User login
MDedge conference coverage features onsite reporting of the latest study results and expert perspectives from leading researchers.
Management, Evaluation of Chronic Itch in Older Adults
WASHINGTON — , Shawn G. Kwatra, MD, said at the ElderDerm conference on dermatology in older patients hosted by the GW School of Medicine & Health Sciences.
“We found a few years ago that eosinophils seem to differentiate this group, and now we’re finding that IgE and CBC [complete blood count] differential can help you get a little better sense of who has an immune-driven itch vs something more neuropathic,” said Dr. Kwatra, professor and chair of dermatology at the University of Maryland, Baltimore, who founded and directed the Johns Hopkins Itch Center before coming to the University of Maryland in 2023. Not all patients with immune-driven itch will have these biomarkers, “but it’s a helpful tool,” he said.
CPUO is the term that is increasingly being used, he said, to describe intense, chronic pruritus without primary skin lesions or rashes and without any known systemic cause. It becomes more common as people get older and is sometimes debilitating. The initial evaluation should be kept “simple and straightforward,” he advised, with heightened concern for underlying malignancy in those who present with an itch of less than 12 months’ duration.
Biologics, JAK Inhibitors: Case Reports, Ongoing Research
Research conducted by Dr. Kwatra and Jaya Manjunath, a fourth-year medical student at The George Washington University, Washington, documented higher levels of Th2-associated cytokines and inflammatory markers in patients with CPUO who had elevated IgE or eosinophil levels, or both than in patients with itch who had low IgE and eosinophil levels. The patients with higher levels also had a greater response to off-label treatment with immunomodulatory therapy.
“Multiple Th2-related inflammatory markers, like IL [interleukin]-5 and eotaxin-3, were reduced after dupilumab” in patients who responded to the therapy, said Ms. Manjunath, who co-presented the meeting session on chronic itch with Dr. Kwatra. Other changes in the plasma cytokine profile included a reduction in the serum level of thymus and activation-regulated chemokine, which is a biomarker for atopic dermatitis. The research is under review for publication.
Meanwhile, a phase 3 trial (LIBERTY-CPUO-CHIC) of dupilumab for CPUO is currently underway, Dr. Kwatra noted. Investigators are randomizing patients with severe pruritus (Worst Itch Numeric Rating Scale [WI-NRS] ≥ 7) to dupilumab or placebo for 12 or 24 weeks.
In one of several cases shared by Dr. Kwatra and Ms. Manjunath, a 71-year-old Black woman with a 6-month history of generalized itch (WI-NRS = 10) and a history of type 2 diabetes, hypertension, and chronic kidney disease was found to have elevated eosinophil levels and a negative malignancy workup. Previous therapies included antihistamines and topical steroids. She was started on a 600-mg loading dose of subcutaneous dupilumab followed by 300 mg every 14 days. At the 2-month follow-up, her WI-NRS score was 0.
Because “dupilumab is off label right now for this form of itch, oftentimes our first line is methotrexate,” Dr. Kwatra said. Patients “can have a good response with this therapeutic.”
He also described the case of a 72-year-old Black woman with total body itch for 2 years (WI-NRS = 10) and a history of seasonal allergies, thyroid disease, and hypertension. Previous therapies included prednisone, antihistamines, topical steroids, and gabapentin. The patient was found to have high IgE (447 kU/L) and eosinophil levels (4.9%), was started on methotrexate, and had an itch score of 0 at the 8-month follow-up.
JAK inhibitors may also have a role in the management of CPUO. A phase 2 nonrandomized controlled trial of abrocitinib for adults with prurigo nodularis (PN) or CPUO, recently published in JAMA Dermatology, showed itch scores decreased by 53.7% in the CPUO group (and 78.3% in the PN group) after 12 weeks of treatment with oral abrocitinib 200 mg daily. Patients had significant improvements in quality of life and no serious adverse events, said Dr. Kwatra, the lead author of the paper.
One of these patients was a 73-year-old White man who had experienced total body itch for 1.5 years (predominantly affecting his upper extremities; WI-NRS = 10) and a history of ascending aortic aneurysm, hypertension, and hyperlipidemia. Previous failed therapies included dupilumab (> 6 months), topical steroids, tacrolimus, and antihistamines. Labs showed elevated IgE (456 kU/L) and eosinophil levels (11.7%). After 12 weeks of treatment with abrocitinib, the WI-NRS decreased to 2.
PD-1 Inhibitors As a Trigger
Chronic pruritus caused by the anticancer PD-1 inhibitors is becoming more common as the utilization of these immune checkpoint inhibitors increases, Dr. Kwatra noted. “You don’t see much in the skin, but [these patients have] very high IgE and eosinophils,” he said. “We’ve been seeing more reports recently of utilizing agents that target type 2 inflammation off label for PD-1 inhibitor–related skin manifestations.”
One such patient with PD-1 inhibitor–induced pruritus was a 65-year-old White man with metastatic melanoma who reported a 6-month history of itching that began 3 weeks after the start of treatment with the PD-1 inhibitor pembrolizumab. His WI-NRS score was 10 despite treatment with topical steroids and antihistamines. He had a history of psoriasis. Labs showed elevated IgE (1350 kU/L) and eosinophil levels (4.5%). At a 4-month follow-up after treatment with off-label dupilumab (a 600-mg subcutaneous loading dose followed by 300 mg every 14 days), his WI-NRS score was 0.
In a paper recently published in JAAD International, Dr. Kwatra, Ms. Manjunath, and coinvestigators reported on a series of 15 patients who developed chronic pruritus following an immune stimulus exposure, including immunotherapy and vaccination (2024 Apr 7:16:97-102. doi: 10.1016/j.jdin.2024.03.022). Most immunotherapy-treated patients experienced pruritus during treatment or after 21-60 days of receiving treatment, and the patients with vaccine-stimulated pruritus (after Tdap and messenger RNA COVID-19 vaccination) developed pruritus within a week of vaccination.
In addition to the elevated levels of IgE and eosinophils, plasma cytokine analysis showed elevated levels of IL-5, thymic stromal lymphopoietin, and other Th2-related cytokines and inflammatory markers in patients with immune-stimulated pruritus compared with healthy controls, Ms. Manjunath said at the meeting.
When a Malignancy Workup Becomes Important
The initial part of any diagnostic workup for CPUO should include CBC with differential, liver function tests, renal function tests, and thyroid function testing, said Kwatra, referring to a diagnostic algorithm he developed, which was published as part of a CME review in the Journal of the American Academy of Dermatology in 2022.
Then, as indicated by risk factors in the history and physical, one could order other tests such as HIV serology, hepatitis B/C serologies, bullous pemphigoid testing, chest x-rays, evaluation for gammopathies, stool examination for ova and parasites, or heavy metal testing. “Do you do everything at once? We like to keep it straightforward,” Dr. Kwatra said. “Depending on the patient’s risk factors, you could order more or less.”
A malignancy workup should be strongly considered in patients whose itch duration is less than 12 months — and especially if the duration is less than 3 months — with an emphasis on cancers more frequently associated with itch: Hematologic and hepatobiliary cancers. This is “when concern should be heightened ... when there should be a lower threshold for workup,” he said.
The 12-month recommendation stems from a Danish cohort study published in 2014 that demonstrated a twofold increased incidence of cancer among patients with pruritus in the first 3 months after the diagnosis of pruritus. The 1-year absolute cancer risk was 1.63%.
Other risk factors for underlying malignancy or malignancy development in patients with CPUO include age older than 60 years, male sex, liver disease, and current or prior smoking, according to another study, noted Dr. Kwatra.
Dr. Kwatra disclosed that he is an advisory board member/consultant for Pfizer, Regeneron, Sanofi, and other companies and an investigator for Galderma, Incyte, Pfizer, and Sanofi. Manjunath served as the codirector of the ElderDerm conference.
A version of this article first appeared on Medscape.com.
WASHINGTON — , Shawn G. Kwatra, MD, said at the ElderDerm conference on dermatology in older patients hosted by the GW School of Medicine & Health Sciences.
“We found a few years ago that eosinophils seem to differentiate this group, and now we’re finding that IgE and CBC [complete blood count] differential can help you get a little better sense of who has an immune-driven itch vs something more neuropathic,” said Dr. Kwatra, professor and chair of dermatology at the University of Maryland, Baltimore, who founded and directed the Johns Hopkins Itch Center before coming to the University of Maryland in 2023. Not all patients with immune-driven itch will have these biomarkers, “but it’s a helpful tool,” he said.
CPUO is the term that is increasingly being used, he said, to describe intense, chronic pruritus without primary skin lesions or rashes and without any known systemic cause. It becomes more common as people get older and is sometimes debilitating. The initial evaluation should be kept “simple and straightforward,” he advised, with heightened concern for underlying malignancy in those who present with an itch of less than 12 months’ duration.
Biologics, JAK Inhibitors: Case Reports, Ongoing Research
Research conducted by Dr. Kwatra and Jaya Manjunath, a fourth-year medical student at The George Washington University, Washington, documented higher levels of Th2-associated cytokines and inflammatory markers in patients with CPUO who had elevated IgE or eosinophil levels, or both than in patients with itch who had low IgE and eosinophil levels. The patients with higher levels also had a greater response to off-label treatment with immunomodulatory therapy.
“Multiple Th2-related inflammatory markers, like IL [interleukin]-5 and eotaxin-3, were reduced after dupilumab” in patients who responded to the therapy, said Ms. Manjunath, who co-presented the meeting session on chronic itch with Dr. Kwatra. Other changes in the plasma cytokine profile included a reduction in the serum level of thymus and activation-regulated chemokine, which is a biomarker for atopic dermatitis. The research is under review for publication.
Meanwhile, a phase 3 trial (LIBERTY-CPUO-CHIC) of dupilumab for CPUO is currently underway, Dr. Kwatra noted. Investigators are randomizing patients with severe pruritus (Worst Itch Numeric Rating Scale [WI-NRS] ≥ 7) to dupilumab or placebo for 12 or 24 weeks.
In one of several cases shared by Dr. Kwatra and Ms. Manjunath, a 71-year-old Black woman with a 6-month history of generalized itch (WI-NRS = 10) and a history of type 2 diabetes, hypertension, and chronic kidney disease was found to have elevated eosinophil levels and a negative malignancy workup. Previous therapies included antihistamines and topical steroids. She was started on a 600-mg loading dose of subcutaneous dupilumab followed by 300 mg every 14 days. At the 2-month follow-up, her WI-NRS score was 0.
Because “dupilumab is off label right now for this form of itch, oftentimes our first line is methotrexate,” Dr. Kwatra said. Patients “can have a good response with this therapeutic.”
He also described the case of a 72-year-old Black woman with total body itch for 2 years (WI-NRS = 10) and a history of seasonal allergies, thyroid disease, and hypertension. Previous therapies included prednisone, antihistamines, topical steroids, and gabapentin. The patient was found to have high IgE (447 kU/L) and eosinophil levels (4.9%), was started on methotrexate, and had an itch score of 0 at the 8-month follow-up.
JAK inhibitors may also have a role in the management of CPUO. A phase 2 nonrandomized controlled trial of abrocitinib for adults with prurigo nodularis (PN) or CPUO, recently published in JAMA Dermatology, showed itch scores decreased by 53.7% in the CPUO group (and 78.3% in the PN group) after 12 weeks of treatment with oral abrocitinib 200 mg daily. Patients had significant improvements in quality of life and no serious adverse events, said Dr. Kwatra, the lead author of the paper.
One of these patients was a 73-year-old White man who had experienced total body itch for 1.5 years (predominantly affecting his upper extremities; WI-NRS = 10) and a history of ascending aortic aneurysm, hypertension, and hyperlipidemia. Previous failed therapies included dupilumab (> 6 months), topical steroids, tacrolimus, and antihistamines. Labs showed elevated IgE (456 kU/L) and eosinophil levels (11.7%). After 12 weeks of treatment with abrocitinib, the WI-NRS decreased to 2.
PD-1 Inhibitors As a Trigger
Chronic pruritus caused by the anticancer PD-1 inhibitors is becoming more common as the utilization of these immune checkpoint inhibitors increases, Dr. Kwatra noted. “You don’t see much in the skin, but [these patients have] very high IgE and eosinophils,” he said. “We’ve been seeing more reports recently of utilizing agents that target type 2 inflammation off label for PD-1 inhibitor–related skin manifestations.”
One such patient with PD-1 inhibitor–induced pruritus was a 65-year-old White man with metastatic melanoma who reported a 6-month history of itching that began 3 weeks after the start of treatment with the PD-1 inhibitor pembrolizumab. His WI-NRS score was 10 despite treatment with topical steroids and antihistamines. He had a history of psoriasis. Labs showed elevated IgE (1350 kU/L) and eosinophil levels (4.5%). At a 4-month follow-up after treatment with off-label dupilumab (a 600-mg subcutaneous loading dose followed by 300 mg every 14 days), his WI-NRS score was 0.
In a paper recently published in JAAD International, Dr. Kwatra, Ms. Manjunath, and coinvestigators reported on a series of 15 patients who developed chronic pruritus following an immune stimulus exposure, including immunotherapy and vaccination (2024 Apr 7:16:97-102. doi: 10.1016/j.jdin.2024.03.022). Most immunotherapy-treated patients experienced pruritus during treatment or after 21-60 days of receiving treatment, and the patients with vaccine-stimulated pruritus (after Tdap and messenger RNA COVID-19 vaccination) developed pruritus within a week of vaccination.
In addition to the elevated levels of IgE and eosinophils, plasma cytokine analysis showed elevated levels of IL-5, thymic stromal lymphopoietin, and other Th2-related cytokines and inflammatory markers in patients with immune-stimulated pruritus compared with healthy controls, Ms. Manjunath said at the meeting.
When a Malignancy Workup Becomes Important
The initial part of any diagnostic workup for CPUO should include CBC with differential, liver function tests, renal function tests, and thyroid function testing, said Kwatra, referring to a diagnostic algorithm he developed, which was published as part of a CME review in the Journal of the American Academy of Dermatology in 2022.
Then, as indicated by risk factors in the history and physical, one could order other tests such as HIV serology, hepatitis B/C serologies, bullous pemphigoid testing, chest x-rays, evaluation for gammopathies, stool examination for ova and parasites, or heavy metal testing. “Do you do everything at once? We like to keep it straightforward,” Dr. Kwatra said. “Depending on the patient’s risk factors, you could order more or less.”
A malignancy workup should be strongly considered in patients whose itch duration is less than 12 months — and especially if the duration is less than 3 months — with an emphasis on cancers more frequently associated with itch: Hematologic and hepatobiliary cancers. This is “when concern should be heightened ... when there should be a lower threshold for workup,” he said.
The 12-month recommendation stems from a Danish cohort study published in 2014 that demonstrated a twofold increased incidence of cancer among patients with pruritus in the first 3 months after the diagnosis of pruritus. The 1-year absolute cancer risk was 1.63%.
Other risk factors for underlying malignancy or malignancy development in patients with CPUO include age older than 60 years, male sex, liver disease, and current or prior smoking, according to another study, noted Dr. Kwatra.
Dr. Kwatra disclosed that he is an advisory board member/consultant for Pfizer, Regeneron, Sanofi, and other companies and an investigator for Galderma, Incyte, Pfizer, and Sanofi. Manjunath served as the codirector of the ElderDerm conference.
A version of this article first appeared on Medscape.com.
WASHINGTON — , Shawn G. Kwatra, MD, said at the ElderDerm conference on dermatology in older patients hosted by the GW School of Medicine & Health Sciences.
“We found a few years ago that eosinophils seem to differentiate this group, and now we’re finding that IgE and CBC [complete blood count] differential can help you get a little better sense of who has an immune-driven itch vs something more neuropathic,” said Dr. Kwatra, professor and chair of dermatology at the University of Maryland, Baltimore, who founded and directed the Johns Hopkins Itch Center before coming to the University of Maryland in 2023. Not all patients with immune-driven itch will have these biomarkers, “but it’s a helpful tool,” he said.
CPUO is the term that is increasingly being used, he said, to describe intense, chronic pruritus without primary skin lesions or rashes and without any known systemic cause. It becomes more common as people get older and is sometimes debilitating. The initial evaluation should be kept “simple and straightforward,” he advised, with heightened concern for underlying malignancy in those who present with an itch of less than 12 months’ duration.
Biologics, JAK Inhibitors: Case Reports, Ongoing Research
Research conducted by Dr. Kwatra and Jaya Manjunath, a fourth-year medical student at The George Washington University, Washington, documented higher levels of Th2-associated cytokines and inflammatory markers in patients with CPUO who had elevated IgE or eosinophil levels, or both than in patients with itch who had low IgE and eosinophil levels. The patients with higher levels also had a greater response to off-label treatment with immunomodulatory therapy.
“Multiple Th2-related inflammatory markers, like IL [interleukin]-5 and eotaxin-3, were reduced after dupilumab” in patients who responded to the therapy, said Ms. Manjunath, who co-presented the meeting session on chronic itch with Dr. Kwatra. Other changes in the plasma cytokine profile included a reduction in the serum level of thymus and activation-regulated chemokine, which is a biomarker for atopic dermatitis. The research is under review for publication.
Meanwhile, a phase 3 trial (LIBERTY-CPUO-CHIC) of dupilumab for CPUO is currently underway, Dr. Kwatra noted. Investigators are randomizing patients with severe pruritus (Worst Itch Numeric Rating Scale [WI-NRS] ≥ 7) to dupilumab or placebo for 12 or 24 weeks.
In one of several cases shared by Dr. Kwatra and Ms. Manjunath, a 71-year-old Black woman with a 6-month history of generalized itch (WI-NRS = 10) and a history of type 2 diabetes, hypertension, and chronic kidney disease was found to have elevated eosinophil levels and a negative malignancy workup. Previous therapies included antihistamines and topical steroids. She was started on a 600-mg loading dose of subcutaneous dupilumab followed by 300 mg every 14 days. At the 2-month follow-up, her WI-NRS score was 0.
Because “dupilumab is off label right now for this form of itch, oftentimes our first line is methotrexate,” Dr. Kwatra said. Patients “can have a good response with this therapeutic.”
He also described the case of a 72-year-old Black woman with total body itch for 2 years (WI-NRS = 10) and a history of seasonal allergies, thyroid disease, and hypertension. Previous therapies included prednisone, antihistamines, topical steroids, and gabapentin. The patient was found to have high IgE (447 kU/L) and eosinophil levels (4.9%), was started on methotrexate, and had an itch score of 0 at the 8-month follow-up.
JAK inhibitors may also have a role in the management of CPUO. A phase 2 nonrandomized controlled trial of abrocitinib for adults with prurigo nodularis (PN) or CPUO, recently published in JAMA Dermatology, showed itch scores decreased by 53.7% in the CPUO group (and 78.3% in the PN group) after 12 weeks of treatment with oral abrocitinib 200 mg daily. Patients had significant improvements in quality of life and no serious adverse events, said Dr. Kwatra, the lead author of the paper.
One of these patients was a 73-year-old White man who had experienced total body itch for 1.5 years (predominantly affecting his upper extremities; WI-NRS = 10) and a history of ascending aortic aneurysm, hypertension, and hyperlipidemia. Previous failed therapies included dupilumab (> 6 months), topical steroids, tacrolimus, and antihistamines. Labs showed elevated IgE (456 kU/L) and eosinophil levels (11.7%). After 12 weeks of treatment with abrocitinib, the WI-NRS decreased to 2.
PD-1 Inhibitors As a Trigger
Chronic pruritus caused by the anticancer PD-1 inhibitors is becoming more common as the utilization of these immune checkpoint inhibitors increases, Dr. Kwatra noted. “You don’t see much in the skin, but [these patients have] very high IgE and eosinophils,” he said. “We’ve been seeing more reports recently of utilizing agents that target type 2 inflammation off label for PD-1 inhibitor–related skin manifestations.”
One such patient with PD-1 inhibitor–induced pruritus was a 65-year-old White man with metastatic melanoma who reported a 6-month history of itching that began 3 weeks after the start of treatment with the PD-1 inhibitor pembrolizumab. His WI-NRS score was 10 despite treatment with topical steroids and antihistamines. He had a history of psoriasis. Labs showed elevated IgE (1350 kU/L) and eosinophil levels (4.5%). At a 4-month follow-up after treatment with off-label dupilumab (a 600-mg subcutaneous loading dose followed by 300 mg every 14 days), his WI-NRS score was 0.
In a paper recently published in JAAD International, Dr. Kwatra, Ms. Manjunath, and coinvestigators reported on a series of 15 patients who developed chronic pruritus following an immune stimulus exposure, including immunotherapy and vaccination (2024 Apr 7:16:97-102. doi: 10.1016/j.jdin.2024.03.022). Most immunotherapy-treated patients experienced pruritus during treatment or after 21-60 days of receiving treatment, and the patients with vaccine-stimulated pruritus (after Tdap and messenger RNA COVID-19 vaccination) developed pruritus within a week of vaccination.
In addition to the elevated levels of IgE and eosinophils, plasma cytokine analysis showed elevated levels of IL-5, thymic stromal lymphopoietin, and other Th2-related cytokines and inflammatory markers in patients with immune-stimulated pruritus compared with healthy controls, Ms. Manjunath said at the meeting.
When a Malignancy Workup Becomes Important
The initial part of any diagnostic workup for CPUO should include CBC with differential, liver function tests, renal function tests, and thyroid function testing, said Kwatra, referring to a diagnostic algorithm he developed, which was published as part of a CME review in the Journal of the American Academy of Dermatology in 2022.
Then, as indicated by risk factors in the history and physical, one could order other tests such as HIV serology, hepatitis B/C serologies, bullous pemphigoid testing, chest x-rays, evaluation for gammopathies, stool examination for ova and parasites, or heavy metal testing. “Do you do everything at once? We like to keep it straightforward,” Dr. Kwatra said. “Depending on the patient’s risk factors, you could order more or less.”
A malignancy workup should be strongly considered in patients whose itch duration is less than 12 months — and especially if the duration is less than 3 months — with an emphasis on cancers more frequently associated with itch: Hematologic and hepatobiliary cancers. This is “when concern should be heightened ... when there should be a lower threshold for workup,” he said.
The 12-month recommendation stems from a Danish cohort study published in 2014 that demonstrated a twofold increased incidence of cancer among patients with pruritus in the first 3 months after the diagnosis of pruritus. The 1-year absolute cancer risk was 1.63%.
Other risk factors for underlying malignancy or malignancy development in patients with CPUO include age older than 60 years, male sex, liver disease, and current or prior smoking, according to another study, noted Dr. Kwatra.
Dr. Kwatra disclosed that he is an advisory board member/consultant for Pfizer, Regeneron, Sanofi, and other companies and an investigator for Galderma, Incyte, Pfizer, and Sanofi. Manjunath served as the codirector of the ElderDerm conference.
A version of this article first appeared on Medscape.com.
FROM ELDERDERM 2024
Skin Dxs in Children in Refugee Camps Include Fungal Infections, Leishmaniasis
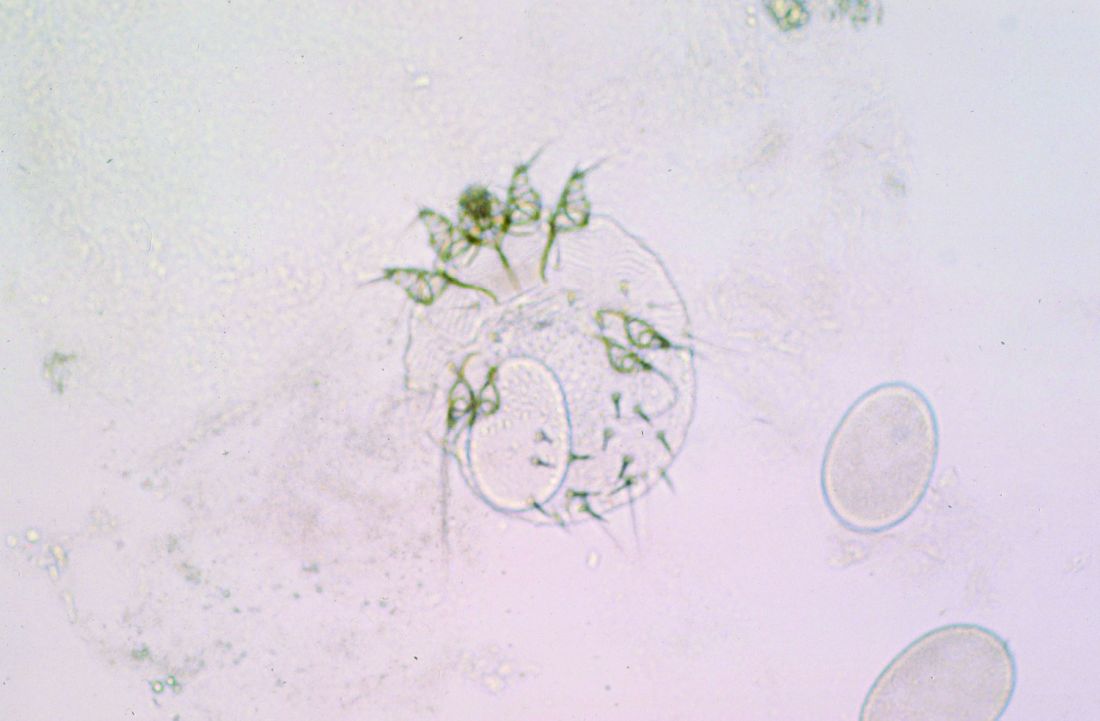
on the topic, a literature review showed. However, likely culprits include infectious diseases with cutaneous manifestations, such as pediculosis, tinea capitis, and scabies.
“Current data indicates that one in two refugees are children,” one of the study investigators, Mehar Maju, MPH, a fourth-year student at of the University of Washington School of Medicine, Seattle, said in an interview following the annual meeting of the Society for Pediatric Dermatology, where the results were presented during a poster session.
“The number of refugees continues to rise to unprecedented levels every year,” and climate change continues to drive increases in migration, “impacting those residing in camps,” she said. “As we continue to think about what this means for best supporting those residing in camps, I think it’s also important to consider how to best support refugees, specifically children, when they arrive in the United States. Part of this is to know what conditions are most prevalent and what type of social support this vulnerable population needs.”
To identify the common dermatologic conditions among children living in refugee camps, Ms. Maju and fellow fourth-year University of Washington medical student Nadia Siddiqui searched PubMed and Google Scholar for studies that were published in English and reported on the skin disease prevalence and management for refugees who are children. Key search terms used included “refugees,” “children,” “dermatology,” and “skin disease.” Of approximately 105 potential studies identified, 19 underwent analysis. Of these, only five were included in the final review.
One of the five studies was conducted in rural Nyala, Sudan. The study found that 88.8% of those living in orphanages and refugee camps were reported to have a skin disorder, commonly fungal or bacterial infections and dermatitis. In a separate case series, researchers found that cutaneous leishmaniasis was rising among Syrian refugee children.
A study that looked at morbidity and disease burden in mainland Greece refugee camps found that the skin was the second-most common site of communicable diseases among children, behind those of the respiratory tract. In another study that investigated the health of children in Australian immigration detention centers, complaints related to skin conditions were significantly elevated among children who were detained offshore, compared with those who were detained onshore.
Finally, in a study of 125 children between the ages of 1 and 15 years at a Sierra Leone–based displacement camp, the prevalence of scabies was 77% among those aged < 5 years and peaked to 86% among those aged 5-9 years.
“It was surprising to see the limited information about dermatologic diseases impacting children in refugee camps,” Ms. Maju said. “I expected that there would be more information on the specific proportion of diseases beyond those of infectious etiology. For example, I had believed that we would have more information on the prevalence of atopic dermatitis, vitiligo, and other more chronic skin diseases.”
