User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Pandemic weighing on physicians’ happiness outside of work: survey
One of the unexpected consequences of the pandemic is that many people are rethinking their priorities and lifestyles, and physicians are no exception.
Pets, prayer, and partners
The pandemic has taken a toll on physicians outside of work as well as on the job. Eight in 10 physicians (82% of men and 80% of women) said they were “somewhat” or “very” happy outside of work before the pandemic. This is almost exactly the same result as in last year’s survey.
However, when asked how happy they are outside of work currently, only 6 in 10 (59%) reported being “somewhat” or “very” happy. While the pandemic has made life difficult for everyone, health care professionals face particular stresses even outside of work. Wayne M. Sotile, PhD, founder of the Center for Physician Resilience, says he has counseled doctors who witnessed COVID-related suffering and death at work, then came home to a partner who didn’t believe that the pandemic was real.
Still, physicians reported that spending time with people they love and engaging in favorite activities helps them stay happy. “Spending time with pets” and “religious practice/prayer” were frequent “other” responses to the question, “What do you do to maintain happiness and mental health?” Seven in 10 physicians reported having some kind of religious or spiritual beliefs.
The majority of physicians (83%) are either married or living with a partner, with male physicians edging out their female peers (89% vs. 75%). Among married physicians, 8 in 10 physicians reported that their union is “good” or “very good.” The pandemic may have helped in this respect. Dr. Sotile says he’s heard physicians say that they’ve connected more with their families in the past 18 months. Specialists with the highest rates of happy marriages were otolaryngologists and immunologists (both 91%), followed closely by dermatologists, rheumatologists, and nephrologists (all 90%).
Among physicians balancing a medical career and parenthood, female physicians reported feeling conflicted more often than males (48% vs. 29%). Nicole A. Sparks, MD, an ob.gyn. and a health and lifestyle blogger, cites not being there for her kids as a source of stress. She notes that her two young children notice when she’s not there to help with homework, read bedtime stories, or make their dinner. “Mom guilt can definitely set in if I have to miss important events,” she says.
Work-life balance is an important, if elusive, goal for physicians, and not just females. Sixty percent of female doctors and 53% of male doctors said they would be willing to take a cut in pay if it meant more free time and a better work-life balance. Many doctors do manage to get away from work occasionally, with one-fifth of all physicians taking 5 or more weeks of vacation each year.
Seeking a ‘balanced life’
Alexis Polles, MD, medical director for the Professionals Resource Network, points out the importance of taking time for personal health and wellness. “When we work with professionals who have problems with mental health or substance abuse, they often don’t have a balanced life,” she says. “They are usually in a workaholic mindset and disregard their own needs.”
Few physicians seem to prioritize self-care, with a third indicating they “always” or “most of the time” spend enough time on their own health and wellness. But of those who do, males (38%) are more likely than females (27%) to spend enough time on their own health and wellness. Dr. Polles adds that exercising after a shift can help physicians better make the transition from professional to personal life. Though they did not report when they exercised, about a third of physicians reported doing so four or more times per week. Controlling weight is an issue as well, with 49% of male and 55% of female physicians saying they are currently trying to lose weight.
Of physicians who drink alcohol, about a third have three or more drinks per week. (The CDC defines “heavy drinking” as consuming 15 drinks or more per week for men and eight drinks or more per week for women.)
Of those surveyed, 92% say they do not regularly use cannabidiol or cannabis, and a mere 4% of respondents said they would use at least one of these substances if they were to become legal in their state.
A version of this article first appeared on Medscape.com.
One of the unexpected consequences of the pandemic is that many people are rethinking their priorities and lifestyles, and physicians are no exception.
Pets, prayer, and partners
The pandemic has taken a toll on physicians outside of work as well as on the job. Eight in 10 physicians (82% of men and 80% of women) said they were “somewhat” or “very” happy outside of work before the pandemic. This is almost exactly the same result as in last year’s survey.
However, when asked how happy they are outside of work currently, only 6 in 10 (59%) reported being “somewhat” or “very” happy. While the pandemic has made life difficult for everyone, health care professionals face particular stresses even outside of work. Wayne M. Sotile, PhD, founder of the Center for Physician Resilience, says he has counseled doctors who witnessed COVID-related suffering and death at work, then came home to a partner who didn’t believe that the pandemic was real.
Still, physicians reported that spending time with people they love and engaging in favorite activities helps them stay happy. “Spending time with pets” and “religious practice/prayer” were frequent “other” responses to the question, “What do you do to maintain happiness and mental health?” Seven in 10 physicians reported having some kind of religious or spiritual beliefs.
The majority of physicians (83%) are either married or living with a partner, with male physicians edging out their female peers (89% vs. 75%). Among married physicians, 8 in 10 physicians reported that their union is “good” or “very good.” The pandemic may have helped in this respect. Dr. Sotile says he’s heard physicians say that they’ve connected more with their families in the past 18 months. Specialists with the highest rates of happy marriages were otolaryngologists and immunologists (both 91%), followed closely by dermatologists, rheumatologists, and nephrologists (all 90%).
Among physicians balancing a medical career and parenthood, female physicians reported feeling conflicted more often than males (48% vs. 29%). Nicole A. Sparks, MD, an ob.gyn. and a health and lifestyle blogger, cites not being there for her kids as a source of stress. She notes that her two young children notice when she’s not there to help with homework, read bedtime stories, or make their dinner. “Mom guilt can definitely set in if I have to miss important events,” she says.
Work-life balance is an important, if elusive, goal for physicians, and not just females. Sixty percent of female doctors and 53% of male doctors said they would be willing to take a cut in pay if it meant more free time and a better work-life balance. Many doctors do manage to get away from work occasionally, with one-fifth of all physicians taking 5 or more weeks of vacation each year.
Seeking a ‘balanced life’
Alexis Polles, MD, medical director for the Professionals Resource Network, points out the importance of taking time for personal health and wellness. “When we work with professionals who have problems with mental health or substance abuse, they often don’t have a balanced life,” she says. “They are usually in a workaholic mindset and disregard their own needs.”
Few physicians seem to prioritize self-care, with a third indicating they “always” or “most of the time” spend enough time on their own health and wellness. But of those who do, males (38%) are more likely than females (27%) to spend enough time on their own health and wellness. Dr. Polles adds that exercising after a shift can help physicians better make the transition from professional to personal life. Though they did not report when they exercised, about a third of physicians reported doing so four or more times per week. Controlling weight is an issue as well, with 49% of male and 55% of female physicians saying they are currently trying to lose weight.
Of physicians who drink alcohol, about a third have three or more drinks per week. (The CDC defines “heavy drinking” as consuming 15 drinks or more per week for men and eight drinks or more per week for women.)
Of those surveyed, 92% say they do not regularly use cannabidiol or cannabis, and a mere 4% of respondents said they would use at least one of these substances if they were to become legal in their state.
A version of this article first appeared on Medscape.com.
One of the unexpected consequences of the pandemic is that many people are rethinking their priorities and lifestyles, and physicians are no exception.
Pets, prayer, and partners
The pandemic has taken a toll on physicians outside of work as well as on the job. Eight in 10 physicians (82% of men and 80% of women) said they were “somewhat” or “very” happy outside of work before the pandemic. This is almost exactly the same result as in last year’s survey.
However, when asked how happy they are outside of work currently, only 6 in 10 (59%) reported being “somewhat” or “very” happy. While the pandemic has made life difficult for everyone, health care professionals face particular stresses even outside of work. Wayne M. Sotile, PhD, founder of the Center for Physician Resilience, says he has counseled doctors who witnessed COVID-related suffering and death at work, then came home to a partner who didn’t believe that the pandemic was real.
Still, physicians reported that spending time with people they love and engaging in favorite activities helps them stay happy. “Spending time with pets” and “religious practice/prayer” were frequent “other” responses to the question, “What do you do to maintain happiness and mental health?” Seven in 10 physicians reported having some kind of religious or spiritual beliefs.
The majority of physicians (83%) are either married or living with a partner, with male physicians edging out their female peers (89% vs. 75%). Among married physicians, 8 in 10 physicians reported that their union is “good” or “very good.” The pandemic may have helped in this respect. Dr. Sotile says he’s heard physicians say that they’ve connected more with their families in the past 18 months. Specialists with the highest rates of happy marriages were otolaryngologists and immunologists (both 91%), followed closely by dermatologists, rheumatologists, and nephrologists (all 90%).
Among physicians balancing a medical career and parenthood, female physicians reported feeling conflicted more often than males (48% vs. 29%). Nicole A. Sparks, MD, an ob.gyn. and a health and lifestyle blogger, cites not being there for her kids as a source of stress. She notes that her two young children notice when she’s not there to help with homework, read bedtime stories, or make their dinner. “Mom guilt can definitely set in if I have to miss important events,” she says.
Work-life balance is an important, if elusive, goal for physicians, and not just females. Sixty percent of female doctors and 53% of male doctors said they would be willing to take a cut in pay if it meant more free time and a better work-life balance. Many doctors do manage to get away from work occasionally, with one-fifth of all physicians taking 5 or more weeks of vacation each year.
Seeking a ‘balanced life’
Alexis Polles, MD, medical director for the Professionals Resource Network, points out the importance of taking time for personal health and wellness. “When we work with professionals who have problems with mental health or substance abuse, they often don’t have a balanced life,” she says. “They are usually in a workaholic mindset and disregard their own needs.”
Few physicians seem to prioritize self-care, with a third indicating they “always” or “most of the time” spend enough time on their own health and wellness. But of those who do, males (38%) are more likely than females (27%) to spend enough time on their own health and wellness. Dr. Polles adds that exercising after a shift can help physicians better make the transition from professional to personal life. Though they did not report when they exercised, about a third of physicians reported doing so four or more times per week. Controlling weight is an issue as well, with 49% of male and 55% of female physicians saying they are currently trying to lose weight.
Of physicians who drink alcohol, about a third have three or more drinks per week. (The CDC defines “heavy drinking” as consuming 15 drinks or more per week for men and eight drinks or more per week for women.)
Of those surveyed, 92% say they do not regularly use cannabidiol or cannabis, and a mere 4% of respondents said they would use at least one of these substances if they were to become legal in their state.
A version of this article first appeared on Medscape.com.
Dramatic increase in driving high after cannabis legislation
Since Canada legalized marijuana in 2018, there has been a dramatic increase in the number of individuals driving while high, new research shows.
Investigators studied over 4,000 drivers treated after a motor vehicle collision in British Columbia trauma centers and found that, before cannabis was legalized, a THC level greater than 0 ng/mL in the blood was present in roughly 10% of drivers. After the drug was legalized this percentage increased to 18%. The percentages of injured drivers with at least 2 ng/mL, the Canadian legal limit, and at least 5 ng/mL more than doubled.
“It’s concerning that we’re seeing such a dramatic increase,” study investigator Jeffrey Brubacher, MD, associate professor, department of emergency medicine, University of British Columbia, Vancouver, said in a press release.
“There are serious risks associated with driving after cannabis use and our findings suggest more [work] is needed to deter this dangerous behavior in light of legalization,” he said.
The study was published online Jan. 12 in the New England Journal of Medicine.
Impact of legalization?
The investigators note that the Canadian government introduced a law aiming to prevent cannabis-impaired driving by establishing penalties and criminal charges for drivers found with a whole-blood THC level of 2 ng/mL, with more severe penalties for those with a THC level of greater than 5 ng/mL or greater than 2.5 ng/mL combined with a blood alcohol level of .05%.
Cannabis use is “associated with cognitive deficits and psychomotor impairment, and there is evidence that it increases the risk of motor vehicle crashes, especially at higher THC levels,” they noted.
“I’m an emergency physician at Vancouver General Hospital’s trauma center. We’ve been measuring drug levels in injured drivers since 2013 here in British Columbia and, in particular, we’ve been measuring THC levels,” Dr. Brubacher said in an interview. “We thought it would be interesting and important to see what would happen after legalization.”
The investigators studied 4,339 drivers – 3,550 whose accident took place before legalization of cannabis, and 789 after legalization – who had been moderately injured in a motor vehicle collision and presented to four British Columbia trauma centers between January 2013 and March 2020.
said Dr. Brubacher. Drivers included in the study had excess blood remaining after the clinical testing had been completed, which was then used for drug analysis.
Insufficient laws
After legalization there was an increased prevalence of drivers with a THC level greater than 0 ng/mL, a TCH level of at least 2 ng/mL, and a THC level of at least 5 ng/mL.
The largest increases in a THC level of at least 2 ng/mL were in drivers 50 years of age or older and among male drivers (adjusted prevalence ratio, 5.18; 95% confidence interval, 2.49-10.78 and aPR, 2.44; 95% CI, 1.60-3.74, respectively).
“There were no significant changes in the prevalence of drivers testing positive for alcohol,” the authors reported.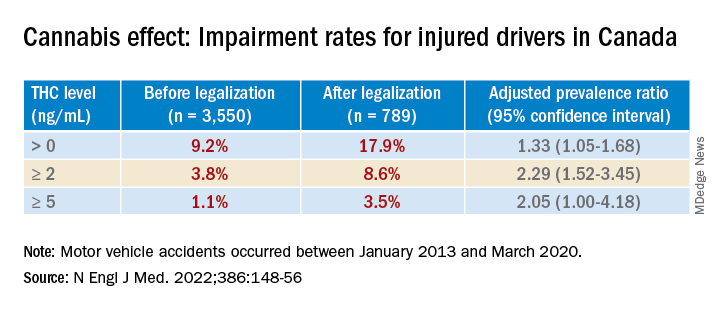
Dr. Brubacher said the evidence suggests these new laws “are not enough to stop everyone from driving after using cannabis.”
The findings have implications for clinicians and patients and for policymakers, he said. “My moderately conservative recommendations are that, if you are going to smoke cannabis, wait at least 4 hours after smoking before you drive. Edibles last longer, and patients should wait least 8 hours after ingesting [edibles] before driving. And of course, if you continue to feel the effects of the THC, you should avoid driving altogether until the time has elapsed and you no longer feel any effects.”
Dr. Brubacher hopes policy makers will use the study’s findings to “design public information campaigns and enforcement measures that encourage drivers, especially older drivers, to separate cannabis use from driving.”
Additionally, “policy makers shouldn’t lose sight of drinking and driving because that’s an even bigger problem than the risk of driving under the influence of cannabis.”
Focus on older adults
In a comment, Anees Bahji, MD, an International Collaborative Addiction Medicine research fellow at the British Columbia Centre on Substance Use, called the study “interesting and relevant.”
He raised several questions regarding the “correlation between the level of a substance in a person’s system and the degree of impairment.” For example, “does the same level of THC in the blood affect us all the same way? And to what extent do the levels detected at the time of the analysis correlate with the level in the person’s system at the time of driving?”
An additional consideration “is for individuals with cannabis use disorder and for those who have developed tolerance to the psychoactive effects of THC: Does it affect their driving skills in the same way as someone who is cannabis naive?” asked Dr. Bahji, a clinical assistant professor at the University of Calgary (Alta.) who was not involved with the study.
Also commenting, Eric Sevigny, PhD, associate professor of criminal justice and criminology at Georgia State University, Atlanta, described it as a “well-designed study that adds yet another data point for considering appropriate road safety policy responses alongside ongoing cannabis liberalization.”
However, the findings “cannot say much about whether cannabis legalization leads to an increase in cannabis-impaired driving, because current research finds little correlation between biological THC concentrations and driving performance,” said Dr. Sevigny, who was not involved with the study.
The finding of “higher THC prevalence among older adults is also relevant for road safety, as this population has a number of concomitant risk factors, such as cognitive decline and prescription drug use,” Dr. Sevigny added.
The study was supported by the Canadian Institutes of Health Research. Dr. Brubacher and Dr. Sevigny disclosed no relevant financial relationships. Dr. Bahji reported receiving research funding from the Canadian Institutes of Health Research, the Calgary Health Trust, the American Psychiatric Association, NIDA, and the University of Calgary.
A version of this article first appeared on Medscape.com.
Since Canada legalized marijuana in 2018, there has been a dramatic increase in the number of individuals driving while high, new research shows.
Investigators studied over 4,000 drivers treated after a motor vehicle collision in British Columbia trauma centers and found that, before cannabis was legalized, a THC level greater than 0 ng/mL in the blood was present in roughly 10% of drivers. After the drug was legalized this percentage increased to 18%. The percentages of injured drivers with at least 2 ng/mL, the Canadian legal limit, and at least 5 ng/mL more than doubled.
“It’s concerning that we’re seeing such a dramatic increase,” study investigator Jeffrey Brubacher, MD, associate professor, department of emergency medicine, University of British Columbia, Vancouver, said in a press release.
“There are serious risks associated with driving after cannabis use and our findings suggest more [work] is needed to deter this dangerous behavior in light of legalization,” he said.
The study was published online Jan. 12 in the New England Journal of Medicine.
Impact of legalization?
The investigators note that the Canadian government introduced a law aiming to prevent cannabis-impaired driving by establishing penalties and criminal charges for drivers found with a whole-blood THC level of 2 ng/mL, with more severe penalties for those with a THC level of greater than 5 ng/mL or greater than 2.5 ng/mL combined with a blood alcohol level of .05%.
Cannabis use is “associated with cognitive deficits and psychomotor impairment, and there is evidence that it increases the risk of motor vehicle crashes, especially at higher THC levels,” they noted.
“I’m an emergency physician at Vancouver General Hospital’s trauma center. We’ve been measuring drug levels in injured drivers since 2013 here in British Columbia and, in particular, we’ve been measuring THC levels,” Dr. Brubacher said in an interview. “We thought it would be interesting and important to see what would happen after legalization.”
The investigators studied 4,339 drivers – 3,550 whose accident took place before legalization of cannabis, and 789 after legalization – who had been moderately injured in a motor vehicle collision and presented to four British Columbia trauma centers between January 2013 and March 2020.
said Dr. Brubacher. Drivers included in the study had excess blood remaining after the clinical testing had been completed, which was then used for drug analysis.
Insufficient laws
After legalization there was an increased prevalence of drivers with a THC level greater than 0 ng/mL, a TCH level of at least 2 ng/mL, and a THC level of at least 5 ng/mL.
