User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
SSRI improves cognition, major depression in early dementia
TOPLINE:
METHODOLOGY:
- The multicenter MEMORY study included 82 subjects with MDD and early-stage dementia, mean age 70.3 years, mostly female (66%) and White (95%).
- Vortioxetine, a modulator of 5-hydroxytryptamine receptor activity and an inhibitor of the 5-HT transporter, initiated at 5 mg/day (recommended starting dose in older adults) with the dose up-titrated to 10 mg/day after a week and flexible dosing thereafter.
- Depression was assessed using the Montgomery-Åsberg Depression Rating Scale (MADRS), and cognition with the Digit Symbol Substitution Test (DSST) and Rey Auditory Verbal Learning Test.
TAKEAWAY:
- There was significant and clinically meaningful improvement in the severity of depressive symptoms, as measured by MADRS total score (the primary outcome), at all assessment time points (P < .0001).
- Improvements in depressive symptoms were irrespective of dementia type.
- There were also significant improvements in DSST total score (P < .0001) and in daily functioning and health-related quality of life (HRQoL).
- Vortioxetine was well tolerated; side effects, including nausea and abdominal pain, were mostly mild to moderate.
IN PRACTICE:
“Vortioxetine demonstrated effectiveness in clinically significantly improving depressive symptoms, cognitive performance, daily and global functioning, and HRQoL in patients with MDD and comorbid early-stage dementia treated for 12 weeks” the researchers noted.
STUDY DETAILS:
The study was conducted by Michael Cronquist Christensen from pharmaceutical company H. Lundbeck, Valby, Denmark, and colleagues. It was published online in the Journal of Affective Disorders.
LIMITATIONS:
The study is open label and lacked a control group. Learning effects were possible, which could contribute to improved cognitive performance, although significant improvement on the RAVLT was not observed until week 4, suggesting earning effects were minimal.
DISCLOSURES:
The study was funded by H. Lundbeck. Mr. Christensen is an employee of H. Lundbeck.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The multicenter MEMORY study included 82 subjects with MDD and early-stage dementia, mean age 70.3 years, mostly female (66%) and White (95%).
- Vortioxetine, a modulator of 5-hydroxytryptamine receptor activity and an inhibitor of the 5-HT transporter, initiated at 5 mg/day (recommended starting dose in older adults) with the dose up-titrated to 10 mg/day after a week and flexible dosing thereafter.
- Depression was assessed using the Montgomery-Åsberg Depression Rating Scale (MADRS), and cognition with the Digit Symbol Substitution Test (DSST) and Rey Auditory Verbal Learning Test.
TAKEAWAY:
- There was significant and clinically meaningful improvement in the severity of depressive symptoms, as measured by MADRS total score (the primary outcome), at all assessment time points (P < .0001).
- Improvements in depressive symptoms were irrespective of dementia type.
- There were also significant improvements in DSST total score (P < .0001) and in daily functioning and health-related quality of life (HRQoL).
- Vortioxetine was well tolerated; side effects, including nausea and abdominal pain, were mostly mild to moderate.
IN PRACTICE:
“Vortioxetine demonstrated effectiveness in clinically significantly improving depressive symptoms, cognitive performance, daily and global functioning, and HRQoL in patients with MDD and comorbid early-stage dementia treated for 12 weeks” the researchers noted.
STUDY DETAILS:
The study was conducted by Michael Cronquist Christensen from pharmaceutical company H. Lundbeck, Valby, Denmark, and colleagues. It was published online in the Journal of Affective Disorders.
LIMITATIONS:
The study is open label and lacked a control group. Learning effects were possible, which could contribute to improved cognitive performance, although significant improvement on the RAVLT was not observed until week 4, suggesting earning effects were minimal.
DISCLOSURES:
The study was funded by H. Lundbeck. Mr. Christensen is an employee of H. Lundbeck.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The multicenter MEMORY study included 82 subjects with MDD and early-stage dementia, mean age 70.3 years, mostly female (66%) and White (95%).
- Vortioxetine, a modulator of 5-hydroxytryptamine receptor activity and an inhibitor of the 5-HT transporter, initiated at 5 mg/day (recommended starting dose in older adults) with the dose up-titrated to 10 mg/day after a week and flexible dosing thereafter.
- Depression was assessed using the Montgomery-Åsberg Depression Rating Scale (MADRS), and cognition with the Digit Symbol Substitution Test (DSST) and Rey Auditory Verbal Learning Test.
TAKEAWAY:
- There was significant and clinically meaningful improvement in the severity of depressive symptoms, as measured by MADRS total score (the primary outcome), at all assessment time points (P < .0001).
- Improvements in depressive symptoms were irrespective of dementia type.
- There were also significant improvements in DSST total score (P < .0001) and in daily functioning and health-related quality of life (HRQoL).
- Vortioxetine was well tolerated; side effects, including nausea and abdominal pain, were mostly mild to moderate.
IN PRACTICE:
“Vortioxetine demonstrated effectiveness in clinically significantly improving depressive symptoms, cognitive performance, daily and global functioning, and HRQoL in patients with MDD and comorbid early-stage dementia treated for 12 weeks” the researchers noted.
STUDY DETAILS:
The study was conducted by Michael Cronquist Christensen from pharmaceutical company H. Lundbeck, Valby, Denmark, and colleagues. It was published online in the Journal of Affective Disorders.
LIMITATIONS:
The study is open label and lacked a control group. Learning effects were possible, which could contribute to improved cognitive performance, although significant improvement on the RAVLT was not observed until week 4, suggesting earning effects were minimal.
DISCLOSURES:
The study was funded by H. Lundbeck. Mr. Christensen is an employee of H. Lundbeck.
A version of this article first appeared on Medscape.com.
Should you dismiss a difficult patient?
Some patients continually cancel their appointments, ignore your medical directions, treat your staff rudely, or send you harassing emails.
Do you have to tolerate their behavior?
No, these are all appropriate reasons to terminate patients, attorneys say. Patients also can be dismissed for misleading doctors about their past medical history, chronic drug-seeking, displaying threatening or seductive behavior toward staff members or physicians, or any criminal behavior in the office, experts say.
But even if a reason seems legitimate, that doesn’t make it legal. Doctors should consider whether the reason is legal, said Chicago-area attorney Ericka Adler, JD, a partner at Roetzel & Andress, who advises doctors about terminating patients.
Ms. Adler said.
Terminating patients for an “illegal” reason such as discrimination based on race or gender or sexual orientation – even if couched as a legitimate patient issue – could open the practice to a lawsuit, Ms. Adler said.
Doctors also want to avoid patient abandonment claims by talking to the patient about problems and documenting them as they arise. If they can’t be resolved, doctors should ensure that there’s continuity of care when patients change physicians, said Ms. Adler.
About 90% of physicians have dismissed at least one patient during their career, according to a study of nearly 800 primary care practices. The most common reasons were legitimate: a patient was “extremely disruptive and/or behaved inappropriately toward clinicians or staff”; a patient had “violated chronic pain and controlled substance policies”; and a patient had “repeatedly missed appointments.”
Jacqui O’Kane, DO, a family physician at South Georgia Medical Center in rural Nashville, said she has dismissed about 15 of 3,000 patients she has seen in the past 3 years at the clinic. Before she dismisses a patient, she looks at whether there has been a pattern of behavior and tries to talk to them about the problem first to find out if there are other reasons for it.
She also gives patients a warning: If the unacceptable behavior continues, it will lead to their dismissal.
When patients cross a line
Dr. O’Kane warned an elderly man who used the N-word with her that she wouldn’t tolerate that language in her office. Then, when he later called her front office employee the N-word, she decided to dismiss him.
“I said, ‘That’s it, you can’t say that to someone in this office. I already told you once, and you did it again. I’m sorry, you have to find another doctor,’ ” said Dr. O’Kane.
Another patient crossed a line when she missed four appointments, refused to come in, and kept sending Dr. O’Kane long messages on MyChart demanding medications and advice. One message was fairly obtrusive: “If you don’t give me something stronger for my nerves TODAY, I am going to LOSE MY MIND!!!” Dr. O’Kane said the patient wrote.
“I then told her that’s not how I run my practice and that she needed to find someone else.”
Another common reason doctors dismiss patients is for nonpayment, says Ms. Adler.
Recently, however, some patients have also begun demanding their money back from doctors for services already received and billed because they were unhappy about something that occurred at the doctor’s office, said Ms. Adler.
“I advise doctors to respond: ‘We disagree that you didn’t get the service, but we will give you your money back, and we’re also terminating you from our practice.’ At that point, the doctor-patient relationship has become impossible,” said Ms. Adler.
How to dismiss difficult patients ethically and legally
According to the AMA’s Council on Ethical and Judicial Affairs, a physician may not discontinue treatment of a patient if further treatment is medically indicated without giving the patient reasonable notice and sufficient opportunity to make alternative arrangements for care.
Terminating a patient abruptly without transferring their care could lead to a claim of patient abandonment and the physician being called before a licensing board for potentially violating the state’s Medical Practice Act, said Ms. Adler.
Doctors can take these six steps to set the stage for dismissal and avoid a claim of patient abandonment.
1. Create written policies. Medical practices can describe the rules and behavior they expect from patients in these policies, which can cover, for example, payment, treating staff with courtesy, and medications. “When the rules are in writing and patients sign off on them, that gives doctors a certain comfort level in being able to refer to them and say that the patient hasn’t been compliant,” said Ms. Adler.
She also recommends that your practice create a policy that doctors should let the patient know about their concerns and meet with them to discuss the problem before receiving a termination letter.
2. Document any consistent problems you’re having with a patient. When you start having problems with a patient, you should document when the problem occurred, how often it occurred, any discussions with the patient about the problem, warnings you gave the patient, and if and when you decided to terminate the patient.
3. Meet with the patient to discuss the problem. “Talking and meeting with a patient also allows the physician to assess whether there’s another issue. For example, is there a mental health concern? Is there a financial reason for nonpayment or no-shows? There are multiple benefits to finding out what the problem is,” said Ms. Adler.
Once you’ve decided to terminate a patient, here’s what you should do:
4. Allow enough time for the patient to find alternative care. Ms. Adler recommends giving patients 30 days’ notice and that physicians offer to provide emergency care during that time. However, if the patient is undergoing treatment or has other challenges, more time may be needed to transfer care.
“It’s important to consider the patient’s context – if the patient is receiving cancer treatment, or is in a late stage of pregnancy, or lives in a rural area where few specialists are available, you may want to treat them longer – at least until they finish their treatment,” said Ms. Adler. Also, states may have their own requirements about minimum notice periods, she said.
5. Provide patients with written notice that you intend to terminate their care. Ms. Adler recommends that each letter be tailored to the patient’s specific circumstances. “You could spell out a patient’s history of noncompliance or nonpayment or inappropriate conduct because it’s been documented and the patient is already aware of it from a previous discussion,” she said.
Ms. Adler also recommends that doctors consult with legal counsel when in doubt or if contacted by the patient’s lawyer. Some lawyers will draft the termination letters, she said.
6. Include the following information in the written letter: The date that they will no longer receive care, how they can obtain copies of their medical records, and how they can find a new physician by providing contact information for a state medical association or similar organization, which often maintains a database of clinicians by specialty and location.
The letter should also state that the doctor will provide emergency care during the 30 days. Ms. Adler also recommends sending the notice by certified mail.
Dr. O’Kane said she may be more likely to give patients a second chance because she practices in a rural underserved area, and she understands that her patients don’t have many other options for health care. She also has developed a reputation for being willing to take on difficult patients that other physicians didn’t want to deal with, she said.
She encourages physicians to talk to patients to find out why, for example, they may not be compliant with medications.
“The patient may say, ‘I had to choose between paying for medications and putting food on the table,’ ” said Dr. O’Kane.
A version of this article first appeared on Medscape.com.
Some patients continually cancel their appointments, ignore your medical directions, treat your staff rudely, or send you harassing emails.
Do you have to tolerate their behavior?
No, these are all appropriate reasons to terminate patients, attorneys say. Patients also can be dismissed for misleading doctors about their past medical history, chronic drug-seeking, displaying threatening or seductive behavior toward staff members or physicians, or any criminal behavior in the office, experts say.
But even if a reason seems legitimate, that doesn’t make it legal. Doctors should consider whether the reason is legal, said Chicago-area attorney Ericka Adler, JD, a partner at Roetzel & Andress, who advises doctors about terminating patients.
Ms. Adler said.
Terminating patients for an “illegal” reason such as discrimination based on race or gender or sexual orientation – even if couched as a legitimate patient issue – could open the practice to a lawsuit, Ms. Adler said.
Doctors also want to avoid patient abandonment claims by talking to the patient about problems and documenting them as they arise. If they can’t be resolved, doctors should ensure that there’s continuity of care when patients change physicians, said Ms. Adler.
About 90% of physicians have dismissed at least one patient during their career, according to a study of nearly 800 primary care practices. The most common reasons were legitimate: a patient was “extremely disruptive and/or behaved inappropriately toward clinicians or staff”; a patient had “violated chronic pain and controlled substance policies”; and a patient had “repeatedly missed appointments.”
Jacqui O’Kane, DO, a family physician at South Georgia Medical Center in rural Nashville, said she has dismissed about 15 of 3,000 patients she has seen in the past 3 years at the clinic. Before she dismisses a patient, she looks at whether there has been a pattern of behavior and tries to talk to them about the problem first to find out if there are other reasons for it.
She also gives patients a warning: If the unacceptable behavior continues, it will lead to their dismissal.
When patients cross a line
Dr. O’Kane warned an elderly man who used the N-word with her that she wouldn’t tolerate that language in her office. Then, when he later called her front office employee the N-word, she decided to dismiss him.
“I said, ‘That’s it, you can’t say that to someone in this office. I already told you once, and you did it again. I’m sorry, you have to find another doctor,’ ” said Dr. O’Kane.
Another patient crossed a line when she missed four appointments, refused to come in, and kept sending Dr. O’Kane long messages on MyChart demanding medications and advice. One message was fairly obtrusive: “If you don’t give me something stronger for my nerves TODAY, I am going to LOSE MY MIND!!!” Dr. O’Kane said the patient wrote.
“I then told her that’s not how I run my practice and that she needed to find someone else.”
Another common reason doctors dismiss patients is for nonpayment, says Ms. Adler.
Recently, however, some patients have also begun demanding their money back from doctors for services already received and billed because they were unhappy about something that occurred at the doctor’s office, said Ms. Adler.
“I advise doctors to respond: ‘We disagree that you didn’t get the service, but we will give you your money back, and we’re also terminating you from our practice.’ At that point, the doctor-patient relationship has become impossible,” said Ms. Adler.
How to dismiss difficult patients ethically and legally
According to the AMA’s Council on Ethical and Judicial Affairs, a physician may not discontinue treatment of a patient if further treatment is medically indicated without giving the patient reasonable notice and sufficient opportunity to make alternative arrangements for care.
Terminating a patient abruptly without transferring their care could lead to a claim of patient abandonment and the physician being called before a licensing board for potentially violating the state’s Medical Practice Act, said Ms. Adler.
Doctors can take these six steps to set the stage for dismissal and avoid a claim of patient abandonment.
1. Create written policies. Medical practices can describe the rules and behavior they expect from patients in these policies, which can cover, for example, payment, treating staff with courtesy, and medications. “When the rules are in writing and patients sign off on them, that gives doctors a certain comfort level in being able to refer to them and say that the patient hasn’t been compliant,” said Ms. Adler.
She also recommends that your practice create a policy that doctors should let the patient know about their concerns and meet with them to discuss the problem before receiving a termination letter.
2. Document any consistent problems you’re having with a patient. When you start having problems with a patient, you should document when the problem occurred, how often it occurred, any discussions with the patient about the problem, warnings you gave the patient, and if and when you decided to terminate the patient.
3. Meet with the patient to discuss the problem. “Talking and meeting with a patient also allows the physician to assess whether there’s another issue. For example, is there a mental health concern? Is there a financial reason for nonpayment or no-shows? There are multiple benefits to finding out what the problem is,” said Ms. Adler.
Once you’ve decided to terminate a patient, here’s what you should do:
4. Allow enough time for the patient to find alternative care. Ms. Adler recommends giving patients 30 days’ notice and that physicians offer to provide emergency care during that time. However, if the patient is undergoing treatment or has other challenges, more time may be needed to transfer care.
“It’s important to consider the patient’s context – if the patient is receiving cancer treatment, or is in a late stage of pregnancy, or lives in a rural area where few specialists are available, you may want to treat them longer – at least until they finish their treatment,” said Ms. Adler. Also, states may have their own requirements about minimum notice periods, she said.
5. Provide patients with written notice that you intend to terminate their care. Ms. Adler recommends that each letter be tailored to the patient’s specific circumstances. “You could spell out a patient’s history of noncompliance or nonpayment or inappropriate conduct because it’s been documented and the patient is already aware of it from a previous discussion,” she said.
Ms. Adler also recommends that doctors consult with legal counsel when in doubt or if contacted by the patient’s lawyer. Some lawyers will draft the termination letters, she said.
6. Include the following information in the written letter: The date that they will no longer receive care, how they can obtain copies of their medical records, and how they can find a new physician by providing contact information for a state medical association or similar organization, which often maintains a database of clinicians by specialty and location.
The letter should also state that the doctor will provide emergency care during the 30 days. Ms. Adler also recommends sending the notice by certified mail.
