues describe in our How We Do It section the process of developing and implementing a psychosocial distress management program at their institution in Puerto Rico. The authors also summarize the results of a pilot study to validate the Patient Health Questionnaire (PHQ-9) as a measure to improve the process of emotional distress management in particular.
In recent years, the number of approvals and new indications for therapies for different cancer types has increased significantly. We highlight two such approvals in this issue. One is the PARP inhibitor, rucaparib, which was approved in both the platinum-sensitive and -resistant settings for BRCA1- and BRCA2-mutant patients with ovarian cancer. The other is the new CD38 antibody daratumumab, which was originally approved as a single-agent therapy for relapsed myeloma and which has now received a second approval with demonstrated improvement of progression-free survival when given with the lenalidomide-dexamethasone or bortezomib-dexamethasone combinations.
When it comes to new therapies, immunotherapies are at the cutting edge. Who hasn’t heard of the new checkpoint inhibitor drugs for a range of cancers that have either been approved or are in trial? Until now, we have used these immunotherapies as single agents, but Jane de Lartigue writes of the potential of combining more than one immunotherapy drug and/or combining an immune checkpoint inhibitor with a chemotherapy drug. The key behind this concept is that the more antigenic differentiation and tumor infiltrating lymphocytes in the system, the better the immunotherapy might work.
In the previous issue of the journal, one of our Editors, Thomas Strouse, discussed the issue of physician aid in dying (PAD)4 and asserted he had come to view “active non-participation” in legal PAD as a “toxic form of patient abandonment.” This is, of course, a very challenging and complex topic, and one that we likely have to address on a weekly basis with some of our cancer patients: if palliative care and end-of-life is the goal, how can we most humanely achieve that ethically and legally in concert with our patients’ wishes? Is it right or wrong to aid in some way in the dying process? Dr Alva Weir responds to Dr Strouse’s editorial, taking the view point that physician-assisted suicide is toxic abandonment. Dr Strauss responds, and I encourage you to read this very interesting exchange that highlights the point-counterpoint views of physician involvement in the dying process.
We round off the issue with a bumper crop of Case Reports. They include two that document diagnostic challenges: one in a patient with pulmonary sarcomatoid carcinoma presenting as a necrotizing cavitary lung lesion and another in which atraumatic splenic rupture is the initial presentation of CML. Also included is a report on a case of primary cardiac prosthetic valve-associated lymphoma and another on how a collaborative effort between oncologists and dermatologists contributed to the resolution of palmoplantar exacerbation of psoriasis in a patient who had been treated with nivolumab.
Going digital
I will close by remarking that the Journal of Community and Supportive Oncology, or JCSO, will be going digital only after this print issue. We will continue publishing the same content as a bimonthly digital issue, posting articles directly to our website, and mailing out our regular electronic newsletters. So visit the website, www.jcso-online.com, where you can read the articles as soon as they are posted and also find instructions for downloading the app for the digital edition – it’s quick, easy, and free, in case you were wondering. For a shortcut to the download the app, you can also use http://bit.ly/2nCEPIa.
Finally, if you would like to submit a paper to us for consideration for publication, you can do so by going to www.editorialmanager.com/jso/. We will consider submissions in original research, reviews, How We Do It, case reports, and tumor board summaries – you’ll find all the information you need to submit a paper at the EditorialManager platform. And let’s not forget social media – we’re on Twitter where our handle is @jcs_onc, my personal Twitter handle is @davidhenrymd, so connect with us – follow us, like us, and retweet us.
1. Pear R, Kelly K. Trump concedes health law overhaul is ‘unbelievably complex.’ https://www.nytimes.com/2017/02/27/us/politics/trump-concedes-health-law-overhaul-is-unbelievably-complex.html?_r=0. New York Times. February 27, 2017. Accessed April 4, 2017.
2. Arkoosh VA. The Patient Protection and Affordable Care Act: no rhetoric, just the facts. Commun Oncol. 2012;9(6):206-209.
3. USPSTF A and B Recommendations. US Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/Page/Name/uspstf-a-and-b-recommendations/. January 2017. Accessed April 4, 2017.
4. Strouse T. End-of-life options and the legal pathways to physician aid in dying. J Community Support Oncol. 2017;15(1):1-3.
1. Pear R, Kelly K. Trump concedes health law overhaul is ‘unbelievably complex.’ https://www.nytimes.com/2017/02/27/us/politics/trump-concedes-health-law-overhaul-is-unbelievably-complex.html?_r=0. New York Times. February 27, 2017. Accessed April 4, 2017.
2. Arkoosh VA. The Patient Protection and Affordable Care Act: no rhetoric, just the facts. Commun Oncol. 2012;9(6):206-209.
3. USPSTF A and B Recommendations. US Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/Page/Name/uspstf-a-and-b-recommendations/. January 2017. Accessed April 4, 2017.
4. Strouse T. End-of-life options and the legal pathways to physician aid in dying. J Community Support Oncol. 2017;15(1):1-3.
End-of-life options and the legal pathways to physician aid in dying
By early 2017, roughly 18% of all US citizens will reside in a state with a legal pathway to physician aid in dying via lethal prescription. When the End of Life Options Act (EOLOA) went into effect in in California in June 2016, it became the fourth state with laws allowing physician aid in dying (PAD). Oregon (1997), Washington (2009), and Vermont (2009) had preceded it, and Montana (2009) operates similarly as a result of a Supreme Court decision there. However, California’s law also legalized PAD in a state that is much larger and more socioeconomically diverse than the other four states – with its 39 million residents, California more than triples the number of Americans who live in PAD legal states. Together, these 5 states represent 16% of the entire US population (roughly 321 million according to the 2015 Census). Most recently, in December 2016, they were joined by Colorado, adding a state population of 5.5 million.
The state laws have much in common: to “qualify” for legal access to a lethal prescription, a patient must make an in-person verbal request to his/her attending physician. The patient must also: be an adult (aged 18 years or older); be a resident of that state; have a terminal illness the course of which is expected to lead to natural death within 6 months; be making a noncoerced, voluntary request; repeat the verbal request no sooner than 15 days after the first request, followed by a witnessed, formal written request; and have the capacity to self-administer the lethal prescription in a private setting.1
In California, as in the other states, additional safeguards are built in: the terminal diagnosis and the patient’s capacity to make the request must be verified by a second, independent consultant physician. If either the attending or the consultant physician finds evidence of a “mental disorder,” they are obligated under the law to refer the patient to a psychiatrist or psychologist for an evaluation. The psychological expert is charged with verifying the patient’s mental capacity and ability to make a voluntary end-of-life choice, with determining whether a mental disorder is in fact present, and if it is, whether that mental disorder is impairing the patient’s judgment. A finding of impaired judgment due to mental disorder halts the legal process until the disorder is rectified by treatment, the passage of time, or other factors.
Many of the themes and concepts outlined in these laws are familiar to oncology clinicians simply because we take care of seriously ill and dying patients. Indeed, access to the Medicare Hospice Benefit requires certification – often by an oncologist – that a patient has a terminal diagnosis with a maximum 6-month expected survival. In addition, oncologists encounter many patients who wish to talk about quality of life while they weigh various treatment options, and it is normative for patients (though often anxiety producing for clinicians) to broach topics related to end of life, symptom management, and even aid in dying. Many patients fear poor quality of life, intractable symptom burden, dependency on others, and loss of control more than they fear their cancers. Their efforts to initiate this discussion often fit into a much larger and more durable set of personal values and ideals about suffering, dependency, futility, and personal autonomy.
Weighing the evidence
And yet there is vigorous objection to PAD laws from many corners. Some religious organizations and faith-based health care delivery systems oppose the laws and, in opting-out of the voluntary legal pathways for participation, prohibit their employed and affiliated physicians and other professionals from doing so as well.2 Some physician organizations, and individual physicians, claim that involvement in aid in dying – such as by providing a legal lethal prescription – violates the Hippocratic oath and that (in effect) there is no circumstance under which it could be ethically permissible.
There are also bioethicists, including physician ethicists, who sincerely reach similar conclusions and warn of the “slippery slope” that might lead beyond aid in dying as currently legalized in the US to assisting in the deaths of those with disabilities, those with depression or other treatable psychiatric illness, and even to active euthanasia, including euthanasia of nonconsenting or incapable individuals.3 These objectors generally remain adamant and cite what we would all agree are excesses in certain European countries, despite the absence of evidence that the European measures could be approved in the United States under current laws and practices.
The largest amount of publicly available evidence to inform this discussion in the US comes from Oregon, which has nearly 20 years of experience with the law and its reporting requirements.4 Very broadly, the Oregon experience supports the view that PAD is pursued and completed by a very small percentage of the population: in 2015 (the most recent year for which data is available) 218 people possessed lethal prescriptions; 132 of them ingested the medications and died. Thus about 61% of those who received the prescription used it for its intended purpose, resulting in a Death with Dignity Act death rate of 0.39% (132 of 34,160 deaths in Oregon) in 2015. Since the law’s inception in 1997, 991 patients are known to have died from lethal ingestion of 1545 prescriptions written (a 64% “use” rate).
Equally important is the evidence from Oregon describing those who seek to use the law. In 2015, as in previous years, most patients were older than the general population (78% aged 65 years or older; median age at death, 73). Of those patients, 93% were white and well educated (43% had at least a college degree), compared with the population at large. In all, 72%-78% of patients had cancer; 6%-8% had ALS (amyotrophic lateral sclerosis); and end-stage heart disease seemed to be increasing, trending up from 2% to 6% in recent years.
In addition, 90% died at home, with 92% on hospice, and more than 99% had health insurance of some kind. These figures provide strong evidence that PAD is not being inappropriately used among historically vulnerable or disempowered ethnic/racial minorities, socioeconomically or educationally disadvantaged groups, or disabled individuals. On the contrary, “uptake” or use of PAD by the disadvantaged in Oregon seems, perhaps not surprisingly, to occur at rates significantly below their representation in the general population of the state.