The largest increases in a THC level of at least 2 ng/mL were in drivers 50 years of age or older and among male drivers (adjusted prevalence ratio, 5.18; 95% confidence interval, 2.49-10.78 and aPR, 2.44; 95% CI, 1.60-3.74, respectively).
“There were no significant changes in the prevalence of drivers testing positive for alcohol,” the authors reported.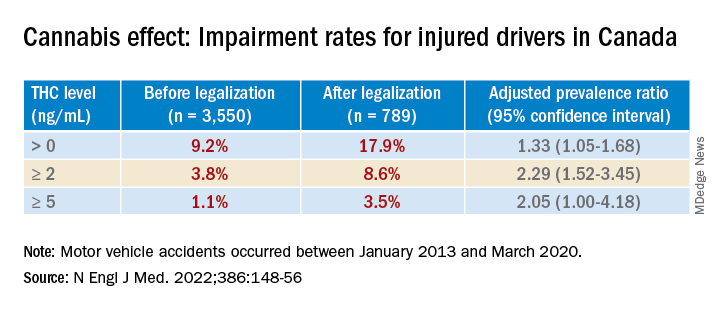
Dr. Brubacher said the evidence suggests these new laws “are not enough to stop everyone from driving after using cannabis.”
The findings have implications for clinicians and patients and for policymakers, he said. “My moderately conservative recommendations are that, if you are going to smoke cannabis, wait at least 4 hours after smoking before you drive. Edibles last longer, and patients should wait least 8 hours after ingesting [edibles] before driving. And of course, if you continue to feel the effects of the THC, you should avoid driving altogether until the time has elapsed and you no longer feel any effects.”
Dr. Brubacher hopes policy makers will use the study’s findings to “design public information campaigns and enforcement measures that encourage drivers, especially older drivers, to separate cannabis use from driving.”
Additionally, “policy makers shouldn’t lose sight of drinking and driving because that’s an even bigger problem than the risk of driving under the influence of cannabis.”
Focus on older adults
In a comment, Anees Bahji, MD, an International Collaborative Addiction Medicine research fellow at the British Columbia Centre on Substance Use, called the study “interesting and relevant.”
He raised several questions regarding the “correlation between the level of a substance in a person’s system and the degree of impairment.” For example, “does the same level of THC in the blood affect us all the same way? And to what extent do the levels detected at the time of the analysis correlate with the level in the person’s system at the time of driving?”
An additional consideration “is for individuals with cannabis use disorder and for those who have developed tolerance to the psychoactive effects of THC: Does it affect their driving skills in the same way as someone who is cannabis naive?” asked Dr. Bahji, a clinical assistant professor at the University of Calgary (Alta.) who was not involved with the study.
Also commenting, Eric Sevigny, PhD, associate professor of criminal justice and criminology at Georgia State University, Atlanta, described it as a “well-designed study that adds yet another data point for considering appropriate road safety policy responses alongside ongoing cannabis liberalization.”
However, the findings “cannot say much about whether cannabis legalization leads to an increase in cannabis-impaired driving, because current research finds little correlation between biological THC concentrations and driving performance,” said Dr. Sevigny, who was not involved with the study.
The finding of “higher THC prevalence among older adults is also relevant for road safety, as this population has a number of concomitant risk factors, such as cognitive decline and prescription drug use,” Dr. Sevigny added.
The study was supported by the Canadian Institutes of Health Research. Dr. Brubacher and Dr. Sevigny disclosed no relevant financial relationships. Dr. Bahji reported receiving research funding from the Canadian Institutes of Health Research, the Calgary Health Trust, the American Psychiatric Association, NIDA, and the University of Calgary.
A version of this article first appeared on Medscape.com.
Since Canada legalized marijuana in 2018, there has been a dramatic increase in the number of individuals driving while high, new research shows.
Investigators studied over 4,000 drivers treated after a motor vehicle collision in British Columbia trauma centers and found that, before cannabis was legalized, a THC level greater than 0 ng/mL in the blood was present in roughly 10% of drivers. After the drug was legalized this percentage increased to 18%. The percentages of injured drivers with at least 2 ng/mL, the Canadian legal limit, and at least 5 ng/mL more than doubled.
“It’s concerning that we’re seeing such a dramatic increase,” study investigator Jeffrey Brubacher, MD, associate professor, department of emergency medicine, University of British Columbia, Vancouver, said in a press release.
“There are serious risks associated with driving after cannabis use and our findings suggest more [work] is needed to deter this dangerous behavior in light of legalization,” he said.
The study was published online Jan. 12 in the New England Journal of Medicine.
Impact of legalization?
The investigators note that the Canadian government introduced a law aiming to prevent cannabis-impaired driving by establishing penalties and criminal charges for drivers found with a whole-blood THC level of 2 ng/mL, with more severe penalties for those with a THC level of greater than 5 ng/mL or greater than 2.5 ng/mL combined with a blood alcohol level of .05%.
Cannabis use is “associated with cognitive deficits and psychomotor impairment, and there is evidence that it increases the risk of motor vehicle crashes, especially at higher THC levels,” they noted.
“I’m an emergency physician at Vancouver General Hospital’s trauma center. We’ve been measuring drug levels in injured drivers since 2013 here in British Columbia and, in particular, we’ve been measuring THC levels,” Dr. Brubacher said in an interview. “We thought it would be interesting and important to see what would happen after legalization.”
The investigators studied 4,339 drivers – 3,550 whose accident took place before legalization of cannabis, and 789 after legalization – who had been moderately injured in a motor vehicle collision and presented to four British Columbia trauma centers between January 2013 and March 2020.
said Dr. Brubacher. Drivers included in the study had excess blood remaining after the clinical testing had been completed, which was then used for drug analysis.
Insufficient laws
After legalization there was an increased prevalence of drivers with a THC level greater than 0 ng/mL, a TCH level of at least 2 ng/mL, and a THC level of at least 5 ng/mL.
The largest increases in a THC level of at least 2 ng/mL were in drivers 50 years of age or older and among male drivers (adjusted prevalence ratio, 5.18; 95% confidence interval, 2.49-10.78 and aPR, 2.44; 95% CI, 1.60-3.74, respectively).
“There were no significant changes in the prevalence of drivers testing positive for alcohol,” the authors reported.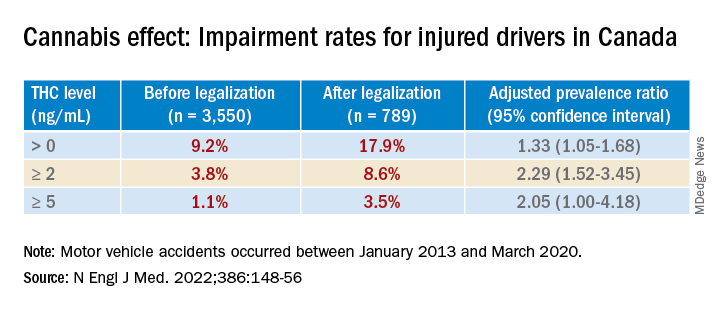
Dr. Brubacher said the evidence suggests these new laws “are not enough to stop everyone from driving after using cannabis.”
The findings have implications for clinicians and patients and for policymakers, he said. “My moderately conservative recommendations are that, if you are going to smoke cannabis, wait at least 4 hours after smoking before you drive. Edibles last longer, and patients should wait least 8 hours after ingesting [edibles] before driving. And of course, if you continue to feel the effects of the THC, you should avoid driving altogether until the time has elapsed and you no longer feel any effects.”
Dr. Brubacher hopes policy makers will use the study’s findings to “design public information campaigns and enforcement measures that encourage drivers, especially older drivers, to separate cannabis use from driving.”
Additionally, “policy makers shouldn’t lose sight of drinking and driving because that’s an even bigger problem than the risk of driving under the influence of cannabis.”
Focus on older adults
In a comment, Anees Bahji, MD, an International Collaborative Addiction Medicine research fellow at the British Columbia Centre on Substance Use, called the study “interesting and relevant.”
He raised several questions regarding the “correlation between the level of a substance in a person’s system and the degree of impairment.” For example, “does the same level of THC in the blood affect us all the same way? And to what extent do the levels detected at the time of the analysis correlate with the level in the person’s system at the time of driving?”
An additional consideration “is for individuals with cannabis use disorder and for those who have developed tolerance to the psychoactive effects of THC: Does it affect their driving skills in the same way as someone who is cannabis naive?” asked Dr. Bahji, a clinical assistant professor at the University of Calgary (Alta.) who was not involved with the study.
Also commenting, Eric Sevigny, PhD, associate professor of criminal justice and criminology at Georgia State University, Atlanta, described it as a “well-designed study that adds yet another data point for considering appropriate road safety policy responses alongside ongoing cannabis liberalization.”
However, the findings “cannot say much about whether cannabis legalization leads to an increase in cannabis-impaired driving, because current research finds little correlation between biological THC concentrations and driving performance,” said Dr. Sevigny, who was not involved with the study.
The finding of “higher THC prevalence among older adults is also relevant for road safety, as this population has a number of concomitant risk factors, such as cognitive decline and prescription drug use,” Dr. Sevigny added.
The study was supported by the Canadian Institutes of Health Research. Dr. Brubacher and Dr. Sevigny disclosed no relevant financial relationships. Dr. Bahji reported receiving research funding from the Canadian Institutes of Health Research, the Calgary Health Trust, the American Psychiatric Association, NIDA, and the University of Calgary.
A version of this article first appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Psychiatry resident’s viral posts reveal his own mental health battle
First-year psychiatry resident Jake Goodman, MD, knew he was taking a chance when he opened up on his popular social media platforms about his personal mental health battle. He mulled over the decision for several weeks before deciding to take the plunge.
As he voiced recently on his TikTok page, his biggest social media fanbase, with 1.3 million followers, it felt freeing to get his personal struggle off his chest.
“I’m a doctor in training, and most doctors would advise me not to post this,” the 29-year-old from Miami said in the video last month, which garnered 1.2 million views on TikTok alone. “They would say it’s risky for my career. But I didn’t join the medical field to continue the toxic status quo. I’m part of a new generation of health care professionals that are not afraid to be vulnerable and talk about mental health.”
“Dr. Jake,” as he calls himself on social media, admitted he was a physician who treats mental illness and also takes medication for it. “It felt good to say that. And by the way, I’m proud of it,” he said in the TikTok post.
A champion of mental health throughout the pandemic, Dr. Goodman called attention to the illness in the medical field. In a message on Instagram, he stated, “Opening up about your mental health as a medical professional, especially as a doctor who treats mental illness, can be taboo ... So here’s me leading by example.”
He also cited statistics on the challenge: “1 in 2 people will be diagnosed with a mental health illness at some point in their life. Yet many of us will never take medication that can help correct the chemical imbalance in our brains due to medication stigma: the fear that taking medications for our mental health somehow makes us weak.”
Mental health remains an issue among residents. Nearly 70% of residents polled by Medscape in its 2021 Residents Lifestyle & Happiness Report said they strongly or somewhat agree there’s a stigma against seeking mental health help. And nearly half, or 47% of those polled, said they sometimes (36%) or always/most of the time (11%) were depressed. The latter category rose in the past year.
Dr. Goodman told this news organization that he became passionate about mental health when he lost a college friend to suicide. “It really exposed the stigma” of mental health, he said. “I always knew it was there, but it took me seeing someone lose his life and [asking] why didn’t he feel comfortable talking to us, and why didn’t I feel comfortable talking to him?”
Stress of medical training
The decision to pursue psychiatry as his specialty came after a rotation in a clinic for people struggling with substance use disorders. “I was enthralled to see people change their life ... just by mental health care.” It’s why he went into medicine, he tells this news organization. “I always wanted to be in a field to help people [before they hit] rock bottom, when no one else could be there for them.”
Dr. Goodman’s personal battle with mental health didn’t arise until he started residency. “I was not really myself.” He said he felt numb and burned out. “I was not getting as much enjoyment out of things.” A friend pointed out that he might be depressed, so he went to see a therapist and then a psychiatrist and started on medication. “It had a profound impact on how I felt.”
Still, it took a while before Dr. Goodman was comfortable sharing his story with the 1.6 million followers he had already built across his social media platforms.
“I started on social media in 2020 with the goal of advocating for mental health and inspiring future doctors.” He said the message seemed to resonate with people struggling during the early part of the pandemic. On his social media accounts, he also talks about medical school, residency, and being a health care provider. His fiancé is also a resident doctor, in internal medicine.
Dr. Goodman is also trying to create a more realistic image of doctors than the superheroes he believed they were growing up. He wants those who grow up wanting to be doctors and who look up to him to see him as a human being with vulnerabilities, such as mental health.
“You can be a doctor and have mental health issues. Seeking treatment for mental health makes you a better doctor, and for other health care workers suffering in the midst of the pandemic, I want to let them know they are not alone.”
He pointed to the statistic that doctors have one of the highest suicide rates of any professions. “It’s better to talk about that in the early stages of training.”
Students, residents, or attending physicians who have mental health challenges shouldn’t allow their symptoms to go untreated, Dr. Goodman added. “Holding in all the stress and anxiety and feelings in a very traumatic field may be dangerous. ”
One of his goals is to campaign for the removal of a question on state medical licensing forms requiring doctors to report any mental health diagnosis. It’s why doctors may be afraid to admit that they are struggling. “I’m still here. It didn’t ruin my career.”
Doctors who seek treatment for mental health are theoretically protected under the Americans With Disabilities Act from being refused a license on the basis of that diagnosis. Dr. Goodman hopes to advocate at the state level to reduce discrimination and increase accessibility for doctors to seek mental health care.
Still, Dr. Goodman concedes he was initially fearful of the repercussions. “I opened up about it because this post could save lives. I was doing what I believed in.”
So if he runs into barriers to receive his medical license because of his admission, “that’s a serious problem,” he said. “There is already a shortage of doctors. We’ll see what happens in a few years. I am not the only one who will answer ‘yes’ to having sought treatment for a mental illness. The questions do not really need to be there.”
A version of this article first appeared on Medscape.com.
First-year psychiatry resident Jake Goodman, MD, knew he was taking a chance when he opened up on his popular social media platforms about his personal mental health battle. He mulled over the decision for several weeks before deciding to take the plunge.
As he voiced recently on his TikTok page, his biggest social media fanbase, with 1.3 million followers, it felt freeing to get his personal struggle off his chest.
“I’m a doctor in training, and most doctors would advise me not to post this,” the 29-year-old from Miami said in the video last month, which garnered 1.2 million views on TikTok alone. “They would say it’s risky for my career. But I didn’t join the medical field to continue the toxic status quo. I’m part of a new generation of health care professionals that are not afraid to be vulnerable and talk about mental health.”
“Dr. Jake,” as he calls himself on social media, admitted he was a physician who treats mental illness and also takes medication for it. “It felt good to say that. And by the way, I’m proud of it,” he said in the TikTok post.
A champion of mental health throughout the pandemic, Dr. Goodman called attention to the illness in the medical field. In a message on Instagram, he stated, “Opening up about your mental health as a medical professional, especially as a doctor who treats mental illness, can be taboo ... So here’s me leading by example.”
He also cited statistics on the challenge: “1 in 2 people will be diagnosed with a mental health illness at some point in their life. Yet many of us will never take medication that can help correct the chemical imbalance in our brains due to medication stigma: the fear that taking medications for our mental health somehow makes us weak.”
Mental health remains an issue among residents. Nearly 70% of residents polled by Medscape in its 2021 Residents Lifestyle & Happiness Report said they strongly or somewhat agree there’s a stigma against seeking mental health help. And nearly half, or 47% of those polled, said they sometimes (36%) or always/most of the time (11%) were depressed. The latter category rose in the past year.
Dr. Goodman told this news organization that he became passionate about mental health when he lost a college friend to suicide. “It really exposed the stigma” of mental health, he said. “I always knew it was there, but it took me seeing someone lose his life and [asking] why didn’t he feel comfortable talking to us, and why didn’t I feel comfortable talking to him?”
Stress of medical training
The decision to pursue psychiatry as his specialty came after a rotation in a clinic for people struggling with substance use disorders. “I was enthralled to see people change their life ... just by mental health care.” It’s why he went into medicine, he tells this news organization. “I always wanted to be in a field to help people [before they hit] rock bottom, when no one else could be there for them.”
Dr. Goodman’s personal battle with mental health didn’t arise until he started residency. “I was not really myself.” He said he felt numb and burned out. “I was not getting as much enjoyment out of things.” A friend pointed out that he might be depressed, so he went to see a therapist and then a psychiatrist and started on medication. “It had a profound impact on how I felt.”
Still, it took a while before Dr. Goodman was comfortable sharing his story with the 1.6 million followers he had already built across his social media platforms.
“I started on social media in 2020 with the goal of advocating for mental health and inspiring future doctors.” He said the message seemed to resonate with people struggling during the early part of the pandemic. On his social media accounts, he also talks about medical school, residency, and being a health care provider. His fiancé is also a resident doctor, in internal medicine.
Dr. Goodman is also trying to create a more realistic image of doctors than the superheroes he believed they were growing up. He wants those who grow up wanting to be doctors and who look up to him to see him as a human being with vulnerabilities, such as mental health.
“You can be a doctor and have mental health issues. Seeking treatment for mental health makes you a better doctor, and for other health care workers suffering in the midst of the pandemic, I want to let them know they are not alone.”
He pointed to the statistic that doctors have one of the highest suicide rates of any professions. “It’s better to talk about that in the early stages of training.”
Students, residents, or attending physicians who have mental health challenges shouldn’t allow their symptoms to go untreated, Dr. Goodman added. “Holding in all the stress and anxiety and feelings in a very traumatic field may be dangerous. ”
One of his goals is to campaign for the removal of a question on state medical licensing forms requiring doctors to report any mental health diagnosis. It’s why doctors may be afraid to admit that they are struggling. “I’m still here. It didn’t ruin my career.”
Doctors who seek treatment for mental health are theoretically protected under the Americans With Disabilities Act from being refused a license on the basis of that diagnosis. Dr. Goodman hopes to advocate at the state level to reduce discrimination and increase accessibility for doctors to seek mental health care.
Still, Dr. Goodman concedes he was initially fearful of the repercussions. “I opened up about it because this post could save lives. I was doing what I believed in.”