She acknowledged certain limitations of the analysis, mainly the lack of published information on the skin health of pediatric refugees. “A study that evaluates the health status and dermatologic prevalence of disease among children residing in camps and those newly arrived in the United States from camps would provide unprecedented insight into this topic,” Ms. Maju said. “The results could guide public health efforts in improving care delivery and preparedness in camps and clinicians serving this particular population when they arrive in the United States.”
She and Ms. Siddiqui reported having no relevant disclosures.
A version of this article first appeared on Medscape.com.
on the topic, a literature review showed. However, likely culprits include infectious diseases with cutaneous manifestations, such as pediculosis, tinea capitis, and scabies.
“Current data indicates that one in two refugees are children,” one of the study investigators, Mehar Maju, MPH, a fourth-year student at of the University of Washington School of Medicine, Seattle, said in an interview following the annual meeting of the Society for Pediatric Dermatology, where the results were presented during a poster session.
“The number of refugees continues to rise to unprecedented levels every year,” and climate change continues to drive increases in migration, “impacting those residing in camps,” she said. “As we continue to think about what this means for best supporting those residing in camps, I think it’s also important to consider how to best support refugees, specifically children, when they arrive in the United States. Part of this is to know what conditions are most prevalent and what type of social support this vulnerable population needs.”
To identify the common dermatologic conditions among children living in refugee camps, Ms. Maju and fellow fourth-year University of Washington medical student Nadia Siddiqui searched PubMed and Google Scholar for studies that were published in English and reported on the skin disease prevalence and management for refugees who are children. Key search terms used included “refugees,” “children,” “dermatology,” and “skin disease.” Of approximately 105 potential studies identified, 19 underwent analysis. Of these, only five were included in the final review.
One of the five studies was conducted in rural Nyala, Sudan. The study found that 88.8% of those living in orphanages and refugee camps were reported to have a skin disorder, commonly fungal or bacterial infections and dermatitis. In a separate case series, researchers found that cutaneous leishmaniasis was rising among Syrian refugee children.
A study that looked at morbidity and disease burden in mainland Greece refugee camps found that the skin was the second-most common site of communicable diseases among children, behind those of the respiratory tract. In another study that investigated the health of children in Australian immigration detention centers, complaints related to skin conditions were significantly elevated among children who were detained offshore, compared with those who were detained onshore.
Finally, in a study of 125 children between the ages of 1 and 15 years at a Sierra Leone–based displacement camp, the prevalence of scabies was 77% among those aged < 5 years and peaked to 86% among those aged 5-9 years.
“It was surprising to see the limited information about dermatologic diseases impacting children in refugee camps,” Ms. Maju said. “I expected that there would be more information on the specific proportion of diseases beyond those of infectious etiology. For example, I had believed that we would have more information on the prevalence of atopic dermatitis, vitiligo, and other more chronic skin diseases.”
She acknowledged certain limitations of the analysis, mainly the lack of published information on the skin health of pediatric refugees. “A study that evaluates the health status and dermatologic prevalence of disease among children residing in camps and those newly arrived in the United States from camps would provide unprecedented insight into this topic,” Ms. Maju said. “The results could guide public health efforts in improving care delivery and preparedness in camps and clinicians serving this particular population when they arrive in the United States.”
She and Ms. Siddiqui reported having no relevant disclosures.
A version of this article first appeared on Medscape.com.
on the topic, a literature review showed. However, likely culprits include infectious diseases with cutaneous manifestations, such as pediculosis, tinea capitis, and scabies.
“Current data indicates that one in two refugees are children,” one of the study investigators, Mehar Maju, MPH, a fourth-year student at of the University of Washington School of Medicine, Seattle, said in an interview following the annual meeting of the Society for Pediatric Dermatology, where the results were presented during a poster session.
“The number of refugees continues to rise to unprecedented levels every year,” and climate change continues to drive increases in migration, “impacting those residing in camps,” she said. “As we continue to think about what this means for best supporting those residing in camps, I think it’s also important to consider how to best support refugees, specifically children, when they arrive in the United States. Part of this is to know what conditions are most prevalent and what type of social support this vulnerable population needs.”
To identify the common dermatologic conditions among children living in refugee camps, Ms. Maju and fellow fourth-year University of Washington medical student Nadia Siddiqui searched PubMed and Google Scholar for studies that were published in English and reported on the skin disease prevalence and management for refugees who are children. Key search terms used included “refugees,” “children,” “dermatology,” and “skin disease.” Of approximately 105 potential studies identified, 19 underwent analysis. Of these, only five were included in the final review.
One of the five studies was conducted in rural Nyala, Sudan. The study found that 88.8% of those living in orphanages and refugee camps were reported to have a skin disorder, commonly fungal or bacterial infections and dermatitis. In a separate case series, researchers found that cutaneous leishmaniasis was rising among Syrian refugee children.
A study that looked at morbidity and disease burden in mainland Greece refugee camps found that the skin was the second-most common site of communicable diseases among children, behind those of the respiratory tract. In another study that investigated the health of children in Australian immigration detention centers, complaints related to skin conditions were significantly elevated among children who were detained offshore, compared with those who were detained onshore.
Finally, in a study of 125 children between the ages of 1 and 15 years at a Sierra Leone–based displacement camp, the prevalence of scabies was 77% among those aged < 5 years and peaked to 86% among those aged 5-9 years.
“It was surprising to see the limited information about dermatologic diseases impacting children in refugee camps,” Ms. Maju said. “I expected that there would be more information on the specific proportion of diseases beyond those of infectious etiology. For example, I had believed that we would have more information on the prevalence of atopic dermatitis, vitiligo, and other more chronic skin diseases.”
She acknowledged certain limitations of the analysis, mainly the lack of published information on the skin health of pediatric refugees. “A study that evaluates the health status and dermatologic prevalence of disease among children residing in camps and those newly arrived in the United States from camps would provide unprecedented insight into this topic,” Ms. Maju said. “The results could guide public health efforts in improving care delivery and preparedness in camps and clinicians serving this particular population when they arrive in the United States.”
She and Ms. Siddiqui reported having no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM SPD 2024
Sjögren Disease Treatments in Early Trials Have Mostly Positive Results
VIENNA — Nipocalimab, iscalimab, and tibulizumab, but not lusvertikimab, appear to be promising new agents for Sjögren disease that warrant further investigation, suggest the results of four separate early clinical trials reported at the recent annual European Congress of Rheumatology (EULAR).
This is potentially good news for patients, as discovering new treatments that work for managing the various symptoms of Sjögren disease is a high priority, Jacques-Eric Gottenberg, MD, PhD, said when he presented the results of the phase 2 DAHLIAS study of nipocalimab during a late-breaking abstract session.
“All patients suffer from high burden of symptoms — pain, fatigue, and dryness; nearly 50% of patients have systemic complications; mortality is increased, so there is a high unmet need since no specific drug has been accepted so far,” said Dr. Gottenberg, who works at Strasbourg University Hospital in Strasbourg, France.
“The pathogenesis of the disease involves high B-cell activation, resulting in high IgG levels, and secretion of autoantibodies,” such as anti-Ro, anti-La, anti-Sjögren’s syndrome type A (anti-SSA), and anti-Sjögren’s syndrome type B antibodies, Dr. Gottenberg said.
Thus, one approach to reducing the disease burden is to try to lower circulating immunoglobulin G (IgG) levels and IgG-associated autoantibodies, which is how the monoclonal antibody nipocalimab works. Nipocalimab essentially blocks the interaction of IgG with the neonatal fragment crystallizable receptor and has already been shown to have efficacy in other autoimmune conditions such as myasthenia gravis and fetal and neonatal hemolytic disease, although not as hoped in rheumatoid arthritis.
The DAHLIAS Phase 2 Study
Now, results from the DAHLIAS study show that nipocalimab may also work in Sjögren disease, with significant improvement vs placebo seen in the primary endpoint of the total EULAR Sjögren’s Syndrome Disease Activity Index (clinESSDAI) at 24 weeks for one of the two doses of the drug that were tested.
The multicenter, placebo-controlled, double-blind study was conducted in 163 patients with moderate to severely active primary Sjögren disease. The latter was determined by having a clinESSDAI of 6 or higher and seropositivity for anti-Ro60, anti-Ro52, or both autoantibodies.
Dr. Gottenberg reported that the mean age of patients was 48 years; the majority (92.6%) were women and of White ethnicity (90.8%). The baseline clinESSDAI was a mean of 9.9; 98.1% had anti-Ro60, 80.6% had anti-Ro52, and 71.9% had anti-La antibodies.
In addition to standard of care, patients were randomly allocated to receive intravenous treatment every 2 weeks with nipocalimab 5 mg/kg or 15 mg/kg, or placebo.
At 24 weeks, the least squares mean (LSM) change in clinESSDAI from baseline was −3.74 for placebo, −4.08 for nipocalimab 5 mg/kg (P = not significant vs placebo), and −6.40 for nipocalimab 15 mg/kg (P = .02 vs placebo).
Nipocalimab 15 mg/kg also “demonstrated similar and consistent trends in other key efficacy endpoints,” Dr. Gottenberg said. This included improvements in the ESSDAI and EULAR Sjögren’s Syndrome Patient Reported Index (ESSPRI) and composite measures such as the Sjögren’s Tool for Assessing Response (STAR), Composite of Relevant Endpoints for Sjögren’s Syndrome (CRESS), and the Disease Activity Level. There were also improvements in the unstimulated salivary flow rate.
Safety findings showed no new concerns, with adverse events reported in 62.5% of placebo-treated patients and by 79.2% and 79.6% of patients receiving nipocalimab 5 mg/kg and 15 mg/kg, respectively. Serious adverse events were reported in a respective 5.4%, 7.5%, and 7.4%, including severe infections or infections requiring intravenous anti-infectives in 1.8%, 3.8%, and 1.9% of participants, although none was thought to be related to the study treatment. No opportunistic infections or any deaths were reported.
Thomas Schindler, PhD, senior clinical scientist at F. Hoffmann-La Roche Ltd., in Basel, Switzerland, commented from the audience: “This was a very impressive set of results, and I’m very surprised that its safety profile is so benign.”
Dr. Schindler wanted to know if there were any changes in the serum albumin level and if this manifested as any laboratory abnormalities, but there were no reported cases of severe hypoalbuminemia in the study.
The TWINSS Phase 2 Study
Similarly hopeful results were reported for iscalimab, a fully human IgG1 anti-CD40 monoclonal antibody that is given by subcutaneous injection, during a clinical abstracts session. Xavier Mariette, MD, PhD, head of the Rheumatology Department at Bicêtre Hospital, Paris-Saclay University in Paris, France, reported updated results of the phase 2b dose-ranging TWINSS study, showing sustained benefits at 48 weeks. The primary endpoint results at 24 weeks were recently published in The Lancet.
TWINSS was set up to assess the safety and efficacy of iscalimab given every 2 weeks vs placebo in two distinct cohorts of patients with Sjögren disease — one with moderate to severe disease with both systemic and symptomatic involvement and the other with low systemic involvement but high symptom burden.
Whereas patients in the first cohort who had moderate to severe disease (n = 173) were randomly allocated to one of three doses (150, 300, and 600 mg) of iscalimab or placebo for the initial 24 weeks, those in the second cohort (n = 100) were randomly allocated to a 600-mg dose or placebo. After the double-blind period ended, patients taking iscalimab continued on the dose they were taking for another 24 weeks, with those in the placebo arms switching to the 600-mg dose in cohort 1 and the 300-mg dose in cohort 2.
Topline results for those in cohort 1 with moderate to severe Sjögren disease were that the significant improvements in ESSDAI that had been seen at week 24 were maintained in those who continued iscalimab and improved in those who had switched from placebo.
LSM change from baseline in ESSDAI vs placebo at week 24 had been −3.0, −1.4, and −2.9 for the 150-, 300-, and 600-mg doses of iscalimab, respectively. Results at week 48 were a respective −7.6, −5.7, and −7.9. The LSM change for the placebo-treated patients who had switched to the 600-mg dose was −6.7.
Dr. Mariette reported “consistent improvement” in patient-reported outcomes, including ESSPRI, the Sjögren’s Syndrome Symptom Diary, Functional Assessment of Chronic Illness Therapy-Fatigue measure, and the Impact of Dry Eye on Everyday Life instrument. There was also a significant improvement in stimulated salivary flow rates.
Similar benefits were seen in the second cohort of patients who did not have systemic involvement but had a high burden of symptoms, with improved ESSPRI scores of a LSM change from baseline vs placebo of −2.29 for patients continuing iscalimab 600 mg treatment and −1.14 for those taking the 300-mg dose after being treated with placebo. Improvements were also seen in the other patient-reported outcomes used.
Regarding safety, Dr. Mariette reported that there were “no specific issues” seen in the patients who switched from placebo to iscalimab, either at the 300-mg or 600-mg dose. Any adverse event occurred in around 80% of placebo-treated patients and roughly 90% of those given iscalimab, and serious adverse events occurred in 11.4%, 14.3%, and 11.4% pf patients treated with iscalimab 150, 300, and 600 mg, and 4.9% of those given placebo and then 600 mg iscalimab.
“The safety seems equivalent to patients having received iscalimab from the beginning of the trial,” Dr. Mariette said, adding “the risk-benefit [analysis] seems positive in patients up to week 48.”
Phase 1 Trial of Tibulizumab
Further positive early trial results were reported by Michael Howell, PhD, chief scientific officer for Zura Bio, a biotech company based in Henderson, Nevada. During a poster tour at EULAR 2024, Dr. Howell presented some preliminary findings from a phase 1 trial of tibulizumab, a dual antagonist of interleukin (IL)-17A and the B-cell–activating factor (BAFF) engineered by fusing elements of ixekizumab (Taltz) and tabalumab together.
“The headline result for me is that the molecule does what it’s supposed to,” Dr. Howell told this news organization. “We have potent engagement of the IL-17 and BAFF pathways, and this sets the tone for additional exploration in rheumatologic diseases where there’s known activation of those two pathways,” he said.
Dr. Howell reported that total B-cell counts and lower levels of type 1 T helper cells were seen during the trial.
Over the years, Dr. Howell, an immunologist, has been involved in the development of many therapeutics, such as risankizumab (Skyrizi) and spesolimab (Spevigo).
“When I look at the molecules and the opportunity we have to do broader antagonism of pathways in a safe aspect, this is probably one of the most exciting,” he said.
The trial he presented included 25 people with a confirmed diagnosis of Sjögren disease and anti-SSA or anti-SSB antibodies. Patients received tibulizumab or a placebo for a total of 12 weeks via a subcutaneous injection. Various doses were tested: 30 mg, 100 mg, or 300 mg every 4 weeks, or 300 mg every 2 weeks.
Serum levels of both BAFF and IL-17A increased as expected in the tibulizumab-treated patients, and Dr. Howell reported that “it’s well tolerated. There’s no adverse event profile that caused any concern.”
As a phase 1 study, it was not powered to look at efficacy, but there were positive signals, Dr. Howell said, meaning that the drug is likely to be tested further in a phase 2 trial.
Lusvertikimab Phase 2 Trial
During the same poster tour, the null findings of a phase 2 trial of the anti-IL-7 monoclonal antibody lusvertikimab were presented by Benjamin Fisher, MD, professor of rheumatology at Birmingham University in Birmingham, England.
Dr. Fisher told this news organization: “It’s a negative study, at least over the 3-month period that we’ve studied it.” Whether longer durations of treatment may be needed is a question that currently cannot be answered, he added.
A total of 48 patients with Sjögren disease had been included in the trial from 19 different centers in Europe, the United States, and Australia. The mean age of the participants was 53.7 years, 87% were women, and the mean duration of disease was 5.0 years. Baseline ESSDAI and ESSPRI were 12.1 and 7.0, respectively. Half were receiving other background treatment, and 72.9% were anti-Ro or anti-SSA positive.
Lusvertikimab 750 mg or a matching placebo was given via intravenous infusion at weeks 0, 2, 4, 7, and 10.
The primary endpoint was the mean change in ESSDAI from baseline to week 13, which was the same, at −3.9, in both groups. There was also no significant difference between the groups in any of the other secondary endpoints that were used, including ESSPRI, Schirmer’s test, the ocular staining score, salivary flow rate, physician and patient global assessment, assessment of fatigue, quality of life, or the composite measures STAR and CRESS.
“This isn’t going anywhere,” said Dr. Fisher, asking what was going to happen next and if this meant the end of IL-7-focused therapy.
“For years, there’s been quite a lot of interest in this,” Dr. Fisher said. Sjögren disease is characterized by a sort of focal inflammation of the saliva glands, which is composed of both T and B cells in the early stages, probably a T-cell component and a B-cell component, he explained.
“IL-7 is thought to be an important cytokine for homeostasis of the T-cell compartment, so for maintenance of T central memory and effector memory cells,” he said. “So, the idea is that, if you block IL-7, you switch off T cells, and you may rebalance the immune system towards a more regulatory phenotype. Just that it didn’t work,” Dr. Fisher said.
“There’s large unmet need,” he said. “Sjögren’s is associated with poor health-related quality of life, [and] a large part that is symptom-driven — dryness and fatigue — which we have no real interventions yet for patients; there’s no licensed therapeutics for it.”
Dr. Fisher cited ianalumab as one of the front-runners for becoming the first licensed treatment for Sjögren disease. The novel BAFF-targeting antibody is already in phase 3 trials and is also showing promise for the treatment of systemic lupus erythematosus.
“Then there are CD40-targeting drugs; the ones most advanced are dazodalibep and iscalimab.” Commenting on the potential of iscalimab, Dr. Fisher said that it “seems to work — it improves systemic disease activity; it also leads to some symptomatic improvement, which has been difficult to demonstrate in Sjögren’s.”
Dr. Fisher added that “the nipocalimab data looks interesting, as do data on TYK2 inhibition.”
The DAHLIAS study was funded by Janssen Research & Development. Dr. Gottenberg has consulted for AbbVie, Bristol Myers Squibb (BMS), Galapagos, Gilead, Janssen, Lilly, Merck Sharp & Dohme, Novartis, Pfizer, Sanofi, and UCB. The TWINSS study was funded by Novartis. Dr. Mariette has consulted for BMS, Galapagos, GlaxoSmithKline, Novartis, Pfizer, and Servier. The tibulizumab phase 1 study was funded by Eli Lilly & Company. Dr. Howell is an employee of the developer, Zura Bio. The Institut de Recherches Internationales Servier sponsored the lusvertikimab trial. Dr. Fisher has consulted for Novartis, Roche, BMS, Galapagos, Janssen, Servier, UCB, and Sanofi and received funding to his institution for collaborative research from Janssen, Celgene, Galapagos, and Servier.
A version of this article first appeared on Medscape.com.
VIENNA — Nipocalimab, iscalimab, and tibulizumab, but not lusvertikimab, appear to be promising new agents for Sjögren disease that warrant further investigation, suggest the results of four separate early clinical trials reported at the recent annual European Congress of Rheumatology (EULAR).
This is potentially good news for patients, as discovering new treatments that work for managing the various symptoms of Sjögren disease is a high priority, Jacques-Eric Gottenberg, MD, PhD, said when he presented the results of the phase 2 DAHLIAS study of nipocalimab during a late-breaking abstract session.
“All patients suffer from high burden of symptoms — pain, fatigue, and dryness; nearly 50% of patients have systemic complications; mortality is increased, so there is a high unmet need since no specific drug has been accepted so far,” said Dr. Gottenberg, who works at Strasbourg University Hospital in Strasbourg, France.
“The pathogenesis of the disease involves high B-cell activation, resulting in high IgG levels, and secretion of autoantibodies,” such as anti-Ro, anti-La, anti-Sjögren’s syndrome type A (anti-SSA), and anti-Sjögren’s syndrome type B antibodies, Dr. Gottenberg said.
Thus, one approach to reducing the disease burden is to try to lower circulating immunoglobulin G (IgG) levels and IgG-associated autoantibodies, which is how the monoclonal antibody nipocalimab works. Nipocalimab essentially blocks the interaction of IgG with the neonatal fragment crystallizable receptor and has already been shown to have efficacy in other autoimmune conditions such as myasthenia gravis and fetal and neonatal hemolytic disease, although not as hoped in rheumatoid arthritis.
The DAHLIAS Phase 2 Study
Now, results from the DAHLIAS study show that nipocalimab may also work in Sjögren disease, with significant improvement vs placebo seen in the primary endpoint of the total EULAR Sjögren’s Syndrome Disease Activity Index (clinESSDAI) at 24 weeks for one of the two doses of the drug that were tested.
The multicenter, placebo-controlled, double-blind study was conducted in 163 patients with moderate to severely active primary Sjögren disease. The latter was determined by having a clinESSDAI of 6 or higher and seropositivity for anti-Ro60, anti-Ro52, or both autoantibodies.
Dr. Gottenberg reported that the mean age of patients was 48 years; the majority (92.6%) were women and of White ethnicity (90.8%). The baseline clinESSDAI was a mean of 9.9; 98.1% had anti-Ro60, 80.6% had anti-Ro52, and 71.9% had anti-La antibodies.
In addition to standard of care, patients were randomly allocated to receive intravenous treatment every 2 weeks with nipocalimab 5 mg/kg or 15 mg/kg, or placebo.
At 24 weeks, the least squares mean (LSM) change in clinESSDAI from baseline was −3.74 for placebo, −4.08 for nipocalimab 5 mg/kg (P = not significant vs placebo), and −6.40 for nipocalimab 15 mg/kg (P = .02 vs placebo).
Nipocalimab 15 mg/kg also “demonstrated similar and consistent trends in other key efficacy endpoints,” Dr. Gottenberg said. This included improvements in the ESSDAI and EULAR Sjögren’s Syndrome Patient Reported Index (ESSPRI) and composite measures such as the Sjögren’s Tool for Assessing Response (STAR), Composite of Relevant Endpoints for Sjögren’s Syndrome (CRESS), and the Disease Activity Level. There were also improvements in the unstimulated salivary flow rate.
Safety findings showed no new concerns, with adverse events reported in 62.5% of placebo-treated patients and by 79.2% and 79.6% of patients receiving nipocalimab 5 mg/kg and 15 mg/kg, respectively. Serious adverse events were reported in a respective 5.4%, 7.5%, and 7.4%, including severe infections or infections requiring intravenous anti-infectives in 1.8%, 3.8%, and 1.9% of participants, although none was thought to be related to the study treatment. No opportunistic infections or any deaths were reported.
Thomas Schindler, PhD, senior clinical scientist at F. Hoffmann-La Roche Ltd., in Basel, Switzerland, commented from the audience: “This was a very impressive set of results, and I’m very surprised that its safety profile is so benign.”
Dr. Schindler wanted to know if there were any changes in the serum albumin level and if this manifested as any laboratory abnormalities, but there were no reported cases of severe hypoalbuminemia in the study.
The TWINSS Phase 2 Study
Similarly hopeful results were reported for iscalimab, a fully human IgG1 anti-CD40 monoclonal antibody that is given by subcutaneous injection, during a clinical abstracts session. Xavier Mariette, MD, PhD, head of the Rheumatology Department at Bicêtre Hospital, Paris-Saclay University in Paris, France, reported updated results of the phase 2b dose-ranging TWINSS study, showing sustained benefits at 48 weeks. The primary endpoint results at 24 weeks were recently published in The Lancet.
TWINSS was set up to assess the safety and efficacy of iscalimab given every 2 weeks vs placebo in two distinct cohorts of patients with Sjögren disease — one with moderate to severe disease with both systemic and symptomatic involvement and the other with low systemic involvement but high symptom burden.
Whereas patients in the first cohort who had moderate to severe disease (n = 173) were randomly allocated to one of three doses (150, 300, and 600 mg) of iscalimab or placebo for the initial 24 weeks, those in the second cohort (n = 100) were randomly allocated to a 600-mg dose or placebo. After the double-blind period ended, patients taking iscalimab continued on the dose they were taking for another 24 weeks, with those in the placebo arms switching to the 600-mg dose in cohort 1 and the 300-mg dose in cohort 2.
Topline results for those in cohort 1 with moderate to severe Sjögren disease were that the significant improvements in ESSDAI that had been seen at week 24 were maintained in those who continued iscalimab and improved in those who had switched from placebo.
LSM change from baseline in ESSDAI vs placebo at week 24 had been −3.0, −1.4, and −2.9 for the 150-, 300-, and 600-mg doses of iscalimab, respectively. Results at week 48 were a respective −7.6, −5.7, and −7.9. The LSM change for the placebo-treated patients who had switched to the 600-mg dose was −6.7.
Dr. Mariette reported “consistent improvement” in patient-reported outcomes, including ESSPRI, the Sjögren’s Syndrome Symptom Diary, Functional Assessment of Chronic Illness Therapy-Fatigue measure, and the Impact of Dry Eye on Everyday Life instrument. There was also a significant improvement in stimulated salivary flow rates.
Similar benefits were seen in the second cohort of patients who did not have systemic involvement but had a high burden of symptoms, with improved ESSPRI scores of a LSM change from baseline vs placebo of −2.29 for patients continuing iscalimab 600 mg treatment and −1.14 for those taking the 300-mg dose after being treated with placebo. Improvements were also seen in the other patient-reported outcomes used.
Regarding safety, Dr. Mariette reported that there were “no specific issues” seen in the patients who switched from placebo to iscalimab, either at the 300-mg or 600-mg dose. Any adverse event occurred in around 80% of placebo-treated patients and roughly 90% of those given iscalimab, and serious adverse events occurred in 11.4%, 14.3%, and 11.4% pf patients treated with iscalimab 150, 300, and 600 mg, and 4.9% of those given placebo and then 600 mg iscalimab.
“The safety seems equivalent to patients having received iscalimab from the beginning of the trial,” Dr. Mariette said, adding “the risk-benefit [analysis] seems positive in patients up to week 48.”
Phase 1 Trial of Tibulizumab
Further positive early trial results were reported by Michael Howell, PhD, chief scientific officer for Zura Bio, a biotech company based in Henderson, Nevada. During a poster tour at EULAR 2024, Dr. Howell presented some preliminary findings from a phase 1 trial of tibulizumab, a dual antagonist of interleukin (IL)-17A and the B-cell–activating factor (BAFF) engineered by fusing elements of ixekizumab (Taltz) and tabalumab together.
“The headline result for me is that the molecule does what it’s supposed to,” Dr. Howell told this news organization. “We have potent engagement of the IL-17 and BAFF pathways, and this sets the tone for additional exploration in rheumatologic diseases where there’s known activation of those two pathways,” he said.
Dr. Howell reported that total B-cell counts and lower levels of type 1 T helper cells were seen during the trial.
Over the years, Dr. Howell, an immunologist, has been involved in the development of many therapeutics, such as risankizumab (Skyrizi) and spesolimab (Spevigo).
“When I look at the molecules and the opportunity we have to do broader antagonism of pathways in a safe aspect, this is probably one of the most exciting,” he said.
The trial he presented included 25 people with a confirmed diagnosis of Sjögren disease and anti-SSA or anti-SSB antibodies. Patients received tibulizumab or a placebo for a total of 12 weeks via a subcutaneous injection. Various doses were tested: 30 mg, 100 mg, or 300 mg every 4 weeks, or 300 mg every 2 weeks.
Serum levels of both BAFF and IL-17A increased as expected in the tibulizumab-treated patients, and Dr. Howell reported that “it’s well tolerated. There’s no adverse event profile that caused any concern.”
As a phase 1 study, it was not powered to look at efficacy, but there were positive signals, Dr. Howell said, meaning that the drug is likely to be tested further in a phase 2 trial.
Lusvertikimab Phase 2 Trial
During the same poster tour, the null findings of a phase 2 trial of the anti-IL-7 monoclonal antibody lusvertikimab were presented by Benjamin Fisher, MD, professor of rheumatology at Birmingham University in Birmingham, England.
Dr. Fisher told this news organization: “It’s a negative study, at least over the 3-month period that we’ve studied it.” Whether longer durations of treatment may be needed is a question that currently cannot be answered, he added.
