User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Powered by CHEST Physician, Clinician Reviews, MDedge Family Medicine, Internal Medicine News, and The Journal of Clinical Outcomes Management.
Summer camps need help managing childhood anaphylaxis
ATLANTA – Summer camp personnel need a refresher course on the recognition, treatment, and prevention of allergic reactions in children, according to an online survey of camps in almost 40 U.S. states and Canadian provinces.
There’s a lot of data about how schools handle allergies but almost nothing about summer camps. To fill the gap, the investigators sent surveys across North America to 158 camp directors, 141 camp medical personnel – mostly registered nurses – and 198 camp staffers. Most of the camps were traditional rural affairs where children stay for several weeks, but there were also suburban and city day camps.
The results weren’t good. About a third of directors and staff, and almost 20% of medical personnel, said they had no education on food allergies. Less than 40% had a good understanding of the different ways that anaphylaxis can present. Less than 80% of camp directors and medical personnel and less than 50% of staff knew the right sequence for anaphylaxis treatment – epinephrine first, followed by a 911 call, and then a call to parents. Many respondents didn’t know the correct injection site for epinephrine.
They also were confused about hand sanitizers versus soap and water. Many mistakenly thought that sanitizers were as good as washing for removing allergens. “Their knowledge about how to clean tables and clean hands of food allergens was limited,” said lead investigator Margaret T. Redmond, MD, an allergist at Nationwide Children’s Hospital in Columbus, Ohio.
It all points to the need for education. “We were surprised at the poor recognition of anaphylactic symptoms. We are trying to identify the weaknesses in camps for targeted interventions. We know from the school data that, with education, people can change,” Dr. Redmond said.
During the 2016 summer session, 51 camps agreed to report epinephrine. Most were rural, with an average of 150 campers per day staying a median of 51 days. There were 12 epinephrine shots over that time, about half for peanut reactions and the rest for bee, wasp, and fire ant stings. None of the children died.
“Families that have kids with food allergies should reach out to camps about their policies and make sure they have epinephrine available at all times and that they have food allergy action plans” that staff know about, Dr. Redmond said.
The work was funded by Mylan and kaleo, both makers of epinephrine autoinjectors. Dr. Lee and Dr. Redmond had no relevant financial disclosures.
ATLANTA – Summer camp personnel need a refresher course on the recognition, treatment, and prevention of allergic reactions in children, according to an online survey of camps in almost 40 U.S. states and Canadian provinces.
There’s a lot of data about how schools handle allergies but almost nothing about summer camps. To fill the gap, the investigators sent surveys across North America to 158 camp directors, 141 camp medical personnel – mostly registered nurses – and 198 camp staffers. Most of the camps were traditional rural affairs where children stay for several weeks, but there were also suburban and city day camps.
The results weren’t good. About a third of directors and staff, and almost 20% of medical personnel, said they had no education on food allergies. Less than 40% had a good understanding of the different ways that anaphylaxis can present. Less than 80% of camp directors and medical personnel and less than 50% of staff knew the right sequence for anaphylaxis treatment – epinephrine first, followed by a 911 call, and then a call to parents. Many respondents didn’t know the correct injection site for epinephrine.
They also were confused about hand sanitizers versus soap and water. Many mistakenly thought that sanitizers were as good as washing for removing allergens. “Their knowledge about how to clean tables and clean hands of food allergens was limited,” said lead investigator Margaret T. Redmond, MD, an allergist at Nationwide Children’s Hospital in Columbus, Ohio.
It all points to the need for education. “We were surprised at the poor recognition of anaphylactic symptoms. We are trying to identify the weaknesses in camps for targeted interventions. We know from the school data that, with education, people can change,” Dr. Redmond said.
During the 2016 summer session, 51 camps agreed to report epinephrine. Most were rural, with an average of 150 campers per day staying a median of 51 days. There were 12 epinephrine shots over that time, about half for peanut reactions and the rest for bee, wasp, and fire ant stings. None of the children died.
“Families that have kids with food allergies should reach out to camps about their policies and make sure they have epinephrine available at all times and that they have food allergy action plans” that staff know about, Dr. Redmond said.
The work was funded by Mylan and kaleo, both makers of epinephrine autoinjectors. Dr. Lee and Dr. Redmond had no relevant financial disclosures.
ATLANTA – Summer camp personnel need a refresher course on the recognition, treatment, and prevention of allergic reactions in children, according to an online survey of camps in almost 40 U.S. states and Canadian provinces.
There’s a lot of data about how schools handle allergies but almost nothing about summer camps. To fill the gap, the investigators sent surveys across North America to 158 camp directors, 141 camp medical personnel – mostly registered nurses – and 198 camp staffers. Most of the camps were traditional rural affairs where children stay for several weeks, but there were also suburban and city day camps.
The results weren’t good. About a third of directors and staff, and almost 20% of medical personnel, said they had no education on food allergies. Less than 40% had a good understanding of the different ways that anaphylaxis can present. Less than 80% of camp directors and medical personnel and less than 50% of staff knew the right sequence for anaphylaxis treatment – epinephrine first, followed by a 911 call, and then a call to parents. Many respondents didn’t know the correct injection site for epinephrine.
They also were confused about hand sanitizers versus soap and water. Many mistakenly thought that sanitizers were as good as washing for removing allergens. “Their knowledge about how to clean tables and clean hands of food allergens was limited,” said lead investigator Margaret T. Redmond, MD, an allergist at Nationwide Children’s Hospital in Columbus, Ohio.
It all points to the need for education. “We were surprised at the poor recognition of anaphylactic symptoms. We are trying to identify the weaknesses in camps for targeted interventions. We know from the school data that, with education, people can change,” Dr. Redmond said.
During the 2016 summer session, 51 camps agreed to report epinephrine. Most were rural, with an average of 150 campers per day staying a median of 51 days. There were 12 epinephrine shots over that time, about half for peanut reactions and the rest for bee, wasp, and fire ant stings. None of the children died.
“Families that have kids with food allergies should reach out to camps about their policies and make sure they have epinephrine available at all times and that they have food allergy action plans” that staff know about, Dr. Redmond said.
The work was funded by Mylan and kaleo, both makers of epinephrine autoinjectors. Dr. Lee and Dr. Redmond had no relevant financial disclosures.
AT AAAAI 2017 ANNUAL MEETING
Key clinical point:
Major finding: About a third of directors and camp staff and almost 20% of medical personnel (mostly registered nurses) said they had no previous education on food allergies.
Data source: An online survey of camps in almost 40 U.S. states and Canadian provinces, including almost 500 personnel.
Disclosures: The work was funded by Mylan and kaleo, both makers of epinephrine autoinjectors. Dr. Lee and Dr. Redmond had no relevant financial disclosures.
Study nixed magnesium for infants with acute bronchiolitis
Intravenous magnesium does not benefit, and may harm, infants with moderate to severe acute bronchiolitis, investigators reported.
Compared with placebo, adding a single intravenous dose of magnesium sulfate (100 mg/kg) to usual care did not reduce time to medical readiness for discharge, even when patients had eczema or a family history of asthma, and was tied to more than a threefold rise in the rate of short-term readmissions, Khalid Al Ansari, MD, of Hamad Medical Corp. in Doha, Qatar, and his associates wrote in Chest. “To our knowledge, this is the first randomized study to investigate the effect of intravenous magnesium in a bronchiolitis population,” they added.
Bronchiolitis lacks new, inexpensive, readily available treatments, despite being a common reason for hospital admission, the researchers noted. For older children with moderate to severe exacerbations of asthma, a meta-analysis found that the addition of magnesium to usual care appeared to cut readmissions and shorten lengths of stay, compared with placebo. To explore magnesium therapy in younger children, the investigators enrolled 162 previously healthy infants up to 18 months old who had been admitted to the short-stay unit of a pediatric emergency center with a diagnosis of moderate to severe viral bronchiolitis. Patients received usual care with oral dexamethasone and nebulized 5% hypertonic saline in 1 mL of 1:1000 epinephrine, plus an intravenous 60-minute infusion with a blinded syringe of either 0.9% saline placebo or magnesium sulfate (100 mg/kg) (Chest. 2017 Mar 9. doi: 10.1016/j.chest.2017.03.002).
The primary endpoint, time to medical readiness for discharge, did not statistically differ between groups, averaging 24.1 (95% confidence interval, 20.0-29.1) hours with magnesium and 25.3 (95% CI, 20.3-31.5) hours with placebo (P = .91). Among patients with a history of eczema or a family history of asthma, mean times to readiness for discharge resembled those for the entire cohort and did not statistically differ based on treatment. Average Wang bronchiolitis severity scores also were similar between groups, as were rates of outpatient clinic visits (33.8% with magnesium and 27.2% with placebo). Thus, the trial identified “no benefit in adding intravenous magnesium for infant bronchiolitis, even in patients characterized to be at a higher risk for asthma,” the researchers concluded.
Strikingly, 2-week readmission rates were 19.5% with magnesium (95% CI, 11.3-30.1) and 6.2% with placebo (95% CI, 0.02-13.8; P = .016). Among patients with eczema or a family history of asthma, 2-week readmission rates also were significantly higher with magnesium (26.3%; 95% CI, 13.4-43.1) than with placebo (7.5%; 95% CI, 1.6-20.4; P = .034) These might have been chance findings, or magnesium might have masked worse bronchiolitis, prolonged the disease course, or interacted with 5% hypertonic saline or systemic corticosteroids, the investigators said. Intravenous magnesium might contribute to secondary relapse, especially among patients with eczema or a family history of asthma, they added.
Patients in this study had a median age of 3.7 months (range, 22 days to 17.6 months), about half had eczema or a family history of asthma, and 86% had positive nasopharyngeal virus swabs. Cardiopulmonary monitoring revealed no acute events during treatment. Of 16 readmissions in the magnesium group, 11 entered the infirmary and 4 entered the hospital. The five placebo readmissions included four to the infirmary and one to the hospital.
“As with other ‘negative studies,’ we may have failed to identify a benefit from intravenous magnesium in a patient subgroup because of our limited sample size,” the investigators wrote. “But we think our findings are generalizable to a similarly heterogeneous group of patients presenting for bronchiolitis care in a busy urban emergency department.”
Hamad Medical Corp. sponsored the study. The investigators reported having no conflicts of interest.
The study authors are correct that there isn’t a “new” treatment for infant bronchiolitis. But the American Academy of Pediatrics published a Clinical Practice Guidelines in 2014 (Pediatrics. Vol 134, Number 5, November 2014).
This study included patients admitted to a short-stay unit within the emergency room and they were receiving both of these therapies as “usual care.” Therefore, it is difficult to say if this may have confounded the results. In any case, intravenous magnesium sulfate doesn’t make sense as an intervention for bronchiolitis.
The study authors are correct that there isn’t a “new” treatment for infant bronchiolitis. But the American Academy of Pediatrics published a Clinical Practice Guidelines in 2014 (Pediatrics. Vol 134, Number 5, November 2014).
This study included patients admitted to a short-stay unit within the emergency room and they were receiving both of these therapies as “usual care.” Therefore, it is difficult to say if this may have confounded the results. In any case, intravenous magnesium sulfate doesn’t make sense as an intervention for bronchiolitis.
The study authors are correct that there isn’t a “new” treatment for infant bronchiolitis. But the American Academy of Pediatrics published a Clinical Practice Guidelines in 2014 (Pediatrics. Vol 134, Number 5, November 2014).
This study included patients admitted to a short-stay unit within the emergency room and they were receiving both of these therapies as “usual care.” Therefore, it is difficult to say if this may have confounded the results. In any case, intravenous magnesium sulfate doesn’t make sense as an intervention for bronchiolitis.
Intravenous magnesium does not benefit, and may harm, infants with moderate to severe acute bronchiolitis, investigators reported.
Compared with placebo, adding a single intravenous dose of magnesium sulfate (100 mg/kg) to usual care did not reduce time to medical readiness for discharge, even when patients had eczema or a family history of asthma, and was tied to more than a threefold rise in the rate of short-term readmissions, Khalid Al Ansari, MD, of Hamad Medical Corp. in Doha, Qatar, and his associates wrote in Chest. “To our knowledge, this is the first randomized study to investigate the effect of intravenous magnesium in a bronchiolitis population,” they added.
Bronchiolitis lacks new, inexpensive, readily available treatments, despite being a common reason for hospital admission, the researchers noted. For older children with moderate to severe exacerbations of asthma, a meta-analysis found that the addition of magnesium to usual care appeared to cut readmissions and shorten lengths of stay, compared with placebo. To explore magnesium therapy in younger children, the investigators enrolled 162 previously healthy infants up to 18 months old who had been admitted to the short-stay unit of a pediatric emergency center with a diagnosis of moderate to severe viral bronchiolitis. Patients received usual care with oral dexamethasone and nebulized 5% hypertonic saline in 1 mL of 1:1000 epinephrine, plus an intravenous 60-minute infusion with a blinded syringe of either 0.9% saline placebo or magnesium sulfate (100 mg/kg) (Chest. 2017 Mar 9. doi: 10.1016/j.chest.2017.03.002).
