User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Harmful emotional hit of antidepressants underappreciated
SAN FRANCISCO – , new research shows.
Emotional blunting can be described as feeling emotionally flat and incapable of finding pleasure. The patient may feel less sadness, guilt, or hopelessness, but that may come at the cost of feeling less joy, surprise, and happiness. Some people with SSRI-induced blunting even report caring less about important relationships.
It’s an issue that needs greater attention, study investigator Mujeeb U. Shad, MD, with Valley Health Services and University of Nevada, Las Vegas, said in an interview.
“Patients may come to the clinic and report feeling emotionally and cognitively flat and not be taken seriously by their provider, but they are genuinely reporting something that is happening to them and decreasing their quality of life,” Dr. Shad explained.
The study was presented at the annual meeting of the American Psychiatric Association.
Something ‘missing’
Dr. Shad said that the genesis for the study came from a resident who noticed that many patients receiving SSRIs reported feeling better and not as bothered by the depression, yet, at the same time, they felt something was “missing. Their families would say, ‘You’re better but you’re not the same person.’ ”
To investigate further, the researchers did a “scoping review” of 25 original studies that assessed antidepressant-related emotional blunting. Until now, there hasn’t been a systematic review of this issue, Dr. Shad said.
Ten of the studies looked at the role of SSRIs in emotional blunting, whereas the other 15 looked at serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and second-generation antipsychotic medications.
The results of the review show that emotional blunting is a significant patient-reported concern. It often presents as a subjective complaint of changed personality, feeling a lesser intensity of overall emotions, and the manifestation of not being oneself often attributed to antidepressant use, the researchers found. Emotional blunting was more commonly associated with SSRIs than with the other medications in the studies.
Common clinical strategies to manage antidepressant-induced emotional blunting reported in the literature include dose reduction or switching to a different antidepressant class; however, the literature did not make the distinction between emotional blunting as a primary symptom of depression or an adverse effect of antidepressants.
Dr. Shad said that there is a need to develop valid and reliable measures to assess emotional blunting related to antidepressants.
He noted that optimal patient care should include pre- and posttreatment assessment of emotional blunting. One useful tool is the Oxford Questionnaire on the Emotional Side-Effects of Antidepressants.
Can’t get to the top
Jacob Cross, MD, who wasn’t involved in the study, said that he has seen the impact of antidepressant-related emotional blunting first-hand.
“I’ve had multiple patients report emotional blunting on antidepressant therapy,” Dr. Cross, with the department of psychiatry, Rush Medical College, Chicago, said.
“These patients feel like their emotions are not as high and not as low; so they experience directional improvement, but they’re still not feeling like they can get that top peak emotion. It’s kind of similar to anhedonia. They’re just feeling like a little cut off, like they’re climbing a cliff and just can’t get to that top,” Dr. Cross said.
For a patient with emotional blunting, Dr. Cross said he might “switch to an antidepressant that’s more stimulating like an SNRI from an SSRI. You could also lower the dose and see if that helps, but I usually change the drug class.”
The study had no specific funding. Dr. Shad and Dr. Cross have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – , new research shows.
Emotional blunting can be described as feeling emotionally flat and incapable of finding pleasure. The patient may feel less sadness, guilt, or hopelessness, but that may come at the cost of feeling less joy, surprise, and happiness. Some people with SSRI-induced blunting even report caring less about important relationships.
It’s an issue that needs greater attention, study investigator Mujeeb U. Shad, MD, with Valley Health Services and University of Nevada, Las Vegas, said in an interview.
“Patients may come to the clinic and report feeling emotionally and cognitively flat and not be taken seriously by their provider, but they are genuinely reporting something that is happening to them and decreasing their quality of life,” Dr. Shad explained.
The study was presented at the annual meeting of the American Psychiatric Association.
Something ‘missing’
Dr. Shad said that the genesis for the study came from a resident who noticed that many patients receiving SSRIs reported feeling better and not as bothered by the depression, yet, at the same time, they felt something was “missing. Their families would say, ‘You’re better but you’re not the same person.’ ”
To investigate further, the researchers did a “scoping review” of 25 original studies that assessed antidepressant-related emotional blunting. Until now, there hasn’t been a systematic review of this issue, Dr. Shad said.
Ten of the studies looked at the role of SSRIs in emotional blunting, whereas the other 15 looked at serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and second-generation antipsychotic medications.
The results of the review show that emotional blunting is a significant patient-reported concern. It often presents as a subjective complaint of changed personality, feeling a lesser intensity of overall emotions, and the manifestation of not being oneself often attributed to antidepressant use, the researchers found. Emotional blunting was more commonly associated with SSRIs than with the other medications in the studies.
Common clinical strategies to manage antidepressant-induced emotional blunting reported in the literature include dose reduction or switching to a different antidepressant class; however, the literature did not make the distinction between emotional blunting as a primary symptom of depression or an adverse effect of antidepressants.
Dr. Shad said that there is a need to develop valid and reliable measures to assess emotional blunting related to antidepressants.
He noted that optimal patient care should include pre- and posttreatment assessment of emotional blunting. One useful tool is the Oxford Questionnaire on the Emotional Side-Effects of Antidepressants.
Can’t get to the top
Jacob Cross, MD, who wasn’t involved in the study, said that he has seen the impact of antidepressant-related emotional blunting first-hand.
“I’ve had multiple patients report emotional blunting on antidepressant therapy,” Dr. Cross, with the department of psychiatry, Rush Medical College, Chicago, said.
“These patients feel like their emotions are not as high and not as low; so they experience directional improvement, but they’re still not feeling like they can get that top peak emotion. It’s kind of similar to anhedonia. They’re just feeling like a little cut off, like they’re climbing a cliff and just can’t get to that top,” Dr. Cross said.
For a patient with emotional blunting, Dr. Cross said he might “switch to an antidepressant that’s more stimulating like an SNRI from an SSRI. You could also lower the dose and see if that helps, but I usually change the drug class.”
The study had no specific funding. Dr. Shad and Dr. Cross have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – , new research shows.
Emotional blunting can be described as feeling emotionally flat and incapable of finding pleasure. The patient may feel less sadness, guilt, or hopelessness, but that may come at the cost of feeling less joy, surprise, and happiness. Some people with SSRI-induced blunting even report caring less about important relationships.
It’s an issue that needs greater attention, study investigator Mujeeb U. Shad, MD, with Valley Health Services and University of Nevada, Las Vegas, said in an interview.
“Patients may come to the clinic and report feeling emotionally and cognitively flat and not be taken seriously by their provider, but they are genuinely reporting something that is happening to them and decreasing their quality of life,” Dr. Shad explained.
The study was presented at the annual meeting of the American Psychiatric Association.
Something ‘missing’
Dr. Shad said that the genesis for the study came from a resident who noticed that many patients receiving SSRIs reported feeling better and not as bothered by the depression, yet, at the same time, they felt something was “missing. Their families would say, ‘You’re better but you’re not the same person.’ ”
To investigate further, the researchers did a “scoping review” of 25 original studies that assessed antidepressant-related emotional blunting. Until now, there hasn’t been a systematic review of this issue, Dr. Shad said.
Ten of the studies looked at the role of SSRIs in emotional blunting, whereas the other 15 looked at serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and second-generation antipsychotic medications.
The results of the review show that emotional blunting is a significant patient-reported concern. It often presents as a subjective complaint of changed personality, feeling a lesser intensity of overall emotions, and the manifestation of not being oneself often attributed to antidepressant use, the researchers found. Emotional blunting was more commonly associated with SSRIs than with the other medications in the studies.
Common clinical strategies to manage antidepressant-induced emotional blunting reported in the literature include dose reduction or switching to a different antidepressant class; however, the literature did not make the distinction between emotional blunting as a primary symptom of depression or an adverse effect of antidepressants.
Dr. Shad said that there is a need to develop valid and reliable measures to assess emotional blunting related to antidepressants.
He noted that optimal patient care should include pre- and posttreatment assessment of emotional blunting. One useful tool is the Oxford Questionnaire on the Emotional Side-Effects of Antidepressants.
Can’t get to the top
Jacob Cross, MD, who wasn’t involved in the study, said that he has seen the impact of antidepressant-related emotional blunting first-hand.
“I’ve had multiple patients report emotional blunting on antidepressant therapy,” Dr. Cross, with the department of psychiatry, Rush Medical College, Chicago, said.
“These patients feel like their emotions are not as high and not as low; so they experience directional improvement, but they’re still not feeling like they can get that top peak emotion. It’s kind of similar to anhedonia. They’re just feeling like a little cut off, like they’re climbing a cliff and just can’t get to that top,” Dr. Cross said.
For a patient with emotional blunting, Dr. Cross said he might “switch to an antidepressant that’s more stimulating like an SNRI from an SSRI. You could also lower the dose and see if that helps, but I usually change the drug class.”
The study had no specific funding. Dr. Shad and Dr. Cross have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
AT APA 2023
People still want their medical intelligence in human form
Doctors or AI? Lukewarm vote of confidence goes to …
Well, we’ve got some good news for the physicians out there, and we’ve got some bad news. Which do you want first? Okay, we’re mostly hearing good news, so here goes: Most people would choose a human doctor over artificial intelligence for the diagnosis and treatment of their medical conditions.
And the bad news? In the survey we’re talking about, “most” was 53%, so not exactly a huge victory for the carbon-based life forms. Yup, about 47% of the 2,472 respondents said they would prefer an AI-based clinic over a human specialist, and that number went up if individuals were told that their primary care physicians were on board with AI, “or otherwise nudged to consider AI as good,” the research team said in a written statement released by the University of Arizona, Tucson.
They went on to add that “this signaled the significance of the human physician in guiding a patient’s decision.” So patients will still need their doctors in the future to … um … this is a bit awkward … tell them how good the AI is?
And yes, we know that ChatGPT is already doing the same thing to journalists, but could it write a medical-humor column? Not a chance. Probably can’t even tell a joke.
How do ghosts get rid of wrinkles? Boo-tox. There, let’s see ChatGPT do that.
Explaining the joke makes it funnier, right?
Here at LOTME headquarters, we live by one simple rule, passed down directly from the Buddha himself: “Never let a good presurgical assessment of refractory epilepsy go to waste. Also, don’t believe everything you read on the Internet.”
This human-created joke has been brought to you by the leading theory of humor, which states that comedy stems from our brain reacting to an incongruous part of reality in a positive way. These positive emotions light up our neurons in a specific fashion, and boom, comedy is achieved.
Previous studies into the science of comedy have typically used functional MRI to analyze the brain while it was gripped in the throes of a comedic reaction. Unfortunately, fMRI cannot detect the entirety of the electromagnetic spectrum generated by the brain during these moments, so observing scientists have been, quite literally, missing out on some of the joke. And that’s where a new study from France comes in.
In the study, the researchers showed a group of patients with epilepsy who were hooked up to deep brain electrodes and a high-tech neuroimaging machine – part of the aforementioned presurgical assessment – a 3-minute excerpt from a Charlie Chaplin movie and analyzed their brain activity. Why Charlie Chaplin? Simple. Slapstick is perhaps the most accessible form of comedy across cultures. We can all appreciate a man getting hit in the head with a coconut. The world’s oldest bar joke or whatever this is? Not so much.
During the funniest scenes, all study participants showed increased high-frequency gamma waves (indicating high cognitive engagement) and a decrease in low-frequency waves (indicating reduced inattention and introspection). During unfunny scenes, such as transition moments, the opposite occurred. Importantly, this inverse relationship occurred in the temporal lobe but not in other regions, supporting previous research that indicated humor was mainly processed in the temporal lobe.
The investigators suggested future research should focus on longer videos with more complex forms of comedy, such as jokes, irony, sarcasm, or reference humor. So, uh, a guy getting hit in the head with two coconuts? That’s high-brow stuff right there.
Hot take: Humans aren’t that special
We humans have always prided ourselves on being different from “the animals” in an exceptional way. News flash! We aren’t. We may be the apex predator, but new research shows that humans, as part of the animal kingdom, just aren’t special.
Not special? How can they say that? Are gorillas doing open-heart surgery? Do wolverines tell jokes? At a more basic level, though, the way we operate as mammals in societies is not unique or even new. Elephants are known to mourn their deceased and to have funeral-like practices, ants invented agriculture, and we’re certainly not the only species that has figured out how to use tools.
This new research just demonstrates another way we aren’t exceptional, and that’s in our mating practices and outcomes.
“Humans appear to resemble mammals that live in monogamous partnerships and to some extent, those classified as cooperative breeders, where breeding individuals have to rely on the help of others to raise their offspring,” Monique Borgerhoff Mulder, PhD, professor emerita of anthropology at the University of California, Davis, said in a written statement.
The research team, which consisted of over 100 investigators, looked at 90 human populations based on data from over 80,000 people globally and compared the human data with 49 different nonhuman mammal species. In polygynous societies in which men take several wives, they found, women have more access to resources like food, shelter, and parenting help. Monogamy, on the other hand, “can drive significant inequalities among women,” Dr. Borgerhoff Mulder said, by promoting large differences in the number of children couples produce.
Human day-to-day behavior and child-rearing habits – one parent taking a daughter to ballet class and fixing dinner so the other parent can get to exercise class before picking up the son from soccer practice – may have us thinking that we are part of an evolved society, but really we are not much different than other mammals that hunt, forage for food, and rear and teach their children, the researchers suggested.
So, yes, humans can travel to the moon, create a vaccine for smallpox, and hit other humans with coconuts, but when it comes to simply having offspring or raising them, we’re not all that special. Get over it.
Doctors or AI? Lukewarm vote of confidence goes to …
Well, we’ve got some good news for the physicians out there, and we’ve got some bad news. Which do you want first? Okay, we’re mostly hearing good news, so here goes: Most people would choose a human doctor over artificial intelligence for the diagnosis and treatment of their medical conditions.
And the bad news? In the survey we’re talking about, “most” was 53%, so not exactly a huge victory for the carbon-based life forms. Yup, about 47% of the 2,472 respondents said they would prefer an AI-based clinic over a human specialist, and that number went up if individuals were told that their primary care physicians were on board with AI, “or otherwise nudged to consider AI as good,” the research team said in a written statement released by the University of Arizona, Tucson.
They went on to add that “this signaled the significance of the human physician in guiding a patient’s decision.” So patients will still need their doctors in the future to … um … this is a bit awkward … tell them how good the AI is?
And yes, we know that ChatGPT is already doing the same thing to journalists, but could it write a medical-humor column? Not a chance. Probably can’t even tell a joke.
How do ghosts get rid of wrinkles? Boo-tox. There, let’s see ChatGPT do that.
Explaining the joke makes it funnier, right?
Here at LOTME headquarters, we live by one simple rule, passed down directly from the Buddha himself: “Never let a good presurgical assessment of refractory epilepsy go to waste. Also, don’t believe everything you read on the Internet.”
This human-created joke has been brought to you by the leading theory of humor, which states that comedy stems from our brain reacting to an incongruous part of reality in a positive way. These positive emotions light up our neurons in a specific fashion, and boom, comedy is achieved.
Previous studies into the science of comedy have typically used functional MRI to analyze the brain while it was gripped in the throes of a comedic reaction. Unfortunately, fMRI cannot detect the entirety of the electromagnetic spectrum generated by the brain during these moments, so observing scientists have been, quite literally, missing out on some of the joke. And that’s where a new study from France comes in.
In the study, the researchers showed a group of patients with epilepsy who were hooked up to deep brain electrodes and a high-tech neuroimaging machine – part of the aforementioned presurgical assessment – a 3-minute excerpt from a Charlie Chaplin movie and analyzed their brain activity. Why Charlie Chaplin? Simple. Slapstick is perhaps the most accessible form of comedy across cultures. We can all appreciate a man getting hit in the head with a coconut. The world’s oldest bar joke or whatever this is? Not so much.
During the funniest scenes, all study participants showed increased high-frequency gamma waves (indicating high cognitive engagement) and a decrease in low-frequency waves (indicating reduced inattention and introspection). During unfunny scenes, such as transition moments, the opposite occurred. Importantly, this inverse relationship occurred in the temporal lobe but not in other regions, supporting previous research that indicated humor was mainly processed in the temporal lobe.
