User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Depressive symptoms tied to higher stroke risk, worse outcomes
new research suggests.
Data from the international INTERSTROKE study also showed that those with depressive symptoms before a stroke had worse outcomes, including a significantly higher mortality rate in the first month after a stroke.
These findings build on prior research on the link between depression and stroke, including one study that showed an increased risk for incident stroke among those with a high number of depressive symptoms and another that found that worsening depression can precede stroke in older adults.
“Depression is an important risk factor for acute stroke and is potentially a modifiable contributor to the global burden of stroke,” lead investigator Robert Murphy, MB, a consultant in stroke and geriatric medicine and a researcher with the clinical research facility at the University of Galway, Ireland, told this news organization. “Even mild depressive symptoms were found in this study to be associated with increased risk of stroke and this adds to the literature that across the full range of depressive symptoms there is an association with increased risk of stroke.”
The findings were published online March 8 in Neurology.
Significant stroke risk
For the analysis, investigators collected data on 26,877 cases and controls across 32 countries who participated in INTERSTROKE, an international case-control study of risk factors for a first acute stroke. Participants were recruited between 2007 and 2015 and completed a series of questionnaires about stroke risk factors, including measures of depressive symptoms experienced in the past 12 months.
After adjustment for occupation, education, wealth index, diet, physical activity, alcohol consumption, and smoking history, having prestroke depressive symptoms was associated with greater odds for acute stroke (adjusted odds ratio [aOR], 1.46; 95% confidence interval [CI], 1.34-1.58), including both intracerebral hemorrhage (aOR, 1.56; 95% CI, 1.28-1.91) and ischemic stroke (aOR, 1.44; 95% CI, 1.31-1.58).
Stroke risk increased with increasing severity of depression, but even those with mild depression had a 35% increased risk (aOR, 1.35; 95% CI, 1.19-1.53).
The increased risk held even after the researchers adjusted further for diabetes, hypertension, atrial fibrillation, and body mass index, and work, home, and financial stress.
The association was consistent across geographical regions and age groups, but was stronger in men and in those without hypertension.
“This study looks at different constructs of depression and identifies that across the spectrum of mild, moderate, and severe depressive symptoms that there is an association present with acute stroke and that a biological gradient emerges with increasing burden of depressive symptoms associated with increasing risk,” Dr. Murphy said.
An antidepressant mediating effect?
While prestroke depressive symptoms were not associated with a greater odds of worse stroke severity, they were associated with worse outcomes (P < .001) and higher mortality (10% vs. 8.1%; P = .003) 1 month after a stroke.
In a subgroup analysis, researchers found no association between depressive symptoms and stroke risk in patients who were taking antidepressants.
While no assumptions of causality can be drawn from these findings, “this subgroup analysis does suggest that an increased risk of stroke in those with depression may be attenuated if a patient is on appropriate treatment,” Dr. Murphy said. “This is an area that warrants further exploration.”
The mechanisms that link depression to stroke are unclear, but these findings offer strong evidence that this link exists, Dr. Murphy said.
“We adjusted for potential confounders in sequential models and after adjusting for traditional cardiovascular risk factors there was a consistent association between depressive symptoms and stroke identifying that there is likely an independent association between depression and stroke,” Dr. Murphy said.
Questions remain
Commenting on the study, Daniel T. Lackland DrPH, professor, division of translational neurosciences and population studies, department of neurology, Medical University of South Carolina, Charleston, said it adds to a growing body of work on the association of stroke and depression.
“In this case, depression may be a risk factor for having a stroke,” said Dr. Lackland, who was not part of the study. In addition, the study suggests that “treating depression can have additional benefits beyond mental health, in this case, reduced stroke risks.”
However, it’s important, as with any observational study, that there may be confounding factors that may offer an alternative explanation for the findings.
“Further, it is often difficult to accurately assess depression in all individuals, and specifically in individuals who have had a stroke,” Dr. Lackland said. “While this particular study adds depression as a risk factor and suggests treatment of depression in reducing risks, it is important to emphasize that the traditional stroke risk factors including hypertension should [be] continually recognized and treat[ed] with high rigor.”
The INTERSTROKE study was funded by the Canadian Institutes of Health Research, the Heart and Stroke Foundation of Canada, the Canadian Stroke Network, the Swedish Research Council, the Swedish Heart Lung Foundation, AFA Insurance, The Health & Medical Care Committee of the Regional Executive Board, Region Västra Götaland, and through unrestricted grants from several pharmaceutical companies with major contributions from AstraZeneca, Boehringer Ingelheim (Canada), Pfizer (Canada), Merck Sharp & Dohme, the Swedish Heart Lung Foundation, Chest Heart & Stroke Scotland, and the Stroke Association (United Kingdom). Dr. Murphy and Dr. Lackland have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
Data from the international INTERSTROKE study also showed that those with depressive symptoms before a stroke had worse outcomes, including a significantly higher mortality rate in the first month after a stroke.
These findings build on prior research on the link between depression and stroke, including one study that showed an increased risk for incident stroke among those with a high number of depressive symptoms and another that found that worsening depression can precede stroke in older adults.
“Depression is an important risk factor for acute stroke and is potentially a modifiable contributor to the global burden of stroke,” lead investigator Robert Murphy, MB, a consultant in stroke and geriatric medicine and a researcher with the clinical research facility at the University of Galway, Ireland, told this news organization. “Even mild depressive symptoms were found in this study to be associated with increased risk of stroke and this adds to the literature that across the full range of depressive symptoms there is an association with increased risk of stroke.”
The findings were published online March 8 in Neurology.
Significant stroke risk
For the analysis, investigators collected data on 26,877 cases and controls across 32 countries who participated in INTERSTROKE, an international case-control study of risk factors for a first acute stroke. Participants were recruited between 2007 and 2015 and completed a series of questionnaires about stroke risk factors, including measures of depressive symptoms experienced in the past 12 months.
After adjustment for occupation, education, wealth index, diet, physical activity, alcohol consumption, and smoking history, having prestroke depressive symptoms was associated with greater odds for acute stroke (adjusted odds ratio [aOR], 1.46; 95% confidence interval [CI], 1.34-1.58), including both intracerebral hemorrhage (aOR, 1.56; 95% CI, 1.28-1.91) and ischemic stroke (aOR, 1.44; 95% CI, 1.31-1.58).
Stroke risk increased with increasing severity of depression, but even those with mild depression had a 35% increased risk (aOR, 1.35; 95% CI, 1.19-1.53).
The increased risk held even after the researchers adjusted further for diabetes, hypertension, atrial fibrillation, and body mass index, and work, home, and financial stress.
The association was consistent across geographical regions and age groups, but was stronger in men and in those without hypertension.
“This study looks at different constructs of depression and identifies that across the spectrum of mild, moderate, and severe depressive symptoms that there is an association present with acute stroke and that a biological gradient emerges with increasing burden of depressive symptoms associated with increasing risk,” Dr. Murphy said.
An antidepressant mediating effect?
While prestroke depressive symptoms were not associated with a greater odds of worse stroke severity, they were associated with worse outcomes (P < .001) and higher mortality (10% vs. 8.1%; P = .003) 1 month after a stroke.
In a subgroup analysis, researchers found no association between depressive symptoms and stroke risk in patients who were taking antidepressants.
While no assumptions of causality can be drawn from these findings, “this subgroup analysis does suggest that an increased risk of stroke in those with depression may be attenuated if a patient is on appropriate treatment,” Dr. Murphy said. “This is an area that warrants further exploration.”
The mechanisms that link depression to stroke are unclear, but these findings offer strong evidence that this link exists, Dr. Murphy said.
“We adjusted for potential confounders in sequential models and after adjusting for traditional cardiovascular risk factors there was a consistent association between depressive symptoms and stroke identifying that there is likely an independent association between depression and stroke,” Dr. Murphy said.
Questions remain
Commenting on the study, Daniel T. Lackland DrPH, professor, division of translational neurosciences and population studies, department of neurology, Medical University of South Carolina, Charleston, said it adds to a growing body of work on the association of stroke and depression.
“In this case, depression may be a risk factor for having a stroke,” said Dr. Lackland, who was not part of the study. In addition, the study suggests that “treating depression can have additional benefits beyond mental health, in this case, reduced stroke risks.”
However, it’s important, as with any observational study, that there may be confounding factors that may offer an alternative explanation for the findings.
“Further, it is often difficult to accurately assess depression in all individuals, and specifically in individuals who have had a stroke,” Dr. Lackland said. “While this particular study adds depression as a risk factor and suggests treatment of depression in reducing risks, it is important to emphasize that the traditional stroke risk factors including hypertension should [be] continually recognized and treat[ed] with high rigor.”
The INTERSTROKE study was funded by the Canadian Institutes of Health Research, the Heart and Stroke Foundation of Canada, the Canadian Stroke Network, the Swedish Research Council, the Swedish Heart Lung Foundation, AFA Insurance, The Health & Medical Care Committee of the Regional Executive Board, Region Västra Götaland, and through unrestricted grants from several pharmaceutical companies with major contributions from AstraZeneca, Boehringer Ingelheim (Canada), Pfizer (Canada), Merck Sharp & Dohme, the Swedish Heart Lung Foundation, Chest Heart & Stroke Scotland, and the Stroke Association (United Kingdom). Dr. Murphy and Dr. Lackland have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
Data from the international INTERSTROKE study also showed that those with depressive symptoms before a stroke had worse outcomes, including a significantly higher mortality rate in the first month after a stroke.
These findings build on prior research on the link between depression and stroke, including one study that showed an increased risk for incident stroke among those with a high number of depressive symptoms and another that found that worsening depression can precede stroke in older adults.
“Depression is an important risk factor for acute stroke and is potentially a modifiable contributor to the global burden of stroke,” lead investigator Robert Murphy, MB, a consultant in stroke and geriatric medicine and a researcher with the clinical research facility at the University of Galway, Ireland, told this news organization. “Even mild depressive symptoms were found in this study to be associated with increased risk of stroke and this adds to the literature that across the full range of depressive symptoms there is an association with increased risk of stroke.”
The findings were published online March 8 in Neurology.
Significant stroke risk
For the analysis, investigators collected data on 26,877 cases and controls across 32 countries who participated in INTERSTROKE, an international case-control study of risk factors for a first acute stroke. Participants were recruited between 2007 and 2015 and completed a series of questionnaires about stroke risk factors, including measures of depressive symptoms experienced in the past 12 months.
After adjustment for occupation, education, wealth index, diet, physical activity, alcohol consumption, and smoking history, having prestroke depressive symptoms was associated with greater odds for acute stroke (adjusted odds ratio [aOR], 1.46; 95% confidence interval [CI], 1.34-1.58), including both intracerebral hemorrhage (aOR, 1.56; 95% CI, 1.28-1.91) and ischemic stroke (aOR, 1.44; 95% CI, 1.31-1.58).
Stroke risk increased with increasing severity of depression, but even those with mild depression had a 35% increased risk (aOR, 1.35; 95% CI, 1.19-1.53).
The increased risk held even after the researchers adjusted further for diabetes, hypertension, atrial fibrillation, and body mass index, and work, home, and financial stress.
The association was consistent across geographical regions and age groups, but was stronger in men and in those without hypertension.
“This study looks at different constructs of depression and identifies that across the spectrum of mild, moderate, and severe depressive symptoms that there is an association present with acute stroke and that a biological gradient emerges with increasing burden of depressive symptoms associated with increasing risk,” Dr. Murphy said.
An antidepressant mediating effect?
While prestroke depressive symptoms were not associated with a greater odds of worse stroke severity, they were associated with worse outcomes (P < .001) and higher mortality (10% vs. 8.1%; P = .003) 1 month after a stroke.
In a subgroup analysis, researchers found no association between depressive symptoms and stroke risk in patients who were taking antidepressants.
While no assumptions of causality can be drawn from these findings, “this subgroup analysis does suggest that an increased risk of stroke in those with depression may be attenuated if a patient is on appropriate treatment,” Dr. Murphy said. “This is an area that warrants further exploration.”
The mechanisms that link depression to stroke are unclear, but these findings offer strong evidence that this link exists, Dr. Murphy said.
“We adjusted for potential confounders in sequential models and after adjusting for traditional cardiovascular risk factors there was a consistent association between depressive symptoms and stroke identifying that there is likely an independent association between depression and stroke,” Dr. Murphy said.
Questions remain
Commenting on the study, Daniel T. Lackland DrPH, professor, division of translational neurosciences and population studies, department of neurology, Medical University of South Carolina, Charleston, said it adds to a growing body of work on the association of stroke and depression.
“In this case, depression may be a risk factor for having a stroke,” said Dr. Lackland, who was not part of the study. In addition, the study suggests that “treating depression can have additional benefits beyond mental health, in this case, reduced stroke risks.”
However, it’s important, as with any observational study, that there may be confounding factors that may offer an alternative explanation for the findings.
“Further, it is often difficult to accurately assess depression in all individuals, and specifically in individuals who have had a stroke,” Dr. Lackland said. “While this particular study adds depression as a risk factor and suggests treatment of depression in reducing risks, it is important to emphasize that the traditional stroke risk factors including hypertension should [be] continually recognized and treat[ed] with high rigor.”
The INTERSTROKE study was funded by the Canadian Institutes of Health Research, the Heart and Stroke Foundation of Canada, the Canadian Stroke Network, the Swedish Research Council, the Swedish Heart Lung Foundation, AFA Insurance, The Health & Medical Care Committee of the Regional Executive Board, Region Västra Götaland, and through unrestricted grants from several pharmaceutical companies with major contributions from AstraZeneca, Boehringer Ingelheim (Canada), Pfizer (Canada), Merck Sharp & Dohme, the Swedish Heart Lung Foundation, Chest Heart & Stroke Scotland, and the Stroke Association (United Kingdom). Dr. Murphy and Dr. Lackland have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY
Telehealth doctor indicted on health care fraud, opioid distribution charges
Sangita Patel, MD, 50, practiced at Advance Medical Home Physicians in Troy.
According to court documents, between July 2020 and June 2022 Patel was responsible for submitting Medicare claims for improper telehealth visits she didn’t conduct herself.
Dr. Patel, who accepted patients who paid in cash as well as those with Medicare and Medicaid coverage, billed approximately $3.4 million to Medicare between 2018 and 2022, according to court documents. An unusual number of these visits were billed using complex codes, an indication of health care fraud. The investigation also found that on many days, Dr. Patel billed for more than 24 hours of services. During this period, according to the document, 76% of Dr. Patel’s Medicare reimbursements were for telehealth.
Prosecutors say that Dr. Patel prescribed Schedule II controlled substances to more than 90% of the patients in these telehealth visits. She delegated her prescription authority to an unlicensed medical assistant. Through undercover visits and cell site search warrant data, the investigation found that Dr. Patel directed patients to contact, via cell phone, this assistant, who then entered electronic prescriptions into the electronic medical records system. Dr. Patel then signed the prescriptions and sent them to the pharmacies without ever interacting with the patients. Prosecutors also used text messages, obtained by search warrant, between Dr. Patel and her assistant and between the assistant and undercover informers to build their case.
