User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Powered by CHEST Physician, Clinician Reviews, MDedge Family Medicine, Internal Medicine News, and The Journal of Clinical Outcomes Management.
Riociguat shows benefit in PAH with poor response to PDE inhibitors
LOS ANGELES – Pulmonary artery hypertension patients who have an insufficient response to phosphodiesterase inhibitors may benefit from a switch to riociguat (Adempas), based on results from a 24-week, open-label investigation from the drug’s maker, Bayer.
The 61 patients – mean age 54 years, 74% of whom were women – had World Health Organization functional class 3 disease, with 6-minute walking distances of 165-440 meters, and cardiac indices below 3 L/min/m2 despite being on a phosphodiesterase inhibitor (PDEi) for 90 days or more, 40 (66%) on sildenafil (Viagra) and 21 (34%) on tadalafil (Cialis).
After PDEi washout, the researchers swapped them for riociguat titrated to a maximum oral dose of 2.5 mg t.i.d. The 50 patients (82%) on concomitant endothelin receptor antagonists (ERA) were allowed to stay on them. At week 24, 16 patients (34% of the 47 evaluable patients) achieved the combined endpoint of no clinical worsening, functional class 1 or 2, and 30 meters or more improvement on their walk test.
“The key point is that it was safe to switch people from a [PDEi] to riociguat, and it seemed to have improved efficacy, but we hesitate on these conclusions because it was an open-label trial, and the results need to be confirmed,” lead investigator James Klinger, MD, professor of medicine at Brown University, Providence, R.I., said at the annual meeting of the American College of Chest Physicians. A randomized, controlled trial is underway, he added.
The usual approach to PAH is to start patients on a PDEi, often with an ERA. If that doesn’t work, a prostacyclin is added. The cost can exceed $200,000 a year.
“This is a study that says, wait a minute, before you add a third drug to the first two, maybe it would be worthwhile to” switch out the PDEi. “You would save the person the addition of a third drug,” and the cost would be comparable or less than a three-drug regimen, Dr. Klinger said.
The researchers also found that after 24 weeks on riociguat, mean plasma cyclic guanosine monophosphate (cGMP) increased by 4.6 pmol/mL, urinary cGMP by 1,005 pmol/mL, and asymmetric dimethylarginine (ADMA) by 0.004 micromol/L.
The biomarkers were important because the team is trying to find a way to identify patients who would benefit most from riociguat. “As a field, we still don’t understand the disease well enough to know” how to best match patients and drugs. “We are trying to find a biomarker that would identify patients who are more likely to respond to one medication versus another,” Dr. Klinger said.
ADMA inhibits the production of nitric oxide, and is a bad player in PAH. The study results were reassuring because riociguat didn’t have much of an effect on ADMA levels, although the “slight difference was not enough to identify people who might do better with” it, Dr. Klinger said.
As for cGMP, “when we raise [levels] with riociguat, patients get better, so we think riociguat is raising cGMP in the right place, which we think is the lungs. Unfortunately, we don’t’ have a biomarker that can distinguish lung cGMP from total body cGMP,” he said.
The work was funded by Bayer, maker of riociguat. Dr. Klinger is an unpaid consultant, and also receives research support from the company.
LOS ANGELES – Pulmonary artery hypertension patients who have an insufficient response to phosphodiesterase inhibitors may benefit from a switch to riociguat (Adempas), based on results from a 24-week, open-label investigation from the drug’s maker, Bayer.
The 61 patients – mean age 54 years, 74% of whom were women – had World Health Organization functional class 3 disease, with 6-minute walking distances of 165-440 meters, and cardiac indices below 3 L/min/m2 despite being on a phosphodiesterase inhibitor (PDEi) for 90 days or more, 40 (66%) on sildenafil (Viagra) and 21 (34%) on tadalafil (Cialis).
After PDEi washout, the researchers swapped them for riociguat titrated to a maximum oral dose of 2.5 mg t.i.d. The 50 patients (82%) on concomitant endothelin receptor antagonists (ERA) were allowed to stay on them. At week 24, 16 patients (34% of the 47 evaluable patients) achieved the combined endpoint of no clinical worsening, functional class 1 or 2, and 30 meters or more improvement on their walk test.
“The key point is that it was safe to switch people from a [PDEi] to riociguat, and it seemed to have improved efficacy, but we hesitate on these conclusions because it was an open-label trial, and the results need to be confirmed,” lead investigator James Klinger, MD, professor of medicine at Brown University, Providence, R.I., said at the annual meeting of the American College of Chest Physicians. A randomized, controlled trial is underway, he added.
The usual approach to PAH is to start patients on a PDEi, often with an ERA. If that doesn’t work, a prostacyclin is added. The cost can exceed $200,000 a year.
“This is a study that says, wait a minute, before you add a third drug to the first two, maybe it would be worthwhile to” switch out the PDEi. “You would save the person the addition of a third drug,” and the cost would be comparable or less than a three-drug regimen, Dr. Klinger said.
The researchers also found that after 24 weeks on riociguat, mean plasma cyclic guanosine monophosphate (cGMP) increased by 4.6 pmol/mL, urinary cGMP by 1,005 pmol/mL, and asymmetric dimethylarginine (ADMA) by 0.004 micromol/L.
The biomarkers were important because the team is trying to find a way to identify patients who would benefit most from riociguat. “As a field, we still don’t understand the disease well enough to know” how to best match patients and drugs. “We are trying to find a biomarker that would identify patients who are more likely to respond to one medication versus another,” Dr. Klinger said.
ADMA inhibits the production of nitric oxide, and is a bad player in PAH. The study results were reassuring because riociguat didn’t have much of an effect on ADMA levels, although the “slight difference was not enough to identify people who might do better with” it, Dr. Klinger said.
As for cGMP, “when we raise [levels] with riociguat, patients get better, so we think riociguat is raising cGMP in the right place, which we think is the lungs. Unfortunately, we don’t’ have a biomarker that can distinguish lung cGMP from total body cGMP,” he said.
The work was funded by Bayer, maker of riociguat. Dr. Klinger is an unpaid consultant, and also receives research support from the company.
LOS ANGELES – Pulmonary artery hypertension patients who have an insufficient response to phosphodiesterase inhibitors may benefit from a switch to riociguat (Adempas), based on results from a 24-week, open-label investigation from the drug’s maker, Bayer.
The 61 patients – mean age 54 years, 74% of whom were women – had World Health Organization functional class 3 disease, with 6-minute walking distances of 165-440 meters, and cardiac indices below 3 L/min/m2 despite being on a phosphodiesterase inhibitor (PDEi) for 90 days or more, 40 (66%) on sildenafil (Viagra) and 21 (34%) on tadalafil (Cialis).
After PDEi washout, the researchers swapped them for riociguat titrated to a maximum oral dose of 2.5 mg t.i.d. The 50 patients (82%) on concomitant endothelin receptor antagonists (ERA) were allowed to stay on them. At week 24, 16 patients (34% of the 47 evaluable patients) achieved the combined endpoint of no clinical worsening, functional class 1 or 2, and 30 meters or more improvement on their walk test.
“The key point is that it was safe to switch people from a [PDEi] to riociguat, and it seemed to have improved efficacy, but we hesitate on these conclusions because it was an open-label trial, and the results need to be confirmed,” lead investigator James Klinger, MD, professor of medicine at Brown University, Providence, R.I., said at the annual meeting of the American College of Chest Physicians. A randomized, controlled trial is underway, he added.
The usual approach to PAH is to start patients on a PDEi, often with an ERA. If that doesn’t work, a prostacyclin is added. The cost can exceed $200,000 a year.
“This is a study that says, wait a minute, before you add a third drug to the first two, maybe it would be worthwhile to” switch out the PDEi. “You would save the person the addition of a third drug,” and the cost would be comparable or less than a three-drug regimen, Dr. Klinger said.
The researchers also found that after 24 weeks on riociguat, mean plasma cyclic guanosine monophosphate (cGMP) increased by 4.6 pmol/mL, urinary cGMP by 1,005 pmol/mL, and asymmetric dimethylarginine (ADMA) by 0.004 micromol/L.
The biomarkers were important because the team is trying to find a way to identify patients who would benefit most from riociguat. “As a field, we still don’t understand the disease well enough to know” how to best match patients and drugs. “We are trying to find a biomarker that would identify patients who are more likely to respond to one medication versus another,” Dr. Klinger said.
