User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Study provides new analysis of isotretinoin and risk for adverse neuropsychiatric outcomes
The use of , in a large retrospective cohort study published in the British Journal of Dermatology.
Although severe neuropsychiatric effects associated with isotretinoin therapy in patients with acne have been reported, “the evidence base ... is mixed and inconclusive,” and many studies are small, Seena Fazel, MBChB, MD, of the department of psychiatry, Oxford University, England, and co-authors write in the study.
The study results suggest that isotretinoin is conferring protection against adverse neuropsychiatric outcomes, particularly when compared with using oral antibiotics to treat acne, Dr. Fazel, professor of forensic psychiatry at Oxford University and the study’s senior author, said in an interview.
In the study, the investigators reviewed electronic health records (2013-2019) from a primarily United States–based dataset (TriNetX) of patients with acne aged 12-27 who had been followed for up to 1 year after their prescriptions had been dispensed.
There were four arms: those prescribed isotretinoin (30,866), oral antibiotics (44,748), topical anti-acne treatments (108,367), and those who had not been prescribed any acne treatment (78,666). The primary outcomes were diagnoses of a neuropsychiatric disorder (psychotic, mood, anxiety, personality, behavioral, and sleep disorders; and non-fatal self-harm) within one year of being prescribed treatment.
After using propensity score matching to adjust for confounders at baseline, the investigators determined that the odds ratio for any incident neuropsychiatric outcomes among patients with acne treated with isotretinoin was 0.80 (95% confidence interval, 0.74-0.87), compared with patients on oral antibiotics; 0.94 (95% CI, 0.87-1.02), compared with patients on topical anti-acne medications; and 1.06 (95% CI, 0.97-1.16), compared with those without a prescription for anti-acne medicines.
Side effects of isotretinoin – such as headache, dry mouth, and fatigue – were higher among those on isotretinoin than in the other three groups.
The authors concluded that isotretinoin was not independently linked to excess adverse neuropsychiatric outcomes at a population level. “We observed a consistent association between increasing acne severity as indicated by anti-acne treatment options and incidence of adverse neuropsychiatric outcomes, but the findings showed that isotretinoin exposure did not add to the risk of neuropsychiatric adverse outcomes over and above what was associated with oral antibiotics,” they write.
Isotretinoin treatment “appeared to mitigate the excess neuropsychiatric risk associated with recalcitrant moderate-to-severe acne,” they add.
The dermatology community has been interested in the impact isotretinoin has on mental health, and “I think clinically, they see that people get better on isotretinoin and their mental health improves,” Dr. Fazel told this news organization.
Asked to comment on the study results, John Barbieri, MD, MBA, director of the Advanced Acne Therapeutics Clinic, Brigham and Women’s Hospital, Boston, commended the investigators for the design of the trial.
“One of the strengths of this study is that they use a technique called propensity-score matching, where you try to make the groups of patients similar with respect to their other characteristics to minimize the risks of confounding and bias in the study, which I think is a real strength,” he told this news organization. “The other thing that they do, which I think is a strength, is to think about the impact of acne severity on these outcomes, because we know acne itself is associated with depression and risk for suicide and other neuropsychiatric outcomes.”
Including a cohort of patients who had acne and received oral antibiotics for comparison “is a nice way to address the potential for confounding by severity and confounding by indication,” Dr. Barbieri said. “Those who get antibiotics usually have more severe acne. They may not have it as severely as those who get isotretinoin, but it is a nice approach to account for background levels of depression and neuropsychiatric outcomes in patients with acne. I think that is a real strength of the study. This is one of the best studies to have looked at this question.”
However, although the study found that isotretinoin decreased the excess psychiatric risk associated with refractory moderate-to-severe acne, it does not rule out the possibility that individuals may experience an adverse psychiatric outcome while on isotretinoin, Dr. Barbieri said.
“While I think on a population level, we absolutely can feel reassured by these data, I do think there are individual patients who have idiosyncratic, unpredictable reactions to isotretinoin where they have mood changes, whether it be irritability, depression, or other mood changes,” he cautioned. “Given the association of acne itself with mental health comorbidities, it is important to screen for comorbidities such as depression in all patients with acne.”
The study was funded by the Wellcome Trust, which provided Dr. Fazel and the first author with financial support for the study. One author is an employee of TriNetX; the other authors had no relevant disclosures. Dr. Barbieri reported no financial disclosures. He is cochair of the AAD’s Acne Guidelines Workgroup and associate editor at JAMA Dermatology.
A version of this article first appeared on Medscape.com.
The use of , in a large retrospective cohort study published in the British Journal of Dermatology.
Although severe neuropsychiatric effects associated with isotretinoin therapy in patients with acne have been reported, “the evidence base ... is mixed and inconclusive,” and many studies are small, Seena Fazel, MBChB, MD, of the department of psychiatry, Oxford University, England, and co-authors write in the study.
The study results suggest that isotretinoin is conferring protection against adverse neuropsychiatric outcomes, particularly when compared with using oral antibiotics to treat acne, Dr. Fazel, professor of forensic psychiatry at Oxford University and the study’s senior author, said in an interview.
In the study, the investigators reviewed electronic health records (2013-2019) from a primarily United States–based dataset (TriNetX) of patients with acne aged 12-27 who had been followed for up to 1 year after their prescriptions had been dispensed.
There were four arms: those prescribed isotretinoin (30,866), oral antibiotics (44,748), topical anti-acne treatments (108,367), and those who had not been prescribed any acne treatment (78,666). The primary outcomes were diagnoses of a neuropsychiatric disorder (psychotic, mood, anxiety, personality, behavioral, and sleep disorders; and non-fatal self-harm) within one year of being prescribed treatment.
After using propensity score matching to adjust for confounders at baseline, the investigators determined that the odds ratio for any incident neuropsychiatric outcomes among patients with acne treated with isotretinoin was 0.80 (95% confidence interval, 0.74-0.87), compared with patients on oral antibiotics; 0.94 (95% CI, 0.87-1.02), compared with patients on topical anti-acne medications; and 1.06 (95% CI, 0.97-1.16), compared with those without a prescription for anti-acne medicines.
Side effects of isotretinoin – such as headache, dry mouth, and fatigue – were higher among those on isotretinoin than in the other three groups.
The authors concluded that isotretinoin was not independently linked to excess adverse neuropsychiatric outcomes at a population level. “We observed a consistent association between increasing acne severity as indicated by anti-acne treatment options and incidence of adverse neuropsychiatric outcomes, but the findings showed that isotretinoin exposure did not add to the risk of neuropsychiatric adverse outcomes over and above what was associated with oral antibiotics,” they write.
Isotretinoin treatment “appeared to mitigate the excess neuropsychiatric risk associated with recalcitrant moderate-to-severe acne,” they add.
The dermatology community has been interested in the impact isotretinoin has on mental health, and “I think clinically, they see that people get better on isotretinoin and their mental health improves,” Dr. Fazel told this news organization.
Asked to comment on the study results, John Barbieri, MD, MBA, director of the Advanced Acne Therapeutics Clinic, Brigham and Women’s Hospital, Boston, commended the investigators for the design of the trial.
“One of the strengths of this study is that they use a technique called propensity-score matching, where you try to make the groups of patients similar with respect to their other characteristics to minimize the risks of confounding and bias in the study, which I think is a real strength,” he told this news organization. “The other thing that they do, which I think is a strength, is to think about the impact of acne severity on these outcomes, because we know acne itself is associated with depression and risk for suicide and other neuropsychiatric outcomes.”
Including a cohort of patients who had acne and received oral antibiotics for comparison “is a nice way to address the potential for confounding by severity and confounding by indication,” Dr. Barbieri said. “Those who get antibiotics usually have more severe acne. They may not have it as severely as those who get isotretinoin, but it is a nice approach to account for background levels of depression and neuropsychiatric outcomes in patients with acne. I think that is a real strength of the study. This is one of the best studies to have looked at this question.”
However, although the study found that isotretinoin decreased the excess psychiatric risk associated with refractory moderate-to-severe acne, it does not rule out the possibility that individuals may experience an adverse psychiatric outcome while on isotretinoin, Dr. Barbieri said.
“While I think on a population level, we absolutely can feel reassured by these data, I do think there are individual patients who have idiosyncratic, unpredictable reactions to isotretinoin where they have mood changes, whether it be irritability, depression, or other mood changes,” he cautioned. “Given the association of acne itself with mental health comorbidities, it is important to screen for comorbidities such as depression in all patients with acne.”
The study was funded by the Wellcome Trust, which provided Dr. Fazel and the first author with financial support for the study. One author is an employee of TriNetX; the other authors had no relevant disclosures. Dr. Barbieri reported no financial disclosures. He is cochair of the AAD’s Acne Guidelines Workgroup and associate editor at JAMA Dermatology.
A version of this article first appeared on Medscape.com.
The use of , in a large retrospective cohort study published in the British Journal of Dermatology.
Although severe neuropsychiatric effects associated with isotretinoin therapy in patients with acne have been reported, “the evidence base ... is mixed and inconclusive,” and many studies are small, Seena Fazel, MBChB, MD, of the department of psychiatry, Oxford University, England, and co-authors write in the study.
The study results suggest that isotretinoin is conferring protection against adverse neuropsychiatric outcomes, particularly when compared with using oral antibiotics to treat acne, Dr. Fazel, professor of forensic psychiatry at Oxford University and the study’s senior author, said in an interview.
In the study, the investigators reviewed electronic health records (2013-2019) from a primarily United States–based dataset (TriNetX) of patients with acne aged 12-27 who had been followed for up to 1 year after their prescriptions had been dispensed.
There were four arms: those prescribed isotretinoin (30,866), oral antibiotics (44,748), topical anti-acne treatments (108,367), and those who had not been prescribed any acne treatment (78,666). The primary outcomes were diagnoses of a neuropsychiatric disorder (psychotic, mood, anxiety, personality, behavioral, and sleep disorders; and non-fatal self-harm) within one year of being prescribed treatment.
After using propensity score matching to adjust for confounders at baseline, the investigators determined that the odds ratio for any incident neuropsychiatric outcomes among patients with acne treated with isotretinoin was 0.80 (95% confidence interval, 0.74-0.87), compared with patients on oral antibiotics; 0.94 (95% CI, 0.87-1.02), compared with patients on topical anti-acne medications; and 1.06 (95% CI, 0.97-1.16), compared with those without a prescription for anti-acne medicines.
Side effects of isotretinoin – such as headache, dry mouth, and fatigue – were higher among those on isotretinoin than in the other three groups.
The authors concluded that isotretinoin was not independently linked to excess adverse neuropsychiatric outcomes at a population level. “We observed a consistent association between increasing acne severity as indicated by anti-acne treatment options and incidence of adverse neuropsychiatric outcomes, but the findings showed that isotretinoin exposure did not add to the risk of neuropsychiatric adverse outcomes over and above what was associated with oral antibiotics,” they write.
Isotretinoin treatment “appeared to mitigate the excess neuropsychiatric risk associated with recalcitrant moderate-to-severe acne,” they add.
The dermatology community has been interested in the impact isotretinoin has on mental health, and “I think clinically, they see that people get better on isotretinoin and their mental health improves,” Dr. Fazel told this news organization.
Asked to comment on the study results, John Barbieri, MD, MBA, director of the Advanced Acne Therapeutics Clinic, Brigham and Women’s Hospital, Boston, commended the investigators for the design of the trial.
“One of the strengths of this study is that they use a technique called propensity-score matching, where you try to make the groups of patients similar with respect to their other characteristics to minimize the risks of confounding and bias in the study, which I think is a real strength,” he told this news organization. “The other thing that they do, which I think is a strength, is to think about the impact of acne severity on these outcomes, because we know acne itself is associated with depression and risk for suicide and other neuropsychiatric outcomes.”
Including a cohort of patients who had acne and received oral antibiotics for comparison “is a nice way to address the potential for confounding by severity and confounding by indication,” Dr. Barbieri said. “Those who get antibiotics usually have more severe acne. They may not have it as severely as those who get isotretinoin, but it is a nice approach to account for background levels of depression and neuropsychiatric outcomes in patients with acne. I think that is a real strength of the study. This is one of the best studies to have looked at this question.”
However, although the study found that isotretinoin decreased the excess psychiatric risk associated with refractory moderate-to-severe acne, it does not rule out the possibility that individuals may experience an adverse psychiatric outcome while on isotretinoin, Dr. Barbieri said.
“While I think on a population level, we absolutely can feel reassured by these data, I do think there are individual patients who have idiosyncratic, unpredictable reactions to isotretinoin where they have mood changes, whether it be irritability, depression, or other mood changes,” he cautioned. “Given the association of acne itself with mental health comorbidities, it is important to screen for comorbidities such as depression in all patients with acne.”
The study was funded by the Wellcome Trust, which provided Dr. Fazel and the first author with financial support for the study. One author is an employee of TriNetX; the other authors had no relevant disclosures. Dr. Barbieri reported no financial disclosures. He is cochair of the AAD’s Acne Guidelines Workgroup and associate editor at JAMA Dermatology.
A version of this article first appeared on Medscape.com.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
FDA clears diagnostic test for early Alzheimer’s
The Lumipulse G β-Amyloid Ratio 1-42/1-40 (Fujirebio Diagnostics) test detects amyloid plaques associated with AD in adults age 55 or older who are under investigation for AD and other causes of cognitive decline.
“The availability of an in vitro diagnostic test that can potentially eliminate the need for time-consuming and expensive [positron emission tomography (PET)] scans is great news for individuals and families concerned with the possibility of an Alzheimer’s disease diagnosis,” Jeff Shuren, MD, JD, director of the FDA’s Center for Devices and Radiological Health, said in a statement.
“With the Lumipulse test, there is a new option that can typically be completed the same day and can give doctors the same information regarding brain amyloid status, without the radiation risk, to help determine if a patient’s cognitive impairment is due to Alzheimer’s disease,” he added.
In its statement, the FDA notes that there is an “unmet need for a reliable and safe test that can accurately identify patients with amyloid plaques consistent with Alzheimer’s disease.”
The agency goes on to state that this new test may eliminate the need to use PET brain scans, a “potentially costly and cumbersome option” to visualize amyloid plaques for the diagnosis of AD.
The Lumipulse test measures the ratio of β-amyloid 1-42 and β-amyloid 1-40 concentrations in human cerebral spinal fluid (CSF). A positive Lumipulse G β-amyloid Ratio (1-42/1-40) test result is consistent with the presence of amyloid plaques, similar to that revealed in a PET scan. A negative result is consistent with a negative amyloid PET scan result.
However, the FDA notes that the test is not a stand-alone assay and should be used in conjunction with other clinical evaluations and additional tests to determine treatment options.
The FDA reports that it evaluated the safety and efficacy of the test in a clinical study of 292 CSF samples from the Alzheimer’s Disease Neuroimaging Initiative sample bank.
The samples were tested by the Lumipulse G β-amyloid Ratio (1-42/1-40) and compared with amyloid PET scan results. In this clinical study, 97% of individuals with Lumipulse G β-amyloid Ratio (1-42/1-40) positive results had the presence of amyloid plaques by PET scan and 84% of individuals with negative results had a negative amyloid PET scan.
The risks associated with the Lumipulse G β-amyloid Ratio (1-42/1-40) test are mainly the possibility of false-positive and false-negative test results.
False-positive results, in conjunction with other clinical information, could lead to an inappropriate diagnosis of, and unnecessary treatment for AD.
False-negative test results could result in additional unnecessary diagnostic tests and potential delay in effective treatment for AD.
The FDA reviewed the device through the De Novo premarket review pathway, a regulatory pathway for low- to moderate-risk devices of a new type.
The agency says this action “creates a new regulatory classification, which means that subsequent devices of the same type with the same intended use may go through FDA’s 510(k) premarket process, whereby devices can obtain marketing authorization by demonstrating substantial equivalence to a predicate device.”
The Lumipulse G β-amyloid Ratio (1-42/1-40) was granted Breakthrough Device designation, a process designed to expedite the development and review of devices that may provide for more effective treatment or diagnosis of life-threatening or irreversibly debilitating diseases or conditions.
A version of this article first appeared on Medscape.com.
The Lumipulse G β-Amyloid Ratio 1-42/1-40 (Fujirebio Diagnostics) test detects amyloid plaques associated with AD in adults age 55 or older who are under investigation for AD and other causes of cognitive decline.
“The availability of an in vitro diagnostic test that can potentially eliminate the need for time-consuming and expensive [positron emission tomography (PET)] scans is great news for individuals and families concerned with the possibility of an Alzheimer’s disease diagnosis,” Jeff Shuren, MD, JD, director of the FDA’s Center for Devices and Radiological Health, said in a statement.
“With the Lumipulse test, there is a new option that can typically be completed the same day and can give doctors the same information regarding brain amyloid status, without the radiation risk, to help determine if a patient’s cognitive impairment is due to Alzheimer’s disease,” he added.
In its statement, the FDA notes that there is an “unmet need for a reliable and safe test that can accurately identify patients with amyloid plaques consistent with Alzheimer’s disease.”
The agency goes on to state that this new test may eliminate the need to use PET brain scans, a “potentially costly and cumbersome option” to visualize amyloid plaques for the diagnosis of AD.