So if he runs into barriers to receive his medical license because of his admission, “that’s a serious problem,” he said. “There is already a shortage of doctors. We’ll see what happens in a few years. I am not the only one who will answer ‘yes’ to having sought treatment for a mental illness. The questions do not really need to be there.”
A version of this article first appeared on Medscape.com.
First-year psychiatry resident Jake Goodman, MD, knew he was taking a chance when he opened up on his popular social media platforms about his personal mental health battle. He mulled over the decision for several weeks before deciding to take the plunge.
As he voiced recently on his TikTok page, his biggest social media fanbase, with 1.3 million followers, it felt freeing to get his personal struggle off his chest.
“I’m a doctor in training, and most doctors would advise me not to post this,” the 29-year-old from Miami said in the video last month, which garnered 1.2 million views on TikTok alone. “They would say it’s risky for my career. But I didn’t join the medical field to continue the toxic status quo. I’m part of a new generation of health care professionals that are not afraid to be vulnerable and talk about mental health.”
“Dr. Jake,” as he calls himself on social media, admitted he was a physician who treats mental illness and also takes medication for it. “It felt good to say that. And by the way, I’m proud of it,” he said in the TikTok post.
A champion of mental health throughout the pandemic, Dr. Goodman called attention to the illness in the medical field. In a message on Instagram, he stated, “Opening up about your mental health as a medical professional, especially as a doctor who treats mental illness, can be taboo ... So here’s me leading by example.”
He also cited statistics on the challenge: “1 in 2 people will be diagnosed with a mental health illness at some point in their life. Yet many of us will never take medication that can help correct the chemical imbalance in our brains due to medication stigma: the fear that taking medications for our mental health somehow makes us weak.”
Mental health remains an issue among residents. Nearly 70% of residents polled by Medscape in its 2021 Residents Lifestyle & Happiness Report said they strongly or somewhat agree there’s a stigma against seeking mental health help. And nearly half, or 47% of those polled, said they sometimes (36%) or always/most of the time (11%) were depressed. The latter category rose in the past year.
Dr. Goodman told this news organization that he became passionate about mental health when he lost a college friend to suicide. “It really exposed the stigma” of mental health, he said. “I always knew it was there, but it took me seeing someone lose his life and [asking] why didn’t he feel comfortable talking to us, and why didn’t I feel comfortable talking to him?”
Stress of medical training
The decision to pursue psychiatry as his specialty came after a rotation in a clinic for people struggling with substance use disorders. “I was enthralled to see people change their life ... just by mental health care.” It’s why he went into medicine, he tells this news organization. “I always wanted to be in a field to help people [before they hit] rock bottom, when no one else could be there for them.”
Dr. Goodman’s personal battle with mental health didn’t arise until he started residency. “I was not really myself.” He said he felt numb and burned out. “I was not getting as much enjoyment out of things.” A friend pointed out that he might be depressed, so he went to see a therapist and then a psychiatrist and started on medication. “It had a profound impact on how I felt.”
Still, it took a while before Dr. Goodman was comfortable sharing his story with the 1.6 million followers he had already built across his social media platforms.
“I started on social media in 2020 with the goal of advocating for mental health and inspiring future doctors.” He said the message seemed to resonate with people struggling during the early part of the pandemic. On his social media accounts, he also talks about medical school, residency, and being a health care provider. His fiancé is also a resident doctor, in internal medicine.
Dr. Goodman is also trying to create a more realistic image of doctors than the superheroes he believed they were growing up. He wants those who grow up wanting to be doctors and who look up to him to see him as a human being with vulnerabilities, such as mental health.
“You can be a doctor and have mental health issues. Seeking treatment for mental health makes you a better doctor, and for other health care workers suffering in the midst of the pandemic, I want to let them know they are not alone.”
He pointed to the statistic that doctors have one of the highest suicide rates of any professions. “It’s better to talk about that in the early stages of training.”
Students, residents, or attending physicians who have mental health challenges shouldn’t allow their symptoms to go untreated, Dr. Goodman added. “Holding in all the stress and anxiety and feelings in a very traumatic field may be dangerous. ”
One of his goals is to campaign for the removal of a question on state medical licensing forms requiring doctors to report any mental health diagnosis. It’s why doctors may be afraid to admit that they are struggling. “I’m still here. It didn’t ruin my career.”
Doctors who seek treatment for mental health are theoretically protected under the Americans With Disabilities Act from being refused a license on the basis of that diagnosis. Dr. Goodman hopes to advocate at the state level to reduce discrimination and increase accessibility for doctors to seek mental health care.
Still, Dr. Goodman concedes he was initially fearful of the repercussions. “I opened up about it because this post could save lives. I was doing what I believed in.”
So if he runs into barriers to receive his medical license because of his admission, “that’s a serious problem,” he said. “There is already a shortage of doctors. We’ll see what happens in a few years. I am not the only one who will answer ‘yes’ to having sought treatment for a mental illness. The questions do not really need to be there.”
A version of this article first appeared on Medscape.com.
When the patient wants to speak to a manager
A patient swore at me the other day. Not as in “she used a curse word.” As in she spewed fury, spitting out a vulgar, adverbial word before “... terrible doctor” while jabbing her finger toward me. In my 15 years of practice, I’d never had that happen before. Equally surprising, I was not surprised by her outburst. The level of incivility from patients is at an all-time high.
Her anger was misdirected. She wanted me to write a letter to her employer excusing her from getting a vaccine. It was neither indicated nor ethical for me to do so. I did my best to redirect her, but without success. As our chief of service, I often help with service concerns and am happy to see patients who want another opinion or want to speak with the department head (aka, “the manager”). Usually I can help. Lately, it’s become harder.
Not only are such rude incidents more frequent, but they are also more dramatic and inappropriate. For example, I cannot imagine writing a complaint against a doctor stating that she must be a foreign medical grad (as it happens, she’s Ivy League-trained) or demanding money back when a biopsy result turned out to be benign, or threatening to report a doctor to the medical board because he failed to schedule a follow-up appointment (that doctor had been retired for months). Patients have hung up on our staff mid-sentence and slammed a clinic door when they left in a huff. Why are so many previously sensible people throwing childlike tantrums?
It’s the same phenomenon happening to our fellow service agents across all industries. The Federal Aviation Administration’s graph of unruly passenger incidents is a flat line from 1995 to 2019, then it goes straight vertical. A recent survey showed that Americans’ sense of civility is low and worse, that people’s expectations that civility will improve is going down. It’s palpable. Last month, I witnessed a man and woman screaming at each other over Christmas lights in a busy store. An army of aproned walkie-talkie staff surrounded them and escorted them out – their coordination and efficiency clearly indicated they’d done this before. Customers everywhere are mad, frustrated, disenfranchised. Lately, a lot of things just are not working out for them. Supplies are out. Kids are sent home from school. No elective surgery appointments are available. The insta-gratification they’ve grown accustomed to from Amazon and DoorDash is colliding with the reality that not everything works that way.
The word “patient’’ you’ll recall comes from the Latin “patior,” meaning to suffer or bear. With virus variants raging, inflation growing, and call center wait times approaching infinity, many of our patients, it seems, cannot bear any more. I’m confident this situation will improve and our patients will be more reasonable in their expectations, but I am afraid that, in the end, we’ll have lost some decorum and dignity that we may never find again in medicine.
For my potty-mouthed patient, I made an excuse to leave the room to get my dermatoscope and walked out. It gave her time to calm down. I returned in a few minutes to do a skin exam. As I was wrapping up, I advised her that she cannot raise her voice or use offensive language and that she should know that I and everyone in our office cares about her and wants to help. She did apologize for her behavior, but then had to add that, if I really cared, I’d write the letter for her.
I guess the customer is not always right.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
A patient swore at me the other day. Not as in “she used a curse word.” As in she spewed fury, spitting out a vulgar, adverbial word before “... terrible doctor” while jabbing her finger toward me. In my 15 years of practice, I’d never had that happen before. Equally surprising, I was not surprised by her outburst. The level of incivility from patients is at an all-time high.
Her anger was misdirected. She wanted me to write a letter to her employer excusing her from getting a vaccine. It was neither indicated nor ethical for me to do so. I did my best to redirect her, but without success. As our chief of service, I often help with service concerns and am happy to see patients who want another opinion or want to speak with the department head (aka, “the manager”). Usually I can help. Lately, it’s become harder.
Not only are such rude incidents more frequent, but they are also more dramatic and inappropriate. For example, I cannot imagine writing a complaint against a doctor stating that she must be a foreign medical grad (as it happens, she’s Ivy League-trained) or demanding money back when a biopsy result turned out to be benign, or threatening to report a doctor to the medical board because he failed to schedule a follow-up appointment (that doctor had been retired for months). Patients have hung up on our staff mid-sentence and slammed a clinic door when they left in a huff. Why are so many previously sensible people throwing childlike tantrums?
It’s the same phenomenon happening to our fellow service agents across all industries. The Federal Aviation Administration’s graph of unruly passenger incidents is a flat line from 1995 to 2019, then it goes straight vertical. A recent survey showed that Americans’ sense of civility is low and worse, that people’s expectations that civility will improve is going down. It’s palpable. Last month, I witnessed a man and woman screaming at each other over Christmas lights in a busy store. An army of aproned walkie-talkie staff surrounded them and escorted them out – their coordination and efficiency clearly indicated they’d done this before. Customers everywhere are mad, frustrated, disenfranchised. Lately, a lot of things just are not working out for them. Supplies are out. Kids are sent home from school. No elective surgery appointments are available. The insta-gratification they’ve grown accustomed to from Amazon and DoorDash is colliding with the reality that not everything works that way.
The word “patient’’ you’ll recall comes from the Latin “patior,” meaning to suffer or bear. With virus variants raging, inflation growing, and call center wait times approaching infinity, many of our patients, it seems, cannot bear any more. I’m confident this situation will improve and our patients will be more reasonable in their expectations, but I am afraid that, in the end, we’ll have lost some decorum and dignity that we may never find again in medicine.
For my potty-mouthed patient, I made an excuse to leave the room to get my dermatoscope and walked out. It gave her time to calm down. I returned in a few minutes to do a skin exam. As I was wrapping up, I advised her that she cannot raise her voice or use offensive language and that she should know that I and everyone in our office cares about her and wants to help. She did apologize for her behavior, but then had to add that, if I really cared, I’d write the letter for her.
I guess the customer is not always right.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
A patient swore at me the other day. Not as in “she used a curse word.” As in she spewed fury, spitting out a vulgar, adverbial word before “... terrible doctor” while jabbing her finger toward me. In my 15 years of practice, I’d never had that happen before. Equally surprising, I was not surprised by her outburst. The level of incivility from patients is at an all-time high.
Her anger was misdirected. She wanted me to write a letter to her employer excusing her from getting a vaccine. It was neither indicated nor ethical for me to do so. I did my best to redirect her, but without success. As our chief of service, I often help with service concerns and am happy to see patients who want another opinion or want to speak with the department head (aka, “the manager”). Usually I can help. Lately, it’s become harder.
Not only are such rude incidents more frequent, but they are also more dramatic and inappropriate. For example, I cannot imagine writing a complaint against a doctor stating that she must be a foreign medical grad (as it happens, she’s Ivy League-trained) or demanding money back when a biopsy result turned out to be benign, or threatening to report a doctor to the medical board because he failed to schedule a follow-up appointment (that doctor had been retired for months). Patients have hung up on our staff mid-sentence and slammed a clinic door when they left in a huff. Why are so many previously sensible people throwing childlike tantrums?
It’s the same phenomenon happening to our fellow service agents across all industries. The Federal Aviation Administration’s graph of unruly passenger incidents is a flat line from 1995 to 2019, then it goes straight vertical. A recent survey showed that Americans’ sense of civility is low and worse, that people’s expectations that civility will improve is going down. It’s palpable. Last month, I witnessed a man and woman screaming at each other over Christmas lights in a busy store. An army of aproned walkie-talkie staff surrounded them and escorted them out – their coordination and efficiency clearly indicated they’d done this before. Customers everywhere are mad, frustrated, disenfranchised. Lately, a lot of things just are not working out for them. Supplies are out. Kids are sent home from school. No elective surgery appointments are available. The insta-gratification they’ve grown accustomed to from Amazon and DoorDash is colliding with the reality that not everything works that way.
The word “patient’’ you’ll recall comes from the Latin “patior,” meaning to suffer or bear. With virus variants raging, inflation growing, and call center wait times approaching infinity, many of our patients, it seems, cannot bear any more. I’m confident this situation will improve and our patients will be more reasonable in their expectations, but I am afraid that, in the end, we’ll have lost some decorum and dignity that we may never find again in medicine.
For my potty-mouthed patient, I made an excuse to leave the room to get my dermatoscope and walked out. It gave her time to calm down. I returned in a few minutes to do a skin exam. As I was wrapping up, I advised her that she cannot raise her voice or use offensive language and that she should know that I and everyone in our office cares about her and wants to help. She did apologize for her behavior, but then had to add that, if I really cared, I’d write the letter for her.
I guess the customer is not always right.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
Mental health problems in kids linked with school closures
Behavior problems, anxiety, and depression in youths were associated with these individuals participating in remote schooling during broader social lockdowns in a new study.
The systematic review, which was published in JAMA Pediatrics on Jan. 18, 2022, was based on data from 36 studies from 11 countries on mental health, physical health, and well-being in children and adolescents aged 0-18 years. The total population included 79,781 children and 18,028 parents or caregivers. The studies reflected the first wave of pandemic school closures and lockdowns from February to July 2020, with the duration of school closure ranging from 1 week to 3 months.
“There are strong theoretical reasons to suggest that school closures may have contributed to a considerable proportion of the harms identified here, particularly mental health harms, through reduction in social contacts with peers and teachers,” Russell Viner, PhD, of UCL Great Ormond St Institute of Child Health, London, and colleagues wrote in their paper.
The researchers included 9 longitudinal pre-post studies, 5 cohort studies, 21 cross-sectional studies, and 1 modeling study in their analysis. Overall, approximately one-third of the studies (36%) were considered high quality, and approximately two-thirds (64%) of the studies were published in journals. Twenty-five of the reports analyzed focused on mental health and well-being.
Schools provide not only education, but also services including meals, health care, and health supplies. Schools also serve as a safety net and source of social support for children, the researchers noted.
The losses children may have experienced during school closures occurred during a time when more than 167,000 children younger than 18 years lost a parent or caregiver to COVID-19, according to a recent report titled “Hidden Pain” by researchers at the University of Pennsylvania, Nemours Children’s Health, and the COVID Collaborative. Although not addressed in the current study, school closures would prevent bereaved children from receiving social-emotional support from friends and teachers. This crisis of loss also prompted the American Academy of Pediatrics to issue a National State of Emergency in Children’s Mental Health in October 2021.
New study results
These studies identified associations between school closures during broader lockdowns and increased emotional and behavioral problems, as well as increased restlessness and inattention. Across these studies, 18%-60% of children and adolescents scored higher than the risk thresholds for diagnoses of distress, especially depressive symptoms and anxiety.
Although two studies showed no significant association with suicide in response to school closures during lockdowns, three studies suggested increased use of screen time, two studies reported increased social media use, and six studies reported lower levels of physical activity.
Three studies of child abuse showed decreases in notifications during lockdowns, likely driven by lack of referrals from schools, the authors noted. A total of 10 studies on sleep and 5 studies on diet showed inconsistent evidence of harm during the specific period of school closures and social lockdowns.
“The contrast of rises in distress with decreases in presentations suggests that there was an escalation of unmet mental health need during lockdowns in already vulnerable children and adolescents,” the researchers wrote. “More troubling still is evidence of a reduction in the ability of the health and social care systems to protect children in many countries, as shown by the large falls in child protection referrals seen in high-quality cohort studies.”
‘Study presents concrete assessments rather than speculation’
“Concerns have been widely expressed in the lay media and beyond that school closures could negatively impact the mental and physical health of children and adolescents,” M. Susan Jay, MD, of the Medical College of Wisconsin, Milwaukee, said in an interview. “The authors presented a narrative synthesis summarizing available evidence for the first wave of COVID-19 on school closures during the broader social lockdown occurring during this period.”
The “importance” of this research is that “it is not a single convenience sample study, but a systematic review from 11 countries including the United States, United Kingdom, China, and Turkey, among others, and that the quality of the information was graded,” Dr. Jay said. “Although not a meta-analysis, the study presents concrete assessments rather than speculation and overviews its limitations so that the clinician can weigh this information. Importantly, the authors excluded closure of schools with transmission of infection.
“Clearly, school lockdowns as a measure of controlling infectious disease needs balance with potential of negative health behaviors in children and adolescents. Ongoing prospective longitudinal studies are needed as sequential waves of the pandemic continue,” she emphasized.
“Clinically, this study highlights the need for clinicians to consider [asking] about the impact of school closures and remote versus hybrid versus in-person education [as part of their] patients and families question inventory,” Dr. Jay said. “Also, the use of depression inventories can be offered to youth to assess their mental health state at a visit, either via telemedicine or in person, and ideally at sequential visits for a more in-depth assessment.”
Schools play key role in social and emotional development
“It was important to conduct this study now, because this current time is unprecedented,” Peter L. Loper Jr., MD, of the University of South Carolina, Columbia, said in an interview. “We know based on evolutionary biology, anthropology, and developmental psychology, among other disciplines, that meaningful interpersonal interactions embedded in the context of community are vital to supporting human well-being.
“In our current time, the primary framework of community for our children is the school setting; it is the predominant space where they engage in the interpersonal interactions necessary for developing resilience, their sense of purpose, belonging, and fidelity,” he emphasized.
“Rarely in the course of human existence have kids been removed from the broader context of community to this extent and for this duration,” Dr. Loper said. “This study capitalizes on this unprecedented moment to begin to further understand how compromises in our sociocultural infrastructure of community, like school closures and lockdowns, may manifest as mental health problems in children and adolescents. More importantly, it contributes to the exploration of potential unintended consequences of our current infection control measures so we can adapt to support the overall well-being of our children in this ‘new normal.’ ”
Dr. Loper added that he was not surprised by the new study’s findings.
“We were already seeing a decline in pediatric mental health and overall well-being in the years preceding COVID-19 because of the ‘isolation epidemic’ involving many of the factors that this study explored,” he said. “I think this review further illustrates the vital necessity of community to support the health and well-being of humans, and specifically children and adolescents.”