ADMA inhibits the production of nitric oxide, and is a bad player in PAH. The study results were reassuring because riociguat didn’t have much of an effect on ADMA levels, although the “slight difference was not enough to identify people who might do better with” it, Dr. Klinger said.
As for cGMP, “when we raise [levels] with riociguat, patients get better, so we think riociguat is raising cGMP in the right place, which we think is the lungs. Unfortunately, we don’t’ have a biomarker that can distinguish lung cGMP from total body cGMP,” he said.
The work was funded by Bayer, maker of riociguat. Dr. Klinger is an unpaid consultant, and also receives research support from the company.
AT CHEST 2016
Key clinical point:
Major finding: At week 24, 34% of 47 evaluable patients (16%) achieved the combined endpoint of no clinical worsening, functional class 1 or 2, and a 30-meter or more improvement on their walk test.
Data source: Open-label, nonrandomized 24-week study of 61 patients
Disclosures: The work was funded by Bayer, maker of riociguat. The lead investigator is an unpaid consultant, and also receives research support from the company.
Inhaled antibiotic for bronchiectasis shows promise
AT CHEST 2016
LOS ANGELES – Long-term inhaled ciprofloxacin therapy appears to be a safe and effective treatment option in patients with bronchiectasis, results from an international phase III trial showed.
“This is really exciting; it’s the first large study of an inhaled antibiotic to show a benefit in this population,” study investigator Kevin Winthrop, MD, said in an interview prior to the annual meeting of the American College of Chest Physicians. “There’s a tremendous unmet need and a lot of these patients have daily struggles and their quality of life is low. To have something that would improve that would be a benefit for patients and physicians alike.”
Compared with patients in the placebo arm, those in the ciprofloxacin dry powder for inhalation (DPI) 14-day on/off arm experienced a significantly prolonged time to first exacerbation (a mean of 336 days versus 186 days, respectively; adjusted hazard ratio, 0.53; P = .0005) and a significantly reduced exacerbation frequency over 48 weeks (a mean of 0.78 vs. 1.42; adjusted incident rate of 0.61; P = .0061). A nonsignificant trend in favor of ciprofloxacin DPI was observed for both primary endpoints among patients in the 28-day on/off arm (time to first exacerbation: HR, 0.73; P = .065; frequency of exacerbations: adjusted incidence rate ratio, 0.98; P = .89).
Treatment-emergent adverse events and adverse events leading to discontinuation were similar across treatment groups (82% in the ciprofloxacin DPI 14-day on/off arm, 83% in the ciprofloxacin DPI 28-day on/off arm, and 83% in the pooled placebo arm. The rates of serious adverse events were also similar in the three treatment groups (17%, 20%, and 23%, respectively). “Tolerability markers like hoarseness, bronchospasm, shortness of breath, or increased cough were similar between the treatment arms,” said Dr. Winthrop, who is an infectious diseases specialist at Oregon Health and Science University, Portland.“The safety profile looks really good. There were no typical fluoroquinolone types of problems such as tendinopathy reported.”
A follow-up trial known as RESPIRE 2 is ongoing. RESPIRE 1 was funded by Bayer. Dr. Winthrop disclosed that he is a consultant for the company.
This article was updated on 10/25/2016 at 9:51 AM Est
AT CHEST 2016
LOS ANGELES – Long-term inhaled ciprofloxacin therapy appears to be a safe and effective treatment option in patients with bronchiectasis, results from an international phase III trial showed.
“This is really exciting; it’s the first large study of an inhaled antibiotic to show a benefit in this population,” study investigator Kevin Winthrop, MD, said in an interview prior to the annual meeting of the American College of Chest Physicians. “There’s a tremendous unmet need and a lot of these patients have daily struggles and their quality of life is low. To have something that would improve that would be a benefit for patients and physicians alike.”
Compared with patients in the placebo arm, those in the ciprofloxacin dry powder for inhalation (DPI) 14-day on/off arm experienced a significantly prolonged time to first exacerbation (a mean of 336 days versus 186 days, respectively; adjusted hazard ratio, 0.53; P = .0005) and a significantly reduced exacerbation frequency over 48 weeks (a mean of 0.78 vs. 1.42; adjusted incident rate of 0.61; P = .0061). A nonsignificant trend in favor of ciprofloxacin DPI was observed for both primary endpoints among patients in the 28-day on/off arm (time to first exacerbation: HR, 0.73; P = .065; frequency of exacerbations: adjusted incidence rate ratio, 0.98; P = .89).
Treatment-emergent adverse events and adverse events leading to discontinuation were similar across treatment groups (82% in the ciprofloxacin DPI 14-day on/off arm, 83% in the ciprofloxacin DPI 28-day on/off arm, and 83% in the pooled placebo arm. The rates of serious adverse events were also similar in the three treatment groups (17%, 20%, and 23%, respectively). “Tolerability markers like hoarseness, bronchospasm, shortness of breath, or increased cough were similar between the treatment arms,” said Dr. Winthrop, who is an infectious diseases specialist at Oregon Health and Science University, Portland.“The safety profile looks really good. There were no typical fluoroquinolone types of problems such as tendinopathy reported.”
A follow-up trial known as RESPIRE 2 is ongoing. RESPIRE 1 was funded by Bayer. Dr. Winthrop disclosed that he is a consultant for the company.
This article was updated on 10/25/2016 at 9:51 AM Est
AT CHEST 2016
LOS ANGELES – Long-term inhaled ciprofloxacin therapy appears to be a safe and effective treatment option in patients with bronchiectasis, results from an international phase III trial showed.
“This is really exciting; it’s the first large study of an inhaled antibiotic to show a benefit in this population,” study investigator Kevin Winthrop, MD, said in an interview prior to the annual meeting of the American College of Chest Physicians. “There’s a tremendous unmet need and a lot of these patients have daily struggles and their quality of life is low. To have something that would improve that would be a benefit for patients and physicians alike.”
Compared with patients in the placebo arm, those in the ciprofloxacin dry powder for inhalation (DPI) 14-day on/off arm experienced a significantly prolonged time to first exacerbation (a mean of 336 days versus 186 days, respectively; adjusted hazard ratio, 0.53; P = .0005) and a significantly reduced exacerbation frequency over 48 weeks (a mean of 0.78 vs. 1.42; adjusted incident rate of 0.61; P = .0061). A nonsignificant trend in favor of ciprofloxacin DPI was observed for both primary endpoints among patients in the 28-day on/off arm (time to first exacerbation: HR, 0.73; P = .065; frequency of exacerbations: adjusted incidence rate ratio, 0.98; P = .89).
Treatment-emergent adverse events and adverse events leading to discontinuation were similar across treatment groups (82% in the ciprofloxacin DPI 14-day on/off arm, 83% in the ciprofloxacin DPI 28-day on/off arm, and 83% in the pooled placebo arm. The rates of serious adverse events were also similar in the three treatment groups (17%, 20%, and 23%, respectively). “Tolerability markers like hoarseness, bronchospasm, shortness of breath, or increased cough were similar between the treatment arms,” said Dr. Winthrop, who is an infectious diseases specialist at Oregon Health and Science University, Portland.“The safety profile looks really good. There were no typical fluoroquinolone types of problems such as tendinopathy reported.”
A follow-up trial known as RESPIRE 2 is ongoing. RESPIRE 1 was funded by Bayer. Dr. Winthrop disclosed that he is a consultant for the company.
This article was updated on 10/25/2016 at 9:51 AM Est
Key clinical point:
Major finding: Compared with patients in the placebo arm, those in the ciprofloxacin 14-day on/off arm experienced a significantly prolonged time to first exacerbation (a mean of 336 days vs. 186 days, respectively; adjusted hazard ratio, 0.53; P = .0005).
Data source: A multicenter study of 416 patients who were randomized 2:1 to ciprofloxacin 32.5 mg or placebo administered twice per day using a pocket-sized inhaler as a cyclical regimen of either 14 days on/off drug or 28 days on/off drug, for 48 weeks.
Disclosures: RESPIRE 1 was funded by Bayer. Dr. Winthrop disclosed that he is a consultant for the company.
COPD spirometry use suboptimal in primary care
LOS ANGELES – Spirometry is the standard for diagnosing chronic obstructive pulmonary disease, but it’s underused and misused in primary care, according to investigators from the Corpus Christi (Tex.) Medical Center.
