User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Joint effort: CBD not just innocent bystander in weed
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
I visited a legal cannabis dispensary in Massachusetts a few years ago, mostly to see what the hype was about. There I was, knowing basically nothing about pot, as the gentle stoner behind the counter explained to me the differences between the various strains. Acapulco Gold is buoyant and energizing; Purple Kush is sleepy, relaxed, dissociative. Here’s a strain that makes you feel nostalgic; here’s one that helps you focus. It was as complicated and as oddly specific as a fancy wine tasting – and, I had a feeling, about as reliable.
It’s a plant, after all, and though delta-9-tetrahydrocannabinol (THC) is the chemical responsible for its euphoric effects, it is far from the only substance in there.
The second most important compound in cannabis is cannabidiol, and most people will tell you that CBD is the gentle yin to THC’s paranoiac yang. Hence your local ganja barista reminding you that, if you don›t want all those anxiety-inducing side effects of THC, grab a strain with a nice CBD balance.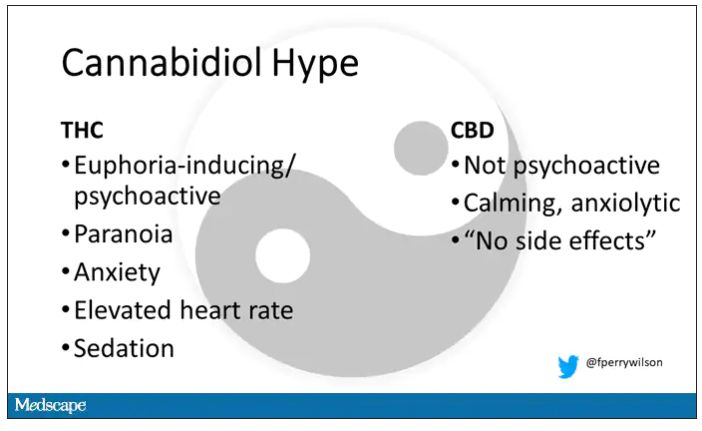
But is it true? A new study appearing in JAMA Network Open suggests, in fact, that it’s quite the opposite. This study is from Austin Zamarripa and colleagues, who clearly sit at the researcher cool kids table.
Eighteen adults who had abstained from marijuana use for at least a month participated in this trial (which is way more fun than anything we do in my lab at Yale). In random order, separated by at least a week, they ate some special brownies.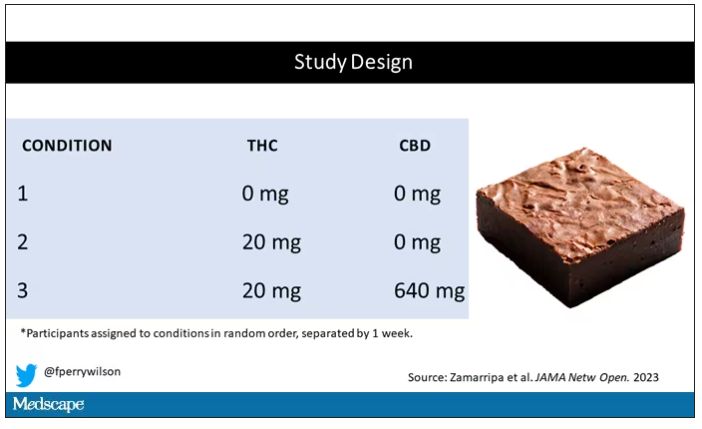
Condition one was a control brownie, condition two was a brownie containing 20 mg of THC, and condition three was a brownie containing 20 mg of THC and 640 mg of CBD. Participants were assigned each condition in random order, separated by at least a week.
A side note on doses for those of you who, like me, are not totally weed literate. A dose of 20 mg of THC is about a third of what you might find in a typical joint these days (though it’s about double the THC content of a joint in the ‘70s – I believe the technical term is “doobie”). And 640 mg of CBD is a decent dose, as 5 mg per kilogram is what some folks start with to achieve therapeutic effects.
Both THC and CBD interact with the cytochrome p450 system in the liver. This matters when you’re ingesting them instead of smoking them because you have first-pass metabolism to contend with. And, because of that p450 inhibition, it’s possible that CBD might actually increase the amount of THC that gets into your bloodstream from the brownie, or gummy, or pizza sauce, or whatever.
Let’s get to the results, starting with blood THC concentration. It’s not subtle. With CBD on board the THC concentration rises higher faster, with roughly double the area under the curve.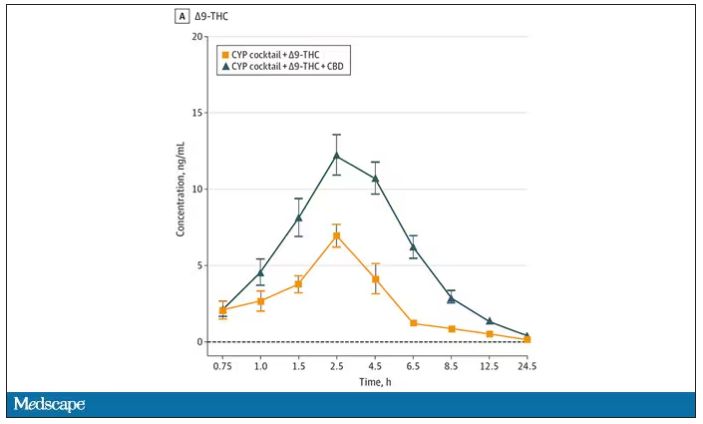
And, unsurprisingly, the subjective experience correlated with those higher levels. Individuals rated the “drug effect” higher with the combo. But, interestingly, the “pleasant” drug effect didn’t change much, while the unpleasant effects were substantially higher. No mitigation of THC anxiety here – quite the opposite. CBD made the anxiety worse.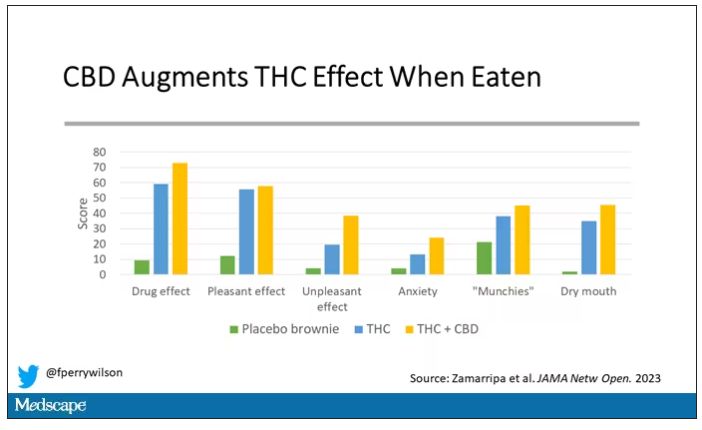
Cognitive effects were equally profound. Scores on a digit symbol substitution test and a paced serial addition task were all substantially worse when CBD was mixed with THC.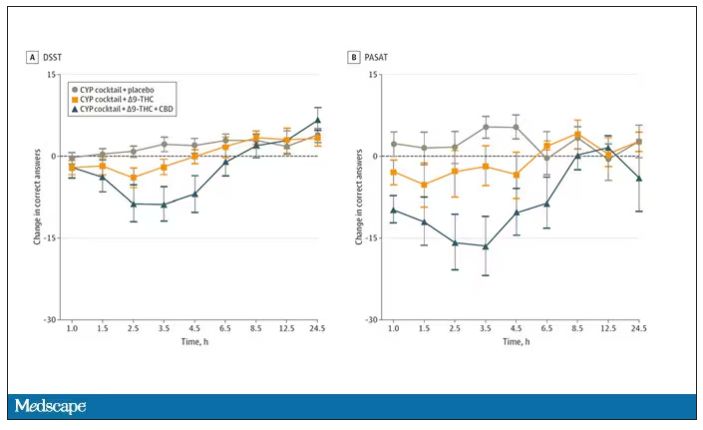
And for those of you who want some more objective measures, check out the heart rate. Despite the purported “calming” nature of CBD, heart rates were way higher when individuals were exposed to both chemicals.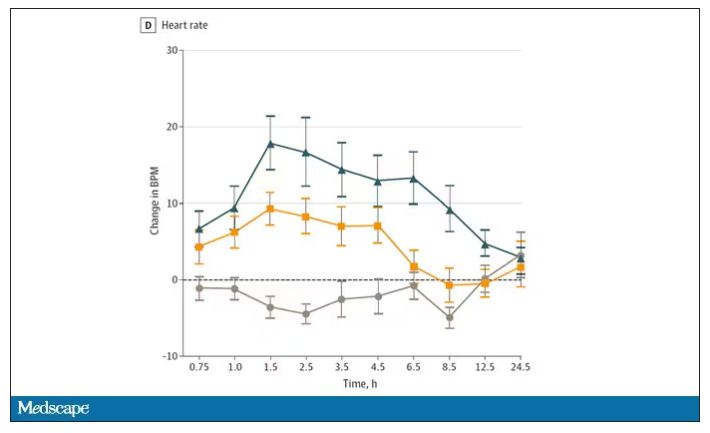
The picture here is quite clear, though the mechanism is not. At least when talking edibles, CBD enhances the effects of THC, and not necessarily for the better. It may be that CBD is competing with some of the proteins that metabolize THC, thus prolonging its effects. CBD may also directly inhibit those enzymes. But whatever the case, I think we can safely say the myth that CBD makes the effects of THC more mild or more tolerable is busted.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator in New Haven, Conn.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
I visited a legal cannabis dispensary in Massachusetts a few years ago, mostly to see what the hype was about. There I was, knowing basically nothing about pot, as the gentle stoner behind the counter explained to me the differences between the various strains. Acapulco Gold is buoyant and energizing; Purple Kush is sleepy, relaxed, dissociative. Here’s a strain that makes you feel nostalgic; here’s one that helps you focus. It was as complicated and as oddly specific as a fancy wine tasting – and, I had a feeling, about as reliable.
It’s a plant, after all, and though delta-9-tetrahydrocannabinol (THC) is the chemical responsible for its euphoric effects, it is far from the only substance in there.
The second most important compound in cannabis is cannabidiol, and most people will tell you that CBD is the gentle yin to THC’s paranoiac yang. Hence your local ganja barista reminding you that, if you don›t want all those anxiety-inducing side effects of THC, grab a strain with a nice CBD balance.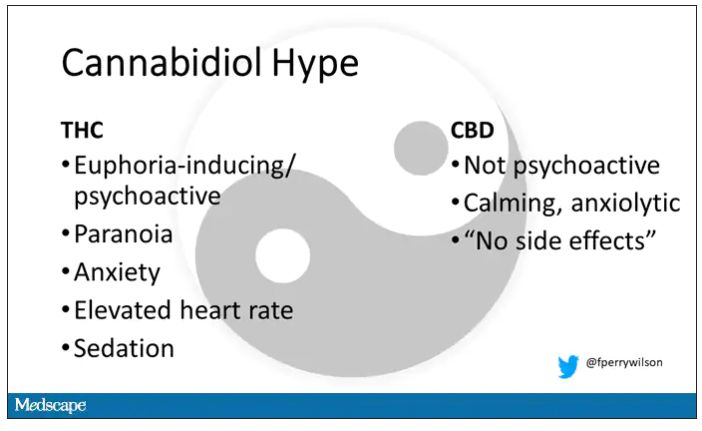
But is it true? A new study appearing in JAMA Network Open suggests, in fact, that it’s quite the opposite. This study is from Austin Zamarripa and colleagues, who clearly sit at the researcher cool kids table.
Eighteen adults who had abstained from marijuana use for at least a month participated in this trial (which is way more fun than anything we do in my lab at Yale). In random order, separated by at least a week, they ate some special brownies.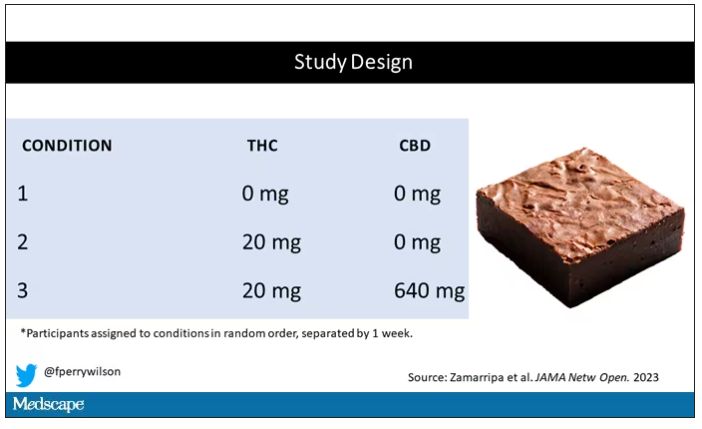
Condition one was a control brownie, condition two was a brownie containing 20 mg of THC, and condition three was a brownie containing 20 mg of THC and 640 mg of CBD. Participants were assigned each condition in random order, separated by at least a week.
A side note on doses for those of you who, like me, are not totally weed literate. A dose of 20 mg of THC is about a third of what you might find in a typical joint these days (though it’s about double the THC content of a joint in the ‘70s – I believe the technical term is “doobie”). And 640 mg of CBD is a decent dose, as 5 mg per kilogram is what some folks start with to achieve therapeutic effects.
Both THC and CBD interact with the cytochrome p450 system in the liver. This matters when you’re ingesting them instead of smoking them because you have first-pass metabolism to contend with. And, because of that p450 inhibition, it’s possible that CBD might actually increase the amount of THC that gets into your bloodstream from the brownie, or gummy, or pizza sauce, or whatever.
Let’s get to the results, starting with blood THC concentration. It’s not subtle. With CBD on board the THC concentration rises higher faster, with roughly double the area under the curve.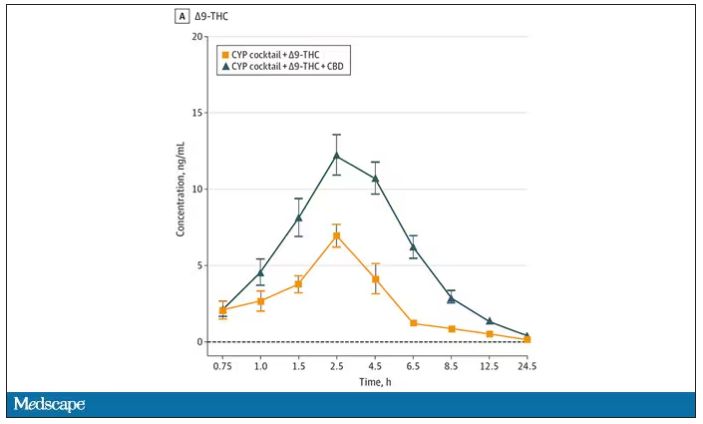
And, unsurprisingly, the subjective experience correlated with those higher levels. Individuals rated the “drug effect” higher with the combo. But, interestingly, the “pleasant” drug effect didn’t change much, while the unpleasant effects were substantially higher. No mitigation of THC anxiety here – quite the opposite. CBD made the anxiety worse.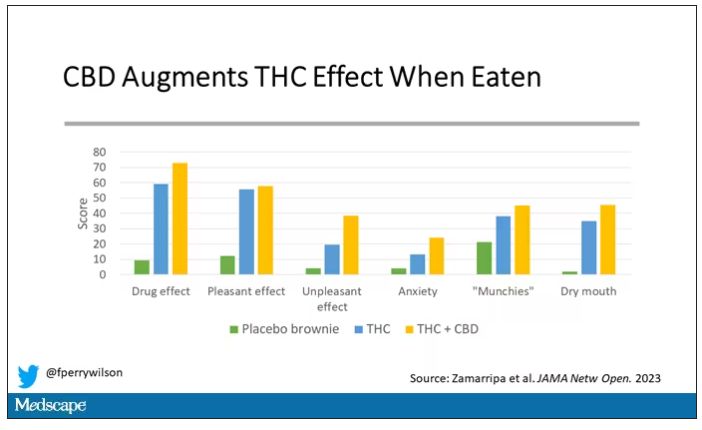
Cognitive effects were equally profound. Scores on a digit symbol substitution test and a paced serial addition task were all substantially worse when CBD was mixed with THC.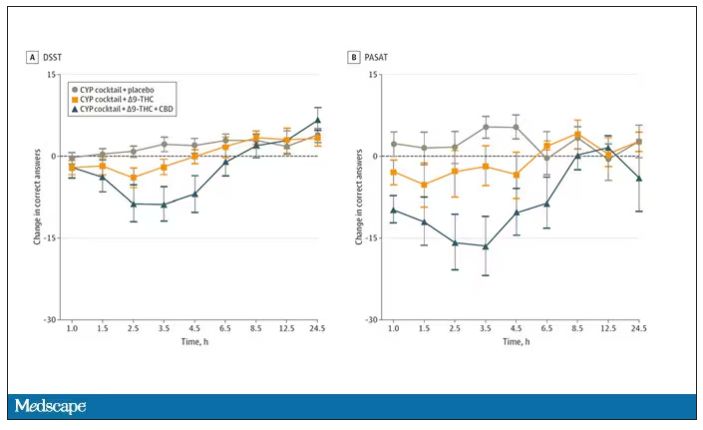
And for those of you who want some more objective measures, check out the heart rate. Despite the purported “calming” nature of CBD, heart rates were way higher when individuals were exposed to both chemicals.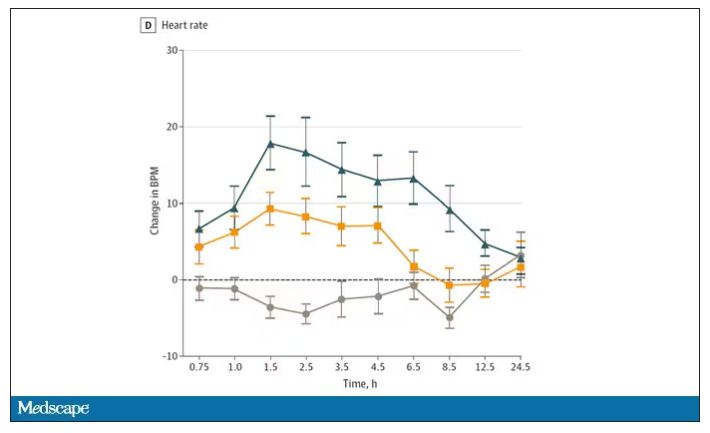
The picture here is quite clear, though the mechanism is not. At least when talking edibles, CBD enhances the effects of THC, and not necessarily for the better. It may be that CBD is competing with some of the proteins that metabolize THC, thus prolonging its effects. CBD may also directly inhibit those enzymes. But whatever the case, I think we can safely say the myth that CBD makes the effects of THC more mild or more tolerable is busted.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator in New Haven, Conn.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
I visited a legal cannabis dispensary in Massachusetts a few years ago, mostly to see what the hype was about. There I was, knowing basically nothing about pot, as the gentle stoner behind the counter explained to me the differences between the various strains. Acapulco Gold is buoyant and energizing; Purple Kush is sleepy, relaxed, dissociative. Here’s a strain that makes you feel nostalgic; here’s one that helps you focus. It was as complicated and as oddly specific as a fancy wine tasting – and, I had a feeling, about as reliable.
It’s a plant, after all, and though delta-9-tetrahydrocannabinol (THC) is the chemical responsible for its euphoric effects, it is far from the only substance in there.
The second most important compound in cannabis is cannabidiol, and most people will tell you that CBD is the gentle yin to THC’s paranoiac yang. Hence your local ganja barista reminding you that, if you don›t want all those anxiety-inducing side effects of THC, grab a strain with a nice CBD balance.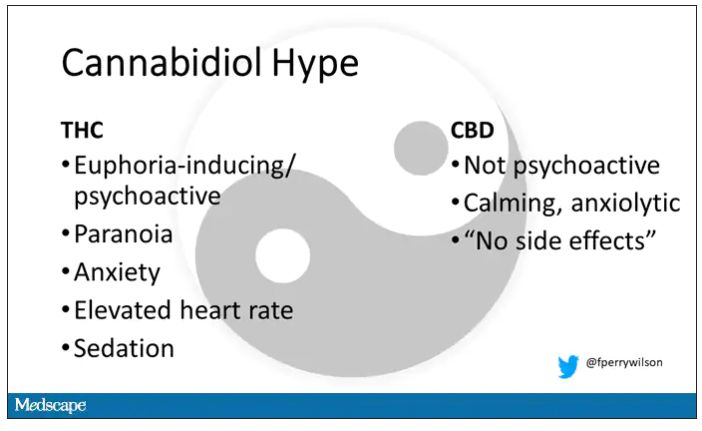
But is it true? A new study appearing in JAMA Network Open suggests, in fact, that it’s quite the opposite. This study is from Austin Zamarripa and colleagues, who clearly sit at the researcher cool kids table.
Eighteen adults who had abstained from marijuana use for at least a month participated in this trial (which is way more fun than anything we do in my lab at Yale). In random order, separated by at least a week, they ate some special brownies.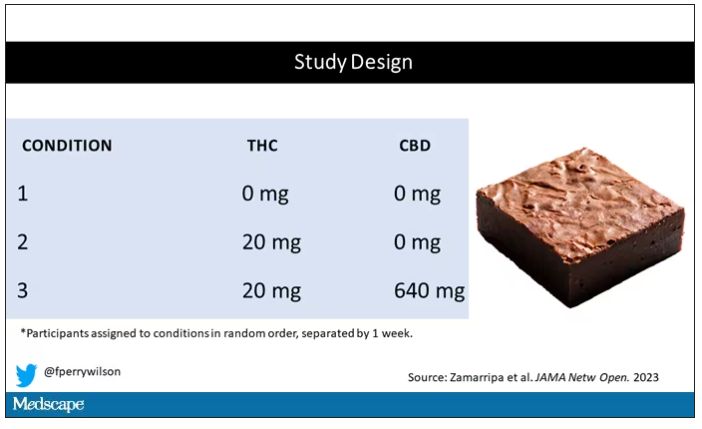
Condition one was a control brownie, condition two was a brownie containing 20 mg of THC, and condition three was a brownie containing 20 mg of THC and 640 mg of CBD. Participants were assigned each condition in random order, separated by at least a week.
A side note on doses for those of you who, like me, are not totally weed literate. A dose of 20 mg of THC is about a third of what you might find in a typical joint these days (though it’s about double the THC content of a joint in the ‘70s – I believe the technical term is “doobie”). And 640 mg of CBD is a decent dose, as 5 mg per kilogram is what some folks start with to achieve therapeutic effects.
Both THC and CBD interact with the cytochrome p450 system in the liver. This matters when you’re ingesting them instead of smoking them because you have first-pass metabolism to contend with. And, because of that p450 inhibition, it’s possible that CBD might actually increase the amount of THC that gets into your bloodstream from the brownie, or gummy, or pizza sauce, or whatever.