Intractable symptom burden (or fear of it) was rated as a minor contributor to the decision to pursue PAD, ranking sixth out of the 7 options and endorsed by about a quarter of patients. The three most frequently cited end-of-life concerns were: decreasing ability to participate in activities that made life enjoyable (96%), loss of autonomy (92%), and loss of dignity (75%).
A broader range of choice
I have worked for nearly 30 years in California oncology clinical settings as a palliative care physician and psychiatrist. During that time I have been involved in the care of two patients who committed violent suicide (self-inflicted gunshot). Both events took place before the passage of the California EOLOA, both patients were educated, professional older white men who were fiercely independent and who saw their progressive cancers as rapidly worsening their quality of life and intolerably increasing their dependency on beloved others (although their judgments about this did not take into account how the others actually felt); neither had a primary psychiatric illness, and neither had intractable symptom burden. Both men had expressed interest in and were denied access to lethal prescription. Sadly, neither had the kind of long-term, trusting relationship with a physician that appears to have provided access to non-legally sanctioned PAD for decades before the first state laws allowing it – and therefore each apparently decided to exert his autonomy in the ultimate act of self-determination. In both cases, it seemed to me that violent suicide was a bad, last recourse – clearly, each man regarded continued living in his intolerable state as even worse – but also the worst possible outcome for their surviving families, for their traumatized clinicians, and for the bystanders who witnessed these deaths and the first responders who were called to the scenes. We cannot know that the availability of lethal prescription would have pre-empted these violent suicides, but I suspect it might have given each man a much broader range of choice about how to deal with circumstances he found entirely unacceptable, and which he simply could not and would not tolerate.
An informed, person-centered approach
It is in the context of these experiences that I have come to view “active non-participation” in legal PAD – that is, decisions by individual physicians and/or health systems not only to not provide, but also not refer patients to possibly willing providers and systems without regard for specific clinical contexts – as a toxic form of patient abandonment. I am also concerned that this rigid stance (like many rigid stances in the service of alleged moral absolutes) may lead to greater suffering and harm – such as the violent suicides I have described – than a more moderate, contextually informed, person-centered approach that does not outlaw certain clinical topics. Indeed, in my participating institution in California, it has become clear that a request for PAD leads (as a result of a carefully and comprehensively constructed “navigator” process) to a level of patient and family care that should be provided to every patient with terminal illness in this country. While that statement is a sad reflection on our society’s general commitment to caring for the dying, it seems that the extra attention required by the process leading to a PAD, and the revelations that emerge in that process, often lead to a withdrawal of the request for a lethal prescription, and/or allows the drug to go unused if provided.
Many leading bioethical treatises, including those emerging from faith-based academic and university settings, also support the view that PAD can be and is morally justified under a certain set of circumstances. Not surprisingly, those circumstances encompass most of what is written into the state laws permitting PAD. They include, according to Beauchamp and Childress:5
- A voluntary request by a competent patient
- An ongoing physician-patient relationship
- Mutual and informed decision-making by patient and physician
- A supportive yet critical and probing environment of decision making
- A considered rejection of alternatives
- Structured consultation with other parties in medicine
- A patient’s expression of a durable preference for death
- Unacceptable suffering by the patient
- Use of a means that is as painless and comfortable as possible
We tell many of our patients that cancer is now treated as a chronic illness. In the context of treating that chronic illness we have the profound opportunity – some would say the obligation – to come to know our patients as whole individuals who often have long-held health values, ideas about what a life worth living looks like, and very personal fears and hopes. We may well come to know them more intimately while serving as their cancer clinicians than any other health professionals do – and even as do any other individuals with whom they will ever interact.
The hours in the infusion chair afford many opportunities for us to understand (and, ideally, document) a patient’s advance care plans, health values, goals, views about end-of-life measures such as artificial ventilation and resuscitation. No one reasonably disputes the “rightness” of learning these things. The evidence shows us that under very rare circumstances, knowing and respecting our patients may include understanding their wishes about physician aid in dying, which requires us to build upon the profound trust that has been established by being able to hear and understand their requests. It seems to me that the end of life is the most inappropriate time for any of us to tell patients they must look elsewhere.
The opinions expressed here are those of the author alone, and do not reflect the view of other individuals, institutions, or professional organizations with which Dr Strouse is affiliated.
1. Gostin LO, Roberts AE. Physician assisted dying: a turning point? JAMA 2016;315;249-250.
2. Buck C. With barbiturates and martini, Sonoma man among first Californians to die under end-of-life law. http://www.sacbee.com/news/local/health-and-medicine/article95676342.html. Published August 16, 2016. Accessed January 17, 2017.
3. Snyder L, Sulmasy DP. Physician-assisted suicide. http://annals.org/aim/article/714672/physician-assisted-suicide. Published August 7, 2001. Accessed January 17, 2017.
4. Oregan Public Health Division. Oregan Death With Dignity Act: 2015 data summary. https://public.health.oregon.gov/ProviderPartnerResources/EvaluationResearch/DeathwithDignityAct/Documents/year18.pdf. Published February 4, 2016. Accessed January 17, 2017.
5. Beauchamp TL, Childress JF. Nonmaleficence. In Principles of biomedical ethics. 7th ed. New York, NY: Oxford University Press; 2013:184.
By early 2017, roughly 18% of all US citizens will reside in a state with a legal pathway to physician aid in dying via lethal prescription. When the End of Life Options Act (EOLOA) went into effect in in California in June 2016, it became the fourth state with laws allowing physician aid in dying (PAD). Oregon (1997), Washington (2009), and Vermont (2009) had preceded it, and Montana (2009) operates similarly as a result of a Supreme Court decision there. However, California’s law also legalized PAD in a state that is much larger and more socioeconomically diverse than the other four states – with its 39 million residents, California more than triples the number of Americans who live in PAD legal states. Together, these 5 states represent 16% of the entire US population (roughly 321 million according to the 2015 Census). Most recently, in December 2016, they were joined by Colorado, adding a state population of 5.5 million.
The state laws have much in common: to “qualify” for legal access to a lethal prescription, a patient must make an in-person verbal request to his/her attending physician. The patient must also: be an adult (aged 18 years or older); be a resident of that state; have a terminal illness the course of which is expected to lead to natural death within 6 months; be making a noncoerced, voluntary request; repeat the verbal request no sooner than 15 days after the first request, followed by a witnessed, formal written request; and have the capacity to self-administer the lethal prescription in a private setting.1
In California, as in the other states, additional safeguards are built in: the terminal diagnosis and the patient’s capacity to make the request must be verified by a second, independent consultant physician. If either the attending or the consultant physician finds evidence of a “mental disorder,” they are obligated under the law to refer the patient to a psychiatrist or psychologist for an evaluation. The psychological expert is charged with verifying the patient’s mental capacity and ability to make a voluntary end-of-life choice, with determining whether a mental disorder is in fact present, and if it is, whether that mental disorder is impairing the patient’s judgment. A finding of impaired judgment due to mental disorder halts the legal process until the disorder is rectified by treatment, the passage of time, or other factors.
Many of the themes and concepts outlined in these laws are familiar to oncology clinicians simply because we take care of seriously ill and dying patients. Indeed, access to the Medicare Hospice Benefit requires certification – often by an oncologist – that a patient has a terminal diagnosis with a maximum 6-month expected survival. In addition, oncologists encounter many patients who wish to talk about quality of life while they weigh various treatment options, and it is normative for patients (though often anxiety producing for clinicians) to broach topics related to end of life, symptom management, and even aid in dying. Many patients fear poor quality of life, intractable symptom burden, dependency on others, and loss of control more than they fear their cancers. Their efforts to initiate this discussion often fit into a much larger and more durable set of personal values and ideals about suffering, dependency, futility, and personal autonomy.
Weighing the evidence
And yet there is vigorous objection to PAD laws from many corners. Some religious organizations and faith-based health care delivery systems oppose the laws and, in opting-out of the voluntary legal pathways for participation, prohibit their employed and affiliated physicians and other professionals from doing so as well.2 Some physician organizations, and individual physicians, claim that involvement in aid in dying – such as by providing a legal lethal prescription – violates the Hippocratic oath and that (in effect) there is no circumstance under which it could be ethically permissible.
There are also bioethicists, including physician ethicists, who sincerely reach similar conclusions and warn of the “slippery slope” that might lead beyond aid in dying as currently legalized in the US to assisting in the deaths of those with disabilities, those with depression or other treatable psychiatric illness, and even to active euthanasia, including euthanasia of nonconsenting or incapable individuals.3 These objectors generally remain adamant and cite what we would all agree are excesses in certain European countries, despite the absence of evidence that the European measures could be approved in the United States under current laws and practices.
The largest amount of publicly available evidence to inform this discussion in the US comes from Oregon, which has nearly 20 years of experience with the law and its reporting requirements.4 Very broadly, the Oregon experience supports the view that PAD is pursued and completed by a very small percentage of the population: in 2015 (the most recent year for which data is available) 218 people possessed lethal prescriptions; 132 of them ingested the medications and died. Thus about 61% of those who received the prescription used it for its intended purpose, resulting in a Death with Dignity Act death rate of 0.39% (132 of 34,160 deaths in Oregon) in 2015. Since the law’s inception in 1997, 991 patients are known to have died from lethal ingestion of 1545 prescriptions written (a 64% “use” rate).
Equally important is the evidence from Oregon describing those who seek to use the law. In 2015, as in previous years, most patients were older than the general population (78% aged 65 years or older; median age at death, 73). Of those patients, 93% were white and well educated (43% had at least a college degree), compared with the population at large. In all, 72%-78% of patients had cancer; 6%-8% had ALS (amyotrophic lateral sclerosis); and end-stage heart disease seemed to be increasing, trending up from 2% to 6% in recent years.