The conclusion is based on a review of just 65 patients from internal medicine and family practice clinics near the medical center, but “I do think this [pattern] is representative of what we are seeing in every primary care office. This has been a problem [documented] in the literature for a decade, and it remains a problem,” said lead investigator Stephen Eikermann, DO, an internal medicine resident at the center.
Meanwhile, of those diagnosed by spirometry, 32% didn’t meet the gold-standard Global Initiative for Chronic Obstructive Lung Disease (GOLD) diagnostic criteria by having a postbronchodilator forced expiratory volume in 1 second/forced vital capacity (FEV1/FVC) of less than 70%. Clinicians might not have known that postbronchodilator values are the ones that matter. “People who have asthma are being tagged as having COPD,” and once that diagnosis is in the chart, it’s hard to remove, even when patients improve. “With the COPD readmission penalty in place, an erroneous diagnosis of COPD [has] significant financial risks,” Dr. Eikermann said.
“Misdiagnosis leads to significant financial consequences and puts patients at risk for osteoporotic fractures and malignant arrhythmias. It’s a problem of education.” Busy practitioners might not have had time to catch the latest 2015 GOLD standards, he said.
The guidelines state that COPD should be considered in any patient who has dyspnea, chronic cough, or sputum production, plus smoking or other risks. “Spirometry is required to make the diagnosis.”
To help, Dr. Eikermann and his colleagues plan lectures and a quick reference handout, and maybe a smartphone app. They also plan to remind practitioners that Medicare pays at a reasonable rate for spirometry.
The 65 patients in the study were about evenly split between men and women, and were 70 years old, on average. They had about 34 pack-years of smoking, and some were still smoking despite being on home oxygen.
Men were less likely to have spirometry than women; older subjects and current smokers – as opposed to former smokers – were, too. The risk of COPD increases with age and smoking, so the finding was puzzling. For unknown reasons, “there appears to be a bias against ordering spirometry” for some patients, Dr. Eikermann said.
There was no outside funding for the work, and the investigators had no disclosures.
LOS ANGELES – Spirometry is the standard for diagnosing chronic obstructive pulmonary disease, but it’s underused and misused in primary care, according to investigators from the Corpus Christi (Tex.) Medical Center.
The conclusion is based on a review of just 65 patients from internal medicine and family practice clinics near the medical center, but “I do think this [pattern] is representative of what we are seeing in every primary care office. This has been a problem [documented] in the literature for a decade, and it remains a problem,” said lead investigator Stephen Eikermann, DO, an internal medicine resident at the center.
Meanwhile, of those diagnosed by spirometry, 32% didn’t meet the gold-standard Global Initiative for Chronic Obstructive Lung Disease (GOLD) diagnostic criteria by having a postbronchodilator forced expiratory volume in 1 second/forced vital capacity (FEV1/FVC) of less than 70%. Clinicians might not have known that postbronchodilator values are the ones that matter. “People who have asthma are being tagged as having COPD,” and once that diagnosis is in the chart, it’s hard to remove, even when patients improve. “With the COPD readmission penalty in place, an erroneous diagnosis of COPD [has] significant financial risks,” Dr. Eikermann said.
“Misdiagnosis leads to significant financial consequences and puts patients at risk for osteoporotic fractures and malignant arrhythmias. It’s a problem of education.” Busy practitioners might not have had time to catch the latest 2015 GOLD standards, he said.
The guidelines state that COPD should be considered in any patient who has dyspnea, chronic cough, or sputum production, plus smoking or other risks. “Spirometry is required to make the diagnosis.”
To help, Dr. Eikermann and his colleagues plan lectures and a quick reference handout, and maybe a smartphone app. They also plan to remind practitioners that Medicare pays at a reasonable rate for spirometry.
The 65 patients in the study were about evenly split between men and women, and were 70 years old, on average. They had about 34 pack-years of smoking, and some were still smoking despite being on home oxygen.
Men were less likely to have spirometry than women; older subjects and current smokers – as opposed to former smokers – were, too. The risk of COPD increases with age and smoking, so the finding was puzzling. For unknown reasons, “there appears to be a bias against ordering spirometry” for some patients, Dr. Eikermann said.
There was no outside funding for the work, and the investigators had no disclosures.
LOS ANGELES – Spirometry is the standard for diagnosing chronic obstructive pulmonary disease, but it’s underused and misused in primary care, according to investigators from the Corpus Christi (Tex.) Medical Center.
The conclusion is based on a review of just 65 patients from internal medicine and family practice clinics near the medical center, but “I do think this [pattern] is representative of what we are seeing in every primary care office. This has been a problem [documented] in the literature for a decade, and it remains a problem,” said lead investigator Stephen Eikermann, DO, an internal medicine resident at the center.
Meanwhile, of those diagnosed by spirometry, 32% didn’t meet the gold-standard Global Initiative for Chronic Obstructive Lung Disease (GOLD) diagnostic criteria by having a postbronchodilator forced expiratory volume in 1 second/forced vital capacity (FEV1/FVC) of less than 70%. Clinicians might not have known that postbronchodilator values are the ones that matter. “People who have asthma are being tagged as having COPD,” and once that diagnosis is in the chart, it’s hard to remove, even when patients improve. “With the COPD readmission penalty in place, an erroneous diagnosis of COPD [has] significant financial risks,” Dr. Eikermann said.
“Misdiagnosis leads to significant financial consequences and puts patients at risk for osteoporotic fractures and malignant arrhythmias. It’s a problem of education.” Busy practitioners might not have had time to catch the latest 2015 GOLD standards, he said.
The guidelines state that COPD should be considered in any patient who has dyspnea, chronic cough, or sputum production, plus smoking or other risks. “Spirometry is required to make the diagnosis.”
To help, Dr. Eikermann and his colleagues plan lectures and a quick reference handout, and maybe a smartphone app. They also plan to remind practitioners that Medicare pays at a reasonable rate for spirometry.
The 65 patients in the study were about evenly split between men and women, and were 70 years old, on average. They had about 34 pack-years of smoking, and some were still smoking despite being on home oxygen.
Men were less likely to have spirometry than women; older subjects and current smokers – as opposed to former smokers – were, too. The risk of COPD increases with age and smoking, so the finding was puzzling. For unknown reasons, “there appears to be a bias against ordering spirometry” for some patients, Dr. Eikermann said.
There was no outside funding for the work, and the investigators had no disclosures.
Key clinical point:
Major finding: Only 29% of patients diagnosed with chronic obstructive pulmonary disease (COPD) at two clinics underwent spirometry. Of those diagnosed by spirometry, 32% didn’t meet the gold-standard Global Initiative for Chronic Obstructive Lung Disease (GOLD) diagnostic criteria by having a postbronchodilator FEV1/FVC of less than 70%.
Data source: Review of 65 COPD cases treated at two primary care clinics.
Disclosures: There was no outside funding for the work, and the investigators had no disclosures.
Lung cancer screening found effective in a community hospital
LOS ANGELES – Lung cancer screening with low-dose CT scans in a community hospital setting replicates results from international and multicenter trials when it comes to diagnosing early-stage lung cancer, findings from a single-center study showed.
“It’s too early in our experience to say that we’re saving lives, but the fact that we’re detecting early lung cancers in the predicted percentages is good for community hospitals that are wondering, ‘Is it worth it to screen for lung cancer? Can we do it?’ ” Richard P. Salzano Jr., MD, said in an interview in advance of the annual meeting of the American College of Chest Physicians.
In July 2013, the 130-bed Griffin Hospital launched a lung cancer screening program codirected by a pulmonologist and a cardiothoracic surgeon. All low-dose CT scans were read by two designated radiologists. Dr. Salzano reported results from 514 patients enrolled in the program between July 2013 and December 2015. A total of nine lung cancers were detected. Seven (78%) were stage I or II lung cancers, and the remaining two (22%) were stage II or IV, results that are in line with data from the I-ELCAP and NLST trials.
In another component of the study, the researchers randomly selected 101 patients from the lung cancer screening program to answer questions by telephone intended to quantify their anxiety about lung cancer before and after participating in the program, attitudes about smoking behaviors, and general impressions of the screening process. On a scale of 0-10, with 10 being “very anxious,” Dr. Salzano reported that the mean anxiety level about lung cancer fell from a level of 4.69 before screening to 3.87 afterward, a difference that reached statistical significance, with a P value of .014. “None of the patients reported negative impacts of the program,” he added. “They reported a general improvement in their well-being as a result of participating in the program.” In addition, of the 53 respondents who were current smokers upon enrolling in the screening program, five quit after intake, and the remaining 48 indicated that they were “more likely to quit” as a result of being enrolled.
