User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Powered by CHEST Physician, Clinician Reviews, MDedge Family Medicine, Internal Medicine News, and The Journal of Clinical Outcomes Management.
GERD and sleep disorders often go hand in glove
DENVER – Gastroesophageal reflux disease is fertile soil for medical and psychiatric comorbid conditions, with sleep disorders leading the way, Maurice M. Ohayon, MD, reported at the annual meeting of the Associated Professional Sleep Societies.
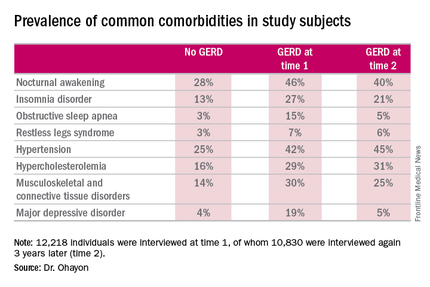
He presented a very large, longitudinal, population-based study of gastroesophageal reflux disease (GERD) and its fellow travelers. The study entailed telephone interviews with 12,218 nationally representative subjects in 8 states at time 1, and reinterviews with 10,830 of them 3 years later. The interviews were guided by Sleep-EVAL, a validated computerized diagnostic interview system.
At time 1, 10.6% of subjects reported that they were told by a physician they have GERD and/or they were taking a medication for it. At time 2 (3 years later), the prevalence had increased to 12.4%, according to Dr. Ohayon, professor of psychiatry and behavioral sciences, chief of the division of public mental health and population sciences, and director of the sleep epidemiology research center at Stanford (Calif.) University.
Chronic GERD – that is, GERD at both time points – was present in 3.9% of subjects; 6% of subjects were remitters, meaning that they had GERD at time 1 but not at time 2. Another 8.5% of the total sample had incident GERD, meaning they had GERD at time 2 but not time 1.
The prevalence of GERD rose stepwise with increasing age, from the low single digits in 18- to 34-year-olds to a peak in the 55- to 64-year-old age group, where the prevalence was 13.5% at time 1 and 17% at time 2.
GERD was significantly more common in women. At time 2, the prevalence was 10% in men and 14.4% in women.
Nocturnal awakening was the sleep disorder symptom most commonly associated with GERD. It was a complaint in 28% of subjects who never had GERD, 46% of those with GERD at time 1, and 40% of those with GERD at time 2.
Insomnia, obstructive sleep apnea, and restless legs syndrome were also significantly more common among subjects with GERD. So were musculoskeletal and connective tissue diseases, hypertension, hypercholesterolemia, and major depressive disorder.
The study was supported by the John Arrillaga Foundation and Takeda Pharmaceuticals. Dr. Ohayon reported no financial conflicts of interest.
DENVER – Gastroesophageal reflux disease is fertile soil for medical and psychiatric comorbid conditions, with sleep disorders leading the way, Maurice M. Ohayon, MD, reported at the annual meeting of the Associated Professional Sleep Societies.
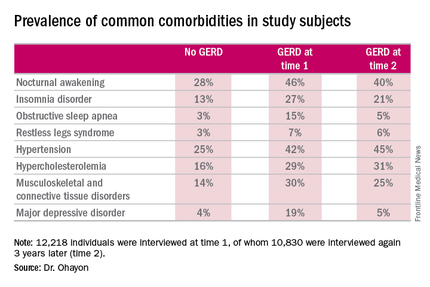
He presented a very large, longitudinal, population-based study of gastroesophageal reflux disease (GERD) and its fellow travelers. The study entailed telephone interviews with 12,218 nationally representative subjects in 8 states at time 1, and reinterviews with 10,830 of them 3 years later. The interviews were guided by Sleep-EVAL, a validated computerized diagnostic interview system.
At time 1, 10.6% of subjects reported that they were told by a physician they have GERD and/or they were taking a medication for it. At time 2 (3 years later), the prevalence had increased to 12.4%, according to Dr. Ohayon, professor of psychiatry and behavioral sciences, chief of the division of public mental health and population sciences, and director of the sleep epidemiology research center at Stanford (Calif.) University.
Chronic GERD – that is, GERD at both time points – was present in 3.9% of subjects; 6% of subjects were remitters, meaning that they had GERD at time 1 but not at time 2. Another 8.5% of the total sample had incident GERD, meaning they had GERD at time 2 but not time 1.
The prevalence of GERD rose stepwise with increasing age, from the low single digits in 18- to 34-year-olds to a peak in the 55- to 64-year-old age group, where the prevalence was 13.5% at time 1 and 17% at time 2.
GERD was significantly more common in women. At time 2, the prevalence was 10% in men and 14.4% in women.
Nocturnal awakening was the sleep disorder symptom most commonly associated with GERD. It was a complaint in 28% of subjects who never had GERD, 46% of those with GERD at time 1, and 40% of those with GERD at time 2.
Insomnia, obstructive sleep apnea, and restless legs syndrome were also significantly more common among subjects with GERD. So were musculoskeletal and connective tissue diseases, hypertension, hypercholesterolemia, and major depressive disorder.
The study was supported by the John Arrillaga Foundation and Takeda Pharmaceuticals. Dr. Ohayon reported no financial conflicts of interest.
DENVER – Gastroesophageal reflux disease is fertile soil for medical and psychiatric comorbid conditions, with sleep disorders leading the way, Maurice M. Ohayon, MD, reported at the annual meeting of the Associated Professional Sleep Societies.
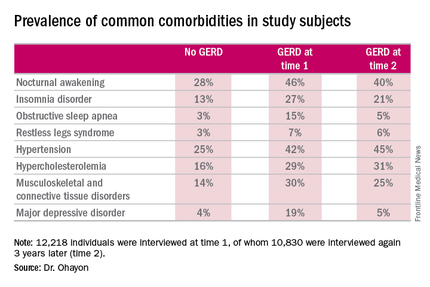
He presented a very large, longitudinal, population-based study of gastroesophageal reflux disease (GERD) and its fellow travelers. The study entailed telephone interviews with 12,218 nationally representative subjects in 8 states at time 1, and reinterviews with 10,830 of them 3 years later. The interviews were guided by Sleep-EVAL, a validated computerized diagnostic interview system.
At time 1, 10.6% of subjects reported that they were told by a physician they have GERD and/or they were taking a medication for it. At time 2 (3 years later), the prevalence had increased to 12.4%, according to Dr. Ohayon, professor of psychiatry and behavioral sciences, chief of the division of public mental health and population sciences, and director of the sleep epidemiology research center at Stanford (Calif.) University.
Chronic GERD – that is, GERD at both time points – was present in 3.9% of subjects; 6% of subjects were remitters, meaning that they had GERD at time 1 but not at time 2. Another 8.5% of the total sample had incident GERD, meaning they had GERD at time 2 but not time 1.
The prevalence of GERD rose stepwise with increasing age, from the low single digits in 18- to 34-year-olds to a peak in the 55- to 64-year-old age group, where the prevalence was 13.5% at time 1 and 17% at time 2.
GERD was significantly more common in women. At time 2, the prevalence was 10% in men and 14.4% in women.
Nocturnal awakening was the sleep disorder symptom most commonly associated with GERD. It was a complaint in 28% of subjects who never had GERD, 46% of those with GERD at time 1, and 40% of those with GERD at time 2.
Insomnia, obstructive sleep apnea, and restless legs syndrome were also significantly more common among subjects with GERD. So were musculoskeletal and connective tissue diseases, hypertension, hypercholesterolemia, and major depressive disorder.
The study was supported by the John Arrillaga Foundation and Takeda Pharmaceuticals. Dr. Ohayon reported no financial conflicts of interest.
AT SLEEP 2016
Key clinical point: Inquire about potentially treatable sleep disturbances in patients with GERD.
Major finding: Nocturnal awakenings were reported to be a problem in 28% of subjects with no history of gastroesophageal reflux disease, but in up to 46% of those with the digestive disease.
Data source: A longitudinal, population-based study of 12,218 nationally representative adults interviewed regarding the prevalence of GERD as well as comorbid sleep, medical, and psychiatric conditions.
Disclosures: The study was supported by the John Arrillaga Foundation and Takeda Pharmaceuticals. The presenter reported having no financial conflicts of interest.
MPT64 rapid test may miss TB caused by M. africanum strain
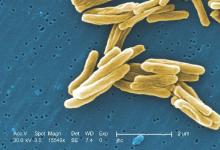
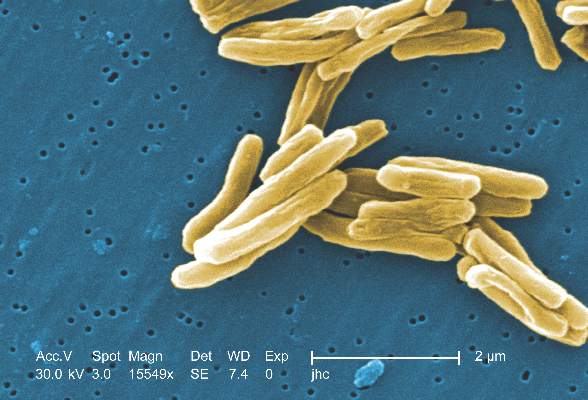
Tuberculosis caused by Mycobacterium africanum West Africa 2 is significantly less likely to be detected by a MPT64 rapid antigen test than is M. tuberculosis, according to a research team based in the Gambia.
A total of 173 MGIT culture-positive sputum samples were included in the study, and the initial MPT64 test was negative in 23 samples. Just over 90% of M. tuberculosis (MTB) samples converted to positive on day 0, while only 78.4% of M. africanum West Africa 2 (MAF2) samples converted. After 10 days, 97.5% of MTB samples were positive, while conversion of MAF2 samples remained low at 84.3%.
In a comparison of the mRNA transcript from samples of six MTB and five MAF2 patients who had not been treated for TB, the MTP64 gene was about 2.5 times more abundant in the MTB samples than the MAF2 samples. No association was found between conversion to positivity and sex, age, therapy, or mycobacterial growth units.
“Given the relatively low cost, limited technical expertise, and shorter turnaround time associated with using rapid speciation tests, compared to alternative speciation methods, MPT64 rapid tests will likely remain one of the preferred options for timely diagnosis of suspected TB despite the possibility of false negative results. Therefore, a negative MPT64 result would require confirmation by an alternative method, such as molecular tests or culture on p-nitrobenzoic acid, depending on laboratory infrastructure and resources,” the investigators noted.
Read the full study in PLoS Neglected Tropical Diseases (doi:10.1371/journal.pntd.0004801).
Tuberculosis caused by Mycobacterium africanum West Africa 2 is significantly less likely to be detected by a MPT64 rapid antigen test than is M. tuberculosis, according to a research team based in the Gambia.
A total of 173 MGIT culture-positive sputum samples were included in the study, and the initial MPT64 test was negative in 23 samples. Just over 90% of M. tuberculosis (MTB) samples converted to positive on day 0, while only 78.4% of M. africanum West Africa 2 (MAF2) samples converted. After 10 days, 97.5% of MTB samples were positive, while conversion of MAF2 samples remained low at 84.3%.
In a comparison of the mRNA transcript from samples of six MTB and five MAF2 patients who had not been treated for TB, the MTP64 gene was about 2.5 times more abundant in the MTB samples than the MAF2 samples. No association was found between conversion to positivity and sex, age, therapy, or mycobacterial growth units.
“Given the relatively low cost, limited technical expertise, and shorter turnaround time associated with using rapid speciation tests, compared to alternative speciation methods, MPT64 rapid tests will likely remain one of the preferred options for timely diagnosis of suspected TB despite the possibility of false negative results. Therefore, a negative MPT64 result would require confirmation by an alternative method, such as molecular tests or culture on p-nitrobenzoic acid, depending on laboratory infrastructure and resources,” the investigators noted.
Read the full study in PLoS Neglected Tropical Diseases (doi:10.1371/journal.pntd.0004801).
Tuberculosis caused by Mycobacterium africanum West Africa 2 is significantly less likely to be detected by a MPT64 rapid antigen test than is M. tuberculosis, according to a research team based in the Gambia.
A total of 173 MGIT culture-positive sputum samples were included in the study, and the initial MPT64 test was negative in 23 samples. Just over 90% of M. tuberculosis (MTB) samples converted to positive on day 0, while only 78.4% of M. africanum West Africa 2 (MAF2) samples converted. After 10 days, 97.5% of MTB samples were positive, while conversion of MAF2 samples remained low at 84.3%.
In a comparison of the mRNA transcript from samples of six MTB and five MAF2 patients who had not been treated for TB, the MTP64 gene was about 2.5 times more abundant in the MTB samples than the MAF2 samples. No association was found between conversion to positivity and sex, age, therapy, or mycobacterial growth units.
“Given the relatively low cost, limited technical expertise, and shorter turnaround time associated with using rapid speciation tests, compared to alternative speciation methods, MPT64 rapid tests will likely remain one of the preferred options for timely diagnosis of suspected TB despite the possibility of false negative results. Therefore, a negative MPT64 result would require confirmation by an alternative method, such as molecular tests or culture on p-nitrobenzoic acid, depending on laboratory infrastructure and resources,” the investigators noted.
Read the full study in PLoS Neglected Tropical Diseases (doi:10.1371/journal.pntd.0004801).
FROM PLOS NEGLECTED TROPICAL DISEASES
MPT64 rapid test may miss TB caused by M. africanum strain
Tuberculosis caused by Mycobacterium africanum West Africa 2 is significantly less likely to be detected by a MPT64 rapid antigen test than is M. tuberculosis, according to a research team based in the Gambia.
A total of 173 MGIT culture-positive sputum samples were included in the study, and the initial MPT64 test was negative in 23 samples. Just over 90% of M. tuberculosis (MTB) samples converted to positive on day 0, while only 78.4% of M. africanum West Africa 2 (MAF2) samples converted. After 10 days, 97.5% of MTB samples were positive, while conversion of MAF2 samples remained low at 84.3%.
In a comparison of the mRNA transcript from samples of six MTB and five MAF2 patients who had not been treated for TB, the MTP64 gene was about 2.5 times more abundant in the MTB samples than the MAF2 samples. No association was found between conversion to positivity and sex, age, therapy, or mycobacterial growth units.
“Given the relatively low cost, limited technical expertise, and shorter turnaround time associated with using rapid speciation tests, compared to alternative speciation methods, MPT64 rapid tests will likely remain one of the preferred options for timely diagnosis of suspected TB despite the possibility of false negative results. Therefore, a negative MPT64 result would require confirmation by an alternative method, such as molecular tests or culture on p-nitrobenzoic acid, depending on laboratory infrastructure and resources,” the investigators noted.
Read the full study in PLoS Neglected Tropical Diseases (doi:10.1371/journal.pntd.0004801).
Tuberculosis caused by Mycobacterium africanum West Africa 2 is significantly less likely to be detected by a MPT64 rapid antigen test than is M. tuberculosis, according to a research team based in the Gambia.
A total of 173 MGIT culture-positive sputum samples were included in the study, and the initial MPT64 test was negative in 23 samples. Just over 90% of M. tuberculosis (MTB) samples converted to positive on day 0, while only 78.4% of M. africanum West Africa 2 (MAF2) samples converted. After 10 days, 97.5% of MTB samples were positive, while conversion of MAF2 samples remained low at 84.3%.
In a comparison of the mRNA transcript from samples of six MTB and five MAF2 patients who had not been treated for TB, the MTP64 gene was about 2.5 times more abundant in the MTB samples than the MAF2 samples. No association was found between conversion to positivity and sex, age, therapy, or mycobacterial growth units.
“Given the relatively low cost, limited technical expertise, and shorter turnaround time associated with using rapid speciation tests, compared to alternative speciation methods, MPT64 rapid tests will likely remain one of the preferred options for timely diagnosis of suspected TB despite the possibility of false negative results. Therefore, a negative MPT64 result would require confirmation by an alternative method, such as molecular tests or culture on p-nitrobenzoic acid, depending on laboratory infrastructure and resources,” the investigators noted.
Read the full study in PLoS Neglected Tropical Diseases (doi:10.1371/journal.pntd.0004801).
Tuberculosis caused by Mycobacterium africanum West Africa 2 is significantly less likely to be detected by a MPT64 rapid antigen test than is M. tuberculosis, according to a research team based in the Gambia.
A total of 173 MGIT culture-positive sputum samples were included in the study, and the initial MPT64 test was negative in 23 samples. Just over 90% of M. tuberculosis (MTB) samples converted to positive on day 0, while only 78.4% of M. africanum West Africa 2 (MAF2) samples converted. After 10 days, 97.5% of MTB samples were positive, while conversion of MAF2 samples remained low at 84.3%.
In a comparison of the mRNA transcript from samples of six MTB and five MAF2 patients who had not been treated for TB, the MTP64 gene was about 2.5 times more abundant in the MTB samples than the MAF2 samples. No association was found between conversion to positivity and sex, age, therapy, or mycobacterial growth units.
“Given the relatively low cost, limited technical expertise, and shorter turnaround time associated with using rapid speciation tests, compared to alternative speciation methods, MPT64 rapid tests will likely remain one of the preferred options for timely diagnosis of suspected TB despite the possibility of false negative results. Therefore, a negative MPT64 result would require confirmation by an alternative method, such as molecular tests or culture on p-nitrobenzoic acid, depending on laboratory infrastructure and resources,” the investigators noted.
Read the full study in PLoS Neglected Tropical Diseases (doi:10.1371/journal.pntd.0004801).
FROM PLOS NEGLECTED TROPICAL DISEASES
Nonwhite race, lower socioeconomic status predicts persistently active AD
SCOTTSDALE, ARIZ. –Among patients with atopic dermatitis, persistently active disease was significantly more common among females of nonwhite race with a history of atopy than among patients without these characteristics, in an analysis of survey data from the Pediatric Elective Eczema Registry.
Annual household income under $50,000 also was a significant predictor of persistently active eczema, according to Katrina Abuabara, MD, of the department of dermatology, University of California, San Francisco, and her associates, who reported their results in a poster at the annual meeting of the Society for Investigative Dermatology.
Atopic dermatitis often persists into adulthood, but few studies have explored contributors to poor disease control. To help fill that gap, the investigators analyzed 65,237 surveys from the Pediatric Eczema Elective Registry (PEER), which tracks children and young adults aged 2-26 years with physician-diagnosed atopic dermatitis. The average age of the 6,237 patients was 7 years at enrollment (standard deviation, 4 years). They were followed at 6-month intervals for up to 10 years, with an average of about 10 surveys per respondent (standard deviation, 6.3 surveys).
In all, 4,607 patients (74% of the cohort) returned surveys spanning early childhood through their mid-20s. Only 15% of patients had “resolving” disease, meaning that as they aged, they increasingly reported complete disease control for periods of 6 months and longer.
The remaining 85% of patients had persistently active disease. In this group, 54% were female, 77% had a household income under $50,000 per year, 71% were nonwhite, and 75% had a history of atopy. Each of these characteristics significantly increased the odds of persistently active atopic dermatitis in the multivariable model (P less than .05 for each association).
Nonwhite race and history of atopy were the strongest predictors of persistently active disease – each lowered the odds of complete disease control by almost 50% (odds ratio, 0.53). Furthermore, females had 37% lower odds of complete disease control compared with males (OR, 0.63), and individuals with household income under $50,000 had 16% lower odds of complete disease control compared with those with higher annual incomes (OR, 0.84).
The link between lower socioeconomic status and persistently active eczema belies previous findings, the researchers noted. Those studies found that individuals of higher socioeconomic status were at greater risk for developing atopic dermatitis, but “failed to account for the chronic nature of the disease. In contrast, our results suggest that atopic dermatitis persistence may be associated with lower income and nonwhite race, and highlight the importance of longitudinal studies that permit analysis of mechanisms of disease control over time.”
Dr. Abuabara received a grant from the Clinical & Translational Science Institute of UCSF. She had no disclosures.
SCOTTSDALE, ARIZ. –Among patients with atopic dermatitis, persistently active disease was significantly more common among females of nonwhite race with a history of atopy than among patients without these characteristics, in an analysis of survey data from the Pediatric Elective Eczema Registry.
