User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
More on AI-generated content
In his recent editorial (“A ‘guest editorial’ … generated by ChatGPT?”
Sara Hartley, MD
Berkeley, California
I just read the “guest editorial” generated by ChatGPT. Thank you for this article. Although this is truly an amazing advancement in artificial intelligence (AI), I feel this guest editorial was very basic. It did not read like scientific writing. It read more like it was written at an 11th- or 12th-grade level, though I am fully aware that the question was simple, and thus the answer was not very deep. I can’t deny that if I had been tested, chances are good I would have fallen among the 32% of my peers who would not have recognized it as AI. I appreciate that you (and your team) are working on a protocol regarding how to include content generated by or with the help of AI. God knows if (most likely, when) people with evil minds will use AI to spread false information that may dispute the accredited scientific data and research that guide the medical world and many other fields. I wonder if AI can serve as a search engine that is better or easier to use than PubMed (for example) and the other services we use for research and learning.
Alex Mustachi, PMHNP-BC
Suffern, New York
I wanted to let you know how much I enjoyed reading your recent editorial on AI and scientific writing. Sharing the 4 AI-generated “articles” with readers (“For artificial intelligence, the future is finally here,”
Martha Sajatovic, MD
Cleveland, Ohio
Continue to: The AI-generated samples...
The Al-generated samples were fascinating. As far as I superficially noted, the spelling, grammar, and punctuation were correct. That is better than one gets from most student compositions. However, the articles were completely lacking in depth or apparent insight. The article on anosognosia mentioned it can be present in up to 50% of cases of schizophrenia. In my experience, it is present in approximately 99.9% of cases. It clearly did not consider if anosognosia is also present in alcoholics, codependents, abusers, or people with bizarre political beliefs. But I guess the “intelligence” wasn’t asked that. The other samples also show shallow thinking and repetitive wording—pretty much like my high school junior compositions.
Maybe an appropriate use for AI is a task such as evaluating suicide notes. AI’s success causes one to feel nonplussed. Much more disconcerting was a recent news article that reported AI made up nonexistent references to a professor’s alleged sexual harassment, and then generated citations to its own made-up reference.1 That is indeed frightening new territory. How does one fight against a machine to clear their own name?
Linda Miller, NP
Harrisonburg, Virginia
References
1. Verma P, Oremus W. ChatGPT invented a sexual harassment scandal and named a real law prof as the accused. The Washington Post. April 5, 2023. Accessed May 8, 2023. https://www.washingtonpost.com/technology/2023/04/05/chatgpt-lies/
Thank you, Dr. Nasrallah, for your latest thought-provoking articles on AI. Time and again you provide the profession with cutting-edge, relevant food for thought. Caveat emptor, indeed.
Lawrence E. Cormier, MD
Denver, Colorado
Continue to: We read with interest...
We read with interest Dr. Nasrallah’s editorial that invited readers to share their take on the quality of an AI-generated writing sample. I (MZP) was a computational neuroscience major at Columbia University and was accepted to medical school in 2022 at age 19. I identify with the character traits common among many young tech entrepreneurs driving the AI revolution—social awkwardness; discomfort with subjective emotions; restricted areas of interest; algorithmic thinking; strict, naive idealism; and an obsession with data. To gain a deeper understanding of Sam Altman, the CEO of OpenAI (the company that created ChatGPT), we analyzed a 2.5-hour interview that MIT research scientist Lex Fridman conducted with Altman.1 As a result, we began to discern why AI-generated text feels so stiff and bland compared to the superior fluidity and expressiveness of human communication. As of now, the creation is a reflection of its creator.
Generally speaking, computer scientists are not warm and fuzzy types. Hence, ChatGPT strives to be neutral, accurate, and objective compared to more biased and fallible humans, and, consequently, its language lacks the emotive flair we have come to relish in normal human interactions. In the interview, Altman discusses several solutions that will soon raise the quality of ChatGPT’s currently deficient emotional quotient to approximate its superior IQ. Altruistically, Altman has opened ChatGPT to all, so we can freely interact and utilize its potential to increase our productivity exponentially. As a result, ChatGPT interfaces with millions of humans through RLHF (reinforcement learning from human feedback), which makes each iteration more in tune with our sensibilities.2 Another initiative Altman is undertaking is to depart his Silicon Valley bubble for a road trip to interact with “regular people” and gain a better sense of how to make ChatGPT more user-friendly.1
What’s so saddening about Dr. Nasrallah’s homework assignment is that he is asking us to evaluate with our mature adult standards an article that was written at the emotional stage of a child in early high school. But our hubris and complacency are entirely unfounded because ChatGPT is learning much faster than we ever could, and it will quickly surpass us all as it continues to evolve.
It is also quite disconcerting to hear how Altman is naively relying upon governmental regulation and corporate responsibility to manage the potential misuse of future artificial general intelligence for social, economic, and political control and upheaval. We know well the harmful effects of the internet and social media, particularly on our youth, yet our laws still lag far behind the fact that these technological innovations are simultaneously enhancing our knowledge while destroying our souls. As custodians of our world, dedicated to promoting and preserving mental well-being, we cannot wait much longer to intervene in properly parenting AI along its wisest developmental trajectory before it is too late.
Maxwell Zachary Price, BA
Nutley, New Jersey
Richard Louis Price, MD
New York, New York
References
1. Sam Altman: OpenAI CEO on GPT-4, ChatGPT, and the Future of AI. Lex Fridman Podcast #367. March 25, 2023. Accessed April 5, 2023. https://www.youtube.com/watch?v=L_Guz73e6fw
2. Heikkilä M. How OpenAI is trying to make ChatGPT safer and less biased. MIT Technology Review. Published February 21, 2023. Accessed April 5, 2023. https://www.technologyreview.com/2023/02/21/1068893/how-openai-is-trying-to-make-chatgpt-safer-and-less-biased/
Disclosures
The authors report no financial relationships with any companies whose products are mentioned in their letters, or with manufacturers of competing products.
In his recent editorial (“A ‘guest editorial’ … generated by ChatGPT?”
Sara Hartley, MD
Berkeley, California
I just read the “guest editorial” generated by ChatGPT. Thank you for this article. Although this is truly an amazing advancement in artificial intelligence (AI), I feel this guest editorial was very basic. It did not read like scientific writing. It read more like it was written at an 11th- or 12th-grade level, though I am fully aware that the question was simple, and thus the answer was not very deep. I can’t deny that if I had been tested, chances are good I would have fallen among the 32% of my peers who would not have recognized it as AI. I appreciate that you (and your team) are working on a protocol regarding how to include content generated by or with the help of AI. God knows if (most likely, when) people with evil minds will use AI to spread false information that may dispute the accredited scientific data and research that guide the medical world and many other fields. I wonder if AI can serve as a search engine that is better or easier to use than PubMed (for example) and the other services we use for research and learning.
Alex Mustachi, PMHNP-BC
Suffern, New York
I wanted to let you know how much I enjoyed reading your recent editorial on AI and scientific writing. Sharing the 4 AI-generated “articles” with readers (“For artificial intelligence, the future is finally here,”
Martha Sajatovic, MD
Cleveland, Ohio
Continue to: The AI-generated samples...
The Al-generated samples were fascinating. As far as I superficially noted, the spelling, grammar, and punctuation were correct. That is better than one gets from most student compositions. However, the articles were completely lacking in depth or apparent insight. The article on anosognosia mentioned it can be present in up to 50% of cases of schizophrenia. In my experience, it is present in approximately 99.9% of cases. It clearly did not consider if anosognosia is also present in alcoholics, codependents, abusers, or people with bizarre political beliefs. But I guess the “intelligence” wasn’t asked that. The other samples also show shallow thinking and repetitive wording—pretty much like my high school junior compositions.
Maybe an appropriate use for AI is a task such as evaluating suicide notes. AI’s success causes one to feel nonplussed. Much more disconcerting was a recent news article that reported AI made up nonexistent references to a professor’s alleged sexual harassment, and then generated citations to its own made-up reference.1 That is indeed frightening new territory. How does one fight against a machine to clear their own name?
Linda Miller, NP
Harrisonburg, Virginia
References
1. Verma P, Oremus W. ChatGPT invented a sexual harassment scandal and named a real law prof as the accused. The Washington Post. April 5, 2023. Accessed May 8, 2023. https://www.washingtonpost.com/technology/2023/04/05/chatgpt-lies/
Thank you, Dr. Nasrallah, for your latest thought-provoking articles on AI. Time and again you provide the profession with cutting-edge, relevant food for thought. Caveat emptor, indeed.
Lawrence E. Cormier, MD
Denver, Colorado
Continue to: We read with interest...
We read with interest Dr. Nasrallah’s editorial that invited readers to share their take on the quality of an AI-generated writing sample. I (MZP) was a computational neuroscience major at Columbia University and was accepted to medical school in 2022 at age 19. I identify with the character traits common among many young tech entrepreneurs driving the AI revolution—social awkwardness; discomfort with subjective emotions; restricted areas of interest; algorithmic thinking; strict, naive idealism; and an obsession with data. To gain a deeper understanding of Sam Altman, the CEO of OpenAI (the company that created ChatGPT), we analyzed a 2.5-hour interview that MIT research scientist Lex Fridman conducted with Altman.1 As a result, we began to discern why AI-generated text feels so stiff and bland compared to the superior fluidity and expressiveness of human communication. As of now, the creation is a reflection of its creator.
Generally speaking, computer scientists are not warm and fuzzy types. Hence, ChatGPT strives to be neutral, accurate, and objective compared to more biased and fallible humans, and, consequently, its language lacks the emotive flair we have come to relish in normal human interactions. In the interview, Altman discusses several solutions that will soon raise the quality of ChatGPT’s currently deficient emotional quotient to approximate its superior IQ. Altruistically, Altman has opened ChatGPT to all, so we can freely interact and utilize its potential to increase our productivity exponentially. As a result, ChatGPT interfaces with millions of humans through RLHF (reinforcement learning from human feedback), which makes each iteration more in tune with our sensibilities.2 Another initiative Altman is undertaking is to depart his Silicon Valley bubble for a road trip to interact with “regular people” and gain a better sense of how to make ChatGPT more user-friendly.1
What’s so saddening about Dr. Nasrallah’s homework assignment is that he is asking us to evaluate with our mature adult standards an article that was written at the emotional stage of a child in early high school. But our hubris and complacency are entirely unfounded because ChatGPT is learning much faster than we ever could, and it will quickly surpass us all as it continues to evolve.
It is also quite disconcerting to hear how Altman is naively relying upon governmental regulation and corporate responsibility to manage the potential misuse of future artificial general intelligence for social, economic, and political control and upheaval. We know well the harmful effects of the internet and social media, particularly on our youth, yet our laws still lag far behind the fact that these technological innovations are simultaneously enhancing our knowledge while destroying our souls. As custodians of our world, dedicated to promoting and preserving mental well-being, we cannot wait much longer to intervene in properly parenting AI along its wisest developmental trajectory before it is too late.
Maxwell Zachary Price, BA
Nutley, New Jersey
Richard Louis Price, MD
New York, New York
References
1. Sam Altman: OpenAI CEO on GPT-4, ChatGPT, and the Future of AI. Lex Fridman Podcast #367. March 25, 2023. Accessed April 5, 2023. https://www.youtube.com/watch?v=L_Guz73e6fw
2. Heikkilä M. How OpenAI is trying to make ChatGPT safer and less biased. MIT Technology Review. Published February 21, 2023. Accessed April 5, 2023. https://www.technologyreview.com/2023/02/21/1068893/how-openai-is-trying-to-make-chatgpt-safer-and-less-biased/
Disclosures
The authors report no financial relationships with any companies whose products are mentioned in their letters, or with manufacturers of competing products.
In his recent editorial (“A ‘guest editorial’ … generated by ChatGPT?”
Sara Hartley, MD
Berkeley, California
I just read the “guest editorial” generated by ChatGPT. Thank you for this article. Although this is truly an amazing advancement in artificial intelligence (AI), I feel this guest editorial was very basic. It did not read like scientific writing. It read more like it was written at an 11th- or 12th-grade level, though I am fully aware that the question was simple, and thus the answer was not very deep. I can’t deny that if I had been tested, chances are good I would have fallen among the 32% of my peers who would not have recognized it as AI. I appreciate that you (and your team) are working on a protocol regarding how to include content generated by or with the help of AI. God knows if (most likely, when) people with evil minds will use AI to spread false information that may dispute the accredited scientific data and research that guide the medical world and many other fields. I wonder if AI can serve as a search engine that is better or easier to use than PubMed (for example) and the other services we use for research and learning.
Alex Mustachi, PMHNP-BC
Suffern, New York
I wanted to let you know how much I enjoyed reading your recent editorial on AI and scientific writing. Sharing the 4 AI-generated “articles” with readers (“For artificial intelligence, the future is finally here,”
Martha Sajatovic, MD
Cleveland, Ohio
Continue to: The AI-generated samples...
The Al-generated samples were fascinating. As far as I superficially noted, the spelling, grammar, and punctuation were correct. That is better than one gets from most student compositions. However, the articles were completely lacking in depth or apparent insight. The article on anosognosia mentioned it can be present in up to 50% of cases of schizophrenia. In my experience, it is present in approximately 99.9% of cases. It clearly did not consider if anosognosia is also present in alcoholics, codependents, abusers, or people with bizarre political beliefs. But I guess the “intelligence” wasn’t asked that. The other samples also show shallow thinking and repetitive wording—pretty much like my high school junior compositions.
Maybe an appropriate use for AI is a task such as evaluating suicide notes. AI’s success causes one to feel nonplussed. Much more disconcerting was a recent news article that reported AI made up nonexistent references to a professor’s alleged sexual harassment, and then generated citations to its own made-up reference.1 That is indeed frightening new territory. How does one fight against a machine to clear their own name?
Linda Miller, NP
Harrisonburg, Virginia
References
1. Verma P, Oremus W. ChatGPT invented a sexual harassment scandal and named a real law prof as the accused. The Washington Post. April 5, 2023. Accessed May 8, 2023. https://www.washingtonpost.com/technology/2023/04/05/chatgpt-lies/
Thank you, Dr. Nasrallah, for your latest thought-provoking articles on AI. Time and again you provide the profession with cutting-edge, relevant food for thought. Caveat emptor, indeed.
Lawrence E. Cormier, MD
Denver, Colorado
Continue to: We read with interest...
We read with interest Dr. Nasrallah’s editorial that invited readers to share their take on the quality of an AI-generated writing sample. I (MZP) was a computational neuroscience major at Columbia University and was accepted to medical school in 2022 at age 19. I identify with the character traits common among many young tech entrepreneurs driving the AI revolution—social awkwardness; discomfort with subjective emotions; restricted areas of interest; algorithmic thinking; strict, naive idealism; and an obsession with data. To gain a deeper understanding of Sam Altman, the CEO of OpenAI (the company that created ChatGPT), we analyzed a 2.5-hour interview that MIT research scientist Lex Fridman conducted with Altman.1 As a result, we began to discern why AI-generated text feels so stiff and bland compared to the superior fluidity and expressiveness of human communication. As of now, the creation is a reflection of its creator.