A total of 48 patients with Sjögren disease had been included in the trial from 19 different centers in Europe, the United States, and Australia. The mean age of the participants was 53.7 years, 87% were women, and the mean duration of disease was 5.0 years. Baseline ESSDAI and ESSPRI were 12.1 and 7.0, respectively. Half were receiving other background treatment, and 72.9% were anti-Ro or anti-SSA positive.
Lusvertikimab 750 mg or a matching placebo was given via intravenous infusion at weeks 0, 2, 4, 7, and 10.
The primary endpoint was the mean change in ESSDAI from baseline to week 13, which was the same, at −3.9, in both groups. There was also no significant difference between the groups in any of the other secondary endpoints that were used, including ESSPRI, Schirmer’s test, the ocular staining score, salivary flow rate, physician and patient global assessment, assessment of fatigue, quality of life, or the composite measures STAR and CRESS.
“This isn’t going anywhere,” said Dr. Fisher, asking what was going to happen next and if this meant the end of IL-7-focused therapy.
“For years, there’s been quite a lot of interest in this,” Dr. Fisher said. Sjögren disease is characterized by a sort of focal inflammation of the saliva glands, which is composed of both T and B cells in the early stages, probably a T-cell component and a B-cell component, he explained.
“IL-7 is thought to be an important cytokine for homeostasis of the T-cell compartment, so for maintenance of T central memory and effector memory cells,” he said. “So, the idea is that, if you block IL-7, you switch off T cells, and you may rebalance the immune system towards a more regulatory phenotype. Just that it didn’t work,” Dr. Fisher said.
“There’s large unmet need,” he said. “Sjögren’s is associated with poor health-related quality of life, [and] a large part that is symptom-driven — dryness and fatigue — which we have no real interventions yet for patients; there’s no licensed therapeutics for it.”
Dr. Fisher cited ianalumab as one of the front-runners for becoming the first licensed treatment for Sjögren disease. The novel BAFF-targeting antibody is already in phase 3 trials and is also showing promise for the treatment of systemic lupus erythematosus.
“Then there are CD40-targeting drugs; the ones most advanced are dazodalibep and iscalimab.” Commenting on the potential of iscalimab, Dr. Fisher said that it “seems to work — it improves systemic disease activity; it also leads to some symptomatic improvement, which has been difficult to demonstrate in Sjögren’s.”
Dr. Fisher added that “the nipocalimab data looks interesting, as do data on TYK2 inhibition.”
The DAHLIAS study was funded by Janssen Research & Development. Dr. Gottenberg has consulted for AbbVie, Bristol Myers Squibb (BMS), Galapagos, Gilead, Janssen, Lilly, Merck Sharp & Dohme, Novartis, Pfizer, Sanofi, and UCB. The TWINSS study was funded by Novartis. Dr. Mariette has consulted for BMS, Galapagos, GlaxoSmithKline, Novartis, Pfizer, and Servier. The tibulizumab phase 1 study was funded by Eli Lilly & Company. Dr. Howell is an employee of the developer, Zura Bio. The Institut de Recherches Internationales Servier sponsored the lusvertikimab trial. Dr. Fisher has consulted for Novartis, Roche, BMS, Galapagos, Janssen, Servier, UCB, and Sanofi and received funding to his institution for collaborative research from Janssen, Celgene, Galapagos, and Servier.
A version of this article first appeared on Medscape.com.
VIENNA — Nipocalimab, iscalimab, and tibulizumab, but not lusvertikimab, appear to be promising new agents for Sjögren disease that warrant further investigation, suggest the results of four separate early clinical trials reported at the recent annual European Congress of Rheumatology (EULAR).
This is potentially good news for patients, as discovering new treatments that work for managing the various symptoms of Sjögren disease is a high priority, Jacques-Eric Gottenberg, MD, PhD, said when he presented the results of the phase 2 DAHLIAS study of nipocalimab during a late-breaking abstract session.
“All patients suffer from high burden of symptoms — pain, fatigue, and dryness; nearly 50% of patients have systemic complications; mortality is increased, so there is a high unmet need since no specific drug has been accepted so far,” said Dr. Gottenberg, who works at Strasbourg University Hospital in Strasbourg, France.
“The pathogenesis of the disease involves high B-cell activation, resulting in high IgG levels, and secretion of autoantibodies,” such as anti-Ro, anti-La, anti-Sjögren’s syndrome type A (anti-SSA), and anti-Sjögren’s syndrome type B antibodies, Dr. Gottenberg said.
Thus, one approach to reducing the disease burden is to try to lower circulating immunoglobulin G (IgG) levels and IgG-associated autoantibodies, which is how the monoclonal antibody nipocalimab works. Nipocalimab essentially blocks the interaction of IgG with the neonatal fragment crystallizable receptor and has already been shown to have efficacy in other autoimmune conditions such as myasthenia gravis and fetal and neonatal hemolytic disease, although not as hoped in rheumatoid arthritis.
The DAHLIAS Phase 2 Study
Now, results from the DAHLIAS study show that nipocalimab may also work in Sjögren disease, with significant improvement vs placebo seen in the primary endpoint of the total EULAR Sjögren’s Syndrome Disease Activity Index (clinESSDAI) at 24 weeks for one of the two doses of the drug that were tested.
The multicenter, placebo-controlled, double-blind study was conducted in 163 patients with moderate to severely active primary Sjögren disease. The latter was determined by having a clinESSDAI of 6 or higher and seropositivity for anti-Ro60, anti-Ro52, or both autoantibodies.
Dr. Gottenberg reported that the mean age of patients was 48 years; the majority (92.6%) were women and of White ethnicity (90.8%). The baseline clinESSDAI was a mean of 9.9; 98.1% had anti-Ro60, 80.6% had anti-Ro52, and 71.9% had anti-La antibodies.
In addition to standard of care, patients were randomly allocated to receive intravenous treatment every 2 weeks with nipocalimab 5 mg/kg or 15 mg/kg, or placebo.
At 24 weeks, the least squares mean (LSM) change in clinESSDAI from baseline was −3.74 for placebo, −4.08 for nipocalimab 5 mg/kg (P = not significant vs placebo), and −6.40 for nipocalimab 15 mg/kg (P = .02 vs placebo).
Nipocalimab 15 mg/kg also “demonstrated similar and consistent trends in other key efficacy endpoints,” Dr. Gottenberg said. This included improvements in the ESSDAI and EULAR Sjögren’s Syndrome Patient Reported Index (ESSPRI) and composite measures such as the Sjögren’s Tool for Assessing Response (STAR), Composite of Relevant Endpoints for Sjögren’s Syndrome (CRESS), and the Disease Activity Level. There were also improvements in the unstimulated salivary flow rate.
Safety findings showed no new concerns, with adverse events reported in 62.5% of placebo-treated patients and by 79.2% and 79.6% of patients receiving nipocalimab 5 mg/kg and 15 mg/kg, respectively. Serious adverse events were reported in a respective 5.4%, 7.5%, and 7.4%, including severe infections or infections requiring intravenous anti-infectives in 1.8%, 3.8%, and 1.9% of participants, although none was thought to be related to the study treatment. No opportunistic infections or any deaths were reported.
Thomas Schindler, PhD, senior clinical scientist at F. Hoffmann-La Roche Ltd., in Basel, Switzerland, commented from the audience: “This was a very impressive set of results, and I’m very surprised that its safety profile is so benign.”
Dr. Schindler wanted to know if there were any changes in the serum albumin level and if this manifested as any laboratory abnormalities, but there were no reported cases of severe hypoalbuminemia in the study.
The TWINSS Phase 2 Study
Similarly hopeful results were reported for iscalimab, a fully human IgG1 anti-CD40 monoclonal antibody that is given by subcutaneous injection, during a clinical abstracts session. Xavier Mariette, MD, PhD, head of the Rheumatology Department at Bicêtre Hospital, Paris-Saclay University in Paris, France, reported updated results of the phase 2b dose-ranging TWINSS study, showing sustained benefits at 48 weeks. The primary endpoint results at 24 weeks were recently published in The Lancet.
TWINSS was set up to assess the safety and efficacy of iscalimab given every 2 weeks vs placebo in two distinct cohorts of patients with Sjögren disease — one with moderate to severe disease with both systemic and symptomatic involvement and the other with low systemic involvement but high symptom burden.
Whereas patients in the first cohort who had moderate to severe disease (n = 173) were randomly allocated to one of three doses (150, 300, and 600 mg) of iscalimab or placebo for the initial 24 weeks, those in the second cohort (n = 100) were randomly allocated to a 600-mg dose or placebo. After the double-blind period ended, patients taking iscalimab continued on the dose they were taking for another 24 weeks, with those in the placebo arms switching to the 600-mg dose in cohort 1 and the 300-mg dose in cohort 2.
Topline results for those in cohort 1 with moderate to severe Sjögren disease were that the significant improvements in ESSDAI that had been seen at week 24 were maintained in those who continued iscalimab and improved in those who had switched from placebo.
LSM change from baseline in ESSDAI vs placebo at week 24 had been −3.0, −1.4, and −2.9 for the 150-, 300-, and 600-mg doses of iscalimab, respectively. Results at week 48 were a respective −7.6, −5.7, and −7.9. The LSM change for the placebo-treated patients who had switched to the 600-mg dose was −6.7.
Dr. Mariette reported “consistent improvement” in patient-reported outcomes, including ESSPRI, the Sjögren’s Syndrome Symptom Diary, Functional Assessment of Chronic Illness Therapy-Fatigue measure, and the Impact of Dry Eye on Everyday Life instrument. There was also a significant improvement in stimulated salivary flow rates.
Similar benefits were seen in the second cohort of patients who did not have systemic involvement but had a high burden of symptoms, with improved ESSPRI scores of a LSM change from baseline vs placebo of −2.29 for patients continuing iscalimab 600 mg treatment and −1.14 for those taking the 300-mg dose after being treated with placebo. Improvements were also seen in the other patient-reported outcomes used.
Regarding safety, Dr. Mariette reported that there were “no specific issues” seen in the patients who switched from placebo to iscalimab, either at the 300-mg or 600-mg dose. Any adverse event occurred in around 80% of placebo-treated patients and roughly 90% of those given iscalimab, and serious adverse events occurred in 11.4%, 14.3%, and 11.4% pf patients treated with iscalimab 150, 300, and 600 mg, and 4.9% of those given placebo and then 600 mg iscalimab.
“The safety seems equivalent to patients having received iscalimab from the beginning of the trial,” Dr. Mariette said, adding “the risk-benefit [analysis] seems positive in patients up to week 48.”
Phase 1 Trial of Tibulizumab
Further positive early trial results were reported by Michael Howell, PhD, chief scientific officer for Zura Bio, a biotech company based in Henderson, Nevada. During a poster tour at EULAR 2024, Dr. Howell presented some preliminary findings from a phase 1 trial of tibulizumab, a dual antagonist of interleukin (IL)-17A and the B-cell–activating factor (BAFF) engineered by fusing elements of ixekizumab (Taltz) and tabalumab together.
“The headline result for me is that the molecule does what it’s supposed to,” Dr. Howell told this news organization. “We have potent engagement of the IL-17 and BAFF pathways, and this sets the tone for additional exploration in rheumatologic diseases where there’s known activation of those two pathways,” he said.
Dr. Howell reported that total B-cell counts and lower levels of type 1 T helper cells were seen during the trial.
Over the years, Dr. Howell, an immunologist, has been involved in the development of many therapeutics, such as risankizumab (Skyrizi) and spesolimab (Spevigo).
“When I look at the molecules and the opportunity we have to do broader antagonism of pathways in a safe aspect, this is probably one of the most exciting,” he said.
The trial he presented included 25 people with a confirmed diagnosis of Sjögren disease and anti-SSA or anti-SSB antibodies. Patients received tibulizumab or a placebo for a total of 12 weeks via a subcutaneous injection. Various doses were tested: 30 mg, 100 mg, or 300 mg every 4 weeks, or 300 mg every 2 weeks.
Serum levels of both BAFF and IL-17A increased as expected in the tibulizumab-treated patients, and Dr. Howell reported that “it’s well tolerated. There’s no adverse event profile that caused any concern.”
As a phase 1 study, it was not powered to look at efficacy, but there were positive signals, Dr. Howell said, meaning that the drug is likely to be tested further in a phase 2 trial.
Lusvertikimab Phase 2 Trial
During the same poster tour, the null findings of a phase 2 trial of the anti-IL-7 monoclonal antibody lusvertikimab were presented by Benjamin Fisher, MD, professor of rheumatology at Birmingham University in Birmingham, England.
Dr. Fisher told this news organization: “It’s a negative study, at least over the 3-month period that we’ve studied it.” Whether longer durations of treatment may be needed is a question that currently cannot be answered, he added.
A total of 48 patients with Sjögren disease had been included in the trial from 19 different centers in Europe, the United States, and Australia. The mean age of the participants was 53.7 years, 87% were women, and the mean duration of disease was 5.0 years. Baseline ESSDAI and ESSPRI were 12.1 and 7.0, respectively. Half were receiving other background treatment, and 72.9% were anti-Ro or anti-SSA positive.
Lusvertikimab 750 mg or a matching placebo was given via intravenous infusion at weeks 0, 2, 4, 7, and 10.
The primary endpoint was the mean change in ESSDAI from baseline to week 13, which was the same, at −3.9, in both groups. There was also no significant difference between the groups in any of the other secondary endpoints that were used, including ESSPRI, Schirmer’s test, the ocular staining score, salivary flow rate, physician and patient global assessment, assessment of fatigue, quality of life, or the composite measures STAR and CRESS.
“This isn’t going anywhere,” said Dr. Fisher, asking what was going to happen next and if this meant the end of IL-7-focused therapy.
“For years, there’s been quite a lot of interest in this,” Dr. Fisher said. Sjögren disease is characterized by a sort of focal inflammation of the saliva glands, which is composed of both T and B cells in the early stages, probably a T-cell component and a B-cell component, he explained.
“IL-7 is thought to be an important cytokine for homeostasis of the T-cell compartment, so for maintenance of T central memory and effector memory cells,” he said. “So, the idea is that, if you block IL-7, you switch off T cells, and you may rebalance the immune system towards a more regulatory phenotype. Just that it didn’t work,” Dr. Fisher said.
“There’s large unmet need,” he said. “Sjögren’s is associated with poor health-related quality of life, [and] a large part that is symptom-driven — dryness and fatigue — which we have no real interventions yet for patients; there’s no licensed therapeutics for it.”
Dr. Fisher cited ianalumab as one of the front-runners for becoming the first licensed treatment for Sjögren disease. The novel BAFF-targeting antibody is already in phase 3 trials and is also showing promise for the treatment of systemic lupus erythematosus.
“Then there are CD40-targeting drugs; the ones most advanced are dazodalibep and iscalimab.” Commenting on the potential of iscalimab, Dr. Fisher said that it “seems to work — it improves systemic disease activity; it also leads to some symptomatic improvement, which has been difficult to demonstrate in Sjögren’s.”
Dr. Fisher added that “the nipocalimab data looks interesting, as do data on TYK2 inhibition.”
The DAHLIAS study was funded by Janssen Research & Development. Dr. Gottenberg has consulted for AbbVie, Bristol Myers Squibb (BMS), Galapagos, Gilead, Janssen, Lilly, Merck Sharp & Dohme, Novartis, Pfizer, Sanofi, and UCB. The TWINSS study was funded by Novartis. Dr. Mariette has consulted for BMS, Galapagos, GlaxoSmithKline, Novartis, Pfizer, and Servier. The tibulizumab phase 1 study was funded by Eli Lilly & Company. Dr. Howell is an employee of the developer, Zura Bio. The Institut de Recherches Internationales Servier sponsored the lusvertikimab trial. Dr. Fisher has consulted for Novartis, Roche, BMS, Galapagos, Janssen, Servier, UCB, and Sanofi and received funding to his institution for collaborative research from Janssen, Celgene, Galapagos, and Servier.
A version of this article first appeared on Medscape.com.
FROM EULAR 2024
Future of Lupus Treatments Looks Brighter With Multiple Promising Therapeutic Approaches
VIENNA — It may have been a while since there have been any major breakthroughs in the treatment of systemic lupus erythematosus (SLE), but there are high hopes that this is a situation that may be about to change, experts agreed at the annual European Congress of Rheumatology.
“It’s an incredibly vivid area of development,” Laurent Arnaud, MD, PhD, professor of rheumatology at the University of Strasbourg in Strasbourg, France, said during one of the first sessions of the meeting. He reported that there were at least 17 phase 2 and 14 phase 3 trials that were expected to start within the next few years, all with investigational agents that target different immune cells or pathways that have been implicated in the pathogenesis of SLE.
In a systematic review published last year, Dr. Arnaud and coauthors found that there were 92 investigational biologic or novel targeted agents in various phases of clinical testing. This included B-cell–targeting agents such as ianalumab, plasma cell-targeting agents such as daratumumab, and drugs with novel mechanisms of action such as KPG-818, which targets the CRL4-Cereblon (CRBN) E3 ubiquitin ligase complex. Phase 2 data on all three of these investigational agents were presented during various sessions at EULAR 2024, all with positive results, suggesting that their further development in SLE is worth pursuing.
There are of course “many more candidates in the pipeline,” Dr. Arnaud said. “I’m very happy that I think we are going to see great days for lupus right in front of our eyes.”
Targeting B Cells
Drugs that target B cells have been at the forefront of lupus treatment for several years, as David Isenberg, MD, professor of rheumatology at University College London, pointed out during an interview for EULAR TV.
“It’s clearly important to target the cells which are likely to be causing the problem in lupus, and in the main, that tends to be B cells,” he said.
Dr. Isenberg, who is renowned for his work with the B-cell–targeting agent rituximab, added: “But we know that obviously T cells integrate with B cells, so anything which interrupts the link between the T cell and the B cell is likely to be important.”
Chimeric Antigen Receptor (CAR) T-Cell Therapy ‘Revolution’
One new way of targeting B cells is with CAR T-cell therapy, which David D’Cruz , MD, PhD, a consultant rheumatologist for Guy’s and St. Thomas’ Hospital NHS Foundation Trust in London, picked as one of the “most striking” topics highlighted at EULAR 2024.
This is “truly personalized medicine,” Dr. D’Cruz said. This is an autologous therapy because a patient’s T cells are removed by leukapheresis, transfected with a CAR T vector directed against a component of the B cell, and then returned to them.
“I do feel that we’re on the cusp of a major revolution,” Dr. D’Cruz told this news organization. Not only in lupus but also in other rheumatic conditions that have proved really difficult to treat, such as systemic sclerosis and myositis, he said.
“Basically, it’s a very powerful B-cell–depleting tool, but it’s much more profound B-cell–depleting tool than, for example, rituximab or belimumab,” explained Dr. D’Cruz. “What you’re doing is reprogramming T cells to attack the B cells.”
Although rituximab and belimumab clear all the B cells in the circulation, there are still some cells left behind in the bone marrow, “and it’s very difficult to get rid of those,” Dr. D’Cruz said. “What CAR T-cell therapy appears to do is wipe out all the CD19-positive B cells everywhere, in the blood and the tissue. So you get a really profound B-cell depletion.”
Eric Morand, MBBS, PhD, head of rheumatology at Monash Health in Melbourne, Australia, told this news organization that there was obviously “a lot of buzz” about CAR T-cell therapy.
“We’re waiting to see if the exciting data from Erlangen can be reproduced in other centers with other CAR T products to show that it is a universal effect. We haven’t seen that yet, but I think we will by next year.”
Cost and expertise are two major considerations and potential limiting factors, however, as Dr. D’Cruz and Dr. Isenberg both pointed out in separate interviews with this news organization.
Dr. D’Cruz said: “It’s very expensive, it takes a while, and it doesn’t always work is what I’m hearing. It’s usually successful, but again, a little bit depends on the technique and the people doing the process.”
Dr. Isenberg said: “CAR T-cell therapy is, I think, very exciting because it does look to be quite promising. But as it costs 350,000 euros per patient, I don’t think that it is going to be widely adopted.”
Even if it could be afforded by certain centers in the West, he added, this just would not be feasible in poorer nations. “So, we’ve got to find other effective, cheaper ways to go,” Dr. Isenberg said.
“I think there are some very interesting ideas with monoclonal antibodies which target at least two different targets — one on the B cell, one on the T cell — and that could well be the way to take this forward,” he suggested.
Ianalumab ‘Double Blocking’ B Cells
Another way could be to develop more potent B-cell–depleting drugs, as Nancy Agmon-Levin , MD, head of the Clinical Immunology, Angioedema and Allergy Unit, Lupus and Autoimmune Diseases Clinic, at Sheba Medical Center, Tel Aviv University in Tel Aviv, Israel, reported during one of the clinical abstract sessions at EULAR 2024.
Dr. Agmon-Levin presented data on 67 individuals with SLE who had participated in a multicenter phase 2 study of ianalumab, a fully human immunoglobulin (Ig) G1 monoclonal antibody that results in a “double blocking of the B-cell lineage.”
Ianalumab targets the B-cell–activating factor receptor (BAFFR), but what makes it distinct from other BAFF-targeting drugs is that it has had a fructose molecule removed from its Fc portion, which renders it more likely to trigger antibody-dependent cellular cytotoxicity.
“This is a B-cell depletion therapy,” Agmon-Levin said, but it also blocks BAFFR-mediated survival of B cells, so the subsequent recuperation process of BAFFR-expressing B cells is affected, leading to continued B-cell depletion.
The phase 2 study she presented consisted of an initial 28-week, double-blind period, during which time participants had been randomly allocated to receive either subcutaneous injections of ianalumab 300 mg or a matching placebo every 4 weeks. This was followed by a 24-week, open-label period where all participants were treated with ianalumab, and then an off-treatment, minimal follow-up period that lasted up to 68 weeks, with continued data collection for safety.
The primary outcome measure was a composite of meeting criteria for the SLE Responder Index 4 and a sustained reduction in corticosteroid use at 28 weeks. This was achieved in 15 of the 34 (44.1%) people treated with ianalumab vs only 3 (9.1%) of the 33 people who had been given a placebo.
Dr. Agmon-Levin reported that the effect on this outcome was sustained to the end of the open-label period, at 1 year, in 15 (45.5%) of 33 participants who had continued treatment with ianalumab and achieved in 13 (40.6%) of 32 participants who had switched from placebo to ianalumab treatment.
Moreover, longer durations of treatment were associated with a host of improved outcomes, Dr. Agmon-Levin said: “Treatment was improved along the 52 weeks, and we can see from the LLDAS [Lupus Low Disease Activity State], DORIS [Definition Of Remission In SLE], and SRI-6 and -8 that as you continue the therapy, you improve the outcomes.”
The potential benefits of ianalumab in the treatment of SLE and lupus nephritis will now be further examined in the phase 3 SIRIUS-SLE1 , SIRIUS-SLE2, and SIRIUS-LN trials, which are estimated to provide initial results in 2027 and complete in early 2029 or 2030.
Targeting Plasma Cells With Daratumumab
Another drug showing signs that it might be useful as a treatment for SLE is daratumumab, as Tobias Alexander, MD, of Charité — Universitätsmedizin Berlin, reported during one of the late-breaking abstract sessions at EULAR 2024.
“Daratumumab is a human, first-in-class anti-CD38 antibody that efficiently depletes plasma cells,” Dr. Alexander said. CD38 is both a receptor and an enzyme, and while it is found on the surface of most immune cells, it’s particularly expressed by plasma cells, he added.
Daratumumab is not a total newcomer, however, as it’s already approved for the treatment of multiple myeloma under the trade name Darzalex. The rationale for using it in SLE comes from two case reports, Dr. Alexander explained. The first, published in 2020 in The New England Journal of Medicine, involved two patients with severe and life-threatening lupus who were given off-label treatment for a period of 4 weeks and experienced good clinical and serologic responses. The second, published last year in Nature Medicine, involved six patients with refractory lupus nephritis, five of whom had a clinical response at 6 months.
“On this background, we conducted an investigator-initiated trial, which was an open-label, single-center, proof-of-concept study,” Dr. Alexander said. A total of 10 female patients whose ages ranged from 24 to 43 years were included in the phase 2 trial that was dubbed DARALUP. For inclusion, all had to have a Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K) of four or more for clinical manifestations, have been treated with at least two prior disease-modifying drugs to no avail, and be anti–double-stranded DNA (anti-dsDNA) antibody positive. Dr. Alexander reported that the median baseline SLEDAI-2K score was 12 and ranged from 8 to 20, with the number of prior therapies ranging from two to nine.
Daratumumab was given at a dose of 1800 mg via subcutaneous injection every week for 8 weeks. This is the same dose that is used to treat multiple myeloma, Dr. Alexander explained, although the dosing is not stopped. The reason for stopping after 8 weeks in the current trial was to be able to see what happened once the treatment was stopped. The follow-up was for 36 weeks.
Dr. Alexander reported that there was a “very dramatic and significant” effect on the primary endpoint of a reduction in anti-dsDNA antibody levels, decreasing from a median of 166.3 U/mL at baseline to 61.1 U/mL at week 12 (P = .002). Alongside, there was a reduction in the SLEDAI-2K score from 12 to 4 within 12 weeks, which was sustained at the 36-week follow-up assessment. Improvements in skin, joint, kidney, and level of proteinuria were also seen.
Although all patients experienced adverse events, none were serious. Infections and infestations (mostly nasopharyngitis, COVID-19, and gastroenteritis) were the most common, experienced by 80% of the participants; 70% had injection site reactions or fatigue, 60% had gastrointestinal symptoms, 50% had a fall of IgG < 5 g/L, 40% had headache, and 20% had back pain.
“This is a positive trial. I think we could demonstrate that [daratumumab] produced very strong, rapid, and durable clinical improvements,” Dr. Alexander said. “We think that targeting CD38 is relevant; plasma cells had been depleted based on the reduction of anti-dsDNA antibodies,” he added.
From the audience, however, Peter Nash, MBBS, of Griffith University in Brisbane, Australia, questioned whether the results could be attributed to “a steroid effect” because patients had been treated with oral dexamethasone throughout the study.
Dr. Alexander noted that steroid use had been part of the treatment schedule but acknowledged it was a possible confounder.
“I think we can be confident that [daratumumab] had a major effect on plasma cells decreasing…because we see that also the vaccine titers decreased,” Dr. Alexander said. “Time will tell, but even more important is the durability of the responses over time, which you don’t achieve under steroids.”
KPG-818’s Novel Mechanism of Action
Elsewhere at EULAR 2024, positive results of another phase 2 study involving a drug with an entirely different mechanism of action, KPG-818, were reported in a poster presentation. KPG-818 modulates CRBN, which results in the degradation of two transcription factors (Aiolos and Ikaros) that are involved in the development, maturation, and proliferation of innate and adaptive immune cells and have been linked to genetic risk in SLE, according to the poster’s authors. It is currently in development for the treatment of SLE, Behçet disease, inflammatory bowel disease, multiple myeloma, and non-Hodgkin lymphoma.
Yao Wang, MD, chief medical officer of KPG-818’s developer Kangpu Biopharmaceuticals, Hefei, China, and associates found that oral doses of 0.15 or 0.6 mg KPG-818 were “generally well-tolerated” and produced immunomodulatory changes that could be beneficial in people with SLE over a 12-week treatment period.
“Only two new agents have been approved for the treatment of SLE in the past five decades in USA and Europe,” Dr. Wang and team wrote, which highlights “a significant unmet need for more effective and safe treatment options.”
They believe that KPG-818 might well fit the bill based on the results of their study, in which 35 of 37 recruited patients completed the treatment. Compared with placebo, they observed reduced numbers of total B cells, Aiolos+ T and B cells, and increased Treg cells.
SLEDAI-2K and Cutaneous Lupus Erythematosus Disease Area and Severity Index activity scores in the 0.15-mg group were improved relative to baseline and placebo.
“The proof-of-concept findings suggest a favorable benefit/risk ratio in SLE for KPG-818,” Dr. Wang and coauthors said, supporting its further development in SLE.