The investigators suggested future research should focus on longer videos with more complex forms of comedy, such as jokes, irony, sarcasm, or reference humor. So, uh, a guy getting hit in the head with two coconuts? That’s high-brow stuff right there.
Hot take: Humans aren’t that special
We humans have always prided ourselves on being different from “the animals” in an exceptional way. News flash! We aren’t. We may be the apex predator, but new research shows that humans, as part of the animal kingdom, just aren’t special.
Not special? How can they say that? Are gorillas doing open-heart surgery? Do wolverines tell jokes? At a more basic level, though, the way we operate as mammals in societies is not unique or even new. Elephants are known to mourn their deceased and to have funeral-like practices, ants invented agriculture, and we’re certainly not the only species that has figured out how to use tools.
This new research just demonstrates another way we aren’t exceptional, and that’s in our mating practices and outcomes.
“Humans appear to resemble mammals that live in monogamous partnerships and to some extent, those classified as cooperative breeders, where breeding individuals have to rely on the help of others to raise their offspring,” Monique Borgerhoff Mulder, PhD, professor emerita of anthropology at the University of California, Davis, said in a written statement.
The research team, which consisted of over 100 investigators, looked at 90 human populations based on data from over 80,000 people globally and compared the human data with 49 different nonhuman mammal species. In polygynous societies in which men take several wives, they found, women have more access to resources like food, shelter, and parenting help. Monogamy, on the other hand, “can drive significant inequalities among women,” Dr. Borgerhoff Mulder said, by promoting large differences in the number of children couples produce.
Human day-to-day behavior and child-rearing habits – one parent taking a daughter to ballet class and fixing dinner so the other parent can get to exercise class before picking up the son from soccer practice – may have us thinking that we are part of an evolved society, but really we are not much different than other mammals that hunt, forage for food, and rear and teach their children, the researchers suggested.
So, yes, humans can travel to the moon, create a vaccine for smallpox, and hit other humans with coconuts, but when it comes to simply having offspring or raising them, we’re not all that special. Get over it.
Doctors or AI? Lukewarm vote of confidence goes to …
Well, we’ve got some good news for the physicians out there, and we’ve got some bad news. Which do you want first? Okay, we’re mostly hearing good news, so here goes: Most people would choose a human doctor over artificial intelligence for the diagnosis and treatment of their medical conditions.
And the bad news? In the survey we’re talking about, “most” was 53%, so not exactly a huge victory for the carbon-based life forms. Yup, about 47% of the 2,472 respondents said they would prefer an AI-based clinic over a human specialist, and that number went up if individuals were told that their primary care physicians were on board with AI, “or otherwise nudged to consider AI as good,” the research team said in a written statement released by the University of Arizona, Tucson.
They went on to add that “this signaled the significance of the human physician in guiding a patient’s decision.” So patients will still need their doctors in the future to … um … this is a bit awkward … tell them how good the AI is?
And yes, we know that ChatGPT is already doing the same thing to journalists, but could it write a medical-humor column? Not a chance. Probably can’t even tell a joke.
How do ghosts get rid of wrinkles? Boo-tox. There, let’s see ChatGPT do that.
Explaining the joke makes it funnier, right?
Here at LOTME headquarters, we live by one simple rule, passed down directly from the Buddha himself: “Never let a good presurgical assessment of refractory epilepsy go to waste. Also, don’t believe everything you read on the Internet.”
This human-created joke has been brought to you by the leading theory of humor, which states that comedy stems from our brain reacting to an incongruous part of reality in a positive way. These positive emotions light up our neurons in a specific fashion, and boom, comedy is achieved.
Previous studies into the science of comedy have typically used functional MRI to analyze the brain while it was gripped in the throes of a comedic reaction. Unfortunately, fMRI cannot detect the entirety of the electromagnetic spectrum generated by the brain during these moments, so observing scientists have been, quite literally, missing out on some of the joke. And that’s where a new study from France comes in.
In the study, the researchers showed a group of patients with epilepsy who were hooked up to deep brain electrodes and a high-tech neuroimaging machine – part of the aforementioned presurgical assessment – a 3-minute excerpt from a Charlie Chaplin movie and analyzed their brain activity. Why Charlie Chaplin? Simple. Slapstick is perhaps the most accessible form of comedy across cultures. We can all appreciate a man getting hit in the head with a coconut. The world’s oldest bar joke or whatever this is? Not so much.
During the funniest scenes, all study participants showed increased high-frequency gamma waves (indicating high cognitive engagement) and a decrease in low-frequency waves (indicating reduced inattention and introspection). During unfunny scenes, such as transition moments, the opposite occurred. Importantly, this inverse relationship occurred in the temporal lobe but not in other regions, supporting previous research that indicated humor was mainly processed in the temporal lobe.
The investigators suggested future research should focus on longer videos with more complex forms of comedy, such as jokes, irony, sarcasm, or reference humor. So, uh, a guy getting hit in the head with two coconuts? That’s high-brow stuff right there.
Hot take: Humans aren’t that special
We humans have always prided ourselves on being different from “the animals” in an exceptional way. News flash! We aren’t. We may be the apex predator, but new research shows that humans, as part of the animal kingdom, just aren’t special.
Not special? How can they say that? Are gorillas doing open-heart surgery? Do wolverines tell jokes? At a more basic level, though, the way we operate as mammals in societies is not unique or even new. Elephants are known to mourn their deceased and to have funeral-like practices, ants invented agriculture, and we’re certainly not the only species that has figured out how to use tools.
This new research just demonstrates another way we aren’t exceptional, and that’s in our mating practices and outcomes.
“Humans appear to resemble mammals that live in monogamous partnerships and to some extent, those classified as cooperative breeders, where breeding individuals have to rely on the help of others to raise their offspring,” Monique Borgerhoff Mulder, PhD, professor emerita of anthropology at the University of California, Davis, said in a written statement.
The research team, which consisted of over 100 investigators, looked at 90 human populations based on data from over 80,000 people globally and compared the human data with 49 different nonhuman mammal species. In polygynous societies in which men take several wives, they found, women have more access to resources like food, shelter, and parenting help. Monogamy, on the other hand, “can drive significant inequalities among women,” Dr. Borgerhoff Mulder said, by promoting large differences in the number of children couples produce.
Human day-to-day behavior and child-rearing habits – one parent taking a daughter to ballet class and fixing dinner so the other parent can get to exercise class before picking up the son from soccer practice – may have us thinking that we are part of an evolved society, but really we are not much different than other mammals that hunt, forage for food, and rear and teach their children, the researchers suggested.
So, yes, humans can travel to the moon, create a vaccine for smallpox, and hit other humans with coconuts, but when it comes to simply having offspring or raising them, we’re not all that special. Get over it.
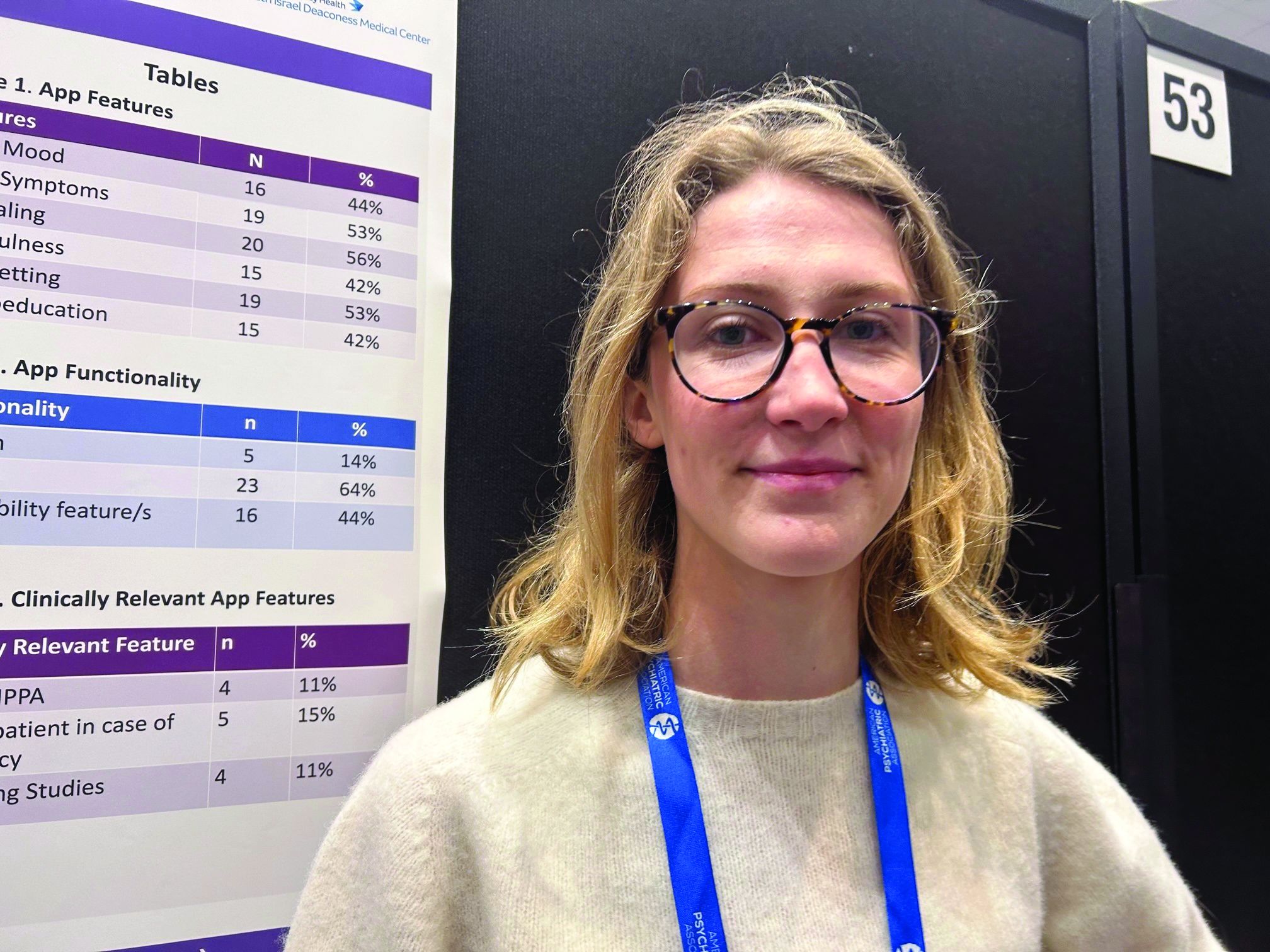
Eating disorder apps fall short when it comes to privacy
SAN FRANCISCO –
Federal laws require those handling sensitive health information to have policies and security safeguards in place to protect such information, whether it’s stored on paper or electronically.
“As it stands right now, there’s not enough evidence to support using these apps as an adjunct to clinical care,” study author Theodora O’Leary, a 4th-year medical student at Tufts University, Boston, said in an interview. “We need more research on the efficacy of these apps because right now not enough of them meet HIPAA [standards] and don’t have privacy and security measures.”
The findings were presented at the annual meeting of the American Psychiatric Association.
Eating disorders (EDs) are a common mental health condition affecting almost 1 in 10 Americans over their lifetime. Yet only about a third of patients with an eating disorder receive adequate treatment.
The pandemic saw a rise in eating disorders and in the use of mental health apps “to kind of fill the gap because people couldn’t be seen in person,” said Ms. O’Leary.
Inexpensive and accessible
Smartphone apps have a lot of advantages for patients with an ED. For one thing, they’re relatively inexpensive and accessible; most Americans already own one or more devices on which these apps can be used.
They’re also a feasible means of delivering psychological interventions, which are often recommended for EDs. Among these interventions, cognitive-behavioral therapy (CBT) has the largest evidence base for this condition.
Also, as many individuals with an ED may be reluctant to seek treatment because of stigma and shame, the anonymity afforded by an app could increase access to the help they seek.
But Ms. O’Leary warned the Food and Drug Administration does not regulate these apps, and people are sharing their personal health information on them.
The researchers conducted a review of commercially available eating disorder apps by searching the Apple and Google play stores using key phrases such as “eating disorder,” “anorexia,” and “binge eating disorder.”
They found 16 relevant apps that they added to the publicly available apps already in a database at Tufts, for a total of about 36 that were evaluated in the study (the number fluctuates as apps are deleted.)
They then reviewed the apps using the 105 questions based on the APA’s app evaluation model, which covers categories such as efficacy, privacy, accessibility, and clinical applicability. And they used filters to group apps by characteristics such as function, cost, and features.
The vast majority were self-help apps, which include things like journaling, meditation, and information on CBT. Others were reference apps that provide related definitions and sometimes include surveys to determine, for example, if the user has an eating disorder.
About 44% of the apps track mood, and 53% track symptoms. Some 56% include journaling, 42% mindfulness, 53% goal setting, and 42% psychoeducation.
Hybrid care
Only 5% of apps allow for “hybrid” care. This, explained Ms. O’Leary, is when clinicians use their own app to access patients’ apps, allowing them to track food restrictions and therapies, and make comments.
“The hybrid is viewed as the best form of app”, she said. “It’s almost like an adjunct to clinical care.”
Hybrid apps also tend to have patient safety features, she added. And these apps meet HIPAA standards, which only 11% of the apps in the study did.
Only 15% of apps advised patients to take steps in case of an emergency, and 11% had supporting studies. And where there was supporting research, much of it was funded by the app creators, said Ms. O’Leary.
For example, an app provided by Noom (the weight loss program that promises to help change habits and mindsets around food) “has a bunch of feasibility studies but they’re all funded by Noom”, which can introduce bias, she explained.
None of the apps were created by an accredited health care institution, she noted. “And I think only one app out of all the eating disorder apps we looked at was from a nonprofit.”
About 17% of the apps offer help with a “coach” or “expert”. However, these apps often fail to disclose the definition of a coach or state they’re not a replacement for medical care.
Coaching apps more expensive
Additionally, these coaching apps are often some of the most expensive, said Ms. O’Leary.
Daniel E. Gih, MD, associate professor at the University of Nebraska Medical Center, Omaha, helped start an eating disorders program at the University of Michigan and continues to treat patients with eating disorders. He said the increase in the use of eating disorder apps isn’t surprising as the incidence of these disorders increased in the wake of pandemic restrictions, especially among young people.
“Patients are likely doing more research on their medical conditions and trying to crowdsource information or self-treat,” Dr. Gih said.
It’s unclear whether “shame or just the general lack of specialized eating disorder professionals,” including physicians, is driving some of the interest in these apps, he added.
Dr. Gih stressed eating disorder apps should not only include screening for suicidality, but also explicitly tell patients to seek immediate attention if they show certain signs – for example, fainting, chest pain, or blood in emesis.
“The apps may be giving patients false hope or delaying medical care,” he said. “Apps are likely not sufficient enough to replace a multidisciplinary team with experience and expertise in eating disorders.”
Ms. O’Leary and Dr. Gih report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO –
Federal laws require those handling sensitive health information to have policies and security safeguards in place to protect such information, whether it’s stored on paper or electronically.
“As it stands right now, there’s not enough evidence to support using these apps as an adjunct to clinical care,” study author Theodora O’Leary, a 4th-year medical student at Tufts University, Boston, said in an interview. “We need more research on the efficacy of these apps because right now not enough of them meet HIPAA [standards] and don’t have privacy and security measures.”
The findings were presented at the annual meeting of the American Psychiatric Association.
Eating disorders (EDs) are a common mental health condition affecting almost 1 in 10 Americans over their lifetime. Yet only about a third of patients with an eating disorder receive adequate treatment.
The pandemic saw a rise in eating disorders and in the use of mental health apps “to kind of fill the gap because people couldn’t be seen in person,” said Ms. O’Leary.
Inexpensive and accessible
Smartphone apps have a lot of advantages for patients with an ED. For one thing, they’re relatively inexpensive and accessible; most Americans already own one or more devices on which these apps can be used.
They’re also a feasible means of delivering psychological interventions, which are often recommended for EDs. Among these interventions, cognitive-behavioral therapy (CBT) has the largest evidence base for this condition.