The primary endpoint, time to medical readiness for discharge, did not statistically differ between groups, averaging 24.1 (95% confidence interval, 20.0-29.1) hours with magnesium and 25.3 (95% CI, 20.3-31.5) hours with placebo (P = .91). Among patients with a history of eczema or a family history of asthma, mean times to readiness for discharge resembled those for the entire cohort and did not statistically differ based on treatment. Average Wang bronchiolitis severity scores also were similar between groups, as were rates of outpatient clinic visits (33.8% with magnesium and 27.2% with placebo). Thus, the trial identified “no benefit in adding intravenous magnesium for infant bronchiolitis, even in patients characterized to be at a higher risk for asthma,” the researchers concluded.
Strikingly, 2-week readmission rates were 19.5% with magnesium (95% CI, 11.3-30.1) and 6.2% with placebo (95% CI, 0.02-13.8; P = .016). Among patients with eczema or a family history of asthma, 2-week readmission rates also were significantly higher with magnesium (26.3%; 95% CI, 13.4-43.1) than with placebo (7.5%; 95% CI, 1.6-20.4; P = .034) These might have been chance findings, or magnesium might have masked worse bronchiolitis, prolonged the disease course, or interacted with 5% hypertonic saline or systemic corticosteroids, the investigators said. Intravenous magnesium might contribute to secondary relapse, especially among patients with eczema or a family history of asthma, they added.
Patients in this study had a median age of 3.7 months (range, 22 days to 17.6 months), about half had eczema or a family history of asthma, and 86% had positive nasopharyngeal virus swabs. Cardiopulmonary monitoring revealed no acute events during treatment. Of 16 readmissions in the magnesium group, 11 entered the infirmary and 4 entered the hospital. The five placebo readmissions included four to the infirmary and one to the hospital.
“As with other ‘negative studies,’ we may have failed to identify a benefit from intravenous magnesium in a patient subgroup because of our limited sample size,” the investigators wrote. “But we think our findings are generalizable to a similarly heterogeneous group of patients presenting for bronchiolitis care in a busy urban emergency department.”
Hamad Medical Corp. sponsored the study. The investigators reported having no conflicts of interest.
Intravenous magnesium does not benefit, and may harm, infants with moderate to severe acute bronchiolitis, investigators reported.
Compared with placebo, adding a single intravenous dose of magnesium sulfate (100 mg/kg) to usual care did not reduce time to medical readiness for discharge, even when patients had eczema or a family history of asthma, and was tied to more than a threefold rise in the rate of short-term readmissions, Khalid Al Ansari, MD, of Hamad Medical Corp. in Doha, Qatar, and his associates wrote in Chest. “To our knowledge, this is the first randomized study to investigate the effect of intravenous magnesium in a bronchiolitis population,” they added.
Bronchiolitis lacks new, inexpensive, readily available treatments, despite being a common reason for hospital admission, the researchers noted. For older children with moderate to severe exacerbations of asthma, a meta-analysis found that the addition of magnesium to usual care appeared to cut readmissions and shorten lengths of stay, compared with placebo. To explore magnesium therapy in younger children, the investigators enrolled 162 previously healthy infants up to 18 months old who had been admitted to the short-stay unit of a pediatric emergency center with a diagnosis of moderate to severe viral bronchiolitis. Patients received usual care with oral dexamethasone and nebulized 5% hypertonic saline in 1 mL of 1:1000 epinephrine, plus an intravenous 60-minute infusion with a blinded syringe of either 0.9% saline placebo or magnesium sulfate (100 mg/kg) (Chest. 2017 Mar 9. doi: 10.1016/j.chest.2017.03.002).
The primary endpoint, time to medical readiness for discharge, did not statistically differ between groups, averaging 24.1 (95% confidence interval, 20.0-29.1) hours with magnesium and 25.3 (95% CI, 20.3-31.5) hours with placebo (P = .91). Among patients with a history of eczema or a family history of asthma, mean times to readiness for discharge resembled those for the entire cohort and did not statistically differ based on treatment. Average Wang bronchiolitis severity scores also were similar between groups, as were rates of outpatient clinic visits (33.8% with magnesium and 27.2% with placebo). Thus, the trial identified “no benefit in adding intravenous magnesium for infant bronchiolitis, even in patients characterized to be at a higher risk for asthma,” the researchers concluded.
Strikingly, 2-week readmission rates were 19.5% with magnesium (95% CI, 11.3-30.1) and 6.2% with placebo (95% CI, 0.02-13.8; P = .016). Among patients with eczema or a family history of asthma, 2-week readmission rates also were significantly higher with magnesium (26.3%; 95% CI, 13.4-43.1) than with placebo (7.5%; 95% CI, 1.6-20.4; P = .034) These might have been chance findings, or magnesium might have masked worse bronchiolitis, prolonged the disease course, or interacted with 5% hypertonic saline or systemic corticosteroids, the investigators said. Intravenous magnesium might contribute to secondary relapse, especially among patients with eczema or a family history of asthma, they added.
Patients in this study had a median age of 3.7 months (range, 22 days to 17.6 months), about half had eczema or a family history of asthma, and 86% had positive nasopharyngeal virus swabs. Cardiopulmonary monitoring revealed no acute events during treatment. Of 16 readmissions in the magnesium group, 11 entered the infirmary and 4 entered the hospital. The five placebo readmissions included four to the infirmary and one to the hospital.
“As with other ‘negative studies,’ we may have failed to identify a benefit from intravenous magnesium in a patient subgroup because of our limited sample size,” the investigators wrote. “But we think our findings are generalizable to a similarly heterogeneous group of patients presenting for bronchiolitis care in a busy urban emergency department.”
Hamad Medical Corp. sponsored the study. The investigators reported having no conflicts of interest.
Key clinical point: Intravenous magnesium does not benefit, and may harm, infants with acute bronchiolitis.
Major finding: Time to medical readiness for discharge averaged 24.1 hours (95% CI, 20.0-29.1) in the magnesium group and 25.3 hours (95% CI, 20.3-31.5) in the placebo group (P = .91). Rates of 2-week readmission were 19.5% with magnesium and 6.2% with placebo (P = .016).
Data source: A single-center, randomized, double-blind, placebo-controlled trial of 162 previously healthy infants diagnosed with viral bronchiolitis.
Disclosures: Hamad Medical Corp. sponsored the study. The investigators reported having no conflicts of interest.
2016-2017 flu season continues to wind down
Influenza activity took another healthy step down as outpatient visits continued to drop, according to the Centers for Disease Control and Prevention.
The proportion of outpatient visits for influenza-like illness (ILI) was down to 3.2% for the week ending March 18, 2017, the CDC reported, compared with 3.6% the week before. (The figure of 3.7% previously reported for last week has been adjusted this week, so the halt in the decline in outpatient visits was actually more of a slowdown.) The national baseline for outpatient ILI visits is 2.2%.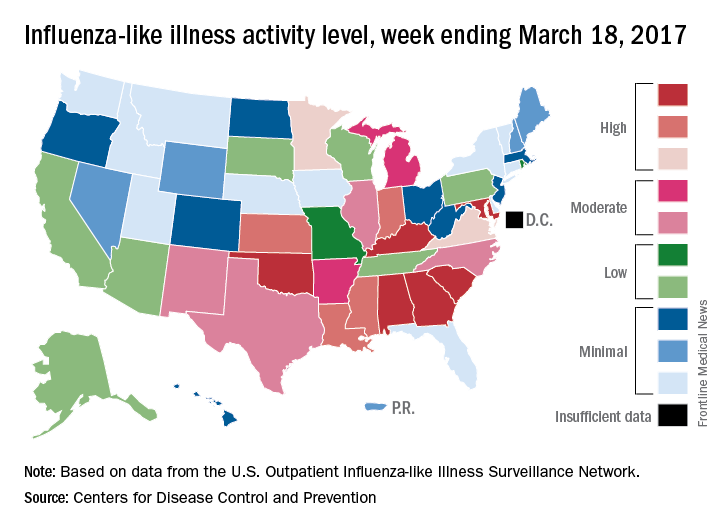
Two flu-related pediatric deaths were reported during the week of March 18, but both occurred earlier: one during the week ending Feb. 18 and the other in the week ending Feb. 25, the CDC reported. The total number of pediatric flu deaths reported is now 55 for the 2016-2017 season.
Influenza activity took another healthy step down as outpatient visits continued to drop, according to the Centers for Disease Control and Prevention.
The proportion of outpatient visits for influenza-like illness (ILI) was down to 3.2% for the week ending March 18, 2017, the CDC reported, compared with 3.6% the week before. (The figure of 3.7% previously reported for last week has been adjusted this week, so the halt in the decline in outpatient visits was actually more of a slowdown.) The national baseline for outpatient ILI visits is 2.2%.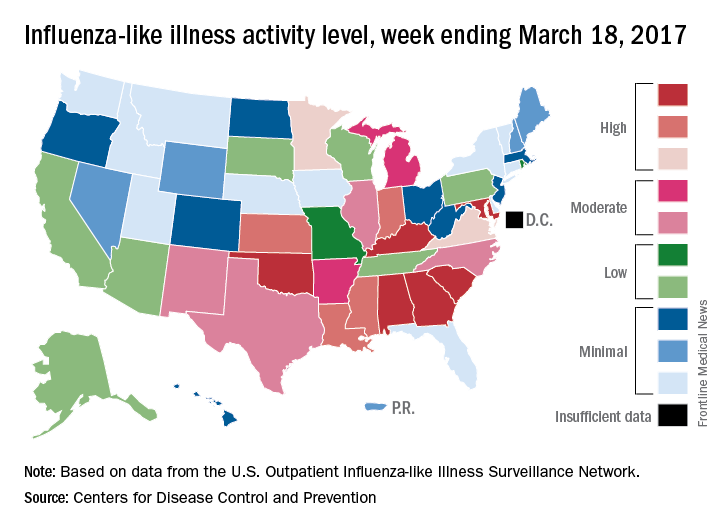
Two flu-related pediatric deaths were reported during the week of March 18, but both occurred earlier: one during the week ending Feb. 18 and the other in the week ending Feb. 25, the CDC reported. The total number of pediatric flu deaths reported is now 55 for the 2016-2017 season.
Influenza activity took another healthy step down as outpatient visits continued to drop, according to the Centers for Disease Control and Prevention.
The proportion of outpatient visits for influenza-like illness (ILI) was down to 3.2% for the week ending March 18, 2017, the CDC reported, compared with 3.6% the week before. (The figure of 3.7% previously reported for last week has been adjusted this week, so the halt in the decline in outpatient visits was actually more of a slowdown.) The national baseline for outpatient ILI visits is 2.2%.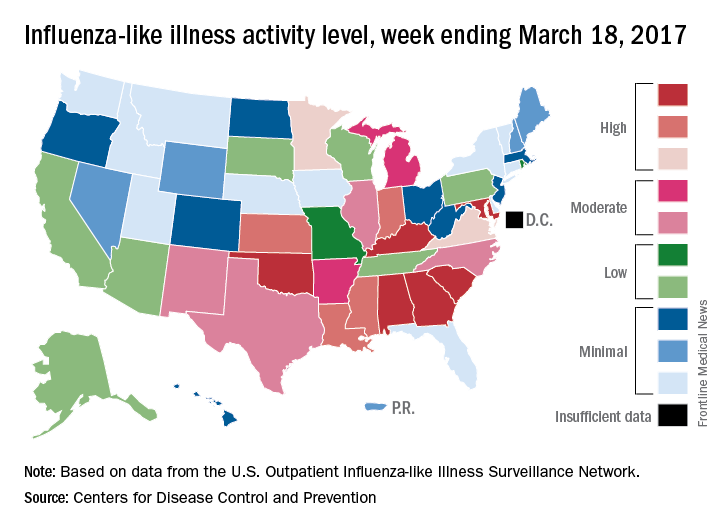
Two flu-related pediatric deaths were reported during the week of March 18, but both occurred earlier: one during the week ending Feb. 18 and the other in the week ending Feb. 25, the CDC reported. The total number of pediatric flu deaths reported is now 55 for the 2016-2017 season.
Parental perception of asthma may predict future acute visits
ATLANTA – For low-income and minority children with asthma, parents’ perception of a child’s asthma control may be an important predictor of future acute visits, independent of guideline-based criteria for asthma control, judging from the results from a prospective cohort study.
The National Asthma Education and Prevention Program (NAEPP)–based assessment of asthma control incorporates symptoms, nighttime awakenings, and activity interference; short-acting beta 2-agonist use, lung function, and history of exacerbations, “but it does not take into account parental perceptions of asthma control,” lead study author Suzanne Rossi, MD, said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “We also know that parental report of symptom frequency and their perception of their child’s asthma control are frequently discordant.”
In an effort to answer these questions, the researchers conducted a prospective cohort study of 150 Baltimore children aged 5-17 years with persistent asthma who had an exacerbation within the past year. After a baseline assessment, clinic visits occurred every 3 months for 1 year. The predictor variable was parental perception of asthma control assessed by the following question: “Do you believe that your child’s asthma was well controlled within the past 4 weeks?” The primary outcome was an acute visit, defined as an unscheduled visit to a physician or an ED visit or a hospitalization. The researchers used generalized estimating equations to relate parental perception of asthma control to future acute visits.
The mean age of patients was 11 years, 57% were male, 91% were African American, and 85% were on public health insurance. In addition, 15% were overweight and 28% were obese. At baseline, patients were using short-acting beta-2 agonists a mean of 4.2 days every 2 weeks, and 96% had an acute visit in the prior 12 months. Only 9% met criteria for well-controlled asthma as defined by NAEPP criteria, 36% were not well controlled, and 55% were poorly controlled.