Dr. O’Kane said she may be more likely to give patients a second chance because she practices in a rural underserved area, and she understands that her patients don’t have many other options for health care. She also has developed a reputation for being willing to take on difficult patients that other physicians didn’t want to deal with, she said.
She encourages physicians to talk to patients to find out why, for example, they may not be compliant with medications.
“The patient may say, ‘I had to choose between paying for medications and putting food on the table,’ ” said Dr. O’Kane.
A version of this article first appeared on Medscape.com.
Some patients continually cancel their appointments, ignore your medical directions, treat your staff rudely, or send you harassing emails.
Do you have to tolerate their behavior?
No, these are all appropriate reasons to terminate patients, attorneys say. Patients also can be dismissed for misleading doctors about their past medical history, chronic drug-seeking, displaying threatening or seductive behavior toward staff members or physicians, or any criminal behavior in the office, experts say.
But even if a reason seems legitimate, that doesn’t make it legal. Doctors should consider whether the reason is legal, said Chicago-area attorney Ericka Adler, JD, a partner at Roetzel & Andress, who advises doctors about terminating patients.
Ms. Adler said.
Terminating patients for an “illegal” reason such as discrimination based on race or gender or sexual orientation – even if couched as a legitimate patient issue – could open the practice to a lawsuit, Ms. Adler said.
Doctors also want to avoid patient abandonment claims by talking to the patient about problems and documenting them as they arise. If they can’t be resolved, doctors should ensure that there’s continuity of care when patients change physicians, said Ms. Adler.
About 90% of physicians have dismissed at least one patient during their career, according to a study of nearly 800 primary care practices. The most common reasons were legitimate: a patient was “extremely disruptive and/or behaved inappropriately toward clinicians or staff”; a patient had “violated chronic pain and controlled substance policies”; and a patient had “repeatedly missed appointments.”
Jacqui O’Kane, DO, a family physician at South Georgia Medical Center in rural Nashville, said she has dismissed about 15 of 3,000 patients she has seen in the past 3 years at the clinic. Before she dismisses a patient, she looks at whether there has been a pattern of behavior and tries to talk to them about the problem first to find out if there are other reasons for it.
She also gives patients a warning: If the unacceptable behavior continues, it will lead to their dismissal.
When patients cross a line
Dr. O’Kane warned an elderly man who used the N-word with her that she wouldn’t tolerate that language in her office. Then, when he later called her front office employee the N-word, she decided to dismiss him.
“I said, ‘That’s it, you can’t say that to someone in this office. I already told you once, and you did it again. I’m sorry, you have to find another doctor,’ ” said Dr. O’Kane.
Another patient crossed a line when she missed four appointments, refused to come in, and kept sending Dr. O’Kane long messages on MyChart demanding medications and advice. One message was fairly obtrusive: “If you don’t give me something stronger for my nerves TODAY, I am going to LOSE MY MIND!!!” Dr. O’Kane said the patient wrote.
“I then told her that’s not how I run my practice and that she needed to find someone else.”
Another common reason doctors dismiss patients is for nonpayment, says Ms. Adler.
Recently, however, some patients have also begun demanding their money back from doctors for services already received and billed because they were unhappy about something that occurred at the doctor’s office, said Ms. Adler.
“I advise doctors to respond: ‘We disagree that you didn’t get the service, but we will give you your money back, and we’re also terminating you from our practice.’ At that point, the doctor-patient relationship has become impossible,” said Ms. Adler.
How to dismiss difficult patients ethically and legally
According to the AMA’s Council on Ethical and Judicial Affairs, a physician may not discontinue treatment of a patient if further treatment is medically indicated without giving the patient reasonable notice and sufficient opportunity to make alternative arrangements for care.
Terminating a patient abruptly without transferring their care could lead to a claim of patient abandonment and the physician being called before a licensing board for potentially violating the state’s Medical Practice Act, said Ms. Adler.
Doctors can take these six steps to set the stage for dismissal and avoid a claim of patient abandonment.
1. Create written policies. Medical practices can describe the rules and behavior they expect from patients in these policies, which can cover, for example, payment, treating staff with courtesy, and medications. “When the rules are in writing and patients sign off on them, that gives doctors a certain comfort level in being able to refer to them and say that the patient hasn’t been compliant,” said Ms. Adler.
She also recommends that your practice create a policy that doctors should let the patient know about their concerns and meet with them to discuss the problem before receiving a termination letter.
2. Document any consistent problems you’re having with a patient. When you start having problems with a patient, you should document when the problem occurred, how often it occurred, any discussions with the patient about the problem, warnings you gave the patient, and if and when you decided to terminate the patient.
3. Meet with the patient to discuss the problem. “Talking and meeting with a patient also allows the physician to assess whether there’s another issue. For example, is there a mental health concern? Is there a financial reason for nonpayment or no-shows? There are multiple benefits to finding out what the problem is,” said Ms. Adler.
Once you’ve decided to terminate a patient, here’s what you should do:
4. Allow enough time for the patient to find alternative care. Ms. Adler recommends giving patients 30 days’ notice and that physicians offer to provide emergency care during that time. However, if the patient is undergoing treatment or has other challenges, more time may be needed to transfer care.
“It’s important to consider the patient’s context – if the patient is receiving cancer treatment, or is in a late stage of pregnancy, or lives in a rural area where few specialists are available, you may want to treat them longer – at least until they finish their treatment,” said Ms. Adler. Also, states may have their own requirements about minimum notice periods, she said.
5. Provide patients with written notice that you intend to terminate their care. Ms. Adler recommends that each letter be tailored to the patient’s specific circumstances. “You could spell out a patient’s history of noncompliance or nonpayment or inappropriate conduct because it’s been documented and the patient is already aware of it from a previous discussion,” she said.
Ms. Adler also recommends that doctors consult with legal counsel when in doubt or if contacted by the patient’s lawyer. Some lawyers will draft the termination letters, she said.
6. Include the following information in the written letter: The date that they will no longer receive care, how they can obtain copies of their medical records, and how they can find a new physician by providing contact information for a state medical association or similar organization, which often maintains a database of clinicians by specialty and location.
The letter should also state that the doctor will provide emergency care during the 30 days. Ms. Adler also recommends sending the notice by certified mail.
Dr. O’Kane said she may be more likely to give patients a second chance because she practices in a rural underserved area, and she understands that her patients don’t have many other options for health care. She also has developed a reputation for being willing to take on difficult patients that other physicians didn’t want to deal with, she said.
She encourages physicians to talk to patients to find out why, for example, they may not be compliant with medications.
“The patient may say, ‘I had to choose between paying for medications and putting food on the table,’ ” said Dr. O’Kane.
A version of this article first appeared on Medscape.com.
Therapists’ oxytocin levels tied to patient outcomes
TOPLINE:
METHODOLOGY:
- Evidence suggests patient experiences of negative emotions predict outcomes of psychotherapy for major depressive disorder (MDD), but mechanisms remain unclear.
- Researchers used a mediation model based on the role of oxytocin (OT) in attachment relationships, such as between parent and infant.
- They collected 435 oxytocin samples pre- and post-session from therapists of 62 patients receiving psychotherapy for MDD.
- Hamilton Rating Scale for Depression (HRSD) was administered to patients before sessions, and patients reported their in-session emotions.
TAKEAWAY:
- Higher negative emotion levels of patients predicted higher therapist oxytocin levels on the post-session assessment, when controlling for the pre-session oxytocin (“a” path [same-session path between negative affect and OT levels]: 0.11; standard error, 0.05; P = 03; 95% confidence interval, 0.003-0.20)
- Higher therapist oxytocin levels predicted lower depression severity in the next session (“b” path [time-lagged association between post-session OT levels and depression severity]: –0.97; SE, 0.34; P = .005; 95 % CI, –1.57 to –0.22)
- An increase in therapists’ oxytocin in response to patients’ negative emotions may represent activation of the therapists’ caregiving system signaling the emergence of a healthy therapeutic interaction.
IN PRACTICE:
“The findings suggest that therapists’ oxytocin responses could potentially serve as a biomarker of an effective therapeutic process,” the researchers write.
STUDY DETAILS:
The study was conducted by Hadar Fisher, department of psychology, University of Haifa, Israel, and colleagues. It was published online in the Journal of Affective Disorders.
LIMITATIONS:
The sample size, while one of the largest in studies looking at oxytocin in psychotherapy, still has limited statistical power. The study used post-session retrospective self-reports to measure negative emotions, which focused on patients’ experiences rather than expression of these emotions.
DISCLOSURES:
The study was supported by a grant from the Israeli Science Foundation. The authors report no competing interests.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Evidence suggests patient experiences of negative emotions predict outcomes of psychotherapy for major depressive disorder (MDD), but mechanisms remain unclear.
- Researchers used a mediation model based on the role of oxytocin (OT) in attachment relationships, such as between parent and infant.
- They collected 435 oxytocin samples pre- and post-session from therapists of 62 patients receiving psychotherapy for MDD.
- Hamilton Rating Scale for Depression (HRSD) was administered to patients before sessions, and patients reported their in-session emotions.
TAKEAWAY:
- Higher negative emotion levels of patients predicted higher therapist oxytocin levels on the post-session assessment, when controlling for the pre-session oxytocin (“a” path [same-session path between negative affect and OT levels]: 0.11; standard error, 0.05; P = 03; 95% confidence interval, 0.003-0.20)
- Higher therapist oxytocin levels predicted lower depression severity in the next session (“b” path [time-lagged association between post-session OT levels and depression severity]: –0.97; SE, 0.34; P = .005; 95 % CI, –1.57 to –0.22)
- An increase in therapists’ oxytocin in response to patients’ negative emotions may represent activation of the therapists’ caregiving system signaling the emergence of a healthy therapeutic interaction.
IN PRACTICE:
“The findings suggest that therapists’ oxytocin responses could potentially serve as a biomarker of an effective therapeutic process,” the researchers write.
STUDY DETAILS:
The study was conducted by Hadar Fisher, department of psychology, University of Haifa, Israel, and colleagues. It was published online in the Journal of Affective Disorders.
LIMITATIONS:
The sample size, while one of the largest in studies looking at oxytocin in psychotherapy, still has limited statistical power. The study used post-session retrospective self-reports to measure negative emotions, which focused on patients’ experiences rather than expression of these emotions.
DISCLOSURES:
The study was supported by a grant from the Israeli Science Foundation. The authors report no competing interests.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Evidence suggests patient experiences of negative emotions predict outcomes of psychotherapy for major depressive disorder (MDD), but mechanisms remain unclear.
- Researchers used a mediation model based on the role of oxytocin (OT) in attachment relationships, such as between parent and infant.
- They collected 435 oxytocin samples pre- and post-session from therapists of 62 patients receiving psychotherapy for MDD.
- Hamilton Rating Scale for Depression (HRSD) was administered to patients before sessions, and patients reported their in-session emotions.
TAKEAWAY:
- Higher negative emotion levels of patients predicted higher therapist oxytocin levels on the post-session assessment, when controlling for the pre-session oxytocin (“a” path [same-session path between negative affect and OT levels]: 0.11; standard error, 0.05; P = 03; 95% confidence interval, 0.003-0.20)
- Higher therapist oxytocin levels predicted lower depression severity in the next session (“b” path [time-lagged association between post-session OT levels and depression severity]: –0.97; SE, 0.34; P = .005; 95 % CI, –1.57 to –0.22)
- An increase in therapists’ oxytocin in response to patients’ negative emotions may represent activation of the therapists’ caregiving system signaling the emergence of a healthy therapeutic interaction.
IN PRACTICE:
“The findings suggest that therapists’ oxytocin responses could potentially serve as a biomarker of an effective therapeutic process,” the researchers write.
STUDY DETAILS:
The study was conducted by Hadar Fisher, department of psychology, University of Haifa, Israel, and colleagues. It was published online in the Journal of Affective Disorders.
LIMITATIONS:
The sample size, while one of the largest in studies looking at oxytocin in psychotherapy, still has limited statistical power. The study used post-session retrospective self-reports to measure negative emotions, which focused on patients’ experiences rather than expression of these emotions.
DISCLOSURES:
The study was supported by a grant from the Israeli Science Foundation. The authors report no competing interests.
A version of this article first appeared on Medscape.com.
Low-calorie tastes sweeter with a little salt
Low-calorie tastes sweeter with a little salt
Diet and sugar-free foods and drinks seem like a good idea, but it’s hard to get past that strange aftertaste, right? It’s the calling card for the noncaloric aspartame- and stevia-containing sweeteners that we consume to make us feel like we can have the best of both worlds.
That weird lingering taste can be a total turn-off for some (raises hand), but researchers have found an almost facepalm solution to the not-so-sweet problem, and it’s salt.
Now, the concept of sweet and salty is not a far-fetched partnership when it comes to snack consumption (try M&Ms in your popcorn). The researchers at Almendra, a manufacturer of stevia sweeteners, put that iconic flavor pair to the test by adding mineral salts that have some nutritional value to lessen the effect of a stevia compound, rebaudioside A, found in noncaloric sweeteners.
The researchers added in magnesium chloride, calcium chloride, and potassium chloride separately to lessen rebaudioside A’s intensity, but they needed so much salt that it killed the sweet taste completely. A blend of the three mineral salts, however, reduced the lingering taste by 79% and improved the real sugar-like taste. The researchers tried this blend in reduced-calorie orange juice and a citrus-flavored soft drink, improving the taste in both.
The salty and sweet match comes in for the win once again. This time helping against the fight of obesity instead of making it worse.
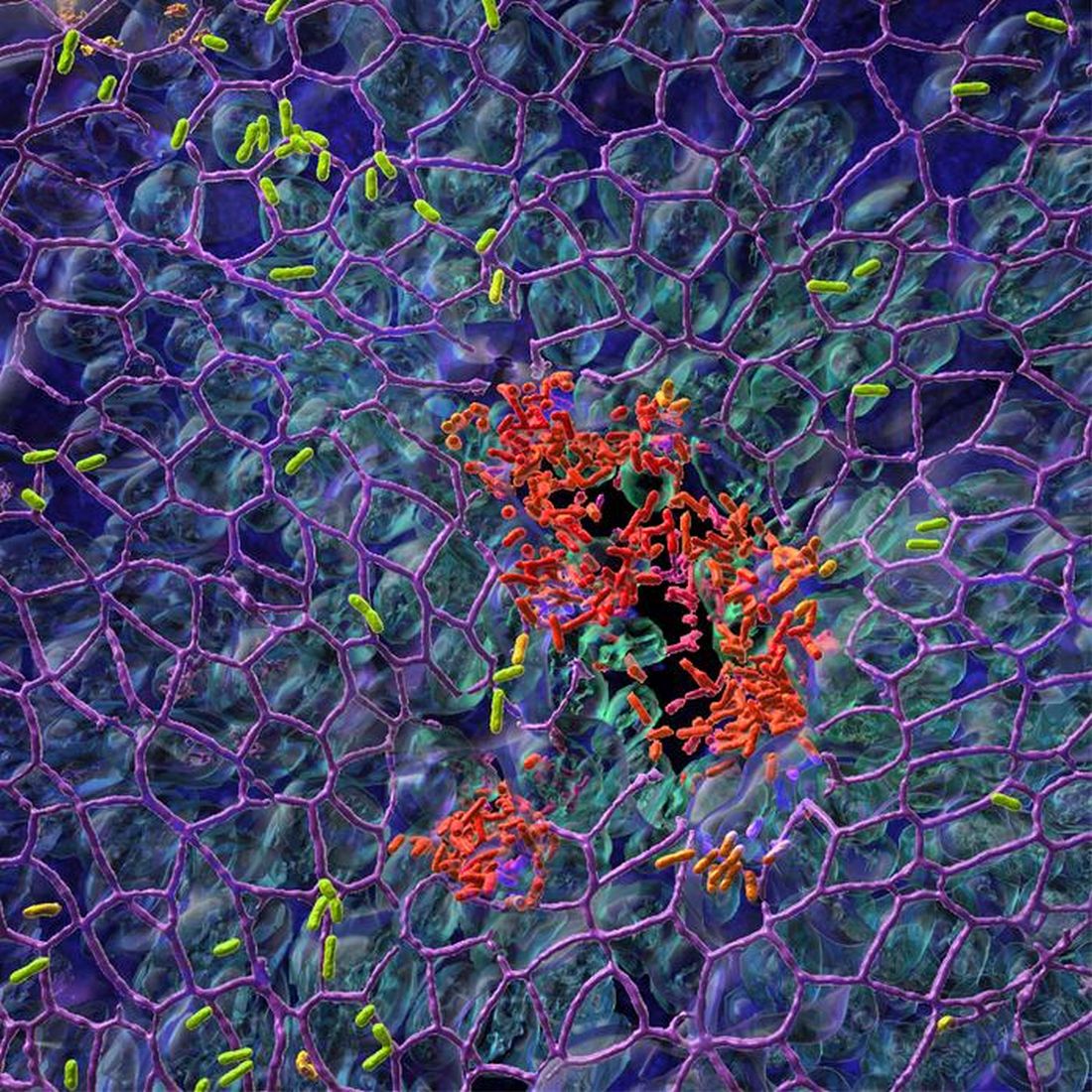
Pseudomonas’ Achilles’ heel is more of an Achilles’ genetic switch
Today, on the long-awaited return of “Bacteria vs. the World,” we meet one of the rock stars of infectious disease.