Also, as many individuals with an ED may be reluctant to seek treatment because of stigma and shame, the anonymity afforded by an app could increase access to the help they seek.
But Ms. O’Leary warned the Food and Drug Administration does not regulate these apps, and people are sharing their personal health information on them.
The researchers conducted a review of commercially available eating disorder apps by searching the Apple and Google play stores using key phrases such as “eating disorder,” “anorexia,” and “binge eating disorder.”
They found 16 relevant apps that they added to the publicly available apps already in a database at Tufts, for a total of about 36 that were evaluated in the study (the number fluctuates as apps are deleted.)
They then reviewed the apps using the 105 questions based on the APA’s app evaluation model, which covers categories such as efficacy, privacy, accessibility, and clinical applicability. And they used filters to group apps by characteristics such as function, cost, and features.
The vast majority were self-help apps, which include things like journaling, meditation, and information on CBT. Others were reference apps that provide related definitions and sometimes include surveys to determine, for example, if the user has an eating disorder.
About 44% of the apps track mood, and 53% track symptoms. Some 56% include journaling, 42% mindfulness, 53% goal setting, and 42% psychoeducation.
Hybrid care
Only 5% of apps allow for “hybrid” care. This, explained Ms. O’Leary, is when clinicians use their own app to access patients’ apps, allowing them to track food restrictions and therapies, and make comments.
“The hybrid is viewed as the best form of app”, she said. “It’s almost like an adjunct to clinical care.”
Hybrid apps also tend to have patient safety features, she added. And these apps meet HIPAA standards, which only 11% of the apps in the study did.
Only 15% of apps advised patients to take steps in case of an emergency, and 11% had supporting studies. And where there was supporting research, much of it was funded by the app creators, said Ms. O’Leary.
For example, an app provided by Noom (the weight loss program that promises to help change habits and mindsets around food) “has a bunch of feasibility studies but they’re all funded by Noom”, which can introduce bias, she explained.
None of the apps were created by an accredited health care institution, she noted. “And I think only one app out of all the eating disorder apps we looked at was from a nonprofit.”
About 17% of the apps offer help with a “coach” or “expert”. However, these apps often fail to disclose the definition of a coach or state they’re not a replacement for medical care.
Coaching apps more expensive
Additionally, these coaching apps are often some of the most expensive, said Ms. O’Leary.
Daniel E. Gih, MD, associate professor at the University of Nebraska Medical Center, Omaha, helped start an eating disorders program at the University of Michigan and continues to treat patients with eating disorders. He said the increase in the use of eating disorder apps isn’t surprising as the incidence of these disorders increased in the wake of pandemic restrictions, especially among young people.
“Patients are likely doing more research on their medical conditions and trying to crowdsource information or self-treat,” Dr. Gih said.
It’s unclear whether “shame or just the general lack of specialized eating disorder professionals,” including physicians, is driving some of the interest in these apps, he added.
Dr. Gih stressed eating disorder apps should not only include screening for suicidality, but also explicitly tell patients to seek immediate attention if they show certain signs – for example, fainting, chest pain, or blood in emesis.
“The apps may be giving patients false hope or delaying medical care,” he said. “Apps are likely not sufficient enough to replace a multidisciplinary team with experience and expertise in eating disorders.”
Ms. O’Leary and Dr. Gih report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO –
Federal laws require those handling sensitive health information to have policies and security safeguards in place to protect such information, whether it’s stored on paper or electronically.
“As it stands right now, there’s not enough evidence to support using these apps as an adjunct to clinical care,” study author Theodora O’Leary, a 4th-year medical student at Tufts University, Boston, said in an interview. “We need more research on the efficacy of these apps because right now not enough of them meet HIPAA [standards] and don’t have privacy and security measures.”
The findings were presented at the annual meeting of the American Psychiatric Association.
Eating disorders (EDs) are a common mental health condition affecting almost 1 in 10 Americans over their lifetime. Yet only about a third of patients with an eating disorder receive adequate treatment.
The pandemic saw a rise in eating disorders and in the use of mental health apps “to kind of fill the gap because people couldn’t be seen in person,” said Ms. O’Leary.
Inexpensive and accessible
Smartphone apps have a lot of advantages for patients with an ED. For one thing, they’re relatively inexpensive and accessible; most Americans already own one or more devices on which these apps can be used.
They’re also a feasible means of delivering psychological interventions, which are often recommended for EDs. Among these interventions, cognitive-behavioral therapy (CBT) has the largest evidence base for this condition.
Also, as many individuals with an ED may be reluctant to seek treatment because of stigma and shame, the anonymity afforded by an app could increase access to the help they seek.
But Ms. O’Leary warned the Food and Drug Administration does not regulate these apps, and people are sharing their personal health information on them.
The researchers conducted a review of commercially available eating disorder apps by searching the Apple and Google play stores using key phrases such as “eating disorder,” “anorexia,” and “binge eating disorder.”
They found 16 relevant apps that they added to the publicly available apps already in a database at Tufts, for a total of about 36 that were evaluated in the study (the number fluctuates as apps are deleted.)
They then reviewed the apps using the 105 questions based on the APA’s app evaluation model, which covers categories such as efficacy, privacy, accessibility, and clinical applicability. And they used filters to group apps by characteristics such as function, cost, and features.
The vast majority were self-help apps, which include things like journaling, meditation, and information on CBT. Others were reference apps that provide related definitions and sometimes include surveys to determine, for example, if the user has an eating disorder.
About 44% of the apps track mood, and 53% track symptoms. Some 56% include journaling, 42% mindfulness, 53% goal setting, and 42% psychoeducation.
Hybrid care
Only 5% of apps allow for “hybrid” care. This, explained Ms. O’Leary, is when clinicians use their own app to access patients’ apps, allowing them to track food restrictions and therapies, and make comments.
“The hybrid is viewed as the best form of app”, she said. “It’s almost like an adjunct to clinical care.”
Hybrid apps also tend to have patient safety features, she added. And these apps meet HIPAA standards, which only 11% of the apps in the study did.
Only 15% of apps advised patients to take steps in case of an emergency, and 11% had supporting studies. And where there was supporting research, much of it was funded by the app creators, said Ms. O’Leary.
For example, an app provided by Noom (the weight loss program that promises to help change habits and mindsets around food) “has a bunch of feasibility studies but they’re all funded by Noom”, which can introduce bias, she explained.
None of the apps were created by an accredited health care institution, she noted. “And I think only one app out of all the eating disorder apps we looked at was from a nonprofit.”
About 17% of the apps offer help with a “coach” or “expert”. However, these apps often fail to disclose the definition of a coach or state they’re not a replacement for medical care.
Coaching apps more expensive
Additionally, these coaching apps are often some of the most expensive, said Ms. O’Leary.
Daniel E. Gih, MD, associate professor at the University of Nebraska Medical Center, Omaha, helped start an eating disorders program at the University of Michigan and continues to treat patients with eating disorders. He said the increase in the use of eating disorder apps isn’t surprising as the incidence of these disorders increased in the wake of pandemic restrictions, especially among young people.
“Patients are likely doing more research on their medical conditions and trying to crowdsource information or self-treat,” Dr. Gih said.
It’s unclear whether “shame or just the general lack of specialized eating disorder professionals,” including physicians, is driving some of the interest in these apps, he added.
Dr. Gih stressed eating disorder apps should not only include screening for suicidality, but also explicitly tell patients to seek immediate attention if they show certain signs – for example, fainting, chest pain, or blood in emesis.
“The apps may be giving patients false hope or delaying medical care,” he said. “Apps are likely not sufficient enough to replace a multidisciplinary team with experience and expertise in eating disorders.”
Ms. O’Leary and Dr. Gih report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT APA 2023
Docs can help combat TikTok misinformation on rare psychiatric disorder
SAN FRANCISCO – , new research shows.
These findings, say investigators, underscore the need for mental health professionals to help counter the spread of false information by creating accurate content and posting it on the popular social media platform.
“Health care professionals need to make engaging content to post on social media platforms like YouTube and especially TikTok, to reach wider audiences and combat misinformation about DID,” study investigator Isreal Bladimir Munoz, a fourth-year medical student at University of Texas, Galveston, said in an interview.
The findings were presented at the annual meeting of the American Psychiatric Association.
Popularized by the media
A rare condition affecting less than 1% of the general population, DID involves two or more distinct personality states, along with changes in behavior and memory gaps.
The condition has been popularized in books and the media. Movies such as “Split,” “Psycho,” and “Fight Club” all feature characters with DID.
“These bring awareness about the condition, but also often sensationalize or stigmatize it and reinforce stereotypes,” said Mr. Munoz.
In recent years, social media has become an integral part of everyday life. An estimated 4.2 billion people actively frequent sites such as YouTube, TikTok, Twitter, and Meta.
Although social media allows for instant communication and the opportunity for self-expression, there are mounting concerns about the spread of misinformation and its potential impact on mental health and privacy, said Mr. Munoz.
To evaluate the quality and accuracy of information about DID on social media, investigators analyzed 60 YouTube and 97 TikTok videos on the condition.
To evaluate the reliability and the intent and reliability of videos, researchers used the modified DISCERN instrument and the Global Quality Scale, a five-point rating system.
Using these tools, the researchers determined whether the selected videos were useful, misleading, or neither. Mr. Munoz said videos were classified as useful if they contained accurate information about the condition and its pathogenesis, treatment, and management.
Researchers determined that for YouTube videos, 51.7% were useful, 6.6% were misleading, and 34.7% were neither. About 43.3% of these videos involved interviews, 21.7% were educational, 15% involved personal stories, 8.3% were films/TV programs, 5% were comedy skits, and 3.3% were another content type.
The highest quality YouTube videos were from educational organizations and health care professionals. The least accurate videos came from independent users and film/TV sources.
As for TikTok videos on DID, only 5.2% were useful, 10.3% were misleading, and 41.7% were neither.
The main sources for TikTok videos were independent organizations, whereas podcasts and film/TV were the least common sources.
The findings, said Mr. Munoz, underscore the need for medical professionals to develop high-quality content about DID and post it on TikTok to counter misinformation on social media.
Call to action
In a comment, Howard Y. Liu, MD, a child and adolescent psychiatrist and chair of the department of psychiatry, University of Nebraska, Omaha, described the study as “compelling.”
When it comes to public health messages, it’s important to know what social media people are using. Today’s parents are on Twitter and Facebook, whereas their children are more likely to be checking out YouTube and TikTok, said Dr. Liu, chair of the APA’s Council on Communications.
“TikTok is critical because that’s where all the youth eyeballs are,” he said.
The medical profession needs to engage with the platform to reach this next-generation audience and help stop the spread of misinformation about DID, said Dr. Liu. He noted that the APA is looking into undertaking such an initiative.
The study investigators report no relevant disclosures. Dr. Liu reports no relevant disclosures.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – , new research shows.
These findings, say investigators, underscore the need for mental health professionals to help counter the spread of false information by creating accurate content and posting it on the popular social media platform.
“Health care professionals need to make engaging content to post on social media platforms like YouTube and especially TikTok, to reach wider audiences and combat misinformation about DID,” study investigator Isreal Bladimir Munoz, a fourth-year medical student at University of Texas, Galveston, said in an interview.
The findings were presented at the annual meeting of the American Psychiatric Association.
Popularized by the media
A rare condition affecting less than 1% of the general population, DID involves two or more distinct personality states, along with changes in behavior and memory gaps.
The condition has been popularized in books and the media. Movies such as “Split,” “Psycho,” and “Fight Club” all feature characters with DID.
“These bring awareness about the condition, but also often sensationalize or stigmatize it and reinforce stereotypes,” said Mr. Munoz.
In recent years, social media has become an integral part of everyday life. An estimated 4.2 billion people actively frequent sites such as YouTube, TikTok, Twitter, and Meta.
Although social media allows for instant communication and the opportunity for self-expression, there are mounting concerns about the spread of misinformation and its potential impact on mental health and privacy, said Mr. Munoz.
To evaluate the quality and accuracy of information about DID on social media, investigators analyzed 60 YouTube and 97 TikTok videos on the condition.
To evaluate the reliability and the intent and reliability of videos, researchers used the modified DISCERN instrument and the Global Quality Scale, a five-point rating system.
Using these tools, the researchers determined whether the selected videos were useful, misleading, or neither. Mr. Munoz said videos were classified as useful if they contained accurate information about the condition and its pathogenesis, treatment, and management.
Researchers determined that for YouTube videos, 51.7% were useful, 6.6% were misleading, and 34.7% were neither. About 43.3% of these videos involved interviews, 21.7% were educational, 15% involved personal stories, 8.3% were films/TV programs, 5% were comedy skits, and 3.3% were another content type.
The highest quality YouTube videos were from educational organizations and health care professionals. The least accurate videos came from independent users and film/TV sources.
As for TikTok videos on DID, only 5.2% were useful, 10.3% were misleading, and 41.7% were neither.
The main sources for TikTok videos were independent organizations, whereas podcasts and film/TV were the least common sources.
The findings, said Mr. Munoz, underscore the need for medical professionals to develop high-quality content about DID and post it on TikTok to counter misinformation on social media.
Call to action
In a comment, Howard Y. Liu, MD, a child and adolescent psychiatrist and chair of the department of psychiatry, University of Nebraska, Omaha, described the study as “compelling.”
When it comes to public health messages, it’s important to know what social media people are using. Today’s parents are on Twitter and Facebook, whereas their children are more likely to be checking out YouTube and TikTok, said Dr. Liu, chair of the APA’s Council on Communications.
“TikTok is critical because that’s where all the youth eyeballs are,” he said.
The medical profession needs to engage with the platform to reach this next-generation audience and help stop the spread of misinformation about DID, said Dr. Liu. He noted that the APA is looking into undertaking such an initiative.
The study investigators report no relevant disclosures. Dr. Liu reports no relevant disclosures.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – , new research shows.
These findings, say investigators, underscore the need for mental health professionals to help counter the spread of false information by creating accurate content and posting it on the popular social media platform.
“Health care professionals need to make engaging content to post on social media platforms like YouTube and especially TikTok, to reach wider audiences and combat misinformation about DID,” study investigator Isreal Bladimir Munoz, a fourth-year medical student at University of Texas, Galveston, said in an interview.
The findings were presented at the annual meeting of the American Psychiatric Association.
Popularized by the media
A rare condition affecting less than 1% of the general population, DID involves two or more distinct personality states, along with changes in behavior and memory gaps.
The condition has been popularized in books and the media. Movies such as “Split,” “Psycho,” and “Fight Club” all feature characters with DID.
“These bring awareness about the condition, but also often sensationalize or stigmatize it and reinforce stereotypes,” said Mr. Munoz.
In recent years, social media has become an integral part of everyday life. An estimated 4.2 billion people actively frequent sites such as YouTube, TikTok, Twitter, and Meta.
Although social media allows for instant communication and the opportunity for self-expression, there are mounting concerns about the spread of misinformation and its potential impact on mental health and privacy, said Mr. Munoz.
To evaluate the quality and accuracy of information about DID on social media, investigators analyzed 60 YouTube and 97 TikTok videos on the condition.
To evaluate the reliability and the intent and reliability of videos, researchers used the modified DISCERN instrument and the Global Quality Scale, a five-point rating system.
Using these tools, the researchers determined whether the selected videos were useful, misleading, or neither. Mr. Munoz said videos were classified as useful if they contained accurate information about the condition and its pathogenesis, treatment, and management.
Researchers determined that for YouTube videos, 51.7% were useful, 6.6% were misleading, and 34.7% were neither. About 43.3% of these videos involved interviews, 21.7% were educational, 15% involved personal stories, 8.3% were films/TV programs, 5% were comedy skits, and 3.3% were another content type.
The highest quality YouTube videos were from educational organizations and health care professionals. The least accurate videos came from independent users and film/TV sources.
As for TikTok videos on DID, only 5.2% were useful, 10.3% were misleading, and 41.7% were neither.
The main sources for TikTok videos were independent organizations, whereas podcasts and film/TV were the least common sources.