The Lumipulse test measures the ratio of β-amyloid 1-42 and β-amyloid 1-40 concentrations in human cerebral spinal fluid (CSF). A positive Lumipulse G β-amyloid Ratio (1-42/1-40) test result is consistent with the presence of amyloid plaques, similar to that revealed in a PET scan. A negative result is consistent with a negative amyloid PET scan result.
However, the FDA notes that the test is not a stand-alone assay and should be used in conjunction with other clinical evaluations and additional tests to determine treatment options.
The FDA reports that it evaluated the safety and efficacy of the test in a clinical study of 292 CSF samples from the Alzheimer’s Disease Neuroimaging Initiative sample bank.
The samples were tested by the Lumipulse G β-amyloid Ratio (1-42/1-40) and compared with amyloid PET scan results. In this clinical study, 97% of individuals with Lumipulse G β-amyloid Ratio (1-42/1-40) positive results had the presence of amyloid plaques by PET scan and 84% of individuals with negative results had a negative amyloid PET scan.
The risks associated with the Lumipulse G β-amyloid Ratio (1-42/1-40) test are mainly the possibility of false-positive and false-negative test results.
False-positive results, in conjunction with other clinical information, could lead to an inappropriate diagnosis of, and unnecessary treatment for AD.
False-negative test results could result in additional unnecessary diagnostic tests and potential delay in effective treatment for AD.
The FDA reviewed the device through the De Novo premarket review pathway, a regulatory pathway for low- to moderate-risk devices of a new type.
The agency says this action “creates a new regulatory classification, which means that subsequent devices of the same type with the same intended use may go through FDA’s 510(k) premarket process, whereby devices can obtain marketing authorization by demonstrating substantial equivalence to a predicate device.”
The Lumipulse G β-amyloid Ratio (1-42/1-40) was granted Breakthrough Device designation, a process designed to expedite the development and review of devices that may provide for more effective treatment or diagnosis of life-threatening or irreversibly debilitating diseases or conditions.
A version of this article first appeared on Medscape.com.
The Lumipulse G β-Amyloid Ratio 1-42/1-40 (Fujirebio Diagnostics) test detects amyloid plaques associated with AD in adults age 55 or older who are under investigation for AD and other causes of cognitive decline.
“The availability of an in vitro diagnostic test that can potentially eliminate the need for time-consuming and expensive [positron emission tomography (PET)] scans is great news for individuals and families concerned with the possibility of an Alzheimer’s disease diagnosis,” Jeff Shuren, MD, JD, director of the FDA’s Center for Devices and Radiological Health, said in a statement.
“With the Lumipulse test, there is a new option that can typically be completed the same day and can give doctors the same information regarding brain amyloid status, without the radiation risk, to help determine if a patient’s cognitive impairment is due to Alzheimer’s disease,” he added.
In its statement, the FDA notes that there is an “unmet need for a reliable and safe test that can accurately identify patients with amyloid plaques consistent with Alzheimer’s disease.”
The agency goes on to state that this new test may eliminate the need to use PET brain scans, a “potentially costly and cumbersome option” to visualize amyloid plaques for the diagnosis of AD.
The Lumipulse test measures the ratio of β-amyloid 1-42 and β-amyloid 1-40 concentrations in human cerebral spinal fluid (CSF). A positive Lumipulse G β-amyloid Ratio (1-42/1-40) test result is consistent with the presence of amyloid plaques, similar to that revealed in a PET scan. A negative result is consistent with a negative amyloid PET scan result.
However, the FDA notes that the test is not a stand-alone assay and should be used in conjunction with other clinical evaluations and additional tests to determine treatment options.
The FDA reports that it evaluated the safety and efficacy of the test in a clinical study of 292 CSF samples from the Alzheimer’s Disease Neuroimaging Initiative sample bank.
The samples were tested by the Lumipulse G β-amyloid Ratio (1-42/1-40) and compared with amyloid PET scan results. In this clinical study, 97% of individuals with Lumipulse G β-amyloid Ratio (1-42/1-40) positive results had the presence of amyloid plaques by PET scan and 84% of individuals with negative results had a negative amyloid PET scan.
The risks associated with the Lumipulse G β-amyloid Ratio (1-42/1-40) test are mainly the possibility of false-positive and false-negative test results.
False-positive results, in conjunction with other clinical information, could lead to an inappropriate diagnosis of, and unnecessary treatment for AD.
False-negative test results could result in additional unnecessary diagnostic tests and potential delay in effective treatment for AD.
The FDA reviewed the device through the De Novo premarket review pathway, a regulatory pathway for low- to moderate-risk devices of a new type.
The agency says this action “creates a new regulatory classification, which means that subsequent devices of the same type with the same intended use may go through FDA’s 510(k) premarket process, whereby devices can obtain marketing authorization by demonstrating substantial equivalence to a predicate device.”
The Lumipulse G β-amyloid Ratio (1-42/1-40) was granted Breakthrough Device designation, a process designed to expedite the development and review of devices that may provide for more effective treatment or diagnosis of life-threatening or irreversibly debilitating diseases or conditions.
A version of this article first appeared on Medscape.com.
Mood instability in childhood as a precursor to bipolar disorder
Mood instability, or sudden, unpredictable, and frequent shifts in emotional states, characterizes many types of psychiatric disorder, including attention-deficit/hyperactivity disorder (ADHD), personality disorders, depression, and posttraumatic stress disorder. To say that individuals with bipolar disorder (BD) have mood instability sounds like a tautology. Nonetheless, mood instability has particular relevance to BD: Many patients have irregular or labile moods even when they are between major episodes of mania and depression.1
Children of parents with BD who have high levels of mood instability are at particularly high risk for developing BD (types I or II) in late adolescence or early adulthood.2 The following case provides an illustration:
Patrick, age 14, entered treatment with diagnoses of ADHD and other specified bipolar disorder. His mother felt that his behavior resembled that of his father, who had been treated for manic episodes. During the COVID-19 pandemic, Patrick had become increasingly difficult at home, with significant oppositionality, impulsive behavior, and difficulty following through on school assignments or household tasks. His mother’s most significant complaints concerned Patrick’s sudden outbursts of anger and abrupt verbal abuse when she asked him to stop playing video games. When interrupted, he cursed loudly and sometimes turned violent; he had broken a window and a door at home and had on one occasion physically attacked his younger brother. Patrick agreed that he became angry at times, but felt that others provoked him. When queried about depression, he described anxiety and worry. He was unable to describe a particular trigger for his anxiety except for being interrupted in online games with his friends, which made him “feel like a total loser.”
His mother reported that Patrick had multiple 1- to 2-day intervals in which he became “really silly, laughing at nothing,” talking rapidly, jumping from one topic to another, and becoming annoyed when others didn’t share his enthusiasm. In these activated intervals, he slept little and seemed to be full of energy; his mother would hear him talking loudly into his phone throughout the night. During one such interval he had become verbally aggressive with a peer, which had ruined their friendship. Both Patrick and his mother reported that they had been fighting constantly and, in her words, “our house has become a war zone.”
In our recent article in the Journal of the American Academy of Child and Adolescent Psychiatry,3 my coauthors and I examined the association between parents’ ratings of mood instability and clinicians’ longitudinal ratings of symptoms and functioning among youth (ages 9-17 years) who were at high risk for BD. The participants met DSM-5 diagnostic criteria for major depressive disorder or other specified BD, defined as recurrent and brief periods of elevation and activation that did not meet syndromal mania or hypomania criteria. All participants had at least one first- or second-degree family member with a history of BD I or II. Following a period of evaluation, participants were randomly assigned to one of two 4-month psychological therapies: Family-focused therapy (12 sessions of psychoeducation, communication training, and problem-solving skills training) or enhanced usual care (6 sessions of family and individual psychoeducation and support). They also received pharmacological management from study-affiliated psychiatrists when warranted.
We measured mood instability at intake and every 4-6 months over an average of 2 years (range 0-255 weeks). We used a brief parent questionnaire – the Children’s Affective Lability Scale4 – which enables measurement of lability on the dimensions of elevation or activation (e.g., bursts of silliness or hilarity, excessive familiarity with others), irritability (e.g., temper outbursts), or anxious-depression (e.g., sudden bouts of crying).
Over the 1- to 4-year period of follow-up, mood instability was associated with poor prognosis indicators in high-risk youth: Being younger, having younger ages at first symptom onset, being diagnosed with other specified BD (vs. major depression), and having more complex patterns of comorbid disorders. Mood instability tracked closely with levels of mania, depression, and global functioning over the follow-up. There was a temporal pathway between a diagnosis of other specified bipolar disorder at intake and higher levels of mood instability at follow-up, which in turn predicted higher levels of parent/child conflict. High levels of mood lability may lead to isolation from peers and tension within family relationships, which may fuel further children’s expressions of frustration, rage, depression, or impulsive behavior.
Youth with higher levels of mood instability required more complex medication regimens over 1 year than did those with lower instability. There was an overall reduction in mood instability as children aged (or spent more time in treatment). Over the 1- to 4-year follow-up, family-focused therapy was associated with longer intervals prior to new mood episodes than was enhanced usual care, but reductions in mood instability were independent of the type of psychosocial treatment assigned to children.
The participants in this study could not be followed long enough to determine whether levels of mood instability were associated with the later development of syndromal BD. Other studies, however, have documented this relationship. Large-scale longitudinal studies of high-risk children find that measures of mood lability – along with early onset manic symptoms, depression, anxiety, and a family history of mania or hypomania – can be combined to calculate the risk that any individual child will develop BD I or II over the next 5-8 years.2,5
Clinicians should include measurement of the severity and psychosocial determinants of persistent mood shifts in youth under their care, particularly those with a family history of BD. Mood instability is associated with more severe symptom trajectories, more social isolation, and greater distress and conflict within the family. It may require a greater intensity of both pharmacological and psychosocial treatments to treat existing symptoms and functional impairments, and to prevent further mood deterioration.
Dr. Miklowitz is Distinguished Professor of Psychiatry and Biobehavioral Sciences, University of California, Los Angeles, Semel Institute for Neuroscience and Human Behavior. He is the author of “The Bipolar Disorder Survival Guide, 3rd Ed.” (New York: Guilford Press, 2019) and “Bipolar Disorder: A Family-Focused Treatment Approach, 2nd Ed” (New York: Guilford Press, 2010). He has no conflicts of interest to disclose. Contact Dr. Miklowitz at [email protected].
References
1. Bonsall MB, et al. Nonlinear time-series approaches in characterizing mood stability and mood instability in bipolar disorder. Proc Biol Sci. Mar 7 2012;279(1730):916-24. doi: 10.1098/rspb.2011.1246.
2. Hafeman DM, et al. Toward the definition of a bipolar prodrome: Dimensional predictors of bipolar spectrum disorders in at-risk youths. Am J Psychiatry. 2016;173(7):695-704. doi: 10.1176/appi.ajp.2015.15040414.
3. Miklowitz DJ, et al. Mood instability in youth at high risk for bipolar disorder. J Am Acad Child Adol Psychiatry. 2022 Mar 17;S0890-8567(22)00118-6. doi: 10.1016/j.jaac.2022.03.009.
4. Gerson AC, et al. The Children’s Affective Lability Scale: a psychometric evaluation of reliability. Psychiatry Res. Dec 20 1996;65(3):189-98. doi: 10.1016/s0165-1781(96)02851-x.
5. Birmaher B, et al. A risk calculator to predict the individual risk of conversion from subthreshold bipolar symptoms to bipolar disorder I or II in youth. J Am Acad Child Adol Psychiatry. 2018;57(10):755-63. doi: 10.1016/j.jaac.2018.05.023.
Mood instability, or sudden, unpredictable, and frequent shifts in emotional states, characterizes many types of psychiatric disorder, including attention-deficit/hyperactivity disorder (ADHD), personality disorders, depression, and posttraumatic stress disorder. To say that individuals with bipolar disorder (BD) have mood instability sounds like a tautology. Nonetheless, mood instability has particular relevance to BD: Many patients have irregular or labile moods even when they are between major episodes of mania and depression.1
Children of parents with BD who have high levels of mood instability are at particularly high risk for developing BD (types I or II) in late adolescence or early adulthood.2 The following case provides an illustration:
Patrick, age 14, entered treatment with diagnoses of ADHD and other specified bipolar disorder. His mother felt that his behavior resembled that of his father, who had been treated for manic episodes. During the COVID-19 pandemic, Patrick had become increasingly difficult at home, with significant oppositionality, impulsive behavior, and difficulty following through on school assignments or household tasks. His mother’s most significant complaints concerned Patrick’s sudden outbursts of anger and abrupt verbal abuse when she asked him to stop playing video games. When interrupted, he cursed loudly and sometimes turned violent; he had broken a window and a door at home and had on one occasion physically attacked his younger brother. Patrick agreed that he became angry at times, but felt that others provoked him. When queried about depression, he described anxiety and worry. He was unable to describe a particular trigger for his anxiety except for being interrupted in online games with his friends, which made him “feel like a total loser.”
His mother reported that Patrick had multiple 1- to 2-day intervals in which he became “really silly, laughing at nothing,” talking rapidly, jumping from one topic to another, and becoming annoyed when others didn’t share his enthusiasm. In these activated intervals, he slept little and seemed to be full of energy; his mother would hear him talking loudly into his phone throughout the night. During one such interval he had become verbally aggressive with a peer, which had ruined their friendship. Both Patrick and his mother reported that they had been fighting constantly and, in her words, “our house has become a war zone.”
In our recent article in the Journal of the American Academy of Child and Adolescent Psychiatry,3 my coauthors and I examined the association between parents’ ratings of mood instability and clinicians’ longitudinal ratings of symptoms and functioning among youth (ages 9-17 years) who were at high risk for BD. The participants met DSM-5 diagnostic criteria for major depressive disorder or other specified BD, defined as recurrent and brief periods of elevation and activation that did not meet syndromal mania or hypomania criteria. All participants had at least one first- or second-degree family member with a history of BD I or II. Following a period of evaluation, participants were randomly assigned to one of two 4-month psychological therapies: Family-focused therapy (12 sessions of psychoeducation, communication training, and problem-solving skills training) or enhanced usual care (6 sessions of family and individual psychoeducation and support). They also received pharmacological management from study-affiliated psychiatrists when warranted.
We measured mood instability at intake and every 4-6 months over an average of 2 years (range 0-255 weeks). We used a brief parent questionnaire – the Children’s Affective Lability Scale4 – which enables measurement of lability on the dimensions of elevation or activation (e.g., bursts of silliness or hilarity, excessive familiarity with others), irritability (e.g., temper outbursts), or anxious-depression (e.g., sudden bouts of crying).
Over the 1- to 4-year period of follow-up, mood instability was associated with poor prognosis indicators in high-risk youth: Being younger, having younger ages at first symptom onset, being diagnosed with other specified BD (vs. major depression), and having more complex patterns of comorbid disorders. Mood instability tracked closely with levels of mania, depression, and global functioning over the follow-up. There was a temporal pathway between a diagnosis of other specified bipolar disorder at intake and higher levels of mood instability at follow-up, which in turn predicted higher levels of parent/child conflict. High levels of mood lability may lead to isolation from peers and tension within family relationships, which may fuel further children’s expressions of frustration, rage, depression, or impulsive behavior.
Youth with higher levels of mood instability required more complex medication regimens over 1 year than did those with lower instability. There was an overall reduction in mood instability as children aged (or spent more time in treatment). Over the 1- to 4-year follow-up, family-focused therapy was associated with longer intervals prior to new mood episodes than was enhanced usual care, but reductions in mood instability were independent of the type of psychosocial treatment assigned to children.
The participants in this study could not be followed long enough to determine whether levels of mood instability were associated with the later development of syndromal BD. Other studies, however, have documented this relationship. Large-scale longitudinal studies of high-risk children find that measures of mood lability – along with early onset manic symptoms, depression, anxiety, and a family history of mania or hypomania – can be combined to calculate the risk that any individual child will develop BD I or II over the next 5-8 years.2,5
Clinicians should include measurement of the severity and psychosocial determinants of persistent mood shifts in youth under their care, particularly those with a family history of BD. Mood instability is associated with more severe symptom trajectories, more social isolation, and greater distress and conflict within the family. It may require a greater intensity of both pharmacological and psychosocial treatments to treat existing symptoms and functional impairments, and to prevent further mood deterioration.
Dr. Miklowitz is Distinguished Professor of Psychiatry and Biobehavioral Sciences, University of California, Los Angeles, Semel Institute for Neuroscience and Human Behavior. He is the author of “The Bipolar Disorder Survival Guide, 3rd Ed.” (New York: Guilford Press, 2019) and “Bipolar Disorder: A Family-Focused Treatment Approach, 2nd Ed” (New York: Guilford Press, 2010). He has no conflicts of interest to disclose. Contact Dr. Miklowitz at [email protected].
References
1. Bonsall MB, et al. Nonlinear time-series approaches in characterizing mood stability and mood instability in bipolar disorder. Proc Biol Sci. Mar 7 2012;279(1730):916-24. doi: 10.1098/rspb.2011.1246.
2. Hafeman DM, et al. Toward the definition of a bipolar prodrome: Dimensional predictors of bipolar spectrum disorders in at-risk youths. Am J Psychiatry. 2016;173(7):695-704. doi: 10.1176/appi.ajp.2015.15040414.
