User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Were these true medical miracles? Doctors disagree
It was a freezing December day, and two young brothers were playing outside near a swimming pool when the younger boy, a 3-year-old toddler, fell into the water.
The 7-year-old immediately jumped into the pool to save his brother and was able to pull the toddler to the pool steps where the boy’s head was above water. But the icy temperatures overcame the older brother and he drifted underwater.
“Despite being at the forefront of medicine, what we don’t understand often exceeds what we do understand,” said Harley Rotbart, MD, author of “Miracles We Have Seen” (Health Communications: Deerfield Beach, Fla., 2016).
Paramedics arrived to find both boys unconscious and rushed them to the Children’s Hospital of Philadelphia. The younger boy regained consciousness in the ICU and recovered. The 7-year-old, however, was unresponsive and remained in a coma, said Dr. Rotbart a pediatrician and author based in Denver.
Family members stayed at the boy’s bedside and prayed. But after several weeks, the child’s condition remained unchanged. His parents began to discuss ending life support and organ donation. Then late one night, as Dr. Rotbart sat reading to the unconscious patient, the little boy squeezed his hand. In disbelief, Dr. Rotbart told all of his colleagues about the squeeze the next morning. Everyone attributed the movement to an involuntary muscle spasm, he said. After all, every test and scan showed the boy had no brain function.
But later that day, the child grasped another staff member’s hand. Shortly after that, he squeezed in response to a command. Dr. Rotbart and his staff were stunned, but cautious about feeling too much hope.
Days later, the child opened his eyes. Then, he smiled. His parents were overjoyed.
“When he walked out of the hospital more than 2 months after the near-drowning and his heroic rescue of his little brother, we all cheered and cried,” Dr. Rotbart wrote in his book. “We cried many times in the weeks preceding, and I still cry whenever I recall this story.”
The experience, which happened years ago when Dr. Rotbart was a trainee, has stayed with the pediatrician his entire career.
“His awakening was seemingly impossible – and then it happened,” Dr. Rotbart said. “Despite being at the forefront of medicine and science, what we don’t understand often exceeds what we do understand. And even when we think we understand, we are frequently proven wrong.”
For many, Dr. Rotbart’s experience raises questions about the existence of medical miracles.
Do physicians believe in medical miracles? The answers are diverse.
“I have no doubt that extraordinary outcomes happen where patients who are overwhelmingly expected not to survive, do,” says Eric Beam, MD, a hospitalist based in San Diego. “That’s one of the reasons we choose our words very carefully in our conversations with patients and their families and remember that nothing is 0%, and nothing is 100%. But doctors tend to treat situations that are 99.9% as absolute. I don’t think you can practice medicine with the hope or expectation that every case you see has the potential to beat the odds – or be a medical miracle.”
Disappearing cancer hailed as ‘miracle’
In 2003, physicians projected that Joseph Rick, 40, had just a few months to live. His mucosal melanoma had spread throughout his body, progressing even after several surgeries, radiation therapy, and a combination of chemotherapy agents, recalled Antoni Ribas, MD, PhD, an oncologist and director of the tumor immunology program at Jonsson Comprehensive Cancer Center in Los Angeles.
Mr. Rick’s melanoma had spread to his intestines with traces on his stomach and bladder. Tumors were present on his liver, lungs, and pancreas. Rick bought a grave and prepared for the worst, he recounted in a Cancer Research Institute video. But his fate took a turn when he enrolled in an experimental drug trial in December 2003. The phase 1 trial was for a new immune modulating antibody, called an anti–CTLA-4 antibody, said Dr. Ribas, who conducted the trial.
Over the next few weeks and months, all areas of Rick’s melanoma metastases disappeared. By 2009, he was in remission. He has lived the rest of his life with no evidence of melanoma, according to Dr. Ribas.
Mr. Rick’s case has been referenced throughout literature and news stories as a “medical miracle” and a “cancer miracle.”
Does Dr. Ribas think the case was a medical miracle?
“The response in Joseph Rick was what happened in 10%-15% of patients who received anti-CTLA-4 therapy,” Dr. Ribas said. “These were not miracles. These patients responded because their immune system trying to attack the cancer had been stuck at the CTLA-4 checkpoint. Blocking this checkpoint allowed their immune system to proceed to attack and kill cancer cells anywhere in the body.”
The scientific basis of this therapy was work by University of Texas MD Anderson Cancer Center immunologist James Allison, PhD, that had been done 5 years earlier in mouse models, where giving an anti–CTLA-4 antibody to mice allowed them to reject several implanted cancers, Dr. Ribas explained. Dr. Allison received the 2018 Nobel Prize in Physiology or Medicine for this work, subsequently opening the door for what we now call “immune checkpoint blockade therapy for cancer.” Dr. Ribas added.
“We tend to call miracles good things that we do not understand how they happened,” Dr. Ribas said. “From the human observation perspective, there have been plenty of medical miracles. However, each one has a specific biological mechanism that led to improvement in a patient. In cancer treatment, early studies using the immune system resulted in occasional patients having tumor responses and long-term benefits.
“With the increased understanding of how the immune system interacts with cancers, which is based on remarkable progress in understanding how the immune system works generated over the past several decades, these ‘miracles’ become specific mechanisms leading to response to cancer, which can then be replicated in other patients.”
Patient defies odds after 45 minutes without heartbeat
Florida ob.gyn. Michael Fleischer, MD, had just performed a routine repeat cesarean birth, delivering a healthy baby girl. His patient, Ruby, had a history of high blood pressure but medication taken during the pregnancy had kept her levels stabilized.
In the waiting room, Dr. Fleischer informed Ruby’s large family of the good news. He was planning to head home early that day when he heard his name being called over the hospital’s loudspeaker. Ruby had stopped breathing.
“The anesthesiologist was with her and had immediately intubated her,” Dr. Fleischer said. “We checked to make sure there was no problems or bleeding from the C-section, but everything was completely fine. However, we couldn’t keep her blood pressure stable.”
Dr. Fleischer suspected the respiratory arrest was caused by either an amniotic fluid embolism or a pulmonary embolism. Intubation continued and physicians gave Ruby medication to stabilize her blood pressure. Then suddenly, Ruby’s heart stopped.
Dr. Fleischer and other doctors began compressions, which they continued for 30 minutes. They shocked Ruby with defibrillator paddles multiple times, but there was no change.
“I was already thinking, this is hopeless, there’s nothing we can do,” he said. “The writing is on the wall. She’s going to die.”
Dr. Fleischer spoke to Ruby’s family and explained the tragic turn of events. Relatives were distraught and tearfully visited Ruby to say their goodbyes. They prayed and cried. Eventually, physicians ceased compressions. Ruby had gone 45 minutes without a pulse. The EKG was still showing some irregularity, FDr. leischer said, but no rhythm. Physicians kept Ruby intubated as they waited for the background electrical activity to fade. As they watched the screen in anguish, there was suddenly a blip on the heart rate monitor. Then another and another. Within seconds, Ruby’s heart went back into sinus rhythm.
“We were in disbelief,” Dr. Fleischer said. “We did some tests and put her in the ICU, and she was fine. Usually, after doing compressions on anyone, you’d have bruising or broken ribs. She had nothing. She just woke up and said: ‘What am I doing here? Let me go see my baby.’ ”
Ruby fully recovered, and 3 days later, she went home with her newborn.
While the recovery was unbelievable, Dr. Fleischer stopped short of calling it a medical miracle. There were scientific contributors to her survival: she was immediately intubated when she stopped breathing and compressions were started as soon as her heart stopped.
However, Dr. Fleischer said the fact that lifesaving measures had ended, and Ruby revived on her own was indeed, miraculous.
“It wasn’t like we were doing compressions and brought her back,” he said. “I can scientifically explain things in my mind, except for that. That when we finally stopped and took our hands off her, that’s when something changed. That’s when she came back.”
How do ‘medical miracles’ impact physicians?
When Dr. Rotbart was writing his book, which includes physician essays from across the world, he was struck by how many of the events happened decades earlier.
“This is another testament to the powerful impact these experiences have on those witnessing them,” he said. “In many cases, physicians describing events occurring years ago noted that those early memories served to give them hope as they encountered new, seemingly hopeless cases in subsequent years. Some contributors wrote that the ‘miracle experience’ actually directed them in their choice of specialty and has influenced much of their professional decision-making throughout their careers. Others draw on those miraculous moments at times when they themselves feel hopeless in the face of adversity and tragedy.”
Dr. Fleischer said that, although Ruby’s story has stayed with him, his mindset or practice style didn’t necessarily change after the experience.
“I’m not sure if it’s affected me because I haven’t been in that situation again,” he said. “I’m in the middle. I would never rule out anything, but I’m not going to base how I practice on the hope for a medical miracle.”
In a recent opinion piece for the New York Times, pulmonary and critical care physician, Daniela Lamas, MD, wrote about the sometimes negative effects of miracle cases on physicians. Such experiences for instance, can lead to a greater drive to beat the odds in future cases, which can sometimes lead to false hope, protracted critical care admissions, and futile procedures.
“After all, in most cases in the ICU, our initial prognoses are correct,” she wrote. “So there’s a risk to standing at the bedside, thinking about that one patient who made it home despite our predictions. We can give that experience too much weight in influencing our decisions and recommendations.”
Dr. Beam said unexpected outcomes – particularly in the age of COVID-19 – can certainly make physicians think differently about life-sustaining measures and when to discuss end-of-life care with family members. In his own practice, Dr. Beam has encountered unexpected COVID recoveries. Now, he generally gives extremely ill COVID patients a little more time to see if their bodies recover.
“It remains true that people who are really sick with COVID, who are on ventilated or who are requiring a lot of up respiratory support, they don’t do well on average,” he said. “But it is [also] true that there are a handful of people who get to that point and do come back to 80% or 90% of where they were. It makes you think twice.”
What to do when parents hope for a miracle
In his palliative care practice, Nashville, Tenn., surgeon Myrick Shinall Jr., MD, PhD, regularly encounters families and patients who wish for a medical miracle.
“It happens pretty often from a palliative care perspective,” he said. “What I have experienced the most is a patient with a severe brain injury who we don’t believe is recoverable. The medical team is discussing with the family that it is probably time to discontinue the ventilator. In those situations, families will often talk about wanting us to continue on [our life-sustaining efforts] in the hopes that a miracle will happen.”
Dr. Shinall and Trevor Bibler, PhD, recently authored two articles about best practices for responding to patients who hope for a miracle. The first one, published in the American Journal of Bioethics, is directed toward bioethicists; the second article, in the Journal of Pain and Symptom Management, targets clinicians.
A primary takeaway from the papers is that health professionals should recognize that hope for a miracle may mean different things to different people, said Dr. Bibler, an ethicist and assistant professor at Baylor College of Medicine, Houston. Some patients may have an innocuous hope for a miracle without a religious connotation, whereas others may have a firm conviction in their idea of God, their spirituality, and a concrete vision of the miracle.
“To hear that a family or patient is hoping for a miracle, one shouldn’t assume they already know what the patient or the family might mean by that,” Dr. Bibler said. “If a patient were to say, ‘I hope for a miracle,’ you might ask: ‘What do you mean by a miracle?’ Health professionals should feel empowered to ask that question.”
Health care professionals should explore a patient’s hope for a miracle, be nonjudgmental, ask clarifying questions, restate what the patient has said, and delve into the patient’s world view on death and dying, according to Dr. Bibler’s analyses. In some cases, it may be helpful to include a chaplain or the presence of a theology outsider in discussions.
When his patients and their families raise the subject of miracles, Dr. Shinall said he inquires what a miracle would look like in their opinion and tries to gauge how much of the assertion is a general hope compared with a firm belief.
“I try to work with them to make sure they understand doctors’ decisions and recommendations are based on what we know and can predict from our medical experience,” he said. “And that there’s nothing we’re going to do to prevent a miracle from happening, but that that can’t be our medical plan – to wait for a miracle.”
Despite the many patients and families Dr. Shinall has encountered who hope for a miracle, he has never experienced a case that he would describe as a medical miracle, he said.
Dr. Rotbart believes all physicians struggle with finding balance in how far to push in hope of a miracle and when to let go.
“Miracles, whether they happen to us, or we hear of them from colleagues or we read about them, should humble us as physicians,” he said. “I have come to believe that what we don’t know or don’t understand about medicine, medical miracles, or life in general, isn‘t necessarily cause for fear, and can even be reason for hope.
“Medicine has come a long way since Hippocrates’ theory of The Four Humors and The Four Temperaments, yet we still have much to learn about the workings of the human body. As physicians, we should take comfort in how much we don’t know because that allows us to share hope with our patients and, occasionally, makes medical miracles possible.”
A version of this article first appeared on Medscape.com.
It was a freezing December day, and two young brothers were playing outside near a swimming pool when the younger boy, a 3-year-old toddler, fell into the water.
The 7-year-old immediately jumped into the pool to save his brother and was able to pull the toddler to the pool steps where the boy’s head was above water. But the icy temperatures overcame the older brother and he drifted underwater.
“Despite being at the forefront of medicine, what we don’t understand often exceeds what we do understand,” said Harley Rotbart, MD, author of “Miracles We Have Seen” (Health Communications: Deerfield Beach, Fla., 2016).
Paramedics arrived to find both boys unconscious and rushed them to the Children’s Hospital of Philadelphia. The younger boy regained consciousness in the ICU and recovered. The 7-year-old, however, was unresponsive and remained in a coma, said Dr. Rotbart a pediatrician and author based in Denver.
Family members stayed at the boy’s bedside and prayed. But after several weeks, the child’s condition remained unchanged. His parents began to discuss ending life support and organ donation. Then late one night, as Dr. Rotbart sat reading to the unconscious patient, the little boy squeezed his hand. In disbelief, Dr. Rotbart told all of his colleagues about the squeeze the next morning. Everyone attributed the movement to an involuntary muscle spasm, he said. After all, every test and scan showed the boy had no brain function.
But later that day, the child grasped another staff member’s hand. Shortly after that, he squeezed in response to a command. Dr. Rotbart and his staff were stunned, but cautious about feeling too much hope.