At the baseline visit, 73% of parents said that their child’s asthma was well controlled, 20% said that it was not well controlled, and 7% were unsure. Of the 136 children who met NAEPP criteria for uncontrolled asthma, 71% had parents who reported that their child’s asthma was well controlled.
The researchers found that on average, children with parents who report uncontrolled asthma were 2.4-fold times more likely to have an acute visit within the next 3 months, compared with children whose parents reported that their child’s asthma was well controlled. The odds ratio remained similar after adjustment for NAEPP-based asthma control, and for age, gender, race, controller medication, insurance, and atopy. Data on hospitalization was excluded because there was insufficient data for analysis.
Dr. Rossi and her associates also found that parental perception of uncontrolled asthma was a predictor of future acute visits among females but not males (odds ratio, 5.3 vs. OR, 1.3, respectively; P = .03), and among those who were overweight or obese but not among those with a normal BMI (OR, 6.2 vs. OR, 1.3; P = .04). Age was not a modifier. She acknowledged certain limitations of the study, including the inability to measure the severity of asthma exacerbation. “Therefore, this primary outcome may reflect parental concern,” Dr. Rossi said. “In addition, these findings may not be generalizable to other pediatric asthma populations. We also had a small sample size for some outcomes such as hospitalization. In terms of future directions, it would be nice to know whether the findings are replicable in other similar populations and in population-based studies. It would be interesting to examine the association with larger study populations to evaluate hospitalizations and to get an assessment of the severity of symptoms associated with the acute visit.”
The National Institute of Allergy and Infectious Diseases, the National Institute of Environmental Health Sciences, and Johns Hopkins University School of Medicine supported the study. Dr. Rossi reported having no financial disclosures.
ATLANTA – For low-income and minority children with asthma, parents’ perception of a child’s asthma control may be an important predictor of future acute visits, independent of guideline-based criteria for asthma control, judging from the results from a prospective cohort study.
The National Asthma Education and Prevention Program (NAEPP)–based assessment of asthma control incorporates symptoms, nighttime awakenings, and activity interference; short-acting beta 2-agonist use, lung function, and history of exacerbations, “but it does not take into account parental perceptions of asthma control,” lead study author Suzanne Rossi, MD, said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “We also know that parental report of symptom frequency and their perception of their child’s asthma control are frequently discordant.”
In an effort to answer these questions, the researchers conducted a prospective cohort study of 150 Baltimore children aged 5-17 years with persistent asthma who had an exacerbation within the past year. After a baseline assessment, clinic visits occurred every 3 months for 1 year. The predictor variable was parental perception of asthma control assessed by the following question: “Do you believe that your child’s asthma was well controlled within the past 4 weeks?” The primary outcome was an acute visit, defined as an unscheduled visit to a physician or an ED visit or a hospitalization. The researchers used generalized estimating equations to relate parental perception of asthma control to future acute visits.
The mean age of patients was 11 years, 57% were male, 91% were African American, and 85% were on public health insurance. In addition, 15% were overweight and 28% were obese. At baseline, patients were using short-acting beta-2 agonists a mean of 4.2 days every 2 weeks, and 96% had an acute visit in the prior 12 months. Only 9% met criteria for well-controlled asthma as defined by NAEPP criteria, 36% were not well controlled, and 55% were poorly controlled.
At the baseline visit, 73% of parents said that their child’s asthma was well controlled, 20% said that it was not well controlled, and 7% were unsure. Of the 136 children who met NAEPP criteria for uncontrolled asthma, 71% had parents who reported that their child’s asthma was well controlled.
The researchers found that on average, children with parents who report uncontrolled asthma were 2.4-fold times more likely to have an acute visit within the next 3 months, compared with children whose parents reported that their child’s asthma was well controlled. The odds ratio remained similar after adjustment for NAEPP-based asthma control, and for age, gender, race, controller medication, insurance, and atopy. Data on hospitalization was excluded because there was insufficient data for analysis.
Dr. Rossi and her associates also found that parental perception of uncontrolled asthma was a predictor of future acute visits among females but not males (odds ratio, 5.3 vs. OR, 1.3, respectively; P = .03), and among those who were overweight or obese but not among those with a normal BMI (OR, 6.2 vs. OR, 1.3; P = .04). Age was not a modifier. She acknowledged certain limitations of the study, including the inability to measure the severity of asthma exacerbation. “Therefore, this primary outcome may reflect parental concern,” Dr. Rossi said. “In addition, these findings may not be generalizable to other pediatric asthma populations. We also had a small sample size for some outcomes such as hospitalization. In terms of future directions, it would be nice to know whether the findings are replicable in other similar populations and in population-based studies. It would be interesting to examine the association with larger study populations to evaluate hospitalizations and to get an assessment of the severity of symptoms associated with the acute visit.”
The National Institute of Allergy and Infectious Diseases, the National Institute of Environmental Health Sciences, and Johns Hopkins University School of Medicine supported the study. Dr. Rossi reported having no financial disclosures.
ATLANTA – For low-income and minority children with asthma, parents’ perception of a child’s asthma control may be an important predictor of future acute visits, independent of guideline-based criteria for asthma control, judging from the results from a prospective cohort study.
The National Asthma Education and Prevention Program (NAEPP)–based assessment of asthma control incorporates symptoms, nighttime awakenings, and activity interference; short-acting beta 2-agonist use, lung function, and history of exacerbations, “but it does not take into account parental perceptions of asthma control,” lead study author Suzanne Rossi, MD, said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “We also know that parental report of symptom frequency and their perception of their child’s asthma control are frequently discordant.”
In an effort to answer these questions, the researchers conducted a prospective cohort study of 150 Baltimore children aged 5-17 years with persistent asthma who had an exacerbation within the past year. After a baseline assessment, clinic visits occurred every 3 months for 1 year. The predictor variable was parental perception of asthma control assessed by the following question: “Do you believe that your child’s asthma was well controlled within the past 4 weeks?” The primary outcome was an acute visit, defined as an unscheduled visit to a physician or an ED visit or a hospitalization. The researchers used generalized estimating equations to relate parental perception of asthma control to future acute visits.
The mean age of patients was 11 years, 57% were male, 91% were African American, and 85% were on public health insurance. In addition, 15% were overweight and 28% were obese. At baseline, patients were using short-acting beta-2 agonists a mean of 4.2 days every 2 weeks, and 96% had an acute visit in the prior 12 months. Only 9% met criteria for well-controlled asthma as defined by NAEPP criteria, 36% were not well controlled, and 55% were poorly controlled.
At the baseline visit, 73% of parents said that their child’s asthma was well controlled, 20% said that it was not well controlled, and 7% were unsure. Of the 136 children who met NAEPP criteria for uncontrolled asthma, 71% had parents who reported that their child’s asthma was well controlled.
The researchers found that on average, children with parents who report uncontrolled asthma were 2.4-fold times more likely to have an acute visit within the next 3 months, compared with children whose parents reported that their child’s asthma was well controlled. The odds ratio remained similar after adjustment for NAEPP-based asthma control, and for age, gender, race, controller medication, insurance, and atopy. Data on hospitalization was excluded because there was insufficient data for analysis.
Dr. Rossi and her associates also found that parental perception of uncontrolled asthma was a predictor of future acute visits among females but not males (odds ratio, 5.3 vs. OR, 1.3, respectively; P = .03), and among those who were overweight or obese but not among those with a normal BMI (OR, 6.2 vs. OR, 1.3; P = .04). Age was not a modifier. She acknowledged certain limitations of the study, including the inability to measure the severity of asthma exacerbation. “Therefore, this primary outcome may reflect parental concern,” Dr. Rossi said. “In addition, these findings may not be generalizable to other pediatric asthma populations. We also had a small sample size for some outcomes such as hospitalization. In terms of future directions, it would be nice to know whether the findings are replicable in other similar populations and in population-based studies. It would be interesting to examine the association with larger study populations to evaluate hospitalizations and to get an assessment of the severity of symptoms associated with the acute visit.”
The National Institute of Allergy and Infectious Diseases, the National Institute of Environmental Health Sciences, and Johns Hopkins University School of Medicine supported the study. Dr. Rossi reported having no financial disclosures.
AT THE 2017 AAAAI ANNUAL MEETING
Key clinical point:
Major finding: Children whose parents reported uncontrolled asthma were 2.4-fold times more likely to have an acute visit within the next 3 months, compared with children whose parents reported that their child’s asthma was well controlled.
Data source: A prospective cohort study of 150 Baltimore children aged 5-17 years with persistent asthma who had an exacerbation within the past year.
Disclosures: The National Institute of Allergy and Infectious Diseases, the National Institute of Environmental Health Sciences, and Johns Hopkins University School of Medicine supported the study. Dr. Rossi reported having no financial disclosures.
Anti-TNF agents show clinical benefit in refractory sarcoidosis
FROM SEMINARS IN ARTHRITIS & RHEUMATISM
Around two-thirds of patients with severe or refractory sarcoidosis show a significant clinical response to tumor necrosis factor (TNF) antagonists, according to findings from a retrospective, multicenter cohort study.
Biologic agents targeting TNF, such as etanercept, infliximab, and adalimumab, have been introduced as a third-line option for patients with disease that is refractory to other treatments. However, Yvan Jamilloux, MD, of the Hospices Civils de Lyon (France) and his coauthors reported that there are still insufficient data available on efficacy and safety of these drugs in the context of sarcoidosis.
Dr. Jamilloux and his colleagues analyzed data from 132 sarcoidosis patients who received TNF antagonists, 122 (92%) of whom had severe sarcoidosis (Semin Arthritis Rheum. 2017 Mar 8. doi: 10.1016/j.semarthrit.2017.03.005).
Overall, 64% of patients showed clinical improvements in response to TNF antagonists; 18% had a complete response, and 46% had a partial response. However, 33 (25%) patients showed no change, and 14 (11%) had continued disease progression despite treatment with TNF antagonists. In another 16 patients who received a second TNF antagonist, 10 (63%) had a complete or partial clinical response. The investigators could find no differences in response between anti-TNF agents or between monotherapy and a combination with an immunosuppressant.
Pulmonary involvement was associated with a significantly lower clinical response, but none of the other factors examined in a multivariate analysis (sex, age, ethnicity, organ involvement, disease duration, steroid dosage, or prior immunosuppressant use) distinguished responders and nonresponders.
The authors noted that these response rates were lower than those seen in the literature and suggested this may be attributable to the multicenter design, more patients with longer-lasting and more refractory disease, and longer times under biologic therapy (median 12 months).
The researchers reported significant improvements in central nervous system, peripheral nervous system, heart, skin, and upper respiratory tract involvements based on declines in Extrapulmonary Physician Organ Severity Tool (ePOST) scores. There were also improvements in the eye, muscle, and lung, but these were not statistically significant.
TNF-antagonist therapy was associated with a high rate of adverse events. Around half of all patients (52%) experienced adverse events, such as pneumonia, urinary tract infections, bacterial sepsis, and herpes zoster. In 31 patients (23%), these led to treatment cessation.
Nine patients also had severe allergic reactions, four had paradoxical granulomatous reactions, three developed neutralizing antibodies against anti-TNF agents, two patients had demyelinating lesions, and one had a serum sickness-like reaction. All of these events led to discontinuation.
Overall, 128 (97%) of the patients in the study had received corticosteroids as first-line therapy, and 125 (95%) had received at least one second-line immunosuppressive drug over a median duration of 16 months. Most were treated with infliximab (91%) as the first-line TNF antagonist, followed by adalimumab (6%), etanercept (2%), and certolizumab pegol (1%).
Treatment with TNF antagonists was associated with significant reductions in corticosteroid use; the mean daily prednisone dose decreased from 23 mg/day to 11 mg/day over the median 20.5-month follow-up. This was seen even in the 33 patients who showed no change in their disease course after TNF-antagonist therapy.
No conflicts of interest were declared.
This uncontrolled, unblinded retrospective observational study reports the outcomes of anti-TNF therapy in a heterogenous group of refractory sarcoid patients, with only 12% of the severe sarcoidosis population studied having the indication for treatment based on lung involvement. Further, it is notable that the patients with primarily pulmonary involvement had a poorer response to anti-TNF therapy. Over half of the patients had an adverse event related to the treatment, with nearly a quarter having to discontinue therapy. Given the limitations of this type of study, the low numbers of pulmonary sarcoid patients included, the lack of an efficacy signal in pulmonary sarcoid, and the high rate of serious adverse events – the role of anti-TNF agents for pulmonary sarcoid remains unclear and limited. However
This uncontrolled, unblinded retrospective observational study reports the outcomes of anti-TNF therapy in a heterogenous group of refractory sarcoid patients, with only 12% of the severe sarcoidosis population studied having the indication for treatment based on lung involvement. Further, it is notable that the patients with primarily pulmonary involvement had a poorer response to anti-TNF therapy. Over half of the patients had an adverse event related to the treatment, with nearly a quarter having to discontinue therapy. Given the limitations of this type of study, the low numbers of pulmonary sarcoid patients included, the lack of an efficacy signal in pulmonary sarcoid, and the high rate of serious adverse events – the role of anti-TNF agents for pulmonary sarcoid remains unclear and limited. However
This uncontrolled, unblinded retrospective observational study reports the outcomes of anti-TNF therapy in a heterogenous group of refractory sarcoid patients, with only 12% of the severe sarcoidosis population studied having the indication for treatment based on lung involvement. Further, it is notable that the patients with primarily pulmonary involvement had a poorer response to anti-TNF therapy. Over half of the patients had an adverse event related to the treatment, with nearly a quarter having to discontinue therapy. Given the limitations of this type of study, the low numbers of pulmonary sarcoid patients included, the lack of an efficacy signal in pulmonary sarcoid, and the high rate of serious adverse events – the role of anti-TNF agents for pulmonary sarcoid remains unclear and limited. However
FROM SEMINARS IN ARTHRITIS & RHEUMATISM
Around two-thirds of patients with severe or refractory sarcoidosis show a significant clinical response to tumor necrosis factor (TNF) antagonists, according to findings from a retrospective, multicenter cohort study.
