User login
MDedge conference coverage features onsite reporting of the latest study results and expert perspectives from leading researchers.
Impact of Stewardship Assistance Pilot Program for Veterans on Adherence and Persistence to Oral mCRPC Therapies
Background
Given the poor prognosis of patients with metastatic castration-resistant prostate cancer (mCRPC), interventions aimed at increasing adherence to oral treatments have the potential to improve patient outcomes. This study evaluates the impact of a patient stewardship assistance pilot program (stewardship program) on the adherence and persistence to oral treatments among patients with mCRPC at VA medical centers (VAMCs).
Methods
A non-randomized controlled study design and data from the VA Corporate Data Warehouse were used. The study included patients treated with an oral mCRPC therapy (i.e., abiraterone acetate or enzalutamide) between 08/2018 and 12/2019. Patients participating in the stewardship program formed the intervention arm and patients not participating the controls. Control patients were selected and matched 1:3 based on age, race and index year. The index date was the date of initiation of abiraterone acetate or enzalutamide. Outcomes included persistence (no gap >60 days of supply) and adherence (proportion of days covered [PDC] ≥80%) to oral mCRPC treatment post-index. Persistence and adherence were compared between the two arms using a Cox proportional hazard model and logistic regression model, respectively, adjusted for baseline characteristics.
Results
The study included 108 intervention patients (mean age: 74.6, 19.4% Black or African American, 44.4% from South, mean Quan-CCI: 6.7) and 324 control patients (mean age: 74.6, 19.4% Black or African American, 31.5% from South, mean Quan-CCI: 6.2). There was no statistically significant difference in persistence between the intervention and control arms (hazard ratio [95% confidence interval]: 0.84 [0.66-1.10], p-value: 0.211), with respective median times to discontinuation of 18 and 19 months. Over the first 12 months post-index, the proportion of adherent patients was not significantly different between the intervention arm and the control arm (50.6% vs. 50.9%; odds ratio [95% confidence interval]: 1.05 [0.80-1.38], p-value: 0.729).
Conclusions
In this racially diverse study of patients treated at VAMCs, high levels of persistence and adherence to oral mCRPC therapy were observed. The absence of any significant difference in adherence and persistence from the study intervention suggests that a stewardship assistance program aimed at improving adherence and persistence of patients with mCRPC may not be required at VAMCs.
Background
Given the poor prognosis of patients with metastatic castration-resistant prostate cancer (mCRPC), interventions aimed at increasing adherence to oral treatments have the potential to improve patient outcomes. This study evaluates the impact of a patient stewardship assistance pilot program (stewardship program) on the adherence and persistence to oral treatments among patients with mCRPC at VA medical centers (VAMCs).
Methods
A non-randomized controlled study design and data from the VA Corporate Data Warehouse were used. The study included patients treated with an oral mCRPC therapy (i.e., abiraterone acetate or enzalutamide) between 08/2018 and 12/2019. Patients participating in the stewardship program formed the intervention arm and patients not participating the controls. Control patients were selected and matched 1:3 based on age, race and index year. The index date was the date of initiation of abiraterone acetate or enzalutamide. Outcomes included persistence (no gap >60 days of supply) and adherence (proportion of days covered [PDC] ≥80%) to oral mCRPC treatment post-index. Persistence and adherence were compared between the two arms using a Cox proportional hazard model and logistic regression model, respectively, adjusted for baseline characteristics.
Results
The study included 108 intervention patients (mean age: 74.6, 19.4% Black or African American, 44.4% from South, mean Quan-CCI: 6.7) and 324 control patients (mean age: 74.6, 19.4% Black or African American, 31.5% from South, mean Quan-CCI: 6.2). There was no statistically significant difference in persistence between the intervention and control arms (hazard ratio [95% confidence interval]: 0.84 [0.66-1.10], p-value: 0.211), with respective median times to discontinuation of 18 and 19 months. Over the first 12 months post-index, the proportion of adherent patients was not significantly different between the intervention arm and the control arm (50.6% vs. 50.9%; odds ratio [95% confidence interval]: 1.05 [0.80-1.38], p-value: 0.729).
Conclusions
In this racially diverse study of patients treated at VAMCs, high levels of persistence and adherence to oral mCRPC therapy were observed. The absence of any significant difference in adherence and persistence from the study intervention suggests that a stewardship assistance program aimed at improving adherence and persistence of patients with mCRPC may not be required at VAMCs.
Background
Given the poor prognosis of patients with metastatic castration-resistant prostate cancer (mCRPC), interventions aimed at increasing adherence to oral treatments have the potential to improve patient outcomes. This study evaluates the impact of a patient stewardship assistance pilot program (stewardship program) on the adherence and persistence to oral treatments among patients with mCRPC at VA medical centers (VAMCs).
Methods
A non-randomized controlled study design and data from the VA Corporate Data Warehouse were used. The study included patients treated with an oral mCRPC therapy (i.e., abiraterone acetate or enzalutamide) between 08/2018 and 12/2019. Patients participating in the stewardship program formed the intervention arm and patients not participating the controls. Control patients were selected and matched 1:3 based on age, race and index year. The index date was the date of initiation of abiraterone acetate or enzalutamide. Outcomes included persistence (no gap >60 days of supply) and adherence (proportion of days covered [PDC] ≥80%) to oral mCRPC treatment post-index. Persistence and adherence were compared between the two arms using a Cox proportional hazard model and logistic regression model, respectively, adjusted for baseline characteristics.
Results
The study included 108 intervention patients (mean age: 74.6, 19.4% Black or African American, 44.4% from South, mean Quan-CCI: 6.7) and 324 control patients (mean age: 74.6, 19.4% Black or African American, 31.5% from South, mean Quan-CCI: 6.2). There was no statistically significant difference in persistence between the intervention and control arms (hazard ratio [95% confidence interval]: 0.84 [0.66-1.10], p-value: 0.211), with respective median times to discontinuation of 18 and 19 months. Over the first 12 months post-index, the proportion of adherent patients was not significantly different between the intervention arm and the control arm (50.6% vs. 50.9%; odds ratio [95% confidence interval]: 1.05 [0.80-1.38], p-value: 0.729).
Conclusions
In this racially diverse study of patients treated at VAMCs, high levels of persistence and adherence to oral mCRPC therapy were observed. The absence of any significant difference in adherence and persistence from the study intervention suggests that a stewardship assistance program aimed at improving adherence and persistence of patients with mCRPC may not be required at VAMCs.
Unexpected Findings: A Rare Case of Signet Ring Cell Adenocarcinoma in the Small Intestine
Introduction
Signet ring cell carcinoma (SRCC) of the small intestine is very rare. It is characterized by the presence of malignant cells that contain mucin that push nuclei to the periphery. It is more aggressive compared to other adenocarcinomas due to early metastasis and poorer prognosis.
Case Presentation
A 59-year-old male with a history of HIV/AIDS, presented with complaints of anorexia, vomiting and weight loss. Initial abdominal CT showed a retroperitoneal mass causing gastric outlet obstruction. The patient elected to go home after supportive treatment and follow up as an outpatient, however, he presented 10 days later with worsening symptoms. Evaluation with CT abdomen and pelvis showed enlarging soft tissue density in the retrocrural space extending into the retroperitoneum around the aorta, as well as a 1.5 cm intraluminal cystic lesion in the duodenum. Endoscopic ultrasound revealed lymphadenopathy of celiac and porta hepatis regions, along with duodenal stenosis, stent placement for decompression was not feasible and biopsies were inconclusive. The decision was made to proceed with laparotomy for decompression and additional biopsies from the retroperitoneal mass and omental lymph nodes, which confirmed poorly differentiated adenocarcinoma with signet ring cells. The presence of a mass in the duodenum strongly suggested adenocarcinoma of small intestine origin. As the patient’s symptoms worsened, imaging revealed progression with lung metastases. The patient continued to deteriorate rapidly requiring dialysis and gangrenous cholecystitis. Given his complex medical history, patient decided to transition to comfort care.
Discussion
SRCC can present with any GI symptoms. Most important step in diagnosing SRCC is biopsy. Current treatment options for small intestinal malignancies include wide resection that includes the mesentery and corresponding lymph nodes. The use of adjuvant chemotherapy has been described only in small retrospective studies. Due to its scarcity, there isn’t sufficient data for optimal treatment strategies compared to gastric SRCC.
Conclusions
This case report highlights the importance of how rare and aggressive signet ring cell adenocarcinoma of the small intestine. There are only a few cases documented in the literature, which is why we lack data on how to manage the disease.
Introduction
Signet ring cell carcinoma (SRCC) of the small intestine is very rare. It is characterized by the presence of malignant cells that contain mucin that push nuclei to the periphery. It is more aggressive compared to other adenocarcinomas due to early metastasis and poorer prognosis.
Case Presentation
A 59-year-old male with a history of HIV/AIDS, presented with complaints of anorexia, vomiting and weight loss. Initial abdominal CT showed a retroperitoneal mass causing gastric outlet obstruction. The patient elected to go home after supportive treatment and follow up as an outpatient, however, he presented 10 days later with worsening symptoms. Evaluation with CT abdomen and pelvis showed enlarging soft tissue density in the retrocrural space extending into the retroperitoneum around the aorta, as well as a 1.5 cm intraluminal cystic lesion in the duodenum. Endoscopic ultrasound revealed lymphadenopathy of celiac and porta hepatis regions, along with duodenal stenosis, stent placement for decompression was not feasible and biopsies were inconclusive. The decision was made to proceed with laparotomy for decompression and additional biopsies from the retroperitoneal mass and omental lymph nodes, which confirmed poorly differentiated adenocarcinoma with signet ring cells. The presence of a mass in the duodenum strongly suggested adenocarcinoma of small intestine origin. As the patient’s symptoms worsened, imaging revealed progression with lung metastases. The patient continued to deteriorate rapidly requiring dialysis and gangrenous cholecystitis. Given his complex medical history, patient decided to transition to comfort care.
Discussion
SRCC can present with any GI symptoms. Most important step in diagnosing SRCC is biopsy. Current treatment options for small intestinal malignancies include wide resection that includes the mesentery and corresponding lymph nodes. The use of adjuvant chemotherapy has been described only in small retrospective studies. Due to its scarcity, there isn’t sufficient data for optimal treatment strategies compared to gastric SRCC.
Conclusions
This case report highlights the importance of how rare and aggressive signet ring cell adenocarcinoma of the small intestine. There are only a few cases documented in the literature, which is why we lack data on how to manage the disease.
Introduction
Signet ring cell carcinoma (SRCC) of the small intestine is very rare. It is characterized by the presence of malignant cells that contain mucin that push nuclei to the periphery. It is more aggressive compared to other adenocarcinomas due to early metastasis and poorer prognosis.
Case Presentation
A 59-year-old male with a history of HIV/AIDS, presented with complaints of anorexia, vomiting and weight loss. Initial abdominal CT showed a retroperitoneal mass causing gastric outlet obstruction. The patient elected to go home after supportive treatment and follow up as an outpatient, however, he presented 10 days later with worsening symptoms. Evaluation with CT abdomen and pelvis showed enlarging soft tissue density in the retrocrural space extending into the retroperitoneum around the aorta, as well as a 1.5 cm intraluminal cystic lesion in the duodenum. Endoscopic ultrasound revealed lymphadenopathy of celiac and porta hepatis regions, along with duodenal stenosis, stent placement for decompression was not feasible and biopsies were inconclusive. The decision was made to proceed with laparotomy for decompression and additional biopsies from the retroperitoneal mass and omental lymph nodes, which confirmed poorly differentiated adenocarcinoma with signet ring cells. The presence of a mass in the duodenum strongly suggested adenocarcinoma of small intestine origin. As the patient’s symptoms worsened, imaging revealed progression with lung metastases. The patient continued to deteriorate rapidly requiring dialysis and gangrenous cholecystitis. Given his complex medical history, patient decided to transition to comfort care.
Discussion
SRCC can present with any GI symptoms. Most important step in diagnosing SRCC is biopsy. Current treatment options for small intestinal malignancies include wide resection that includes the mesentery and corresponding lymph nodes. The use of adjuvant chemotherapy has been described only in small retrospective studies. Due to its scarcity, there isn’t sufficient data for optimal treatment strategies compared to gastric SRCC.
Conclusions
This case report highlights the importance of how rare and aggressive signet ring cell adenocarcinoma of the small intestine. There are only a few cases documented in the literature, which is why we lack data on how to manage the disease.
Registered Dietitian Staffing and Nutrition Practices in High-Risk Cancer Patients Across the Veterans Health Administration
Background
Nutrition disorders, such as sarcopenia, malnutrition, and cachexia are prevalent in cancer patients and correlated with negative outcomes, increased costs, and reduced quality of life (QOL). Registered dietitians (RDs) effectively diagnose and treat nutrition disorders. RD staffing guidelines in outpatient cancer centers are non-specific and unvalidated. This study explored RD staffing ratios to determine trends which may indicate best practices.
Methods
Facility-level measures including full time equivalents (FTE), referral practices, RD participation interdisciplinary round participation, and nutrition referral practices were obtained from survey data of RDs working in oncology clinics and from cancer registries across VHA between 2016-2017. A proactive score was calculated based on interdisciplinary meeting attendances, use of validated screening tools, and standardized protocols for nutrition referrals. Chart review was conducted for 681 Veterans from 13 VHA cancer centers and 207 oncology providers (OPs) to determine weight change, malnutrition, oral nutrition supplement (ONS) use, time to RD referral, and survival. Logistic regression was used for statistical analysis.
Results
Mean and median RD FTE assigned to oncology clinics was 0.5. The total RD:OP ratio ranged from 1:4 to 1:850 with an average of 1 RD to 48.5 OP. An increase in RD:OP ratio from 0:1 to 1:1 was associated with a 16-fold increased odds of weight maintenance during cancer treatment (95% CI: 2.01, 127.53). A 10% increase in the RD:OP ratio increased probability of weight maintenance by 32%. Being seen by an RD was associated with 2.87 times odds of being diagnosed with malnutrition (95% CI: 1.62, 5.08). Each unit increase in a facility’s proactive score was associated with 38% increased odds of a patient being seen by an RD (95% CI: 1.08, 1.76), and 21% reduced odds of being prescribed an ONS (95% CI: 0.63, 0.98).
