User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Hormone therapy in transgender teens linked to better adult mental health
In another salvo in the heated debate over treatment for kids who believe they’re transgender, a study published in PLoS One suggests that transgender adults who received hormone therapy as teenagers are mentally healthier in a pair of ways than those who didn’t.
The study, which only looks at transgender adults, doesn’t confirm that hormone therapy in childhood is a beneficial treatment. Still, “we found that for all age groups, access to [adolescent] gender-affirming hormone initiation was associated with lower odds of past-year suicidal ideation and past-month severe psychological distress measured in adulthood,” said lead author Jack Turban, MD, chief fellow in child and adolescent psychiatry at Stanford (Calif.) University, in an interview. “We also found better mental-health outcomes for those who started gender-affirming hormones as adolescents when compared to those who didn’t start them until they were adults.”
The use of hormone treatment and puberty blockers by transgender teens is extremely controversial. Critics say the treatments are harmful and unnecessary, and Republican politicians are trying to ban their use in some states. Last spring, Arkansas became the first state to ban the treatments. The law is on hold amid a legal challenge.
The researchers launched the study to gain more insight into the impact of hormone therapy on children. “There have been several longitudinal studies showing that mental health improves following gender-affirming medical care for transgender youth, but there has been less research looking at the relationship between when these medications are started and adult mental health outcomes,” Dr. Turban said. “This is the first study to look at various ages of initiation of gender-affirming hormones and compare outcomes between those who started gender-affirming hormones during adolescence and those who did not start them until adulthood.”
For the new study, the authors analyzed the findings of the 2015 U.S. Transgender Survey of 27,715 adults and focused on 21,598 who said they’d wanted hormone therapy (40% aged 18-24, 83% White, 35% transgender male, 41% transgender female, with the rest using other terms such as “queer” or “nonbinary” to describe themselves).
Of these subjects, 41.0% never received hormone therapy, 0.6% underwent therapy in early adolescence, 1.7% received it in late adolescence, and 56.8% got it as adults.
The researchers made various adjustments for confounders – age, partnership status, employment status, K-12 harassment, and experience of gender identity conversion efforts. Those who received hormone therapy had lower odds of past-year suicidal ideation vs. those who didn’t: adjusted odds ratio, 0.4; 95% confidence interval, 0.2-0.6; P < .0001 for therapy that occurred from age 14 to 15, aOR, 0.5; 95% CI, 0.4-0.7; P < .0001, for therapy that occurred from age 16 to 17, and aOR, 0.8; 95% CI, 0.7-0.8; P < .0001 for therapy that occurred in adulthood.
However, there was no statistically significant link between hormone therapy and past-year suicidal ideation with a plan or past-year suicide attempt.
The study also found lower rates of past-month severe psychological distress: aOR. 0.3; 95% CI, 0.2-0.4; P < .0001 for therapy from age 14 to 15, aOR, 0.3; 95% CI, 0.3-0.4; P < .0001 for therapy from age 16 to 17, and aOR, 0.6 (95% CI, 0.5-0.6; P < .0001) for therapy in adulthood.
There was no statistically significant link between hormone therapy and past-month binge drinking or lifetime illicit drug use.
“The findings indicate that clinicians caring for adolescents need to be properly trained in gender-affirming medical care, including hormone therapy, in order to help promote good mental health outcomes for transgender people. Comprehensive training in gender-affirming care is currently not part of standard medical education curricula,” said study coauthor Alex Keuroghlian, MD, MPH, director of the National LGBTQIA+ Health Education Center at the Fenway Institute and associate professor of psychiatry at Harvard Medical School, Boston, in an interview.
The study has limitations. The survey population doesn’t include anyone who committed suicide, nor does it include people who had gender dysphoria as children but didn’t go on to identify as transgender as adults. It is also retrospective. “There is a general consensus that, given the data we have so far, it would be unethical to conduct a randomized controlled trial in this space,” said study lead author Dr. Turban.
Several critics of hormone therapy in teens support a psychotherapy-based approach to gender dysphoria that considers whether other factors are at play than transgender orientation. They’ve united to attack research based on the 2015 transgender survey. In a 2021 report in Archives of Sexual Behavior, they called it “a highly skewed sample” and objected to “a conflation of ethical nonaffirmative psychotherapy with conversion therapy.”
In an interview, one of the critics – developmental psychologist and retired University of Sydney professor Dianna Kenny, PhD – said the new study’s “serious problem of recall bias” about hormone therapy in the survey is “insurmountable.” The survey, she said, also fails to explore why participants who wanted hormone therapy didn’t get it.
Dr. Kenny, who believes all hormone therapy in teens with gender dysphoria outside of clinical trials is inappropriate, also pointed out that hormone therapy has many side effects. She added that young people with gender dysphoria often “realize through a process of cognitive and psychosocial maturation that they were not ‘genuinely’ trans but suffering from other conditions that needed treatment – e.g., internalized homophobia, trauma, including sexual abuse, attention-deficit/hyperactivity disorder, autism spectrum disorder, etc.”
No specific funding is reported, although two of the authors report receiving various grants, fellowship and research funding. Dr. Turban discloses textbook royalties from Springer Nature and expert witness payments from the ACLU. Dr. Keuroghlian discloses textbook royalties from McGraw Hill. Dr. Kenny reports no disclosures.
In another salvo in the heated debate over treatment for kids who believe they’re transgender, a study published in PLoS One suggests that transgender adults who received hormone therapy as teenagers are mentally healthier in a pair of ways than those who didn’t.
The study, which only looks at transgender adults, doesn’t confirm that hormone therapy in childhood is a beneficial treatment. Still, “we found that for all age groups, access to [adolescent] gender-affirming hormone initiation was associated with lower odds of past-year suicidal ideation and past-month severe psychological distress measured in adulthood,” said lead author Jack Turban, MD, chief fellow in child and adolescent psychiatry at Stanford (Calif.) University, in an interview. “We also found better mental-health outcomes for those who started gender-affirming hormones as adolescents when compared to those who didn’t start them until they were adults.”
The use of hormone treatment and puberty blockers by transgender teens is extremely controversial. Critics say the treatments are harmful and unnecessary, and Republican politicians are trying to ban their use in some states. Last spring, Arkansas became the first state to ban the treatments. The law is on hold amid a legal challenge.
The researchers launched the study to gain more insight into the impact of hormone therapy on children. “There have been several longitudinal studies showing that mental health improves following gender-affirming medical care for transgender youth, but there has been less research looking at the relationship between when these medications are started and adult mental health outcomes,” Dr. Turban said. “This is the first study to look at various ages of initiation of gender-affirming hormones and compare outcomes between those who started gender-affirming hormones during adolescence and those who did not start them until adulthood.”
For the new study, the authors analyzed the findings of the 2015 U.S. Transgender Survey of 27,715 adults and focused on 21,598 who said they’d wanted hormone therapy (40% aged 18-24, 83% White, 35% transgender male, 41% transgender female, with the rest using other terms such as “queer” or “nonbinary” to describe themselves).
Of these subjects, 41.0% never received hormone therapy, 0.6% underwent therapy in early adolescence, 1.7% received it in late adolescence, and 56.8% got it as adults.
The researchers made various adjustments for confounders – age, partnership status, employment status, K-12 harassment, and experience of gender identity conversion efforts. Those who received hormone therapy had lower odds of past-year suicidal ideation vs. those who didn’t: adjusted odds ratio, 0.4; 95% confidence interval, 0.2-0.6; P < .0001 for therapy that occurred from age 14 to 15, aOR, 0.5; 95% CI, 0.4-0.7; P < .0001, for therapy that occurred from age 16 to 17, and aOR, 0.8; 95% CI, 0.7-0.8; P < .0001 for therapy that occurred in adulthood.
However, there was no statistically significant link between hormone therapy and past-year suicidal ideation with a plan or past-year suicide attempt.
The study also found lower rates of past-month severe psychological distress: aOR. 0.3; 95% CI, 0.2-0.4; P < .0001 for therapy from age 14 to 15, aOR, 0.3; 95% CI, 0.3-0.4; P < .0001 for therapy from age 16 to 17, and aOR, 0.6 (95% CI, 0.5-0.6; P < .0001) for therapy in adulthood.
There was no statistically significant link between hormone therapy and past-month binge drinking or lifetime illicit drug use.
“The findings indicate that clinicians caring for adolescents need to be properly trained in gender-affirming medical care, including hormone therapy, in order to help promote good mental health outcomes for transgender people. Comprehensive training in gender-affirming care is currently not part of standard medical education curricula,” said study coauthor Alex Keuroghlian, MD, MPH, director of the National LGBTQIA+ Health Education Center at the Fenway Institute and associate professor of psychiatry at Harvard Medical School, Boston, in an interview.
The study has limitations. The survey population doesn’t include anyone who committed suicide, nor does it include people who had gender dysphoria as children but didn’t go on to identify as transgender as adults. It is also retrospective. “There is a general consensus that, given the data we have so far, it would be unethical to conduct a randomized controlled trial in this space,” said study lead author Dr. Turban.
Several critics of hormone therapy in teens support a psychotherapy-based approach to gender dysphoria that considers whether other factors are at play than transgender orientation. They’ve united to attack research based on the 2015 transgender survey. In a 2021 report in Archives of Sexual Behavior, they called it “a highly skewed sample” and objected to “a conflation of ethical nonaffirmative psychotherapy with conversion therapy.”
In an interview, one of the critics – developmental psychologist and retired University of Sydney professor Dianna Kenny, PhD – said the new study’s “serious problem of recall bias” about hormone therapy in the survey is “insurmountable.” The survey, she said, also fails to explore why participants who wanted hormone therapy didn’t get it.
Dr. Kenny, who believes all hormone therapy in teens with gender dysphoria outside of clinical trials is inappropriate, also pointed out that hormone therapy has many side effects. She added that young people with gender dysphoria often “realize through a process of cognitive and psychosocial maturation that they were not ‘genuinely’ trans but suffering from other conditions that needed treatment – e.g., internalized homophobia, trauma, including sexual abuse, attention-deficit/hyperactivity disorder, autism spectrum disorder, etc.”
No specific funding is reported, although two of the authors report receiving various grants, fellowship and research funding. Dr. Turban discloses textbook royalties from Springer Nature and expert witness payments from the ACLU. Dr. Keuroghlian discloses textbook royalties from McGraw Hill. Dr. Kenny reports no disclosures.
In another salvo in the heated debate over treatment for kids who believe they’re transgender, a study published in PLoS One suggests that transgender adults who received hormone therapy as teenagers are mentally healthier in a pair of ways than those who didn’t.
The study, which only looks at transgender adults, doesn’t confirm that hormone therapy in childhood is a beneficial treatment. Still, “we found that for all age groups, access to [adolescent] gender-affirming hormone initiation was associated with lower odds of past-year suicidal ideation and past-month severe psychological distress measured in adulthood,” said lead author Jack Turban, MD, chief fellow in child and adolescent psychiatry at Stanford (Calif.) University, in an interview. “We also found better mental-health outcomes for those who started gender-affirming hormones as adolescents when compared to those who didn’t start them until they were adults.”
The use of hormone treatment and puberty blockers by transgender teens is extremely controversial. Critics say the treatments are harmful and unnecessary, and Republican politicians are trying to ban their use in some states. Last spring, Arkansas became the first state to ban the treatments. The law is on hold amid a legal challenge.
The researchers launched the study to gain more insight into the impact of hormone therapy on children. “There have been several longitudinal studies showing that mental health improves following gender-affirming medical care for transgender youth, but there has been less research looking at the relationship between when these medications are started and adult mental health outcomes,” Dr. Turban said. “This is the first study to look at various ages of initiation of gender-affirming hormones and compare outcomes between those who started gender-affirming hormones during adolescence and those who did not start them until adulthood.”
For the new study, the authors analyzed the findings of the 2015 U.S. Transgender Survey of 27,715 adults and focused on 21,598 who said they’d wanted hormone therapy (40% aged 18-24, 83% White, 35% transgender male, 41% transgender female, with the rest using other terms such as “queer” or “nonbinary” to describe themselves).
Of these subjects, 41.0% never received hormone therapy, 0.6% underwent therapy in early adolescence, 1.7% received it in late adolescence, and 56.8% got it as adults.
The researchers made various adjustments for confounders – age, partnership status, employment status, K-12 harassment, and experience of gender identity conversion efforts. Those who received hormone therapy had lower odds of past-year suicidal ideation vs. those who didn’t: adjusted odds ratio, 0.4; 95% confidence interval, 0.2-0.6; P < .0001 for therapy that occurred from age 14 to 15, aOR, 0.5; 95% CI, 0.4-0.7; P < .0001, for therapy that occurred from age 16 to 17, and aOR, 0.8; 95% CI, 0.7-0.8; P < .0001 for therapy that occurred in adulthood.
However, there was no statistically significant link between hormone therapy and past-year suicidal ideation with a plan or past-year suicide attempt.
The study also found lower rates of past-month severe psychological distress: aOR. 0.3; 95% CI, 0.2-0.4; P < .0001 for therapy from age 14 to 15, aOR, 0.3; 95% CI, 0.3-0.4; P < .0001 for therapy from age 16 to 17, and aOR, 0.6 (95% CI, 0.5-0.6; P < .0001) for therapy in adulthood.
There was no statistically significant link between hormone therapy and past-month binge drinking or lifetime illicit drug use.
“The findings indicate that clinicians caring for adolescents need to be properly trained in gender-affirming medical care, including hormone therapy, in order to help promote good mental health outcomes for transgender people. Comprehensive training in gender-affirming care is currently not part of standard medical education curricula,” said study coauthor Alex Keuroghlian, MD, MPH, director of the National LGBTQIA+ Health Education Center at the Fenway Institute and associate professor of psychiatry at Harvard Medical School, Boston, in an interview.
The study has limitations. The survey population doesn’t include anyone who committed suicide, nor does it include people who had gender dysphoria as children but didn’t go on to identify as transgender as adults. It is also retrospective. “There is a general consensus that, given the data we have so far, it would be unethical to conduct a randomized controlled trial in this space,” said study lead author Dr. Turban.
Several critics of hormone therapy in teens support a psychotherapy-based approach to gender dysphoria that considers whether other factors are at play than transgender orientation. They’ve united to attack research based on the 2015 transgender survey. In a 2021 report in Archives of Sexual Behavior, they called it “a highly skewed sample” and objected to “a conflation of ethical nonaffirmative psychotherapy with conversion therapy.”
In an interview, one of the critics – developmental psychologist and retired University of Sydney professor Dianna Kenny, PhD – said the new study’s “serious problem of recall bias” about hormone therapy in the survey is “insurmountable.” The survey, she said, also fails to explore why participants who wanted hormone therapy didn’t get it.
Dr. Kenny, who believes all hormone therapy in teens with gender dysphoria outside of clinical trials is inappropriate, also pointed out that hormone therapy has many side effects. She added that young people with gender dysphoria often “realize through a process of cognitive and psychosocial maturation that they were not ‘genuinely’ trans but suffering from other conditions that needed treatment – e.g., internalized homophobia, trauma, including sexual abuse, attention-deficit/hyperactivity disorder, autism spectrum disorder, etc.”
No specific funding is reported, although two of the authors report receiving various grants, fellowship and research funding. Dr. Turban discloses textbook royalties from Springer Nature and expert witness payments from the ACLU. Dr. Keuroghlian discloses textbook royalties from McGraw Hill. Dr. Kenny reports no disclosures.
FROM PLOS ONE
OTC cannabidiol products tied to improved pain, sleep, anxiety
Interim findings from Advancing CBD Education and Science, a 100% virtual, open label, randomized, controlled trial, show study participants experienced various degrees of “clinically meaningful” improvements in sleep quality, anxiety, and pain.
“ACES is the largest clinical trial ever conducted on commercially available CBD products and provides first-of-its-kind real world evidence into what conditions users may experience benefit from CBD usage, whether these benefits are clinically meaningful, what attributes of CBD products may impact health outcomes, and what side effects may occur,” study coinvestigator Jessica Saleska, PhD, MPH, director of research at Radicle Science, the company that conducted the study, told this news organization.
Scant evidence
Despite the growing market size of commercially available CBD products “there is still scant data on the effectiveness of over-the-counter cannabinoid products due to the cost, speed, and scale limitations of the current approach to scientific research,” Jeff Chen, MD, MBA, cofounder and CEO of Radicle Science, told this news organization.
One of the study’s goals, said Ethan Russo, MD, a neurologist, founder/CEO of CReDO Science, and scientific adviser for Radicle, is to help consumers make informed decisions before purchasing and using commercially available oral CBD products.
Designed to eliminate all physical infrastructure, which minimizes costs and facilitates faster execution, ACES was conducted much like a phase 4 clinical trial, collating real-world data gathered over 4 weeks.
“The process that Radicle scientists [have] advanced is sort of a crowdsourcing approach to doing clinical science,” Dr. Russo said. “Hopefully, there is going to be a considerable amount of data generated that [will] affect people’s buying options.”
The study also aimed to evaluate product attributes, including composition, mode of use, dosage, dosage timing and frequency, and their correlation to degrees of outcomes.
Dr. Russo explained why product composition is an important factor, especially when dealing with CBD. “What happens with any given [CBD] preparation is going to be totally a function of other components, if any.
“For example, there’s this mistaken notion that cannabidiol is sedating; it is not. Pure cannabidiol is stimulating in low and moderate amounts. Where the confusion has arisen is that the early chemovars containing cannabidiol were also predominant in myrcene, the sedating terpene, [thereby] creating this misimpression that it is good for sleep,” he added.
However, CBD might also affect sleep by reducing anxiety that interferes with it. “What’s clear is that cannabidiol is an antianxiety agent, if you have a sufficient dose,” Dr. Russo said.
The 4-week study included 2,704 participants aged 21 years and older, self-reporting anxiety, chronic pain, or sleep disturbances as a primary reason for taking CBD. Study participants were randomly assigned to receive 1 of 13 commercially available oral CBD extracts.
Participants were allocated to 1 of 14 cohorts, comprising 13 treatment groups with 208 participants each who received a single CBD product, or a wait-list control group of 296 participants who received product at the study’s end.
The primary outcome focused on “clinically meaningful” changes, which were defined as “distinct and palpable improvements in quality of life through improvements in respective health outcomes.”
Secondary outcomes included changes in sleep, anxiety, and pain based on several validated indices, including the PROMIS (Patient-Reported Outcome Measurement Information System) Sleep Short Form; the PROMIS Anxiety Scale; the Patient Global Impression of Change; the Pain, Enjoyment, General Activity scale; and the General Anxiety Disorder–7 scale.
The interim study results are promising, with participants reporting, on average, a 71% improvement in well-being. Additionally, 63% reported clinically meaningful improvements in anxiety, and 61% in sleep quality. The CBD products provided smaller benefits in pain management, with less than half (47%) experiencing meaningful improvements.
In addition to improvement in sleep, pain, and anxiety, these data highlight how rapidly benefits occurred; most were realized during the first week of the study, with up to 61% of treatment group participants reporting a therapeutic effect within 1-4 hours of taking their assigned product.
Overcoming the placebo effect
Commenting on the research, Justin Strickland, PhD, an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore, who was not involved in the research, said without knowing a lot about the pharmacology of the products being tested, early dramatic improvements in these measures, such as sleep impairment, are common.
“There are some data to suggest that there is an expectancy effect when we talk about the therapeutic benefit of cannabinoid products, (i.e., when someone has the expectation that they are going to experience a stronger effect) but this is true of any drug in an open label trial,” Dr. Strickland added.
Dr. Russo took the point a step further. “It’s getting near impossible to look at cannabinoid compounds, even with randomized, controlled trials because of the burgeoning placebo responses. When you couple it with the fact that consumers have the mistaken notion that cannabis-based drugs are miraculous, the expectations are so high that everyone thinks that they’re on the real stuff, even if it’s a placebo group.”
Still, both Dr. Strickland and Dr. Russo highlighted the fact that ACES mirrors real-world experience, which will they hope will inform the use of CBD and CBD-based preparations moving forward. By removing certain barriers like institutional bureaucracy or federal funding restrictions inherent to more traditional randomized controlled trial design, ACES might provide data that bridge the gap between efficacy and effectiveness.
ACES was funded by Radicle Science. Dr. Chen is cofounder and CEO of Radicle Science. Dr. Russo and Dr. Strickland disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Interim findings from Advancing CBD Education and Science, a 100% virtual, open label, randomized, controlled trial, show study participants experienced various degrees of “clinically meaningful” improvements in sleep quality, anxiety, and pain.
“ACES is the largest clinical trial ever conducted on commercially available CBD products and provides first-of-its-kind real world evidence into what conditions users may experience benefit from CBD usage, whether these benefits are clinically meaningful, what attributes of CBD products may impact health outcomes, and what side effects may occur,” study coinvestigator Jessica Saleska, PhD, MPH, director of research at Radicle Science, the company that conducted the study, told this news organization.
Scant evidence
Despite the growing market size of commercially available CBD products “there is still scant data on the effectiveness of over-the-counter cannabinoid products due to the cost, speed, and scale limitations of the current approach to scientific research,” Jeff Chen, MD, MBA, cofounder and CEO of Radicle Science, told this news organization.
One of the study’s goals, said Ethan Russo, MD, a neurologist, founder/CEO of CReDO Science, and scientific adviser for Radicle, is to help consumers make informed decisions before purchasing and using commercially available oral CBD products.
Designed to eliminate all physical infrastructure, which minimizes costs and facilitates faster execution, ACES was conducted much like a phase 4 clinical trial, collating real-world data gathered over 4 weeks.
“The process that Radicle scientists [have] advanced is sort of a crowdsourcing approach to doing clinical science,” Dr. Russo said. “Hopefully, there is going to be a considerable amount of data generated that [will] affect people’s buying options.”
The study also aimed to evaluate product attributes, including composition, mode of use, dosage, dosage timing and frequency, and their correlation to degrees of outcomes.
Dr. Russo explained why product composition is an important factor, especially when dealing with CBD. “What happens with any given [CBD] preparation is going to be totally a function of other components, if any.
“For example, there’s this mistaken notion that cannabidiol is sedating; it is not. Pure cannabidiol is stimulating in low and moderate amounts. Where the confusion has arisen is that the early chemovars containing cannabidiol were also predominant in myrcene, the sedating terpene, [thereby] creating this misimpression that it is good for sleep,” he added.
However, CBD might also affect sleep by reducing anxiety that interferes with it. “What’s clear is that cannabidiol is an antianxiety agent, if you have a sufficient dose,” Dr. Russo said.
The 4-week study included 2,704 participants aged 21 years and older, self-reporting anxiety, chronic pain, or sleep disturbances as a primary reason for taking CBD. Study participants were randomly assigned to receive 1 of 13 commercially available oral CBD extracts.
Participants were allocated to 1 of 14 cohorts, comprising 13 treatment groups with 208 participants each who received a single CBD product, or a wait-list control group of 296 participants who received product at the study’s end.
The primary outcome focused on “clinically meaningful” changes, which were defined as “distinct and palpable improvements in quality of life through improvements in respective health outcomes.”
Secondary outcomes included changes in sleep, anxiety, and pain based on several validated indices, including the PROMIS (Patient-Reported Outcome Measurement Information System) Sleep Short Form; the PROMIS Anxiety Scale; the Patient Global Impression of Change; the Pain, Enjoyment, General Activity scale; and the General Anxiety Disorder–7 scale.
The interim study results are promising, with participants reporting, on average, a 71% improvement in well-being. Additionally, 63% reported clinically meaningful improvements in anxiety, and 61% in sleep quality. The CBD products provided smaller benefits in pain management, with less than half (47%) experiencing meaningful improvements.
In addition to improvement in sleep, pain, and anxiety, these data highlight how rapidly benefits occurred; most were realized during the first week of the study, with up to 61% of treatment group participants reporting a therapeutic effect within 1-4 hours of taking their assigned product.
Overcoming the placebo effect
Commenting on the research, Justin Strickland, PhD, an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore, who was not involved in the research, said without knowing a lot about the pharmacology of the products being tested, early dramatic improvements in these measures, such as sleep impairment, are common.
“There are some data to suggest that there is an expectancy effect when we talk about the therapeutic benefit of cannabinoid products, (i.e., when someone has the expectation that they are going to experience a stronger effect) but this is true of any drug in an open label trial,” Dr. Strickland added.
Dr. Russo took the point a step further. “It’s getting near impossible to look at cannabinoid compounds, even with randomized, controlled trials because of the burgeoning placebo responses. When you couple it with the fact that consumers have the mistaken notion that cannabis-based drugs are miraculous, the expectations are so high that everyone thinks that they’re on the real stuff, even if it’s a placebo group.”
Still, both Dr. Strickland and Dr. Russo highlighted the fact that ACES mirrors real-world experience, which will they hope will inform the use of CBD and CBD-based preparations moving forward. By removing certain barriers like institutional bureaucracy or federal funding restrictions inherent to more traditional randomized controlled trial design, ACES might provide data that bridge the gap between efficacy and effectiveness.
ACES was funded by Radicle Science. Dr. Chen is cofounder and CEO of Radicle Science. Dr. Russo and Dr. Strickland disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Interim findings from Advancing CBD Education and Science, a 100% virtual, open label, randomized, controlled trial, show study participants experienced various degrees of “clinically meaningful” improvements in sleep quality, anxiety, and pain.
“ACES is the largest clinical trial ever conducted on commercially available CBD products and provides first-of-its-kind real world evidence into what conditions users may experience benefit from CBD usage, whether these benefits are clinically meaningful, what attributes of CBD products may impact health outcomes, and what side effects may occur,” study coinvestigator Jessica Saleska, PhD, MPH, director of research at Radicle Science, the company that conducted the study, told this news organization.
Scant evidence
Despite the growing market size of commercially available CBD products “there is still scant data on the effectiveness of over-the-counter cannabinoid products due to the cost, speed, and scale limitations of the current approach to scientific research,” Jeff Chen, MD, MBA, cofounder and CEO of Radicle Science, told this news organization.
One of the study’s goals, said Ethan Russo, MD, a neurologist, founder/CEO of CReDO Science, and scientific adviser for Radicle, is to help consumers make informed decisions before purchasing and using commercially available oral CBD products.
Designed to eliminate all physical infrastructure, which minimizes costs and facilitates faster execution, ACES was conducted much like a phase 4 clinical trial, collating real-world data gathered over 4 weeks.
“The process that Radicle scientists [have] advanced is sort of a crowdsourcing approach to doing clinical science,” Dr. Russo said. “Hopefully, there is going to be a considerable amount of data generated that [will] affect people’s buying options.”
The study also aimed to evaluate product attributes, including composition, mode of use, dosage, dosage timing and frequency, and their correlation to degrees of outcomes.
Dr. Russo explained why product composition is an important factor, especially when dealing with CBD. “What happens with any given [CBD] preparation is going to be totally a function of other components, if any.
“For example, there’s this mistaken notion that cannabidiol is sedating; it is not. Pure cannabidiol is stimulating in low and moderate amounts. Where the confusion has arisen is that the early chemovars containing cannabidiol were also predominant in myrcene, the sedating terpene, [thereby] creating this misimpression that it is good for sleep,” he added.
However, CBD might also affect sleep by reducing anxiety that interferes with it. “What’s clear is that cannabidiol is an antianxiety agent, if you have a sufficient dose,” Dr. Russo said.
The 4-week study included 2,704 participants aged 21 years and older, self-reporting anxiety, chronic pain, or sleep disturbances as a primary reason for taking CBD. Study participants were randomly assigned to receive 1 of 13 commercially available oral CBD extracts.
Participants were allocated to 1 of 14 cohorts, comprising 13 treatment groups with 208 participants each who received a single CBD product, or a wait-list control group of 296 participants who received product at the study’s end.
The primary outcome focused on “clinically meaningful” changes, which were defined as “distinct and palpable improvements in quality of life through improvements in respective health outcomes.”
Secondary outcomes included changes in sleep, anxiety, and pain based on several validated indices, including the PROMIS (Patient-Reported Outcome Measurement Information System) Sleep Short Form; the PROMIS Anxiety Scale; the Patient Global Impression of Change; the Pain, Enjoyment, General Activity scale; and the General Anxiety Disorder–7 scale.
The interim study results are promising, with participants reporting, on average, a 71% improvement in well-being. Additionally, 63% reported clinically meaningful improvements in anxiety, and 61% in sleep quality. The CBD products provided smaller benefits in pain management, with less than half (47%) experiencing meaningful improvements.
In addition to improvement in sleep, pain, and anxiety, these data highlight how rapidly benefits occurred; most were realized during the first week of the study, with up to 61% of treatment group participants reporting a therapeutic effect within 1-4 hours of taking their assigned product.
Overcoming the placebo effect
Commenting on the research, Justin Strickland, PhD, an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore, who was not involved in the research, said without knowing a lot about the pharmacology of the products being tested, early dramatic improvements in these measures, such as sleep impairment, are common.
“There are some data to suggest that there is an expectancy effect when we talk about the therapeutic benefit of cannabinoid products, (i.e., when someone has the expectation that they are going to experience a stronger effect) but this is true of any drug in an open label trial,” Dr. Strickland added.
Dr. Russo took the point a step further. “It’s getting near impossible to look at cannabinoid compounds, even with randomized, controlled trials because of the burgeoning placebo responses. When you couple it with the fact that consumers have the mistaken notion that cannabis-based drugs are miraculous, the expectations are so high that everyone thinks that they’re on the real stuff, even if it’s a placebo group.”
Still, both Dr. Strickland and Dr. Russo highlighted the fact that ACES mirrors real-world experience, which will they hope will inform the use of CBD and CBD-based preparations moving forward. By removing certain barriers like institutional bureaucracy or federal funding restrictions inherent to more traditional randomized controlled trial design, ACES might provide data that bridge the gap between efficacy and effectiveness.
ACES was funded by Radicle Science. Dr. Chen is cofounder and CEO of Radicle Science. Dr. Russo and Dr. Strickland disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Physician burnout, depression compounded by COVID: Survey
In 2020, it was hard to imagine that the situation could get worse for doctors.
But 2021 presented a new set of challenges. As quarantines lifted and physicians tried to get back to work, they were forced to deal with reduced staff, continuing COVID stress, and pandemic-related anxieties about family and loved ones.
Medscape’s National Burnout and Depression Report 2022 asked more than 13,000 physicians from 29 specialties to share details about their lives and struggles with burnout and depression in 2021. The results paint a picture of physicians trying to fulfill their mission to care for patients, but struggling to maintain their own well-being amid a global pandemic.
Burnout bump
In 2021’s report, 42% of physicians said they were burned out. In 2022, that number increased to 47%. Perhaps not surprisingly, burnout among emergency physicians took the biggest leap, increasing from 43% to 60%. Critical care (56%), ob.gyn. (53%), and infectious disease and family medicine (both at 51%) rounded out the top five specialties with doctors experiencing burnout in 2021.
Burnout has typically been a greater problem for women than men physicians, and the pandemic hasn’t changed that. “There’s no question that women have reported far more role strain during the pandemic than men,” says Carol A. Bernstein, MD, psychiatrist at Montefiore Health System and professor and vice chair for faculty development and well-being at the Albert Einstein College of Medicine, both in New York. And indeed, 56% of women and 41% of men reported burnout in the 2022 survey.
The causes, however, weren’t especially pandemic related – or at least not directly. As in previous surveys, the major contributing factor to burnout was too much paperwork (60%), such as charting and other bureaucratic tasks. Treating COVID-19 patients was cited as the major source of stress by 10% of respondents. About 34% said too many hours at work was the biggest contributing factor to burnout.
The nature of the beast
What is burnout like for these doctors? One described the conditions that lead to burnout like this: “I barely spend enough time with most patients, just running from one to the next; and then after work, I spend hours documenting, charting, dealing with reports. I feel like an overpaid clerk.” Another said: “Where’s the relationships with patients that used to make this worthwhile?” Others fingered staffing shortages at work or an overwhelming home life: “Staff calls in sick; we’re all running around trying to find things and get things done. It never ends.”
Of those who do experience burnout, the problem reaches beyond the workplace, with 54% saying that their burnout has a strong/severe impact on life and 68% reporting that burnout affects their relationships. One respondent said: “I’m always tired; I have trouble concentrating, no time for the children, more arguments with my hubby.” Another put it this way: “Home is just as busy and chaotic as work. I can never relax.”
It doesn’t help matters that physicians are likely to think they’re the only professionals experiencing job burnout. For example, only 36% of respondents believe teachers experience comparable burnout, yet more than 41% of teachers leave the profession within 5 years of starting – often because of burnout.
When it comes to methods for coping with burnout, exercise is the clear favorite, with 63% of respondents saying exercise helps maintain their mental health. About 41% talk with family members or close friends. However, less healthy coping mechanisms were cited as well, such as isolating themselves from others (45%), sleeping (41%), and eating junk food (35%) or drinking alcohol (24%).
When it comes to trying to alleviate burnout, 29% have tried meditation or similar stress-reduction techniques, while others have reduced their work hours (29%) or changed their work settings (19%).
‘Now I feel like there’s no hope’
About a fifth of physicians (21%) said they suffered from clinical depression, and 64% reported feeling “blue, down, or sad.” One physician characterized their depression this way: “I used to think my life would be great. Now I feel like there’s no hope, this will never get better, I’ll never be happy.”
Of doctors reporting depression, 53% said their illness did not affect their interactions with patients, while 34% said depression caused them to be more easily exasperated by patients.
When asked about seeking help for depression, about half (49%) said they believed they could deal with emotional stress on their own. Unfortunately, fear of medical boards finding out keeps 43% of physicians from reaching out for help, according to the survey.
A version of this article first appeared on Medscape.com.
In 2020, it was hard to imagine that the situation could get worse for doctors.
But 2021 presented a new set of challenges. As quarantines lifted and physicians tried to get back to work, they were forced to deal with reduced staff, continuing COVID stress, and pandemic-related anxieties about family and loved ones.
Medscape’s National Burnout and Depression Report 2022 asked more than 13,000 physicians from 29 specialties to share details about their lives and struggles with burnout and depression in 2021. The results paint a picture of physicians trying to fulfill their mission to care for patients, but struggling to maintain their own well-being amid a global pandemic.
Burnout bump
In 2021’s report, 42% of physicians said they were burned out. In 2022, that number increased to 47%. Perhaps not surprisingly, burnout among emergency physicians took the biggest leap, increasing from 43% to 60%. Critical care (56%), ob.gyn. (53%), and infectious disease and family medicine (both at 51%) rounded out the top five specialties with doctors experiencing burnout in 2021.
Burnout has typically been a greater problem for women than men physicians, and the pandemic hasn’t changed that. “There’s no question that women have reported far more role strain during the pandemic than men,” says Carol A. Bernstein, MD, psychiatrist at Montefiore Health System and professor and vice chair for faculty development and well-being at the Albert Einstein College of Medicine, both in New York. And indeed, 56% of women and 41% of men reported burnout in the 2022 survey.
The causes, however, weren’t especially pandemic related – or at least not directly. As in previous surveys, the major contributing factor to burnout was too much paperwork (60%), such as charting and other bureaucratic tasks. Treating COVID-19 patients was cited as the major source of stress by 10% of respondents. About 34% said too many hours at work was the biggest contributing factor to burnout.
The nature of the beast
What is burnout like for these doctors? One described the conditions that lead to burnout like this: “I barely spend enough time with most patients, just running from one to the next; and then after work, I spend hours documenting, charting, dealing with reports. I feel like an overpaid clerk.” Another said: “Where’s the relationships with patients that used to make this worthwhile?” Others fingered staffing shortages at work or an overwhelming home life: “Staff calls in sick; we’re all running around trying to find things and get things done. It never ends.”
Of those who do experience burnout, the problem reaches beyond the workplace, with 54% saying that their burnout has a strong/severe impact on life and 68% reporting that burnout affects their relationships. One respondent said: “I’m always tired; I have trouble concentrating, no time for the children, more arguments with my hubby.” Another put it this way: “Home is just as busy and chaotic as work. I can never relax.”
It doesn’t help matters that physicians are likely to think they’re the only professionals experiencing job burnout. For example, only 36% of respondents believe teachers experience comparable burnout, yet more than 41% of teachers leave the profession within 5 years of starting – often because of burnout.
When it comes to methods for coping with burnout, exercise is the clear favorite, with 63% of respondents saying exercise helps maintain their mental health. About 41% talk with family members or close friends. However, less healthy coping mechanisms were cited as well, such as isolating themselves from others (45%), sleeping (41%), and eating junk food (35%) or drinking alcohol (24%).
When it comes to trying to alleviate burnout, 29% have tried meditation or similar stress-reduction techniques, while others have reduced their work hours (29%) or changed their work settings (19%).
‘Now I feel like there’s no hope’
About a fifth of physicians (21%) said they suffered from clinical depression, and 64% reported feeling “blue, down, or sad.” One physician characterized their depression this way: “I used to think my life would be great. Now I feel like there’s no hope, this will never get better, I’ll never be happy.”
Of doctors reporting depression, 53% said their illness did not affect their interactions with patients, while 34% said depression caused them to be more easily exasperated by patients.
When asked about seeking help for depression, about half (49%) said they believed they could deal with emotional stress on their own. Unfortunately, fear of medical boards finding out keeps 43% of physicians from reaching out for help, according to the survey.
A version of this article first appeared on Medscape.com.
In 2020, it was hard to imagine that the situation could get worse for doctors.
But 2021 presented a new set of challenges. As quarantines lifted and physicians tried to get back to work, they were forced to deal with reduced staff, continuing COVID stress, and pandemic-related anxieties about family and loved ones.
Medscape’s National Burnout and Depression Report 2022 asked more than 13,000 physicians from 29 specialties to share details about their lives and struggles with burnout and depression in 2021. The results paint a picture of physicians trying to fulfill their mission to care for patients, but struggling to maintain their own well-being amid a global pandemic.
Burnout bump
In 2021’s report, 42% of physicians said they were burned out. In 2022, that number increased to 47%. Perhaps not surprisingly, burnout among emergency physicians took the biggest leap, increasing from 43% to 60%. Critical care (56%), ob.gyn. (53%), and infectious disease and family medicine (both at 51%) rounded out the top five specialties with doctors experiencing burnout in 2021.
Burnout has typically been a greater problem for women than men physicians, and the pandemic hasn’t changed that. “There’s no question that women have reported far more role strain during the pandemic than men,” says Carol A. Bernstein, MD, psychiatrist at Montefiore Health System and professor and vice chair for faculty development and well-being at the Albert Einstein College of Medicine, both in New York. And indeed, 56% of women and 41% of men reported burnout in the 2022 survey.
The causes, however, weren’t especially pandemic related – or at least not directly. As in previous surveys, the major contributing factor to burnout was too much paperwork (60%), such as charting and other bureaucratic tasks. Treating COVID-19 patients was cited as the major source of stress by 10% of respondents. About 34% said too many hours at work was the biggest contributing factor to burnout.
The nature of the beast
What is burnout like for these doctors? One described the conditions that lead to burnout like this: “I barely spend enough time with most patients, just running from one to the next; and then after work, I spend hours documenting, charting, dealing with reports. I feel like an overpaid clerk.” Another said: “Where’s the relationships with patients that used to make this worthwhile?” Others fingered staffing shortages at work or an overwhelming home life: “Staff calls in sick; we’re all running around trying to find things and get things done. It never ends.”
Of those who do experience burnout, the problem reaches beyond the workplace, with 54% saying that their burnout has a strong/severe impact on life and 68% reporting that burnout affects their relationships. One respondent said: “I’m always tired; I have trouble concentrating, no time for the children, more arguments with my hubby.” Another put it this way: “Home is just as busy and chaotic as work. I can never relax.”
It doesn’t help matters that physicians are likely to think they’re the only professionals experiencing job burnout. For example, only 36% of respondents believe teachers experience comparable burnout, yet more than 41% of teachers leave the profession within 5 years of starting – often because of burnout.
When it comes to methods for coping with burnout, exercise is the clear favorite, with 63% of respondents saying exercise helps maintain their mental health. About 41% talk with family members or close friends. However, less healthy coping mechanisms were cited as well, such as isolating themselves from others (45%), sleeping (41%), and eating junk food (35%) or drinking alcohol (24%).
When it comes to trying to alleviate burnout, 29% have tried meditation or similar stress-reduction techniques, while others have reduced their work hours (29%) or changed their work settings (19%).
‘Now I feel like there’s no hope’
About a fifth of physicians (21%) said they suffered from clinical depression, and 64% reported feeling “blue, down, or sad.” One physician characterized their depression this way: “I used to think my life would be great. Now I feel like there’s no hope, this will never get better, I’ll never be happy.”
Of doctors reporting depression, 53% said their illness did not affect their interactions with patients, while 34% said depression caused them to be more easily exasperated by patients.
When asked about seeking help for depression, about half (49%) said they believed they could deal with emotional stress on their own. Unfortunately, fear of medical boards finding out keeps 43% of physicians from reaching out for help, according to the survey.
A version of this article first appeared on Medscape.com.
Things reproductive psychiatrists might ‘always’ or ‘never’ do in 2022
The experience of practicing reproductive psychiatry in the context of the pandemic has highlighted unique situations I’ve written about in previous columns that have affected pregnant and postpartum women during the pandemic, such as the management of anxiety and insomnia.
The pandemic has also seen a shift to telemedicine and an opportunity to use virtual platforms to engage with colleagues in our subspecialty across the country. These forums of engagement, which we realize virtually with so many of our colleagues, has prompted me to refine and galvanize what I consider to be some principles that guide frequently encountered clinical scenarios in reproductive psychiatry.
To open 2022, I wanted to revisit the practices I nearly “always” (or conversely, “never”) follow as a reproductive psychiatrist across the numerous clinical situations and variations on the associated clinical themes encountered as we see patients during pregnancy and the postpartum period.
Things we ‘always’ do
1. I continue to make maternal euthymia the North Star of treatment before, during, and after pregnancy.
Before pregnancy, maternal euthymia may be realized through optimization of pharmacologic and nonpharmacologic treatments and waiting to conceive until patients are emotionally well. Sustaining euthymia during pregnancy is a critical issue because of the extent to which euthymia during pregnancy predicts postpartum course. According to many studies, postpartum euthymia is the strongest predictor of long-term neurobehavioral outcome and risk for later child psychopathology. At the end of the day, there are few things I would not do with respect to treatment of maternal psychiatric disorder if the upside afforded maternal euthymia.
2. I almost always treat with consistency of medication across the peripartum period.
Although there have been discussions about the wisdom of changing medications, such as antidepressants, benzodiazepines, and mood stabilizers, that have afforded euthymia during pregnancy as patients approach their delivery date, the evidence base supporting switching medications at that time is exceedingly sparse. The time to adjust or to modify is typically not just prior to delivery unless it is to prevent postpartum psychiatric disorder (see below).
3. I simplify regimens before pregnancy if it’s unclear which medications have afforded patients euthymia.
We have a growing appreciation that polypharmacy is the rule in treatment of affective disorder for both unipolar and bipolar illness. Consultation before pregnancy is the ideal time to take a particularly careful history and think about simplifying regimens where adding medicines hasn’t clearly provided enhanced clinical benefit to the patient.
4. When making a treatment plan for psychiatric disorder during pregnancy, I consider the impact of untreated psychiatric disorder (even if not absolutely quantifiable) on fetal, neonatal, and maternal well-being.
Perhaps now more than even 5-10 years ago, we have better data describing the adverse effects of untreated psychiatric illness on fetal, neonatal, and maternal well-being.
We always try to deliberately consider the effect of a specific treatment on fetal well-being. Less attention (and science) has focused on the effect on pregnancy of deferring treatment; historically, this has not been adequately quantified in the risk-benefit decision. Yet, there is growing evidence of the increased adverse effects of activating the stress axis on everything from intrauterine fetal programming in the brain to effects on obstetrical outcomes such as preterm labor and delivery.
5. I appreciate the value of postpartum prophylaxis for pregnant women with bipolar disorder to mitigate risk of relapse.
We have spoken over the last 20 months of the pandemic, particularly in reproductive psychiatry circles, about the importance of keeping reproductive-age women with bipolar disorder emotionally well as they plan to conceive, during pregnancy, and in the postpartum period. The management of bipolar disorder during this time can be a humbling experience. Clinical roughening can be quick and severe, and so we do everything that we can for these women.
The area in which we have the strongest evidence base for mitigating risk with bipolar women is the value of postpartum prophylaxis during the peripartum period, regardless of what patients have done with their mood-stabilizing medications during pregnancy. Given the risk for postpartum disease, even though there are varying amounts of evidence on prophylactic benefit of specific mood stabilizers (i.e., lithium vs. atypical antipsychotics), the value of prophylaxis against worsening of bipolar disorder postpartum is widely accepted.
The importance of this has been particularly underscored during the pandemic where postpartum support, although available, has been more tenuous given the fluctuations in COVID-19 status around the country. The availability of friends and loved ones as support during the postpartum period has become less reliable in certain circumstances during the pandemic. In some cases, COVID-19 surges have wreaked havoc on travel plans and support persons have contracted the virus, rendering on-site support nonviable given safety concerns. Last-minute shifts of support plans have been responsible for disruption of care plans for new moms and by extension, have affected the ability to protect the sleep of bipolar women, which is critical. Keeping bipolar women well during the postpartum period with plans and backup plans for management remains critical.
Things we ‘never’ do
1. I never taper antidepressants (just prior to delivery), I never check plasma levels of selective serotonin reuptake inhibitors (across pregnancy, or just prior to labor and delivery), and I never use sodium valproate (during pregnancy).
Although there has been some discussion about the potential to mitigate risk for maternal or neonatal toxicity with lowering of agents such as lithium or lamotrigine during pregnancy, I do not routinely check plasma levels or arbitrarily change the dose of antidepressants, lithium, or lamotrigine during pregnancy in the absence of clinical symptoms.
We know full well that plasma levels of medications decline during pregnancy because of hemodilution with lithium and antidepressants and, in the case of lamotrigine, the effects of rising estrogen concentration during pregnancy on the metabolism of lamotrigine. While several studies have shown the decrease of SSRI concentration during pregnancy absent a change in dose of medication, these data have not correlated changes in plasma concentration of SSRI with a frank change in clinical status across pregnancy. Unlike what we see in conditions like epilepsy, where doses are increased to maintain therapeutic plasma levels to mitigate risk for seizure, those therapeutic plasma levels do not clearly exist for the psychiatric medications most widely used to treat psychiatric disorders.
We also almost never use sodium valproate in reproductive-age women despite its efficacy in both the acute and maintenance treatment of bipolar disorder given the risk of both major malformations associated with first-trimester fetal exposure to valproate and the data suggesting longer-term adverse neurobehavioral effects associated with its use during pregnancy.
2. We never suggest patients defer pregnancy based on their underlying psychiatric disorder.
Our role is to provide the best information regarding reproductive safety of psychiatric medications and risks of untreated psychiatric disorder to patients as they and relevant parties weigh the risks of pursuing one treatment or another. Those are private choices, and women and their partners make private decisions applying their own calculus with respect to moving forward with plans to conceive.
3. We never switch antidepressants once a woman has become pregnant.
Although we continue to see patients switched to older SSRIs such as sertraline with documentation of pregnancy, a patient’s road to getting well is sometimes very lengthy. In the absence of indicting reproductive safety data for any particular antidepressant, for patients who have gotten well on an antidepressant, even one for which we have less information, we stay the course and do not switch arbitrarily to an older SSRI for which we may have more reproductive safety data.
If we have the luxury prior to pregnancy to switch a patient to an untried and better studied antidepressant with more data supporting safety, we do so. But this is rarely the case. More often, we see women presenting with a newly documented pregnancy (frequently unplanned, with half of pregnancies across the country still being unplanned across sociodemographic lines) on an antidepressant with varying amounts of reproductive safety information available for the medicine being taken, and frequently after failed previous trials of other antidepressants. In this scenario, we rarely see the time of a newly documented pregnancy as an opportunity to pursue a new trial of an antidepressant without known efficacy for that patient; we stay the course and hope for sustained euthymia on the drug which has afforded euthymia to date.
Final thoughts
Dos and don’ts are relative in reproductive psychiatry. We tend to apply available data and clinical experience as we guide patients on a case-by-case basis, considering the most currently available rigorous reproductive safety data, as well as the individual patient’s clinical status and her personal wishes.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital (MGH) in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at [email protected].
The experience of practicing reproductive psychiatry in the context of the pandemic has highlighted unique situations I’ve written about in previous columns that have affected pregnant and postpartum women during the pandemic, such as the management of anxiety and insomnia.
The pandemic has also seen a shift to telemedicine and an opportunity to use virtual platforms to engage with colleagues in our subspecialty across the country. These forums of engagement, which we realize virtually with so many of our colleagues, has prompted me to refine and galvanize what I consider to be some principles that guide frequently encountered clinical scenarios in reproductive psychiatry.
To open 2022, I wanted to revisit the practices I nearly “always” (or conversely, “never”) follow as a reproductive psychiatrist across the numerous clinical situations and variations on the associated clinical themes encountered as we see patients during pregnancy and the postpartum period.
Things we ‘always’ do
1. I continue to make maternal euthymia the North Star of treatment before, during, and after pregnancy.
Before pregnancy, maternal euthymia may be realized through optimization of pharmacologic and nonpharmacologic treatments and waiting to conceive until patients are emotionally well. Sustaining euthymia during pregnancy is a critical issue because of the extent to which euthymia during pregnancy predicts postpartum course. According to many studies, postpartum euthymia is the strongest predictor of long-term neurobehavioral outcome and risk for later child psychopathology. At the end of the day, there are few things I would not do with respect to treatment of maternal psychiatric disorder if the upside afforded maternal euthymia.
2. I almost always treat with consistency of medication across the peripartum period.
Although there have been discussions about the wisdom of changing medications, such as antidepressants, benzodiazepines, and mood stabilizers, that have afforded euthymia during pregnancy as patients approach their delivery date, the evidence base supporting switching medications at that time is exceedingly sparse. The time to adjust or to modify is typically not just prior to delivery unless it is to prevent postpartum psychiatric disorder (see below).
3. I simplify regimens before pregnancy if it’s unclear which medications have afforded patients euthymia.
We have a growing appreciation that polypharmacy is the rule in treatment of affective disorder for both unipolar and bipolar illness. Consultation before pregnancy is the ideal time to take a particularly careful history and think about simplifying regimens where adding medicines hasn’t clearly provided enhanced clinical benefit to the patient.
4. When making a treatment plan for psychiatric disorder during pregnancy, I consider the impact of untreated psychiatric disorder (even if not absolutely quantifiable) on fetal, neonatal, and maternal well-being.
Perhaps now more than even 5-10 years ago, we have better data describing the adverse effects of untreated psychiatric illness on fetal, neonatal, and maternal well-being.
We always try to deliberately consider the effect of a specific treatment on fetal well-being. Less attention (and science) has focused on the effect on pregnancy of deferring treatment; historically, this has not been adequately quantified in the risk-benefit decision. Yet, there is growing evidence of the increased adverse effects of activating the stress axis on everything from intrauterine fetal programming in the brain to effects on obstetrical outcomes such as preterm labor and delivery.
5. I appreciate the value of postpartum prophylaxis for pregnant women with bipolar disorder to mitigate risk of relapse.
We have spoken over the last 20 months of the pandemic, particularly in reproductive psychiatry circles, about the importance of keeping reproductive-age women with bipolar disorder emotionally well as they plan to conceive, during pregnancy, and in the postpartum period. The management of bipolar disorder during this time can be a humbling experience. Clinical roughening can be quick and severe, and so we do everything that we can for these women.
The area in which we have the strongest evidence base for mitigating risk with bipolar women is the value of postpartum prophylaxis during the peripartum period, regardless of what patients have done with their mood-stabilizing medications during pregnancy. Given the risk for postpartum disease, even though there are varying amounts of evidence on prophylactic benefit of specific mood stabilizers (i.e., lithium vs. atypical antipsychotics), the value of prophylaxis against worsening of bipolar disorder postpartum is widely accepted.
The importance of this has been particularly underscored during the pandemic where postpartum support, although available, has been more tenuous given the fluctuations in COVID-19 status around the country. The availability of friends and loved ones as support during the postpartum period has become less reliable in certain circumstances during the pandemic. In some cases, COVID-19 surges have wreaked havoc on travel plans and support persons have contracted the virus, rendering on-site support nonviable given safety concerns. Last-minute shifts of support plans have been responsible for disruption of care plans for new moms and by extension, have affected the ability to protect the sleep of bipolar women, which is critical. Keeping bipolar women well during the postpartum period with plans and backup plans for management remains critical.
Things we ‘never’ do
1. I never taper antidepressants (just prior to delivery), I never check plasma levels of selective serotonin reuptake inhibitors (across pregnancy, or just prior to labor and delivery), and I never use sodium valproate (during pregnancy).
Although there has been some discussion about the potential to mitigate risk for maternal or neonatal toxicity with lowering of agents such as lithium or lamotrigine during pregnancy, I do not routinely check plasma levels or arbitrarily change the dose of antidepressants, lithium, or lamotrigine during pregnancy in the absence of clinical symptoms.
We know full well that plasma levels of medications decline during pregnancy because of hemodilution with lithium and antidepressants and, in the case of lamotrigine, the effects of rising estrogen concentration during pregnancy on the metabolism of lamotrigine. While several studies have shown the decrease of SSRI concentration during pregnancy absent a change in dose of medication, these data have not correlated changes in plasma concentration of SSRI with a frank change in clinical status across pregnancy. Unlike what we see in conditions like epilepsy, where doses are increased to maintain therapeutic plasma levels to mitigate risk for seizure, those therapeutic plasma levels do not clearly exist for the psychiatric medications most widely used to treat psychiatric disorders.
We also almost never use sodium valproate in reproductive-age women despite its efficacy in both the acute and maintenance treatment of bipolar disorder given the risk of both major malformations associated with first-trimester fetal exposure to valproate and the data suggesting longer-term adverse neurobehavioral effects associated with its use during pregnancy.
2. We never suggest patients defer pregnancy based on their underlying psychiatric disorder.
Our role is to provide the best information regarding reproductive safety of psychiatric medications and risks of untreated psychiatric disorder to patients as they and relevant parties weigh the risks of pursuing one treatment or another. Those are private choices, and women and their partners make private decisions applying their own calculus with respect to moving forward with plans to conceive.
3. We never switch antidepressants once a woman has become pregnant.
Although we continue to see patients switched to older SSRIs such as sertraline with documentation of pregnancy, a patient’s road to getting well is sometimes very lengthy. In the absence of indicting reproductive safety data for any particular antidepressant, for patients who have gotten well on an antidepressant, even one for which we have less information, we stay the course and do not switch arbitrarily to an older SSRI for which we may have more reproductive safety data.
If we have the luxury prior to pregnancy to switch a patient to an untried and better studied antidepressant with more data supporting safety, we do so. But this is rarely the case. More often, we see women presenting with a newly documented pregnancy (frequently unplanned, with half of pregnancies across the country still being unplanned across sociodemographic lines) on an antidepressant with varying amounts of reproductive safety information available for the medicine being taken, and frequently after failed previous trials of other antidepressants. In this scenario, we rarely see the time of a newly documented pregnancy as an opportunity to pursue a new trial of an antidepressant without known efficacy for that patient; we stay the course and hope for sustained euthymia on the drug which has afforded euthymia to date.
Final thoughts
Dos and don’ts are relative in reproductive psychiatry. We tend to apply available data and clinical experience as we guide patients on a case-by-case basis, considering the most currently available rigorous reproductive safety data, as well as the individual patient’s clinical status and her personal wishes.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital (MGH) in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at [email protected].
The experience of practicing reproductive psychiatry in the context of the pandemic has highlighted unique situations I’ve written about in previous columns that have affected pregnant and postpartum women during the pandemic, such as the management of anxiety and insomnia.
The pandemic has also seen a shift to telemedicine and an opportunity to use virtual platforms to engage with colleagues in our subspecialty across the country. These forums of engagement, which we realize virtually with so many of our colleagues, has prompted me to refine and galvanize what I consider to be some principles that guide frequently encountered clinical scenarios in reproductive psychiatry.
To open 2022, I wanted to revisit the practices I nearly “always” (or conversely, “never”) follow as a reproductive psychiatrist across the numerous clinical situations and variations on the associated clinical themes encountered as we see patients during pregnancy and the postpartum period.
Things we ‘always’ do
1. I continue to make maternal euthymia the North Star of treatment before, during, and after pregnancy.
Before pregnancy, maternal euthymia may be realized through optimization of pharmacologic and nonpharmacologic treatments and waiting to conceive until patients are emotionally well. Sustaining euthymia during pregnancy is a critical issue because of the extent to which euthymia during pregnancy predicts postpartum course. According to many studies, postpartum euthymia is the strongest predictor of long-term neurobehavioral outcome and risk for later child psychopathology. At the end of the day, there are few things I would not do with respect to treatment of maternal psychiatric disorder if the upside afforded maternal euthymia.
2. I almost always treat with consistency of medication across the peripartum period.
Although there have been discussions about the wisdom of changing medications, such as antidepressants, benzodiazepines, and mood stabilizers, that have afforded euthymia during pregnancy as patients approach their delivery date, the evidence base supporting switching medications at that time is exceedingly sparse. The time to adjust or to modify is typically not just prior to delivery unless it is to prevent postpartum psychiatric disorder (see below).
3. I simplify regimens before pregnancy if it’s unclear which medications have afforded patients euthymia.
We have a growing appreciation that polypharmacy is the rule in treatment of affective disorder for both unipolar and bipolar illness. Consultation before pregnancy is the ideal time to take a particularly careful history and think about simplifying regimens where adding medicines hasn’t clearly provided enhanced clinical benefit to the patient.
4. When making a treatment plan for psychiatric disorder during pregnancy, I consider the impact of untreated psychiatric disorder (even if not absolutely quantifiable) on fetal, neonatal, and maternal well-being.
Perhaps now more than even 5-10 years ago, we have better data describing the adverse effects of untreated psychiatric illness on fetal, neonatal, and maternal well-being.
We always try to deliberately consider the effect of a specific treatment on fetal well-being. Less attention (and science) has focused on the effect on pregnancy of deferring treatment; historically, this has not been adequately quantified in the risk-benefit decision. Yet, there is growing evidence of the increased adverse effects of activating the stress axis on everything from intrauterine fetal programming in the brain to effects on obstetrical outcomes such as preterm labor and delivery.
5. I appreciate the value of postpartum prophylaxis for pregnant women with bipolar disorder to mitigate risk of relapse.
We have spoken over the last 20 months of the pandemic, particularly in reproductive psychiatry circles, about the importance of keeping reproductive-age women with bipolar disorder emotionally well as they plan to conceive, during pregnancy, and in the postpartum period. The management of bipolar disorder during this time can be a humbling experience. Clinical roughening can be quick and severe, and so we do everything that we can for these women.
The area in which we have the strongest evidence base for mitigating risk with bipolar women is the value of postpartum prophylaxis during the peripartum period, regardless of what patients have done with their mood-stabilizing medications during pregnancy. Given the risk for postpartum disease, even though there are varying amounts of evidence on prophylactic benefit of specific mood stabilizers (i.e., lithium vs. atypical antipsychotics), the value of prophylaxis against worsening of bipolar disorder postpartum is widely accepted.
The importance of this has been particularly underscored during the pandemic where postpartum support, although available, has been more tenuous given the fluctuations in COVID-19 status around the country. The availability of friends and loved ones as support during the postpartum period has become less reliable in certain circumstances during the pandemic. In some cases, COVID-19 surges have wreaked havoc on travel plans and support persons have contracted the virus, rendering on-site support nonviable given safety concerns. Last-minute shifts of support plans have been responsible for disruption of care plans for new moms and by extension, have affected the ability to protect the sleep of bipolar women, which is critical. Keeping bipolar women well during the postpartum period with plans and backup plans for management remains critical.
Things we ‘never’ do
1. I never taper antidepressants (just prior to delivery), I never check plasma levels of selective serotonin reuptake inhibitors (across pregnancy, or just prior to labor and delivery), and I never use sodium valproate (during pregnancy).
Although there has been some discussion about the potential to mitigate risk for maternal or neonatal toxicity with lowering of agents such as lithium or lamotrigine during pregnancy, I do not routinely check plasma levels or arbitrarily change the dose of antidepressants, lithium, or lamotrigine during pregnancy in the absence of clinical symptoms.
We know full well that plasma levels of medications decline during pregnancy because of hemodilution with lithium and antidepressants and, in the case of lamotrigine, the effects of rising estrogen concentration during pregnancy on the metabolism of lamotrigine. While several studies have shown the decrease of SSRI concentration during pregnancy absent a change in dose of medication, these data have not correlated changes in plasma concentration of SSRI with a frank change in clinical status across pregnancy. Unlike what we see in conditions like epilepsy, where doses are increased to maintain therapeutic plasma levels to mitigate risk for seizure, those therapeutic plasma levels do not clearly exist for the psychiatric medications most widely used to treat psychiatric disorders.
We also almost never use sodium valproate in reproductive-age women despite its efficacy in both the acute and maintenance treatment of bipolar disorder given the risk of both major malformations associated with first-trimester fetal exposure to valproate and the data suggesting longer-term adverse neurobehavioral effects associated with its use during pregnancy.
2. We never suggest patients defer pregnancy based on their underlying psychiatric disorder.
Our role is to provide the best information regarding reproductive safety of psychiatric medications and risks of untreated psychiatric disorder to patients as they and relevant parties weigh the risks of pursuing one treatment or another. Those are private choices, and women and their partners make private decisions applying their own calculus with respect to moving forward with plans to conceive.
3. We never switch antidepressants once a woman has become pregnant.
Although we continue to see patients switched to older SSRIs such as sertraline with documentation of pregnancy, a patient’s road to getting well is sometimes very lengthy. In the absence of indicting reproductive safety data for any particular antidepressant, for patients who have gotten well on an antidepressant, even one for which we have less information, we stay the course and do not switch arbitrarily to an older SSRI for which we may have more reproductive safety data.
If we have the luxury prior to pregnancy to switch a patient to an untried and better studied antidepressant with more data supporting safety, we do so. But this is rarely the case. More often, we see women presenting with a newly documented pregnancy (frequently unplanned, with half of pregnancies across the country still being unplanned across sociodemographic lines) on an antidepressant with varying amounts of reproductive safety information available for the medicine being taken, and frequently after failed previous trials of other antidepressants. In this scenario, we rarely see the time of a newly documented pregnancy as an opportunity to pursue a new trial of an antidepressant without known efficacy for that patient; we stay the course and hope for sustained euthymia on the drug which has afforded euthymia to date.
Final thoughts
Dos and don’ts are relative in reproductive psychiatry. We tend to apply available data and clinical experience as we guide patients on a case-by-case basis, considering the most currently available rigorous reproductive safety data, as well as the individual patient’s clinical status and her personal wishes.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital (MGH) in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at [email protected].
GAP looks back on 75 years of shaping psychiatry
Almost 4 years had passed since Pearl Harbor forced the United States into the Second World War when three military and government services members went to the American Psychiatric Association with a plea: They needed soldiers who could pass the military’s mental and emotional health screening.
The military had rejected or discharged more than 2.5 million servicemen and volunteers on mental health grounds, and frustrated psychiatrists in the service didn’t know where else to turn but to their century-old professional psychiatric organization.
But the APA had grown so large and unwieldy by then that its size, bureaucracy, and singular focus on research left few resources for helping solve an urgent national mental health problem, no matter how worthy it was.
“At the time, the APA was kind of the face of organized psychiatry, but it was organized in a way that did not lend itself to addressing the needs of the military,” said Jack W. Bonner III, MD, professor emeritus of psychiatry at the University of South Carolina, Greenville. “It was considered sort of a stodgy organization that really wasn’t nimble enough to reorganize to look at those needs at that point in time.”
And that, the military psychiatrists decided, would not do. Desperate to solve the problem, they took matters into their own hands.
Nearly 2 years later, 15 psychiatrists, mostly military or ex-military, gathered in the hotel room of the U.S. Army Medical Corps chief of neuropsychiatry the night before the annual APA conference. It was 1946, and America had won the war – but with a huge toll on mental health, both in and out of the military. Aside from veterans’ “shell shock” and the specter of inadequate troops for potential future conflicts, huge social shifts had occurred during the war, and public mental health hospitals and community resources had deteriorated just as demand for psychiatrists and mental health personnel well outstripped supply.
If the APA wasn’t going to tackle these problems head on, the 15 psychiatrists decided, they would force it to, and they enshrined that goal in the name they gave themselves: the Group for the Advancement of Psychiatry. Two days later, three of them challenged incumbent APA officers in elections and won. The infiltration of these “Young Turks,” as they thought of themselves, had begun. From that point forward, GAP members have frequently held APA leadership positions, and APA leaders have often gone on to join GAP. Gradually, the smaller upstart organization nudged the behemoth toward more involvement with social issues, but GAP remains more nimble given its size.
“The APA is a pretty leviathan organization and can’t deal with issues in the same way a smaller organization can, and GAP can fulfill that role of being much more responsive to contemporary issues,” said Dr. Bonner, who is a member of GAP’s planning, marketing, and communications committee.
The think tank of psychiatry
If it seems strange today that such progressivism arose from military medical officers, equally striking is how that nascent group has improbably grown from its modest, pragmatic beginnings into a psychiatry “think tank” today. from mental health care in prisons to use of controversial treatments such as shock therapy, from racial tensions to gender inequality, from medical school curricula to mental institution standards, from LBGTQ rights to climate change.
“We’re not here to do the latest double-blind, placebo-controlled research on things,” said Lawrence S. Gross, MD, president of GAP, professor of clinical psychiatry and the behavioral sciences at the University of Southern California, Los Angeles, and a member of the committee on psychopharmacology. “It’s more for leaders to think about issues in different areas that affect the field of psychiatry and how they interface with society.”
Or, more simply, “GAP is a group that predominantly exists for one major purpose, and that is to add to the body of knowledge in the field,” said Sy Saeed, MD, MS, chair of the department of psychiatry at East Carolina University, Greenville, N.C., and chair of the group’s administration and leadership committee.
And the organization doesn’t shy from controversial topics, either, such as examining direct-to-consumer marketing and when patients should stop antidepressant therapy.
“We’re very good at getting marketed to on when to start medications, but how good are we at actually timing when to cut back on them? How long is long enough to treat?” Dr. Gross asked. The organization continues to have “an undercurrent of recognizing and fostering change and making people aware of things that may be controversial at times but also further the field by looking at these different areas of psychiatry.”
Despite the group’s relatively small size of about 200 members, its impact touches nearly everyone in the profession, whether they realize it or not. And though the group certainly has its weaknesses – such as steep membership fees that may deter some from joining and its need to improve membership diversity – GAP actively seeks ways to address these internal challenges just as it does external ones.
“It’s probably one of the best-kept secrets in psychiatry,” Dr. Gross said. But it’s a secret the members want out. That’s one reason members consider the organization’s crown jewel to be its fellowship program. In fact, Steven S. Sharfstein, MD, MPA, a former GAP president, clinical professor of psychiatry at the University of Maryland, Baltimore, and chair of the planning, marketing, and communications committee, did not formally join GAP until the 1980s. But he first became involved with the group as a resident in the fellowship program in 1969.
In its current incarnation, 12 fellows spend 2 years as working members of GAP, assigned to one of its committees to put in work just like every other member is expected to do, but they reap the wisdom and mentorship of its members at the same time.
One thing that makes GAP so special to its members is the ability “to mentor young psychiatrists, going from generation to generation trying to identify leaders and facilitate their growth,” Dr. Gross said. And that process, through not only the fellowship program but also through the members’ diversity of ages and career stages, sustains the organization’s vigor.
“Its strength is that you create this continuum where senior people get to mentor people who are early in their career, and this way, the knowledge continues,” Dr. Saaed said.
Creation, not death, by committee
In the early years, GAP’s longevity was in question. Once it had successfully steered the APA toward taking more action to address social problems, did it still have a role to play? A majority of members decided that it did. “New problems arose as old ones were solved,” wrote the late Albert Deutsch in an early history of GAP, and “some steps which were confidently expected to repair an ill or defect did not turn out to be completely effective.” In its first decade, GAP members led the APA to establish new medical director and director of information positions, to improve professional standards and facilitate improvement of mental health facilities, and to expand training.
But where GAP really excelled was in developing projects, something the APA wasn’t well-suited to do, explained Carol C. Nadelson, MD, professor of psychiatry at Harvard Medical School, Boston, a member of the gender and mental health committee, and a past president of GAP. And the breadth of those projects has “expanded as the field has changed and evolved,” said Dr. Nadelson, the first woman president of the APA.
Those projects, the beating heart of GAP’s work, come from its specialized working committees, groups of 6-12 members who spend a couple years focused on a single question or problem in psychiatry that the committee has decided needs attention. The number of committees has grown from 9 at its founding to 32 today, shrinking and expanding as society’s needs demand. Each committee looks for an area it thinks is important and needs attention or updating and then decides how to proceed in addressing it. This structure as a confederation of committees differs greatly from other medical organizations.
“Committees really function in an autonomous, almost independent manner,” Dr. Bonner said. “They control their work, what they do, and how they do it, and the executive structure of the organization has very little impact on those individual committees.”
It’s only when a committee produces whatever project it’s working on that it’s disseminated to the rest of the organization for review.
“The fact that it’s such a federated organization is both a strength and a weakness,” said Roberto Lewis-Fernández, MD, professor of clinical psychiatry at Columbia University, New York, and chair of the cultural psychiatry committee. The tension between becoming too siloed within a committee and needing some sense of greater unity and the cross-pollination that provides is always present, but it’s perhaps also part of the organization’s vibrancy as it constantly seeks the right balance.
It also sometimes allows for fruitful collaborations, such as a recent publication produced by both the religion committee and the LGBTQ+ committee on helping LGBTQ+ teenagers and communities of faith, pointed out Jack Drescher, MD, a GAP past president who serves as clinical professor of psychiatry at Columbia University, and a member of the LGBTQ and media committees.
GAP is also unique in expecting every member to actively put in work toward its mission.
“If you join the APA, you can do absolutely nothing, or you can go to a conference once a year and learn from other people, but you don’t have to be active,” said Gail Robinson, MD, professor of psychiatry and ob.gyn. at the University of Toronto and chair of GAP’s gender and mental health committee. But if you’re a GAP member who isn’t contributing, expect to hear from someone asking how they can help you figure out how you can contribute.
Expecting that much work from members means meeting more often than most medical societies. Except during the pandemic, GAP members have always met twice a year for a long weekend in White Plains, N.Y., to focus almost exclusively on the committees’ current projects. Each meeting allows members “to immerse themselves in thinking about topics that the various committees find of interest and think might be of interest to the rest of the world,” said David Adler, MD, a professor of psychiatry and medicine at Tufts Medical Center in Boston, and chair of the GAP publication board. Whereas APA meetings are massive, frenetic events focused primarily on new research and continuing education for tens of thousands of attendees, GAP meetings are more intimidate and meditative, “a time in which the leaders can exchange ideas in a more private setting,” Dr. Adler said.
What makes GAP’s meetings so special is that they provide a temporary refuge with the explicit goal of encouraging unhurried discussion and deliberation about big ideas that matter, Dr. Robinson said.
“One of the enjoyable parts of GAP is that you have time to think,” Dr. Robinson said. “In your regular life, you’re seeing patients, you’re doing research or organizing things, but in GAP, you can sit with a group of like-minded, interested people and toss some ideas around about what’s important right now. What should we be looking at? What is the field not paying enough attention to? And then the ideas bubble up. In a lot of other organizations, you’re doing specific work, some of it political, some in terms of the organization, but to just sort of sit and think about what’s important in your field and what people should know more about is a different kind of feeling.”
A force for change
The work GAP produces has had a substantial impact on the field of psychiatry and society in general over the past 7 and a half decades. Consider this list of just a handful of GAP contributions in its first decade.
- Guidance regarding electroconvulsive therapy in 1947, followed by an update, in response to reaction to the first document, in 1950.
- A guide to school integration after Brown v. Board of Education that considered the psychiatric challenges of integration.
- A report for employers on workers with epilepsy for occupational health and safety.
- Publications that raised mental hospital standards in the 1950s.
- A range of action documents used by medical schools, psychology and social work departments and agencies, governmental bodies, courts, industry, public schools, and community health and welfare agencies.
Over the years, GAP’s influence has sometimes been overt – such as publishing the only diagnostic and statistical manual for child psychiatry for years before that material was incorporated into the official DSM. Sometimes it’s just ahead of the curve, such as the women’s mental health committee publishing a paper that reviewed the evidence on “abortion trauma syndrome” and concluding that it doesn’t exist shortly before the American Psychological Association and the U.K.’s Royal College of Psychiatrists published reviews with similar conclusions. In a few instances, GAP has caused shifts in how the APA operates, such as encouraging the larger organization to publish books on mental health, said Dr. Sharfstein, a past president of the APA.
Much of the organization’s impact occurs through its effects on education, which affects clinical psychiatry at large.“Some reports are very much designed to have an impact on psychiatry education, residency training and curriculum development, which would have a big impact on practice,” Dr. Sharfstein said. An example is the committee on disasters, which examines the best ways for mental health professionals to respond to and mitigate the mental health fallout from the consequences of natural and manmade disasters.
Most often, though, GAP’s influence is akin to strategically planting very carefully cultivated seeds throughout the academic and clinical media ecosystems and letting them bloom how they will. For example, Dr. Lewis-Fernández described a project the cultural committee published in 2013: a checklist for how a psychiatry research article should address topics related to race, ethnicity, and culture. After reviewing articles in the field and their methodologies, the group developed a checklist of best practices and tested them with articles in the field to see how the checklist held up before publishing it.
“Initially, some people read it, some people didn’t, but over time, it’s gotten picked up, and it’s now about to be used in a journal on psychiatric services as a guide to authors and reviews on the appropriate use of these concepts,” Dr. Lewis-Fernández said.
GAP’s influence also blooms through the cross-pollination that occurs at meetings, where leaders in psychiatry from all across the country come together, discuss ideas, and then take new ideas back to their universities, where they teach them to their residents. Perhaps the best example of this influence in recent years has been a increasing shift in teaching about LGBTQ+ issues.
“There’s an underrepresentation of teaching about LGBTQ+ issues in many psychiatric training programs in many medical schools,” Dr. Drescher said. The organization has worked to raise awareness about these gaps in the education of medical students and mental health professionals and then address it, such as designing an online module curriculum in the early 2000s for how to teach residents about LGBTQ+ mental health issues and then updating it as needed.
Perhaps GAP’s greatest lifetime achievement is forcing the field of psychiatry to confront the fact that it – and its patients – do not stand apart from the society in which they exist.
“People aren’t just psychiatric disorders. They live in society, and society has an impact on them, and that affects how people cope,” Dr. Robinson said. That was once a radical concept, but now “psychiatry as a whole has moved to be more broadly expansive” just as GAP itself has broadened its scope, as evidenced by the wide range of committees, more than triple what the organization had at its founding. “GAP was really at the vanguard of that expansion into the recognizing the need to consider the interaction between the individual and the environment they live in socially.”
That’s never been more true than during the COVID-19 pandemic, contributing to perhaps the greatest mental health crisis in the nation’s history since World War II. But the pandemic hasn’t slowed down GAP’s work. In fact, in some ways, the pandemic has facilitated the group’s ability to meet more often virtually and focus on acute issues the pandemic itself has caused. The psychopathology committee published one paper on the impact of telehealth on treating the chronic mentally ill during COVID, and another delved into rethinking where things stand with institutional racism within psychiatry. The women’s mental health committee published articles on the impact of COVID on pregnant and postpartum women, and the impact of COVID on minority women.
Confronting challenges within, too
For all its positive influence, GAP has its weaknesses as well. Two of the biggest barriers to membership, for example, are the steep dues and travel to the twice annual meetings, Dr. Lewis-Fernández said.
The membership dues are not needlessly high: The organization relies on philanthropy and dues for all of its activities, most recently, secured endowments from institutional and individual donors to fund all of the GAP fellows, Dr. Gross said.
“With a low number of members, the cost is larger per member,” Dr. Bonner explained. In fact, GAP has only recently overcome a period of financial uncertainty, now finally on solid ground in terms of fundings.
While the dues can be onerous, Dr. Lewis-Fernández said the organization has been actively thinking about ways to reduce it, particularly for those who may need help if traveling from farther away or younger-career individuals, such as those without tenure or with young families.
It can also be difficult for the organization to attract diverse members from different racial and ethnic groups when leaders in psychiatry from those backgrounds are courted by many other groups, or just to attract younger members in general, but GAP continues to seek ways to overcome those challenges.
“The majority of people in GAP have some kind of academic interest, and the nature of being an early career psychiatrist in academia is that you have to publish to get promoted,” Dr. Bonner said. GAP’s historical practice of producing publications by committee without individual attribution was a disincentive to those early-career folks. “More recently, we’ve changed that so that now individuals can put their names on their product, which has eliminated that particular barriers for young people.”
As the organization continues to seek ways to address those issues, it also faces the same challenges as every other scientific group: Staying relevant in the new, and constantly changing, media landscape.
“It’s an interesting evolution because it started off with books and monographs for many, many years,” Dr. Robinson said, “and then it kind of moved away from that to more articles.” More recently, some committees have returned to writing books while others explore other forms of media to keep up with the times. Long gone are the days when a committee might spend 2-10 years producing one monograph.
“In today’s world, you can’t be relevant operating that way,” said Dr. Bonner, noting that some committees have produced videos or podcasts.
But the sheer amount of information out there is intimidating as well. “Nowadays, a lot of people get their information off the Internet, and how do you actually sift through that?” Dr. Saeed said. “How you find signal in this noise is a whole different thing now, so how GAP produces its information is at that trajectory right now. Should we be producing more electronic books? What should be our peer-review process? How do we make sure the information is current? If we are about sharing information and generating new knowledge, what’s the best way of disseminating that?”
A testament to the organization’s willingness to confront that challenge, however, is its exploration of every possible platform – even those well outside the traditional ones. The climate committee, for example, recently set about addressing climate anxiety in children, but they didn’t produce a report or develop a teaching module or even develop a series of podcasts. Instead, the committee collaborated with Jeremy D. Wortzel, MPhil, an MD and MPH candidate at the University of Pennsylvania, Philadelphia, and Lena K. Champlin, a doctoral candidate in environmental science at Drexel University, Philadelpha, to write a children’s book. “Coco’s Fire: Changing Climate Anxiety into Climate Action” was published in October 2021.
GAP continues to leave its mark
For all the work that members put into the organization, members say they reap substantial benefits as well. Dr. Saaed recalls feeling flattered when invited to join the organization because of how influential it is and the opportunity to work with so many leaders in psychiatry. “When you come to GAP committee meetings, you would run into people whose book or research you might have read and who are very prominent in the field,” he said.
Dr. Drescher credited GAP with helping him develop his voice and polish his editing skills, which later aided him when he became editor of the Journal of Gay and Lesbian Mental Health. When the LGBTQ+ committee shifted from reports to writing op-eds, members learned how to write opinion pieces and then teach members of other committees those skills, resulting in GAP-produced op-eds in consumer and trade publications. And then there are the intangible rewards that leave a profound impact on members.
Some members see GAP as central to their professional lives and perhaps legacies.
“Outside of the medical center, this has probably been the most important professional organization of my career, and I think there are a lot of people who feel that way,” Dr. Adler said. “It’s a very unique experience, and the goal is to examine today’s critical issues and say something about them in a way in which maybe the world will take notice.”
Almost 4 years had passed since Pearl Harbor forced the United States into the Second World War when three military and government services members went to the American Psychiatric Association with a plea: They needed soldiers who could pass the military’s mental and emotional health screening.
The military had rejected or discharged more than 2.5 million servicemen and volunteers on mental health grounds, and frustrated psychiatrists in the service didn’t know where else to turn but to their century-old professional psychiatric organization.
But the APA had grown so large and unwieldy by then that its size, bureaucracy, and singular focus on research left few resources for helping solve an urgent national mental health problem, no matter how worthy it was.
“At the time, the APA was kind of the face of organized psychiatry, but it was organized in a way that did not lend itself to addressing the needs of the military,” said Jack W. Bonner III, MD, professor emeritus of psychiatry at the University of South Carolina, Greenville. “It was considered sort of a stodgy organization that really wasn’t nimble enough to reorganize to look at those needs at that point in time.”
And that, the military psychiatrists decided, would not do. Desperate to solve the problem, they took matters into their own hands.
Nearly 2 years later, 15 psychiatrists, mostly military or ex-military, gathered in the hotel room of the U.S. Army Medical Corps chief of neuropsychiatry the night before the annual APA conference. It was 1946, and America had won the war – but with a huge toll on mental health, both in and out of the military. Aside from veterans’ “shell shock” and the specter of inadequate troops for potential future conflicts, huge social shifts had occurred during the war, and public mental health hospitals and community resources had deteriorated just as demand for psychiatrists and mental health personnel well outstripped supply.
If the APA wasn’t going to tackle these problems head on, the 15 psychiatrists decided, they would force it to, and they enshrined that goal in the name they gave themselves: the Group for the Advancement of Psychiatry. Two days later, three of them challenged incumbent APA officers in elections and won. The infiltration of these “Young Turks,” as they thought of themselves, had begun. From that point forward, GAP members have frequently held APA leadership positions, and APA leaders have often gone on to join GAP. Gradually, the smaller upstart organization nudged the behemoth toward more involvement with social issues, but GAP remains more nimble given its size.
“The APA is a pretty leviathan organization and can’t deal with issues in the same way a smaller organization can, and GAP can fulfill that role of being much more responsive to contemporary issues,” said Dr. Bonner, who is a member of GAP’s planning, marketing, and communications committee.
The think tank of psychiatry
If it seems strange today that such progressivism arose from military medical officers, equally striking is how that nascent group has improbably grown from its modest, pragmatic beginnings into a psychiatry “think tank” today. from mental health care in prisons to use of controversial treatments such as shock therapy, from racial tensions to gender inequality, from medical school curricula to mental institution standards, from LBGTQ rights to climate change.
“We’re not here to do the latest double-blind, placebo-controlled research on things,” said Lawrence S. Gross, MD, president of GAP, professor of clinical psychiatry and the behavioral sciences at the University of Southern California, Los Angeles, and a member of the committee on psychopharmacology. “It’s more for leaders to think about issues in different areas that affect the field of psychiatry and how they interface with society.”
Or, more simply, “GAP is a group that predominantly exists for one major purpose, and that is to add to the body of knowledge in the field,” said Sy Saeed, MD, MS, chair of the department of psychiatry at East Carolina University, Greenville, N.C., and chair of the group’s administration and leadership committee.
And the organization doesn’t shy from controversial topics, either, such as examining direct-to-consumer marketing and when patients should stop antidepressant therapy.
“We’re very good at getting marketed to on when to start medications, but how good are we at actually timing when to cut back on them? How long is long enough to treat?” Dr. Gross asked. The organization continues to have “an undercurrent of recognizing and fostering change and making people aware of things that may be controversial at times but also further the field by looking at these different areas of psychiatry.”
Despite the group’s relatively small size of about 200 members, its impact touches nearly everyone in the profession, whether they realize it or not. And though the group certainly has its weaknesses – such as steep membership fees that may deter some from joining and its need to improve membership diversity – GAP actively seeks ways to address these internal challenges just as it does external ones.
“It’s probably one of the best-kept secrets in psychiatry,” Dr. Gross said. But it’s a secret the members want out. That’s one reason members consider the organization’s crown jewel to be its fellowship program. In fact, Steven S. Sharfstein, MD, MPA, a former GAP president, clinical professor of psychiatry at the University of Maryland, Baltimore, and chair of the planning, marketing, and communications committee, did not formally join GAP until the 1980s. But he first became involved with the group as a resident in the fellowship program in 1969.
In its current incarnation, 12 fellows spend 2 years as working members of GAP, assigned to one of its committees to put in work just like every other member is expected to do, but they reap the wisdom and mentorship of its members at the same time.
One thing that makes GAP so special to its members is the ability “to mentor young psychiatrists, going from generation to generation trying to identify leaders and facilitate their growth,” Dr. Gross said. And that process, through not only the fellowship program but also through the members’ diversity of ages and career stages, sustains the organization’s vigor.
“Its strength is that you create this continuum where senior people get to mentor people who are early in their career, and this way, the knowledge continues,” Dr. Saaed said.
Creation, not death, by committee
In the early years, GAP’s longevity was in question. Once it had successfully steered the APA toward taking more action to address social problems, did it still have a role to play? A majority of members decided that it did. “New problems arose as old ones were solved,” wrote the late Albert Deutsch in an early history of GAP, and “some steps which were confidently expected to repair an ill or defect did not turn out to be completely effective.” In its first decade, GAP members led the APA to establish new medical director and director of information positions, to improve professional standards and facilitate improvement of mental health facilities, and to expand training.
But where GAP really excelled was in developing projects, something the APA wasn’t well-suited to do, explained Carol C. Nadelson, MD, professor of psychiatry at Harvard Medical School, Boston, a member of the gender and mental health committee, and a past president of GAP. And the breadth of those projects has “expanded as the field has changed and evolved,” said Dr. Nadelson, the first woman president of the APA.
Those projects, the beating heart of GAP’s work, come from its specialized working committees, groups of 6-12 members who spend a couple years focused on a single question or problem in psychiatry that the committee has decided needs attention. The number of committees has grown from 9 at its founding to 32 today, shrinking and expanding as society’s needs demand. Each committee looks for an area it thinks is important and needs attention or updating and then decides how to proceed in addressing it. This structure as a confederation of committees differs greatly from other medical organizations.
“Committees really function in an autonomous, almost independent manner,” Dr. Bonner said. “They control their work, what they do, and how they do it, and the executive structure of the organization has very little impact on those individual committees.”
It’s only when a committee produces whatever project it’s working on that it’s disseminated to the rest of the organization for review.
“The fact that it’s such a federated organization is both a strength and a weakness,” said Roberto Lewis-Fernández, MD, professor of clinical psychiatry at Columbia University, New York, and chair of the cultural psychiatry committee. The tension between becoming too siloed within a committee and needing some sense of greater unity and the cross-pollination that provides is always present, but it’s perhaps also part of the organization’s vibrancy as it constantly seeks the right balance.
It also sometimes allows for fruitful collaborations, such as a recent publication produced by both the religion committee and the LGBTQ+ committee on helping LGBTQ+ teenagers and communities of faith, pointed out Jack Drescher, MD, a GAP past president who serves as clinical professor of psychiatry at Columbia University, and a member of the LGBTQ and media committees.
GAP is also unique in expecting every member to actively put in work toward its mission.
“If you join the APA, you can do absolutely nothing, or you can go to a conference once a year and learn from other people, but you don’t have to be active,” said Gail Robinson, MD, professor of psychiatry and ob.gyn. at the University of Toronto and chair of GAP’s gender and mental health committee. But if you’re a GAP member who isn’t contributing, expect to hear from someone asking how they can help you figure out how you can contribute.
Expecting that much work from members means meeting more often than most medical societies. Except during the pandemic, GAP members have always met twice a year for a long weekend in White Plains, N.Y., to focus almost exclusively on the committees’ current projects. Each meeting allows members “to immerse themselves in thinking about topics that the various committees find of interest and think might be of interest to the rest of the world,” said David Adler, MD, a professor of psychiatry and medicine at Tufts Medical Center in Boston, and chair of the GAP publication board. Whereas APA meetings are massive, frenetic events focused primarily on new research and continuing education for tens of thousands of attendees, GAP meetings are more intimidate and meditative, “a time in which the leaders can exchange ideas in a more private setting,” Dr. Adler said.
What makes GAP’s meetings so special is that they provide a temporary refuge with the explicit goal of encouraging unhurried discussion and deliberation about big ideas that matter, Dr. Robinson said.
“One of the enjoyable parts of GAP is that you have time to think,” Dr. Robinson said. “In your regular life, you’re seeing patients, you’re doing research or organizing things, but in GAP, you can sit with a group of like-minded, interested people and toss some ideas around about what’s important right now. What should we be looking at? What is the field not paying enough attention to? And then the ideas bubble up. In a lot of other organizations, you’re doing specific work, some of it political, some in terms of the organization, but to just sort of sit and think about what’s important in your field and what people should know more about is a different kind of feeling.”
A force for change
The work GAP produces has had a substantial impact on the field of psychiatry and society in general over the past 7 and a half decades. Consider this list of just a handful of GAP contributions in its first decade.
- Guidance regarding electroconvulsive therapy in 1947, followed by an update, in response to reaction to the first document, in 1950.
- A guide to school integration after Brown v. Board of Education that considered the psychiatric challenges of integration.
- A report for employers on workers with epilepsy for occupational health and safety.
- Publications that raised mental hospital standards in the 1950s.
- A range of action documents used by medical schools, psychology and social work departments and agencies, governmental bodies, courts, industry, public schools, and community health and welfare agencies.
Over the years, GAP’s influence has sometimes been overt – such as publishing the only diagnostic and statistical manual for child psychiatry for years before that material was incorporated into the official DSM. Sometimes it’s just ahead of the curve, such as the women’s mental health committee publishing a paper that reviewed the evidence on “abortion trauma syndrome” and concluding that it doesn’t exist shortly before the American Psychological Association and the U.K.’s Royal College of Psychiatrists published reviews with similar conclusions. In a few instances, GAP has caused shifts in how the APA operates, such as encouraging the larger organization to publish books on mental health, said Dr. Sharfstein, a past president of the APA.
Much of the organization’s impact occurs through its effects on education, which affects clinical psychiatry at large.“Some reports are very much designed to have an impact on psychiatry education, residency training and curriculum development, which would have a big impact on practice,” Dr. Sharfstein said. An example is the committee on disasters, which examines the best ways for mental health professionals to respond to and mitigate the mental health fallout from the consequences of natural and manmade disasters.
Most often, though, GAP’s influence is akin to strategically planting very carefully cultivated seeds throughout the academic and clinical media ecosystems and letting them bloom how they will. For example, Dr. Lewis-Fernández described a project the cultural committee published in 2013: a checklist for how a psychiatry research article should address topics related to race, ethnicity, and culture. After reviewing articles in the field and their methodologies, the group developed a checklist of best practices and tested them with articles in the field to see how the checklist held up before publishing it.
“Initially, some people read it, some people didn’t, but over time, it’s gotten picked up, and it’s now about to be used in a journal on psychiatric services as a guide to authors and reviews on the appropriate use of these concepts,” Dr. Lewis-Fernández said.
GAP’s influence also blooms through the cross-pollination that occurs at meetings, where leaders in psychiatry from all across the country come together, discuss ideas, and then take new ideas back to their universities, where they teach them to their residents. Perhaps the best example of this influence in recent years has been a increasing shift in teaching about LGBTQ+ issues.
“There’s an underrepresentation of teaching about LGBTQ+ issues in many psychiatric training programs in many medical schools,” Dr. Drescher said. The organization has worked to raise awareness about these gaps in the education of medical students and mental health professionals and then address it, such as designing an online module curriculum in the early 2000s for how to teach residents about LGBTQ+ mental health issues and then updating it as needed.
Perhaps GAP’s greatest lifetime achievement is forcing the field of psychiatry to confront the fact that it – and its patients – do not stand apart from the society in which they exist.
“People aren’t just psychiatric disorders. They live in society, and society has an impact on them, and that affects how people cope,” Dr. Robinson said. That was once a radical concept, but now “psychiatry as a whole has moved to be more broadly expansive” just as GAP itself has broadened its scope, as evidenced by the wide range of committees, more than triple what the organization had at its founding. “GAP was really at the vanguard of that expansion into the recognizing the need to consider the interaction between the individual and the environment they live in socially.”
That’s never been more true than during the COVID-19 pandemic, contributing to perhaps the greatest mental health crisis in the nation’s history since World War II. But the pandemic hasn’t slowed down GAP’s work. In fact, in some ways, the pandemic has facilitated the group’s ability to meet more often virtually and focus on acute issues the pandemic itself has caused. The psychopathology committee published one paper on the impact of telehealth on treating the chronic mentally ill during COVID, and another delved into rethinking where things stand with institutional racism within psychiatry. The women’s mental health committee published articles on the impact of COVID on pregnant and postpartum women, and the impact of COVID on minority women.
Confronting challenges within, too
For all its positive influence, GAP has its weaknesses as well. Two of the biggest barriers to membership, for example, are the steep dues and travel to the twice annual meetings, Dr. Lewis-Fernández said.
The membership dues are not needlessly high: The organization relies on philanthropy and dues for all of its activities, most recently, secured endowments from institutional and individual donors to fund all of the GAP fellows, Dr. Gross said.
“With a low number of members, the cost is larger per member,” Dr. Bonner explained. In fact, GAP has only recently overcome a period of financial uncertainty, now finally on solid ground in terms of fundings.
While the dues can be onerous, Dr. Lewis-Fernández said the organization has been actively thinking about ways to reduce it, particularly for those who may need help if traveling from farther away or younger-career individuals, such as those without tenure or with young families.
It can also be difficult for the organization to attract diverse members from different racial and ethnic groups when leaders in psychiatry from those backgrounds are courted by many other groups, or just to attract younger members in general, but GAP continues to seek ways to overcome those challenges.
“The majority of people in GAP have some kind of academic interest, and the nature of being an early career psychiatrist in academia is that you have to publish to get promoted,” Dr. Bonner said. GAP’s historical practice of producing publications by committee without individual attribution was a disincentive to those early-career folks. “More recently, we’ve changed that so that now individuals can put their names on their product, which has eliminated that particular barriers for young people.”
As the organization continues to seek ways to address those issues, it also faces the same challenges as every other scientific group: Staying relevant in the new, and constantly changing, media landscape.
“It’s an interesting evolution because it started off with books and monographs for many, many years,” Dr. Robinson said, “and then it kind of moved away from that to more articles.” More recently, some committees have returned to writing books while others explore other forms of media to keep up with the times. Long gone are the days when a committee might spend 2-10 years producing one monograph.
“In today’s world, you can’t be relevant operating that way,” said Dr. Bonner, noting that some committees have produced videos or podcasts.
But the sheer amount of information out there is intimidating as well. “Nowadays, a lot of people get their information off the Internet, and how do you actually sift through that?” Dr. Saeed said. “How you find signal in this noise is a whole different thing now, so how GAP produces its information is at that trajectory right now. Should we be producing more electronic books? What should be our peer-review process? How do we make sure the information is current? If we are about sharing information and generating new knowledge, what’s the best way of disseminating that?”
A testament to the organization’s willingness to confront that challenge, however, is its exploration of every possible platform – even those well outside the traditional ones. The climate committee, for example, recently set about addressing climate anxiety in children, but they didn’t produce a report or develop a teaching module or even develop a series of podcasts. Instead, the committee collaborated with Jeremy D. Wortzel, MPhil, an MD and MPH candidate at the University of Pennsylvania, Philadelphia, and Lena K. Champlin, a doctoral candidate in environmental science at Drexel University, Philadelpha, to write a children’s book. “Coco’s Fire: Changing Climate Anxiety into Climate Action” was published in October 2021.
GAP continues to leave its mark
For all the work that members put into the organization, members say they reap substantial benefits as well. Dr. Saaed recalls feeling flattered when invited to join the organization because of how influential it is and the opportunity to work with so many leaders in psychiatry. “When you come to GAP committee meetings, you would run into people whose book or research you might have read and who are very prominent in the field,” he said.
Dr. Drescher credited GAP with helping him develop his voice and polish his editing skills, which later aided him when he became editor of the Journal of Gay and Lesbian Mental Health. When the LGBTQ+ committee shifted from reports to writing op-eds, members learned how to write opinion pieces and then teach members of other committees those skills, resulting in GAP-produced op-eds in consumer and trade publications. And then there are the intangible rewards that leave a profound impact on members.
Some members see GAP as central to their professional lives and perhaps legacies.
“Outside of the medical center, this has probably been the most important professional organization of my career, and I think there are a lot of people who feel that way,” Dr. Adler said. “It’s a very unique experience, and the goal is to examine today’s critical issues and say something about them in a way in which maybe the world will take notice.”
Almost 4 years had passed since Pearl Harbor forced the United States into the Second World War when three military and government services members went to the American Psychiatric Association with a plea: They needed soldiers who could pass the military’s mental and emotional health screening.
The military had rejected or discharged more than 2.5 million servicemen and volunteers on mental health grounds, and frustrated psychiatrists in the service didn’t know where else to turn but to their century-old professional psychiatric organization.
But the APA had grown so large and unwieldy by then that its size, bureaucracy, and singular focus on research left few resources for helping solve an urgent national mental health problem, no matter how worthy it was.
“At the time, the APA was kind of the face of organized psychiatry, but it was organized in a way that did not lend itself to addressing the needs of the military,” said Jack W. Bonner III, MD, professor emeritus of psychiatry at the University of South Carolina, Greenville. “It was considered sort of a stodgy organization that really wasn’t nimble enough to reorganize to look at those needs at that point in time.”
And that, the military psychiatrists decided, would not do. Desperate to solve the problem, they took matters into their own hands.
Nearly 2 years later, 15 psychiatrists, mostly military or ex-military, gathered in the hotel room of the U.S. Army Medical Corps chief of neuropsychiatry the night before the annual APA conference. It was 1946, and America had won the war – but with a huge toll on mental health, both in and out of the military. Aside from veterans’ “shell shock” and the specter of inadequate troops for potential future conflicts, huge social shifts had occurred during the war, and public mental health hospitals and community resources had deteriorated just as demand for psychiatrists and mental health personnel well outstripped supply.
If the APA wasn’t going to tackle these problems head on, the 15 psychiatrists decided, they would force it to, and they enshrined that goal in the name they gave themselves: the Group for the Advancement of Psychiatry. Two days later, three of them challenged incumbent APA officers in elections and won. The infiltration of these “Young Turks,” as they thought of themselves, had begun. From that point forward, GAP members have frequently held APA leadership positions, and APA leaders have often gone on to join GAP. Gradually, the smaller upstart organization nudged the behemoth toward more involvement with social issues, but GAP remains more nimble given its size.
“The APA is a pretty leviathan organization and can’t deal with issues in the same way a smaller organization can, and GAP can fulfill that role of being much more responsive to contemporary issues,” said Dr. Bonner, who is a member of GAP’s planning, marketing, and communications committee.
The think tank of psychiatry
If it seems strange today that such progressivism arose from military medical officers, equally striking is how that nascent group has improbably grown from its modest, pragmatic beginnings into a psychiatry “think tank” today. from mental health care in prisons to use of controversial treatments such as shock therapy, from racial tensions to gender inequality, from medical school curricula to mental institution standards, from LBGTQ rights to climate change.
“We’re not here to do the latest double-blind, placebo-controlled research on things,” said Lawrence S. Gross, MD, president of GAP, professor of clinical psychiatry and the behavioral sciences at the University of Southern California, Los Angeles, and a member of the committee on psychopharmacology. “It’s more for leaders to think about issues in different areas that affect the field of psychiatry and how they interface with society.”
Or, more simply, “GAP is a group that predominantly exists for one major purpose, and that is to add to the body of knowledge in the field,” said Sy Saeed, MD, MS, chair of the department of psychiatry at East Carolina University, Greenville, N.C., and chair of the group’s administration and leadership committee.
And the organization doesn’t shy from controversial topics, either, such as examining direct-to-consumer marketing and when patients should stop antidepressant therapy.
“We’re very good at getting marketed to on when to start medications, but how good are we at actually timing when to cut back on them? How long is long enough to treat?” Dr. Gross asked. The organization continues to have “an undercurrent of recognizing and fostering change and making people aware of things that may be controversial at times but also further the field by looking at these different areas of psychiatry.”
Despite the group’s relatively small size of about 200 members, its impact touches nearly everyone in the profession, whether they realize it or not. And though the group certainly has its weaknesses – such as steep membership fees that may deter some from joining and its need to improve membership diversity – GAP actively seeks ways to address these internal challenges just as it does external ones.
“It’s probably one of the best-kept secrets in psychiatry,” Dr. Gross said. But it’s a secret the members want out. That’s one reason members consider the organization’s crown jewel to be its fellowship program. In fact, Steven S. Sharfstein, MD, MPA, a former GAP president, clinical professor of psychiatry at the University of Maryland, Baltimore, and chair of the planning, marketing, and communications committee, did not formally join GAP until the 1980s. But he first became involved with the group as a resident in the fellowship program in 1969.
In its current incarnation, 12 fellows spend 2 years as working members of GAP, assigned to one of its committees to put in work just like every other member is expected to do, but they reap the wisdom and mentorship of its members at the same time.
One thing that makes GAP so special to its members is the ability “to mentor young psychiatrists, going from generation to generation trying to identify leaders and facilitate their growth,” Dr. Gross said. And that process, through not only the fellowship program but also through the members’ diversity of ages and career stages, sustains the organization’s vigor.
“Its strength is that you create this continuum where senior people get to mentor people who are early in their career, and this way, the knowledge continues,” Dr. Saaed said.
Creation, not death, by committee
In the early years, GAP’s longevity was in question. Once it had successfully steered the APA toward taking more action to address social problems, did it still have a role to play? A majority of members decided that it did. “New problems arose as old ones were solved,” wrote the late Albert Deutsch in an early history of GAP, and “some steps which were confidently expected to repair an ill or defect did not turn out to be completely effective.” In its first decade, GAP members led the APA to establish new medical director and director of information positions, to improve professional standards and facilitate improvement of mental health facilities, and to expand training.
But where GAP really excelled was in developing projects, something the APA wasn’t well-suited to do, explained Carol C. Nadelson, MD, professor of psychiatry at Harvard Medical School, Boston, a member of the gender and mental health committee, and a past president of GAP. And the breadth of those projects has “expanded as the field has changed and evolved,” said Dr. Nadelson, the first woman president of the APA.
Those projects, the beating heart of GAP’s work, come from its specialized working committees, groups of 6-12 members who spend a couple years focused on a single question or problem in psychiatry that the committee has decided needs attention. The number of committees has grown from 9 at its founding to 32 today, shrinking and expanding as society’s needs demand. Each committee looks for an area it thinks is important and needs attention or updating and then decides how to proceed in addressing it. This structure as a confederation of committees differs greatly from other medical organizations.
“Committees really function in an autonomous, almost independent manner,” Dr. Bonner said. “They control their work, what they do, and how they do it, and the executive structure of the organization has very little impact on those individual committees.”
It’s only when a committee produces whatever project it’s working on that it’s disseminated to the rest of the organization for review.
“The fact that it’s such a federated organization is both a strength and a weakness,” said Roberto Lewis-Fernández, MD, professor of clinical psychiatry at Columbia University, New York, and chair of the cultural psychiatry committee. The tension between becoming too siloed within a committee and needing some sense of greater unity and the cross-pollination that provides is always present, but it’s perhaps also part of the organization’s vibrancy as it constantly seeks the right balance.
It also sometimes allows for fruitful collaborations, such as a recent publication produced by both the religion committee and the LGBTQ+ committee on helping LGBTQ+ teenagers and communities of faith, pointed out Jack Drescher, MD, a GAP past president who serves as clinical professor of psychiatry at Columbia University, and a member of the LGBTQ and media committees.
GAP is also unique in expecting every member to actively put in work toward its mission.
“If you join the APA, you can do absolutely nothing, or you can go to a conference once a year and learn from other people, but you don’t have to be active,” said Gail Robinson, MD, professor of psychiatry and ob.gyn. at the University of Toronto and chair of GAP’s gender and mental health committee. But if you’re a GAP member who isn’t contributing, expect to hear from someone asking how they can help you figure out how you can contribute.
Expecting that much work from members means meeting more often than most medical societies. Except during the pandemic, GAP members have always met twice a year for a long weekend in White Plains, N.Y., to focus almost exclusively on the committees’ current projects. Each meeting allows members “to immerse themselves in thinking about topics that the various committees find of interest and think might be of interest to the rest of the world,” said David Adler, MD, a professor of psychiatry and medicine at Tufts Medical Center in Boston, and chair of the GAP publication board. Whereas APA meetings are massive, frenetic events focused primarily on new research and continuing education for tens of thousands of attendees, GAP meetings are more intimidate and meditative, “a time in which the leaders can exchange ideas in a more private setting,” Dr. Adler said.
What makes GAP’s meetings so special is that they provide a temporary refuge with the explicit goal of encouraging unhurried discussion and deliberation about big ideas that matter, Dr. Robinson said.
“One of the enjoyable parts of GAP is that you have time to think,” Dr. Robinson said. “In your regular life, you’re seeing patients, you’re doing research or organizing things, but in GAP, you can sit with a group of like-minded, interested people and toss some ideas around about what’s important right now. What should we be looking at? What is the field not paying enough attention to? And then the ideas bubble up. In a lot of other organizations, you’re doing specific work, some of it political, some in terms of the organization, but to just sort of sit and think about what’s important in your field and what people should know more about is a different kind of feeling.”
A force for change
The work GAP produces has had a substantial impact on the field of psychiatry and society in general over the past 7 and a half decades. Consider this list of just a handful of GAP contributions in its first decade.
- Guidance regarding electroconvulsive therapy in 1947, followed by an update, in response to reaction to the first document, in 1950.
- A guide to school integration after Brown v. Board of Education that considered the psychiatric challenges of integration.
- A report for employers on workers with epilepsy for occupational health and safety.
- Publications that raised mental hospital standards in the 1950s.
- A range of action documents used by medical schools, psychology and social work departments and agencies, governmental bodies, courts, industry, public schools, and community health and welfare agencies.
Over the years, GAP’s influence has sometimes been overt – such as publishing the only diagnostic and statistical manual for child psychiatry for years before that material was incorporated into the official DSM. Sometimes it’s just ahead of the curve, such as the women’s mental health committee publishing a paper that reviewed the evidence on “abortion trauma syndrome” and concluding that it doesn’t exist shortly before the American Psychological Association and the U.K.’s Royal College of Psychiatrists published reviews with similar conclusions. In a few instances, GAP has caused shifts in how the APA operates, such as encouraging the larger organization to publish books on mental health, said Dr. Sharfstein, a past president of the APA.
Much of the organization’s impact occurs through its effects on education, which affects clinical psychiatry at large.“Some reports are very much designed to have an impact on psychiatry education, residency training and curriculum development, which would have a big impact on practice,” Dr. Sharfstein said. An example is the committee on disasters, which examines the best ways for mental health professionals to respond to and mitigate the mental health fallout from the consequences of natural and manmade disasters.
Most often, though, GAP’s influence is akin to strategically planting very carefully cultivated seeds throughout the academic and clinical media ecosystems and letting them bloom how they will. For example, Dr. Lewis-Fernández described a project the cultural committee published in 2013: a checklist for how a psychiatry research article should address topics related to race, ethnicity, and culture. After reviewing articles in the field and their methodologies, the group developed a checklist of best practices and tested them with articles in the field to see how the checklist held up before publishing it.
“Initially, some people read it, some people didn’t, but over time, it’s gotten picked up, and it’s now about to be used in a journal on psychiatric services as a guide to authors and reviews on the appropriate use of these concepts,” Dr. Lewis-Fernández said.
GAP’s influence also blooms through the cross-pollination that occurs at meetings, where leaders in psychiatry from all across the country come together, discuss ideas, and then take new ideas back to their universities, where they teach them to their residents. Perhaps the best example of this influence in recent years has been a increasing shift in teaching about LGBTQ+ issues.
“There’s an underrepresentation of teaching about LGBTQ+ issues in many psychiatric training programs in many medical schools,” Dr. Drescher said. The organization has worked to raise awareness about these gaps in the education of medical students and mental health professionals and then address it, such as designing an online module curriculum in the early 2000s for how to teach residents about LGBTQ+ mental health issues and then updating it as needed.
Perhaps GAP’s greatest lifetime achievement is forcing the field of psychiatry to confront the fact that it – and its patients – do not stand apart from the society in which they exist.
“People aren’t just psychiatric disorders. They live in society, and society has an impact on them, and that affects how people cope,” Dr. Robinson said. That was once a radical concept, but now “psychiatry as a whole has moved to be more broadly expansive” just as GAP itself has broadened its scope, as evidenced by the wide range of committees, more than triple what the organization had at its founding. “GAP was really at the vanguard of that expansion into the recognizing the need to consider the interaction between the individual and the environment they live in socially.”
That’s never been more true than during the COVID-19 pandemic, contributing to perhaps the greatest mental health crisis in the nation’s history since World War II. But the pandemic hasn’t slowed down GAP’s work. In fact, in some ways, the pandemic has facilitated the group’s ability to meet more often virtually and focus on acute issues the pandemic itself has caused. The psychopathology committee published one paper on the impact of telehealth on treating the chronic mentally ill during COVID, and another delved into rethinking where things stand with institutional racism within psychiatry. The women’s mental health committee published articles on the impact of COVID on pregnant and postpartum women, and the impact of COVID on minority women.
Confronting challenges within, too
For all its positive influence, GAP has its weaknesses as well. Two of the biggest barriers to membership, for example, are the steep dues and travel to the twice annual meetings, Dr. Lewis-Fernández said.
The membership dues are not needlessly high: The organization relies on philanthropy and dues for all of its activities, most recently, secured endowments from institutional and individual donors to fund all of the GAP fellows, Dr. Gross said.
“With a low number of members, the cost is larger per member,” Dr. Bonner explained. In fact, GAP has only recently overcome a period of financial uncertainty, now finally on solid ground in terms of fundings.
While the dues can be onerous, Dr. Lewis-Fernández said the organization has been actively thinking about ways to reduce it, particularly for those who may need help if traveling from farther away or younger-career individuals, such as those without tenure or with young families.
It can also be difficult for the organization to attract diverse members from different racial and ethnic groups when leaders in psychiatry from those backgrounds are courted by many other groups, or just to attract younger members in general, but GAP continues to seek ways to overcome those challenges.
“The majority of people in GAP have some kind of academic interest, and the nature of being an early career psychiatrist in academia is that you have to publish to get promoted,” Dr. Bonner said. GAP’s historical practice of producing publications by committee without individual attribution was a disincentive to those early-career folks. “More recently, we’ve changed that so that now individuals can put their names on their product, which has eliminated that particular barriers for young people.”
As the organization continues to seek ways to address those issues, it also faces the same challenges as every other scientific group: Staying relevant in the new, and constantly changing, media landscape.
“It’s an interesting evolution because it started off with books and monographs for many, many years,” Dr. Robinson said, “and then it kind of moved away from that to more articles.” More recently, some committees have returned to writing books while others explore other forms of media to keep up with the times. Long gone are the days when a committee might spend 2-10 years producing one monograph.
“In today’s world, you can’t be relevant operating that way,” said Dr. Bonner, noting that some committees have produced videos or podcasts.
But the sheer amount of information out there is intimidating as well. “Nowadays, a lot of people get their information off the Internet, and how do you actually sift through that?” Dr. Saeed said. “How you find signal in this noise is a whole different thing now, so how GAP produces its information is at that trajectory right now. Should we be producing more electronic books? What should be our peer-review process? How do we make sure the information is current? If we are about sharing information and generating new knowledge, what’s the best way of disseminating that?”
A testament to the organization’s willingness to confront that challenge, however, is its exploration of every possible platform – even those well outside the traditional ones. The climate committee, for example, recently set about addressing climate anxiety in children, but they didn’t produce a report or develop a teaching module or even develop a series of podcasts. Instead, the committee collaborated with Jeremy D. Wortzel, MPhil, an MD and MPH candidate at the University of Pennsylvania, Philadelphia, and Lena K. Champlin, a doctoral candidate in environmental science at Drexel University, Philadelpha, to write a children’s book. “Coco’s Fire: Changing Climate Anxiety into Climate Action” was published in October 2021.
GAP continues to leave its mark
For all the work that members put into the organization, members say they reap substantial benefits as well. Dr. Saaed recalls feeling flattered when invited to join the organization because of how influential it is and the opportunity to work with so many leaders in psychiatry. “When you come to GAP committee meetings, you would run into people whose book or research you might have read and who are very prominent in the field,” he said.
Dr. Drescher credited GAP with helping him develop his voice and polish his editing skills, which later aided him when he became editor of the Journal of Gay and Lesbian Mental Health. When the LGBTQ+ committee shifted from reports to writing op-eds, members learned how to write opinion pieces and then teach members of other committees those skills, resulting in GAP-produced op-eds in consumer and trade publications. And then there are the intangible rewards that leave a profound impact on members.
Some members see GAP as central to their professional lives and perhaps legacies.
“Outside of the medical center, this has probably been the most important professional organization of my career, and I think there are a lot of people who feel that way,” Dr. Adler said. “It’s a very unique experience, and the goal is to examine today’s critical issues and say something about them in a way in which maybe the world will take notice.”
Five things you should know about ‘free’ at-home COVID tests
Americans keep hearing that it is important to test frequently for COVID-19 at home. But just try to find an “at-home” rapid COVID test in a store and at a price that makes frequent tests affordable.
Testing, as well as mask-wearing, is an important measure if the country ever hopes to beat COVID, restore normal routines and get the economy running efficiently. To get Americans cheaper tests, the federal government now plans to have insurance companies pay for them.
You can either get one without any out-of-pocket expense from retail pharmacies that are part of an insurance company’s network or buy it at any store and get reimbursed by the insurer.
Congress said private insurers must cover all COVID testing and any associated medical services when it passed the Families First Coronavirus Response Act and the Coronavirus Aid, Relief and Economic Security, or CARES, Act. The have-insurance-pay-for-it solution has been used frequently through the pandemic. Insurance companies have been told to pay for polymerase chain reaction tests, COVID treatments and the administration of vaccines. (Taxpayers are paying for the cost of the vaccines themselves.) It appears to be an elegant solution for a politician because it looks free and isn’t using taxpayer money.
1. Are the tests really free?
Well, no. As many an economist will tell you, there ain’t no such thing as a free lunch. Someone has to pick up the tab. Initially, the insurance companies bear the cost. Cynthia Cox, a vice president at KFF who studies the Affordable Care Act and private insurers, said the total bill could amount to billions of dollars. Exactly how much depends on “how easy it is to get them, and how many will be reimbursed,” she said.
2. Will the insurance company just swallow those imposed costs?
If companies draw from the time-tested insurance giants’ playbook, they’ll pass along those costs to customers. “This will put upward pressure on premiums,” said Emily Gee, vice president and coordinator for health policy at the Center for American Progress.
Major insurance companies like Cigna, Anthem, UnitedHealthcare, and Aetna did not respond to requests to discuss this issue.
3. If that’s the case, why haven’t I been hit with higher premiums already?
Insurance companies had the chance last year to raise premiums but, mostly, they did not.
Why? Perhaps because insurers have so far made so much money during the pandemic they didn’t need to. For example, the industry’s profits in 2020 increased 41% to $31 billion from $22 billion, according to the National Association of Insurance Commissioners. The NAIC said the industry has continued its “tremendous growth trend” that started before COVID emerged. Companies will be reporting 2021 results soon.
The reason behind these profits is clear. You were paying premiums based on projections your insurance company made about how much health care consumers would use that year. Because people stayed home, had fewer accidents, postponed surgeries and often avoided going to visit the doctor or the hospital, insurers paid out less. They rebated some of their earnings back to customers, but they pocketed a lot more.
As the companies’ actuaries work on predicting 2023 expenditures, premiums could go up if they foresee more claims and expenses. Paying for millions of rapid tests is something they would include in their calculations.
4. Regardless of my premiums, will the tests cost me money directly?
It’s quite possible. If your insurance company doesn’t have an arrangement with a retailer where you can simply pick up your allotted tests, you’ll have to pay for them – at whatever price the store sets. If that’s the case, you’ll need to fill out a form to request a reimbursement from the insurance company. How many times have you lost receipts or just plain neglected to mail in for rebates on something you bought? A lot, right?
Here’s another thing: The reimbursement is set at $12 per test. If you pay $30 for a test – and that is not unheard of – your insurer is only on the hook for $12. You eat the $18.
And by the way, people on Medicare will have to pay for their tests themselves. People who get their health care covered by Medicaid can obtain free test kits at community centers.
A few free tests are supposed to arrive at every American home via the U.S. Postal Service. And the Biden administration has activated a website where Americans can order free tests from a cache of a billion the federal government ordered.
5. Will this help bring down the costs of at-home tests and make them easier to find?
The free COVID tests are unlikely to have much immediate impact on general cost and availability. You will still need to search for them. The federal measures likely will stimulate the demand for tests, which in the short term may make them harder to find.
But the demand, and some government guarantees to manufacturers, may induce test makers to make more of them faster. The increased competition and supply theoretically could bring down the price. There is certainly room for prices to decline since the wholesale cost of the test is between $5 and $7, analysts estimate. “It’s a big step in the right direction,” Ms. Gee said.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Americans keep hearing that it is important to test frequently for COVID-19 at home. But just try to find an “at-home” rapid COVID test in a store and at a price that makes frequent tests affordable.
Testing, as well as mask-wearing, is an important measure if the country ever hopes to beat COVID, restore normal routines and get the economy running efficiently. To get Americans cheaper tests, the federal government now plans to have insurance companies pay for them.
You can either get one without any out-of-pocket expense from retail pharmacies that are part of an insurance company’s network or buy it at any store and get reimbursed by the insurer.
Congress said private insurers must cover all COVID testing and any associated medical services when it passed the Families First Coronavirus Response Act and the Coronavirus Aid, Relief and Economic Security, or CARES, Act. The have-insurance-pay-for-it solution has been used frequently through the pandemic. Insurance companies have been told to pay for polymerase chain reaction tests, COVID treatments and the administration of vaccines. (Taxpayers are paying for the cost of the vaccines themselves.) It appears to be an elegant solution for a politician because it looks free and isn’t using taxpayer money.
1. Are the tests really free?
Well, no. As many an economist will tell you, there ain’t no such thing as a free lunch. Someone has to pick up the tab. Initially, the insurance companies bear the cost. Cynthia Cox, a vice president at KFF who studies the Affordable Care Act and private insurers, said the total bill could amount to billions of dollars. Exactly how much depends on “how easy it is to get them, and how many will be reimbursed,” she said.
2. Will the insurance company just swallow those imposed costs?
If companies draw from the time-tested insurance giants’ playbook, they’ll pass along those costs to customers. “This will put upward pressure on premiums,” said Emily Gee, vice president and coordinator for health policy at the Center for American Progress.
Major insurance companies like Cigna, Anthem, UnitedHealthcare, and Aetna did not respond to requests to discuss this issue.
3. If that’s the case, why haven’t I been hit with higher premiums already?
Insurance companies had the chance last year to raise premiums but, mostly, they did not.
Why? Perhaps because insurers have so far made so much money during the pandemic they didn’t need to. For example, the industry’s profits in 2020 increased 41% to $31 billion from $22 billion, according to the National Association of Insurance Commissioners. The NAIC said the industry has continued its “tremendous growth trend” that started before COVID emerged. Companies will be reporting 2021 results soon.
The reason behind these profits is clear. You were paying premiums based on projections your insurance company made about how much health care consumers would use that year. Because people stayed home, had fewer accidents, postponed surgeries and often avoided going to visit the doctor or the hospital, insurers paid out less. They rebated some of their earnings back to customers, but they pocketed a lot more.
As the companies’ actuaries work on predicting 2023 expenditures, premiums could go up if they foresee more claims and expenses. Paying for millions of rapid tests is something they would include in their calculations.
4. Regardless of my premiums, will the tests cost me money directly?
It’s quite possible. If your insurance company doesn’t have an arrangement with a retailer where you can simply pick up your allotted tests, you’ll have to pay for them – at whatever price the store sets. If that’s the case, you’ll need to fill out a form to request a reimbursement from the insurance company. How many times have you lost receipts or just plain neglected to mail in for rebates on something you bought? A lot, right?
Here’s another thing: The reimbursement is set at $12 per test. If you pay $30 for a test – and that is not unheard of – your insurer is only on the hook for $12. You eat the $18.
And by the way, people on Medicare will have to pay for their tests themselves. People who get their health care covered by Medicaid can obtain free test kits at community centers.
A few free tests are supposed to arrive at every American home via the U.S. Postal Service. And the Biden administration has activated a website where Americans can order free tests from a cache of a billion the federal government ordered.
5. Will this help bring down the costs of at-home tests and make them easier to find?
The free COVID tests are unlikely to have much immediate impact on general cost and availability. You will still need to search for them. The federal measures likely will stimulate the demand for tests, which in the short term may make them harder to find.
But the demand, and some government guarantees to manufacturers, may induce test makers to make more of them faster. The increased competition and supply theoretically could bring down the price. There is certainly room for prices to decline since the wholesale cost of the test is between $5 and $7, analysts estimate. “It’s a big step in the right direction,” Ms. Gee said.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Americans keep hearing that it is important to test frequently for COVID-19 at home. But just try to find an “at-home” rapid COVID test in a store and at a price that makes frequent tests affordable.
Testing, as well as mask-wearing, is an important measure if the country ever hopes to beat COVID, restore normal routines and get the economy running efficiently. To get Americans cheaper tests, the federal government now plans to have insurance companies pay for them.
You can either get one without any out-of-pocket expense from retail pharmacies that are part of an insurance company’s network or buy it at any store and get reimbursed by the insurer.
Congress said private insurers must cover all COVID testing and any associated medical services when it passed the Families First Coronavirus Response Act and the Coronavirus Aid, Relief and Economic Security, or CARES, Act. The have-insurance-pay-for-it solution has been used frequently through the pandemic. Insurance companies have been told to pay for polymerase chain reaction tests, COVID treatments and the administration of vaccines. (Taxpayers are paying for the cost of the vaccines themselves.) It appears to be an elegant solution for a politician because it looks free and isn’t using taxpayer money.
1. Are the tests really free?
Well, no. As many an economist will tell you, there ain’t no such thing as a free lunch. Someone has to pick up the tab. Initially, the insurance companies bear the cost. Cynthia Cox, a vice president at KFF who studies the Affordable Care Act and private insurers, said the total bill could amount to billions of dollars. Exactly how much depends on “how easy it is to get them, and how many will be reimbursed,” she said.
2. Will the insurance company just swallow those imposed costs?
If companies draw from the time-tested insurance giants’ playbook, they’ll pass along those costs to customers. “This will put upward pressure on premiums,” said Emily Gee, vice president and coordinator for health policy at the Center for American Progress.
Major insurance companies like Cigna, Anthem, UnitedHealthcare, and Aetna did not respond to requests to discuss this issue.
3. If that’s the case, why haven’t I been hit with higher premiums already?
Insurance companies had the chance last year to raise premiums but, mostly, they did not.
Why? Perhaps because insurers have so far made so much money during the pandemic they didn’t need to. For example, the industry’s profits in 2020 increased 41% to $31 billion from $22 billion, according to the National Association of Insurance Commissioners. The NAIC said the industry has continued its “tremendous growth trend” that started before COVID emerged. Companies will be reporting 2021 results soon.
The reason behind these profits is clear. You were paying premiums based on projections your insurance company made about how much health care consumers would use that year. Because people stayed home, had fewer accidents, postponed surgeries and often avoided going to visit the doctor or the hospital, insurers paid out less. They rebated some of their earnings back to customers, but they pocketed a lot more.
As the companies’ actuaries work on predicting 2023 expenditures, premiums could go up if they foresee more claims and expenses. Paying for millions of rapid tests is something they would include in their calculations.
4. Regardless of my premiums, will the tests cost me money directly?
It’s quite possible. If your insurance company doesn’t have an arrangement with a retailer where you can simply pick up your allotted tests, you’ll have to pay for them – at whatever price the store sets. If that’s the case, you’ll need to fill out a form to request a reimbursement from the insurance company. How many times have you lost receipts or just plain neglected to mail in for rebates on something you bought? A lot, right?
Here’s another thing: The reimbursement is set at $12 per test. If you pay $30 for a test – and that is not unheard of – your insurer is only on the hook for $12. You eat the $18.
And by the way, people on Medicare will have to pay for their tests themselves. People who get their health care covered by Medicaid can obtain free test kits at community centers.
A few free tests are supposed to arrive at every American home via the U.S. Postal Service. And the Biden administration has activated a website where Americans can order free tests from a cache of a billion the federal government ordered.
5. Will this help bring down the costs of at-home tests and make them easier to find?
The free COVID tests are unlikely to have much immediate impact on general cost and availability. You will still need to search for them. The federal measures likely will stimulate the demand for tests, which in the short term may make them harder to find.
But the demand, and some government guarantees to manufacturers, may induce test makers to make more of them faster. The increased competition and supply theoretically could bring down the price. There is certainly room for prices to decline since the wholesale cost of the test is between $5 and $7, analysts estimate. “It’s a big step in the right direction,” Ms. Gee said.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Siblings of people with bipolar disorder have higher cancer risk
, according to new research from Taiwan.
“To our knowledge, our study is the first to report an increased overall cancer risk as well as increased risks of breast and ectodermal cancer among the unaffected siblings aged < 50 years of patients with bipolar disorder,” Ya-Mei Bai, MD, PhD, of National Yang-Ming University, Taipei, Taiwan, and colleagues write in an article published online in the International Journal of Cancer.
Most, but not all, previous studies have shown a link between bipolar disorder and cancer. Whether the elevated risk of malignancy extends to family members without the mental health condition has not been elucidated.
To investigate, the researchers turned to the National Health Insurance Research Database of Taiwan. They identified 25,356 individuals diagnosed with bipolar disorder by a psychiatrist between 1996 and 2010 and the same number of unaffected siblings, as well as more than 100,000 age-, sex-, income-, and residence-matched controls without severe mental illness.
Compared with the control group, people with bipolar disorder (odds ratio, 1.22) and their unaffected siblings (OR, 1.17) both had a higher risk of developing malignant cancer of any kind. The researchers also found that both groups were at higher risk for breast cancer, with odds ratios of 1.98 in individuals with bipolar disorder and 1.73 in their unaffected siblings.
However, the risk of skin cancer was only high in people with bipolar disorder (OR, 2.70) and not in their siblings (OR, 0.62). And conversely, the risk of kidney cancer was significantly increased in unaffected siblings (OR, 2.45) but not in people with bipolar disorder (OR, 0.47).
When stratified by the embryonic developmental layer from which tumors had originated – ectodermal, mesodermal, or endodermal – the authors observed a significantly increased risk for only ectodermal cancers. In addition, only people under age 50 in both groups (OR, 1.90 for those with bipolar disorder; OR, 1.65 for siblings) were more likely to develop an ectodermal cancer, especially of the breast, compared with the control group. The risks remained elevated after excluding breast cancer but were no longer significant.
When stratified by age, the risk of developing any cancer in both groups also only appeared to be greater for those under age 50 (OR, 1.34 in people with bipolar disorder; OR, 1.32 in siblings) compared with those aged 50 and over (OR, 0.97 and 0.99, respectively). The authors highlighted these figures in the supplemental data set but did not discuss it further in the study beyond a brief mention that “younger patients with bipolar disorder and younger unaffected siblings (< 50 years), but not older ones (≥ 50 years), were more likely to develop any malignancy during the follow-up than matched controls.”
“This paper essentially finds what we have found in our previous work – that people with bipolar disorder have a greater risk of cancer,” said Michael Berk, MBBCh, PhD, a professor of psychiatry at the Deakin University School of Medicine in Geelong, Australia, who published a systematic review and meta-analysis last spring on cancer risk and the role of lithium treatment in bipolar disorder.
“The interesting finding in our work,” Dr. Berk told this news organization, “is that this risk is attenuated by use of lithium but not other agents.”
The Taiwanese researchers propose a “biopsychosocial explanation” for their results, noting that both the nervous system and the breast and skin develop from the ectoderm, and that cancer risk factors such as smoking and obesity are more common in people with bipolar disorder and their unaffected siblings.
“The findings,” they write, “imply a genetic overlap in neurodevelopment and malignancy pathogenesis and may encourage clinicians to closely monitor patients with bipolar disorder and their unaffected siblings for cancer warning signs.”
The authors, however, caution that their study needs validation and had several limitations, including lack of adjustment for drug treatment and lifestyle and environmental factors.
“Our findings may persuade clinicians and researchers to reevaluate the cancer risk among the unaffected siblings of patients with schizophrenia and bipolar disorder because these two severe mental disorders may have a common biopsychosocial pathophysiology,” the team writes.
The study was supported by a grant from Taipei Veterans General Hospital, Yen Tjing Ling Medical Foundation, and the Ministry of Science and Technology, Taiwan.
A version of this article first appeared on Medscape.com.
, according to new research from Taiwan.
“To our knowledge, our study is the first to report an increased overall cancer risk as well as increased risks of breast and ectodermal cancer among the unaffected siblings aged < 50 years of patients with bipolar disorder,” Ya-Mei Bai, MD, PhD, of National Yang-Ming University, Taipei, Taiwan, and colleagues write in an article published online in the International Journal of Cancer.
Most, but not all, previous studies have shown a link between bipolar disorder and cancer. Whether the elevated risk of malignancy extends to family members without the mental health condition has not been elucidated.
To investigate, the researchers turned to the National Health Insurance Research Database of Taiwan. They identified 25,356 individuals diagnosed with bipolar disorder by a psychiatrist between 1996 and 2010 and the same number of unaffected siblings, as well as more than 100,000 age-, sex-, income-, and residence-matched controls without severe mental illness.
Compared with the control group, people with bipolar disorder (odds ratio, 1.22) and their unaffected siblings (OR, 1.17) both had a higher risk of developing malignant cancer of any kind. The researchers also found that both groups were at higher risk for breast cancer, with odds ratios of 1.98 in individuals with bipolar disorder and 1.73 in their unaffected siblings.
However, the risk of skin cancer was only high in people with bipolar disorder (OR, 2.70) and not in their siblings (OR, 0.62). And conversely, the risk of kidney cancer was significantly increased in unaffected siblings (OR, 2.45) but not in people with bipolar disorder (OR, 0.47).
When stratified by the embryonic developmental layer from which tumors had originated – ectodermal, mesodermal, or endodermal – the authors observed a significantly increased risk for only ectodermal cancers. In addition, only people under age 50 in both groups (OR, 1.90 for those with bipolar disorder; OR, 1.65 for siblings) were more likely to develop an ectodermal cancer, especially of the breast, compared with the control group. The risks remained elevated after excluding breast cancer but were no longer significant.
When stratified by age, the risk of developing any cancer in both groups also only appeared to be greater for those under age 50 (OR, 1.34 in people with bipolar disorder; OR, 1.32 in siblings) compared with those aged 50 and over (OR, 0.97 and 0.99, respectively). The authors highlighted these figures in the supplemental data set but did not discuss it further in the study beyond a brief mention that “younger patients with bipolar disorder and younger unaffected siblings (< 50 years), but not older ones (≥ 50 years), were more likely to develop any malignancy during the follow-up than matched controls.”
“This paper essentially finds what we have found in our previous work – that people with bipolar disorder have a greater risk of cancer,” said Michael Berk, MBBCh, PhD, a professor of psychiatry at the Deakin University School of Medicine in Geelong, Australia, who published a systematic review and meta-analysis last spring on cancer risk and the role of lithium treatment in bipolar disorder.
“The interesting finding in our work,” Dr. Berk told this news organization, “is that this risk is attenuated by use of lithium but not other agents.”
The Taiwanese researchers propose a “biopsychosocial explanation” for their results, noting that both the nervous system and the breast and skin develop from the ectoderm, and that cancer risk factors such as smoking and obesity are more common in people with bipolar disorder and their unaffected siblings.
“The findings,” they write, “imply a genetic overlap in neurodevelopment and malignancy pathogenesis and may encourage clinicians to closely monitor patients with bipolar disorder and their unaffected siblings for cancer warning signs.”
The authors, however, caution that their study needs validation and had several limitations, including lack of adjustment for drug treatment and lifestyle and environmental factors.
“Our findings may persuade clinicians and researchers to reevaluate the cancer risk among the unaffected siblings of patients with schizophrenia and bipolar disorder because these two severe mental disorders may have a common biopsychosocial pathophysiology,” the team writes.
The study was supported by a grant from Taipei Veterans General Hospital, Yen Tjing Ling Medical Foundation, and the Ministry of Science and Technology, Taiwan.
A version of this article first appeared on Medscape.com.
, according to new research from Taiwan.
“To our knowledge, our study is the first to report an increased overall cancer risk as well as increased risks of breast and ectodermal cancer among the unaffected siblings aged < 50 years of patients with bipolar disorder,” Ya-Mei Bai, MD, PhD, of National Yang-Ming University, Taipei, Taiwan, and colleagues write in an article published online in the International Journal of Cancer.
Most, but not all, previous studies have shown a link between bipolar disorder and cancer. Whether the elevated risk of malignancy extends to family members without the mental health condition has not been elucidated.
To investigate, the researchers turned to the National Health Insurance Research Database of Taiwan. They identified 25,356 individuals diagnosed with bipolar disorder by a psychiatrist between 1996 and 2010 and the same number of unaffected siblings, as well as more than 100,000 age-, sex-, income-, and residence-matched controls without severe mental illness.
Compared with the control group, people with bipolar disorder (odds ratio, 1.22) and their unaffected siblings (OR, 1.17) both had a higher risk of developing malignant cancer of any kind. The researchers also found that both groups were at higher risk for breast cancer, with odds ratios of 1.98 in individuals with bipolar disorder and 1.73 in their unaffected siblings.
However, the risk of skin cancer was only high in people with bipolar disorder (OR, 2.70) and not in their siblings (OR, 0.62). And conversely, the risk of kidney cancer was significantly increased in unaffected siblings (OR, 2.45) but not in people with bipolar disorder (OR, 0.47).
When stratified by the embryonic developmental layer from which tumors had originated – ectodermal, mesodermal, or endodermal – the authors observed a significantly increased risk for only ectodermal cancers. In addition, only people under age 50 in both groups (OR, 1.90 for those with bipolar disorder; OR, 1.65 for siblings) were more likely to develop an ectodermal cancer, especially of the breast, compared with the control group. The risks remained elevated after excluding breast cancer but were no longer significant.
When stratified by age, the risk of developing any cancer in both groups also only appeared to be greater for those under age 50 (OR, 1.34 in people with bipolar disorder; OR, 1.32 in siblings) compared with those aged 50 and over (OR, 0.97 and 0.99, respectively). The authors highlighted these figures in the supplemental data set but did not discuss it further in the study beyond a brief mention that “younger patients with bipolar disorder and younger unaffected siblings (< 50 years), but not older ones (≥ 50 years), were more likely to develop any malignancy during the follow-up than matched controls.”
“This paper essentially finds what we have found in our previous work – that people with bipolar disorder have a greater risk of cancer,” said Michael Berk, MBBCh, PhD, a professor of psychiatry at the Deakin University School of Medicine in Geelong, Australia, who published a systematic review and meta-analysis last spring on cancer risk and the role of lithium treatment in bipolar disorder.
“The interesting finding in our work,” Dr. Berk told this news organization, “is that this risk is attenuated by use of lithium but not other agents.”
The Taiwanese researchers propose a “biopsychosocial explanation” for their results, noting that both the nervous system and the breast and skin develop from the ectoderm, and that cancer risk factors such as smoking and obesity are more common in people with bipolar disorder and their unaffected siblings.
“The findings,” they write, “imply a genetic overlap in neurodevelopment and malignancy pathogenesis and may encourage clinicians to closely monitor patients with bipolar disorder and their unaffected siblings for cancer warning signs.”
The authors, however, caution that their study needs validation and had several limitations, including lack of adjustment for drug treatment and lifestyle and environmental factors.
“Our findings may persuade clinicians and researchers to reevaluate the cancer risk among the unaffected siblings of patients with schizophrenia and bipolar disorder because these two severe mental disorders may have a common biopsychosocial pathophysiology,” the team writes.
The study was supported by a grant from Taipei Veterans General Hospital, Yen Tjing Ling Medical Foundation, and the Ministry of Science and Technology, Taiwan.
A version of this article first appeared on Medscape.com.
FROM INTERNATIONAL JOURNAL OF CANCER
Novel biomarker found for Alzheimer’s disease
The study covered in this summary was published in medRxiv.org as a preprint and has not yet been peer reviewed.
Key takeaways
- Estimated beta-amyloid (Aβ42) cellular uptake can be more than two times greater in AD patients compared to cognitively normal subjects. A less pronounced yet increased uptake rate was also observed in patients with late-onset mild cognitive impairment (MCI). This increased uptake may prove to be a key mechanism defining age-related AD progression.
- The increased cellular amyloid uptake in AD and LMCI may lead to quicker disease progression, but early-onset MCI may result from increased production of toxic amyloid metabolites.
Why this matters
- Additional biomarkers for AD could greatly aid diagnosis and course prediction, as they are currently limited to PET scan analysis of amyloid plaque deposits and concentration of Aβ42 in cerebrospinal fluid (CSF).
- Amyloid deposits found by PET have a positive correlation with AD diagnosis. In contrast, CSF-Aβ42 and AD diagnosis or cognitive decline are negatively correlated. Normal cognition (NC) is associated with higher CSF beta-amyloid levels, but previous research has not explained why CSF-Aβ42 levels can be equivalent in patients with NC but high amyloid load and patients with AD and low amyloid load.
Study design
- The authors of this retrospective study used anonymized data obtained from the Alzheimer’s’s Disease Neuroimaging Initiative (ADNI). ADNI’s goal has been to test whether serial MRI scans, PET scans, biomarkers, and clinical/neuropsychological assessment can be combined to measure the progression of MCI and AD.
- Study subjects had either an AD diagnosis or NC and were divided into two groups: low amyloid load and high amyloid load. The fraction of patients with an AD diagnosis was calculated as a function of CSF-Aβ42.
- Calculations and statistical comparisons were performed using Microsoft Excel and custom-written C++ programs.
Key results
- The lowest levels of CSF-Aβ42 correlated with the highest percentage of AD-diagnosed patients, estimated to be 27% in subjects with low amyloid deposit density and 65% in those with high deposit density.
- The relationship between CSF-Aβ42 levels and amyloid load can be described using a simple mathematical model: Amyloid concentration in the interstitial cells is equal to the synthesis rate divided by the density of amyloid deposits plus the sum of the rate of amyloid removal through the CSF and the cellular amyloid uptake rate.
- AD and late-onset MCI patients had a significantly higher amyloid removal rate compared to NC subjects.
- Early-onset MCI patients had Aβ42 turnover similar to that of NC subjects, pointing to a different underlying mechanism such as enzymatic disbalance.
Limitations
- The model used to explain amyloid exchange between the interstitial space and the CSF is oversimplified; the actual process is more complex.
- Synthesis and uptake rates of Aβ42 vary throughout areas of the brain. The model assumes a homogeneous distribution within the interstitial compartment.
Study disclosures
- Research reported in this publication was not supported by any external funding. Data collection and sharing for this project were funded by ADNI.
A version of this article first appeared on Medscape.com.
The study covered in this summary was published in medRxiv.org as a preprint and has not yet been peer reviewed.
Key takeaways
- Estimated beta-amyloid (Aβ42) cellular uptake can be more than two times greater in AD patients compared to cognitively normal subjects. A less pronounced yet increased uptake rate was also observed in patients with late-onset mild cognitive impairment (MCI). This increased uptake may prove to be a key mechanism defining age-related AD progression.
- The increased cellular amyloid uptake in AD and LMCI may lead to quicker disease progression, but early-onset MCI may result from increased production of toxic amyloid metabolites.
Why this matters
- Additional biomarkers for AD could greatly aid diagnosis and course prediction, as they are currently limited to PET scan analysis of amyloid plaque deposits and concentration of Aβ42 in cerebrospinal fluid (CSF).
- Amyloid deposits found by PET have a positive correlation with AD diagnosis. In contrast, CSF-Aβ42 and AD diagnosis or cognitive decline are negatively correlated. Normal cognition (NC) is associated with higher CSF beta-amyloid levels, but previous research has not explained why CSF-Aβ42 levels can be equivalent in patients with NC but high amyloid load and patients with AD and low amyloid load.
Study design
- The authors of this retrospective study used anonymized data obtained from the Alzheimer’s’s Disease Neuroimaging Initiative (ADNI). ADNI’s goal has been to test whether serial MRI scans, PET scans, biomarkers, and clinical/neuropsychological assessment can be combined to measure the progression of MCI and AD.
- Study subjects had either an AD diagnosis or NC and were divided into two groups: low amyloid load and high amyloid load. The fraction of patients with an AD diagnosis was calculated as a function of CSF-Aβ42.
- Calculations and statistical comparisons were performed using Microsoft Excel and custom-written C++ programs.
Key results
- The lowest levels of CSF-Aβ42 correlated with the highest percentage of AD-diagnosed patients, estimated to be 27% in subjects with low amyloid deposit density and 65% in those with high deposit density.
- The relationship between CSF-Aβ42 levels and amyloid load can be described using a simple mathematical model: Amyloid concentration in the interstitial cells is equal to the synthesis rate divided by the density of amyloid deposits plus the sum of the rate of amyloid removal through the CSF and the cellular amyloid uptake rate.
- AD and late-onset MCI patients had a significantly higher amyloid removal rate compared to NC subjects.
- Early-onset MCI patients had Aβ42 turnover similar to that of NC subjects, pointing to a different underlying mechanism such as enzymatic disbalance.
Limitations
- The model used to explain amyloid exchange between the interstitial space and the CSF is oversimplified; the actual process is more complex.
- Synthesis and uptake rates of Aβ42 vary throughout areas of the brain. The model assumes a homogeneous distribution within the interstitial compartment.
Study disclosures
- Research reported in this publication was not supported by any external funding. Data collection and sharing for this project were funded by ADNI.
A version of this article first appeared on Medscape.com.
The study covered in this summary was published in medRxiv.org as a preprint and has not yet been peer reviewed.
Key takeaways
- Estimated beta-amyloid (Aβ42) cellular uptake can be more than two times greater in AD patients compared to cognitively normal subjects. A less pronounced yet increased uptake rate was also observed in patients with late-onset mild cognitive impairment (MCI). This increased uptake may prove to be a key mechanism defining age-related AD progression.
- The increased cellular amyloid uptake in AD and LMCI may lead to quicker disease progression, but early-onset MCI may result from increased production of toxic amyloid metabolites.
Why this matters
- Additional biomarkers for AD could greatly aid diagnosis and course prediction, as they are currently limited to PET scan analysis of amyloid plaque deposits and concentration of Aβ42 in cerebrospinal fluid (CSF).
- Amyloid deposits found by PET have a positive correlation with AD diagnosis. In contrast, CSF-Aβ42 and AD diagnosis or cognitive decline are negatively correlated. Normal cognition (NC) is associated with higher CSF beta-amyloid levels, but previous research has not explained why CSF-Aβ42 levels can be equivalent in patients with NC but high amyloid load and patients with AD and low amyloid load.
Study design
- The authors of this retrospective study used anonymized data obtained from the Alzheimer’s’s Disease Neuroimaging Initiative (ADNI). ADNI’s goal has been to test whether serial MRI scans, PET scans, biomarkers, and clinical/neuropsychological assessment can be combined to measure the progression of MCI and AD.
- Study subjects had either an AD diagnosis or NC and were divided into two groups: low amyloid load and high amyloid load. The fraction of patients with an AD diagnosis was calculated as a function of CSF-Aβ42.
- Calculations and statistical comparisons were performed using Microsoft Excel and custom-written C++ programs.
Key results
- The lowest levels of CSF-Aβ42 correlated with the highest percentage of AD-diagnosed patients, estimated to be 27% in subjects with low amyloid deposit density and 65% in those with high deposit density.
- The relationship between CSF-Aβ42 levels and amyloid load can be described using a simple mathematical model: Amyloid concentration in the interstitial cells is equal to the synthesis rate divided by the density of amyloid deposits plus the sum of the rate of amyloid removal through the CSF and the cellular amyloid uptake rate.
- AD and late-onset MCI patients had a significantly higher amyloid removal rate compared to NC subjects.
- Early-onset MCI patients had Aβ42 turnover similar to that of NC subjects, pointing to a different underlying mechanism such as enzymatic disbalance.
Limitations
- The model used to explain amyloid exchange between the interstitial space and the CSF is oversimplified; the actual process is more complex.
- Synthesis and uptake rates of Aβ42 vary throughout areas of the brain. The model assumes a homogeneous distribution within the interstitial compartment.
Study disclosures
- Research reported in this publication was not supported by any external funding. Data collection and sharing for this project were funded by ADNI.
A version of this article first appeared on Medscape.com.
COVID at 2 years: Preparing for a different ‘normal’
Two years into the COVID-19 pandemic, the United States is still breaking records in hospital overcrowding and new cases.
The United States is logging nearly 800,000 cases a day, hospitals are starting to fray, and deaths have topped 850,000. Schools oscillate from remote to in-person learning, polarizing communities.
The vaccines are lifesaving for many, yet frustration mounts as the numbers of unvaccinated people in this country stays relatively stagnant (63% in the United States are fully vaccinated) and other parts of the world have seen hardly a single dose. Africa has the slowest vaccination rate among continents, with only 14% of the population receiving one shot, according to the New York Times tracker.
Yet
Effective vaccines and treatments that can keep people out of the hospital were developed at an astounding pace, and advances in tracking and testing – in both access and effectiveness – are starting to pay off.
Some experts say it’s possible that the raging Omicron surge will slow by late spring, providing some relief and maybe shifting the pandemic to a slower-burning endemic.
But other experts caution to keep our guard up, saying it’s time to settle into a “new normal” and upend the strategy for fighting COVID-19.
Time to change COVID thinking
Three former members of the Biden-Harris Transition COVID-19 Advisory Board wrote recently in JAMA that COVID-19 has now become one of the many viral respiratory diseases that health care providers and patients will manage each year.
The group of experts from the University of Pennsylvania, University of Minnesota, and New York University write that “many of the measures to reduce transmission of SARS-CoV-2 (for example, ventilation) will also reduce transmission of other respiratory viruses. Thus, policy makers should retire previous public health categorizations, including deaths from pneumonia and influenza or pneumonia, influenza, and COVID-19, and focus on a new category: the aggregate risk of all respiratory virus infections.”
Other experts, including Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security, Baltimore, have said it’s been clear since the early days of SARS-CoV-2 that we must learn to live with the virus because it “will be ever present for the remaining history of our species.”
But that doesn’t mean the virus will always have the upper hand. Although the United States has been reaching record numbers of hospitalizations in January, these hospitalizations differ from those of last year – marked by fewer extreme lifesaving measures, fewer deaths, and shorter hospital stays – caused in part by medical and therapeutic advances and in part to the nature of the Omicron variant itself.
One sign of progress, Dr. Adalja said, will be the widespread decoupling of cases from hospitalizations, something that has already happened in countries such as the United Kingdom.
“That’s a reflection of how well they have vaccinated their high-risk population and how poorly we have vaccinated our high-risk population,” he said.
Omicron will bump up natural immunity
Dr. Adalja said though the numbers of unvaccinated in the United States appear to be stuck, Omicron’s sweep will make the difference, leaving behind more natural immunity in the population.
Currently, hospitals are struggling with staffing concerns as a “direct result” of too many unvaccinated people, he said.
Andrew Badley, MD, an infectious diseases specialist at Mayo Clinic in Rochester, Minn., and director of the clinic’s COVID-19 Task Force, said the good news with Omicron is that nearly all people it infects will recover.
Over time, when the body sees foreign antigens repeatedly, the quantity and quality of the antibodies the immune system produces increase and the body becomes better at fighting disease.
So “a large amount of the population will have recovered and have a degree of immunity,” Dr. Badley said.
His optimism is tempered by his belief that “it’s going to get worse before it gets better.”
But Dr. Badley still predicts a turnaround. “We’ll see a downturn in COVID in late spring or early summer,” and well into the second quarter of 2022, “we’ll see a reemergence of control.”
Right now, with Omicron, one infected person is infecting three to five others, he said. The hope is that it will eventually reach one-to-one endemic levels.
As for the threat of new variants, Badley said, “it’s not predictable whether they will be stronger or weaker.”
Masks may be around for years
Many experts predict that masks will continue to be part of the national wardrobe for the foreseeable future.
“We will continue to see new cases for years and years to come. Some will respond to that with masks in public places for a very long time. I personally will do so,” Dr. Badley said.
Two mindsets: Inside/outside the hospital
Emily Landon, MD, an infectious disease doctor and the executive medical director of infection prevention and control at University of Chicago Medicine, told this news organization she views the pandemic from two different vantage points.
As a health care provider, she sees her hospital, like others worldwide, overwhelmed. Supplies of a major weapon to help prevent hospitalization, the monoclonal antibody sotrovimab, are running out. Dr. Landon said she has been calling other hospitals to see if they have supplies and, if so, whether Omicron patients can transfer there.
Bottom line: The things they relied on a month ago to keep people out of the hospital are no longer there, she said.
Meanwhile, “We have more COVID patients than we have ever had,” Dr. Landon said.
Last year, UChicago hit a high of 170 people hospitalized with COVID. This year, so far, the peak was 270.
Dr. Landon said she is frustrated when she leaves that overburdened world inside the hospital for the outside world, where people wear no masks or ineffective face coverings and gather unsafely. Although some of that behavior reflects an intention to flout the advice of medical experts, some is caused in part, she said, by the lack of a clear national health strategy and garbled communication from those in charge of public safety.
Americans are deciding for themselves, on an a la carte basis, whether to wear a mask or get tested or travel, and school districts decide individually when it’s time to go virtual.
“People are exhausted from having to do a risk-benefit analysis for every single activity they, their friends, their kids want to participate in,” she said.
U.S. behind in several areas
Despite our self-image as the global leader in science and medicine, the United States stumbled badly in its response to the pandemic, with grave consequences both at home and abroad, experts say.
In a recent commentary in JAMA, Lawrence Gostin, JD, from Georgetown University, Washington, and Jennifer Nuzzo, DrPH, at Johns Hopkins University, Baltimore, pointed to several critical shortfalls in the nation’s efforts to control the disease.
One such shortfall is public trust.
This news organization reported in June 2021 that a poll of its readers found that 44% said their trust in the CDC had waned during the pandemic, and 33% said their trust in the FDA had eroded as well.
Health care providers who responded to the poll lost trust as well. About half of the doctors and nurses who responded said they disagreed with the FDA’s decision-making during the pandemic. Nearly 60% of doctors and 65% of nurses said they disagreed with the CDC’s overall pandemic guidance.
Lack of trust can make people resist vaccines and efforts to fight the virus, the authors wrote.
“This will become really relevant when we have ample supply of Pfizer’s antiviral medication,” Mr. Gostin, who directs the O’Neill Institute for National and Global Health Law at Georgetown, told this news organization. “The next phase of the pandemic is not to link testing to contact tracing, because we’re way past that, but to link testing to treatment.”
Lack of regional manufacturing of products is also thwarting global progress.
“It is extraordinarily important that our pharmaceutical industry transfer technology in a pandemic,” Mr. Gostin said. “The most glaring failure to do that is the mRNA vaccines. We’ve got this enormously effective vaccine and the two manufacturers – Pfizer and Moderna – are refusing to share the technology with producers in other countries. That keeps coming back to haunt us.”
Another problem: When the vaccines are shared with other countries, they are being delivered close to the date they expire or arriving at a shipyards without warning, so even some of the doses that get delivered are going to waste, Mr. Gostin said.
“It’s one of the greatest moral failures of my lifetime,” he said.
Also a failure is the “jaw-dropping” state of testing 2 years into the pandemic, he said, as people continue to pay high prices for tests or endure long lines.
The U.S. government updated its calculations and ordered 1 billion tests for the general public. The COVIDtests.gov website to order the free tests is now live.
It’s a step in the right direction. Mr. Gostin and Dr. Nuzzo wrote that there is every reason to expect future epidemics that are as serious or more serious than COVID.
“Failure to address clearly observed weaknesses in the COVID-19 response will have preventable adverse health, social, and economic consequences when the next novel outbreak occurs,” they wrote.
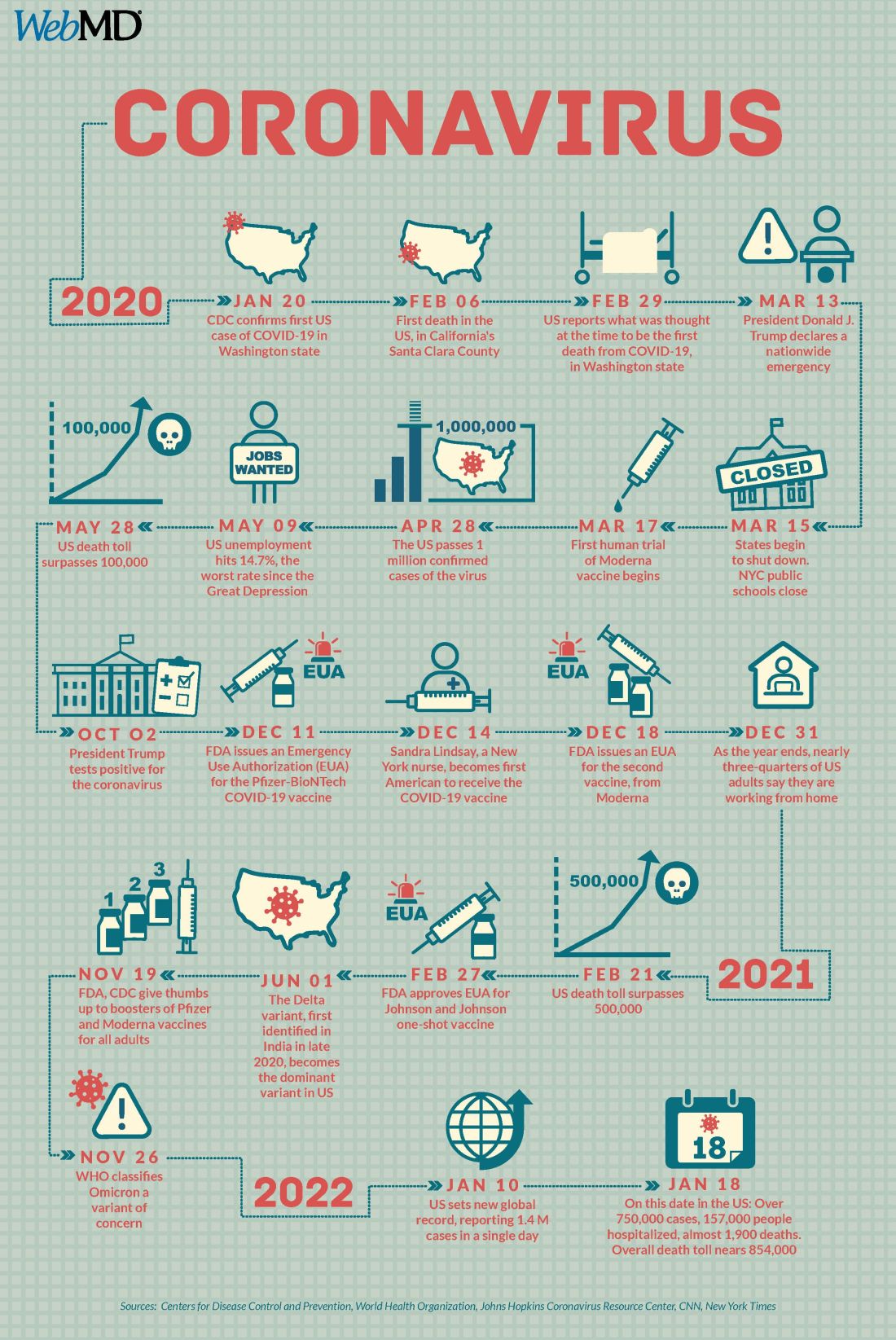
A version of this article first appeared on WebMD.com.
Two years into the COVID-19 pandemic, the United States is still breaking records in hospital overcrowding and new cases.
The United States is logging nearly 800,000 cases a day, hospitals are starting to fray, and deaths have topped 850,000. Schools oscillate from remote to in-person learning, polarizing communities.
The vaccines are lifesaving for many, yet frustration mounts as the numbers of unvaccinated people in this country stays relatively stagnant (63% in the United States are fully vaccinated) and other parts of the world have seen hardly a single dose. Africa has the slowest vaccination rate among continents, with only 14% of the population receiving one shot, according to the New York Times tracker.
Yet
Effective vaccines and treatments that can keep people out of the hospital were developed at an astounding pace, and advances in tracking and testing – in both access and effectiveness – are starting to pay off.
Some experts say it’s possible that the raging Omicron surge will slow by late spring, providing some relief and maybe shifting the pandemic to a slower-burning endemic.
But other experts caution to keep our guard up, saying it’s time to settle into a “new normal” and upend the strategy for fighting COVID-19.
Time to change COVID thinking
Three former members of the Biden-Harris Transition COVID-19 Advisory Board wrote recently in JAMA that COVID-19 has now become one of the many viral respiratory diseases that health care providers and patients will manage each year.
The group of experts from the University of Pennsylvania, University of Minnesota, and New York University write that “many of the measures to reduce transmission of SARS-CoV-2 (for example, ventilation) will also reduce transmission of other respiratory viruses. Thus, policy makers should retire previous public health categorizations, including deaths from pneumonia and influenza or pneumonia, influenza, and COVID-19, and focus on a new category: the aggregate risk of all respiratory virus infections.”
Other experts, including Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security, Baltimore, have said it’s been clear since the early days of SARS-CoV-2 that we must learn to live with the virus because it “will be ever present for the remaining history of our species.”
But that doesn’t mean the virus will always have the upper hand. Although the United States has been reaching record numbers of hospitalizations in January, these hospitalizations differ from those of last year – marked by fewer extreme lifesaving measures, fewer deaths, and shorter hospital stays – caused in part by medical and therapeutic advances and in part to the nature of the Omicron variant itself.
One sign of progress, Dr. Adalja said, will be the widespread decoupling of cases from hospitalizations, something that has already happened in countries such as the United Kingdom.
“That’s a reflection of how well they have vaccinated their high-risk population and how poorly we have vaccinated our high-risk population,” he said.
Omicron will bump up natural immunity
Dr. Adalja said though the numbers of unvaccinated in the United States appear to be stuck, Omicron’s sweep will make the difference, leaving behind more natural immunity in the population.
Currently, hospitals are struggling with staffing concerns as a “direct result” of too many unvaccinated people, he said.
Andrew Badley, MD, an infectious diseases specialist at Mayo Clinic in Rochester, Minn., and director of the clinic’s COVID-19 Task Force, said the good news with Omicron is that nearly all people it infects will recover.
Over time, when the body sees foreign antigens repeatedly, the quantity and quality of the antibodies the immune system produces increase and the body becomes better at fighting disease.
So “a large amount of the population will have recovered and have a degree of immunity,” Dr. Badley said.
His optimism is tempered by his belief that “it’s going to get worse before it gets better.”
But Dr. Badley still predicts a turnaround. “We’ll see a downturn in COVID in late spring or early summer,” and well into the second quarter of 2022, “we’ll see a reemergence of control.”
Right now, with Omicron, one infected person is infecting three to five others, he said. The hope is that it will eventually reach one-to-one endemic levels.
As for the threat of new variants, Badley said, “it’s not predictable whether they will be stronger or weaker.”
Masks may be around for years
Many experts predict that masks will continue to be part of the national wardrobe for the foreseeable future.
“We will continue to see new cases for years and years to come. Some will respond to that with masks in public places for a very long time. I personally will do so,” Dr. Badley said.
Two mindsets: Inside/outside the hospital
Emily Landon, MD, an infectious disease doctor and the executive medical director of infection prevention and control at University of Chicago Medicine, told this news organization she views the pandemic from two different vantage points.
As a health care provider, she sees her hospital, like others worldwide, overwhelmed. Supplies of a major weapon to help prevent hospitalization, the monoclonal antibody sotrovimab, are running out. Dr. Landon said she has been calling other hospitals to see if they have supplies and, if so, whether Omicron patients can transfer there.
Bottom line: The things they relied on a month ago to keep people out of the hospital are no longer there, she said.
Meanwhile, “We have more COVID patients than we have ever had,” Dr. Landon said.
Last year, UChicago hit a high of 170 people hospitalized with COVID. This year, so far, the peak was 270.
Dr. Landon said she is frustrated when she leaves that overburdened world inside the hospital for the outside world, where people wear no masks or ineffective face coverings and gather unsafely. Although some of that behavior reflects an intention to flout the advice of medical experts, some is caused in part, she said, by the lack of a clear national health strategy and garbled communication from those in charge of public safety.
Americans are deciding for themselves, on an a la carte basis, whether to wear a mask or get tested or travel, and school districts decide individually when it’s time to go virtual.
“People are exhausted from having to do a risk-benefit analysis for every single activity they, their friends, their kids want to participate in,” she said.
U.S. behind in several areas
Despite our self-image as the global leader in science and medicine, the United States stumbled badly in its response to the pandemic, with grave consequences both at home and abroad, experts say.
In a recent commentary in JAMA, Lawrence Gostin, JD, from Georgetown University, Washington, and Jennifer Nuzzo, DrPH, at Johns Hopkins University, Baltimore, pointed to several critical shortfalls in the nation’s efforts to control the disease.
One such shortfall is public trust.
This news organization reported in June 2021 that a poll of its readers found that 44% said their trust in the CDC had waned during the pandemic, and 33% said their trust in the FDA had eroded as well.
Health care providers who responded to the poll lost trust as well. About half of the doctors and nurses who responded said they disagreed with the FDA’s decision-making during the pandemic. Nearly 60% of doctors and 65% of nurses said they disagreed with the CDC’s overall pandemic guidance.
Lack of trust can make people resist vaccines and efforts to fight the virus, the authors wrote.
“This will become really relevant when we have ample supply of Pfizer’s antiviral medication,” Mr. Gostin, who directs the O’Neill Institute for National and Global Health Law at Georgetown, told this news organization. “The next phase of the pandemic is not to link testing to contact tracing, because we’re way past that, but to link testing to treatment.”
Lack of regional manufacturing of products is also thwarting global progress.
“It is extraordinarily important that our pharmaceutical industry transfer technology in a pandemic,” Mr. Gostin said. “The most glaring failure to do that is the mRNA vaccines. We’ve got this enormously effective vaccine and the two manufacturers – Pfizer and Moderna – are refusing to share the technology with producers in other countries. That keeps coming back to haunt us.”
Another problem: When the vaccines are shared with other countries, they are being delivered close to the date they expire or arriving at a shipyards without warning, so even some of the doses that get delivered are going to waste, Mr. Gostin said.
“It’s one of the greatest moral failures of my lifetime,” he said.
Also a failure is the “jaw-dropping” state of testing 2 years into the pandemic, he said, as people continue to pay high prices for tests or endure long lines.
The U.S. government updated its calculations and ordered 1 billion tests for the general public. The COVIDtests.gov website to order the free tests is now live.
It’s a step in the right direction. Mr. Gostin and Dr. Nuzzo wrote that there is every reason to expect future epidemics that are as serious or more serious than COVID.
“Failure to address clearly observed weaknesses in the COVID-19 response will have preventable adverse health, social, and economic consequences when the next novel outbreak occurs,” they wrote.
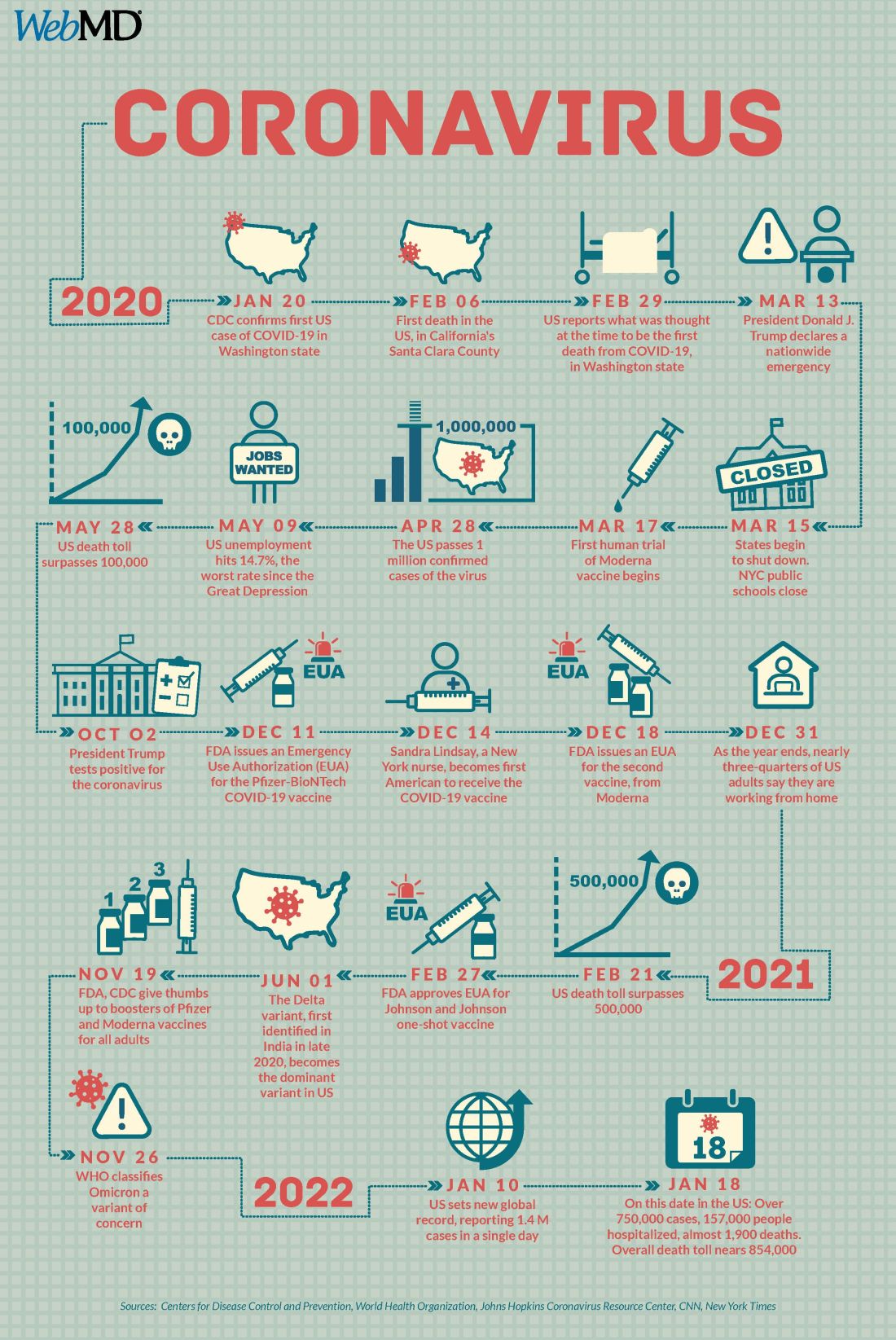
A version of this article first appeared on WebMD.com.
Two years into the COVID-19 pandemic, the United States is still breaking records in hospital overcrowding and new cases.
The United States is logging nearly 800,000 cases a day, hospitals are starting to fray, and deaths have topped 850,000. Schools oscillate from remote to in-person learning, polarizing communities.
The vaccines are lifesaving for many, yet frustration mounts as the numbers of unvaccinated people in this country stays relatively stagnant (63% in the United States are fully vaccinated) and other parts of the world have seen hardly a single dose. Africa has the slowest vaccination rate among continents, with only 14% of the population receiving one shot, according to the New York Times tracker.
Yet
Effective vaccines and treatments that can keep people out of the hospital were developed at an astounding pace, and advances in tracking and testing – in both access and effectiveness – are starting to pay off.
Some experts say it’s possible that the raging Omicron surge will slow by late spring, providing some relief and maybe shifting the pandemic to a slower-burning endemic.
But other experts caution to keep our guard up, saying it’s time to settle into a “new normal” and upend the strategy for fighting COVID-19.
Time to change COVID thinking
Three former members of the Biden-Harris Transition COVID-19 Advisory Board wrote recently in JAMA that COVID-19 has now become one of the many viral respiratory diseases that health care providers and patients will manage each year.
The group of experts from the University of Pennsylvania, University of Minnesota, and New York University write that “many of the measures to reduce transmission of SARS-CoV-2 (for example, ventilation) will also reduce transmission of other respiratory viruses. Thus, policy makers should retire previous public health categorizations, including deaths from pneumonia and influenza or pneumonia, influenza, and COVID-19, and focus on a new category: the aggregate risk of all respiratory virus infections.”
Other experts, including Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security, Baltimore, have said it’s been clear since the early days of SARS-CoV-2 that we must learn to live with the virus because it “will be ever present for the remaining history of our species.”
But that doesn’t mean the virus will always have the upper hand. Although the United States has been reaching record numbers of hospitalizations in January, these hospitalizations differ from those of last year – marked by fewer extreme lifesaving measures, fewer deaths, and shorter hospital stays – caused in part by medical and therapeutic advances and in part to the nature of the Omicron variant itself.
One sign of progress, Dr. Adalja said, will be the widespread decoupling of cases from hospitalizations, something that has already happened in countries such as the United Kingdom.
“That’s a reflection of how well they have vaccinated their high-risk population and how poorly we have vaccinated our high-risk population,” he said.
Omicron will bump up natural immunity
Dr. Adalja said though the numbers of unvaccinated in the United States appear to be stuck, Omicron’s sweep will make the difference, leaving behind more natural immunity in the population.
Currently, hospitals are struggling with staffing concerns as a “direct result” of too many unvaccinated people, he said.
Andrew Badley, MD, an infectious diseases specialist at Mayo Clinic in Rochester, Minn., and director of the clinic’s COVID-19 Task Force, said the good news with Omicron is that nearly all people it infects will recover.
Over time, when the body sees foreign antigens repeatedly, the quantity and quality of the antibodies the immune system produces increase and the body becomes better at fighting disease.
So “a large amount of the population will have recovered and have a degree of immunity,” Dr. Badley said.
His optimism is tempered by his belief that “it’s going to get worse before it gets better.”
But Dr. Badley still predicts a turnaround. “We’ll see a downturn in COVID in late spring or early summer,” and well into the second quarter of 2022, “we’ll see a reemergence of control.”
Right now, with Omicron, one infected person is infecting three to five others, he said. The hope is that it will eventually reach one-to-one endemic levels.
As for the threat of new variants, Badley said, “it’s not predictable whether they will be stronger or weaker.”
Masks may be around for years
Many experts predict that masks will continue to be part of the national wardrobe for the foreseeable future.
“We will continue to see new cases for years and years to come. Some will respond to that with masks in public places for a very long time. I personally will do so,” Dr. Badley said.
Two mindsets: Inside/outside the hospital
Emily Landon, MD, an infectious disease doctor and the executive medical director of infection prevention and control at University of Chicago Medicine, told this news organization she views the pandemic from two different vantage points.
As a health care provider, she sees her hospital, like others worldwide, overwhelmed. Supplies of a major weapon to help prevent hospitalization, the monoclonal antibody sotrovimab, are running out. Dr. Landon said she has been calling other hospitals to see if they have supplies and, if so, whether Omicron patients can transfer there.
Bottom line: The things they relied on a month ago to keep people out of the hospital are no longer there, she said.
Meanwhile, “We have more COVID patients than we have ever had,” Dr. Landon said.
Last year, UChicago hit a high of 170 people hospitalized with COVID. This year, so far, the peak was 270.
Dr. Landon said she is frustrated when she leaves that overburdened world inside the hospital for the outside world, where people wear no masks or ineffective face coverings and gather unsafely. Although some of that behavior reflects an intention to flout the advice of medical experts, some is caused in part, she said, by the lack of a clear national health strategy and garbled communication from those in charge of public safety.
Americans are deciding for themselves, on an a la carte basis, whether to wear a mask or get tested or travel, and school districts decide individually when it’s time to go virtual.
“People are exhausted from having to do a risk-benefit analysis for every single activity they, their friends, their kids want to participate in,” she said.
U.S. behind in several areas
Despite our self-image as the global leader in science and medicine, the United States stumbled badly in its response to the pandemic, with grave consequences both at home and abroad, experts say.
In a recent commentary in JAMA, Lawrence Gostin, JD, from Georgetown University, Washington, and Jennifer Nuzzo, DrPH, at Johns Hopkins University, Baltimore, pointed to several critical shortfalls in the nation’s efforts to control the disease.
One such shortfall is public trust.
This news organization reported in June 2021 that a poll of its readers found that 44% said their trust in the CDC had waned during the pandemic, and 33% said their trust in the FDA had eroded as well.
Health care providers who responded to the poll lost trust as well. About half of the doctors and nurses who responded said they disagreed with the FDA’s decision-making during the pandemic. Nearly 60% of doctors and 65% of nurses said they disagreed with the CDC’s overall pandemic guidance.
Lack of trust can make people resist vaccines and efforts to fight the virus, the authors wrote.
“This will become really relevant when we have ample supply of Pfizer’s antiviral medication,” Mr. Gostin, who directs the O’Neill Institute for National and Global Health Law at Georgetown, told this news organization. “The next phase of the pandemic is not to link testing to contact tracing, because we’re way past that, but to link testing to treatment.”
Lack of regional manufacturing of products is also thwarting global progress.
“It is extraordinarily important that our pharmaceutical industry transfer technology in a pandemic,” Mr. Gostin said. “The most glaring failure to do that is the mRNA vaccines. We’ve got this enormously effective vaccine and the two manufacturers – Pfizer and Moderna – are refusing to share the technology with producers in other countries. That keeps coming back to haunt us.”
Another problem: When the vaccines are shared with other countries, they are being delivered close to the date they expire or arriving at a shipyards without warning, so even some of the doses that get delivered are going to waste, Mr. Gostin said.
“It’s one of the greatest moral failures of my lifetime,” he said.
Also a failure is the “jaw-dropping” state of testing 2 years into the pandemic, he said, as people continue to pay high prices for tests or endure long lines.
The U.S. government updated its calculations and ordered 1 billion tests for the general public. The COVIDtests.gov website to order the free tests is now live.
It’s a step in the right direction. Mr. Gostin and Dr. Nuzzo wrote that there is every reason to expect future epidemics that are as serious or more serious than COVID.
“Failure to address clearly observed weaknesses in the COVID-19 response will have preventable adverse health, social, and economic consequences when the next novel outbreak occurs,” they wrote.
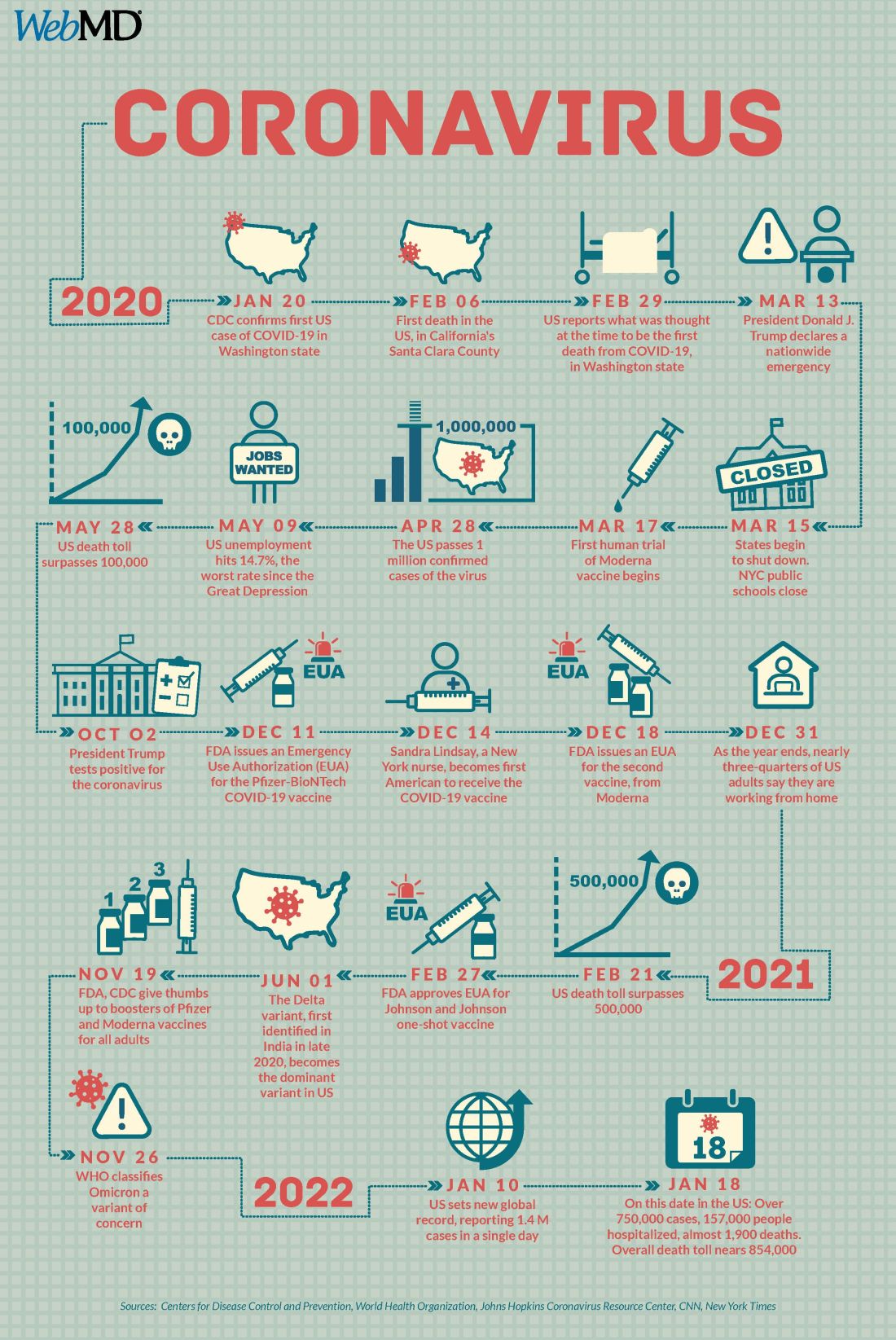
A version of this article first appeared on WebMD.com.
Make America beautiful: Support mask mandates
In space, no one can hear your red blood cells scream
There are many reasons why space is the final frontier, not least of which are the major health issues space travel places on the human body. So until a shady billionaire finds an alien protomolecule on a Saturnian moon and starts splicing it with human DNA so we can hang out in space all day without a spacesuit, we’re stuck with things like space anemia, a condition many astronauts develop after extended time in space.
Space anemia has been known for many years, but it was assumed that it developed as a reaction to microgravity and was a short-term phenomenon only – a temporary compensation as fluids and blood volume adjusted themselves. But as new research shows, that assumption seems to be wrong.
For the study, published in Nature Medicine, 13 astronauts who were in space for at least 120 days – long enough for all their red blood cells to have been produced in space – had their blood tested consistently. Before their flights, the astronauts created and destroyed 2 million red blood cells per second, but while they were in space, they destroyed 3 million cells per second. Notably, this process continued for the entire duration of the space flight. So, not a temporary reaction.
Consequently, 5 of the 13 astronauts developed anemia when they returned to Earth. (Interesting space fact: Having fewer blood cells isn’t a problem while you’re in space; the effects of anemia only manifest when the body returns to full gravity.) The anemia disappeared after a few months, but the astronauts were still destroying 30% more red blood cells a year after their spaceflight than they were before leaving Earth.
You may be thinking: Well, if they were destroying 50% more red blood cells while in space, how come they didn’t all develop severe anemia? The researchers theorized that production was boosted as well, which sounds like a good thing. The body is compensating, as it should. Unfortunately, that increased production stresses bone marrow function and the demand for energy spikes. That’s not such a good thing. And of course, many of the astronauts got anemia anyway.
To tackle the issue, the researchers emphasized the importance of feeding astronauts a proper diet, plus potential supplements before spaceflight. So don’t worry, Captain Kirk will be able to arm wrestle Klingons and romance suspiciously human-looking aliens without fear of keeling over from anemia-induced fatigue. Earth will stay safe.
Tell me with your eyes
Communication can be hard, even under the best of circumstances, but for many nonverbal patients in the intensive care unit who can’t move, getting a point across to the health care team can be a huge struggle in itself.
Health care professionals have been making do with eye-blinking or head-nodding, but what if that’s just not enough? New research shows that it’s not, and there’s a more effective way for patients to say what they mean just by looking.
In a study published in the Journal of Trauma and Acute Care Surgery, researchers looked into using eye-tracking systems for nonverbal ICU patients to communicate. Eye-tracking isn’t anything new, but using it as a form of communication among nonverbal patients with critical illness hasn’t been looked at before.
How does it work? The eye-tracking system is set up in the patient’s line of sight and its various algorithms and software collect data to calculate where exactly the patient is looking. Established scores and scales assess the patient’s mood, quality of life, pain, and self-esteem.
The researchers found that participating patients were actually experiencing more negative moods, pain, and feelings of frustration than was once believed. Making this tool even more valuable for treatment adjustment and meeting patients’ needs.
In this case, it means that health care providers are getting an eyeful … of communication.
Make America grave again
Here we go again. Somebody just found something else that the United States is not the best at. To go along with math and science education, infrastructure investment, quality of life …
That’s going to go on for a while, so let’s get to the new stuff. An international group of researchers surveyed end-of-life care in 81 countries and ranked them based on the assessment of 181 experts in those countries. They looked at 13 different factors, including proper management of pain and comfort, having a clean and safe space, being treated kindly, lack of cost barriers to appropriate care, and treatments that address quality of life and don’t just extend life.
… press freedom, industrial production, racial equality, Internet connectivity …
Their report card, published in the Journal of Pain and Symptom Management, gave six countries an A, with Great Britain at the top. The other five were Ireland, Taiwan, Australia, South Korea, and Costa Rica. The lowest grade went to Paraguay in 81st place, with Lebanon, Brazil, Senegal, and Haiti just ahead.
… environmental stewardship, body-mass index, social mobility, COVID safeness …
The United States, getting a firm grasp on mediocrity, ranked 43rd. Here are some countries that did better: North Macedonia (7th), Sri Lanka (16th), Uganda (31st), and Uruguay 33rd). In the United States, “we spend so much money trying to get people to live longer, but we don’t spend enough money in helping people die better,” lead author Eric A. Finkelstein, PhD, said in a written statement.
… economic stability, and soccer; we’re also not the best at dying. Wait, did we already say that?
The face mask that launched a thousand ships
Face masks, clearly, have been a source of social strife during the pandemic. People may not agree on mandates, but a mask can be a pretty-low-maintenance face shield if you don’t feel like putting on make-up or want to cover up some blemishes.
Before the pandemic, people thought that those wearing face masks were less attractive because the masks represented illness or disease, according to Dr. Michael Lewis of Cardiff (Wales) University. Back then, no one really wore masks besides doctors and nurses, so if you saw someone wearing one on the street, you probably wondered what they were trying to hide.
Now, though, the subject of face mask attractiveness has been revisited by Dr. Lewis and his associate, Oliver Hies, who found that face masks now make people more attractive.
“Our study suggests faces are considered most attractive when covered by medical face masks. … At a time when we feel vulnerable, we may find the wearing of medical masks reassuring and so feel more positive towards the wearer,” Dr. Lewis told the Guardian.
He suggested that we’re no longer looking at people wearing a mask as disease riddled, but rather doing their part to protect society. Or maybe we focus more on someone’s eyes when that’s all there is to look at. Or, maybe we wind up making up what the rest of someone’s face looks like to meet our attractiveness criteria.
However you feel about masks, they’re cheaper than plastic surgery. And you can go out wearing a new face every day.
In space, no one can hear your red blood cells scream
There are many reasons why space is the final frontier, not least of which are the major health issues space travel places on the human body. So until a shady billionaire finds an alien protomolecule on a Saturnian moon and starts splicing it with human DNA so we can hang out in space all day without a spacesuit, we’re stuck with things like space anemia, a condition many astronauts develop after extended time in space.
Space anemia has been known for many years, but it was assumed that it developed as a reaction to microgravity and was a short-term phenomenon only – a temporary compensation as fluids and blood volume adjusted themselves. But as new research shows, that assumption seems to be wrong.
For the study, published in Nature Medicine, 13 astronauts who were in space for at least 120 days – long enough for all their red blood cells to have been produced in space – had their blood tested consistently. Before their flights, the astronauts created and destroyed 2 million red blood cells per second, but while they were in space, they destroyed 3 million cells per second. Notably, this process continued for the entire duration of the space flight. So, not a temporary reaction.
Consequently, 5 of the 13 astronauts developed anemia when they returned to Earth. (Interesting space fact: Having fewer blood cells isn’t a problem while you’re in space; the effects of anemia only manifest when the body returns to full gravity.) The anemia disappeared after a few months, but the astronauts were still destroying 30% more red blood cells a year after their spaceflight than they were before leaving Earth.
You may be thinking: Well, if they were destroying 50% more red blood cells while in space, how come they didn’t all develop severe anemia? The researchers theorized that production was boosted as well, which sounds like a good thing. The body is compensating, as it should. Unfortunately, that increased production stresses bone marrow function and the demand for energy spikes. That’s not such a good thing. And of course, many of the astronauts got anemia anyway.
To tackle the issue, the researchers emphasized the importance of feeding astronauts a proper diet, plus potential supplements before spaceflight. So don’t worry, Captain Kirk will be able to arm wrestle Klingons and romance suspiciously human-looking aliens without fear of keeling over from anemia-induced fatigue. Earth will stay safe.
Tell me with your eyes
Communication can be hard, even under the best of circumstances, but for many nonverbal patients in the intensive care unit who can’t move, getting a point across to the health care team can be a huge struggle in itself.
Health care professionals have been making do with eye-blinking or head-nodding, but what if that’s just not enough? New research shows that it’s not, and there’s a more effective way for patients to say what they mean just by looking.
In a study published in the Journal of Trauma and Acute Care Surgery, researchers looked into using eye-tracking systems for nonverbal ICU patients to communicate. Eye-tracking isn’t anything new, but using it as a form of communication among nonverbal patients with critical illness hasn’t been looked at before.
How does it work? The eye-tracking system is set up in the patient’s line of sight and its various algorithms and software collect data to calculate where exactly the patient is looking. Established scores and scales assess the patient’s mood, quality of life, pain, and self-esteem.
The researchers found that participating patients were actually experiencing more negative moods, pain, and feelings of frustration than was once believed. Making this tool even more valuable for treatment adjustment and meeting patients’ needs.
In this case, it means that health care providers are getting an eyeful … of communication.
Make America grave again
Here we go again. Somebody just found something else that the United States is not the best at. To go along with math and science education, infrastructure investment, quality of life …
That’s going to go on for a while, so let’s get to the new stuff. An international group of researchers surveyed end-of-life care in 81 countries and ranked them based on the assessment of 181 experts in those countries. They looked at 13 different factors, including proper management of pain and comfort, having a clean and safe space, being treated kindly, lack of cost barriers to appropriate care, and treatments that address quality of life and don’t just extend life.
… press freedom, industrial production, racial equality, Internet connectivity …
Their report card, published in the Journal of Pain and Symptom Management, gave six countries an A, with Great Britain at the top. The other five were Ireland, Taiwan, Australia, South Korea, and Costa Rica. The lowest grade went to Paraguay in 81st place, with Lebanon, Brazil, Senegal, and Haiti just ahead.
… environmental stewardship, body-mass index, social mobility, COVID safeness …
The United States, getting a firm grasp on mediocrity, ranked 43rd. Here are some countries that did better: North Macedonia (7th), Sri Lanka (16th), Uganda (31st), and Uruguay 33rd). In the United States, “we spend so much money trying to get people to live longer, but we don’t spend enough money in helping people die better,” lead author Eric A. Finkelstein, PhD, said in a written statement.
… economic stability, and soccer; we’re also not the best at dying. Wait, did we already say that?
The face mask that launched a thousand ships
Face masks, clearly, have been a source of social strife during the pandemic. People may not agree on mandates, but a mask can be a pretty-low-maintenance face shield if you don’t feel like putting on make-up or want to cover up some blemishes.
Before the pandemic, people thought that those wearing face masks were less attractive because the masks represented illness or disease, according to Dr. Michael Lewis of Cardiff (Wales) University. Back then, no one really wore masks besides doctors and nurses, so if you saw someone wearing one on the street, you probably wondered what they were trying to hide.
Now, though, the subject of face mask attractiveness has been revisited by Dr. Lewis and his associate, Oliver Hies, who found that face masks now make people more attractive.
“Our study suggests faces are considered most attractive when covered by medical face masks. … At a time when we feel vulnerable, we may find the wearing of medical masks reassuring and so feel more positive towards the wearer,” Dr. Lewis told the Guardian.
He suggested that we’re no longer looking at people wearing a mask as disease riddled, but rather doing their part to protect society. Or maybe we focus more on someone’s eyes when that’s all there is to look at. Or, maybe we wind up making up what the rest of someone’s face looks like to meet our attractiveness criteria.
However you feel about masks, they’re cheaper than plastic surgery. And you can go out wearing a new face every day.
In space, no one can hear your red blood cells scream
There are many reasons why space is the final frontier, not least of which are the major health issues space travel places on the human body. So until a shady billionaire finds an alien protomolecule on a Saturnian moon and starts splicing it with human DNA so we can hang out in space all day without a spacesuit, we’re stuck with things like space anemia, a condition many astronauts develop after extended time in space.
Space anemia has been known for many years, but it was assumed that it developed as a reaction to microgravity and was a short-term phenomenon only – a temporary compensation as fluids and blood volume adjusted themselves. But as new research shows, that assumption seems to be wrong.
For the study, published in Nature Medicine, 13 astronauts who were in space for at least 120 days – long enough for all their red blood cells to have been produced in space – had their blood tested consistently. Before their flights, the astronauts created and destroyed 2 million red blood cells per second, but while they were in space, they destroyed 3 million cells per second. Notably, this process continued for the entire duration of the space flight. So, not a temporary reaction.
Consequently, 5 of the 13 astronauts developed anemia when they returned to Earth. (Interesting space fact: Having fewer blood cells isn’t a problem while you’re in space; the effects of anemia only manifest when the body returns to full gravity.) The anemia disappeared after a few months, but the astronauts were still destroying 30% more red blood cells a year after their spaceflight than they were before leaving Earth.
You may be thinking: Well, if they were destroying 50% more red blood cells while in space, how come they didn’t all develop severe anemia? The researchers theorized that production was boosted as well, which sounds like a good thing. The body is compensating, as it should. Unfortunately, that increased production stresses bone marrow function and the demand for energy spikes. That’s not such a good thing. And of course, many of the astronauts got anemia anyway.
To tackle the issue, the researchers emphasized the importance of feeding astronauts a proper diet, plus potential supplements before spaceflight. So don’t worry, Captain Kirk will be able to arm wrestle Klingons and romance suspiciously human-looking aliens without fear of keeling over from anemia-induced fatigue. Earth will stay safe.
Tell me with your eyes
Communication can be hard, even under the best of circumstances, but for many nonverbal patients in the intensive care unit who can’t move, getting a point across to the health care team can be a huge struggle in itself.
Health care professionals have been making do with eye-blinking or head-nodding, but what if that’s just not enough? New research shows that it’s not, and there’s a more effective way for patients to say what they mean just by looking.
In a study published in the Journal of Trauma and Acute Care Surgery, researchers looked into using eye-tracking systems for nonverbal ICU patients to communicate. Eye-tracking isn’t anything new, but using it as a form of communication among nonverbal patients with critical illness hasn’t been looked at before.
How does it work? The eye-tracking system is set up in the patient’s line of sight and its various algorithms and software collect data to calculate where exactly the patient is looking. Established scores and scales assess the patient’s mood, quality of life, pain, and self-esteem.
The researchers found that participating patients were actually experiencing more negative moods, pain, and feelings of frustration than was once believed. Making this tool even more valuable for treatment adjustment and meeting patients’ needs.
In this case, it means that health care providers are getting an eyeful … of communication.
Make America grave again
Here we go again. Somebody just found something else that the United States is not the best at. To go along with math and science education, infrastructure investment, quality of life …
That’s going to go on for a while, so let’s get to the new stuff. An international group of researchers surveyed end-of-life care in 81 countries and ranked them based on the assessment of 181 experts in those countries. They looked at 13 different factors, including proper management of pain and comfort, having a clean and safe space, being treated kindly, lack of cost barriers to appropriate care, and treatments that address quality of life and don’t just extend life.
… press freedom, industrial production, racial equality, Internet connectivity …
Their report card, published in the Journal of Pain and Symptom Management, gave six countries an A, with Great Britain at the top. The other five were Ireland, Taiwan, Australia, South Korea, and Costa Rica. The lowest grade went to Paraguay in 81st place, with Lebanon, Brazil, Senegal, and Haiti just ahead.
… environmental stewardship, body-mass index, social mobility, COVID safeness …
The United States, getting a firm grasp on mediocrity, ranked 43rd. Here are some countries that did better: North Macedonia (7th), Sri Lanka (16th), Uganda (31st), and Uruguay 33rd). In the United States, “we spend so much money trying to get people to live longer, but we don’t spend enough money in helping people die better,” lead author Eric A. Finkelstein, PhD, said in a written statement.
… economic stability, and soccer; we’re also not the best at dying. Wait, did we already say that?
The face mask that launched a thousand ships
Face masks, clearly, have been a source of social strife during the pandemic. People may not agree on mandates, but a mask can be a pretty-low-maintenance face shield if you don’t feel like putting on make-up or want to cover up some blemishes.
Before the pandemic, people thought that those wearing face masks were less attractive because the masks represented illness or disease, according to Dr. Michael Lewis of Cardiff (Wales) University. Back then, no one really wore masks besides doctors and nurses, so if you saw someone wearing one on the street, you probably wondered what they were trying to hide.
Now, though, the subject of face mask attractiveness has been revisited by Dr. Lewis and his associate, Oliver Hies, who found that face masks now make people more attractive.
“Our study suggests faces are considered most attractive when covered by medical face masks. … At a time when we feel vulnerable, we may find the wearing of medical masks reassuring and so feel more positive towards the wearer,” Dr. Lewis told the Guardian.
He suggested that we’re no longer looking at people wearing a mask as disease riddled, but rather doing their part to protect society. Or maybe we focus more on someone’s eyes when that’s all there is to look at. Or, maybe we wind up making up what the rest of someone’s face looks like to meet our attractiveness criteria.
However you feel about masks, they’re cheaper than plastic surgery. And you can go out wearing a new face every day.