Biologic agents targeting TNF, such as etanercept, infliximab, and adalimumab, have been introduced as a third-line option for patients with disease that is refractory to other treatments. However, Yvan Jamilloux, MD, of the Hospices Civils de Lyon (France) and his coauthors reported that there are still insufficient data available on efficacy and safety of these drugs in the context of sarcoidosis.
Dr. Jamilloux and his colleagues analyzed data from 132 sarcoidosis patients who received TNF antagonists, 122 (92%) of whom had severe sarcoidosis (Semin Arthritis Rheum. 2017 Mar 8. doi: 10.1016/j.semarthrit.2017.03.005).
Overall, 64% of patients showed clinical improvements in response to TNF antagonists; 18% had a complete response, and 46% had a partial response. However, 33 (25%) patients showed no change, and 14 (11%) had continued disease progression despite treatment with TNF antagonists. In another 16 patients who received a second TNF antagonist, 10 (63%) had a complete or partial clinical response. The investigators could find no differences in response between anti-TNF agents or between monotherapy and a combination with an immunosuppressant.
Pulmonary involvement was associated with a significantly lower clinical response, but none of the other factors examined in a multivariate analysis (sex, age, ethnicity, organ involvement, disease duration, steroid dosage, or prior immunosuppressant use) distinguished responders and nonresponders.
The authors noted that these response rates were lower than those seen in the literature and suggested this may be attributable to the multicenter design, more patients with longer-lasting and more refractory disease, and longer times under biologic therapy (median 12 months).
The researchers reported significant improvements in central nervous system, peripheral nervous system, heart, skin, and upper respiratory tract involvements based on declines in Extrapulmonary Physician Organ Severity Tool (ePOST) scores. There were also improvements in the eye, muscle, and lung, but these were not statistically significant.
TNF-antagonist therapy was associated with a high rate of adverse events. Around half of all patients (52%) experienced adverse events, such as pneumonia, urinary tract infections, bacterial sepsis, and herpes zoster. In 31 patients (23%), these led to treatment cessation.
Nine patients also had severe allergic reactions, four had paradoxical granulomatous reactions, three developed neutralizing antibodies against anti-TNF agents, two patients had demyelinating lesions, and one had a serum sickness-like reaction. All of these events led to discontinuation.
Overall, 128 (97%) of the patients in the study had received corticosteroids as first-line therapy, and 125 (95%) had received at least one second-line immunosuppressive drug over a median duration of 16 months. Most were treated with infliximab (91%) as the first-line TNF antagonist, followed by adalimumab (6%), etanercept (2%), and certolizumab pegol (1%).
Treatment with TNF antagonists was associated with significant reductions in corticosteroid use; the mean daily prednisone dose decreased from 23 mg/day to 11 mg/day over the median 20.5-month follow-up. This was seen even in the 33 patients who showed no change in their disease course after TNF-antagonist therapy.
No conflicts of interest were declared.
FROM SEMINARS IN ARTHRITIS & RHEUMATISM
Around two-thirds of patients with severe or refractory sarcoidosis show a significant clinical response to tumor necrosis factor (TNF) antagonists, according to findings from a retrospective, multicenter cohort study.
Biologic agents targeting TNF, such as etanercept, infliximab, and adalimumab, have been introduced as a third-line option for patients with disease that is refractory to other treatments. However, Yvan Jamilloux, MD, of the Hospices Civils de Lyon (France) and his coauthors reported that there are still insufficient data available on efficacy and safety of these drugs in the context of sarcoidosis.
Dr. Jamilloux and his colleagues analyzed data from 132 sarcoidosis patients who received TNF antagonists, 122 (92%) of whom had severe sarcoidosis (Semin Arthritis Rheum. 2017 Mar 8. doi: 10.1016/j.semarthrit.2017.03.005).
Overall, 64% of patients showed clinical improvements in response to TNF antagonists; 18% had a complete response, and 46% had a partial response. However, 33 (25%) patients showed no change, and 14 (11%) had continued disease progression despite treatment with TNF antagonists. In another 16 patients who received a second TNF antagonist, 10 (63%) had a complete or partial clinical response. The investigators could find no differences in response between anti-TNF agents or between monotherapy and a combination with an immunosuppressant.
Pulmonary involvement was associated with a significantly lower clinical response, but none of the other factors examined in a multivariate analysis (sex, age, ethnicity, organ involvement, disease duration, steroid dosage, or prior immunosuppressant use) distinguished responders and nonresponders.
The authors noted that these response rates were lower than those seen in the literature and suggested this may be attributable to the multicenter design, more patients with longer-lasting and more refractory disease, and longer times under biologic therapy (median 12 months).
The researchers reported significant improvements in central nervous system, peripheral nervous system, heart, skin, and upper respiratory tract involvements based on declines in Extrapulmonary Physician Organ Severity Tool (ePOST) scores. There were also improvements in the eye, muscle, and lung, but these were not statistically significant.
TNF-antagonist therapy was associated with a high rate of adverse events. Around half of all patients (52%) experienced adverse events, such as pneumonia, urinary tract infections, bacterial sepsis, and herpes zoster. In 31 patients (23%), these led to treatment cessation.
Nine patients also had severe allergic reactions, four had paradoxical granulomatous reactions, three developed neutralizing antibodies against anti-TNF agents, two patients had demyelinating lesions, and one had a serum sickness-like reaction. All of these events led to discontinuation.
Overall, 128 (97%) of the patients in the study had received corticosteroids as first-line therapy, and 125 (95%) had received at least one second-line immunosuppressive drug over a median duration of 16 months. Most were treated with infliximab (91%) as the first-line TNF antagonist, followed by adalimumab (6%), etanercept (2%), and certolizumab pegol (1%).
Treatment with TNF antagonists was associated with significant reductions in corticosteroid use; the mean daily prednisone dose decreased from 23 mg/day to 11 mg/day over the median 20.5-month follow-up. This was seen even in the 33 patients who showed no change in their disease course after TNF-antagonist therapy.
No conflicts of interest were declared.
Key clinical point:
Major finding: A total of 18% had a complete response, and 46% had a partial response, to TNF antagonists.
Data source: A retrospective, multicenter study in 132 sarcoidosis patients who received TNF antagonists.
Disclosures: No conflicts of interest were declared.
U.S. influenza activity remains steady
The decline in U.S. influenza activity that started in February paused during the week ending March 11, according to the U.S. Centers for Disease Control and Prevention.
The proportion of outpatient visits for influenza-like illness (ILI) stayed at 3.7% for a second consecutive week after declining for 3 weeks in a row. The peak for the season, 5.2%, came during the week ending Feb. 11, CDC data show. The national baseline is 2.2%.
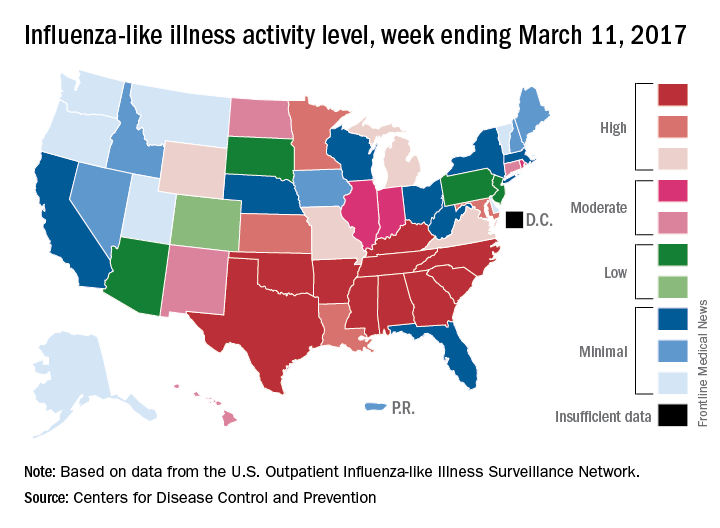
Five ILI-related pediatric deaths were reported to the CDC for the week – all of which occurred during previous weeks – bringing the total to 53 for the 2016-2017 season, the CDC said.
The decline in U.S. influenza activity that started in February paused during the week ending March 11, according to the U.S. Centers for Disease Control and Prevention.
The proportion of outpatient visits for influenza-like illness (ILI) stayed at 3.7% for a second consecutive week after declining for 3 weeks in a row. The peak for the season, 5.2%, came during the week ending Feb. 11, CDC data show. The national baseline is 2.2%.
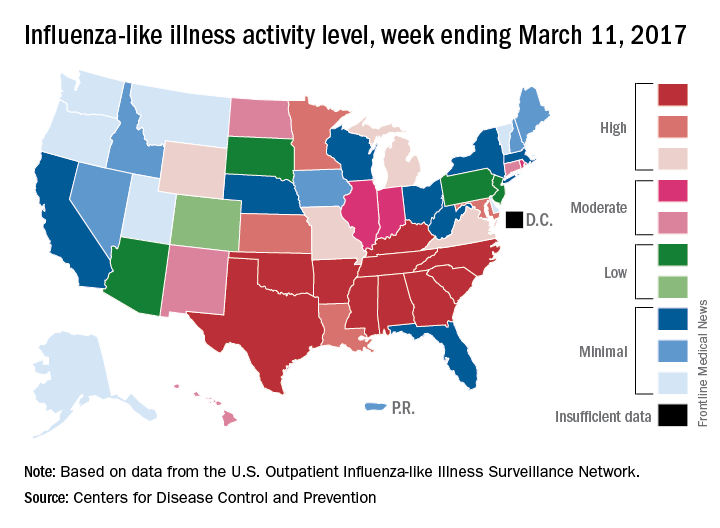
Five ILI-related pediatric deaths were reported to the CDC for the week – all of which occurred during previous weeks – bringing the total to 53 for the 2016-2017 season, the CDC said.
The decline in U.S. influenza activity that started in February paused during the week ending March 11, according to the U.S. Centers for Disease Control and Prevention.
The proportion of outpatient visits for influenza-like illness (ILI) stayed at 3.7% for a second consecutive week after declining for 3 weeks in a row. The peak for the season, 5.2%, came during the week ending Feb. 11, CDC data show. The national baseline is 2.2%.
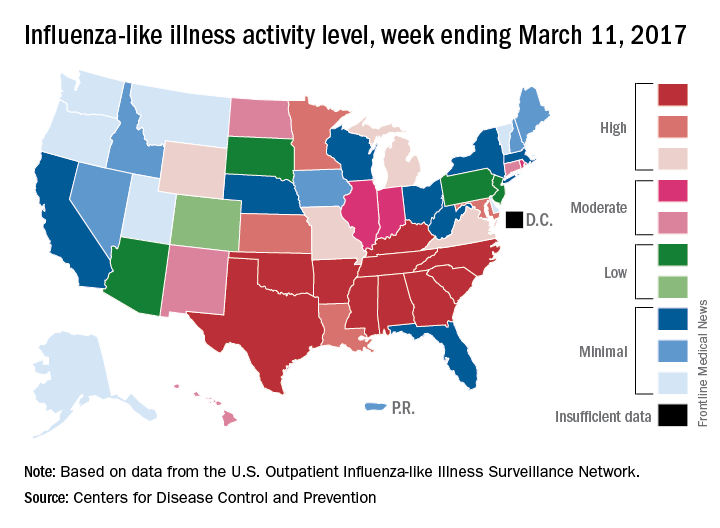
Five ILI-related pediatric deaths were reported to the CDC for the week – all of which occurred during previous weeks – bringing the total to 53 for the 2016-2017 season, the CDC said.
Hold your breath
“Exercising my ‘reasoned judgment,’ I have no doubt that the right to a climate system capable of sustaining human life is fundamental to a free and ordered society.”
– U.S. District Judge Ann Aiken in Kelsey Cascadia Rose Juliana vs. United States of America, et al.
In many areas of the world, the simple act of breathing has become hazardous to people’s health.
According to the World Health Organization, more people die every day from air pollution than from HIV/AIDS, tuberculosis, and road injuries combined. In China, more than 1 million deaths annually are linked to polluted air (76/100,000); in India the number of deaths is more than 600,000 annually (49/100,000); and in the United States, that figure comes to more than 38,000 (12/100,000).
And yet, nonpolluting, alternative options – such as sun and wind power – are readily available.
Dirty air is visible on a hot summer day – when, mixed with other substances, it forms smog. Higher temperatures can then speed up the chemical reactions that form smog. We breathe in that polluted air, especially on days when the air is stagnant or there is temperature inversion.