Conclusions
Few cancer centers employ dedicated fulltime RDs and nutrition practices vary across cancer centers. Improved RD:OP ratios may contribute to improved nutrition outcomes for this population. When RDs are active in interdisciplinary cancer teams, nutrition treatment improves. These efforts support patient complexity, facility funding, and QOL. These data may be used to support cancer care guidelines across VHA.
Background
Nutrition disorders, such as sarcopenia, malnutrition, and cachexia are prevalent in cancer patients and correlated with negative outcomes, increased costs, and reduced quality of life (QOL). Registered dietitians (RDs) effectively diagnose and treat nutrition disorders. RD staffing guidelines in outpatient cancer centers are non-specific and unvalidated. This study explored RD staffing ratios to determine trends which may indicate best practices.
Methods
Facility-level measures including full time equivalents (FTE), referral practices, RD participation interdisciplinary round participation, and nutrition referral practices were obtained from survey data of RDs working in oncology clinics and from cancer registries across VHA between 2016-2017. A proactive score was calculated based on interdisciplinary meeting attendances, use of validated screening tools, and standardized protocols for nutrition referrals. Chart review was conducted for 681 Veterans from 13 VHA cancer centers and 207 oncology providers (OPs) to determine weight change, malnutrition, oral nutrition supplement (ONS) use, time to RD referral, and survival. Logistic regression was used for statistical analysis.
Results
Mean and median RD FTE assigned to oncology clinics was 0.5. The total RD:OP ratio ranged from 1:4 to 1:850 with an average of 1 RD to 48.5 OP. An increase in RD:OP ratio from 0:1 to 1:1 was associated with a 16-fold increased odds of weight maintenance during cancer treatment (95% CI: 2.01, 127.53). A 10% increase in the RD:OP ratio increased probability of weight maintenance by 32%. Being seen by an RD was associated with 2.87 times odds of being diagnosed with malnutrition (95% CI: 1.62, 5.08). Each unit increase in a facility’s proactive score was associated with 38% increased odds of a patient being seen by an RD (95% CI: 1.08, 1.76), and 21% reduced odds of being prescribed an ONS (95% CI: 0.63, 0.98).
Conclusions
Few cancer centers employ dedicated fulltime RDs and nutrition practices vary across cancer centers. Improved RD:OP ratios may contribute to improved nutrition outcomes for this population. When RDs are active in interdisciplinary cancer teams, nutrition treatment improves. These efforts support patient complexity, facility funding, and QOL. These data may be used to support cancer care guidelines across VHA.
Background
Nutrition disorders, such as sarcopenia, malnutrition, and cachexia are prevalent in cancer patients and correlated with negative outcomes, increased costs, and reduced quality of life (QOL). Registered dietitians (RDs) effectively diagnose and treat nutrition disorders. RD staffing guidelines in outpatient cancer centers are non-specific and unvalidated. This study explored RD staffing ratios to determine trends which may indicate best practices.
Methods
Facility-level measures including full time equivalents (FTE), referral practices, RD participation interdisciplinary round participation, and nutrition referral practices were obtained from survey data of RDs working in oncology clinics and from cancer registries across VHA between 2016-2017. A proactive score was calculated based on interdisciplinary meeting attendances, use of validated screening tools, and standardized protocols for nutrition referrals. Chart review was conducted for 681 Veterans from 13 VHA cancer centers and 207 oncology providers (OPs) to determine weight change, malnutrition, oral nutrition supplement (ONS) use, time to RD referral, and survival. Logistic regression was used for statistical analysis.
Results
Mean and median RD FTE assigned to oncology clinics was 0.5. The total RD:OP ratio ranged from 1:4 to 1:850 with an average of 1 RD to 48.5 OP. An increase in RD:OP ratio from 0:1 to 1:1 was associated with a 16-fold increased odds of weight maintenance during cancer treatment (95% CI: 2.01, 127.53). A 10% increase in the RD:OP ratio increased probability of weight maintenance by 32%. Being seen by an RD was associated with 2.87 times odds of being diagnosed with malnutrition (95% CI: 1.62, 5.08). Each unit increase in a facility’s proactive score was associated with 38% increased odds of a patient being seen by an RD (95% CI: 1.08, 1.76), and 21% reduced odds of being prescribed an ONS (95% CI: 0.63, 0.98).
Conclusions
Few cancer centers employ dedicated fulltime RDs and nutrition practices vary across cancer centers. Improved RD:OP ratios may contribute to improved nutrition outcomes for this population. When RDs are active in interdisciplinary cancer teams, nutrition treatment improves. These efforts support patient complexity, facility funding, and QOL. These data may be used to support cancer care guidelines across VHA.
Telehealth Research and Innovation for Veterans With Cancer (THRIVE): Understanding Experiences of National TeleOncology Service Providers
Background
Currently within the Veterans Health Administration, nearly 38% of VA users reside in rural areas. Approximately 70% of rural areas do not have an oncologist, resulting in a high proportion of Veterans who lack access to specialized cancer services. The National TeleOncology Service (NTO) was designed to increase access to specialty and subspecialty cancer care for Veterans regardless of geographical location, and for those who may experience additional barriers to in-person care due to medical complexity or other social determinants of health. Purpose: THRIVE focuses on health equity for telehealth-delivered cancer care. We are specifically interested in the intersection of poverty, rurality, and race. As part of this inquiry, we examined provider experiences of the NTO to better understand the benefits, drawbacks, facilitators and barriers to implementing NTO care.
Methods
We conducted two focus groups with NTO providers. We developed guides using the Consolidated Framework for Implementation Research (CFIR 2.0) and utilized rapid qualitative analysis. We arrayed data in matrices based on CFIR 2.0-based guide for analysis.
Results
The focus groups included NTO physicians (n=4) and non-physicians (n=19). Providers agreed that NTO provides valuable cancer care to Veterans facing in-person access issues. The technology is easy to use for many patients, but those in rural areas experiencing poverty struggle most. NTO’s technical support resources reduce technical skill and equipment barriers and facilitate connection for both patients and providers. Providers enjoyed the team-based approach of NTO and believed it increases care quality through access to multiple providers and resources within the clinical encounter. The NTO’s work could be strengthened by standardizing technology to facilitate records transfer and enable sharing of documentation and education between NTO and patients. Implications: This study examined providers’ perceived acceptability, feasibility, barriers, and facilitators of NTO-delivered cancer care within VA, demonstrating that NTO service is well-liked and a valuable emerging resource of VA care.
Conclusions
In an era when CMMS shifts away from reimbursing telehealth, VA has committed to continue such care providing a variety of patient-centered approaches. NTO may serve as a model for expanding telehealth-delivered care for other serious and chronic diseases and conditions.
Background
Currently within the Veterans Health Administration, nearly 38% of VA users reside in rural areas. Approximately 70% of rural areas do not have an oncologist, resulting in a high proportion of Veterans who lack access to specialized cancer services. The National TeleOncology Service (NTO) was designed to increase access to specialty and subspecialty cancer care for Veterans regardless of geographical location, and for those who may experience additional barriers to in-person care due to medical complexity or other social determinants of health. Purpose: THRIVE focuses on health equity for telehealth-delivered cancer care. We are specifically interested in the intersection of poverty, rurality, and race. As part of this inquiry, we examined provider experiences of the NTO to better understand the benefits, drawbacks, facilitators and barriers to implementing NTO care.
Methods
We conducted two focus groups with NTO providers. We developed guides using the Consolidated Framework for Implementation Research (CFIR 2.0) and utilized rapid qualitative analysis. We arrayed data in matrices based on CFIR 2.0-based guide for analysis.
Results
The focus groups included NTO physicians (n=4) and non-physicians (n=19). Providers agreed that NTO provides valuable cancer care to Veterans facing in-person access issues. The technology is easy to use for many patients, but those in rural areas experiencing poverty struggle most. NTO’s technical support resources reduce technical skill and equipment barriers and facilitate connection for both patients and providers. Providers enjoyed the team-based approach of NTO and believed it increases care quality through access to multiple providers and resources within the clinical encounter. The NTO’s work could be strengthened by standardizing technology to facilitate records transfer and enable sharing of documentation and education between NTO and patients. Implications: This study examined providers’ perceived acceptability, feasibility, barriers, and facilitators of NTO-delivered cancer care within VA, demonstrating that NTO service is well-liked and a valuable emerging resource of VA care.
Conclusions
In an era when CMMS shifts away from reimbursing telehealth, VA has committed to continue such care providing a variety of patient-centered approaches. NTO may serve as a model for expanding telehealth-delivered care for other serious and chronic diseases and conditions.
Background
Currently within the Veterans Health Administration, nearly 38% of VA users reside in rural areas. Approximately 70% of rural areas do not have an oncologist, resulting in a high proportion of Veterans who lack access to specialized cancer services. The National TeleOncology Service (NTO) was designed to increase access to specialty and subspecialty cancer care for Veterans regardless of geographical location, and for those who may experience additional barriers to in-person care due to medical complexity or other social determinants of health. Purpose: THRIVE focuses on health equity for telehealth-delivered cancer care. We are specifically interested in the intersection of poverty, rurality, and race. As part of this inquiry, we examined provider experiences of the NTO to better understand the benefits, drawbacks, facilitators and barriers to implementing NTO care.
Methods
We conducted two focus groups with NTO providers. We developed guides using the Consolidated Framework for Implementation Research (CFIR 2.0) and utilized rapid qualitative analysis. We arrayed data in matrices based on CFIR 2.0-based guide for analysis.
Results
The focus groups included NTO physicians (n=4) and non-physicians (n=19). Providers agreed that NTO provides valuable cancer care to Veterans facing in-person access issues. The technology is easy to use for many patients, but those in rural areas experiencing poverty struggle most. NTO’s technical support resources reduce technical skill and equipment barriers and facilitate connection for both patients and providers. Providers enjoyed the team-based approach of NTO and believed it increases care quality through access to multiple providers and resources within the clinical encounter. The NTO’s work could be strengthened by standardizing technology to facilitate records transfer and enable sharing of documentation and education between NTO and patients. Implications: This study examined providers’ perceived acceptability, feasibility, barriers, and facilitators of NTO-delivered cancer care within VA, demonstrating that NTO service is well-liked and a valuable emerging resource of VA care.
Conclusions
In an era when CMMS shifts away from reimbursing telehealth, VA has committed to continue such care providing a variety of patient-centered approaches. NTO may serve as a model for expanding telehealth-delivered care for other serious and chronic diseases and conditions.
Support for Laser Treatment to Reduce NMSC Risk is Increasing
CARLSBAD, CALIFORNIA — and a key 2017 publication laid the groundwork for current approaches, according to Elizabeth Tanzi, MD.
In the article, which was published in Molecules, Mike Kemp, PhD, and Jeffrey Bryant Travers, MD, PhD, at Wright State University, Dayton, Ohio, and Dan F. Spandau, PhD, at Indiana University School of Medicine, Indianapolis, demonstrated that geriatric skin responds to ultraviolet B (UVB) differently than young skin because of differences in insulin-like growth factor 1 (IGF-1) levels produced by dermal fibroblasts.
“As we age, our fibroblasts become senescent, inactive,” Dr. Tanzi, associate clinical professor of dermatology at George Washington University, Washington, DC, said at the Controversies and Conversations in Laser and Cosmetic Surgery symposium. “They don’t make as many growth factors, particularly IGF-1, and therefore we don’t stimulate the responses. We need more of our growth factors.”
In later, separate work, Dr. Travers, Dr. Spandau, and colleagues found that using dermabrasion or fractionated laser resurfacing to wound the skin can result in increased dermal IGF-1 levels and normalization of the abnormal pro-carcinogenic UV response associated with geriatric skin — a treatment that has the potential to prevent NMSC. That study “was the epiphany” for fostering interest among researchers in the field of lasers and medicine, Dr. Tanzi said.
In a retrospective cohort study, Mathew Avram, MD, JD, and colleagues reviewed patients with a history of facial keratinocyte carcinoma (KC) who were treated at Massachusetts General Hospital in Boston between 2005 and 2021. The study population included 43 patients treated with either the 1927- or the 1550-nm nonablative fractional laser (NAFL) and 52 matched controls. The rate of subsequent facial KC development was 20.9% in NAFL-treated patients and 40.4% in controls (relative risk, 0.52, P = .049).
During a separate presentation at the meeting, Dr. Avram, director of lasers and cosmetics at Massachusetts General Hospital, Boston, said that, when he and his colleagues controlled for age, gender, and skin type, controls were 2.65 times more likely to develop new facial KC, compared with those treated with NAFL (P = .0169). “This enhanced effect was seen with the 1550-nm device, compared with the 1927-nm device. The study shows us that 1550-nm/1927-nm NAFL may have a protective effect for patients with a history of KC, but the role of each wavelength is to be determined. We also need a prospective, controlled study to verify the results.”
In an ongoing study first presented at the 2023 annual meeting of the American Society for Dermatologic Surgery, Dr. Tanzi and colleagues enrolled 15 patients aged ≥ 55 years to evaluate the restoration of physiologic features and biomarkers in skin treated with 25% trichloroacetic acid (TCA), plus the 1550-nm or 1927-nm NAFL. Four sites on the back were treated and biopsies were taken at baseline and at 3 months post treatment. The protocol involved TCA 25% to speckled frost, with the 1550-nm device set to level 6 at 70 mJ and the 1927-nm device set to level 8 at 20 mJ. Immunohistochemical stains are still pending; however, physiologic changes were noted.
Three months after a single treatment, the 1927-nm treated areas showed statistically significant elongation of fibroblasts (consistent with younger fibroblasts) on histology. “Although not a large study, it supports the growing body of research that demonstrates we are improving the health of our patients’ skin with certain types of laser treatments, not just beautifying it,” Dr. Tanzi said.
Dr. Tanzi disclosed being a member of the advisory board for AbbVie/Allergan and Sciton, and is a consultant for Alastin/Galderma, Candesant Biomedical, Cytrellis, Revance, and Solta Medical. Dr. Avram disclosed that he receives intellectual property royalties from and holds stock options in Cytrellis, and is a consultant to Allergan and holds stock options in BAI Biosciences, Sofwave, and La Jolla NanoMedical.
A version of this article first appeared on Medscape.com.
CARLSBAD, CALIFORNIA — and a key 2017 publication laid the groundwork for current approaches, according to Elizabeth Tanzi, MD.
