User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Sexual dysfunction, hair loss linked with long COVID
according to findings of a large study.
Anuradhaa Subramanian, PhD, with the Institute of Applied Health Research at the University of Birmingham (England), led the research published online in Nature Medicine.
The team analyzed 486,149 electronic health records from adult patients with confirmed COVID in the United Kingdom, compared with 1.9 million people with no history of COVID, from January 2020 to April 2021. Researchers matched both groups closely in terms of demographic, social, and clinical traits.
New symptoms
The team identified 62 symptoms, including the well-known indicators of long COVID, such as fatigue, loss of sense of smell, shortness of breath, and brain fog, but also hair loss, sexual dysfunction, chest pain, fever, loss of control of bowel movements, and limb swelling.
“These differences in symptoms reported between the infected and uninfected groups remained even after we accounted for age, sex, ethnic group, socioeconomic status, body mass index, smoking status, the presence of more than 80 health conditions, and past reporting of the same symptom,” Dr. Subramanian and coresearcher Shamil Haroon, PhD, wrote in a summary of their research in The Conversation.
They pointed out that only 20 of the symptoms they found are included in the World Health Organization’s clinical case definition for long COVID.
They also found that people more likely to have persistent symptoms 3 months after COVID infection were also more likely to be young, female, smokers, to belong to certain minority ethnic groups, and to have lower socioeconomic status. They were also more likely to be obese and have a wide range of health conditions.
Dr. Haroon, an associate clinical professor at the University of Birmingham, said that one reason it appeared that younger people were more likely to get symptoms of long COVID may be that older adults with COVID were more likely to be hospitalized and weren’t included in this study.
“Since we only considered nonhospitalized adults, the older adults we included in our study may have been relatively healthier and thus had a lower symptom burden,” he said.
Dr. Subramania noted that older patients were more likely to report lasting COVID-related symptoms in the study, but when researchers accounted for a wide range of other conditions that patients had before infection (which generally more commonly happen in older adults), they found younger age as a risk factor for long-term COVID-related symptoms.
In the study period, most patients were unvaccinated, and results came before the widespread Delta and Omicron variants.
More than half (56.6%) of the patients infected with the virus that causes COVID had been diagnosed in 2020, and 43.4% in 2021. Less than 5% (4.5%) of the patients infected with the virus and 4.7% of the patients with no recorded evidence of a COVID infection had received at least a single dose of a COVID vaccine before the study started.
Eric Topol, MD, founder and director of the Scripps Research Translational Institute in La Jolla, Calif., and editor-in-chief of Medscape, said more studies need to be done to see whether results would be different with vaccination status and evolving variants.
But he noted that this study has several strengths: “The hair loss, libido loss, and ejaculation difficulty are all new symptoms,” and the study – large and carefully controlled – shows these issues were among those more likely to occur.
A loss of sense of smell – which is not a new observation – was still the most likely risk shown in the study, followed by hair loss, sneezing, ejaculation difficulty, and reduced sex drive; followed by shortness of breath, fatigue, chest pain associated with breathing difficulties, hoarseness, and fever.
Three main clusters of symptoms
Given the wide range of symptoms, long COVID likely represents a group of conditions, the authors wrote.
They found three main clusters. The largest, with roughly 80% of people with long COVID in the study, faced a broad spectrum of symptoms, ranging from fatigue to headache and pain. The second-largest group, (15%) mostly had symptoms having to do with mental health and thinking skills, including depression, anxiety, brain fog, and insomnia. The smallest group (5%) had mainly respiratory symptoms such as shortness of breath, coughing, and wheezing.
Putting symptoms in clusters will be important to start understanding what leads to long COVID, said Farha Ikramuddin, MD, a rehabilitation specialist at the University of Minnesota, Minneapolis.
She added that, while the symptoms listed in this paper are new in published research, she has certainly been seeing them over time in her long COVID clinic. (The researchers also used only coded health care data, so they were limited in what symptoms they could discover, she notes.)
Dr. Ikramuddin said a strength of the paper is its large size, but she also cautioned that it’s difficult to determine whether members of the comparison group truly had no COVID infection when the information is taken from their medical records. Often, people test at home or assume they have COVID and don’t test; therefore the information wouldn’t be recorded.
Evaluating nonhospitalized patients is also important, she said, as much of the research on long COVID has come from hospitalized patients, so little has been known about the symptoms of those with milder infections.
“Patients who have been hospitalized and have long COVID look very different from the patients who were not hospitalized,” Dr. Ikramuddin said.
One clear message from the paper, she said, is that listening and asking extensive questions about symptoms are important with patients who have had COVID.
“Counseling has also become very important for our patients in the pandemic,” she said.
It will also be important to do studies on returning to work for patients with long COVID to see how many are able to return and at what capacity, Dr. Ikramuddin said.
A version of this article first appeared on WebMD.com.
according to findings of a large study.
Anuradhaa Subramanian, PhD, with the Institute of Applied Health Research at the University of Birmingham (England), led the research published online in Nature Medicine.
The team analyzed 486,149 electronic health records from adult patients with confirmed COVID in the United Kingdom, compared with 1.9 million people with no history of COVID, from January 2020 to April 2021. Researchers matched both groups closely in terms of demographic, social, and clinical traits.
New symptoms
The team identified 62 symptoms, including the well-known indicators of long COVID, such as fatigue, loss of sense of smell, shortness of breath, and brain fog, but also hair loss, sexual dysfunction, chest pain, fever, loss of control of bowel movements, and limb swelling.
“These differences in symptoms reported between the infected and uninfected groups remained even after we accounted for age, sex, ethnic group, socioeconomic status, body mass index, smoking status, the presence of more than 80 health conditions, and past reporting of the same symptom,” Dr. Subramanian and coresearcher Shamil Haroon, PhD, wrote in a summary of their research in The Conversation.
They pointed out that only 20 of the symptoms they found are included in the World Health Organization’s clinical case definition for long COVID.
They also found that people more likely to have persistent symptoms 3 months after COVID infection were also more likely to be young, female, smokers, to belong to certain minority ethnic groups, and to have lower socioeconomic status. They were also more likely to be obese and have a wide range of health conditions.
Dr. Haroon, an associate clinical professor at the University of Birmingham, said that one reason it appeared that younger people were more likely to get symptoms of long COVID may be that older adults with COVID were more likely to be hospitalized and weren’t included in this study.
“Since we only considered nonhospitalized adults, the older adults we included in our study may have been relatively healthier and thus had a lower symptom burden,” he said.
Dr. Subramania noted that older patients were more likely to report lasting COVID-related symptoms in the study, but when researchers accounted for a wide range of other conditions that patients had before infection (which generally more commonly happen in older adults), they found younger age as a risk factor for long-term COVID-related symptoms.
In the study period, most patients were unvaccinated, and results came before the widespread Delta and Omicron variants.
More than half (56.6%) of the patients infected with the virus that causes COVID had been diagnosed in 2020, and 43.4% in 2021. Less than 5% (4.5%) of the patients infected with the virus and 4.7% of the patients with no recorded evidence of a COVID infection had received at least a single dose of a COVID vaccine before the study started.
Eric Topol, MD, founder and director of the Scripps Research Translational Institute in La Jolla, Calif., and editor-in-chief of Medscape, said more studies need to be done to see whether results would be different with vaccination status and evolving variants.
But he noted that this study has several strengths: “The hair loss, libido loss, and ejaculation difficulty are all new symptoms,” and the study – large and carefully controlled – shows these issues were among those more likely to occur.
A loss of sense of smell – which is not a new observation – was still the most likely risk shown in the study, followed by hair loss, sneezing, ejaculation difficulty, and reduced sex drive; followed by shortness of breath, fatigue, chest pain associated with breathing difficulties, hoarseness, and fever.
Three main clusters of symptoms
Given the wide range of symptoms, long COVID likely represents a group of conditions, the authors wrote.
They found three main clusters. The largest, with roughly 80% of people with long COVID in the study, faced a broad spectrum of symptoms, ranging from fatigue to headache and pain. The second-largest group, (15%) mostly had symptoms having to do with mental health and thinking skills, including depression, anxiety, brain fog, and insomnia. The smallest group (5%) had mainly respiratory symptoms such as shortness of breath, coughing, and wheezing.
Putting symptoms in clusters will be important to start understanding what leads to long COVID, said Farha Ikramuddin, MD, a rehabilitation specialist at the University of Minnesota, Minneapolis.
She added that, while the symptoms listed in this paper are new in published research, she has certainly been seeing them over time in her long COVID clinic. (The researchers also used only coded health care data, so they were limited in what symptoms they could discover, she notes.)
Dr. Ikramuddin said a strength of the paper is its large size, but she also cautioned that it’s difficult to determine whether members of the comparison group truly had no COVID infection when the information is taken from their medical records. Often, people test at home or assume they have COVID and don’t test; therefore the information wouldn’t be recorded.
Evaluating nonhospitalized patients is also important, she said, as much of the research on long COVID has come from hospitalized patients, so little has been known about the symptoms of those with milder infections.
“Patients who have been hospitalized and have long COVID look very different from the patients who were not hospitalized,” Dr. Ikramuddin said.
One clear message from the paper, she said, is that listening and asking extensive questions about symptoms are important with patients who have had COVID.
“Counseling has also become very important for our patients in the pandemic,” she said.
It will also be important to do studies on returning to work for patients with long COVID to see how many are able to return and at what capacity, Dr. Ikramuddin said.
A version of this article first appeared on WebMD.com.
according to findings of a large study.
Anuradhaa Subramanian, PhD, with the Institute of Applied Health Research at the University of Birmingham (England), led the research published online in Nature Medicine.
The team analyzed 486,149 electronic health records from adult patients with confirmed COVID in the United Kingdom, compared with 1.9 million people with no history of COVID, from January 2020 to April 2021. Researchers matched both groups closely in terms of demographic, social, and clinical traits.
New symptoms
The team identified 62 symptoms, including the well-known indicators of long COVID, such as fatigue, loss of sense of smell, shortness of breath, and brain fog, but also hair loss, sexual dysfunction, chest pain, fever, loss of control of bowel movements, and limb swelling.
“These differences in symptoms reported between the infected and uninfected groups remained even after we accounted for age, sex, ethnic group, socioeconomic status, body mass index, smoking status, the presence of more than 80 health conditions, and past reporting of the same symptom,” Dr. Subramanian and coresearcher Shamil Haroon, PhD, wrote in a summary of their research in The Conversation.
They pointed out that only 20 of the symptoms they found are included in the World Health Organization’s clinical case definition for long COVID.
They also found that people more likely to have persistent symptoms 3 months after COVID infection were also more likely to be young, female, smokers, to belong to certain minority ethnic groups, and to have lower socioeconomic status. They were also more likely to be obese and have a wide range of health conditions.
Dr. Haroon, an associate clinical professor at the University of Birmingham, said that one reason it appeared that younger people were more likely to get symptoms of long COVID may be that older adults with COVID were more likely to be hospitalized and weren’t included in this study.
“Since we only considered nonhospitalized adults, the older adults we included in our study may have been relatively healthier and thus had a lower symptom burden,” he said.
Dr. Subramania noted that older patients were more likely to report lasting COVID-related symptoms in the study, but when researchers accounted for a wide range of other conditions that patients had before infection (which generally more commonly happen in older adults), they found younger age as a risk factor for long-term COVID-related symptoms.
In the study period, most patients were unvaccinated, and results came before the widespread Delta and Omicron variants.
More than half (56.6%) of the patients infected with the virus that causes COVID had been diagnosed in 2020, and 43.4% in 2021. Less than 5% (4.5%) of the patients infected with the virus and 4.7% of the patients with no recorded evidence of a COVID infection had received at least a single dose of a COVID vaccine before the study started.
Eric Topol, MD, founder and director of the Scripps Research Translational Institute in La Jolla, Calif., and editor-in-chief of Medscape, said more studies need to be done to see whether results would be different with vaccination status and evolving variants.
But he noted that this study has several strengths: “The hair loss, libido loss, and ejaculation difficulty are all new symptoms,” and the study – large and carefully controlled – shows these issues were among those more likely to occur.
A loss of sense of smell – which is not a new observation – was still the most likely risk shown in the study, followed by hair loss, sneezing, ejaculation difficulty, and reduced sex drive; followed by shortness of breath, fatigue, chest pain associated with breathing difficulties, hoarseness, and fever.
Three main clusters of symptoms
Given the wide range of symptoms, long COVID likely represents a group of conditions, the authors wrote.
They found three main clusters. The largest, with roughly 80% of people with long COVID in the study, faced a broad spectrum of symptoms, ranging from fatigue to headache and pain. The second-largest group, (15%) mostly had symptoms having to do with mental health and thinking skills, including depression, anxiety, brain fog, and insomnia. The smallest group (5%) had mainly respiratory symptoms such as shortness of breath, coughing, and wheezing.
Putting symptoms in clusters will be important to start understanding what leads to long COVID, said Farha Ikramuddin, MD, a rehabilitation specialist at the University of Minnesota, Minneapolis.
She added that, while the symptoms listed in this paper are new in published research, she has certainly been seeing them over time in her long COVID clinic. (The researchers also used only coded health care data, so they were limited in what symptoms they could discover, she notes.)
Dr. Ikramuddin said a strength of the paper is its large size, but she also cautioned that it’s difficult to determine whether members of the comparison group truly had no COVID infection when the information is taken from their medical records. Often, people test at home or assume they have COVID and don’t test; therefore the information wouldn’t be recorded.
Evaluating nonhospitalized patients is also important, she said, as much of the research on long COVID has come from hospitalized patients, so little has been known about the symptoms of those with milder infections.
“Patients who have been hospitalized and have long COVID look very different from the patients who were not hospitalized,” Dr. Ikramuddin said.
One clear message from the paper, she said, is that listening and asking extensive questions about symptoms are important with patients who have had COVID.
“Counseling has also become very important for our patients in the pandemic,” she said.
It will also be important to do studies on returning to work for patients with long COVID to see how many are able to return and at what capacity, Dr. Ikramuddin said.
A version of this article first appeared on WebMD.com.
FROM NATURE MEDICINE
Should you sell your practice to a private equity firm?
More and more physicians are being wooed by private equity firms that want to buy their practices. The total value of private equity deals in health care in 2019 is estimated at about $120 billion, and it’s expected to grow over the coming years.
While the potential profit may seem alluring, physicians have mixed feelings as to whether this will be a boon or a disappointment.
Angelo Falcone, MD, a former emergency physician in Rockville, Md., found that a private equity investment transformed his career path.
For 19 years, Dr. Falcone was CEO of an emergency medicine group with 35 partners that staffed 10 emergency departments, mostly in Maryland. “We were a pretty small operation looking to get bigger, but to do that would require a substantial investment,” he said.
In 2015, after checking out all their options, the partners decided to sell to US Acute Care Solutions (USACS), a new private equity company founded by Welsh, Carson, Anderson & Stowe, an investment firm in New York. Private equity can be used to expand practices and pay for new equipment. Dr. Falcone, serving as a USACS board member and its operational president, helped spur the company’s astounding growth. Today, USACS has about 5,000 physicians and other clinicians operating in 30 states.
In 2019, Dr. Falcone stepped down from his management post at USACS, took training in integrative medicine, and 2 years later opened a solo integrative medicine practice in Rockville. The new practice, which operates on a concierge model, is not connected with USACS, but Dr, Falcone still sits on the USACS board.
“I had a great experience at USACS. I believe in the power of private equity to support our patients and physicians,” Dr. Falcone said. “Now, at age 58, I have a second career in integrative medicine.”
Private equity is still controversial
David Fleeger, MD, has a different opinion of private equity. “I get offers from private equity firms fairly often, but I’m not seriously interested,” said Dr. Fleeger, a surgeon with Central Texas Colon and Rectal Surgeons in Austin.
“We don’t want to sell to anybody; we want to control our destiny,” he said. “We don’t have to borrow money or repay loans, and we don’t expect to get a windfall for the practice. The profits in medicine are too narrow for that to be realistic. There is no free lunch.”
Some of the doctors who sign up for private equity deals become dissatisfied and want to end the arrangement, according to John Pinto, an ophthalmic practice management consultant in San Diego.
“I get calls about once a month from doctors who want to get out of a private equity deal or revise the terms,” he said. “Some complaints are that the PE firm was too tight with the budget, wouldn’t hire needed staff, mismanaged operations, or otherwise mishandled their investment in the practice.”
It’s difficult for disgruntled physicians to exit a private equity deal, Mr. Pinto said. They commonly have to give up part of the payment they had received for their practice if they leave prematurely, and depending on the jurisdiction, stiff noncompete clauses in their contract won’t allow them to practice nearby.
Disillusioned physicians – and even many physicians who had good experiences with private equity – usually don’t want to air their complaints in public. One reason most of these doctors keep silent is that they have signed nondisclosure and nondisparagement agreements that are part of most private equity deals.
The private equity proposition
Private equity firms typically pay a great deal more for practices than hospitals or even many large private practices, according to James D. Wall, an attorney in Winston-Salem, N.C., who has handled many private equity deals. Mr. Wall said private equity often organizes physicians around one specialty. One advantage these physicians have over hospital-employed physicians is that they aren’t under pressure to refer within a network.
Private equity companies set values for practices on the basis of their earnings before interest, taxes, depreciation, and amortization (EBITDA), said Howard Bogard, an attorney with Burr & Forman in Raleigh, N.C., who has handled many deals. Mr. Bogard said the amount physicians are paid is usually between 4 and 12 times’ EBITDA, so if your practice is earning $1 million a year in EBITDA, you would get $4 million to $12 million for it.
Of the total price tag, “Doctors get a hefty immediate payment when they sell,” Mr. Bogard said. “It might be 70% of the purchase price up front, and the 30% left over is equity in the buyer. The private equity firm then sells the practice 5-7 years later, and at that time, the physician’s equity is converted to cash and equity in the new buyer, often at the same 70/30 ratio. The idea is to keep the doctor interested in staying.”
Private equity firms expand practices to receive more favorable reimbursements and achieve economies of scale, according to Jane Zhu, MD, an assistant professor of medicine at Oregon Health & Science University, Portland, who has studied the phenomenon. Dr. Zhu said these firms may enhance profits by contracting with Medicare Advantage plans, joining accountable care organizations (ACOs), having their physicians work longer hours, and using advanced-practice clinicians instead of physicians.
“They want to make a large return in the order of 20% per year over several years, but they don’t want to strip the practice of value, because they’ll need to sell it to a new investor,” Dr. Zhu said.
When doctors sell to a private equity firm, they become employees and often have to take a pay cut, but their pay may rise again as new efficiencies are instituted. This occurred for partners in Minnesota Eye Consultants (MEC), an 11-member ophthalmology practice in Bloomington, Minn., that helped found Unifeye Vision Partners (UVP), a private equity company financed by Chicago-based Waud Capital Partners.
“When we sold the practice in 2017, we expected to see a 30% cut in the partners’ personal income,” said Richard L. Lindstrom, MD, who headed MEC until he retired last year. “Now, coming into the 6th year, all of the former partners who are still working are earning 10% above presale levels, except for one doctor who wanted to work fewer hours.” These doctors aren’t working longer hours but rather are benefiting from efficiencies, such as adding scribes and improving scheduling, he said.
Private equity brought discipline to the practice, said Dr. Lindstrom, who still sits on the Unifeye board. “In an independent practice, the partners may decide on a new piece of equipment because it would be fun to have, not because they’ve done a financial analysis,” he said. “We don’t wing it anymore.”
On the other hand, according to Dr. Zhu, some private equity firms may use draconian methods to improve efficiency. “Doctors may be expected to order or perform more services or work faster or longer to reach a certain threshold,” she said.
Can private equity uphold your interests?
To win over doctors, a private equity firm may agree to finance projects that the doctors want. For example, Dr. Lindstrom said after his group joined Unifeye, Waud Capital agreed to finance the doctors’ plan to open a new $6 million office. Before the deal, the partners would have had to take out a $6 million loan and personally guarantee it, he said.
A private equity firm may even agree to support the selling doctors’ practice philosophy, such as serving low-income patients – as long as it has a revenue stream. Luis Benavides, MD, is part of a seven-physician family medicine practice that treats many low-income patients in Laredo, Tex. “There is a lot of poverty here,” he said. This March, the group sold to a large private equity company, whose name Dr. Benavides preferred not to reveal.
One reason they made the new arrangement, Dr. Benavides said, was to qualify for ACO REACH, a new Medicare payment program that is mostly used in underserved areas and that allows more distribution of shared savings payments. “Our goal has always been better care,” he said. “We want to know how we can best serve our community.”
Dr. Benavides acknowledges that he has less independence in the new arrangement, but “I already lost my independence when I went from solo practice to a group,” he said. “The upside of a larger organization is that other people may have better ideas than you have.”
Private equity firms often set up governance structures to give physicians some measure of control. Dr. Lindstrom said the governing board of his former practice is solely made up of physicians and deals with local issues such as what office doctors will work in and how many patients they will see. Waud Capital has control of the Unifeye board of directors, but it mainly deals with larger issues, such as acquisition of more practices, he said.
In rare instances, private equity gives doctors control. Dr. Falcone said that from the start of USACS, doctors owned 65% of the company, and in 2020, the physician partners bought out Welsh Carson. “Then we engaged the private equity firm Apollo Global Management, which lent us money for the buyout and became our capital partner, with the doctors now owning 98% of the company,” he said.
On the other hand, some private equity arrangements reportedly have little regard for doctors’ well-being, especially if they are new doctors who didn’t participate in the deal and don’t have equity in it. Dr. Zhu recalled that a new physician was recruited by a practice and was promised a partnership track, but she wasn’t told that the partners were negotiating a private equity deal. “She didn’t find out until the practice was sold months later,” Dr. Zhu said. “The chances of her getting any equity now are unclear.”
Making sure that you pick a company that has your interests at heart requires a lot of digging. Dr. Lindstrom said he and his partners took 3 years to make a decision. They hired a broker to pick the 10 best private equity firms. Then they met with those companies and hired a law firm and an accounting firm to assess them. As the partners inched toward a deal, they voted on each of five critical steps in the decision-making process, he said. He noted that each vote was unanimous.
Impact of private equity
“Private equity deals are changing the health care landscape,” Mr. Wall said. “They are creating large, independent practices that help physicians remain independent from hospital systems and potentially have the clout to get more favorable reimbursements.”
“There is a lot of misunderstanding and mistrust among physicians about private equity,” Dr. Benavides said. “I imagine it will take a while for it to be accepted.”
Until the COVID pandemic, the annual number of private equity deals for doctors had been rising. Will it recover that pace? Mr. Pinto said rising interest rates may dampen activity in the near future.
“The private equity firm often performs a leveraged buyout using borrowed money,” he explained. “This works better when interest rates are low, but interest rates are trending higher. Private equity firms aren’t going away, but they may have to be less generous as the cost of money rises.”
A version of this article first appeared on Medscape.com.
More and more physicians are being wooed by private equity firms that want to buy their practices. The total value of private equity deals in health care in 2019 is estimated at about $120 billion, and it’s expected to grow over the coming years.
While the potential profit may seem alluring, physicians have mixed feelings as to whether this will be a boon or a disappointment.
Angelo Falcone, MD, a former emergency physician in Rockville, Md., found that a private equity investment transformed his career path.
For 19 years, Dr. Falcone was CEO of an emergency medicine group with 35 partners that staffed 10 emergency departments, mostly in Maryland. “We were a pretty small operation looking to get bigger, but to do that would require a substantial investment,” he said.
In 2015, after checking out all their options, the partners decided to sell to US Acute Care Solutions (USACS), a new private equity company founded by Welsh, Carson, Anderson & Stowe, an investment firm in New York. Private equity can be used to expand practices and pay for new equipment. Dr. Falcone, serving as a USACS board member and its operational president, helped spur the company’s astounding growth. Today, USACS has about 5,000 physicians and other clinicians operating in 30 states.
In 2019, Dr. Falcone stepped down from his management post at USACS, took training in integrative medicine, and 2 years later opened a solo integrative medicine practice in Rockville. The new practice, which operates on a concierge model, is not connected with USACS, but Dr, Falcone still sits on the USACS board.
“I had a great experience at USACS. I believe in the power of private equity to support our patients and physicians,” Dr. Falcone said. “Now, at age 58, I have a second career in integrative medicine.”
Private equity is still controversial
David Fleeger, MD, has a different opinion of private equity. “I get offers from private equity firms fairly often, but I’m not seriously interested,” said Dr. Fleeger, a surgeon with Central Texas Colon and Rectal Surgeons in Austin.
“We don’t want to sell to anybody; we want to control our destiny,” he said. “We don’t have to borrow money or repay loans, and we don’t expect to get a windfall for the practice. The profits in medicine are too narrow for that to be realistic. There is no free lunch.”
Some of the doctors who sign up for private equity deals become dissatisfied and want to end the arrangement, according to John Pinto, an ophthalmic practice management consultant in San Diego.
“I get calls about once a month from doctors who want to get out of a private equity deal or revise the terms,” he said. “Some complaints are that the PE firm was too tight with the budget, wouldn’t hire needed staff, mismanaged operations, or otherwise mishandled their investment in the practice.”
It’s difficult for disgruntled physicians to exit a private equity deal, Mr. Pinto said. They commonly have to give up part of the payment they had received for their practice if they leave prematurely, and depending on the jurisdiction, stiff noncompete clauses in their contract won’t allow them to practice nearby.
Disillusioned physicians – and even many physicians who had good experiences with private equity – usually don’t want to air their complaints in public. One reason most of these doctors keep silent is that they have signed nondisclosure and nondisparagement agreements that are part of most private equity deals.