LOTME: Through the use of imaginary technology, we’re talking to Pseudomonas aeruginosa. Thanks for joining us on such short notice, after Neisseria gonorrhoeae canceled at the last minute.
P. aeruginosa: No problem. I think we can all guess what that little devil is up to.
LOTME: Bacterial resistance to antibiotics is a huge problem for our species. What makes you so hard to fight?
P. aeruginosa: We’ve been trying to keep that a secret, actually, but now that researchers in Switzerland and Denmark seem to have figured it out, I guess it’s okay for me to spill the beans.
LOTME: Beans? What do beans have to do with it?
P. aeruginosa: Nothing, it’s just a colloquial expression that means I’m sharing previously private information.
LOTME: Sure, we knew that. Please, continue your spilling.
P. aeruginosa: The secret is … Well, let’s just say we were a little worried when the Clash released “Should I Stay or Should I Go” back in the 1980s.
LOTME: The Clash? Now we’re really confused.
P. aeruginosa: The answer to their question, “Should I stay or should I go? is yes. Successful invasion of a human is all about division of labor. “While one fraction of the bacterial population adheres to the mucosal surface and forms a biofilm, the other subpopulation spreads to distant tissue sites,” is how the investigators described it. We can increase surface colonization by using a “job-sharing” process, they said, and even resist antibiotics because most of us remain in the protective biofilm.
LOTME: And they say you guys don’t have brains.
P. aeruginosa: But wait, there’s more. We don’t just divide the labor randomly. After the initial colonization we form two functionally distinct subpopulations. One has high levels of the bacterial signaling molecule c-di-GMP and stays put to work on the biofilm. The other group, with low levels of c-di-GMP, heads out to the surrounding tissue to continue the colonization. As project leader Urs Jenal put it, “By identifying the genetic switch, we have tracked down the Achilles heel of the pathogen.”
LOTME: Pretty clever stuff, for humans, anyway.
P. aeruginosa: We agree, but now that you know our secret, we can’t let you share it.
LOTME: Wait! The journal article’s already been published. Your secret is out. You can’t stop that by infecting me.
P. aeruginosa: True enough, but are you familiar with the fable of the scorpion and the frog? It’s our nature.
LOTME: Nooooo! N. gonorrhoeae wouldn’t have done this!
What a pain in the Butt
Businesses rise and businesses fall. We all know that one cursed location, that spot in town where we see businesses move in and close up in a matter of months. At the same time, though, there are also businesses that have been around as long as anyone can remember, pillars of the community.
Corydon, IN., likely has a few such long-lived shops, but it is officially down one 70-year-old family business as of late April, with the unfortunate passing of beloved local pharmacy Butt Drugs. Prescription pick-up in rear.
The business dates back to 1952, when it was founded as William H. Butt Drugs. We’re sure William Butt was never teased about his last name. Nope. No one would ever do that. After he passed the store to his children, it underwent a stint as Butt Rexall Drugs. When the shop was passed down to its third-generation and ultimately final owner, Katie Butt Beckort, she decided to simplify the name. Get right down to the bottom of things, as it were.
Butt Drugs was a popular spot, featuring an old-school soda fountain and themed souvenirs. According to Ms. Butt Beckort, people would come from miles away to buy “I love Butt Drugs” T-shirts, magnets, and so on. Yes, they knew perfectly well what they were sitting on.
So, if was such a hit, why did it close? Butt Drugs may have a hilarious name and merchandise to match, but the pharmacy portion of the pharmacy had been losing money for years. You know, the actual point of the business. As with so many things, we can blame it on the insurance companies. More than half the drugs that passed through Butt Drugs’ doors were sold at a loss, because the insurance companies refused to reimburse the store more than the wholesale price of the drug. Not even a good butt drug could clear up that financial diarrhea.
And so, we’ve lost Butt Drugs forever. Spicy food enthusiasts, coffee drinkers, and all patrons of Taco Bell, take a moment to reflect and mourn on what you’ve lost. No more Butt Drugs to relieve your suffering. A true kick in the butt indeed.
Low-calorie tastes sweeter with a little salt
Diet and sugar-free foods and drinks seem like a good idea, but it’s hard to get past that strange aftertaste, right? It’s the calling card for the noncaloric aspartame- and stevia-containing sweeteners that we consume to make us feel like we can have the best of both worlds.
That weird lingering taste can be a total turn-off for some (raises hand), but researchers have found an almost facepalm solution to the not-so-sweet problem, and it’s salt.
Now, the concept of sweet and salty is not a far-fetched partnership when it comes to snack consumption (try M&Ms in your popcorn). The researchers at Almendra, a manufacturer of stevia sweeteners, put that iconic flavor pair to the test by adding mineral salts that have some nutritional value to lessen the effect of a stevia compound, rebaudioside A, found in noncaloric sweeteners.
The researchers added in magnesium chloride, calcium chloride, and potassium chloride separately to lessen rebaudioside A’s intensity, but they needed so much salt that it killed the sweet taste completely. A blend of the three mineral salts, however, reduced the lingering taste by 79% and improved the real sugar-like taste. The researchers tried this blend in reduced-calorie orange juice and a citrus-flavored soft drink, improving the taste in both.
The salty and sweet match comes in for the win once again. This time helping against the fight of obesity instead of making it worse.
Pseudomonas’ Achilles’ heel is more of an Achilles’ genetic switch
Today, on the long-awaited return of “Bacteria vs. the World,” we meet one of the rock stars of infectious disease.
LOTME: Through the use of imaginary technology, we’re talking to Pseudomonas aeruginosa. Thanks for joining us on such short notice, after Neisseria gonorrhoeae canceled at the last minute.
P. aeruginosa: No problem. I think we can all guess what that little devil is up to.
LOTME: Bacterial resistance to antibiotics is a huge problem for our species. What makes you so hard to fight?
P. aeruginosa: We’ve been trying to keep that a secret, actually, but now that researchers in Switzerland and Denmark seem to have figured it out, I guess it’s okay for me to spill the beans.
LOTME: Beans? What do beans have to do with it?
P. aeruginosa: Nothing, it’s just a colloquial expression that means I’m sharing previously private information.
LOTME: Sure, we knew that. Please, continue your spilling.
P. aeruginosa: The secret is … Well, let’s just say we were a little worried when the Clash released “Should I Stay or Should I Go” back in the 1980s.
LOTME: The Clash? Now we’re really confused.
P. aeruginosa: The answer to their question, “Should I stay or should I go? is yes. Successful invasion of a human is all about division of labor. “While one fraction of the bacterial population adheres to the mucosal surface and forms a biofilm, the other subpopulation spreads to distant tissue sites,” is how the investigators described it. We can increase surface colonization by using a “job-sharing” process, they said, and even resist antibiotics because most of us remain in the protective biofilm.
LOTME: And they say you guys don’t have brains.
P. aeruginosa: But wait, there’s more. We don’t just divide the labor randomly. After the initial colonization we form two functionally distinct subpopulations. One has high levels of the bacterial signaling molecule c-di-GMP and stays put to work on the biofilm. The other group, with low levels of c-di-GMP, heads out to the surrounding tissue to continue the colonization. As project leader Urs Jenal put it, “By identifying the genetic switch, we have tracked down the Achilles heel of the pathogen.”
LOTME: Pretty clever stuff, for humans, anyway.
P. aeruginosa: We agree, but now that you know our secret, we can’t let you share it.
LOTME: Wait! The journal article’s already been published. Your secret is out. You can’t stop that by infecting me.
P. aeruginosa: True enough, but are you familiar with the fable of the scorpion and the frog? It’s our nature.
LOTME: Nooooo! N. gonorrhoeae wouldn’t have done this!
What a pain in the Butt
Businesses rise and businesses fall. We all know that one cursed location, that spot in town where we see businesses move in and close up in a matter of months. At the same time, though, there are also businesses that have been around as long as anyone can remember, pillars of the community.
Corydon, IN., likely has a few such long-lived shops, but it is officially down one 70-year-old family business as of late April, with the unfortunate passing of beloved local pharmacy Butt Drugs. Prescription pick-up in rear.
The business dates back to 1952, when it was founded as William H. Butt Drugs. We’re sure William Butt was never teased about his last name. Nope. No one would ever do that. After he passed the store to his children, it underwent a stint as Butt Rexall Drugs. When the shop was passed down to its third-generation and ultimately final owner, Katie Butt Beckort, she decided to simplify the name. Get right down to the bottom of things, as it were.
Butt Drugs was a popular spot, featuring an old-school soda fountain and themed souvenirs. According to Ms. Butt Beckort, people would come from miles away to buy “I love Butt Drugs” T-shirts, magnets, and so on. Yes, they knew perfectly well what they were sitting on.
So, if was such a hit, why did it close? Butt Drugs may have a hilarious name and merchandise to match, but the pharmacy portion of the pharmacy had been losing money for years. You know, the actual point of the business. As with so many things, we can blame it on the insurance companies. More than half the drugs that passed through Butt Drugs’ doors were sold at a loss, because the insurance companies refused to reimburse the store more than the wholesale price of the drug. Not even a good butt drug could clear up that financial diarrhea.
And so, we’ve lost Butt Drugs forever. Spicy food enthusiasts, coffee drinkers, and all patrons of Taco Bell, take a moment to reflect and mourn on what you’ve lost. No more Butt Drugs to relieve your suffering. A true kick in the butt indeed.
Low-calorie tastes sweeter with a little salt
Diet and sugar-free foods and drinks seem like a good idea, but it’s hard to get past that strange aftertaste, right? It’s the calling card for the noncaloric aspartame- and stevia-containing sweeteners that we consume to make us feel like we can have the best of both worlds.
That weird lingering taste can be a total turn-off for some (raises hand), but researchers have found an almost facepalm solution to the not-so-sweet problem, and it’s salt.
Now, the concept of sweet and salty is not a far-fetched partnership when it comes to snack consumption (try M&Ms in your popcorn). The researchers at Almendra, a manufacturer of stevia sweeteners, put that iconic flavor pair to the test by adding mineral salts that have some nutritional value to lessen the effect of a stevia compound, rebaudioside A, found in noncaloric sweeteners.
The researchers added in magnesium chloride, calcium chloride, and potassium chloride separately to lessen rebaudioside A’s intensity, but they needed so much salt that it killed the sweet taste completely. A blend of the three mineral salts, however, reduced the lingering taste by 79% and improved the real sugar-like taste. The researchers tried this blend in reduced-calorie orange juice and a citrus-flavored soft drink, improving the taste in both.
The salty and sweet match comes in for the win once again. This time helping against the fight of obesity instead of making it worse.
Pseudomonas’ Achilles’ heel is more of an Achilles’ genetic switch
Today, on the long-awaited return of “Bacteria vs. the World,” we meet one of the rock stars of infectious disease.
LOTME: Through the use of imaginary technology, we’re talking to Pseudomonas aeruginosa. Thanks for joining us on such short notice, after Neisseria gonorrhoeae canceled at the last minute.
P. aeruginosa: No problem. I think we can all guess what that little devil is up to.
LOTME: Bacterial resistance to antibiotics is a huge problem for our species. What makes you so hard to fight?
P. aeruginosa: We’ve been trying to keep that a secret, actually, but now that researchers in Switzerland and Denmark seem to have figured it out, I guess it’s okay for me to spill the beans.
LOTME: Beans? What do beans have to do with it?
P. aeruginosa: Nothing, it’s just a colloquial expression that means I’m sharing previously private information.
LOTME: Sure, we knew that. Please, continue your spilling.
P. aeruginosa: The secret is … Well, let’s just say we were a little worried when the Clash released “Should I Stay or Should I Go” back in the 1980s.
LOTME: The Clash? Now we’re really confused.
P. aeruginosa: The answer to their question, “Should I stay or should I go? is yes. Successful invasion of a human is all about division of labor. “While one fraction of the bacterial population adheres to the mucosal surface and forms a biofilm, the other subpopulation spreads to distant tissue sites,” is how the investigators described it. We can increase surface colonization by using a “job-sharing” process, they said, and even resist antibiotics because most of us remain in the protective biofilm.
LOTME: And they say you guys don’t have brains.
P. aeruginosa: But wait, there’s more. We don’t just divide the labor randomly. After the initial colonization we form two functionally distinct subpopulations. One has high levels of the bacterial signaling molecule c-di-GMP and stays put to work on the biofilm. The other group, with low levels of c-di-GMP, heads out to the surrounding tissue to continue the colonization. As project leader Urs Jenal put it, “By identifying the genetic switch, we have tracked down the Achilles heel of the pathogen.”
LOTME: Pretty clever stuff, for humans, anyway.
P. aeruginosa: We agree, but now that you know our secret, we can’t let you share it.
LOTME: Wait! The journal article’s already been published. Your secret is out. You can’t stop that by infecting me.
P. aeruginosa: True enough, but are you familiar with the fable of the scorpion and the frog? It’s our nature.
LOTME: Nooooo! N. gonorrhoeae wouldn’t have done this!
What a pain in the Butt
Businesses rise and businesses fall. We all know that one cursed location, that spot in town where we see businesses move in and close up in a matter of months. At the same time, though, there are also businesses that have been around as long as anyone can remember, pillars of the community.
Corydon, IN., likely has a few such long-lived shops, but it is officially down one 70-year-old family business as of late April, with the unfortunate passing of beloved local pharmacy Butt Drugs. Prescription pick-up in rear.
The business dates back to 1952, when it was founded as William H. Butt Drugs. We’re sure William Butt was never teased about his last name. Nope. No one would ever do that. After he passed the store to his children, it underwent a stint as Butt Rexall Drugs. When the shop was passed down to its third-generation and ultimately final owner, Katie Butt Beckort, she decided to simplify the name. Get right down to the bottom of things, as it were.
Butt Drugs was a popular spot, featuring an old-school soda fountain and themed souvenirs. According to Ms. Butt Beckort, people would come from miles away to buy “I love Butt Drugs” T-shirts, magnets, and so on. Yes, they knew perfectly well what they were sitting on.
So, if was such a hit, why did it close? Butt Drugs may have a hilarious name and merchandise to match, but the pharmacy portion of the pharmacy had been losing money for years. You know, the actual point of the business. As with so many things, we can blame it on the insurance companies. More than half the drugs that passed through Butt Drugs’ doors were sold at a loss, because the insurance companies refused to reimburse the store more than the wholesale price of the drug. Not even a good butt drug could clear up that financial diarrhea.
And so, we’ve lost Butt Drugs forever. Spicy food enthusiasts, coffee drinkers, and all patrons of Taco Bell, take a moment to reflect and mourn on what you’ve lost. No more Butt Drugs to relieve your suffering. A true kick in the butt indeed.
How not to establish rapport with your patient
1. Stride confidently into the room to greet your 84-year-old female patient.
2. Introduce yourself saying, “Hi, I’m Dr. Jeff Benabio.”
3. Extend your clenched fist toward her chest and wait for her to reciprocate.
4. Smile awkwardly behind your mask while you wait.
5. Advise that you are doing a fist bump instead of a handshake to prevent the spread of viruses.
6. Wait.
7. Explain that she can bump, also known as “dap,” you back by extending her clenched fist and bumping into yours.
8. Wait a bit more.
9. Lower your fist and pat her on the shoulder with your left hand. Do so gently so it doesn’t seem like you just did a quick right jab followed by a left hook.
10. Sit down diffidently and pray that you can help her so this office visit is not an utter disaster.
It seemed a good idea for 2020: Let’s stop shaking hands while we wait out this viral apocalypse. Sensible, but entering a patient room and just sitting down didn’t work. It felt cold, impolite – this isn’t the DMV. In medicine, a complete stranger has to trust us to get naked, tell intimate secrets, even be stuck by needles all within minutes of meeting. We needed a trust-building substitute greeting.
There was the Muslim hand-on-my-heart greeting. Or the Hindu “namaste” or Buddhist “amituofo” folded hands. Or perhaps the paternalistic shoulder pat? I went with the fist bump. With some of my partner docs, my old MBA squad, my neighbor, the fist bump felt natural, reciprocated without hesitation. But it fails with many patients. To understand why, it’s helpful to know the history of the fist bump, also known as the dap.
Dap is an acronym for Dignity And Pride. It’s a variation of a handshake that originated among Black soldiers in the Vietnam war as a means of showing fraternity and establishing connectedness. In Vietnam, 30% of the combat battalions were Black. Marginalized in the military and at home, they created a greeting that was meaningful and unique. The dap was a series of shakes, bumps, slaps, and hugs that was symbolic. It was a means of showing respect and humility, that no one is above others, that I’ve got your back and you’ve got mine. It was a powerful recognition of humanity and effective means of personal connection. It spread from the Black community to the general population and it exists still today. The choreographed pregame handshake you see so many NBA players engage in is a descendant of the dap. Like many rituals, it reinforces bonds with those who are your people, your team, those you trust.
The more generalized version is the simple fist bump. It is widely used, notably by President Obama, and in the appropriate circumstance, will almost always be reciprocated. But it doesn’t work well to create trust with a stranger. With a patient for example, you are not showing them respect for some accomplishment. Nor are we connecting with them as a member of your team. Unless this is a patient whom you’ve seen many times before, a fist bump attempt might be met with “are you serious?” In fact, a survey done in 2016 asking infectious disease professionals what they thought of fist bumps as a greeting, very few replied it was a good idea. Most felt it was unprofessional. Not to mention that a fist bump does not symbolize an agreement in the way that a handshake does (and has done since at least the 9th century BC).
