User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Powered by CHEST Physician, Clinician Reviews, MDedge Family Medicine, Internal Medicine News, and The Journal of Clinical Outcomes Management.
July 2015: Click for Credit
Here are 7 articles in the July issue of Clinician Reviews (accreditation valid until January 1, 2016):
1. BSR: Multiple Benefits Seen With Intensive Psoriatic Arthritis Therapy
Multiple joint and skin benefits can be achieved by intensively treating patients with psoriatic arthritis (PsA) until they achieve a set of minimal disease activity (MDA) criteria (see Table), an expert said at the British Society for Rheumatology annual conference.
To take the posttest, go to: http://bit.ly/1KaikxW
2. Subclinical Hyperthyroidism Linked to Higher Fracture Risk
Individuals with subclinical hyperthyroidism are at increased risk for hip and other fractures, according to the authors of a meta-analysis. The researchers examined data from 70,298 individuals—4,092 with subclinical hypothyroidism and 2,219 with subclinical hyperthyroidism—enrolled in 13 prospective cohort studies.
To take the posttest, go to: http://bit.ly/1H13j0t
3. Newer Oral Contraceptives Pose Higher VTE Risk
The risk for venous thromboembolism (VTE) is generally greater for women using oral contraceptives with newer types of progestogen hormones than for those taking older, second-generation birth control pills, study results showed.
To take the posttest, go to: http://bit.ly/1AKQert
4. Statins, Fibrates Lower Stroke Risk in Elderly
Both statin and fibrate therapies taken to improve lipid profiles decreased risk for stroke by 30% in a community-dwelling population of elderly people, according to a prospective European study published online in the British Medical Journal.
To take the posttest, go to: http://bit.ly/1FuyYCb
5. Cystic Fibrosis–related Diabetes Requires Different Approach
Cystic fibrosis–related diabetes (CFRD) is a unique disease that requires a different mindset on the part of the treating clinician.
To take the posttest, go to: http://bit.ly/1BKGZCm
6. CVD Risk Persists for 40 Years in Hodgkin Survivors
People who survive Hodgkin lymphoma in adolescence or young adulthood remain at very high risk for cardiovascular disease (CVD) for at least 40 years—the longest period for which they have been followed, according to the results of a retrospective cohort study of more than 2,500 patients.
To take the posttest, go to: http://bit.ly/1M5ymYG
7. Asymptomatic Carotid Stenosis and Central Sleep Apnea Linked
More than two-thirds of patients with asymptomatic carotid stenosis are likely to have sleep apnea, according to an observational study. The polysomnography results of 96 patients with asymptomatic extracranial carotid stenosis revealed that 69% had sleep apnea: 42% had obstructive sleep apnea (OSA) and 27%, central sleep apnea (CSA).
To take the posttest, go to: http://bit.ly/1SWGPmb
Here are 7 articles in the July issue of Clinician Reviews (accreditation valid until January 1, 2016):
1. BSR: Multiple Benefits Seen With Intensive Psoriatic Arthritis Therapy
Multiple joint and skin benefits can be achieved by intensively treating patients with psoriatic arthritis (PsA) until they achieve a set of minimal disease activity (MDA) criteria (see Table), an expert said at the British Society for Rheumatology annual conference.
To take the posttest, go to: http://bit.ly/1KaikxW
2. Subclinical Hyperthyroidism Linked to Higher Fracture Risk
Individuals with subclinical hyperthyroidism are at increased risk for hip and other fractures, according to the authors of a meta-analysis. The researchers examined data from 70,298 individuals—4,092 with subclinical hypothyroidism and 2,219 with subclinical hyperthyroidism—enrolled in 13 prospective cohort studies.
To take the posttest, go to: http://bit.ly/1H13j0t
3. Newer Oral Contraceptives Pose Higher VTE Risk
The risk for venous thromboembolism (VTE) is generally greater for women using oral contraceptives with newer types of progestogen hormones than for those taking older, second-generation birth control pills, study results showed.
To take the posttest, go to: http://bit.ly/1AKQert
4. Statins, Fibrates Lower Stroke Risk in Elderly
Both statin and fibrate therapies taken to improve lipid profiles decreased risk for stroke by 30% in a community-dwelling population of elderly people, according to a prospective European study published online in the British Medical Journal.
To take the posttest, go to: http://bit.ly/1FuyYCb
5. Cystic Fibrosis–related Diabetes Requires Different Approach
Cystic fibrosis–related diabetes (CFRD) is a unique disease that requires a different mindset on the part of the treating clinician.
To take the posttest, go to: http://bit.ly/1BKGZCm
6. CVD Risk Persists for 40 Years in Hodgkin Survivors
People who survive Hodgkin lymphoma in adolescence or young adulthood remain at very high risk for cardiovascular disease (CVD) for at least 40 years—the longest period for which they have been followed, according to the results of a retrospective cohort study of more than 2,500 patients.
To take the posttest, go to: http://bit.ly/1M5ymYG
7. Asymptomatic Carotid Stenosis and Central Sleep Apnea Linked
More than two-thirds of patients with asymptomatic carotid stenosis are likely to have sleep apnea, according to an observational study. The polysomnography results of 96 patients with asymptomatic extracranial carotid stenosis revealed that 69% had sleep apnea: 42% had obstructive sleep apnea (OSA) and 27%, central sleep apnea (CSA).
To take the posttest, go to: http://bit.ly/1SWGPmb
Here are 7 articles in the July issue of Clinician Reviews (accreditation valid until January 1, 2016):
1. BSR: Multiple Benefits Seen With Intensive Psoriatic Arthritis Therapy
Multiple joint and skin benefits can be achieved by intensively treating patients with psoriatic arthritis (PsA) until they achieve a set of minimal disease activity (MDA) criteria (see Table), an expert said at the British Society for Rheumatology annual conference.
To take the posttest, go to: http://bit.ly/1KaikxW
2. Subclinical Hyperthyroidism Linked to Higher Fracture Risk
Individuals with subclinical hyperthyroidism are at increased risk for hip and other fractures, according to the authors of a meta-analysis. The researchers examined data from 70,298 individuals—4,092 with subclinical hypothyroidism and 2,219 with subclinical hyperthyroidism—enrolled in 13 prospective cohort studies.
To take the posttest, go to: http://bit.ly/1H13j0t
3. Newer Oral Contraceptives Pose Higher VTE Risk
The risk for venous thromboembolism (VTE) is generally greater for women using oral contraceptives with newer types of progestogen hormones than for those taking older, second-generation birth control pills, study results showed.
To take the posttest, go to: http://bit.ly/1AKQert
4. Statins, Fibrates Lower Stroke Risk in Elderly
Both statin and fibrate therapies taken to improve lipid profiles decreased risk for stroke by 30% in a community-dwelling population of elderly people, according to a prospective European study published online in the British Medical Journal.
To take the posttest, go to: http://bit.ly/1FuyYCb
5. Cystic Fibrosis–related Diabetes Requires Different Approach
Cystic fibrosis–related diabetes (CFRD) is a unique disease that requires a different mindset on the part of the treating clinician.
To take the posttest, go to: http://bit.ly/1BKGZCm
6. CVD Risk Persists for 40 Years in Hodgkin Survivors
People who survive Hodgkin lymphoma in adolescence or young adulthood remain at very high risk for cardiovascular disease (CVD) for at least 40 years—the longest period for which they have been followed, according to the results of a retrospective cohort study of more than 2,500 patients.
To take the posttest, go to: http://bit.ly/1M5ymYG
7. Asymptomatic Carotid Stenosis and Central Sleep Apnea Linked
More than two-thirds of patients with asymptomatic carotid stenosis are likely to have sleep apnea, according to an observational study. The polysomnography results of 96 patients with asymptomatic extracranial carotid stenosis revealed that 69% had sleep apnea: 42% had obstructive sleep apnea (OSA) and 27%, central sleep apnea (CSA).
To take the posttest, go to: http://bit.ly/1SWGPmb
VIDEO: Helping patients sleep better can be simple
WASHINGTON – Sleep disorders can be treated easily in the primary care setting, although there are times when it’s best to refer to a sleep clinic. Dr. Raman K. Malhotra of the department of neurology at Saint Louis University, shares ways to help determine when a patient is presenting with sleep disorders vs. mood disorders. He also offers tips for patients, who can get the rest they need, once their sleep habits are adjusted. Also discussed in this video, recorded at the meeting held by the Global Academy for Medical Education, is the use of melatonin and iron supplementation to combat restless legs syndrome. Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
WASHINGTON – Sleep disorders can be treated easily in the primary care setting, although there are times when it’s best to refer to a sleep clinic. Dr. Raman K. Malhotra of the department of neurology at Saint Louis University, shares ways to help determine when a patient is presenting with sleep disorders vs. mood disorders. He also offers tips for patients, who can get the rest they need, once their sleep habits are adjusted. Also discussed in this video, recorded at the meeting held by the Global Academy for Medical Education, is the use of melatonin and iron supplementation to combat restless legs syndrome. Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
WASHINGTON – Sleep disorders can be treated easily in the primary care setting, although there are times when it’s best to refer to a sleep clinic. Dr. Raman K. Malhotra of the department of neurology at Saint Louis University, shares ways to help determine when a patient is presenting with sleep disorders vs. mood disorders. He also offers tips for patients, who can get the rest they need, once their sleep habits are adjusted. Also discussed in this video, recorded at the meeting held by the Global Academy for Medical Education, is the use of melatonin and iron supplementation to combat restless legs syndrome. Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
AT THE SUMMIT IN NEUROLOGY & PSYCHIATRY
Mind the Gap
An 8-month-old boy with a history of hypotonia, developmental delay, and seizure disorder refractory to multiple anticonvulsant medications was brought to the ED with a two-week history of intermittent fever and poor oral intake. His current medications included sodium bromide (185 mg bid, orally) for his seizure disorder.
On physical examination, the boy appeared small for his age, with diffuse hypotonia and diminished reflexes. He was able to track with his eyes but was otherwise unresponsive. No rash was present. Results of initial laboratory studies were sodium, 144 mEq/L; potassium, 4.8 mEq/L; chloride, 179 mEq/L; bicarbonate, 21 mEq/L; blood urea nitrogen, 6 mg/dL; creatinine, 0.1 mg/dL; and glucose, 63 mg/dL. His anion gap (AG) was −56.
WHAT DOES THE ANION GAP REPRESENT?
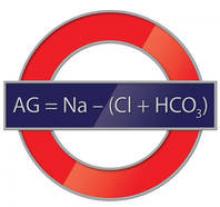
The AG is a valuable clinical calculation derived from the measured extracellular electrolytes and provides an index of acid-base status.1 Due to the necessity of electroneutrality, the sum of positive charges (cations) in the extracellular fluid must be balanced exactly with the sum of negative charges (anions). However, to routinely measure all of the cations and anions in the serum would be time-consuming and is also unnecessary. Because most clinical laboratories commonly only measure one relevant cation (sodium) and two anions (chloride and bicarbonate), the positive and negative sums are not completely balanced. The AG therefore refers to this difference (ie, AG = Na – [Cl + HCO3]).
Of course, electroneutrality exists in vivo and is accomplished by the presence of unmeasured anions (UA; eg, lactate and phosphate) and unmeasured cations (UC; eg, potassium and calcium) not accounted for in the AG (ie, AG = UA – UC). In other words, the sum of measured plus unmeasured anions must equal the sum of the measured plus unmeasured cations.
WHAT CAUSES A LOW OR NEGATIVE ANION GAP?
While most health care providers are well versed in the clinical significance of an elevated AG (eg, MUDPILES [methanol, uremia, diabetic ketoacidosis, propylene glycol or phenformin, iron or isoniazid, lactate, ethylene glycol, salicylates]), the meaning of a low or negative AG is underappreciated. There are several scenarios that could potentially yield a low or negative AG, including decreased concentration of UA, increased concentrations of nonsodium cations (UC), and overestimation of serum chloride.
Decreased concentration of unmeasured anions. This most commonly occurs by two mechanisms: dilution of the extracellular fluid or hypoalbuminemia. The addition of water to the extracellular fluid will cause a proportionate dilution of all the measured electrolytes. Since the concentration of measured cations is higher than that of the measured anions, there is a small and relatively insignificant decrease in the AG.
Alternatively, hypoalbuminemia results in a low AG due to the change in UA; albumin is negatively charged. At physiologic pH, the overwhelming majority of serum proteins are anionic and counter-balanced by the positive charge of sodium. Albumin, the most abundant serum protein, accounts for approximately 75% of the normal AG. Hypoalbuminemic states, such as cirrhosis or nephrotic syndrome, can therefore cause low AG due to the retention of chloride to replace the lost negative charge. The albumin concentration can be corrected to calculate the AG.2
Nonsodium cations. There are a number of clinical conditions that result in the retention of nonsodium cations. For example, the excess positively charged paraproteins associated with IgG myeloma raise the UC concentration, resulting in a low AG. Similarly, elevations of unmeasured cationic electrolytes, such as calcium and magnesium, may also result in a lower AG. Significant changes in AG, though, are caused only by profound (and often life-threatening) hypercalcemia or hypermagnesemia.
Overestimation of serum chloride. Overestimation of serum chloride most commonly occurs in the clinical scenario of bromide exposure. In normal physiologic conditions, chloride is the only halide present in the extracellular fluid. With intake of brominated products, chloride may be partially replaced by bromide. As there is greater renal tubular avidity for bromide, chronic ingestion of bromide results in a gradual rise in serum bromide concentrations with a proportional fall in chloride.