Days later, the child opened his eyes. Then, he smiled. His parents were overjoyed.
“When he walked out of the hospital more than 2 months after the near-drowning and his heroic rescue of his little brother, we all cheered and cried,” Dr. Rotbart wrote in his book. “We cried many times in the weeks preceding, and I still cry whenever I recall this story.”
The experience, which happened years ago when Dr. Rotbart was a trainee, has stayed with the pediatrician his entire career.
“His awakening was seemingly impossible – and then it happened,” Dr. Rotbart said. “Despite being at the forefront of medicine and science, what we don’t understand often exceeds what we do understand. And even when we think we understand, we are frequently proven wrong.”
For many, Dr. Rotbart’s experience raises questions about the existence of medical miracles.
Do physicians believe in medical miracles? The answers are diverse.
“I have no doubt that extraordinary outcomes happen where patients who are overwhelmingly expected not to survive, do,” says Eric Beam, MD, a hospitalist based in San Diego. “That’s one of the reasons we choose our words very carefully in our conversations with patients and their families and remember that nothing is 0%, and nothing is 100%. But doctors tend to treat situations that are 99.9% as absolute. I don’t think you can practice medicine with the hope or expectation that every case you see has the potential to beat the odds – or be a medical miracle.”
Disappearing cancer hailed as ‘miracle’
In 2003, physicians projected that Joseph Rick, 40, had just a few months to live. His mucosal melanoma had spread throughout his body, progressing even after several surgeries, radiation therapy, and a combination of chemotherapy agents, recalled Antoni Ribas, MD, PhD, an oncologist and director of the tumor immunology program at Jonsson Comprehensive Cancer Center in Los Angeles.
Mr. Rick’s melanoma had spread to his intestines with traces on his stomach and bladder. Tumors were present on his liver, lungs, and pancreas. Rick bought a grave and prepared for the worst, he recounted in a Cancer Research Institute video. But his fate took a turn when he enrolled in an experimental drug trial in December 2003. The phase 1 trial was for a new immune modulating antibody, called an anti–CTLA-4 antibody, said Dr. Ribas, who conducted the trial.
Over the next few weeks and months, all areas of Rick’s melanoma metastases disappeared. By 2009, he was in remission. He has lived the rest of his life with no evidence of melanoma, according to Dr. Ribas.
Mr. Rick’s case has been referenced throughout literature and news stories as a “medical miracle” and a “cancer miracle.”
Does Dr. Ribas think the case was a medical miracle?
“The response in Joseph Rick was what happened in 10%-15% of patients who received anti-CTLA-4 therapy,” Dr. Ribas said. “These were not miracles. These patients responded because their immune system trying to attack the cancer had been stuck at the CTLA-4 checkpoint. Blocking this checkpoint allowed their immune system to proceed to attack and kill cancer cells anywhere in the body.”
The scientific basis of this therapy was work by University of Texas MD Anderson Cancer Center immunologist James Allison, PhD, that had been done 5 years earlier in mouse models, where giving an anti–CTLA-4 antibody to mice allowed them to reject several implanted cancers, Dr. Ribas explained. Dr. Allison received the 2018 Nobel Prize in Physiology or Medicine for this work, subsequently opening the door for what we now call “immune checkpoint blockade therapy for cancer.” Dr. Ribas added.
“We tend to call miracles good things that we do not understand how they happened,” Dr. Ribas said. “From the human observation perspective, there have been plenty of medical miracles. However, each one has a specific biological mechanism that led to improvement in a patient. In cancer treatment, early studies using the immune system resulted in occasional patients having tumor responses and long-term benefits.
“With the increased understanding of how the immune system interacts with cancers, which is based on remarkable progress in understanding how the immune system works generated over the past several decades, these ‘miracles’ become specific mechanisms leading to response to cancer, which can then be replicated in other patients.”
Patient defies odds after 45 minutes without heartbeat
Florida ob.gyn. Michael Fleischer, MD, had just performed a routine repeat cesarean birth, delivering a healthy baby girl. His patient, Ruby, had a history of high blood pressure but medication taken during the pregnancy had kept her levels stabilized.
In the waiting room, Dr. Fleischer informed Ruby’s large family of the good news. He was planning to head home early that day when he heard his name being called over the hospital’s loudspeaker. Ruby had stopped breathing.
“The anesthesiologist was with her and had immediately intubated her,” Dr. Fleischer said. “We checked to make sure there was no problems or bleeding from the C-section, but everything was completely fine. However, we couldn’t keep her blood pressure stable.”
Dr. Fleischer suspected the respiratory arrest was caused by either an amniotic fluid embolism or a pulmonary embolism. Intubation continued and physicians gave Ruby medication to stabilize her blood pressure. Then suddenly, Ruby’s heart stopped.
Dr. Fleischer and other doctors began compressions, which they continued for 30 minutes. They shocked Ruby with defibrillator paddles multiple times, but there was no change.
“I was already thinking, this is hopeless, there’s nothing we can do,” he said. “The writing is on the wall. She’s going to die.”
Dr. Fleischer spoke to Ruby’s family and explained the tragic turn of events. Relatives were distraught and tearfully visited Ruby to say their goodbyes. They prayed and cried. Eventually, physicians ceased compressions. Ruby had gone 45 minutes without a pulse. The EKG was still showing some irregularity, FDr. leischer said, but no rhythm. Physicians kept Ruby intubated as they waited for the background electrical activity to fade. As they watched the screen in anguish, there was suddenly a blip on the heart rate monitor. Then another and another. Within seconds, Ruby’s heart went back into sinus rhythm.
“We were in disbelief,” Dr. Fleischer said. “We did some tests and put her in the ICU, and she was fine. Usually, after doing compressions on anyone, you’d have bruising or broken ribs. She had nothing. She just woke up and said: ‘What am I doing here? Let me go see my baby.’ ”
Ruby fully recovered, and 3 days later, she went home with her newborn.
While the recovery was unbelievable, Dr. Fleischer stopped short of calling it a medical miracle. There were scientific contributors to her survival: she was immediately intubated when she stopped breathing and compressions were started as soon as her heart stopped.
However, Dr. Fleischer said the fact that lifesaving measures had ended, and Ruby revived on her own was indeed, miraculous.
“It wasn’t like we were doing compressions and brought her back,” he said. “I can scientifically explain things in my mind, except for that. That when we finally stopped and took our hands off her, that’s when something changed. That’s when she came back.”
How do ‘medical miracles’ impact physicians?
When Dr. Rotbart was writing his book, which includes physician essays from across the world, he was struck by how many of the events happened decades earlier.
“This is another testament to the powerful impact these experiences have on those witnessing them,” he said. “In many cases, physicians describing events occurring years ago noted that those early memories served to give them hope as they encountered new, seemingly hopeless cases in subsequent years. Some contributors wrote that the ‘miracle experience’ actually directed them in their choice of specialty and has influenced much of their professional decision-making throughout their careers. Others draw on those miraculous moments at times when they themselves feel hopeless in the face of adversity and tragedy.”
Dr. Fleischer said that, although Ruby’s story has stayed with him, his mindset or practice style didn’t necessarily change after the experience.
“I’m not sure if it’s affected me because I haven’t been in that situation again,” he said. “I’m in the middle. I would never rule out anything, but I’m not going to base how I practice on the hope for a medical miracle.”
In a recent opinion piece for the New York Times, pulmonary and critical care physician, Daniela Lamas, MD, wrote about the sometimes negative effects of miracle cases on physicians. Such experiences for instance, can lead to a greater drive to beat the odds in future cases, which can sometimes lead to false hope, protracted critical care admissions, and futile procedures.
“After all, in most cases in the ICU, our initial prognoses are correct,” she wrote. “So there’s a risk to standing at the bedside, thinking about that one patient who made it home despite our predictions. We can give that experience too much weight in influencing our decisions and recommendations.”
Dr. Beam said unexpected outcomes – particularly in the age of COVID-19 – can certainly make physicians think differently about life-sustaining measures and when to discuss end-of-life care with family members. In his own practice, Dr. Beam has encountered unexpected COVID recoveries. Now, he generally gives extremely ill COVID patients a little more time to see if their bodies recover.
“It remains true that people who are really sick with COVID, who are on ventilated or who are requiring a lot of up respiratory support, they don’t do well on average,” he said. “But it is [also] true that there are a handful of people who get to that point and do come back to 80% or 90% of where they were. It makes you think twice.”
What to do when parents hope for a miracle
In his palliative care practice, Nashville, Tenn., surgeon Myrick Shinall Jr., MD, PhD, regularly encounters families and patients who wish for a medical miracle.
“It happens pretty often from a palliative care perspective,” he said. “What I have experienced the most is a patient with a severe brain injury who we don’t believe is recoverable. The medical team is discussing with the family that it is probably time to discontinue the ventilator. In those situations, families will often talk about wanting us to continue on [our life-sustaining efforts] in the hopes that a miracle will happen.”
Dr. Shinall and Trevor Bibler, PhD, recently authored two articles about best practices for responding to patients who hope for a miracle. The first one, published in the American Journal of Bioethics, is directed toward bioethicists; the second article, in the Journal of Pain and Symptom Management, targets clinicians.
A primary takeaway from the papers is that health professionals should recognize that hope for a miracle may mean different things to different people, said Dr. Bibler, an ethicist and assistant professor at Baylor College of Medicine, Houston. Some patients may have an innocuous hope for a miracle without a religious connotation, whereas others may have a firm conviction in their idea of God, their spirituality, and a concrete vision of the miracle.
“To hear that a family or patient is hoping for a miracle, one shouldn’t assume they already know what the patient or the family might mean by that,” Dr. Bibler said. “If a patient were to say, ‘I hope for a miracle,’ you might ask: ‘What do you mean by a miracle?’ Health professionals should feel empowered to ask that question.”
Health care professionals should explore a patient’s hope for a miracle, be nonjudgmental, ask clarifying questions, restate what the patient has said, and delve into the patient’s world view on death and dying, according to Dr. Bibler’s analyses. In some cases, it may be helpful to include a chaplain or the presence of a theology outsider in discussions.
When his patients and their families raise the subject of miracles, Dr. Shinall said he inquires what a miracle would look like in their opinion and tries to gauge how much of the assertion is a general hope compared with a firm belief.
“I try to work with them to make sure they understand doctors’ decisions and recommendations are based on what we know and can predict from our medical experience,” he said. “And that there’s nothing we’re going to do to prevent a miracle from happening, but that that can’t be our medical plan – to wait for a miracle.”
Despite the many patients and families Dr. Shinall has encountered who hope for a miracle, he has never experienced a case that he would describe as a medical miracle, he said.
Dr. Rotbart believes all physicians struggle with finding balance in how far to push in hope of a miracle and when to let go.
“Miracles, whether they happen to us, or we hear of them from colleagues or we read about them, should humble us as physicians,” he said. “I have come to believe that what we don’t know or don’t understand about medicine, medical miracles, or life in general, isn‘t necessarily cause for fear, and can even be reason for hope.
“Medicine has come a long way since Hippocrates’ theory of The Four Humors and The Four Temperaments, yet we still have much to learn about the workings of the human body. As physicians, we should take comfort in how much we don’t know because that allows us to share hope with our patients and, occasionally, makes medical miracles possible.”
A version of this article first appeared on Medscape.com.
It was a freezing December day, and two young brothers were playing outside near a swimming pool when the younger boy, a 3-year-old toddler, fell into the water.
The 7-year-old immediately jumped into the pool to save his brother and was able to pull the toddler to the pool steps where the boy’s head was above water. But the icy temperatures overcame the older brother and he drifted underwater.
“Despite being at the forefront of medicine, what we don’t understand often exceeds what we do understand,” said Harley Rotbart, MD, author of “Miracles We Have Seen” (Health Communications: Deerfield Beach, Fla., 2016).
Paramedics arrived to find both boys unconscious and rushed them to the Children’s Hospital of Philadelphia. The younger boy regained consciousness in the ICU and recovered. The 7-year-old, however, was unresponsive and remained in a coma, said Dr. Rotbart a pediatrician and author based in Denver.
Family members stayed at the boy’s bedside and prayed. But after several weeks, the child’s condition remained unchanged. His parents began to discuss ending life support and organ donation. Then late one night, as Dr. Rotbart sat reading to the unconscious patient, the little boy squeezed his hand. In disbelief, Dr. Rotbart told all of his colleagues about the squeeze the next morning. Everyone attributed the movement to an involuntary muscle spasm, he said. After all, every test and scan showed the boy had no brain function.
But later that day, the child grasped another staff member’s hand. Shortly after that, he squeezed in response to a command. Dr. Rotbart and his staff were stunned, but cautious about feeling too much hope.
Days later, the child opened his eyes. Then, he smiled. His parents were overjoyed.
“When he walked out of the hospital more than 2 months after the near-drowning and his heroic rescue of his little brother, we all cheered and cried,” Dr. Rotbart wrote in his book. “We cried many times in the weeks preceding, and I still cry whenever I recall this story.”
The experience, which happened years ago when Dr. Rotbart was a trainee, has stayed with the pediatrician his entire career.
“His awakening was seemingly impossible – and then it happened,” Dr. Rotbart said. “Despite being at the forefront of medicine and science, what we don’t understand often exceeds what we do understand. And even when we think we understand, we are frequently proven wrong.”
For many, Dr. Rotbart’s experience raises questions about the existence of medical miracles.
Do physicians believe in medical miracles? The answers are diverse.
“I have no doubt that extraordinary outcomes happen where patients who are overwhelmingly expected not to survive, do,” says Eric Beam, MD, a hospitalist based in San Diego. “That’s one of the reasons we choose our words very carefully in our conversations with patients and their families and remember that nothing is 0%, and nothing is 100%. But doctors tend to treat situations that are 99.9% as absolute. I don’t think you can practice medicine with the hope or expectation that every case you see has the potential to beat the odds – or be a medical miracle.”
Disappearing cancer hailed as ‘miracle’
In 2003, physicians projected that Joseph Rick, 40, had just a few months to live. His mucosal melanoma had spread throughout his body, progressing even after several surgeries, radiation therapy, and a combination of chemotherapy agents, recalled Antoni Ribas, MD, PhD, an oncologist and director of the tumor immunology program at Jonsson Comprehensive Cancer Center in Los Angeles.