With COVID waning and masks doffed, I’ve found myself back to handshaking. Yes, I sanitize before and after, another ritual that has symbolic as well as practical significance. I get fewer sideways glances from my geriatric patients for sure. But I do still offer a little dap for my liquid nitrogen–survivor kids and for the occasional fellow Gen Xer. “Wonder Twin powers, activate!”
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
1. Stride confidently into the room to greet your 84-year-old female patient.
2. Introduce yourself saying, “Hi, I’m Dr. Jeff Benabio.”
3. Extend your clenched fist toward her chest and wait for her to reciprocate.
4. Smile awkwardly behind your mask while you wait.
5. Advise that you are doing a fist bump instead of a handshake to prevent the spread of viruses.
6. Wait.
7. Explain that she can bump, also known as “dap,” you back by extending her clenched fist and bumping into yours.
8. Wait a bit more.
9. Lower your fist and pat her on the shoulder with your left hand. Do so gently so it doesn’t seem like you just did a quick right jab followed by a left hook.
10. Sit down diffidently and pray that you can help her so this office visit is not an utter disaster.
It seemed a good idea for 2020: Let’s stop shaking hands while we wait out this viral apocalypse. Sensible, but entering a patient room and just sitting down didn’t work. It felt cold, impolite – this isn’t the DMV. In medicine, a complete stranger has to trust us to get naked, tell intimate secrets, even be stuck by needles all within minutes of meeting. We needed a trust-building substitute greeting.
There was the Muslim hand-on-my-heart greeting. Or the Hindu “namaste” or Buddhist “amituofo” folded hands. Or perhaps the paternalistic shoulder pat? I went with the fist bump. With some of my partner docs, my old MBA squad, my neighbor, the fist bump felt natural, reciprocated without hesitation. But it fails with many patients. To understand why, it’s helpful to know the history of the fist bump, also known as the dap.
Dap is an acronym for Dignity And Pride. It’s a variation of a handshake that originated among Black soldiers in the Vietnam war as a means of showing fraternity and establishing connectedness. In Vietnam, 30% of the combat battalions were Black. Marginalized in the military and at home, they created a greeting that was meaningful and unique. The dap was a series of shakes, bumps, slaps, and hugs that was symbolic. It was a means of showing respect and humility, that no one is above others, that I’ve got your back and you’ve got mine. It was a powerful recognition of humanity and effective means of personal connection. It spread from the Black community to the general population and it exists still today. The choreographed pregame handshake you see so many NBA players engage in is a descendant of the dap. Like many rituals, it reinforces bonds with those who are your people, your team, those you trust.
The more generalized version is the simple fist bump. It is widely used, notably by President Obama, and in the appropriate circumstance, will almost always be reciprocated. But it doesn’t work well to create trust with a stranger. With a patient for example, you are not showing them respect for some accomplishment. Nor are we connecting with them as a member of your team. Unless this is a patient whom you’ve seen many times before, a fist bump attempt might be met with “are you serious?” In fact, a survey done in 2016 asking infectious disease professionals what they thought of fist bumps as a greeting, very few replied it was a good idea. Most felt it was unprofessional. Not to mention that a fist bump does not symbolize an agreement in the way that a handshake does (and has done since at least the 9th century BC).
With COVID waning and masks doffed, I’ve found myself back to handshaking. Yes, I sanitize before and after, another ritual that has symbolic as well as practical significance. I get fewer sideways glances from my geriatric patients for sure. But I do still offer a little dap for my liquid nitrogen–survivor kids and for the occasional fellow Gen Xer. “Wonder Twin powers, activate!”
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
1. Stride confidently into the room to greet your 84-year-old female patient.
2. Introduce yourself saying, “Hi, I’m Dr. Jeff Benabio.”
3. Extend your clenched fist toward her chest and wait for her to reciprocate.
4. Smile awkwardly behind your mask while you wait.
5. Advise that you are doing a fist bump instead of a handshake to prevent the spread of viruses.
6. Wait.
7. Explain that she can bump, also known as “dap,” you back by extending her clenched fist and bumping into yours.
8. Wait a bit more.
9. Lower your fist and pat her on the shoulder with your left hand. Do so gently so it doesn’t seem like you just did a quick right jab followed by a left hook.
10. Sit down diffidently and pray that you can help her so this office visit is not an utter disaster.
It seemed a good idea for 2020: Let’s stop shaking hands while we wait out this viral apocalypse. Sensible, but entering a patient room and just sitting down didn’t work. It felt cold, impolite – this isn’t the DMV. In medicine, a complete stranger has to trust us to get naked, tell intimate secrets, even be stuck by needles all within minutes of meeting. We needed a trust-building substitute greeting.
There was the Muslim hand-on-my-heart greeting. Or the Hindu “namaste” or Buddhist “amituofo” folded hands. Or perhaps the paternalistic shoulder pat? I went with the fist bump. With some of my partner docs, my old MBA squad, my neighbor, the fist bump felt natural, reciprocated without hesitation. But it fails with many patients. To understand why, it’s helpful to know the history of the fist bump, also known as the dap.
Dap is an acronym for Dignity And Pride. It’s a variation of a handshake that originated among Black soldiers in the Vietnam war as a means of showing fraternity and establishing connectedness. In Vietnam, 30% of the combat battalions were Black. Marginalized in the military and at home, they created a greeting that was meaningful and unique. The dap was a series of shakes, bumps, slaps, and hugs that was symbolic. It was a means of showing respect and humility, that no one is above others, that I’ve got your back and you’ve got mine. It was a powerful recognition of humanity and effective means of personal connection. It spread from the Black community to the general population and it exists still today. The choreographed pregame handshake you see so many NBA players engage in is a descendant of the dap. Like many rituals, it reinforces bonds with those who are your people, your team, those you trust.
The more generalized version is the simple fist bump. It is widely used, notably by President Obama, and in the appropriate circumstance, will almost always be reciprocated. But it doesn’t work well to create trust with a stranger. With a patient for example, you are not showing them respect for some accomplishment. Nor are we connecting with them as a member of your team. Unless this is a patient whom you’ve seen many times before, a fist bump attempt might be met with “are you serious?” In fact, a survey done in 2016 asking infectious disease professionals what they thought of fist bumps as a greeting, very few replied it was a good idea. Most felt it was unprofessional. Not to mention that a fist bump does not symbolize an agreement in the way that a handshake does (and has done since at least the 9th century BC).
With COVID waning and masks doffed, I’ve found myself back to handshaking. Yes, I sanitize before and after, another ritual that has symbolic as well as practical significance. I get fewer sideways glances from my geriatric patients for sure. But I do still offer a little dap for my liquid nitrogen–survivor kids and for the occasional fellow Gen Xer. “Wonder Twin powers, activate!”
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
Final USPSTF recommendations on anxiety, depression, suicide risk
In line with draft recommendations, the task force for the first time has endorsed screening for anxiety disorders in all adults younger than age 65 without recognized signs or symptoms of anxiety.
This “B” recommendation reflects “moderate certainty” evidence that screening for anxiety in this population has a moderate net benefit. There currently is not enough evidence to recommend for or against screening for anxiety disorders in adults 65 and older, the task force said.
The USPSTF final recommendation statements and corresponding evidence summaries were published online in the Journal of the American Medical Association, as well as on the task force website.
Jury out on screening for suicide risk
The task force continues to recommend screening all adults for depression. This “B” recommendation reflects moderate-certainty evidence that screening for major depression in adults has a moderate net benefit.
However, there is not enough evidence to recommend for or against screening for suicide risk in all adults. Therefore, the task issued an “I” statement, indicating that the balance of benefits and harms cannot be determined at present.
“We are urgently calling for more research to determine the effectiveness of screening all adults for suicide risk and screening adults 65 and older for anxiety disorders,” task force member Gbenga Ogedegbe, MD, MPH, founding director of the Institute for Excellence in Health Equity at NYU Langone Health, New York, said in a statement.
The authors of an accompanying editorial noted that a positive screen result for anxiety “should be immediately followed with clinical evaluation for suicidality”.
Murray Stein, MD, MPH, and Linda Hill, MD, MPH, both with University of California, San Diego, also noted that a positive screen for anxiety could be indicative of posttraumatic stress disorder (PTSD) and clinicians should “be prepared to follow up with requisite questions about traumatic experiences that will be needed to home in on a diagnosis of PTSD that may require additional follow-up, referral, or both.
“Anxiety disorders can be distressing and disabling, and appropriate recognition and treatment can be life-altering and, in some cases, lifesaving, for patients,” Dr. Stein and Dr. Hill pointed out.
Effective, evidence-based psychological and pharmacologic treatments for anxiety disorders are available, they added. But the recommendation to routinely screen for anxiety disorder “must be accompanied by the recognition that there are too few mental health specialists available to manage the care of all patients with anxiety disorders, and even fewer who provide services for low-income and non-English-speaking populations,” they wrote.
This research report received no commercial funding. Disclosures for task force members and editorial writers are listed with the original articles.
A version of this article originally appeared on Medscape.com.
In line with draft recommendations, the task force for the first time has endorsed screening for anxiety disorders in all adults younger than age 65 without recognized signs or symptoms of anxiety.
This “B” recommendation reflects “moderate certainty” evidence that screening for anxiety in this population has a moderate net benefit. There currently is not enough evidence to recommend for or against screening for anxiety disorders in adults 65 and older, the task force said.
The USPSTF final recommendation statements and corresponding evidence summaries were published online in the Journal of the American Medical Association, as well as on the task force website.
Jury out on screening for suicide risk
The task force continues to recommend screening all adults for depression. This “B” recommendation reflects moderate-certainty evidence that screening for major depression in adults has a moderate net benefit.
However, there is not enough evidence to recommend for or against screening for suicide risk in all adults. Therefore, the task issued an “I” statement, indicating that the balance of benefits and harms cannot be determined at present.
“We are urgently calling for more research to determine the effectiveness of screening all adults for suicide risk and screening adults 65 and older for anxiety disorders,” task force member Gbenga Ogedegbe, MD, MPH, founding director of the Institute for Excellence in Health Equity at NYU Langone Health, New York, said in a statement.
The authors of an accompanying editorial noted that a positive screen result for anxiety “should be immediately followed with clinical evaluation for suicidality”.
Murray Stein, MD, MPH, and Linda Hill, MD, MPH, both with University of California, San Diego, also noted that a positive screen for anxiety could be indicative of posttraumatic stress disorder (PTSD) and clinicians should “be prepared to follow up with requisite questions about traumatic experiences that will be needed to home in on a diagnosis of PTSD that may require additional follow-up, referral, or both.
“Anxiety disorders can be distressing and disabling, and appropriate recognition and treatment can be life-altering and, in some cases, lifesaving, for patients,” Dr. Stein and Dr. Hill pointed out.
Effective, evidence-based psychological and pharmacologic treatments for anxiety disorders are available, they added. But the recommendation to routinely screen for anxiety disorder “must be accompanied by the recognition that there are too few mental health specialists available to manage the care of all patients with anxiety disorders, and even fewer who provide services for low-income and non-English-speaking populations,” they wrote.
This research report received no commercial funding. Disclosures for task force members and editorial writers are listed with the original articles.
A version of this article originally appeared on Medscape.com.
In line with draft recommendations, the task force for the first time has endorsed screening for anxiety disorders in all adults younger than age 65 without recognized signs or symptoms of anxiety.
This “B” recommendation reflects “moderate certainty” evidence that screening for anxiety in this population has a moderate net benefit. There currently is not enough evidence to recommend for or against screening for anxiety disorders in adults 65 and older, the task force said.
The USPSTF final recommendation statements and corresponding evidence summaries were published online in the Journal of the American Medical Association, as well as on the task force website.
Jury out on screening for suicide risk
The task force continues to recommend screening all adults for depression. This “B” recommendation reflects moderate-certainty evidence that screening for major depression in adults has a moderate net benefit.
However, there is not enough evidence to recommend for or against screening for suicide risk in all adults. Therefore, the task issued an “I” statement, indicating that the balance of benefits and harms cannot be determined at present.
“We are urgently calling for more research to determine the effectiveness of screening all adults for suicide risk and screening adults 65 and older for anxiety disorders,” task force member Gbenga Ogedegbe, MD, MPH, founding director of the Institute for Excellence in Health Equity at NYU Langone Health, New York, said in a statement.
The authors of an accompanying editorial noted that a positive screen result for anxiety “should be immediately followed with clinical evaluation for suicidality”.
Murray Stein, MD, MPH, and Linda Hill, MD, MPH, both with University of California, San Diego, also noted that a positive screen for anxiety could be indicative of posttraumatic stress disorder (PTSD) and clinicians should “be prepared to follow up with requisite questions about traumatic experiences that will be needed to home in on a diagnosis of PTSD that may require additional follow-up, referral, or both.
“Anxiety disorders can be distressing and disabling, and appropriate recognition and treatment can be life-altering and, in some cases, lifesaving, for patients,” Dr. Stein and Dr. Hill pointed out.
Effective, evidence-based psychological and pharmacologic treatments for anxiety disorders are available, they added. But the recommendation to routinely screen for anxiety disorder “must be accompanied by the recognition that there are too few mental health specialists available to manage the care of all patients with anxiety disorders, and even fewer who provide services for low-income and non-English-speaking populations,” they wrote.
This research report received no commercial funding. Disclosures for task force members and editorial writers are listed with the original articles.
A version of this article originally appeared on Medscape.com.
Book review: “Sexual Citizens”
The Sexual Health Initiative to Foster Transformation (SHIFT)1 is a landmark study about sexual assault at college, which has generated 20 scientific articles and several chapters in books, but unfortunately, has not made its way into the psychiatric literature.
“Sexual Citizens: Sex, Power and Assault on Campus,” by Jennifer Hirsch and Shamus Khan, (available in audio book and paperback) was written as a follow up to the SHIFT study, so the rest of us can absorb the findings.2 This mixed-methods study included a survey of over 1,600 students aged 18-29 from Columbia University and Barnard College regarding their relationships and sexual histories, including assault. Data were collected using daily diaries, focus groups, and hundreds of hours of field work observation by young researchers. One- to 3-hour in-depth interviews exploring sexual experiences on campus were conducted with 151 students. These interviews are the focus of the book. It is a well-written, provocative story brimming with insights for those of us who lack the time to scour social science literature.
“Sexual Citizens” and the SHIFT study confirmed much of what we know. Sexual assault is common and has enduring effects. The study found that 36% of women and 15% of men had experienced unwanted, nonconsensual sexual contact by senior year. Twenty percent of women and 6% of men were rape survivors. Freshman, LGBTQ, and minority students were found at highest risk of assault. SHIFT reaffirmed that abstinence-only education is not a protective factor against college sexual assault, but neither was knowledge of affirmative consent (the practice of “ongoing and explicit” checking-in with partners) which few students ever employed. Encouragingly, students taught refusal skills were less likely to experience sexual assault.
Many of the book’s valuable lessons fall under the umbrella of failures of language and communication. For example, after drinking, they went to his room. She was expecting a social interaction, but with no other place to sit, they sat on his bed where she was coaxed or pressured into a sexual encounter. Afterward, she leaves, and it is never discussed again. One partner desires emotional intimacy, and the other, bragging rights in the fraternity or at the girls’ weekly brunch. Numerous personal stories like these, though at times heart wrenching, provide perspective on the barriers to addressing assault.
Subjects relayed experiences of assault by strangers or friends, and some provided details of their own actions as perpetrators. Stumbling around words and emotions, an avoidance of explicit language stemmed from shame, a fear of personal responsibility, the desire to maintain social cohesion, and concern for potential consequences for the perpetrator. Many subjects were resistant to calling nonconsensual sexual activity rape or even assault. Some who had perpetrated were unaware their behavior may have been experienced as assault, with recognition of this fact dawning during interviews.
This apparent limitation in self-reflective capacity may be in part due to the conceptualization of what assault is. Focus groups identified a discernible difference in how men and women understood assaults, with men believing rapes looked like a woman fighting back and screaming for help ... which is rarely what happens.
Notably absent among the interviewed are any flagrant perpetrators. The methodology section theorizes that individuals who intentionally harmed their peers were unlikely to choose to participate in this study. In addition, the characterization of assailants as “sociopathic predators” is based in a history of racialized imagery that leads us astray from the truth about campus sexual assault. Most assaults do not involve force, and SHIFT data showed 75% of victims knew their assailants. Ultimately, a major aim of the research was to study assault alongside healthy sex to “understand those pivotal moments when encounters change from being sex, to being assault.” Doing this requires understanding the where, how, and why students have sex, a more complicated undertaking than we may think.
In discussing their sexual lives, subjects frequently noted they did not have space to talk about their assaults. Though 81% of students discussed their experiences with someone, friend groups were often overburdened with stories, which minimized the victim’s experience. Furthermore, most had not sought help from the student counseling centers. Students navigating this complex field were frequently doing so in isolation. SHIFT found subjects to be eager to participate; they would often express thankfulness, and a sense of freedom in sharing with researchers. Commonly, students expressly did not want retribution for perpetrators, but simply a place to be heard without challenge. The current legal system precludes that possibility, leaving individuals without the option to confront perpetrators, and perpetrators often not knowing the extent of the damage they caused.