From a clinical standpoint, “we need to be intentional and consistent in balancing infection control measures with our kids’ fundamental psychosocial needs,” Dr. Loper said.
“We need to recognize that, when children and adolescents are isolated from community, their fundamental psychosocial needs go unmet,” he emphasized. “If children and adolescents cannot access the meaningful interpersonal interactions necessary for resilience, then they cannot overcome or navigate distress. They will exhibit the avoidance and withdrawal behaviors that accumulate to manifest as adverse mental health symptoms like anxiety and depression.
“Additional research is needed to further explore how compromises in the psychosocial infrastructure of community manifest as downstream symptom indicators such as anxiety and depression,” which are often manifestations of unmet needs, Dr. Loper said.
Limitations and strengths, according to authors
The findings were limited by several factors, including a lack of examination of school closures’ effects on mental health independent of broader social lockdowns, according to the researchers. Other limitations included the authors potentially having missed studies, inclusion of cross-sectional studies with relatively weak evidence, potential bias from studies using parent reports, and a focus on the first COVID-19 wave, during which many school closures were of limited duration. Also, the researchers said they did not include studies focused on particular groups, such as children with learning difficulties or autism.
The use of large databases from education as well as health care in studies analyzed were strengths of the new research, they said. The investigators received no outside funding for their study. The researchers, Dr. Jay, and Dr. Loper had no financial conflicts to disclose. Dr. Jay serves on the editorial advisory board of Pediatric News.
Behavior problems, anxiety, and depression in youths were associated with these individuals participating in remote schooling during broader social lockdowns in a new study.
The systematic review, which was published in JAMA Pediatrics on Jan. 18, 2022, was based on data from 36 studies from 11 countries on mental health, physical health, and well-being in children and adolescents aged 0-18 years. The total population included 79,781 children and 18,028 parents or caregivers. The studies reflected the first wave of pandemic school closures and lockdowns from February to July 2020, with the duration of school closure ranging from 1 week to 3 months.
“There are strong theoretical reasons to suggest that school closures may have contributed to a considerable proportion of the harms identified here, particularly mental health harms, through reduction in social contacts with peers and teachers,” Russell Viner, PhD, of UCL Great Ormond St Institute of Child Health, London, and colleagues wrote in their paper.
The researchers included 9 longitudinal pre-post studies, 5 cohort studies, 21 cross-sectional studies, and 1 modeling study in their analysis. Overall, approximately one-third of the studies (36%) were considered high quality, and approximately two-thirds (64%) of the studies were published in journals. Twenty-five of the reports analyzed focused on mental health and well-being.
Schools provide not only education, but also services including meals, health care, and health supplies. Schools also serve as a safety net and source of social support for children, the researchers noted.
The losses children may have experienced during school closures occurred during a time when more than 167,000 children younger than 18 years lost a parent or caregiver to COVID-19, according to a recent report titled “Hidden Pain” by researchers at the University of Pennsylvania, Nemours Children’s Health, and the COVID Collaborative. Although not addressed in the current study, school closures would prevent bereaved children from receiving social-emotional support from friends and teachers. This crisis of loss also prompted the American Academy of Pediatrics to issue a National State of Emergency in Children’s Mental Health in October 2021.
New study results
These studies identified associations between school closures during broader lockdowns and increased emotional and behavioral problems, as well as increased restlessness and inattention. Across these studies, 18%-60% of children and adolescents scored higher than the risk thresholds for diagnoses of distress, especially depressive symptoms and anxiety.
Although two studies showed no significant association with suicide in response to school closures during lockdowns, three studies suggested increased use of screen time, two studies reported increased social media use, and six studies reported lower levels of physical activity.
Three studies of child abuse showed decreases in notifications during lockdowns, likely driven by lack of referrals from schools, the authors noted. A total of 10 studies on sleep and 5 studies on diet showed inconsistent evidence of harm during the specific period of school closures and social lockdowns.
“The contrast of rises in distress with decreases in presentations suggests that there was an escalation of unmet mental health need during lockdowns in already vulnerable children and adolescents,” the researchers wrote. “More troubling still is evidence of a reduction in the ability of the health and social care systems to protect children in many countries, as shown by the large falls in child protection referrals seen in high-quality cohort studies.”
‘Study presents concrete assessments rather than speculation’
“Concerns have been widely expressed in the lay media and beyond that school closures could negatively impact the mental and physical health of children and adolescents,” M. Susan Jay, MD, of the Medical College of Wisconsin, Milwaukee, said in an interview. “The authors presented a narrative synthesis summarizing available evidence for the first wave of COVID-19 on school closures during the broader social lockdown occurring during this period.”
The “importance” of this research is that “it is not a single convenience sample study, but a systematic review from 11 countries including the United States, United Kingdom, China, and Turkey, among others, and that the quality of the information was graded,” Dr. Jay said. “Although not a meta-analysis, the study presents concrete assessments rather than speculation and overviews its limitations so that the clinician can weigh this information. Importantly, the authors excluded closure of schools with transmission of infection.
“Clearly, school lockdowns as a measure of controlling infectious disease needs balance with potential of negative health behaviors in children and adolescents. Ongoing prospective longitudinal studies are needed as sequential waves of the pandemic continue,” she emphasized.
“Clinically, this study highlights the need for clinicians to consider [asking] about the impact of school closures and remote versus hybrid versus in-person education [as part of their] patients and families question inventory,” Dr. Jay said. “Also, the use of depression inventories can be offered to youth to assess their mental health state at a visit, either via telemedicine or in person, and ideally at sequential visits for a more in-depth assessment.”
Schools play key role in social and emotional development
“It was important to conduct this study now, because this current time is unprecedented,” Peter L. Loper Jr., MD, of the University of South Carolina, Columbia, said in an interview. “We know based on evolutionary biology, anthropology, and developmental psychology, among other disciplines, that meaningful interpersonal interactions embedded in the context of community are vital to supporting human well-being.
“In our current time, the primary framework of community for our children is the school setting; it is the predominant space where they engage in the interpersonal interactions necessary for developing resilience, their sense of purpose, belonging, and fidelity,” he emphasized.
“Rarely in the course of human existence have kids been removed from the broader context of community to this extent and for this duration,” Dr. Loper said. “This study capitalizes on this unprecedented moment to begin to further understand how compromises in our sociocultural infrastructure of community, like school closures and lockdowns, may manifest as mental health problems in children and adolescents. More importantly, it contributes to the exploration of potential unintended consequences of our current infection control measures so we can adapt to support the overall well-being of our children in this ‘new normal.’ ”
Dr. Loper added that he was not surprised by the new study’s findings.
“We were already seeing a decline in pediatric mental health and overall well-being in the years preceding COVID-19 because of the ‘isolation epidemic’ involving many of the factors that this study explored,” he said. “I think this review further illustrates the vital necessity of community to support the health and well-being of humans, and specifically children and adolescents.”
From a clinical standpoint, “we need to be intentional and consistent in balancing infection control measures with our kids’ fundamental psychosocial needs,” Dr. Loper said.
“We need to recognize that, when children and adolescents are isolated from community, their fundamental psychosocial needs go unmet,” he emphasized. “If children and adolescents cannot access the meaningful interpersonal interactions necessary for resilience, then they cannot overcome or navigate distress. They will exhibit the avoidance and withdrawal behaviors that accumulate to manifest as adverse mental health symptoms like anxiety and depression.
“Additional research is needed to further explore how compromises in the psychosocial infrastructure of community manifest as downstream symptom indicators such as anxiety and depression,” which are often manifestations of unmet needs, Dr. Loper said.
Limitations and strengths, according to authors
The findings were limited by several factors, including a lack of examination of school closures’ effects on mental health independent of broader social lockdowns, according to the researchers. Other limitations included the authors potentially having missed studies, inclusion of cross-sectional studies with relatively weak evidence, potential bias from studies using parent reports, and a focus on the first COVID-19 wave, during which many school closures were of limited duration. Also, the researchers said they did not include studies focused on particular groups, such as children with learning difficulties or autism.
The use of large databases from education as well as health care in studies analyzed were strengths of the new research, they said. The investigators received no outside funding for their study. The researchers, Dr. Jay, and Dr. Loper had no financial conflicts to disclose. Dr. Jay serves on the editorial advisory board of Pediatric News.
Behavior problems, anxiety, and depression in youths were associated with these individuals participating in remote schooling during broader social lockdowns in a new study.
The systematic review, which was published in JAMA Pediatrics on Jan. 18, 2022, was based on data from 36 studies from 11 countries on mental health, physical health, and well-being in children and adolescents aged 0-18 years. The total population included 79,781 children and 18,028 parents or caregivers. The studies reflected the first wave of pandemic school closures and lockdowns from February to July 2020, with the duration of school closure ranging from 1 week to 3 months.
“There are strong theoretical reasons to suggest that school closures may have contributed to a considerable proportion of the harms identified here, particularly mental health harms, through reduction in social contacts with peers and teachers,” Russell Viner, PhD, of UCL Great Ormond St Institute of Child Health, London, and colleagues wrote in their paper.
The researchers included 9 longitudinal pre-post studies, 5 cohort studies, 21 cross-sectional studies, and 1 modeling study in their analysis. Overall, approximately one-third of the studies (36%) were considered high quality, and approximately two-thirds (64%) of the studies were published in journals. Twenty-five of the reports analyzed focused on mental health and well-being.
Schools provide not only education, but also services including meals, health care, and health supplies. Schools also serve as a safety net and source of social support for children, the researchers noted.
The losses children may have experienced during school closures occurred during a time when more than 167,000 children younger than 18 years lost a parent or caregiver to COVID-19, according to a recent report titled “Hidden Pain” by researchers at the University of Pennsylvania, Nemours Children’s Health, and the COVID Collaborative. Although not addressed in the current study, school closures would prevent bereaved children from receiving social-emotional support from friends and teachers. This crisis of loss also prompted the American Academy of Pediatrics to issue a National State of Emergency in Children’s Mental Health in October 2021.
New study results
These studies identified associations between school closures during broader lockdowns and increased emotional and behavioral problems, as well as increased restlessness and inattention. Across these studies, 18%-60% of children and adolescents scored higher than the risk thresholds for diagnoses of distress, especially depressive symptoms and anxiety.
Although two studies showed no significant association with suicide in response to school closures during lockdowns, three studies suggested increased use of screen time, two studies reported increased social media use, and six studies reported lower levels of physical activity.
Three studies of child abuse showed decreases in notifications during lockdowns, likely driven by lack of referrals from schools, the authors noted. A total of 10 studies on sleep and 5 studies on diet showed inconsistent evidence of harm during the specific period of school closures and social lockdowns.
“The contrast of rises in distress with decreases in presentations suggests that there was an escalation of unmet mental health need during lockdowns in already vulnerable children and adolescents,” the researchers wrote. “More troubling still is evidence of a reduction in the ability of the health and social care systems to protect children in many countries, as shown by the large falls in child protection referrals seen in high-quality cohort studies.”
‘Study presents concrete assessments rather than speculation’
“Concerns have been widely expressed in the lay media and beyond that school closures could negatively impact the mental and physical health of children and adolescents,” M. Susan Jay, MD, of the Medical College of Wisconsin, Milwaukee, said in an interview. “The authors presented a narrative synthesis summarizing available evidence for the first wave of COVID-19 on school closures during the broader social lockdown occurring during this period.”
The “importance” of this research is that “it is not a single convenience sample study, but a systematic review from 11 countries including the United States, United Kingdom, China, and Turkey, among others, and that the quality of the information was graded,” Dr. Jay said. “Although not a meta-analysis, the study presents concrete assessments rather than speculation and overviews its limitations so that the clinician can weigh this information. Importantly, the authors excluded closure of schools with transmission of infection.
“Clearly, school lockdowns as a measure of controlling infectious disease needs balance with potential of negative health behaviors in children and adolescents. Ongoing prospective longitudinal studies are needed as sequential waves of the pandemic continue,” she emphasized.
“Clinically, this study highlights the need for clinicians to consider [asking] about the impact of school closures and remote versus hybrid versus in-person education [as part of their] patients and families question inventory,” Dr. Jay said. “Also, the use of depression inventories can be offered to youth to assess their mental health state at a visit, either via telemedicine or in person, and ideally at sequential visits for a more in-depth assessment.”
Schools play key role in social and emotional development
“It was important to conduct this study now, because this current time is unprecedented,” Peter L. Loper Jr., MD, of the University of South Carolina, Columbia, said in an interview. “We know based on evolutionary biology, anthropology, and developmental psychology, among other disciplines, that meaningful interpersonal interactions embedded in the context of community are vital to supporting human well-being.
“In our current time, the primary framework of community for our children is the school setting; it is the predominant space where they engage in the interpersonal interactions necessary for developing resilience, their sense of purpose, belonging, and fidelity,” he emphasized.
“Rarely in the course of human existence have kids been removed from the broader context of community to this extent and for this duration,” Dr. Loper said. “This study capitalizes on this unprecedented moment to begin to further understand how compromises in our sociocultural infrastructure of community, like school closures and lockdowns, may manifest as mental health problems in children and adolescents. More importantly, it contributes to the exploration of potential unintended consequences of our current infection control measures so we can adapt to support the overall well-being of our children in this ‘new normal.’ ”
Dr. Loper added that he was not surprised by the new study’s findings.
“We were already seeing a decline in pediatric mental health and overall well-being in the years preceding COVID-19 because of the ‘isolation epidemic’ involving many of the factors that this study explored,” he said. “I think this review further illustrates the vital necessity of community to support the health and well-being of humans, and specifically children and adolescents.”
From a clinical standpoint, “we need to be intentional and consistent in balancing infection control measures with our kids’ fundamental psychosocial needs,” Dr. Loper said.
“We need to recognize that, when children and adolescents are isolated from community, their fundamental psychosocial needs go unmet,” he emphasized. “If children and adolescents cannot access the meaningful interpersonal interactions necessary for resilience, then they cannot overcome or navigate distress. They will exhibit the avoidance and withdrawal behaviors that accumulate to manifest as adverse mental health symptoms like anxiety and depression.
“Additional research is needed to further explore how compromises in the psychosocial infrastructure of community manifest as downstream symptom indicators such as anxiety and depression,” which are often manifestations of unmet needs, Dr. Loper said.
Limitations and strengths, according to authors
The findings were limited by several factors, including a lack of examination of school closures’ effects on mental health independent of broader social lockdowns, according to the researchers. Other limitations included the authors potentially having missed studies, inclusion of cross-sectional studies with relatively weak evidence, potential bias from studies using parent reports, and a focus on the first COVID-19 wave, during which many school closures were of limited duration. Also, the researchers said they did not include studies focused on particular groups, such as children with learning difficulties or autism.
The use of large databases from education as well as health care in studies analyzed were strengths of the new research, they said. The investigators received no outside funding for their study. The researchers, Dr. Jay, and Dr. Loper had no financial conflicts to disclose. Dr. Jay serves on the editorial advisory board of Pediatric News.
FROM JAMA PEDIATRICS
Study finds genetic factor for COVID smell and taste loss
, according to a new study published in the journal Nature Genetics
The finding could eventually help the 1.6 million people in the United States who still can’t smell or have had a change in their ability to smell more than 6 months after getting the coronavirus. The exact cause related to COVID-19 is still unknown, but researchers believe it could be because of damage in a part of the nose called the olfactory epithelium.
“How we get from infection to smell loss remains unclear,” Justin Turner, MD, an associate professor of otolaryngology at Vanderbilt University, Nashville, Tenn., told NBC News. Dr. Turner was not part of the research team.
“Early data suggest that supporting cells of the olfactory epithelium are the ones mostly being infected by the virus, and presumably this leads to the death of the neurons themselves,” he said. “But we don’t really, really know why and when that happens, and why it seems to preferentially happen in certain individuals.”
Researchers at 23andMe, a genomics and biotechnology company, did the study as part of a larger COVID-19 project, which includes people in the United States and the United Kingdom. They analyzed data from nearly 70,000 people who took online surveys after receiving a positive coronavirus test. Among those, 68% reported a loss of smell or taste as a symptom.
The study team compared the genetic differences between those who lost their sense of smell and taste and those who didn’t. They found that a location near two olfactory genes – UGT2A1 and UGT2A2 – is associated with COVID-19 loss of smell and taste. The genetic risk factor makes it 11% more likely for a person with COVID-19 to lose their sense of smell or taste.
The research team also found that women were 11% more likely than men to report a loss of smell and taste. About 73% of those who reported a loss of smell and taste were ages 26-35.
The researchers aren’t sure how the genes are involved, though they suspect that infected cells could lead to smell loss. Typically, the genes are expressed in tissue inside the nose involved with smell and play a role in processing things that have an odor. To use the findings, researchers need to learn more about the genes, how they are expressed, and what their functions are, NBC News reported.
The findings could help lead to treatments. Other research has shown that the loss of taste and smell is related to a “failure to protect the sensory cells of the nose and tongue from viral infection,” Danielle Reed, PhD, associate director of the Monell Chemical Senses Center in Philadelphia, told NBC News. She was not part of the research team but studies person-to-person differences in the loss of these senses because of COVID-19.
“This study suggests a different direction,” she said. “The pathways that break down the chemicals that cause taste and smell in the first place might be over or underactive, reducing or distorting the ability to taste and smell.”
A version of this article first appeared on WebMD.com.
, according to a new study published in the journal Nature Genetics
The finding could eventually help the 1.6 million people in the United States who still can’t smell or have had a change in their ability to smell more than 6 months after getting the coronavirus. The exact cause related to COVID-19 is still unknown, but researchers believe it could be because of damage in a part of the nose called the olfactory epithelium.
“How we get from infection to smell loss remains unclear,” Justin Turner, MD, an associate professor of otolaryngology at Vanderbilt University, Nashville, Tenn., told NBC News. Dr. Turner was not part of the research team.
“Early data suggest that supporting cells of the olfactory epithelium are the ones mostly being infected by the virus, and presumably this leads to the death of the neurons themselves,” he said. “But we don’t really, really know why and when that happens, and why it seems to preferentially happen in certain individuals.”