In addition, 90% died at home, with 92% on hospice, and more than 99% had health insurance of some kind. These figures provide strong evidence that PAD is not being inappropriately used among historically vulnerable or disempowered ethnic/racial minorities, socioeconomically or educationally disadvantaged groups, or disabled individuals. On the contrary, “uptake” or use of PAD by the disadvantaged in Oregon seems, perhaps not surprisingly, to occur at rates significantly below their representation in the general population of the state.
Intractable symptom burden (or fear of it) was rated as a minor contributor to the decision to pursue PAD, ranking sixth out of the 7 options and endorsed by about a quarter of patients. The three most frequently cited end-of-life concerns were: decreasing ability to participate in activities that made life enjoyable (96%), loss of autonomy (92%), and loss of dignity (75%).
A broader range of choice
I have worked for nearly 30 years in California oncology clinical settings as a palliative care physician and psychiatrist. During that time I have been involved in the care of two patients who committed violent suicide (self-inflicted gunshot). Both events took place before the passage of the California EOLOA, both patients were educated, professional older white men who were fiercely independent and who saw their progressive cancers as rapidly worsening their quality of life and intolerably increasing their dependency on beloved others (although their judgments about this did not take into account how the others actually felt); neither had a primary psychiatric illness, and neither had intractable symptom burden. Both men had expressed interest in and were denied access to lethal prescription. Sadly, neither had the kind of long-term, trusting relationship with a physician that appears to have provided access to non-legally sanctioned PAD for decades before the first state laws allowing it – and therefore each apparently decided to exert his autonomy in the ultimate act of self-determination. In both cases, it seemed to me that violent suicide was a bad, last recourse – clearly, each man regarded continued living in his intolerable state as even worse – but also the worst possible outcome for their surviving families, for their traumatized clinicians, and for the bystanders who witnessed these deaths and the first responders who were called to the scenes. We cannot know that the availability of lethal prescription would have pre-empted these violent suicides, but I suspect it might have given each man a much broader range of choice about how to deal with circumstances he found entirely unacceptable, and which he simply could not and would not tolerate.
An informed, person-centered approach
It is in the context of these experiences that I have come to view “active non-participation” in legal PAD – that is, decisions by individual physicians and/or health systems not only to not provide, but also not refer patients to possibly willing providers and systems without regard for specific clinical contexts – as a toxic form of patient abandonment. I am also concerned that this rigid stance (like many rigid stances in the service of alleged moral absolutes) may lead to greater suffering and harm – such as the violent suicides I have described – than a more moderate, contextually informed, person-centered approach that does not outlaw certain clinical topics. Indeed, in my participating institution in California, it has become clear that a request for PAD leads (as a result of a carefully and comprehensively constructed “navigator” process) to a level of patient and family care that should be provided to every patient with terminal illness in this country. While that statement is a sad reflection on our society’s general commitment to caring for the dying, it seems that the extra attention required by the process leading to a PAD, and the revelations that emerge in that process, often lead to a withdrawal of the request for a lethal prescription, and/or allows the drug to go unused if provided.
Many leading bioethical treatises, including those emerging from faith-based academic and university settings, also support the view that PAD can be and is morally justified under a certain set of circumstances. Not surprisingly, those circumstances encompass most of what is written into the state laws permitting PAD. They include, according to Beauchamp and Childress:5
- A voluntary request by a competent patient
- An ongoing physician-patient relationship
- Mutual and informed decision-making by patient and physician
- A supportive yet critical and probing environment of decision making
- A considered rejection of alternatives
- Structured consultation with other parties in medicine
- A patient’s expression of a durable preference for death
- Unacceptable suffering by the patient
- Use of a means that is as painless and comfortable as possible
We tell many of our patients that cancer is now treated as a chronic illness. In the context of treating that chronic illness we have the profound opportunity – some would say the obligation – to come to know our patients as whole individuals who often have long-held health values, ideas about what a life worth living looks like, and very personal fears and hopes. We may well come to know them more intimately while serving as their cancer clinicians than any other health professionals do – and even as do any other individuals with whom they will ever interact.
The hours in the infusion chair afford many opportunities for us to understand (and, ideally, document) a patient’s advance care plans, health values, goals, views about end-of-life measures such as artificial ventilation and resuscitation. No one reasonably disputes the “rightness” of learning these things. The evidence shows us that under very rare circumstances, knowing and respecting our patients may include understanding their wishes about physician aid in dying, which requires us to build upon the profound trust that has been established by being able to hear and understand their requests. It seems to me that the end of life is the most inappropriate time for any of us to tell patients they must look elsewhere.
The opinions expressed here are those of the author alone, and do not reflect the view of other individuals, institutions, or professional organizations with which Dr Strouse is affiliated.
By early 2017, roughly 18% of all US citizens will reside in a state with a legal pathway to physician aid in dying via lethal prescription. When the End of Life Options Act (EOLOA) went into effect in in California in June 2016, it became the fourth state with laws allowing physician aid in dying (PAD). Oregon (1997), Washington (2009), and Vermont (2009) had preceded it, and Montana (2009) operates similarly as a result of a Supreme Court decision there. However, California’s law also legalized PAD in a state that is much larger and more socioeconomically diverse than the other four states – with its 39 million residents, California more than triples the number of Americans who live in PAD legal states. Together, these 5 states represent 16% of the entire US population (roughly 321 million according to the 2015 Census). Most recently, in December 2016, they were joined by Colorado, adding a state population of 5.5 million.
The state laws have much in common: to “qualify” for legal access to a lethal prescription, a patient must make an in-person verbal request to his/her attending physician. The patient must also: be an adult (aged 18 years or older); be a resident of that state; have a terminal illness the course of which is expected to lead to natural death within 6 months; be making a noncoerced, voluntary request; repeat the verbal request no sooner than 15 days after the first request, followed by a witnessed, formal written request; and have the capacity to self-administer the lethal prescription in a private setting.1
In California, as in the other states, additional safeguards are built in: the terminal diagnosis and the patient’s capacity to make the request must be verified by a second, independent consultant physician. If either the attending or the consultant physician finds evidence of a “mental disorder,” they are obligated under the law to refer the patient to a psychiatrist or psychologist for an evaluation. The psychological expert is charged with verifying the patient’s mental capacity and ability to make a voluntary end-of-life choice, with determining whether a mental disorder is in fact present, and if it is, whether that mental disorder is impairing the patient’s judgment. A finding of impaired judgment due to mental disorder halts the legal process until the disorder is rectified by treatment, the passage of time, or other factors.
Many of the themes and concepts outlined in these laws are familiar to oncology clinicians simply because we take care of seriously ill and dying patients. Indeed, access to the Medicare Hospice Benefit requires certification – often by an oncologist – that a patient has a terminal diagnosis with a maximum 6-month expected survival. In addition, oncologists encounter many patients who wish to talk about quality of life while they weigh various treatment options, and it is normative for patients (though often anxiety producing for clinicians) to broach topics related to end of life, symptom management, and even aid in dying. Many patients fear poor quality of life, intractable symptom burden, dependency on others, and loss of control more than they fear their cancers. Their efforts to initiate this discussion often fit into a much larger and more durable set of personal values and ideals about suffering, dependency, futility, and personal autonomy.
Weighing the evidence
And yet there is vigorous objection to PAD laws from many corners. Some religious organizations and faith-based health care delivery systems oppose the laws and, in opting-out of the voluntary legal pathways for participation, prohibit their employed and affiliated physicians and other professionals from doing so as well.2 Some physician organizations, and individual physicians, claim that involvement in aid in dying – such as by providing a legal lethal prescription – violates the Hippocratic oath and that (in effect) there is no circumstance under which it could be ethically permissible.
There are also bioethicists, including physician ethicists, who sincerely reach similar conclusions and warn of the “slippery slope” that might lead beyond aid in dying as currently legalized in the US to assisting in the deaths of those with disabilities, those with depression or other treatable psychiatric illness, and even to active euthanasia, including euthanasia of nonconsenting or incapable individuals.3 These objectors generally remain adamant and cite what we would all agree are excesses in certain European countries, despite the absence of evidence that the European measures could be approved in the United States under current laws and practices.
The largest amount of publicly available evidence to inform this discussion in the US comes from Oregon, which has nearly 20 years of experience with the law and its reporting requirements.4 Very broadly, the Oregon experience supports the view that PAD is pursued and completed by a very small percentage of the population: in 2015 (the most recent year for which data is available) 218 people possessed lethal prescriptions; 132 of them ingested the medications and died. Thus about 61% of those who received the prescription used it for its intended purpose, resulting in a Death with Dignity Act death rate of 0.39% (132 of 34,160 deaths in Oregon) in 2015. Since the law’s inception in 1997, 991 patients are known to have died from lethal ingestion of 1545 prescriptions written (a 64% “use” rate).
Equally important is the evidence from Oregon describing those who seek to use the law. In 2015, as in previous years, most patients were older than the general population (78% aged 65 years or older; median age at death, 73). Of those patients, 93% were white and well educated (43% had at least a college degree), compared with the population at large. In all, 72%-78% of patients had cancer; 6%-8% had ALS (amyotrophic lateral sclerosis); and end-stage heart disease seemed to be increasing, trending up from 2% to 6% in recent years.
In addition, 90% died at home, with 92% on hospice, and more than 99% had health insurance of some kind. These figures provide strong evidence that PAD is not being inappropriately used among historically vulnerable or disempowered ethnic/racial minorities, socioeconomically or educationally disadvantaged groups, or disabled individuals. On the contrary, “uptake” or use of PAD by the disadvantaged in Oregon seems, perhaps not surprisingly, to occur at rates significantly below their representation in the general population of the state.
Intractable symptom burden (or fear of it) was rated as a minor contributor to the decision to pursue PAD, ranking sixth out of the 7 options and endorsed by about a quarter of patients. The three most frequently cited end-of-life concerns were: decreasing ability to participate in activities that made life enjoyable (96%), loss of autonomy (92%), and loss of dignity (75%).