Generally speaking, computer scientists are not warm and fuzzy types. Hence, ChatGPT strives to be neutral, accurate, and objective compared to more biased and fallible humans, and, consequently, its language lacks the emotive flair we have come to relish in normal human interactions. In the interview, Altman discusses several solutions that will soon raise the quality of ChatGPT’s currently deficient emotional quotient to approximate its superior IQ. Altruistically, Altman has opened ChatGPT to all, so we can freely interact and utilize its potential to increase our productivity exponentially. As a result, ChatGPT interfaces with millions of humans through RLHF (reinforcement learning from human feedback), which makes each iteration more in tune with our sensibilities.2 Another initiative Altman is undertaking is to depart his Silicon Valley bubble for a road trip to interact with “regular people” and gain a better sense of how to make ChatGPT more user-friendly.1
What’s so saddening about Dr. Nasrallah’s homework assignment is that he is asking us to evaluate with our mature adult standards an article that was written at the emotional stage of a child in early high school. But our hubris and complacency are entirely unfounded because ChatGPT is learning much faster than we ever could, and it will quickly surpass us all as it continues to evolve.
It is also quite disconcerting to hear how Altman is naively relying upon governmental regulation and corporate responsibility to manage the potential misuse of future artificial general intelligence for social, economic, and political control and upheaval. We know well the harmful effects of the internet and social media, particularly on our youth, yet our laws still lag far behind the fact that these technological innovations are simultaneously enhancing our knowledge while destroying our souls. As custodians of our world, dedicated to promoting and preserving mental well-being, we cannot wait much longer to intervene in properly parenting AI along its wisest developmental trajectory before it is too late.
Maxwell Zachary Price, BA
Nutley, New Jersey
Richard Louis Price, MD
New York, New York
References
1. Sam Altman: OpenAI CEO on GPT-4, ChatGPT, and the Future of AI. Lex Fridman Podcast #367. March 25, 2023. Accessed April 5, 2023. https://www.youtube.com/watch?v=L_Guz73e6fw
2. Heikkilä M. How OpenAI is trying to make ChatGPT safer and less biased. MIT Technology Review. Published February 21, 2023. Accessed April 5, 2023. https://www.technologyreview.com/2023/02/21/1068893/how-openai-is-trying-to-make-chatgpt-safer-and-less-biased/
Disclosures
The authors report no financial relationships with any companies whose products are mentioned in their letters, or with manufacturers of competing products.
Quick medication, better communication linked to less violence at inpatient psych unit
SAN FRANCISCO – Physically violent events at an inpatient psychiatric unit in Pennsylvania dropped by 59.8% in the months after it implemented a plan to administer antipsychotic medications to patients more quickly – both in the emergency department and in the unit – and improve handoffs between providers and nurses, researchers reported.
“We were able to significantly reduce violence,” said Michael Chen, MD, Lehigh Valley Health Network psychiatry resident and lead author of an abstract presented at the annual meeting of the American Psychiatric Association. “Furthermore, the interventions were effective in reducing episodes of violence rather than redirecting it. And the overall feeling of safety on the inpatient psychiatric unit improved.”
Violence is common in psychiatric units, although it’s not clear how often it occurs. “The data has shown that patients with a psychotic disorder such as schizophrenia or a mood disorder with psychotic features such as bipolar disorder tend to account for most of the episodes of violence on the unit,” Dr. Chen said in an interview. “This inevitably results in a higher risk for violence on inpatient psychiatric units as a large portion of patients admitted to inpatient psychiatric units have these diagnoses.”
Enlisting the pharmacy department
For the new study, investigators tracked episodes of violence – including verbal attacks – at an Allentown, Penn.–area inpatient psychiatric unit from December 2021 to September 2022. According to Dr. Chen, unit leaders implemented the new plan in May 2022 in the wake of higher levels of violence during the COVID-19 pandemic and the concurrent staff shortages.
Clinic leaders sought to identify potentially aggressive patients in the emergency department and treat them with antipsychotics prior to admission to the psychiatric unit, ensure that the pharmacy provides access to as-needed or standing medications, and develop “standardized huddles to ensure proper handoffs between providers and nurses.”
Medical staff relied on the Dynamic Appraisal of Situational Aggression scale, risk factors, and clinical judgment to determine which patients had the potential to be violent, Dr. Chen said.
As for treatment, first-line antipsychotics are typically given orally, but they can be injected if patients must be treated over their objections, he said. “We would only consider starting standing medications against objections in patients who are involuntarily committed.”
During the 5 months before the intervention was implemented versus the following 5 months, the average monthly number of physically violent events in the psychiatric unit fell from 12.4 to 4.8 (–61.1%, P = .04), and verbal threats dipped from 7.2 to 4 (–44.4%, P = .15). The total average number of violent events per month, including violence against property, fell from an average of 25.4 to 10.2 (–59.8%, P = .03).
The total patient population didn’t vary significantly over time, Dr. Chen said. “Thus, the decrease in violence was not correlated with a decrease in patient load.”
While “there were concerns that there would just be higher episodes of violence in the ED while psychiatry patients awaited placement,” Dr. Chen said, the numbers actually showed reductions in violence in that setting. The average number of physically violent events per month in the ED fell from 49.6 to 39.4 (–20.6%, P = .03). Verbal threats dropped from 38 to 34.6 (–8.9%, P = .5) and overall violent events dipped from 87.6 to 74 (–15.6%, P = .08).
Why did the interventions seem to work? “Standing doses as well as as-needed medications started for psychiatric patients in the emergency department have been crucial to prevent delay of care,” Dr. Chen said. Enlisting the pharmacy department “helped ensure all patients had appropriate as-needed medications to prevent them from decompensating on the units,” he added, and “involvement of nursing and ancillary staff in high-risk rounds allowed the treatment team to rapidly anticipate and address concerns.”
The study authors also reported that nursing staff felt safer. Scores on a perception-of-safety scale – with 1 most unsafe and 7 most safe – improved from 3.3 to 4.2 (+27%, P < .01).
Dr. Chen said there was a “minimal” increase in cost to implement the intervention, although coordination is necessary. “The emergency department and psychiatry department have to work together to initiate treatment in the ED while awaiting beds,” he said. “The treatment team needs to communicate concerns during rounds. The pharmacist and psychiatrist need to work together to ensure that proper as-needed medications are available.”
‘Good clinical practice’
In an interview, psychiatrist Mark J. Russ, MD, of NewYork-Presbyterian/Westchester Behavioral Health and Weill Cornell Medical College, said violent incidents in inpatient psychiatric units are influenced by many factors, such as history of violence, substance use, history of trauma, psychosis/paranoia, and medical problems.
The units themselves can contribute to the risk of violence through power struggles and lack of attention paid to respect and dignity, he said. “Attention to these issues is important in reducing violence,” he noted. “Generalized training for staff in de-escalation techniques and trauma-informed care is imperative. There may be value in developing specialized psychiatric ICUs where staff are meticulously trained in these and other approaches.”
The new study, Dr. Russ said, suggests that “early identification of patients at risk of engaging in violent behavior on the inpatient unit, pharmacologic treatment, and good communication helps reduce violence.” The findings, he added, suggest that “interventions known to constitute good clinical practice are indeed helpful.”
However, he cautioned that “treating all at-risk patients with antipsychotics, regardless of their psychiatric diagnosis, might well be considered chemical restraint, depending on [the] circumstances.”
There was no study funding. The study authors and Dr. Russ have no disclosures.
SAN FRANCISCO – Physically violent events at an inpatient psychiatric unit in Pennsylvania dropped by 59.8% in the months after it implemented a plan to administer antipsychotic medications to patients more quickly – both in the emergency department and in the unit – and improve handoffs between providers and nurses, researchers reported.
“We were able to significantly reduce violence,” said Michael Chen, MD, Lehigh Valley Health Network psychiatry resident and lead author of an abstract presented at the annual meeting of the American Psychiatric Association. “Furthermore, the interventions were effective in reducing episodes of violence rather than redirecting it. And the overall feeling of safety on the inpatient psychiatric unit improved.”
Violence is common in psychiatric units, although it’s not clear how often it occurs. “The data has shown that patients with a psychotic disorder such as schizophrenia or a mood disorder with psychotic features such as bipolar disorder tend to account for most of the episodes of violence on the unit,” Dr. Chen said in an interview. “This inevitably results in a higher risk for violence on inpatient psychiatric units as a large portion of patients admitted to inpatient psychiatric units have these diagnoses.”
Enlisting the pharmacy department
For the new study, investigators tracked episodes of violence – including verbal attacks – at an Allentown, Penn.–area inpatient psychiatric unit from December 2021 to September 2022. According to Dr. Chen, unit leaders implemented the new plan in May 2022 in the wake of higher levels of violence during the COVID-19 pandemic and the concurrent staff shortages.
Clinic leaders sought to identify potentially aggressive patients in the emergency department and treat them with antipsychotics prior to admission to the psychiatric unit, ensure that the pharmacy provides access to as-needed or standing medications, and develop “standardized huddles to ensure proper handoffs between providers and nurses.”
Medical staff relied on the Dynamic Appraisal of Situational Aggression scale, risk factors, and clinical judgment to determine which patients had the potential to be violent, Dr. Chen said.
As for treatment, first-line antipsychotics are typically given orally, but they can be injected if patients must be treated over their objections, he said. “We would only consider starting standing medications against objections in patients who are involuntarily committed.”
During the 5 months before the intervention was implemented versus the following 5 months, the average monthly number of physically violent events in the psychiatric unit fell from 12.4 to 4.8 (–61.1%, P = .04), and verbal threats dipped from 7.2 to 4 (–44.4%, P = .15). The total average number of violent events per month, including violence against property, fell from an average of 25.4 to 10.2 (–59.8%, P = .03).
The total patient population didn’t vary significantly over time, Dr. Chen said. “Thus, the decrease in violence was not correlated with a decrease in patient load.”
While “there were concerns that there would just be higher episodes of violence in the ED while psychiatry patients awaited placement,” Dr. Chen said, the numbers actually showed reductions in violence in that setting. The average number of physically violent events per month in the ED fell from 49.6 to 39.4 (–20.6%, P = .03). Verbal threats dropped from 38 to 34.6 (–8.9%, P = .5) and overall violent events dipped from 87.6 to 74 (–15.6%, P = .08).
Why did the interventions seem to work? “Standing doses as well as as-needed medications started for psychiatric patients in the emergency department have been crucial to prevent delay of care,” Dr. Chen said. Enlisting the pharmacy department “helped ensure all patients had appropriate as-needed medications to prevent them from decompensating on the units,” he added, and “involvement of nursing and ancillary staff in high-risk rounds allowed the treatment team to rapidly anticipate and address concerns.”
The study authors also reported that nursing staff felt safer. Scores on a perception-of-safety scale – with 1 most unsafe and 7 most safe – improved from 3.3 to 4.2 (+27%, P < .01).
Dr. Chen said there was a “minimal” increase in cost to implement the intervention, although coordination is necessary. “The emergency department and psychiatry department have to work together to initiate treatment in the ED while awaiting beds,” he said. “The treatment team needs to communicate concerns during rounds. The pharmacist and psychiatrist need to work together to ensure that proper as-needed medications are available.”
‘Good clinical practice’
In an interview, psychiatrist Mark J. Russ, MD, of NewYork-Presbyterian/Westchester Behavioral Health and Weill Cornell Medical College, said violent incidents in inpatient psychiatric units are influenced by many factors, such as history of violence, substance use, history of trauma, psychosis/paranoia, and medical problems.
The units themselves can contribute to the risk of violence through power struggles and lack of attention paid to respect and dignity, he said. “Attention to these issues is important in reducing violence,” he noted. “Generalized training for staff in de-escalation techniques and trauma-informed care is imperative. There may be value in developing specialized psychiatric ICUs where staff are meticulously trained in these and other approaches.”
The new study, Dr. Russ said, suggests that “early identification of patients at risk of engaging in violent behavior on the inpatient unit, pharmacologic treatment, and good communication helps reduce violence.” The findings, he added, suggest that “interventions known to constitute good clinical practice are indeed helpful.”
However, he cautioned that “treating all at-risk patients with antipsychotics, regardless of their psychiatric diagnosis, might well be considered chemical restraint, depending on [the] circumstances.”
There was no study funding. The study authors and Dr. Russ have no disclosures.
SAN FRANCISCO – Physically violent events at an inpatient psychiatric unit in Pennsylvania dropped by 59.8% in the months after it implemented a plan to administer antipsychotic medications to patients more quickly – both in the emergency department and in the unit – and improve handoffs between providers and nurses, researchers reported.
“We were able to significantly reduce violence,” said Michael Chen, MD, Lehigh Valley Health Network psychiatry resident and lead author of an abstract presented at the annual meeting of the American Psychiatric Association. “Furthermore, the interventions were effective in reducing episodes of violence rather than redirecting it. And the overall feeling of safety on the inpatient psychiatric unit improved.”
Violence is common in psychiatric units, although it’s not clear how often it occurs. “The data has shown that patients with a psychotic disorder such as schizophrenia or a mood disorder with psychotic features such as bipolar disorder tend to account for most of the episodes of violence on the unit,” Dr. Chen said in an interview. “This inevitably results in a higher risk for violence on inpatient psychiatric units as a large portion of patients admitted to inpatient psychiatric units have these diagnoses.”
Enlisting the pharmacy department
For the new study, investigators tracked episodes of violence – including verbal attacks – at an Allentown, Penn.–area inpatient psychiatric unit from December 2021 to September 2022. According to Dr. Chen, unit leaders implemented the new plan in May 2022 in the wake of higher levels of violence during the COVID-19 pandemic and the concurrent staff shortages.
Clinic leaders sought to identify potentially aggressive patients in the emergency department and treat them with antipsychotics prior to admission to the psychiatric unit, ensure that the pharmacy provides access to as-needed or standing medications, and develop “standardized huddles to ensure proper handoffs between providers and nurses.”
Medical staff relied on the Dynamic Appraisal of Situational Aggression scale, risk factors, and clinical judgment to determine which patients had the potential to be violent, Dr. Chen said.
As for treatment, first-line antipsychotics are typically given orally, but they can be injected if patients must be treated over their objections, he said. “We would only consider starting standing medications against objections in patients who are involuntarily committed.”
During the 5 months before the intervention was implemented versus the following 5 months, the average monthly number of physically violent events in the psychiatric unit fell from 12.4 to 4.8 (–61.1%, P = .04), and verbal threats dipped from 7.2 to 4 (–44.4%, P = .15). The total average number of violent events per month, including violence against property, fell from an average of 25.4 to 10.2 (–59.8%, P = .03).
The total patient population didn’t vary significantly over time, Dr. Chen said. “Thus, the decrease in violence was not correlated with a decrease in patient load.”
While “there were concerns that there would just be higher episodes of violence in the ED while psychiatry patients awaited placement,” Dr. Chen said, the numbers actually showed reductions in violence in that setting. The average number of physically violent events per month in the ED fell from 49.6 to 39.4 (–20.6%, P = .03). Verbal threats dropped from 38 to 34.6 (–8.9%, P = .5) and overall violent events dipped from 87.6 to 74 (–15.6%, P = .08).
Why did the interventions seem to work? “Standing doses as well as as-needed medications started for psychiatric patients in the emergency department have been crucial to prevent delay of care,” Dr. Chen said. Enlisting the pharmacy department “helped ensure all patients had appropriate as-needed medications to prevent them from decompensating on the units,” he added, and “involvement of nursing and ancillary staff in high-risk rounds allowed the treatment team to rapidly anticipate and address concerns.”
The study authors also reported that nursing staff felt safer. Scores on a perception-of-safety scale – with 1 most unsafe and 7 most safe – improved from 3.3 to 4.2 (+27%, P < .01).