Dr. Patel is also accused of referring patients to other providers, who in turn billed Medicare for claims associated with those patients. Advance Medical received $143,000 from these providers, potentially in violation of anti-kickback laws, according to bank records obtained by subpoena.
If convicted, Dr. Patel could be sentenced to up to 10 years in federal prison.
A version of this article first appeared on Medscape.com.
Sangita Patel, MD, 50, practiced at Advance Medical Home Physicians in Troy.
According to court documents, between July 2020 and June 2022 Patel was responsible for submitting Medicare claims for improper telehealth visits she didn’t conduct herself.
Dr. Patel, who accepted patients who paid in cash as well as those with Medicare and Medicaid coverage, billed approximately $3.4 million to Medicare between 2018 and 2022, according to court documents. An unusual number of these visits were billed using complex codes, an indication of health care fraud. The investigation also found that on many days, Dr. Patel billed for more than 24 hours of services. During this period, according to the document, 76% of Dr. Patel’s Medicare reimbursements were for telehealth.
Prosecutors say that Dr. Patel prescribed Schedule II controlled substances to more than 90% of the patients in these telehealth visits. She delegated her prescription authority to an unlicensed medical assistant. Through undercover visits and cell site search warrant data, the investigation found that Dr. Patel directed patients to contact, via cell phone, this assistant, who then entered electronic prescriptions into the electronic medical records system. Dr. Patel then signed the prescriptions and sent them to the pharmacies without ever interacting with the patients. Prosecutors also used text messages, obtained by search warrant, between Dr. Patel and her assistant and between the assistant and undercover informers to build their case.
Dr. Patel is also accused of referring patients to other providers, who in turn billed Medicare for claims associated with those patients. Advance Medical received $143,000 from these providers, potentially in violation of anti-kickback laws, according to bank records obtained by subpoena.
If convicted, Dr. Patel could be sentenced to up to 10 years in federal prison.
A version of this article first appeared on Medscape.com.
Sangita Patel, MD, 50, practiced at Advance Medical Home Physicians in Troy.
According to court documents, between July 2020 and June 2022 Patel was responsible for submitting Medicare claims for improper telehealth visits she didn’t conduct herself.
Dr. Patel, who accepted patients who paid in cash as well as those with Medicare and Medicaid coverage, billed approximately $3.4 million to Medicare between 2018 and 2022, according to court documents. An unusual number of these visits were billed using complex codes, an indication of health care fraud. The investigation also found that on many days, Dr. Patel billed for more than 24 hours of services. During this period, according to the document, 76% of Dr. Patel’s Medicare reimbursements were for telehealth.
Prosecutors say that Dr. Patel prescribed Schedule II controlled substances to more than 90% of the patients in these telehealth visits. She delegated her prescription authority to an unlicensed medical assistant. Through undercover visits and cell site search warrant data, the investigation found that Dr. Patel directed patients to contact, via cell phone, this assistant, who then entered electronic prescriptions into the electronic medical records system. Dr. Patel then signed the prescriptions and sent them to the pharmacies without ever interacting with the patients. Prosecutors also used text messages, obtained by search warrant, between Dr. Patel and her assistant and between the assistant and undercover informers to build their case.
Dr. Patel is also accused of referring patients to other providers, who in turn billed Medicare for claims associated with those patients. Advance Medical received $143,000 from these providers, potentially in violation of anti-kickback laws, according to bank records obtained by subpoena.
If convicted, Dr. Patel could be sentenced to up to 10 years in federal prison.
A version of this article first appeared on Medscape.com.
Migraine after concussion linked to worse outcomes
researchers have found.
“Early assessment of headache – and whether it has migraine features – after concussion can be helpful in predicting which children are at risk for poor outcomes and identifying children who require targeted intervention,” said senior author Keith Owen Yeates, PhD, the Ronald and Irene Ward Chair in Pediatric Brain Injury Professor and head of the department of psychology at the University of Calgary (Alta.). “Posttraumatic headache, especially when it involves migraine features, is a strong predictor of persisting symptoms and poorer quality of life after childhood concussion.”
Approximately 840,000 children per year visit an emergency department in the United States after having a traumatic brain injury. As many as 90% of those visits are considered to involve a concussion, according to the investigators. Although most children recover quickly, approximately one-third continue to report symptoms a month after the event.
Posttraumatic headache occurs in up to 90% of children, most commonly with features of migraine.
The new study, published in JAMA Network Open, was a secondary analysis of the Advancing Concussion Assessment in Pediatrics (A-CAP) prospective cohort study. The study was conducted at five emergency departments in Canada from September 2016 to July 2019 and included children and adolescents aged 8-17 years who presented with acute concussion or an orthopedic injury.
Children were included in the concussion group if they had a history of blunt head trauma resulting in at least one of three criteria consistent with the World Health Organization definition of mild traumatic brain injury. The criteria include loss of consciousness for less than 30 minutes, a Glasgow Coma Scale score of 13 or 14, or at least one acute sign or symptom of concussion, as noted by emergency clinicians.
Patients were excluded from the concussion group if they had deteriorating neurologic status, underwent neurosurgical intervention, had posttraumatic amnesia that lasted more than 24 hours, or had a score higher than 4 on the Abbreviated Injury Scale (AIS). The orthopedic injury group included patients without symptoms of concussion and with blunt trauma associated with an AIS 13 score of 4 or less. Patients were excluded from both groups if they had an overnight hospitalization for traumatic brain injury, a concussion within the past 3 months, or a neurodevelopmental disorder.
The researchers analyzed data from 928 children of 967 enrolled in the study. The median age was 12.2 years, and 41.3% were female. The final study cohort included 239 children with orthopedic injuries but no headache, 160 with a concussion and no headache, 134 with a concussion and nonmigraine headaches, and 254 with a concussion and migraine headaches.
Children with posttraumatic migraines 10 days after a concussion had the most severe symptoms and worst quality of life 3 months following their head trauma, the researchers found. Children without headaches within 10 days after concussion had the best 3-month outcomes, comparable to those with orthopedic injuries alone.
The researchers said the strengths of their study included its large population and its inclusion of various causes of head trauma, not just sports-related concussions. Limitations included self-reports of headaches instead of a physician diagnosis and lack of control for clinical interventions that might have affected the outcomes.
Charles Tator, MD, PhD, director of the Canadian Concussion Centre at Toronto Western Hospital, said the findings were unsurprising.
“Headaches are the most common symptom after concussion,” Dr. Tator, who was not involved in the latest research, told this news organization. “In my practice and research with concussed kids 11 and up and with adults, those with preconcussion history of migraine are the most difficult to treat because their headaches don’t improve unless specific measures are taken.”
Dr. Tator, who also is a professor of neurosurgery at the University of Toronto, said clinicians who treat concussions must determine which type of headaches children are experiencing – and refer as early as possible for migraine prevention or treatment and medication, as warranted.
“Early recognition after concussion that migraine headaches are occurring will save kids a lot of suffering,” he said.
The study was supported by a Canadian Institute of Health Research Foundation Grant and by funds from the Alberta Children’s Hospital Foundation and the Alberta Children’s Hospital Research Institute. Dr. Tator has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
researchers have found.
“Early assessment of headache – and whether it has migraine features – after concussion can be helpful in predicting which children are at risk for poor outcomes and identifying children who require targeted intervention,” said senior author Keith Owen Yeates, PhD, the Ronald and Irene Ward Chair in Pediatric Brain Injury Professor and head of the department of psychology at the University of Calgary (Alta.). “Posttraumatic headache, especially when it involves migraine features, is a strong predictor of persisting symptoms and poorer quality of life after childhood concussion.”
Approximately 840,000 children per year visit an emergency department in the United States after having a traumatic brain injury. As many as 90% of those visits are considered to involve a concussion, according to the investigators. Although most children recover quickly, approximately one-third continue to report symptoms a month after the event.
Posttraumatic headache occurs in up to 90% of children, most commonly with features of migraine.
The new study, published in JAMA Network Open, was a secondary analysis of the Advancing Concussion Assessment in Pediatrics (A-CAP) prospective cohort study. The study was conducted at five emergency departments in Canada from September 2016 to July 2019 and included children and adolescents aged 8-17 years who presented with acute concussion or an orthopedic injury.
Children were included in the concussion group if they had a history of blunt head trauma resulting in at least one of three criteria consistent with the World Health Organization definition of mild traumatic brain injury. The criteria include loss of consciousness for less than 30 minutes, a Glasgow Coma Scale score of 13 or 14, or at least one acute sign or symptom of concussion, as noted by emergency clinicians.
Patients were excluded from the concussion group if they had deteriorating neurologic status, underwent neurosurgical intervention, had posttraumatic amnesia that lasted more than 24 hours, or had a score higher than 4 on the Abbreviated Injury Scale (AIS). The orthopedic injury group included patients without symptoms of concussion and with blunt trauma associated with an AIS 13 score of 4 or less. Patients were excluded from both groups if they had an overnight hospitalization for traumatic brain injury, a concussion within the past 3 months, or a neurodevelopmental disorder.
The researchers analyzed data from 928 children of 967 enrolled in the study. The median age was 12.2 years, and 41.3% were female. The final study cohort included 239 children with orthopedic injuries but no headache, 160 with a concussion and no headache, 134 with a concussion and nonmigraine headaches, and 254 with a concussion and migraine headaches.
Children with posttraumatic migraines 10 days after a concussion had the most severe symptoms and worst quality of life 3 months following their head trauma, the researchers found. Children without headaches within 10 days after concussion had the best 3-month outcomes, comparable to those with orthopedic injuries alone.
The researchers said the strengths of their study included its large population and its inclusion of various causes of head trauma, not just sports-related concussions. Limitations included self-reports of headaches instead of a physician diagnosis and lack of control for clinical interventions that might have affected the outcomes.
Charles Tator, MD, PhD, director of the Canadian Concussion Centre at Toronto Western Hospital, said the findings were unsurprising.
“Headaches are the most common symptom after concussion,” Dr. Tator, who was not involved in the latest research, told this news organization. “In my practice and research with concussed kids 11 and up and with adults, those with preconcussion history of migraine are the most difficult to treat because their headaches don’t improve unless specific measures are taken.”
Dr. Tator, who also is a professor of neurosurgery at the University of Toronto, said clinicians who treat concussions must determine which type of headaches children are experiencing – and refer as early as possible for migraine prevention or treatment and medication, as warranted.
“Early recognition after concussion that migraine headaches are occurring will save kids a lot of suffering,” he said.
The study was supported by a Canadian Institute of Health Research Foundation Grant and by funds from the Alberta Children’s Hospital Foundation and the Alberta Children’s Hospital Research Institute. Dr. Tator has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
researchers have found.
“Early assessment of headache – and whether it has migraine features – after concussion can be helpful in predicting which children are at risk for poor outcomes and identifying children who require targeted intervention,” said senior author Keith Owen Yeates, PhD, the Ronald and Irene Ward Chair in Pediatric Brain Injury Professor and head of the department of psychology at the University of Calgary (Alta.). “Posttraumatic headache, especially when it involves migraine features, is a strong predictor of persisting symptoms and poorer quality of life after childhood concussion.”
Approximately 840,000 children per year visit an emergency department in the United States after having a traumatic brain injury. As many as 90% of those visits are considered to involve a concussion, according to the investigators. Although most children recover quickly, approximately one-third continue to report symptoms a month after the event.
Posttraumatic headache occurs in up to 90% of children, most commonly with features of migraine.
The new study, published in JAMA Network Open, was a secondary analysis of the Advancing Concussion Assessment in Pediatrics (A-CAP) prospective cohort study. The study was conducted at five emergency departments in Canada from September 2016 to July 2019 and included children and adolescents aged 8-17 years who presented with acute concussion or an orthopedic injury.
Children were included in the concussion group if they had a history of blunt head trauma resulting in at least one of three criteria consistent with the World Health Organization definition of mild traumatic brain injury. The criteria include loss of consciousness for less than 30 minutes, a Glasgow Coma Scale score of 13 or 14, or at least one acute sign or symptom of concussion, as noted by emergency clinicians.
Patients were excluded from the concussion group if they had deteriorating neurologic status, underwent neurosurgical intervention, had posttraumatic amnesia that lasted more than 24 hours, or had a score higher than 4 on the Abbreviated Injury Scale (AIS). The orthopedic injury group included patients without symptoms of concussion and with blunt trauma associated with an AIS 13 score of 4 or less. Patients were excluded from both groups if they had an overnight hospitalization for traumatic brain injury, a concussion within the past 3 months, or a neurodevelopmental disorder.
The researchers analyzed data from 928 children of 967 enrolled in the study. The median age was 12.2 years, and 41.3% were female. The final study cohort included 239 children with orthopedic injuries but no headache, 160 with a concussion and no headache, 134 with a concussion and nonmigraine headaches, and 254 with a concussion and migraine headaches.
Children with posttraumatic migraines 10 days after a concussion had the most severe symptoms and worst quality of life 3 months following their head trauma, the researchers found. Children without headaches within 10 days after concussion had the best 3-month outcomes, comparable to those with orthopedic injuries alone.
The researchers said the strengths of their study included its large population and its inclusion of various causes of head trauma, not just sports-related concussions. Limitations included self-reports of headaches instead of a physician diagnosis and lack of control for clinical interventions that might have affected the outcomes.
Charles Tator, MD, PhD, director of the Canadian Concussion Centre at Toronto Western Hospital, said the findings were unsurprising.
“Headaches are the most common symptom after concussion,” Dr. Tator, who was not involved in the latest research, told this news organization. “In my practice and research with concussed kids 11 and up and with adults, those with preconcussion history of migraine are the most difficult to treat because their headaches don’t improve unless specific measures are taken.”
Dr. Tator, who also is a professor of neurosurgery at the University of Toronto, said clinicians who treat concussions must determine which type of headaches children are experiencing – and refer as early as possible for migraine prevention or treatment and medication, as warranted.
“Early recognition after concussion that migraine headaches are occurring will save kids a lot of suffering,” he said.
The study was supported by a Canadian Institute of Health Research Foundation Grant and by funds from the Alberta Children’s Hospital Foundation and the Alberta Children’s Hospital Research Institute. Dr. Tator has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Modified ECT lowers dental, skeletal fracture risk
“ECT is associated with a very low risk of skeletal fractures, even in high-risk patients, and is also associated with a low risk of dental fractures,” said study investigator Chittaranjan Andrade, MD, noting that preexisting bone and dental disease increase this risk.
Overall, clinicians who provide ECT “need to be aware of rare adverse effects, as well as the common ones,” Dr. Andrade, senior professor of clinical psychopharmacology and neurotoxicology, National Institute of Mental Health and Neurosciences, Bangalore, India, told this news organization. He added they also “need data to be able to provide reassurance.”
The findings were published online in The Journal of Clinical Psychiatry.
Avoid unmodified ECT
Dr. Andrade conducted the study because the risk of skeletal and dental fractures associated with ECT is “not commonly discussed.”