Where can psychiatrists have an impact right now? “Sexual Citizens” identifies four key areas for intervention to work toward a world with less sexual assault. These are:
- Improving diversity, inequality, and power distortions.
- Education about sex and sexual assault.
- Substance use.
- Mental health.
Substance use and mental health are especially relevant for psychiatrists (That substance use contributes to sexual assault is known by approximately ... everybody!). Unwanted sexual contact prior to college (20% of students) increased the odds of experiencing assault during college. Harm reduction strategies should be introduced before college, according to the SHIFT research, particularly in skills-based training on how to say “No” to unwanted sex. Psychiatrists are likely used to asking brief history questions related to sexual assault and rape. “Sexual Citizens” highlights the inadequacy of this blunt language and guides the reader toward a refined knowledge of the language needed to address sexual assault.
Dr. Whisler is a child and adolescent psychiatry fellow at the Stanford (Calif.) University. Dr. Higgins is affiliate associate professor of psychiatry and family medicine at the Medical University of South Carolina, Charleston.
References
1. Hirsch JS et al. Social dimensions of sexual consent among cisgender heterosexual college students: Insights from ethnographic research. J Adolesc Health. 2019 Jan;64(1):26-35. doi: 10.1016/j.jadohealth.2018.06.011.
2. Hirsch JS and Khan S. Sexual citizens: Sex, power, and assault on campus. New York: W.W. Norton & Company, 2020.
The Sexual Health Initiative to Foster Transformation (SHIFT)1 is a landmark study about sexual assault at college, which has generated 20 scientific articles and several chapters in books, but unfortunately, has not made its way into the psychiatric literature.
“Sexual Citizens: Sex, Power and Assault on Campus,” by Jennifer Hirsch and Shamus Khan, (available in audio book and paperback) was written as a follow up to the SHIFT study, so the rest of us can absorb the findings.2 This mixed-methods study included a survey of over 1,600 students aged 18-29 from Columbia University and Barnard College regarding their relationships and sexual histories, including assault. Data were collected using daily diaries, focus groups, and hundreds of hours of field work observation by young researchers. One- to 3-hour in-depth interviews exploring sexual experiences on campus were conducted with 151 students. These interviews are the focus of the book. It is a well-written, provocative story brimming with insights for those of us who lack the time to scour social science literature.
“Sexual Citizens” and the SHIFT study confirmed much of what we know. Sexual assault is common and has enduring effects. The study found that 36% of women and 15% of men had experienced unwanted, nonconsensual sexual contact by senior year. Twenty percent of women and 6% of men were rape survivors. Freshman, LGBTQ, and minority students were found at highest risk of assault. SHIFT reaffirmed that abstinence-only education is not a protective factor against college sexual assault, but neither was knowledge of affirmative consent (the practice of “ongoing and explicit” checking-in with partners) which few students ever employed. Encouragingly, students taught refusal skills were less likely to experience sexual assault.
Many of the book’s valuable lessons fall under the umbrella of failures of language and communication. For example, after drinking, they went to his room. She was expecting a social interaction, but with no other place to sit, they sat on his bed where she was coaxed or pressured into a sexual encounter. Afterward, she leaves, and it is never discussed again. One partner desires emotional intimacy, and the other, bragging rights in the fraternity or at the girls’ weekly brunch. Numerous personal stories like these, though at times heart wrenching, provide perspective on the barriers to addressing assault.
Subjects relayed experiences of assault by strangers or friends, and some provided details of their own actions as perpetrators. Stumbling around words and emotions, an avoidance of explicit language stemmed from shame, a fear of personal responsibility, the desire to maintain social cohesion, and concern for potential consequences for the perpetrator. Many subjects were resistant to calling nonconsensual sexual activity rape or even assault. Some who had perpetrated were unaware their behavior may have been experienced as assault, with recognition of this fact dawning during interviews.
This apparent limitation in self-reflective capacity may be in part due to the conceptualization of what assault is. Focus groups identified a discernible difference in how men and women understood assaults, with men believing rapes looked like a woman fighting back and screaming for help ... which is rarely what happens.
Notably absent among the interviewed are any flagrant perpetrators. The methodology section theorizes that individuals who intentionally harmed their peers were unlikely to choose to participate in this study. In addition, the characterization of assailants as “sociopathic predators” is based in a history of racialized imagery that leads us astray from the truth about campus sexual assault. Most assaults do not involve force, and SHIFT data showed 75% of victims knew their assailants. Ultimately, a major aim of the research was to study assault alongside healthy sex to “understand those pivotal moments when encounters change from being sex, to being assault.” Doing this requires understanding the where, how, and why students have sex, a more complicated undertaking than we may think.
In discussing their sexual lives, subjects frequently noted they did not have space to talk about their assaults. Though 81% of students discussed their experiences with someone, friend groups were often overburdened with stories, which minimized the victim’s experience. Furthermore, most had not sought help from the student counseling centers. Students navigating this complex field were frequently doing so in isolation. SHIFT found subjects to be eager to participate; they would often express thankfulness, and a sense of freedom in sharing with researchers. Commonly, students expressly did not want retribution for perpetrators, but simply a place to be heard without challenge. The current legal system precludes that possibility, leaving individuals without the option to confront perpetrators, and perpetrators often not knowing the extent of the damage they caused.
Where can psychiatrists have an impact right now? “Sexual Citizens” identifies four key areas for intervention to work toward a world with less sexual assault. These are:
- Improving diversity, inequality, and power distortions.
- Education about sex and sexual assault.
- Substance use.
- Mental health.
Substance use and mental health are especially relevant for psychiatrists (That substance use contributes to sexual assault is known by approximately ... everybody!). Unwanted sexual contact prior to college (20% of students) increased the odds of experiencing assault during college. Harm reduction strategies should be introduced before college, according to the SHIFT research, particularly in skills-based training on how to say “No” to unwanted sex. Psychiatrists are likely used to asking brief history questions related to sexual assault and rape. “Sexual Citizens” highlights the inadequacy of this blunt language and guides the reader toward a refined knowledge of the language needed to address sexual assault.
Dr. Whisler is a child and adolescent psychiatry fellow at the Stanford (Calif.) University. Dr. Higgins is affiliate associate professor of psychiatry and family medicine at the Medical University of South Carolina, Charleston.
References
1. Hirsch JS et al. Social dimensions of sexual consent among cisgender heterosexual college students: Insights from ethnographic research. J Adolesc Health. 2019 Jan;64(1):26-35. doi: 10.1016/j.jadohealth.2018.06.011.
2. Hirsch JS and Khan S. Sexual citizens: Sex, power, and assault on campus. New York: W.W. Norton & Company, 2020.
The Sexual Health Initiative to Foster Transformation (SHIFT)1 is a landmark study about sexual assault at college, which has generated 20 scientific articles and several chapters in books, but unfortunately, has not made its way into the psychiatric literature.
“Sexual Citizens: Sex, Power and Assault on Campus,” by Jennifer Hirsch and Shamus Khan, (available in audio book and paperback) was written as a follow up to the SHIFT study, so the rest of us can absorb the findings.2 This mixed-methods study included a survey of over 1,600 students aged 18-29 from Columbia University and Barnard College regarding their relationships and sexual histories, including assault. Data were collected using daily diaries, focus groups, and hundreds of hours of field work observation by young researchers. One- to 3-hour in-depth interviews exploring sexual experiences on campus were conducted with 151 students. These interviews are the focus of the book. It is a well-written, provocative story brimming with insights for those of us who lack the time to scour social science literature.
“Sexual Citizens” and the SHIFT study confirmed much of what we know. Sexual assault is common and has enduring effects. The study found that 36% of women and 15% of men had experienced unwanted, nonconsensual sexual contact by senior year. Twenty percent of women and 6% of men were rape survivors. Freshman, LGBTQ, and minority students were found at highest risk of assault. SHIFT reaffirmed that abstinence-only education is not a protective factor against college sexual assault, but neither was knowledge of affirmative consent (the practice of “ongoing and explicit” checking-in with partners) which few students ever employed. Encouragingly, students taught refusal skills were less likely to experience sexual assault.
Many of the book’s valuable lessons fall under the umbrella of failures of language and communication. For example, after drinking, they went to his room. She was expecting a social interaction, but with no other place to sit, they sat on his bed where she was coaxed or pressured into a sexual encounter. Afterward, she leaves, and it is never discussed again. One partner desires emotional intimacy, and the other, bragging rights in the fraternity or at the girls’ weekly brunch. Numerous personal stories like these, though at times heart wrenching, provide perspective on the barriers to addressing assault.
Subjects relayed experiences of assault by strangers or friends, and some provided details of their own actions as perpetrators. Stumbling around words and emotions, an avoidance of explicit language stemmed from shame, a fear of personal responsibility, the desire to maintain social cohesion, and concern for potential consequences for the perpetrator. Many subjects were resistant to calling nonconsensual sexual activity rape or even assault. Some who had perpetrated were unaware their behavior may have been experienced as assault, with recognition of this fact dawning during interviews.
This apparent limitation in self-reflective capacity may be in part due to the conceptualization of what assault is. Focus groups identified a discernible difference in how men and women understood assaults, with men believing rapes looked like a woman fighting back and screaming for help ... which is rarely what happens.
Notably absent among the interviewed are any flagrant perpetrators. The methodology section theorizes that individuals who intentionally harmed their peers were unlikely to choose to participate in this study. In addition, the characterization of assailants as “sociopathic predators” is based in a history of racialized imagery that leads us astray from the truth about campus sexual assault. Most assaults do not involve force, and SHIFT data showed 75% of victims knew their assailants. Ultimately, a major aim of the research was to study assault alongside healthy sex to “understand those pivotal moments when encounters change from being sex, to being assault.” Doing this requires understanding the where, how, and why students have sex, a more complicated undertaking than we may think.
In discussing their sexual lives, subjects frequently noted they did not have space to talk about their assaults. Though 81% of students discussed their experiences with someone, friend groups were often overburdened with stories, which minimized the victim’s experience. Furthermore, most had not sought help from the student counseling centers. Students navigating this complex field were frequently doing so in isolation. SHIFT found subjects to be eager to participate; they would often express thankfulness, and a sense of freedom in sharing with researchers. Commonly, students expressly did not want retribution for perpetrators, but simply a place to be heard without challenge. The current legal system precludes that possibility, leaving individuals without the option to confront perpetrators, and perpetrators often not knowing the extent of the damage they caused.
Where can psychiatrists have an impact right now? “Sexual Citizens” identifies four key areas for intervention to work toward a world with less sexual assault. These are:
- Improving diversity, inequality, and power distortions.
- Education about sex and sexual assault.
- Substance use.
- Mental health.
Substance use and mental health are especially relevant for psychiatrists (That substance use contributes to sexual assault is known by approximately ... everybody!). Unwanted sexual contact prior to college (20% of students) increased the odds of experiencing assault during college. Harm reduction strategies should be introduced before college, according to the SHIFT research, particularly in skills-based training on how to say “No” to unwanted sex. Psychiatrists are likely used to asking brief history questions related to sexual assault and rape. “Sexual Citizens” highlights the inadequacy of this blunt language and guides the reader toward a refined knowledge of the language needed to address sexual assault.
Dr. Whisler is a child and adolescent psychiatry fellow at the Stanford (Calif.) University. Dr. Higgins is affiliate associate professor of psychiatry and family medicine at the Medical University of South Carolina, Charleston.
References
1. Hirsch JS et al. Social dimensions of sexual consent among cisgender heterosexual college students: Insights from ethnographic research. J Adolesc Health. 2019 Jan;64(1):26-35. doi: 10.1016/j.jadohealth.2018.06.011.
2. Hirsch JS and Khan S. Sexual citizens: Sex, power, and assault on campus. New York: W.W. Norton & Company, 2020.
Tips for addressing uptick in mental health visits: Primary care providers collaborate, innovate
This growth in the number of patients needing behavioral health–related care is likely driven by multiple factors, including a shortage of mental health care providers, an increasing incidence of psychiatric illness, and destigmatization of mental health in general, suggested Swetha P. Iruku, MD, MPH, associate professor of family medicine and community health at the University of Pennsylvania and Penn Medicine family physician in Philadelphia.
The Centers for Disease Control and Prevention noted that “the COVID-19 pandemic has been associated with mental health challenges related to the morbidity and mortality caused by the disease and to mitigation activities, including the impact of physical distancing and stay-at-home orders,” in a Morbidity and Mortality Weekly Report.
From June 24 to 30, 2020, U.S. adults reported considerably elevated adverse mental health conditions associated with COVID-19, and symptoms of anxiety disorder and depressive disorder climbed during the months of April through June of the same year, compared with the same period in 2019, they wrote.
Even before the pandemic got underway, multiple studies of national data published this year suggested mental issues were on the rise in the United States. For example, the proportion of adult patient visits to primary care providers that addressed mental health concerns rose from 10.7% to 15.9% from 2006 to 2018, according to research published in Health Affairs. Plus, the number and proportion of pediatric acute care hospitalizations because of mental health diagnoses increased significantly between 2009 and 2019, according to a paper published in JAMA.
“I truly believe that we can’t, as primary care physicians, take care of someone’s physical health without also taking care of their mental health,” Dr. Iruku said in an interview. “It’s all intertwined.”
To rise to this challenge, PCPs first need a collaborative mindset, she suggested, as well as familiarity with available resources, both locally and virtually.
This article examines strategies for managing mental illness in primary care, outlines clinical resources, and reviews related educational opportunities.
In addition, clinical pearls are shared by Dr. Iruku and five other clinicians who provide or have provided mental health care to primary care patients or work in close collaboration with a primary care practice, including a clinical psychologist, a nurse practitioner licensed in psychiatric health, a pediatrician, and a licensed clinical social worker.
Build a network
Most of the providers interviewed cited the importance of collaboration in mental health care, particularly for complex cases.
“I would recommend [that primary care providers get] to know the psychiatric providers [in their area],” said Jessica Viton, DNP, FNP, PMHNP, who delivers mental health care through a community-based primary care practice in Colorado which she requested remain anonymous.
Dr. Iruku suggested making an in-person connection first, if possible.
“So much of what we do is ‘see one, do one, teach one,’ so learn a little bit, then go off and trial,” she said. “[It can be valuable] having someone in your back pocket that you can contact in the case of an emergency, or in a situation where you just don’t know how to tackle it.”
Screen for depression and anxiety
William J. Sieber, PhD, a clinical psychologist, director of integrated behavioral health, and professor in the department of family medicine and public health and the department of psychiatry at the University of California, San Diego, said primary care providers should screen all adult patients for depression and anxiety with the Patient Health Questionnaire (PHQ-9) and General Anxiety Disorder Assessment (GAD-7), respectively.
To save time, he suggested a cascading approach.
“In primary care, everybody’s in a hurry,” Dr. Sieber said. “[With the cascading approach,] the first two items [from each questionnaire] are given, and if a person endorses either of those items … then they are asked to complete the other items.”
Jennifer Mullally, MD, a pediatrician at Sanford Health in Fargo, N.D., uses this cascading approach to depression and anxiety screening with all her patients aged 13-18. For younger kids, she screens only those who present with signs or symptoms of mental health issues, or if the parent shares a concern.
This approach differs slightly from U.S. Preventive Services Task Force recommendations, which suggest screening for anxiety in patients aged 8-18 years and depression in patients aged 12-18 years.
Use other screening tools only as needed
Dr. Sieber, the research director for the division of family medicine at UC San Diego, collaborates regularly with primary care providers via hallway consultations, by sharing cases, and through providing oversight of psychiatric care at 13 primary care practices within the UC San Diego network. He recommended against routine screening beyond depression and anxiety in the primary care setting.
“There are a lot of screening tools,” Dr. Sieber said. “It depends on what you’re presented with. The challenge in primary care is you’re going to see all kinds of things. It’s not like running a depression clinic.”
Other than the PHQ-9 and GAD-7, he suggested primary care providers establish familiarity with screening tools for posttraumatic stress disorder and attention-deficit/hyperactivity disorder, noting again that these should be used only when one of the conditions is already suspected.
Dr. Mullally follows a similar approach with her pediatric population. In addition to the GAD-7, she investigates whether a patient has anxiety with the Screen for Child Anxiety Related Disorders (SCARED). For depression, she couples the PHQ-9 with the Columbia Suicide Severity Rating Scale.
While additional screening tools like these are readily available online, Dr. Viton suggested that they should be employed only if the provider is trained to interpret and respond to those findings, and only if they know which tool to use, and when.
For example, she has recently observed PCPs diagnosing adults with ADHD using a three-question test, when in fact a full-length, standardized instrument should be administered by a provider with necessary training.
She also pointed out that bipolar disorder continues to be underdiagnosed, possibly because of providers detecting depression using a questionnaire like the PHQ-9, while failing to inquire about manic episodes.
Leverage online resources
If depression is confirmed, Dr. Iruku often directs the patient to the Mayo Clinic Depression Medication Choice Decision Aid. This website steers patients through medication options based on their answers to a questionnaire. Choices are listed alongside possible adverse effects.
For clinician use, Dr. Iruku recommended The Waco Guide to Psychopharmacology in Primary Care, which aids clinical decision-making for mental illness and substance abuse. The app processes case details to suggest first-, second-, and third-line pharmacotherapies, as well as modifications based on patient needs.
Even with tools like these, however, a referral may be needed.
“[Primary care providers] may not be the best fit for what the patient is looking for, from a mental health or behavioral standpoint,” Dr. Sieber said.