Dr. Chen said there was a “minimal” increase in cost to implement the intervention, although coordination is necessary. “The emergency department and psychiatry department have to work together to initiate treatment in the ED while awaiting beds,” he said. “The treatment team needs to communicate concerns during rounds. The pharmacist and psychiatrist need to work together to ensure that proper as-needed medications are available.”
‘Good clinical practice’
In an interview, psychiatrist Mark J. Russ, MD, of NewYork-Presbyterian/Westchester Behavioral Health and Weill Cornell Medical College, said violent incidents in inpatient psychiatric units are influenced by many factors, such as history of violence, substance use, history of trauma, psychosis/paranoia, and medical problems.
The units themselves can contribute to the risk of violence through power struggles and lack of attention paid to respect and dignity, he said. “Attention to these issues is important in reducing violence,” he noted. “Generalized training for staff in de-escalation techniques and trauma-informed care is imperative. There may be value in developing specialized psychiatric ICUs where staff are meticulously trained in these and other approaches.”
The new study, Dr. Russ said, suggests that “early identification of patients at risk of engaging in violent behavior on the inpatient unit, pharmacologic treatment, and good communication helps reduce violence.” The findings, he added, suggest that “interventions known to constitute good clinical practice are indeed helpful.”
However, he cautioned that “treating all at-risk patients with antipsychotics, regardless of their psychiatric diagnosis, might well be considered chemical restraint, depending on [the] circumstances.”
There was no study funding. The study authors and Dr. Russ have no disclosures.
AT APA 2023
PTSD, anxiety linked to out-of-hospital cardiac arrest
Investigators compared more than 35,000 OHCA case patients with a similar number of matched control persons and found an almost 1.5 times higher hazard of long-term stress conditions among OHCA case patients, compared with control persons, with a similar hazard for anxiety. Posttraumatic stress disorder was associated with an almost twofold higher risk of OHCA.
The findings applied equally to men and women and were independent of the presence of cardiovascular disease (CVD).
“This study raises awareness of the higher risks of OHCA and early risk monitoring to prevent OHCA in patients with stress-related disorders and anxiety,” write Talip Eroglu, of the department of cardiology, Copenhagen University Hospital, and colleagues.
The study was published online in BMJ Open Heart.
Stress disorders and anxiety overrepresented
OHCA “predominantly arises from lethal cardiac arrhythmias ... that occur most frequently in the setting of coronary heart disease,” the authors write. However, increasing evidence suggests that rates of OHCA may also be increased in association with noncardiac diseases.
Individuals with stress-related disorders and anxiety are “overrepresented” among victims of cardiac arrest as well as those with multiple CVDs. But previous studies of OHCA have been limited by small numbers of cardiac arrests. In addition, those studies involved only data from selected populations or used in-hospital diagnosis to identify cardiac arrest, thereby potentially omitting OHCA patients who died prior to hospital admission.
The researchers therefore turned to data from Danish health registries that include a large, unselected cohort of patients with OHCA to investigate whether long-term stress conditions (that is, PTSD and adjustment disorder) or anxiety disorder were associated with OHCA.
They stratified the cohort according to sex, age, and CVD to identify which risk factor confers the highest risk of OHCA in patients with long-term stress conditions or anxiety, and they conducted sensitivity analyses of potential confounders, such as depression.
The design was a nested-case control model in which records at an individual patient level across registries were cross-linked to data from other national registries and were compared to matched control persons from the general population (35,195 OHCAs and 351,950 matched control persons; median IQR age, 72 [62-81] years; 66.82% men).
The prevalence of comorbidities and use of cardiovascular drugs were higher among OHCA case patients than among non-OHCA control persons.
Keep aware of stress and anxiety as risk factors
Among OHCA and non-OHCA participants, long-term stress conditions were diagnosed in 0.92% and 0.45%, respectively. Anxiety was diagnosed in 0.85% of OHCA case patients and in 0.37% of non-OHCA control persons.
These conditions were associated with a higher rate of OHCA after adjustment for common OHCA risk factors.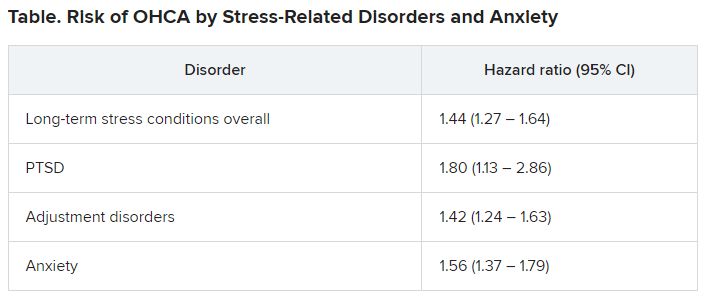
There were no significant differences in results when the researchers adjusted for the use of anxiolytics and antidepressants.
When they examined the prevalence of concomitant medication use or comorbidities, they found that depression was more frequent among patients with long-term stress and anxiety, compared with individuals with neither of those diagnoses. Additionally, patients with long-term stress and anxiety more often used anxiolytics, antidepressants, and QT-prolonging drugs.
Stratification of the analyses according to sex revealed that the OHCA rate was increased in both women and men with long-term stress and anxiety. There were no significant differences between the sexes. There were also no significant differences between the association among different age groups, nor between patients with and those without CVD, ischemic heart disease, or heart failure.
Previous research has shown associations of stress-related disorders or anxiety with cardiovascular outcomes, including myocardial infarction, heart failure, and cerebrovascular disease. These disorders might be “biological mediators in the causal pathway of OHCA” and contribute to the increased OHCA rate associated with stress-related disorders and anxiety, the authors suggest.
Nevertheless, they note, stress-related disorders and anxiety remained significantly associated with OHCA after controlling for these variables, “suggesting that it is unlikely that traditional risk factors of OHCA alone explain this relationship.”
They suggest several potential mechanisms. One is that the relationship is likely mediated by the activity of the sympathetic autonomic nervous system, which “leads to an increase in heart rate, release of neurotransmitters into the circulation, and local release of neurotransmitters in the heart.”
Each of these factors “may potentially influence cardiac electrophysiology and facilitate ventricular arrhythmias and OHCA.”
In addition to a biological mechanism, behavioral and psychosocial factors may also contribute to OHCA risk, since stress-related disorders and anxiety “often lead to unhealthy lifestyle, such as smoking and lower physical activity, which in turn may increase the risk of OHCA.” Given the absence of data on these features in the registries the investigators used, they were unable to account for them.
However, “it is unlikely that knowledge of these factors would have altered our conclusions considering that we have adjusted for all the relevant cardiovascular comorbidities.”
Similarly, other psychiatric disorders, such as depression, can contribute to OHCA risk, but they adjusted for depression in their multivariable analyses.
“Awareness of the higher risks of OHCA in patients with stress-related disorders and anxiety is important when treating these patients,” they conclude.
Detrimental to the heart, not just the psyche
Glenn Levine, MD, master clinician and professor of medicine, Baylor College of Medicine, Houston, called it an “important study in that it is a large, nationwide cohort study and thus provides important information to complement much smaller, focused studies.”
Like those other studies, “it finds that negative psychological health, specifically, long-term stress (as well as anxiety), is associated with a significantly increased risk of out-of-hospital cardiac arrest,” continued Dr. Levine, who is the chief of the cardiology section at Michael E. DeBakey VA Medical Center, Houston, and was not involved with the study.
Dr. Levine thinks the study “does a good job, as best one can for such a study, in trying to control for other factors, and zeroing in specifically on stress (and anxiety), trying to assess their independent contributions to the risk of developing cardiac arrest.”
The take-home message for clinicians and patients “is that negative psychological stress factors, such as stress and anxiety, are not only detrimental to one’s psychological health but likely increase one’s risk for adverse cardiac events, such as cardiac arrest,” he stated.
No specific funding for the study was disclosed. Mr. Eroglu has disclosed no relevant financial relationships. The other authors’ disclosures are listed in the original article. Dr. Levine reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators compared more than 35,000 OHCA case patients with a similar number of matched control persons and found an almost 1.5 times higher hazard of long-term stress conditions among OHCA case patients, compared with control persons, with a similar hazard for anxiety. Posttraumatic stress disorder was associated with an almost twofold higher risk of OHCA.
The findings applied equally to men and women and were independent of the presence of cardiovascular disease (CVD).
“This study raises awareness of the higher risks of OHCA and early risk monitoring to prevent OHCA in patients with stress-related disorders and anxiety,” write Talip Eroglu, of the department of cardiology, Copenhagen University Hospital, and colleagues.
The study was published online in BMJ Open Heart.
Stress disorders and anxiety overrepresented
OHCA “predominantly arises from lethal cardiac arrhythmias ... that occur most frequently in the setting of coronary heart disease,” the authors write. However, increasing evidence suggests that rates of OHCA may also be increased in association with noncardiac diseases.
Individuals with stress-related disorders and anxiety are “overrepresented” among victims of cardiac arrest as well as those with multiple CVDs. But previous studies of OHCA have been limited by small numbers of cardiac arrests. In addition, those studies involved only data from selected populations or used in-hospital diagnosis to identify cardiac arrest, thereby potentially omitting OHCA patients who died prior to hospital admission.
The researchers therefore turned to data from Danish health registries that include a large, unselected cohort of patients with OHCA to investigate whether long-term stress conditions (that is, PTSD and adjustment disorder) or anxiety disorder were associated with OHCA.
They stratified the cohort according to sex, age, and CVD to identify which risk factor confers the highest risk of OHCA in patients with long-term stress conditions or anxiety, and they conducted sensitivity analyses of potential confounders, such as depression.
The design was a nested-case control model in which records at an individual patient level across registries were cross-linked to data from other national registries and were compared to matched control persons from the general population (35,195 OHCAs and 351,950 matched control persons; median IQR age, 72 [62-81] years; 66.82% men).
The prevalence of comorbidities and use of cardiovascular drugs were higher among OHCA case patients than among non-OHCA control persons.
Keep aware of stress and anxiety as risk factors
Among OHCA and non-OHCA participants, long-term stress conditions were diagnosed in 0.92% and 0.45%, respectively. Anxiety was diagnosed in 0.85% of OHCA case patients and in 0.37% of non-OHCA control persons.
These conditions were associated with a higher rate of OHCA after adjustment for common OHCA risk factors.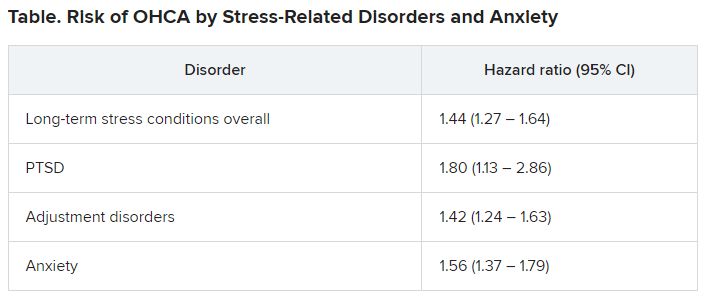
There were no significant differences in results when the researchers adjusted for the use of anxiolytics and antidepressants.
When they examined the prevalence of concomitant medication use or comorbidities, they found that depression was more frequent among patients with long-term stress and anxiety, compared with individuals with neither of those diagnoses. Additionally, patients with long-term stress and anxiety more often used anxiolytics, antidepressants, and QT-prolonging drugs.
Stratification of the analyses according to sex revealed that the OHCA rate was increased in both women and men with long-term stress and anxiety. There were no significant differences between the sexes. There were also no significant differences between the association among different age groups, nor between patients with and those without CVD, ischemic heart disease, or heart failure.
Previous research has shown associations of stress-related disorders or anxiety with cardiovascular outcomes, including myocardial infarction, heart failure, and cerebrovascular disease. These disorders might be “biological mediators in the causal pathway of OHCA” and contribute to the increased OHCA rate associated with stress-related disorders and anxiety, the authors suggest.
Nevertheless, they note, stress-related disorders and anxiety remained significantly associated with OHCA after controlling for these variables, “suggesting that it is unlikely that traditional risk factors of OHCA alone explain this relationship.”
They suggest several potential mechanisms. One is that the relationship is likely mediated by the activity of the sympathetic autonomic nervous system, which “leads to an increase in heart rate, release of neurotransmitters into the circulation, and local release of neurotransmitters in the heart.”
Each of these factors “may potentially influence cardiac electrophysiology and facilitate ventricular arrhythmias and OHCA.”
In addition to a biological mechanism, behavioral and psychosocial factors may also contribute to OHCA risk, since stress-related disorders and anxiety “often lead to unhealthy lifestyle, such as smoking and lower physical activity, which in turn may increase the risk of OHCA.” Given the absence of data on these features in the registries the investigators used, they were unable to account for them.
However, “it is unlikely that knowledge of these factors would have altered our conclusions considering that we have adjusted for all the relevant cardiovascular comorbidities.”
Similarly, other psychiatric disorders, such as depression, can contribute to OHCA risk, but they adjusted for depression in their multivariable analyses.
“Awareness of the higher risks of OHCA in patients with stress-related disorders and anxiety is important when treating these patients,” they conclude.
Detrimental to the heart, not just the psyche
Glenn Levine, MD, master clinician and professor of medicine, Baylor College of Medicine, Houston, called it an “important study in that it is a large, nationwide cohort study and thus provides important information to complement much smaller, focused studies.”
Like those other studies, “it finds that negative psychological health, specifically, long-term stress (as well as anxiety), is associated with a significantly increased risk of out-of-hospital cardiac arrest,” continued Dr. Levine, who is the chief of the cardiology section at Michael E. DeBakey VA Medical Center, Houston, and was not involved with the study.
Dr. Levine thinks the study “does a good job, as best one can for such a study, in trying to control for other factors, and zeroing in specifically on stress (and anxiety), trying to assess their independent contributions to the risk of developing cardiac arrest.”
The take-home message for clinicians and patients “is that negative psychological stress factors, such as stress and anxiety, are not only detrimental to one’s psychological health but likely increase one’s risk for adverse cardiac events, such as cardiac arrest,” he stated.
No specific funding for the study was disclosed. Mr. Eroglu has disclosed no relevant financial relationships. The other authors’ disclosures are listed in the original article. Dr. Levine reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators compared more than 35,000 OHCA case patients with a similar number of matched control persons and found an almost 1.5 times higher hazard of long-term stress conditions among OHCA case patients, compared with control persons, with a similar hazard for anxiety. Posttraumatic stress disorder was associated with an almost twofold higher risk of OHCA.
The findings applied equally to men and women and were independent of the presence of cardiovascular disease (CVD).
“This study raises awareness of the higher risks of OHCA and early risk monitoring to prevent OHCA in patients with stress-related disorders and anxiety,” write Talip Eroglu, of the department of cardiology, Copenhagen University Hospital, and colleagues.
The study was published online in BMJ Open Heart.
Stress disorders and anxiety overrepresented
OHCA “predominantly arises from lethal cardiac arrhythmias ... that occur most frequently in the setting of coronary heart disease,” the authors write. However, increasing evidence suggests that rates of OHCA may also be increased in association with noncardiac diseases.
Individuals with stress-related disorders and anxiety are “overrepresented” among victims of cardiac arrest as well as those with multiple CVDs. But previous studies of OHCA have been limited by small numbers of cardiac arrests. In addition, those studies involved only data from selected populations or used in-hospital diagnosis to identify cardiac arrest, thereby potentially omitting OHCA patients who died prior to hospital admission.