Although ECT is perhaps the most effective available treatment for major mental illness, it is associated with several adverse effects, including those associated with delivery of an electrical stimulus to the brain, which results in central and peripheral seizure, he noted.
“The central seizure is essential for the efficacy of ECT,” said Dr. Andrade. In contrast, “the motor seizure has no therapeutic value, is cosmetically displeasing, and may rarely be associated with peripheral adverse effects affecting muscles, joints, teeth, and bones,” he added.
The musculoskeletal and dental injuries are caused by stretching, twisting, compression, or direct injury. Particularly during the motor seizure, the “sudden jerk” associated with the tonic contraction of muscles as well as the repeated jerks associated with each clonic contraction can result in injuries, including skeletal and dental fractures.
To address this concern, the motor seizure is “modified” or attenuated through use of an intravenous muscle relaxant administered with other ECT premedication.
“How effectively the musculoskeletal and dental adverse effects are minimized depends on how well the motor seizure is modified,” Dr. Andrade said. He emphasized that the “use of unmodified ECT is strongly discouraged.”
Dr. Andrade reviewed prior research into the skeletal and dental risks of ECT. The infrequency of cases and ethical difficulties in conducting randomized clinical trials with such patients require reliance on anecdotal reports, he said.
Bite blocks, seizure modifiers
Population-based data showed that the fracture risk with modified ECT is two events per 100,000 ECTs. However, the risk may be as low as 0.36 events per 100,000 ECTs if calculated only with recent data, Dr. Andrade noted.
Population-based studies also suggest that the dental fracture risk with modified ECT is .02% per ECT and .17% per ECT course.
Although fractures have been reported under “unusual circumstances” among patients receiving modified ECT, many other reports point to the safety of this treatment, even in ultrahigh-risk patients.
Such patients include those with severe osteoporosis, metastatic bone disease, osteogenesis imperfecta, Ehlers-Danlos syndrome, Harrington rod implants, recent long bone fractures, multiple bone fractures, surgical repair of hip fracture, vertebroplasty, and maxillofacial repair.
Dr. Andrade noted that oral health is “poor” among patients with major mental illness for multiple reasons, including poor nutrition, self-neglect, and decreased salivation caused by the anticholinergic effects of medications.
This places these patients at increased risk for dental adverse effects during ECT because the muscles of the jaw contract forcefully during the motor seizure, causing sudden impact and, subsequently, sustained pressure on the teeth, Dr. Andrade said.
Moreover, because ECT is typically administered through repeated sessions, dental injuries may accumulate over the course of treatment.
ECT-associated skeletal risks arise from the tonic-clonic contractions of the muscles of the trunk and limbs, which need to be addressed via use of succinylcholine or other muscle relaxants included in ECT premedication.
Dr. Andrade noted that succinylcholine is effective at modifying the motor seizure at the common dose of 0.5-1.0 mg/kg. However, about 5% of patients require a higher dose (>1.5 mg/kg). If the dose is 1-2 mg/kg for patients at high risk for orthopedic complications, “muscle relaxation during ECT could be expected to be reasonably complete,” he said.
“Because of wide interpersonal variation, a neurostimulator may need to be used to identify the ideal dose for an individual patient,” he added.
In addition, use of bite blocks and effective jaw immobilization during ECT can reduce the risk. “Careful assessment of preexisting risk and good ECT practice can minimize the risk of skeletal and dental complications during ECT,” Dr. Andrade said.
Risks vs. benefits
Commenting on the study, Mark S. George, MD, distinguished professor of psychiatry, radiology, and neurology, and director of the brain stimulation division, Medical University of South Carolina, Charleston, said this was a “well-written review of how frequently patients who are undergoing modern ECT have bone fractures or dental fractures during the procedure.”
Dr. George, who was not involved with the research, added that modern medications and management “make ECT a truly safe procedure.”
“It is not without some risk, but these risks are low, especially when compared to the risks of untreated or undertreated depression or catatonia, like suicide,” he said.
Dr. Andrade publishes an e-newsletter supported by Sun Pharmaceuticals, with payments made directly to registered charities, but does not benefit financially from the relationship. His travel expenses for delivering lectures and workshops have been supported by the organizers themselves or pharmaceutical companies at the behest of the organizers. He has provided advice to various pharmaceutical companies and has received “nominal compensation.” He has also received payments for developing educational materials for scientific initiatives and programs, such as for the Behavioral and Neurosciences Foundation of India, PsyBase India, Texas Tech University USA, the Nordic Association for Convulsive Therapy, and the American Society of Clinical Psychopharmacology. Dr. George reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
“ECT is associated with a very low risk of skeletal fractures, even in high-risk patients, and is also associated with a low risk of dental fractures,” said study investigator Chittaranjan Andrade, MD, noting that preexisting bone and dental disease increase this risk.
Overall, clinicians who provide ECT “need to be aware of rare adverse effects, as well as the common ones,” Dr. Andrade, senior professor of clinical psychopharmacology and neurotoxicology, National Institute of Mental Health and Neurosciences, Bangalore, India, told this news organization. He added they also “need data to be able to provide reassurance.”
The findings were published online in The Journal of Clinical Psychiatry.
Avoid unmodified ECT
Dr. Andrade conducted the study because the risk of skeletal and dental fractures associated with ECT is “not commonly discussed.”
Although ECT is perhaps the most effective available treatment for major mental illness, it is associated with several adverse effects, including those associated with delivery of an electrical stimulus to the brain, which results in central and peripheral seizure, he noted.
“The central seizure is essential for the efficacy of ECT,” said Dr. Andrade. In contrast, “the motor seizure has no therapeutic value, is cosmetically displeasing, and may rarely be associated with peripheral adverse effects affecting muscles, joints, teeth, and bones,” he added.
The musculoskeletal and dental injuries are caused by stretching, twisting, compression, or direct injury. Particularly during the motor seizure, the “sudden jerk” associated with the tonic contraction of muscles as well as the repeated jerks associated with each clonic contraction can result in injuries, including skeletal and dental fractures.
To address this concern, the motor seizure is “modified” or attenuated through use of an intravenous muscle relaxant administered with other ECT premedication.
“How effectively the musculoskeletal and dental adverse effects are minimized depends on how well the motor seizure is modified,” Dr. Andrade said. He emphasized that the “use of unmodified ECT is strongly discouraged.”
Dr. Andrade reviewed prior research into the skeletal and dental risks of ECT. The infrequency of cases and ethical difficulties in conducting randomized clinical trials with such patients require reliance on anecdotal reports, he said.
Bite blocks, seizure modifiers
Population-based data showed that the fracture risk with modified ECT is two events per 100,000 ECTs. However, the risk may be as low as 0.36 events per 100,000 ECTs if calculated only with recent data, Dr. Andrade noted.
Population-based studies also suggest that the dental fracture risk with modified ECT is .02% per ECT and .17% per ECT course.
Although fractures have been reported under “unusual circumstances” among patients receiving modified ECT, many other reports point to the safety of this treatment, even in ultrahigh-risk patients.
Such patients include those with severe osteoporosis, metastatic bone disease, osteogenesis imperfecta, Ehlers-Danlos syndrome, Harrington rod implants, recent long bone fractures, multiple bone fractures, surgical repair of hip fracture, vertebroplasty, and maxillofacial repair.
Dr. Andrade noted that oral health is “poor” among patients with major mental illness for multiple reasons, including poor nutrition, self-neglect, and decreased salivation caused by the anticholinergic effects of medications.
This places these patients at increased risk for dental adverse effects during ECT because the muscles of the jaw contract forcefully during the motor seizure, causing sudden impact and, subsequently, sustained pressure on the teeth, Dr. Andrade said.
Moreover, because ECT is typically administered through repeated sessions, dental injuries may accumulate over the course of treatment.
ECT-associated skeletal risks arise from the tonic-clonic contractions of the muscles of the trunk and limbs, which need to be addressed via use of succinylcholine or other muscle relaxants included in ECT premedication.
Dr. Andrade noted that succinylcholine is effective at modifying the motor seizure at the common dose of 0.5-1.0 mg/kg. However, about 5% of patients require a higher dose (>1.5 mg/kg). If the dose is 1-2 mg/kg for patients at high risk for orthopedic complications, “muscle relaxation during ECT could be expected to be reasonably complete,” he said.
“Because of wide interpersonal variation, a neurostimulator may need to be used to identify the ideal dose for an individual patient,” he added.
In addition, use of bite blocks and effective jaw immobilization during ECT can reduce the risk. “Careful assessment of preexisting risk and good ECT practice can minimize the risk of skeletal and dental complications during ECT,” Dr. Andrade said.
Risks vs. benefits
Commenting on the study, Mark S. George, MD, distinguished professor of psychiatry, radiology, and neurology, and director of the brain stimulation division, Medical University of South Carolina, Charleston, said this was a “well-written review of how frequently patients who are undergoing modern ECT have bone fractures or dental fractures during the procedure.”
Dr. George, who was not involved with the research, added that modern medications and management “make ECT a truly safe procedure.”
“It is not without some risk, but these risks are low, especially when compared to the risks of untreated or undertreated depression or catatonia, like suicide,” he said.
Dr. Andrade publishes an e-newsletter supported by Sun Pharmaceuticals, with payments made directly to registered charities, but does not benefit financially from the relationship. His travel expenses for delivering lectures and workshops have been supported by the organizers themselves or pharmaceutical companies at the behest of the organizers. He has provided advice to various pharmaceutical companies and has received “nominal compensation.” He has also received payments for developing educational materials for scientific initiatives and programs, such as for the Behavioral and Neurosciences Foundation of India, PsyBase India, Texas Tech University USA, the Nordic Association for Convulsive Therapy, and the American Society of Clinical Psychopharmacology. Dr. George reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
“ECT is associated with a very low risk of skeletal fractures, even in high-risk patients, and is also associated with a low risk of dental fractures,” said study investigator Chittaranjan Andrade, MD, noting that preexisting bone and dental disease increase this risk.
Overall, clinicians who provide ECT “need to be aware of rare adverse effects, as well as the common ones,” Dr. Andrade, senior professor of clinical psychopharmacology and neurotoxicology, National Institute of Mental Health and Neurosciences, Bangalore, India, told this news organization. He added they also “need data to be able to provide reassurance.”
The findings were published online in The Journal of Clinical Psychiatry.
Avoid unmodified ECT
Dr. Andrade conducted the study because the risk of skeletal and dental fractures associated with ECT is “not commonly discussed.”
Although ECT is perhaps the most effective available treatment for major mental illness, it is associated with several adverse effects, including those associated with delivery of an electrical stimulus to the brain, which results in central and peripheral seizure, he noted.
“The central seizure is essential for the efficacy of ECT,” said Dr. Andrade. In contrast, “the motor seizure has no therapeutic value, is cosmetically displeasing, and may rarely be associated with peripheral adverse effects affecting muscles, joints, teeth, and bones,” he added.
The musculoskeletal and dental injuries are caused by stretching, twisting, compression, or direct injury. Particularly during the motor seizure, the “sudden jerk” associated with the tonic contraction of muscles as well as the repeated jerks associated with each clonic contraction can result in injuries, including skeletal and dental fractures.
To address this concern, the motor seizure is “modified” or attenuated through use of an intravenous muscle relaxant administered with other ECT premedication.
“How effectively the musculoskeletal and dental adverse effects are minimized depends on how well the motor seizure is modified,” Dr. Andrade said. He emphasized that the “use of unmodified ECT is strongly discouraged.”
Dr. Andrade reviewed prior research into the skeletal and dental risks of ECT. The infrequency of cases and ethical difficulties in conducting randomized clinical trials with such patients require reliance on anecdotal reports, he said.
Bite blocks, seizure modifiers
Population-based data showed that the fracture risk with modified ECT is two events per 100,000 ECTs. However, the risk may be as low as 0.36 events per 100,000 ECTs if calculated only with recent data, Dr. Andrade noted.
Population-based studies also suggest that the dental fracture risk with modified ECT is .02% per ECT and .17% per ECT course.
Although fractures have been reported under “unusual circumstances” among patients receiving modified ECT, many other reports point to the safety of this treatment, even in ultrahigh-risk patients.
Such patients include those with severe osteoporosis, metastatic bone disease, osteogenesis imperfecta, Ehlers-Danlos syndrome, Harrington rod implants, recent long bone fractures, multiple bone fractures, surgical repair of hip fracture, vertebroplasty, and maxillofacial repair.
Dr. Andrade noted that oral health is “poor” among patients with major mental illness for multiple reasons, including poor nutrition, self-neglect, and decreased salivation caused by the anticholinergic effects of medications.
This places these patients at increased risk for dental adverse effects during ECT because the muscles of the jaw contract forcefully during the motor seizure, causing sudden impact and, subsequently, sustained pressure on the teeth, Dr. Andrade said.
Moreover, because ECT is typically administered through repeated sessions, dental injuries may accumulate over the course of treatment.
ECT-associated skeletal risks arise from the tonic-clonic contractions of the muscles of the trunk and limbs, which need to be addressed via use of succinylcholine or other muscle relaxants included in ECT premedication.
Dr. Andrade noted that succinylcholine is effective at modifying the motor seizure at the common dose of 0.5-1.0 mg/kg. However, about 5% of patients require a higher dose (>1.5 mg/kg). If the dose is 1-2 mg/kg for patients at high risk for orthopedic complications, “muscle relaxation during ECT could be expected to be reasonably complete,” he said.
“Because of wide interpersonal variation, a neurostimulator may need to be used to identify the ideal dose for an individual patient,” he added.
In addition, use of bite blocks and effective jaw immobilization during ECT can reduce the risk. “Careful assessment of preexisting risk and good ECT practice can minimize the risk of skeletal and dental complications during ECT,” Dr. Andrade said.
Risks vs. benefits
Commenting on the study, Mark S. George, MD, distinguished professor of psychiatry, radiology, and neurology, and director of the brain stimulation division, Medical University of South Carolina, Charleston, said this was a “well-written review of how frequently patients who are undergoing modern ECT have bone fractures or dental fractures during the procedure.”
Dr. George, who was not involved with the research, added that modern medications and management “make ECT a truly safe procedure.”
“It is not without some risk, but these risks are low, especially when compared to the risks of untreated or undertreated depression or catatonia, like suicide,” he said.
Dr. Andrade publishes an e-newsletter supported by Sun Pharmaceuticals, with payments made directly to registered charities, but does not benefit financially from the relationship. His travel expenses for delivering lectures and workshops have been supported by the organizers themselves or pharmaceutical companies at the behest of the organizers. He has provided advice to various pharmaceutical companies and has received “nominal compensation.” He has also received payments for developing educational materials for scientific initiatives and programs, such as for the Behavioral and Neurosciences Foundation of India, PsyBase India, Texas Tech University USA, the Nordic Association for Convulsive Therapy, and the American Society of Clinical Psychopharmacology. Dr. George reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL PSYCHIATRY
We have seen the future of healthy muffins, and its name is Roselle
Get ‘em while they’re hot … for your health
Today on the Eating Channel, it’s a very special episode of “Much Ado About Muffin.”