Researchers at 23andMe, a genomics and biotechnology company, did the study as part of a larger COVID-19 project, which includes people in the United States and the United Kingdom. They analyzed data from nearly 70,000 people who took online surveys after receiving a positive coronavirus test. Among those, 68% reported a loss of smell or taste as a symptom.
The study team compared the genetic differences between those who lost their sense of smell and taste and those who didn’t. They found that a location near two olfactory genes – UGT2A1 and UGT2A2 – is associated with COVID-19 loss of smell and taste. The genetic risk factor makes it 11% more likely for a person with COVID-19 to lose their sense of smell or taste.
The research team also found that women were 11% more likely than men to report a loss of smell and taste. About 73% of those who reported a loss of smell and taste were ages 26-35.
The researchers aren’t sure how the genes are involved, though they suspect that infected cells could lead to smell loss. Typically, the genes are expressed in tissue inside the nose involved with smell and play a role in processing things that have an odor. To use the findings, researchers need to learn more about the genes, how they are expressed, and what their functions are, NBC News reported.
The findings could help lead to treatments. Other research has shown that the loss of taste and smell is related to a “failure to protect the sensory cells of the nose and tongue from viral infection,” Danielle Reed, PhD, associate director of the Monell Chemical Senses Center in Philadelphia, told NBC News. She was not part of the research team but studies person-to-person differences in the loss of these senses because of COVID-19.
“This study suggests a different direction,” she said. “The pathways that break down the chemicals that cause taste and smell in the first place might be over or underactive, reducing or distorting the ability to taste and smell.”
A version of this article first appeared on WebMD.com.
, according to a new study published in the journal Nature Genetics
The finding could eventually help the 1.6 million people in the United States who still can’t smell or have had a change in their ability to smell more than 6 months after getting the coronavirus. The exact cause related to COVID-19 is still unknown, but researchers believe it could be because of damage in a part of the nose called the olfactory epithelium.
“How we get from infection to smell loss remains unclear,” Justin Turner, MD, an associate professor of otolaryngology at Vanderbilt University, Nashville, Tenn., told NBC News. Dr. Turner was not part of the research team.
“Early data suggest that supporting cells of the olfactory epithelium are the ones mostly being infected by the virus, and presumably this leads to the death of the neurons themselves,” he said. “But we don’t really, really know why and when that happens, and why it seems to preferentially happen in certain individuals.”
Researchers at 23andMe, a genomics and biotechnology company, did the study as part of a larger COVID-19 project, which includes people in the United States and the United Kingdom. They analyzed data from nearly 70,000 people who took online surveys after receiving a positive coronavirus test. Among those, 68% reported a loss of smell or taste as a symptom.
The study team compared the genetic differences between those who lost their sense of smell and taste and those who didn’t. They found that a location near two olfactory genes – UGT2A1 and UGT2A2 – is associated with COVID-19 loss of smell and taste. The genetic risk factor makes it 11% more likely for a person with COVID-19 to lose their sense of smell or taste.
The research team also found that women were 11% more likely than men to report a loss of smell and taste. About 73% of those who reported a loss of smell and taste were ages 26-35.
The researchers aren’t sure how the genes are involved, though they suspect that infected cells could lead to smell loss. Typically, the genes are expressed in tissue inside the nose involved with smell and play a role in processing things that have an odor. To use the findings, researchers need to learn more about the genes, how they are expressed, and what their functions are, NBC News reported.
The findings could help lead to treatments. Other research has shown that the loss of taste and smell is related to a “failure to protect the sensory cells of the nose and tongue from viral infection,” Danielle Reed, PhD, associate director of the Monell Chemical Senses Center in Philadelphia, told NBC News. She was not part of the research team but studies person-to-person differences in the loss of these senses because of COVID-19.
“This study suggests a different direction,” she said. “The pathways that break down the chemicals that cause taste and smell in the first place might be over or underactive, reducing or distorting the ability to taste and smell.”
A version of this article first appeared on WebMD.com.
FROM NATURE GENETICS
Fourth vaccine shot less effective against Omicron, Israeli study says
, according to new research at an Israeli hospital.
The preliminary results, released on Jan. 17, challenge the idea of giving a second booster dose to slow the spread of the coronavirus, according to USA Today.
“Despite increased antibody levels, the fourth vaccine only offers a partial defense against the virus,” Gili Regev-Yochay, MD, director of the hospital’s infection prevention and control units, told reporters.
“The vaccines, which were more effective against previous variants, offer less protection versus Omicron,” she said.
In a clinical trial, 274 medical workers at Sheba Medical Center near Tel Aviv received a fourth vaccine dose in December – 154 got the Pfizer vaccine and 120 got the Moderna vaccine – after previously getting three Pfizer shots.
Both groups received a boost in antibodies that was “slightly higher” than after the third shot, Dr. Regev-Yochay said. But when compared with a control group that didn’t receive the fourth dose, the extra boost didn’t prevent the spread of Omicron.
“We see many infected with Omicron who received the fourth dose,” Dr. Regev-Yochay said. “Granted, a bit less than in the control group, but still a lot of infections.”
Some public health officials in Israel say the campaign for fourth doses is still worthwhile, according to The Times of Israel. The vaccine still works well against the Alpha and Delta variants, Dr. Regev-Yochay said, and a fourth shot should go to older adults and those who face higher risks for severe COVID-19.
Hours after releasing the preliminary results, Sheba Medical Center published a statement calling for “continuing the vaccination drive for risk groups at this time, even though the vaccine doesn’t provide optimal protection against getting infected with the variant.” News outlets reported that the hospital was pressured into issuing the statement after Israel’s Health Ministry didn’t like the release of the early study results, The Times of Israel reported.
The second booster “returns the level of antibodies to what it was at the beginning of the third booster,” Nachman Ash, MD, director of Israel’s Health Ministry, told Channel 13 TV in Israel, according to The Associated Press.
“That has great importance, especially among the older population,” he said.
As of Sunday, more than 500,000 people in Israel had received fourth doses since the country began offering them last month to medical workers, immunocompromised patients, and people ages 60 years and older, the AP reported. At the same time, the country has faced a recent coronavirus surge that has led to record-breaking numbers of cases and rising hospitalizations.
On Tuesday, the Israeli government said it would shorten the mandatory quarantine period from 7 days to 5 days, the AP reported.
“This decision will enable us to continue safeguarding public health on the one hand and to keep the economy going at this time on the other, even though it is difficult, so that we can get through this wave safely,” Prime Minister Naftali Bennett said.
A version of this article first appeared on WebMD.com.
, according to new research at an Israeli hospital.
The preliminary results, released on Jan. 17, challenge the idea of giving a second booster dose to slow the spread of the coronavirus, according to USA Today.
“Despite increased antibody levels, the fourth vaccine only offers a partial defense against the virus,” Gili Regev-Yochay, MD, director of the hospital’s infection prevention and control units, told reporters.
“The vaccines, which were more effective against previous variants, offer less protection versus Omicron,” she said.
In a clinical trial, 274 medical workers at Sheba Medical Center near Tel Aviv received a fourth vaccine dose in December – 154 got the Pfizer vaccine and 120 got the Moderna vaccine – after previously getting three Pfizer shots.
Both groups received a boost in antibodies that was “slightly higher” than after the third shot, Dr. Regev-Yochay said. But when compared with a control group that didn’t receive the fourth dose, the extra boost didn’t prevent the spread of Omicron.
“We see many infected with Omicron who received the fourth dose,” Dr. Regev-Yochay said. “Granted, a bit less than in the control group, but still a lot of infections.”
Some public health officials in Israel say the campaign for fourth doses is still worthwhile, according to The Times of Israel. The vaccine still works well against the Alpha and Delta variants, Dr. Regev-Yochay said, and a fourth shot should go to older adults and those who face higher risks for severe COVID-19.
Hours after releasing the preliminary results, Sheba Medical Center published a statement calling for “continuing the vaccination drive for risk groups at this time, even though the vaccine doesn’t provide optimal protection against getting infected with the variant.” News outlets reported that the hospital was pressured into issuing the statement after Israel’s Health Ministry didn’t like the release of the early study results, The Times of Israel reported.
The second booster “returns the level of antibodies to what it was at the beginning of the third booster,” Nachman Ash, MD, director of Israel’s Health Ministry, told Channel 13 TV in Israel, according to The Associated Press.
“That has great importance, especially among the older population,” he said.
As of Sunday, more than 500,000 people in Israel had received fourth doses since the country began offering them last month to medical workers, immunocompromised patients, and people ages 60 years and older, the AP reported. At the same time, the country has faced a recent coronavirus surge that has led to record-breaking numbers of cases and rising hospitalizations.
On Tuesday, the Israeli government said it would shorten the mandatory quarantine period from 7 days to 5 days, the AP reported.
“This decision will enable us to continue safeguarding public health on the one hand and to keep the economy going at this time on the other, even though it is difficult, so that we can get through this wave safely,” Prime Minister Naftali Bennett said.
A version of this article first appeared on WebMD.com.
, according to new research at an Israeli hospital.
The preliminary results, released on Jan. 17, challenge the idea of giving a second booster dose to slow the spread of the coronavirus, according to USA Today.
“Despite increased antibody levels, the fourth vaccine only offers a partial defense against the virus,” Gili Regev-Yochay, MD, director of the hospital’s infection prevention and control units, told reporters.
“The vaccines, which were more effective against previous variants, offer less protection versus Omicron,” she said.
In a clinical trial, 274 medical workers at Sheba Medical Center near Tel Aviv received a fourth vaccine dose in December – 154 got the Pfizer vaccine and 120 got the Moderna vaccine – after previously getting three Pfizer shots.
Both groups received a boost in antibodies that was “slightly higher” than after the third shot, Dr. Regev-Yochay said. But when compared with a control group that didn’t receive the fourth dose, the extra boost didn’t prevent the spread of Omicron.
“We see many infected with Omicron who received the fourth dose,” Dr. Regev-Yochay said. “Granted, a bit less than in the control group, but still a lot of infections.”
Some public health officials in Israel say the campaign for fourth doses is still worthwhile, according to The Times of Israel. The vaccine still works well against the Alpha and Delta variants, Dr. Regev-Yochay said, and a fourth shot should go to older adults and those who face higher risks for severe COVID-19.
Hours after releasing the preliminary results, Sheba Medical Center published a statement calling for “continuing the vaccination drive for risk groups at this time, even though the vaccine doesn’t provide optimal protection against getting infected with the variant.” News outlets reported that the hospital was pressured into issuing the statement after Israel’s Health Ministry didn’t like the release of the early study results, The Times of Israel reported.
The second booster “returns the level of antibodies to what it was at the beginning of the third booster,” Nachman Ash, MD, director of Israel’s Health Ministry, told Channel 13 TV in Israel, according to The Associated Press.
“That has great importance, especially among the older population,” he said.
As of Sunday, more than 500,000 people in Israel had received fourth doses since the country began offering them last month to medical workers, immunocompromised patients, and people ages 60 years and older, the AP reported. At the same time, the country has faced a recent coronavirus surge that has led to record-breaking numbers of cases and rising hospitalizations.
On Tuesday, the Israeli government said it would shorten the mandatory quarantine period from 7 days to 5 days, the AP reported.
“This decision will enable us to continue safeguarding public health on the one hand and to keep the economy going at this time on the other, even though it is difficult, so that we can get through this wave safely,” Prime Minister Naftali Bennett said.
A version of this article first appeared on WebMD.com.
Family-oriented care in adult psychiatric residency
The Group for the Advancement of Psychiatry’s Committee on the Family published an updated curriculum in October 2021 on family-oriented care. The first curriculum, published in 2006, was nominated as the American Association of Directors of Psychiatric Residency Training model curriculum for family-oriented care. The updated curriculum, produced by the GAP family committee and guests, is shorter and more focused.
The following is a summary of the introduction and the highlights.
Introduction
Use of family systems–based techniques in the diagnosis and care of patients is a key evidence-based tool for psychiatric disorders. However, it is not a current Accreditation Council for Graduate Medical Education Training training requirement, and it is possible to complete psychiatry residency without exposure to this key framework.
Here, we highlight the importance of considering patients through a “family systems” lens and the incorporation of multiple individuals from an individual patient’s identified system in their care.
Current medicine curricula emphasize patient autonomy, one of the core pillars of ethics. Autonomy is the cornerstone of the everyday practice within medicine of communicating all risks, benefits, and alternatives of a proposed treatment to a patient making decisions about desired paths forward. This prevents paternalistic care in which the doctor “knows best” and makes decisions for the patient. Unfortunately, the emphasis of this pillar has morphed over time into the idea that the individual patient is the only person to whom this information should be provided or from whom information should be obtained.
Extensive research proves conclusively that family support, education, and psychoeducation improve both patient and family functioning in medical and psychiatric illness. as well as overlook the opportunity to use the structure and support system around a patient to strengthen their care and improve treatment outcomes.
The network and family dynamics around a patient can be critical to providing accurate information on medication adherence and symptoms, supporting recovery, and handling emergencies. Markedly improved patient outcomes occur when family members are seen as allies and offered support, assessment, and psychoeducation. In fact, the American Psychiatric Association’s Practice Guidelines on the treatment of schizophrenia (2020), major depressive disorder (2010), and bipolar disorder (2002) include the expectation that patients’ family members will be involved in the assessment and treatment of patients. Yet, training in how to incorporate these practices is often minimal or nonexistent during residency.
A family systems orientation is distinguished by its view of the family as a transactional system. Stressful events and problems of an individual member affect the whole family as a functional unit, with ripple effects for all members and their relationships. In turn, the family response – how the family handles problems – contributes significantly to positive adaptation or to individual and relational dysfunction. Thus, individual problems are assessed and addressed in the context of the family, with attention to socioeconomic and other environmental stressors.
A family systems approach is distinguished less by who is in the room and more by the clinician’s attention to relationship systems in assessment and treatment planning. We need to consider how family members may contribute to – and be affected by – problem situations. Most importantly, regardless of the source of difficulties, we involve key family members who can contribute to needed changes. Interventions are aimed at modifying dysfunctional patterns, tapping family resources, and strengthening both individual and family functioning.
A family systemic lens is useful for working with all types of families, for example: refugee families, thinking through child adoption processes, working with families with specific social disadvantages, etc. Incorporating issues of race, gender, and sexual orientation is important in this work, as is working with larger systems such as schools, workplaces, and health care settings.
As opposed to previous viewpoints that family therapy is the only “family” skill to be taught during residency, the GAP committee proposes that psychiatric residents should be trained in skills of family inclusion, support, and psychoeducation, and that these skills should be taught throughout the residency. Our goal is to have residents be able to consider any case through a family systems lens, to understand how patients’ illnesses and their family systems have bidirectional effects on each other, to perform a basic assessment of family system functioning, and to use this information in diagnostic and treatment planning.
Training goals
Systems-based thinking will enable trainees to:
1. Ally with family members to work with the patient to comply with goals of care (for example, taking medications, complying with lifestyle changes, and maintaining sobriety).
- Teachers focus on engagement, joining with families.
2. Help patients understand the influences of their families in their own lives, such as intergenerational transmission of trauma and resilience.
- Teachers focus on the creation of a genogram, and the location of the individual within their family system.
3. Understand that mental health includes the creation and maintenance of healthy relationships.
- Teachers focus on assessing a willingness to listen to others’ points of view and the cocreation of a shared reality and belief system: a belief that relationships can change over time and how to create new family narratives.
4. Understand the impact of illness on the family unit and the impact of the family unit on illness.
- Teachers focus on the concept of a family system, clarifying the roles within the family, including caregiving responsibilities.
5. Assess the family for strengths and weaknesses.
- Teachers focus on how families maintain a healthy emotional climate, allocate roles, decide on rules, problem-solving abilities, and so on.
6. Gather information from multiple informants in the same room.
- Teachers focus on using communication techniques to elicit, guide, and redirect information from multiple individuals of a system with varying perspectives in the same room. Teachers help students understand that there are multiple realities in families and learn how to maintain multidirectional partiality.
Knowledge, skills, and attitudes across all treatment settings
Knowledge: Beginning level
- Healthy family functioning at the various phases of the family life cycle. Systems concepts are applicable to families, multidisciplinary teams in clinical settings, and medical/government organizations. However, family systems are distinguished by deep attachment bonds, specific generational hierarchy, goals of emotional safety and, for many families, child rearing.
- Systemic thinking, unlike a linear cause and effect model, examines the feedback loops by which multiple persons or groups arrive at a specific way of functioning.
- Understanding boundaries, subsystems, and feedback loops is critical to understanding interpersonal connections. Understand how the family affects and is affected by psychiatric and medical illnesses. Impact of interpersonal stress on biological systems. The role of expressed emotion (EE) in psychiatric illness. EE describes the level of criticism, hostility, and emotional overinvolvement in families. It has been studied extensively across the health care spectrum, and cultural variance is significant.
- The components of family psychoeducation, and its associated research in improving patient and family outcomes.
Knowledge: Advanced level
- Principles of adaptive and maladaptive relational functioning in family life and family organization, communication, problem solving, and emotional regulation. Role of family strengths, resilience in reducing vulnerability.
- Couple and family development over the life cycle.
- Understanding multigenerational patterns.
- How age, gender, class, culture, and spirituality affect family life.
- The variety of family forms (for example, single parent, stepfamilies, same-sex parents).
- Special issues in couples and families, including loss, divorce and remarriage, immigration, illness, secrets, affairs, violence, alcohol and substance abuse, sexuality, including LGBTQi. Relationship of families to larger systems, for example, schools, work, health care systems, government agencies.
Skills
- Family-interviewing skills, especially managing high levels of emotion and making room for multiple points of view.
- Promoting resilience, hope, and strength.
- Basic psychoeducation techniques, which includes providing a therapeutic space for emotional processing, providing information about the illness, skills such as better communication, problem-solving, and relapse drill and support.
- Collaborative treatment planning with family members and other helping professionals. Treatment planning should include all members of the system: patient, family members, and members of the treatment team. Good planning establishes a role for family members, helps define criteria for managing emergencies, looks for areas of strength and resilience and provides clear and realistic goals for treatment.
- Knowledge of, and referral to, local and national resources, both in the community and online.
Attitudes
- Appreciate the multiple points of view in a family.
- Interest in family members as people with their own needs and history.
- Including family members as a resource in recovery.