In the article, which was published in Molecules, Mike Kemp, PhD, and Jeffrey Bryant Travers, MD, PhD, at Wright State University, Dayton, Ohio, and Dan F. Spandau, PhD, at Indiana University School of Medicine, Indianapolis, demonstrated that geriatric skin responds to ultraviolet B (UVB) differently than young skin because of differences in insulin-like growth factor 1 (IGF-1) levels produced by dermal fibroblasts.
“As we age, our fibroblasts become senescent, inactive,” Dr. Tanzi, associate clinical professor of dermatology at George Washington University, Washington, DC, said at the Controversies and Conversations in Laser and Cosmetic Surgery symposium. “They don’t make as many growth factors, particularly IGF-1, and therefore we don’t stimulate the responses. We need more of our growth factors.”
In later, separate work, Dr. Travers, Dr. Spandau, and colleagues found that using dermabrasion or fractionated laser resurfacing to wound the skin can result in increased dermal IGF-1 levels and normalization of the abnormal pro-carcinogenic UV response associated with geriatric skin — a treatment that has the potential to prevent NMSC. That study “was the epiphany” for fostering interest among researchers in the field of lasers and medicine, Dr. Tanzi said.
In a retrospective cohort study, Mathew Avram, MD, JD, and colleagues reviewed patients with a history of facial keratinocyte carcinoma (KC) who were treated at Massachusetts General Hospital in Boston between 2005 and 2021. The study population included 43 patients treated with either the 1927- or the 1550-nm nonablative fractional laser (NAFL) and 52 matched controls. The rate of subsequent facial KC development was 20.9% in NAFL-treated patients and 40.4% in controls (relative risk, 0.52, P = .049).
During a separate presentation at the meeting, Dr. Avram, director of lasers and cosmetics at Massachusetts General Hospital, Boston, said that, when he and his colleagues controlled for age, gender, and skin type, controls were 2.65 times more likely to develop new facial KC, compared with those treated with NAFL (P = .0169). “This enhanced effect was seen with the 1550-nm device, compared with the 1927-nm device. The study shows us that 1550-nm/1927-nm NAFL may have a protective effect for patients with a history of KC, but the role of each wavelength is to be determined. We also need a prospective, controlled study to verify the results.”
In an ongoing study first presented at the 2023 annual meeting of the American Society for Dermatologic Surgery, Dr. Tanzi and colleagues enrolled 15 patients aged ≥ 55 years to evaluate the restoration of physiologic features and biomarkers in skin treated with 25% trichloroacetic acid (TCA), plus the 1550-nm or 1927-nm NAFL. Four sites on the back were treated and biopsies were taken at baseline and at 3 months post treatment. The protocol involved TCA 25% to speckled frost, with the 1550-nm device set to level 6 at 70 mJ and the 1927-nm device set to level 8 at 20 mJ. Immunohistochemical stains are still pending; however, physiologic changes were noted.
Three months after a single treatment, the 1927-nm treated areas showed statistically significant elongation of fibroblasts (consistent with younger fibroblasts) on histology. “Although not a large study, it supports the growing body of research that demonstrates we are improving the health of our patients’ skin with certain types of laser treatments, not just beautifying it,” Dr. Tanzi said.
Dr. Tanzi disclosed being a member of the advisory board for AbbVie/Allergan and Sciton, and is a consultant for Alastin/Galderma, Candesant Biomedical, Cytrellis, Revance, and Solta Medical. Dr. Avram disclosed that he receives intellectual property royalties from and holds stock options in Cytrellis, and is a consultant to Allergan and holds stock options in BAI Biosciences, Sofwave, and La Jolla NanoMedical.
A version of this article first appeared on Medscape.com.
CARLSBAD, CALIFORNIA — and a key 2017 publication laid the groundwork for current approaches, according to Elizabeth Tanzi, MD.
In the article, which was published in Molecules, Mike Kemp, PhD, and Jeffrey Bryant Travers, MD, PhD, at Wright State University, Dayton, Ohio, and Dan F. Spandau, PhD, at Indiana University School of Medicine, Indianapolis, demonstrated that geriatric skin responds to ultraviolet B (UVB) differently than young skin because of differences in insulin-like growth factor 1 (IGF-1) levels produced by dermal fibroblasts.
“As we age, our fibroblasts become senescent, inactive,” Dr. Tanzi, associate clinical professor of dermatology at George Washington University, Washington, DC, said at the Controversies and Conversations in Laser and Cosmetic Surgery symposium. “They don’t make as many growth factors, particularly IGF-1, and therefore we don’t stimulate the responses. We need more of our growth factors.”
In later, separate work, Dr. Travers, Dr. Spandau, and colleagues found that using dermabrasion or fractionated laser resurfacing to wound the skin can result in increased dermal IGF-1 levels and normalization of the abnormal pro-carcinogenic UV response associated with geriatric skin — a treatment that has the potential to prevent NMSC. That study “was the epiphany” for fostering interest among researchers in the field of lasers and medicine, Dr. Tanzi said.
In a retrospective cohort study, Mathew Avram, MD, JD, and colleagues reviewed patients with a history of facial keratinocyte carcinoma (KC) who were treated at Massachusetts General Hospital in Boston between 2005 and 2021. The study population included 43 patients treated with either the 1927- or the 1550-nm nonablative fractional laser (NAFL) and 52 matched controls. The rate of subsequent facial KC development was 20.9% in NAFL-treated patients and 40.4% in controls (relative risk, 0.52, P = .049).
During a separate presentation at the meeting, Dr. Avram, director of lasers and cosmetics at Massachusetts General Hospital, Boston, said that, when he and his colleagues controlled for age, gender, and skin type, controls were 2.65 times more likely to develop new facial KC, compared with those treated with NAFL (P = .0169). “This enhanced effect was seen with the 1550-nm device, compared with the 1927-nm device. The study shows us that 1550-nm/1927-nm NAFL may have a protective effect for patients with a history of KC, but the role of each wavelength is to be determined. We also need a prospective, controlled study to verify the results.”
In an ongoing study first presented at the 2023 annual meeting of the American Society for Dermatologic Surgery, Dr. Tanzi and colleagues enrolled 15 patients aged ≥ 55 years to evaluate the restoration of physiologic features and biomarkers in skin treated with 25% trichloroacetic acid (TCA), plus the 1550-nm or 1927-nm NAFL. Four sites on the back were treated and biopsies were taken at baseline and at 3 months post treatment. The protocol involved TCA 25% to speckled frost, with the 1550-nm device set to level 6 at 70 mJ and the 1927-nm device set to level 8 at 20 mJ. Immunohistochemical stains are still pending; however, physiologic changes were noted.
Three months after a single treatment, the 1927-nm treated areas showed statistically significant elongation of fibroblasts (consistent with younger fibroblasts) on histology. “Although not a large study, it supports the growing body of research that demonstrates we are improving the health of our patients’ skin with certain types of laser treatments, not just beautifying it,” Dr. Tanzi said.
Dr. Tanzi disclosed being a member of the advisory board for AbbVie/Allergan and Sciton, and is a consultant for Alastin/Galderma, Candesant Biomedical, Cytrellis, Revance, and Solta Medical. Dr. Avram disclosed that he receives intellectual property royalties from and holds stock options in Cytrellis, and is a consultant to Allergan and holds stock options in BAI Biosciences, Sofwave, and La Jolla NanoMedical.
A version of this article first appeared on Medscape.com.
Diagnosing, Treating Rashes In Patients on Immune Checkpoint Inhibitors
WASHINGTON, DC — and with judicious usage and dosing of prednisone when deemed necessary, Blair Allais, MD, said during a session on supportive oncodermatology at the ElderDerm conference on dermatology in the older patient hosted by the George Washington University School of Medicine and Health Sciences, Washington, DC.
“It’s important when you see these patients to be as specific as possible” based on morphology and histopathology, and to treat the rashes in a similar way as in the non-ICI setting,” said Dr. Allais, a dermato-oncologist at the Inova Schar Cancer Institute, Fairfax, Virginia.
cirAEs are the most frequently reported and most visible adverse effects of checkpoint inhibition — a treatment that has emerged as a standard therapy for many malignancies since the first ICI was approved in 2011 for metastatic melanoma.
And contrary to what the phenomenon of immunosenescence might suggest, older patients are no less prone to cirAEs than younger patients. “You’d think you’d have fewer rashes and side effects as you age, but that’s not true,” said Dr. Allais, who completed a fellowship in cutaneous oncology after her dermatology residency.
A 2021 multicenter international cohort study of over 900 patients aged ≥ 80 years treated with single-agent ICIs for cancer did not find any significant differences in the development of immune-related adverse events among those younger than 85, those aged 85-89 years, and those 90 and older. Neither did the ELDERS study in the United Kingdom; this prospective observational study found similar rates of high-grade and low-grade immune toxicity in its two cohorts of patients ≥ 70 and < 70 years of age.
At the meeting, Dr. Allais, who coauthored a 2023 review of cirAEs from ICIs, reviewed recent developments and provided the following advice:
New diagnostic criteria: “Really exciting” news for more precise diagnosis and optimal therapy of cirAEs, Dr. Allais said, is a position paper published in the Journal for ImmunoTherapy of Cancer that offers consensus-based diagnostic criteria for the 10 most common types of dermatologic immune-related adverse events and an overall diagnostic framework. “Luckily, through the work of a Delphi consensus group, we can now have [more diagnostic specificity],” which is important for both clinical care and research, she said.
Most cirAEs have typically been reported nonspecifically as “rash,” but diagnosing a rash subtype is “critical in tailoring appropriate therapy that it is both effective and the least detrimental to the oncology treatment plan for patients with cancer,” the group’s coauthors wrote.
The 10 core diagnoses include psoriasis, eczematous dermatitis, vitiligo, Grover disease, eruptive atypical squamous proliferation, and bullous pemphigoid. Outside of the core diagnoses are other nonspecific presentations that require evaluation to arrive at a diagnosis, if possible, or to reveal data that can allow for targeted therapy and severity grading, the group explains in its paper.
“To prednisone or not to prednisone”: The development of cirAEs is associated with reduced mortality and improved cancer outcomes, making the use of immunosuppressants such as corticosteroids a therapeutic dilemma. “Patients who get these rashes usually do better with respect to their cancer, so the concern has been, if we affect how they respond to their immunotherapy, we may minimize that improvement in mortality,” said Dr. Allais, also assistant professor at the University of Virginia, Charlottesville, and clinical assistant professor of dermatology at George Washington University.
A widely discussed study published in 2015 reported on 254 patients with melanoma who developed an immune-related adverse event during treatment with ipilimumab — approximately one third of whom required systemic corticosteroids — and concluded that systemic corticosteroids did not affect overall survival or time to (cancer) treatment failure. This study from Memorial Sloan Kettering Cancer Center, New York City, “was the first large study looking at this question,” she said, and the subsequent message for several years in conferences and the literature was that steroids do not affect the efficacy of checkpoint inhibitors.
“But the study was not without limitations,” Dr. Allais said, “because the patients who got prednisone were mainly those with higher-grade toxicities,” while those not treated with corticosteroids had either no toxicities or low-grade toxicities. “If higher-grade toxicities were associated with better (antitumor) response, the steroids may have just [blunted] that benefit.”
The current totality of data available in the literature suggests that corticosteroids may indeed have an impact on the efficacy of ICI therapy. “Subsequent studies have come out in the community that have shown that we should probably think twice about giving prednisone to some patients, particularly within the first 50 days of ICI treatment, and that we should be mindful of the dose,” Dr. Allais said.
The takeaways from these studies — all published in the past few years — are to use prednisone early and liberally for life-threatening toxicity, to use it at the lowest dose and for the shortest course when there is not an appropriate alternative, to avoid it for diagnoses that are not treated with prednisone outside the ICI setting, and to “have a plan” for a steroid-sparing agent to use after prednisone, she said.
Dr. Allais recommends heightened consideration during the first 50 days of ICI treatment based on a multicenter retrospective study that found a significant association between use of high-dose glucocorticoids (≥ 60 mg prednisone equivalent once a day) within 8 weeks of anti–programmed cell death protein 1 (PD-1) monotherapy initiation and poorer progression-free and overall survival. The study covered a cohort of 947 patients with advanced melanoma treated with anti–PD-1 monotherapy between 2009 and 2019, 54% of whom developed immune-related adverse events.
This study and other recent studies addressing the association between steroids and survival outcomes in patients with immune-related adverse events during ICI therapy are described in Dr. Allais’ 2023 review of cirAEs from ICIs.
Approach to morbilliform eruptions: This rash is “super common” in patients on ICIs, occurring generally within 2-3 weeks of starting treatment. “It tends to be self-limited and can recur with future infusions,” Dr. Allais said.
Systemic steroids should be reserved for severe or refractory eruptions. “Usually, I treat the patients with topical steroids, and I manage their expectations (that the rash may recur with subsequent infusions), but I closely follow them up” within 2-3 weeks, she said. It’s important to rule out a severe cutaneous adverse drug eruption, of course, and to start high-dose systemic steroids immediately if necessary. “Antibiotics are a big culprit” and often can be discontinued.
Soak and smear: “I’m obsessed” with this technique of a 20-minute soak in plain water followed by application of steroid ointment, said Dr. Allais, referring to a small study published in 2005 that reported a complete response after 2 weeks in 60% of patients with psoriasis, atopic dermatitis, and other inflammatory skin conditions (none had cancer), who had failed prior systemic therapy. All patients had at least a 75% response.
The method offers a way to “avoid the systemic immunosuppression we’d get with prednisone,” she said. One just needs to make sure the older patient can get in and out of their tub safely.
ICI-induced bullous pemphigoid (BP): BP occurs more frequently in the ICI setting, compared with the general population, with a median time to development of 8.5 months after ICI initiation. It is associated in this setting with improved tumor response, but “many oncologists stop anticancer treatment because of this diagnosis,” she said.
In the supportive oncodermatology space, however, ICI-induced BP exemplifies the value of tailored treatment regimens, she said. A small multi-institutional retrospective cohort study published in 2023 identified 35 cases of ICI-BP among 5636 ICI-treated patients and found that 8 out of 11 patients who received biologic therapy (rituximab, omalizumab, or dupilumab) had a complete response to ICI-BP without flares following subsequent ICI cycles. And while statistical significance was not reached, the study showed that no cancer-related outcomes were worsened.
“If you see someone with ICI-induced BP and they have a lot of involvement, you could start them on steroids and get that steroid-sparing agent initiated for approval. ... And if IgE is elevated, you might reach for omalizumab,” said Dr. Allais, noting that her favored treatment overall is dupilumab.
Risk factors for the development of ICI-induced BP include age > 70, skin cancer, and having an initial response to ICI on first imaging, the latter of which “I find fascinating ... because imaging occurs within the first 12 weeks of treatment, but we don’t see BP popping up until 8.5 months into treatment,” she noted. “So maybe there’s a baseline risk factor that could predispose them.”
Caution with antibiotics: “I try to avoid antibiotics in the ICI setting,” Dr. Allais said, in deference to the “ever-important microbiome.” Studies have demonstrated that the microbiomes of responders to ICI treatment are different from those of nonresponders, she said.
And a “fascinating” study of patients with melanoma undergoing ICI therapy showed not only a higher abundance of Ruminococcaceae bacteria in responders vs nonresponders but a significant impact of dietary fiber. High dietary fiber was associated with significantly improved overall survival in the patients on ICI, with the most pronounced benefit in patients with good fiber intake and no probiotic use. “Even wilder, their T cells changed,” she said. “They had a high expression of genes related to T-cell activation ... so more tumor-infiltrating lymphocytes.”
A retrospective study of 568 patients with stages III and IV melanoma treated with ICI showed that those exposed to antibiotics prior to ICI had significantly worse overall survival than those not exposed to antibiotics. “Think before you give them,” Dr. Allais said. “And try to tell your older patients to eat beans and greens.”
Dr. Allais reported having no relevant disclosures.
A version of this article first appeared on Medscape.com.
WASHINGTON, DC — and with judicious usage and dosing of prednisone when deemed necessary, Blair Allais, MD, said during a session on supportive oncodermatology at the ElderDerm conference on dermatology in the older patient hosted by the George Washington University School of Medicine and Health Sciences, Washington, DC.
“It’s important when you see these patients to be as specific as possible” based on morphology and histopathology, and to treat the rashes in a similar way as in the non-ICI setting,” said Dr. Allais, a dermato-oncologist at the Inova Schar Cancer Institute, Fairfax, Virginia.
cirAEs are the most frequently reported and most visible adverse effects of checkpoint inhibition — a treatment that has emerged as a standard therapy for many malignancies since the first ICI was approved in 2011 for metastatic melanoma.
And contrary to what the phenomenon of immunosenescence might suggest, older patients are no less prone to cirAEs than younger patients. “You’d think you’d have fewer rashes and side effects as you age, but that’s not true,” said Dr. Allais, who completed a fellowship in cutaneous oncology after her dermatology residency.
A 2021 multicenter international cohort study of over 900 patients aged ≥ 80 years treated with single-agent ICIs for cancer did not find any significant differences in the development of immune-related adverse events among those younger than 85, those aged 85-89 years, and those 90 and older. Neither did the ELDERS study in the United Kingdom; this prospective observational study found similar rates of high-grade and low-grade immune toxicity in its two cohorts of patients ≥ 70 and < 70 years of age.
At the meeting, Dr. Allais, who coauthored a 2023 review of cirAEs from ICIs, reviewed recent developments and provided the following advice:
New diagnostic criteria: “Really exciting” news for more precise diagnosis and optimal therapy of cirAEs, Dr. Allais said, is a position paper published in the Journal for ImmunoTherapy of Cancer that offers consensus-based diagnostic criteria for the 10 most common types of dermatologic immune-related adverse events and an overall diagnostic framework. “Luckily, through the work of a Delphi consensus group, we can now have [more diagnostic specificity],” which is important for both clinical care and research, she said.
Most cirAEs have typically been reported nonspecifically as “rash,” but diagnosing a rash subtype is “critical in tailoring appropriate therapy that it is both effective and the least detrimental to the oncology treatment plan for patients with cancer,” the group’s coauthors wrote.
The 10 core diagnoses include psoriasis, eczematous dermatitis, vitiligo, Grover disease, eruptive atypical squamous proliferation, and bullous pemphigoid. Outside of the core diagnoses are other nonspecific presentations that require evaluation to arrive at a diagnosis, if possible, or to reveal data that can allow for targeted therapy and severity grading, the group explains in its paper.
“To prednisone or not to prednisone”: The development of cirAEs is associated with reduced mortality and improved cancer outcomes, making the use of immunosuppressants such as corticosteroids a therapeutic dilemma. “Patients who get these rashes usually do better with respect to their cancer, so the concern has been, if we affect how they respond to their immunotherapy, we may minimize that improvement in mortality,” said Dr. Allais, also assistant professor at the University of Virginia, Charlottesville, and clinical assistant professor of dermatology at George Washington University.
A widely discussed study published in 2015 reported on 254 patients with melanoma who developed an immune-related adverse event during treatment with ipilimumab — approximately one third of whom required systemic corticosteroids — and concluded that systemic corticosteroids did not affect overall survival or time to (cancer) treatment failure. This study from Memorial Sloan Kettering Cancer Center, New York City, “was the first large study looking at this question,” she said, and the subsequent message for several years in conferences and the literature was that steroids do not affect the efficacy of checkpoint inhibitors.
“But the study was not without limitations,” Dr. Allais said, “because the patients who got prednisone were mainly those with higher-grade toxicities,” while those not treated with corticosteroids had either no toxicities or low-grade toxicities. “If higher-grade toxicities were associated with better (antitumor) response, the steroids may have just [blunted] that benefit.”
The current totality of data available in the literature suggests that corticosteroids may indeed have an impact on the efficacy of ICI therapy. “Subsequent studies have come out in the community that have shown that we should probably think twice about giving prednisone to some patients, particularly within the first 50 days of ICI treatment, and that we should be mindful of the dose,” Dr. Allais said.
The takeaways from these studies — all published in the past few years — are to use prednisone early and liberally for life-threatening toxicity, to use it at the lowest dose and for the shortest course when there is not an appropriate alternative, to avoid it for diagnoses that are not treated with prednisone outside the ICI setting, and to “have a plan” for a steroid-sparing agent to use after prednisone, she said.
Dr. Allais recommends heightened consideration during the first 50 days of ICI treatment based on a multicenter retrospective study that found a significant association between use of high-dose glucocorticoids (≥ 60 mg prednisone equivalent once a day) within 8 weeks of anti–programmed cell death protein 1 (PD-1) monotherapy initiation and poorer progression-free and overall survival. The study covered a cohort of 947 patients with advanced melanoma treated with anti–PD-1 monotherapy between 2009 and 2019, 54% of whom developed immune-related adverse events.
This study and other recent studies addressing the association between steroids and survival outcomes in patients with immune-related adverse events during ICI therapy are described in Dr. Allais’ 2023 review of cirAEs from ICIs.
Approach to morbilliform eruptions: This rash is “super common” in patients on ICIs, occurring generally within 2-3 weeks of starting treatment. “It tends to be self-limited and can recur with future infusions,” Dr. Allais said.
Systemic steroids should be reserved for severe or refractory eruptions. “Usually, I treat the patients with topical steroids, and I manage their expectations (that the rash may recur with subsequent infusions), but I closely follow them up” within 2-3 weeks, she said. It’s important to rule out a severe cutaneous adverse drug eruption, of course, and to start high-dose systemic steroids immediately if necessary. “Antibiotics are a big culprit” and often can be discontinued.
Soak and smear: “I’m obsessed” with this technique of a 20-minute soak in plain water followed by application of steroid ointment, said Dr. Allais, referring to a small study published in 2005 that reported a complete response after 2 weeks in 60% of patients with psoriasis, atopic dermatitis, and other inflammatory skin conditions (none had cancer), who had failed prior systemic therapy. All patients had at least a 75% response.
The method offers a way to “avoid the systemic immunosuppression we’d get with prednisone,” she said. One just needs to make sure the older patient can get in and out of their tub safely.
ICI-induced bullous pemphigoid (BP): BP occurs more frequently in the ICI setting, compared with the general population, with a median time to development of 8.5 months after ICI initiation. It is associated in this setting with improved tumor response, but “many oncologists stop anticancer treatment because of this diagnosis,” she said.
In the supportive oncodermatology space, however, ICI-induced BP exemplifies the value of tailored treatment regimens, she said. A small multi-institutional retrospective cohort study published in 2023 identified 35 cases of ICI-BP among 5636 ICI-treated patients and found that 8 out of 11 patients who received biologic therapy (rituximab, omalizumab, or dupilumab) had a complete response to ICI-BP without flares following subsequent ICI cycles. And while statistical significance was not reached, the study showed that no cancer-related outcomes were worsened.
“If you see someone with ICI-induced BP and they have a lot of involvement, you could start them on steroids and get that steroid-sparing agent initiated for approval. ... And if IgE is elevated, you might reach for omalizumab,” said Dr. Allais, noting that her favored treatment overall is dupilumab.
Risk factors for the development of ICI-induced BP include age > 70, skin cancer, and having an initial response to ICI on first imaging, the latter of which “I find fascinating ... because imaging occurs within the first 12 weeks of treatment, but we don’t see BP popping up until 8.5 months into treatment,” she noted. “So maybe there’s a baseline risk factor that could predispose them.”
Caution with antibiotics: “I try to avoid antibiotics in the ICI setting,” Dr. Allais said, in deference to the “ever-important microbiome.” Studies have demonstrated that the microbiomes of responders to ICI treatment are different from those of nonresponders, she said.
And a “fascinating” study of patients with melanoma undergoing ICI therapy showed not only a higher abundance of Ruminococcaceae bacteria in responders vs nonresponders but a significant impact of dietary fiber. High dietary fiber was associated with significantly improved overall survival in the patients on ICI, with the most pronounced benefit in patients with good fiber intake and no probiotic use. “Even wilder, their T cells changed,” she said. “They had a high expression of genes related to T-cell activation ... so more tumor-infiltrating lymphocytes.”
A retrospective study of 568 patients with stages III and IV melanoma treated with ICI showed that those exposed to antibiotics prior to ICI had significantly worse overall survival than those not exposed to antibiotics. “Think before you give them,” Dr. Allais said. “And try to tell your older patients to eat beans and greens.”
Dr. Allais reported having no relevant disclosures.
A version of this article first appeared on Medscape.com.
WASHINGTON, DC — and with judicious usage and dosing of prednisone when deemed necessary, Blair Allais, MD, said during a session on supportive oncodermatology at the ElderDerm conference on dermatology in the older patient hosted by the George Washington University School of Medicine and Health Sciences, Washington, DC.
“It’s important when you see these patients to be as specific as possible” based on morphology and histopathology, and to treat the rashes in a similar way as in the non-ICI setting,” said Dr. Allais, a dermato-oncologist at the Inova Schar Cancer Institute, Fairfax, Virginia.
cirAEs are the most frequently reported and most visible adverse effects of checkpoint inhibition — a treatment that has emerged as a standard therapy for many malignancies since the first ICI was approved in 2011 for metastatic melanoma.
And contrary to what the phenomenon of immunosenescence might suggest, older patients are no less prone to cirAEs than younger patients. “You’d think you’d have fewer rashes and side effects as you age, but that’s not true,” said Dr. Allais, who completed a fellowship in cutaneous oncology after her dermatology residency.
A 2021 multicenter international cohort study of over 900 patients aged ≥ 80 years treated with single-agent ICIs for cancer did not find any significant differences in the development of immune-related adverse events among those younger than 85, those aged 85-89 years, and those 90 and older. Neither did the ELDERS study in the United Kingdom; this prospective observational study found similar rates of high-grade and low-grade immune toxicity in its two cohorts of patients ≥ 70 and < 70 years of age.
At the meeting, Dr. Allais, who coauthored a 2023 review of cirAEs from ICIs, reviewed recent developments and provided the following advice:
New diagnostic criteria: “Really exciting” news for more precise diagnosis and optimal therapy of cirAEs, Dr. Allais said, is a position paper published in the Journal for ImmunoTherapy of Cancer that offers consensus-based diagnostic criteria for the 10 most common types of dermatologic immune-related adverse events and an overall diagnostic framework. “Luckily, through the work of a Delphi consensus group, we can now have [more diagnostic specificity],” which is important for both clinical care and research, she said.
Most cirAEs have typically been reported nonspecifically as “rash,” but diagnosing a rash subtype is “critical in tailoring appropriate therapy that it is both effective and the least detrimental to the oncology treatment plan for patients with cancer,” the group’s coauthors wrote.
The 10 core diagnoses include psoriasis, eczematous dermatitis, vitiligo, Grover disease, eruptive atypical squamous proliferation, and bullous pemphigoid. Outside of the core diagnoses are other nonspecific presentations that require evaluation to arrive at a diagnosis, if possible, or to reveal data that can allow for targeted therapy and severity grading, the group explains in its paper.
“To prednisone or not to prednisone”: The development of cirAEs is associated with reduced mortality and improved cancer outcomes, making the use of immunosuppressants such as corticosteroids a therapeutic dilemma. “Patients who get these rashes usually do better with respect to their cancer, so the concern has been, if we affect how they respond to their immunotherapy, we may minimize that improvement in mortality,” said Dr. Allais, also assistant professor at the University of Virginia, Charlottesville, and clinical assistant professor of dermatology at George Washington University.
A widely discussed study published in 2015 reported on 254 patients with melanoma who developed an immune-related adverse event during treatment with ipilimumab — approximately one third of whom required systemic corticosteroids — and concluded that systemic corticosteroids did not affect overall survival or time to (cancer) treatment failure. This study from Memorial Sloan Kettering Cancer Center, New York City, “was the first large study looking at this question,” she said, and the subsequent message for several years in conferences and the literature was that steroids do not affect the efficacy of checkpoint inhibitors.
“But the study was not without limitations,” Dr. Allais said, “because the patients who got prednisone were mainly those with higher-grade toxicities,” while those not treated with corticosteroids had either no toxicities or low-grade toxicities. “If higher-grade toxicities were associated with better (antitumor) response, the steroids may have just [blunted] that benefit.”
The current totality of data available in the literature suggests that corticosteroids may indeed have an impact on the efficacy of ICI therapy. “Subsequent studies have come out in the community that have shown that we should probably think twice about giving prednisone to some patients, particularly within the first 50 days of ICI treatment, and that we should be mindful of the dose,” Dr. Allais said.
The takeaways from these studies — all published in the past few years — are to use prednisone early and liberally for life-threatening toxicity, to use it at the lowest dose and for the shortest course when there is not an appropriate alternative, to avoid it for diagnoses that are not treated with prednisone outside the ICI setting, and to “have a plan” for a steroid-sparing agent to use after prednisone, she said.
Dr. Allais recommends heightened consideration during the first 50 days of ICI treatment based on a multicenter retrospective study that found a significant association between use of high-dose glucocorticoids (≥ 60 mg prednisone equivalent once a day) within 8 weeks of anti–programmed cell death protein 1 (PD-1) monotherapy initiation and poorer progression-free and overall survival. The study covered a cohort of 947 patients with advanced melanoma treated with anti–PD-1 monotherapy between 2009 and 2019, 54% of whom developed immune-related adverse events.
This study and other recent studies addressing the association between steroids and survival outcomes in patients with immune-related adverse events during ICI therapy are described in Dr. Allais’ 2023 review of cirAEs from ICIs.
Approach to morbilliform eruptions: This rash is “super common” in patients on ICIs, occurring generally within 2-3 weeks of starting treatment. “It tends to be self-limited and can recur with future infusions,” Dr. Allais said.
Systemic steroids should be reserved for severe or refractory eruptions. “Usually, I treat the patients with topical steroids, and I manage their expectations (that the rash may recur with subsequent infusions), but I closely follow them up” within 2-3 weeks, she said. It’s important to rule out a severe cutaneous adverse drug eruption, of course, and to start high-dose systemic steroids immediately if necessary. “Antibiotics are a big culprit” and often can be discontinued.
Soak and smear: “I’m obsessed” with this technique of a 20-minute soak in plain water followed by application of steroid ointment, said Dr. Allais, referring to a small study published in 2005 that reported a complete response after 2 weeks in 60% of patients with psoriasis, atopic dermatitis, and other inflammatory skin conditions (none had cancer), who had failed prior systemic therapy. All patients had at least a 75% response.
The method offers a way to “avoid the systemic immunosuppression we’d get with prednisone,” she said. One just needs to make sure the older patient can get in and out of their tub safely.
ICI-induced bullous pemphigoid (BP): BP occurs more frequently in the ICI setting, compared with the general population, with a median time to development of 8.5 months after ICI initiation. It is associated in this setting with improved tumor response, but “many oncologists stop anticancer treatment because of this diagnosis,” she said.
In the supportive oncodermatology space, however, ICI-induced BP exemplifies the value of tailored treatment regimens, she said. A small multi-institutional retrospective cohort study published in 2023 identified 35 cases of ICI-BP among 5636 ICI-treated patients and found that 8 out of 11 patients who received biologic therapy (rituximab, omalizumab, or dupilumab) had a complete response to ICI-BP without flares following subsequent ICI cycles. And while statistical significance was not reached, the study showed that no cancer-related outcomes were worsened.
“If you see someone with ICI-induced BP and they have a lot of involvement, you could start them on steroids and get that steroid-sparing agent initiated for approval. ... And if IgE is elevated, you might reach for omalizumab,” said Dr. Allais, noting that her favored treatment overall is dupilumab.
Risk factors for the development of ICI-induced BP include age > 70, skin cancer, and having an initial response to ICI on first imaging, the latter of which “I find fascinating ... because imaging occurs within the first 12 weeks of treatment, but we don’t see BP popping up until 8.5 months into treatment,” she noted. “So maybe there’s a baseline risk factor that could predispose them.”
Caution with antibiotics: “I try to avoid antibiotics in the ICI setting,” Dr. Allais said, in deference to the “ever-important microbiome.” Studies have demonstrated that the microbiomes of responders to ICI treatment are different from those of nonresponders, she said.
And a “fascinating” study of patients with melanoma undergoing ICI therapy showed not only a higher abundance of Ruminococcaceae bacteria in responders vs nonresponders but a significant impact of dietary fiber. High dietary fiber was associated with significantly improved overall survival in the patients on ICI, with the most pronounced benefit in patients with good fiber intake and no probiotic use. “Even wilder, their T cells changed,” she said. “They had a high expression of genes related to T-cell activation ... so more tumor-infiltrating lymphocytes.”
A retrospective study of 568 patients with stages III and IV melanoma treated with ICI showed that those exposed to antibiotics prior to ICI had significantly worse overall survival than those not exposed to antibiotics. “Think before you give them,” Dr. Allais said. “And try to tell your older patients to eat beans and greens.”
Dr. Allais reported having no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM ELDERDERM 2024
Storybooks Can Help Children Deal with Skin Conditions
TORONTO —
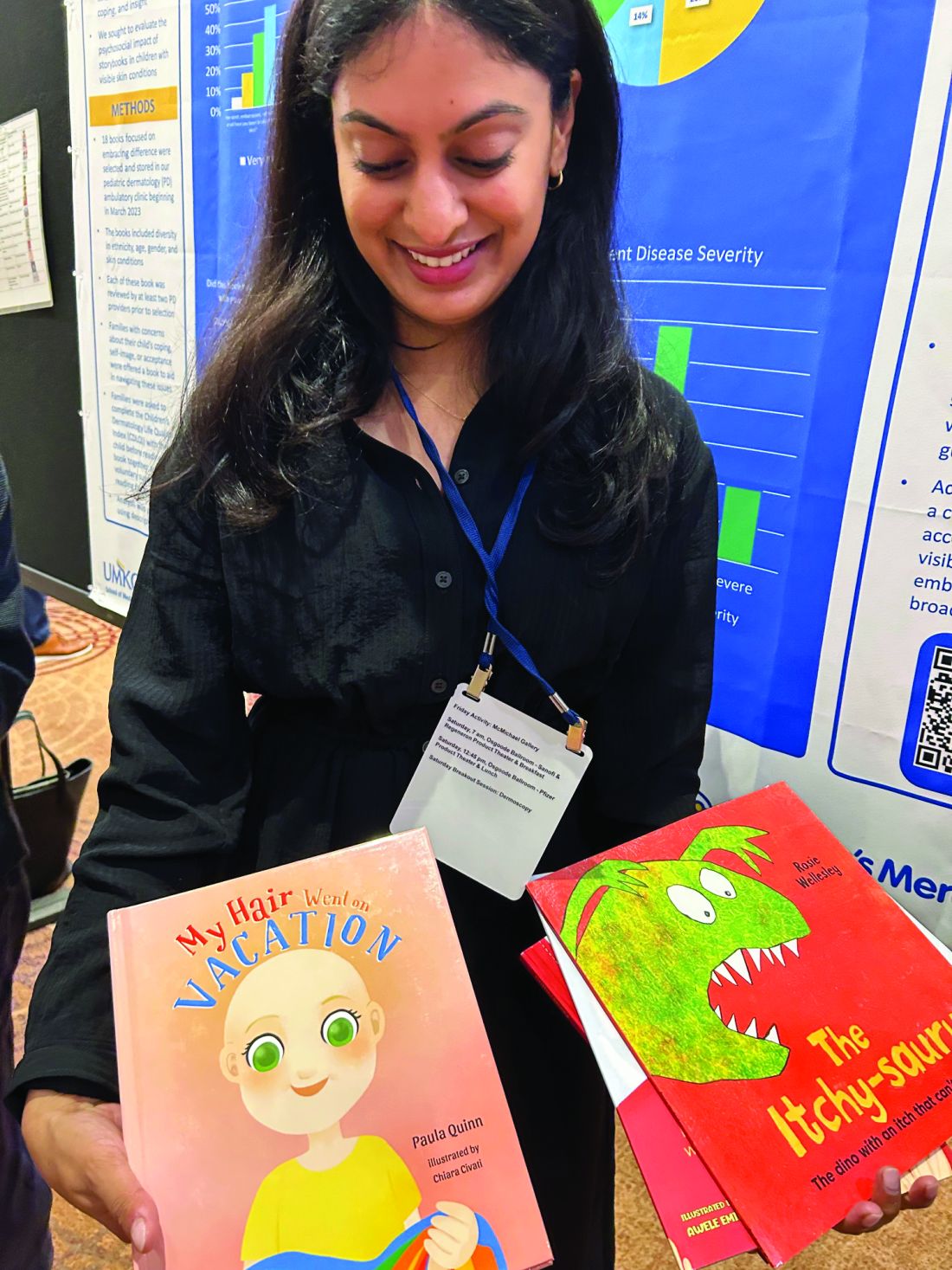
So far, “the study demonstrates that these books have value to patients and families,” one of the study authors, Sonia Havele, MD, a pediatrician and dermatology resident at Children’s Mercy Hospital Kansas City, Kansas City, Missouri, said in an interview.
“There are tools to help kids cope with their skin conditions, but we’re underutilizing them,” she added. “And part of the reason we’re underutilizing storybooks is that we just don’t know what’s out there.” For the study, the researchers received funding to purchase 18 “creative and thoughtful” storybooks related to pediatric skin conditions, reviewed by at least two pediatric dermatologists before being selected, which are just a sample of related books that are available.
The study results were presented as a poster at the annual meeting of the Society for Pediatric Dermatology.
Children with visible skin conditions, which can include port-wine stains, capillary malformations, and congenital moles, may be subjected to teasing or bullying at school, and the conditions can also affect their quality of life.
Beauty and the Birthmark
The books include one titled “Beauty with a Birthmark” and another, “My Hair Went on Vacation.” An illustrated book, “Just Ask: Be Different, Be Brave, Be You,” by US Supreme Court Justice Sonia Sotomayor, offers tips on how to answer common questions about someone’s appearance.
Dr. Havele said that Justice Sotomayor’s book “empowers kids, their siblings, their classmates ... to ask questions, and it teaches patients not to be afraid of those questions, and to really lean into educating their peers, and their family members.”
“Kids are really just curious,” she added. “They’ll make comments like: ‘Hey, what’s that spot on your face?’ Or, they’ll ask about vitiligo because they’ve never seen somebody with it before.”
To evaluate the psychosocial impact of these types of books for children with visible skin conditions, Dr. Havele and colleagues designed a study that includes patients aged 2-12 years dealing with issues related to self-esteem, acceptance, coping, or bullying. Parents are provided with a relevant storybook to read at home with their child in a “safe and comfortable space” and “at their own pace and their own time,” said Dr. Havele.
Inside the book is a QR code to access the validated Children’s Dermatology Life Quality Index (CDLQI). Families complete the survey at baseline and provide feedback after reading the book. Researchers collect information about demographics, age, gender, and skin conditions, which included atopic dermatitis, alopecia areata, vitiligo, hemangioma, and port-wine stain.
The response rate so far is 34%, and close to 80 parents have completed the survey with their child, Dr. Havele said.
At baseline, many of the children were either moderately or severely affected in terms of their quality of life (45% scored ≥ 6 on the CDLQI).
After reading the book, about 80% of parents reported it had a positive impact, and about 20% said it had a somewhat positive impact on their child’s self-image or confidence. Almost 80% agreed, and the remainder somewhat agreed it encouraged their child to embrace differences.
Most respondents also said the book helped the parent and child cope with the child’s condition. “So really, it was overall a positive response,” said Dr. Havele. “We are able to demonstrate that these books have value in a more scientific or objective way.”
This may not be surprising. Dr. Havele referred to more formal bibliotherapy (book therapy), which has been studied in other pediatric populations, including patients with cancer and those who have experienced trauma.
Awesome Space
Pediatric dermatologists are perfectly positioned to play a role in improving the lives of their patients with skin issues. “We see the impact of visible skin disease on children all the time,” said Dr. Havele. “The dermatology visit is an awesome space and opportunity to introduce these books to families and potentially help them talk about the skin condition with their child.”
In addition to prescribing therapies, “we’re also with these kids through an emotional journey, and I think giving them tools for that emotional journey is very helpful,” she added.
Such books would have been a great help to Dr. Havele herself. Growing up, she had severe atopic dermatitis covering much of her body. “Having such a resource would have helped me better cope with my reality of being different than everyone else.”
She hopes a database will be established to house these resources so other providers can refer patients to the list of books. Other books include “The Itchy-saurus: The Dino with an itch that can’t be scratched,” “Hair in My Brush,” and “I am Unique!”
Dr. Havele had no relevant disclosures.
A version of this article first appeared on Medscape.com.
TORONTO —
So far, “the study demonstrates that these books have value to patients and families,” one of the study authors, Sonia Havele, MD, a pediatrician and dermatology resident at Children’s Mercy Hospital Kansas City, Kansas City, Missouri, said in an interview.
“There are tools to help kids cope with their skin conditions, but we’re underutilizing them,” she added. “And part of the reason we’re underutilizing storybooks is that we just don’t know what’s out there.” For the study, the researchers received funding to purchase 18 “creative and thoughtful” storybooks related to pediatric skin conditions, reviewed by at least two pediatric dermatologists before being selected, which are just a sample of related books that are available.
The study results were presented as a poster at the annual meeting of the Society for Pediatric Dermatology.
Children with visible skin conditions, which can include port-wine stains, capillary malformations, and congenital moles, may be subjected to teasing or bullying at school, and the conditions can also affect their quality of life.
Beauty and the Birthmark
The books include one titled “Beauty with a Birthmark” and another, “My Hair Went on Vacation.” An illustrated book, “Just Ask: Be Different, Be Brave, Be You,” by US Supreme Court Justice Sonia Sotomayor, offers tips on how to answer common questions about someone’s appearance.
Dr. Havele said that Justice Sotomayor’s book “empowers kids, their siblings, their classmates ... to ask questions, and it teaches patients not to be afraid of those questions, and to really lean into educating their peers, and their family members.”
“Kids are really just curious,” she added. “They’ll make comments like: ‘Hey, what’s that spot on your face?’ Or, they’ll ask about vitiligo because they’ve never seen somebody with it before.”
To evaluate the psychosocial impact of these types of books for children with visible skin conditions, Dr. Havele and colleagues designed a study that includes patients aged 2-12 years dealing with issues related to self-esteem, acceptance, coping, or bullying. Parents are provided with a relevant storybook to read at home with their child in a “safe and comfortable space” and “at their own pace and their own time,” said Dr. Havele.
Inside the book is a QR code to access the validated Children’s Dermatology Life Quality Index (CDLQI). Families complete the survey at baseline and provide feedback after reading the book. Researchers collect information about demographics, age, gender, and skin conditions, which included atopic dermatitis, alopecia areata, vitiligo, hemangioma, and port-wine stain.