However, and more importantly, bromide interferes with a number of laboratory techniques measuring chloride concentrations, resulting in a spuriously elevated chloride, or pseudohyperchloremia. Because the measured sodium and bicarbonate concentrations will remain unchanged, this falsely elevated chloride measurement will result in a negative AG.
Continue for causes of the falsely elevated chloride >>
WHAT CAUSES THE FALSELY ELEVATED CHLORIDE?
All of the current laboratory techniques for measurement of serum chloride concentration can potentially result in a falsely elevated value. However, the degree of pseudohyperchloremia will depend on the specific assay used for measurement. The ion-selective electrode method used by many common laboratory analyzers appears to have the greatest interference on chloride measurement in the presence of bromide. This is simply due to the molecular similarity of bromide and chloride.
Conversely, the coulometry method, often used as a reference standard, has the least interference of current laboratory methods.3 This is because coulometry does not completely rely on molecular structure to measure concentration; rather, it measures the amount of energy produced or consumed in an electrolysis reaction. Iodide, another halide compound, has also been described as a cause of pseudohyperchloremia, whereas fluoride does not seem to have significant interference.4
HOW ARE PATIENTS EXPOSED TO BROMIDE SALTS?
Bromide salts, specifically sodium bromide, are infrequently used to treat seizure disorders but are generally reserved for patients with epilepsy refractory to other, less toxic anticonvulsant medications. During the era when bromide salts were more commonly used to treat epilepsy, bromide intoxication, or bromism, was frequently observed.
Bromism may manifest as a constellation of nonspecific neurologic and psychiatric symptoms. These most commonly include headache, weakness, agitation, confusion, and hallucinations. In more severe cases of bromism, stupor and coma may occur.3,5
Although bromide salts are no longer commonly prescribed, a number of products still contain brominated ingredients. Symptoms of bromide intoxication can occur with chronic use of a cough syrup containing dextromethorphan hydrobromide, as well as the brominated vegetable oils found in some soft drinks.5
Continue for how bromism is treated >>
HOW IS BROMISM TREATED?
The treatment of bromism involves preventing further exposure to bromide and promoting bromide excretion. Bromide has a long half-life (10 to 12 days), but in patients with normal renal function, it is possible to reduce this half-life to approximately three days with hydration and diuresis with sodium chloride.3
Alternatively, in patients with impaired renal function or severe intoxication, hemodialysis has been used effectively.5
CASE CONCLUSION
The patient was admitted for observation and treated with IV sodium chloride. After consultation with his neurologist, he was discharged home in the care of his parents, who were advised to continue him on sodium bromide (185 mg bid, orally) since his seizures were refractory to other anticonvulsant medications.
REFERENCES
1. Emmett M, Narins RG. Clinical use of the anion gap. Medicine (Baltimore). 1977;56(1):38-54.
2. Figge J, Jabor A, Kazda A, Fencl V. Anion gap and hypoalbuminemia. Crit Care Med. 1998;26(11):1807-1810.
3. Vasuyattakul S, Lertpattanasuwan N, Vareesangthip K, et al. A negative anion gap as a clue to diagnose bromide intoxication. Nephron. 1995;69(3):311-313.
4. Yamamoto K, Kobayashi H, Kobayashi T, Murakami S. False hyperchloremia in bromism. J Anesth. 1991;5(1):88-91.
5. Ng YY, Lin WL, Chen TW. Spurious hyperchloremia and decreased anion gap in a patient with dextromethorphan bromide. Am J Nephrol. 1992;12(4):268-270.
An 8-month-old boy with a history of hypotonia, developmental delay, and seizure disorder refractory to multiple anticonvulsant medications was brought to the ED with a two-week history of intermittent fever and poor oral intake. His current medications included sodium bromide (185 mg bid, orally) for his seizure disorder.
On physical examination, the boy appeared small for his age, with diffuse hypotonia and diminished reflexes. He was able to track with his eyes but was otherwise unresponsive. No rash was present. Results of initial laboratory studies were sodium, 144 mEq/L; potassium, 4.8 mEq/L; chloride, 179 mEq/L; bicarbonate, 21 mEq/L; blood urea nitrogen, 6 mg/dL; creatinine, 0.1 mg/dL; and glucose, 63 mg/dL. His anion gap (AG) was −56.
WHAT DOES THE ANION GAP REPRESENT?
The AG is a valuable clinical calculation derived from the measured extracellular electrolytes and provides an index of acid-base status.1 Due to the necessity of electroneutrality, the sum of positive charges (cations) in the extracellular fluid must be balanced exactly with the sum of negative charges (anions). However, to routinely measure all of the cations and anions in the serum would be time-consuming and is also unnecessary. Because most clinical laboratories commonly only measure one relevant cation (sodium) and two anions (chloride and bicarbonate), the positive and negative sums are not completely balanced. The AG therefore refers to this difference (ie, AG = Na – [Cl + HCO3]).
Of course, electroneutrality exists in vivo and is accomplished by the presence of unmeasured anions (UA; eg, lactate and phosphate) and unmeasured cations (UC; eg, potassium and calcium) not accounted for in the AG (ie, AG = UA – UC). In other words, the sum of measured plus unmeasured anions must equal the sum of the measured plus unmeasured cations.
WHAT CAUSES A LOW OR NEGATIVE ANION GAP?
While most health care providers are well versed in the clinical significance of an elevated AG (eg, MUDPILES [methanol, uremia, diabetic ketoacidosis, propylene glycol or phenformin, iron or isoniazid, lactate, ethylene glycol, salicylates]), the meaning of a low or negative AG is underappreciated. There are several scenarios that could potentially yield a low or negative AG, including decreased concentration of UA, increased concentrations of nonsodium cations (UC), and overestimation of serum chloride.
Decreased concentration of unmeasured anions. This most commonly occurs by two mechanisms: dilution of the extracellular fluid or hypoalbuminemia. The addition of water to the extracellular fluid will cause a proportionate dilution of all the measured electrolytes. Since the concentration of measured cations is higher than that of the measured anions, there is a small and relatively insignificant decrease in the AG.
Alternatively, hypoalbuminemia results in a low AG due to the change in UA; albumin is negatively charged. At physiologic pH, the overwhelming majority of serum proteins are anionic and counter-balanced by the positive charge of sodium. Albumin, the most abundant serum protein, accounts for approximately 75% of the normal AG. Hypoalbuminemic states, such as cirrhosis or nephrotic syndrome, can therefore cause low AG due to the retention of chloride to replace the lost negative charge. The albumin concentration can be corrected to calculate the AG.2
Nonsodium cations. There are a number of clinical conditions that result in the retention of nonsodium cations. For example, the excess positively charged paraproteins associated with IgG myeloma raise the UC concentration, resulting in a low AG. Similarly, elevations of unmeasured cationic electrolytes, such as calcium and magnesium, may also result in a lower AG. Significant changes in AG, though, are caused only by profound (and often life-threatening) hypercalcemia or hypermagnesemia.
Overestimation of serum chloride. Overestimation of serum chloride most commonly occurs in the clinical scenario of bromide exposure. In normal physiologic conditions, chloride is the only halide present in the extracellular fluid. With intake of brominated products, chloride may be partially replaced by bromide. As there is greater renal tubular avidity for bromide, chronic ingestion of bromide results in a gradual rise in serum bromide concentrations with a proportional fall in chloride.
However, and more importantly, bromide interferes with a number of laboratory techniques measuring chloride concentrations, resulting in a spuriously elevated chloride, or pseudohyperchloremia. Because the measured sodium and bicarbonate concentrations will remain unchanged, this falsely elevated chloride measurement will result in a negative AG.
Continue for causes of the falsely elevated chloride >>
WHAT CAUSES THE FALSELY ELEVATED CHLORIDE?
All of the current laboratory techniques for measurement of serum chloride concentration can potentially result in a falsely elevated value. However, the degree of pseudohyperchloremia will depend on the specific assay used for measurement. The ion-selective electrode method used by many common laboratory analyzers appears to have the greatest interference on chloride measurement in the presence of bromide. This is simply due to the molecular similarity of bromide and chloride.
Conversely, the coulometry method, often used as a reference standard, has the least interference of current laboratory methods.3 This is because coulometry does not completely rely on molecular structure to measure concentration; rather, it measures the amount of energy produced or consumed in an electrolysis reaction. Iodide, another halide compound, has also been described as a cause of pseudohyperchloremia, whereas fluoride does not seem to have significant interference.4
HOW ARE PATIENTS EXPOSED TO BROMIDE SALTS?
Bromide salts, specifically sodium bromide, are infrequently used to treat seizure disorders but are generally reserved for patients with epilepsy refractory to other, less toxic anticonvulsant medications. During the era when bromide salts were more commonly used to treat epilepsy, bromide intoxication, or bromism, was frequently observed.
Bromism may manifest as a constellation of nonspecific neurologic and psychiatric symptoms. These most commonly include headache, weakness, agitation, confusion, and hallucinations. In more severe cases of bromism, stupor and coma may occur.3,5
Although bromide salts are no longer commonly prescribed, a number of products still contain brominated ingredients. Symptoms of bromide intoxication can occur with chronic use of a cough syrup containing dextromethorphan hydrobromide, as well as the brominated vegetable oils found in some soft drinks.5
Continue for how bromism is treated >>
HOW IS BROMISM TREATED?
The treatment of bromism involves preventing further exposure to bromide and promoting bromide excretion. Bromide has a long half-life (10 to 12 days), but in patients with normal renal function, it is possible to reduce this half-life to approximately three days with hydration and diuresis with sodium chloride.3
Alternatively, in patients with impaired renal function or severe intoxication, hemodialysis has been used effectively.5
CASE CONCLUSION
The patient was admitted for observation and treated with IV sodium chloride. After consultation with his neurologist, he was discharged home in the care of his parents, who were advised to continue him on sodium bromide (185 mg bid, orally) since his seizures were refractory to other anticonvulsant medications.
REFERENCES
1. Emmett M, Narins RG. Clinical use of the anion gap. Medicine (Baltimore). 1977;56(1):38-54.
2. Figge J, Jabor A, Kazda A, Fencl V. Anion gap and hypoalbuminemia. Crit Care Med. 1998;26(11):1807-1810.
3. Vasuyattakul S, Lertpattanasuwan N, Vareesangthip K, et al. A negative anion gap as a clue to diagnose bromide intoxication. Nephron. 1995;69(3):311-313.
4. Yamamoto K, Kobayashi H, Kobayashi T, Murakami S. False hyperchloremia in bromism. J Anesth. 1991;5(1):88-91.
5. Ng YY, Lin WL, Chen TW. Spurious hyperchloremia and decreased anion gap in a patient with dextromethorphan bromide. Am J Nephrol. 1992;12(4):268-270.
An 8-month-old boy with a history of hypotonia, developmental delay, and seizure disorder refractory to multiple anticonvulsant medications was brought to the ED with a two-week history of intermittent fever and poor oral intake. His current medications included sodium bromide (185 mg bid, orally) for his seizure disorder.
On physical examination, the boy appeared small for his age, with diffuse hypotonia and diminished reflexes. He was able to track with his eyes but was otherwise unresponsive. No rash was present. Results of initial laboratory studies were sodium, 144 mEq/L; potassium, 4.8 mEq/L; chloride, 179 mEq/L; bicarbonate, 21 mEq/L; blood urea nitrogen, 6 mg/dL; creatinine, 0.1 mg/dL; and glucose, 63 mg/dL. His anion gap (AG) was −56.
WHAT DOES THE ANION GAP REPRESENT?
The AG is a valuable clinical calculation derived from the measured extracellular electrolytes and provides an index of acid-base status.1 Due to the necessity of electroneutrality, the sum of positive charges (cations) in the extracellular fluid must be balanced exactly with the sum of negative charges (anions). However, to routinely measure all of the cations and anions in the serum would be time-consuming and is also unnecessary. Because most clinical laboratories commonly only measure one relevant cation (sodium) and two anions (chloride and bicarbonate), the positive and negative sums are not completely balanced. The AG therefore refers to this difference (ie, AG = Na – [Cl + HCO3]).
Of course, electroneutrality exists in vivo and is accomplished by the presence of unmeasured anions (UA; eg, lactate and phosphate) and unmeasured cations (UC; eg, potassium and calcium) not accounted for in the AG (ie, AG = UA – UC). In other words, the sum of measured plus unmeasured anions must equal the sum of the measured plus unmeasured cations.
WHAT CAUSES A LOW OR NEGATIVE ANION GAP?
While most health care providers are well versed in the clinical significance of an elevated AG (eg, MUDPILES [methanol, uremia, diabetic ketoacidosis, propylene glycol or phenformin, iron or isoniazid, lactate, ethylene glycol, salicylates]), the meaning of a low or negative AG is underappreciated. There are several scenarios that could potentially yield a low or negative AG, including decreased concentration of UA, increased concentrations of nonsodium cations (UC), and overestimation of serum chloride.
Decreased concentration of unmeasured anions. This most commonly occurs by two mechanisms: dilution of the extracellular fluid or hypoalbuminemia. The addition of water to the extracellular fluid will cause a proportionate dilution of all the measured electrolytes. Since the concentration of measured cations is higher than that of the measured anions, there is a small and relatively insignificant decrease in the AG.