The private equity proposition
Private equity firms typically pay a great deal more for practices than hospitals or even many large private practices, according to James D. Wall, an attorney in Winston-Salem, N.C., who has handled many private equity deals. Mr. Wall said private equity often organizes physicians around one specialty. One advantage these physicians have over hospital-employed physicians is that they aren’t under pressure to refer within a network.
Private equity companies set values for practices on the basis of their earnings before interest, taxes, depreciation, and amortization (EBITDA), said Howard Bogard, an attorney with Burr & Forman in Raleigh, N.C., who has handled many deals. Mr. Bogard said the amount physicians are paid is usually between 4 and 12 times’ EBITDA, so if your practice is earning $1 million a year in EBITDA, you would get $4 million to $12 million for it.
Of the total price tag, “Doctors get a hefty immediate payment when they sell,” Mr. Bogard said. “It might be 70% of the purchase price up front, and the 30% left over is equity in the buyer. The private equity firm then sells the practice 5-7 years later, and at that time, the physician’s equity is converted to cash and equity in the new buyer, often at the same 70/30 ratio. The idea is to keep the doctor interested in staying.”
Private equity firms expand practices to receive more favorable reimbursements and achieve economies of scale, according to Jane Zhu, MD, an assistant professor of medicine at Oregon Health & Science University, Portland, who has studied the phenomenon. Dr. Zhu said these firms may enhance profits by contracting with Medicare Advantage plans, joining accountable care organizations (ACOs), having their physicians work longer hours, and using advanced-practice clinicians instead of physicians.
“They want to make a large return in the order of 20% per year over several years, but they don’t want to strip the practice of value, because they’ll need to sell it to a new investor,” Dr. Zhu said.
When doctors sell to a private equity firm, they become employees and often have to take a pay cut, but their pay may rise again as new efficiencies are instituted. This occurred for partners in Minnesota Eye Consultants (MEC), an 11-member ophthalmology practice in Bloomington, Minn., that helped found Unifeye Vision Partners (UVP), a private equity company financed by Chicago-based Waud Capital Partners.
“When we sold the practice in 2017, we expected to see a 30% cut in the partners’ personal income,” said Richard L. Lindstrom, MD, who headed MEC until he retired last year. “Now, coming into the 6th year, all of the former partners who are still working are earning 10% above presale levels, except for one doctor who wanted to work fewer hours.” These doctors aren’t working longer hours but rather are benefiting from efficiencies, such as adding scribes and improving scheduling, he said.
Private equity brought discipline to the practice, said Dr. Lindstrom, who still sits on the Unifeye board. “In an independent practice, the partners may decide on a new piece of equipment because it would be fun to have, not because they’ve done a financial analysis,” he said. “We don’t wing it anymore.”
On the other hand, according to Dr. Zhu, some private equity firms may use draconian methods to improve efficiency. “Doctors may be expected to order or perform more services or work faster or longer to reach a certain threshold,” she said.
Can private equity uphold your interests?
To win over doctors, a private equity firm may agree to finance projects that the doctors want. For example, Dr. Lindstrom said after his group joined Unifeye, Waud Capital agreed to finance the doctors’ plan to open a new $6 million office. Before the deal, the partners would have had to take out a $6 million loan and personally guarantee it, he said.
A private equity firm may even agree to support the selling doctors’ practice philosophy, such as serving low-income patients – as long as it has a revenue stream. Luis Benavides, MD, is part of a seven-physician family medicine practice that treats many low-income patients in Laredo, Tex. “There is a lot of poverty here,” he said. This March, the group sold to a large private equity company, whose name Dr. Benavides preferred not to reveal.
One reason they made the new arrangement, Dr. Benavides said, was to qualify for ACO REACH, a new Medicare payment program that is mostly used in underserved areas and that allows more distribution of shared savings payments. “Our goal has always been better care,” he said. “We want to know how we can best serve our community.”
Dr. Benavides acknowledges that he has less independence in the new arrangement, but “I already lost my independence when I went from solo practice to a group,” he said. “The upside of a larger organization is that other people may have better ideas than you have.”
Private equity firms often set up governance structures to give physicians some measure of control. Dr. Lindstrom said the governing board of his former practice is solely made up of physicians and deals with local issues such as what office doctors will work in and how many patients they will see. Waud Capital has control of the Unifeye board of directors, but it mainly deals with larger issues, such as acquisition of more practices, he said.
In rare instances, private equity gives doctors control. Dr. Falcone said that from the start of USACS, doctors owned 65% of the company, and in 2020, the physician partners bought out Welsh Carson. “Then we engaged the private equity firm Apollo Global Management, which lent us money for the buyout and became our capital partner, with the doctors now owning 98% of the company,” he said.
On the other hand, some private equity arrangements reportedly have little regard for doctors’ well-being, especially if they are new doctors who didn’t participate in the deal and don’t have equity in it. Dr. Zhu recalled that a new physician was recruited by a practice and was promised a partnership track, but she wasn’t told that the partners were negotiating a private equity deal. “She didn’t find out until the practice was sold months later,” Dr. Zhu said. “The chances of her getting any equity now are unclear.”
Making sure that you pick a company that has your interests at heart requires a lot of digging. Dr. Lindstrom said he and his partners took 3 years to make a decision. They hired a broker to pick the 10 best private equity firms. Then they met with those companies and hired a law firm and an accounting firm to assess them. As the partners inched toward a deal, they voted on each of five critical steps in the decision-making process, he said. He noted that each vote was unanimous.
Impact of private equity
“Private equity deals are changing the health care landscape,” Mr. Wall said. “They are creating large, independent practices that help physicians remain independent from hospital systems and potentially have the clout to get more favorable reimbursements.”
“There is a lot of misunderstanding and mistrust among physicians about private equity,” Dr. Benavides said. “I imagine it will take a while for it to be accepted.”
Until the COVID pandemic, the annual number of private equity deals for doctors had been rising. Will it recover that pace? Mr. Pinto said rising interest rates may dampen activity in the near future.
“The private equity firm often performs a leveraged buyout using borrowed money,” he explained. “This works better when interest rates are low, but interest rates are trending higher. Private equity firms aren’t going away, but they may have to be less generous as the cost of money rises.”
A version of this article first appeared on Medscape.com.
More and more physicians are being wooed by private equity firms that want to buy their practices. The total value of private equity deals in health care in 2019 is estimated at about $120 billion, and it’s expected to grow over the coming years.
While the potential profit may seem alluring, physicians have mixed feelings as to whether this will be a boon or a disappointment.
Angelo Falcone, MD, a former emergency physician in Rockville, Md., found that a private equity investment transformed his career path.
For 19 years, Dr. Falcone was CEO of an emergency medicine group with 35 partners that staffed 10 emergency departments, mostly in Maryland. “We were a pretty small operation looking to get bigger, but to do that would require a substantial investment,” he said.
In 2015, after checking out all their options, the partners decided to sell to US Acute Care Solutions (USACS), a new private equity company founded by Welsh, Carson, Anderson & Stowe, an investment firm in New York. Private equity can be used to expand practices and pay for new equipment. Dr. Falcone, serving as a USACS board member and its operational president, helped spur the company’s astounding growth. Today, USACS has about 5,000 physicians and other clinicians operating in 30 states.
In 2019, Dr. Falcone stepped down from his management post at USACS, took training in integrative medicine, and 2 years later opened a solo integrative medicine practice in Rockville. The new practice, which operates on a concierge model, is not connected with USACS, but Dr, Falcone still sits on the USACS board.
“I had a great experience at USACS. I believe in the power of private equity to support our patients and physicians,” Dr. Falcone said. “Now, at age 58, I have a second career in integrative medicine.”
Private equity is still controversial
David Fleeger, MD, has a different opinion of private equity. “I get offers from private equity firms fairly often, but I’m not seriously interested,” said Dr. Fleeger, a surgeon with Central Texas Colon and Rectal Surgeons in Austin.
“We don’t want to sell to anybody; we want to control our destiny,” he said. “We don’t have to borrow money or repay loans, and we don’t expect to get a windfall for the practice. The profits in medicine are too narrow for that to be realistic. There is no free lunch.”
Some of the doctors who sign up for private equity deals become dissatisfied and want to end the arrangement, according to John Pinto, an ophthalmic practice management consultant in San Diego.
“I get calls about once a month from doctors who want to get out of a private equity deal or revise the terms,” he said. “Some complaints are that the PE firm was too tight with the budget, wouldn’t hire needed staff, mismanaged operations, or otherwise mishandled their investment in the practice.”
It’s difficult for disgruntled physicians to exit a private equity deal, Mr. Pinto said. They commonly have to give up part of the payment they had received for their practice if they leave prematurely, and depending on the jurisdiction, stiff noncompete clauses in their contract won’t allow them to practice nearby.
Disillusioned physicians – and even many physicians who had good experiences with private equity – usually don’t want to air their complaints in public. One reason most of these doctors keep silent is that they have signed nondisclosure and nondisparagement agreements that are part of most private equity deals.
The private equity proposition
Private equity firms typically pay a great deal more for practices than hospitals or even many large private practices, according to James D. Wall, an attorney in Winston-Salem, N.C., who has handled many private equity deals. Mr. Wall said private equity often organizes physicians around one specialty. One advantage these physicians have over hospital-employed physicians is that they aren’t under pressure to refer within a network.
Private equity companies set values for practices on the basis of their earnings before interest, taxes, depreciation, and amortization (EBITDA), said Howard Bogard, an attorney with Burr & Forman in Raleigh, N.C., who has handled many deals. Mr. Bogard said the amount physicians are paid is usually between 4 and 12 times’ EBITDA, so if your practice is earning $1 million a year in EBITDA, you would get $4 million to $12 million for it.
Of the total price tag, “Doctors get a hefty immediate payment when they sell,” Mr. Bogard said. “It might be 70% of the purchase price up front, and the 30% left over is equity in the buyer. The private equity firm then sells the practice 5-7 years later, and at that time, the physician’s equity is converted to cash and equity in the new buyer, often at the same 70/30 ratio. The idea is to keep the doctor interested in staying.”
Private equity firms expand practices to receive more favorable reimbursements and achieve economies of scale, according to Jane Zhu, MD, an assistant professor of medicine at Oregon Health & Science University, Portland, who has studied the phenomenon. Dr. Zhu said these firms may enhance profits by contracting with Medicare Advantage plans, joining accountable care organizations (ACOs), having their physicians work longer hours, and using advanced-practice clinicians instead of physicians.
“They want to make a large return in the order of 20% per year over several years, but they don’t want to strip the practice of value, because they’ll need to sell it to a new investor,” Dr. Zhu said.
When doctors sell to a private equity firm, they become employees and often have to take a pay cut, but their pay may rise again as new efficiencies are instituted. This occurred for partners in Minnesota Eye Consultants (MEC), an 11-member ophthalmology practice in Bloomington, Minn., that helped found Unifeye Vision Partners (UVP), a private equity company financed by Chicago-based Waud Capital Partners.
“When we sold the practice in 2017, we expected to see a 30% cut in the partners’ personal income,” said Richard L. Lindstrom, MD, who headed MEC until he retired last year. “Now, coming into the 6th year, all of the former partners who are still working are earning 10% above presale levels, except for one doctor who wanted to work fewer hours.” These doctors aren’t working longer hours but rather are benefiting from efficiencies, such as adding scribes and improving scheduling, he said.
Private equity brought discipline to the practice, said Dr. Lindstrom, who still sits on the Unifeye board. “In an independent practice, the partners may decide on a new piece of equipment because it would be fun to have, not because they’ve done a financial analysis,” he said. “We don’t wing it anymore.”
On the other hand, according to Dr. Zhu, some private equity firms may use draconian methods to improve efficiency. “Doctors may be expected to order or perform more services or work faster or longer to reach a certain threshold,” she said.
Can private equity uphold your interests?
To win over doctors, a private equity firm may agree to finance projects that the doctors want. For example, Dr. Lindstrom said after his group joined Unifeye, Waud Capital agreed to finance the doctors’ plan to open a new $6 million office. Before the deal, the partners would have had to take out a $6 million loan and personally guarantee it, he said.
A private equity firm may even agree to support the selling doctors’ practice philosophy, such as serving low-income patients – as long as it has a revenue stream. Luis Benavides, MD, is part of a seven-physician family medicine practice that treats many low-income patients in Laredo, Tex. “There is a lot of poverty here,” he said. This March, the group sold to a large private equity company, whose name Dr. Benavides preferred not to reveal.
One reason they made the new arrangement, Dr. Benavides said, was to qualify for ACO REACH, a new Medicare payment program that is mostly used in underserved areas and that allows more distribution of shared savings payments. “Our goal has always been better care,” he said. “We want to know how we can best serve our community.”
Dr. Benavides acknowledges that he has less independence in the new arrangement, but “I already lost my independence when I went from solo practice to a group,” he said. “The upside of a larger organization is that other people may have better ideas than you have.”
Private equity firms often set up governance structures to give physicians some measure of control. Dr. Lindstrom said the governing board of his former practice is solely made up of physicians and deals with local issues such as what office doctors will work in and how many patients they will see. Waud Capital has control of the Unifeye board of directors, but it mainly deals with larger issues, such as acquisition of more practices, he said.
In rare instances, private equity gives doctors control. Dr. Falcone said that from the start of USACS, doctors owned 65% of the company, and in 2020, the physician partners bought out Welsh Carson. “Then we engaged the private equity firm Apollo Global Management, which lent us money for the buyout and became our capital partner, with the doctors now owning 98% of the company,” he said.
On the other hand, some private equity arrangements reportedly have little regard for doctors’ well-being, especially if they are new doctors who didn’t participate in the deal and don’t have equity in it. Dr. Zhu recalled that a new physician was recruited by a practice and was promised a partnership track, but she wasn’t told that the partners were negotiating a private equity deal. “She didn’t find out until the practice was sold months later,” Dr. Zhu said. “The chances of her getting any equity now are unclear.”
Making sure that you pick a company that has your interests at heart requires a lot of digging. Dr. Lindstrom said he and his partners took 3 years to make a decision. They hired a broker to pick the 10 best private equity firms. Then they met with those companies and hired a law firm and an accounting firm to assess them. As the partners inched toward a deal, they voted on each of five critical steps in the decision-making process, he said. He noted that each vote was unanimous.
Impact of private equity
“Private equity deals are changing the health care landscape,” Mr. Wall said. “They are creating large, independent practices that help physicians remain independent from hospital systems and potentially have the clout to get more favorable reimbursements.”
“There is a lot of misunderstanding and mistrust among physicians about private equity,” Dr. Benavides said. “I imagine it will take a while for it to be accepted.”
Until the COVID pandemic, the annual number of private equity deals for doctors had been rising. Will it recover that pace? Mr. Pinto said rising interest rates may dampen activity in the near future.
“The private equity firm often performs a leveraged buyout using borrowed money,” he explained. “This works better when interest rates are low, but interest rates are trending higher. Private equity firms aren’t going away, but they may have to be less generous as the cost of money rises.”
A version of this article first appeared on Medscape.com.
Patients who engage in risky ‘chemsex’ benefit from appropriate treatment
Chemsex combines sex, drugs, and smartphones, and physicians know very little about it. Dedicated consultations were instituted in the fall of 2019 at the Infectious Diseases Department at the Saint-Louis Hospital in Paris. It’s estimated that 1,000 persons who were patients there practice chemsex.
Alexandre Aslan, MD, is one of the department’s physicians; he is also a sexologist and psychotherapist-psychoanalyst. At the ALBATROS International Congress of Addiction, which took place in the French capital in June, he presented the results of a study of patients who engage in chemsex and who regularly attend those consultations. Through this research, light is being shed on the phenomenon.
This news organization invited Dr. Aslan to discuss the issues connected with this practice.
Question: What exactly is chemsex, also known as party ‘n’ play (PnP)?
Dr. Aslan: Hearing the word “chemsex,” one would automatically think that it is what it sounds like it is: having sex while on drugs. That’s not really what it is. According to the definition that’s been published in the scientific literature, chemsex is a practice seen among men who have sex with men, where they take some very specific substances during sexual activity to sustain, enhance, or intensify the sexual experience, but also to “manage” issues related to intimacy, performance, and concerns about sexually transmitted infections (STIs). The substances are most commonly a cocktail of three drugs: GHB [gamma-hydroxybutyrate], cathinones, and crystal meth. In chemsex, smartphones play a central role as well, through the use of social networking and dating applications – those location-based apps that allow users to instantly find partners.
Question: In what ways does meeting through apps influence the sexual relationship and the use of substances?
Dr. Aslan: Because the plan to meet up for sex is being made through these kinds of apps, the promise to have sex is often implied – and this is before the individuals even meet up in real life. Let me explain. It’s not an encounter or a person that’s going to trigger sexual desire. Instead, it’s something within – the sexual “urge” inside of the individual – that’s going to drive them toward sexual activity. Now, finding yourself promising to have sex with someone – someone you don’t know, haven’t spoken to, and haven’t actually met – in an environment where it’s possible that you’ll meet several people and where the moments in which the sexual acts take place are predominantly characterized by pornography-related performance scripts: This can push you to take substances so you can “let go” and get to the point where you’re able to adapt to the requirements of the situation. Seeking to perform well and to not be overly inhibited, these individuals have found that this drug cocktail proves to be quite explosive, imparting a very strong capacity for experiencing excitement and even bringing about new sexual practices.
Question: Can you speak a bit about drug-enhanced sex?
Dr. Aslan: We sexologists consider it to be a very particular type of sex. People who engage in it feel that the sex is very intense, with unbelievable experiences, and that they have a deeper connection with their partner. In fact, it’s a type of sex where taking these substances does away with the very principles of sexual physiology – in other words, desire followed by excitement, plateau, orgasm, and resolution. Little by little, one’s sexual partner is no longer going to exist in the sex session, and the benefit is a succession of partners whose sole purpose is to keep the fire of excitement burning, an excitement that’s also reinforced by the substances taken. It’s “sex” under the influence rather than a sexual encounter linked to desire.
Question: What impact does it have on health?
Dr. Aslan: This practice brings with it numerous complications, such as STIs, but also physical injuries, as these sessions can last for 24 to more than 48 hours. There are also psychological complications, because these drugs can bring about depression, paranoia, self-harm, and even episodes of decompensation. And then, it should be noted that later on, the spotlight gets pulled away from the sex – the pretext from the very beginning – and shifts toward the taking of drugs: The individuals will no longer be able to separate the sexual encounter from the taking of drugs. Then, in a few years, there’s no longer the sexual encounter, only the taking of drugs. In the United States, between 2021 and 2022, there was a decrease in the number of deaths caused by heroin and prescription opioids. On the other hand, since 2020, the overdoses that have exploded in number are those related to fentanyl, nonprescription opioids, and stimulants – cocaine and methamphetamine, which can come back into the practices particularly through the seemingly “playful” arena of sex.
Question: How is it that things have gone from being a practice that’s under control to full-on drug addiction?
Dr. Aslan: You still have people who manage to keep things under control. But the kinds of drugs that are taken are highly addictive and compel the individual to take even more. It’s one big circle: The exciting sexual relationship itself, to which you add substances that cause even more dopamine to be released, and a smartphone screen with excitatory pornographic images on it all the time. In all the patients we see, we notice a trajectory that looks like the trajectory of every drug. When they’re at the beginning – in other words, the first year – after a first experience that they consider to be explosive, they may not return to the scene right away, and then they do return to it. They realize that it’s perhaps not as marvelous as the first time, but they’re going to give it another try. During this novelty phase, a strategy is pursued whereby they adapt and make adjustments in an attempt to feel again what they felt the first time. At the end of a year or two, they become disillusioned and they refocus on all activities having to do with drug use. Our hospital department conducted a survey where we asked detailed questions to over 100 individuals. It showed that people noticed the negative consequences that chemsex had on their work (60%), on their private lives and sex lives (55%), and on their relationships with friends and family (63%). This means that people are well aware of the negative effects that this practice has in very important areas of their lives. But even if they notice all of that, even if they resolve to have a certain number of sexual relations without drugs involved, these substances are so powerful in releasing a rush of dopamine that that very fact can sweep away any capacity the individual may have had to make a decision and stick to it, and they’re going to feel practically “compelled” to use. This is what’s called a craving.
Question: How do you identify patients who engage in chemsex among the patients in your infectious diseases department?
Dr. Aslan: As a rule, all patients admitted to our department are asked a series of questions. Do you use drugs to engage in sexual relations? Which drug do you prefer? How do you take it? Do you have a good time? Do you find that it’s good for you? Are you okay with how much you’re using? We also ask patients to tell us when they last had drug-free sex. It’s a very important question, because if we can identify someone who has had 10 or so partners a month but hasn’t had drug-free sex for over a month, we’ll try to steer the conversation to where they’ll come to think that it might not be such a bad idea to talk about it.
Question: Should a physician be asking younger patients whether they’re engaging in chemsex?
Dr. Aslan: Yes, but the physician has to be very careful. We often have a tendency to believe that we’re capable of speaking with our patients about relevant matters related to sex. We see ourselves as that kind of person, not to mention we’re open-minded. Now, as in all fields of medicine, we have to educate ourselves about how best to approach patients – in this case, about their sexual health. Because sometimes, despite our best intentions, we can do harm. The idea that we have of our own sexual behavior does not necessarily help provide counsel regarding another person’s sexual behavior, particularly when there are differences between the two. If you’re interested in the issue, you need to be trained on all the answers that could come up. There are training courses online. There’s a module on sexual health and chemsex at a site designed to give private practice physicians guidance about PrEP. It’s at least a place to start. This way, physicians will know what questions they can ask and when they should reach out to a specialist, such as a sexologist with training in these specific issues.
Question: What is the treatment based on?
Dr. Aslan: The traditional approach taken by addiction medicine physicians may not be comprehensive enough. Likewise, a sexologist’s approach alone can only go so far. It’s impossible to get by thinking that a single discipline can hold the solution, all the answers. So, it’s a multidisciplinary sexual health treatment. There should be a psychiatrist or addiction medicine physician who knows the drugs and is capable of navigating through this landscape of psychiatric comorbidities (such as psychoses and ADHD).
There also has to be a sexologist for the treatment of any sexual dysfunctions there may be. At Saint-Louis Hospital, 60% of patients who engage in chemsex said that engaging in the practice was related to a sexual problem that they noted – but never went to see a doctor about – before the first time they used. Be that as it may, it’s still the case that if these patients had been able to see a sexologist – who would have treated the problem – the drug may perhaps not have taken hold.
There also has to be a practitioner who can focus on risk reduction. In other words, someone capable of helping the patient get to the desired level of use where the craving, the need for instant gratification, can be kept in check.
In practice, one can sometimes, in addition to all of that, turn to medical treatments to manage the craving or medical comorbidities, an approach based on sexology to provide care for the sexual dysfunction or even to help the person learn how to evoke sexual or erotic fantasies without drugs, and an approach based on addiction medicine or psychotherapy, as some of our patients experienced sexual abuse in childhood. In the end, chemsex is just the outer layer – a problem that only seems to pertain to sex but that, in reality, covers up a wide range of issues. And not only sexual issues or issues that are related to drugs like chemsex is.
Question: What are the outcomes of this multidisciplinary treatment?
Dr. Aslan: Before we finish, I must point out and just state that the patients, when they’re cared for and when they’re provided with the appropriate treatment, change their practices. Some of our patients, even those with more advanced cases in terms of frequency, how often they’re injecting drugs – every 30 minutes over the course of 24 or 48 hours, with complications such as thrombosis, sepsis, and abscesses – they’ve completely stopped after several months of treatment. They now lead lives that, as they’ve told us, work better for them. So, those of us in the health care industry, we have to get organized and set things up in a way that will allow us to focus our efforts on treating these patients.
A version of this article first appeared on Medscape.com. This article was translated from the Medscape French edition.
Chemsex combines sex, drugs, and smartphones, and physicians know very little about it. Dedicated consultations were instituted in the fall of 2019 at the Infectious Diseases Department at the Saint-Louis Hospital in Paris. It’s estimated that 1,000 persons who were patients there practice chemsex.
Alexandre Aslan, MD, is one of the department’s physicians; he is also a sexologist and psychotherapist-psychoanalyst. At the ALBATROS International Congress of Addiction, which took place in the French capital in June, he presented the results of a study of patients who engage in chemsex and who regularly attend those consultations. Through this research, light is being shed on the phenomenon.
This news organization invited Dr. Aslan to discuss the issues connected with this practice.
Question: What exactly is chemsex, also known as party ‘n’ play (PnP)?
Dr. Aslan: Hearing the word “chemsex,” one would automatically think that it is what it sounds like it is: having sex while on drugs. That’s not really what it is. According to the definition that’s been published in the scientific literature, chemsex is a practice seen among men who have sex with men, where they take some very specific substances during sexual activity to sustain, enhance, or intensify the sexual experience, but also to “manage” issues related to intimacy, performance, and concerns about sexually transmitted infections (STIs). The substances are most commonly a cocktail of three drugs: GHB [gamma-hydroxybutyrate], cathinones, and crystal meth. In chemsex, smartphones play a central role as well, through the use of social networking and dating applications – those location-based apps that allow users to instantly find partners.
Question: In what ways does meeting through apps influence the sexual relationship and the use of substances?
Dr. Aslan: Because the plan to meet up for sex is being made through these kinds of apps, the promise to have sex is often implied – and this is before the individuals even meet up in real life. Let me explain. It’s not an encounter or a person that’s going to trigger sexual desire. Instead, it’s something within – the sexual “urge” inside of the individual – that’s going to drive them toward sexual activity. Now, finding yourself promising to have sex with someone – someone you don’t know, haven’t spoken to, and haven’t actually met – in an environment where it’s possible that you’ll meet several people and where the moments in which the sexual acts take place are predominantly characterized by pornography-related performance scripts: This can push you to take substances so you can “let go” and get to the point where you’re able to adapt to the requirements of the situation. Seeking to perform well and to not be overly inhibited, these individuals have found that this drug cocktail proves to be quite explosive, imparting a very strong capacity for experiencing excitement and even bringing about new sexual practices.