- Understand caregiver burden and rewards and that stress extends to all family members.
Training techniques
Most learning takes place at the level of patient, supervisor, and resident. It is critical that the resident sees faculty members dealing with patients in observed or shared family sessions, and /or sees videos made by faculty or professionally made videos. Attitudes are best learned by modeling.
Areas of focus can include time management, addressing the fear that family sessions may get out of control, and the influence of the residents’ own life experiences and background including potential generational or cultural differences on their assessment and interactions with patient family dynamics. In skill development, our goal is efficient interviewing, history taking, and support in controlling sessions.
It is difficult to specify which techniques are most useful in didactic sessions as each presenter will have a different skill set for engaging the class. The techniques that work best are the ones most comfortable to the presenter. Any technique that gets emotions involved, such as role play, sculpting, discussing movie clips, bringing in family members to discuss their experiences, or self-exploration, will generate the most powerful learning. If time permits, exploration of the resident’s own family, including a genogram, is an exceptionally helpful technique, especially if accompanied by asking the residents to interview their own families.
Adult didactic curriculum
The curriculum represents basic concepts. We have vignettes by the authors, if needed, but it is best if the class, including the supervisor, uses vignettes from their own experiences. Material for use in class is in references, but the class is urged to draw on their own experiences as this supports strength-based teaching. The following are key topics and concepts for each of the training years.
Basic concepts for PGY1 and PGY2
1. Where are you in the family and individual life cycles? What are your experiences with psychiatric illness in family/friends? Open discussion about how individual and family life cycles interact. Draw genograms of s/o in the class or with the supervisor.
2. Healthy family functioning and family resilience. Recommend asking residents to talk to their parents/elders about their lives and family life cycle when they were your age. Open discussion about what makes a healthy resilient family.
3. How do I connect with the family rather than just one person? How do you learn to hold multiple perspectives? How do I try not to take sides/multidirectional partiality? How do I see each person in a positive way? How do I focus on family strengths, rather than focusing on someone behaving badly (which is really hard because it is overlearned in individual therapy).
4. What are the common factors used across all therapies, both individual and family? When is it best to use an individual relational approach versus a family systemic approach?
5. How do I decide if a family needs support or education or family therapy?
6. Psychoeducation: Research, current use and cultural adaptations.
7. Attachment styles and couples therapy.
8. What is the evidence base behind our work?
System practice for PGY 3 and 4
These seminars follow the basic seminars. The focus is on clarification of what systems thinking means. Systems thinking or relational thinking is to be differentiated from systems-based practice. These lectures require knowledge of systemic practice. If there are no local experts, residency programs can reach out to national experts at the Association of Family Psychiatrists, for help with virtual/remote or in-person teaching.
Here is a list of other topics that should be covered:
- Relational formulation, nested subsystems, boundaries, history of these concepts, contributions to the development of family therapy.
- How to define and identify common systems concepts, such as circular patterns, feedback loops, and triangulation. Teach circular questioning. Framing. This concept is the family systems equivalent of insight. How to intervene to effect communication change and behavior change?
- Working at interfaces: community, legal, government, agencies, and so on, and other treaters, consultation. Include systemic and individual racism.
- Understanding the complexity of intimacy.
- Emergency situations. When to report regarding abuse. Dealing with family trauma.
- Varieties of family therapy; assumptions and major concepts.
*The new curriculum was written by The GAP Committee on the Family: Ellen Berman, MD; John Rolland, MD, MPH; John Sargent, MD; and me, and with guests Chayanin Foongsathaporn, MD; Sarah Nguyen, MD, MPH; Neha Sharma, DO; and Jodi Zik, MD. For the full curriculum, which includes residency milestones, site-specific training goals, references, and case studies, please access the Association of Family Psychiatry’s website: www.familypsychiatrists.org.Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at [email protected].
The Group for the Advancement of Psychiatry’s Committee on the Family published an updated curriculum in October 2021 on family-oriented care. The first curriculum, published in 2006, was nominated as the American Association of Directors of Psychiatric Residency Training model curriculum for family-oriented care. The updated curriculum, produced by the GAP family committee and guests, is shorter and more focused.
The following is a summary of the introduction and the highlights.
Introduction
Use of family systems–based techniques in the diagnosis and care of patients is a key evidence-based tool for psychiatric disorders. However, it is not a current Accreditation Council for Graduate Medical Education Training training requirement, and it is possible to complete psychiatry residency without exposure to this key framework.
Here, we highlight the importance of considering patients through a “family systems” lens and the incorporation of multiple individuals from an individual patient’s identified system in their care.
Current medicine curricula emphasize patient autonomy, one of the core pillars of ethics. Autonomy is the cornerstone of the everyday practice within medicine of communicating all risks, benefits, and alternatives of a proposed treatment to a patient making decisions about desired paths forward. This prevents paternalistic care in which the doctor “knows best” and makes decisions for the patient. Unfortunately, the emphasis of this pillar has morphed over time into the idea that the individual patient is the only person to whom this information should be provided or from whom information should be obtained.
Extensive research proves conclusively that family support, education, and psychoeducation improve both patient and family functioning in medical and psychiatric illness. as well as overlook the opportunity to use the structure and support system around a patient to strengthen their care and improve treatment outcomes.
The network and family dynamics around a patient can be critical to providing accurate information on medication adherence and symptoms, supporting recovery, and handling emergencies. Markedly improved patient outcomes occur when family members are seen as allies and offered support, assessment, and psychoeducation. In fact, the American Psychiatric Association’s Practice Guidelines on the treatment of schizophrenia (2020), major depressive disorder (2010), and bipolar disorder (2002) include the expectation that patients’ family members will be involved in the assessment and treatment of patients. Yet, training in how to incorporate these practices is often minimal or nonexistent during residency.
A family systems orientation is distinguished by its view of the family as a transactional system. Stressful events and problems of an individual member affect the whole family as a functional unit, with ripple effects for all members and their relationships. In turn, the family response – how the family handles problems – contributes significantly to positive adaptation or to individual and relational dysfunction. Thus, individual problems are assessed and addressed in the context of the family, with attention to socioeconomic and other environmental stressors.
A family systems approach is distinguished less by who is in the room and more by the clinician’s attention to relationship systems in assessment and treatment planning. We need to consider how family members may contribute to – and be affected by – problem situations. Most importantly, regardless of the source of difficulties, we involve key family members who can contribute to needed changes. Interventions are aimed at modifying dysfunctional patterns, tapping family resources, and strengthening both individual and family functioning.
A family systemic lens is useful for working with all types of families, for example: refugee families, thinking through child adoption processes, working with families with specific social disadvantages, etc. Incorporating issues of race, gender, and sexual orientation is important in this work, as is working with larger systems such as schools, workplaces, and health care settings.
As opposed to previous viewpoints that family therapy is the only “family” skill to be taught during residency, the GAP committee proposes that psychiatric residents should be trained in skills of family inclusion, support, and psychoeducation, and that these skills should be taught throughout the residency. Our goal is to have residents be able to consider any case through a family systems lens, to understand how patients’ illnesses and their family systems have bidirectional effects on each other, to perform a basic assessment of family system functioning, and to use this information in diagnostic and treatment planning.
Training goals
Systems-based thinking will enable trainees to:
1. Ally with family members to work with the patient to comply with goals of care (for example, taking medications, complying with lifestyle changes, and maintaining sobriety).
- Teachers focus on engagement, joining with families.
2. Help patients understand the influences of their families in their own lives, such as intergenerational transmission of trauma and resilience.
- Teachers focus on the creation of a genogram, and the location of the individual within their family system.
3. Understand that mental health includes the creation and maintenance of healthy relationships.
- Teachers focus on assessing a willingness to listen to others’ points of view and the cocreation of a shared reality and belief system: a belief that relationships can change over time and how to create new family narratives.
4. Understand the impact of illness on the family unit and the impact of the family unit on illness.
- Teachers focus on the concept of a family system, clarifying the roles within the family, including caregiving responsibilities.
5. Assess the family for strengths and weaknesses.
- Teachers focus on how families maintain a healthy emotional climate, allocate roles, decide on rules, problem-solving abilities, and so on.
6. Gather information from multiple informants in the same room.
- Teachers focus on using communication techniques to elicit, guide, and redirect information from multiple individuals of a system with varying perspectives in the same room. Teachers help students understand that there are multiple realities in families and learn how to maintain multidirectional partiality.
Knowledge, skills, and attitudes across all treatment settings
Knowledge: Beginning level
- Healthy family functioning at the various phases of the family life cycle. Systems concepts are applicable to families, multidisciplinary teams in clinical settings, and medical/government organizations. However, family systems are distinguished by deep attachment bonds, specific generational hierarchy, goals of emotional safety and, for many families, child rearing.
- Systemic thinking, unlike a linear cause and effect model, examines the feedback loops by which multiple persons or groups arrive at a specific way of functioning.
- Understanding boundaries, subsystems, and feedback loops is critical to understanding interpersonal connections. Understand how the family affects and is affected by psychiatric and medical illnesses. Impact of interpersonal stress on biological systems. The role of expressed emotion (EE) in psychiatric illness. EE describes the level of criticism, hostility, and emotional overinvolvement in families. It has been studied extensively across the health care spectrum, and cultural variance is significant.
- The components of family psychoeducation, and its associated research in improving patient and family outcomes.
Knowledge: Advanced level
- Principles of adaptive and maladaptive relational functioning in family life and family organization, communication, problem solving, and emotional regulation. Role of family strengths, resilience in reducing vulnerability.
- Couple and family development over the life cycle.
- Understanding multigenerational patterns.
- How age, gender, class, culture, and spirituality affect family life.
- The variety of family forms (for example, single parent, stepfamilies, same-sex parents).
- Special issues in couples and families, including loss, divorce and remarriage, immigration, illness, secrets, affairs, violence, alcohol and substance abuse, sexuality, including LGBTQi. Relationship of families to larger systems, for example, schools, work, health care systems, government agencies.
Skills
- Family-interviewing skills, especially managing high levels of emotion and making room for multiple points of view.
- Promoting resilience, hope, and strength.
- Basic psychoeducation techniques, which includes providing a therapeutic space for emotional processing, providing information about the illness, skills such as better communication, problem-solving, and relapse drill and support.
- Collaborative treatment planning with family members and other helping professionals. Treatment planning should include all members of the system: patient, family members, and members of the treatment team. Good planning establishes a role for family members, helps define criteria for managing emergencies, looks for areas of strength and resilience and provides clear and realistic goals for treatment.
- Knowledge of, and referral to, local and national resources, both in the community and online.
Attitudes
- Appreciate the multiple points of view in a family.
- Interest in family members as people with their own needs and history.
- Including family members as a resource in recovery.
- Understand caregiver burden and rewards and that stress extends to all family members.
Training techniques
Most learning takes place at the level of patient, supervisor, and resident. It is critical that the resident sees faculty members dealing with patients in observed or shared family sessions, and /or sees videos made by faculty or professionally made videos. Attitudes are best learned by modeling.
Areas of focus can include time management, addressing the fear that family sessions may get out of control, and the influence of the residents’ own life experiences and background including potential generational or cultural differences on their assessment and interactions with patient family dynamics. In skill development, our goal is efficient interviewing, history taking, and support in controlling sessions.
It is difficult to specify which techniques are most useful in didactic sessions as each presenter will have a different skill set for engaging the class. The techniques that work best are the ones most comfortable to the presenter. Any technique that gets emotions involved, such as role play, sculpting, discussing movie clips, bringing in family members to discuss their experiences, or self-exploration, will generate the most powerful learning. If time permits, exploration of the resident’s own family, including a genogram, is an exceptionally helpful technique, especially if accompanied by asking the residents to interview their own families.
Adult didactic curriculum
The curriculum represents basic concepts. We have vignettes by the authors, if needed, but it is best if the class, including the supervisor, uses vignettes from their own experiences. Material for use in class is in references, but the class is urged to draw on their own experiences as this supports strength-based teaching. The following are key topics and concepts for each of the training years.
Basic concepts for PGY1 and PGY2
1. Where are you in the family and individual life cycles? What are your experiences with psychiatric illness in family/friends? Open discussion about how individual and family life cycles interact. Draw genograms of s/o in the class or with the supervisor.
2. Healthy family functioning and family resilience. Recommend asking residents to talk to their parents/elders about their lives and family life cycle when they were your age. Open discussion about what makes a healthy resilient family.
3. How do I connect with the family rather than just one person? How do you learn to hold multiple perspectives? How do I try not to take sides/multidirectional partiality? How do I see each person in a positive way? How do I focus on family strengths, rather than focusing on someone behaving badly (which is really hard because it is overlearned in individual therapy).
4. What are the common factors used across all therapies, both individual and family? When is it best to use an individual relational approach versus a family systemic approach?
5. How do I decide if a family needs support or education or family therapy?
6. Psychoeducation: Research, current use and cultural adaptations.
7. Attachment styles and couples therapy.
8. What is the evidence base behind our work?
System practice for PGY 3 and 4
These seminars follow the basic seminars. The focus is on clarification of what systems thinking means. Systems thinking or relational thinking is to be differentiated from systems-based practice. These lectures require knowledge of systemic practice. If there are no local experts, residency programs can reach out to national experts at the Association of Family Psychiatrists, for help with virtual/remote or in-person teaching.
Here is a list of other topics that should be covered:
- Relational formulation, nested subsystems, boundaries, history of these concepts, contributions to the development of family therapy.
- How to define and identify common systems concepts, such as circular patterns, feedback loops, and triangulation. Teach circular questioning. Framing. This concept is the family systems equivalent of insight. How to intervene to effect communication change and behavior change?
- Working at interfaces: community, legal, government, agencies, and so on, and other treaters, consultation. Include systemic and individual racism.
- Understanding the complexity of intimacy.
- Emergency situations. When to report regarding abuse. Dealing with family trauma.
- Varieties of family therapy; assumptions and major concepts.
*The new curriculum was written by The GAP Committee on the Family: Ellen Berman, MD; John Rolland, MD, MPH; John Sargent, MD; and me, and with guests Chayanin Foongsathaporn, MD; Sarah Nguyen, MD, MPH; Neha Sharma, DO; and Jodi Zik, MD. For the full curriculum, which includes residency milestones, site-specific training goals, references, and case studies, please access the Association of Family Psychiatry’s website: www.familypsychiatrists.org.Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at [email protected].
The Group for the Advancement of Psychiatry’s Committee on the Family published an updated curriculum in October 2021 on family-oriented care. The first curriculum, published in 2006, was nominated as the American Association of Directors of Psychiatric Residency Training model curriculum for family-oriented care. The updated curriculum, produced by the GAP family committee and guests, is shorter and more focused.
The following is a summary of the introduction and the highlights.
Introduction
Use of family systems–based techniques in the diagnosis and care of patients is a key evidence-based tool for psychiatric disorders. However, it is not a current Accreditation Council for Graduate Medical Education Training training requirement, and it is possible to complete psychiatry residency without exposure to this key framework.
Here, we highlight the importance of considering patients through a “family systems” lens and the incorporation of multiple individuals from an individual patient’s identified system in their care.
Current medicine curricula emphasize patient autonomy, one of the core pillars of ethics. Autonomy is the cornerstone of the everyday practice within medicine of communicating all risks, benefits, and alternatives of a proposed treatment to a patient making decisions about desired paths forward. This prevents paternalistic care in which the doctor “knows best” and makes decisions for the patient. Unfortunately, the emphasis of this pillar has morphed over time into the idea that the individual patient is the only person to whom this information should be provided or from whom information should be obtained.
Extensive research proves conclusively that family support, education, and psychoeducation improve both patient and family functioning in medical and psychiatric illness. as well as overlook the opportunity to use the structure and support system around a patient to strengthen their care and improve treatment outcomes.
The network and family dynamics around a patient can be critical to providing accurate information on medication adherence and symptoms, supporting recovery, and handling emergencies. Markedly improved patient outcomes occur when family members are seen as allies and offered support, assessment, and psychoeducation. In fact, the American Psychiatric Association’s Practice Guidelines on the treatment of schizophrenia (2020), major depressive disorder (2010), and bipolar disorder (2002) include the expectation that patients’ family members will be involved in the assessment and treatment of patients. Yet, training in how to incorporate these practices is often minimal or nonexistent during residency.
A family systems orientation is distinguished by its view of the family as a transactional system. Stressful events and problems of an individual member affect the whole family as a functional unit, with ripple effects for all members and their relationships. In turn, the family response – how the family handles problems – contributes significantly to positive adaptation or to individual and relational dysfunction. Thus, individual problems are assessed and addressed in the context of the family, with attention to socioeconomic and other environmental stressors.
A family systems approach is distinguished less by who is in the room and more by the clinician’s attention to relationship systems in assessment and treatment planning. We need to consider how family members may contribute to – and be affected by – problem situations. Most importantly, regardless of the source of difficulties, we involve key family members who can contribute to needed changes. Interventions are aimed at modifying dysfunctional patterns, tapping family resources, and strengthening both individual and family functioning.
A family systemic lens is useful for working with all types of families, for example: refugee families, thinking through child adoption processes, working with families with specific social disadvantages, etc. Incorporating issues of race, gender, and sexual orientation is important in this work, as is working with larger systems such as schools, workplaces, and health care settings.
As opposed to previous viewpoints that family therapy is the only “family” skill to be taught during residency, the GAP committee proposes that psychiatric residents should be trained in skills of family inclusion, support, and psychoeducation, and that these skills should be taught throughout the residency. Our goal is to have residents be able to consider any case through a family systems lens, to understand how patients’ illnesses and their family systems have bidirectional effects on each other, to perform a basic assessment of family system functioning, and to use this information in diagnostic and treatment planning.
Training goals
Systems-based thinking will enable trainees to:
1. Ally with family members to work with the patient to comply with goals of care (for example, taking medications, complying with lifestyle changes, and maintaining sobriety).
- Teachers focus on engagement, joining with families.
2. Help patients understand the influences of their families in their own lives, such as intergenerational transmission of trauma and resilience.
- Teachers focus on the creation of a genogram, and the location of the individual within their family system.
3. Understand that mental health includes the creation and maintenance of healthy relationships.
- Teachers focus on assessing a willingness to listen to others’ points of view and the cocreation of a shared reality and belief system: a belief that relationships can change over time and how to create new family narratives.