3. Miklowitz DJ, et al. Mood instability in youth at high risk for bipolar disorder. J Am Acad Child Adol Psychiatry. 2022 Mar 17;S0890-8567(22)00118-6. doi: 10.1016/j.jaac.2022.03.009.
4. Gerson AC, et al. The Children’s Affective Lability Scale: a psychometric evaluation of reliability. Psychiatry Res. Dec 20 1996;65(3):189-98. doi: 10.1016/s0165-1781(96)02851-x.
5. Birmaher B, et al. A risk calculator to predict the individual risk of conversion from subthreshold bipolar symptoms to bipolar disorder I or II in youth. J Am Acad Child Adol Psychiatry. 2018;57(10):755-63. doi: 10.1016/j.jaac.2018.05.023.
Mood instability, or sudden, unpredictable, and frequent shifts in emotional states, characterizes many types of psychiatric disorder, including attention-deficit/hyperactivity disorder (ADHD), personality disorders, depression, and posttraumatic stress disorder. To say that individuals with bipolar disorder (BD) have mood instability sounds like a tautology. Nonetheless, mood instability has particular relevance to BD: Many patients have irregular or labile moods even when they are between major episodes of mania and depression.1
Children of parents with BD who have high levels of mood instability are at particularly high risk for developing BD (types I or II) in late adolescence or early adulthood.2 The following case provides an illustration:
Patrick, age 14, entered treatment with diagnoses of ADHD and other specified bipolar disorder. His mother felt that his behavior resembled that of his father, who had been treated for manic episodes. During the COVID-19 pandemic, Patrick had become increasingly difficult at home, with significant oppositionality, impulsive behavior, and difficulty following through on school assignments or household tasks. His mother’s most significant complaints concerned Patrick’s sudden outbursts of anger and abrupt verbal abuse when she asked him to stop playing video games. When interrupted, he cursed loudly and sometimes turned violent; he had broken a window and a door at home and had on one occasion physically attacked his younger brother. Patrick agreed that he became angry at times, but felt that others provoked him. When queried about depression, he described anxiety and worry. He was unable to describe a particular trigger for his anxiety except for being interrupted in online games with his friends, which made him “feel like a total loser.”
His mother reported that Patrick had multiple 1- to 2-day intervals in which he became “really silly, laughing at nothing,” talking rapidly, jumping from one topic to another, and becoming annoyed when others didn’t share his enthusiasm. In these activated intervals, he slept little and seemed to be full of energy; his mother would hear him talking loudly into his phone throughout the night. During one such interval he had become verbally aggressive with a peer, which had ruined their friendship. Both Patrick and his mother reported that they had been fighting constantly and, in her words, “our house has become a war zone.”
In our recent article in the Journal of the American Academy of Child and Adolescent Psychiatry,3 my coauthors and I examined the association between parents’ ratings of mood instability and clinicians’ longitudinal ratings of symptoms and functioning among youth (ages 9-17 years) who were at high risk for BD. The participants met DSM-5 diagnostic criteria for major depressive disorder or other specified BD, defined as recurrent and brief periods of elevation and activation that did not meet syndromal mania or hypomania criteria. All participants had at least one first- or second-degree family member with a history of BD I or II. Following a period of evaluation, participants were randomly assigned to one of two 4-month psychological therapies: Family-focused therapy (12 sessions of psychoeducation, communication training, and problem-solving skills training) or enhanced usual care (6 sessions of family and individual psychoeducation and support). They also received pharmacological management from study-affiliated psychiatrists when warranted.
We measured mood instability at intake and every 4-6 months over an average of 2 years (range 0-255 weeks). We used a brief parent questionnaire – the Children’s Affective Lability Scale4 – which enables measurement of lability on the dimensions of elevation or activation (e.g., bursts of silliness or hilarity, excessive familiarity with others), irritability (e.g., temper outbursts), or anxious-depression (e.g., sudden bouts of crying).
Over the 1- to 4-year period of follow-up, mood instability was associated with poor prognosis indicators in high-risk youth: Being younger, having younger ages at first symptom onset, being diagnosed with other specified BD (vs. major depression), and having more complex patterns of comorbid disorders. Mood instability tracked closely with levels of mania, depression, and global functioning over the follow-up. There was a temporal pathway between a diagnosis of other specified bipolar disorder at intake and higher levels of mood instability at follow-up, which in turn predicted higher levels of parent/child conflict. High levels of mood lability may lead to isolation from peers and tension within family relationships, which may fuel further children’s expressions of frustration, rage, depression, or impulsive behavior.
Youth with higher levels of mood instability required more complex medication regimens over 1 year than did those with lower instability. There was an overall reduction in mood instability as children aged (or spent more time in treatment). Over the 1- to 4-year follow-up, family-focused therapy was associated with longer intervals prior to new mood episodes than was enhanced usual care, but reductions in mood instability were independent of the type of psychosocial treatment assigned to children.
The participants in this study could not be followed long enough to determine whether levels of mood instability were associated with the later development of syndromal BD. Other studies, however, have documented this relationship. Large-scale longitudinal studies of high-risk children find that measures of mood lability – along with early onset manic symptoms, depression, anxiety, and a family history of mania or hypomania – can be combined to calculate the risk that any individual child will develop BD I or II over the next 5-8 years.2,5
Clinicians should include measurement of the severity and psychosocial determinants of persistent mood shifts in youth under their care, particularly those with a family history of BD. Mood instability is associated with more severe symptom trajectories, more social isolation, and greater distress and conflict within the family. It may require a greater intensity of both pharmacological and psychosocial treatments to treat existing symptoms and functional impairments, and to prevent further mood deterioration.
Dr. Miklowitz is Distinguished Professor of Psychiatry and Biobehavioral Sciences, University of California, Los Angeles, Semel Institute for Neuroscience and Human Behavior. He is the author of “The Bipolar Disorder Survival Guide, 3rd Ed.” (New York: Guilford Press, 2019) and “Bipolar Disorder: A Family-Focused Treatment Approach, 2nd Ed” (New York: Guilford Press, 2010). He has no conflicts of interest to disclose. Contact Dr. Miklowitz at [email protected].
References
1. Bonsall MB, et al. Nonlinear time-series approaches in characterizing mood stability and mood instability in bipolar disorder. Proc Biol Sci. Mar 7 2012;279(1730):916-24. doi: 10.1098/rspb.2011.1246.
2. Hafeman DM, et al. Toward the definition of a bipolar prodrome: Dimensional predictors of bipolar spectrum disorders in at-risk youths. Am J Psychiatry. 2016;173(7):695-704. doi: 10.1176/appi.ajp.2015.15040414.
3. Miklowitz DJ, et al. Mood instability in youth at high risk for bipolar disorder. J Am Acad Child Adol Psychiatry. 2022 Mar 17;S0890-8567(22)00118-6. doi: 10.1016/j.jaac.2022.03.009.
4. Gerson AC, et al. The Children’s Affective Lability Scale: a psychometric evaluation of reliability. Psychiatry Res. Dec 20 1996;65(3):189-98. doi: 10.1016/s0165-1781(96)02851-x.
5. Birmaher B, et al. A risk calculator to predict the individual risk of conversion from subthreshold bipolar symptoms to bipolar disorder I or II in youth. J Am Acad Child Adol Psychiatry. 2018;57(10):755-63. doi: 10.1016/j.jaac.2018.05.023.
Fecal transfer could be the transplant of youth
Fecal matter may be in the fountain of youth
Yes, you read that headline correctly. New research by scientists at Quadram Institute and the University of East Anglia, both in Norwich, England, supports the claim that transferring fecal microbes might actually have some positive effects on reversing the aging process in the eyes, brain, and gut.
How do they know? Mice, of course. In the study, scientists took the gut microbes from older mice and transferred them into the younger mince. The young mice displayed inflamed signs of aging in their guts, brains, and eyes, which, we all know, decline in function as we age. What happens is a chronic inflammation of cells as we get older that can be found in the brain or gut that leads to a degenerative state over time.
When the older mice received the gut microbes from younger mice, the investigators saw the reverse: Gut, brain, and eye functionality improved. In a way, minimizing the inflammation.
There’s tons of research out there that suggests gut health is the key to a healthy life, but this study points directly to an improvement in brain and vision functionality as a result of the transfer.
Now, we’re not insinuating you get a poo transfer as you reach old age. And the shift to human studies on microbiota replacement therapy is still in the works. But this definitely is a topic to watch and could be a game changer in the age-old quest to bottle youth or at least improve quality of life as we age.
For now, the scientists did find some connections between the beneficial bacteria in the transplants and the human diet that could have similar effects, like changes in the metabolism of certain fats and vitamin that could have effects on the inflammatory cells in the eye and brain.
The more you know!
It’s not lying, it’s preemptive truth
Lying is bad. Bold statement, we know, but a true one. After all, God spent an entire commandment telling people not to do the whole bearing false witness thing, and God is generally known for not joking around. He’s a pretty serious dude.
In case you’ve been wandering around the desert for a while and haven’t had wifi, we have a bit of a misinformation problem these days. People lie all the time about a lot of things, and a lot of people believe the lies. According to new research, however, there are also a lot of people who recognize the lies but accept them anyway because they believe that the lies will become true in the future.
Imagine the following scenario: A friend gets a job he’s not qualified for because he listed a skill he doesn’t have. That’s bad, right? And the people the researchers interviewed agreed, at least initially. But when informed that our friend is planning on obtaining the skill in summer classes in the near future, the study participants became far more willing to excuse the initial lie.
A friend jumping the gun on training he doesn’t have yet is fairly innocuous as far as lying goes, but as the researchers found, this willingness to forgive lies because they could become true extends far further. For example, millions of people do not vote illegally in U.S. elections, nor do White people get approved for mortgages at rates 300% higher than minorities, but when asked to imagine scenarios in which those statements could be true, study participants were less likely to condemn the lie and prevent it from spreading further, especially if their political viewpoints aligned with the respective falsehood.
It seems, then, that while we may aspire to not tell lies, we take after another guy with magic powers who spent too much time in the desert: “What I told you was true, from a certain point of view.”
It tastes like feng shui, but it’s not
You know about biomes. You’ve read about various microbiomes. Allow us to introduce you to the envirome,
The envirome “includes all the natural and man-made elements of our environment throughout the lifespan, notably the built environment,” said Robert Schneider, dean of the College of Integrative Medicine at Maharishi International University. Located in – you guessed it – Fairfield, Iowa, and home of the Fighting Transcendentalists. MAHARISHI RULES!
[Editor’s note: You made that up, right? Well, it really is in Iowa, but they don’t seem to have an athletic program.]
In an effort to maximize the envirome’s potential to improve quality of life, Dr. Schneider and his associates systematically integrated the principles of Maharishi Vastu architecture (MVA) into a comprehensive building system. MVA is “a holistic wellness architectural system that aligns buildings with nature’s intelligence, creating balanced, orderly, and integrated living environments with the goal of improving occupants’ lives,” the university explained in a written statement.
Since “modern medicine now recognizes the powerful effects of the ‘envirome’ on health,” Dr. Schneider said in that statement, the researchers reviewed 40 years’ worth of published studies on MVA’s benefits – an analysis that appears in Global Advances in Health and Medicine.
As far as our homes are concerned, here are some of the things MVA says we should be doing:
- The headboard of a bed should be oriented to the east or south when you sleep. This will improve mental health.
- While sitting at a desk or work area, a person should face east or north to improve brain coherence.
- The main entrance of a house should face east because morning light is superior to afternoon light.
And you were worried about feng shui. Well, forget feng shui. Feng shui is for amateurs. MVA is the way to go. MVA is the GOAT. MAHARISHI RULES!
Fecal matter may be in the fountain of youth
Yes, you read that headline correctly. New research by scientists at Quadram Institute and the University of East Anglia, both in Norwich, England, supports the claim that transferring fecal microbes might actually have some positive effects on reversing the aging process in the eyes, brain, and gut.
How do they know? Mice, of course. In the study, scientists took the gut microbes from older mice and transferred them into the younger mince. The young mice displayed inflamed signs of aging in their guts, brains, and eyes, which, we all know, decline in function as we age. What happens is a chronic inflammation of cells as we get older that can be found in the brain or gut that leads to a degenerative state over time.
When the older mice received the gut microbes from younger mice, the investigators saw the reverse: Gut, brain, and eye functionality improved. In a way, minimizing the inflammation.
There’s tons of research out there that suggests gut health is the key to a healthy life, but this study points directly to an improvement in brain and vision functionality as a result of the transfer.
Now, we’re not insinuating you get a poo transfer as you reach old age. And the shift to human studies on microbiota replacement therapy is still in the works. But this definitely is a topic to watch and could be a game changer in the age-old quest to bottle youth or at least improve quality of life as we age.
For now, the scientists did find some connections between the beneficial bacteria in the transplants and the human diet that could have similar effects, like changes in the metabolism of certain fats and vitamin that could have effects on the inflammatory cells in the eye and brain.
The more you know!
It’s not lying, it’s preemptive truth
Lying is bad. Bold statement, we know, but a true one. After all, God spent an entire commandment telling people not to do the whole bearing false witness thing, and God is generally known for not joking around. He’s a pretty serious dude.
In case you’ve been wandering around the desert for a while and haven’t had wifi, we have a bit of a misinformation problem these days. People lie all the time about a lot of things, and a lot of people believe the lies. According to new research, however, there are also a lot of people who recognize the lies but accept them anyway because they believe that the lies will become true in the future.
Imagine the following scenario: A friend gets a job he’s not qualified for because he listed a skill he doesn’t have. That’s bad, right? And the people the researchers interviewed agreed, at least initially. But when informed that our friend is planning on obtaining the skill in summer classes in the near future, the study participants became far more willing to excuse the initial lie.
A friend jumping the gun on training he doesn’t have yet is fairly innocuous as far as lying goes, but as the researchers found, this willingness to forgive lies because they could become true extends far further. For example, millions of people do not vote illegally in U.S. elections, nor do White people get approved for mortgages at rates 300% higher than minorities, but when asked to imagine scenarios in which those statements could be true, study participants were less likely to condemn the lie and prevent it from spreading further, especially if their political viewpoints aligned with the respective falsehood.
It seems, then, that while we may aspire to not tell lies, we take after another guy with magic powers who spent too much time in the desert: “What I told you was true, from a certain point of view.”
It tastes like feng shui, but it’s not
You know about biomes. You’ve read about various microbiomes. Allow us to introduce you to the envirome,
The envirome “includes all the natural and man-made elements of our environment throughout the lifespan, notably the built environment,” said Robert Schneider, dean of the College of Integrative Medicine at Maharishi International University. Located in – you guessed it – Fairfield, Iowa, and home of the Fighting Transcendentalists. MAHARISHI RULES!
[Editor’s note: You made that up, right? Well, it really is in Iowa, but they don’t seem to have an athletic program.]
In an effort to maximize the envirome’s potential to improve quality of life, Dr. Schneider and his associates systematically integrated the principles of Maharishi Vastu architecture (MVA) into a comprehensive building system. MVA is “a holistic wellness architectural system that aligns buildings with nature’s intelligence, creating balanced, orderly, and integrated living environments with the goal of improving occupants’ lives,” the university explained in a written statement.
Since “modern medicine now recognizes the powerful effects of the ‘envirome’ on health,” Dr. Schneider said in that statement, the researchers reviewed 40 years’ worth of published studies on MVA’s benefits – an analysis that appears in Global Advances in Health and Medicine.
As far as our homes are concerned, here are some of the things MVA says we should be doing:
- The headboard of a bed should be oriented to the east or south when you sleep. This will improve mental health.
- While sitting at a desk or work area, a person should face east or north to improve brain coherence.
- The main entrance of a house should face east because morning light is superior to afternoon light.
And you were worried about feng shui. Well, forget feng shui. Feng shui is for amateurs. MVA is the way to go. MVA is the GOAT. MAHARISHI RULES!
Fecal matter may be in the fountain of youth
Yes, you read that headline correctly. New research by scientists at Quadram Institute and the University of East Anglia, both in Norwich, England, supports the claim that transferring fecal microbes might actually have some positive effects on reversing the aging process in the eyes, brain, and gut.
How do they know? Mice, of course. In the study, scientists took the gut microbes from older mice and transferred them into the younger mince. The young mice displayed inflamed signs of aging in their guts, brains, and eyes, which, we all know, decline in function as we age. What happens is a chronic inflammation of cells as we get older that can be found in the brain or gut that leads to a degenerative state over time.
When the older mice received the gut microbes from younger mice, the investigators saw the reverse: Gut, brain, and eye functionality improved. In a way, minimizing the inflammation.
There’s tons of research out there that suggests gut health is the key to a healthy life, but this study points directly to an improvement in brain and vision functionality as a result of the transfer.
Now, we’re not insinuating you get a poo transfer as you reach old age. And the shift to human studies on microbiota replacement therapy is still in the works. But this definitely is a topic to watch and could be a game changer in the age-old quest to bottle youth or at least improve quality of life as we age.
For now, the scientists did find some connections between the beneficial bacteria in the transplants and the human diet that could have similar effects, like changes in the metabolism of certain fats and vitamin that could have effects on the inflammatory cells in the eye and brain.
The more you know!
It’s not lying, it’s preemptive truth
Lying is bad. Bold statement, we know, but a true one. After all, God spent an entire commandment telling people not to do the whole bearing false witness thing, and God is generally known for not joking around. He’s a pretty serious dude.