Mr. Rick’s melanoma had spread to his intestines with traces on his stomach and bladder. Tumors were present on his liver, lungs, and pancreas. Rick bought a grave and prepared for the worst, he recounted in a Cancer Research Institute video. But his fate took a turn when he enrolled in an experimental drug trial in December 2003. The phase 1 trial was for a new immune modulating antibody, called an anti–CTLA-4 antibody, said Dr. Ribas, who conducted the trial.
Over the next few weeks and months, all areas of Rick’s melanoma metastases disappeared. By 2009, he was in remission. He has lived the rest of his life with no evidence of melanoma, according to Dr. Ribas.
Mr. Rick’s case has been referenced throughout literature and news stories as a “medical miracle” and a “cancer miracle.”
Does Dr. Ribas think the case was a medical miracle?
“The response in Joseph Rick was what happened in 10%-15% of patients who received anti-CTLA-4 therapy,” Dr. Ribas said. “These were not miracles. These patients responded because their immune system trying to attack the cancer had been stuck at the CTLA-4 checkpoint. Blocking this checkpoint allowed their immune system to proceed to attack and kill cancer cells anywhere in the body.”
The scientific basis of this therapy was work by University of Texas MD Anderson Cancer Center immunologist James Allison, PhD, that had been done 5 years earlier in mouse models, where giving an anti–CTLA-4 antibody to mice allowed them to reject several implanted cancers, Dr. Ribas explained. Dr. Allison received the 2018 Nobel Prize in Physiology or Medicine for this work, subsequently opening the door for what we now call “immune checkpoint blockade therapy for cancer.” Dr. Ribas added.
“We tend to call miracles good things that we do not understand how they happened,” Dr. Ribas said. “From the human observation perspective, there have been plenty of medical miracles. However, each one has a specific biological mechanism that led to improvement in a patient. In cancer treatment, early studies using the immune system resulted in occasional patients having tumor responses and long-term benefits.
“With the increased understanding of how the immune system interacts with cancers, which is based on remarkable progress in understanding how the immune system works generated over the past several decades, these ‘miracles’ become specific mechanisms leading to response to cancer, which can then be replicated in other patients.”
Patient defies odds after 45 minutes without heartbeat
Florida ob.gyn. Michael Fleischer, MD, had just performed a routine repeat cesarean birth, delivering a healthy baby girl. His patient, Ruby, had a history of high blood pressure but medication taken during the pregnancy had kept her levels stabilized.
In the waiting room, Dr. Fleischer informed Ruby’s large family of the good news. He was planning to head home early that day when he heard his name being called over the hospital’s loudspeaker. Ruby had stopped breathing.
“The anesthesiologist was with her and had immediately intubated her,” Dr. Fleischer said. “We checked to make sure there was no problems or bleeding from the C-section, but everything was completely fine. However, we couldn’t keep her blood pressure stable.”
Dr. Fleischer suspected the respiratory arrest was caused by either an amniotic fluid embolism or a pulmonary embolism. Intubation continued and physicians gave Ruby medication to stabilize her blood pressure. Then suddenly, Ruby’s heart stopped.
Dr. Fleischer and other doctors began compressions, which they continued for 30 minutes. They shocked Ruby with defibrillator paddles multiple times, but there was no change.
“I was already thinking, this is hopeless, there’s nothing we can do,” he said. “The writing is on the wall. She’s going to die.”
Dr. Fleischer spoke to Ruby’s family and explained the tragic turn of events. Relatives were distraught and tearfully visited Ruby to say their goodbyes. They prayed and cried. Eventually, physicians ceased compressions. Ruby had gone 45 minutes without a pulse. The EKG was still showing some irregularity, FDr. leischer said, but no rhythm. Physicians kept Ruby intubated as they waited for the background electrical activity to fade. As they watched the screen in anguish, there was suddenly a blip on the heart rate monitor. Then another and another. Within seconds, Ruby’s heart went back into sinus rhythm.
“We were in disbelief,” Dr. Fleischer said. “We did some tests and put her in the ICU, and she was fine. Usually, after doing compressions on anyone, you’d have bruising or broken ribs. She had nothing. She just woke up and said: ‘What am I doing here? Let me go see my baby.’ ”
Ruby fully recovered, and 3 days later, she went home with her newborn.
While the recovery was unbelievable, Dr. Fleischer stopped short of calling it a medical miracle. There were scientific contributors to her survival: she was immediately intubated when she stopped breathing and compressions were started as soon as her heart stopped.
However, Dr. Fleischer said the fact that lifesaving measures had ended, and Ruby revived on her own was indeed, miraculous.
“It wasn’t like we were doing compressions and brought her back,” he said. “I can scientifically explain things in my mind, except for that. That when we finally stopped and took our hands off her, that’s when something changed. That’s when she came back.”
How do ‘medical miracles’ impact physicians?
When Dr. Rotbart was writing his book, which includes physician essays from across the world, he was struck by how many of the events happened decades earlier.
“This is another testament to the powerful impact these experiences have on those witnessing them,” he said. “In many cases, physicians describing events occurring years ago noted that those early memories served to give them hope as they encountered new, seemingly hopeless cases in subsequent years. Some contributors wrote that the ‘miracle experience’ actually directed them in their choice of specialty and has influenced much of their professional decision-making throughout their careers. Others draw on those miraculous moments at times when they themselves feel hopeless in the face of adversity and tragedy.”
Dr. Fleischer said that, although Ruby’s story has stayed with him, his mindset or practice style didn’t necessarily change after the experience.
“I’m not sure if it’s affected me because I haven’t been in that situation again,” he said. “I’m in the middle. I would never rule out anything, but I’m not going to base how I practice on the hope for a medical miracle.”
In a recent opinion piece for the New York Times, pulmonary and critical care physician, Daniela Lamas, MD, wrote about the sometimes negative effects of miracle cases on physicians. Such experiences for instance, can lead to a greater drive to beat the odds in future cases, which can sometimes lead to false hope, protracted critical care admissions, and futile procedures.
“After all, in most cases in the ICU, our initial prognoses are correct,” she wrote. “So there’s a risk to standing at the bedside, thinking about that one patient who made it home despite our predictions. We can give that experience too much weight in influencing our decisions and recommendations.”
Dr. Beam said unexpected outcomes – particularly in the age of COVID-19 – can certainly make physicians think differently about life-sustaining measures and when to discuss end-of-life care with family members. In his own practice, Dr. Beam has encountered unexpected COVID recoveries. Now, he generally gives extremely ill COVID patients a little more time to see if their bodies recover.
“It remains true that people who are really sick with COVID, who are on ventilated or who are requiring a lot of up respiratory support, they don’t do well on average,” he said. “But it is [also] true that there are a handful of people who get to that point and do come back to 80% or 90% of where they were. It makes you think twice.”
What to do when parents hope for a miracle
In his palliative care practice, Nashville, Tenn., surgeon Myrick Shinall Jr., MD, PhD, regularly encounters families and patients who wish for a medical miracle.
“It happens pretty often from a palliative care perspective,” he said. “What I have experienced the most is a patient with a severe brain injury who we don’t believe is recoverable. The medical team is discussing with the family that it is probably time to discontinue the ventilator. In those situations, families will often talk about wanting us to continue on [our life-sustaining efforts] in the hopes that a miracle will happen.”
Dr. Shinall and Trevor Bibler, PhD, recently authored two articles about best practices for responding to patients who hope for a miracle. The first one, published in the American Journal of Bioethics, is directed toward bioethicists; the second article, in the Journal of Pain and Symptom Management, targets clinicians.
A primary takeaway from the papers is that health professionals should recognize that hope for a miracle may mean different things to different people, said Dr. Bibler, an ethicist and assistant professor at Baylor College of Medicine, Houston. Some patients may have an innocuous hope for a miracle without a religious connotation, whereas others may have a firm conviction in their idea of God, their spirituality, and a concrete vision of the miracle.
“To hear that a family or patient is hoping for a miracle, one shouldn’t assume they already know what the patient or the family might mean by that,” Dr. Bibler said. “If a patient were to say, ‘I hope for a miracle,’ you might ask: ‘What do you mean by a miracle?’ Health professionals should feel empowered to ask that question.”
Health care professionals should explore a patient’s hope for a miracle, be nonjudgmental, ask clarifying questions, restate what the patient has said, and delve into the patient’s world view on death and dying, according to Dr. Bibler’s analyses. In some cases, it may be helpful to include a chaplain or the presence of a theology outsider in discussions.
When his patients and their families raise the subject of miracles, Dr. Shinall said he inquires what a miracle would look like in their opinion and tries to gauge how much of the assertion is a general hope compared with a firm belief.
“I try to work with them to make sure they understand doctors’ decisions and recommendations are based on what we know and can predict from our medical experience,” he said. “And that there’s nothing we’re going to do to prevent a miracle from happening, but that that can’t be our medical plan – to wait for a miracle.”
Despite the many patients and families Dr. Shinall has encountered who hope for a miracle, he has never experienced a case that he would describe as a medical miracle, he said.
Dr. Rotbart believes all physicians struggle with finding balance in how far to push in hope of a miracle and when to let go.
“Miracles, whether they happen to us, or we hear of them from colleagues or we read about them, should humble us as physicians,” he said. “I have come to believe that what we don’t know or don’t understand about medicine, medical miracles, or life in general, isn‘t necessarily cause for fear, and can even be reason for hope.
“Medicine has come a long way since Hippocrates’ theory of The Four Humors and The Four Temperaments, yet we still have much to learn about the workings of the human body. As physicians, we should take comfort in how much we don’t know because that allows us to share hope with our patients and, occasionally, makes medical miracles possible.”
A version of this article first appeared on Medscape.com.
Why mRNA COVID vaccines are preferred (and why patients should be reassured)
On December 16, 2021, the Advisory Committee on Immunization Practices (ACIP) voted to preferentially recommend messenger RNA (mRNA) vaccines over the Johnson & Johnson/Janssen (J&J) COVID-19 (Ad.26.COV2.S) adenovirus vector vaccine for prevention of COVID-19.1 The mRNA vaccines include Pfizer-BioNTech COVID-19 (BNT162b2) and Moderna COVID-19 (mRNA-1273).
The reason for this preferential recommendation is a rare but serious adverse reaction—thrombosis with thrombocytopenia (TTS) —that has been associated with the J&J vaccine. As of December 8, 2021, more than 16.9 million doses of the J&J COVID-19 vaccine have been given in the United States. The CDC has identified 57 confirmed reports of people who received this vaccine and later developed TTS.2 The known incidence of TTS is thus 1 per ~ 300,000 doses, although the rate may actually be higher.2 All cases have been documented as having occurred after administration of the J&J primary single-dose vaccine; none have been documented (so far) after the booster—although the number of booster doses of the J&J COVID-19 vaccine has been small.
Women between the ages of 30 and 50 years have the highest risk for TTS, with rates of 1 per 94,000 in those ages 30-39 and 1 per 111,000 for those ages 40-49.2,3 All those with TTS have been hospitalized, and 9 have died.2,3 While this adverse reaction is rare, the seriousness of it led the ACIP to state a preference for the mRNA vaccines.
The significance of the recommendation:
- Unless a person has a contraindication to an mRNA vaccine, they should receive 1 of these 2 vaccines for their primary series and boosters.
- The only “Mix and Match” that should occur with boosters is to follow a J&J/Janssen COVID-19 vaccine with an mRNA booster. At this time, booster doses following a 2-dose mRNA primary series should be with an mRNA vaccine.
- The recommendation is for adults ages 18 and older; however, the J&J/Janssen COVID-19 vaccine is not yet approved for younger age-groups.
- The J&J/Janssen COVID-19 vaccine remains an option for those who cannot receive an mRNA vaccine, but it should be administered only after full informed consent.
The J&J/Janssen COVID-19 vaccine initially looked promising a year ago because of its single-dose primary series and its much less stringent storage requirements. However, things have not quite panned out for the vaccine. Its effectiveness after a single dose has proven to be significantly inferior to the 2-dose mRNA vaccines, and it has now been associated with a very serious, albeit rare, adverse reaction.
The major take-home point for physicians to pass on to their patients is that the nation’s system for monitoring vaccine safety works. It can pick up serious adverse reactions that occur at a rate as low as 1/300,000. This should be reassuring.
1. CDC. CDC Endorses ACIP’s Updated COVID-19 Vaccine Recommendations [press release]. December 16, 2021. Accessed December 22, 2021. www.cdc.gov/media/releases/2021/s1216-covid-19-vaccines.html
2. CDC. Selected Adverse Events Reported after COVID-19 Vaccination. December 20, 2021. Accessed December 22, 2021. www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/adverse-events.html
3. See I. Updates on thrombosis with thrombocytopenia syndrome (TTS). Presented to the Advisory Committee on Immunization Practices. December 16, 2021. Accessed December 22, 2021. www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-12-16/02-COVID-See-508.pdf
On December 16, 2021, the Advisory Committee on Immunization Practices (ACIP) voted to preferentially recommend messenger RNA (mRNA) vaccines over the Johnson & Johnson/Janssen (J&J) COVID-19 (Ad.26.COV2.S) adenovirus vector vaccine for prevention of COVID-19.1 The mRNA vaccines include Pfizer-BioNTech COVID-19 (BNT162b2) and Moderna COVID-19 (mRNA-1273).
The reason for this preferential recommendation is a rare but serious adverse reaction—thrombosis with thrombocytopenia (TTS) —that has been associated with the J&J vaccine. As of December 8, 2021, more than 16.9 million doses of the J&J COVID-19 vaccine have been given in the United States. The CDC has identified 57 confirmed reports of people who received this vaccine and later developed TTS.2 The known incidence of TTS is thus 1 per ~ 300,000 doses, although the rate may actually be higher.2 All cases have been documented as having occurred after administration of the J&J primary single-dose vaccine; none have been documented (so far) after the booster—although the number of booster doses of the J&J COVID-19 vaccine has been small.