The muffin. For some of us, it’s a good way to pretend we’re not having dessert for breakfast. A bran muffin can be loaded with calcium and fiber, and our beloved blueberry is full of yummy antioxidants and vitamins. Definitely not dessert.
Well, the muffin denial can stop there because there’s a new flavor on the scene, and research suggests it may actually be healthy. (Disclaimer: Muffin may not be considered healthy in Norway.) This new muffin has a name, Roselle, that comes from the calyx extract used in it, which is found in the Hibiscus sabdariffa plant of the same name.
Now, when it comes to new foods, especially ones that are supposed to be healthy, the No. 1 criteria is the same: It has to taste good. Researchers at the Norwegian University of Science and Technology and Amity University in India agreed, but they also set out to make it nutritionally valuable and give it a long shelf life without the addition of preservatives.
Sounds like a tall order, but they figured it out.
Not only is it tasty, but the properties of it could rival your morning multivitamin. Hibiscus extract has huge amounts of antioxidants, like phenolics, which are believed to help prevent cell membrane damage. Foods like vegetables, flax seed, and whole grains also have these antioxidants, but why not just have a Roselle muffin instead? You also get a dose of ascorbic acid without the glass of OJ in the morning.
The ascorbic acid, however, is not there just to help you. It also helps to check the researcher’s third box, shelf life. These naturally rosy-colored pastries will stay mold-free for 6 days without refrigeration at room temperature and without added preservatives.
Our guess, though, is they won’t be on the kitchen counter long enough to find out.
A sobering proposition
If Hollywood is to be believed, there’s no amount of drunkenness that can’t be cured with a cup of coffee or a stern slap in the face. Unfortunately, here in the real world the only thing that can make you less drunk is time. Maybe next time you’ll stop after that seventh Manhattan.
But what if we could beat time? What if there’s an actual sobriety drug out there?
Say hello to fibroblast growth factor 21. Although the liver already does good work filtering out what is essentially poison, it then goes the extra mile and produces fibroblast growth factor 21 (or, as her friends call her, FGF21), a hormone that suppresses the desire to drink, makes you desire water, and protects the liver all at the same time.
Now, FGF21 in its current role is great, but if you’ve ever seen or been a drunk person before, you’ve experienced the lack of interest in listening to reason, especially when it comes from within our own bodies. Who are you to tell us what to do, body? You’re not the boss of us! So a group of scientists decided to push the limits of FGF21. Could it do more than it already does?
First off, they genetically altered a group of mice so that they didn’t produce FGF21 on their own. Then they got them drunk. We’re going to assume they built a scale model of the bar from Cheers and had the mice filter in through the front door as they served their subjects beer out of tiny little glasses.
Once the mice were nice and liquored up, some were given a treatment of FGF21 while others were given a placebo. Lo and behold, the mice given FGF21 recovered about 50% faster than those that received the control treatment. Not exactly instant, but 50% is nothing to sniff at.
Before you bring your FGF21 supplement to the bar, though, this research only applies to mice. We don’t know if it works in people. And make sure you stick to booze. If your choice of intoxication is a bit more exotic, FGF21 isn’t going to do anything for you. Yes, the scientists tried. Yes, those mice are living a very interesting life. And yes, we are jealous of drugged-up lab mice.
Supersize your imagination, shrink your snacks
Have you ever heard of the meal-recall effect? Did you know that, in England, a biscuit is really a cookie? Did you also know that the magazine Bon Appétit is not the same as the peer-reviewed journal Appetite? We do … now.
The meal-recall effect is the subsequent reduction in snacking that comes from remembering a recent meal. It was used to great effect in a recent study conducted at the University of Cambridge, which is in England, where they feed their experimental humans cookies but, for some reason, call them biscuits.
For the first part of the study, the participants were invited to dine at Che Laboratory, where they “were given a microwave ready meal of rice and sauce and a cup of water,” according to a statement from the university. As our Uncle Ernie would say, “Gourmet all the way.”
The test subjects were instructed not to eat anything for 3 hours and “then invited back to the lab to perform imagination tasks.” Those who did come back were randomly divided into five different groups, each with a different task:
- Imagine moving their recent lunch at the lab around a plate.
- Recall eating their recent lunch in detail.
- Imagine that the lunch was twice as big and filling as it really was.
- Look at a photograph of spaghetti hoops in tomato sauce and write a description of it before imagining moving the food around a plate.
- Look at a photo of paper clips and rubber bands and imagine moving them around.
Now, at last, we get to the biscuits/cookies, which were the subject of a taste test that “was simply a rouse for covertly assessing snacking,” the investigators explained. As part of that test, participants were told they could eat as many biscuits as they wanted.
When the tables were cleared and the leftovers examined, the group that imagined spaghetti hoops had eaten the most biscuits (75.9 g), followed by the group that imagined paper clips (75.5 g), the moving-their-lunch-around-the-plate group (72.0 g), and the group that relived eating their lunch (70.0 g).
In a victory for the meal-recall effect, the people who imagined their meal being twice as big ate the fewest biscuits (51.1 g). “Your mind can be more powerful than your stomach in dictating how much you eat,” lead author Joanna Szypula, PhD, said in the university statement.
Oh! One more thing. The study appeared in Appetite, which is a peer-reviewed journal, not in Bon Appétit, which is not a peer-reviewed journal. Thanks to the fine folks at both publications for pointing that out to us.
Get ‘em while they’re hot … for your health
Today on the Eating Channel, it’s a very special episode of “Much Ado About Muffin.”
The muffin. For some of us, it’s a good way to pretend we’re not having dessert for breakfast. A bran muffin can be loaded with calcium and fiber, and our beloved blueberry is full of yummy antioxidants and vitamins. Definitely not dessert.
Well, the muffin denial can stop there because there’s a new flavor on the scene, and research suggests it may actually be healthy. (Disclaimer: Muffin may not be considered healthy in Norway.) This new muffin has a name, Roselle, that comes from the calyx extract used in it, which is found in the Hibiscus sabdariffa plant of the same name.
Now, when it comes to new foods, especially ones that are supposed to be healthy, the No. 1 criteria is the same: It has to taste good. Researchers at the Norwegian University of Science and Technology and Amity University in India agreed, but they also set out to make it nutritionally valuable and give it a long shelf life without the addition of preservatives.
Sounds like a tall order, but they figured it out.
Not only is it tasty, but the properties of it could rival your morning multivitamin. Hibiscus extract has huge amounts of antioxidants, like phenolics, which are believed to help prevent cell membrane damage. Foods like vegetables, flax seed, and whole grains also have these antioxidants, but why not just have a Roselle muffin instead? You also get a dose of ascorbic acid without the glass of OJ in the morning.
The ascorbic acid, however, is not there just to help you. It also helps to check the researcher’s third box, shelf life. These naturally rosy-colored pastries will stay mold-free for 6 days without refrigeration at room temperature and without added preservatives.
Our guess, though, is they won’t be on the kitchen counter long enough to find out.
A sobering proposition
If Hollywood is to be believed, there’s no amount of drunkenness that can’t be cured with a cup of coffee or a stern slap in the face. Unfortunately, here in the real world the only thing that can make you less drunk is time. Maybe next time you’ll stop after that seventh Manhattan.
But what if we could beat time? What if there’s an actual sobriety drug out there?
Say hello to fibroblast growth factor 21. Although the liver already does good work filtering out what is essentially poison, it then goes the extra mile and produces fibroblast growth factor 21 (or, as her friends call her, FGF21), a hormone that suppresses the desire to drink, makes you desire water, and protects the liver all at the same time.
Now, FGF21 in its current role is great, but if you’ve ever seen or been a drunk person before, you’ve experienced the lack of interest in listening to reason, especially when it comes from within our own bodies. Who are you to tell us what to do, body? You’re not the boss of us! So a group of scientists decided to push the limits of FGF21. Could it do more than it already does?
First off, they genetically altered a group of mice so that they didn’t produce FGF21 on their own. Then they got them drunk. We’re going to assume they built a scale model of the bar from Cheers and had the mice filter in through the front door as they served their subjects beer out of tiny little glasses.
Once the mice were nice and liquored up, some were given a treatment of FGF21 while others were given a placebo. Lo and behold, the mice given FGF21 recovered about 50% faster than those that received the control treatment. Not exactly instant, but 50% is nothing to sniff at.
Before you bring your FGF21 supplement to the bar, though, this research only applies to mice. We don’t know if it works in people. And make sure you stick to booze. If your choice of intoxication is a bit more exotic, FGF21 isn’t going to do anything for you. Yes, the scientists tried. Yes, those mice are living a very interesting life. And yes, we are jealous of drugged-up lab mice.
Supersize your imagination, shrink your snacks
Have you ever heard of the meal-recall effect? Did you know that, in England, a biscuit is really a cookie? Did you also know that the magazine Bon Appétit is not the same as the peer-reviewed journal Appetite? We do … now.
The meal-recall effect is the subsequent reduction in snacking that comes from remembering a recent meal. It was used to great effect in a recent study conducted at the University of Cambridge, which is in England, where they feed their experimental humans cookies but, for some reason, call them biscuits.
For the first part of the study, the participants were invited to dine at Che Laboratory, where they “were given a microwave ready meal of rice and sauce and a cup of water,” according to a statement from the university. As our Uncle Ernie would say, “Gourmet all the way.”
The test subjects were instructed not to eat anything for 3 hours and “then invited back to the lab to perform imagination tasks.” Those who did come back were randomly divided into five different groups, each with a different task:
- Imagine moving their recent lunch at the lab around a plate.
- Recall eating their recent lunch in detail.
- Imagine that the lunch was twice as big and filling as it really was.
- Look at a photograph of spaghetti hoops in tomato sauce and write a description of it before imagining moving the food around a plate.
- Look at a photo of paper clips and rubber bands and imagine moving them around.
Now, at last, we get to the biscuits/cookies, which were the subject of a taste test that “was simply a rouse for covertly assessing snacking,” the investigators explained. As part of that test, participants were told they could eat as many biscuits as they wanted.
When the tables were cleared and the leftovers examined, the group that imagined spaghetti hoops had eaten the most biscuits (75.9 g), followed by the group that imagined paper clips (75.5 g), the moving-their-lunch-around-the-plate group (72.0 g), and the group that relived eating their lunch (70.0 g).
In a victory for the meal-recall effect, the people who imagined their meal being twice as big ate the fewest biscuits (51.1 g). “Your mind can be more powerful than your stomach in dictating how much you eat,” lead author Joanna Szypula, PhD, said in the university statement.
Oh! One more thing. The study appeared in Appetite, which is a peer-reviewed journal, not in Bon Appétit, which is not a peer-reviewed journal. Thanks to the fine folks at both publications for pointing that out to us.
Get ‘em while they’re hot … for your health
Today on the Eating Channel, it’s a very special episode of “Much Ado About Muffin.”
The muffin. For some of us, it’s a good way to pretend we’re not having dessert for breakfast. A bran muffin can be loaded with calcium and fiber, and our beloved blueberry is full of yummy antioxidants and vitamins. Definitely not dessert.
Well, the muffin denial can stop there because there’s a new flavor on the scene, and research suggests it may actually be healthy. (Disclaimer: Muffin may not be considered healthy in Norway.) This new muffin has a name, Roselle, that comes from the calyx extract used in it, which is found in the Hibiscus sabdariffa plant of the same name.
Now, when it comes to new foods, especially ones that are supposed to be healthy, the No. 1 criteria is the same: It has to taste good. Researchers at the Norwegian University of Science and Technology and Amity University in India agreed, but they also set out to make it nutritionally valuable and give it a long shelf life without the addition of preservatives.
Sounds like a tall order, but they figured it out.
Not only is it tasty, but the properties of it could rival your morning multivitamin. Hibiscus extract has huge amounts of antioxidants, like phenolics, which are believed to help prevent cell membrane damage. Foods like vegetables, flax seed, and whole grains also have these antioxidants, but why not just have a Roselle muffin instead? You also get a dose of ascorbic acid without the glass of OJ in the morning.
The ascorbic acid, however, is not there just to help you. It also helps to check the researcher’s third box, shelf life. These naturally rosy-colored pastries will stay mold-free for 6 days without refrigeration at room temperature and without added preservatives.
Our guess, though, is they won’t be on the kitchen counter long enough to find out.
A sobering proposition
If Hollywood is to be believed, there’s no amount of drunkenness that can’t be cured with a cup of coffee or a stern slap in the face. Unfortunately, here in the real world the only thing that can make you less drunk is time. Maybe next time you’ll stop after that seventh Manhattan.
But what if we could beat time? What if there’s an actual sobriety drug out there?
Say hello to fibroblast growth factor 21. Although the liver already does good work filtering out what is essentially poison, it then goes the extra mile and produces fibroblast growth factor 21 (or, as her friends call her, FGF21), a hormone that suppresses the desire to drink, makes you desire water, and protects the liver all at the same time.
Now, FGF21 in its current role is great, but if you’ve ever seen or been a drunk person before, you’ve experienced the lack of interest in listening to reason, especially when it comes from within our own bodies. Who are you to tell us what to do, body? You’re not the boss of us! So a group of scientists decided to push the limits of FGF21. Could it do more than it already does?
First off, they genetically altered a group of mice so that they didn’t produce FGF21 on their own. Then they got them drunk. We’re going to assume they built a scale model of the bar from Cheers and had the mice filter in through the front door as they served their subjects beer out of tiny little glasses.
Once the mice were nice and liquored up, some were given a treatment of FGF21 while others were given a placebo. Lo and behold, the mice given FGF21 recovered about 50% faster than those that received the control treatment. Not exactly instant, but 50% is nothing to sniff at.
Before you bring your FGF21 supplement to the bar, though, this research only applies to mice. We don’t know if it works in people. And make sure you stick to booze. If your choice of intoxication is a bit more exotic, FGF21 isn’t going to do anything for you. Yes, the scientists tried. Yes, those mice are living a very interesting life. And yes, we are jealous of drugged-up lab mice.
Supersize your imagination, shrink your snacks
Have you ever heard of the meal-recall effect? Did you know that, in England, a biscuit is really a cookie? Did you also know that the magazine Bon Appétit is not the same as the peer-reviewed journal Appetite? We do … now.
The meal-recall effect is the subsequent reduction in snacking that comes from remembering a recent meal. It was used to great effect in a recent study conducted at the University of Cambridge, which is in England, where they feed their experimental humans cookies but, for some reason, call them biscuits.
For the first part of the study, the participants were invited to dine at Che Laboratory, where they “were given a microwave ready meal of rice and sauce and a cup of water,” according to a statement from the university. As our Uncle Ernie would say, “Gourmet all the way.”
The test subjects were instructed not to eat anything for 3 hours and “then invited back to the lab to perform imagination tasks.” Those who did come back were randomly divided into five different groups, each with a different task:
- Imagine moving their recent lunch at the lab around a plate.
- Recall eating their recent lunch in detail.
- Imagine that the lunch was twice as big and filling as it really was.
- Look at a photograph of spaghetti hoops in tomato sauce and write a description of it before imagining moving the food around a plate.