The researchers therefore turned to data from Danish health registries that include a large, unselected cohort of patients with OHCA to investigate whether long-term stress conditions (that is, PTSD and adjustment disorder) or anxiety disorder were associated with OHCA.
They stratified the cohort according to sex, age, and CVD to identify which risk factor confers the highest risk of OHCA in patients with long-term stress conditions or anxiety, and they conducted sensitivity analyses of potential confounders, such as depression.
The design was a nested-case control model in which records at an individual patient level across registries were cross-linked to data from other national registries and were compared to matched control persons from the general population (35,195 OHCAs and 351,950 matched control persons; median IQR age, 72 [62-81] years; 66.82% men).
The prevalence of comorbidities and use of cardiovascular drugs were higher among OHCA case patients than among non-OHCA control persons.
Keep aware of stress and anxiety as risk factors
Among OHCA and non-OHCA participants, long-term stress conditions were diagnosed in 0.92% and 0.45%, respectively. Anxiety was diagnosed in 0.85% of OHCA case patients and in 0.37% of non-OHCA control persons.
These conditions were associated with a higher rate of OHCA after adjustment for common OHCA risk factors.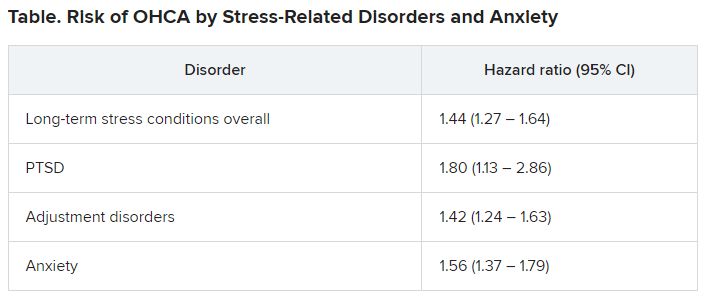
There were no significant differences in results when the researchers adjusted for the use of anxiolytics and antidepressants.
When they examined the prevalence of concomitant medication use or comorbidities, they found that depression was more frequent among patients with long-term stress and anxiety, compared with individuals with neither of those diagnoses. Additionally, patients with long-term stress and anxiety more often used anxiolytics, antidepressants, and QT-prolonging drugs.
Stratification of the analyses according to sex revealed that the OHCA rate was increased in both women and men with long-term stress and anxiety. There were no significant differences between the sexes. There were also no significant differences between the association among different age groups, nor between patients with and those without CVD, ischemic heart disease, or heart failure.
Previous research has shown associations of stress-related disorders or anxiety with cardiovascular outcomes, including myocardial infarction, heart failure, and cerebrovascular disease. These disorders might be “biological mediators in the causal pathway of OHCA” and contribute to the increased OHCA rate associated with stress-related disorders and anxiety, the authors suggest.
Nevertheless, they note, stress-related disorders and anxiety remained significantly associated with OHCA after controlling for these variables, “suggesting that it is unlikely that traditional risk factors of OHCA alone explain this relationship.”
They suggest several potential mechanisms. One is that the relationship is likely mediated by the activity of the sympathetic autonomic nervous system, which “leads to an increase in heart rate, release of neurotransmitters into the circulation, and local release of neurotransmitters in the heart.”
Each of these factors “may potentially influence cardiac electrophysiology and facilitate ventricular arrhythmias and OHCA.”
In addition to a biological mechanism, behavioral and psychosocial factors may also contribute to OHCA risk, since stress-related disorders and anxiety “often lead to unhealthy lifestyle, such as smoking and lower physical activity, which in turn may increase the risk of OHCA.” Given the absence of data on these features in the registries the investigators used, they were unable to account for them.
However, “it is unlikely that knowledge of these factors would have altered our conclusions considering that we have adjusted for all the relevant cardiovascular comorbidities.”
Similarly, other psychiatric disorders, such as depression, can contribute to OHCA risk, but they adjusted for depression in their multivariable analyses.
“Awareness of the higher risks of OHCA in patients with stress-related disorders and anxiety is important when treating these patients,” they conclude.
Detrimental to the heart, not just the psyche
Glenn Levine, MD, master clinician and professor of medicine, Baylor College of Medicine, Houston, called it an “important study in that it is a large, nationwide cohort study and thus provides important information to complement much smaller, focused studies.”
Like those other studies, “it finds that negative psychological health, specifically, long-term stress (as well as anxiety), is associated with a significantly increased risk of out-of-hospital cardiac arrest,” continued Dr. Levine, who is the chief of the cardiology section at Michael E. DeBakey VA Medical Center, Houston, and was not involved with the study.
Dr. Levine thinks the study “does a good job, as best one can for such a study, in trying to control for other factors, and zeroing in specifically on stress (and anxiety), trying to assess their independent contributions to the risk of developing cardiac arrest.”
The take-home message for clinicians and patients “is that negative psychological stress factors, such as stress and anxiety, are not only detrimental to one’s psychological health but likely increase one’s risk for adverse cardiac events, such as cardiac arrest,” he stated.
No specific funding for the study was disclosed. Mr. Eroglu has disclosed no relevant financial relationships. The other authors’ disclosures are listed in the original article. Dr. Levine reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM BMJ OPEN HEART
States move to curb insurers’ prior authorization requirements as federal reforms lag
Amid growing criticism of health insurers’ onerous prior authorization practices, lawmakers in 30 states have introduced bills this year that aim to rein in insurer gatekeeping and improve patient care.
“This is something that goes on in every doctor’s office every day; the frustrations, the delays, and the use of office staff time are just unbelievable,” said Steven Orland, MD, a board-certified urologist and president of the Medical Society of New Jersey.
The bills, which cover private health plans and insurers that states regulate, may provide some relief for physicians as federal efforts to streamline prior authorization for some Medicare patients have lagged.
Last year, Congress failed to pass the Improving Seniors’ Timely Access to Care Act of 2021, despite 326 co-sponsors. The bill would have compelled insurers covering Medicare Advantage enrollees to speed up prior authorizations, make the process more transparent, and remove obstacles such as requiring fax machine submissions.
Last month, however, the Centers for Medicare & Medicaid Services issued a final rule that will improve some aspects of prior authorizations in Medicare Advantage insurance plans and ensure that enrollees have the same access to necessary care as traditional Medicare enrollees.
The insurance industry has long defended prior authorization requirements and opposed legislation that would limit them.
America’s Health Insurance Plans (AHIP) and the Blue Cross Blue Shield Association said in a 2019 letter to a congressional committee when the federal legislation was first introduced, “Prior authorizations enforce best practices and guidelines for care management and help physicians identify and avoid care techniques that would harm patient outcomes, such as designating prescriptions that could feed into an opioid addiction.” AHIP didn’t respond to repeated requests for comment.
But some major insurers now appear willing to compromise and voluntarily reduce the volume of prior authorizations they require. Days before the federal final rule was released, three major insurers – United HealthCare, Cigna, and Aetna CVS Health – announced they plan to drop some prior authorization requirements and automate processes.
United HealthCare said it will eliminate almost 20% of its prior authorizations for some nonurgent surgeries and procedures starting this summer. It also will create a national Gold Card program in 2024 for physicians who meet its eligibility requirements, which would eliminate prior authorization requirements for most procedures. Both initiatives will apply to commercial, Medicare Advantage, and Medicaid businesses, said the insurer in a statement.
However, United HealthCare also announced that in June it will start requiring prior authorization for diagnostic (not screening) gastrointestinal endoscopies for its nearly 27 million privately insured patients, citing data it says shows potentially harmful overuse of scopes. Physician groups have publicly criticized the move, saying it could delay lifesaving treatment, and have asked the insurer to reconsider.
Cigna and Aetna also have moved to pare back prior authorization processes. Scott Josephs, national medical officer for Cigna, told Healthcare Dive that Cigna has removed prior authorization reviews from nearly 500 services since 2020.
An Aetna spokesperson told Healthcare Dive that the CVS-owned payer has implemented a gold card program and rolled back prior authorization requirements on cataract surgeries, video EEGs, and home infusion for some drugs, according to Healthcare Dive.
Cigna has faced increased scrutiny from some state regulators since a ProPublica/The Capitol Forum article revealed in March that its doctors were denying claims without opening patients’ files, contrary to what insurance laws and regulations require in many states.
Over a period of 2 months last year, Cigna doctors denied over 300,000 requests for payments using this method, spending an average of 1.2 seconds on each case, the investigation found. In a written response, Cigna said the reporting by ProPublica and The Capitol Forum was “biased and incomplete.”
States aim to reduce prior authorization volume
The American Medical Association said it has been tracking nearly 90 prior authorization reform bills in 30 states. More than a dozen bills are still being considered in this legislative session, including in Arkansas, California, New Jersey, North Carolina, Maryland, and Washington, D.C.
“The groundswell of activity in the states reflects how big a problem this is,” said an AMA legislative expert. “The issue used to be ‘how can we automate and streamline processes’; now the issue is focused on reducing the volume of prior authorizations and the harm that can cause patients.”
The state bills use different strategies to reduce excessive prior authorization requirements. Maryland’s proposed bill, for example, would require just one prior authorization to stay on a prescription drug, if the insurer has previously approved the drug and the patient continues to successfully be treated by the drug.
Washington, D.C. and New Jersey have introduced comprehensive reform bills that include a “grace period” of 60 days, to ensure continuity of care when a patient switches health plans. They also would eliminate repeat authorizations for chronic and long-term conditions, set explicit timelines for insurers to respond to prior authorization requests and appeals, and require that practicing physicians review denials that are appealed.
Many state bills also would require insurers to be more transparent by posting information on their websites about which services and drugs require prior authorization and what their approval rates are for them, said AMA’s legislative expert.
“There’s a black hole of information that insurers have access to. We would really like to know how many prior authorization requests are denied, the time it takes to deny them, and the reasons for denial,” said Josh Bengal, JD, the director of government relations for the Medical Society of New Jersey.
The legislation in New Jersey and other states faces stiff opposition from the insurance lobby, especially state associations of health plans affiliated with AHIP. The California Association of Health Plans, for example, opposes a “gold card” bill (SB 598), introduced in February, that would allow a select group of high-performing doctors to skip prior authorizations for 1 year.
The CAHP states, “Californians deserve safe, high quality, high-value health care. Yet SB 598 will derail the progress we have made in our health care system by lowering the value and safety that Californians should expect from their health care providers,” according to a fact sheet.
The fact-sheet defines “low-value care” as medical services for which there is little to no benefit and poses potential physical or financial harm to patients, such as unnecessary CT scans or MRIs for uncomplicated conditions.
California is one of about a dozen states that have introduced gold card legislation this year. If enacted, they would join five states with gold card laws: West Virginia, Texas, Vermont, Michigan, and Louisiana.
How do gold cards work?
Physicians who achieve a high approval rate of prior authorizations from insurers for 1 year are eligible to be exempted from obtaining prior authorizations the following year.
The approval rate is at least 90% for a certain number of eligible health services, but the number of prior authorizations required to qualify can range from 5 to 30, depending on the state law.
Gold card legislation typically also gives the treating physician the right to have an appeal of a prior authorization denial by a physician peer of the same or similar specialty.
California’s bill would also apply to all covered health services, which is broader than what United HealthCare has proposed for its gold card exemption. The bill would also require a plan or insurer to annually monitor rates of prior authorization approval, modification, appeal, and denial, and to discontinue services, items, and supplies that are approved 95% of the time.
“These are important reforms that will help ensure that patients can receive the care they need, when they need it,” said CMA president Donaldo Hernandez, MD.
However, it’s not clear how many physicians will meet “gold card” status based on Texas’ recent experience with its own “gold card” law.
The Texas Department of Insurance estimated that only 3.3% of licensed physicians in the state have met “gold card” status since the bill became law in 2021, said Zeke Silva, MD, an interventional radiologist who serves on the Council of Legislation for the Texas Medical Association.
He noted that the legislation has had a limited effect for several reasons. Commercial health plans only make up only about 20% of all health plans in Texas. Also, the final regulations didn’t go into effect until last May and physicians are evaluated by health plans for “gold card” status every 6 months, said Dr. Silva.
In addition, physicians must have at least five prior authorizations approved for the same health service, which the law left up to the health plans to define, said Dr. Silva.
Now, the Texas Medical Association is lobbying for legislative improvements. “We want to reduce the number of eligible services that health plans require for prior authorizations and have more oversight of prior authorization denials by the Texas Department of Insurance and the Texas Medical Board,” said Dr. Silva.
He’s optimistic that if the bill becomes law, the number of physicians eligible for gold cards may increase.
Meanwhile, the AMA’s legislative expert, who declined to be identified because of organization policy, acknowledged the possibility that some prior authorization bills will die in state legislatures this year.
“We remain hopeful, but it’s an uphill battle. The state medical associations face a lot of opposition from health plans who don’t want to see these reforms become law.”
A version of this article originally appeared on Medscape.com.
Amid growing criticism of health insurers’ onerous prior authorization practices, lawmakers in 30 states have introduced bills this year that aim to rein in insurer gatekeeping and improve patient care.
“This is something that goes on in every doctor’s office every day; the frustrations, the delays, and the use of office staff time are just unbelievable,” said Steven Orland, MD, a board-certified urologist and president of the Medical Society of New Jersey.
The bills, which cover private health plans and insurers that states regulate, may provide some relief for physicians as federal efforts to streamline prior authorization for some Medicare patients have lagged.
Last year, Congress failed to pass the Improving Seniors’ Timely Access to Care Act of 2021, despite 326 co-sponsors. The bill would have compelled insurers covering Medicare Advantage enrollees to speed up prior authorizations, make the process more transparent, and remove obstacles such as requiring fax machine submissions.
Last month, however, the Centers for Medicare & Medicaid Services issued a final rule that will improve some aspects of prior authorizations in Medicare Advantage insurance plans and ensure that enrollees have the same access to necessary care as traditional Medicare enrollees.
The insurance industry has long defended prior authorization requirements and opposed legislation that would limit them.
America’s Health Insurance Plans (AHIP) and the Blue Cross Blue Shield Association said in a 2019 letter to a congressional committee when the federal legislation was first introduced, “Prior authorizations enforce best practices and guidelines for care management and help physicians identify and avoid care techniques that would harm patient outcomes, such as designating prescriptions that could feed into an opioid addiction.” AHIP didn’t respond to repeated requests for comment.
But some major insurers now appear willing to compromise and voluntarily reduce the volume of prior authorizations they require. Days before the federal final rule was released, three major insurers – United HealthCare, Cigna, and Aetna CVS Health – announced they plan to drop some prior authorization requirements and automate processes.
United HealthCare said it will eliminate almost 20% of its prior authorizations for some nonurgent surgeries and procedures starting this summer. It also will create a national Gold Card program in 2024 for physicians who meet its eligibility requirements, which would eliminate prior authorization requirements for most procedures. Both initiatives will apply to commercial, Medicare Advantage, and Medicaid businesses, said the insurer in a statement.
However, United HealthCare also announced that in June it will start requiring prior authorization for diagnostic (not screening) gastrointestinal endoscopies for its nearly 27 million privately insured patients, citing data it says shows potentially harmful overuse of scopes. Physician groups have publicly criticized the move, saying it could delay lifesaving treatment, and have asked the insurer to reconsider.
Cigna and Aetna also have moved to pare back prior authorization processes. Scott Josephs, national medical officer for Cigna, told Healthcare Dive that Cigna has removed prior authorization reviews from nearly 500 services since 2020.