Alternatively, hypoalbuminemia results in a low AG due to the change in UA; albumin is negatively charged. At physiologic pH, the overwhelming majority of serum proteins are anionic and counter-balanced by the positive charge of sodium. Albumin, the most abundant serum protein, accounts for approximately 75% of the normal AG. Hypoalbuminemic states, such as cirrhosis or nephrotic syndrome, can therefore cause low AG due to the retention of chloride to replace the lost negative charge. The albumin concentration can be corrected to calculate the AG.2
Nonsodium cations. There are a number of clinical conditions that result in the retention of nonsodium cations. For example, the excess positively charged paraproteins associated with IgG myeloma raise the UC concentration, resulting in a low AG. Similarly, elevations of unmeasured cationic electrolytes, such as calcium and magnesium, may also result in a lower AG. Significant changes in AG, though, are caused only by profound (and often life-threatening) hypercalcemia or hypermagnesemia.
Overestimation of serum chloride. Overestimation of serum chloride most commonly occurs in the clinical scenario of bromide exposure. In normal physiologic conditions, chloride is the only halide present in the extracellular fluid. With intake of brominated products, chloride may be partially replaced by bromide. As there is greater renal tubular avidity for bromide, chronic ingestion of bromide results in a gradual rise in serum bromide concentrations with a proportional fall in chloride.
However, and more importantly, bromide interferes with a number of laboratory techniques measuring chloride concentrations, resulting in a spuriously elevated chloride, or pseudohyperchloremia. Because the measured sodium and bicarbonate concentrations will remain unchanged, this falsely elevated chloride measurement will result in a negative AG.
Continue for causes of the falsely elevated chloride >>
WHAT CAUSES THE FALSELY ELEVATED CHLORIDE?
All of the current laboratory techniques for measurement of serum chloride concentration can potentially result in a falsely elevated value. However, the degree of pseudohyperchloremia will depend on the specific assay used for measurement. The ion-selective electrode method used by many common laboratory analyzers appears to have the greatest interference on chloride measurement in the presence of bromide. This is simply due to the molecular similarity of bromide and chloride.
Conversely, the coulometry method, often used as a reference standard, has the least interference of current laboratory methods.3 This is because coulometry does not completely rely on molecular structure to measure concentration; rather, it measures the amount of energy produced or consumed in an electrolysis reaction. Iodide, another halide compound, has also been described as a cause of pseudohyperchloremia, whereas fluoride does not seem to have significant interference.4
HOW ARE PATIENTS EXPOSED TO BROMIDE SALTS?
Bromide salts, specifically sodium bromide, are infrequently used to treat seizure disorders but are generally reserved for patients with epilepsy refractory to other, less toxic anticonvulsant medications. During the era when bromide salts were more commonly used to treat epilepsy, bromide intoxication, or bromism, was frequently observed.
Bromism may manifest as a constellation of nonspecific neurologic and psychiatric symptoms. These most commonly include headache, weakness, agitation, confusion, and hallucinations. In more severe cases of bromism, stupor and coma may occur.3,5
Although bromide salts are no longer commonly prescribed, a number of products still contain brominated ingredients. Symptoms of bromide intoxication can occur with chronic use of a cough syrup containing dextromethorphan hydrobromide, as well as the brominated vegetable oils found in some soft drinks.5
Continue for how bromism is treated >>
HOW IS BROMISM TREATED?
The treatment of bromism involves preventing further exposure to bromide and promoting bromide excretion. Bromide has a long half-life (10 to 12 days), but in patients with normal renal function, it is possible to reduce this half-life to approximately three days with hydration and diuresis with sodium chloride.3
Alternatively, in patients with impaired renal function or severe intoxication, hemodialysis has been used effectively.5
CASE CONCLUSION
The patient was admitted for observation and treated with IV sodium chloride. After consultation with his neurologist, he was discharged home in the care of his parents, who were advised to continue him on sodium bromide (185 mg bid, orally) since his seizures were refractory to other anticonvulsant medications.
REFERENCES
1. Emmett M, Narins RG. Clinical use of the anion gap. Medicine (Baltimore). 1977;56(1):38-54.
2. Figge J, Jabor A, Kazda A, Fencl V. Anion gap and hypoalbuminemia. Crit Care Med. 1998;26(11):1807-1810.
3. Vasuyattakul S, Lertpattanasuwan N, Vareesangthip K, et al. A negative anion gap as a clue to diagnose bromide intoxication. Nephron. 1995;69(3):311-313.
4. Yamamoto K, Kobayashi H, Kobayashi T, Murakami S. False hyperchloremia in bromism. J Anesth. 1991;5(1):88-91.
5. Ng YY, Lin WL, Chen TW. Spurious hyperchloremia and decreased anion gap in a patient with dextromethorphan bromide. Am J Nephrol. 1992;12(4):268-270.
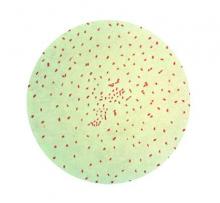
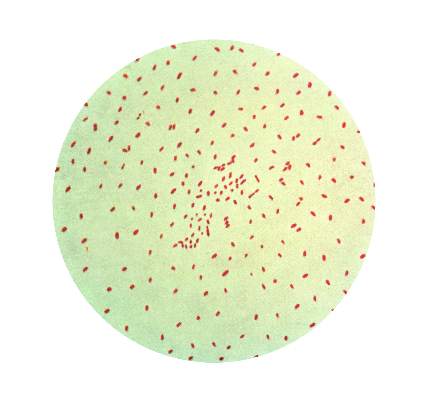
Rise in Bordetella pertussis associated with asymptomatic transmission
Asymptomatic transmission may help explain the recent rise in incidence of Bordetella pertussis, according to a new study.
Both the United States and the United Kingdom have witnessed increased rates of whooping cough diagnosis, despite high vaccination for B. pertussis. “It may be that aP [acellular pertussis]–vaccinated infected people are less efficient at transmitting B. pertussis, compared with unvaccinated infected people, though it is not clear to what extent,” said Dr. Benjamin M. Althouse and Dr. Samuel V. Scarpino of the Santa Fe (N.M.) Institute (BMC Medicine 2015 [doi:10.1186/s12916-015-0382-8]). “The results on vaccination have important public health and clinical implications, especially related to recommendations for isolating unvaccinated or partially vaccinated infants.”
The researchers analyzed reported cases and incidence of B. pertussis from the United States and United Kingdom with data obtained from the Centers for Disease Control and Prevention (1922-2012) and Public Health England (1940-2013), respectively.
Using 36 U.S. B. pertussis isolates from 1935 to 2005, the researchers created a phylodynamic model and used a mathematical model to apply the data to understand the public health and clinical impact of asymptomatic transmission.
Utilizing a wavelet analysis, the incidence of B. pertussis in the United Kingdom returned to a 4-year cyclic pattern similar to the prevaccine era after switching to the acellular B. pertussis vaccine. Both countries demonstrated age-specific attack rate changes after switching from the whole-cell to the acellular B. pertussis vaccine.
Dr. Althouse and Dr. Scarpino noted these observations may be a result of asymptomatic transmission in acellular-vaccinated individuals and cannot be fully explained by B. pertussis evolution or waning immunity.
Finally, as the percentage of acellular vaccination increases, the number of asymptomatic cases of B. pertussis increases. Vaccination levels in the low to moderate range were associated with a 5- to 15-fold increase in symptomatic cases, whereas very high levels (greater than 99%) of vaccination demonstrated no change in the rate of symptomatic cases. The researchers suggest the results are consistent with the increased B. pertussis incidence in 2012 that was 5.4-folder higher than in 1985-1995.
Dr. Althouse and Dr. Scarpino concluded that the models demonstrate that an acellular B. pertussis vaccination that does not prevent transmission in asymptomatic individuals could account for the increased incidence and failure of unvaccinated infant cocooning.
The research was supported by the Omidyar Group and the Santa Fe Institute. The researchers report no competing interests.
Asymptomatic transmission may help explain the recent rise in incidence of Bordetella pertussis, according to a new study.
Both the United States and the United Kingdom have witnessed increased rates of whooping cough diagnosis, despite high vaccination for B. pertussis. “It may be that aP [acellular pertussis]–vaccinated infected people are less efficient at transmitting B. pertussis, compared with unvaccinated infected people, though it is not clear to what extent,” said Dr. Benjamin M. Althouse and Dr. Samuel V. Scarpino of the Santa Fe (N.M.) Institute (BMC Medicine 2015 [doi:10.1186/s12916-015-0382-8]). “The results on vaccination have important public health and clinical implications, especially related to recommendations for isolating unvaccinated or partially vaccinated infants.”
The researchers analyzed reported cases and incidence of B. pertussis from the United States and United Kingdom with data obtained from the Centers for Disease Control and Prevention (1922-2012) and Public Health England (1940-2013), respectively.
Using 36 U.S. B. pertussis isolates from 1935 to 2005, the researchers created a phylodynamic model and used a mathematical model to apply the data to understand the public health and clinical impact of asymptomatic transmission.
Utilizing a wavelet analysis, the incidence of B. pertussis in the United Kingdom returned to a 4-year cyclic pattern similar to the prevaccine era after switching to the acellular B. pertussis vaccine. Both countries demonstrated age-specific attack rate changes after switching from the whole-cell to the acellular B. pertussis vaccine.
Dr. Althouse and Dr. Scarpino noted these observations may be a result of asymptomatic transmission in acellular-vaccinated individuals and cannot be fully explained by B. pertussis evolution or waning immunity.
Finally, as the percentage of acellular vaccination increases, the number of asymptomatic cases of B. pertussis increases. Vaccination levels in the low to moderate range were associated with a 5- to 15-fold increase in symptomatic cases, whereas very high levels (greater than 99%) of vaccination demonstrated no change in the rate of symptomatic cases. The researchers suggest the results are consistent with the increased B. pertussis incidence in 2012 that was 5.4-folder higher than in 1985-1995.
Dr. Althouse and Dr. Scarpino concluded that the models demonstrate that an acellular B. pertussis vaccination that does not prevent transmission in asymptomatic individuals could account for the increased incidence and failure of unvaccinated infant cocooning.
The research was supported by the Omidyar Group and the Santa Fe Institute. The researchers report no competing interests.
Asymptomatic transmission may help explain the recent rise in incidence of Bordetella pertussis, according to a new study.
Both the United States and the United Kingdom have witnessed increased rates of whooping cough diagnosis, despite high vaccination for B. pertussis. “It may be that aP [acellular pertussis]–vaccinated infected people are less efficient at transmitting B. pertussis, compared with unvaccinated infected people, though it is not clear to what extent,” said Dr. Benjamin M. Althouse and Dr. Samuel V. Scarpino of the Santa Fe (N.M.) Institute (BMC Medicine 2015 [doi:10.1186/s12916-015-0382-8]). “The results on vaccination have important public health and clinical implications, especially related to recommendations for isolating unvaccinated or partially vaccinated infants.”
The researchers analyzed reported cases and incidence of B. pertussis from the United States and United Kingdom with data obtained from the Centers for Disease Control and Prevention (1922-2012) and Public Health England (1940-2013), respectively.
Using 36 U.S. B. pertussis isolates from 1935 to 2005, the researchers created a phylodynamic model and used a mathematical model to apply the data to understand the public health and clinical impact of asymptomatic transmission.
Utilizing a wavelet analysis, the incidence of B. pertussis in the United Kingdom returned to a 4-year cyclic pattern similar to the prevaccine era after switching to the acellular B. pertussis vaccine. Both countries demonstrated age-specific attack rate changes after switching from the whole-cell to the acellular B. pertussis vaccine.
Dr. Althouse and Dr. Scarpino noted these observations may be a result of asymptomatic transmission in acellular-vaccinated individuals and cannot be fully explained by B. pertussis evolution or waning immunity.
Finally, as the percentage of acellular vaccination increases, the number of asymptomatic cases of B. pertussis increases. Vaccination levels in the low to moderate range were associated with a 5- to 15-fold increase in symptomatic cases, whereas very high levels (greater than 99%) of vaccination demonstrated no change in the rate of symptomatic cases. The researchers suggest the results are consistent with the increased B. pertussis incidence in 2012 that was 5.4-folder higher than in 1985-1995.
Dr. Althouse and Dr. Scarpino concluded that the models demonstrate that an acellular B. pertussis vaccination that does not prevent transmission in asymptomatic individuals could account for the increased incidence and failure of unvaccinated infant cocooning.
The research was supported by the Omidyar Group and the Santa Fe Institute. The researchers report no competing interests.
FROM BMC MEDICINE
Key clinical point: Asymptomatic transmission of B. pertussis by vaccinated individuals may explain rise in whooping cough.
Major finding: Phylodynamic and wavelet analyses of data are consistent with asymptomatic transmission of B. pertussis.
Data source: Data of reported cases of B. pertussis was obtained from the Centers for Disease Control and Prevention and Public Health England and analysis of 36 U.S. isolates from 1935 to 2005.
Disclosures: The researchers report no competing interests and were supported by the Omidyar Group and the Santa Fe Institute.