Need for Treatments
Dr. Isenberg told this news organization that both daratumumab and KPG-818 would be welcome additions as treatment options if further trials proved their worth.
“The great frustration about lupus is that, compared to patients with rheumatoid arthritis, the choice has been so limited,” Dr. Isenberg said. Aside from rituximab (Rituxan) and belimumab (Benlysta), which are used with certain restrictions, there are no other biologic targeted treatments available in the United Kingdom. Anifrolumab (Saphnelo) has a license in the United States and some European countries but is not yet available for him to use in his practice.
Daratumumab and KPG-818 are “different types of molecules, and if they work that will be great. It would be nice to have the choice,” Dr. Isenberg said. “Whether they will be as effective as I think rituximab is, I don’t know, but these are some very encouraging results.”
Of course, these are all phase 2 trials, and the “big problem” is that such positive results do not always translate when it comes to phase 3, as Dr. D’Cruz told this news organization.
“Until a few years ago, there had been about 25 or 30 industry-led trails, and they’d all failed, except for belimumab and anifrolumab,” Dr. D’Cruz said. These drugs were found to work and be generally safe in phase 1 and 2 trials, but “when they come to phase 3, they all seem to fail, and we don’t know why.”
These are large global studies, D’Cruz added, observing that problems with patient selection, steroid use, and choice of outcome measures were possible factors for why the EXPLORER and LUNAR studies had shown no benefit for rituximab despite the drug being widely used to treat SLE.
Dr. Isenberg, who has coauthored an article on the topic of why drugs seem to fail at the final hurdle, noted: “I think it has a lot to do with the nature of the disease. It’s a complicated disease.” From having “savvy physicians doing the trials for you” to the placebo response, there are “a whole bunch or reasons why these things haven’t worked in lupus.”
Dr. Morand commented: “We’ve got many programs in phase 2 and 3, and because there’s so many, they’re all facing recruitment challenges, and as a consequence of so much activity, every program is going a little slower than hoped for.”
As for other drugs on the horizon, Dr. Morand noted: “We’re very optimistic about things like litifilimab and deucravacitinib; that’s two examples that are in phase 3. Earlier in the program of development, [there are] a huge range of targets being addressed. The future looks bright. But we might have to wait a while.”
Dr. Arnaud has consulted for AstraZeneca, AbbVie, Alpine Immune Sciences, Biogen, Bristol Myers Squibb, Boehringer Ingelheim, Chugai Pharmaceutical, GlaxoSmithKline, Grifols, Janssen, Kezar Life Sciences, LFB, Lilly, Medac, Merck, Novartis, Pfizer, Roche, and UCB. Dr. Isenberg has served as an adviser to Merck Serono, AstraZeneca, Eli Lilly, Servier, and ImmuPharma. Any honoraria received is passed on to a local arthritis charity connected to his hospital. Dr. D’Cruz has served as a consultant and advisory board member for GlaxoSmithKline and CSL Vifor. Dr. Morand has received research support, consultancy fees, or both from multiple pharmaceutical companies paid to his institution including AbbVie, Amgen, AstraZeneca, Biogen, Bristol Myers Squibb, Eli Lilly, EMD Serono, Dragonfly, Genentech, GlaxoSmithKline, Janssen, Novartis, RemeGen, Takeda, UCB, and Zenas. The ianalumab trial presented by Dr. Agmon-Levin was sponsored by Novartis Pharma; however, she reported having no conflicts of interest. The DARALUP study was an investigator-initiated trial supported by Janssen. Dr. Alexander has received consulting fees, study support, honoraria, and travel grants from various pharmaceutical companies including AbbVie, Amgen, AstraZeneca, Bayer, GlaxoSmithKline, Janssen, and Lilly. Dr. Nash has consulted for The Rheumatology Education Group Consultants. The KPG-818 study reported by Dr. Wang was sponsored by Kangpu Biopharmaceuticals.
A version of this article first appeared on Medscape.com.
VIENNA — It may have been a while since there have been any major breakthroughs in the treatment of systemic lupus erythematosus (SLE), but there are high hopes that this is a situation that may be about to change, experts agreed at the annual European Congress of Rheumatology.
“It’s an incredibly vivid area of development,” Laurent Arnaud, MD, PhD, professor of rheumatology at the University of Strasbourg in Strasbourg, France, said during one of the first sessions of the meeting. He reported that there were at least 17 phase 2 and 14 phase 3 trials that were expected to start within the next few years, all with investigational agents that target different immune cells or pathways that have been implicated in the pathogenesis of SLE.
In a systematic review published last year, Dr. Arnaud and coauthors found that there were 92 investigational biologic or novel targeted agents in various phases of clinical testing. This included B-cell–targeting agents such as ianalumab, plasma cell-targeting agents such as daratumumab, and drugs with novel mechanisms of action such as KPG-818, which targets the CRL4-Cereblon (CRBN) E3 ubiquitin ligase complex. Phase 2 data on all three of these investigational agents were presented during various sessions at EULAR 2024, all with positive results, suggesting that their further development in SLE is worth pursuing.
There are of course “many more candidates in the pipeline,” Dr. Arnaud said. “I’m very happy that I think we are going to see great days for lupus right in front of our eyes.”
Targeting B Cells
Drugs that target B cells have been at the forefront of lupus treatment for several years, as David Isenberg, MD, professor of rheumatology at University College London, pointed out during an interview for EULAR TV.
“It’s clearly important to target the cells which are likely to be causing the problem in lupus, and in the main, that tends to be B cells,” he said.
Dr. Isenberg, who is renowned for his work with the B-cell–targeting agent rituximab, added: “But we know that obviously T cells integrate with B cells, so anything which interrupts the link between the T cell and the B cell is likely to be important.”
Chimeric Antigen Receptor (CAR) T-Cell Therapy ‘Revolution’
One new way of targeting B cells is with CAR T-cell therapy, which David D’Cruz , MD, PhD, a consultant rheumatologist for Guy’s and St. Thomas’ Hospital NHS Foundation Trust in London, picked as one of the “most striking” topics highlighted at EULAR 2024.
This is “truly personalized medicine,” Dr. D’Cruz said. This is an autologous therapy because a patient’s T cells are removed by leukapheresis, transfected with a CAR T vector directed against a component of the B cell, and then returned to them.
“I do feel that we’re on the cusp of a major revolution,” Dr. D’Cruz told this news organization. Not only in lupus but also in other rheumatic conditions that have proved really difficult to treat, such as systemic sclerosis and myositis, he said.
“Basically, it’s a very powerful B-cell–depleting tool, but it’s much more profound B-cell–depleting tool than, for example, rituximab or belimumab,” explained Dr. D’Cruz. “What you’re doing is reprogramming T cells to attack the B cells.”
Although rituximab and belimumab clear all the B cells in the circulation, there are still some cells left behind in the bone marrow, “and it’s very difficult to get rid of those,” Dr. D’Cruz said. “What CAR T-cell therapy appears to do is wipe out all the CD19-positive B cells everywhere, in the blood and the tissue. So you get a really profound B-cell depletion.”
Eric Morand, MBBS, PhD, head of rheumatology at Monash Health in Melbourne, Australia, told this news organization that there was obviously “a lot of buzz” about CAR T-cell therapy.
“We’re waiting to see if the exciting data from Erlangen can be reproduced in other centers with other CAR T products to show that it is a universal effect. We haven’t seen that yet, but I think we will by next year.”
Cost and expertise are two major considerations and potential limiting factors, however, as Dr. D’Cruz and Dr. Isenberg both pointed out in separate interviews with this news organization.
Dr. D’Cruz said: “It’s very expensive, it takes a while, and it doesn’t always work is what I’m hearing. It’s usually successful, but again, a little bit depends on the technique and the people doing the process.”
Dr. Isenberg said: “CAR T-cell therapy is, I think, very exciting because it does look to be quite promising. But as it costs 350,000 euros per patient, I don’t think that it is going to be widely adopted.”
Even if it could be afforded by certain centers in the West, he added, this just would not be feasible in poorer nations. “So, we’ve got to find other effective, cheaper ways to go,” Dr. Isenberg said.
“I think there are some very interesting ideas with monoclonal antibodies which target at least two different targets — one on the B cell, one on the T cell — and that could well be the way to take this forward,” he suggested.
Ianalumab ‘Double Blocking’ B Cells
Another way could be to develop more potent B-cell–depleting drugs, as Nancy Agmon-Levin , MD, head of the Clinical Immunology, Angioedema and Allergy Unit, Lupus and Autoimmune Diseases Clinic, at Sheba Medical Center, Tel Aviv University in Tel Aviv, Israel, reported during one of the clinical abstract sessions at EULAR 2024.
Dr. Agmon-Levin presented data on 67 individuals with SLE who had participated in a multicenter phase 2 study of ianalumab, a fully human immunoglobulin (Ig) G1 monoclonal antibody that results in a “double blocking of the B-cell lineage.”
Ianalumab targets the B-cell–activating factor receptor (BAFFR), but what makes it distinct from other BAFF-targeting drugs is that it has had a fructose molecule removed from its Fc portion, which renders it more likely to trigger antibody-dependent cellular cytotoxicity.
“This is a B-cell depletion therapy,” Agmon-Levin said, but it also blocks BAFFR-mediated survival of B cells, so the subsequent recuperation process of BAFFR-expressing B cells is affected, leading to continued B-cell depletion.
The phase 2 study she presented consisted of an initial 28-week, double-blind period, during which time participants had been randomly allocated to receive either subcutaneous injections of ianalumab 300 mg or a matching placebo every 4 weeks. This was followed by a 24-week, open-label period where all participants were treated with ianalumab, and then an off-treatment, minimal follow-up period that lasted up to 68 weeks, with continued data collection for safety.
The primary outcome measure was a composite of meeting criteria for the SLE Responder Index 4 and a sustained reduction in corticosteroid use at 28 weeks. This was achieved in 15 of the 34 (44.1%) people treated with ianalumab vs only 3 (9.1%) of the 33 people who had been given a placebo.
Dr. Agmon-Levin reported that the effect on this outcome was sustained to the end of the open-label period, at 1 year, in 15 (45.5%) of 33 participants who had continued treatment with ianalumab and achieved in 13 (40.6%) of 32 participants who had switched from placebo to ianalumab treatment.
Moreover, longer durations of treatment were associated with a host of improved outcomes, Dr. Agmon-Levin said: “Treatment was improved along the 52 weeks, and we can see from the LLDAS [Lupus Low Disease Activity State], DORIS [Definition Of Remission In SLE], and SRI-6 and -8 that as you continue the therapy, you improve the outcomes.”
The potential benefits of ianalumab in the treatment of SLE and lupus nephritis will now be further examined in the phase 3 SIRIUS-SLE1 , SIRIUS-SLE2, and SIRIUS-LN trials, which are estimated to provide initial results in 2027 and complete in early 2029 or 2030.
Targeting Plasma Cells With Daratumumab
Another drug showing signs that it might be useful as a treatment for SLE is daratumumab, as Tobias Alexander, MD, of Charité — Universitätsmedizin Berlin, reported during one of the late-breaking abstract sessions at EULAR 2024.
“Daratumumab is a human, first-in-class anti-CD38 antibody that efficiently depletes plasma cells,” Dr. Alexander said. CD38 is both a receptor and an enzyme, and while it is found on the surface of most immune cells, it’s particularly expressed by plasma cells, he added.
Daratumumab is not a total newcomer, however, as it’s already approved for the treatment of multiple myeloma under the trade name Darzalex. The rationale for using it in SLE comes from two case reports, Dr. Alexander explained. The first, published in 2020 in The New England Journal of Medicine, involved two patients with severe and life-threatening lupus who were given off-label treatment for a period of 4 weeks and experienced good clinical and serologic responses. The second, published last year in Nature Medicine, involved six patients with refractory lupus nephritis, five of whom had a clinical response at 6 months.
“On this background, we conducted an investigator-initiated trial, which was an open-label, single-center, proof-of-concept study,” Dr. Alexander said. A total of 10 female patients whose ages ranged from 24 to 43 years were included in the phase 2 trial that was dubbed DARALUP. For inclusion, all had to have a Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K) of four or more for clinical manifestations, have been treated with at least two prior disease-modifying drugs to no avail, and be anti–double-stranded DNA (anti-dsDNA) antibody positive. Dr. Alexander reported that the median baseline SLEDAI-2K score was 12 and ranged from 8 to 20, with the number of prior therapies ranging from two to nine.
Daratumumab was given at a dose of 1800 mg via subcutaneous injection every week for 8 weeks. This is the same dose that is used to treat multiple myeloma, Dr. Alexander explained, although the dosing is not stopped. The reason for stopping after 8 weeks in the current trial was to be able to see what happened once the treatment was stopped. The follow-up was for 36 weeks.
Dr. Alexander reported that there was a “very dramatic and significant” effect on the primary endpoint of a reduction in anti-dsDNA antibody levels, decreasing from a median of 166.3 U/mL at baseline to 61.1 U/mL at week 12 (P = .002). Alongside, there was a reduction in the SLEDAI-2K score from 12 to 4 within 12 weeks, which was sustained at the 36-week follow-up assessment. Improvements in skin, joint, kidney, and level of proteinuria were also seen.
Although all patients experienced adverse events, none were serious. Infections and infestations (mostly nasopharyngitis, COVID-19, and gastroenteritis) were the most common, experienced by 80% of the participants; 70% had injection site reactions or fatigue, 60% had gastrointestinal symptoms, 50% had a fall of IgG < 5 g/L, 40% had headache, and 20% had back pain.
“This is a positive trial. I think we could demonstrate that [daratumumab] produced very strong, rapid, and durable clinical improvements,” Dr. Alexander said. “We think that targeting CD38 is relevant; plasma cells had been depleted based on the reduction of anti-dsDNA antibodies,” he added.
From the audience, however, Peter Nash, MBBS, of Griffith University in Brisbane, Australia, questioned whether the results could be attributed to “a steroid effect” because patients had been treated with oral dexamethasone throughout the study.
Dr. Alexander noted that steroid use had been part of the treatment schedule but acknowledged it was a possible confounder.
“I think we can be confident that [daratumumab] had a major effect on plasma cells decreasing…because we see that also the vaccine titers decreased,” Dr. Alexander said. “Time will tell, but even more important is the durability of the responses over time, which you don’t achieve under steroids.”
KPG-818’s Novel Mechanism of Action
Elsewhere at EULAR 2024, positive results of another phase 2 study involving a drug with an entirely different mechanism of action, KPG-818, were reported in a poster presentation. KPG-818 modulates CRBN, which results in the degradation of two transcription factors (Aiolos and Ikaros) that are involved in the development, maturation, and proliferation of innate and adaptive immune cells and have been linked to genetic risk in SLE, according to the poster’s authors. It is currently in development for the treatment of SLE, Behçet disease, inflammatory bowel disease, multiple myeloma, and non-Hodgkin lymphoma.
Yao Wang, MD, chief medical officer of KPG-818’s developer Kangpu Biopharmaceuticals, Hefei, China, and associates found that oral doses of 0.15 or 0.6 mg KPG-818 were “generally well-tolerated” and produced immunomodulatory changes that could be beneficial in people with SLE over a 12-week treatment period.
“Only two new agents have been approved for the treatment of SLE in the past five decades in USA and Europe,” Dr. Wang and team wrote, which highlights “a significant unmet need for more effective and safe treatment options.”
They believe that KPG-818 might well fit the bill based on the results of their study, in which 35 of 37 recruited patients completed the treatment. Compared with placebo, they observed reduced numbers of total B cells, Aiolos+ T and B cells, and increased Treg cells.
SLEDAI-2K and Cutaneous Lupus Erythematosus Disease Area and Severity Index activity scores in the 0.15-mg group were improved relative to baseline and placebo.
“The proof-of-concept findings suggest a favorable benefit/risk ratio in SLE for KPG-818,” Dr. Wang and coauthors said, supporting its further development in SLE.
Need for Treatments
Dr. Isenberg told this news organization that both daratumumab and KPG-818 would be welcome additions as treatment options if further trials proved their worth.
“The great frustration about lupus is that, compared to patients with rheumatoid arthritis, the choice has been so limited,” Dr. Isenberg said. Aside from rituximab (Rituxan) and belimumab (Benlysta), which are used with certain restrictions, there are no other biologic targeted treatments available in the United Kingdom. Anifrolumab (Saphnelo) has a license in the United States and some European countries but is not yet available for him to use in his practice.
Daratumumab and KPG-818 are “different types of molecules, and if they work that will be great. It would be nice to have the choice,” Dr. Isenberg said. “Whether they will be as effective as I think rituximab is, I don’t know, but these are some very encouraging results.”
Of course, these are all phase 2 trials, and the “big problem” is that such positive results do not always translate when it comes to phase 3, as Dr. D’Cruz told this news organization.
“Until a few years ago, there had been about 25 or 30 industry-led trails, and they’d all failed, except for belimumab and anifrolumab,” Dr. D’Cruz said. These drugs were found to work and be generally safe in phase 1 and 2 trials, but “when they come to phase 3, they all seem to fail, and we don’t know why.”
These are large global studies, D’Cruz added, observing that problems with patient selection, steroid use, and choice of outcome measures were possible factors for why the EXPLORER and LUNAR studies had shown no benefit for rituximab despite the drug being widely used to treat SLE.
Dr. Isenberg, who has coauthored an article on the topic of why drugs seem to fail at the final hurdle, noted: “I think it has a lot to do with the nature of the disease. It’s a complicated disease.” From having “savvy physicians doing the trials for you” to the placebo response, there are “a whole bunch or reasons why these things haven’t worked in lupus.”
Dr. Morand commented: “We’ve got many programs in phase 2 and 3, and because there’s so many, they’re all facing recruitment challenges, and as a consequence of so much activity, every program is going a little slower than hoped for.”
As for other drugs on the horizon, Dr. Morand noted: “We’re very optimistic about things like litifilimab and deucravacitinib; that’s two examples that are in phase 3. Earlier in the program of development, [there are] a huge range of targets being addressed. The future looks bright. But we might have to wait a while.”
Dr. Arnaud has consulted for AstraZeneca, AbbVie, Alpine Immune Sciences, Biogen, Bristol Myers Squibb, Boehringer Ingelheim, Chugai Pharmaceutical, GlaxoSmithKline, Grifols, Janssen, Kezar Life Sciences, LFB, Lilly, Medac, Merck, Novartis, Pfizer, Roche, and UCB. Dr. Isenberg has served as an adviser to Merck Serono, AstraZeneca, Eli Lilly, Servier, and ImmuPharma. Any honoraria received is passed on to a local arthritis charity connected to his hospital. Dr. D’Cruz has served as a consultant and advisory board member for GlaxoSmithKline and CSL Vifor. Dr. Morand has received research support, consultancy fees, or both from multiple pharmaceutical companies paid to his institution including AbbVie, Amgen, AstraZeneca, Biogen, Bristol Myers Squibb, Eli Lilly, EMD Serono, Dragonfly, Genentech, GlaxoSmithKline, Janssen, Novartis, RemeGen, Takeda, UCB, and Zenas. The ianalumab trial presented by Dr. Agmon-Levin was sponsored by Novartis Pharma; however, she reported having no conflicts of interest. The DARALUP study was an investigator-initiated trial supported by Janssen. Dr. Alexander has received consulting fees, study support, honoraria, and travel grants from various pharmaceutical companies including AbbVie, Amgen, AstraZeneca, Bayer, GlaxoSmithKline, Janssen, and Lilly. Dr. Nash has consulted for The Rheumatology Education Group Consultants. The KPG-818 study reported by Dr. Wang was sponsored by Kangpu Biopharmaceuticals.
A version of this article first appeared on Medscape.com.
VIENNA — It may have been a while since there have been any major breakthroughs in the treatment of systemic lupus erythematosus (SLE), but there are high hopes that this is a situation that may be about to change, experts agreed at the annual European Congress of Rheumatology.
“It’s an incredibly vivid area of development,” Laurent Arnaud, MD, PhD, professor of rheumatology at the University of Strasbourg in Strasbourg, France, said during one of the first sessions of the meeting. He reported that there were at least 17 phase 2 and 14 phase 3 trials that were expected to start within the next few years, all with investigational agents that target different immune cells or pathways that have been implicated in the pathogenesis of SLE.
In a systematic review published last year, Dr. Arnaud and coauthors found that there were 92 investigational biologic or novel targeted agents in various phases of clinical testing. This included B-cell–targeting agents such as ianalumab, plasma cell-targeting agents such as daratumumab, and drugs with novel mechanisms of action such as KPG-818, which targets the CRL4-Cereblon (CRBN) E3 ubiquitin ligase complex. Phase 2 data on all three of these investigational agents were presented during various sessions at EULAR 2024, all with positive results, suggesting that their further development in SLE is worth pursuing.
There are of course “many more candidates in the pipeline,” Dr. Arnaud said. “I’m very happy that I think we are going to see great days for lupus right in front of our eyes.”
Targeting B Cells
Drugs that target B cells have been at the forefront of lupus treatment for several years, as David Isenberg, MD, professor of rheumatology at University College London, pointed out during an interview for EULAR TV.
“It’s clearly important to target the cells which are likely to be causing the problem in lupus, and in the main, that tends to be B cells,” he said.
Dr. Isenberg, who is renowned for his work with the B-cell–targeting agent rituximab, added: “But we know that obviously T cells integrate with B cells, so anything which interrupts the link between the T cell and the B cell is likely to be important.”
Chimeric Antigen Receptor (CAR) T-Cell Therapy ‘Revolution’
One new way of targeting B cells is with CAR T-cell therapy, which David D’Cruz , MD, PhD, a consultant rheumatologist for Guy’s and St. Thomas’ Hospital NHS Foundation Trust in London, picked as one of the “most striking” topics highlighted at EULAR 2024.
This is “truly personalized medicine,” Dr. D’Cruz said. This is an autologous therapy because a patient’s T cells are removed by leukapheresis, transfected with a CAR T vector directed against a component of the B cell, and then returned to them.
“I do feel that we’re on the cusp of a major revolution,” Dr. D’Cruz told this news organization. Not only in lupus but also in other rheumatic conditions that have proved really difficult to treat, such as systemic sclerosis and myositis, he said.
“Basically, it’s a very powerful B-cell–depleting tool, but it’s much more profound B-cell–depleting tool than, for example, rituximab or belimumab,” explained Dr. D’Cruz. “What you’re doing is reprogramming T cells to attack the B cells.”
Although rituximab and belimumab clear all the B cells in the circulation, there are still some cells left behind in the bone marrow, “and it’s very difficult to get rid of those,” Dr. D’Cruz said. “What CAR T-cell therapy appears to do is wipe out all the CD19-positive B cells everywhere, in the blood and the tissue. So you get a really profound B-cell depletion.”
Eric Morand, MBBS, PhD, head of rheumatology at Monash Health in Melbourne, Australia, told this news organization that there was obviously “a lot of buzz” about CAR T-cell therapy.
“We’re waiting to see if the exciting data from Erlangen can be reproduced in other centers with other CAR T products to show that it is a universal effect. We haven’t seen that yet, but I think we will by next year.”
Cost and expertise are two major considerations and potential limiting factors, however, as Dr. D’Cruz and Dr. Isenberg both pointed out in separate interviews with this news organization.
Dr. D’Cruz said: “It’s very expensive, it takes a while, and it doesn’t always work is what I’m hearing. It’s usually successful, but again, a little bit depends on the technique and the people doing the process.”
Dr. Isenberg said: “CAR T-cell therapy is, I think, very exciting because it does look to be quite promising. But as it costs 350,000 euros per patient, I don’t think that it is going to be widely adopted.”
Even if it could be afforded by certain centers in the West, he added, this just would not be feasible in poorer nations. “So, we’ve got to find other effective, cheaper ways to go,” Dr. Isenberg said.
“I think there are some very interesting ideas with monoclonal antibodies which target at least two different targets — one on the B cell, one on the T cell — and that could well be the way to take this forward,” he suggested.
Ianalumab ‘Double Blocking’ B Cells
Another way could be to develop more potent B-cell–depleting drugs, as Nancy Agmon-Levin , MD, head of the Clinical Immunology, Angioedema and Allergy Unit, Lupus and Autoimmune Diseases Clinic, at Sheba Medical Center, Tel Aviv University in Tel Aviv, Israel, reported during one of the clinical abstract sessions at EULAR 2024.
Dr. Agmon-Levin presented data on 67 individuals with SLE who had participated in a multicenter phase 2 study of ianalumab, a fully human immunoglobulin (Ig) G1 monoclonal antibody that results in a “double blocking of the B-cell lineage.”
Ianalumab targets the B-cell–activating factor receptor (BAFFR), but what makes it distinct from other BAFF-targeting drugs is that it has had a fructose molecule removed from its Fc portion, which renders it more likely to trigger antibody-dependent cellular cytotoxicity.
“This is a B-cell depletion therapy,” Agmon-Levin said, but it also blocks BAFFR-mediated survival of B cells, so the subsequent recuperation process of BAFFR-expressing B cells is affected, leading to continued B-cell depletion.
The phase 2 study she presented consisted of an initial 28-week, double-blind period, during which time participants had been randomly allocated to receive either subcutaneous injections of ianalumab 300 mg or a matching placebo every 4 weeks. This was followed by a 24-week, open-label period where all participants were treated with ianalumab, and then an off-treatment, minimal follow-up period that lasted up to 68 weeks, with continued data collection for safety.
The primary outcome measure was a composite of meeting criteria for the SLE Responder Index 4 and a sustained reduction in corticosteroid use at 28 weeks. This was achieved in 15 of the 34 (44.1%) people treated with ianalumab vs only 3 (9.1%) of the 33 people who had been given a placebo.
Dr. Agmon-Levin reported that the effect on this outcome was sustained to the end of the open-label period, at 1 year, in 15 (45.5%) of 33 participants who had continued treatment with ianalumab and achieved in 13 (40.6%) of 32 participants who had switched from placebo to ianalumab treatment.
Moreover, longer durations of treatment were associated with a host of improved outcomes, Dr. Agmon-Levin said: “Treatment was improved along the 52 weeks, and we can see from the LLDAS [Lupus Low Disease Activity State], DORIS [Definition Of Remission In SLE], and SRI-6 and -8 that as you continue the therapy, you improve the outcomes.”
The potential benefits of ianalumab in the treatment of SLE and lupus nephritis will now be further examined in the phase 3 SIRIUS-SLE1 , SIRIUS-SLE2, and SIRIUS-LN trials, which are estimated to provide initial results in 2027 and complete in early 2029 or 2030.
Targeting Plasma Cells With Daratumumab
Another drug showing signs that it might be useful as a treatment for SLE is daratumumab, as Tobias Alexander, MD, of Charité — Universitätsmedizin Berlin, reported during one of the late-breaking abstract sessions at EULAR 2024.
“Daratumumab is a human, first-in-class anti-CD38 antibody that efficiently depletes plasma cells,” Dr. Alexander said. CD38 is both a receptor and an enzyme, and while it is found on the surface of most immune cells, it’s particularly expressed by plasma cells, he added.
Daratumumab is not a total newcomer, however, as it’s already approved for the treatment of multiple myeloma under the trade name Darzalex. The rationale for using it in SLE comes from two case reports, Dr. Alexander explained. The first, published in 2020 in The New England Journal of Medicine, involved two patients with severe and life-threatening lupus who were given off-label treatment for a period of 4 weeks and experienced good clinical and serologic responses. The second, published last year in Nature Medicine, involved six patients with refractory lupus nephritis, five of whom had a clinical response at 6 months.
“On this background, we conducted an investigator-initiated trial, which was an open-label, single-center, proof-of-concept study,” Dr. Alexander said. A total of 10 female patients whose ages ranged from 24 to 43 years were included in the phase 2 trial that was dubbed DARALUP. For inclusion, all had to have a Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K) of four or more for clinical manifestations, have been treated with at least two prior disease-modifying drugs to no avail, and be anti–double-stranded DNA (anti-dsDNA) antibody positive. Dr. Alexander reported that the median baseline SLEDAI-2K score was 12 and ranged from 8 to 20, with the number of prior therapies ranging from two to nine.