The findings, said Mr. Munoz, underscore the need for medical professionals to develop high-quality content about DID and post it on TikTok to counter misinformation on social media.
Call to action
In a comment, Howard Y. Liu, MD, a child and adolescent psychiatrist and chair of the department of psychiatry, University of Nebraska, Omaha, described the study as “compelling.”
When it comes to public health messages, it’s important to know what social media people are using. Today’s parents are on Twitter and Facebook, whereas their children are more likely to be checking out YouTube and TikTok, said Dr. Liu, chair of the APA’s Council on Communications.
“TikTok is critical because that’s where all the youth eyeballs are,” he said.
The medical profession needs to engage with the platform to reach this next-generation audience and help stop the spread of misinformation about DID, said Dr. Liu. He noted that the APA is looking into undertaking such an initiative.
The study investigators report no relevant disclosures. Dr. Liu reports no relevant disclosures.
A version of this article first appeared on Medscape.com.
AT APA 2023
The family firearm often used in youth suicide
SAN FRANCISCO – , according to results of a novel “psychological autopsy study” of loved ones of youth who died by gun-related suicide.
Yet, families don’t always recognize the danger firearms pose to a young person with suicide risk factors, even when there is a young person in the house with a mental health condition, the data show.
Perhaps most importantly, many parents indicated that they would have removed firearms from the home if it had been suggested by their health care professionals.
The study was presented at the American Psychiatric Association annual meeting.
The message is very clear: Clinicians need to ask about guns and gun safety with patients and families, said study investigator Paul Nestadt, MD, of Johns Hopkins Bloomberg School of Public Health in Baltimore.
“It’s never illegal to ask about gun access and it’s medically relevant. Just do it,” he said during a briefing with reporters.
Grim statistics
Suicide rates have been climbing in the United States for the majority of the past 20 years. Suicide is the second most common cause of death among youth.
Dr. Nestadt noted that overall about 8% of suicide attempts result in death, but when an attempt involves a firearm the percentage jumps astronomically to 90%.
Research has shown that for every 10% increase in household firearms in a given community there is a 27% increase in youth suicide deaths.
“In the world of public health and mental health, we think about having access to firearms as an important risk factor for completed suicide. But in the United States, guns have become an important part of how many Americans see themselves,” Dr. Nestadt told reporters.
Research has shown that half of gun owners say owning a gun is central to their identity and three quarters say it’s essential to their freedom, he noted.
To explore these attitudes further, Dr. Nestadt and colleagues did 11 “psychological autopsy interviews” with the loved ones of nine young people aged 17-21 who died by gun-related suicide. They interviewed six mothers, three fathers, one sibling, and one close friend.
Most of the families had some level of “familial engagement” with firearms, Dr. Nestadt reported.
In more than two-thirds of the families, the youth used a family-owned firearm to commit suicide.
Notably, more than three-quarters of the youth had received mental health care before taking their lives, with many receiving care in the weeks prior to their suicide; 44% had made a prior suicide attempt.
In many cases, parents shared that they had not considered their family-owned firearms to be sources of danger and indicated that had their clinicians expressed concern about the gun in the home, they may have acted to reduce the risk by removing it.
Several also shared that they would have considered using Maryland’s Extreme Risk Protective Order Law if it had existed at the time and they had been made aware of it.
Extreme risk protection order (ERPO) laws, or “red flag laws,” prohibit individuals at risk for harming themselves or others from purchasing or owning a firearm.
Dr. Nestadt said youth suicide interventions “must acknowledge culturally embedded roots of identity formation while rescripting firearms from expressions of family cohesion to instruments that may undermine that cohesion.”
‘Courageous study’
Dr. Nestadt noted that while this study was challenging on many fronts, it took no convincing to get these grieving families to participate.
“They wanted to talk to us, especially because they were hopeful that our work could help prevent future suicides, but also they wanted to talk about their loved ones,” he said.
“When you lose someone to cancer, people give you hugs and flowers. When you lose someone to suicide, people don’t discuss it. Suicide has a stigma to it.”
Briefing moderator Howard Liu, MD, MBA, chair of the department of psychiatry, University of Nebraska Medical Center, Omaha, praised the study team for a “courageous study that really required a tremendous amount of vulnerability from the research team and clearly from the survivors as well.”
This is an “important and timely public health discussion,” said Dr. Liu, chair of the APA Council on Communications.
“We’re all facing this challenge of how do we reduce suicide across all ages, from youth to adults as well. This is a really vital discussion and such an important clue about access and trying to reduce access in a moment of impulsivity,” he added.
The study had no commercial funding. Dr. Nestadt and Dr. Liu report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – , according to results of a novel “psychological autopsy study” of loved ones of youth who died by gun-related suicide.
Yet, families don’t always recognize the danger firearms pose to a young person with suicide risk factors, even when there is a young person in the house with a mental health condition, the data show.
Perhaps most importantly, many parents indicated that they would have removed firearms from the home if it had been suggested by their health care professionals.
The study was presented at the American Psychiatric Association annual meeting.
The message is very clear: Clinicians need to ask about guns and gun safety with patients and families, said study investigator Paul Nestadt, MD, of Johns Hopkins Bloomberg School of Public Health in Baltimore.
“It’s never illegal to ask about gun access and it’s medically relevant. Just do it,” he said during a briefing with reporters.
Grim statistics
Suicide rates have been climbing in the United States for the majority of the past 20 years. Suicide is the second most common cause of death among youth.
Dr. Nestadt noted that overall about 8% of suicide attempts result in death, but when an attempt involves a firearm the percentage jumps astronomically to 90%.
Research has shown that for every 10% increase in household firearms in a given community there is a 27% increase in youth suicide deaths.
“In the world of public health and mental health, we think about having access to firearms as an important risk factor for completed suicide. But in the United States, guns have become an important part of how many Americans see themselves,” Dr. Nestadt told reporters.
Research has shown that half of gun owners say owning a gun is central to their identity and three quarters say it’s essential to their freedom, he noted.
To explore these attitudes further, Dr. Nestadt and colleagues did 11 “psychological autopsy interviews” with the loved ones of nine young people aged 17-21 who died by gun-related suicide. They interviewed six mothers, three fathers, one sibling, and one close friend.
Most of the families had some level of “familial engagement” with firearms, Dr. Nestadt reported.
In more than two-thirds of the families, the youth used a family-owned firearm to commit suicide.
Notably, more than three-quarters of the youth had received mental health care before taking their lives, with many receiving care in the weeks prior to their suicide; 44% had made a prior suicide attempt.
In many cases, parents shared that they had not considered their family-owned firearms to be sources of danger and indicated that had their clinicians expressed concern about the gun in the home, they may have acted to reduce the risk by removing it.
Several also shared that they would have considered using Maryland’s Extreme Risk Protective Order Law if it had existed at the time and they had been made aware of it.
Extreme risk protection order (ERPO) laws, or “red flag laws,” prohibit individuals at risk for harming themselves or others from purchasing or owning a firearm.
Dr. Nestadt said youth suicide interventions “must acknowledge culturally embedded roots of identity formation while rescripting firearms from expressions of family cohesion to instruments that may undermine that cohesion.”
‘Courageous study’
Dr. Nestadt noted that while this study was challenging on many fronts, it took no convincing to get these grieving families to participate.
“They wanted to talk to us, especially because they were hopeful that our work could help prevent future suicides, but also they wanted to talk about their loved ones,” he said.
“When you lose someone to cancer, people give you hugs and flowers. When you lose someone to suicide, people don’t discuss it. Suicide has a stigma to it.”
Briefing moderator Howard Liu, MD, MBA, chair of the department of psychiatry, University of Nebraska Medical Center, Omaha, praised the study team for a “courageous study that really required a tremendous amount of vulnerability from the research team and clearly from the survivors as well.”
This is an “important and timely public health discussion,” said Dr. Liu, chair of the APA Council on Communications.
“We’re all facing this challenge of how do we reduce suicide across all ages, from youth to adults as well. This is a really vital discussion and such an important clue about access and trying to reduce access in a moment of impulsivity,” he added.
The study had no commercial funding. Dr. Nestadt and Dr. Liu report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – , according to results of a novel “psychological autopsy study” of loved ones of youth who died by gun-related suicide.
Yet, families don’t always recognize the danger firearms pose to a young person with suicide risk factors, even when there is a young person in the house with a mental health condition, the data show.
Perhaps most importantly, many parents indicated that they would have removed firearms from the home if it had been suggested by their health care professionals.
The study was presented at the American Psychiatric Association annual meeting.
The message is very clear: Clinicians need to ask about guns and gun safety with patients and families, said study investigator Paul Nestadt, MD, of Johns Hopkins Bloomberg School of Public Health in Baltimore.
“It’s never illegal to ask about gun access and it’s medically relevant. Just do it,” he said during a briefing with reporters.
Grim statistics
Suicide rates have been climbing in the United States for the majority of the past 20 years. Suicide is the second most common cause of death among youth.
Dr. Nestadt noted that overall about 8% of suicide attempts result in death, but when an attempt involves a firearm the percentage jumps astronomically to 90%.
Research has shown that for every 10% increase in household firearms in a given community there is a 27% increase in youth suicide deaths.
“In the world of public health and mental health, we think about having access to firearms as an important risk factor for completed suicide. But in the United States, guns have become an important part of how many Americans see themselves,” Dr. Nestadt told reporters.
Research has shown that half of gun owners say owning a gun is central to their identity and three quarters say it’s essential to their freedom, he noted.
To explore these attitudes further, Dr. Nestadt and colleagues did 11 “psychological autopsy interviews” with the loved ones of nine young people aged 17-21 who died by gun-related suicide. They interviewed six mothers, three fathers, one sibling, and one close friend.
Most of the families had some level of “familial engagement” with firearms, Dr. Nestadt reported.
In more than two-thirds of the families, the youth used a family-owned firearm to commit suicide.
Notably, more than three-quarters of the youth had received mental health care before taking their lives, with many receiving care in the weeks prior to their suicide; 44% had made a prior suicide attempt.
In many cases, parents shared that they had not considered their family-owned firearms to be sources of danger and indicated that had their clinicians expressed concern about the gun in the home, they may have acted to reduce the risk by removing it.
Several also shared that they would have considered using Maryland’s Extreme Risk Protective Order Law if it had existed at the time and they had been made aware of it.
Extreme risk protection order (ERPO) laws, or “red flag laws,” prohibit individuals at risk for harming themselves or others from purchasing or owning a firearm.
Dr. Nestadt said youth suicide interventions “must acknowledge culturally embedded roots of identity formation while rescripting firearms from expressions of family cohesion to instruments that may undermine that cohesion.”
‘Courageous study’
Dr. Nestadt noted that while this study was challenging on many fronts, it took no convincing to get these grieving families to participate.
“They wanted to talk to us, especially because they were hopeful that our work could help prevent future suicides, but also they wanted to talk about their loved ones,” he said.
“When you lose someone to cancer, people give you hugs and flowers. When you lose someone to suicide, people don’t discuss it. Suicide has a stigma to it.”
Briefing moderator Howard Liu, MD, MBA, chair of the department of psychiatry, University of Nebraska Medical Center, Omaha, praised the study team for a “courageous study that really required a tremendous amount of vulnerability from the research team and clearly from the survivors as well.”
This is an “important and timely public health discussion,” said Dr. Liu, chair of the APA Council on Communications.
“We’re all facing this challenge of how do we reduce suicide across all ages, from youth to adults as well. This is a really vital discussion and such an important clue about access and trying to reduce access in a moment of impulsivity,” he added.
The study had no commercial funding. Dr. Nestadt and Dr. Liu report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT APA 2023
Black patients most likely to be restrained in EDs, Latino patients least likely
SAN FRANCISCO – .
In contrast, Hispanic/Latino patients were less likely to be restrained than both Black and White patients, researchers reported in a poster presented at the annual meeting of the American Psychiatric Association. The study authors also found that clinicians rarely turned to restraints, using them in just 2,712 of 882,390 ED visits (0.3%) over a 7-year period.
The study doesn’t examine why the disparities exist. But lead author Erika Chang-Sing, a medical student at Yale University, New Haven, Conn., said in an interview that it’s clear that racial bias is the cause of the differences in restraint rates among White, Black, and Hispanics/Latino patients. “We think that there are multiple contributing factors to the higher rates of restraint for Black patients brought to the hospital by police, and all of them are rooted in systemic racism,” she said, adding that “the lower odds of restraint in the Hispanic or Latino group are also rooted in systemic racism and inequity.”
According to Ms. Chang-Sing, researchers launched the study to gain insight into the use of the restraints in the Southeast and to see what’s happening in light of the recent publicizing of killings of Black people by police. Being taken to the hospital by police “might contribute both to the individual patient’s behavior and the health care provider’s assessment of risk in determining whether or not to apply restraints,” she said.
Other research has linked ethnicity to higher rates of restraint use. For example, a 2021 study of 32,054 cases of patients under mandatory psychiatric hold in 11 Massachusetts emergency rooms found that Black (adjusted odds ratio, 1.22) and Hispanic (aOR, 1.45) patients were more likely to be restrained than White patients.
For the new study, researchers retrospectively tracked 885,102 emergency room visits at three North Carolina emergency departments from 2015 to 2022, including 9,130 who were brought in by police and 2,712 who were physically restrained because of the perceived risk of violence. “Providers use restraints, or straps, to secure the patient’s wrists and ankles to the bed,” Ms. Chang-Sing said.
Among all patients, 52.5% were Black, but 66% of those who were restrained were Black. The numbers for White patients were 35.7% and 23.9%, respectively, and 5.7% and 3.2% for Hispanics/Latino patients. Black patients were less likely than White patients to get a psychiatric primary emergency department diagnosis (aOR, 0.67), but those in that category were more likely than their White counterparts to be restrained (aOR, 1.36).
The higher risk of restraint use in Black patients overall disappeared when researchers adjusted their statistics to account for the effects of sex, age, and type of insurance (aOR, 0.86). Ms. Chang-Sing said the study team is reanalyzing the data since they think insurance may not be a confounder.
Why might Hispanic/Latino ethnicity be protective against restraint use? “This may be due to language barriers, fear of law enforcement, and avoidance of the hospital in the first place,” Ms. Chang-Sing said.
Emergency physician Wendy Macias-Konstantopoulos, MD, MPH, MBA, of Harvard Medical School and Massachusetts General Hospital, both in Boston, coauthored the 2021 study on police restraints. In an interview, she said the new findings add to previous research by providing data about the role played by the police who bring patients to the ED. She added that there is no evidence that certain populations simply need more restraints.
What can be done to reduce disparities in restraint use? Mental health teams can make a difference by responding to mental health emergencies, Ms. Chang-Sing said. “These providers can be instrumental in communicating to patients that the intention is to care for them, not to punish them.”
Another strategy is to increase the number of clinics and crisis response centers, she said. Hospital-based crisis response teams can also be helpful, she said. “Because these teams are focused only on behavioral emergencies, they can be more thoughtful in avoiding the use of restraints.”
No study funding was reported. The study authors and Dr. Macias-Konstantopoulos have no disclosures.
SAN FRANCISCO – .
In contrast, Hispanic/Latino patients were less likely to be restrained than both Black and White patients, researchers reported in a poster presented at the annual meeting of the American Psychiatric Association. The study authors also found that clinicians rarely turned to restraints, using them in just 2,712 of 882,390 ED visits (0.3%) over a 7-year period.
The study doesn’t examine why the disparities exist. But lead author Erika Chang-Sing, a medical student at Yale University, New Haven, Conn., said in an interview that it’s clear that racial bias is the cause of the differences in restraint rates among White, Black, and Hispanics/Latino patients. “We think that there are multiple contributing factors to the higher rates of restraint for Black patients brought to the hospital by police, and all of them are rooted in systemic racism,” she said, adding that “the lower odds of restraint in the Hispanic or Latino group are also rooted in systemic racism and inequity.”
According to Ms. Chang-Sing, researchers launched the study to gain insight into the use of the restraints in the Southeast and to see what’s happening in light of the recent publicizing of killings of Black people by police. Being taken to the hospital by police “might contribute both to the individual patient’s behavior and the health care provider’s assessment of risk in determining whether or not to apply restraints,” she said.
Other research has linked ethnicity to higher rates of restraint use. For example, a 2021 study of 32,054 cases of patients under mandatory psychiatric hold in 11 Massachusetts emergency rooms found that Black (adjusted odds ratio, 1.22) and Hispanic (aOR, 1.45) patients were more likely to be restrained than White patients.
For the new study, researchers retrospectively tracked 885,102 emergency room visits at three North Carolina emergency departments from 2015 to 2022, including 9,130 who were brought in by police and 2,712 who were physically restrained because of the perceived risk of violence. “Providers use restraints, or straps, to secure the patient’s wrists and ankles to the bed,” Ms. Chang-Sing said.
Among all patients, 52.5% were Black, but 66% of those who were restrained were Black. The numbers for White patients were 35.7% and 23.9%, respectively, and 5.7% and 3.2% for Hispanics/Latino patients. Black patients were less likely than White patients to get a psychiatric primary emergency department diagnosis (aOR, 0.67), but those in that category were more likely than their White counterparts to be restrained (aOR, 1.36).
The higher risk of restraint use in Black patients overall disappeared when researchers adjusted their statistics to account for the effects of sex, age, and type of insurance (aOR, 0.86). Ms. Chang-Sing said the study team is reanalyzing the data since they think insurance may not be a confounder.
Why might Hispanic/Latino ethnicity be protective against restraint use? “This may be due to language barriers, fear of law enforcement, and avoidance of the hospital in the first place,” Ms. Chang-Sing said.
Emergency physician Wendy Macias-Konstantopoulos, MD, MPH, MBA, of Harvard Medical School and Massachusetts General Hospital, both in Boston, coauthored the 2021 study on police restraints. In an interview, she said the new findings add to previous research by providing data about the role played by the police who bring patients to the ED. She added that there is no evidence that certain populations simply need more restraints.
What can be done to reduce disparities in restraint use? Mental health teams can make a difference by responding to mental health emergencies, Ms. Chang-Sing said. “These providers can be instrumental in communicating to patients that the intention is to care for them, not to punish them.”
Another strategy is to increase the number of clinics and crisis response centers, she said. Hospital-based crisis response teams can also be helpful, she said. “Because these teams are focused only on behavioral emergencies, they can be more thoughtful in avoiding the use of restraints.”
No study funding was reported. The study authors and Dr. Macias-Konstantopoulos have no disclosures.
SAN FRANCISCO – .
In contrast, Hispanic/Latino patients were less likely to be restrained than both Black and White patients, researchers reported in a poster presented at the annual meeting of the American Psychiatric Association. The study authors also found that clinicians rarely turned to restraints, using them in just 2,712 of 882,390 ED visits (0.3%) over a 7-year period.
The study doesn’t examine why the disparities exist. But lead author Erika Chang-Sing, a medical student at Yale University, New Haven, Conn., said in an interview that it’s clear that racial bias is the cause of the differences in restraint rates among White, Black, and Hispanics/Latino patients. “We think that there are multiple contributing factors to the higher rates of restraint for Black patients brought to the hospital by police, and all of them are rooted in systemic racism,” she said, adding that “the lower odds of restraint in the Hispanic or Latino group are also rooted in systemic racism and inequity.”
According to Ms. Chang-Sing, researchers launched the study to gain insight into the use of the restraints in the Southeast and to see what’s happening in light of the recent publicizing of killings of Black people by police. Being taken to the hospital by police “might contribute both to the individual patient’s behavior and the health care provider’s assessment of risk in determining whether or not to apply restraints,” she said.
Other research has linked ethnicity to higher rates of restraint use. For example, a 2021 study of 32,054 cases of patients under mandatory psychiatric hold in 11 Massachusetts emergency rooms found that Black (adjusted odds ratio, 1.22) and Hispanic (aOR, 1.45) patients were more likely to be restrained than White patients.
For the new study, researchers retrospectively tracked 885,102 emergency room visits at three North Carolina emergency departments from 2015 to 2022, including 9,130 who were brought in by police and 2,712 who were physically restrained because of the perceived risk of violence. “Providers use restraints, or straps, to secure the patient’s wrists and ankles to the bed,” Ms. Chang-Sing said.
Among all patients, 52.5% were Black, but 66% of those who were restrained were Black. The numbers for White patients were 35.7% and 23.9%, respectively, and 5.7% and 3.2% for Hispanics/Latino patients. Black patients were less likely than White patients to get a psychiatric primary emergency department diagnosis (aOR, 0.67), but those in that category were more likely than their White counterparts to be restrained (aOR, 1.36).
The higher risk of restraint use in Black patients overall disappeared when researchers adjusted their statistics to account for the effects of sex, age, and type of insurance (aOR, 0.86). Ms. Chang-Sing said the study team is reanalyzing the data since they think insurance may not be a confounder.
Why might Hispanic/Latino ethnicity be protective against restraint use? “This may be due to language barriers, fear of law enforcement, and avoidance of the hospital in the first place,” Ms. Chang-Sing said.
Emergency physician Wendy Macias-Konstantopoulos, MD, MPH, MBA, of Harvard Medical School and Massachusetts General Hospital, both in Boston, coauthored the 2021 study on police restraints. In an interview, she said the new findings add to previous research by providing data about the role played by the police who bring patients to the ED. She added that there is no evidence that certain populations simply need more restraints.
What can be done to reduce disparities in restraint use? Mental health teams can make a difference by responding to mental health emergencies, Ms. Chang-Sing said. “These providers can be instrumental in communicating to patients that the intention is to care for them, not to punish them.”
Another strategy is to increase the number of clinics and crisis response centers, she said. Hospital-based crisis response teams can also be helpful, she said. “Because these teams are focused only on behavioral emergencies, they can be more thoughtful in avoiding the use of restraints.”
No study funding was reported. The study authors and Dr. Macias-Konstantopoulos have no disclosures.
AT APA 2023
We can reduce suicide with enforced treatment and eyesight supervision
The old man was restrained at the last moment from jumping off the hospital’s fifth floor atrium parapet. He was suffering from terminal cancer and had been racked with chronic, severe pain for months.
The consult recognized symptoms of depression arising from his continuous physical suffering, advising that a male aide be dispatched to sit with the man and that he be put on a regimen of 10 mg of methadone twice a day to alleviate the pain. The following day the man was calm; he no longer wanted to kill himself. He expressed a strong desire to go home, return to gardening, and to play with his grandchildren.
Most of the 47,000 suicides that occur in the United States every year are preventable.1 Our national policy on this front has been nothing short of an abject failure. The government implemented a system with limited effect on completed suicides – a telephone hotline. This hotline is not called by the most common suicide victims: male, old, and quiet.2
The consequences of this national policy disaster have been profound, resulting in the biggest loss of productive years of life for any fatal condition.3 The grief experienced by the families of those who commit suicide is far greater than normal bereavement: The cause of death of their loved ones was not an unfortunate accident or a disease, it was an intentional act, and families take it personally.
One of the greatest achievements of psychiatry during the 20th century was the lowering of suicide rates in prisons by 70% with no treatment, no additional staffing, and no additional expenditures of funds. Today if inmates threaten suicide, they are immediately placed under eyesight supervision by guards. The federal pamphlet that describes this protocol was published in 1995 and is freely available online.4
Half of all suicide attempts are made by individuals who are legally drunk.5 Watch them for 6 hours and then ask them if they want to kill themselves and the response will almost invariably be “Of course not,” with the risk of further attempts dissipating in step with their blood alcohol level. The best resources to provide this kind of intervention are responsible adult family members, at no cost to the government. Indeed, in many cases family supervision is superior to that provided by a locked psychiatric ward with three staff members chasing after 20 agitated people all night long. The one-on-one attention that a family member can provide is free as well as far more personal and insightful, and more sincerely caring.
Guarantees in the field of medicine are rare. But, one such guarantee is that after their mood has improved, 100% of people will be thankful that they did not hurt themselves.6 This means that successful treatment will prevent 100% of all suicides.7 Not all treatments are successful, but 95% can be.8 At autopsy, few successful suicide victims have psychiatric medications in their system.9 The urge to kill oneself might best be characterized as a temporary chemical alteration of the brain causing delusional thoughts, including the ultimate delusion that life is not worth living.10 This alteration suppresses the strongest, most fundamental urge of all, namely, the survival instinct.
We must overturn the catastrophic decision of the U.S. Supreme Court that requires the showing of a dangerous act and the holding of a trial employing at least three lawyers for involuntary commitment to be authorized. Rather, involuntary treatment is justified by medical necessity as determined by two licensed professionals with no conflicts of interest. It can be outpatient.
The Supreme Court’s decision in O’Connor v. Donaldson in 1975 remedied an illusory wrong, addressing an act of blatant malpractice, not policy inequity.11 The superintendent of the state facility in that case was not even a doctor. He kept O’Connor prisoner for more than a decade, perhaps to keep a bed filled. Over the past half-century, this one decision has resulted in 1 million preventable suicides12 and half a million senseless murders by paranoid individuals, including many rampage shootings.13
More than two-thirds of homeless individuals suffer from an untreated mental condition.14 The vast majority of them will refuse all offers of treatment because they also have anosognosia, a brain-based disorder causing denial of illness.15 By referring to these individuals as “homeless,” we are also lowering real estate values for a square block around where they happen to be camped out. That cost has never been calculated, but it is another real consequence of this devastating Supreme Court decision.16
Detractors and mental health rights activists may argue that individual rights cannot be infringed. In that case, those same detractors and mental health rights activists must take responsibility for the thousands of lives and billions of dollars in economic damage caused by their refusal to allow an effective solution to the suicide epidemic to be implemented. Enforced outpatient treatment by the U.S. Air Force dropped its suicide rate by 60%. As an unintended benefit, the murder rate dropped by 50%.17
It is high time we did so.
Dr. Behar is a psychiatrist in Lower Merion, Pa. He graduated from Hahnemann Medical College, Philadelphia, in 1975, and has had postgraduate training at SUNY Stony Brook, University of Iowa, the National Institute of Mental Health, and Columbia University. His practice focuses on difficult, treatment-resistant cases.
References
1. U.S. Centers for Disease Control and Prevention. Suicide Prevention. 2020.
2. Luoma JB et al. Contact with mental health and primary care providers before suicide: A review of the evidence. Am J Psychiatry. 2002 Jun 1. doi: 10.1176/appi.ajp.159.6.909.
3. World Health Organization. Suicide. 2021 Jun 17.
4. National Institute of Corrections. Correctional suicide prevention: Policies and procedures. 1995.
5. Hufford MR. Alcohol and suicidal behavior. Clin Psychol Rev. 2001 Jul;21(5):797-811.
6. Stanley B and Brown GK. Safety planning intervention: A brief intervention to mitigate suicide risk. Cogn Behav Pract. 2012 May;19(2):256-64.
7. Ibid.
8. Brown GK and Jager-Hyman S. Evidence-based psychotherapies for suicide prevention: Future directions. Am J Prev Med. 2014 Sep;47(3 Suppl 2):S186-94.
9. Isometsä ET. Psychological autopsy studies – A review. Eur Psychiatry. 2001 Nov;16(7):379-85.
10. Van Orden KA et al. The interpersonal theory of suicide. Psychol Rev. 2010 Apr; 117(2):575-600.
11. O’Connor v. Donaldson, 422 U.S. 563 (1975).
12. Calculated based on annual suicide statistics from the CDC and the time elapsed since the Supreme Court decision in O’Connor v. Donaldson.
13. Metzl JM and MacLeish KT. Mental illness, mass shootings, and the politics of American firearms. Am J Public Health. 2015 Feb;105(2):240-9.
14. Fazel S et al. The prevalence of mental disorders among the homeless in western countries: Systematic review and meta-regression analysis. PLoS Med. 2008 Dec 2;5(12):e225.
15. Amador XF and David AS. (eds.) Insight and psychosis: Awareness of illness in schizophrenia and related disorders (2nd ed.). Oxford Univ Press. 2004.
16. Calculated based on the potential impact of homelessness on property values and the relationship between untreated mental illness and homelessness.
17. Armed Forces Health Surveillance Branch. Surveillance snapshot: Manner and cause of death, active component, U.S. Armed Forces, 1998-2015. Medical Surveillance Monthly Report. 2016 Apr;23(4):19.
The old man was restrained at the last moment from jumping off the hospital’s fifth floor atrium parapet. He was suffering from terminal cancer and had been racked with chronic, severe pain for months.
The consult recognized symptoms of depression arising from his continuous physical suffering, advising that a male aide be dispatched to sit with the man and that he be put on a regimen of 10 mg of methadone twice a day to alleviate the pain. The following day the man was calm; he no longer wanted to kill himself. He expressed a strong desire to go home, return to gardening, and to play with his grandchildren.
Most of the 47,000 suicides that occur in the United States every year are preventable.1 Our national policy on this front has been nothing short of an abject failure. The government implemented a system with limited effect on completed suicides – a telephone hotline. This hotline is not called by the most common suicide victims: male, old, and quiet.2
The consequences of this national policy disaster have been profound, resulting in the biggest loss of productive years of life for any fatal condition.3 The grief experienced by the families of those who commit suicide is far greater than normal bereavement: The cause of death of their loved ones was not an unfortunate accident or a disease, it was an intentional act, and families take it personally.
One of the greatest achievements of psychiatry during the 20th century was the lowering of suicide rates in prisons by 70% with no treatment, no additional staffing, and no additional expenditures of funds. Today if inmates threaten suicide, they are immediately placed under eyesight supervision by guards. The federal pamphlet that describes this protocol was published in 1995 and is freely available online.4
Half of all suicide attempts are made by individuals who are legally drunk.5 Watch them for 6 hours and then ask them if they want to kill themselves and the response will almost invariably be “Of course not,” with the risk of further attempts dissipating in step with their blood alcohol level. The best resources to provide this kind of intervention are responsible adult family members, at no cost to the government. Indeed, in many cases family supervision is superior to that provided by a locked psychiatric ward with three staff members chasing after 20 agitated people all night long. The one-on-one attention that a family member can provide is free as well as far more personal and insightful, and more sincerely caring.
Guarantees in the field of medicine are rare. But, one such guarantee is that after their mood has improved, 100% of people will be thankful that they did not hurt themselves.6 This means that successful treatment will prevent 100% of all suicides.7 Not all treatments are successful, but 95% can be.8 At autopsy, few successful suicide victims have psychiatric medications in their system.9 The urge to kill oneself might best be characterized as a temporary chemical alteration of the brain causing delusional thoughts, including the ultimate delusion that life is not worth living.10 This alteration suppresses the strongest, most fundamental urge of all, namely, the survival instinct.
We must overturn the catastrophic decision of the U.S. Supreme Court that requires the showing of a dangerous act and the holding of a trial employing at least three lawyers for involuntary commitment to be authorized. Rather, involuntary treatment is justified by medical necessity as determined by two licensed professionals with no conflicts of interest. It can be outpatient.
The Supreme Court’s decision in O’Connor v. Donaldson in 1975 remedied an illusory wrong, addressing an act of blatant malpractice, not policy inequity.11 The superintendent of the state facility in that case was not even a doctor. He kept O’Connor prisoner for more than a decade, perhaps to keep a bed filled. Over the past half-century, this one decision has resulted in 1 million preventable suicides12 and half a million senseless murders by paranoid individuals, including many rampage shootings.13
More than two-thirds of homeless individuals suffer from an untreated mental condition.14 The vast majority of them will refuse all offers of treatment because they also have anosognosia, a brain-based disorder causing denial of illness.15 By referring to these individuals as “homeless,” we are also lowering real estate values for a square block around where they happen to be camped out. That cost has never been calculated, but it is another real consequence of this devastating Supreme Court decision.16
Detractors and mental health rights activists may argue that individual rights cannot be infringed. In that case, those same detractors and mental health rights activists must take responsibility for the thousands of lives and billions of dollars in economic damage caused by their refusal to allow an effective solution to the suicide epidemic to be implemented. Enforced outpatient treatment by the U.S. Air Force dropped its suicide rate by 60%. As an unintended benefit, the murder rate dropped by 50%.17
It is high time we did so.