An Aetna spokesperson told Healthcare Dive that the CVS-owned payer has implemented a gold card program and rolled back prior authorization requirements on cataract surgeries, video EEGs, and home infusion for some drugs, according to Healthcare Dive.
Cigna has faced increased scrutiny from some state regulators since a ProPublica/The Capitol Forum article revealed in March that its doctors were denying claims without opening patients’ files, contrary to what insurance laws and regulations require in many states.
Over a period of 2 months last year, Cigna doctors denied over 300,000 requests for payments using this method, spending an average of 1.2 seconds on each case, the investigation found. In a written response, Cigna said the reporting by ProPublica and The Capitol Forum was “biased and incomplete.”
States aim to reduce prior authorization volume
The American Medical Association said it has been tracking nearly 90 prior authorization reform bills in 30 states. More than a dozen bills are still being considered in this legislative session, including in Arkansas, California, New Jersey, North Carolina, Maryland, and Washington, D.C.
“The groundswell of activity in the states reflects how big a problem this is,” said an AMA legislative expert. “The issue used to be ‘how can we automate and streamline processes’; now the issue is focused on reducing the volume of prior authorizations and the harm that can cause patients.”
The state bills use different strategies to reduce excessive prior authorization requirements. Maryland’s proposed bill, for example, would require just one prior authorization to stay on a prescription drug, if the insurer has previously approved the drug and the patient continues to successfully be treated by the drug.
Washington, D.C. and New Jersey have introduced comprehensive reform bills that include a “grace period” of 60 days, to ensure continuity of care when a patient switches health plans. They also would eliminate repeat authorizations for chronic and long-term conditions, set explicit timelines for insurers to respond to prior authorization requests and appeals, and require that practicing physicians review denials that are appealed.
Many state bills also would require insurers to be more transparent by posting information on their websites about which services and drugs require prior authorization and what their approval rates are for them, said AMA’s legislative expert.
“There’s a black hole of information that insurers have access to. We would really like to know how many prior authorization requests are denied, the time it takes to deny them, and the reasons for denial,” said Josh Bengal, JD, the director of government relations for the Medical Society of New Jersey.
The legislation in New Jersey and other states faces stiff opposition from the insurance lobby, especially state associations of health plans affiliated with AHIP. The California Association of Health Plans, for example, opposes a “gold card” bill (SB 598), introduced in February, that would allow a select group of high-performing doctors to skip prior authorizations for 1 year.
The CAHP states, “Californians deserve safe, high quality, high-value health care. Yet SB 598 will derail the progress we have made in our health care system by lowering the value and safety that Californians should expect from their health care providers,” according to a fact sheet.
The fact-sheet defines “low-value care” as medical services for which there is little to no benefit and poses potential physical or financial harm to patients, such as unnecessary CT scans or MRIs for uncomplicated conditions.
California is one of about a dozen states that have introduced gold card legislation this year. If enacted, they would join five states with gold card laws: West Virginia, Texas, Vermont, Michigan, and Louisiana.
How do gold cards work?
Physicians who achieve a high approval rate of prior authorizations from insurers for 1 year are eligible to be exempted from obtaining prior authorizations the following year.
The approval rate is at least 90% for a certain number of eligible health services, but the number of prior authorizations required to qualify can range from 5 to 30, depending on the state law.
Gold card legislation typically also gives the treating physician the right to have an appeal of a prior authorization denial by a physician peer of the same or similar specialty.
California’s bill would also apply to all covered health services, which is broader than what United HealthCare has proposed for its gold card exemption. The bill would also require a plan or insurer to annually monitor rates of prior authorization approval, modification, appeal, and denial, and to discontinue services, items, and supplies that are approved 95% of the time.
“These are important reforms that will help ensure that patients can receive the care they need, when they need it,” said CMA president Donaldo Hernandez, MD.
However, it’s not clear how many physicians will meet “gold card” status based on Texas’ recent experience with its own “gold card” law.
The Texas Department of Insurance estimated that only 3.3% of licensed physicians in the state have met “gold card” status since the bill became law in 2021, said Zeke Silva, MD, an interventional radiologist who serves on the Council of Legislation for the Texas Medical Association.
He noted that the legislation has had a limited effect for several reasons. Commercial health plans only make up only about 20% of all health plans in Texas. Also, the final regulations didn’t go into effect until last May and physicians are evaluated by health plans for “gold card” status every 6 months, said Dr. Silva.
In addition, physicians must have at least five prior authorizations approved for the same health service, which the law left up to the health plans to define, said Dr. Silva.
Now, the Texas Medical Association is lobbying for legislative improvements. “We want to reduce the number of eligible services that health plans require for prior authorizations and have more oversight of prior authorization denials by the Texas Department of Insurance and the Texas Medical Board,” said Dr. Silva.
He’s optimistic that if the bill becomes law, the number of physicians eligible for gold cards may increase.
Meanwhile, the AMA’s legislative expert, who declined to be identified because of organization policy, acknowledged the possibility that some prior authorization bills will die in state legislatures this year.
“We remain hopeful, but it’s an uphill battle. The state medical associations face a lot of opposition from health plans who don’t want to see these reforms become law.”
A version of this article originally appeared on Medscape.com.
Amid growing criticism of health insurers’ onerous prior authorization practices, lawmakers in 30 states have introduced bills this year that aim to rein in insurer gatekeeping and improve patient care.
“This is something that goes on in every doctor’s office every day; the frustrations, the delays, and the use of office staff time are just unbelievable,” said Steven Orland, MD, a board-certified urologist and president of the Medical Society of New Jersey.
The bills, which cover private health plans and insurers that states regulate, may provide some relief for physicians as federal efforts to streamline prior authorization for some Medicare patients have lagged.
Last year, Congress failed to pass the Improving Seniors’ Timely Access to Care Act of 2021, despite 326 co-sponsors. The bill would have compelled insurers covering Medicare Advantage enrollees to speed up prior authorizations, make the process more transparent, and remove obstacles such as requiring fax machine submissions.
Last month, however, the Centers for Medicare & Medicaid Services issued a final rule that will improve some aspects of prior authorizations in Medicare Advantage insurance plans and ensure that enrollees have the same access to necessary care as traditional Medicare enrollees.
The insurance industry has long defended prior authorization requirements and opposed legislation that would limit them.
America’s Health Insurance Plans (AHIP) and the Blue Cross Blue Shield Association said in a 2019 letter to a congressional committee when the federal legislation was first introduced, “Prior authorizations enforce best practices and guidelines for care management and help physicians identify and avoid care techniques that would harm patient outcomes, such as designating prescriptions that could feed into an opioid addiction.” AHIP didn’t respond to repeated requests for comment.
But some major insurers now appear willing to compromise and voluntarily reduce the volume of prior authorizations they require. Days before the federal final rule was released, three major insurers – United HealthCare, Cigna, and Aetna CVS Health – announced they plan to drop some prior authorization requirements and automate processes.
United HealthCare said it will eliminate almost 20% of its prior authorizations for some nonurgent surgeries and procedures starting this summer. It also will create a national Gold Card program in 2024 for physicians who meet its eligibility requirements, which would eliminate prior authorization requirements for most procedures. Both initiatives will apply to commercial, Medicare Advantage, and Medicaid businesses, said the insurer in a statement.
However, United HealthCare also announced that in June it will start requiring prior authorization for diagnostic (not screening) gastrointestinal endoscopies for its nearly 27 million privately insured patients, citing data it says shows potentially harmful overuse of scopes. Physician groups have publicly criticized the move, saying it could delay lifesaving treatment, and have asked the insurer to reconsider.
Cigna and Aetna also have moved to pare back prior authorization processes. Scott Josephs, national medical officer for Cigna, told Healthcare Dive that Cigna has removed prior authorization reviews from nearly 500 services since 2020.
An Aetna spokesperson told Healthcare Dive that the CVS-owned payer has implemented a gold card program and rolled back prior authorization requirements on cataract surgeries, video EEGs, and home infusion for some drugs, according to Healthcare Dive.
Cigna has faced increased scrutiny from some state regulators since a ProPublica/The Capitol Forum article revealed in March that its doctors were denying claims without opening patients’ files, contrary to what insurance laws and regulations require in many states.
Over a period of 2 months last year, Cigna doctors denied over 300,000 requests for payments using this method, spending an average of 1.2 seconds on each case, the investigation found. In a written response, Cigna said the reporting by ProPublica and The Capitol Forum was “biased and incomplete.”
States aim to reduce prior authorization volume
The American Medical Association said it has been tracking nearly 90 prior authorization reform bills in 30 states. More than a dozen bills are still being considered in this legislative session, including in Arkansas, California, New Jersey, North Carolina, Maryland, and Washington, D.C.
“The groundswell of activity in the states reflects how big a problem this is,” said an AMA legislative expert. “The issue used to be ‘how can we automate and streamline processes’; now the issue is focused on reducing the volume of prior authorizations and the harm that can cause patients.”
The state bills use different strategies to reduce excessive prior authorization requirements. Maryland’s proposed bill, for example, would require just one prior authorization to stay on a prescription drug, if the insurer has previously approved the drug and the patient continues to successfully be treated by the drug.
Washington, D.C. and New Jersey have introduced comprehensive reform bills that include a “grace period” of 60 days, to ensure continuity of care when a patient switches health plans. They also would eliminate repeat authorizations for chronic and long-term conditions, set explicit timelines for insurers to respond to prior authorization requests and appeals, and require that practicing physicians review denials that are appealed.
Many state bills also would require insurers to be more transparent by posting information on their websites about which services and drugs require prior authorization and what their approval rates are for them, said AMA’s legislative expert.
“There’s a black hole of information that insurers have access to. We would really like to know how many prior authorization requests are denied, the time it takes to deny them, and the reasons for denial,” said Josh Bengal, JD, the director of government relations for the Medical Society of New Jersey.
The legislation in New Jersey and other states faces stiff opposition from the insurance lobby, especially state associations of health plans affiliated with AHIP. The California Association of Health Plans, for example, opposes a “gold card” bill (SB 598), introduced in February, that would allow a select group of high-performing doctors to skip prior authorizations for 1 year.
The CAHP states, “Californians deserve safe, high quality, high-value health care. Yet SB 598 will derail the progress we have made in our health care system by lowering the value and safety that Californians should expect from their health care providers,” according to a fact sheet.
The fact-sheet defines “low-value care” as medical services for which there is little to no benefit and poses potential physical or financial harm to patients, such as unnecessary CT scans or MRIs for uncomplicated conditions.
California is one of about a dozen states that have introduced gold card legislation this year. If enacted, they would join five states with gold card laws: West Virginia, Texas, Vermont, Michigan, and Louisiana.
How do gold cards work?
Physicians who achieve a high approval rate of prior authorizations from insurers for 1 year are eligible to be exempted from obtaining prior authorizations the following year.
The approval rate is at least 90% for a certain number of eligible health services, but the number of prior authorizations required to qualify can range from 5 to 30, depending on the state law.
Gold card legislation typically also gives the treating physician the right to have an appeal of a prior authorization denial by a physician peer of the same or similar specialty.
California’s bill would also apply to all covered health services, which is broader than what United HealthCare has proposed for its gold card exemption. The bill would also require a plan or insurer to annually monitor rates of prior authorization approval, modification, appeal, and denial, and to discontinue services, items, and supplies that are approved 95% of the time.
“These are important reforms that will help ensure that patients can receive the care they need, when they need it,” said CMA president Donaldo Hernandez, MD.
However, it’s not clear how many physicians will meet “gold card” status based on Texas’ recent experience with its own “gold card” law.
The Texas Department of Insurance estimated that only 3.3% of licensed physicians in the state have met “gold card” status since the bill became law in 2021, said Zeke Silva, MD, an interventional radiologist who serves on the Council of Legislation for the Texas Medical Association.
He noted that the legislation has had a limited effect for several reasons. Commercial health plans only make up only about 20% of all health plans in Texas. Also, the final regulations didn’t go into effect until last May and physicians are evaluated by health plans for “gold card” status every 6 months, said Dr. Silva.
In addition, physicians must have at least five prior authorizations approved for the same health service, which the law left up to the health plans to define, said Dr. Silva.
Now, the Texas Medical Association is lobbying for legislative improvements. “We want to reduce the number of eligible services that health plans require for prior authorizations and have more oversight of prior authorization denials by the Texas Department of Insurance and the Texas Medical Board,” said Dr. Silva.
He’s optimistic that if the bill becomes law, the number of physicians eligible for gold cards may increase.
Meanwhile, the AMA’s legislative expert, who declined to be identified because of organization policy, acknowledged the possibility that some prior authorization bills will die in state legislatures this year.
“We remain hopeful, but it’s an uphill battle. The state medical associations face a lot of opposition from health plans who don’t want to see these reforms become law.”
A version of this article originally appeared on Medscape.com.
Researchers locate signals in brain related to chronic pain
a new study in Nature Neuroscience concluded.
The researchers used the devices on four patients who had felt endless nerve pain for more than a year. The devices recorded several times a day, which could pave “the way for implanted devices to one day predict pain signals or even short-circuit them,” The New York Times reported.
The study says the pain “was associated with electrical fluctuations in the orbitofrontal cortex, an area involved in emotion regulation, self-evaluation, and decision-making,” The Times reported. “The research suggests that such patterns of brain activity could serve as biomarkers to guide diagnosis and treatment for millions of people with shooting or burning chronic pain linked to a damaged nervous system.”
Ajay Wasan, MD, and a pain specialist at the University of Pittsburgh who was not involved in the study praised it to the Times.
“The study really advances a whole generation of research that has shown that the functioning of the brain is really important to processing and perceiving pain,” he said.
Chronic pain is defined as persistent or recurring and lasting more than three months. The Centers for Disease Control and Prevention says about 20% of Americans experience it. It has been linked with depression, Alzheimer’s disease and other dementias, suicide, and substance use.
Yet, the study’s authors noted, “pain severity is often measured through subjective report, while objective biomarkers that may guide diagnosis and treatment are lacking.”
Medtronic provided devices for the study. The study authors reported no conflicts of interest.
A version of this article first appeared on WebMD.com.
a new study in Nature Neuroscience concluded.
The researchers used the devices on four patients who had felt endless nerve pain for more than a year. The devices recorded several times a day, which could pave “the way for implanted devices to one day predict pain signals or even short-circuit them,” The New York Times reported.
The study says the pain “was associated with electrical fluctuations in the orbitofrontal cortex, an area involved in emotion regulation, self-evaluation, and decision-making,” The Times reported. “The research suggests that such patterns of brain activity could serve as biomarkers to guide diagnosis and treatment for millions of people with shooting or burning chronic pain linked to a damaged nervous system.”
Ajay Wasan, MD, and a pain specialist at the University of Pittsburgh who was not involved in the study praised it to the Times.
“The study really advances a whole generation of research that has shown that the functioning of the brain is really important to processing and perceiving pain,” he said.
Chronic pain is defined as persistent or recurring and lasting more than three months. The Centers for Disease Control and Prevention says about 20% of Americans experience it. It has been linked with depression, Alzheimer’s disease and other dementias, suicide, and substance use.
Yet, the study’s authors noted, “pain severity is often measured through subjective report, while objective biomarkers that may guide diagnosis and treatment are lacking.”
Medtronic provided devices for the study. The study authors reported no conflicts of interest.
A version of this article first appeared on WebMD.com.
a new study in Nature Neuroscience concluded.