In this case, he encourages patients to visit Psychology Today, a “quite popular portal” that helps patients locate a suitable provider based on location, insurance, driving radius, and mental health concern. This usually generates 10-20 options, Dr. Sieber said, although results can vary.
“It may be discouraging, because maybe only three [providers] pop up based on your criteria, and the closest one is miles away,” he said.
Consider virtual support
If no local psychiatric help is available, Dr. Sieber suggested virtual support, highlighting that “it’s much easier now than it was 3 or 4 years ago” to connect patients with external mental health care.
But this strategy should be reserved for cases of actual need instead of pure convenience, cautioned Dr. Viton, who noted that virtual visits may fail to capture the nuance of an in-person meeting, as body language, mode of dress, and other clues can provide insights into mental health status.
“Occasionally, I think you do have to have an in-person visit, especially when you’re developing a rapport with someone,” Dr. Viton said.
Claire McArdle, a licensed clinical social worker in Fort Collins, Colo., noted that virtual care from an outside provider may also impede the collaboration needed to effectively address mental illness.
In her 11 years in primary care at Associates in Family Medicine, Ms. McArdle had countless interactions with colleagues seeking support when managing a complex case. “I’m coaching providers, front desk staff, and nursing staff on how to interact with patients [with] behavioral health needs,” she said, citing the multitude of nonmedical factors that need to be considered, such as family relationships and patient preferences.
These unscheduled conversations with colleagues throughout the day are impossible to have when sharing a case with an unknown, remote peer.
Ms. McArdle speaks from experience. She recently resigned from Associates in Family Medicine to start her own private therapy practice after her former employer was acquired by VillageMD, a national provider that terminated employment of most other social workers in the practice and began outsourcing mental health care to Mindoula Health, a virtual provider.
Dr. Sieber offered a similar perspective on in-person collaboration as the psychiatric specialist at his center. He routinely offers on-site support for both providers and patients, serving as “another set of eyes and ears” when there is a concern about patient safety or directly managing care when a patient is hospitalized for mental illness.
While virtual solutions may fall short of in-person management, they can offer care at a scale and cost impossible through traditional practice.
This could even be free. Zero-cost, automated software now allows individuals who are uninsured or unable to afford care at least one avenue to manage their mental health concerns.
For example, Bliss is a free, 8-session, interactive online therapy program for depression that was created by the Centre for Interactive Mental Health Solutions. The program offers a tool for monitoring mood and quizzes to test understanding of personal mental health management, among other features.
More advanced programs are emerging as artificial intelligence (AI) enables dialogues between humans and machines. This is the case with Woebot, an app that asks the user about their mood throughout the day, and responds with evidence-based strategies for managing concerns, all for free at press time.
Keep learning
A range of educational options and professional resources are available for primary care providers who would like to improve their knowledge of mental health care. These include formal fellowships in primary care psychiatry/behavioral health integration, free mental health webinars, and various other opportunities.
Eric Eschweiler, DNP, APRN, FNP-C, PHN, completed the University of California, Irvine, Train New Trainers (TNT) Primary Care Psychiatry (PCP) Fellowship in 2016, when he was working as a solo nurse practitioner.
“I was drowning in practice,” said Dr. Eschweiler, director of nursing and public health outreach services at Riverside-San Bernardino County Indian Health, Grand Terrace, Calif., in an interview. “I was a solo NP. There was no physician on site. We were seeing a lot of [individuals with] schizoaffective [disorder] in downtown San Bernardino, the homeless, unhoused – a lot of substance use. I felt I needed to have the skills to be able to treat them effectively. That’s what the fellowship did.”
The skills Dr. Eschweiler learned from participating in his fellowship allowed him to manage more cases of mental illness without need for referral. When a referral was needed for a complex or severe case, he had the confidence to bridge care and collaborate more effectively with psychiatric specialists.
“It was awesome, because we were able to communicate using the same language,” Dr. Eschweiler said of these collaborations. “It’s [about] talking that same language, starting those initial treatments, and then moving forward with specialty care, and vice versa. [Psychiatric specialists] would send me patients that needed medical care because of the types of medications they were taking. And I was then very well aware of those side effects and other issues that might come up from those treatments. So it’s a two-way street.”
Dr. Eschweiler was so impressed by his fellowship that he has since ushered multiple providers through the program since transitioning to an administrative role as director of nursing.
In Fargo, where psychiatric care is sparse and wait times for referral can be months long, Dr. Mullally, like Dr. Eschweiler, knew that she needed more training in mental health.
“I don’t feel like we get enough training in residency,” Dr. Mullally said. “So you do need to look at your options for further CME.”
Out of several CME courses she has taken to further her understanding of pediatric psychiatry, Dr. Mullally recommended The Reach Institute above all others, as their courses involve in-depth discussions and valuable handouts, particularly for medication selection.
“I think that a lot of the other CMEs tend to involve a lot more PowerPoint presentations,” Dr. Mullally said. “And you don’t necessarily leave with a lot of good documents. I still use my Reach handouts. I have them sitting right next to me. I use them every single day.”
Providers interested in The Reach Institute, however, should be prepared to invest both time and money, she added, citing a 2-3 day commitment, and calling it “not cheap.” To overcome these barriers, she suggested that providers get their institution to support their attendance.
For a lighter commitment, Dr. Iruku recommended the American Academy of Family Physicians CME portal, as this offers 13 online, accredited courses covering a range of topics, from adolescent health to substance abuse disorders.
Dr. Sieber suggested that primary care providers join the Collaborative Family Healthcare Association, which aims to integrate physical and behavioral health in routine practice. CFHA, of which he is a member, offers a “bevy of different resources” for interested providers, including a conference in Phoenix this October.
The interviewees disclosed no conflicts of interest.
This growth in the number of patients needing behavioral health–related care is likely driven by multiple factors, including a shortage of mental health care providers, an increasing incidence of psychiatric illness, and destigmatization of mental health in general, suggested Swetha P. Iruku, MD, MPH, associate professor of family medicine and community health at the University of Pennsylvania and Penn Medicine family physician in Philadelphia.
The Centers for Disease Control and Prevention noted that “the COVID-19 pandemic has been associated with mental health challenges related to the morbidity and mortality caused by the disease and to mitigation activities, including the impact of physical distancing and stay-at-home orders,” in a Morbidity and Mortality Weekly Report.
From June 24 to 30, 2020, U.S. adults reported considerably elevated adverse mental health conditions associated with COVID-19, and symptoms of anxiety disorder and depressive disorder climbed during the months of April through June of the same year, compared with the same period in 2019, they wrote.
Even before the pandemic got underway, multiple studies of national data published this year suggested mental issues were on the rise in the United States. For example, the proportion of adult patient visits to primary care providers that addressed mental health concerns rose from 10.7% to 15.9% from 2006 to 2018, according to research published in Health Affairs. Plus, the number and proportion of pediatric acute care hospitalizations because of mental health diagnoses increased significantly between 2009 and 2019, according to a paper published in JAMA.
“I truly believe that we can’t, as primary care physicians, take care of someone’s physical health without also taking care of their mental health,” Dr. Iruku said in an interview. “It’s all intertwined.”
To rise to this challenge, PCPs first need a collaborative mindset, she suggested, as well as familiarity with available resources, both locally and virtually.
This article examines strategies for managing mental illness in primary care, outlines clinical resources, and reviews related educational opportunities.
In addition, clinical pearls are shared by Dr. Iruku and five other clinicians who provide or have provided mental health care to primary care patients or work in close collaboration with a primary care practice, including a clinical psychologist, a nurse practitioner licensed in psychiatric health, a pediatrician, and a licensed clinical social worker.
Build a network
Most of the providers interviewed cited the importance of collaboration in mental health care, particularly for complex cases.
“I would recommend [that primary care providers get] to know the psychiatric providers [in their area],” said Jessica Viton, DNP, FNP, PMHNP, who delivers mental health care through a community-based primary care practice in Colorado which she requested remain anonymous.
Dr. Iruku suggested making an in-person connection first, if possible.
“So much of what we do is ‘see one, do one, teach one,’ so learn a little bit, then go off and trial,” she said. “[It can be valuable] having someone in your back pocket that you can contact in the case of an emergency, or in a situation where you just don’t know how to tackle it.”
Screen for depression and anxiety
William J. Sieber, PhD, a clinical psychologist, director of integrated behavioral health, and professor in the department of family medicine and public health and the department of psychiatry at the University of California, San Diego, said primary care providers should screen all adult patients for depression and anxiety with the Patient Health Questionnaire (PHQ-9) and General Anxiety Disorder Assessment (GAD-7), respectively.
To save time, he suggested a cascading approach.
“In primary care, everybody’s in a hurry,” Dr. Sieber said. “[With the cascading approach,] the first two items [from each questionnaire] are given, and if a person endorses either of those items … then they are asked to complete the other items.”
Jennifer Mullally, MD, a pediatrician at Sanford Health in Fargo, N.D., uses this cascading approach to depression and anxiety screening with all her patients aged 13-18. For younger kids, she screens only those who present with signs or symptoms of mental health issues, or if the parent shares a concern.
This approach differs slightly from U.S. Preventive Services Task Force recommendations, which suggest screening for anxiety in patients aged 8-18 years and depression in patients aged 12-18 years.
Use other screening tools only as needed
Dr. Sieber, the research director for the division of family medicine at UC San Diego, collaborates regularly with primary care providers via hallway consultations, by sharing cases, and through providing oversight of psychiatric care at 13 primary care practices within the UC San Diego network. He recommended against routine screening beyond depression and anxiety in the primary care setting.
“There are a lot of screening tools,” Dr. Sieber said. “It depends on what you’re presented with. The challenge in primary care is you’re going to see all kinds of things. It’s not like running a depression clinic.”
Other than the PHQ-9 and GAD-7, he suggested primary care providers establish familiarity with screening tools for posttraumatic stress disorder and attention-deficit/hyperactivity disorder, noting again that these should be used only when one of the conditions is already suspected.
Dr. Mullally follows a similar approach with her pediatric population. In addition to the GAD-7, she investigates whether a patient has anxiety with the Screen for Child Anxiety Related Disorders (SCARED). For depression, she couples the PHQ-9 with the Columbia Suicide Severity Rating Scale.
While additional screening tools like these are readily available online, Dr. Viton suggested that they should be employed only if the provider is trained to interpret and respond to those findings, and only if they know which tool to use, and when.
For example, she has recently observed PCPs diagnosing adults with ADHD using a three-question test, when in fact a full-length, standardized instrument should be administered by a provider with necessary training.
She also pointed out that bipolar disorder continues to be underdiagnosed, possibly because of providers detecting depression using a questionnaire like the PHQ-9, while failing to inquire about manic episodes.
Leverage online resources
If depression is confirmed, Dr. Iruku often directs the patient to the Mayo Clinic Depression Medication Choice Decision Aid. This website steers patients through medication options based on their answers to a questionnaire. Choices are listed alongside possible adverse effects.
For clinician use, Dr. Iruku recommended The Waco Guide to Psychopharmacology in Primary Care, which aids clinical decision-making for mental illness and substance abuse. The app processes case details to suggest first-, second-, and third-line pharmacotherapies, as well as modifications based on patient needs.
Even with tools like these, however, a referral may be needed.
“[Primary care providers] may not be the best fit for what the patient is looking for, from a mental health or behavioral standpoint,” Dr. Sieber said.
In this case, he encourages patients to visit Psychology Today, a “quite popular portal” that helps patients locate a suitable provider based on location, insurance, driving radius, and mental health concern. This usually generates 10-20 options, Dr. Sieber said, although results can vary.
“It may be discouraging, because maybe only three [providers] pop up based on your criteria, and the closest one is miles away,” he said.
Consider virtual support
If no local psychiatric help is available, Dr. Sieber suggested virtual support, highlighting that “it’s much easier now than it was 3 or 4 years ago” to connect patients with external mental health care.
But this strategy should be reserved for cases of actual need instead of pure convenience, cautioned Dr. Viton, who noted that virtual visits may fail to capture the nuance of an in-person meeting, as body language, mode of dress, and other clues can provide insights into mental health status.
“Occasionally, I think you do have to have an in-person visit, especially when you’re developing a rapport with someone,” Dr. Viton said.
Claire McArdle, a licensed clinical social worker in Fort Collins, Colo., noted that virtual care from an outside provider may also impede the collaboration needed to effectively address mental illness.
In her 11 years in primary care at Associates in Family Medicine, Ms. McArdle had countless interactions with colleagues seeking support when managing a complex case. “I’m coaching providers, front desk staff, and nursing staff on how to interact with patients [with] behavioral health needs,” she said, citing the multitude of nonmedical factors that need to be considered, such as family relationships and patient preferences.
These unscheduled conversations with colleagues throughout the day are impossible to have when sharing a case with an unknown, remote peer.
Ms. McArdle speaks from experience. She recently resigned from Associates in Family Medicine to start her own private therapy practice after her former employer was acquired by VillageMD, a national provider that terminated employment of most other social workers in the practice and began outsourcing mental health care to Mindoula Health, a virtual provider.
Dr. Sieber offered a similar perspective on in-person collaboration as the psychiatric specialist at his center. He routinely offers on-site support for both providers and patients, serving as “another set of eyes and ears” when there is a concern about patient safety or directly managing care when a patient is hospitalized for mental illness.
While virtual solutions may fall short of in-person management, they can offer care at a scale and cost impossible through traditional practice.
This could even be free. Zero-cost, automated software now allows individuals who are uninsured or unable to afford care at least one avenue to manage their mental health concerns.
For example, Bliss is a free, 8-session, interactive online therapy program for depression that was created by the Centre for Interactive Mental Health Solutions. The program offers a tool for monitoring mood and quizzes to test understanding of personal mental health management, among other features.
More advanced programs are emerging as artificial intelligence (AI) enables dialogues between humans and machines. This is the case with Woebot, an app that asks the user about their mood throughout the day, and responds with evidence-based strategies for managing concerns, all for free at press time.
Keep learning
A range of educational options and professional resources are available for primary care providers who would like to improve their knowledge of mental health care. These include formal fellowships in primary care psychiatry/behavioral health integration, free mental health webinars, and various other opportunities.
Eric Eschweiler, DNP, APRN, FNP-C, PHN, completed the University of California, Irvine, Train New Trainers (TNT) Primary Care Psychiatry (PCP) Fellowship in 2016, when he was working as a solo nurse practitioner.
“I was drowning in practice,” said Dr. Eschweiler, director of nursing and public health outreach services at Riverside-San Bernardino County Indian Health, Grand Terrace, Calif., in an interview. “I was a solo NP. There was no physician on site. We were seeing a lot of [individuals with] schizoaffective [disorder] in downtown San Bernardino, the homeless, unhoused – a lot of substance use. I felt I needed to have the skills to be able to treat them effectively. That’s what the fellowship did.”
The skills Dr. Eschweiler learned from participating in his fellowship allowed him to manage more cases of mental illness without need for referral. When a referral was needed for a complex or severe case, he had the confidence to bridge care and collaborate more effectively with psychiatric specialists.
“It was awesome, because we were able to communicate using the same language,” Dr. Eschweiler said of these collaborations. “It’s [about] talking that same language, starting those initial treatments, and then moving forward with specialty care, and vice versa. [Psychiatric specialists] would send me patients that needed medical care because of the types of medications they were taking. And I was then very well aware of those side effects and other issues that might come up from those treatments. So it’s a two-way street.”
Dr. Eschweiler was so impressed by his fellowship that he has since ushered multiple providers through the program since transitioning to an administrative role as director of nursing.
In Fargo, where psychiatric care is sparse and wait times for referral can be months long, Dr. Mullally, like Dr. Eschweiler, knew that she needed more training in mental health.
“I don’t feel like we get enough training in residency,” Dr. Mullally said. “So you do need to look at your options for further CME.”
Out of several CME courses she has taken to further her understanding of pediatric psychiatry, Dr. Mullally recommended The Reach Institute above all others, as their courses involve in-depth discussions and valuable handouts, particularly for medication selection.
“I think that a lot of the other CMEs tend to involve a lot more PowerPoint presentations,” Dr. Mullally said. “And you don’t necessarily leave with a lot of good documents. I still use my Reach handouts. I have them sitting right next to me. I use them every single day.”
Providers interested in The Reach Institute, however, should be prepared to invest both time and money, she added, citing a 2-3 day commitment, and calling it “not cheap.” To overcome these barriers, she suggested that providers get their institution to support their attendance.
For a lighter commitment, Dr. Iruku recommended the American Academy of Family Physicians CME portal, as this offers 13 online, accredited courses covering a range of topics, from adolescent health to substance abuse disorders.
Dr. Sieber suggested that primary care providers join the Collaborative Family Healthcare Association, which aims to integrate physical and behavioral health in routine practice. CFHA, of which he is a member, offers a “bevy of different resources” for interested providers, including a conference in Phoenix this October.
The interviewees disclosed no conflicts of interest.
This growth in the number of patients needing behavioral health–related care is likely driven by multiple factors, including a shortage of mental health care providers, an increasing incidence of psychiatric illness, and destigmatization of mental health in general, suggested Swetha P. Iruku, MD, MPH, associate professor of family medicine and community health at the University of Pennsylvania and Penn Medicine family physician in Philadelphia.