Daratumumab was given at a dose of 1800 mg via subcutaneous injection every week for 8 weeks. This is the same dose that is used to treat multiple myeloma, Dr. Alexander explained, although the dosing is not stopped. The reason for stopping after 8 weeks in the current trial was to be able to see what happened once the treatment was stopped. The follow-up was for 36 weeks.
Dr. Alexander reported that there was a “very dramatic and significant” effect on the primary endpoint of a reduction in anti-dsDNA antibody levels, decreasing from a median of 166.3 U/mL at baseline to 61.1 U/mL at week 12 (P = .002). Alongside, there was a reduction in the SLEDAI-2K score from 12 to 4 within 12 weeks, which was sustained at the 36-week follow-up assessment. Improvements in skin, joint, kidney, and level of proteinuria were also seen.
Although all patients experienced adverse events, none were serious. Infections and infestations (mostly nasopharyngitis, COVID-19, and gastroenteritis) were the most common, experienced by 80% of the participants; 70% had injection site reactions or fatigue, 60% had gastrointestinal symptoms, 50% had a fall of IgG < 5 g/L, 40% had headache, and 20% had back pain.
“This is a positive trial. I think we could demonstrate that [daratumumab] produced very strong, rapid, and durable clinical improvements,” Dr. Alexander said. “We think that targeting CD38 is relevant; plasma cells had been depleted based on the reduction of anti-dsDNA antibodies,” he added.
From the audience, however, Peter Nash, MBBS, of Griffith University in Brisbane, Australia, questioned whether the results could be attributed to “a steroid effect” because patients had been treated with oral dexamethasone throughout the study.
Dr. Alexander noted that steroid use had been part of the treatment schedule but acknowledged it was a possible confounder.
“I think we can be confident that [daratumumab] had a major effect on plasma cells decreasing…because we see that also the vaccine titers decreased,” Dr. Alexander said. “Time will tell, but even more important is the durability of the responses over time, which you don’t achieve under steroids.”
KPG-818’s Novel Mechanism of Action
Elsewhere at EULAR 2024, positive results of another phase 2 study involving a drug with an entirely different mechanism of action, KPG-818, were reported in a poster presentation. KPG-818 modulates CRBN, which results in the degradation of two transcription factors (Aiolos and Ikaros) that are involved in the development, maturation, and proliferation of innate and adaptive immune cells and have been linked to genetic risk in SLE, according to the poster’s authors. It is currently in development for the treatment of SLE, Behçet disease, inflammatory bowel disease, multiple myeloma, and non-Hodgkin lymphoma.
Yao Wang, MD, chief medical officer of KPG-818’s developer Kangpu Biopharmaceuticals, Hefei, China, and associates found that oral doses of 0.15 or 0.6 mg KPG-818 were “generally well-tolerated” and produced immunomodulatory changes that could be beneficial in people with SLE over a 12-week treatment period.
“Only two new agents have been approved for the treatment of SLE in the past five decades in USA and Europe,” Dr. Wang and team wrote, which highlights “a significant unmet need for more effective and safe treatment options.”
They believe that KPG-818 might well fit the bill based on the results of their study, in which 35 of 37 recruited patients completed the treatment. Compared with placebo, they observed reduced numbers of total B cells, Aiolos+ T and B cells, and increased Treg cells.
SLEDAI-2K and Cutaneous Lupus Erythematosus Disease Area and Severity Index activity scores in the 0.15-mg group were improved relative to baseline and placebo.
“The proof-of-concept findings suggest a favorable benefit/risk ratio in SLE for KPG-818,” Dr. Wang and coauthors said, supporting its further development in SLE.
Need for Treatments
Dr. Isenberg told this news organization that both daratumumab and KPG-818 would be welcome additions as treatment options if further trials proved their worth.
“The great frustration about lupus is that, compared to patients with rheumatoid arthritis, the choice has been so limited,” Dr. Isenberg said. Aside from rituximab (Rituxan) and belimumab (Benlysta), which are used with certain restrictions, there are no other biologic targeted treatments available in the United Kingdom. Anifrolumab (Saphnelo) has a license in the United States and some European countries but is not yet available for him to use in his practice.
Daratumumab and KPG-818 are “different types of molecules, and if they work that will be great. It would be nice to have the choice,” Dr. Isenberg said. “Whether they will be as effective as I think rituximab is, I don’t know, but these are some very encouraging results.”
Of course, these are all phase 2 trials, and the “big problem” is that such positive results do not always translate when it comes to phase 3, as Dr. D’Cruz told this news organization.
“Until a few years ago, there had been about 25 or 30 industry-led trails, and they’d all failed, except for belimumab and anifrolumab,” Dr. D’Cruz said. These drugs were found to work and be generally safe in phase 1 and 2 trials, but “when they come to phase 3, they all seem to fail, and we don’t know why.”
These are large global studies, D’Cruz added, observing that problems with patient selection, steroid use, and choice of outcome measures were possible factors for why the EXPLORER and LUNAR studies had shown no benefit for rituximab despite the drug being widely used to treat SLE.
Dr. Isenberg, who has coauthored an article on the topic of why drugs seem to fail at the final hurdle, noted: “I think it has a lot to do with the nature of the disease. It’s a complicated disease.” From having “savvy physicians doing the trials for you” to the placebo response, there are “a whole bunch or reasons why these things haven’t worked in lupus.”
Dr. Morand commented: “We’ve got many programs in phase 2 and 3, and because there’s so many, they’re all facing recruitment challenges, and as a consequence of so much activity, every program is going a little slower than hoped for.”
As for other drugs on the horizon, Dr. Morand noted: “We’re very optimistic about things like litifilimab and deucravacitinib; that’s two examples that are in phase 3. Earlier in the program of development, [there are] a huge range of targets being addressed. The future looks bright. But we might have to wait a while.”
Dr. Arnaud has consulted for AstraZeneca, AbbVie, Alpine Immune Sciences, Biogen, Bristol Myers Squibb, Boehringer Ingelheim, Chugai Pharmaceutical, GlaxoSmithKline, Grifols, Janssen, Kezar Life Sciences, LFB, Lilly, Medac, Merck, Novartis, Pfizer, Roche, and UCB. Dr. Isenberg has served as an adviser to Merck Serono, AstraZeneca, Eli Lilly, Servier, and ImmuPharma. Any honoraria received is passed on to a local arthritis charity connected to his hospital. Dr. D’Cruz has served as a consultant and advisory board member for GlaxoSmithKline and CSL Vifor. Dr. Morand has received research support, consultancy fees, or both from multiple pharmaceutical companies paid to his institution including AbbVie, Amgen, AstraZeneca, Biogen, Bristol Myers Squibb, Eli Lilly, EMD Serono, Dragonfly, Genentech, GlaxoSmithKline, Janssen, Novartis, RemeGen, Takeda, UCB, and Zenas. The ianalumab trial presented by Dr. Agmon-Levin was sponsored by Novartis Pharma; however, she reported having no conflicts of interest. The DARALUP study was an investigator-initiated trial supported by Janssen. Dr. Alexander has received consulting fees, study support, honoraria, and travel grants from various pharmaceutical companies including AbbVie, Amgen, AstraZeneca, Bayer, GlaxoSmithKline, Janssen, and Lilly. Dr. Nash has consulted for The Rheumatology Education Group Consultants. The KPG-818 study reported by Dr. Wang was sponsored by Kangpu Biopharmaceuticals.
A version of this article first appeared on Medscape.com.
FROM EULAR 2024
Consider Risks, Toxicity of Some Topical Ingredients in Infants, Young Children
TORONTO — Lawrence A. Schachner, MD, would like pediatric dermatologists to adopt a “toxic agent of the year” to raise awareness about the potential harm related to certain topical treatments in babies and young children.
Dr. Schachner, director of the Division of Pediatric Dermatology in the Department of Dermatology & Cutaneous Surgery at the University of Miami, Coral Gables, Florida, said he got the idea from the American Contact Dermatitis Society, which annually names the “Allergen of the Year.”
, said Dr. Schachner, professor of pediatrics and dermatology at the University of Miami.
“Any one of those would be excellent toxic substances of the year” that could be the focus of an educational campaign, he told this news organization following his presentation on “Toxicology of Topical Ingredients in Pediatric Dermatology” at the annual meeting of the Society for Pediatric Dermatology on July 14.
Benzene might also be a good candidate for the list, although the jury seems to be still out on its toxicity, said Dr. Schachner.
He talked about the “four Ps” of poisoning — the physician, pharmacy, parents, and pharmaceutical manufacturing — which all have some responsibility for errors that lead to adverse outcomes but can also take steps to prevent them.
During his presentation, Dr. Schachner discussed how babies are especially sensitive to topical therapies, noting that a baby’s skin is thinner and more permeable than that of an adult. And children have a greater body surface-to-weight ratio, so they absorb more substances through their skin.
He also noted that babies lack natural moisturizing factors, and their skin barrier isn’t mature until about age 3-5 years, stressing the need for extreme care when applying a topical agent to a baby’s skin.
Tragic Stories
Dr. Schachner pointed to some instances of mishaps related to toxic topical substances in children. There was the outbreak in the early 1980s of accidental hexachlorophene poisoning among children in France exposed to talc “baby powder.” Of the 204 affected children, 36 died.
The cause was a manufacturing error; the product contained 6.3% hexachlorophene, as opposed to the 0.1% limit recommended by the US Food and Drug Administration (FDA).
Local anesthetics, including lidocaine, dibucaine, and prilocaine, can cause local anesthetic systemic toxicity, a syndrome with symptoms that include central nervous system depression, seizures, and cardiotoxicity. Dr. Schachner described the case of a 3-year-old who developed methemoglobinemia, with seizures, after treatment with an excessive amount of eutectic mixture of local anesthetics (EMLA) cream, which contains both lidocaine and prilocaine.
EMLA shouldn’t be used with methemoglobinemia-inducing agents, such as some antimalarials, analgesics, anesthetics, and antineoplastic agents. It’s not recommended in neonates or for those under 12 months if receiving methemoglobinemia-inducing agents, “and I would keep an eye on it after 12 months of age,” said Dr. Schachner.
He cited a retrospective review of topical lidocaine toxicity in pediatric patients reported to the National Poison Data System from 2000 to 2020. It found 37 cases of toxicity, the most common from application prior to dermatologic procedures (37.5%), which led to two deaths.
Not Benign Agents
“These are not benign agents; we have to use them correctly,” Dr. Schachner stressed. When discussing alcohols and antiseptics, he noted that phenol is found in a variety of household disinfectants, gargling products, ointments, and lip balms. Phenol can be used as a chemical peel and is the antiseptic component of Castellani paint. He also referred to cases of alcohol intoxication linked to umbilical care in newborns.
Benzene at elevated levels has been found in some topical benzoyl peroxide acne products and in some sunscreens. There have been suggestions, not strongly substantiated, that benzene may increase the risk for cancer, especially leukemias.
But there is sparse data on the absorption and toxicity of benzene exposure with sunscreen use. The data, he said, include an analysis of National Health and Nutrition Examination Survey data, which found that people who regularly used sunscreens were less likely to have elevated benzene levels compared with those who didn’t use sunscreens.
Turning to insecticides, Dr. Schachner discussed N,N-diethyl-m-toluamide (DEET), the active ingredient in many insect repellents. It helps avoid “some terrible diseases,” including mosquito-borne illnesses such as malaria and tick-borne conditions such as Lyme disease, and is available in several convenient formulations, he said.
When used on children, the American Academy of Pediatrics (AAP) recommends products with no more than 30% DEET. And insect repellents are not recommended for children younger than 2 months, or under clothing or damaged skin, he said.
Dr. Schachner referred to a case series of 18 children who developed DEET-induced encephalopathy; 13 (72%) involved dermal exposure. Three of those with cutaneous exposure died, mostly from neurologic, respiratory, and cardiac issues. “What’s very striking is that 55% of the kids were exposed to DEET of 20% or less, even though the AAP approves DEET at 30%, so maybe that’s something we have to look at,” he said.
Medication Patches
With medication patches, especially fentanyl transdermal patches, much can go wrong when it comes to children. This was highlighted by the cases Schachner cited, including an infant who developed acute cytotoxic cerebellar edema from fentanyl patch intoxication.
In another case, emergency room staff found a fentanyl patch stuck to the back of a 3-year-old girl. A CT scan showed global cerebral edema, and the patient progressed to brain death. “This is not a unique case; there have been over 10 such cases in the United States,” said Dr. Schachner. “We should be doing better with fentanyl.”
Nicotine patches can also be dangerous to children, he added. As for other topical agents, there have been reports of toxicity and deaths linked to salicylic acid, commonly used by dermatologists because of its bacteriostatic, fungicidal, keratolytic, and photoprotective properties.
Dr. Schachner cited the case of a 2-month-old where the pediatrician prescribed 50% salicylic acid for seborrheic dermatitis of the scalp, under occlusion. “It’s amazing this child survived; that’s clearly a physician error,” he said.
Henna, a reddish-brown dye derived from the crushed leaves of Lawsonia alba, is used cosmetically for the hair, skin, and nails. Many henna products are mixed with additives, including para-phenylenediamine, which has been associated with dermatitis, asthma, renal failure, and permanent vision loss.
Asked to comment on the presentation, Sheilagh Maguiness, MD, professor of dermatology and pediatrics and chair of pediatric dermatology at the University of Minnesota, Minneapolis, recalled a particularly concerning story in 2008, when the FDA issued a warning about Mommy’s Bliss, a cream containing chlorphenesin and phenoxyethanol as preservatives, promoted to nursing mothers for soothing cracked nipples. There were reports of the cream causing respiratory distress, vomiting, and diarrhea in nursing infants.
Dr. Schachner is chair of Stiefel Laboratories and is an investigator with: Astellas, Berg Pharma, Celgene, Ferndale Labs, Lilly, Medimetriks Pharmaceuticals, Novartis, Organogenesis, Pfizer, Sciton; is a consultant for: Alphyn, Amryt Pharma, Beiersdorf, Brickell, Cutanea, Hoth, Lexington, Mustela, TopMD, Noble Pharma; a speaker for: Novartis, Sanofi-Regeneron, CeraVe; is on the advisory boards of: Almirall, Alphyn, Apogee, Aslan, Biofrontera, CeraVe, Krystal Biotech, Mustela, Noble Pharma, Pfizer, Pierre Fabre, Sanofi-Regeneron; and owns stocks in: TopMD and Alphyn. Dr. Maguiness had no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
TORONTO — Lawrence A. Schachner, MD, would like pediatric dermatologists to adopt a “toxic agent of the year” to raise awareness about the potential harm related to certain topical treatments in babies and young children.
Dr. Schachner, director of the Division of Pediatric Dermatology in the Department of Dermatology & Cutaneous Surgery at the University of Miami, Coral Gables, Florida, said he got the idea from the American Contact Dermatitis Society, which annually names the “Allergen of the Year.”
, said Dr. Schachner, professor of pediatrics and dermatology at the University of Miami.
“Any one of those would be excellent toxic substances of the year” that could be the focus of an educational campaign, he told this news organization following his presentation on “Toxicology of Topical Ingredients in Pediatric Dermatology” at the annual meeting of the Society for Pediatric Dermatology on July 14.
Benzene might also be a good candidate for the list, although the jury seems to be still out on its toxicity, said Dr. Schachner.
He talked about the “four Ps” of poisoning — the physician, pharmacy, parents, and pharmaceutical manufacturing — which all have some responsibility for errors that lead to adverse outcomes but can also take steps to prevent them.
During his presentation, Dr. Schachner discussed how babies are especially sensitive to topical therapies, noting that a baby’s skin is thinner and more permeable than that of an adult. And children have a greater body surface-to-weight ratio, so they absorb more substances through their skin.
He also noted that babies lack natural moisturizing factors, and their skin barrier isn’t mature until about age 3-5 years, stressing the need for extreme care when applying a topical agent to a baby’s skin.
Tragic Stories
Dr. Schachner pointed to some instances of mishaps related to toxic topical substances in children. There was the outbreak in the early 1980s of accidental hexachlorophene poisoning among children in France exposed to talc “baby powder.” Of the 204 affected children, 36 died.
The cause was a manufacturing error; the product contained 6.3% hexachlorophene, as opposed to the 0.1% limit recommended by the US Food and Drug Administration (FDA).
Local anesthetics, including lidocaine, dibucaine, and prilocaine, can cause local anesthetic systemic toxicity, a syndrome with symptoms that include central nervous system depression, seizures, and cardiotoxicity. Dr. Schachner described the case of a 3-year-old who developed methemoglobinemia, with seizures, after treatment with an excessive amount of eutectic mixture of local anesthetics (EMLA) cream, which contains both lidocaine and prilocaine.
EMLA shouldn’t be used with methemoglobinemia-inducing agents, such as some antimalarials, analgesics, anesthetics, and antineoplastic agents. It’s not recommended in neonates or for those under 12 months if receiving methemoglobinemia-inducing agents, “and I would keep an eye on it after 12 months of age,” said Dr. Schachner.
He cited a retrospective review of topical lidocaine toxicity in pediatric patients reported to the National Poison Data System from 2000 to 2020. It found 37 cases of toxicity, the most common from application prior to dermatologic procedures (37.5%), which led to two deaths.
Not Benign Agents
“These are not benign agents; we have to use them correctly,” Dr. Schachner stressed. When discussing alcohols and antiseptics, he noted that phenol is found in a variety of household disinfectants, gargling products, ointments, and lip balms. Phenol can be used as a chemical peel and is the antiseptic component of Castellani paint. He also referred to cases of alcohol intoxication linked to umbilical care in newborns.
Benzene at elevated levels has been found in some topical benzoyl peroxide acne products and in some sunscreens. There have been suggestions, not strongly substantiated, that benzene may increase the risk for cancer, especially leukemias.
But there is sparse data on the absorption and toxicity of benzene exposure with sunscreen use. The data, he said, include an analysis of National Health and Nutrition Examination Survey data, which found that people who regularly used sunscreens were less likely to have elevated benzene levels compared with those who didn’t use sunscreens.
Turning to insecticides, Dr. Schachner discussed N,N-diethyl-m-toluamide (DEET), the active ingredient in many insect repellents. It helps avoid “some terrible diseases,” including mosquito-borne illnesses such as malaria and tick-borne conditions such as Lyme disease, and is available in several convenient formulations, he said.
When used on children, the American Academy of Pediatrics (AAP) recommends products with no more than 30% DEET. And insect repellents are not recommended for children younger than 2 months, or under clothing or damaged skin, he said.
Dr. Schachner referred to a case series of 18 children who developed DEET-induced encephalopathy; 13 (72%) involved dermal exposure. Three of those with cutaneous exposure died, mostly from neurologic, respiratory, and cardiac issues. “What’s very striking is that 55% of the kids were exposed to DEET of 20% or less, even though the AAP approves DEET at 30%, so maybe that’s something we have to look at,” he said.
Medication Patches
With medication patches, especially fentanyl transdermal patches, much can go wrong when it comes to children. This was highlighted by the cases Schachner cited, including an infant who developed acute cytotoxic cerebellar edema from fentanyl patch intoxication.
In another case, emergency room staff found a fentanyl patch stuck to the back of a 3-year-old girl. A CT scan showed global cerebral edema, and the patient progressed to brain death. “This is not a unique case; there have been over 10 such cases in the United States,” said Dr. Schachner. “We should be doing better with fentanyl.”
Nicotine patches can also be dangerous to children, he added. As for other topical agents, there have been reports of toxicity and deaths linked to salicylic acid, commonly used by dermatologists because of its bacteriostatic, fungicidal, keratolytic, and photoprotective properties.
Dr. Schachner cited the case of a 2-month-old where the pediatrician prescribed 50% salicylic acid for seborrheic dermatitis of the scalp, under occlusion. “It’s amazing this child survived; that’s clearly a physician error,” he said.
Henna, a reddish-brown dye derived from the crushed leaves of Lawsonia alba, is used cosmetically for the hair, skin, and nails. Many henna products are mixed with additives, including para-phenylenediamine, which has been associated with dermatitis, asthma, renal failure, and permanent vision loss.
Asked to comment on the presentation, Sheilagh Maguiness, MD, professor of dermatology and pediatrics and chair of pediatric dermatology at the University of Minnesota, Minneapolis, recalled a particularly concerning story in 2008, when the FDA issued a warning about Mommy’s Bliss, a cream containing chlorphenesin and phenoxyethanol as preservatives, promoted to nursing mothers for soothing cracked nipples. There were reports of the cream causing respiratory distress, vomiting, and diarrhea in nursing infants.
Dr. Schachner is chair of Stiefel Laboratories and is an investigator with: Astellas, Berg Pharma, Celgene, Ferndale Labs, Lilly, Medimetriks Pharmaceuticals, Novartis, Organogenesis, Pfizer, Sciton; is a consultant for: Alphyn, Amryt Pharma, Beiersdorf, Brickell, Cutanea, Hoth, Lexington, Mustela, TopMD, Noble Pharma; a speaker for: Novartis, Sanofi-Regeneron, CeraVe; is on the advisory boards of: Almirall, Alphyn, Apogee, Aslan, Biofrontera, CeraVe, Krystal Biotech, Mustela, Noble Pharma, Pfizer, Pierre Fabre, Sanofi-Regeneron; and owns stocks in: TopMD and Alphyn. Dr. Maguiness had no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
TORONTO — Lawrence A. Schachner, MD, would like pediatric dermatologists to adopt a “toxic agent of the year” to raise awareness about the potential harm related to certain topical treatments in babies and young children.
Dr. Schachner, director of the Division of Pediatric Dermatology in the Department of Dermatology & Cutaneous Surgery at the University of Miami, Coral Gables, Florida, said he got the idea from the American Contact Dermatitis Society, which annually names the “Allergen of the Year.”
, said Dr. Schachner, professor of pediatrics and dermatology at the University of Miami.
“Any one of those would be excellent toxic substances of the year” that could be the focus of an educational campaign, he told this news organization following his presentation on “Toxicology of Topical Ingredients in Pediatric Dermatology” at the annual meeting of the Society for Pediatric Dermatology on July 14.
Benzene might also be a good candidate for the list, although the jury seems to be still out on its toxicity, said Dr. Schachner.
He talked about the “four Ps” of poisoning — the physician, pharmacy, parents, and pharmaceutical manufacturing — which all have some responsibility for errors that lead to adverse outcomes but can also take steps to prevent them.
During his presentation, Dr. Schachner discussed how babies are especially sensitive to topical therapies, noting that a baby’s skin is thinner and more permeable than that of an adult. And children have a greater body surface-to-weight ratio, so they absorb more substances through their skin.
He also noted that babies lack natural moisturizing factors, and their skin barrier isn’t mature until about age 3-5 years, stressing the need for extreme care when applying a topical agent to a baby’s skin.
Tragic Stories
Dr. Schachner pointed to some instances of mishaps related to toxic topical substances in children. There was the outbreak in the early 1980s of accidental hexachlorophene poisoning among children in France exposed to talc “baby powder.” Of the 204 affected children, 36 died.
The cause was a manufacturing error; the product contained 6.3% hexachlorophene, as opposed to the 0.1% limit recommended by the US Food and Drug Administration (FDA).
Local anesthetics, including lidocaine, dibucaine, and prilocaine, can cause local anesthetic systemic toxicity, a syndrome with symptoms that include central nervous system depression, seizures, and cardiotoxicity. Dr. Schachner described the case of a 3-year-old who developed methemoglobinemia, with seizures, after treatment with an excessive amount of eutectic mixture of local anesthetics (EMLA) cream, which contains both lidocaine and prilocaine.
EMLA shouldn’t be used with methemoglobinemia-inducing agents, such as some antimalarials, analgesics, anesthetics, and antineoplastic agents. It’s not recommended in neonates or for those under 12 months if receiving methemoglobinemia-inducing agents, “and I would keep an eye on it after 12 months of age,” said Dr. Schachner.
He cited a retrospective review of topical lidocaine toxicity in pediatric patients reported to the National Poison Data System from 2000 to 2020. It found 37 cases of toxicity, the most common from application prior to dermatologic procedures (37.5%), which led to two deaths.
Not Benign Agents
“These are not benign agents; we have to use them correctly,” Dr. Schachner stressed. When discussing alcohols and antiseptics, he noted that phenol is found in a variety of household disinfectants, gargling products, ointments, and lip balms. Phenol can be used as a chemical peel and is the antiseptic component of Castellani paint. He also referred to cases of alcohol intoxication linked to umbilical care in newborns.
Benzene at elevated levels has been found in some topical benzoyl peroxide acne products and in some sunscreens. There have been suggestions, not strongly substantiated, that benzene may increase the risk for cancer, especially leukemias.
But there is sparse data on the absorption and toxicity of benzene exposure with sunscreen use. The data, he said, include an analysis of National Health and Nutrition Examination Survey data, which found that people who regularly used sunscreens were less likely to have elevated benzene levels compared with those who didn’t use sunscreens.
Turning to insecticides, Dr. Schachner discussed N,N-diethyl-m-toluamide (DEET), the active ingredient in many insect repellents. It helps avoid “some terrible diseases,” including mosquito-borne illnesses such as malaria and tick-borne conditions such as Lyme disease, and is available in several convenient formulations, he said.
When used on children, the American Academy of Pediatrics (AAP) recommends products with no more than 30% DEET. And insect repellents are not recommended for children younger than 2 months, or under clothing or damaged skin, he said.
Dr. Schachner referred to a case series of 18 children who developed DEET-induced encephalopathy; 13 (72%) involved dermal exposure. Three of those with cutaneous exposure died, mostly from neurologic, respiratory, and cardiac issues. “What’s very striking is that 55% of the kids were exposed to DEET of 20% or less, even though the AAP approves DEET at 30%, so maybe that’s something we have to look at,” he said.
Medication Patches
With medication patches, especially fentanyl transdermal patches, much can go wrong when it comes to children. This was highlighted by the cases Schachner cited, including an infant who developed acute cytotoxic cerebellar edema from fentanyl patch intoxication.
In another case, emergency room staff found a fentanyl patch stuck to the back of a 3-year-old girl. A CT scan showed global cerebral edema, and the patient progressed to brain death. “This is not a unique case; there have been over 10 such cases in the United States,” said Dr. Schachner. “We should be doing better with fentanyl.”
Nicotine patches can also be dangerous to children, he added. As for other topical agents, there have been reports of toxicity and deaths linked to salicylic acid, commonly used by dermatologists because of its bacteriostatic, fungicidal, keratolytic, and photoprotective properties.
Dr. Schachner cited the case of a 2-month-old where the pediatrician prescribed 50% salicylic acid for seborrheic dermatitis of the scalp, under occlusion. “It’s amazing this child survived; that’s clearly a physician error,” he said.
Henna, a reddish-brown dye derived from the crushed leaves of Lawsonia alba, is used cosmetically for the hair, skin, and nails. Many henna products are mixed with additives, including para-phenylenediamine, which has been associated with dermatitis, asthma, renal failure, and permanent vision loss.
Asked to comment on the presentation, Sheilagh Maguiness, MD, professor of dermatology and pediatrics and chair of pediatric dermatology at the University of Minnesota, Minneapolis, recalled a particularly concerning story in 2008, when the FDA issued a warning about Mommy’s Bliss, a cream containing chlorphenesin and phenoxyethanol as preservatives, promoted to nursing mothers for soothing cracked nipples. There were reports of the cream causing respiratory distress, vomiting, and diarrhea in nursing infants.