ACIP: Tdap during pregnancy optimal strategy for protecting infants
Based on the available evidence of the impact “cocooning” has on transmission of pertussis to infants, no changes are currently recommended in the use of Tdap vaccine for close contacts of infants, Jennifer Liang, D.V.M., said at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
Presenting the conclusions of ACIP’s pertussis vaccines work group review on the impact of cocooning strategies, Dr. Liang, the CDC’s lead member of the work group, said that pertussis vaccination programs should be focused on vaccinating women during every pregnancy, maintaining high levels of DTap coverage, sustaining Tdap coverage in adolescents, and improving Tdap coverage in adults.
In 2005, ACIP recommended the “cocooning” strategy: vaccinating with Tdap for all close contacts of infants under age 12 months to reduce the risk of transmitting pertussis, including parents, siblings, grandparents, child care providers, and health care personnel, in addition to vaccinating pregnant women immediately post partum. In 2011, ACIP recommended Tdap during pregnancy for women who had not previously received the vaccine, or a postpartum dose for women who did not receive the vaccine during pregnancy and had not previously received the vaccine. In 2012, the recommendation was expanded to every pregnancy, whether or not the woman had received the vaccine before.
The optimal strategy to prevent the transmission of pertussis is vaccinating women during pregnancy, which has been shown to be highly effective in reducing transmission to infants, but rates of vaccination in pregnant women have not been high, said Dr. Liang, an epidemiologist in the CDC’s National Center for Immunization and Respiratory Diseases.
Rates of Tdap coverage, however, among pregnant women in the United States have ranged from 14% to 23% in studies using different sources, including a Michigan Medicaid study, she said.
Implementing and sustaining cocooning programs remain a challenge. Although uptake of Tdap has been highest in postpartum women, there has been limited success in vaccinating fathers or other family members, she said, noting that, in 2012, the rate of Tdap coverage among adults aged 19-64 years who reported living with an infant under age 1 year was 26%.
The effect of cocooning in preventing infant pertussis also is “unclear and inconclusive,” and evidence of the effectiveness of the postpartum dose in preventing infant pertussis is limited and the data are conflicting, Dr. Liang said. Another issue is that, over the past decade, the source of transmission to infants has shifted from parents (usually mothers) as the most common source to siblings, who have more recently been identified as the most common source, she said. A CDC study determined that, between 2006 and 2013, family members were the source of the infection in 66%-85% of infant pertussis cases in which the source of infection was known. Siblings were the most common source, linked to almost 40% of cases.
“Even if additional Tdap doses are recommended, this would not address the observed shift to siblings as the source of pertussis to infants and puts greater emphasis on the importance of providing newborns with antipertussis antibodies, and there is an optimal strategy in place – vaccinating women during pregnancy,” she said.
This message is emphasized in a recently launched CDC campaign to improve Tdap vaccination rates during pregnancy, which includes fact sheets for health care professionals that point out that Tdap during pregnancy provides the best protection for infants, postpartum Tdap administration is not optimal, and “cocooning alone may not be effective and is hard to implement.”
Several meeting participants pointed out that vaccine uptake during pregnancy is higher in settings where the vaccine is available on site, as high as 80%-90% of pregnancies, and that having to get the vaccine outside of the office, such as at a pharmacy, can markedly reduce the likelihood of vaccination. The CDC’s updated materials, including fact sheets and posters, are available for health care professionals at http://www.cdc.gov/pertussis/materials/hcp.html.
A single dose of Tdap is recommended for people aged 11-64 years: one dose is routinely administered at age 11 or 12 years and one dose of Tdap is recommended for pregnant women during every pregnancy. DTaP vaccine is used to vaccinate younger children starting at age 2 months and is not licensed for adolescents, adults, or children 7 years of age and older.
Based on the available evidence of the impact “cocooning” has on transmission of pertussis to infants, no changes are currently recommended in the use of Tdap vaccine for close contacts of infants, Jennifer Liang, D.V.M., said at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
Presenting the conclusions of ACIP’s pertussis vaccines work group review on the impact of cocooning strategies, Dr. Liang, the CDC’s lead member of the work group, said that pertussis vaccination programs should be focused on vaccinating women during every pregnancy, maintaining high levels of DTap coverage, sustaining Tdap coverage in adolescents, and improving Tdap coverage in adults.
In 2005, ACIP recommended the “cocooning” strategy: vaccinating with Tdap for all close contacts of infants under age 12 months to reduce the risk of transmitting pertussis, including parents, siblings, grandparents, child care providers, and health care personnel, in addition to vaccinating pregnant women immediately post partum. In 2011, ACIP recommended Tdap during pregnancy for women who had not previously received the vaccine, or a postpartum dose for women who did not receive the vaccine during pregnancy and had not previously received the vaccine. In 2012, the recommendation was expanded to every pregnancy, whether or not the woman had received the vaccine before.
The optimal strategy to prevent the transmission of pertussis is vaccinating women during pregnancy, which has been shown to be highly effective in reducing transmission to infants, but rates of vaccination in pregnant women have not been high, said Dr. Liang, an epidemiologist in the CDC’s National Center for Immunization and Respiratory Diseases.
Rates of Tdap coverage, however, among pregnant women in the United States have ranged from 14% to 23% in studies using different sources, including a Michigan Medicaid study, she said.
Implementing and sustaining cocooning programs remain a challenge. Although uptake of Tdap has been highest in postpartum women, there has been limited success in vaccinating fathers or other family members, she said, noting that, in 2012, the rate of Tdap coverage among adults aged 19-64 years who reported living with an infant under age 1 year was 26%.
The effect of cocooning in preventing infant pertussis also is “unclear and inconclusive,” and evidence of the effectiveness of the postpartum dose in preventing infant pertussis is limited and the data are conflicting, Dr. Liang said. Another issue is that, over the past decade, the source of transmission to infants has shifted from parents (usually mothers) as the most common source to siblings, who have more recently been identified as the most common source, she said. A CDC study determined that, between 2006 and 2013, family members were the source of the infection in 66%-85% of infant pertussis cases in which the source of infection was known. Siblings were the most common source, linked to almost 40% of cases.
“Even if additional Tdap doses are recommended, this would not address the observed shift to siblings as the source of pertussis to infants and puts greater emphasis on the importance of providing newborns with antipertussis antibodies, and there is an optimal strategy in place – vaccinating women during pregnancy,” she said.
This message is emphasized in a recently launched CDC campaign to improve Tdap vaccination rates during pregnancy, which includes fact sheets for health care professionals that point out that Tdap during pregnancy provides the best protection for infants, postpartum Tdap administration is not optimal, and “cocooning alone may not be effective and is hard to implement.”
Several meeting participants pointed out that vaccine uptake during pregnancy is higher in settings where the vaccine is available on site, as high as 80%-90% of pregnancies, and that having to get the vaccine outside of the office, such as at a pharmacy, can markedly reduce the likelihood of vaccination. The CDC’s updated materials, including fact sheets and posters, are available for health care professionals at http://www.cdc.gov/pertussis/materials/hcp.html.
A single dose of Tdap is recommended for people aged 11-64 years: one dose is routinely administered at age 11 or 12 years and one dose of Tdap is recommended for pregnant women during every pregnancy. DTaP vaccine is used to vaccinate younger children starting at age 2 months and is not licensed for adolescents, adults, or children 7 years of age and older.
Based on the available evidence of the impact “cocooning” has on transmission of pertussis to infants, no changes are currently recommended in the use of Tdap vaccine for close contacts of infants, Jennifer Liang, D.V.M., said at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
Presenting the conclusions of ACIP’s pertussis vaccines work group review on the impact of cocooning strategies, Dr. Liang, the CDC’s lead member of the work group, said that pertussis vaccination programs should be focused on vaccinating women during every pregnancy, maintaining high levels of DTap coverage, sustaining Tdap coverage in adolescents, and improving Tdap coverage in adults.
In 2005, ACIP recommended the “cocooning” strategy: vaccinating with Tdap for all close contacts of infants under age 12 months to reduce the risk of transmitting pertussis, including parents, siblings, grandparents, child care providers, and health care personnel, in addition to vaccinating pregnant women immediately post partum. In 2011, ACIP recommended Tdap during pregnancy for women who had not previously received the vaccine, or a postpartum dose for women who did not receive the vaccine during pregnancy and had not previously received the vaccine. In 2012, the recommendation was expanded to every pregnancy, whether or not the woman had received the vaccine before.
The optimal strategy to prevent the transmission of pertussis is vaccinating women during pregnancy, which has been shown to be highly effective in reducing transmission to infants, but rates of vaccination in pregnant women have not been high, said Dr. Liang, an epidemiologist in the CDC’s National Center for Immunization and Respiratory Diseases.
Rates of Tdap coverage, however, among pregnant women in the United States have ranged from 14% to 23% in studies using different sources, including a Michigan Medicaid study, she said.
Implementing and sustaining cocooning programs remain a challenge. Although uptake of Tdap has been highest in postpartum women, there has been limited success in vaccinating fathers or other family members, she said, noting that, in 2012, the rate of Tdap coverage among adults aged 19-64 years who reported living with an infant under age 1 year was 26%.
The effect of cocooning in preventing infant pertussis also is “unclear and inconclusive,” and evidence of the effectiveness of the postpartum dose in preventing infant pertussis is limited and the data are conflicting, Dr. Liang said. Another issue is that, over the past decade, the source of transmission to infants has shifted from parents (usually mothers) as the most common source to siblings, who have more recently been identified as the most common source, she said. A CDC study determined that, between 2006 and 2013, family members were the source of the infection in 66%-85% of infant pertussis cases in which the source of infection was known. Siblings were the most common source, linked to almost 40% of cases.
“Even if additional Tdap doses are recommended, this would not address the observed shift to siblings as the source of pertussis to infants and puts greater emphasis on the importance of providing newborns with antipertussis antibodies, and there is an optimal strategy in place – vaccinating women during pregnancy,” she said.
This message is emphasized in a recently launched CDC campaign to improve Tdap vaccination rates during pregnancy, which includes fact sheets for health care professionals that point out that Tdap during pregnancy provides the best protection for infants, postpartum Tdap administration is not optimal, and “cocooning alone may not be effective and is hard to implement.”
Several meeting participants pointed out that vaccine uptake during pregnancy is higher in settings where the vaccine is available on site, as high as 80%-90% of pregnancies, and that having to get the vaccine outside of the office, such as at a pharmacy, can markedly reduce the likelihood of vaccination. The CDC’s updated materials, including fact sheets and posters, are available for health care professionals at http://www.cdc.gov/pertussis/materials/hcp.html.
A single dose of Tdap is recommended for people aged 11-64 years: one dose is routinely administered at age 11 or 12 years and one dose of Tdap is recommended for pregnant women during every pregnancy. DTaP vaccine is used to vaccinate younger children starting at age 2 months and is not licensed for adolescents, adults, or children 7 years of age and older.
FROM AN ACIP MEETING
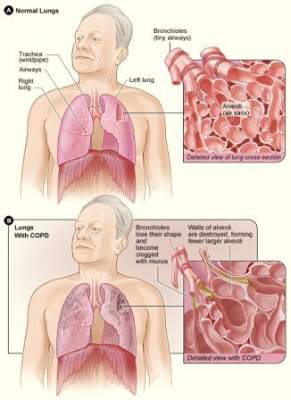
ATS: Glycopyrronium improves lung function, health status in COPD
DENVER – Twice-daily treatment with the long-acting muscarinic antagonist glycopyrronium improved lung function and health status in patients with chronic obstructive pulmonary disorder (COPD) and moderate to severe airflow limitation in the randomized, double-blind, placebo-controlled GEM2 study.
In patients with stable symptomatic COPD with moderate to severe airflow limitation, twice-daily 12.5-mcg dosing of glycopyrronium provides clinically meaningful improvement in lung function over the 12-hour dosing interval, has early onset, is sustained over 12 weeks when compared with placebo, and is associated with significant improvements in COPD symptoms, health status, and rescue medication use, as well as numerical improvement in dyspnea scores, Dr. Edward Kerwin of the Clinical Research Institute of Southern Oregon, PC, Medford, and his colleagues reported in a poster at an international conference of the American Thoracic Society.
Lung function – as measured by forced expiratory volume in 1 second (FEV1) area under the curve from 0-12 hours (AUC 0-12h) – was significantly better both at day 1 and at week 12 of treatment in 216 patients who were randomized to receive a 12.5 mcg twice daily dose of the fast-onset, long-acting muscarinic antagonist (Novartis), compared with 216 patients who received placebo; there was a “significant and clinically meaningful between-treatment difference of 119 and 123 mL, respectively,” the researchers wrote.
“Glycopyrronium also showed consistently significant improvements in trough FEV1 vs. placebo at all assessed time points,” they said, adding that glycopyrronium showed an early onset of bronchodilation with significant improvements in FEV1 at 5 and 15 minutes post dose, compared with placebo at day 1 and week 12.
The least squares mean treatment differences for glycopyrronium vs. placebo for change from baseline in trough forced vital capacity (FVC) were 171 mL on day 2, and 130 mL at week 12. Peak FEV1 and peak FVC were significantly improved with glycopyrronium vs. placebo on day 1 (least squares mean treatment differences of 137 and 223 mL, respectively) and at week 12 (least squares mean treatment differences of 148 and 201 mL, respectively).
