User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Powered by CHEST Physician, Clinician Reviews, MDedge Family Medicine, Internal Medicine News, and The Journal of Clinical Outcomes Management.
ACOS under-recognized, under-treated
Exacerbations in bronchodilator-responsive asthma–chronic obstructive pulmonary disease overlap syndrome (ACOS) were more frequent and severe than in COPD with emphysema, but only a minority of patients were treated to prevent them, in a review of 1,005 patients from the Annals of the American Thoracic Society.
All the subjects were current or former smokers culled from the COPDGene Study, a multicenter observational study looking for the genetic roots of COPD susceptibility; 385 patients met the investigators’ criteria for ACOS with bronchodilator response (ACOS-BDR), which included a history of asthma or hay fever, airway obstruction with significant bronchodilator responsiveness, and less then 15% emphysema on chest CT.
Another 620 subjects met criteria for COPD with emphysema, including airway obstruction without bronchodilator reversibility, and more than 15% emphysema on chest CT (Ann Am Thorac Soc. 2016 Sep;13(9):1483-9).
Although the ACOS patients had better lung function, they had similar severity and frequency of exacerbations, compared with the COPD group. After adjustment for forced expiratory volume in 1 second percent predicted and other factors, the patients with ACOS-BDR were actually more likely to have severe and frequent exacerbations. Possible explanations for this are that they were more likely to smoke and have gastroesophageal reflux disease and obstructive sleep apnea, all of which increase the risk of exacerbations.
Even so, ACOS-BDR patients were less likely to be on a long-acting beta-agonist (6.8% versus 13.9%); a long-acting muscarinic antagonist (20% versus 60.8%); or a combination long-acting beta-agonist/inhaled corticosteroid (29.9% versus 55.6%).
“Only a small percentage of them were being treated ... Early and aggressive treatment with combination therapy may help alleviate symptoms and decrease exacerbations,” said investigators led by James Cosentino, DO, of Temple University School of Medicine, Philadelphia. Patients with ACOS “are a particularly high-risk group.” They deserve “special attention, and practitioners need to be diligent in evaluation of them.”
ACOS is being increasingly recognized as a distinct clinical entity with perhaps a worse prognosis than either asthma or COPD alone. The goal of the study was to better characterize the disease.
To that end, the team found four features that seemed to distinguish ACOS-BDR from COPD with emphysema: ACOS-BDR patients were younger (60.6 versus 65.9 years old); heavier (body mass index 29.6 versus 25.1 kg/m2; more likely to be African American (26.8% versus 14.4%); and more likely to be current smokers (50.9% versus 20.7%).
It’s “likely that current smoking in subjects with ACOS, coupled with the long duration of asthma, leads to inflammation and small airway remodeling with development of symptoms earlier in the disease course than that seen in those with COPD with emphysema,” the investigators said.
“Early and aggressive treatment with combination therapy may help alleviate symptoms and decrease exacerbations. Recognition and treatment of comorbidities and aggressive smoking cessation may also play a key role in preventing exacerbations and alleviating the morbidity associated with ACOS; however, future studies on the treatment of ACOS are needed,” they said.
The majority of subjects with ACOS-BDR met criteria for Global Initiative for Chronic Obstructive Lung Disease grade B, indicating a high degree of symptoms despite less severe airflow obstruction.
The funding source wasn’t reported. Dr. Cosentino had no conflicts. Other authors disclosed personal fees from Concert Pharmaceuticals, CSA Medical, CSL Behring, Gala Therapeutics, and Novartis.
The importance of this study is that it used readily available metrics to define ACOS in a COPD population. Although diffusion capacity was not reported, quantification of emphysema on chest CT scans combined with history and spirometry provide a reasonable approach to distinguishing ACOS-BDR from COPD with emphysema.
Although subjects with COPD had smoked more heavily as measured by cigarette pack-years, subjects with ACOS were much more likely to be current smokers... Subjects with ACOS also had a higher prevalence of comorbidities such as sleep apnea, diabetes mellitus, hypertension, and hypercholesterolemia as compared with patients with COPD. Having a higher BMI, to near obesity, and a greater prevalence of gastroesophageal reflux disease raises questions related to diet, lifestyle, and nutrition as potential contributors to ACOS pathophysiology.
In the future, the use of diagnostic terms such as “asthma,” “COPD,” and “ACOS,” will likely give way to the more unifying diagnosis of obstructive airway disease (OAD)... OAD would be further delineated on the basis of molecular phenotyping, genomic, and systems biology approaches, in combination with more traditional clinical and physiological parameters... This new mindset can help us solve the problem of obstructive airway disease taxonomy and develop not only better treatments, but eventually invent lasting cures – if we are so lucky.
Amir Zeki, MD , is an assistant professor in the Division of Pulmonary, Critical Care, and Sleep Medicine at the University of California, Davis. Nizar Jarjour, MD , is a professor of medicine and head of the allergy, pulmonary, and critical care division at the University of Wisconsin, Madison. Dr. Zeki had no disclosures. Dr. Jarjour reported consulting fees from AstraZeneca, Daiichi Sankyo, and Teva. They made their comments in an editorial ( Ann Am Thorac Soc. 2016 Sep;13(9):1440-2 ).
The importance of this study is that it used readily available metrics to define ACOS in a COPD population. Although diffusion capacity was not reported, quantification of emphysema on chest CT scans combined with history and spirometry provide a reasonable approach to distinguishing ACOS-BDR from COPD with emphysema.
Although subjects with COPD had smoked more heavily as measured by cigarette pack-years, subjects with ACOS were much more likely to be current smokers... Subjects with ACOS also had a higher prevalence of comorbidities such as sleep apnea, diabetes mellitus, hypertension, and hypercholesterolemia as compared with patients with COPD. Having a higher BMI, to near obesity, and a greater prevalence of gastroesophageal reflux disease raises questions related to diet, lifestyle, and nutrition as potential contributors to ACOS pathophysiology.
In the future, the use of diagnostic terms such as “asthma,” “COPD,” and “ACOS,” will likely give way to the more unifying diagnosis of obstructive airway disease (OAD)... OAD would be further delineated on the basis of molecular phenotyping, genomic, and systems biology approaches, in combination with more traditional clinical and physiological parameters... This new mindset can help us solve the problem of obstructive airway disease taxonomy and develop not only better treatments, but eventually invent lasting cures – if we are so lucky.
Amir Zeki, MD , is an assistant professor in the Division of Pulmonary, Critical Care, and Sleep Medicine at the University of California, Davis. Nizar Jarjour, MD , is a professor of medicine and head of the allergy, pulmonary, and critical care division at the University of Wisconsin, Madison. Dr. Zeki had no disclosures. Dr. Jarjour reported consulting fees from AstraZeneca, Daiichi Sankyo, and Teva. They made their comments in an editorial ( Ann Am Thorac Soc. 2016 Sep;13(9):1440-2 ).
The importance of this study is that it used readily available metrics to define ACOS in a COPD population. Although diffusion capacity was not reported, quantification of emphysema on chest CT scans combined with history and spirometry provide a reasonable approach to distinguishing ACOS-BDR from COPD with emphysema.
Although subjects with COPD had smoked more heavily as measured by cigarette pack-years, subjects with ACOS were much more likely to be current smokers... Subjects with ACOS also had a higher prevalence of comorbidities such as sleep apnea, diabetes mellitus, hypertension, and hypercholesterolemia as compared with patients with COPD. Having a higher BMI, to near obesity, and a greater prevalence of gastroesophageal reflux disease raises questions related to diet, lifestyle, and nutrition as potential contributors to ACOS pathophysiology.
In the future, the use of diagnostic terms such as “asthma,” “COPD,” and “ACOS,” will likely give way to the more unifying diagnosis of obstructive airway disease (OAD)... OAD would be further delineated on the basis of molecular phenotyping, genomic, and systems biology approaches, in combination with more traditional clinical and physiological parameters... This new mindset can help us solve the problem of obstructive airway disease taxonomy and develop not only better treatments, but eventually invent lasting cures – if we are so lucky.
Amir Zeki, MD , is an assistant professor in the Division of Pulmonary, Critical Care, and Sleep Medicine at the University of California, Davis. Nizar Jarjour, MD , is a professor of medicine and head of the allergy, pulmonary, and critical care division at the University of Wisconsin, Madison. Dr. Zeki had no disclosures. Dr. Jarjour reported consulting fees from AstraZeneca, Daiichi Sankyo, and Teva. They made their comments in an editorial ( Ann Am Thorac Soc. 2016 Sep;13(9):1440-2 ).
Exacerbations in bronchodilator-responsive asthma–chronic obstructive pulmonary disease overlap syndrome (ACOS) were more frequent and severe than in COPD with emphysema, but only a minority of patients were treated to prevent them, in a review of 1,005 patients from the Annals of the American Thoracic Society.
All the subjects were current or former smokers culled from the COPDGene Study, a multicenter observational study looking for the genetic roots of COPD susceptibility; 385 patients met the investigators’ criteria for ACOS with bronchodilator response (ACOS-BDR), which included a history of asthma or hay fever, airway obstruction with significant bronchodilator responsiveness, and less then 15% emphysema on chest CT.
Another 620 subjects met criteria for COPD with emphysema, including airway obstruction without bronchodilator reversibility, and more than 15% emphysema on chest CT (Ann Am Thorac Soc. 2016 Sep;13(9):1483-9).
Although the ACOS patients had better lung function, they had similar severity and frequency of exacerbations, compared with the COPD group. After adjustment for forced expiratory volume in 1 second percent predicted and other factors, the patients with ACOS-BDR were actually more likely to have severe and frequent exacerbations. Possible explanations for this are that they were more likely to smoke and have gastroesophageal reflux disease and obstructive sleep apnea, all of which increase the risk of exacerbations.
Even so, ACOS-BDR patients were less likely to be on a long-acting beta-agonist (6.8% versus 13.9%); a long-acting muscarinic antagonist (20% versus 60.8%); or a combination long-acting beta-agonist/inhaled corticosteroid (29.9% versus 55.6%).
“Only a small percentage of them were being treated ... Early and aggressive treatment with combination therapy may help alleviate symptoms and decrease exacerbations,” said investigators led by James Cosentino, DO, of Temple University School of Medicine, Philadelphia. Patients with ACOS “are a particularly high-risk group.” They deserve “special attention, and practitioners need to be diligent in evaluation of them.”
ACOS is being increasingly recognized as a distinct clinical entity with perhaps a worse prognosis than either asthma or COPD alone. The goal of the study was to better characterize the disease.
To that end, the team found four features that seemed to distinguish ACOS-BDR from COPD with emphysema: ACOS-BDR patients were younger (60.6 versus 65.9 years old); heavier (body mass index 29.6 versus 25.1 kg/m2; more likely to be African American (26.8% versus 14.4%); and more likely to be current smokers (50.9% versus 20.7%).
It’s “likely that current smoking in subjects with ACOS, coupled with the long duration of asthma, leads to inflammation and small airway remodeling with development of symptoms earlier in the disease course than that seen in those with COPD with emphysema,” the investigators said.
“Early and aggressive treatment with combination therapy may help alleviate symptoms and decrease exacerbations. Recognition and treatment of comorbidities and aggressive smoking cessation may also play a key role in preventing exacerbations and alleviating the morbidity associated with ACOS; however, future studies on the treatment of ACOS are needed,” they said.
The majority of subjects with ACOS-BDR met criteria for Global Initiative for Chronic Obstructive Lung Disease grade B, indicating a high degree of symptoms despite less severe airflow obstruction.
The funding source wasn’t reported. Dr. Cosentino had no conflicts. Other authors disclosed personal fees from Concert Pharmaceuticals, CSA Medical, CSL Behring, Gala Therapeutics, and Novartis.
Exacerbations in bronchodilator-responsive asthma–chronic obstructive pulmonary disease overlap syndrome (ACOS) were more frequent and severe than in COPD with emphysema, but only a minority of patients were treated to prevent them, in a review of 1,005 patients from the Annals of the American Thoracic Society.
All the subjects were current or former smokers culled from the COPDGene Study, a multicenter observational study looking for the genetic roots of COPD susceptibility; 385 patients met the investigators’ criteria for ACOS with bronchodilator response (ACOS-BDR), which included a history of asthma or hay fever, airway obstruction with significant bronchodilator responsiveness, and less then 15% emphysema on chest CT.
Another 620 subjects met criteria for COPD with emphysema, including airway obstruction without bronchodilator reversibility, and more than 15% emphysema on chest CT (Ann Am Thorac Soc. 2016 Sep;13(9):1483-9).
Although the ACOS patients had better lung function, they had similar severity and frequency of exacerbations, compared with the COPD group. After adjustment for forced expiratory volume in 1 second percent predicted and other factors, the patients with ACOS-BDR were actually more likely to have severe and frequent exacerbations. Possible explanations for this are that they were more likely to smoke and have gastroesophageal reflux disease and obstructive sleep apnea, all of which increase the risk of exacerbations.
Even so, ACOS-BDR patients were less likely to be on a long-acting beta-agonist (6.8% versus 13.9%); a long-acting muscarinic antagonist (20% versus 60.8%); or a combination long-acting beta-agonist/inhaled corticosteroid (29.9% versus 55.6%).
“Only a small percentage of them were being treated ... Early and aggressive treatment with combination therapy may help alleviate symptoms and decrease exacerbations,” said investigators led by James Cosentino, DO, of Temple University School of Medicine, Philadelphia. Patients with ACOS “are a particularly high-risk group.” They deserve “special attention, and practitioners need to be diligent in evaluation of them.”
ACOS is being increasingly recognized as a distinct clinical entity with perhaps a worse prognosis than either asthma or COPD alone. The goal of the study was to better characterize the disease.
To that end, the team found four features that seemed to distinguish ACOS-BDR from COPD with emphysema: ACOS-BDR patients were younger (60.6 versus 65.9 years old); heavier (body mass index 29.6 versus 25.1 kg/m2; more likely to be African American (26.8% versus 14.4%); and more likely to be current smokers (50.9% versus 20.7%).
It’s “likely that current smoking in subjects with ACOS, coupled with the long duration of asthma, leads to inflammation and small airway remodeling with development of symptoms earlier in the disease course than that seen in those with COPD with emphysema,” the investigators said.
“Early and aggressive treatment with combination therapy may help alleviate symptoms and decrease exacerbations. Recognition and treatment of comorbidities and aggressive smoking cessation may also play a key role in preventing exacerbations and alleviating the morbidity associated with ACOS; however, future studies on the treatment of ACOS are needed,” they said.
The majority of subjects with ACOS-BDR met criteria for Global Initiative for Chronic Obstructive Lung Disease grade B, indicating a high degree of symptoms despite less severe airflow obstruction.
The funding source wasn’t reported. Dr. Cosentino had no conflicts. Other authors disclosed personal fees from Concert Pharmaceuticals, CSA Medical, CSL Behring, Gala Therapeutics, and Novartis.
FROM THE ANNALS OF THE AMERICAN THORACIC SOCIETY
Key clinical point:
Major finding: ACOS-BDR patients were less likely to be on a long-acting beta-agonist (6.8% versus 13.9%); a long-acting muscarinic antagonist (20% versus 60.8%); or a combination long-acting beta-agonist/inhaled corticosteroid (29.9% versus 55.6%).
Data source: 1,005 patients from the COPDGene study.
Disclosures: The funding source wasn’t reported. Authors disclosed personal fees from Concert Pharmaceuticals, CSA Medical, CSL Behring, Gala Therapeutics, and Novartis.
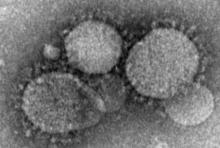
Health care workers at risk for mild MERS-CoV infections
Health care workers directly caring for patients with Middle East respiratory syndrome coronavirus (MERS-CoV) are more highly predisposed to contracting the virus, but in a milder form than that of their patients, thus making it difficult to diagnose and treat.
In a study published in Emerging Infectious Diseases, health care professionals (HCP) from the King Faisal Specialist Hospital and Research Centre in Riyadh, Saudi Arabia, were examined to determine their likelihood for getting MERS-CoV based on their proximity to patients who already had it.
“Healthcare settings are important amplifiers of transmission,” explained the investigators, led by Basem M. Alraddadi, MD. “Current MERS-CoV infection control recommendations are based on experience with other viruses rather than on a complete understanding of the epidemiology of MERS-CoV transmission.”