Question: Can you speak a bit about drug-enhanced sex?
Dr. Aslan: We sexologists consider it to be a very particular type of sex. People who engage in it feel that the sex is very intense, with unbelievable experiences, and that they have a deeper connection with their partner. In fact, it’s a type of sex where taking these substances does away with the very principles of sexual physiology – in other words, desire followed by excitement, plateau, orgasm, and resolution. Little by little, one’s sexual partner is no longer going to exist in the sex session, and the benefit is a succession of partners whose sole purpose is to keep the fire of excitement burning, an excitement that’s also reinforced by the substances taken. It’s “sex” under the influence rather than a sexual encounter linked to desire.
Question: What impact does it have on health?
Dr. Aslan: This practice brings with it numerous complications, such as STIs, but also physical injuries, as these sessions can last for 24 to more than 48 hours. There are also psychological complications, because these drugs can bring about depression, paranoia, self-harm, and even episodes of decompensation. And then, it should be noted that later on, the spotlight gets pulled away from the sex – the pretext from the very beginning – and shifts toward the taking of drugs: The individuals will no longer be able to separate the sexual encounter from the taking of drugs. Then, in a few years, there’s no longer the sexual encounter, only the taking of drugs. In the United States, between 2021 and 2022, there was a decrease in the number of deaths caused by heroin and prescription opioids. On the other hand, since 2020, the overdoses that have exploded in number are those related to fentanyl, nonprescription opioids, and stimulants – cocaine and methamphetamine, which can come back into the practices particularly through the seemingly “playful” arena of sex.
Question: How is it that things have gone from being a practice that’s under control to full-on drug addiction?
Dr. Aslan: You still have people who manage to keep things under control. But the kinds of drugs that are taken are highly addictive and compel the individual to take even more. It’s one big circle: The exciting sexual relationship itself, to which you add substances that cause even more dopamine to be released, and a smartphone screen with excitatory pornographic images on it all the time. In all the patients we see, we notice a trajectory that looks like the trajectory of every drug. When they’re at the beginning – in other words, the first year – after a first experience that they consider to be explosive, they may not return to the scene right away, and then they do return to it. They realize that it’s perhaps not as marvelous as the first time, but they’re going to give it another try. During this novelty phase, a strategy is pursued whereby they adapt and make adjustments in an attempt to feel again what they felt the first time. At the end of a year or two, they become disillusioned and they refocus on all activities having to do with drug use. Our hospital department conducted a survey where we asked detailed questions to over 100 individuals. It showed that people noticed the negative consequences that chemsex had on their work (60%), on their private lives and sex lives (55%), and on their relationships with friends and family (63%). This means that people are well aware of the negative effects that this practice has in very important areas of their lives. But even if they notice all of that, even if they resolve to have a certain number of sexual relations without drugs involved, these substances are so powerful in releasing a rush of dopamine that that very fact can sweep away any capacity the individual may have had to make a decision and stick to it, and they’re going to feel practically “compelled” to use. This is what’s called a craving.
Question: How do you identify patients who engage in chemsex among the patients in your infectious diseases department?
Dr. Aslan: As a rule, all patients admitted to our department are asked a series of questions. Do you use drugs to engage in sexual relations? Which drug do you prefer? How do you take it? Do you have a good time? Do you find that it’s good for you? Are you okay with how much you’re using? We also ask patients to tell us when they last had drug-free sex. It’s a very important question, because if we can identify someone who has had 10 or so partners a month but hasn’t had drug-free sex for over a month, we’ll try to steer the conversation to where they’ll come to think that it might not be such a bad idea to talk about it.
Question: Should a physician be asking younger patients whether they’re engaging in chemsex?
Dr. Aslan: Yes, but the physician has to be very careful. We often have a tendency to believe that we’re capable of speaking with our patients about relevant matters related to sex. We see ourselves as that kind of person, not to mention we’re open-minded. Now, as in all fields of medicine, we have to educate ourselves about how best to approach patients – in this case, about their sexual health. Because sometimes, despite our best intentions, we can do harm. The idea that we have of our own sexual behavior does not necessarily help provide counsel regarding another person’s sexual behavior, particularly when there are differences between the two. If you’re interested in the issue, you need to be trained on all the answers that could come up. There are training courses online. There’s a module on sexual health and chemsex at a site designed to give private practice physicians guidance about PrEP. It’s at least a place to start. This way, physicians will know what questions they can ask and when they should reach out to a specialist, such as a sexologist with training in these specific issues.
Question: What is the treatment based on?
Dr. Aslan: The traditional approach taken by addiction medicine physicians may not be comprehensive enough. Likewise, a sexologist’s approach alone can only go so far. It’s impossible to get by thinking that a single discipline can hold the solution, all the answers. So, it’s a multidisciplinary sexual health treatment. There should be a psychiatrist or addiction medicine physician who knows the drugs and is capable of navigating through this landscape of psychiatric comorbidities (such as psychoses and ADHD).
There also has to be a sexologist for the treatment of any sexual dysfunctions there may be. At Saint-Louis Hospital, 60% of patients who engage in chemsex said that engaging in the practice was related to a sexual problem that they noted – but never went to see a doctor about – before the first time they used. Be that as it may, it’s still the case that if these patients had been able to see a sexologist – who would have treated the problem – the drug may perhaps not have taken hold.
There also has to be a practitioner who can focus on risk reduction. In other words, someone capable of helping the patient get to the desired level of use where the craving, the need for instant gratification, can be kept in check.
In practice, one can sometimes, in addition to all of that, turn to medical treatments to manage the craving or medical comorbidities, an approach based on sexology to provide care for the sexual dysfunction or even to help the person learn how to evoke sexual or erotic fantasies without drugs, and an approach based on addiction medicine or psychotherapy, as some of our patients experienced sexual abuse in childhood. In the end, chemsex is just the outer layer – a problem that only seems to pertain to sex but that, in reality, covers up a wide range of issues. And not only sexual issues or issues that are related to drugs like chemsex is.
Question: What are the outcomes of this multidisciplinary treatment?
Dr. Aslan: Before we finish, I must point out and just state that the patients, when they’re cared for and when they’re provided with the appropriate treatment, change their practices. Some of our patients, even those with more advanced cases in terms of frequency, how often they’re injecting drugs – every 30 minutes over the course of 24 or 48 hours, with complications such as thrombosis, sepsis, and abscesses – they’ve completely stopped after several months of treatment. They now lead lives that, as they’ve told us, work better for them. So, those of us in the health care industry, we have to get organized and set things up in a way that will allow us to focus our efforts on treating these patients.
A version of this article first appeared on Medscape.com. This article was translated from the Medscape French edition.
Chemsex combines sex, drugs, and smartphones, and physicians know very little about it. Dedicated consultations were instituted in the fall of 2019 at the Infectious Diseases Department at the Saint-Louis Hospital in Paris. It’s estimated that 1,000 persons who were patients there practice chemsex.
Alexandre Aslan, MD, is one of the department’s physicians; he is also a sexologist and psychotherapist-psychoanalyst. At the ALBATROS International Congress of Addiction, which took place in the French capital in June, he presented the results of a study of patients who engage in chemsex and who regularly attend those consultations. Through this research, light is being shed on the phenomenon.
This news organization invited Dr. Aslan to discuss the issues connected with this practice.
Question: What exactly is chemsex, also known as party ‘n’ play (PnP)?
Dr. Aslan: Hearing the word “chemsex,” one would automatically think that it is what it sounds like it is: having sex while on drugs. That’s not really what it is. According to the definition that’s been published in the scientific literature, chemsex is a practice seen among men who have sex with men, where they take some very specific substances during sexual activity to sustain, enhance, or intensify the sexual experience, but also to “manage” issues related to intimacy, performance, and concerns about sexually transmitted infections (STIs). The substances are most commonly a cocktail of three drugs: GHB [gamma-hydroxybutyrate], cathinones, and crystal meth. In chemsex, smartphones play a central role as well, through the use of social networking and dating applications – those location-based apps that allow users to instantly find partners.
Question: In what ways does meeting through apps influence the sexual relationship and the use of substances?
Dr. Aslan: Because the plan to meet up for sex is being made through these kinds of apps, the promise to have sex is often implied – and this is before the individuals even meet up in real life. Let me explain. It’s not an encounter or a person that’s going to trigger sexual desire. Instead, it’s something within – the sexual “urge” inside of the individual – that’s going to drive them toward sexual activity. Now, finding yourself promising to have sex with someone – someone you don’t know, haven’t spoken to, and haven’t actually met – in an environment where it’s possible that you’ll meet several people and where the moments in which the sexual acts take place are predominantly characterized by pornography-related performance scripts: This can push you to take substances so you can “let go” and get to the point where you’re able to adapt to the requirements of the situation. Seeking to perform well and to not be overly inhibited, these individuals have found that this drug cocktail proves to be quite explosive, imparting a very strong capacity for experiencing excitement and even bringing about new sexual practices.
Question: Can you speak a bit about drug-enhanced sex?
Dr. Aslan: We sexologists consider it to be a very particular type of sex. People who engage in it feel that the sex is very intense, with unbelievable experiences, and that they have a deeper connection with their partner. In fact, it’s a type of sex where taking these substances does away with the very principles of sexual physiology – in other words, desire followed by excitement, plateau, orgasm, and resolution. Little by little, one’s sexual partner is no longer going to exist in the sex session, and the benefit is a succession of partners whose sole purpose is to keep the fire of excitement burning, an excitement that’s also reinforced by the substances taken. It’s “sex” under the influence rather than a sexual encounter linked to desire.
Question: What impact does it have on health?
Dr. Aslan: This practice brings with it numerous complications, such as STIs, but also physical injuries, as these sessions can last for 24 to more than 48 hours. There are also psychological complications, because these drugs can bring about depression, paranoia, self-harm, and even episodes of decompensation. And then, it should be noted that later on, the spotlight gets pulled away from the sex – the pretext from the very beginning – and shifts toward the taking of drugs: The individuals will no longer be able to separate the sexual encounter from the taking of drugs. Then, in a few years, there’s no longer the sexual encounter, only the taking of drugs. In the United States, between 2021 and 2022, there was a decrease in the number of deaths caused by heroin and prescription opioids. On the other hand, since 2020, the overdoses that have exploded in number are those related to fentanyl, nonprescription opioids, and stimulants – cocaine and methamphetamine, which can come back into the practices particularly through the seemingly “playful” arena of sex.
Question: How is it that things have gone from being a practice that’s under control to full-on drug addiction?
Dr. Aslan: You still have people who manage to keep things under control. But the kinds of drugs that are taken are highly addictive and compel the individual to take even more. It’s one big circle: The exciting sexual relationship itself, to which you add substances that cause even more dopamine to be released, and a smartphone screen with excitatory pornographic images on it all the time. In all the patients we see, we notice a trajectory that looks like the trajectory of every drug. When they’re at the beginning – in other words, the first year – after a first experience that they consider to be explosive, they may not return to the scene right away, and then they do return to it. They realize that it’s perhaps not as marvelous as the first time, but they’re going to give it another try. During this novelty phase, a strategy is pursued whereby they adapt and make adjustments in an attempt to feel again what they felt the first time. At the end of a year or two, they become disillusioned and they refocus on all activities having to do with drug use. Our hospital department conducted a survey where we asked detailed questions to over 100 individuals. It showed that people noticed the negative consequences that chemsex had on their work (60%), on their private lives and sex lives (55%), and on their relationships with friends and family (63%). This means that people are well aware of the negative effects that this practice has in very important areas of their lives. But even if they notice all of that, even if they resolve to have a certain number of sexual relations without drugs involved, these substances are so powerful in releasing a rush of dopamine that that very fact can sweep away any capacity the individual may have had to make a decision and stick to it, and they’re going to feel practically “compelled” to use. This is what’s called a craving.
Question: How do you identify patients who engage in chemsex among the patients in your infectious diseases department?
Dr. Aslan: As a rule, all patients admitted to our department are asked a series of questions. Do you use drugs to engage in sexual relations? Which drug do you prefer? How do you take it? Do you have a good time? Do you find that it’s good for you? Are you okay with how much you’re using? We also ask patients to tell us when they last had drug-free sex. It’s a very important question, because if we can identify someone who has had 10 or so partners a month but hasn’t had drug-free sex for over a month, we’ll try to steer the conversation to where they’ll come to think that it might not be such a bad idea to talk about it.
Question: Should a physician be asking younger patients whether they’re engaging in chemsex?
Dr. Aslan: Yes, but the physician has to be very careful. We often have a tendency to believe that we’re capable of speaking with our patients about relevant matters related to sex. We see ourselves as that kind of person, not to mention we’re open-minded. Now, as in all fields of medicine, we have to educate ourselves about how best to approach patients – in this case, about their sexual health. Because sometimes, despite our best intentions, we can do harm. The idea that we have of our own sexual behavior does not necessarily help provide counsel regarding another person’s sexual behavior, particularly when there are differences between the two. If you’re interested in the issue, you need to be trained on all the answers that could come up. There are training courses online. There’s a module on sexual health and chemsex at a site designed to give private practice physicians guidance about PrEP. It’s at least a place to start. This way, physicians will know what questions they can ask and when they should reach out to a specialist, such as a sexologist with training in these specific issues.
Question: What is the treatment based on?
Dr. Aslan: The traditional approach taken by addiction medicine physicians may not be comprehensive enough. Likewise, a sexologist’s approach alone can only go so far. It’s impossible to get by thinking that a single discipline can hold the solution, all the answers. So, it’s a multidisciplinary sexual health treatment. There should be a psychiatrist or addiction medicine physician who knows the drugs and is capable of navigating through this landscape of psychiatric comorbidities (such as psychoses and ADHD).
There also has to be a sexologist for the treatment of any sexual dysfunctions there may be. At Saint-Louis Hospital, 60% of patients who engage in chemsex said that engaging in the practice was related to a sexual problem that they noted – but never went to see a doctor about – before the first time they used. Be that as it may, it’s still the case that if these patients had been able to see a sexologist – who would have treated the problem – the drug may perhaps not have taken hold.
There also has to be a practitioner who can focus on risk reduction. In other words, someone capable of helping the patient get to the desired level of use where the craving, the need for instant gratification, can be kept in check.
In practice, one can sometimes, in addition to all of that, turn to medical treatments to manage the craving or medical comorbidities, an approach based on sexology to provide care for the sexual dysfunction or even to help the person learn how to evoke sexual or erotic fantasies without drugs, and an approach based on addiction medicine or psychotherapy, as some of our patients experienced sexual abuse in childhood. In the end, chemsex is just the outer layer – a problem that only seems to pertain to sex but that, in reality, covers up a wide range of issues. And not only sexual issues or issues that are related to drugs like chemsex is.
Question: What are the outcomes of this multidisciplinary treatment?
Dr. Aslan: Before we finish, I must point out and just state that the patients, when they’re cared for and when they’re provided with the appropriate treatment, change their practices. Some of our patients, even those with more advanced cases in terms of frequency, how often they’re injecting drugs – every 30 minutes over the course of 24 or 48 hours, with complications such as thrombosis, sepsis, and abscesses – they’ve completely stopped after several months of treatment. They now lead lives that, as they’ve told us, work better for them. So, those of us in the health care industry, we have to get organized and set things up in a way that will allow us to focus our efforts on treating these patients.
A version of this article first appeared on Medscape.com. This article was translated from the Medscape French edition.
Which factors fuel sexual violence in health care?
At the beginning of July, Brazilians across the country were appalled when they heard that an anesthesiologist was accused of sexually abusing a woman he had been treating during cesarean delivery. The incident was recorded on video by nurses and nurse technicians who, having become suspicious of the excessive amount of sedatives given to mothers-to-be by this particular anesthesiologist, decided to film him during a procedure. To do this, they made a last-minute change, switching delivery rooms to one in which they had hidden a cell phone in a cabinet.
What the footage showed was horrifying and the assailant, Giovanni Quintella Bezerra, was arrested on the spot. He’s a 32-year-old, White, successful physician, and he’s now accused of rape. The authorities are looking into whether there are more victims, others who may have been abused by the physician. The police are investigating about 40 surgeries in which Dr. Bezerra participated. That same month saw the arrest of another physician, gynecologist Ricardo Teles Martins, who was arrested after being accused of sexually harassing and abusing several women in Hidrolândia, in the northeastern state of Ceará.
In gathering information about these incidents, this news organization interviewed four Brazilian specialists to get their insights on the issues that have been brought to light by these recent cases and the factors that play a role in these kinds of criminal acts. Claudio Cohen, MD, PhD, is a psychiatrist, bioethicist, and professor at the University of São Paulo in Brazil. Daniela Pedroso, MA, is a psychologist who has 25 years’ experience working with victims of sexual violence. Gynecologist and obstetrician Jefferson Drezett, MD, PhD, is a professor in the field of population genetics and reproductive and sexual health at the Federal University of ABC, São Paulo, and in the department of health, life cycles, and society at the University of São Paulo School of Public Health. Maria Alice Scardoelli, MD, is a psychiatrist who also serves as vice-chair of the São Paulo Regional Council of Medicine (Cremesp).
Accusations and investigations
Not all incidents of sexual violence in health care institutions are reported, and precise numbers are difficult to obtain. The fact that there are any cases at all is troubling. In 2019, journalists from The Intercept found that over a period of 6 years (2014-2019), 1,734 such attacks were recorded in nine Brazilian states. They were able to get that information from the states’ Public Security Secretariats by using the Information Access Act, a law that regulates the right to access public information.
Efforts to determine how widespread this type of sexual violence is are further complicated by the difficulties in collating the accusations filed at each state’s regional council of medicine, police stations, and public prosecutor’s office. Which investigative steps are taken depends upon where the report was filed, and only occasionally do these entities communicate with each other. According to its data, Cremesp received 78 accusations in 2019. In 2020, that number increased to 84. In 2021, it was 83; these types of attacks were the seventh most common among the investigations opened that year. In the first 6 months of 2022, there were 36 complaints. The number includes investigations opened on the basis of press reports. In such cases, enough information must be available in the press reports make it possible to initiate an evaluation and assessment of the matter. There is no information about how many accusations became the subject of professional ethics proceedings and how many were formally adjudicated.
“Each accusation received is investigated by a technical committee made up of professionals from various specialties. There really needs to be a rigorous evaluation and assessment during the investigation. We cannot be unfair: It may turn out that there was no truth to the accusation after all, and yet someone’s career may already have been destroyed,” explained Dr. Scardoelli.
After the accusation is investigated and accepted by Cremesp, there is no deadline by which the proceedings must end. They can take up to 5 years, and sometimes longer. Since March, however, a deadline for the investigation period has been in effect, after which the proceedings can commence.
“We now have 90 days to make an evaluation and assessment in the investigation phase; that time period can be extended by 3 months, starting from the date the accusation is submitted to the council. If the case is accepted, then the proceedings are opened,” Dr. Scardoelli said.
Some incidents are not reported by victims. And there are incidents that are reported only after many years have passed. This was the case with Nina Marqueti, the actress at the center of #OndeDói — “Where It Hurts” — a campaign that was launched to raise awareness about sexual violence committed by health care professionals. When she was 16, her pediatrician sexually abused her. It wasn’t until 2019, more than a decade later, that she felt able to make this accusation known publicly.
Almost immediately, the campaign received over 4,000 posts online. Most of them were people’s accounts of acts of violence committed by physicians during appointments in their offices or during treatment in a hospital. These are available on Twitter under the hashtag #ondedoi.
Inadequate sex education?
News reports about physicians who abuse patients have a tremendous impact on the public. People are genuinely surprised when they hear the words “health care professional” and “sex attack” in the same sentence. “One of the most disturbing aspects is that health care professionals are committing these acts of violence against women who are in a vulnerable state, typically when they’re under anesthesia, they’ve fallen ill, or when the health care professional introduces an element of deception into the procedure so as to create the opportunity to abuse the patient in some way,” said Dr. Drezett.
As Dr. Cohen sees it, to perpetrate these acts of sexual violence, physicians – as well as lawyers, religious leaders, judges, politicians, police officers, and other persons in a position of trust – make use of their power to take advantage of a person’s vulnerability. “Physicians, lawyers, police officers, religious leaders, dads, bosses, husbands – the people who commit sexual abuse all have something in common,” he said. “In terms of the emotional aspect, all of them are taking advantage of both the power that their position holds in society and the asymmetrical power dynamics that exist between them and the other person.”
Indeed, anyone who knocks on a physician’s door seeking a diagnosis or treatment, anyone who knocks on a lawyer’s door seeking assistance, is putting themselves in a fragile situation. “The abuser considers the other person an object, not a human being who has rights,” said Dr. Cohen. People who fit the psychological and behavioral profile of a sexual assailant find in these “powerful” professions and in the circumstances and opportunities these professions provide a means to fulfill their desires. In medicine, however, there is yet another imbalance, one involving consent to touch a person’s body.
The age of the recently arrested anesthesiologist is something that caught Dr. Cohen’s attention. As noted in one of his many books, Bioética e Sexualidade nas Relações Profissionais [Bioethics and Sexuality in Professional Relationships], published in 1999 by the São Paulo Medical Association, age is a characteristic that repeatedly came up in his analysis of 150 sexual abuse proceedings handled by Cremesp.
“When I looked over the cases, I saw that most of the abusers were not right out of med school in their twenties – a time when sex is at the forefront of one’s life – nor were the abusers on the older end of the age spectrum. The abusers were, in fact, those who had already had several years of experience – as was the case with this 32-year-old anesthesiologist who, at a particular moment in time, breached all prohibitions and betrayed the expectations that society had of him as a physician: to care for people’s well-being and to alleviate their suffering. There was nothing that could hold him back from fulfilling his desire, not even the presence of nurses and other physicians in the operating room.” As for the findings of Dr. Cohen’s review, the majority of the 150 cases were dismissed because of lack of evidence.
To Ms. Pedroso, who has treated more than 12,000 victims of sexual harassment, it’s the questioning and intimidation that women feel in relationship to the male physician – a person who is viewed as holding knowledge about her body – that leaves them vulnerable and more subject to acts of violence, especially in more remote places. “We’re speaking, yet again, about rape culture. Not many people know what that term means, but, generally speaking, it has to do with the objectification of women’s bodies and the issue of boys growing up thinking they have the right to touch girls and women and that they will go unpunished for doing so.”
The lack of sex education and efforts to prevent sexual abuse are contributing factors for why the situation remains unchanged. “We are long overdue. We live in a country where there’s this completely mistaken belief that talking about sex education involves teaching children how to have sex, as opposed to teaching them how to protect themselves. We teach girls that they have to protect themselves from being raped, but we don’t teach boys not to rape.”
Another point highlighted by Ms. Pedroso is the fact that to carry out their actions, sexual assailants seek out-of-the-way places, places where they believe the rules can be bent and where they won’t be caught. This is what may have happened with Dr. Bezerra. During a recent press conference, the coordinator of the Health Section of the Rio de Janeiro Public Defender’s Office, Thaísa Guerreiro, stated that although the Women’s Hospital in São João do Meriti – one of the places where the assailant worked as an anesthesiologist – had adopted protocols to protect patients, it failed to enforce them. Another observation was that the health care professionals normalized violations of a woman’s right to have a companion present throughout labor and delivery, a right guaranteed by federal law. Ms. Guerreiro went on to say that the hospital’s chief of anesthesia and the state’s health coordination office did not question this, nor did they find it strange or surprising. According to witness statements, Dr. Bezerra would ask the patients’ husbands to leave the room in the middle of the procedure.
It should be clarified, Dr. Drezett mentioned, that although obstetric violence and sexual abuse overlap in places, they do not have the same root cause or definition. “There are two sets of situations that we term ‘obstetric violence.’ One involves any type of disrespectful treatment, whether comments or neglect, during pregnancy, delivery, or the postpartum period. The other refers to health care professionals’ attitudes in imposing inadequate and outdated medical procedures at the time of birth, such as keeping the woman fasting, having her pubic hair removed, and inducing labor or speeding up the delivery with oxytocin and [routine] episiotomy, among other things.”
Early education crucial
How are health care institutions dealing with this problem? “Very poorly. Sexual violence perpetrated by physicians and other health care professionals is a taboo subject that people are still afraid to talk about,” Dr. Cohen observed. “Regrettably, sexual violence happens all too often. Before, maybe we weren’t talking about it much because, from our viewpoint, health care professionals, such as physicians and nurses, weren’t likely to commit acts of violence while performing their duties,” noted Dr. Drezett.
Dr. Drezett also spoke about schools and what role they can play. “Of course, schools should discuss violence against women, especially in the field of health care. This has been done for a long time now, though it’s not in every curriculum in every medical school or nursing school, nor in every school of social work or of psychology,” said Dr. Drezett. For example, in the bioethics classes taken in the third and fourth years of the University of São Paolo’s medical degree program, Dr. Cohen asks students to reflect on the significance of being in a position where you ask a patient you’ve never met to undress so you can perform an exam, and the patient promptly and readily complies. “This is not about the physician, it’s about the power of the institution,” the professor pointed out. Sexual violence is a problem on the university campus as well. Another front in the battle has formed across various schools, where groups of students have created feminist collectives to have sexual violence and other issues related to gender-based violence added to the agenda.
Dr. Drezett said it’s very unlikely that efforts made during a degree program are going to succeed in preventing students who are prone to commit sexual violence from engaging in such behavior. “We’re talking about gender-specific lessons, where discussions about gender-based violence should be started much, much earlier – parents talking to their children, teachers talking to their pupils.” He also doesn’t believe that the molesters are dissuaded by the fact that these accusations get publicized in the media. “If they were, the Roger Abdelmassih case would have done away with the problem.”
On the other hand, Dr. Drezett suggested, publicizing these stories can help to bring very positive issues out into the open. What the Bezerra case made clear was that laws were not followed and rights were not protected. An environment was thus created in which the sexual crime could be perpetrated, with nurses coming to suspect acts of obstetric violence, such as use of sedation, which prevented the woman from having skin-to-skin contact with the newborn and from breastfeeding within the first few hours of birth – two clinical practices that are recommended the world over.
“Health care professionals who act properly, in accordance with best practices for interacting with others and performing daily duties, at all times, in public or private practice – they remove themselves from situations like those described in the Bezerra case; they don’t practice medicine in a reckless manner,” said Dr. Drezett.
Another negative aspect of all this, he said, is that the suspicion and wariness that patients feel may spread far and wide. “Among my colleagues are anesthetists and anesthesiologists with impeccable ethical and professional records. They are very upset that people are now regarding them with doubt and uncertainty. We need to make it clear that those horrifying cases are the exceptions, not the rule,” he said. There is also a need to correct the misconception that such abuse is always in some way associated with obstetrics and gynecology.
“This is not true. These incidents can happen in any doctor’s office. It all depends on the physician – whether he or she has designs on committing a criminal act,” Dr. Drezett noted. He did point out that there are few sexual molesters among health care professionals, though there are numerous cases. Yet this in no way diminishes the seriousness of the incidents. “Of course, we’re speaking again about the exceptions, but in my experience of treating victims, I’ve seen, for example, more cases where it’s been a police officer, not a physician, committing an act of sexual violence against a woman,” he stated.
The nurses and nurse technicians at São João do Meriti Hospital who reported the abuser acted very assertively. If they hadn’t gathered the evidence to back up their accusations, it’s possible that the physician wouldn’t have been caught in the act and that the case would have taken a different course – including pressure being put on them and their becoming the target of retaliation.
A version of this article first appeared on Medscape.com. This article was translated from the Medscape Portuguese edition.
At the beginning of July, Brazilians across the country were appalled when they heard that an anesthesiologist was accused of sexually abusing a woman he had been treating during cesarean delivery. The incident was recorded on video by nurses and nurse technicians who, having become suspicious of the excessive amount of sedatives given to mothers-to-be by this particular anesthesiologist, decided to film him during a procedure. To do this, they made a last-minute change, switching delivery rooms to one in which they had hidden a cell phone in a cabinet.
What the footage showed was horrifying and the assailant, Giovanni Quintella Bezerra, was arrested on the spot. He’s a 32-year-old, White, successful physician, and he’s now accused of rape. The authorities are looking into whether there are more victims, others who may have been abused by the physician. The police are investigating about 40 surgeries in which Dr. Bezerra participated. That same month saw the arrest of another physician, gynecologist Ricardo Teles Martins, who was arrested after being accused of sexually harassing and abusing several women in Hidrolândia, in the northeastern state of Ceará.
In gathering information about these incidents, this news organization interviewed four Brazilian specialists to get their insights on the issues that have been brought to light by these recent cases and the factors that play a role in these kinds of criminal acts. Claudio Cohen, MD, PhD, is a psychiatrist, bioethicist, and professor at the University of São Paulo in Brazil. Daniela Pedroso, MA, is a psychologist who has 25 years’ experience working with victims of sexual violence. Gynecologist and obstetrician Jefferson Drezett, MD, PhD, is a professor in the field of population genetics and reproductive and sexual health at the Federal University of ABC, São Paulo, and in the department of health, life cycles, and society at the University of São Paulo School of Public Health. Maria Alice Scardoelli, MD, is a psychiatrist who also serves as vice-chair of the São Paulo Regional Council of Medicine (Cremesp).
Accusations and investigations
Not all incidents of sexual violence in health care institutions are reported, and precise numbers are difficult to obtain. The fact that there are any cases at all is troubling. In 2019, journalists from The Intercept found that over a period of 6 years (2014-2019), 1,734 such attacks were recorded in nine Brazilian states. They were able to get that information from the states’ Public Security Secretariats by using the Information Access Act, a law that regulates the right to access public information.
Efforts to determine how widespread this type of sexual violence is are further complicated by the difficulties in collating the accusations filed at each state’s regional council of medicine, police stations, and public prosecutor’s office. Which investigative steps are taken depends upon where the report was filed, and only occasionally do these entities communicate with each other. According to its data, Cremesp received 78 accusations in 2019. In 2020, that number increased to 84. In 2021, it was 83; these types of attacks were the seventh most common among the investigations opened that year. In the first 6 months of 2022, there were 36 complaints. The number includes investigations opened on the basis of press reports. In such cases, enough information must be available in the press reports make it possible to initiate an evaluation and assessment of the matter. There is no information about how many accusations became the subject of professional ethics proceedings and how many were formally adjudicated.
“Each accusation received is investigated by a technical committee made up of professionals from various specialties. There really needs to be a rigorous evaluation and assessment during the investigation. We cannot be unfair: It may turn out that there was no truth to the accusation after all, and yet someone’s career may already have been destroyed,” explained Dr. Scardoelli.
After the accusation is investigated and accepted by Cremesp, there is no deadline by which the proceedings must end. They can take up to 5 years, and sometimes longer. Since March, however, a deadline for the investigation period has been in effect, after which the proceedings can commence.
“We now have 90 days to make an evaluation and assessment in the investigation phase; that time period can be extended by 3 months, starting from the date the accusation is submitted to the council. If the case is accepted, then the proceedings are opened,” Dr. Scardoelli said.
Some incidents are not reported by victims. And there are incidents that are reported only after many years have passed. This was the case with Nina Marqueti, the actress at the center of #OndeDói — “Where It Hurts” — a campaign that was launched to raise awareness about sexual violence committed by health care professionals. When she was 16, her pediatrician sexually abused her. It wasn’t until 2019, more than a decade later, that she felt able to make this accusation known publicly.
Almost immediately, the campaign received over 4,000 posts online. Most of them were people’s accounts of acts of violence committed by physicians during appointments in their offices or during treatment in a hospital. These are available on Twitter under the hashtag #ondedoi.
Inadequate sex education?
News reports about physicians who abuse patients have a tremendous impact on the public. People are genuinely surprised when they hear the words “health care professional” and “sex attack” in the same sentence. “One of the most disturbing aspects is that health care professionals are committing these acts of violence against women who are in a vulnerable state, typically when they’re under anesthesia, they’ve fallen ill, or when the health care professional introduces an element of deception into the procedure so as to create the opportunity to abuse the patient in some way,” said Dr. Drezett.
As Dr. Cohen sees it, to perpetrate these acts of sexual violence, physicians – as well as lawyers, religious leaders, judges, politicians, police officers, and other persons in a position of trust – make use of their power to take advantage of a person’s vulnerability. “Physicians, lawyers, police officers, religious leaders, dads, bosses, husbands – the people who commit sexual abuse all have something in common,” he said. “In terms of the emotional aspect, all of them are taking advantage of both the power that their position holds in society and the asymmetrical power dynamics that exist between them and the other person.”
Indeed, anyone who knocks on a physician’s door seeking a diagnosis or treatment, anyone who knocks on a lawyer’s door seeking assistance, is putting themselves in a fragile situation. “The abuser considers the other person an object, not a human being who has rights,” said Dr. Cohen. People who fit the psychological and behavioral profile of a sexual assailant find in these “powerful” professions and in the circumstances and opportunities these professions provide a means to fulfill their desires. In medicine, however, there is yet another imbalance, one involving consent to touch a person’s body.
The age of the recently arrested anesthesiologist is something that caught Dr. Cohen’s attention. As noted in one of his many books, Bioética e Sexualidade nas Relações Profissionais [Bioethics and Sexuality in Professional Relationships], published in 1999 by the São Paulo Medical Association, age is a characteristic that repeatedly came up in his analysis of 150 sexual abuse proceedings handled by Cremesp.
“When I looked over the cases, I saw that most of the abusers were not right out of med school in their twenties – a time when sex is at the forefront of one’s life – nor were the abusers on the older end of the age spectrum. The abusers were, in fact, those who had already had several years of experience – as was the case with this 32-year-old anesthesiologist who, at a particular moment in time, breached all prohibitions and betrayed the expectations that society had of him as a physician: to care for people’s well-being and to alleviate their suffering. There was nothing that could hold him back from fulfilling his desire, not even the presence of nurses and other physicians in the operating room.” As for the findings of Dr. Cohen’s review, the majority of the 150 cases were dismissed because of lack of evidence.
To Ms. Pedroso, who has treated more than 12,000 victims of sexual harassment, it’s the questioning and intimidation that women feel in relationship to the male physician – a person who is viewed as holding knowledge about her body – that leaves them vulnerable and more subject to acts of violence, especially in more remote places. “We’re speaking, yet again, about rape culture. Not many people know what that term means, but, generally speaking, it has to do with the objectification of women’s bodies and the issue of boys growing up thinking they have the right to touch girls and women and that they will go unpunished for doing so.”
The lack of sex education and efforts to prevent sexual abuse are contributing factors for why the situation remains unchanged. “We are long overdue. We live in a country where there’s this completely mistaken belief that talking about sex education involves teaching children how to have sex, as opposed to teaching them how to protect themselves. We teach girls that they have to protect themselves from being raped, but we don’t teach boys not to rape.”
Another point highlighted by Ms. Pedroso is the fact that to carry out their actions, sexual assailants seek out-of-the-way places, places where they believe the rules can be bent and where they won’t be caught. This is what may have happened with Dr. Bezerra. During a recent press conference, the coordinator of the Health Section of the Rio de Janeiro Public Defender’s Office, Thaísa Guerreiro, stated that although the Women’s Hospital in São João do Meriti – one of the places where the assailant worked as an anesthesiologist – had adopted protocols to protect patients, it failed to enforce them. Another observation was that the health care professionals normalized violations of a woman’s right to have a companion present throughout labor and delivery, a right guaranteed by federal law. Ms. Guerreiro went on to say that the hospital’s chief of anesthesia and the state’s health coordination office did not question this, nor did they find it strange or surprising. According to witness statements, Dr. Bezerra would ask the patients’ husbands to leave the room in the middle of the procedure.
It should be clarified, Dr. Drezett mentioned, that although obstetric violence and sexual abuse overlap in places, they do not have the same root cause or definition. “There are two sets of situations that we term ‘obstetric violence.’ One involves any type of disrespectful treatment, whether comments or neglect, during pregnancy, delivery, or the postpartum period. The other refers to health care professionals’ attitudes in imposing inadequate and outdated medical procedures at the time of birth, such as keeping the woman fasting, having her pubic hair removed, and inducing labor or speeding up the delivery with oxytocin and [routine] episiotomy, among other things.”
Early education crucial
How are health care institutions dealing with this problem? “Very poorly. Sexual violence perpetrated by physicians and other health care professionals is a taboo subject that people are still afraid to talk about,” Dr. Cohen observed. “Regrettably, sexual violence happens all too often. Before, maybe we weren’t talking about it much because, from our viewpoint, health care professionals, such as physicians and nurses, weren’t likely to commit acts of violence while performing their duties,” noted Dr. Drezett.
Dr. Drezett also spoke about schools and what role they can play. “Of course, schools should discuss violence against women, especially in the field of health care. This has been done for a long time now, though it’s not in every curriculum in every medical school or nursing school, nor in every school of social work or of psychology,” said Dr. Drezett. For example, in the bioethics classes taken in the third and fourth years of the University of São Paolo’s medical degree program, Dr. Cohen asks students to reflect on the significance of being in a position where you ask a patient you’ve never met to undress so you can perform an exam, and the patient promptly and readily complies. “This is not about the physician, it’s about the power of the institution,” the professor pointed out. Sexual violence is a problem on the university campus as well. Another front in the battle has formed across various schools, where groups of students have created feminist collectives to have sexual violence and other issues related to gender-based violence added to the agenda.
Dr. Drezett said it’s very unlikely that efforts made during a degree program are going to succeed in preventing students who are prone to commit sexual violence from engaging in such behavior. “We’re talking about gender-specific lessons, where discussions about gender-based violence should be started much, much earlier – parents talking to their children, teachers talking to their pupils.” He also doesn’t believe that the molesters are dissuaded by the fact that these accusations get publicized in the media. “If they were, the Roger Abdelmassih case would have done away with the problem.”
On the other hand, Dr. Drezett suggested, publicizing these stories can help to bring very positive issues out into the open. What the Bezerra case made clear was that laws were not followed and rights were not protected. An environment was thus created in which the sexual crime could be perpetrated, with nurses coming to suspect acts of obstetric violence, such as use of sedation, which prevented the woman from having skin-to-skin contact with the newborn and from breastfeeding within the first few hours of birth – two clinical practices that are recommended the world over.
“Health care professionals who act properly, in accordance with best practices for interacting with others and performing daily duties, at all times, in public or private practice – they remove themselves from situations like those described in the Bezerra case; they don’t practice medicine in a reckless manner,” said Dr. Drezett.
Another negative aspect of all this, he said, is that the suspicion and wariness that patients feel may spread far and wide. “Among my colleagues are anesthetists and anesthesiologists with impeccable ethical and professional records. They are very upset that people are now regarding them with doubt and uncertainty. We need to make it clear that those horrifying cases are the exceptions, not the rule,” he said. There is also a need to correct the misconception that such abuse is always in some way associated with obstetrics and gynecology.
“This is not true. These incidents can happen in any doctor’s office. It all depends on the physician – whether he or she has designs on committing a criminal act,” Dr. Drezett noted. He did point out that there are few sexual molesters among health care professionals, though there are numerous cases. Yet this in no way diminishes the seriousness of the incidents. “Of course, we’re speaking again about the exceptions, but in my experience of treating victims, I’ve seen, for example, more cases where it’s been a police officer, not a physician, committing an act of sexual violence against a woman,” he stated.
The nurses and nurse technicians at São João do Meriti Hospital who reported the abuser acted very assertively. If they hadn’t gathered the evidence to back up their accusations, it’s possible that the physician wouldn’t have been caught in the act and that the case would have taken a different course – including pressure being put on them and their becoming the target of retaliation.
A version of this article first appeared on Medscape.com. This article was translated from the Medscape Portuguese edition.
At the beginning of July, Brazilians across the country were appalled when they heard that an anesthesiologist was accused of sexually abusing a woman he had been treating during cesarean delivery. The incident was recorded on video by nurses and nurse technicians who, having become suspicious of the excessive amount of sedatives given to mothers-to-be by this particular anesthesiologist, decided to film him during a procedure. To do this, they made a last-minute change, switching delivery rooms to one in which they had hidden a cell phone in a cabinet.
What the footage showed was horrifying and the assailant, Giovanni Quintella Bezerra, was arrested on the spot. He’s a 32-year-old, White, successful physician, and he’s now accused of rape. The authorities are looking into whether there are more victims, others who may have been abused by the physician. The police are investigating about 40 surgeries in which Dr. Bezerra participated. That same month saw the arrest of another physician, gynecologist Ricardo Teles Martins, who was arrested after being accused of sexually harassing and abusing several women in Hidrolândia, in the northeastern state of Ceará.
In gathering information about these incidents, this news organization interviewed four Brazilian specialists to get their insights on the issues that have been brought to light by these recent cases and the factors that play a role in these kinds of criminal acts. Claudio Cohen, MD, PhD, is a psychiatrist, bioethicist, and professor at the University of São Paulo in Brazil. Daniela Pedroso, MA, is a psychologist who has 25 years’ experience working with victims of sexual violence. Gynecologist and obstetrician Jefferson Drezett, MD, PhD, is a professor in the field of population genetics and reproductive and sexual health at the Federal University of ABC, São Paulo, and in the department of health, life cycles, and society at the University of São Paulo School of Public Health. Maria Alice Scardoelli, MD, is a psychiatrist who also serves as vice-chair of the São Paulo Regional Council of Medicine (Cremesp).
Accusations and investigations
Not all incidents of sexual violence in health care institutions are reported, and precise numbers are difficult to obtain. The fact that there are any cases at all is troubling. In 2019, journalists from The Intercept found that over a period of 6 years (2014-2019), 1,734 such attacks were recorded in nine Brazilian states. They were able to get that information from the states’ Public Security Secretariats by using the Information Access Act, a law that regulates the right to access public information.
Efforts to determine how widespread this type of sexual violence is are further complicated by the difficulties in collating the accusations filed at each state’s regional council of medicine, police stations, and public prosecutor’s office. Which investigative steps are taken depends upon where the report was filed, and only occasionally do these entities communicate with each other. According to its data, Cremesp received 78 accusations in 2019. In 2020, that number increased to 84. In 2021, it was 83; these types of attacks were the seventh most common among the investigations opened that year. In the first 6 months of 2022, there were 36 complaints. The number includes investigations opened on the basis of press reports. In such cases, enough information must be available in the press reports make it possible to initiate an evaluation and assessment of the matter. There is no information about how many accusations became the subject of professional ethics proceedings and how many were formally adjudicated.
“Each accusation received is investigated by a technical committee made up of professionals from various specialties. There really needs to be a rigorous evaluation and assessment during the investigation. We cannot be unfair: It may turn out that there was no truth to the accusation after all, and yet someone’s career may already have been destroyed,” explained Dr. Scardoelli.
After the accusation is investigated and accepted by Cremesp, there is no deadline by which the proceedings must end. They can take up to 5 years, and sometimes longer. Since March, however, a deadline for the investigation period has been in effect, after which the proceedings can commence.
“We now have 90 days to make an evaluation and assessment in the investigation phase; that time period can be extended by 3 months, starting from the date the accusation is submitted to the council. If the case is accepted, then the proceedings are opened,” Dr. Scardoelli said.
Some incidents are not reported by victims. And there are incidents that are reported only after many years have passed. This was the case with Nina Marqueti, the actress at the center of #OndeDói — “Where It Hurts” — a campaign that was launched to raise awareness about sexual violence committed by health care professionals. When she was 16, her pediatrician sexually abused her. It wasn’t until 2019, more than a decade later, that she felt able to make this accusation known publicly.
Almost immediately, the campaign received over 4,000 posts online. Most of them were people’s accounts of acts of violence committed by physicians during appointments in their offices or during treatment in a hospital. These are available on Twitter under the hashtag #ondedoi.
Inadequate sex education?
News reports about physicians who abuse patients have a tremendous impact on the public. People are genuinely surprised when they hear the words “health care professional” and “sex attack” in the same sentence. “One of the most disturbing aspects is that health care professionals are committing these acts of violence against women who are in a vulnerable state, typically when they’re under anesthesia, they’ve fallen ill, or when the health care professional introduces an element of deception into the procedure so as to create the opportunity to abuse the patient in some way,” said Dr. Drezett.
As Dr. Cohen sees it, to perpetrate these acts of sexual violence, physicians – as well as lawyers, religious leaders, judges, politicians, police officers, and other persons in a position of trust – make use of their power to take advantage of a person’s vulnerability. “Physicians, lawyers, police officers, religious leaders, dads, bosses, husbands – the people who commit sexual abuse all have something in common,” he said. “In terms of the emotional aspect, all of them are taking advantage of both the power that their position holds in society and the asymmetrical power dynamics that exist between them and the other person.”
Indeed, anyone who knocks on a physician’s door seeking a diagnosis or treatment, anyone who knocks on a lawyer’s door seeking assistance, is putting themselves in a fragile situation. “The abuser considers the other person an object, not a human being who has rights,” said Dr. Cohen. People who fit the psychological and behavioral profile of a sexual assailant find in these “powerful” professions and in the circumstances and opportunities these professions provide a means to fulfill their desires. In medicine, however, there is yet another imbalance, one involving consent to touch a person’s body.
The age of the recently arrested anesthesiologist is something that caught Dr. Cohen’s attention. As noted in one of his many books, Bioética e Sexualidade nas Relações Profissionais [Bioethics and Sexuality in Professional Relationships], published in 1999 by the São Paulo Medical Association, age is a characteristic that repeatedly came up in his analysis of 150 sexual abuse proceedings handled by Cremesp.
“When I looked over the cases, I saw that most of the abusers were not right out of med school in their twenties – a time when sex is at the forefront of one’s life – nor were the abusers on the older end of the age spectrum. The abusers were, in fact, those who had already had several years of experience – as was the case with this 32-year-old anesthesiologist who, at a particular moment in time, breached all prohibitions and betrayed the expectations that society had of him as a physician: to care for people’s well-being and to alleviate their suffering. There was nothing that could hold him back from fulfilling his desire, not even the presence of nurses and other physicians in the operating room.” As for the findings of Dr. Cohen’s review, the majority of the 150 cases were dismissed because of lack of evidence.
To Ms. Pedroso, who has treated more than 12,000 victims of sexual harassment, it’s the questioning and intimidation that women feel in relationship to the male physician – a person who is viewed as holding knowledge about her body – that leaves them vulnerable and more subject to acts of violence, especially in more remote places. “We’re speaking, yet again, about rape culture. Not many people know what that term means, but, generally speaking, it has to do with the objectification of women’s bodies and the issue of boys growing up thinking they have the right to touch girls and women and that they will go unpunished for doing so.”
The lack of sex education and efforts to prevent sexual abuse are contributing factors for why the situation remains unchanged. “We are long overdue. We live in a country where there’s this completely mistaken belief that talking about sex education involves teaching children how to have sex, as opposed to teaching them how to protect themselves. We teach girls that they have to protect themselves from being raped, but we don’t teach boys not to rape.”
Another point highlighted by Ms. Pedroso is the fact that to carry out their actions, sexual assailants seek out-of-the-way places, places where they believe the rules can be bent and where they won’t be caught. This is what may have happened with Dr. Bezerra. During a recent press conference, the coordinator of the Health Section of the Rio de Janeiro Public Defender’s Office, Thaísa Guerreiro, stated that although the Women’s Hospital in São João do Meriti – one of the places where the assailant worked as an anesthesiologist – had adopted protocols to protect patients, it failed to enforce them. Another observation was that the health care professionals normalized violations of a woman’s right to have a companion present throughout labor and delivery, a right guaranteed by federal law. Ms. Guerreiro went on to say that the hospital’s chief of anesthesia and the state’s health coordination office did not question this, nor did they find it strange or surprising. According to witness statements, Dr. Bezerra would ask the patients’ husbands to leave the room in the middle of the procedure.
It should be clarified, Dr. Drezett mentioned, that although obstetric violence and sexual abuse overlap in places, they do not have the same root cause or definition. “There are two sets of situations that we term ‘obstetric violence.’ One involves any type of disrespectful treatment, whether comments or neglect, during pregnancy, delivery, or the postpartum period. The other refers to health care professionals’ attitudes in imposing inadequate and outdated medical procedures at the time of birth, such as keeping the woman fasting, having her pubic hair removed, and inducing labor or speeding up the delivery with oxytocin and [routine] episiotomy, among other things.”
Early education crucial
How are health care institutions dealing with this problem? “Very poorly. Sexual violence perpetrated by physicians and other health care professionals is a taboo subject that people are still afraid to talk about,” Dr. Cohen observed. “Regrettably, sexual violence happens all too often. Before, maybe we weren’t talking about it much because, from our viewpoint, health care professionals, such as physicians and nurses, weren’t likely to commit acts of violence while performing their duties,” noted Dr. Drezett.
Dr. Drezett also spoke about schools and what role they can play. “Of course, schools should discuss violence against women, especially in the field of health care. This has been done for a long time now, though it’s not in every curriculum in every medical school or nursing school, nor in every school of social work or of psychology,” said Dr. Drezett. For example, in the bioethics classes taken in the third and fourth years of the University of São Paolo’s medical degree program, Dr. Cohen asks students to reflect on the significance of being in a position where you ask a patient you’ve never met to undress so you can perform an exam, and the patient promptly and readily complies. “This is not about the physician, it’s about the power of the institution,” the professor pointed out. Sexual violence is a problem on the university campus as well. Another front in the battle has formed across various schools, where groups of students have created feminist collectives to have sexual violence and other issues related to gender-based violence added to the agenda.
Dr. Drezett said it’s very unlikely that efforts made during a degree program are going to succeed in preventing students who are prone to commit sexual violence from engaging in such behavior. “We’re talking about gender-specific lessons, where discussions about gender-based violence should be started much, much earlier – parents talking to their children, teachers talking to their pupils.” He also doesn’t believe that the molesters are dissuaded by the fact that these accusations get publicized in the media. “If they were, the Roger Abdelmassih case would have done away with the problem.”
On the other hand, Dr. Drezett suggested, publicizing these stories can help to bring very positive issues out into the open. What the Bezerra case made clear was that laws were not followed and rights were not protected. An environment was thus created in which the sexual crime could be perpetrated, with nurses coming to suspect acts of obstetric violence, such as use of sedation, which prevented the woman from having skin-to-skin contact with the newborn and from breastfeeding within the first few hours of birth – two clinical practices that are recommended the world over.
“Health care professionals who act properly, in accordance with best practices for interacting with others and performing daily duties, at all times, in public or private practice – they remove themselves from situations like those described in the Bezerra case; they don’t practice medicine in a reckless manner,” said Dr. Drezett.
Another negative aspect of all this, he said, is that the suspicion and wariness that patients feel may spread far and wide. “Among my colleagues are anesthetists and anesthesiologists with impeccable ethical and professional records. They are very upset that people are now regarding them with doubt and uncertainty. We need to make it clear that those horrifying cases are the exceptions, not the rule,” he said. There is also a need to correct the misconception that such abuse is always in some way associated with obstetrics and gynecology.
“This is not true. These incidents can happen in any doctor’s office. It all depends on the physician – whether he or she has designs on committing a criminal act,” Dr. Drezett noted. He did point out that there are few sexual molesters among health care professionals, though there are numerous cases. Yet this in no way diminishes the seriousness of the incidents. “Of course, we’re speaking again about the exceptions, but in my experience of treating victims, I’ve seen, for example, more cases where it’s been a police officer, not a physician, committing an act of sexual violence against a woman,” he stated.
The nurses and nurse technicians at São João do Meriti Hospital who reported the abuser acted very assertively. If they hadn’t gathered the evidence to back up their accusations, it’s possible that the physician wouldn’t have been caught in the act and that the case would have taken a different course – including pressure being put on them and their becoming the target of retaliation.
A version of this article first appeared on Medscape.com. This article was translated from the Medscape Portuguese edition.
Alzheimer’s disease: Alternative mechanisms make clinical progress
SAN DIEGO – In 1906, a neuroanatomist and psychiatrist named Alois Alzheimer examined the brain of a 50-year-old woman whom he had treated for paranoia, sleep and memory problems, aggression, and confusion. His autopsy revealed plaques and tangles in her brain. The most common components of these tangles are beta-amyloid peptide (A-beta) and the microtubule binding protein tau. Over the past few decades, that finding has launched many clinical development programs and dozens of clinical trials.
To date, all but one program has failed. In 2021, amidst much controversy, FDA granted accelerated approval to Biogen’s Aduhelm, which effectively clears A-beta and tau deposits from patients’ brains. The problem is that the clinical benefit is small, and uptake has been so low that the company was forced to abandon a planned postmarketing observational trial.
Chasing the wrong target?
At a session at the 2022 Alzheimer’s Association International Conference, Raymond J. Tesi, MD, rather forcefully refuted that approach. “Amyloid and tau therapies have had 20 years to prove themselves. We have multiple cases where we’ve been able to decrease amyloid, maybe not so much tau, but certainly amyloid, and the benefits are mild at best. So I think that the Alzheimer’s drug development community, whether you look at the NIH, whether you look at academia, whether you look at biopharma, has focused on a target that has not proven itself, and it’s time to move on,” said Dr. Tesi, who is president, CEO, and chief medical officer at INmune Bio.
Later in the session,
One audience member defended the potential importance of A-beta and tau, especially in astrogliosis, which is a reaction to stress by astrocytes that attempts to limit tissue damage. The questioner suggested that it was still important to measure the effect of a novel drug on A-beta and tau. “What would be the cause of the reactive astrogliosis and microglia activation, if we are not giving a damn about amyloid and tau?” he asked.
After a bit of back and forth, Dr. Tesi replied: “We both have a religious belief here, and sooner or later we’ll get the answer.”
A diverse clinical pipeline
The session itself focused on four companies, including Dr. Tesi’s INmune Bio, which have drugs with alternative mechanisms entering the advanced stages of clinical development. That’s good news, according to Heather Snyder, PhD, who is vice president of Medical & Scientific Relations at the Alzheimer’s Association. “One of the things that I think is really important is the diversity of what’s in the clinical pipeline, and it’s not just in the very beginning anymore. We’re seeing [companies] now reporting phase 2 [studies] and planning their next stage. That’s something that as a field we should be excited about. As we understand more and more about the biology, we’re now seeing that translating into clinical trials and we’re seeing that translate through the clinical pipeline of development,” said Dr. Snyder in an interview.
Targeting neuroinflammation
Dr. Tesi kicked off the session describing INmune Bio’s focus on neuroinflammation. The company’s drug candidate targets soluble tumor necrosis factor (TNF), which the company believes is a direct cause of Alzheimer’s disease through promotion of inflammation. He noted that TNF is a primary mediator of inflammation in rheumatoid arthritis, and patients with RA have an eightfold increased risk of developing Alzheimer’s disease, compared with the general population, while patients with RA who are taking anti-TNF medication have a 60% lower risk than the general population.
The company’s TNF inhibitor XPro is also unique in that it induces remyelination in mice, while other TNF inhibitors potentially “abuse” the brain by causing demyelination. Earlier research showed that it reduces neuroinflammation, improves nerve cell survival, and improves synaptic function. The company is conducting two phase 2 clinical trials, one in patients with mild cognitive impairment (MCI) and one in mild Alzheimer’s disease. They also use the MCI Alzheimer’s Cognitive Composite (EMACC) tool for assessing outcomes rather than the more commonly used Alzheimer’s Disease Assessment Scale-Cognitive subscale (ADAS-Cog). “ADAS-Cog is like trying to make sushi with an axe. It is designed for moderate to severe disease, and trying to use it for mild (Alzheimer’s disease) or MCI is a mistake. EMACC is purpose built for mild [AD] and MCI patients,” said Dr. Tesi.
Maintaining homeostatis
Next, Hans Moebius, MD, PhD, chief medical officer of Athira Pharma, described his company’s focus on the hepatocyte growth factor (HGF) receptor, also known as tyrosine kinase MET (HGF/MET). It plays an important role in brain development and homeostasis, and it is expressed at lower levels in the frontal cortex and hippocampus of patients with Alzheimer’s disease. The company’s small-molecule drug candidate boosts the HGF/MET pathway, leading to downstream neuroprotection and neurotrophic effects. It also promotes formation of new synapses.
Dr. Moebius presented the results of a phase 2 trial showing that the drug, called fosgonimeton, led to significant cognitive improvement compared with placebo. The company is conducting a phase 3 clinical trial.
Type 3 diabetes?
In his talk, John Didsbury, PhD, founder and CEO of T3D Therapeutics, framed Alzheimer’s disease as a disease of metabolic dysfunction. He believes alterations to glucose and lipids in the brain cause structural changes that lead to symptoms. He pointed out that the strongest genetic Alzheimer’s disease risk factor is a mutant form of the lipid transport protein APOE4.
“What we have is dysregulated glucose energy metabolism and lipid metabolism that really cause, in our mind, the structural event changes and the stress event changes – plaques, tangles, inflammation, etc. – but these events perpetuate the dysregulated metabolism. It’s a massive positive feedback loop that many have called type 3 diabetes – a brain-specific form of diabetes,” said Dr. Didsbury.
The company’s approach is to use systems biology to identify a drug target that can bypass multiple aberrant insulin signaling pathways. Its drug candidate regulates the expression of multiple genes involved in glucose metabolism. Dr. Didsbury presented interim results from a phase 2 study showing improvement over placebo.
Focusing on neurotoxic proteins
The final presentation of the session was by Maria Maccecchini, PhD, founder, president, and CEO of Annovis Bio. The company’s drug, buntanetap, reduces expression of a range of neurotoxic proteins. The downstream effects include restoration of axonal transport, reduction of inflammation, and protection of nerve cells. The company believes that Alzheimer’s disease results from acute and chronic stress events that lead to high levels of neurotoxic proteins, which include A-beta, tau, alpha-synuclein, and TDP43. The proteins aren’t just players in Alzheimer’s disease – they are present in abnormal levels in Parkinson’s disease and a range of other brain pathologies.
“In the brain of an Alzheimer’s and of a Parkinson’s [patient], you’re going to find all four proteins. You’ll find them in different concentrations, at different time points, in different brain areas. If you just remove one, you still have the other three that cause impairment in axonal transport, and that leads to inflammation that leads to neurodegeneration,” said Dr. Maccecchini.
The company’s drug manages to reduce levels of all four proteins by binding to a segment of messenger RNA (mRNA) shared by all of them. mRNA serves as a template for protein synthesis. Under normal conditions, the neurotoxic protein concentrations are kept low because the mRNA segment remains bound to a regulatory protein that prevents synthesis from occurring. However, when stress leads to high levels of iron, this regulatory binding protein releases the mRNA segment (along with the rest of the mRNA). The freed mRNA becomes available to the cell’s protein synthesis machinery, which starts producing high levels of neurotoxic proteins. Annovis Bio’s drug improves the ability of the regulatory protein to bind to the mRNA segment, preventing protein expression even in high-iron conditions. It works on all four neurotoxic proteins because they all have the regulatory segment in their mRNA.
The drug led to improvements in phase 2 studies of Alzheimer’s disease and Parkinson’s disease, and the company is currently recruiting for a phase 3 study in Parkinson’s disease and a phase 2/3 dose-response study in Alzheimer’s disease.
Combination treatments for a complex disease
Taken together, the presentations provided a snapshot of the post–A-beta/tau Alzheimer’s development world, and the future could be messy. Alzheimer’s disease and other dementias are likely to require combination treatments, according to Dr. Snyder. “This is a complex disease, not just Alzheimer’s but other dementias. It’s not going to be a single drug, a single target. It’s going to require some type of combinatorial approach, whether that be with medication and lifestyle interventions, or risk reduction, and different medications,” she said.
The latest results are good news for that approach: “We’re seeing that maturation of the science in these trials,” said Dr. Snyder.
Cheng Fang, PhD, senior vice president of research and development at Annovis Bio, agreed with that sentiment. “I believe [Alzheimer’s disease and dementia] is a very complicated disease. I always call them diseases instead of a disease because it’s a spectrum. I don’t believe one drug can cure them all, as much as I am confident in our drug. I think it’s extremely important to encourage this kind of diverse thinking,” said Dr. Fang.
Dr. Snyder has no relevant financial disclosures. Dr. Tesi, Dr. Moebius, Dr. Didsbury, Dr. Maccecchini, and Dr. Fang are employees and in some cases stockholders of their respective companies.
SAN DIEGO – In 1906, a neuroanatomist and psychiatrist named Alois Alzheimer examined the brain of a 50-year-old woman whom he had treated for paranoia, sleep and memory problems, aggression, and confusion. His autopsy revealed plaques and tangles in her brain. The most common components of these tangles are beta-amyloid peptide (A-beta) and the microtubule binding protein tau. Over the past few decades, that finding has launched many clinical development programs and dozens of clinical trials.
To date, all but one program has failed. In 2021, amidst much controversy, FDA granted accelerated approval to Biogen’s Aduhelm, which effectively clears A-beta and tau deposits from patients’ brains. The problem is that the clinical benefit is small, and uptake has been so low that the company was forced to abandon a planned postmarketing observational trial.
Chasing the wrong target?
At a session at the 2022 Alzheimer’s Association International Conference, Raymond J. Tesi, MD, rather forcefully refuted that approach. “Amyloid and tau therapies have had 20 years to prove themselves. We have multiple cases where we’ve been able to decrease amyloid, maybe not so much tau, but certainly amyloid, and the benefits are mild at best. So I think that the Alzheimer’s drug development community, whether you look at the NIH, whether you look at academia, whether you look at biopharma, has focused on a target that has not proven itself, and it’s time to move on,” said Dr. Tesi, who is president, CEO, and chief medical officer at INmune Bio.
Later in the session,
One audience member defended the potential importance of A-beta and tau, especially in astrogliosis, which is a reaction to stress by astrocytes that attempts to limit tissue damage. The questioner suggested that it was still important to measure the effect of a novel drug on A-beta and tau. “What would be the cause of the reactive astrogliosis and microglia activation, if we are not giving a damn about amyloid and tau?” he asked.
After a bit of back and forth, Dr. Tesi replied: “We both have a religious belief here, and sooner or later we’ll get the answer.”
A diverse clinical pipeline
The session itself focused on four companies, including Dr. Tesi’s INmune Bio, which have drugs with alternative mechanisms entering the advanced stages of clinical development. That’s good news, according to Heather Snyder, PhD, who is vice president of Medical & Scientific Relations at the Alzheimer’s Association. “One of the things that I think is really important is the diversity of what’s in the clinical pipeline, and it’s not just in the very beginning anymore. We’re seeing [companies] now reporting phase 2 [studies] and planning their next stage. That’s something that as a field we should be excited about. As we understand more and more about the biology, we’re now seeing that translating into clinical trials and we’re seeing that translate through the clinical pipeline of development,” said Dr. Snyder in an interview.
Targeting neuroinflammation
Dr. Tesi kicked off the session describing INmune Bio’s focus on neuroinflammation. The company’s drug candidate targets soluble tumor necrosis factor (TNF), which the company believes is a direct cause of Alzheimer’s disease through promotion of inflammation. He noted that TNF is a primary mediator of inflammation in rheumatoid arthritis, and patients with RA have an eightfold increased risk of developing Alzheimer’s disease, compared with the general population, while patients with RA who are taking anti-TNF medication have a 60% lower risk than the general population.
The company’s TNF inhibitor XPro is also unique in that it induces remyelination in mice, while other TNF inhibitors potentially “abuse” the brain by causing demyelination. Earlier research showed that it reduces neuroinflammation, improves nerve cell survival, and improves synaptic function. The company is conducting two phase 2 clinical trials, one in patients with mild cognitive impairment (MCI) and one in mild Alzheimer’s disease. They also use the MCI Alzheimer’s Cognitive Composite (EMACC) tool for assessing outcomes rather than the more commonly used Alzheimer’s Disease Assessment Scale-Cognitive subscale (ADAS-Cog). “ADAS-Cog is like trying to make sushi with an axe. It is designed for moderate to severe disease, and trying to use it for mild (Alzheimer’s disease) or MCI is a mistake. EMACC is purpose built for mild [AD] and MCI patients,” said Dr. Tesi.
Maintaining homeostatis
Next, Hans Moebius, MD, PhD, chief medical officer of Athira Pharma, described his company’s focus on the hepatocyte growth factor (HGF) receptor, also known as tyrosine kinase MET (HGF/MET). It plays an important role in brain development and homeostasis, and it is expressed at lower levels in the frontal cortex and hippocampus of patients with Alzheimer’s disease. The company’s small-molecule drug candidate boosts the HGF/MET pathway, leading to downstream neuroprotection and neurotrophic effects. It also promotes formation of new synapses.
Dr. Moebius presented the results of a phase 2 trial showing that the drug, called fosgonimeton, led to significant cognitive improvement compared with placebo. The company is conducting a phase 3 clinical trial.
Type 3 diabetes?
In his talk, John Didsbury, PhD, founder and CEO of T3D Therapeutics, framed Alzheimer’s disease as a disease of metabolic dysfunction. He believes alterations to glucose and lipids in the brain cause structural changes that lead to symptoms. He pointed out that the strongest genetic Alzheimer’s disease risk factor is a mutant form of the lipid transport protein APOE4.
“What we have is dysregulated glucose energy metabolism and lipid metabolism that really cause, in our mind, the structural event changes and the stress event changes – plaques, tangles, inflammation, etc. – but these events perpetuate the dysregulated metabolism. It’s a massive positive feedback loop that many have called type 3 diabetes – a brain-specific form of diabetes,” said Dr. Didsbury.
The company’s approach is to use systems biology to identify a drug target that can bypass multiple aberrant insulin signaling pathways. Its drug candidate regulates the expression of multiple genes involved in glucose metabolism. Dr. Didsbury presented interim results from a phase 2 study showing improvement over placebo.
Focusing on neurotoxic proteins
The final presentation of the session was by Maria Maccecchini, PhD, founder, president, and CEO of Annovis Bio. The company’s drug, buntanetap, reduces expression of a range of neurotoxic proteins. The downstream effects include restoration of axonal transport, reduction of inflammation, and protection of nerve cells. The company believes that Alzheimer’s disease results from acute and chronic stress events that lead to high levels of neurotoxic proteins, which include A-beta, tau, alpha-synuclein, and TDP43. The proteins aren’t just players in Alzheimer’s disease – they are present in abnormal levels in Parkinson’s disease and a range of other brain pathologies.
“In the brain of an Alzheimer’s and of a Parkinson’s [patient], you’re going to find all four proteins. You’ll find them in different concentrations, at different time points, in different brain areas. If you just remove one, you still have the other three that cause impairment in axonal transport, and that leads to inflammation that leads to neurodegeneration,” said Dr. Maccecchini.
The company’s drug manages to reduce levels of all four proteins by binding to a segment of messenger RNA (mRNA) shared by all of them. mRNA serves as a template for protein synthesis. Under normal conditions, the neurotoxic protein concentrations are kept low because the mRNA segment remains bound to a regulatory protein that prevents synthesis from occurring. However, when stress leads to high levels of iron, this regulatory binding protein releases the mRNA segment (along with the rest of the mRNA). The freed mRNA becomes available to the cell’s protein synthesis machinery, which starts producing high levels of neurotoxic proteins. Annovis Bio’s drug improves the ability of the regulatory protein to bind to the mRNA segment, preventing protein expression even in high-iron conditions. It works on all four neurotoxic proteins because they all have the regulatory segment in their mRNA.
The drug led to improvements in phase 2 studies of Alzheimer’s disease and Parkinson’s disease, and the company is currently recruiting for a phase 3 study in Parkinson’s disease and a phase 2/3 dose-response study in Alzheimer’s disease.
Combination treatments for a complex disease
Taken together, the presentations provided a snapshot of the post–A-beta/tau Alzheimer’s development world, and the future could be messy. Alzheimer’s disease and other dementias are likely to require combination treatments, according to Dr. Snyder. “This is a complex disease, not just Alzheimer’s but other dementias. It’s not going to be a single drug, a single target. It’s going to require some type of combinatorial approach, whether that be with medication and lifestyle interventions, or risk reduction, and different medications,” she said.
The latest results are good news for that approach: “We’re seeing that maturation of the science in these trials,” said Dr. Snyder.
Cheng Fang, PhD, senior vice president of research and development at Annovis Bio, agreed with that sentiment. “I believe [Alzheimer’s disease and dementia] is a very complicated disease. I always call them diseases instead of a disease because it’s a spectrum. I don’t believe one drug can cure them all, as much as I am confident in our drug. I think it’s extremely important to encourage this kind of diverse thinking,” said Dr. Fang.
Dr. Snyder has no relevant financial disclosures. Dr. Tesi, Dr. Moebius, Dr. Didsbury, Dr. Maccecchini, and Dr. Fang are employees and in some cases stockholders of their respective companies.
SAN DIEGO – In 1906, a neuroanatomist and psychiatrist named Alois Alzheimer examined the brain of a 50-year-old woman whom he had treated for paranoia, sleep and memory problems, aggression, and confusion. His autopsy revealed plaques and tangles in her brain. The most common components of these tangles are beta-amyloid peptide (A-beta) and the microtubule binding protein tau. Over the past few decades, that finding has launched many clinical development programs and dozens of clinical trials.
To date, all but one program has failed. In 2021, amidst much controversy, FDA granted accelerated approval to Biogen’s Aduhelm, which effectively clears A-beta and tau deposits from patients’ brains. The problem is that the clinical benefit is small, and uptake has been so low that the company was forced to abandon a planned postmarketing observational trial.
Chasing the wrong target?
At a session at the 2022 Alzheimer’s Association International Conference, Raymond J. Tesi, MD, rather forcefully refuted that approach. “Amyloid and tau therapies have had 20 years to prove themselves. We have multiple cases where we’ve been able to decrease amyloid, maybe not so much tau, but certainly amyloid, and the benefits are mild at best. So I think that the Alzheimer’s drug development community, whether you look at the NIH, whether you look at academia, whether you look at biopharma, has focused on a target that has not proven itself, and it’s time to move on,” said Dr. Tesi, who is president, CEO, and chief medical officer at INmune Bio.
Later in the session,
One audience member defended the potential importance of A-beta and tau, especially in astrogliosis, which is a reaction to stress by astrocytes that attempts to limit tissue damage. The questioner suggested that it was still important to measure the effect of a novel drug on A-beta and tau. “What would be the cause of the reactive astrogliosis and microglia activation, if we are not giving a damn about amyloid and tau?” he asked.
After a bit of back and forth, Dr. Tesi replied: “We both have a religious belief here, and sooner or later we’ll get the answer.”
A diverse clinical pipeline
The session itself focused on four companies, including Dr. Tesi’s INmune Bio, which have drugs with alternative mechanisms entering the advanced stages of clinical development. That’s good news, according to Heather Snyder, PhD, who is vice president of Medical & Scientific Relations at the Alzheimer’s Association. “One of the things that I think is really important is the diversity of what’s in the clinical pipeline, and it’s not just in the very beginning anymore. We’re seeing [companies] now reporting phase 2 [studies] and planning their next stage. That’s something that as a field we should be excited about. As we understand more and more about the biology, we’re now seeing that translating into clinical trials and we’re seeing that translate through the clinical pipeline of development,” said Dr. Snyder in an interview.
Targeting neuroinflammation
Dr. Tesi kicked off the session describing INmune Bio’s focus on neuroinflammation. The company’s drug candidate targets soluble tumor necrosis factor (TNF), which the company believes is a direct cause of Alzheimer’s disease through promotion of inflammation. He noted that TNF is a primary mediator of inflammation in rheumatoid arthritis, and patients with RA have an eightfold increased risk of developing Alzheimer’s disease, compared with the general population, while patients with RA who are taking anti-TNF medication have a 60% lower risk than the general population.
The company’s TNF inhibitor XPro is also unique in that it induces remyelination in mice, while other TNF inhibitors potentially “abuse” the brain by causing demyelination. Earlier research showed that it reduces neuroinflammation, improves nerve cell survival, and improves synaptic function. The company is conducting two phase 2 clinical trials, one in patients with mild cognitive impairment (MCI) and one in mild Alzheimer’s disease. They also use the MCI Alzheimer’s Cognitive Composite (EMACC) tool for assessing outcomes rather than the more commonly used Alzheimer’s Disease Assessment Scale-Cognitive subscale (ADAS-Cog). “ADAS-Cog is like trying to make sushi with an axe. It is designed for moderate to severe disease, and trying to use it for mild (Alzheimer’s disease) or MCI is a mistake. EMACC is purpose built for mild [AD] and MCI patients,” said Dr. Tesi.
Maintaining homeostatis
Next, Hans Moebius, MD, PhD, chief medical officer of Athira Pharma, described his company’s focus on the hepatocyte growth factor (HGF) receptor, also known as tyrosine kinase MET (HGF/MET). It plays an important role in brain development and homeostasis, and it is expressed at lower levels in the frontal cortex and hippocampus of patients with Alzheimer’s disease. The company’s small-molecule drug candidate boosts the HGF/MET pathway, leading to downstream neuroprotection and neurotrophic effects. It also promotes formation of new synapses.
Dr. Moebius presented the results of a phase 2 trial showing that the drug, called fosgonimeton, led to significant cognitive improvement compared with placebo. The company is conducting a phase 3 clinical trial.
Type 3 diabetes?
In his talk, John Didsbury, PhD, founder and CEO of T3D Therapeutics, framed Alzheimer’s disease as a disease of metabolic dysfunction. He believes alterations to glucose and lipids in the brain cause structural changes that lead to symptoms. He pointed out that the strongest genetic Alzheimer’s disease risk factor is a mutant form of the lipid transport protein APOE4.
“What we have is dysregulated glucose energy metabolism and lipid metabolism that really cause, in our mind, the structural event changes and the stress event changes – plaques, tangles, inflammation, etc. – but these events perpetuate the dysregulated metabolism. It’s a massive positive feedback loop that many have called type 3 diabetes – a brain-specific form of diabetes,” said Dr. Didsbury.
The company’s approach is to use systems biology to identify a drug target that can bypass multiple aberrant insulin signaling pathways. Its drug candidate regulates the expression of multiple genes involved in glucose metabolism. Dr. Didsbury presented interim results from a phase 2 study showing improvement over placebo.
Focusing on neurotoxic proteins
The final presentation of the session was by Maria Maccecchini, PhD, founder, president, and CEO of Annovis Bio. The company’s drug, buntanetap, reduces expression of a range of neurotoxic proteins. The downstream effects include restoration of axonal transport, reduction of inflammation, and protection of nerve cells. The company believes that Alzheimer’s disease results from acute and chronic stress events that lead to high levels of neurotoxic proteins, which include A-beta, tau, alpha-synuclein, and TDP43. The proteins aren’t just players in Alzheimer’s disease – they are present in abnormal levels in Parkinson’s disease and a range of other brain pathologies.
“In the brain of an Alzheimer’s and of a Parkinson’s [patient], you’re going to find all four proteins. You’ll find them in different concentrations, at different time points, in different brain areas. If you just remove one, you still have the other three that cause impairment in axonal transport, and that leads to inflammation that leads to neurodegeneration,” said Dr. Maccecchini.
The company’s drug manages to reduce levels of all four proteins by binding to a segment of messenger RNA (mRNA) shared by all of them. mRNA serves as a template for protein synthesis. Under normal conditions, the neurotoxic protein concentrations are kept low because the mRNA segment remains bound to a regulatory protein that prevents synthesis from occurring. However, when stress leads to high levels of iron, this regulatory binding protein releases the mRNA segment (along with the rest of the mRNA). The freed mRNA becomes available to the cell’s protein synthesis machinery, which starts producing high levels of neurotoxic proteins. Annovis Bio’s drug improves the ability of the regulatory protein to bind to the mRNA segment, preventing protein expression even in high-iron conditions. It works on all four neurotoxic proteins because they all have the regulatory segment in their mRNA.
The drug led to improvements in phase 2 studies of Alzheimer’s disease and Parkinson’s disease, and the company is currently recruiting for a phase 3 study in Parkinson’s disease and a phase 2/3 dose-response study in Alzheimer’s disease.
Combination treatments for a complex disease
Taken together, the presentations provided a snapshot of the post–A-beta/tau Alzheimer’s development world, and the future could be messy. Alzheimer’s disease and other dementias are likely to require combination treatments, according to Dr. Snyder. “This is a complex disease, not just Alzheimer’s but other dementias. It’s not going to be a single drug, a single target. It’s going to require some type of combinatorial approach, whether that be with medication and lifestyle interventions, or risk reduction, and different medications,” she said.
The latest results are good news for that approach: “We’re seeing that maturation of the science in these trials,” said Dr. Snyder.
Cheng Fang, PhD, senior vice president of research and development at Annovis Bio, agreed with that sentiment. “I believe [Alzheimer’s disease and dementia] is a very complicated disease. I always call them diseases instead of a disease because it’s a spectrum. I don’t believe one drug can cure them all, as much as I am confident in our drug. I think it’s extremely important to encourage this kind of diverse thinking,” said Dr. Fang.
Dr. Snyder has no relevant financial disclosures. Dr. Tesi, Dr. Moebius, Dr. Didsbury, Dr. Maccecchini, and Dr. Fang are employees and in some cases stockholders of their respective companies.
AT AAIC 2022
Saddled with med school debt, yet left out of loan forgiveness plans
In a recently obtained plan by Politico, the Biden administration is zeroing in on a broad student loan forgiveness plan to be released imminently. The plan would broadly forgive $10,000 in federal student loans, including graduate and PLUS loans. However, there’s a rub: The plan restricts the forgiveness to those with incomes below $150,000.
This would unfairly exclude many in health care from receiving this forgiveness, an egregious oversight given how much health care providers have sacrificed during the pandemic.
What was proposed?
Previously, it was reported that the Biden administration was considering this same amount of forgiveness, but with plans to exclude borrowers by either career or income. Student loan payments have been on an extended CARES Act forbearance since March 2020, with payment resumption planned for Aug. 31. The administration has said that they would deliver a plan for further extensions before this date and have repeatedly teased including forgiveness.
Forgiveness for some ...
Forgiving $10,000 of federal student loans would relieve some 15 million borrowers of student debt, roughly one-third of the 45 million borrowers with debt.
This would provide a massive boost to these borrowers (who disproportionately are female, low-income, and non-White), many of whom were targeted by predatory institutions whose education didn’t offer any actual tangible benefit to their earnings. While this is a group that absolutely ought to have their loans forgiven, drawing an income line inappropriately restricts those in health care from receiving any forgiveness.
... But not for others
Someone making an annual gross income of $150,000 is in the 80th percentile of earners in the United States (for comparison, the top 1% took home more than $505,000 in 2021). What student loan borrowers make up the remaining 20%? Overwhelmingly, health care providers occupy that tier: physicians, dentists, veterinarians, and advanced-practice nurses.
These schools leave their graduates with some of the highest student loan burdens, with veterinarians, dentists, and physicians having the highest debt-to-income ratios of any professional careers.
Flat forgiveness is regressive
Forgiving any student debt is the right direction. Too may have fallen victim to an industry without quality control, appropriate regulation, or price control. Quite the opposite, the blank-check model of student loan financing has led to an arms race as it comes to capital improvements in university spending.
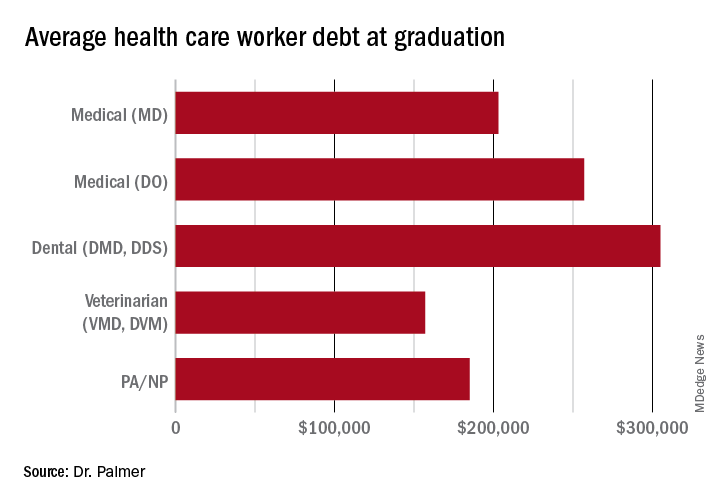
The price of medical schools has risen more than four times as fast as inflation over the past 30 years, with dental and veterinary schools and nursing education showing similarly exaggerated price increases. Trainees in these fields are more likely to have taken on six-figure debt, with average debt loads at graduation in the table below. While $10,000 will move the proverbial needle less for these borrowers, does that mean they should be excluded?
Health care workers’ income declines during the pandemic
Now, over 2½ years since the start of the COVID pandemic, multiple reports have demonstrated that health care workers have suffered a loss in income. This loss in income was never compensated for, as the Paycheck Protection Program and the individual economic stimuli typically excluded doctors and high earners.
COVID and the hazard tax
As a provider during the COVID-19 pandemic, I didn’t ask for hazard pay. I supported those who did but recognized their requests were more ceremonial than they were likely to be successful.
However, I flatly reject the idea that my fellow health care practitioners are not deserving of student loan forgiveness simply based on an arbitrary income threshold. Health care providers are saddled with high debt burden, have suffered lost income, and have given of themselves during a devastating pandemic, where more than 1 million perished in the United States.
Bottom line
Health care workers should not be excluded from student loan forgiveness. Sadly, the Biden administration has signaled that they are dropping career-based exclusions in favor of more broadly harmful income-based forgiveness restrictions. This will disproportionately harm physicians and other health care workers.
These practitioners have suffered financially as a result of working through the COVID pandemic; should they also be forced to shoulder another financial injury by being excluded from student loan forgiveness?
Dr. Palmer is the chief operating officer and cofounder of Panacea Financial. He is also a practicing pediatric hospitalist at Boston Children’s Hospital and is on faculty at Harvard Medical School, also in Boston.
A version of this article first appeared on Medscape.com.
In a recently obtained plan by Politico, the Biden administration is zeroing in on a broad student loan forgiveness plan to be released imminently. The plan would broadly forgive $10,000 in federal student loans, including graduate and PLUS loans. However, there’s a rub: The plan restricts the forgiveness to those with incomes below $150,000.
This would unfairly exclude many in health care from receiving this forgiveness, an egregious oversight given how much health care providers have sacrificed during the pandemic.
What was proposed?
Previously, it was reported that the Biden administration was considering this same amount of forgiveness, but with plans to exclude borrowers by either career or income. Student loan payments have been on an extended CARES Act forbearance since March 2020, with payment resumption planned for Aug. 31. The administration has said that they would deliver a plan for further extensions before this date and have repeatedly teased including forgiveness.
Forgiveness for some ...
Forgiving $10,000 of federal student loans would relieve some 15 million borrowers of student debt, roughly one-third of the 45 million borrowers with debt.
This would provide a massive boost to these borrowers (who disproportionately are female, low-income, and non-White), many of whom were targeted by predatory institutions whose education didn’t offer any actual tangible benefit to their earnings. While this is a group that absolutely ought to have their loans forgiven, drawing an income line inappropriately restricts those in health care from receiving any forgiveness.
... But not for others
Someone making an annual gross income of $150,000 is in the 80th percentile of earners in the United States (for comparison, the top 1% took home more than $505,000 in 2021). What student loan borrowers make up the remaining 20%? Overwhelmingly, health care providers occupy that tier: physicians, dentists, veterinarians, and advanced-practice nurses.
These schools leave their graduates with some of the highest student loan burdens, with veterinarians, dentists, and physicians having the highest debt-to-income ratios of any professional careers.
Flat forgiveness is regressive
Forgiving any student debt is the right direction. Too may have fallen victim to an industry without quality control, appropriate regulation, or price control. Quite the opposite, the blank-check model of student loan financing has led to an arms race as it comes to capital improvements in university spending.
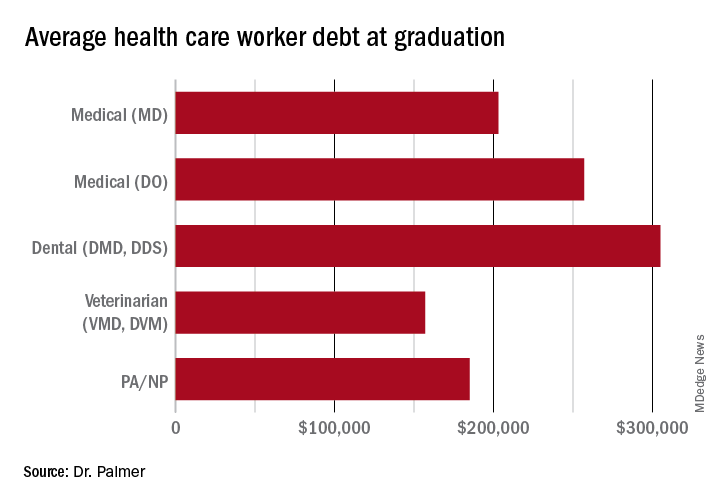
The price of medical schools has risen more than four times as fast as inflation over the past 30 years, with dental and veterinary schools and nursing education showing similarly exaggerated price increases. Trainees in these fields are more likely to have taken on six-figure debt, with average debt loads at graduation in the table below. While $10,000 will move the proverbial needle less for these borrowers, does that mean they should be excluded?
Health care workers’ income declines during the pandemic
Now, over 2½ years since the start of the COVID pandemic, multiple reports have demonstrated that health care workers have suffered a loss in income. This loss in income was never compensated for, as the Paycheck Protection Program and the individual economic stimuli typically excluded doctors and high earners.
COVID and the hazard tax
As a provider during the COVID-19 pandemic, I didn’t ask for hazard pay. I supported those who did but recognized their requests were more ceremonial than they were likely to be successful.
However, I flatly reject the idea that my fellow health care practitioners are not deserving of student loan forgiveness simply based on an arbitrary income threshold. Health care providers are saddled with high debt burden, have suffered lost income, and have given of themselves during a devastating pandemic, where more than 1 million perished in the United States.
Bottom line
Health care workers should not be excluded from student loan forgiveness. Sadly, the Biden administration has signaled that they are dropping career-based exclusions in favor of more broadly harmful income-based forgiveness restrictions. This will disproportionately harm physicians and other health care workers.
These practitioners have suffered financially as a result of working through the COVID pandemic; should they also be forced to shoulder another financial injury by being excluded from student loan forgiveness?
Dr. Palmer is the chief operating officer and cofounder of Panacea Financial. He is also a practicing pediatric hospitalist at Boston Children’s Hospital and is on faculty at Harvard Medical School, also in Boston.
A version of this article first appeared on Medscape.com.
In a recently obtained plan by Politico, the Biden administration is zeroing in on a broad student loan forgiveness plan to be released imminently. The plan would broadly forgive $10,000 in federal student loans, including graduate and PLUS loans. However, there’s a rub: The plan restricts the forgiveness to those with incomes below $150,000.
This would unfairly exclude many in health care from receiving this forgiveness, an egregious oversight given how much health care providers have sacrificed during the pandemic.
What was proposed?
Previously, it was reported that the Biden administration was considering this same amount of forgiveness, but with plans to exclude borrowers by either career or income. Student loan payments have been on an extended CARES Act forbearance since March 2020, with payment resumption planned for Aug. 31. The administration has said that they would deliver a plan for further extensions before this date and have repeatedly teased including forgiveness.
Forgiveness for some ...
Forgiving $10,000 of federal student loans would relieve some 15 million borrowers of student debt, roughly one-third of the 45 million borrowers with debt.
This would provide a massive boost to these borrowers (who disproportionately are female, low-income, and non-White), many of whom were targeted by predatory institutions whose education didn’t offer any actual tangible benefit to their earnings. While this is a group that absolutely ought to have their loans forgiven, drawing an income line inappropriately restricts those in health care from receiving any forgiveness.
... But not for others
Someone making an annual gross income of $150,000 is in the 80th percentile of earners in the United States (for comparison, the top 1% took home more than $505,000 in 2021). What student loan borrowers make up the remaining 20%? Overwhelmingly, health care providers occupy that tier: physicians, dentists, veterinarians, and advanced-practice nurses.
These schools leave their graduates with some of the highest student loan burdens, with veterinarians, dentists, and physicians having the highest debt-to-income ratios of any professional careers.
Flat forgiveness is regressive
Forgiving any student debt is the right direction. Too may have fallen victim to an industry without quality control, appropriate regulation, or price control. Quite the opposite, the blank-check model of student loan financing has led to an arms race as it comes to capital improvements in university spending.
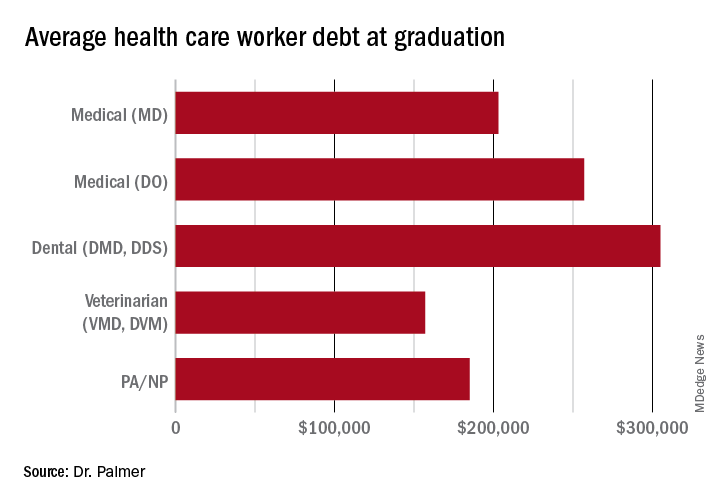
The price of medical schools has risen more than four times as fast as inflation over the past 30 years, with dental and veterinary schools and nursing education showing similarly exaggerated price increases. Trainees in these fields are more likely to have taken on six-figure debt, with average debt loads at graduation in the table below. While $10,000 will move the proverbial needle less for these borrowers, does that mean they should be excluded?
Health care workers’ income declines during the pandemic
Now, over 2½ years since the start of the COVID pandemic, multiple reports have demonstrated that health care workers have suffered a loss in income. This loss in income was never compensated for, as the Paycheck Protection Program and the individual economic stimuli typically excluded doctors and high earners.
COVID and the hazard tax
As a provider during the COVID-19 pandemic, I didn’t ask for hazard pay. I supported those who did but recognized their requests were more ceremonial than they were likely to be successful.
However, I flatly reject the idea that my fellow health care practitioners are not deserving of student loan forgiveness simply based on an arbitrary income threshold. Health care providers are saddled with high debt burden, have suffered lost income, and have given of themselves during a devastating pandemic, where more than 1 million perished in the United States.
Bottom line
Health care workers should not be excluded from student loan forgiveness. Sadly, the Biden administration has signaled that they are dropping career-based exclusions in favor of more broadly harmful income-based forgiveness restrictions. This will disproportionately harm physicians and other health care workers.
These practitioners have suffered financially as a result of working through the COVID pandemic; should they also be forced to shoulder another financial injury by being excluded from student loan forgiveness?
Dr. Palmer is the chief operating officer and cofounder of Panacea Financial. He is also a practicing pediatric hospitalist at Boston Children’s Hospital and is on faculty at Harvard Medical School, also in Boston.
A version of this article first appeared on Medscape.com.
Weight-loss surgery has a big effect on marriage
Kristal was only in her mid-30s when she decided to have surgery. Her doctor said it was too early. But the Oregon mom of three had found herself in the hospital twice for obesity-related lung complications before her 35th birthday. So she got the gastric sleeve.
And at first it seemed like the best decision for her and her family. She was losing weight – 100 pounds in 16 months – and so was her husband. The whole family was more active and seemed to have more energy. But then her husband’s weight began to creep back up.
While she joined a running group and signed up for half-marathons, her husband’s depression and drinking worsened. The healthier lifestyle they’d shared was now an unspoken wedge between them.
And the added attention Kristal was getting from men and women because of her thinner size only added to the tension. After 30 years together and 22 years of marriage, the high school sweethearts divorced in June 2021. Kristal’s weight loss wasn’t the only problem, but she and her ex-husband believe it was the beginning of the end.
An unexpected outcome?
New research from the University of Pittsburgh found that Kristal’s experience is a common one. The study looked at data from 1,441 bariatric surgery patients and found that never-married patients were over 50% more likely to get married, and married patients were more than twice as likely to get divorced, compared to the general U.S. population.
This U.S. data follows two Scandinavian studies from 2018 and 2020 that found similar relationship changes after bariatric surgery. But the postsurgery divorce rate in the United States was only about half that found in the Danish and Swedish studies, according to the new study published in Annals of Surgery.
It’s important to note that even with an increase in the divorce rate, most marriages in the study were unchanged, said epidemiologist and lead author Wendy King, PhD. In fact, 81% of couples were still married 5 years after surgery. But where the U.S. population has a divorce rate of 3.5%, bariatric patients in the study had an 8% divorce rate. Likewise, those who’d never been married before the surgery had a marriage rate of 18%, compared to 7% in the U.S. population.
Surgery certainly isn’t a death sentence for a patient’s love life. But the uptick in marriage and divorce suggests bariatric surgery significantly impacts how people engage in relationships.
“It makes sense,” said clinical psychologist Rachel Goldman, PhD, who specializes in health and wellness issues and bariatric surgery cases in New York City. “People are changing their lifestyle.” And those changes don’t start or stop the day of surgery, they begin as soon as someone decides to have surgery and continue as a lifelong process, she said.
For some patients, these healthy habits may offer a “new lease on life,” said Dr. King. According to the study, patients who had better physical health after surgery were more likely to get married.
But the continual lifestyle changes can dramatically impact the rituals of existing relationships, said Dr. Goldman. Maybe a couple loved to go out and enjoy an extravagant meal before surgery, or they had ice cream and watched a movie every Friday. The habit changes that come with bariatric surgery can require one partner to focus less on those rituals.
These sorts of changes may leave one or both people feeling like their partner is turning away from them, said Don Cole, DMin, a relationship therapist and clinical director at the Gottman Institute in Seattle, a think tank focused on the science of relationships. The person who had surgery may feel unsupported in the new journey if the partner keeps advocating for unhealthy habits, he said. And the person who didn’t have surgery may feel cast aside by the partner’s new health priorities.
Changes, even those that are positive and healthy, create a kind of crisis for relationships, Dr. Cole said. It’s not just bariatric surgery. Bringing a baby into the home, infertility treatments, and substance abuse recovery are all considered positive changes that are also predictors of relationship dissatisfaction and divorce, he said.
A couple could have a range of emotions after one partner gets bariatric surgery, Dr. Cole said. Unfortunately, “my experience as a therapist says they aren’t that good [at talking about it],” he said.
But bariatric surgery isn’t the only thing at play in these relationship changes, according to the study. Married patients had a much lower chance of separation or divorce (13%) than patients who were unmarried but living together (44%) by 5 years after surgery. Similarly, most people who were already separated either got divorced or resumed being married. It’s as if the surgery and lifestyle changes served as a catalyst for people who already had one foot out of (or in) the door, Dr. Goldman said.
A high sexual desire after surgery was also a predictor of divorce. In fact, there were more things before surgery that impacted divorce than surgery-related changes. It’s possible that many of these patients are “on the path toward change already,” Dr. King said. “Who knows how much the surgery had to do with it.”
Dr. Goldman recalled a patient who, before surgery, had very low self-worth. She wasn’t satisfied with her relationship but admitted to staying because she didn’t believe she could do any better than her current partner. After surgery, her perspective radically changed. She started to get healthier, invested in her education, and changed jobs. And when her partner refused to join her in making changes, she left. Maybe some of these patients “were already thinking about leaving but just didn’t have the confidence,” Dr. Goldman said.
Still, it’s critical that patients receive more counseling on how choosing to have bariatric surgery can impact their relationship before and after their weight loss procedure, Dr. King said. It should be the standard of care.
Currently, relationship-specific counseling isn’t required, Dr. Goldman said. Most programs do require a psychosocial evaluation before surgery, “but they are quite varied.” And even in programs where relationships are mentioned, there often isn’t a psychologist or licensed mental health professional on the team.
Since Dr. King’s previous research on substance abuse after bariatric surgery changed common practice in the field, Dr. Goldman said she hopes the new data will have a similar influence and relationship counseling will become the norm.
Dr. Cole actually had bariatric surgery. He recalled potential relationship issues were briefly mentioned. Someone at the clinic said if his marriage felt challenged, he should seek help from a professional, and that was it.
For Dr. Cole, there were unexpected negative feelings of shame and disappointment after surgery. He felt the extreme weight loss was all his colleagues could talk about and was very disappointed when there was no change in his chronic pain, a primary reason he had the procedure.
Fortunately, he could talk to his wife – also is a relationship therapist at Gottman – about the range of emotions. “One of the things that we know that creates a deep sense of trust is [when] I know my partner is there for me when I’m not well,” Dr. Cole said.
But these negative emotions can be the very things that feel most difficult to talk about or hear from a partner. It’s hard to share our own negative feelings and to hear someone else’s, Dr. Cole said.
He advises creating a new “ritual of connection: moments in time when you plan to turn toward one another.”
That could be a daily walk, where you intentionally talk about the surgery-related changes that both of you have had. Dr. Cole said to ask yourself, “Are we intentional about turning toward one another in those [challenging] moments?”
A version of this article first appeared on WebMD.com.
Kristal was only in her mid-30s when she decided to have surgery. Her doctor said it was too early. But the Oregon mom of three had found herself in the hospital twice for obesity-related lung complications before her 35th birthday. So she got the gastric sleeve.
And at first it seemed like the best decision for her and her family. She was losing weight – 100 pounds in 16 months – and so was her husband. The whole family was more active and seemed to have more energy. But then her husband’s weight began to creep back up.
While she joined a running group and signed up for half-marathons, her husband’s depression and drinking worsened. The healthier lifestyle they’d shared was now an unspoken wedge between them.
And the added attention Kristal was getting from men and women because of her thinner size only added to the tension. After 30 years together and 22 years of marriage, the high school sweethearts divorced in June 2021. Kristal’s weight loss wasn’t the only problem, but she and her ex-husband believe it was the beginning of the end.
An unexpected outcome?
New research from the University of Pittsburgh found that Kristal’s experience is a common one. The study looked at data from 1,441 bariatric surgery patients and found that never-married patients were over 50% more likely to get married, and married patients were more than twice as likely to get divorced, compared to the general U.S. population.
This U.S. data follows two Scandinavian studies from 2018 and 2020 that found similar relationship changes after bariatric surgery. But the postsurgery divorce rate in the United States was only about half that found in the Danish and Swedish studies, according to the new study published in Annals of Surgery.
It’s important to note that even with an increase in the divorce rate, most marriages in the study were unchanged, said epidemiologist and lead author Wendy King, PhD. In fact, 81% of couples were still married 5 years after surgery. But where the U.S. population has a divorce rate of 3.5%, bariatric patients in the study had an 8% divorce rate. Likewise, those who’d never been married before the surgery had a marriage rate of 18%, compared to 7% in the U.S. population.
Surgery certainly isn’t a death sentence for a patient’s love life. But the uptick in marriage and divorce suggests bariatric surgery significantly impacts how people engage in relationships.
“It makes sense,” said clinical psychologist Rachel Goldman, PhD, who specializes in health and wellness issues and bariatric surgery cases in New York City. “People are changing their lifestyle.” And those changes don’t start or stop the day of surgery, they begin as soon as someone decides to have surgery and continue as a lifelong process, she said.
For some patients, these healthy habits may offer a “new lease on life,” said Dr. King. According to the study, patients who had better physical health after surgery were more likely to get married.
But the continual lifestyle changes can dramatically impact the rituals of existing relationships, said Dr. Goldman. Maybe a couple loved to go out and enjoy an extravagant meal before surgery, or they had ice cream and watched a movie every Friday. The habit changes that come with bariatric surgery can require one partner to focus less on those rituals.
These sorts of changes may leave one or both people feeling like their partner is turning away from them, said Don Cole, DMin, a relationship therapist and clinical director at the Gottman Institute in Seattle, a think tank focused on the science of relationships. The person who had surgery may feel unsupported in the new journey if the partner keeps advocating for unhealthy habits, he said. And the person who didn’t have surgery may feel cast aside by the partner’s new health priorities.
Changes, even those that are positive and healthy, create a kind of crisis for relationships, Dr. Cole said. It’s not just bariatric surgery. Bringing a baby into the home, infertility treatments, and substance abuse recovery are all considered positive changes that are also predictors of relationship dissatisfaction and divorce, he said.
A couple could have a range of emotions after one partner gets bariatric surgery, Dr. Cole said. Unfortunately, “my experience as a therapist says they aren’t that good [at talking about it],” he said.
But bariatric surgery isn’t the only thing at play in these relationship changes, according to the study. Married patients had a much lower chance of separation or divorce (13%) than patients who were unmarried but living together (44%) by 5 years after surgery. Similarly, most people who were already separated either got divorced or resumed being married. It’s as if the surgery and lifestyle changes served as a catalyst for people who already had one foot out of (or in) the door, Dr. Goldman said.
A high sexual desire after surgery was also a predictor of divorce. In fact, there were more things before surgery that impacted divorce than surgery-related changes. It’s possible that many of these patients are “on the path toward change already,” Dr. King said. “Who knows how much the surgery had to do with it.”
Dr. Goldman recalled a patient who, before surgery, had very low self-worth. She wasn’t satisfied with her relationship but admitted to staying because she didn’t believe she could do any better than her current partner. After surgery, her perspective radically changed. She started to get healthier, invested in her education, and changed jobs. And when her partner refused to join her in making changes, she left. Maybe some of these patients “were already thinking about leaving but just didn’t have the confidence,” Dr. Goldman said.
Still, it’s critical that patients receive more counseling on how choosing to have bariatric surgery can impact their relationship before and after their weight loss procedure, Dr. King said. It should be the standard of care.
Currently, relationship-specific counseling isn’t required, Dr. Goldman said. Most programs do require a psychosocial evaluation before surgery, “but they are quite varied.” And even in programs where relationships are mentioned, there often isn’t a psychologist or licensed mental health professional on the team.
Since Dr. King’s previous research on substance abuse after bariatric surgery changed common practice in the field, Dr. Goldman said she hopes the new data will have a similar influence and relationship counseling will become the norm.
Dr. Cole actually had bariatric surgery. He recalled potential relationship issues were briefly mentioned. Someone at the clinic said if his marriage felt challenged, he should seek help from a professional, and that was it.
For Dr. Cole, there were unexpected negative feelings of shame and disappointment after surgery. He felt the extreme weight loss was all his colleagues could talk about and was very disappointed when there was no change in his chronic pain, a primary reason he had the procedure.
Fortunately, he could talk to his wife – also is a relationship therapist at Gottman – about the range of emotions. “One of the things that we know that creates a deep sense of trust is [when] I know my partner is there for me when I’m not well,” Dr. Cole said.
But these negative emotions can be the very things that feel most difficult to talk about or hear from a partner. It’s hard to share our own negative feelings and to hear someone else’s, Dr. Cole said.
He advises creating a new “ritual of connection: moments in time when you plan to turn toward one another.”
That could be a daily walk, where you intentionally talk about the surgery-related changes that both of you have had. Dr. Cole said to ask yourself, “Are we intentional about turning toward one another in those [challenging] moments?”
A version of this article first appeared on WebMD.com.
Kristal was only in her mid-30s when she decided to have surgery. Her doctor said it was too early. But the Oregon mom of three had found herself in the hospital twice for obesity-related lung complications before her 35th birthday. So she got the gastric sleeve.
And at first it seemed like the best decision for her and her family. She was losing weight – 100 pounds in 16 months – and so was her husband. The whole family was more active and seemed to have more energy. But then her husband’s weight began to creep back up.
While she joined a running group and signed up for half-marathons, her husband’s depression and drinking worsened. The healthier lifestyle they’d shared was now an unspoken wedge between them.
And the added attention Kristal was getting from men and women because of her thinner size only added to the tension. After 30 years together and 22 years of marriage, the high school sweethearts divorced in June 2021. Kristal’s weight loss wasn’t the only problem, but she and her ex-husband believe it was the beginning of the end.
An unexpected outcome?
New research from the University of Pittsburgh found that Kristal’s experience is a common one. The study looked at data from 1,441 bariatric surgery patients and found that never-married patients were over 50% more likely to get married, and married patients were more than twice as likely to get divorced, compared to the general U.S. population.
This U.S. data follows two Scandinavian studies from 2018 and 2020 that found similar relationship changes after bariatric surgery. But the postsurgery divorce rate in the United States was only about half that found in the Danish and Swedish studies, according to the new study published in Annals of Surgery.
It’s important to note that even with an increase in the divorce rate, most marriages in the study were unchanged, said epidemiologist and lead author Wendy King, PhD. In fact, 81% of couples were still married 5 years after surgery. But where the U.S. population has a divorce rate of 3.5%, bariatric patients in the study had an 8% divorce rate. Likewise, those who’d never been married before the surgery had a marriage rate of 18%, compared to 7% in the U.S. population.
Surgery certainly isn’t a death sentence for a patient’s love life. But the uptick in marriage and divorce suggests bariatric surgery significantly impacts how people engage in relationships.
“It makes sense,” said clinical psychologist Rachel Goldman, PhD, who specializes in health and wellness issues and bariatric surgery cases in New York City. “People are changing their lifestyle.” And those changes don’t start or stop the day of surgery, they begin as soon as someone decides to have surgery and continue as a lifelong process, she said.
For some patients, these healthy habits may offer a “new lease on life,” said Dr. King. According to the study, patients who had better physical health after surgery were more likely to get married.
But the continual lifestyle changes can dramatically impact the rituals of existing relationships, said Dr. Goldman. Maybe a couple loved to go out and enjoy an extravagant meal before surgery, or they had ice cream and watched a movie every Friday. The habit changes that come with bariatric surgery can require one partner to focus less on those rituals.
These sorts of changes may leave one or both people feeling like their partner is turning away from them, said Don Cole, DMin, a relationship therapist and clinical director at the Gottman Institute in Seattle, a think tank focused on the science of relationships. The person who had surgery may feel unsupported in the new journey if the partner keeps advocating for unhealthy habits, he said. And the person who didn’t have surgery may feel cast aside by the partner’s new health priorities.
Changes, even those that are positive and healthy, create a kind of crisis for relationships, Dr. Cole said. It’s not just bariatric surgery. Bringing a baby into the home, infertility treatments, and substance abuse recovery are all considered positive changes that are also predictors of relationship dissatisfaction and divorce, he said.
A couple could have a range of emotions after one partner gets bariatric surgery, Dr. Cole said. Unfortunately, “my experience as a therapist says they aren’t that good [at talking about it],” he said.
But bariatric surgery isn’t the only thing at play in these relationship changes, according to the study. Married patients had a much lower chance of separation or divorce (13%) than patients who were unmarried but living together (44%) by 5 years after surgery. Similarly, most people who were already separated either got divorced or resumed being married. It’s as if the surgery and lifestyle changes served as a catalyst for people who already had one foot out of (or in) the door, Dr. Goldman said.
A high sexual desire after surgery was also a predictor of divorce. In fact, there were more things before surgery that impacted divorce than surgery-related changes. It’s possible that many of these patients are “on the path toward change already,” Dr. King said. “Who knows how much the surgery had to do with it.”
Dr. Goldman recalled a patient who, before surgery, had very low self-worth. She wasn’t satisfied with her relationship but admitted to staying because she didn’t believe she could do any better than her current partner. After surgery, her perspective radically changed. She started to get healthier, invested in her education, and changed jobs. And when her partner refused to join her in making changes, she left. Maybe some of these patients “were already thinking about leaving but just didn’t have the confidence,” Dr. Goldman said.
Still, it’s critical that patients receive more counseling on how choosing to have bariatric surgery can impact their relationship before and after their weight loss procedure, Dr. King said. It should be the standard of care.
Currently, relationship-specific counseling isn’t required, Dr. Goldman said. Most programs do require a psychosocial evaluation before surgery, “but they are quite varied.” And even in programs where relationships are mentioned, there often isn’t a psychologist or licensed mental health professional on the team.
Since Dr. King’s previous research on substance abuse after bariatric surgery changed common practice in the field, Dr. Goldman said she hopes the new data will have a similar influence and relationship counseling will become the norm.
Dr. Cole actually had bariatric surgery. He recalled potential relationship issues were briefly mentioned. Someone at the clinic said if his marriage felt challenged, he should seek help from a professional, and that was it.
For Dr. Cole, there were unexpected negative feelings of shame and disappointment after surgery. He felt the extreme weight loss was all his colleagues could talk about and was very disappointed when there was no change in his chronic pain, a primary reason he had the procedure.
Fortunately, he could talk to his wife – also is a relationship therapist at Gottman – about the range of emotions. “One of the things that we know that creates a deep sense of trust is [when] I know my partner is there for me when I’m not well,” Dr. Cole said.
But these negative emotions can be the very things that feel most difficult to talk about or hear from a partner. It’s hard to share our own negative feelings and to hear someone else’s, Dr. Cole said.
He advises creating a new “ritual of connection: moments in time when you plan to turn toward one another.”
That could be a daily walk, where you intentionally talk about the surgery-related changes that both of you have had. Dr. Cole said to ask yourself, “Are we intentional about turning toward one another in those [challenging] moments?”
A version of this article first appeared on WebMD.com.
FROM ANNALS OF SURGERY
Long COVID’s grip will likely tighten as infections continue
COVID-19 is far from done in the United States, with more than 111,000 new cases being recorded a day in the second week of August, according to Johns Hopkins University, and 625 deaths being reported every day. , a condition that already has affected between 7.7 million and 23 million Americans, according to U.S. government estimates.
“It is evident that long COVID is real, that it already impacts a substantial number of people, and that this number may continue to grow as new infections occur,” the U.S. Department of Health and Human Services (HHS) said in a research action plan released Aug. 4.
“We are heading towards a big problem on our hands,” says Ziyad Al-Aly, MD, chief of research and development at the Veterans Affairs Hospital in St. Louis. “It’s like if we are falling in a plane, hurtling towards the ground. It doesn’t matter at what speed we are falling; what matters is that we are all falling, and falling fast. It’s a real problem. We needed to bring attention to this, yesterday,” he said.
Bryan Lau, PhD, professor of epidemiology at Johns Hopkins Bloomberg School of Public Health, Baltimore, and co-lead of a long COVID study there, says whether it’s 5% of the 92 million officially recorded U.S. COVID-19 cases, or 30% – on the higher end of estimates – that means anywhere between 4.5 million and 27 million Americans will have the effects of long COVID.
Other experts put the estimates even higher.
“If we conservatively assume 100 million working-age adults have been infected, that implies 10 to 33 million may have long COVID,” Alice Burns, PhD, associate director for the Kaiser Family Foundation’s Program on Medicaid and the Uninsured, wrote in an analysis.
And even the Centers for Disease Control and Prevention says only a fraction of cases have been recorded.
That, in turn, means tens of millions of people who struggle to work, to get to school, and to take care of their families – and who will be making demands on an already stressed U.S. health care system.
The HHS said in its Aug. 4 report that long COVID could keep 1 million people a day out of work, with a loss of $50 billion in annual pay.
Dr. Lau said health workers and policymakers are woefully unprepared.
“If you have a family unit, and the mom or dad can’t work, or has trouble taking their child to activities, where does the question of support come into play? Where is there potential for food issues, or housing issues?” he asked. “I see the potential for the burden to be extremely large in that capacity.”
Dr. Lau said he has yet to see any strong estimates of how many cases of long COVID might develop. Because a person has to get COVID-19 to ultimately get long COVID, the two are linked. In other words, as COVID-19 cases rise, so will cases of long COVID, and vice versa.
Evidence from the Kaiser Family Foundation analysis suggests a significant impact on employment: Surveys showed more than half of adults with long COVID who worked before becoming infected are either out of work or working fewer hours. Conditions associated with long COVID – such as fatigue, malaise, or problems concentrating – limit people’s ability to work, even if they have jobs that allow for accommodations.
Two surveys of people with long COVID who had worked before becoming infected showed that between 22% and 27% of them were out of work after getting long COVID. In comparison, among all working-age adults in 2019, only 7% were out of work. Given the sheer number of working-age adults with long COVID, the effects on employment may be profound and are likely to involve more people over time. One study estimates that long COVID already accounts for 15% of unfilled jobs.
The most severe symptoms of long COVID include brain fog and heart complications, known to persist for weeks for months after a COVID-19 infection.
A study from the University of Norway published in Open Forum Infectious Diseases found 53% of people tested had at least one symptom of thinking problems 13 months after infection with COVID-19. According to the HHS’ latest report on long COVID, people with thinking problems, heart conditions, mobility issues, and other symptoms are going to need a considerable amount of care. Many will need lengthy periods of rehabilitation.
Dr. Al-Aly worries that long COVID has already severely affected the labor force and the job market, all while burdening the country’s health care system.
“While there are variations in how individuals respond and cope with long COVID, the unifying thread is that with the level of disability it causes, more people will be struggling to keep up with the demands of the workforce and more people will be out on disability than ever before,” he said.
Studies from Johns Hopkins and the University of Washington estimate that 5%-30% of people could get long COVID in the future. Projections beyond that are hazy.
“So far, all the studies we have done on long COVID have been reactionary. Much of the activism around long COVID has been patient led. We are seeing more and more people with lasting symptoms. We need our research to catch up,” Dr. Lau said.
Theo Vos, MD, PhD, professor of health sciences at University of Washington, Seattle, said the main reasons for the huge range of predictions are the variety of methods used, as well as differences in sample size. Also, much long COVID data is self-reported, making it difficult for epidemiologists to track.
“With self-reported data, you can’t plug people into a machine and say this is what they have or this is what they don’t have. At the population level, the only thing you can do is ask questions. There is no systematic way to define long COVID,” he said.
Dr. Vos’s most recent study, which is being peer-reviewed and revised, found that most people with long COVID have symptoms similar to those seen in other autoimmune diseases. But sometimes the immune system can overreact, causing the more severe symptoms, such as brain fog and heart problems, associated with long COVID.
One reason that researchers struggle to come up with numbers, said Dr. Al-Aly, is the rapid rise of new variants. These variants appear to sometimes cause less severe disease than previous ones, but it’s not clear whether that means different risks for long COVID.
“There’s a wide diversity in severity. Someone can have long COVID and be fully functional, while others are not functional at all. We still have a long way to go before we figure out why,” Dr. Lau said.
A version of this article first appeared on WebMD.com.
COVID-19 is far from done in the United States, with more than 111,000 new cases being recorded a day in the second week of August, according to Johns Hopkins University, and 625 deaths being reported every day. , a condition that already has affected between 7.7 million and 23 million Americans, according to U.S. government estimates.
“It is evident that long COVID is real, that it already impacts a substantial number of people, and that this number may continue to grow as new infections occur,” the U.S. Department of Health and Human Services (HHS) said in a research action plan released Aug. 4.
“We are heading towards a big problem on our hands,” says Ziyad Al-Aly, MD, chief of research and development at the Veterans Affairs Hospital in St. Louis. “It’s like if we are falling in a plane, hurtling towards the ground. It doesn’t matter at what speed we are falling; what matters is that we are all falling, and falling fast. It’s a real problem. We needed to bring attention to this, yesterday,” he said.
Bryan Lau, PhD, professor of epidemiology at Johns Hopkins Bloomberg School of Public Health, Baltimore, and co-lead of a long COVID study there, says whether it’s 5% of the 92 million officially recorded U.S. COVID-19 cases, or 30% – on the higher end of estimates – that means anywhere between 4.5 million and 27 million Americans will have the effects of long COVID.
Other experts put the estimates even higher.
“If we conservatively assume 100 million working-age adults have been infected, that implies 10 to 33 million may have long COVID,” Alice Burns, PhD, associate director for the Kaiser Family Foundation’s Program on Medicaid and the Uninsured, wrote in an analysis.
And even the Centers for Disease Control and Prevention says only a fraction of cases have been recorded.
That, in turn, means tens of millions of people who struggle to work, to get to school, and to take care of their families – and who will be making demands on an already stressed U.S. health care system.
The HHS said in its Aug. 4 report that long COVID could keep 1 million people a day out of work, with a loss of $50 billion in annual pay.
Dr. Lau said health workers and policymakers are woefully unprepared.
“If you have a family unit, and the mom or dad can’t work, or has trouble taking their child to activities, where does the question of support come into play? Where is there potential for food issues, or housing issues?” he asked. “I see the potential for the burden to be extremely large in that capacity.”
Dr. Lau said he has yet to see any strong estimates of how many cases of long COVID might develop. Because a person has to get COVID-19 to ultimately get long COVID, the two are linked. In other words, as COVID-19 cases rise, so will cases of long COVID, and vice versa.
Evidence from the Kaiser Family Foundation analysis suggests a significant impact on employment: Surveys showed more than half of adults with long COVID who worked before becoming infected are either out of work or working fewer hours. Conditions associated with long COVID – such as fatigue, malaise, or problems concentrating – limit people’s ability to work, even if they have jobs that allow for accommodations.
Two surveys of people with long COVID who had worked before becoming infected showed that between 22% and 27% of them were out of work after getting long COVID. In comparison, among all working-age adults in 2019, only 7% were out of work. Given the sheer number of working-age adults with long COVID, the effects on employment may be profound and are likely to involve more people over time. One study estimates that long COVID already accounts for 15% of unfilled jobs.
The most severe symptoms of long COVID include brain fog and heart complications, known to persist for weeks for months after a COVID-19 infection.
A study from the University of Norway published in Open Forum Infectious Diseases found 53% of people tested had at least one symptom of thinking problems 13 months after infection with COVID-19. According to the HHS’ latest report on long COVID, people with thinking problems, heart conditions, mobility issues, and other symptoms are going to need a considerable amount of care. Many will need lengthy periods of rehabilitation.
Dr. Al-Aly worries that long COVID has already severely affected the labor force and the job market, all while burdening the country’s health care system.
“While there are variations in how individuals respond and cope with long COVID, the unifying thread is that with the level of disability it causes, more people will be struggling to keep up with the demands of the workforce and more people will be out on disability than ever before,” he said.
Studies from Johns Hopkins and the University of Washington estimate that 5%-30% of people could get long COVID in the future. Projections beyond that are hazy.
“So far, all the studies we have done on long COVID have been reactionary. Much of the activism around long COVID has been patient led. We are seeing more and more people with lasting symptoms. We need our research to catch up,” Dr. Lau said.
Theo Vos, MD, PhD, professor of health sciences at University of Washington, Seattle, said the main reasons for the huge range of predictions are the variety of methods used, as well as differences in sample size. Also, much long COVID data is self-reported, making it difficult for epidemiologists to track.
“With self-reported data, you can’t plug people into a machine and say this is what they have or this is what they don’t have. At the population level, the only thing you can do is ask questions. There is no systematic way to define long COVID,” he said.
Dr. Vos’s most recent study, which is being peer-reviewed and revised, found that most people with long COVID have symptoms similar to those seen in other autoimmune diseases. But sometimes the immune system can overreact, causing the more severe symptoms, such as brain fog and heart problems, associated with long COVID.
One reason that researchers struggle to come up with numbers, said Dr. Al-Aly, is the rapid rise of new variants. These variants appear to sometimes cause less severe disease than previous ones, but it’s not clear whether that means different risks for long COVID.
“There’s a wide diversity in severity. Someone can have long COVID and be fully functional, while others are not functional at all. We still have a long way to go before we figure out why,” Dr. Lau said.
A version of this article first appeared on WebMD.com.
COVID-19 is far from done in the United States, with more than 111,000 new cases being recorded a day in the second week of August, according to Johns Hopkins University, and 625 deaths being reported every day. , a condition that already has affected between 7.7 million and 23 million Americans, according to U.S. government estimates.
“It is evident that long COVID is real, that it already impacts a substantial number of people, and that this number may continue to grow as new infections occur,” the U.S. Department of Health and Human Services (HHS) said in a research action plan released Aug. 4.
“We are heading towards a big problem on our hands,” says Ziyad Al-Aly, MD, chief of research and development at the Veterans Affairs Hospital in St. Louis. “It’s like if we are falling in a plane, hurtling towards the ground. It doesn’t matter at what speed we are falling; what matters is that we are all falling, and falling fast. It’s a real problem. We needed to bring attention to this, yesterday,” he said.
Bryan Lau, PhD, professor of epidemiology at Johns Hopkins Bloomberg School of Public Health, Baltimore, and co-lead of a long COVID study there, says whether it’s 5% of the 92 million officially recorded U.S. COVID-19 cases, or 30% – on the higher end of estimates – that means anywhere between 4.5 million and 27 million Americans will have the effects of long COVID.
Other experts put the estimates even higher.
“If we conservatively assume 100 million working-age adults have been infected, that implies 10 to 33 million may have long COVID,” Alice Burns, PhD, associate director for the Kaiser Family Foundation’s Program on Medicaid and the Uninsured, wrote in an analysis.
And even the Centers for Disease Control and Prevention says only a fraction of cases have been recorded.
That, in turn, means tens of millions of people who struggle to work, to get to school, and to take care of their families – and who will be making demands on an already stressed U.S. health care system.
The HHS said in its Aug. 4 report that long COVID could keep 1 million people a day out of work, with a loss of $50 billion in annual pay.
Dr. Lau said health workers and policymakers are woefully unprepared.
“If you have a family unit, and the mom or dad can’t work, or has trouble taking their child to activities, where does the question of support come into play? Where is there potential for food issues, or housing issues?” he asked. “I see the potential for the burden to be extremely large in that capacity.”
Dr. Lau said he has yet to see any strong estimates of how many cases of long COVID might develop. Because a person has to get COVID-19 to ultimately get long COVID, the two are linked. In other words, as COVID-19 cases rise, so will cases of long COVID, and vice versa.
Evidence from the Kaiser Family Foundation analysis suggests a significant impact on employment: Surveys showed more than half of adults with long COVID who worked before becoming infected are either out of work or working fewer hours. Conditions associated with long COVID – such as fatigue, malaise, or problems concentrating – limit people’s ability to work, even if they have jobs that allow for accommodations.
Two surveys of people with long COVID who had worked before becoming infected showed that between 22% and 27% of them were out of work after getting long COVID. In comparison, among all working-age adults in 2019, only 7% were out of work. Given the sheer number of working-age adults with long COVID, the effects on employment may be profound and are likely to involve more people over time. One study estimates that long COVID already accounts for 15% of unfilled jobs.
The most severe symptoms of long COVID include brain fog and heart complications, known to persist for weeks for months after a COVID-19 infection.
A study from the University of Norway published in Open Forum Infectious Diseases found 53% of people tested had at least one symptom of thinking problems 13 months after infection with COVID-19. According to the HHS’ latest report on long COVID, people with thinking problems, heart conditions, mobility issues, and other symptoms are going to need a considerable amount of care. Many will need lengthy periods of rehabilitation.
Dr. Al-Aly worries that long COVID has already severely affected the labor force and the job market, all while burdening the country’s health care system.
“While there are variations in how individuals respond and cope with long COVID, the unifying thread is that with the level of disability it causes, more people will be struggling to keep up with the demands of the workforce and more people will be out on disability than ever before,” he said.
Studies from Johns Hopkins and the University of Washington estimate that 5%-30% of people could get long COVID in the future. Projections beyond that are hazy.
“So far, all the studies we have done on long COVID have been reactionary. Much of the activism around long COVID has been patient led. We are seeing more and more people with lasting symptoms. We need our research to catch up,” Dr. Lau said.
Theo Vos, MD, PhD, professor of health sciences at University of Washington, Seattle, said the main reasons for the huge range of predictions are the variety of methods used, as well as differences in sample size. Also, much long COVID data is self-reported, making it difficult for epidemiologists to track.
“With self-reported data, you can’t plug people into a machine and say this is what they have or this is what they don’t have. At the population level, the only thing you can do is ask questions. There is no systematic way to define long COVID,” he said.
Dr. Vos’s most recent study, which is being peer-reviewed and revised, found that most people with long COVID have symptoms similar to those seen in other autoimmune diseases. But sometimes the immune system can overreact, causing the more severe symptoms, such as brain fog and heart problems, associated with long COVID.
One reason that researchers struggle to come up with numbers, said Dr. Al-Aly, is the rapid rise of new variants. These variants appear to sometimes cause less severe disease than previous ones, but it’s not clear whether that means different risks for long COVID.
“There’s a wide diversity in severity. Someone can have long COVID and be fully functional, while others are not functional at all. We still have a long way to go before we figure out why,” Dr. Lau said.
A version of this article first appeared on WebMD.com.
‘Shocking’ and persistent gap in treatment for opioid addiction
The vast majority of Americans with opioid use disorder (OUD) do not receive potentially lifesaving medications.
Drugs such as methadone, buprenorphine, and extended-release naltrexone have been shown to reduce opioid overdoses by more than 50%. Yet a new analysis shows that only about 1 in 10 people living with OUD receive these medications.
“Even though it’s not especially surprising, it’s still disturbing and shocking in a way that we have just made such little progress on this huge issue,” study investigator Noa Krawczyk, PhD, with the Center for Opioid Epidemiology and Policy, department of population health, NYU Langone, told this news organization.
The study was published online in the International Journal of Drug Policy.
Increased urgency
Despite efforts to increase capacity for OUD treatment in the United States, how receipt of treatment compares to need for treatment remains unclear.
Dr. Krawczyk and colleagues examined the gap between new estimates of OUD prevalence and treatment at the national and state levels from 2010 through 2019.
“,” the investigators write.
Adjusted estimates suggest that past-year OUD affected roughly 7.63 million individuals in the United States (2,773 per 100,000), yet only about 1.02 million received medication (365 per 100,000), they note.
Overall, there was a 106% increase in receipt of medications for OUD across the United States from 2010 to 2019 and a 5% increase from 2018 to 2019.
Yet, as of 2019, 87% of people with OUD were not receiving medication.
“While the number of people getting treatment doubled over the last decade, it’s nowhere near the amount of people who are still struggling with an opioid use disorder, and the urgency of the problem has become much worse because of the worsening fentanyl crisis and the lethality of the drug supply,” said Dr. Krawczyk.
The study also showed wide variation in past-year OUD prevalence and treatment across the United States.
Past-year OUD rates were highest in Washington, D.C., and lowest in Minnesota. Receipt of treatment was lowest in South Dakota and highest in Vermont.
However, in all 50 states and Washington, D.C., past-year OUD prevalence was greater than rates of medication use. As of 2019, the largest treatment gaps were in Iowa, North Dakota, and Washington, D.C. The smallest treatment gaps were in Connecticut, Maryland, and Rhode Island.
Long road ahead
“Even in states with the smallest treatment gaps, at least 50% of people who could benefit from medications for opioid use disorder are still not receiving them,” senior author Magdalena Cerdá, DrPH, director of the Center for Opioid Epidemiology and Policy in the department of population health at NYU Langone Health, said in a statement.
“We have a long way to go in reducing stigma surrounding treatment and in devising the types of policies and programs we need to ensure these medications reach the people who need them the most,” Dr. Cerdá added.
Access to OUD treatment is an ongoing problem in the United States.
“A lot of areas don’t have specialty treatment programs that provide methadone, or they might not have addiction-trained providers who are willing to prescribe buprenorphine or have a waiver to prescribe buprenorphine, so a lot places are really struggling with where people can get treatment,” said Dr. Krawczyk.
Recent data show that 46% of counties lack an OUD medication provider, and 32% have no specialty programs to treat substance use disorders.
Dr. Krawczyk and colleagues note that COVID-19–related policy changes and recently proposed legislation to allow more flexible and convenient access to OUD treatment may be a first step toward expanding access to this lifesaving treatment.
But improving initial access to medication for OUD is “only the first step – our research and health systems have a long way to go in addressing the needs of people with OUD to support retention in treatment and services to effectively reduce overdose and improve long-term health and well-being,” the researchers write.
The study was supported by the NYU Center for Epidemiology and Policy. Dr. Krawczyk has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The vast majority of Americans with opioid use disorder (OUD) do not receive potentially lifesaving medications.
Drugs such as methadone, buprenorphine, and extended-release naltrexone have been shown to reduce opioid overdoses by more than 50%. Yet a new analysis shows that only about 1 in 10 people living with OUD receive these medications.
“Even though it’s not especially surprising, it’s still disturbing and shocking in a way that we have just made such little progress on this huge issue,” study investigator Noa Krawczyk, PhD, with the Center for Opioid Epidemiology and Policy, department of population health, NYU Langone, told this news organization.
The study was published online in the International Journal of Drug Policy.
Increased urgency
Despite efforts to increase capacity for OUD treatment in the United States, how receipt of treatment compares to need for treatment remains unclear.
Dr. Krawczyk and colleagues examined the gap between new estimates of OUD prevalence and treatment at the national and state levels from 2010 through 2019.
“,” the investigators write.
Adjusted estimates suggest that past-year OUD affected roughly 7.63 million individuals in the United States (2,773 per 100,000), yet only about 1.02 million received medication (365 per 100,000), they note.
Overall, there was a 106% increase in receipt of medications for OUD across the United States from 2010 to 2019 and a 5% increase from 2018 to 2019.
Yet, as of 2019, 87% of people with OUD were not receiving medication.
“While the number of people getting treatment doubled over the last decade, it’s nowhere near the amount of people who are still struggling with an opioid use disorder, and the urgency of the problem has become much worse because of the worsening fentanyl crisis and the lethality of the drug supply,” said Dr. Krawczyk.
The study also showed wide variation in past-year OUD prevalence and treatment across the United States.
Past-year OUD rates were highest in Washington, D.C., and lowest in Minnesota. Receipt of treatment was lowest in South Dakota and highest in Vermont.
However, in all 50 states and Washington, D.C., past-year OUD prevalence was greater than rates of medication use. As of 2019, the largest treatment gaps were in Iowa, North Dakota, and Washington, D.C. The smallest treatment gaps were in Connecticut, Maryland, and Rhode Island.
Long road ahead
“Even in states with the smallest treatment gaps, at least 50% of people who could benefit from medications for opioid use disorder are still not receiving them,” senior author Magdalena Cerdá, DrPH, director of the Center for Opioid Epidemiology and Policy in the department of population health at NYU Langone Health, said in a statement.
“We have a long way to go in reducing stigma surrounding treatment and in devising the types of policies and programs we need to ensure these medications reach the people who need them the most,” Dr. Cerdá added.
Access to OUD treatment is an ongoing problem in the United States.
“A lot of areas don’t have specialty treatment programs that provide methadone, or they might not have addiction-trained providers who are willing to prescribe buprenorphine or have a waiver to prescribe buprenorphine, so a lot places are really struggling with where people can get treatment,” said Dr. Krawczyk.
Recent data show that 46% of counties lack an OUD medication provider, and 32% have no specialty programs to treat substance use disorders.
Dr. Krawczyk and colleagues note that COVID-19–related policy changes and recently proposed legislation to allow more flexible and convenient access to OUD treatment may be a first step toward expanding access to this lifesaving treatment.
But improving initial access to medication for OUD is “only the first step – our research and health systems have a long way to go in addressing the needs of people with OUD to support retention in treatment and services to effectively reduce overdose and improve long-term health and well-being,” the researchers write.
The study was supported by the NYU Center for Epidemiology and Policy. Dr. Krawczyk has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The vast majority of Americans with opioid use disorder (OUD) do not receive potentially lifesaving medications.
Drugs such as methadone, buprenorphine, and extended-release naltrexone have been shown to reduce opioid overdoses by more than 50%. Yet a new analysis shows that only about 1 in 10 people living with OUD receive these medications.
“Even though it’s not especially surprising, it’s still disturbing and shocking in a way that we have just made such little progress on this huge issue,” study investigator Noa Krawczyk, PhD, with the Center for Opioid Epidemiology and Policy, department of population health, NYU Langone, told this news organization.
The study was published online in the International Journal of Drug Policy.
Increased urgency
Despite efforts to increase capacity for OUD treatment in the United States, how receipt of treatment compares to need for treatment remains unclear.
Dr. Krawczyk and colleagues examined the gap between new estimates of OUD prevalence and treatment at the national and state levels from 2010 through 2019.
“,” the investigators write.
Adjusted estimates suggest that past-year OUD affected roughly 7.63 million individuals in the United States (2,773 per 100,000), yet only about 1.02 million received medication (365 per 100,000), they note.
Overall, there was a 106% increase in receipt of medications for OUD across the United States from 2010 to 2019 and a 5% increase from 2018 to 2019.
Yet, as of 2019, 87% of people with OUD were not receiving medication.
“While the number of people getting treatment doubled over the last decade, it’s nowhere near the amount of people who are still struggling with an opioid use disorder, and the urgency of the problem has become much worse because of the worsening fentanyl crisis and the lethality of the drug supply,” said Dr. Krawczyk.
The study also showed wide variation in past-year OUD prevalence and treatment across the United States.
Past-year OUD rates were highest in Washington, D.C., and lowest in Minnesota. Receipt of treatment was lowest in South Dakota and highest in Vermont.
However, in all 50 states and Washington, D.C., past-year OUD prevalence was greater than rates of medication use. As of 2019, the largest treatment gaps were in Iowa, North Dakota, and Washington, D.C. The smallest treatment gaps were in Connecticut, Maryland, and Rhode Island.
Long road ahead
“Even in states with the smallest treatment gaps, at least 50% of people who could benefit from medications for opioid use disorder are still not receiving them,” senior author Magdalena Cerdá, DrPH, director of the Center for Opioid Epidemiology and Policy in the department of population health at NYU Langone Health, said in a statement.
“We have a long way to go in reducing stigma surrounding treatment and in devising the types of policies and programs we need to ensure these medications reach the people who need them the most,” Dr. Cerdá added.
Access to OUD treatment is an ongoing problem in the United States.
“A lot of areas don’t have specialty treatment programs that provide methadone, or they might not have addiction-trained providers who are willing to prescribe buprenorphine or have a waiver to prescribe buprenorphine, so a lot places are really struggling with where people can get treatment,” said Dr. Krawczyk.
Recent data show that 46% of counties lack an OUD medication provider, and 32% have no specialty programs to treat substance use disorders.
Dr. Krawczyk and colleagues note that COVID-19–related policy changes and recently proposed legislation to allow more flexible and convenient access to OUD treatment may be a first step toward expanding access to this lifesaving treatment.
But improving initial access to medication for OUD is “only the first step – our research and health systems have a long way to go in addressing the needs of people with OUD to support retention in treatment and services to effectively reduce overdose and improve long-term health and well-being,” the researchers write.
The study was supported by the NYU Center for Epidemiology and Policy. Dr. Krawczyk has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE INTERNATIONAL JOURNAL OF DRUG POLICY
Stressed about weight gain? Well, stress causes weight gain
Stress, meet weight gain. Weight gain, meet stress
You’re not eating differently and you’re keeping active, but your waistline is expanding. How is that happening? Since eating healthy and exercising shouldn’t make you gain weight, there may be a hidden factor getting in your way. Stress. The one thing that can have a grip on your circadian rhythm stronger than any bodybuilder.
Investigators at Weill Cornell Medicine published two mouse studies that suggest stress and other factors that throw the body’s circadian clocks out of rhythm may contribute to weight gain.
In the first study, the researchers imitated disruptive condition effects like high cortisol exposure and chronic stress by implanting pellets under the skin that released glucocorticoid at a constant rate for 21 days. Mice that received the pellets had twice as much white and brown fat, as well as much higher insulin levels, regardless of their unchanged and still-healthy diet.
In the second study, they used tagged proteins as markers to monitor the daily fluctuations of a protein that regulates fat cell production and circadian gene expression in mouse fat cell precursors. The results showed “that fat cell precursors commit to becoming fat cells only during the circadian cycle phase corresponding to evening in humans,” they said in a written statement.
“Every cell in our body has an intrinsic cell clock, just like the fat cells, and we have a master clock in our brain, which controls hormone secretion,” said senior author Mary Teruel of Cornell University. “A lot of forces are working against a healthy metabolism when we are out of circadian rhythm. The more we understand, the more likely we will be able to do something about it.”
So if you’re stressing out that the scale is or isn’t moving in the direction you want, you could be standing in your own way. Take a chill pill.
Who can smell cancer? The locust nose
If you need to smell some gas, there’s nothing better than a nose. Just ask a scientist: “Noses are still state of the art,” said Debajit Saha, PhD, of Michigan State University. “There’s really nothing like them when it comes to gas sensing.”
And when it comes to noses, dogs are best, right? After all, there’s a reason we don’t have bomb-sniffing wombats and drug-sniffing ostriches. Dogs are better. Better, but not perfect. And if they’re not perfect, then human technology can do better.
Enter the electronic nose. Which is better than dogs … except that it isn’t. “People have been working on ‘electronic noses’ for more than 15 years, but they’re still not close to achieving what biology can do seamlessly,” Dr. Saha explained in a statement from the university.
Which brings us back to dogs. If you want to detect early-stage cancer using smell, you go to the dogs, right? Nope.
Here’s Christopher Contag, PhD, also of Michigan State, who recruited Dr. Saha to the university: “I told him, ‘When you come here, we’ll detect cancer. I’m sure your locusts can do it.’ ”
Yes, locusts. Dr. Contag and his research team were looking at mouth cancers and noticed that different cell lines had different appearances. Then they discovered that those different-looking cell lines produced different metabolites, some of which were volatile.
Enter Dr. Saha’s locusts. They were able to tell the difference between normal cells and cancer cells and could even distinguish between the different cell lines. And how they were able to share this information? Not voluntarily, that’s for sure. The researchers attached electrodes to the insects’ brains and recorded their responses to gas samples from both healthy and cancer cells. Those brain signals were then used to create chemical profiles of the different cells. Piece of cake.
The whole getting-electrodes-attached-to-their-brains thing seemed at least a bit ethically ambiguous, so we contacted the locusts’ PR office, which offered some positive spin: “Humans get their early cancer detection and we get that whole swarms-that-devour-entire-countrysides thing off our backs. Win win.”
Bad news for vampires everywhere
Pop culture has been extraordinarily kind to the vampire. A few hundred years ago, vampires were demon-possessed, often-inhuman monsters. Now? They’re suave, sophisticated, beautiful, and oh-so dramatic and angst-filled about their “curse.” Drink a little human blood, live and look young forever. Such monsters they are.
It does make sense in a morbid sort of way. An old person receiving the blood of the young does seem like a good idea for rejuvenation, right? A team of Ukrainian researchers sought to find out, conducting a study in which older mice were linked with young mice via heterochronic parabiosis. For 3 months, old-young mice pairs were surgically connected and shared blood. After 3 months, the mice were disconnected from each other and the effects of the blood link were studied.
For all the vampire enthusiasts out there, we have bad news and worse news. The bad news first: The older mice received absolutely no benefit from heterochronic parabiosis. No youthfulness, no increased lifespan, nothing. The worse news is that the younger mice were adversely affected by the older blood. They aged more and experienced a shortened lifespan, even after the connection was severed. The old blood, according to the investigators, contains factors capable of inducing aging in younger mice, but the opposite is not true. Further research into aging, they added, should focus on suppressing the aging factors in older blood.
Of note, the paper was written by doctors who are currently refugees, fleeing the war in Ukraine. We don’t want to speculate on the true cause of the war, but we’re onto you, Putin. We know you wanted the vampire research for yourself, but it won’t work. Your dream of becoming Vlad “Dracula” Putin will never come to pass.
Hearing is not always believing
Have you ever heard yourself on a voice mail, or from a recording you did at work? No matter how good you sound, you still might feel like the recording sounds nothing like you. It may even cause low self-esteem for those who don’t like how their voice sounds or don’t recognize it when it’s played back to them.
Since one possible symptom of schizophrenia is not recognizing one’s own speech and having a false sense of control over actions, and those with schizophrenia may hallucinate or hear voices, not being able to recognize their own voices may be alarming.
A recent study on the sense of agency, or sense of control, involved having volunteers speak with different pitches in their voices and then having it played back to them to gauge their reactions.
“Our results demonstrate that hearing one’s own voice is a critical factor to increased self-agency over speech. In other words, we do not strongly feel that ‘I’ am generating the speech if we hear someone else’s voice as an outcome of the speech. Our study provides empirical evidence of the tight link between the sense of agency and self-voice identity,” lead author Ryu Ohata, PhD, of the University of Tokyo, said in a written statement.
As social interaction becomes more digital through platforms such as FaceTime, Zoom, and voicemail, especially since the pandemic has promoted social distancing, it makes sense that people may be more aware and more surprised by how they sound on recordings.
So, if you ever promised someone something that you don’t want to do, and they play it back to you from the recording you made, maybe you can just say you don’t recognize the voice. And if it’s not you, then you don’t have to do it.
Stress, meet weight gain. Weight gain, meet stress
You’re not eating differently and you’re keeping active, but your waistline is expanding. How is that happening? Since eating healthy and exercising shouldn’t make you gain weight, there may be a hidden factor getting in your way. Stress. The one thing that can have a grip on your circadian rhythm stronger than any bodybuilder.
Investigators at Weill Cornell Medicine published two mouse studies that suggest stress and other factors that throw the body’s circadian clocks out of rhythm may contribute to weight gain.
In the first study, the researchers imitated disruptive condition effects like high cortisol exposure and chronic stress by implanting pellets under the skin that released glucocorticoid at a constant rate for 21 days. Mice that received the pellets had twice as much white and brown fat, as well as much higher insulin levels, regardless of their unchanged and still-healthy diet.
In the second study, they used tagged proteins as markers to monitor the daily fluctuations of a protein that regulates fat cell production and circadian gene expression in mouse fat cell precursors. The results showed “that fat cell precursors commit to becoming fat cells only during the circadian cycle phase corresponding to evening in humans,” they said in a written statement.
“Every cell in our body has an intrinsic cell clock, just like the fat cells, and we have a master clock in our brain, which controls hormone secretion,” said senior author Mary Teruel of Cornell University. “A lot of forces are working against a healthy metabolism when we are out of circadian rhythm. The more we understand, the more likely we will be able to do something about it.”
So if you’re stressing out that the scale is or isn’t moving in the direction you want, you could be standing in your own way. Take a chill pill.
Who can smell cancer? The locust nose
If you need to smell some gas, there’s nothing better than a nose. Just ask a scientist: “Noses are still state of the art,” said Debajit Saha, PhD, of Michigan State University. “There’s really nothing like them when it comes to gas sensing.”
And when it comes to noses, dogs are best, right? After all, there’s a reason we don’t have bomb-sniffing wombats and drug-sniffing ostriches. Dogs are better. Better, but not perfect. And if they’re not perfect, then human technology can do better.
Enter the electronic nose. Which is better than dogs … except that it isn’t. “People have been working on ‘electronic noses’ for more than 15 years, but they’re still not close to achieving what biology can do seamlessly,” Dr. Saha explained in a statement from the university.
Which brings us back to dogs. If you want to detect early-stage cancer using smell, you go to the dogs, right? Nope.
Here’s Christopher Contag, PhD, also of Michigan State, who recruited Dr. Saha to the university: “I told him, ‘When you come here, we’ll detect cancer. I’m sure your locusts can do it.’ ”
Yes, locusts. Dr. Contag and his research team were looking at mouth cancers and noticed that different cell lines had different appearances. Then they discovered that those different-looking cell lines produced different metabolites, some of which were volatile.
Enter Dr. Saha’s locusts. They were able to tell the difference between normal cells and cancer cells and could even distinguish between the different cell lines. And how they were able to share this information? Not voluntarily, that’s for sure. The researchers attached electrodes to the insects’ brains and recorded their responses to gas samples from both healthy and cancer cells. Those brain signals were then used to create chemical profiles of the different cells. Piece of cake.
The whole getting-electrodes-attached-to-their-brains thing seemed at least a bit ethically ambiguous, so we contacted the locusts’ PR office, which offered some positive spin: “Humans get their early cancer detection and we get that whole swarms-that-devour-entire-countrysides thing off our backs. Win win.”
Bad news for vampires everywhere
Pop culture has been extraordinarily kind to the vampire. A few hundred years ago, vampires were demon-possessed, often-inhuman monsters. Now? They’re suave, sophisticated, beautiful, and oh-so dramatic and angst-filled about their “curse.” Drink a little human blood, live and look young forever. Such monsters they are.
It does make sense in a morbid sort of way. An old person receiving the blood of the young does seem like a good idea for rejuvenation, right? A team of Ukrainian researchers sought to find out, conducting a study in which older mice were linked with young mice via heterochronic parabiosis. For 3 months, old-young mice pairs were surgically connected and shared blood. After 3 months, the mice were disconnected from each other and the effects of the blood link were studied.
For all the vampire enthusiasts out there, we have bad news and worse news. The bad news first: The older mice received absolutely no benefit from heterochronic parabiosis. No youthfulness, no increased lifespan, nothing. The worse news is that the younger mice were adversely affected by the older blood. They aged more and experienced a shortened lifespan, even after the connection was severed. The old blood, according to the investigators, contains factors capable of inducing aging in younger mice, but the opposite is not true. Further research into aging, they added, should focus on suppressing the aging factors in older blood.
Of note, the paper was written by doctors who are currently refugees, fleeing the war in Ukraine. We don’t want to speculate on the true cause of the war, but we’re onto you, Putin. We know you wanted the vampire research for yourself, but it won’t work. Your dream of becoming Vlad “Dracula” Putin will never come to pass.
Hearing is not always believing
Have you ever heard yourself on a voice mail, or from a recording you did at work? No matter how good you sound, you still might feel like the recording sounds nothing like you. It may even cause low self-esteem for those who don’t like how their voice sounds or don’t recognize it when it’s played back to them.
Since one possible symptom of schizophrenia is not recognizing one’s own speech and having a false sense of control over actions, and those with schizophrenia may hallucinate or hear voices, not being able to recognize their own voices may be alarming.
A recent study on the sense of agency, or sense of control, involved having volunteers speak with different pitches in their voices and then having it played back to them to gauge their reactions.
“Our results demonstrate that hearing one’s own voice is a critical factor to increased self-agency over speech. In other words, we do not strongly feel that ‘I’ am generating the speech if we hear someone else’s voice as an outcome of the speech. Our study provides empirical evidence of the tight link between the sense of agency and self-voice identity,” lead author Ryu Ohata, PhD, of the University of Tokyo, said in a written statement.
As social interaction becomes more digital through platforms such as FaceTime, Zoom, and voicemail, especially since the pandemic has promoted social distancing, it makes sense that people may be more aware and more surprised by how they sound on recordings.
So, if you ever promised someone something that you don’t want to do, and they play it back to you from the recording you made, maybe you can just say you don’t recognize the voice. And if it’s not you, then you don’t have to do it.
Stress, meet weight gain. Weight gain, meet stress
You’re not eating differently and you’re keeping active, but your waistline is expanding. How is that happening? Since eating healthy and exercising shouldn’t make you gain weight, there may be a hidden factor getting in your way. Stress. The one thing that can have a grip on your circadian rhythm stronger than any bodybuilder.
Investigators at Weill Cornell Medicine published two mouse studies that suggest stress and other factors that throw the body’s circadian clocks out of rhythm may contribute to weight gain.
In the first study, the researchers imitated disruptive condition effects like high cortisol exposure and chronic stress by implanting pellets under the skin that released glucocorticoid at a constant rate for 21 days. Mice that received the pellets had twice as much white and brown fat, as well as much higher insulin levels, regardless of their unchanged and still-healthy diet.
In the second study, they used tagged proteins as markers to monitor the daily fluctuations of a protein that regulates fat cell production and circadian gene expression in mouse fat cell precursors. The results showed “that fat cell precursors commit to becoming fat cells only during the circadian cycle phase corresponding to evening in humans,” they said in a written statement.
“Every cell in our body has an intrinsic cell clock, just like the fat cells, and we have a master clock in our brain, which controls hormone secretion,” said senior author Mary Teruel of Cornell University. “A lot of forces are working against a healthy metabolism when we are out of circadian rhythm. The more we understand, the more likely we will be able to do something about it.”
So if you’re stressing out that the scale is or isn’t moving in the direction you want, you could be standing in your own way. Take a chill pill.
Who can smell cancer? The locust nose
If you need to smell some gas, there’s nothing better than a nose. Just ask a scientist: “Noses are still state of the art,” said Debajit Saha, PhD, of Michigan State University. “There’s really nothing like them when it comes to gas sensing.”
And when it comes to noses, dogs are best, right? After all, there’s a reason we don’t have bomb-sniffing wombats and drug-sniffing ostriches. Dogs are better. Better, but not perfect. And if they’re not perfect, then human technology can do better.
Enter the electronic nose. Which is better than dogs … except that it isn’t. “People have been working on ‘electronic noses’ for more than 15 years, but they’re still not close to achieving what biology can do seamlessly,” Dr. Saha explained in a statement from the university.
Which brings us back to dogs. If you want to detect early-stage cancer using smell, you go to the dogs, right? Nope.
Here’s Christopher Contag, PhD, also of Michigan State, who recruited Dr. Saha to the university: “I told him, ‘When you come here, we’ll detect cancer. I’m sure your locusts can do it.’ ”
Yes, locusts. Dr. Contag and his research team were looking at mouth cancers and noticed that different cell lines had different appearances. Then they discovered that those different-looking cell lines produced different metabolites, some of which were volatile.
Enter Dr. Saha’s locusts. They were able to tell the difference between normal cells and cancer cells and could even distinguish between the different cell lines. And how they were able to share this information? Not voluntarily, that’s for sure. The researchers attached electrodes to the insects’ brains and recorded their responses to gas samples from both healthy and cancer cells. Those brain signals were then used to create chemical profiles of the different cells. Piece of cake.
The whole getting-electrodes-attached-to-their-brains thing seemed at least a bit ethically ambiguous, so we contacted the locusts’ PR office, which offered some positive spin: “Humans get their early cancer detection and we get that whole swarms-that-devour-entire-countrysides thing off our backs. Win win.”
Bad news for vampires everywhere
Pop culture has been extraordinarily kind to the vampire. A few hundred years ago, vampires were demon-possessed, often-inhuman monsters. Now? They’re suave, sophisticated, beautiful, and oh-so dramatic and angst-filled about their “curse.” Drink a little human blood, live and look young forever. Such monsters they are.
It does make sense in a morbid sort of way. An old person receiving the blood of the young does seem like a good idea for rejuvenation, right? A team of Ukrainian researchers sought to find out, conducting a study in which older mice were linked with young mice via heterochronic parabiosis. For 3 months, old-young mice pairs were surgically connected and shared blood. After 3 months, the mice were disconnected from each other and the effects of the blood link were studied.
For all the vampire enthusiasts out there, we have bad news and worse news. The bad news first: The older mice received absolutely no benefit from heterochronic parabiosis. No youthfulness, no increased lifespan, nothing. The worse news is that the younger mice were adversely affected by the older blood. They aged more and experienced a shortened lifespan, even after the connection was severed. The old blood, according to the investigators, contains factors capable of inducing aging in younger mice, but the opposite is not true. Further research into aging, they added, should focus on suppressing the aging factors in older blood.
Of note, the paper was written by doctors who are currently refugees, fleeing the war in Ukraine. We don’t want to speculate on the true cause of the war, but we’re onto you, Putin. We know you wanted the vampire research for yourself, but it won’t work. Your dream of becoming Vlad “Dracula” Putin will never come to pass.
Hearing is not always believing
Have you ever heard yourself on a voice mail, or from a recording you did at work? No matter how good you sound, you still might feel like the recording sounds nothing like you. It may even cause low self-esteem for those who don’t like how their voice sounds or don’t recognize it when it’s played back to them.
Since one possible symptom of schizophrenia is not recognizing one’s own speech and having a false sense of control over actions, and those with schizophrenia may hallucinate or hear voices, not being able to recognize their own voices may be alarming.
A recent study on the sense of agency, or sense of control, involved having volunteers speak with different pitches in their voices and then having it played back to them to gauge their reactions.
“Our results demonstrate that hearing one’s own voice is a critical factor to increased self-agency over speech. In other words, we do not strongly feel that ‘I’ am generating the speech if we hear someone else’s voice as an outcome of the speech. Our study provides empirical evidence of the tight link between the sense of agency and self-voice identity,” lead author Ryu Ohata, PhD, of the University of Tokyo, said in a written statement.
As social interaction becomes more digital through platforms such as FaceTime, Zoom, and voicemail, especially since the pandemic has promoted social distancing, it makes sense that people may be more aware and more surprised by how they sound on recordings.
So, if you ever promised someone something that you don’t want to do, and they play it back to you from the recording you made, maybe you can just say you don’t recognize the voice. And if it’s not you, then you don’t have to do it.