A broader range of choice
I have worked for nearly 30 years in California oncology clinical settings as a palliative care physician and psychiatrist. During that time I have been involved in the care of two patients who committed violent suicide (self-inflicted gunshot). Both events took place before the passage of the California EOLOA, both patients were educated, professional older white men who were fiercely independent and who saw their progressive cancers as rapidly worsening their quality of life and intolerably increasing their dependency on beloved others (although their judgments about this did not take into account how the others actually felt); neither had a primary psychiatric illness, and neither had intractable symptom burden. Both men had expressed interest in and were denied access to lethal prescription. Sadly, neither had the kind of long-term, trusting relationship with a physician that appears to have provided access to non-legally sanctioned PAD for decades before the first state laws allowing it – and therefore each apparently decided to exert his autonomy in the ultimate act of self-determination. In both cases, it seemed to me that violent suicide was a bad, last recourse – clearly, each man regarded continued living in his intolerable state as even worse – but also the worst possible outcome for their surviving families, for their traumatized clinicians, and for the bystanders who witnessed these deaths and the first responders who were called to the scenes. We cannot know that the availability of lethal prescription would have pre-empted these violent suicides, but I suspect it might have given each man a much broader range of choice about how to deal with circumstances he found entirely unacceptable, and which he simply could not and would not tolerate.
An informed, person-centered approach
It is in the context of these experiences that I have come to view “active non-participation” in legal PAD – that is, decisions by individual physicians and/or health systems not only to not provide, but also not refer patients to possibly willing providers and systems without regard for specific clinical contexts – as a toxic form of patient abandonment. I am also concerned that this rigid stance (like many rigid stances in the service of alleged moral absolutes) may lead to greater suffering and harm – such as the violent suicides I have described – than a more moderate, contextually informed, person-centered approach that does not outlaw certain clinical topics. Indeed, in my participating institution in California, it has become clear that a request for PAD leads (as a result of a carefully and comprehensively constructed “navigator” process) to a level of patient and family care that should be provided to every patient with terminal illness in this country. While that statement is a sad reflection on our society’s general commitment to caring for the dying, it seems that the extra attention required by the process leading to a PAD, and the revelations that emerge in that process, often lead to a withdrawal of the request for a lethal prescription, and/or allows the drug to go unused if provided.
Many leading bioethical treatises, including those emerging from faith-based academic and university settings, also support the view that PAD can be and is morally justified under a certain set of circumstances. Not surprisingly, those circumstances encompass most of what is written into the state laws permitting PAD. They include, according to Beauchamp and Childress:5
- A voluntary request by a competent patient
- An ongoing physician-patient relationship
- Mutual and informed decision-making by patient and physician
- A supportive yet critical and probing environment of decision making
- A considered rejection of alternatives
- Structured consultation with other parties in medicine
- A patient’s expression of a durable preference for death
- Unacceptable suffering by the patient
- Use of a means that is as painless and comfortable as possible
We tell many of our patients that cancer is now treated as a chronic illness. In the context of treating that chronic illness we have the profound opportunity – some would say the obligation – to come to know our patients as whole individuals who often have long-held health values, ideas about what a life worth living looks like, and very personal fears and hopes. We may well come to know them more intimately while serving as their cancer clinicians than any other health professionals do – and even as do any other individuals with whom they will ever interact.
The hours in the infusion chair afford many opportunities for us to understand (and, ideally, document) a patient’s advance care plans, health values, goals, views about end-of-life measures such as artificial ventilation and resuscitation. No one reasonably disputes the “rightness” of learning these things. The evidence shows us that under very rare circumstances, knowing and respecting our patients may include understanding their wishes about physician aid in dying, which requires us to build upon the profound trust that has been established by being able to hear and understand their requests. It seems to me that the end of life is the most inappropriate time for any of us to tell patients they must look elsewhere.
The opinions expressed here are those of the author alone, and do not reflect the view of other individuals, institutions, or professional organizations with which Dr Strouse is affiliated.
1. Gostin LO, Roberts AE. Physician assisted dying: a turning point? JAMA 2016;315;249-250.
2. Buck C. With barbiturates and martini, Sonoma man among first Californians to die under end-of-life law. http://www.sacbee.com/news/local/health-and-medicine/article95676342.html. Published August 16, 2016. Accessed January 17, 2017.
3. Snyder L, Sulmasy DP. Physician-assisted suicide. http://annals.org/aim/article/714672/physician-assisted-suicide. Published August 7, 2001. Accessed January 17, 2017.
4. Oregan Public Health Division. Oregan Death With Dignity Act: 2015 data summary. https://public.health.oregon.gov/ProviderPartnerResources/EvaluationResearch/DeathwithDignityAct/Documents/year18.pdf. Published February 4, 2016. Accessed January 17, 2017.
5. Beauchamp TL, Childress JF. Nonmaleficence. In Principles of biomedical ethics. 7th ed. New York, NY: Oxford University Press; 2013:184.
1. Gostin LO, Roberts AE. Physician assisted dying: a turning point? JAMA 2016;315;249-250.
2. Buck C. With barbiturates and martini, Sonoma man among first Californians to die under end-of-life law. http://www.sacbee.com/news/local/health-and-medicine/article95676342.html. Published August 16, 2016. Accessed January 17, 2017.
3. Snyder L, Sulmasy DP. Physician-assisted suicide. http://annals.org/aim/article/714672/physician-assisted-suicide. Published August 7, 2001. Accessed January 17, 2017.
4. Oregan Public Health Division. Oregan Death With Dignity Act: 2015 data summary. https://public.health.oregon.gov/ProviderPartnerResources/EvaluationResearch/DeathwithDignityAct/Documents/year18.pdf. Published February 4, 2016. Accessed January 17, 2017.
5. Beauchamp TL, Childress JF. Nonmaleficence. In Principles of biomedical ethics. 7th ed. New York, NY: Oxford University Press; 2013:184.
Start offering antenatal corticosteroids to women delivering between 34 0/7 and 36 6/7 weeks of gestation to improve newborn outcomes
Antenatal corticosteroid treat-ment prior to preterm birth is the most important pharmacologic intervention available to obstetricians to improve newborn health. Antenatal corticosteroids reduce preterm newborn morbidity and mortality.1 The American College of Obstetricians and Gynecologists (ACOG) recently has summarized updated recommendations for the use of antenatal steroid treatment.2
ACOG guidance includes:
- “A single course of corticosteroids is recommended for pregnant women between 24 0/7 weeks and 33 6/7 weeks of gestation, including for those with ruptured membranes and multiple gestations.” This guidance is supported by many high-quality trials and meta-analyses.1
- A single course of corticosteroids “may be considered for pregnant women starting at 23 0/7 weeks of gestation who are at risk of preterm delivery within 7 days.”
- “A single repeat course of antenatal corticosteroids should be considered in women who are less than 34 0/7 weeks of gestation who have an imminent risk of preterm delivery within the next 7 days and whose prior course of antenatal corticosteroids was administered more than 14 days previously.” A repeat course of corticosteroids could be considered as early as 7 days from the prior dose.
- No more than 2 courses of antenatal steroids should be administered.
An important new ACOG recommendation is:
- “A single course of betamethasone is recommended for pregnant women between 34 0/7 and 36 6/7 weeks of gestation at risk of preterm birth within 7 days, and who have not received a previous course of antenatal corticosteroids.”
This recommendation is based, in part, on a high-quality, randomized trial including 2,831 women at high risk for preterm birth between 34 0/7 and 36 6/7 weeks of gestation who were randomly assigned to receive a course of betamethasone or placebo. The newborn and maternal outcomes observed in this study are summarized in the TABLE.3

A few points relevant to the Antenatal Late Preterm Steroids study bear emphasizing. The women enrolled in this trial were at high risk for preterm delivery based on preterm labor with a cervical dilation of ≥3 cm or 75% effacement, spontaneous rupture of the membranes, or a planned late preterm delivery by cesarean or induction. No tocolytics were administered to women in this study, and approximately 40% of the women delivered within 24 hours of entry into the trial and only received 1 dose of corticosteroid or placebo.
Women with multiple gestations, pregestational diabetes, or a prior course of corticosteroids were not included in the trial; therefore, this study cannot guide our clinical practice for these subgroups of women. Of note, betamethasone should not be administered to women in the late preterm who have chorioamnionitis.
Related article:
When could use of antenatal corticosteroids in the late preterm birth period be beneficial?
The investigators calculated that 35 women would need to be treated to prevent one case of the primary outcome: a composite score of the use of respiratory support. Consequently, 34 fetuses who do not benefit from treatment are exposed in utero to betamethasone. Long-term follow-up of infants born to mothers participating in this study is currently underway.
A recent meta-analysis of 3 trials including 3,200 women at high risk for preterm delivery at 34 0/7 to 36 6/7 weeks of gestation reported that the corticosteroid administration reduced newborn risk for transient tachypnea of the newborn (relative risk [RR], 0.72; 95% confidence interval [CI], 0.56−0.92), severe respiratory distress syndrome (RR, 0.60; 95% CI, 0.33−0.94), and use of surfactant (RR, 0.61; 95% CI, 0.38−0.99).4
The recommendation to offer a single course of betamethasone for pregnant women between 34 0/7 and 36 6/7 weeks of gestation at risk for preterm birth has not been embraced enthusiastically by all obstetricians. Many experts have emphasized that the known risks of late preterm betamethasone, including neonatal hypoglycemia and the unknown long-term risks of treatment, including suboptimal neurodevelopmental, cardiovascular, and metabolic outcomes should dampen enthusiasm for embracing the new ACOG recommendation.5 Experts also emphasize that late preterm newborns are less likely to benefit from antenatal corticosteroid treatment than babies born at less than 34 weeks. Hence, many late preterm newborns will be exposed to a potentially harmful intervention and have only a small chance of benefiting from the treatment.6
Many neonatologists believe that for the newborn, the benefits of maternal corticosteroid treatment outweigh the risks.7–9 In a 30-year follow-up of 534 newborns participating in antenatal corticosteroid trials, treatment had no effect on body size, blood lipids, blood pressure, plasma cortisol, prevalence of diabetes, lung function, history of cardiovascular disease, educational attainment, or socioeconomic status. Corticosteroid treatment was associated with increased insulin secretion in response to a glucose load.10 In this study, the mothers received treatment at a median of 33 weeks of gestation and births occurred at a median of 35 weeks. Hence this study is relevant to the issue of late preterm corticosteroid treatment.