In case you’ve been wandering around the desert for a while and haven’t had wifi, we have a bit of a misinformation problem these days. People lie all the time about a lot of things, and a lot of people believe the lies. According to new research, however, there are also a lot of people who recognize the lies but accept them anyway because they believe that the lies will become true in the future.
Imagine the following scenario: A friend gets a job he’s not qualified for because he listed a skill he doesn’t have. That’s bad, right? And the people the researchers interviewed agreed, at least initially. But when informed that our friend is planning on obtaining the skill in summer classes in the near future, the study participants became far more willing to excuse the initial lie.
A friend jumping the gun on training he doesn’t have yet is fairly innocuous as far as lying goes, but as the researchers found, this willingness to forgive lies because they could become true extends far further. For example, millions of people do not vote illegally in U.S. elections, nor do White people get approved for mortgages at rates 300% higher than minorities, but when asked to imagine scenarios in which those statements could be true, study participants were less likely to condemn the lie and prevent it from spreading further, especially if their political viewpoints aligned with the respective falsehood.
It seems, then, that while we may aspire to not tell lies, we take after another guy with magic powers who spent too much time in the desert: “What I told you was true, from a certain point of view.”
It tastes like feng shui, but it’s not
You know about biomes. You’ve read about various microbiomes. Allow us to introduce you to the envirome,
The envirome “includes all the natural and man-made elements of our environment throughout the lifespan, notably the built environment,” said Robert Schneider, dean of the College of Integrative Medicine at Maharishi International University. Located in – you guessed it – Fairfield, Iowa, and home of the Fighting Transcendentalists. MAHARISHI RULES!
[Editor’s note: You made that up, right? Well, it really is in Iowa, but they don’t seem to have an athletic program.]
In an effort to maximize the envirome’s potential to improve quality of life, Dr. Schneider and his associates systematically integrated the principles of Maharishi Vastu architecture (MVA) into a comprehensive building system. MVA is “a holistic wellness architectural system that aligns buildings with nature’s intelligence, creating balanced, orderly, and integrated living environments with the goal of improving occupants’ lives,” the university explained in a written statement.
Since “modern medicine now recognizes the powerful effects of the ‘envirome’ on health,” Dr. Schneider said in that statement, the researchers reviewed 40 years’ worth of published studies on MVA’s benefits – an analysis that appears in Global Advances in Health and Medicine.
As far as our homes are concerned, here are some of the things MVA says we should be doing:
- The headboard of a bed should be oriented to the east or south when you sleep. This will improve mental health.
- While sitting at a desk or work area, a person should face east or north to improve brain coherence.
- The main entrance of a house should face east because morning light is superior to afternoon light.
And you were worried about feng shui. Well, forget feng shui. Feng shui is for amateurs. MVA is the way to go. MVA is the GOAT. MAHARISHI RULES!
Depression biomarkers: Which ones matter most?
Multiple biomarkers of depression involved in several brain circuits are altered in patients with unipolar depression.
because they suggest neuroimmunological alterations, disturbances in the blood-brain-barrier, hyperactivity in the hypothalamic-pituitary-adrenal (HPA) axis, and impaired neuroplasticity as factors in depression pathophysiology.
However, said study investigator Michael E. Benros, MD, PhD, professor and head of research at Mental Health Centre Copenhagen and University of Copenhagen, this is on a group level. “So in order to be relevant in a clinical context, the results need to be validated by further high-quality studies identifying subgroups with different biological underpinnings,” he told this news organization.
Identification of potential subgroups of depression with different biomarkers might help explain the diverse symptomatology and variability in treatment response observed in patients with depression, he noted.
The study was published online in JAMA Psychiatry.
Multiple pathways to depression
The systematic review and meta-analysis included 97 studies investigating 165 CSF biomarkers.
Of the 42 biomarkers investigated in at least two studies, patients with unipolar depression had higher CSF levels of interleukin 6, a marker of chronic inflammation; total protein, which signals blood-brain barrier dysfunction and increased permeability; and cortisol, which is linked to psychological stress, compared with healthy controls.
Depression was also associated with:
- Lower CSF levels of homovanillic acid, the major terminal metabolite of dopamine.
- Gamma-aminobutyric acid (GABA), the major inhibitory neurotransmitter in the CNS thought to play a vital role in the control of stress and depression.
- Somatostatin, a neuropeptide often coexpressed with GABA.
- Brain-derived neurotrophic factor (BDNF), a protein involved in neurogenesis, synaptic plasticity, and neurotransmission.
- Amyloid-β 40, implicated in Alzheimer’s disease.
- Transthyretin, involved in transport of thyroxine across the blood-brain barrier.
Collectively, the findings point toward a “dysregulated dopaminergic system, a compromised inhibitory system, HPA axis hyperactivity, increased neuroinflammation and blood-brain barrier permeability, and impaired neuroplasticity as important factors in depression pathophysiology,” the investigators wrote.
“It is notable that we did not find significant difference in the metabolite levels of serotonin and noradrenalin, which are the most targeted neurotransmitters in modern antidepressant treatment,” said Dr. Benros.
However, this could be explained by substantial heterogeneity between studies and the fact that quantification of total CSF biomarker concentrations does not reflect local alteration within the brain, he explained.
Many of the studies had small cohorts and most quantified only a few biomarkers, making it hard to examine potential interactions between biomarkers or identify specific phenotypes of depression.
“Novel high-quality studies including larger cohorts with an integrative approach and extensive numbers of biomarkers are needed to validate these potential biomarkers of depression and set the stage for the development of more effective and precise treatments,” the researchers noted.
Which ones hold water?
Reached for comment, Dean MacKinnon, MD, associate professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore, noted that this analysis “extracts the vast amount of knowledge” gained from different studies on biomarkers in the CSF for depression.
“They were able to identify 97 papers that have enough information in them that they could sort of lump them together and see which ones still hold water. It’s always useful to be able to look at patterns in the research and see if you can find some consistent trends,” he told this news organization.
Dr. MacKinnon, who was not part of the research team, also noted that “nonreplicability” is a problem in psychiatry and psychology research, “so being able to show that at least some studies were sufficiently well done, to get a good result, and that they could be replicated in at least one other good study is useful information.”
When it comes to depression, Dr. MacKinnon said, “We just don’t know enough to really pin down a physiologic pathway to explain it. The fact that some people seem to have high cortisol and some people seem to have high permeability of blood-brain barrier, and others have abnormalities in dopamine, is interesting and suggests that depression is likely not a unitary disease with a single cause.”
He cautioned, however, that the findings don’t have immediate clinical implications for individual patients with depression.
“Theoretically, down the road, if you extrapolate from what they found, and if it’s truly the case that this research maps to something that could suggest a different clinical approach, you might be able to determine whether one patient might respond better to an SSRI or an SNRI or something like that,” Dr. MacKinnon said.
Dr. Benros reported grants from Lundbeck Foundation during the conduct of the study. Dr. MacKinnon has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Multiple biomarkers of depression involved in several brain circuits are altered in patients with unipolar depression.
because they suggest neuroimmunological alterations, disturbances in the blood-brain-barrier, hyperactivity in the hypothalamic-pituitary-adrenal (HPA) axis, and impaired neuroplasticity as factors in depression pathophysiology.
However, said study investigator Michael E. Benros, MD, PhD, professor and head of research at Mental Health Centre Copenhagen and University of Copenhagen, this is on a group level. “So in order to be relevant in a clinical context, the results need to be validated by further high-quality studies identifying subgroups with different biological underpinnings,” he told this news organization.
Identification of potential subgroups of depression with different biomarkers might help explain the diverse symptomatology and variability in treatment response observed in patients with depression, he noted.
The study was published online in JAMA Psychiatry.
Multiple pathways to depression
The systematic review and meta-analysis included 97 studies investigating 165 CSF biomarkers.
Of the 42 biomarkers investigated in at least two studies, patients with unipolar depression had higher CSF levels of interleukin 6, a marker of chronic inflammation; total protein, which signals blood-brain barrier dysfunction and increased permeability; and cortisol, which is linked to psychological stress, compared with healthy controls.
Depression was also associated with:
- Lower CSF levels of homovanillic acid, the major terminal metabolite of dopamine.
- Gamma-aminobutyric acid (GABA), the major inhibitory neurotransmitter in the CNS thought to play a vital role in the control of stress and depression.
- Somatostatin, a neuropeptide often coexpressed with GABA.
- Brain-derived neurotrophic factor (BDNF), a protein involved in neurogenesis, synaptic plasticity, and neurotransmission.
- Amyloid-β 40, implicated in Alzheimer’s disease.
- Transthyretin, involved in transport of thyroxine across the blood-brain barrier.
Collectively, the findings point toward a “dysregulated dopaminergic system, a compromised inhibitory system, HPA axis hyperactivity, increased neuroinflammation and blood-brain barrier permeability, and impaired neuroplasticity as important factors in depression pathophysiology,” the investigators wrote.
“It is notable that we did not find significant difference in the metabolite levels of serotonin and noradrenalin, which are the most targeted neurotransmitters in modern antidepressant treatment,” said Dr. Benros.
However, this could be explained by substantial heterogeneity between studies and the fact that quantification of total CSF biomarker concentrations does not reflect local alteration within the brain, he explained.
Many of the studies had small cohorts and most quantified only a few biomarkers, making it hard to examine potential interactions between biomarkers or identify specific phenotypes of depression.
“Novel high-quality studies including larger cohorts with an integrative approach and extensive numbers of biomarkers are needed to validate these potential biomarkers of depression and set the stage for the development of more effective and precise treatments,” the researchers noted.
Which ones hold water?
Reached for comment, Dean MacKinnon, MD, associate professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore, noted that this analysis “extracts the vast amount of knowledge” gained from different studies on biomarkers in the CSF for depression.
“They were able to identify 97 papers that have enough information in them that they could sort of lump them together and see which ones still hold water. It’s always useful to be able to look at patterns in the research and see if you can find some consistent trends,” he told this news organization.
Dr. MacKinnon, who was not part of the research team, also noted that “nonreplicability” is a problem in psychiatry and psychology research, “so being able to show that at least some studies were sufficiently well done, to get a good result, and that they could be replicated in at least one other good study is useful information.”
When it comes to depression, Dr. MacKinnon said, “We just don’t know enough to really pin down a physiologic pathway to explain it. The fact that some people seem to have high cortisol and some people seem to have high permeability of blood-brain barrier, and others have abnormalities in dopamine, is interesting and suggests that depression is likely not a unitary disease with a single cause.”
He cautioned, however, that the findings don’t have immediate clinical implications for individual patients with depression.
“Theoretically, down the road, if you extrapolate from what they found, and if it’s truly the case that this research maps to something that could suggest a different clinical approach, you might be able to determine whether one patient might respond better to an SSRI or an SNRI or something like that,” Dr. MacKinnon said.
Dr. Benros reported grants from Lundbeck Foundation during the conduct of the study. Dr. MacKinnon has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Multiple biomarkers of depression involved in several brain circuits are altered in patients with unipolar depression.
because they suggest neuroimmunological alterations, disturbances in the blood-brain-barrier, hyperactivity in the hypothalamic-pituitary-adrenal (HPA) axis, and impaired neuroplasticity as factors in depression pathophysiology.
However, said study investigator Michael E. Benros, MD, PhD, professor and head of research at Mental Health Centre Copenhagen and University of Copenhagen, this is on a group level. “So in order to be relevant in a clinical context, the results need to be validated by further high-quality studies identifying subgroups with different biological underpinnings,” he told this news organization.
Identification of potential subgroups of depression with different biomarkers might help explain the diverse symptomatology and variability in treatment response observed in patients with depression, he noted.
The study was published online in JAMA Psychiatry.
Multiple pathways to depression
The systematic review and meta-analysis included 97 studies investigating 165 CSF biomarkers.
Of the 42 biomarkers investigated in at least two studies, patients with unipolar depression had higher CSF levels of interleukin 6, a marker of chronic inflammation; total protein, which signals blood-brain barrier dysfunction and increased permeability; and cortisol, which is linked to psychological stress, compared with healthy controls.
Depression was also associated with:
- Lower CSF levels of homovanillic acid, the major terminal metabolite of dopamine.
- Gamma-aminobutyric acid (GABA), the major inhibitory neurotransmitter in the CNS thought to play a vital role in the control of stress and depression.
- Somatostatin, a neuropeptide often coexpressed with GABA.
- Brain-derived neurotrophic factor (BDNF), a protein involved in neurogenesis, synaptic plasticity, and neurotransmission.
- Amyloid-β 40, implicated in Alzheimer’s disease.
- Transthyretin, involved in transport of thyroxine across the blood-brain barrier.
Collectively, the findings point toward a “dysregulated dopaminergic system, a compromised inhibitory system, HPA axis hyperactivity, increased neuroinflammation and blood-brain barrier permeability, and impaired neuroplasticity as important factors in depression pathophysiology,” the investigators wrote.
“It is notable that we did not find significant difference in the metabolite levels of serotonin and noradrenalin, which are the most targeted neurotransmitters in modern antidepressant treatment,” said Dr. Benros.
However, this could be explained by substantial heterogeneity between studies and the fact that quantification of total CSF biomarker concentrations does not reflect local alteration within the brain, he explained.
Many of the studies had small cohorts and most quantified only a few biomarkers, making it hard to examine potential interactions between biomarkers or identify specific phenotypes of depression.
“Novel high-quality studies including larger cohorts with an integrative approach and extensive numbers of biomarkers are needed to validate these potential biomarkers of depression and set the stage for the development of more effective and precise treatments,” the researchers noted.
Which ones hold water?
Reached for comment, Dean MacKinnon, MD, associate professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore, noted that this analysis “extracts the vast amount of knowledge” gained from different studies on biomarkers in the CSF for depression.
“They were able to identify 97 papers that have enough information in them that they could sort of lump them together and see which ones still hold water. It’s always useful to be able to look at patterns in the research and see if you can find some consistent trends,” he told this news organization.
Dr. MacKinnon, who was not part of the research team, also noted that “nonreplicability” is a problem in psychiatry and psychology research, “so being able to show that at least some studies were sufficiently well done, to get a good result, and that they could be replicated in at least one other good study is useful information.”
When it comes to depression, Dr. MacKinnon said, “We just don’t know enough to really pin down a physiologic pathway to explain it. The fact that some people seem to have high cortisol and some people seem to have high permeability of blood-brain barrier, and others have abnormalities in dopamine, is interesting and suggests that depression is likely not a unitary disease with a single cause.”
He cautioned, however, that the findings don’t have immediate clinical implications for individual patients with depression.
“Theoretically, down the road, if you extrapolate from what they found, and if it’s truly the case that this research maps to something that could suggest a different clinical approach, you might be able to determine whether one patient might respond better to an SSRI or an SNRI or something like that,” Dr. MacKinnon said.
Dr. Benros reported grants from Lundbeck Foundation during the conduct of the study. Dr. MacKinnon has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Burnout ‘highly prevalent’ in psychiatrists across the globe
Burnout in psychiatrists is “highly prevalent” across the globe, new research shows.
In a review and meta-analysis of 36 studies and more than 5,000 psychiatrists in European countries, as well as the United States, Australia, New Zealand, India, Turkey, and Thailand,
“Our review showed that regardless of the identification method of burnout, its prevalence among psychiatrists is high and ranges from 25% to 50%,” lead author Kirill Bykov, MD, a PhD candidate at the Peoples’ Friendship University of Russia (RUDN University), Moscow, Russian Federation, told this news organization.
There was a “high heterogeneity of studies in terms of statistics, screening methods, burnout definitions, and cutoff points in the included studies, which necessitates the unification of future research methodology, but not to the detriment of the development of the theoretical background,” Dr. Bykov said.
The findings were published online in the Journal of Affective Disorders.
‘Unresolved problem’
Although burnout is a serious and prevalent problem among health care workers, little research has focused on burnout in mental health workers compared with other professionals, the investigators noted.
A previous systematic review and meta-analysis that focused specifically on burnout in psychiatrists was limited by methodologic concerns, including that the only burnout screening instrument used in the included studies was the full-length (22-item) MBI.
The current researchers surmised that “the integration of different empirical studies of psychiatrists’ burnout prevalence [remained] an unresolved problem.”
Dr. Bykov noted the current review was “investigator-initiated” and was a part of his PhD dissertation.
“Studying the works devoted to the burnout of psychiatrists, I drew attention to the varying prevalence rates of this phenomenon among them. This prompted me to conduct a systematic review of the literature and summarize the available data,” he said.
Unlike the previous review, the current one “does not contain restrictions regarding the place of research, publication language, covered burnout concepts, definitions, and screening instruments. Thus, its results will be helpful for practitioners and scientists around the world,” Dr. Bykov added.
Among the inclusion criteria was that a study should be empirical and quantitative, contain at least 20 practicing psychiatrists as participants, use a valid and reliable burnout screening instrument, have at least one burnout metric extractable specifically with regard to psychiatrists, and have a national survey or a response rate among psychiatrists of 20% or greater.
Qualitative or review articles or studies consisting of psychiatric trainees (such as medical students or residents) or nonpracticing psychiatrists were excluded.
Pooled prevalence
The researchers included 36 studies that comprised 5,481 participants (51.3% were women; mean age, 46.7 years). All studies had from 20 to 1,157 participants. They were employed in an array of settings in 19 countries.
In 22 studies, survey years ranged from 1996 to 2018; 14 studies did not report the year of data collection.
Most studies (75%) used some version of the MBI, and 19 studies used the full-length 22-item MBI Human Service Survey (MBI-HSS) . The survey rates emotional exhaustion (EE), depersonalization (DP), and low personal achievement (PA) on a 7-point Likert scale from 0 (“never”) to 6 (“almost every day”).
Other instruments included the CBI, the 16-item Oldenburg Burnout Inventory, the 21-item Tedium Measure, the 30-item Professional Quality of Life measure, the Rohland et al. Single-Item Measure of Self-Perceived Burnout, and the 21-item Brief Burnout Questionnaire.
Only three studies were free of methodologic limitations. The remaining 33 studies had some problems, such as not reporting the response rate or comparability between responders and nonresponders.
Results showed that the overall prevalence of burnout, as measured by the MBI and the CBI, was 25.9% (range, 11.1%-40.75%) and 50.3% (range, 30.9%-69.8%), respectively.
The pooled prevalence for burnout components is shown in the table.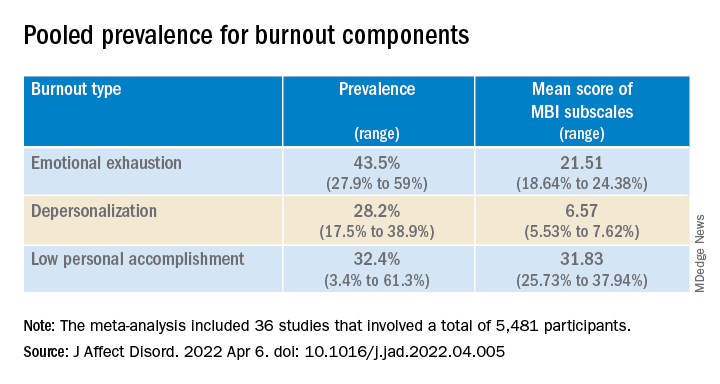
European psychiatrists had lower EE scores (20.82; 95% confidence interval, 7.24-4.41) compared with their non-European counterparts (24.99; 95% CI, 23.05-26.94; P = .045).
‘Carry the hope’
In a comment, Christine Crawford, MD, associate medical director of the National Alliance on Mental Illness (NAMI), said she was surprised the burnout numbers weren’t higher.
Many colleagues she interacts with “have been experiencing pretty significant burnout that has only been exacerbated by the pandemic and ever-growing demand for mental health providers, and there aren’t enough to meet that demand,” said Dr. Crawford, a psychiatrist at Boston Medical Center’s Outpatient Child and Adolescent Psychiatry Clinic and at Codman Square Health Center. She was not involved with the current research.
Dr. Crawford noted that much of the data was from Europeans. Speaking to the experience of U.S.-based psychiatrists, she said there is a “greater appreciation for what we do as mental health providers, due to the growing conversations around mental health and normalizing mental health conditions.”
On the other hand, there is “a lack of parity in reimbursement rates. Although the general public values mental health, the medical system doesn’t value mental health providers in the same way as physicians in other specialties,” Dr. Crawford said. Feeling devalued can contribute to burnout, she added.
One way to counter burnout is to remember “that our role is to carry the hope. We can be hopeful for the patient that the treatment will work or the medications can provide some relief,” Dr. Crawford noted.
Psychiatrists “may need to hold on tightly to that hope because we may not receive that instant gratification from the patient or receive praise or see the change from the patient during that time, which can be challenging,” she said.
“But it’s important for us to keep in mind that, even in that moment when the patient can’t see it, we can work alongside the patient to create the vision of hope and what it will look like in the future,” said Dr. Crawford.
In the 2022 Medscape Psychiatrist Lifestyle, Happiness & Burnout Report, an annual online survey of Medscape member physicians, 47% of respondents reported burnout – which was up from 42% the previous year.
The investigators received no funding for this work. They and Dr. Crawford report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Burnout in psychiatrists is “highly prevalent” across the globe, new research shows.
In a review and meta-analysis of 36 studies and more than 5,000 psychiatrists in European countries, as well as the United States, Australia, New Zealand, India, Turkey, and Thailand,
“Our review showed that regardless of the identification method of burnout, its prevalence among psychiatrists is high and ranges from 25% to 50%,” lead author Kirill Bykov, MD, a PhD candidate at the Peoples’ Friendship University of Russia (RUDN University), Moscow, Russian Federation, told this news organization.
There was a “high heterogeneity of studies in terms of statistics, screening methods, burnout definitions, and cutoff points in the included studies, which necessitates the unification of future research methodology, but not to the detriment of the development of the theoretical background,” Dr. Bykov said.
The findings were published online in the Journal of Affective Disorders.
‘Unresolved problem’
Although burnout is a serious and prevalent problem among health care workers, little research has focused on burnout in mental health workers compared with other professionals, the investigators noted.
A previous systematic review and meta-analysis that focused specifically on burnout in psychiatrists was limited by methodologic concerns, including that the only burnout screening instrument used in the included studies was the full-length (22-item) MBI.
The current researchers surmised that “the integration of different empirical studies of psychiatrists’ burnout prevalence [remained] an unresolved problem.”
Dr. Bykov noted the current review was “investigator-initiated” and was a part of his PhD dissertation.
“Studying the works devoted to the burnout of psychiatrists, I drew attention to the varying prevalence rates of this phenomenon among them. This prompted me to conduct a systematic review of the literature and summarize the available data,” he said.
Unlike the previous review, the current one “does not contain restrictions regarding the place of research, publication language, covered burnout concepts, definitions, and screening instruments. Thus, its results will be helpful for practitioners and scientists around the world,” Dr. Bykov added.
Among the inclusion criteria was that a study should be empirical and quantitative, contain at least 20 practicing psychiatrists as participants, use a valid and reliable burnout screening instrument, have at least one burnout metric extractable specifically with regard to psychiatrists, and have a national survey or a response rate among psychiatrists of 20% or greater.
Qualitative or review articles or studies consisting of psychiatric trainees (such as medical students or residents) or nonpracticing psychiatrists were excluded.
Pooled prevalence
The researchers included 36 studies that comprised 5,481 participants (51.3% were women; mean age, 46.7 years). All studies had from 20 to 1,157 participants. They were employed in an array of settings in 19 countries.
In 22 studies, survey years ranged from 1996 to 2018; 14 studies did not report the year of data collection.
Most studies (75%) used some version of the MBI, and 19 studies used the full-length 22-item MBI Human Service Survey (MBI-HSS) . The survey rates emotional exhaustion (EE), depersonalization (DP), and low personal achievement (PA) on a 7-point Likert scale from 0 (“never”) to 6 (“almost every day”).
Other instruments included the CBI, the 16-item Oldenburg Burnout Inventory, the 21-item Tedium Measure, the 30-item Professional Quality of Life measure, the Rohland et al. Single-Item Measure of Self-Perceived Burnout, and the 21-item Brief Burnout Questionnaire.
Only three studies were free of methodologic limitations. The remaining 33 studies had some problems, such as not reporting the response rate or comparability between responders and nonresponders.
Results showed that the overall prevalence of burnout, as measured by the MBI and the CBI, was 25.9% (range, 11.1%-40.75%) and 50.3% (range, 30.9%-69.8%), respectively.
The pooled prevalence for burnout components is shown in the table.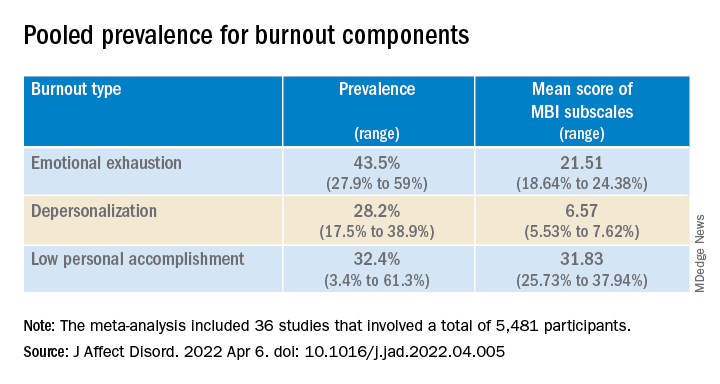
European psychiatrists had lower EE scores (20.82; 95% confidence interval, 7.24-4.41) compared with their non-European counterparts (24.99; 95% CI, 23.05-26.94; P = .045).
‘Carry the hope’
In a comment, Christine Crawford, MD, associate medical director of the National Alliance on Mental Illness (NAMI), said she was surprised the burnout numbers weren’t higher.
Many colleagues she interacts with “have been experiencing pretty significant burnout that has only been exacerbated by the pandemic and ever-growing demand for mental health providers, and there aren’t enough to meet that demand,” said Dr. Crawford, a psychiatrist at Boston Medical Center’s Outpatient Child and Adolescent Psychiatry Clinic and at Codman Square Health Center. She was not involved with the current research.
Dr. Crawford noted that much of the data was from Europeans. Speaking to the experience of U.S.-based psychiatrists, she said there is a “greater appreciation for what we do as mental health providers, due to the growing conversations around mental health and normalizing mental health conditions.”
On the other hand, there is “a lack of parity in reimbursement rates. Although the general public values mental health, the medical system doesn’t value mental health providers in the same way as physicians in other specialties,” Dr. Crawford said. Feeling devalued can contribute to burnout, she added.
One way to counter burnout is to remember “that our role is to carry the hope. We can be hopeful for the patient that the treatment will work or the medications can provide some relief,” Dr. Crawford noted.
Psychiatrists “may need to hold on tightly to that hope because we may not receive that instant gratification from the patient or receive praise or see the change from the patient during that time, which can be challenging,” she said.
“But it’s important for us to keep in mind that, even in that moment when the patient can’t see it, we can work alongside the patient to create the vision of hope and what it will look like in the future,” said Dr. Crawford.
In the 2022 Medscape Psychiatrist Lifestyle, Happiness & Burnout Report, an annual online survey of Medscape member physicians, 47% of respondents reported burnout – which was up from 42% the previous year.
The investigators received no funding for this work. They and Dr. Crawford report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Burnout in psychiatrists is “highly prevalent” across the globe, new research shows.
In a review and meta-analysis of 36 studies and more than 5,000 psychiatrists in European countries, as well as the United States, Australia, New Zealand, India, Turkey, and Thailand,
“Our review showed that regardless of the identification method of burnout, its prevalence among psychiatrists is high and ranges from 25% to 50%,” lead author Kirill Bykov, MD, a PhD candidate at the Peoples’ Friendship University of Russia (RUDN University), Moscow, Russian Federation, told this news organization.
There was a “high heterogeneity of studies in terms of statistics, screening methods, burnout definitions, and cutoff points in the included studies, which necessitates the unification of future research methodology, but not to the detriment of the development of the theoretical background,” Dr. Bykov said.
The findings were published online in the Journal of Affective Disorders.
‘Unresolved problem’
Although burnout is a serious and prevalent problem among health care workers, little research has focused on burnout in mental health workers compared with other professionals, the investigators noted.
A previous systematic review and meta-analysis that focused specifically on burnout in psychiatrists was limited by methodologic concerns, including that the only burnout screening instrument used in the included studies was the full-length (22-item) MBI.
The current researchers surmised that “the integration of different empirical studies of psychiatrists’ burnout prevalence [remained] an unresolved problem.”
Dr. Bykov noted the current review was “investigator-initiated” and was a part of his PhD dissertation.
“Studying the works devoted to the burnout of psychiatrists, I drew attention to the varying prevalence rates of this phenomenon among them. This prompted me to conduct a systematic review of the literature and summarize the available data,” he said.
Unlike the previous review, the current one “does not contain restrictions regarding the place of research, publication language, covered burnout concepts, definitions, and screening instruments. Thus, its results will be helpful for practitioners and scientists around the world,” Dr. Bykov added.
Among the inclusion criteria was that a study should be empirical and quantitative, contain at least 20 practicing psychiatrists as participants, use a valid and reliable burnout screening instrument, have at least one burnout metric extractable specifically with regard to psychiatrists, and have a national survey or a response rate among psychiatrists of 20% or greater.
Qualitative or review articles or studies consisting of psychiatric trainees (such as medical students or residents) or nonpracticing psychiatrists were excluded.
Pooled prevalence
The researchers included 36 studies that comprised 5,481 participants (51.3% were women; mean age, 46.7 years). All studies had from 20 to 1,157 participants. They were employed in an array of settings in 19 countries.
In 22 studies, survey years ranged from 1996 to 2018; 14 studies did not report the year of data collection.
Most studies (75%) used some version of the MBI, and 19 studies used the full-length 22-item MBI Human Service Survey (MBI-HSS) . The survey rates emotional exhaustion (EE), depersonalization (DP), and low personal achievement (PA) on a 7-point Likert scale from 0 (“never”) to 6 (“almost every day”).
Other instruments included the CBI, the 16-item Oldenburg Burnout Inventory, the 21-item Tedium Measure, the 30-item Professional Quality of Life measure, the Rohland et al. Single-Item Measure of Self-Perceived Burnout, and the 21-item Brief Burnout Questionnaire.
Only three studies were free of methodologic limitations. The remaining 33 studies had some problems, such as not reporting the response rate or comparability between responders and nonresponders.
Results showed that the overall prevalence of burnout, as measured by the MBI and the CBI, was 25.9% (range, 11.1%-40.75%) and 50.3% (range, 30.9%-69.8%), respectively.
The pooled prevalence for burnout components is shown in the table.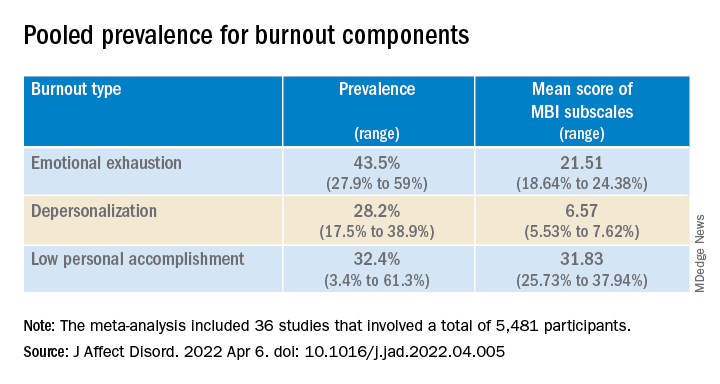
European psychiatrists had lower EE scores (20.82; 95% confidence interval, 7.24-4.41) compared with their non-European counterparts (24.99; 95% CI, 23.05-26.94; P = .045).
‘Carry the hope’
In a comment, Christine Crawford, MD, associate medical director of the National Alliance on Mental Illness (NAMI), said she was surprised the burnout numbers weren’t higher.
Many colleagues she interacts with “have been experiencing pretty significant burnout that has only been exacerbated by the pandemic and ever-growing demand for mental health providers, and there aren’t enough to meet that demand,” said Dr. Crawford, a psychiatrist at Boston Medical Center’s Outpatient Child and Adolescent Psychiatry Clinic and at Codman Square Health Center. She was not involved with the current research.
Dr. Crawford noted that much of the data was from Europeans. Speaking to the experience of U.S.-based psychiatrists, she said there is a “greater appreciation for what we do as mental health providers, due to the growing conversations around mental health and normalizing mental health conditions.”
On the other hand, there is “a lack of parity in reimbursement rates. Although the general public values mental health, the medical system doesn’t value mental health providers in the same way as physicians in other specialties,” Dr. Crawford said. Feeling devalued can contribute to burnout, she added.
One way to counter burnout is to remember “that our role is to carry the hope. We can be hopeful for the patient that the treatment will work or the medications can provide some relief,” Dr. Crawford noted.
Psychiatrists “may need to hold on tightly to that hope because we may not receive that instant gratification from the patient or receive praise or see the change from the patient during that time, which can be challenging,” she said.
“But it’s important for us to keep in mind that, even in that moment when the patient can’t see it, we can work alongside the patient to create the vision of hope and what it will look like in the future,” said Dr. Crawford.
In the 2022 Medscape Psychiatrist Lifestyle, Happiness & Burnout Report, an annual online survey of Medscape member physicians, 47% of respondents reported burnout – which was up from 42% the previous year.
The investigators received no funding for this work. They and Dr. Crawford report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF AFFECTIVE DISORDERS
Seven hours of sleep is ideal for middle aged and older
Sleep disturbances are common in older age, and previous studies have shown associations between too much or too little sleep and increased risk of cognitive decline, but the ideal amount of sleep for preserving mental health has not been well described, according to the authors of the new paper.
In the study published in Nature Aging, the team of researchers from China and the United Kingdom reviewed data from the UK Biobank, a national database of individuals in the United Kingdom that includes cognitive assessments, mental health questionnaires, and brain imaging data, as well as genetic information.
Sleep is important for physical and psychological health, and also serves a neuroprotective function by clearing waste products from the brain, lead author Yuzhu Li of Fudan University, Shanghai, China, and colleagues wrote.
The study population included 498,277 participants, aged 38-73 years, who completed touchscreen questionnaires about sleep duration between 2006 and 2010. The average age at baseline was 56.5 years, 54% were female, and the mean sleep duration was 7.15 hours.
The researchers also reviewed brain imaging data and genetic data from 39,692 participants in 2014 to examine the relationships between sleep duration and brain structure and between sleep duration and genetic risk. In addition, 156,884 participants completed an online follow-up mental health questionnaire in 2016-2017 to assess the longitudinal impact of sleep on mental health.
Both excessive and insufficient sleep was associated with impaired cognitive performance, evidenced by the U-shaped curve found by the researchers in their data analysis, which used quadratic associations.
Specific cognitive functions including pair matching, trail making, prospective memory, and reaction time were significantly impaired with too much or too little sleep, the researchers said. “This demonstrated the positive association of both insufficient and excessive sleep duration with inferior performance on cognitive tasks.”
When the researchers analyzed the association between sleep duration and mental health, sleep duration also showed a U-shaped association with symptoms of anxiety, depression, mental distress, mania, and self-harm, while well-being showed an inverted U-shape. All associations between sleep duration and mental health were statistically significant after controlling for confounding variables (P < .001).
On further analysis (using two-line tests), the researchers determined that consistent sleep duration of approximately 7 hours per night was optimal for cognitive performance and for good mental health.
The researchers also used neuroimaging data to examine the relationship between sleep duration and brain structure. Overall, greater changes were seen in the regions of the brain involved in cognitive processing and memory.
“The most significant cortical volumes nonlinearly associated with sleep duration included the precentral cortex, the superior frontal gyrus, the lateral orbitofrontal cortex, the pars orbitalis, the frontal pole, and the middle temporal cortex,” the researchers wrote (P < .05 for all).
The association between sleep duration and cognitive function diminished among individuals older than 65 years, compared with those aged approximately 40 years, which suggests that optimal sleep duration may be more beneficial in middle age, the researchers noted. However, no similar impact of age was seen for mental health. For brain structure, the nonlinear relationship between sleep duration and cortical volumes was greatest in those aged 44-59 years, and gradually flattened with older age.
Research supports sleep discussions with patients
“Primary care physicians can use this study in their discussions with middle-aged and older patients to recommend optimal sleep duration and measures to achieve this sleep target,” Noel Deep, MD, a general internist in group practice in Antigo, Wisc., who was not involved in the study, said in an interview.
“This study is important because it demonstrated that both inadequate and excessive sleep patterns were associated with cognitive and mental health changes,” said Dr. Deep. “It supported previous observations of cognitive decline and mental health disorders being linked to disturbed sleep. But this study was unique because it provides data supporting an optimal sleep duration of 7 hours and the ill effects of both insufficient and excessive sleep duration.
“The usual thought process has been to assume that older individuals may not require as much sleep as the younger individuals, but this study supports an optimal time duration of sleep of 7 hours that benefits the older individuals. It was also interesting to note the mental health effects caused by the inadequate and excessive sleep durations,” he added.
As for additional research, “I would like to look into the quality of the sleep, in addition to the duration of sleep,” said Dr. Deep. For example, whether the excessive sleep was caused by poor quality sleep or fragmented sleep leading to the structural and subsequent cognitive decline.
Study limitations
“The current study relied on self-reporting of the sleep duration and was not observed and recorded data,” Dr. Deep noted. “It would also be beneficial to not only rely on healthy volunteers reporting the sleep duration, but also obtain sleep data from individuals with known brain disorders.”
The study findings were limited by several other factors, including the use of total sleep duration only, without other measures of sleep hygiene, the researchers noted. More research is needed to investigate the mechanisms driving the association between too much and not enough sleep and poor mental health and cognitive function.
The study was supported by the National Key R&D Program of China, the Shanghai Municipal Science and Technology Major Project, the Shanghai Center for Brain Science and Brain-Inspired Technology, the 111 Project, the National Natural Sciences Foundation of China and the Shanghai Rising Star Program.
The researchers had no financial conflicts to disclose. Dr. Deep had no financial conflicts to disclose, but serves on the editorial advisory board of Internal Medicine News.
Sleep disturbances are common in older age, and previous studies have shown associations between too much or too little sleep and increased risk of cognitive decline, but the ideal amount of sleep for preserving mental health has not been well described, according to the authors of the new paper.
In the study published in Nature Aging, the team of researchers from China and the United Kingdom reviewed data from the UK Biobank, a national database of individuals in the United Kingdom that includes cognitive assessments, mental health questionnaires, and brain imaging data, as well as genetic information.
Sleep is important for physical and psychological health, and also serves a neuroprotective function by clearing waste products from the brain, lead author Yuzhu Li of Fudan University, Shanghai, China, and colleagues wrote.
The study population included 498,277 participants, aged 38-73 years, who completed touchscreen questionnaires about sleep duration between 2006 and 2010. The average age at baseline was 56.5 years, 54% were female, and the mean sleep duration was 7.15 hours.
The researchers also reviewed brain imaging data and genetic data from 39,692 participants in 2014 to examine the relationships between sleep duration and brain structure and between sleep duration and genetic risk. In addition, 156,884 participants completed an online follow-up mental health questionnaire in 2016-2017 to assess the longitudinal impact of sleep on mental health.
Both excessive and insufficient sleep was associated with impaired cognitive performance, evidenced by the U-shaped curve found by the researchers in their data analysis, which used quadratic associations.
Specific cognitive functions including pair matching, trail making, prospective memory, and reaction time were significantly impaired with too much or too little sleep, the researchers said. “This demonstrated the positive association of both insufficient and excessive sleep duration with inferior performance on cognitive tasks.”
When the researchers analyzed the association between sleep duration and mental health, sleep duration also showed a U-shaped association with symptoms of anxiety, depression, mental distress, mania, and self-harm, while well-being showed an inverted U-shape. All associations between sleep duration and mental health were statistically significant after controlling for confounding variables (P < .001).
On further analysis (using two-line tests), the researchers determined that consistent sleep duration of approximately 7 hours per night was optimal for cognitive performance and for good mental health.
The researchers also used neuroimaging data to examine the relationship between sleep duration and brain structure. Overall, greater changes were seen in the regions of the brain involved in cognitive processing and memory.
“The most significant cortical volumes nonlinearly associated with sleep duration included the precentral cortex, the superior frontal gyrus, the lateral orbitofrontal cortex, the pars orbitalis, the frontal pole, and the middle temporal cortex,” the researchers wrote (P < .05 for all).
The association between sleep duration and cognitive function diminished among individuals older than 65 years, compared with those aged approximately 40 years, which suggests that optimal sleep duration may be more beneficial in middle age, the researchers noted. However, no similar impact of age was seen for mental health. For brain structure, the nonlinear relationship between sleep duration and cortical volumes was greatest in those aged 44-59 years, and gradually flattened with older age.
Research supports sleep discussions with patients
“Primary care physicians can use this study in their discussions with middle-aged and older patients to recommend optimal sleep duration and measures to achieve this sleep target,” Noel Deep, MD, a general internist in group practice in Antigo, Wisc., who was not involved in the study, said in an interview.
“This study is important because it demonstrated that both inadequate and excessive sleep patterns were associated with cognitive and mental health changes,” said Dr. Deep. “It supported previous observations of cognitive decline and mental health disorders being linked to disturbed sleep. But this study was unique because it provides data supporting an optimal sleep duration of 7 hours and the ill effects of both insufficient and excessive sleep duration.
“The usual thought process has been to assume that older individuals may not require as much sleep as the younger individuals, but this study supports an optimal time duration of sleep of 7 hours that benefits the older individuals. It was also interesting to note the mental health effects caused by the inadequate and excessive sleep durations,” he added.
As for additional research, “I would like to look into the quality of the sleep, in addition to the duration of sleep,” said Dr. Deep. For example, whether the excessive sleep was caused by poor quality sleep or fragmented sleep leading to the structural and subsequent cognitive decline.
Study limitations
“The current study relied on self-reporting of the sleep duration and was not observed and recorded data,” Dr. Deep noted. “It would also be beneficial to not only rely on healthy volunteers reporting the sleep duration, but also obtain sleep data from individuals with known brain disorders.”
The study findings were limited by several other factors, including the use of total sleep duration only, without other measures of sleep hygiene, the researchers noted. More research is needed to investigate the mechanisms driving the association between too much and not enough sleep and poor mental health and cognitive function.
The study was supported by the National Key R&D Program of China, the Shanghai Municipal Science and Technology Major Project, the Shanghai Center for Brain Science and Brain-Inspired Technology, the 111 Project, the National Natural Sciences Foundation of China and the Shanghai Rising Star Program.
The researchers had no financial conflicts to disclose. Dr. Deep had no financial conflicts to disclose, but serves on the editorial advisory board of Internal Medicine News.
Sleep disturbances are common in older age, and previous studies have shown associations between too much or too little sleep and increased risk of cognitive decline, but the ideal amount of sleep for preserving mental health has not been well described, according to the authors of the new paper.
In the study published in Nature Aging, the team of researchers from China and the United Kingdom reviewed data from the UK Biobank, a national database of individuals in the United Kingdom that includes cognitive assessments, mental health questionnaires, and brain imaging data, as well as genetic information.
Sleep is important for physical and psychological health, and also serves a neuroprotective function by clearing waste products from the brain, lead author Yuzhu Li of Fudan University, Shanghai, China, and colleagues wrote.
The study population included 498,277 participants, aged 38-73 years, who completed touchscreen questionnaires about sleep duration between 2006 and 2010. The average age at baseline was 56.5 years, 54% were female, and the mean sleep duration was 7.15 hours.
The researchers also reviewed brain imaging data and genetic data from 39,692 participants in 2014 to examine the relationships between sleep duration and brain structure and between sleep duration and genetic risk. In addition, 156,884 participants completed an online follow-up mental health questionnaire in 2016-2017 to assess the longitudinal impact of sleep on mental health.
Both excessive and insufficient sleep was associated with impaired cognitive performance, evidenced by the U-shaped curve found by the researchers in their data analysis, which used quadratic associations.
Specific cognitive functions including pair matching, trail making, prospective memory, and reaction time were significantly impaired with too much or too little sleep, the researchers said. “This demonstrated the positive association of both insufficient and excessive sleep duration with inferior performance on cognitive tasks.”
When the researchers analyzed the association between sleep duration and mental health, sleep duration also showed a U-shaped association with symptoms of anxiety, depression, mental distress, mania, and self-harm, while well-being showed an inverted U-shape. All associations between sleep duration and mental health were statistically significant after controlling for confounding variables (P < .001).
On further analysis (using two-line tests), the researchers determined that consistent sleep duration of approximately 7 hours per night was optimal for cognitive performance and for good mental health.
The researchers also used neuroimaging data to examine the relationship between sleep duration and brain structure. Overall, greater changes were seen in the regions of the brain involved in cognitive processing and memory.
“The most significant cortical volumes nonlinearly associated with sleep duration included the precentral cortex, the superior frontal gyrus, the lateral orbitofrontal cortex, the pars orbitalis, the frontal pole, and the middle temporal cortex,” the researchers wrote (P < .05 for all).
The association between sleep duration and cognitive function diminished among individuals older than 65 years, compared with those aged approximately 40 years, which suggests that optimal sleep duration may be more beneficial in middle age, the researchers noted. However, no similar impact of age was seen for mental health. For brain structure, the nonlinear relationship between sleep duration and cortical volumes was greatest in those aged 44-59 years, and gradually flattened with older age.
Research supports sleep discussions with patients
“Primary care physicians can use this study in their discussions with middle-aged and older patients to recommend optimal sleep duration and measures to achieve this sleep target,” Noel Deep, MD, a general internist in group practice in Antigo, Wisc., who was not involved in the study, said in an interview.
“This study is important because it demonstrated that both inadequate and excessive sleep patterns were associated with cognitive and mental health changes,” said Dr. Deep. “It supported previous observations of cognitive decline and mental health disorders being linked to disturbed sleep. But this study was unique because it provides data supporting an optimal sleep duration of 7 hours and the ill effects of both insufficient and excessive sleep duration.
“The usual thought process has been to assume that older individuals may not require as much sleep as the younger individuals, but this study supports an optimal time duration of sleep of 7 hours that benefits the older individuals. It was also interesting to note the mental health effects caused by the inadequate and excessive sleep durations,” he added.
As for additional research, “I would like to look into the quality of the sleep, in addition to the duration of sleep,” said Dr. Deep. For example, whether the excessive sleep was caused by poor quality sleep or fragmented sleep leading to the structural and subsequent cognitive decline.
Study limitations
“The current study relied on self-reporting of the sleep duration and was not observed and recorded data,” Dr. Deep noted. “It would also be beneficial to not only rely on healthy volunteers reporting the sleep duration, but also obtain sleep data from individuals with known brain disorders.”
The study findings were limited by several other factors, including the use of total sleep duration only, without other measures of sleep hygiene, the researchers noted. More research is needed to investigate the mechanisms driving the association between too much and not enough sleep and poor mental health and cognitive function.
The study was supported by the National Key R&D Program of China, the Shanghai Municipal Science and Technology Major Project, the Shanghai Center for Brain Science and Brain-Inspired Technology, the 111 Project, the National Natural Sciences Foundation of China and the Shanghai Rising Star Program.
The researchers had no financial conflicts to disclose. Dr. Deep had no financial conflicts to disclose, but serves on the editorial advisory board of Internal Medicine News.
FROM NATURE AGING
Severe COVID-19 adds 20 years of cognitive aging: Study
adding that the impairment is “equivalent to losing 10 IQ points.”
In their study, published in eClinicalMedicine, a team of scientists from the University of Cambridge and Imperial College London said there is growing evidence that COVID-19 can cause lasting cognitive and mental health problems. Patients report fatigue, “brain fog,” problems recalling words, sleep disturbances, anxiety, and even posttraumatic stress disorder months after infection.
The researchers analyzed data from 46 individuals who received critical care for COVID-19 at Addenbrooke’s Hospital between March and July 2020 (27 females, 19 males, mean age 51 years, 16 of whom had mechanical ventilation) and were recruited to the NIHR COVID-19 BioResource project.
At an average of 6 months after acute COVID-19 illness, the study participants underwent detailed computerized cognitive tests via the Cognitron platform, comprising eight tasks deployed on an iPad measuring mental function such as memory, attention, and reasoning. Also assessed were anxiety, depression, and posttraumatic stress disorder via standard mood, anxiety, and posttraumatic stress scales – specifically the Generalized Anxiety Disorder 7 (GAD-7), the Patient Health Questionnaire 9 (PHQ-9), and the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders 5 (PCL-5). Their data were compared against 460 controls – matched for age, sex, education, and first language – and the pattern of deficits across tasks was qualitatively compared with normal age-related decline and early-stage dementia.
Less accurate and slower response times
The authors highlighted how this was the first time a “rigorous assessment and comparison” had been carried out in relation to the after-effects of severe COVID-19.
“Cognitive impairment is common to a wide range of neurological disorders, including dementia, and even routine aging, but the patterns we saw – the cognitive ‘fingerprint’ of COVID-19 – was distinct from all of these,” said David Menon, MD, division of anesthesia at the University of Cambridge, England, and the study’s senior author.
The scientists found that COVID-19 survivors were less accurate and had slower response times than the control population, and added that survivors scored particularly poorly on verbal analogical reasoning and showed slower processing speeds.
Critically, the scale of the cognitive deficits correlated with acute illness severity, but not fatigue or mental health status at the time of cognitive assessment, said the authors.
Recovery ‘at best gradual’
The effects were strongest for those with more severe acute illness, and who required mechanical ventilation, said the authors, who found that acute illness severity was “better at predicting the cognitive deficits.”
The authors pointed out how these deficits were still detectable when patients were followed up 6 months later, and that, although patients’ scores and reaction times began to improve over time, any recovery was “at best gradual” and likely to be influenced by factors such as illness severity and its neurological or psychological impacts.
“We followed some patients up as late as 10 months after their acute infection, so were able to see a very slow improvement,” Dr. Menon said. He explained how, while this improvement was not statistically significant, it was “at least heading in the right direction.”
However, he warned it is very possible that some of these individuals “will never fully recover.”
The cognitive deficits observed may be due to several factors in combination, said the authors, including inadequate oxygen or blood supply to the brain, blockage of large or small blood vessels due to clotting, and microscopic bleeds. They highlighted how the most important mechanism, however, may be “damage caused by the body’s own inflammatory response and immune system.”
Adam Hampshire, PhD, of the department of brain sciences at Imperial College London, one of the study’s authors, described how around 40,000 people have been through intensive care with COVID-19 in England alone, with many more despite having been very sick not admitted to hospital. This means there is a “large number of people out there still experiencing problems with cognition many months later,” he said. “We urgently need to look at what can be done to help these people.”
A version of this article first appeared on Univadis.
adding that the impairment is “equivalent to losing 10 IQ points.”
In their study, published in eClinicalMedicine, a team of scientists from the University of Cambridge and Imperial College London said there is growing evidence that COVID-19 can cause lasting cognitive and mental health problems. Patients report fatigue, “brain fog,” problems recalling words, sleep disturbances, anxiety, and even posttraumatic stress disorder months after infection.
The researchers analyzed data from 46 individuals who received critical care for COVID-19 at Addenbrooke’s Hospital between March and July 2020 (27 females, 19 males, mean age 51 years, 16 of whom had mechanical ventilation) and were recruited to the NIHR COVID-19 BioResource project.
At an average of 6 months after acute COVID-19 illness, the study participants underwent detailed computerized cognitive tests via the Cognitron platform, comprising eight tasks deployed on an iPad measuring mental function such as memory, attention, and reasoning. Also assessed were anxiety, depression, and posttraumatic stress disorder via standard mood, anxiety, and posttraumatic stress scales – specifically the Generalized Anxiety Disorder 7 (GAD-7), the Patient Health Questionnaire 9 (PHQ-9), and the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders 5 (PCL-5). Their data were compared against 460 controls – matched for age, sex, education, and first language – and the pattern of deficits across tasks was qualitatively compared with normal age-related decline and early-stage dementia.
Less accurate and slower response times
The authors highlighted how this was the first time a “rigorous assessment and comparison” had been carried out in relation to the after-effects of severe COVID-19.
“Cognitive impairment is common to a wide range of neurological disorders, including dementia, and even routine aging, but the patterns we saw – the cognitive ‘fingerprint’ of COVID-19 – was distinct from all of these,” said David Menon, MD, division of anesthesia at the University of Cambridge, England, and the study’s senior author.
The scientists found that COVID-19 survivors were less accurate and had slower response times than the control population, and added that survivors scored particularly poorly on verbal analogical reasoning and showed slower processing speeds.
Critically, the scale of the cognitive deficits correlated with acute illness severity, but not fatigue or mental health status at the time of cognitive assessment, said the authors.
Recovery ‘at best gradual’
The effects were strongest for those with more severe acute illness, and who required mechanical ventilation, said the authors, who found that acute illness severity was “better at predicting the cognitive deficits.”
The authors pointed out how these deficits were still detectable when patients were followed up 6 months later, and that, although patients’ scores and reaction times began to improve over time, any recovery was “at best gradual” and likely to be influenced by factors such as illness severity and its neurological or psychological impacts.
“We followed some patients up as late as 10 months after their acute infection, so were able to see a very slow improvement,” Dr. Menon said. He explained how, while this improvement was not statistically significant, it was “at least heading in the right direction.”
However, he warned it is very possible that some of these individuals “will never fully recover.”
The cognitive deficits observed may be due to several factors in combination, said the authors, including inadequate oxygen or blood supply to the brain, blockage of large or small blood vessels due to clotting, and microscopic bleeds. They highlighted how the most important mechanism, however, may be “damage caused by the body’s own inflammatory response and immune system.”
Adam Hampshire, PhD, of the department of brain sciences at Imperial College London, one of the study’s authors, described how around 40,000 people have been through intensive care with COVID-19 in England alone, with many more despite having been very sick not admitted to hospital. This means there is a “large number of people out there still experiencing problems with cognition many months later,” he said. “We urgently need to look at what can be done to help these people.”
A version of this article first appeared on Univadis.
adding that the impairment is “equivalent to losing 10 IQ points.”
In their study, published in eClinicalMedicine, a team of scientists from the University of Cambridge and Imperial College London said there is growing evidence that COVID-19 can cause lasting cognitive and mental health problems. Patients report fatigue, “brain fog,” problems recalling words, sleep disturbances, anxiety, and even posttraumatic stress disorder months after infection.
The researchers analyzed data from 46 individuals who received critical care for COVID-19 at Addenbrooke’s Hospital between March and July 2020 (27 females, 19 males, mean age 51 years, 16 of whom had mechanical ventilation) and were recruited to the NIHR COVID-19 BioResource project.
At an average of 6 months after acute COVID-19 illness, the study participants underwent detailed computerized cognitive tests via the Cognitron platform, comprising eight tasks deployed on an iPad measuring mental function such as memory, attention, and reasoning. Also assessed were anxiety, depression, and posttraumatic stress disorder via standard mood, anxiety, and posttraumatic stress scales – specifically the Generalized Anxiety Disorder 7 (GAD-7), the Patient Health Questionnaire 9 (PHQ-9), and the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders 5 (PCL-5). Their data were compared against 460 controls – matched for age, sex, education, and first language – and the pattern of deficits across tasks was qualitatively compared with normal age-related decline and early-stage dementia.
Less accurate and slower response times
The authors highlighted how this was the first time a “rigorous assessment and comparison” had been carried out in relation to the after-effects of severe COVID-19.
“Cognitive impairment is common to a wide range of neurological disorders, including dementia, and even routine aging, but the patterns we saw – the cognitive ‘fingerprint’ of COVID-19 – was distinct from all of these,” said David Menon, MD, division of anesthesia at the University of Cambridge, England, and the study’s senior author.
The scientists found that COVID-19 survivors were less accurate and had slower response times than the control population, and added that survivors scored particularly poorly on verbal analogical reasoning and showed slower processing speeds.
Critically, the scale of the cognitive deficits correlated with acute illness severity, but not fatigue or mental health status at the time of cognitive assessment, said the authors.
Recovery ‘at best gradual’
The effects were strongest for those with more severe acute illness, and who required mechanical ventilation, said the authors, who found that acute illness severity was “better at predicting the cognitive deficits.”
The authors pointed out how these deficits were still detectable when patients were followed up 6 months later, and that, although patients’ scores and reaction times began to improve over time, any recovery was “at best gradual” and likely to be influenced by factors such as illness severity and its neurological or psychological impacts.
“We followed some patients up as late as 10 months after their acute infection, so were able to see a very slow improvement,” Dr. Menon said. He explained how, while this improvement was not statistically significant, it was “at least heading in the right direction.”
However, he warned it is very possible that some of these individuals “will never fully recover.”
The cognitive deficits observed may be due to several factors in combination, said the authors, including inadequate oxygen or blood supply to the brain, blockage of large or small blood vessels due to clotting, and microscopic bleeds. They highlighted how the most important mechanism, however, may be “damage caused by the body’s own inflammatory response and immune system.”
Adam Hampshire, PhD, of the department of brain sciences at Imperial College London, one of the study’s authors, described how around 40,000 people have been through intensive care with COVID-19 in England alone, with many more despite having been very sick not admitted to hospital. This means there is a “large number of people out there still experiencing problems with cognition many months later,” he said. “We urgently need to look at what can be done to help these people.”
A version of this article first appeared on Univadis.
FROM ECLINICAL MEDICINE
Few children with early social gender transition change their minds
Approximately 7% of youth who chose gender identity social transition in early childhood had retransitioned 5 years later, based on data from 317 individuals.
“Increasing numbers of children are socially transitioning to live in line with their gender identity, rather than the gender assumed by their sex at birth – a process that typically involves changing a child’s pronouns, first name, hairstyle, and clothing,” wrote Kristina R. Olson, PhD, of Princeton (N.J.) University, and colleagues.
The question of whether early childhood social transitions will result in high rates of retransition continues to be a subject for debate, and long-term data on retransition rates and identity outcomes in children who transition are limited, they said.
To examine retransition in early-transitioning children, the researchers identified 317 binary socially transitioned transgender children to participate in a longitudinal study known as the Trans Youth Project (TYP) between July 2013 and December 2017. The study was published in Pediatrics. The mean age at baseline was 8 years. At study entry, participants had to have made a complete binary social transition, including changing their pronouns from those used at birth. During the 5-year follow-up period, children and parents were asked about use of puberty blockers and/or gender-affirming hormones. At study entry, 37 children had begun some type of puberty blockers. A total of 124 children initially socially transitioned before 6 years of age, and 193 initially socially transitioned at 6 years or older.
The study did not evaluate whether the participants met the DSM-5 criteria for gender dysphoria in childhood, the researchers noted. “Based on data collected at their initial visit, we do know that these participants showed signs of gender identification and gender-typed preferences commonly associated with their gender, not their sex assigned at birth,” they wrote.
Participants were classified as binary transgender, nonbinary, or cisgender based on their pronouns at follow-up. Binary transgender pronouns were associated with the other binary assigned sex, nonbinary pronouns were they/them or a mix of they/them and binary pronouns, and cisgender pronouns were those associated with assigned sex.
Overall, 7.3% of the participants had retransitioned at least once by 5 years after their initial binary social transition. The majority (94%) were living as binary transgender youth, including 1.3% who retransitioned to cisgender or nonbinary and then back to binary transgender during the follow-up period. A total of 2.5% were living as cisgender youth and 3.5% were living as nonbinary youth. These rates were similar across the initial population, as well as the 291 participants who continue to be in contact with the researchers, the 200 who had gone at least 5 years since their initial social transition, and the 280 participants who began the study before starting puberty blockers.
The researchers found no differences in retransition rates related to participant sex at birth. Rates of retransition were slightly higher among participants who made their initial social transition before 6 years of age, but these rates were low, the researchers noted.
The study findings were limited by several factors including the use of a volunteer community sample, with the potential for bias that may not generalize to the population at large, the researchers noted. Other limitations included the use of pronouns as the main criteria for retransition, and the classification of a change from binary transgender to nonbinary as a transition, they said. “Many nonbinary people consider themselves to be transgender,” they noted.
“If we had used a stricter criterion of retransition, more similar to the common use of terms like “detransition” or “desistence,” referring only to youth who are living as cisgender, then our retransition rate would have been lower (2.5%),” the researchers explained. Another limitation was the disproportionate number of trans girls, the researchers said. However, because no significant gender effect appeared in terms of retransition rates, “we do not predict any change in pattern of results if we had a different ratio of participants by sex at birth,” they said.
The researchers stated that they intend to follow the cohort through adolescence and into adulthood.
“As more youth are coming out and being supported in their transitions early in development, it is increasingly critical that clinicians understand the experiences of this cohort and not make assumptions about them as a function of older data from youth who lived under different circumstances,” the researchers emphasized. “Though we can never predict the exact gender trajectory of any child, these data suggest that many youth who identify as transgender early, and are supported through a social transition, will continue to identify as transgender 5 years after initial social transition.” They concluded that more research is needed to determine how best to support initial and later gender transitions in youth.
Study offers support for family discussions
“This study is important to help provide more data regarding the experiences of gender-diverse youth,” M. Brett Cooper, MD, of UT Southwestern Medical Center, Dallas, said in an interview. “The results of a study like this can be used by clinicians to help provide advice and guidance to parents and families as they support their children through their gender journey,” said Dr. Cooper, who was not involved in the study. The current study “also provides evidence to support that persistent, insistent, and consistent youth have an extremely low rate of retransition to a gender that aligns with their sex assigned at birth. This refutes suggestions by politicians and others that those who seek medical care have a high rate of regret or retransition,” Dr. Cooper emphasized.
“I was not surprised at all by their findings,” said Dr. Cooper. “These are very similar to what I have seen in my own panel of gender-diverse patients and what has been seen in other studies,” he noted.
The take-home message of the current study does not suggest any change in clinical practice, Dr. Cooper said. “Guidance already suggests supporting these youth on their gender journey and that for some youth, this may mean retransitioning to identify with their sex assigned at birth,” he explained.
The study was supported in part by grants to the researchers from the National Institutes of Health, the National Science Foundation, the Arcus Foundation, and the MacArthur Foundation. The researchers had no financial conflicts to disclose.
Approximately 7% of youth who chose gender identity social transition in early childhood had retransitioned 5 years later, based on data from 317 individuals.
“Increasing numbers of children are socially transitioning to live in line with their gender identity, rather than the gender assumed by their sex at birth – a process that typically involves changing a child’s pronouns, first name, hairstyle, and clothing,” wrote Kristina R. Olson, PhD, of Princeton (N.J.) University, and colleagues.
The question of whether early childhood social transitions will result in high rates of retransition continues to be a subject for debate, and long-term data on retransition rates and identity outcomes in children who transition are limited, they said.
To examine retransition in early-transitioning children, the researchers identified 317 binary socially transitioned transgender children to participate in a longitudinal study known as the Trans Youth Project (TYP) between July 2013 and December 2017. The study was published in Pediatrics. The mean age at baseline was 8 years. At study entry, participants had to have made a complete binary social transition, including changing their pronouns from those used at birth. During the 5-year follow-up period, children and parents were asked about use of puberty blockers and/or gender-affirming hormones. At study entry, 37 children had begun some type of puberty blockers. A total of 124 children initially socially transitioned before 6 years of age, and 193 initially socially transitioned at 6 years or older.
The study did not evaluate whether the participants met the DSM-5 criteria for gender dysphoria in childhood, the researchers noted. “Based on data collected at their initial visit, we do know that these participants showed signs of gender identification and gender-typed preferences commonly associated with their gender, not their sex assigned at birth,” they wrote.
Participants were classified as binary transgender, nonbinary, or cisgender based on their pronouns at follow-up. Binary transgender pronouns were associated with the other binary assigned sex, nonbinary pronouns were they/them or a mix of they/them and binary pronouns, and cisgender pronouns were those associated with assigned sex.
Overall, 7.3% of the participants had retransitioned at least once by 5 years after their initial binary social transition. The majority (94%) were living as binary transgender youth, including 1.3% who retransitioned to cisgender or nonbinary and then back to binary transgender during the follow-up period. A total of 2.5% were living as cisgender youth and 3.5% were living as nonbinary youth. These rates were similar across the initial population, as well as the 291 participants who continue to be in contact with the researchers, the 200 who had gone at least 5 years since their initial social transition, and the 280 participants who began the study before starting puberty blockers.
The researchers found no differences in retransition rates related to participant sex at birth. Rates of retransition were slightly higher among participants who made their initial social transition before 6 years of age, but these rates were low, the researchers noted.
The study findings were limited by several factors including the use of a volunteer community sample, with the potential for bias that may not generalize to the population at large, the researchers noted. Other limitations included the use of pronouns as the main criteria for retransition, and the classification of a change from binary transgender to nonbinary as a transition, they said. “Many nonbinary people consider themselves to be transgender,” they noted.
“If we had used a stricter criterion of retransition, more similar to the common use of terms like “detransition” or “desistence,” referring only to youth who are living as cisgender, then our retransition rate would have been lower (2.5%),” the researchers explained. Another limitation was the disproportionate number of trans girls, the researchers said. However, because no significant gender effect appeared in terms of retransition rates, “we do not predict any change in pattern of results if we had a different ratio of participants by sex at birth,” they said.
The researchers stated that they intend to follow the cohort through adolescence and into adulthood.
“As more youth are coming out and being supported in their transitions early in development, it is increasingly critical that clinicians understand the experiences of this cohort and not make assumptions about them as a function of older data from youth who lived under different circumstances,” the researchers emphasized. “Though we can never predict the exact gender trajectory of any child, these data suggest that many youth who identify as transgender early, and are supported through a social transition, will continue to identify as transgender 5 years after initial social transition.” They concluded that more research is needed to determine how best to support initial and later gender transitions in youth.
Study offers support for family discussions
“This study is important to help provide more data regarding the experiences of gender-diverse youth,” M. Brett Cooper, MD, of UT Southwestern Medical Center, Dallas, said in an interview. “The results of a study like this can be used by clinicians to help provide advice and guidance to parents and families as they support their children through their gender journey,” said Dr. Cooper, who was not involved in the study. The current study “also provides evidence to support that persistent, insistent, and consistent youth have an extremely low rate of retransition to a gender that aligns with their sex assigned at birth. This refutes suggestions by politicians and others that those who seek medical care have a high rate of regret or retransition,” Dr. Cooper emphasized.
“I was not surprised at all by their findings,” said Dr. Cooper. “These are very similar to what I have seen in my own panel of gender-diverse patients and what has been seen in other studies,” he noted.
The take-home message of the current study does not suggest any change in clinical practice, Dr. Cooper said. “Guidance already suggests supporting these youth on their gender journey and that for some youth, this may mean retransitioning to identify with their sex assigned at birth,” he explained.
The study was supported in part by grants to the researchers from the National Institutes of Health, the National Science Foundation, the Arcus Foundation, and the MacArthur Foundation. The researchers had no financial conflicts to disclose.
Approximately 7% of youth who chose gender identity social transition in early childhood had retransitioned 5 years later, based on data from 317 individuals.
“Increasing numbers of children are socially transitioning to live in line with their gender identity, rather than the gender assumed by their sex at birth – a process that typically involves changing a child’s pronouns, first name, hairstyle, and clothing,” wrote Kristina R. Olson, PhD, of Princeton (N.J.) University, and colleagues.
The question of whether early childhood social transitions will result in high rates of retransition continues to be a subject for debate, and long-term data on retransition rates and identity outcomes in children who transition are limited, they said.
To examine retransition in early-transitioning children, the researchers identified 317 binary socially transitioned transgender children to participate in a longitudinal study known as the Trans Youth Project (TYP) between July 2013 and December 2017. The study was published in Pediatrics. The mean age at baseline was 8 years. At study entry, participants had to have made a complete binary social transition, including changing their pronouns from those used at birth. During the 5-year follow-up period, children and parents were asked about use of puberty blockers and/or gender-affirming hormones. At study entry, 37 children had begun some type of puberty blockers. A total of 124 children initially socially transitioned before 6 years of age, and 193 initially socially transitioned at 6 years or older.
The study did not evaluate whether the participants met the DSM-5 criteria for gender dysphoria in childhood, the researchers noted. “Based on data collected at their initial visit, we do know that these participants showed signs of gender identification and gender-typed preferences commonly associated with their gender, not their sex assigned at birth,” they wrote.
Participants were classified as binary transgender, nonbinary, or cisgender based on their pronouns at follow-up. Binary transgender pronouns were associated with the other binary assigned sex, nonbinary pronouns were they/them or a mix of they/them and binary pronouns, and cisgender pronouns were those associated with assigned sex.
Overall, 7.3% of the participants had retransitioned at least once by 5 years after their initial binary social transition. The majority (94%) were living as binary transgender youth, including 1.3% who retransitioned to cisgender or nonbinary and then back to binary transgender during the follow-up period. A total of 2.5% were living as cisgender youth and 3.5% were living as nonbinary youth. These rates were similar across the initial population, as well as the 291 participants who continue to be in contact with the researchers, the 200 who had gone at least 5 years since their initial social transition, and the 280 participants who began the study before starting puberty blockers.
The researchers found no differences in retransition rates related to participant sex at birth. Rates of retransition were slightly higher among participants who made their initial social transition before 6 years of age, but these rates were low, the researchers noted.
The study findings were limited by several factors including the use of a volunteer community sample, with the potential for bias that may not generalize to the population at large, the researchers noted. Other limitations included the use of pronouns as the main criteria for retransition, and the classification of a change from binary transgender to nonbinary as a transition, they said. “Many nonbinary people consider themselves to be transgender,” they noted.
“If we had used a stricter criterion of retransition, more similar to the common use of terms like “detransition” or “desistence,” referring only to youth who are living as cisgender, then our retransition rate would have been lower (2.5%),” the researchers explained. Another limitation was the disproportionate number of trans girls, the researchers said. However, because no significant gender effect appeared in terms of retransition rates, “we do not predict any change in pattern of results if we had a different ratio of participants by sex at birth,” they said.
The researchers stated that they intend to follow the cohort through adolescence and into adulthood.
“As more youth are coming out and being supported in their transitions early in development, it is increasingly critical that clinicians understand the experiences of this cohort and not make assumptions about them as a function of older data from youth who lived under different circumstances,” the researchers emphasized. “Though we can never predict the exact gender trajectory of any child, these data suggest that many youth who identify as transgender early, and are supported through a social transition, will continue to identify as transgender 5 years after initial social transition.” They concluded that more research is needed to determine how best to support initial and later gender transitions in youth.
Study offers support for family discussions
“This study is important to help provide more data regarding the experiences of gender-diverse youth,” M. Brett Cooper, MD, of UT Southwestern Medical Center, Dallas, said in an interview. “The results of a study like this can be used by clinicians to help provide advice and guidance to parents and families as they support their children through their gender journey,” said Dr. Cooper, who was not involved in the study. The current study “also provides evidence to support that persistent, insistent, and consistent youth have an extremely low rate of retransition to a gender that aligns with their sex assigned at birth. This refutes suggestions by politicians and others that those who seek medical care have a high rate of regret or retransition,” Dr. Cooper emphasized.
“I was not surprised at all by their findings,” said Dr. Cooper. “These are very similar to what I have seen in my own panel of gender-diverse patients and what has been seen in other studies,” he noted.
The take-home message of the current study does not suggest any change in clinical practice, Dr. Cooper said. “Guidance already suggests supporting these youth on their gender journey and that for some youth, this may mean retransitioning to identify with their sex assigned at birth,” he explained.
The study was supported in part by grants to the researchers from the National Institutes of Health, the National Science Foundation, the Arcus Foundation, and the MacArthur Foundation. The researchers had no financial conflicts to disclose.
FROM PEDIATRICS
CBT or hypnotherapy may help kids’ functional abdominal pain
Functional abdominal pain in childhood and adolescence is extremely stressful for patients and a therapeutic challenge for the physicians treating them. A meta-analysis of 33 randomized-controlled studies published in JAMA Pediatrics shows that cognitive-behavioral therapy or hypnotherapy promises the greatest therapy success.
“If children or adolescents complain about chronic abdominal pain and a detailed diagnostic does not reveal any somatic cause, this is referred to as functional abdominal pain,” Burkhard Rodeck, MD, general secretary of the German Society of Pediatrics and Adolescent Medicine in Berlin, told this news organization.
Signal perception disorder
“These patients are experiencing a signal perception disorder: normal body signals, such as a slight stomach rumble, are assigned to the pain category for them much more quickly than for other people,” said Dr. Rodeck. “The meta-analysis provides confirmation of this – functional abdominal pain is actually a biopsychosocial matter.”
In the standard therapy of functional abdominal pain, however, it is also possible to choose a medicinal approach. “Studies show that herbal preparations such as peppermint oil capsules have some efficacy, since they attenuate the strength of the signals being sent from the gastrointestinal tract to the brain, with the result that they are not perceived so quickly as pain. Probiotics can also potentially help,” added Dr. Rodeck.
“If this is unsuccessful, the child must be offered a psychologic/psychotherapeutic measure, usually cognitive-behavioral therapy.”
Comparison of psychosocial therapies
The meta-analysis was carried out by a research team at the University of Central Lancashire, Preston, United Kingdom. It included 2,657 children and adolescents between the ages of 7 and 17 years, of which two-thirds were girls.
Various psychosocial therapy approaches for functional abdominal pain, such as cognitive-behavioral therapy, educational assistance, hypnotherapy (directed at the digestive system), guided meditation with relaxation, yoga, or (visceral) osteopathy were investigated and compared in the studies – sometimes against each other and sometimes against no intervention.
Lead author Morris Gordon, MBChB, PhD, professor of evidence synthesis and systematic review at the University of Central Lancashire, and his colleagues reported that cognitive-behavioral therapy was 2.37-times more likely to result in therapy success than no intervention. To treat functional abdominal pain successfully in one child or adolescent, five children needed to be treated with cognitive-behavioral therapy.
Rarer, milder pain
The children and adolescents treated with cognitive-behavioral therapy also experienced less frequent and less severe abdominal pain than the children and adolescents who did not receive any intervention. The rate of side effect–related therapy discontinuations did not differ between the groups.
Hypnotherapy could also be associated with an improved outcome, compared with no intervention, added Dr. Gordon and his colleagues. Hypnotherapy was 2.86-times more likely to result in therapy success, and the number needed to treat was five.
The other therapeutic approaches investigated did not perform any better in the studies than no intervention. However, the authors noted that evidence of the effectiveness of cognitive-behavioral therapy and hypnotherapy is moderate or weak, especially owing to the high bias risk.
“The therapy for functional abdominal pain cannot be compared with the therapy for scarlet fever, for example, where penicillin is administered in the knowledge that recovery is guaranteed. There is evidence that cognitive-behavioral therapy and possibly also hypnotherapy may help, but this is not true for every patient,” said Dr. Rodeck.
Start with the pediatrician
Dr. Gordon and his co-authors suggested considering cognitive-behavioral therapy and hypnotherapy for the treatment of functional abdominal pain in children and adolescents. But they added that further randomized controlled studies are necessary to improve the quality of evidence and therefore the reliability of these results.
Children and adolescents with functional abdominal pain do not need to be sent directly to the psychologist for treatment, said Dr. Rodeck. The pediatric or adolescent medicine specialist can also administer the initial behavioral therapy measures. “Some patients manage with the behavioral therapy approaches we offer as pediatric and adolescent medicine specialists; others require professional support with psychologic expertise,” said Dr. Rodeck. Should outpatient treatment be unsuccessful, inpatient therapy in special psychosomatic clinics or wards remains an option.
Education offers relief
For many patients, being informed about the connections and mechanisms that play a role in functional abdominal pain can offer a lot of relief, said Dr. Rodeck. Offering coping strategies that can be used in the event of acute symptoms is also a part of this education.
“If patients have functional abdominal pain for which no organic cause can be found, this can lead to frustration, sadness, and despair. The problem can become even worse if they feel that they are not being taken seriously by the physician,” said Dr. Rodeck. These negative experiences can further exacerbate the pain perception disorder. The aim of behavioral therapy measures is therefore to interrupt and downregulate this vicious cycle.
“Constant investigations are not always helpful for patients with functional abdominal pain. Time must be taken with these patients to talk and explore the options. They have definite abdominal pain, they are not imagining it. They must be taken seriously,” he emphasized.
A version of this article first appeared on Medscape.com.
Functional abdominal pain in childhood and adolescence is extremely stressful for patients and a therapeutic challenge for the physicians treating them. A meta-analysis of 33 randomized-controlled studies published in JAMA Pediatrics shows that cognitive-behavioral therapy or hypnotherapy promises the greatest therapy success.
“If children or adolescents complain about chronic abdominal pain and a detailed diagnostic does not reveal any somatic cause, this is referred to as functional abdominal pain,” Burkhard Rodeck, MD, general secretary of the German Society of Pediatrics and Adolescent Medicine in Berlin, told this news organization.
Signal perception disorder
“These patients are experiencing a signal perception disorder: normal body signals, such as a slight stomach rumble, are assigned to the pain category for them much more quickly than for other people,” said Dr. Rodeck. “The meta-analysis provides confirmation of this – functional abdominal pain is actually a biopsychosocial matter.”
In the standard therapy of functional abdominal pain, however, it is also possible to choose a medicinal approach. “Studies show that herbal preparations such as peppermint oil capsules have some efficacy, since they attenuate the strength of the signals being sent from the gastrointestinal tract to the brain, with the result that they are not perceived so quickly as pain. Probiotics can also potentially help,” added Dr. Rodeck.
“If this is unsuccessful, the child must be offered a psychologic/psychotherapeutic measure, usually cognitive-behavioral therapy.”
Comparison of psychosocial therapies
The meta-analysis was carried out by a research team at the University of Central Lancashire, Preston, United Kingdom. It included 2,657 children and adolescents between the ages of 7 and 17 years, of which two-thirds were girls.
Various psychosocial therapy approaches for functional abdominal pain, such as cognitive-behavioral therapy, educational assistance, hypnotherapy (directed at the digestive system), guided meditation with relaxation, yoga, or (visceral) osteopathy were investigated and compared in the studies – sometimes against each other and sometimes against no intervention.
Lead author Morris Gordon, MBChB, PhD, professor of evidence synthesis and systematic review at the University of Central Lancashire, and his colleagues reported that cognitive-behavioral therapy was 2.37-times more likely to result in therapy success than no intervention. To treat functional abdominal pain successfully in one child or adolescent, five children needed to be treated with cognitive-behavioral therapy.
Rarer, milder pain
The children and adolescents treated with cognitive-behavioral therapy also experienced less frequent and less severe abdominal pain than the children and adolescents who did not receive any intervention. The rate of side effect–related therapy discontinuations did not differ between the groups.
Hypnotherapy could also be associated with an improved outcome, compared with no intervention, added Dr. Gordon and his colleagues. Hypnotherapy was 2.86-times more likely to result in therapy success, and the number needed to treat was five.
The other therapeutic approaches investigated did not perform any better in the studies than no intervention. However, the authors noted that evidence of the effectiveness of cognitive-behavioral therapy and hypnotherapy is moderate or weak, especially owing to the high bias risk.
“The therapy for functional abdominal pain cannot be compared with the therapy for scarlet fever, for example, where penicillin is administered in the knowledge that recovery is guaranteed. There is evidence that cognitive-behavioral therapy and possibly also hypnotherapy may help, but this is not true for every patient,” said Dr. Rodeck.
Start with the pediatrician
Dr. Gordon and his co-authors suggested considering cognitive-behavioral therapy and hypnotherapy for the treatment of functional abdominal pain in children and adolescents. But they added that further randomized controlled studies are necessary to improve the quality of evidence and therefore the reliability of these results.
Children and adolescents with functional abdominal pain do not need to be sent directly to the psychologist for treatment, said Dr. Rodeck. The pediatric or adolescent medicine specialist can also administer the initial behavioral therapy measures. “Some patients manage with the behavioral therapy approaches we offer as pediatric and adolescent medicine specialists; others require professional support with psychologic expertise,” said Dr. Rodeck. Should outpatient treatment be unsuccessful, inpatient therapy in special psychosomatic clinics or wards remains an option.
Education offers relief
For many patients, being informed about the connections and mechanisms that play a role in functional abdominal pain can offer a lot of relief, said Dr. Rodeck. Offering coping strategies that can be used in the event of acute symptoms is also a part of this education.
“If patients have functional abdominal pain for which no organic cause can be found, this can lead to frustration, sadness, and despair. The problem can become even worse if they feel that they are not being taken seriously by the physician,” said Dr. Rodeck. These negative experiences can further exacerbate the pain perception disorder. The aim of behavioral therapy measures is therefore to interrupt and downregulate this vicious cycle.
“Constant investigations are not always helpful for patients with functional abdominal pain. Time must be taken with these patients to talk and explore the options. They have definite abdominal pain, they are not imagining it. They must be taken seriously,” he emphasized.
A version of this article first appeared on Medscape.com.
Functional abdominal pain in childhood and adolescence is extremely stressful for patients and a therapeutic challenge for the physicians treating them. A meta-analysis of 33 randomized-controlled studies published in JAMA Pediatrics shows that cognitive-behavioral therapy or hypnotherapy promises the greatest therapy success.
“If children or adolescents complain about chronic abdominal pain and a detailed diagnostic does not reveal any somatic cause, this is referred to as functional abdominal pain,” Burkhard Rodeck, MD, general secretary of the German Society of Pediatrics and Adolescent Medicine in Berlin, told this news organization.
Signal perception disorder
“These patients are experiencing a signal perception disorder: normal body signals, such as a slight stomach rumble, are assigned to the pain category for them much more quickly than for other people,” said Dr. Rodeck. “The meta-analysis provides confirmation of this – functional abdominal pain is actually a biopsychosocial matter.”
In the standard therapy of functional abdominal pain, however, it is also possible to choose a medicinal approach. “Studies show that herbal preparations such as peppermint oil capsules have some efficacy, since they attenuate the strength of the signals being sent from the gastrointestinal tract to the brain, with the result that they are not perceived so quickly as pain. Probiotics can also potentially help,” added Dr. Rodeck.
“If this is unsuccessful, the child must be offered a psychologic/psychotherapeutic measure, usually cognitive-behavioral therapy.”
Comparison of psychosocial therapies
The meta-analysis was carried out by a research team at the University of Central Lancashire, Preston, United Kingdom. It included 2,657 children and adolescents between the ages of 7 and 17 years, of which two-thirds were girls.
Various psychosocial therapy approaches for functional abdominal pain, such as cognitive-behavioral therapy, educational assistance, hypnotherapy (directed at the digestive system), guided meditation with relaxation, yoga, or (visceral) osteopathy were investigated and compared in the studies – sometimes against each other and sometimes against no intervention.
Lead author Morris Gordon, MBChB, PhD, professor of evidence synthesis and systematic review at the University of Central Lancashire, and his colleagues reported that cognitive-behavioral therapy was 2.37-times more likely to result in therapy success than no intervention. To treat functional abdominal pain successfully in one child or adolescent, five children needed to be treated with cognitive-behavioral therapy.
Rarer, milder pain
The children and adolescents treated with cognitive-behavioral therapy also experienced less frequent and less severe abdominal pain than the children and adolescents who did not receive any intervention. The rate of side effect–related therapy discontinuations did not differ between the groups.
Hypnotherapy could also be associated with an improved outcome, compared with no intervention, added Dr. Gordon and his colleagues. Hypnotherapy was 2.86-times more likely to result in therapy success, and the number needed to treat was five.
The other therapeutic approaches investigated did not perform any better in the studies than no intervention. However, the authors noted that evidence of the effectiveness of cognitive-behavioral therapy and hypnotherapy is moderate or weak, especially owing to the high bias risk.
“The therapy for functional abdominal pain cannot be compared with the therapy for scarlet fever, for example, where penicillin is administered in the knowledge that recovery is guaranteed. There is evidence that cognitive-behavioral therapy and possibly also hypnotherapy may help, but this is not true for every patient,” said Dr. Rodeck.
Start with the pediatrician
Dr. Gordon and his co-authors suggested considering cognitive-behavioral therapy and hypnotherapy for the treatment of functional abdominal pain in children and adolescents. But they added that further randomized controlled studies are necessary to improve the quality of evidence and therefore the reliability of these results.
Children and adolescents with functional abdominal pain do not need to be sent directly to the psychologist for treatment, said Dr. Rodeck. The pediatric or adolescent medicine specialist can also administer the initial behavioral therapy measures. “Some patients manage with the behavioral therapy approaches we offer as pediatric and adolescent medicine specialists; others require professional support with psychologic expertise,” said Dr. Rodeck. Should outpatient treatment be unsuccessful, inpatient therapy in special psychosomatic clinics or wards remains an option.
Education offers relief
For many patients, being informed about the connections and mechanisms that play a role in functional abdominal pain can offer a lot of relief, said Dr. Rodeck. Offering coping strategies that can be used in the event of acute symptoms is also a part of this education.
“If patients have functional abdominal pain for which no organic cause can be found, this can lead to frustration, sadness, and despair. The problem can become even worse if they feel that they are not being taken seriously by the physician,” said Dr. Rodeck. These negative experiences can further exacerbate the pain perception disorder. The aim of behavioral therapy measures is therefore to interrupt and downregulate this vicious cycle.
“Constant investigations are not always helpful for patients with functional abdominal pain. Time must be taken with these patients to talk and explore the options. They have definite abdominal pain, they are not imagining it. They must be taken seriously,” he emphasized.
A version of this article first appeared on Medscape.com.