The health effects of climate change
Black carbon found in air pollution leads to drug-resistant bacteria and alters antibiotic tolerance.1 The pollution also is associated with multiple cancers: lung, liver, ovarian, and, possibly, breast.2,3,4,5 It causes inflammation linked to the development of coronary artery disease (seen even in children!) and plaque formation leading to heart attacks and cardiac arrhythmias – including atrial fibrillation. Air pollution causes, triggers, or worsens respiratory illnesses – chronic obstructive pulmonary disease, emphysema, asthma, infections – and is responsible for lifelong diminished lung volume in children (a reason families are leaving Beijing.) Exponentially increased rates of autism are linked to bad air quality, as are autoimmune diseases, which also are on the rise.6,7 Polluted air causes brain inflammation – living near sources of air pollution increases the risk of dementia – and other neurodegenerative diseases such as Alzheimer’s disease, Parkinson’s, and amyotrophic lateral sclerosis.8 The blood brain barrier protects the brain from most foreign matter, but particulate matter, especially ultrafine particulate matter of less than 1 mcm such as magnetite, can cross directly into the brain via the olfactory nerve. (Magnetite has been identified in the brain tissue of residents living in areas where the substance is produced as a result of industrial waste.) While particulate matter of 2.5 mcmis measured in the United States, ultrafine particulate matter is not.
Psychiatric symptoms and chronic psychiatric disorders also are associated with polluted air: On days with poor air quality, a statistically significant increase is seen in suicide threats and visits to emergency departments for panic attacks.9,10
A rise in aggression occurs when there are abnormally high temperatures and significant changes in rainfall. More assaults, murders, suicides, domestic violence, and child abuse can be expected, and a rise in unrest around the world should come as no surprise.
As a consequence of increased CO2 in the atmosphere, temperatures have already risen by 2° F: Sixteen of the hottest years on record have occurred in the last 17 years, with 2016 as the hottest year ever recorded. In Iraq and Kuwait, the temperature last summer reached 129.2° F.
We are experiencing more frequent and extreme weather events, chronic climate conditions, and the cascading disruption of ecosystems. Drought and sea level rise are leading to physical and psychological impacts – both direct and indirect. Some regions of the world have become destabilized, triggering migrations and the refugee crisis.
Along with these psychological impacts, CO2 affects cognition: A recent study by the Harvard School of Public Health, Boston, shows that the indoor levels of CO2 to which American workers typically are exposed impair cognitive functioning, particularly in the areas of strategic thinking, information processing, and crisis management.11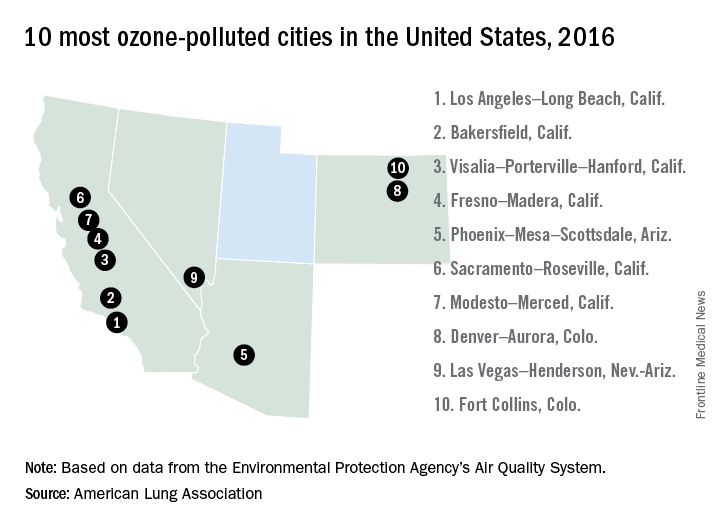
What do we do about it?
As mental health professionals, we know that aggression can be overt or passive (from inaction). Overwhelming evidence shows harm to public health from burning fossil fuels, and yet, though we are making progress, resistance still exists in the transition to clean, renewable energy critical for the health of our families and communities. When political will is what stands between us and getting back on a path to breathing clean air, how can inaction be understood as anything but an act of aggression?
This issue has reached U.S. courts: In a landmark case, 21 youths aged 9-20 years represented by “Our Children’s Trust” are suing the U.S. government in the Oregon U.S. District Court for failure to act on climate. The case, heard by Judge Ann Aiken, is now headed to trial.
All of us have a duty to collectively, repeatedly, and forcefully call on policy makers to take action.
That leads me to what we can do as doctors. In this effort to quickly transition to safe, clean renewable energy, we all have a role to play. The notion that we can’t do anything as individuals is no more credible than saying “my vote doesn’t matter.” Just as our actions as voters in a democracy demonstrate the collective civic responsibility we owe one another, so too do our actions on climate. As global citizens, all actions that we take to help us live within the planet’s means are opportunities to restore balance.
What we do collectively drives markets and determines the social norms that powerfully influence the decisions of others – sometimes even unconsciously.
As doctors, we have a unique role to play in the places we work – urging hospitals, clinics, academic centers, and other organizations and facilities to lead by example, become role models for energy efficiency, and choose clean renewable energy sources over the ones harming our health. We can start by choosing wind and solar to power our homes and influencing others to do the same.
We are the voices because this is a health message.
Dr. Van Susteren is a practicing general and forensic psychiatrist in Washington. She serves on the advisory board of the Center for Health and the Global Environment at Harvard T.H. Chan School of Public Health, Boston. Dr. Van Susteren is a former member of the board of directors of the National Wildlife Federation and coauthor of group’s report, “The Psychological Effects of Global Warming on the United States – Why the U.S. Mental Health System is Not Prepared.” In 2006, Dr. Van Susteren sought the Democratic nomination for a U.S. Senate seat in Maryland. She also founded Lucky Planet Foods, a company that provides plant-based, low carbon foods.
References
1. Environ Microbiol. 2017 Feb 14. doi: 10.1111/1462-2920.13686.
2. Environ Health Perspect. 2017 Mar;125[3]:378-84.
3. J Hepatol. 2015;63[6]:1397-1404.
4. J Toxicol Environ Health A. 2012;75[3]:174-82.
5. Environ Health Perspect. 2012 Nov; 118[11]:1578-83.
6. J Child Psychol Psychiatry. 2016; 57[3]:271-92.
7. Curr Opin Pediatr. 2010;22[2]219-25.
8. Inhal Toxicol. 2008;20[5]:499-506.
9. J Psychiatr Res. 2015 Mar;62:130-5.
10. Schizophr Res. 2016 Oct 5. doi: 10.1016/j.schres.2016.10.003.
11. Environ Health Perspect. 2016 Jun;124[6]:805-12.
“Exercising my ‘reasoned judgment,’ I have no doubt that the right to a climate system capable of sustaining human life is fundamental to a free and ordered society.”
– U.S. District Judge Ann Aiken in Kelsey Cascadia Rose Juliana vs. United States of America, et al.
In many areas of the world, the simple act of breathing has become hazardous to people’s health.
According to the World Health Organization, more people die every day from air pollution than from HIV/AIDS, tuberculosis, and road injuries combined. In China, more than 1 million deaths annually are linked to polluted air (76/100,000); in India the number of deaths is more than 600,000 annually (49/100,000); and in the United States, that figure comes to more than 38,000 (12/100,000).
And yet, nonpolluting, alternative options – such as sun and wind power – are readily available.
Dirty air is visible on a hot summer day – when, mixed with other substances, it forms smog. Higher temperatures can then speed up the chemical reactions that form smog. We breathe in that polluted air, especially on days when the air is stagnant or there is temperature inversion.
The health effects of climate change
Black carbon found in air pollution leads to drug-resistant bacteria and alters antibiotic tolerance.1 The pollution also is associated with multiple cancers: lung, liver, ovarian, and, possibly, breast.2,3,4,5 It causes inflammation linked to the development of coronary artery disease (seen even in children!) and plaque formation leading to heart attacks and cardiac arrhythmias – including atrial fibrillation. Air pollution causes, triggers, or worsens respiratory illnesses – chronic obstructive pulmonary disease, emphysema, asthma, infections – and is responsible for lifelong diminished lung volume in children (a reason families are leaving Beijing.) Exponentially increased rates of autism are linked to bad air quality, as are autoimmune diseases, which also are on the rise.6,7 Polluted air causes brain inflammation – living near sources of air pollution increases the risk of dementia – and other neurodegenerative diseases such as Alzheimer’s disease, Parkinson’s, and amyotrophic lateral sclerosis.8 The blood brain barrier protects the brain from most foreign matter, but particulate matter, especially ultrafine particulate matter of less than 1 mcm such as magnetite, can cross directly into the brain via the olfactory nerve. (Magnetite has been identified in the brain tissue of residents living in areas where the substance is produced as a result of industrial waste.) While particulate matter of 2.5 mcmis measured in the United States, ultrafine particulate matter is not.
Psychiatric symptoms and chronic psychiatric disorders also are associated with polluted air: On days with poor air quality, a statistically significant increase is seen in suicide threats and visits to emergency departments for panic attacks.9,10
A rise in aggression occurs when there are abnormally high temperatures and significant changes in rainfall. More assaults, murders, suicides, domestic violence, and child abuse can be expected, and a rise in unrest around the world should come as no surprise.
As a consequence of increased CO2 in the atmosphere, temperatures have already risen by 2° F: Sixteen of the hottest years on record have occurred in the last 17 years, with 2016 as the hottest year ever recorded. In Iraq and Kuwait, the temperature last summer reached 129.2° F.
We are experiencing more frequent and extreme weather events, chronic climate conditions, and the cascading disruption of ecosystems. Drought and sea level rise are leading to physical and psychological impacts – both direct and indirect. Some regions of the world have become destabilized, triggering migrations and the refugee crisis.
Along with these psychological impacts, CO2 affects cognition: A recent study by the Harvard School of Public Health, Boston, shows that the indoor levels of CO2 to which American workers typically are exposed impair cognitive functioning, particularly in the areas of strategic thinking, information processing, and crisis management.11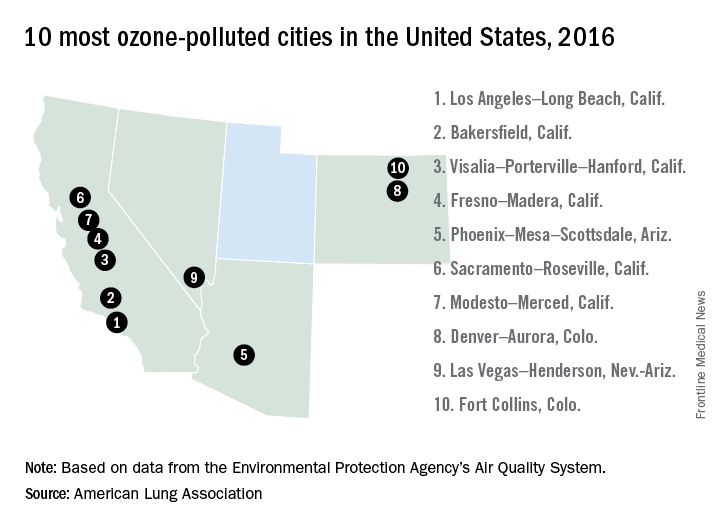
What do we do about it?
As mental health professionals, we know that aggression can be overt or passive (from inaction). Overwhelming evidence shows harm to public health from burning fossil fuels, and yet, though we are making progress, resistance still exists in the transition to clean, renewable energy critical for the health of our families and communities. When political will is what stands between us and getting back on a path to breathing clean air, how can inaction be understood as anything but an act of aggression?
This issue has reached U.S. courts: In a landmark case, 21 youths aged 9-20 years represented by “Our Children’s Trust” are suing the U.S. government in the Oregon U.S. District Court for failure to act on climate. The case, heard by Judge Ann Aiken, is now headed to trial.
All of us have a duty to collectively, repeatedly, and forcefully call on policy makers to take action.
That leads me to what we can do as doctors. In this effort to quickly transition to safe, clean renewable energy, we all have a role to play. The notion that we can’t do anything as individuals is no more credible than saying “my vote doesn’t matter.” Just as our actions as voters in a democracy demonstrate the collective civic responsibility we owe one another, so too do our actions on climate. As global citizens, all actions that we take to help us live within the planet’s means are opportunities to restore balance.
What we do collectively drives markets and determines the social norms that powerfully influence the decisions of others – sometimes even unconsciously.
As doctors, we have a unique role to play in the places we work – urging hospitals, clinics, academic centers, and other organizations and facilities to lead by example, become role models for energy efficiency, and choose clean renewable energy sources over the ones harming our health. We can start by choosing wind and solar to power our homes and influencing others to do the same.
We are the voices because this is a health message.
Dr. Van Susteren is a practicing general and forensic psychiatrist in Washington. She serves on the advisory board of the Center for Health and the Global Environment at Harvard T.H. Chan School of Public Health, Boston. Dr. Van Susteren is a former member of the board of directors of the National Wildlife Federation and coauthor of group’s report, “The Psychological Effects of Global Warming on the United States – Why the U.S. Mental Health System is Not Prepared.” In 2006, Dr. Van Susteren sought the Democratic nomination for a U.S. Senate seat in Maryland. She also founded Lucky Planet Foods, a company that provides plant-based, low carbon foods.