Health status was improved at week 12, with both significant and clinically meaningful improvements in St. George’s Respiratory Questionnaire total score in the treatment vs. placebo group (–6.4 vs. –1.2), and the percentage of patients achieving minimal clinically important differences (MCID), defined as at least 4 units, was significantly higher in the treatment vs. placebo group (54.9% vs. 42.3%), the investigators said.
Additionally, numerical improvements in transition dyspnea index total score, and percentage of patients achieving a MCID, defined as at least 1 unit, were observed at week 12 in the glycopyrronium vs. placebo group.
Patients in the glycopyrronium group showed improvement on all symptoms scores and endpoints, according to data recorded in patient e-diaries, and those in the treatment group also were able to perform usual daily activities significantly more often than those in the placebo group.
“A statistically significant decrease in daily, daytime, and nighttime number of puffs, and a significant increase in the percentage of days with no rescue medication use were observed,” the investigators noted.
Patients included in the multicenter GEM2 (Glycopyrronium Effect on Symptoms and Lung Function) study were adults aged 40 years and older with moderate to severe airflow limitation (GOLD 2011 strategy level 2 or 3), who were either current or former smokers with a smoking history of at least 10 pack-years. All had postbronchodilator FEV1 of at least 30% and less than 80% of the predicted value, and postbronchodilator FEV1/forced vital capacity ratio of less than 0.70 at a run-in visit. They also all had a modified Medical Research Council grade of 2 or greater at the run-in visit. Patients with a history of asthma or with a COPD exacerbation requiring treatment with antibiotics and/or systemic corticosteroids, and/or with hospitalization within 6 weeks of the screening and run-in periods were excluded, as were those with a history of long QT syndrome or whose corrected QT was greater than 450 ms at the run-in visit.
All underwent an initial 1- to 7-day washout period and a 2-week run-in period prior to randomization, as well as a safety follow-up period. Patients received either glycopyrronium 12. 5 mcg or placebo twice daily delivered via the Neohaler device for 12 weeks.
Treatment was generally well tolerated; of the 430 patients included in the safety set, 44 permanently discontinued treatment due to adverse events (4.6% and 4.2% in the treatment and placebo groups, respectively). The number who experienced at least one adverse event during the treatment period was similar in the two groups; COPD was the most common adverse event, occurring in 20.8% of those in the treatment group and 21.5% in the placebo group.
A nonfatal myocardial infraction occurred in one patient in the treatment group.
Laboratory parameters and vital sign findings were comparable in the two groups.
Based on the findings of the GEM studies, Novartis has submitted a New Drug Application to the Food and Drug Administration; glycopyrronium is already approved in more than 70 countries, including countries in Latin America and the European Union, as a once-daily treatment marketed as the Seebri Breezhaler.
The GEM2 study was sponsored by Novartis Pharmaceuticals. Two of the study researchers are Novartis employees.
DENVER – Twice-daily treatment with the long-acting muscarinic antagonist glycopyrronium improved lung function and health status in patients with chronic obstructive pulmonary disorder (COPD) and moderate to severe airflow limitation in the randomized, double-blind, placebo-controlled GEM2 study.
In patients with stable symptomatic COPD with moderate to severe airflow limitation, twice-daily 12.5-mcg dosing of glycopyrronium provides clinically meaningful improvement in lung function over the 12-hour dosing interval, has early onset, is sustained over 12 weeks when compared with placebo, and is associated with significant improvements in COPD symptoms, health status, and rescue medication use, as well as numerical improvement in dyspnea scores, Dr. Edward Kerwin of the Clinical Research Institute of Southern Oregon, PC, Medford, and his colleagues reported in a poster at an international conference of the American Thoracic Society.
Lung function – as measured by forced expiratory volume in 1 second (FEV1) area under the curve from 0-12 hours (AUC 0-12h) – was significantly better both at day 1 and at week 12 of treatment in 216 patients who were randomized to receive a 12.5 mcg twice daily dose of the fast-onset, long-acting muscarinic antagonist (Novartis), compared with 216 patients who received placebo; there was a “significant and clinically meaningful between-treatment difference of 119 and 123 mL, respectively,” the researchers wrote.
“Glycopyrronium also showed consistently significant improvements in trough FEV1 vs. placebo at all assessed time points,” they said, adding that glycopyrronium showed an early onset of bronchodilation with significant improvements in FEV1 at 5 and 15 minutes post dose, compared with placebo at day 1 and week 12.
The least squares mean treatment differences for glycopyrronium vs. placebo for change from baseline in trough forced vital capacity (FVC) were 171 mL on day 2, and 130 mL at week 12. Peak FEV1 and peak FVC were significantly improved with glycopyrronium vs. placebo on day 1 (least squares mean treatment differences of 137 and 223 mL, respectively) and at week 12 (least squares mean treatment differences of 148 and 201 mL, respectively).
Health status was improved at week 12, with both significant and clinically meaningful improvements in St. George’s Respiratory Questionnaire total score in the treatment vs. placebo group (–6.4 vs. –1.2), and the percentage of patients achieving minimal clinically important differences (MCID), defined as at least 4 units, was significantly higher in the treatment vs. placebo group (54.9% vs. 42.3%), the investigators said.
Additionally, numerical improvements in transition dyspnea index total score, and percentage of patients achieving a MCID, defined as at least 1 unit, were observed at week 12 in the glycopyrronium vs. placebo group.
Patients in the glycopyrronium group showed improvement on all symptoms scores and endpoints, according to data recorded in patient e-diaries, and those in the treatment group also were able to perform usual daily activities significantly more often than those in the placebo group.
“A statistically significant decrease in daily, daytime, and nighttime number of puffs, and a significant increase in the percentage of days with no rescue medication use were observed,” the investigators noted.
Patients included in the multicenter GEM2 (Glycopyrronium Effect on Symptoms and Lung Function) study were adults aged 40 years and older with moderate to severe airflow limitation (GOLD 2011 strategy level 2 or 3), who were either current or former smokers with a smoking history of at least 10 pack-years. All had postbronchodilator FEV1 of at least 30% and less than 80% of the predicted value, and postbronchodilator FEV1/forced vital capacity ratio of less than 0.70 at a run-in visit. They also all had a modified Medical Research Council grade of 2 or greater at the run-in visit. Patients with a history of asthma or with a COPD exacerbation requiring treatment with antibiotics and/or systemic corticosteroids, and/or with hospitalization within 6 weeks of the screening and run-in periods were excluded, as were those with a history of long QT syndrome or whose corrected QT was greater than 450 ms at the run-in visit.
All underwent an initial 1- to 7-day washout period and a 2-week run-in period prior to randomization, as well as a safety follow-up period. Patients received either glycopyrronium 12. 5 mcg or placebo twice daily delivered via the Neohaler device for 12 weeks.
Treatment was generally well tolerated; of the 430 patients included in the safety set, 44 permanently discontinued treatment due to adverse events (4.6% and 4.2% in the treatment and placebo groups, respectively). The number who experienced at least one adverse event during the treatment period was similar in the two groups; COPD was the most common adverse event, occurring in 20.8% of those in the treatment group and 21.5% in the placebo group.
A nonfatal myocardial infraction occurred in one patient in the treatment group.
Laboratory parameters and vital sign findings were comparable in the two groups.
Based on the findings of the GEM studies, Novartis has submitted a New Drug Application to the Food and Drug Administration; glycopyrronium is already approved in more than 70 countries, including countries in Latin America and the European Union, as a once-daily treatment marketed as the Seebri Breezhaler.
The GEM2 study was sponsored by Novartis Pharmaceuticals. Two of the study researchers are Novartis employees.
DENVER – Twice-daily treatment with the long-acting muscarinic antagonist glycopyrronium improved lung function and health status in patients with chronic obstructive pulmonary disorder (COPD) and moderate to severe airflow limitation in the randomized, double-blind, placebo-controlled GEM2 study.
In patients with stable symptomatic COPD with moderate to severe airflow limitation, twice-daily 12.5-mcg dosing of glycopyrronium provides clinically meaningful improvement in lung function over the 12-hour dosing interval, has early onset, is sustained over 12 weeks when compared with placebo, and is associated with significant improvements in COPD symptoms, health status, and rescue medication use, as well as numerical improvement in dyspnea scores, Dr. Edward Kerwin of the Clinical Research Institute of Southern Oregon, PC, Medford, and his colleagues reported in a poster at an international conference of the American Thoracic Society.
Lung function – as measured by forced expiratory volume in 1 second (FEV1) area under the curve from 0-12 hours (AUC 0-12h) – was significantly better both at day 1 and at week 12 of treatment in 216 patients who were randomized to receive a 12.5 mcg twice daily dose of the fast-onset, long-acting muscarinic antagonist (Novartis), compared with 216 patients who received placebo; there was a “significant and clinically meaningful between-treatment difference of 119 and 123 mL, respectively,” the researchers wrote.
“Glycopyrronium also showed consistently significant improvements in trough FEV1 vs. placebo at all assessed time points,” they said, adding that glycopyrronium showed an early onset of bronchodilation with significant improvements in FEV1 at 5 and 15 minutes post dose, compared with placebo at day 1 and week 12.
The least squares mean treatment differences for glycopyrronium vs. placebo for change from baseline in trough forced vital capacity (FVC) were 171 mL on day 2, and 130 mL at week 12. Peak FEV1 and peak FVC were significantly improved with glycopyrronium vs. placebo on day 1 (least squares mean treatment differences of 137 and 223 mL, respectively) and at week 12 (least squares mean treatment differences of 148 and 201 mL, respectively).
Health status was improved at week 12, with both significant and clinically meaningful improvements in St. George’s Respiratory Questionnaire total score in the treatment vs. placebo group (–6.4 vs. –1.2), and the percentage of patients achieving minimal clinically important differences (MCID), defined as at least 4 units, was significantly higher in the treatment vs. placebo group (54.9% vs. 42.3%), the investigators said.
Additionally, numerical improvements in transition dyspnea index total score, and percentage of patients achieving a MCID, defined as at least 1 unit, were observed at week 12 in the glycopyrronium vs. placebo group.
Patients in the glycopyrronium group showed improvement on all symptoms scores and endpoints, according to data recorded in patient e-diaries, and those in the treatment group also were able to perform usual daily activities significantly more often than those in the placebo group.
“A statistically significant decrease in daily, daytime, and nighttime number of puffs, and a significant increase in the percentage of days with no rescue medication use were observed,” the investigators noted.
Patients included in the multicenter GEM2 (Glycopyrronium Effect on Symptoms and Lung Function) study were adults aged 40 years and older with moderate to severe airflow limitation (GOLD 2011 strategy level 2 or 3), who were either current or former smokers with a smoking history of at least 10 pack-years. All had postbronchodilator FEV1 of at least 30% and less than 80% of the predicted value, and postbronchodilator FEV1/forced vital capacity ratio of less than 0.70 at a run-in visit. They also all had a modified Medical Research Council grade of 2 or greater at the run-in visit. Patients with a history of asthma or with a COPD exacerbation requiring treatment with antibiotics and/or systemic corticosteroids, and/or with hospitalization within 6 weeks of the screening and run-in periods were excluded, as were those with a history of long QT syndrome or whose corrected QT was greater than 450 ms at the run-in visit.
All underwent an initial 1- to 7-day washout period and a 2-week run-in period prior to randomization, as well as a safety follow-up period. Patients received either glycopyrronium 12. 5 mcg or placebo twice daily delivered via the Neohaler device for 12 weeks.
Treatment was generally well tolerated; of the 430 patients included in the safety set, 44 permanently discontinued treatment due to adverse events (4.6% and 4.2% in the treatment and placebo groups, respectively). The number who experienced at least one adverse event during the treatment period was similar in the two groups; COPD was the most common adverse event, occurring in 20.8% of those in the treatment group and 21.5% in the placebo group.
A nonfatal myocardial infraction occurred in one patient in the treatment group.
Laboratory parameters and vital sign findings were comparable in the two groups.
Based on the findings of the GEM studies, Novartis has submitted a New Drug Application to the Food and Drug Administration; glycopyrronium is already approved in more than 70 countries, including countries in Latin America and the European Union, as a once-daily treatment marketed as the Seebri Breezhaler.
The GEM2 study was sponsored by Novartis Pharmaceuticals. Two of the study researchers are Novartis employees.
AT ATS 2015
Key clinical point: Glycopyrronium provides fast-onset, clinically meaningful improvement in lung function vs. placebo in COPD patients with moderate to severe airflow limitation.
Major finding: The between-treatment differences in FEV1 AUC (0-12 h) at day 1 and week 12 of treatment were 119 and 123 mL, respectively.
Data source: A randomized, double-blind, placebo-controlled trial of 432 patients.
Disclosures: The GEM2 study was sponsored by Novartis Pharmaceuticals. Two of the study researchers are Novartis employees.
COPDGene: Millions of smokers may have undiagnosed COPD
More than half of smokers with normal spirometry had some form of respiratory-related impairment associated with COPD, Dr. Elizabeth A. Regan and the Genetic Epidemiology of COPD (COPDGene) investigators reported in JAMA Internal Medicine.
The findings imply that up to 35 million current and former smokers older than age 55 years in the United States may have some form of respiratory-related impairment associated with COPD that has gone undiagnosed with standard spirometry, the researchers wrote (JAMA Internal Med. 2015 June 22 (doi:10.1001/jamainternmed.2015.2735).
They found that 55% of current and former smokers older than age 55 years in the study who did not meet the spirometric criteria for COPD (GOLD [Global Initiative for Chronic Obstructive Lung Disease] 0 score) had significant respiratory disease. Their conclusion was based on seven metrics: chronic bronchitis (seen in 12.6% of the GOLD 0 participants), history of severe respiratory exacerbations (seen in 4.3%), dyspnea score of at least 2 (seen in 23.5%), quantitative emphysema exceeding 5% (seen in 9.8%), quantitative gas trapping exceeding 20%, (seen in 12.2%), St. George’s Respiratory Questionnaire (SGRQ) total score exceeding 25 (seen in 26%), and a 6-minute walk distance of less than 350 m (seen in 15.4%).
In 108 never smokers, none had chronic bronchitis or respiratory exacerbations, 3.7% had dyspnea, 8.3% had quantitative emphysema exceeding 5%, 10.2% had quantitative gas trapping exceeding 20%, 3.7% had SGRQ scores above 25, and 3.7% had a 6-minute walk distance of less than 350 m.
Dr. Regan of National Jewish Health and the University of Colorado, Denver, and her associates gathered data from 21 sites across the United States regarding 8,872 current or former smokers who were between the ages of 45 and 80 years and were classified using GOLD spirometric criteria based on postbronchodilator spirometry: 4,388 had a GOLD 0 score, defined as a normal postbronchodilator ratio of FEV1 to forced vital capacity exceeding 0.7 and an FEV1 percentage of at least 80% predicted; 794 patients had a GOLD 1 score, defined as mild COPD; and 3,690 had a GOLD 2-4 score, defined as moderate to severe COPD.
Compared with 108 never smokers, the GOLD 0 group had a worse quality of life score (mean SGRQ total score 17.6 for GOLD 0 and 7 for never smokers) and a lower 6-minute walk distance (447 m vs. 493 m). In a subset of 300 patients in the GOLD 0 group whose CT scans were visually scored, 42% (127) had evidence of emphysema or airway thickening. In a subset of 100 never smokers, 10% had evidence of emphysema or airway thickening.
Current guidelines do not include treating smokers with normal spirometry, but physicians recognize the role of medication in treating symptoms and effective treatments need to be determined for GOLD 0 patients, the researchers said. Respiratory medications were being prescribed to 20% of the GOLD 0 participants in COPDGene who had at least one impairment, yet these patients reported more symptoms.
The COPDGene study is sponsored by funding from the National Heart, Lung, and Blood Institute and the COPD Foundation through contributions made to an industry advisory board representing AstraZeneca, Boehringer Ingelheim, Novartis, Pfizer, Siemens, Sunovian, and GlaxoSmithKline.
More than half of smokers with normal spirometry had some form of respiratory-related impairment associated with COPD, Dr. Elizabeth A. Regan and the Genetic Epidemiology of COPD (COPDGene) investigators reported in JAMA Internal Medicine.
The findings imply that up to 35 million current and former smokers older than age 55 years in the United States may have some form of respiratory-related impairment associated with COPD that has gone undiagnosed with standard spirometry, the researchers wrote (JAMA Internal Med. 2015 June 22 (doi:10.1001/jamainternmed.2015.2735).
They found that 55% of current and former smokers older than age 55 years in the study who did not meet the spirometric criteria for COPD (GOLD [Global Initiative for Chronic Obstructive Lung Disease] 0 score) had significant respiratory disease. Their conclusion was based on seven metrics: chronic bronchitis (seen in 12.6% of the GOLD 0 participants), history of severe respiratory exacerbations (seen in 4.3%), dyspnea score of at least 2 (seen in 23.5%), quantitative emphysema exceeding 5% (seen in 9.8%), quantitative gas trapping exceeding 20%, (seen in 12.2%), St. George’s Respiratory Questionnaire (SGRQ) total score exceeding 25 (seen in 26%), and a 6-minute walk distance of less than 350 m (seen in 15.4%).
In 108 never smokers, none had chronic bronchitis or respiratory exacerbations, 3.7% had dyspnea, 8.3% had quantitative emphysema exceeding 5%, 10.2% had quantitative gas trapping exceeding 20%, 3.7% had SGRQ scores above 25, and 3.7% had a 6-minute walk distance of less than 350 m.
Dr. Regan of National Jewish Health and the University of Colorado, Denver, and her associates gathered data from 21 sites across the United States regarding 8,872 current or former smokers who were between the ages of 45 and 80 years and were classified using GOLD spirometric criteria based on postbronchodilator spirometry: 4,388 had a GOLD 0 score, defined as a normal postbronchodilator ratio of FEV1 to forced vital capacity exceeding 0.7 and an FEV1 percentage of at least 80% predicted; 794 patients had a GOLD 1 score, defined as mild COPD; and 3,690 had a GOLD 2-4 score, defined as moderate to severe COPD.
Compared with 108 never smokers, the GOLD 0 group had a worse quality of life score (mean SGRQ total score 17.6 for GOLD 0 and 7 for never smokers) and a lower 6-minute walk distance (447 m vs. 493 m). In a subset of 300 patients in the GOLD 0 group whose CT scans were visually scored, 42% (127) had evidence of emphysema or airway thickening. In a subset of 100 never smokers, 10% had evidence of emphysema or airway thickening.
Current guidelines do not include treating smokers with normal spirometry, but physicians recognize the role of medication in treating symptoms and effective treatments need to be determined for GOLD 0 patients, the researchers said. Respiratory medications were being prescribed to 20% of the GOLD 0 participants in COPDGene who had at least one impairment, yet these patients reported more symptoms.
The COPDGene study is sponsored by funding from the National Heart, Lung, and Blood Institute and the COPD Foundation through contributions made to an industry advisory board representing AstraZeneca, Boehringer Ingelheim, Novartis, Pfizer, Siemens, Sunovian, and GlaxoSmithKline.
More than half of smokers with normal spirometry had some form of respiratory-related impairment associated with COPD, Dr. Elizabeth A. Regan and the Genetic Epidemiology of COPD (COPDGene) investigators reported in JAMA Internal Medicine.
The findings imply that up to 35 million current and former smokers older than age 55 years in the United States may have some form of respiratory-related impairment associated with COPD that has gone undiagnosed with standard spirometry, the researchers wrote (JAMA Internal Med. 2015 June 22 (doi:10.1001/jamainternmed.2015.2735).
They found that 55% of current and former smokers older than age 55 years in the study who did not meet the spirometric criteria for COPD (GOLD [Global Initiative for Chronic Obstructive Lung Disease] 0 score) had significant respiratory disease. Their conclusion was based on seven metrics: chronic bronchitis (seen in 12.6% of the GOLD 0 participants), history of severe respiratory exacerbations (seen in 4.3%), dyspnea score of at least 2 (seen in 23.5%), quantitative emphysema exceeding 5% (seen in 9.8%), quantitative gas trapping exceeding 20%, (seen in 12.2%), St. George’s Respiratory Questionnaire (SGRQ) total score exceeding 25 (seen in 26%), and a 6-minute walk distance of less than 350 m (seen in 15.4%).
In 108 never smokers, none had chronic bronchitis or respiratory exacerbations, 3.7% had dyspnea, 8.3% had quantitative emphysema exceeding 5%, 10.2% had quantitative gas trapping exceeding 20%, 3.7% had SGRQ scores above 25, and 3.7% had a 6-minute walk distance of less than 350 m.
Dr. Regan of National Jewish Health and the University of Colorado, Denver, and her associates gathered data from 21 sites across the United States regarding 8,872 current or former smokers who were between the ages of 45 and 80 years and were classified using GOLD spirometric criteria based on postbronchodilator spirometry: 4,388 had a GOLD 0 score, defined as a normal postbronchodilator ratio of FEV1 to forced vital capacity exceeding 0.7 and an FEV1 percentage of at least 80% predicted; 794 patients had a GOLD 1 score, defined as mild COPD; and 3,690 had a GOLD 2-4 score, defined as moderate to severe COPD.
Compared with 108 never smokers, the GOLD 0 group had a worse quality of life score (mean SGRQ total score 17.6 for GOLD 0 and 7 for never smokers) and a lower 6-minute walk distance (447 m vs. 493 m). In a subset of 300 patients in the GOLD 0 group whose CT scans were visually scored, 42% (127) had evidence of emphysema or airway thickening. In a subset of 100 never smokers, 10% had evidence of emphysema or airway thickening.
Current guidelines do not include treating smokers with normal spirometry, but physicians recognize the role of medication in treating symptoms and effective treatments need to be determined for GOLD 0 patients, the researchers said. Respiratory medications were being prescribed to 20% of the GOLD 0 participants in COPDGene who had at least one impairment, yet these patients reported more symptoms.
The COPDGene study is sponsored by funding from the National Heart, Lung, and Blood Institute and the COPD Foundation through contributions made to an industry advisory board representing AstraZeneca, Boehringer Ingelheim, Novartis, Pfizer, Siemens, Sunovian, and GlaxoSmithKline.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Up to 35 million current and former smokers older than age 55 years may have COPD-like respiratory-related impairment.
Major finding: Of 4,388 current and former smokers older than age 55 years who did not meet the spirometric criteria for COPD (GOLD 0 score), 55% had significant respiratory disease.
Data source: The COPDGene study, one of the largest studies ever to investigate the underlying genetic factors of COPD, plans to enroll 10,000 individuals.
Disclosures: The COPDGene study is sponsored by funding from the National Heart, Lung, and Blood Institute and the COPD Foundation through contributions made to an industry advisory board representing AstraZeneca, Boehringer Ingelheim, Novartis, Pfizer, Siemens, Sunovian, and GlaxoSmithKline.
Invasive approaches ‘overused’ for evaluating pulmonary nodules
One in four intermediate-sized (8-20 mm) pulmonary nodules were found to be malignant, based on results from a retrospective study of 377 patients seen in 18 community pulmonology practices.
Malignant nodules were more likely to be found in current or former smokers and to be larger than the benign nodules.
Further, despite guideline recommendations for surveillance of pulmonary nodules with less than a 5% pretest probability of malignancy, 44% of 36 patients with low-risk pulmonary nodules underwent at least one invasive procedure.
“To our knowledge, this is the first study that documents the prevalence of cancer (25%) in patients with intermediate-sized nodules referred to community-based pulmonologists,” wrote Dr. Nichole T. Tanner of the Medical University of South Carolina, Charleston, and her coauthors in the study published online (Chest 2015 June 18 [doi:10.1378/chest.15-0630]). “This finding has implications for managing pulmonary nodules in the community; because the risk of cancer is substantial, patients should be managed based on their individualized risk for malignancy.”
Biopsy – either by transthoracic needle aspiration or bronchoscopy – was performed in 33% (125) of patients, of whom 35% were found to have a malignancy and 57% had a specific benign diagnosis; biopsies in 8% were nondiagnostic and those patients were followed for 2 years.
Referrals for surgery were given to 20% (77) of patients; 19 had previously undergone a biopsy, with 11 having a nondiagnostic biopsy and eight having a received a benign result. Of patients who underwent surgery, 65% were diagnosed with a malignancy, and 35% had benign disease. However, the rate of surgical resection was similar regardless of patients’ pretest probability of malignancy.
PET scanning, performed in 37% of patients, was more likely in those who had a biopsy or surgery. The overall accuracy of PET was 74%, and the false-negative rate decreased slightly as the size of the nodule increased.
“Guidelines recommend surgery if the pretest probability of cancer is high (pCA > 65%) because a negative biopsy would not dissuade the clinician from pursuing a definitive diagnosis and a positive biopsy would lead to surgery anyway.”
The researchers pointed out that there are a range of noninvasive options now available to determine the likelihood that a nodule is malignant, such as CT scanning with the use of volumetric software to measure diameter and volume-doubling time of a nodule in between scans.
The study was supported by Integrated Diagnostics. All but one study author declared consulting fees, grant funding, stock options, or employment with Integrated Diagnostics.
One in four intermediate-sized (8-20 mm) pulmonary nodules were found to be malignant, based on results from a retrospective study of 377 patients seen in 18 community pulmonology practices.
Malignant nodules were more likely to be found in current or former smokers and to be larger than the benign nodules.
Further, despite guideline recommendations for surveillance of pulmonary nodules with less than a 5% pretest probability of malignancy, 44% of 36 patients with low-risk pulmonary nodules underwent at least one invasive procedure.
“To our knowledge, this is the first study that documents the prevalence of cancer (25%) in patients with intermediate-sized nodules referred to community-based pulmonologists,” wrote Dr. Nichole T. Tanner of the Medical University of South Carolina, Charleston, and her coauthors in the study published online (Chest 2015 June 18 [doi:10.1378/chest.15-0630]). “This finding has implications for managing pulmonary nodules in the community; because the risk of cancer is substantial, patients should be managed based on their individualized risk for malignancy.”
Biopsy – either by transthoracic needle aspiration or bronchoscopy – was performed in 33% (125) of patients, of whom 35% were found to have a malignancy and 57% had a specific benign diagnosis; biopsies in 8% were nondiagnostic and those patients were followed for 2 years.
Referrals for surgery were given to 20% (77) of patients; 19 had previously undergone a biopsy, with 11 having a nondiagnostic biopsy and eight having a received a benign result. Of patients who underwent surgery, 65% were diagnosed with a malignancy, and 35% had benign disease. However, the rate of surgical resection was similar regardless of patients’ pretest probability of malignancy.
PET scanning, performed in 37% of patients, was more likely in those who had a biopsy or surgery. The overall accuracy of PET was 74%, and the false-negative rate decreased slightly as the size of the nodule increased.
“Guidelines recommend surgery if the pretest probability of cancer is high (pCA > 65%) because a negative biopsy would not dissuade the clinician from pursuing a definitive diagnosis and a positive biopsy would lead to surgery anyway.”
The researchers pointed out that there are a range of noninvasive options now available to determine the likelihood that a nodule is malignant, such as CT scanning with the use of volumetric software to measure diameter and volume-doubling time of a nodule in between scans.
The study was supported by Integrated Diagnostics. All but one study author declared consulting fees, grant funding, stock options, or employment with Integrated Diagnostics.
One in four intermediate-sized (8-20 mm) pulmonary nodules were found to be malignant, based on results from a retrospective study of 377 patients seen in 18 community pulmonology practices.
Malignant nodules were more likely to be found in current or former smokers and to be larger than the benign nodules.
Further, despite guideline recommendations for surveillance of pulmonary nodules with less than a 5% pretest probability of malignancy, 44% of 36 patients with low-risk pulmonary nodules underwent at least one invasive procedure.
“To our knowledge, this is the first study that documents the prevalence of cancer (25%) in patients with intermediate-sized nodules referred to community-based pulmonologists,” wrote Dr. Nichole T. Tanner of the Medical University of South Carolina, Charleston, and her coauthors in the study published online (Chest 2015 June 18 [doi:10.1378/chest.15-0630]). “This finding has implications for managing pulmonary nodules in the community; because the risk of cancer is substantial, patients should be managed based on their individualized risk for malignancy.”
Biopsy – either by transthoracic needle aspiration or bronchoscopy – was performed in 33% (125) of patients, of whom 35% were found to have a malignancy and 57% had a specific benign diagnosis; biopsies in 8% were nondiagnostic and those patients were followed for 2 years.
Referrals for surgery were given to 20% (77) of patients; 19 had previously undergone a biopsy, with 11 having a nondiagnostic biopsy and eight having a received a benign result. Of patients who underwent surgery, 65% were diagnosed with a malignancy, and 35% had benign disease. However, the rate of surgical resection was similar regardless of patients’ pretest probability of malignancy.
PET scanning, performed in 37% of patients, was more likely in those who had a biopsy or surgery. The overall accuracy of PET was 74%, and the false-negative rate decreased slightly as the size of the nodule increased.
“Guidelines recommend surgery if the pretest probability of cancer is high (pCA > 65%) because a negative biopsy would not dissuade the clinician from pursuing a definitive diagnosis and a positive biopsy would lead to surgery anyway.”
The researchers pointed out that there are a range of noninvasive options now available to determine the likelihood that a nodule is malignant, such as CT scanning with the use of volumetric software to measure diameter and volume-doubling time of a nodule in between scans.
The study was supported by Integrated Diagnostics. All but one study author declared consulting fees, grant funding, stock options, or employment with Integrated Diagnostics.
FROM CHEST
Key clinical point: One in four pulmonary nodules 8-20 mm in size are malignant, and invasive tests are being overused in low-risk patients in community settings.
Major finding: Despite guidelines recommending pulmonary nodes with a less than 5% pretest probability of malignancy be managed with surveillance only, 44% of low-risk patients in the study underwent at least one invasive procedure for what proved to be a benign nodule.
Data source: A multicenter, retrospective study in 377 patients.
Disclosures: The study was supported by Integrated Diagnostics. All but one author declared consulting fees, grant funding, stock options, or employment with Integrated Diagnostics.
Carrots and sticks lead to smoking cessation
Rewarding smokers for quitting was a more popular option for smoking cessation compared to sanctions-based treatment, but about the same number of participants in either group had quit smoking after 1 year.
Reward-based smoking cessation programs were accepted by 90% of those randomized, compared with 13.7% acceptance of deposit-based programs, and at 6 months, significantly more reward-based participants had ceased smoking, compared with deposit-based participants (15.2% vs. 10.2%). However, as with most such studies, at 1 year, nearly 50% of those who had achieved abstinence at 6 months had returned to smoking in all groups, according to a randomized controlled study of 2,538 CVS Caremark employees and their friends and relatives (ClinicalTrials.gov number, NCT01526265).
Participants were assigned to one of five groups: 468 to usual care only as the control, reported Dr. Scott D. Halpern of the University of Pennsylvania and his colleagues (N. Engl. J. Med. 2015;372:2108-17). They and all participants received information about local smoking cessation resources, cessation guides produced by the American Cancer Society, and, the 41% of the participants receiving health benefits through CVS Caremark had free access to a behavioral-modification program and nicotine-replacement therapy.
In addition, 498 were assigned to individual reward (eligible to receive $200 if they had biochemically confirmed abstinence at each of three times: 14 days, 30 days, and 6 months after quitting, with an additional $200 bonus at 6 months, for a total of $800); 519 to collaborative reward (in addition to the $800, patients were grouped into cohorts of six individuals who would receive an additional $100 per time point if one participant quit smoking to $600 per time point per participant if all six quit); 582 to individual deposit (the $800 dollars included a $150 deposit that would be refunded to participants who quit smoking), and 471 to competitive deposit (included the $150 deposit with the addition of a $450 matching reward per member ($3,600 total), which was redistributed among members who quit at each time point).
In intention-to-treat analyses, all four programs yielded greater rates of sustained cessation through 6 months (range, 9.4%-16.0%) than did usual care (6.0%) (P < .05 for all comparisons).
At 6 months, sustained abstinence was greater with reward-based incentives (15.7%) than with deposit-based (10.2%) (P < .001) and was similar between individual-incentive programs and group-incentive ones (12.1% vs. 13.7%, P = 0.29).
In addition, in instrumental-variable analyses that accounted for differential acceptance, the rate of abstinence at 6 months was 13.2% higher in the deposit-based programs than in the reward-based programs among those who would accept participation in either type of program, the authors stated, indicating that the use of such a program might be of great cost-effectiveness to a health care provider.
Dr. Halpern reported having no relevant conflicts of interest. The National Cancer Institute, the National Institute on Aging, and CVS Caremark supported the study.
Smoking remains the leading cause of preventable deaths in America. It is estimated that employing a smoker costs nearly $6,000 more per year than employing nonsmokers. The article cited, in the New England Journal of Medicine, describes a randomized controlled trial of CVS Caremark employees, their families, and friends who smoke more than five cigarettes per day. The trial compared usual care to four different interventions designed to assess whether a financial incentive would entice greater quitting and abstinence rates.
The researchers looked at whether group participation with potential peer pressure would improve quitting rates. The group-oriented arms were not more effective than individual incentive arms. The psychology of loss aversion versus cash incentive was addressed by asking participants in one group to deposit money and get it back after 6 months of being smoking free. Requiring deposits resulted in decreased participation overall but in those who committed to this arm higher abstinence rates were seen. Overall, incentive rewards over 6 months of participation nearly tripled the rate of smoking cessation compared to usual care.

|
Dr. Michael Liptay |
The severity of cigarette smoking addiction was highlighted by a maximum success rate of around 15% in the best arm as well as a 50% return to smoking rate in those original quitters at 1 year after trial inception. Future innovations in employee benefit design must address the need for shared participation in health maintenance and some form of lifelong risk/reward system that engages people to be responsible for their own health choices.
Dr. Michael Liptay is the medical editor for Thoracic Surgery News.
Smoking remains the leading cause of preventable deaths in America. It is estimated that employing a smoker costs nearly $6,000 more per year than employing nonsmokers. The article cited, in the New England Journal of Medicine, describes a randomized controlled trial of CVS Caremark employees, their families, and friends who smoke more than five cigarettes per day. The trial compared usual care to four different interventions designed to assess whether a financial incentive would entice greater quitting and abstinence rates.
The researchers looked at whether group participation with potential peer pressure would improve quitting rates. The group-oriented arms were not more effective than individual incentive arms. The psychology of loss aversion versus cash incentive was addressed by asking participants in one group to deposit money and get it back after 6 months of being smoking free. Requiring deposits resulted in decreased participation overall but in those who committed to this arm higher abstinence rates were seen. Overall, incentive rewards over 6 months of participation nearly tripled the rate of smoking cessation compared to usual care.

|
Dr. Michael Liptay |
The severity of cigarette smoking addiction was highlighted by a maximum success rate of around 15% in the best arm as well as a 50% return to smoking rate in those original quitters at 1 year after trial inception. Future innovations in employee benefit design must address the need for shared participation in health maintenance and some form of lifelong risk/reward system that engages people to be responsible for their own health choices.
Dr. Michael Liptay is the medical editor for Thoracic Surgery News.
Smoking remains the leading cause of preventable deaths in America. It is estimated that employing a smoker costs nearly $6,000 more per year than employing nonsmokers. The article cited, in the New England Journal of Medicine, describes a randomized controlled trial of CVS Caremark employees, their families, and friends who smoke more than five cigarettes per day. The trial compared usual care to four different interventions designed to assess whether a financial incentive would entice greater quitting and abstinence rates.
The researchers looked at whether group participation with potential peer pressure would improve quitting rates. The group-oriented arms were not more effective than individual incentive arms. The psychology of loss aversion versus cash incentive was addressed by asking participants in one group to deposit money and get it back after 6 months of being smoking free. Requiring deposits resulted in decreased participation overall but in those who committed to this arm higher abstinence rates were seen. Overall, incentive rewards over 6 months of participation nearly tripled the rate of smoking cessation compared to usual care.

|
Dr. Michael Liptay |
The severity of cigarette smoking addiction was highlighted by a maximum success rate of around 15% in the best arm as well as a 50% return to smoking rate in those original quitters at 1 year after trial inception. Future innovations in employee benefit design must address the need for shared participation in health maintenance and some form of lifelong risk/reward system that engages people to be responsible for their own health choices.
Dr. Michael Liptay is the medical editor for Thoracic Surgery News.
Rewarding smokers for quitting was a more popular option for smoking cessation compared to sanctions-based treatment, but about the same number of participants in either group had quit smoking after 1 year.
Reward-based smoking cessation programs were accepted by 90% of those randomized, compared with 13.7% acceptance of deposit-based programs, and at 6 months, significantly more reward-based participants had ceased smoking, compared with deposit-based participants (15.2% vs. 10.2%). However, as with most such studies, at 1 year, nearly 50% of those who had achieved abstinence at 6 months had returned to smoking in all groups, according to a randomized controlled study of 2,538 CVS Caremark employees and their friends and relatives (ClinicalTrials.gov number, NCT01526265).
Participants were assigned to one of five groups: 468 to usual care only as the control, reported Dr. Scott D. Halpern of the University of Pennsylvania and his colleagues (N. Engl. J. Med. 2015;372:2108-17). They and all participants received information about local smoking cessation resources, cessation guides produced by the American Cancer Society, and, the 41% of the participants receiving health benefits through CVS Caremark had free access to a behavioral-modification program and nicotine-replacement therapy.
In addition, 498 were assigned to individual reward (eligible to receive $200 if they had biochemically confirmed abstinence at each of three times: 14 days, 30 days, and 6 months after quitting, with an additional $200 bonus at 6 months, for a total of $800); 519 to collaborative reward (in addition to the $800, patients were grouped into cohorts of six individuals who would receive an additional $100 per time point if one participant quit smoking to $600 per time point per participant if all six quit); 582 to individual deposit (the $800 dollars included a $150 deposit that would be refunded to participants who quit smoking), and 471 to competitive deposit (included the $150 deposit with the addition of a $450 matching reward per member ($3,600 total), which was redistributed among members who quit at each time point).
In intention-to-treat analyses, all four programs yielded greater rates of sustained cessation through 6 months (range, 9.4%-16.0%) than did usual care (6.0%) (P < .05 for all comparisons).
At 6 months, sustained abstinence was greater with reward-based incentives (15.7%) than with deposit-based (10.2%) (P < .001) and was similar between individual-incentive programs and group-incentive ones (12.1% vs. 13.7%, P = 0.29).
In addition, in instrumental-variable analyses that accounted for differential acceptance, the rate of abstinence at 6 months was 13.2% higher in the deposit-based programs than in the reward-based programs among those who would accept participation in either type of program, the authors stated, indicating that the use of such a program might be of great cost-effectiveness to a health care provider.
Dr. Halpern reported having no relevant conflicts of interest. The National Cancer Institute, the National Institute on Aging, and CVS Caremark supported the study.
Rewarding smokers for quitting was a more popular option for smoking cessation compared to sanctions-based treatment, but about the same number of participants in either group had quit smoking after 1 year.
Reward-based smoking cessation programs were accepted by 90% of those randomized, compared with 13.7% acceptance of deposit-based programs, and at 6 months, significantly more reward-based participants had ceased smoking, compared with deposit-based participants (15.2% vs. 10.2%). However, as with most such studies, at 1 year, nearly 50% of those who had achieved abstinence at 6 months had returned to smoking in all groups, according to a randomized controlled study of 2,538 CVS Caremark employees and their friends and relatives (ClinicalTrials.gov number, NCT01526265).
Participants were assigned to one of five groups: 468 to usual care only as the control, reported Dr. Scott D. Halpern of the University of Pennsylvania and his colleagues (N. Engl. J. Med. 2015;372:2108-17). They and all participants received information about local smoking cessation resources, cessation guides produced by the American Cancer Society, and, the 41% of the participants receiving health benefits through CVS Caremark had free access to a behavioral-modification program and nicotine-replacement therapy.
In addition, 498 were assigned to individual reward (eligible to receive $200 if they had biochemically confirmed abstinence at each of three times: 14 days, 30 days, and 6 months after quitting, with an additional $200 bonus at 6 months, for a total of $800); 519 to collaborative reward (in addition to the $800, patients were grouped into cohorts of six individuals who would receive an additional $100 per time point if one participant quit smoking to $600 per time point per participant if all six quit); 582 to individual deposit (the $800 dollars included a $150 deposit that would be refunded to participants who quit smoking), and 471 to competitive deposit (included the $150 deposit with the addition of a $450 matching reward per member ($3,600 total), which was redistributed among members who quit at each time point).
In intention-to-treat analyses, all four programs yielded greater rates of sustained cessation through 6 months (range, 9.4%-16.0%) than did usual care (6.0%) (P < .05 for all comparisons).
At 6 months, sustained abstinence was greater with reward-based incentives (15.7%) than with deposit-based (10.2%) (P < .001) and was similar between individual-incentive programs and group-incentive ones (12.1% vs. 13.7%, P = 0.29).
In addition, in instrumental-variable analyses that accounted for differential acceptance, the rate of abstinence at 6 months was 13.2% higher in the deposit-based programs than in the reward-based programs among those who would accept participation in either type of program, the authors stated, indicating that the use of such a program might be of great cost-effectiveness to a health care provider.
Dr. Halpern reported having no relevant conflicts of interest. The National Cancer Institute, the National Institute on Aging, and CVS Caremark supported the study.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Reward-based smoking cessation incentive programs were more acceptable and effective than were reward plus penalty-based programs.
Major finding: At 6 months, significantly more reward-based participants had ceased smoking compared with deposit-based participants (15.2% vs. 10.2%).
Data source: A five-group randomized, controlled trial of 2,538 CVS-Caremark employees comparing usual care with four incentive programs aimed at sustained abstinence from smoking.
Disclosures: Dr. Halpern reported having no relevant conflicts of interest. The National Cancer Institute, the National Institute on Aging, and CVS Caremark supported the study.
Only moderate-quality evidence supports medical cannabinoids
At best, only moderate-quality evidence supports the use of medical cannabinoids, and for only two conditions. And low-quality evidence only “suggests” that these agents may improve other medical conditions, but that limited effectiveness applies only to the four conditions that have been studied, according to a report published online June 23 in JAMA.
This doesn’t necessarily mean that cannabinoids have poor efficacy but instead likely reflects the dearth of high-quality research into their medical usefulness.
In what they described as the first comprehensive review to evaluate the efficacy of numerous cannabinoids across a broad range of indications, researchers analyzed data from 79 studies involving 6,462 participants performed from 1975 to early 2015. The studies assessed nabilone, dronabinol, nabiximols, levonantradol, THC, THC/CBD, and ajuvenic acid, delivered via oral capsules, cigarettes, vaporizers, oromucosal sprays, or intramuscular injection, said Penny F. Whiting, Ph.D., of University Hospitals Bristol (England) and her associates.
Most of the studies suggested that cannabinoids improved symptoms for nearly all the 10 medical conditions included in this meta-analysis, but most of the studies were of poor quality so their conclusions were questionable. These agents’ efficacy did not vary according to the type of cannabinoid assessed or the mode of delivery.
Moderate-quality evidence indicated that cannabinoids may be beneficial for chronic neuropathic or cancer pain, and moderate-quality evidence indicated that they may also be beneficial for spasticity due to multiple sclerosis or traumatic paraplegia. Low-quality evidence suggested that cannabinoids may improve nausea and vomiting due to chemotherapy, may improve appetite and induce weight gain in HIV infection, and may improve sleep in primary sleep disorders as well as in conditions that disrupt sleep such as fibromyalgia, multiple sclerosis, and chronic pain. Very low-quality evidence (due to extremely small sample sizes) suggested that cannabinoids may greatly improve tic severity in Tourette’s syndrome, Dr. Whiting and her associates said (JAMA 2015 June 23 [doi:10.1001/jama.2015.6358]).
Otherwise, the evidence did not support cannabinoids’ efficacy in anxiety, depression, psychosis, or glaucoma. Adverse events included asthenia, problems with balance, confusion, dizziness, disorientation, dry mouth, fatigue, and somnolence.
It is unclear why medical marijuana has averted the usual Food and Drug Administration approval process required of other medications.
Adequately powered, double-blind, randomized, placebo- or treatment-controlled clinical trials are critical to establish cannabinoids’ short- and long-term efficacy and safety. Yet they already qualify by state law for use in conditions as varied as hepatitis C, Crohn’s disease, Parkinson’s disease, psoriasis, sickle cell disease, and posttraumatic stress disorder.
In particular, the risks of repeated exposure to cannabinoids needs further study. Addiction, tolerance, and a distinct withdrawal syndrome have been documented, and there is also a small but definite risk of psychotic disorder.
Dr. Deepak Cyril D’Souza and Dr. Mohini Ranganathan are in the department of psychiatry at Yale University, New Haven; in the psychiatry service at Veterans Affairs Connecticut Healthcare System, West Haven; and at Abraham Ribicoff Research Facilities at the Connecticut Mental Health Center, New Haven. Dr. D’Souza reported receiving grants from AbbVie and Pfizer, and serves on the Connecticut Board of Physicians that advises the Commissioner of Consumer Protection about the Act Concerning the Palliative Use of Marijuana. Dr. Ranganathan reported receiving grants from Insys Therapeutics. Dr. D’Souza and Dr. Ranganathan made these remarks in an editorial accompanying Dr. Whiting’s report (JAMA 2015;313:2431-2).
It is unclear why medical marijuana has averted the usual Food and Drug Administration approval process required of other medications.
Adequately powered, double-blind, randomized, placebo- or treatment-controlled clinical trials are critical to establish cannabinoids’ short- and long-term efficacy and safety. Yet they already qualify by state law for use in conditions as varied as hepatitis C, Crohn’s disease, Parkinson’s disease, psoriasis, sickle cell disease, and posttraumatic stress disorder.
In particular, the risks of repeated exposure to cannabinoids needs further study. Addiction, tolerance, and a distinct withdrawal syndrome have been documented, and there is also a small but definite risk of psychotic disorder.
Dr. Deepak Cyril D’Souza and Dr. Mohini Ranganathan are in the department of psychiatry at Yale University, New Haven; in the psychiatry service at Veterans Affairs Connecticut Healthcare System, West Haven; and at Abraham Ribicoff Research Facilities at the Connecticut Mental Health Center, New Haven. Dr. D’Souza reported receiving grants from AbbVie and Pfizer, and serves on the Connecticut Board of Physicians that advises the Commissioner of Consumer Protection about the Act Concerning the Palliative Use of Marijuana. Dr. Ranganathan reported receiving grants from Insys Therapeutics. Dr. D’Souza and Dr. Ranganathan made these remarks in an editorial accompanying Dr. Whiting’s report (JAMA 2015;313:2431-2).
It is unclear why medical marijuana has averted the usual Food and Drug Administration approval process required of other medications.
Adequately powered, double-blind, randomized, placebo- or treatment-controlled clinical trials are critical to establish cannabinoids’ short- and long-term efficacy and safety. Yet they already qualify by state law for use in conditions as varied as hepatitis C, Crohn’s disease, Parkinson’s disease, psoriasis, sickle cell disease, and posttraumatic stress disorder.
In particular, the risks of repeated exposure to cannabinoids needs further study. Addiction, tolerance, and a distinct withdrawal syndrome have been documented, and there is also a small but definite risk of psychotic disorder.
Dr. Deepak Cyril D’Souza and Dr. Mohini Ranganathan are in the department of psychiatry at Yale University, New Haven; in the psychiatry service at Veterans Affairs Connecticut Healthcare System, West Haven; and at Abraham Ribicoff Research Facilities at the Connecticut Mental Health Center, New Haven. Dr. D’Souza reported receiving grants from AbbVie and Pfizer, and serves on the Connecticut Board of Physicians that advises the Commissioner of Consumer Protection about the Act Concerning the Palliative Use of Marijuana. Dr. Ranganathan reported receiving grants from Insys Therapeutics. Dr. D’Souza and Dr. Ranganathan made these remarks in an editorial accompanying Dr. Whiting’s report (JAMA 2015;313:2431-2).
At best, only moderate-quality evidence supports the use of medical cannabinoids, and for only two conditions. And low-quality evidence only “suggests” that these agents may improve other medical conditions, but that limited effectiveness applies only to the four conditions that have been studied, according to a report published online June 23 in JAMA.
This doesn’t necessarily mean that cannabinoids have poor efficacy but instead likely reflects the dearth of high-quality research into their medical usefulness.
In what they described as the first comprehensive review to evaluate the efficacy of numerous cannabinoids across a broad range of indications, researchers analyzed data from 79 studies involving 6,462 participants performed from 1975 to early 2015. The studies assessed nabilone, dronabinol, nabiximols, levonantradol, THC, THC/CBD, and ajuvenic acid, delivered via oral capsules, cigarettes, vaporizers, oromucosal sprays, or intramuscular injection, said Penny F. Whiting, Ph.D., of University Hospitals Bristol (England) and her associates.
Most of the studies suggested that cannabinoids improved symptoms for nearly all the 10 medical conditions included in this meta-analysis, but most of the studies were of poor quality so their conclusions were questionable. These agents’ efficacy did not vary according to the type of cannabinoid assessed or the mode of delivery.
Moderate-quality evidence indicated that cannabinoids may be beneficial for chronic neuropathic or cancer pain, and moderate-quality evidence indicated that they may also be beneficial for spasticity due to multiple sclerosis or traumatic paraplegia. Low-quality evidence suggested that cannabinoids may improve nausea and vomiting due to chemotherapy, may improve appetite and induce weight gain in HIV infection, and may improve sleep in primary sleep disorders as well as in conditions that disrupt sleep such as fibromyalgia, multiple sclerosis, and chronic pain. Very low-quality evidence (due to extremely small sample sizes) suggested that cannabinoids may greatly improve tic severity in Tourette’s syndrome, Dr. Whiting and her associates said (JAMA 2015 June 23 [doi:10.1001/jama.2015.6358]).
Otherwise, the evidence did not support cannabinoids’ efficacy in anxiety, depression, psychosis, or glaucoma. Adverse events included asthenia, problems with balance, confusion, dizziness, disorientation, dry mouth, fatigue, and somnolence.
At best, only moderate-quality evidence supports the use of medical cannabinoids, and for only two conditions. And low-quality evidence only “suggests” that these agents may improve other medical conditions, but that limited effectiveness applies only to the four conditions that have been studied, according to a report published online June 23 in JAMA.
This doesn’t necessarily mean that cannabinoids have poor efficacy but instead likely reflects the dearth of high-quality research into their medical usefulness.
In what they described as the first comprehensive review to evaluate the efficacy of numerous cannabinoids across a broad range of indications, researchers analyzed data from 79 studies involving 6,462 participants performed from 1975 to early 2015. The studies assessed nabilone, dronabinol, nabiximols, levonantradol, THC, THC/CBD, and ajuvenic acid, delivered via oral capsules, cigarettes, vaporizers, oromucosal sprays, or intramuscular injection, said Penny F. Whiting, Ph.D., of University Hospitals Bristol (England) and her associates.
Most of the studies suggested that cannabinoids improved symptoms for nearly all the 10 medical conditions included in this meta-analysis, but most of the studies were of poor quality so their conclusions were questionable. These agents’ efficacy did not vary according to the type of cannabinoid assessed or the mode of delivery.
Moderate-quality evidence indicated that cannabinoids may be beneficial for chronic neuropathic or cancer pain, and moderate-quality evidence indicated that they may also be beneficial for spasticity due to multiple sclerosis or traumatic paraplegia. Low-quality evidence suggested that cannabinoids may improve nausea and vomiting due to chemotherapy, may improve appetite and induce weight gain in HIV infection, and may improve sleep in primary sleep disorders as well as in conditions that disrupt sleep such as fibromyalgia, multiple sclerosis, and chronic pain. Very low-quality evidence (due to extremely small sample sizes) suggested that cannabinoids may greatly improve tic severity in Tourette’s syndrome, Dr. Whiting and her associates said (JAMA 2015 June 23 [doi:10.1001/jama.2015.6358]).
Otherwise, the evidence did not support cannabinoids’ efficacy in anxiety, depression, psychosis, or glaucoma. Adverse events included asthenia, problems with balance, confusion, dizziness, disorientation, dry mouth, fatigue, and somnolence.
FROM JAMA
Key clinical point: Only moderate-quality evidence supports the use of medical cannabinoids, and only for two conditions.
Major finding: Moderate-quality evidence indicated that cannabinoids may be beneficial for chronic neuropathic or cancer pain and for spasticity due to multiple sclerosis or traumatic paraplegia.
Data source: A comprehensive review of the literature since 1975 and a meta-analysis of 79 clinical trials involving 6,462 participants.
Disclosures: This study was funded by the Swiss Federal Office of Public Health. Dr. Whiting and her associates reported having no relevant financial conflicts of interest.