The Centers for Disease Control and Prevention noted that “the COVID-19 pandemic has been associated with mental health challenges related to the morbidity and mortality caused by the disease and to mitigation activities, including the impact of physical distancing and stay-at-home orders,” in a Morbidity and Mortality Weekly Report.
From June 24 to 30, 2020, U.S. adults reported considerably elevated adverse mental health conditions associated with COVID-19, and symptoms of anxiety disorder and depressive disorder climbed during the months of April through June of the same year, compared with the same period in 2019, they wrote.
Even before the pandemic got underway, multiple studies of national data published this year suggested mental issues were on the rise in the United States. For example, the proportion of adult patient visits to primary care providers that addressed mental health concerns rose from 10.7% to 15.9% from 2006 to 2018, according to research published in Health Affairs. Plus, the number and proportion of pediatric acute care hospitalizations because of mental health diagnoses increased significantly between 2009 and 2019, according to a paper published in JAMA.
“I truly believe that we can’t, as primary care physicians, take care of someone’s physical health without also taking care of their mental health,” Dr. Iruku said in an interview. “It’s all intertwined.”
To rise to this challenge, PCPs first need a collaborative mindset, she suggested, as well as familiarity with available resources, both locally and virtually.
This article examines strategies for managing mental illness in primary care, outlines clinical resources, and reviews related educational opportunities.
In addition, clinical pearls are shared by Dr. Iruku and five other clinicians who provide or have provided mental health care to primary care patients or work in close collaboration with a primary care practice, including a clinical psychologist, a nurse practitioner licensed in psychiatric health, a pediatrician, and a licensed clinical social worker.
Build a network
Most of the providers interviewed cited the importance of collaboration in mental health care, particularly for complex cases.
“I would recommend [that primary care providers get] to know the psychiatric providers [in their area],” said Jessica Viton, DNP, FNP, PMHNP, who delivers mental health care through a community-based primary care practice in Colorado which she requested remain anonymous.
Dr. Iruku suggested making an in-person connection first, if possible.
“So much of what we do is ‘see one, do one, teach one,’ so learn a little bit, then go off and trial,” she said. “[It can be valuable] having someone in your back pocket that you can contact in the case of an emergency, or in a situation where you just don’t know how to tackle it.”
Screen for depression and anxiety
William J. Sieber, PhD, a clinical psychologist, director of integrated behavioral health, and professor in the department of family medicine and public health and the department of psychiatry at the University of California, San Diego, said primary care providers should screen all adult patients for depression and anxiety with the Patient Health Questionnaire (PHQ-9) and General Anxiety Disorder Assessment (GAD-7), respectively.
To save time, he suggested a cascading approach.
“In primary care, everybody’s in a hurry,” Dr. Sieber said. “[With the cascading approach,] the first two items [from each questionnaire] are given, and if a person endorses either of those items … then they are asked to complete the other items.”
Jennifer Mullally, MD, a pediatrician at Sanford Health in Fargo, N.D., uses this cascading approach to depression and anxiety screening with all her patients aged 13-18. For younger kids, she screens only those who present with signs or symptoms of mental health issues, or if the parent shares a concern.
This approach differs slightly from U.S. Preventive Services Task Force recommendations, which suggest screening for anxiety in patients aged 8-18 years and depression in patients aged 12-18 years.
Use other screening tools only as needed
Dr. Sieber, the research director for the division of family medicine at UC San Diego, collaborates regularly with primary care providers via hallway consultations, by sharing cases, and through providing oversight of psychiatric care at 13 primary care practices within the UC San Diego network. He recommended against routine screening beyond depression and anxiety in the primary care setting.
“There are a lot of screening tools,” Dr. Sieber said. “It depends on what you’re presented with. The challenge in primary care is you’re going to see all kinds of things. It’s not like running a depression clinic.”
Other than the PHQ-9 and GAD-7, he suggested primary care providers establish familiarity with screening tools for posttraumatic stress disorder and attention-deficit/hyperactivity disorder, noting again that these should be used only when one of the conditions is already suspected.
Dr. Mullally follows a similar approach with her pediatric population. In addition to the GAD-7, she investigates whether a patient has anxiety with the Screen for Child Anxiety Related Disorders (SCARED). For depression, she couples the PHQ-9 with the Columbia Suicide Severity Rating Scale.
While additional screening tools like these are readily available online, Dr. Viton suggested that they should be employed only if the provider is trained to interpret and respond to those findings, and only if they know which tool to use, and when.
For example, she has recently observed PCPs diagnosing adults with ADHD using a three-question test, when in fact a full-length, standardized instrument should be administered by a provider with necessary training.
She also pointed out that bipolar disorder continues to be underdiagnosed, possibly because of providers detecting depression using a questionnaire like the PHQ-9, while failing to inquire about manic episodes.
Leverage online resources
If depression is confirmed, Dr. Iruku often directs the patient to the Mayo Clinic Depression Medication Choice Decision Aid. This website steers patients through medication options based on their answers to a questionnaire. Choices are listed alongside possible adverse effects.
For clinician use, Dr. Iruku recommended The Waco Guide to Psychopharmacology in Primary Care, which aids clinical decision-making for mental illness and substance abuse. The app processes case details to suggest first-, second-, and third-line pharmacotherapies, as well as modifications based on patient needs.
Even with tools like these, however, a referral may be needed.
“[Primary care providers] may not be the best fit for what the patient is looking for, from a mental health or behavioral standpoint,” Dr. Sieber said.
In this case, he encourages patients to visit Psychology Today, a “quite popular portal” that helps patients locate a suitable provider based on location, insurance, driving radius, and mental health concern. This usually generates 10-20 options, Dr. Sieber said, although results can vary.
“It may be discouraging, because maybe only three [providers] pop up based on your criteria, and the closest one is miles away,” he said.
Consider virtual support
If no local psychiatric help is available, Dr. Sieber suggested virtual support, highlighting that “it’s much easier now than it was 3 or 4 years ago” to connect patients with external mental health care.
But this strategy should be reserved for cases of actual need instead of pure convenience, cautioned Dr. Viton, who noted that virtual visits may fail to capture the nuance of an in-person meeting, as body language, mode of dress, and other clues can provide insights into mental health status.
“Occasionally, I think you do have to have an in-person visit, especially when you’re developing a rapport with someone,” Dr. Viton said.
Claire McArdle, a licensed clinical social worker in Fort Collins, Colo., noted that virtual care from an outside provider may also impede the collaboration needed to effectively address mental illness.
In her 11 years in primary care at Associates in Family Medicine, Ms. McArdle had countless interactions with colleagues seeking support when managing a complex case. “I’m coaching providers, front desk staff, and nursing staff on how to interact with patients [with] behavioral health needs,” she said, citing the multitude of nonmedical factors that need to be considered, such as family relationships and patient preferences.
These unscheduled conversations with colleagues throughout the day are impossible to have when sharing a case with an unknown, remote peer.
Ms. McArdle speaks from experience. She recently resigned from Associates in Family Medicine to start her own private therapy practice after her former employer was acquired by VillageMD, a national provider that terminated employment of most other social workers in the practice and began outsourcing mental health care to Mindoula Health, a virtual provider.
Dr. Sieber offered a similar perspective on in-person collaboration as the psychiatric specialist at his center. He routinely offers on-site support for both providers and patients, serving as “another set of eyes and ears” when there is a concern about patient safety or directly managing care when a patient is hospitalized for mental illness.
While virtual solutions may fall short of in-person management, they can offer care at a scale and cost impossible through traditional practice.
This could even be free. Zero-cost, automated software now allows individuals who are uninsured or unable to afford care at least one avenue to manage their mental health concerns.
For example, Bliss is a free, 8-session, interactive online therapy program for depression that was created by the Centre for Interactive Mental Health Solutions. The program offers a tool for monitoring mood and quizzes to test understanding of personal mental health management, among other features.
More advanced programs are emerging as artificial intelligence (AI) enables dialogues between humans and machines. This is the case with Woebot, an app that asks the user about their mood throughout the day, and responds with evidence-based strategies for managing concerns, all for free at press time.
Keep learning
A range of educational options and professional resources are available for primary care providers who would like to improve their knowledge of mental health care. These include formal fellowships in primary care psychiatry/behavioral health integration, free mental health webinars, and various other opportunities.
Eric Eschweiler, DNP, APRN, FNP-C, PHN, completed the University of California, Irvine, Train New Trainers (TNT) Primary Care Psychiatry (PCP) Fellowship in 2016, when he was working as a solo nurse practitioner.
“I was drowning in practice,” said Dr. Eschweiler, director of nursing and public health outreach services at Riverside-San Bernardino County Indian Health, Grand Terrace, Calif., in an interview. “I was a solo NP. There was no physician on site. We were seeing a lot of [individuals with] schizoaffective [disorder] in downtown San Bernardino, the homeless, unhoused – a lot of substance use. I felt I needed to have the skills to be able to treat them effectively. That’s what the fellowship did.”
The skills Dr. Eschweiler learned from participating in his fellowship allowed him to manage more cases of mental illness without need for referral. When a referral was needed for a complex or severe case, he had the confidence to bridge care and collaborate more effectively with psychiatric specialists.
“It was awesome, because we were able to communicate using the same language,” Dr. Eschweiler said of these collaborations. “It’s [about] talking that same language, starting those initial treatments, and then moving forward with specialty care, and vice versa. [Psychiatric specialists] would send me patients that needed medical care because of the types of medications they were taking. And I was then very well aware of those side effects and other issues that might come up from those treatments. So it’s a two-way street.”
Dr. Eschweiler was so impressed by his fellowship that he has since ushered multiple providers through the program since transitioning to an administrative role as director of nursing.
In Fargo, where psychiatric care is sparse and wait times for referral can be months long, Dr. Mullally, like Dr. Eschweiler, knew that she needed more training in mental health.
“I don’t feel like we get enough training in residency,” Dr. Mullally said. “So you do need to look at your options for further CME.”
Out of several CME courses she has taken to further her understanding of pediatric psychiatry, Dr. Mullally recommended The Reach Institute above all others, as their courses involve in-depth discussions and valuable handouts, particularly for medication selection.
“I think that a lot of the other CMEs tend to involve a lot more PowerPoint presentations,” Dr. Mullally said. “And you don’t necessarily leave with a lot of good documents. I still use my Reach handouts. I have them sitting right next to me. I use them every single day.”
Providers interested in The Reach Institute, however, should be prepared to invest both time and money, she added, citing a 2-3 day commitment, and calling it “not cheap.” To overcome these barriers, she suggested that providers get their institution to support their attendance.
For a lighter commitment, Dr. Iruku recommended the American Academy of Family Physicians CME portal, as this offers 13 online, accredited courses covering a range of topics, from adolescent health to substance abuse disorders.
Dr. Sieber suggested that primary care providers join the Collaborative Family Healthcare Association, which aims to integrate physical and behavioral health in routine practice. CFHA, of which he is a member, offers a “bevy of different resources” for interested providers, including a conference in Phoenix this October.
The interviewees disclosed no conflicts of interest.
Altered gut bacteria a biomarker of preclinical Alzheimer’s?
The findings open up the possibility of analyzing the gut microbiome to identify individuals at a higher risk for dementia and perhaps designing microbiome-altering preventive treatments to help stave off cognitive decline, researchers noted.
Study investigator Gautam Dantas, PhD, cautioned that it’s not known whether the gut is influencing the brain, or the brain is influencing the gut, “but this association is valuable to know in either case.
“It could be that the changes in the gut microbiome are just a readout of pathological changes in the brain. The other alternative is that the gut microbiome is contributing to AD, in which case, altering the gut microbiome with probiotics or fecal transfers might help change the course of the disease,” Dr. Dantas, Washington University, St. Louis, said in a news release.
The study was published online in Science Translational Medicine.
Stool test?
Multiple lines of evidence suggest a role for gut microbes in the evolution of AD pathogenesis. However, less is known about gut microbiome changes in the preclinical (presymptomatic) phase of AD.
To investigate, Dr. Dantas and colleagues studied 164 cognitively normal adults, 49 of whom had biomarker evidence of preclinical AD.
After the researchers accounted for clinical covariates and diet, those with preclinical AD had distinct gut microbial taxonomic profiles compared with their healthy controls.
The observed microbiome features correlated with amyloid and tau but not neurodegeneration biomarkers, “suggesting that the gut microbial community changes early in the disease process,” the researchers suggested.
They identified specific taxa that were associated with preclinical AD and including these microbiome features improved the accuracy, sensitivity, and specificity of machine learning classifiers for predicting preclinical AD status.
The findings suggest “markers in the stool might complement early screening measures for preclinical AD,” the researchers noted.
“The nice thing about using the gut microbiome as a screening tool is its simplicity and ease,” Beau Ances, MD, PhD, professor of neurology, at Washington University, St. Louis, said in the release.
“One day, individuals may be able to provide a stool sample and find out if they are at increased risk for developing AD. It would be much easier and less invasive and more accessible for a large proportion of the population, especially underrepresented groups, compared to brain scans or spinal taps,” Dr. Ances added.
The researchers have launched a 5-year follow-up study designed to help determine whether the differences in the gut microbiome are a cause or a result of the brain changes seen in early AD.
Caveats, cautionary notes
In a comment, Claire Sexton, DPhil, Alzheimer’s Association senior director of scientific programs and outreach, cautioned that the study design means that it’s “not possible to prove one thing causes another. What it can show is that two or more aspects are in some way related, thus setting the stage for further research.”
Dr. Sexton noted that though the authors accounted for a number of variables in their models, including age, sex, race, education, body mass index, hypertension, and diabetes, and observed no differences in intake of any major nutrient group, “it’s still not possible to rule out that additional factors beyond the variations in gut microbiome contributed to the changes in brain markers of Alzheimer’s.”
Dr. Sexton also noted that the study population is not representative of all people living with AD, with the vast majority of those with preclinical AD in the study being White.
“If these findings are replicated and confirmed in study groups that are representative of our communities, it is possible that gut microbiome signatures could be a further addition to the suite of diagnostic tools employed in certain settings,” Dr. Sexton said.
This research was supported by the Infection Disease Society of America Foundation, the National Institute on Aging, the Brennan Fund and the Paula and Rodger Riney Foundation. Dr. Dantas, Dr. Ances and Dr. Sexton have no relevant disclosures.
A version of this article first appeared on Medscape.com.
The findings open up the possibility of analyzing the gut microbiome to identify individuals at a higher risk for dementia and perhaps designing microbiome-altering preventive treatments to help stave off cognitive decline, researchers noted.
Study investigator Gautam Dantas, PhD, cautioned that it’s not known whether the gut is influencing the brain, or the brain is influencing the gut, “but this association is valuable to know in either case.
“It could be that the changes in the gut microbiome are just a readout of pathological changes in the brain. The other alternative is that the gut microbiome is contributing to AD, in which case, altering the gut microbiome with probiotics or fecal transfers might help change the course of the disease,” Dr. Dantas, Washington University, St. Louis, said in a news release.
The study was published online in Science Translational Medicine.
Stool test?
Multiple lines of evidence suggest a role for gut microbes in the evolution of AD pathogenesis. However, less is known about gut microbiome changes in the preclinical (presymptomatic) phase of AD.
To investigate, Dr. Dantas and colleagues studied 164 cognitively normal adults, 49 of whom had biomarker evidence of preclinical AD.
After the researchers accounted for clinical covariates and diet, those with preclinical AD had distinct gut microbial taxonomic profiles compared with their healthy controls.
The observed microbiome features correlated with amyloid and tau but not neurodegeneration biomarkers, “suggesting that the gut microbial community changes early in the disease process,” the researchers suggested.
They identified specific taxa that were associated with preclinical AD and including these microbiome features improved the accuracy, sensitivity, and specificity of machine learning classifiers for predicting preclinical AD status.
The findings suggest “markers in the stool might complement early screening measures for preclinical AD,” the researchers noted.
“The nice thing about using the gut microbiome as a screening tool is its simplicity and ease,” Beau Ances, MD, PhD, professor of neurology, at Washington University, St. Louis, said in the release.
“One day, individuals may be able to provide a stool sample and find out if they are at increased risk for developing AD. It would be much easier and less invasive and more accessible for a large proportion of the population, especially underrepresented groups, compared to brain scans or spinal taps,” Dr. Ances added.
The researchers have launched a 5-year follow-up study designed to help determine whether the differences in the gut microbiome are a cause or a result of the brain changes seen in early AD.
Caveats, cautionary notes
In a comment, Claire Sexton, DPhil, Alzheimer’s Association senior director of scientific programs and outreach, cautioned that the study design means that it’s “not possible to prove one thing causes another. What it can show is that two or more aspects are in some way related, thus setting the stage for further research.”
Dr. Sexton noted that though the authors accounted for a number of variables in their models, including age, sex, race, education, body mass index, hypertension, and diabetes, and observed no differences in intake of any major nutrient group, “it’s still not possible to rule out that additional factors beyond the variations in gut microbiome contributed to the changes in brain markers of Alzheimer’s.”
Dr. Sexton also noted that the study population is not representative of all people living with AD, with the vast majority of those with preclinical AD in the study being White.
“If these findings are replicated and confirmed in study groups that are representative of our communities, it is possible that gut microbiome signatures could be a further addition to the suite of diagnostic tools employed in certain settings,” Dr. Sexton said.