4. Understand the impact of illness on the family unit and the impact of the family unit on illness.
- Teachers focus on the concept of a family system, clarifying the roles within the family, including caregiving responsibilities.
5. Assess the family for strengths and weaknesses.
- Teachers focus on how families maintain a healthy emotional climate, allocate roles, decide on rules, problem-solving abilities, and so on.
6. Gather information from multiple informants in the same room.
- Teachers focus on using communication techniques to elicit, guide, and redirect information from multiple individuals of a system with varying perspectives in the same room. Teachers help students understand that there are multiple realities in families and learn how to maintain multidirectional partiality.
Knowledge, skills, and attitudes across all treatment settings
Knowledge: Beginning level
- Healthy family functioning at the various phases of the family life cycle. Systems concepts are applicable to families, multidisciplinary teams in clinical settings, and medical/government organizations. However, family systems are distinguished by deep attachment bonds, specific generational hierarchy, goals of emotional safety and, for many families, child rearing.
- Systemic thinking, unlike a linear cause and effect model, examines the feedback loops by which multiple persons or groups arrive at a specific way of functioning.
- Understanding boundaries, subsystems, and feedback loops is critical to understanding interpersonal connections. Understand how the family affects and is affected by psychiatric and medical illnesses. Impact of interpersonal stress on biological systems. The role of expressed emotion (EE) in psychiatric illness. EE describes the level of criticism, hostility, and emotional overinvolvement in families. It has been studied extensively across the health care spectrum, and cultural variance is significant.
- The components of family psychoeducation, and its associated research in improving patient and family outcomes.
Knowledge: Advanced level
- Principles of adaptive and maladaptive relational functioning in family life and family organization, communication, problem solving, and emotional regulation. Role of family strengths, resilience in reducing vulnerability.
- Couple and family development over the life cycle.
- Understanding multigenerational patterns.
- How age, gender, class, culture, and spirituality affect family life.
- The variety of family forms (for example, single parent, stepfamilies, same-sex parents).
- Special issues in couples and families, including loss, divorce and remarriage, immigration, illness, secrets, affairs, violence, alcohol and substance abuse, sexuality, including LGBTQi. Relationship of families to larger systems, for example, schools, work, health care systems, government agencies.
Skills
- Family-interviewing skills, especially managing high levels of emotion and making room for multiple points of view.
- Promoting resilience, hope, and strength.
- Basic psychoeducation techniques, which includes providing a therapeutic space for emotional processing, providing information about the illness, skills such as better communication, problem-solving, and relapse drill and support.
- Collaborative treatment planning with family members and other helping professionals. Treatment planning should include all members of the system: patient, family members, and members of the treatment team. Good planning establishes a role for family members, helps define criteria for managing emergencies, looks for areas of strength and resilience and provides clear and realistic goals for treatment.
- Knowledge of, and referral to, local and national resources, both in the community and online.
Attitudes
- Appreciate the multiple points of view in a family.
- Interest in family members as people with their own needs and history.
- Including family members as a resource in recovery.
- Understand caregiver burden and rewards and that stress extends to all family members.
Training techniques
Most learning takes place at the level of patient, supervisor, and resident. It is critical that the resident sees faculty members dealing with patients in observed or shared family sessions, and /or sees videos made by faculty or professionally made videos. Attitudes are best learned by modeling.
Areas of focus can include time management, addressing the fear that family sessions may get out of control, and the influence of the residents’ own life experiences and background including potential generational or cultural differences on their assessment and interactions with patient family dynamics. In skill development, our goal is efficient interviewing, history taking, and support in controlling sessions.
It is difficult to specify which techniques are most useful in didactic sessions as each presenter will have a different skill set for engaging the class. The techniques that work best are the ones most comfortable to the presenter. Any technique that gets emotions involved, such as role play, sculpting, discussing movie clips, bringing in family members to discuss their experiences, or self-exploration, will generate the most powerful learning. If time permits, exploration of the resident’s own family, including a genogram, is an exceptionally helpful technique, especially if accompanied by asking the residents to interview their own families.
Adult didactic curriculum
The curriculum represents basic concepts. We have vignettes by the authors, if needed, but it is best if the class, including the supervisor, uses vignettes from their own experiences. Material for use in class is in references, but the class is urged to draw on their own experiences as this supports strength-based teaching. The following are key topics and concepts for each of the training years.
Basic concepts for PGY1 and PGY2
1. Where are you in the family and individual life cycles? What are your experiences with psychiatric illness in family/friends? Open discussion about how individual and family life cycles interact. Draw genograms of s/o in the class or with the supervisor.
2. Healthy family functioning and family resilience. Recommend asking residents to talk to their parents/elders about their lives and family life cycle when they were your age. Open discussion about what makes a healthy resilient family.
3. How do I connect with the family rather than just one person? How do you learn to hold multiple perspectives? How do I try not to take sides/multidirectional partiality? How do I see each person in a positive way? How do I focus on family strengths, rather than focusing on someone behaving badly (which is really hard because it is overlearned in individual therapy).
4. What are the common factors used across all therapies, both individual and family? When is it best to use an individual relational approach versus a family systemic approach?
5. How do I decide if a family needs support or education or family therapy?
6. Psychoeducation: Research, current use and cultural adaptations.
7. Attachment styles and couples therapy.
8. What is the evidence base behind our work?
System practice for PGY 3 and 4
These seminars follow the basic seminars. The focus is on clarification of what systems thinking means. Systems thinking or relational thinking is to be differentiated from systems-based practice. These lectures require knowledge of systemic practice. If there are no local experts, residency programs can reach out to national experts at the Association of Family Psychiatrists, for help with virtual/remote or in-person teaching.
Here is a list of other topics that should be covered:
- Relational formulation, nested subsystems, boundaries, history of these concepts, contributions to the development of family therapy.
- How to define and identify common systems concepts, such as circular patterns, feedback loops, and triangulation. Teach circular questioning. Framing. This concept is the family systems equivalent of insight. How to intervene to effect communication change and behavior change?
- Working at interfaces: community, legal, government, agencies, and so on, and other treaters, consultation. Include systemic and individual racism.
- Understanding the complexity of intimacy.
- Emergency situations. When to report regarding abuse. Dealing with family trauma.
- Varieties of family therapy; assumptions and major concepts.
*The new curriculum was written by The GAP Committee on the Family: Ellen Berman, MD; John Rolland, MD, MPH; John Sargent, MD; and me, and with guests Chayanin Foongsathaporn, MD; Sarah Nguyen, MD, MPH; Neha Sharma, DO; and Jodi Zik, MD. For the full curriculum, which includes residency milestones, site-specific training goals, references, and case studies, please access the Association of Family Psychiatry’s website: www.familypsychiatrists.org.Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at [email protected].
Feds’ website for free at-home COVID tests launches day early
The Biden administration’s new no-cost, at-home testing program launched Jan. 18, a day ahead of schedule.
The administration said 500 million tests are available to be delivered to homes across the country. This accounts for half of the president’s recent pledge to purchase 1 billion free at-home COVID-19 tests to distribute to the American public.
On a Jan. 14 call with reporters, senior White House officials offered some details about the new program.
Here’s what we know so far.
How do I order my free tests?
Americans can visit COVIDtests.gov to order their rapid at-home tests. You can also order directly from the U.S. Postal Service website. After you order, you’ll receive a confirmation email that promises to send tracking information once your order ships.
What information do I need to order the tests?
You only need your name and home mailing address.
There is also an option to provide your email address to get updates on the status of your order.
What if someone needs help ordering the tests?
There will be a free call-in line for people needing more help, including those having trouble accessing the internet, according to White House officials.
What tests will be available?
There are nine at-home tests available through FDA emergency use authorization. According to the Frequently Asked Questions section of COVIDtests.gov, "You will not be able to choose the brand you order as part of this program.”
How long will it take to get the tests once I order them?
Tests are expected to ship 7 to 12 days after you order them.
But White House officials say that the time frame will likely shorten as the program gains steam.
How many can I order?
There’s a limit of four tests per residential mailing address.
For larger families, White House officials suggest trying other free testing options, like visiting COVID-19 testing sites or your local health center.
Is this a one-time opportunity?
The White House doesn’t say, but officials did mention that if you run out of your four free tests, there are many other ways to access free at-home tests, such as COVID-19 testing sites, pharmacies, and community health centers.
The free tests available through COVIDtests.gov are in addition to an estimated 375 million at-home rapid tests on the market in the U.S. this month.
When should people use a rapid at-home test?
The CDC and experts with other public health groups agree that Americans should consider using at-home rapid tests in the following situations:
- If they begin to have symptoms consistent with COVID-19;
- At least 5 days after close contact with someone who has COVID;
- If someone is indoors with a group of people who are at risk of severe disease or are unvaccinated.
Are at-home rapid tests accurate?
The U.S. Department of Health and Human Services and other federal officials confirmed through studies that all tests distributed through this program can detect the Omicron variant. These agencies also confirmed that their performance is consistent with the FDA’s emergency use authorization.
Is the website designed to handle high demand?
After the original website to sign up for health insurance under the Affordable Care Act crashed repeatedly at launch, the government says it has prepared for high demand for ordering at-home rapid tests.
The U.S. Digital Service (USDS), an organization founded after Healthcare.gov, has partnered with the Postal Service to plan for the launch.
The Postal Service has expanded its staffing, similar to what’s done during the holidays.
All orders in the continental United States will be shipped through first-class mail, with shipments to Alaska, Hawaii, U.S. territories, and military and overseas addresses sent through priority mail.
A version of this article first appeared on WebMD.com.
The Biden administration’s new no-cost, at-home testing program launched Jan. 18, a day ahead of schedule.
The administration said 500 million tests are available to be delivered to homes across the country. This accounts for half of the president’s recent pledge to purchase 1 billion free at-home COVID-19 tests to distribute to the American public.
On a Jan. 14 call with reporters, senior White House officials offered some details about the new program.
Here’s what we know so far.
How do I order my free tests?
Americans can visit COVIDtests.gov to order their rapid at-home tests. You can also order directly from the U.S. Postal Service website. After you order, you’ll receive a confirmation email that promises to send tracking information once your order ships.
What information do I need to order the tests?
You only need your name and home mailing address.
There is also an option to provide your email address to get updates on the status of your order.
What if someone needs help ordering the tests?
There will be a free call-in line for people needing more help, including those having trouble accessing the internet, according to White House officials.
What tests will be available?
There are nine at-home tests available through FDA emergency use authorization. According to the Frequently Asked Questions section of COVIDtests.gov, "You will not be able to choose the brand you order as part of this program.”
How long will it take to get the tests once I order them?
Tests are expected to ship 7 to 12 days after you order them.
But White House officials say that the time frame will likely shorten as the program gains steam.
How many can I order?
There’s a limit of four tests per residential mailing address.
For larger families, White House officials suggest trying other free testing options, like visiting COVID-19 testing sites or your local health center.
Is this a one-time opportunity?
The White House doesn’t say, but officials did mention that if you run out of your four free tests, there are many other ways to access free at-home tests, such as COVID-19 testing sites, pharmacies, and community health centers.
The free tests available through COVIDtests.gov are in addition to an estimated 375 million at-home rapid tests on the market in the U.S. this month.
When should people use a rapid at-home test?
The CDC and experts with other public health groups agree that Americans should consider using at-home rapid tests in the following situations:
- If they begin to have symptoms consistent with COVID-19;
- At least 5 days after close contact with someone who has COVID;
- If someone is indoors with a group of people who are at risk of severe disease or are unvaccinated.
Are at-home rapid tests accurate?
The U.S. Department of Health and Human Services and other federal officials confirmed through studies that all tests distributed through this program can detect the Omicron variant. These agencies also confirmed that their performance is consistent with the FDA’s emergency use authorization.
Is the website designed to handle high demand?
After the original website to sign up for health insurance under the Affordable Care Act crashed repeatedly at launch, the government says it has prepared for high demand for ordering at-home rapid tests.
The U.S. Digital Service (USDS), an organization founded after Healthcare.gov, has partnered with the Postal Service to plan for the launch.
The Postal Service has expanded its staffing, similar to what’s done during the holidays.
All orders in the continental United States will be shipped through first-class mail, with shipments to Alaska, Hawaii, U.S. territories, and military and overseas addresses sent through priority mail.
A version of this article first appeared on WebMD.com.
The Biden administration’s new no-cost, at-home testing program launched Jan. 18, a day ahead of schedule.
The administration said 500 million tests are available to be delivered to homes across the country. This accounts for half of the president’s recent pledge to purchase 1 billion free at-home COVID-19 tests to distribute to the American public.
On a Jan. 14 call with reporters, senior White House officials offered some details about the new program.
Here’s what we know so far.
How do I order my free tests?
Americans can visit COVIDtests.gov to order their rapid at-home tests. You can also order directly from the U.S. Postal Service website. After you order, you’ll receive a confirmation email that promises to send tracking information once your order ships.
What information do I need to order the tests?
You only need your name and home mailing address.
There is also an option to provide your email address to get updates on the status of your order.
What if someone needs help ordering the tests?
There will be a free call-in line for people needing more help, including those having trouble accessing the internet, according to White House officials.
What tests will be available?
There are nine at-home tests available through FDA emergency use authorization. According to the Frequently Asked Questions section of COVIDtests.gov, "You will not be able to choose the brand you order as part of this program.”
How long will it take to get the tests once I order them?
Tests are expected to ship 7 to 12 days after you order them.
But White House officials say that the time frame will likely shorten as the program gains steam.
How many can I order?
There’s a limit of four tests per residential mailing address.
For larger families, White House officials suggest trying other free testing options, like visiting COVID-19 testing sites or your local health center.
Is this a one-time opportunity?
The White House doesn’t say, but officials did mention that if you run out of your four free tests, there are many other ways to access free at-home tests, such as COVID-19 testing sites, pharmacies, and community health centers.
The free tests available through COVIDtests.gov are in addition to an estimated 375 million at-home rapid tests on the market in the U.S. this month.
When should people use a rapid at-home test?
The CDC and experts with other public health groups agree that Americans should consider using at-home rapid tests in the following situations:
- If they begin to have symptoms consistent with COVID-19;
- At least 5 days after close contact with someone who has COVID;
- If someone is indoors with a group of people who are at risk of severe disease or are unvaccinated.
Are at-home rapid tests accurate?
The U.S. Department of Health and Human Services and other federal officials confirmed through studies that all tests distributed through this program can detect the Omicron variant. These agencies also confirmed that their performance is consistent with the FDA’s emergency use authorization.
Is the website designed to handle high demand?
After the original website to sign up for health insurance under the Affordable Care Act crashed repeatedly at launch, the government says it has prepared for high demand for ordering at-home rapid tests.
The U.S. Digital Service (USDS), an organization founded after Healthcare.gov, has partnered with the Postal Service to plan for the launch.
The Postal Service has expanded its staffing, similar to what’s done during the holidays.
All orders in the continental United States will be shipped through first-class mail, with shipments to Alaska, Hawaii, U.S. territories, and military and overseas addresses sent through priority mail.
A version of this article first appeared on WebMD.com.
Emotions, science, and the politics of COVID
A social worker called with a plea in April 2020, when the hospital was filled with COVID-19 patients, some so sick they were on ventilators. “I need your help with a family. Mom is in the ICU, intubated; her son died here 2 weeks ago of COVID and her daughters are overwhelmed, unable to visit because of restrictions. The staff anticipates extubating Elvira imminently, but she will be fragile and alone. When is the right time to tell Elvira that Tony died?”
That happened at the beginning of the COVID pandemic. I handled the case remotely with heroic help from overburdened nurses and doctors who were acting as medical staff, social workers, and substitute family to an isolated patient in the hospital. Such was the confusion with the new virus before vaccines and treatments.
The impact of pandemics: A historical perspective
Beginning in antiquity, there were pandemics that decimated populations. Before antibiotics, vaccines or awareness of microorganisms, people feared contagion and sought isolation from the sick. People also thought that those who recovered were less likely to fall ill again, and if they did get sick, the illness would be milder.
There is abundant documentation of bubonic plague outbreaks, such as the “Black Death” in the Middle Ages. The Spanish flu of 1918 struck down robust young Americans and spread worldwide. Although the bubonic plague was at the center of major infectious outbreaks, including the pandemic of the Justinian era (500s) and the Great Plague of London (1665-1666), other infectious diseases, untreatable at the time, prevailed simultaneously. Wars, world trade, unsanitary conditions, and urban crowding enhanced the spread. Pandemics shaped history. Some historians attribute the fall of the Roman Empire to unrelenting infectious disease carried in migratory battles.
Even in the earliest outbreaks, the poor populace died more readily than the well off, who had means to escape and seclude themselves from congested areas. Samuel Pepys, a diarist of the London Plague, was a famed businessman and government official; he wrote of seeing the suffering in his city, but he escaped to live with his wife in their country home. What Samuel Pepys wrote of London during the Plague can apply to the early period of the COVID pandemic: “How few people I see, and those looking like people that had taken leave of the world.”
There are lurid descriptions of the chaos of pandemics, especially of the Black Death and the Plague of London. First published in 1722, Daniel Defoe’s “A Journal of the Plague Year” describes the suffering of the sick that included people abandoning the afflicted and others running rampant with delirium in the streets, screaming in pain. City officials took cruel measures that they considered necessary, such as locking away families in their homes, sick and well together, when an individual member showed symptoms. The Middle Ages saw deadly anti-Semitism. During the Black Death, fanatics murdered Jews in the belief that they brought on the pestilence. Ignorance created panic.
As happens in tragedy, there was also bravery. Some stayed to tend to the sick; charities provided food for poor people during the London Plague.
Back to the 21st century
After 3 weeks on the ventilator, Elvira got extubated. A team including her doctor, nurse, and Connie, one of her daughters, told Elvira that her 28-year-old son had died of COVID. I began telepsychiatry with Elvira and her two daughters. Treatment continued after Elvira returned home. In telephone sessions, we discussed bereavement and how to cope with the emotional and physical challenges in recovery.
Before he contracted COVID, Tony, Elvira’s son, had compromised health. He was on dialysis awaiting a kidney transplant. His mother prepared his meals and often accompanied Tony to doctor appointments. Still, Elvira said, “I wasn’t there to hold his hand.” At age 71, Elvira was also at high risk. She suffered from diabetes, high blood pressure, hyperlipidemia, and had coronary stents. Elvira was compliant with medications for her conditions.
What we know; where we are
“Infectious diseases are not static conditions but depend upon a constantly changing relationship between parasite and invaded species which is bound to result in modifications of both clinical and epidemiological manifestations.”
Hans Zinsser, Rats, Lice and History
We need to be informed by history and grateful to the geniuses who brought us into the modern age of medicine. We can prevent diseases with public health measures, and by understanding and treating crises. Edward Jenner, who recognized the protective effect of cowpox against smallpox, developed inoculations beginning in 1796; he ushered in immunology and saved the lives of millions. Smallpox is now eradicated. A succession of microbe hunters, including Louis Pasteur and Robert Koch, benefited from the development of the microscope by Antonie van Leeuwenhoek. With the advent and use of penicillin in the early 1940s, Alexander Fleming welcomed antibiotics; by the 1960s this modality became widespread. In the mid-20th century, immunologists recognized that bacteria and viruses change and adapt to the environment.
The planet has seen ravaging pandemics that then dissipated and, although untreatable at the time, disappeared into a reservoir, such as rats or lice. People also developed herd immunity from exposure to the offending microorganisms within the population. Less toxic, these agents no longer kill those who get infected but they can be transmissible and endemic to humans.
The mental health consequences of pandemics are reminiscent of other severe illnesses. The seriously ill develop cognitive aberrations and can become delirious. The population at risk and those who get sick can experience depression, PTSD, and anxiety – including panic.
Update on Elvira
Elvira continues to improve. She also participates in support groups, including one that addresses bereavement for parents of children who died of COVID and other causes. “I didn’t have a chance to say goodbye,” she said. But what she calls her “brain fog” has dissipated. She walks better, and she is getting evaluation of radiculopathy, probably from nerve root injury during her 3 weeks in bed on the ventilator. She’s still experiencing pain in her feet.
With regard to her symptoms she said: “I cry almost every day.” Her PTSD has abated, but she sometimes has nightmares. Elvira is writing a book about the induced coma and the “hallucinations from hell to heaven” she experienced. She wonders:“Did Tony go through the same thing?” Her empathy is enhanced by her background as a retired social worker with the Administration for Children’s Services in New York.
The role of psychiatry
In its early, most virulent form, SARS-CoV-2 devastated thousands of people, especially the elderly medically vulnerable. With scientific tools we developed vaccines and treatments and continue to study the dynamics of this virus.
As Andy Miller, MD, chief of the division of infectious diseases at the Hospital for Special Surgery, said when I spoke with him about the virus, because of the way in which viruses mutate, “we must remain aware” of the trajectory of SARS-CoV-2 and “counter irrational beliefs.”
How should psychiatry deal with COVID? As scientists, we seek the truth without bias and politics. Mental illness is our domain. Other specialties have the expertise to treat and even prevent infectious disease. We can assist our doctor colleagues to understand depression, anxiety, PTSD, and cognitive issues when they occur. Our medical mission should be, as always, to treat those who suffer mental illness. Now that extends to the consequences of COVID.
Suggested reading
Camus A. The Plague. New York: Vintage Books,. 1991.
Defoe D. A Journal of the Plague Year. Mineola, N.Y.: Dover Publications, 2001.
Kelly J. The Great Mortality: An Intimate History of the Black Death, The Most Devastating Plague of All Time. New York: Harper Perennial, 2005.
Pepys S. The Diary of Samuel Pepys: The Great Plague of London & The Great Fire of London, 1665-1666. Oxford, England: Benediction Classics, 2020.
Emerg Infect Dis. 2005 Mar 11(3):402-96.
Zinsser H. Rats, Lice and History. Boston/Toronto: Little Brown and Co., 1935.
Dr. Cohen is in private practice of psychotherapy and medication management in New York. She has been a consultant at the Hospital for Special Surgery and at New York–Presbyterian, and a forensic psychiatry expert. She changed key facts about Elvira’s case to protect her anonymity.
A social worker called with a plea in April 2020, when the hospital was filled with COVID-19 patients, some so sick they were on ventilators. “I need your help with a family. Mom is in the ICU, intubated; her son died here 2 weeks ago of COVID and her daughters are overwhelmed, unable to visit because of restrictions. The staff anticipates extubating Elvira imminently, but she will be fragile and alone. When is the right time to tell Elvira that Tony died?”
That happened at the beginning of the COVID pandemic. I handled the case remotely with heroic help from overburdened nurses and doctors who were acting as medical staff, social workers, and substitute family to an isolated patient in the hospital. Such was the confusion with the new virus before vaccines and treatments.
The impact of pandemics: A historical perspective
Beginning in antiquity, there were pandemics that decimated populations. Before antibiotics, vaccines or awareness of microorganisms, people feared contagion and sought isolation from the sick. People also thought that those who recovered were less likely to fall ill again, and if they did get sick, the illness would be milder.
There is abundant documentation of bubonic plague outbreaks, such as the “Black Death” in the Middle Ages. The Spanish flu of 1918 struck down robust young Americans and spread worldwide. Although the bubonic plague was at the center of major infectious outbreaks, including the pandemic of the Justinian era (500s) and the Great Plague of London (1665-1666), other infectious diseases, untreatable at the time, prevailed simultaneously. Wars, world trade, unsanitary conditions, and urban crowding enhanced the spread. Pandemics shaped history. Some historians attribute the fall of the Roman Empire to unrelenting infectious disease carried in migratory battles.
Even in the earliest outbreaks, the poor populace died more readily than the well off, who had means to escape and seclude themselves from congested areas. Samuel Pepys, a diarist of the London Plague, was a famed businessman and government official; he wrote of seeing the suffering in his city, but he escaped to live with his wife in their country home. What Samuel Pepys wrote of London during the Plague can apply to the early period of the COVID pandemic: “How few people I see, and those looking like people that had taken leave of the world.”
There are lurid descriptions of the chaos of pandemics, especially of the Black Death and the Plague of London. First published in 1722, Daniel Defoe’s “A Journal of the Plague Year” describes the suffering of the sick that included people abandoning the afflicted and others running rampant with delirium in the streets, screaming in pain. City officials took cruel measures that they considered necessary, such as locking away families in their homes, sick and well together, when an individual member showed symptoms. The Middle Ages saw deadly anti-Semitism. During the Black Death, fanatics murdered Jews in the belief that they brought on the pestilence. Ignorance created panic.
As happens in tragedy, there was also bravery. Some stayed to tend to the sick; charities provided food for poor people during the London Plague.
Back to the 21st century
After 3 weeks on the ventilator, Elvira got extubated. A team including her doctor, nurse, and Connie, one of her daughters, told Elvira that her 28-year-old son had died of COVID. I began telepsychiatry with Elvira and her two daughters. Treatment continued after Elvira returned home. In telephone sessions, we discussed bereavement and how to cope with the emotional and physical challenges in recovery.
Before he contracted COVID, Tony, Elvira’s son, had compromised health. He was on dialysis awaiting a kidney transplant. His mother prepared his meals and often accompanied Tony to doctor appointments. Still, Elvira said, “I wasn’t there to hold his hand.” At age 71, Elvira was also at high risk. She suffered from diabetes, high blood pressure, hyperlipidemia, and had coronary stents. Elvira was compliant with medications for her conditions.
What we know; where we are
“Infectious diseases are not static conditions but depend upon a constantly changing relationship between parasite and invaded species which is bound to result in modifications of both clinical and epidemiological manifestations.”
Hans Zinsser, Rats, Lice and History
We need to be informed by history and grateful to the geniuses who brought us into the modern age of medicine. We can prevent diseases with public health measures, and by understanding and treating crises. Edward Jenner, who recognized the protective effect of cowpox against smallpox, developed inoculations beginning in 1796; he ushered in immunology and saved the lives of millions. Smallpox is now eradicated. A succession of microbe hunters, including Louis Pasteur and Robert Koch, benefited from the development of the microscope by Antonie van Leeuwenhoek. With the advent and use of penicillin in the early 1940s, Alexander Fleming welcomed antibiotics; by the 1960s this modality became widespread. In the mid-20th century, immunologists recognized that bacteria and viruses change and adapt to the environment.
The planet has seen ravaging pandemics that then dissipated and, although untreatable at the time, disappeared into a reservoir, such as rats or lice. People also developed herd immunity from exposure to the offending microorganisms within the population. Less toxic, these agents no longer kill those who get infected but they can be transmissible and endemic to humans.
The mental health consequences of pandemics are reminiscent of other severe illnesses. The seriously ill develop cognitive aberrations and can become delirious. The population at risk and those who get sick can experience depression, PTSD, and anxiety – including panic.
Update on Elvira
Elvira continues to improve. She also participates in support groups, including one that addresses bereavement for parents of children who died of COVID and other causes. “I didn’t have a chance to say goodbye,” she said. But what she calls her “brain fog” has dissipated. She walks better, and she is getting evaluation of radiculopathy, probably from nerve root injury during her 3 weeks in bed on the ventilator. She’s still experiencing pain in her feet.
With regard to her symptoms she said: “I cry almost every day.” Her PTSD has abated, but she sometimes has nightmares. Elvira is writing a book about the induced coma and the “hallucinations from hell to heaven” she experienced. She wonders:“Did Tony go through the same thing?” Her empathy is enhanced by her background as a retired social worker with the Administration for Children’s Services in New York.
The role of psychiatry
In its early, most virulent form, SARS-CoV-2 devastated thousands of people, especially the elderly medically vulnerable. With scientific tools we developed vaccines and treatments and continue to study the dynamics of this virus.
As Andy Miller, MD, chief of the division of infectious diseases at the Hospital for Special Surgery, said when I spoke with him about the virus, because of the way in which viruses mutate, “we must remain aware” of the trajectory of SARS-CoV-2 and “counter irrational beliefs.”
How should psychiatry deal with COVID? As scientists, we seek the truth without bias and politics. Mental illness is our domain. Other specialties have the expertise to treat and even prevent infectious disease. We can assist our doctor colleagues to understand depression, anxiety, PTSD, and cognitive issues when they occur. Our medical mission should be, as always, to treat those who suffer mental illness. Now that extends to the consequences of COVID.
Suggested reading
Camus A. The Plague. New York: Vintage Books,. 1991.
Defoe D. A Journal of the Plague Year. Mineola, N.Y.: Dover Publications, 2001.
Kelly J. The Great Mortality: An Intimate History of the Black Death, The Most Devastating Plague of All Time. New York: Harper Perennial, 2005.
Pepys S. The Diary of Samuel Pepys: The Great Plague of London & The Great Fire of London, 1665-1666. Oxford, England: Benediction Classics, 2020.
Emerg Infect Dis. 2005 Mar 11(3):402-96.
Zinsser H. Rats, Lice and History. Boston/Toronto: Little Brown and Co., 1935.
Dr. Cohen is in private practice of psychotherapy and medication management in New York. She has been a consultant at the Hospital for Special Surgery and at New York–Presbyterian, and a forensic psychiatry expert. She changed key facts about Elvira’s case to protect her anonymity.
A social worker called with a plea in April 2020, when the hospital was filled with COVID-19 patients, some so sick they were on ventilators. “I need your help with a family. Mom is in the ICU, intubated; her son died here 2 weeks ago of COVID and her daughters are overwhelmed, unable to visit because of restrictions. The staff anticipates extubating Elvira imminently, but she will be fragile and alone. When is the right time to tell Elvira that Tony died?”
That happened at the beginning of the COVID pandemic. I handled the case remotely with heroic help from overburdened nurses and doctors who were acting as medical staff, social workers, and substitute family to an isolated patient in the hospital. Such was the confusion with the new virus before vaccines and treatments.
The impact of pandemics: A historical perspective
Beginning in antiquity, there were pandemics that decimated populations. Before antibiotics, vaccines or awareness of microorganisms, people feared contagion and sought isolation from the sick. People also thought that those who recovered were less likely to fall ill again, and if they did get sick, the illness would be milder.
There is abundant documentation of bubonic plague outbreaks, such as the “Black Death” in the Middle Ages. The Spanish flu of 1918 struck down robust young Americans and spread worldwide. Although the bubonic plague was at the center of major infectious outbreaks, including the pandemic of the Justinian era (500s) and the Great Plague of London (1665-1666), other infectious diseases, untreatable at the time, prevailed simultaneously. Wars, world trade, unsanitary conditions, and urban crowding enhanced the spread. Pandemics shaped history. Some historians attribute the fall of the Roman Empire to unrelenting infectious disease carried in migratory battles.
Even in the earliest outbreaks, the poor populace died more readily than the well off, who had means to escape and seclude themselves from congested areas. Samuel Pepys, a diarist of the London Plague, was a famed businessman and government official; he wrote of seeing the suffering in his city, but he escaped to live with his wife in their country home. What Samuel Pepys wrote of London during the Plague can apply to the early period of the COVID pandemic: “How few people I see, and those looking like people that had taken leave of the world.”
There are lurid descriptions of the chaos of pandemics, especially of the Black Death and the Plague of London. First published in 1722, Daniel Defoe’s “A Journal of the Plague Year” describes the suffering of the sick that included people abandoning the afflicted and others running rampant with delirium in the streets, screaming in pain. City officials took cruel measures that they considered necessary, such as locking away families in their homes, sick and well together, when an individual member showed symptoms. The Middle Ages saw deadly anti-Semitism. During the Black Death, fanatics murdered Jews in the belief that they brought on the pestilence. Ignorance created panic.
As happens in tragedy, there was also bravery. Some stayed to tend to the sick; charities provided food for poor people during the London Plague.
Back to the 21st century
After 3 weeks on the ventilator, Elvira got extubated. A team including her doctor, nurse, and Connie, one of her daughters, told Elvira that her 28-year-old son had died of COVID. I began telepsychiatry with Elvira and her two daughters. Treatment continued after Elvira returned home. In telephone sessions, we discussed bereavement and how to cope with the emotional and physical challenges in recovery.
Before he contracted COVID, Tony, Elvira’s son, had compromised health. He was on dialysis awaiting a kidney transplant. His mother prepared his meals and often accompanied Tony to doctor appointments. Still, Elvira said, “I wasn’t there to hold his hand.” At age 71, Elvira was also at high risk. She suffered from diabetes, high blood pressure, hyperlipidemia, and had coronary stents. Elvira was compliant with medications for her conditions.
What we know; where we are
“Infectious diseases are not static conditions but depend upon a constantly changing relationship between parasite and invaded species which is bound to result in modifications of both clinical and epidemiological manifestations.”
Hans Zinsser, Rats, Lice and History
We need to be informed by history and grateful to the geniuses who brought us into the modern age of medicine. We can prevent diseases with public health measures, and by understanding and treating crises. Edward Jenner, who recognized the protective effect of cowpox against smallpox, developed inoculations beginning in 1796; he ushered in immunology and saved the lives of millions. Smallpox is now eradicated. A succession of microbe hunters, including Louis Pasteur and Robert Koch, benefited from the development of the microscope by Antonie van Leeuwenhoek. With the advent and use of penicillin in the early 1940s, Alexander Fleming welcomed antibiotics; by the 1960s this modality became widespread. In the mid-20th century, immunologists recognized that bacteria and viruses change and adapt to the environment.
The planet has seen ravaging pandemics that then dissipated and, although untreatable at the time, disappeared into a reservoir, such as rats or lice. People also developed herd immunity from exposure to the offending microorganisms within the population. Less toxic, these agents no longer kill those who get infected but they can be transmissible and endemic to humans.
The mental health consequences of pandemics are reminiscent of other severe illnesses. The seriously ill develop cognitive aberrations and can become delirious. The population at risk and those who get sick can experience depression, PTSD, and anxiety – including panic.
Update on Elvira
Elvira continues to improve. She also participates in support groups, including one that addresses bereavement for parents of children who died of COVID and other causes. “I didn’t have a chance to say goodbye,” she said. But what she calls her “brain fog” has dissipated. She walks better, and she is getting evaluation of radiculopathy, probably from nerve root injury during her 3 weeks in bed on the ventilator. She’s still experiencing pain in her feet.
With regard to her symptoms she said: “I cry almost every day.” Her PTSD has abated, but she sometimes has nightmares. Elvira is writing a book about the induced coma and the “hallucinations from hell to heaven” she experienced. She wonders:“Did Tony go through the same thing?” Her empathy is enhanced by her background as a retired social worker with the Administration for Children’s Services in New York.
The role of psychiatry
In its early, most virulent form, SARS-CoV-2 devastated thousands of people, especially the elderly medically vulnerable. With scientific tools we developed vaccines and treatments and continue to study the dynamics of this virus.
As Andy Miller, MD, chief of the division of infectious diseases at the Hospital for Special Surgery, said when I spoke with him about the virus, because of the way in which viruses mutate, “we must remain aware” of the trajectory of SARS-CoV-2 and “counter irrational beliefs.”
How should psychiatry deal with COVID? As scientists, we seek the truth without bias and politics. Mental illness is our domain. Other specialties have the expertise to treat and even prevent infectious disease. We can assist our doctor colleagues to understand depression, anxiety, PTSD, and cognitive issues when they occur. Our medical mission should be, as always, to treat those who suffer mental illness. Now that extends to the consequences of COVID.
Suggested reading
Camus A. The Plague. New York: Vintage Books,. 1991.
Defoe D. A Journal of the Plague Year. Mineola, N.Y.: Dover Publications, 2001.
Kelly J. The Great Mortality: An Intimate History of the Black Death, The Most Devastating Plague of All Time. New York: Harper Perennial, 2005.
Pepys S. The Diary of Samuel Pepys: The Great Plague of London & The Great Fire of London, 1665-1666. Oxford, England: Benediction Classics, 2020.
Emerg Infect Dis. 2005 Mar 11(3):402-96.
Zinsser H. Rats, Lice and History. Boston/Toronto: Little Brown and Co., 1935.
Dr. Cohen is in private practice of psychotherapy and medication management in New York. She has been a consultant at the Hospital for Special Surgery and at New York–Presbyterian, and a forensic psychiatry expert. She changed key facts about Elvira’s case to protect her anonymity.