The researchers used the devices on four patients who had felt endless nerve pain for more than a year. The devices recorded several times a day, which could pave “the way for implanted devices to one day predict pain signals or even short-circuit them,” The New York Times reported.
The study says the pain “was associated with electrical fluctuations in the orbitofrontal cortex, an area involved in emotion regulation, self-evaluation, and decision-making,” The Times reported. “The research suggests that such patterns of brain activity could serve as biomarkers to guide diagnosis and treatment for millions of people with shooting or burning chronic pain linked to a damaged nervous system.”
Ajay Wasan, MD, and a pain specialist at the University of Pittsburgh who was not involved in the study praised it to the Times.
“The study really advances a whole generation of research that has shown that the functioning of the brain is really important to processing and perceiving pain,” he said.
Chronic pain is defined as persistent or recurring and lasting more than three months. The Centers for Disease Control and Prevention says about 20% of Americans experience it. It has been linked with depression, Alzheimer’s disease and other dementias, suicide, and substance use.
Yet, the study’s authors noted, “pain severity is often measured through subjective report, while objective biomarkers that may guide diagnosis and treatment are lacking.”
Medtronic provided devices for the study. The study authors reported no conflicts of interest.
A version of this article first appeared on WebMD.com.
FROM NATURE NEUROSCIENCE
Serious mental illness not a factor in most mass school shootings
Mass shootings, often on school campuses, have become a regular and sad reality in the United States.
The statistics are grim. Every day 12 children die from gun violence in America and another 32 are shot and injured. Since the Columbine High School shooting in 1999, more than 338,000 students in the United States have experienced school gun violence, according to the nonprofit organization Sandy Hook Promise.
A new analysis from the Columbia Mass Murder Database (CMMD) sheds fresh light on the debate over whether mental illness or easy access to guns is the key driver of mass shootings.
The findings, which are published in the Journal of Forensic Sciences, show that most perpetrators of mass school shootings are young, White men without serious mental illness.
A ‘straw man’
Mental health is often used as a “straw man” in debates about mass shootings, lead investigator Ragy Girgis, MD, told this news organization.
“There are many factors that contribute to the mass shooting epidemic, including gun access, criminality, substance use and misuse, and many others. Mental illness is incidental in the vast majority of cases,” said Dr. Girgis, with Columbia University Irving Medical Center, New York, and the New York State Psychiatric Institute.
“People with serious mental illness constitute only a small portion of the perpetrators of gun violence in this country,” coinvestigator Paul Appelbaum, MD, professor of psychiatry, medicine, and law at Columbia University, New York, told this news organization.
Using the CMMD, the researchers examined 82 incidents of mass murder perpetrated in academic settings including schools, colleges, and universities. The average number of victims of these incidents was eight. More than half (60%) of mass school shootings involved at least one semi- or fully automatic firearm.
All 82 incidents were initiated by men (mean age, 28), and 67% were White. About two-thirds (63%) involved guns.
More than three-quarters (77%) of all perpetrators of mass murders in academic settings had no recorded history of psychotic symptoms.
Despite the absence of serious mental illness, almost half (46%) of the mass school shooters took their own lives at the scene, suggesting that they viewed themselves as engaging in some form of “final act,” the researchers note.
“The major difference between mass shooters in school settings and elsewhere is the higher rate of suicide by the perpetrators in school settings. That suggests that the shootings are often part of a preexisting intent to die on the part of the shooter,” said Dr. Appelbaum.
Epidemic of emptiness
He noted that the typical profile of a mass school shooter is that of “a young male with anger problems, often as a result of bullying or abuse, frequently described as a loner, who has signaled a desire to kill other people.”
“If we only focus on mental illness, we will miss the warning signs in the majority of cases associated with victimization (such as bullying) and consequent anger,” Dr. Appelbaum said.
Dr. Girgis said there is a need to deal with the “epidemic of emptiness, narcissism, anger, and societal rejection felt by many young men/boys who, when combined with a desire to take their own lives and a great need for notoriety, feel that perpetrating a mass school shooting is their only option.”
“We also need to understand why it is so easy for so many mass school shooters to obtain firearms that are not theirs – either illegally or from someone else who themselves may have obtained the firearm legally,” Dr. Girgis said.
“All countries have people with mental illness,” Dr. Appelbaum said, “but among developed countries the U.S. is unique in the easy availability of weapons and in our disproportionate rate of murders.”
He also noted that school shootings are not a problem that clinicians are going to solve.
“Although they can be alert to signals from their patients of an intent to harm people in a school (or other) setting, the vast majority of shooters are not receiving treatment for a mental disorder,” Dr. Appelbaum said.
“This is a problem that can only be substantially diminished by reducing access to firearms, which includes requirements for safe storage, universal background checks, waiting periods to purchase firearms, and similar means-oriented interventions,” he added.
Need for regular mental health checks
Thea Gallagher, PsyD, who was not involved in the study, noted that mass school shooters may not have a psychotic illness, but with mental health there is a “spectrum, and obviously, that individual is struggling to some extent, most likely, mentally, if they are at a place where they are willing to take the lives of others and themselves.”
“We need to understand more about how people get to this place and the issues people are struggling with. We need to push for yearly mental health checks just like the yearly physical,” Dr. Gallagher, with the department of psychiatry at NYU Langone Health, New York, told this news organization.
“The more that we create conversation and moments to talk about how people are feeling internally, the better chance we have to give people who are struggling healthy coping strategies and the opportunity to process their emotions and not bury them,” Dr. Gallagher said.
Support for the study was provided in part by the New York State Office of Mental Hygiene, and the Elizabeth K. Dollard Charitable Trust. Dr. Girgis has received royalties and/or advances from books on mental health published by Wipf and Stock, and Routledge/Taylor and Francis. He has consulted for Noble Insights, IMS Expert Services, and Fowler White Burnett. Dr. Appelbaum and Dr. Gallagher report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Mass shootings, often on school campuses, have become a regular and sad reality in the United States.
The statistics are grim. Every day 12 children die from gun violence in America and another 32 are shot and injured. Since the Columbine High School shooting in 1999, more than 338,000 students in the United States have experienced school gun violence, according to the nonprofit organization Sandy Hook Promise.
A new analysis from the Columbia Mass Murder Database (CMMD) sheds fresh light on the debate over whether mental illness or easy access to guns is the key driver of mass shootings.
The findings, which are published in the Journal of Forensic Sciences, show that most perpetrators of mass school shootings are young, White men without serious mental illness.
A ‘straw man’
Mental health is often used as a “straw man” in debates about mass shootings, lead investigator Ragy Girgis, MD, told this news organization.
“There are many factors that contribute to the mass shooting epidemic, including gun access, criminality, substance use and misuse, and many others. Mental illness is incidental in the vast majority of cases,” said Dr. Girgis, with Columbia University Irving Medical Center, New York, and the New York State Psychiatric Institute.
“People with serious mental illness constitute only a small portion of the perpetrators of gun violence in this country,” coinvestigator Paul Appelbaum, MD, professor of psychiatry, medicine, and law at Columbia University, New York, told this news organization.
Using the CMMD, the researchers examined 82 incidents of mass murder perpetrated in academic settings including schools, colleges, and universities. The average number of victims of these incidents was eight. More than half (60%) of mass school shootings involved at least one semi- or fully automatic firearm.
All 82 incidents were initiated by men (mean age, 28), and 67% were White. About two-thirds (63%) involved guns.
More than three-quarters (77%) of all perpetrators of mass murders in academic settings had no recorded history of psychotic symptoms.
Despite the absence of serious mental illness, almost half (46%) of the mass school shooters took their own lives at the scene, suggesting that they viewed themselves as engaging in some form of “final act,” the researchers note.
“The major difference between mass shooters in school settings and elsewhere is the higher rate of suicide by the perpetrators in school settings. That suggests that the shootings are often part of a preexisting intent to die on the part of the shooter,” said Dr. Appelbaum.
Epidemic of emptiness
He noted that the typical profile of a mass school shooter is that of “a young male with anger problems, often as a result of bullying or abuse, frequently described as a loner, who has signaled a desire to kill other people.”
“If we only focus on mental illness, we will miss the warning signs in the majority of cases associated with victimization (such as bullying) and consequent anger,” Dr. Appelbaum said.
Dr. Girgis said there is a need to deal with the “epidemic of emptiness, narcissism, anger, and societal rejection felt by many young men/boys who, when combined with a desire to take their own lives and a great need for notoriety, feel that perpetrating a mass school shooting is their only option.”
“We also need to understand why it is so easy for so many mass school shooters to obtain firearms that are not theirs – either illegally or from someone else who themselves may have obtained the firearm legally,” Dr. Girgis said.
“All countries have people with mental illness,” Dr. Appelbaum said, “but among developed countries the U.S. is unique in the easy availability of weapons and in our disproportionate rate of murders.”
He also noted that school shootings are not a problem that clinicians are going to solve.
“Although they can be alert to signals from their patients of an intent to harm people in a school (or other) setting, the vast majority of shooters are not receiving treatment for a mental disorder,” Dr. Appelbaum said.
“This is a problem that can only be substantially diminished by reducing access to firearms, which includes requirements for safe storage, universal background checks, waiting periods to purchase firearms, and similar means-oriented interventions,” he added.
Need for regular mental health checks
Thea Gallagher, PsyD, who was not involved in the study, noted that mass school shooters may not have a psychotic illness, but with mental health there is a “spectrum, and obviously, that individual is struggling to some extent, most likely, mentally, if they are at a place where they are willing to take the lives of others and themselves.”
“We need to understand more about how people get to this place and the issues people are struggling with. We need to push for yearly mental health checks just like the yearly physical,” Dr. Gallagher, with the department of psychiatry at NYU Langone Health, New York, told this news organization.
“The more that we create conversation and moments to talk about how people are feeling internally, the better chance we have to give people who are struggling healthy coping strategies and the opportunity to process their emotions and not bury them,” Dr. Gallagher said.
Support for the study was provided in part by the New York State Office of Mental Hygiene, and the Elizabeth K. Dollard Charitable Trust. Dr. Girgis has received royalties and/or advances from books on mental health published by Wipf and Stock, and Routledge/Taylor and Francis. He has consulted for Noble Insights, IMS Expert Services, and Fowler White Burnett. Dr. Appelbaum and Dr. Gallagher report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Mass shootings, often on school campuses, have become a regular and sad reality in the United States.
The statistics are grim. Every day 12 children die from gun violence in America and another 32 are shot and injured. Since the Columbine High School shooting in 1999, more than 338,000 students in the United States have experienced school gun violence, according to the nonprofit organization Sandy Hook Promise.
A new analysis from the Columbia Mass Murder Database (CMMD) sheds fresh light on the debate over whether mental illness or easy access to guns is the key driver of mass shootings.
The findings, which are published in the Journal of Forensic Sciences, show that most perpetrators of mass school shootings are young, White men without serious mental illness.
A ‘straw man’
Mental health is often used as a “straw man” in debates about mass shootings, lead investigator Ragy Girgis, MD, told this news organization.
“There are many factors that contribute to the mass shooting epidemic, including gun access, criminality, substance use and misuse, and many others. Mental illness is incidental in the vast majority of cases,” said Dr. Girgis, with Columbia University Irving Medical Center, New York, and the New York State Psychiatric Institute.
“People with serious mental illness constitute only a small portion of the perpetrators of gun violence in this country,” coinvestigator Paul Appelbaum, MD, professor of psychiatry, medicine, and law at Columbia University, New York, told this news organization.
Using the CMMD, the researchers examined 82 incidents of mass murder perpetrated in academic settings including schools, colleges, and universities. The average number of victims of these incidents was eight. More than half (60%) of mass school shootings involved at least one semi- or fully automatic firearm.
All 82 incidents were initiated by men (mean age, 28), and 67% were White. About two-thirds (63%) involved guns.
More than three-quarters (77%) of all perpetrators of mass murders in academic settings had no recorded history of psychotic symptoms.
Despite the absence of serious mental illness, almost half (46%) of the mass school shooters took their own lives at the scene, suggesting that they viewed themselves as engaging in some form of “final act,” the researchers note.
“The major difference between mass shooters in school settings and elsewhere is the higher rate of suicide by the perpetrators in school settings. That suggests that the shootings are often part of a preexisting intent to die on the part of the shooter,” said Dr. Appelbaum.
Epidemic of emptiness
He noted that the typical profile of a mass school shooter is that of “a young male with anger problems, often as a result of bullying or abuse, frequently described as a loner, who has signaled a desire to kill other people.”
“If we only focus on mental illness, we will miss the warning signs in the majority of cases associated with victimization (such as bullying) and consequent anger,” Dr. Appelbaum said.
Dr. Girgis said there is a need to deal with the “epidemic of emptiness, narcissism, anger, and societal rejection felt by many young men/boys who, when combined with a desire to take their own lives and a great need for notoriety, feel that perpetrating a mass school shooting is their only option.”
“We also need to understand why it is so easy for so many mass school shooters to obtain firearms that are not theirs – either illegally or from someone else who themselves may have obtained the firearm legally,” Dr. Girgis said.
“All countries have people with mental illness,” Dr. Appelbaum said, “but among developed countries the U.S. is unique in the easy availability of weapons and in our disproportionate rate of murders.”
He also noted that school shootings are not a problem that clinicians are going to solve.
“Although they can be alert to signals from their patients of an intent to harm people in a school (or other) setting, the vast majority of shooters are not receiving treatment for a mental disorder,” Dr. Appelbaum said.
“This is a problem that can only be substantially diminished by reducing access to firearms, which includes requirements for safe storage, universal background checks, waiting periods to purchase firearms, and similar means-oriented interventions,” he added.
Need for regular mental health checks
Thea Gallagher, PsyD, who was not involved in the study, noted that mass school shooters may not have a psychotic illness, but with mental health there is a “spectrum, and obviously, that individual is struggling to some extent, most likely, mentally, if they are at a place where they are willing to take the lives of others and themselves.”
“We need to understand more about how people get to this place and the issues people are struggling with. We need to push for yearly mental health checks just like the yearly physical,” Dr. Gallagher, with the department of psychiatry at NYU Langone Health, New York, told this news organization.
“The more that we create conversation and moments to talk about how people are feeling internally, the better chance we have to give people who are struggling healthy coping strategies and the opportunity to process their emotions and not bury them,” Dr. Gallagher said.
Support for the study was provided in part by the New York State Office of Mental Hygiene, and the Elizabeth K. Dollard Charitable Trust. Dr. Girgis has received royalties and/or advances from books on mental health published by Wipf and Stock, and Routledge/Taylor and Francis. He has consulted for Noble Insights, IMS Expert Services, and Fowler White Burnett. Dr. Appelbaum and Dr. Gallagher report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Younger age of type 2 diabetes onset linked to dementia risk
, new findings suggest.
Moreover, the new data from the prospective Atherosclerosis Risk in Communities (ARIC) cohort also suggest that the previously identified increased risk for dementia among people with prediabetes appears to be entirely explained by the subset who go on to develop type 2 diabetes.
“Our findings suggest that preventing prediabetes progression, especially in younger individuals, may be an important way to reduce the dementia burden,” wrote PhD student Jiaqi Hu of Johns Hopkins University, Baltimore, and colleagues. Their article was published online in Diabetologia.
The result builds on previous findings linking dysglycemia and cognitive decline, the study’s lead author, Elizabeth Selvin, PhD, of the Bloomberg School of Public Health at Johns Hopkins, said in an interview.