Women between the ages of 30 and 50 years have the highest risk for TTS, with rates of 1 per 94,000 in those ages 30-39 and 1 per 111,000 for those ages 40-49.2,3 All those with TTS have been hospitalized, and 9 have died.2,3 While this adverse reaction is rare, the seriousness of it led the ACIP to state a preference for the mRNA vaccines.
The significance of the recommendation:
- Unless a person has a contraindication to an mRNA vaccine, they should receive 1 of these 2 vaccines for their primary series and boosters.
- The only “Mix and Match” that should occur with boosters is to follow a J&J/Janssen COVID-19 vaccine with an mRNA booster. At this time, booster doses following a 2-dose mRNA primary series should be with an mRNA vaccine.
- The recommendation is for adults ages 18 and older; however, the J&J/Janssen COVID-19 vaccine is not yet approved for younger age-groups.
- The J&J/Janssen COVID-19 vaccine remains an option for those who cannot receive an mRNA vaccine, but it should be administered only after full informed consent.
The J&J/Janssen COVID-19 vaccine initially looked promising a year ago because of its single-dose primary series and its much less stringent storage requirements. However, things have not quite panned out for the vaccine. Its effectiveness after a single dose has proven to be significantly inferior to the 2-dose mRNA vaccines, and it has now been associated with a very serious, albeit rare, adverse reaction.
The major take-home point for physicians to pass on to their patients is that the nation’s system for monitoring vaccine safety works. It can pick up serious adverse reactions that occur at a rate as low as 1/300,000. This should be reassuring.
On December 16, 2021, the Advisory Committee on Immunization Practices (ACIP) voted to preferentially recommend messenger RNA (mRNA) vaccines over the Johnson & Johnson/Janssen (J&J) COVID-19 (Ad.26.COV2.S) adenovirus vector vaccine for prevention of COVID-19.1 The mRNA vaccines include Pfizer-BioNTech COVID-19 (BNT162b2) and Moderna COVID-19 (mRNA-1273).
The reason for this preferential recommendation is a rare but serious adverse reaction—thrombosis with thrombocytopenia (TTS) —that has been associated with the J&J vaccine. As of December 8, 2021, more than 16.9 million doses of the J&J COVID-19 vaccine have been given in the United States. The CDC has identified 57 confirmed reports of people who received this vaccine and later developed TTS.2 The known incidence of TTS is thus 1 per ~ 300,000 doses, although the rate may actually be higher.2 All cases have been documented as having occurred after administration of the J&J primary single-dose vaccine; none have been documented (so far) after the booster—although the number of booster doses of the J&J COVID-19 vaccine has been small.
Women between the ages of 30 and 50 years have the highest risk for TTS, with rates of 1 per 94,000 in those ages 30-39 and 1 per 111,000 for those ages 40-49.2,3 All those with TTS have been hospitalized, and 9 have died.2,3 While this adverse reaction is rare, the seriousness of it led the ACIP to state a preference for the mRNA vaccines.
The significance of the recommendation:
- Unless a person has a contraindication to an mRNA vaccine, they should receive 1 of these 2 vaccines for their primary series and boosters.
- The only “Mix and Match” that should occur with boosters is to follow a J&J/Janssen COVID-19 vaccine with an mRNA booster. At this time, booster doses following a 2-dose mRNA primary series should be with an mRNA vaccine.
- The recommendation is for adults ages 18 and older; however, the J&J/Janssen COVID-19 vaccine is not yet approved for younger age-groups.
- The J&J/Janssen COVID-19 vaccine remains an option for those who cannot receive an mRNA vaccine, but it should be administered only after full informed consent.
The J&J/Janssen COVID-19 vaccine initially looked promising a year ago because of its single-dose primary series and its much less stringent storage requirements. However, things have not quite panned out for the vaccine. Its effectiveness after a single dose has proven to be significantly inferior to the 2-dose mRNA vaccines, and it has now been associated with a very serious, albeit rare, adverse reaction.
The major take-home point for physicians to pass on to their patients is that the nation’s system for monitoring vaccine safety works. It can pick up serious adverse reactions that occur at a rate as low as 1/300,000. This should be reassuring.
1. CDC. CDC Endorses ACIP’s Updated COVID-19 Vaccine Recommendations [press release]. December 16, 2021. Accessed December 22, 2021. www.cdc.gov/media/releases/2021/s1216-covid-19-vaccines.html
2. CDC. Selected Adverse Events Reported after COVID-19 Vaccination. December 20, 2021. Accessed December 22, 2021. www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/adverse-events.html
3. See I. Updates on thrombosis with thrombocytopenia syndrome (TTS). Presented to the Advisory Committee on Immunization Practices. December 16, 2021. Accessed December 22, 2021. www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-12-16/02-COVID-See-508.pdf
1. CDC. CDC Endorses ACIP’s Updated COVID-19 Vaccine Recommendations [press release]. December 16, 2021. Accessed December 22, 2021. www.cdc.gov/media/releases/2021/s1216-covid-19-vaccines.html
2. CDC. Selected Adverse Events Reported after COVID-19 Vaccination. December 20, 2021. Accessed December 22, 2021. www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/adverse-events.html
3. See I. Updates on thrombosis with thrombocytopenia syndrome (TTS). Presented to the Advisory Committee on Immunization Practices. December 16, 2021. Accessed December 22, 2021. www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-12-16/02-COVID-See-508.pdf
FDA to review PDE4-inhibitor roflumilast for psoriasis
The , according to a statement from the manufacturer.
Roflumilast cream (also known as ARQ-151) is a small molecule inhibitor of PDE4, an enzyme that increases proinflammatory mediators and decreases anti-inflammatory mediators. PDE4 is an established treatment target in dermatology: The FDA approved PDE-4 inhibitor crisaborole (Eucrisa) as a topical treatment for mild to moderate atopic dermatitis in 2016, and an oral PDE-4 inhibitor, orismilast, is being studied for the treatment of plaque psoriasis.
Topical roflumilast, if approved, would be the first topical PDE4 inhibitor for psoriasis in particular, according to the Arcutis Biotherapeutics statement. The cream is designed for use on the entire body, including the face and sensitive intertriginous areas.
The NDA is based on data from a pair of phase 3 randomized, double-blind 8-week studies known as DERMIS 1 and DERMIS 2 (Trials of PDE4 Inhibition with Roflumilast for the Management of Plaque Psoriasis” One and Two) and a long-term phase 2b open-label study.
DERMIS 1 and DERMIS 2 were identical multinational, multicenter studies designed to assess the safety and efficacy of 0.3% roflumilast cream. In the studies, roflumilast met its primary endpoint and patients treated with it demonstrated an Investigator Global Assessment (IGA) success rate of 42.4% compared with 6.1% for the vehicle control (P < .0001), and 37.5% compared with 6.9% for the vehicle control (P < .0001), in the DERMIS 1 and 2 trials, respectively, according to Arcutis.
In the phase 2b study, the treatment effect lasted for 52-64 weeks. Roflumilast was well tolerated across the three studies.
Overall, the most common adverse events reported in the studies were diarrhea (3%), headache (2%), insomnia (1%), nausea (1%), upper respiratory tract infections (1%), and urinary tract infections (1%).
Roflumilast also showed statistically significant improvement compared to a vehicle on secondary endpoints including Intertriginous IGA (I-IGA) Success, Psoriasis Area Severity Index-75 (PASI-75), reductions in itch as measured by the Worst Itch-Numerical Rating Scale (WI-NRS), and patient perceptions of symptoms based on the Psoriasis Symptoms Diary (PSD).
The FDA has set a Prescription Drug User Fee Act (PDUFA) target action date of July 29, 2022, according to the manufacturer’s statement. An oral formulation of roflumilast was approved by the FDA in 2011, for reducing the risk of exacerbations of chronic obstructive pulmonary disease (COPD) in patients with severe COPD.
The , according to a statement from the manufacturer.
Roflumilast cream (also known as ARQ-151) is a small molecule inhibitor of PDE4, an enzyme that increases proinflammatory mediators and decreases anti-inflammatory mediators. PDE4 is an established treatment target in dermatology: The FDA approved PDE-4 inhibitor crisaborole (Eucrisa) as a topical treatment for mild to moderate atopic dermatitis in 2016, and an oral PDE-4 inhibitor, orismilast, is being studied for the treatment of plaque psoriasis.
Topical roflumilast, if approved, would be the first topical PDE4 inhibitor for psoriasis in particular, according to the Arcutis Biotherapeutics statement. The cream is designed for use on the entire body, including the face and sensitive intertriginous areas.
The NDA is based on data from a pair of phase 3 randomized, double-blind 8-week studies known as DERMIS 1 and DERMIS 2 (Trials of PDE4 Inhibition with Roflumilast for the Management of Plaque Psoriasis” One and Two) and a long-term phase 2b open-label study.
DERMIS 1 and DERMIS 2 were identical multinational, multicenter studies designed to assess the safety and efficacy of 0.3% roflumilast cream. In the studies, roflumilast met its primary endpoint and patients treated with it demonstrated an Investigator Global Assessment (IGA) success rate of 42.4% compared with 6.1% for the vehicle control (P < .0001), and 37.5% compared with 6.9% for the vehicle control (P < .0001), in the DERMIS 1 and 2 trials, respectively, according to Arcutis.
In the phase 2b study, the treatment effect lasted for 52-64 weeks. Roflumilast was well tolerated across the three studies.
Overall, the most common adverse events reported in the studies were diarrhea (3%), headache (2%), insomnia (1%), nausea (1%), upper respiratory tract infections (1%), and urinary tract infections (1%).
Roflumilast also showed statistically significant improvement compared to a vehicle on secondary endpoints including Intertriginous IGA (I-IGA) Success, Psoriasis Area Severity Index-75 (PASI-75), reductions in itch as measured by the Worst Itch-Numerical Rating Scale (WI-NRS), and patient perceptions of symptoms based on the Psoriasis Symptoms Diary (PSD).
The FDA has set a Prescription Drug User Fee Act (PDUFA) target action date of July 29, 2022, according to the manufacturer’s statement. An oral formulation of roflumilast was approved by the FDA in 2011, for reducing the risk of exacerbations of chronic obstructive pulmonary disease (COPD) in patients with severe COPD.
The , according to a statement from the manufacturer.
Roflumilast cream (also known as ARQ-151) is a small molecule inhibitor of PDE4, an enzyme that increases proinflammatory mediators and decreases anti-inflammatory mediators. PDE4 is an established treatment target in dermatology: The FDA approved PDE-4 inhibitor crisaborole (Eucrisa) as a topical treatment for mild to moderate atopic dermatitis in 2016, and an oral PDE-4 inhibitor, orismilast, is being studied for the treatment of plaque psoriasis.
Topical roflumilast, if approved, would be the first topical PDE4 inhibitor for psoriasis in particular, according to the Arcutis Biotherapeutics statement. The cream is designed for use on the entire body, including the face and sensitive intertriginous areas.
The NDA is based on data from a pair of phase 3 randomized, double-blind 8-week studies known as DERMIS 1 and DERMIS 2 (Trials of PDE4 Inhibition with Roflumilast for the Management of Plaque Psoriasis” One and Two) and a long-term phase 2b open-label study.
DERMIS 1 and DERMIS 2 were identical multinational, multicenter studies designed to assess the safety and efficacy of 0.3% roflumilast cream. In the studies, roflumilast met its primary endpoint and patients treated with it demonstrated an Investigator Global Assessment (IGA) success rate of 42.4% compared with 6.1% for the vehicle control (P < .0001), and 37.5% compared with 6.9% for the vehicle control (P < .0001), in the DERMIS 1 and 2 trials, respectively, according to Arcutis.
In the phase 2b study, the treatment effect lasted for 52-64 weeks. Roflumilast was well tolerated across the three studies.
Overall, the most common adverse events reported in the studies were diarrhea (3%), headache (2%), insomnia (1%), nausea (1%), upper respiratory tract infections (1%), and urinary tract infections (1%).
Roflumilast also showed statistically significant improvement compared to a vehicle on secondary endpoints including Intertriginous IGA (I-IGA) Success, Psoriasis Area Severity Index-75 (PASI-75), reductions in itch as measured by the Worst Itch-Numerical Rating Scale (WI-NRS), and patient perceptions of symptoms based on the Psoriasis Symptoms Diary (PSD).
The FDA has set a Prescription Drug User Fee Act (PDUFA) target action date of July 29, 2022, according to the manufacturer’s statement. An oral formulation of roflumilast was approved by the FDA in 2011, for reducing the risk of exacerbations of chronic obstructive pulmonary disease (COPD) in patients with severe COPD.
COVID-19, sure, but what else will we remember 2021 for?
who answered a recent Medscape Medical News poll. Perhaps no surprise there.
Coming in distant second, at 26%, was the new law requiring that patients be granted electronic access to clinical notes. The controversial Food and Drug Administration approval of aducanumab (Aduhelm, Biogen/Eisai) to treat Alzheimer’s disease was next, cited by almost 16% when asked what they would remember most about 2021.
Coming in at 10% or less were the permanent end to the Step 2 Clinical Skills test, the JAMA deputy editor resignation over controversial comments, and an “other” option that allowed for write-in responses.
It should be noted respondents could choose up to three answers to this and other questions in this survey, except for questions about profession and specialty.
Exciting news in 2021
Widespread availability of COVID-19 vaccines was the No. 1 response – chosen by 85% – when asked what medical news or events excited them in 2021.
FDA clearance of a 5-minute test for early dementia was selected by 22%, followed by almost 16% citing approval in October 2021 of abemaciclib (Verzenio, Lilly) “described as the first advance for early breast cancer in 20 years.”
The resignation of JAMA editors over a podcast on race rounded out the list of exciting medical news or events – coming in fourth at 11%. A total 5% of readers chose “other” and were asked to specify what news or events excited them in 2021.
A frustrating year?
Medscape also asked readers what medical news or events frustrated them in 2021. A majority, 81%, chose COVID-19 vaccine hesitancy or refusal. Almost one-third, 31%, chose the effect of climate change on health worldwide.