- Look at a photo of paper clips and rubber bands and imagine moving them around.
Now, at last, we get to the biscuits/cookies, which were the subject of a taste test that “was simply a rouse for covertly assessing snacking,” the investigators explained. As part of that test, participants were told they could eat as many biscuits as they wanted.
When the tables were cleared and the leftovers examined, the group that imagined spaghetti hoops had eaten the most biscuits (75.9 g), followed by the group that imagined paper clips (75.5 g), the moving-their-lunch-around-the-plate group (72.0 g), and the group that relived eating their lunch (70.0 g).
In a victory for the meal-recall effect, the people who imagined their meal being twice as big ate the fewest biscuits (51.1 g). “Your mind can be more powerful than your stomach in dictating how much you eat,” lead author Joanna Szypula, PhD, said in the university statement.
Oh! One more thing. The study appeared in Appetite, which is a peer-reviewed journal, not in Bon Appétit, which is not a peer-reviewed journal. Thanks to the fine folks at both publications for pointing that out to us.
New insight into preventing antipsychotic-induced weight gain
In the first dose-response meta-analysis focusing on antipsychotic-induced weight gain, researchers provide data on the trajectory of this risk associated with individual agents.
Investigators analyzed 52 randomized controlled trials (RCTs) encompassing more than 22,500 participants with schizophrenia treated with antipsychotics. They found that, with the exception of aripiprazole long-acting injectable (LAI), all of the other antipsychotics has significant dose-response effect on weight gain. Furthermore, weight gain occurred with some antipsychotics even at relatively low doses.
“We found significant dose-response associations for weight and metabolic variables, with a unique signature for each antipsychotic,” write the investigators, led by Michel Sabé, MD, of the division of adult psychiatry, department of psychiatry, Geneva University Hospitals.
“Despite several limitations, including the limited number of available studies, our results may provide useful information for preventing weight gain and metabolic disturbances by adapting antipsychotic doses,” they add.
The study was published online in The Journal of Clinical Psychiatry.
Balancing risks and benefits
Antipsychotics are first-line therapy for schizophrenia and are associated with weight gain, lipid disturbances, and glucose dysregulation – especially second-generation antipsychotics (SGAs), which can lead to obesity, type 2 diabetes, and metabolic syndrome.
Given that people with schizophrenia also tend to have lifestyle-related cardiovascular risk factors, it’s important to find “a balance between beneficial and adverse effects of antipsychotics,” the investigators note
The question of whether weight gain and metabolic dysregulation are dose-dependent “remains controversial.” The effect of specific SGAs on weight gain has been investigated, but only one study has been conducted using a dose-response meta-analysis, and that study did not address metabolic disturbance.
The investigators conducted a systematic review and a dose-response meta-analysis of fixed-dose randomized controlled trials (RCTs) investigating antipsychotic-induced weight gain and metabolic disturbance in adults with acute schizophrenia.
To be included in the analysis, RCTs had to focus on adult patients with schizophrenia or related disorders and include a placebo as a comparator to the drug.
Studies involved only short-term administration of antipsychotics (2-13 weeks) rather than maintenance therapy.
The mean (SD) change in weight (body weight and/or body mass index) between baseline and the study endpoint constituted the primary outcome, with secondary outcomes including changes in metabolic parameters.
The researchers characterized the dose-response relationship using a nonlinear restricted cubic spline model, with three “knots” located at the 10th, 50th, and 90th percentiles of overall dose distribution.
They also calculated dose-response curves and estimated 50% and 95% effective doses (ED50 and ED95, respectively), extracted from the estimated dose-response curves for each antipsychotic.
The researchers then calculated the weight gain at each effective dose (ED50 and ED95) in milligrams and the weight gain corresponding to the ED95 value in kilograms.
Shared decision-making
Of 6,812 citations, the researchers selected 52 RCTs that met inclusion criteria (n = 22,588 participants, with 16,311 receiving antipsychotics and 6,277 receiving placebo; mean age, 38.5 years, 69.2% male). The studies were conducted between1996 and 2021.
The risk for bias in most studies was “low,” although 21% of the studies “presented a high risk.”
With the exception of aripiprazole LAI, all of the other antipsychotics had a “significant dose-response” association with weight.
For example, oral aripiprazole exhibited a significant dose-response association for weight, but there was no significant association found for aripiprazole LAI (c2 = 8.744; P = .0126 vs. c2 = 3.107; P = .2115). However, both curves were still ascending at maximum doses, the authors note.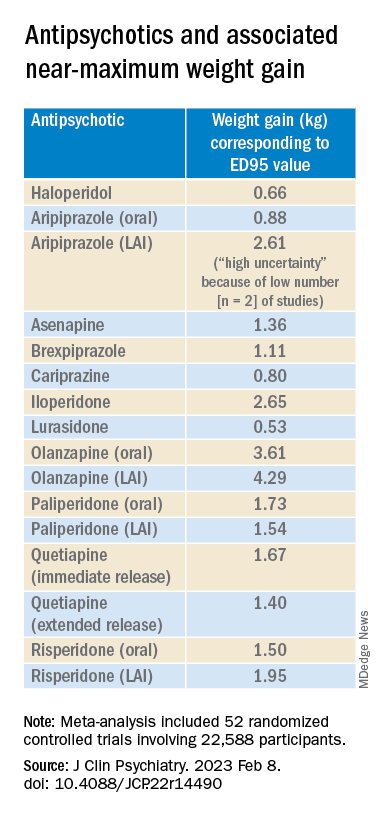
Metabolically neutral
Antipsychotics with a decreasing or quasi-parabolic dose-response curve for weight included brexpiprazole, cariprazine, haloperidol, lurasidone, and quetiapine ER: for these antipsychotics, the ED95 weight gain ranged from 0.53 kg to 1.40 kg.
These antipsychotics “reach their weight gain ED95 at relatively low median effective doses, and higher doses, which mostly correspond to near-maximum effective doses, may even be associated with less weight gain,” the authors note.
In addition, only doses higher than the near-maximum effective dose of brexpiprazole were associated with a small increase in total cholesterol. And cariprazine presented “significantly decreasing curves” at higher doses for LDL cholesterol.
With the exception of quetiapine, this group of medications might be regarded as “metabolically neutral” in terms of weight gain and metabolic disturbances.
Antipsychotics with a plateau-shaped curve were asenapine, iloperidone, paliperidone LAI, quetiapine IR, and risperidone, with a weight gain ED95 ranging from 1.36 to 2.65 kg.
Aripiprazole and olanzapine (oral and LAI formulations), as well as risperidone LAI and oral paliperidone, presented weight gain curves that continued climbing at higher doses (especially olanzapine). However, the drugs have different metabolic profiles, ranging from 0.88 kg ED95 for oral aripiprazole to 4.29 kg for olanzapine LAI.
Olanzapine had the most pronounced weight gain, in addition to associations with all metabolic outcomes.
For some drugs with important metabolic side effects, “a lower dose might provide a better combination of high efficacy and reduced metabolic side effects,” the authors write.
The findings might “provide additional information for clinicians aiming to determine the most suitable dose to prevent weight gain and metabolic disturbance in a shared decision-making process with their patients,” they note.
The results add to “existing concerns about the use of olanzapine as a first-line drug,” they add.
Lowest effective dose
Commenting on the study, Roger S. McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the mood disorders psychopharmacology unit, said clinicians “not infrequently increase doses to achieve better symptom control, [but] this decision should be informed by the additional observation herein that the increase in those could be accompanied by weight increase.”
Moreover, many patients “take concomitant medications that could possibly increase the bioavailability of antipsychotics, which may also increase the risk for weight gain,” said Dr. McIntyre, chairman and executive director of the Brain and Cognitive Discover Foundation, Toronto. He was not involved with this study.
“These data provide a reason to believe that for many people antipsychotic-associated weight gain could be mitigated by using the lowest effective dose, and rather than censor the use of some medications out of concern for weight gain, perhaps using the lowest effective dose of the medication will provide the opportunity for mitigation,” he added. “So I think it really guides clinicians to provide the lowest effective dose as a potential therapeutic and preventive strategy.”
The study received no financial support. Dr. Sabé reports no relevant financial relationships. Three coauthors report relationships with industry; the full list is contained in the original article.
Dr. McIntyre is a CEO of Braxia Scientific Corp. He has received research grant support from CIHR/GACD/National Natural Science Foundation of China (NSFC) and the Milken Institute; speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Boehringer Ingelheim, Sage, Biogen, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Viatris, Abbvie, and Atai Life Sciences.
A version of this article first appeared on Medscape.com.
In the first dose-response meta-analysis focusing on antipsychotic-induced weight gain, researchers provide data on the trajectory of this risk associated with individual agents.
Investigators analyzed 52 randomized controlled trials (RCTs) encompassing more than 22,500 participants with schizophrenia treated with antipsychotics. They found that, with the exception of aripiprazole long-acting injectable (LAI), all of the other antipsychotics has significant dose-response effect on weight gain. Furthermore, weight gain occurred with some antipsychotics even at relatively low doses.
“We found significant dose-response associations for weight and metabolic variables, with a unique signature for each antipsychotic,” write the investigators, led by Michel Sabé, MD, of the division of adult psychiatry, department of psychiatry, Geneva University Hospitals.
“Despite several limitations, including the limited number of available studies, our results may provide useful information for preventing weight gain and metabolic disturbances by adapting antipsychotic doses,” they add.
The study was published online in The Journal of Clinical Psychiatry.
Balancing risks and benefits
Antipsychotics are first-line therapy for schizophrenia and are associated with weight gain, lipid disturbances, and glucose dysregulation – especially second-generation antipsychotics (SGAs), which can lead to obesity, type 2 diabetes, and metabolic syndrome.
Given that people with schizophrenia also tend to have lifestyle-related cardiovascular risk factors, it’s important to find “a balance between beneficial and adverse effects of antipsychotics,” the investigators note
The question of whether weight gain and metabolic dysregulation are dose-dependent “remains controversial.” The effect of specific SGAs on weight gain has been investigated, but only one study has been conducted using a dose-response meta-analysis, and that study did not address metabolic disturbance.
The investigators conducted a systematic review and a dose-response meta-analysis of fixed-dose randomized controlled trials (RCTs) investigating antipsychotic-induced weight gain and metabolic disturbance in adults with acute schizophrenia.
To be included in the analysis, RCTs had to focus on adult patients with schizophrenia or related disorders and include a placebo as a comparator to the drug.
Studies involved only short-term administration of antipsychotics (2-13 weeks) rather than maintenance therapy.
The mean (SD) change in weight (body weight and/or body mass index) between baseline and the study endpoint constituted the primary outcome, with secondary outcomes including changes in metabolic parameters.
The researchers characterized the dose-response relationship using a nonlinear restricted cubic spline model, with three “knots” located at the 10th, 50th, and 90th percentiles of overall dose distribution.
They also calculated dose-response curves and estimated 50% and 95% effective doses (ED50 and ED95, respectively), extracted from the estimated dose-response curves for each antipsychotic.
The researchers then calculated the weight gain at each effective dose (ED50 and ED95) in milligrams and the weight gain corresponding to the ED95 value in kilograms.
Shared decision-making
Of 6,812 citations, the researchers selected 52 RCTs that met inclusion criteria (n = 22,588 participants, with 16,311 receiving antipsychotics and 6,277 receiving placebo; mean age, 38.5 years, 69.2% male). The studies were conducted between1996 and 2021.
The risk for bias in most studies was “low,” although 21% of the studies “presented a high risk.”
With the exception of aripiprazole LAI, all of the other antipsychotics had a “significant dose-response” association with weight.
For example, oral aripiprazole exhibited a significant dose-response association for weight, but there was no significant association found for aripiprazole LAI (c2 = 8.744; P = .0126 vs. c2 = 3.107; P = .2115). However, both curves were still ascending at maximum doses, the authors note.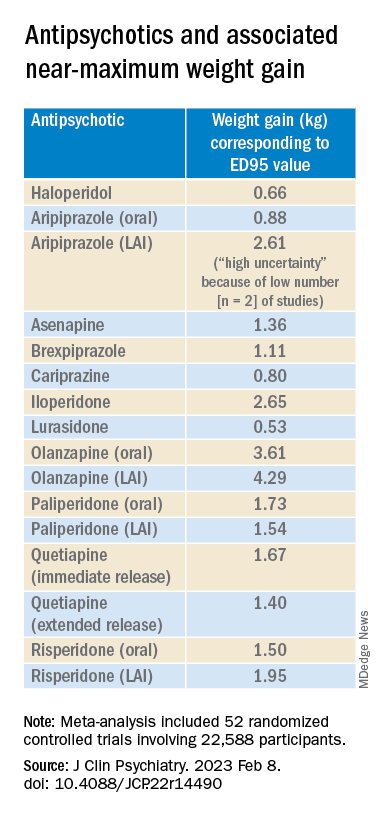
Metabolically neutral
Antipsychotics with a decreasing or quasi-parabolic dose-response curve for weight included brexpiprazole, cariprazine, haloperidol, lurasidone, and quetiapine ER: for these antipsychotics, the ED95 weight gain ranged from 0.53 kg to 1.40 kg.
These antipsychotics “reach their weight gain ED95 at relatively low median effective doses, and higher doses, which mostly correspond to near-maximum effective doses, may even be associated with less weight gain,” the authors note.
In addition, only doses higher than the near-maximum effective dose of brexpiprazole were associated with a small increase in total cholesterol. And cariprazine presented “significantly decreasing curves” at higher doses for LDL cholesterol.
With the exception of quetiapine, this group of medications might be regarded as “metabolically neutral” in terms of weight gain and metabolic disturbances.
Antipsychotics with a plateau-shaped curve were asenapine, iloperidone, paliperidone LAI, quetiapine IR, and risperidone, with a weight gain ED95 ranging from 1.36 to 2.65 kg.
Aripiprazole and olanzapine (oral and LAI formulations), as well as risperidone LAI and oral paliperidone, presented weight gain curves that continued climbing at higher doses (especially olanzapine). However, the drugs have different metabolic profiles, ranging from 0.88 kg ED95 for oral aripiprazole to 4.29 kg for olanzapine LAI.
Olanzapine had the most pronounced weight gain, in addition to associations with all metabolic outcomes.
For some drugs with important metabolic side effects, “a lower dose might provide a better combination of high efficacy and reduced metabolic side effects,” the authors write.
The findings might “provide additional information for clinicians aiming to determine the most suitable dose to prevent weight gain and metabolic disturbance in a shared decision-making process with their patients,” they note.
The results add to “existing concerns about the use of olanzapine as a first-line drug,” they add.
Lowest effective dose
Commenting on the study, Roger S. McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the mood disorders psychopharmacology unit, said clinicians “not infrequently increase doses to achieve better symptom control, [but] this decision should be informed by the additional observation herein that the increase in those could be accompanied by weight increase.”
Moreover, many patients “take concomitant medications that could possibly increase the bioavailability of antipsychotics, which may also increase the risk for weight gain,” said Dr. McIntyre, chairman and executive director of the Brain and Cognitive Discover Foundation, Toronto. He was not involved with this study.