Annual household income under $50,000 also was a significant predictor of persistently active eczema, according to Katrina Abuabara, MD, of the department of dermatology, University of California, San Francisco, and her associates, who reported their results in a poster at the annual meeting of the Society for Investigative Dermatology.
Atopic dermatitis often persists into adulthood, but few studies have explored contributors to poor disease control. To help fill that gap, the investigators analyzed 65,237 surveys from the Pediatric Eczema Elective Registry (PEER), which tracks children and young adults aged 2-26 years with physician-diagnosed atopic dermatitis. The average age of the 6,237 patients was 7 years at enrollment (standard deviation, 4 years). They were followed at 6-month intervals for up to 10 years, with an average of about 10 surveys per respondent (standard deviation, 6.3 surveys).
In all, 4,607 patients (74% of the cohort) returned surveys spanning early childhood through their mid-20s. Only 15% of patients had “resolving” disease, meaning that as they aged, they increasingly reported complete disease control for periods of 6 months and longer.
The remaining 85% of patients had persistently active disease. In this group, 54% were female, 77% had a household income under $50,000 per year, 71% were nonwhite, and 75% had a history of atopy. Each of these characteristics significantly increased the odds of persistently active atopic dermatitis in the multivariable model (P less than .05 for each association).
Nonwhite race and history of atopy were the strongest predictors of persistently active disease – each lowered the odds of complete disease control by almost 50% (odds ratio, 0.53). Furthermore, females had 37% lower odds of complete disease control compared with males (OR, 0.63), and individuals with household income under $50,000 had 16% lower odds of complete disease control compared with those with higher annual incomes (OR, 0.84).
The link between lower socioeconomic status and persistently active eczema belies previous findings, the researchers noted. Those studies found that individuals of higher socioeconomic status were at greater risk for developing atopic dermatitis, but “failed to account for the chronic nature of the disease. In contrast, our results suggest that atopic dermatitis persistence may be associated with lower income and nonwhite race, and highlight the importance of longitudinal studies that permit analysis of mechanisms of disease control over time.”
Dr. Abuabara received a grant from the Clinical & Translational Science Institute of UCSF. She had no disclosures.
SCOTTSDALE, ARIZ. –Among patients with atopic dermatitis, persistently active disease was significantly more common among females of nonwhite race with a history of atopy than among patients without these characteristics, in an analysis of survey data from the Pediatric Elective Eczema Registry.
Annual household income under $50,000 also was a significant predictor of persistently active eczema, according to Katrina Abuabara, MD, of the department of dermatology, University of California, San Francisco, and her associates, who reported their results in a poster at the annual meeting of the Society for Investigative Dermatology.
Atopic dermatitis often persists into adulthood, but few studies have explored contributors to poor disease control. To help fill that gap, the investigators analyzed 65,237 surveys from the Pediatric Eczema Elective Registry (PEER), which tracks children and young adults aged 2-26 years with physician-diagnosed atopic dermatitis. The average age of the 6,237 patients was 7 years at enrollment (standard deviation, 4 years). They were followed at 6-month intervals for up to 10 years, with an average of about 10 surveys per respondent (standard deviation, 6.3 surveys).
In all, 4,607 patients (74% of the cohort) returned surveys spanning early childhood through their mid-20s. Only 15% of patients had “resolving” disease, meaning that as they aged, they increasingly reported complete disease control for periods of 6 months and longer.
The remaining 85% of patients had persistently active disease. In this group, 54% were female, 77% had a household income under $50,000 per year, 71% were nonwhite, and 75% had a history of atopy. Each of these characteristics significantly increased the odds of persistently active atopic dermatitis in the multivariable model (P less than .05 for each association).
Nonwhite race and history of atopy were the strongest predictors of persistently active disease – each lowered the odds of complete disease control by almost 50% (odds ratio, 0.53). Furthermore, females had 37% lower odds of complete disease control compared with males (OR, 0.63), and individuals with household income under $50,000 had 16% lower odds of complete disease control compared with those with higher annual incomes (OR, 0.84).
The link between lower socioeconomic status and persistently active eczema belies previous findings, the researchers noted. Those studies found that individuals of higher socioeconomic status were at greater risk for developing atopic dermatitis, but “failed to account for the chronic nature of the disease. In contrast, our results suggest that atopic dermatitis persistence may be associated with lower income and nonwhite race, and highlight the importance of longitudinal studies that permit analysis of mechanisms of disease control over time.”
Dr. Abuabara received a grant from the Clinical & Translational Science Institute of UCSF. She had no disclosures.
AT THE 2016 SID ANNUAL MEETING
Key clinical point: Persistently active atopic dermatitis is associated with nonwhite race, annual household income under $50,000, female sex, and history of atopy.
Major finding: Nonwhite race and history of atopy each lowered the odds of complete disease control by about 43% (odds ratios, 0.53; P less than .05).
Data source: A longitudinal cohort study of 6,237 patients aged 2-26 years from the Pediatric Eczema Elective Registry (PEER).
Disclosures: Dr. Abuabara received a grant from the Clinical & Translational Science Institute of UCSF. She had no disclosures.
Nonwhite race, lower socioeconomic status predicts persistently active AD
SCOTTSDALE, ARIZ. –Among patients with atopic dermatitis, persistently active disease was significantly more common among females of nonwhite race with a history of atopy than among patients without these characteristics, in an analysis of survey data from the Pediatric Elective Eczema Registry.
Annual household income under $50,000 also was a significant predictor of persistently active eczema, according to Katrina Abuabara, MD, of the department of dermatology, University of California, San Francisco, and her associates, who reported their results in a poster at the annual meeting of the Society for Investigative Dermatology.
Atopic dermatitis often persists into adulthood, but few studies have explored contributors to poor disease control. To help fill that gap, the investigators analyzed 65,237 surveys from the Pediatric Eczema Elective Registry (PEER), which tracks children and young adults aged 2-26 years with physician-diagnosed atopic dermatitis. The average age of the 6,237 patients was 7 years at enrollment (standard deviation, 4 years). They were followed at 6-month intervals for up to 10 years, with an average of about 10 surveys per respondent (standard deviation, 6.3 surveys).
In all, 4,607 patients (74% of the cohort) returned surveys spanning early childhood through their mid-20s. Only 15% of patients had “resolving” disease, meaning that as they aged, they increasingly reported complete disease control for periods of 6 months and longer.
The remaining 85% of patients had persistently active disease. In this group, 54% were female, 77% had a household income under $50,000 per year, 71% were nonwhite, and 75% had a history of atopy. Each of these characteristics significantly increased the odds of persistently active atopic dermatitis in the multivariable model (P less than .05 for each association).
Nonwhite race and history of atopy were the strongest predictors of persistently active disease – each lowered the odds of complete disease control by almost 50% (odds ratio, 0.53). Furthermore, females had 37% lower odds of complete disease control compared with males (OR, 0.63), and individuals with household income under $50,000 had 16% lower odds of complete disease control compared with those with higher annual incomes (OR, 0.84).
The link between lower socioeconomic status and persistently active eczema belies previous findings, the researchers noted. Those studies found that individuals of higher socioeconomic status were at greater risk for developing atopic dermatitis, but “failed to account for the chronic nature of the disease. In contrast, our results suggest that atopic dermatitis persistence may be associated with lower income and nonwhite race, and highlight the importance of longitudinal studies that permit analysis of mechanisms of disease control over time.”
Dr. Abuabara received a grant from the Clinical & Translational Science Institute of UCSF. She had no disclosures.
SCOTTSDALE, ARIZ. –Among patients with atopic dermatitis, persistently active disease was significantly more common among females of nonwhite race with a history of atopy than among patients without these characteristics, in an analysis of survey data from the Pediatric Elective Eczema Registry.
Annual household income under $50,000 also was a significant predictor of persistently active eczema, according to Katrina Abuabara, MD, of the department of dermatology, University of California, San Francisco, and her associates, who reported their results in a poster at the annual meeting of the Society for Investigative Dermatology.
Atopic dermatitis often persists into adulthood, but few studies have explored contributors to poor disease control. To help fill that gap, the investigators analyzed 65,237 surveys from the Pediatric Eczema Elective Registry (PEER), which tracks children and young adults aged 2-26 years with physician-diagnosed atopic dermatitis. The average age of the 6,237 patients was 7 years at enrollment (standard deviation, 4 years). They were followed at 6-month intervals for up to 10 years, with an average of about 10 surveys per respondent (standard deviation, 6.3 surveys).
In all, 4,607 patients (74% of the cohort) returned surveys spanning early childhood through their mid-20s. Only 15% of patients had “resolving” disease, meaning that as they aged, they increasingly reported complete disease control for periods of 6 months and longer.
The remaining 85% of patients had persistently active disease. In this group, 54% were female, 77% had a household income under $50,000 per year, 71% were nonwhite, and 75% had a history of atopy. Each of these characteristics significantly increased the odds of persistently active atopic dermatitis in the multivariable model (P less than .05 for each association).
Nonwhite race and history of atopy were the strongest predictors of persistently active disease – each lowered the odds of complete disease control by almost 50% (odds ratio, 0.53). Furthermore, females had 37% lower odds of complete disease control compared with males (OR, 0.63), and individuals with household income under $50,000 had 16% lower odds of complete disease control compared with those with higher annual incomes (OR, 0.84).
The link between lower socioeconomic status and persistently active eczema belies previous findings, the researchers noted. Those studies found that individuals of higher socioeconomic status were at greater risk for developing atopic dermatitis, but “failed to account for the chronic nature of the disease. In contrast, our results suggest that atopic dermatitis persistence may be associated with lower income and nonwhite race, and highlight the importance of longitudinal studies that permit analysis of mechanisms of disease control over time.”
Dr. Abuabara received a grant from the Clinical & Translational Science Institute of UCSF. She had no disclosures.
SCOTTSDALE, ARIZ. –Among patients with atopic dermatitis, persistently active disease was significantly more common among females of nonwhite race with a history of atopy than among patients without these characteristics, in an analysis of survey data from the Pediatric Elective Eczema Registry.
Annual household income under $50,000 also was a significant predictor of persistently active eczema, according to Katrina Abuabara, MD, of the department of dermatology, University of California, San Francisco, and her associates, who reported their results in a poster at the annual meeting of the Society for Investigative Dermatology.
Atopic dermatitis often persists into adulthood, but few studies have explored contributors to poor disease control. To help fill that gap, the investigators analyzed 65,237 surveys from the Pediatric Eczema Elective Registry (PEER), which tracks children and young adults aged 2-26 years with physician-diagnosed atopic dermatitis. The average age of the 6,237 patients was 7 years at enrollment (standard deviation, 4 years). They were followed at 6-month intervals for up to 10 years, with an average of about 10 surveys per respondent (standard deviation, 6.3 surveys).
In all, 4,607 patients (74% of the cohort) returned surveys spanning early childhood through their mid-20s. Only 15% of patients had “resolving” disease, meaning that as they aged, they increasingly reported complete disease control for periods of 6 months and longer.
The remaining 85% of patients had persistently active disease. In this group, 54% were female, 77% had a household income under $50,000 per year, 71% were nonwhite, and 75% had a history of atopy. Each of these characteristics significantly increased the odds of persistently active atopic dermatitis in the multivariable model (P less than .05 for each association).
Nonwhite race and history of atopy were the strongest predictors of persistently active disease – each lowered the odds of complete disease control by almost 50% (odds ratio, 0.53). Furthermore, females had 37% lower odds of complete disease control compared with males (OR, 0.63), and individuals with household income under $50,000 had 16% lower odds of complete disease control compared with those with higher annual incomes (OR, 0.84).
The link between lower socioeconomic status and persistently active eczema belies previous findings, the researchers noted. Those studies found that individuals of higher socioeconomic status were at greater risk for developing atopic dermatitis, but “failed to account for the chronic nature of the disease. In contrast, our results suggest that atopic dermatitis persistence may be associated with lower income and nonwhite race, and highlight the importance of longitudinal studies that permit analysis of mechanisms of disease control over time.”
Dr. Abuabara received a grant from the Clinical & Translational Science Institute of UCSF. She had no disclosures.
AT THE 2016 SID ANNUAL MEETING
Key clinical point: Persistently active atopic dermatitis is associated with nonwhite race, annual household income under $50,000, female sex, and history of atopy.
Major finding: Nonwhite race and history of atopy each lowered the odds of complete disease control by about 43% (odds ratios, 0.53; P less than .05).
Data source: A longitudinal cohort study of 6,237 patients aged 2-26 years from the Pediatric Eczema Elective Registry (PEER).
Disclosures: Dr. Abuabara received a grant from the Clinical & Translational Science Institute of UCSF. She had no disclosures.
Sleep apnea in pregnancy linked to preterm birth
DENVER – Pregnant women with sleep apnea are more likely to have planned obstetric interventions, results of an Australian population-based cohort study suggest.
The study included all 636,227 in-hospital births during 2002-2012 in New South Wales, Australia’s most populous state. Maternal sleep apnea was also associated with increased rates of planned preterm birth, even though preterm birth is widely considered the greatest contributor to neonatal morbidity and mortality, Yu Sun Bin, PhD, said at the annual meeting of the Associated Professional Sleep Societies.
“Somewhere along the line, clinicians decided that the risks of preterm birth to the baby were outweighed by the risks to the mother of delivering at term,” said Dr. Bin of the University of Sydney.
She and her coinvestigators undertook this study because even though previous studies have linked maternal sleep apnea to increased risks of gestational diabetes and gestational hypertension, most of the prior studies were small, cross-sectional, and/or relied upon snoring as a proxy for sleep apnea, which many sleep specialists consider invalid.
The investigators compared maternal and infant outcomes for mothers with a documented diagnosis of sleep apnea – either central or obstructive – in the year before or during pregnancy with outcomes for mothers without that diagnosis.
There were 519 mothers with diagnosed sleep apnea, for a prevalence of 0.08%. That figure is low in light of other evidence, making it likely that the 635,708 women in the no-sleep-apnea group actually included a substantial number of mothers with undiagnosed sleep apnea. Thus, the investigators’ estimates of the adverse impacts of sleep apnea in pregnancy are “rather conservative,” according to Dr. Bin.
Australian women with sleep apnea were older and less healthy than mothers without sleep apnea were. They had higher baseline rates of obesity, preexisting diabetes, chronic hypertension, and were more likely to be smokers.
The incidence of pregnancy hypertension was 19.7% in the sleep apnea group and 8.7% in controls. In a multivariate regression analysis adjusted for potential confounders, the maternal sleep apnea group had a 40% greater risk of developing hypertension than did controls. However, contrary to previous smaller studies, they did not have a significantly increased rate of gestational diabetes.
Even after controlling for both pregnancy hypertension and gestational diabetes, the sleep apnea group still had a significant 15% increase in the relative likelihood of a planned delivery.
The rate of preterm birth at 36 weeks or earlier was 14.5% in the maternal sleep apnea group, compared with 6.9% in controls, for an adjusted 1.5-fold increased relative risk.
Perinatal death occurred in 1.9% of the sleep apnea group and 0.9% of controls; however, the resultant adjusted 1.73-fold increased risk didn’t attain statistical significance because of the small number of deaths in the study. Dr. Bin said she and her colleagues plan to further investigate this signal to learn whether it is real or an artifact of small numbers.
The incidence of 5-minute Apgar scores below 7 was 4.6% in the sleep apnea group, compared with 2.4% in controls, for an adjusted 1.6-fold increased risk. The rate of neonatal intensive care unit admission in the sleep apnea group was 27.9%, versus 16% in controls, for a 1.61-fold increased relative risk.
The NICU admission rate for preterm infants didn’t differ between the two groups. The difference occurred in term babies, whose NICU admission rate was 20.3% if they were in the sleep apnea group, but just 12.1% in the control group.
“This suggests that maternal sleep apnea is contributing to some condition in the baby that requires additional support,” Dr. Bin observed.
The nature of that condition, however, remains unclear, since all patient data available to the investigators was deidentified.
The incidence of small-for-gestational-age babies was similar in the sleep apnea and control groups. In contrast, the large-for-gestational-age rate was 15.2% in the sleep apnea group, compared with 9.1% in controls, for an adjusted 1.27-fold increased risk.
The two main limitations of the Australian study were the likely underdiagnosis of sleep apnea and the lack of any information on treatment of affected patients, according to Dr. Bin. A key unresolved question, she added, is whether interventions for maternal sleep apnea reduce the risks identified in the New South Wales study. She noted that one 16-patient randomized study of nasal continuous positive airway pressure suggests the answer is yes (Sleep Med. 2007 Dec;9:15-21).
The Australian National Health and Medical Research Council supported the study. Dr. Bin reported having no financial conflicts.
DENVER – Pregnant women with sleep apnea are more likely to have planned obstetric interventions, results of an Australian population-based cohort study suggest.
The study included all 636,227 in-hospital births during 2002-2012 in New South Wales, Australia’s most populous state. Maternal sleep apnea was also associated with increased rates of planned preterm birth, even though preterm birth is widely considered the greatest contributor to neonatal morbidity and mortality, Yu Sun Bin, PhD, said at the annual meeting of the Associated Professional Sleep Societies.
“Somewhere along the line, clinicians decided that the risks of preterm birth to the baby were outweighed by the risks to the mother of delivering at term,” said Dr. Bin of the University of Sydney.
She and her coinvestigators undertook this study because even though previous studies have linked maternal sleep apnea to increased risks of gestational diabetes and gestational hypertension, most of the prior studies were small, cross-sectional, and/or relied upon snoring as a proxy for sleep apnea, which many sleep specialists consider invalid.
The investigators compared maternal and infant outcomes for mothers with a documented diagnosis of sleep apnea – either central or obstructive – in the year before or during pregnancy with outcomes for mothers without that diagnosis.
There were 519 mothers with diagnosed sleep apnea, for a prevalence of 0.08%. That figure is low in light of other evidence, making it likely that the 635,708 women in the no-sleep-apnea group actually included a substantial number of mothers with undiagnosed sleep apnea. Thus, the investigators’ estimates of the adverse impacts of sleep apnea in pregnancy are “rather conservative,” according to Dr. Bin.
Australian women with sleep apnea were older and less healthy than mothers without sleep apnea were. They had higher baseline rates of obesity, preexisting diabetes, chronic hypertension, and were more likely to be smokers.
The incidence of pregnancy hypertension was 19.7% in the sleep apnea group and 8.7% in controls. In a multivariate regression analysis adjusted for potential confounders, the maternal sleep apnea group had a 40% greater risk of developing hypertension than did controls. However, contrary to previous smaller studies, they did not have a significantly increased rate of gestational diabetes.
Even after controlling for both pregnancy hypertension and gestational diabetes, the sleep apnea group still had a significant 15% increase in the relative likelihood of a planned delivery.
The rate of preterm birth at 36 weeks or earlier was 14.5% in the maternal sleep apnea group, compared with 6.9% in controls, for an adjusted 1.5-fold increased relative risk.
Perinatal death occurred in 1.9% of the sleep apnea group and 0.9% of controls; however, the resultant adjusted 1.73-fold increased risk didn’t attain statistical significance because of the small number of deaths in the study. Dr. Bin said she and her colleagues plan to further investigate this signal to learn whether it is real or an artifact of small numbers.
The incidence of 5-minute Apgar scores below 7 was 4.6% in the sleep apnea group, compared with 2.4% in controls, for an adjusted 1.6-fold increased risk. The rate of neonatal intensive care unit admission in the sleep apnea group was 27.9%, versus 16% in controls, for a 1.61-fold increased relative risk.
The NICU admission rate for preterm infants didn’t differ between the two groups. The difference occurred in term babies, whose NICU admission rate was 20.3% if they were in the sleep apnea group, but just 12.1% in the control group.
“This suggests that maternal sleep apnea is contributing to some condition in the baby that requires additional support,” Dr. Bin observed.
The nature of that condition, however, remains unclear, since all patient data available to the investigators was deidentified.
The incidence of small-for-gestational-age babies was similar in the sleep apnea and control groups. In contrast, the large-for-gestational-age rate was 15.2% in the sleep apnea group, compared with 9.1% in controls, for an adjusted 1.27-fold increased risk.
The two main limitations of the Australian study were the likely underdiagnosis of sleep apnea and the lack of any information on treatment of affected patients, according to Dr. Bin. A key unresolved question, she added, is whether interventions for maternal sleep apnea reduce the risks identified in the New South Wales study. She noted that one 16-patient randomized study of nasal continuous positive airway pressure suggests the answer is yes (Sleep Med. 2007 Dec;9:15-21).
The Australian National Health and Medical Research Council supported the study. Dr. Bin reported having no financial conflicts.
DENVER – Pregnant women with sleep apnea are more likely to have planned obstetric interventions, results of an Australian population-based cohort study suggest.
The study included all 636,227 in-hospital births during 2002-2012 in New South Wales, Australia’s most populous state. Maternal sleep apnea was also associated with increased rates of planned preterm birth, even though preterm birth is widely considered the greatest contributor to neonatal morbidity and mortality, Yu Sun Bin, PhD, said at the annual meeting of the Associated Professional Sleep Societies.
“Somewhere along the line, clinicians decided that the risks of preterm birth to the baby were outweighed by the risks to the mother of delivering at term,” said Dr. Bin of the University of Sydney.
She and her coinvestigators undertook this study because even though previous studies have linked maternal sleep apnea to increased risks of gestational diabetes and gestational hypertension, most of the prior studies were small, cross-sectional, and/or relied upon snoring as a proxy for sleep apnea, which many sleep specialists consider invalid.
The investigators compared maternal and infant outcomes for mothers with a documented diagnosis of sleep apnea – either central or obstructive – in the year before or during pregnancy with outcomes for mothers without that diagnosis.
There were 519 mothers with diagnosed sleep apnea, for a prevalence of 0.08%. That figure is low in light of other evidence, making it likely that the 635,708 women in the no-sleep-apnea group actually included a substantial number of mothers with undiagnosed sleep apnea. Thus, the investigators’ estimates of the adverse impacts of sleep apnea in pregnancy are “rather conservative,” according to Dr. Bin.
Australian women with sleep apnea were older and less healthy than mothers without sleep apnea were. They had higher baseline rates of obesity, preexisting diabetes, chronic hypertension, and were more likely to be smokers.
The incidence of pregnancy hypertension was 19.7% in the sleep apnea group and 8.7% in controls. In a multivariate regression analysis adjusted for potential confounders, the maternal sleep apnea group had a 40% greater risk of developing hypertension than did controls. However, contrary to previous smaller studies, they did not have a significantly increased rate of gestational diabetes.
Even after controlling for both pregnancy hypertension and gestational diabetes, the sleep apnea group still had a significant 15% increase in the relative likelihood of a planned delivery.
The rate of preterm birth at 36 weeks or earlier was 14.5% in the maternal sleep apnea group, compared with 6.9% in controls, for an adjusted 1.5-fold increased relative risk.
Perinatal death occurred in 1.9% of the sleep apnea group and 0.9% of controls; however, the resultant adjusted 1.73-fold increased risk didn’t attain statistical significance because of the small number of deaths in the study. Dr. Bin said she and her colleagues plan to further investigate this signal to learn whether it is real or an artifact of small numbers.
The incidence of 5-minute Apgar scores below 7 was 4.6% in the sleep apnea group, compared with 2.4% in controls, for an adjusted 1.6-fold increased risk. The rate of neonatal intensive care unit admission in the sleep apnea group was 27.9%, versus 16% in controls, for a 1.61-fold increased relative risk.
The NICU admission rate for preterm infants didn’t differ between the two groups. The difference occurred in term babies, whose NICU admission rate was 20.3% if they were in the sleep apnea group, but just 12.1% in the control group.
“This suggests that maternal sleep apnea is contributing to some condition in the baby that requires additional support,” Dr. Bin observed.
The nature of that condition, however, remains unclear, since all patient data available to the investigators was deidentified.
The incidence of small-for-gestational-age babies was similar in the sleep apnea and control groups. In contrast, the large-for-gestational-age rate was 15.2% in the sleep apnea group, compared with 9.1% in controls, for an adjusted 1.27-fold increased risk.
The two main limitations of the Australian study were the likely underdiagnosis of sleep apnea and the lack of any information on treatment of affected patients, according to Dr. Bin. A key unresolved question, she added, is whether interventions for maternal sleep apnea reduce the risks identified in the New South Wales study. She noted that one 16-patient randomized study of nasal continuous positive airway pressure suggests the answer is yes (Sleep Med. 2007 Dec;9:15-21).
The Australian National Health and Medical Research Council supported the study. Dr. Bin reported having no financial conflicts.
AT SLEEP 2016
Key clinical point: Maternal sleep apnea is associated with increased rates of obstetric intervention and preterm birth.
Major finding: The rate of preterm birth at 36 weeks or earlier was 14.5% in the group with maternal sleep apnea, compared with 6.9% in controls.
Data source: A population-based cohort study of 636,227 women who gave birth in a New South Wales, Australia, hospital during 2002-2012.
Disclosures: The Australian National Health and Medical Research Council supported the study. Dr. Bin reported having no financial conflicts.
Insomnia severity more pronounced in older Hispanics
Insomnia is a more pronounced problem than expected among Hispanics over age 50, according to results of a study by Christopher N. Kaufmann, PhD, and his coauthors.
Dr. Kaufmann and his colleagues studied 22,252 participants of white, Non-Hispanic black, Hispanic, or other race/ethnicity. Participant data came from a nationally representative survey from 2002 to 2010, in which patients rated the severity of four insomnia symptoms. All participants were adults older than 50 years.
Insomnia severity scores increased 0.19 points over time after the investigators controlled for sex, race/ethnicity, education, and baseline age (95% CI, 0.14-0.24; t = 7.52; design df = 56; P less than .001). After adjustment for accumulated health conditions and body mass index, this trend decreased, Dr. Kaufmann and his colleagues added. However, the increasing trajectory of insomnia severity was “significantly more pronounced” among Hispanics, compared with non-Hispanic whites, after adjustment for accumulated health conditions, body mass index, and number of depressive symptoms, the investigators said in the report.
Although health conditions can result in greater insomnia severity with age, “further research is needed to determine the reasons for a different insomnia trajectory among Hispanics,” the authors concluded.
Read the full article in the American Journal of Geriatric Psychiatry.
Insomnia is a more pronounced problem than expected among Hispanics over age 50, according to results of a study by Christopher N. Kaufmann, PhD, and his coauthors.
Dr. Kaufmann and his colleagues studied 22,252 participants of white, Non-Hispanic black, Hispanic, or other race/ethnicity. Participant data came from a nationally representative survey from 2002 to 2010, in which patients rated the severity of four insomnia symptoms. All participants were adults older than 50 years.
Insomnia severity scores increased 0.19 points over time after the investigators controlled for sex, race/ethnicity, education, and baseline age (95% CI, 0.14-0.24; t = 7.52; design df = 56; P less than .001). After adjustment for accumulated health conditions and body mass index, this trend decreased, Dr. Kaufmann and his colleagues added. However, the increasing trajectory of insomnia severity was “significantly more pronounced” among Hispanics, compared with non-Hispanic whites, after adjustment for accumulated health conditions, body mass index, and number of depressive symptoms, the investigators said in the report.
Although health conditions can result in greater insomnia severity with age, “further research is needed to determine the reasons for a different insomnia trajectory among Hispanics,” the authors concluded.
Read the full article in the American Journal of Geriatric Psychiatry.
Insomnia is a more pronounced problem than expected among Hispanics over age 50, according to results of a study by Christopher N. Kaufmann, PhD, and his coauthors.
Dr. Kaufmann and his colleagues studied 22,252 participants of white, Non-Hispanic black, Hispanic, or other race/ethnicity. Participant data came from a nationally representative survey from 2002 to 2010, in which patients rated the severity of four insomnia symptoms. All participants were adults older than 50 years.
Insomnia severity scores increased 0.19 points over time after the investigators controlled for sex, race/ethnicity, education, and baseline age (95% CI, 0.14-0.24; t = 7.52; design df = 56; P less than .001). After adjustment for accumulated health conditions and body mass index, this trend decreased, Dr. Kaufmann and his colleagues added. However, the increasing trajectory of insomnia severity was “significantly more pronounced” among Hispanics, compared with non-Hispanic whites, after adjustment for accumulated health conditions, body mass index, and number of depressive symptoms, the investigators said in the report.
Although health conditions can result in greater insomnia severity with age, “further research is needed to determine the reasons for a different insomnia trajectory among Hispanics,” the authors concluded.
Read the full article in the American Journal of Geriatric Psychiatry.
FROM THE AMERICAN JOURNAL OF GERIATRIC PSYCHIATRY
Staffing, work environment drive VAP risk in the ICU
SAN FRANCISCO – The work environment for nurses and the physician staffing model in the intensive care unit influence patients’ likelihood of acquiring ventilator-associated pneumonia (VAP), based on a cohort study of 25 ICUs.
Overall, each 1-point increase in the score for the nurse work environment – indicating that nurses had a greater sense of playing an important role in patient care – was unexpectedly associated with a roughly sixfold higher rate of VAP among the ICU’s patients, according to data reported in a session and press briefing at an international conference of the American Thoracic Society. However, additional analyses showed that the rate of VAP was higher in closed units where a board-certified critical care physician (intensivist) managed and led care rather than an open unit where care is shared.
“We think that the organization of the ICU is actually influencing nursing practice, which is a really novel finding,” commented first author Deena Kelly Costa, PhD, RN, of the University of Michigan School of Nursing in Ann Arbor. “In closed ICUs, when you have a board-certified physician and an ICU team managing and leading care, even if the work environment is better, nurses may not feel as empowered to standardize their care or practice.”
“ICU nurses are the ones who are primarily responsible for VAP preventive practices: they keep the head of the bed higher than 45 degrees, they conduct oral care, they conduct (patient) surveillance. ICU physicians are involved with writing the orders and ventilator setting management. So how these providers work together could theoretically influence the risk for patients developing VAP,” Dr. Costa said.
“We need to be thinking a little bit more critically about not only the care that’s happening at the bedside... but also at an organizational level. How are these providers organized, and can we work together to improve patient outcomes?”
“I’m not suggesting that we get rid of all closed ICUs because I don’t think that’s the solution,” Dr. Costa maintained. “I think from an administrative perspective, we need to be considering what’s the organization of these clinicians and this unit, and [in a context-specific manner], how can we improve it for better patient outcomes? That may be both working on improving the work environment and making the nurses feel more empowered, or it could be potentially considering other staffing models.”
Some data have already linked a more favorable nurse work environment and the presence of a board-certified critical care physician independently with better patient outcomes in the ICU. But studies of their joint impact are lacking.
The investigators performed a secondary, unit-level analysis of nurse survey data collected during 2005 and 2006 in ICUs in southern Michigan.
In all, 462 nurses working in 25 ICUs completed the Practice Environment Scale of the Nursing Work Index, on which averaged summary scores range between 1 (unfavorable) and 4 (favorable). The scale captures environmental factors such as the adequacy of resources for nurses, support from their managers, and their level of involvement in hospital policy decisions.
The rate of VAP during the same period was assessed using data from more than 1,000 patients from each ICU.
The summary nurse work environment score averaged 2.69 points in the 21 ICUs that had a closed physician staffing model and 2.62 points in the 4 ICUs that had an open physician staffing model. The respective rates of VAP were 7.5% and 2.5%.
In adjusted analysis among all 25 ICUs, each 1-point increase in an ICU’s Practice Environment Scale score was associated with a sharply higher rate of VAP on the unit (adjusted incidence rate ratio, 5.76; P = .02).
However, there was a strong interaction between the score and physician staffing model (P less than .001). In open ICUs, as the score rose, the rate of VAP fell (from about 16% to 5%), whereas in closed ICUs, as the score rose, so did the rate of VAP (from about 3% to 14%).
Dr. Costa disclosed that she had no relevant conflicts of interest. The parent survey was funded by the Blue Cross Blue Shield Foundation of Michigan.
SAN FRANCISCO – The work environment for nurses and the physician staffing model in the intensive care unit influence patients’ likelihood of acquiring ventilator-associated pneumonia (VAP), based on a cohort study of 25 ICUs.
Overall, each 1-point increase in the score for the nurse work environment – indicating that nurses had a greater sense of playing an important role in patient care – was unexpectedly associated with a roughly sixfold higher rate of VAP among the ICU’s patients, according to data reported in a session and press briefing at an international conference of the American Thoracic Society. However, additional analyses showed that the rate of VAP was higher in closed units where a board-certified critical care physician (intensivist) managed and led care rather than an open unit where care is shared.
“We think that the organization of the ICU is actually influencing nursing practice, which is a really novel finding,” commented first author Deena Kelly Costa, PhD, RN, of the University of Michigan School of Nursing in Ann Arbor. “In closed ICUs, when you have a board-certified physician and an ICU team managing and leading care, even if the work environment is better, nurses may not feel as empowered to standardize their care or practice.”
“ICU nurses are the ones who are primarily responsible for VAP preventive practices: they keep the head of the bed higher than 45 degrees, they conduct oral care, they conduct (patient) surveillance. ICU physicians are involved with writing the orders and ventilator setting management. So how these providers work together could theoretically influence the risk for patients developing VAP,” Dr. Costa said.
“We need to be thinking a little bit more critically about not only the care that’s happening at the bedside... but also at an organizational level. How are these providers organized, and can we work together to improve patient outcomes?”
“I’m not suggesting that we get rid of all closed ICUs because I don’t think that’s the solution,” Dr. Costa maintained. “I think from an administrative perspective, we need to be considering what’s the organization of these clinicians and this unit, and [in a context-specific manner], how can we improve it for better patient outcomes? That may be both working on improving the work environment and making the nurses feel more empowered, or it could be potentially considering other staffing models.”
Some data have already linked a more favorable nurse work environment and the presence of a board-certified critical care physician independently with better patient outcomes in the ICU. But studies of their joint impact are lacking.
The investigators performed a secondary, unit-level analysis of nurse survey data collected during 2005 and 2006 in ICUs in southern Michigan.
In all, 462 nurses working in 25 ICUs completed the Practice Environment Scale of the Nursing Work Index, on which averaged summary scores range between 1 (unfavorable) and 4 (favorable). The scale captures environmental factors such as the adequacy of resources for nurses, support from their managers, and their level of involvement in hospital policy decisions.
The rate of VAP during the same period was assessed using data from more than 1,000 patients from each ICU.
The summary nurse work environment score averaged 2.69 points in the 21 ICUs that had a closed physician staffing model and 2.62 points in the 4 ICUs that had an open physician staffing model. The respective rates of VAP were 7.5% and 2.5%.
In adjusted analysis among all 25 ICUs, each 1-point increase in an ICU’s Practice Environment Scale score was associated with a sharply higher rate of VAP on the unit (adjusted incidence rate ratio, 5.76; P = .02).
However, there was a strong interaction between the score and physician staffing model (P less than .001). In open ICUs, as the score rose, the rate of VAP fell (from about 16% to 5%), whereas in closed ICUs, as the score rose, so did the rate of VAP (from about 3% to 14%).
Dr. Costa disclosed that she had no relevant conflicts of interest. The parent survey was funded by the Blue Cross Blue Shield Foundation of Michigan.
SAN FRANCISCO – The work environment for nurses and the physician staffing model in the intensive care unit influence patients’ likelihood of acquiring ventilator-associated pneumonia (VAP), based on a cohort study of 25 ICUs.
Overall, each 1-point increase in the score for the nurse work environment – indicating that nurses had a greater sense of playing an important role in patient care – was unexpectedly associated with a roughly sixfold higher rate of VAP among the ICU’s patients, according to data reported in a session and press briefing at an international conference of the American Thoracic Society. However, additional analyses showed that the rate of VAP was higher in closed units where a board-certified critical care physician (intensivist) managed and led care rather than an open unit where care is shared.
“We think that the organization of the ICU is actually influencing nursing practice, which is a really novel finding,” commented first author Deena Kelly Costa, PhD, RN, of the University of Michigan School of Nursing in Ann Arbor. “In closed ICUs, when you have a board-certified physician and an ICU team managing and leading care, even if the work environment is better, nurses may not feel as empowered to standardize their care or practice.”
“ICU nurses are the ones who are primarily responsible for VAP preventive practices: they keep the head of the bed higher than 45 degrees, they conduct oral care, they conduct (patient) surveillance. ICU physicians are involved with writing the orders and ventilator setting management. So how these providers work together could theoretically influence the risk for patients developing VAP,” Dr. Costa said.
“We need to be thinking a little bit more critically about not only the care that’s happening at the bedside... but also at an organizational level. How are these providers organized, and can we work together to improve patient outcomes?”
“I’m not suggesting that we get rid of all closed ICUs because I don’t think that’s the solution,” Dr. Costa maintained. “I think from an administrative perspective, we need to be considering what’s the organization of these clinicians and this unit, and [in a context-specific manner], how can we improve it for better patient outcomes? That may be both working on improving the work environment and making the nurses feel more empowered, or it could be potentially considering other staffing models.”
Some data have already linked a more favorable nurse work environment and the presence of a board-certified critical care physician independently with better patient outcomes in the ICU. But studies of their joint impact are lacking.
The investigators performed a secondary, unit-level analysis of nurse survey data collected during 2005 and 2006 in ICUs in southern Michigan.
In all, 462 nurses working in 25 ICUs completed the Practice Environment Scale of the Nursing Work Index, on which averaged summary scores range between 1 (unfavorable) and 4 (favorable). The scale captures environmental factors such as the adequacy of resources for nurses, support from their managers, and their level of involvement in hospital policy decisions.
The rate of VAP during the same period was assessed using data from more than 1,000 patients from each ICU.
The summary nurse work environment score averaged 2.69 points in the 21 ICUs that had a closed physician staffing model and 2.62 points in the 4 ICUs that had an open physician staffing model. The respective rates of VAP were 7.5% and 2.5%.
In adjusted analysis among all 25 ICUs, each 1-point increase in an ICU’s Practice Environment Scale score was associated with a sharply higher rate of VAP on the unit (adjusted incidence rate ratio, 5.76; P = .02).
However, there was a strong interaction between the score and physician staffing model (P less than .001). In open ICUs, as the score rose, the rate of VAP fell (from about 16% to 5%), whereas in closed ICUs, as the score rose, so did the rate of VAP (from about 3% to 14%).
Dr. Costa disclosed that she had no relevant conflicts of interest. The parent survey was funded by the Blue Cross Blue Shield Foundation of Michigan.
AT ATS 2016
Key clinical point: The impact of nurse work environment on risk of VAP in the ICU depends on the unit’s physician staffing model.
Major finding: A better nurse work environment was associated with a higher rate of VAP overall (incidence rate ratio, 5.76), but there was an interaction whereby it was positively associated with rate in closed units but negatively so in open units.
Data source: A cohort study of 25 ICUs, 462 nurses, and more than 25,000 patients in southern Michigan between 2005 and 2006.
Disclosures: Dr. Costa disclosed that she had no relevant conflicts of interest. The parent study was funded by the Blue Cross Blue Shield Foundation of Michigan.
Insomnia in young men boosts cardiovascular and cerebrovascular risk
DENVER – Young to early middle-aged men with insomnia symptoms are at increased risk for cardiovascular and cerebrovascular events, according to an analysis from the landmark CARDIA study.
“We found that younger to mid-life men with difficulty initiating sleep or with more than one insomnia symptom were at greater risk for incident cardiovascular disease events. And despite the fact that women in general seemed to be more prone to report those sleep difficulties, those that did were not at increased risk,” Megan E. Petrov, PhD, reported at the annual meeting of the Associated Professional Sleep Societies.
It is well established that insomnia in older adults is associated with increased cardiovascular risk. For example, a meta-analysis of 13 prospective studies with more than 123,000 subjects concluded that insomnia was associated with a 45% increased risk of fatal and nonfatal cardiovascular events (Eur J Prev Cardiol. 2014 Jan;21[1]:57-64). But those studies typically involved older individuals, which makes cause and effect more difficult to determine because so many chronic conditions become more prevalent with advancing age, noted Dr. Petrov of Arizona State University in Phoenix.
“We wanted to see if insomnia is truly an early risk factor in the pathogenesis of cardiovascular disease and stroke,” she said.
To do so, she and her coinvestigators turned to the CARDIA database. CARDIA (the Coronary Artery Risk Development in Young Adults study), is a National Heart, Lung, and Blood Institute–sponsored prospective, epidemiologic study.
She reported on 2,950 non-Hispanic black or white participants aged 33-45 and free of any history of cardiovascular disease in 2000-2001, when they answered questions about insomnia symptoms. Difficulty in initiating sleep was reported by 16.3% of men and 20.7% of women. Difficulty maintaining sleep was a problem for 9.3% of men and 14.5% of women. And 20.6% of men and 20.1% of women reported frequent early morning awakening.
During a mean 11.5 years of prospective follow-up, 4.1% of men and 2.3% of women had a fatal or nonfatal MI, stroke, transient ischemic attack, heart failure, peripheral vascular disease, or hospitalization for an acute coronary syndrome.
In a multivariate logistic regression analysis fully adjusted for demographics, socioeconomic status, body mass index, blood pressure, diabetes, depression, health behaviors, medications, thyroid disease, and kidney problems, men who reported difficulty in getting to sleep had a 2.64-fold increased risk of one of these adverse outcomes. That was the only insomnia symptom associated with significantly increased risk. However, men but not women who reported having more than one insomnia symptom had a 39% increased risk of a cardiovascular event for each additional symptom.
Prior studies have shown that insomnia is associated with cardiac sympathetic hyperactivation. That observation suggests a plausible mechanism for increased cardiovascular and cerebrovascular risk, but it doesn’t explain why that risk was confined to young men in CARDIA. One possibility is that because of gender-related differences in perception, men tend to report having insomnia symptoms only when the insomnia is more severe, Dr. Petrov suggested.
The strengths of the CARDIA study are that all cardiovascular endpoints had to be physician certified, and the study includes a large black population. A study limitation is the relatively small number of cardiovascular events, as to be expected in a younger population. Thus, confirmation of the new findings in another large data set will be important, she noted.
As a next step in her research, Dr. Petrov said she plans to drill down in the CARDIA data to see if race modified the impact of insomnia symptoms on cardiovascular outcomes. Black participants reported all insomnia symptoms more frequently than did whites. For example, difficulty initiating sleep was reported by 25.7% of blacks, compared with just 13.5% of whites, and early morning awakening was twice as prevalent among the black participants.
Also, CARDIA participants provided self-reported sleep duration data. It will be illuminating to see if sleep duration had a modifying effect upon the insomnia/cardiovascular risk association observed in men, she said.
Dr. Petrov reported having no relevant financial conflicts.
DENVER – Young to early middle-aged men with insomnia symptoms are at increased risk for cardiovascular and cerebrovascular events, according to an analysis from the landmark CARDIA study.
“We found that younger to mid-life men with difficulty initiating sleep or with more than one insomnia symptom were at greater risk for incident cardiovascular disease events. And despite the fact that women in general seemed to be more prone to report those sleep difficulties, those that did were not at increased risk,” Megan E. Petrov, PhD, reported at the annual meeting of the Associated Professional Sleep Societies.
It is well established that insomnia in older adults is associated with increased cardiovascular risk. For example, a meta-analysis of 13 prospective studies with more than 123,000 subjects concluded that insomnia was associated with a 45% increased risk of fatal and nonfatal cardiovascular events (Eur J Prev Cardiol. 2014 Jan;21[1]:57-64). But those studies typically involved older individuals, which makes cause and effect more difficult to determine because so many chronic conditions become more prevalent with advancing age, noted Dr. Petrov of Arizona State University in Phoenix.
“We wanted to see if insomnia is truly an early risk factor in the pathogenesis of cardiovascular disease and stroke,” she said.
To do so, she and her coinvestigators turned to the CARDIA database. CARDIA (the Coronary Artery Risk Development in Young Adults study), is a National Heart, Lung, and Blood Institute–sponsored prospective, epidemiologic study.
She reported on 2,950 non-Hispanic black or white participants aged 33-45 and free of any history of cardiovascular disease in 2000-2001, when they answered questions about insomnia symptoms. Difficulty in initiating sleep was reported by 16.3% of men and 20.7% of women. Difficulty maintaining sleep was a problem for 9.3% of men and 14.5% of women. And 20.6% of men and 20.1% of women reported frequent early morning awakening.
During a mean 11.5 years of prospective follow-up, 4.1% of men and 2.3% of women had a fatal or nonfatal MI, stroke, transient ischemic attack, heart failure, peripheral vascular disease, or hospitalization for an acute coronary syndrome.
In a multivariate logistic regression analysis fully adjusted for demographics, socioeconomic status, body mass index, blood pressure, diabetes, depression, health behaviors, medications, thyroid disease, and kidney problems, men who reported difficulty in getting to sleep had a 2.64-fold increased risk of one of these adverse outcomes. That was the only insomnia symptom associated with significantly increased risk. However, men but not women who reported having more than one insomnia symptom had a 39% increased risk of a cardiovascular event for each additional symptom.
Prior studies have shown that insomnia is associated with cardiac sympathetic hyperactivation. That observation suggests a plausible mechanism for increased cardiovascular and cerebrovascular risk, but it doesn’t explain why that risk was confined to young men in CARDIA. One possibility is that because of gender-related differences in perception, men tend to report having insomnia symptoms only when the insomnia is more severe, Dr. Petrov suggested.
The strengths of the CARDIA study are that all cardiovascular endpoints had to be physician certified, and the study includes a large black population. A study limitation is the relatively small number of cardiovascular events, as to be expected in a younger population. Thus, confirmation of the new findings in another large data set will be important, she noted.
As a next step in her research, Dr. Petrov said she plans to drill down in the CARDIA data to see if race modified the impact of insomnia symptoms on cardiovascular outcomes. Black participants reported all insomnia symptoms more frequently than did whites. For example, difficulty initiating sleep was reported by 25.7% of blacks, compared with just 13.5% of whites, and early morning awakening was twice as prevalent among the black participants.
Also, CARDIA participants provided self-reported sleep duration data. It will be illuminating to see if sleep duration had a modifying effect upon the insomnia/cardiovascular risk association observed in men, she said.
Dr. Petrov reported having no relevant financial conflicts.
DENVER – Young to early middle-aged men with insomnia symptoms are at increased risk for cardiovascular and cerebrovascular events, according to an analysis from the landmark CARDIA study.
“We found that younger to mid-life men with difficulty initiating sleep or with more than one insomnia symptom were at greater risk for incident cardiovascular disease events. And despite the fact that women in general seemed to be more prone to report those sleep difficulties, those that did were not at increased risk,” Megan E. Petrov, PhD, reported at the annual meeting of the Associated Professional Sleep Societies.
It is well established that insomnia in older adults is associated with increased cardiovascular risk. For example, a meta-analysis of 13 prospective studies with more than 123,000 subjects concluded that insomnia was associated with a 45% increased risk of fatal and nonfatal cardiovascular events (Eur J Prev Cardiol. 2014 Jan;21[1]:57-64). But those studies typically involved older individuals, which makes cause and effect more difficult to determine because so many chronic conditions become more prevalent with advancing age, noted Dr. Petrov of Arizona State University in Phoenix.
“We wanted to see if insomnia is truly an early risk factor in the pathogenesis of cardiovascular disease and stroke,” she said.
To do so, she and her coinvestigators turned to the CARDIA database. CARDIA (the Coronary Artery Risk Development in Young Adults study), is a National Heart, Lung, and Blood Institute–sponsored prospective, epidemiologic study.
She reported on 2,950 non-Hispanic black or white participants aged 33-45 and free of any history of cardiovascular disease in 2000-2001, when they answered questions about insomnia symptoms. Difficulty in initiating sleep was reported by 16.3% of men and 20.7% of women. Difficulty maintaining sleep was a problem for 9.3% of men and 14.5% of women. And 20.6% of men and 20.1% of women reported frequent early morning awakening.
During a mean 11.5 years of prospective follow-up, 4.1% of men and 2.3% of women had a fatal or nonfatal MI, stroke, transient ischemic attack, heart failure, peripheral vascular disease, or hospitalization for an acute coronary syndrome.
In a multivariate logistic regression analysis fully adjusted for demographics, socioeconomic status, body mass index, blood pressure, diabetes, depression, health behaviors, medications, thyroid disease, and kidney problems, men who reported difficulty in getting to sleep had a 2.64-fold increased risk of one of these adverse outcomes. That was the only insomnia symptom associated with significantly increased risk. However, men but not women who reported having more than one insomnia symptom had a 39% increased risk of a cardiovascular event for each additional symptom.
Prior studies have shown that insomnia is associated with cardiac sympathetic hyperactivation. That observation suggests a plausible mechanism for increased cardiovascular and cerebrovascular risk, but it doesn’t explain why that risk was confined to young men in CARDIA. One possibility is that because of gender-related differences in perception, men tend to report having insomnia symptoms only when the insomnia is more severe, Dr. Petrov suggested.
The strengths of the CARDIA study are that all cardiovascular endpoints had to be physician certified, and the study includes a large black population. A study limitation is the relatively small number of cardiovascular events, as to be expected in a younger population. Thus, confirmation of the new findings in another large data set will be important, she noted.
As a next step in her research, Dr. Petrov said she plans to drill down in the CARDIA data to see if race modified the impact of insomnia symptoms on cardiovascular outcomes. Black participants reported all insomnia symptoms more frequently than did whites. For example, difficulty initiating sleep was reported by 25.7% of blacks, compared with just 13.5% of whites, and early morning awakening was twice as prevalent among the black participants.
Also, CARDIA participants provided self-reported sleep duration data. It will be illuminating to see if sleep duration had a modifying effect upon the insomnia/cardiovascular risk association observed in men, she said.
Dr. Petrov reported having no relevant financial conflicts.
AT SLEEP 2016
Key clinical point: Insomnia symptoms are associated with increased cardiovascular and cerebrovascular event rates in young to middle-aged men.
Major finding: Men aged 33-45 who reported frequent difficulty in falling asleep were at an adjusted 2.64-fold increased risk of a major cardiovascular or cerebrovascular event during subsequent follow-up.
Data source: The prospective, epidemiologic CARDIA study including 2,950 black or white subjects aged 33-45 at enrollment who were followed for a mean of 11.5 years.
Disclosures: The CARDIA study is supported by the National Institutes of Health. The presenter reported having no relevant financial conflicts.
Restless sleep in 11-year-olds predicts earlier substance use
DENVER – Poor sleep quality and shorter sleep duration in boys at age 11 years is associated with subsequent accelerated use and misuse of alcohol and cannabis during adolescence and emerging adulthood, Thomas B. Mike reported at the annual meeting of the Associated Professional Sleep Societies.
This association has been reported before in cross-sectional studies. But Mr. Mike presented new findings from the longitudinal prospective Pitt Mother and Child Project.
The study comprised 170 boys aged 11 years whose mothers filled out the Child Sleep Questionnaire, modified for pediatric use from the well known Pittsburgh Sleep Quality Index. At that time, the boys also were assessed for internalizing and externalizing behaviors, neighborhood dangerousness, and socioeconomic status – all of which are factors known to influence teen substance use.
When participants reached ages 20 and 22 years, they underwent detailed interviews including assessment via the validated Lifetime Drinking History and Lifetime Drug History questionnaires.
In a multivariate Cox regression analysis controlling for a history of child internalizing and externalizing problem behavior as well as socioeconomic factors, every hour of sleep duration less than 9.5 hours at age 11 years was associated with a 21% acceleration in the time to first use of alcohol and a 22% acceleration in first use of cannabis, reported Mr. Mike, a medical student at the University of Pittsburgh.
Moreover, every 1 point worse score for sleep quality on the Child Sleep Questionnaire, scored from 0 (best) to 21 (worst), was associated with a 9% acceleration in time to alcohol use and an 8% acceleration to cannabis use.
Subjects with poor sleep duration and quality as 11-year-olds by parental report also experienced intoxication at a younger age than did those who had been better sleepers at that age. And they reported more frequent use of alcohol and cannabis during adolescence.
In an interview, Mr. Mike, who is planning a career in pediatrics, said the study findings contain an important message for pediatricians and family physicians when they meet with the parents of young boys entering adolescence.
“Probably the biggest take-home message is, ‘sleep more, sleep better.’ We don’t have a lot of ways to intervene right now for kids who have poor sleep, but we know based on this and other studies that kids who don’t sleep enough are more likely to use drugs and more likely to engage in other risky behaviors. So any way the parents can intervene will help, perhaps by getting them to bed earlier or trying to get them on a more regular schedule. At a social policy level, having school start later would probably be the most effective measure, but that probably won’t happen for a very long time,” he said.
“The vast majority of people who end up addicted to drugs later in life started when they were kids, so any way we can reduce adolescent substance use should have a downstream effect, including a decreased total substance use burden,” Mr. Mike added.
Possible mechanisms for the observed longitudinal association between poor quality and duration of sleep at age 11 years and earlier and heavier use of alcohol and cannabis later in adolescence include attempted self-medication for sleep problems, reward regulation, and alterations in brain chemistry, making the boys more susceptible to using drugs later in life, perhaps because they obtain a bigger high than their peers do. The investigators plan to delve deeper into the role of self-regulation and mental health as possible mechanisms linking childhood sleep and later substance use, he said.
The Pitt Mother and Child Project is supported by the National Institutes of Health. Mr. Mike reported having no financial conflicts.
DENVER – Poor sleep quality and shorter sleep duration in boys at age 11 years is associated with subsequent accelerated use and misuse of alcohol and cannabis during adolescence and emerging adulthood, Thomas B. Mike reported at the annual meeting of the Associated Professional Sleep Societies.
This association has been reported before in cross-sectional studies. But Mr. Mike presented new findings from the longitudinal prospective Pitt Mother and Child Project.
The study comprised 170 boys aged 11 years whose mothers filled out the Child Sleep Questionnaire, modified for pediatric use from the well known Pittsburgh Sleep Quality Index. At that time, the boys also were assessed for internalizing and externalizing behaviors, neighborhood dangerousness, and socioeconomic status – all of which are factors known to influence teen substance use.
When participants reached ages 20 and 22 years, they underwent detailed interviews including assessment via the validated Lifetime Drinking History and Lifetime Drug History questionnaires.
In a multivariate Cox regression analysis controlling for a history of child internalizing and externalizing problem behavior as well as socioeconomic factors, every hour of sleep duration less than 9.5 hours at age 11 years was associated with a 21% acceleration in the time to first use of alcohol and a 22% acceleration in first use of cannabis, reported Mr. Mike, a medical student at the University of Pittsburgh.
Moreover, every 1 point worse score for sleep quality on the Child Sleep Questionnaire, scored from 0 (best) to 21 (worst), was associated with a 9% acceleration in time to alcohol use and an 8% acceleration to cannabis use.
Subjects with poor sleep duration and quality as 11-year-olds by parental report also experienced intoxication at a younger age than did those who had been better sleepers at that age. And they reported more frequent use of alcohol and cannabis during adolescence.
In an interview, Mr. Mike, who is planning a career in pediatrics, said the study findings contain an important message for pediatricians and family physicians when they meet with the parents of young boys entering adolescence.
“Probably the biggest take-home message is, ‘sleep more, sleep better.’ We don’t have a lot of ways to intervene right now for kids who have poor sleep, but we know based on this and other studies that kids who don’t sleep enough are more likely to use drugs and more likely to engage in other risky behaviors. So any way the parents can intervene will help, perhaps by getting them to bed earlier or trying to get them on a more regular schedule. At a social policy level, having school start later would probably be the most effective measure, but that probably won’t happen for a very long time,” he said.
“The vast majority of people who end up addicted to drugs later in life started when they were kids, so any way we can reduce adolescent substance use should have a downstream effect, including a decreased total substance use burden,” Mr. Mike added.
Possible mechanisms for the observed longitudinal association between poor quality and duration of sleep at age 11 years and earlier and heavier use of alcohol and cannabis later in adolescence include attempted self-medication for sleep problems, reward regulation, and alterations in brain chemistry, making the boys more susceptible to using drugs later in life, perhaps because they obtain a bigger high than their peers do. The investigators plan to delve deeper into the role of self-regulation and mental health as possible mechanisms linking childhood sleep and later substance use, he said.
The Pitt Mother and Child Project is supported by the National Institutes of Health. Mr. Mike reported having no financial conflicts.
DENVER – Poor sleep quality and shorter sleep duration in boys at age 11 years is associated with subsequent accelerated use and misuse of alcohol and cannabis during adolescence and emerging adulthood, Thomas B. Mike reported at the annual meeting of the Associated Professional Sleep Societies.
This association has been reported before in cross-sectional studies. But Mr. Mike presented new findings from the longitudinal prospective Pitt Mother and Child Project.
The study comprised 170 boys aged 11 years whose mothers filled out the Child Sleep Questionnaire, modified for pediatric use from the well known Pittsburgh Sleep Quality Index. At that time, the boys also were assessed for internalizing and externalizing behaviors, neighborhood dangerousness, and socioeconomic status – all of which are factors known to influence teen substance use.
When participants reached ages 20 and 22 years, they underwent detailed interviews including assessment via the validated Lifetime Drinking History and Lifetime Drug History questionnaires.
In a multivariate Cox regression analysis controlling for a history of child internalizing and externalizing problem behavior as well as socioeconomic factors, every hour of sleep duration less than 9.5 hours at age 11 years was associated with a 21% acceleration in the time to first use of alcohol and a 22% acceleration in first use of cannabis, reported Mr. Mike, a medical student at the University of Pittsburgh.
Moreover, every 1 point worse score for sleep quality on the Child Sleep Questionnaire, scored from 0 (best) to 21 (worst), was associated with a 9% acceleration in time to alcohol use and an 8% acceleration to cannabis use.
Subjects with poor sleep duration and quality as 11-year-olds by parental report also experienced intoxication at a younger age than did those who had been better sleepers at that age. And they reported more frequent use of alcohol and cannabis during adolescence.
In an interview, Mr. Mike, who is planning a career in pediatrics, said the study findings contain an important message for pediatricians and family physicians when they meet with the parents of young boys entering adolescence.
“Probably the biggest take-home message is, ‘sleep more, sleep better.’ We don’t have a lot of ways to intervene right now for kids who have poor sleep, but we know based on this and other studies that kids who don’t sleep enough are more likely to use drugs and more likely to engage in other risky behaviors. So any way the parents can intervene will help, perhaps by getting them to bed earlier or trying to get them on a more regular schedule. At a social policy level, having school start later would probably be the most effective measure, but that probably won’t happen for a very long time,” he said.
“The vast majority of people who end up addicted to drugs later in life started when they were kids, so any way we can reduce adolescent substance use should have a downstream effect, including a decreased total substance use burden,” Mr. Mike added.
Possible mechanisms for the observed longitudinal association between poor quality and duration of sleep at age 11 years and earlier and heavier use of alcohol and cannabis later in adolescence include attempted self-medication for sleep problems, reward regulation, and alterations in brain chemistry, making the boys more susceptible to using drugs later in life, perhaps because they obtain a bigger high than their peers do. The investigators plan to delve deeper into the role of self-regulation and mental health as possible mechanisms linking childhood sleep and later substance use, he said.
The Pitt Mother and Child Project is supported by the National Institutes of Health. Mr. Mike reported having no financial conflicts.
AT SLEEP 2016
Key clinical point: Boys with poor sleep quality and quantity start using alcohol and cannabis earlier as teens.
Major finding: Every hour less of sleep duration at age 11 years was associated with a 21% acceleration in time to first use of alcohol and a 22% acceleration in first use of cannabis.
Data source: An analysis from the Pitt Mother and Child Project of 170 boys with sleep data recorded at age 11 and lifetime alcohol and cannabis use recalled at ages 20 and 22.
Disclosures: The Pitt Mother and Child Project is supported by the National Institutes of Health. The presenter reported having no financial conflicts.