The response rate so far is 34%, and close to 80 parents have completed the survey with their child, Dr. Havele said.
At baseline, many of the children were either moderately or severely affected in terms of their quality of life (45% scored ≥ 6 on the CDLQI).
After reading the book, about 80% of parents reported it had a positive impact, and about 20% said it had a somewhat positive impact on their child’s self-image or confidence. Almost 80% agreed, and the remainder somewhat agreed it encouraged their child to embrace differences.
Most respondents also said the book helped the parent and child cope with the child’s condition. “So really, it was overall a positive response,” said Dr. Havele. “We are able to demonstrate that these books have value in a more scientific or objective way.”
This may not be surprising. Dr. Havele referred to more formal bibliotherapy (book therapy), which has been studied in other pediatric populations, including patients with cancer and those who have experienced trauma.
Awesome Space
Pediatric dermatologists are perfectly positioned to play a role in improving the lives of their patients with skin issues. “We see the impact of visible skin disease on children all the time,” said Dr. Havele. “The dermatology visit is an awesome space and opportunity to introduce these books to families and potentially help them talk about the skin condition with their child.”
In addition to prescribing therapies, “we’re also with these kids through an emotional journey, and I think giving them tools for that emotional journey is very helpful,” she added.
Such books would have been a great help to Dr. Havele herself. Growing up, she had severe atopic dermatitis covering much of her body. “Having such a resource would have helped me better cope with my reality of being different than everyone else.”
She hopes a database will be established to house these resources so other providers can refer patients to the list of books. Other books include “The Itchy-saurus: The Dino with an itch that can’t be scratched,” “Hair in My Brush,” and “I am Unique!”
Dr. Havele had no relevant disclosures.
A version of this article first appeared on Medscape.com.
TORONTO —
So far, “the study demonstrates that these books have value to patients and families,” one of the study authors, Sonia Havele, MD, a pediatrician and dermatology resident at Children’s Mercy Hospital Kansas City, Kansas City, Missouri, said in an interview.
“There are tools to help kids cope with their skin conditions, but we’re underutilizing them,” she added. “And part of the reason we’re underutilizing storybooks is that we just don’t know what’s out there.” For the study, the researchers received funding to purchase 18 “creative and thoughtful” storybooks related to pediatric skin conditions, reviewed by at least two pediatric dermatologists before being selected, which are just a sample of related books that are available.
The study results were presented as a poster at the annual meeting of the Society for Pediatric Dermatology.
Children with visible skin conditions, which can include port-wine stains, capillary malformations, and congenital moles, may be subjected to teasing or bullying at school, and the conditions can also affect their quality of life.
Beauty and the Birthmark
The books include one titled “Beauty with a Birthmark” and another, “My Hair Went on Vacation.” An illustrated book, “Just Ask: Be Different, Be Brave, Be You,” by US Supreme Court Justice Sonia Sotomayor, offers tips on how to answer common questions about someone’s appearance.
Dr. Havele said that Justice Sotomayor’s book “empowers kids, their siblings, their classmates ... to ask questions, and it teaches patients not to be afraid of those questions, and to really lean into educating their peers, and their family members.”
“Kids are really just curious,” she added. “They’ll make comments like: ‘Hey, what’s that spot on your face?’ Or, they’ll ask about vitiligo because they’ve never seen somebody with it before.”
To evaluate the psychosocial impact of these types of books for children with visible skin conditions, Dr. Havele and colleagues designed a study that includes patients aged 2-12 years dealing with issues related to self-esteem, acceptance, coping, or bullying. Parents are provided with a relevant storybook to read at home with their child in a “safe and comfortable space” and “at their own pace and their own time,” said Dr. Havele.
Inside the book is a QR code to access the validated Children’s Dermatology Life Quality Index (CDLQI). Families complete the survey at baseline and provide feedback after reading the book. Researchers collect information about demographics, age, gender, and skin conditions, which included atopic dermatitis, alopecia areata, vitiligo, hemangioma, and port-wine stain.
The response rate so far is 34%, and close to 80 parents have completed the survey with their child, Dr. Havele said.
At baseline, many of the children were either moderately or severely affected in terms of their quality of life (45% scored ≥ 6 on the CDLQI).
After reading the book, about 80% of parents reported it had a positive impact, and about 20% said it had a somewhat positive impact on their child’s self-image or confidence. Almost 80% agreed, and the remainder somewhat agreed it encouraged their child to embrace differences.
Most respondents also said the book helped the parent and child cope with the child’s condition. “So really, it was overall a positive response,” said Dr. Havele. “We are able to demonstrate that these books have value in a more scientific or objective way.”
This may not be surprising. Dr. Havele referred to more formal bibliotherapy (book therapy), which has been studied in other pediatric populations, including patients with cancer and those who have experienced trauma.
Awesome Space
Pediatric dermatologists are perfectly positioned to play a role in improving the lives of their patients with skin issues. “We see the impact of visible skin disease on children all the time,” said Dr. Havele. “The dermatology visit is an awesome space and opportunity to introduce these books to families and potentially help them talk about the skin condition with their child.”
In addition to prescribing therapies, “we’re also with these kids through an emotional journey, and I think giving them tools for that emotional journey is very helpful,” she added.
Such books would have been a great help to Dr. Havele herself. Growing up, she had severe atopic dermatitis covering much of her body. “Having such a resource would have helped me better cope with my reality of being different than everyone else.”
She hopes a database will be established to house these resources so other providers can refer patients to the list of books. Other books include “The Itchy-saurus: The Dino with an itch that can’t be scratched,” “Hair in My Brush,” and “I am Unique!”
Dr. Havele had no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM SPD 2024
Who’s Behind Cosmetic Procedures at MedSpas?
CARLSBAD, CALIFORNIA — according to Sara Hogan, MD.
“I’m not anti-MedSpa; I’m pro-patient safety,” Dr. Hogan, clinical assistant professor of dermatology at George Washington University, Washington, DC, said at the Controversies & Conversations in Laser & Cosmetic Surgery symposium. “The MedSpa industry is booming; it brought in $17 billion in 2023. There are as many MedSpas in the United States as there are practicing dermatologists, and that number is set to exceed the number of dermatologists.”
According to industry data from the American Med Spa Association, 63% of member MedSpas have non-MD ownership. Among MedSpas owned by physicians, 80% are of a non–core specialty, meaning a specialty other than dermatology, plastic surgery, otorhinolaryngology, or ophthalmology. Of MedSpa medical directors, 69% are from non–core physician specialties. “There’s an increasing amount of data that shows a relatively higher incidence of complications from cosmetic procedures that are delivered at MedSpas,” Dr. Hogan said. “A 2020 study suggested that this is likely due to improper training, improper technique, and/or improper device settings.”
Dr. Hogan also cited adverse effects linked to counterfeit or mishandled botulinum toxin injections that prompted the Centers for Disease Control and Prevention to issue an alert to clinicians in April 2024. Clusters of 22 people in 11 states reported adverse effects after receiving injections with counterfeit botulinum toxin or injections administered by unlicensed or untrained individuals or in non-healthcare settings, such as homes or spas.
To better understand who performs cosmetic procedures, provides medical supervision, and follows safety protocols at MedSpas, Dr. Hogan and colleagues conducted a “truth in advertising” study of 127 MedSpas in the greater Chicago area. They chose this geographic location because an analysis published in 2021 identified Chicago as having the third highest number of aesthetic physicians and the fifth highest number of MedSpas in the United States. The researchers enlisted help from “secret shoppers” who contacted the MedSpas by telephone to ask about the level of training, if patients underwent a review of medical history, the level of on-site physician supervision, and the protocol for complications.
The top five cosmetic procedures offered by the 127 surveyed MedSpas were facials (85.0%), hair removal (85.0%), botulinum toxin injections (83.5%), dermal fillers (82.7%), and chemical peels (76.4%). About two thirds of cosmetic procedures were performed by aestheticians (66.9%), followed by registered nurses or licensed practical nurses (52.8%), board-certified physicians (48.8%, mostly plastic and reconstructive surgeons), nurse practitioners (27.6%), and physician assistants (9.4%).
In the realm of supervision, 16.5% of MedSpas surveyed reported that a medical director or supervising physician is always on site. “If not located on site, when asked where the physicians are, the majority of the time they were at the physician’s primary practice, clinic, or hospital,” Dr. Hogan said. “Only 65% of the MedSpas surveyed stated that they informed the patient that the supervising physician is not on site. In addition, a patient’s medical history is reviewed at only 40% of the MedSpas. To give context, in Illinois, a physician can only deliver care after a physician-patient relationship has been established, meaning that a good faith exam has been performed. And if they are to delegate any type of service, they must always be on site to provide assistance.”
Dr. Hogan noted that there are no federal statutes or agencies that regulate or oversee MedSpas. “Regulation and oversight are often delegated to state licensing agencies that are overwhelmed and often stretched thin regarding personnel and budgets,” she said. To raise awareness of this issue, the American Society for Dermatologic Surgery Association (ASDSA) launched the Medical Spa Safety Coalition, which aims to promote model legislation for states known as the Medical Spa Safety Act. Highlights of the bill include clear definitions of medical spa and medical director, as well as the requirement of an on-site medical director who must be a physician trained in all procedures performed at the MedSpa. Coalition members include 16 state dermatology boards as well as the ASDSA, the American Academy of Dermatology Association, the American Society for Laser Medicine & Surgery, and the American Society of Plastic Surgeons.
The ASDSA provided funding to support the published study. Dr. Hogan reported having no financial disclosures.
A version of this article appeared on Medscape.com.
CARLSBAD, CALIFORNIA — according to Sara Hogan, MD.
“I’m not anti-MedSpa; I’m pro-patient safety,” Dr. Hogan, clinical assistant professor of dermatology at George Washington University, Washington, DC, said at the Controversies & Conversations in Laser & Cosmetic Surgery symposium. “The MedSpa industry is booming; it brought in $17 billion in 2023. There are as many MedSpas in the United States as there are practicing dermatologists, and that number is set to exceed the number of dermatologists.”
According to industry data from the American Med Spa Association, 63% of member MedSpas have non-MD ownership. Among MedSpas owned by physicians, 80% are of a non–core specialty, meaning a specialty other than dermatology, plastic surgery, otorhinolaryngology, or ophthalmology. Of MedSpa medical directors, 69% are from non–core physician specialties. “There’s an increasing amount of data that shows a relatively higher incidence of complications from cosmetic procedures that are delivered at MedSpas,” Dr. Hogan said. “A 2020 study suggested that this is likely due to improper training, improper technique, and/or improper device settings.”
Dr. Hogan also cited adverse effects linked to counterfeit or mishandled botulinum toxin injections that prompted the Centers for Disease Control and Prevention to issue an alert to clinicians in April 2024. Clusters of 22 people in 11 states reported adverse effects after receiving injections with counterfeit botulinum toxin or injections administered by unlicensed or untrained individuals or in non-healthcare settings, such as homes or spas.
To better understand who performs cosmetic procedures, provides medical supervision, and follows safety protocols at MedSpas, Dr. Hogan and colleagues conducted a “truth in advertising” study of 127 MedSpas in the greater Chicago area. They chose this geographic location because an analysis published in 2021 identified Chicago as having the third highest number of aesthetic physicians and the fifth highest number of MedSpas in the United States. The researchers enlisted help from “secret shoppers” who contacted the MedSpas by telephone to ask about the level of training, if patients underwent a review of medical history, the level of on-site physician supervision, and the protocol for complications.
The top five cosmetic procedures offered by the 127 surveyed MedSpas were facials (85.0%), hair removal (85.0%), botulinum toxin injections (83.5%), dermal fillers (82.7%), and chemical peels (76.4%). About two thirds of cosmetic procedures were performed by aestheticians (66.9%), followed by registered nurses or licensed practical nurses (52.8%), board-certified physicians (48.8%, mostly plastic and reconstructive surgeons), nurse practitioners (27.6%), and physician assistants (9.4%).
In the realm of supervision, 16.5% of MedSpas surveyed reported that a medical director or supervising physician is always on site. “If not located on site, when asked where the physicians are, the majority of the time they were at the physician’s primary practice, clinic, or hospital,” Dr. Hogan said. “Only 65% of the MedSpas surveyed stated that they informed the patient that the supervising physician is not on site. In addition, a patient’s medical history is reviewed at only 40% of the MedSpas. To give context, in Illinois, a physician can only deliver care after a physician-patient relationship has been established, meaning that a good faith exam has been performed. And if they are to delegate any type of service, they must always be on site to provide assistance.”
Dr. Hogan noted that there are no federal statutes or agencies that regulate or oversee MedSpas. “Regulation and oversight are often delegated to state licensing agencies that are overwhelmed and often stretched thin regarding personnel and budgets,” she said. To raise awareness of this issue, the American Society for Dermatologic Surgery Association (ASDSA) launched the Medical Spa Safety Coalition, which aims to promote model legislation for states known as the Medical Spa Safety Act. Highlights of the bill include clear definitions of medical spa and medical director, as well as the requirement of an on-site medical director who must be a physician trained in all procedures performed at the MedSpa. Coalition members include 16 state dermatology boards as well as the ASDSA, the American Academy of Dermatology Association, the American Society for Laser Medicine & Surgery, and the American Society of Plastic Surgeons.
The ASDSA provided funding to support the published study. Dr. Hogan reported having no financial disclosures.
A version of this article appeared on Medscape.com.
CARLSBAD, CALIFORNIA — according to Sara Hogan, MD.
“I’m not anti-MedSpa; I’m pro-patient safety,” Dr. Hogan, clinical assistant professor of dermatology at George Washington University, Washington, DC, said at the Controversies & Conversations in Laser & Cosmetic Surgery symposium. “The MedSpa industry is booming; it brought in $17 billion in 2023. There are as many MedSpas in the United States as there are practicing dermatologists, and that number is set to exceed the number of dermatologists.”
According to industry data from the American Med Spa Association, 63% of member MedSpas have non-MD ownership. Among MedSpas owned by physicians, 80% are of a non–core specialty, meaning a specialty other than dermatology, plastic surgery, otorhinolaryngology, or ophthalmology. Of MedSpa medical directors, 69% are from non–core physician specialties. “There’s an increasing amount of data that shows a relatively higher incidence of complications from cosmetic procedures that are delivered at MedSpas,” Dr. Hogan said. “A 2020 study suggested that this is likely due to improper training, improper technique, and/or improper device settings.”