“These data provide a reason to believe that for many people antipsychotic-associated weight gain could be mitigated by using the lowest effective dose, and rather than censor the use of some medications out of concern for weight gain, perhaps using the lowest effective dose of the medication will provide the opportunity for mitigation,” he added. “So I think it really guides clinicians to provide the lowest effective dose as a potential therapeutic and preventive strategy.”
The study received no financial support. Dr. Sabé reports no relevant financial relationships. Three coauthors report relationships with industry; the full list is contained in the original article.
Dr. McIntyre is a CEO of Braxia Scientific Corp. He has received research grant support from CIHR/GACD/National Natural Science Foundation of China (NSFC) and the Milken Institute; speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Boehringer Ingelheim, Sage, Biogen, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Viatris, Abbvie, and Atai Life Sciences.
A version of this article first appeared on Medscape.com.
In the first dose-response meta-analysis focusing on antipsychotic-induced weight gain, researchers provide data on the trajectory of this risk associated with individual agents.
Investigators analyzed 52 randomized controlled trials (RCTs) encompassing more than 22,500 participants with schizophrenia treated with antipsychotics. They found that, with the exception of aripiprazole long-acting injectable (LAI), all of the other antipsychotics has significant dose-response effect on weight gain. Furthermore, weight gain occurred with some antipsychotics even at relatively low doses.
“We found significant dose-response associations for weight and metabolic variables, with a unique signature for each antipsychotic,” write the investigators, led by Michel Sabé, MD, of the division of adult psychiatry, department of psychiatry, Geneva University Hospitals.
“Despite several limitations, including the limited number of available studies, our results may provide useful information for preventing weight gain and metabolic disturbances by adapting antipsychotic doses,” they add.
The study was published online in The Journal of Clinical Psychiatry.
Balancing risks and benefits
Antipsychotics are first-line therapy for schizophrenia and are associated with weight gain, lipid disturbances, and glucose dysregulation – especially second-generation antipsychotics (SGAs), which can lead to obesity, type 2 diabetes, and metabolic syndrome.
Given that people with schizophrenia also tend to have lifestyle-related cardiovascular risk factors, it’s important to find “a balance between beneficial and adverse effects of antipsychotics,” the investigators note
The question of whether weight gain and metabolic dysregulation are dose-dependent “remains controversial.” The effect of specific SGAs on weight gain has been investigated, but only one study has been conducted using a dose-response meta-analysis, and that study did not address metabolic disturbance.
The investigators conducted a systematic review and a dose-response meta-analysis of fixed-dose randomized controlled trials (RCTs) investigating antipsychotic-induced weight gain and metabolic disturbance in adults with acute schizophrenia.
To be included in the analysis, RCTs had to focus on adult patients with schizophrenia or related disorders and include a placebo as a comparator to the drug.
Studies involved only short-term administration of antipsychotics (2-13 weeks) rather than maintenance therapy.
The mean (SD) change in weight (body weight and/or body mass index) between baseline and the study endpoint constituted the primary outcome, with secondary outcomes including changes in metabolic parameters.
The researchers characterized the dose-response relationship using a nonlinear restricted cubic spline model, with three “knots” located at the 10th, 50th, and 90th percentiles of overall dose distribution.
They also calculated dose-response curves and estimated 50% and 95% effective doses (ED50 and ED95, respectively), extracted from the estimated dose-response curves for each antipsychotic.
The researchers then calculated the weight gain at each effective dose (ED50 and ED95) in milligrams and the weight gain corresponding to the ED95 value in kilograms.
Shared decision-making
Of 6,812 citations, the researchers selected 52 RCTs that met inclusion criteria (n = 22,588 participants, with 16,311 receiving antipsychotics and 6,277 receiving placebo; mean age, 38.5 years, 69.2% male). The studies were conducted between1996 and 2021.
The risk for bias in most studies was “low,” although 21% of the studies “presented a high risk.”
With the exception of aripiprazole LAI, all of the other antipsychotics had a “significant dose-response” association with weight.
For example, oral aripiprazole exhibited a significant dose-response association for weight, but there was no significant association found for aripiprazole LAI (c2 = 8.744; P = .0126 vs. c2 = 3.107; P = .2115). However, both curves were still ascending at maximum doses, the authors note.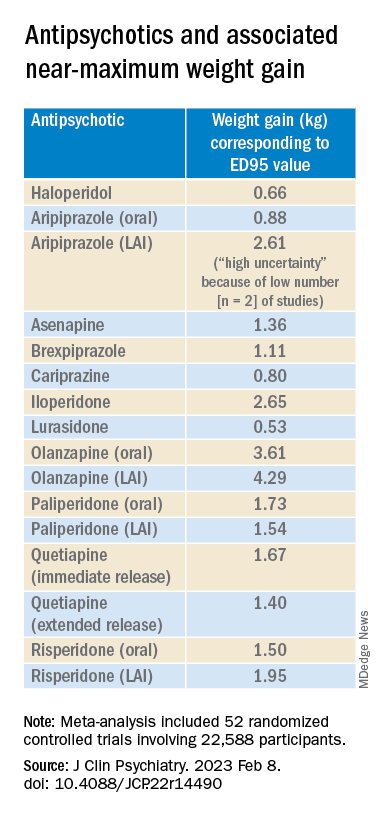
Metabolically neutral
Antipsychotics with a decreasing or quasi-parabolic dose-response curve for weight included brexpiprazole, cariprazine, haloperidol, lurasidone, and quetiapine ER: for these antipsychotics, the ED95 weight gain ranged from 0.53 kg to 1.40 kg.
These antipsychotics “reach their weight gain ED95 at relatively low median effective doses, and higher doses, which mostly correspond to near-maximum effective doses, may even be associated with less weight gain,” the authors note.
In addition, only doses higher than the near-maximum effective dose of brexpiprazole were associated with a small increase in total cholesterol. And cariprazine presented “significantly decreasing curves” at higher doses for LDL cholesterol.
With the exception of quetiapine, this group of medications might be regarded as “metabolically neutral” in terms of weight gain and metabolic disturbances.
Antipsychotics with a plateau-shaped curve were asenapine, iloperidone, paliperidone LAI, quetiapine IR, and risperidone, with a weight gain ED95 ranging from 1.36 to 2.65 kg.
Aripiprazole and olanzapine (oral and LAI formulations), as well as risperidone LAI and oral paliperidone, presented weight gain curves that continued climbing at higher doses (especially olanzapine). However, the drugs have different metabolic profiles, ranging from 0.88 kg ED95 for oral aripiprazole to 4.29 kg for olanzapine LAI.
Olanzapine had the most pronounced weight gain, in addition to associations with all metabolic outcomes.
For some drugs with important metabolic side effects, “a lower dose might provide a better combination of high efficacy and reduced metabolic side effects,” the authors write.
The findings might “provide additional information for clinicians aiming to determine the most suitable dose to prevent weight gain and metabolic disturbance in a shared decision-making process with their patients,” they note.
The results add to “existing concerns about the use of olanzapine as a first-line drug,” they add.
Lowest effective dose
Commenting on the study, Roger S. McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the mood disorders psychopharmacology unit, said clinicians “not infrequently increase doses to achieve better symptom control, [but] this decision should be informed by the additional observation herein that the increase in those could be accompanied by weight increase.”
Moreover, many patients “take concomitant medications that could possibly increase the bioavailability of antipsychotics, which may also increase the risk for weight gain,” said Dr. McIntyre, chairman and executive director of the Brain and Cognitive Discover Foundation, Toronto. He was not involved with this study.
“These data provide a reason to believe that for many people antipsychotic-associated weight gain could be mitigated by using the lowest effective dose, and rather than censor the use of some medications out of concern for weight gain, perhaps using the lowest effective dose of the medication will provide the opportunity for mitigation,” he added. “So I think it really guides clinicians to provide the lowest effective dose as a potential therapeutic and preventive strategy.”
The study received no financial support. Dr. Sabé reports no relevant financial relationships. Three coauthors report relationships with industry; the full list is contained in the original article.
Dr. McIntyre is a CEO of Braxia Scientific Corp. He has received research grant support from CIHR/GACD/National Natural Science Foundation of China (NSFC) and the Milken Institute; speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Boehringer Ingelheim, Sage, Biogen, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Viatris, Abbvie, and Atai Life Sciences.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL PSYCHIATRY
APA releases updated eating disorder guidelines
The updated guidelines focus primarily on anorexia nervosa (AN), bulimia nervosa (BN), and binge-eating disorder (BED) and include recommendations for screening and treatment.
“Eating disorders often are unrecognized and untreated,” Catherine Crone, MD, chair of the guideline writing group, said in a statement from APA. “This guideline and supplementary resources are intended to serve as a practical tool for clinicians, to help with screening, diagnosis, and providing evidence-based treatment for eating disorders.”
Approximately one in five children worldwide are at risk for developing an eating disorder and U.S. medical admissions for adolescents with restrictive eating disorders more than doubled during the pandemic.
The economic cost of eating disorders in the United States from 2018 to 2019 was an estimated $64.7 billion, the report notes, with an additional $326.5 billion attributable to reductions in well-being associated with eating disorders.
The executive summary of the updated guidelines was published online in The American Journal of Psychiatry.
The practice guideline, which was approved at the 2021 APA annual meeting, features 16 recommendations for clinicians, including screening patients for eating disorders as part of an initial psychiatric evaluation and conducting comprehensive patient evaluations that incorporate laboratory tests and electrocardiograms.
Recommendations also include setting individualized weight goals for patients with anorexia and incorporating family-based therapy as part of a treatment plan for adolescents with anorexia or bulimia.
“This practice guideline aims to help clinicians improve care for their patients by reviewing current evidence and providing evidence-based statements that are intended to enhance knowledge, increase assessment, and optimize treatment of eating disorders,” the authors wrote.
A range of other resources were released with the new guidelines to provide clinicians with support to implement the recommendations, including a pocket guide for clinicians, continuing medical education activities, and slides. The association is also launching a pocket guide for patients and families and an interactive tool kit with a screening assessment calculator.
The APA guidelines follow the 2021 release by the American Academy of Pediatrics on diagnosing and managing eating disorders in children and adolescents.
The development of the guidelines was supported by a grant from the Council of Medical Specialty Societies.
A version of this article first appeared on Medscape.com.
The updated guidelines focus primarily on anorexia nervosa (AN), bulimia nervosa (BN), and binge-eating disorder (BED) and include recommendations for screening and treatment.
“Eating disorders often are unrecognized and untreated,” Catherine Crone, MD, chair of the guideline writing group, said in a statement from APA. “This guideline and supplementary resources are intended to serve as a practical tool for clinicians, to help with screening, diagnosis, and providing evidence-based treatment for eating disorders.”
Approximately one in five children worldwide are at risk for developing an eating disorder and U.S. medical admissions for adolescents with restrictive eating disorders more than doubled during the pandemic.
The economic cost of eating disorders in the United States from 2018 to 2019 was an estimated $64.7 billion, the report notes, with an additional $326.5 billion attributable to reductions in well-being associated with eating disorders.
The executive summary of the updated guidelines was published online in The American Journal of Psychiatry.
The practice guideline, which was approved at the 2021 APA annual meeting, features 16 recommendations for clinicians, including screening patients for eating disorders as part of an initial psychiatric evaluation and conducting comprehensive patient evaluations that incorporate laboratory tests and electrocardiograms.
Recommendations also include setting individualized weight goals for patients with anorexia and incorporating family-based therapy as part of a treatment plan for adolescents with anorexia or bulimia.
“This practice guideline aims to help clinicians improve care for their patients by reviewing current evidence and providing evidence-based statements that are intended to enhance knowledge, increase assessment, and optimize treatment of eating disorders,” the authors wrote.
A range of other resources were released with the new guidelines to provide clinicians with support to implement the recommendations, including a pocket guide for clinicians, continuing medical education activities, and slides. The association is also launching a pocket guide for patients and families and an interactive tool kit with a screening assessment calculator.
The APA guidelines follow the 2021 release by the American Academy of Pediatrics on diagnosing and managing eating disorders in children and adolescents.
The development of the guidelines was supported by a grant from the Council of Medical Specialty Societies.
A version of this article first appeared on Medscape.com.
The updated guidelines focus primarily on anorexia nervosa (AN), bulimia nervosa (BN), and binge-eating disorder (BED) and include recommendations for screening and treatment.
“Eating disorders often are unrecognized and untreated,” Catherine Crone, MD, chair of the guideline writing group, said in a statement from APA. “This guideline and supplementary resources are intended to serve as a practical tool for clinicians, to help with screening, diagnosis, and providing evidence-based treatment for eating disorders.”
Approximately one in five children worldwide are at risk for developing an eating disorder and U.S. medical admissions for adolescents with restrictive eating disorders more than doubled during the pandemic.
The economic cost of eating disorders in the United States from 2018 to 2019 was an estimated $64.7 billion, the report notes, with an additional $326.5 billion attributable to reductions in well-being associated with eating disorders.
The executive summary of the updated guidelines was published online in The American Journal of Psychiatry.
The practice guideline, which was approved at the 2021 APA annual meeting, features 16 recommendations for clinicians, including screening patients for eating disorders as part of an initial psychiatric evaluation and conducting comprehensive patient evaluations that incorporate laboratory tests and electrocardiograms.
Recommendations also include setting individualized weight goals for patients with anorexia and incorporating family-based therapy as part of a treatment plan for adolescents with anorexia or bulimia.
“This practice guideline aims to help clinicians improve care for their patients by reviewing current evidence and providing evidence-based statements that are intended to enhance knowledge, increase assessment, and optimize treatment of eating disorders,” the authors wrote.
A range of other resources were released with the new guidelines to provide clinicians with support to implement the recommendations, including a pocket guide for clinicians, continuing medical education activities, and slides. The association is also launching a pocket guide for patients and families and an interactive tool kit with a screening assessment calculator.
The APA guidelines follow the 2021 release by the American Academy of Pediatrics on diagnosing and managing eating disorders in children and adolescents.
The development of the guidelines was supported by a grant from the Council of Medical Specialty Societies.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF PSYCHIATRY
Specialty and age may contribute to suicidal thoughts among physicians
A physician’s specialty can make a difference when it comes to having suicidal thoughts. Doctors who specialize in family medicine, obstetrics-gynecology, and psychiatry reported double the rates of suicidal thoughts than doctors in oncology, rheumatology, and pulmonary medicine, according to Doctors’ Burden: Medscape Physician Suicide Report 2023.
“The specialties with the highest reporting of physician suicidal thoughts are also those with the greatest physician shortages, based on the number of job openings posted by recruiting sites,” said Peter Yellowlees, MD, professor of psychiatry and chief wellness officer at UC Davis Health.
Doctors in those specialties are overworked, which can lead to burnout, he said.
There’s also a generational divide among physicians who reported suicidal thoughts. Millennials (age 27-41) and Gen-X physicians (age 42-56) were more likely to report these thoughts than were Baby Boomers (age 57-75) and the Silent Generation (age 76-95).
