User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Long COVID is real, and many real questions remain
Long story short, we still have a lot to learn about long COVID-19.
But it is a real phenomenon with real long-term health effects for people recovering from coronavirus infections. And diagnosing and managing it can get tricky, as some symptoms of long COVID-19 overlap with those of other conditions – and what many people have as they recover from any challenging stay in the ICU.
Risk factors remain largely unknown as well: What makes one person more likely to have symptoms like fatigue, “brain fog,” or headaches versus someone else? Researchers are just starting to offer some intriguing answers, but the evidence is preliminary at this point, experts said at a media briefing sponsored by the Infectious Diseases Society of America.
Unanswered questions include: Does an autoimmune reaction drive long COVID? Does the coronavirus linger in reservoirs within the body and reactivate later? What protection against long COVID do vaccines and treatments offer, if any?
To get a handle on these and other questions, nailing down a standard definition of long COVID would be a good start.
“Studies so far have used different definitions of long COVID,” Nahid Bhadelia, MD, founding director of the Boston University Center for Emerging Infectious Diseases Policy and Research, said during the briefing.
Fatigue is the most commonly symptom of long COVID in research so far, said Dr. Bhadelia, who is also an associate professor of medicine at Boston University.
“What’s difficult in this situation is it’s been 2 years in a global pandemic. We’re all fatigued. How do you tease this apart?” she asked.
Other common symptoms are a hard time thinking quickly – also known as “brain fog” – and the feeling that, despite normal oxygen levels, breathing is difficult, said Kathleen Bell, MD.
Headache, joint and muscle pain, and persistent loss of smell and taste are also widely reported, said Dr. Bell, a professor and chair of the department of physical medicine and rehabilitation at the University of Texas Southwestern Medical Center in Dallas.
Not all the symptoms are physical either.
“Pretty prominent things that we’re seeing are very high levels of anxiety, depression, and insomnia,” Dr. Bell said. These “actually seem to be associated independently with the virus as opposed to just being a completely reactive component.”
More research will be needed to distinguish the causes of these conditions.
A difficult diagnosis
the experts said.
“We are starting to see some interesting features of inaccurate attributions to COVID, both on the part of perhaps the person with long COVID symptoms and health care providers,” Dr. Bell said.“It’s sometimes a little difficult to sort it out.”
Dr. Bell said she was not suggesting misdiagnoses are common, “but it is difficult for physicians that don’t see a lot of people with long COVID.”
The advice is to consider other conditions. “You can have both a long COVID syndrome and other syndromes as well,” she said. “As one of my teachers used to say: ‘You can have both ticks and fleas.’ ”
Predicting long COVID
In a study getting attention, researchers identified four early things linked to greater chances that someone with COVID-19 will have long-term effects: type 2 diabetes at the time of diagnosis, the presence of specific autoantibodies, unusual levels of SARS-CoV-2 RNA in the blood, and signs of the Epstein-Barr virus in the blood.
The study, published in Cell, followed 309 people 2-3 months after COVID-19.
“That’s important work, but it’s early work,” Dr. Bhadelia said. “I think we still have a while to go in terms of understanding the mechanism of long COVID.”
Unexpected patients getting long COVID care
“We are seeing different populations than we all expected to see when this pandemic first started,” Dr. Bell said.
Instead of seeing primarily patients who had severe COVID-19, “the preponderance of people that we’re seeing in long COVID clinics are people who are enabled, were never hospitalized, and have what people might call mild to moderate cases of coronavirus infection,” she said.
Also, instead of just older patients, people of all ages are seeking long COVID care.
One thing that appears more certain is a lack of diversity in people seeking care at long COVID clinics nationwide.
“Many of us who have long COVID specialty clinics will tell you that we are tending to see fairly educated, socioeconomically stable population in these clinics,” Dr. Bell said. “We know that based on the early statistics of who’s getting COVID and having significant COVID that we may not be seeing those populations for follow-up.”
Is an autoinflammatory process to blame?
It remains unclear if a hyperinflammatory response is driving persistent post–COVID-19 symptoms. Children and some adults have developed multisystem inflammatory conditions associated with COVID-19, for example.
There is a signal, and “I think there is enough data now to show something does happen,” Dr. Bhadelia said. “The question is, how often does it happen?”
Spending time in critical care, even without COVID-19, can result in persistent symptoms after a hospital stay, such as acute respiratory distress syndrome. Recovery can take time because being in an ICU is “basically the physiologically equivalent of a car crash,” Dr. Bhadelia said. “So you’re recovering from that, too.”
Dr. Bell agreed. “You’re not only recovering from the virus itself, you’re recovering from intubation, secondary infections, secondary lung conditions, perhaps other organ failure, and prolonged bed rest. There are so many things that go into that, that it’s a little bit hard to sort that out from what long COVID is and what the direct effects of the virus are.”
Also a research opportunity
“I hate to call it this, but we’ve never had an opportunity [where] we have so many people in such a short amount of time with the same viral disorder,” Dr. Bell said. “We also have the technology to investigate it. This has never happened.
“SARS-CoV-2 is not the only virus. This is just the only one we’ve gotten whacked with in such a huge quantity at one time,” she said.
What researchers learn now about COVID-19 and long COVID “is a model that’s going to be able to be applied in the future to infectious diseases in general,” Dr. Bell predicted.
How long will long COVID last?
The vast majority of people with long COVID will get better over time, given enough support and relief of their symptoms, Dr. Bell said.
Type 2 diabetes, preexisting pulmonary disease, and other things could affect how long it takes to recover from long COVID, she said, although more evidence is needed.
“I don’t think at this point that anyone can say how long this long COVID will last because there are a variety of factors,” Dr. Bell said.
A version of this article first appeared on WebMD.com.
Long story short, we still have a lot to learn about long COVID-19.
But it is a real phenomenon with real long-term health effects for people recovering from coronavirus infections. And diagnosing and managing it can get tricky, as some symptoms of long COVID-19 overlap with those of other conditions – and what many people have as they recover from any challenging stay in the ICU.
Risk factors remain largely unknown as well: What makes one person more likely to have symptoms like fatigue, “brain fog,” or headaches versus someone else? Researchers are just starting to offer some intriguing answers, but the evidence is preliminary at this point, experts said at a media briefing sponsored by the Infectious Diseases Society of America.
Unanswered questions include: Does an autoimmune reaction drive long COVID? Does the coronavirus linger in reservoirs within the body and reactivate later? What protection against long COVID do vaccines and treatments offer, if any?
To get a handle on these and other questions, nailing down a standard definition of long COVID would be a good start.
“Studies so far have used different definitions of long COVID,” Nahid Bhadelia, MD, founding director of the Boston University Center for Emerging Infectious Diseases Policy and Research, said during the briefing.
Fatigue is the most commonly symptom of long COVID in research so far, said Dr. Bhadelia, who is also an associate professor of medicine at Boston University.
“What’s difficult in this situation is it’s been 2 years in a global pandemic. We’re all fatigued. How do you tease this apart?” she asked.
Other common symptoms are a hard time thinking quickly – also known as “brain fog” – and the feeling that, despite normal oxygen levels, breathing is difficult, said Kathleen Bell, MD.
Headache, joint and muscle pain, and persistent loss of smell and taste are also widely reported, said Dr. Bell, a professor and chair of the department of physical medicine and rehabilitation at the University of Texas Southwestern Medical Center in Dallas.
Not all the symptoms are physical either.
“Pretty prominent things that we’re seeing are very high levels of anxiety, depression, and insomnia,” Dr. Bell said. These “actually seem to be associated independently with the virus as opposed to just being a completely reactive component.”
More research will be needed to distinguish the causes of these conditions.
A difficult diagnosis
the experts said.
“We are starting to see some interesting features of inaccurate attributions to COVID, both on the part of perhaps the person with long COVID symptoms and health care providers,” Dr. Bell said.“It’s sometimes a little difficult to sort it out.”
Dr. Bell said she was not suggesting misdiagnoses are common, “but it is difficult for physicians that don’t see a lot of people with long COVID.”
The advice is to consider other conditions. “You can have both a long COVID syndrome and other syndromes as well,” she said. “As one of my teachers used to say: ‘You can have both ticks and fleas.’ ”
Predicting long COVID
In a study getting attention, researchers identified four early things linked to greater chances that someone with COVID-19 will have long-term effects: type 2 diabetes at the time of diagnosis, the presence of specific autoantibodies, unusual levels of SARS-CoV-2 RNA in the blood, and signs of the Epstein-Barr virus in the blood.
The study, published in Cell, followed 309 people 2-3 months after COVID-19.
“That’s important work, but it’s early work,” Dr. Bhadelia said. “I think we still have a while to go in terms of understanding the mechanism of long COVID.”
Unexpected patients getting long COVID care
“We are seeing different populations than we all expected to see when this pandemic first started,” Dr. Bell said.
Instead of seeing primarily patients who had severe COVID-19, “the preponderance of people that we’re seeing in long COVID clinics are people who are enabled, were never hospitalized, and have what people might call mild to moderate cases of coronavirus infection,” she said.
Also, instead of just older patients, people of all ages are seeking long COVID care.
One thing that appears more certain is a lack of diversity in people seeking care at long COVID clinics nationwide.
“Many of us who have long COVID specialty clinics will tell you that we are tending to see fairly educated, socioeconomically stable population in these clinics,” Dr. Bell said. “We know that based on the early statistics of who’s getting COVID and having significant COVID that we may not be seeing those populations for follow-up.”
Is an autoinflammatory process to blame?
It remains unclear if a hyperinflammatory response is driving persistent post–COVID-19 symptoms. Children and some adults have developed multisystem inflammatory conditions associated with COVID-19, for example.
There is a signal, and “I think there is enough data now to show something does happen,” Dr. Bhadelia said. “The question is, how often does it happen?”
Spending time in critical care, even without COVID-19, can result in persistent symptoms after a hospital stay, such as acute respiratory distress syndrome. Recovery can take time because being in an ICU is “basically the physiologically equivalent of a car crash,” Dr. Bhadelia said. “So you’re recovering from that, too.”
Dr. Bell agreed. “You’re not only recovering from the virus itself, you’re recovering from intubation, secondary infections, secondary lung conditions, perhaps other organ failure, and prolonged bed rest. There are so many things that go into that, that it’s a little bit hard to sort that out from what long COVID is and what the direct effects of the virus are.”
Also a research opportunity
“I hate to call it this, but we’ve never had an opportunity [where] we have so many people in such a short amount of time with the same viral disorder,” Dr. Bell said. “We also have the technology to investigate it. This has never happened.
“SARS-CoV-2 is not the only virus. This is just the only one we’ve gotten whacked with in such a huge quantity at one time,” she said.
What researchers learn now about COVID-19 and long COVID “is a model that’s going to be able to be applied in the future to infectious diseases in general,” Dr. Bell predicted.
How long will long COVID last?
The vast majority of people with long COVID will get better over time, given enough support and relief of their symptoms, Dr. Bell said.
Type 2 diabetes, preexisting pulmonary disease, and other things could affect how long it takes to recover from long COVID, she said, although more evidence is needed.
“I don’t think at this point that anyone can say how long this long COVID will last because there are a variety of factors,” Dr. Bell said.
A version of this article first appeared on WebMD.com.
Long story short, we still have a lot to learn about long COVID-19.
But it is a real phenomenon with real long-term health effects for people recovering from coronavirus infections. And diagnosing and managing it can get tricky, as some symptoms of long COVID-19 overlap with those of other conditions – and what many people have as they recover from any challenging stay in the ICU.
Risk factors remain largely unknown as well: What makes one person more likely to have symptoms like fatigue, “brain fog,” or headaches versus someone else? Researchers are just starting to offer some intriguing answers, but the evidence is preliminary at this point, experts said at a media briefing sponsored by the Infectious Diseases Society of America.
Unanswered questions include: Does an autoimmune reaction drive long COVID? Does the coronavirus linger in reservoirs within the body and reactivate later? What protection against long COVID do vaccines and treatments offer, if any?
To get a handle on these and other questions, nailing down a standard definition of long COVID would be a good start.
“Studies so far have used different definitions of long COVID,” Nahid Bhadelia, MD, founding director of the Boston University Center for Emerging Infectious Diseases Policy and Research, said during the briefing.
Fatigue is the most commonly symptom of long COVID in research so far, said Dr. Bhadelia, who is also an associate professor of medicine at Boston University.
“What’s difficult in this situation is it’s been 2 years in a global pandemic. We’re all fatigued. How do you tease this apart?” she asked.
Other common symptoms are a hard time thinking quickly – also known as “brain fog” – and the feeling that, despite normal oxygen levels, breathing is difficult, said Kathleen Bell, MD.
Headache, joint and muscle pain, and persistent loss of smell and taste are also widely reported, said Dr. Bell, a professor and chair of the department of physical medicine and rehabilitation at the University of Texas Southwestern Medical Center in Dallas.
Not all the symptoms are physical either.
“Pretty prominent things that we’re seeing are very high levels of anxiety, depression, and insomnia,” Dr. Bell said. These “actually seem to be associated independently with the virus as opposed to just being a completely reactive component.”
More research will be needed to distinguish the causes of these conditions.
A difficult diagnosis
the experts said.
“We are starting to see some interesting features of inaccurate attributions to COVID, both on the part of perhaps the person with long COVID symptoms and health care providers,” Dr. Bell said.“It’s sometimes a little difficult to sort it out.”
Dr. Bell said she was not suggesting misdiagnoses are common, “but it is difficult for physicians that don’t see a lot of people with long COVID.”
The advice is to consider other conditions. “You can have both a long COVID syndrome and other syndromes as well,” she said. “As one of my teachers used to say: ‘You can have both ticks and fleas.’ ”
Predicting long COVID
In a study getting attention, researchers identified four early things linked to greater chances that someone with COVID-19 will have long-term effects: type 2 diabetes at the time of diagnosis, the presence of specific autoantibodies, unusual levels of SARS-CoV-2 RNA in the blood, and signs of the Epstein-Barr virus in the blood.
The study, published in Cell, followed 309 people 2-3 months after COVID-19.
“That’s important work, but it’s early work,” Dr. Bhadelia said. “I think we still have a while to go in terms of understanding the mechanism of long COVID.”
Unexpected patients getting long COVID care
“We are seeing different populations than we all expected to see when this pandemic first started,” Dr. Bell said.
Instead of seeing primarily patients who had severe COVID-19, “the preponderance of people that we’re seeing in long COVID clinics are people who are enabled, were never hospitalized, and have what people might call mild to moderate cases of coronavirus infection,” she said.
Also, instead of just older patients, people of all ages are seeking long COVID care.
One thing that appears more certain is a lack of diversity in people seeking care at long COVID clinics nationwide.
“Many of us who have long COVID specialty clinics will tell you that we are tending to see fairly educated, socioeconomically stable population in these clinics,” Dr. Bell said. “We know that based on the early statistics of who’s getting COVID and having significant COVID that we may not be seeing those populations for follow-up.”
Is an autoinflammatory process to blame?
It remains unclear if a hyperinflammatory response is driving persistent post–COVID-19 symptoms. Children and some adults have developed multisystem inflammatory conditions associated with COVID-19, for example.
There is a signal, and “I think there is enough data now to show something does happen,” Dr. Bhadelia said. “The question is, how often does it happen?”
Spending time in critical care, even without COVID-19, can result in persistent symptoms after a hospital stay, such as acute respiratory distress syndrome. Recovery can take time because being in an ICU is “basically the physiologically equivalent of a car crash,” Dr. Bhadelia said. “So you’re recovering from that, too.”
Dr. Bell agreed. “You’re not only recovering from the virus itself, you’re recovering from intubation, secondary infections, secondary lung conditions, perhaps other organ failure, and prolonged bed rest. There are so many things that go into that, that it’s a little bit hard to sort that out from what long COVID is and what the direct effects of the virus are.”
Also a research opportunity
“I hate to call it this, but we’ve never had an opportunity [where] we have so many people in such a short amount of time with the same viral disorder,” Dr. Bell said. “We also have the technology to investigate it. This has never happened.
“SARS-CoV-2 is not the only virus. This is just the only one we’ve gotten whacked with in such a huge quantity at one time,” she said.
What researchers learn now about COVID-19 and long COVID “is a model that’s going to be able to be applied in the future to infectious diseases in general,” Dr. Bell predicted.
How long will long COVID last?
The vast majority of people with long COVID will get better over time, given enough support and relief of their symptoms, Dr. Bell said.
Type 2 diabetes, preexisting pulmonary disease, and other things could affect how long it takes to recover from long COVID, she said, although more evidence is needed.
“I don’t think at this point that anyone can say how long this long COVID will last because there are a variety of factors,” Dr. Bell said.
A version of this article first appeared on WebMD.com.
Immunocompromised patients should receive fourth COVID shot: CDC
The Centers for Disease Control and Prevention contacted pharmacies on Jan. 26 to reinforce the message that people with moderate to severe immune suppression should receive a fourth COVID-19 vaccine, according to Kaiser Health News.
The conference call came a day after the news outlet reported that immunocompromised people were being turned away by pharmacies. White House officials also emphasized on Jan. 26 that immunocompromised people should receive an additional shot.
During the call, the CDC “reiterated the recommendations, running through case examples,” Mitchel Rothholz, RPh, MBA, chief of governance and state affiliates for the American Pharmacists Association, told KHN.
While on the call, Mr. Rothholz asked for a “prepared document” with the CDC’s recommendations “so we can clearly and consistently communicate the message.” The CDC officials on the call said they would create a document but “don’t know how long that will take,” Mr. Rothholz told KHN.
The CDC recommends an additional shot -– or a fourth shot – for those who have weak immune systems, which makes them more at risk for severe COVID-19 and death. About 7 million American adults are considered immunocompromised, KHN reported, which includes people who have certain medical conditions that impair their immune response or who take immune-suppressing drugs because of organ transplants, cancer, or autoimmune diseases.
The CDC first recommended fourth shots for immunocompromised people in October. This month, the CDC shortened the time for booster shots from 6 months to 5 months, and some immunocompromised people who are due for another shot have begun to seek them. The agency has been educating pharmacists and other health providers since then, a CDC spokesperson told KHN.
While patients don’t need to provide proof that they are immunocompromised, according to the CDC, some have been turned away, KHN reported.
To improve communication with the public, large pharmacies could issue news releases and update their websites “explicitly stating that they are offering fourth doses” to immunocompromised people, Ameet Kini, MD, a professor of pathology and laboratory medicine at Loyola University Medical Center in Chicago, told KHN.
Pharmacies should also update their patient portals and provide “clear guidance for their pharmacists,” he said.
A version of this article first appeared on WebMD.com.
The Centers for Disease Control and Prevention contacted pharmacies on Jan. 26 to reinforce the message that people with moderate to severe immune suppression should receive a fourth COVID-19 vaccine, according to Kaiser Health News.
The conference call came a day after the news outlet reported that immunocompromised people were being turned away by pharmacies. White House officials also emphasized on Jan. 26 that immunocompromised people should receive an additional shot.
During the call, the CDC “reiterated the recommendations, running through case examples,” Mitchel Rothholz, RPh, MBA, chief of governance and state affiliates for the American Pharmacists Association, told KHN.
While on the call, Mr. Rothholz asked for a “prepared document” with the CDC’s recommendations “so we can clearly and consistently communicate the message.” The CDC officials on the call said they would create a document but “don’t know how long that will take,” Mr. Rothholz told KHN.
The CDC recommends an additional shot -– or a fourth shot – for those who have weak immune systems, which makes them more at risk for severe COVID-19 and death. About 7 million American adults are considered immunocompromised, KHN reported, which includes people who have certain medical conditions that impair their immune response or who take immune-suppressing drugs because of organ transplants, cancer, or autoimmune diseases.
The CDC first recommended fourth shots for immunocompromised people in October. This month, the CDC shortened the time for booster shots from 6 months to 5 months, and some immunocompromised people who are due for another shot have begun to seek them. The agency has been educating pharmacists and other health providers since then, a CDC spokesperson told KHN.
While patients don’t need to provide proof that they are immunocompromised, according to the CDC, some have been turned away, KHN reported.
To improve communication with the public, large pharmacies could issue news releases and update their websites “explicitly stating that they are offering fourth doses” to immunocompromised people, Ameet Kini, MD, a professor of pathology and laboratory medicine at Loyola University Medical Center in Chicago, told KHN.
Pharmacies should also update their patient portals and provide “clear guidance for their pharmacists,” he said.
A version of this article first appeared on WebMD.com.
The Centers for Disease Control and Prevention contacted pharmacies on Jan. 26 to reinforce the message that people with moderate to severe immune suppression should receive a fourth COVID-19 vaccine, according to Kaiser Health News.
The conference call came a day after the news outlet reported that immunocompromised people were being turned away by pharmacies. White House officials also emphasized on Jan. 26 that immunocompromised people should receive an additional shot.
During the call, the CDC “reiterated the recommendations, running through case examples,” Mitchel Rothholz, RPh, MBA, chief of governance and state affiliates for the American Pharmacists Association, told KHN.
While on the call, Mr. Rothholz asked for a “prepared document” with the CDC’s recommendations “so we can clearly and consistently communicate the message.” The CDC officials on the call said they would create a document but “don’t know how long that will take,” Mr. Rothholz told KHN.
The CDC recommends an additional shot -– or a fourth shot – for those who have weak immune systems, which makes them more at risk for severe COVID-19 and death. About 7 million American adults are considered immunocompromised, KHN reported, which includes people who have certain medical conditions that impair their immune response or who take immune-suppressing drugs because of organ transplants, cancer, or autoimmune diseases.
The CDC first recommended fourth shots for immunocompromised people in October. This month, the CDC shortened the time for booster shots from 6 months to 5 months, and some immunocompromised people who are due for another shot have begun to seek them. The agency has been educating pharmacists and other health providers since then, a CDC spokesperson told KHN.
While patients don’t need to provide proof that they are immunocompromised, according to the CDC, some have been turned away, KHN reported.
To improve communication with the public, large pharmacies could issue news releases and update their websites “explicitly stating that they are offering fourth doses” to immunocompromised people, Ameet Kini, MD, a professor of pathology and laboratory medicine at Loyola University Medical Center in Chicago, told KHN.
Pharmacies should also update their patient portals and provide “clear guidance for their pharmacists,” he said.
A version of this article first appeared on WebMD.com.
Get free masks at grocery stores and pharmacies starting Jan. 28
The first batches are expected to arrive in some stores on Jan. 27, and many locations will begin offering them to customers on Jan. 28, according to NPR.
Meijer, which operates more than 250 groceries and pharmacies throughout the Midwest, has received about 3 million masks. Customers can pick up masks from the greeter stand at the store entrance.
More than 2,200 Kroger stores with pharmacies will give out free masks, with the first shipment expected to arrive on Jan. 27, a spokeswoman told NPR.
Walgreens will likely begin offering masks in some stores on Jan. 28, which will continue “on a rolling basis in the days and weeks following,” a spokesman told NPR.
Masks should arrive by Jan. 28 at Southeastern Grocers locations with in-store pharmacies, including Fresco y Mas, Harveys, and Winn-Dixie, according to CNN.
Hy-Vee received and began giving out masks on Jan. 21, and most stores with pharmacies were giving them out Jan. 26, according to Today.
CVS Pharmacy locations will offer free masks as early as Jan. 27, a spokesman told Today. That will include CVS Pharmacy locations inside Target and Schnucks.
Albertsons is “currently working to finalize details regarding inventory and distribution,” the chain told Today.
Rite Aid will have free masks in some stores at the end of the week, with all stores receiving them by early February, Today reported.
Walmart and Sam’s Club will offer free masks late next week at the earliest, according to NBC Chicago.
The Biden administration is sending out 400 million N95 masks from the Strategic National Stockpile. Each person can take up to three free masks, if they’re available, the Department of Health and Human Services has said.
The distribution of masks is meant to align with the CDC’s latest recommendation to wear an N95 or KN95 mask to prevent the spread of the highly transmissible Omicron variant. When worn correctly over the mouth and nose, the high-filtration masks are made to filter out 95% or more of airborne particles.
The Biden administration is also sending masks to community health centers and COVID-19 test kits directly to Americans. The programs are ramping up now and should be fully running by early February, NPR reported.
A version of this article first appeared on WebMD.com.
The first batches are expected to arrive in some stores on Jan. 27, and many locations will begin offering them to customers on Jan. 28, according to NPR.
Meijer, which operates more than 250 groceries and pharmacies throughout the Midwest, has received about 3 million masks. Customers can pick up masks from the greeter stand at the store entrance.
More than 2,200 Kroger stores with pharmacies will give out free masks, with the first shipment expected to arrive on Jan. 27, a spokeswoman told NPR.
Walgreens will likely begin offering masks in some stores on Jan. 28, which will continue “on a rolling basis in the days and weeks following,” a spokesman told NPR.
Masks should arrive by Jan. 28 at Southeastern Grocers locations with in-store pharmacies, including Fresco y Mas, Harveys, and Winn-Dixie, according to CNN.
Hy-Vee received and began giving out masks on Jan. 21, and most stores with pharmacies were giving them out Jan. 26, according to Today.
CVS Pharmacy locations will offer free masks as early as Jan. 27, a spokesman told Today. That will include CVS Pharmacy locations inside Target and Schnucks.
Albertsons is “currently working to finalize details regarding inventory and distribution,” the chain told Today.
Rite Aid will have free masks in some stores at the end of the week, with all stores receiving them by early February, Today reported.
Walmart and Sam’s Club will offer free masks late next week at the earliest, according to NBC Chicago.
The Biden administration is sending out 400 million N95 masks from the Strategic National Stockpile. Each person can take up to three free masks, if they’re available, the Department of Health and Human Services has said.
The distribution of masks is meant to align with the CDC’s latest recommendation to wear an N95 or KN95 mask to prevent the spread of the highly transmissible Omicron variant. When worn correctly over the mouth and nose, the high-filtration masks are made to filter out 95% or more of airborne particles.
The Biden administration is also sending masks to community health centers and COVID-19 test kits directly to Americans. The programs are ramping up now and should be fully running by early February, NPR reported.
A version of this article first appeared on WebMD.com.
The first batches are expected to arrive in some stores on Jan. 27, and many locations will begin offering them to customers on Jan. 28, according to NPR.
Meijer, which operates more than 250 groceries and pharmacies throughout the Midwest, has received about 3 million masks. Customers can pick up masks from the greeter stand at the store entrance.
More than 2,200 Kroger stores with pharmacies will give out free masks, with the first shipment expected to arrive on Jan. 27, a spokeswoman told NPR.
Walgreens will likely begin offering masks in some stores on Jan. 28, which will continue “on a rolling basis in the days and weeks following,” a spokesman told NPR.
Masks should arrive by Jan. 28 at Southeastern Grocers locations with in-store pharmacies, including Fresco y Mas, Harveys, and Winn-Dixie, according to CNN.
Hy-Vee received and began giving out masks on Jan. 21, and most stores with pharmacies were giving them out Jan. 26, according to Today.
CVS Pharmacy locations will offer free masks as early as Jan. 27, a spokesman told Today. That will include CVS Pharmacy locations inside Target and Schnucks.
Albertsons is “currently working to finalize details regarding inventory and distribution,” the chain told Today.
Rite Aid will have free masks in some stores at the end of the week, with all stores receiving them by early February, Today reported.
Walmart and Sam’s Club will offer free masks late next week at the earliest, according to NBC Chicago.
The Biden administration is sending out 400 million N95 masks from the Strategic National Stockpile. Each person can take up to three free masks, if they’re available, the Department of Health and Human Services has said.
The distribution of masks is meant to align with the CDC’s latest recommendation to wear an N95 or KN95 mask to prevent the spread of the highly transmissible Omicron variant. When worn correctly over the mouth and nose, the high-filtration masks are made to filter out 95% or more of airborne particles.
The Biden administration is also sending masks to community health centers and COVID-19 test kits directly to Americans. The programs are ramping up now and should be fully running by early February, NPR reported.
A version of this article first appeared on WebMD.com.
Kids’ mask use linked with fewer childcare closings
Mask-wearing in childcare programs is linked with fewer COVID-19–related program closures, new data released suggest.
Researchers included 6,654 childcare professionals in a prospective, 1-year, longitudinal electronic survey study of home- and center-based childcare programs in all 50 states.
Findings by Thomas S. Murray, MD, PhD, with the department of pediatrics, Yale University, New Haven, Conn., and coauthors, were published in JAMA Network Open on Jan. 28, 2022.
They found that mask-wearing from the May 22, 2020, baseline to June 8, 2020, was associated with a 13% reduction in program closures within the following year (adjusted relative risk, 0.87; 95% confidence interval, 0.77-0.99). Continued mask-wearing throughout the 1-year follow-up was associated with a 14% reduction in program closures (aRR, 0.86; 95% CI, 0.74-1.00).
The authors said the evidence supports current masking recommendation in younger children provided by the Centers for Disease Control and Prevention.
They wrote: “This finding has important public health policy implications for families that rely on childcare to sustain employment.”
The benefits of masking in preventing COVID-19 transmission within kindergarten through 12th-grade classes are well documented. Masks are particularly important in areas where vaccinations are not widespread.
Masks can be worn safely by young children without harming respiratory function, studies have shown.
William Schaffner, MD, an infectious disease expert at Vanderbilt University, Nashville, Tenn., pointed out that the American Academy of Pediatrics has said there are no noteworthy effects on breathing function for most children.
“There’s been so much discussion about the contribution of masks to reducing the risk of COVID that it’s nice to have the data,” he said, adding that this is a relationship that has been difficult to study, but this analysis was able to make the connection with hard numbers.
“It’s an important outcome,” he said in an interview.
The authors pointed out there is evidence that school-age children can identify most emotions in masked faces.
They added that “2-year-old children recognize spoken words better through an opaque mask, compared with a clear face shield, suggesting verbal communication to infants is not harmed by face masks.”
Studies have shown that childhood infection with other respiratory viruses also decreased and asthma symptoms were not reported when preschool children wore masks and used other preventative steps.
The authors wrote that a potential reason for that may be that those who wear masks have less face touching, known to increase the spread of COVID-19.
Paloma Beamer, PhD, an engineer and exposure scientist at University of Arizona, Tucson, who also has a 3-year-old son who wears masks at his daycare center, said in an interview that she works closely with his school on training kids how to wear their masks because getting young children to keep them on and finding ones that fit is challenging.
“We need layered controls and protections in place at schools as much as possible,” she said, adding that the authors didn’t mention ventilation, but that’s another important component as well.
“We’re fortunate in Arizona that we are in an old school and the windows are open as much as possible,” she said.
She said this study shows that “masks are a great form of additional control.” Her son is on his third quarantine this month after three kids tested positive, she added.
She said: “I think these newer variants perhaps make the findings of this study more compelling and it will be interesting to see if the researchers do a follow-up study.”
Strengths of the study include that it utilized prospective data from a large national cohort of childcare professionals. Additionally, the retention rate was high at 1 year. And the self-reported information likely gives better information than looking at policies that may or may not be well followed.
Limitations include potential reporting bias because the self-reports were not independently confirmed. Also, family behavior outside childcare, such as social gatherings where masking is not enforced, also influence COVID-19 cases when children gather and may affect the numbers of closures.
Having the option of childcare centers benefits kids with in-person early education and social interactions with staff, the authors noted. The centers also help parents return to work without interruptions at home.
“Our findings support current national recommendations endorsed by many local and state governments for masking children 2 years and older in childcare programs when community COVID-19 transmission levels are elevated,” the authors wrote.
Dr. Schaffner said the results have implications outside of childcare centers and should be included in discussions of masking in schools and in the general public.
All phases of this study were supported by and coauthors report grants from the Andrew & Julie Klingenstein Family Fund, Esther A. & Joseph Klingenstein Fund, Heising-Simons Foundation, W.K. Kellogg Foundation, Foundation for Child Development, Early Educator Investment Collaborative, and Scholastic. The study was partially funded by the Yale Institute for Global Health. Dr. Schaffner and Dr. Beamer reported no relevant financial relationships.
Mask-wearing in childcare programs is linked with fewer COVID-19–related program closures, new data released suggest.
Researchers included 6,654 childcare professionals in a prospective, 1-year, longitudinal electronic survey study of home- and center-based childcare programs in all 50 states.
Findings by Thomas S. Murray, MD, PhD, with the department of pediatrics, Yale University, New Haven, Conn., and coauthors, were published in JAMA Network Open on Jan. 28, 2022.
They found that mask-wearing from the May 22, 2020, baseline to June 8, 2020, was associated with a 13% reduction in program closures within the following year (adjusted relative risk, 0.87; 95% confidence interval, 0.77-0.99). Continued mask-wearing throughout the 1-year follow-up was associated with a 14% reduction in program closures (aRR, 0.86; 95% CI, 0.74-1.00).
The authors said the evidence supports current masking recommendation in younger children provided by the Centers for Disease Control and Prevention.
They wrote: “This finding has important public health policy implications for families that rely on childcare to sustain employment.”
The benefits of masking in preventing COVID-19 transmission within kindergarten through 12th-grade classes are well documented. Masks are particularly important in areas where vaccinations are not widespread.
Masks can be worn safely by young children without harming respiratory function, studies have shown.
William Schaffner, MD, an infectious disease expert at Vanderbilt University, Nashville, Tenn., pointed out that the American Academy of Pediatrics has said there are no noteworthy effects on breathing function for most children.
“There’s been so much discussion about the contribution of masks to reducing the risk of COVID that it’s nice to have the data,” he said, adding that this is a relationship that has been difficult to study, but this analysis was able to make the connection with hard numbers.
“It’s an important outcome,” he said in an interview.
The authors pointed out there is evidence that school-age children can identify most emotions in masked faces.
They added that “2-year-old children recognize spoken words better through an opaque mask, compared with a clear face shield, suggesting verbal communication to infants is not harmed by face masks.”
Studies have shown that childhood infection with other respiratory viruses also decreased and asthma symptoms were not reported when preschool children wore masks and used other preventative steps.
The authors wrote that a potential reason for that may be that those who wear masks have less face touching, known to increase the spread of COVID-19.
Paloma Beamer, PhD, an engineer and exposure scientist at University of Arizona, Tucson, who also has a 3-year-old son who wears masks at his daycare center, said in an interview that she works closely with his school on training kids how to wear their masks because getting young children to keep them on and finding ones that fit is challenging.
“We need layered controls and protections in place at schools as much as possible,” she said, adding that the authors didn’t mention ventilation, but that’s another important component as well.
“We’re fortunate in Arizona that we are in an old school and the windows are open as much as possible,” she said.
She said this study shows that “masks are a great form of additional control.” Her son is on his third quarantine this month after three kids tested positive, she added.
She said: “I think these newer variants perhaps make the findings of this study more compelling and it will be interesting to see if the researchers do a follow-up study.”
Strengths of the study include that it utilized prospective data from a large national cohort of childcare professionals. Additionally, the retention rate was high at 1 year. And the self-reported information likely gives better information than looking at policies that may or may not be well followed.
Limitations include potential reporting bias because the self-reports were not independently confirmed. Also, family behavior outside childcare, such as social gatherings where masking is not enforced, also influence COVID-19 cases when children gather and may affect the numbers of closures.
Having the option of childcare centers benefits kids with in-person early education and social interactions with staff, the authors noted. The centers also help parents return to work without interruptions at home.
“Our findings support current national recommendations endorsed by many local and state governments for masking children 2 years and older in childcare programs when community COVID-19 transmission levels are elevated,” the authors wrote.
Dr. Schaffner said the results have implications outside of childcare centers and should be included in discussions of masking in schools and in the general public.
All phases of this study were supported by and coauthors report grants from the Andrew & Julie Klingenstein Family Fund, Esther A. & Joseph Klingenstein Fund, Heising-Simons Foundation, W.K. Kellogg Foundation, Foundation for Child Development, Early Educator Investment Collaborative, and Scholastic. The study was partially funded by the Yale Institute for Global Health. Dr. Schaffner and Dr. Beamer reported no relevant financial relationships.
Mask-wearing in childcare programs is linked with fewer COVID-19–related program closures, new data released suggest.
Researchers included 6,654 childcare professionals in a prospective, 1-year, longitudinal electronic survey study of home- and center-based childcare programs in all 50 states.
Findings by Thomas S. Murray, MD, PhD, with the department of pediatrics, Yale University, New Haven, Conn., and coauthors, were published in JAMA Network Open on Jan. 28, 2022.
They found that mask-wearing from the May 22, 2020, baseline to June 8, 2020, was associated with a 13% reduction in program closures within the following year (adjusted relative risk, 0.87; 95% confidence interval, 0.77-0.99). Continued mask-wearing throughout the 1-year follow-up was associated with a 14% reduction in program closures (aRR, 0.86; 95% CI, 0.74-1.00).
The authors said the evidence supports current masking recommendation in younger children provided by the Centers for Disease Control and Prevention.
They wrote: “This finding has important public health policy implications for families that rely on childcare to sustain employment.”
The benefits of masking in preventing COVID-19 transmission within kindergarten through 12th-grade classes are well documented. Masks are particularly important in areas where vaccinations are not widespread.
Masks can be worn safely by young children without harming respiratory function, studies have shown.
William Schaffner, MD, an infectious disease expert at Vanderbilt University, Nashville, Tenn., pointed out that the American Academy of Pediatrics has said there are no noteworthy effects on breathing function for most children.
“There’s been so much discussion about the contribution of masks to reducing the risk of COVID that it’s nice to have the data,” he said, adding that this is a relationship that has been difficult to study, but this analysis was able to make the connection with hard numbers.
“It’s an important outcome,” he said in an interview.
The authors pointed out there is evidence that school-age children can identify most emotions in masked faces.
They added that “2-year-old children recognize spoken words better through an opaque mask, compared with a clear face shield, suggesting verbal communication to infants is not harmed by face masks.”
Studies have shown that childhood infection with other respiratory viruses also decreased and asthma symptoms were not reported when preschool children wore masks and used other preventative steps.
The authors wrote that a potential reason for that may be that those who wear masks have less face touching, known to increase the spread of COVID-19.
Paloma Beamer, PhD, an engineer and exposure scientist at University of Arizona, Tucson, who also has a 3-year-old son who wears masks at his daycare center, said in an interview that she works closely with his school on training kids how to wear their masks because getting young children to keep them on and finding ones that fit is challenging.
“We need layered controls and protections in place at schools as much as possible,” she said, adding that the authors didn’t mention ventilation, but that’s another important component as well.
“We’re fortunate in Arizona that we are in an old school and the windows are open as much as possible,” she said.
She said this study shows that “masks are a great form of additional control.” Her son is on his third quarantine this month after three kids tested positive, she added.
She said: “I think these newer variants perhaps make the findings of this study more compelling and it will be interesting to see if the researchers do a follow-up study.”
Strengths of the study include that it utilized prospective data from a large national cohort of childcare professionals. Additionally, the retention rate was high at 1 year. And the self-reported information likely gives better information than looking at policies that may or may not be well followed.
Limitations include potential reporting bias because the self-reports were not independently confirmed. Also, family behavior outside childcare, such as social gatherings where masking is not enforced, also influence COVID-19 cases when children gather and may affect the numbers of closures.
Having the option of childcare centers benefits kids with in-person early education and social interactions with staff, the authors noted. The centers also help parents return to work without interruptions at home.
“Our findings support current national recommendations endorsed by many local and state governments for masking children 2 years and older in childcare programs when community COVID-19 transmission levels are elevated,” the authors wrote.
Dr. Schaffner said the results have implications outside of childcare centers and should be included in discussions of masking in schools and in the general public.
All phases of this study were supported by and coauthors report grants from the Andrew & Julie Klingenstein Family Fund, Esther A. & Joseph Klingenstein Fund, Heising-Simons Foundation, W.K. Kellogg Foundation, Foundation for Child Development, Early Educator Investment Collaborative, and Scholastic. The study was partially funded by the Yale Institute for Global Health. Dr. Schaffner and Dr. Beamer reported no relevant financial relationships.
FROM JAMA NETWORK OPEN
Another winter for our discontent
Here we are. Again. It’s cold and it’s gray. The sun rises late and sets early, so that it feels like midnight by 8 p.m. Indoor venues are risky with the highly contagious Omicron variant, and I feel like we are all pushing the replay button on 2021’s miserable winter.
In some ways, it’s worse: In 2021 we had the hope that vaccines would pull us out of the pandemic and we had guidance on all that we should not be doing. In January, we were gaming the various Internet sites to get a coveted vaccine for ourselves or our family and friends, then lining up to get jabbed. We did not yet know that it wouldn’t be enough – that we’d need boosters, that Delta and Omicron would defy the vaccines. Yes, the vaccines work miracles to prevent severe disease and death, but the worry of passing the virus to someone who is vulnerable or unvaccinated(!), or both, remains – and now we can wonder how we’ll ever get out of this mess with hopeful talk of an endemic, while we wait on the next variant. I like certainty, and this pandemic is one big screaming reminder that certainty about anything is just a pleasant notion, death and taxes excluded, of course.
Kris Lukish, vice president of human resources at Johns Hopkins Hospital in Baltimore, started an update to the hospital employees with: “As we begin 2022, it feels like we are experiencing dejà vu, or ‘Groundhog Day,’ or ‘50 First Dates.’ In ‘50 First Dates,’ Drew Barrymore wakes up each day reliving one specific day. It never changes. I realize our world may seem a little like that right now. We thought we’d turned a corner with COVID, and instead we saw a rapid rise in cases and hospitalizations due to the Omicron variant, higher than in previous surges.”
In 2021, many of us skipped holiday travel and ate outdoors. My morning coffee group moved to Zoom and it wasn’t until late spring, when community rates of COVID nose-dived, that I began seeing patients in my office for the first time in over a year. Since many of my patients are over 60, I tested myself with a home antigen test before going into the office. I changed my schedule so sessions began on the half-hour to be sure the suite’s waiting room would be empty, and I purchased an air purifier, cracked the window open, and figured everyone was as safe as we could reasonably be.
By the first Monday in January 2022, the positivity rate in Maryland was just shy of 30%. Twitter circulated anecdotes about false negatives with the home antigen test kits, and I decided it was safest to return to all-virtual appointments.
Mona Masood, DO, is cofounder of the Physician Support Line, a call-in service for doctors that started in March 2020. She has noted a change in the problems physicians face.
“We’re seeing a lot of empathy fatigue,” Dr. Masood said. “It’s not unexpected with a prolonged situation like this – the trauma has doctors in survival mode and they need to be present for themselves, their families, and their patients. People are emotionally drained, and we’re stretching them to the limit. Now at the front lines, doctors are getting a lot of backlash. There are the conspiracy theories, and people who challenge their knowledge and training and it leads them to ask if they should be doing this work. and these are large decisions that are being made in a specific context.
“The other thing we’re hearing is from trainees – residents and fellows – who are expected to carry a lot of work on the COVID units. Some are being told that they can’t graduate because they haven’t finished their other training requirements. This type of systemic issue produces moral injury.”
Dr. Masood talked about what running the support line has been like for her. “I know people want to give more in a catastrophe, and I was realistic that the enthusiasm might die off. I would go as long as psychiatrists volunteer, and the most incredible thing is that it hasn’t stopped. Some of the original people are no longer with us, but others have come aboard, and it’s been incredible to be a part of this.”
In her Jan. 26, 2022, newsletter, epidemiologist Katelyn Jetelina, PhD, MPH, tried to be reassuring about the future. “In order to know how this will end, we need to look at how other pandemics ended,” Dr. Jetelina wrote. “First, recognize the last part of that sentence ... pandemics end. Every epi curve comes down. This pandemic will end, too. Hold that fact close to you.”
She wrote about the three ways that pandemics end. The SARS pandemic of 2002 lasted 1.5 years as public health measures were effective, in large part because the disease was spread only by symptomatic patients. Vaccines offer a second way to end pandemics, as they have for polio and smallpox. “If the globe works together, we could possibly eradicate SARS-CoV-2 with vaccines. [Now that we have numerous animal reservoirs, though, this is close to impossible.]”
Finally, Dr. Jetelina noted that the 1918 flu changed from a pandemic situation to being endemic. “Over time, the virus attenuated, it became less severe.” Society acclimates to a virus with a low mortality rate. “The vast majority of scientists think an endemic state is the future of SARS-CoV-2. I agree.” And she goes on to define endemic as a steady state, but not the absence of suffering. She likens it to malaria and tuberculosis, illnesses with high global mortality.
“An endemic will come without an announcement or headlines, we won’t know we’re there until well after we’ve arrived.” She wrote of the uncertainty that faces us moving forward: We don’t know how much, or how long, immunity from Omicron infections will last, or if future variants will cause more or less severe disease. She casted her vote for global vaccinations, boosters, masks, better ventilation, communication, empathy, and tolerance to end the pandemic.
In Maryland, hospitalizations and positivity are starting to decline from the postholiday surge. I have figured out that I am not good at predicting what will happen next, and the experts don’t seem to be much better. I’d like a headline ending, the kind we looked to be heading toward last June.
I’ve told my patients who want to come in person that I will reassess in March. We have written our own rules, and mine are somewhere in the middle – I don’t go to public indoor spaces unmasked, but I do see vaccinated family and friends in our homes without masks. I don’t want to be responsible for transmitting a potentially fatal illness to a vulnerable patient. Honestly, this makes no sense, but since there is a video option, I feel I should not risk passing a potentially lethal virus to my patients. I just hope I’m not writing this same article again in January 2023.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins. Dr. Miller has no conflicts of interest.
Here we are. Again. It’s cold and it’s gray. The sun rises late and sets early, so that it feels like midnight by 8 p.m. Indoor venues are risky with the highly contagious Omicron variant, and I feel like we are all pushing the replay button on 2021’s miserable winter.
In some ways, it’s worse: In 2021 we had the hope that vaccines would pull us out of the pandemic and we had guidance on all that we should not be doing. In January, we were gaming the various Internet sites to get a coveted vaccine for ourselves or our family and friends, then lining up to get jabbed. We did not yet know that it wouldn’t be enough – that we’d need boosters, that Delta and Omicron would defy the vaccines. Yes, the vaccines work miracles to prevent severe disease and death, but the worry of passing the virus to someone who is vulnerable or unvaccinated(!), or both, remains – and now we can wonder how we’ll ever get out of this mess with hopeful talk of an endemic, while we wait on the next variant. I like certainty, and this pandemic is one big screaming reminder that certainty about anything is just a pleasant notion, death and taxes excluded, of course.
Kris Lukish, vice president of human resources at Johns Hopkins Hospital in Baltimore, started an update to the hospital employees with: “As we begin 2022, it feels like we are experiencing dejà vu, or ‘Groundhog Day,’ or ‘50 First Dates.’ In ‘50 First Dates,’ Drew Barrymore wakes up each day reliving one specific day. It never changes. I realize our world may seem a little like that right now. We thought we’d turned a corner with COVID, and instead we saw a rapid rise in cases and hospitalizations due to the Omicron variant, higher than in previous surges.”
In 2021, many of us skipped holiday travel and ate outdoors. My morning coffee group moved to Zoom and it wasn’t until late spring, when community rates of COVID nose-dived, that I began seeing patients in my office for the first time in over a year. Since many of my patients are over 60, I tested myself with a home antigen test before going into the office. I changed my schedule so sessions began on the half-hour to be sure the suite’s waiting room would be empty, and I purchased an air purifier, cracked the window open, and figured everyone was as safe as we could reasonably be.
By the first Monday in January 2022, the positivity rate in Maryland was just shy of 30%. Twitter circulated anecdotes about false negatives with the home antigen test kits, and I decided it was safest to return to all-virtual appointments.
Mona Masood, DO, is cofounder of the Physician Support Line, a call-in service for doctors that started in March 2020. She has noted a change in the problems physicians face.
“We’re seeing a lot of empathy fatigue,” Dr. Masood said. “It’s not unexpected with a prolonged situation like this – the trauma has doctors in survival mode and they need to be present for themselves, their families, and their patients. People are emotionally drained, and we’re stretching them to the limit. Now at the front lines, doctors are getting a lot of backlash. There are the conspiracy theories, and people who challenge their knowledge and training and it leads them to ask if they should be doing this work. and these are large decisions that are being made in a specific context.
“The other thing we’re hearing is from trainees – residents and fellows – who are expected to carry a lot of work on the COVID units. Some are being told that they can’t graduate because they haven’t finished their other training requirements. This type of systemic issue produces moral injury.”
Dr. Masood talked about what running the support line has been like for her. “I know people want to give more in a catastrophe, and I was realistic that the enthusiasm might die off. I would go as long as psychiatrists volunteer, and the most incredible thing is that it hasn’t stopped. Some of the original people are no longer with us, but others have come aboard, and it’s been incredible to be a part of this.”
In her Jan. 26, 2022, newsletter, epidemiologist Katelyn Jetelina, PhD, MPH, tried to be reassuring about the future. “In order to know how this will end, we need to look at how other pandemics ended,” Dr. Jetelina wrote. “First, recognize the last part of that sentence ... pandemics end. Every epi curve comes down. This pandemic will end, too. Hold that fact close to you.”
She wrote about the three ways that pandemics end. The SARS pandemic of 2002 lasted 1.5 years as public health measures were effective, in large part because the disease was spread only by symptomatic patients. Vaccines offer a second way to end pandemics, as they have for polio and smallpox. “If the globe works together, we could possibly eradicate SARS-CoV-2 with vaccines. [Now that we have numerous animal reservoirs, though, this is close to impossible.]”
Finally, Dr. Jetelina noted that the 1918 flu changed from a pandemic situation to being endemic. “Over time, the virus attenuated, it became less severe.” Society acclimates to a virus with a low mortality rate. “The vast majority of scientists think an endemic state is the future of SARS-CoV-2. I agree.” And she goes on to define endemic as a steady state, but not the absence of suffering. She likens it to malaria and tuberculosis, illnesses with high global mortality.
“An endemic will come without an announcement or headlines, we won’t know we’re there until well after we’ve arrived.” She wrote of the uncertainty that faces us moving forward: We don’t know how much, or how long, immunity from Omicron infections will last, or if future variants will cause more or less severe disease. She casted her vote for global vaccinations, boosters, masks, better ventilation, communication, empathy, and tolerance to end the pandemic.
In Maryland, hospitalizations and positivity are starting to decline from the postholiday surge. I have figured out that I am not good at predicting what will happen next, and the experts don’t seem to be much better. I’d like a headline ending, the kind we looked to be heading toward last June.
I’ve told my patients who want to come in person that I will reassess in March. We have written our own rules, and mine are somewhere in the middle – I don’t go to public indoor spaces unmasked, but I do see vaccinated family and friends in our homes without masks. I don’t want to be responsible for transmitting a potentially fatal illness to a vulnerable patient. Honestly, this makes no sense, but since there is a video option, I feel I should not risk passing a potentially lethal virus to my patients. I just hope I’m not writing this same article again in January 2023.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins. Dr. Miller has no conflicts of interest.
Here we are. Again. It’s cold and it’s gray. The sun rises late and sets early, so that it feels like midnight by 8 p.m. Indoor venues are risky with the highly contagious Omicron variant, and I feel like we are all pushing the replay button on 2021’s miserable winter.
In some ways, it’s worse: In 2021 we had the hope that vaccines would pull us out of the pandemic and we had guidance on all that we should not be doing. In January, we were gaming the various Internet sites to get a coveted vaccine for ourselves or our family and friends, then lining up to get jabbed. We did not yet know that it wouldn’t be enough – that we’d need boosters, that Delta and Omicron would defy the vaccines. Yes, the vaccines work miracles to prevent severe disease and death, but the worry of passing the virus to someone who is vulnerable or unvaccinated(!), or both, remains – and now we can wonder how we’ll ever get out of this mess with hopeful talk of an endemic, while we wait on the next variant. I like certainty, and this pandemic is one big screaming reminder that certainty about anything is just a pleasant notion, death and taxes excluded, of course.
Kris Lukish, vice president of human resources at Johns Hopkins Hospital in Baltimore, started an update to the hospital employees with: “As we begin 2022, it feels like we are experiencing dejà vu, or ‘Groundhog Day,’ or ‘50 First Dates.’ In ‘50 First Dates,’ Drew Barrymore wakes up each day reliving one specific day. It never changes. I realize our world may seem a little like that right now. We thought we’d turned a corner with COVID, and instead we saw a rapid rise in cases and hospitalizations due to the Omicron variant, higher than in previous surges.”
In 2021, many of us skipped holiday travel and ate outdoors. My morning coffee group moved to Zoom and it wasn’t until late spring, when community rates of COVID nose-dived, that I began seeing patients in my office for the first time in over a year. Since many of my patients are over 60, I tested myself with a home antigen test before going into the office. I changed my schedule so sessions began on the half-hour to be sure the suite’s waiting room would be empty, and I purchased an air purifier, cracked the window open, and figured everyone was as safe as we could reasonably be.
By the first Monday in January 2022, the positivity rate in Maryland was just shy of 30%. Twitter circulated anecdotes about false negatives with the home antigen test kits, and I decided it was safest to return to all-virtual appointments.
Mona Masood, DO, is cofounder of the Physician Support Line, a call-in service for doctors that started in March 2020. She has noted a change in the problems physicians face.
“We’re seeing a lot of empathy fatigue,” Dr. Masood said. “It’s not unexpected with a prolonged situation like this – the trauma has doctors in survival mode and they need to be present for themselves, their families, and their patients. People are emotionally drained, and we’re stretching them to the limit. Now at the front lines, doctors are getting a lot of backlash. There are the conspiracy theories, and people who challenge their knowledge and training and it leads them to ask if they should be doing this work. and these are large decisions that are being made in a specific context.
“The other thing we’re hearing is from trainees – residents and fellows – who are expected to carry a lot of work on the COVID units. Some are being told that they can’t graduate because they haven’t finished their other training requirements. This type of systemic issue produces moral injury.”
Dr. Masood talked about what running the support line has been like for her. “I know people want to give more in a catastrophe, and I was realistic that the enthusiasm might die off. I would go as long as psychiatrists volunteer, and the most incredible thing is that it hasn’t stopped. Some of the original people are no longer with us, but others have come aboard, and it’s been incredible to be a part of this.”
In her Jan. 26, 2022, newsletter, epidemiologist Katelyn Jetelina, PhD, MPH, tried to be reassuring about the future. “In order to know how this will end, we need to look at how other pandemics ended,” Dr. Jetelina wrote. “First, recognize the last part of that sentence ... pandemics end. Every epi curve comes down. This pandemic will end, too. Hold that fact close to you.”
She wrote about the three ways that pandemics end. The SARS pandemic of 2002 lasted 1.5 years as public health measures were effective, in large part because the disease was spread only by symptomatic patients. Vaccines offer a second way to end pandemics, as they have for polio and smallpox. “If the globe works together, we could possibly eradicate SARS-CoV-2 with vaccines. [Now that we have numerous animal reservoirs, though, this is close to impossible.]”
Finally, Dr. Jetelina noted that the 1918 flu changed from a pandemic situation to being endemic. “Over time, the virus attenuated, it became less severe.” Society acclimates to a virus with a low mortality rate. “The vast majority of scientists think an endemic state is the future of SARS-CoV-2. I agree.” And she goes on to define endemic as a steady state, but not the absence of suffering. She likens it to malaria and tuberculosis, illnesses with high global mortality.
“An endemic will come without an announcement or headlines, we won’t know we’re there until well after we’ve arrived.” She wrote of the uncertainty that faces us moving forward: We don’t know how much, or how long, immunity from Omicron infections will last, or if future variants will cause more or less severe disease. She casted her vote for global vaccinations, boosters, masks, better ventilation, communication, empathy, and tolerance to end the pandemic.
In Maryland, hospitalizations and positivity are starting to decline from the postholiday surge. I have figured out that I am not good at predicting what will happen next, and the experts don’t seem to be much better. I’d like a headline ending, the kind we looked to be heading toward last June.
I’ve told my patients who want to come in person that I will reassess in March. We have written our own rules, and mine are somewhere in the middle – I don’t go to public indoor spaces unmasked, but I do see vaccinated family and friends in our homes without masks. I don’t want to be responsible for transmitting a potentially fatal illness to a vulnerable patient. Honestly, this makes no sense, but since there is a video option, I feel I should not risk passing a potentially lethal virus to my patients. I just hope I’m not writing this same article again in January 2023.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins. Dr. Miller has no conflicts of interest.
We’re dying to tell you about fatigability
Are you tired? Or are you death tired?
When we’re feeling that burnout monster creep in we sometimes say that we’re being worked to death or that we’re dead tired, but what if that feeling could predict when it’s your actual time to go?
In a recent study published in the Journals of Gerontology: Series A, epidemiologists from the University of Pittsburgh were able to associate a level of “physical fatigability” with mortality.
The researchers administered the Pittsburgh Fatigability Scale to almost 3,000 participants aged ≥ 60 years, who ranked from 0 to 5 on how tired they thought they would be after doing activities like light housework or a leisurely 30-minute walk. After accounting for factors such as preexisting conditions and mental health, the researchers found that people who scored 25 or more points were 2.3 times more likely to die in the next 2.7 years, compared with those who scored under 25.
So what does that tell us about the importance of being continuously active? It’s pretty important.
“Previous research indicates that getting more physical activity can reduce a person’s fatigability. Our study is the first to link more severe physical fatigability to an earlier death,” lead author Nancy W. Glynn, PhD, said in a separate statement. The best way to keep physically active, she suggested, is to set manageable goals and a routine.
A nice walk around the neighborhood during golden hour or a little bit of yoga before breakfast could be a great way to keep the body moving, because you know what they say: Use it or lose it.
This work is NFT protected: Do not screenshot
If you’ve been following the nonmedical news, you’ve likely heard the term “NFT” explode in the past few months. Standing for nonfungible token, NFTs are, at least theoretically, a proof of ownership for digital creations that prevents anyone other than the buyer from reselling the artwork. Sounds like a great idea: It protects artists and buyers alike.
Much like its cousin cryptocurrency, however, the NFT world is rife with speculation, scams, misunderstanding, and drawings of bored monkeys. It’s the Wild West out there in the digital art universe: One poor unfortunate accidentally sold a $300k NFT image for $3,000, a group of investors spent $3 million buying an NFT for a rare version of Dune believing it gave them the copyright (it did not), and an Indonesian engineering student’s 5-year series of expressionless selfies is now worth a million dollars.
This is a column detailing weird medical news, however, so with our setup complete (though our understanding of NFTs is very much not), we move to France and meet our hero (?), Emmanuel Masmejean, an orthopedic surgeon who apparently wasn’t making enough money in his lucrative medical career.
In a move of apocalyptic madness, he threw ethics out the window, delved into his archive, and found an x-ray of a young woman with a bullet lodged in her arm. The woman was a survivor of the Bataclan mass shooting and bombing in 2015, and don’t you worry, our intrepid entrepreneur made sure to identify her as such when he tried selling the x-ray as an NFT on an online art website for $2,776. Yes, this is very much a violation of doctor-patient confidentiality, and no, that’s not a lot of money to risk your medical career on.
Naturally, the woman was horrified and shocked to learn that the image was being sold, her lawyer told the Guardian. When the doctor called her, he merely attempted to justify his action, rather than apologizing or showing any remorse. Dr. Masmejean is now facing legal action and a disciplinary charge for his attempted entry into the NFT world for publishing the image without permission, and the NFT has been removed from the website. Should have stuck with the bored monkeys.
Avatars could be the future
Zoom, FaceTime, and Skype are great when people can’t be together in the same room, state, or country. Not the same as being somewhere in person, but a pretty good replacement during a global pandemic. But what if you had a robot that could be present for you?
Seven-year-old Joshua Martinangeli of Berlin has a severe lung disease and needs to wear a tube in his neck, so he cannot attend school. A robot avatar, donated to Joshua through a private initiative, sits in his seat in the classroom and is able to interact with the students and teacher, according to Reuters. A light on the avatar blinks when Joshua wants to speak and the children can talk with him too. Joshua and his classmates agree that it’s not the same as him really being there to talk and learn, but it’s a great way to keep him included.
“We are the only district in Berlin that has bought four avatars for its schools. The impetus was COVID-19, but I think this will be the future well beyond the pandemic,” Torsten Kuehne, district education councilor, told Reuters.
So where do we get an avatar to go out and run errands? Can we send it to the office instead of Zooming the next meeting? Or maybe our avatar could go to the gym for us. But how do we get the results to show up on our bodies? C’mon science, figure this out.
Futility, thy name is Kiribati
Before we get to the rest of our regularly scheduled hilarity, a brief geography lesson is in order: Kiribati is an island nation – actually 32 atolls and one coral island – in the central Pacific Ocean. Those atolls are spread out across 1.4 million square miles around the intersection of the equator and the International Date Line, so Kiribati is the only country in the world located in all four hemispheres.
Now, back to the news.
Kiribati closed its borders early in the COVID-19 pandemic and recorded only two cases in almost 2 years. Things were going so well that the authorities recently decided to reopen the country to international travelers. Silly authorities.
The first plane was set to arrive on Jan. 14 from Fiji. This being the age of COVID, plans were made and precautions were taken. All 54 passengers quarantined for 2 weeks before the flight and underwent regular testing, the Guardian noted, and “they were only allowed on the flight after returning negative tests.”
You guessed it. Two-thirds of those 54 people tested positive for COVID-19 after landing in Kiribati.
All of the passengers were quarantined, but since then a security guard at the quarantine center has tested positive, as has someone who was not involved in the quarantine. According to NPR, the government said that “there is now an assumption that COVID-19 is now spreading in the community on South Tarawa and Betio.”
Moral of the story? You can’t beat COVID, so never try.
[EDITOR: Is that really the message we want to send to our readers?]
If you can’t beat them, join them.
[EDITOR: Nope. Try again.]
Resistance is futile?
[EDITOR: Sigh. Close enough.]
Are you tired? Or are you death tired?
When we’re feeling that burnout monster creep in we sometimes say that we’re being worked to death or that we’re dead tired, but what if that feeling could predict when it’s your actual time to go?
In a recent study published in the Journals of Gerontology: Series A, epidemiologists from the University of Pittsburgh were able to associate a level of “physical fatigability” with mortality.
The researchers administered the Pittsburgh Fatigability Scale to almost 3,000 participants aged ≥ 60 years, who ranked from 0 to 5 on how tired they thought they would be after doing activities like light housework or a leisurely 30-minute walk. After accounting for factors such as preexisting conditions and mental health, the researchers found that people who scored 25 or more points were 2.3 times more likely to die in the next 2.7 years, compared with those who scored under 25.
So what does that tell us about the importance of being continuously active? It’s pretty important.
“Previous research indicates that getting more physical activity can reduce a person’s fatigability. Our study is the first to link more severe physical fatigability to an earlier death,” lead author Nancy W. Glynn, PhD, said in a separate statement. The best way to keep physically active, she suggested, is to set manageable goals and a routine.
A nice walk around the neighborhood during golden hour or a little bit of yoga before breakfast could be a great way to keep the body moving, because you know what they say: Use it or lose it.
This work is NFT protected: Do not screenshot
If you’ve been following the nonmedical news, you’ve likely heard the term “NFT” explode in the past few months. Standing for nonfungible token, NFTs are, at least theoretically, a proof of ownership for digital creations that prevents anyone other than the buyer from reselling the artwork. Sounds like a great idea: It protects artists and buyers alike.
Much like its cousin cryptocurrency, however, the NFT world is rife with speculation, scams, misunderstanding, and drawings of bored monkeys. It’s the Wild West out there in the digital art universe: One poor unfortunate accidentally sold a $300k NFT image for $3,000, a group of investors spent $3 million buying an NFT for a rare version of Dune believing it gave them the copyright (it did not), and an Indonesian engineering student’s 5-year series of expressionless selfies is now worth a million dollars.
This is a column detailing weird medical news, however, so with our setup complete (though our understanding of NFTs is very much not), we move to France and meet our hero (?), Emmanuel Masmejean, an orthopedic surgeon who apparently wasn’t making enough money in his lucrative medical career.
In a move of apocalyptic madness, he threw ethics out the window, delved into his archive, and found an x-ray of a young woman with a bullet lodged in her arm. The woman was a survivor of the Bataclan mass shooting and bombing in 2015, and don’t you worry, our intrepid entrepreneur made sure to identify her as such when he tried selling the x-ray as an NFT on an online art website for $2,776. Yes, this is very much a violation of doctor-patient confidentiality, and no, that’s not a lot of money to risk your medical career on.
Naturally, the woman was horrified and shocked to learn that the image was being sold, her lawyer told the Guardian. When the doctor called her, he merely attempted to justify his action, rather than apologizing or showing any remorse. Dr. Masmejean is now facing legal action and a disciplinary charge for his attempted entry into the NFT world for publishing the image without permission, and the NFT has been removed from the website. Should have stuck with the bored monkeys.
Avatars could be the future
Zoom, FaceTime, and Skype are great when people can’t be together in the same room, state, or country. Not the same as being somewhere in person, but a pretty good replacement during a global pandemic. But what if you had a robot that could be present for you?
Seven-year-old Joshua Martinangeli of Berlin has a severe lung disease and needs to wear a tube in his neck, so he cannot attend school. A robot avatar, donated to Joshua through a private initiative, sits in his seat in the classroom and is able to interact with the students and teacher, according to Reuters. A light on the avatar blinks when Joshua wants to speak and the children can talk with him too. Joshua and his classmates agree that it’s not the same as him really being there to talk and learn, but it’s a great way to keep him included.
“We are the only district in Berlin that has bought four avatars for its schools. The impetus was COVID-19, but I think this will be the future well beyond the pandemic,” Torsten Kuehne, district education councilor, told Reuters.
So where do we get an avatar to go out and run errands? Can we send it to the office instead of Zooming the next meeting? Or maybe our avatar could go to the gym for us. But how do we get the results to show up on our bodies? C’mon science, figure this out.
Futility, thy name is Kiribati
Before we get to the rest of our regularly scheduled hilarity, a brief geography lesson is in order: Kiribati is an island nation – actually 32 atolls and one coral island – in the central Pacific Ocean. Those atolls are spread out across 1.4 million square miles around the intersection of the equator and the International Date Line, so Kiribati is the only country in the world located in all four hemispheres.
Now, back to the news.
Kiribati closed its borders early in the COVID-19 pandemic and recorded only two cases in almost 2 years. Things were going so well that the authorities recently decided to reopen the country to international travelers. Silly authorities.
The first plane was set to arrive on Jan. 14 from Fiji. This being the age of COVID, plans were made and precautions were taken. All 54 passengers quarantined for 2 weeks before the flight and underwent regular testing, the Guardian noted, and “they were only allowed on the flight after returning negative tests.”
You guessed it. Two-thirds of those 54 people tested positive for COVID-19 after landing in Kiribati.
All of the passengers were quarantined, but since then a security guard at the quarantine center has tested positive, as has someone who was not involved in the quarantine. According to NPR, the government said that “there is now an assumption that COVID-19 is now spreading in the community on South Tarawa and Betio.”
Moral of the story? You can’t beat COVID, so never try.
[EDITOR: Is that really the message we want to send to our readers?]
If you can’t beat them, join them.
[EDITOR: Nope. Try again.]
Resistance is futile?
[EDITOR: Sigh. Close enough.]
Are you tired? Or are you death tired?
When we’re feeling that burnout monster creep in we sometimes say that we’re being worked to death or that we’re dead tired, but what if that feeling could predict when it’s your actual time to go?
In a recent study published in the Journals of Gerontology: Series A, epidemiologists from the University of Pittsburgh were able to associate a level of “physical fatigability” with mortality.
The researchers administered the Pittsburgh Fatigability Scale to almost 3,000 participants aged ≥ 60 years, who ranked from 0 to 5 on how tired they thought they would be after doing activities like light housework or a leisurely 30-minute walk. After accounting for factors such as preexisting conditions and mental health, the researchers found that people who scored 25 or more points were 2.3 times more likely to die in the next 2.7 years, compared with those who scored under 25.
So what does that tell us about the importance of being continuously active? It’s pretty important.
“Previous research indicates that getting more physical activity can reduce a person’s fatigability. Our study is the first to link more severe physical fatigability to an earlier death,” lead author Nancy W. Glynn, PhD, said in a separate statement. The best way to keep physically active, she suggested, is to set manageable goals and a routine.
A nice walk around the neighborhood during golden hour or a little bit of yoga before breakfast could be a great way to keep the body moving, because you know what they say: Use it or lose it.
This work is NFT protected: Do not screenshot
If you’ve been following the nonmedical news, you’ve likely heard the term “NFT” explode in the past few months. Standing for nonfungible token, NFTs are, at least theoretically, a proof of ownership for digital creations that prevents anyone other than the buyer from reselling the artwork. Sounds like a great idea: It protects artists and buyers alike.
Much like its cousin cryptocurrency, however, the NFT world is rife with speculation, scams, misunderstanding, and drawings of bored monkeys. It’s the Wild West out there in the digital art universe: One poor unfortunate accidentally sold a $300k NFT image for $3,000, a group of investors spent $3 million buying an NFT for a rare version of Dune believing it gave them the copyright (it did not), and an Indonesian engineering student’s 5-year series of expressionless selfies is now worth a million dollars.
This is a column detailing weird medical news, however, so with our setup complete (though our understanding of NFTs is very much not), we move to France and meet our hero (?), Emmanuel Masmejean, an orthopedic surgeon who apparently wasn’t making enough money in his lucrative medical career.
In a move of apocalyptic madness, he threw ethics out the window, delved into his archive, and found an x-ray of a young woman with a bullet lodged in her arm. The woman was a survivor of the Bataclan mass shooting and bombing in 2015, and don’t you worry, our intrepid entrepreneur made sure to identify her as such when he tried selling the x-ray as an NFT on an online art website for $2,776. Yes, this is very much a violation of doctor-patient confidentiality, and no, that’s not a lot of money to risk your medical career on.
Naturally, the woman was horrified and shocked to learn that the image was being sold, her lawyer told the Guardian. When the doctor called her, he merely attempted to justify his action, rather than apologizing or showing any remorse. Dr. Masmejean is now facing legal action and a disciplinary charge for his attempted entry into the NFT world for publishing the image without permission, and the NFT has been removed from the website. Should have stuck with the bored monkeys.
Avatars could be the future
Zoom, FaceTime, and Skype are great when people can’t be together in the same room, state, or country. Not the same as being somewhere in person, but a pretty good replacement during a global pandemic. But what if you had a robot that could be present for you?
Seven-year-old Joshua Martinangeli of Berlin has a severe lung disease and needs to wear a tube in his neck, so he cannot attend school. A robot avatar, donated to Joshua through a private initiative, sits in his seat in the classroom and is able to interact with the students and teacher, according to Reuters. A light on the avatar blinks when Joshua wants to speak and the children can talk with him too. Joshua and his classmates agree that it’s not the same as him really being there to talk and learn, but it’s a great way to keep him included.
“We are the only district in Berlin that has bought four avatars for its schools. The impetus was COVID-19, but I think this will be the future well beyond the pandemic,” Torsten Kuehne, district education councilor, told Reuters.
So where do we get an avatar to go out and run errands? Can we send it to the office instead of Zooming the next meeting? Or maybe our avatar could go to the gym for us. But how do we get the results to show up on our bodies? C’mon science, figure this out.
Futility, thy name is Kiribati
Before we get to the rest of our regularly scheduled hilarity, a brief geography lesson is in order: Kiribati is an island nation – actually 32 atolls and one coral island – in the central Pacific Ocean. Those atolls are spread out across 1.4 million square miles around the intersection of the equator and the International Date Line, so Kiribati is the only country in the world located in all four hemispheres.
Now, back to the news.
Kiribati closed its borders early in the COVID-19 pandemic and recorded only two cases in almost 2 years. Things were going so well that the authorities recently decided to reopen the country to international travelers. Silly authorities.
The first plane was set to arrive on Jan. 14 from Fiji. This being the age of COVID, plans were made and precautions were taken. All 54 passengers quarantined for 2 weeks before the flight and underwent regular testing, the Guardian noted, and “they were only allowed on the flight after returning negative tests.”
You guessed it. Two-thirds of those 54 people tested positive for COVID-19 after landing in Kiribati.
All of the passengers were quarantined, but since then a security guard at the quarantine center has tested positive, as has someone who was not involved in the quarantine. According to NPR, the government said that “there is now an assumption that COVID-19 is now spreading in the community on South Tarawa and Betio.”
Moral of the story? You can’t beat COVID, so never try.
[EDITOR: Is that really the message we want to send to our readers?]
If you can’t beat them, join them.
[EDITOR: Nope. Try again.]
Resistance is futile?
[EDITOR: Sigh. Close enough.]
35% of employers to proceed with vaccine mandate, poll shows
despite a recent U.S. Supreme Court ruling that blocked the Biden administration’s vaccine-or-test rule for big businesses.
But the poll by Gartner Inc. showed no consensus among employers. About 4% of polled executives said they’re dropping their vaccine mandate, 29% are in a wait-and-see position, and 12% are less likely to impose a mandate now, Bloomberg reported.
Executives were divided on how a vaccine mandate would affect absenteeism and employee morale. Almost 40% of polled employers said they thought a mandate would attract workers, but about 25% said it would do the opposite, Bloomberg said.
“What is more attractive -- to have a mandate or not?” Brian Kropp, PhD, Gartner’s chief of human resources research, said in an interview with Bloomberg. “Most are not exactly sure what to do.”
Big companies have reacted differently since the court’s ruling.
Starbucks announced it was dropping its vaccine-or-test rule for the company’s approximately 228,000 employees. General Electric dropped its mandate after the ruling, but Honeywell International Inc. announced it was staying with its vaccination policy, Bloomberg said.
The Supreme Court ruled Jan. 13 against the Biden administration’s mandate for businesses. The Occupational Safety and Health Administration had proposed that every company with more than 100 employees would be required to ensure workers were either vaccinated or tested weekly for COVID-19.
State governments and business groups immediately appealed, and the court ruled 6-3 against the mandate. The Biden administration officially dropped its rule on Wednesday.
A version of this article first appeared on WebMD.com.
despite a recent U.S. Supreme Court ruling that blocked the Biden administration’s vaccine-or-test rule for big businesses.
But the poll by Gartner Inc. showed no consensus among employers. About 4% of polled executives said they’re dropping their vaccine mandate, 29% are in a wait-and-see position, and 12% are less likely to impose a mandate now, Bloomberg reported.
Executives were divided on how a vaccine mandate would affect absenteeism and employee morale. Almost 40% of polled employers said they thought a mandate would attract workers, but about 25% said it would do the opposite, Bloomberg said.
“What is more attractive -- to have a mandate or not?” Brian Kropp, PhD, Gartner’s chief of human resources research, said in an interview with Bloomberg. “Most are not exactly sure what to do.”
Big companies have reacted differently since the court’s ruling.
Starbucks announced it was dropping its vaccine-or-test rule for the company’s approximately 228,000 employees. General Electric dropped its mandate after the ruling, but Honeywell International Inc. announced it was staying with its vaccination policy, Bloomberg said.
The Supreme Court ruled Jan. 13 against the Biden administration’s mandate for businesses. The Occupational Safety and Health Administration had proposed that every company with more than 100 employees would be required to ensure workers were either vaccinated or tested weekly for COVID-19.
State governments and business groups immediately appealed, and the court ruled 6-3 against the mandate. The Biden administration officially dropped its rule on Wednesday.
A version of this article first appeared on WebMD.com.
despite a recent U.S. Supreme Court ruling that blocked the Biden administration’s vaccine-or-test rule for big businesses.
But the poll by Gartner Inc. showed no consensus among employers. About 4% of polled executives said they’re dropping their vaccine mandate, 29% are in a wait-and-see position, and 12% are less likely to impose a mandate now, Bloomberg reported.
Executives were divided on how a vaccine mandate would affect absenteeism and employee morale. Almost 40% of polled employers said they thought a mandate would attract workers, but about 25% said it would do the opposite, Bloomberg said.
“What is more attractive -- to have a mandate or not?” Brian Kropp, PhD, Gartner’s chief of human resources research, said in an interview with Bloomberg. “Most are not exactly sure what to do.”
Big companies have reacted differently since the court’s ruling.
Starbucks announced it was dropping its vaccine-or-test rule for the company’s approximately 228,000 employees. General Electric dropped its mandate after the ruling, but Honeywell International Inc. announced it was staying with its vaccination policy, Bloomberg said.
The Supreme Court ruled Jan. 13 against the Biden administration’s mandate for businesses. The Occupational Safety and Health Administration had proposed that every company with more than 100 employees would be required to ensure workers were either vaccinated or tested weekly for COVID-19.
State governments and business groups immediately appealed, and the court ruled 6-3 against the mandate. The Biden administration officially dropped its rule on Wednesday.
A version of this article first appeared on WebMD.com.
Omicron survives longer on plastic, skin than other COVID variants
, one possible explanation for why Omicron has spread so rapidly around the world.
In a lab experiment, samples of different variants were applied to pieces of plastic and human skin collected from autopsies, researchers from Kyoto Prefectural University of Medicine wrote in bioRxiv. A variant “survived” until it could no longer be detected on the surface.
“This study showed that the Omicron variant also has the highest environmental stability among VOCs (variants of concern), which suggests that this high stability might also be one of the factors that have allowed the Omicron variant to replace the Delta variant and spread rapidly,” the researchers wrote.
On plastic, the Omicron variant samples survived an average of 193.5 hours, a little more than 8 days. By comparison, the other survival times on plastic were 56 hours for the original COVID strain, 191.3 hours for Alpha, 156.6 hours for Beta, 59.3 hours for Gamma, and 114 hours for Delta.
On skin samples, the Omicron samples survived an average of 21.1 hours. The other variants had these average survival times on skin: 8.6 hours for the original version, 19.6 hours for Alpha, 19.1 hours for Beta, 11 hours for Gamma, and 16.8 hours for Delta.
The study found that the variants had more resistance to ethanol than the original strain of COVID. That said, all COVID samples were inactivated after being exposed to alcohol-based hand sanitizers for 15 seconds.
“Therefore, it is highly recommended that current infection control (hand hygiene) practices use disinfectants ... as proposed by the World Health Organization,” the researchers said.
The study has not been peer-reviewed.
A version of this article first appeared on WebMD.com.
, one possible explanation for why Omicron has spread so rapidly around the world.
In a lab experiment, samples of different variants were applied to pieces of plastic and human skin collected from autopsies, researchers from Kyoto Prefectural University of Medicine wrote in bioRxiv. A variant “survived” until it could no longer be detected on the surface.
“This study showed that the Omicron variant also has the highest environmental stability among VOCs (variants of concern), which suggests that this high stability might also be one of the factors that have allowed the Omicron variant to replace the Delta variant and spread rapidly,” the researchers wrote.
On plastic, the Omicron variant samples survived an average of 193.5 hours, a little more than 8 days. By comparison, the other survival times on plastic were 56 hours for the original COVID strain, 191.3 hours for Alpha, 156.6 hours for Beta, 59.3 hours for Gamma, and 114 hours for Delta.
On skin samples, the Omicron samples survived an average of 21.1 hours. The other variants had these average survival times on skin: 8.6 hours for the original version, 19.6 hours for Alpha, 19.1 hours for Beta, 11 hours for Gamma, and 16.8 hours for Delta.
The study found that the variants had more resistance to ethanol than the original strain of COVID. That said, all COVID samples were inactivated after being exposed to alcohol-based hand sanitizers for 15 seconds.
“Therefore, it is highly recommended that current infection control (hand hygiene) practices use disinfectants ... as proposed by the World Health Organization,” the researchers said.
The study has not been peer-reviewed.
A version of this article first appeared on WebMD.com.
, one possible explanation for why Omicron has spread so rapidly around the world.
In a lab experiment, samples of different variants were applied to pieces of plastic and human skin collected from autopsies, researchers from Kyoto Prefectural University of Medicine wrote in bioRxiv. A variant “survived” until it could no longer be detected on the surface.
“This study showed that the Omicron variant also has the highest environmental stability among VOCs (variants of concern), which suggests that this high stability might also be one of the factors that have allowed the Omicron variant to replace the Delta variant and spread rapidly,” the researchers wrote.
On plastic, the Omicron variant samples survived an average of 193.5 hours, a little more than 8 days. By comparison, the other survival times on plastic were 56 hours for the original COVID strain, 191.3 hours for Alpha, 156.6 hours for Beta, 59.3 hours for Gamma, and 114 hours for Delta.
On skin samples, the Omicron samples survived an average of 21.1 hours. The other variants had these average survival times on skin: 8.6 hours for the original version, 19.6 hours for Alpha, 19.1 hours for Beta, 11 hours for Gamma, and 16.8 hours for Delta.
The study found that the variants had more resistance to ethanol than the original strain of COVID. That said, all COVID samples were inactivated after being exposed to alcohol-based hand sanitizers for 15 seconds.
“Therefore, it is highly recommended that current infection control (hand hygiene) practices use disinfectants ... as proposed by the World Health Organization,” the researchers said.
The study has not been peer-reviewed.
A version of this article first appeared on WebMD.com.
Presence of autoantibodies most predictive of long COVID in study
Other significant early predictors of prolonged COVID symptoms – which the researchers called postacute sequelae – were having type 2 diabetes, SARS-CoV-2 RNAemia, and Epstein-Barr virus (EBV) viremia, Yapeng Su, PhD, of the Institute for Systems Biology (ISB) in Seattle, and colleagues wrote in Cell.
Having EBV viremia suggested that latent EBV has been reactivated, the authors noted.
“The most important postacute sequelae [that is conditions that are consequences of a disease] of COVID is the presence of autoantibodies,” James R. Heath, PhD, president of ISB and a bioengineering professor at the University of Washington, Seattle, said in an interview. “It’s about two times more important than the others.”
Dr. Heath and coauthors said early detection of this and other variables could prompt earlier aggressive treatment in patients susceptible to long COVID and ward off lingering symptoms.
“These predictive measures of long COVID can also help to better inform patients of their possible disease course,” study coauthor Daniel G. Chen, an undergraduate researcher at ISB, said in an interview. “We were also able to partially resolve the immunological underpinnings of some postacute sequelae of COVID in a way that suggested potential therapies, and the timing of those therapies.”
For example, he continued, the use of antivirals very early in the infectious course may mitigate the later development of long COVID. “This will, of course, have to be explored in an appropriately designed clinical trial.
“We also identified biomarkers of certain types of long COVID, such as neurological sequelae. Those biomarkers can help define the condition, which is a first step towards developing treatments.”
Study findings
With COVID patients monitored for 2 or 3 months, the study findings of the international “multiomic profiling” analysis include:
- Subclinical patient autoantibodies that reduce anti–SARS-CoV-2 antibodies suggest there is immune dysregulation during COVID-19 infection.
- Reactivation of latent other viruses during initial infection may be contributing to long COVID.
- Gastrointestinal postacute sequelae of COVID presents with a unique postacute expansion of cytotoxic T cells.
- SARS-CoV-2–specific and cytomegalovirus-specific CD8+ T cells displayed unique dynamics during recovery from infection.
According to the authors, as many as 69% of COVID-19 patients suffer from long COVID – a range of new, recurrent, or ongoing problems 4 or more weeks following initial SARS-CoV-2 infection. These may include memory loss, gastrointestinal distress, fatigue, anosmia, and shortness of breath.
Long COVID has been associated with acute disease severity, and is suspected to be related to autoimmune factors and unresolved viral fragments, according to the paper.
Research methods
The international study did a deep and detailed dive into multiple molecular markers of long COVID. It enrolled 209 COVID-19 patients with varying degrees of disease severity and matched them to 457 healthy controls. The researchers’ goal was to identify discrete and quantifiable long COVID factors and guide possible preemptive treatment.
Patients were assessed at three time points: at initial diagnosis, during the acute disease phase about a week later, and again 2 to 3 months post onset of symptoms after recovery from the acute phase of COVID. At the third assessment, some patients had lingering symptoms such as fatigue (52% ), cough (25%), and loss of taste or sense of smell (18%).
Blood draws were analyzed for autoantibodies and SARS-CoV-2–specific antibodies, global plasma proteomic and metabolomic profiles, and single-cell multiomic characterizations of peripheral blood mononuclear cells.
Each blood draw was paired with nasal-swab and plasma measurements of SARS-CoV-2 viral load and the data sets were integrated with electronic health records and self-reported patient symptoms to guide the interpretation of the molecular signatures of long COVID.
Author conclusions
The authors found an association between T2 hyperinflammation and long COVID–anticipating autoantibodies. This association further implies that hyperinflammation-controlling therapies in the acute stage of COVID may influence whether a patient experiences long COVID. “However, the detailed timing and context of these therapies matter, and, thus, future well-controlled studies will be needed to test these and other therapeutic implications,” Dr. Su and colleagues wrote.
Moreover, the negative correlations between anti–SARS-CoV-2 IgG and certain autoantibodies may suggest that patients with elevated autoantibody levels are more susceptible to breakthrough infections, the authors said.
“Many patients with high autoantibodies simultaneously have low protective antibodies that neutralize SARS-CoV-2, and that’s going to make them more susceptible to breakthrough infections,” Mr. Chen explained.*
“Detectability of most [long COVID-19 factors] at COVID diagnosis emphasizes the importance of early disease measurements for understanding emergent chronic conditions and suggests [long COVID] treatment strategies,” they wrote.
According to Mr. Chen, there are clear similarities in underlying immunobiology between patients with COVID autoantibodies and patients with systemic lupus erythematosus.
“These findings are also helping us frame our thinking around other chronic autoimmune conditions, such as postacute Lyme syndrome, for example,” said Dr. Heath.
The bottom line, said Mr. Chen, is that measuring early long COVID indicators may result in preventive treatments. “An example is the cortisol deficiency we see in certain long COVID patients. There are known treatments such as cortisol replacement therapy that should be explored for this group.”
Outside expert’s take on findings
Commenting on the study, Sherry Hsiang-Yi Chou, MD, who was not involved in the research, called the study a very important first step in understanding the path of this complex phenomenon and perhaps other conditions with long-term side effects.
“The researchers have done huge amount of innovative scientific work. They’ve shown the DNA signature of how our bodies respond to this disease,” said Dr. Chou, who is chief of the division of neurocritical care at Northwestern Medicine in Chicago.
“This type of research will help us scientifically understand and differentiate the various syndromes within long COVID. It will help identify who’s at risk for different aspects of this syndrome and lead to following them for longer periods in clinical trials,” she added.
The authors acknowledged that lengthier studies in larger cohorts were needed to see which patients will develop long-term chronic postacute sequelae of COVID.
This research was supported by the Wilke Family Foundation, the Parker Institute for Cancer Immunotherapy, Merck, and the Biomedical Advanced Research and Development Authority. Other support came from the National Institutes of Health, the Bill and Melinda Gates Foundation, Saint John’s Cancer Center, Fred Hutchinson Cancer Research Center, and the European Union’s Horizon 2020 research and innovation program. Dr. Heath is a cofounder of Pact Pharma. He and several coauthors disclosed various ties to multiple private-sector companies. Mr. Chen and Dr. Chou had no competing interests.
*Correction, 1/28: An earlier version of this story misidentified Daniel G. Chen, an undergraduate researcher at ISB.
Other significant early predictors of prolonged COVID symptoms – which the researchers called postacute sequelae – were having type 2 diabetes, SARS-CoV-2 RNAemia, and Epstein-Barr virus (EBV) viremia, Yapeng Su, PhD, of the Institute for Systems Biology (ISB) in Seattle, and colleagues wrote in Cell.
Having EBV viremia suggested that latent EBV has been reactivated, the authors noted.
“The most important postacute sequelae [that is conditions that are consequences of a disease] of COVID is the presence of autoantibodies,” James R. Heath, PhD, president of ISB and a bioengineering professor at the University of Washington, Seattle, said in an interview. “It’s about two times more important than the others.”
Dr. Heath and coauthors said early detection of this and other variables could prompt earlier aggressive treatment in patients susceptible to long COVID and ward off lingering symptoms.
“These predictive measures of long COVID can also help to better inform patients of their possible disease course,” study coauthor Daniel G. Chen, an undergraduate researcher at ISB, said in an interview. “We were also able to partially resolve the immunological underpinnings of some postacute sequelae of COVID in a way that suggested potential therapies, and the timing of those therapies.”
For example, he continued, the use of antivirals very early in the infectious course may mitigate the later development of long COVID. “This will, of course, have to be explored in an appropriately designed clinical trial.
“We also identified biomarkers of certain types of long COVID, such as neurological sequelae. Those biomarkers can help define the condition, which is a first step towards developing treatments.”
Study findings
With COVID patients monitored for 2 or 3 months, the study findings of the international “multiomic profiling” analysis include:
- Subclinical patient autoantibodies that reduce anti–SARS-CoV-2 antibodies suggest there is immune dysregulation during COVID-19 infection.
- Reactivation of latent other viruses during initial infection may be contributing to long COVID.
- Gastrointestinal postacute sequelae of COVID presents with a unique postacute expansion of cytotoxic T cells.
- SARS-CoV-2–specific and cytomegalovirus-specific CD8+ T cells displayed unique dynamics during recovery from infection.
According to the authors, as many as 69% of COVID-19 patients suffer from long COVID – a range of new, recurrent, or ongoing problems 4 or more weeks following initial SARS-CoV-2 infection. These may include memory loss, gastrointestinal distress, fatigue, anosmia, and shortness of breath.
Long COVID has been associated with acute disease severity, and is suspected to be related to autoimmune factors and unresolved viral fragments, according to the paper.
Research methods
The international study did a deep and detailed dive into multiple molecular markers of long COVID. It enrolled 209 COVID-19 patients with varying degrees of disease severity and matched them to 457 healthy controls. The researchers’ goal was to identify discrete and quantifiable long COVID factors and guide possible preemptive treatment.
Patients were assessed at three time points: at initial diagnosis, during the acute disease phase about a week later, and again 2 to 3 months post onset of symptoms after recovery from the acute phase of COVID. At the third assessment, some patients had lingering symptoms such as fatigue (52% ), cough (25%), and loss of taste or sense of smell (18%).
Blood draws were analyzed for autoantibodies and SARS-CoV-2–specific antibodies, global plasma proteomic and metabolomic profiles, and single-cell multiomic characterizations of peripheral blood mononuclear cells.
Each blood draw was paired with nasal-swab and plasma measurements of SARS-CoV-2 viral load and the data sets were integrated with electronic health records and self-reported patient symptoms to guide the interpretation of the molecular signatures of long COVID.
Author conclusions
The authors found an association between T2 hyperinflammation and long COVID–anticipating autoantibodies. This association further implies that hyperinflammation-controlling therapies in the acute stage of COVID may influence whether a patient experiences long COVID. “However, the detailed timing and context of these therapies matter, and, thus, future well-controlled studies will be needed to test these and other therapeutic implications,” Dr. Su and colleagues wrote.
Moreover, the negative correlations between anti–SARS-CoV-2 IgG and certain autoantibodies may suggest that patients with elevated autoantibody levels are more susceptible to breakthrough infections, the authors said.
“Many patients with high autoantibodies simultaneously have low protective antibodies that neutralize SARS-CoV-2, and that’s going to make them more susceptible to breakthrough infections,” Mr. Chen explained.*
“Detectability of most [long COVID-19 factors] at COVID diagnosis emphasizes the importance of early disease measurements for understanding emergent chronic conditions and suggests [long COVID] treatment strategies,” they wrote.
According to Mr. Chen, there are clear similarities in underlying immunobiology between patients with COVID autoantibodies and patients with systemic lupus erythematosus.
“These findings are also helping us frame our thinking around other chronic autoimmune conditions, such as postacute Lyme syndrome, for example,” said Dr. Heath.
The bottom line, said Mr. Chen, is that measuring early long COVID indicators may result in preventive treatments. “An example is the cortisol deficiency we see in certain long COVID patients. There are known treatments such as cortisol replacement therapy that should be explored for this group.”
Outside expert’s take on findings
Commenting on the study, Sherry Hsiang-Yi Chou, MD, who was not involved in the research, called the study a very important first step in understanding the path of this complex phenomenon and perhaps other conditions with long-term side effects.
“The researchers have done huge amount of innovative scientific work. They’ve shown the DNA signature of how our bodies respond to this disease,” said Dr. Chou, who is chief of the division of neurocritical care at Northwestern Medicine in Chicago.
“This type of research will help us scientifically understand and differentiate the various syndromes within long COVID. It will help identify who’s at risk for different aspects of this syndrome and lead to following them for longer periods in clinical trials,” she added.
The authors acknowledged that lengthier studies in larger cohorts were needed to see which patients will develop long-term chronic postacute sequelae of COVID.
This research was supported by the Wilke Family Foundation, the Parker Institute for Cancer Immunotherapy, Merck, and the Biomedical Advanced Research and Development Authority. Other support came from the National Institutes of Health, the Bill and Melinda Gates Foundation, Saint John’s Cancer Center, Fred Hutchinson Cancer Research Center, and the European Union’s Horizon 2020 research and innovation program. Dr. Heath is a cofounder of Pact Pharma. He and several coauthors disclosed various ties to multiple private-sector companies. Mr. Chen and Dr. Chou had no competing interests.
*Correction, 1/28: An earlier version of this story misidentified Daniel G. Chen, an undergraduate researcher at ISB.
Other significant early predictors of prolonged COVID symptoms – which the researchers called postacute sequelae – were having type 2 diabetes, SARS-CoV-2 RNAemia, and Epstein-Barr virus (EBV) viremia, Yapeng Su, PhD, of the Institute for Systems Biology (ISB) in Seattle, and colleagues wrote in Cell.
Having EBV viremia suggested that latent EBV has been reactivated, the authors noted.
“The most important postacute sequelae [that is conditions that are consequences of a disease] of COVID is the presence of autoantibodies,” James R. Heath, PhD, president of ISB and a bioengineering professor at the University of Washington, Seattle, said in an interview. “It’s about two times more important than the others.”
Dr. Heath and coauthors said early detection of this and other variables could prompt earlier aggressive treatment in patients susceptible to long COVID and ward off lingering symptoms.
“These predictive measures of long COVID can also help to better inform patients of their possible disease course,” study coauthor Daniel G. Chen, an undergraduate researcher at ISB, said in an interview. “We were also able to partially resolve the immunological underpinnings of some postacute sequelae of COVID in a way that suggested potential therapies, and the timing of those therapies.”
For example, he continued, the use of antivirals very early in the infectious course may mitigate the later development of long COVID. “This will, of course, have to be explored in an appropriately designed clinical trial.
“We also identified biomarkers of certain types of long COVID, such as neurological sequelae. Those biomarkers can help define the condition, which is a first step towards developing treatments.”
Study findings
With COVID patients monitored for 2 or 3 months, the study findings of the international “multiomic profiling” analysis include:
- Subclinical patient autoantibodies that reduce anti–SARS-CoV-2 antibodies suggest there is immune dysregulation during COVID-19 infection.
- Reactivation of latent other viruses during initial infection may be contributing to long COVID.
- Gastrointestinal postacute sequelae of COVID presents with a unique postacute expansion of cytotoxic T cells.
- SARS-CoV-2–specific and cytomegalovirus-specific CD8+ T cells displayed unique dynamics during recovery from infection.
According to the authors, as many as 69% of COVID-19 patients suffer from long COVID – a range of new, recurrent, or ongoing problems 4 or more weeks following initial SARS-CoV-2 infection. These may include memory loss, gastrointestinal distress, fatigue, anosmia, and shortness of breath.
Long COVID has been associated with acute disease severity, and is suspected to be related to autoimmune factors and unresolved viral fragments, according to the paper.
Research methods
The international study did a deep and detailed dive into multiple molecular markers of long COVID. It enrolled 209 COVID-19 patients with varying degrees of disease severity and matched them to 457 healthy controls. The researchers’ goal was to identify discrete and quantifiable long COVID factors and guide possible preemptive treatment.
Patients were assessed at three time points: at initial diagnosis, during the acute disease phase about a week later, and again 2 to 3 months post onset of symptoms after recovery from the acute phase of COVID. At the third assessment, some patients had lingering symptoms such as fatigue (52% ), cough (25%), and loss of taste or sense of smell (18%).
Blood draws were analyzed for autoantibodies and SARS-CoV-2–specific antibodies, global plasma proteomic and metabolomic profiles, and single-cell multiomic characterizations of peripheral blood mononuclear cells.
Each blood draw was paired with nasal-swab and plasma measurements of SARS-CoV-2 viral load and the data sets were integrated with electronic health records and self-reported patient symptoms to guide the interpretation of the molecular signatures of long COVID.
Author conclusions
The authors found an association between T2 hyperinflammation and long COVID–anticipating autoantibodies. This association further implies that hyperinflammation-controlling therapies in the acute stage of COVID may influence whether a patient experiences long COVID. “However, the detailed timing and context of these therapies matter, and, thus, future well-controlled studies will be needed to test these and other therapeutic implications,” Dr. Su and colleagues wrote.
Moreover, the negative correlations between anti–SARS-CoV-2 IgG and certain autoantibodies may suggest that patients with elevated autoantibody levels are more susceptible to breakthrough infections, the authors said.
“Many patients with high autoantibodies simultaneously have low protective antibodies that neutralize SARS-CoV-2, and that’s going to make them more susceptible to breakthrough infections,” Mr. Chen explained.*
“Detectability of most [long COVID-19 factors] at COVID diagnosis emphasizes the importance of early disease measurements for understanding emergent chronic conditions and suggests [long COVID] treatment strategies,” they wrote.
According to Mr. Chen, there are clear similarities in underlying immunobiology between patients with COVID autoantibodies and patients with systemic lupus erythematosus.
“These findings are also helping us frame our thinking around other chronic autoimmune conditions, such as postacute Lyme syndrome, for example,” said Dr. Heath.
The bottom line, said Mr. Chen, is that measuring early long COVID indicators may result in preventive treatments. “An example is the cortisol deficiency we see in certain long COVID patients. There are known treatments such as cortisol replacement therapy that should be explored for this group.”
Outside expert’s take on findings
Commenting on the study, Sherry Hsiang-Yi Chou, MD, who was not involved in the research, called the study a very important first step in understanding the path of this complex phenomenon and perhaps other conditions with long-term side effects.
“The researchers have done huge amount of innovative scientific work. They’ve shown the DNA signature of how our bodies respond to this disease,” said Dr. Chou, who is chief of the division of neurocritical care at Northwestern Medicine in Chicago.
“This type of research will help us scientifically understand and differentiate the various syndromes within long COVID. It will help identify who’s at risk for different aspects of this syndrome and lead to following them for longer periods in clinical trials,” she added.
The authors acknowledged that lengthier studies in larger cohorts were needed to see which patients will develop long-term chronic postacute sequelae of COVID.
This research was supported by the Wilke Family Foundation, the Parker Institute for Cancer Immunotherapy, Merck, and the Biomedical Advanced Research and Development Authority. Other support came from the National Institutes of Health, the Bill and Melinda Gates Foundation, Saint John’s Cancer Center, Fred Hutchinson Cancer Research Center, and the European Union’s Horizon 2020 research and innovation program. Dr. Heath is a cofounder of Pact Pharma. He and several coauthors disclosed various ties to multiple private-sector companies. Mr. Chen and Dr. Chou had no competing interests.
*Correction, 1/28: An earlier version of this story misidentified Daniel G. Chen, an undergraduate researcher at ISB.
FROM CELL
Children and COVID: United States passes 10 million total cases
Weekly COVID-19 cases in children topped 1 million for the first time as the cumulative count surpassed 10 million since the start of the pandemic, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
the AAP and CHA said in their weekly COVID report. Those 10.6 million child cases represent 18.4% of all cases, and the latest 1.15 million represented 25.5% of all cases for the week.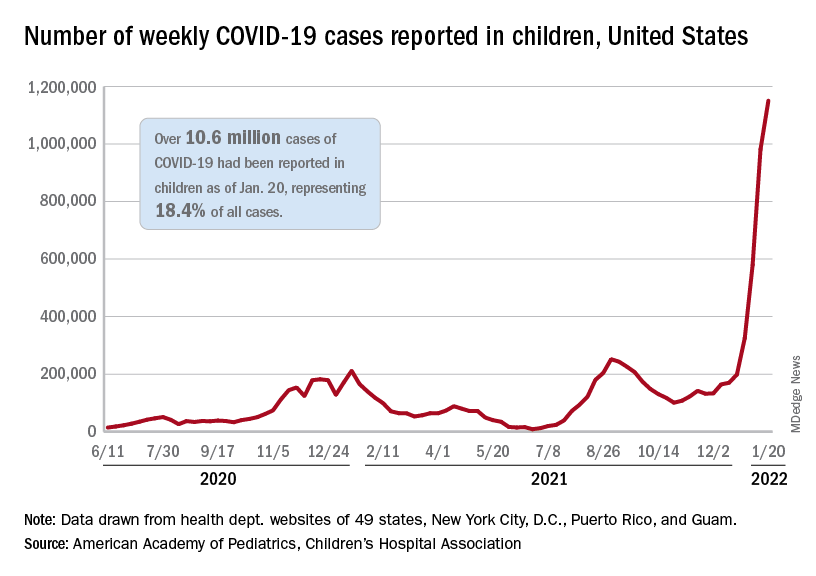
Regionally, the South had the most cases with over 380,000 for the week of Jan. 14-20, while the West was next with close to 350,000, followed by the Midwest and then the East. Among the states, the largest percent increases – on the order of 30% – came in New England (Massachusetts, Rhode Island, and Vermont), as well as Virginia and California, the AAP and CHA said.
Examining all those cases by vaccination status shows an obvious difference between the Omicron and Delta variants: The fully vaccinated have been hit much harder than before. For the week ending Dec. 25, 2021, the incidence of COVID-19 in children aged 12-17 years was 704 per 100,000 among those were unvaccinated and 384 per 100,000 in those who were fully vaccinated. During the Delta surge in the summer of 2021, the peak rates were 938 (unvaccinated) and 79 (vaccinated), the Centers for Disease Control and Prevention said.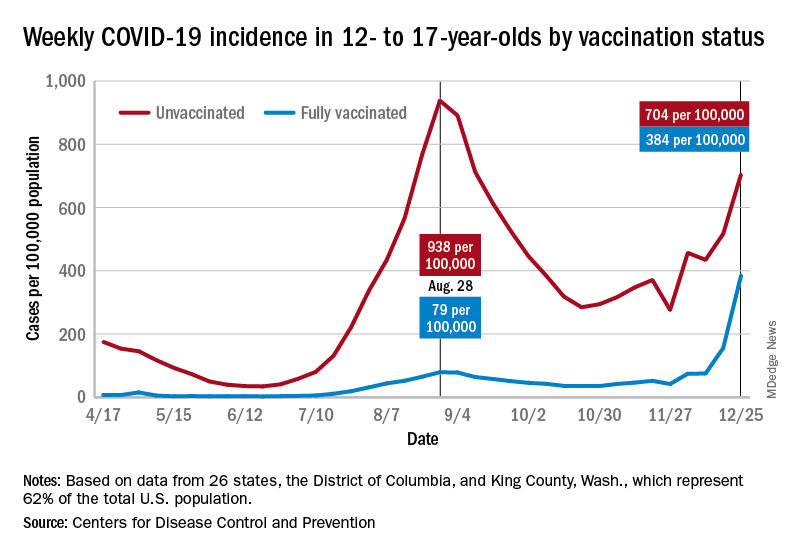
Hospitalizations are also at record levels, but two separate CDC databases seem to show a decline in child admissions over the last available week or so of data, which follows the trend among all ages. The peak among children aged 0-17 years came on Jan. 15, when the rate of new admissions reached 1.25 per 100,000, based on reporting to the CDC from 5,265 hospitals nationwide.
The second database, the COVID-19–Associated Hospitalization Surveillance Network (COVID-NET), indicates that children aged 0-4 years had the highest admission rate, 14.5 per 100,000, for the week ending Jan. 8, compared with 5.5 per 100,000 for 12- to 17-year-olds and 2.3 per 100,000 for those aged 5-11 years. COVID-NET covers almost 100 counties in 10 states, along with 4 entire states, and represents about 10% of the U.S. population.
Vaccinations rose briefly in late December and into January to meet the Omicron surge, but the numbers for the latest week show a return to their earlier levels. In children aged 5-11 years, new vaccinations went from 381,000 for the week of Dec. 20-26 to 524,000 for Jan. 3-9, but fell to just 260,000 during Jan. 17-23. The response was a little later for those aged 12-17, with the big week coming Jan. 10-16, but there was still a 38% drop for Jan. 17-23, according to the CDC’s COVID Data Tracker.
Currently, 29.3% of all 5- to 11-year-olds have received at least one dose of the COVID vaccine, and an even 20.0% are fully vaccinated. For children aged 12-17, the corresponding figures are 65.8% and 55.1%, the CDC said.
Statewide vaccination rates vary from Vermont’s high of 61% for those aged 5-11 to 12% for Alabama, Louisiana, and Mississippi, while Hawaii has the highest rate for 12- to 17-year-olds at 92% and Wyoming has the lowest at 39%, the AAP reported.
Weekly COVID-19 cases in children topped 1 million for the first time as the cumulative count surpassed 10 million since the start of the pandemic, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
the AAP and CHA said in their weekly COVID report. Those 10.6 million child cases represent 18.4% of all cases, and the latest 1.15 million represented 25.5% of all cases for the week.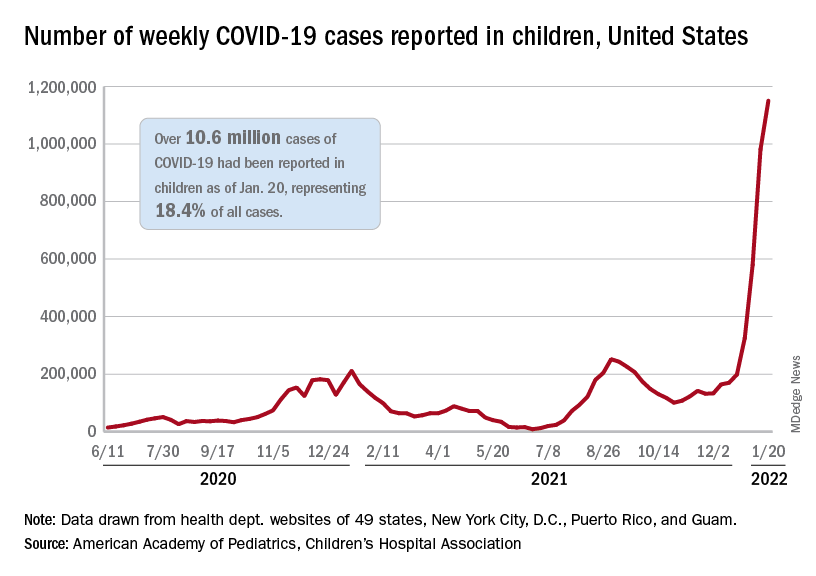
Regionally, the South had the most cases with over 380,000 for the week of Jan. 14-20, while the West was next with close to 350,000, followed by the Midwest and then the East. Among the states, the largest percent increases – on the order of 30% – came in New England (Massachusetts, Rhode Island, and Vermont), as well as Virginia and California, the AAP and CHA said.
Examining all those cases by vaccination status shows an obvious difference between the Omicron and Delta variants: The fully vaccinated have been hit much harder than before. For the week ending Dec. 25, 2021, the incidence of COVID-19 in children aged 12-17 years was 704 per 100,000 among those were unvaccinated and 384 per 100,000 in those who were fully vaccinated. During the Delta surge in the summer of 2021, the peak rates were 938 (unvaccinated) and 79 (vaccinated), the Centers for Disease Control and Prevention said.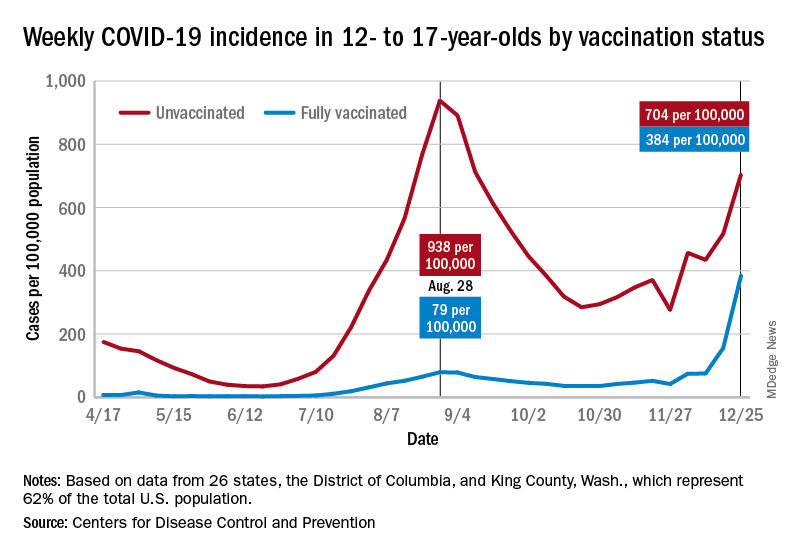
Hospitalizations are also at record levels, but two separate CDC databases seem to show a decline in child admissions over the last available week or so of data, which follows the trend among all ages. The peak among children aged 0-17 years came on Jan. 15, when the rate of new admissions reached 1.25 per 100,000, based on reporting to the CDC from 5,265 hospitals nationwide.
The second database, the COVID-19–Associated Hospitalization Surveillance Network (COVID-NET), indicates that children aged 0-4 years had the highest admission rate, 14.5 per 100,000, for the week ending Jan. 8, compared with 5.5 per 100,000 for 12- to 17-year-olds and 2.3 per 100,000 for those aged 5-11 years. COVID-NET covers almost 100 counties in 10 states, along with 4 entire states, and represents about 10% of the U.S. population.
Vaccinations rose briefly in late December and into January to meet the Omicron surge, but the numbers for the latest week show a return to their earlier levels. In children aged 5-11 years, new vaccinations went from 381,000 for the week of Dec. 20-26 to 524,000 for Jan. 3-9, but fell to just 260,000 during Jan. 17-23. The response was a little later for those aged 12-17, with the big week coming Jan. 10-16, but there was still a 38% drop for Jan. 17-23, according to the CDC’s COVID Data Tracker.
Currently, 29.3% of all 5- to 11-year-olds have received at least one dose of the COVID vaccine, and an even 20.0% are fully vaccinated. For children aged 12-17, the corresponding figures are 65.8% and 55.1%, the CDC said.
Statewide vaccination rates vary from Vermont’s high of 61% for those aged 5-11 to 12% for Alabama, Louisiana, and Mississippi, while Hawaii has the highest rate for 12- to 17-year-olds at 92% and Wyoming has the lowest at 39%, the AAP reported.
Weekly COVID-19 cases in children topped 1 million for the first time as the cumulative count surpassed 10 million since the start of the pandemic, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
the AAP and CHA said in their weekly COVID report. Those 10.6 million child cases represent 18.4% of all cases, and the latest 1.15 million represented 25.5% of all cases for the week.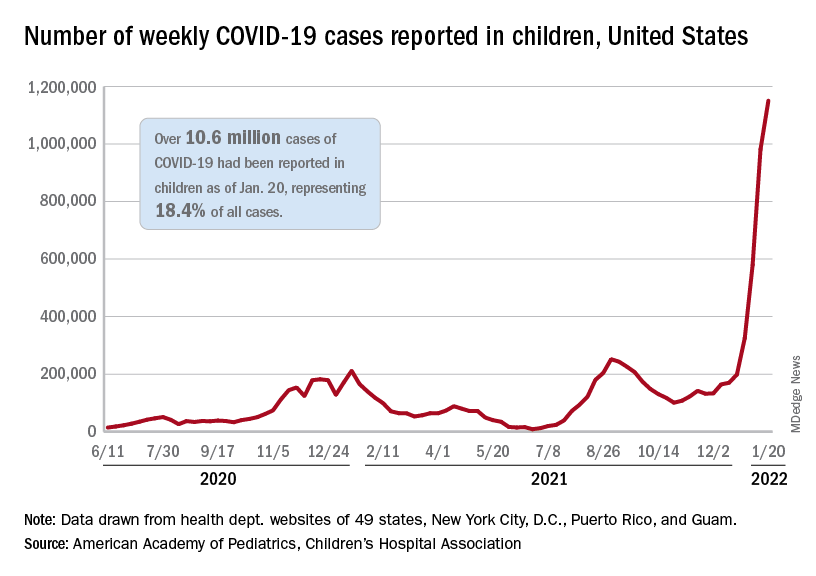
Regionally, the South had the most cases with over 380,000 for the week of Jan. 14-20, while the West was next with close to 350,000, followed by the Midwest and then the East. Among the states, the largest percent increases – on the order of 30% – came in New England (Massachusetts, Rhode Island, and Vermont), as well as Virginia and California, the AAP and CHA said.
Examining all those cases by vaccination status shows an obvious difference between the Omicron and Delta variants: The fully vaccinated have been hit much harder than before. For the week ending Dec. 25, 2021, the incidence of COVID-19 in children aged 12-17 years was 704 per 100,000 among those were unvaccinated and 384 per 100,000 in those who were fully vaccinated. During the Delta surge in the summer of 2021, the peak rates were 938 (unvaccinated) and 79 (vaccinated), the Centers for Disease Control and Prevention said.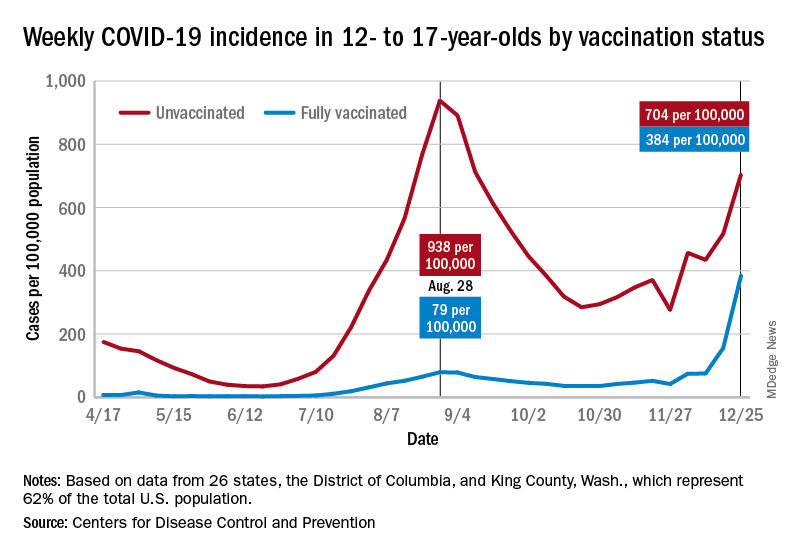
Hospitalizations are also at record levels, but two separate CDC databases seem to show a decline in child admissions over the last available week or so of data, which follows the trend among all ages. The peak among children aged 0-17 years came on Jan. 15, when the rate of new admissions reached 1.25 per 100,000, based on reporting to the CDC from 5,265 hospitals nationwide.
The second database, the COVID-19–Associated Hospitalization Surveillance Network (COVID-NET), indicates that children aged 0-4 years had the highest admission rate, 14.5 per 100,000, for the week ending Jan. 8, compared with 5.5 per 100,000 for 12- to 17-year-olds and 2.3 per 100,000 for those aged 5-11 years. COVID-NET covers almost 100 counties in 10 states, along with 4 entire states, and represents about 10% of the U.S. population.
Vaccinations rose briefly in late December and into January to meet the Omicron surge, but the numbers for the latest week show a return to their earlier levels. In children aged 5-11 years, new vaccinations went from 381,000 for the week of Dec. 20-26 to 524,000 for Jan. 3-9, but fell to just 260,000 during Jan. 17-23. The response was a little later for those aged 12-17, with the big week coming Jan. 10-16, but there was still a 38% drop for Jan. 17-23, according to the CDC’s COVID Data Tracker.
Currently, 29.3% of all 5- to 11-year-olds have received at least one dose of the COVID vaccine, and an even 20.0% are fully vaccinated. For children aged 12-17, the corresponding figures are 65.8% and 55.1%, the CDC said.
Statewide vaccination rates vary from Vermont’s high of 61% for those aged 5-11 to 12% for Alabama, Louisiana, and Mississippi, while Hawaii has the highest rate for 12- to 17-year-olds at 92% and Wyoming has the lowest at 39%, the AAP reported.