References
1. Environ Microbiol. 2017 Feb 14. doi: 10.1111/1462-2920.13686.
2. Environ Health Perspect. 2017 Mar;125[3]:378-84.
3. J Hepatol. 2015;63[6]:1397-1404.
4. J Toxicol Environ Health A. 2012;75[3]:174-82.
5. Environ Health Perspect. 2012 Nov; 118[11]:1578-83.
6. J Child Psychol Psychiatry. 2016; 57[3]:271-92.
7. Curr Opin Pediatr. 2010;22[2]219-25.
8. Inhal Toxicol. 2008;20[5]:499-506.
9. J Psychiatr Res. 2015 Mar;62:130-5.
10. Schizophr Res. 2016 Oct 5. doi: 10.1016/j.schres.2016.10.003.
11. Environ Health Perspect. 2016 Jun;124[6]:805-12.
“Exercising my ‘reasoned judgment,’ I have no doubt that the right to a climate system capable of sustaining human life is fundamental to a free and ordered society.”
– U.S. District Judge Ann Aiken in Kelsey Cascadia Rose Juliana vs. United States of America, et al.
In many areas of the world, the simple act of breathing has become hazardous to people’s health.
According to the World Health Organization, more people die every day from air pollution than from HIV/AIDS, tuberculosis, and road injuries combined. In China, more than 1 million deaths annually are linked to polluted air (76/100,000); in India the number of deaths is more than 600,000 annually (49/100,000); and in the United States, that figure comes to more than 38,000 (12/100,000).
And yet, nonpolluting, alternative options – such as sun and wind power – are readily available.
Dirty air is visible on a hot summer day – when, mixed with other substances, it forms smog. Higher temperatures can then speed up the chemical reactions that form smog. We breathe in that polluted air, especially on days when the air is stagnant or there is temperature inversion.
The health effects of climate change
Black carbon found in air pollution leads to drug-resistant bacteria and alters antibiotic tolerance.1 The pollution also is associated with multiple cancers: lung, liver, ovarian, and, possibly, breast.2,3,4,5 It causes inflammation linked to the development of coronary artery disease (seen even in children!) and plaque formation leading to heart attacks and cardiac arrhythmias – including atrial fibrillation. Air pollution causes, triggers, or worsens respiratory illnesses – chronic obstructive pulmonary disease, emphysema, asthma, infections – and is responsible for lifelong diminished lung volume in children (a reason families are leaving Beijing.) Exponentially increased rates of autism are linked to bad air quality, as are autoimmune diseases, which also are on the rise.6,7 Polluted air causes brain inflammation – living near sources of air pollution increases the risk of dementia – and other neurodegenerative diseases such as Alzheimer’s disease, Parkinson’s, and amyotrophic lateral sclerosis.8 The blood brain barrier protects the brain from most foreign matter, but particulate matter, especially ultrafine particulate matter of less than 1 mcm such as magnetite, can cross directly into the brain via the olfactory nerve. (Magnetite has been identified in the brain tissue of residents living in areas where the substance is produced as a result of industrial waste.) While particulate matter of 2.5 mcmis measured in the United States, ultrafine particulate matter is not.
Psychiatric symptoms and chronic psychiatric disorders also are associated with polluted air: On days with poor air quality, a statistically significant increase is seen in suicide threats and visits to emergency departments for panic attacks.9,10
A rise in aggression occurs when there are abnormally high temperatures and significant changes in rainfall. More assaults, murders, suicides, domestic violence, and child abuse can be expected, and a rise in unrest around the world should come as no surprise.
As a consequence of increased CO2 in the atmosphere, temperatures have already risen by 2° F: Sixteen of the hottest years on record have occurred in the last 17 years, with 2016 as the hottest year ever recorded. In Iraq and Kuwait, the temperature last summer reached 129.2° F.
We are experiencing more frequent and extreme weather events, chronic climate conditions, and the cascading disruption of ecosystems. Drought and sea level rise are leading to physical and psychological impacts – both direct and indirect. Some regions of the world have become destabilized, triggering migrations and the refugee crisis.
Along with these psychological impacts, CO2 affects cognition: A recent study by the Harvard School of Public Health, Boston, shows that the indoor levels of CO2 to which American workers typically are exposed impair cognitive functioning, particularly in the areas of strategic thinking, information processing, and crisis management.11
What do we do about it?
As mental health professionals, we know that aggression can be overt or passive (from inaction). Overwhelming evidence shows harm to public health from burning fossil fuels, and yet, though we are making progress, resistance still exists in the transition to clean, renewable energy critical for the health of our families and communities. When political will is what stands between us and getting back on a path to breathing clean air, how can inaction be understood as anything but an act of aggression?
This issue has reached U.S. courts: In a landmark case, 21 youths aged 9-20 years represented by “Our Children’s Trust” are suing the U.S. government in the Oregon U.S. District Court for failure to act on climate. The case, heard by Judge Ann Aiken, is now headed to trial.
All of us have a duty to collectively, repeatedly, and forcefully call on policy makers to take action.
That leads me to what we can do as doctors. In this effort to quickly transition to safe, clean renewable energy, we all have a role to play. The notion that we can’t do anything as individuals is no more credible than saying “my vote doesn’t matter.” Just as our actions as voters in a democracy demonstrate the collective civic responsibility we owe one another, so too do our actions on climate. As global citizens, all actions that we take to help us live within the planet’s means are opportunities to restore balance.
What we do collectively drives markets and determines the social norms that powerfully influence the decisions of others – sometimes even unconsciously.
As doctors, we have a unique role to play in the places we work – urging hospitals, clinics, academic centers, and other organizations and facilities to lead by example, become role models for energy efficiency, and choose clean renewable energy sources over the ones harming our health. We can start by choosing wind and solar to power our homes and influencing others to do the same.
We are the voices because this is a health message.
Dr. Van Susteren is a practicing general and forensic psychiatrist in Washington. She serves on the advisory board of the Center for Health and the Global Environment at Harvard T.H. Chan School of Public Health, Boston. Dr. Van Susteren is a former member of the board of directors of the National Wildlife Federation and coauthor of group’s report, “The Psychological Effects of Global Warming on the United States – Why the U.S. Mental Health System is Not Prepared.” In 2006, Dr. Van Susteren sought the Democratic nomination for a U.S. Senate seat in Maryland. She also founded Lucky Planet Foods, a company that provides plant-based, low carbon foods.
References
1. Environ Microbiol. 2017 Feb 14. doi: 10.1111/1462-2920.13686.
2. Environ Health Perspect. 2017 Mar;125[3]:378-84.
3. J Hepatol. 2015;63[6]:1397-1404.
4. J Toxicol Environ Health A. 2012;75[3]:174-82.
5. Environ Health Perspect. 2012 Nov; 118[11]:1578-83.
6. J Child Psychol Psychiatry. 2016; 57[3]:271-92.
7. Curr Opin Pediatr. 2010;22[2]219-25.
8. Inhal Toxicol. 2008;20[5]:499-506.
9. J Psychiatr Res. 2015 Mar;62:130-5.
10. Schizophr Res. 2016 Oct 5. doi: 10.1016/j.schres.2016.10.003.
11. Environ Health Perspect. 2016 Jun;124[6]:805-12.
Preoperative variables can predict prolonged air leak
Prolonged air leak is a well-known complication after lung cancer surgery that can worsen patient outcomes and drive up costs, and while international authors have developed tools to calculate the risk of PAL, their use has been limited in the United States for various reasons. Researchers at the University of Pittsburgh have reported on a predictive model that uses easy-to-obtain patient factors, such as forced expiratory volume and smoking history, to help surgeons identify patients at greatest risk for complications and implement preventative measures.
Adam Attaar and his coauthors reported that their nomogram had an accuracy rate of 76%, with a 95% confidence interval, for predicting PAL after surgery (J Thorac Cardiovasc Surg. 2017 March;153[3]:690-9). “Using readily available candidate variables, our nomogram predicts increasing risk of prolonged air leak with good discriminatory ability,” noted Mr. Attaar, a student at University of Pittsburgh, and his coauthors.
Previously published reports put the incidence of PAL complications at 6%-18%, they noted. In the University of Pittsburgh series of 2,317 patients who had pulmonary resection for lung cancer or nodules from January 2009 to June 2014, the incidence was 8.6%.
In this series, patients with PAL were more likely to be older, men, and smokers, and to have a lower body mass index, peripheral vascular disease, chronic obstructive pulmonary disease, a history of steroid use, a high Zubrod score and lower forced expiratory volume.“They were less likely to have diabetes or to be hospitalized before surgery,” the researchers said. Surgical factors that characterized patients with PAL were resection for primary lung cancer rather than benign or metastatic tumors; lobectomy/segmentectomy or bilobectomy rather than wedge resection; a right-sided resection; thoracotomy; and a surgeon with higher annual caseloads.
Not all those factors made it into the nomogram, however. The nomogram scores each of these 10 variables to calculate the risk of PAL, in order of their weighting: lower forced expiratory volume, procedure type, BMI, right-sided thoracotomy, preoperative hospitalization, annual surgeon caseload, wedge resection by thoracotomy, reoperation, smoking history, and Zubrod score. A second nomogram drops out surgeon volume to make it more generalizable to other institutions.
In explaining higher surgeon volume as a risk factor for PAL, the researchers said that high-volume surgeons may be operating on patients with variables not accounted for in the Society of Thoracic Surgeons General Thoracic Surgery Database. “These unmeasured variables … could reveal modifiable technical factors to reduce the incidence of PAL and require further study,” the researchers said.
Fast-track discharge has gained acceptance in recent years as a way to spare patients a prolonged hospital stay and cut costs, but in this series the median hospital stay for patients with PAL was 10 days vs. 4 days for non-PAL patients (P less than 0.001).
“An accurate and generalizable PAL risk stratification tool could facilitate surgical decision making and patient-specific care” and aid in the design of trials to evaluate air-leak reduction methods such as sealants, buttressed staple lines, and pneumoperitoneum the researchers wrote.
Going forward, further development of the model would involve a multicenter study and inclusion of risk factors not accounted for in the thoracic surgery database, they noted.
The researchers had no relevant financial relationships to disclose.
The authors of this study “have performed a rigorous set of analyses to create this model,” Chi-Fu Jeffrey Yang, MD, of Duke University, Durham, N.C., noted in his invited commentary (J Thorac Cardiovasc Surg. 2017 March;53[3]:700-1). “The strengths of this study include its sound statistical analysis and study design,” Dr. Yang wrote. He gave the authors credit for using bootstrapping to internally validate the model.
However, Dr. Yang said that the database used by the researchers did not account for “numerous important variables,” including presence of pleural adhesions and emphysema status. The analysis also grouped lobectomy and segmentectomy together, and did not consider intraoperative variables such as sealant use, or postoperative management.
While Dr. Yang commended the study authors for developing a “reliable nomogram,” getting it implemented in the clinic is another hurdle. “It is commonly cited that it takes approximately 17 years for research evidence to translate into daily practice,” he said. To shorten that time line, he suggested the authors take a cue from various tech groups: Develop an app that surgeons can use.
Dr. Yang had no relevant financial relationships to disclose.
The authors of this study “have performed a rigorous set of analyses to create this model,” Chi-Fu Jeffrey Yang, MD, of Duke University, Durham, N.C., noted in his invited commentary (J Thorac Cardiovasc Surg. 2017 March;53[3]:700-1). “The strengths of this study include its sound statistical analysis and study design,” Dr. Yang wrote. He gave the authors credit for using bootstrapping to internally validate the model.
However, Dr. Yang said that the database used by the researchers did not account for “numerous important variables,” including presence of pleural adhesions and emphysema status. The analysis also grouped lobectomy and segmentectomy together, and did not consider intraoperative variables such as sealant use, or postoperative management.
While Dr. Yang commended the study authors for developing a “reliable nomogram,” getting it implemented in the clinic is another hurdle. “It is commonly cited that it takes approximately 17 years for research evidence to translate into daily practice,” he said. To shorten that time line, he suggested the authors take a cue from various tech groups: Develop an app that surgeons can use.
Dr. Yang had no relevant financial relationships to disclose.
The authors of this study “have performed a rigorous set of analyses to create this model,” Chi-Fu Jeffrey Yang, MD, of Duke University, Durham, N.C., noted in his invited commentary (J Thorac Cardiovasc Surg. 2017 March;53[3]:700-1). “The strengths of this study include its sound statistical analysis and study design,” Dr. Yang wrote. He gave the authors credit for using bootstrapping to internally validate the model.
However, Dr. Yang said that the database used by the researchers did not account for “numerous important variables,” including presence of pleural adhesions and emphysema status. The analysis also grouped lobectomy and segmentectomy together, and did not consider intraoperative variables such as sealant use, or postoperative management.
While Dr. Yang commended the study authors for developing a “reliable nomogram,” getting it implemented in the clinic is another hurdle. “It is commonly cited that it takes approximately 17 years for research evidence to translate into daily practice,” he said. To shorten that time line, he suggested the authors take a cue from various tech groups: Develop an app that surgeons can use.
Dr. Yang had no relevant financial relationships to disclose.
Prolonged air leak is a well-known complication after lung cancer surgery that can worsen patient outcomes and drive up costs, and while international authors have developed tools to calculate the risk of PAL, their use has been limited in the United States for various reasons. Researchers at the University of Pittsburgh have reported on a predictive model that uses easy-to-obtain patient factors, such as forced expiratory volume and smoking history, to help surgeons identify patients at greatest risk for complications and implement preventative measures.