Dr. Alraddadi and his coinvestigators identified 363 HCP, all of whom would be placed into one of three cohorts based on the department in which they worked most extensively: the Medical Intensive Care Unit (MICU), the emergency department (ED), and the neurology unit. A total of 292 HCP were ultimately enrolled in the study: 131 in MICU, 127 in ED, and 34 in neurology. After 9 subjects were excluded because of unavailability of serum specimens, 128 MICU, 122 ED, and 33 neurology unit workers remained.
While none of the neurology unit workers contracted the virus, 15 MICU workers (11.7%) and 5 ED workers (4.1%) did, for a total of 20 out of the 250 subjects in those two cohorts (8%). Radiology technicians were the most susceptible, as 5 of 17 (29.4%) got the virus, followed by 13 of 138 nurses (9.4%), 1 of 31 respiratory therapists (3.2%), and 1 of 41 physicians (2.4%).
“HCP who reported always covering their nose and mouth with either a medical mask or N95 respirator had lower risk for infection than did HCP reporting not always or never doing so, [while] those who reported always using N95 respirators for direct patient contact were less likely to be seropositive, a trend that approached statistical significance (P = .07),” the authors noted.
The most frequent symptoms reported by those surveyed were muscle pain, fevers, headaches, dry cough, and shortness of breath. In the 20-case HCP sample, however, 12 subjects (60%) only had mild illness while 3 (15%) were asymptomatic, making it very hard to diagnose and treat their infection. Three subjects (15%) had severe illness, while another two (10%) had moderate illness, meaning they were admitted to hospital but did not require any mechanical ventilation.
“Our study did not identify strong associations with underlying chronic illnesses, most likely because the prevalence of such conditions was low ([less than] 10%) in this population, [but] HCPs with a history of smoking had a risk for infection almost 3 times that of nonsmokers,” the authors wrote (Emerg Infect Dis. 2016 Nov. doi: 10.3201/eid2211.160920).
The Ministry of Health of Saudi Arabia and the Centers for Disease Control and Prevention funded the study. Dr. Alraddadi and his coauthors did not report any disclosures.
Health care workers directly caring for patients with Middle East respiratory syndrome coronavirus (MERS-CoV) are more highly predisposed to contracting the virus, but in a milder form than that of their patients, thus making it difficult to diagnose and treat.
In a study published in Emerging Infectious Diseases, health care professionals (HCP) from the King Faisal Specialist Hospital and Research Centre in Riyadh, Saudi Arabia, were examined to determine their likelihood for getting MERS-CoV based on their proximity to patients who already had it.
“Healthcare settings are important amplifiers of transmission,” explained the investigators, led by Basem M. Alraddadi, MD. “Current MERS-CoV infection control recommendations are based on experience with other viruses rather than on a complete understanding of the epidemiology of MERS-CoV transmission.”
Dr. Alraddadi and his coinvestigators identified 363 HCP, all of whom would be placed into one of three cohorts based on the department in which they worked most extensively: the Medical Intensive Care Unit (MICU), the emergency department (ED), and the neurology unit. A total of 292 HCP were ultimately enrolled in the study: 131 in MICU, 127 in ED, and 34 in neurology. After 9 subjects were excluded because of unavailability of serum specimens, 128 MICU, 122 ED, and 33 neurology unit workers remained.
While none of the neurology unit workers contracted the virus, 15 MICU workers (11.7%) and 5 ED workers (4.1%) did, for a total of 20 out of the 250 subjects in those two cohorts (8%). Radiology technicians were the most susceptible, as 5 of 17 (29.4%) got the virus, followed by 13 of 138 nurses (9.4%), 1 of 31 respiratory therapists (3.2%), and 1 of 41 physicians (2.4%).
“HCP who reported always covering their nose and mouth with either a medical mask or N95 respirator had lower risk for infection than did HCP reporting not always or never doing so, [while] those who reported always using N95 respirators for direct patient contact were less likely to be seropositive, a trend that approached statistical significance (P = .07),” the authors noted.
The most frequent symptoms reported by those surveyed were muscle pain, fevers, headaches, dry cough, and shortness of breath. In the 20-case HCP sample, however, 12 subjects (60%) only had mild illness while 3 (15%) were asymptomatic, making it very hard to diagnose and treat their infection. Three subjects (15%) had severe illness, while another two (10%) had moderate illness, meaning they were admitted to hospital but did not require any mechanical ventilation.
“Our study did not identify strong associations with underlying chronic illnesses, most likely because the prevalence of such conditions was low ([less than] 10%) in this population, [but] HCPs with a history of smoking had a risk for infection almost 3 times that of nonsmokers,” the authors wrote (Emerg Infect Dis. 2016 Nov. doi: 10.3201/eid2211.160920).
The Ministry of Health of Saudi Arabia and the Centers for Disease Control and Prevention funded the study. Dr. Alraddadi and his coauthors did not report any disclosures.
Health care workers directly caring for patients with Middle East respiratory syndrome coronavirus (MERS-CoV) are more highly predisposed to contracting the virus, but in a milder form than that of their patients, thus making it difficult to diagnose and treat.
In a study published in Emerging Infectious Diseases, health care professionals (HCP) from the King Faisal Specialist Hospital and Research Centre in Riyadh, Saudi Arabia, were examined to determine their likelihood for getting MERS-CoV based on their proximity to patients who already had it.
“Healthcare settings are important amplifiers of transmission,” explained the investigators, led by Basem M. Alraddadi, MD. “Current MERS-CoV infection control recommendations are based on experience with other viruses rather than on a complete understanding of the epidemiology of MERS-CoV transmission.”
Dr. Alraddadi and his coinvestigators identified 363 HCP, all of whom would be placed into one of three cohorts based on the department in which they worked most extensively: the Medical Intensive Care Unit (MICU), the emergency department (ED), and the neurology unit. A total of 292 HCP were ultimately enrolled in the study: 131 in MICU, 127 in ED, and 34 in neurology. After 9 subjects were excluded because of unavailability of serum specimens, 128 MICU, 122 ED, and 33 neurology unit workers remained.
While none of the neurology unit workers contracted the virus, 15 MICU workers (11.7%) and 5 ED workers (4.1%) did, for a total of 20 out of the 250 subjects in those two cohorts (8%). Radiology technicians were the most susceptible, as 5 of 17 (29.4%) got the virus, followed by 13 of 138 nurses (9.4%), 1 of 31 respiratory therapists (3.2%), and 1 of 41 physicians (2.4%).
“HCP who reported always covering their nose and mouth with either a medical mask or N95 respirator had lower risk for infection than did HCP reporting not always or never doing so, [while] those who reported always using N95 respirators for direct patient contact were less likely to be seropositive, a trend that approached statistical significance (P = .07),” the authors noted.
The most frequent symptoms reported by those surveyed were muscle pain, fevers, headaches, dry cough, and shortness of breath. In the 20-case HCP sample, however, 12 subjects (60%) only had mild illness while 3 (15%) were asymptomatic, making it very hard to diagnose and treat their infection. Three subjects (15%) had severe illness, while another two (10%) had moderate illness, meaning they were admitted to hospital but did not require any mechanical ventilation.
“Our study did not identify strong associations with underlying chronic illnesses, most likely because the prevalence of such conditions was low ([less than] 10%) in this population, [but] HCPs with a history of smoking had a risk for infection almost 3 times that of nonsmokers,” the authors wrote (Emerg Infect Dis. 2016 Nov. doi: 10.3201/eid2211.160920).
The Ministry of Health of Saudi Arabia and the Centers for Disease Control and Prevention funded the study. Dr. Alraddadi and his coauthors did not report any disclosures.
Key clinical point:
Major finding: Among workers who actually treated MERS-CoV patients, 20 out of 250 (8%) contracted the virus, while none of the clerical staff or patient transporters did.
Data source: Retrospective, single-center study of 363 health care personnel during May-June 2014.
Disclosures: The Ministry of Health of Saudi Arabia and the Centers for Disease Control and Prevention funded the study. The authors reported no financial disclosures.
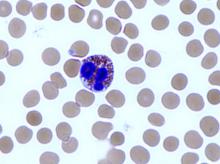
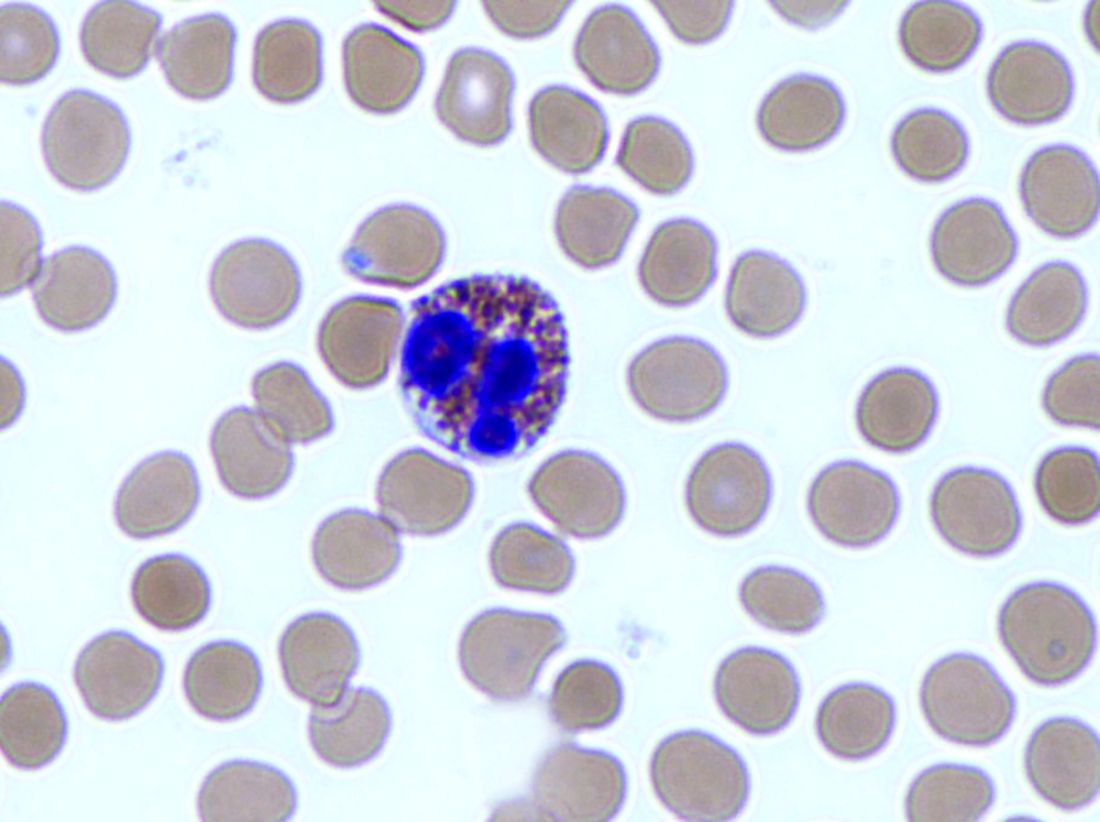
Reslizumab performance tied to eosinophil count
Reslizumab was most effective in patients with high baseline eosinophil counts, two randomized, placebo-controlled studies have determined. The companion studies were simultaneously published in the October issue of Chest.
The drug reslizumab, an anti–interleukin-5 monoclonal antibody, is made by Teva Branded Pharmaceutical Products R&D, who sponsored both studies.
The larger study, comprising 492 patients, found no significant benefit of reslizumab over placebo, Jonathan Corren, MD, and his colleagues wrote (Chest. 2016;150:799-810). But this study didn’t stratify patients by baseline eosinophil levels; a post-hoc subanalysis found a significant benefit in forced expiratory volume in 69 of the patients who had at least 400 eosinophils/microliter (mcL) when treatment began.
In these patients, the drug significantly improved not only lung function, but asthma symptoms and asthma-related quality of life scores.
“These efficacy findings are consistent with results from other reslizumab trials and combined with the favorable safety profile observed, support the use of reslizumab in patients with asthma and elevated blood eosinophils, uncontrolled by an inhaled corticosteroid-based regimen,” Dr. Bjermer and his coauthors wrote.
The unstratified trial was conducted at 66 sites in the U.S. All of the patients had poorly controlled asthma despite using at least a medium-dosed inhaled corticosteroid. They were randomized to infusions of reslizumab 3.0 mg/kg or placebo given once every 4 weeks for 16 weeks.*
The primary endpoint was the change in forced expiratory volume in one second (FEV1); secondary endpoints included quality of life scores; the need for rescue medication; forced vital capacity; and eosinophil count.
Patients in the placebo and reslizumab groups were an average age of 45.1 years and 44.9 years, respectively. The mean disease duration of patients in both groups was 26 years.
At week 16, the mean change in FEV1 from baseline was 255 ml in the active group and 187 ml in the placebo group – not a significant difference.
The team performed a post-hoc subgroup analysis that dichotomized the cohort based on baseline eosinophil levels. For the 343 with counts of less than 400 cells/mcL, there was no difference in FEV1 at 16 weeks, between the patients who received treatment and the patients who received a placebo. The FEV1s of these two groups were separated by just 33 mL.
The story was different for the 82 patients with at least 400 cells/mcL, with 69 of such patients receiving the drug and 13 of such patients receiving the placebo. At 16 weeks, the difference in FEV1 change was 270 mL, in favor of the active group. The strength of these findings may be weakened by the large difference in size between the treatment and placebo groups and the “near complete lack of response in the small number of placebo-treated patients.”
“Interpretation of the results in the [400 or more cells/mcL] subgroup is limited as the study was not designed or statistically powered to specifically test this group of patients,” the team wrote. Nevertheless, they concluded that reslizumab is a reasonable treatment option for this group. “These findings support an acceptable benefit-risk profile for reslizumab in asthma patients with a blood eosinophil threshold” of at least 400 cells/mcL.
The stratified study examined more endpoints: pre-bronchodilator spirometry (forced expiratory volume in one second FEV1, forced vital capacity, and forced expiratory flow), asthma symptoms, quality of life, rescue inhaler use, and blood eosinophil levels.
The 315 patients in this study all had a baseline eosinophil count of at least 400 cells/mcL. They were randomized to placebo or to 0.3 or 3.0 mg/kg reslizumab dose once every 4 weeks for 16 weeks. The mean ages for the patients taking the placebo, reslizumab 0.3 mg/kg, and reslizumab 3.0 mg/kg were 44.2, 44.5, and 43.0, respectively. The range of average disease durations for patients in the placebo group and two reslizumab groups was 20 to 20.7 years.
The final FEV1 was significantly improved over placebo in both active groups, although the change was much more pronounced in those taking 3.0 mg/kg, compared with those taking 0.3 mg/kg (160 mL and 115 mL, respectively, relative to placebo). Forced vital capacity also improved significantly in the 3.0 mg/kg dose group (130 mL relative to placebo).
Reslizumab was generally well tolerated in both studies. The most frequent adverse events in the stratified study were asthma worsening, headache, nasopharyngitis, upper respiratory infections, and sinusitis.
In the unstratified study, there were two anaphylactic reactions, but only one was related to the study drug. No deaths occurred in either treatment group of this study.
Both trials were sponsored by Teva. Dr. Bjermer has served on advisory boards or provided lectures for Aerocrine, Airsonett, ALK, Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, Genentech, GlaxoSmithKline, Meda, Mundipharma, Nigaard, Novartis, Regeneron, Sanofi-Aventis, Takeda, and Teva. Dr. Corren has been involved in speaker bureau activities for Genentech and Merck; he has served on advisory boards for Genentech, Merck, Novartis, and Vectura.
*CORRECTION 12/9/16: An earlier version of this article misstated the infusion frequency.
[email protected]
On Twitter @Alz_Gal
Persistent eosinophilic inflammation is present in about half of patients with severe asthma, and the studies by Corren and Bjermer represent important advances in learning how to target this inflammatory pathway, Richard Russell, MBBS, MRCP, and Christopher Brightling, PhD, FCCP, wrote in an accompanying editorial (Chest. 2016;150:766-8).
“The most advanced therapeutic target is IL-5, which is an attractive target because it is an obligate cytokine for eosinophil maturation and survival. Its inhibition is thus predicted to reduce bone marrow production of eosinophils and promote apoptosis,” wrote Dr. Russell, a clinical research fellow, and Dr. Brightling, a professor, both at the University of Leicester (England).