“Community hospitals need to embrace lung screening,” Dr. Salzano concluded. “The findings from the large studies are transferable. It’s helping your patients in terms of their attitudes about lung cancer, about smoking cessation, and about improving their wellness.”
He reported having no relevant financial disclosures.
LOS ANGELES – Lung cancer screening with low-dose CT scans in a community hospital setting replicates results from international and multicenter trials when it comes to diagnosing early-stage lung cancer, findings from a single-center study showed.
“It’s too early in our experience to say that we’re saving lives, but the fact that we’re detecting early lung cancers in the predicted percentages is good for community hospitals that are wondering, ‘Is it worth it to screen for lung cancer? Can we do it?’ ” Richard P. Salzano Jr., MD, said in an interview in advance of the annual meeting of the American College of Chest Physicians.
In July 2013, the 130-bed Griffin Hospital launched a lung cancer screening program codirected by a pulmonologist and a cardiothoracic surgeon. All low-dose CT scans were read by two designated radiologists. Dr. Salzano reported results from 514 patients enrolled in the program between July 2013 and December 2015. A total of nine lung cancers were detected. Seven (78%) were stage I or II lung cancers, and the remaining two (22%) were stage II or IV, results that are in line with data from the I-ELCAP and NLST trials.
In another component of the study, the researchers randomly selected 101 patients from the lung cancer screening program to answer questions by telephone intended to quantify their anxiety about lung cancer before and after participating in the program, attitudes about smoking behaviors, and general impressions of the screening process. On a scale of 0-10, with 10 being “very anxious,” Dr. Salzano reported that the mean anxiety level about lung cancer fell from a level of 4.69 before screening to 3.87 afterward, a difference that reached statistical significance, with a P value of .014. “None of the patients reported negative impacts of the program,” he added. “They reported a general improvement in their well-being as a result of participating in the program.” In addition, of the 53 respondents who were current smokers upon enrolling in the screening program, five quit after intake, and the remaining 48 indicated that they were “more likely to quit” as a result of being enrolled.
“Community hospitals need to embrace lung screening,” Dr. Salzano concluded. “The findings from the large studies are transferable. It’s helping your patients in terms of their attitudes about lung cancer, about smoking cessation, and about improving their wellness.”
He reported having no relevant financial disclosures.
LOS ANGELES – Lung cancer screening with low-dose CT scans in a community hospital setting replicates results from international and multicenter trials when it comes to diagnosing early-stage lung cancer, findings from a single-center study showed.
“It’s too early in our experience to say that we’re saving lives, but the fact that we’re detecting early lung cancers in the predicted percentages is good for community hospitals that are wondering, ‘Is it worth it to screen for lung cancer? Can we do it?’ ” Richard P. Salzano Jr., MD, said in an interview in advance of the annual meeting of the American College of Chest Physicians.
In July 2013, the 130-bed Griffin Hospital launched a lung cancer screening program codirected by a pulmonologist and a cardiothoracic surgeon. All low-dose CT scans were read by two designated radiologists. Dr. Salzano reported results from 514 patients enrolled in the program between July 2013 and December 2015. A total of nine lung cancers were detected. Seven (78%) were stage I or II lung cancers, and the remaining two (22%) were stage II or IV, results that are in line with data from the I-ELCAP and NLST trials.
In another component of the study, the researchers randomly selected 101 patients from the lung cancer screening program to answer questions by telephone intended to quantify their anxiety about lung cancer before and after participating in the program, attitudes about smoking behaviors, and general impressions of the screening process. On a scale of 0-10, with 10 being “very anxious,” Dr. Salzano reported that the mean anxiety level about lung cancer fell from a level of 4.69 before screening to 3.87 afterward, a difference that reached statistical significance, with a P value of .014. “None of the patients reported negative impacts of the program,” he added. “They reported a general improvement in their well-being as a result of participating in the program.” In addition, of the 53 respondents who were current smokers upon enrolling in the screening program, five quit after intake, and the remaining 48 indicated that they were “more likely to quit” as a result of being enrolled.
“Community hospitals need to embrace lung screening,” Dr. Salzano concluded. “The findings from the large studies are transferable. It’s helping your patients in terms of their attitudes about lung cancer, about smoking cessation, and about improving their wellness.”
He reported having no relevant financial disclosures.
AT CHEST 2016
Key clinical point:
Major finding: Of nine lung cancers detected, seven (78%) were stage I or II lung cancers and the remaining two (22%) were stage II or IV.
Data source: Results from 514 patients enrolled in a community hospital–based lung cancer screening program between July 2013 and December 2015.
Disclosures: Dr. Salzano reported having no relevant financial disclosures.
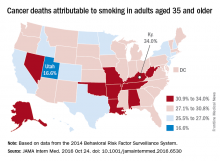
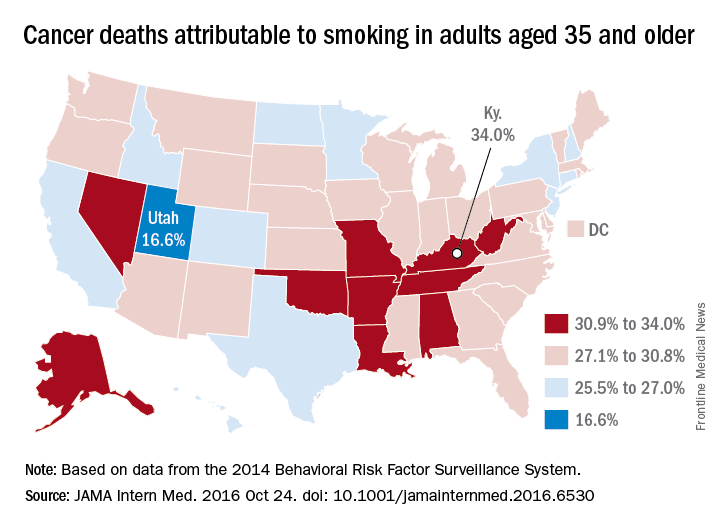
Smoking-attributable cancer mortality highest in Kentucky
Almost 29% of cancer deaths among U.S. adults aged 35 years and older were attributable to cigarette smoking in 2014, according to investigators from the American Cancer Society.
Of the 585,000 cancer deaths among those 35 years and older that year, more than 167,000 (28.6%) were estimated to be the result of cigarette smoking, reported Joannie Lortet-Tieulent, MSc, and her associates at the ACS in Atlanta (JAMA Intern Med. 2016 Oct 24. doi: 10.1001/jamainternmed.2016.6530).
Among men aged 35 years and older, 33.7% of U.S. cancer deaths were attributable to cigarette smoking, compared with 22.9% for women. Arkansas had the highest rate (39.5%) for men and Kentucky had the highest rate (29.0%) for women. Not surprisingly, Utah had the lowest rate for both men (21.8%) and women (11.1%), according to the analysis of data from the 2014 Behavioral Risk Factor Surveillance System. For men, Utah was the only state with a rate below 30%.
The investigators did not report any conflicts of interest. The study was supported by the intramural research department of the American Cancer Society.
Almost 29% of cancer deaths among U.S. adults aged 35 years and older were attributable to cigarette smoking in 2014, according to investigators from the American Cancer Society.
Of the 585,000 cancer deaths among those 35 years and older that year, more than 167,000 (28.6%) were estimated to be the result of cigarette smoking, reported Joannie Lortet-Tieulent, MSc, and her associates at the ACS in Atlanta (JAMA Intern Med. 2016 Oct 24. doi: 10.1001/jamainternmed.2016.6530).
Among men aged 35 years and older, 33.7% of U.S. cancer deaths were attributable to cigarette smoking, compared with 22.9% for women. Arkansas had the highest rate (39.5%) for men and Kentucky had the highest rate (29.0%) for women. Not surprisingly, Utah had the lowest rate for both men (21.8%) and women (11.1%), according to the analysis of data from the 2014 Behavioral Risk Factor Surveillance System. For men, Utah was the only state with a rate below 30%.
The investigators did not report any conflicts of interest. The study was supported by the intramural research department of the American Cancer Society.
Almost 29% of cancer deaths among U.S. adults aged 35 years and older were attributable to cigarette smoking in 2014, according to investigators from the American Cancer Society.