“Our prior work in the ARIC study suggests that improving glucose control could help prevent dementia in later life,” she said.
Other studies have also linked higher A1c levels and diabetes in midlife to increased rates of cognitive decline. In addition, Dr. Selvin noted, “There is growing evidence that focusing on vascular health, especially focusing on diabetes and blood pressure, in midlife can stave off dementia in later life.”
This new study is the first to examine the effect of diabetes in the relationship between prediabetes and dementia, as well as the age of diabetes onset on subsequent dementia.
Prediabetes linked to dementia via diabetes development
Of the 11,656 ARIC participants without diabetes at baseline during 1990-1992 (age 46-70 years), 20.0% had prediabetes (defined as A1c 5.7%-6.4% or 39-46 mmol/mol). During a median follow-up of 15.9 years, 3,143 participants developed diabetes. The proportions of patients who developed diabetes were 44.6% among those with prediabetes at baseline versus 22.5% of those without.
Dementia developed in 2,247 participants over a median follow-up of 24.7 years. The cumulative incidence of dementia was 23.9% among those who developed diabetes versus 20.5% among those who did not.
After adjustment for demographics and for the Alzheimer’s disease–linked apolipoprotein E (APOE) gene, prediabetes was significantly associated with incident dementia (hazard ratio [HR], 1.19). However, significance disappeared after adjustment for incident diabetes (HR, 1.09), the researchers reported.
Younger age at diabetes diagnosis raises dementia risk
Age at diabetes diagnosis made a difference in dementia risk. With adjustments for lifestyle, demographic, and clinical factors, those diagnosed with diabetes before age 60 years had a nearly threefold increased risk for dementia compared with those who never developed diabetes (HR, 2.92; P < .001).
The dementia risk was also significantly increased, although to a lesser degree, among those aged 60-69 years at diabetes diagnosis (HR, 1.73; P < .001) and age 70-79 years at diabetes diagnosis (HR, 1.23; P < .001). The relationship was not significant for those aged 80 years and older (HR, 1.13).
“Prevention efforts in people with diabetes diagnosed younger than 65 years should be a high priority,” the authors urged.
Taken together, the data suggest that prolonged exposure to hyperglycemia plays a major role in dementia development.
“Putative mechanisms include acute and chronic hyperglycemia, glucose toxicity, insulin resistance, and microvascular dysfunction of the central nervous system. ... Glucose toxicity and microvascular dysfunction are associated with increased inflammatory and oxidative stress, leading to increased blood–brain permeability,” the researchers wrote.
Dr. Selvin said that her group is pursuing further work in this area using continuous glucose monitoring. “We plan to look at ... how glycemic control and different patterns of glucose in older adults may be linked to cognitive decline and other neurocognitive outcomes.”
The researchers reported no relevant financial relationships. Dr. Selvin has reported being on the advisory board for Diabetologia; she had no role in peer review of the manuscript.
A version of this article first appeared on Medscape.com.
, new findings suggest.
Moreover, the new data from the prospective Atherosclerosis Risk in Communities (ARIC) cohort also suggest that the previously identified increased risk for dementia among people with prediabetes appears to be entirely explained by the subset who go on to develop type 2 diabetes.
“Our findings suggest that preventing prediabetes progression, especially in younger individuals, may be an important way to reduce the dementia burden,” wrote PhD student Jiaqi Hu of Johns Hopkins University, Baltimore, and colleagues. Their article was published online in Diabetologia.
The result builds on previous findings linking dysglycemia and cognitive decline, the study’s lead author, Elizabeth Selvin, PhD, of the Bloomberg School of Public Health at Johns Hopkins, said in an interview.
“Our prior work in the ARIC study suggests that improving glucose control could help prevent dementia in later life,” she said.
Other studies have also linked higher A1c levels and diabetes in midlife to increased rates of cognitive decline. In addition, Dr. Selvin noted, “There is growing evidence that focusing on vascular health, especially focusing on diabetes and blood pressure, in midlife can stave off dementia in later life.”
This new study is the first to examine the effect of diabetes in the relationship between prediabetes and dementia, as well as the age of diabetes onset on subsequent dementia.
Prediabetes linked to dementia via diabetes development
Of the 11,656 ARIC participants without diabetes at baseline during 1990-1992 (age 46-70 years), 20.0% had prediabetes (defined as A1c 5.7%-6.4% or 39-46 mmol/mol). During a median follow-up of 15.9 years, 3,143 participants developed diabetes. The proportions of patients who developed diabetes were 44.6% among those with prediabetes at baseline versus 22.5% of those without.
Dementia developed in 2,247 participants over a median follow-up of 24.7 years. The cumulative incidence of dementia was 23.9% among those who developed diabetes versus 20.5% among those who did not.
After adjustment for demographics and for the Alzheimer’s disease–linked apolipoprotein E (APOE) gene, prediabetes was significantly associated with incident dementia (hazard ratio [HR], 1.19). However, significance disappeared after adjustment for incident diabetes (HR, 1.09), the researchers reported.
Younger age at diabetes diagnosis raises dementia risk
Age at diabetes diagnosis made a difference in dementia risk. With adjustments for lifestyle, demographic, and clinical factors, those diagnosed with diabetes before age 60 years had a nearly threefold increased risk for dementia compared with those who never developed diabetes (HR, 2.92; P < .001).
The dementia risk was also significantly increased, although to a lesser degree, among those aged 60-69 years at diabetes diagnosis (HR, 1.73; P < .001) and age 70-79 years at diabetes diagnosis (HR, 1.23; P < .001). The relationship was not significant for those aged 80 years and older (HR, 1.13).
“Prevention efforts in people with diabetes diagnosed younger than 65 years should be a high priority,” the authors urged.
Taken together, the data suggest that prolonged exposure to hyperglycemia plays a major role in dementia development.
“Putative mechanisms include acute and chronic hyperglycemia, glucose toxicity, insulin resistance, and microvascular dysfunction of the central nervous system. ... Glucose toxicity and microvascular dysfunction are associated with increased inflammatory and oxidative stress, leading to increased blood–brain permeability,” the researchers wrote.
Dr. Selvin said that her group is pursuing further work in this area using continuous glucose monitoring. “We plan to look at ... how glycemic control and different patterns of glucose in older adults may be linked to cognitive decline and other neurocognitive outcomes.”
The researchers reported no relevant financial relationships. Dr. Selvin has reported being on the advisory board for Diabetologia; she had no role in peer review of the manuscript.
A version of this article first appeared on Medscape.com.
, new findings suggest.
Moreover, the new data from the prospective Atherosclerosis Risk in Communities (ARIC) cohort also suggest that the previously identified increased risk for dementia among people with prediabetes appears to be entirely explained by the subset who go on to develop type 2 diabetes.
“Our findings suggest that preventing prediabetes progression, especially in younger individuals, may be an important way to reduce the dementia burden,” wrote PhD student Jiaqi Hu of Johns Hopkins University, Baltimore, and colleagues. Their article was published online in Diabetologia.
The result builds on previous findings linking dysglycemia and cognitive decline, the study’s lead author, Elizabeth Selvin, PhD, of the Bloomberg School of Public Health at Johns Hopkins, said in an interview.
“Our prior work in the ARIC study suggests that improving glucose control could help prevent dementia in later life,” she said.
Other studies have also linked higher A1c levels and diabetes in midlife to increased rates of cognitive decline. In addition, Dr. Selvin noted, “There is growing evidence that focusing on vascular health, especially focusing on diabetes and blood pressure, in midlife can stave off dementia in later life.”
This new study is the first to examine the effect of diabetes in the relationship between prediabetes and dementia, as well as the age of diabetes onset on subsequent dementia.
Prediabetes linked to dementia via diabetes development
Of the 11,656 ARIC participants without diabetes at baseline during 1990-1992 (age 46-70 years), 20.0% had prediabetes (defined as A1c 5.7%-6.4% or 39-46 mmol/mol). During a median follow-up of 15.9 years, 3,143 participants developed diabetes. The proportions of patients who developed diabetes were 44.6% among those with prediabetes at baseline versus 22.5% of those without.
Dementia developed in 2,247 participants over a median follow-up of 24.7 years. The cumulative incidence of dementia was 23.9% among those who developed diabetes versus 20.5% among those who did not.
After adjustment for demographics and for the Alzheimer’s disease–linked apolipoprotein E (APOE) gene, prediabetes was significantly associated with incident dementia (hazard ratio [HR], 1.19). However, significance disappeared after adjustment for incident diabetes (HR, 1.09), the researchers reported.
Younger age at diabetes diagnosis raises dementia risk
Age at diabetes diagnosis made a difference in dementia risk. With adjustments for lifestyle, demographic, and clinical factors, those diagnosed with diabetes before age 60 years had a nearly threefold increased risk for dementia compared with those who never developed diabetes (HR, 2.92; P < .001).
The dementia risk was also significantly increased, although to a lesser degree, among those aged 60-69 years at diabetes diagnosis (HR, 1.73; P < .001) and age 70-79 years at diabetes diagnosis (HR, 1.23; P < .001). The relationship was not significant for those aged 80 years and older (HR, 1.13).
“Prevention efforts in people with diabetes diagnosed younger than 65 years should be a high priority,” the authors urged.
Taken together, the data suggest that prolonged exposure to hyperglycemia plays a major role in dementia development.
“Putative mechanisms include acute and chronic hyperglycemia, glucose toxicity, insulin resistance, and microvascular dysfunction of the central nervous system. ... Glucose toxicity and microvascular dysfunction are associated with increased inflammatory and oxidative stress, leading to increased blood–brain permeability,” the researchers wrote.
Dr. Selvin said that her group is pursuing further work in this area using continuous glucose monitoring. “We plan to look at ... how glycemic control and different patterns of glucose in older adults may be linked to cognitive decline and other neurocognitive outcomes.”
The researchers reported no relevant financial relationships. Dr. Selvin has reported being on the advisory board for Diabetologia; she had no role in peer review of the manuscript.
A version of this article first appeared on Medscape.com.
FROM DIABETOLOGIA
FDA approves buprenorphine injection for opioid use disorder
The medication comes in two formulations: a weekly and a monthly version. The weekly treatment is indicated in patients who have initiated treatment with a single dose of transmucosal buprenorphine or who are already being treated with the drug. The monthly version is for patients already receiving buprenorphine.
“Buprenorphine is an important treatment option for opioid use disorder. Today’s approval expands dosing options and provides people with opioid use disorder a greater opportunity to sustain long-term recovery,” said FDA Commissioner Robert M. Califf, MD, in a release. “The FDA will continue to take the critical steps necessary to pursue efforts that advance evidence-based treatments for substance use disorders, which is a strategic priority under the FDA’s Overdose Prevention Framework,” Dr. Califf added.
The Substance Abuse and Mental Health Services Administration reports that patients receiving medication for OUD have their risk for all-cause mortality cut by 50%.
In its release, the FDA said that it remains committed to increasing treatment options for OUD. Earlier this month, the agency issued a joint letter with SAMHSA to underscore the importance of counseling and other services as part of a comprehensive treatment plan the disorder. It also emphasized that receiving buprenorphine should not be contingent on participating in such services.
Brixadi is approved in both weekly and monthly subcutaneous injectable formulations at varying doses, including lower doses that may be appropriate for patients who do not tolerate higher doses of extended-release buprenorphine that are currently available.
The drug will be available through a Risk Evaluation and Mitigation Strategy program and administered only by health care providers in a health care setting.
The most common adverse reactions associated with the drug include injection-site pain, headache, constipation, nausea, injection-site erythema, injection-site pruritus, insomnia, and urinary tract infections. The FDA reports that such side effects occur in at least 5% of patients.
A version of this article originally appeared on Medscape.com.
The medication comes in two formulations: a weekly and a monthly version. The weekly treatment is indicated in patients who have initiated treatment with a single dose of transmucosal buprenorphine or who are already being treated with the drug. The monthly version is for patients already receiving buprenorphine.
“Buprenorphine is an important treatment option for opioid use disorder. Today’s approval expands dosing options and provides people with opioid use disorder a greater opportunity to sustain long-term recovery,” said FDA Commissioner Robert M. Califf, MD, in a release. “The FDA will continue to take the critical steps necessary to pursue efforts that advance evidence-based treatments for substance use disorders, which is a strategic priority under the FDA’s Overdose Prevention Framework,” Dr. Califf added.
The Substance Abuse and Mental Health Services Administration reports that patients receiving medication for OUD have their risk for all-cause mortality cut by 50%.
In its release, the FDA said that it remains committed to increasing treatment options for OUD. Earlier this month, the agency issued a joint letter with SAMHSA to underscore the importance of counseling and other services as part of a comprehensive treatment plan the disorder. It also emphasized that receiving buprenorphine should not be contingent on participating in such services.
Brixadi is approved in both weekly and monthly subcutaneous injectable formulations at varying doses, including lower doses that may be appropriate for patients who do not tolerate higher doses of extended-release buprenorphine that are currently available.
The drug will be available through a Risk Evaluation and Mitigation Strategy program and administered only by health care providers in a health care setting.
The most common adverse reactions associated with the drug include injection-site pain, headache, constipation, nausea, injection-site erythema, injection-site pruritus, insomnia, and urinary tract infections. The FDA reports that such side effects occur in at least 5% of patients.
A version of this article originally appeared on Medscape.com.
The medication comes in two formulations: a weekly and a monthly version. The weekly treatment is indicated in patients who have initiated treatment with a single dose of transmucosal buprenorphine or who are already being treated with the drug. The monthly version is for patients already receiving buprenorphine.
“Buprenorphine is an important treatment option for opioid use disorder. Today’s approval expands dosing options and provides people with opioid use disorder a greater opportunity to sustain long-term recovery,” said FDA Commissioner Robert M. Califf, MD, in a release. “The FDA will continue to take the critical steps necessary to pursue efforts that advance evidence-based treatments for substance use disorders, which is a strategic priority under the FDA’s Overdose Prevention Framework,” Dr. Califf added.
The Substance Abuse and Mental Health Services Administration reports that patients receiving medication for OUD have their risk for all-cause mortality cut by 50%.
In its release, the FDA said that it remains committed to increasing treatment options for OUD. Earlier this month, the agency issued a joint letter with SAMHSA to underscore the importance of counseling and other services as part of a comprehensive treatment plan the disorder. It also emphasized that receiving buprenorphine should not be contingent on participating in such services.
Brixadi is approved in both weekly and monthly subcutaneous injectable formulations at varying doses, including lower doses that may be appropriate for patients who do not tolerate higher doses of extended-release buprenorphine that are currently available.
The drug will be available through a Risk Evaluation and Mitigation Strategy program and administered only by health care providers in a health care setting.
The most common adverse reactions associated with the drug include injection-site pain, headache, constipation, nausea, injection-site erythema, injection-site pruritus, insomnia, and urinary tract infections. The FDA reports that such side effects occur in at least 5% of patients.
A version of this article originally appeared on Medscape.com.
Can online mindfulness and self-compassion training improve quality of life for patients with atopic dermatitis?
, according to results of a small randomized controlled trial in Japan.
“We found that skin disease–specific QOL improved over time with a large effect size,” lead study author Sanae Kishimoto, MHS, MPH, of the School of Public Health, Graduate School of Medicine at Kyoto University and colleagues write in JAMA Dermatology. “These findings suggest that mindfulness and self-compassion training is an effective treatment option for adults with AD.”