“These findings support the view that an elevated blood eosinophil count is associated with a good clinical response [to the antibody reslizumab] but [the studies] did not find a clear correlation between the intensity of the baseline eosinophil count and response,” the colleagues wrote. “Thus, the best cut-off for the blood eosinophil count to apply clinically remains uncertain.”
Clinicians and patients may find a different answer to this riddle than do payers.
“From a patient perspective there is an argument to select a low or no cut-off as there is some benefit even with low baseline eosinophil counts, whereas from a payer’s perspective the health economic benefit is better with a higher cut-off.”
As is often the case, more study will help clarify these new concerns.
“We are moving into a new era of Type-2 immunity-mediated therapies that will bring new opportunities for clinicians and our patients, but with this opportunity comes new challenges. Biomarkers will increase in importance to help drive precision medicine, but we need to understand how to use them, and, in particular, what cut-points to apply. For anti-IL-5 approaches, we probably need to look towards elevated blood eosinophil counts, as aiming for a high cut-off is most likely the best way we shall achieve success.”
Dr. Russell had no financial disclosures. Mr. Brightling reported financial relationships with several pharmaceutical companies, but not with Teva.
Persistent eosinophilic inflammation is present in about half of patients with severe asthma, and the studies by Corren and Bjermer represent important advances in learning how to target this inflammatory pathway, Richard Russell, MBBS, MRCP, and Christopher Brightling, PhD, FCCP, wrote in an accompanying editorial (Chest. 2016;150:766-8).
“The most advanced therapeutic target is IL-5, which is an attractive target because it is an obligate cytokine for eosinophil maturation and survival. Its inhibition is thus predicted to reduce bone marrow production of eosinophils and promote apoptosis,” wrote Dr. Russell, a clinical research fellow, and Dr. Brightling, a professor, both at the University of Leicester (England).
“These findings support the view that an elevated blood eosinophil count is associated with a good clinical response [to the antibody reslizumab] but [the studies] did not find a clear correlation between the intensity of the baseline eosinophil count and response,” the colleagues wrote. “Thus, the best cut-off for the blood eosinophil count to apply clinically remains uncertain.”
Clinicians and patients may find a different answer to this riddle than do payers.
“From a patient perspective there is an argument to select a low or no cut-off as there is some benefit even with low baseline eosinophil counts, whereas from a payer’s perspective the health economic benefit is better with a higher cut-off.”
As is often the case, more study will help clarify these new concerns.
“We are moving into a new era of Type-2 immunity-mediated therapies that will bring new opportunities for clinicians and our patients, but with this opportunity comes new challenges. Biomarkers will increase in importance to help drive precision medicine, but we need to understand how to use them, and, in particular, what cut-points to apply. For anti-IL-5 approaches, we probably need to look towards elevated blood eosinophil counts, as aiming for a high cut-off is most likely the best way we shall achieve success.”
Dr. Russell had no financial disclosures. Mr. Brightling reported financial relationships with several pharmaceutical companies, but not with Teva.
Persistent eosinophilic inflammation is present in about half of patients with severe asthma, and the studies by Corren and Bjermer represent important advances in learning how to target this inflammatory pathway, Richard Russell, MBBS, MRCP, and Christopher Brightling, PhD, FCCP, wrote in an accompanying editorial (Chest. 2016;150:766-8).
“The most advanced therapeutic target is IL-5, which is an attractive target because it is an obligate cytokine for eosinophil maturation and survival. Its inhibition is thus predicted to reduce bone marrow production of eosinophils and promote apoptosis,” wrote Dr. Russell, a clinical research fellow, and Dr. Brightling, a professor, both at the University of Leicester (England).
“These findings support the view that an elevated blood eosinophil count is associated with a good clinical response [to the antibody reslizumab] but [the studies] did not find a clear correlation between the intensity of the baseline eosinophil count and response,” the colleagues wrote. “Thus, the best cut-off for the blood eosinophil count to apply clinically remains uncertain.”
Clinicians and patients may find a different answer to this riddle than do payers.
“From a patient perspective there is an argument to select a low or no cut-off as there is some benefit even with low baseline eosinophil counts, whereas from a payer’s perspective the health economic benefit is better with a higher cut-off.”
As is often the case, more study will help clarify these new concerns.
“We are moving into a new era of Type-2 immunity-mediated therapies that will bring new opportunities for clinicians and our patients, but with this opportunity comes new challenges. Biomarkers will increase in importance to help drive precision medicine, but we need to understand how to use them, and, in particular, what cut-points to apply. For anti-IL-5 approaches, we probably need to look towards elevated blood eosinophil counts, as aiming for a high cut-off is most likely the best way we shall achieve success.”
Dr. Russell had no financial disclosures. Mr. Brightling reported financial relationships with several pharmaceutical companies, but not with Teva.
Reslizumab was most effective in patients with high baseline eosinophil counts, two randomized, placebo-controlled studies have determined. The companion studies were simultaneously published in the October issue of Chest.
The drug reslizumab, an anti–interleukin-5 monoclonal antibody, is made by Teva Branded Pharmaceutical Products R&D, who sponsored both studies.
The larger study, comprising 492 patients, found no significant benefit of reslizumab over placebo, Jonathan Corren, MD, and his colleagues wrote (Chest. 2016;150:799-810). But this study didn’t stratify patients by baseline eosinophil levels; a post-hoc subanalysis found a significant benefit in forced expiratory volume in 69 of the patients who had at least 400 eosinophils/microliter (mcL) when treatment began.
In these patients, the drug significantly improved not only lung function, but asthma symptoms and asthma-related quality of life scores.
“These efficacy findings are consistent with results from other reslizumab trials and combined with the favorable safety profile observed, support the use of reslizumab in patients with asthma and elevated blood eosinophils, uncontrolled by an inhaled corticosteroid-based regimen,” Dr. Bjermer and his coauthors wrote.
The unstratified trial was conducted at 66 sites in the U.S. All of the patients had poorly controlled asthma despite using at least a medium-dosed inhaled corticosteroid. They were randomized to infusions of reslizumab 3.0 mg/kg or placebo given once every 4 weeks for 16 weeks.*
The primary endpoint was the change in forced expiratory volume in one second (FEV1); secondary endpoints included quality of life scores; the need for rescue medication; forced vital capacity; and eosinophil count.
Patients in the placebo and reslizumab groups were an average age of 45.1 years and 44.9 years, respectively. The mean disease duration of patients in both groups was 26 years.
At week 16, the mean change in FEV1 from baseline was 255 ml in the active group and 187 ml in the placebo group – not a significant difference.
The team performed a post-hoc subgroup analysis that dichotomized the cohort based on baseline eosinophil levels. For the 343 with counts of less than 400 cells/mcL, there was no difference in FEV1 at 16 weeks, between the patients who received treatment and the patients who received a placebo. The FEV1s of these two groups were separated by just 33 mL.
The story was different for the 82 patients with at least 400 cells/mcL, with 69 of such patients receiving the drug and 13 of such patients receiving the placebo. At 16 weeks, the difference in FEV1 change was 270 mL, in favor of the active group. The strength of these findings may be weakened by the large difference in size between the treatment and placebo groups and the “near complete lack of response in the small number of placebo-treated patients.”
“Interpretation of the results in the [400 or more cells/mcL] subgroup is limited as the study was not designed or statistically powered to specifically test this group of patients,” the team wrote. Nevertheless, they concluded that reslizumab is a reasonable treatment option for this group. “These findings support an acceptable benefit-risk profile for reslizumab in asthma patients with a blood eosinophil threshold” of at least 400 cells/mcL.
The stratified study examined more endpoints: pre-bronchodilator spirometry (forced expiratory volume in one second FEV1, forced vital capacity, and forced expiratory flow), asthma symptoms, quality of life, rescue inhaler use, and blood eosinophil levels.
The 315 patients in this study all had a baseline eosinophil count of at least 400 cells/mcL. They were randomized to placebo or to 0.3 or 3.0 mg/kg reslizumab dose once every 4 weeks for 16 weeks. The mean ages for the patients taking the placebo, reslizumab 0.3 mg/kg, and reslizumab 3.0 mg/kg were 44.2, 44.5, and 43.0, respectively. The range of average disease durations for patients in the placebo group and two reslizumab groups was 20 to 20.7 years.
The final FEV1 was significantly improved over placebo in both active groups, although the change was much more pronounced in those taking 3.0 mg/kg, compared with those taking 0.3 mg/kg (160 mL and 115 mL, respectively, relative to placebo). Forced vital capacity also improved significantly in the 3.0 mg/kg dose group (130 mL relative to placebo).
Reslizumab was generally well tolerated in both studies. The most frequent adverse events in the stratified study were asthma worsening, headache, nasopharyngitis, upper respiratory infections, and sinusitis.
In the unstratified study, there were two anaphylactic reactions, but only one was related to the study drug. No deaths occurred in either treatment group of this study.
Both trials were sponsored by Teva. Dr. Bjermer has served on advisory boards or provided lectures for Aerocrine, Airsonett, ALK, Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, Genentech, GlaxoSmithKline, Meda, Mundipharma, Nigaard, Novartis, Regeneron, Sanofi-Aventis, Takeda, and Teva. Dr. Corren has been involved in speaker bureau activities for Genentech and Merck; he has served on advisory boards for Genentech, Merck, Novartis, and Vectura.
*CORRECTION 12/9/16: An earlier version of this article misstated the infusion frequency.
[email protected]
On Twitter @Alz_Gal
Reslizumab was most effective in patients with high baseline eosinophil counts, two randomized, placebo-controlled studies have determined. The companion studies were simultaneously published in the October issue of Chest.
The drug reslizumab, an anti–interleukin-5 monoclonal antibody, is made by Teva Branded Pharmaceutical Products R&D, who sponsored both studies.
The larger study, comprising 492 patients, found no significant benefit of reslizumab over placebo, Jonathan Corren, MD, and his colleagues wrote (Chest. 2016;150:799-810). But this study didn’t stratify patients by baseline eosinophil levels; a post-hoc subanalysis found a significant benefit in forced expiratory volume in 69 of the patients who had at least 400 eosinophils/microliter (mcL) when treatment began.
In these patients, the drug significantly improved not only lung function, but asthma symptoms and asthma-related quality of life scores.
“These efficacy findings are consistent with results from other reslizumab trials and combined with the favorable safety profile observed, support the use of reslizumab in patients with asthma and elevated blood eosinophils, uncontrolled by an inhaled corticosteroid-based regimen,” Dr. Bjermer and his coauthors wrote.
The unstratified trial was conducted at 66 sites in the U.S. All of the patients had poorly controlled asthma despite using at least a medium-dosed inhaled corticosteroid. They were randomized to infusions of reslizumab 3.0 mg/kg or placebo given once every 4 weeks for 16 weeks.*
The primary endpoint was the change in forced expiratory volume in one second (FEV1); secondary endpoints included quality of life scores; the need for rescue medication; forced vital capacity; and eosinophil count.
Patients in the placebo and reslizumab groups were an average age of 45.1 years and 44.9 years, respectively. The mean disease duration of patients in both groups was 26 years.
At week 16, the mean change in FEV1 from baseline was 255 ml in the active group and 187 ml in the placebo group – not a significant difference.
The team performed a post-hoc subgroup analysis that dichotomized the cohort based on baseline eosinophil levels. For the 343 with counts of less than 400 cells/mcL, there was no difference in FEV1 at 16 weeks, between the patients who received treatment and the patients who received a placebo. The FEV1s of these two groups were separated by just 33 mL.
The story was different for the 82 patients with at least 400 cells/mcL, with 69 of such patients receiving the drug and 13 of such patients receiving the placebo. At 16 weeks, the difference in FEV1 change was 270 mL, in favor of the active group. The strength of these findings may be weakened by the large difference in size between the treatment and placebo groups and the “near complete lack of response in the small number of placebo-treated patients.”
“Interpretation of the results in the [400 or more cells/mcL] subgroup is limited as the study was not designed or statistically powered to specifically test this group of patients,” the team wrote. Nevertheless, they concluded that reslizumab is a reasonable treatment option for this group. “These findings support an acceptable benefit-risk profile for reslizumab in asthma patients with a blood eosinophil threshold” of at least 400 cells/mcL.
The stratified study examined more endpoints: pre-bronchodilator spirometry (forced expiratory volume in one second FEV1, forced vital capacity, and forced expiratory flow), asthma symptoms, quality of life, rescue inhaler use, and blood eosinophil levels.
The 315 patients in this study all had a baseline eosinophil count of at least 400 cells/mcL. They were randomized to placebo or to 0.3 or 3.0 mg/kg reslizumab dose once every 4 weeks for 16 weeks. The mean ages for the patients taking the placebo, reslizumab 0.3 mg/kg, and reslizumab 3.0 mg/kg were 44.2, 44.5, and 43.0, respectively. The range of average disease durations for patients in the placebo group and two reslizumab groups was 20 to 20.7 years.
The final FEV1 was significantly improved over placebo in both active groups, although the change was much more pronounced in those taking 3.0 mg/kg, compared with those taking 0.3 mg/kg (160 mL and 115 mL, respectively, relative to placebo). Forced vital capacity also improved significantly in the 3.0 mg/kg dose group (130 mL relative to placebo).
Reslizumab was generally well tolerated in both studies. The most frequent adverse events in the stratified study were asthma worsening, headache, nasopharyngitis, upper respiratory infections, and sinusitis.
In the unstratified study, there were two anaphylactic reactions, but only one was related to the study drug. No deaths occurred in either treatment group of this study.
Both trials were sponsored by Teva. Dr. Bjermer has served on advisory boards or provided lectures for Aerocrine, Airsonett, ALK, Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, Genentech, GlaxoSmithKline, Meda, Mundipharma, Nigaard, Novartis, Regeneron, Sanofi-Aventis, Takeda, and Teva. Dr. Corren has been involved in speaker bureau activities for Genentech and Merck; he has served on advisory boards for Genentech, Merck, Novartis, and Vectura.
*CORRECTION 12/9/16: An earlier version of this article misstated the infusion frequency.
[email protected]
On Twitter @Alz_Gal
FROM CHEST
Key clinical point:
Major finding: Forced expiratory volume in 1 second (FEV1) improved by 160 mL with reslizumab 3.0 mg/kg relative to placebo.
Data source: The two randomized, placebo-controlled studies comprised about 800 patients.
Disclosures: Both trials were sponsored by Teva Branded Pharmaceutical Products R&D. Dr. Bjermer has served on an advisory board or provided lectures for Teva. Dr. Corren has served on advisory boards and has been involved in speaker bureau activities for various pharmaceutical companies.
Procalcitonin helps ID pneumonia patients needing intubation
Procalcitonin can help predict which patients with community-acquired pneumonia may require intubation for respiratory failure during a hospital admission.
Compared to those with undetectable levels, patients with a procalcitonin of 5 ng/mL were three times more likely to require invasive respiratory support, and those with a 10 ng/mL level were five times more likely, reported Wesley Self, MD, and his colleagues (Chest. 2016;150[4]:819-28. doi: 10.1016/j.chest.2016.04.010).
While predictive accuracy isn’t good enough to merit use of procalcitonin as a stand-alone test, adding it to existing clinical management tools “is likely to improve identification of patients needing intensive care,” wrote Dr. Self of Vanderbilt University, Nashville, and his colleagues. “An elevated procalcitonin level may help identify these patients without overt clinical signs of impending respiratory failure or shock but who would benefit from early [intensive care unit] admission.”
The team examined serum procalcitonin as a biomarker in a subgroup of patients included in the Etiology of Pneumonia in the Community (EPIC) study of adults hospitalized with community-acquire pneumonia. The primary outcome was the need for invasive respiratory and/or vasopressor support (IRVS) within 72 hours.
Secondarily, they looked at whether adding procalcitonin boosted the performance of accepted pneumonia risk scores, including the American Thoracic Society minor criteria (ATS).
The cohort comprised 1,770 patients with a median age of 57 years. Of these, 115 (6.5%) needed IRVS within 72 hours of admission. Almost 16% were admitted directly into an intensive care unit; almost 7% experienced a delayed transfer from a medical unit into an ICU. The in-hospital mortality was about 2%.