Adam Attaar and his coauthors reported that their nomogram had an accuracy rate of 76%, with a 95% confidence interval, for predicting PAL after surgery (J Thorac Cardiovasc Surg. 2017 March;153[3]:690-9). “Using readily available candidate variables, our nomogram predicts increasing risk of prolonged air leak with good discriminatory ability,” noted Mr. Attaar, a student at University of Pittsburgh, and his coauthors.
Previously published reports put the incidence of PAL complications at 6%-18%, they noted. In the University of Pittsburgh series of 2,317 patients who had pulmonary resection for lung cancer or nodules from January 2009 to June 2014, the incidence was 8.6%.
In this series, patients with PAL were more likely to be older, men, and smokers, and to have a lower body mass index, peripheral vascular disease, chronic obstructive pulmonary disease, a history of steroid use, a high Zubrod score and lower forced expiratory volume.“They were less likely to have diabetes or to be hospitalized before surgery,” the researchers said. Surgical factors that characterized patients with PAL were resection for primary lung cancer rather than benign or metastatic tumors; lobectomy/segmentectomy or bilobectomy rather than wedge resection; a right-sided resection; thoracotomy; and a surgeon with higher annual caseloads.
Not all those factors made it into the nomogram, however. The nomogram scores each of these 10 variables to calculate the risk of PAL, in order of their weighting: lower forced expiratory volume, procedure type, BMI, right-sided thoracotomy, preoperative hospitalization, annual surgeon caseload, wedge resection by thoracotomy, reoperation, smoking history, and Zubrod score. A second nomogram drops out surgeon volume to make it more generalizable to other institutions.
In explaining higher surgeon volume as a risk factor for PAL, the researchers said that high-volume surgeons may be operating on patients with variables not accounted for in the Society of Thoracic Surgeons General Thoracic Surgery Database. “These unmeasured variables … could reveal modifiable technical factors to reduce the incidence of PAL and require further study,” the researchers said.
Fast-track discharge has gained acceptance in recent years as a way to spare patients a prolonged hospital stay and cut costs, but in this series the median hospital stay for patients with PAL was 10 days vs. 4 days for non-PAL patients (P less than 0.001).
“An accurate and generalizable PAL risk stratification tool could facilitate surgical decision making and patient-specific care” and aid in the design of trials to evaluate air-leak reduction methods such as sealants, buttressed staple lines, and pneumoperitoneum the researchers wrote.
Going forward, further development of the model would involve a multicenter study and inclusion of risk factors not accounted for in the thoracic surgery database, they noted.
The researchers had no relevant financial relationships to disclose.
Prolonged air leak is a well-known complication after lung cancer surgery that can worsen patient outcomes and drive up costs, and while international authors have developed tools to calculate the risk of PAL, their use has been limited in the United States for various reasons. Researchers at the University of Pittsburgh have reported on a predictive model that uses easy-to-obtain patient factors, such as forced expiratory volume and smoking history, to help surgeons identify patients at greatest risk for complications and implement preventative measures.
Adam Attaar and his coauthors reported that their nomogram had an accuracy rate of 76%, with a 95% confidence interval, for predicting PAL after surgery (J Thorac Cardiovasc Surg. 2017 March;153[3]:690-9). “Using readily available candidate variables, our nomogram predicts increasing risk of prolonged air leak with good discriminatory ability,” noted Mr. Attaar, a student at University of Pittsburgh, and his coauthors.
Previously published reports put the incidence of PAL complications at 6%-18%, they noted. In the University of Pittsburgh series of 2,317 patients who had pulmonary resection for lung cancer or nodules from January 2009 to June 2014, the incidence was 8.6%.
In this series, patients with PAL were more likely to be older, men, and smokers, and to have a lower body mass index, peripheral vascular disease, chronic obstructive pulmonary disease, a history of steroid use, a high Zubrod score and lower forced expiratory volume.“They were less likely to have diabetes or to be hospitalized before surgery,” the researchers said. Surgical factors that characterized patients with PAL were resection for primary lung cancer rather than benign or metastatic tumors; lobectomy/segmentectomy or bilobectomy rather than wedge resection; a right-sided resection; thoracotomy; and a surgeon with higher annual caseloads.
Not all those factors made it into the nomogram, however. The nomogram scores each of these 10 variables to calculate the risk of PAL, in order of their weighting: lower forced expiratory volume, procedure type, BMI, right-sided thoracotomy, preoperative hospitalization, annual surgeon caseload, wedge resection by thoracotomy, reoperation, smoking history, and Zubrod score. A second nomogram drops out surgeon volume to make it more generalizable to other institutions.
In explaining higher surgeon volume as a risk factor for PAL, the researchers said that high-volume surgeons may be operating on patients with variables not accounted for in the Society of Thoracic Surgeons General Thoracic Surgery Database. “These unmeasured variables … could reveal modifiable technical factors to reduce the incidence of PAL and require further study,” the researchers said.
Fast-track discharge has gained acceptance in recent years as a way to spare patients a prolonged hospital stay and cut costs, but in this series the median hospital stay for patients with PAL was 10 days vs. 4 days for non-PAL patients (P less than 0.001).
“An accurate and generalizable PAL risk stratification tool could facilitate surgical decision making and patient-specific care” and aid in the design of trials to evaluate air-leak reduction methods such as sealants, buttressed staple lines, and pneumoperitoneum the researchers wrote.
Going forward, further development of the model would involve a multicenter study and inclusion of risk factors not accounted for in the thoracic surgery database, they noted.
The researchers had no relevant financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Preoperative variables can be evaluated to determine patient risk for prolonged air leak (PAL) in lung resection for cancer.
Major finding: A nomogram demonstrated 76% discriminatory accuracy in predicting PAL after lung resection.
Data source: Analysis of 2,522 pulmonary resections performed at eight hospitals within the University of Pittsburgh health system from January 2009 to June 2014.
Disclosures: The researchers had no conflicts of interest to disclose.
Genetic variant linked to more antibiotics, corticosteroid use in COPD
A genetic variant associated with a poorer therapeutic response in patients with asthma may also be linked to more severe chronic obstructive pulmonary disease, researchers have found.
The polymorphisms at codons 16 and 27 of the beta-2-adrenoreceptor (ADRB2) gene are responsible for enhanced down-regulation of the beta-2-adrenoreceptor, and research suggests that Arg/Arg homozygosity at position 16 is associated with worse control of disease in patients with bronchial asthma.
However, the results of studies exploring the impact of this variant “on the clinical response to the administration of the beta-2-adrenoreceptor agonists in COPD patients are “parse and inconclusive,” according to Justyna Emeryk-Maksymiuk and colleagues at the Medical University of Lublin in Poland.
In a study published in the April issue of Pulmonary Pharmacology & Therapeutics, the researchers looked for variants of the ADRB2 gene in blood samples taken from 92 patients with stable grade COPD.
They collected data on each patient’s disease course during the previous 12 months, including the frequency of exacerbations requiring hospitalization, and antibiotic and systemic corticosteroid use.
They found significant differences between patients with either the Arg/Arg (n = 18), Arg/Gly (n = 61) and Gly/Gly (n = 13) polymorphism at codon 16 of the ADRB2 gene (Pulm Pharmacol Ther. 2017. doi: 10.1016/j.pupt.2017.01.005).
Those who were Arg/Arg homozygotes were significantly more likely to require two or more courses of antibiotic therapy: 33% of this group required two courses of antibiotics compared to 16.4% of those with the Arg/Gly polymorphism and none of those with the Gly/Gly polymorphism.
Those with the Arg/Arg polymorphism also required significantly more corticosteroid therapy; 16.7% needed three or more courses of systemic corticosteroid therapy, compared to none of the patients with the other polymorphisms.
However there were no significant differences between the three groups in the number of hospitalizations over the prior 12 months.
The researchers did not see any significant effects on hospitalizations, courses of corticosteroids or antibiotics from polymorphisms at codon 27 of the ADRB2 gene.
“The majority of researchers focus on the bronchodilator effect brought by the activation of the beta-2-adrenoreceptors, with less emphasis on the facts that these receptors are also involved in the inhibition of mast cell degranulation, chemotaxis, adhesion and activation of leukocytes, as well as in the improvement of mucociliary clearance of respiratory epithelium,” the authors wrote.
“The results of these studies confirmed that the Arg/Arg genotype at codon 16 predisposes patients to clinically more severe manifestation of obstructive respiratory disorders.”
The authors noted that the differences in the effect of genetic polymorphisms in the ADRB2 gene could also be the result of differences in the use of inhaled glucocorticoids, as these can prevent the desensitization of the beta-2-adrenoreceptor.
Previous research has found that nonusage of inhaled glucocorticoids in asthma patients with the Arg/Arg phenotype is associated with a twofold greater odds of uncontrolled asthma, when compared with patients with the Gly/Gly phenotype.
While patients with asthma are recommended to have inhaled glucocorticoids in conjunction with beta-2-mimetics, a considerable fraction of patients with COPD would not be administered glucocorticoids.
“Therefore, it cannot be excluded that a more severe course of asthma and COPD in patients with [the] Arg/Arg genotype of [the] ADRB2 gene at codon 16 does not result solely from the polymorphism itself, but also from the lack of [inhaled glucocorticoids].”
The Ministry of Science and Education supported the study. No conflicts of interest were declared.
A genetic variant associated with a poorer therapeutic response in patients with asthma may also be linked to more severe chronic obstructive pulmonary disease, researchers have found.
The polymorphisms at codons 16 and 27 of the beta-2-adrenoreceptor (ADRB2) gene are responsible for enhanced down-regulation of the beta-2-adrenoreceptor, and research suggests that Arg/Arg homozygosity at position 16 is associated with worse control of disease in patients with bronchial asthma.
However, the results of studies exploring the impact of this variant “on the clinical response to the administration of the beta-2-adrenoreceptor agonists in COPD patients are “parse and inconclusive,” according to Justyna Emeryk-Maksymiuk and colleagues at the Medical University of Lublin in Poland.
In a study published in the April issue of Pulmonary Pharmacology & Therapeutics, the researchers looked for variants of the ADRB2 gene in blood samples taken from 92 patients with stable grade COPD.
They collected data on each patient’s disease course during the previous 12 months, including the frequency of exacerbations requiring hospitalization, and antibiotic and systemic corticosteroid use.
They found significant differences between patients with either the Arg/Arg (n = 18), Arg/Gly (n = 61) and Gly/Gly (n = 13) polymorphism at codon 16 of the ADRB2 gene (Pulm Pharmacol Ther. 2017. doi: 10.1016/j.pupt.2017.01.005).
Those who were Arg/Arg homozygotes were significantly more likely to require two or more courses of antibiotic therapy: 33% of this group required two courses of antibiotics compared to 16.4% of those with the Arg/Gly polymorphism and none of those with the Gly/Gly polymorphism.
Those with the Arg/Arg polymorphism also required significantly more corticosteroid therapy; 16.7% needed three or more courses of systemic corticosteroid therapy, compared to none of the patients with the other polymorphisms.
However there were no significant differences between the three groups in the number of hospitalizations over the prior 12 months.
The researchers did not see any significant effects on hospitalizations, courses of corticosteroids or antibiotics from polymorphisms at codon 27 of the ADRB2 gene.
“The majority of researchers focus on the bronchodilator effect brought by the activation of the beta-2-adrenoreceptors, with less emphasis on the facts that these receptors are also involved in the inhibition of mast cell degranulation, chemotaxis, adhesion and activation of leukocytes, as well as in the improvement of mucociliary clearance of respiratory epithelium,” the authors wrote.
“The results of these studies confirmed that the Arg/Arg genotype at codon 16 predisposes patients to clinically more severe manifestation of obstructive respiratory disorders.”
The authors noted that the differences in the effect of genetic polymorphisms in the ADRB2 gene could also be the result of differences in the use of inhaled glucocorticoids, as these can prevent the desensitization of the beta-2-adrenoreceptor.
Previous research has found that nonusage of inhaled glucocorticoids in asthma patients with the Arg/Arg phenotype is associated with a twofold greater odds of uncontrolled asthma, when compared with patients with the Gly/Gly phenotype.
While patients with asthma are recommended to have inhaled glucocorticoids in conjunction with beta-2-mimetics, a considerable fraction of patients with COPD would not be administered glucocorticoids.
“Therefore, it cannot be excluded that a more severe course of asthma and COPD in patients with [the] Arg/Arg genotype of [the] ADRB2 gene at codon 16 does not result solely from the polymorphism itself, but also from the lack of [inhaled glucocorticoids].”
The Ministry of Science and Education supported the study. No conflicts of interest were declared.
A genetic variant associated with a poorer therapeutic response in patients with asthma may also be linked to more severe chronic obstructive pulmonary disease, researchers have found.
The polymorphisms at codons 16 and 27 of the beta-2-adrenoreceptor (ADRB2) gene are responsible for enhanced down-regulation of the beta-2-adrenoreceptor, and research suggests that Arg/Arg homozygosity at position 16 is associated with worse control of disease in patients with bronchial asthma.
However, the results of studies exploring the impact of this variant “on the clinical response to the administration of the beta-2-adrenoreceptor agonists in COPD patients are “parse and inconclusive,” according to Justyna Emeryk-Maksymiuk and colleagues at the Medical University of Lublin in Poland.
In a study published in the April issue of Pulmonary Pharmacology & Therapeutics, the researchers looked for variants of the ADRB2 gene in blood samples taken from 92 patients with stable grade COPD.
They collected data on each patient’s disease course during the previous 12 months, including the frequency of exacerbations requiring hospitalization, and antibiotic and systemic corticosteroid use.
They found significant differences between patients with either the Arg/Arg (n = 18), Arg/Gly (n = 61) and Gly/Gly (n = 13) polymorphism at codon 16 of the ADRB2 gene (Pulm Pharmacol Ther. 2017. doi: 10.1016/j.pupt.2017.01.005).
Those who were Arg/Arg homozygotes were significantly more likely to require two or more courses of antibiotic therapy: 33% of this group required two courses of antibiotics compared to 16.4% of those with the Arg/Gly polymorphism and none of those with the Gly/Gly polymorphism.
Those with the Arg/Arg polymorphism also required significantly more corticosteroid therapy; 16.7% needed three or more courses of systemic corticosteroid therapy, compared to none of the patients with the other polymorphisms.
However there were no significant differences between the three groups in the number of hospitalizations over the prior 12 months.
The researchers did not see any significant effects on hospitalizations, courses of corticosteroids or antibiotics from polymorphisms at codon 27 of the ADRB2 gene.
“The majority of researchers focus on the bronchodilator effect brought by the activation of the beta-2-adrenoreceptors, with less emphasis on the facts that these receptors are also involved in the inhibition of mast cell degranulation, chemotaxis, adhesion and activation of leukocytes, as well as in the improvement of mucociliary clearance of respiratory epithelium,” the authors wrote.
“The results of these studies confirmed that the Arg/Arg genotype at codon 16 predisposes patients to clinically more severe manifestation of obstructive respiratory disorders.”
The authors noted that the differences in the effect of genetic polymorphisms in the ADRB2 gene could also be the result of differences in the use of inhaled glucocorticoids, as these can prevent the desensitization of the beta-2-adrenoreceptor.
Previous research has found that nonusage of inhaled glucocorticoids in asthma patients with the Arg/Arg phenotype is associated with a twofold greater odds of uncontrolled asthma, when compared with patients with the Gly/Gly phenotype.
While patients with asthma are recommended to have inhaled glucocorticoids in conjunction with beta-2-mimetics, a considerable fraction of patients with COPD would not be administered glucocorticoids.
“Therefore, it cannot be excluded that a more severe course of asthma and COPD in patients with [the] Arg/Arg genotype of [the] ADRB2 gene at codon 16 does not result solely from the polymorphism itself, but also from the lack of [inhaled glucocorticoids].”
The Ministry of Science and Education supported the study. No conflicts of interest were declared.
FROM PULMONARY PHARMACOLOGY & THERAPEUTICS
Key clinical point: A genetic variation linked to poorer disease control in asthma is associated with a similar effect in patients with chronic obstructive pulmonary disease.
Major finding: Patients with COPD who are Arg/Arg homozygotes at codon 16 of the beta-2-adrenoreceptor gene were significantly more likely to require two or more courses of antibiotic therapy and more systemic corticosteroid therapy than were patients with other polymorphisms.
Data source: A retrospective cohort study of 92 patients with stable grade COPD.
Disclosures: The Ministry of Science and Education supported the study. No conflicts of interest were declared.
EBUS scope, EUS-FNA similarly effective
When assessing a patient for lung cancer, a procedure involving the insertion of an EBUS scope in the esophagus – EUS-B-FNA – can achieve similarly accurate results as endoscopic ultrasound guided–fine-needle aspiration (EUS-FNA), according to a new study.
This finding could lead patients to choose EUS-B-FNA over EUS-FNA – the standard of care for analyzing potential metastasis of the left adrenal glands (LAGs) – resulting in both time and cost savings for patients.
“A recent report showed that LAG visualization using the EBUS scope was possible in 85% of patients,” according to the authors of this study, including Prof. Jouke T. Annema, MD of the University of Amsterdam. Prior to this new research, it was unknown to what extent a single EBUS scope adequately assess and sample the LAGs and how its performance related to the use of a conventional endoscopic ultrasound–guided scope (Lung Cancer. 2017. doi: org/10.1016/j.lungcan.2017.02.011).
Dr. Annema and his coauthors recruited patients from four centers – three in the Netherlands, one in Poland – and followed them prospectively. Patients with “(suspected) lung cancer [who] had an indication for both mediastinal lymph node and LAG sampling” were recruited for the study. The researchers followed 44 patients through final diagnosis to determine if they ultimately had lung cancer.
Subjects first received complete mediastinal and hilar staging of lung cancer and any present tumors via an EBUS and EUS-B procedure. Following an EBUS examination of the mediastinum, the EBUS scope was retracted from the trachea and positioned into the esophagus for an examination of the mediastinal nodes. Then, the EBUS scope was advanced into the stomach for identification of the LAG. Afterward, the routine EUS-FNA was performed. LAG analysis across both methods involved visualizing the LAG and collecting an adequate tissue sample for testing.
“In short, in order to locate the LAG, a structured three step approach was used according to the EUS assessment tool (EUS-AT): identification of the liver, abdominal aorta, coeliac trunk, left kidney, and LAG,” the authors noted. “By turning the EBUS scope clockwise from the liver, the abdominal aorta and coeliac trun[k] are identified. By subsequently turning the EBUS scope gently in caudal direction, the left kidney and LAG are identified.”
Endoscopists then evaluated both procedures in each subject according to feasibility and practicability to determine if the findings of the experimental procedure were usable. Finally, a cytologic exam was conducted, using Giemsa or Papanicolaou staining to determine if any present cancer had metastasized, and a final diagnosis was made.
LAG analysis had a success rate of 89% (39/44; 95% confidence interval, 76-95%) for EUS-B-FNA, compared with 93% (41/44; 95% CI, 82-98%) for EUS-FNA. Similarly, when looking at the rate of sensitivity for LAG metastases, EUS-B had a rate of sensitivity for LAG metastases of at least 87% (95% CI, 65-97%), while EUS-FNA was found to be at least 83% (95% CI, 62-95%. Endoscopists were equally satisfied with both procedures in the “majority” of cases in this study.
“In [five] cases (11%), the EUS-B-FNA procedure was unsuccessful, due to the inability to make good contact of the ultrasound transducer and the stomach wall,” the authors explained. “The conventional EUS scope is more stable as a result of the increased tube diameter. Another advantage of the conventional echo-endoscope is its wider scanning angle. ... The conventional EUS scope is also longer than the EBUS scope, [but that] does not seem to be the limiting factor.”
No funding source was disclosed for this study. The authors reported no relevant financial disclosures.
When assessing a patient for lung cancer, a procedure involving the insertion of an EBUS scope in the esophagus – EUS-B-FNA – can achieve similarly accurate results as endoscopic ultrasound guided–fine-needle aspiration (EUS-FNA), according to a new study.
This finding could lead patients to choose EUS-B-FNA over EUS-FNA – the standard of care for analyzing potential metastasis of the left adrenal glands (LAGs) – resulting in both time and cost savings for patients.
“A recent report showed that LAG visualization using the EBUS scope was possible in 85% of patients,” according to the authors of this study, including Prof. Jouke T. Annema, MD of the University of Amsterdam. Prior to this new research, it was unknown to what extent a single EBUS scope adequately assess and sample the LAGs and how its performance related to the use of a conventional endoscopic ultrasound–guided scope (Lung Cancer. 2017. doi: org/10.1016/j.lungcan.2017.02.011).
Dr. Annema and his coauthors recruited patients from four centers – three in the Netherlands, one in Poland – and followed them prospectively. Patients with “(suspected) lung cancer [who] had an indication for both mediastinal lymph node and LAG sampling” were recruited for the study. The researchers followed 44 patients through final diagnosis to determine if they ultimately had lung cancer.
Subjects first received complete mediastinal and hilar staging of lung cancer and any present tumors via an EBUS and EUS-B procedure. Following an EBUS examination of the mediastinum, the EBUS scope was retracted from the trachea and positioned into the esophagus for an examination of the mediastinal nodes. Then, the EBUS scope was advanced into the stomach for identification of the LAG. Afterward, the routine EUS-FNA was performed. LAG analysis across both methods involved visualizing the LAG and collecting an adequate tissue sample for testing.
“In short, in order to locate the LAG, a structured three step approach was used according to the EUS assessment tool (EUS-AT): identification of the liver, abdominal aorta, coeliac trunk, left kidney, and LAG,” the authors noted. “By turning the EBUS scope clockwise from the liver, the abdominal aorta and coeliac trun[k] are identified. By subsequently turning the EBUS scope gently in caudal direction, the left kidney and LAG are identified.”
Endoscopists then evaluated both procedures in each subject according to feasibility and practicability to determine if the findings of the experimental procedure were usable. Finally, a cytologic exam was conducted, using Giemsa or Papanicolaou staining to determine if any present cancer had metastasized, and a final diagnosis was made.
LAG analysis had a success rate of 89% (39/44; 95% confidence interval, 76-95%) for EUS-B-FNA, compared with 93% (41/44; 95% CI, 82-98%) for EUS-FNA. Similarly, when looking at the rate of sensitivity for LAG metastases, EUS-B had a rate of sensitivity for LAG metastases of at least 87% (95% CI, 65-97%), while EUS-FNA was found to be at least 83% (95% CI, 62-95%. Endoscopists were equally satisfied with both procedures in the “majority” of cases in this study.
“In [five] cases (11%), the EUS-B-FNA procedure was unsuccessful, due to the inability to make good contact of the ultrasound transducer and the stomach wall,” the authors explained. “The conventional EUS scope is more stable as a result of the increased tube diameter. Another advantage of the conventional echo-endoscope is its wider scanning angle. ... The conventional EUS scope is also longer than the EBUS scope, [but that] does not seem to be the limiting factor.”
No funding source was disclosed for this study. The authors reported no relevant financial disclosures.
When assessing a patient for lung cancer, a procedure involving the insertion of an EBUS scope in the esophagus – EUS-B-FNA – can achieve similarly accurate results as endoscopic ultrasound guided–fine-needle aspiration (EUS-FNA), according to a new study.
This finding could lead patients to choose EUS-B-FNA over EUS-FNA – the standard of care for analyzing potential metastasis of the left adrenal glands (LAGs) – resulting in both time and cost savings for patients.
“A recent report showed that LAG visualization using the EBUS scope was possible in 85% of patients,” according to the authors of this study, including Prof. Jouke T. Annema, MD of the University of Amsterdam. Prior to this new research, it was unknown to what extent a single EBUS scope adequately assess and sample the LAGs and how its performance related to the use of a conventional endoscopic ultrasound–guided scope (Lung Cancer. 2017. doi: org/10.1016/j.lungcan.2017.02.011).
Dr. Annema and his coauthors recruited patients from four centers – three in the Netherlands, one in Poland – and followed them prospectively. Patients with “(suspected) lung cancer [who] had an indication for both mediastinal lymph node and LAG sampling” were recruited for the study. The researchers followed 44 patients through final diagnosis to determine if they ultimately had lung cancer.
Subjects first received complete mediastinal and hilar staging of lung cancer and any present tumors via an EBUS and EUS-B procedure. Following an EBUS examination of the mediastinum, the EBUS scope was retracted from the trachea and positioned into the esophagus for an examination of the mediastinal nodes. Then, the EBUS scope was advanced into the stomach for identification of the LAG. Afterward, the routine EUS-FNA was performed. LAG analysis across both methods involved visualizing the LAG and collecting an adequate tissue sample for testing.
“In short, in order to locate the LAG, a structured three step approach was used according to the EUS assessment tool (EUS-AT): identification of the liver, abdominal aorta, coeliac trunk, left kidney, and LAG,” the authors noted. “By turning the EBUS scope clockwise from the liver, the abdominal aorta and coeliac trun[k] are identified. By subsequently turning the EBUS scope gently in caudal direction, the left kidney and LAG are identified.”
Endoscopists then evaluated both procedures in each subject according to feasibility and practicability to determine if the findings of the experimental procedure were usable. Finally, a cytologic exam was conducted, using Giemsa or Papanicolaou staining to determine if any present cancer had metastasized, and a final diagnosis was made.
LAG analysis had a success rate of 89% (39/44; 95% confidence interval, 76-95%) for EUS-B-FNA, compared with 93% (41/44; 95% CI, 82-98%) for EUS-FNA. Similarly, when looking at the rate of sensitivity for LAG metastases, EUS-B had a rate of sensitivity for LAG metastases of at least 87% (95% CI, 65-97%), while EUS-FNA was found to be at least 83% (95% CI, 62-95%. Endoscopists were equally satisfied with both procedures in the “majority” of cases in this study.
“In [five] cases (11%), the EUS-B-FNA procedure was unsuccessful, due to the inability to make good contact of the ultrasound transducer and the stomach wall,” the authors explained. “The conventional EUS scope is more stable as a result of the increased tube diameter. Another advantage of the conventional echo-endoscope is its wider scanning angle. ... The conventional EUS scope is also longer than the EBUS scope, [but that] does not seem to be the limiting factor.”
No funding source was disclosed for this study. The authors reported no relevant financial disclosures.
FROM LUNG CANCER
Key clinical point:
Major finding: EUS-B-FNA had a success rate of 89%, versus 93% for EUS-FNA, while sensitivity for LAG metastases were 87% and 83%, respectively.
Data source: Multicenter, prospective study of 44 consecutive suspected lung cancer patients.
Disclosures: No funding source disclosed. Authors reported no relevant financial disclosures.