“Younger physicians are more burned out – they may have less control over their lives and less meaning than some older doctors who can do what they want,” said Dr. Yellowlees.
One millennial respondent commented that being on call and being required to chart detailed notes in the EHR has contributed to her burnout. “I’m more impatient and make less time and effort to see my friends and family.”
One Silent Generation respondent commented, “I am semi-retired, I take no call, I work no weekends, I provide anesthesia care in my area of special expertise, I work clinically about 46 days a year. Life is good, particularly compared to my younger colleagues who are working 60-plus hours a week with evening work, weekend work, and call. I feel really sorry for them.”
When young people enter medical school, they’re quite healthy, with low rates of depression and burnout, said Dr. Yellowlees. Yet, studies have shown that rates of burnout and suicidal thoughts increased within 2 years. “That reflects what happens when a group of idealistic young people hit a horrible system,” he said.
Who’s responsible?
Millennials were three times as likely as baby boomers to say that a medical school or health care organization should be responsible when a student or physician commits suicide.
“Young physicians may expect more of their employers than my generation did, which we see in residency programs that have unionized,” said Dr. Yellowlees, a Baby Boomer.
“As more young doctors are employed by health care organizations, they also may expect more resources to be available to them, such as wellness programs,” he added.
Younger doctors also focus more on work-life balance than older doctors, including time off and having hobbies, he said. “They are much more rational in terms of their overall beliefs and expectations than the older generation.”
Whom doctors confide in
Nearly 60% of physician-respondents with suicidal thoughts said they confided in a professional or someone they knew. Men were just as likely as women to reach out to a therapist (38%), whereas men were slightly more likely to confide in a family member and women were slightly more likely to confide in a colleague.
“It’s interesting that women are more active in seeking support at work – they often have developed a network of colleagues to support each other’s careers and whom they can confide in,” said Dr. Yellowlees.
He emphasized that 40% of physicians said they didn’t confide in anyone when they had suicidal thoughts. Of those, just over half said they could cope without professional help.
One respondent commented, “It’s just a thought; nothing I would actually do.” Another commented, “Mental health professionals can’t fix the underlying reason for the problem.”
Many doctors were concerned about risking disclosure to their medical boards (42%); that it would show up on their insurance records (33%); and that their colleagues would find out (25%), according to the report.
One respondent commented, “I don’t trust doctors to keep it to themselves.”
Another barrier doctors mentioned was a lack of time to seek help. One commented, “Time. I have none, when am I supposed to find an hour for counseling?”
A version of this article originally appeared on Medscape.com.
A physician’s specialty can make a difference when it comes to having suicidal thoughts. Doctors who specialize in family medicine, obstetrics-gynecology, and psychiatry reported double the rates of suicidal thoughts than doctors in oncology, rheumatology, and pulmonary medicine, according to Doctors’ Burden: Medscape Physician Suicide Report 2023.
“The specialties with the highest reporting of physician suicidal thoughts are also those with the greatest physician shortages, based on the number of job openings posted by recruiting sites,” said Peter Yellowlees, MD, professor of psychiatry and chief wellness officer at UC Davis Health.
Doctors in those specialties are overworked, which can lead to burnout, he said.
There’s also a generational divide among physicians who reported suicidal thoughts. Millennials (age 27-41) and Gen-X physicians (age 42-56) were more likely to report these thoughts than were Baby Boomers (age 57-75) and the Silent Generation (age 76-95).
“Younger physicians are more burned out – they may have less control over their lives and less meaning than some older doctors who can do what they want,” said Dr. Yellowlees.
One millennial respondent commented that being on call and being required to chart detailed notes in the EHR has contributed to her burnout. “I’m more impatient and make less time and effort to see my friends and family.”
One Silent Generation respondent commented, “I am semi-retired, I take no call, I work no weekends, I provide anesthesia care in my area of special expertise, I work clinically about 46 days a year. Life is good, particularly compared to my younger colleagues who are working 60-plus hours a week with evening work, weekend work, and call. I feel really sorry for them.”
When young people enter medical school, they’re quite healthy, with low rates of depression and burnout, said Dr. Yellowlees. Yet, studies have shown that rates of burnout and suicidal thoughts increased within 2 years. “That reflects what happens when a group of idealistic young people hit a horrible system,” he said.
Who’s responsible?
Millennials were three times as likely as baby boomers to say that a medical school or health care organization should be responsible when a student or physician commits suicide.
“Young physicians may expect more of their employers than my generation did, which we see in residency programs that have unionized,” said Dr. Yellowlees, a Baby Boomer.
“As more young doctors are employed by health care organizations, they also may expect more resources to be available to them, such as wellness programs,” he added.
Younger doctors also focus more on work-life balance than older doctors, including time off and having hobbies, he said. “They are much more rational in terms of their overall beliefs and expectations than the older generation.”
Whom doctors confide in
Nearly 60% of physician-respondents with suicidal thoughts said they confided in a professional or someone they knew. Men were just as likely as women to reach out to a therapist (38%), whereas men were slightly more likely to confide in a family member and women were slightly more likely to confide in a colleague.
“It’s interesting that women are more active in seeking support at work – they often have developed a network of colleagues to support each other’s careers and whom they can confide in,” said Dr. Yellowlees.
He emphasized that 40% of physicians said they didn’t confide in anyone when they had suicidal thoughts. Of those, just over half said they could cope without professional help.
One respondent commented, “It’s just a thought; nothing I would actually do.” Another commented, “Mental health professionals can’t fix the underlying reason for the problem.”
Many doctors were concerned about risking disclosure to their medical boards (42%); that it would show up on their insurance records (33%); and that their colleagues would find out (25%), according to the report.
One respondent commented, “I don’t trust doctors to keep it to themselves.”
Another barrier doctors mentioned was a lack of time to seek help. One commented, “Time. I have none, when am I supposed to find an hour for counseling?”
A version of this article originally appeared on Medscape.com.
A physician’s specialty can make a difference when it comes to having suicidal thoughts. Doctors who specialize in family medicine, obstetrics-gynecology, and psychiatry reported double the rates of suicidal thoughts than doctors in oncology, rheumatology, and pulmonary medicine, according to Doctors’ Burden: Medscape Physician Suicide Report 2023.
“The specialties with the highest reporting of physician suicidal thoughts are also those with the greatest physician shortages, based on the number of job openings posted by recruiting sites,” said Peter Yellowlees, MD, professor of psychiatry and chief wellness officer at UC Davis Health.
Doctors in those specialties are overworked, which can lead to burnout, he said.
There’s also a generational divide among physicians who reported suicidal thoughts. Millennials (age 27-41) and Gen-X physicians (age 42-56) were more likely to report these thoughts than were Baby Boomers (age 57-75) and the Silent Generation (age 76-95).
“Younger physicians are more burned out – they may have less control over their lives and less meaning than some older doctors who can do what they want,” said Dr. Yellowlees.
One millennial respondent commented that being on call and being required to chart detailed notes in the EHR has contributed to her burnout. “I’m more impatient and make less time and effort to see my friends and family.”
One Silent Generation respondent commented, “I am semi-retired, I take no call, I work no weekends, I provide anesthesia care in my area of special expertise, I work clinically about 46 days a year. Life is good, particularly compared to my younger colleagues who are working 60-plus hours a week with evening work, weekend work, and call. I feel really sorry for them.”
When young people enter medical school, they’re quite healthy, with low rates of depression and burnout, said Dr. Yellowlees. Yet, studies have shown that rates of burnout and suicidal thoughts increased within 2 years. “That reflects what happens when a group of idealistic young people hit a horrible system,” he said.
Who’s responsible?
Millennials were three times as likely as baby boomers to say that a medical school or health care organization should be responsible when a student or physician commits suicide.
“Young physicians may expect more of their employers than my generation did, which we see in residency programs that have unionized,” said Dr. Yellowlees, a Baby Boomer.
“As more young doctors are employed by health care organizations, they also may expect more resources to be available to them, such as wellness programs,” he added.
Younger doctors also focus more on work-life balance than older doctors, including time off and having hobbies, he said. “They are much more rational in terms of their overall beliefs and expectations than the older generation.”
Whom doctors confide in
Nearly 60% of physician-respondents with suicidal thoughts said they confided in a professional or someone they knew. Men were just as likely as women to reach out to a therapist (38%), whereas men were slightly more likely to confide in a family member and women were slightly more likely to confide in a colleague.
“It’s interesting that women are more active in seeking support at work – they often have developed a network of colleagues to support each other’s careers and whom they can confide in,” said Dr. Yellowlees.
He emphasized that 40% of physicians said they didn’t confide in anyone when they had suicidal thoughts. Of those, just over half said they could cope without professional help.
One respondent commented, “It’s just a thought; nothing I would actually do.” Another commented, “Mental health professionals can’t fix the underlying reason for the problem.”
Many doctors were concerned about risking disclosure to their medical boards (42%); that it would show up on their insurance records (33%); and that their colleagues would find out (25%), according to the report.
One respondent commented, “I don’t trust doctors to keep it to themselves.”
Another barrier doctors mentioned was a lack of time to seek help. One commented, “Time. I have none, when am I supposed to find an hour for counseling?”
A version of this article originally appeared on Medscape.com.
Black people are less likely to receive dementia meds
, preliminary data from a retrospective study show.
“There have been disparities regarding the use of cognition-enhancing medications in the treatment of dementia described in the literature, and disparities in the use of adjunctive treatments for other neuropsychiatric symptoms of dementia described in hospital and nursing home settings,” said study investigator Alice Hawkins, MD, with the department of neurology, Icahn School of Medicine at Mount Sinai, New York. “However, less is known about use of dementia medications that people take at home. Our study found disparities in this area as well,” Dr. Hawkins said.
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology.
More research needed
The researchers analyzed data on 3,655 Black and 12,885 White patients with a diagnosis of dementia who were seen at Mount Sinai. They evaluated utilization of five medication classes:
- cholinesterase inhibitors.
- N-methyl D-aspartate (NMDA) receptor antagonists.
- selective serotonin reuptake inhibitors (SSRIs).
- antipsychotics.
- benzodiazepines.
They found that Black patients with dementia received cognitive enhancers less often than White patients with dementia (20% vs. 30% for cholinesterase inhibitors; 10% vs. 17% for NMDA antagonists).
Black patients with dementia were also less likely to receive medications for behavioral and psychological symptom management, compared with White peers (24% vs. 40% for SSRIs; 18% vs. 22% for antipsychotics; and 18% vs. 37% for benzodiazepines).
These disparities remained even after controlling for factors such as demographics and insurance coverage.
“Larger systemic forces such as systemic racism, quality of care, and provider bias are harder to pin down, particularly in the medical record, though they all may be playing a role in perpetuating these inequities. More research will be needed to pinpoint all the factors that are contributing to these disparities,” said Dr. Hawkins.
The researchers found Black patients who were referred to a neurologist received cholinesterase inhibitors and NMDA antagonists at rates comparable with White patients. “Therefore, referrals to specialists such as neurologists may decrease the disparities for these prescriptions,” Dr. Hawkins said.
Crucial research
Commenting on the findings, Carl V. Hill, PhD, MPH, Alzheimer’s Association chief diversity, equity, and inclusion officer, said the study “adds to previous research that points to inequities in the administering of medications for dementia symptoms, and highlights the inequities we know exist in dementia care.”
“Cognitive enhancers and other behavioral/psychological management drugs, while they don’t stop, slow, or cure dementia, can offer relief for some of the challenging symptoms associated with diseases caused by dementia. If people aren’t being appropriately prescribed medications that may offer symptom relief from this challenging disease, it could lead to poorer health outcomes,” said Dr. Hill.
“These data underscore the importance of health disparities research that is crucial in uncovering inequities in dementia treatment, care, and research for Black individuals, as well as all underrepresented populations.
“We must create a society in which the underserved, disproportionately affected, and underrepresented are safe, cared for, and valued. This can be done through enhancing cultural competence in health care settings, improving representation within the health care system, and engaging and building trust with diverse communities,” Dr. Hill said.
The Alzheimer’s Association has partnered with more than 500 diverse community-based groups on disease education programs to ensure families have information and resources to navigate this devastating disease.
The study was supported by the American Academy of Neurology Resident Research Scholarship. Dr. Hawkins and Dr. Hill reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, preliminary data from a retrospective study show.
“There have been disparities regarding the use of cognition-enhancing medications in the treatment of dementia described in the literature, and disparities in the use of adjunctive treatments for other neuropsychiatric symptoms of dementia described in hospital and nursing home settings,” said study investigator Alice Hawkins, MD, with the department of neurology, Icahn School of Medicine at Mount Sinai, New York. “However, less is known about use of dementia medications that people take at home. Our study found disparities in this area as well,” Dr. Hawkins said.
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology.
More research needed
The researchers analyzed data on 3,655 Black and 12,885 White patients with a diagnosis of dementia who were seen at Mount Sinai. They evaluated utilization of five medication classes:
- cholinesterase inhibitors.
- N-methyl D-aspartate (NMDA) receptor antagonists.
- selective serotonin reuptake inhibitors (SSRIs).
- antipsychotics.
- benzodiazepines.
They found that Black patients with dementia received cognitive enhancers less often than White patients with dementia (20% vs. 30% for cholinesterase inhibitors; 10% vs. 17% for NMDA antagonists).
Black patients with dementia were also less likely to receive medications for behavioral and psychological symptom management, compared with White peers (24% vs. 40% for SSRIs; 18% vs. 22% for antipsychotics; and 18% vs. 37% for benzodiazepines).
These disparities remained even after controlling for factors such as demographics and insurance coverage.
“Larger systemic forces such as systemic racism, quality of care, and provider bias are harder to pin down, particularly in the medical record, though they all may be playing a role in perpetuating these inequities. More research will be needed to pinpoint all the factors that are contributing to these disparities,” said Dr. Hawkins.
The researchers found Black patients who were referred to a neurologist received cholinesterase inhibitors and NMDA antagonists at rates comparable with White patients. “Therefore, referrals to specialists such as neurologists may decrease the disparities for these prescriptions,” Dr. Hawkins said.
Crucial research
Commenting on the findings, Carl V. Hill, PhD, MPH, Alzheimer’s Association chief diversity, equity, and inclusion officer, said the study “adds to previous research that points to inequities in the administering of medications for dementia symptoms, and highlights the inequities we know exist in dementia care.”
“Cognitive enhancers and other behavioral/psychological management drugs, while they don’t stop, slow, or cure dementia, can offer relief for some of the challenging symptoms associated with diseases caused by dementia. If people aren’t being appropriately prescribed medications that may offer symptom relief from this challenging disease, it could lead to poorer health outcomes,” said Dr. Hill.
“These data underscore the importance of health disparities research that is crucial in uncovering inequities in dementia treatment, care, and research for Black individuals, as well as all underrepresented populations.
“We must create a society in which the underserved, disproportionately affected, and underrepresented are safe, cared for, and valued. This can be done through enhancing cultural competence in health care settings, improving representation within the health care system, and engaging and building trust with diverse communities,” Dr. Hill said.