Balancing risks and benefits is complex. Balancing immediate benefits against long-term risks is most challenging. Regarding antenatal steroid use there are many unknowns, including optimal dose, drug formulation, and timing from treatment to delivery. In addition we need more high-quality data delineating the long-term effects of antenatal corticosteroids on childhood and adult health.
Read about 3 options to use in your practice
Consider these 3 options for your practice
As noted, the Antenatal Late Preterm Steroids trial investigators are pursuing long-term follow-up of the children born after maternal treatment with antenatal glucocorticoids. Both ACOG and the Society for Maternal-Fetal Medicine (SMFM)11 recommend administration of antenatal glucocorticoids to women at high risk for late preterm delivery. However, since some experts are concerned that a great number of babies born late preterm will have been exposed to glucocorticoids, whose long-term risks are not well known, with only a few babies having a modest short-term benefit, 3 options could be considered for your clinical practice.
Related article:
Need for caution before extending the use of antenatal corticosteroids beyond 34 weeks’ gestation
Option 1
Follow the ACOG and SMFM suggestion that all women with a high risk of late preterm birth be offered antenatal corticosteroids. Counsel the mother and family about the potential risks and benefits and involve them in the decision.
Two alternative options are to limit antenatal corticosteroid treatment to subgroups of late preterm babies most likely to benefit from treatment, those born by cesarean delivery and those born at the earliest gestational ages.
Option 2
Limit the use of antenatal corticosteroids in the late preterm to women who are scheduled for a cesarean delivery for an obstetric indication between 34 0/7 weeks and 36 6/7 weeks of gestation. This approach greatly reduces the number of babies born in the late preterm that will be exposed to antenatal corticosteroids and focuses the treatment on a subset of babies who are certain to be born preterm and most likely to benefit.
Option 3
Limit the use of antenatal corticosteroids to women at high risk for preterm birth whose newborns are most likely to benefit from treatment—women at 34 0/7 to 35 6/7 weeks of gestation. Neonates born in the 34th or 35th week of gestation are at higher risk for morbidity than those born in the 36th week of gestation and are likely to derive the greatest benefit from antenatal corticosteroid treatment.3,12
My advice
Yogi Berra advised, “It is tough to make predictions, especially about the future.” Although ACOG and SMFM have recommended administration of glucocorticoids to women at high risk for late preterm birth, many experts caution that until the long-term effects of antenatal corticosteroids are better characterized we should limit the use of corticosteroids in the late preterm.5,6,13 My prediction is that long-term follow-up studies will not document significant adverse effects of one course of late preterm antenatal glucocorticoid treatment on children. My advice is to start offering antenatal corticosteroids to some women at high risk for late preterm delivery.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Roberts D, Dalziel S. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2006;CD004454.
- American College of Obstetricians and Gynecologists' Committee on Obstetrics Practice; Society for Maternal−Fetal Medicine. Committee Opinion No. 677: Antenatal corticosteroid therapy for fetal maturation. Obstet Gynecol. 2016;128(4):e187−e194.
- Gyamfi-Bannerman C, Thom EA, Blackwell SC, et al; NICHD Maternal-Fetal Medicine Units Network. Antenatal betamethasone for women at risk for late preterm delivery. N Engl J Med. 2016;374(14):1311−1320.
- Saccone G, Berghella V. Antenatal corticosteroids for maturity of term or near term fetuses: systematic review and meta-analysis of randomized controlled trials. BMJ. 2016;355:i5044.
- Kamath-Rayne BD, Rozance PJ, Goldenberg RL, Jobe AH. Antenatal corticosteroids beyond 34 weeks gestation: What do we do now? Am J Obstet Gynecol. 2016;215(4):423−430.
- Vidaeff AC, Belfort MA, Steer PJ. Antenatal corticosteroids: a time for more careful scrutiny of the indications? BJOG. 2016;123(7):1067−1069.
- Dalziel SR, Lim VK, Lambert A, McCarthy D, et al. Antenatal exposure to betamethasone: psychological functioning and health related quality of life 31 years after inclusion in randomised controlled trial. BMJ. 2005;331(7518):665.
- Dalziel SR, Rea HH, Walker NK, et al. Long term effects of antenatal betamethasone on lung function: 30 year follow up of a randomised controlled trial. Thorax. 2006;61(8):678−683.
- McKinlay CJ, Cutfield WS, Battin MR, Dalziel SR, Crowther CA, Harding JE; ACTORDS Study Group. Cardiovascular risk factors in children after repeat doses of antenatal glucocorticoids: an RCT. Pediatrics. 2015;135(2):e405−e415.
- Dalziel SR, Walker NK, Parag V, et al. Cardiovascular risk factors after antenatal exposure to betamethasone: 30-year follow-up of a randomised controlled trial. Lancet. 2005;365(9474):1856−1862.
- Society for Maternal-Fetal Medicine (SMFM) Publications Committee. Implementation of the use of antenatal corticosteroids in the later preterm birth period in women at risk for preterm delivery. Am J Obstet Gynecol. 2016;215(2):B13−B15.
- Bastek JA, Langmuir H, Kondapalli LA, Pare E, Adamczak JE, Srinivas SK. Antenatal corticosteroids for late-preterm infants: a decision-analytic and economic analysis. ISRN Obstet Gynecol. 2012;2012:491595.
- Nowik CM, Davies GA, Smith GN. We should proceed with caution when it comes to antenatal corticosteroids after 34 weeks. J Obstet Gynaecol Can. 2018;39(1):49−51.
Antenatal corticosteroid treat-ment prior to preterm birth is the most important pharmacologic intervention available to obstetricians to improve newborn health. Antenatal corticosteroids reduce preterm newborn morbidity and mortality.1 The American College of Obstetricians and Gynecologists (ACOG) recently has summarized updated recommendations for the use of antenatal steroid treatment.2
ACOG guidance includes:
- “A single course of corticosteroids is recommended for pregnant women between 24 0/7 weeks and 33 6/7 weeks of gestation, including for those with ruptured membranes and multiple gestations.” This guidance is supported by many high-quality trials and meta-analyses.1
- A single course of corticosteroids “may be considered for pregnant women starting at 23 0/7 weeks of gestation who are at risk of preterm delivery within 7 days.”
- “A single repeat course of antenatal corticosteroids should be considered in women who are less than 34 0/7 weeks of gestation who have an imminent risk of preterm delivery within the next 7 days and whose prior course of antenatal corticosteroids was administered more than 14 days previously.” A repeat course of corticosteroids could be considered as early as 7 days from the prior dose.
- No more than 2 courses of antenatal steroids should be administered.
An important new ACOG recommendation is:
- “A single course of betamethasone is recommended for pregnant women between 34 0/7 and 36 6/7 weeks of gestation at risk of preterm birth within 7 days, and who have not received a previous course of antenatal corticosteroids.”
This recommendation is based, in part, on a high-quality, randomized trial including 2,831 women at high risk for preterm birth between 34 0/7 and 36 6/7 weeks of gestation who were randomly assigned to receive a course of betamethasone or placebo. The newborn and maternal outcomes observed in this study are summarized in the TABLE.3

A few points relevant to the Antenatal Late Preterm Steroids study bear emphasizing. The women enrolled in this trial were at high risk for preterm delivery based on preterm labor with a cervical dilation of ≥3 cm or 75% effacement, spontaneous rupture of the membranes, or a planned late preterm delivery by cesarean or induction. No tocolytics were administered to women in this study, and approximately 40% of the women delivered within 24 hours of entry into the trial and only received 1 dose of corticosteroid or placebo.
Women with multiple gestations, pregestational diabetes, or a prior course of corticosteroids were not included in the trial; therefore, this study cannot guide our clinical practice for these subgroups of women. Of note, betamethasone should not be administered to women in the late preterm who have chorioamnionitis.
Related article:
When could use of antenatal corticosteroids in the late preterm birth period be beneficial?
The investigators calculated that 35 women would need to be treated to prevent one case of the primary outcome: a composite score of the use of respiratory support. Consequently, 34 fetuses who do not benefit from treatment are exposed in utero to betamethasone. Long-term follow-up of infants born to mothers participating in this study is currently underway.
A recent meta-analysis of 3 trials including 3,200 women at high risk for preterm delivery at 34 0/7 to 36 6/7 weeks of gestation reported that the corticosteroid administration reduced newborn risk for transient tachypnea of the newborn (relative risk [RR], 0.72; 95% confidence interval [CI], 0.56−0.92), severe respiratory distress syndrome (RR, 0.60; 95% CI, 0.33−0.94), and use of surfactant (RR, 0.61; 95% CI, 0.38−0.99).4
The recommendation to offer a single course of betamethasone for pregnant women between 34 0/7 and 36 6/7 weeks of gestation at risk for preterm birth has not been embraced enthusiastically by all obstetricians. Many experts have emphasized that the known risks of late preterm betamethasone, including neonatal hypoglycemia and the unknown long-term risks of treatment, including suboptimal neurodevelopmental, cardiovascular, and metabolic outcomes should dampen enthusiasm for embracing the new ACOG recommendation.5 Experts also emphasize that late preterm newborns are less likely to benefit from antenatal corticosteroid treatment than babies born at less than 34 weeks. Hence, many late preterm newborns will be exposed to a potentially harmful intervention and have only a small chance of benefiting from the treatment.6
Many neonatologists believe that for the newborn, the benefits of maternal corticosteroid treatment outweigh the risks.7–9 In a 30-year follow-up of 534 newborns participating in antenatal corticosteroid trials, treatment had no effect on body size, blood lipids, blood pressure, plasma cortisol, prevalence of diabetes, lung function, history of cardiovascular disease, educational attainment, or socioeconomic status. Corticosteroid treatment was associated with increased insulin secretion in response to a glucose load.10 In this study, the mothers received treatment at a median of 33 weeks of gestation and births occurred at a median of 35 weeks. Hence this study is relevant to the issue of late preterm corticosteroid treatment.