Most (1,642) had an ATS score of less than 3; among these, about 5% needed IRVS. The remainder had a score of 3 or higher; about 30% required IRVS. All had procalcitonin levels pulled at admission. The levels were significantly higher among patients who required IRVS than those who didn’t (1.43 ng/mL vs. 0.14 ng/mL).
A multivariate analysis found that procalcitonin was strongly associated with the risk of IRVS. In patients with undetectable levels, the risk was 4%. At 5-10 ng/mL, the overall risk of IRVS was about 14%. Every 1-ng/mL increase in this range boosted the risk of IRVS by 1%-2%.
Adding the measurement of procalcitonin to traditional pneumonia severity risk scores significantly improved the patients’ performance. When stratified by ATS minor criteria, the risk of IRVS was 4.7% among low-risk patients. That decreased to 2.4% with the addition of undetectable procalcitonin, and increased to 12% with the addition of a 10 ng/mL level.
Conversely, without considering procalcitonin, ATS high-risk patients had almost a 30% risk of IRVS. Among these high-risk patients, IRVS risk dropped to 13% with undetectable procalcitonin and increased to 36% with high procalcitonin.
Adding the biomarker level to the ATS system improved its ability to correctly classify patients, the team said. “Using at least 3 ATS minor criteria alone to indicate high risk, 77 (4.4%) of the 1,770 total patients were misclassified as low-risk and experienced IRVS. Including procalcitonin of at least 0.83 ng/ml in addition … as a high-risk indicator reduced the number of patients with IRVS misclassified as low risk to 44 (2.5%). Adding procalcitonin of at least 0.83 ng/mL as a high-risk indicator resulted in 370 additional patients being classified as high risk, with 33 correctly classified as having IRVS.”
Dr. Self reported financial relationships with multiple pharmaceutical companies.
[email protected]
On Twitter @Alz_Gal
While measuring procalcitonin adds valuable information to pneumonia risk stratification schemes, this process lacks the accuracy needed to enable the diagnosis of pneumonia as a stand-alone test, Daiana Stolz, MD, MPH, FCCP, wrote in an editorial.
“This study further supports the notion that procalcitonin has a limited prognostic accuracy as a stand-alone test. It also does not seem to outperform the risk estimation of a combination of clinical and laboratorial parameters. However, it also emphasizes its potential to capture nuances elusive to the clinical assessment, which do not seem to be consistently reflected even in elaborated severity scores recommended for clinical routine use,” she said (Chest. 2016;150[4]:769-71. doi: 10.1016/j.chest.2016.07.017).
[Procalcitonin] values vary according to the pneumonia severity and this association is stronger than the one between disease severity and other clinical and laboratory variables,” she said.
Risk scores like the ATS system can be weak, “in particular with regard to positive predictive values,” Dr. Stolz wrote. And this is an important issue. “It is clear that patients fulfilling major criteria (endotracheal intubation and mechanical ventilation; shock-requiring vasopressors) should be considered for ICU admission; however, there is still controversy about the value of the minor criteria. ICU care is costly and a limited resource worldwide.”
She called for “a randomized study evaluating the outcome and cost-effectiveness of a procalcitonin-refined clinical score in severe [community acquired pneumonia].”
Dr. Stolz is a pulmonologist at the University Hospital Basel, Switzerland. She reported financial relationships with several pharmaceutical companies.
While measuring procalcitonin adds valuable information to pneumonia risk stratification schemes, this process lacks the accuracy needed to enable the diagnosis of pneumonia as a stand-alone test, Daiana Stolz, MD, MPH, FCCP, wrote in an editorial.
“This study further supports the notion that procalcitonin has a limited prognostic accuracy as a stand-alone test. It also does not seem to outperform the risk estimation of a combination of clinical and laboratorial parameters. However, it also emphasizes its potential to capture nuances elusive to the clinical assessment, which do not seem to be consistently reflected even in elaborated severity scores recommended for clinical routine use,” she said (Chest. 2016;150[4]:769-71. doi: 10.1016/j.chest.2016.07.017).
[Procalcitonin] values vary according to the pneumonia severity and this association is stronger than the one between disease severity and other clinical and laboratory variables,” she said.
Risk scores like the ATS system can be weak, “in particular with regard to positive predictive values,” Dr. Stolz wrote. And this is an important issue. “It is clear that patients fulfilling major criteria (endotracheal intubation and mechanical ventilation; shock-requiring vasopressors) should be considered for ICU admission; however, there is still controversy about the value of the minor criteria. ICU care is costly and a limited resource worldwide.”
She called for “a randomized study evaluating the outcome and cost-effectiveness of a procalcitonin-refined clinical score in severe [community acquired pneumonia].”
Dr. Stolz is a pulmonologist at the University Hospital Basel, Switzerland. She reported financial relationships with several pharmaceutical companies.
While measuring procalcitonin adds valuable information to pneumonia risk stratification schemes, this process lacks the accuracy needed to enable the diagnosis of pneumonia as a stand-alone test, Daiana Stolz, MD, MPH, FCCP, wrote in an editorial.
“This study further supports the notion that procalcitonin has a limited prognostic accuracy as a stand-alone test. It also does not seem to outperform the risk estimation of a combination of clinical and laboratorial parameters. However, it also emphasizes its potential to capture nuances elusive to the clinical assessment, which do not seem to be consistently reflected even in elaborated severity scores recommended for clinical routine use,” she said (Chest. 2016;150[4]:769-71. doi: 10.1016/j.chest.2016.07.017).
[Procalcitonin] values vary according to the pneumonia severity and this association is stronger than the one between disease severity and other clinical and laboratory variables,” she said.
Risk scores like the ATS system can be weak, “in particular with regard to positive predictive values,” Dr. Stolz wrote. And this is an important issue. “It is clear that patients fulfilling major criteria (endotracheal intubation and mechanical ventilation; shock-requiring vasopressors) should be considered for ICU admission; however, there is still controversy about the value of the minor criteria. ICU care is costly and a limited resource worldwide.”
She called for “a randomized study evaluating the outcome and cost-effectiveness of a procalcitonin-refined clinical score in severe [community acquired pneumonia].”
Dr. Stolz is a pulmonologist at the University Hospital Basel, Switzerland. She reported financial relationships with several pharmaceutical companies.
Procalcitonin can help predict which patients with community-acquired pneumonia may require intubation for respiratory failure during a hospital admission.
Compared to those with undetectable levels, patients with a procalcitonin of 5 ng/mL were three times more likely to require invasive respiratory support, and those with a 10 ng/mL level were five times more likely, reported Wesley Self, MD, and his colleagues (Chest. 2016;150[4]:819-28. doi: 10.1016/j.chest.2016.04.010).
While predictive accuracy isn’t good enough to merit use of procalcitonin as a stand-alone test, adding it to existing clinical management tools “is likely to improve identification of patients needing intensive care,” wrote Dr. Self of Vanderbilt University, Nashville, and his colleagues. “An elevated procalcitonin level may help identify these patients without overt clinical signs of impending respiratory failure or shock but who would benefit from early [intensive care unit] admission.”
The team examined serum procalcitonin as a biomarker in a subgroup of patients included in the Etiology of Pneumonia in the Community (EPIC) study of adults hospitalized with community-acquire pneumonia. The primary outcome was the need for invasive respiratory and/or vasopressor support (IRVS) within 72 hours.
Secondarily, they looked at whether adding procalcitonin boosted the performance of accepted pneumonia risk scores, including the American Thoracic Society minor criteria (ATS).
The cohort comprised 1,770 patients with a median age of 57 years. Of these, 115 (6.5%) needed IRVS within 72 hours of admission. Almost 16% were admitted directly into an intensive care unit; almost 7% experienced a delayed transfer from a medical unit into an ICU. The in-hospital mortality was about 2%.
Most (1,642) had an ATS score of less than 3; among these, about 5% needed IRVS. The remainder had a score of 3 or higher; about 30% required IRVS. All had procalcitonin levels pulled at admission. The levels were significantly higher among patients who required IRVS than those who didn’t (1.43 ng/mL vs. 0.14 ng/mL).
A multivariate analysis found that procalcitonin was strongly associated with the risk of IRVS. In patients with undetectable levels, the risk was 4%. At 5-10 ng/mL, the overall risk of IRVS was about 14%. Every 1-ng/mL increase in this range boosted the risk of IRVS by 1%-2%.
Adding the measurement of procalcitonin to traditional pneumonia severity risk scores significantly improved the patients’ performance. When stratified by ATS minor criteria, the risk of IRVS was 4.7% among low-risk patients. That decreased to 2.4% with the addition of undetectable procalcitonin, and increased to 12% with the addition of a 10 ng/mL level.
Conversely, without considering procalcitonin, ATS high-risk patients had almost a 30% risk of IRVS. Among these high-risk patients, IRVS risk dropped to 13% with undetectable procalcitonin and increased to 36% with high procalcitonin.
Adding the biomarker level to the ATS system improved its ability to correctly classify patients, the team said. “Using at least 3 ATS minor criteria alone to indicate high risk, 77 (4.4%) of the 1,770 total patients were misclassified as low-risk and experienced IRVS. Including procalcitonin of at least 0.83 ng/ml in addition … as a high-risk indicator reduced the number of patients with IRVS misclassified as low risk to 44 (2.5%). Adding procalcitonin of at least 0.83 ng/mL as a high-risk indicator resulted in 370 additional patients being classified as high risk, with 33 correctly classified as having IRVS.”
Dr. Self reported financial relationships with multiple pharmaceutical companies.
[email protected]
On Twitter @Alz_Gal
Procalcitonin can help predict which patients with community-acquired pneumonia may require intubation for respiratory failure during a hospital admission.
Compared to those with undetectable levels, patients with a procalcitonin of 5 ng/mL were three times more likely to require invasive respiratory support, and those with a 10 ng/mL level were five times more likely, reported Wesley Self, MD, and his colleagues (Chest. 2016;150[4]:819-28. doi: 10.1016/j.chest.2016.04.010).
While predictive accuracy isn’t good enough to merit use of procalcitonin as a stand-alone test, adding it to existing clinical management tools “is likely to improve identification of patients needing intensive care,” wrote Dr. Self of Vanderbilt University, Nashville, and his colleagues. “An elevated procalcitonin level may help identify these patients without overt clinical signs of impending respiratory failure or shock but who would benefit from early [intensive care unit] admission.”
The team examined serum procalcitonin as a biomarker in a subgroup of patients included in the Etiology of Pneumonia in the Community (EPIC) study of adults hospitalized with community-acquire pneumonia. The primary outcome was the need for invasive respiratory and/or vasopressor support (IRVS) within 72 hours.
Secondarily, they looked at whether adding procalcitonin boosted the performance of accepted pneumonia risk scores, including the American Thoracic Society minor criteria (ATS).
The cohort comprised 1,770 patients with a median age of 57 years. Of these, 115 (6.5%) needed IRVS within 72 hours of admission. Almost 16% were admitted directly into an intensive care unit; almost 7% experienced a delayed transfer from a medical unit into an ICU. The in-hospital mortality was about 2%.
Most (1,642) had an ATS score of less than 3; among these, about 5% needed IRVS. The remainder had a score of 3 or higher; about 30% required IRVS. All had procalcitonin levels pulled at admission. The levels were significantly higher among patients who required IRVS than those who didn’t (1.43 ng/mL vs. 0.14 ng/mL).
A multivariate analysis found that procalcitonin was strongly associated with the risk of IRVS. In patients with undetectable levels, the risk was 4%. At 5-10 ng/mL, the overall risk of IRVS was about 14%. Every 1-ng/mL increase in this range boosted the risk of IRVS by 1%-2%.
Adding the measurement of procalcitonin to traditional pneumonia severity risk scores significantly improved the patients’ performance. When stratified by ATS minor criteria, the risk of IRVS was 4.7% among low-risk patients. That decreased to 2.4% with the addition of undetectable procalcitonin, and increased to 12% with the addition of a 10 ng/mL level.
Conversely, without considering procalcitonin, ATS high-risk patients had almost a 30% risk of IRVS. Among these high-risk patients, IRVS risk dropped to 13% with undetectable procalcitonin and increased to 36% with high procalcitonin.
Adding the biomarker level to the ATS system improved its ability to correctly classify patients, the team said. “Using at least 3 ATS minor criteria alone to indicate high risk, 77 (4.4%) of the 1,770 total patients were misclassified as low-risk and experienced IRVS. Including procalcitonin of at least 0.83 ng/ml in addition … as a high-risk indicator reduced the number of patients with IRVS misclassified as low risk to 44 (2.5%). Adding procalcitonin of at least 0.83 ng/mL as a high-risk indicator resulted in 370 additional patients being classified as high risk, with 33 correctly classified as having IRVS.”
Dr. Self reported financial relationships with multiple pharmaceutical companies.
[email protected]
On Twitter @Alz_Gal
FROM CHEST
Key clinical point:
Major finding: At a procalcitonin level of 5-10 ng/mL, the overall risk of invasive respiratory and/or vasopressor support was about 14%.
Data source: The analysis comprised 1,770 patients.
Disclosures: Dr. Self reported financial relationships with several pharmaceutical companies.
Depression drops COPD medication adherence
Chronic obstructive pulmonary disease (COPD) patients with depression are less likely to take their maintenance medications, according to a review of Medicare claims by the University of Maryland, Baltimore.
“Clinicians who treat older adults newly diagnosed with COPD should be aware of the development of depression, especially during the first 6 months. As such, clinicians should consider the need to monitor their patients with COPD for … depression [treatment], as well as use of and adherence to prescribed COPD medications. Close management of these and other aspects of newly diagnosed older adults with COPD will help to ensure optimal clinical outcomes,” said the investigators, led by Jennifer Albrecht, PhD, of the department of epidemiology and public health at the University of Maryland.
The researchers ran a random sampling of Medicare data and identified 31,033 beneficiaries diagnosed with COPD between 2006 and 2010; 6,227 patients (20% of the study sample) were diagnosed with depression within 2 years of being diagnosed with COPD.
The investigators found that depression reduced the likelihood of chronic obstructive pulmonary disease patients filling their prescriptions. Maintenance medication adherence was low overall, peaking at 57% in the month after the first fill and decreasing every month for the next 9 months for both the patients with depression and those patients who had not been diagnosed with the condition. Depression made things worse; 20% of depressed patients filled 80% or more of their medications at the pharmacy, vs. 22% of nondepressed patients. Patients with newly diagnosed depression were about 7% less likely to have good adherence (odds ratio, 0.93; 95% confidence interval, 0.89-0.98). Women – 65% of the study sample and 75% of those with depression – were less likely than men to fill their scripts.
Meanwhile, adherence to COPD maintenance medication was more likely among patients on short-term inhalers and supplemental oxygen, as well as among nursing home patients and those with low-income subsidies.
Patients were 83% white. Those diagnosed with depression were slightly younger on average than those who were not (67 vs. 69 years old) and were more likely to have more than three comorbid conditions (33% vs. 23%). With the exception of asthma, comorbid conditions made adherence worse. Depressed patients also had more severe COPD symptoms, based on their higher rates of oxygen use (10% vs. 8%).
Dr. Albrecht reported receiving grants from the National Institutes of Health during the conduct of the study.
Chronic obstructive pulmonary disease (COPD) patients with depression are less likely to take their maintenance medications, according to a review of Medicare claims by the University of Maryland, Baltimore.
“Clinicians who treat older adults newly diagnosed with COPD should be aware of the development of depression, especially during the first 6 months. As such, clinicians should consider the need to monitor their patients with COPD for … depression [treatment], as well as use of and adherence to prescribed COPD medications. Close management of these and other aspects of newly diagnosed older adults with COPD will help to ensure optimal clinical outcomes,” said the investigators, led by Jennifer Albrecht, PhD, of the department of epidemiology and public health at the University of Maryland.
The researchers ran a random sampling of Medicare data and identified 31,033 beneficiaries diagnosed with COPD between 2006 and 2010; 6,227 patients (20% of the study sample) were diagnosed with depression within 2 years of being diagnosed with COPD.
The investigators found that depression reduced the likelihood of chronic obstructive pulmonary disease patients filling their prescriptions. Maintenance medication adherence was low overall, peaking at 57% in the month after the first fill and decreasing every month for the next 9 months for both the patients with depression and those patients who had not been diagnosed with the condition. Depression made things worse; 20% of depressed patients filled 80% or more of their medications at the pharmacy, vs. 22% of nondepressed patients. Patients with newly diagnosed depression were about 7% less likely to have good adherence (odds ratio, 0.93; 95% confidence interval, 0.89-0.98). Women – 65% of the study sample and 75% of those with depression – were less likely than men to fill their scripts.
Meanwhile, adherence to COPD maintenance medication was more likely among patients on short-term inhalers and supplemental oxygen, as well as among nursing home patients and those with low-income subsidies.
Patients were 83% white. Those diagnosed with depression were slightly younger on average than those who were not (67 vs. 69 years old) and were more likely to have more than three comorbid conditions (33% vs. 23%). With the exception of asthma, comorbid conditions made adherence worse. Depressed patients also had more severe COPD symptoms, based on their higher rates of oxygen use (10% vs. 8%).
Dr. Albrecht reported receiving grants from the National Institutes of Health during the conduct of the study.
Chronic obstructive pulmonary disease (COPD) patients with depression are less likely to take their maintenance medications, according to a review of Medicare claims by the University of Maryland, Baltimore.
“Clinicians who treat older adults newly diagnosed with COPD should be aware of the development of depression, especially during the first 6 months. As such, clinicians should consider the need to monitor their patients with COPD for … depression [treatment], as well as use of and adherence to prescribed COPD medications. Close management of these and other aspects of newly diagnosed older adults with COPD will help to ensure optimal clinical outcomes,” said the investigators, led by Jennifer Albrecht, PhD, of the department of epidemiology and public health at the University of Maryland.
The researchers ran a random sampling of Medicare data and identified 31,033 beneficiaries diagnosed with COPD between 2006 and 2010; 6,227 patients (20% of the study sample) were diagnosed with depression within 2 years of being diagnosed with COPD.
The investigators found that depression reduced the likelihood of chronic obstructive pulmonary disease patients filling their prescriptions. Maintenance medication adherence was low overall, peaking at 57% in the month after the first fill and decreasing every month for the next 9 months for both the patients with depression and those patients who had not been diagnosed with the condition. Depression made things worse; 20% of depressed patients filled 80% or more of their medications at the pharmacy, vs. 22% of nondepressed patients. Patients with newly diagnosed depression were about 7% less likely to have good adherence (odds ratio, 0.93; 95% confidence interval, 0.89-0.98). Women – 65% of the study sample and 75% of those with depression – were less likely than men to fill their scripts.
Meanwhile, adherence to COPD maintenance medication was more likely among patients on short-term inhalers and supplemental oxygen, as well as among nursing home patients and those with low-income subsidies.
Patients were 83% white. Those diagnosed with depression were slightly younger on average than those who were not (67 vs. 69 years old) and were more likely to have more than three comorbid conditions (33% vs. 23%). With the exception of asthma, comorbid conditions made adherence worse. Depressed patients also had more severe COPD symptoms, based on their higher rates of oxygen use (10% vs. 8%).
Dr. Albrecht reported receiving grants from the National Institutes of Health during the conduct of the study.
FROM THE ANNALS OF THE AMERICAN THORACIC SOCIETY
Key clinical point:
Major finding: Patients with newly diagnosed depression were about 7% less likely to have good adherence to their medications (OR 0.93; 95% CI, 0.89–0.98).
Data source: A review of 31,033 Medicare COPD patients, who had filled their COPD maintenance medication at least twice.
Disclosures: Dr. Albrecht reported receiving grants from the National Institutes of Health during the conduct of the study.
Conservative oxygen therapy in the ICU reduces mortality
A strategy of conservatively controlling oxygen delivery to patients in the intensive care unit results in lower mortality than the conventional, more liberal approach whereby patients are often kept in a hyperoxemic state, finds a randomized controlled trial.
The trial, known as Oxygen-ICU, enrolled more than 400 adult ICU patients from an Italian center. Initially planned to last 2 years, it was terminated early because of slow enrollment after an earthquake reduced ICU capacity, with the decision supported by positive results of an interim analysis.
Patients had an absolute nearly 9% lower risk of dying in the ICU with use of the conservative oxygen strategy as compared with the conventional one, according to data reported at the annual congress of the European Society of Intensive Care Medicine and simultaneously published (JAMA. 2016 Oct 5. doi: 10.1001/jama.2016.11993).
“To our knowledge, this is the first randomized clinical trial to evaluate the effect of a conservative oxygen therapy on mortality compared with a standard, more liberal approach in a medical-surgical population of adult critically ill patients,” write the investigators, who were led by Massimo Girardis, MD, of the Intensive Care Unit, Department of Anesthesiology and Intensive Care, University Hospital of Modena (Italy).
Among critically ill patients with an ICU length of stay of 72 hours or longer, a conservative protocol for oxygen therapy compared with conventional therapy resulted in a lower ICU mortality,” they conclude. “However, these preliminary findings were based on unplanned early termination of the trial, and a larger multicenter trial is needed to evaluate the potential benefit of such conservative oxygen therapy in critically ill patients.”
In the trial, consecutive patients were randomized evenly to receive conservative oxygen therapy (maintenance of PaO2 between 70 and 100 mm Hg or arterial oxyhemoglobin saturation [SpO2] between 94% and 98%) or conventional oxygen therapy (allowance of PaO2 values up to 150 mm Hg or SpO2 values between 97% and 100%) on an open-label basis.
The originally targeted enrollment was 660 patients, but the study was stopped early after only 480 patients had been enrolled.
Results of modified intent-to-treat analyses showed that daily time-weighted PaO2 averages during patients’ ICU stays were higher in the conventional group than in the conservative group (median PaO2, 102 vs. 87 mm Hg; P less than .001).
The rate of ICU mortality, the trial’s primary endpoint, was 11.6% with conservative therapy, about half of the 20.2% seen with conventional therapy (absolute mean difference, 0.086; P = .01).
The conservative group also had lower rates of shock (3.7% vs. 10.6%, P = .006), liver failure (1.9% vs. 6.4%, P = .02), and bacteremia (5.1% vs. 10.1%, P = .049). And they spent a day less on the ventilator (median mechanical ventilation–free hours, 72 vs. 48; P = .02).
Lengths of ICU stay and hospital stay did not differ between the two groups.
One of the study authors reports serving as the data monitoring chair for a phase II study sponsored by InflaRx, on the antibiotic advisory board for Bayer, and on sepsis advisory boards for Biotest and Merck. The study was supported by the National Fund for Scientific Research of the University of Modena and Reggio Emilia.
The reduction in mortality seen with conservative oxygen therapy in the Oxygen-ICU trial was “striking,” according to editorialist Dr. Niall D. Ferguson. However, “it is likely that to some extent, this trial has overestimated the true treatment effect of conservative oxygen therapy,” he cautions, given baseline imbalances between groups, early stopping based in part on an unplanned interim analysis, and the small number of deaths. The editorialist noted that the study was underpowered and criticized its use of a modified intent-to-treat analysis.
The trial’s findings contrast with those of a pilot study conducted by the ANZICS clinical trials group that did not find better outcomes with use of lower oxygen targets, according to Dr. Ferguson. However, in that trial, both arms had lower target and actual PaO2 levels. Thus, the optimal clinical approach remains uncertain.
“Until the results of further trials addressing this issue are available, there appears to be little downside in the careful titration and monitoring of supplemental oxygen in the ICU to achieve physiologically normal levels of PaO2 while avoiding potentially dangerous hyperoxia,” he concludes.
Dr. Ferguson disclosed that he has no relevant conflicts of interest.
Niall D. Ferguson, MD, MSc, is with the Interdepartmental Division of Critical Care Medicine and Departments of Medicine and Physiology, University of Toronto; the Institute of Health Policy, Management, & Evaluation, University of Toronto; the Division of Respirology, Department of Medicine, University Health Network and Mount Sinai Hospital; and the Toronto General Research Institute.
The reduction in mortality seen with conservative oxygen therapy in the Oxygen-ICU trial was “striking,” according to editorialist Dr. Niall D. Ferguson. However, “it is likely that to some extent, this trial has overestimated the true treatment effect of conservative oxygen therapy,” he cautions, given baseline imbalances between groups, early stopping based in part on an unplanned interim analysis, and the small number of deaths. The editorialist noted that the study was underpowered and criticized its use of a modified intent-to-treat analysis.
The trial’s findings contrast with those of a pilot study conducted by the ANZICS clinical trials group that did not find better outcomes with use of lower oxygen targets, according to Dr. Ferguson. However, in that trial, both arms had lower target and actual PaO2 levels. Thus, the optimal clinical approach remains uncertain.
“Until the results of further trials addressing this issue are available, there appears to be little downside in the careful titration and monitoring of supplemental oxygen in the ICU to achieve physiologically normal levels of PaO2 while avoiding potentially dangerous hyperoxia,” he concludes.
Dr. Ferguson disclosed that he has no relevant conflicts of interest.
Niall D. Ferguson, MD, MSc, is with the Interdepartmental Division of Critical Care Medicine and Departments of Medicine and Physiology, University of Toronto; the Institute of Health Policy, Management, & Evaluation, University of Toronto; the Division of Respirology, Department of Medicine, University Health Network and Mount Sinai Hospital; and the Toronto General Research Institute.
The reduction in mortality seen with conservative oxygen therapy in the Oxygen-ICU trial was “striking,” according to editorialist Dr. Niall D. Ferguson. However, “it is likely that to some extent, this trial has overestimated the true treatment effect of conservative oxygen therapy,” he cautions, given baseline imbalances between groups, early stopping based in part on an unplanned interim analysis, and the small number of deaths. The editorialist noted that the study was underpowered and criticized its use of a modified intent-to-treat analysis.
The trial’s findings contrast with those of a pilot study conducted by the ANZICS clinical trials group that did not find better outcomes with use of lower oxygen targets, according to Dr. Ferguson. However, in that trial, both arms had lower target and actual PaO2 levels. Thus, the optimal clinical approach remains uncertain.
“Until the results of further trials addressing this issue are available, there appears to be little downside in the careful titration and monitoring of supplemental oxygen in the ICU to achieve physiologically normal levels of PaO2 while avoiding potentially dangerous hyperoxia,” he concludes.
Dr. Ferguson disclosed that he has no relevant conflicts of interest.
Niall D. Ferguson, MD, MSc, is with the Interdepartmental Division of Critical Care Medicine and Departments of Medicine and Physiology, University of Toronto; the Institute of Health Policy, Management, & Evaluation, University of Toronto; the Division of Respirology, Department of Medicine, University Health Network and Mount Sinai Hospital; and the Toronto General Research Institute.
A strategy of conservatively controlling oxygen delivery to patients in the intensive care unit results in lower mortality than the conventional, more liberal approach whereby patients are often kept in a hyperoxemic state, finds a randomized controlled trial.
The trial, known as Oxygen-ICU, enrolled more than 400 adult ICU patients from an Italian center. Initially planned to last 2 years, it was terminated early because of slow enrollment after an earthquake reduced ICU capacity, with the decision supported by positive results of an interim analysis.
Patients had an absolute nearly 9% lower risk of dying in the ICU with use of the conservative oxygen strategy as compared with the conventional one, according to data reported at the annual congress of the European Society of Intensive Care Medicine and simultaneously published (JAMA. 2016 Oct 5. doi: 10.1001/jama.2016.11993).
“To our knowledge, this is the first randomized clinical trial to evaluate the effect of a conservative oxygen therapy on mortality compared with a standard, more liberal approach in a medical-surgical population of adult critically ill patients,” write the investigators, who were led by Massimo Girardis, MD, of the Intensive Care Unit, Department of Anesthesiology and Intensive Care, University Hospital of Modena (Italy).
Among critically ill patients with an ICU length of stay of 72 hours or longer, a conservative protocol for oxygen therapy compared with conventional therapy resulted in a lower ICU mortality,” they conclude. “However, these preliminary findings were based on unplanned early termination of the trial, and a larger multicenter trial is needed to evaluate the potential benefit of such conservative oxygen therapy in critically ill patients.”
In the trial, consecutive patients were randomized evenly to receive conservative oxygen therapy (maintenance of PaO2 between 70 and 100 mm Hg or arterial oxyhemoglobin saturation [SpO2] between 94% and 98%) or conventional oxygen therapy (allowance of PaO2 values up to 150 mm Hg or SpO2 values between 97% and 100%) on an open-label basis.
The originally targeted enrollment was 660 patients, but the study was stopped early after only 480 patients had been enrolled.
Results of modified intent-to-treat analyses showed that daily time-weighted PaO2 averages during patients’ ICU stays were higher in the conventional group than in the conservative group (median PaO2, 102 vs. 87 mm Hg; P less than .001).
The rate of ICU mortality, the trial’s primary endpoint, was 11.6% with conservative therapy, about half of the 20.2% seen with conventional therapy (absolute mean difference, 0.086; P = .01).
The conservative group also had lower rates of shock (3.7% vs. 10.6%, P = .006), liver failure (1.9% vs. 6.4%, P = .02), and bacteremia (5.1% vs. 10.1%, P = .049). And they spent a day less on the ventilator (median mechanical ventilation–free hours, 72 vs. 48; P = .02).
Lengths of ICU stay and hospital stay did not differ between the two groups.
One of the study authors reports serving as the data monitoring chair for a phase II study sponsored by InflaRx, on the antibiotic advisory board for Bayer, and on sepsis advisory boards for Biotest and Merck. The study was supported by the National Fund for Scientific Research of the University of Modena and Reggio Emilia.
A strategy of conservatively controlling oxygen delivery to patients in the intensive care unit results in lower mortality than the conventional, more liberal approach whereby patients are often kept in a hyperoxemic state, finds a randomized controlled trial.
The trial, known as Oxygen-ICU, enrolled more than 400 adult ICU patients from an Italian center. Initially planned to last 2 years, it was terminated early because of slow enrollment after an earthquake reduced ICU capacity, with the decision supported by positive results of an interim analysis.
Patients had an absolute nearly 9% lower risk of dying in the ICU with use of the conservative oxygen strategy as compared with the conventional one, according to data reported at the annual congress of the European Society of Intensive Care Medicine and simultaneously published (JAMA. 2016 Oct 5. doi: 10.1001/jama.2016.11993).
“To our knowledge, this is the first randomized clinical trial to evaluate the effect of a conservative oxygen therapy on mortality compared with a standard, more liberal approach in a medical-surgical population of adult critically ill patients,” write the investigators, who were led by Massimo Girardis, MD, of the Intensive Care Unit, Department of Anesthesiology and Intensive Care, University Hospital of Modena (Italy).
Among critically ill patients with an ICU length of stay of 72 hours or longer, a conservative protocol for oxygen therapy compared with conventional therapy resulted in a lower ICU mortality,” they conclude. “However, these preliminary findings were based on unplanned early termination of the trial, and a larger multicenter trial is needed to evaluate the potential benefit of such conservative oxygen therapy in critically ill patients.”
In the trial, consecutive patients were randomized evenly to receive conservative oxygen therapy (maintenance of PaO2 between 70 and 100 mm Hg or arterial oxyhemoglobin saturation [SpO2] between 94% and 98%) or conventional oxygen therapy (allowance of PaO2 values up to 150 mm Hg or SpO2 values between 97% and 100%) on an open-label basis.
The originally targeted enrollment was 660 patients, but the study was stopped early after only 480 patients had been enrolled.
Results of modified intent-to-treat analyses showed that daily time-weighted PaO2 averages during patients’ ICU stays were higher in the conventional group than in the conservative group (median PaO2, 102 vs. 87 mm Hg; P less than .001).
The rate of ICU mortality, the trial’s primary endpoint, was 11.6% with conservative therapy, about half of the 20.2% seen with conventional therapy (absolute mean difference, 0.086; P = .01).
The conservative group also had lower rates of shock (3.7% vs. 10.6%, P = .006), liver failure (1.9% vs. 6.4%, P = .02), and bacteremia (5.1% vs. 10.1%, P = .049). And they spent a day less on the ventilator (median mechanical ventilation–free hours, 72 vs. 48; P = .02).
Lengths of ICU stay and hospital stay did not differ between the two groups.
One of the study authors reports serving as the data monitoring chair for a phase II study sponsored by InflaRx, on the antibiotic advisory board for Bayer, and on sepsis advisory boards for Biotest and Merck. The study was supported by the National Fund for Scientific Research of the University of Modena and Reggio Emilia.
FROM ESICM CONGRESS 2016
Key clinical point:
Major finding: Relative to conventional therapy, conservative therapy was associated with a lower ICU mortality (absolute risk reduction, 0.086; P = .01).
Data source: A randomized controlled trial among 434 patients admitted to a medical-surgical ICU and expected to stay at least 72 hours (Oxygen-ICU trial).
Disclosures: One of the study authors reports serving as the data monitoring chair for a phase II study sponsored by InflaRx, on the antibiotic advisory board for Bayer, and on sepsis advisory boards for Biotest and Merck. The study was supported by the National Fund for Scientific Research of the University of Modena and Reggio Emilia. Dr. Ferguson disclosed that he has no relevant conflicts of interest.
Benefits of lebrikizumab in asthma inconsistent
LONDON – Two large phase III trials with lebrikizumab, a monoclonal antibody that blocks the activity of interleukin-13 (IL-13), produced inconsistent evidence of benefit in patients with uncontrolled asthma, according to a presentation of both sets of data at the annual congress of the European Respiratory Society.
The two phase III studies compared lebrikizumab in doses of 37.5 mg and 125 mg to placebo, each administered subcutaneously every 4 weeks. The results were mixed not only for the primary endpoint, which was a reduction in the rate of exacerbations, but also for several secondary outcomes.
Evenly randomized into three treatment arms, 1,081 patients were enrolled in LAVOLTA I and 1,081 in LAVOLTA II. For entry, patients were required to have a forced expiratory volume in 1 second (FEV1) between 40% and 80% of predicted. Lebrikizumab was added on top of stable background therapy. For the efficacy analyses, patients were divided into those who were biomarker high, defined as having levels of periostin greater than 50 ng/mL or blood eosinophils greater than 300 mcg/L, or biomarker low, defined as having lower levels of periostin and blood eosinophils.
Over the 52-week study period in the biomarker high patients enrolled in LAVOLTA I, the rate of exacerbations was 51% lower among those randomized to the 37.5 mg dose (P less than .001) and 30% lower (P = .0232) among those randomized to the 125-mg dose relative to placebo. In the biomarker low group, a statistically significant 45% reduction in exacerbations was achieved with the 37.5 mg dose relative to placebo (P = .0318), but a 28% reduction in exacerbations, which was achieved in patients taking the 125-mg dose, was not statistically significant.
In the biomarker high patients enrolled in LAVOLTA II, both the 37.5-mg and the 125-mg doses reduced the rate of exacerbations by 26% relative to placebo, but neither reduction reached statistical significance. In the biomarker low patients, the 37.5-mg dose was associated with a 46% increase in exacerbations and the 125-mg dose was associated with a 6% increase in exacerbations relative to placebo.
In LAVOLTA I, lung function (as measured by FEV1) improved in biomarker high patients in both active treatment arms relative to placebo. The relative advantage of taking lebrikizumab was seen only in the biomarker low patients who took the 125-mg dose.
In LAVOLTA II, a similar advantage was observed in biomarker high patients who took both doses of lebrikizumab over biomarker high patients who took the placebo. There were no significant differences in outcomes observed between any treatment arms in the biomarker low group of LAVOLTA II.
Changes in other secondary endpoints were also inconsistent between the two studies. For example, the time to first exacerbation was significantly increased by lebrikizumab in LAVOLTA I but not in LAVOLTA II. Although use of rescue medications was significantly lower in patients receiving lebrikizumab in both studies, the rate of urgent health care utilization, such as emergency department visits, was lower in patients who took lebrikizumab in LAVOLTA 1, but not in those patients who too the drug in LAVOLTA II.
One consistency between the two studies’ outcomes was a lack of “meaningful improvements” having occurred in patients’ quality of life, as measured by the Asthma Quality of Life Questionnaire and the 5-item Asthma Control Questionnaire, according to Dr. Hanania.
The only difference in the occurrences of events associated with impaired immune function observed between any of the groups was a slight increase in the rate of herpes zoster among those treated with lebrikizumab relative to placebo (1.1% vs. 0.3%), Dr. Hanania reported. The only death that occurred in either study involved a patient in a placebo group. The rates of other side effects were comparable among patients in the active treatment and placebo groups.
An improvement in exacerbations would be consistent with the purported mechanism of lebrikizumab, because IL-13 is believed to induce expression of periostin, which, in turn, is thought to mediate bronchial hyper-responsiveness. In previously completed phase II trials, lebrikizumab was associated with a significant reduction in the rate of exacerbations over 24 weeks among patients with moderate to severe asthma (Thorax. 2015;80:748-56).
Asked in the discussion period whether the results of LAVOLTA I and II signaled the end of lebrikizumab studies in asthma control, Dr. Hanania deferred the question to Roche, which is developing this agent.
He noted that additional studies in a more select group of patients may be warranted and that lebrikizumab is still being evaluated for use in other lung diseases, such as idiopathic pulmonary fibrosis.
Dr. Hanania reports financial relationships with Forest, GlaxoSmithKline, Novartis, Pfizer, and Roche.
LONDON – Two large phase III trials with lebrikizumab, a monoclonal antibody that blocks the activity of interleukin-13 (IL-13), produced inconsistent evidence of benefit in patients with uncontrolled asthma, according to a presentation of both sets of data at the annual congress of the European Respiratory Society.
The two phase III studies compared lebrikizumab in doses of 37.5 mg and 125 mg to placebo, each administered subcutaneously every 4 weeks. The results were mixed not only for the primary endpoint, which was a reduction in the rate of exacerbations, but also for several secondary outcomes.
Evenly randomized into three treatment arms, 1,081 patients were enrolled in LAVOLTA I and 1,081 in LAVOLTA II. For entry, patients were required to have a forced expiratory volume in 1 second (FEV1) between 40% and 80% of predicted. Lebrikizumab was added on top of stable background therapy. For the efficacy analyses, patients were divided into those who were biomarker high, defined as having levels of periostin greater than 50 ng/mL or blood eosinophils greater than 300 mcg/L, or biomarker low, defined as having lower levels of periostin and blood eosinophils.
Over the 52-week study period in the biomarker high patients enrolled in LAVOLTA I, the rate of exacerbations was 51% lower among those randomized to the 37.5 mg dose (P less than .001) and 30% lower (P = .0232) among those randomized to the 125-mg dose relative to placebo. In the biomarker low group, a statistically significant 45% reduction in exacerbations was achieved with the 37.5 mg dose relative to placebo (P = .0318), but a 28% reduction in exacerbations, which was achieved in patients taking the 125-mg dose, was not statistically significant.
In the biomarker high patients enrolled in LAVOLTA II, both the 37.5-mg and the 125-mg doses reduced the rate of exacerbations by 26% relative to placebo, but neither reduction reached statistical significance. In the biomarker low patients, the 37.5-mg dose was associated with a 46% increase in exacerbations and the 125-mg dose was associated with a 6% increase in exacerbations relative to placebo.
In LAVOLTA I, lung function (as measured by FEV1) improved in biomarker high patients in both active treatment arms relative to placebo. The relative advantage of taking lebrikizumab was seen only in the biomarker low patients who took the 125-mg dose.
In LAVOLTA II, a similar advantage was observed in biomarker high patients who took both doses of lebrikizumab over biomarker high patients who took the placebo. There were no significant differences in outcomes observed between any treatment arms in the biomarker low group of LAVOLTA II.
Changes in other secondary endpoints were also inconsistent between the two studies. For example, the time to first exacerbation was significantly increased by lebrikizumab in LAVOLTA I but not in LAVOLTA II. Although use of rescue medications was significantly lower in patients receiving lebrikizumab in both studies, the rate of urgent health care utilization, such as emergency department visits, was lower in patients who took lebrikizumab in LAVOLTA 1, but not in those patients who too the drug in LAVOLTA II.
One consistency between the two studies’ outcomes was a lack of “meaningful improvements” having occurred in patients’ quality of life, as measured by the Asthma Quality of Life Questionnaire and the 5-item Asthma Control Questionnaire, according to Dr. Hanania.
The only difference in the occurrences of events associated with impaired immune function observed between any of the groups was a slight increase in the rate of herpes zoster among those treated with lebrikizumab relative to placebo (1.1% vs. 0.3%), Dr. Hanania reported. The only death that occurred in either study involved a patient in a placebo group. The rates of other side effects were comparable among patients in the active treatment and placebo groups.
An improvement in exacerbations would be consistent with the purported mechanism of lebrikizumab, because IL-13 is believed to induce expression of periostin, which, in turn, is thought to mediate bronchial hyper-responsiveness. In previously completed phase II trials, lebrikizumab was associated with a significant reduction in the rate of exacerbations over 24 weeks among patients with moderate to severe asthma (Thorax. 2015;80:748-56).
Asked in the discussion period whether the results of LAVOLTA I and II signaled the end of lebrikizumab studies in asthma control, Dr. Hanania deferred the question to Roche, which is developing this agent.
He noted that additional studies in a more select group of patients may be warranted and that lebrikizumab is still being evaluated for use in other lung diseases, such as idiopathic pulmonary fibrosis.
Dr. Hanania reports financial relationships with Forest, GlaxoSmithKline, Novartis, Pfizer, and Roche.
LONDON – Two large phase III trials with lebrikizumab, a monoclonal antibody that blocks the activity of interleukin-13 (IL-13), produced inconsistent evidence of benefit in patients with uncontrolled asthma, according to a presentation of both sets of data at the annual congress of the European Respiratory Society.
The two phase III studies compared lebrikizumab in doses of 37.5 mg and 125 mg to placebo, each administered subcutaneously every 4 weeks. The results were mixed not only for the primary endpoint, which was a reduction in the rate of exacerbations, but also for several secondary outcomes.
Evenly randomized into three treatment arms, 1,081 patients were enrolled in LAVOLTA I and 1,081 in LAVOLTA II. For entry, patients were required to have a forced expiratory volume in 1 second (FEV1) between 40% and 80% of predicted. Lebrikizumab was added on top of stable background therapy. For the efficacy analyses, patients were divided into those who were biomarker high, defined as having levels of periostin greater than 50 ng/mL or blood eosinophils greater than 300 mcg/L, or biomarker low, defined as having lower levels of periostin and blood eosinophils.
Over the 52-week study period in the biomarker high patients enrolled in LAVOLTA I, the rate of exacerbations was 51% lower among those randomized to the 37.5 mg dose (P less than .001) and 30% lower (P = .0232) among those randomized to the 125-mg dose relative to placebo. In the biomarker low group, a statistically significant 45% reduction in exacerbations was achieved with the 37.5 mg dose relative to placebo (P = .0318), but a 28% reduction in exacerbations, which was achieved in patients taking the 125-mg dose, was not statistically significant.
In the biomarker high patients enrolled in LAVOLTA II, both the 37.5-mg and the 125-mg doses reduced the rate of exacerbations by 26% relative to placebo, but neither reduction reached statistical significance. In the biomarker low patients, the 37.5-mg dose was associated with a 46% increase in exacerbations and the 125-mg dose was associated with a 6% increase in exacerbations relative to placebo.
In LAVOLTA I, lung function (as measured by FEV1) improved in biomarker high patients in both active treatment arms relative to placebo. The relative advantage of taking lebrikizumab was seen only in the biomarker low patients who took the 125-mg dose.
In LAVOLTA II, a similar advantage was observed in biomarker high patients who took both doses of lebrikizumab over biomarker high patients who took the placebo. There were no significant differences in outcomes observed between any treatment arms in the biomarker low group of LAVOLTA II.
Changes in other secondary endpoints were also inconsistent between the two studies. For example, the time to first exacerbation was significantly increased by lebrikizumab in LAVOLTA I but not in LAVOLTA II. Although use of rescue medications was significantly lower in patients receiving lebrikizumab in both studies, the rate of urgent health care utilization, such as emergency department visits, was lower in patients who took lebrikizumab in LAVOLTA 1, but not in those patients who too the drug in LAVOLTA II.
One consistency between the two studies’ outcomes was a lack of “meaningful improvements” having occurred in patients’ quality of life, as measured by the Asthma Quality of Life Questionnaire and the 5-item Asthma Control Questionnaire, according to Dr. Hanania.
The only difference in the occurrences of events associated with impaired immune function observed between any of the groups was a slight increase in the rate of herpes zoster among those treated with lebrikizumab relative to placebo (1.1% vs. 0.3%), Dr. Hanania reported. The only death that occurred in either study involved a patient in a placebo group. The rates of other side effects were comparable among patients in the active treatment and placebo groups.
An improvement in exacerbations would be consistent with the purported mechanism of lebrikizumab, because IL-13 is believed to induce expression of periostin, which, in turn, is thought to mediate bronchial hyper-responsiveness. In previously completed phase II trials, lebrikizumab was associated with a significant reduction in the rate of exacerbations over 24 weeks among patients with moderate to severe asthma (Thorax. 2015;80:748-56).
Asked in the discussion period whether the results of LAVOLTA I and II signaled the end of lebrikizumab studies in asthma control, Dr. Hanania deferred the question to Roche, which is developing this agent.
He noted that additional studies in a more select group of patients may be warranted and that lebrikizumab is still being evaluated for use in other lung diseases, such as idiopathic pulmonary fibrosis.
Dr. Hanania reports financial relationships with Forest, GlaxoSmithKline, Novartis, Pfizer, and Roche.
AT THE ERS CONGRESS 2016
Key clinical point: The primary efficacy endpoint was achieved in only one of two phase III trials of lebrikizumab for treatment of uncontrolled asthma.
Major finding: For lebrikizumab, which targets IL-13, the inconsistency of significant benefit clouds its future as an asthma treatment.
Data source: A placebo-controlled multicenter phase III program.
Disclosures: Dr. Hanania reports financial relationships with Forest, GlaxoSmithKline, Novartis, Pfizer, and Roche.
CT evidence of emphysema in ever smokers predicts activity limitation
LONDON – Recent evidence of ever smokers having measurable deficits in activity even when lung function is preserved has been further expanded by findings suggesting a different phenotype for patients in this group with radiologic evidence of emphysema, according to data from SPIROMICS (Subpopulations and Intermediate Outcome Measures In COPD Study).
The most recent data were presented at the annual congress of the European Respiratory Society.
Earlier this year, published data drawn from SPIROMICS demonstrated that current and former smokers with preserved lung function (forced expiratory volume in 1 second:forced vital capacity greater than or equal to 0.70) had activity limitations, respiratory symptoms, and exacerbations even though they did not meet the current definition of chronic obstructive pulmonary disease (COPD) (N Engl J Med. 2016;374:1811-21). In the new analysis, further distinctions could be made for patients in this subgroup who also had emphysema on computed tomography (CT).
“Among smokers with preserved lung function, emphysema on CT was associated with reduced activity levels and desaturation on the 6-minute walk test (6MWT),” reported Christian M. Lo Cascio, MD, Columbia University, New York. Compared with smokers with preserved lung function without CT evidence of emphysema, the patients with emphysema on CT did not have more symptoms or exacerbations.
“These and prior findings suggest two distinct but overlapping phenotypes in ever smokers with preserved lung function: an airway disease with respiratory symptoms and frequent exacerbations and emphysema characterized by activity limitation and increased mortality,” said Dr. Lo Cascio.
SPIROMICS, an observational study supported by the National Heart, Lung, and Blood Institute, has enrolled current and former smokers at six centers in the United States to prospectively analyze biomarker, genetic, and clinical data. In the previously published analysis, the focus was on the difference between 849 ever smokers with preserved lung function and 963 patients with mild to moderate COPD. In the data presented by Dr. Lo Cascio, 901 SPIROMICS patients with preserved lung function were analyzed with the focus on the difference between the 66 (7%) who had radiologic evidence of emphysema and the 835 (93%) who had undergone CT indicating that they did not have emphysema.
“Our hypothesis was that the subgroup of patients with emphysema on CT would have lower activity levels, greater desaturation of at least 4% on the 6MWT, more respiratory symptoms, and more exacerbations,” Dr. Lo Cascio reported.
The hypothesis was only half correct. As measured on the activity component of the St. Georges Respiratory Questionnaire, there was about a 10-point (P less than .001) greater reduction in reported activity levels among those with emphysema on CT relative to those without. In addition, the odds ratio (OR) for significant oxygen desaturation, defined as a 4% fall in oxygen saturation of hemoglobin during the 6MWD, was approximately two times greater (P less than .001) for the patients with CT evidence of emphysema.
There were no significant differences between the two groups in walking distance on the 6MWD. Both sets of patients had the same rate of exacerbations and scores on the symptom component of the St. Georges Respiratory Questionnaire, which captures cough, phlegm, wheezing, shortness of breath, and symptom-free days.
Overall, when ever smokers with preserved lung function were subdivided into those with and without CT evidence of emphysema, several similarities were found between the two groups. For those with CT evidence of emphysema and those with no CT evidence of emphysema, mean pack-years of smoking were 43 years and 40 years, respectively, and average body mass indexes were 28.1 and 29.1, respectively. The percentage of patients who had a COPD Assessment Test score of greater than or equal to 10 was 61% among those with CT evidence of emphysema, vs. 50% among those patients without CT evidence of emphysema.
When asked if looking for emphysema on CT in ever smokers with preserved lung function might have clinical utility, Dr. Lo Cascio suggested that it is not yet clear how this information might change management. These data strengthen other evidence from SPIROMICS that ever smokers who do not meet the definition of COPD already have a significant disease burden, he said.
Dr. Lo Cascio reports no relevant financial relationships.
LONDON – Recent evidence of ever smokers having measurable deficits in activity even when lung function is preserved has been further expanded by findings suggesting a different phenotype for patients in this group with radiologic evidence of emphysema, according to data from SPIROMICS (Subpopulations and Intermediate Outcome Measures In COPD Study).
The most recent data were presented at the annual congress of the European Respiratory Society.
Earlier this year, published data drawn from SPIROMICS demonstrated that current and former smokers with preserved lung function (forced expiratory volume in 1 second:forced vital capacity greater than or equal to 0.70) had activity limitations, respiratory symptoms, and exacerbations even though they did not meet the current definition of chronic obstructive pulmonary disease (COPD) (N Engl J Med. 2016;374:1811-21). In the new analysis, further distinctions could be made for patients in this subgroup who also had emphysema on computed tomography (CT).
“Among smokers with preserved lung function, emphysema on CT was associated with reduced activity levels and desaturation on the 6-minute walk test (6MWT),” reported Christian M. Lo Cascio, MD, Columbia University, New York. Compared with smokers with preserved lung function without CT evidence of emphysema, the patients with emphysema on CT did not have more symptoms or exacerbations.
“These and prior findings suggest two distinct but overlapping phenotypes in ever smokers with preserved lung function: an airway disease with respiratory symptoms and frequent exacerbations and emphysema characterized by activity limitation and increased mortality,” said Dr. Lo Cascio.
SPIROMICS, an observational study supported by the National Heart, Lung, and Blood Institute, has enrolled current and former smokers at six centers in the United States to prospectively analyze biomarker, genetic, and clinical data. In the previously published analysis, the focus was on the difference between 849 ever smokers with preserved lung function and 963 patients with mild to moderate COPD. In the data presented by Dr. Lo Cascio, 901 SPIROMICS patients with preserved lung function were analyzed with the focus on the difference between the 66 (7%) who had radiologic evidence of emphysema and the 835 (93%) who had undergone CT indicating that they did not have emphysema.
“Our hypothesis was that the subgroup of patients with emphysema on CT would have lower activity levels, greater desaturation of at least 4% on the 6MWT, more respiratory symptoms, and more exacerbations,” Dr. Lo Cascio reported.
The hypothesis was only half correct. As measured on the activity component of the St. Georges Respiratory Questionnaire, there was about a 10-point (P less than .001) greater reduction in reported activity levels among those with emphysema on CT relative to those without. In addition, the odds ratio (OR) for significant oxygen desaturation, defined as a 4% fall in oxygen saturation of hemoglobin during the 6MWD, was approximately two times greater (P less than .001) for the patients with CT evidence of emphysema.
There were no significant differences between the two groups in walking distance on the 6MWD. Both sets of patients had the same rate of exacerbations and scores on the symptom component of the St. Georges Respiratory Questionnaire, which captures cough, phlegm, wheezing, shortness of breath, and symptom-free days.
Overall, when ever smokers with preserved lung function were subdivided into those with and without CT evidence of emphysema, several similarities were found between the two groups. For those with CT evidence of emphysema and those with no CT evidence of emphysema, mean pack-years of smoking were 43 years and 40 years, respectively, and average body mass indexes were 28.1 and 29.1, respectively. The percentage of patients who had a COPD Assessment Test score of greater than or equal to 10 was 61% among those with CT evidence of emphysema, vs. 50% among those patients without CT evidence of emphysema.
When asked if looking for emphysema on CT in ever smokers with preserved lung function might have clinical utility, Dr. Lo Cascio suggested that it is not yet clear how this information might change management. These data strengthen other evidence from SPIROMICS that ever smokers who do not meet the definition of COPD already have a significant disease burden, he said.
Dr. Lo Cascio reports no relevant financial relationships.
LONDON – Recent evidence of ever smokers having measurable deficits in activity even when lung function is preserved has been further expanded by findings suggesting a different phenotype for patients in this group with radiologic evidence of emphysema, according to data from SPIROMICS (Subpopulations and Intermediate Outcome Measures In COPD Study).
The most recent data were presented at the annual congress of the European Respiratory Society.
Earlier this year, published data drawn from SPIROMICS demonstrated that current and former smokers with preserved lung function (forced expiratory volume in 1 second:forced vital capacity greater than or equal to 0.70) had activity limitations, respiratory symptoms, and exacerbations even though they did not meet the current definition of chronic obstructive pulmonary disease (COPD) (N Engl J Med. 2016;374:1811-21). In the new analysis, further distinctions could be made for patients in this subgroup who also had emphysema on computed tomography (CT).
“Among smokers with preserved lung function, emphysema on CT was associated with reduced activity levels and desaturation on the 6-minute walk test (6MWT),” reported Christian M. Lo Cascio, MD, Columbia University, New York. Compared with smokers with preserved lung function without CT evidence of emphysema, the patients with emphysema on CT did not have more symptoms or exacerbations.
“These and prior findings suggest two distinct but overlapping phenotypes in ever smokers with preserved lung function: an airway disease with respiratory symptoms and frequent exacerbations and emphysema characterized by activity limitation and increased mortality,” said Dr. Lo Cascio.
SPIROMICS, an observational study supported by the National Heart, Lung, and Blood Institute, has enrolled current and former smokers at six centers in the United States to prospectively analyze biomarker, genetic, and clinical data. In the previously published analysis, the focus was on the difference between 849 ever smokers with preserved lung function and 963 patients with mild to moderate COPD. In the data presented by Dr. Lo Cascio, 901 SPIROMICS patients with preserved lung function were analyzed with the focus on the difference between the 66 (7%) who had radiologic evidence of emphysema and the 835 (93%) who had undergone CT indicating that they did not have emphysema.
“Our hypothesis was that the subgroup of patients with emphysema on CT would have lower activity levels, greater desaturation of at least 4% on the 6MWT, more respiratory symptoms, and more exacerbations,” Dr. Lo Cascio reported.
The hypothesis was only half correct. As measured on the activity component of the St. Georges Respiratory Questionnaire, there was about a 10-point (P less than .001) greater reduction in reported activity levels among those with emphysema on CT relative to those without. In addition, the odds ratio (OR) for significant oxygen desaturation, defined as a 4% fall in oxygen saturation of hemoglobin during the 6MWD, was approximately two times greater (P less than .001) for the patients with CT evidence of emphysema.
There were no significant differences between the two groups in walking distance on the 6MWD. Both sets of patients had the same rate of exacerbations and scores on the symptom component of the St. Georges Respiratory Questionnaire, which captures cough, phlegm, wheezing, shortness of breath, and symptom-free days.
Overall, when ever smokers with preserved lung function were subdivided into those with and without CT evidence of emphysema, several similarities were found between the two groups. For those with CT evidence of emphysema and those with no CT evidence of emphysema, mean pack-years of smoking were 43 years and 40 years, respectively, and average body mass indexes were 28.1 and 29.1, respectively. The percentage of patients who had a COPD Assessment Test score of greater than or equal to 10 was 61% among those with CT evidence of emphysema, vs. 50% among those patients without CT evidence of emphysema.
When asked if looking for emphysema on CT in ever smokers with preserved lung function might have clinical utility, Dr. Lo Cascio suggested that it is not yet clear how this information might change management. These data strengthen other evidence from SPIROMICS that ever smokers who do not meet the definition of COPD already have a significant disease burden, he said.
Dr. Lo Cascio reports no relevant financial relationships.
AT THE ERS CONGRESS 2016
Key clinical point: Among ever smokers with preserved lung function, CT evidence of emphysema identifies a group with even greater functional impairment.
Major finding: Despite preserved lung function in both groups, physical activity and desaturation on exercise was greater (P less than .001) in patients with emphysema.
Data source: Subpopulation analysis of prospective registry study.
Disclosures: Dr. Lo Cascio reports no relevant financial relationships.
Inhaled antibiotic regimen reduces bronchiectasis exacerbations
LONDON – In patients with non–cystic fibrosis bronchiectasis (NCFB), use of inhaled ciprofloxacin on a schedule of 14 days on and 14 days off significantly reduced the rate of exacerbations, in a multicenter placebo-controlled trial. The results were presented at the annual congress of the European Respiratory Society.
“At last, an antibiotic intervention trial [in NCFB] with a positive outcome,” reported Anthony De Soyza, MBChB, PhD, senior lecturer in respiratory medicine, Newcastle (England) University. Dr. De Soyza was the study’s principal investigator.
In this study, called RESPIRE 1, the researchers conducted two placebo-controlled arms simultaneously. In one, patients randomized to inhaled ciprofloxacin or placebo took their assigned treatment twice daily for 14 days on and then 14 days off. In the other, patients took their assigned treatment of ciprofloxacin or placebo twice daily, but for 28 days on and then 28 days off. The on-off schedules were maintained for 48 weeks. The ratio of randomization of active therapy to placebo was 2:1.
There were two co-primary endpoints. One was the number of exacerbations over the 48 weeks of follow-up. Exacerbations were strictly defined as the worsening of at least three respiratory symptoms (dyspnea, wheezing, cough, increased sputum volume over 24 hours, or increased sputum purulence) plus fever with malaise or fatigue, and systemic antibiotic use. The other endpoint was the time to first exacerbation.
When the 111 patients randomized to the 14-day on-off regimen of inhaled ciprofloxacin were compared to 49 placebo patients, the mean number of exacerbations over 48 weeks of follow-up was 0.6 in the active treatment group, versus 1.0 in the placebo group (adjusted hazard ratio of 0.61, P = .0061), according to Dr. De Soyza.
The mean time to first exacerbation approached 1 year in those randomized to the 14-day on-off schedule of inhaled ciprofloxacin. In the two placebo arms (pooled for this analysis), the mean time to first exacerbation was 186 days. This difference was highly significant (HR = 0.53; P = .0005).
On the 28-day schedule, for 174 patients, there was a trend for a delay in the time to first exacerbation (HR 0.73; P = .0650) for those randomized to inhaled ciprofloxacin relative to placebo. The difference in the mean number of exacerbations between patients in the experimental group and the placebo group did not approach significance, which Dr. De Soyza said may have been caused by a lack of protection from antibiotics during the off period.
Ciprofloxacin, which was delivered in a dose of 32.5 mg in a proprietary dry powder inhalation device, was well tolerated. The overall rate of adverse events was similar across the study arms. The rates of discontinuation for adverse events in the 14-day and 28-day arms of ciprofloxacin were 12.5% and 10.6%, respectively. These rates were numerically lower than the 13.9% rate of adverse events that occurred among the patients receiving placebos.
According to previously published data cited by Dr. De Soyza, the proportion of NCFB patients with chronic lung infections is 70%, and approximately 40% of these patients have at least two exacerbations per year. In patients with at least two exacerbations per year, the 4-year mortality rate is 15%, Dr. De Soyza reported.
“There is an urgent medical need for better therapeutic strategies to improve outcome in patients with this disease,” he emphasized.
In this particular study, enrolled patients had relatively advanced NCFB. About 30% had a baseline forced expiratory volume in one second of less than 50% of predicted, about 55% had experienced two or more exacerbations in the past 12 months, 20% had been hospitalized in the last year, and more than 15% were on long-term oral macrolides, Dr. De Soyza reported.
These data will be rendered even more compelling if the similarly designed and nearly completed RESPIRE 2 trial produces similar results, he said. If both studies demonstrate protection from exacerbations, they might lead to “a paradigm shift” in the treatment of NCFB, he added.
In the context of the limited strategies currently available for NCFB, “the punch line is that this is a really exciting outcome,” he said.
Dr. De Soyza has financial relationships with AstraZeneca, Bayer, Chiesi, Forrest Labs, GlaxoSmithKline, Novartis, and Teva.
LONDON – In patients with non–cystic fibrosis bronchiectasis (NCFB), use of inhaled ciprofloxacin on a schedule of 14 days on and 14 days off significantly reduced the rate of exacerbations, in a multicenter placebo-controlled trial. The results were presented at the annual congress of the European Respiratory Society.
“At last, an antibiotic intervention trial [in NCFB] with a positive outcome,” reported Anthony De Soyza, MBChB, PhD, senior lecturer in respiratory medicine, Newcastle (England) University. Dr. De Soyza was the study’s principal investigator.
In this study, called RESPIRE 1, the researchers conducted two placebo-controlled arms simultaneously. In one, patients randomized to inhaled ciprofloxacin or placebo took their assigned treatment twice daily for 14 days on and then 14 days off. In the other, patients took their assigned treatment of ciprofloxacin or placebo twice daily, but for 28 days on and then 28 days off. The on-off schedules were maintained for 48 weeks. The ratio of randomization of active therapy to placebo was 2:1.
There were two co-primary endpoints. One was the number of exacerbations over the 48 weeks of follow-up. Exacerbations were strictly defined as the worsening of at least three respiratory symptoms (dyspnea, wheezing, cough, increased sputum volume over 24 hours, or increased sputum purulence) plus fever with malaise or fatigue, and systemic antibiotic use. The other endpoint was the time to first exacerbation.
When the 111 patients randomized to the 14-day on-off regimen of inhaled ciprofloxacin were compared to 49 placebo patients, the mean number of exacerbations over 48 weeks of follow-up was 0.6 in the active treatment group, versus 1.0 in the placebo group (adjusted hazard ratio of 0.61, P = .0061), according to Dr. De Soyza.
The mean time to first exacerbation approached 1 year in those randomized to the 14-day on-off schedule of inhaled ciprofloxacin. In the two placebo arms (pooled for this analysis), the mean time to first exacerbation was 186 days. This difference was highly significant (HR = 0.53; P = .0005).
On the 28-day schedule, for 174 patients, there was a trend for a delay in the time to first exacerbation (HR 0.73; P = .0650) for those randomized to inhaled ciprofloxacin relative to placebo. The difference in the mean number of exacerbations between patients in the experimental group and the placebo group did not approach significance, which Dr. De Soyza said may have been caused by a lack of protection from antibiotics during the off period.
Ciprofloxacin, which was delivered in a dose of 32.5 mg in a proprietary dry powder inhalation device, was well tolerated. The overall rate of adverse events was similar across the study arms. The rates of discontinuation for adverse events in the 14-day and 28-day arms of ciprofloxacin were 12.5% and 10.6%, respectively. These rates were numerically lower than the 13.9% rate of adverse events that occurred among the patients receiving placebos.
According to previously published data cited by Dr. De Soyza, the proportion of NCFB patients with chronic lung infections is 70%, and approximately 40% of these patients have at least two exacerbations per year. In patients with at least two exacerbations per year, the 4-year mortality rate is 15%, Dr. De Soyza reported.
“There is an urgent medical need for better therapeutic strategies to improve outcome in patients with this disease,” he emphasized.
In this particular study, enrolled patients had relatively advanced NCFB. About 30% had a baseline forced expiratory volume in one second of less than 50% of predicted, about 55% had experienced two or more exacerbations in the past 12 months, 20% had been hospitalized in the last year, and more than 15% were on long-term oral macrolides, Dr. De Soyza reported.
These data will be rendered even more compelling if the similarly designed and nearly completed RESPIRE 2 trial produces similar results, he said. If both studies demonstrate protection from exacerbations, they might lead to “a paradigm shift” in the treatment of NCFB, he added.
In the context of the limited strategies currently available for NCFB, “the punch line is that this is a really exciting outcome,” he said.
Dr. De Soyza has financial relationships with AstraZeneca, Bayer, Chiesi, Forrest Labs, GlaxoSmithKline, Novartis, and Teva.
LONDON – In patients with non–cystic fibrosis bronchiectasis (NCFB), use of inhaled ciprofloxacin on a schedule of 14 days on and 14 days off significantly reduced the rate of exacerbations, in a multicenter placebo-controlled trial. The results were presented at the annual congress of the European Respiratory Society.
“At last, an antibiotic intervention trial [in NCFB] with a positive outcome,” reported Anthony De Soyza, MBChB, PhD, senior lecturer in respiratory medicine, Newcastle (England) University. Dr. De Soyza was the study’s principal investigator.
In this study, called RESPIRE 1, the researchers conducted two placebo-controlled arms simultaneously. In one, patients randomized to inhaled ciprofloxacin or placebo took their assigned treatment twice daily for 14 days on and then 14 days off. In the other, patients took their assigned treatment of ciprofloxacin or placebo twice daily, but for 28 days on and then 28 days off. The on-off schedules were maintained for 48 weeks. The ratio of randomization of active therapy to placebo was 2:1.
There were two co-primary endpoints. One was the number of exacerbations over the 48 weeks of follow-up. Exacerbations were strictly defined as the worsening of at least three respiratory symptoms (dyspnea, wheezing, cough, increased sputum volume over 24 hours, or increased sputum purulence) plus fever with malaise or fatigue, and systemic antibiotic use. The other endpoint was the time to first exacerbation.
When the 111 patients randomized to the 14-day on-off regimen of inhaled ciprofloxacin were compared to 49 placebo patients, the mean number of exacerbations over 48 weeks of follow-up was 0.6 in the active treatment group, versus 1.0 in the placebo group (adjusted hazard ratio of 0.61, P = .0061), according to Dr. De Soyza.
The mean time to first exacerbation approached 1 year in those randomized to the 14-day on-off schedule of inhaled ciprofloxacin. In the two placebo arms (pooled for this analysis), the mean time to first exacerbation was 186 days. This difference was highly significant (HR = 0.53; P = .0005).
On the 28-day schedule, for 174 patients, there was a trend for a delay in the time to first exacerbation (HR 0.73; P = .0650) for those randomized to inhaled ciprofloxacin relative to placebo. The difference in the mean number of exacerbations between patients in the experimental group and the placebo group did not approach significance, which Dr. De Soyza said may have been caused by a lack of protection from antibiotics during the off period.
Ciprofloxacin, which was delivered in a dose of 32.5 mg in a proprietary dry powder inhalation device, was well tolerated. The overall rate of adverse events was similar across the study arms. The rates of discontinuation for adverse events in the 14-day and 28-day arms of ciprofloxacin were 12.5% and 10.6%, respectively. These rates were numerically lower than the 13.9% rate of adverse events that occurred among the patients receiving placebos.
According to previously published data cited by Dr. De Soyza, the proportion of NCFB patients with chronic lung infections is 70%, and approximately 40% of these patients have at least two exacerbations per year. In patients with at least two exacerbations per year, the 4-year mortality rate is 15%, Dr. De Soyza reported.
“There is an urgent medical need for better therapeutic strategies to improve outcome in patients with this disease,” he emphasized.
In this particular study, enrolled patients had relatively advanced NCFB. About 30% had a baseline forced expiratory volume in one second of less than 50% of predicted, about 55% had experienced two or more exacerbations in the past 12 months, 20% had been hospitalized in the last year, and more than 15% were on long-term oral macrolides, Dr. De Soyza reported.
These data will be rendered even more compelling if the similarly designed and nearly completed RESPIRE 2 trial produces similar results, he said. If both studies demonstrate protection from exacerbations, they might lead to “a paradigm shift” in the treatment of NCFB, he added.
In the context of the limited strategies currently available for NCFB, “the punch line is that this is a really exciting outcome,” he said.
Dr. De Soyza has financial relationships with AstraZeneca, Bayer, Chiesi, Forrest Labs, GlaxoSmithKline, Novartis, and Teva.
AT THE ERS CONGRESS 2016
Key clinical point: An every-14-day regimen of inhaled ciprofloxacin reduced the number of and the rate of exacerbations in non–cystic fibrosis bronchiectasis patients.
Major finding: The rate of exacerbations was reduced by 39% over a 48-week period in those randomized to the inhaled antibiotic relative to placebo.
Data source: A multicenter double-blind, placebo-controlled trial.
Disclosures: Dr. De Soyza has financial relationships with AstraZeneca, Bayer, Chiesi, Forrest Labs, GlaxoSmithKline, Novartis, and Teva.
Periostin level may indicate upper-airway disease in asthmatics
LONDON – Measuring serum levels of the extracellular protein periostin could help identify patients with asthma who have comorbid upper-airway disease, according to research from a late-breaking oral abstract presented at the annual congress of the European Respiratory Society.
Periostin is known to be involved in the pathophysiology of upper-airway disease, linked to both airway remodeling and inflammation. Levels of periostin have been shown to be higher in patients with asthma, allergic rhinitis, and chronic rhinosinusitis than in healthy individuals, and there are data suggesting that it could be linked to severity. However, little is known about whether serum periostin can be used to detect and perhaps monitor upper-airway disease in patients with asthma.
Serum periostin levels were found to be higher in asthma patients with comorbid chronic rhinosinusitis, compared with those with no comorbid upper-airway disease (119.8 vs. 86.3 ng/mL; P = .04).
Levels of periostin in the serum were also significantly higher in asthma patients with chronic rhinosinusitis who also had nasal polyps than in those who did not have nasal polyps (143.3 vs. 94.0 ng/mL; P = .01).
“Serum periostin is a sensitive biomarker for detecting comorbid chronic rhinosinusitis, especially in patients with chronic rhinosinusitis with nasal polyps,” said Dr. Takamitsu Asano, who reported the findings at the meeting. Dr. Asano of Nagoya (Japan) City University Graduate School of Medical Sciences noted that the serum periostin could also reflect the severity of chronic rhinosinusitis in patients with asthma.
“Upper-airway diseases are considered risk factors for the exacerbation and poor control of asthma,” Dr. Asano explained. It is thought, he said, that 40%-50% of patients with asthma have comorbid chronic rhinosinusitis, and 57%-70% have comorbid allergic rhinitis.
Dr. Asano and colleagues at Nagoya City University and Saga (Japan) Medical School recruited 65 patients with stable asthma, with or without comorbid upper-airway disease, between July 2014 and December 2015. Of these patients, 20 had no comorbid upper-airway disease, 22 had rhinitis, 21 had chronic rhinosinusitis, and two had confirmed nasal polyps. Of the 21 patients with chronic rhinosinusitis, 10 had and 11 did not have nasal polyps. Patients’ diagnoses were checked by otorhinolaryngology specialists.
The recruited patients, who were a mean age of 56 years, with an asthma disease duration of 9 years, underwent the following tests: fractional exhaled nitric oxide testing, spirometry, sputum induction, and sinus computed tomography scanning. They also had their blood tested for serum periostin, eosinophils, eotaxin, and immunoglobulin E levels.
Serum periostin levels were found to correlate with the results of fractional exhaled nitric oxide testing, and with blood and sputum eosinophil counts, with respective correlation coefficients of 0.36 (P = .003), 0.35 (P = .005), and 0.44 (P = .004).
In a separate study presented by Dr. Cecile Holweg of Genentech, several patient factors were found to influence the level of serum periostin. Using data from trials of the experimental asthma therapy lebrikizumab and the asthma therapy omalizumab (Xolair), the biologic variability in serum periostin and blood eosinophils was characterized according to patient demographics, asthma severity, concomitant medication use, and comorbidities, including upper-airway diseases.
Multivariate analysis showed that serum periostin levels were higher in patients with nasal polyps and in patients from South America and Asia. Conversely, serum periostin levels were lower in patients with high body mass index and in patients who were current smokers.
Raised eosinophil counts were also seen in patients with nasal polyps and lower eosinophil counts were observed in current smokers.
“These factors should be taken into account when making treatment decisions based on these biomarkers,” Dr. Holweg concluded.
Dr. Asano has received financial support from Novartis, AstraZeneca, Merck Sharp & Dohme, and Eisai Co. Dr. Holweg is an employee of Genentech.
LONDON – Measuring serum levels of the extracellular protein periostin could help identify patients with asthma who have comorbid upper-airway disease, according to research from a late-breaking oral abstract presented at the annual congress of the European Respiratory Society.
Periostin is known to be involved in the pathophysiology of upper-airway disease, linked to both airway remodeling and inflammation. Levels of periostin have been shown to be higher in patients with asthma, allergic rhinitis, and chronic rhinosinusitis than in healthy individuals, and there are data suggesting that it could be linked to severity. However, little is known about whether serum periostin can be used to detect and perhaps monitor upper-airway disease in patients with asthma.
Serum periostin levels were found to be higher in asthma patients with comorbid chronic rhinosinusitis, compared with those with no comorbid upper-airway disease (119.8 vs. 86.3 ng/mL; P = .04).
Levels of periostin in the serum were also significantly higher in asthma patients with chronic rhinosinusitis who also had nasal polyps than in those who did not have nasal polyps (143.3 vs. 94.0 ng/mL; P = .01).
“Serum periostin is a sensitive biomarker for detecting comorbid chronic rhinosinusitis, especially in patients with chronic rhinosinusitis with nasal polyps,” said Dr. Takamitsu Asano, who reported the findings at the meeting. Dr. Asano of Nagoya (Japan) City University Graduate School of Medical Sciences noted that the serum periostin could also reflect the severity of chronic rhinosinusitis in patients with asthma.
“Upper-airway diseases are considered risk factors for the exacerbation and poor control of asthma,” Dr. Asano explained. It is thought, he said, that 40%-50% of patients with asthma have comorbid chronic rhinosinusitis, and 57%-70% have comorbid allergic rhinitis.
Dr. Asano and colleagues at Nagoya City University and Saga (Japan) Medical School recruited 65 patients with stable asthma, with or without comorbid upper-airway disease, between July 2014 and December 2015. Of these patients, 20 had no comorbid upper-airway disease, 22 had rhinitis, 21 had chronic rhinosinusitis, and two had confirmed nasal polyps. Of the 21 patients with chronic rhinosinusitis, 10 had and 11 did not have nasal polyps. Patients’ diagnoses were checked by otorhinolaryngology specialists.
The recruited patients, who were a mean age of 56 years, with an asthma disease duration of 9 years, underwent the following tests: fractional exhaled nitric oxide testing, spirometry, sputum induction, and sinus computed tomography scanning. They also had their blood tested for serum periostin, eosinophils, eotaxin, and immunoglobulin E levels.
Serum periostin levels were found to correlate with the results of fractional exhaled nitric oxide testing, and with blood and sputum eosinophil counts, with respective correlation coefficients of 0.36 (P = .003), 0.35 (P = .005), and 0.44 (P = .004).
In a separate study presented by Dr. Cecile Holweg of Genentech, several patient factors were found to influence the level of serum periostin. Using data from trials of the experimental asthma therapy lebrikizumab and the asthma therapy omalizumab (Xolair), the biologic variability in serum periostin and blood eosinophils was characterized according to patient demographics, asthma severity, concomitant medication use, and comorbidities, including upper-airway diseases.
Multivariate analysis showed that serum periostin levels were higher in patients with nasal polyps and in patients from South America and Asia. Conversely, serum periostin levels were lower in patients with high body mass index and in patients who were current smokers.
Raised eosinophil counts were also seen in patients with nasal polyps and lower eosinophil counts were observed in current smokers.
“These factors should be taken into account when making treatment decisions based on these biomarkers,” Dr. Holweg concluded.
Dr. Asano has received financial support from Novartis, AstraZeneca, Merck Sharp & Dohme, and Eisai Co. Dr. Holweg is an employee of Genentech.
LONDON – Measuring serum levels of the extracellular protein periostin could help identify patients with asthma who have comorbid upper-airway disease, according to research from a late-breaking oral abstract presented at the annual congress of the European Respiratory Society.
Periostin is known to be involved in the pathophysiology of upper-airway disease, linked to both airway remodeling and inflammation. Levels of periostin have been shown to be higher in patients with asthma, allergic rhinitis, and chronic rhinosinusitis than in healthy individuals, and there are data suggesting that it could be linked to severity. However, little is known about whether serum periostin can be used to detect and perhaps monitor upper-airway disease in patients with asthma.
Serum periostin levels were found to be higher in asthma patients with comorbid chronic rhinosinusitis, compared with those with no comorbid upper-airway disease (119.8 vs. 86.3 ng/mL; P = .04).
Levels of periostin in the serum were also significantly higher in asthma patients with chronic rhinosinusitis who also had nasal polyps than in those who did not have nasal polyps (143.3 vs. 94.0 ng/mL; P = .01).
“Serum periostin is a sensitive biomarker for detecting comorbid chronic rhinosinusitis, especially in patients with chronic rhinosinusitis with nasal polyps,” said Dr. Takamitsu Asano, who reported the findings at the meeting. Dr. Asano of Nagoya (Japan) City University Graduate School of Medical Sciences noted that the serum periostin could also reflect the severity of chronic rhinosinusitis in patients with asthma.
“Upper-airway diseases are considered risk factors for the exacerbation and poor control of asthma,” Dr. Asano explained. It is thought, he said, that 40%-50% of patients with asthma have comorbid chronic rhinosinusitis, and 57%-70% have comorbid allergic rhinitis.
Dr. Asano and colleagues at Nagoya City University and Saga (Japan) Medical School recruited 65 patients with stable asthma, with or without comorbid upper-airway disease, between July 2014 and December 2015. Of these patients, 20 had no comorbid upper-airway disease, 22 had rhinitis, 21 had chronic rhinosinusitis, and two had confirmed nasal polyps. Of the 21 patients with chronic rhinosinusitis, 10 had and 11 did not have nasal polyps. Patients’ diagnoses were checked by otorhinolaryngology specialists.
The recruited patients, who were a mean age of 56 years, with an asthma disease duration of 9 years, underwent the following tests: fractional exhaled nitric oxide testing, spirometry, sputum induction, and sinus computed tomography scanning. They also had their blood tested for serum periostin, eosinophils, eotaxin, and immunoglobulin E levels.
Serum periostin levels were found to correlate with the results of fractional exhaled nitric oxide testing, and with blood and sputum eosinophil counts, with respective correlation coefficients of 0.36 (P = .003), 0.35 (P = .005), and 0.44 (P = .004).
In a separate study presented by Dr. Cecile Holweg of Genentech, several patient factors were found to influence the level of serum periostin. Using data from trials of the experimental asthma therapy lebrikizumab and the asthma therapy omalizumab (Xolair), the biologic variability in serum periostin and blood eosinophils was characterized according to patient demographics, asthma severity, concomitant medication use, and comorbidities, including upper-airway diseases.
Multivariate analysis showed that serum periostin levels were higher in patients with nasal polyps and in patients from South America and Asia. Conversely, serum periostin levels were lower in patients with high body mass index and in patients who were current smokers.
Raised eosinophil counts were also seen in patients with nasal polyps and lower eosinophil counts were observed in current smokers.
“These factors should be taken into account when making treatment decisions based on these biomarkers,” Dr. Holweg concluded.
Dr. Asano has received financial support from Novartis, AstraZeneca, Merck Sharp & Dohme, and Eisai Co. Dr. Holweg is an employee of Genentech.
AT THE ERS CONGRESS 2016
Key clinical point: Measuring serum periostin could be useful for chronic rhinosinusitis detection in asthma patients.
Major finding: Serum periostin levels were higher in patients with comorbid chronic rhinosinusitis, compared with those with no comorbid upper-airway disease (119.8 vs. 86.3 ng/mL, P = .04).
Data source: Prospective study of comorbid upper-airway disease, rhinitis, and chronic rhinosinusitis in 65 patients with asthma.
Disclosures: Dr. Asano has received financial support from Novartis, AstraZeneca, Merck Sharp & Dohme, and Eisai Co.