Dr. Hogan also cited adverse effects linked to counterfeit or mishandled botulinum toxin injections that prompted the Centers for Disease Control and Prevention to issue an alert to clinicians in April 2024. Clusters of 22 people in 11 states reported adverse effects after receiving injections with counterfeit botulinum toxin or injections administered by unlicensed or untrained individuals or in non-healthcare settings, such as homes or spas.
To better understand who performs cosmetic procedures, provides medical supervision, and follows safety protocols at MedSpas, Dr. Hogan and colleagues conducted a “truth in advertising” study of 127 MedSpas in the greater Chicago area. They chose this geographic location because an analysis published in 2021 identified Chicago as having the third highest number of aesthetic physicians and the fifth highest number of MedSpas in the United States. The researchers enlisted help from “secret shoppers” who contacted the MedSpas by telephone to ask about the level of training, if patients underwent a review of medical history, the level of on-site physician supervision, and the protocol for complications.
The top five cosmetic procedures offered by the 127 surveyed MedSpas were facials (85.0%), hair removal (85.0%), botulinum toxin injections (83.5%), dermal fillers (82.7%), and chemical peels (76.4%). About two thirds of cosmetic procedures were performed by aestheticians (66.9%), followed by registered nurses or licensed practical nurses (52.8%), board-certified physicians (48.8%, mostly plastic and reconstructive surgeons), nurse practitioners (27.6%), and physician assistants (9.4%).
In the realm of supervision, 16.5% of MedSpas surveyed reported that a medical director or supervising physician is always on site. “If not located on site, when asked where the physicians are, the majority of the time they were at the physician’s primary practice, clinic, or hospital,” Dr. Hogan said. “Only 65% of the MedSpas surveyed stated that they informed the patient that the supervising physician is not on site. In addition, a patient’s medical history is reviewed at only 40% of the MedSpas. To give context, in Illinois, a physician can only deliver care after a physician-patient relationship has been established, meaning that a good faith exam has been performed. And if they are to delegate any type of service, they must always be on site to provide assistance.”
Dr. Hogan noted that there are no federal statutes or agencies that regulate or oversee MedSpas. “Regulation and oversight are often delegated to state licensing agencies that are overwhelmed and often stretched thin regarding personnel and budgets,” she said. To raise awareness of this issue, the American Society for Dermatologic Surgery Association (ASDSA) launched the Medical Spa Safety Coalition, which aims to promote model legislation for states known as the Medical Spa Safety Act. Highlights of the bill include clear definitions of medical spa and medical director, as well as the requirement of an on-site medical director who must be a physician trained in all procedures performed at the MedSpa. Coalition members include 16 state dermatology boards as well as the ASDSA, the American Academy of Dermatology Association, the American Society for Laser Medicine & Surgery, and the American Society of Plastic Surgeons.
The ASDSA provided funding to support the published study. Dr. Hogan reported having no financial disclosures.
A version of this article appeared on Medscape.com.
Fillers, Hyaluronidase Relieve Orofacial Changes in Patients with Scleroderma
CARLSBAD, CALIFORNIA — In 2003, researchers asked 303 patients with systemic sclerosis (scleroderma) what bothered them most about their disease from an aesthetic standpoint: Orofacial features, such as thin lips and mouth furrows, or non-facial features, such as fingertip ulceration and waxy changes to the skin.
Respondents expressed significant concern about specific orofacial features, including thin lips (73%), mouth furrows (80%), loss of facial lines (68%), and a smaller, tighter mouth (77%).
“Patients with systemic sclerosis may have loss of vermilion lip, microstomia, and perioral rhytids,” Kathleen Cook Suozzi, MD, who directs the Aesthetic Dermatology Program at Yale University School of Medicine, New Haven, Connecticut, said at the Controversies and Conversations in Laser and Cosmetic Surgery annual symposium. “How can we address these changes for our patients?”
Recent research has shown that hyaluronidase injections can help improve orofacial changes commonly experienced by patients with scleroderma. In 2019, researchers in Alabama reported the case of a 53-year-old woman treated with hyaluronidase for scleroderma-induced microstomia. After four visits over 7 months and a total hyaluronidase dose of 470 IU, the patient reported an improved Mouth Handicap in Systemic Sclerosis (MHISS) score (38 of 48); subjective improvement of symptoms, including greater ease in eating and undergoing dental treatment; and improved mouth closure.
In 2023, researchers published a cohort study of four women between the ages of 43 and 61 with autoimmune sclerosing conditions that resulted in oral microstomia. Following hyaluronidase injections, all improved in mouth opening capacity and MHISS, with change stabilizing between three and five treatments. More recently, in a study pending publication in JAAD Case Reports, Dr. Suozzi and colleagues retrospectively evaluated 12 women with scleroderma who received between 150 and 300 units of hyaluronic acid (HA) filler for microstomia between 2020 and 2023. Of the 12 women, 58% had diffuse disease, and 42% had limited disease. Overall, oral aperture width increased by 0.65 cm (P = .0027) and oral aperture height increased by 0.88 cm (P < .0001). “In general, patients needed three to four treatments to reach peak effect, and then they reached a plateau,” Dr. Suozzi said. “It wasn’t that the treatment wasn’t working anymore, but it was because their oral aperture had gotten to a size of around 5 cm, which is clinically normal. Interestingly, we found that if the patient’s disease flared and their microstomia started to return, when you rechallenged them, they continued to respond. So, patients can continue to use this treatment over time.”
In a separate case series of seven patients, Dr. Suozzi and colleagues prospectively evaluated the effect of HA soft tissue filler with Restylane Silk for lip augmentation. Study participants experienced statistically significant increases in the difference between pre- and postinjection fullness in both upper and lower lips. Also, the mean posttreatment score fell between “much improved” (2) and “improved” (3) on both the Investigator Global Aesthetic Improvement Scale and the Subject Global Aesthetic Improvement Scale.
Dr. Suozzi recommends using nerve blocks for injecting HA filler or hyaluronidase in patients with scleroderma and minimizing the injection points. “Initially, we were using 30% lidocaine preparations around the mouth for an hour before the procedure, and patients were still having pain, so now we use nerve blocks,” she said. “For hyaluronidase, we do perform a test dose of 75-100 units, usually in the commissure. It’s amazing how well it works; people will usually come back after their test dose and have improvements in their measurements. This is a really easy treatment to perform, and I think it can be done in the office of a general dermatologist. There is concern about cross-reactivity with bee venom, so you want to ask patients about that.”
Dr. Suozzi reported having no relevant financial relationships.
A version of this article first appeared on Medscape.com.
CARLSBAD, CALIFORNIA — In 2003, researchers asked 303 patients with systemic sclerosis (scleroderma) what bothered them most about their disease from an aesthetic standpoint: Orofacial features, such as thin lips and mouth furrows, or non-facial features, such as fingertip ulceration and waxy changes to the skin.
Respondents expressed significant concern about specific orofacial features, including thin lips (73%), mouth furrows (80%), loss of facial lines (68%), and a smaller, tighter mouth (77%).
“Patients with systemic sclerosis may have loss of vermilion lip, microstomia, and perioral rhytids,” Kathleen Cook Suozzi, MD, who directs the Aesthetic Dermatology Program at Yale University School of Medicine, New Haven, Connecticut, said at the Controversies and Conversations in Laser and Cosmetic Surgery annual symposium. “How can we address these changes for our patients?”
Recent research has shown that hyaluronidase injections can help improve orofacial changes commonly experienced by patients with scleroderma. In 2019, researchers in Alabama reported the case of a 53-year-old woman treated with hyaluronidase for scleroderma-induced microstomia. After four visits over 7 months and a total hyaluronidase dose of 470 IU, the patient reported an improved Mouth Handicap in Systemic Sclerosis (MHISS) score (38 of 48); subjective improvement of symptoms, including greater ease in eating and undergoing dental treatment; and improved mouth closure.
In 2023, researchers published a cohort study of four women between the ages of 43 and 61 with autoimmune sclerosing conditions that resulted in oral microstomia. Following hyaluronidase injections, all improved in mouth opening capacity and MHISS, with change stabilizing between three and five treatments. More recently, in a study pending publication in JAAD Case Reports, Dr. Suozzi and colleagues retrospectively evaluated 12 women with scleroderma who received between 150 and 300 units of hyaluronic acid (HA) filler for microstomia between 2020 and 2023. Of the 12 women, 58% had diffuse disease, and 42% had limited disease. Overall, oral aperture width increased by 0.65 cm (P = .0027) and oral aperture height increased by 0.88 cm (P < .0001). “In general, patients needed three to four treatments to reach peak effect, and then they reached a plateau,” Dr. Suozzi said. “It wasn’t that the treatment wasn’t working anymore, but it was because their oral aperture had gotten to a size of around 5 cm, which is clinically normal. Interestingly, we found that if the patient’s disease flared and their microstomia started to return, when you rechallenged them, they continued to respond. So, patients can continue to use this treatment over time.”
In a separate case series of seven patients, Dr. Suozzi and colleagues prospectively evaluated the effect of HA soft tissue filler with Restylane Silk for lip augmentation. Study participants experienced statistically significant increases in the difference between pre- and postinjection fullness in both upper and lower lips. Also, the mean posttreatment score fell between “much improved” (2) and “improved” (3) on both the Investigator Global Aesthetic Improvement Scale and the Subject Global Aesthetic Improvement Scale.
Dr. Suozzi recommends using nerve blocks for injecting HA filler or hyaluronidase in patients with scleroderma and minimizing the injection points. “Initially, we were using 30% lidocaine preparations around the mouth for an hour before the procedure, and patients were still having pain, so now we use nerve blocks,” she said. “For hyaluronidase, we do perform a test dose of 75-100 units, usually in the commissure. It’s amazing how well it works; people will usually come back after their test dose and have improvements in their measurements. This is a really easy treatment to perform, and I think it can be done in the office of a general dermatologist. There is concern about cross-reactivity with bee venom, so you want to ask patients about that.”
Dr. Suozzi reported having no relevant financial relationships.
A version of this article first appeared on Medscape.com.
CARLSBAD, CALIFORNIA — In 2003, researchers asked 303 patients with systemic sclerosis (scleroderma) what bothered them most about their disease from an aesthetic standpoint: Orofacial features, such as thin lips and mouth furrows, or non-facial features, such as fingertip ulceration and waxy changes to the skin.
Respondents expressed significant concern about specific orofacial features, including thin lips (73%), mouth furrows (80%), loss of facial lines (68%), and a smaller, tighter mouth (77%).
“Patients with systemic sclerosis may have loss of vermilion lip, microstomia, and perioral rhytids,” Kathleen Cook Suozzi, MD, who directs the Aesthetic Dermatology Program at Yale University School of Medicine, New Haven, Connecticut, said at the Controversies and Conversations in Laser and Cosmetic Surgery annual symposium. “How can we address these changes for our patients?”
Recent research has shown that hyaluronidase injections can help improve orofacial changes commonly experienced by patients with scleroderma. In 2019, researchers in Alabama reported the case of a 53-year-old woman treated with hyaluronidase for scleroderma-induced microstomia. After four visits over 7 months and a total hyaluronidase dose of 470 IU, the patient reported an improved Mouth Handicap in Systemic Sclerosis (MHISS) score (38 of 48); subjective improvement of symptoms, including greater ease in eating and undergoing dental treatment; and improved mouth closure.
In 2023, researchers published a cohort study of four women between the ages of 43 and 61 with autoimmune sclerosing conditions that resulted in oral microstomia. Following hyaluronidase injections, all improved in mouth opening capacity and MHISS, with change stabilizing between three and five treatments. More recently, in a study pending publication in JAAD Case Reports, Dr. Suozzi and colleagues retrospectively evaluated 12 women with scleroderma who received between 150 and 300 units of hyaluronic acid (HA) filler for microstomia between 2020 and 2023. Of the 12 women, 58% had diffuse disease, and 42% had limited disease. Overall, oral aperture width increased by 0.65 cm (P = .0027) and oral aperture height increased by 0.88 cm (P < .0001). “In general, patients needed three to four treatments to reach peak effect, and then they reached a plateau,” Dr. Suozzi said. “It wasn’t that the treatment wasn’t working anymore, but it was because their oral aperture had gotten to a size of around 5 cm, which is clinically normal. Interestingly, we found that if the patient’s disease flared and their microstomia started to return, when you rechallenged them, they continued to respond. So, patients can continue to use this treatment over time.”
In a separate case series of seven patients, Dr. Suozzi and colleagues prospectively evaluated the effect of HA soft tissue filler with Restylane Silk for lip augmentation. Study participants experienced statistically significant increases in the difference between pre- and postinjection fullness in both upper and lower lips. Also, the mean posttreatment score fell between “much improved” (2) and “improved” (3) on both the Investigator Global Aesthetic Improvement Scale and the Subject Global Aesthetic Improvement Scale.
Dr. Suozzi recommends using nerve blocks for injecting HA filler or hyaluronidase in patients with scleroderma and minimizing the injection points. “Initially, we were using 30% lidocaine preparations around the mouth for an hour before the procedure, and patients were still having pain, so now we use nerve blocks,” she said. “For hyaluronidase, we do perform a test dose of 75-100 units, usually in the commissure. It’s amazing how well it works; people will usually come back after their test dose and have improvements in their measurements. This is a really easy treatment to perform, and I think it can be done in the office of a general dermatologist. There is concern about cross-reactivity with bee venom, so you want to ask patients about that.”
Dr. Suozzi reported having no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Recommendations From a Pediatric Dermatologist on Using AI in Daily Practice
TORONTO — with the various AI models.
He reminds doctors that many of their colleagues and patients and their families are already using these systems, “and you don’t want to be left behind.”
In an interview following his presentation on AI at the annual meeting of the Society for Pediatric Dermatology (SPD), Dr. Yan discussed his tips for using AI.
Changing Fast
From the outset, most generative AI systems have been very good at processing language — for example, generating letters of medical necessity and summarizing disease processes into lay terms. But now they’re becoming “truly multimodal,” said Dr. Yan. “You can enter images; you could have it process audio; you can even start to have it refine video.”