Some of the most memorable news or events of 2021 were also selected as frustrating by readers. For example, 22% were frustrated by the law requiring that patients be granted electronic access to clinical notes, followed by 19% who referred to the aducanumab approval in June. Furthermore, about 12% selected the JAMA resignations.
A shocking survey question
Asked what medical news or event from 2021 shocked readers, COVID-19 vaccine hesitancy or refusal was the most common answer, at 69%.
The U.S. Preventive Services Task Force ruling out aspirin in people over age 60 for primary prevention of cardiovascular disease shocked 36% of respondents.
Coming in third and fourth on the survey were the two JAMA editors resigning after a podcast on race, chosen by 19%, and the demise of the Step 2 Clinical Skills test, selected by 18%.
Interestingly, almost 96% of respondents were physicians. Less than 1% were residents, physician assistants, or nurses. Respondents also represented a wide range of specialties. From a list of 29 possible specialties, including “other,” family medicine, internal medicine, and psychiatry were the most common.
For more on the year that was 2021, see the Medscape Year in Medicine 2021: News That Made a Difference slideshow. Read Medscape’s full Year in Medicine report.
Wondering what stood out most to our readers in 2020? Here is a story about the results of a similar survey 1 year ago.
A version of this article first appeared on Medscape.com.
who answered a recent Medscape Medical News poll. Perhaps no surprise there.
Coming in distant second, at 26%, was the new law requiring that patients be granted electronic access to clinical notes. The controversial Food and Drug Administration approval of aducanumab (Aduhelm, Biogen/Eisai) to treat Alzheimer’s disease was next, cited by almost 16% when asked what they would remember most about 2021.
Coming in at 10% or less were the permanent end to the Step 2 Clinical Skills test, the JAMA deputy editor resignation over controversial comments, and an “other” option that allowed for write-in responses.
It should be noted respondents could choose up to three answers to this and other questions in this survey, except for questions about profession and specialty.
Exciting news in 2021
Widespread availability of COVID-19 vaccines was the No. 1 response – chosen by 85% – when asked what medical news or events excited them in 2021.
FDA clearance of a 5-minute test for early dementia was selected by 22%, followed by almost 16% citing approval in October 2021 of abemaciclib (Verzenio, Lilly) “described as the first advance for early breast cancer in 20 years.”
The resignation of JAMA editors over a podcast on race rounded out the list of exciting medical news or events – coming in fourth at 11%. A total 5% of readers chose “other” and were asked to specify what news or events excited them in 2021.
A frustrating year?
Medscape also asked readers what medical news or events frustrated them in 2021. A majority, 81%, chose COVID-19 vaccine hesitancy or refusal. Almost one-third, 31%, chose the effect of climate change on health worldwide.
Some of the most memorable news or events of 2021 were also selected as frustrating by readers. For example, 22% were frustrated by the law requiring that patients be granted electronic access to clinical notes, followed by 19% who referred to the aducanumab approval in June. Furthermore, about 12% selected the JAMA resignations.
A shocking survey question
Asked what medical news or event from 2021 shocked readers, COVID-19 vaccine hesitancy or refusal was the most common answer, at 69%.
The U.S. Preventive Services Task Force ruling out aspirin in people over age 60 for primary prevention of cardiovascular disease shocked 36% of respondents.
Coming in third and fourth on the survey were the two JAMA editors resigning after a podcast on race, chosen by 19%, and the demise of the Step 2 Clinical Skills test, selected by 18%.
Interestingly, almost 96% of respondents were physicians. Less than 1% were residents, physician assistants, or nurses. Respondents also represented a wide range of specialties. From a list of 29 possible specialties, including “other,” family medicine, internal medicine, and psychiatry were the most common.
For more on the year that was 2021, see the Medscape Year in Medicine 2021: News That Made a Difference slideshow. Read Medscape’s full Year in Medicine report.
Wondering what stood out most to our readers in 2020? Here is a story about the results of a similar survey 1 year ago.
A version of this article first appeared on Medscape.com.
who answered a recent Medscape Medical News poll. Perhaps no surprise there.
Coming in distant second, at 26%, was the new law requiring that patients be granted electronic access to clinical notes. The controversial Food and Drug Administration approval of aducanumab (Aduhelm, Biogen/Eisai) to treat Alzheimer’s disease was next, cited by almost 16% when asked what they would remember most about 2021.
Coming in at 10% or less were the permanent end to the Step 2 Clinical Skills test, the JAMA deputy editor resignation over controversial comments, and an “other” option that allowed for write-in responses.
It should be noted respondents could choose up to three answers to this and other questions in this survey, except for questions about profession and specialty.
Exciting news in 2021
Widespread availability of COVID-19 vaccines was the No. 1 response – chosen by 85% – when asked what medical news or events excited them in 2021.
FDA clearance of a 5-minute test for early dementia was selected by 22%, followed by almost 16% citing approval in October 2021 of abemaciclib (Verzenio, Lilly) “described as the first advance for early breast cancer in 20 years.”
The resignation of JAMA editors over a podcast on race rounded out the list of exciting medical news or events – coming in fourth at 11%. A total 5% of readers chose “other” and were asked to specify what news or events excited them in 2021.
A frustrating year?
Medscape also asked readers what medical news or events frustrated them in 2021. A majority, 81%, chose COVID-19 vaccine hesitancy or refusal. Almost one-third, 31%, chose the effect of climate change on health worldwide.
Some of the most memorable news or events of 2021 were also selected as frustrating by readers. For example, 22% were frustrated by the law requiring that patients be granted electronic access to clinical notes, followed by 19% who referred to the aducanumab approval in June. Furthermore, about 12% selected the JAMA resignations.
A shocking survey question
Asked what medical news or event from 2021 shocked readers, COVID-19 vaccine hesitancy or refusal was the most common answer, at 69%.
The U.S. Preventive Services Task Force ruling out aspirin in people over age 60 for primary prevention of cardiovascular disease shocked 36% of respondents.
Coming in third and fourth on the survey were the two JAMA editors resigning after a podcast on race, chosen by 19%, and the demise of the Step 2 Clinical Skills test, selected by 18%.
Interestingly, almost 96% of respondents were physicians. Less than 1% were residents, physician assistants, or nurses. Respondents also represented a wide range of specialties. From a list of 29 possible specialties, including “other,” family medicine, internal medicine, and psychiatry were the most common.
For more on the year that was 2021, see the Medscape Year in Medicine 2021: News That Made a Difference slideshow. Read Medscape’s full Year in Medicine report.
Wondering what stood out most to our readers in 2020? Here is a story about the results of a similar survey 1 year ago.
A version of this article first appeared on Medscape.com.
Why patients should ditch cloth masks
Are you still wearing a cloth face mask?
Amid the rapidly spreading Omicron variant, experts stress that we all should swap cloth masks for N95 respirators or 3-ply surgical masks.
For background: N95 respirators are tightly fitting masks that cover your mouth and nose and help prevent contact with droplets and tiny particles in the air from people talking, coughing, sneezing, and spreading in other ways. Usually worn by health care workers and first responders, these masks can filter up to 95% of air droplets and particles, according to the CDC.
KN95 and KN94 masks are similar but are designed to meet international standards, unlike N95s that are approved by the Centers for Disease Control and Prevention’s National Institute for Occupational Safety and Health.
Meanwhile, a 3-ply surgical mask is a looser-fitting mask that can help prevent contact with infected droplets in the air.
But recommendations to opt for N95 and 3-ply surgical masks over cloth masks are nothing new, says Leana Wen, MD, an emergency doctor and public health professor at George Washington University, Washington.
In fact, public health experts have been urging stronger mask protection for months.
“It’s not just with Omicron that we need better masks, it was with Delta, it was with Alpha before that,” Dr. Wen said. “We have known for many months that COVID-19 is airborne, and therefore, a simple cloth mask is not going to cut it.”
Here’s what to know about these protective masks.
They’re necessary
Omicron is spreading much faster than previous COVID-19 variants. As it’s up to three times as likely to spread as the Delta variant, mask-wearing is paramount right now, says Anita Gupta, DO, an adjunct assistant professor of anesthesiology and critical care medicine and pain medicine at Johns Hopkins University, Baltimore.
The quality of a mask also matters a lot, said Dr. Wen.
“Double masking, including a well-fitting cloth mask on top of a surgical mask, adds additional protection,” she said. “Ideally, though, people should be wearing an N95, KN95, or KF94 when in indoor settings around other people with unknown vaccination status.”
If wearing an N95 mask causes extreme discomfort, wear it in high-risk settings where there are lots of people, like crowded restaurants and busy commuter trains, says Dr. Wen. “If you’re in a grocery store, there’s plenty of space and ventilation. You may not need an N95. I recommend that people obtain different masks and practice with them in low-risk settings before they go out in public in a high-risk setting.”
But people should wear a 3-ply surgical mask at the very least.
Three-ply surgical and N95 mask qualities
With 3-ply surgical masks, the fit of the mask is often more of an issue than its comfort, Dr. Wen said. But there are ways to adjust these masks, especially for those who have smaller heads.
“You can put a rubber band around the ear loops and make them a bit tighter,” said Dr. Wen. “Some people have found that using pins in their hair, that’s another way of keeping the loops in place.”
Another important tip on 3-ply surgical masks and N95s: These masks are reusable.
But how many times you should use them varies, Dr. Wen said. “As an example, if you are sweating a lot, and the mask is now really damp. Or putting it in your purse or backpack, and now it’s misshapen, and you cannot get it back to fit on your face, then it’s time to throw it away.”
Protection first
For some, cloth masks became somewhat of a statement, with people sporting logos of their favorite NFL team, or maybe even a fun animal print.
But you should always keep in mind the purpose of wearing a mask, Dr. Wen said. “Mask wearing is very functional and is about reducing your likelihood of contracting COVID. People should also use whatever methods inspire them, too, but for me, it’s purely a functional exercise.”
Mask wearing is not always enjoyable, but it remains critical in keeping people safe from COVID-19, especially the elderly and other high-risk people, Gupta says.
“There is lots of research and experts working hard to stop COVID-19,” she says. “It is important for all of us to remember that wearing a mask alone doesn’t make us safe.”
“We all need to keep washing our hands frequently and maintaining a distance from people, as well.”
For more information on where to find 3-ply surgical masks and N95s, check here or here to start.
A version of this article first appeared on WebMD.com.
Are you still wearing a cloth face mask?
Amid the rapidly spreading Omicron variant, experts stress that we all should swap cloth masks for N95 respirators or 3-ply surgical masks.
For background: N95 respirators are tightly fitting masks that cover your mouth and nose and help prevent contact with droplets and tiny particles in the air from people talking, coughing, sneezing, and spreading in other ways. Usually worn by health care workers and first responders, these masks can filter up to 95% of air droplets and particles, according to the CDC.
KN95 and KN94 masks are similar but are designed to meet international standards, unlike N95s that are approved by the Centers for Disease Control and Prevention’s National Institute for Occupational Safety and Health.
Meanwhile, a 3-ply surgical mask is a looser-fitting mask that can help prevent contact with infected droplets in the air.
But recommendations to opt for N95 and 3-ply surgical masks over cloth masks are nothing new, says Leana Wen, MD, an emergency doctor and public health professor at George Washington University, Washington.
In fact, public health experts have been urging stronger mask protection for months.
“It’s not just with Omicron that we need better masks, it was with Delta, it was with Alpha before that,” Dr. Wen said. “We have known for many months that COVID-19 is airborne, and therefore, a simple cloth mask is not going to cut it.”
Here’s what to know about these protective masks.
They’re necessary
Omicron is spreading much faster than previous COVID-19 variants. As it’s up to three times as likely to spread as the Delta variant, mask-wearing is paramount right now, says Anita Gupta, DO, an adjunct assistant professor of anesthesiology and critical care medicine and pain medicine at Johns Hopkins University, Baltimore.
The quality of a mask also matters a lot, said Dr. Wen.
“Double masking, including a well-fitting cloth mask on top of a surgical mask, adds additional protection,” she said. “Ideally, though, people should be wearing an N95, KN95, or KF94 when in indoor settings around other people with unknown vaccination status.”
If wearing an N95 mask causes extreme discomfort, wear it in high-risk settings where there are lots of people, like crowded restaurants and busy commuter trains, says Dr. Wen. “If you’re in a grocery store, there’s plenty of space and ventilation. You may not need an N95. I recommend that people obtain different masks and practice with them in low-risk settings before they go out in public in a high-risk setting.”
But people should wear a 3-ply surgical mask at the very least.
Three-ply surgical and N95 mask qualities
With 3-ply surgical masks, the fit of the mask is often more of an issue than its comfort, Dr. Wen said. But there are ways to adjust these masks, especially for those who have smaller heads.
“You can put a rubber band around the ear loops and make them a bit tighter,” said Dr. Wen. “Some people have found that using pins in their hair, that’s another way of keeping the loops in place.”
Another important tip on 3-ply surgical masks and N95s: These masks are reusable.
But how many times you should use them varies, Dr. Wen said. “As an example, if you are sweating a lot, and the mask is now really damp. Or putting it in your purse or backpack, and now it’s misshapen, and you cannot get it back to fit on your face, then it’s time to throw it away.”
Protection first
For some, cloth masks became somewhat of a statement, with people sporting logos of their favorite NFL team, or maybe even a fun animal print.
But you should always keep in mind the purpose of wearing a mask, Dr. Wen said. “Mask wearing is very functional and is about reducing your likelihood of contracting COVID. People should also use whatever methods inspire them, too, but for me, it’s purely a functional exercise.”
Mask wearing is not always enjoyable, but it remains critical in keeping people safe from COVID-19, especially the elderly and other high-risk people, Gupta says.
“There is lots of research and experts working hard to stop COVID-19,” she says. “It is important for all of us to remember that wearing a mask alone doesn’t make us safe.”
“We all need to keep washing our hands frequently and maintaining a distance from people, as well.”
For more information on where to find 3-ply surgical masks and N95s, check here or here to start.
A version of this article first appeared on WebMD.com.
Are you still wearing a cloth face mask?