Let’s get to the results, starting with blood THC concentration. It’s not subtle. With CBD on board the THC concentration rises higher faster, with roughly double the area under the curve.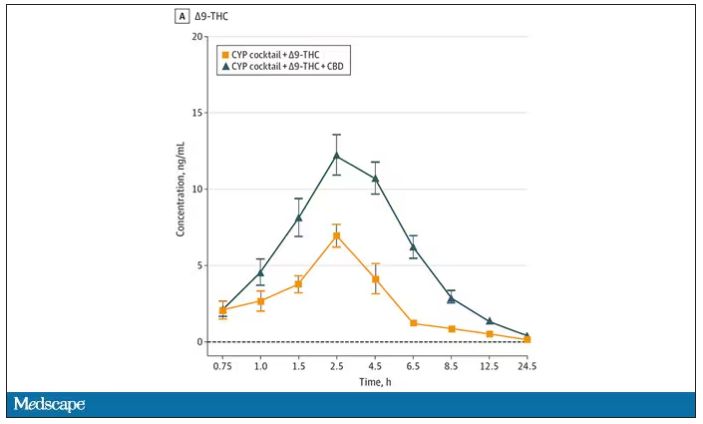
And, unsurprisingly, the subjective experience correlated with those higher levels. Individuals rated the “drug effect” higher with the combo. But, interestingly, the “pleasant” drug effect didn’t change much, while the unpleasant effects were substantially higher. No mitigation of THC anxiety here – quite the opposite. CBD made the anxiety worse.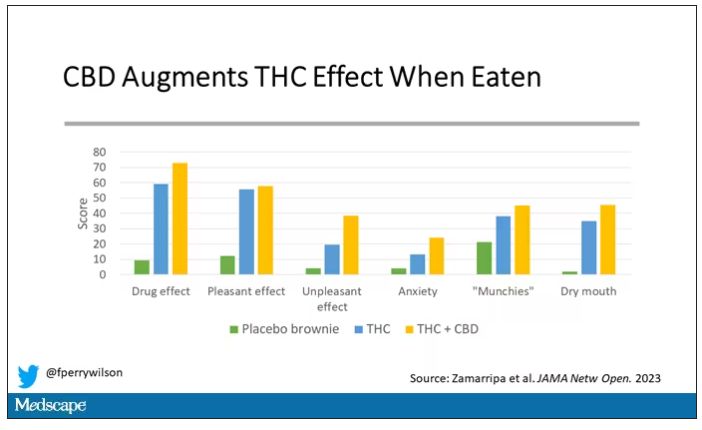
Cognitive effects were equally profound. Scores on a digit symbol substitution test and a paced serial addition task were all substantially worse when CBD was mixed with THC.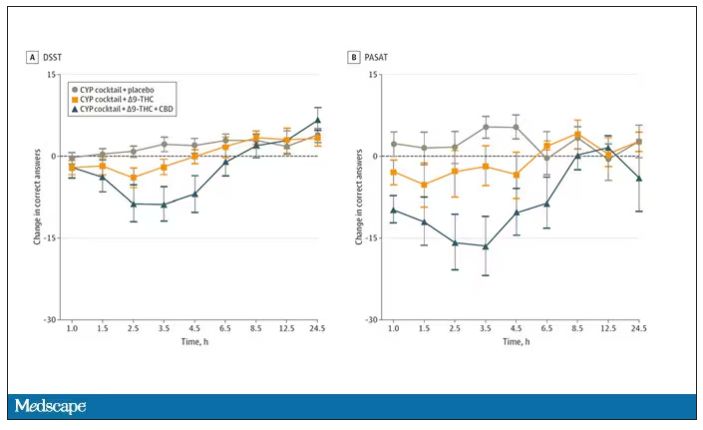
And for those of you who want some more objective measures, check out the heart rate. Despite the purported “calming” nature of CBD, heart rates were way higher when individuals were exposed to both chemicals.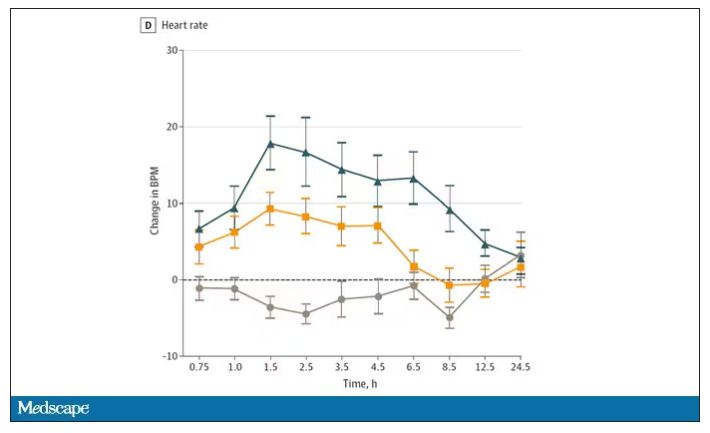
The picture here is quite clear, though the mechanism is not. At least when talking edibles, CBD enhances the effects of THC, and not necessarily for the better. It may be that CBD is competing with some of the proteins that metabolize THC, thus prolonging its effects. CBD may also directly inhibit those enzymes. But whatever the case, I think we can safely say the myth that CBD makes the effects of THC more mild or more tolerable is busted.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator in New Haven, Conn.
A version of this article first appeared on Medscape.com.
Doctors are disappearing from emergency departments as hospitals look to cut costs
She didn’t know much about miscarriage, but this seemed like one.
In the emergency department, she was examined then sent home, she said. She went back when her cramping became excruciating. Then home again. It ultimately took three trips to the ED on 3 consecutive days, generating three separate bills, before she saw a doctor who looked at her blood work and confirmed her fears.
“At the time I wasn’t thinking, ‘Oh, I need to see a doctor,’ ” Ms. Valle recalled. “But when you think about it, it’s like, ‘Well, dang – why didn’t I see a doctor?’ ” It’s unclear whether the repeat visits were due to delays in seeing a physician, but the experience worried her. And she’s still paying the bills.
The hospital declined to discuss Ms. Valle’s care, citing patient privacy. But 17 months before her 3-day ordeal, Tennova had outsourced its emergency departments to American Physician Partners, a medical staffing company owned by private equity investors. APP employs fewer doctors in its EDs as one of its cost-saving initiatives to increase earnings, according to a confidential company document obtained by KHN and NPR.
This staffing strategy has permeated hospitals, and particularly emergency departments, that seek to reduce their top expense: physician labor. While diagnosing and treating patients was once their domain, doctors are increasingly being replaced by nurse practitioners and physician assistants, collectively known as “midlevel practitioners,” who can perform many of the same duties and generate much of the same revenue for less than half of the pay.
“APP has numerous cost saving initiatives underway as part of the Company’s continual focus on cost optimization,” the document says, including a “shift of staffing” between doctors and midlevel practitioners.
In a statement to KHN, American Physician Partners said this strategy is a way to ensure all EDs remain fully staffed, calling it a “blended model” that allows doctors, nurse practitioners, and physician assistants “to provide care to their fullest potential.”
Critics of this strategy say the quest to save money results in treatment meted out by someone with far less training than a physician, leaving patients vulnerable to misdiagnoses, higher medical bills, and inadequate care. And these fears are bolstered by evidence that suggests dropping doctors from EDs may not be good for patients.
A working paper, published in October by the National Bureau of Economic Research, analyzed roughly 1.1 million visits to 44 EDs throughout the Veterans Health Administration, where nurse practitioners can treat patients without oversight from doctors.
Researchers found that treatment by a nurse practitioner resulted on average in a 7% increase in cost of care and an 11% increase in length of stay, extending patients’ time in the ED by minutes for minor visits and hours for longer ones. These gaps widened among patients with more severe diagnoses, the study said, but could be somewhat mitigated by nurse practitioners with more experience.
The study also found that ED patients treated by a nurse practitioner were 20% more likely to be readmitted to the hospital for a preventable reason within 30 days, although the overall risk of readmission remained very small.
Yiqun Chen, PhD, who is an assistant professor of economics at the University of Illinois at Chicago and coauthored the study, said these findings are not an indictment of nurse practitioners in the ED. Instead, she said, she hopes the study will guide how to best deploy nurse practitioners: in treatment of simpler patients or circumstances when no doctor is available.
“It’s not just a simple question of if we can substitute physicians with nurse practitioners or not,” Dr. Chen said. “It depends on how we use them. If we just use them as independent providers, especially ... for relatively complicated patients, it doesn’t seem to be a very good use.”
Dr. Chen’s research echoes smaller studies, like one from The Harvey L. Neiman Health Policy Institute that found nonphysician practitioners in EDs were associated with a 5.3% increase in imaging, which could unnecessarily increase bills for patients. Separately, a study at the Hattiesburg Clinic in Mississippi found that midlevel practitioners in primary care – not in the emergency department – increased the out-of-pocket costs to patients while also leading to worse performance on 9 of 10 quality-of-care metrics, including cancer screenings and vaccination rates.
But definitive evidence remains elusive that replacing ER doctors with nonphysicians has a negative impact on patients, said Cameron Gettel, MD, an assistant professor of emergency medicine at Yale University, New Haven, Conn. Private equity investment and the use of midlevel practitioners rose in lockstep in the ED, Dr. Gettel said, and in the absence of game-changing research, the pattern will likely continue.
“Worse patient outcomes haven’t really been shown across the board,” he said. “And I think until that is shown, then they will continue to play an increasing role.”
For private equity, dropping ED docs is a “simple equation”
Private equity companies pool money from wealthy investors to buy their way into various industries, often slashing spending and seeking to flip businesses in 3 to 7 years. While this business model is a proven moneymaker on Wall Street, it raises concerns in health care, where critics worry the pressure to turn big profits will influence life-or-death decisions that were once left solely to medical professionals.
Nearly $1 trillion in private equity funds have gone into almost 8,000 health care transactions over the past decade, according to industry tracker PitchBook, including buying into medical staffing companies that many hospitals hire to manage their emergency departments.
Two firms dominate the ED staffing industry: TeamHealth, bought by private equity firm Blackstone in 2016, and Envision Healthcare, bought by KKR in 2018. Trying to undercut these staffing giants is American Physician Partners, a rapidly expanding company that runs EDs in at least 17 states and is 50% owned by private equity firm BBH Capital Partners.
These staffing companies have been among the most aggressive in replacing doctors to cut costs, said Robert McNamara, MD, a founder of the American Academy of Emergency Medicine and chair of emergency medicine at Temple University, Philadelphia.
“It’s a relatively simple equation,” Dr. McNamara said. “Their No. 1 expense is the board-certified emergency physician. So they are going to want to keep that expense as low as possible.”
Not everyone sees the trend of private equity in ED staffing in a negative light. Jennifer Orozco, president of the American Academy of Physician Associates, which represents physician assistants, said even if the change – to use more nonphysician providers – is driven by the staffing firms’ desire to make more money, patients are still well served by a team approach that includes nurse practitioners and physician assistants.
“Though I see that shift, it’s not about profits at the end of the day,” Ms. Orozco said. “It’s about the patient.”
The “shift” is nearly invisible to patients because hospitals rarely promote branding from their ED staffing firms and there is little public documentation of private equity investments.
Arthur Smolensky, MD, a Tennessee emergency medicine specialist attempting to measure private equity’s intrusion into EDs, said his review of hospital job postings and employment contracts in 14 major metropolitan areas found that 43% of ED patients were seen in EDs staffed by companies with nonphysician owners, nearly all of whom are private equity investors.
Dr. Smolensky hopes to publish his full study, expanding to 55 metro areas, later this year. But this research will merely quantify what many doctors already know: The ED has changed. Demoralized by an increased focus on profit, and wary of a looming surplus of emergency medicine residents because there are fewer jobs to fill, many experienced doctors are leaving the ED on their own, he said.
“Most of us didn’t go into medicine to supervise an army of people that are not as well trained as we are,” Dr. Smolensky said. “We want to take care of patients.”
“I guess we’re the first guinea pigs for our ER”
Joshua Allen, a nurse practitioner at a small Kentucky hospital, snaked a rubber hose through a rack of pork ribs to practice inserting a chest tube to fix a collapsed lung.
It was 2020, and American Physician Partners was restructuring the ED where Mr. Allen worked, reducing shifts from two doctors to one. Once Mr. Allen had placed 10 tubes under a doctor’s supervision, he would be allowed to do it on his own.
“I guess we’re the first guinea pigs for our ER,” he said. “If we do have a major trauma and multiple victims come in, there’s only one doctor there. ... We need to be prepared.”
Mr. Allen is one of many midlevel practitioners finding work in emergency departments. Nurse practitioners and physician assistants are among the fastest-growing occupations in the nation, according to the U.S. Bureau of Labor Statistics.
Generally, they have master’s degrees and receive several years of specialized schooling but have significantly less training than doctors. Many are permitted to diagnose patients and prescribe medication with little or no supervision from a doctor, although limitations vary by state.
The Neiman Institute found that the share of ED visits in which a midlevel practitioner was the main clinician increased by more than 172% between 2005 and 2020. Another study, in the Journal of Emergency Medicine, reported that if trends continue there may be equal numbers of midlevel practitioners and doctors in EDs by 2030.
There is little mystery as to why. Federal data shows emergency medicine doctors are paid about $310,000 a year on average, while nurse practitioners and physician assistants earn less than $120,000. Generally, hospitals can bill for care by a midlevel practitioner at 85% the rate of a doctor while paying them less than half as much.
Private equity can make millions in the gap.
For example, Envision once encouraged EDs to employ “the least expensive resource” and treat up to 35% of patients with midlevel practitioners, according to a 2017 PowerPoint presentation. The presentation drew scorn on social media and disappeared from Envision’s website.
Envision declined a request for a phone interview. In a written statement to KHN, spokesperson Aliese Polk said the company does not direct its physician leaders on how to care for patients and called the presentation a “concept guide” that does not represent current views.
American Physician Partners touted roughly the same staffing strategy in 2021 in response to the No Surprises Act, which threatened the company’s profits by outlawing surprise medical bills. In its confidential pitch to lenders, the company estimated it could cut almost $6 million by shifting more staffing from physicians to midlevel practitioners.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
She didn’t know much about miscarriage, but this seemed like one.
In the emergency department, she was examined then sent home, she said. She went back when her cramping became excruciating. Then home again. It ultimately took three trips to the ED on 3 consecutive days, generating three separate bills, before she saw a doctor who looked at her blood work and confirmed her fears.
“At the time I wasn’t thinking, ‘Oh, I need to see a doctor,’ ” Ms. Valle recalled. “But when you think about it, it’s like, ‘Well, dang – why didn’t I see a doctor?’ ” It’s unclear whether the repeat visits were due to delays in seeing a physician, but the experience worried her. And she’s still paying the bills.
The hospital declined to discuss Ms. Valle’s care, citing patient privacy. But 17 months before her 3-day ordeal, Tennova had outsourced its emergency departments to American Physician Partners, a medical staffing company owned by private equity investors. APP employs fewer doctors in its EDs as one of its cost-saving initiatives to increase earnings, according to a confidential company document obtained by KHN and NPR.
This staffing strategy has permeated hospitals, and particularly emergency departments, that seek to reduce their top expense: physician labor. While diagnosing and treating patients was once their domain, doctors are increasingly being replaced by nurse practitioners and physician assistants, collectively known as “midlevel practitioners,” who can perform many of the same duties and generate much of the same revenue for less than half of the pay.
“APP has numerous cost saving initiatives underway as part of the Company’s continual focus on cost optimization,” the document says, including a “shift of staffing” between doctors and midlevel practitioners.
In a statement to KHN, American Physician Partners said this strategy is a way to ensure all EDs remain fully staffed, calling it a “blended model” that allows doctors, nurse practitioners, and physician assistants “to provide care to their fullest potential.”
Critics of this strategy say the quest to save money results in treatment meted out by someone with far less training than a physician, leaving patients vulnerable to misdiagnoses, higher medical bills, and inadequate care. And these fears are bolstered by evidence that suggests dropping doctors from EDs may not be good for patients.
A working paper, published in October by the National Bureau of Economic Research, analyzed roughly 1.1 million visits to 44 EDs throughout the Veterans Health Administration, where nurse practitioners can treat patients without oversight from doctors.
Researchers found that treatment by a nurse practitioner resulted on average in a 7% increase in cost of care and an 11% increase in length of stay, extending patients’ time in the ED by minutes for minor visits and hours for longer ones. These gaps widened among patients with more severe diagnoses, the study said, but could be somewhat mitigated by nurse practitioners with more experience.
The study also found that ED patients treated by a nurse practitioner were 20% more likely to be readmitted to the hospital for a preventable reason within 30 days, although the overall risk of readmission remained very small.
Yiqun Chen, PhD, who is an assistant professor of economics at the University of Illinois at Chicago and coauthored the study, said these findings are not an indictment of nurse practitioners in the ED. Instead, she said, she hopes the study will guide how to best deploy nurse practitioners: in treatment of simpler patients or circumstances when no doctor is available.
“It’s not just a simple question of if we can substitute physicians with nurse practitioners or not,” Dr. Chen said. “It depends on how we use them. If we just use them as independent providers, especially ... for relatively complicated patients, it doesn’t seem to be a very good use.”
Dr. Chen’s research echoes smaller studies, like one from The Harvey L. Neiman Health Policy Institute that found nonphysician practitioners in EDs were associated with a 5.3% increase in imaging, which could unnecessarily increase bills for patients. Separately, a study at the Hattiesburg Clinic in Mississippi found that midlevel practitioners in primary care – not in the emergency department – increased the out-of-pocket costs to patients while also leading to worse performance on 9 of 10 quality-of-care metrics, including cancer screenings and vaccination rates.
But definitive evidence remains elusive that replacing ER doctors with nonphysicians has a negative impact on patients, said Cameron Gettel, MD, an assistant professor of emergency medicine at Yale University, New Haven, Conn. Private equity investment and the use of midlevel practitioners rose in lockstep in the ED, Dr. Gettel said, and in the absence of game-changing research, the pattern will likely continue.
“Worse patient outcomes haven’t really been shown across the board,” he said. “And I think until that is shown, then they will continue to play an increasing role.”
For private equity, dropping ED docs is a “simple equation”
Private equity companies pool money from wealthy investors to buy their way into various industries, often slashing spending and seeking to flip businesses in 3 to 7 years. While this business model is a proven moneymaker on Wall Street, it raises concerns in health care, where critics worry the pressure to turn big profits will influence life-or-death decisions that were once left solely to medical professionals.
Nearly $1 trillion in private equity funds have gone into almost 8,000 health care transactions over the past decade, according to industry tracker PitchBook, including buying into medical staffing companies that many hospitals hire to manage their emergency departments.
Two firms dominate the ED staffing industry: TeamHealth, bought by private equity firm Blackstone in 2016, and Envision Healthcare, bought by KKR in 2018. Trying to undercut these staffing giants is American Physician Partners, a rapidly expanding company that runs EDs in at least 17 states and is 50% owned by private equity firm BBH Capital Partners.
These staffing companies have been among the most aggressive in replacing doctors to cut costs, said Robert McNamara, MD, a founder of the American Academy of Emergency Medicine and chair of emergency medicine at Temple University, Philadelphia.
“It’s a relatively simple equation,” Dr. McNamara said. “Their No. 1 expense is the board-certified emergency physician. So they are going to want to keep that expense as low as possible.”
Not everyone sees the trend of private equity in ED staffing in a negative light. Jennifer Orozco, president of the American Academy of Physician Associates, which represents physician assistants, said even if the change – to use more nonphysician providers – is driven by the staffing firms’ desire to make more money, patients are still well served by a team approach that includes nurse practitioners and physician assistants.
“Though I see that shift, it’s not about profits at the end of the day,” Ms. Orozco said. “It’s about the patient.”
The “shift” is nearly invisible to patients because hospitals rarely promote branding from their ED staffing firms and there is little public documentation of private equity investments.
Arthur Smolensky, MD, a Tennessee emergency medicine specialist attempting to measure private equity’s intrusion into EDs, said his review of hospital job postings and employment contracts in 14 major metropolitan areas found that 43% of ED patients were seen in EDs staffed by companies with nonphysician owners, nearly all of whom are private equity investors.
Dr. Smolensky hopes to publish his full study, expanding to 55 metro areas, later this year. But this research will merely quantify what many doctors already know: The ED has changed. Demoralized by an increased focus on profit, and wary of a looming surplus of emergency medicine residents because there are fewer jobs to fill, many experienced doctors are leaving the ED on their own, he said.
“Most of us didn’t go into medicine to supervise an army of people that are not as well trained as we are,” Dr. Smolensky said. “We want to take care of patients.”
“I guess we’re the first guinea pigs for our ER”
Joshua Allen, a nurse practitioner at a small Kentucky hospital, snaked a rubber hose through a rack of pork ribs to practice inserting a chest tube to fix a collapsed lung.
It was 2020, and American Physician Partners was restructuring the ED where Mr. Allen worked, reducing shifts from two doctors to one. Once Mr. Allen had placed 10 tubes under a doctor’s supervision, he would be allowed to do it on his own.
“I guess we’re the first guinea pigs for our ER,” he said. “If we do have a major trauma and multiple victims come in, there’s only one doctor there. ... We need to be prepared.”
Mr. Allen is one of many midlevel practitioners finding work in emergency departments. Nurse practitioners and physician assistants are among the fastest-growing occupations in the nation, according to the U.S. Bureau of Labor Statistics.
Generally, they have master’s degrees and receive several years of specialized schooling but have significantly less training than doctors. Many are permitted to diagnose patients and prescribe medication with little or no supervision from a doctor, although limitations vary by state.
The Neiman Institute found that the share of ED visits in which a midlevel practitioner was the main clinician increased by more than 172% between 2005 and 2020. Another study, in the Journal of Emergency Medicine, reported that if trends continue there may be equal numbers of midlevel practitioners and doctors in EDs by 2030.
There is little mystery as to why. Federal data shows emergency medicine doctors are paid about $310,000 a year on average, while nurse practitioners and physician assistants earn less than $120,000. Generally, hospitals can bill for care by a midlevel practitioner at 85% the rate of a doctor while paying them less than half as much.
Private equity can make millions in the gap.
For example, Envision once encouraged EDs to employ “the least expensive resource” and treat up to 35% of patients with midlevel practitioners, according to a 2017 PowerPoint presentation. The presentation drew scorn on social media and disappeared from Envision’s website.
Envision declined a request for a phone interview. In a written statement to KHN, spokesperson Aliese Polk said the company does not direct its physician leaders on how to care for patients and called the presentation a “concept guide” that does not represent current views.
American Physician Partners touted roughly the same staffing strategy in 2021 in response to the No Surprises Act, which threatened the company’s profits by outlawing surprise medical bills. In its confidential pitch to lenders, the company estimated it could cut almost $6 million by shifting more staffing from physicians to midlevel practitioners.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
She didn’t know much about miscarriage, but this seemed like one.
In the emergency department, she was examined then sent home, she said. She went back when her cramping became excruciating. Then home again. It ultimately took three trips to the ED on 3 consecutive days, generating three separate bills, before she saw a doctor who looked at her blood work and confirmed her fears.
“At the time I wasn’t thinking, ‘Oh, I need to see a doctor,’ ” Ms. Valle recalled. “But when you think about it, it’s like, ‘Well, dang – why didn’t I see a doctor?’ ” It’s unclear whether the repeat visits were due to delays in seeing a physician, but the experience worried her. And she’s still paying the bills.
The hospital declined to discuss Ms. Valle’s care, citing patient privacy. But 17 months before her 3-day ordeal, Tennova had outsourced its emergency departments to American Physician Partners, a medical staffing company owned by private equity investors. APP employs fewer doctors in its EDs as one of its cost-saving initiatives to increase earnings, according to a confidential company document obtained by KHN and NPR.
This staffing strategy has permeated hospitals, and particularly emergency departments, that seek to reduce their top expense: physician labor. While diagnosing and treating patients was once their domain, doctors are increasingly being replaced by nurse practitioners and physician assistants, collectively known as “midlevel practitioners,” who can perform many of the same duties and generate much of the same revenue for less than half of the pay.
“APP has numerous cost saving initiatives underway as part of the Company’s continual focus on cost optimization,” the document says, including a “shift of staffing” between doctors and midlevel practitioners.
In a statement to KHN, American Physician Partners said this strategy is a way to ensure all EDs remain fully staffed, calling it a “blended model” that allows doctors, nurse practitioners, and physician assistants “to provide care to their fullest potential.”
Critics of this strategy say the quest to save money results in treatment meted out by someone with far less training than a physician, leaving patients vulnerable to misdiagnoses, higher medical bills, and inadequate care. And these fears are bolstered by evidence that suggests dropping doctors from EDs may not be good for patients.