Of the 585,000 cancer deaths among those 35 years and older that year, more than 167,000 (28.6%) were estimated to be the result of cigarette smoking, reported Joannie Lortet-Tieulent, MSc, and her associates at the ACS in Atlanta (JAMA Intern Med. 2016 Oct 24. doi: 10.1001/jamainternmed.2016.6530).
Among men aged 35 years and older, 33.7% of U.S. cancer deaths were attributable to cigarette smoking, compared with 22.9% for women. Arkansas had the highest rate (39.5%) for men and Kentucky had the highest rate (29.0%) for women. Not surprisingly, Utah had the lowest rate for both men (21.8%) and women (11.1%), according to the analysis of data from the 2014 Behavioral Risk Factor Surveillance System. For men, Utah was the only state with a rate below 30%.
The investigators did not report any conflicts of interest. The study was supported by the intramural research department of the American Cancer Society.
COPD: Diagnostic and Treatment Update for the Primary Care Setting
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Smokers’ hand grip strength predicts risk for respiratory events
LOS ANGELES – Hand grip strength is independently predictive of risk for respiratory events in smokers who have or are at risk for chronic obstructive pulmonary disease, results from a single-center study showed.
“Measures of lung function, including spirometry, are used as the main descriptors of COPD severity and prognosis,” Carlos H. Martinez, MD, MPH, said in an interview in advance of the annual meeting of the American College of Chest Physicians. “These measurements, as important as they are, need to be improved, in order to develop better risk and prognostic models of the disease, to identify subgroups at higher risk of poor outcomes ... With our work, we have proved that simple physical tests could be part of future prognostic models.”
Interest has grown in developing multidimensional models to predict respiratory prognosis. Such models include BODE (body mass index, airflow obstruction, dyspnea and exercise capacity), ADO (age, dyspnea and airflow obstruction), and DOSE (dyspnea, airflow obstruction, smoking status, and exacerbation frequency).
In patients with or at risk for COPD, Dr. Martinez, of the University of Michigan Health System, Ann Arbor, and his colleagues tested the associations of hand grip strength with measures of body composition such as pectoralis muscle area and extent of subcutaneous fat, imaging phenotypes, and lung function.
The researchers obtained demographic, clinical, lung function, hand grip strength, and imaging data from 441 smokers with and without COPD participating in the Genetic Epidemiology of COPD Study (COPDGene) at the National Jewish Health in Denver. Imaging methods used in the study were developed by George R. Washko, MD, and his associates at Brigham and Women’s Hospital, Boston, to evaluate patients’ body composition, including chest CTs to obtain measures of airway thickness, emphysema percentage, pectoralis muscle area, and subcutaneous adipose tissue area.
Correlations between measures of lung function, imaging phenotypes, body composition, and hand grip strength were analyzed in univariate analysis and in multivariate linear models. The association between hand grip strength and exacerbations was analyzed at enrollment and during an average follow-up of 2.6 years.
Hand grip strength was similar across groups categorized by spirometry severity and was not associated with emphysema severity.
After adjustment for demographics, smoking history, smoking intensity, comorbidities and lung imaging phenotypes, however, grip strength was associated with pectoralis muscle area (increase of 3.9 kg per one standard deviation of pectoral muscle area) and subcutaneous adipose tissue (a decrement of 5.1 kg per one standard deviation of subcutaneous adipose tissue). These associations were independent of body mass index and the presence of emphysema.
During follow-up, hand grip strength was associated with exacerbations (risk ratio 0.94 per one kg increment on grip strength) and incident exacerbations (incident risk ratio 0.92 per one kg increment on grip strength) in models adjusted for other factors known to be associated with exacerbations.
Research in body composition has mostly relied on dual absorptiometry and bioelectrical impedance, tools not routinely used in clinical practice, Dr. Martinez said. “We were surprised by the ability to show similar results using imaging data that are available from regular chest CTs.”
“We have confirmed prior hypotheses that it is not just weight or BMI that matters (to risk of exacerbations), but how much muscle and how much fat are contributing to our patient’s high or low BMI,” Dr. Martinez said.
Hand grip testing can be challenging in this patient population, he said. Still, “asking relevant questions about (patients’) physical fitness will help us to understand better our patients’ needs. We can also give more attention to the extrapulmonary structures included in the numerous chest CT scans that we order for our patients. These imaging studies, besides the information that they provide about parenchymal and mediastinal structures, include important and easy to discover clues to identify patients at higher risk of exacerbations – those with low muscle and low hand grip could benefit from close follow-up.”
Dr. Martinez acknowledged certain limitations of the study, including the selection of the measures of body composition. “We used analysis of chest CTs, instead of the gold standard of dual absorptiometry (DXA) or other methods such as bioelectrical impedance,” he said. “A final limitation is that we tested a selected group of participants in a cohort study, not a representative sample of the population, [with a] low burden of emphysema and fewer African American participants.”
Dr. Martinez disclosed that his work is supported by the National Institutes of Health and that COPDGene also receives NIH funding. He acknowledged the support and effort of all COPDGene investigators and participants.
LOS ANGELES – Hand grip strength is independently predictive of risk for respiratory events in smokers who have or are at risk for chronic obstructive pulmonary disease, results from a single-center study showed.
“Measures of lung function, including spirometry, are used as the main descriptors of COPD severity and prognosis,” Carlos H. Martinez, MD, MPH, said in an interview in advance of the annual meeting of the American College of Chest Physicians. “These measurements, as important as they are, need to be improved, in order to develop better risk and prognostic models of the disease, to identify subgroups at higher risk of poor outcomes ... With our work, we have proved that simple physical tests could be part of future prognostic models.”
Interest has grown in developing multidimensional models to predict respiratory prognosis. Such models include BODE (body mass index, airflow obstruction, dyspnea and exercise capacity), ADO (age, dyspnea and airflow obstruction), and DOSE (dyspnea, airflow obstruction, smoking status, and exacerbation frequency).
In patients with or at risk for COPD, Dr. Martinez, of the University of Michigan Health System, Ann Arbor, and his colleagues tested the associations of hand grip strength with measures of body composition such as pectoralis muscle area and extent of subcutaneous fat, imaging phenotypes, and lung function.
The researchers obtained demographic, clinical, lung function, hand grip strength, and imaging data from 441 smokers with and without COPD participating in the Genetic Epidemiology of COPD Study (COPDGene) at the National Jewish Health in Denver. Imaging methods used in the study were developed by George R. Washko, MD, and his associates at Brigham and Women’s Hospital, Boston, to evaluate patients’ body composition, including chest CTs to obtain measures of airway thickness, emphysema percentage, pectoralis muscle area, and subcutaneous adipose tissue area.
Correlations between measures of lung function, imaging phenotypes, body composition, and hand grip strength were analyzed in univariate analysis and in multivariate linear models. The association between hand grip strength and exacerbations was analyzed at enrollment and during an average follow-up of 2.6 years.
Hand grip strength was similar across groups categorized by spirometry severity and was not associated with emphysema severity.
After adjustment for demographics, smoking history, smoking intensity, comorbidities and lung imaging phenotypes, however, grip strength was associated with pectoralis muscle area (increase of 3.9 kg per one standard deviation of pectoral muscle area) and subcutaneous adipose tissue (a decrement of 5.1 kg per one standard deviation of subcutaneous adipose tissue). These associations were independent of body mass index and the presence of emphysema.
During follow-up, hand grip strength was associated with exacerbations (risk ratio 0.94 per one kg increment on grip strength) and incident exacerbations (incident risk ratio 0.92 per one kg increment on grip strength) in models adjusted for other factors known to be associated with exacerbations.
Research in body composition has mostly relied on dual absorptiometry and bioelectrical impedance, tools not routinely used in clinical practice, Dr. Martinez said. “We were surprised by the ability to show similar results using imaging data that are available from regular chest CTs.”
“We have confirmed prior hypotheses that it is not just weight or BMI that matters (to risk of exacerbations), but how much muscle and how much fat are contributing to our patient’s high or low BMI,” Dr. Martinez said.
Hand grip testing can be challenging in this patient population, he said. Still, “asking relevant questions about (patients’) physical fitness will help us to understand better our patients’ needs. We can also give more attention to the extrapulmonary structures included in the numerous chest CT scans that we order for our patients. These imaging studies, besides the information that they provide about parenchymal and mediastinal structures, include important and easy to discover clues to identify patients at higher risk of exacerbations – those with low muscle and low hand grip could benefit from close follow-up.”