Amid the rapidly spreading Omicron variant, experts stress that we all should swap cloth masks for N95 respirators or 3-ply surgical masks.
For background: N95 respirators are tightly fitting masks that cover your mouth and nose and help prevent contact with droplets and tiny particles in the air from people talking, coughing, sneezing, and spreading in other ways. Usually worn by health care workers and first responders, these masks can filter up to 95% of air droplets and particles, according to the CDC.
KN95 and KN94 masks are similar but are designed to meet international standards, unlike N95s that are approved by the Centers for Disease Control and Prevention’s National Institute for Occupational Safety and Health.
Meanwhile, a 3-ply surgical mask is a looser-fitting mask that can help prevent contact with infected droplets in the air.
But recommendations to opt for N95 and 3-ply surgical masks over cloth masks are nothing new, says Leana Wen, MD, an emergency doctor and public health professor at George Washington University, Washington.
In fact, public health experts have been urging stronger mask protection for months.
“It’s not just with Omicron that we need better masks, it was with Delta, it was with Alpha before that,” Dr. Wen said. “We have known for many months that COVID-19 is airborne, and therefore, a simple cloth mask is not going to cut it.”
Here’s what to know about these protective masks.
They’re necessary
Omicron is spreading much faster than previous COVID-19 variants. As it’s up to three times as likely to spread as the Delta variant, mask-wearing is paramount right now, says Anita Gupta, DO, an adjunct assistant professor of anesthesiology and critical care medicine and pain medicine at Johns Hopkins University, Baltimore.
The quality of a mask also matters a lot, said Dr. Wen.
“Double masking, including a well-fitting cloth mask on top of a surgical mask, adds additional protection,” she said. “Ideally, though, people should be wearing an N95, KN95, or KF94 when in indoor settings around other people with unknown vaccination status.”
If wearing an N95 mask causes extreme discomfort, wear it in high-risk settings where there are lots of people, like crowded restaurants and busy commuter trains, says Dr. Wen. “If you’re in a grocery store, there’s plenty of space and ventilation. You may not need an N95. I recommend that people obtain different masks and practice with them in low-risk settings before they go out in public in a high-risk setting.”
But people should wear a 3-ply surgical mask at the very least.
Three-ply surgical and N95 mask qualities
With 3-ply surgical masks, the fit of the mask is often more of an issue than its comfort, Dr. Wen said. But there are ways to adjust these masks, especially for those who have smaller heads.
“You can put a rubber band around the ear loops and make them a bit tighter,” said Dr. Wen. “Some people have found that using pins in their hair, that’s another way of keeping the loops in place.”
Another important tip on 3-ply surgical masks and N95s: These masks are reusable.
But how many times you should use them varies, Dr. Wen said. “As an example, if you are sweating a lot, and the mask is now really damp. Or putting it in your purse or backpack, and now it’s misshapen, and you cannot get it back to fit on your face, then it’s time to throw it away.”
Protection first
For some, cloth masks became somewhat of a statement, with people sporting logos of their favorite NFL team, or maybe even a fun animal print.
But you should always keep in mind the purpose of wearing a mask, Dr. Wen said. “Mask wearing is very functional and is about reducing your likelihood of contracting COVID. People should also use whatever methods inspire them, too, but for me, it’s purely a functional exercise.”
Mask wearing is not always enjoyable, but it remains critical in keeping people safe from COVID-19, especially the elderly and other high-risk people, Gupta says.
“There is lots of research and experts working hard to stop COVID-19,” she says. “It is important for all of us to remember that wearing a mask alone doesn’t make us safe.”
“We all need to keep washing our hands frequently and maintaining a distance from people, as well.”
For more information on where to find 3-ply surgical masks and N95s, check here or here to start.
A version of this article first appeared on WebMD.com.
COVID-19–positive or exposed? What to do next
With new cases of COVID-19 skyrocketing to more than 240,000 a day recently in the U.S., many people are facing the same situation: A family member or friend tests positive or was exposed to someone who did, and the holiday gathering, visit, or return to work is just days or hours away. Now what?
New guidance issued Dec. 27 by the Centers for Disease Control and Prevention shortens the recommended isolation and quarantine period for the general population, coming after the agency shortened the isolation period for health care workers.
This news organization reached out to two infectious disease specialists to get answers to questions that are frequently asked in these situations.
If you have tested positive for COVID-19, what do you do next?
“If you have tested positive, you are infected. At the moment, you are [either] symptomatically affected or presymptomatically infected,’’ said Paul A. Offit, MD, director of the Vaccine Education Center and professor of pediatrics at Children’s Hospital of Philadelphia. At that point, you need to isolate for 5 days, according to the new CDC guidance. (That period has been shortened from 10 days.)
Isolation means separating the infected person from others. Quarantine refers to things you should do if you’re exposed to the virus or you have a close contact infected with COVID-19.
Under the new CDC guidelines, after the 5-day isolation, if the infected person then has no symptoms, he or she can leave isolation and then wear a mask for 5 days.
Those who test positive also need to tell their close contacts they are positive, said Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security.
According to the CDC, the change to a shortened quarantine time is motivated by science ‘’demonstrating that the majority of SARS-CoV-2 transmission occurs early in the course of the illness, generally in the 1-2 days prior to onset of symptoms and the 2-3 days after.”
If you have been exposed to someone with COVID-19, what do you do next?
“If they are vaccinated and boosted, the guidance says there is no need to quarantine,” Dr. Adalja said. But the CDC guidance does recommend these people wear a well-fitting mask at all times when around others for 10 days after exposure.
For everyone else, including the unvaccinated and those who are more than 6 months out from their second Pfizer or Moderna vaccine dose, or more than 2 months from their J&J dose, the CDC recommends a quarantine for 5 days – and wearing a mask for the 5 days after that.
On a practical level, Dr. Adalja said he thinks those who are vaccinated but not boosted could also skip the quarantine and wear a mask for 10 days. Dr. Offit agrees. Because many people exposed have trouble quarantining, Dr. Offit advises those exposed who can’t follow that guidance to be sure to wear a mask for 10 days when indoors. The CDC guidance also offers that as another strategy – that if a 5-day quarantine is not feasible, the exposed person should wear a mask for 10 days when around others.
But if someone who was exposed gets symptoms, that person then enters the infected category and follows that guidance, Dr. Offit said.
When should the person who has been exposed get tested?
After the exposure, ‘’you should probably wait 2-3 days,” Dr. Offit said. “The virus has to reproduce itself.”
Testing should be done by those exposed at least once, Dr. Adalja said.
“But there’s data to support daily testing to guide their activities, but this is not CDC guidance. Home tests are sufficient for this purpose.”
At what point can the infected person mingle safely with others?
“Technically, if asymptomatic, 10 days without a mask, 5 days with a mask,” said Dr. Adalja. “I think this could also be guided with home test negativity being a gauge [as to whether to mingle].”
A version of this article first appeared on WebMD.com.
With new cases of COVID-19 skyrocketing to more than 240,000 a day recently in the U.S., many people are facing the same situation: A family member or friend tests positive or was exposed to someone who did, and the holiday gathering, visit, or return to work is just days or hours away. Now what?
New guidance issued Dec. 27 by the Centers for Disease Control and Prevention shortens the recommended isolation and quarantine period for the general population, coming after the agency shortened the isolation period for health care workers.
This news organization reached out to two infectious disease specialists to get answers to questions that are frequently asked in these situations.
If you have tested positive for COVID-19, what do you do next?
“If you have tested positive, you are infected. At the moment, you are [either] symptomatically affected or presymptomatically infected,’’ said Paul A. Offit, MD, director of the Vaccine Education Center and professor of pediatrics at Children’s Hospital of Philadelphia. At that point, you need to isolate for 5 days, according to the new CDC guidance. (That period has been shortened from 10 days.)
Isolation means separating the infected person from others. Quarantine refers to things you should do if you’re exposed to the virus or you have a close contact infected with COVID-19.
Under the new CDC guidelines, after the 5-day isolation, if the infected person then has no symptoms, he or she can leave isolation and then wear a mask for 5 days.
Those who test positive also need to tell their close contacts they are positive, said Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security.
According to the CDC, the change to a shortened quarantine time is motivated by science ‘’demonstrating that the majority of SARS-CoV-2 transmission occurs early in the course of the illness, generally in the 1-2 days prior to onset of symptoms and the 2-3 days after.”
If you have been exposed to someone with COVID-19, what do you do next?
“If they are vaccinated and boosted, the guidance says there is no need to quarantine,” Dr. Adalja said. But the CDC guidance does recommend these people wear a well-fitting mask at all times when around others for 10 days after exposure.
For everyone else, including the unvaccinated and those who are more than 6 months out from their second Pfizer or Moderna vaccine dose, or more than 2 months from their J&J dose, the CDC recommends a quarantine for 5 days – and wearing a mask for the 5 days after that.
On a practical level, Dr. Adalja said he thinks those who are vaccinated but not boosted could also skip the quarantine and wear a mask for 10 days. Dr. Offit agrees. Because many people exposed have trouble quarantining, Dr. Offit advises those exposed who can’t follow that guidance to be sure to wear a mask for 10 days when indoors. The CDC guidance also offers that as another strategy – that if a 5-day quarantine is not feasible, the exposed person should wear a mask for 10 days when around others.
But if someone who was exposed gets symptoms, that person then enters the infected category and follows that guidance, Dr. Offit said.
When should the person who has been exposed get tested?
After the exposure, ‘’you should probably wait 2-3 days,” Dr. Offit said. “The virus has to reproduce itself.”
Testing should be done by those exposed at least once, Dr. Adalja said.
“But there’s data to support daily testing to guide their activities, but this is not CDC guidance. Home tests are sufficient for this purpose.”
At what point can the infected person mingle safely with others?
“Technically, if asymptomatic, 10 days without a mask, 5 days with a mask,” said Dr. Adalja. “I think this could also be guided with home test negativity being a gauge [as to whether to mingle].”
A version of this article first appeared on WebMD.com.
With new cases of COVID-19 skyrocketing to more than 240,000 a day recently in the U.S., many people are facing the same situation: A family member or friend tests positive or was exposed to someone who did, and the holiday gathering, visit, or return to work is just days or hours away. Now what?
New guidance issued Dec. 27 by the Centers for Disease Control and Prevention shortens the recommended isolation and quarantine period for the general population, coming after the agency shortened the isolation period for health care workers.
This news organization reached out to two infectious disease specialists to get answers to questions that are frequently asked in these situations.
If you have tested positive for COVID-19, what do you do next?
“If you have tested positive, you are infected. At the moment, you are [either] symptomatically affected or presymptomatically infected,’’ said Paul A. Offit, MD, director of the Vaccine Education Center and professor of pediatrics at Children’s Hospital of Philadelphia. At that point, you need to isolate for 5 days, according to the new CDC guidance. (That period has been shortened from 10 days.)
Isolation means separating the infected person from others. Quarantine refers to things you should do if you’re exposed to the virus or you have a close contact infected with COVID-19.
Under the new CDC guidelines, after the 5-day isolation, if the infected person then has no symptoms, he or she can leave isolation and then wear a mask for 5 days.
Those who test positive also need to tell their close contacts they are positive, said Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security.
According to the CDC, the change to a shortened quarantine time is motivated by science ‘’demonstrating that the majority of SARS-CoV-2 transmission occurs early in the course of the illness, generally in the 1-2 days prior to onset of symptoms and the 2-3 days after.”
If you have been exposed to someone with COVID-19, what do you do next?
“If they are vaccinated and boosted, the guidance says there is no need to quarantine,” Dr. Adalja said. But the CDC guidance does recommend these people wear a well-fitting mask at all times when around others for 10 days after exposure.
For everyone else, including the unvaccinated and those who are more than 6 months out from their second Pfizer or Moderna vaccine dose, or more than 2 months from their J&J dose, the CDC recommends a quarantine for 5 days – and wearing a mask for the 5 days after that.
On a practical level, Dr. Adalja said he thinks those who are vaccinated but not boosted could also skip the quarantine and wear a mask for 10 days. Dr. Offit agrees. Because many people exposed have trouble quarantining, Dr. Offit advises those exposed who can’t follow that guidance to be sure to wear a mask for 10 days when indoors. The CDC guidance also offers that as another strategy – that if a 5-day quarantine is not feasible, the exposed person should wear a mask for 10 days when around others.
But if someone who was exposed gets symptoms, that person then enters the infected category and follows that guidance, Dr. Offit said.
When should the person who has been exposed get tested?
After the exposure, ‘’you should probably wait 2-3 days,” Dr. Offit said. “The virus has to reproduce itself.”
Testing should be done by those exposed at least once, Dr. Adalja said.
“But there’s data to support daily testing to guide their activities, but this is not CDC guidance. Home tests are sufficient for this purpose.”
At what point can the infected person mingle safely with others?
“Technically, if asymptomatic, 10 days without a mask, 5 days with a mask,” said Dr. Adalja. “I think this could also be guided with home test negativity being a gauge [as to whether to mingle].”
A version of this article first appeared on WebMD.com.
COVID-19 antigen tests may be less sensitive to Omicron: FDA
Rapid antigen tests for COVID-19 might be less effective at detecting the Omicron variant that is spreading rapidly across the United States, according to the Food and Drug Administration.
Early data suggest that COVID-19 antigen tests “do detect the Omicron variant but may have reduced sensitivity,” the FDA said in a statement posted Dec. 28 on its website.
The FDA is working with the National Institutes of Health’s Rapid Acceleration of Diagnostics (RADx) initiative to assess the performance of antigen tests with patient samples that have the Omicron variant.
The potential for antigen tests to be less sensitive for the Omicron variant emerged in tests using patient samples containing live virus, “which represents the best way to evaluate true test performance in the short term,” the FDA said.
Initial laboratory tests using heat-activated (killed) virus samples found that antigen tests were able to detect the Omicron variant.
“It is important to note that these laboratory data are not a replacement for clinical study evaluations using patient samples with live virus, which are ongoing. The FDA and RADx are continuing to further evaluate the performance of antigen tests using patient samples with live virus,” the FDA said.
Testing still important
The agency continues to recommend use of antigen tests as directed in the authorized labeling and in accordance with the instructions included with the tests.