This research was supported by the Infection Disease Society of America Foundation, the National Institute on Aging, the Brennan Fund and the Paula and Rodger Riney Foundation. Dr. Dantas, Dr. Ances and Dr. Sexton have no relevant disclosures.
A version of this article first appeared on Medscape.com.
The findings open up the possibility of analyzing the gut microbiome to identify individuals at a higher risk for dementia and perhaps designing microbiome-altering preventive treatments to help stave off cognitive decline, researchers noted.
Study investigator Gautam Dantas, PhD, cautioned that it’s not known whether the gut is influencing the brain, or the brain is influencing the gut, “but this association is valuable to know in either case.
“It could be that the changes in the gut microbiome are just a readout of pathological changes in the brain. The other alternative is that the gut microbiome is contributing to AD, in which case, altering the gut microbiome with probiotics or fecal transfers might help change the course of the disease,” Dr. Dantas, Washington University, St. Louis, said in a news release.
The study was published online in Science Translational Medicine.
Stool test?
Multiple lines of evidence suggest a role for gut microbes in the evolution of AD pathogenesis. However, less is known about gut microbiome changes in the preclinical (presymptomatic) phase of AD.
To investigate, Dr. Dantas and colleagues studied 164 cognitively normal adults, 49 of whom had biomarker evidence of preclinical AD.
After the researchers accounted for clinical covariates and diet, those with preclinical AD had distinct gut microbial taxonomic profiles compared with their healthy controls.
The observed microbiome features correlated with amyloid and tau but not neurodegeneration biomarkers, “suggesting that the gut microbial community changes early in the disease process,” the researchers suggested.
They identified specific taxa that were associated with preclinical AD and including these microbiome features improved the accuracy, sensitivity, and specificity of machine learning classifiers for predicting preclinical AD status.
The findings suggest “markers in the stool might complement early screening measures for preclinical AD,” the researchers noted.
“The nice thing about using the gut microbiome as a screening tool is its simplicity and ease,” Beau Ances, MD, PhD, professor of neurology, at Washington University, St. Louis, said in the release.
“One day, individuals may be able to provide a stool sample and find out if they are at increased risk for developing AD. It would be much easier and less invasive and more accessible for a large proportion of the population, especially underrepresented groups, compared to brain scans or spinal taps,” Dr. Ances added.
The researchers have launched a 5-year follow-up study designed to help determine whether the differences in the gut microbiome are a cause or a result of the brain changes seen in early AD.
Caveats, cautionary notes
In a comment, Claire Sexton, DPhil, Alzheimer’s Association senior director of scientific programs and outreach, cautioned that the study design means that it’s “not possible to prove one thing causes another. What it can show is that two or more aspects are in some way related, thus setting the stage for further research.”
Dr. Sexton noted that though the authors accounted for a number of variables in their models, including age, sex, race, education, body mass index, hypertension, and diabetes, and observed no differences in intake of any major nutrient group, “it’s still not possible to rule out that additional factors beyond the variations in gut microbiome contributed to the changes in brain markers of Alzheimer’s.”
Dr. Sexton also noted that the study population is not representative of all people living with AD, with the vast majority of those with preclinical AD in the study being White.
“If these findings are replicated and confirmed in study groups that are representative of our communities, it is possible that gut microbiome signatures could be a further addition to the suite of diagnostic tools employed in certain settings,” Dr. Sexton said.
This research was supported by the Infection Disease Society of America Foundation, the National Institute on Aging, the Brennan Fund and the Paula and Rodger Riney Foundation. Dr. Dantas, Dr. Ances and Dr. Sexton have no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM SCIENCE TRANSLATIONAL MEDICINE
Probiotics an effective adjunct to antidepressants for major depression
By the end of the 8-week pilot study, participants who had an incomplete response to antidepressants prior to taking probiotics scored better on measures of anxiety and depression versus placebo.
“This was a pilot study, designed as an initial exploration of whether improving gut health with probiotics could act as a new pathway for supporting mood and mental health,” study investigator Viktoriya Nikolova, PhD, Institute of Psychiatry, Psychology and Neuroscience at King’s College London, said in an interview.
“While very promising and exciting, our findings are only the first step, and larger trials are needed,” she noted.
The findings were published online in JAMA Psychiatry.
Gut-brain axis
It is estimated that up to 60% of people taking antidepressants for major depressive disorder (MDD) do not achieve full response.
With an eye on the so-called gut-brain axis as a treatment target for depression, the researchers conducted a meta-analysis of seven randomized controlled trials (RCT) in 2021 and found that probiotics appeared effective in reducing depressive symptoms when taken alongside antidepressants. The studies in this meta-analysis either reported poor adherence rates or did not investigate how well study participants tolerated probiotics.
To further investigate, Dr. Nikolova and team launched a pilot RCT by recruiting study participants from primary and secondary health care services, and through general advertising in London. Data were collected from September 2019 to May 2022.
They included 49 adults diagnosed with MDD with an incomplete antidepressant response, indicated by a score of greater than 13 on the Hamilton Depression Rating Scale-17 (HAMD-17).
Half of the participants were randomly assigned to receive a widely available, proprietary, 14-strain blend probiotic supplement, and half received placebo. Both groups took their study drug four times per day during the 8-week trial.
At baseline, 4 weeks, and 8 weeks, investigators assessed the participants for depression with the HAMD-17, the Inventory of Depressive Symptomatology (IDS) Self-Report, and anxiety with the Hamilton Anxiety Rating Scale (HAMA).
The majority of participants (80%) were female with a mean age of 32 years. Adherence was high, with 97% of the doses taken as required, and no adverse events were reported.
Standardized effect sizes from linear mixed models demonstrated that, when compared with the placebo group, the probiotic group had more improvement in depressive symptoms according to the HAMD-17 (week 4: SES, 0.70; 95% confidence interval, 0.01-0.98) and IDS Self Report (week 8: SES, 0.64; 95% CI, 0.03-0.87).
When compared with the placebo group, the probiotic group also experienced greater improvements in anxiety symptoms according to the HAMA (week 4: SES, 0.67; 95% CI, 0-0.95; week 8: SES, 0.79; 95% CI, 0.06-1.05).
Dr. Nikolova said a large follow-up trial is planned to further confirm the results.
Nutritional psychiatrist Drew Ramsey, MD, author of Eat to Beat Depression and Anxiety and assistant clinical professor of psychiatry at Columbia University, New York, said in an interview: “This randomized clinical trial adds to the considerable evidence that food choices impact depression outcomes.”
He further noted that, “in nutritional psychiatry, we recommend eating fermented foods as they have been shown to improve microbiome diversity and decrease markers of inflammation.”
Dr. Ramsey noted that the RCT used the equivalent colony-forming unit of a “single serving of kombucha.”
“In our clinical group and our nutritional psychiatry course for clinicians, we recommend fermented foods over probiotics as this is the most sustainable, evidence-based way to improve microbiome diversity,” said Dr. Ramsey, citing recent research by Gardner and colleagues at Stanford (Calif.) University.
“This is an industry-funded trial that adds to the evidence base but should be interpreted by patients and clinicians as promoting consumption of more kefir, kimchi, and kombucha, not that patients should take probiotics,” he said.
A key place for probiotics in mental health
Commenting on the study, Uma Naidoo, MD, said: “As I shared throughout my first book, This is Your Brain on Food, there is a real place for the use of probiotics in mental health, including the importance of the gut-brain connection.”
Dr. Naidoo is the director of nutritional and metabolic psychiatry at Massachusetts General Hospital and of nutritional psychiatry at the MGH Academy, both in Boston.
She noted that, when a person stops using a probiotic after trying it out, the positive changes in the gut are reversed, so “remaining consistent in taking the probiotic is important if you have found it helpful for your mood.”
Dr. Naidoo added that “each person’s gut microbiome is so unique that it is likely not every human being will have the same reaction to a probiotic.”
“Eating foods with live probiotics may also benefit gut health and, therefore, mood,” she said. The same goes with eating fermented foods with live active cultures.”
The study was funded by a Medical Research Council Industrial CASE PhD Studentship with ADM Protexin (supplier of the probiotics) as the industry partner and additional support from Freya Green. Dr. Nikolova has received grants from the Medical Research Council and ADM Protexin during the conduct of the study as well as personal fees from Janssen outside the submitted work.
A version of this article first appeared on Medscape.com.
By the end of the 8-week pilot study, participants who had an incomplete response to antidepressants prior to taking probiotics scored better on measures of anxiety and depression versus placebo.
“This was a pilot study, designed as an initial exploration of whether improving gut health with probiotics could act as a new pathway for supporting mood and mental health,” study investigator Viktoriya Nikolova, PhD, Institute of Psychiatry, Psychology and Neuroscience at King’s College London, said in an interview.
“While very promising and exciting, our findings are only the first step, and larger trials are needed,” she noted.
The findings were published online in JAMA Psychiatry.
Gut-brain axis
It is estimated that up to 60% of people taking antidepressants for major depressive disorder (MDD) do not achieve full response.
With an eye on the so-called gut-brain axis as a treatment target for depression, the researchers conducted a meta-analysis of seven randomized controlled trials (RCT) in 2021 and found that probiotics appeared effective in reducing depressive symptoms when taken alongside antidepressants. The studies in this meta-analysis either reported poor adherence rates or did not investigate how well study participants tolerated probiotics.
To further investigate, Dr. Nikolova and team launched a pilot RCT by recruiting study participants from primary and secondary health care services, and through general advertising in London. Data were collected from September 2019 to May 2022.
They included 49 adults diagnosed with MDD with an incomplete antidepressant response, indicated by a score of greater than 13 on the Hamilton Depression Rating Scale-17 (HAMD-17).
Half of the participants were randomly assigned to receive a widely available, proprietary, 14-strain blend probiotic supplement, and half received placebo. Both groups took their study drug four times per day during the 8-week trial.
At baseline, 4 weeks, and 8 weeks, investigators assessed the participants for depression with the HAMD-17, the Inventory of Depressive Symptomatology (IDS) Self-Report, and anxiety with the Hamilton Anxiety Rating Scale (HAMA).
The majority of participants (80%) were female with a mean age of 32 years. Adherence was high, with 97% of the doses taken as required, and no adverse events were reported.
Standardized effect sizes from linear mixed models demonstrated that, when compared with the placebo group, the probiotic group had more improvement in depressive symptoms according to the HAMD-17 (week 4: SES, 0.70; 95% confidence interval, 0.01-0.98) and IDS Self Report (week 8: SES, 0.64; 95% CI, 0.03-0.87).
When compared with the placebo group, the probiotic group also experienced greater improvements in anxiety symptoms according to the HAMA (week 4: SES, 0.67; 95% CI, 0-0.95; week 8: SES, 0.79; 95% CI, 0.06-1.05).
Dr. Nikolova said a large follow-up trial is planned to further confirm the results.
Nutritional psychiatrist Drew Ramsey, MD, author of Eat to Beat Depression and Anxiety and assistant clinical professor of psychiatry at Columbia University, New York, said in an interview: “This randomized clinical trial adds to the considerable evidence that food choices impact depression outcomes.”
He further noted that, “in nutritional psychiatry, we recommend eating fermented foods as they have been shown to improve microbiome diversity and decrease markers of inflammation.”
Dr. Ramsey noted that the RCT used the equivalent colony-forming unit of a “single serving of kombucha.”
“In our clinical group and our nutritional psychiatry course for clinicians, we recommend fermented foods over probiotics as this is the most sustainable, evidence-based way to improve microbiome diversity,” said Dr. Ramsey, citing recent research by Gardner and colleagues at Stanford (Calif.) University.
“This is an industry-funded trial that adds to the evidence base but should be interpreted by patients and clinicians as promoting consumption of more kefir, kimchi, and kombucha, not that patients should take probiotics,” he said.
A key place for probiotics in mental health
Commenting on the study, Uma Naidoo, MD, said: “As I shared throughout my first book, This is Your Brain on Food, there is a real place for the use of probiotics in mental health, including the importance of the gut-brain connection.”
Dr. Naidoo is the director of nutritional and metabolic psychiatry at Massachusetts General Hospital and of nutritional psychiatry at the MGH Academy, both in Boston.
She noted that, when a person stops using a probiotic after trying it out, the positive changes in the gut are reversed, so “remaining consistent in taking the probiotic is important if you have found it helpful for your mood.”
Dr. Naidoo added that “each person’s gut microbiome is so unique that it is likely not every human being will have the same reaction to a probiotic.”
“Eating foods with live probiotics may also benefit gut health and, therefore, mood,” she said. The same goes with eating fermented foods with live active cultures.”
The study was funded by a Medical Research Council Industrial CASE PhD Studentship with ADM Protexin (supplier of the probiotics) as the industry partner and additional support from Freya Green. Dr. Nikolova has received grants from the Medical Research Council and ADM Protexin during the conduct of the study as well as personal fees from Janssen outside the submitted work.
A version of this article first appeared on Medscape.com.
By the end of the 8-week pilot study, participants who had an incomplete response to antidepressants prior to taking probiotics scored better on measures of anxiety and depression versus placebo.
“This was a pilot study, designed as an initial exploration of whether improving gut health with probiotics could act as a new pathway for supporting mood and mental health,” study investigator Viktoriya Nikolova, PhD, Institute of Psychiatry, Psychology and Neuroscience at King’s College London, said in an interview.
“While very promising and exciting, our findings are only the first step, and larger trials are needed,” she noted.
The findings were published online in JAMA Psychiatry.
Gut-brain axis
It is estimated that up to 60% of people taking antidepressants for major depressive disorder (MDD) do not achieve full response.
With an eye on the so-called gut-brain axis as a treatment target for depression, the researchers conducted a meta-analysis of seven randomized controlled trials (RCT) in 2021 and found that probiotics appeared effective in reducing depressive symptoms when taken alongside antidepressants. The studies in this meta-analysis either reported poor adherence rates or did not investigate how well study participants tolerated probiotics.
To further investigate, Dr. Nikolova and team launched a pilot RCT by recruiting study participants from primary and secondary health care services, and through general advertising in London. Data were collected from September 2019 to May 2022.
They included 49 adults diagnosed with MDD with an incomplete antidepressant response, indicated by a score of greater than 13 on the Hamilton Depression Rating Scale-17 (HAMD-17).
Half of the participants were randomly assigned to receive a widely available, proprietary, 14-strain blend probiotic supplement, and half received placebo. Both groups took their study drug four times per day during the 8-week trial.
At baseline, 4 weeks, and 8 weeks, investigators assessed the participants for depression with the HAMD-17, the Inventory of Depressive Symptomatology (IDS) Self-Report, and anxiety with the Hamilton Anxiety Rating Scale (HAMA).
The majority of participants (80%) were female with a mean age of 32 years. Adherence was high, with 97% of the doses taken as required, and no adverse events were reported.
Standardized effect sizes from linear mixed models demonstrated that, when compared with the placebo group, the probiotic group had more improvement in depressive symptoms according to the HAMD-17 (week 4: SES, 0.70; 95% confidence interval, 0.01-0.98) and IDS Self Report (week 8: SES, 0.64; 95% CI, 0.03-0.87).
When compared with the placebo group, the probiotic group also experienced greater improvements in anxiety symptoms according to the HAMA (week 4: SES, 0.67; 95% CI, 0-0.95; week 8: SES, 0.79; 95% CI, 0.06-1.05).
Dr. Nikolova said a large follow-up trial is planned to further confirm the results.
Nutritional psychiatrist Drew Ramsey, MD, author of Eat to Beat Depression and Anxiety and assistant clinical professor of psychiatry at Columbia University, New York, said in an interview: “This randomized clinical trial adds to the considerable evidence that food choices impact depression outcomes.”
He further noted that, “in nutritional psychiatry, we recommend eating fermented foods as they have been shown to improve microbiome diversity and decrease markers of inflammation.”
Dr. Ramsey noted that the RCT used the equivalent colony-forming unit of a “single serving of kombucha.”
“In our clinical group and our nutritional psychiatry course for clinicians, we recommend fermented foods over probiotics as this is the most sustainable, evidence-based way to improve microbiome diversity,” said Dr. Ramsey, citing recent research by Gardner and colleagues at Stanford (Calif.) University.
“This is an industry-funded trial that adds to the evidence base but should be interpreted by patients and clinicians as promoting consumption of more kefir, kimchi, and kombucha, not that patients should take probiotics,” he said.
A key place for probiotics in mental health
Commenting on the study, Uma Naidoo, MD, said: “As I shared throughout my first book, This is Your Brain on Food, there is a real place for the use of probiotics in mental health, including the importance of the gut-brain connection.”
Dr. Naidoo is the director of nutritional and metabolic psychiatry at Massachusetts General Hospital and of nutritional psychiatry at the MGH Academy, both in Boston.
She noted that, when a person stops using a probiotic after trying it out, the positive changes in the gut are reversed, so “remaining consistent in taking the probiotic is important if you have found it helpful for your mood.”
Dr. Naidoo added that “each person’s gut microbiome is so unique that it is likely not every human being will have the same reaction to a probiotic.”
“Eating foods with live probiotics may also benefit gut health and, therefore, mood,” she said. The same goes with eating fermented foods with live active cultures.”
The study was funded by a Medical Research Council Industrial CASE PhD Studentship with ADM Protexin (supplier of the probiotics) as the industry partner and additional support from Freya Green. Dr. Nikolova has received grants from the Medical Research Council and ADM Protexin during the conduct of the study as well as personal fees from Janssen outside the submitted work.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY