User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Men with hypersexual disorder may have oxytocin overload
Men with hypersexual disorder showed higher levels of oxytocin in their blood than did healthy control men without the disorder, in a study with 102 participants.
Hypersexual disorder (HD) is characterized by “excessive and persistent sexual behaviors in relation to various mood states, with an impulsivity component and experienced loss of control,” John Flanagan, MD, of the Karolinska Institutet in Stockholm and colleagues wrote. Although HD is not included as a separate diagnosis in the current DSM, the similar disorder of compulsive sexual behavior is included in the ICD.
Data on the pathophysiology of HD are limited, although a previous study by corresponding author Andreas Chatzittofis, MD, and colleagues showed evidence of neuroendocrine dysregulation in men with HD, and prompted the current study to explore the possible involvement of the oxytocinergic system in HD.
In the current study, published in the Journal of Clinical Endocrinology & Metabolism, the researchers identified 64 men with HD and 38 healthy male controls. The patients were help-seeking men older than 18 years diagnosed with HD who presented to a single center in Sweden during 2013-2014. The men were included in a randomized clinical trial of cognitive-behavioral therapy for HD, and 30 of them participated in a 7-week CBT program.
Oxytocin, secreted by the pituitary gland, is known to play a role in sexual behavior, but has not been examined in HD men, the researchers said. At baseline, the mean plasma oxytocin was 31.0 pM in the HD patients, which was significantly higher than the mean 16.9 pM in healthy controls (P < .001). However, the 30 HD men who underwent CBT showed significant improvement in oxytocin levels, from a mean pretreatment level of 30.5 to a mean posttreatment level of 20.2 pM (P = .0000019).
The study findings were limited by several factors, including the lack of data on oxytocin for a wait list or control group, as well as the inability to control for confounding factors such as diet, physical activity, ethnicity, and stress, and a lack of data on sexual activity prior to oxytocin measurements, the researchers noted.
However, “although there is no clear consensus at this point, previous studies support the use of oxytocin plasma levels as a surrogate variable for [cerebrospinal fluid] oxytocin activity,” the researchers wrote in their discussion. The current study findings support the potential of oxytocin as a biomarker for HD diagnostics and also as a measure of disease severity. Larger studies to confirm the findings, especially those that exclude potential confounders, would be valuable.
Oxytocin may be treatment target
The study is important because of the lack of knowledge regarding the pathophysiology underlying hypersexual disorder, Dr. Chatzittofis of the University of Cyprus, Nicosia, said in an interview. “This is the first study to indicate a role for oxytocin’s involvement” in hypersexual disorder in men. Dr. Chatzittofis led a team in a previous study that showed an association between HD in men and dysregulation of the hypothalamic pituitary adrenal axis.
In the current study, “we discovered that men with compulsive sexual behavior disorder had higher oxytocin levels, compared with healthy men,” said Dr. Chatzittofis, adding that the take-home message for clinicians is the potential of CBT for treatment. “Cognitive-behavior therapy led to a reduction in both hypersexual behavior and oxytocin levels.” The results suggest that oxytocin plays an important role in sex addiction.
Consequently, oxytocin may be a potential drug target for future pharmacologic treatment of hypersexual disorder, he added.
The study was supported by the Swedish Research Council, the Stockholm County Council, and by a partnership between Umeå University and Västerbotten County Council. The researchers had no financial conflicts to disclose.
Men with hypersexual disorder showed higher levels of oxytocin in their blood than did healthy control men without the disorder, in a study with 102 participants.
Hypersexual disorder (HD) is characterized by “excessive and persistent sexual behaviors in relation to various mood states, with an impulsivity component and experienced loss of control,” John Flanagan, MD, of the Karolinska Institutet in Stockholm and colleagues wrote. Although HD is not included as a separate diagnosis in the current DSM, the similar disorder of compulsive sexual behavior is included in the ICD.
Data on the pathophysiology of HD are limited, although a previous study by corresponding author Andreas Chatzittofis, MD, and colleagues showed evidence of neuroendocrine dysregulation in men with HD, and prompted the current study to explore the possible involvement of the oxytocinergic system in HD.
In the current study, published in the Journal of Clinical Endocrinology & Metabolism, the researchers identified 64 men with HD and 38 healthy male controls. The patients were help-seeking men older than 18 years diagnosed with HD who presented to a single center in Sweden during 2013-2014. The men were included in a randomized clinical trial of cognitive-behavioral therapy for HD, and 30 of them participated in a 7-week CBT program.
Oxytocin, secreted by the pituitary gland, is known to play a role in sexual behavior, but has not been examined in HD men, the researchers said. At baseline, the mean plasma oxytocin was 31.0 pM in the HD patients, which was significantly higher than the mean 16.9 pM in healthy controls (P < .001). However, the 30 HD men who underwent CBT showed significant improvement in oxytocin levels, from a mean pretreatment level of 30.5 to a mean posttreatment level of 20.2 pM (P = .0000019).
The study findings were limited by several factors, including the lack of data on oxytocin for a wait list or control group, as well as the inability to control for confounding factors such as diet, physical activity, ethnicity, and stress, and a lack of data on sexual activity prior to oxytocin measurements, the researchers noted.
However, “although there is no clear consensus at this point, previous studies support the use of oxytocin plasma levels as a surrogate variable for [cerebrospinal fluid] oxytocin activity,” the researchers wrote in their discussion. The current study findings support the potential of oxytocin as a biomarker for HD diagnostics and also as a measure of disease severity. Larger studies to confirm the findings, especially those that exclude potential confounders, would be valuable.
Oxytocin may be treatment target
The study is important because of the lack of knowledge regarding the pathophysiology underlying hypersexual disorder, Dr. Chatzittofis of the University of Cyprus, Nicosia, said in an interview. “This is the first study to indicate a role for oxytocin’s involvement” in hypersexual disorder in men. Dr. Chatzittofis led a team in a previous study that showed an association between HD in men and dysregulation of the hypothalamic pituitary adrenal axis.
In the current study, “we discovered that men with compulsive sexual behavior disorder had higher oxytocin levels, compared with healthy men,” said Dr. Chatzittofis, adding that the take-home message for clinicians is the potential of CBT for treatment. “Cognitive-behavior therapy led to a reduction in both hypersexual behavior and oxytocin levels.” The results suggest that oxytocin plays an important role in sex addiction.
Consequently, oxytocin may be a potential drug target for future pharmacologic treatment of hypersexual disorder, he added.
The study was supported by the Swedish Research Council, the Stockholm County Council, and by a partnership between Umeå University and Västerbotten County Council. The researchers had no financial conflicts to disclose.
Men with hypersexual disorder showed higher levels of oxytocin in their blood than did healthy control men without the disorder, in a study with 102 participants.
Hypersexual disorder (HD) is characterized by “excessive and persistent sexual behaviors in relation to various mood states, with an impulsivity component and experienced loss of control,” John Flanagan, MD, of the Karolinska Institutet in Stockholm and colleagues wrote. Although HD is not included as a separate diagnosis in the current DSM, the similar disorder of compulsive sexual behavior is included in the ICD.
Data on the pathophysiology of HD are limited, although a previous study by corresponding author Andreas Chatzittofis, MD, and colleagues showed evidence of neuroendocrine dysregulation in men with HD, and prompted the current study to explore the possible involvement of the oxytocinergic system in HD.
In the current study, published in the Journal of Clinical Endocrinology & Metabolism, the researchers identified 64 men with HD and 38 healthy male controls. The patients were help-seeking men older than 18 years diagnosed with HD who presented to a single center in Sweden during 2013-2014. The men were included in a randomized clinical trial of cognitive-behavioral therapy for HD, and 30 of them participated in a 7-week CBT program.
Oxytocin, secreted by the pituitary gland, is known to play a role in sexual behavior, but has not been examined in HD men, the researchers said. At baseline, the mean plasma oxytocin was 31.0 pM in the HD patients, which was significantly higher than the mean 16.9 pM in healthy controls (P < .001). However, the 30 HD men who underwent CBT showed significant improvement in oxytocin levels, from a mean pretreatment level of 30.5 to a mean posttreatment level of 20.2 pM (P = .0000019).
The study findings were limited by several factors, including the lack of data on oxytocin for a wait list or control group, as well as the inability to control for confounding factors such as diet, physical activity, ethnicity, and stress, and a lack of data on sexual activity prior to oxytocin measurements, the researchers noted.
However, “although there is no clear consensus at this point, previous studies support the use of oxytocin plasma levels as a surrogate variable for [cerebrospinal fluid] oxytocin activity,” the researchers wrote in their discussion. The current study findings support the potential of oxytocin as a biomarker for HD diagnostics and also as a measure of disease severity. Larger studies to confirm the findings, especially those that exclude potential confounders, would be valuable.
Oxytocin may be treatment target
The study is important because of the lack of knowledge regarding the pathophysiology underlying hypersexual disorder, Dr. Chatzittofis of the University of Cyprus, Nicosia, said in an interview. “This is the first study to indicate a role for oxytocin’s involvement” in hypersexual disorder in men. Dr. Chatzittofis led a team in a previous study that showed an association between HD in men and dysregulation of the hypothalamic pituitary adrenal axis.
In the current study, “we discovered that men with compulsive sexual behavior disorder had higher oxytocin levels, compared with healthy men,” said Dr. Chatzittofis, adding that the take-home message for clinicians is the potential of CBT for treatment. “Cognitive-behavior therapy led to a reduction in both hypersexual behavior and oxytocin levels.” The results suggest that oxytocin plays an important role in sex addiction.
Consequently, oxytocin may be a potential drug target for future pharmacologic treatment of hypersexual disorder, he added.
The study was supported by the Swedish Research Council, the Stockholm County Council, and by a partnership between Umeå University and Västerbotten County Council. The researchers had no financial conflicts to disclose.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM
OTC melatonin supplement use rises fivefold over 20 years
, a new study finds, although only 2% of a recent group of survey respondents said they had taken the sleep aid within the past month.
The findings, reported Feb. 1 in a research letter in the Journal of the American Medical Association, suggest that “millions of U.S. individuals are using melatonin,” study coauthor Naima Covassin, PhD, an associate consultant at Mayo Clinic in Rochester, Minn., told this news organization. “It is important to ask patients who report sleep problems whether they consume melatonin supplements, and these findings should certainly prompt more research in this area.”
The supplements boost the levels of melatonin, a hormone that is linked to the sleep-wake cycle. “Melatonin facilitates our ability to fall asleep at our bedtime by decreasing the natural early evening circadian arousal that helps keep us alert despite our having been awake since the morning,” said David N. Neubauer, MD, a sleep specialist at Johns Hopkins University, Baltimore. “It isn’t so much that melatonin is sedating, but rather that it turns off arousal.”
For the new study, researchers tracked data from the National Health and Nutrition Examination Survey from 1999-2000 to 2017-2018 and focused on respondents aged 20 and older (n = 55,021, mean age, 47.5, 52% women). As the researchers noted, response rates dipped mightily from a high of 84% in 2001-2002 to just 51.9% in 2017-2018.
The study found that the overall reported weighted prevalence of melatonin use grew from 0.4% (95% confidence interval, 0.2%-1.0%) in 1999-2000 to 2.1% (95% CI, 1.5%-2.9%) in 2017-2018 (linear P = .004). In 93.9% of cases of reported melatonin use, the surveyors confirmed it by checking for supplement bottles.
“These trends were similar in men and women and across age groups,” Dr. Covassin said. “We also found that use of more than 5 mg/day melatonin was not reported till 2005-2006, and it has been increasing since.”
Melatonin supplements are now available in tablets, capsules, gummies, powders, liquids, sprays, and other formulations. Users can even buy CBD-melatonin combos.
The survey doesn’t explore why the respondents used melatonin nor whether they thought it actually helped them. “The study was designed to evaluate the breadth of use of melatonin, rather than its effectiveness as a sleep aid,” Dr. Covassin said.
Dr. Neubauer, who wasn’t associated with the study, said the research seems valid. According to him, melatonin use has likely grown because of marketing and a higher number of products. He added that melatonin products are being manufactured at higher doses, although melatonin has a flat dose-response curve. “Higher doses typically do not have a greater effect,” he said.
According to Dr. Covassin, melatonin is generally considered to be safe, although side effects such as fatigue, dizziness, and headaches have been reported in clinical trials. “This is especially evident when high doses are administered,” Dr. Covassin said. “Other potentially more harmful consequences have also been noted. For instance, it has been found that acute administration of melatonin may decrease glucose tolerance, which may be especially problematic in patients with preexisting vulnerabilities such in those with diabetes. There are also very limited data on whether sustained use is safe in the long run.”
Moving forward, Dr. Covassin said, “we are interested in better understanding consumption of melatonin supplements across different populations as well as the impact of chronic use.”
The study authors are supported by grants from the National Natural Science Foundation of China, National Institutes of Health, Sleep Number Corporation (to Mayo Clinic), the Alice Sheets Marriott Professorship, and the Mayo Clinic Marie Ingalls Research Career Development Award.
Dr. Covassin and Dr. Neubauer have disclosed no relevant financial relationships. Study coauthor Virend K. Somers, MD, PhD, reports having served as a consultant for Respicardia, Baker Tilly, Bayer, and Jazz Pharmaceuticals and serving on the Sleep Number Research Advisory Board.
A version of this article first appeared on Medscape.com.
, a new study finds, although only 2% of a recent group of survey respondents said they had taken the sleep aid within the past month.
The findings, reported Feb. 1 in a research letter in the Journal of the American Medical Association, suggest that “millions of U.S. individuals are using melatonin,” study coauthor Naima Covassin, PhD, an associate consultant at Mayo Clinic in Rochester, Minn., told this news organization. “It is important to ask patients who report sleep problems whether they consume melatonin supplements, and these findings should certainly prompt more research in this area.”
The supplements boost the levels of melatonin, a hormone that is linked to the sleep-wake cycle. “Melatonin facilitates our ability to fall asleep at our bedtime by decreasing the natural early evening circadian arousal that helps keep us alert despite our having been awake since the morning,” said David N. Neubauer, MD, a sleep specialist at Johns Hopkins University, Baltimore. “It isn’t so much that melatonin is sedating, but rather that it turns off arousal.”
For the new study, researchers tracked data from the National Health and Nutrition Examination Survey from 1999-2000 to 2017-2018 and focused on respondents aged 20 and older (n = 55,021, mean age, 47.5, 52% women). As the researchers noted, response rates dipped mightily from a high of 84% in 2001-2002 to just 51.9% in 2017-2018.
The study found that the overall reported weighted prevalence of melatonin use grew from 0.4% (95% confidence interval, 0.2%-1.0%) in 1999-2000 to 2.1% (95% CI, 1.5%-2.9%) in 2017-2018 (linear P = .004). In 93.9% of cases of reported melatonin use, the surveyors confirmed it by checking for supplement bottles.
“These trends were similar in men and women and across age groups,” Dr. Covassin said. “We also found that use of more than 5 mg/day melatonin was not reported till 2005-2006, and it has been increasing since.”
Melatonin supplements are now available in tablets, capsules, gummies, powders, liquids, sprays, and other formulations. Users can even buy CBD-melatonin combos.
The survey doesn’t explore why the respondents used melatonin nor whether they thought it actually helped them. “The study was designed to evaluate the breadth of use of melatonin, rather than its effectiveness as a sleep aid,” Dr. Covassin said.
Dr. Neubauer, who wasn’t associated with the study, said the research seems valid. According to him, melatonin use has likely grown because of marketing and a higher number of products. He added that melatonin products are being manufactured at higher doses, although melatonin has a flat dose-response curve. “Higher doses typically do not have a greater effect,” he said.
According to Dr. Covassin, melatonin is generally considered to be safe, although side effects such as fatigue, dizziness, and headaches have been reported in clinical trials. “This is especially evident when high doses are administered,” Dr. Covassin said. “Other potentially more harmful consequences have also been noted. For instance, it has been found that acute administration of melatonin may decrease glucose tolerance, which may be especially problematic in patients with preexisting vulnerabilities such in those with diabetes. There are also very limited data on whether sustained use is safe in the long run.”
Moving forward, Dr. Covassin said, “we are interested in better understanding consumption of melatonin supplements across different populations as well as the impact of chronic use.”
The study authors are supported by grants from the National Natural Science Foundation of China, National Institutes of Health, Sleep Number Corporation (to Mayo Clinic), the Alice Sheets Marriott Professorship, and the Mayo Clinic Marie Ingalls Research Career Development Award.
Dr. Covassin and Dr. Neubauer have disclosed no relevant financial relationships. Study coauthor Virend K. Somers, MD, PhD, reports having served as a consultant for Respicardia, Baker Tilly, Bayer, and Jazz Pharmaceuticals and serving on the Sleep Number Research Advisory Board.
A version of this article first appeared on Medscape.com.
, a new study finds, although only 2% of a recent group of survey respondents said they had taken the sleep aid within the past month.
The findings, reported Feb. 1 in a research letter in the Journal of the American Medical Association, suggest that “millions of U.S. individuals are using melatonin,” study coauthor Naima Covassin, PhD, an associate consultant at Mayo Clinic in Rochester, Minn., told this news organization. “It is important to ask patients who report sleep problems whether they consume melatonin supplements, and these findings should certainly prompt more research in this area.”
The supplements boost the levels of melatonin, a hormone that is linked to the sleep-wake cycle. “Melatonin facilitates our ability to fall asleep at our bedtime by decreasing the natural early evening circadian arousal that helps keep us alert despite our having been awake since the morning,” said David N. Neubauer, MD, a sleep specialist at Johns Hopkins University, Baltimore. “It isn’t so much that melatonin is sedating, but rather that it turns off arousal.”
For the new study, researchers tracked data from the National Health and Nutrition Examination Survey from 1999-2000 to 2017-2018 and focused on respondents aged 20 and older (n = 55,021, mean age, 47.5, 52% women). As the researchers noted, response rates dipped mightily from a high of 84% in 2001-2002 to just 51.9% in 2017-2018.
The study found that the overall reported weighted prevalence of melatonin use grew from 0.4% (95% confidence interval, 0.2%-1.0%) in 1999-2000 to 2.1% (95% CI, 1.5%-2.9%) in 2017-2018 (linear P = .004). In 93.9% of cases of reported melatonin use, the surveyors confirmed it by checking for supplement bottles.
“These trends were similar in men and women and across age groups,” Dr. Covassin said. “We also found that use of more than 5 mg/day melatonin was not reported till 2005-2006, and it has been increasing since.”
Melatonin supplements are now available in tablets, capsules, gummies, powders, liquids, sprays, and other formulations. Users can even buy CBD-melatonin combos.
The survey doesn’t explore why the respondents used melatonin nor whether they thought it actually helped them. “The study was designed to evaluate the breadth of use of melatonin, rather than its effectiveness as a sleep aid,” Dr. Covassin said.
Dr. Neubauer, who wasn’t associated with the study, said the research seems valid. According to him, melatonin use has likely grown because of marketing and a higher number of products. He added that melatonin products are being manufactured at higher doses, although melatonin has a flat dose-response curve. “Higher doses typically do not have a greater effect,” he said.
According to Dr. Covassin, melatonin is generally considered to be safe, although side effects such as fatigue, dizziness, and headaches have been reported in clinical trials. “This is especially evident when high doses are administered,” Dr. Covassin said. “Other potentially more harmful consequences have also been noted. For instance, it has been found that acute administration of melatonin may decrease glucose tolerance, which may be especially problematic in patients with preexisting vulnerabilities such in those with diabetes. There are also very limited data on whether sustained use is safe in the long run.”
Moving forward, Dr. Covassin said, “we are interested in better understanding consumption of melatonin supplements across different populations as well as the impact of chronic use.”
The study authors are supported by grants from the National Natural Science Foundation of China, National Institutes of Health, Sleep Number Corporation (to Mayo Clinic), the Alice Sheets Marriott Professorship, and the Mayo Clinic Marie Ingalls Research Career Development Award.
Dr. Covassin and Dr. Neubauer have disclosed no relevant financial relationships. Study coauthor Virend K. Somers, MD, PhD, reports having served as a consultant for Respicardia, Baker Tilly, Bayer, and Jazz Pharmaceuticals and serving on the Sleep Number Research Advisory Board.
A version of this article first appeared on Medscape.com.
FROM JAMA
The cell that might trigger Alzheimer’s disease
It all started with genetic data. A gene here, a gene there. Eventually the story became clearer: If scientists are to one day find a cure for Alzheimer’s disease, they should look to the immune system.
Over the past couple decades, researchers have identified numerous genes involved in various immune system functions that may also contribute to Alzheimer’s disease. Some of the prime suspects are genes that control microglia, now the focus of intense research in developing new Alzheimer’s drugs.
Microglia are amoeba-like cells that scour the brain for injuries and invaders. They help clear dead or impaired brain cells and literally gobble up invading microbes. Without them, we’d be in trouble.
In a normal brain, a protein called beta-amyloid is cleared away through our lymphatic system by microglia as molecular junk. But sometimes it builds up. Certain gene mutations are one culprit in this toxic accumulation. Traumatic brain injury is another, and, perhaps, impaired microglial function.
One thing everyone agrees on is that in people with Alzheimer’s disease, too much amyloid accumulates between their brain cells and in the vessels that supply the brain with blood. Once amyloid begins to clog networks of neurons, it triggers the accumulation of another protein, called tau, inside of these brain cells. The presence of tau sends microglia and other immune mechanisms into overdrive, resulting in the inflammatory immune response that many experts believe ultimately saps brain vitality in Alzheimer’s disease.
The gene scene
To date, nearly a dozen genes involved in immune and microglial function have been tied to Alzheimer’s disease. The first was CD33, identified in 2008.
“When we got the results, I literally ran to my colleague’s office next door and said, you gotta see this!” said Harvard neuroscientist Rudolph Tanzi. Dr. Tanzi, who goes by Rudy, led the CD33 research. The discovery was quickly named a top medical breakthrough of 2008 by Time magazine.
“We were laughing because what they didn’t know is we had no idea what this gene did,” he joked. But over time, research by Dr. Tanzi and his group revealed that CD33 is a kind of microglial on-off switch, activating the cells as part of an inflammatory pathway.
“We kind of got it all going when it came to the genetics,” he said.
Microglia normally recognize molecular patterns associated with microbes and cellular damage as unwanted. This is how they know to take action – to devour unfamiliar pathogens and dead tissue. Dr. Tanzi believes microglia sense any sign of brain damage as an infection, which causes them to become hyperactive.
Much of our modern human immune system, he explained, evolved many hundreds of thousands of years ago. Our lifespans at the time were far shorter than they are today, and the majority of people didn’t live long enough to develop dementia or the withered brain cells that come with it. So our immune system, he said, assumes any faulty brain tissue is due to a microbe, not dementia. Microglia react aggressively, clearing the area to prevent the spread of infection.
“They say, ‘We better wipe out this part of the brain that’s infected, even if it’s not.’ They don’t know,” quipped Dr. Tanzi. “That’s what causes neuroinflammation. And CD33 turns this response on. The microglia become killers, not just janitors.”
A brake on overactive microglia
If CD33 is the yin, a gene called TREM2 is the yang. Discovered a few years after CD33, TREM2 reins in microglial activation, returning them to their role as cellular housekeepers.
Neurologist David Holtzman, MD, of Washington University in St. Louis, who studies TREM2, agrees that wherever you find amyloid, tau, or dead brain cells, there are microglia raring to go and ready to scavenge.
“I think at first a lot of people thought these cells were reacting to Alzheimer’s pathology, and not necessarily a cause of the disease,” he said.
It was the discovery of TREM2 on the heels of CD33 that really shifted the thinking, in part because it produces a protein that in the brain is only found in microglia. “Many of us [in the field] immediately said, ‘Look, there’s now a risk factor that is only expressed in microglia. It must be that innate immune cells are important in some way in the pathogenesis of the disease,’ “ he added.
Dr. Holtzman sees microglial activation in impending dementia as a double-edged sword. In the beginning, microglia clear unwanted amyloid to maintain brain health. But once accumulated amyloid and tau have done enough damage, the neuroinflammation that comes with microglial activation does more harm than good. Neurons die en masse and dementia sets in.
But not all researchers are convinced.
Serge Revist, PhD, is a professor in the department of molecular medicine at the Laval University Medical School in Quebec. Based on his lab’s research, he believes that while impaired immune activity is involved in Alzheimer’s disease, it is not the root cause. “I don’t think it is the immune cells that do the damage, I still think it is the beta-amyloid itself,” he said, “In my lab, in mouse studies, we’ve never found that immune cells were directly responsible for killing neurons.”
He does believe that in some patients with Alzheimer’s disease, microglia may not be able to handle the excess amyloid that accumulates in the disease and that developing treatments that improve the ability of microglia and the immune system to clear the protein could be effective.
Microglial medicines
The biological cascade leading to Alzheimer’s disease is a tangled one. Gene variants influencing the accumulation and clearance of amyloid are likely a major contributor. But immune activity caused by early life infection might also be involved, at least in some cases. This infectious theory of Alzheimer’s disease was first proposed by Dr. Tanzi’s now-deceased colleague Robert Moir, PhD. Dr. Tanzi’s group even has evidence that amyloid itself is antimicrobial and evolved to protect us from pathogens, only to become a problem when overactive and aggregated.
And the same goes for microglia, cells whose over-ambition might cause much of the brain degeneration seen in Alzheimer’s disease.
In theory, if a treatment could decrease CD33 activity or increase that of TREM2, doctors might one day may be able to slow or even stop the progression of dementia. Instead of going after amyloid itself – the mechanism behind so many failed investigational Alzheimer’s drugs – a therapy that quells the immune response to amyloid might be the answer in treating dementia.
“There are a number of scientists and companies trying to figure out how to influence genes like TREM2 and CD33 and to both decrease amyloid and act on the downstream consequences of the protein,” said Dr. Holtzman. “All of this is to say that somewhere in the biology that causes Alzheimer’s disease, the immune system is involved.”
It seems that in many cases, the most common form of a dementia might be due to a well-intentioned immune cell going rogue. “I think you’d hear this from basically any researcher worth their salt,” said Dr. Tanzi. “I feel strongly that without microglial activation, you will not get Alzheimer’s disease.”
A version of this article first appeared on Medscape.com.
It all started with genetic data. A gene here, a gene there. Eventually the story became clearer: If scientists are to one day find a cure for Alzheimer’s disease, they should look to the immune system.
Over the past couple decades, researchers have identified numerous genes involved in various immune system functions that may also contribute to Alzheimer’s disease. Some of the prime suspects are genes that control microglia, now the focus of intense research in developing new Alzheimer’s drugs.
Microglia are amoeba-like cells that scour the brain for injuries and invaders. They help clear dead or impaired brain cells and literally gobble up invading microbes. Without them, we’d be in trouble.
In a normal brain, a protein called beta-amyloid is cleared away through our lymphatic system by microglia as molecular junk. But sometimes it builds up. Certain gene mutations are one culprit in this toxic accumulation. Traumatic brain injury is another, and, perhaps, impaired microglial function.
One thing everyone agrees on is that in people with Alzheimer’s disease, too much amyloid accumulates between their brain cells and in the vessels that supply the brain with blood. Once amyloid begins to clog networks of neurons, it triggers the accumulation of another protein, called tau, inside of these brain cells. The presence of tau sends microglia and other immune mechanisms into overdrive, resulting in the inflammatory immune response that many experts believe ultimately saps brain vitality in Alzheimer’s disease.
The gene scene
To date, nearly a dozen genes involved in immune and microglial function have been tied to Alzheimer’s disease. The first was CD33, identified in 2008.
“When we got the results, I literally ran to my colleague’s office next door and said, you gotta see this!” said Harvard neuroscientist Rudolph Tanzi. Dr. Tanzi, who goes by Rudy, led the CD33 research. The discovery was quickly named a top medical breakthrough of 2008 by Time magazine.
“We were laughing because what they didn’t know is we had no idea what this gene did,” he joked. But over time, research by Dr. Tanzi and his group revealed that CD33 is a kind of microglial on-off switch, activating the cells as part of an inflammatory pathway.
“We kind of got it all going when it came to the genetics,” he said.
Microglia normally recognize molecular patterns associated with microbes and cellular damage as unwanted. This is how they know to take action – to devour unfamiliar pathogens and dead tissue. Dr. Tanzi believes microglia sense any sign of brain damage as an infection, which causes them to become hyperactive.
Much of our modern human immune system, he explained, evolved many hundreds of thousands of years ago. Our lifespans at the time were far shorter than they are today, and the majority of people didn’t live long enough to develop dementia or the withered brain cells that come with it. So our immune system, he said, assumes any faulty brain tissue is due to a microbe, not dementia. Microglia react aggressively, clearing the area to prevent the spread of infection.
“They say, ‘We better wipe out this part of the brain that’s infected, even if it’s not.’ They don’t know,” quipped Dr. Tanzi. “That’s what causes neuroinflammation. And CD33 turns this response on. The microglia become killers, not just janitors.”
A brake on overactive microglia
If CD33 is the yin, a gene called TREM2 is the yang. Discovered a few years after CD33, TREM2 reins in microglial activation, returning them to their role as cellular housekeepers.
Neurologist David Holtzman, MD, of Washington University in St. Louis, who studies TREM2, agrees that wherever you find amyloid, tau, or dead brain cells, there are microglia raring to go and ready to scavenge.
“I think at first a lot of people thought these cells were reacting to Alzheimer’s pathology, and not necessarily a cause of the disease,” he said.
It was the discovery of TREM2 on the heels of CD33 that really shifted the thinking, in part because it produces a protein that in the brain is only found in microglia. “Many of us [in the field] immediately said, ‘Look, there’s now a risk factor that is only expressed in microglia. It must be that innate immune cells are important in some way in the pathogenesis of the disease,’ “ he added.
Dr. Holtzman sees microglial activation in impending dementia as a double-edged sword. In the beginning, microglia clear unwanted amyloid to maintain brain health. But once accumulated amyloid and tau have done enough damage, the neuroinflammation that comes with microglial activation does more harm than good. Neurons die en masse and dementia sets in.
But not all researchers are convinced.
Serge Revist, PhD, is a professor in the department of molecular medicine at the Laval University Medical School in Quebec. Based on his lab’s research, he believes that while impaired immune activity is involved in Alzheimer’s disease, it is not the root cause. “I don’t think it is the immune cells that do the damage, I still think it is the beta-amyloid itself,” he said, “In my lab, in mouse studies, we’ve never found that immune cells were directly responsible for killing neurons.”
He does believe that in some patients with Alzheimer’s disease, microglia may not be able to handle the excess amyloid that accumulates in the disease and that developing treatments that improve the ability of microglia and the immune system to clear the protein could be effective.
Microglial medicines
The biological cascade leading to Alzheimer’s disease is a tangled one. Gene variants influencing the accumulation and clearance of amyloid are likely a major contributor. But immune activity caused by early life infection might also be involved, at least in some cases. This infectious theory of Alzheimer’s disease was first proposed by Dr. Tanzi’s now-deceased colleague Robert Moir, PhD. Dr. Tanzi’s group even has evidence that amyloid itself is antimicrobial and evolved to protect us from pathogens, only to become a problem when overactive and aggregated.
And the same goes for microglia, cells whose over-ambition might cause much of the brain degeneration seen in Alzheimer’s disease.
In theory, if a treatment could decrease CD33 activity or increase that of TREM2, doctors might one day may be able to slow or even stop the progression of dementia. Instead of going after amyloid itself – the mechanism behind so many failed investigational Alzheimer’s drugs – a therapy that quells the immune response to amyloid might be the answer in treating dementia.
“There are a number of scientists and companies trying to figure out how to influence genes like TREM2 and CD33 and to both decrease amyloid and act on the downstream consequences of the protein,” said Dr. Holtzman. “All of this is to say that somewhere in the biology that causes Alzheimer’s disease, the immune system is involved.”
It seems that in many cases, the most common form of a dementia might be due to a well-intentioned immune cell going rogue. “I think you’d hear this from basically any researcher worth their salt,” said Dr. Tanzi. “I feel strongly that without microglial activation, you will not get Alzheimer’s disease.”
A version of this article first appeared on Medscape.com.
It all started with genetic data. A gene here, a gene there. Eventually the story became clearer: If scientists are to one day find a cure for Alzheimer’s disease, they should look to the immune system.
Over the past couple decades, researchers have identified numerous genes involved in various immune system functions that may also contribute to Alzheimer’s disease. Some of the prime suspects are genes that control microglia, now the focus of intense research in developing new Alzheimer’s drugs.
Microglia are amoeba-like cells that scour the brain for injuries and invaders. They help clear dead or impaired brain cells and literally gobble up invading microbes. Without them, we’d be in trouble.
In a normal brain, a protein called beta-amyloid is cleared away through our lymphatic system by microglia as molecular junk. But sometimes it builds up. Certain gene mutations are one culprit in this toxic accumulation. Traumatic brain injury is another, and, perhaps, impaired microglial function.
One thing everyone agrees on is that in people with Alzheimer’s disease, too much amyloid accumulates between their brain cells and in the vessels that supply the brain with blood. Once amyloid begins to clog networks of neurons, it triggers the accumulation of another protein, called tau, inside of these brain cells. The presence of tau sends microglia and other immune mechanisms into overdrive, resulting in the inflammatory immune response that many experts believe ultimately saps brain vitality in Alzheimer’s disease.
The gene scene
To date, nearly a dozen genes involved in immune and microglial function have been tied to Alzheimer’s disease. The first was CD33, identified in 2008.
“When we got the results, I literally ran to my colleague’s office next door and said, you gotta see this!” said Harvard neuroscientist Rudolph Tanzi. Dr. Tanzi, who goes by Rudy, led the CD33 research. The discovery was quickly named a top medical breakthrough of 2008 by Time magazine.
“We were laughing because what they didn’t know is we had no idea what this gene did,” he joked. But over time, research by Dr. Tanzi and his group revealed that CD33 is a kind of microglial on-off switch, activating the cells as part of an inflammatory pathway.
“We kind of got it all going when it came to the genetics,” he said.
Microglia normally recognize molecular patterns associated with microbes and cellular damage as unwanted. This is how they know to take action – to devour unfamiliar pathogens and dead tissue. Dr. Tanzi believes microglia sense any sign of brain damage as an infection, which causes them to become hyperactive.
Much of our modern human immune system, he explained, evolved many hundreds of thousands of years ago. Our lifespans at the time were far shorter than they are today, and the majority of people didn’t live long enough to develop dementia or the withered brain cells that come with it. So our immune system, he said, assumes any faulty brain tissue is due to a microbe, not dementia. Microglia react aggressively, clearing the area to prevent the spread of infection.
“They say, ‘We better wipe out this part of the brain that’s infected, even if it’s not.’ They don’t know,” quipped Dr. Tanzi. “That’s what causes neuroinflammation. And CD33 turns this response on. The microglia become killers, not just janitors.”
A brake on overactive microglia
If CD33 is the yin, a gene called TREM2 is the yang. Discovered a few years after CD33, TREM2 reins in microglial activation, returning them to their role as cellular housekeepers.
Neurologist David Holtzman, MD, of Washington University in St. Louis, who studies TREM2, agrees that wherever you find amyloid, tau, or dead brain cells, there are microglia raring to go and ready to scavenge.
“I think at first a lot of people thought these cells were reacting to Alzheimer’s pathology, and not necessarily a cause of the disease,” he said.
It was the discovery of TREM2 on the heels of CD33 that really shifted the thinking, in part because it produces a protein that in the brain is only found in microglia. “Many of us [in the field] immediately said, ‘Look, there’s now a risk factor that is only expressed in microglia. It must be that innate immune cells are important in some way in the pathogenesis of the disease,’ “ he added.
Dr. Holtzman sees microglial activation in impending dementia as a double-edged sword. In the beginning, microglia clear unwanted amyloid to maintain brain health. But once accumulated amyloid and tau have done enough damage, the neuroinflammation that comes with microglial activation does more harm than good. Neurons die en masse and dementia sets in.
But not all researchers are convinced.
Serge Revist, PhD, is a professor in the department of molecular medicine at the Laval University Medical School in Quebec. Based on his lab’s research, he believes that while impaired immune activity is involved in Alzheimer’s disease, it is not the root cause. “I don’t think it is the immune cells that do the damage, I still think it is the beta-amyloid itself,” he said, “In my lab, in mouse studies, we’ve never found that immune cells were directly responsible for killing neurons.”
He does believe that in some patients with Alzheimer’s disease, microglia may not be able to handle the excess amyloid that accumulates in the disease and that developing treatments that improve the ability of microglia and the immune system to clear the protein could be effective.
Microglial medicines
The biological cascade leading to Alzheimer’s disease is a tangled one. Gene variants influencing the accumulation and clearance of amyloid are likely a major contributor. But immune activity caused by early life infection might also be involved, at least in some cases. This infectious theory of Alzheimer’s disease was first proposed by Dr. Tanzi’s now-deceased colleague Robert Moir, PhD. Dr. Tanzi’s group even has evidence that amyloid itself is antimicrobial and evolved to protect us from pathogens, only to become a problem when overactive and aggregated.
And the same goes for microglia, cells whose over-ambition might cause much of the brain degeneration seen in Alzheimer’s disease.
In theory, if a treatment could decrease CD33 activity or increase that of TREM2, doctors might one day may be able to slow or even stop the progression of dementia. Instead of going after amyloid itself – the mechanism behind so many failed investigational Alzheimer’s drugs – a therapy that quells the immune response to amyloid might be the answer in treating dementia.
“There are a number of scientists and companies trying to figure out how to influence genes like TREM2 and CD33 and to both decrease amyloid and act on the downstream consequences of the protein,” said Dr. Holtzman. “All of this is to say that somewhere in the biology that causes Alzheimer’s disease, the immune system is involved.”
It seems that in many cases, the most common form of a dementia might be due to a well-intentioned immune cell going rogue. “I think you’d hear this from basically any researcher worth their salt,” said Dr. Tanzi. “I feel strongly that without microglial activation, you will not get Alzheimer’s disease.”
A version of this article first appeared on Medscape.com.
Psychedelic therapy and suicide: A myth busted?
A commonly held belief that classic psychedelic therapy can trigger suicidal thoughts, actions, or other types of self-harm is not supported by research, and, in fact, the opposite may be true.
Results from a meta-analysis of individual patient data showed that psychedelic therapy was associated with large, acute, and sustained decreases in suicidality across a range of clinical patient populations.
“ It gives us a better understanding of the effects of psychedelics on suicidality in the context of clinical trials,” study investigator Cory Weissman, MD, department of psychiatry, University of Toronto, told this news organization.
The evidence suggests psychedelic therapy “may reduce suicidal ideation when administered in the appropriate setting and offered to carefully screened patients,” Dr. Weissman said.
The findings were published online Jan. 18 in The Journal of Clinical Psychiatry.
More research needed
The analysis included seven psychedelic therapy clinical trials that had data on suicidality. Five of the trials used psilocybin plus psychotherapy and two used ayahuasca plus psychotherapy. All seven trials had a “low” risk of bias.
Patients included in the trials had treatment-resistant major depressive disorder (MDD), recurrent MDD, AIDS-related demoralization, and distress related to life-threatening cancer.
The meta-analytic results showed significant decreases in suicidality at all acute time points (80 to 240 minutes post administration) and at most post-acute time points (1 day to 4 months post administration).
Effect sizes for reductions in suicidality were “large” at all acute time points, with standardized mean differences (SMD) ranging from -1.48 to -1.72, and remained large from 1 day to 3-4 months after therapy (SMD range, -1.50 to -2.36).
At 6 months, the effect size for reductions in suicidality with psychedelic therapy was “medium” (SMD, -0.65).
Large effect sizes for reductions in suicidality occurred across the different patient populations represented in the trial, the investigators note.
No study reported any suicide-related adverse events because of administration of a psychedelic. There were also “very few” acute (6.5%) or postacute (3.0%) elevations in suicidality, “providing support for the safety of psychedelic therapy within controlled contexts,” the researchers write.
They caution, however, that large controlled trials that specifically evaluate the effect of psychedelic therapy on suicidality are needed.
Promising avenue
In an accompanying editorial, Daniel Grossman, BS, and Peter Hendricks, PhD, department of health behavior, University of Alabama at Birmingham, note that results of this review warrant “optimism” for use of psychedelics for treatment of suicidality.
Based on this study and others, classic psychedelic therapy for suicidality appears to be a “promising avenue” for further investigation, they write.
However, research and anecdotes about increased suicidality and other self-harm attributed to psychedelic therapy, “though evidently rare, remain a critical concern” for further research to address, Dr. Grossman and Dr. Hendricks add.
The hope is that future research “clarifies who is most subject to these risks, what factors best identify them, and how best to navigate their treatment safely,” they write.
The meta-analysis had no funding. Dr. Weissman receives funding from the Brain and Behavior Research Foundation and serves on the advisory board of GoodCap Pharmaceuticals. Dr. Hendricks is on the scientific advisory board of Bright Minds Biosciences, Eleusis Benefit Corporation, and Rest Pharmaceuticals.
A version of this article first appeared on Medscape.com.
A commonly held belief that classic psychedelic therapy can trigger suicidal thoughts, actions, or other types of self-harm is not supported by research, and, in fact, the opposite may be true.
Results from a meta-analysis of individual patient data showed that psychedelic therapy was associated with large, acute, and sustained decreases in suicidality across a range of clinical patient populations.
“ It gives us a better understanding of the effects of psychedelics on suicidality in the context of clinical trials,” study investigator Cory Weissman, MD, department of psychiatry, University of Toronto, told this news organization.
The evidence suggests psychedelic therapy “may reduce suicidal ideation when administered in the appropriate setting and offered to carefully screened patients,” Dr. Weissman said.
The findings were published online Jan. 18 in The Journal of Clinical Psychiatry.
More research needed
The analysis included seven psychedelic therapy clinical trials that had data on suicidality. Five of the trials used psilocybin plus psychotherapy and two used ayahuasca plus psychotherapy. All seven trials had a “low” risk of bias.
Patients included in the trials had treatment-resistant major depressive disorder (MDD), recurrent MDD, AIDS-related demoralization, and distress related to life-threatening cancer.
The meta-analytic results showed significant decreases in suicidality at all acute time points (80 to 240 minutes post administration) and at most post-acute time points (1 day to 4 months post administration).
Effect sizes for reductions in suicidality were “large” at all acute time points, with standardized mean differences (SMD) ranging from -1.48 to -1.72, and remained large from 1 day to 3-4 months after therapy (SMD range, -1.50 to -2.36).
At 6 months, the effect size for reductions in suicidality with psychedelic therapy was “medium” (SMD, -0.65).
Large effect sizes for reductions in suicidality occurred across the different patient populations represented in the trial, the investigators note.
No study reported any suicide-related adverse events because of administration of a psychedelic. There were also “very few” acute (6.5%) or postacute (3.0%) elevations in suicidality, “providing support for the safety of psychedelic therapy within controlled contexts,” the researchers write.
They caution, however, that large controlled trials that specifically evaluate the effect of psychedelic therapy on suicidality are needed.
Promising avenue
In an accompanying editorial, Daniel Grossman, BS, and Peter Hendricks, PhD, department of health behavior, University of Alabama at Birmingham, note that results of this review warrant “optimism” for use of psychedelics for treatment of suicidality.
Based on this study and others, classic psychedelic therapy for suicidality appears to be a “promising avenue” for further investigation, they write.
However, research and anecdotes about increased suicidality and other self-harm attributed to psychedelic therapy, “though evidently rare, remain a critical concern” for further research to address, Dr. Grossman and Dr. Hendricks add.
The hope is that future research “clarifies who is most subject to these risks, what factors best identify them, and how best to navigate their treatment safely,” they write.
The meta-analysis had no funding. Dr. Weissman receives funding from the Brain and Behavior Research Foundation and serves on the advisory board of GoodCap Pharmaceuticals. Dr. Hendricks is on the scientific advisory board of Bright Minds Biosciences, Eleusis Benefit Corporation, and Rest Pharmaceuticals.
A version of this article first appeared on Medscape.com.
A commonly held belief that classic psychedelic therapy can trigger suicidal thoughts, actions, or other types of self-harm is not supported by research, and, in fact, the opposite may be true.
Results from a meta-analysis of individual patient data showed that psychedelic therapy was associated with large, acute, and sustained decreases in suicidality across a range of clinical patient populations.
“ It gives us a better understanding of the effects of psychedelics on suicidality in the context of clinical trials,” study investigator Cory Weissman, MD, department of psychiatry, University of Toronto, told this news organization.
The evidence suggests psychedelic therapy “may reduce suicidal ideation when administered in the appropriate setting and offered to carefully screened patients,” Dr. Weissman said.
The findings were published online Jan. 18 in The Journal of Clinical Psychiatry.
More research needed
The analysis included seven psychedelic therapy clinical trials that had data on suicidality. Five of the trials used psilocybin plus psychotherapy and two used ayahuasca plus psychotherapy. All seven trials had a “low” risk of bias.
Patients included in the trials had treatment-resistant major depressive disorder (MDD), recurrent MDD, AIDS-related demoralization, and distress related to life-threatening cancer.
The meta-analytic results showed significant decreases in suicidality at all acute time points (80 to 240 minutes post administration) and at most post-acute time points (1 day to 4 months post administration).
Effect sizes for reductions in suicidality were “large” at all acute time points, with standardized mean differences (SMD) ranging from -1.48 to -1.72, and remained large from 1 day to 3-4 months after therapy (SMD range, -1.50 to -2.36).
At 6 months, the effect size for reductions in suicidality with psychedelic therapy was “medium” (SMD, -0.65).
Large effect sizes for reductions in suicidality occurred across the different patient populations represented in the trial, the investigators note.
No study reported any suicide-related adverse events because of administration of a psychedelic. There were also “very few” acute (6.5%) or postacute (3.0%) elevations in suicidality, “providing support for the safety of psychedelic therapy within controlled contexts,” the researchers write.
They caution, however, that large controlled trials that specifically evaluate the effect of psychedelic therapy on suicidality are needed.
Promising avenue
In an accompanying editorial, Daniel Grossman, BS, and Peter Hendricks, PhD, department of health behavior, University of Alabama at Birmingham, note that results of this review warrant “optimism” for use of psychedelics for treatment of suicidality.
Based on this study and others, classic psychedelic therapy for suicidality appears to be a “promising avenue” for further investigation, they write.
However, research and anecdotes about increased suicidality and other self-harm attributed to psychedelic therapy, “though evidently rare, remain a critical concern” for further research to address, Dr. Grossman and Dr. Hendricks add.
The hope is that future research “clarifies who is most subject to these risks, what factors best identify them, and how best to navigate their treatment safely,” they write.
The meta-analysis had no funding. Dr. Weissman receives funding from the Brain and Behavior Research Foundation and serves on the advisory board of GoodCap Pharmaceuticals. Dr. Hendricks is on the scientific advisory board of Bright Minds Biosciences, Eleusis Benefit Corporation, and Rest Pharmaceuticals.
A version of this article first appeared on Medscape.com.
What docs don’t know about the Disabilities Act can hurt them and patients
Lisa Iezzoni, MD, a professor of medicine at Harvard Medical School and a disability researcher at Massachusetts General Hospital, both in Boston, has used a wheelchair for more than 30 years because of multiple sclerosis. When she visits her primary care doctor, she doesn’t get weighed because the scales are not wheelchair accessible.
This failure to weigh her and other patients in wheelchairs could lead to serious medical problems. Weight is used to monitor a person’s overall health and prenatal health and to determine accurate doses for medications such as some chemotherapies, said Dr. Iezzoni.
In another situation, a man who used a wheelchair said that his primary care doctor never got him out of it for a complete physical exam. The patient later developed lymphoma, which first appeared in his groin. The doctor should have accommodated his disability and used a height-adjustable exam table or a portable lift to transfer him onto the table.
When physicians don’t provide access to medical care that patients with disabilities need, they put themselves at greater risk of lawsuits, fines, and settlements.
Yet, a new study in Health Affairs suggests that a large percentage of doctors are not fully aware of what they are legally required to do.
Under federal nondiscrimination laws (Americans With Disabilities Act, American Rehabilitation Act, and ADA Amendments Act), medical practices must provide equal access to people with disabilities, accommodate their disability-related needs, and not refuse them medical services because of their disabilities, say disability experts.
Where doctors go wrong with disability laws
What doctors don’t know about providing reasonable accommodations makes them vulnerable to lawsuits, which worries more than two-thirds of the 714 outpatient doctors surveyed.
Not only are they required to provide reasonable accommodations, but they also have to pay for them, the researchers said. One-fifth of the surveyed doctors said they didn’t know that practice owners have to pay.
More than one practice has made patients pay for services needed for their disability, such as sign language interpreters – the patients later complained this violated the ADA to enforcement agencies.
Doctors also don’t know that they have to collaborate with patients to determine what reasonable accommodations they need – over two-thirds of those surveyed said they didn’t know it was a joint responsibility, the study found.
When doctors fail to accommodate patients’ disability needs, they engage in discrimination and violate the ADA, says Elizabeth Pendo, JD, a coauthor of the study and the Joseph J. Simeone Professor of Law at Saint Louis University.
The Department of Justice has investigated several patient complaints of alleged disability discrimination recently and resolved the disputes with agreements and small fines in some cases. “The goal is not to get large financial settlements but to work with practices to get the correct procedures in place to be compliant,” said Ms. Pendo.
Physicians would be wise to check out whether their practices are as accessible as they think. Even if there’s a ramp to the office building, the parking lot may not have a van-accessible space or enough handicapped parking signs, or the exam room may be too narrow for a wheelchair to navigate.
These practices violated the ADA and agreed to make changes:
- Hamden, Conn., has two buildings that patients with physical disabilities couldn’t easily enter. The physician owners agreed to change the buildings’ entrances and access routes and add features to make it easier to use examination rooms and restrooms and the check-in and check-out areas.
- Seven medical offices in Riverside, Calif., failed to communicate effectively with deaf and hard-of-hearing patients. They should have had a qualified sign language interpreter, an assistive listening device, or another appropriate aid or service available to a deaf patient and her family. Instead, the office relied on a video remote interpretation system that often failed to work. The agreement requires the clinic to provide those aids and services to patients and their companions who are deaf or hard of hearing, advertise their availability, assess each patient who is deaf or hard of hearing to determine the best aids and services for their needs, and pay $5,000 in compensation to the complainant and a $1,000 civil penalty to the United States.
- Springfield, Mass., refused to provide full joint replacements to two patients being treated with buprenorphine, a medication used to treat opioid use disorder. Rather than accommodate the patients, the surgeons referred them elsewhere because they were uncomfortable with the postoperative pain management protocol for patients prescribed buprenorphine. “The Americans With Disabilities Act protects health care access for people under medical treatment for opioid use disorder,” said Acting U.S. Attorney Nathaniel R. Mendell. “Health care providers must comply with the ADA, even when doing so is inconvenient or makes them uncomfortable.” The agreement requires the practice to adopt a nondiscrimination policy, provide training on the ADA and opioid use disorder, and pay two complainants $15,000 each for pain and suffering.
The DOJ has filed civil lawsuits against medical practices when they failed to resolve the allegations. Recent cases include an ophthalmology practice with 24 facilities in Arizona that refused to help transfer patients in wheelchairs to surgery tables for eye surgery and required them to pay for transfer support services and two obstetricians-gynecologists in Bakersfield, Calif., who refused to provide routine medical care to a patient because of her HIV status.
What doctors should know
Many people tend to think of a person with a disability as being in a wheelchair. But the ADA has a very broad definition of disability, which includes any physical or mental impairment that substantially limits any major life activity, said Ms. Pendo.
“It was amended in 2008 to clarify that the definition includes people with chronic diseases such as diabetes and cancer, cognitive and neurological disorders, substance abuse disorders, vision and hearing loss, and learning and other disabilities,” she said.
That means that doctors have to accommodate many types of disabilities, which can be challenging. The ADA only specifies that fixed structures need to be accessible, such as parking lots, driveways, and buildings, said Dr. Iezzoni.
When it comes to “reasonable accommodations,” doctors should decide that on a case-by-case basis, she said.
“We can say based on our study that 71% of doctors don’t know the right way to think about the accommodations – they don’t know they need to talk to patients so they can explain to them exactly what they need to accommodate their disability,” said Dr. Iezzoni.
Doctors are also required to provide effective communication for patients with sensory or cognitive disabilities, which can depend on the severity, said Ms. Pendo. Is the person deaf or hard of hearing, blind or partially sighted – is the dementia mild or severe?
“The requirement is there, but what that looks like will vary by patient. That’s what’s challenging,” said Ms. Pendo.
Dr. Iezzoni recommends that doctor’s offices ask patients whether they need special help or individual assistance when they make appointments and enter their responses in their records. She also suggests that patients be asked at follow-up appointments whether they still need the same help or not.
“Disabilities can change over time – a person with bad arthritis may need help getting onto an exam table, but later get a knee or hip replacement that is effective and no longer need that help,” said Dr. Iezzoni.
Benefits outweigh costs
Physicians have made progress in meeting the ADA’s physical accessibility requirements, said Dr. Iezzoni. “The literature suggests that doctors have done a good job at fixing the structural barriers people with mobility issues face, such as ramps and bathrooms.”
However, there are exceptions in rural older buildings which can be harder to retrofit for wheelchair accessibility, she said. “I recall interviewing a rural doctor several years ago who said that he knew his patients well and when a patient visits with mobility problems, he goes down and carries the patient up the steps to his office. My response was that is not respectful of the patient or safe for the patient or you. That doctor has since changed the location of his practice,” said Dr. Iezzoni.
Some doctors may resist paying for accessible medical equipment because of cost, but she said the benefits are worth it. These include preventing staff injuries when they transfer patients and being used by patients with temporary disabilities and aging people with bad knees, backs, hearing and sight. In addition, businesses may be eligible for federal and state tax credits.
Dr. Iezzoni recently visited her doctor where they finally got height-adjustable exam tables. “I asked the assistant, who really likes these tables? She said it’s the elderly ladies of short stature – the table is lowered and they sit down and get on it.”
But, Dr. Iezonni’s main message to doctors is that patients with disabilities deserve equal quality of care. “Just because we have a disability doesn’t mean we should get worse care than other people. It’s a matter of professionalism that doctors should want to give the same quality care to all their patients.”
A version of this article first appeared on Medscape.com.
Lisa Iezzoni, MD, a professor of medicine at Harvard Medical School and a disability researcher at Massachusetts General Hospital, both in Boston, has used a wheelchair for more than 30 years because of multiple sclerosis. When she visits her primary care doctor, she doesn’t get weighed because the scales are not wheelchair accessible.
This failure to weigh her and other patients in wheelchairs could lead to serious medical problems. Weight is used to monitor a person’s overall health and prenatal health and to determine accurate doses for medications such as some chemotherapies, said Dr. Iezzoni.
In another situation, a man who used a wheelchair said that his primary care doctor never got him out of it for a complete physical exam. The patient later developed lymphoma, which first appeared in his groin. The doctor should have accommodated his disability and used a height-adjustable exam table or a portable lift to transfer him onto the table.
When physicians don’t provide access to medical care that patients with disabilities need, they put themselves at greater risk of lawsuits, fines, and settlements.
Yet, a new study in Health Affairs suggests that a large percentage of doctors are not fully aware of what they are legally required to do.
Under federal nondiscrimination laws (Americans With Disabilities Act, American Rehabilitation Act, and ADA Amendments Act), medical practices must provide equal access to people with disabilities, accommodate their disability-related needs, and not refuse them medical services because of their disabilities, say disability experts.
Where doctors go wrong with disability laws
What doctors don’t know about providing reasonable accommodations makes them vulnerable to lawsuits, which worries more than two-thirds of the 714 outpatient doctors surveyed.
Not only are they required to provide reasonable accommodations, but they also have to pay for them, the researchers said. One-fifth of the surveyed doctors said they didn’t know that practice owners have to pay.
More than one practice has made patients pay for services needed for their disability, such as sign language interpreters – the patients later complained this violated the ADA to enforcement agencies.
Doctors also don’t know that they have to collaborate with patients to determine what reasonable accommodations they need – over two-thirds of those surveyed said they didn’t know it was a joint responsibility, the study found.
When doctors fail to accommodate patients’ disability needs, they engage in discrimination and violate the ADA, says Elizabeth Pendo, JD, a coauthor of the study and the Joseph J. Simeone Professor of Law at Saint Louis University.
The Department of Justice has investigated several patient complaints of alleged disability discrimination recently and resolved the disputes with agreements and small fines in some cases. “The goal is not to get large financial settlements but to work with practices to get the correct procedures in place to be compliant,” said Ms. Pendo.
Physicians would be wise to check out whether their practices are as accessible as they think. Even if there’s a ramp to the office building, the parking lot may not have a van-accessible space or enough handicapped parking signs, or the exam room may be too narrow for a wheelchair to navigate.
These practices violated the ADA and agreed to make changes:
- Hamden, Conn., has two buildings that patients with physical disabilities couldn’t easily enter. The physician owners agreed to change the buildings’ entrances and access routes and add features to make it easier to use examination rooms and restrooms and the check-in and check-out areas.
- Seven medical offices in Riverside, Calif., failed to communicate effectively with deaf and hard-of-hearing patients. They should have had a qualified sign language interpreter, an assistive listening device, or another appropriate aid or service available to a deaf patient and her family. Instead, the office relied on a video remote interpretation system that often failed to work. The agreement requires the clinic to provide those aids and services to patients and their companions who are deaf or hard of hearing, advertise their availability, assess each patient who is deaf or hard of hearing to determine the best aids and services for their needs, and pay $5,000 in compensation to the complainant and a $1,000 civil penalty to the United States.
- Springfield, Mass., refused to provide full joint replacements to two patients being treated with buprenorphine, a medication used to treat opioid use disorder. Rather than accommodate the patients, the surgeons referred them elsewhere because they were uncomfortable with the postoperative pain management protocol for patients prescribed buprenorphine. “The Americans With Disabilities Act protects health care access for people under medical treatment for opioid use disorder,” said Acting U.S. Attorney Nathaniel R. Mendell. “Health care providers must comply with the ADA, even when doing so is inconvenient or makes them uncomfortable.” The agreement requires the practice to adopt a nondiscrimination policy, provide training on the ADA and opioid use disorder, and pay two complainants $15,000 each for pain and suffering.
The DOJ has filed civil lawsuits against medical practices when they failed to resolve the allegations. Recent cases include an ophthalmology practice with 24 facilities in Arizona that refused to help transfer patients in wheelchairs to surgery tables for eye surgery and required them to pay for transfer support services and two obstetricians-gynecologists in Bakersfield, Calif., who refused to provide routine medical care to a patient because of her HIV status.
What doctors should know
Many people tend to think of a person with a disability as being in a wheelchair. But the ADA has a very broad definition of disability, which includes any physical or mental impairment that substantially limits any major life activity, said Ms. Pendo.
“It was amended in 2008 to clarify that the definition includes people with chronic diseases such as diabetes and cancer, cognitive and neurological disorders, substance abuse disorders, vision and hearing loss, and learning and other disabilities,” she said.
That means that doctors have to accommodate many types of disabilities, which can be challenging. The ADA only specifies that fixed structures need to be accessible, such as parking lots, driveways, and buildings, said Dr. Iezzoni.
When it comes to “reasonable accommodations,” doctors should decide that on a case-by-case basis, she said.
“We can say based on our study that 71% of doctors don’t know the right way to think about the accommodations – they don’t know they need to talk to patients so they can explain to them exactly what they need to accommodate their disability,” said Dr. Iezzoni.
Doctors are also required to provide effective communication for patients with sensory or cognitive disabilities, which can depend on the severity, said Ms. Pendo. Is the person deaf or hard of hearing, blind or partially sighted – is the dementia mild or severe?
“The requirement is there, but what that looks like will vary by patient. That’s what’s challenging,” said Ms. Pendo.
Dr. Iezzoni recommends that doctor’s offices ask patients whether they need special help or individual assistance when they make appointments and enter their responses in their records. She also suggests that patients be asked at follow-up appointments whether they still need the same help or not.
“Disabilities can change over time – a person with bad arthritis may need help getting onto an exam table, but later get a knee or hip replacement that is effective and no longer need that help,” said Dr. Iezzoni.
Benefits outweigh costs
Physicians have made progress in meeting the ADA’s physical accessibility requirements, said Dr. Iezzoni. “The literature suggests that doctors have done a good job at fixing the structural barriers people with mobility issues face, such as ramps and bathrooms.”
However, there are exceptions in rural older buildings which can be harder to retrofit for wheelchair accessibility, she said. “I recall interviewing a rural doctor several years ago who said that he knew his patients well and when a patient visits with mobility problems, he goes down and carries the patient up the steps to his office. My response was that is not respectful of the patient or safe for the patient or you. That doctor has since changed the location of his practice,” said Dr. Iezzoni.
Some doctors may resist paying for accessible medical equipment because of cost, but she said the benefits are worth it. These include preventing staff injuries when they transfer patients and being used by patients with temporary disabilities and aging people with bad knees, backs, hearing and sight. In addition, businesses may be eligible for federal and state tax credits.
Dr. Iezzoni recently visited her doctor where they finally got height-adjustable exam tables. “I asked the assistant, who really likes these tables? She said it’s the elderly ladies of short stature – the table is lowered and they sit down and get on it.”
But, Dr. Iezonni’s main message to doctors is that patients with disabilities deserve equal quality of care. “Just because we have a disability doesn’t mean we should get worse care than other people. It’s a matter of professionalism that doctors should want to give the same quality care to all their patients.”
A version of this article first appeared on Medscape.com.
Lisa Iezzoni, MD, a professor of medicine at Harvard Medical School and a disability researcher at Massachusetts General Hospital, both in Boston, has used a wheelchair for more than 30 years because of multiple sclerosis. When she visits her primary care doctor, she doesn’t get weighed because the scales are not wheelchair accessible.
This failure to weigh her and other patients in wheelchairs could lead to serious medical problems. Weight is used to monitor a person’s overall health and prenatal health and to determine accurate doses for medications such as some chemotherapies, said Dr. Iezzoni.
In another situation, a man who used a wheelchair said that his primary care doctor never got him out of it for a complete physical exam. The patient later developed lymphoma, which first appeared in his groin. The doctor should have accommodated his disability and used a height-adjustable exam table or a portable lift to transfer him onto the table.
When physicians don’t provide access to medical care that patients with disabilities need, they put themselves at greater risk of lawsuits, fines, and settlements.
Yet, a new study in Health Affairs suggests that a large percentage of doctors are not fully aware of what they are legally required to do.
Under federal nondiscrimination laws (Americans With Disabilities Act, American Rehabilitation Act, and ADA Amendments Act), medical practices must provide equal access to people with disabilities, accommodate their disability-related needs, and not refuse them medical services because of their disabilities, say disability experts.
Where doctors go wrong with disability laws
What doctors don’t know about providing reasonable accommodations makes them vulnerable to lawsuits, which worries more than two-thirds of the 714 outpatient doctors surveyed.
Not only are they required to provide reasonable accommodations, but they also have to pay for them, the researchers said. One-fifth of the surveyed doctors said they didn’t know that practice owners have to pay.
More than one practice has made patients pay for services needed for their disability, such as sign language interpreters – the patients later complained this violated the ADA to enforcement agencies.
Doctors also don’t know that they have to collaborate with patients to determine what reasonable accommodations they need – over two-thirds of those surveyed said they didn’t know it was a joint responsibility, the study found.
When doctors fail to accommodate patients’ disability needs, they engage in discrimination and violate the ADA, says Elizabeth Pendo, JD, a coauthor of the study and the Joseph J. Simeone Professor of Law at Saint Louis University.
The Department of Justice has investigated several patient complaints of alleged disability discrimination recently and resolved the disputes with agreements and small fines in some cases. “The goal is not to get large financial settlements but to work with practices to get the correct procedures in place to be compliant,” said Ms. Pendo.
Physicians would be wise to check out whether their practices are as accessible as they think. Even if there’s a ramp to the office building, the parking lot may not have a van-accessible space or enough handicapped parking signs, or the exam room may be too narrow for a wheelchair to navigate.
These practices violated the ADA and agreed to make changes:
- Hamden, Conn., has two buildings that patients with physical disabilities couldn’t easily enter. The physician owners agreed to change the buildings’ entrances and access routes and add features to make it easier to use examination rooms and restrooms and the check-in and check-out areas.
- Seven medical offices in Riverside, Calif., failed to communicate effectively with deaf and hard-of-hearing patients. They should have had a qualified sign language interpreter, an assistive listening device, or another appropriate aid or service available to a deaf patient and her family. Instead, the office relied on a video remote interpretation system that often failed to work. The agreement requires the clinic to provide those aids and services to patients and their companions who are deaf or hard of hearing, advertise their availability, assess each patient who is deaf or hard of hearing to determine the best aids and services for their needs, and pay $5,000 in compensation to the complainant and a $1,000 civil penalty to the United States.
- Springfield, Mass., refused to provide full joint replacements to two patients being treated with buprenorphine, a medication used to treat opioid use disorder. Rather than accommodate the patients, the surgeons referred them elsewhere because they were uncomfortable with the postoperative pain management protocol for patients prescribed buprenorphine. “The Americans With Disabilities Act protects health care access for people under medical treatment for opioid use disorder,” said Acting U.S. Attorney Nathaniel R. Mendell. “Health care providers must comply with the ADA, even when doing so is inconvenient or makes them uncomfortable.” The agreement requires the practice to adopt a nondiscrimination policy, provide training on the ADA and opioid use disorder, and pay two complainants $15,000 each for pain and suffering.
The DOJ has filed civil lawsuits against medical practices when they failed to resolve the allegations. Recent cases include an ophthalmology practice with 24 facilities in Arizona that refused to help transfer patients in wheelchairs to surgery tables for eye surgery and required them to pay for transfer support services and two obstetricians-gynecologists in Bakersfield, Calif., who refused to provide routine medical care to a patient because of her HIV status.
What doctors should know
Many people tend to think of a person with a disability as being in a wheelchair. But the ADA has a very broad definition of disability, which includes any physical or mental impairment that substantially limits any major life activity, said Ms. Pendo.
“It was amended in 2008 to clarify that the definition includes people with chronic diseases such as diabetes and cancer, cognitive and neurological disorders, substance abuse disorders, vision and hearing loss, and learning and other disabilities,” she said.
That means that doctors have to accommodate many types of disabilities, which can be challenging. The ADA only specifies that fixed structures need to be accessible, such as parking lots, driveways, and buildings, said Dr. Iezzoni.
When it comes to “reasonable accommodations,” doctors should decide that on a case-by-case basis, she said.
“We can say based on our study that 71% of doctors don’t know the right way to think about the accommodations – they don’t know they need to talk to patients so they can explain to them exactly what they need to accommodate their disability,” said Dr. Iezzoni.
Doctors are also required to provide effective communication for patients with sensory or cognitive disabilities, which can depend on the severity, said Ms. Pendo. Is the person deaf or hard of hearing, blind or partially sighted – is the dementia mild or severe?
“The requirement is there, but what that looks like will vary by patient. That’s what’s challenging,” said Ms. Pendo.
Dr. Iezzoni recommends that doctor’s offices ask patients whether they need special help or individual assistance when they make appointments and enter their responses in their records. She also suggests that patients be asked at follow-up appointments whether they still need the same help or not.
“Disabilities can change over time – a person with bad arthritis may need help getting onto an exam table, but later get a knee or hip replacement that is effective and no longer need that help,” said Dr. Iezzoni.
Benefits outweigh costs
Physicians have made progress in meeting the ADA’s physical accessibility requirements, said Dr. Iezzoni. “The literature suggests that doctors have done a good job at fixing the structural barriers people with mobility issues face, such as ramps and bathrooms.”
However, there are exceptions in rural older buildings which can be harder to retrofit for wheelchair accessibility, she said. “I recall interviewing a rural doctor several years ago who said that he knew his patients well and when a patient visits with mobility problems, he goes down and carries the patient up the steps to his office. My response was that is not respectful of the patient or safe for the patient or you. That doctor has since changed the location of his practice,” said Dr. Iezzoni.
Some doctors may resist paying for accessible medical equipment because of cost, but she said the benefits are worth it. These include preventing staff injuries when they transfer patients and being used by patients with temporary disabilities and aging people with bad knees, backs, hearing and sight. In addition, businesses may be eligible for federal and state tax credits.
Dr. Iezzoni recently visited her doctor where they finally got height-adjustable exam tables. “I asked the assistant, who really likes these tables? She said it’s the elderly ladies of short stature – the table is lowered and they sit down and get on it.”
But, Dr. Iezonni’s main message to doctors is that patients with disabilities deserve equal quality of care. “Just because we have a disability doesn’t mean we should get worse care than other people. It’s a matter of professionalism that doctors should want to give the same quality care to all their patients.”
A version of this article first appeared on Medscape.com.
Newly approved drug improves sleep onset in insomnia
In the first of two studies, a 50-mg dose of daridorexant was associated with a reduction in latency to persistent sleep (LPS) of 11.7 minutes at month 3 versus placebo. The drug also was associated with improved daytime function.
Based on these results, the Food and Drug Administration approved daridorexant for the treatment of insomnia in adults earlier in January.
“The study shows that it is a really good drug that works differently from most other drugs,” said Emmanuel Mignot, MD, PhD, professor of sleep medicine at Stanford (Calif.) University. “It’s more specific to sleep,” Dr. Mignot added.
The findings were published in the February issue of The Lancet Neurology.
Two trials, three doses
Daridorexant is a dual orexin receptor antagonist intended to reduce excessive wakefulness. The investigators hypothesized that, because of its therapeutic target, the drug would not cause sleepiness on the morning after administration.
To examine daridorexant’s safety and efficacy, the researchers conducted two double-blind, parallel-group, phase 3 trials. Eligible participants were aged 18 years or older, had moderate to severe insomnia disorder, and had a self-reported history of disturbed sleep at least 3 nights per week for at least 3 months before screening.
In study 1, investigators randomly assigned participants in groups of equal size to daridorexant 25 mg, 50 mg, or placebo. In study 2, participants were randomly assigned to daridorexant 10 mg, 25 mg, or placebo.
During a placebo run-in period, participants underwent polysomnography on two consecutive nights to define baseline values. At the end of months 1 and 3 of the treatment period, participants again underwent 2 nights of polysomnography. A final night of polysomnography occurred during the placebo run-out period.
Self-assessments included the Insomnia Daytime Symptoms and Impacts Questionnaire (IDSIQ). This questionnaire, to which participants responded daily, is designed to measure the daytime impairments related to insomnia. The IDSIQ questions focus on sleepiness, mood, alertness, and cognition.
The study’s primary endpoints were change from baseline in wake after sleep onset (WASO) and LPS at months 1 and 3. Secondary endpoints were change from baseline in self-reported total sleep time and change in the IDSIQ sleepiness domain score at months 1 and 3.
The investigators enrolled 930 participants in study 1 and 924 in study 2. In each study, more than two-thirds of participants were women, 39% were aged 65 or older, and demographic and baseline characteristics were similar between treatment groups.
Dose-dependent effects
At month 1 in study 1, WASO was reduced by 22.8 minutes (P < .0001) in patients who received the 50-mg dose and by 12.2 minutes (P < .0001) in the 25-mg dose. At month 3, WASO was reduced by 18.3 minutes (P < .0001) in those assigned to 50 mg and by 11.9 minutes (P < .0001) in those assigned to 25 mg.
LPS was reduced by 11.4 minutes (P < .0001) at month 1 and by 11.7 minutes (P < .0001) at month 3 with the 50-mg dose versus placebo. LPS was reduced by 8.3 minutes (P = .0005) at month 1 and by 7.6 minutes (P = .0015) at month 3 with the 25-mg dose versus placebo.
At both time points, self-reported total sleep time was significantly increased and the IDSIQ sleepiness score significantly improved with the 50-mg dose. The 25-mg dose was associated with significant improvements in self-reported total sleep time at both time points, but not with significant improvements in IDSIQ sleepiness score.
In study 2, the 25-mg dose was associated with significant reductions in WASO at month 1 (11.6 minutes, P = .0001) and month 3 (10.3 minutes, P = .0028) compared with placebo. The 25-mg dose was not associated with significant differences in LPS at either time point, however.
Similarly, the 25-mg dose was associated with improvements in self-reported total sleep time, but not with the IDSIQ sleepiness score. The 10-mg dose was not associated with improvements on any endpoint compared with placebo.
Longer studies needed
In an accompanying editorial, Kai Spiegelhalder, PhD, University of Freiburg, Germany, and colleagues pointed out that although insomnia disorder is defined by self-reported difficulty initiating or maintaining sleep, none of the primary or secondary endpoints in these trials addressed these symptoms.
However, Dr. Mignot noted the use of the IDSIQ scale is the most interesting aspect of the study. Although difficulty with concentration and mood impairment are major symptoms of insomnia, they are often neglected. “This drug was reversing the daytime impairment that insomniacs have,” said Dr. Mignot. “We now need to systematically study people not only for the effect on sleep, but also that it makes them feel better the day after.”
He added that most of the current hypnotics were not developed to treat insomnia. Daridorexant, in contrast, targets the wake-promoting orexin system. “It works more selectively on sleep and not on other things. Most of the other sleeping pills have more complex effects on the brain,” Dr. Mignot said.
Commenting on the study, John Winkelman, MD, PhD, professor of psychiatry at Harvard Medical School, Boston, said the low prevalence of side effects associated with daridorexant was remarkable. “This is not what most of the benzodiazepine receptor agonists looked like,” said Dr. Winkelman, who was not involved with the research.
Many insomnia drugs affect transmitter systems that are widespread in the brain, thus provoking side effects. But orexin-receptor antagonists “don’t seem to produce a lot of side effects,” he noted.
Although the study duration was reasonable, longer studies will be necessary, he added. “And it would be nice to see comparative data. Prescribers want to see some context.” said Dr. Winkelman.
The study was funded by Idorsia Pharmaceuticals. Dr. Mignot reported receiving research or clinical trial funding from Axsome, Jazz Pharmaceuticals, Avadel, Apple, Huami, Sunovion, and Takeda. He has also received consulting fees or speakers’ conference reimbursement from Idorsia, Centessa Pharmaceuticals, Jazz Pharmaceuticals, Avadel, Dreem, and Takeda. Dr. Winkelman has consulted for Idorsia and has participated in investigator-initiated studies supported by Merck.
A version of this article first appeared on Medscape.com.
In the first of two studies, a 50-mg dose of daridorexant was associated with a reduction in latency to persistent sleep (LPS) of 11.7 minutes at month 3 versus placebo. The drug also was associated with improved daytime function.
Based on these results, the Food and Drug Administration approved daridorexant for the treatment of insomnia in adults earlier in January.
“The study shows that it is a really good drug that works differently from most other drugs,” said Emmanuel Mignot, MD, PhD, professor of sleep medicine at Stanford (Calif.) University. “It’s more specific to sleep,” Dr. Mignot added.
The findings were published in the February issue of The Lancet Neurology.
Two trials, three doses
Daridorexant is a dual orexin receptor antagonist intended to reduce excessive wakefulness. The investigators hypothesized that, because of its therapeutic target, the drug would not cause sleepiness on the morning after administration.
To examine daridorexant’s safety and efficacy, the researchers conducted two double-blind, parallel-group, phase 3 trials. Eligible participants were aged 18 years or older, had moderate to severe insomnia disorder, and had a self-reported history of disturbed sleep at least 3 nights per week for at least 3 months before screening.
In study 1, investigators randomly assigned participants in groups of equal size to daridorexant 25 mg, 50 mg, or placebo. In study 2, participants were randomly assigned to daridorexant 10 mg, 25 mg, or placebo.
During a placebo run-in period, participants underwent polysomnography on two consecutive nights to define baseline values. At the end of months 1 and 3 of the treatment period, participants again underwent 2 nights of polysomnography. A final night of polysomnography occurred during the placebo run-out period.
Self-assessments included the Insomnia Daytime Symptoms and Impacts Questionnaire (IDSIQ). This questionnaire, to which participants responded daily, is designed to measure the daytime impairments related to insomnia. The IDSIQ questions focus on sleepiness, mood, alertness, and cognition.
The study’s primary endpoints were change from baseline in wake after sleep onset (WASO) and LPS at months 1 and 3. Secondary endpoints were change from baseline in self-reported total sleep time and change in the IDSIQ sleepiness domain score at months 1 and 3.
The investigators enrolled 930 participants in study 1 and 924 in study 2. In each study, more than two-thirds of participants were women, 39% were aged 65 or older, and demographic and baseline characteristics were similar between treatment groups.
Dose-dependent effects
At month 1 in study 1, WASO was reduced by 22.8 minutes (P < .0001) in patients who received the 50-mg dose and by 12.2 minutes (P < .0001) in the 25-mg dose. At month 3, WASO was reduced by 18.3 minutes (P < .0001) in those assigned to 50 mg and by 11.9 minutes (P < .0001) in those assigned to 25 mg.
LPS was reduced by 11.4 minutes (P < .0001) at month 1 and by 11.7 minutes (P < .0001) at month 3 with the 50-mg dose versus placebo. LPS was reduced by 8.3 minutes (P = .0005) at month 1 and by 7.6 minutes (P = .0015) at month 3 with the 25-mg dose versus placebo.
At both time points, self-reported total sleep time was significantly increased and the IDSIQ sleepiness score significantly improved with the 50-mg dose. The 25-mg dose was associated with significant improvements in self-reported total sleep time at both time points, but not with significant improvements in IDSIQ sleepiness score.
In study 2, the 25-mg dose was associated with significant reductions in WASO at month 1 (11.6 minutes, P = .0001) and month 3 (10.3 minutes, P = .0028) compared with placebo. The 25-mg dose was not associated with significant differences in LPS at either time point, however.
Similarly, the 25-mg dose was associated with improvements in self-reported total sleep time, but not with the IDSIQ sleepiness score. The 10-mg dose was not associated with improvements on any endpoint compared with placebo.
Longer studies needed
In an accompanying editorial, Kai Spiegelhalder, PhD, University of Freiburg, Germany, and colleagues pointed out that although insomnia disorder is defined by self-reported difficulty initiating or maintaining sleep, none of the primary or secondary endpoints in these trials addressed these symptoms.
However, Dr. Mignot noted the use of the IDSIQ scale is the most interesting aspect of the study. Although difficulty with concentration and mood impairment are major symptoms of insomnia, they are often neglected. “This drug was reversing the daytime impairment that insomniacs have,” said Dr. Mignot. “We now need to systematically study people not only for the effect on sleep, but also that it makes them feel better the day after.”
He added that most of the current hypnotics were not developed to treat insomnia. Daridorexant, in contrast, targets the wake-promoting orexin system. “It works more selectively on sleep and not on other things. Most of the other sleeping pills have more complex effects on the brain,” Dr. Mignot said.
Commenting on the study, John Winkelman, MD, PhD, professor of psychiatry at Harvard Medical School, Boston, said the low prevalence of side effects associated with daridorexant was remarkable. “This is not what most of the benzodiazepine receptor agonists looked like,” said Dr. Winkelman, who was not involved with the research.
Many insomnia drugs affect transmitter systems that are widespread in the brain, thus provoking side effects. But orexin-receptor antagonists “don’t seem to produce a lot of side effects,” he noted.
Although the study duration was reasonable, longer studies will be necessary, he added. “And it would be nice to see comparative data. Prescribers want to see some context.” said Dr. Winkelman.
The study was funded by Idorsia Pharmaceuticals. Dr. Mignot reported receiving research or clinical trial funding from Axsome, Jazz Pharmaceuticals, Avadel, Apple, Huami, Sunovion, and Takeda. He has also received consulting fees or speakers’ conference reimbursement from Idorsia, Centessa Pharmaceuticals, Jazz Pharmaceuticals, Avadel, Dreem, and Takeda. Dr. Winkelman has consulted for Idorsia and has participated in investigator-initiated studies supported by Merck.
A version of this article first appeared on Medscape.com.
In the first of two studies, a 50-mg dose of daridorexant was associated with a reduction in latency to persistent sleep (LPS) of 11.7 minutes at month 3 versus placebo. The drug also was associated with improved daytime function.
Based on these results, the Food and Drug Administration approved daridorexant for the treatment of insomnia in adults earlier in January.
“The study shows that it is a really good drug that works differently from most other drugs,” said Emmanuel Mignot, MD, PhD, professor of sleep medicine at Stanford (Calif.) University. “It’s more specific to sleep,” Dr. Mignot added.
The findings were published in the February issue of The Lancet Neurology.
Two trials, three doses
Daridorexant is a dual orexin receptor antagonist intended to reduce excessive wakefulness. The investigators hypothesized that, because of its therapeutic target, the drug would not cause sleepiness on the morning after administration.
To examine daridorexant’s safety and efficacy, the researchers conducted two double-blind, parallel-group, phase 3 trials. Eligible participants were aged 18 years or older, had moderate to severe insomnia disorder, and had a self-reported history of disturbed sleep at least 3 nights per week for at least 3 months before screening.
In study 1, investigators randomly assigned participants in groups of equal size to daridorexant 25 mg, 50 mg, or placebo. In study 2, participants were randomly assigned to daridorexant 10 mg, 25 mg, or placebo.
During a placebo run-in period, participants underwent polysomnography on two consecutive nights to define baseline values. At the end of months 1 and 3 of the treatment period, participants again underwent 2 nights of polysomnography. A final night of polysomnography occurred during the placebo run-out period.
Self-assessments included the Insomnia Daytime Symptoms and Impacts Questionnaire (IDSIQ). This questionnaire, to which participants responded daily, is designed to measure the daytime impairments related to insomnia. The IDSIQ questions focus on sleepiness, mood, alertness, and cognition.
The study’s primary endpoints were change from baseline in wake after sleep onset (WASO) and LPS at months 1 and 3. Secondary endpoints were change from baseline in self-reported total sleep time and change in the IDSIQ sleepiness domain score at months 1 and 3.
The investigators enrolled 930 participants in study 1 and 924 in study 2. In each study, more than two-thirds of participants were women, 39% were aged 65 or older, and demographic and baseline characteristics were similar between treatment groups.
Dose-dependent effects
At month 1 in study 1, WASO was reduced by 22.8 minutes (P < .0001) in patients who received the 50-mg dose and by 12.2 minutes (P < .0001) in the 25-mg dose. At month 3, WASO was reduced by 18.3 minutes (P < .0001) in those assigned to 50 mg and by 11.9 minutes (P < .0001) in those assigned to 25 mg.
LPS was reduced by 11.4 minutes (P < .0001) at month 1 and by 11.7 minutes (P < .0001) at month 3 with the 50-mg dose versus placebo. LPS was reduced by 8.3 minutes (P = .0005) at month 1 and by 7.6 minutes (P = .0015) at month 3 with the 25-mg dose versus placebo.
At both time points, self-reported total sleep time was significantly increased and the IDSIQ sleepiness score significantly improved with the 50-mg dose. The 25-mg dose was associated with significant improvements in self-reported total sleep time at both time points, but not with significant improvements in IDSIQ sleepiness score.
In study 2, the 25-mg dose was associated with significant reductions in WASO at month 1 (11.6 minutes, P = .0001) and month 3 (10.3 minutes, P = .0028) compared with placebo. The 25-mg dose was not associated with significant differences in LPS at either time point, however.
Similarly, the 25-mg dose was associated with improvements in self-reported total sleep time, but not with the IDSIQ sleepiness score. The 10-mg dose was not associated with improvements on any endpoint compared with placebo.
Longer studies needed
In an accompanying editorial, Kai Spiegelhalder, PhD, University of Freiburg, Germany, and colleagues pointed out that although insomnia disorder is defined by self-reported difficulty initiating or maintaining sleep, none of the primary or secondary endpoints in these trials addressed these symptoms.
However, Dr. Mignot noted the use of the IDSIQ scale is the most interesting aspect of the study. Although difficulty with concentration and mood impairment are major symptoms of insomnia, they are often neglected. “This drug was reversing the daytime impairment that insomniacs have,” said Dr. Mignot. “We now need to systematically study people not only for the effect on sleep, but also that it makes them feel better the day after.”
He added that most of the current hypnotics were not developed to treat insomnia. Daridorexant, in contrast, targets the wake-promoting orexin system. “It works more selectively on sleep and not on other things. Most of the other sleeping pills have more complex effects on the brain,” Dr. Mignot said.
Commenting on the study, John Winkelman, MD, PhD, professor of psychiatry at Harvard Medical School, Boston, said the low prevalence of side effects associated with daridorexant was remarkable. “This is not what most of the benzodiazepine receptor agonists looked like,” said Dr. Winkelman, who was not involved with the research.
Many insomnia drugs affect transmitter systems that are widespread in the brain, thus provoking side effects. But orexin-receptor antagonists “don’t seem to produce a lot of side effects,” he noted.
Although the study duration was reasonable, longer studies will be necessary, he added. “And it would be nice to see comparative data. Prescribers want to see some context.” said Dr. Winkelman.
The study was funded by Idorsia Pharmaceuticals. Dr. Mignot reported receiving research or clinical trial funding from Axsome, Jazz Pharmaceuticals, Avadel, Apple, Huami, Sunovion, and Takeda. He has also received consulting fees or speakers’ conference reimbursement from Idorsia, Centessa Pharmaceuticals, Jazz Pharmaceuticals, Avadel, Dreem, and Takeda. Dr. Winkelman has consulted for Idorsia and has participated in investigator-initiated studies supported by Merck.
A version of this article first appeared on Medscape.com.
FROM THE LANCET NEUROLOGY
Omicron subvariant 1.5 times more contagious than Omicron
according to CNBC.
The Statens Serum Institut, which monitors infectious diseases in Denmark, said that BA.2 is more contagious, but it doesn’t appear to increase hospitalizations or reduce how well the vaccine works.
BA.2 overtook BA.1 as the primary variant in Denmark within a few weeks, Troels Lillebaek, director of the institute, told CNBC. The subvariant has five unique mutations on a key part of the spike protein, which is what the coronavirus uses to invade human cells. This often means a higher rate of spreading.
The Omicron subvariant has been detected in at least 29 states in the United States and 56 countries, according to the latest update from Outbreak.info. The United States has detected 188 infections, with the worldwide total nearing 25,000.
Denmark has reported the highest number of cases, followed by the United Kingdom and India. Both Denmark and India have reported that BA.2 now accounts for about half of new COVID-19 cases in those countries.
On Jan. 28, the U.K. Health Security Agency said BA.2 has a “substantial” growth advantage over the original Omicron strain. The subvariant has spread faster in all regions of England where there were enough cases to conduct an analysis, the agency said in a report.
A preliminary evaluation found that BA.2 doesn’t appear to change how well the vaccine works compared to the original Omicron strain, the agency said. A booster dose was 70% effective at preventing symptomatic illness for BA.2, compared with 63% for the original Omicron strain.
The Centers for Disease Control and Prevention also said on Jan. 28 that, although the subvariant has become more common in some countries, it is currently at a low level in the United States and doesn’t appear to be more serious.
“Currently there is no evidence that the BA.2 lineage is more severe than the BA.1 lineage,” Kristen Nordlund, a CDC spokesperson, told CNBC.
The World Health Organization hasn’t labeled BA.2 a “variant of concern” so far but will continue to monitor it. WHO officials have said that new variants will arise as Omicron spreads across the world.
“The next variant of concern will be more fit, and what we mean by that is it will be more transmissible because it will have to overtake what is currently circulating,” Maria Van Kerkhove, the WHO’s COVID-19 technical lead, said during a livestream on Jan. 25.
“The big question is whether or not future variants will be more or less severe,” she said.
A version of this article first appeared on WebMD.com.
according to CNBC.
The Statens Serum Institut, which monitors infectious diseases in Denmark, said that BA.2 is more contagious, but it doesn’t appear to increase hospitalizations or reduce how well the vaccine works.
BA.2 overtook BA.1 as the primary variant in Denmark within a few weeks, Troels Lillebaek, director of the institute, told CNBC. The subvariant has five unique mutations on a key part of the spike protein, which is what the coronavirus uses to invade human cells. This often means a higher rate of spreading.
The Omicron subvariant has been detected in at least 29 states in the United States and 56 countries, according to the latest update from Outbreak.info. The United States has detected 188 infections, with the worldwide total nearing 25,000.
Denmark has reported the highest number of cases, followed by the United Kingdom and India. Both Denmark and India have reported that BA.2 now accounts for about half of new COVID-19 cases in those countries.
On Jan. 28, the U.K. Health Security Agency said BA.2 has a “substantial” growth advantage over the original Omicron strain. The subvariant has spread faster in all regions of England where there were enough cases to conduct an analysis, the agency said in a report.
A preliminary evaluation found that BA.2 doesn’t appear to change how well the vaccine works compared to the original Omicron strain, the agency said. A booster dose was 70% effective at preventing symptomatic illness for BA.2, compared with 63% for the original Omicron strain.
The Centers for Disease Control and Prevention also said on Jan. 28 that, although the subvariant has become more common in some countries, it is currently at a low level in the United States and doesn’t appear to be more serious.
“Currently there is no evidence that the BA.2 lineage is more severe than the BA.1 lineage,” Kristen Nordlund, a CDC spokesperson, told CNBC.
The World Health Organization hasn’t labeled BA.2 a “variant of concern” so far but will continue to monitor it. WHO officials have said that new variants will arise as Omicron spreads across the world.
“The next variant of concern will be more fit, and what we mean by that is it will be more transmissible because it will have to overtake what is currently circulating,” Maria Van Kerkhove, the WHO’s COVID-19 technical lead, said during a livestream on Jan. 25.
“The big question is whether or not future variants will be more or less severe,” she said.
A version of this article first appeared on WebMD.com.
according to CNBC.
The Statens Serum Institut, which monitors infectious diseases in Denmark, said that BA.2 is more contagious, but it doesn’t appear to increase hospitalizations or reduce how well the vaccine works.
BA.2 overtook BA.1 as the primary variant in Denmark within a few weeks, Troels Lillebaek, director of the institute, told CNBC. The subvariant has five unique mutations on a key part of the spike protein, which is what the coronavirus uses to invade human cells. This often means a higher rate of spreading.
The Omicron subvariant has been detected in at least 29 states in the United States and 56 countries, according to the latest update from Outbreak.info. The United States has detected 188 infections, with the worldwide total nearing 25,000.
Denmark has reported the highest number of cases, followed by the United Kingdom and India. Both Denmark and India have reported that BA.2 now accounts for about half of new COVID-19 cases in those countries.
On Jan. 28, the U.K. Health Security Agency said BA.2 has a “substantial” growth advantage over the original Omicron strain. The subvariant has spread faster in all regions of England where there were enough cases to conduct an analysis, the agency said in a report.
A preliminary evaluation found that BA.2 doesn’t appear to change how well the vaccine works compared to the original Omicron strain, the agency said. A booster dose was 70% effective at preventing symptomatic illness for BA.2, compared with 63% for the original Omicron strain.
The Centers for Disease Control and Prevention also said on Jan. 28 that, although the subvariant has become more common in some countries, it is currently at a low level in the United States and doesn’t appear to be more serious.
“Currently there is no evidence that the BA.2 lineage is more severe than the BA.1 lineage,” Kristen Nordlund, a CDC spokesperson, told CNBC.
The World Health Organization hasn’t labeled BA.2 a “variant of concern” so far but will continue to monitor it. WHO officials have said that new variants will arise as Omicron spreads across the world.
“The next variant of concern will be more fit, and what we mean by that is it will be more transmissible because it will have to overtake what is currently circulating,” Maria Van Kerkhove, the WHO’s COVID-19 technical lead, said during a livestream on Jan. 25.
“The big question is whether or not future variants will be more or less severe,” she said.
A version of this article first appeared on WebMD.com.
Assessing imminent suicide risk: What about future planning?
A patient who has the ability to plan for their future can be reassuring for a clinician who is conducting an imminent suicide risk evaluation. However, that patient may report future plans even as they are contemplating suicide. Therefore, this variable should not be simplified categorically to the mere presence or absence of future plans. Such plans, and the process by which they are produced, should be examined more closely. In this article, we explore the relationship between a patient’s intent to die by suicide in the near future and their ability to maintain future planning. We also use case examples to highlight certain characteristics that may allow future planning to be integrated more reliably into the assessment of imminent risk of suicide.
An inherent challenge
Suicide risk assessment can be challenging due to the numerous factors that can contribute to a patient’s suicidal intent.1 Some individuals don’t seek help when they develop suicidal thoughts, and even among those who do, recognizing who may be at greater risk is not an easy task. Sometimes, this leads to inadequate interventions and a subsequent failure to ensure safety, or to an overreaction and unnecessary hospitalization.
A common difficulty is a patient’s unwillingness to cooperate with the examination.2 Some patients do not present voluntarily, while others may seek help but then conceal suicidal intent. In a sample of 66 psychotherapy patients who reported concealing suicidal ideation from their therapist and provided short essay responses explaining their motives for doing so, approximately 70% said fear of involuntary hospitalization was their motive to hide those thoughts from their doctor.3 Other reasons for concealment are shame, stigma, embarrassment, fear of rejection, and loss of autonomy.3-5 Moreover, higher levels of suicidal ideation are associated with treatment avoidance.6 Therefore, it is important to improve suicide predictability independent of the patient report. In a survey of 1,150 emergency physicians in Australasia, Canada, the United Kingdom, and the United States, the need for evidence-based guidelines on when to hospitalize a patient at risk for suicide was ranked as the 7th-highest priority.7 There are limitations to using suicide risk assessment scales,8,9 because scales designed to have high sensitivity are less specific, and those with high specificity fail to identify individuals at high risk.9,10 Most of the research conducted in this area has focused on the risk of suicide in 2 to 6 months, and not on imminent risk.11
What is ‘imminent’ risk?
There is no specific time definition for “imminent risk,” but the Lifeline Standards, Trainings, and Practices Subcommittee, a group of national and international experts in suicide prevention, defines imminent risk of suicide as the belief that there is a “close temporal connection between the person’s current risk status and actions that could lead to his/her suicide.”12 Practically, suicide could be considered imminent when it occurs within a few days of the evaluation. However, suicide may take place within a few days of an evaluation due to new life events or impulsive actions, which may explain why imminent risk of suicide can be difficult to define and predict. In clinical practice, there is little evidence-based knowledge about estimating imminent risk. Recent studies have explored certain aspects of a patient’s history in the attempt to improve imminent risk predictability.13 In light of the complexity of this matter and the lack of widely validated tools, clinicians are encouraged to share their experience with other clinicians while the efforts to advance evidence-based knowledge and tools continue.
The function of future planning
Future planning is a mental process embedded in several crucial executive functions. It operates on a daily basis to organize, prioritize, and carry out tasks to achieve day-to-day and more distant future goals. Some research has found that a decreased ability to generate positive future thoughts is linked to increased suicide risk in the long term.14-17 Positive future planning can be affected by even minor fluctuations in mood because the additional processing capacity needed during these mood changes may limit one’s ability to generate positive future thoughts.18 Patients experiencing mood episodes are known to experience cognitive dysfunctions.19-21 However, additional measurable cognitive changes have been detected in patients who are suicidal. For example, in a small study (N = 33) of patients with depression, those who were experiencing suicidal thoughts underperformed on several measures of executive functioning compared to patients with no suicidal ideation.22
However, when addressing imminent rather than future suicide risk, even neutral future plans—such as day-to-day plans or those addressing barriers to treatment—can be a meaningful indicator of the investment in one’s future beyond a potential near-term suicide, and therefore can be explored to further inform the risk evaluation. Significant mental resources can be consumed due to the level of distress associated with contemplating suicide, and therefore patients may have a reduced capacity for day-to-day planning. Thus, serious suicide contemplation is less likely in the presence of typical future planning.
Continue to: Characteristics of future planning...
Characteristics of future planning
Some patients may pretend to engage in future planning to indicate the absence of suicidal intent. This necessitates a more nuanced assessment of future plans beyond whether they exist or not by examining the genuineness of such plans, and the authenticity of the process by which they are produced. The Table lists 3 characteristics of future plans/future planning that, based on our clinical experience, can be helpful to evaluate during an imminent suicide risk evaluation. These are described in the following case examples.
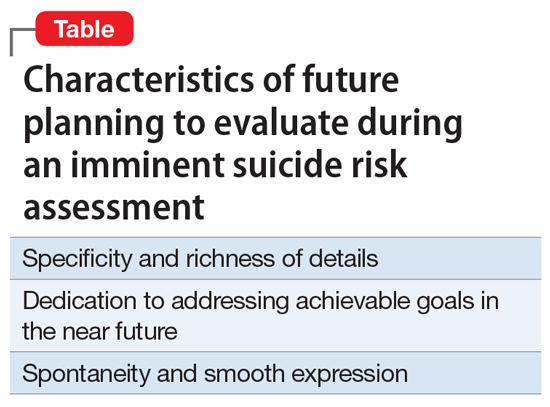
Specificity and richness of details
CASE 1
Mr. A, a college student, presents to the emergency department (ED) complaining of depression and suicidal thoughts that he is able to dismiss. He would like to avoid starting a medication because he has finals in 2 weeks and is worried about adverse effects. He learned about cognitive-behavioral therapy and is interested in getting a referral to a specific office because it is located within a walking distance from campus and easy for him to access because he does not own a car.
The volume of details expressed in a patient’s future plans is important. The more detailed these plans are, the more likely the patient is invested in them. Attendance to the details, especially when addressing expected barriers to treatment, such as transportation, can be evidence of genuine future planning and subsequently of low imminent suicide risk. Spreng et al23 found that autobiographic plans that are more specific and richer in detail recruit additional brain regions that are not recruited in plans that are sparsely detailed or constructed from more generalized representations.
CASE 2
An ambulance transports Ms. B, age 42, from a primary care clinic to the ED because she has been having suicidal thoughts, with a plan to hang herself, for the past 2 days. During the evaluation, Ms. B denies having further suicidal thoughts and declines inpatient admission. She claims that she cannot be away from her children because she is their primary caretaker. Collateral information reveals that Ms. B’s mother has been caring for her children for the last 2 weeks because Ms. B has been too depressed to do so. She continues to refuse admission and is in tears while trying to explain how her absence due to inpatient treatment will be detrimental to her children. Eventually, she angrily accuses the clinician of abusing her children by forcing her to be hospitalized.
In an effort to conceal suicidal intent, patients may present obligations or excuses that would be an obstacle to psychiatric hospitalization. This might give a false perception of intact future planning. However, in these cases, patients often fail to volunteer details about their future plans or show evidence for actual attendance to their obligations. Due to the lack of tangible details to explain the negative effects of inpatient treatment, patients may compensate by using an exaggerated emotional response, with a strong emotional attachment to the obligation and severe distress over their potential inability to fulfill it due to a psychiatric hospitalization. This may contribute to concealing suicidal intent in a different way. A patient may be distressed by the prospect of losing their autonomy or ability to attempt suicide if hospitalized, and they may employ a false excuse as a substitute for the actual reason underlying their distress. A clinician may be falsely reassured if they do not accurately perceive the true cause of the emotional distress. Upon deeper exploration, the expressed emotional attachment is often found to be superficial and has little substantive support.
Continue to: Dedication to addressing acheivable goals in the near future...
Dedication to addressing achievable goals in the near future
CASE 3
Ms. C, age 15, survived a suicide attempt via a medication overdose. She says that she regrets what she did and is not planning to attempt suicide again. Ms. C says she no longer wants to die because in the future she wants to help people by becoming a nurse. She adds that there is a lot waiting for her because she wants to travel all over the world.
Ms. D, age 15, also survived a suicide attempt via a medication overdose. She also says that she regrets what she did and is not planning to attempt suicide again. Ms. D asks whether the physician would be willing to contact the school on her behalf to explain why she had to miss class and to ask for accommodations at school to assist with her panic attacks.
Future planning that involves a patient generating new plans to address current circumstances or the near future may be more reliable than future planning in which a patient repeats their previously constructed plans for the distant future. Eliciting more distant plans, such as a career or family-oriented decisions, indicates the ability to access these “memorized” plans rather than the ability to generate future plans.
Plans that address the distant future, such as those expressed by Ms. C, may have stronger neurologic imprints as a result of repeated memorization and modifications over the years, which may allow a patient to access these plans even while under the stress associated with suicidal thinking. On the other hand, plans that address the near future, such as those expressed by Ms. D, are likely generated in response to current circumstances, which indicates the presence of adequate mental capacity to attend to the current situation, and hence, less preoccupation with suicidal thinking. There might be a neurologic basis for this: some evidence suggests that executive frontoparietal control is recruited in achievable, near-future planning, whereas abstract, difficult-to-achieve, more distant planning fails to engage these additional brain regions.23,24
Spontaneity and smooth expression
CASE 4
Mr. E, age 48, reassures his psychiatrist that he has no intent to act on his suicidal thoughts. When he is offered treatment options, he explains that he would like to start pharmacologic treatment because he only has a few weeks left before he relocates for a new job. The clinician discusses starting a specific medication, and Mr. E expresses interest unless the medication will interfere with his future position as a machine operator. Later, he declines social work assistance to establish care in his new location, preferring to first get the new health care insurance.
A smooth and noncalculated flow of future plans in a patient’s speech allows their plans to be more believable. Plans that naturally flow in response to a verbal exchange and without direct inquiry from the clinician are less likely to be confabulated. This leaves clinicians with the burden of improving the skill of subtly eliciting a patient’s future plans while avoiding directly asking about them. Directly inquiring about such plans may easily tip off the patient that their future planning is under investigation, which may result in misleading responses.
Although future plans that are expressed abruptly, without introductory verbal exchange, or are explicitly linked to why the patient doesn’t intend to kill themselves, can be genuine, the clinician may need to be skeptical about their significance during the risk evaluation. While facing such challenges, clinicians could attempt to shift the patient’s attention away from a safety and disposition-focused conversation toward a less goal-directed verbal exchange during which other opportunities for smooth expression of future plans may emerge. For example, if a patient suddenly discusses how much they care about X in attempt to emphasize why they are not contemplating suicide, the clinician may respond by gently asking the patient to talk more about X.
Continue to: Adopt a more nuanced approach...
Adopt a more nuanced approach
Assessment of the imminent risk of suicide is complicated and not well researched. A patient’s future planning can be used to better inform the evaluation. A patient may have a limited ability to generate future plans while contemplating suicide. Future plans that are specific, rich in details, achievable, dedicated to addressing the near future, and expressed smoothly and in a noncalculated fashion may be more reliable than other types of plans. The process of future planning may indicate low imminent suicide risk when it leads the patient to generate new plans to address current circumstances or the near future. When evaluating a patient’s imminent suicide risk, clinicians should consider abandoning a binary “is there future planning or not” approach and adopting a more complex, nuanced understanding to appropriately utilize this important factor in the risk assessment.
Bottom Line
A patient’s ability to plan for the future should be explored during an assessment of imminent suicide risk. Future plans that are specific, rich in details, achievable, dedicated to addressing the near future, and expressed smoothly and in a noncalculated fashion may be more reliable than other types of plans.
1. Gilbert AM, Garno JL, Braga RJ, et al. Clinical and cognitive correlates of suicide attempts in bipolar disorder: is suicide predictable? J Clin Psychiatry. 2011;72(8):1027-1033.
2. Obegi JH. Your patient refuses a suicide risk assessment. Now what? Current Psychiatry. 2021;20(4):45.
3. Blanchard M, Farber BA. “It is never okay to talk about suicide”: Patients’ reasons for concealing suicidal ideation in psychotherapy. Psychother Res. 2020;30(1):124-136.
4. Richards JE, Whiteside U, Ludman EJ, et al. Understanding why patients may not report suicidal ideation at a health care visit prior to a suicide attempt: a qualitative study. Psychiatr Serv. 2019;70(1):40-45.
5. Fulginiti A, Frey LM. Exploring suicide-related disclosure motivation and the impact on mechanisms linked to suicide. Death Stud. 2019;43(9):562-569.
6. Wilson CJ, Deane FP, Marshall KL, et al. Adolescents’ suicidal thinking and reluctance to consult general medical practitioners. J Youth Adolesc. 2010;39(4):343-356.
7. Eagles D, Stiell IG, Clement CM, et al. International survey of emergency physicians’ priorities for clinical decision rules. Acad Emerg Med. 2008;15(2):177-182.
8. Swedish Council on Health Technology Assessment (SBU): SBU Systematic Review Summaries. Instruments for Suicide Risk Assessment. Summary and Conclusions. SBU Yellow Report No. 242. 2015. Accessed January 6, 2021. https://www.ncbi.nlm.nih.gov/books/NBK350492/
9. Runeson B, Odeberg J, Pettersson A, et al. Instruments for the assessment of suicide risk: a systematic review evaluating the certainty of the evidence. PLoS One. 2017;12(7):e0180292. doi:10.1371/journal.pone.0180292
10. Steeg S, Quinlivan L, Nowland R, et al. Accuracy of risk scales for predicting repeat self-harm and suicide: a multicentre, population-level cohort study using routine clinical data. BMC Psychiatry. 2018;18(1):113.
11. Nock MK, Banaji MR. Prediction of suicide ideation and attempts among adolescents using a brief performance-based test. J Consult Clin Psychol. 2007;75(5):707-715.
12. Draper J, Murphy G, Vega E, et al. Helping callers to the National Suicide Prevention Lifeline who are at imminent risk of suicide: the importance of active engagement, active rescue, and collaboration between crisis and emergency services. Suicide Life Threat Behav. 2015;45(3):261-270.
13. Glenn CR, Nock MK. Improving the short-term prediction of suicidal behavior. Am J Prev Med. 2014;47(3 Suppl 2):S176-S180.
14. MacLeod AK, Pankhania B, Lee M, et al. Parasuicide, depression and the anticipation of positive and negative future experiences. Psychol Med. 1997;27(4):973-977.
15. MacLeod AK, Tata P, Evans K, et al. Recovery of positive future thinking within a high-risk parasuicide group: results from a pilot randomized controlled trial. Br J Clin Psychol. 1998;37(4):371-379.
16. MacLeod AK, Tata P, Tyrer P, et al. Hopelessness and positive and negative future thinking in parasuicide. Br J Clin Psychol. 2005;44(Pt 4):495-504.
17. O’Connor RC, Smyth R, Williams JM. Intrapersonal positive future thinking predicts repeat suicide attempts in hospital-treated suicide attempters. J Consult Clin Psychol. 2015;83(1):169-176.
18. O’Connor RC, Williams JMG. The relationship between positive future thinking, brooding, defeat and entrapment. Personality and Individual Differences. 2014;70:29-34.
19. Castaneda AE, Tuulio-Henriksson A, Marttunen M, et al. A review on cognitive impairments in depressive and anxiety disorders with a focus on young adults. J Affect Disord. 2008;106(1-2):1-27.
20. Austin MP, Mitchell P, Goodwin GM. Cognitive deficits in depression: possible implications for functional neuropathology. Br J Psychiatry. 2001;178:200-206.
21. Buoli M, Caldiroli A, Caletti E, et al. The impact of mood episodes and duration of illness on cognition in bipolar disorder. Compr Psychiatry. 2014;55(7):1561-1566.
22. Marzuk PM, Hartwell N, Leon AC, et al. Executive functioning in depressed patients with suicidal ideation. Acta Psychiatr Scand. 2005;112(4):294-301.
23. Spreng RN, Gerlach KD, Turner GR, et al. Autobiographical planning and the brain: activation and its modulation by qualitative features. J Cogn Neurosci. 2015;27(11):2147-2157.
24. Spreng RN, Sepulcre J, Turner GR, et al. Intrinsic architecture underlying the relations among the default, dorsal attention, and frontoparietal control networks of the human brain. J Cogn Neurosci. 2013;25(1):74-86.
A patient who has the ability to plan for their future can be reassuring for a clinician who is conducting an imminent suicide risk evaluation. However, that patient may report future plans even as they are contemplating suicide. Therefore, this variable should not be simplified categorically to the mere presence or absence of future plans. Such plans, and the process by which they are produced, should be examined more closely. In this article, we explore the relationship between a patient’s intent to die by suicide in the near future and their ability to maintain future planning. We also use case examples to highlight certain characteristics that may allow future planning to be integrated more reliably into the assessment of imminent risk of suicide.
An inherent challenge
Suicide risk assessment can be challenging due to the numerous factors that can contribute to a patient’s suicidal intent.1 Some individuals don’t seek help when they develop suicidal thoughts, and even among those who do, recognizing who may be at greater risk is not an easy task. Sometimes, this leads to inadequate interventions and a subsequent failure to ensure safety, or to an overreaction and unnecessary hospitalization.
A common difficulty is a patient’s unwillingness to cooperate with the examination.2 Some patients do not present voluntarily, while others may seek help but then conceal suicidal intent. In a sample of 66 psychotherapy patients who reported concealing suicidal ideation from their therapist and provided short essay responses explaining their motives for doing so, approximately 70% said fear of involuntary hospitalization was their motive to hide those thoughts from their doctor.3 Other reasons for concealment are shame, stigma, embarrassment, fear of rejection, and loss of autonomy.3-5 Moreover, higher levels of suicidal ideation are associated with treatment avoidance.6 Therefore, it is important to improve suicide predictability independent of the patient report. In a survey of 1,150 emergency physicians in Australasia, Canada, the United Kingdom, and the United States, the need for evidence-based guidelines on when to hospitalize a patient at risk for suicide was ranked as the 7th-highest priority.7 There are limitations to using suicide risk assessment scales,8,9 because scales designed to have high sensitivity are less specific, and those with high specificity fail to identify individuals at high risk.9,10 Most of the research conducted in this area has focused on the risk of suicide in 2 to 6 months, and not on imminent risk.11
What is ‘imminent’ risk?
There is no specific time definition for “imminent risk,” but the Lifeline Standards, Trainings, and Practices Subcommittee, a group of national and international experts in suicide prevention, defines imminent risk of suicide as the belief that there is a “close temporal connection between the person’s current risk status and actions that could lead to his/her suicide.”12 Practically, suicide could be considered imminent when it occurs within a few days of the evaluation. However, suicide may take place within a few days of an evaluation due to new life events or impulsive actions, which may explain why imminent risk of suicide can be difficult to define and predict. In clinical practice, there is little evidence-based knowledge about estimating imminent risk. Recent studies have explored certain aspects of a patient’s history in the attempt to improve imminent risk predictability.13 In light of the complexity of this matter and the lack of widely validated tools, clinicians are encouraged to share their experience with other clinicians while the efforts to advance evidence-based knowledge and tools continue.
The function of future planning
Future planning is a mental process embedded in several crucial executive functions. It operates on a daily basis to organize, prioritize, and carry out tasks to achieve day-to-day and more distant future goals. Some research has found that a decreased ability to generate positive future thoughts is linked to increased suicide risk in the long term.14-17 Positive future planning can be affected by even minor fluctuations in mood because the additional processing capacity needed during these mood changes may limit one’s ability to generate positive future thoughts.18 Patients experiencing mood episodes are known to experience cognitive dysfunctions.19-21 However, additional measurable cognitive changes have been detected in patients who are suicidal. For example, in a small study (N = 33) of patients with depression, those who were experiencing suicidal thoughts underperformed on several measures of executive functioning compared to patients with no suicidal ideation.22
However, when addressing imminent rather than future suicide risk, even neutral future plans—such as day-to-day plans or those addressing barriers to treatment—can be a meaningful indicator of the investment in one’s future beyond a potential near-term suicide, and therefore can be explored to further inform the risk evaluation. Significant mental resources can be consumed due to the level of distress associated with contemplating suicide, and therefore patients may have a reduced capacity for day-to-day planning. Thus, serious suicide contemplation is less likely in the presence of typical future planning.
Continue to: Characteristics of future planning...
Characteristics of future planning
Some patients may pretend to engage in future planning to indicate the absence of suicidal intent. This necessitates a more nuanced assessment of future plans beyond whether they exist or not by examining the genuineness of such plans, and the authenticity of the process by which they are produced. The Table lists 3 characteristics of future plans/future planning that, based on our clinical experience, can be helpful to evaluate during an imminent suicide risk evaluation. These are described in the following case examples.
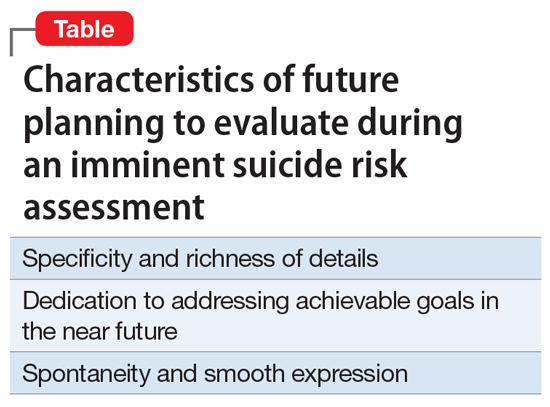
Specificity and richness of details
CASE 1
Mr. A, a college student, presents to the emergency department (ED) complaining of depression and suicidal thoughts that he is able to dismiss. He would like to avoid starting a medication because he has finals in 2 weeks and is worried about adverse effects. He learned about cognitive-behavioral therapy and is interested in getting a referral to a specific office because it is located within a walking distance from campus and easy for him to access because he does not own a car.
The volume of details expressed in a patient’s future plans is important. The more detailed these plans are, the more likely the patient is invested in them. Attendance to the details, especially when addressing expected barriers to treatment, such as transportation, can be evidence of genuine future planning and subsequently of low imminent suicide risk. Spreng et al23 found that autobiographic plans that are more specific and richer in detail recruit additional brain regions that are not recruited in plans that are sparsely detailed or constructed from more generalized representations.
CASE 2
An ambulance transports Ms. B, age 42, from a primary care clinic to the ED because she has been having suicidal thoughts, with a plan to hang herself, for the past 2 days. During the evaluation, Ms. B denies having further suicidal thoughts and declines inpatient admission. She claims that she cannot be away from her children because she is their primary caretaker. Collateral information reveals that Ms. B’s mother has been caring for her children for the last 2 weeks because Ms. B has been too depressed to do so. She continues to refuse admission and is in tears while trying to explain how her absence due to inpatient treatment will be detrimental to her children. Eventually, she angrily accuses the clinician of abusing her children by forcing her to be hospitalized.
In an effort to conceal suicidal intent, patients may present obligations or excuses that would be an obstacle to psychiatric hospitalization. This might give a false perception of intact future planning. However, in these cases, patients often fail to volunteer details about their future plans or show evidence for actual attendance to their obligations. Due to the lack of tangible details to explain the negative effects of inpatient treatment, patients may compensate by using an exaggerated emotional response, with a strong emotional attachment to the obligation and severe distress over their potential inability to fulfill it due to a psychiatric hospitalization. This may contribute to concealing suicidal intent in a different way. A patient may be distressed by the prospect of losing their autonomy or ability to attempt suicide if hospitalized, and they may employ a false excuse as a substitute for the actual reason underlying their distress. A clinician may be falsely reassured if they do not accurately perceive the true cause of the emotional distress. Upon deeper exploration, the expressed emotional attachment is often found to be superficial and has little substantive support.
Continue to: Dedication to addressing acheivable goals in the near future...
Dedication to addressing achievable goals in the near future
CASE 3
Ms. C, age 15, survived a suicide attempt via a medication overdose. She says that she regrets what she did and is not planning to attempt suicide again. Ms. C says she no longer wants to die because in the future she wants to help people by becoming a nurse. She adds that there is a lot waiting for her because she wants to travel all over the world.
Ms. D, age 15, also survived a suicide attempt via a medication overdose. She also says that she regrets what she did and is not planning to attempt suicide again. Ms. D asks whether the physician would be willing to contact the school on her behalf to explain why she had to miss class and to ask for accommodations at school to assist with her panic attacks.
Future planning that involves a patient generating new plans to address current circumstances or the near future may be more reliable than future planning in which a patient repeats their previously constructed plans for the distant future. Eliciting more distant plans, such as a career or family-oriented decisions, indicates the ability to access these “memorized” plans rather than the ability to generate future plans.
Plans that address the distant future, such as those expressed by Ms. C, may have stronger neurologic imprints as a result of repeated memorization and modifications over the years, which may allow a patient to access these plans even while under the stress associated with suicidal thinking. On the other hand, plans that address the near future, such as those expressed by Ms. D, are likely generated in response to current circumstances, which indicates the presence of adequate mental capacity to attend to the current situation, and hence, less preoccupation with suicidal thinking. There might be a neurologic basis for this: some evidence suggests that executive frontoparietal control is recruited in achievable, near-future planning, whereas abstract, difficult-to-achieve, more distant planning fails to engage these additional brain regions.23,24
Spontaneity and smooth expression
CASE 4
Mr. E, age 48, reassures his psychiatrist that he has no intent to act on his suicidal thoughts. When he is offered treatment options, he explains that he would like to start pharmacologic treatment because he only has a few weeks left before he relocates for a new job. The clinician discusses starting a specific medication, and Mr. E expresses interest unless the medication will interfere with his future position as a machine operator. Later, he declines social work assistance to establish care in his new location, preferring to first get the new health care insurance.
A smooth and noncalculated flow of future plans in a patient’s speech allows their plans to be more believable. Plans that naturally flow in response to a verbal exchange and without direct inquiry from the clinician are less likely to be confabulated. This leaves clinicians with the burden of improving the skill of subtly eliciting a patient’s future plans while avoiding directly asking about them. Directly inquiring about such plans may easily tip off the patient that their future planning is under investigation, which may result in misleading responses.
Although future plans that are expressed abruptly, without introductory verbal exchange, or are explicitly linked to why the patient doesn’t intend to kill themselves, can be genuine, the clinician may need to be skeptical about their significance during the risk evaluation. While facing such challenges, clinicians could attempt to shift the patient’s attention away from a safety and disposition-focused conversation toward a less goal-directed verbal exchange during which other opportunities for smooth expression of future plans may emerge. For example, if a patient suddenly discusses how much they care about X in attempt to emphasize why they are not contemplating suicide, the clinician may respond by gently asking the patient to talk more about X.
Continue to: Adopt a more nuanced approach...
Adopt a more nuanced approach
Assessment of the imminent risk of suicide is complicated and not well researched. A patient’s future planning can be used to better inform the evaluation. A patient may have a limited ability to generate future plans while contemplating suicide. Future plans that are specific, rich in details, achievable, dedicated to addressing the near future, and expressed smoothly and in a noncalculated fashion may be more reliable than other types of plans. The process of future planning may indicate low imminent suicide risk when it leads the patient to generate new plans to address current circumstances or the near future. When evaluating a patient’s imminent suicide risk, clinicians should consider abandoning a binary “is there future planning or not” approach and adopting a more complex, nuanced understanding to appropriately utilize this important factor in the risk assessment.
Bottom Line
A patient’s ability to plan for the future should be explored during an assessment of imminent suicide risk. Future plans that are specific, rich in details, achievable, dedicated to addressing the near future, and expressed smoothly and in a noncalculated fashion may be more reliable than other types of plans.
A patient who has the ability to plan for their future can be reassuring for a clinician who is conducting an imminent suicide risk evaluation. However, that patient may report future plans even as they are contemplating suicide. Therefore, this variable should not be simplified categorically to the mere presence or absence of future plans. Such plans, and the process by which they are produced, should be examined more closely. In this article, we explore the relationship between a patient’s intent to die by suicide in the near future and their ability to maintain future planning. We also use case examples to highlight certain characteristics that may allow future planning to be integrated more reliably into the assessment of imminent risk of suicide.
An inherent challenge
Suicide risk assessment can be challenging due to the numerous factors that can contribute to a patient’s suicidal intent.1 Some individuals don’t seek help when they develop suicidal thoughts, and even among those who do, recognizing who may be at greater risk is not an easy task. Sometimes, this leads to inadequate interventions and a subsequent failure to ensure safety, or to an overreaction and unnecessary hospitalization.
A common difficulty is a patient’s unwillingness to cooperate with the examination.2 Some patients do not present voluntarily, while others may seek help but then conceal suicidal intent. In a sample of 66 psychotherapy patients who reported concealing suicidal ideation from their therapist and provided short essay responses explaining their motives for doing so, approximately 70% said fear of involuntary hospitalization was their motive to hide those thoughts from their doctor.3 Other reasons for concealment are shame, stigma, embarrassment, fear of rejection, and loss of autonomy.3-5 Moreover, higher levels of suicidal ideation are associated with treatment avoidance.6 Therefore, it is important to improve suicide predictability independent of the patient report. In a survey of 1,150 emergency physicians in Australasia, Canada, the United Kingdom, and the United States, the need for evidence-based guidelines on when to hospitalize a patient at risk for suicide was ranked as the 7th-highest priority.7 There are limitations to using suicide risk assessment scales,8,9 because scales designed to have high sensitivity are less specific, and those with high specificity fail to identify individuals at high risk.9,10 Most of the research conducted in this area has focused on the risk of suicide in 2 to 6 months, and not on imminent risk.11
What is ‘imminent’ risk?
There is no specific time definition for “imminent risk,” but the Lifeline Standards, Trainings, and Practices Subcommittee, a group of national and international experts in suicide prevention, defines imminent risk of suicide as the belief that there is a “close temporal connection between the person’s current risk status and actions that could lead to his/her suicide.”12 Practically, suicide could be considered imminent when it occurs within a few days of the evaluation. However, suicide may take place within a few days of an evaluation due to new life events or impulsive actions, which may explain why imminent risk of suicide can be difficult to define and predict. In clinical practice, there is little evidence-based knowledge about estimating imminent risk. Recent studies have explored certain aspects of a patient’s history in the attempt to improve imminent risk predictability.13 In light of the complexity of this matter and the lack of widely validated tools, clinicians are encouraged to share their experience with other clinicians while the efforts to advance evidence-based knowledge and tools continue.
The function of future planning
Future planning is a mental process embedded in several crucial executive functions. It operates on a daily basis to organize, prioritize, and carry out tasks to achieve day-to-day and more distant future goals. Some research has found that a decreased ability to generate positive future thoughts is linked to increased suicide risk in the long term.14-17 Positive future planning can be affected by even minor fluctuations in mood because the additional processing capacity needed during these mood changes may limit one’s ability to generate positive future thoughts.18 Patients experiencing mood episodes are known to experience cognitive dysfunctions.19-21 However, additional measurable cognitive changes have been detected in patients who are suicidal. For example, in a small study (N = 33) of patients with depression, those who were experiencing suicidal thoughts underperformed on several measures of executive functioning compared to patients with no suicidal ideation.22
However, when addressing imminent rather than future suicide risk, even neutral future plans—such as day-to-day plans or those addressing barriers to treatment—can be a meaningful indicator of the investment in one’s future beyond a potential near-term suicide, and therefore can be explored to further inform the risk evaluation. Significant mental resources can be consumed due to the level of distress associated with contemplating suicide, and therefore patients may have a reduced capacity for day-to-day planning. Thus, serious suicide contemplation is less likely in the presence of typical future planning.
Continue to: Characteristics of future planning...
Characteristics of future planning
Some patients may pretend to engage in future planning to indicate the absence of suicidal intent. This necessitates a more nuanced assessment of future plans beyond whether they exist or not by examining the genuineness of such plans, and the authenticity of the process by which they are produced. The Table lists 3 characteristics of future plans/future planning that, based on our clinical experience, can be helpful to evaluate during an imminent suicide risk evaluation. These are described in the following case examples.
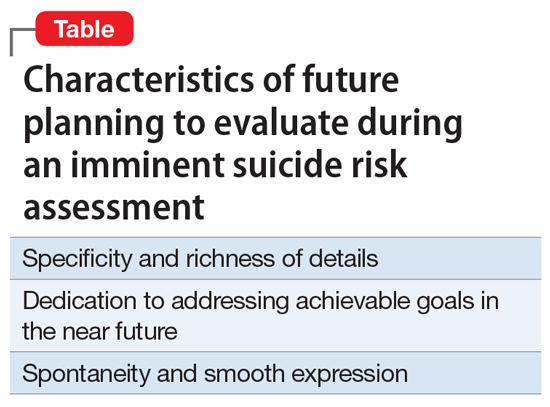
Specificity and richness of details
CASE 1
Mr. A, a college student, presents to the emergency department (ED) complaining of depression and suicidal thoughts that he is able to dismiss. He would like to avoid starting a medication because he has finals in 2 weeks and is worried about adverse effects. He learned about cognitive-behavioral therapy and is interested in getting a referral to a specific office because it is located within a walking distance from campus and easy for him to access because he does not own a car.
The volume of details expressed in a patient’s future plans is important. The more detailed these plans are, the more likely the patient is invested in them. Attendance to the details, especially when addressing expected barriers to treatment, such as transportation, can be evidence of genuine future planning and subsequently of low imminent suicide risk. Spreng et al23 found that autobiographic plans that are more specific and richer in detail recruit additional brain regions that are not recruited in plans that are sparsely detailed or constructed from more generalized representations.
CASE 2
An ambulance transports Ms. B, age 42, from a primary care clinic to the ED because she has been having suicidal thoughts, with a plan to hang herself, for the past 2 days. During the evaluation, Ms. B denies having further suicidal thoughts and declines inpatient admission. She claims that she cannot be away from her children because she is their primary caretaker. Collateral information reveals that Ms. B’s mother has been caring for her children for the last 2 weeks because Ms. B has been too depressed to do so. She continues to refuse admission and is in tears while trying to explain how her absence due to inpatient treatment will be detrimental to her children. Eventually, she angrily accuses the clinician of abusing her children by forcing her to be hospitalized.
In an effort to conceal suicidal intent, patients may present obligations or excuses that would be an obstacle to psychiatric hospitalization. This might give a false perception of intact future planning. However, in these cases, patients often fail to volunteer details about their future plans or show evidence for actual attendance to their obligations. Due to the lack of tangible details to explain the negative effects of inpatient treatment, patients may compensate by using an exaggerated emotional response, with a strong emotional attachment to the obligation and severe distress over their potential inability to fulfill it due to a psychiatric hospitalization. This may contribute to concealing suicidal intent in a different way. A patient may be distressed by the prospect of losing their autonomy or ability to attempt suicide if hospitalized, and they may employ a false excuse as a substitute for the actual reason underlying their distress. A clinician may be falsely reassured if they do not accurately perceive the true cause of the emotional distress. Upon deeper exploration, the expressed emotional attachment is often found to be superficial and has little substantive support.
Continue to: Dedication to addressing acheivable goals in the near future...
Dedication to addressing achievable goals in the near future
CASE 3
Ms. C, age 15, survived a suicide attempt via a medication overdose. She says that she regrets what she did and is not planning to attempt suicide again. Ms. C says she no longer wants to die because in the future she wants to help people by becoming a nurse. She adds that there is a lot waiting for her because she wants to travel all over the world.
Ms. D, age 15, also survived a suicide attempt via a medication overdose. She also says that she regrets what she did and is not planning to attempt suicide again. Ms. D asks whether the physician would be willing to contact the school on her behalf to explain why she had to miss class and to ask for accommodations at school to assist with her panic attacks.
Future planning that involves a patient generating new plans to address current circumstances or the near future may be more reliable than future planning in which a patient repeats their previously constructed plans for the distant future. Eliciting more distant plans, such as a career or family-oriented decisions, indicates the ability to access these “memorized” plans rather than the ability to generate future plans.
Plans that address the distant future, such as those expressed by Ms. C, may have stronger neurologic imprints as a result of repeated memorization and modifications over the years, which may allow a patient to access these plans even while under the stress associated with suicidal thinking. On the other hand, plans that address the near future, such as those expressed by Ms. D, are likely generated in response to current circumstances, which indicates the presence of adequate mental capacity to attend to the current situation, and hence, less preoccupation with suicidal thinking. There might be a neurologic basis for this: some evidence suggests that executive frontoparietal control is recruited in achievable, near-future planning, whereas abstract, difficult-to-achieve, more distant planning fails to engage these additional brain regions.23,24
Spontaneity and smooth expression
CASE 4
Mr. E, age 48, reassures his psychiatrist that he has no intent to act on his suicidal thoughts. When he is offered treatment options, he explains that he would like to start pharmacologic treatment because he only has a few weeks left before he relocates for a new job. The clinician discusses starting a specific medication, and Mr. E expresses interest unless the medication will interfere with his future position as a machine operator. Later, he declines social work assistance to establish care in his new location, preferring to first get the new health care insurance.
A smooth and noncalculated flow of future plans in a patient’s speech allows their plans to be more believable. Plans that naturally flow in response to a verbal exchange and without direct inquiry from the clinician are less likely to be confabulated. This leaves clinicians with the burden of improving the skill of subtly eliciting a patient’s future plans while avoiding directly asking about them. Directly inquiring about such plans may easily tip off the patient that their future planning is under investigation, which may result in misleading responses.
Although future plans that are expressed abruptly, without introductory verbal exchange, or are explicitly linked to why the patient doesn’t intend to kill themselves, can be genuine, the clinician may need to be skeptical about their significance during the risk evaluation. While facing such challenges, clinicians could attempt to shift the patient’s attention away from a safety and disposition-focused conversation toward a less goal-directed verbal exchange during which other opportunities for smooth expression of future plans may emerge. For example, if a patient suddenly discusses how much they care about X in attempt to emphasize why they are not contemplating suicide, the clinician may respond by gently asking the patient to talk more about X.
Continue to: Adopt a more nuanced approach...
Adopt a more nuanced approach
Assessment of the imminent risk of suicide is complicated and not well researched. A patient’s future planning can be used to better inform the evaluation. A patient may have a limited ability to generate future plans while contemplating suicide. Future plans that are specific, rich in details, achievable, dedicated to addressing the near future, and expressed smoothly and in a noncalculated fashion may be more reliable than other types of plans. The process of future planning may indicate low imminent suicide risk when it leads the patient to generate new plans to address current circumstances or the near future. When evaluating a patient’s imminent suicide risk, clinicians should consider abandoning a binary “is there future planning or not” approach and adopting a more complex, nuanced understanding to appropriately utilize this important factor in the risk assessment.
Bottom Line
A patient’s ability to plan for the future should be explored during an assessment of imminent suicide risk. Future plans that are specific, rich in details, achievable, dedicated to addressing the near future, and expressed smoothly and in a noncalculated fashion may be more reliable than other types of plans.
1. Gilbert AM, Garno JL, Braga RJ, et al. Clinical and cognitive correlates of suicide attempts in bipolar disorder: is suicide predictable? J Clin Psychiatry. 2011;72(8):1027-1033.
2. Obegi JH. Your patient refuses a suicide risk assessment. Now what? Current Psychiatry. 2021;20(4):45.
3. Blanchard M, Farber BA. “It is never okay to talk about suicide”: Patients’ reasons for concealing suicidal ideation in psychotherapy. Psychother Res. 2020;30(1):124-136.
4. Richards JE, Whiteside U, Ludman EJ, et al. Understanding why patients may not report suicidal ideation at a health care visit prior to a suicide attempt: a qualitative study. Psychiatr Serv. 2019;70(1):40-45.
5. Fulginiti A, Frey LM. Exploring suicide-related disclosure motivation and the impact on mechanisms linked to suicide. Death Stud. 2019;43(9):562-569.
6. Wilson CJ, Deane FP, Marshall KL, et al. Adolescents’ suicidal thinking and reluctance to consult general medical practitioners. J Youth Adolesc. 2010;39(4):343-356.
7. Eagles D, Stiell IG, Clement CM, et al. International survey of emergency physicians’ priorities for clinical decision rules. Acad Emerg Med. 2008;15(2):177-182.
8. Swedish Council on Health Technology Assessment (SBU): SBU Systematic Review Summaries. Instruments for Suicide Risk Assessment. Summary and Conclusions. SBU Yellow Report No. 242. 2015. Accessed January 6, 2021. https://www.ncbi.nlm.nih.gov/books/NBK350492/
9. Runeson B, Odeberg J, Pettersson A, et al. Instruments for the assessment of suicide risk: a systematic review evaluating the certainty of the evidence. PLoS One. 2017;12(7):e0180292. doi:10.1371/journal.pone.0180292
10. Steeg S, Quinlivan L, Nowland R, et al. Accuracy of risk scales for predicting repeat self-harm and suicide: a multicentre, population-level cohort study using routine clinical data. BMC Psychiatry. 2018;18(1):113.
11. Nock MK, Banaji MR. Prediction of suicide ideation and attempts among adolescents using a brief performance-based test. J Consult Clin Psychol. 2007;75(5):707-715.
12. Draper J, Murphy G, Vega E, et al. Helping callers to the National Suicide Prevention Lifeline who are at imminent risk of suicide: the importance of active engagement, active rescue, and collaboration between crisis and emergency services. Suicide Life Threat Behav. 2015;45(3):261-270.
13. Glenn CR, Nock MK. Improving the short-term prediction of suicidal behavior. Am J Prev Med. 2014;47(3 Suppl 2):S176-S180.
14. MacLeod AK, Pankhania B, Lee M, et al. Parasuicide, depression and the anticipation of positive and negative future experiences. Psychol Med. 1997;27(4):973-977.
15. MacLeod AK, Tata P, Evans K, et al. Recovery of positive future thinking within a high-risk parasuicide group: results from a pilot randomized controlled trial. Br J Clin Psychol. 1998;37(4):371-379.
16. MacLeod AK, Tata P, Tyrer P, et al. Hopelessness and positive and negative future thinking in parasuicide. Br J Clin Psychol. 2005;44(Pt 4):495-504.
17. O’Connor RC, Smyth R, Williams JM. Intrapersonal positive future thinking predicts repeat suicide attempts in hospital-treated suicide attempters. J Consult Clin Psychol. 2015;83(1):169-176.
18. O’Connor RC, Williams JMG. The relationship between positive future thinking, brooding, defeat and entrapment. Personality and Individual Differences. 2014;70:29-34.
19. Castaneda AE, Tuulio-Henriksson A, Marttunen M, et al. A review on cognitive impairments in depressive and anxiety disorders with a focus on young adults. J Affect Disord. 2008;106(1-2):1-27.
20. Austin MP, Mitchell P, Goodwin GM. Cognitive deficits in depression: possible implications for functional neuropathology. Br J Psychiatry. 2001;178:200-206.
21. Buoli M, Caldiroli A, Caletti E, et al. The impact of mood episodes and duration of illness on cognition in bipolar disorder. Compr Psychiatry. 2014;55(7):1561-1566.
22. Marzuk PM, Hartwell N, Leon AC, et al. Executive functioning in depressed patients with suicidal ideation. Acta Psychiatr Scand. 2005;112(4):294-301.
23. Spreng RN, Gerlach KD, Turner GR, et al. Autobiographical planning and the brain: activation and its modulation by qualitative features. J Cogn Neurosci. 2015;27(11):2147-2157.
24. Spreng RN, Sepulcre J, Turner GR, et al. Intrinsic architecture underlying the relations among the default, dorsal attention, and frontoparietal control networks of the human brain. J Cogn Neurosci. 2013;25(1):74-86.
1. Gilbert AM, Garno JL, Braga RJ, et al. Clinical and cognitive correlates of suicide attempts in bipolar disorder: is suicide predictable? J Clin Psychiatry. 2011;72(8):1027-1033.
2. Obegi JH. Your patient refuses a suicide risk assessment. Now what? Current Psychiatry. 2021;20(4):45.
3. Blanchard M, Farber BA. “It is never okay to talk about suicide”: Patients’ reasons for concealing suicidal ideation in psychotherapy. Psychother Res. 2020;30(1):124-136.
4. Richards JE, Whiteside U, Ludman EJ, et al. Understanding why patients may not report suicidal ideation at a health care visit prior to a suicide attempt: a qualitative study. Psychiatr Serv. 2019;70(1):40-45.
5. Fulginiti A, Frey LM. Exploring suicide-related disclosure motivation and the impact on mechanisms linked to suicide. Death Stud. 2019;43(9):562-569.
6. Wilson CJ, Deane FP, Marshall KL, et al. Adolescents’ suicidal thinking and reluctance to consult general medical practitioners. J Youth Adolesc. 2010;39(4):343-356.
7. Eagles D, Stiell IG, Clement CM, et al. International survey of emergency physicians’ priorities for clinical decision rules. Acad Emerg Med. 2008;15(2):177-182.
8. Swedish Council on Health Technology Assessment (SBU): SBU Systematic Review Summaries. Instruments for Suicide Risk Assessment. Summary and Conclusions. SBU Yellow Report No. 242. 2015. Accessed January 6, 2021. https://www.ncbi.nlm.nih.gov/books/NBK350492/
9. Runeson B, Odeberg J, Pettersson A, et al. Instruments for the assessment of suicide risk: a systematic review evaluating the certainty of the evidence. PLoS One. 2017;12(7):e0180292. doi:10.1371/journal.pone.0180292
10. Steeg S, Quinlivan L, Nowland R, et al. Accuracy of risk scales for predicting repeat self-harm and suicide: a multicentre, population-level cohort study using routine clinical data. BMC Psychiatry. 2018;18(1):113.
11. Nock MK, Banaji MR. Prediction of suicide ideation and attempts among adolescents using a brief performance-based test. J Consult Clin Psychol. 2007;75(5):707-715.
12. Draper J, Murphy G, Vega E, et al. Helping callers to the National Suicide Prevention Lifeline who are at imminent risk of suicide: the importance of active engagement, active rescue, and collaboration between crisis and emergency services. Suicide Life Threat Behav. 2015;45(3):261-270.
13. Glenn CR, Nock MK. Improving the short-term prediction of suicidal behavior. Am J Prev Med. 2014;47(3 Suppl 2):S176-S180.
14. MacLeod AK, Pankhania B, Lee M, et al. Parasuicide, depression and the anticipation of positive and negative future experiences. Psychol Med. 1997;27(4):973-977.
15. MacLeod AK, Tata P, Evans K, et al. Recovery of positive future thinking within a high-risk parasuicide group: results from a pilot randomized controlled trial. Br J Clin Psychol. 1998;37(4):371-379.
16. MacLeod AK, Tata P, Tyrer P, et al. Hopelessness and positive and negative future thinking in parasuicide. Br J Clin Psychol. 2005;44(Pt 4):495-504.
17. O’Connor RC, Smyth R, Williams JM. Intrapersonal positive future thinking predicts repeat suicide attempts in hospital-treated suicide attempters. J Consult Clin Psychol. 2015;83(1):169-176.
18. O’Connor RC, Williams JMG. The relationship between positive future thinking, brooding, defeat and entrapment. Personality and Individual Differences. 2014;70:29-34.
19. Castaneda AE, Tuulio-Henriksson A, Marttunen M, et al. A review on cognitive impairments in depressive and anxiety disorders with a focus on young adults. J Affect Disord. 2008;106(1-2):1-27.
20. Austin MP, Mitchell P, Goodwin GM. Cognitive deficits in depression: possible implications for functional neuropathology. Br J Psychiatry. 2001;178:200-206.
21. Buoli M, Caldiroli A, Caletti E, et al. The impact of mood episodes and duration of illness on cognition in bipolar disorder. Compr Psychiatry. 2014;55(7):1561-1566.
22. Marzuk PM, Hartwell N, Leon AC, et al. Executive functioning in depressed patients with suicidal ideation. Acta Psychiatr Scand. 2005;112(4):294-301.
23. Spreng RN, Gerlach KD, Turner GR, et al. Autobiographical planning and the brain: activation and its modulation by qualitative features. J Cogn Neurosci. 2015;27(11):2147-2157.
24. Spreng RN, Sepulcre J, Turner GR, et al. Intrinsic architecture underlying the relations among the default, dorsal attention, and frontoparietal control networks of the human brain. J Cogn Neurosci. 2013;25(1):74-86.
Borderline personality disorder: 6 studies of psychosocial interventions
SECOND OF 2 PARTS
Borderline personality disorder (BPD) is associated with serious impairment in psychosocial functioning.1 It is characterized by an ongoing pattern of mood instability, cognitive distortions, problems with self-image, and impulsive behavior that often results in problems in relationships. As a result, patients with BPD tend to utilize more mental health services than patients with other personality disorders or major depressive disorder.2
Some clinicians believe BPD is difficult to treat. While historically there has been little consensus on the best treatments for this disorder, current options include both pharmacologic and psychological interventions. In Part 1 of this 2-part article, we focused on 6 studies that evaluated biological interventions.3 Here in Part 2, we focus on findings from 6 recent randomized controlled trials (RCTs) of psychosocial interventions for BPD
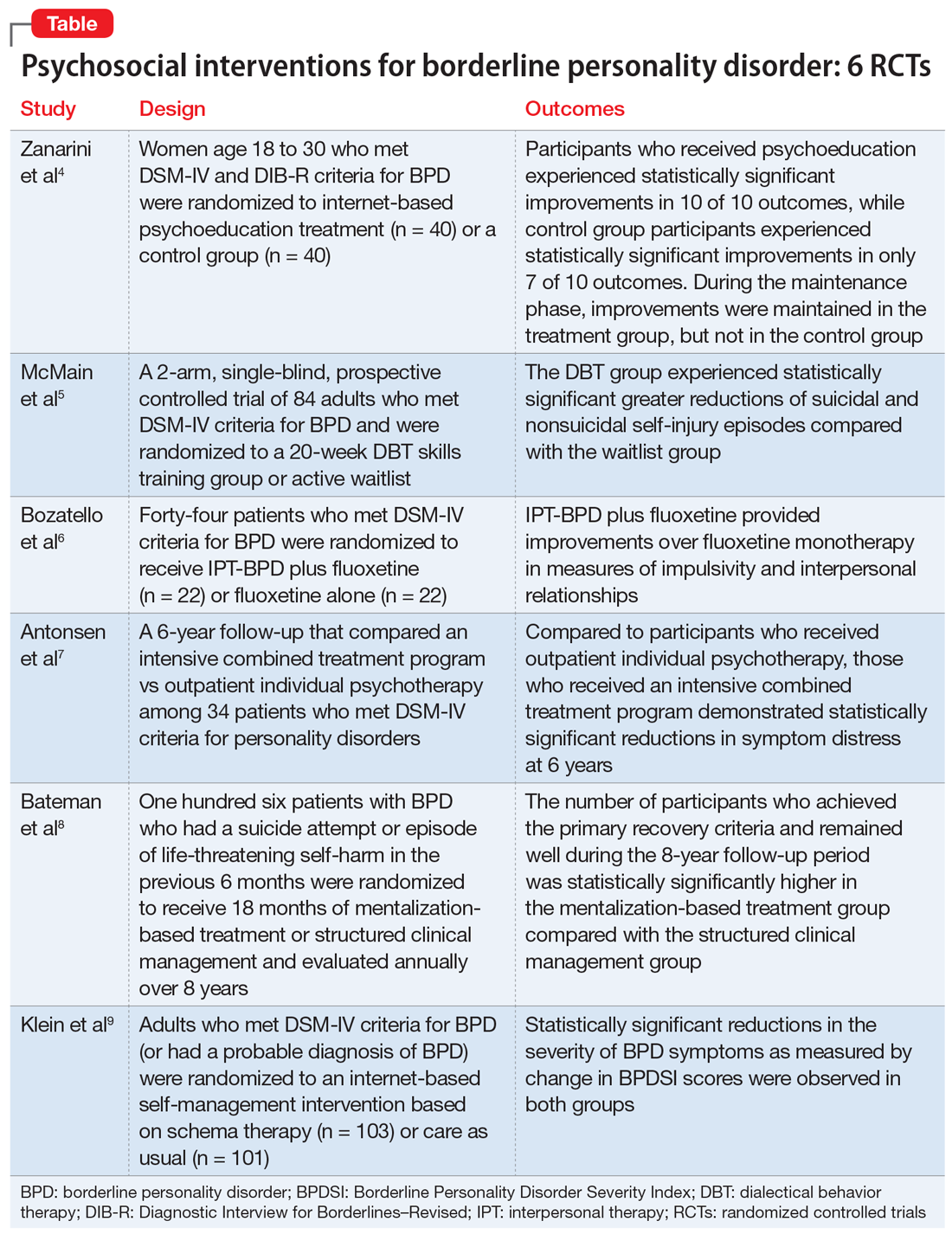
1. Zanarini MC, Conkey LC, Temes CM, et al. Randomized controlled trial of web-based psychoeducation for women with borderline personality disorder. J Clin Psychiatry. 2018;79(3):16m11153. doi: 10.4088/JCP.16m11153
Research has shown that BPD is a treatable illness with a more favorable prognosis than previously believed. Despite this, patients often experience difficulty accessing the most up-to-date information on BPD, which can impede their treatment. A 2008 study by Zanarini et al10 of younger female patients with BPD demonstrated that immediate, in-person psychoeducation improved impulsivity and relationships. Widespread implementation of this program proved problematic, however, due to cost and personnel constraints. To resolve this issue, researchers developed an internet-based version of the program. In a 2018 follow-up study, Zanarini et al4 examined the effect of this internet-based psychoeducation program on symptoms of BPD.
Continue to: Study design...
Study design
- Women (age 18 to 30) who met DSM-IV and Diagnostic Interview for Borderlines–Revised criteria for BPD were randomized to an internet-based psychoeducation treatment group (n = 40) or a control group (n = 40).
- Ten outcomes concerning symptom severity and psychosocial functioning were assessed during weeks 1 to 12 (acute phase) and at months 6, 9, and 12 (maintenance phase) using the self-report version of the Zanarini Rating Scale for BPD (ZAN-BPD), the Borderline Evaluation of Severity over Time, the Sheehan Disability Scale, the Clinically Useful Depression Outcome Scale, the Clinically Useful Anxiety Outcome Scale, and Weissman’s Social Adjustment Scale (SAS).
Outcomes
- In the acute phase, treatment group participants experienced statistically significant improvements in all 10 outcomes. Control group participants demonstrated similar results, achieving statistically significant improvements in 7 of 10 outcomes.
- Compared to the control group, the treatment group experienced a more significant reduction in impulsivity and improvement in psychosocial functioning as measured by the ZAN-BPD and SAS.
- In the maintenance phase, treatment group participants achieved statistically significant improvements in 9 of 10 outcomes, whereas control group participants demonstrated statistically significant improvements in only 3 of 10 outcomes.
- Compared to the control group, the treatment group also demonstrated a significantly greater improvement in all 4 sector scores and the total score of the ZAN-BP
Conclusions/limitations
- In patients with BPD, internet-based psychoeducation reduced symptom severity and improved psychosocial functioning, with effects lasting 1 year. Treatment group participants experienced clinically significant improvements in all outcomes measured during the acute phase of the study; most improvements were maintained over 1 year.
- While the control group initially saw similar improvements in most measurements, these improvements were not maintained as effectively over 1 year.
- Limitations include a female-only population, the restricted age range of participants, and recruitment exclusively from volunteers.
2. McMain SF, Guimond T, Barnhart R, et al. A randomized trial of brief dialectical behaviour therapy skills training in suicidal patients suffering from borderline disorder. Acta Psychiatr Scand. 2017;135(2):138-148.
Standard dialectical behavior therapy (DBT) is an effective treatment for BPD; however, access is often limited by shortages of clinicians and resources. Therefore, it has become increasingly common for clinical settings to offer patients only the skills training component of DBT, which requires fewer resources. While several clinical trials examining brief DBT skills–only treatment for BPD have shown promising results, it is unclear how effective this intervention is at reducing suicidal or nonsuicidal self-injury (NSSI) episodes. McMain et al5 explored the effectiveness of brief DBT skills–only adjunctive treatment on the rates of suicidal and NSSI episodes in patients with BPD.
Study design
- In this 2-arm, single-blind, prospective controlled trial, 84 adults who met DSM-IV criteria for BPD were randomized to a 20-week DBT skills training group (DBT group) or an active waitlist (WL group). No restrictions on additional psychosocial or pharmacologic treatments were imposed on either group.
- The primary outcome was the frequency of suicidal and NSSI episodes as measured by the Lifetime Suicide Attempt Self-Injury Interview and the Deliberate Self-Harm Inventory (DSHI). Measurements occurred at baseline, 10 weeks, 20 weeks, and 3 months posttreatment (32 weeks).
- Secondary outcomes included changes in health care utilization, BPD symptoms, and coping. These were assessed using the Treatment History Interview-2, Borderline Symptom List-23, State-Trait Anger Expression Inventory, Symptom Checklist-90-revised (SCL-90-R), Barratt Impulsiveness Scale-11, Beck Depression Inventory (BDI)-II, Social Adjustment Scale Self-report, Difficulties in Emotion Regulation Scale, Distress Tolerance Scale, and Kentucky Inventory of Mindfulness Scale.
Outcomes
- At Week 32, compared to the WL group, the DBT group showed statistically significant greater reductions in the frequency of suicidal and NSSI episodes as measured by the LSASI but not by the DSHI. The DBT group experienced statistically significant improvements in distress tolerance and emotion regulation over the WL group at all points, but no difference on mindfulness. The DBT group achieved greater reductions in anger over time as compared to the WL group.
- At Week 20, compared to the WL group, the DBT group showed significant improvements in social adjustment, symptom distress, and borderline symptoms. There were no significant group differences on impulsivity. Between-group differences in the number of hospital admissions favored the DBT group at 10 and 20 weeks, but not at 32 weeks. There was no statistically significant difference between the groups with respect to the number of emergency department visits.
- Analyses of group differences in clinical improvement as measured by the SCL-90-R revealed statistically reliable and clinically significant changes in the DBT group over the WL group at 20 weeks, but not at 32 weeks.
Conclusions/limitations
- Brief DBT skills training reduced suicidal and NSSI episodes in patients with BPD. Participants in the DBT group also demonstrated greater improvement in anger, distress tolerance, and emotion regulation compared to the control group. These results were evident 3 months after treatment. However, any gains in health care utilization, social adjustment, symptom distress, and borderline symptoms diminished or did not differ from waitlist participants at Week 32. At that time, participants in the DBT group demonstrated a similar level of symptomatology as the WL group.
- Limitations include the use of an active waitlist control group, allowance of concurrent treatments, the absence of an active therapeutic comparator group, use of self-report measures, use of an instrument with unknown psychometric properties, and a relatively short 3-month follow-up period.
3. Bozzatello P, Bellino S. Combined therapy with interpersonal psychotherapy adapted for borderline personality disorder: a two-years follow-up. Psychiatry Res. 2016;240:151-156.
Psychotherapeutic options for treating BPD include DBT, mentalization-based treatment, schema-focused therapy, transference-based psychotherapy, and systems training for emotional predictability and problem solving. More recently, interpersonal therapy also has been adapted for BPD (IPT-BPD). However, thus far no trials have investigated the long-term effects of this therapy on BPD. In 2010, Bellino et al11 published a 32-week RCT examining the effect of IPT-BPD on BPD. They concluded that IPT-BPD plus fluoxetine was superior to fluoxetine alone in improving symptoms and quality of life. The present study by Bozzatello et al6 examined whether the benefits of IPT-BPD plus fluoxetine demonstrated in the 2010 study persisted over a 24-month follow-up.
Continue to: Study design...
Study design
- In the 2010 study by Bellino et al,11 55 outpatients who met DSM-IV criteria for BPD were randomized to receive IPT-BPD plus fluoxetine (combined therapy) or fluoxetine alone for 32 weeks. Forty-four participants completed a 24-month follow-up study (n = 22 for IPT-BPD plus fluoxetine, n = 22 for fluoxetine only).
- Clinical assessments were performed at 6, 12, and 24 months, and used the same instruments as the original study, including the Clinical Global Impression Scale–Severity item, Hamilton Depression Rating Scale, Hamilton Anxiety Rating Scale (HARS), Social and Occupational Functioning Assessment, Satisfaction Profile (SAT-P), and the Borderline Personality Disorder Severity Index (BPDSI).
Outcomes
- While the original study demonstrated that combined therapy had a clinically significant effect over fluoxetine alone on both HARS score and the BPDSI item “affective instability” at 32 weeks, this advantage was maintained only at the 6-month assessment.
- The improvements that the combined therapy provided over fluoxetine monotherapy on the BPDSI items of “impulsivity” and “interpersonal relationships” as well as the SAT-P factors of social and psychological functioning at 32 weeks were preserved at 24 months. No additional improvements were seen.
Conclusions/limitations
- The improvements in impulsivity, interpersonal functioning, social functioning, and psychological functioning at 32 weeks seen with IPT-BPD plus fluoxetine compared with fluoxetine alone persisted for 2 years after completing therapy; no further improvements were seen.
- The improvements to anxiety and affective instability that combined therapy demonstrated over fluoxetine monotherapy at 32 weeks were not maintained at 24 months.
- Limitations include a small sample size, exclusion of psychiatric comorbidities, and a lack of assessment of session or medication adherence.
4. Antonsen BT, Kvarstein EH, Urnes Ø, et al. Favourable outcome of long-term combined psychotherapy for patients with borderline personality disorder: six-year follow-up of a randomized study. Psychother Res. 2017;27(1):51-63.
While many studies have demonstrated the benefits of psychotherapy for treating personality disorders, there is limited research of how different levels of psychotherapy may impact treatment outcomes. An RCT called the Ullevål Personality Project (UPP)12 compared an intensive combined treatment program (CP) with outpatient individual psychotherapy (OIP) in patients with personality disorders. The CP program consisted of short-term day-hospital treatment followed by outpatient combined group and individual psychotherapy. The outcomes this RCT evaluated included suicide attempts, suicidal thoughts, self-injury, psychosocial functioning, symptom distress, and interpersonal and personality problems. A 6-year follow-up concluded there were no differences in outcomes between the 2 treatment groups. However, in this RCT, Antonsen et al7 examined whether CP produced statistically significant benefits over OIP in a subset of patients with BPD.
Study design
- In the UPP trial,12 117 patients who met DSM-IV criteria for personality disorders (excluding antisocial and schizotypal personality disorder) were randomized to receive 18 weeks of day hospital psychotherapy followed by CP or OIP. Fifty-two participants in the UPP were diagnosed with BPD, and 34 of these participants completed the 6-year follow-up investigation.
- Symptom distress, psychosocial functioning, interpersonal problems, quality of life, personality functioning, and self-harm/suicidal thoughts/suicide attempts were assessed at baseline, 8 months, 18 months, 3 years, and 6 years using the SCL-90-R Global Severity Index (GSI), BDI, Global Assessment of Functioning (GAF), Work and Social Adjustment Scale (WSAS), Quality of Life 10-point scale (QOL), Circumplex of Interpersonal Problems (CIP), and the 60-item short form of the Severity Indices of Personality Problems (SIPP-118) questionnaire.
Outcomes
- Compared to the OIP group, the CP group demonstrated statistically significant reductions in symptom distress at Year 6 as measured by the SCL-90-R GSI. Between Years 3 and 6, the CP group continued to show improvements in psychosocial functioning as demonstrated by improvements in GAF and WSAS scores. The OIP group’s scores worsened during this time. Compared to the OIP group, participants in the CP group also had significantly better outcomes on the SIPP-118 domains of self-control and identity integration.
- There were no significant differences between groups on the proportion of participants who engaged in self-harm or experienced suicidal thoughts or attempts. There were no significant differences in outcomes between the treatment groups on the CIP, BDI, or QOL.
- Participants in CP group tended to use fewer psychotropic medications than those in the OIP group over time, but this difference was not statistically significant. The 2 groups did not differ in use of health care services over the last year.
- Avoidant personality disorder (AVPD) did not have a significant moderator effect on GAF score. Comorbid AVPD was a negative predictor of GAF score, independent of the group.
Conclusions/limitations
- Both groups experienced a remission rate of 90% at 6-year follow-up. Compared with the OIP group, participants in the CP group experienced significantly greater reductions in symptom distress and improvements in self-control and identity integration at 6 years. Between Years 3 and 6, participants in the CP group experienced significant improvements in psychosocial functioning compared with OIP group participants. The 2 groups did not differ on other outcomes, including the CIP, BDI, QOL, suicidal thoughts, suicidal attempts, self-harm, and health care utilization.
- Despite statistically significant differences in GAF scores favoring the CP group over the OIP group during Years 3 to 6, GAF scores did not differ significantly in the final year, which suggests that symptomatic remission does not equal functional improvement.
- Limitations include a lack of control for intensity or length of treatment in statistical analyses, small sample size, lack of correction for multiple testing, lack of an a priori power analysis, missing data and potential violation of the missing at random assumption, use of therapists’ preferred treatment method/practice, and a lack of control for other treatments.
5. Bateman A, Constantinou MP, Fonagy P, et al. Eight-year prospective follow-up of mentalization-based treatment versus structured clinical management for people with borderline personality disorder. Personal Disord. 2021;12(4):291-299.
The efficacy of various psychotherapies for symptoms of BPD has been well established. However, there is limited evidence that these effects persist over time. In 2009, Bateman et al13 conducted an 18-month RCT comparing the effectiveness of outpatient mentalization-based treatment (MBT) against structured clinical management (SCM) for patients with BPD. Both groups experienced substantial improvements, but patients assigned to MBT demonstrated greater improvement in clinically significant problems, including suicide attempts and hospitalizations. In a 2021 follow-up to this study, Bateman et al8 investigated whether the MBT group’s gains in the primary outcomes (absence of severe self-harm, suicide attempts, and inpatient admissions in the previous 12 months), social functioning, vocational engagement, and mental health service usage were maintained throughout an 8-year follow-up period.
Continue to: Study design...
Study design
- In the 2009 trial, Bateman et al13 randomized adult participants who met DSM-IV criteria for BPD and had a suicide attempt or episode of life-threatening self-harm in the past 6 months to receive 18 months of MBT or SCM. The primary outcome was crisis events, defined as a composite of suicidal and severe self-injurious behaviors and hospitalizations. The 2021 Bateman et al8 study expanded this investigation by collecting additional data on a yearly basis for 8 years.
- Of the 134 original participants, 98 agreed to complete the follow-up. Due to attrition, the follow-up period was limited to 8 years. At each yearly visit, researchers collected information on the primary outcome, the absence of severe self-harm, suicide attempts, and inpatient admissions in the previous 12 months.
- Secondary measures were collected mainly through a modified version of the Client Service Receipt Inventory and included critical incidents, psychiatric and medical hospital and community services, employment and other personally meaningful activity, psychoactive medication, and other mental health treatments.
Outcomes
- The number of participants who met diagnostic criteria for BPD at the 1-year follow-up was significantly lower in the MBT group compared with the SCM group. To improve participant retention, this outcome was not evaluated at later visits.
- The number of participants who achieved the primary recovery criteria of the original trial (absence of severe self-harm, suicide attempts, and inpatient admissions in the previous 12 months) and remained well throughout the entire follow-up period was significantly higher in the MBT group compared with the SCM group. The average number of years during which participants failed to meet recovery criteria was significantly greater in the SCM group compared with the MBT group.
- When controlling for age, treatment group was a significant predictor of recovery during the follow-up period. Overall, significantly fewer participants in the MBT group experienced critical incidents during the follow-up period.
- The SCM group used crisis mental health services for a significantly greater number of follow-up years than the MBT group, although the likelihood of ever using crisis services did not statistically differ between the groups. Both groups had similar use of outpatient mental health services, primary care services, and nonmental health medical services. Compared to the SCM group, the MBT group had significantly fewer professional support service visits and significantly fewer outpatient psychiatrist visits.
- MBT group participants spent more time in education, were less likely to be unemployed, and were less likely to use social care interventions than SCM group participants. Although those in the MBT group spent more months engaged in purposeful activity, there was no significant difference between the groups in the proportion of participants who did not engage in purposeful activity.
- The MBT group spent fewer months receiving psychotherapeutic medication compared with the SCM group. The variables that yielded significant 2-way interactions were eating disorder, substance use disorder, and physical abuse, suggesting greater benefit from MBT with these concurrent diagnoses. Younger age was associated with better outcomes.
Conclusions/limitations
- This study demonstrated that patients with BPD significantly benefited from specialized therapies such as MBT.
- At the 1 follow-up visit, the number of participants who met diagnostic criteria for BPD was significantly lower in the MBT group compared with the SCM group.
- The number of participants who had achieved the primary recovery criteria and remained well during the 8-year follow-up period was significantly higher in the MBT group compared to the SCM group.
- Limitations include increasing attrition over time, possible allegiance effects and unmasking of research assistants, lack of self-report questionnaires, and the potentially erroneous conclusion that increased use of services equates to poorer treatment response and greater need for support.
6. Klein JP, Hauer-von Mauschwitz A, Berger T, et al. Effectiveness and safety of the adjunctive use of an internet-based self-management intervention for borderline personality disorder in addition to care as usual: results from a randomised controlled trial. BMJ Open. 2021;11(9):e047771.
Fewer than 1 in 4 patients with BPD have access to effective psychotherapies. The use of internet-based self-management interventions (SMIs) developed from evidence-based psychotherapies can help close this treatment gap. Although the efficacy of SMIs for several mental disorders has been demonstrated in multiple meta-analyses, results for BPD are mixed. In this study, Klein et al9 examined the effectiveness and safety of the adjunctive use of an SMI based on schema therapy in addition to care as usual (CAU) in patients with BPD.
Study design
- In a 12-month, rater-blind, controlled parallel group trial, adults who had a total BPDSI score ≥15 and either a diagnosis of BPD according to DSM-IV criteria or a probable diagnosis of BPD (if they had also received a BPD diagnosis from their treating physician) were randomized to an internet-based SMI based on schema therapy called priovi (n = 103) or CAU (n = 101). Participants could complete the SMI content in approximately 6 months but were recommended to use the intervention for the entire year.
- Participation in psychotherapy and psychiatric treatment, including pharmacotherapy, was permitted. At baseline, 74% of participants were receiving psychotherapy and 88% were receiving psychiatric treatment.
- The primary outcome was change in BPDSI score at 12 months. The primary safety outcome was the number of serious adverse events at 12 months. Secondary outcomes included BPD severity, depressive symptoms, anxiety symptoms, quality of life, uncontrolled internet use, negative treatment effects, and satisfaction with the intervention. Most assessments were measured at baseline, 3 months, 6 months, 9 months, and 12 months.
Outcomes
- Large reductions in the severity of BPD symptoms as measured by change in BPDSI score was observed in both groups. Although the average reduction in BPDSI score was greater in the SMI group, this difference was not statistically significant from the CAU group.
- There was no statistically significant difference in the number of serious adverse events between groups at any time.
Conclusions/limitations
- Treatment with SMI did not result in improved outcomes over CAU. Although the average reduction in BPDSI score was greater in the SMI group compared to the CAU group, this difference was not statistically significant.
- The authors cautioned that the smaller-than-expected between-groups effect size must be interpreted against the background of an unexpectedly large effect in the CAU group. In fact, the CAU group pre/post effect was comparable to the pre/post effect of intensive specialized DBT treatment groups in previous RCTs.
- The authors also suggested that the high percentage of participants who received psychotherapy did not allow for an additional benefit from SMI.
- Limitations include recruitment method, lack of systematic assessment of accidental unblinding, high exclusion rate due to failure of the participant or treating clinician to provide confirmation of diagnosis, and the use of a serious adverse events assessment that is not psychometrically validated.
Bottom Line
Evidence from randomized controlled trials suggests that internet-based psychoeducation, brief dialectical behavior therapy skills-only treatment, interpersonal therapy, a program that combines day treatment with individual and group psychotherapy, and mentalization-based treatment can improve symptoms and quality of life for patients with borderline personality disorder.
1. Skodol AE, Gunderson JG, McGlashan TM, et al. Functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder. Am J Psychiatry. 2002;159(2):276-83.
2. Bender DS, Dolan RT, Skodol AE, et al. Treatment utilization by patients with personality disorders. Am J Psychiatry. 2001;158(2):295-302.
3. Saeed SA, Kallis AC. Borderline personality disorder: 6 studies of biological interventions. Current Psychiatry. 2021;20(11):26-30,34-36.
4. Zanarini MC, Conkey LC, Temes CM, et al. Randomized controlled trial of web-based psychoeducation for women with borderline personality disorder. J Clin Psychiatry. 2018;79(3):16m11153. doi:10.4088/JCP.16m11153
5. McMain SF, Guimond T, Barnhart R, et al. A randomized trial of brief dialectical behaviour therapy skills training in suicidal patients suffering from borderline disorder. Acta Psychiatr Scand. 2017;135(2):138-148. doi:10.1111/acps.12664
6. Bozzatello P, Bellino S. Combined therapy with interpersonal psychotherapy adapted for borderline personality disorder: a two-years follow-up. Psychiatry Res. 2016;240:151-156. doi:10.1016/j.psychres.2016.04.014
7. Antonsen BT, Kvarstein EH, Urnes Ø, et al. Favourable outcome of long-term combined psychotherapy for patients with borderline personality disorder: six-year follow-up of a randomized study. Psychother Res. 2017;27(1):51-63. doi:10.1080/10503307.2015.1072283
8. Bateman A, Constantinou MP, Fonagy P, et al. Eight-year prospective follow-up of mentalization-based treatment versus structured clinical management for people with borderline personality disorder. Personal Disord. 2021;12(4):291-299. doi:10.1037/per0000422
9. Klein JP, Hauer-von Mauschwitz A, Berger T, et al. Effectiveness and safety of the adjunctive use of an internet-based self-management intervention for borderline personality disorder in addition to care as usual: results from a randomised controlled trial. BMJ Open. 2021;11(9):e047771. doi:10.1136/bmjopen-2020-047771
10. Zanarini MC, Frankenburg FR. A preliminary, randomized trial of psychoeducation for women with borderline personality disorder. J Pers Disord. 2008;22(3):284-290.
11. Bellino S, Rinaldi C, Bogetto F. Adaptation of interpersonal psychotherapy to borderline personality disorder: a comparison of combined therapy and single pharmacotherapy. Can J Psychiatry. 2010;55(2):74-81.
12. Arnevik E, Wilberg T, Urnes Ø, et al. Psychotherapy for personality disorders: short-term day hospital psychotherapy versus outpatient individual therapy – a randomized controlled study. Eur Psychiatry. 2009,24(2):71-78. doi:10.1016/j.eurpsy.2008.09.004
13. Bateman A, Fonagy P. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. Am J Psychiatry. 2009;166(12):1355-1364.
SECOND OF 2 PARTS
Borderline personality disorder (BPD) is associated with serious impairment in psychosocial functioning.1 It is characterized by an ongoing pattern of mood instability, cognitive distortions, problems with self-image, and impulsive behavior that often results in problems in relationships. As a result, patients with BPD tend to utilize more mental health services than patients with other personality disorders or major depressive disorder.2
Some clinicians believe BPD is difficult to treat. While historically there has been little consensus on the best treatments for this disorder, current options include both pharmacologic and psychological interventions. In Part 1 of this 2-part article, we focused on 6 studies that evaluated biological interventions.3 Here in Part 2, we focus on findings from 6 recent randomized controlled trials (RCTs) of psychosocial interventions for BPD
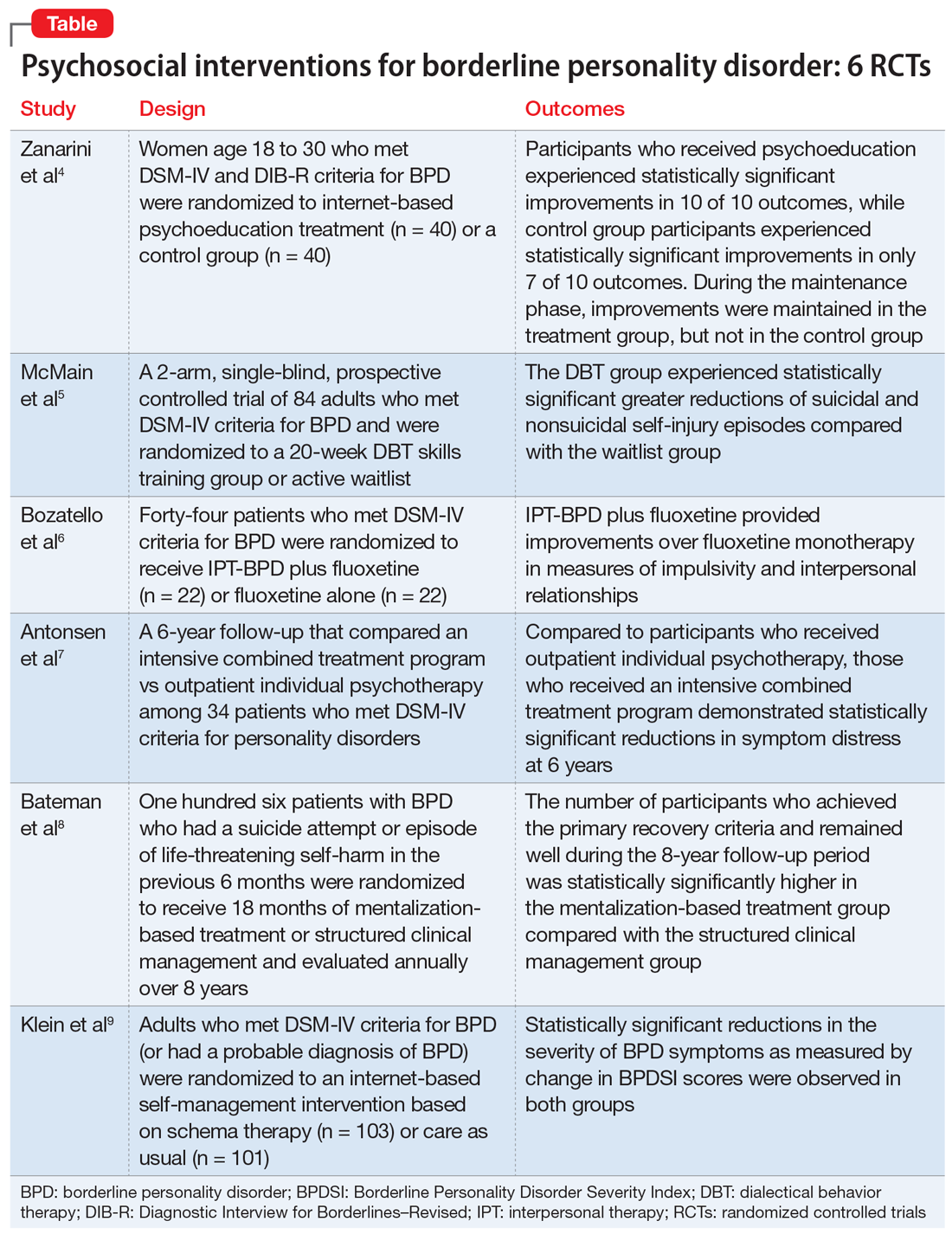
1. Zanarini MC, Conkey LC, Temes CM, et al. Randomized controlled trial of web-based psychoeducation for women with borderline personality disorder. J Clin Psychiatry. 2018;79(3):16m11153. doi: 10.4088/JCP.16m11153
Research has shown that BPD is a treatable illness with a more favorable prognosis than previously believed. Despite this, patients often experience difficulty accessing the most up-to-date information on BPD, which can impede their treatment. A 2008 study by Zanarini et al10 of younger female patients with BPD demonstrated that immediate, in-person psychoeducation improved impulsivity and relationships. Widespread implementation of this program proved problematic, however, due to cost and personnel constraints. To resolve this issue, researchers developed an internet-based version of the program. In a 2018 follow-up study, Zanarini et al4 examined the effect of this internet-based psychoeducation program on symptoms of BPD.
Continue to: Study design...
Study design
- Women (age 18 to 30) who met DSM-IV and Diagnostic Interview for Borderlines–Revised criteria for BPD were randomized to an internet-based psychoeducation treatment group (n = 40) or a control group (n = 40).
- Ten outcomes concerning symptom severity and psychosocial functioning were assessed during weeks 1 to 12 (acute phase) and at months 6, 9, and 12 (maintenance phase) using the self-report version of the Zanarini Rating Scale for BPD (ZAN-BPD), the Borderline Evaluation of Severity over Time, the Sheehan Disability Scale, the Clinically Useful Depression Outcome Scale, the Clinically Useful Anxiety Outcome Scale, and Weissman’s Social Adjustment Scale (SAS).
Outcomes
- In the acute phase, treatment group participants experienced statistically significant improvements in all 10 outcomes. Control group participants demonstrated similar results, achieving statistically significant improvements in 7 of 10 outcomes.
- Compared to the control group, the treatment group experienced a more significant reduction in impulsivity and improvement in psychosocial functioning as measured by the ZAN-BPD and SAS.
- In the maintenance phase, treatment group participants achieved statistically significant improvements in 9 of 10 outcomes, whereas control group participants demonstrated statistically significant improvements in only 3 of 10 outcomes.
- Compared to the control group, the treatment group also demonstrated a significantly greater improvement in all 4 sector scores and the total score of the ZAN-BP
Conclusions/limitations
- In patients with BPD, internet-based psychoeducation reduced symptom severity and improved psychosocial functioning, with effects lasting 1 year. Treatment group participants experienced clinically significant improvements in all outcomes measured during the acute phase of the study; most improvements were maintained over 1 year.
- While the control group initially saw similar improvements in most measurements, these improvements were not maintained as effectively over 1 year.
- Limitations include a female-only population, the restricted age range of participants, and recruitment exclusively from volunteers.
2. McMain SF, Guimond T, Barnhart R, et al. A randomized trial of brief dialectical behaviour therapy skills training in suicidal patients suffering from borderline disorder. Acta Psychiatr Scand. 2017;135(2):138-148.
Standard dialectical behavior therapy (DBT) is an effective treatment for BPD; however, access is often limited by shortages of clinicians and resources. Therefore, it has become increasingly common for clinical settings to offer patients only the skills training component of DBT, which requires fewer resources. While several clinical trials examining brief DBT skills–only treatment for BPD have shown promising results, it is unclear how effective this intervention is at reducing suicidal or nonsuicidal self-injury (NSSI) episodes. McMain et al5 explored the effectiveness of brief DBT skills–only adjunctive treatment on the rates of suicidal and NSSI episodes in patients with BPD.
Study design
- In this 2-arm, single-blind, prospective controlled trial, 84 adults who met DSM-IV criteria for BPD were randomized to a 20-week DBT skills training group (DBT group) or an active waitlist (WL group). No restrictions on additional psychosocial or pharmacologic treatments were imposed on either group.
- The primary outcome was the frequency of suicidal and NSSI episodes as measured by the Lifetime Suicide Attempt Self-Injury Interview and the Deliberate Self-Harm Inventory (DSHI). Measurements occurred at baseline, 10 weeks, 20 weeks, and 3 months posttreatment (32 weeks).
- Secondary outcomes included changes in health care utilization, BPD symptoms, and coping. These were assessed using the Treatment History Interview-2, Borderline Symptom List-23, State-Trait Anger Expression Inventory, Symptom Checklist-90-revised (SCL-90-R), Barratt Impulsiveness Scale-11, Beck Depression Inventory (BDI)-II, Social Adjustment Scale Self-report, Difficulties in Emotion Regulation Scale, Distress Tolerance Scale, and Kentucky Inventory of Mindfulness Scale.
Outcomes
- At Week 32, compared to the WL group, the DBT group showed statistically significant greater reductions in the frequency of suicidal and NSSI episodes as measured by the LSASI but not by the DSHI. The DBT group experienced statistically significant improvements in distress tolerance and emotion regulation over the WL group at all points, but no difference on mindfulness. The DBT group achieved greater reductions in anger over time as compared to the WL group.
- At Week 20, compared to the WL group, the DBT group showed significant improvements in social adjustment, symptom distress, and borderline symptoms. There were no significant group differences on impulsivity. Between-group differences in the number of hospital admissions favored the DBT group at 10 and 20 weeks, but not at 32 weeks. There was no statistically significant difference between the groups with respect to the number of emergency department visits.
- Analyses of group differences in clinical improvement as measured by the SCL-90-R revealed statistically reliable and clinically significant changes in the DBT group over the WL group at 20 weeks, but not at 32 weeks.
Conclusions/limitations
- Brief DBT skills training reduced suicidal and NSSI episodes in patients with BPD. Participants in the DBT group also demonstrated greater improvement in anger, distress tolerance, and emotion regulation compared to the control group. These results were evident 3 months after treatment. However, any gains in health care utilization, social adjustment, symptom distress, and borderline symptoms diminished or did not differ from waitlist participants at Week 32. At that time, participants in the DBT group demonstrated a similar level of symptomatology as the WL group.
- Limitations include the use of an active waitlist control group, allowance of concurrent treatments, the absence of an active therapeutic comparator group, use of self-report measures, use of an instrument with unknown psychometric properties, and a relatively short 3-month follow-up period.
3. Bozzatello P, Bellino S. Combined therapy with interpersonal psychotherapy adapted for borderline personality disorder: a two-years follow-up. Psychiatry Res. 2016;240:151-156.
Psychotherapeutic options for treating BPD include DBT, mentalization-based treatment, schema-focused therapy, transference-based psychotherapy, and systems training for emotional predictability and problem solving. More recently, interpersonal therapy also has been adapted for BPD (IPT-BPD). However, thus far no trials have investigated the long-term effects of this therapy on BPD. In 2010, Bellino et al11 published a 32-week RCT examining the effect of IPT-BPD on BPD. They concluded that IPT-BPD plus fluoxetine was superior to fluoxetine alone in improving symptoms and quality of life. The present study by Bozzatello et al6 examined whether the benefits of IPT-BPD plus fluoxetine demonstrated in the 2010 study persisted over a 24-month follow-up.
Continue to: Study design...
Study design
- In the 2010 study by Bellino et al,11 55 outpatients who met DSM-IV criteria for BPD were randomized to receive IPT-BPD plus fluoxetine (combined therapy) or fluoxetine alone for 32 weeks. Forty-four participants completed a 24-month follow-up study (n = 22 for IPT-BPD plus fluoxetine, n = 22 for fluoxetine only).
- Clinical assessments were performed at 6, 12, and 24 months, and used the same instruments as the original study, including the Clinical Global Impression Scale–Severity item, Hamilton Depression Rating Scale, Hamilton Anxiety Rating Scale (HARS), Social and Occupational Functioning Assessment, Satisfaction Profile (SAT-P), and the Borderline Personality Disorder Severity Index (BPDSI).
Outcomes
- While the original study demonstrated that combined therapy had a clinically significant effect over fluoxetine alone on both HARS score and the BPDSI item “affective instability” at 32 weeks, this advantage was maintained only at the 6-month assessment.
- The improvements that the combined therapy provided over fluoxetine monotherapy on the BPDSI items of “impulsivity” and “interpersonal relationships” as well as the SAT-P factors of social and psychological functioning at 32 weeks were preserved at 24 months. No additional improvements were seen.
Conclusions/limitations
- The improvements in impulsivity, interpersonal functioning, social functioning, and psychological functioning at 32 weeks seen with IPT-BPD plus fluoxetine compared with fluoxetine alone persisted for 2 years after completing therapy; no further improvements were seen.
- The improvements to anxiety and affective instability that combined therapy demonstrated over fluoxetine monotherapy at 32 weeks were not maintained at 24 months.
- Limitations include a small sample size, exclusion of psychiatric comorbidities, and a lack of assessment of session or medication adherence.
4. Antonsen BT, Kvarstein EH, Urnes Ø, et al. Favourable outcome of long-term combined psychotherapy for patients with borderline personality disorder: six-year follow-up of a randomized study. Psychother Res. 2017;27(1):51-63.
While many studies have demonstrated the benefits of psychotherapy for treating personality disorders, there is limited research of how different levels of psychotherapy may impact treatment outcomes. An RCT called the Ullevål Personality Project (UPP)12 compared an intensive combined treatment program (CP) with outpatient individual psychotherapy (OIP) in patients with personality disorders. The CP program consisted of short-term day-hospital treatment followed by outpatient combined group and individual psychotherapy. The outcomes this RCT evaluated included suicide attempts, suicidal thoughts, self-injury, psychosocial functioning, symptom distress, and interpersonal and personality problems. A 6-year follow-up concluded there were no differences in outcomes between the 2 treatment groups. However, in this RCT, Antonsen et al7 examined whether CP produced statistically significant benefits over OIP in a subset of patients with BPD.
Study design
- In the UPP trial,12 117 patients who met DSM-IV criteria for personality disorders (excluding antisocial and schizotypal personality disorder) were randomized to receive 18 weeks of day hospital psychotherapy followed by CP or OIP. Fifty-two participants in the UPP were diagnosed with BPD, and 34 of these participants completed the 6-year follow-up investigation.
- Symptom distress, psychosocial functioning, interpersonal problems, quality of life, personality functioning, and self-harm/suicidal thoughts/suicide attempts were assessed at baseline, 8 months, 18 months, 3 years, and 6 years using the SCL-90-R Global Severity Index (GSI), BDI, Global Assessment of Functioning (GAF), Work and Social Adjustment Scale (WSAS), Quality of Life 10-point scale (QOL), Circumplex of Interpersonal Problems (CIP), and the 60-item short form of the Severity Indices of Personality Problems (SIPP-118) questionnaire.
Outcomes
- Compared to the OIP group, the CP group demonstrated statistically significant reductions in symptom distress at Year 6 as measured by the SCL-90-R GSI. Between Years 3 and 6, the CP group continued to show improvements in psychosocial functioning as demonstrated by improvements in GAF and WSAS scores. The OIP group’s scores worsened during this time. Compared to the OIP group, participants in the CP group also had significantly better outcomes on the SIPP-118 domains of self-control and identity integration.
- There were no significant differences between groups on the proportion of participants who engaged in self-harm or experienced suicidal thoughts or attempts. There were no significant differences in outcomes between the treatment groups on the CIP, BDI, or QOL.
- Participants in CP group tended to use fewer psychotropic medications than those in the OIP group over time, but this difference was not statistically significant. The 2 groups did not differ in use of health care services over the last year.
- Avoidant personality disorder (AVPD) did not have a significant moderator effect on GAF score. Comorbid AVPD was a negative predictor of GAF score, independent of the group.
Conclusions/limitations
- Both groups experienced a remission rate of 90% at 6-year follow-up. Compared with the OIP group, participants in the CP group experienced significantly greater reductions in symptom distress and improvements in self-control and identity integration at 6 years. Between Years 3 and 6, participants in the CP group experienced significant improvements in psychosocial functioning compared with OIP group participants. The 2 groups did not differ on other outcomes, including the CIP, BDI, QOL, suicidal thoughts, suicidal attempts, self-harm, and health care utilization.
- Despite statistically significant differences in GAF scores favoring the CP group over the OIP group during Years 3 to 6, GAF scores did not differ significantly in the final year, which suggests that symptomatic remission does not equal functional improvement.
- Limitations include a lack of control for intensity or length of treatment in statistical analyses, small sample size, lack of correction for multiple testing, lack of an a priori power analysis, missing data and potential violation of the missing at random assumption, use of therapists’ preferred treatment method/practice, and a lack of control for other treatments.
5. Bateman A, Constantinou MP, Fonagy P, et al. Eight-year prospective follow-up of mentalization-based treatment versus structured clinical management for people with borderline personality disorder. Personal Disord. 2021;12(4):291-299.
The efficacy of various psychotherapies for symptoms of BPD has been well established. However, there is limited evidence that these effects persist over time. In 2009, Bateman et al13 conducted an 18-month RCT comparing the effectiveness of outpatient mentalization-based treatment (MBT) against structured clinical management (SCM) for patients with BPD. Both groups experienced substantial improvements, but patients assigned to MBT demonstrated greater improvement in clinically significant problems, including suicide attempts and hospitalizations. In a 2021 follow-up to this study, Bateman et al8 investigated whether the MBT group’s gains in the primary outcomes (absence of severe self-harm, suicide attempts, and inpatient admissions in the previous 12 months), social functioning, vocational engagement, and mental health service usage were maintained throughout an 8-year follow-up period.
Continue to: Study design...
Study design
- In the 2009 trial, Bateman et al13 randomized adult participants who met DSM-IV criteria for BPD and had a suicide attempt or episode of life-threatening self-harm in the past 6 months to receive 18 months of MBT or SCM. The primary outcome was crisis events, defined as a composite of suicidal and severe self-injurious behaviors and hospitalizations. The 2021 Bateman et al8 study expanded this investigation by collecting additional data on a yearly basis for 8 years.
- Of the 134 original participants, 98 agreed to complete the follow-up. Due to attrition, the follow-up period was limited to 8 years. At each yearly visit, researchers collected information on the primary outcome, the absence of severe self-harm, suicide attempts, and inpatient admissions in the previous 12 months.
- Secondary measures were collected mainly through a modified version of the Client Service Receipt Inventory and included critical incidents, psychiatric and medical hospital and community services, employment and other personally meaningful activity, psychoactive medication, and other mental health treatments.
Outcomes
- The number of participants who met diagnostic criteria for BPD at the 1-year follow-up was significantly lower in the MBT group compared with the SCM group. To improve participant retention, this outcome was not evaluated at later visits.
- The number of participants who achieved the primary recovery criteria of the original trial (absence of severe self-harm, suicide attempts, and inpatient admissions in the previous 12 months) and remained well throughout the entire follow-up period was significantly higher in the MBT group compared with the SCM group. The average number of years during which participants failed to meet recovery criteria was significantly greater in the SCM group compared with the MBT group.
- When controlling for age, treatment group was a significant predictor of recovery during the follow-up period. Overall, significantly fewer participants in the MBT group experienced critical incidents during the follow-up period.
- The SCM group used crisis mental health services for a significantly greater number of follow-up years than the MBT group, although the likelihood of ever using crisis services did not statistically differ between the groups. Both groups had similar use of outpatient mental health services, primary care services, and nonmental health medical services. Compared to the SCM group, the MBT group had significantly fewer professional support service visits and significantly fewer outpatient psychiatrist visits.
- MBT group participants spent more time in education, were less likely to be unemployed, and were less likely to use social care interventions than SCM group participants. Although those in the MBT group spent more months engaged in purposeful activity, there was no significant difference between the groups in the proportion of participants who did not engage in purposeful activity.
- The MBT group spent fewer months receiving psychotherapeutic medication compared with the SCM group. The variables that yielded significant 2-way interactions were eating disorder, substance use disorder, and physical abuse, suggesting greater benefit from MBT with these concurrent diagnoses. Younger age was associated with better outcomes.
Conclusions/limitations
- This study demonstrated that patients with BPD significantly benefited from specialized therapies such as MBT.
- At the 1 follow-up visit, the number of participants who met diagnostic criteria for BPD was significantly lower in the MBT group compared with the SCM group.
- The number of participants who had achieved the primary recovery criteria and remained well during the 8-year follow-up period was significantly higher in the MBT group compared to the SCM group.
- Limitations include increasing attrition over time, possible allegiance effects and unmasking of research assistants, lack of self-report questionnaires, and the potentially erroneous conclusion that increased use of services equates to poorer treatment response and greater need for support.
6. Klein JP, Hauer-von Mauschwitz A, Berger T, et al. Effectiveness and safety of the adjunctive use of an internet-based self-management intervention for borderline personality disorder in addition to care as usual: results from a randomised controlled trial. BMJ Open. 2021;11(9):e047771.
Fewer than 1 in 4 patients with BPD have access to effective psychotherapies. The use of internet-based self-management interventions (SMIs) developed from evidence-based psychotherapies can help close this treatment gap. Although the efficacy of SMIs for several mental disorders has been demonstrated in multiple meta-analyses, results for BPD are mixed. In this study, Klein et al9 examined the effectiveness and safety of the adjunctive use of an SMI based on schema therapy in addition to care as usual (CAU) in patients with BPD.
Study design
- In a 12-month, rater-blind, controlled parallel group trial, adults who had a total BPDSI score ≥15 and either a diagnosis of BPD according to DSM-IV criteria or a probable diagnosis of BPD (if they had also received a BPD diagnosis from their treating physician) were randomized to an internet-based SMI based on schema therapy called priovi (n = 103) or CAU (n = 101). Participants could complete the SMI content in approximately 6 months but were recommended to use the intervention for the entire year.
- Participation in psychotherapy and psychiatric treatment, including pharmacotherapy, was permitted. At baseline, 74% of participants were receiving psychotherapy and 88% were receiving psychiatric treatment.
- The primary outcome was change in BPDSI score at 12 months. The primary safety outcome was the number of serious adverse events at 12 months. Secondary outcomes included BPD severity, depressive symptoms, anxiety symptoms, quality of life, uncontrolled internet use, negative treatment effects, and satisfaction with the intervention. Most assessments were measured at baseline, 3 months, 6 months, 9 months, and 12 months.
Outcomes
- Large reductions in the severity of BPD symptoms as measured by change in BPDSI score was observed in both groups. Although the average reduction in BPDSI score was greater in the SMI group, this difference was not statistically significant from the CAU group.
- There was no statistically significant difference in the number of serious adverse events between groups at any time.
Conclusions/limitations
- Treatment with SMI did not result in improved outcomes over CAU. Although the average reduction in BPDSI score was greater in the SMI group compared to the CAU group, this difference was not statistically significant.
- The authors cautioned that the smaller-than-expected between-groups effect size must be interpreted against the background of an unexpectedly large effect in the CAU group. In fact, the CAU group pre/post effect was comparable to the pre/post effect of intensive specialized DBT treatment groups in previous RCTs.
- The authors also suggested that the high percentage of participants who received psychotherapy did not allow for an additional benefit from SMI.
- Limitations include recruitment method, lack of systematic assessment of accidental unblinding, high exclusion rate due to failure of the participant or treating clinician to provide confirmation of diagnosis, and the use of a serious adverse events assessment that is not psychometrically validated.
Bottom Line
Evidence from randomized controlled trials suggests that internet-based psychoeducation, brief dialectical behavior therapy skills-only treatment, interpersonal therapy, a program that combines day treatment with individual and group psychotherapy, and mentalization-based treatment can improve symptoms and quality of life for patients with borderline personality disorder.
SECOND OF 2 PARTS
Borderline personality disorder (BPD) is associated with serious impairment in psychosocial functioning.1 It is characterized by an ongoing pattern of mood instability, cognitive distortions, problems with self-image, and impulsive behavior that often results in problems in relationships. As a result, patients with BPD tend to utilize more mental health services than patients with other personality disorders or major depressive disorder.2
Some clinicians believe BPD is difficult to treat. While historically there has been little consensus on the best treatments for this disorder, current options include both pharmacologic and psychological interventions. In Part 1 of this 2-part article, we focused on 6 studies that evaluated biological interventions.3 Here in Part 2, we focus on findings from 6 recent randomized controlled trials (RCTs) of psychosocial interventions for BPD
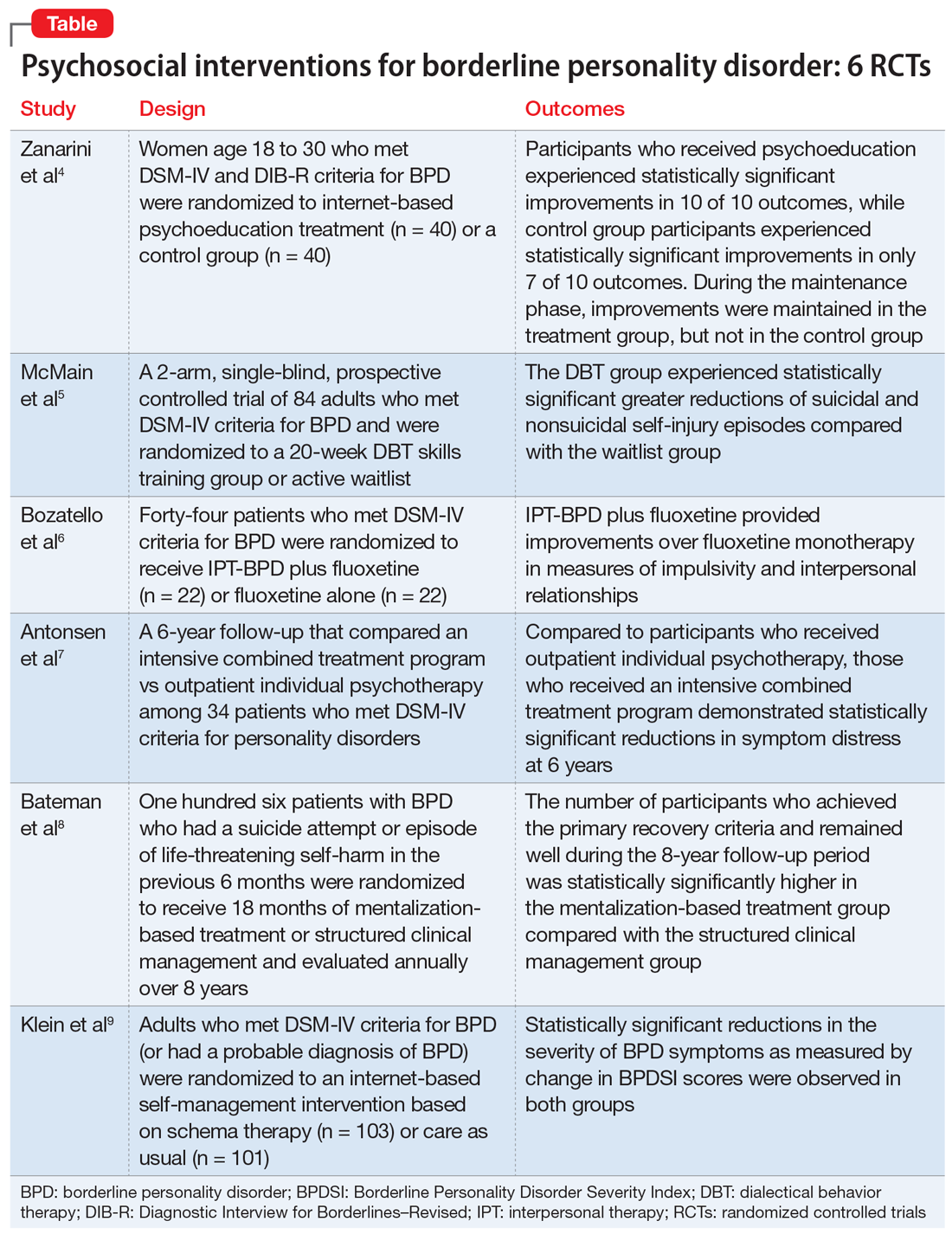
1. Zanarini MC, Conkey LC, Temes CM, et al. Randomized controlled trial of web-based psychoeducation for women with borderline personality disorder. J Clin Psychiatry. 2018;79(3):16m11153. doi: 10.4088/JCP.16m11153
Research has shown that BPD is a treatable illness with a more favorable prognosis than previously believed. Despite this, patients often experience difficulty accessing the most up-to-date information on BPD, which can impede their treatment. A 2008 study by Zanarini et al10 of younger female patients with BPD demonstrated that immediate, in-person psychoeducation improved impulsivity and relationships. Widespread implementation of this program proved problematic, however, due to cost and personnel constraints. To resolve this issue, researchers developed an internet-based version of the program. In a 2018 follow-up study, Zanarini et al4 examined the effect of this internet-based psychoeducation program on symptoms of BPD.
Continue to: Study design...
Study design
- Women (age 18 to 30) who met DSM-IV and Diagnostic Interview for Borderlines–Revised criteria for BPD were randomized to an internet-based psychoeducation treatment group (n = 40) or a control group (n = 40).
- Ten outcomes concerning symptom severity and psychosocial functioning were assessed during weeks 1 to 12 (acute phase) and at months 6, 9, and 12 (maintenance phase) using the self-report version of the Zanarini Rating Scale for BPD (ZAN-BPD), the Borderline Evaluation of Severity over Time, the Sheehan Disability Scale, the Clinically Useful Depression Outcome Scale, the Clinically Useful Anxiety Outcome Scale, and Weissman’s Social Adjustment Scale (SAS).
Outcomes
- In the acute phase, treatment group participants experienced statistically significant improvements in all 10 outcomes. Control group participants demonstrated similar results, achieving statistically significant improvements in 7 of 10 outcomes.
- Compared to the control group, the treatment group experienced a more significant reduction in impulsivity and improvement in psychosocial functioning as measured by the ZAN-BPD and SAS.
- In the maintenance phase, treatment group participants achieved statistically significant improvements in 9 of 10 outcomes, whereas control group participants demonstrated statistically significant improvements in only 3 of 10 outcomes.
- Compared to the control group, the treatment group also demonstrated a significantly greater improvement in all 4 sector scores and the total score of the ZAN-BP
Conclusions/limitations
- In patients with BPD, internet-based psychoeducation reduced symptom severity and improved psychosocial functioning, with effects lasting 1 year. Treatment group participants experienced clinically significant improvements in all outcomes measured during the acute phase of the study; most improvements were maintained over 1 year.
- While the control group initially saw similar improvements in most measurements, these improvements were not maintained as effectively over 1 year.
- Limitations include a female-only population, the restricted age range of participants, and recruitment exclusively from volunteers.
2. McMain SF, Guimond T, Barnhart R, et al. A randomized trial of brief dialectical behaviour therapy skills training in suicidal patients suffering from borderline disorder. Acta Psychiatr Scand. 2017;135(2):138-148.
Standard dialectical behavior therapy (DBT) is an effective treatment for BPD; however, access is often limited by shortages of clinicians and resources. Therefore, it has become increasingly common for clinical settings to offer patients only the skills training component of DBT, which requires fewer resources. While several clinical trials examining brief DBT skills–only treatment for BPD have shown promising results, it is unclear how effective this intervention is at reducing suicidal or nonsuicidal self-injury (NSSI) episodes. McMain et al5 explored the effectiveness of brief DBT skills–only adjunctive treatment on the rates of suicidal and NSSI episodes in patients with BPD.
Study design
- In this 2-arm, single-blind, prospective controlled trial, 84 adults who met DSM-IV criteria for BPD were randomized to a 20-week DBT skills training group (DBT group) or an active waitlist (WL group). No restrictions on additional psychosocial or pharmacologic treatments were imposed on either group.
- The primary outcome was the frequency of suicidal and NSSI episodes as measured by the Lifetime Suicide Attempt Self-Injury Interview and the Deliberate Self-Harm Inventory (DSHI). Measurements occurred at baseline, 10 weeks, 20 weeks, and 3 months posttreatment (32 weeks).
- Secondary outcomes included changes in health care utilization, BPD symptoms, and coping. These were assessed using the Treatment History Interview-2, Borderline Symptom List-23, State-Trait Anger Expression Inventory, Symptom Checklist-90-revised (SCL-90-R), Barratt Impulsiveness Scale-11, Beck Depression Inventory (BDI)-II, Social Adjustment Scale Self-report, Difficulties in Emotion Regulation Scale, Distress Tolerance Scale, and Kentucky Inventory of Mindfulness Scale.
Outcomes
- At Week 32, compared to the WL group, the DBT group showed statistically significant greater reductions in the frequency of suicidal and NSSI episodes as measured by the LSASI but not by the DSHI. The DBT group experienced statistically significant improvements in distress tolerance and emotion regulation over the WL group at all points, but no difference on mindfulness. The DBT group achieved greater reductions in anger over time as compared to the WL group.
- At Week 20, compared to the WL group, the DBT group showed significant improvements in social adjustment, symptom distress, and borderline symptoms. There were no significant group differences on impulsivity. Between-group differences in the number of hospital admissions favored the DBT group at 10 and 20 weeks, but not at 32 weeks. There was no statistically significant difference between the groups with respect to the number of emergency department visits.
- Analyses of group differences in clinical improvement as measured by the SCL-90-R revealed statistically reliable and clinically significant changes in the DBT group over the WL group at 20 weeks, but not at 32 weeks.
Conclusions/limitations
- Brief DBT skills training reduced suicidal and NSSI episodes in patients with BPD. Participants in the DBT group also demonstrated greater improvement in anger, distress tolerance, and emotion regulation compared to the control group. These results were evident 3 months after treatment. However, any gains in health care utilization, social adjustment, symptom distress, and borderline symptoms diminished or did not differ from waitlist participants at Week 32. At that time, participants in the DBT group demonstrated a similar level of symptomatology as the WL group.
- Limitations include the use of an active waitlist control group, allowance of concurrent treatments, the absence of an active therapeutic comparator group, use of self-report measures, use of an instrument with unknown psychometric properties, and a relatively short 3-month follow-up period.
3. Bozzatello P, Bellino S. Combined therapy with interpersonal psychotherapy adapted for borderline personality disorder: a two-years follow-up. Psychiatry Res. 2016;240:151-156.
Psychotherapeutic options for treating BPD include DBT, mentalization-based treatment, schema-focused therapy, transference-based psychotherapy, and systems training for emotional predictability and problem solving. More recently, interpersonal therapy also has been adapted for BPD (IPT-BPD). However, thus far no trials have investigated the long-term effects of this therapy on BPD. In 2010, Bellino et al11 published a 32-week RCT examining the effect of IPT-BPD on BPD. They concluded that IPT-BPD plus fluoxetine was superior to fluoxetine alone in improving symptoms and quality of life. The present study by Bozzatello et al6 examined whether the benefits of IPT-BPD plus fluoxetine demonstrated in the 2010 study persisted over a 24-month follow-up.
Continue to: Study design...
Study design
- In the 2010 study by Bellino et al,11 55 outpatients who met DSM-IV criteria for BPD were randomized to receive IPT-BPD plus fluoxetine (combined therapy) or fluoxetine alone for 32 weeks. Forty-four participants completed a 24-month follow-up study (n = 22 for IPT-BPD plus fluoxetine, n = 22 for fluoxetine only).
- Clinical assessments were performed at 6, 12, and 24 months, and used the same instruments as the original study, including the Clinical Global Impression Scale–Severity item, Hamilton Depression Rating Scale, Hamilton Anxiety Rating Scale (HARS), Social and Occupational Functioning Assessment, Satisfaction Profile (SAT-P), and the Borderline Personality Disorder Severity Index (BPDSI).
Outcomes
- While the original study demonstrated that combined therapy had a clinically significant effect over fluoxetine alone on both HARS score and the BPDSI item “affective instability” at 32 weeks, this advantage was maintained only at the 6-month assessment.
- The improvements that the combined therapy provided over fluoxetine monotherapy on the BPDSI items of “impulsivity” and “interpersonal relationships” as well as the SAT-P factors of social and psychological functioning at 32 weeks were preserved at 24 months. No additional improvements were seen.
Conclusions/limitations
- The improvements in impulsivity, interpersonal functioning, social functioning, and psychological functioning at 32 weeks seen with IPT-BPD plus fluoxetine compared with fluoxetine alone persisted for 2 years after completing therapy; no further improvements were seen.
- The improvements to anxiety and affective instability that combined therapy demonstrated over fluoxetine monotherapy at 32 weeks were not maintained at 24 months.
- Limitations include a small sample size, exclusion of psychiatric comorbidities, and a lack of assessment of session or medication adherence.
4. Antonsen BT, Kvarstein EH, Urnes Ø, et al. Favourable outcome of long-term combined psychotherapy for patients with borderline personality disorder: six-year follow-up of a randomized study. Psychother Res. 2017;27(1):51-63.
While many studies have demonstrated the benefits of psychotherapy for treating personality disorders, there is limited research of how different levels of psychotherapy may impact treatment outcomes. An RCT called the Ullevål Personality Project (UPP)12 compared an intensive combined treatment program (CP) with outpatient individual psychotherapy (OIP) in patients with personality disorders. The CP program consisted of short-term day-hospital treatment followed by outpatient combined group and individual psychotherapy. The outcomes this RCT evaluated included suicide attempts, suicidal thoughts, self-injury, psychosocial functioning, symptom distress, and interpersonal and personality problems. A 6-year follow-up concluded there were no differences in outcomes between the 2 treatment groups. However, in this RCT, Antonsen et al7 examined whether CP produced statistically significant benefits over OIP in a subset of patients with BPD.
Study design
- In the UPP trial,12 117 patients who met DSM-IV criteria for personality disorders (excluding antisocial and schizotypal personality disorder) were randomized to receive 18 weeks of day hospital psychotherapy followed by CP or OIP. Fifty-two participants in the UPP were diagnosed with BPD, and 34 of these participants completed the 6-year follow-up investigation.
- Symptom distress, psychosocial functioning, interpersonal problems, quality of life, personality functioning, and self-harm/suicidal thoughts/suicide attempts were assessed at baseline, 8 months, 18 months, 3 years, and 6 years using the SCL-90-R Global Severity Index (GSI), BDI, Global Assessment of Functioning (GAF), Work and Social Adjustment Scale (WSAS), Quality of Life 10-point scale (QOL), Circumplex of Interpersonal Problems (CIP), and the 60-item short form of the Severity Indices of Personality Problems (SIPP-118) questionnaire.
Outcomes
- Compared to the OIP group, the CP group demonstrated statistically significant reductions in symptom distress at Year 6 as measured by the SCL-90-R GSI. Between Years 3 and 6, the CP group continued to show improvements in psychosocial functioning as demonstrated by improvements in GAF and WSAS scores. The OIP group’s scores worsened during this time. Compared to the OIP group, participants in the CP group also had significantly better outcomes on the SIPP-118 domains of self-control and identity integration.
- There were no significant differences between groups on the proportion of participants who engaged in self-harm or experienced suicidal thoughts or attempts. There were no significant differences in outcomes between the treatment groups on the CIP, BDI, or QOL.
- Participants in CP group tended to use fewer psychotropic medications than those in the OIP group over time, but this difference was not statistically significant. The 2 groups did not differ in use of health care services over the last year.
- Avoidant personality disorder (AVPD) did not have a significant moderator effect on GAF score. Comorbid AVPD was a negative predictor of GAF score, independent of the group.
Conclusions/limitations
- Both groups experienced a remission rate of 90% at 6-year follow-up. Compared with the OIP group, participants in the CP group experienced significantly greater reductions in symptom distress and improvements in self-control and identity integration at 6 years. Between Years 3 and 6, participants in the CP group experienced significant improvements in psychosocial functioning compared with OIP group participants. The 2 groups did not differ on other outcomes, including the CIP, BDI, QOL, suicidal thoughts, suicidal attempts, self-harm, and health care utilization.
- Despite statistically significant differences in GAF scores favoring the CP group over the OIP group during Years 3 to 6, GAF scores did not differ significantly in the final year, which suggests that symptomatic remission does not equal functional improvement.
- Limitations include a lack of control for intensity or length of treatment in statistical analyses, small sample size, lack of correction for multiple testing, lack of an a priori power analysis, missing data and potential violation of the missing at random assumption, use of therapists’ preferred treatment method/practice, and a lack of control for other treatments.
5. Bateman A, Constantinou MP, Fonagy P, et al. Eight-year prospective follow-up of mentalization-based treatment versus structured clinical management for people with borderline personality disorder. Personal Disord. 2021;12(4):291-299.
The efficacy of various psychotherapies for symptoms of BPD has been well established. However, there is limited evidence that these effects persist over time. In 2009, Bateman et al13 conducted an 18-month RCT comparing the effectiveness of outpatient mentalization-based treatment (MBT) against structured clinical management (SCM) for patients with BPD. Both groups experienced substantial improvements, but patients assigned to MBT demonstrated greater improvement in clinically significant problems, including suicide attempts and hospitalizations. In a 2021 follow-up to this study, Bateman et al8 investigated whether the MBT group’s gains in the primary outcomes (absence of severe self-harm, suicide attempts, and inpatient admissions in the previous 12 months), social functioning, vocational engagement, and mental health service usage were maintained throughout an 8-year follow-up period.
Continue to: Study design...
Study design
- In the 2009 trial, Bateman et al13 randomized adult participants who met DSM-IV criteria for BPD and had a suicide attempt or episode of life-threatening self-harm in the past 6 months to receive 18 months of MBT or SCM. The primary outcome was crisis events, defined as a composite of suicidal and severe self-injurious behaviors and hospitalizations. The 2021 Bateman et al8 study expanded this investigation by collecting additional data on a yearly basis for 8 years.
- Of the 134 original participants, 98 agreed to complete the follow-up. Due to attrition, the follow-up period was limited to 8 years. At each yearly visit, researchers collected information on the primary outcome, the absence of severe self-harm, suicide attempts, and inpatient admissions in the previous 12 months.
- Secondary measures were collected mainly through a modified version of the Client Service Receipt Inventory and included critical incidents, psychiatric and medical hospital and community services, employment and other personally meaningful activity, psychoactive medication, and other mental health treatments.
Outcomes
- The number of participants who met diagnostic criteria for BPD at the 1-year follow-up was significantly lower in the MBT group compared with the SCM group. To improve participant retention, this outcome was not evaluated at later visits.
- The number of participants who achieved the primary recovery criteria of the original trial (absence of severe self-harm, suicide attempts, and inpatient admissions in the previous 12 months) and remained well throughout the entire follow-up period was significantly higher in the MBT group compared with the SCM group. The average number of years during which participants failed to meet recovery criteria was significantly greater in the SCM group compared with the MBT group.
- When controlling for age, treatment group was a significant predictor of recovery during the follow-up period. Overall, significantly fewer participants in the MBT group experienced critical incidents during the follow-up period.
- The SCM group used crisis mental health services for a significantly greater number of follow-up years than the MBT group, although the likelihood of ever using crisis services did not statistically differ between the groups. Both groups had similar use of outpatient mental health services, primary care services, and nonmental health medical services. Compared to the SCM group, the MBT group had significantly fewer professional support service visits and significantly fewer outpatient psychiatrist visits.
- MBT group participants spent more time in education, were less likely to be unemployed, and were less likely to use social care interventions than SCM group participants. Although those in the MBT group spent more months engaged in purposeful activity, there was no significant difference between the groups in the proportion of participants who did not engage in purposeful activity.
- The MBT group spent fewer months receiving psychotherapeutic medication compared with the SCM group. The variables that yielded significant 2-way interactions were eating disorder, substance use disorder, and physical abuse, suggesting greater benefit from MBT with these concurrent diagnoses. Younger age was associated with better outcomes.
Conclusions/limitations
- This study demonstrated that patients with BPD significantly benefited from specialized therapies such as MBT.
- At the 1 follow-up visit, the number of participants who met diagnostic criteria for BPD was significantly lower in the MBT group compared with the SCM group.
- The number of participants who had achieved the primary recovery criteria and remained well during the 8-year follow-up period was significantly higher in the MBT group compared to the SCM group.
- Limitations include increasing attrition over time, possible allegiance effects and unmasking of research assistants, lack of self-report questionnaires, and the potentially erroneous conclusion that increased use of services equates to poorer treatment response and greater need for support.
6. Klein JP, Hauer-von Mauschwitz A, Berger T, et al. Effectiveness and safety of the adjunctive use of an internet-based self-management intervention for borderline personality disorder in addition to care as usual: results from a randomised controlled trial. BMJ Open. 2021;11(9):e047771.
Fewer than 1 in 4 patients with BPD have access to effective psychotherapies. The use of internet-based self-management interventions (SMIs) developed from evidence-based psychotherapies can help close this treatment gap. Although the efficacy of SMIs for several mental disorders has been demonstrated in multiple meta-analyses, results for BPD are mixed. In this study, Klein et al9 examined the effectiveness and safety of the adjunctive use of an SMI based on schema therapy in addition to care as usual (CAU) in patients with BPD.
Study design
- In a 12-month, rater-blind, controlled parallel group trial, adults who had a total BPDSI score ≥15 and either a diagnosis of BPD according to DSM-IV criteria or a probable diagnosis of BPD (if they had also received a BPD diagnosis from their treating physician) were randomized to an internet-based SMI based on schema therapy called priovi (n = 103) or CAU (n = 101). Participants could complete the SMI content in approximately 6 months but were recommended to use the intervention for the entire year.
- Participation in psychotherapy and psychiatric treatment, including pharmacotherapy, was permitted. At baseline, 74% of participants were receiving psychotherapy and 88% were receiving psychiatric treatment.
- The primary outcome was change in BPDSI score at 12 months. The primary safety outcome was the number of serious adverse events at 12 months. Secondary outcomes included BPD severity, depressive symptoms, anxiety symptoms, quality of life, uncontrolled internet use, negative treatment effects, and satisfaction with the intervention. Most assessments were measured at baseline, 3 months, 6 months, 9 months, and 12 months.
Outcomes
- Large reductions in the severity of BPD symptoms as measured by change in BPDSI score was observed in both groups. Although the average reduction in BPDSI score was greater in the SMI group, this difference was not statistically significant from the CAU group.
- There was no statistically significant difference in the number of serious adverse events between groups at any time.
Conclusions/limitations
- Treatment with SMI did not result in improved outcomes over CAU. Although the average reduction in BPDSI score was greater in the SMI group compared to the CAU group, this difference was not statistically significant.
- The authors cautioned that the smaller-than-expected between-groups effect size must be interpreted against the background of an unexpectedly large effect in the CAU group. In fact, the CAU group pre/post effect was comparable to the pre/post effect of intensive specialized DBT treatment groups in previous RCTs.
- The authors also suggested that the high percentage of participants who received psychotherapy did not allow for an additional benefit from SMI.
- Limitations include recruitment method, lack of systematic assessment of accidental unblinding, high exclusion rate due to failure of the participant or treating clinician to provide confirmation of diagnosis, and the use of a serious adverse events assessment that is not psychometrically validated.
Bottom Line
Evidence from randomized controlled trials suggests that internet-based psychoeducation, brief dialectical behavior therapy skills-only treatment, interpersonal therapy, a program that combines day treatment with individual and group psychotherapy, and mentalization-based treatment can improve symptoms and quality of life for patients with borderline personality disorder.
1. Skodol AE, Gunderson JG, McGlashan TM, et al. Functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder. Am J Psychiatry. 2002;159(2):276-83.
2. Bender DS, Dolan RT, Skodol AE, et al. Treatment utilization by patients with personality disorders. Am J Psychiatry. 2001;158(2):295-302.
3. Saeed SA, Kallis AC. Borderline personality disorder: 6 studies of biological interventions. Current Psychiatry. 2021;20(11):26-30,34-36.
4. Zanarini MC, Conkey LC, Temes CM, et al. Randomized controlled trial of web-based psychoeducation for women with borderline personality disorder. J Clin Psychiatry. 2018;79(3):16m11153. doi:10.4088/JCP.16m11153
5. McMain SF, Guimond T, Barnhart R, et al. A randomized trial of brief dialectical behaviour therapy skills training in suicidal patients suffering from borderline disorder. Acta Psychiatr Scand. 2017;135(2):138-148. doi:10.1111/acps.12664
6. Bozzatello P, Bellino S. Combined therapy with interpersonal psychotherapy adapted for borderline personality disorder: a two-years follow-up. Psychiatry Res. 2016;240:151-156. doi:10.1016/j.psychres.2016.04.014
7. Antonsen BT, Kvarstein EH, Urnes Ø, et al. Favourable outcome of long-term combined psychotherapy for patients with borderline personality disorder: six-year follow-up of a randomized study. Psychother Res. 2017;27(1):51-63. doi:10.1080/10503307.2015.1072283
8. Bateman A, Constantinou MP, Fonagy P, et al. Eight-year prospective follow-up of mentalization-based treatment versus structured clinical management for people with borderline personality disorder. Personal Disord. 2021;12(4):291-299. doi:10.1037/per0000422
9. Klein JP, Hauer-von Mauschwitz A, Berger T, et al. Effectiveness and safety of the adjunctive use of an internet-based self-management intervention for borderline personality disorder in addition to care as usual: results from a randomised controlled trial. BMJ Open. 2021;11(9):e047771. doi:10.1136/bmjopen-2020-047771
10. Zanarini MC, Frankenburg FR. A preliminary, randomized trial of psychoeducation for women with borderline personality disorder. J Pers Disord. 2008;22(3):284-290.
11. Bellino S, Rinaldi C, Bogetto F. Adaptation of interpersonal psychotherapy to borderline personality disorder: a comparison of combined therapy and single pharmacotherapy. Can J Psychiatry. 2010;55(2):74-81.
12. Arnevik E, Wilberg T, Urnes Ø, et al. Psychotherapy for personality disorders: short-term day hospital psychotherapy versus outpatient individual therapy – a randomized controlled study. Eur Psychiatry. 2009,24(2):71-78. doi:10.1016/j.eurpsy.2008.09.004
13. Bateman A, Fonagy P. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. Am J Psychiatry. 2009;166(12):1355-1364.
1. Skodol AE, Gunderson JG, McGlashan TM, et al. Functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder. Am J Psychiatry. 2002;159(2):276-83.
2. Bender DS, Dolan RT, Skodol AE, et al. Treatment utilization by patients with personality disorders. Am J Psychiatry. 2001;158(2):295-302.
3. Saeed SA, Kallis AC. Borderline personality disorder: 6 studies of biological interventions. Current Psychiatry. 2021;20(11):26-30,34-36.
4. Zanarini MC, Conkey LC, Temes CM, et al. Randomized controlled trial of web-based psychoeducation for women with borderline personality disorder. J Clin Psychiatry. 2018;79(3):16m11153. doi:10.4088/JCP.16m11153
5. McMain SF, Guimond T, Barnhart R, et al. A randomized trial of brief dialectical behaviour therapy skills training in suicidal patients suffering from borderline disorder. Acta Psychiatr Scand. 2017;135(2):138-148. doi:10.1111/acps.12664
6. Bozzatello P, Bellino S. Combined therapy with interpersonal psychotherapy adapted for borderline personality disorder: a two-years follow-up. Psychiatry Res. 2016;240:151-156. doi:10.1016/j.psychres.2016.04.014
7. Antonsen BT, Kvarstein EH, Urnes Ø, et al. Favourable outcome of long-term combined psychotherapy for patients with borderline personality disorder: six-year follow-up of a randomized study. Psychother Res. 2017;27(1):51-63. doi:10.1080/10503307.2015.1072283
8. Bateman A, Constantinou MP, Fonagy P, et al. Eight-year prospective follow-up of mentalization-based treatment versus structured clinical management for people with borderline personality disorder. Personal Disord. 2021;12(4):291-299. doi:10.1037/per0000422
9. Klein JP, Hauer-von Mauschwitz A, Berger T, et al. Effectiveness and safety of the adjunctive use of an internet-based self-management intervention for borderline personality disorder in addition to care as usual: results from a randomised controlled trial. BMJ Open. 2021;11(9):e047771. doi:10.1136/bmjopen-2020-047771
10. Zanarini MC, Frankenburg FR. A preliminary, randomized trial of psychoeducation for women with borderline personality disorder. J Pers Disord. 2008;22(3):284-290.
11. Bellino S, Rinaldi C, Bogetto F. Adaptation of interpersonal psychotherapy to borderline personality disorder: a comparison of combined therapy and single pharmacotherapy. Can J Psychiatry. 2010;55(2):74-81.
12. Arnevik E, Wilberg T, Urnes Ø, et al. Psychotherapy for personality disorders: short-term day hospital psychotherapy versus outpatient individual therapy – a randomized controlled study. Eur Psychiatry. 2009,24(2):71-78. doi:10.1016/j.eurpsy.2008.09.004
13. Bateman A, Fonagy P. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. Am J Psychiatry. 2009;166(12):1355-1364.
Psychiatric partial hospitalization programs: What you need to know
Psychiatric partial hospitalization programs (PHPs), previously known as “day hospitals,” serve to bridge the gap between inpatient and outpatient facilities by providing intensive, highly structured outpatient behavioral health services (typically several hours of psychotherapy each weekday for most days of the week). The concept of PHPs has existed since at least the 1950s, but such programs started to become more common in the United States as the result of legislation passed in 1963 (Box1-3). In this article, I provide a brief introductory review of PHPs, while acknowledging that most research on PHPs was conducted years ago and is rather limited.
Box
The concept of partial hospitalization programs (PHPs) was developed before the 1950s.1 However, in the United States, PHPs did not take hold until Congress passed the Community Mental Health Act of 1963, which required that PHPs must be a core component of Community Mental Health Centers (CMHCs). The Omnibus Budget Reconciliation Acts of 1987 and 1990 required Medicare to pay for PHPs affiliated with or based in CMHCs and psychiatric hospitals, which resulted in a proliferation of PHPs across the country. The number of CMHCbased PHPs grew from 296 in 1993 to 769 in 1997.2 By 2016, more than one-third (38.7%) of all metropolitan hospitals and 11.4% of nonmetropolitan hospitals in the United States provided PHP services.3 This growth was also partially the result of private health insurance companies and the managed care industry clamping down on inpatient hospital stays and approving PHP care to reduce costs. In recent years, freestanding PHPs that are not affiliated with a CMHC or hospital have opened to serve high-functioning patients who do not want inpatient hospitalization or the stigma associated with it.
PHPs: What they are, and how they work
The term “partial hospitalization” is fraught with confusion because initially it was used to contrast such services from full hospitalization. Historically, it was used to describe services for patients who had been discharged home from a state hospital and attended a program on the hospital grounds during the day as outpatients. In reality, today’s PHPs are “day treatment” programs, but the terminology has stuck.
PHPs are neither an inpatient service nor a strict outpatient service, but rather a midground along the continuum of treatment intensity between the 2 traditional types of psychiatric services for patients with a range of mental illness of varying severity. The Association for Ambulatory Behavioral Healthcare, which has set standards and guidelines for PHPs, defines a PHP as “an ambulatory treatment program that includes the major diagnostic, medical, psychiatric, psychosocial, and prevocational treatment modalities designed for patients with serious mental disorders who require coordinated intensive, comprehensive, and multidisciplinary treatment not provided in an outpatient clinical setting.”4 PHPs can render acute care as an alternative to inpatient treatment, provide transitional stabilization treatment between an inpatient stay and traditional outpatient treatment (once a week or less frequent), and function as a supplement to traditional outpatient treatment.
Medicare has established criteria that PHPs must meet to qualify for reimbursement5; these criteria are now widely accepted as standards of care by the insurance industry. To meet the Medicare criteria, PHP treatment must be active and structured to provide an individualized treatment plan that incorporates coordination of services to meet the particular needs of the patient.5 It must include a multidisciplinary team approach to patient care under the direction of a physician, and the treatment goals must be measurable, functional, time-framed, medically necessary, and directly related to the reason for admission.5 The physician must certify the medical necessity for admission by documenting that the patient has a diagnosis of an acute Axis I mental disorder, a level of functioning that includes severe impairments in multiple areas of daily life, and a “reasonable expectation” that the disorder and level of functioning will improve as a result of the treatment.5
The Joint Commission (formerly JCAHO) lumps day treatment, intensive outpatient, partial hospitalization, and adult day care services into a single category of an ambulatory health care environment offering an organized day or night program of assessment, treatment, care, services, habilitation, or rehabilitation for individuals who do not require 24-hour care.6 For behavioral health, this may be a structured, ongoing program that typically meets 2 to 5 times a week for 2 to 5 hours per day.6
Most PHPs for adult patients provide services during the day 5 days per week and average 5 to 6 hours of programming per day. Night or evening programming may be a good option for patients who work during the day. Typically, treatment is provided in a group therapy format, with individual therapy at least once a week. Group therapy may include cognitive-behavioral therapy, coping with grief and loss, trauma recovery, conflict resolution, stress management, anger control, and behavioral modification. Family therapy is provided as needed, but usually is mandatory for children and adolescents. Many PHPs offer intensive outpatient programs (IOPs) as a step down to further facilitate a patient’s adjustment to psychosocial and family functioning while returning to work on a part-time basis. IOPs typically provide 3 to 4 hours of service per day 3 days per week. While not evidence-based, the typical duration of PHP treatment is 4 to 6 weeks, followed by an additional 2 to 4 weeks of IOP.
Continue to: Advantages and disadvantages...
Advantages and disadvantages
Based on a qualitative literature review, Neffinger1 outlined potential advantages and disadvantages of PHPs vs inpatient hospitalization (Table1). While these have not been empirically studied, they may be useful to consider when determining if a PHP would be beneficial for a specific patient.
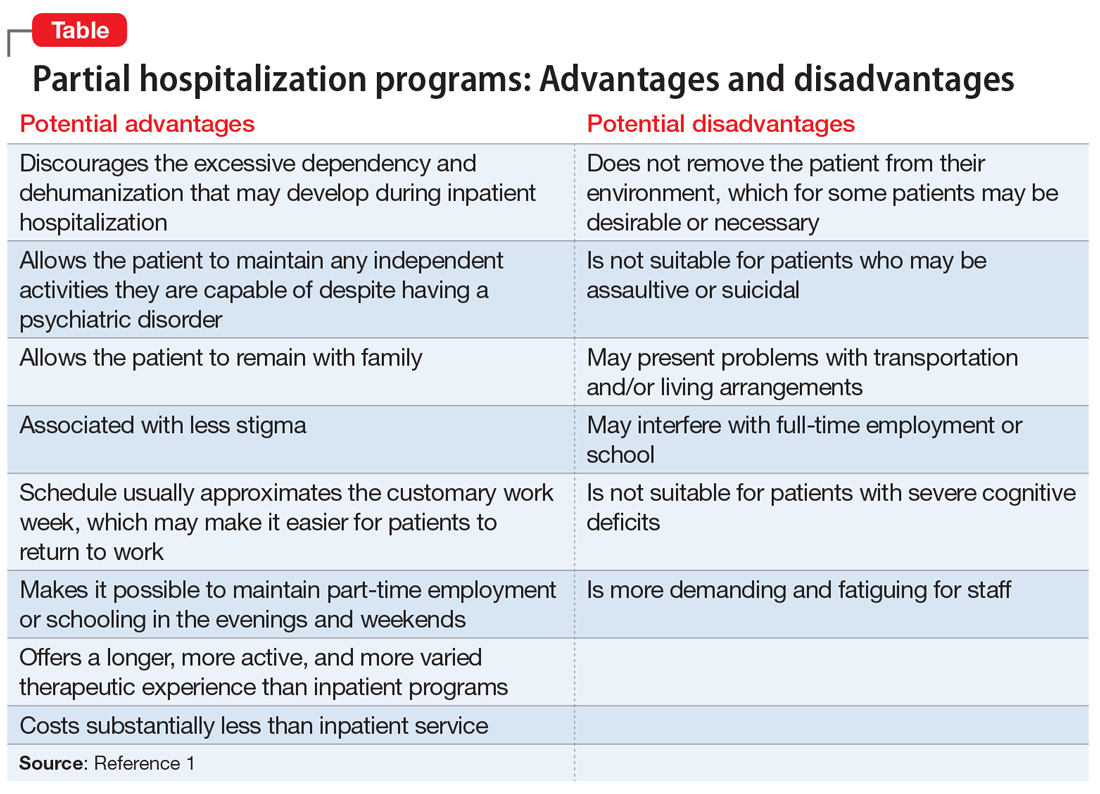
Which factors are most therapeutic?
Research on which factors of PHPs are of therapeutic value is quite limited and primarily consists of surveys of small numbers of participants. Hoge et al7 explored the active therapeutic factors responsible for change in the Connecticut Mental Health Center PHP by comparing responses of 20 patients with those of their clinicians. Ninety-five percent of patients rated structure as the top therapeutic factor, followed by interpersonal contact, medication, and altruism. Other factors that were rated as important by 40% or fewer participants were catharsis, learning, mobilization of family support, connection to community, universality, patient autonomy, successful completion, security, feedback on behavior, and practice at home. In a British study8 that used a similar method, patients reported that counseling was the most helpful aspect of treatment, followed by medical treatment, while staff picked groups followed by a planned approach.
Evidence supports PHPs’ effectiveness
Some research has suggested that PHPs can be effective, both clinically and in terms of cost. Marshall et al9 conducted a systematic review of the effectiveness of an acute day hospital vs inpatient admission vs outpatient care that included 9 trials. They concluded that psychiatric inpatient admissions could be reduced by at least 23% if patients were diverted to an acute day hospital. They also found some evidence that day treatment programs may be superior to outpatient care in improving symptoms in nonpsychotic patients who are refractory to outpatient treatment. In a systematic review of 18 studies, high rates of satisfaction with PHP services suggested PHPs have an advantage over inpatient treatment within 1 year of discharge; patients and families were more satisfied with PHPs.10 In a study of 197 urban, socioeconomically disadvantaged, severely ill patients, Sledge et al11 compared the clinical outcomes of those who participated in day hospital programs with those of patients who received inpatient care. They found that while overall the 2 approaches produced similar outcomes, there were slightly more positive effects for day hospital programs in measures of symptoms, overall functioning, and social functioning. In terms of cost effectiveness, a 1978 study found that even after correcting for differences in treatment days between inpatient and PHP services, there was a significant financial advantage with PHP (costs were one-third less), primarily because of lower costs per day.12 In another study, PHP cost savings were 20%, and potential savings were higher for nonpsychotic patients.13
Are PHPs appropriate for children and adolescents?
Studies of PHPs for adolescents found that patients made gains in peer relationships, behavioral and academic performance, and control of their emotions.14,15 A review of PHPs’ effectiveness for children suggested that 66% to 99% of treated patients demonstrated improvement and successful return to community-based schools, and family functioning was a major factor in improvement.14 In a follow-up study that surveyed patients via telephone >1 year after discharge from a PHP, almost 80% of the children and adolescents were either “doing OK” or were “well-adjusted.”14 Only 22.5% required inpatient or residential treatment; the majority were doing well in school, with only 7% failing.14 In addition, 60% of parents reported satisfaction with treatment, and 85% reported functional improvement in their children.
Factors that predict PHP success or failure
In an analysis of a day treatment program that provided 4 months of intensive psychodynamic, group-oriented milieu treatment for patients with long-standing personality disorders, Rosie et al16 found 3 factors that contributed to the success of the PHP:
- optimal treatment-patient matching
- judicious use of authority in milieu therapy
- maintaining close relationships with referral sources.
In a study that compared 58 patients who completed an Ottawa hospital PHP and 44 who did not complete the program, psychological mindedness and chronicity of psychiatric illness were found to predict completion.17 However, a study of 59 females with anorexia nervosa who were transferred from inpatient care to an eating disorder day hospital program found that a longer duration of illness, amenorrhea, and a lower body mass index were associated with PHP treatment failure and inpatient rehospitalization.18 One study found that for individuals who were referred to a PHP from inpatient care, suicidal ideation and greater psychotic symptoms were associated with acute inpatient rehospitalization.19 Other factors associated with PHP nonattendance and treatment failure include limited personal and economic resources, high rates of substance abuse disorders, multiple admissions, and disability.20 In a study of 103 alcohol-dependent patients who completed IOP treatment, 64% were abstinent at 6 months follow-up; relapse was associated with a longer duration of alcohol dependence and a higher number of prior treatments, while favorable outcomes were associated with a lower degree of depression, anxiety, and craving.21 Patients with cocaine dependence who completed an IOP showed significant improvements in addiction scores and had more favorable outcomes in employment status and psychological problems if they stayed longer in treatment.22
Bottom Line
Psychiatric partial hospitalization programs (PHPs) provide a transition from inpatient hospitalization to outpatient treatment for patients who need further stabilization, or serve as an alternative to inpatient treatment for patients who don’t need or want inpatient hospitalization. PHPs can be as effective as inpatient treatment for all but the most seriously ill patients, and are more cost-effective than inpatient treatment.
1. Neffinger GG. Partial hospitalization: an overview. J Community Psychol. 1981;9(3):262-269.
2. Leung MY, Drozd EM, Healy DA, et al. Impacts associated with the Medicare Psychiatric PPS: a study of partial hospitalization programs. February 2009. Accessed January 8, 2022. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Reports/downloads/Leung_PHP_PPS_2010.pdf
3. Williams T, Borders TF, Jasinski L. Partial Psychiatric Hospitalization Program Availability in Non-Metropolitan and Non-Metropolitan Hospitals Nationally. Rural and Underserved Health Research Center; 2019.
4. Rosser J, Michael S, eds. Standards and guidelines for partial hospital programs and intensive outpatient programs. Association for Ambulatory Behavioral Healthcare. 2018. Accessed January 8, 2022. https://aabh.org/wp-content/uploads/2021/05/2021-SandG-Final.pdf
5. CMS Manual System PUB. 100-02 Medicare Benefit Policy: Partial Hospitalization Services, Department of Health and Human Services. Centers for Medicare & Medicaid Services; 2004:6-9.
6. Joint Commission. Guide to Joint Commission Behavioral Healthcare Accreditation. Joint Commission; 2007:36.
7. Hoge MA, Farrell SP, Munchel ME, et al. Therapeutic factors in partial hospitalization. Psychiatry. 1988;51(2):199-210.
8. Ricketts T, Kirshbaum MN. Helpfulness of mental health day care: client and staff views. J Adv Nurs. 1994;20(2):297-306.
9. Marshall M, Crowther R, Almaraz-Serrano A, et al. Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) acute day hospital versus admission; (2) vocational rehabilitation; (3) day hospital versus outpatient care. Health Technol Assess. 2001;5(21):1-75.
10. Horvitz-Lennon M, Normand SL, Gaccione P, et al. Partial versus full hospitalization for adults in psychiatric distress: a systematic review of the published literature (1957-1997). Am J Psychiatry. 2001;158(5):676-685.
11. Sledge WH, Tebes J, Rakfeldt J, et al. Day hospital/crisis respite care versus inpatient care, Part I: Clinical outcomes. Am J Psychiatry. 1996;153(8):1065-1073.
12. Fink EB, Longabaugh R, Stout R. The paradoxical underutilization of partial hospitalization. Am J Psychiatry. 1978;135(6):713-716.
13. Sledge WH, Tebes J, Wolff N, et al. Day hospital/crisis respite care versus inpatient care, Part II: service utilization and costs. Am J Psychiatry. 1996;153(8):1074-1083.
14. Kiser LJ. Treatment-effectiveness research in child and adolescent partial hospitalization. Psychiatr Hosp. 1991;22(2):51-8.
15. Milin R, Coupland K, Walker S, et al. Outcome and follow-up study of an adolescent psychiatric day treatment school program. J Am Acad Child Adolesc Psychiatry. 2000;39(3):320-328.
16. Rosie JS, Azim HF, Piper WE, et al. Effective psychiatric day treatment: historical lessons. Psychiatr Serv. 1995;46(10):1019-1026.
17. Tasca GA, Balfour L, Bissada H, et al. Treatment completion and outcome in a partial hospitalization program: interactions among patient variables. Psychotherapy Res. 1999;9(2):232-247.
18. Howard WT, Evans KK, Quintero-Howard CV, et al. Predictors of success or failure of transition to day hospital treatment for inpatients with anorexia nervosa. Am J Psychiatry. 1999;156(11):1697-1702.
19. Beard C, Hearon BA, Lee J, et al. When partial hospitalization fails: risk factors for inpatient hospitalization. J Nerv Ment Dis. 2016;204(6):431-436.
20. Lieberman PB, Guggenheim FG. Reasons for patient nonattendance during acute partial hospitalization. Psychiatr Serv. 2016;67(6):684-687.
21. Bottlender M, Soyka M. Efficacy of an intensive outpatient rehabilitation program in alcoholism: predictors of outcome 6 months after treatment. Eur Addict Res. 2005;11(3):132-137.
22. Gottheil E, Weinstein SP, Sterling RC, et al. A randomized controlled study of the effectiveness of intensive outpatient treatment for cocaine dependence. Psychiatr Serv. 1998;49(6):782-787.
Psychiatric partial hospitalization programs (PHPs), previously known as “day hospitals,” serve to bridge the gap between inpatient and outpatient facilities by providing intensive, highly structured outpatient behavioral health services (typically several hours of psychotherapy each weekday for most days of the week). The concept of PHPs has existed since at least the 1950s, but such programs started to become more common in the United States as the result of legislation passed in 1963 (Box1-3). In this article, I provide a brief introductory review of PHPs, while acknowledging that most research on PHPs was conducted years ago and is rather limited.
Box
The concept of partial hospitalization programs (PHPs) was developed before the 1950s.1 However, in the United States, PHPs did not take hold until Congress passed the Community Mental Health Act of 1963, which required that PHPs must be a core component of Community Mental Health Centers (CMHCs). The Omnibus Budget Reconciliation Acts of 1987 and 1990 required Medicare to pay for PHPs affiliated with or based in CMHCs and psychiatric hospitals, which resulted in a proliferation of PHPs across the country. The number of CMHCbased PHPs grew from 296 in 1993 to 769 in 1997.2 By 2016, more than one-third (38.7%) of all metropolitan hospitals and 11.4% of nonmetropolitan hospitals in the United States provided PHP services.3 This growth was also partially the result of private health insurance companies and the managed care industry clamping down on inpatient hospital stays and approving PHP care to reduce costs. In recent years, freestanding PHPs that are not affiliated with a CMHC or hospital have opened to serve high-functioning patients who do not want inpatient hospitalization or the stigma associated with it.
PHPs: What they are, and how they work
The term “partial hospitalization” is fraught with confusion because initially it was used to contrast such services from full hospitalization. Historically, it was used to describe services for patients who had been discharged home from a state hospital and attended a program on the hospital grounds during the day as outpatients. In reality, today’s PHPs are “day treatment” programs, but the terminology has stuck.
PHPs are neither an inpatient service nor a strict outpatient service, but rather a midground along the continuum of treatment intensity between the 2 traditional types of psychiatric services for patients with a range of mental illness of varying severity. The Association for Ambulatory Behavioral Healthcare, which has set standards and guidelines for PHPs, defines a PHP as “an ambulatory treatment program that includes the major diagnostic, medical, psychiatric, psychosocial, and prevocational treatment modalities designed for patients with serious mental disorders who require coordinated intensive, comprehensive, and multidisciplinary treatment not provided in an outpatient clinical setting.”4 PHPs can render acute care as an alternative to inpatient treatment, provide transitional stabilization treatment between an inpatient stay and traditional outpatient treatment (once a week or less frequent), and function as a supplement to traditional outpatient treatment.
Medicare has established criteria that PHPs must meet to qualify for reimbursement5; these criteria are now widely accepted as standards of care by the insurance industry. To meet the Medicare criteria, PHP treatment must be active and structured to provide an individualized treatment plan that incorporates coordination of services to meet the particular needs of the patient.5 It must include a multidisciplinary team approach to patient care under the direction of a physician, and the treatment goals must be measurable, functional, time-framed, medically necessary, and directly related to the reason for admission.5 The physician must certify the medical necessity for admission by documenting that the patient has a diagnosis of an acute Axis I mental disorder, a level of functioning that includes severe impairments in multiple areas of daily life, and a “reasonable expectation” that the disorder and level of functioning will improve as a result of the treatment.5
The Joint Commission (formerly JCAHO) lumps day treatment, intensive outpatient, partial hospitalization, and adult day care services into a single category of an ambulatory health care environment offering an organized day or night program of assessment, treatment, care, services, habilitation, or rehabilitation for individuals who do not require 24-hour care.6 For behavioral health, this may be a structured, ongoing program that typically meets 2 to 5 times a week for 2 to 5 hours per day.6
Most PHPs for adult patients provide services during the day 5 days per week and average 5 to 6 hours of programming per day. Night or evening programming may be a good option for patients who work during the day. Typically, treatment is provided in a group therapy format, with individual therapy at least once a week. Group therapy may include cognitive-behavioral therapy, coping with grief and loss, trauma recovery, conflict resolution, stress management, anger control, and behavioral modification. Family therapy is provided as needed, but usually is mandatory for children and adolescents. Many PHPs offer intensive outpatient programs (IOPs) as a step down to further facilitate a patient’s adjustment to psychosocial and family functioning while returning to work on a part-time basis. IOPs typically provide 3 to 4 hours of service per day 3 days per week. While not evidence-based, the typical duration of PHP treatment is 4 to 6 weeks, followed by an additional 2 to 4 weeks of IOP.
Continue to: Advantages and disadvantages...
Advantages and disadvantages
Based on a qualitative literature review, Neffinger1 outlined potential advantages and disadvantages of PHPs vs inpatient hospitalization (Table1). While these have not been empirically studied, they may be useful to consider when determining if a PHP would be beneficial for a specific patient.
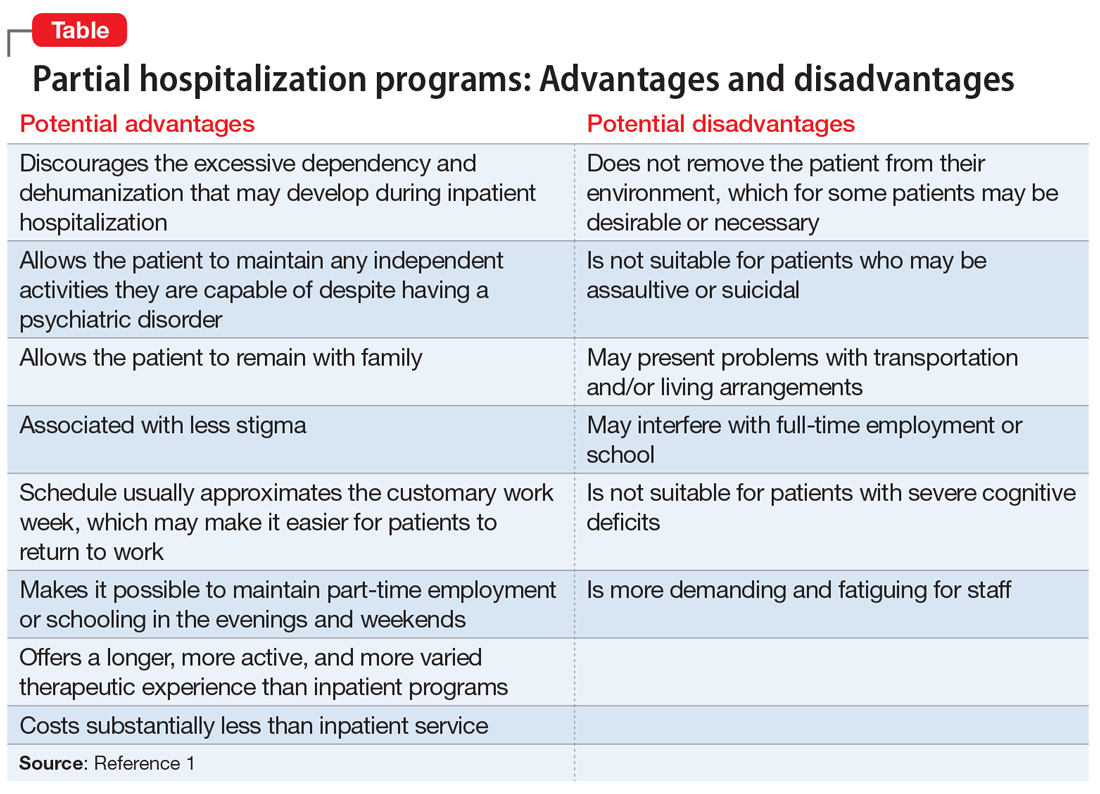
Which factors are most therapeutic?
Research on which factors of PHPs are of therapeutic value is quite limited and primarily consists of surveys of small numbers of participants. Hoge et al7 explored the active therapeutic factors responsible for change in the Connecticut Mental Health Center PHP by comparing responses of 20 patients with those of their clinicians. Ninety-five percent of patients rated structure as the top therapeutic factor, followed by interpersonal contact, medication, and altruism. Other factors that were rated as important by 40% or fewer participants were catharsis, learning, mobilization of family support, connection to community, universality, patient autonomy, successful completion, security, feedback on behavior, and practice at home. In a British study8 that used a similar method, patients reported that counseling was the most helpful aspect of treatment, followed by medical treatment, while staff picked groups followed by a planned approach.
Evidence supports PHPs’ effectiveness
Some research has suggested that PHPs can be effective, both clinically and in terms of cost. Marshall et al9 conducted a systematic review of the effectiveness of an acute day hospital vs inpatient admission vs outpatient care that included 9 trials. They concluded that psychiatric inpatient admissions could be reduced by at least 23% if patients were diverted to an acute day hospital. They also found some evidence that day treatment programs may be superior to outpatient care in improving symptoms in nonpsychotic patients who are refractory to outpatient treatment. In a systematic review of 18 studies, high rates of satisfaction with PHP services suggested PHPs have an advantage over inpatient treatment within 1 year of discharge; patients and families were more satisfied with PHPs.10 In a study of 197 urban, socioeconomically disadvantaged, severely ill patients, Sledge et al11 compared the clinical outcomes of those who participated in day hospital programs with those of patients who received inpatient care. They found that while overall the 2 approaches produced similar outcomes, there were slightly more positive effects for day hospital programs in measures of symptoms, overall functioning, and social functioning. In terms of cost effectiveness, a 1978 study found that even after correcting for differences in treatment days between inpatient and PHP services, there was a significant financial advantage with PHP (costs were one-third less), primarily because of lower costs per day.12 In another study, PHP cost savings were 20%, and potential savings were higher for nonpsychotic patients.13
Are PHPs appropriate for children and adolescents?
Studies of PHPs for adolescents found that patients made gains in peer relationships, behavioral and academic performance, and control of their emotions.14,15 A review of PHPs’ effectiveness for children suggested that 66% to 99% of treated patients demonstrated improvement and successful return to community-based schools, and family functioning was a major factor in improvement.14 In a follow-up study that surveyed patients via telephone >1 year after discharge from a PHP, almost 80% of the children and adolescents were either “doing OK” or were “well-adjusted.”14 Only 22.5% required inpatient or residential treatment; the majority were doing well in school, with only 7% failing.14 In addition, 60% of parents reported satisfaction with treatment, and 85% reported functional improvement in their children.
Factors that predict PHP success or failure
In an analysis of a day treatment program that provided 4 months of intensive psychodynamic, group-oriented milieu treatment for patients with long-standing personality disorders, Rosie et al16 found 3 factors that contributed to the success of the PHP:
- optimal treatment-patient matching
- judicious use of authority in milieu therapy
- maintaining close relationships with referral sources.
In a study that compared 58 patients who completed an Ottawa hospital PHP and 44 who did not complete the program, psychological mindedness and chronicity of psychiatric illness were found to predict completion.17 However, a study of 59 females with anorexia nervosa who were transferred from inpatient care to an eating disorder day hospital program found that a longer duration of illness, amenorrhea, and a lower body mass index were associated with PHP treatment failure and inpatient rehospitalization.18 One study found that for individuals who were referred to a PHP from inpatient care, suicidal ideation and greater psychotic symptoms were associated with acute inpatient rehospitalization.19 Other factors associated with PHP nonattendance and treatment failure include limited personal and economic resources, high rates of substance abuse disorders, multiple admissions, and disability.20 In a study of 103 alcohol-dependent patients who completed IOP treatment, 64% were abstinent at 6 months follow-up; relapse was associated with a longer duration of alcohol dependence and a higher number of prior treatments, while favorable outcomes were associated with a lower degree of depression, anxiety, and craving.21 Patients with cocaine dependence who completed an IOP showed significant improvements in addiction scores and had more favorable outcomes in employment status and psychological problems if they stayed longer in treatment.22
Bottom Line
Psychiatric partial hospitalization programs (PHPs) provide a transition from inpatient hospitalization to outpatient treatment for patients who need further stabilization, or serve as an alternative to inpatient treatment for patients who don’t need or want inpatient hospitalization. PHPs can be as effective as inpatient treatment for all but the most seriously ill patients, and are more cost-effective than inpatient treatment.
Psychiatric partial hospitalization programs (PHPs), previously known as “day hospitals,” serve to bridge the gap between inpatient and outpatient facilities by providing intensive, highly structured outpatient behavioral health services (typically several hours of psychotherapy each weekday for most days of the week). The concept of PHPs has existed since at least the 1950s, but such programs started to become more common in the United States as the result of legislation passed in 1963 (Box1-3). In this article, I provide a brief introductory review of PHPs, while acknowledging that most research on PHPs was conducted years ago and is rather limited.
Box
The concept of partial hospitalization programs (PHPs) was developed before the 1950s.1 However, in the United States, PHPs did not take hold until Congress passed the Community Mental Health Act of 1963, which required that PHPs must be a core component of Community Mental Health Centers (CMHCs). The Omnibus Budget Reconciliation Acts of 1987 and 1990 required Medicare to pay for PHPs affiliated with or based in CMHCs and psychiatric hospitals, which resulted in a proliferation of PHPs across the country. The number of CMHCbased PHPs grew from 296 in 1993 to 769 in 1997.2 By 2016, more than one-third (38.7%) of all metropolitan hospitals and 11.4% of nonmetropolitan hospitals in the United States provided PHP services.3 This growth was also partially the result of private health insurance companies and the managed care industry clamping down on inpatient hospital stays and approving PHP care to reduce costs. In recent years, freestanding PHPs that are not affiliated with a CMHC or hospital have opened to serve high-functioning patients who do not want inpatient hospitalization or the stigma associated with it.
PHPs: What they are, and how they work
The term “partial hospitalization” is fraught with confusion because initially it was used to contrast such services from full hospitalization. Historically, it was used to describe services for patients who had been discharged home from a state hospital and attended a program on the hospital grounds during the day as outpatients. In reality, today’s PHPs are “day treatment” programs, but the terminology has stuck.
PHPs are neither an inpatient service nor a strict outpatient service, but rather a midground along the continuum of treatment intensity between the 2 traditional types of psychiatric services for patients with a range of mental illness of varying severity. The Association for Ambulatory Behavioral Healthcare, which has set standards and guidelines for PHPs, defines a PHP as “an ambulatory treatment program that includes the major diagnostic, medical, psychiatric, psychosocial, and prevocational treatment modalities designed for patients with serious mental disorders who require coordinated intensive, comprehensive, and multidisciplinary treatment not provided in an outpatient clinical setting.”4 PHPs can render acute care as an alternative to inpatient treatment, provide transitional stabilization treatment between an inpatient stay and traditional outpatient treatment (once a week or less frequent), and function as a supplement to traditional outpatient treatment.
Medicare has established criteria that PHPs must meet to qualify for reimbursement5; these criteria are now widely accepted as standards of care by the insurance industry. To meet the Medicare criteria, PHP treatment must be active and structured to provide an individualized treatment plan that incorporates coordination of services to meet the particular needs of the patient.5 It must include a multidisciplinary team approach to patient care under the direction of a physician, and the treatment goals must be measurable, functional, time-framed, medically necessary, and directly related to the reason for admission.5 The physician must certify the medical necessity for admission by documenting that the patient has a diagnosis of an acute Axis I mental disorder, a level of functioning that includes severe impairments in multiple areas of daily life, and a “reasonable expectation” that the disorder and level of functioning will improve as a result of the treatment.5
The Joint Commission (formerly JCAHO) lumps day treatment, intensive outpatient, partial hospitalization, and adult day care services into a single category of an ambulatory health care environment offering an organized day or night program of assessment, treatment, care, services, habilitation, or rehabilitation for individuals who do not require 24-hour care.6 For behavioral health, this may be a structured, ongoing program that typically meets 2 to 5 times a week for 2 to 5 hours per day.6
Most PHPs for adult patients provide services during the day 5 days per week and average 5 to 6 hours of programming per day. Night or evening programming may be a good option for patients who work during the day. Typically, treatment is provided in a group therapy format, with individual therapy at least once a week. Group therapy may include cognitive-behavioral therapy, coping with grief and loss, trauma recovery, conflict resolution, stress management, anger control, and behavioral modification. Family therapy is provided as needed, but usually is mandatory for children and adolescents. Many PHPs offer intensive outpatient programs (IOPs) as a step down to further facilitate a patient’s adjustment to psychosocial and family functioning while returning to work on a part-time basis. IOPs typically provide 3 to 4 hours of service per day 3 days per week. While not evidence-based, the typical duration of PHP treatment is 4 to 6 weeks, followed by an additional 2 to 4 weeks of IOP.
Continue to: Advantages and disadvantages...
Advantages and disadvantages
Based on a qualitative literature review, Neffinger1 outlined potential advantages and disadvantages of PHPs vs inpatient hospitalization (Table1). While these have not been empirically studied, they may be useful to consider when determining if a PHP would be beneficial for a specific patient.
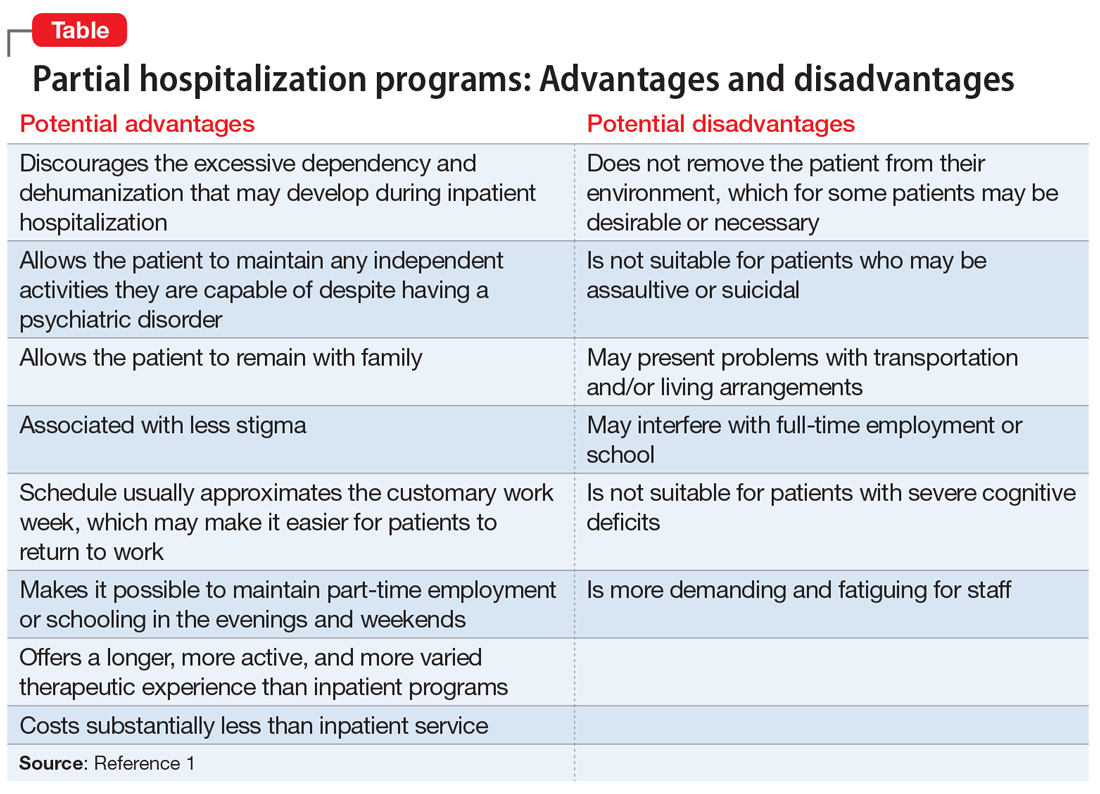
Which factors are most therapeutic?
Research on which factors of PHPs are of therapeutic value is quite limited and primarily consists of surveys of small numbers of participants. Hoge et al7 explored the active therapeutic factors responsible for change in the Connecticut Mental Health Center PHP by comparing responses of 20 patients with those of their clinicians. Ninety-five percent of patients rated structure as the top therapeutic factor, followed by interpersonal contact, medication, and altruism. Other factors that were rated as important by 40% or fewer participants were catharsis, learning, mobilization of family support, connection to community, universality, patient autonomy, successful completion, security, feedback on behavior, and practice at home. In a British study8 that used a similar method, patients reported that counseling was the most helpful aspect of treatment, followed by medical treatment, while staff picked groups followed by a planned approach.
Evidence supports PHPs’ effectiveness
Some research has suggested that PHPs can be effective, both clinically and in terms of cost. Marshall et al9 conducted a systematic review of the effectiveness of an acute day hospital vs inpatient admission vs outpatient care that included 9 trials. They concluded that psychiatric inpatient admissions could be reduced by at least 23% if patients were diverted to an acute day hospital. They also found some evidence that day treatment programs may be superior to outpatient care in improving symptoms in nonpsychotic patients who are refractory to outpatient treatment. In a systematic review of 18 studies, high rates of satisfaction with PHP services suggested PHPs have an advantage over inpatient treatment within 1 year of discharge; patients and families were more satisfied with PHPs.10 In a study of 197 urban, socioeconomically disadvantaged, severely ill patients, Sledge et al11 compared the clinical outcomes of those who participated in day hospital programs with those of patients who received inpatient care. They found that while overall the 2 approaches produced similar outcomes, there were slightly more positive effects for day hospital programs in measures of symptoms, overall functioning, and social functioning. In terms of cost effectiveness, a 1978 study found that even after correcting for differences in treatment days between inpatient and PHP services, there was a significant financial advantage with PHP (costs were one-third less), primarily because of lower costs per day.12 In another study, PHP cost savings were 20%, and potential savings were higher for nonpsychotic patients.13
Are PHPs appropriate for children and adolescents?
Studies of PHPs for adolescents found that patients made gains in peer relationships, behavioral and academic performance, and control of their emotions.14,15 A review of PHPs’ effectiveness for children suggested that 66% to 99% of treated patients demonstrated improvement and successful return to community-based schools, and family functioning was a major factor in improvement.14 In a follow-up study that surveyed patients via telephone >1 year after discharge from a PHP, almost 80% of the children and adolescents were either “doing OK” or were “well-adjusted.”14 Only 22.5% required inpatient or residential treatment; the majority were doing well in school, with only 7% failing.14 In addition, 60% of parents reported satisfaction with treatment, and 85% reported functional improvement in their children.
Factors that predict PHP success or failure
In an analysis of a day treatment program that provided 4 months of intensive psychodynamic, group-oriented milieu treatment for patients with long-standing personality disorders, Rosie et al16 found 3 factors that contributed to the success of the PHP:
- optimal treatment-patient matching
- judicious use of authority in milieu therapy
- maintaining close relationships with referral sources.
In a study that compared 58 patients who completed an Ottawa hospital PHP and 44 who did not complete the program, psychological mindedness and chronicity of psychiatric illness were found to predict completion.17 However, a study of 59 females with anorexia nervosa who were transferred from inpatient care to an eating disorder day hospital program found that a longer duration of illness, amenorrhea, and a lower body mass index were associated with PHP treatment failure and inpatient rehospitalization.18 One study found that for individuals who were referred to a PHP from inpatient care, suicidal ideation and greater psychotic symptoms were associated with acute inpatient rehospitalization.19 Other factors associated with PHP nonattendance and treatment failure include limited personal and economic resources, high rates of substance abuse disorders, multiple admissions, and disability.20 In a study of 103 alcohol-dependent patients who completed IOP treatment, 64% were abstinent at 6 months follow-up; relapse was associated with a longer duration of alcohol dependence and a higher number of prior treatments, while favorable outcomes were associated with a lower degree of depression, anxiety, and craving.21 Patients with cocaine dependence who completed an IOP showed significant improvements in addiction scores and had more favorable outcomes in employment status and psychological problems if they stayed longer in treatment.22
Bottom Line
Psychiatric partial hospitalization programs (PHPs) provide a transition from inpatient hospitalization to outpatient treatment for patients who need further stabilization, or serve as an alternative to inpatient treatment for patients who don’t need or want inpatient hospitalization. PHPs can be as effective as inpatient treatment for all but the most seriously ill patients, and are more cost-effective than inpatient treatment.
1. Neffinger GG. Partial hospitalization: an overview. J Community Psychol. 1981;9(3):262-269.
2. Leung MY, Drozd EM, Healy DA, et al. Impacts associated with the Medicare Psychiatric PPS: a study of partial hospitalization programs. February 2009. Accessed January 8, 2022. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Reports/downloads/Leung_PHP_PPS_2010.pdf
3. Williams T, Borders TF, Jasinski L. Partial Psychiatric Hospitalization Program Availability in Non-Metropolitan and Non-Metropolitan Hospitals Nationally. Rural and Underserved Health Research Center; 2019.
4. Rosser J, Michael S, eds. Standards and guidelines for partial hospital programs and intensive outpatient programs. Association for Ambulatory Behavioral Healthcare. 2018. Accessed January 8, 2022. https://aabh.org/wp-content/uploads/2021/05/2021-SandG-Final.pdf
5. CMS Manual System PUB. 100-02 Medicare Benefit Policy: Partial Hospitalization Services, Department of Health and Human Services. Centers for Medicare & Medicaid Services; 2004:6-9.
6. Joint Commission. Guide to Joint Commission Behavioral Healthcare Accreditation. Joint Commission; 2007:36.
7. Hoge MA, Farrell SP, Munchel ME, et al. Therapeutic factors in partial hospitalization. Psychiatry. 1988;51(2):199-210.
8. Ricketts T, Kirshbaum MN. Helpfulness of mental health day care: client and staff views. J Adv Nurs. 1994;20(2):297-306.
9. Marshall M, Crowther R, Almaraz-Serrano A, et al. Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) acute day hospital versus admission; (2) vocational rehabilitation; (3) day hospital versus outpatient care. Health Technol Assess. 2001;5(21):1-75.
10. Horvitz-Lennon M, Normand SL, Gaccione P, et al. Partial versus full hospitalization for adults in psychiatric distress: a systematic review of the published literature (1957-1997). Am J Psychiatry. 2001;158(5):676-685.
11. Sledge WH, Tebes J, Rakfeldt J, et al. Day hospital/crisis respite care versus inpatient care, Part I: Clinical outcomes. Am J Psychiatry. 1996;153(8):1065-1073.
12. Fink EB, Longabaugh R, Stout R. The paradoxical underutilization of partial hospitalization. Am J Psychiatry. 1978;135(6):713-716.
13. Sledge WH, Tebes J, Wolff N, et al. Day hospital/crisis respite care versus inpatient care, Part II: service utilization and costs. Am J Psychiatry. 1996;153(8):1074-1083.
14. Kiser LJ. Treatment-effectiveness research in child and adolescent partial hospitalization. Psychiatr Hosp. 1991;22(2):51-8.
15. Milin R, Coupland K, Walker S, et al. Outcome and follow-up study of an adolescent psychiatric day treatment school program. J Am Acad Child Adolesc Psychiatry. 2000;39(3):320-328.
16. Rosie JS, Azim HF, Piper WE, et al. Effective psychiatric day treatment: historical lessons. Psychiatr Serv. 1995;46(10):1019-1026.
17. Tasca GA, Balfour L, Bissada H, et al. Treatment completion and outcome in a partial hospitalization program: interactions among patient variables. Psychotherapy Res. 1999;9(2):232-247.
18. Howard WT, Evans KK, Quintero-Howard CV, et al. Predictors of success or failure of transition to day hospital treatment for inpatients with anorexia nervosa. Am J Psychiatry. 1999;156(11):1697-1702.
19. Beard C, Hearon BA, Lee J, et al. When partial hospitalization fails: risk factors for inpatient hospitalization. J Nerv Ment Dis. 2016;204(6):431-436.
20. Lieberman PB, Guggenheim FG. Reasons for patient nonattendance during acute partial hospitalization. Psychiatr Serv. 2016;67(6):684-687.
21. Bottlender M, Soyka M. Efficacy of an intensive outpatient rehabilitation program in alcoholism: predictors of outcome 6 months after treatment. Eur Addict Res. 2005;11(3):132-137.
22. Gottheil E, Weinstein SP, Sterling RC, et al. A randomized controlled study of the effectiveness of intensive outpatient treatment for cocaine dependence. Psychiatr Serv. 1998;49(6):782-787.
1. Neffinger GG. Partial hospitalization: an overview. J Community Psychol. 1981;9(3):262-269.
2. Leung MY, Drozd EM, Healy DA, et al. Impacts associated with the Medicare Psychiatric PPS: a study of partial hospitalization programs. February 2009. Accessed January 8, 2022. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Reports/downloads/Leung_PHP_PPS_2010.pdf
3. Williams T, Borders TF, Jasinski L. Partial Psychiatric Hospitalization Program Availability in Non-Metropolitan and Non-Metropolitan Hospitals Nationally. Rural and Underserved Health Research Center; 2019.
4. Rosser J, Michael S, eds. Standards and guidelines for partial hospital programs and intensive outpatient programs. Association for Ambulatory Behavioral Healthcare. 2018. Accessed January 8, 2022. https://aabh.org/wp-content/uploads/2021/05/2021-SandG-Final.pdf
5. CMS Manual System PUB. 100-02 Medicare Benefit Policy: Partial Hospitalization Services, Department of Health and Human Services. Centers for Medicare & Medicaid Services; 2004:6-9.
6. Joint Commission. Guide to Joint Commission Behavioral Healthcare Accreditation. Joint Commission; 2007:36.
7. Hoge MA, Farrell SP, Munchel ME, et al. Therapeutic factors in partial hospitalization. Psychiatry. 1988;51(2):199-210.
8. Ricketts T, Kirshbaum MN. Helpfulness of mental health day care: client and staff views. J Adv Nurs. 1994;20(2):297-306.
9. Marshall M, Crowther R, Almaraz-Serrano A, et al. Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) acute day hospital versus admission; (2) vocational rehabilitation; (3) day hospital versus outpatient care. Health Technol Assess. 2001;5(21):1-75.
10. Horvitz-Lennon M, Normand SL, Gaccione P, et al. Partial versus full hospitalization for adults in psychiatric distress: a systematic review of the published literature (1957-1997). Am J Psychiatry. 2001;158(5):676-685.
11. Sledge WH, Tebes J, Rakfeldt J, et al. Day hospital/crisis respite care versus inpatient care, Part I: Clinical outcomes. Am J Psychiatry. 1996;153(8):1065-1073.
12. Fink EB, Longabaugh R, Stout R. The paradoxical underutilization of partial hospitalization. Am J Psychiatry. 1978;135(6):713-716.
13. Sledge WH, Tebes J, Wolff N, et al. Day hospital/crisis respite care versus inpatient care, Part II: service utilization and costs. Am J Psychiatry. 1996;153(8):1074-1083.
14. Kiser LJ. Treatment-effectiveness research in child and adolescent partial hospitalization. Psychiatr Hosp. 1991;22(2):51-8.
15. Milin R, Coupland K, Walker S, et al. Outcome and follow-up study of an adolescent psychiatric day treatment school program. J Am Acad Child Adolesc Psychiatry. 2000;39(3):320-328.
16. Rosie JS, Azim HF, Piper WE, et al. Effective psychiatric day treatment: historical lessons. Psychiatr Serv. 1995;46(10):1019-1026.
17. Tasca GA, Balfour L, Bissada H, et al. Treatment completion and outcome in a partial hospitalization program: interactions among patient variables. Psychotherapy Res. 1999;9(2):232-247.
18. Howard WT, Evans KK, Quintero-Howard CV, et al. Predictors of success or failure of transition to day hospital treatment for inpatients with anorexia nervosa. Am J Psychiatry. 1999;156(11):1697-1702.
19. Beard C, Hearon BA, Lee J, et al. When partial hospitalization fails: risk factors for inpatient hospitalization. J Nerv Ment Dis. 2016;204(6):431-436.
20. Lieberman PB, Guggenheim FG. Reasons for patient nonattendance during acute partial hospitalization. Psychiatr Serv. 2016;67(6):684-687.
21. Bottlender M, Soyka M. Efficacy of an intensive outpatient rehabilitation program in alcoholism: predictors of outcome 6 months after treatment. Eur Addict Res. 2005;11(3):132-137.
22. Gottheil E, Weinstein SP, Sterling RC, et al. A randomized controlled study of the effectiveness of intensive outpatient treatment for cocaine dependence. Psychiatr Serv. 1998;49(6):782-787.