Balancing risks and benefits is complex. Balancing immediate benefits against long-term risks is most challenging. Regarding antenatal steroid use there are many unknowns, including optimal dose, drug formulation, and timing from treatment to delivery. In addition we need more high-quality data delineating the long-term effects of antenatal corticosteroids on childhood and adult health.
Read about 3 options to use in your practice
Consider these 3 options for your practice
As noted, the Antenatal Late Preterm Steroids trial investigators are pursuing long-term follow-up of the children born after maternal treatment with antenatal glucocorticoids. Both ACOG and the Society for Maternal-Fetal Medicine (SMFM)11 recommend administration of antenatal glucocorticoids to women at high risk for late preterm delivery. However, since some experts are concerned that a great number of babies born late preterm will have been exposed to glucocorticoids, whose long-term risks are not well known, with only a few babies having a modest short-term benefit, 3 options could be considered for your clinical practice.
Related article:
Need for caution before extending the use of antenatal corticosteroids beyond 34 weeks’ gestation
Option 1
Follow the ACOG and SMFM suggestion that all women with a high risk of late preterm birth be offered antenatal corticosteroids. Counsel the mother and family about the potential risks and benefits and involve them in the decision.
Two alternative options are to limit antenatal corticosteroid treatment to subgroups of late preterm babies most likely to benefit from treatment, those born by cesarean delivery and those born at the earliest gestational ages.
Option 2
Limit the use of antenatal corticosteroids in the late preterm to women who are scheduled for a cesarean delivery for an obstetric indication between 34 0/7 weeks and 36 6/7 weeks of gestation. This approach greatly reduces the number of babies born in the late preterm that will be exposed to antenatal corticosteroids and focuses the treatment on a subset of babies who are certain to be born preterm and most likely to benefit.
Option 3
Limit the use of antenatal corticosteroids to women at high risk for preterm birth whose newborns are most likely to benefit from treatment—women at 34 0/7 to 35 6/7 weeks of gestation. Neonates born in the 34th or 35th week of gestation are at higher risk for morbidity than those born in the 36th week of gestation and are likely to derive the greatest benefit from antenatal corticosteroid treatment.3,12
My advice
Yogi Berra advised, “It is tough to make predictions, especially about the future.” Although ACOG and SMFM have recommended administration of glucocorticoids to women at high risk for late preterm birth, many experts caution that until the long-term effects of antenatal corticosteroids are better characterized we should limit the use of corticosteroids in the late preterm.5,6,13 My prediction is that long-term follow-up studies will not document significant adverse effects of one course of late preterm antenatal glucocorticoid treatment on children. My advice is to start offering antenatal corticosteroids to some women at high risk for late preterm delivery.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Antenatal corticosteroid treat-ment prior to preterm birth is the most important pharmacologic intervention available to obstetricians to improve newborn health. Antenatal corticosteroids reduce preterm newborn morbidity and mortality.1 The American College of Obstetricians and Gynecologists (ACOG) recently has summarized updated recommendations for the use of antenatal steroid treatment.2
ACOG guidance includes:
- “A single course of corticosteroids is recommended for pregnant women between 24 0/7 weeks and 33 6/7 weeks of gestation, including for those with ruptured membranes and multiple gestations.” This guidance is supported by many high-quality trials and meta-analyses.1
- A single course of corticosteroids “may be considered for pregnant women starting at 23 0/7 weeks of gestation who are at risk of preterm delivery within 7 days.”
- “A single repeat course of antenatal corticosteroids should be considered in women who are less than 34 0/7 weeks of gestation who have an imminent risk of preterm delivery within the next 7 days and whose prior course of antenatal corticosteroids was administered more than 14 days previously.” A repeat course of corticosteroids could be considered as early as 7 days from the prior dose.
- No more than 2 courses of antenatal steroids should be administered.
An important new ACOG recommendation is:
- “A single course of betamethasone is recommended for pregnant women between 34 0/7 and 36 6/7 weeks of gestation at risk of preterm birth within 7 days, and who have not received a previous course of antenatal corticosteroids.”
This recommendation is based, in part, on a high-quality, randomized trial including 2,831 women at high risk for preterm birth between 34 0/7 and 36 6/7 weeks of gestation who were randomly assigned to receive a course of betamethasone or placebo. The newborn and maternal outcomes observed in this study are summarized in the TABLE.3

A few points relevant to the Antenatal Late Preterm Steroids study bear emphasizing. The women enrolled in this trial were at high risk for preterm delivery based on preterm labor with a cervical dilation of ≥3 cm or 75% effacement, spontaneous rupture of the membranes, or a planned late preterm delivery by cesarean or induction. No tocolytics were administered to women in this study, and approximately 40% of the women delivered within 24 hours of entry into the trial and only received 1 dose of corticosteroid or placebo.
Women with multiple gestations, pregestational diabetes, or a prior course of corticosteroids were not included in the trial; therefore, this study cannot guide our clinical practice for these subgroups of women. Of note, betamethasone should not be administered to women in the late preterm who have chorioamnionitis.
Related article:
When could use of antenatal corticosteroids in the late preterm birth period be beneficial?
The investigators calculated that 35 women would need to be treated to prevent one case of the primary outcome: a composite score of the use of respiratory support. Consequently, 34 fetuses who do not benefit from treatment are exposed in utero to betamethasone. Long-term follow-up of infants born to mothers participating in this study is currently underway.
A recent meta-analysis of 3 trials including 3,200 women at high risk for preterm delivery at 34 0/7 to 36 6/7 weeks of gestation reported that the corticosteroid administration reduced newborn risk for transient tachypnea of the newborn (relative risk [RR], 0.72; 95% confidence interval [CI], 0.56−0.92), severe respiratory distress syndrome (RR, 0.60; 95% CI, 0.33−0.94), and use of surfactant (RR, 0.61; 95% CI, 0.38−0.99).4
The recommendation to offer a single course of betamethasone for pregnant women between 34 0/7 and 36 6/7 weeks of gestation at risk for preterm birth has not been embraced enthusiastically by all obstetricians. Many experts have emphasized that the known risks of late preterm betamethasone, including neonatal hypoglycemia and the unknown long-term risks of treatment, including suboptimal neurodevelopmental, cardiovascular, and metabolic outcomes should dampen enthusiasm for embracing the new ACOG recommendation.5 Experts also emphasize that late preterm newborns are less likely to benefit from antenatal corticosteroid treatment than babies born at less than 34 weeks. Hence, many late preterm newborns will be exposed to a potentially harmful intervention and have only a small chance of benefiting from the treatment.6
Many neonatologists believe that for the newborn, the benefits of maternal corticosteroid treatment outweigh the risks.7–9 In a 30-year follow-up of 534 newborns participating in antenatal corticosteroid trials, treatment had no effect on body size, blood lipids, blood pressure, plasma cortisol, prevalence of diabetes, lung function, history of cardiovascular disease, educational attainment, or socioeconomic status. Corticosteroid treatment was associated with increased insulin secretion in response to a glucose load.10 In this study, the mothers received treatment at a median of 33 weeks of gestation and births occurred at a median of 35 weeks. Hence this study is relevant to the issue of late preterm corticosteroid treatment.
Balancing risks and benefits is complex. Balancing immediate benefits against long-term risks is most challenging. Regarding antenatal steroid use there are many unknowns, including optimal dose, drug formulation, and timing from treatment to delivery. In addition we need more high-quality data delineating the long-term effects of antenatal corticosteroids on childhood and adult health.
Read about 3 options to use in your practice
Consider these 3 options for your practice
As noted, the Antenatal Late Preterm Steroids trial investigators are pursuing long-term follow-up of the children born after maternal treatment with antenatal glucocorticoids. Both ACOG and the Society for Maternal-Fetal Medicine (SMFM)11 recommend administration of antenatal glucocorticoids to women at high risk for late preterm delivery. However, since some experts are concerned that a great number of babies born late preterm will have been exposed to glucocorticoids, whose long-term risks are not well known, with only a few babies having a modest short-term benefit, 3 options could be considered for your clinical practice.
Related article:
Need for caution before extending the use of antenatal corticosteroids beyond 34 weeks’ gestation
Option 1
Follow the ACOG and SMFM suggestion that all women with a high risk of late preterm birth be offered antenatal corticosteroids. Counsel the mother and family about the potential risks and benefits and involve them in the decision.
Two alternative options are to limit antenatal corticosteroid treatment to subgroups of late preterm babies most likely to benefit from treatment, those born by cesarean delivery and those born at the earliest gestational ages.
Option 2
Limit the use of antenatal corticosteroids in the late preterm to women who are scheduled for a cesarean delivery for an obstetric indication between 34 0/7 weeks and 36 6/7 weeks of gestation. This approach greatly reduces the number of babies born in the late preterm that will be exposed to antenatal corticosteroids and focuses the treatment on a subset of babies who are certain to be born preterm and most likely to benefit.
Option 3
Limit the use of antenatal corticosteroids to women at high risk for preterm birth whose newborns are most likely to benefit from treatment—women at 34 0/7 to 35 6/7 weeks of gestation. Neonates born in the 34th or 35th week of gestation are at higher risk for morbidity than those born in the 36th week of gestation and are likely to derive the greatest benefit from antenatal corticosteroid treatment.3,12
My advice
Yogi Berra advised, “It is tough to make predictions, especially about the future.” Although ACOG and SMFM have recommended administration of glucocorticoids to women at high risk for late preterm birth, many experts caution that until the long-term effects of antenatal corticosteroids are better characterized we should limit the use of corticosteroids in the late preterm.5,6,13 My prediction is that long-term follow-up studies will not document significant adverse effects of one course of late preterm antenatal glucocorticoid treatment on children. My advice is to start offering antenatal corticosteroids to some women at high risk for late preterm delivery.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Roberts D, Dalziel S. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2006;CD004454.