Dr. Martinez acknowledged certain limitations of the study, including the selection of the measures of body composition. “We used analysis of chest CTs, instead of the gold standard of dual absorptiometry (DXA) or other methods such as bioelectrical impedance,” he said. “A final limitation is that we tested a selected group of participants in a cohort study, not a representative sample of the population, [with a] low burden of emphysema and fewer African American participants.”
Dr. Martinez disclosed that his work is supported by the National Institutes of Health and that COPDGene also receives NIH funding. He acknowledged the support and effort of all COPDGene investigators and participants.
LOS ANGELES – Hand grip strength is independently predictive of risk for respiratory events in smokers who have or are at risk for chronic obstructive pulmonary disease, results from a single-center study showed.
“Measures of lung function, including spirometry, are used as the main descriptors of COPD severity and prognosis,” Carlos H. Martinez, MD, MPH, said in an interview in advance of the annual meeting of the American College of Chest Physicians. “These measurements, as important as they are, need to be improved, in order to develop better risk and prognostic models of the disease, to identify subgroups at higher risk of poor outcomes ... With our work, we have proved that simple physical tests could be part of future prognostic models.”
Interest has grown in developing multidimensional models to predict respiratory prognosis. Such models include BODE (body mass index, airflow obstruction, dyspnea and exercise capacity), ADO (age, dyspnea and airflow obstruction), and DOSE (dyspnea, airflow obstruction, smoking status, and exacerbation frequency).
In patients with or at risk for COPD, Dr. Martinez, of the University of Michigan Health System, Ann Arbor, and his colleagues tested the associations of hand grip strength with measures of body composition such as pectoralis muscle area and extent of subcutaneous fat, imaging phenotypes, and lung function.
The researchers obtained demographic, clinical, lung function, hand grip strength, and imaging data from 441 smokers with and without COPD participating in the Genetic Epidemiology of COPD Study (COPDGene) at the National Jewish Health in Denver. Imaging methods used in the study were developed by George R. Washko, MD, and his associates at Brigham and Women’s Hospital, Boston, to evaluate patients’ body composition, including chest CTs to obtain measures of airway thickness, emphysema percentage, pectoralis muscle area, and subcutaneous adipose tissue area.
Correlations between measures of lung function, imaging phenotypes, body composition, and hand grip strength were analyzed in univariate analysis and in multivariate linear models. The association between hand grip strength and exacerbations was analyzed at enrollment and during an average follow-up of 2.6 years.
Hand grip strength was similar across groups categorized by spirometry severity and was not associated with emphysema severity.
After adjustment for demographics, smoking history, smoking intensity, comorbidities and lung imaging phenotypes, however, grip strength was associated with pectoralis muscle area (increase of 3.9 kg per one standard deviation of pectoral muscle area) and subcutaneous adipose tissue (a decrement of 5.1 kg per one standard deviation of subcutaneous adipose tissue). These associations were independent of body mass index and the presence of emphysema.
During follow-up, hand grip strength was associated with exacerbations (risk ratio 0.94 per one kg increment on grip strength) and incident exacerbations (incident risk ratio 0.92 per one kg increment on grip strength) in models adjusted for other factors known to be associated with exacerbations.
Research in body composition has mostly relied on dual absorptiometry and bioelectrical impedance, tools not routinely used in clinical practice, Dr. Martinez said. “We were surprised by the ability to show similar results using imaging data that are available from regular chest CTs.”
“We have confirmed prior hypotheses that it is not just weight or BMI that matters (to risk of exacerbations), but how much muscle and how much fat are contributing to our patient’s high or low BMI,” Dr. Martinez said.
Hand grip testing can be challenging in this patient population, he said. Still, “asking relevant questions about (patients’) physical fitness will help us to understand better our patients’ needs. We can also give more attention to the extrapulmonary structures included in the numerous chest CT scans that we order for our patients. These imaging studies, besides the information that they provide about parenchymal and mediastinal structures, include important and easy to discover clues to identify patients at higher risk of exacerbations – those with low muscle and low hand grip could benefit from close follow-up.”
Dr. Martinez acknowledged certain limitations of the study, including the selection of the measures of body composition. “We used analysis of chest CTs, instead of the gold standard of dual absorptiometry (DXA) or other methods such as bioelectrical impedance,” he said. “A final limitation is that we tested a selected group of participants in a cohort study, not a representative sample of the population, [with a] low burden of emphysema and fewer African American participants.”
Dr. Martinez disclosed that his work is supported by the National Institutes of Health and that COPDGene also receives NIH funding. He acknowledged the support and effort of all COPDGene investigators and participants.
AT CHEST 2016
Key clinical point:
Major finding: During an average follow-up of 2.6 years, hand grip strength was associated with cross-sectional exacerbations (risk ratio 0.94 per one kg increment on grip strength) and incident exacerbations (incident risk ratio 0.92 per one kg increment on grip strength).
Data source: Data from 441 smokers with and without COPD participating in the Genetic Epidemiology of COPD Study (COPDGene) at National Jewish Health in Denver.
Disclosures: Dr. Martinez disclosed that his work is supported by the National Institutes of Health and that COPDGene also receives NIH funding.
Chest physician perceptions of e-cigarettes mixed
AT CHEST 2016
LOS ANGELES – Chest physicians in the United States are likely to encounter electronic cigarette users in clinical practice, yet there is no consensus regarding how to advise them, results from a survey suggest.
“There is controversy in the community of physicians we surveyed on whether e-cigarettes would be useful for smoking cessation and whether they can reduce harm from tobacco smoking,” lead study author Stephen R. Baldassarri, MD, said in an interview in advance of the annual meeting of the American College of Chest Physicians. “Our results suggest that we need more high quality scientific data regarding potential harms and benefits of e-cigarettes in order to inform both health professionals and the general public.”
When asked if ECs promote tobacco cessation, respondents were split (33% agreed or strongly agreed while 32% disagreed or strongly disagreed); only 13% believed that ECs were at least as effective as Food and Drug Administration–approved treatments to promote smoking cessation, and 11% reported that ECs should be used in an initial quit attempt. Dr. Baldassarri also reported that 6% of respondents thought ECs are more harmful than smoking, 21% thought switching from daily tobacco smoking to EC use would improve a patient’s health, and 55% reported feeling comfortable discussing health effects of ECs with their patients.
“In light of the fact that the long-term health risks of ECs remain unknown, we were surprised to find that more than half of the survey respondents reported feeling comfortable discussing health effects of ECs,” Dr. Baldassarri commented. “This proportion was higher than we expected given the current state of the scientific evidence.”
He acknowledged certain limitations of the survey, including its low response rate, “which limits the degree to which we can generalize our findings to account for the perceptions of all chest physicians,” he said. “We surveyed providers only within CHEST, and opinions and experiences of physicians outside of the organization and in other specialties may vary. And finally, since knowledge regarding e-cigarettes is rapidly evolving, the perceptions and opinions here are likely subject to change over the next few years as more becomes known.”
Dr. Baldassarri reported having no financial disclosures.
AT CHEST 2016
LOS ANGELES – Chest physicians in the United States are likely to encounter electronic cigarette users in clinical practice, yet there is no consensus regarding how to advise them, results from a survey suggest.
“There is controversy in the community of physicians we surveyed on whether e-cigarettes would be useful for smoking cessation and whether they can reduce harm from tobacco smoking,” lead study author Stephen R. Baldassarri, MD, said in an interview in advance of the annual meeting of the American College of Chest Physicians. “Our results suggest that we need more high quality scientific data regarding potential harms and benefits of e-cigarettes in order to inform both health professionals and the general public.”
When asked if ECs promote tobacco cessation, respondents were split (33% agreed or strongly agreed while 32% disagreed or strongly disagreed); only 13% believed that ECs were at least as effective as Food and Drug Administration–approved treatments to promote smoking cessation, and 11% reported that ECs should be used in an initial quit attempt. Dr. Baldassarri also reported that 6% of respondents thought ECs are more harmful than smoking, 21% thought switching from daily tobacco smoking to EC use would improve a patient’s health, and 55% reported feeling comfortable discussing health effects of ECs with their patients.
“In light of the fact that the long-term health risks of ECs remain unknown, we were surprised to find that more than half of the survey respondents reported feeling comfortable discussing health effects of ECs,” Dr. Baldassarri commented. “This proportion was higher than we expected given the current state of the scientific evidence.”
He acknowledged certain limitations of the survey, including its low response rate, “which limits the degree to which we can generalize our findings to account for the perceptions of all chest physicians,” he said. “We surveyed providers only within CHEST, and opinions and experiences of physicians outside of the organization and in other specialties may vary. And finally, since knowledge regarding e-cigarettes is rapidly evolving, the perceptions and opinions here are likely subject to change over the next few years as more becomes known.”
Dr. Baldassarri reported having no financial disclosures.
AT CHEST 2016
LOS ANGELES – Chest physicians in the United States are likely to encounter electronic cigarette users in clinical practice, yet there is no consensus regarding how to advise them, results from a survey suggest.
“There is controversy in the community of physicians we surveyed on whether e-cigarettes would be useful for smoking cessation and whether they can reduce harm from tobacco smoking,” lead study author Stephen R. Baldassarri, MD, said in an interview in advance of the annual meeting of the American College of Chest Physicians. “Our results suggest that we need more high quality scientific data regarding potential harms and benefits of e-cigarettes in order to inform both health professionals and the general public.”
When asked if ECs promote tobacco cessation, respondents were split (33% agreed or strongly agreed while 32% disagreed or strongly disagreed); only 13% believed that ECs were at least as effective as Food and Drug Administration–approved treatments to promote smoking cessation, and 11% reported that ECs should be used in an initial quit attempt. Dr. Baldassarri also reported that 6% of respondents thought ECs are more harmful than smoking, 21% thought switching from daily tobacco smoking to EC use would improve a patient’s health, and 55% reported feeling comfortable discussing health effects of ECs with their patients.
“In light of the fact that the long-term health risks of ECs remain unknown, we were surprised to find that more than half of the survey respondents reported feeling comfortable discussing health effects of ECs,” Dr. Baldassarri commented. “This proportion was higher than we expected given the current state of the scientific evidence.”
He acknowledged certain limitations of the survey, including its low response rate, “which limits the degree to which we can generalize our findings to account for the perceptions of all chest physicians,” he said. “We surveyed providers only within CHEST, and opinions and experiences of physicians outside of the organization and in other specialties may vary. And finally, since knowledge regarding e-cigarettes is rapidly evolving, the perceptions and opinions here are likely subject to change over the next few years as more becomes known.”
Dr. Baldassarri reported having no financial disclosures.
Key clinical point:
Major finding: When asked if electronic cigarettes (ECs) promote tobacco cessation, respondents were split (33% agreed or strongly agreed, while 32% disagreed or strongly disagreed).
Data source: Responses from 994 members of the American College of Chest Physicians who completed a brief online questionnaire about practice patterns and perceptions regarding EC use and tobacco smoking among their patients.
Disclosures: Dr. Baldassarri reported having no financial disclosures.
High resting heart rate may signal exacerbation risk in COPD patients
LOS ANGELES – Higher resting heart rate may predict future risk of exacerbation in patients with recent chronic obstructive pulmonary disease (COPD) exacerbation, results from a multicenter study suggest.
“Resting heart [rate] is often a readily available clinical data,” lead study author Ahmad Ismail, MD, said in an interview in advance of the annual meeting of the American College of Chest Physicians. “Its significance is often overlooked in daily clinical practice until tachycardia or bradycardia happens. In COPD patients, it has been shown that the resting heart rate can predict mortality. However, there is a lack of data showing its association with the rates of exacerbations, the major player in determining overall outcome in patients with COPD.”
The mean age of the study population was 67 years, and 77% of them had higher resting heart rates, defined as one that exceeded 80 beats per minute (BPM). The mean resting heart rate in the higher resting heart rate group was 92, compared with a mean of 70 BPM in the lower resting heart rate group. Dr. Ismail reported that at month 3, patients with higher resting heart rates had significantly higher proportion of exacerbations, compared with those who had a lower resting heart rates (54% vs. 27%; P = .013). The trend was followed through until month 9. There was also a statistically significant moderate strength linear correlation between resting heart rate and exacerbation frequency at 3, 6, and 9 months (r = 0.400; P less than .001: r = 0.440; P less than .001: and r = 0.416; P = .004, respectively). The mean exacerbation frequency was also significantly higher in the higher resting heart rate group at month 3 and month 6 (2.00 vs. 0.48; P less than .001: and 3.42 vs. 1.14; P = .004).
“Higher resting heart rate may predict future risk of exacerbation in patients with recent COPD exacerbation,” Dr. Ismail concluded. “Further study however is required to determine the effect of lowering resting heart rate on the future risk of exacerbation.” He acknowledged certain limitations of the study, including the fact that it excluded patients who were on beta-blockers or any rate-modifying drugs, and those with history of cardiac failure and ischemic heart disease, and that there was no baseline echocardiogram performed to ensure the absence of ischemic heart disease and other possible causes of the higher resting heart rates. “We also had slightly higher than expected dropouts giving a nonsignificant result at 12 months follow-up, though the trend follows the overall results of the study,” he said.
The study was funded by a grant from the Malaysian Thoracic Society. Dr. Ismail reported having no financial disclosures.
LOS ANGELES – Higher resting heart rate may predict future risk of exacerbation in patients with recent chronic obstructive pulmonary disease (COPD) exacerbation, results from a multicenter study suggest.
“Resting heart [rate] is often a readily available clinical data,” lead study author Ahmad Ismail, MD, said in an interview in advance of the annual meeting of the American College of Chest Physicians. “Its significance is often overlooked in daily clinical practice until tachycardia or bradycardia happens. In COPD patients, it has been shown that the resting heart rate can predict mortality. However, there is a lack of data showing its association with the rates of exacerbations, the major player in determining overall outcome in patients with COPD.”
The mean age of the study population was 67 years, and 77% of them had higher resting heart rates, defined as one that exceeded 80 beats per minute (BPM). The mean resting heart rate in the higher resting heart rate group was 92, compared with a mean of 70 BPM in the lower resting heart rate group. Dr. Ismail reported that at month 3, patients with higher resting heart rates had significantly higher proportion of exacerbations, compared with those who had a lower resting heart rates (54% vs. 27%; P = .013). The trend was followed through until month 9. There was also a statistically significant moderate strength linear correlation between resting heart rate and exacerbation frequency at 3, 6, and 9 months (r = 0.400; P less than .001: r = 0.440; P less than .001: and r = 0.416; P = .004, respectively). The mean exacerbation frequency was also significantly higher in the higher resting heart rate group at month 3 and month 6 (2.00 vs. 0.48; P less than .001: and 3.42 vs. 1.14; P = .004).
“Higher resting heart rate may predict future risk of exacerbation in patients with recent COPD exacerbation,” Dr. Ismail concluded. “Further study however is required to determine the effect of lowering resting heart rate on the future risk of exacerbation.” He acknowledged certain limitations of the study, including the fact that it excluded patients who were on beta-blockers or any rate-modifying drugs, and those with history of cardiac failure and ischemic heart disease, and that there was no baseline echocardiogram performed to ensure the absence of ischemic heart disease and other possible causes of the higher resting heart rates. “We also had slightly higher than expected dropouts giving a nonsignificant result at 12 months follow-up, though the trend follows the overall results of the study,” he said.
The study was funded by a grant from the Malaysian Thoracic Society. Dr. Ismail reported having no financial disclosures.
LOS ANGELES – Higher resting heart rate may predict future risk of exacerbation in patients with recent chronic obstructive pulmonary disease (COPD) exacerbation, results from a multicenter study suggest.
“Resting heart [rate] is often a readily available clinical data,” lead study author Ahmad Ismail, MD, said in an interview in advance of the annual meeting of the American College of Chest Physicians. “Its significance is often overlooked in daily clinical practice until tachycardia or bradycardia happens. In COPD patients, it has been shown that the resting heart rate can predict mortality. However, there is a lack of data showing its association with the rates of exacerbations, the major player in determining overall outcome in patients with COPD.”
The mean age of the study population was 67 years, and 77% of them had higher resting heart rates, defined as one that exceeded 80 beats per minute (BPM). The mean resting heart rate in the higher resting heart rate group was 92, compared with a mean of 70 BPM in the lower resting heart rate group. Dr. Ismail reported that at month 3, patients with higher resting heart rates had significantly higher proportion of exacerbations, compared with those who had a lower resting heart rates (54% vs. 27%; P = .013). The trend was followed through until month 9. There was also a statistically significant moderate strength linear correlation between resting heart rate and exacerbation frequency at 3, 6, and 9 months (r = 0.400; P less than .001: r = 0.440; P less than .001: and r = 0.416; P = .004, respectively). The mean exacerbation frequency was also significantly higher in the higher resting heart rate group at month 3 and month 6 (2.00 vs. 0.48; P less than .001: and 3.42 vs. 1.14; P = .004).
“Higher resting heart rate may predict future risk of exacerbation in patients with recent COPD exacerbation,” Dr. Ismail concluded. “Further study however is required to determine the effect of lowering resting heart rate on the future risk of exacerbation.” He acknowledged certain limitations of the study, including the fact that it excluded patients who were on beta-blockers or any rate-modifying drugs, and those with history of cardiac failure and ischemic heart disease, and that there was no baseline echocardiogram performed to ensure the absence of ischemic heart disease and other possible causes of the higher resting heart rates. “We also had slightly higher than expected dropouts giving a nonsignificant result at 12 months follow-up, though the trend follows the overall results of the study,” he said.
The study was funded by a grant from the Malaysian Thoracic Society. Dr. Ismail reported having no financial disclosures.
AT CHEST 2016
Key clinical point:
Major finding: At month 3, patients with higher resting heart rates had significantly higher proportion of exacerbations, compared with those who had a lower resting heart rates (54% vs. 27%; P = .013).
Data source: An evaluation of 147 COPD patients at 10 centers who were hospitalized for acute exacerbation of COPD between April 2012 and September 2015.
Disclosures: The study was funded by a grant from the Malaysian Thoracic Society. Dr. Ismail reported having no financial disclosures.
Pulmonary embolism common in patients hospitalized for syncope
When specifically looked for, pulmonary embolism was identified in approximately 17% of adults hospitalized for a first episode of syncope, according to a report published in the New England Journal of Medicine.
Most medical textbooks include pulmonary embolism (PE) in the differential diagnosis of syncope, but “current international guidelines, including those from the European Society of Cardiology and the American Heart Association, pay little attention to establishing a diagnostic workup for PE in these patients. Hence, when a patient is admitted to a hospital for an episode of syncope, PE – a potentially fatal disease that can be effectively treated – is rarely considered as a possible cause,” said Paolo Prandoni, MD, PhD, of the vascular medicine unit, University of Padua (Italy), and his associates in the PESY (Prevalence of Pulmonary Embolism in Patients With Syncope) trial.
The investigators used a systematic diagnostic work-up to determine the prevalence of PE in a cross-sectional study involving 560 adults hospitalized for syncope at 11 medical centers across Italy during a 2.5-year period. Most of these patients were elderly (mean age, 76 years), and most had clinical evidence indicating that a factor other than PE had caused their fainting. For this study, syncope was defined as a transient loss of consciousness with rapid onset, short duration (less than 1 minute), and spontaneous resolution, with obvious causes ruled out (such as epileptic seizure, stroke, or head trauma).
The “unexpectedly high” prevalence of PE was 17.3% overall, and it was consistent, ranging from 15% to 20%, across all 11 hospitals. The prevalence was even higher, at 25.4%, in the subgroup of 205 patients who had syncope of undetermined origin, as well as in 12.7% of the subgroup of 355 patients considered to have an alternative explanation for the disorder, Dr. Prandoni and his associates wrote (N Engl J Med. 2016 Oct 20. doi: 10.1056/NEJMoa1602172).
The researchers noted that this study likely underestimates the actual prevalence of PE among patients with syncope because it did not include patients who were not hospitalized, such as those who received only ambulatory care and those who presented to an emergency department but were not admitted.
The study was supported by the University of Padua. Dr. Prandoni and his associates reported having no relevant financial disclosures.
When specifically looked for, pulmonary embolism was identified in approximately 17% of adults hospitalized for a first episode of syncope, according to a report published in the New England Journal of Medicine.
Most medical textbooks include pulmonary embolism (PE) in the differential diagnosis of syncope, but “current international guidelines, including those from the European Society of Cardiology and the American Heart Association, pay little attention to establishing a diagnostic workup for PE in these patients. Hence, when a patient is admitted to a hospital for an episode of syncope, PE – a potentially fatal disease that can be effectively treated – is rarely considered as a possible cause,” said Paolo Prandoni, MD, PhD, of the vascular medicine unit, University of Padua (Italy), and his associates in the PESY (Prevalence of Pulmonary Embolism in Patients With Syncope) trial.
The investigators used a systematic diagnostic work-up to determine the prevalence of PE in a cross-sectional study involving 560 adults hospitalized for syncope at 11 medical centers across Italy during a 2.5-year period. Most of these patients were elderly (mean age, 76 years), and most had clinical evidence indicating that a factor other than PE had caused their fainting. For this study, syncope was defined as a transient loss of consciousness with rapid onset, short duration (less than 1 minute), and spontaneous resolution, with obvious causes ruled out (such as epileptic seizure, stroke, or head trauma).
The “unexpectedly high” prevalence of PE was 17.3% overall, and it was consistent, ranging from 15% to 20%, across all 11 hospitals. The prevalence was even higher, at 25.4%, in the subgroup of 205 patients who had syncope of undetermined origin, as well as in 12.7% of the subgroup of 355 patients considered to have an alternative explanation for the disorder, Dr. Prandoni and his associates wrote (N Engl J Med. 2016 Oct 20. doi: 10.1056/NEJMoa1602172).
The researchers noted that this study likely underestimates the actual prevalence of PE among patients with syncope because it did not include patients who were not hospitalized, such as those who received only ambulatory care and those who presented to an emergency department but were not admitted.
The study was supported by the University of Padua. Dr. Prandoni and his associates reported having no relevant financial disclosures.
When specifically looked for, pulmonary embolism was identified in approximately 17% of adults hospitalized for a first episode of syncope, according to a report published in the New England Journal of Medicine.
Most medical textbooks include pulmonary embolism (PE) in the differential diagnosis of syncope, but “current international guidelines, including those from the European Society of Cardiology and the American Heart Association, pay little attention to establishing a diagnostic workup for PE in these patients. Hence, when a patient is admitted to a hospital for an episode of syncope, PE – a potentially fatal disease that can be effectively treated – is rarely considered as a possible cause,” said Paolo Prandoni, MD, PhD, of the vascular medicine unit, University of Padua (Italy), and his associates in the PESY (Prevalence of Pulmonary Embolism in Patients With Syncope) trial.
The investigators used a systematic diagnostic work-up to determine the prevalence of PE in a cross-sectional study involving 560 adults hospitalized for syncope at 11 medical centers across Italy during a 2.5-year period. Most of these patients were elderly (mean age, 76 years), and most had clinical evidence indicating that a factor other than PE had caused their fainting. For this study, syncope was defined as a transient loss of consciousness with rapid onset, short duration (less than 1 minute), and spontaneous resolution, with obvious causes ruled out (such as epileptic seizure, stroke, or head trauma).
The “unexpectedly high” prevalence of PE was 17.3% overall, and it was consistent, ranging from 15% to 20%, across all 11 hospitals. The prevalence was even higher, at 25.4%, in the subgroup of 205 patients who had syncope of undetermined origin, as well as in 12.7% of the subgroup of 355 patients considered to have an alternative explanation for the disorder, Dr. Prandoni and his associates wrote (N Engl J Med. 2016 Oct 20. doi: 10.1056/NEJMoa1602172).
The researchers noted that this study likely underestimates the actual prevalence of PE among patients with syncope because it did not include patients who were not hospitalized, such as those who received only ambulatory care and those who presented to an emergency department but were not admitted.
The study was supported by the University of Padua. Dr. Prandoni and his associates reported having no relevant financial disclosures.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: When specifically looked for, pulmonary embolism was identified in approximately 17% of adults hospitalized for a first episode of syncope.
Major finding: The “unexpectedly high” prevalence of PE was 17.3% overall, and it was consistent, ranging from 15% to 20%, across all 11 hospitals in the study.
Data source: A cross-sectional study involving 560 adults hospitalized for syncope at 11 Italian medical centers during a 2.5 year period.
Disclosures: This study was supported by the University of Padua (Italy). Dr. Prandoni and his associates reported having no relevant financial disclosures.