Dr. Schachner is chair of Stiefel Laboratories and is an investigator with: Astellas, Berg Pharma, Celgene, Ferndale Labs, Lilly, Medimetriks Pharmaceuticals, Novartis, Organogenesis, Pfizer, Sciton; is a consultant for: Alphyn, Amryt Pharma, Beiersdorf, Brickell, Cutanea, Hoth, Lexington, Mustela, TopMD, Noble Pharma; a speaker for: Novartis, Sanofi-Regeneron, CeraVe; is on the advisory boards of: Almirall, Alphyn, Apogee, Aslan, Biofrontera, CeraVe, Krystal Biotech, Mustela, Noble Pharma, Pfizer, Pierre Fabre, Sanofi-Regeneron; and owns stocks in: TopMD and Alphyn. Dr. Maguiness had no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
FROM SPD 2024
Too Much Coffee Linked to Accelerated Cognitive Decline
PHILADELPHIA – results from a large study suggest.
Investigators examined the impact of different amounts of coffee and tea on fluid intelligence — a measure of cognitive functions including abstract reasoning, pattern recognition, and logical thinking.
“It’s the old adage that too much of anything isn’t good. It’s all about balance, so moderate coffee consumption is okay but too much is probably not recommended,” said study investigator Kelsey R. Sewell, PhD, Advent Health Research Institute, Orlando, Florida.
The findings of the study were presented at the 2024 Alzheimer’s Association International Conference (AAIC).
One of the World’s Most Widely Consumed Beverages
Coffee is one of the most widely consumed beverages around the world. The beans contain a range of bioactive compounds, including caffeine, chlorogenic acid, and small amounts of vitamins and minerals.
Consistent evidence from observational and epidemiologic studies indicates that intake of both coffee and tea has beneficial effects on stroke, heart failure, cancers, diabetes, and Parkinson’s disease.
Several studies also suggest that coffee may reduce the risk for Alzheimer’s disease, said Dr. Sewell. However, there are limited longitudinal data on associations between coffee and tea intake and cognitive decline, particularly in distinct cognitive domains.
Dr. Sewell’s group previously published a study of cognitively unimpaired older adults that found greater coffee consumption was associated with slower cognitive decline and slower accumulation of brain beta-amyloid.
Their current study extends some of the prior findings and investigates the relationship between both coffee and tea intake and cognitive decline over time in a larger sample of older adults.
This new study included 8451 mostly female (60%) and White (97%) cognitively unimpaired adults older than 60 (mean age, 67.8 years) in the UK Biobank, a large-scale research resource containing in-depth, deidentified genetic and health information from half a million UK participants. Study subjects had a mean body mass index (BMI) of 26, and about 26% were apolipoprotein epsilon 4 (APOE e4) gene carriers.
Researchers divided coffee and tea consumption into tertiles: high, moderate, and no consumption.
For daily coffee consumption, 18% reported drinking four or more cups (high consumption), 58% reported drinking one to three cups (moderate consumption), and 25% reported that they never drink coffee. For daily tea consumption, 47% reported drinking four or more cups (high consumption), 38% reported drinking one to three cups (moderate consumption), and 15% reported that they never drink tea.
The study assessed cognitive function at baseline and at least two additional patient visits.
Researchers used linear mixed models to assess the relationships between coffee and tea intake and cognitive outcomes. The models adjusted for age, sex, Townsend deprivation index (reflecting socioeconomic status), ethnicity, APOE e4 status, and BMI.
Steeper Decline
Compared with high coffee consumption (four or more cups daily), people who never consumed coffee (beta, 0.06; standard error [SE], 0.02; P = .005) and those with moderate consumption (beta, 0.07; SE, 0.02; P = < .001) had slower decline in fluid intelligence after an average of 8.83 years of follow-up.
“We can see that those with high coffee consumption showed the steepest decline in fluid intelligence across the follow up, compared to those with moderate coffee consumption and those never consuming coffee,” said Dr. Sewell, referring to illustrative graphs.
At the same time, “our data suggest that across this time period, moderate coffee consumption can serve as some kind of protective factor against cognitive decline,” she added.
For tea, there was a somewhat different pattern. People who never drank tea had a greater decline in fluid intelligence, compared with those who had moderate consumption (beta, 0.06; SE, 0.02; P = .0090) or high consumption (beta, 0.06; SE, 0.02; P = .003).
Because this is an observational study, “we still need randomized controlled trials to better understand the neuroprotective mechanism of coffee and tea compounds,” said Dr. Sewell.
Responding later to a query from a meeting delegate about how moderate coffee drinking could be protective, Dr. Sewell said there are probably “different levels of mechanisms,” including at the molecular level (possibly involving amyloid toxicity) and the behavioral level (possibly involving sleep patterns).
Dr. Sewell said that she hopes this line of investigation will lead to new avenues of research in preventive strategies for Alzheimer’s disease.
“We hope that coffee and tea intake could contribute to the development of a safe and inexpensive strategy for delaying the onset and reducing the incidence for Alzheimer’s disease.”
A limitation of the study is possible recall bias, because coffee and tea consumption were self-reported. However, this may not be much of an issue because coffee and tea consumption “is usually quite a habitual behavior,” said Dr. Sewell.
The study also had no data on midlife coffee or tea consumption and did not compare the effect of different preparation methods or types of coffee and tea — for example, green tea versus black tea.
When asked if the study controlled for smoking, Dr. Sewell said it didn’t but added that it would be interesting to explore its impact on cognition.
Dr. Sewell reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
PHILADELPHIA – results from a large study suggest.
Investigators examined the impact of different amounts of coffee and tea on fluid intelligence — a measure of cognitive functions including abstract reasoning, pattern recognition, and logical thinking.
“It’s the old adage that too much of anything isn’t good. It’s all about balance, so moderate coffee consumption is okay but too much is probably not recommended,” said study investigator Kelsey R. Sewell, PhD, Advent Health Research Institute, Orlando, Florida.
The findings of the study were presented at the 2024 Alzheimer’s Association International Conference (AAIC).
One of the World’s Most Widely Consumed Beverages
Coffee is one of the most widely consumed beverages around the world. The beans contain a range of bioactive compounds, including caffeine, chlorogenic acid, and small amounts of vitamins and minerals.
Consistent evidence from observational and epidemiologic studies indicates that intake of both coffee and tea has beneficial effects on stroke, heart failure, cancers, diabetes, and Parkinson’s disease.
Several studies also suggest that coffee may reduce the risk for Alzheimer’s disease, said Dr. Sewell. However, there are limited longitudinal data on associations between coffee and tea intake and cognitive decline, particularly in distinct cognitive domains.
Dr. Sewell’s group previously published a study of cognitively unimpaired older adults that found greater coffee consumption was associated with slower cognitive decline and slower accumulation of brain beta-amyloid.
Their current study extends some of the prior findings and investigates the relationship between both coffee and tea intake and cognitive decline over time in a larger sample of older adults.
This new study included 8451 mostly female (60%) and White (97%) cognitively unimpaired adults older than 60 (mean age, 67.8 years) in the UK Biobank, a large-scale research resource containing in-depth, deidentified genetic and health information from half a million UK participants. Study subjects had a mean body mass index (BMI) of 26, and about 26% were apolipoprotein epsilon 4 (APOE e4) gene carriers.
Researchers divided coffee and tea consumption into tertiles: high, moderate, and no consumption.
For daily coffee consumption, 18% reported drinking four or more cups (high consumption), 58% reported drinking one to three cups (moderate consumption), and 25% reported that they never drink coffee. For daily tea consumption, 47% reported drinking four or more cups (high consumption), 38% reported drinking one to three cups (moderate consumption), and 15% reported that they never drink tea.
The study assessed cognitive function at baseline and at least two additional patient visits.
Researchers used linear mixed models to assess the relationships between coffee and tea intake and cognitive outcomes. The models adjusted for age, sex, Townsend deprivation index (reflecting socioeconomic status), ethnicity, APOE e4 status, and BMI.
Steeper Decline
Compared with high coffee consumption (four or more cups daily), people who never consumed coffee (beta, 0.06; standard error [SE], 0.02; P = .005) and those with moderate consumption (beta, 0.07; SE, 0.02; P = < .001) had slower decline in fluid intelligence after an average of 8.83 years of follow-up.
“We can see that those with high coffee consumption showed the steepest decline in fluid intelligence across the follow up, compared to those with moderate coffee consumption and those never consuming coffee,” said Dr. Sewell, referring to illustrative graphs.
At the same time, “our data suggest that across this time period, moderate coffee consumption can serve as some kind of protective factor against cognitive decline,” she added.
For tea, there was a somewhat different pattern. People who never drank tea had a greater decline in fluid intelligence, compared with those who had moderate consumption (beta, 0.06; SE, 0.02; P = .0090) or high consumption (beta, 0.06; SE, 0.02; P = .003).
Because this is an observational study, “we still need randomized controlled trials to better understand the neuroprotective mechanism of coffee and tea compounds,” said Dr. Sewell.
Responding later to a query from a meeting delegate about how moderate coffee drinking could be protective, Dr. Sewell said there are probably “different levels of mechanisms,” including at the molecular level (possibly involving amyloid toxicity) and the behavioral level (possibly involving sleep patterns).
Dr. Sewell said that she hopes this line of investigation will lead to new avenues of research in preventive strategies for Alzheimer’s disease.
“We hope that coffee and tea intake could contribute to the development of a safe and inexpensive strategy for delaying the onset and reducing the incidence for Alzheimer’s disease.”
A limitation of the study is possible recall bias, because coffee and tea consumption were self-reported. However, this may not be much of an issue because coffee and tea consumption “is usually quite a habitual behavior,” said Dr. Sewell.
The study also had no data on midlife coffee or tea consumption and did not compare the effect of different preparation methods or types of coffee and tea — for example, green tea versus black tea.
When asked if the study controlled for smoking, Dr. Sewell said it didn’t but added that it would be interesting to explore its impact on cognition.
Dr. Sewell reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
PHILADELPHIA – results from a large study suggest.
Investigators examined the impact of different amounts of coffee and tea on fluid intelligence — a measure of cognitive functions including abstract reasoning, pattern recognition, and logical thinking.
“It’s the old adage that too much of anything isn’t good. It’s all about balance, so moderate coffee consumption is okay but too much is probably not recommended,” said study investigator Kelsey R. Sewell, PhD, Advent Health Research Institute, Orlando, Florida.
The findings of the study were presented at the 2024 Alzheimer’s Association International Conference (AAIC).
One of the World’s Most Widely Consumed Beverages
Coffee is one of the most widely consumed beverages around the world. The beans contain a range of bioactive compounds, including caffeine, chlorogenic acid, and small amounts of vitamins and minerals.
Consistent evidence from observational and epidemiologic studies indicates that intake of both coffee and tea has beneficial effects on stroke, heart failure, cancers, diabetes, and Parkinson’s disease.
Several studies also suggest that coffee may reduce the risk for Alzheimer’s disease, said Dr. Sewell. However, there are limited longitudinal data on associations between coffee and tea intake and cognitive decline, particularly in distinct cognitive domains.
Dr. Sewell’s group previously published a study of cognitively unimpaired older adults that found greater coffee consumption was associated with slower cognitive decline and slower accumulation of brain beta-amyloid.
Their current study extends some of the prior findings and investigates the relationship between both coffee and tea intake and cognitive decline over time in a larger sample of older adults.
This new study included 8451 mostly female (60%) and White (97%) cognitively unimpaired adults older than 60 (mean age, 67.8 years) in the UK Biobank, a large-scale research resource containing in-depth, deidentified genetic and health information from half a million UK participants. Study subjects had a mean body mass index (BMI) of 26, and about 26% were apolipoprotein epsilon 4 (APOE e4) gene carriers.
Researchers divided coffee and tea consumption into tertiles: high, moderate, and no consumption.
For daily coffee consumption, 18% reported drinking four or more cups (high consumption), 58% reported drinking one to three cups (moderate consumption), and 25% reported that they never drink coffee. For daily tea consumption, 47% reported drinking four or more cups (high consumption), 38% reported drinking one to three cups (moderate consumption), and 15% reported that they never drink tea.
The study assessed cognitive function at baseline and at least two additional patient visits.
Researchers used linear mixed models to assess the relationships between coffee and tea intake and cognitive outcomes. The models adjusted for age, sex, Townsend deprivation index (reflecting socioeconomic status), ethnicity, APOE e4 status, and BMI.
Steeper Decline
Compared with high coffee consumption (four or more cups daily), people who never consumed coffee (beta, 0.06; standard error [SE], 0.02; P = .005) and those with moderate consumption (beta, 0.07; SE, 0.02; P = < .001) had slower decline in fluid intelligence after an average of 8.83 years of follow-up.
“We can see that those with high coffee consumption showed the steepest decline in fluid intelligence across the follow up, compared to those with moderate coffee consumption and those never consuming coffee,” said Dr. Sewell, referring to illustrative graphs.
At the same time, “our data suggest that across this time period, moderate coffee consumption can serve as some kind of protective factor against cognitive decline,” she added.
For tea, there was a somewhat different pattern. People who never drank tea had a greater decline in fluid intelligence, compared with those who had moderate consumption (beta, 0.06; SE, 0.02; P = .0090) or high consumption (beta, 0.06; SE, 0.02; P = .003).
Because this is an observational study, “we still need randomized controlled trials to better understand the neuroprotective mechanism of coffee and tea compounds,” said Dr. Sewell.
Responding later to a query from a meeting delegate about how moderate coffee drinking could be protective, Dr. Sewell said there are probably “different levels of mechanisms,” including at the molecular level (possibly involving amyloid toxicity) and the behavioral level (possibly involving sleep patterns).
Dr. Sewell said that she hopes this line of investigation will lead to new avenues of research in preventive strategies for Alzheimer’s disease.
“We hope that coffee and tea intake could contribute to the development of a safe and inexpensive strategy for delaying the onset and reducing the incidence for Alzheimer’s disease.”
A limitation of the study is possible recall bias, because coffee and tea consumption were self-reported. However, this may not be much of an issue because coffee and tea consumption “is usually quite a habitual behavior,” said Dr. Sewell.
The study also had no data on midlife coffee or tea consumption and did not compare the effect of different preparation methods or types of coffee and tea — for example, green tea versus black tea.
When asked if the study controlled for smoking, Dr. Sewell said it didn’t but added that it would be interesting to explore its impact on cognition.
Dr. Sewell reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM AAIC 2024
Almost 50% of Global Dementia Cases May Be Preventable
PHILADELPHIA – a report from the Lancet Commission on dementia prevention, intervention, and care.
The report adds two new modifiable risk factors for dementia — high cholesterol and vision loss — to the 12 risk factors identified in the 2020 Lancet Commission report, which were linked to about 40% of all dementia cases.
The original Lancet Commission report, published in 2017, identified nine modifiable risk factors that were estimated to be responsible for one third of dementia cases.
“Our new report reveals that there is much more that can and should be done to reduce the risk of dementia. It’s never too early or too late to act, with opportunities to make an impact at any stage of life,” lead author Gill Livingston, MD, from University College London in England, said in a statement.
The 57-page report was published online in The Lancet Neurology (to coincide with its presentation at the 2024 Alzheimer’s Association International Conference (AAIC).
‘Compelling’ New Evidence
The 12 risk factors cited in the 2020 report are lower levels of education, hearing loss, hypertension, smoking, obesity, depression, physical inactivity, diabetes, excessive alcohol consumption, traumatic brain injury (TBI), air pollution, and social isolation.
According to the authors of the current report, there is “new compelling evidence” that untreated vision loss and elevated low-density lipoprotein (LDL) cholesterol are also risk factors for dementia.
These two added risk factors are associated with 9% of all dementia cases — with an estimated 7% of cases caused by high LDL cholesterol from about age 40 years, and 2% of cases caused by untreated vision loss in later life, the authors said.
Out of all 14 risk factors, those tied to the greatest proportion of dementia in the global population are hearing impairment and high LDL cholesterol (7% each), along with less education in early life, and social isolation in later life (5% each), the report estimates.
The new report also outlines 13 recommendations aimed at individuals and governments to help guard against dementia. They include preventing and treating hearing loss, vision loss, and depression; being cognitively active throughout life; using head protection in contact sports; reducing vascular risk factors (high cholesterol, diabetes, obesity, hypertension); improving air quality; and providing supportive community environments to increase social contact.
Tara Spires-Jones, PhD, president of the British Neuroscience Association, emphasized that, while this research doesn’t directly link specific factors to dementia, it supports evidence that a healthy lifestyle — encompassing education, social activities, exercise, cognitive engagement, and avoiding head injuries and harmful factors for heart and lung health — can enhance brain resilience and prevent dementia.
In an interview, Heather M. Snyder, PhD, senior vice president of medical and scientific relations, Alzheimer’s Association, said: “Our brains are complex and what happens throughout our lives may increase or decrease our risk for dementia as we age. Protecting brain health as we age requires a comprehensive approach that includes discussions on diet, exercise, heart health, hearing, and vision.”
Also weighing in on the new report, Shaheen Lakhan, MD, PhD, neurologist and researcher based in Miami, Florida, said the addition of high cholesterol is “particularly noteworthy as it reinforces the intricate connection between vascular health and brain health — a link we’ve long suspected but can now target more effectively.”
As for vision loss, “it’s not just a matter of seeing clearly; it’s a matter of thinking clearly. Untreated vision loss can lead to social isolation, reduced physical activity, and cognitive decline,” said Dr. Lakhan.
Dementia Is Not Inevitable
In his view, “the potential to prevent or delay nearly half of dementia cases by addressing these risk factors is nothing short of revolutionary. It shifts our perspective from viewing dementia as an inevitable part of aging to seeing it as a condition we can actively work to prevent,” Dr. Lakhan added.
He said the report’s emphasis on health equity is also important.
“Dementia risk factors disproportionately affect socioeconomically disadvantaged groups and low- and middle-income countries. Addressing these disparities isn’t just a matter of fairness in the fight against dementia, equality in prevention is as important as equality in treatment,” Dr. Lakhan commented.
While the report offers hope, it also presents a challenge, he said.
Implementing the recommended preventive measures requires a “coordinated effort from individuals, healthcare systems, and policymakers. The potential benefits, both in terms of quality of life and economic savings, make this effort not just worthwhile but imperative. Preventing dementia is not just a medical imperative — it’s an economic and humanitarian one,” Dr. Lakhan said.
Masud Husain, PhD, with the University of Oxford in England, agreed.
The conclusions in this report are “very important for all of us, but particularly for health policy makers and government,” he said.
“If we did simple things well such as screening for some of the factors identified in this report, with adequate resources to perform this, we have the potential to prevent dementia on a national scale. This would be far more cost effective than developing high-tech treatments, which so far have been disappointing in their impacts on people with established dementia,” Dr. Husain said.
The Lancet Commission was funded by University College London, Alzheimer’s Society, Alzheimer’s Research UK, and the Economic and Social Research Council. A complete list of author disclosures is available with the original article. Dr. Snyder, Dr. Lakhan, Dr. Husain and Dr. Spires-Jones have no relevant disclosures.
A version of this article appeared on Medscape.com.
PHILADELPHIA – a report from the Lancet Commission on dementia prevention, intervention, and care.
The report adds two new modifiable risk factors for dementia — high cholesterol and vision loss — to the 12 risk factors identified in the 2020 Lancet Commission report, which were linked to about 40% of all dementia cases.
The original Lancet Commission report, published in 2017, identified nine modifiable risk factors that were estimated to be responsible for one third of dementia cases.
“Our new report reveals that there is much more that can and should be done to reduce the risk of dementia. It’s never too early or too late to act, with opportunities to make an impact at any stage of life,” lead author Gill Livingston, MD, from University College London in England, said in a statement.
The 57-page report was published online in The Lancet Neurology (to coincide with its presentation at the 2024 Alzheimer’s Association International Conference (AAIC).
‘Compelling’ New Evidence
The 12 risk factors cited in the 2020 report are lower levels of education, hearing loss, hypertension, smoking, obesity, depression, physical inactivity, diabetes, excessive alcohol consumption, traumatic brain injury (TBI), air pollution, and social isolation.
According to the authors of the current report, there is “new compelling evidence” that untreated vision loss and elevated low-density lipoprotein (LDL) cholesterol are also risk factors for dementia.
These two added risk factors are associated with 9% of all dementia cases — with an estimated 7% of cases caused by high LDL cholesterol from about age 40 years, and 2% of cases caused by untreated vision loss in later life, the authors said.
Out of all 14 risk factors, those tied to the greatest proportion of dementia in the global population are hearing impairment and high LDL cholesterol (7% each), along with less education in early life, and social isolation in later life (5% each), the report estimates.
The new report also outlines 13 recommendations aimed at individuals and governments to help guard against dementia. They include preventing and treating hearing loss, vision loss, and depression; being cognitively active throughout life; using head protection in contact sports; reducing vascular risk factors (high cholesterol, diabetes, obesity, hypertension); improving air quality; and providing supportive community environments to increase social contact.
Tara Spires-Jones, PhD, president of the British Neuroscience Association, emphasized that, while this research doesn’t directly link specific factors to dementia, it supports evidence that a healthy lifestyle — encompassing education, social activities, exercise, cognitive engagement, and avoiding head injuries and harmful factors for heart and lung health — can enhance brain resilience and prevent dementia.
In an interview, Heather M. Snyder, PhD, senior vice president of medical and scientific relations, Alzheimer’s Association, said: “Our brains are complex and what happens throughout our lives may increase or decrease our risk for dementia as we age. Protecting brain health as we age requires a comprehensive approach that includes discussions on diet, exercise, heart health, hearing, and vision.”
Also weighing in on the new report, Shaheen Lakhan, MD, PhD, neurologist and researcher based in Miami, Florida, said the addition of high cholesterol is “particularly noteworthy as it reinforces the intricate connection between vascular health and brain health — a link we’ve long suspected but can now target more effectively.”
As for vision loss, “it’s not just a matter of seeing clearly; it’s a matter of thinking clearly. Untreated vision loss can lead to social isolation, reduced physical activity, and cognitive decline,” said Dr. Lakhan.
Dementia Is Not Inevitable
In his view, “the potential to prevent or delay nearly half of dementia cases by addressing these risk factors is nothing short of revolutionary. It shifts our perspective from viewing dementia as an inevitable part of aging to seeing it as a condition we can actively work to prevent,” Dr. Lakhan added.
He said the report’s emphasis on health equity is also important.
“Dementia risk factors disproportionately affect socioeconomically disadvantaged groups and low- and middle-income countries. Addressing these disparities isn’t just a matter of fairness in the fight against dementia, equality in prevention is as important as equality in treatment,” Dr. Lakhan commented.
While the report offers hope, it also presents a challenge, he said.
Implementing the recommended preventive measures requires a “coordinated effort from individuals, healthcare systems, and policymakers. The potential benefits, both in terms of quality of life and economic savings, make this effort not just worthwhile but imperative. Preventing dementia is not just a medical imperative — it’s an economic and humanitarian one,” Dr. Lakhan said.
Masud Husain, PhD, with the University of Oxford in England, agreed.
The conclusions in this report are “very important for all of us, but particularly for health policy makers and government,” he said.
“If we did simple things well such as screening for some of the factors identified in this report, with adequate resources to perform this, we have the potential to prevent dementia on a national scale. This would be far more cost effective than developing high-tech treatments, which so far have been disappointing in their impacts on people with established dementia,” Dr. Husain said.
The Lancet Commission was funded by University College London, Alzheimer’s Society, Alzheimer’s Research UK, and the Economic and Social Research Council. A complete list of author disclosures is available with the original article. Dr. Snyder, Dr. Lakhan, Dr. Husain and Dr. Spires-Jones have no relevant disclosures.
A version of this article appeared on Medscape.com.
PHILADELPHIA – a report from the Lancet Commission on dementia prevention, intervention, and care.
The report adds two new modifiable risk factors for dementia — high cholesterol and vision loss — to the 12 risk factors identified in the 2020 Lancet Commission report, which were linked to about 40% of all dementia cases.
The original Lancet Commission report, published in 2017, identified nine modifiable risk factors that were estimated to be responsible for one third of dementia cases.
“Our new report reveals that there is much more that can and should be done to reduce the risk of dementia. It’s never too early or too late to act, with opportunities to make an impact at any stage of life,” lead author Gill Livingston, MD, from University College London in England, said in a statement.
The 57-page report was published online in The Lancet Neurology (to coincide with its presentation at the 2024 Alzheimer’s Association International Conference (AAIC).
‘Compelling’ New Evidence
The 12 risk factors cited in the 2020 report are lower levels of education, hearing loss, hypertension, smoking, obesity, depression, physical inactivity, diabetes, excessive alcohol consumption, traumatic brain injury (TBI), air pollution, and social isolation.
According to the authors of the current report, there is “new compelling evidence” that untreated vision loss and elevated low-density lipoprotein (LDL) cholesterol are also risk factors for dementia.
These two added risk factors are associated with 9% of all dementia cases — with an estimated 7% of cases caused by high LDL cholesterol from about age 40 years, and 2% of cases caused by untreated vision loss in later life, the authors said.
Out of all 14 risk factors, those tied to the greatest proportion of dementia in the global population are hearing impairment and high LDL cholesterol (7% each), along with less education in early life, and social isolation in later life (5% each), the report estimates.
The new report also outlines 13 recommendations aimed at individuals and governments to help guard against dementia. They include preventing and treating hearing loss, vision loss, and depression; being cognitively active throughout life; using head protection in contact sports; reducing vascular risk factors (high cholesterol, diabetes, obesity, hypertension); improving air quality; and providing supportive community environments to increase social contact.
Tara Spires-Jones, PhD, president of the British Neuroscience Association, emphasized that, while this research doesn’t directly link specific factors to dementia, it supports evidence that a healthy lifestyle — encompassing education, social activities, exercise, cognitive engagement, and avoiding head injuries and harmful factors for heart and lung health — can enhance brain resilience and prevent dementia.
In an interview, Heather M. Snyder, PhD, senior vice president of medical and scientific relations, Alzheimer’s Association, said: “Our brains are complex and what happens throughout our lives may increase or decrease our risk for dementia as we age. Protecting brain health as we age requires a comprehensive approach that includes discussions on diet, exercise, heart health, hearing, and vision.”
Also weighing in on the new report, Shaheen Lakhan, MD, PhD, neurologist and researcher based in Miami, Florida, said the addition of high cholesterol is “particularly noteworthy as it reinforces the intricate connection between vascular health and brain health — a link we’ve long suspected but can now target more effectively.”
As for vision loss, “it’s not just a matter of seeing clearly; it’s a matter of thinking clearly. Untreated vision loss can lead to social isolation, reduced physical activity, and cognitive decline,” said Dr. Lakhan.
Dementia Is Not Inevitable
In his view, “the potential to prevent or delay nearly half of dementia cases by addressing these risk factors is nothing short of revolutionary. It shifts our perspective from viewing dementia as an inevitable part of aging to seeing it as a condition we can actively work to prevent,” Dr. Lakhan added.
He said the report’s emphasis on health equity is also important.
“Dementia risk factors disproportionately affect socioeconomically disadvantaged groups and low- and middle-income countries. Addressing these disparities isn’t just a matter of fairness in the fight against dementia, equality in prevention is as important as equality in treatment,” Dr. Lakhan commented.
While the report offers hope, it also presents a challenge, he said.
Implementing the recommended preventive measures requires a “coordinated effort from individuals, healthcare systems, and policymakers. The potential benefits, both in terms of quality of life and economic savings, make this effort not just worthwhile but imperative. Preventing dementia is not just a medical imperative — it’s an economic and humanitarian one,” Dr. Lakhan said.
Masud Husain, PhD, with the University of Oxford in England, agreed.
The conclusions in this report are “very important for all of us, but particularly for health policy makers and government,” he said.
“If we did simple things well such as screening for some of the factors identified in this report, with adequate resources to perform this, we have the potential to prevent dementia on a national scale. This would be far more cost effective than developing high-tech treatments, which so far have been disappointing in their impacts on people with established dementia,” Dr. Husain said.
The Lancet Commission was funded by University College London, Alzheimer’s Society, Alzheimer’s Research UK, and the Economic and Social Research Council. A complete list of author disclosures is available with the original article. Dr. Snyder, Dr. Lakhan, Dr. Husain and Dr. Spires-Jones have no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM AAIC 2024
‘Psychological Weight’ Crucial in Patients With Obesity
Increasingly recognized as a multifactorial disease, obesity demands an approach that involves multiple healthcare professionals. For psychologist Andréa Levy, coordinator and founder of the nongovernmental organization Obesity Brazil, addressing the patient’s “psychological weight” is crucial.
In an interview with this news organization, Ms. Levy, who was one of the speakers at the International Congress on Obesity in 2024, emphasized the importance of integrating emotional and behavioral aspects into treatment, because these factors often influence eating habits and weight gain.
She also highlighted the essential collaboration between endocrinologists, nutritionists, psychiatrists, and psychologists, who must work together to provide comprehensive and effective care to patients.
How do psychological factors affect the treatment of obesity?
Psychological factors are important triggers for weight gain. As the degree of obesity increases, so does the predisposition to mental health problems such as anxiety, mood disorders, personality disorders, and eating disorders. Understanding these factors is important because accurate psychodiagnosis is essential for effective disease treatment.
Without a proper diagnosis, the treatment may be incomplete and omit relevant factors. For example, a person with undiagnosed depression who is starting treatment for weight loss may feel discouraged and low on energy. He or she may wrongly attribute these symptoms to the diet or surgery. Similarly, someone undergoing bariatric surgery may confuse malnutrition symptoms with depression, resulting in inadequate treatment with antidepressants and possible iatrogenic complications.
Furthermore, psychotherapy and psychological follow-up are essential to help the individual organize better and understand the treatment and the disease itself. This is especially important in stigmatized diseases and those subject to prejudice such as obesity, where understanding and acceptance are often challenging, which affects treatment adherence.
Is the collaboration between psychologist and psychiatrist always necessary?
Often, it is necessary to have the support of both a psychologist and a psychiatrist. The process generally begins with a good psychodiagnosis. Initially, there may not be a case that requires treatment, but it is important to perform this evaluation to rule out any issues.
The follow-up, unlike weekly psychotherapy, can be monthly or at an interval agreed on with the patient. It is crucial to help him or her navigate the various stages of obesity treatment. For example, the patient may be going through a period of mourning or separation, or a happier moment, such as the beginning of a relationship or the birth of a child in the family. These moments affect eating habits and need to be well managed.
Depending on the degree of the pathology, such as depression, severe binge-eating disorder, or personality disorders, the psychologist works in conjunction with the psychiatrist. When we talk about obesity, we are possibly also talking about a psychiatric population because it is a disease that, besides being highly recurrent, involves many other factors, such as the gaze of others, difficulty with dressing, body pains, mobility, and relationships. Therefore, having this disease alone is already a trigger for disorders such as depression.
What is the main evidence regarding the psychological follow-up of patients with obesity?
Several studies have investigated the relationship between obesity and mental health. Research indicates that the greater the obesity, the higher the likelihood of a positive diagnosis for a psychiatric disorder. Additionally, there is evidence of the benefits of psychological treatment for patients with obesity.
A study published in the Journal of Clinical Endocrinology and Metabolism addressed the impact of cognitive-behavioral therapy (CBT), which helps patients manage goals and treat maladaptive behaviors such as binge-eating disorders. CBT has a modest effect on weight loss, but its integration as part of a lifestyle modification amplifies the results of this loss.
Recent research also shows that weight loss through bariatric surgery offers significant psychological benefits. In the past, it was believed that this procedure could cause depression and other severe psychiatric disorders, but it is now more than proven that weight loss, when done properly and without misconduct or malnutrition, improves psychological and psychiatric issues.
How does psychological follow-up affect the use of medication during obesity treatment?
Many people who take medications, such as corticosteroids for chronic pain or psychiatric medications, may experience weight gain. It is essential to discuss these issues with the psychiatrist because if the patient already has a predisposition to weight gain, medication X should be chosen instead of medication Y, or the dosage should be adjusted. The psychiatrist needs to understand obesity to medicate correctly. Other types of medication, such as chemotherapeutics, may also cause weight gain, often resulting in more abdominal obesity.
There is also lipedema, a hormone-dependent disease that is different from obesity. In this disease, the person gains weight mainly in the legs and arms. In this case, bariatric surgery may result in weight loss only in specific areas, causing disproportionality and difficulty in understanding for the patient. Therefore, when treating obesity, it is important to analyze the patient from all angles: psychological, physiologic, and physical, considering the diversity of the body, its functioning, and hormonal reactions.
Although psychologists do not prescribe medications, they often explain their functioning to the patient. For example, if a patient is taking a glucagon-like peptide 1 analog and experiences initial nausea, he or she may stop using the treatment because the wrong dose had been started. In this case, the psychologist can explain how the medication works and encourage the patient to discuss adjustments with the doctor, avoiding premature discontinuation.
How has the mental health follow-up of patients with obesity evolved over the years?
I started working with people with obesity 25 years ago, when I myself underwent bariatric surgery. At that time, surgeons were used to “solving” the problem and sending the person home. Often, the patient did not even return for surgical follow-up because, in theory, the problem was solved.
Over time, I believe that surgeons learned to talk to the patient, understanding that there is a whole process that even involves creating a bond with the individual who underwent the surgical procedure. Within this process, the importance of the mental health of patients was recognized, and how common it is to confuse a degree of malnutrition with a mental disorder.
Even though I am not a nutritionist, I need to know the difference between a case of malnutrition and depression. So, it is a whole set of factors that needs to be worked on like an orchestra. It is not necessary for this work to be done in the same physical space, but dialogue is important.
Of course, there are things that the patient will only share with the psychologist or with the surgeon, but there are also pieces of information that need to be shared for positive management. I have had patients who were afraid to go back to the nutritionist because they did not lose weight. If they are afraid, it is because the professional is guiding them incorrectly.
What tips would you give to clinicians regarding the psychological approach to people with obesity?
Accessibility is crucial. When someone tells me they are dealing with obesity and depression, I usually ask, “Did you know you have two chronic diseases?” It is essential to explain these concepts because the patient may often think they are free after a successful diet and weight loss, which is not true because of the high relapse associated with obesity. Depression and anxiety follow similar patterns. If the same person wears prescription glasses, I interact by saying, “Did you know you have three chronic diseases?” This question often causes surprise. “I hadn’t thought of that.”
It is essential to use accessible language for the patient to understand the functioning of the disease. More important than choosing a treatment approach is understanding the pathophysiology of obesity and its psychological impact. This avoids a one-size-fits-all approach for all patients.
For example, the impact on someone who developed obesity in childhood after suffering physical, moral, or sexual abuse will probably be deeper than on someone in a healthy family who gained weight after becoming sedentary. Each life story requires a personalized approach.
Sometimes, a patient with mild obesity (grade 1) may not seem to need specific interventions at first glance, but it is crucial to listen to his or her story. Similarly, patients with severe obesity (grades 3 or 4) who resist surgery are entitled to other treatment options, and this is perfectly valid. Therefore, it is always important to ask, “Who is this person? What does obesity represent in their story?” Then propose the most appropriate treatment.
Ms. Levy reported having no relevant financial relationships.
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Increasingly recognized as a multifactorial disease, obesity demands an approach that involves multiple healthcare professionals. For psychologist Andréa Levy, coordinator and founder of the nongovernmental organization Obesity Brazil, addressing the patient’s “psychological weight” is crucial.
In an interview with this news organization, Ms. Levy, who was one of the speakers at the International Congress on Obesity in 2024, emphasized the importance of integrating emotional and behavioral aspects into treatment, because these factors often influence eating habits and weight gain.
She also highlighted the essential collaboration between endocrinologists, nutritionists, psychiatrists, and psychologists, who must work together to provide comprehensive and effective care to patients.
How do psychological factors affect the treatment of obesity?
Psychological factors are important triggers for weight gain. As the degree of obesity increases, so does the predisposition to mental health problems such as anxiety, mood disorders, personality disorders, and eating disorders. Understanding these factors is important because accurate psychodiagnosis is essential for effective disease treatment.
Without a proper diagnosis, the treatment may be incomplete and omit relevant factors. For example, a person with undiagnosed depression who is starting treatment for weight loss may feel discouraged and low on energy. He or she may wrongly attribute these symptoms to the diet or surgery. Similarly, someone undergoing bariatric surgery may confuse malnutrition symptoms with depression, resulting in inadequate treatment with antidepressants and possible iatrogenic complications.
Furthermore, psychotherapy and psychological follow-up are essential to help the individual organize better and understand the treatment and the disease itself. This is especially important in stigmatized diseases and those subject to prejudice such as obesity, where understanding and acceptance are often challenging, which affects treatment adherence.
Is the collaboration between psychologist and psychiatrist always necessary?
Often, it is necessary to have the support of both a psychologist and a psychiatrist. The process generally begins with a good psychodiagnosis. Initially, there may not be a case that requires treatment, but it is important to perform this evaluation to rule out any issues.
The follow-up, unlike weekly psychotherapy, can be monthly or at an interval agreed on with the patient. It is crucial to help him or her navigate the various stages of obesity treatment. For example, the patient may be going through a period of mourning or separation, or a happier moment, such as the beginning of a relationship or the birth of a child in the family. These moments affect eating habits and need to be well managed.
Depending on the degree of the pathology, such as depression, severe binge-eating disorder, or personality disorders, the psychologist works in conjunction with the psychiatrist. When we talk about obesity, we are possibly also talking about a psychiatric population because it is a disease that, besides being highly recurrent, involves many other factors, such as the gaze of others, difficulty with dressing, body pains, mobility, and relationships. Therefore, having this disease alone is already a trigger for disorders such as depression.
What is the main evidence regarding the psychological follow-up of patients with obesity?
Several studies have investigated the relationship between obesity and mental health. Research indicates that the greater the obesity, the higher the likelihood of a positive diagnosis for a psychiatric disorder. Additionally, there is evidence of the benefits of psychological treatment for patients with obesity.
A study published in the Journal of Clinical Endocrinology and Metabolism addressed the impact of cognitive-behavioral therapy (CBT), which helps patients manage goals and treat maladaptive behaviors such as binge-eating disorders. CBT has a modest effect on weight loss, but its integration as part of a lifestyle modification amplifies the results of this loss.
Recent research also shows that weight loss through bariatric surgery offers significant psychological benefits. In the past, it was believed that this procedure could cause depression and other severe psychiatric disorders, but it is now more than proven that weight loss, when done properly and without misconduct or malnutrition, improves psychological and psychiatric issues.
How does psychological follow-up affect the use of medication during obesity treatment?
Many people who take medications, such as corticosteroids for chronic pain or psychiatric medications, may experience weight gain. It is essential to discuss these issues with the psychiatrist because if the patient already has a predisposition to weight gain, medication X should be chosen instead of medication Y, or the dosage should be adjusted. The psychiatrist needs to understand obesity to medicate correctly. Other types of medication, such as chemotherapeutics, may also cause weight gain, often resulting in more abdominal obesity.
There is also lipedema, a hormone-dependent disease that is different from obesity. In this disease, the person gains weight mainly in the legs and arms. In this case, bariatric surgery may result in weight loss only in specific areas, causing disproportionality and difficulty in understanding for the patient. Therefore, when treating obesity, it is important to analyze the patient from all angles: psychological, physiologic, and physical, considering the diversity of the body, its functioning, and hormonal reactions.
Although psychologists do not prescribe medications, they often explain their functioning to the patient. For example, if a patient is taking a glucagon-like peptide 1 analog and experiences initial nausea, he or she may stop using the treatment because the wrong dose had been started. In this case, the psychologist can explain how the medication works and encourage the patient to discuss adjustments with the doctor, avoiding premature discontinuation.
How has the mental health follow-up of patients with obesity evolved over the years?
I started working with people with obesity 25 years ago, when I myself underwent bariatric surgery. At that time, surgeons were used to “solving” the problem and sending the person home. Often, the patient did not even return for surgical follow-up because, in theory, the problem was solved.
Over time, I believe that surgeons learned to talk to the patient, understanding that there is a whole process that even involves creating a bond with the individual who underwent the surgical procedure. Within this process, the importance of the mental health of patients was recognized, and how common it is to confuse a degree of malnutrition with a mental disorder.
Even though I am not a nutritionist, I need to know the difference between a case of malnutrition and depression. So, it is a whole set of factors that needs to be worked on like an orchestra. It is not necessary for this work to be done in the same physical space, but dialogue is important.
Of course, there are things that the patient will only share with the psychologist or with the surgeon, but there are also pieces of information that need to be shared for positive management. I have had patients who were afraid to go back to the nutritionist because they did not lose weight. If they are afraid, it is because the professional is guiding them incorrectly.
What tips would you give to clinicians regarding the psychological approach to people with obesity?
Accessibility is crucial. When someone tells me they are dealing with obesity and depression, I usually ask, “Did you know you have two chronic diseases?” It is essential to explain these concepts because the patient may often think they are free after a successful diet and weight loss, which is not true because of the high relapse associated with obesity. Depression and anxiety follow similar patterns. If the same person wears prescription glasses, I interact by saying, “Did you know you have three chronic diseases?” This question often causes surprise. “I hadn’t thought of that.”
It is essential to use accessible language for the patient to understand the functioning of the disease. More important than choosing a treatment approach is understanding the pathophysiology of obesity and its psychological impact. This avoids a one-size-fits-all approach for all patients.
For example, the impact on someone who developed obesity in childhood after suffering physical, moral, or sexual abuse will probably be deeper than on someone in a healthy family who gained weight after becoming sedentary. Each life story requires a personalized approach.
Sometimes, a patient with mild obesity (grade 1) may not seem to need specific interventions at first glance, but it is crucial to listen to his or her story. Similarly, patients with severe obesity (grades 3 or 4) who resist surgery are entitled to other treatment options, and this is perfectly valid. Therefore, it is always important to ask, “Who is this person? What does obesity represent in their story?” Then propose the most appropriate treatment.
Ms. Levy reported having no relevant financial relationships.
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Increasingly recognized as a multifactorial disease, obesity demands an approach that involves multiple healthcare professionals. For psychologist Andréa Levy, coordinator and founder of the nongovernmental organization Obesity Brazil, addressing the patient’s “psychological weight” is crucial.
In an interview with this news organization, Ms. Levy, who was one of the speakers at the International Congress on Obesity in 2024, emphasized the importance of integrating emotional and behavioral aspects into treatment, because these factors often influence eating habits and weight gain.
She also highlighted the essential collaboration between endocrinologists, nutritionists, psychiatrists, and psychologists, who must work together to provide comprehensive and effective care to patients.
How do psychological factors affect the treatment of obesity?
Psychological factors are important triggers for weight gain. As the degree of obesity increases, so does the predisposition to mental health problems such as anxiety, mood disorders, personality disorders, and eating disorders. Understanding these factors is important because accurate psychodiagnosis is essential for effective disease treatment.
Without a proper diagnosis, the treatment may be incomplete and omit relevant factors. For example, a person with undiagnosed depression who is starting treatment for weight loss may feel discouraged and low on energy. He or she may wrongly attribute these symptoms to the diet or surgery. Similarly, someone undergoing bariatric surgery may confuse malnutrition symptoms with depression, resulting in inadequate treatment with antidepressants and possible iatrogenic complications.
Furthermore, psychotherapy and psychological follow-up are essential to help the individual organize better and understand the treatment and the disease itself. This is especially important in stigmatized diseases and those subject to prejudice such as obesity, where understanding and acceptance are often challenging, which affects treatment adherence.
Is the collaboration between psychologist and psychiatrist always necessary?
Often, it is necessary to have the support of both a psychologist and a psychiatrist. The process generally begins with a good psychodiagnosis. Initially, there may not be a case that requires treatment, but it is important to perform this evaluation to rule out any issues.
The follow-up, unlike weekly psychotherapy, can be monthly or at an interval agreed on with the patient. It is crucial to help him or her navigate the various stages of obesity treatment. For example, the patient may be going through a period of mourning or separation, or a happier moment, such as the beginning of a relationship or the birth of a child in the family. These moments affect eating habits and need to be well managed.
Depending on the degree of the pathology, such as depression, severe binge-eating disorder, or personality disorders, the psychologist works in conjunction with the psychiatrist. When we talk about obesity, we are possibly also talking about a psychiatric population because it is a disease that, besides being highly recurrent, involves many other factors, such as the gaze of others, difficulty with dressing, body pains, mobility, and relationships. Therefore, having this disease alone is already a trigger for disorders such as depression.
What is the main evidence regarding the psychological follow-up of patients with obesity?
Several studies have investigated the relationship between obesity and mental health. Research indicates that the greater the obesity, the higher the likelihood of a positive diagnosis for a psychiatric disorder. Additionally, there is evidence of the benefits of psychological treatment for patients with obesity.
A study published in the Journal of Clinical Endocrinology and Metabolism addressed the impact of cognitive-behavioral therapy (CBT), which helps patients manage goals and treat maladaptive behaviors such as binge-eating disorders. CBT has a modest effect on weight loss, but its integration as part of a lifestyle modification amplifies the results of this loss.
Recent research also shows that weight loss through bariatric surgery offers significant psychological benefits. In the past, it was believed that this procedure could cause depression and other severe psychiatric disorders, but it is now more than proven that weight loss, when done properly and without misconduct or malnutrition, improves psychological and psychiatric issues.
How does psychological follow-up affect the use of medication during obesity treatment?
Many people who take medications, such as corticosteroids for chronic pain or psychiatric medications, may experience weight gain. It is essential to discuss these issues with the psychiatrist because if the patient already has a predisposition to weight gain, medication X should be chosen instead of medication Y, or the dosage should be adjusted. The psychiatrist needs to understand obesity to medicate correctly. Other types of medication, such as chemotherapeutics, may also cause weight gain, often resulting in more abdominal obesity.
There is also lipedema, a hormone-dependent disease that is different from obesity. In this disease, the person gains weight mainly in the legs and arms. In this case, bariatric surgery may result in weight loss only in specific areas, causing disproportionality and difficulty in understanding for the patient. Therefore, when treating obesity, it is important to analyze the patient from all angles: psychological, physiologic, and physical, considering the diversity of the body, its functioning, and hormonal reactions.
Although psychologists do not prescribe medications, they often explain their functioning to the patient. For example, if a patient is taking a glucagon-like peptide 1 analog and experiences initial nausea, he or she may stop using the treatment because the wrong dose had been started. In this case, the psychologist can explain how the medication works and encourage the patient to discuss adjustments with the doctor, avoiding premature discontinuation.
How has the mental health follow-up of patients with obesity evolved over the years?
I started working with people with obesity 25 years ago, when I myself underwent bariatric surgery. At that time, surgeons were used to “solving” the problem and sending the person home. Often, the patient did not even return for surgical follow-up because, in theory, the problem was solved.
Over time, I believe that surgeons learned to talk to the patient, understanding that there is a whole process that even involves creating a bond with the individual who underwent the surgical procedure. Within this process, the importance of the mental health of patients was recognized, and how common it is to confuse a degree of malnutrition with a mental disorder.
Even though I am not a nutritionist, I need to know the difference between a case of malnutrition and depression. So, it is a whole set of factors that needs to be worked on like an orchestra. It is not necessary for this work to be done in the same physical space, but dialogue is important.
Of course, there are things that the patient will only share with the psychologist or with the surgeon, but there are also pieces of information that need to be shared for positive management. I have had patients who were afraid to go back to the nutritionist because they did not lose weight. If they are afraid, it is because the professional is guiding them incorrectly.
What tips would you give to clinicians regarding the psychological approach to people with obesity?
Accessibility is crucial. When someone tells me they are dealing with obesity and depression, I usually ask, “Did you know you have two chronic diseases?” It is essential to explain these concepts because the patient may often think they are free after a successful diet and weight loss, which is not true because of the high relapse associated with obesity. Depression and anxiety follow similar patterns. If the same person wears prescription glasses, I interact by saying, “Did you know you have three chronic diseases?” This question often causes surprise. “I hadn’t thought of that.”
It is essential to use accessible language for the patient to understand the functioning of the disease. More important than choosing a treatment approach is understanding the pathophysiology of obesity and its psychological impact. This avoids a one-size-fits-all approach for all patients.
For example, the impact on someone who developed obesity in childhood after suffering physical, moral, or sexual abuse will probably be deeper than on someone in a healthy family who gained weight after becoming sedentary. Each life story requires a personalized approach.
Sometimes, a patient with mild obesity (grade 1) may not seem to need specific interventions at first glance, but it is crucial to listen to his or her story. Similarly, patients with severe obesity (grades 3 or 4) who resist surgery are entitled to other treatment options, and this is perfectly valid. Therefore, it is always important to ask, “Who is this person? What does obesity represent in their story?” Then propose the most appropriate treatment.
Ms. Levy reported having no relevant financial relationships.
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Promising New Data Support GLP-1s for Dementia Prevention
PHILADELPHIA –
In the phase 2b ELAD clinical trial, adults with early-stage Alzheimer’s disease taking the GLP-1 receptor agonist liraglutide exhibited slower decline in memory and thinking and experienced less brain atrophy over 12 months, compared with placebo.
“The slower loss of brain volume suggests liraglutide protects the brain, much like statins protect the heart,” study chief Paul Edison, MD, PhD, with Imperial College London, London, England, said in a statement.
“While further research is needed, liraglutide may work through various mechanisms, such as reducing inflammation in the brain, lowering insulin resistance and the toxic effects of Alzheimer’s biomarkers amyloid beta and tau, and improving how the brain’s nerve cells communicate,” Dr. Edison said.
He presented the study results at the 2024 Alzheimer’s Association International Conference (AAIC).
Brain Benefits
Liraglutide has previously demonstrated promising neuroprotective effects in animal models of Alzheimer’s disease and epidemiologic studies.
In ELAD, 204 patients with mild to moderate Alzheimer’s disease were randomly allocated (1:1) to a daily subcutaneous injection of up to 1.8 mg of liraglutide or placebo for 12 months; 80 patients in the liraglutide group and 89 in the placebo group completed the study.
Brain MRI was performed at baseline and at 12 months, along with neuropsychometric evaluation and 18F-fludeoxyglucose PET.
The study’s primary endpoint — change in the cerebral glucose metabolic rate in the cortical regions of the brain (hippocampus, medial temporal lobe, and posterior cingulate) — was not met.
However, patients taking liraglutide experienced a significant slowing of cognitive decline, compared with placebo group (P = .01), which was a key secondary outcome, calculated as a composite score of 18 different tests of memory, comprehension, language, and spatial orientation.
Although the study was not powered to assess cognitive changes, adults taking liraglutide had an 18% slower decline in cognitive function over 12 months, compared with those on placebo, Dr. Edison reported.
In addition, patients treated with liraglutide had nearly 50% less volume loss in several areas of the brain involved in memory, language, and decision-making, including frontal, temporal, parietal, and total gray matter, as measured by MRI.
Liraglutide daily subcutaneous injections were safe and well tolerated in patients with Alzheimer’s disease, Dr. Edison reported. There were 25 serious side effects — 18 in the placebo group and 7 in the liraglutide group — and most were considered unlikely to be related to the study treatment. There were no deaths.
Promising, Preliminary
This study shows a positive effect of liraglutide on the brain in terms of “slowing down of brain atrophy and slowing down the rate of cognitive decline,” said Howard Fillit, MD, founding executive director of the Alzheimer’s Drug Discovery Foundation, who wasn’t involved in the study.
Heather Snyder, PhD, vice-president of medical and scientific relations at the Alzheimer’s Association, said it’s “interesting” to see slowing of brain volume loss and some cognitive benefit “especially as the study was not powered necessarily to see some of those changes. The fact that they did see these changes in this small study provides a window into what may happen, but we certainly need larger phase 3 studies.”
In a statement from the UK nonprofit Science Media Centre, Tara Spires-Jones, PhD, president of the British Neuroscience Association and group leader at the UK Dementia Research Institute, called the data “promising.”
“There are clear links from strong data in the field between vascular risk factors including diabetes and obesity being associated with increased risk of dementia. The GLP-1 drug should help reduce these risk factors as well as potentially directly protecting brain cells,” Dr. Spires-Jones said.
However, she said “more research in bigger trials is needed to confirm whether this type of treatment will be effective in people with Alzheimer’s disease.”
Stephen Evans, MSc, emeritus professor, London School of Hygiene and Tropical Medicine, noted that the repurposing of drugs is “an important avenue of research but there is a lot of uncertainty here.”
He cautioned that the “50% brain volume change may not translate to important cognitive effects, and reporting only on those who completed the full 52 weeks of treatment could bring bias into the results. It sounds like it is worth pursuing a larger trial, but these results cannot demonstrate that liraglutide can protect against dementia.”
The ongoing phase 3 EVOKE trial is investigating the effects of the GLP-1 receptor agonist semaglutide in early Alzheimer’s disease.
Funding for the study was provided by Alzheimer’s Society UK, Alzheimer’s Drug Discovery Foundation, Novo Nordisk, John and Lucille Van Geest Foundation, and the National Institute for Health and Care Research Biomedical Research Centre. Dr. Edison, Dr. Fillit, Dr. Snyder, Mr. Evans, and Dr. Spires-Jones had no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
PHILADELPHIA –
In the phase 2b ELAD clinical trial, adults with early-stage Alzheimer’s disease taking the GLP-1 receptor agonist liraglutide exhibited slower decline in memory and thinking and experienced less brain atrophy over 12 months, compared with placebo.
“The slower loss of brain volume suggests liraglutide protects the brain, much like statins protect the heart,” study chief Paul Edison, MD, PhD, with Imperial College London, London, England, said in a statement.
“While further research is needed, liraglutide may work through various mechanisms, such as reducing inflammation in the brain, lowering insulin resistance and the toxic effects of Alzheimer’s biomarkers amyloid beta and tau, and improving how the brain’s nerve cells communicate,” Dr. Edison said.
He presented the study results at the 2024 Alzheimer’s Association International Conference (AAIC).
Brain Benefits
Liraglutide has previously demonstrated promising neuroprotective effects in animal models of Alzheimer’s disease and epidemiologic studies.
In ELAD, 204 patients with mild to moderate Alzheimer’s disease were randomly allocated (1:1) to a daily subcutaneous injection of up to 1.8 mg of liraglutide or placebo for 12 months; 80 patients in the liraglutide group and 89 in the placebo group completed the study.
Brain MRI was performed at baseline and at 12 months, along with neuropsychometric evaluation and 18F-fludeoxyglucose PET.
The study’s primary endpoint — change in the cerebral glucose metabolic rate in the cortical regions of the brain (hippocampus, medial temporal lobe, and posterior cingulate) — was not met.
However, patients taking liraglutide experienced a significant slowing of cognitive decline, compared with placebo group (P = .01), which was a key secondary outcome, calculated as a composite score of 18 different tests of memory, comprehension, language, and spatial orientation.
Although the study was not powered to assess cognitive changes, adults taking liraglutide had an 18% slower decline in cognitive function over 12 months, compared with those on placebo, Dr. Edison reported.
In addition, patients treated with liraglutide had nearly 50% less volume loss in several areas of the brain involved in memory, language, and decision-making, including frontal, temporal, parietal, and total gray matter, as measured by MRI.
Liraglutide daily subcutaneous injections were safe and well tolerated in patients with Alzheimer’s disease, Dr. Edison reported. There were 25 serious side effects — 18 in the placebo group and 7 in the liraglutide group — and most were considered unlikely to be related to the study treatment. There were no deaths.
Promising, Preliminary
This study shows a positive effect of liraglutide on the brain in terms of “slowing down of brain atrophy and slowing down the rate of cognitive decline,” said Howard Fillit, MD, founding executive director of the Alzheimer’s Drug Discovery Foundation, who wasn’t involved in the study.
Heather Snyder, PhD, vice-president of medical and scientific relations at the Alzheimer’s Association, said it’s “interesting” to see slowing of brain volume loss and some cognitive benefit “especially as the study was not powered necessarily to see some of those changes. The fact that they did see these changes in this small study provides a window into what may happen, but we certainly need larger phase 3 studies.”
In a statement from the UK nonprofit Science Media Centre, Tara Spires-Jones, PhD, president of the British Neuroscience Association and group leader at the UK Dementia Research Institute, called the data “promising.”
“There are clear links from strong data in the field between vascular risk factors including diabetes and obesity being associated with increased risk of dementia. The GLP-1 drug should help reduce these risk factors as well as potentially directly protecting brain cells,” Dr. Spires-Jones said.
However, she said “more research in bigger trials is needed to confirm whether this type of treatment will be effective in people with Alzheimer’s disease.”
Stephen Evans, MSc, emeritus professor, London School of Hygiene and Tropical Medicine, noted that the repurposing of drugs is “an important avenue of research but there is a lot of uncertainty here.”
He cautioned that the “50% brain volume change may not translate to important cognitive effects, and reporting only on those who completed the full 52 weeks of treatment could bring bias into the results. It sounds like it is worth pursuing a larger trial, but these results cannot demonstrate that liraglutide can protect against dementia.”
The ongoing phase 3 EVOKE trial is investigating the effects of the GLP-1 receptor agonist semaglutide in early Alzheimer’s disease.
Funding for the study was provided by Alzheimer’s Society UK, Alzheimer’s Drug Discovery Foundation, Novo Nordisk, John and Lucille Van Geest Foundation, and the National Institute for Health and Care Research Biomedical Research Centre. Dr. Edison, Dr. Fillit, Dr. Snyder, Mr. Evans, and Dr. Spires-Jones had no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
PHILADELPHIA –
In the phase 2b ELAD clinical trial, adults with early-stage Alzheimer’s disease taking the GLP-1 receptor agonist liraglutide exhibited slower decline in memory and thinking and experienced less brain atrophy over 12 months, compared with placebo.
“The slower loss of brain volume suggests liraglutide protects the brain, much like statins protect the heart,” study chief Paul Edison, MD, PhD, with Imperial College London, London, England, said in a statement.
“While further research is needed, liraglutide may work through various mechanisms, such as reducing inflammation in the brain, lowering insulin resistance and the toxic effects of Alzheimer’s biomarkers amyloid beta and tau, and improving how the brain’s nerve cells communicate,” Dr. Edison said.
He presented the study results at the 2024 Alzheimer’s Association International Conference (AAIC).
Brain Benefits
Liraglutide has previously demonstrated promising neuroprotective effects in animal models of Alzheimer’s disease and epidemiologic studies.
In ELAD, 204 patients with mild to moderate Alzheimer’s disease were randomly allocated (1:1) to a daily subcutaneous injection of up to 1.8 mg of liraglutide or placebo for 12 months; 80 patients in the liraglutide group and 89 in the placebo group completed the study.
Brain MRI was performed at baseline and at 12 months, along with neuropsychometric evaluation and 18F-fludeoxyglucose PET.
The study’s primary endpoint — change in the cerebral glucose metabolic rate in the cortical regions of the brain (hippocampus, medial temporal lobe, and posterior cingulate) — was not met.
However, patients taking liraglutide experienced a significant slowing of cognitive decline, compared with placebo group (P = .01), which was a key secondary outcome, calculated as a composite score of 18 different tests of memory, comprehension, language, and spatial orientation.
Although the study was not powered to assess cognitive changes, adults taking liraglutide had an 18% slower decline in cognitive function over 12 months, compared with those on placebo, Dr. Edison reported.
In addition, patients treated with liraglutide had nearly 50% less volume loss in several areas of the brain involved in memory, language, and decision-making, including frontal, temporal, parietal, and total gray matter, as measured by MRI.
Liraglutide daily subcutaneous injections were safe and well tolerated in patients with Alzheimer’s disease, Dr. Edison reported. There were 25 serious side effects — 18 in the placebo group and 7 in the liraglutide group — and most were considered unlikely to be related to the study treatment. There were no deaths.
Promising, Preliminary
This study shows a positive effect of liraglutide on the brain in terms of “slowing down of brain atrophy and slowing down the rate of cognitive decline,” said Howard Fillit, MD, founding executive director of the Alzheimer’s Drug Discovery Foundation, who wasn’t involved in the study.
Heather Snyder, PhD, vice-president of medical and scientific relations at the Alzheimer’s Association, said it’s “interesting” to see slowing of brain volume loss and some cognitive benefit “especially as the study was not powered necessarily to see some of those changes. The fact that they did see these changes in this small study provides a window into what may happen, but we certainly need larger phase 3 studies.”
In a statement from the UK nonprofit Science Media Centre, Tara Spires-Jones, PhD, president of the British Neuroscience Association and group leader at the UK Dementia Research Institute, called the data “promising.”
“There are clear links from strong data in the field between vascular risk factors including diabetes and obesity being associated with increased risk of dementia. The GLP-1 drug should help reduce these risk factors as well as potentially directly protecting brain cells,” Dr. Spires-Jones said.
However, she said “more research in bigger trials is needed to confirm whether this type of treatment will be effective in people with Alzheimer’s disease.”
Stephen Evans, MSc, emeritus professor, London School of Hygiene and Tropical Medicine, noted that the repurposing of drugs is “an important avenue of research but there is a lot of uncertainty here.”
He cautioned that the “50% brain volume change may not translate to important cognitive effects, and reporting only on those who completed the full 52 weeks of treatment could bring bias into the results. It sounds like it is worth pursuing a larger trial, but these results cannot demonstrate that liraglutide can protect against dementia.”
The ongoing phase 3 EVOKE trial is investigating the effects of the GLP-1 receptor agonist semaglutide in early Alzheimer’s disease.
Funding for the study was provided by Alzheimer’s Society UK, Alzheimer’s Drug Discovery Foundation, Novo Nordisk, John and Lucille Van Geest Foundation, and the National Institute for Health and Care Research Biomedical Research Centre. Dr. Edison, Dr. Fillit, Dr. Snyder, Mr. Evans, and Dr. Spires-Jones had no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM AAIC 2024
Red Meat Tied to Increased Dementia Risk
PHILADELPHIA – preliminary research shows.
Study participants who consumed 0.25 or more servings of processed meat per day, or roughly two servings per week, had a 15% higher risk for dementia, compared with those who consumed less than 0.10 serving per day, which is about three servings per month.
“Our study found a higher intake of red meat — particularly processed red meat — was associated with a higher risk of developing dementia, as well as worse cognition,” said study author Yuhan Li, MHS, research assistant, Channing Division of Network Medicine, Brigham and Women’s Hospital, Boston, Massachusetts.
However, the study also showed that replacing processed red meat with nuts and legumes could potentially lower this increased risk.
The findings were presented on at the 2024 Alzheimer’s Association International Conference (AAIC).
Inconsistent Research
Previous studies have shown an inconsistent association between red meat intake and cognitive health.
To assess the relationship between diet and dementia, the researchers used data from the Nurses’ Health Study, which began recruiting female registered nurses aged 30-55 years in 1976, and the Health Professionals Follow-Up Study, which began recruiting male health professionals aged 40-75 in 1986.
They assessed processed red meat intake by validated semi-quantitative food frequency questionnaires administered every 2-4 years. Participants were asked how often they consumed a serving of processed red meat.
Investigators also assessed intake of unprocessed red meat, including beef, pork, or lamb as a main dish, in a sandwich or hamburger, or in a mixed dish.
The investigators also looked at participants’ intake of nuts and legumes.
Dementia outcome was a composite endpoint of self-reported dementia and dementia-related death. “Specifically, participants reported a physician diagnosis of Alzheimer’s disease or other forms of dementia by questionnaire. Deaths were identified through state vital statistics records, the National Death Index, family reports, and the postal system,” said Ms. Li.
Three Cognitive Outcomes
Researchers examined three outcomes: dementia, subjective cognitive decline, and objective cognitive function. For dementia, they ascertained incident cases in 87,424 individuals in the UK’s National Health Service database without Parkinson’s disease or baseline dementia, stroke, or cancer.
They longitudinally collected information on subjective cognitive decline from 33,908 Nurses’ Health Study participants and 10,058 participants in the Health Professionals Follow-Up Study.
Cognitive function was assessed using the Telephone Interview for Cognitive Status (1995-2008) in a subset of 17,458 Nurses’ Health Study participants.
Over a follow-up of 38 years (1980-2018), there were 6856 dementia cases in the Nurses’ Health Study. Participants with processed red meat intake of 0.25 or more serving/day, compared with less than 0.10 serving/day, had 15% higher risk for dementia (hazard ratio [HR], 1.15; 95% CI, 1.08-1.23; P < .001).
In addition to an increased risk for dementia, intake of processed red meat was associated with accelerated cognitive aging in global cognition (1.61 years per 1–serving/day increment; 95% CI, 0.20, 3.03) and verbal memory (1.69 years per 1–serving/day increment; 95% CI, 0.13, 3.25; both P = .03).
Participants with processed red meat intake of 0.25 or more serving/day had a 14% higher likelihood of subjective cognitive decline, compared with those with intake less than 0.10 serving/day (odds ratio [OR], 1.14; 95% CI, 1.04-1.24; P = .004).
For unprocessed red meat, consuming 1.00 or more serving/day versus less than 0.50 serving/day was associated with a 16% higher likelihood of subjective cognitive decline (OR, 1.16; 95% CI, 1.04-1.30; P = .02).
Substitution Analysis
Researchers modeled the effects of replacing 1 serving/day of processed red meat with 1 serving/day of nuts and legumes on cognitive outcomes. They did this by treating food intakes as continuous variables and calculating the differences in coefficients of the two food items.
They found that substituting legumes and nuts was associated with a 23% lower risk for dementia (HR, 0.77; 95% CI, 0.69-0.86), 1.37 fewer years of cognitive aging (95% CI, –2.49 to –0.25), and 20% lower odds of subjective cognitive decline (OR, 0.80, 95% CI, 0.69-0.92).
The research cannot determine whether it’s the processing method itself or the type of red meat that affects cognition, Ms. Li cautioned.
“Our study is an epidemiologic study, not a biological mechanism study, but based on our findings, red meat may be related to worse cognition, and processed red meat may add additional risk,” she said.
She also noted that because the study focused solely on red meats, the study cannot determine the potential on the impact of other processed meats on cognition.
Although the study doesn’t address a possible mechanism linking processed red meat with cognition, Ms. Li said it’s possible such meats have high levels of relatively harmful substances, such as nitrites, N-nitroso compounds, and sodium, and that “these carry the additional risk to brain health.”
There are currently no specific guidelines regarding the “safe” amount of processed meat consumption specifically related to cognition, she said.
The study is important because of its large sample size, long follow-up period, and inclusion of repeated measurements of diet, the investigators noted. In addition, researchers assessed both processed and unprocessed red meat and evaluated multiple cognitive outcomes.
The investigators plan to assess the association between other modifiable factors and cognitive health.
Experts Weigh In
In a comment, Claire Sexton, DPhil, senior director of scientific programs and outreach at the Alzheimer’s Association, agreed past studies on the topic have been “mixed,” with only some studies reporting links between cognition or dementia and processed red meat.
Another unique aspect of the study, said Dr. Sexton, was the replacement analysis showing the brain benefits of eating nuts and legumes in place of processed red meat. “So, it’s not just suggesting to people what not to do, but also what they can be doing instead.”
That’s why this large study with more than 130,000 adults that tracked individuals for close to 40 years in some cases “is so valuable,” she added.
In a release from the Science Media Centre in the United Kingdom, several other experts commented on the study. Among them, Kevin McConway, PhD, emeritus professor of applied statistics at the Open University, Milton Keynes, England, said that “it’s pretty well impossible to get a clear message from the information that is available so far about this research. It is a conference paper, and all we have seen so far is a press release, a brief summary of the research, and a diagram. There isn’t a detailed, peer-reviewed research report, not yet anyway. Putting out limited information like this isn’t the right way to report science.”
Dr. McConway also noted that the observational study recorded participants’ diets and dementia diagnoses over several years without assigning specific diets. Those who ate more red processed meat had higher rates of dementia and cognitive decline. However, it’s unclear if these differences are caused by red meat consumption or other factors, such as diet, age, ethnicity, or location.
Researchers typically adjust for these factors, but the available information doesn’t specify what adjustments were made or their impact, he noted, and without detailed data, it’s impossible to evaluate the study’s quality. Although eating more red processed meat might increase dementia risk, more research is needed to confirm this, Dr. McConway added.
Also commenting, Sebastian Walsh, a National Institute for Health and Care Research doctoral fellow who researches population-level approaches to dementia risk reduction at University of Cambridge, Cambridge, England, said that without seeing the full paper, it’s difficult to know exactly what to make of the study’s findings.
“On the surface, this is a large and long study. But it isn’t clear how the analysis was done — specifically what other factors were taken into account when looking at this apparent relationship between red meat and dementia.
“Despite a lot of research looking at specific foods and different diseases, the basic public health advice that eating a healthy, balanced diet is good for health is essentially unchanged. Most people know and accept this. What is most important is to find ways of supporting people, particularly those from poorer backgrounds, to follow this advice and address the obesity epidemic,” said Mr. Walsh.
The study was funded by a National Institutes of Health research grant. Ms. Li reports no relevant conflicts of interest. Dr. Sexton, Dr. McConway, and Mr. Walsh report no relevant disclosures.
A version of this article first appeared on Medscape.com.
PHILADELPHIA – preliminary research shows.
Study participants who consumed 0.25 or more servings of processed meat per day, or roughly two servings per week, had a 15% higher risk for dementia, compared with those who consumed less than 0.10 serving per day, which is about three servings per month.
“Our study found a higher intake of red meat — particularly processed red meat — was associated with a higher risk of developing dementia, as well as worse cognition,” said study author Yuhan Li, MHS, research assistant, Channing Division of Network Medicine, Brigham and Women’s Hospital, Boston, Massachusetts.
However, the study also showed that replacing processed red meat with nuts and legumes could potentially lower this increased risk.
The findings were presented on at the 2024 Alzheimer’s Association International Conference (AAIC).
Inconsistent Research
Previous studies have shown an inconsistent association between red meat intake and cognitive health.
To assess the relationship between diet and dementia, the researchers used data from the Nurses’ Health Study, which began recruiting female registered nurses aged 30-55 years in 1976, and the Health Professionals Follow-Up Study, which began recruiting male health professionals aged 40-75 in 1986.
They assessed processed red meat intake by validated semi-quantitative food frequency questionnaires administered every 2-4 years. Participants were asked how often they consumed a serving of processed red meat.
Investigators also assessed intake of unprocessed red meat, including beef, pork, or lamb as a main dish, in a sandwich or hamburger, or in a mixed dish.
The investigators also looked at participants’ intake of nuts and legumes.
Dementia outcome was a composite endpoint of self-reported dementia and dementia-related death. “Specifically, participants reported a physician diagnosis of Alzheimer’s disease or other forms of dementia by questionnaire. Deaths were identified through state vital statistics records, the National Death Index, family reports, and the postal system,” said Ms. Li.
Three Cognitive Outcomes
Researchers examined three outcomes: dementia, subjective cognitive decline, and objective cognitive function. For dementia, they ascertained incident cases in 87,424 individuals in the UK’s National Health Service database without Parkinson’s disease or baseline dementia, stroke, or cancer.
They longitudinally collected information on subjective cognitive decline from 33,908 Nurses’ Health Study participants and 10,058 participants in the Health Professionals Follow-Up Study.
Cognitive function was assessed using the Telephone Interview for Cognitive Status (1995-2008) in a subset of 17,458 Nurses’ Health Study participants.
Over a follow-up of 38 years (1980-2018), there were 6856 dementia cases in the Nurses’ Health Study. Participants with processed red meat intake of 0.25 or more serving/day, compared with less than 0.10 serving/day, had 15% higher risk for dementia (hazard ratio [HR], 1.15; 95% CI, 1.08-1.23; P < .001).
In addition to an increased risk for dementia, intake of processed red meat was associated with accelerated cognitive aging in global cognition (1.61 years per 1–serving/day increment; 95% CI, 0.20, 3.03) and verbal memory (1.69 years per 1–serving/day increment; 95% CI, 0.13, 3.25; both P = .03).
Participants with processed red meat intake of 0.25 or more serving/day had a 14% higher likelihood of subjective cognitive decline, compared with those with intake less than 0.10 serving/day (odds ratio [OR], 1.14; 95% CI, 1.04-1.24; P = .004).
For unprocessed red meat, consuming 1.00 or more serving/day versus less than 0.50 serving/day was associated with a 16% higher likelihood of subjective cognitive decline (OR, 1.16; 95% CI, 1.04-1.30; P = .02).
Substitution Analysis
Researchers modeled the effects of replacing 1 serving/day of processed red meat with 1 serving/day of nuts and legumes on cognitive outcomes. They did this by treating food intakes as continuous variables and calculating the differences in coefficients of the two food items.
They found that substituting legumes and nuts was associated with a 23% lower risk for dementia (HR, 0.77; 95% CI, 0.69-0.86), 1.37 fewer years of cognitive aging (95% CI, –2.49 to –0.25), and 20% lower odds of subjective cognitive decline (OR, 0.80, 95% CI, 0.69-0.92).
The research cannot determine whether it’s the processing method itself or the type of red meat that affects cognition, Ms. Li cautioned.
“Our study is an epidemiologic study, not a biological mechanism study, but based on our findings, red meat may be related to worse cognition, and processed red meat may add additional risk,” she said.
She also noted that because the study focused solely on red meats, the study cannot determine the potential on the impact of other processed meats on cognition.
Although the study doesn’t address a possible mechanism linking processed red meat with cognition, Ms. Li said it’s possible such meats have high levels of relatively harmful substances, such as nitrites, N-nitroso compounds, and sodium, and that “these carry the additional risk to brain health.”
There are currently no specific guidelines regarding the “safe” amount of processed meat consumption specifically related to cognition, she said.
The study is important because of its large sample size, long follow-up period, and inclusion of repeated measurements of diet, the investigators noted. In addition, researchers assessed both processed and unprocessed red meat and evaluated multiple cognitive outcomes.
The investigators plan to assess the association between other modifiable factors and cognitive health.
Experts Weigh In
In a comment, Claire Sexton, DPhil, senior director of scientific programs and outreach at the Alzheimer’s Association, agreed past studies on the topic have been “mixed,” with only some studies reporting links between cognition or dementia and processed red meat.
Another unique aspect of the study, said Dr. Sexton, was the replacement analysis showing the brain benefits of eating nuts and legumes in place of processed red meat. “So, it’s not just suggesting to people what not to do, but also what they can be doing instead.”
That’s why this large study with more than 130,000 adults that tracked individuals for close to 40 years in some cases “is so valuable,” she added.
In a release from the Science Media Centre in the United Kingdom, several other experts commented on the study. Among them, Kevin McConway, PhD, emeritus professor of applied statistics at the Open University, Milton Keynes, England, said that “it’s pretty well impossible to get a clear message from the information that is available so far about this research. It is a conference paper, and all we have seen so far is a press release, a brief summary of the research, and a diagram. There isn’t a detailed, peer-reviewed research report, not yet anyway. Putting out limited information like this isn’t the right way to report science.”
Dr. McConway also noted that the observational study recorded participants’ diets and dementia diagnoses over several years without assigning specific diets. Those who ate more red processed meat had higher rates of dementia and cognitive decline. However, it’s unclear if these differences are caused by red meat consumption or other factors, such as diet, age, ethnicity, or location.
Researchers typically adjust for these factors, but the available information doesn’t specify what adjustments were made or their impact, he noted, and without detailed data, it’s impossible to evaluate the study’s quality. Although eating more red processed meat might increase dementia risk, more research is needed to confirm this, Dr. McConway added.
Also commenting, Sebastian Walsh, a National Institute for Health and Care Research doctoral fellow who researches population-level approaches to dementia risk reduction at University of Cambridge, Cambridge, England, said that without seeing the full paper, it’s difficult to know exactly what to make of the study’s findings.
“On the surface, this is a large and long study. But it isn’t clear how the analysis was done — specifically what other factors were taken into account when looking at this apparent relationship between red meat and dementia.
“Despite a lot of research looking at specific foods and different diseases, the basic public health advice that eating a healthy, balanced diet is good for health is essentially unchanged. Most people know and accept this. What is most important is to find ways of supporting people, particularly those from poorer backgrounds, to follow this advice and address the obesity epidemic,” said Mr. Walsh.
The study was funded by a National Institutes of Health research grant. Ms. Li reports no relevant conflicts of interest. Dr. Sexton, Dr. McConway, and Mr. Walsh report no relevant disclosures.
A version of this article first appeared on Medscape.com.
PHILADELPHIA – preliminary research shows.
Study participants who consumed 0.25 or more servings of processed meat per day, or roughly two servings per week, had a 15% higher risk for dementia, compared with those who consumed less than 0.10 serving per day, which is about three servings per month.
“Our study found a higher intake of red meat — particularly processed red meat — was associated with a higher risk of developing dementia, as well as worse cognition,” said study author Yuhan Li, MHS, research assistant, Channing Division of Network Medicine, Brigham and Women’s Hospital, Boston, Massachusetts.
However, the study also showed that replacing processed red meat with nuts and legumes could potentially lower this increased risk.
The findings were presented on at the 2024 Alzheimer’s Association International Conference (AAIC).
Inconsistent Research
Previous studies have shown an inconsistent association between red meat intake and cognitive health.
To assess the relationship between diet and dementia, the researchers used data from the Nurses’ Health Study, which began recruiting female registered nurses aged 30-55 years in 1976, and the Health Professionals Follow-Up Study, which began recruiting male health professionals aged 40-75 in 1986.
They assessed processed red meat intake by validated semi-quantitative food frequency questionnaires administered every 2-4 years. Participants were asked how often they consumed a serving of processed red meat.
Investigators also assessed intake of unprocessed red meat, including beef, pork, or lamb as a main dish, in a sandwich or hamburger, or in a mixed dish.
The investigators also looked at participants’ intake of nuts and legumes.
Dementia outcome was a composite endpoint of self-reported dementia and dementia-related death. “Specifically, participants reported a physician diagnosis of Alzheimer’s disease or other forms of dementia by questionnaire. Deaths were identified through state vital statistics records, the National Death Index, family reports, and the postal system,” said Ms. Li.
Three Cognitive Outcomes
Researchers examined three outcomes: dementia, subjective cognitive decline, and objective cognitive function. For dementia, they ascertained incident cases in 87,424 individuals in the UK’s National Health Service database without Parkinson’s disease or baseline dementia, stroke, or cancer.
They longitudinally collected information on subjective cognitive decline from 33,908 Nurses’ Health Study participants and 10,058 participants in the Health Professionals Follow-Up Study.
Cognitive function was assessed using the Telephone Interview for Cognitive Status (1995-2008) in a subset of 17,458 Nurses’ Health Study participants.
Over a follow-up of 38 years (1980-2018), there were 6856 dementia cases in the Nurses’ Health Study. Participants with processed red meat intake of 0.25 or more serving/day, compared with less than 0.10 serving/day, had 15% higher risk for dementia (hazard ratio [HR], 1.15; 95% CI, 1.08-1.23; P < .001).
In addition to an increased risk for dementia, intake of processed red meat was associated with accelerated cognitive aging in global cognition (1.61 years per 1–serving/day increment; 95% CI, 0.20, 3.03) and verbal memory (1.69 years per 1–serving/day increment; 95% CI, 0.13, 3.25; both P = .03).
Participants with processed red meat intake of 0.25 or more serving/day had a 14% higher likelihood of subjective cognitive decline, compared with those with intake less than 0.10 serving/day (odds ratio [OR], 1.14; 95% CI, 1.04-1.24; P = .004).
For unprocessed red meat, consuming 1.00 or more serving/day versus less than 0.50 serving/day was associated with a 16% higher likelihood of subjective cognitive decline (OR, 1.16; 95% CI, 1.04-1.30; P = .02).
Substitution Analysis
Researchers modeled the effects of replacing 1 serving/day of processed red meat with 1 serving/day of nuts and legumes on cognitive outcomes. They did this by treating food intakes as continuous variables and calculating the differences in coefficients of the two food items.
They found that substituting legumes and nuts was associated with a 23% lower risk for dementia (HR, 0.77; 95% CI, 0.69-0.86), 1.37 fewer years of cognitive aging (95% CI, –2.49 to –0.25), and 20% lower odds of subjective cognitive decline (OR, 0.80, 95% CI, 0.69-0.92).
The research cannot determine whether it’s the processing method itself or the type of red meat that affects cognition, Ms. Li cautioned.
“Our study is an epidemiologic study, not a biological mechanism study, but based on our findings, red meat may be related to worse cognition, and processed red meat may add additional risk,” she said.
She also noted that because the study focused solely on red meats, the study cannot determine the potential on the impact of other processed meats on cognition.
Although the study doesn’t address a possible mechanism linking processed red meat with cognition, Ms. Li said it’s possible such meats have high levels of relatively harmful substances, such as nitrites, N-nitroso compounds, and sodium, and that “these carry the additional risk to brain health.”
There are currently no specific guidelines regarding the “safe” amount of processed meat consumption specifically related to cognition, she said.
The study is important because of its large sample size, long follow-up period, and inclusion of repeated measurements of diet, the investigators noted. In addition, researchers assessed both processed and unprocessed red meat and evaluated multiple cognitive outcomes.
The investigators plan to assess the association between other modifiable factors and cognitive health.
Experts Weigh In
In a comment, Claire Sexton, DPhil, senior director of scientific programs and outreach at the Alzheimer’s Association, agreed past studies on the topic have been “mixed,” with only some studies reporting links between cognition or dementia and processed red meat.
Another unique aspect of the study, said Dr. Sexton, was the replacement analysis showing the brain benefits of eating nuts and legumes in place of processed red meat. “So, it’s not just suggesting to people what not to do, but also what they can be doing instead.”
That’s why this large study with more than 130,000 adults that tracked individuals for close to 40 years in some cases “is so valuable,” she added.
In a release from the Science Media Centre in the United Kingdom, several other experts commented on the study. Among them, Kevin McConway, PhD, emeritus professor of applied statistics at the Open University, Milton Keynes, England, said that “it’s pretty well impossible to get a clear message from the information that is available so far about this research. It is a conference paper, and all we have seen so far is a press release, a brief summary of the research, and a diagram. There isn’t a detailed, peer-reviewed research report, not yet anyway. Putting out limited information like this isn’t the right way to report science.”
Dr. McConway also noted that the observational study recorded participants’ diets and dementia diagnoses over several years without assigning specific diets. Those who ate more red processed meat had higher rates of dementia and cognitive decline. However, it’s unclear if these differences are caused by red meat consumption or other factors, such as diet, age, ethnicity, or location.
Researchers typically adjust for these factors, but the available information doesn’t specify what adjustments were made or their impact, he noted, and without detailed data, it’s impossible to evaluate the study’s quality. Although eating more red processed meat might increase dementia risk, more research is needed to confirm this, Dr. McConway added.
Also commenting, Sebastian Walsh, a National Institute for Health and Care Research doctoral fellow who researches population-level approaches to dementia risk reduction at University of Cambridge, Cambridge, England, said that without seeing the full paper, it’s difficult to know exactly what to make of the study’s findings.
“On the surface, this is a large and long study. But it isn’t clear how the analysis was done — specifically what other factors were taken into account when looking at this apparent relationship between red meat and dementia.
“Despite a lot of research looking at specific foods and different diseases, the basic public health advice that eating a healthy, balanced diet is good for health is essentially unchanged. Most people know and accept this. What is most important is to find ways of supporting people, particularly those from poorer backgrounds, to follow this advice and address the obesity epidemic,” said Mr. Walsh.
The study was funded by a National Institutes of Health research grant. Ms. Li reports no relevant conflicts of interest. Dr. Sexton, Dr. McConway, and Mr. Walsh report no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM AAIC 2024