They note that antigen tests are generally less sensitive and less likely to pick up very early infections, compared with molecular tests.
The FDA continues to recommend that an individual with a negative antigen test who has symptoms or a high likelihood of infection because of exposure follow-up with a molecular test to determine if they have COVID-19.
An individual with a positive antigen test should self-isolate and seek follow-up care with a health care provider to determine the next steps.
The FDA, with partners and test developers, are continuing to evaluate test sensitivity, as well as the best timing and frequency of antigen testing.
The agency said that it will provide updated information and any needed recommendations when appropriate.
A version of this article first appeared on Medscape.com.
Rapid antigen tests for COVID-19 might be less effective at detecting the Omicron variant that is spreading rapidly across the United States, according to the Food and Drug Administration.
Early data suggest that COVID-19 antigen tests “do detect the Omicron variant but may have reduced sensitivity,” the FDA said in a statement posted Dec. 28 on its website.
The FDA is working with the National Institutes of Health’s Rapid Acceleration of Diagnostics (RADx) initiative to assess the performance of antigen tests with patient samples that have the Omicron variant.
The potential for antigen tests to be less sensitive for the Omicron variant emerged in tests using patient samples containing live virus, “which represents the best way to evaluate true test performance in the short term,” the FDA said.
Initial laboratory tests using heat-activated (killed) virus samples found that antigen tests were able to detect the Omicron variant.
“It is important to note that these laboratory data are not a replacement for clinical study evaluations using patient samples with live virus, which are ongoing. The FDA and RADx are continuing to further evaluate the performance of antigen tests using patient samples with live virus,” the FDA said.
Testing still important
The agency continues to recommend use of antigen tests as directed in the authorized labeling and in accordance with the instructions included with the tests.
They note that antigen tests are generally less sensitive and less likely to pick up very early infections, compared with molecular tests.
The FDA continues to recommend that an individual with a negative antigen test who has symptoms or a high likelihood of infection because of exposure follow-up with a molecular test to determine if they have COVID-19.
An individual with a positive antigen test should self-isolate and seek follow-up care with a health care provider to determine the next steps.
The FDA, with partners and test developers, are continuing to evaluate test sensitivity, as well as the best timing and frequency of antigen testing.
The agency said that it will provide updated information and any needed recommendations when appropriate.
A version of this article first appeared on Medscape.com.
Rapid antigen tests for COVID-19 might be less effective at detecting the Omicron variant that is spreading rapidly across the United States, according to the Food and Drug Administration.
Early data suggest that COVID-19 antigen tests “do detect the Omicron variant but may have reduced sensitivity,” the FDA said in a statement posted Dec. 28 on its website.
The FDA is working with the National Institutes of Health’s Rapid Acceleration of Diagnostics (RADx) initiative to assess the performance of antigen tests with patient samples that have the Omicron variant.
The potential for antigen tests to be less sensitive for the Omicron variant emerged in tests using patient samples containing live virus, “which represents the best way to evaluate true test performance in the short term,” the FDA said.
Initial laboratory tests using heat-activated (killed) virus samples found that antigen tests were able to detect the Omicron variant.
“It is important to note that these laboratory data are not a replacement for clinical study evaluations using patient samples with live virus, which are ongoing. The FDA and RADx are continuing to further evaluate the performance of antigen tests using patient samples with live virus,” the FDA said.
Testing still important
The agency continues to recommend use of antigen tests as directed in the authorized labeling and in accordance with the instructions included with the tests.
They note that antigen tests are generally less sensitive and less likely to pick up very early infections, compared with molecular tests.
The FDA continues to recommend that an individual with a negative antigen test who has symptoms or a high likelihood of infection because of exposure follow-up with a molecular test to determine if they have COVID-19.
An individual with a positive antigen test should self-isolate and seek follow-up care with a health care provider to determine the next steps.
The FDA, with partners and test developers, are continuing to evaluate test sensitivity, as well as the best timing and frequency of antigen testing.
The agency said that it will provide updated information and any needed recommendations when appropriate.
A version of this article first appeared on Medscape.com.
Coronavirus can spread to heart, brain days after infection
The coronavirus that causes COVID-19 can spread to the heart and brain within days of infection and can survive for months in organs, according to a new study by the National Institutes of Health.
The virus can spread to almost every organ system in the body, which could contribute to the ongoing symptoms seen in “long COVID” patients, the study authors wrote. The study is considered one of the most comprehensive reviews of how the virus replicates in human cells and persists in the human body. It is under review for publication in the journal Nature.
“This is remarkably important work,” Ziyad Al-Aly, MD, director of the Clinical Epidemiology Center at the Veterans Affairs St. Louis Health Care System, told Bloomberg News. Dr. Al-Aly wasn’t involved with the NIH study but has researched the long-term effects of COVID-19.
“For a long time now, we have been scratching our heads and asking why long COVID seems to affect so many organ systems,” he said. “This paper sheds some light and may help explain why long COVID can occur even in people who had mild or asymptomatic acute disease.”
The NIH researchers sampled and analyzed tissues from autopsies on 44 patients who died after contracting the coronavirus during the first year of the pandemic. They found persistent virus particles in multiple parts of the body, including the heart and brain, for as long as 230 days after symptoms began. This could represent infection with defective virus particles, they said, which has also been seen in persistent infections among measles patients.
“We don’t yet know what burden of chronic illness will result in years to come,” Raina MacIntyre, PhD, a professor of global biosecurity at the University of New South Wales, Sydney, told Bloomberg News.
“Will we see young-onset cardiac failure in survivors or early-onset dementia?” she asked. “These are unanswered questions which call for a precautionary public health approach to mitigation of the spread of this virus.”
Unlike other COVID-19 autopsy research, the NIH team had a more comprehensive postmortem tissue collection process, which typically occurred within a day of the patient’s death, Bloomberg News reported. The researchers also used a variety of ways to preserve tissue to figure out viral levels. They were able to grow the virus collected from several tissues, including the heart, lungs, small intestine, and adrenal glands.
“Our results collectively show that, while the highest burden of SARS-CoV-2 is in the airways and lung, the virus can disseminate early during infection and infect cells throughout the entire body, including widely throughout the brain,” the study authors wrote.
A version of this article first appeared on WebMD.com.
The coronavirus that causes COVID-19 can spread to the heart and brain within days of infection and can survive for months in organs, according to a new study by the National Institutes of Health.
The virus can spread to almost every organ system in the body, which could contribute to the ongoing symptoms seen in “long COVID” patients, the study authors wrote. The study is considered one of the most comprehensive reviews of how the virus replicates in human cells and persists in the human body. It is under review for publication in the journal Nature.
“This is remarkably important work,” Ziyad Al-Aly, MD, director of the Clinical Epidemiology Center at the Veterans Affairs St. Louis Health Care System, told Bloomberg News. Dr. Al-Aly wasn’t involved with the NIH study but has researched the long-term effects of COVID-19.
“For a long time now, we have been scratching our heads and asking why long COVID seems to affect so many organ systems,” he said. “This paper sheds some light and may help explain why long COVID can occur even in people who had mild or asymptomatic acute disease.”
The NIH researchers sampled and analyzed tissues from autopsies on 44 patients who died after contracting the coronavirus during the first year of the pandemic. They found persistent virus particles in multiple parts of the body, including the heart and brain, for as long as 230 days after symptoms began. This could represent infection with defective virus particles, they said, which has also been seen in persistent infections among measles patients.
“We don’t yet know what burden of chronic illness will result in years to come,” Raina MacIntyre, PhD, a professor of global biosecurity at the University of New South Wales, Sydney, told Bloomberg News.
“Will we see young-onset cardiac failure in survivors or early-onset dementia?” she asked. “These are unanswered questions which call for a precautionary public health approach to mitigation of the spread of this virus.”
Unlike other COVID-19 autopsy research, the NIH team had a more comprehensive postmortem tissue collection process, which typically occurred within a day of the patient’s death, Bloomberg News reported. The researchers also used a variety of ways to preserve tissue to figure out viral levels. They were able to grow the virus collected from several tissues, including the heart, lungs, small intestine, and adrenal glands.
“Our results collectively show that, while the highest burden of SARS-CoV-2 is in the airways and lung, the virus can disseminate early during infection and infect cells throughout the entire body, including widely throughout the brain,” the study authors wrote.
A version of this article first appeared on WebMD.com.
The coronavirus that causes COVID-19 can spread to the heart and brain within days of infection and can survive for months in organs, according to a new study by the National Institutes of Health.
The virus can spread to almost every organ system in the body, which could contribute to the ongoing symptoms seen in “long COVID” patients, the study authors wrote. The study is considered one of the most comprehensive reviews of how the virus replicates in human cells and persists in the human body. It is under review for publication in the journal Nature.
“This is remarkably important work,” Ziyad Al-Aly, MD, director of the Clinical Epidemiology Center at the Veterans Affairs St. Louis Health Care System, told Bloomberg News. Dr. Al-Aly wasn’t involved with the NIH study but has researched the long-term effects of COVID-19.
“For a long time now, we have been scratching our heads and asking why long COVID seems to affect so many organ systems,” he said. “This paper sheds some light and may help explain why long COVID can occur even in people who had mild or asymptomatic acute disease.”
The NIH researchers sampled and analyzed tissues from autopsies on 44 patients who died after contracting the coronavirus during the first year of the pandemic. They found persistent virus particles in multiple parts of the body, including the heart and brain, for as long as 230 days after symptoms began. This could represent infection with defective virus particles, they said, which has also been seen in persistent infections among measles patients.
“We don’t yet know what burden of chronic illness will result in years to come,” Raina MacIntyre, PhD, a professor of global biosecurity at the University of New South Wales, Sydney, told Bloomberg News.
“Will we see young-onset cardiac failure in survivors or early-onset dementia?” she asked. “These are unanswered questions which call for a precautionary public health approach to mitigation of the spread of this virus.”
Unlike other COVID-19 autopsy research, the NIH team had a more comprehensive postmortem tissue collection process, which typically occurred within a day of the patient’s death, Bloomberg News reported. The researchers also used a variety of ways to preserve tissue to figure out viral levels. They were able to grow the virus collected from several tissues, including the heart, lungs, small intestine, and adrenal glands.
“Our results collectively show that, while the highest burden of SARS-CoV-2 is in the airways and lung, the virus can disseminate early during infection and infect cells throughout the entire body, including widely throughout the brain,” the study authors wrote.
A version of this article first appeared on WebMD.com.
Children and COVID: Nearly 200,000 new cases reported in 1 week
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
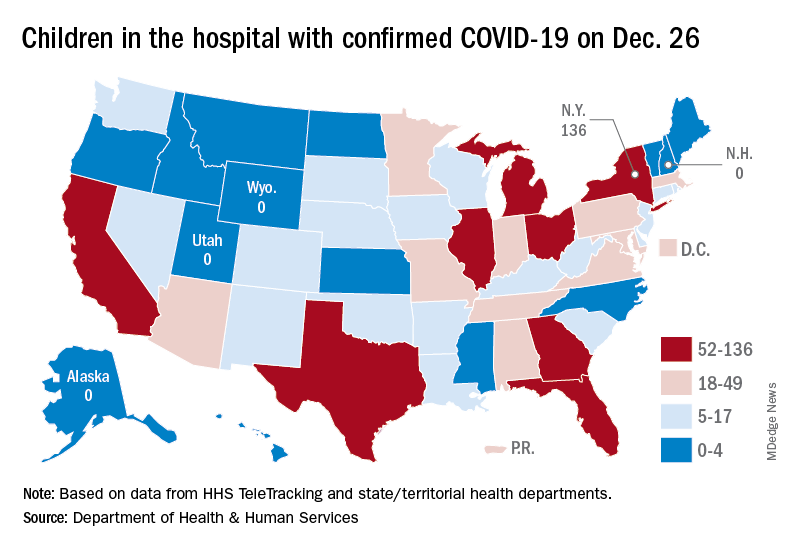
Available state data show that 198,551 child COVID cases were added during the week of Dec. 17-23 – up by 16.8% from the nearly 170,000 new cases reported the previous week and the highest 7-day figure since Sept. 17-23, when 207,000 cases were reported, the AAP and the CHA said in their weekly COVID report. Since Oct. 22-28, when the weekly count dropped to a seasonal low, the weekly count has nearly doubled.
The largest shares of the nearly 199,000 new cases were divided pretty equally between the Northeast and the South, while the West had just a small bump in cases and the Midwest was in the middle. The largest statewide percent increases came in the New England states, along with New Jersey, the District of Columbia, and Puerto Rico. New York State does not report age ranges for COVID cases, the AAP/CHA report noted.
Emergency department visits and hospital admissions are following a similar trend, as both have risen considerably over the last 2 months, data from the Centers for Disease Control and Prevention show.
COVID-related ED visits for children aged 0-11 years – measured as a proportion of all ED visits – are nearing the pandemic high of 4.1% set in late August, while visits in 12- to 15-year-olds have risen from 1.4% in early November to 5.6% on Dec. 24 and 16- to 17-year-olds have gone from 1.5% to 6% over the same period of time, the CDC reported on its COVID Data Tracker.
As for hospital admissions in children aged 0-17 years, the rate was down to 0.19 per 100,000 population on Nov. 11 but had risen to 0.38 per 100,000 as of Dec. 24. The highest point reached in children during the pandemic was 0.46 per 100,000 in early September, the CDC said.
On Dec. 23, 367 children were admitted to hospitals in the United States, the highest number since Sept. 7, when 374 were hospitalized. The highest 1-day total over the course of the pandemic, 394, came just a week before that, Aug. 31, according to the Department of Health & Human Services.
A look at the most recent HHS data shows that 1,161 children were being hospitalized in pediatric inpatient beds with confirmed COVID-19 on Dec. 26. The highest number by state was in New York (136), followed by Texas (90) and Illinois and Ohio, both with 83. There were four states – Alaska, New Hampshire, Utah, and Wyoming – with no hospitalized children, the HHS said. Puerto Rico, meanwhile, had 28 children in the hospital with COVID, more than 38 states.
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
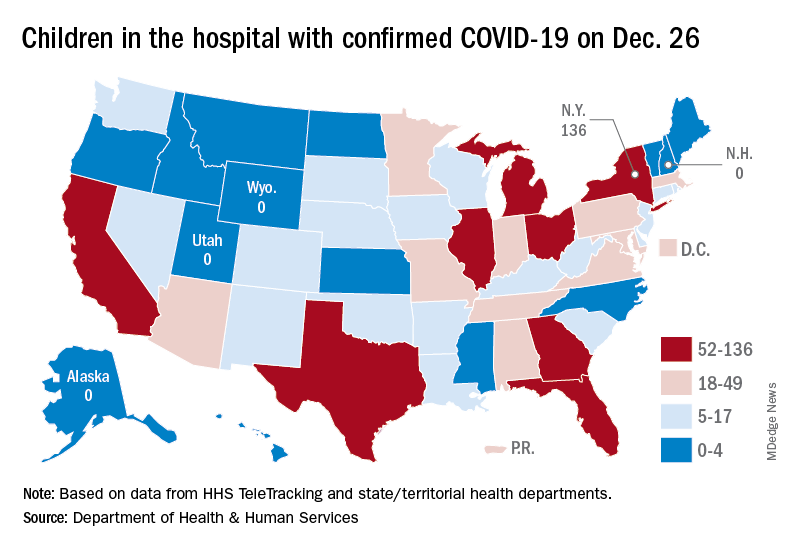
Available state data show that 198,551 child COVID cases were added during the week of Dec. 17-23 – up by 16.8% from the nearly 170,000 new cases reported the previous week and the highest 7-day figure since Sept. 17-23, when 207,000 cases were reported, the AAP and the CHA said in their weekly COVID report. Since Oct. 22-28, when the weekly count dropped to a seasonal low, the weekly count has nearly doubled.
The largest shares of the nearly 199,000 new cases were divided pretty equally between the Northeast and the South, while the West had just a small bump in cases and the Midwest was in the middle. The largest statewide percent increases came in the New England states, along with New Jersey, the District of Columbia, and Puerto Rico. New York State does not report age ranges for COVID cases, the AAP/CHA report noted.
Emergency department visits and hospital admissions are following a similar trend, as both have risen considerably over the last 2 months, data from the Centers for Disease Control and Prevention show.
COVID-related ED visits for children aged 0-11 years – measured as a proportion of all ED visits – are nearing the pandemic high of 4.1% set in late August, while visits in 12- to 15-year-olds have risen from 1.4% in early November to 5.6% on Dec. 24 and 16- to 17-year-olds have gone from 1.5% to 6% over the same period of time, the CDC reported on its COVID Data Tracker.
As for hospital admissions in children aged 0-17 years, the rate was down to 0.19 per 100,000 population on Nov. 11 but had risen to 0.38 per 100,000 as of Dec. 24. The highest point reached in children during the pandemic was 0.46 per 100,000 in early September, the CDC said.
On Dec. 23, 367 children were admitted to hospitals in the United States, the highest number since Sept. 7, when 374 were hospitalized. The highest 1-day total over the course of the pandemic, 394, came just a week before that, Aug. 31, according to the Department of Health & Human Services.
A look at the most recent HHS data shows that 1,161 children were being hospitalized in pediatric inpatient beds with confirmed COVID-19 on Dec. 26. The highest number by state was in New York (136), followed by Texas (90) and Illinois and Ohio, both with 83. There were four states – Alaska, New Hampshire, Utah, and Wyoming – with no hospitalized children, the HHS said. Puerto Rico, meanwhile, had 28 children in the hospital with COVID, more than 38 states.
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
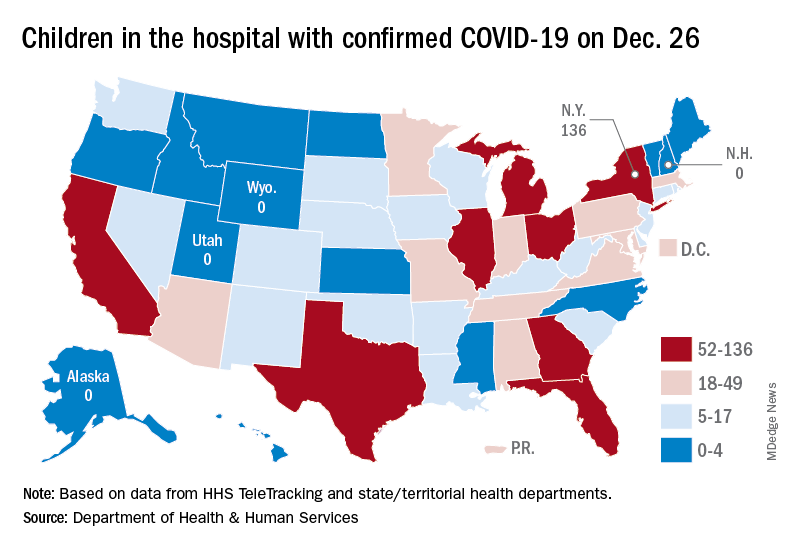
Available state data show that 198,551 child COVID cases were added during the week of Dec. 17-23 – up by 16.8% from the nearly 170,000 new cases reported the previous week and the highest 7-day figure since Sept. 17-23, when 207,000 cases were reported, the AAP and the CHA said in their weekly COVID report. Since Oct. 22-28, when the weekly count dropped to a seasonal low, the weekly count has nearly doubled.
The largest shares of the nearly 199,000 new cases were divided pretty equally between the Northeast and the South, while the West had just a small bump in cases and the Midwest was in the middle. The largest statewide percent increases came in the New England states, along with New Jersey, the District of Columbia, and Puerto Rico. New York State does not report age ranges for COVID cases, the AAP/CHA report noted.
Emergency department visits and hospital admissions are following a similar trend, as both have risen considerably over the last 2 months, data from the Centers for Disease Control and Prevention show.
COVID-related ED visits for children aged 0-11 years – measured as a proportion of all ED visits – are nearing the pandemic high of 4.1% set in late August, while visits in 12- to 15-year-olds have risen from 1.4% in early November to 5.6% on Dec. 24 and 16- to 17-year-olds have gone from 1.5% to 6% over the same period of time, the CDC reported on its COVID Data Tracker.
As for hospital admissions in children aged 0-17 years, the rate was down to 0.19 per 100,000 population on Nov. 11 but had risen to 0.38 per 100,000 as of Dec. 24. The highest point reached in children during the pandemic was 0.46 per 100,000 in early September, the CDC said.
On Dec. 23, 367 children were admitted to hospitals in the United States, the highest number since Sept. 7, when 374 were hospitalized. The highest 1-day total over the course of the pandemic, 394, came just a week before that, Aug. 31, according to the Department of Health & Human Services.
A look at the most recent HHS data shows that 1,161 children were being hospitalized in pediatric inpatient beds with confirmed COVID-19 on Dec. 26. The highest number by state was in New York (136), followed by Texas (90) and Illinois and Ohio, both with 83. There were four states – Alaska, New Hampshire, Utah, and Wyoming – with no hospitalized children, the HHS said. Puerto Rico, meanwhile, had 28 children in the hospital with COVID, more than 38 states.
COVID booster protection may wane in about 10 weeks, new data show
, according to new data from Britain.
U.K. health officials shared the data just before Christmas and noted that there haven’t been enough severe cases of the Omicron variant to calculate how well boosters protect against severe disease. But they believe the extra shots provide significant protection against hospitalization and death.
“It will be a few weeks before effectiveness against severe disease with Omicron can be estimated,” U.K. Health Security Agency officials wrote in the report. “However, based on experience with previous variants, this is likely to be substantially higher than the estimates against symptomatic disease.”
Since countries began reporting Omicron cases in November, multiple studies have suggested the variant is better at escaping antibodies from vaccination and previous infection, according to the New York Times. The U.K. report adds to that, noting that both the initial vaccine series and booster doses were less effective and faded faster against the Omicron variant than the Delta variant.
Among those who received two doses of the AstraZeneca vaccine, a booster of the Pfizer or Moderna vaccine was 60% effective at preventing symptomatic disease 2 to 4 weeks after the shot. But after 10 weeks, the Pfizer booster was 35% effective, and the Moderna booster was 45% effective. (The AstraZeneca vaccine is not authorized in the United States, but the Johnson & Johnson shot uses a similar technology, the New York Times reported.)
Among those who received three Pfizer doses, vaccine effectiveness was 70% about a week after the booster but dropped to 45% after 10 weeks. At the same time, those who received an initial two-dose series of the Pfizer vaccine and then a Moderna booster seemed to have 75% effectiveness up to 9 weeks.
The report was based on an analysis of 148,000 Delta cases and 68,000 Omicron cases in the United Kingdom through Dec. 20. So far, the U.K. health officials wrote, Omicron infections appear to be less severe and less likely to lead to hospitalization than Delta infections. At that time, 132 people with lab-confirmed Omicron had been admitted to hospitals, and 14 deaths had been reported among ages 52-96.
“This analysis is preliminary because of the small numbers of Omicron cases currently in hospital and the limited spread of Omicron into older age groups as yet,” the report said.
The reinfection rate has also increased for the Omicron variant, the report found. Among the 116,000 people who had an Omicron infection, about 11,000 -- or 9.5% -- were linked to a previously confirmed infection, which is likely an undercount of reinfections. In the data analyzed, 69 Omicron cases were a third episode of COVID-19 infection, and 290 cases occurred 60-89 days after a first infection.
A version of this article first appeared on WebMD.com.
, according to new data from Britain.
U.K. health officials shared the data just before Christmas and noted that there haven’t been enough severe cases of the Omicron variant to calculate how well boosters protect against severe disease. But they believe the extra shots provide significant protection against hospitalization and death.
“It will be a few weeks before effectiveness against severe disease with Omicron can be estimated,” U.K. Health Security Agency officials wrote in the report. “However, based on experience with previous variants, this is likely to be substantially higher than the estimates against symptomatic disease.”
Since countries began reporting Omicron cases in November, multiple studies have suggested the variant is better at escaping antibodies from vaccination and previous infection, according to the New York Times. The U.K. report adds to that, noting that both the initial vaccine series and booster doses were less effective and faded faster against the Omicron variant than the Delta variant.
Among those who received two doses of the AstraZeneca vaccine, a booster of the Pfizer or Moderna vaccine was 60% effective at preventing symptomatic disease 2 to 4 weeks after the shot. But after 10 weeks, the Pfizer booster was 35% effective, and the Moderna booster was 45% effective. (The AstraZeneca vaccine is not authorized in the United States, but the Johnson & Johnson shot uses a similar technology, the New York Times reported.)
Among those who received three Pfizer doses, vaccine effectiveness was 70% about a week after the booster but dropped to 45% after 10 weeks. At the same time, those who received an initial two-dose series of the Pfizer vaccine and then a Moderna booster seemed to have 75% effectiveness up to 9 weeks.
The report was based on an analysis of 148,000 Delta cases and 68,000 Omicron cases in the United Kingdom through Dec. 20. So far, the U.K. health officials wrote, Omicron infections appear to be less severe and less likely to lead to hospitalization than Delta infections. At that time, 132 people with lab-confirmed Omicron had been admitted to hospitals, and 14 deaths had been reported among ages 52-96.
“This analysis is preliminary because of the small numbers of Omicron cases currently in hospital and the limited spread of Omicron into older age groups as yet,” the report said.
The reinfection rate has also increased for the Omicron variant, the report found. Among the 116,000 people who had an Omicron infection, about 11,000 -- or 9.5% -- were linked to a previously confirmed infection, which is likely an undercount of reinfections. In the data analyzed, 69 Omicron cases were a third episode of COVID-19 infection, and 290 cases occurred 60-89 days after a first infection.
A version of this article first appeared on WebMD.com.
, according to new data from Britain.
U.K. health officials shared the data just before Christmas and noted that there haven’t been enough severe cases of the Omicron variant to calculate how well boosters protect against severe disease. But they believe the extra shots provide significant protection against hospitalization and death.
“It will be a few weeks before effectiveness against severe disease with Omicron can be estimated,” U.K. Health Security Agency officials wrote in the report. “However, based on experience with previous variants, this is likely to be substantially higher than the estimates against symptomatic disease.”
Since countries began reporting Omicron cases in November, multiple studies have suggested the variant is better at escaping antibodies from vaccination and previous infection, according to the New York Times. The U.K. report adds to that, noting that both the initial vaccine series and booster doses were less effective and faded faster against the Omicron variant than the Delta variant.
Among those who received two doses of the AstraZeneca vaccine, a booster of the Pfizer or Moderna vaccine was 60% effective at preventing symptomatic disease 2 to 4 weeks after the shot. But after 10 weeks, the Pfizer booster was 35% effective, and the Moderna booster was 45% effective. (The AstraZeneca vaccine is not authorized in the United States, but the Johnson & Johnson shot uses a similar technology, the New York Times reported.)
Among those who received three Pfizer doses, vaccine effectiveness was 70% about a week after the booster but dropped to 45% after 10 weeks. At the same time, those who received an initial two-dose series of the Pfizer vaccine and then a Moderna booster seemed to have 75% effectiveness up to 9 weeks.
The report was based on an analysis of 148,000 Delta cases and 68,000 Omicron cases in the United Kingdom through Dec. 20. So far, the U.K. health officials wrote, Omicron infections appear to be less severe and less likely to lead to hospitalization than Delta infections. At that time, 132 people with lab-confirmed Omicron had been admitted to hospitals, and 14 deaths had been reported among ages 52-96.
“This analysis is preliminary because of the small numbers of Omicron cases currently in hospital and the limited spread of Omicron into older age groups as yet,” the report said.
The reinfection rate has also increased for the Omicron variant, the report found. Among the 116,000 people who had an Omicron infection, about 11,000 -- or 9.5% -- were linked to a previously confirmed infection, which is likely an undercount of reinfections. In the data analyzed, 69 Omicron cases were a third episode of COVID-19 infection, and 290 cases occurred 60-89 days after a first infection.
A version of this article first appeared on WebMD.com.