Dr. Behar is a psychiatrist in Lower Merion, Pa. He graduated from Hahnemann Medical College, Philadelphia, in 1975, and has had postgraduate training at SUNY Stony Brook, University of Iowa, the National Institute of Mental Health, and Columbia University. His practice focuses on difficult, treatment-resistant cases.
References
1. U.S. Centers for Disease Control and Prevention. Suicide Prevention. 2020.
2. Luoma JB et al. Contact with mental health and primary care providers before suicide: A review of the evidence. Am J Psychiatry. 2002 Jun 1. doi: 10.1176/appi.ajp.159.6.909.
3. World Health Organization. Suicide. 2021 Jun 17.
4. National Institute of Corrections. Correctional suicide prevention: Policies and procedures. 1995.
5. Hufford MR. Alcohol and suicidal behavior. Clin Psychol Rev. 2001 Jul;21(5):797-811.
6. Stanley B and Brown GK. Safety planning intervention: A brief intervention to mitigate suicide risk. Cogn Behav Pract. 2012 May;19(2):256-64.
7. Ibid.
8. Brown GK and Jager-Hyman S. Evidence-based psychotherapies for suicide prevention: Future directions. Am J Prev Med. 2014 Sep;47(3 Suppl 2):S186-94.
9. Isometsä ET. Psychological autopsy studies – A review. Eur Psychiatry. 2001 Nov;16(7):379-85.
10. Van Orden KA et al. The interpersonal theory of suicide. Psychol Rev. 2010 Apr; 117(2):575-600.
11. O’Connor v. Donaldson, 422 U.S. 563 (1975).
12. Calculated based on annual suicide statistics from the CDC and the time elapsed since the Supreme Court decision in O’Connor v. Donaldson.
13. Metzl JM and MacLeish KT. Mental illness, mass shootings, and the politics of American firearms. Am J Public Health. 2015 Feb;105(2):240-9.
14. Fazel S et al. The prevalence of mental disorders among the homeless in western countries: Systematic review and meta-regression analysis. PLoS Med. 2008 Dec 2;5(12):e225.
15. Amador XF and David AS. (eds.) Insight and psychosis: Awareness of illness in schizophrenia and related disorders (2nd ed.). Oxford Univ Press. 2004.
16. Calculated based on the potential impact of homelessness on property values and the relationship between untreated mental illness and homelessness.
17. Armed Forces Health Surveillance Branch. Surveillance snapshot: Manner and cause of death, active component, U.S. Armed Forces, 1998-2015. Medical Surveillance Monthly Report. 2016 Apr;23(4):19.
The old man was restrained at the last moment from jumping off the hospital’s fifth floor atrium parapet. He was suffering from terminal cancer and had been racked with chronic, severe pain for months.
The consult recognized symptoms of depression arising from his continuous physical suffering, advising that a male aide be dispatched to sit with the man and that he be put on a regimen of 10 mg of methadone twice a day to alleviate the pain. The following day the man was calm; he no longer wanted to kill himself. He expressed a strong desire to go home, return to gardening, and to play with his grandchildren.
Most of the 47,000 suicides that occur in the United States every year are preventable.1 Our national policy on this front has been nothing short of an abject failure. The government implemented a system with limited effect on completed suicides – a telephone hotline. This hotline is not called by the most common suicide victims: male, old, and quiet.2
The consequences of this national policy disaster have been profound, resulting in the biggest loss of productive years of life for any fatal condition.3 The grief experienced by the families of those who commit suicide is far greater than normal bereavement: The cause of death of their loved ones was not an unfortunate accident or a disease, it was an intentional act, and families take it personally.
One of the greatest achievements of psychiatry during the 20th century was the lowering of suicide rates in prisons by 70% with no treatment, no additional staffing, and no additional expenditures of funds. Today if inmates threaten suicide, they are immediately placed under eyesight supervision by guards. The federal pamphlet that describes this protocol was published in 1995 and is freely available online.4
Half of all suicide attempts are made by individuals who are legally drunk.5 Watch them for 6 hours and then ask them if they want to kill themselves and the response will almost invariably be “Of course not,” with the risk of further attempts dissipating in step with their blood alcohol level. The best resources to provide this kind of intervention are responsible adult family members, at no cost to the government. Indeed, in many cases family supervision is superior to that provided by a locked psychiatric ward with three staff members chasing after 20 agitated people all night long. The one-on-one attention that a family member can provide is free as well as far more personal and insightful, and more sincerely caring.
Guarantees in the field of medicine are rare. But, one such guarantee is that after their mood has improved, 100% of people will be thankful that they did not hurt themselves.6 This means that successful treatment will prevent 100% of all suicides.7 Not all treatments are successful, but 95% can be.8 At autopsy, few successful suicide victims have psychiatric medications in their system.9 The urge to kill oneself might best be characterized as a temporary chemical alteration of the brain causing delusional thoughts, including the ultimate delusion that life is not worth living.10 This alteration suppresses the strongest, most fundamental urge of all, namely, the survival instinct.
We must overturn the catastrophic decision of the U.S. Supreme Court that requires the showing of a dangerous act and the holding of a trial employing at least three lawyers for involuntary commitment to be authorized. Rather, involuntary treatment is justified by medical necessity as determined by two licensed professionals with no conflicts of interest. It can be outpatient.
The Supreme Court’s decision in O’Connor v. Donaldson in 1975 remedied an illusory wrong, addressing an act of blatant malpractice, not policy inequity.11 The superintendent of the state facility in that case was not even a doctor. He kept O’Connor prisoner for more than a decade, perhaps to keep a bed filled. Over the past half-century, this one decision has resulted in 1 million preventable suicides12 and half a million senseless murders by paranoid individuals, including many rampage shootings.13
More than two-thirds of homeless individuals suffer from an untreated mental condition.14 The vast majority of them will refuse all offers of treatment because they also have anosognosia, a brain-based disorder causing denial of illness.15 By referring to these individuals as “homeless,” we are also lowering real estate values for a square block around where they happen to be camped out. That cost has never been calculated, but it is another real consequence of this devastating Supreme Court decision.16
Detractors and mental health rights activists may argue that individual rights cannot be infringed. In that case, those same detractors and mental health rights activists must take responsibility for the thousands of lives and billions of dollars in economic damage caused by their refusal to allow an effective solution to the suicide epidemic to be implemented. Enforced outpatient treatment by the U.S. Air Force dropped its suicide rate by 60%. As an unintended benefit, the murder rate dropped by 50%.17
It is high time we did so.
Dr. Behar is a psychiatrist in Lower Merion, Pa. He graduated from Hahnemann Medical College, Philadelphia, in 1975, and has had postgraduate training at SUNY Stony Brook, University of Iowa, the National Institute of Mental Health, and Columbia University. His practice focuses on difficult, treatment-resistant cases.
References
1. U.S. Centers for Disease Control and Prevention. Suicide Prevention. 2020.
2. Luoma JB et al. Contact with mental health and primary care providers before suicide: A review of the evidence. Am J Psychiatry. 2002 Jun 1. doi: 10.1176/appi.ajp.159.6.909.
3. World Health Organization. Suicide. 2021 Jun 17.
4. National Institute of Corrections. Correctional suicide prevention: Policies and procedures. 1995.
5. Hufford MR. Alcohol and suicidal behavior. Clin Psychol Rev. 2001 Jul;21(5):797-811.
6. Stanley B and Brown GK. Safety planning intervention: A brief intervention to mitigate suicide risk. Cogn Behav Pract. 2012 May;19(2):256-64.
7. Ibid.
8. Brown GK and Jager-Hyman S. Evidence-based psychotherapies for suicide prevention: Future directions. Am J Prev Med. 2014 Sep;47(3 Suppl 2):S186-94.
9. Isometsä ET. Psychological autopsy studies – A review. Eur Psychiatry. 2001 Nov;16(7):379-85.
10. Van Orden KA et al. The interpersonal theory of suicide. Psychol Rev. 2010 Apr; 117(2):575-600.
11. O’Connor v. Donaldson, 422 U.S. 563 (1975).
12. Calculated based on annual suicide statistics from the CDC and the time elapsed since the Supreme Court decision in O’Connor v. Donaldson.
13. Metzl JM and MacLeish KT. Mental illness, mass shootings, and the politics of American firearms. Am J Public Health. 2015 Feb;105(2):240-9.
14. Fazel S et al. The prevalence of mental disorders among the homeless in western countries: Systematic review and meta-regression analysis. PLoS Med. 2008 Dec 2;5(12):e225.
15. Amador XF and David AS. (eds.) Insight and psychosis: Awareness of illness in schizophrenia and related disorders (2nd ed.). Oxford Univ Press. 2004.
16. Calculated based on the potential impact of homelessness on property values and the relationship between untreated mental illness and homelessness.
17. Armed Forces Health Surveillance Branch. Surveillance snapshot: Manner and cause of death, active component, U.S. Armed Forces, 1998-2015. Medical Surveillance Monthly Report. 2016 Apr;23(4):19.
Which interventions could lessen the burden of dementia?
Using a microsimulation algorithm that accounts for the effect on mortality, a team from Marseille, France, has shown that interventions targeting the three main vascular risk factors for dementia – hypertension, diabetes, and physical inactivity – could significantly reduce the burden of dementia by 2040.
Although these modeling results could appear too optimistic, since total disappearance of the risk factors was assumed, the authors say the results do show that targeted interventions for these factors could be effective in reducing the future burden of dementia.
Increasing prevalence
According to the World Alzheimer Report 2018, 50 million people around the world were living with dementia; a population roughly around the size of South Korea or Spain. That community is likely to rise to about 152 million people by 2050, which is similar to the size of Russia or Bangladesh, the result of an aging population.
Among modifiable risk factors, many studies support a deleterious effect of hypertension, diabetes, and physical inactivity on the risk of dementia. However, since the distribution of these risk factors could have a direct impact on mortality, reducing it should increase life expectancy and the number of cases of dementia.
The team, headed by Hélène Jacqmin-Gadda, PhD, research director at the University of Bordeaux (France), has developed a microsimulation model capable of predicting the burden of dementia while accounting for the impact on mortality. The team used this approach to assess the impact of interventions targeting these three main risk factors on the burden of dementia in France by 2040.
Removing risk factors
The researchers estimated the incidence of dementia for men and women using data from the 2020 PAQUID cohort, and these data were combined with the projections forecast by the French National Institute of Statistics and Economic Studies to account for mortality with and without dementia.
Without intervention, the prevalence rate of dementia in 2040 would be 9.6% among men and 14% among women older than 65 years.
These figures would decrease to 6.4% (−33%) and 10.4% (−26%), respectively, under the intervention scenario whereby the three modifiable vascular risk factors (hypertension, diabetes, and physical inactivity) would be removed simultaneously beginning in 2020. The prevalence rates are significantly reduced for men and women from age 75 years. In this scenario, life expectancy without dementia would increase by 3.4 years in men and 2.6 years in women, the result of men being more exposed to these three risk factors.
Other scenarios have estimated dementia prevalence with the disappearance of just one of these risk factors. For example, the disappearance of hypertension alone from 2020 could decrease dementia prevalence by 21% in men and 16% in women (because this risk factor is less common in women than in men) by 2040. This reduction would be associated with a decrease in the lifelong probability of dementia among men and women and a gain in life expectancy without dementia of 2 years in men and 1.4 years in women.
Among the three factors, hypertension has the largest impact on dementia burden in the French population, since this is, by far, the most prevalent (69% in men and 49% in women), while intervention targeting only diabetes or physical inactivity would lead to a reduction in dementia prevalence of only 4%-7%.
The authors reported no conflicts of interest.
This article was translated from Univadis France. A version appeared on Medscape.com.
Using a microsimulation algorithm that accounts for the effect on mortality, a team from Marseille, France, has shown that interventions targeting the three main vascular risk factors for dementia – hypertension, diabetes, and physical inactivity – could significantly reduce the burden of dementia by 2040.
Although these modeling results could appear too optimistic, since total disappearance of the risk factors was assumed, the authors say the results do show that targeted interventions for these factors could be effective in reducing the future burden of dementia.
Increasing prevalence
According to the World Alzheimer Report 2018, 50 million people around the world were living with dementia; a population roughly around the size of South Korea or Spain. That community is likely to rise to about 152 million people by 2050, which is similar to the size of Russia or Bangladesh, the result of an aging population.
Among modifiable risk factors, many studies support a deleterious effect of hypertension, diabetes, and physical inactivity on the risk of dementia. However, since the distribution of these risk factors could have a direct impact on mortality, reducing it should increase life expectancy and the number of cases of dementia.
The team, headed by Hélène Jacqmin-Gadda, PhD, research director at the University of Bordeaux (France), has developed a microsimulation model capable of predicting the burden of dementia while accounting for the impact on mortality. The team used this approach to assess the impact of interventions targeting these three main risk factors on the burden of dementia in France by 2040.
Removing risk factors
The researchers estimated the incidence of dementia for men and women using data from the 2020 PAQUID cohort, and these data were combined with the projections forecast by the French National Institute of Statistics and Economic Studies to account for mortality with and without dementia.
Without intervention, the prevalence rate of dementia in 2040 would be 9.6% among men and 14% among women older than 65 years.
These figures would decrease to 6.4% (−33%) and 10.4% (−26%), respectively, under the intervention scenario whereby the three modifiable vascular risk factors (hypertension, diabetes, and physical inactivity) would be removed simultaneously beginning in 2020. The prevalence rates are significantly reduced for men and women from age 75 years. In this scenario, life expectancy without dementia would increase by 3.4 years in men and 2.6 years in women, the result of men being more exposed to these three risk factors.
Other scenarios have estimated dementia prevalence with the disappearance of just one of these risk factors. For example, the disappearance of hypertension alone from 2020 could decrease dementia prevalence by 21% in men and 16% in women (because this risk factor is less common in women than in men) by 2040. This reduction would be associated with a decrease in the lifelong probability of dementia among men and women and a gain in life expectancy without dementia of 2 years in men and 1.4 years in women.
Among the three factors, hypertension has the largest impact on dementia burden in the French population, since this is, by far, the most prevalent (69% in men and 49% in women), while intervention targeting only diabetes or physical inactivity would lead to a reduction in dementia prevalence of only 4%-7%.
The authors reported no conflicts of interest.
This article was translated from Univadis France. A version appeared on Medscape.com.
Using a microsimulation algorithm that accounts for the effect on mortality, a team from Marseille, France, has shown that interventions targeting the three main vascular risk factors for dementia – hypertension, diabetes, and physical inactivity – could significantly reduce the burden of dementia by 2040.
Although these modeling results could appear too optimistic, since total disappearance of the risk factors was assumed, the authors say the results do show that targeted interventions for these factors could be effective in reducing the future burden of dementia.
Increasing prevalence
According to the World Alzheimer Report 2018, 50 million people around the world were living with dementia; a population roughly around the size of South Korea or Spain. That community is likely to rise to about 152 million people by 2050, which is similar to the size of Russia or Bangladesh, the result of an aging population.
Among modifiable risk factors, many studies support a deleterious effect of hypertension, diabetes, and physical inactivity on the risk of dementia. However, since the distribution of these risk factors could have a direct impact on mortality, reducing it should increase life expectancy and the number of cases of dementia.
The team, headed by Hélène Jacqmin-Gadda, PhD, research director at the University of Bordeaux (France), has developed a microsimulation model capable of predicting the burden of dementia while accounting for the impact on mortality. The team used this approach to assess the impact of interventions targeting these three main risk factors on the burden of dementia in France by 2040.
Removing risk factors
The researchers estimated the incidence of dementia for men and women using data from the 2020 PAQUID cohort, and these data were combined with the projections forecast by the French National Institute of Statistics and Economic Studies to account for mortality with and without dementia.
Without intervention, the prevalence rate of dementia in 2040 would be 9.6% among men and 14% among women older than 65 years.
These figures would decrease to 6.4% (−33%) and 10.4% (−26%), respectively, under the intervention scenario whereby the three modifiable vascular risk factors (hypertension, diabetes, and physical inactivity) would be removed simultaneously beginning in 2020. The prevalence rates are significantly reduced for men and women from age 75 years. In this scenario, life expectancy without dementia would increase by 3.4 years in men and 2.6 years in women, the result of men being more exposed to these three risk factors.