- American College of Obstetricians and Gynecologists' Committee on Obstetrics Practice; Society for Maternal−Fetal Medicine. Committee Opinion No. 677: Antenatal corticosteroid therapy for fetal maturation. Obstet Gynecol. 2016;128(4):e187−e194.
- Gyamfi-Bannerman C, Thom EA, Blackwell SC, et al; NICHD Maternal-Fetal Medicine Units Network. Antenatal betamethasone for women at risk for late preterm delivery. N Engl J Med. 2016;374(14):1311−1320.
- Saccone G, Berghella V. Antenatal corticosteroids for maturity of term or near term fetuses: systematic review and meta-analysis of randomized controlled trials. BMJ. 2016;355:i5044.
- Kamath-Rayne BD, Rozance PJ, Goldenberg RL, Jobe AH. Antenatal corticosteroids beyond 34 weeks gestation: What do we do now? Am J Obstet Gynecol. 2016;215(4):423−430.
- Vidaeff AC, Belfort MA, Steer PJ. Antenatal corticosteroids: a time for more careful scrutiny of the indications? BJOG. 2016;123(7):1067−1069.
- Dalziel SR, Lim VK, Lambert A, McCarthy D, et al. Antenatal exposure to betamethasone: psychological functioning and health related quality of life 31 years after inclusion in randomised controlled trial. BMJ. 2005;331(7518):665.
- Dalziel SR, Rea HH, Walker NK, et al. Long term effects of antenatal betamethasone on lung function: 30 year follow up of a randomised controlled trial. Thorax. 2006;61(8):678−683.
- McKinlay CJ, Cutfield WS, Battin MR, Dalziel SR, Crowther CA, Harding JE; ACTORDS Study Group. Cardiovascular risk factors in children after repeat doses of antenatal glucocorticoids: an RCT. Pediatrics. 2015;135(2):e405−e415.
- Dalziel SR, Walker NK, Parag V, et al. Cardiovascular risk factors after antenatal exposure to betamethasone: 30-year follow-up of a randomised controlled trial. Lancet. 2005;365(9474):1856−1862.
- Society for Maternal-Fetal Medicine (SMFM) Publications Committee. Implementation of the use of antenatal corticosteroids in the later preterm birth period in women at risk for preterm delivery. Am J Obstet Gynecol. 2016;215(2):B13−B15.
- Bastek JA, Langmuir H, Kondapalli LA, Pare E, Adamczak JE, Srinivas SK. Antenatal corticosteroids for late-preterm infants: a decision-analytic and economic analysis. ISRN Obstet Gynecol. 2012;2012:491595.
- Nowik CM, Davies GA, Smith GN. We should proceed with caution when it comes to antenatal corticosteroids after 34 weeks. J Obstet Gynaecol Can. 2018;39(1):49−51.
- Roberts D, Dalziel S. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2006;CD004454.
- American College of Obstetricians and Gynecologists' Committee on Obstetrics Practice; Society for Maternal−Fetal Medicine. Committee Opinion No. 677: Antenatal corticosteroid therapy for fetal maturation. Obstet Gynecol. 2016;128(4):e187−e194.
- Gyamfi-Bannerman C, Thom EA, Blackwell SC, et al; NICHD Maternal-Fetal Medicine Units Network. Antenatal betamethasone for women at risk for late preterm delivery. N Engl J Med. 2016;374(14):1311−1320.
- Saccone G, Berghella V. Antenatal corticosteroids for maturity of term or near term fetuses: systematic review and meta-analysis of randomized controlled trials. BMJ. 2016;355:i5044.
- Kamath-Rayne BD, Rozance PJ, Goldenberg RL, Jobe AH. Antenatal corticosteroids beyond 34 weeks gestation: What do we do now? Am J Obstet Gynecol. 2016;215(4):423−430.
- Vidaeff AC, Belfort MA, Steer PJ. Antenatal corticosteroids: a time for more careful scrutiny of the indications? BJOG. 2016;123(7):1067−1069.
- Dalziel SR, Lim VK, Lambert A, McCarthy D, et al. Antenatal exposure to betamethasone: psychological functioning and health related quality of life 31 years after inclusion in randomised controlled trial. BMJ. 2005;331(7518):665.
- Dalziel SR, Rea HH, Walker NK, et al. Long term effects of antenatal betamethasone on lung function: 30 year follow up of a randomised controlled trial. Thorax. 2006;61(8):678−683.
- McKinlay CJ, Cutfield WS, Battin MR, Dalziel SR, Crowther CA, Harding JE; ACTORDS Study Group. Cardiovascular risk factors in children after repeat doses of antenatal glucocorticoids: an RCT. Pediatrics. 2015;135(2):e405−e415.
- Dalziel SR, Walker NK, Parag V, et al. Cardiovascular risk factors after antenatal exposure to betamethasone: 30-year follow-up of a randomised controlled trial. Lancet. 2005;365(9474):1856−1862.
- Society for Maternal-Fetal Medicine (SMFM) Publications Committee. Implementation of the use of antenatal corticosteroids in the later preterm birth period in women at risk for preterm delivery. Am J Obstet Gynecol. 2016;215(2):B13−B15.
- Bastek JA, Langmuir H, Kondapalli LA, Pare E, Adamczak JE, Srinivas SK. Antenatal corticosteroids for late-preterm infants: a decision-analytic and economic analysis. ISRN Obstet Gynecol. 2012;2012:491595.
- Nowik CM, Davies GA, Smith GN. We should proceed with caution when it comes to antenatal corticosteroids after 34 weeks. J Obstet Gynaecol Can. 2018;39(1):49−51.
Thoughtful vaccination
Few in mainstream medicine doubt the efficacy of vaccination and the net positive value of a thoughtful vaccination policy. We have witnessed within a professional lifetime the virtual eradication, at least regionally, of a number of previously devastating infectious diseases including polio, smallpox, pertussis, and measles. With growing understanding of disease mechanisms, the potential value of vaccination has expanded to include preventing sequelae of certain infections and malignancy—a holy grail in oncology, the true prevention of cancer. Sporadic local resistance to uniform vaccination against measles has resulted in geographic reappearance of the disease, providing further support for a uniform approach to vaccination against communicable diseases, with some potential to opt out, perhaps with associated societal repercussions for those who do so.
For most clinicians, certainly those of us dealing with chronically ill or immunosuppressed patients, the decision to recommend annual influenza vaccination and pneumococcal vaccinations per guidelines is an easy one. Vaccination against certain infections provides some protection for the individual patient and for the population, contributing to “herd immunity” and helping to protect against the occurrence of pandemics. But this is not the case for all vaccines. For some vaccines the issues of immunity and vaccination are more individual and complicated and warrant more education, reflection, and conversation.
The vaccine to protect against human papillomavirus is effective at reducing the incidence of cervical and anal cancers triggered by infection with certain strains of human papillomavirus. The viral infection itself is not immediately life-threatening. Thus, patients (and their parents) are asked to consider vaccination against a sexually transmitted virus (before sexual transmission of infection) to prevent a possible malignancy later in life. This decision can create social angst. Perhaps less socially challenging, but medically more complicated, is vaccination against the hepatitis B virus (HBV). HBV is also sexually transmissible, but the source in many patients infected with this virus is unclear. The HBV vaccine helps protect against clinically meaningful hepatitis and chronic liver disease from HBV and also will reduce the occurrence of HBV-associated hepatocellular carcinoma and progression of cirrhosis in patients coinfected with hepatitis C virus.
More complex yet is vaccination against the varicella-zoster virus (VZV) to reduce the likelihood of shingles and its possible consequence, postherpetic neuralgia. Le, Sabella, and Rothberg, in this issue of the Journal, review clinical and public health challenges affecting the use of this vaccine.
We are almost all exposed to this virus as children, through natural infection (chickenpox) or vaccination; many infections are seemingly subclinical. My older son had the distinct misfortune of getting chickenpox in a quite memorable way, developing a concentrated collection of the pruritic vesicles underneath a newly placed arm cast. Whether we remember the initial infection or not, VZV sets up housekeeping and lies dormant for decades within sensory neurons. Decades later, it may erupt as shingles along the distribution of the infected nerves with characteristic painful vesicles, sometimes with persistent, extremely painful, and debilitating residua within the same dermatomal distribution: postherpetic neuralgia. The triggers for this fairly common scenario are only generically understood and include waning cellular immunity attributed to aging, malignancy, immunosuppressive medications, human immunodeficiency virus, and perhaps stress and depression.
The zoster vaccine is unique in that it is given to bolster already present cellular immunity to prevent clinical recurrence of the earlier infection, decades after the virus has been dormant—not, as for the other vaccines noted above, to prevent primary infection. It doesn’t matter if the patient has already experienced an episode of shingles. The currently available vaccine is a live-attenuated strain (Oka) of VZV. Another vaccine in clinical testing uses isolated viral components with adjuvant and thus eliminates current concerns of giving the live-attenuated vaccine to immunosuppressed and elderly patients, those who may benefit the most from it.
Fortunately, it seems that even significantly immunosuppressed and elderly patients tolerate the current vaccine, but at present it is suggested that these groups not receive the vaccine, and vaccination rates in these patients is low. Hopefully, additional data will accumulate regarding the safety of the vaccine and will permit its more widespread use within these patient groups, or a replacement “dead” vaccine will become available.
As Le et al nicely discuss, the current vaccine efficacy wanes over about 10 years, and then a booster vaccine should be considered, but there are few data to provide safety and efficacy outcome measures from patients who received a booster vaccination. The potential need to receive a booster injection after about a decade, the demonstrated greater efficacy against zoster when the initial vaccination is provided to patients ages 60 through 69 than in those over 70, and the lower absolute impact when given to patients ages 50 through 59 (baseline zoster incidence increases with age) should enter into the conversation with patients as to when they should receive the vaccine.
Additionally, there are the extremely provocative and as yet unanswered questions surrounding the implications of vaccination if VZV infection is a trigger of inflammatory vascular diseases such as giant cell arteritis in the elderly, as was proposed by the late Dr. Don Gilden.1
And yes, I did get the vaccine. I was 64 at the time.
- Gilden D, Nagel MA. Varicella zoster virus triggers the immunopathology of giant cell arteritis. Curr Opin Rheumatol 2016; 28:376–382.
Few in mainstream medicine doubt the efficacy of vaccination and the net positive value of a thoughtful vaccination policy. We have witnessed within a professional lifetime the virtual eradication, at least regionally, of a number of previously devastating infectious diseases including polio, smallpox, pertussis, and measles. With growing understanding of disease mechanisms, the potential value of vaccination has expanded to include preventing sequelae of certain infections and malignancy—a holy grail in oncology, the true prevention of cancer. Sporadic local resistance to uniform vaccination against measles has resulted in geographic reappearance of the disease, providing further support for a uniform approach to vaccination against communicable diseases, with some potential to opt out, perhaps with associated societal repercussions for those who do so.
For most clinicians, certainly those of us dealing with chronically ill or immunosuppressed patients, the decision to recommend annual influenza vaccination and pneumococcal vaccinations per guidelines is an easy one. Vaccination against certain infections provides some protection for the individual patient and for the population, contributing to “herd immunity” and helping to protect against the occurrence of pandemics. But this is not the case for all vaccines. For some vaccines the issues of immunity and vaccination are more individual and complicated and warrant more education, reflection, and conversation.
The vaccine to protect against human papillomavirus is effective at reducing the incidence of cervical and anal cancers triggered by infection with certain strains of human papillomavirus. The viral infection itself is not immediately life-threatening. Thus, patients (and their parents) are asked to consider vaccination against a sexually transmitted virus (before sexual transmission of infection) to prevent a possible malignancy later in life. This decision can create social angst. Perhaps less socially challenging, but medically more complicated, is vaccination against the hepatitis B virus (HBV). HBV is also sexually transmissible, but the source in many patients infected with this virus is unclear. The HBV vaccine helps protect against clinically meaningful hepatitis and chronic liver disease from HBV and also will reduce the occurrence of HBV-associated hepatocellular carcinoma and progression of cirrhosis in patients coinfected with hepatitis C virus.
More complex yet is vaccination against the varicella-zoster virus (VZV) to reduce the likelihood of shingles and its possible consequence, postherpetic neuralgia. Le, Sabella, and Rothberg, in this issue of the Journal, review clinical and public health challenges affecting the use of this vaccine.
We are almost all exposed to this virus as children, through natural infection (chickenpox) or vaccination; many infections are seemingly subclinical. My older son had the distinct misfortune of getting chickenpox in a quite memorable way, developing a concentrated collection of the pruritic vesicles underneath a newly placed arm cast. Whether we remember the initial infection or not, VZV sets up housekeeping and lies dormant for decades within sensory neurons. Decades later, it may erupt as shingles along the distribution of the infected nerves with characteristic painful vesicles, sometimes with persistent, extremely painful, and debilitating residua within the same dermatomal distribution: postherpetic neuralgia. The triggers for this fairly common scenario are only generically understood and include waning cellular immunity attributed to aging, malignancy, immunosuppressive medications, human immunodeficiency virus, and perhaps stress and depression.
The zoster vaccine is unique in that it is given to bolster already present cellular immunity to prevent clinical recurrence of the earlier infection, decades after the virus has been dormant—not, as for the other vaccines noted above, to prevent primary infection. It doesn’t matter if the patient has already experienced an episode of shingles. The currently available vaccine is a live-attenuated strain (Oka) of VZV. Another vaccine in clinical testing uses isolated viral components with adjuvant and thus eliminates current concerns of giving the live-attenuated vaccine to immunosuppressed and elderly patients, those who may benefit the most from it.
Fortunately, it seems that even significantly immunosuppressed and elderly patients tolerate the current vaccine, but at present it is suggested that these groups not receive the vaccine, and vaccination rates in these patients is low. Hopefully, additional data will accumulate regarding the safety of the vaccine and will permit its more widespread use within these patient groups, or a replacement “dead” vaccine will become available.
As Le et al nicely discuss, the current vaccine efficacy wanes over about 10 years, and then a booster vaccine should be considered, but there are few data to provide safety and efficacy outcome measures from patients who received a booster vaccination. The potential need to receive a booster injection after about a decade, the demonstrated greater efficacy against zoster when the initial vaccination is provided to patients ages 60 through 69 than in those over 70, and the lower absolute impact when given to patients ages 50 through 59 (baseline zoster incidence increases with age) should enter into the conversation with patients as to when they should receive the vaccine.
Additionally, there are the extremely provocative and as yet unanswered questions surrounding the implications of vaccination if VZV infection is a trigger of inflammatory vascular diseases such as giant cell arteritis in the elderly, as was proposed by the late Dr. Don Gilden.1
And yes, I did get the vaccine. I was 64 at the time.
Few in mainstream medicine doubt the efficacy of vaccination and the net positive value of a thoughtful vaccination policy. We have witnessed within a professional lifetime the virtual eradication, at least regionally, of a number of previously devastating infectious diseases including polio, smallpox, pertussis, and measles. With growing understanding of disease mechanisms, the potential value of vaccination has expanded to include preventing sequelae of certain infections and malignancy—a holy grail in oncology, the true prevention of cancer. Sporadic local resistance to uniform vaccination against measles has resulted in geographic reappearance of the disease, providing further support for a uniform approach to vaccination against communicable diseases, with some potential to opt out, perhaps with associated societal repercussions for those who do so.
For most clinicians, certainly those of us dealing with chronically ill or immunosuppressed patients, the decision to recommend annual influenza vaccination and pneumococcal vaccinations per guidelines is an easy one. Vaccination against certain infections provides some protection for the individual patient and for the population, contributing to “herd immunity” and helping to protect against the occurrence of pandemics. But this is not the case for all vaccines. For some vaccines the issues of immunity and vaccination are more individual and complicated and warrant more education, reflection, and conversation.
The vaccine to protect against human papillomavirus is effective at reducing the incidence of cervical and anal cancers triggered by infection with certain strains of human papillomavirus. The viral infection itself is not immediately life-threatening. Thus, patients (and their parents) are asked to consider vaccination against a sexually transmitted virus (before sexual transmission of infection) to prevent a possible malignancy later in life. This decision can create social angst. Perhaps less socially challenging, but medically more complicated, is vaccination against the hepatitis B virus (HBV). HBV is also sexually transmissible, but the source in many patients infected with this virus is unclear. The HBV vaccine helps protect against clinically meaningful hepatitis and chronic liver disease from HBV and also will reduce the occurrence of HBV-associated hepatocellular carcinoma and progression of cirrhosis in patients coinfected with hepatitis C virus.
More complex yet is vaccination against the varicella-zoster virus (VZV) to reduce the likelihood of shingles and its possible consequence, postherpetic neuralgia. Le, Sabella, and Rothberg, in this issue of the Journal, review clinical and public health challenges affecting the use of this vaccine.
We are almost all exposed to this virus as children, through natural infection (chickenpox) or vaccination; many infections are seemingly subclinical. My older son had the distinct misfortune of getting chickenpox in a quite memorable way, developing a concentrated collection of the pruritic vesicles underneath a newly placed arm cast. Whether we remember the initial infection or not, VZV sets up housekeeping and lies dormant for decades within sensory neurons. Decades later, it may erupt as shingles along the distribution of the infected nerves with characteristic painful vesicles, sometimes with persistent, extremely painful, and debilitating residua within the same dermatomal distribution: postherpetic neuralgia. The triggers for this fairly common scenario are only generically understood and include waning cellular immunity attributed to aging, malignancy, immunosuppressive medications, human immunodeficiency virus, and perhaps stress and depression.
The zoster vaccine is unique in that it is given to bolster already present cellular immunity to prevent clinical recurrence of the earlier infection, decades after the virus has been dormant—not, as for the other vaccines noted above, to prevent primary infection. It doesn’t matter if the patient has already experienced an episode of shingles. The currently available vaccine is a live-attenuated strain (Oka) of VZV. Another vaccine in clinical testing uses isolated viral components with adjuvant and thus eliminates current concerns of giving the live-attenuated vaccine to immunosuppressed and elderly patients, those who may benefit the most from it.
Fortunately, it seems that even significantly immunosuppressed and elderly patients tolerate the current vaccine, but at present it is suggested that these groups not receive the vaccine, and vaccination rates in these patients is low. Hopefully, additional data will accumulate regarding the safety of the vaccine and will permit its more widespread use within these patient groups, or a replacement “dead” vaccine will become available.
As Le et al nicely discuss, the current vaccine efficacy wanes over about 10 years, and then a booster vaccine should be considered, but there are few data to provide safety and efficacy outcome measures from patients who received a booster vaccination. The potential need to receive a booster injection after about a decade, the demonstrated greater efficacy against zoster when the initial vaccination is provided to patients ages 60 through 69 than in those over 70, and the lower absolute impact when given to patients ages 50 through 59 (baseline zoster incidence increases with age) should enter into the conversation with patients as to when they should receive the vaccine.
Additionally, there are the extremely provocative and as yet unanswered questions surrounding the implications of vaccination if VZV infection is a trigger of inflammatory vascular diseases such as giant cell arteritis in the elderly, as was proposed by the late Dr. Don Gilden.1
And yes, I did get the vaccine. I was 64 at the time.
- Gilden D, Nagel MA. Varicella zoster virus triggers the immunopathology of giant cell arteritis. Curr Opin Rheumatol 2016; 28:376–382.
- Gilden D, Nagel MA. Varicella zoster virus triggers the immunopathology of giant cell arteritis. Curr Opin Rheumatol 2016; 28:376–382.