To get started, he recommends signing up for a free account with ChatGPT, Gemini, Perplexity, Claude, and/or Microsoft Copilot. “To make the best choice, you have to try them out yourself because they each have their own kind of flavor and strengths and weaknesses,” said Dr. Yan.
Personally, he finds that ChatGPT is the most versatile, Gemini perhaps a little better in terms of image generation, and Perplexity probably the best at references because it was designed as an online library.
Once you figure out which platforms you prefer, consider signing up for a premium subscription, which is typically month to month and can be canceled at any time, Dr. Yan said. “This will allow you to get the most out of the AI model.”
As these AI systems are based on large language models, they are excellent at text, Dr. Yan noted. He suggests asking one to generate a letter or patient instruction sheet. “If you have a premium model, give it a PDF to summarize an article or take a photo of something that you want its opinion on.”
Privacy Critical
Always pay attention to privacy issues and avoid entering any private health information that would violate the Health Insurance Portability and Accountability Act (HIPAA), he said.
“We have to be very careful about how we interact with AI,” said Dr. Yan. “We can’t be posting private patient health information into these systems, no matter how useful these systems are.” Many academic institutions are creating “walled gardens” — private areas of AI access that don’t allow patient information to “leak out,” he said. “These AI models may have HIPAA protections in place and come with specific guidelines of use.”
The AI “scribe,” which helps with electronic health record documentation, is one of the most useful tools for clinicians, he said. He referred to a recent study showing that an AI scribe saved users an average of 1 hour at the keyboard every day, and a small patient survey showing 71% reported that it led to spending more time with their physician.
When entering requests into a prompt line with an AI system, Dr. Yan stressed that these prompts need to be clear and concise. For a complicated calculation or multistep problem, try adding the words “let’s do this step by step,” he said. “This is a technique invoking a ‘chain of thought’ that allows the system to enhance its accuracy when solving problems.”
If the response is not satisfactory, try being more detailed in the request, he advised, and consider giving the system examples of what you’re looking for and telling it what you don’t want in the output.
“For instance, if you’re asking for a differential diagnosis of rashes that affect the hands and feet, you can stipulate that you only want rashes that are vesicular or that arise in neonates, so you can get a more focused answer,” said Dr. Yan.
If there are “long-winded verbose” responses, add the phrase “be concise,” and it will shorten the response by about 50%, he added.
AI Hallucinations
Dr. Yan broached an issue that occasionally comes up, AI hallucinations, which refer to inaccurate or misleading responses on the basis of incomplete training or intrinsic biases within the model. He pointed to the case of a doctor discussing issues related to a patient’s hands, feet, and mouth, which the AI-generated model summarized as “the patient being diagnosed with hand, foot, and mouth disease.”
Another example he provided was a request to generate a letter of medical necessity for using ustekinumab (Stelara) for treating hidradenitis suppurative in a child that included references for its effectiveness and safety in children. The AI system generated “false references that sounded like they should be real because the authors are often people who have written in that field or on that subject,” said Dr. Yan.
When pressed, the system did acknowledge the references were hypothetical but were meant to illustrate the types of studies that would typically support the use of this drug in pediatric patients with HS. “ It’s well meaning, in the sense that it’s trying to help you achieve your goals using this training system,” said Dr. Yan.
“If you’re skeptical about a response, double-check the answer with a Google search or run the response through another AI [tool] asking it to check if the response is accurate,” he added.
While AI systems won’t replace the clinician, they are continuing to improve and becoming more sophisticated. Dr. Yan advises keeping up with emerging developments and engaging and adapting the most appropriate AI tool for an individual clinician’s work.
Asked to comment on the presentation at the SPD meeting, Sheilagh Maguiness, MD, director of the Division of Pediatric Dermatology at the University of Minnesota, Minneapolis, who, like other doctors, is increasingly testing AI, said she foresees a time when AI scribes fully replace humans for completing tasks during patient interactions.
“The hope is that if the AI scribes get good enough, we can just open our phone, have them translate the interaction, and create the notes for us.”
While she likes the idea of using ChatGPT to help with tasks like letters of recommendation for medications, Dr. Yan’s comments reiterated the importance of “checking and double-checking ChatGPT because it’s not correct all the time.” She particularly welcomed the advice “that we can just go back and ask it again to clarify, and that may improve its answers.”
Dr. Yan’s disclosures included an investment portfolio that includes companies working in the AI space, including Google, Apple, Nvidia, Amazon, Microsoft, and Arm. Dr. Maguiness had no relevant disclosures.
A version of this article first appeared on Medscape.com.
TORONTO — with the various AI models.
He reminds doctors that many of their colleagues and patients and their families are already using these systems, “and you don’t want to be left behind.”
In an interview following his presentation on AI at the annual meeting of the Society for Pediatric Dermatology (SPD), Dr. Yan discussed his tips for using AI.
Changing Fast
From the outset, most generative AI systems have been very good at processing language — for example, generating letters of medical necessity and summarizing disease processes into lay terms. But now they’re becoming “truly multimodal,” said Dr. Yan. “You can enter images; you could have it process audio; you can even start to have it refine video.”
To get started, he recommends signing up for a free account with ChatGPT, Gemini, Perplexity, Claude, and/or Microsoft Copilot. “To make the best choice, you have to try them out yourself because they each have their own kind of flavor and strengths and weaknesses,” said Dr. Yan.
Personally, he finds that ChatGPT is the most versatile, Gemini perhaps a little better in terms of image generation, and Perplexity probably the best at references because it was designed as an online library.
Once you figure out which platforms you prefer, consider signing up for a premium subscription, which is typically month to month and can be canceled at any time, Dr. Yan said. “This will allow you to get the most out of the AI model.”
As these AI systems are based on large language models, they are excellent at text, Dr. Yan noted. He suggests asking one to generate a letter or patient instruction sheet. “If you have a premium model, give it a PDF to summarize an article or take a photo of something that you want its opinion on.”
Privacy Critical
Always pay attention to privacy issues and avoid entering any private health information that would violate the Health Insurance Portability and Accountability Act (HIPAA), he said.
“We have to be very careful about how we interact with AI,” said Dr. Yan. “We can’t be posting private patient health information into these systems, no matter how useful these systems are.” Many academic institutions are creating “walled gardens” — private areas of AI access that don’t allow patient information to “leak out,” he said. “These AI models may have HIPAA protections in place and come with specific guidelines of use.”
The AI “scribe,” which helps with electronic health record documentation, is one of the most useful tools for clinicians, he said. He referred to a recent study showing that an AI scribe saved users an average of 1 hour at the keyboard every day, and a small patient survey showing 71% reported that it led to spending more time with their physician.
When entering requests into a prompt line with an AI system, Dr. Yan stressed that these prompts need to be clear and concise. For a complicated calculation or multistep problem, try adding the words “let’s do this step by step,” he said. “This is a technique invoking a ‘chain of thought’ that allows the system to enhance its accuracy when solving problems.”
If the response is not satisfactory, try being more detailed in the request, he advised, and consider giving the system examples of what you’re looking for and telling it what you don’t want in the output.
“For instance, if you’re asking for a differential diagnosis of rashes that affect the hands and feet, you can stipulate that you only want rashes that are vesicular or that arise in neonates, so you can get a more focused answer,” said Dr. Yan.
If there are “long-winded verbose” responses, add the phrase “be concise,” and it will shorten the response by about 50%, he added.
AI Hallucinations
Dr. Yan broached an issue that occasionally comes up, AI hallucinations, which refer to inaccurate or misleading responses on the basis of incomplete training or intrinsic biases within the model. He pointed to the case of a doctor discussing issues related to a patient’s hands, feet, and mouth, which the AI-generated model summarized as “the patient being diagnosed with hand, foot, and mouth disease.”
Another example he provided was a request to generate a letter of medical necessity for using ustekinumab (Stelara) for treating hidradenitis suppurative in a child that included references for its effectiveness and safety in children. The AI system generated “false references that sounded like they should be real because the authors are often people who have written in that field or on that subject,” said Dr. Yan.
When pressed, the system did acknowledge the references were hypothetical but were meant to illustrate the types of studies that would typically support the use of this drug in pediatric patients with HS. “ It’s well meaning, in the sense that it’s trying to help you achieve your goals using this training system,” said Dr. Yan.
“If you’re skeptical about a response, double-check the answer with a Google search or run the response through another AI [tool] asking it to check if the response is accurate,” he added.
While AI systems won’t replace the clinician, they are continuing to improve and becoming more sophisticated. Dr. Yan advises keeping up with emerging developments and engaging and adapting the most appropriate AI tool for an individual clinician’s work.
Asked to comment on the presentation at the SPD meeting, Sheilagh Maguiness, MD, director of the Division of Pediatric Dermatology at the University of Minnesota, Minneapolis, who, like other doctors, is increasingly testing AI, said she foresees a time when AI scribes fully replace humans for completing tasks during patient interactions.
“The hope is that if the AI scribes get good enough, we can just open our phone, have them translate the interaction, and create the notes for us.”
While she likes the idea of using ChatGPT to help with tasks like letters of recommendation for medications, Dr. Yan’s comments reiterated the importance of “checking and double-checking ChatGPT because it’s not correct all the time.” She particularly welcomed the advice “that we can just go back and ask it again to clarify, and that may improve its answers.”
Dr. Yan’s disclosures included an investment portfolio that includes companies working in the AI space, including Google, Apple, Nvidia, Amazon, Microsoft, and Arm. Dr. Maguiness had no relevant disclosures.
A version of this article first appeared on Medscape.com.
TORONTO — with the various AI models.
He reminds doctors that many of their colleagues and patients and their families are already using these systems, “and you don’t want to be left behind.”
In an interview following his presentation on AI at the annual meeting of the Society for Pediatric Dermatology (SPD), Dr. Yan discussed his tips for using AI.
Changing Fast
From the outset, most generative AI systems have been very good at processing language — for example, generating letters of medical necessity and summarizing disease processes into lay terms. But now they’re becoming “truly multimodal,” said Dr. Yan. “You can enter images; you could have it process audio; you can even start to have it refine video.”
To get started, he recommends signing up for a free account with ChatGPT, Gemini, Perplexity, Claude, and/or Microsoft Copilot. “To make the best choice, you have to try them out yourself because they each have their own kind of flavor and strengths and weaknesses,” said Dr. Yan.
Personally, he finds that ChatGPT is the most versatile, Gemini perhaps a little better in terms of image generation, and Perplexity probably the best at references because it was designed as an online library.
Once you figure out which platforms you prefer, consider signing up for a premium subscription, which is typically month to month and can be canceled at any time, Dr. Yan said. “This will allow you to get the most out of the AI model.”
As these AI systems are based on large language models, they are excellent at text, Dr. Yan noted. He suggests asking one to generate a letter or patient instruction sheet. “If you have a premium model, give it a PDF to summarize an article or take a photo of something that you want its opinion on.”
Privacy Critical
Always pay attention to privacy issues and avoid entering any private health information that would violate the Health Insurance Portability and Accountability Act (HIPAA), he said.
“We have to be very careful about how we interact with AI,” said Dr. Yan. “We can’t be posting private patient health information into these systems, no matter how useful these systems are.” Many academic institutions are creating “walled gardens” — private areas of AI access that don’t allow patient information to “leak out,” he said. “These AI models may have HIPAA protections in place and come with specific guidelines of use.”
The AI “scribe,” which helps with electronic health record documentation, is one of the most useful tools for clinicians, he said. He referred to a recent study showing that an AI scribe saved users an average of 1 hour at the keyboard every day, and a small patient survey showing 71% reported that it led to spending more time with their physician.
When entering requests into a prompt line with an AI system, Dr. Yan stressed that these prompts need to be clear and concise. For a complicated calculation or multistep problem, try adding the words “let’s do this step by step,” he said. “This is a technique invoking a ‘chain of thought’ that allows the system to enhance its accuracy when solving problems.”
If the response is not satisfactory, try being more detailed in the request, he advised, and consider giving the system examples of what you’re looking for and telling it what you don’t want in the output.
“For instance, if you’re asking for a differential diagnosis of rashes that affect the hands and feet, you can stipulate that you only want rashes that are vesicular or that arise in neonates, so you can get a more focused answer,” said Dr. Yan.
If there are “long-winded verbose” responses, add the phrase “be concise,” and it will shorten the response by about 50%, he added.
AI Hallucinations
Dr. Yan broached an issue that occasionally comes up, AI hallucinations, which refer to inaccurate or misleading responses on the basis of incomplete training or intrinsic biases within the model. He pointed to the case of a doctor discussing issues related to a patient’s hands, feet, and mouth, which the AI-generated model summarized as “the patient being diagnosed with hand, foot, and mouth disease.”
Another example he provided was a request to generate a letter of medical necessity for using ustekinumab (Stelara) for treating hidradenitis suppurative in a child that included references for its effectiveness and safety in children. The AI system generated “false references that sounded like they should be real because the authors are often people who have written in that field or on that subject,” said Dr. Yan.
When pressed, the system did acknowledge the references were hypothetical but were meant to illustrate the types of studies that would typically support the use of this drug in pediatric patients with HS. “ It’s well meaning, in the sense that it’s trying to help you achieve your goals using this training system,” said Dr. Yan.
“If you’re skeptical about a response, double-check the answer with a Google search or run the response through another AI [tool] asking it to check if the response is accurate,” he added.
While AI systems won’t replace the clinician, they are continuing to improve and becoming more sophisticated. Dr. Yan advises keeping up with emerging developments and engaging and adapting the most appropriate AI tool for an individual clinician’s work.
Asked to comment on the presentation at the SPD meeting, Sheilagh Maguiness, MD, director of the Division of Pediatric Dermatology at the University of Minnesota, Minneapolis, who, like other doctors, is increasingly testing AI, said she foresees a time when AI scribes fully replace humans for completing tasks during patient interactions.
“The hope is that if the AI scribes get good enough, we can just open our phone, have them translate the interaction, and create the notes for us.”
While she likes the idea of using ChatGPT to help with tasks like letters of recommendation for medications, Dr. Yan’s comments reiterated the importance of “checking and double-checking ChatGPT because it’s not correct all the time.” She particularly welcomed the advice “that we can just go back and ask it again to clarify, and that may improve its answers.”
Dr. Yan’s disclosures included an investment portfolio that includes companies working in the AI space, including Google, Apple, Nvidia, Amazon, Microsoft, and Arm. Dr. Maguiness had no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM SPD 2024