A working paper, published in October by the National Bureau of Economic Research, analyzed roughly 1.1 million visits to 44 EDs throughout the Veterans Health Administration, where nurse practitioners can treat patients without oversight from doctors.
Researchers found that treatment by a nurse practitioner resulted on average in a 7% increase in cost of care and an 11% increase in length of stay, extending patients’ time in the ED by minutes for minor visits and hours for longer ones. These gaps widened among patients with more severe diagnoses, the study said, but could be somewhat mitigated by nurse practitioners with more experience.
The study also found that ED patients treated by a nurse practitioner were 20% more likely to be readmitted to the hospital for a preventable reason within 30 days, although the overall risk of readmission remained very small.
Yiqun Chen, PhD, who is an assistant professor of economics at the University of Illinois at Chicago and coauthored the study, said these findings are not an indictment of nurse practitioners in the ED. Instead, she said, she hopes the study will guide how to best deploy nurse practitioners: in treatment of simpler patients or circumstances when no doctor is available.
“It’s not just a simple question of if we can substitute physicians with nurse practitioners or not,” Dr. Chen said. “It depends on how we use them. If we just use them as independent providers, especially ... for relatively complicated patients, it doesn’t seem to be a very good use.”
Dr. Chen’s research echoes smaller studies, like one from The Harvey L. Neiman Health Policy Institute that found nonphysician practitioners in EDs were associated with a 5.3% increase in imaging, which could unnecessarily increase bills for patients. Separately, a study at the Hattiesburg Clinic in Mississippi found that midlevel practitioners in primary care – not in the emergency department – increased the out-of-pocket costs to patients while also leading to worse performance on 9 of 10 quality-of-care metrics, including cancer screenings and vaccination rates.
But definitive evidence remains elusive that replacing ER doctors with nonphysicians has a negative impact on patients, said Cameron Gettel, MD, an assistant professor of emergency medicine at Yale University, New Haven, Conn. Private equity investment and the use of midlevel practitioners rose in lockstep in the ED, Dr. Gettel said, and in the absence of game-changing research, the pattern will likely continue.
“Worse patient outcomes haven’t really been shown across the board,” he said. “And I think until that is shown, then they will continue to play an increasing role.”
For private equity, dropping ED docs is a “simple equation”
Private equity companies pool money from wealthy investors to buy their way into various industries, often slashing spending and seeking to flip businesses in 3 to 7 years. While this business model is a proven moneymaker on Wall Street, it raises concerns in health care, where critics worry the pressure to turn big profits will influence life-or-death decisions that were once left solely to medical professionals.
Nearly $1 trillion in private equity funds have gone into almost 8,000 health care transactions over the past decade, according to industry tracker PitchBook, including buying into medical staffing companies that many hospitals hire to manage their emergency departments.
Two firms dominate the ED staffing industry: TeamHealth, bought by private equity firm Blackstone in 2016, and Envision Healthcare, bought by KKR in 2018. Trying to undercut these staffing giants is American Physician Partners, a rapidly expanding company that runs EDs in at least 17 states and is 50% owned by private equity firm BBH Capital Partners.
These staffing companies have been among the most aggressive in replacing doctors to cut costs, said Robert McNamara, MD, a founder of the American Academy of Emergency Medicine and chair of emergency medicine at Temple University, Philadelphia.
“It’s a relatively simple equation,” Dr. McNamara said. “Their No. 1 expense is the board-certified emergency physician. So they are going to want to keep that expense as low as possible.”
Not everyone sees the trend of private equity in ED staffing in a negative light. Jennifer Orozco, president of the American Academy of Physician Associates, which represents physician assistants, said even if the change – to use more nonphysician providers – is driven by the staffing firms’ desire to make more money, patients are still well served by a team approach that includes nurse practitioners and physician assistants.
“Though I see that shift, it’s not about profits at the end of the day,” Ms. Orozco said. “It’s about the patient.”
The “shift” is nearly invisible to patients because hospitals rarely promote branding from their ED staffing firms and there is little public documentation of private equity investments.
Arthur Smolensky, MD, a Tennessee emergency medicine specialist attempting to measure private equity’s intrusion into EDs, said his review of hospital job postings and employment contracts in 14 major metropolitan areas found that 43% of ED patients were seen in EDs staffed by companies with nonphysician owners, nearly all of whom are private equity investors.
Dr. Smolensky hopes to publish his full study, expanding to 55 metro areas, later this year. But this research will merely quantify what many doctors already know: The ED has changed. Demoralized by an increased focus on profit, and wary of a looming surplus of emergency medicine residents because there are fewer jobs to fill, many experienced doctors are leaving the ED on their own, he said.
“Most of us didn’t go into medicine to supervise an army of people that are not as well trained as we are,” Dr. Smolensky said. “We want to take care of patients.”
“I guess we’re the first guinea pigs for our ER”
Joshua Allen, a nurse practitioner at a small Kentucky hospital, snaked a rubber hose through a rack of pork ribs to practice inserting a chest tube to fix a collapsed lung.
It was 2020, and American Physician Partners was restructuring the ED where Mr. Allen worked, reducing shifts from two doctors to one. Once Mr. Allen had placed 10 tubes under a doctor’s supervision, he would be allowed to do it on his own.
“I guess we’re the first guinea pigs for our ER,” he said. “If we do have a major trauma and multiple victims come in, there’s only one doctor there. ... We need to be prepared.”
Mr. Allen is one of many midlevel practitioners finding work in emergency departments. Nurse practitioners and physician assistants are among the fastest-growing occupations in the nation, according to the U.S. Bureau of Labor Statistics.
Generally, they have master’s degrees and receive several years of specialized schooling but have significantly less training than doctors. Many are permitted to diagnose patients and prescribe medication with little or no supervision from a doctor, although limitations vary by state.
The Neiman Institute found that the share of ED visits in which a midlevel practitioner was the main clinician increased by more than 172% between 2005 and 2020. Another study, in the Journal of Emergency Medicine, reported that if trends continue there may be equal numbers of midlevel practitioners and doctors in EDs by 2030.
There is little mystery as to why. Federal data shows emergency medicine doctors are paid about $310,000 a year on average, while nurse practitioners and physician assistants earn less than $120,000. Generally, hospitals can bill for care by a midlevel practitioner at 85% the rate of a doctor while paying them less than half as much.
Private equity can make millions in the gap.
For example, Envision once encouraged EDs to employ “the least expensive resource” and treat up to 35% of patients with midlevel practitioners, according to a 2017 PowerPoint presentation. The presentation drew scorn on social media and disappeared from Envision’s website.
Envision declined a request for a phone interview. In a written statement to KHN, spokesperson Aliese Polk said the company does not direct its physician leaders on how to care for patients and called the presentation a “concept guide” that does not represent current views.
American Physician Partners touted roughly the same staffing strategy in 2021 in response to the No Surprises Act, which threatened the company’s profits by outlawing surprise medical bills. In its confidential pitch to lenders, the company estimated it could cut almost $6 million by shifting more staffing from physicians to midlevel practitioners.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
New report says suicide rates rising among young Black people
Significant increases in suicide occurred among Native American, Black and Hispanic people, with a startling rise among young Black people. Meanwhile, the rate of suicide among older people declined between 2018 and 2021, the Centers for Disease Control and Prevention has reported.
In 2021, 48,183 people died by suicide in the United States, which equates to a suicide rate of 14.1 per 100,000 people. That level equals the 2018 suicide rate, which had seen a peak that was followed by declines associated with the pandemic.
Experts said rebounding suicide rates are common following times of crisis, such as the COVID-19 pandemic. Suicide declines have also occurred during times of war and natural disaster, when psychological resilience tends to increase and people work together to overcome shared adversity.
“That will wane, and then you will see rebounding in suicide rates. That is, in fact, what we feared would happen. And it has happened, at least in 2021,” Christine Moutier, MD, chief medical officer of the American Foundation for Suicide Prevention, told the New York Times.
The new CDC report found that the largest increase was among Black people aged 10-24 years, who experienced a 36.6% increase in suicide rate between 2018 and 2021. While Black people experience mental illness at the same rates as that of the general population, historically they have disproportionately limited access to mental health care, according to the American Psychiatric Association.
CDC report authors noted that some of the biggest increases in suicide rates occurred among groups most affected by the pandemic.
From 2018 to 2021, the suicide rate for people aged 25-44 increased among Native Americans by 33.7% and among Black people by 22.9%. Suicide increased among multiracial people by 20.6% and among Hispanic or Latinx people by 19.4%. Among White people of all ages, the suicide rate declined or remained steady.
“As the nation continues to respond to the short- and long-term impacts of the COVID-19 pandemic, remaining vigilant in prevention efforts is critical, especially among disproportionately affected populations where longer-term impacts might compound preexisting inequities in suicide risk,” the CDC researchers wrote.
A version of this article first appeared on WebMD.com.
Significant increases in suicide occurred among Native American, Black and Hispanic people, with a startling rise among young Black people. Meanwhile, the rate of suicide among older people declined between 2018 and 2021, the Centers for Disease Control and Prevention has reported.
In 2021, 48,183 people died by suicide in the United States, which equates to a suicide rate of 14.1 per 100,000 people. That level equals the 2018 suicide rate, which had seen a peak that was followed by declines associated with the pandemic.
Experts said rebounding suicide rates are common following times of crisis, such as the COVID-19 pandemic. Suicide declines have also occurred during times of war and natural disaster, when psychological resilience tends to increase and people work together to overcome shared adversity.
“That will wane, and then you will see rebounding in suicide rates. That is, in fact, what we feared would happen. And it has happened, at least in 2021,” Christine Moutier, MD, chief medical officer of the American Foundation for Suicide Prevention, told the New York Times.
The new CDC report found that the largest increase was among Black people aged 10-24 years, who experienced a 36.6% increase in suicide rate between 2018 and 2021. While Black people experience mental illness at the same rates as that of the general population, historically they have disproportionately limited access to mental health care, according to the American Psychiatric Association.
CDC report authors noted that some of the biggest increases in suicide rates occurred among groups most affected by the pandemic.
From 2018 to 2021, the suicide rate for people aged 25-44 increased among Native Americans by 33.7% and among Black people by 22.9%. Suicide increased among multiracial people by 20.6% and among Hispanic or Latinx people by 19.4%. Among White people of all ages, the suicide rate declined or remained steady.
“As the nation continues to respond to the short- and long-term impacts of the COVID-19 pandemic, remaining vigilant in prevention efforts is critical, especially among disproportionately affected populations where longer-term impacts might compound preexisting inequities in suicide risk,” the CDC researchers wrote.
A version of this article first appeared on WebMD.com.
Significant increases in suicide occurred among Native American, Black and Hispanic people, with a startling rise among young Black people. Meanwhile, the rate of suicide among older people declined between 2018 and 2021, the Centers for Disease Control and Prevention has reported.
In 2021, 48,183 people died by suicide in the United States, which equates to a suicide rate of 14.1 per 100,000 people. That level equals the 2018 suicide rate, which had seen a peak that was followed by declines associated with the pandemic.
Experts said rebounding suicide rates are common following times of crisis, such as the COVID-19 pandemic. Suicide declines have also occurred during times of war and natural disaster, when psychological resilience tends to increase and people work together to overcome shared adversity.
“That will wane, and then you will see rebounding in suicide rates. That is, in fact, what we feared would happen. And it has happened, at least in 2021,” Christine Moutier, MD, chief medical officer of the American Foundation for Suicide Prevention, told the New York Times.
The new CDC report found that the largest increase was among Black people aged 10-24 years, who experienced a 36.6% increase in suicide rate between 2018 and 2021. While Black people experience mental illness at the same rates as that of the general population, historically they have disproportionately limited access to mental health care, according to the American Psychiatric Association.
CDC report authors noted that some of the biggest increases in suicide rates occurred among groups most affected by the pandemic.
From 2018 to 2021, the suicide rate for people aged 25-44 increased among Native Americans by 33.7% and among Black people by 22.9%. Suicide increased among multiracial people by 20.6% and among Hispanic or Latinx people by 19.4%. Among White people of all ages, the suicide rate declined or remained steady.
“As the nation continues to respond to the short- and long-term impacts of the COVID-19 pandemic, remaining vigilant in prevention efforts is critical, especially among disproportionately affected populations where longer-term impacts might compound preexisting inequities in suicide risk,” the CDC researchers wrote.
A version of this article first appeared on WebMD.com.
Repetitive TMS effective for comorbid depression, substance use
In a retrospective observational study, participants receiving 20-30 rTMS sessions delivered over a course of 4-6 weeks showed significant reductions in both craving and depression symptom scores.
In addition, the researchers found that the number of rTMS sessions significantly predicted the number of days of drug abstinence, even after controlling for confounders.
“For each additional TMS session, there was an additional 10 days of abstinence in the community,” principal investigator Wael Foad, MD, medical director, Erada Center for Treatment and Rehabilitation, Dubai, United Arab Emirates, told this news organization.
However, Dr. Foad noted that he would need to construct a randomized controlled trial to further explore that “interesting” finding.
The results were published in the Annals of Clinical Psychiatry.
Inpatient program
The researchers retrospectively analyzed medical records of men admitted to the inpatient unit at the Erada Center between June 2019 and September 2020. The vast majority were native to the UAE.
The inpatient program focuses on treating patients with SUDs and is the only dedicated addiction rehabilitation service in Dubai, the investigators noted.
They analyzed outcomes for 55 men with mild to moderate MDD who received rTMS as standard treatment.
Participants were excluded from the data analysis if they had another comorbid diagnosis from the DSM-5 other than SUD or MDD. They were also excluded if they used an illicit substance 2 weeks before the study or used certain medications, including antipsychotics, benzodiazepines, or mood stabilizers.
When patients first arrived on the unit, they were detoxed for a period of time before they began receiving rTMS sessions.
The 55 men received 20-30 high-frequency rTMS sessions over the course of 4-6 weeks in the area of the dorsolateral prefrontal cortex. Each session consisted of 3,000 pulses delivered over a period of 37.5 minutes. Severity of depression was measured with the Clinical Global Impression–Severity Scale (CGI-S), which uses a 7-point Likert scale.
In addition, participants’ scores were tracked on the Brief Substance Craving Scale (BSCS), a self-report scale that measures craving for primary and secondary substances of abuse over a 24-hr period.
Of all participants, 47% said opiates and 35% said methamphetamine were their primary substances of abuse.
Significant improvement
Results showed a statistically significant improvement (P < .05) between baseline and post-rTMS treatment scores in severity of depression and drug craving, as measured by the BSCS and the CGI-S.
The researchers noted that eight participants dropped out of the study after their first rTMS session for various reasons.
Dr. Foad explained that investigators contracted with study participants to receive 20 rTMS sessions; if the sessions were not fully completed during the inpatient stay, the rTMS sessions were continued on an outpatient basis. A study clinician closely monitored patients until they finished their sessions.
For each additional rTMS session the patients completed beyond 20 sessions, there was an associated excess of 10 more days of abstinence from the primary drug in the community.
The investigators speculated that rTMS may reduce drug craving by increasing dopaminergic binding in the striatum, or by releasing dopamine in the caudate nucleus.
Study limitations cited include the lack of a control group and the fact that the study sample was limited to male inpatients, which limits generalizability of the findings to other populations.
Promising intervention
Commenting on the study, Colleen Ann Hanlon, PhD, noted that, from years of work using TMS for depression, “we know that more sessions of TMS during the acute treatment phase tends to lead to stronger and possibly more durable results long-term.”
Dr. Hanlon, who was not involved with the current research, formerly headed a clinical neuromodulation lab at Wake Forest University, Winston-Salem, N.C. She is now vice president of medical affairs at BrainsWay, an international health technology company specializing in Deep TMS.
She noted that Deep TMS was approved by the Food and Drug Administration for smoking cessation in 2020, “which was a tremendous win for our field at large, and requires only 15 acute sessions followed by 3 weekly sessions” of deep TMS.
“I suspect this is just the beginning of a new era in neuromodulation-based therapeutics for people struggling with drug and alcohol use disorders,” Dr. Hanlon said.
The study behind the FDA approval for smoking approval was a large double-blind, sham-controlled multisite clinical trial where investigators used an H4 coil – a TMS coil that modulates multiple brain areas involved in addictive behaviors simultaneously.
Results from that study showed that 15 sessions of deep TMS significantly improved smoking cessation rates relative to sham (10 Hz, 120% motor threshold, H4 coil, 1,800 pulses/session).
“The difference in cigarette consumption and craving was significant as early as 2 weeks after treatment initiation,” said Dr. Hanlon. “I am looking forward to the future of this field for all people suffering from drug and alcohol use disorders.”
The study and services provided through the Erada Center were funded by the government of Dubai. The investigators reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a retrospective observational study, participants receiving 20-30 rTMS sessions delivered over a course of 4-6 weeks showed significant reductions in both craving and depression symptom scores.
In addition, the researchers found that the number of rTMS sessions significantly predicted the number of days of drug abstinence, even after controlling for confounders.
“For each additional TMS session, there was an additional 10 days of abstinence in the community,” principal investigator Wael Foad, MD, medical director, Erada Center for Treatment and Rehabilitation, Dubai, United Arab Emirates, told this news organization.
However, Dr. Foad noted that he would need to construct a randomized controlled trial to further explore that “interesting” finding.
The results were published in the Annals of Clinical Psychiatry.
Inpatient program
The researchers retrospectively analyzed medical records of men admitted to the inpatient unit at the Erada Center between June 2019 and September 2020. The vast majority were native to the UAE.
The inpatient program focuses on treating patients with SUDs and is the only dedicated addiction rehabilitation service in Dubai, the investigators noted.
They analyzed outcomes for 55 men with mild to moderate MDD who received rTMS as standard treatment.
Participants were excluded from the data analysis if they had another comorbid diagnosis from the DSM-5 other than SUD or MDD. They were also excluded if they used an illicit substance 2 weeks before the study or used certain medications, including antipsychotics, benzodiazepines, or mood stabilizers.
When patients first arrived on the unit, they were detoxed for a period of time before they began receiving rTMS sessions.
The 55 men received 20-30 high-frequency rTMS sessions over the course of 4-6 weeks in the area of the dorsolateral prefrontal cortex. Each session consisted of 3,000 pulses delivered over a period of 37.5 minutes. Severity of depression was measured with the Clinical Global Impression–Severity Scale (CGI-S), which uses a 7-point Likert scale.
In addition, participants’ scores were tracked on the Brief Substance Craving Scale (BSCS), a self-report scale that measures craving for primary and secondary substances of abuse over a 24-hr period.
Of all participants, 47% said opiates and 35% said methamphetamine were their primary substances of abuse.
Significant improvement
Results showed a statistically significant improvement (P < .05) between baseline and post-rTMS treatment scores in severity of depression and drug craving, as measured by the BSCS and the CGI-S.
The researchers noted that eight participants dropped out of the study after their first rTMS session for various reasons.
Dr. Foad explained that investigators contracted with study participants to receive 20 rTMS sessions; if the sessions were not fully completed during the inpatient stay, the rTMS sessions were continued on an outpatient basis. A study clinician closely monitored patients until they finished their sessions.
For each additional rTMS session the patients completed beyond 20 sessions, there was an associated excess of 10 more days of abstinence from the primary drug in the community.
The investigators speculated that rTMS may reduce drug craving by increasing dopaminergic binding in the striatum, or by releasing dopamine in the caudate nucleus.
Study limitations cited include the lack of a control group and the fact that the study sample was limited to male inpatients, which limits generalizability of the findings to other populations.
Promising intervention
Commenting on the study, Colleen Ann Hanlon, PhD, noted that, from years of work using TMS for depression, “we know that more sessions of TMS during the acute treatment phase tends to lead to stronger and possibly more durable results long-term.”
Dr. Hanlon, who was not involved with the current research, formerly headed a clinical neuromodulation lab at Wake Forest University, Winston-Salem, N.C. She is now vice president of medical affairs at BrainsWay, an international health technology company specializing in Deep TMS.
She noted that Deep TMS was approved by the Food and Drug Administration for smoking cessation in 2020, “which was a tremendous win for our field at large, and requires only 15 acute sessions followed by 3 weekly sessions” of deep TMS.
“I suspect this is just the beginning of a new era in neuromodulation-based therapeutics for people struggling with drug and alcohol use disorders,” Dr. Hanlon said.
The study behind the FDA approval for smoking approval was a large double-blind, sham-controlled multisite clinical trial where investigators used an H4 coil – a TMS coil that modulates multiple brain areas involved in addictive behaviors simultaneously.
Results from that study showed that 15 sessions of deep TMS significantly improved smoking cessation rates relative to sham (10 Hz, 120% motor threshold, H4 coil, 1,800 pulses/session).
“The difference in cigarette consumption and craving was significant as early as 2 weeks after treatment initiation,” said Dr. Hanlon. “I am looking forward to the future of this field for all people suffering from drug and alcohol use disorders.”
The study and services provided through the Erada Center were funded by the government of Dubai. The investigators reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a retrospective observational study, participants receiving 20-30 rTMS sessions delivered over a course of 4-6 weeks showed significant reductions in both craving and depression symptom scores.
In addition, the researchers found that the number of rTMS sessions significantly predicted the number of days of drug abstinence, even after controlling for confounders.
“For each additional TMS session, there was an additional 10 days of abstinence in the community,” principal investigator Wael Foad, MD, medical director, Erada Center for Treatment and Rehabilitation, Dubai, United Arab Emirates, told this news organization.
However, Dr. Foad noted that he would need to construct a randomized controlled trial to further explore that “interesting” finding.
The results were published in the Annals of Clinical Psychiatry.
Inpatient program
The researchers retrospectively analyzed medical records of men admitted to the inpatient unit at the Erada Center between June 2019 and September 2020. The vast majority were native to the UAE.
The inpatient program focuses on treating patients with SUDs and is the only dedicated addiction rehabilitation service in Dubai, the investigators noted.
They analyzed outcomes for 55 men with mild to moderate MDD who received rTMS as standard treatment.
Participants were excluded from the data analysis if they had another comorbid diagnosis from the DSM-5 other than SUD or MDD. They were also excluded if they used an illicit substance 2 weeks before the study or used certain medications, including antipsychotics, benzodiazepines, or mood stabilizers.
When patients first arrived on the unit, they were detoxed for a period of time before they began receiving rTMS sessions.
The 55 men received 20-30 high-frequency rTMS sessions over the course of 4-6 weeks in the area of the dorsolateral prefrontal cortex. Each session consisted of 3,000 pulses delivered over a period of 37.5 minutes. Severity of depression was measured with the Clinical Global Impression–Severity Scale (CGI-S), which uses a 7-point Likert scale.
In addition, participants’ scores were tracked on the Brief Substance Craving Scale (BSCS), a self-report scale that measures craving for primary and secondary substances of abuse over a 24-hr period.
Of all participants, 47% said opiates and 35% said methamphetamine were their primary substances of abuse.
Significant improvement
Results showed a statistically significant improvement (P < .05) between baseline and post-rTMS treatment scores in severity of depression and drug craving, as measured by the BSCS and the CGI-S.
The researchers noted that eight participants dropped out of the study after their first rTMS session for various reasons.
Dr. Foad explained that investigators contracted with study participants to receive 20 rTMS sessions; if the sessions were not fully completed during the inpatient stay, the rTMS sessions were continued on an outpatient basis. A study clinician closely monitored patients until they finished their sessions.
For each additional rTMS session the patients completed beyond 20 sessions, there was an associated excess of 10 more days of abstinence from the primary drug in the community.
The investigators speculated that rTMS may reduce drug craving by increasing dopaminergic binding in the striatum, or by releasing dopamine in the caudate nucleus.
Study limitations cited include the lack of a control group and the fact that the study sample was limited to male inpatients, which limits generalizability of the findings to other populations.
Promising intervention
Commenting on the study, Colleen Ann Hanlon, PhD, noted that, from years of work using TMS for depression, “we know that more sessions of TMS during the acute treatment phase tends to lead to stronger and possibly more durable results long-term.”