The Alzheimer’s Association has partnered with more than 500 diverse community-based groups on disease education programs to ensure families have information and resources to navigate this devastating disease.
The study was supported by the American Academy of Neurology Resident Research Scholarship. Dr. Hawkins and Dr. Hill reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, preliminary data from a retrospective study show.
“There have been disparities regarding the use of cognition-enhancing medications in the treatment of dementia described in the literature, and disparities in the use of adjunctive treatments for other neuropsychiatric symptoms of dementia described in hospital and nursing home settings,” said study investigator Alice Hawkins, MD, with the department of neurology, Icahn School of Medicine at Mount Sinai, New York. “However, less is known about use of dementia medications that people take at home. Our study found disparities in this area as well,” Dr. Hawkins said.
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology.
More research needed
The researchers analyzed data on 3,655 Black and 12,885 White patients with a diagnosis of dementia who were seen at Mount Sinai. They evaluated utilization of five medication classes:
- cholinesterase inhibitors.
- N-methyl D-aspartate (NMDA) receptor antagonists.
- selective serotonin reuptake inhibitors (SSRIs).
- antipsychotics.
- benzodiazepines.
They found that Black patients with dementia received cognitive enhancers less often than White patients with dementia (20% vs. 30% for cholinesterase inhibitors; 10% vs. 17% for NMDA antagonists).
Black patients with dementia were also less likely to receive medications for behavioral and psychological symptom management, compared with White peers (24% vs. 40% for SSRIs; 18% vs. 22% for antipsychotics; and 18% vs. 37% for benzodiazepines).
These disparities remained even after controlling for factors such as demographics and insurance coverage.
“Larger systemic forces such as systemic racism, quality of care, and provider bias are harder to pin down, particularly in the medical record, though they all may be playing a role in perpetuating these inequities. More research will be needed to pinpoint all the factors that are contributing to these disparities,” said Dr. Hawkins.
The researchers found Black patients who were referred to a neurologist received cholinesterase inhibitors and NMDA antagonists at rates comparable with White patients. “Therefore, referrals to specialists such as neurologists may decrease the disparities for these prescriptions,” Dr. Hawkins said.
Crucial research
Commenting on the findings, Carl V. Hill, PhD, MPH, Alzheimer’s Association chief diversity, equity, and inclusion officer, said the study “adds to previous research that points to inequities in the administering of medications for dementia symptoms, and highlights the inequities we know exist in dementia care.”
“Cognitive enhancers and other behavioral/psychological management drugs, while they don’t stop, slow, or cure dementia, can offer relief for some of the challenging symptoms associated with diseases caused by dementia. If people aren’t being appropriately prescribed medications that may offer symptom relief from this challenging disease, it could lead to poorer health outcomes,” said Dr. Hill.
“These data underscore the importance of health disparities research that is crucial in uncovering inequities in dementia treatment, care, and research for Black individuals, as well as all underrepresented populations.
“We must create a society in which the underserved, disproportionately affected, and underrepresented are safe, cared for, and valued. This can be done through enhancing cultural competence in health care settings, improving representation within the health care system, and engaging and building trust with diverse communities,” Dr. Hill said.
The Alzheimer’s Association has partnered with more than 500 diverse community-based groups on disease education programs to ensure families have information and resources to navigate this devastating disease.
The study was supported by the American Academy of Neurology Resident Research Scholarship. Dr. Hawkins and Dr. Hill reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Mental health risks higher among young people with IBD
, a new U.K. study suggests.
The retrospective, observational study of young people with IBD versus those without assessed the incidence of a wide range of mental health conditions in people aged 5-25 years.
“Anxiety and depression will not be a surprise to most of us. But we also saw changes for eating disorders, PTSD, and sleep changes,” said Richard K. Russell, MD, a pediatric gastroenterologist at the Royal Hospital for Sick Children, Edinburgh.
Dr. Russell presented the research at the annual congress of the European Crohn’s and Colitis Organisation, held in Copenhagen and virtually.
The findings indicate an unmet need for mental health care for young patients with IBD, he said. “All of us at ECCO need to address this gap.”
Key findings
Dr. Russell and colleagues identified 3,898 young people diagnosed with IBD in the 10-year period Jan. 1, 2010, through Jan. 1, 2020, using the Optimum Patient Care Research Database, which includes de-identified data from more than 1,000 general practices across the United Kingdom. They used propensity score matching to create a control group of 15,571 people without IBD, controlling for age, sex, socioeconomic status, ethnicity, and health conditions other than IBD.
Median follow-up was about 3 years.
The cumulative lifetime risk for developing any mental health condition by age 25 was 31.1% in the IBD group versus 25.1% in controls, a statistically significant difference.
Compared with the control group, the people with incident IBD were significantly more likely to develop the following:
- PTSD.
- Eating disorders.
- Self-harm.
- Sleep disturbance.
- Depression.
- Anxiety disorder.
- ‘Any mental health condition.’
Those most are risk included males overall, and specifically boys aged 12-17 years. Those with Crohn’s disease versus other types of IBD were also most at risk.
In a subgroup analysis, presented as a poster at the meeting, Dr. Russell and colleagues also found that mental health comorbidity in children and young adults with IBD is associated with increased IBD symptoms and health care utilization, as well as time off work.
Children and young adults with both IBD and mental health conditions should be monitored and receive appropriate mental health support as part of their multidisciplinary care, Dr. Russell said.
Dr. Russell added that the study period ended a few months before the COVID-19 pandemic began, so the research does not reflect its impact on mental health in the study population.
“The number of children and young adults we’re seeing in our clinic with mental health issues has rocketed through the roof because of the pandemic,” he said.
Dr. Russell suggested that the organization create a psychology subgroup called Proactive Psychologists of ECCO, or Prosecco for short.
Clinical implications
The study is important for highlighting the increased burden of mental health problems in young people with IBD, said session comoderator Nick Kennedy, MD, a consultant gastroenterologist and chief research information officer with the Royal Devon University Healthcare NHS Foundation Trust in England.
Dr. Kennedy, who was not affiliated with the research, is also supportive of the idea of a psychological subgroup within ECCO.
The peak age for developing mental health disorders found by the study (12-17 years) “is a unique and very sensitive time,” said Sara Mesilhy, MBBS, a gastroenterologist with the Royal College of Physicians in London.
“These results highlight the need for development of early screening psychiatric programs starting from time of diagnosis and continuing on periodic intervals to offer the best management plan for IBD patients, especially those with childhood-onset IBD,” said Dr. Mesilhy, who was not affiliated with the research.
Such programs would “improve the patient’s quality of life, protecting them from a lot of suffering and preventing the bad sequelae for these disorders,” said Dr. Mesilhy. “Moreover, we still need further studies to identify the most efficient monitoring and treatment protocols.”
Dr. Kennedy applauded the researchers for conducting a population-based study because it ensured an adequate cohort size and maximized identification of mental health disorders.
“It was interesting to see that there were a range of conditions where risk was increased, and that males with IBD were at particularly increased risk,” he added.
Researchers’ use of coded primary care data was a study limitation, but it was “appropriately acknowledged by the presenter,” Dr. Kennedy said.
The study was supported by Pfizer. Dr. Russell disclosed he is a consultant and member of a speakers’ bureau for Pfizer outside the submitted work. Dr. Kennedy and Dr. Mesilhy report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, a new U.K. study suggests.
The retrospective, observational study of young people with IBD versus those without assessed the incidence of a wide range of mental health conditions in people aged 5-25 years.
“Anxiety and depression will not be a surprise to most of us. But we also saw changes for eating disorders, PTSD, and sleep changes,” said Richard K. Russell, MD, a pediatric gastroenterologist at the Royal Hospital for Sick Children, Edinburgh.
Dr. Russell presented the research at the annual congress of the European Crohn’s and Colitis Organisation, held in Copenhagen and virtually.
The findings indicate an unmet need for mental health care for young patients with IBD, he said. “All of us at ECCO need to address this gap.”
Key findings
Dr. Russell and colleagues identified 3,898 young people diagnosed with IBD in the 10-year period Jan. 1, 2010, through Jan. 1, 2020, using the Optimum Patient Care Research Database, which includes de-identified data from more than 1,000 general practices across the United Kingdom. They used propensity score matching to create a control group of 15,571 people without IBD, controlling for age, sex, socioeconomic status, ethnicity, and health conditions other than IBD.
Median follow-up was about 3 years.
The cumulative lifetime risk for developing any mental health condition by age 25 was 31.1% in the IBD group versus 25.1% in controls, a statistically significant difference.
Compared with the control group, the people with incident IBD were significantly more likely to develop the following:
- PTSD.
- Eating disorders.
- Self-harm.
- Sleep disturbance.
- Depression.
- Anxiety disorder.
- ‘Any mental health condition.’
Those most are risk included males overall, and specifically boys aged 12-17 years. Those with Crohn’s disease versus other types of IBD were also most at risk.
In a subgroup analysis, presented as a poster at the meeting, Dr. Russell and colleagues also found that mental health comorbidity in children and young adults with IBD is associated with increased IBD symptoms and health care utilization, as well as time off work.
Children and young adults with both IBD and mental health conditions should be monitored and receive appropriate mental health support as part of their multidisciplinary care, Dr. Russell said.
Dr. Russell added that the study period ended a few months before the COVID-19 pandemic began, so the research does not reflect its impact on mental health in the study population.
“The number of children and young adults we’re seeing in our clinic with mental health issues has rocketed through the roof because of the pandemic,” he said.
Dr. Russell suggested that the organization create a psychology subgroup called Proactive Psychologists of ECCO, or Prosecco for short.
Clinical implications
The study is important for highlighting the increased burden of mental health problems in young people with IBD, said session comoderator Nick Kennedy, MD, a consultant gastroenterologist and chief research information officer with the Royal Devon University Healthcare NHS Foundation Trust in England.
Dr. Kennedy, who was not affiliated with the research, is also supportive of the idea of a psychological subgroup within ECCO.
The peak age for developing mental health disorders found by the study (12-17 years) “is a unique and very sensitive time,” said Sara Mesilhy, MBBS, a gastroenterologist with the Royal College of Physicians in London.
“These results highlight the need for development of early screening psychiatric programs starting from time of diagnosis and continuing on periodic intervals to offer the best management plan for IBD patients, especially those with childhood-onset IBD,” said Dr. Mesilhy, who was not affiliated with the research.
Such programs would “improve the patient’s quality of life, protecting them from a lot of suffering and preventing the bad sequelae for these disorders,” said Dr. Mesilhy. “Moreover, we still need further studies to identify the most efficient monitoring and treatment protocols.”
Dr. Kennedy applauded the researchers for conducting a population-based study because it ensured an adequate cohort size and maximized identification of mental health disorders.
“It was interesting to see that there were a range of conditions where risk was increased, and that males with IBD were at particularly increased risk,” he added.
Researchers’ use of coded primary care data was a study limitation, but it was “appropriately acknowledged by the presenter,” Dr. Kennedy said.
The study was supported by Pfizer. Dr. Russell disclosed he is a consultant and member of a speakers’ bureau for Pfizer outside the submitted work. Dr. Kennedy and Dr. Mesilhy report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, a new U.K. study suggests.
The retrospective, observational study of young people with IBD versus those without assessed the incidence of a wide range of mental health conditions in people aged 5-25 years.
“Anxiety and depression will not be a surprise to most of us. But we also saw changes for eating disorders, PTSD, and sleep changes,” said Richard K. Russell, MD, a pediatric gastroenterologist at the Royal Hospital for Sick Children, Edinburgh.
Dr. Russell presented the research at the annual congress of the European Crohn’s and Colitis Organisation, held in Copenhagen and virtually.
The findings indicate an unmet need for mental health care for young patients with IBD, he said. “All of us at ECCO need to address this gap.”
Key findings
Dr. Russell and colleagues identified 3,898 young people diagnosed with IBD in the 10-year period Jan. 1, 2010, through Jan. 1, 2020, using the Optimum Patient Care Research Database, which includes de-identified data from more than 1,000 general practices across the United Kingdom. They used propensity score matching to create a control group of 15,571 people without IBD, controlling for age, sex, socioeconomic status, ethnicity, and health conditions other than IBD.
Median follow-up was about 3 years.
The cumulative lifetime risk for developing any mental health condition by age 25 was 31.1% in the IBD group versus 25.1% in controls, a statistically significant difference.
Compared with the control group, the people with incident IBD were significantly more likely to develop the following:
- PTSD.
- Eating disorders.
- Self-harm.
- Sleep disturbance.
- Depression.
- Anxiety disorder.
- ‘Any mental health condition.’
Those most are risk included males overall, and specifically boys aged 12-17 years. Those with Crohn’s disease versus other types of IBD were also most at risk.
In a subgroup analysis, presented as a poster at the meeting, Dr. Russell and colleagues also found that mental health comorbidity in children and young adults with IBD is associated with increased IBD symptoms and health care utilization, as well as time off work.
Children and young adults with both IBD and mental health conditions should be monitored and receive appropriate mental health support as part of their multidisciplinary care, Dr. Russell said.
Dr. Russell added that the study period ended a few months before the COVID-19 pandemic began, so the research does not reflect its impact on mental health in the study population.
“The number of children and young adults we’re seeing in our clinic with mental health issues has rocketed through the roof because of the pandemic,” he said.
Dr. Russell suggested that the organization create a psychology subgroup called Proactive Psychologists of ECCO, or Prosecco for short.
Clinical implications
The study is important for highlighting the increased burden of mental health problems in young people with IBD, said session comoderator Nick Kennedy, MD, a consultant gastroenterologist and chief research information officer with the Royal Devon University Healthcare NHS Foundation Trust in England.
Dr. Kennedy, who was not affiliated with the research, is also supportive of the idea of a psychological subgroup within ECCO.
The peak age for developing mental health disorders found by the study (12-17 years) “is a unique and very sensitive time,” said Sara Mesilhy, MBBS, a gastroenterologist with the Royal College of Physicians in London.
“These results highlight the need for development of early screening psychiatric programs starting from time of diagnosis and continuing on periodic intervals to offer the best management plan for IBD patients, especially those with childhood-onset IBD,” said Dr. Mesilhy, who was not affiliated with the research.
Such programs would “improve the patient’s quality of life, protecting them from a lot of suffering and preventing the bad sequelae for these disorders,” said Dr. Mesilhy. “Moreover, we still need further studies to identify the most efficient monitoring and treatment protocols.”
Dr. Kennedy applauded the researchers for conducting a population-based study because it ensured an adequate cohort size and maximized identification of mental health disorders.
“It was interesting to see that there were a range of conditions where risk was increased, and that males with IBD were at particularly increased risk,” he added.
Researchers’ use of coded primary care data was a study limitation, but it was “appropriately acknowledged by the presenter,” Dr. Kennedy said.
The study was supported by Pfizer. Dr. Russell disclosed he is a consultant and member of a speakers’ bureau for Pfizer outside the submitted work. Dr. Kennedy and Dr. Mesilhy report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ECCO 2023