Other scenarios have estimated dementia prevalence with the disappearance of just one of these risk factors. For example, the disappearance of hypertension alone from 2020 could decrease dementia prevalence by 21% in men and 16% in women (because this risk factor is less common in women than in men) by 2040. This reduction would be associated with a decrease in the lifelong probability of dementia among men and women and a gain in life expectancy without dementia of 2 years in men and 1.4 years in women.
Among the three factors, hypertension has the largest impact on dementia burden in the French population, since this is, by far, the most prevalent (69% in men and 49% in women), while intervention targeting only diabetes or physical inactivity would lead to a reduction in dementia prevalence of only 4%-7%.
The authors reported no conflicts of interest.
This article was translated from Univadis France. A version appeared on Medscape.com.
FROM THE EUROPEAN JOURNAL OF EPIDEMIOLOGY
Eating disorders in children is a global public health emergency
The high figures are concerning from a public health perspective and highlight the need to implement strategies for preventing eating disorders.
These disorders include anorexia nervosa, bulimia nervosa, binge eating disorder, and eating disorder–not otherwise specified. The prevalence of these disorders in young people has markedly increased globally over the past 50 years. Eating disorders are among the most life-threatening mental disorders; they were responsible for 318 deaths worldwide in 2019.
Because some individuals with eating disorders conceal core symptoms and avoid or delay seeking specialist care because of feelings of embarrassment, stigma, or ambivalence toward treatment, most cases of eating disorders remain undetected and untreated.
Brazilian researchers conducted studies to assess risky behaviors and predisposing factors among young people. The researchers observed that the probability of experiencing eating disorders was higher among young people who had an intense fear of gaining weight, who experienced thin-ideal internalization, who were excessively concerned about food, who experienced compulsive eating episodes, or who used laxatives. As previously reported, most participants in these studies had never sought professional help.
A study conducted in 2020 concluded that the media greatly influences the construction of one’s body image and the creation of aesthetic standards, particularly for adolescents. Adolescents then change their eating patterns and become more vulnerable to mental disorders related to eating.
A group of researchers from several countries, including Brazilians connected to the State University of Londrina, conducted the Global Proportion of Disordered Eating in Children and Adolescents – A Systematic Review and Meta-analysis. The study was coordinated by José Francisco López-Gil, PhD, of the University of Castilla–La Mancha (Spain). The investigators determined the rate of disordered eating among children and adolescents using the SCOFF (Sick, Control, One, Fat, Food) questionnaire, which is the most widely used screening measure for eating disorders.
Methods and results
Four databases were systematically searched (PubMed, Scopus, Web of Science, and the Cochrane Library); date limits were from January 1999 to November 2022. Studies were required to meet the following criteria: participants – studies of community samples of children and adolescents aged 6-18 years – and outcome – disordered eating assessed by the SCOFF questionnaire. The exclusion criteria were studies conducted with young people who had been diagnosed with physical or mental disorders; studies that were published before 1999, because the SCOFF questionnaire was designed in that year; studies in which data were collected during the COVID-19 pandemic, because of the possibility of selection bias; studies that employed data from the same surveys/studies, to avoid duplication; and systematic reviews and/or meta-analyses and qualitative and case studies.
In all, 32 studies, which involved a total of 63,181 participants from 16 countries, were included in the systematic review and meta-analysis, according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines. The overall proportion of children and adolescents with disordered eating was 22.36% (95% confidence interval, 18.84%-26.09%; P < .001; n = 63,181). According to the researchers, girls were significantly more likely to report disordered eating (30.03%; 95% CI, 25.61%-34.65%; n = 27,548) than boys (16.98%; 95% CI, 13.46%-20.81%; n = 26,170; P < .001). It was also observed that disordered eating became more elevated with increasing age (B, 0.03; 95% CI, 0-0.06; P = .049) and BMI (B, 0.03; 95% CI, 0.01-0.05; P < .001).
Translation of outcomes
According to the authors, this was the first meta-analysis that comprehensively examined the overall proportion of children and adolescents with disordered eating in terms of gender, mean age, and BMI. They identified 14,856 (22.36%) children and adolescents with disordered eating in the population analyzed (n = 63,181). A relevant consideration made by the researchers is that, in general, disordered eating and eating disorders are not similar. “Not all children and adolescents who reported disordered eating behaviors (for example, selective eating) will necessarily be diagnosed with an eating disorder.” However, disordered eating in childhood or adolescence may predict outcomes associated with eating disorders in early adulthood. “For this reason, this high proportion found is worrisome and calls for urgent action to try to address this situation.”
The study also found that the proportion of children and adolescents with disordered eating was higher among girls than boys. The reasons for the difference in the prevalence with respect to the sex of the participants are not well understood. Boys are presumed to underreport the problem because of the societal perception that these disorders mostly affect girls and because disordered eating has usually been thought by the general population to be exclusive to girls and women. In addition, it has been noted that the current diagnostic criteria for eating disorders fail to detect disordered eating behaviors more commonly observed in boys than girls, such as intensely engaging in muscle mass gain and weight gain with the goal of improving body image satisfaction. On the other hand, the proportion of young people with disordered eating increased with increasing age and BMI. This finding is in line with the scientific literature worldwide.
The study has certain limitations. First, only studies that analyzed disordered eating using the SCOFF questionnaire were included. Second, because of the cross-sectional nature of most of the included studies, a causal relationship cannot be established. Third, owing to the inclusion of binge eating disorder and other eating disorders specified in the DSM-5, there is not enough evidence to support the use of SCOFF in primary care and community-based settings for screening for the range of eating disorders. Fourth, the meta-analysis included studies in which self-report questionnaires were used to assess disordered eating, and consequently, social desirability and recall bias could have influenced the findings.
Quick measures required
Identifying the magnitude of disordered eating and its distribution in at-risk populations is crucial for planning and executing actions aimed at preventing, detecting, and treating them. Eating disorders are a global public health problem that health care professionals, families, and other community members involved in caring for children and adolescents must not ignore, the researchers said. In addition to diagnosed eating disorders, parents, guardians, and health care professionals should be aware of symptoms of disordered eating, which include behaviors such as weight-loss dieting, binge eating, self-induced vomiting, excessive exercise, and the use of laxatives or diuretics without medical prescription.
This article was translated from the Medscape Portuguese Edition. A version of this article appeared on Medscape.com.
The high figures are concerning from a public health perspective and highlight the need to implement strategies for preventing eating disorders.
These disorders include anorexia nervosa, bulimia nervosa, binge eating disorder, and eating disorder–not otherwise specified. The prevalence of these disorders in young people has markedly increased globally over the past 50 years. Eating disorders are among the most life-threatening mental disorders; they were responsible for 318 deaths worldwide in 2019.
Because some individuals with eating disorders conceal core symptoms and avoid or delay seeking specialist care because of feelings of embarrassment, stigma, or ambivalence toward treatment, most cases of eating disorders remain undetected and untreated.
Brazilian researchers conducted studies to assess risky behaviors and predisposing factors among young people. The researchers observed that the probability of experiencing eating disorders was higher among young people who had an intense fear of gaining weight, who experienced thin-ideal internalization, who were excessively concerned about food, who experienced compulsive eating episodes, or who used laxatives. As previously reported, most participants in these studies had never sought professional help.
A study conducted in 2020 concluded that the media greatly influences the construction of one’s body image and the creation of aesthetic standards, particularly for adolescents. Adolescents then change their eating patterns and become more vulnerable to mental disorders related to eating.
A group of researchers from several countries, including Brazilians connected to the State University of Londrina, conducted the Global Proportion of Disordered Eating in Children and Adolescents – A Systematic Review and Meta-analysis. The study was coordinated by José Francisco López-Gil, PhD, of the University of Castilla–La Mancha (Spain). The investigators determined the rate of disordered eating among children and adolescents using the SCOFF (Sick, Control, One, Fat, Food) questionnaire, which is the most widely used screening measure for eating disorders.
Methods and results
Four databases were systematically searched (PubMed, Scopus, Web of Science, and the Cochrane Library); date limits were from January 1999 to November 2022. Studies were required to meet the following criteria: participants – studies of community samples of children and adolescents aged 6-18 years – and outcome – disordered eating assessed by the SCOFF questionnaire. The exclusion criteria were studies conducted with young people who had been diagnosed with physical or mental disorders; studies that were published before 1999, because the SCOFF questionnaire was designed in that year; studies in which data were collected during the COVID-19 pandemic, because of the possibility of selection bias; studies that employed data from the same surveys/studies, to avoid duplication; and systematic reviews and/or meta-analyses and qualitative and case studies.
In all, 32 studies, which involved a total of 63,181 participants from 16 countries, were included in the systematic review and meta-analysis, according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines. The overall proportion of children and adolescents with disordered eating was 22.36% (95% confidence interval, 18.84%-26.09%; P < .001; n = 63,181). According to the researchers, girls were significantly more likely to report disordered eating (30.03%; 95% CI, 25.61%-34.65%; n = 27,548) than boys (16.98%; 95% CI, 13.46%-20.81%; n = 26,170; P < .001). It was also observed that disordered eating became more elevated with increasing age (B, 0.03; 95% CI, 0-0.06; P = .049) and BMI (B, 0.03; 95% CI, 0.01-0.05; P < .001).
Translation of outcomes
According to the authors, this was the first meta-analysis that comprehensively examined the overall proportion of children and adolescents with disordered eating in terms of gender, mean age, and BMI. They identified 14,856 (22.36%) children and adolescents with disordered eating in the population analyzed (n = 63,181). A relevant consideration made by the researchers is that, in general, disordered eating and eating disorders are not similar. “Not all children and adolescents who reported disordered eating behaviors (for example, selective eating) will necessarily be diagnosed with an eating disorder.” However, disordered eating in childhood or adolescence may predict outcomes associated with eating disorders in early adulthood. “For this reason, this high proportion found is worrisome and calls for urgent action to try to address this situation.”
The study also found that the proportion of children and adolescents with disordered eating was higher among girls than boys. The reasons for the difference in the prevalence with respect to the sex of the participants are not well understood. Boys are presumed to underreport the problem because of the societal perception that these disorders mostly affect girls and because disordered eating has usually been thought by the general population to be exclusive to girls and women. In addition, it has been noted that the current diagnostic criteria for eating disorders fail to detect disordered eating behaviors more commonly observed in boys than girls, such as intensely engaging in muscle mass gain and weight gain with the goal of improving body image satisfaction. On the other hand, the proportion of young people with disordered eating increased with increasing age and BMI. This finding is in line with the scientific literature worldwide.
The study has certain limitations. First, only studies that analyzed disordered eating using the SCOFF questionnaire were included. Second, because of the cross-sectional nature of most of the included studies, a causal relationship cannot be established. Third, owing to the inclusion of binge eating disorder and other eating disorders specified in the DSM-5, there is not enough evidence to support the use of SCOFF in primary care and community-based settings for screening for the range of eating disorders. Fourth, the meta-analysis included studies in which self-report questionnaires were used to assess disordered eating, and consequently, social desirability and recall bias could have influenced the findings.
Quick measures required
Identifying the magnitude of disordered eating and its distribution in at-risk populations is crucial for planning and executing actions aimed at preventing, detecting, and treating them. Eating disorders are a global public health problem that health care professionals, families, and other community members involved in caring for children and adolescents must not ignore, the researchers said. In addition to diagnosed eating disorders, parents, guardians, and health care professionals should be aware of symptoms of disordered eating, which include behaviors such as weight-loss dieting, binge eating, self-induced vomiting, excessive exercise, and the use of laxatives or diuretics without medical prescription.
This article was translated from the Medscape Portuguese Edition. A version of this article appeared on Medscape.com.
The high figures are concerning from a public health perspective and highlight the need to implement strategies for preventing eating disorders.
These disorders include anorexia nervosa, bulimia nervosa, binge eating disorder, and eating disorder–not otherwise specified. The prevalence of these disorders in young people has markedly increased globally over the past 50 years. Eating disorders are among the most life-threatening mental disorders; they were responsible for 318 deaths worldwide in 2019.
Because some individuals with eating disorders conceal core symptoms and avoid or delay seeking specialist care because of feelings of embarrassment, stigma, or ambivalence toward treatment, most cases of eating disorders remain undetected and untreated.
Brazilian researchers conducted studies to assess risky behaviors and predisposing factors among young people. The researchers observed that the probability of experiencing eating disorders was higher among young people who had an intense fear of gaining weight, who experienced thin-ideal internalization, who were excessively concerned about food, who experienced compulsive eating episodes, or who used laxatives. As previously reported, most participants in these studies had never sought professional help.
A study conducted in 2020 concluded that the media greatly influences the construction of one’s body image and the creation of aesthetic standards, particularly for adolescents. Adolescents then change their eating patterns and become more vulnerable to mental disorders related to eating.
A group of researchers from several countries, including Brazilians connected to the State University of Londrina, conducted the Global Proportion of Disordered Eating in Children and Adolescents – A Systematic Review and Meta-analysis. The study was coordinated by José Francisco López-Gil, PhD, of the University of Castilla–La Mancha (Spain). The investigators determined the rate of disordered eating among children and adolescents using the SCOFF (Sick, Control, One, Fat, Food) questionnaire, which is the most widely used screening measure for eating disorders.
Methods and results
Four databases were systematically searched (PubMed, Scopus, Web of Science, and the Cochrane Library); date limits were from January 1999 to November 2022. Studies were required to meet the following criteria: participants – studies of community samples of children and adolescents aged 6-18 years – and outcome – disordered eating assessed by the SCOFF questionnaire. The exclusion criteria were studies conducted with young people who had been diagnosed with physical or mental disorders; studies that were published before 1999, because the SCOFF questionnaire was designed in that year; studies in which data were collected during the COVID-19 pandemic, because of the possibility of selection bias; studies that employed data from the same surveys/studies, to avoid duplication; and systematic reviews and/or meta-analyses and qualitative and case studies.
In all, 32 studies, which involved a total of 63,181 participants from 16 countries, were included in the systematic review and meta-analysis, according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines. The overall proportion of children and adolescents with disordered eating was 22.36% (95% confidence interval, 18.84%-26.09%; P < .001; n = 63,181). According to the researchers, girls were significantly more likely to report disordered eating (30.03%; 95% CI, 25.61%-34.65%; n = 27,548) than boys (16.98%; 95% CI, 13.46%-20.81%; n = 26,170; P < .001). It was also observed that disordered eating became more elevated with increasing age (B, 0.03; 95% CI, 0-0.06; P = .049) and BMI (B, 0.03; 95% CI, 0.01-0.05; P < .001).
Translation of outcomes
According to the authors, this was the first meta-analysis that comprehensively examined the overall proportion of children and adolescents with disordered eating in terms of gender, mean age, and BMI. They identified 14,856 (22.36%) children and adolescents with disordered eating in the population analyzed (n = 63,181). A relevant consideration made by the researchers is that, in general, disordered eating and eating disorders are not similar. “Not all children and adolescents who reported disordered eating behaviors (for example, selective eating) will necessarily be diagnosed with an eating disorder.” However, disordered eating in childhood or adolescence may predict outcomes associated with eating disorders in early adulthood. “For this reason, this high proportion found is worrisome and calls for urgent action to try to address this situation.”
The study also found that the proportion of children and adolescents with disordered eating was higher among girls than boys. The reasons for the difference in the prevalence with respect to the sex of the participants are not well understood. Boys are presumed to underreport the problem because of the societal perception that these disorders mostly affect girls and because disordered eating has usually been thought by the general population to be exclusive to girls and women. In addition, it has been noted that the current diagnostic criteria for eating disorders fail to detect disordered eating behaviors more commonly observed in boys than girls, such as intensely engaging in muscle mass gain and weight gain with the goal of improving body image satisfaction. On the other hand, the proportion of young people with disordered eating increased with increasing age and BMI. This finding is in line with the scientific literature worldwide.