A bothersome disease that worsens quality of life
AD, a chronic, relapsing, inflammatory, multifactorial skin disease involving intense itching, affects an estimated 15%-30% of children and 2%-10% of adults, with the incidence increasing in industrialized countries, the authors state.
Measured by disability-adjusted life years, AD has the highest disease burden among skin diseases, and people with AD commonly have anxiety, depression, and sleep problems. Treatments include medications, other skin care, and lifestyle changes. New biologics appear to be effective but are expensive and need to be studied for their long-term safety, the authors add.
“Stress can make the skin worse, but at the same time the skin disease and symptoms cause stress,” Peter A. Lio, MD, who was not involved in the study, told this news organization by email. “This vicious cycle contributes greatly to impairing quality of life.”
A program focused on wise, kind self-care
In the SMiLE study, the authors recruited adults with moderate to severe AD and Dermatology Life Quality Index (DLQI) score above 6 from dermatology clinics and through online announcements over 1 year beginning in July 2019.
Participants averaged 36.3 years of age, 80% were women, and their mean AD duration was 26.6 years. Everyone was allowed to receive usual care during the study, except for dupilumab (a newly marketed drug when the study started), psychotherapy, or other mindfulness training.
The researchers randomly assigned 56 adults to receive mindfulness training in addition to their usual care and 51 to the wait list plus usual care. Those in the training group received eight weekly 90-minute online mindfulness and self-compassion sessions. Each group-based session was conducted at the same time and day of the week and included meditation, informal psychoeducation, inquiry, and a short lecture, along with an optional 1-day silent meditation retreat at week 7 and an optional 2-hour videoconferencing booster session at week 13.
The intervention encouraged a nonjudgmental relationship with stress using mindfulness-based stress reduction (MBSR) and emphasized a compassionate relationship with oneself during suffering using mindful self-compassion (MSC). The program was developed and taught by lead author Dr. Kishimoto, a Japanese licensed clinical psychologist who has a history of AD, the paper notes.
At 13 weeks, after completing electronic assessments, patients in the training group showed greater improvement in the DLQI score than those on the wait list (between-group difference estimate, –6.34; 95% confidence interval, –8.27 to –4.41; P < .001). The standardized effect size (Cohen’s d) at 13 weeks was –1.06 (95% CI, –1.39 to –0.74).
Patients in the training group also improved more in all secondary outcomes: severity, itch- and scratch-related visual analog scales, self-compassion, mindfulness, psychological symptoms, and adherence to dermatologist-advised treatments.
They were also more likely to follow their dermatologist’s medical treatment plans, including moisturizer and topical steroid use.
One serious adverse event, endometrial cancer in one patient, was judged to be unrelated to the intervention.
Online format may give more patients access to treatment
“With relatively limited data in the literature, this particularly well-done, important study is likely to positively shape thinking around this topic,” said Dr. Lio, of the departments of dermatology and pediatrics at Northwestern University, Chicago. “This study nicely demonstrates that an online approach can be effective.
“In theory, these methods or techniques could democratize treatments like this, and open them up to many more patients,” he added. He would like to see partially or entirely automated apps (free of cost), similar to meditation “apps,” to treat patients more cost-effectively.
Dr. Lio explained that excluding participants on dupilumab (Dupixent) makes the results slightly less generalizable to patients with moderate to severe AD, who may have the most serious QOL challenges and who are often candidates for dupilumab.
“However, given that we almost never have all the known variables for a study, we are generally comfortable extrapolating that the intervention would likely be helpful for patients taking dupilumab as well, despite it not being specifically evaluated in that group,” he said.
Susan Massick, MD, of the department of dermatology at the Ohio State University Wexner Medical Center in Columbus, advises clinicians to take a multipronged approach to treating the physical and behavioral components of AD and to embrace therapies beyond prescription medications.
“Self-compassion training is another tool in our toolbox toward finding the right fix for our patients,” Dr. Massick said by email. She was not involved with this research.
“I applaud the focus of this study on behavioral health training as a means toward wellness and improved mindfulness,” she added. “I was impressed by the extent to which these simple measures helped improve the quality of life for patients who used the training.”
U.S. patients can benefit from these findings
“My sense is that AD patients the world over have many similar characteristics and concerns, so I would anticipate that the results would be comparable in a U.S. population,” Dr. Lio said. “Other studies performed in the U.S. also support this line of thinking.”
Although the study involved highly motivated patients in Japan, the suffering that patients with AD experience is universal regardless of race or ethnicity, Dr. Massick said. “Americans may be even more willing to embrace mindfulness and self-compassion training as a path toward better health and wellness.”
The study was funded by the Japan Agency for Medical Research and Development and the Mental Health Okamoto Memorial Foundation, the KDDI Foundation, the Pfizer Health Research Foundation, and the Japan Society for the Promotion of Science.
Dr. Kishimoto and several coauthors report relevant financial relationships with pharmaceutical companies. Dr. Lio reports financial relationships with Sanofi and Regeneron, the joint developers of dupilumab. Dr. Massick reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to results of a small randomized controlled trial in Japan.
“We found that skin disease–specific QOL improved over time with a large effect size,” lead study author Sanae Kishimoto, MHS, MPH, of the School of Public Health, Graduate School of Medicine at Kyoto University and colleagues write in JAMA Dermatology. “These findings suggest that mindfulness and self-compassion training is an effective treatment option for adults with AD.”
A bothersome disease that worsens quality of life
AD, a chronic, relapsing, inflammatory, multifactorial skin disease involving intense itching, affects an estimated 15%-30% of children and 2%-10% of adults, with the incidence increasing in industrialized countries, the authors state.
Measured by disability-adjusted life years, AD has the highest disease burden among skin diseases, and people with AD commonly have anxiety, depression, and sleep problems. Treatments include medications, other skin care, and lifestyle changes. New biologics appear to be effective but are expensive and need to be studied for their long-term safety, the authors add.
“Stress can make the skin worse, but at the same time the skin disease and symptoms cause stress,” Peter A. Lio, MD, who was not involved in the study, told this news organization by email. “This vicious cycle contributes greatly to impairing quality of life.”
A program focused on wise, kind self-care
In the SMiLE study, the authors recruited adults with moderate to severe AD and Dermatology Life Quality Index (DLQI) score above 6 from dermatology clinics and through online announcements over 1 year beginning in July 2019.
Participants averaged 36.3 years of age, 80% were women, and their mean AD duration was 26.6 years. Everyone was allowed to receive usual care during the study, except for dupilumab (a newly marketed drug when the study started), psychotherapy, or other mindfulness training.
The researchers randomly assigned 56 adults to receive mindfulness training in addition to their usual care and 51 to the wait list plus usual care. Those in the training group received eight weekly 90-minute online mindfulness and self-compassion sessions. Each group-based session was conducted at the same time and day of the week and included meditation, informal psychoeducation, inquiry, and a short lecture, along with an optional 1-day silent meditation retreat at week 7 and an optional 2-hour videoconferencing booster session at week 13.
The intervention encouraged a nonjudgmental relationship with stress using mindfulness-based stress reduction (MBSR) and emphasized a compassionate relationship with oneself during suffering using mindful self-compassion (MSC). The program was developed and taught by lead author Dr. Kishimoto, a Japanese licensed clinical psychologist who has a history of AD, the paper notes.
At 13 weeks, after completing electronic assessments, patients in the training group showed greater improvement in the DLQI score than those on the wait list (between-group difference estimate, –6.34; 95% confidence interval, –8.27 to –4.41; P < .001). The standardized effect size (Cohen’s d) at 13 weeks was –1.06 (95% CI, –1.39 to –0.74).
Patients in the training group also improved more in all secondary outcomes: severity, itch- and scratch-related visual analog scales, self-compassion, mindfulness, psychological symptoms, and adherence to dermatologist-advised treatments.
They were also more likely to follow their dermatologist’s medical treatment plans, including moisturizer and topical steroid use.
One serious adverse event, endometrial cancer in one patient, was judged to be unrelated to the intervention.
Online format may give more patients access to treatment
“With relatively limited data in the literature, this particularly well-done, important study is likely to positively shape thinking around this topic,” said Dr. Lio, of the departments of dermatology and pediatrics at Northwestern University, Chicago. “This study nicely demonstrates that an online approach can be effective.
“In theory, these methods or techniques could democratize treatments like this, and open them up to many more patients,” he added. He would like to see partially or entirely automated apps (free of cost), similar to meditation “apps,” to treat patients more cost-effectively.
Dr. Lio explained that excluding participants on dupilumab (Dupixent) makes the results slightly less generalizable to patients with moderate to severe AD, who may have the most serious QOL challenges and who are often candidates for dupilumab.
“However, given that we almost never have all the known variables for a study, we are generally comfortable extrapolating that the intervention would likely be helpful for patients taking dupilumab as well, despite it not being specifically evaluated in that group,” he said.
Susan Massick, MD, of the department of dermatology at the Ohio State University Wexner Medical Center in Columbus, advises clinicians to take a multipronged approach to treating the physical and behavioral components of AD and to embrace therapies beyond prescription medications.
“Self-compassion training is another tool in our toolbox toward finding the right fix for our patients,” Dr. Massick said by email. She was not involved with this research.
“I applaud the focus of this study on behavioral health training as a means toward wellness and improved mindfulness,” she added. “I was impressed by the extent to which these simple measures helped improve the quality of life for patients who used the training.”
U.S. patients can benefit from these findings
“My sense is that AD patients the world over have many similar characteristics and concerns, so I would anticipate that the results would be comparable in a U.S. population,” Dr. Lio said. “Other studies performed in the U.S. also support this line of thinking.”
Although the study involved highly motivated patients in Japan, the suffering that patients with AD experience is universal regardless of race or ethnicity, Dr. Massick said. “Americans may be even more willing to embrace mindfulness and self-compassion training as a path toward better health and wellness.”
The study was funded by the Japan Agency for Medical Research and Development and the Mental Health Okamoto Memorial Foundation, the KDDI Foundation, the Pfizer Health Research Foundation, and the Japan Society for the Promotion of Science.
Dr. Kishimoto and several coauthors report relevant financial relationships with pharmaceutical companies. Dr. Lio reports financial relationships with Sanofi and Regeneron, the joint developers of dupilumab. Dr. Massick reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to results of a small randomized controlled trial in Japan.
“We found that skin disease–specific QOL improved over time with a large effect size,” lead study author Sanae Kishimoto, MHS, MPH, of the School of Public Health, Graduate School of Medicine at Kyoto University and colleagues write in JAMA Dermatology. “These findings suggest that mindfulness and self-compassion training is an effective treatment option for adults with AD.”
A bothersome disease that worsens quality of life
AD, a chronic, relapsing, inflammatory, multifactorial skin disease involving intense itching, affects an estimated 15%-30% of children and 2%-10% of adults, with the incidence increasing in industrialized countries, the authors state.
Measured by disability-adjusted life years, AD has the highest disease burden among skin diseases, and people with AD commonly have anxiety, depression, and sleep problems. Treatments include medications, other skin care, and lifestyle changes. New biologics appear to be effective but are expensive and need to be studied for their long-term safety, the authors add.
“Stress can make the skin worse, but at the same time the skin disease and symptoms cause stress,” Peter A. Lio, MD, who was not involved in the study, told this news organization by email. “This vicious cycle contributes greatly to impairing quality of life.”
A program focused on wise, kind self-care
In the SMiLE study, the authors recruited adults with moderate to severe AD and Dermatology Life Quality Index (DLQI) score above 6 from dermatology clinics and through online announcements over 1 year beginning in July 2019.
Participants averaged 36.3 years of age, 80% were women, and their mean AD duration was 26.6 years. Everyone was allowed to receive usual care during the study, except for dupilumab (a newly marketed drug when the study started), psychotherapy, or other mindfulness training.
The researchers randomly assigned 56 adults to receive mindfulness training in addition to their usual care and 51 to the wait list plus usual care. Those in the training group received eight weekly 90-minute online mindfulness and self-compassion sessions. Each group-based session was conducted at the same time and day of the week and included meditation, informal psychoeducation, inquiry, and a short lecture, along with an optional 1-day silent meditation retreat at week 7 and an optional 2-hour videoconferencing booster session at week 13.
The intervention encouraged a nonjudgmental relationship with stress using mindfulness-based stress reduction (MBSR) and emphasized a compassionate relationship with oneself during suffering using mindful self-compassion (MSC). The program was developed and taught by lead author Dr. Kishimoto, a Japanese licensed clinical psychologist who has a history of AD, the paper notes.
At 13 weeks, after completing electronic assessments, patients in the training group showed greater improvement in the DLQI score than those on the wait list (between-group difference estimate, –6.34; 95% confidence interval, –8.27 to –4.41; P < .001). The standardized effect size (Cohen’s d) at 13 weeks was –1.06 (95% CI, –1.39 to –0.74).
Patients in the training group also improved more in all secondary outcomes: severity, itch- and scratch-related visual analog scales, self-compassion, mindfulness, psychological symptoms, and adherence to dermatologist-advised treatments.
They were also more likely to follow their dermatologist’s medical treatment plans, including moisturizer and topical steroid use.
One serious adverse event, endometrial cancer in one patient, was judged to be unrelated to the intervention.
Online format may give more patients access to treatment
“With relatively limited data in the literature, this particularly well-done, important study is likely to positively shape thinking around this topic,” said Dr. Lio, of the departments of dermatology and pediatrics at Northwestern University, Chicago. “This study nicely demonstrates that an online approach can be effective.
“In theory, these methods or techniques could democratize treatments like this, and open them up to many more patients,” he added. He would like to see partially or entirely automated apps (free of cost), similar to meditation “apps,” to treat patients more cost-effectively.
Dr. Lio explained that excluding participants on dupilumab (Dupixent) makes the results slightly less generalizable to patients with moderate to severe AD, who may have the most serious QOL challenges and who are often candidates for dupilumab.
“However, given that we almost never have all the known variables for a study, we are generally comfortable extrapolating that the intervention would likely be helpful for patients taking dupilumab as well, despite it not being specifically evaluated in that group,” he said.
Susan Massick, MD, of the department of dermatology at the Ohio State University Wexner Medical Center in Columbus, advises clinicians to take a multipronged approach to treating the physical and behavioral components of AD and to embrace therapies beyond prescription medications.
“Self-compassion training is another tool in our toolbox toward finding the right fix for our patients,” Dr. Massick said by email. She was not involved with this research.
“I applaud the focus of this study on behavioral health training as a means toward wellness and improved mindfulness,” she added. “I was impressed by the extent to which these simple measures helped improve the quality of life for patients who used the training.”
U.S. patients can benefit from these findings
“My sense is that AD patients the world over have many similar characteristics and concerns, so I would anticipate that the results would be comparable in a U.S. population,” Dr. Lio said. “Other studies performed in the U.S. also support this line of thinking.”
Although the study involved highly motivated patients in Japan, the suffering that patients with AD experience is universal regardless of race or ethnicity, Dr. Massick said. “Americans may be even more willing to embrace mindfulness and self-compassion training as a path toward better health and wellness.”
The study was funded by the Japan Agency for Medical Research and Development and the Mental Health Okamoto Memorial Foundation, the KDDI Foundation, the Pfizer Health Research Foundation, and the Japan Society for the Promotion of Science.
Dr. Kishimoto and several coauthors report relevant financial relationships with pharmaceutical companies. Dr. Lio reports financial relationships with Sanofi and Regeneron, the joint developers of dupilumab. Dr. Massick reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA DERMATOLOGY