Dr. Hanlon, who was not involved with the current research, formerly headed a clinical neuromodulation lab at Wake Forest University, Winston-Salem, N.C. She is now vice president of medical affairs at BrainsWay, an international health technology company specializing in Deep TMS.
She noted that Deep TMS was approved by the Food and Drug Administration for smoking cessation in 2020, “which was a tremendous win for our field at large, and requires only 15 acute sessions followed by 3 weekly sessions” of deep TMS.
“I suspect this is just the beginning of a new era in neuromodulation-based therapeutics for people struggling with drug and alcohol use disorders,” Dr. Hanlon said.
The study behind the FDA approval for smoking approval was a large double-blind, sham-controlled multisite clinical trial where investigators used an H4 coil – a TMS coil that modulates multiple brain areas involved in addictive behaviors simultaneously.
Results from that study showed that 15 sessions of deep TMS significantly improved smoking cessation rates relative to sham (10 Hz, 120% motor threshold, H4 coil, 1,800 pulses/session).
“The difference in cigarette consumption and craving was significant as early as 2 weeks after treatment initiation,” said Dr. Hanlon. “I am looking forward to the future of this field for all people suffering from drug and alcohol use disorders.”
The study and services provided through the Erada Center were funded by the government of Dubai. The investigators reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE ANNALS OF CLINICAL PSYCHIATRY
Forced hospitalization for mental illness not a permanent solution
I met Eleanor when I was writing a book on involuntary psychiatric treatment. She was very ill when she presented to an emergency department in Northern California. She was looking for help and would have signed herself in, but after waiting 8 hours with no food or medical attention, she walked out and went to another hospital.
At this point, she was agitated and distressed and began screaming uncontrollably. The physician in the second ED did not offer her the option of signing in, and she was placed on a 72-hour hold and subsequently held in the hospital for 3 weeks after a judge committed her.
Like so many issues, involuntary psychiatric care is highly polarized. Some groups favor legislation to make involuntary treatment easier, while patient advocacy and civil rights groups vehemently oppose such legislation.
We don’t hear from these combatants as much as we hear from those who trumpet their views on abortion or gun control, yet this battlefield exists. It is not surprising that when New York City Mayor Eric Adams announced a plan to hospitalize homeless people with mental illnesses – involuntarily if necessary, and at the discretion of the police – people were outraged.
New York City is not the only place using this strategy to address the problem of mental illness and homelessness; California has enacted similar legislation, and every major city has homeless citizens.
Eleanor was not homeless, and fortunately, she recovered and returned to her family. However, she remained distressed and traumatized by her hospitalization for years. “It sticks with you,” she told me. “I would rather die than go in again.”
I wish I could tell you that Eleanor is unique in saying that she would rather die than go to a hospital unit for treatment, but it is not an uncommon sentiment for patients. Some people who are charged with crimes and end up in the judicial system will opt to go to jail rather than to a psychiatric hospital. It is also not easy to access outpatient psychiatric treatment.
Barriers to care
Many psychiatrists don’t participate with insurance networks, and publicly funded clinics may have long waiting lists, so illnesses escalate until there is a crisis and hospitalization is necessary. For many, stigma and fear of potential professional repercussions are significant barriers to care.
What are the issues that legislation attempts to address? The first is the standard for hospitalizing individuals against their will. In some states, the patient must be dangerous, while in others there is a lower standard of “gravely disabled,” and finally there are those that promote a standard of a “need for treatment.”
The second is related to medicating people against their will, a process that can be rightly perceived as an assault if the patient refuses to take oral medications and must be held down for injections. Next, the use of outpatient civil commitment – legally requiring people to get treatment if they are not in the hospital – has been increasingly invoked as a way to prevent mass murders and random violence against strangers.
All but four states have some legislation for outpatient commitment, euphemistically called Assisted Outpatient Treatment (AOT), yet these laws are difficult to enforce and expensive to enact. They are also not fully effective.
In New York City, Kendra’s Law has not eliminated subway violence by people with psychiatric disturbances, and the shooter who killed 32 people and wounded 17 others at Virginia Tech in 2007 had previously been ordered by a judge to go to outpatient treatment, but he simply never showed up for his appointment.
Finally, the battle includes the right of patients to refuse to have their psychiatric information released to their caretakers under the Health Insurance Portability and Accountability Act of 1996 – a measure that many families believe would help them to get loved ones to take medications and go to appointments.
The concern about how to negotiate the needs of society and the civil rights of people with psychiatric disorders has been with us for centuries. There is a strong antipsychiatry movement that asserts that psychotropic medications are ineffective or harmful and refers to patients as “psychiatric survivors.” We value the right to medical autonomy, and when there is controversy over the validity of a treatment, there is even more controversy over forcing it upon people.
Psychiatric medications are very effective and benefit many people, but they don’t help everyone, and some people experience side effects. Also, we can’t deny that involuntary care can go wrong; the conservatorship of Britney Spears for 13 years is a very public example.
Multiple stakeholders
Many have a stake in how this plays out. There are the patients, who may be suffering and unable to recognize that they are ill, who may have valid reasons for not wanting the treatments, and who ideally should have the right to refuse care.
There are the families who watch their loved ones suffer, deteriorate, and miss the opportunities that life has to offer; who do not want their children to be homeless or incarcerated; and who may be at risk from violent behavior.
There are the mental health professionals who want to do what’s in the best interest of their patients while following legal and ethical mandates, who worry about being sued for tragic outcomes, and who can’t meet the current demand for services.
There is the taxpayer who foots the bill for disability payments, lost productivity, and institutionalization. There is our society that worries that people with psychiatric disorders will commit random acts of violence.
Finally, there are the insurers, who want to pay for as little care as possible and throw up constant hurdles in the treatment process. We must acknowledge that resources used for involuntary treatment are diverted away from those who want care.
Eleanor had many advantages that unhoused people don’t have: a supportive family, health insurance, and the financial means to pay a psychiatrist who respected her wishes to wean off her medications. She returned to a comfortable home and to personal and occupational success.
It is tragic that we have people living on the streets because of a psychiatric disorder, addiction, poverty, or some combination of these. No one should be unhoused. If the rationale of hospitalization is to decrease violence, I am not hopeful. The Epidemiologic Catchment Area study shows that people with psychiatric disorders are responsible for only 4% of all violence.
The logistics of determining which people living on the streets have psychiatric disorders, transporting them safely to medical facilities, and then finding the resources to provide for compassionate and thoughtful care in meaningful and sustained ways are very challenging.
If we don’t want people living on the streets, we need to create supports, including infrastructure to facilitate housing, access to mental health care, and addiction treatment before we resort to involuntary hospitalization.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
I met Eleanor when I was writing a book on involuntary psychiatric treatment. She was very ill when she presented to an emergency department in Northern California. She was looking for help and would have signed herself in, but after waiting 8 hours with no food or medical attention, she walked out and went to another hospital.
At this point, she was agitated and distressed and began screaming uncontrollably. The physician in the second ED did not offer her the option of signing in, and she was placed on a 72-hour hold and subsequently held in the hospital for 3 weeks after a judge committed her.
Like so many issues, involuntary psychiatric care is highly polarized. Some groups favor legislation to make involuntary treatment easier, while patient advocacy and civil rights groups vehemently oppose such legislation.
We don’t hear from these combatants as much as we hear from those who trumpet their views on abortion or gun control, yet this battlefield exists. It is not surprising that when New York City Mayor Eric Adams announced a plan to hospitalize homeless people with mental illnesses – involuntarily if necessary, and at the discretion of the police – people were outraged.
New York City is not the only place using this strategy to address the problem of mental illness and homelessness; California has enacted similar legislation, and every major city has homeless citizens.
Eleanor was not homeless, and fortunately, she recovered and returned to her family. However, she remained distressed and traumatized by her hospitalization for years. “It sticks with you,” she told me. “I would rather die than go in again.”
I wish I could tell you that Eleanor is unique in saying that she would rather die than go to a hospital unit for treatment, but it is not an uncommon sentiment for patients. Some people who are charged with crimes and end up in the judicial system will opt to go to jail rather than to a psychiatric hospital. It is also not easy to access outpatient psychiatric treatment.
Barriers to care
Many psychiatrists don’t participate with insurance networks, and publicly funded clinics may have long waiting lists, so illnesses escalate until there is a crisis and hospitalization is necessary. For many, stigma and fear of potential professional repercussions are significant barriers to care.
What are the issues that legislation attempts to address? The first is the standard for hospitalizing individuals against their will. In some states, the patient must be dangerous, while in others there is a lower standard of “gravely disabled,” and finally there are those that promote a standard of a “need for treatment.”
The second is related to medicating people against their will, a process that can be rightly perceived as an assault if the patient refuses to take oral medications and must be held down for injections. Next, the use of outpatient civil commitment – legally requiring people to get treatment if they are not in the hospital – has been increasingly invoked as a way to prevent mass murders and random violence against strangers.
All but four states have some legislation for outpatient commitment, euphemistically called Assisted Outpatient Treatment (AOT), yet these laws are difficult to enforce and expensive to enact. They are also not fully effective.
In New York City, Kendra’s Law has not eliminated subway violence by people with psychiatric disturbances, and the shooter who killed 32 people and wounded 17 others at Virginia Tech in 2007 had previously been ordered by a judge to go to outpatient treatment, but he simply never showed up for his appointment.
Finally, the battle includes the right of patients to refuse to have their psychiatric information released to their caretakers under the Health Insurance Portability and Accountability Act of 1996 – a measure that many families believe would help them to get loved ones to take medications and go to appointments.
The concern about how to negotiate the needs of society and the civil rights of people with psychiatric disorders has been with us for centuries. There is a strong antipsychiatry movement that asserts that psychotropic medications are ineffective or harmful and refers to patients as “psychiatric survivors.” We value the right to medical autonomy, and when there is controversy over the validity of a treatment, there is even more controversy over forcing it upon people.
Psychiatric medications are very effective and benefit many people, but they don’t help everyone, and some people experience side effects. Also, we can’t deny that involuntary care can go wrong; the conservatorship of Britney Spears for 13 years is a very public example.
Multiple stakeholders
Many have a stake in how this plays out. There are the patients, who may be suffering and unable to recognize that they are ill, who may have valid reasons for not wanting the treatments, and who ideally should have the right to refuse care.
There are the families who watch their loved ones suffer, deteriorate, and miss the opportunities that life has to offer; who do not want their children to be homeless or incarcerated; and who may be at risk from violent behavior.
There are the mental health professionals who want to do what’s in the best interest of their patients while following legal and ethical mandates, who worry about being sued for tragic outcomes, and who can’t meet the current demand for services.
There is the taxpayer who foots the bill for disability payments, lost productivity, and institutionalization. There is our society that worries that people with psychiatric disorders will commit random acts of violence.
Finally, there are the insurers, who want to pay for as little care as possible and throw up constant hurdles in the treatment process. We must acknowledge that resources used for involuntary treatment are diverted away from those who want care.
Eleanor had many advantages that unhoused people don’t have: a supportive family, health insurance, and the financial means to pay a psychiatrist who respected her wishes to wean off her medications. She returned to a comfortable home and to personal and occupational success.
It is tragic that we have people living on the streets because of a psychiatric disorder, addiction, poverty, or some combination of these. No one should be unhoused. If the rationale of hospitalization is to decrease violence, I am not hopeful. The Epidemiologic Catchment Area study shows that people with psychiatric disorders are responsible for only 4% of all violence.
The logistics of determining which people living on the streets have psychiatric disorders, transporting them safely to medical facilities, and then finding the resources to provide for compassionate and thoughtful care in meaningful and sustained ways are very challenging.
If we don’t want people living on the streets, we need to create supports, including infrastructure to facilitate housing, access to mental health care, and addiction treatment before we resort to involuntary hospitalization.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
I met Eleanor when I was writing a book on involuntary psychiatric treatment. She was very ill when she presented to an emergency department in Northern California. She was looking for help and would have signed herself in, but after waiting 8 hours with no food or medical attention, she walked out and went to another hospital.
At this point, she was agitated and distressed and began screaming uncontrollably. The physician in the second ED did not offer her the option of signing in, and she was placed on a 72-hour hold and subsequently held in the hospital for 3 weeks after a judge committed her.
Like so many issues, involuntary psychiatric care is highly polarized. Some groups favor legislation to make involuntary treatment easier, while patient advocacy and civil rights groups vehemently oppose such legislation.
We don’t hear from these combatants as much as we hear from those who trumpet their views on abortion or gun control, yet this battlefield exists. It is not surprising that when New York City Mayor Eric Adams announced a plan to hospitalize homeless people with mental illnesses – involuntarily if necessary, and at the discretion of the police – people were outraged.
New York City is not the only place using this strategy to address the problem of mental illness and homelessness; California has enacted similar legislation, and every major city has homeless citizens.
Eleanor was not homeless, and fortunately, she recovered and returned to her family. However, she remained distressed and traumatized by her hospitalization for years. “It sticks with you,” she told me. “I would rather die than go in again.”
I wish I could tell you that Eleanor is unique in saying that she would rather die than go to a hospital unit for treatment, but it is not an uncommon sentiment for patients. Some people who are charged with crimes and end up in the judicial system will opt to go to jail rather than to a psychiatric hospital. It is also not easy to access outpatient psychiatric treatment.
Barriers to care
Many psychiatrists don’t participate with insurance networks, and publicly funded clinics may have long waiting lists, so illnesses escalate until there is a crisis and hospitalization is necessary. For many, stigma and fear of potential professional repercussions are significant barriers to care.
What are the issues that legislation attempts to address? The first is the standard for hospitalizing individuals against their will. In some states, the patient must be dangerous, while in others there is a lower standard of “gravely disabled,” and finally there are those that promote a standard of a “need for treatment.”
The second is related to medicating people against their will, a process that can be rightly perceived as an assault if the patient refuses to take oral medications and must be held down for injections. Next, the use of outpatient civil commitment – legally requiring people to get treatment if they are not in the hospital – has been increasingly invoked as a way to prevent mass murders and random violence against strangers.
All but four states have some legislation for outpatient commitment, euphemistically called Assisted Outpatient Treatment (AOT), yet these laws are difficult to enforce and expensive to enact. They are also not fully effective.
In New York City, Kendra’s Law has not eliminated subway violence by people with psychiatric disturbances, and the shooter who killed 32 people and wounded 17 others at Virginia Tech in 2007 had previously been ordered by a judge to go to outpatient treatment, but he simply never showed up for his appointment.
Finally, the battle includes the right of patients to refuse to have their psychiatric information released to their caretakers under the Health Insurance Portability and Accountability Act of 1996 – a measure that many families believe would help them to get loved ones to take medications and go to appointments.
The concern about how to negotiate the needs of society and the civil rights of people with psychiatric disorders has been with us for centuries. There is a strong antipsychiatry movement that asserts that psychotropic medications are ineffective or harmful and refers to patients as “psychiatric survivors.” We value the right to medical autonomy, and when there is controversy over the validity of a treatment, there is even more controversy over forcing it upon people.
Psychiatric medications are very effective and benefit many people, but they don’t help everyone, and some people experience side effects. Also, we can’t deny that involuntary care can go wrong; the conservatorship of Britney Spears for 13 years is a very public example.
Multiple stakeholders
Many have a stake in how this plays out. There are the patients, who may be suffering and unable to recognize that they are ill, who may have valid reasons for not wanting the treatments, and who ideally should have the right to refuse care.
There are the families who watch their loved ones suffer, deteriorate, and miss the opportunities that life has to offer; who do not want their children to be homeless or incarcerated; and who may be at risk from violent behavior.
There are the mental health professionals who want to do what’s in the best interest of their patients while following legal and ethical mandates, who worry about being sued for tragic outcomes, and who can’t meet the current demand for services.
There is the taxpayer who foots the bill for disability payments, lost productivity, and institutionalization. There is our society that worries that people with psychiatric disorders will commit random acts of violence.
Finally, there are the insurers, who want to pay for as little care as possible and throw up constant hurdles in the treatment process. We must acknowledge that resources used for involuntary treatment are diverted away from those who want care.
Eleanor had many advantages that unhoused people don’t have: a supportive family, health insurance, and the financial means to pay a psychiatrist who respected her wishes to wean off her medications. She returned to a comfortable home and to personal and occupational success.
It is tragic that we have people living on the streets because of a psychiatric disorder, addiction, poverty, or some combination of these. No one should be unhoused. If the rationale of hospitalization is to decrease violence, I am not hopeful. The Epidemiologic Catchment Area study shows that people with psychiatric disorders are responsible for only 4% of all violence.
The logistics of determining which people living on the streets have psychiatric disorders, transporting them safely to medical facilities, and then finding the resources to provide for compassionate and thoughtful care in meaningful and sustained ways are very challenging.
If we don’t want people living on the streets, we need to create supports, including infrastructure to facilitate housing, access to mental health care, and addiction treatment before we resort to involuntary hospitalization.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
Doctors and dating: There’s an app (or three) for that
Pounding heart, sweating, insomnia. Surges of dopamine, norepinephrine, and adrenaline. All symptoms of a very common yet frustrating condition: Falling in love.
The prognosis is vague. A prescription pad and knowledge of biochemistry aren’t helpful when it comes to relationships.
Medical training can consume decades when others are exploring relationships and starting families. There are few recent data on this, but
But there is hope! By age 36, the number of doctors in long-term relationships had overtaken everyone else by more than 10% for women and 20% for men. The Medscape 2022 Physician Happiness & Lifestyle Report found that 83% were in committed relationships, and even better, happy ones. At least three-quarters of doctors in every specialty described their partnerships as “very good” or “good.”
How should a single medical student, resident, or attending physician find happiness ever after in 2023? Sometimes Mr./Ms. Right can be found in the anatomy lab or hospital, with sparks flying between students or colleagues. But for many in health care, along with millions of others looking for love, the solution is dating apps.
When ‘MD’ is a turnoff
Dr. M, a psychiatry resident in California who prefers not to give her name, hadn’t found a life partner during college, grad school, or medical school. When she passed her final Step 3 board exam, she decided it was time to take the plunge. She signed up for popular dating apps like Hinge, Bumble, and Coffee Meets Bagel, but her dates seemed to follow a disappointing pattern.
“I met lots of guys, but it was incredibly rare to find another physician,” said Dr. M. “I found myself always wanting to talk about my life as a resident. More often than not, the guys would give me this blank stare as I complained about being on call or spoke about spending 12 hours a day studying for a board exam, or even the process of The Match and how I ended up in California.”
Both of Dr. M’s parents are physicians, and she grew up watching how they supported each other through residency, exams, and exhausting schedules. A relationship with another physician, her parents told her, would give both partners the best chance to understand each other’s lives. The problem was how to find one.
That was when Dr. M saw an ad for a dating app with a cute medical name: DownToDate, a play on the clinical evidence resource UpToDate. “I thought it was a meme,” she said. “It was this doctors-only app. I remember thinking, ‘this has to be a joke,’ but then it was very real.”
She signed up and was required to provide a photo of her ID and her NPI number. Immediately, men began “requesting a consult,” the app’s form of “liking” her profile, and sending her “pages” (messages).
DownToDate was created by another physician, Robin Boyer, MD, MBA, a pediatrics resident in Loma Linda, Calif. The inspiration came in 2020 during the initial COVID crisis. Exhausted from long and often heartbreaking shifts, Dr. Boyer was grateful for her husband’s unwavering support. But many of her coresidents weren’t so lucky. The women in particular talked about their dating struggles, and there was a recurring theme. They didn’t feel confident putting “physician” on a dating site profile.
“If you’re male and you tell people you’re a doctor, it seems like it really attracts people,” Dr. Boyer said. “But if you’re female, it brings up a lot of stereotypes where you’re perceived as too intimidating either as the breadwinner, being more educated, or having a [demanding] career. It does make it more difficult.”
Dr. Boyer met her husband in high school, and she had never used a dating app. She convinced a coresident, Celestine Odigwe, MD, to pursue the idea as partners. They began researching the market within their network and heard from over a thousand interested physicians, both men and women, heterosexual and LGBTQ+. They even created fake accounts on other sites to gauge how easy it is to falsify a profile. From these insights, the app took shape. It launched in 2021 and currently has more than 5000 verified users.
Branches from the same tree
Around the same time that DownToDate began, Shivani Shah, DO, a pediatric neurology resident at Duke University, Durham, N.C., and her brother, Sagar Shah, an entrepreneur, had a similar idea.
At the time, Dr. Shah was a fourth-year medical student about to move from New Jersey to North Carolina. Friends who were internal medicine residents described the grueling reality of the early COVID pandemic.
“It was just horrible,” said Dr. Shah. “You were isolated from your family, your support system, everything. ... I think the pandemic really pushed us into realizing that this is a very important need, and sometimes it feels like community is lacking in the health care field.”
The sibling duo developed ForeverX, an app for health care workers to find meaningful and long-term romantic connections. It launched in 2021.
Concerned that the medical field was “siloed,” the Shahs chose to open the app to physicians, dentists, nurses, physical therapists, and other health care professionals. “Opening up the doors to more communication” between the health care branches was a priority.
To prevent catfishing, the app uses a twofold vetting system. Each user submits a photo of their driver’s license and a selfie that must match. There is also health care verification through an NPI number, nurse’s ID, or a manual process for those without either. None of the information is stored.
Through personal experience with dating apps, Dr. Shah hopes ForeverX can improve on some of their flaws, particularly the problem of matches being overly filtered by preferences. The “natural way” of meeting people is not filtered. And while most people have a dating checklist in mind, meeting someone face to face might send some of those prerequisites “out the window.”
“You can’t really put into words how you feel with someone ... the vibe,” Dr. Shah said. That is why her goal is to get people off the app and on an actual date IRL. “Something we’ve discussed internally is, how do we make this experience that’s virtual more human?”
She acknowledged that certain requirements, like a desire for children, might be crucial to some users. Many female doctors in their 30’s feel the “time crunch” of a ticking biological clock.
Optimize your date-ability
“I think people either love or hate dating apps, and I love them,” said Kevin Jubbal, MD. “I get to meet cool people and schedule dates from the comfort of my home.”
Dr. Jubbal, a former plastic surgery resident who left medicine to become an entrepreneur, is the founder of Med School Insiders, a tutoring and advising resource for premeds, medical students, and residents. His YouTube channel has more than 1.5 million subscribers, and he often receives questions about whether dating is feasible in medical school and how to balance a personal and academic/professional life.
Those who hate dating apps or receive few matches would do well to look inward instead of blaming the process, he said. It helps to view the experience as a learning tool that provides feedback very quickly.
“If you want to find a really amazing person, then you need to be what you want to find,” said Dr. Jubbal. “If you want to find someone who’s fit and intelligent and well read and well traveled, you need to be that. Otherwise, you’re probably not going to attract that person.”
An app designed to help single female MDs
Ifie Williams, MD, a psychiatrist in Washington, D.C., believes a wider dating pool is key – provided everyone understands the situation up front. When Dr. Williams started residency in 2014, she was “as single as can be.” She tried many dating apps, but they were extremely time consuming. Even when she set specific preferences, she found herself sifting through “matches” that didn’t fit her criteria.
“Dating nowadays has become almost like a second job,” said Dr. Williams. “Just the amount of time that people are having to spend on apps, swiping left and right and then meeting people. You think they’re interested and then you deal with all these games.”
By 2017, Dr. Williams had invented Miss Doctor, a dating app that would connect female physicians and other doctoral-level professionals with men or women on a similar achievement level.
By definition, these people would not be intimidated by ambitious, busy women. They would be heavily screened and vetted. And one other proviso: they would have to pay for “likes.”
Most dating apps charge a subscription fee. Users are allowed to “like” numerous profiles and perhaps not bother responding to many matches. By contrast, Miss Doctor accounts are free and include a limited number of “likes” to indicate interest. Beyond that, there’s a price.
“We wanted to find a way to make people a little more intentional with how they like people on the app, so they give a little more thought to it,” Dr. Williams said. “So, we monetize it and use that to change behavior.”
After an initial launch in 2017, the app had to take a back seat while Dr. Williams started her psychiatry practice and got married herself. She plans to relaunch it in spring 2023.
Male or female, there is general agreement that finding time to date as a young physician isn’t easy. While DownToDate has had “doctor meets doctor” success stories, many users are still searching for “the one.”
Dr. Boyer believes that career challenges are not a reason to give up. “There are so many single and available people out there,” she said. “And everyone’s deserving of love. Even if you only have an hour a week.”
A version of this article first appeared on Medscape.com.
Pounding heart, sweating, insomnia. Surges of dopamine, norepinephrine, and adrenaline. All symptoms of a very common yet frustrating condition: Falling in love.
The prognosis is vague. A prescription pad and knowledge of biochemistry aren’t helpful when it comes to relationships.
Medical training can consume decades when others are exploring relationships and starting families. There are few recent data on this, but
But there is hope! By age 36, the number of doctors in long-term relationships had overtaken everyone else by more than 10% for women and 20% for men. The Medscape 2022 Physician Happiness & Lifestyle Report found that 83% were in committed relationships, and even better, happy ones. At least three-quarters of doctors in every specialty described their partnerships as “very good” or “good.”
How should a single medical student, resident, or attending physician find happiness ever after in 2023? Sometimes Mr./Ms. Right can be found in the anatomy lab or hospital, with sparks flying between students or colleagues. But for many in health care, along with millions of others looking for love, the solution is dating apps.
When ‘MD’ is a turnoff
Dr. M, a psychiatry resident in California who prefers not to give her name, hadn’t found a life partner during college, grad school, or medical school. When she passed her final Step 3 board exam, she decided it was time to take the plunge. She signed up for popular dating apps like Hinge, Bumble, and Coffee Meets Bagel, but her dates seemed to follow a disappointing pattern.
“I met lots of guys, but it was incredibly rare to find another physician,” said Dr. M. “I found myself always wanting to talk about my life as a resident. More often than not, the guys would give me this blank stare as I complained about being on call or spoke about spending 12 hours a day studying for a board exam, or even the process of The Match and how I ended up in California.”
Both of Dr. M’s parents are physicians, and she grew up watching how they supported each other through residency, exams, and exhausting schedules. A relationship with another physician, her parents told her, would give both partners the best chance to understand each other’s lives. The problem was how to find one.
That was when Dr. M saw an ad for a dating app with a cute medical name: DownToDate, a play on the clinical evidence resource UpToDate. “I thought it was a meme,” she said. “It was this doctors-only app. I remember thinking, ‘this has to be a joke,’ but then it was very real.”
She signed up and was required to provide a photo of her ID and her NPI number. Immediately, men began “requesting a consult,” the app’s form of “liking” her profile, and sending her “pages” (messages).
DownToDate was created by another physician, Robin Boyer, MD, MBA, a pediatrics resident in Loma Linda, Calif. The inspiration came in 2020 during the initial COVID crisis. Exhausted from long and often heartbreaking shifts, Dr. Boyer was grateful for her husband’s unwavering support. But many of her coresidents weren’t so lucky. The women in particular talked about their dating struggles, and there was a recurring theme. They didn’t feel confident putting “physician” on a dating site profile.
“If you’re male and you tell people you’re a doctor, it seems like it really attracts people,” Dr. Boyer said. “But if you’re female, it brings up a lot of stereotypes where you’re perceived as too intimidating either as the breadwinner, being more educated, or having a [demanding] career. It does make it more difficult.”
Dr. Boyer met her husband in high school, and she had never used a dating app. She convinced a coresident, Celestine Odigwe, MD, to pursue the idea as partners. They began researching the market within their network and heard from over a thousand interested physicians, both men and women, heterosexual and LGBTQ+. They even created fake accounts on other sites to gauge how easy it is to falsify a profile. From these insights, the app took shape. It launched in 2021 and currently has more than 5000 verified users.
Branches from the same tree
Around the same time that DownToDate began, Shivani Shah, DO, a pediatric neurology resident at Duke University, Durham, N.C., and her brother, Sagar Shah, an entrepreneur, had a similar idea.
At the time, Dr. Shah was a fourth-year medical student about to move from New Jersey to North Carolina. Friends who were internal medicine residents described the grueling reality of the early COVID pandemic.
“It was just horrible,” said Dr. Shah. “You were isolated from your family, your support system, everything. ... I think the pandemic really pushed us into realizing that this is a very important need, and sometimes it feels like community is lacking in the health care field.”
The sibling duo developed ForeverX, an app for health care workers to find meaningful and long-term romantic connections. It launched in 2021.
Concerned that the medical field was “siloed,” the Shahs chose to open the app to physicians, dentists, nurses, physical therapists, and other health care professionals. “Opening up the doors to more communication” between the health care branches was a priority.
To prevent catfishing, the app uses a twofold vetting system. Each user submits a photo of their driver’s license and a selfie that must match. There is also health care verification through an NPI number, nurse’s ID, or a manual process for those without either. None of the information is stored.
Through personal experience with dating apps, Dr. Shah hopes ForeverX can improve on some of their flaws, particularly the problem of matches being overly filtered by preferences. The “natural way” of meeting people is not filtered. And while most people have a dating checklist in mind, meeting someone face to face might send some of those prerequisites “out the window.”
“You can’t really put into words how you feel with someone ... the vibe,” Dr. Shah said. That is why her goal is to get people off the app and on an actual date IRL. “Something we’ve discussed internally is, how do we make this experience that’s virtual more human?”
She acknowledged that certain requirements, like a desire for children, might be crucial to some users. Many female doctors in their 30’s feel the “time crunch” of a ticking biological clock.
Optimize your date-ability
“I think people either love or hate dating apps, and I love them,” said Kevin Jubbal, MD. “I get to meet cool people and schedule dates from the comfort of my home.”
Dr. Jubbal, a former plastic surgery resident who left medicine to become an entrepreneur, is the founder of Med School Insiders, a tutoring and advising resource for premeds, medical students, and residents. His YouTube channel has more than 1.5 million subscribers, and he often receives questions about whether dating is feasible in medical school and how to balance a personal and academic/professional life.
Those who hate dating apps or receive few matches would do well to look inward instead of blaming the process, he said. It helps to view the experience as a learning tool that provides feedback very quickly.
“If you want to find a really amazing person, then you need to be what you want to find,” said Dr. Jubbal. “If you want to find someone who’s fit and intelligent and well read and well traveled, you need to be that. Otherwise, you’re probably not going to attract that person.”
An app designed to help single female MDs
Ifie Williams, MD, a psychiatrist in Washington, D.C., believes a wider dating pool is key – provided everyone understands the situation up front. When Dr. Williams started residency in 2014, she was “as single as can be.” She tried many dating apps, but they were extremely time consuming. Even when she set specific preferences, she found herself sifting through “matches” that didn’t fit her criteria.
“Dating nowadays has become almost like a second job,” said Dr. Williams. “Just the amount of time that people are having to spend on apps, swiping left and right and then meeting people. You think they’re interested and then you deal with all these games.”
By 2017, Dr. Williams had invented Miss Doctor, a dating app that would connect female physicians and other doctoral-level professionals with men or women on a similar achievement level.
By definition, these people would not be intimidated by ambitious, busy women. They would be heavily screened and vetted. And one other proviso: they would have to pay for “likes.”
Most dating apps charge a subscription fee. Users are allowed to “like” numerous profiles and perhaps not bother responding to many matches. By contrast, Miss Doctor accounts are free and include a limited number of “likes” to indicate interest. Beyond that, there’s a price.
“We wanted to find a way to make people a little more intentional with how they like people on the app, so they give a little more thought to it,” Dr. Williams said. “So, we monetize it and use that to change behavior.”
After an initial launch in 2017, the app had to take a back seat while Dr. Williams started her psychiatry practice and got married herself. She plans to relaunch it in spring 2023.
Male or female, there is general agreement that finding time to date as a young physician isn’t easy. While DownToDate has had “doctor meets doctor” success stories, many users are still searching for “the one.”
Dr. Boyer believes that career challenges are not a reason to give up. “There are so many single and available people out there,” she said. “And everyone’s deserving of love. Even if you only have an hour a week.”
A version of this article first appeared on Medscape.com.
Pounding heart, sweating, insomnia. Surges of dopamine, norepinephrine, and adrenaline. All symptoms of a very common yet frustrating condition: Falling in love.
The prognosis is vague. A prescription pad and knowledge of biochemistry aren’t helpful when it comes to relationships.
Medical training can consume decades when others are exploring relationships and starting families. There are few recent data on this, but
But there is hope! By age 36, the number of doctors in long-term relationships had overtaken everyone else by more than 10% for women and 20% for men. The Medscape 2022 Physician Happiness & Lifestyle Report found that 83% were in committed relationships, and even better, happy ones. At least three-quarters of doctors in every specialty described their partnerships as “very good” or “good.”
How should a single medical student, resident, or attending physician find happiness ever after in 2023? Sometimes Mr./Ms. Right can be found in the anatomy lab or hospital, with sparks flying between students or colleagues. But for many in health care, along with millions of others looking for love, the solution is dating apps.
When ‘MD’ is a turnoff
Dr. M, a psychiatry resident in California who prefers not to give her name, hadn’t found a life partner during college, grad school, or medical school. When she passed her final Step 3 board exam, she decided it was time to take the plunge. She signed up for popular dating apps like Hinge, Bumble, and Coffee Meets Bagel, but her dates seemed to follow a disappointing pattern.
“I met lots of guys, but it was incredibly rare to find another physician,” said Dr. M. “I found myself always wanting to talk about my life as a resident. More often than not, the guys would give me this blank stare as I complained about being on call or spoke about spending 12 hours a day studying for a board exam, or even the process of The Match and how I ended up in California.”
Both of Dr. M’s parents are physicians, and she grew up watching how they supported each other through residency, exams, and exhausting schedules. A relationship with another physician, her parents told her, would give both partners the best chance to understand each other’s lives. The problem was how to find one.
That was when Dr. M saw an ad for a dating app with a cute medical name: DownToDate, a play on the clinical evidence resource UpToDate. “I thought it was a meme,” she said. “It was this doctors-only app. I remember thinking, ‘this has to be a joke,’ but then it was very real.”
She signed up and was required to provide a photo of her ID and her NPI number. Immediately, men began “requesting a consult,” the app’s form of “liking” her profile, and sending her “pages” (messages).
DownToDate was created by another physician, Robin Boyer, MD, MBA, a pediatrics resident in Loma Linda, Calif. The inspiration came in 2020 during the initial COVID crisis. Exhausted from long and often heartbreaking shifts, Dr. Boyer was grateful for her husband’s unwavering support. But many of her coresidents weren’t so lucky. The women in particular talked about their dating struggles, and there was a recurring theme. They didn’t feel confident putting “physician” on a dating site profile.
“If you’re male and you tell people you’re a doctor, it seems like it really attracts people,” Dr. Boyer said. “But if you’re female, it brings up a lot of stereotypes where you’re perceived as too intimidating either as the breadwinner, being more educated, or having a [demanding] career. It does make it more difficult.”
Dr. Boyer met her husband in high school, and she had never used a dating app. She convinced a coresident, Celestine Odigwe, MD, to pursue the idea as partners. They began researching the market within their network and heard from over a thousand interested physicians, both men and women, heterosexual and LGBTQ+. They even created fake accounts on other sites to gauge how easy it is to falsify a profile. From these insights, the app took shape. It launched in 2021 and currently has more than 5000 verified users.
Branches from the same tree
Around the same time that DownToDate began, Shivani Shah, DO, a pediatric neurology resident at Duke University, Durham, N.C., and her brother, Sagar Shah, an entrepreneur, had a similar idea.
At the time, Dr. Shah was a fourth-year medical student about to move from New Jersey to North Carolina. Friends who were internal medicine residents described the grueling reality of the early COVID pandemic.
“It was just horrible,” said Dr. Shah. “You were isolated from your family, your support system, everything. ... I think the pandemic really pushed us into realizing that this is a very important need, and sometimes it feels like community is lacking in the health care field.”
The sibling duo developed ForeverX, an app for health care workers to find meaningful and long-term romantic connections. It launched in 2021.
Concerned that the medical field was “siloed,” the Shahs chose to open the app to physicians, dentists, nurses, physical therapists, and other health care professionals. “Opening up the doors to more communication” between the health care branches was a priority.
To prevent catfishing, the app uses a twofold vetting system. Each user submits a photo of their driver’s license and a selfie that must match. There is also health care verification through an NPI number, nurse’s ID, or a manual process for those without either. None of the information is stored.
Through personal experience with dating apps, Dr. Shah hopes ForeverX can improve on some of their flaws, particularly the problem of matches being overly filtered by preferences. The “natural way” of meeting people is not filtered. And while most people have a dating checklist in mind, meeting someone face to face might send some of those prerequisites “out the window.”
“You can’t really put into words how you feel with someone ... the vibe,” Dr. Shah said. That is why her goal is to get people off the app and on an actual date IRL. “Something we’ve discussed internally is, how do we make this experience that’s virtual more human?”
She acknowledged that certain requirements, like a desire for children, might be crucial to some users. Many female doctors in their 30’s feel the “time crunch” of a ticking biological clock.
Optimize your date-ability
“I think people either love or hate dating apps, and I love them,” said Kevin Jubbal, MD. “I get to meet cool people and schedule dates from the comfort of my home.”
Dr. Jubbal, a former plastic surgery resident who left medicine to become an entrepreneur, is the founder of Med School Insiders, a tutoring and advising resource for premeds, medical students, and residents. His YouTube channel has more than 1.5 million subscribers, and he often receives questions about whether dating is feasible in medical school and how to balance a personal and academic/professional life.
Those who hate dating apps or receive few matches would do well to look inward instead of blaming the process, he said. It helps to view the experience as a learning tool that provides feedback very quickly.
“If you want to find a really amazing person, then you need to be what you want to find,” said Dr. Jubbal. “If you want to find someone who’s fit and intelligent and well read and well traveled, you need to be that. Otherwise, you’re probably not going to attract that person.”
An app designed to help single female MDs
Ifie Williams, MD, a psychiatrist in Washington, D.C., believes a wider dating pool is key – provided everyone understands the situation up front. When Dr. Williams started residency in 2014, she was “as single as can be.” She tried many dating apps, but they were extremely time consuming. Even when she set specific preferences, she found herself sifting through “matches” that didn’t fit her criteria.
“Dating nowadays has become almost like a second job,” said Dr. Williams. “Just the amount of time that people are having to spend on apps, swiping left and right and then meeting people. You think they’re interested and then you deal with all these games.”
By 2017, Dr. Williams had invented Miss Doctor, a dating app that would connect female physicians and other doctoral-level professionals with men or women on a similar achievement level.
By definition, these people would not be intimidated by ambitious, busy women. They would be heavily screened and vetted. And one other proviso: they would have to pay for “likes.”
Most dating apps charge a subscription fee. Users are allowed to “like” numerous profiles and perhaps not bother responding to many matches. By contrast, Miss Doctor accounts are free and include a limited number of “likes” to indicate interest. Beyond that, there’s a price.
“We wanted to find a way to make people a little more intentional with how they like people on the app, so they give a little more thought to it,” Dr. Williams said. “So, we monetize it and use that to change behavior.”
After an initial launch in 2017, the app had to take a back seat while Dr. Williams started her psychiatry practice and got married herself. She plans to relaunch it in spring 2023.
Male or female, there is general agreement that finding time to date as a young physician isn’t easy. While DownToDate has had “doctor meets doctor” success stories, many users are still searching for “the one.”
Dr. Boyer believes that career challenges are not a reason to give up. “There are so many single and available people out there,” she said. “And everyone’s deserving of love. Even if you only have an hour a week.”
A version of this article first appeared on Medscape.com.
Differences in brain structure linked to social disadvantage
Brain volume disparities among young children of different races may be attributable to adverse childhood experiences related to socioeconomic conditions and structural racism, new research suggests.
Investigators from the Belmont, Mass.–based McLean Hospital, an affiliate of Mass General Brigham, found that 9- and 10-year-old children of different racial and socioeconomic backgrounds have subtle neurobiological differences in gray matter volume in certain brain regions associated with trauma and stress.
Lead investigator Nathaniel Harnett, PhD, of the department of psychiatry at Harvard Medical School, Boston, believes this research shows evidence that “structural racism” – broad socioeconomic disadvantages that lead to poverty and emotional trauma – may affect brain structures and growth and ultimately may lead to psychiatric illness.
“For clinicians, I think the take-home message is that we really need to be more aware about the ways in which the disproportionate burden of stress might impact some groups,” Dr. Harnett told this news organization.
“This in turn can affect the way they respond either to later stress or maybe even treatment outcomes.” He added that other brain regions and compensatory mechanisms are likely to be involved, and more work needs to explore these connections.
The study was published online in the American Journal of Psychiatry.
‘Toxic stressor’
Dr. Harnett and colleagues used MRI and survey data from the 2019 Adolescent Brain Cognitive Development (ABCD) study involving over 12,000 children from 21 sites across the United States.
Participating children provided information about emotional and physical conflicts in the household. The ABCD study also surveyed the parents about their race and ethnicity, parental education, employment, and family income. Another factor in the analysis was neighborhood disadvantage, based on the Area Deprivation Index utilizing 17 socioeconomic indicators from the U.S. Census, including poverty and housing.
Comparing brain MRI findings from approximately 7,300 White children and 1,800 Black children in the ABCD study, Dr. Harnett’s group found that Black children had lower gray matter volume in the amygdala, hippocampus, and other subregions of the prefrontal cortex.
Experience of adversity was the “sole factor” explaining brain volume differences, with household income being the predominant factor.
Compared with White children, Black children were three times less likely to have parents who were currently employed. In addition, White parents were more likely than Black parents to have higher education at 75.2% versus 40.6%. Black families had significantly lower household income than White families and experienced more family conflict, material hardship, neighborhood disadvantage, and traumatic events.
The researchers analyzed race-related differences in posttraumatic stress disorder symptoms and the relationship with adversity and found that Black children had significantly greater PTSD symptom severity, and that symptom severity was “further predicted by adversity.”
“Taken together, early-life adversity may act as a toxic stressor that disproportionately impacts Black children as a result of their significantly greater exposure to adversity and contributes to differential neural development of key threat-processing regions,” the investigators write.
“These parts of the brain are involved in what we typically call threat learning,” Dr. Harnett explained. “Threat learning is basically learning to recognize potential dangers in our environment and selecting behaviors to keep us safe, whether we’re going to run away from a danger or face it head on. When you have chronic exposure to things that can be dangerous or can make you feel unsafe, that might have an impact on how these brain regions develop, with potential implications for how these regions function later on in life.”
A consequence of toxic stress
This study is part of a growing body of work on the influence of “toxic stress” and other forms of PTSD on brain architecture. The authors note that prolonged exposure to adverse experiences leads to excessive activation of stress-response systems and accumulation of stress hormones. This disrupts immune and metabolic regulatory systems that influence the developing structures of the brain.
The study helps to contradict the “pseudoscientific falsehood” of biologic race-related differences in brain volume, instead emphasizing the role of adversity brought on by structural racism, the authors add.
In an accompanying editor’s note, the publication’s Editor-in-Chief Ned H. Kalin, MD, called childhood adversity, maltreatment, and stress, “significant risk factors for the development of psychopathology.”
These findings are “critically important, as they speak to the need for psychiatry as a field to be outspoken about the detrimental psychological impacts of race-related disparities in childhood adversity, to call out the fact that these disparities stem from structural racism, and to vigorously support rectifying efforts by pursuing policy changes,” he stated in a news release.
Social construct?
Joan Luby, MD, coauthor of an accompanying editorial, said she and her coauthor “really appreciate the study and think the findings are overall very consistent with the emerging literature, increasing the confidence [in the findings].”
Dr. Luby, a professor of child psychiatry and director of the Early Emotional Development Program, Washington University, St. Louis, noted that she “takes issue” with the fact that the study “makes inferences regarding race, when we think those inferences aren’t well justified, are misinterpretations, and could be misleading.”
Race is a “social construct” and there are many sources of adversity that the authors didn’t measure in the study and are likely the source of any remaining variance they found, including experiences of structural racism and discrimination,” said Dr. Luby, who was not involved in the study.
“How people look doesn’t have any bearing on their inherent biological characteristics, and more [needs to be studied] on how they experience the psychosocial environment and how the psychosocial environment rejects or reacts to them.”
These psychosocial issues “have to be taken into account and measured in a very comprehensive way,” she added.
The ABCD study was supported by the National Institutes of Health and additional federal partners. Dr. Harnett reports no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Dr. Luby receives royalties from Guilford Press. Her coauthor reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Brain volume disparities among young children of different races may be attributable to adverse childhood experiences related to socioeconomic conditions and structural racism, new research suggests.
Investigators from the Belmont, Mass.–based McLean Hospital, an affiliate of Mass General Brigham, found that 9- and 10-year-old children of different racial and socioeconomic backgrounds have subtle neurobiological differences in gray matter volume in certain brain regions associated with trauma and stress.
Lead investigator Nathaniel Harnett, PhD, of the department of psychiatry at Harvard Medical School, Boston, believes this research shows evidence that “structural racism” – broad socioeconomic disadvantages that lead to poverty and emotional trauma – may affect brain structures and growth and ultimately may lead to psychiatric illness.
“For clinicians, I think the take-home message is that we really need to be more aware about the ways in which the disproportionate burden of stress might impact some groups,” Dr. Harnett told this news organization.
“This in turn can affect the way they respond either to later stress or maybe even treatment outcomes.” He added that other brain regions and compensatory mechanisms are likely to be involved, and more work needs to explore these connections.
The study was published online in the American Journal of Psychiatry.
‘Toxic stressor’
Dr. Harnett and colleagues used MRI and survey data from the 2019 Adolescent Brain Cognitive Development (ABCD) study involving over 12,000 children from 21 sites across the United States.
Participating children provided information about emotional and physical conflicts in the household. The ABCD study also surveyed the parents about their race and ethnicity, parental education, employment, and family income. Another factor in the analysis was neighborhood disadvantage, based on the Area Deprivation Index utilizing 17 socioeconomic indicators from the U.S. Census, including poverty and housing.
Comparing brain MRI findings from approximately 7,300 White children and 1,800 Black children in the ABCD study, Dr. Harnett’s group found that Black children had lower gray matter volume in the amygdala, hippocampus, and other subregions of the prefrontal cortex.
Experience of adversity was the “sole factor” explaining brain volume differences, with household income being the predominant factor.
Compared with White children, Black children were three times less likely to have parents who were currently employed. In addition, White parents were more likely than Black parents to have higher education at 75.2% versus 40.6%. Black families had significantly lower household income than White families and experienced more family conflict, material hardship, neighborhood disadvantage, and traumatic events.
The researchers analyzed race-related differences in posttraumatic stress disorder symptoms and the relationship with adversity and found that Black children had significantly greater PTSD symptom severity, and that symptom severity was “further predicted by adversity.”
“Taken together, early-life adversity may act as a toxic stressor that disproportionately impacts Black children as a result of their significantly greater exposure to adversity and contributes to differential neural development of key threat-processing regions,” the investigators write.
“These parts of the brain are involved in what we typically call threat learning,” Dr. Harnett explained. “Threat learning is basically learning to recognize potential dangers in our environment and selecting behaviors to keep us safe, whether we’re going to run away from a danger or face it head on. When you have chronic exposure to things that can be dangerous or can make you feel unsafe, that might have an impact on how these brain regions develop, with potential implications for how these regions function later on in life.”
A consequence of toxic stress
This study is part of a growing body of work on the influence of “toxic stress” and other forms of PTSD on brain architecture. The authors note that prolonged exposure to adverse experiences leads to excessive activation of stress-response systems and accumulation of stress hormones. This disrupts immune and metabolic regulatory systems that influence the developing structures of the brain.
The study helps to contradict the “pseudoscientific falsehood” of biologic race-related differences in brain volume, instead emphasizing the role of adversity brought on by structural racism, the authors add.
In an accompanying editor’s note, the publication’s Editor-in-Chief Ned H. Kalin, MD, called childhood adversity, maltreatment, and stress, “significant risk factors for the development of psychopathology.”
These findings are “critically important, as they speak to the need for psychiatry as a field to be outspoken about the detrimental psychological impacts of race-related disparities in childhood adversity, to call out the fact that these disparities stem from structural racism, and to vigorously support rectifying efforts by pursuing policy changes,” he stated in a news release.
Social construct?
Joan Luby, MD, coauthor of an accompanying editorial, said she and her coauthor “really appreciate the study and think the findings are overall very consistent with the emerging literature, increasing the confidence [in the findings].”
Dr. Luby, a professor of child psychiatry and director of the Early Emotional Development Program, Washington University, St. Louis, noted that she “takes issue” with the fact that the study “makes inferences regarding race, when we think those inferences aren’t well justified, are misinterpretations, and could be misleading.”
Race is a “social construct” and there are many sources of adversity that the authors didn’t measure in the study and are likely the source of any remaining variance they found, including experiences of structural racism and discrimination,” said Dr. Luby, who was not involved in the study.
“How people look doesn’t have any bearing on their inherent biological characteristics, and more [needs to be studied] on how they experience the psychosocial environment and how the psychosocial environment rejects or reacts to them.”
These psychosocial issues “have to be taken into account and measured in a very comprehensive way,” she added.
The ABCD study was supported by the National Institutes of Health and additional federal partners. Dr. Harnett reports no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Dr. Luby receives royalties from Guilford Press. Her coauthor reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Brain volume disparities among young children of different races may be attributable to adverse childhood experiences related to socioeconomic conditions and structural racism, new research suggests.
Investigators from the Belmont, Mass.–based McLean Hospital, an affiliate of Mass General Brigham, found that 9- and 10-year-old children of different racial and socioeconomic backgrounds have subtle neurobiological differences in gray matter volume in certain brain regions associated with trauma and stress.
Lead investigator Nathaniel Harnett, PhD, of the department of psychiatry at Harvard Medical School, Boston, believes this research shows evidence that “structural racism” – broad socioeconomic disadvantages that lead to poverty and emotional trauma – may affect brain structures and growth and ultimately may lead to psychiatric illness.
“For clinicians, I think the take-home message is that we really need to be more aware about the ways in which the disproportionate burden of stress might impact some groups,” Dr. Harnett told this news organization.
“This in turn can affect the way they respond either to later stress or maybe even treatment outcomes.” He added that other brain regions and compensatory mechanisms are likely to be involved, and more work needs to explore these connections.
The study was published online in the American Journal of Psychiatry.
‘Toxic stressor’
Dr. Harnett and colleagues used MRI and survey data from the 2019 Adolescent Brain Cognitive Development (ABCD) study involving over 12,000 children from 21 sites across the United States.
Participating children provided information about emotional and physical conflicts in the household. The ABCD study also surveyed the parents about their race and ethnicity, parental education, employment, and family income. Another factor in the analysis was neighborhood disadvantage, based on the Area Deprivation Index utilizing 17 socioeconomic indicators from the U.S. Census, including poverty and housing.
Comparing brain MRI findings from approximately 7,300 White children and 1,800 Black children in the ABCD study, Dr. Harnett’s group found that Black children had lower gray matter volume in the amygdala, hippocampus, and other subregions of the prefrontal cortex.
Experience of adversity was the “sole factor” explaining brain volume differences, with household income being the predominant factor.
Compared with White children, Black children were three times less likely to have parents who were currently employed. In addition, White parents were more likely than Black parents to have higher education at 75.2% versus 40.6%. Black families had significantly lower household income than White families and experienced more family conflict, material hardship, neighborhood disadvantage, and traumatic events.
The researchers analyzed race-related differences in posttraumatic stress disorder symptoms and the relationship with adversity and found that Black children had significantly greater PTSD symptom severity, and that symptom severity was “further predicted by adversity.”
“Taken together, early-life adversity may act as a toxic stressor that disproportionately impacts Black children as a result of their significantly greater exposure to adversity and contributes to differential neural development of key threat-processing regions,” the investigators write.
“These parts of the brain are involved in what we typically call threat learning,” Dr. Harnett explained. “Threat learning is basically learning to recognize potential dangers in our environment and selecting behaviors to keep us safe, whether we’re going to run away from a danger or face it head on. When you have chronic exposure to things that can be dangerous or can make you feel unsafe, that might have an impact on how these brain regions develop, with potential implications for how these regions function later on in life.”
A consequence of toxic stress
This study is part of a growing body of work on the influence of “toxic stress” and other forms of PTSD on brain architecture. The authors note that prolonged exposure to adverse experiences leads to excessive activation of stress-response systems and accumulation of stress hormones. This disrupts immune and metabolic regulatory systems that influence the developing structures of the brain.
The study helps to contradict the “pseudoscientific falsehood” of biologic race-related differences in brain volume, instead emphasizing the role of adversity brought on by structural racism, the authors add.
In an accompanying editor’s note, the publication’s Editor-in-Chief Ned H. Kalin, MD, called childhood adversity, maltreatment, and stress, “significant risk factors for the development of psychopathology.”
These findings are “critically important, as they speak to the need for psychiatry as a field to be outspoken about the detrimental psychological impacts of race-related disparities in childhood adversity, to call out the fact that these disparities stem from structural racism, and to vigorously support rectifying efforts by pursuing policy changes,” he stated in a news release.
Social construct?
Joan Luby, MD, coauthor of an accompanying editorial, said she and her coauthor “really appreciate the study and think the findings are overall very consistent with the emerging literature, increasing the confidence [in the findings].”
Dr. Luby, a professor of child psychiatry and director of the Early Emotional Development Program, Washington University, St. Louis, noted that she “takes issue” with the fact that the study “makes inferences regarding race, when we think those inferences aren’t well justified, are misinterpretations, and could be misleading.”
Race is a “social construct” and there are many sources of adversity that the authors didn’t measure in the study and are likely the source of any remaining variance they found, including experiences of structural racism and discrimination,” said Dr. Luby, who was not involved in the study.
“How people look doesn’t have any bearing on their inherent biological characteristics, and more [needs to be studied] on how they experience the psychosocial environment and how the psychosocial environment rejects or reacts to them.”
These psychosocial issues “have to be taken into account and measured in a very comprehensive way,” she added.
The ABCD study was supported by the National Institutes of Health and additional federal partners. Dr. Harnett reports no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Dr. Luby receives royalties from Guilford Press. Her coauthor reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Bright light therapy boosts therapeutic response
Both depression and bipolar disorder are leading causes of disability worldwide, and data show that only 50%-60% of these patients respond to first-line antidepressants, wrote Alessandro Cuomo, MD, of the University of Siena Medical Center, Italy, and colleagues.
Bright light therapy (BLT) was originally introduced as a treatment for seasonal affective disorder, but its use has been expanded to treat nonseasonal depression and bipolar disorder, they said. However, the impact of BLT on depressive symptoms in bipolar depression in particular has not been examined, they noted.
In a study published in the Journal of Affective Disorders, the researchers identified 18 men and 23 women aged 18 years and older with bipolar depression based on DSM-5 criteria who had already been treated with antidepressants. The participants were randomized to antidepressants combined with BLT or antidepressants combined with red light exposure (controls). The participants were positioned at 30-80 cm from the 10,000-lux light source for 30 minutes daily. The mean age of the participants was 49.1 years.
The primary outcome was scores on the Montgomery-Åsberg Depression Scale (MADRS), Hamilton Depression Rating Scale (HAMD-17), and CGI-Severity of illness (CGI-S), Fatigue Severity Scale (FSS), and Quality of Life Scale (QOLS) after the 8 weeks of treatment.
After 4 weeks, MADRS scores and HAMD-17 scores were significantly lower in the treatment group, compared with the controls (20 and 18 vs. 27.5 and 24.9, respectively; P < .001). Quality of life scores increased in the treatment group, compared with controls, with median scores of 39 vs. 29.50, respectively.
After 8 weeks, the treatment group continued to show significant improvement, compared with the control group, with scores on the MADRS, HAMD-17, CGI-S, and QOLS of 14.0, 9.0, 1.0, and 62.0 vs. 16.0, 15.5, 2.0, and 40.0, respectively. No side effects were reported.
“From our findings, BLT [proved] particularly effective in bipolar patients without triggering any manic switch, as evidenced instead in some similar studies,” the researchers wrote in their discussion.
Although the mechanism of action for BLT remains unclear, the current study findings confirm the existing knowledge of BLT, they noted. The positive effect of BLT on quality of life “might be attributable to the ability of BLT to reduce the latency times of antidepressants and increase the production of serotonin and melatonin,” as shown in previous work, they said.
The study findings were limited by several factors including the small sample size, which prevents definitive conclusions about the effectiveness of BLT in combination with different antidepressants, and the heterogeneity of the antidepressant treatments, the researchers noted. Larger, prospective studies and randomized, controlled trials are needed, as are studies of special populations such as older adults or those with degenerative diseases, they said.
However, the results suggest BLT has value as a safe and effective treatment and a way to boost therapeutic response and reduce the impact of long-lasting therapies, they concluded.
The study received no outside funding. Dr. Cuomo disclosed serving as a consultant and/or a speaker for Angelini, Glaxo Smith Kline, Lundbeck, Janssen, Otsuka, Pfizer, and Recordati.
Both depression and bipolar disorder are leading causes of disability worldwide, and data show that only 50%-60% of these patients respond to first-line antidepressants, wrote Alessandro Cuomo, MD, of the University of Siena Medical Center, Italy, and colleagues.
Bright light therapy (BLT) was originally introduced as a treatment for seasonal affective disorder, but its use has been expanded to treat nonseasonal depression and bipolar disorder, they said. However, the impact of BLT on depressive symptoms in bipolar depression in particular has not been examined, they noted.
In a study published in the Journal of Affective Disorders, the researchers identified 18 men and 23 women aged 18 years and older with bipolar depression based on DSM-5 criteria who had already been treated with antidepressants. The participants were randomized to antidepressants combined with BLT or antidepressants combined with red light exposure (controls). The participants were positioned at 30-80 cm from the 10,000-lux light source for 30 minutes daily. The mean age of the participants was 49.1 years.
The primary outcome was scores on the Montgomery-Åsberg Depression Scale (MADRS), Hamilton Depression Rating Scale (HAMD-17), and CGI-Severity of illness (CGI-S), Fatigue Severity Scale (FSS), and Quality of Life Scale (QOLS) after the 8 weeks of treatment.
After 4 weeks, MADRS scores and HAMD-17 scores were significantly lower in the treatment group, compared with the controls (20 and 18 vs. 27.5 and 24.9, respectively; P < .001). Quality of life scores increased in the treatment group, compared with controls, with median scores of 39 vs. 29.50, respectively.
After 8 weeks, the treatment group continued to show significant improvement, compared with the control group, with scores on the MADRS, HAMD-17, CGI-S, and QOLS of 14.0, 9.0, 1.0, and 62.0 vs. 16.0, 15.5, 2.0, and 40.0, respectively. No side effects were reported.
“From our findings, BLT [proved] particularly effective in bipolar patients without triggering any manic switch, as evidenced instead in some similar studies,” the researchers wrote in their discussion.
Although the mechanism of action for BLT remains unclear, the current study findings confirm the existing knowledge of BLT, they noted. The positive effect of BLT on quality of life “might be attributable to the ability of BLT to reduce the latency times of antidepressants and increase the production of serotonin and melatonin,” as shown in previous work, they said.
The study findings were limited by several factors including the small sample size, which prevents definitive conclusions about the effectiveness of BLT in combination with different antidepressants, and the heterogeneity of the antidepressant treatments, the researchers noted. Larger, prospective studies and randomized, controlled trials are needed, as are studies of special populations such as older adults or those with degenerative diseases, they said.
However, the results suggest BLT has value as a safe and effective treatment and a way to boost therapeutic response and reduce the impact of long-lasting therapies, they concluded.
The study received no outside funding. Dr. Cuomo disclosed serving as a consultant and/or a speaker for Angelini, Glaxo Smith Kline, Lundbeck, Janssen, Otsuka, Pfizer, and Recordati.
Both depression and bipolar disorder are leading causes of disability worldwide, and data show that only 50%-60% of these patients respond to first-line antidepressants, wrote Alessandro Cuomo, MD, of the University of Siena Medical Center, Italy, and colleagues.
Bright light therapy (BLT) was originally introduced as a treatment for seasonal affective disorder, but its use has been expanded to treat nonseasonal depression and bipolar disorder, they said. However, the impact of BLT on depressive symptoms in bipolar depression in particular has not been examined, they noted.
In a study published in the Journal of Affective Disorders, the researchers identified 18 men and 23 women aged 18 years and older with bipolar depression based on DSM-5 criteria who had already been treated with antidepressants. The participants were randomized to antidepressants combined with BLT or antidepressants combined with red light exposure (controls). The participants were positioned at 30-80 cm from the 10,000-lux light source for 30 minutes daily. The mean age of the participants was 49.1 years.
The primary outcome was scores on the Montgomery-Åsberg Depression Scale (MADRS), Hamilton Depression Rating Scale (HAMD-17), and CGI-Severity of illness (CGI-S), Fatigue Severity Scale (FSS), and Quality of Life Scale (QOLS) after the 8 weeks of treatment.
After 4 weeks, MADRS scores and HAMD-17 scores were significantly lower in the treatment group, compared with the controls (20 and 18 vs. 27.5 and 24.9, respectively; P < .001). Quality of life scores increased in the treatment group, compared with controls, with median scores of 39 vs. 29.50, respectively.
After 8 weeks, the treatment group continued to show significant improvement, compared with the control group, with scores on the MADRS, HAMD-17, CGI-S, and QOLS of 14.0, 9.0, 1.0, and 62.0 vs. 16.0, 15.5, 2.0, and 40.0, respectively. No side effects were reported.
“From our findings, BLT [proved] particularly effective in bipolar patients without triggering any manic switch, as evidenced instead in some similar studies,” the researchers wrote in their discussion.
Although the mechanism of action for BLT remains unclear, the current study findings confirm the existing knowledge of BLT, they noted. The positive effect of BLT on quality of life “might be attributable to the ability of BLT to reduce the latency times of antidepressants and increase the production of serotonin and melatonin,” as shown in previous work, they said.
The study findings were limited by several factors including the small sample size, which prevents definitive conclusions about the effectiveness of BLT in combination with different antidepressants, and the heterogeneity of the antidepressant treatments, the researchers noted. Larger, prospective studies and randomized, controlled trials are needed, as are studies of special populations such as older adults or those with degenerative diseases, they said.
However, the results suggest BLT has value as a safe and effective treatment and a way to boost therapeutic response and reduce the impact of long-lasting therapies, they concluded.
The study received no outside funding. Dr. Cuomo disclosed serving as a consultant and/or a speaker for Angelini, Glaxo Smith Kline, Lundbeck, Janssen, Otsuka, Pfizer, and Recordati.
FROM THE JOURNAL OF AFFECTIVE DISORDERS
How a concussion led a former football player/WWE star to a pioneering neuroscience career
On Oct. 5, 2022, at 10:24 a.m., Chris Nowinski, PhD, cofounder of the Boston-based Concussion Legacy Foundation (CLF), was in his home office when the email came through.
“I pounded my desk, shouted YES! and went to find my wife so I could pick her up and give her a big hug,” he recalled. “It was the culmination of 15 years of research and hard work.”
Robert Cantu, MD, who has been studying head trauma for 50+ years and has published more than 500 papers about it, compares the announcement to the 1964 Surgeon General’s report that linked cigarette smoking with lung cancer and heart disease. With the NIH and the Centers of Disease Control and Prevention (CDC) now in agreement about the risks of participating in impact sports and activities, he said, “We’ve reached a tipping point that should finally prompt deniers such as the NHL, NCAA, FIFA, World Rugby, the International Olympic Committee, and other [sports organizations] to remove all unnecessary head trauma from their sports.”
“A lot of the credit for this must go to Chris,” added Dr. Cantu, medical director and director of clinical research at the Cantu Concussion Center at Emerson Hospital in Concord, Mass. “Clinicians like myself can reach only so many people by writing papers and giving speeches at medical conferences. For this to happen, the message needed to get out to parents, athletes, and society in general. And Chris was the vehicle for doing that.”
Dr. Nowinski didn’t set out to be the messenger. He played football at Harvard in the late 1990s, making second-team All-Ivy as a defensive tackle his senior year. In 2000, he enrolled in Killer Kowalski’s Wrestling Institute and eventually joined Vince McMahon’s World Wrestling Entertainment (WWE).
There he played the role of 295-pound villain “Chris Harvard,” an intellectual snob who dressed in crimson tights and insulted the crowd’s IQ. “Roses are red. Violets are blue. The reason I’m talking so slowly is because no one in [insert name of town he was appearing in] has passed grade 2!”
“I’d often apply my education during a match,” he wrote in his book, “Head Games: Football’s Concussion Crisis.“ In a match in Bridgeport, Conn., I assaulted [my opponent] with a human skeleton, ripped off the skull, got down on bended knee, and began reciting Hamlet. Those were good times.”
Those good times ended abruptly, however, during a match with Bubba Ray Dudley at the Hartford Civic Center in Connecticut in 2003. Even though pro wrestling matches are rehearsed, and the blows aren’t real, accidents happen. Mr. Dudley mistakenly kicked Dr. Nowinski in the jaw with enough force to put him on his back and make the whole ring shake.
“Holy shit, kid! You okay?” asked the referee. Before a foggy Dr. Nowinski could reply, 300-pound Mr. Dudley crashed down on him, hooked his leg, and the ref began counting, “One! Two! …” Dr. Nowinski instinctively kicked out but had forgotten the rest of the script. He managed to finish the match and stagger backstage.
His coherence and awareness gradually returned, but a “throbbing headache” persisted. A locker room doctor said he might have a concussion and recommended he wait to see how he felt before wrestling in Albany, N.Y., the next evening.
The following day the headache had subsided, but he still felt “a little strange.” Nonetheless, he told the doctor he was fine and strutted out to again battle Bubba Ray, this time in a match where he eventually got thrown through a ringside table and suffered the Dudley Death Drop. Afterward, “I crawled backstage and laid down. The headache was much, much worse.”
An event and a process
Dr. Nowinski continued to insist he was “fine” and wrestled a few more matches in the following days before finally acknowledging something was wrong. He’d had his bell rung numerous times in football, but this was different. Even more worrisome, none of the doctors he consulted could give him any definitive answers. He finally found his way to Emerson Hospital, where Dr. Cantu was the chief of neurosurgery.
“I remember that day vividly,” said Dr. Cantu. “Chris was this big, strapping, handsome guy – a hell of an athlete whose star was rising. He didn’t realize that he’d suffered a series of concussions and that trying to push through them was the worst thing he could be doing.”
Concussions and their effects were misunderstood by many athletes, coaches, and even physicians back then. It was assumed that the quarter inch of bone surrounding the adult brain provided adequate protection from common sports impacts and that any aftereffects were temporary. A common treatment was smelling salts and a pat on the back as the athlete returned to action.
However, the brain floats inside the skull in a bath of cerebral fluid. Any significant impact causes it to slosh violently from side to side, damaging tissue, synapses, and cells resulting in inflammation that can manifest as confusion and brain fog.
“A concussion is actually not defined by a physical injury,” explained Dr. Nowinski, “but by a loss of brain function that is induced by trauma. Concussion is not just an event, but also a process.” It’s almost as if the person has suffered a small seizure.
Fortunately, most concussion symptoms resolve within 2 weeks, but in some cases, especially if there’s been additional head trauma, they can persist, causing anxiety, depression, anger, and/or sleep disorders. Known as postconcussion syndrome (PCS), this is what Dr. Nowinski was unknowingly suffering from when he consulted Dr. Cantu.
In fact, one night it an Indianapolis hotel, weeks after his initial concussion, he awoke to find himself on the floor and the room in shambles. His girlfriend was yelling his name and shaking him. She told him he’d been having a nightmare and had suddenly started screaming and tearing up the room. “I didn’t remember any of it,” he said.
Dr. Cantu eventually advised Dr. Nowinski against ever returning to the ring or any activity with the risk for head injury. Research shows that sustaining a single significant concussion increases the risk of subsequent more-severe brain injuries.
“My diagnosis could have sent Chris off the deep end because he could no longer do what he wanted to do with this life,” said Dr. Cantu. “But instead, he used it as a tool to find meaning for his life.”
Dr. Nowinski decided to use his experience as a teaching opportunity, not just for other athletes but also for sports organizations and the medical community.
His book, which focused on the NFL’s “tobacco-industry-like refusal to acknowledge the depths of the problem,” was published in 2006. A year later, Dr. Nowinski partnered with Dr. Cantu to found the Sports Legacy Institute, which eventually became the Concussion Legacy Foundation (CLF).
Cold calling for brain donations
Robert Stern, PhD, is another highly respected authority in the study of neurodegenerative disease. In 2007, he was directing the clinical core of Boston University’s Alzheimer’s Disease Center. After giving a lecture to a group of financial planners and elder-law attorneys one morning, he got a request for a private meeting from a fellow named Chris Nowinski.
“I’d never heard of him, but I agreed,” recalled Dr. Stern, a professor of neurology, neurosurgery, anatomy, and neurobiology at Boston University. “A few days later, this larger-than-life guy walked into our conference room at the BU School of Medicine, exuding a great deal of passion, intellect, and determination. He told me his story and then started talking about the long-term consequences of concussions in sports.”
Dr. Stern had seen patients with dementia pugilistica, the old-school term for CTE. These were mostly boxers with cognitive and behavioral impairment. “But I had not heard about football players,” he said. “I hadn’t put the two together. And as I was listening to Chris, I realized if what he was saying was true then it was not only a potentially huge public health issue, but it was also a potentially huge scientific issue in the field of neurodegenerative disease.”
Dr. Nowinski introduced Dr. Stern to Dr. Cantu, and together with Ann McKee, MD, professor of neurology and pathology at BU, they cofounded the Center for the Study of Traumatic Encephalopathy (CSTE) in 2008. It was the first center of its kind devoted to the study of CTE in the world.
One of Dr. Nowinski’s first jobs at the CSTE was soliciting and procuring brain donations. Since CTE is generally a progressive condition that can take decades to manifest, autopsy was the only way to detect it.
The brains of two former Pittsburgh Steelers, Mike Webster and Terry Long, had been examined after their untimely deaths. After immunostaining, investigators found both former NFL players had “protein misfolds” characteristic of CTE.
This finding drew a lot of public and scientific attention, given that Mr. Long died by suicide and Mr. Webster was homeless when he died of a heart attack. But more scientific evidence was needed to prove a causal link between the head trauma and CTE.
Dr. Nowinski scoured obituaries looking for potential brains to study. When he found one, he would cold call the family and try to convince them to donate it to science. The first brain he secured for the center belonged to John Grimsley, a former NFL linebacker who in 2008 died at age 45 of an accidental gunshot wound. Often, Dr. Nowinski would even be the courier, traveling to pick up the brain after it had been harvested.
Over the next 10 years, Dr. Nowinski and his research team secured 500 brain donations. The research that resulted was staggering. In the beginning only 45 cases of CTE had been identified in the world, but in the first 111 NFL players who were autopsied, 110 had the disorder.
Of the first 53 college football players autopsied, 48 had CTE. Although Dr. Nowinski’s initial focus was football, evidence of CTE was soon detected among athletes in boxing, hockey, soccer, and rugby, as well as in combat veterans. However, the National Football League and other governing sports bodies initially denied any connection between sport-related head trauma and CTE.
Cumulative damage
In 2017, after 7 years of study, Dr. Nowinski earned a PhD in neurology. As the scientific evidence continued to accumulate, two shifts occurred that Dr. Stern said represent Dr. Nowinski’s greatest contributions. First, concussion is now widely recognized as an acute brain injury with symptoms that need to be immediately diagnosed and addressed.
“This is a completely different story from where things were just 10 years ago,” said Dr. Stern, “and Chris played a central role, if not the central role, in raising awareness about that.”
All 50 states and the District of Columbia now have laws regarding sports-related concussion. And there are brain banks in Australia, Canada, New Zealand, Brazil, and the United Kingdom studying CTE. More than 2,500 athletes in a variety of sports, including NASCAR’s Dale Earnhardt Jr. and NFL hall of famer Nick Buoniconti, have publicly pledged to donate their brains to science after their deaths.
Second, said Dr. Stern, we now know that although concussions can contribute to CTE, they are not the sole cause. It’s repetitive subconcussive trauma, without symptoms of concussion, that do the most damage.
“These happen during every practice and in every game,” said Dr. Stern. In fact, it’s estimated that pro football players suffer thousands of subconcussive incidents over the course of their careers. So, a player doesn’t have to see stars or lose consciousness to suffer brain damage; small impacts can accumulate over time.
Understanding this point is crucial for making youth sports safer. “Chris has played a critical role in raising awareness here, too,” said Dr. Stern. “Allowing our kids to get hit in the head over and over can put them at greater risk for later problems, plus it just doesn’t make common sense.”
“The biggest misconception surrounding head trauma in sports,” said Dr. Nowinski, “is the belief among players, coaches, and even the medical and scientific communities that if you get hit in the head and don’t have any symptoms then you’re okay and there hasn’t been any damage. That couldn’t be further from the truth. We now know that people are suffering serious brain injuries due to the accumulated effect of subconcussive impacts, and we need to get the word out about that.”
A major initiative from the Concussion Legacy Foundation called “Stop Hitting Kids in the Head” has the goal of convincing every sport to eliminate repetitive head impacts in players under age 14 – the time when the skull and brain are still developing and most vulnerable – by 2026. In fact, Dr. Nowinski wrote that “there could be a lot of kids who are misdiagnosed and medicated for various behavioral or emotional problems that may actually be head injury–related.”
Starting in 2009, the NFL adopted a series of rule changes designed to better protect its players against repeated head trauma. Among them is a ban on spearing or leading with the helmet, penalties for hitting defenseless players, and more stringent return-to-play guidelines, including concussion protocols.
The NFL has also put more emphasis on flag football options for youngsters and, for the first time, showcased this alternative in the 2023 Pro Bowl. But Dr. Nowinski is pressuring the league to go further. “While acknowledging that the game causes CTE, the NFL still underwrites recruiting 5-year-olds to play tackle football,” he said. “In my opinion, that’s unethical, and it needs to be addressed.”
WWE one of the most responsive organizations
Dr. Nowinski said WWE has been one of the most responsive sports organizations for protecting athletes. A doctor is now ringside at every match as is an observer who knows the script, thereby allowing for instant medical intervention if something goes wrong. “Since everyone is trying to look like they have a concussion all the time, it takes a deep understanding of the business to recognize a real one,” he said.
But this hasn’t been the case with other sports. “I am eternally disappointed in the response of the professional sports industry to the knowledge of CTE and long-term concussion symptoms,” said Dr. Nowinski.
“For example, FIFA [international soccer’s governing body] still doesn’t allow doctors to evaluate [potentially concussed] players on the sidelines and put them back in the game with a free substitution [if they’re deemed okay]. Not giving players proper medical care for a brain injury is unethical,” he said. BU’s Center for the Study of Traumatic Encephalopathy diagnosed the first CTE case in soccer in 2012, and in 2015 Dr. Nowinski successfully lobbied U.S. Soccer to ban heading the ball before age 11.
“Unfortunately, many governing bodies have circled the wagons in denying their sport causes CTE,” he continued. “FIFA, World Rugby, the NHL, even the NCAA and International Olympic Committee refuse to acknowledge it and, therefore, aren’t taking any steps to prevent it. They see it as a threat to their business model. Hopefully, now that the NIH and CDC are aligned about the risks of head impact in sports, this will begin to change.”
Meanwhile, research is continuing. Scientists are getting closer to being able to diagnose CTE in living humans, with ongoing studies using PET scans, blood markers, and spinal fluid markers. In 2019, researchers identified tau proteins specific to CTE that they believe are distinct from those of Alzheimer’s and other neurodegenerative diseases. Next step would be developing a drug to slow the development of CTE once detected.
Nonetheless, athletes at all levels in impact sports still don’t fully appreciate the risks of repeated head trauma and especially subconcussive blows. “I talk to former NFL and college players every week,” said Dr. Stern. “Some tell me, ‘I love the sport, it gave me so much, and I would do it again, but I’m not letting my grandchildren play.’ But others say, ‘As long as they know the risks, they can make their own decision.’ “
Dr. Nowinski has a daughter who is 4 and a son who’s 2. Both play soccer but, thanks to dad, heading isn’t allowed in their age groups. If they continue playing sports, Dr. Nowinski said he’ll make sure they understand the risks and how to protect themselves. This is a conversation all parents should have with their kids at every level to make sure they play safe, he added.
Those in the medical community can also volunteer their time to explain head trauma to athletes, coaches, and school administrators to be sure they understand its seriousness and are doing everything to protect players.
As you watch this year’s Super Bowl, Dr. Nowinski and his team would like you to keep something in mind. Those young men on the field for your entertainment are receiving mild brain trauma repeatedly throughout the game.
Even if it’s not a huge hit that gets replayed and makes everyone gasp, even if no one gets ushered into the little sideline tent for a concussion screening, even if no one loses consciousness, brain damage is still occurring. Watch the heads of the players during every play and think about what’s going on inside their skulls regardless of how big and strong those helmets look.
A version of this article first appeared on Medscape.com.
On Oct. 5, 2022, at 10:24 a.m., Chris Nowinski, PhD, cofounder of the Boston-based Concussion Legacy Foundation (CLF), was in his home office when the email came through.
“I pounded my desk, shouted YES! and went to find my wife so I could pick her up and give her a big hug,” he recalled. “It was the culmination of 15 years of research and hard work.”
Robert Cantu, MD, who has been studying head trauma for 50+ years and has published more than 500 papers about it, compares the announcement to the 1964 Surgeon General’s report that linked cigarette smoking with lung cancer and heart disease. With the NIH and the Centers of Disease Control and Prevention (CDC) now in agreement about the risks of participating in impact sports and activities, he said, “We’ve reached a tipping point that should finally prompt deniers such as the NHL, NCAA, FIFA, World Rugby, the International Olympic Committee, and other [sports organizations] to remove all unnecessary head trauma from their sports.”
“A lot of the credit for this must go to Chris,” added Dr. Cantu, medical director and director of clinical research at the Cantu Concussion Center at Emerson Hospital in Concord, Mass. “Clinicians like myself can reach only so many people by writing papers and giving speeches at medical conferences. For this to happen, the message needed to get out to parents, athletes, and society in general. And Chris was the vehicle for doing that.”
Dr. Nowinski didn’t set out to be the messenger. He played football at Harvard in the late 1990s, making second-team All-Ivy as a defensive tackle his senior year. In 2000, he enrolled in Killer Kowalski’s Wrestling Institute and eventually joined Vince McMahon’s World Wrestling Entertainment (WWE).
There he played the role of 295-pound villain “Chris Harvard,” an intellectual snob who dressed in crimson tights and insulted the crowd’s IQ. “Roses are red. Violets are blue. The reason I’m talking so slowly is because no one in [insert name of town he was appearing in] has passed grade 2!”
“I’d often apply my education during a match,” he wrote in his book, “Head Games: Football’s Concussion Crisis.“ In a match in Bridgeport, Conn., I assaulted [my opponent] with a human skeleton, ripped off the skull, got down on bended knee, and began reciting Hamlet. Those were good times.”
Those good times ended abruptly, however, during a match with Bubba Ray Dudley at the Hartford Civic Center in Connecticut in 2003. Even though pro wrestling matches are rehearsed, and the blows aren’t real, accidents happen. Mr. Dudley mistakenly kicked Dr. Nowinski in the jaw with enough force to put him on his back and make the whole ring shake.
“Holy shit, kid! You okay?” asked the referee. Before a foggy Dr. Nowinski could reply, 300-pound Mr. Dudley crashed down on him, hooked his leg, and the ref began counting, “One! Two! …” Dr. Nowinski instinctively kicked out but had forgotten the rest of the script. He managed to finish the match and stagger backstage.
His coherence and awareness gradually returned, but a “throbbing headache” persisted. A locker room doctor said he might have a concussion and recommended he wait to see how he felt before wrestling in Albany, N.Y., the next evening.
The following day the headache had subsided, but he still felt “a little strange.” Nonetheless, he told the doctor he was fine and strutted out to again battle Bubba Ray, this time in a match where he eventually got thrown through a ringside table and suffered the Dudley Death Drop. Afterward, “I crawled backstage and laid down. The headache was much, much worse.”
An event and a process
Dr. Nowinski continued to insist he was “fine” and wrestled a few more matches in the following days before finally acknowledging something was wrong. He’d had his bell rung numerous times in football, but this was different. Even more worrisome, none of the doctors he consulted could give him any definitive answers. He finally found his way to Emerson Hospital, where Dr. Cantu was the chief of neurosurgery.
“I remember that day vividly,” said Dr. Cantu. “Chris was this big, strapping, handsome guy – a hell of an athlete whose star was rising. He didn’t realize that he’d suffered a series of concussions and that trying to push through them was the worst thing he could be doing.”
Concussions and their effects were misunderstood by many athletes, coaches, and even physicians back then. It was assumed that the quarter inch of bone surrounding the adult brain provided adequate protection from common sports impacts and that any aftereffects were temporary. A common treatment was smelling salts and a pat on the back as the athlete returned to action.
However, the brain floats inside the skull in a bath of cerebral fluid. Any significant impact causes it to slosh violently from side to side, damaging tissue, synapses, and cells resulting in inflammation that can manifest as confusion and brain fog.
“A concussion is actually not defined by a physical injury,” explained Dr. Nowinski, “but by a loss of brain function that is induced by trauma. Concussion is not just an event, but also a process.” It’s almost as if the person has suffered a small seizure.
Fortunately, most concussion symptoms resolve within 2 weeks, but in some cases, especially if there’s been additional head trauma, they can persist, causing anxiety, depression, anger, and/or sleep disorders. Known as postconcussion syndrome (PCS), this is what Dr. Nowinski was unknowingly suffering from when he consulted Dr. Cantu.
In fact, one night it an Indianapolis hotel, weeks after his initial concussion, he awoke to find himself on the floor and the room in shambles. His girlfriend was yelling his name and shaking him. She told him he’d been having a nightmare and had suddenly started screaming and tearing up the room. “I didn’t remember any of it,” he said.
Dr. Cantu eventually advised Dr. Nowinski against ever returning to the ring or any activity with the risk for head injury. Research shows that sustaining a single significant concussion increases the risk of subsequent more-severe brain injuries.
“My diagnosis could have sent Chris off the deep end because he could no longer do what he wanted to do with this life,” said Dr. Cantu. “But instead, he used it as a tool to find meaning for his life.”
Dr. Nowinski decided to use his experience as a teaching opportunity, not just for other athletes but also for sports organizations and the medical community.
His book, which focused on the NFL’s “tobacco-industry-like refusal to acknowledge the depths of the problem,” was published in 2006. A year later, Dr. Nowinski partnered with Dr. Cantu to found the Sports Legacy Institute, which eventually became the Concussion Legacy Foundation (CLF).
Cold calling for brain donations
Robert Stern, PhD, is another highly respected authority in the study of neurodegenerative disease. In 2007, he was directing the clinical core of Boston University’s Alzheimer’s Disease Center. After giving a lecture to a group of financial planners and elder-law attorneys one morning, he got a request for a private meeting from a fellow named Chris Nowinski.
“I’d never heard of him, but I agreed,” recalled Dr. Stern, a professor of neurology, neurosurgery, anatomy, and neurobiology at Boston University. “A few days later, this larger-than-life guy walked into our conference room at the BU School of Medicine, exuding a great deal of passion, intellect, and determination. He told me his story and then started talking about the long-term consequences of concussions in sports.”
Dr. Stern had seen patients with dementia pugilistica, the old-school term for CTE. These were mostly boxers with cognitive and behavioral impairment. “But I had not heard about football players,” he said. “I hadn’t put the two together. And as I was listening to Chris, I realized if what he was saying was true then it was not only a potentially huge public health issue, but it was also a potentially huge scientific issue in the field of neurodegenerative disease.”
Dr. Nowinski introduced Dr. Stern to Dr. Cantu, and together with Ann McKee, MD, professor of neurology and pathology at BU, they cofounded the Center for the Study of Traumatic Encephalopathy (CSTE) in 2008. It was the first center of its kind devoted to the study of CTE in the world.
One of Dr. Nowinski’s first jobs at the CSTE was soliciting and procuring brain donations. Since CTE is generally a progressive condition that can take decades to manifest, autopsy was the only way to detect it.
The brains of two former Pittsburgh Steelers, Mike Webster and Terry Long, had been examined after their untimely deaths. After immunostaining, investigators found both former NFL players had “protein misfolds” characteristic of CTE.
This finding drew a lot of public and scientific attention, given that Mr. Long died by suicide and Mr. Webster was homeless when he died of a heart attack. But more scientific evidence was needed to prove a causal link between the head trauma and CTE.
Dr. Nowinski scoured obituaries looking for potential brains to study. When he found one, he would cold call the family and try to convince them to donate it to science. The first brain he secured for the center belonged to John Grimsley, a former NFL linebacker who in 2008 died at age 45 of an accidental gunshot wound. Often, Dr. Nowinski would even be the courier, traveling to pick up the brain after it had been harvested.
Over the next 10 years, Dr. Nowinski and his research team secured 500 brain donations. The research that resulted was staggering. In the beginning only 45 cases of CTE had been identified in the world, but in the first 111 NFL players who were autopsied, 110 had the disorder.
Of the first 53 college football players autopsied, 48 had CTE. Although Dr. Nowinski’s initial focus was football, evidence of CTE was soon detected among athletes in boxing, hockey, soccer, and rugby, as well as in combat veterans. However, the National Football League and other governing sports bodies initially denied any connection between sport-related head trauma and CTE.
Cumulative damage
In 2017, after 7 years of study, Dr. Nowinski earned a PhD in neurology. As the scientific evidence continued to accumulate, two shifts occurred that Dr. Stern said represent Dr. Nowinski’s greatest contributions. First, concussion is now widely recognized as an acute brain injury with symptoms that need to be immediately diagnosed and addressed.
“This is a completely different story from where things were just 10 years ago,” said Dr. Stern, “and Chris played a central role, if not the central role, in raising awareness about that.”
All 50 states and the District of Columbia now have laws regarding sports-related concussion. And there are brain banks in Australia, Canada, New Zealand, Brazil, and the United Kingdom studying CTE. More than 2,500 athletes in a variety of sports, including NASCAR’s Dale Earnhardt Jr. and NFL hall of famer Nick Buoniconti, have publicly pledged to donate their brains to science after their deaths.
Second, said Dr. Stern, we now know that although concussions can contribute to CTE, they are not the sole cause. It’s repetitive subconcussive trauma, without symptoms of concussion, that do the most damage.
“These happen during every practice and in every game,” said Dr. Stern. In fact, it’s estimated that pro football players suffer thousands of subconcussive incidents over the course of their careers. So, a player doesn’t have to see stars or lose consciousness to suffer brain damage; small impacts can accumulate over time.
Understanding this point is crucial for making youth sports safer. “Chris has played a critical role in raising awareness here, too,” said Dr. Stern. “Allowing our kids to get hit in the head over and over can put them at greater risk for later problems, plus it just doesn’t make common sense.”
“The biggest misconception surrounding head trauma in sports,” said Dr. Nowinski, “is the belief among players, coaches, and even the medical and scientific communities that if you get hit in the head and don’t have any symptoms then you’re okay and there hasn’t been any damage. That couldn’t be further from the truth. We now know that people are suffering serious brain injuries due to the accumulated effect of subconcussive impacts, and we need to get the word out about that.”
A major initiative from the Concussion Legacy Foundation called “Stop Hitting Kids in the Head” has the goal of convincing every sport to eliminate repetitive head impacts in players under age 14 – the time when the skull and brain are still developing and most vulnerable – by 2026. In fact, Dr. Nowinski wrote that “there could be a lot of kids who are misdiagnosed and medicated for various behavioral or emotional problems that may actually be head injury–related.”
Starting in 2009, the NFL adopted a series of rule changes designed to better protect its players against repeated head trauma. Among them is a ban on spearing or leading with the helmet, penalties for hitting defenseless players, and more stringent return-to-play guidelines, including concussion protocols.
The NFL has also put more emphasis on flag football options for youngsters and, for the first time, showcased this alternative in the 2023 Pro Bowl. But Dr. Nowinski is pressuring the league to go further. “While acknowledging that the game causes CTE, the NFL still underwrites recruiting 5-year-olds to play tackle football,” he said. “In my opinion, that’s unethical, and it needs to be addressed.”
WWE one of the most responsive organizations
Dr. Nowinski said WWE has been one of the most responsive sports organizations for protecting athletes. A doctor is now ringside at every match as is an observer who knows the script, thereby allowing for instant medical intervention if something goes wrong. “Since everyone is trying to look like they have a concussion all the time, it takes a deep understanding of the business to recognize a real one,” he said.
But this hasn’t been the case with other sports. “I am eternally disappointed in the response of the professional sports industry to the knowledge of CTE and long-term concussion symptoms,” said Dr. Nowinski.
“For example, FIFA [international soccer’s governing body] still doesn’t allow doctors to evaluate [potentially concussed] players on the sidelines and put them back in the game with a free substitution [if they’re deemed okay]. Not giving players proper medical care for a brain injury is unethical,” he said. BU’s Center for the Study of Traumatic Encephalopathy diagnosed the first CTE case in soccer in 2012, and in 2015 Dr. Nowinski successfully lobbied U.S. Soccer to ban heading the ball before age 11.
“Unfortunately, many governing bodies have circled the wagons in denying their sport causes CTE,” he continued. “FIFA, World Rugby, the NHL, even the NCAA and International Olympic Committee refuse to acknowledge it and, therefore, aren’t taking any steps to prevent it. They see it as a threat to their business model. Hopefully, now that the NIH and CDC are aligned about the risks of head impact in sports, this will begin to change.”
Meanwhile, research is continuing. Scientists are getting closer to being able to diagnose CTE in living humans, with ongoing studies using PET scans, blood markers, and spinal fluid markers. In 2019, researchers identified tau proteins specific to CTE that they believe are distinct from those of Alzheimer’s and other neurodegenerative diseases. Next step would be developing a drug to slow the development of CTE once detected.
Nonetheless, athletes at all levels in impact sports still don’t fully appreciate the risks of repeated head trauma and especially subconcussive blows. “I talk to former NFL and college players every week,” said Dr. Stern. “Some tell me, ‘I love the sport, it gave me so much, and I would do it again, but I’m not letting my grandchildren play.’ But others say, ‘As long as they know the risks, they can make their own decision.’ “
Dr. Nowinski has a daughter who is 4 and a son who’s 2. Both play soccer but, thanks to dad, heading isn’t allowed in their age groups. If they continue playing sports, Dr. Nowinski said he’ll make sure they understand the risks and how to protect themselves. This is a conversation all parents should have with their kids at every level to make sure they play safe, he added.
Those in the medical community can also volunteer their time to explain head trauma to athletes, coaches, and school administrators to be sure they understand its seriousness and are doing everything to protect players.
As you watch this year’s Super Bowl, Dr. Nowinski and his team would like you to keep something in mind. Those young men on the field for your entertainment are receiving mild brain trauma repeatedly throughout the game.
Even if it’s not a huge hit that gets replayed and makes everyone gasp, even if no one gets ushered into the little sideline tent for a concussion screening, even if no one loses consciousness, brain damage is still occurring. Watch the heads of the players during every play and think about what’s going on inside their skulls regardless of how big and strong those helmets look.
A version of this article first appeared on Medscape.com.
On Oct. 5, 2022, at 10:24 a.m., Chris Nowinski, PhD, cofounder of the Boston-based Concussion Legacy Foundation (CLF), was in his home office when the email came through.
“I pounded my desk, shouted YES! and went to find my wife so I could pick her up and give her a big hug,” he recalled. “It was the culmination of 15 years of research and hard work.”
Robert Cantu, MD, who has been studying head trauma for 50+ years and has published more than 500 papers about it, compares the announcement to the 1964 Surgeon General’s report that linked cigarette smoking with lung cancer and heart disease. With the NIH and the Centers of Disease Control and Prevention (CDC) now in agreement about the risks of participating in impact sports and activities, he said, “We’ve reached a tipping point that should finally prompt deniers such as the NHL, NCAA, FIFA, World Rugby, the International Olympic Committee, and other [sports organizations] to remove all unnecessary head trauma from their sports.”
“A lot of the credit for this must go to Chris,” added Dr. Cantu, medical director and director of clinical research at the Cantu Concussion Center at Emerson Hospital in Concord, Mass. “Clinicians like myself can reach only so many people by writing papers and giving speeches at medical conferences. For this to happen, the message needed to get out to parents, athletes, and society in general. And Chris was the vehicle for doing that.”
Dr. Nowinski didn’t set out to be the messenger. He played football at Harvard in the late 1990s, making second-team All-Ivy as a defensive tackle his senior year. In 2000, he enrolled in Killer Kowalski’s Wrestling Institute and eventually joined Vince McMahon’s World Wrestling Entertainment (WWE).
There he played the role of 295-pound villain “Chris Harvard,” an intellectual snob who dressed in crimson tights and insulted the crowd’s IQ. “Roses are red. Violets are blue. The reason I’m talking so slowly is because no one in [insert name of town he was appearing in] has passed grade 2!”
“I’d often apply my education during a match,” he wrote in his book, “Head Games: Football’s Concussion Crisis.“ In a match in Bridgeport, Conn., I assaulted [my opponent] with a human skeleton, ripped off the skull, got down on bended knee, and began reciting Hamlet. Those were good times.”
Those good times ended abruptly, however, during a match with Bubba Ray Dudley at the Hartford Civic Center in Connecticut in 2003. Even though pro wrestling matches are rehearsed, and the blows aren’t real, accidents happen. Mr. Dudley mistakenly kicked Dr. Nowinski in the jaw with enough force to put him on his back and make the whole ring shake.
“Holy shit, kid! You okay?” asked the referee. Before a foggy Dr. Nowinski could reply, 300-pound Mr. Dudley crashed down on him, hooked his leg, and the ref began counting, “One! Two! …” Dr. Nowinski instinctively kicked out but had forgotten the rest of the script. He managed to finish the match and stagger backstage.
His coherence and awareness gradually returned, but a “throbbing headache” persisted. A locker room doctor said he might have a concussion and recommended he wait to see how he felt before wrestling in Albany, N.Y., the next evening.
The following day the headache had subsided, but he still felt “a little strange.” Nonetheless, he told the doctor he was fine and strutted out to again battle Bubba Ray, this time in a match where he eventually got thrown through a ringside table and suffered the Dudley Death Drop. Afterward, “I crawled backstage and laid down. The headache was much, much worse.”
An event and a process
Dr. Nowinski continued to insist he was “fine” and wrestled a few more matches in the following days before finally acknowledging something was wrong. He’d had his bell rung numerous times in football, but this was different. Even more worrisome, none of the doctors he consulted could give him any definitive answers. He finally found his way to Emerson Hospital, where Dr. Cantu was the chief of neurosurgery.
“I remember that day vividly,” said Dr. Cantu. “Chris was this big, strapping, handsome guy – a hell of an athlete whose star was rising. He didn’t realize that he’d suffered a series of concussions and that trying to push through them was the worst thing he could be doing.”
Concussions and their effects were misunderstood by many athletes, coaches, and even physicians back then. It was assumed that the quarter inch of bone surrounding the adult brain provided adequate protection from common sports impacts and that any aftereffects were temporary. A common treatment was smelling salts and a pat on the back as the athlete returned to action.
However, the brain floats inside the skull in a bath of cerebral fluid. Any significant impact causes it to slosh violently from side to side, damaging tissue, synapses, and cells resulting in inflammation that can manifest as confusion and brain fog.
“A concussion is actually not defined by a physical injury,” explained Dr. Nowinski, “but by a loss of brain function that is induced by trauma. Concussion is not just an event, but also a process.” It’s almost as if the person has suffered a small seizure.
Fortunately, most concussion symptoms resolve within 2 weeks, but in some cases, especially if there’s been additional head trauma, they can persist, causing anxiety, depression, anger, and/or sleep disorders. Known as postconcussion syndrome (PCS), this is what Dr. Nowinski was unknowingly suffering from when he consulted Dr. Cantu.
In fact, one night it an Indianapolis hotel, weeks after his initial concussion, he awoke to find himself on the floor and the room in shambles. His girlfriend was yelling his name and shaking him. She told him he’d been having a nightmare and had suddenly started screaming and tearing up the room. “I didn’t remember any of it,” he said.
Dr. Cantu eventually advised Dr. Nowinski against ever returning to the ring or any activity with the risk for head injury. Research shows that sustaining a single significant concussion increases the risk of subsequent more-severe brain injuries.
“My diagnosis could have sent Chris off the deep end because he could no longer do what he wanted to do with this life,” said Dr. Cantu. “But instead, he used it as a tool to find meaning for his life.”
Dr. Nowinski decided to use his experience as a teaching opportunity, not just for other athletes but also for sports organizations and the medical community.
His book, which focused on the NFL’s “tobacco-industry-like refusal to acknowledge the depths of the problem,” was published in 2006. A year later, Dr. Nowinski partnered with Dr. Cantu to found the Sports Legacy Institute, which eventually became the Concussion Legacy Foundation (CLF).
Cold calling for brain donations
Robert Stern, PhD, is another highly respected authority in the study of neurodegenerative disease. In 2007, he was directing the clinical core of Boston University’s Alzheimer’s Disease Center. After giving a lecture to a group of financial planners and elder-law attorneys one morning, he got a request for a private meeting from a fellow named Chris Nowinski.
“I’d never heard of him, but I agreed,” recalled Dr. Stern, a professor of neurology, neurosurgery, anatomy, and neurobiology at Boston University. “A few days later, this larger-than-life guy walked into our conference room at the BU School of Medicine, exuding a great deal of passion, intellect, and determination. He told me his story and then started talking about the long-term consequences of concussions in sports.”
Dr. Stern had seen patients with dementia pugilistica, the old-school term for CTE. These were mostly boxers with cognitive and behavioral impairment. “But I had not heard about football players,” he said. “I hadn’t put the two together. And as I was listening to Chris, I realized if what he was saying was true then it was not only a potentially huge public health issue, but it was also a potentially huge scientific issue in the field of neurodegenerative disease.”
Dr. Nowinski introduced Dr. Stern to Dr. Cantu, and together with Ann McKee, MD, professor of neurology and pathology at BU, they cofounded the Center for the Study of Traumatic Encephalopathy (CSTE) in 2008. It was the first center of its kind devoted to the study of CTE in the world.
One of Dr. Nowinski’s first jobs at the CSTE was soliciting and procuring brain donations. Since CTE is generally a progressive condition that can take decades to manifest, autopsy was the only way to detect it.
The brains of two former Pittsburgh Steelers, Mike Webster and Terry Long, had been examined after their untimely deaths. After immunostaining, investigators found both former NFL players had “protein misfolds” characteristic of CTE.
This finding drew a lot of public and scientific attention, given that Mr. Long died by suicide and Mr. Webster was homeless when he died of a heart attack. But more scientific evidence was needed to prove a causal link between the head trauma and CTE.
Dr. Nowinski scoured obituaries looking for potential brains to study. When he found one, he would cold call the family and try to convince them to donate it to science. The first brain he secured for the center belonged to John Grimsley, a former NFL linebacker who in 2008 died at age 45 of an accidental gunshot wound. Often, Dr. Nowinski would even be the courier, traveling to pick up the brain after it had been harvested.
Over the next 10 years, Dr. Nowinski and his research team secured 500 brain donations. The research that resulted was staggering. In the beginning only 45 cases of CTE had been identified in the world, but in the first 111 NFL players who were autopsied, 110 had the disorder.
Of the first 53 college football players autopsied, 48 had CTE. Although Dr. Nowinski’s initial focus was football, evidence of CTE was soon detected among athletes in boxing, hockey, soccer, and rugby, as well as in combat veterans. However, the National Football League and other governing sports bodies initially denied any connection between sport-related head trauma and CTE.
Cumulative damage
In 2017, after 7 years of study, Dr. Nowinski earned a PhD in neurology. As the scientific evidence continued to accumulate, two shifts occurred that Dr. Stern said represent Dr. Nowinski’s greatest contributions. First, concussion is now widely recognized as an acute brain injury with symptoms that need to be immediately diagnosed and addressed.
“This is a completely different story from where things were just 10 years ago,” said Dr. Stern, “and Chris played a central role, if not the central role, in raising awareness about that.”
All 50 states and the District of Columbia now have laws regarding sports-related concussion. And there are brain banks in Australia, Canada, New Zealand, Brazil, and the United Kingdom studying CTE. More than 2,500 athletes in a variety of sports, including NASCAR’s Dale Earnhardt Jr. and NFL hall of famer Nick Buoniconti, have publicly pledged to donate their brains to science after their deaths.
Second, said Dr. Stern, we now know that although concussions can contribute to CTE, they are not the sole cause. It’s repetitive subconcussive trauma, without symptoms of concussion, that do the most damage.
“These happen during every practice and in every game,” said Dr. Stern. In fact, it’s estimated that pro football players suffer thousands of subconcussive incidents over the course of their careers. So, a player doesn’t have to see stars or lose consciousness to suffer brain damage; small impacts can accumulate over time.
Understanding this point is crucial for making youth sports safer. “Chris has played a critical role in raising awareness here, too,” said Dr. Stern. “Allowing our kids to get hit in the head over and over can put them at greater risk for later problems, plus it just doesn’t make common sense.”
“The biggest misconception surrounding head trauma in sports,” said Dr. Nowinski, “is the belief among players, coaches, and even the medical and scientific communities that if you get hit in the head and don’t have any symptoms then you’re okay and there hasn’t been any damage. That couldn’t be further from the truth. We now know that people are suffering serious brain injuries due to the accumulated effect of subconcussive impacts, and we need to get the word out about that.”
A major initiative from the Concussion Legacy Foundation called “Stop Hitting Kids in the Head” has the goal of convincing every sport to eliminate repetitive head impacts in players under age 14 – the time when the skull and brain are still developing and most vulnerable – by 2026. In fact, Dr. Nowinski wrote that “there could be a lot of kids who are misdiagnosed and medicated for various behavioral or emotional problems that may actually be head injury–related.”
Starting in 2009, the NFL adopted a series of rule changes designed to better protect its players against repeated head trauma. Among them is a ban on spearing or leading with the helmet, penalties for hitting defenseless players, and more stringent return-to-play guidelines, including concussion protocols.
The NFL has also put more emphasis on flag football options for youngsters and, for the first time, showcased this alternative in the 2023 Pro Bowl. But Dr. Nowinski is pressuring the league to go further. “While acknowledging that the game causes CTE, the NFL still underwrites recruiting 5-year-olds to play tackle football,” he said. “In my opinion, that’s unethical, and it needs to be addressed.”
WWE one of the most responsive organizations
Dr. Nowinski said WWE has been one of the most responsive sports organizations for protecting athletes. A doctor is now ringside at every match as is an observer who knows the script, thereby allowing for instant medical intervention if something goes wrong. “Since everyone is trying to look like they have a concussion all the time, it takes a deep understanding of the business to recognize a real one,” he said.
But this hasn’t been the case with other sports. “I am eternally disappointed in the response of the professional sports industry to the knowledge of CTE and long-term concussion symptoms,” said Dr. Nowinski.
“For example, FIFA [international soccer’s governing body] still doesn’t allow doctors to evaluate [potentially concussed] players on the sidelines and put them back in the game with a free substitution [if they’re deemed okay]. Not giving players proper medical care for a brain injury is unethical,” he said. BU’s Center for the Study of Traumatic Encephalopathy diagnosed the first CTE case in soccer in 2012, and in 2015 Dr. Nowinski successfully lobbied U.S. Soccer to ban heading the ball before age 11.
“Unfortunately, many governing bodies have circled the wagons in denying their sport causes CTE,” he continued. “FIFA, World Rugby, the NHL, even the NCAA and International Olympic Committee refuse to acknowledge it and, therefore, aren’t taking any steps to prevent it. They see it as a threat to their business model. Hopefully, now that the NIH and CDC are aligned about the risks of head impact in sports, this will begin to change.”
Meanwhile, research is continuing. Scientists are getting closer to being able to diagnose CTE in living humans, with ongoing studies using PET scans, blood markers, and spinal fluid markers. In 2019, researchers identified tau proteins specific to CTE that they believe are distinct from those of Alzheimer’s and other neurodegenerative diseases. Next step would be developing a drug to slow the development of CTE once detected.
Nonetheless, athletes at all levels in impact sports still don’t fully appreciate the risks of repeated head trauma and especially subconcussive blows. “I talk to former NFL and college players every week,” said Dr. Stern. “Some tell me, ‘I love the sport, it gave me so much, and I would do it again, but I’m not letting my grandchildren play.’ But others say, ‘As long as they know the risks, they can make their own decision.’ “
Dr. Nowinski has a daughter who is 4 and a son who’s 2. Both play soccer but, thanks to dad, heading isn’t allowed in their age groups. If they continue playing sports, Dr. Nowinski said he’ll make sure they understand the risks and how to protect themselves. This is a conversation all parents should have with their kids at every level to make sure they play safe, he added.
Those in the medical community can also volunteer their time to explain head trauma to athletes, coaches, and school administrators to be sure they understand its seriousness and are doing everything to protect players.
As you watch this year’s Super Bowl, Dr. Nowinski and his team would like you to keep something in mind. Those young men on the field for your entertainment are receiving mild brain trauma repeatedly throughout the game.
Even if it’s not a huge hit that gets replayed and makes everyone gasp, even if no one gets ushered into the little sideline tent for a concussion screening, even if no one loses consciousness, brain damage is still occurring. Watch the heads of the players during every play and think about what’s going on inside their skulls regardless of how big and strong those helmets look.
A version of this article first appeared on Medscape.com.
Mental health system failing kids leaving ED
Only 56% of children enrolled in Medicaid received any outpatient follow-up within 30 days after a mental health emergency department discharge, according to results of a large study released in Pediatrics.
Fewer than one-third (31.2%) had an outpatient visit within a week after a mental health ED discharge.
Researchers conducted a retrospective study of 28,551 children ages 6-17 years old who had mental health discharges from EDs from January 2018 to June 2019.
The researchers, led by Jennifer A. Hoffmann, MD, MS, with the division of emergency medicine, Ann & Robert H. Lurie Children’s Hospital of Chicago and Northwestern University, Chicago, also analyzed the effect that having a timely follow-up had on whether the child was likely to return to the ED.
Follow-up within 30 days cuts risk of quick return to ED
They found that follow-up within 30 days was linked with a 26% decreased risk of return within 5 days of the initial ED discharge (hazard ratio, 0.74; 95% confidence interval, 0.63-0.91).
The researchers also found racial disparities in the data. The odds for getting follow-up outpatient care were lower for non-Hispanic Black children, for children with fee-for-service insurance, and for children with no previous mental health outpatient visits.
The numbers were particularly striking for Black children, who were 10% less likely to get outpatient follow-up than their White counterparts.
In addition, 27% of all children in this sample returned to the ED for mental health-related symptoms within 6 months, 20% spent more than 48 hours in the ED for their initial mental health visit, and children with 14 or more mental health outpatient visits had five times higher adjusted odds of follow-up within 7 days and 9.5 times higher adjusted odds of follow-up within 30 days, compared with children with no outpatient mental health visits in the previous year.
A ‘mental health system of care in crisis’
In an accompanying editorial, Hannah E. Karpman, MSW, PhD, with the department of pediatrics, University of Massachusetts, Worcester, and colleagues said those statistics help expose other signs of “a pediatric mental health system of care in crisis.”
If one in five children are spending more than 2 days in the ED for their initial mental health visit, they wrote, that signals the follow-up care they need is not readily available.
The 27% returning to the ED shows that, even if the children are getting outpatient services, that environment is failing them, they noted.
Additionally, 28% of children presented with more than four mental health diagnoses, “suggesting poor diagnostic specificity or perhaps inadequate diagnostic categories to characterize their needs.”
The authors called for interventions that link patients to outpatient care within 5 days of a mental health ED discharge.
The editorialists wrote: “We believe it is time for a “child mental health moonshot,” and call on the field and its funders to come together to launch the next wave of bold mental health research for the benefit of these children and their families who so desperately need our support.”
Things may even be worse in light of COVID
David Rettew, MD, a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland, said in an interview the numbers won’t surprise clinicians who support these children or the patients’ families.
He added that he wouldn’t be surprised if things are even worse now after this study’s data collection, “as COVID and other factors have driven more mental health professionals away from many of the people who need them the most.”
The study does present new evidence that quick access to care is particularly tough for young people who aren’t already established in care, he noted.
“As wait lists grow at outpatient clinics, we are seeing ever stronger need for centers willing and able to provide actual mental health assessment and treatment for people right ‘off the street,’” he said.
Dr. Rettew emphasized that, because mental health conditions rarely improve quickly, having a timely follow-up appointment is important, but won’t likely bring quick improvement.
He agreed with the editorialists’ argument and emphasized, “not only do we need to focus on more rapid care, but also more comprehensive and effective care.
“For an adolescent in crisis, achieving stability often involves more than a medication tweak and a supportive conversation,” Dr. Rettew said. “Rather, it can require an intensive multimodal approach that addresses things like family financial stressors, parental mental health and substance use concerns, school supports, and health promotion or lifestyle changes. What we desperately need are more teams that can quickly intervene on all these levels.”
Addressing problems before crisis is essential
Ideally, teams would address these issues before a crisis. That helps support the “moonshot” charge the editorialists suggest, which “would significantly disrupt the current way we value different components of our health care system,” Dr. Rettew said.
He highlighted a statistic that may get lost in the data: Nearly 40% of youth in enough danger to need an ED visit had no more than one health-related appointment of any kind in the previous year.
“To me, this speaks volumes about the need for earlier involvement before things escalate to the level of an emergency,” Dr. Rettew said.
The authors and editorialists declared no relevant financial relationships. Dr. Rettew is author of the book, “Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.”
Only 56% of children enrolled in Medicaid received any outpatient follow-up within 30 days after a mental health emergency department discharge, according to results of a large study released in Pediatrics.
Fewer than one-third (31.2%) had an outpatient visit within a week after a mental health ED discharge.
Researchers conducted a retrospective study of 28,551 children ages 6-17 years old who had mental health discharges from EDs from January 2018 to June 2019.
The researchers, led by Jennifer A. Hoffmann, MD, MS, with the division of emergency medicine, Ann & Robert H. Lurie Children’s Hospital of Chicago and Northwestern University, Chicago, also analyzed the effect that having a timely follow-up had on whether the child was likely to return to the ED.
Follow-up within 30 days cuts risk of quick return to ED
They found that follow-up within 30 days was linked with a 26% decreased risk of return within 5 days of the initial ED discharge (hazard ratio, 0.74; 95% confidence interval, 0.63-0.91).
The researchers also found racial disparities in the data. The odds for getting follow-up outpatient care were lower for non-Hispanic Black children, for children with fee-for-service insurance, and for children with no previous mental health outpatient visits.
The numbers were particularly striking for Black children, who were 10% less likely to get outpatient follow-up than their White counterparts.
In addition, 27% of all children in this sample returned to the ED for mental health-related symptoms within 6 months, 20% spent more than 48 hours in the ED for their initial mental health visit, and children with 14 or more mental health outpatient visits had five times higher adjusted odds of follow-up within 7 days and 9.5 times higher adjusted odds of follow-up within 30 days, compared with children with no outpatient mental health visits in the previous year.
A ‘mental health system of care in crisis’
In an accompanying editorial, Hannah E. Karpman, MSW, PhD, with the department of pediatrics, University of Massachusetts, Worcester, and colleagues said those statistics help expose other signs of “a pediatric mental health system of care in crisis.”
If one in five children are spending more than 2 days in the ED for their initial mental health visit, they wrote, that signals the follow-up care they need is not readily available.
The 27% returning to the ED shows that, even if the children are getting outpatient services, that environment is failing them, they noted.
Additionally, 28% of children presented with more than four mental health diagnoses, “suggesting poor diagnostic specificity or perhaps inadequate diagnostic categories to characterize their needs.”
The authors called for interventions that link patients to outpatient care within 5 days of a mental health ED discharge.
The editorialists wrote: “We believe it is time for a “child mental health moonshot,” and call on the field and its funders to come together to launch the next wave of bold mental health research for the benefit of these children and their families who so desperately need our support.”
Things may even be worse in light of COVID
David Rettew, MD, a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland, said in an interview the numbers won’t surprise clinicians who support these children or the patients’ families.
He added that he wouldn’t be surprised if things are even worse now after this study’s data collection, “as COVID and other factors have driven more mental health professionals away from many of the people who need them the most.”
The study does present new evidence that quick access to care is particularly tough for young people who aren’t already established in care, he noted.
“As wait lists grow at outpatient clinics, we are seeing ever stronger need for centers willing and able to provide actual mental health assessment and treatment for people right ‘off the street,’” he said.
Dr. Rettew emphasized that, because mental health conditions rarely improve quickly, having a timely follow-up appointment is important, but won’t likely bring quick improvement.
He agreed with the editorialists’ argument and emphasized, “not only do we need to focus on more rapid care, but also more comprehensive and effective care.
“For an adolescent in crisis, achieving stability often involves more than a medication tweak and a supportive conversation,” Dr. Rettew said. “Rather, it can require an intensive multimodal approach that addresses things like family financial stressors, parental mental health and substance use concerns, school supports, and health promotion or lifestyle changes. What we desperately need are more teams that can quickly intervene on all these levels.”
Addressing problems before crisis is essential
Ideally, teams would address these issues before a crisis. That helps support the “moonshot” charge the editorialists suggest, which “would significantly disrupt the current way we value different components of our health care system,” Dr. Rettew said.
He highlighted a statistic that may get lost in the data: Nearly 40% of youth in enough danger to need an ED visit had no more than one health-related appointment of any kind in the previous year.
“To me, this speaks volumes about the need for earlier involvement before things escalate to the level of an emergency,” Dr. Rettew said.
The authors and editorialists declared no relevant financial relationships. Dr. Rettew is author of the book, “Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.”
Only 56% of children enrolled in Medicaid received any outpatient follow-up within 30 days after a mental health emergency department discharge, according to results of a large study released in Pediatrics.
Fewer than one-third (31.2%) had an outpatient visit within a week after a mental health ED discharge.
Researchers conducted a retrospective study of 28,551 children ages 6-17 years old who had mental health discharges from EDs from January 2018 to June 2019.
The researchers, led by Jennifer A. Hoffmann, MD, MS, with the division of emergency medicine, Ann & Robert H. Lurie Children’s Hospital of Chicago and Northwestern University, Chicago, also analyzed the effect that having a timely follow-up had on whether the child was likely to return to the ED.
Follow-up within 30 days cuts risk of quick return to ED
They found that follow-up within 30 days was linked with a 26% decreased risk of return within 5 days of the initial ED discharge (hazard ratio, 0.74; 95% confidence interval, 0.63-0.91).
The researchers also found racial disparities in the data. The odds for getting follow-up outpatient care were lower for non-Hispanic Black children, for children with fee-for-service insurance, and for children with no previous mental health outpatient visits.
The numbers were particularly striking for Black children, who were 10% less likely to get outpatient follow-up than their White counterparts.
In addition, 27% of all children in this sample returned to the ED for mental health-related symptoms within 6 months, 20% spent more than 48 hours in the ED for their initial mental health visit, and children with 14 or more mental health outpatient visits had five times higher adjusted odds of follow-up within 7 days and 9.5 times higher adjusted odds of follow-up within 30 days, compared with children with no outpatient mental health visits in the previous year.
A ‘mental health system of care in crisis’
In an accompanying editorial, Hannah E. Karpman, MSW, PhD, with the department of pediatrics, University of Massachusetts, Worcester, and colleagues said those statistics help expose other signs of “a pediatric mental health system of care in crisis.”
If one in five children are spending more than 2 days in the ED for their initial mental health visit, they wrote, that signals the follow-up care they need is not readily available.
The 27% returning to the ED shows that, even if the children are getting outpatient services, that environment is failing them, they noted.
Additionally, 28% of children presented with more than four mental health diagnoses, “suggesting poor diagnostic specificity or perhaps inadequate diagnostic categories to characterize their needs.”
The authors called for interventions that link patients to outpatient care within 5 days of a mental health ED discharge.
The editorialists wrote: “We believe it is time for a “child mental health moonshot,” and call on the field and its funders to come together to launch the next wave of bold mental health research for the benefit of these children and their families who so desperately need our support.”
Things may even be worse in light of COVID
David Rettew, MD, a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland, said in an interview the numbers won’t surprise clinicians who support these children or the patients’ families.
He added that he wouldn’t be surprised if things are even worse now after this study’s data collection, “as COVID and other factors have driven more mental health professionals away from many of the people who need them the most.”
The study does present new evidence that quick access to care is particularly tough for young people who aren’t already established in care, he noted.
“As wait lists grow at outpatient clinics, we are seeing ever stronger need for centers willing and able to provide actual mental health assessment and treatment for people right ‘off the street,’” he said.
Dr. Rettew emphasized that, because mental health conditions rarely improve quickly, having a timely follow-up appointment is important, but won’t likely bring quick improvement.
He agreed with the editorialists’ argument and emphasized, “not only do we need to focus on more rapid care, but also more comprehensive and effective care.
“For an adolescent in crisis, achieving stability often involves more than a medication tweak and a supportive conversation,” Dr. Rettew said. “Rather, it can require an intensive multimodal approach that addresses things like family financial stressors, parental mental health and substance use concerns, school supports, and health promotion or lifestyle changes. What we desperately need are more teams that can quickly intervene on all these levels.”
Addressing problems before crisis is essential
Ideally, teams would address these issues before a crisis. That helps support the “moonshot” charge the editorialists suggest, which “would significantly disrupt the current way we value different components of our health care system,” Dr. Rettew said.
He highlighted a statistic that may get lost in the data: Nearly 40% of youth in enough danger to need an ED visit had no more than one health-related appointment of any kind in the previous year.
“To me, this speaks volumes about the need for earlier involvement before things escalate to the level of an emergency,” Dr. Rettew said.
The authors and editorialists declared no relevant financial relationships. Dr. Rettew is author of the book, “Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.”
FROM PEDIATRICS