The study has certain limitations. First, only studies that analyzed disordered eating using the SCOFF questionnaire were included. Second, because of the cross-sectional nature of most of the included studies, a causal relationship cannot be established. Third, owing to the inclusion of binge eating disorder and other eating disorders specified in the DSM-5, there is not enough evidence to support the use of SCOFF in primary care and community-based settings for screening for the range of eating disorders. Fourth, the meta-analysis included studies in which self-report questionnaires were used to assess disordered eating, and consequently, social desirability and recall bias could have influenced the findings.
Quick measures required
Identifying the magnitude of disordered eating and its distribution in at-risk populations is crucial for planning and executing actions aimed at preventing, detecting, and treating them. Eating disorders are a global public health problem that health care professionals, families, and other community members involved in caring for children and adolescents must not ignore, the researchers said. In addition to diagnosed eating disorders, parents, guardians, and health care professionals should be aware of symptoms of disordered eating, which include behaviors such as weight-loss dieting, binge eating, self-induced vomiting, excessive exercise, and the use of laxatives or diuretics without medical prescription.
This article was translated from the Medscape Portuguese Edition. A version of this article appeared on Medscape.com.
FROM JAMA PEDIATRICS
Which drug best reduces sleepiness in patients with OSA?
Solriamfetol who have residual daytime sleepiness after conventional treatment, according to a systematic review and meta-analysis.
In a systematic review of 14 trials that included more than 3,000 patients, solriamfetol was associated with improvements of 3.85 points on the Epworth Sleepiness Scale (ESS) score, compared with placebo.
“We found that solriamfetol is almost twice as effective as modafinil-armodafinil – the cheaper, older option – in improving the ESS score and much more effective at improving the Maintenance of Wakefulness Test (MWT),” study author Tyler Pitre, MD, an internal medicine physician at McMaster University, Hamilton, Ont., said in an interview.
The findings were published online in Annals of Internal Medicine.
High-certainty evidence
The analysis included 3,085 adults with excessive daytime sleepiness (EDS) who were receiving or were eligible for conventional OSA treatment such as positive airway pressure. Participants were randomly assigned to either placebo or any EDS pharmacotherapy (armodafinil, modafinil, solriamfetol, or pitolisant). The primary outcomes of the analysis were change in ESS and MWT. Secondary outcomes were drug-related adverse events.
The trials had a median follow-up time of 4 weeks. The meta-analysis showed that solriamfetol improves ESS to a greater extent than placebo (high certainty), armodafinil-modafinil and pitolisant (moderate certainty). Compared with placebo, the mean difference in ESS scores for solriamfetol, armodafinil-modafinil, and pitolisant was –3.85, –2.25, and –2.78, respectively.
The analysis yielded high-certainty evidence that solriamfetol and armodafinil-modafinil improved MWT, compared with placebo. The former was “probably superior,” while pitolisant “may have little to no effect on MWT, compared with placebo,” write the authors. The standardized mean difference in MWT scores, compared with placebo, was 0.90 for solriamfetol and 0.41 for armodafinil-modafinil. “Solriamfetol is probably superior to armodafinil-modafinil in improving MWT (SMD, 0.49),” say the authors.
Compared with placebo, armodafinil-modafinil probably increases the risk for discontinuation due to adverse events (relative risk, 2.01), and solriamfetol may increase the risk for discontinuation (RR, 2.04), according to the authors. Pitolisant “may have little to no effect on drug discontinuations due to adverse events,” write the authors.
Although solriamfetol may have led to more discontinuations than armodafinil-modafinil, “we did not find convincing evidence of serious adverse events, albeit with very short-term follow-up,” they add.
The most common side effects for all interventions were headaches, insomnia, and anxiety. Headaches were most likely with armodafinil-modafinil (RR, 1.87), and insomnia was most likely with pitolisant (RR, 7.25).
“Although solriamfetol appears most effective, comorbid hypertension and costs may be barriers to its use,” say the researchers. “Furthermore, there are potentially effective candidate therapies such as methylphenidate, atomoxetine, or caffeine, which have not been examined in randomized clinical trials.”
Although EDS is reported in 40%-58% of patients with OSA and can persist in 6%-18% despite PAP therapy, most non-sleep specialists may not be aware of pharmacologic options, said Dr. Pitre. “I have not seen a study that looks at the prescribing habits of physicians for this condition, but I suspect that primary care physicians are not prescribing modafinil-armodafinil frequently for this and less so for solriamfetol,” he said. “I hope this paper builds awareness of this condition and also informs clinicians on the options available to patients, as well as common side effects to counsel them on before starting treatment.”
Dr. Pitre was surprised at the magnitude of solriamfetol’s superiority to modafinil-armodafinil but cautioned that solriamfetol has been shown to increase blood pressure in higher doses. It therefore must be prescribed carefully, “especially to a population of patients who often have comorbid hypertension,” he said.
Some limitations of the analysis were that all trials were conducted in high-income countries (most commonly the United States). Moreover, 77% of participants were White, and 71% were male.
Beneficial adjunctive therapy
Commenting on the findings, Sogol Javaheri, MD, MPH, who was not involved in the research, said that they confirm those of prior studies and are “consistent with what my colleagues and I experience in our clinical practices.”
Dr. Javaheri is associate program director of the sleep medicine fellowship at Brigham and Women’s Hospital and assistant professor of medicine at Harvard Medical School, both in Boston.
While sleep medicine specialists are more likely than others to prescribe these medications, “any clinician may use these medications, ideally if they have ruled out other potential reversible causes of EDS,” said Dr. Javaheri. “The medications do not treat the underlying cause, which is why it’s important to use them as an adjunct to conventional therapy that actually treats the underlying sleep disorder and to rule out additional potential causes of sleepiness that are treatable.”
These potential causes might include insufficient sleep (less than 7 hours per night), untreated anemia, and incompletely treated sleep disorders, she explained. In sleep medicine, modafinil is usually the treatment of choice because of its lower cost, but it may reduce the efficacy of hormonal contraception. Solriamfetol, however, does not. “Additionally, I look forward to validation of pitolisant for treatment of EDS in OSA patients, as it is not a controlled substance and may benefit patients with a history of substance abuse or who may be at higher risk of addiction,” said Dr. Javaheri.
The study was conducted without outside funding. Dr. Pitre and Dr. Javaheri report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Solriamfetol who have residual daytime sleepiness after conventional treatment, according to a systematic review and meta-analysis.
In a systematic review of 14 trials that included more than 3,000 patients, solriamfetol was associated with improvements of 3.85 points on the Epworth Sleepiness Scale (ESS) score, compared with placebo.
“We found that solriamfetol is almost twice as effective as modafinil-armodafinil – the cheaper, older option – in improving the ESS score and much more effective at improving the Maintenance of Wakefulness Test (MWT),” study author Tyler Pitre, MD, an internal medicine physician at McMaster University, Hamilton, Ont., said in an interview.
The findings were published online in Annals of Internal Medicine.
High-certainty evidence
The analysis included 3,085 adults with excessive daytime sleepiness (EDS) who were receiving or were eligible for conventional OSA treatment such as positive airway pressure. Participants were randomly assigned to either placebo or any EDS pharmacotherapy (armodafinil, modafinil, solriamfetol, or pitolisant). The primary outcomes of the analysis were change in ESS and MWT. Secondary outcomes were drug-related adverse events.
The trials had a median follow-up time of 4 weeks. The meta-analysis showed that solriamfetol improves ESS to a greater extent than placebo (high certainty), armodafinil-modafinil and pitolisant (moderate certainty). Compared with placebo, the mean difference in ESS scores for solriamfetol, armodafinil-modafinil, and pitolisant was –3.85, –2.25, and –2.78, respectively.
The analysis yielded high-certainty evidence that solriamfetol and armodafinil-modafinil improved MWT, compared with placebo. The former was “probably superior,” while pitolisant “may have little to no effect on MWT, compared with placebo,” write the authors. The standardized mean difference in MWT scores, compared with placebo, was 0.90 for solriamfetol and 0.41 for armodafinil-modafinil. “Solriamfetol is probably superior to armodafinil-modafinil in improving MWT (SMD, 0.49),” say the authors.
Compared with placebo, armodafinil-modafinil probably increases the risk for discontinuation due to adverse events (relative risk, 2.01), and solriamfetol may increase the risk for discontinuation (RR, 2.04), according to the authors. Pitolisant “may have little to no effect on drug discontinuations due to adverse events,” write the authors.
Although solriamfetol may have led to more discontinuations than armodafinil-modafinil, “we did not find convincing evidence of serious adverse events, albeit with very short-term follow-up,” they add.
The most common side effects for all interventions were headaches, insomnia, and anxiety. Headaches were most likely with armodafinil-modafinil (RR, 1.87), and insomnia was most likely with pitolisant (RR, 7.25).
“Although solriamfetol appears most effective, comorbid hypertension and costs may be barriers to its use,” say the researchers. “Furthermore, there are potentially effective candidate therapies such as methylphenidate, atomoxetine, or caffeine, which have not been examined in randomized clinical trials.”
Although EDS is reported in 40%-58% of patients with OSA and can persist in 6%-18% despite PAP therapy, most non-sleep specialists may not be aware of pharmacologic options, said Dr. Pitre. “I have not seen a study that looks at the prescribing habits of physicians for this condition, but I suspect that primary care physicians are not prescribing modafinil-armodafinil frequently for this and less so for solriamfetol,” he said. “I hope this paper builds awareness of this condition and also informs clinicians on the options available to patients, as well as common side effects to counsel them on before starting treatment.”
Dr. Pitre was surprised at the magnitude of solriamfetol’s superiority to modafinil-armodafinil but cautioned that solriamfetol has been shown to increase blood pressure in higher doses. It therefore must be prescribed carefully, “especially to a population of patients who often have comorbid hypertension,” he said.
Some limitations of the analysis were that all trials were conducted in high-income countries (most commonly the United States). Moreover, 77% of participants were White, and 71% were male.
Beneficial adjunctive therapy
Commenting on the findings, Sogol Javaheri, MD, MPH, who was not involved in the research, said that they confirm those of prior studies and are “consistent with what my colleagues and I experience in our clinical practices.”
Dr. Javaheri is associate program director of the sleep medicine fellowship at Brigham and Women’s Hospital and assistant professor of medicine at Harvard Medical School, both in Boston.
While sleep medicine specialists are more likely than others to prescribe these medications, “any clinician may use these medications, ideally if they have ruled out other potential reversible causes of EDS,” said Dr. Javaheri. “The medications do not treat the underlying cause, which is why it’s important to use them as an adjunct to conventional therapy that actually treats the underlying sleep disorder and to rule out additional potential causes of sleepiness that are treatable.”
These potential causes might include insufficient sleep (less than 7 hours per night), untreated anemia, and incompletely treated sleep disorders, she explained. In sleep medicine, modafinil is usually the treatment of choice because of its lower cost, but it may reduce the efficacy of hormonal contraception. Solriamfetol, however, does not. “Additionally, I look forward to validation of pitolisant for treatment of EDS in OSA patients, as it is not a controlled substance and may benefit patients with a history of substance abuse or who may be at higher risk of addiction,” said Dr. Javaheri.
The study was conducted without outside funding. Dr. Pitre and Dr. Javaheri report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Solriamfetol who have residual daytime sleepiness after conventional treatment, according to a systematic review and meta-analysis.
In a systematic review of 14 trials that included more than 3,000 patients, solriamfetol was associated with improvements of 3.85 points on the Epworth Sleepiness Scale (ESS) score, compared with placebo.
“We found that solriamfetol is almost twice as effective as modafinil-armodafinil – the cheaper, older option – in improving the ESS score and much more effective at improving the Maintenance of Wakefulness Test (MWT),” study author Tyler Pitre, MD, an internal medicine physician at McMaster University, Hamilton, Ont., said in an interview.
The findings were published online in Annals of Internal Medicine.
High-certainty evidence
The analysis included 3,085 adults with excessive daytime sleepiness (EDS) who were receiving or were eligible for conventional OSA treatment such as positive airway pressure. Participants were randomly assigned to either placebo or any EDS pharmacotherapy (armodafinil, modafinil, solriamfetol, or pitolisant). The primary outcomes of the analysis were change in ESS and MWT. Secondary outcomes were drug-related adverse events.
The trials had a median follow-up time of 4 weeks. The meta-analysis showed that solriamfetol improves ESS to a greater extent than placebo (high certainty), armodafinil-modafinil and pitolisant (moderate certainty). Compared with placebo, the mean difference in ESS scores for solriamfetol, armodafinil-modafinil, and pitolisant was –3.85, –2.25, and –2.78, respectively.
The analysis yielded high-certainty evidence that solriamfetol and armodafinil-modafinil improved MWT, compared with placebo. The former was “probably superior,” while pitolisant “may have little to no effect on MWT, compared with placebo,” write the authors. The standardized mean difference in MWT scores, compared with placebo, was 0.90 for solriamfetol and 0.41 for armodafinil-modafinil. “Solriamfetol is probably superior to armodafinil-modafinil in improving MWT (SMD, 0.49),” say the authors.
Compared with placebo, armodafinil-modafinil probably increases the risk for discontinuation due to adverse events (relative risk, 2.01), and solriamfetol may increase the risk for discontinuation (RR, 2.04), according to the authors. Pitolisant “may have little to no effect on drug discontinuations due to adverse events,” write the authors.
Although solriamfetol may have led to more discontinuations than armodafinil-modafinil, “we did not find convincing evidence of serious adverse events, albeit with very short-term follow-up,” they add.
The most common side effects for all interventions were headaches, insomnia, and anxiety. Headaches were most likely with armodafinil-modafinil (RR, 1.87), and insomnia was most likely with pitolisant (RR, 7.25).
“Although solriamfetol appears most effective, comorbid hypertension and costs may be barriers to its use,” say the researchers. “Furthermore, there are potentially effective candidate therapies such as methylphenidate, atomoxetine, or caffeine, which have not been examined in randomized clinical trials.”
Although EDS is reported in 40%-58% of patients with OSA and can persist in 6%-18% despite PAP therapy, most non-sleep specialists may not be aware of pharmacologic options, said Dr. Pitre. “I have not seen a study that looks at the prescribing habits of physicians for this condition, but I suspect that primary care physicians are not prescribing modafinil-armodafinil frequently for this and less so for solriamfetol,” he said. “I hope this paper builds awareness of this condition and also informs clinicians on the options available to patients, as well as common side effects to counsel them on before starting treatment.”
Dr. Pitre was surprised at the magnitude of solriamfetol’s superiority to modafinil-armodafinil but cautioned that solriamfetol has been shown to increase blood pressure in higher doses. It therefore must be prescribed carefully, “especially to a population of patients who often have comorbid hypertension,” he said.
Some limitations of the analysis were that all trials were conducted in high-income countries (most commonly the United States). Moreover, 77% of participants were White, and 71% were male.
Beneficial adjunctive therapy
Commenting on the findings, Sogol Javaheri, MD, MPH, who was not involved in the research, said that they confirm those of prior studies and are “consistent with what my colleagues and I experience in our clinical practices.”
Dr. Javaheri is associate program director of the sleep medicine fellowship at Brigham and Women’s Hospital and assistant professor of medicine at Harvard Medical School, both in Boston.
While sleep medicine specialists are more likely than others to prescribe these medications, “any clinician may use these medications, ideally if they have ruled out other potential reversible causes of EDS,” said Dr. Javaheri. “The medications do not treat the underlying cause, which is why it’s important to use them as an adjunct to conventional therapy that actually treats the underlying sleep disorder and to rule out additional potential causes of sleepiness that are treatable.”
These potential causes might include insufficient sleep (less than 7 hours per night), untreated anemia, and incompletely treated sleep disorders, she explained. In sleep medicine, modafinil is usually the treatment of choice because of its lower cost, but it may reduce the efficacy of hormonal contraception. Solriamfetol, however, does not. “Additionally, I look forward to validation of pitolisant for treatment of EDS in OSA patients, as it is not a controlled substance and may benefit patients with a history of substance abuse or who may be at higher risk of addiction,” said Dr. Javaheri.
The study was conducted without outside funding. Dr. Pitre and Dr. Javaheri report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE