User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
School shootings rose to highest number in 20 years, data shows
School shootings from 2020 to 2021 climbed to the highest point in 2 decades, according to a new report from the National Center for Education Statistics and the Bureau of Justice Statistics.
There were 93 shootings with casualties at public and private K-12 schools across the United States from 2020 to 2021, as compared with 23 in the 2000-2001 school year. The latest number included 43 incidents with deaths.
The annual report, which examines crime and safety in schools and colleges, also found a rise in cyberbullying and verbal abuse or disrespect of teachers during the past decade.
“While the lasting impact of these crime and safety issues cannot be measured in statistics alone, these data are valuable to the efforts of our policymakers, school officials and community members to identify and implement preventive and responsive measures,” Peggy Carr, PhD, the commissioner for the National Center for Education Statistics, said in a statement.
The report used a broad definition of shootings, which included instances when guns were fired or flashed on school property, as well as when a bullet hit school grounds for any reason and shootings that happened on school property during remote instruction throughout the COVID-19 pandemic.
More than 311,000 children at 331 schools have gone through gun violence since the shooting at Columbine High School in 1999, according to The Washington Post.
“The increase in shootings in schools is likely a consequence of an overall increase in gun violence and not specific to schools,” Dewey Cornell, PhD, a professor of education at the University of Virginia, Charlottesville, told the newspaper.
“However, most schools will never have a shooting, and their main problems will be fighting and bullying,” he said.
Between 2009 and 2020, the rate of nonfatal criminal victimization, including theft and violent crimes, decreased for ages 12-18, the report found. The rate fell from 51 victimizations per 1,000 students to 11. A major portion of the decline happened during the first year of the pandemic.
Lower percentages of public schools reported certain issues from 2019 to 2020 than from 2009 to 2010, the report found. For instance, 15% of schools reported student bullying at least once a week, as compared with 23% a decade ago. Student sexual harassment of other students dropped from 3% to 2%, and student harassment of other students based on sexual orientation or gender identity dropped from 3% to 2%.
At the same time, teachers faced more hardships, the report found. Schools reporting verbal abuse of teachers at least once a week rose to 10% in the 2019-2020 school year, as compared with 5% in the 2009-2010 school year. Schools reporting acts of disrespect for teachers climbed from 9% to 15%.
The percentage of schools that reported cyberbullying at least once a week doubled during the decade, rising from 8% in 2009-2010 to 16% in 2019-2020, the report found. The prominence of social media has likely added to that increase, the Post reported.
What’s more, about 55% of public schools offered mental health assessments in 2019-2020, and 42% offered mental health treatment services, the report found. The low rates could be linked to not having enough funding or access to licensed professionals, the newspaper reported.
A version of this article first appeared on WebMD.com.
School shootings from 2020 to 2021 climbed to the highest point in 2 decades, according to a new report from the National Center for Education Statistics and the Bureau of Justice Statistics.
There were 93 shootings with casualties at public and private K-12 schools across the United States from 2020 to 2021, as compared with 23 in the 2000-2001 school year. The latest number included 43 incidents with deaths.
The annual report, which examines crime and safety in schools and colleges, also found a rise in cyberbullying and verbal abuse or disrespect of teachers during the past decade.
“While the lasting impact of these crime and safety issues cannot be measured in statistics alone, these data are valuable to the efforts of our policymakers, school officials and community members to identify and implement preventive and responsive measures,” Peggy Carr, PhD, the commissioner for the National Center for Education Statistics, said in a statement.
The report used a broad definition of shootings, which included instances when guns were fired or flashed on school property, as well as when a bullet hit school grounds for any reason and shootings that happened on school property during remote instruction throughout the COVID-19 pandemic.
More than 311,000 children at 331 schools have gone through gun violence since the shooting at Columbine High School in 1999, according to The Washington Post.
“The increase in shootings in schools is likely a consequence of an overall increase in gun violence and not specific to schools,” Dewey Cornell, PhD, a professor of education at the University of Virginia, Charlottesville, told the newspaper.
“However, most schools will never have a shooting, and their main problems will be fighting and bullying,” he said.
Between 2009 and 2020, the rate of nonfatal criminal victimization, including theft and violent crimes, decreased for ages 12-18, the report found. The rate fell from 51 victimizations per 1,000 students to 11. A major portion of the decline happened during the first year of the pandemic.
Lower percentages of public schools reported certain issues from 2019 to 2020 than from 2009 to 2010, the report found. For instance, 15% of schools reported student bullying at least once a week, as compared with 23% a decade ago. Student sexual harassment of other students dropped from 3% to 2%, and student harassment of other students based on sexual orientation or gender identity dropped from 3% to 2%.
At the same time, teachers faced more hardships, the report found. Schools reporting verbal abuse of teachers at least once a week rose to 10% in the 2019-2020 school year, as compared with 5% in the 2009-2010 school year. Schools reporting acts of disrespect for teachers climbed from 9% to 15%.
The percentage of schools that reported cyberbullying at least once a week doubled during the decade, rising from 8% in 2009-2010 to 16% in 2019-2020, the report found. The prominence of social media has likely added to that increase, the Post reported.
What’s more, about 55% of public schools offered mental health assessments in 2019-2020, and 42% offered mental health treatment services, the report found. The low rates could be linked to not having enough funding or access to licensed professionals, the newspaper reported.
A version of this article first appeared on WebMD.com.
School shootings from 2020 to 2021 climbed to the highest point in 2 decades, according to a new report from the National Center for Education Statistics and the Bureau of Justice Statistics.
There were 93 shootings with casualties at public and private K-12 schools across the United States from 2020 to 2021, as compared with 23 in the 2000-2001 school year. The latest number included 43 incidents with deaths.
The annual report, which examines crime and safety in schools and colleges, also found a rise in cyberbullying and verbal abuse or disrespect of teachers during the past decade.
“While the lasting impact of these crime and safety issues cannot be measured in statistics alone, these data are valuable to the efforts of our policymakers, school officials and community members to identify and implement preventive and responsive measures,” Peggy Carr, PhD, the commissioner for the National Center for Education Statistics, said in a statement.
The report used a broad definition of shootings, which included instances when guns were fired or flashed on school property, as well as when a bullet hit school grounds for any reason and shootings that happened on school property during remote instruction throughout the COVID-19 pandemic.
More than 311,000 children at 331 schools have gone through gun violence since the shooting at Columbine High School in 1999, according to The Washington Post.
“The increase in shootings in schools is likely a consequence of an overall increase in gun violence and not specific to schools,” Dewey Cornell, PhD, a professor of education at the University of Virginia, Charlottesville, told the newspaper.
“However, most schools will never have a shooting, and their main problems will be fighting and bullying,” he said.
Between 2009 and 2020, the rate of nonfatal criminal victimization, including theft and violent crimes, decreased for ages 12-18, the report found. The rate fell from 51 victimizations per 1,000 students to 11. A major portion of the decline happened during the first year of the pandemic.
Lower percentages of public schools reported certain issues from 2019 to 2020 than from 2009 to 2010, the report found. For instance, 15% of schools reported student bullying at least once a week, as compared with 23% a decade ago. Student sexual harassment of other students dropped from 3% to 2%, and student harassment of other students based on sexual orientation or gender identity dropped from 3% to 2%.
At the same time, teachers faced more hardships, the report found. Schools reporting verbal abuse of teachers at least once a week rose to 10% in the 2019-2020 school year, as compared with 5% in the 2009-2010 school year. Schools reporting acts of disrespect for teachers climbed from 9% to 15%.
The percentage of schools that reported cyberbullying at least once a week doubled during the decade, rising from 8% in 2009-2010 to 16% in 2019-2020, the report found. The prominence of social media has likely added to that increase, the Post reported.
What’s more, about 55% of public schools offered mental health assessments in 2019-2020, and 42% offered mental health treatment services, the report found. The low rates could be linked to not having enough funding or access to licensed professionals, the newspaper reported.
A version of this article first appeared on WebMD.com.
Pandemic stress tied to increased headache burden in teens
Contrary to previous research findings, the stress of the COVID-19 pandemic has been linked to an increased headache burden in teens.
Investigators found factors contributing to headache for preteens and teens during the pandemic included increased screen time for online learning, depression, anxiety, female sex, and weight gain.
“The stressors and pressures of the pandemic may have eventually taken their toll,” lead author Ayşe Nur Özdağ Acarli, MD, Ermenek State Hospital, department of neurology, Karaman, Turkey, told this news organization.
“Limiting screen time and providing more psychosocial supports would help lessen the burden of the COVID-19 pandemic on adolescents with headache.”
The findings were presented at the Congress of the European Academy of Neurology (EAN) 2022.
Most common neurological problem in kids
Headache is the most common neurological problem in children and adolescents. Potential factors contributing to headache in this population include lack of sleep and physical activity, mental health problems, and socioeconomic conditions.
The COVID-19 pandemic has had a “striking” impact on every aspect of life for young people, said Dr. Acarli.
Some studies reported an improvement in headache prevalence among adolescents during COVID-19, which was attributed to less school-related stress. However, said Dr. Acarli in her personal clinical experience, young patients suffered more frequent and severe headaches during the pandemic.
She noted previous research examining the impact of the pandemic on headache in youth was conducted only in the early days of the pandemic and examined shorter-term effects. Research examining the long-term effects of the pandemic on headache in this patient population has been “lacking,” she said.
The study included 851 participants aged 10-18 years (mean age 14.9 years and 62% female) who were seen at a neurology or pediatric outpatient clinic from August-December 2021. The study excluded subjects with neurological problems, intellectual deficits, autism spectrum disorder, and epilepsy.
Participants completed detailed questionnaires providing data on demographics, exposure to COVID-19, and electronics, as well as information on depressive symptoms as assessed by the Patient Health Questionnaire-9 and anxiety symptoms using the Generalized Anxiety Disorder-7 and COVID-related anxiety.
“We used two distinct scales for anxiety: one for generalized anxiety and the other for COVID-related anxiety,” said Dr. Acarli.
Of the total study population, 756 (89%) reported headaches. This headache prevalence in children and adolescents is like that found in other studies.
Dr. Acarli noted several differences in the headache group versus the non-headache group. The female/male ratio was 2:1 versus 1:1, the mean age was 15.0 versus 14.4, and depression and generalized anxiety scores were significantly higher. There was no significant difference in COVID-19 history in those with and without headache.
Researchers categorized those with headache into four groups: worsening headaches (27%), improved headaches (3%), new onset headaches (10%), and stable headaches (61%).
Compared with the other groups, the worsened headache group included significantly more females and older individuals with more severe and frequent headaches. This group also had more participants reporting at least 15 headache attacks a month and using painkillers at least once a month.
The study showed headache severity was significantly increased with age, headache duration, depression, generalized anxiety (all P < .001), and COVID-19 anxiety (P < .01). Headache frequency, measured as attacks per month, was significantly increased with age, depression, and generalized anxiety (all P < .001).
Worsening headache outcomes during the pandemic were associated with longer exposure to computer screens (odds ratio, 1.7; 95% confidence interval, 1.2-2.3; P < .01), lack of suitable conditions for online learning (OR, 2.6; 95% CI, 1.8-3.8; P < .001), depression (OR, 2.0; 95% CI, 1.4-2.8; P < .001); and COVID-19 anxiety (OR, 3.2; 95% CI, 1.3-8.0; P < .01). Other contributing factors included school exams, living in a city, female sex, and weight gain.
There may be a link between COVID-related headaches and anxiety or depression, but it’s unclear what’s causing what. “We don’t know which is the chicken and which is the egg,” said Dr. Acarli.
Headache triggers
Commenting for this news organization, Raquel Gil-Gouveia, MD, PhD, head of the neurology department, Hospital da Luz, Lisbon, Portugal, who co-chaired the session where the research was presented, said the information collected for the study was “extensive.”
Some results were expected, including the fact that patients with headaches were more anxious and depressed, said Dr. Gil-Gouveia.
“Anxiety and depression are frequent comorbidities of headache and can act as a triggering factor for headache attacks but can also be a consequence of intense or chronic pain,” she said.
She agreed the new results differ from those of studies carried out during the first pandemic lockdown, which showed an improvement in headache, but noted online learning was not fully implemented at that time, “so it was much like being on vacation.”
In addition to isolation, anxiety, and prolonged screen exposure, the lack of peer contact and fewer sports and leisure activities may also have contributed to worsening headaches during the COVID lockdown, but these were not explored in this study, said Dr. Gil-Gouveia.
The study was supported by the Global Migraine and Pain Society. The investigators and Dr. Gil-Gouveia report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Contrary to previous research findings, the stress of the COVID-19 pandemic has been linked to an increased headache burden in teens.
Investigators found factors contributing to headache for preteens and teens during the pandemic included increased screen time for online learning, depression, anxiety, female sex, and weight gain.
“The stressors and pressures of the pandemic may have eventually taken their toll,” lead author Ayşe Nur Özdağ Acarli, MD, Ermenek State Hospital, department of neurology, Karaman, Turkey, told this news organization.
“Limiting screen time and providing more psychosocial supports would help lessen the burden of the COVID-19 pandemic on adolescents with headache.”
The findings were presented at the Congress of the European Academy of Neurology (EAN) 2022.
Most common neurological problem in kids
Headache is the most common neurological problem in children and adolescents. Potential factors contributing to headache in this population include lack of sleep and physical activity, mental health problems, and socioeconomic conditions.
The COVID-19 pandemic has had a “striking” impact on every aspect of life for young people, said Dr. Acarli.
Some studies reported an improvement in headache prevalence among adolescents during COVID-19, which was attributed to less school-related stress. However, said Dr. Acarli in her personal clinical experience, young patients suffered more frequent and severe headaches during the pandemic.
She noted previous research examining the impact of the pandemic on headache in youth was conducted only in the early days of the pandemic and examined shorter-term effects. Research examining the long-term effects of the pandemic on headache in this patient population has been “lacking,” she said.
The study included 851 participants aged 10-18 years (mean age 14.9 years and 62% female) who were seen at a neurology or pediatric outpatient clinic from August-December 2021. The study excluded subjects with neurological problems, intellectual deficits, autism spectrum disorder, and epilepsy.
Participants completed detailed questionnaires providing data on demographics, exposure to COVID-19, and electronics, as well as information on depressive symptoms as assessed by the Patient Health Questionnaire-9 and anxiety symptoms using the Generalized Anxiety Disorder-7 and COVID-related anxiety.
“We used two distinct scales for anxiety: one for generalized anxiety and the other for COVID-related anxiety,” said Dr. Acarli.
Of the total study population, 756 (89%) reported headaches. This headache prevalence in children and adolescents is like that found in other studies.
Dr. Acarli noted several differences in the headache group versus the non-headache group. The female/male ratio was 2:1 versus 1:1, the mean age was 15.0 versus 14.4, and depression and generalized anxiety scores were significantly higher. There was no significant difference in COVID-19 history in those with and without headache.
Researchers categorized those with headache into four groups: worsening headaches (27%), improved headaches (3%), new onset headaches (10%), and stable headaches (61%).
Compared with the other groups, the worsened headache group included significantly more females and older individuals with more severe and frequent headaches. This group also had more participants reporting at least 15 headache attacks a month and using painkillers at least once a month.
The study showed headache severity was significantly increased with age, headache duration, depression, generalized anxiety (all P < .001), and COVID-19 anxiety (P < .01). Headache frequency, measured as attacks per month, was significantly increased with age, depression, and generalized anxiety (all P < .001).
Worsening headache outcomes during the pandemic were associated with longer exposure to computer screens (odds ratio, 1.7; 95% confidence interval, 1.2-2.3; P < .01), lack of suitable conditions for online learning (OR, 2.6; 95% CI, 1.8-3.8; P < .001), depression (OR, 2.0; 95% CI, 1.4-2.8; P < .001); and COVID-19 anxiety (OR, 3.2; 95% CI, 1.3-8.0; P < .01). Other contributing factors included school exams, living in a city, female sex, and weight gain.
There may be a link between COVID-related headaches and anxiety or depression, but it’s unclear what’s causing what. “We don’t know which is the chicken and which is the egg,” said Dr. Acarli.
Headache triggers
Commenting for this news organization, Raquel Gil-Gouveia, MD, PhD, head of the neurology department, Hospital da Luz, Lisbon, Portugal, who co-chaired the session where the research was presented, said the information collected for the study was “extensive.”
Some results were expected, including the fact that patients with headaches were more anxious and depressed, said Dr. Gil-Gouveia.
“Anxiety and depression are frequent comorbidities of headache and can act as a triggering factor for headache attacks but can also be a consequence of intense or chronic pain,” she said.
She agreed the new results differ from those of studies carried out during the first pandemic lockdown, which showed an improvement in headache, but noted online learning was not fully implemented at that time, “so it was much like being on vacation.”
In addition to isolation, anxiety, and prolonged screen exposure, the lack of peer contact and fewer sports and leisure activities may also have contributed to worsening headaches during the COVID lockdown, but these were not explored in this study, said Dr. Gil-Gouveia.
The study was supported by the Global Migraine and Pain Society. The investigators and Dr. Gil-Gouveia report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Contrary to previous research findings, the stress of the COVID-19 pandemic has been linked to an increased headache burden in teens.
Investigators found factors contributing to headache for preteens and teens during the pandemic included increased screen time for online learning, depression, anxiety, female sex, and weight gain.
“The stressors and pressures of the pandemic may have eventually taken their toll,” lead author Ayşe Nur Özdağ Acarli, MD, Ermenek State Hospital, department of neurology, Karaman, Turkey, told this news organization.
“Limiting screen time and providing more psychosocial supports would help lessen the burden of the COVID-19 pandemic on adolescents with headache.”
The findings were presented at the Congress of the European Academy of Neurology (EAN) 2022.
Most common neurological problem in kids
Headache is the most common neurological problem in children and adolescents. Potential factors contributing to headache in this population include lack of sleep and physical activity, mental health problems, and socioeconomic conditions.
The COVID-19 pandemic has had a “striking” impact on every aspect of life for young people, said Dr. Acarli.
Some studies reported an improvement in headache prevalence among adolescents during COVID-19, which was attributed to less school-related stress. However, said Dr. Acarli in her personal clinical experience, young patients suffered more frequent and severe headaches during the pandemic.
She noted previous research examining the impact of the pandemic on headache in youth was conducted only in the early days of the pandemic and examined shorter-term effects. Research examining the long-term effects of the pandemic on headache in this patient population has been “lacking,” she said.
The study included 851 participants aged 10-18 years (mean age 14.9 years and 62% female) who were seen at a neurology or pediatric outpatient clinic from August-December 2021. The study excluded subjects with neurological problems, intellectual deficits, autism spectrum disorder, and epilepsy.
Participants completed detailed questionnaires providing data on demographics, exposure to COVID-19, and electronics, as well as information on depressive symptoms as assessed by the Patient Health Questionnaire-9 and anxiety symptoms using the Generalized Anxiety Disorder-7 and COVID-related anxiety.
“We used two distinct scales for anxiety: one for generalized anxiety and the other for COVID-related anxiety,” said Dr. Acarli.
Of the total study population, 756 (89%) reported headaches. This headache prevalence in children and adolescents is like that found in other studies.
Dr. Acarli noted several differences in the headache group versus the non-headache group. The female/male ratio was 2:1 versus 1:1, the mean age was 15.0 versus 14.4, and depression and generalized anxiety scores were significantly higher. There was no significant difference in COVID-19 history in those with and without headache.
Researchers categorized those with headache into four groups: worsening headaches (27%), improved headaches (3%), new onset headaches (10%), and stable headaches (61%).
Compared with the other groups, the worsened headache group included significantly more females and older individuals with more severe and frequent headaches. This group also had more participants reporting at least 15 headache attacks a month and using painkillers at least once a month.
The study showed headache severity was significantly increased with age, headache duration, depression, generalized anxiety (all P < .001), and COVID-19 anxiety (P < .01). Headache frequency, measured as attacks per month, was significantly increased with age, depression, and generalized anxiety (all P < .001).
Worsening headache outcomes during the pandemic were associated with longer exposure to computer screens (odds ratio, 1.7; 95% confidence interval, 1.2-2.3; P < .01), lack of suitable conditions for online learning (OR, 2.6; 95% CI, 1.8-3.8; P < .001), depression (OR, 2.0; 95% CI, 1.4-2.8; P < .001); and COVID-19 anxiety (OR, 3.2; 95% CI, 1.3-8.0; P < .01). Other contributing factors included school exams, living in a city, female sex, and weight gain.
There may be a link between COVID-related headaches and anxiety or depression, but it’s unclear what’s causing what. “We don’t know which is the chicken and which is the egg,” said Dr. Acarli.
Headache triggers
Commenting for this news organization, Raquel Gil-Gouveia, MD, PhD, head of the neurology department, Hospital da Luz, Lisbon, Portugal, who co-chaired the session where the research was presented, said the information collected for the study was “extensive.”
Some results were expected, including the fact that patients with headaches were more anxious and depressed, said Dr. Gil-Gouveia.
“Anxiety and depression are frequent comorbidities of headache and can act as a triggering factor for headache attacks but can also be a consequence of intense or chronic pain,” she said.
She agreed the new results differ from those of studies carried out during the first pandemic lockdown, which showed an improvement in headache, but noted online learning was not fully implemented at that time, “so it was much like being on vacation.”
In addition to isolation, anxiety, and prolonged screen exposure, the lack of peer contact and fewer sports and leisure activities may also have contributed to worsening headaches during the COVID lockdown, but these were not explored in this study, said Dr. Gil-Gouveia.
The study was supported by the Global Migraine and Pain Society. The investigators and Dr. Gil-Gouveia report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM EAN 2022
White House expands access to monkeypox vaccines
The White House is scaling up its response to the monkeypox outbreak, expanding access to vaccines to more at-risk individuals, officials said in a press call. More than 56,000 doses of the monkeypox vaccine JYNNEOS will be made available immediately, and more than 240,000 doses will be allocated in the coming weeks.
“The administration’s current strategy is focused on containing the outbreak by providing vaccines to those most in need to prevent further spread of monkeypox in the communities most impacted,” CDC Director Rochelle Walensky, MD, MPH, said on a June 28 press call. “As additional supply becomes available, we will further expand our efforts making vaccines available to a wider population.”
As of June 28, there were 4,700 detected cases of monkeypox globally in 49 countries. Since the first U.S. case of monkeypox was identified on May 17, there have been 306 confirmed cases across 28 jurisdictions.
Prior to this announcement, vaccination against monkeypox was recommended only for people with known exposures to the virus. Now, the vaccine is available to people who are likely to be exposed to the virus, including:
- People who have had close physical contact with someone diagnosed with monkeypox.
- People with a sexual partner diagnosed with monkeypox.
- Men who have sex with men who have had multiple sex partners in a venue where monkeypox was identified.
The JYNNEOS vaccine is administered in two doses, delivered 28 days apart. People will have maximum immunity 2 weeks after the second dose. People should be vaccinated within 2 weeks of a possible monkeypox exposure, Dr. Walensky said, adding, “The sooner you can get vaccinated after exposure, the better.”
The U.S. Department of Health and Human Services will immediately allocate the 56,000 JYNNEOS doses across the country, prioritizing jurisdictions to areas of high transmission. A second vaccine, ACAM2000, can also be requested, but it has a greater risk for serious side effects and is not appropriate for immunocompromised individuals or people with heart disease. In the coming weeks, 240,000 JYNNEOS doses will be made available for second doses as well as first doses “as the vaccine strategy broadens,” said David Boucher, director of infectious disease preparedness and response for HHS. There are currently 800,000 JYNNEOS doses that have been manufactured and approved for release, he said, and awaiting inspection by the Food and Drug Administration, which should be completed in the beginning of July.
At the same time, the administration is focusing on increasing access to testing. Monkeypox testing is now available in 78 state public health labs in 48 states that can collectively conduct 10,000 tests per week. In addition, the administration announced on June 23 that HHS began shipping monkeypox tests to five commercial lab companies to expand testing capacity as well as make testing more accessible.
“We continue to work very closely with the community and with public health partners and clinicians to increase awareness of the monkey pox outbreak and to facilitate adequate capacity and equitable access to testing,” Dr. Walensky said. “I strongly encourage all health care providers to have a high clinical suspicion for monkeypox among their patients. Patients presenting with a suspicious rash should be tested.”
A version of this article first appeared on Medscape.com.
The White House is scaling up its response to the monkeypox outbreak, expanding access to vaccines to more at-risk individuals, officials said in a press call. More than 56,000 doses of the monkeypox vaccine JYNNEOS will be made available immediately, and more than 240,000 doses will be allocated in the coming weeks.
“The administration’s current strategy is focused on containing the outbreak by providing vaccines to those most in need to prevent further spread of monkeypox in the communities most impacted,” CDC Director Rochelle Walensky, MD, MPH, said on a June 28 press call. “As additional supply becomes available, we will further expand our efforts making vaccines available to a wider population.”
As of June 28, there were 4,700 detected cases of monkeypox globally in 49 countries. Since the first U.S. case of monkeypox was identified on May 17, there have been 306 confirmed cases across 28 jurisdictions.
Prior to this announcement, vaccination against monkeypox was recommended only for people with known exposures to the virus. Now, the vaccine is available to people who are likely to be exposed to the virus, including:
- People who have had close physical contact with someone diagnosed with monkeypox.
- People with a sexual partner diagnosed with monkeypox.
- Men who have sex with men who have had multiple sex partners in a venue where monkeypox was identified.
The JYNNEOS vaccine is administered in two doses, delivered 28 days apart. People will have maximum immunity 2 weeks after the second dose. People should be vaccinated within 2 weeks of a possible monkeypox exposure, Dr. Walensky said, adding, “The sooner you can get vaccinated after exposure, the better.”
The U.S. Department of Health and Human Services will immediately allocate the 56,000 JYNNEOS doses across the country, prioritizing jurisdictions to areas of high transmission. A second vaccine, ACAM2000, can also be requested, but it has a greater risk for serious side effects and is not appropriate for immunocompromised individuals or people with heart disease. In the coming weeks, 240,000 JYNNEOS doses will be made available for second doses as well as first doses “as the vaccine strategy broadens,” said David Boucher, director of infectious disease preparedness and response for HHS. There are currently 800,000 JYNNEOS doses that have been manufactured and approved for release, he said, and awaiting inspection by the Food and Drug Administration, which should be completed in the beginning of July.
At the same time, the administration is focusing on increasing access to testing. Monkeypox testing is now available in 78 state public health labs in 48 states that can collectively conduct 10,000 tests per week. In addition, the administration announced on June 23 that HHS began shipping monkeypox tests to five commercial lab companies to expand testing capacity as well as make testing more accessible.
“We continue to work very closely with the community and with public health partners and clinicians to increase awareness of the monkey pox outbreak and to facilitate adequate capacity and equitable access to testing,” Dr. Walensky said. “I strongly encourage all health care providers to have a high clinical suspicion for monkeypox among their patients. Patients presenting with a suspicious rash should be tested.”
A version of this article first appeared on Medscape.com.
The White House is scaling up its response to the monkeypox outbreak, expanding access to vaccines to more at-risk individuals, officials said in a press call. More than 56,000 doses of the monkeypox vaccine JYNNEOS will be made available immediately, and more than 240,000 doses will be allocated in the coming weeks.
“The administration’s current strategy is focused on containing the outbreak by providing vaccines to those most in need to prevent further spread of monkeypox in the communities most impacted,” CDC Director Rochelle Walensky, MD, MPH, said on a June 28 press call. “As additional supply becomes available, we will further expand our efforts making vaccines available to a wider population.”
As of June 28, there were 4,700 detected cases of monkeypox globally in 49 countries. Since the first U.S. case of monkeypox was identified on May 17, there have been 306 confirmed cases across 28 jurisdictions.
Prior to this announcement, vaccination against monkeypox was recommended only for people with known exposures to the virus. Now, the vaccine is available to people who are likely to be exposed to the virus, including:
- People who have had close physical contact with someone diagnosed with monkeypox.
- People with a sexual partner diagnosed with monkeypox.
- Men who have sex with men who have had multiple sex partners in a venue where monkeypox was identified.
The JYNNEOS vaccine is administered in two doses, delivered 28 days apart. People will have maximum immunity 2 weeks after the second dose. People should be vaccinated within 2 weeks of a possible monkeypox exposure, Dr. Walensky said, adding, “The sooner you can get vaccinated after exposure, the better.”
The U.S. Department of Health and Human Services will immediately allocate the 56,000 JYNNEOS doses across the country, prioritizing jurisdictions to areas of high transmission. A second vaccine, ACAM2000, can also be requested, but it has a greater risk for serious side effects and is not appropriate for immunocompromised individuals or people with heart disease. In the coming weeks, 240,000 JYNNEOS doses will be made available for second doses as well as first doses “as the vaccine strategy broadens,” said David Boucher, director of infectious disease preparedness and response for HHS. There are currently 800,000 JYNNEOS doses that have been manufactured and approved for release, he said, and awaiting inspection by the Food and Drug Administration, which should be completed in the beginning of July.
At the same time, the administration is focusing on increasing access to testing. Monkeypox testing is now available in 78 state public health labs in 48 states that can collectively conduct 10,000 tests per week. In addition, the administration announced on June 23 that HHS began shipping monkeypox tests to five commercial lab companies to expand testing capacity as well as make testing more accessible.
“We continue to work very closely with the community and with public health partners and clinicians to increase awareness of the monkey pox outbreak and to facilitate adequate capacity and equitable access to testing,” Dr. Walensky said. “I strongly encourage all health care providers to have a high clinical suspicion for monkeypox among their patients. Patients presenting with a suspicious rash should be tested.”
A version of this article first appeared on Medscape.com.
Study finds higher risk of skin cancer after childhood organ transplant
A large study showing an increased risk of keratinocyte carcinoma (KC) in children who receive a solid-organ transplant highlights the need for early education about risk reduction and more research to determine optimal timing for screening, say an investigator and two dermatologists with expertise in transplant-related skin issues.
The increased incidence of KC in pediatric transplant recipients is “really high, so we definitely know there’s risk there,” just as there is for adult recipients of solid-organ transplants, said Cathryn Sibbald, MD, MSc, a dermatologist at the Hospital for Sick Children in Toronto and coauthor of a research letter published in June in JAMA Dermatology.
For their study, Dr. Sibbald and her coinvestigators turned to the Ontario Health Insurance plan database, which covers health care for Canadian citizens and qualified residents in the province. They identified 951 patients younger than the age of 18 who received a solid-organ transplant between 1991 and 2004 at an Ontario hospital
They then used a validated health insurance claims–based algorithm to identify diagnoses of KC for the transplant recipients and for more than 5 million age-matched controls. KC, including squamous and basal cell carcinoma, is the most prevalent skin cancer for people who have had a solid-organ transplant.
Fifteen posttransplant KCs (10 patients, 1.1%) were reported a mean of 13.1 years after transplant, with none reported in the first 4 years. The mean age at transplant was 7.8 years, and the mean age at KC diagnosis was 25.2 years. Kidney transplants were the most common (42.1% of transplantations). Most of the transplants recipients (eight patients) who developed KC had kidney transplantation, and most of them had functional graft at the time of KC diagnosis.
Researchers found an increased incidence of KC compared with that of the general population (standardized incidence ratio, 9.09; 95% confidence interval, 5.48-15.08). And the risk for KC increased with time since transplant, with adjusted hazard ratios for KC of 3.63 (95% CI, 0.51-25.77) for 1-5 years, 5.14 (95% CI, 1.28-20.55) for 5-10 years, and 4.80 (95% CI, 2.29-10.08) for 10 years or more, compared with the control population.
Several years ago, another research team performed a similar population-based cohort study of adult transplant recipients in Ontario and found a 6.6-times increased risk of KC in transplant recipients compared with the general population.
Sun protection and skin cancer screening
In commenting on the study, Sarah Arron, MD, PhD, a San Francisco Bay area dermatologist and immediate past president of the International Immunosuppression and Transplant Skin Cancer Collaborative (www.itscc.org), said she feels “reassured” that young transplant patients tend not to develop the skin cancer until young adulthood.
A ”large study like this is important because the overall rate of KC is low in this age group,” she noted.
The findings “suggest that we can focus our efforts on prevention during childhood, with sun protection and skin cancer education,” she said. “Then, as these children move into adulthood, we can begin screening with skin examinations. Of course, [any child] with a skin lesion or mole that concerns their parents or transplant team should be referred to dermatology for evaluation.”
Pediatric transplant recipients and their parents are most interested in learning about skin cancer prevention either before or immediately after transplantation, according to a survey by other researchers.
Intervention studies needed
The increased risk of KC probably stems largely from immunosuppression, said Dr. Sibbald in an interview. “We know [this is the case] in the older population, and it’s likely true in the younger population as well that it’s one of the primary drivers,” she said.
More research to extensively analyze risk factors should come next, she said. This includes “the granularity of what [immunosuppressants and other] medications are received, and at what dose and for what periods of time, so we can calculate cumulative exposure and its relation to risk,” she said.
Kristin Bibee, MD, PhD, assistant professor of dermatology at Johns Hopkins University in Baltimore, said she’d like to see further studies “evaluate appropriate interventions, like sun-protective behavior in childhood and adolescence or immunosuppression modulation, to prevent malignancy development.”
The optimal time and intensity of screening for young transplant recipients must still be determined, both Dr. Bibee and Dr. Arron said. Patients deemed through further research to be at higher risk may need earlier and/or more intensive surveillance.
The role of race in skin cancer risk in this population is “one question the study leaves open,” said Dr. Arron. U.S. studies have shown that among adult transplant recipients White patients are “at highest risk for the ultraviolet-associated melanoma and squamous cell carcinoma, followed by Asian and Latino patients. African Americans have had the lowest risk, but some still developed skin cancer after transplant,” she said.
Prior studies of cancer in pediatric transplant recipients have reported primarily on internal malignant neoplasms, with limited data on KC, Dr. Sibbald and coauthors wrote. It is possible the incidence of KS is underestimated in the new study because of “undiagnosed or unreported KCs,” they noted.
The new study was funded by a grant from the Pediatric Dermatology Research Alliance and a Hospital for Sick Children grant. In disclosures, Dr. Sibbald reported to JAMA Dermatology receiving grants from the alliance and from Paediatric Consultants Partnership during the conduct of the study. Dr. Arron and Dr. Bibee both said they have no disclosures relevant to the study and its content.
A large study showing an increased risk of keratinocyte carcinoma (KC) in children who receive a solid-organ transplant highlights the need for early education about risk reduction and more research to determine optimal timing for screening, say an investigator and two dermatologists with expertise in transplant-related skin issues.
The increased incidence of KC in pediatric transplant recipients is “really high, so we definitely know there’s risk there,” just as there is for adult recipients of solid-organ transplants, said Cathryn Sibbald, MD, MSc, a dermatologist at the Hospital for Sick Children in Toronto and coauthor of a research letter published in June in JAMA Dermatology.
For their study, Dr. Sibbald and her coinvestigators turned to the Ontario Health Insurance plan database, which covers health care for Canadian citizens and qualified residents in the province. They identified 951 patients younger than the age of 18 who received a solid-organ transplant between 1991 and 2004 at an Ontario hospital
They then used a validated health insurance claims–based algorithm to identify diagnoses of KC for the transplant recipients and for more than 5 million age-matched controls. KC, including squamous and basal cell carcinoma, is the most prevalent skin cancer for people who have had a solid-organ transplant.
Fifteen posttransplant KCs (10 patients, 1.1%) were reported a mean of 13.1 years after transplant, with none reported in the first 4 years. The mean age at transplant was 7.8 years, and the mean age at KC diagnosis was 25.2 years. Kidney transplants were the most common (42.1% of transplantations). Most of the transplants recipients (eight patients) who developed KC had kidney transplantation, and most of them had functional graft at the time of KC diagnosis.
Researchers found an increased incidence of KC compared with that of the general population (standardized incidence ratio, 9.09; 95% confidence interval, 5.48-15.08). And the risk for KC increased with time since transplant, with adjusted hazard ratios for KC of 3.63 (95% CI, 0.51-25.77) for 1-5 years, 5.14 (95% CI, 1.28-20.55) for 5-10 years, and 4.80 (95% CI, 2.29-10.08) for 10 years or more, compared with the control population.
Several years ago, another research team performed a similar population-based cohort study of adult transplant recipients in Ontario and found a 6.6-times increased risk of KC in transplant recipients compared with the general population.
Sun protection and skin cancer screening
In commenting on the study, Sarah Arron, MD, PhD, a San Francisco Bay area dermatologist and immediate past president of the International Immunosuppression and Transplant Skin Cancer Collaborative (www.itscc.org), said she feels “reassured” that young transplant patients tend not to develop the skin cancer until young adulthood.
A ”large study like this is important because the overall rate of KC is low in this age group,” she noted.
The findings “suggest that we can focus our efforts on prevention during childhood, with sun protection and skin cancer education,” she said. “Then, as these children move into adulthood, we can begin screening with skin examinations. Of course, [any child] with a skin lesion or mole that concerns their parents or transplant team should be referred to dermatology for evaluation.”
Pediatric transplant recipients and their parents are most interested in learning about skin cancer prevention either before or immediately after transplantation, according to a survey by other researchers.
Intervention studies needed
The increased risk of KC probably stems largely from immunosuppression, said Dr. Sibbald in an interview. “We know [this is the case] in the older population, and it’s likely true in the younger population as well that it’s one of the primary drivers,” she said.
More research to extensively analyze risk factors should come next, she said. This includes “the granularity of what [immunosuppressants and other] medications are received, and at what dose and for what periods of time, so we can calculate cumulative exposure and its relation to risk,” she said.
Kristin Bibee, MD, PhD, assistant professor of dermatology at Johns Hopkins University in Baltimore, said she’d like to see further studies “evaluate appropriate interventions, like sun-protective behavior in childhood and adolescence or immunosuppression modulation, to prevent malignancy development.”
The optimal time and intensity of screening for young transplant recipients must still be determined, both Dr. Bibee and Dr. Arron said. Patients deemed through further research to be at higher risk may need earlier and/or more intensive surveillance.
The role of race in skin cancer risk in this population is “one question the study leaves open,” said Dr. Arron. U.S. studies have shown that among adult transplant recipients White patients are “at highest risk for the ultraviolet-associated melanoma and squamous cell carcinoma, followed by Asian and Latino patients. African Americans have had the lowest risk, but some still developed skin cancer after transplant,” she said.
Prior studies of cancer in pediatric transplant recipients have reported primarily on internal malignant neoplasms, with limited data on KC, Dr. Sibbald and coauthors wrote. It is possible the incidence of KS is underestimated in the new study because of “undiagnosed or unreported KCs,” they noted.
The new study was funded by a grant from the Pediatric Dermatology Research Alliance and a Hospital for Sick Children grant. In disclosures, Dr. Sibbald reported to JAMA Dermatology receiving grants from the alliance and from Paediatric Consultants Partnership during the conduct of the study. Dr. Arron and Dr. Bibee both said they have no disclosures relevant to the study and its content.
A large study showing an increased risk of keratinocyte carcinoma (KC) in children who receive a solid-organ transplant highlights the need for early education about risk reduction and more research to determine optimal timing for screening, say an investigator and two dermatologists with expertise in transplant-related skin issues.
The increased incidence of KC in pediatric transplant recipients is “really high, so we definitely know there’s risk there,” just as there is for adult recipients of solid-organ transplants, said Cathryn Sibbald, MD, MSc, a dermatologist at the Hospital for Sick Children in Toronto and coauthor of a research letter published in June in JAMA Dermatology.
For their study, Dr. Sibbald and her coinvestigators turned to the Ontario Health Insurance plan database, which covers health care for Canadian citizens and qualified residents in the province. They identified 951 patients younger than the age of 18 who received a solid-organ transplant between 1991 and 2004 at an Ontario hospital
They then used a validated health insurance claims–based algorithm to identify diagnoses of KC for the transplant recipients and for more than 5 million age-matched controls. KC, including squamous and basal cell carcinoma, is the most prevalent skin cancer for people who have had a solid-organ transplant.
Fifteen posttransplant KCs (10 patients, 1.1%) were reported a mean of 13.1 years after transplant, with none reported in the first 4 years. The mean age at transplant was 7.8 years, and the mean age at KC diagnosis was 25.2 years. Kidney transplants were the most common (42.1% of transplantations). Most of the transplants recipients (eight patients) who developed KC had kidney transplantation, and most of them had functional graft at the time of KC diagnosis.
Researchers found an increased incidence of KC compared with that of the general population (standardized incidence ratio, 9.09; 95% confidence interval, 5.48-15.08). And the risk for KC increased with time since transplant, with adjusted hazard ratios for KC of 3.63 (95% CI, 0.51-25.77) for 1-5 years, 5.14 (95% CI, 1.28-20.55) for 5-10 years, and 4.80 (95% CI, 2.29-10.08) for 10 years or more, compared with the control population.
Several years ago, another research team performed a similar population-based cohort study of adult transplant recipients in Ontario and found a 6.6-times increased risk of KC in transplant recipients compared with the general population.
Sun protection and skin cancer screening
In commenting on the study, Sarah Arron, MD, PhD, a San Francisco Bay area dermatologist and immediate past president of the International Immunosuppression and Transplant Skin Cancer Collaborative (www.itscc.org), said she feels “reassured” that young transplant patients tend not to develop the skin cancer until young adulthood.
A ”large study like this is important because the overall rate of KC is low in this age group,” she noted.
The findings “suggest that we can focus our efforts on prevention during childhood, with sun protection and skin cancer education,” she said. “Then, as these children move into adulthood, we can begin screening with skin examinations. Of course, [any child] with a skin lesion or mole that concerns their parents or transplant team should be referred to dermatology for evaluation.”
Pediatric transplant recipients and their parents are most interested in learning about skin cancer prevention either before or immediately after transplantation, according to a survey by other researchers.
Intervention studies needed
The increased risk of KC probably stems largely from immunosuppression, said Dr. Sibbald in an interview. “We know [this is the case] in the older population, and it’s likely true in the younger population as well that it’s one of the primary drivers,” she said.
More research to extensively analyze risk factors should come next, she said. This includes “the granularity of what [immunosuppressants and other] medications are received, and at what dose and for what periods of time, so we can calculate cumulative exposure and its relation to risk,” she said.
Kristin Bibee, MD, PhD, assistant professor of dermatology at Johns Hopkins University in Baltimore, said she’d like to see further studies “evaluate appropriate interventions, like sun-protective behavior in childhood and adolescence or immunosuppression modulation, to prevent malignancy development.”
The optimal time and intensity of screening for young transplant recipients must still be determined, both Dr. Bibee and Dr. Arron said. Patients deemed through further research to be at higher risk may need earlier and/or more intensive surveillance.
The role of race in skin cancer risk in this population is “one question the study leaves open,” said Dr. Arron. U.S. studies have shown that among adult transplant recipients White patients are “at highest risk for the ultraviolet-associated melanoma and squamous cell carcinoma, followed by Asian and Latino patients. African Americans have had the lowest risk, but some still developed skin cancer after transplant,” she said.
Prior studies of cancer in pediatric transplant recipients have reported primarily on internal malignant neoplasms, with limited data on KC, Dr. Sibbald and coauthors wrote. It is possible the incidence of KS is underestimated in the new study because of “undiagnosed or unreported KCs,” they noted.
The new study was funded by a grant from the Pediatric Dermatology Research Alliance and a Hospital for Sick Children grant. In disclosures, Dr. Sibbald reported to JAMA Dermatology receiving grants from the alliance and from Paediatric Consultants Partnership during the conduct of the study. Dr. Arron and Dr. Bibee both said they have no disclosures relevant to the study and its content.
FROM JAMA DERMATOLOGY
Children and COVID: Vaccination off to slow start for the newly eligible
New cases of COVID-19 continue to drop among children, but the vaccination effort in those under age 5 years began with something less than a bang.
In the first 2 days after their respective approvals, almost 99,000 children aged 5-11 years and over 675,000 children aged 12-15 were vaccinated, according to data from the Centers for Disease Control and Prevention. Children aged 0-4 years represent almost 6% of the overall population, compared with 8.7% for the 5- to 11-year-olds and 5.1% for those aged 12-15.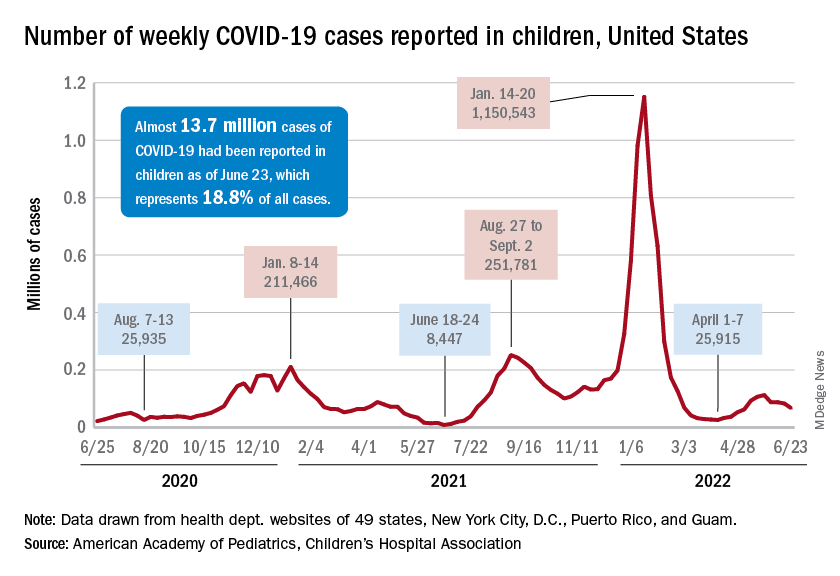
The recent decline in new cases over the past 4 weeks and the substantial decline since the Omicron surge could be a factor in the lack of response, but it is worth noting that the almost 68,000 new child cases reported in the past week, June 17-23, are “far higher than 1 year ago, June 24, 2021, when 8,400 child cases were reported,” the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID report.
That total for June 17-23 was 19% lower than the previous week and down by 40% since new cases hit a spring peak of 112,000 in late May. Regionally, new cases were down in the Midwest, the South, and the West, the AAP/CHA report showed, but the Northeast saw a small increase, which could be a signal of things to come for the summer.
The decline in new cases, however, has not been accompanied by decreases in hospitalizations or emergency department visits. New admissions of children aged 0-17 with confirmed COVID were at 0.31 per 100,000 population on June 24 after reaching that level on June 15, so no drop-off has occurred yet but there are signs of leveling off, based on CDC data.
The ED visit rates have been fairly steady through June, although COVID-related visits were up to 3.4% of all ED visits on June 22 for children aged 0-11 years, after being below 3% for the first 2 weeks of the month. The rate for children aged 12-15 has been between 1.6% and 1.9% for the past 3 weeks and the rate for 16- and 17-year-olds has been hovering between 1.7% and 2.2% for most of June, after going as high as 2.7% in late May, the CDC said on its COVID Data Tracker.
New cases of COVID-19 continue to drop among children, but the vaccination effort in those under age 5 years began with something less than a bang.
In the first 2 days after their respective approvals, almost 99,000 children aged 5-11 years and over 675,000 children aged 12-15 were vaccinated, according to data from the Centers for Disease Control and Prevention. Children aged 0-4 years represent almost 6% of the overall population, compared with 8.7% for the 5- to 11-year-olds and 5.1% for those aged 12-15.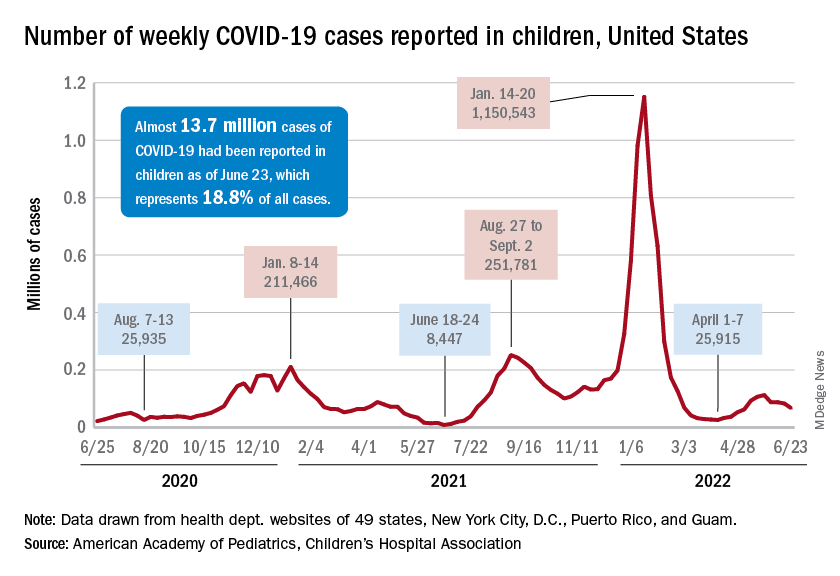
The recent decline in new cases over the past 4 weeks and the substantial decline since the Omicron surge could be a factor in the lack of response, but it is worth noting that the almost 68,000 new child cases reported in the past week, June 17-23, are “far higher than 1 year ago, June 24, 2021, when 8,400 child cases were reported,” the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID report.
That total for June 17-23 was 19% lower than the previous week and down by 40% since new cases hit a spring peak of 112,000 in late May. Regionally, new cases were down in the Midwest, the South, and the West, the AAP/CHA report showed, but the Northeast saw a small increase, which could be a signal of things to come for the summer.
The decline in new cases, however, has not been accompanied by decreases in hospitalizations or emergency department visits. New admissions of children aged 0-17 with confirmed COVID were at 0.31 per 100,000 population on June 24 after reaching that level on June 15, so no drop-off has occurred yet but there are signs of leveling off, based on CDC data.
The ED visit rates have been fairly steady through June, although COVID-related visits were up to 3.4% of all ED visits on June 22 for children aged 0-11 years, after being below 3% for the first 2 weeks of the month. The rate for children aged 12-15 has been between 1.6% and 1.9% for the past 3 weeks and the rate for 16- and 17-year-olds has been hovering between 1.7% and 2.2% for most of June, after going as high as 2.7% in late May, the CDC said on its COVID Data Tracker.
New cases of COVID-19 continue to drop among children, but the vaccination effort in those under age 5 years began with something less than a bang.
In the first 2 days after their respective approvals, almost 99,000 children aged 5-11 years and over 675,000 children aged 12-15 were vaccinated, according to data from the Centers for Disease Control and Prevention. Children aged 0-4 years represent almost 6% of the overall population, compared with 8.7% for the 5- to 11-year-olds and 5.1% for those aged 12-15.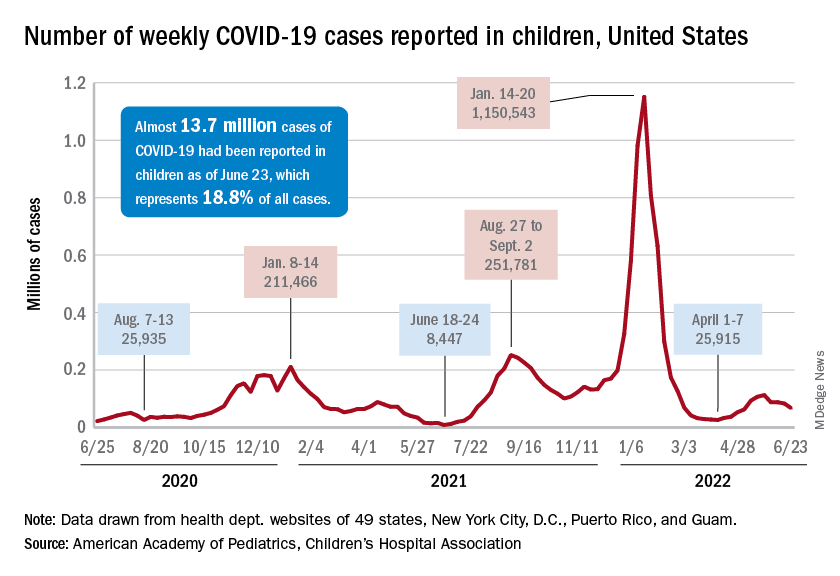
The recent decline in new cases over the past 4 weeks and the substantial decline since the Omicron surge could be a factor in the lack of response, but it is worth noting that the almost 68,000 new child cases reported in the past week, June 17-23, are “far higher than 1 year ago, June 24, 2021, when 8,400 child cases were reported,” the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID report.
That total for June 17-23 was 19% lower than the previous week and down by 40% since new cases hit a spring peak of 112,000 in late May. Regionally, new cases were down in the Midwest, the South, and the West, the AAP/CHA report showed, but the Northeast saw a small increase, which could be a signal of things to come for the summer.
The decline in new cases, however, has not been accompanied by decreases in hospitalizations or emergency department visits. New admissions of children aged 0-17 with confirmed COVID were at 0.31 per 100,000 population on June 24 after reaching that level on June 15, so no drop-off has occurred yet but there are signs of leveling off, based on CDC data.
The ED visit rates have been fairly steady through June, although COVID-related visits were up to 3.4% of all ED visits on June 22 for children aged 0-11 years, after being below 3% for the first 2 weeks of the month. The rate for children aged 12-15 has been between 1.6% and 1.9% for the past 3 weeks and the rate for 16- and 17-year-olds has been hovering between 1.7% and 2.2% for most of June, after going as high as 2.7% in late May, the CDC said on its COVID Data Tracker.
FDA approves Qsymia for treating teens with obesity
The indication is for use as additional therapy along with a reduced-calorie diet and increased physical activity in youth with obesity, defined as a body mass index of the 95th percentile or greater when standardized for age and sex.
Qsymia was first approved in July 2012 for chronic weight management in adults with an initial BMI of 30 kg/m2 or greater (obese) or 27 kg/m2 or greater (overweight) with one or more weight-related comorbidities, as an adjunct to lifestyle modification.
About 1 in 5 adolescents in the United States has obesity, according to the FDA.
The drug is the fourth to be approved for treating obesity in youth, along with liraglutide (Saxenda) and orlistat (Alli, Xenical), both approved down to age 12, and phentermine for those aged 16 and older.
The Qsymia approval was based on data from a phase 4 double-blind, placebo-controlled trial of 223 youth aged 12-16 with obesity who had not lost weight with lifestyle modifications. They were randomly assigned to Qsymia in doses of 7.5 mg phentermine/46 mg topiramate, 15 mg phentermine/92 mg topiramate, or placebo once daily, along with lifestyle counseling for all.
At 56 weeks, those taking the lower Qsymia dose lost an average of 4.8% of their BMI, and those on the higher dose lost 7.1%. In contrast, the placebo group gained about 3.3% of their BMI.
Because Qsymia increases the risk for oral clefts (lip and palate) in a fetus if taken during pregnancy, female patients should obtain negative pregnancy tests before starting the drug, take monthly pregnancy tests while on the drug, and use effective contraception throughout. Also because of the oral cleft risk, Qsymia is available only through an FDA program called a Risk Evaluation and Mitigation Strategy.
Additional potential adverse effects with Qsymia include increased heart rate and suicidal behavior/ideation. Patients should be advised to monitor for mood changes and discontinue the drug if depression or suicidal thoughts develop. The drug has also been linked to slowing of linear growth, so growth should be monitored in adolescents taking the drug, according to the FDA.
Qsymia is also associated with acute myopia, secondary angle closure glaucoma, visual problems, sleep disorders, cognitive impairment, metabolic acidosis, and decreased renal function.
The most common adverse reactions reported in the pediatric clinical trial included depression, dizziness, joint pain, fever, flu, and ankle sprain.
A version of this article first appeared on Medscape.com.
The indication is for use as additional therapy along with a reduced-calorie diet and increased physical activity in youth with obesity, defined as a body mass index of the 95th percentile or greater when standardized for age and sex.
Qsymia was first approved in July 2012 for chronic weight management in adults with an initial BMI of 30 kg/m2 or greater (obese) or 27 kg/m2 or greater (overweight) with one or more weight-related comorbidities, as an adjunct to lifestyle modification.
About 1 in 5 adolescents in the United States has obesity, according to the FDA.
The drug is the fourth to be approved for treating obesity in youth, along with liraglutide (Saxenda) and orlistat (Alli, Xenical), both approved down to age 12, and phentermine for those aged 16 and older.
The Qsymia approval was based on data from a phase 4 double-blind, placebo-controlled trial of 223 youth aged 12-16 with obesity who had not lost weight with lifestyle modifications. They were randomly assigned to Qsymia in doses of 7.5 mg phentermine/46 mg topiramate, 15 mg phentermine/92 mg topiramate, or placebo once daily, along with lifestyle counseling for all.
At 56 weeks, those taking the lower Qsymia dose lost an average of 4.8% of their BMI, and those on the higher dose lost 7.1%. In contrast, the placebo group gained about 3.3% of their BMI.
Because Qsymia increases the risk for oral clefts (lip and palate) in a fetus if taken during pregnancy, female patients should obtain negative pregnancy tests before starting the drug, take monthly pregnancy tests while on the drug, and use effective contraception throughout. Also because of the oral cleft risk, Qsymia is available only through an FDA program called a Risk Evaluation and Mitigation Strategy.
Additional potential adverse effects with Qsymia include increased heart rate and suicidal behavior/ideation. Patients should be advised to monitor for mood changes and discontinue the drug if depression or suicidal thoughts develop. The drug has also been linked to slowing of linear growth, so growth should be monitored in adolescents taking the drug, according to the FDA.
Qsymia is also associated with acute myopia, secondary angle closure glaucoma, visual problems, sleep disorders, cognitive impairment, metabolic acidosis, and decreased renal function.
The most common adverse reactions reported in the pediatric clinical trial included depression, dizziness, joint pain, fever, flu, and ankle sprain.
A version of this article first appeared on Medscape.com.
The indication is for use as additional therapy along with a reduced-calorie diet and increased physical activity in youth with obesity, defined as a body mass index of the 95th percentile or greater when standardized for age and sex.
Qsymia was first approved in July 2012 for chronic weight management in adults with an initial BMI of 30 kg/m2 or greater (obese) or 27 kg/m2 or greater (overweight) with one or more weight-related comorbidities, as an adjunct to lifestyle modification.
About 1 in 5 adolescents in the United States has obesity, according to the FDA.
The drug is the fourth to be approved for treating obesity in youth, along with liraglutide (Saxenda) and orlistat (Alli, Xenical), both approved down to age 12, and phentermine for those aged 16 and older.
The Qsymia approval was based on data from a phase 4 double-blind, placebo-controlled trial of 223 youth aged 12-16 with obesity who had not lost weight with lifestyle modifications. They were randomly assigned to Qsymia in doses of 7.5 mg phentermine/46 mg topiramate, 15 mg phentermine/92 mg topiramate, or placebo once daily, along with lifestyle counseling for all.
At 56 weeks, those taking the lower Qsymia dose lost an average of 4.8% of their BMI, and those on the higher dose lost 7.1%. In contrast, the placebo group gained about 3.3% of their BMI.
Because Qsymia increases the risk for oral clefts (lip and palate) in a fetus if taken during pregnancy, female patients should obtain negative pregnancy tests before starting the drug, take monthly pregnancy tests while on the drug, and use effective contraception throughout. Also because of the oral cleft risk, Qsymia is available only through an FDA program called a Risk Evaluation and Mitigation Strategy.
Additional potential adverse effects with Qsymia include increased heart rate and suicidal behavior/ideation. Patients should be advised to monitor for mood changes and discontinue the drug if depression or suicidal thoughts develop. The drug has also been linked to slowing of linear growth, so growth should be monitored in adolescents taking the drug, according to the FDA.
Qsymia is also associated with acute myopia, secondary angle closure glaucoma, visual problems, sleep disorders, cognitive impairment, metabolic acidosis, and decreased renal function.
The most common adverse reactions reported in the pediatric clinical trial included depression, dizziness, joint pain, fever, flu, and ankle sprain.
A version of this article first appeared on Medscape.com.
Suicide risk rises for cyberbullying victims
Experiencing cyberbullying as a victim was a significant risk factor for suicidality in early adolescents aged 10-13 years, based on data from more than 10,000 individuals.
Adolescent suicidality, defined as suicidal ideation or suicide attempts, remains a major public health issue, Shay Arnon, MA, of Reichman University, Herzliya, Israel, and colleagues wrote.
Although cyberbullying experiences and perpetration have been associated with mental health issues, their roles as specific suicidality risk factors have not been explored, they said.
In a study published in JAMA Network Open, the researchers analyzed data on cyberbullying experiences collected between July 2018 and January 2021 as part of the Adolescent Brain Cognitive Development (ABCD) study, with a diverse population of young adolescents aged 10-13 years.
The study population included 10,414 participants; the mean age was 12 years, 47.6% were female.
Overall, 7.6% of the participants had reported suicidality during the study period. A total of 930 (8.9%) reported experiencing cyberbullying as victims, and 96 (0.9%) reported perpetrating cyberbullying; 66 (69%) of the perpetrators also experienced cyberbullying.
Experiencing cyberbullying was associated with a fourfold increased risk of suicidality (odds ratio, 4.2), that remained significant after controlling for factors including demographics and multiple environmental risk and protective factors, including negative life events, family conflict, parental monitoring, school environment, and racial/ethnic discrimination (OR, 2.5), and after controlling for internalizing and externalizing psychopathology (OR, 1.8).
Adolescents who were both target and perpetrator of offline peer aggression had an increased risk of suicidality (OR, 1.5 for both), and cyberbullying experiences also remained associated with suicidality when included with offline bullying as target and perpetrator (OR, 1.7).
The results contradict previous studies showing an increased risk of suicidality in cyberbullying perpetrators as well as victims, the researchers noted. Some possible reasons for this difference are the anonymity of many cyberbullying perpetrators, and the tendency of many adolescents on social media to make quick-turn comments without thinking of their actions as offensive to others.
The study findings were limited by several factors including the cross-sectional design, which prevented conclusions about causality, a low-resolution screening for cyberbullying experiences, and the effect of unmeasured confounding variables, the researchers noted. Other limitations include the collection of data before the COVID-19 pandemic, so the effects of the pandemic on peer online communication and cyberbullying could not be determined.
However, the results suggest that experiencing cyberbullying is significantly associated with suicidality in young adolescents independent of other peer aggression experiences. “Assessment of cyberbullying experiences among children and adolescents should be a component of the comprehensive suicide risk assessment,” they concluded.
Pandemic pushed existing cyberbullying problems
“Electronic media use has increased significantly in the early adolescent demographic, particularly during the COVID-19 pandemic,” Peter L. Loper Jr., MD, of the University of South Carolina, Columbia, said in an interview.
“In many cases, the majority of an adolescent’s peer-peer interactions are now occurring on electronic devices. This has dramatically increased the incidence and prevalence of cyberbullying, making this study very timely and relevant,” said Dr. Loper, who was not involved in the study.
“From an experiential, ethnographic standpoint working on a psychiatric acute crisis stabilization unit, we have consistently recognized cyberbullying as a common and frequent etiology of suicidal ideation or attempt in the adolescents admitted to our unit,” said Dr. Loper.
“Unfortunately, much of the peer-peer interactions vital to supporting healthy adolescent development are now occurring on electronic devices instead of real-time and in person,” said Dr. Loper. “This comes with great risk to our adolescents and makes them susceptible to multiple potential dangers, not the least of which is cyberbullying.
“The biggest challenge in mitigating the impact of cyberbullying is that most adolescences want to have access to electronic media,” he said. “Limiting adolescents’ access to electronic media, and monitoring adolescents’ electronic media use are vital steps to preventing cyberbullying. Apps such as ‘Bark’ can used by parents to monitor their adolescents’ electronic media activity to ensure their safety and well-being.”
Additional research is needed to focus on other areas in which electronic media use may be affecting adolescents’ social, emotional, and psychological well-being and development, “which will become more and more important as electronic media use in this demographic continues to increase,” Dr. Loper said.
The study was supported by the National Institute of Mental Health and the Lifespan Brain Institute of Children’s Hospital of Philadelphia and Penn Medicine, University of Pennsylvania. The researchers had no financial conflicts to disclose. Dr. Loper had no financial conflicts to disclose.
Experiencing cyberbullying as a victim was a significant risk factor for suicidality in early adolescents aged 10-13 years, based on data from more than 10,000 individuals.
Adolescent suicidality, defined as suicidal ideation or suicide attempts, remains a major public health issue, Shay Arnon, MA, of Reichman University, Herzliya, Israel, and colleagues wrote.
Although cyberbullying experiences and perpetration have been associated with mental health issues, their roles as specific suicidality risk factors have not been explored, they said.
In a study published in JAMA Network Open, the researchers analyzed data on cyberbullying experiences collected between July 2018 and January 2021 as part of the Adolescent Brain Cognitive Development (ABCD) study, with a diverse population of young adolescents aged 10-13 years.
The study population included 10,414 participants; the mean age was 12 years, 47.6% were female.
Overall, 7.6% of the participants had reported suicidality during the study period. A total of 930 (8.9%) reported experiencing cyberbullying as victims, and 96 (0.9%) reported perpetrating cyberbullying; 66 (69%) of the perpetrators also experienced cyberbullying.
Experiencing cyberbullying was associated with a fourfold increased risk of suicidality (odds ratio, 4.2), that remained significant after controlling for factors including demographics and multiple environmental risk and protective factors, including negative life events, family conflict, parental monitoring, school environment, and racial/ethnic discrimination (OR, 2.5), and after controlling for internalizing and externalizing psychopathology (OR, 1.8).
Adolescents who were both target and perpetrator of offline peer aggression had an increased risk of suicidality (OR, 1.5 for both), and cyberbullying experiences also remained associated with suicidality when included with offline bullying as target and perpetrator (OR, 1.7).
The results contradict previous studies showing an increased risk of suicidality in cyberbullying perpetrators as well as victims, the researchers noted. Some possible reasons for this difference are the anonymity of many cyberbullying perpetrators, and the tendency of many adolescents on social media to make quick-turn comments without thinking of their actions as offensive to others.
The study findings were limited by several factors including the cross-sectional design, which prevented conclusions about causality, a low-resolution screening for cyberbullying experiences, and the effect of unmeasured confounding variables, the researchers noted. Other limitations include the collection of data before the COVID-19 pandemic, so the effects of the pandemic on peer online communication and cyberbullying could not be determined.
However, the results suggest that experiencing cyberbullying is significantly associated with suicidality in young adolescents independent of other peer aggression experiences. “Assessment of cyberbullying experiences among children and adolescents should be a component of the comprehensive suicide risk assessment,” they concluded.
Pandemic pushed existing cyberbullying problems
“Electronic media use has increased significantly in the early adolescent demographic, particularly during the COVID-19 pandemic,” Peter L. Loper Jr., MD, of the University of South Carolina, Columbia, said in an interview.
“In many cases, the majority of an adolescent’s peer-peer interactions are now occurring on electronic devices. This has dramatically increased the incidence and prevalence of cyberbullying, making this study very timely and relevant,” said Dr. Loper, who was not involved in the study.
“From an experiential, ethnographic standpoint working on a psychiatric acute crisis stabilization unit, we have consistently recognized cyberbullying as a common and frequent etiology of suicidal ideation or attempt in the adolescents admitted to our unit,” said Dr. Loper.
“Unfortunately, much of the peer-peer interactions vital to supporting healthy adolescent development are now occurring on electronic devices instead of real-time and in person,” said Dr. Loper. “This comes with great risk to our adolescents and makes them susceptible to multiple potential dangers, not the least of which is cyberbullying.
“The biggest challenge in mitigating the impact of cyberbullying is that most adolescences want to have access to electronic media,” he said. “Limiting adolescents’ access to electronic media, and monitoring adolescents’ electronic media use are vital steps to preventing cyberbullying. Apps such as ‘Bark’ can used by parents to monitor their adolescents’ electronic media activity to ensure their safety and well-being.”
Additional research is needed to focus on other areas in which electronic media use may be affecting adolescents’ social, emotional, and psychological well-being and development, “which will become more and more important as electronic media use in this demographic continues to increase,” Dr. Loper said.
The study was supported by the National Institute of Mental Health and the Lifespan Brain Institute of Children’s Hospital of Philadelphia and Penn Medicine, University of Pennsylvania. The researchers had no financial conflicts to disclose. Dr. Loper had no financial conflicts to disclose.
Experiencing cyberbullying as a victim was a significant risk factor for suicidality in early adolescents aged 10-13 years, based on data from more than 10,000 individuals.
Adolescent suicidality, defined as suicidal ideation or suicide attempts, remains a major public health issue, Shay Arnon, MA, of Reichman University, Herzliya, Israel, and colleagues wrote.
Although cyberbullying experiences and perpetration have been associated with mental health issues, their roles as specific suicidality risk factors have not been explored, they said.
In a study published in JAMA Network Open, the researchers analyzed data on cyberbullying experiences collected between July 2018 and January 2021 as part of the Adolescent Brain Cognitive Development (ABCD) study, with a diverse population of young adolescents aged 10-13 years.
The study population included 10,414 participants; the mean age was 12 years, 47.6% were female.
Overall, 7.6% of the participants had reported suicidality during the study period. A total of 930 (8.9%) reported experiencing cyberbullying as victims, and 96 (0.9%) reported perpetrating cyberbullying; 66 (69%) of the perpetrators also experienced cyberbullying.
Experiencing cyberbullying was associated with a fourfold increased risk of suicidality (odds ratio, 4.2), that remained significant after controlling for factors including demographics and multiple environmental risk and protective factors, including negative life events, family conflict, parental monitoring, school environment, and racial/ethnic discrimination (OR, 2.5), and after controlling for internalizing and externalizing psychopathology (OR, 1.8).
Adolescents who were both target and perpetrator of offline peer aggression had an increased risk of suicidality (OR, 1.5 for both), and cyberbullying experiences also remained associated with suicidality when included with offline bullying as target and perpetrator (OR, 1.7).
The results contradict previous studies showing an increased risk of suicidality in cyberbullying perpetrators as well as victims, the researchers noted. Some possible reasons for this difference are the anonymity of many cyberbullying perpetrators, and the tendency of many adolescents on social media to make quick-turn comments without thinking of their actions as offensive to others.
The study findings were limited by several factors including the cross-sectional design, which prevented conclusions about causality, a low-resolution screening for cyberbullying experiences, and the effect of unmeasured confounding variables, the researchers noted. Other limitations include the collection of data before the COVID-19 pandemic, so the effects of the pandemic on peer online communication and cyberbullying could not be determined.
However, the results suggest that experiencing cyberbullying is significantly associated with suicidality in young adolescents independent of other peer aggression experiences. “Assessment of cyberbullying experiences among children and adolescents should be a component of the comprehensive suicide risk assessment,” they concluded.
Pandemic pushed existing cyberbullying problems
“Electronic media use has increased significantly in the early adolescent demographic, particularly during the COVID-19 pandemic,” Peter L. Loper Jr., MD, of the University of South Carolina, Columbia, said in an interview.
“In many cases, the majority of an adolescent’s peer-peer interactions are now occurring on electronic devices. This has dramatically increased the incidence and prevalence of cyberbullying, making this study very timely and relevant,” said Dr. Loper, who was not involved in the study.
“From an experiential, ethnographic standpoint working on a psychiatric acute crisis stabilization unit, we have consistently recognized cyberbullying as a common and frequent etiology of suicidal ideation or attempt in the adolescents admitted to our unit,” said Dr. Loper.
“Unfortunately, much of the peer-peer interactions vital to supporting healthy adolescent development are now occurring on electronic devices instead of real-time and in person,” said Dr. Loper. “This comes with great risk to our adolescents and makes them susceptible to multiple potential dangers, not the least of which is cyberbullying.
“The biggest challenge in mitigating the impact of cyberbullying is that most adolescences want to have access to electronic media,” he said. “Limiting adolescents’ access to electronic media, and monitoring adolescents’ electronic media use are vital steps to preventing cyberbullying. Apps such as ‘Bark’ can used by parents to monitor their adolescents’ electronic media activity to ensure their safety and well-being.”
Additional research is needed to focus on other areas in which electronic media use may be affecting adolescents’ social, emotional, and psychological well-being and development, “which will become more and more important as electronic media use in this demographic continues to increase,” Dr. Loper said.
The study was supported by the National Institute of Mental Health and the Lifespan Brain Institute of Children’s Hospital of Philadelphia and Penn Medicine, University of Pennsylvania. The researchers had no financial conflicts to disclose. Dr. Loper had no financial conflicts to disclose.
FROM JAMA NETWORK OPEN
Obesity linked to smaller testes and possible infertility
new data suggest.
Testicular volume is a fertility marker directly related to sperm count that has halved in the past 40 years worldwide for unknown reasons. At the same time, childhood obesity has risen dramatically and infertility appears to have risen as well, Rossella Cannarella, MD, of the department of endocrinology and andrology, University of Catania (Italy), said at the annual meeting of the Endocrine Society.
According to recent Italian studies, between 14% and 23% of young men aged 18-19 had testicular hypotrophy. “Worryingly, we don’t know the reason for this hypotrophy. And therefore, they are at risk for future infertility,” Dr. Cannarella said during a press briefing.
Her study, which included a total of 264 male children and adolescents, also linked lower testicular volume to hyperinsulinemia and insulin resistance. “The testis is not quiescent in childhood and is sensitive to the hormone insulin. Obesity and metabolic impairment actually can have an effect and negative impact on Sertoli cell proliferation,” Dr. Cannarella said.
Screen testicular volume at all visits
If other studies confirm these results, she said that pediatricians should begin routinely assessing testicular volume at all visits as is now done with height and weight to identify early deflection of the testicular growth curve.
In addition, “include male infertility as a possible consequence of obesity in counseling of male obese children,” she advised.
Asked to comment, Amin Sedaghat Herati, MD, director of male infertility and men’s health at Johns Hopkins Hospital, and assistant professor of urology at Johns Hopkins Medicine, both in Baltimore, said in an interview: “I think what’s really interesting about this study is the association that they’ve made between testicular volume and obesity.”
But, he noted, “it does not implicate necessarily the development of infertility. It’s an extrapolation. So it’s a step towards the link between obesity and infertility, and it’s an important study to establish the association, but changes in testicular volume and even changes in semen panel don’t necessarily indicate fertility or infertility.”
The findings are “consistent with what we know as far as what obesity can potentially do to the activity of the cells in the testes. The authors are postulating that it’s more the support cells, called Sertoli cells, but I would say it’s probably all of the cells that are being affected by obesity and specifically elevated leptin levels,” Dr. Herati said.
He agrees with the recommendation that pediatricians screen all boys for testicular volume. “I agree it’s a good idea so they don’t miss any cases in which the testes don’t develop the way they should or any other conditions,” Dr. Herati said. “I think in general it’s a good practice, especially in the peripubertal stage, to make sure that kids are on the same growth curve and that they’re meeting their Tanner staging. [Pediatricians] should be looking at the size of the testes and tracking, maybe not at every visit, but at least on an annual basis.”
And, he noted, “I think any study that establishes a link that we can point to when we’re educating patients and parents is important.”
Links found between overweight/obesity, testicular hypotrophy
The study population included 61 male children and adolescents with normal weight, 53 with overweight, and 150 with obesity. Insulin resistance (Homeostatic Model Assessment for Insulin Resistance index ≥ 2.5) was present in 97 participants, 22 had prediabetes, and 3 had type 2 diabetes. Clinical data were collected retrospectively.
Among the boys aged 9-14 years, those with overweight and obesity had significantly lower testicular volume, compared with those of normal weight.
Those who were in Tanner Stage 1 were more likely to have overweight and obesity than those with normal weight, suggesting that “overweight and obese adolescents start puberty later than those of normal weight,” Dr. Cannarella said.
In the 14- to 16-year-old age group, those with insulin resistance had lower testicular volume, compared with those without insulin resistance (HOMA index < 2.5). The number of insulin-resistant adolescents was greater than that of controls in the Tanner stage 2 group.
In both the prepubertal (< 9 years) and pubertal (14-16 years) groups, hyperinsulinemia was associated with lower levels of testicular volume.
Hyperinsulinemia did not influence the timing of puberty onset.
No way to quantify the effect of obesity on fertility just yet
During a press briefing, Dr. Cannarella commented that obesity is likely just one of several factors influencing what appears to be an increase in male infertility over time. “It isn’t of course the only reason, but many factors in our environment have drastically changed, compared to 40 years ago, including the prevalence of heavy metals and endocrine disruptors, and of course, the change in habits and higher prevalence of metabolic disease. All of this has an impact on the proliferation of Sertoli cells in childhood and this may explain the trend toward the decline of sperm concentration and count.”
Longitudinal data are needed to establish cause and effect, she noted. “We need longitudinal studies that link the degrees of testicular volume with the degree of the sperm concentration and count starting from childhood and ending with the adult age. This is the missing link so far.”
Dr. Cannarella has reported no relevant financial relationships. Dr. Herati has reported being an advisor for Dadi, LiNA Medical, and Teleflex.
A version of this article first appeared on Medscape.com.
new data suggest.
Testicular volume is a fertility marker directly related to sperm count that has halved in the past 40 years worldwide for unknown reasons. At the same time, childhood obesity has risen dramatically and infertility appears to have risen as well, Rossella Cannarella, MD, of the department of endocrinology and andrology, University of Catania (Italy), said at the annual meeting of the Endocrine Society.
According to recent Italian studies, between 14% and 23% of young men aged 18-19 had testicular hypotrophy. “Worryingly, we don’t know the reason for this hypotrophy. And therefore, they are at risk for future infertility,” Dr. Cannarella said during a press briefing.
Her study, which included a total of 264 male children and adolescents, also linked lower testicular volume to hyperinsulinemia and insulin resistance. “The testis is not quiescent in childhood and is sensitive to the hormone insulin. Obesity and metabolic impairment actually can have an effect and negative impact on Sertoli cell proliferation,” Dr. Cannarella said.
Screen testicular volume at all visits
If other studies confirm these results, she said that pediatricians should begin routinely assessing testicular volume at all visits as is now done with height and weight to identify early deflection of the testicular growth curve.
In addition, “include male infertility as a possible consequence of obesity in counseling of male obese children,” she advised.
Asked to comment, Amin Sedaghat Herati, MD, director of male infertility and men’s health at Johns Hopkins Hospital, and assistant professor of urology at Johns Hopkins Medicine, both in Baltimore, said in an interview: “I think what’s really interesting about this study is the association that they’ve made between testicular volume and obesity.”
But, he noted, “it does not implicate necessarily the development of infertility. It’s an extrapolation. So it’s a step towards the link between obesity and infertility, and it’s an important study to establish the association, but changes in testicular volume and even changes in semen panel don’t necessarily indicate fertility or infertility.”
The findings are “consistent with what we know as far as what obesity can potentially do to the activity of the cells in the testes. The authors are postulating that it’s more the support cells, called Sertoli cells, but I would say it’s probably all of the cells that are being affected by obesity and specifically elevated leptin levels,” Dr. Herati said.
He agrees with the recommendation that pediatricians screen all boys for testicular volume. “I agree it’s a good idea so they don’t miss any cases in which the testes don’t develop the way they should or any other conditions,” Dr. Herati said. “I think in general it’s a good practice, especially in the peripubertal stage, to make sure that kids are on the same growth curve and that they’re meeting their Tanner staging. [Pediatricians] should be looking at the size of the testes and tracking, maybe not at every visit, but at least on an annual basis.”
And, he noted, “I think any study that establishes a link that we can point to when we’re educating patients and parents is important.”
Links found between overweight/obesity, testicular hypotrophy
The study population included 61 male children and adolescents with normal weight, 53 with overweight, and 150 with obesity. Insulin resistance (Homeostatic Model Assessment for Insulin Resistance index ≥ 2.5) was present in 97 participants, 22 had prediabetes, and 3 had type 2 diabetes. Clinical data were collected retrospectively.
Among the boys aged 9-14 years, those with overweight and obesity had significantly lower testicular volume, compared with those of normal weight.
Those who were in Tanner Stage 1 were more likely to have overweight and obesity than those with normal weight, suggesting that “overweight and obese adolescents start puberty later than those of normal weight,” Dr. Cannarella said.
In the 14- to 16-year-old age group, those with insulin resistance had lower testicular volume, compared with those without insulin resistance (HOMA index < 2.5). The number of insulin-resistant adolescents was greater than that of controls in the Tanner stage 2 group.
In both the prepubertal (< 9 years) and pubertal (14-16 years) groups, hyperinsulinemia was associated with lower levels of testicular volume.
Hyperinsulinemia did not influence the timing of puberty onset.
No way to quantify the effect of obesity on fertility just yet
During a press briefing, Dr. Cannarella commented that obesity is likely just one of several factors influencing what appears to be an increase in male infertility over time. “It isn’t of course the only reason, but many factors in our environment have drastically changed, compared to 40 years ago, including the prevalence of heavy metals and endocrine disruptors, and of course, the change in habits and higher prevalence of metabolic disease. All of this has an impact on the proliferation of Sertoli cells in childhood and this may explain the trend toward the decline of sperm concentration and count.”
Longitudinal data are needed to establish cause and effect, she noted. “We need longitudinal studies that link the degrees of testicular volume with the degree of the sperm concentration and count starting from childhood and ending with the adult age. This is the missing link so far.”
Dr. Cannarella has reported no relevant financial relationships. Dr. Herati has reported being an advisor for Dadi, LiNA Medical, and Teleflex.
A version of this article first appeared on Medscape.com.
new data suggest.
Testicular volume is a fertility marker directly related to sperm count that has halved in the past 40 years worldwide for unknown reasons. At the same time, childhood obesity has risen dramatically and infertility appears to have risen as well, Rossella Cannarella, MD, of the department of endocrinology and andrology, University of Catania (Italy), said at the annual meeting of the Endocrine Society.
According to recent Italian studies, between 14% and 23% of young men aged 18-19 had testicular hypotrophy. “Worryingly, we don’t know the reason for this hypotrophy. And therefore, they are at risk for future infertility,” Dr. Cannarella said during a press briefing.
Her study, which included a total of 264 male children and adolescents, also linked lower testicular volume to hyperinsulinemia and insulin resistance. “The testis is not quiescent in childhood and is sensitive to the hormone insulin. Obesity and metabolic impairment actually can have an effect and negative impact on Sertoli cell proliferation,” Dr. Cannarella said.
Screen testicular volume at all visits
If other studies confirm these results, she said that pediatricians should begin routinely assessing testicular volume at all visits as is now done with height and weight to identify early deflection of the testicular growth curve.
In addition, “include male infertility as a possible consequence of obesity in counseling of male obese children,” she advised.
Asked to comment, Amin Sedaghat Herati, MD, director of male infertility and men’s health at Johns Hopkins Hospital, and assistant professor of urology at Johns Hopkins Medicine, both in Baltimore, said in an interview: “I think what’s really interesting about this study is the association that they’ve made between testicular volume and obesity.”
But, he noted, “it does not implicate necessarily the development of infertility. It’s an extrapolation. So it’s a step towards the link between obesity and infertility, and it’s an important study to establish the association, but changes in testicular volume and even changes in semen panel don’t necessarily indicate fertility or infertility.”
The findings are “consistent with what we know as far as what obesity can potentially do to the activity of the cells in the testes. The authors are postulating that it’s more the support cells, called Sertoli cells, but I would say it’s probably all of the cells that are being affected by obesity and specifically elevated leptin levels,” Dr. Herati said.
He agrees with the recommendation that pediatricians screen all boys for testicular volume. “I agree it’s a good idea so they don’t miss any cases in which the testes don’t develop the way they should or any other conditions,” Dr. Herati said. “I think in general it’s a good practice, especially in the peripubertal stage, to make sure that kids are on the same growth curve and that they’re meeting their Tanner staging. [Pediatricians] should be looking at the size of the testes and tracking, maybe not at every visit, but at least on an annual basis.”
And, he noted, “I think any study that establishes a link that we can point to when we’re educating patients and parents is important.”
Links found between overweight/obesity, testicular hypotrophy
The study population included 61 male children and adolescents with normal weight, 53 with overweight, and 150 with obesity. Insulin resistance (Homeostatic Model Assessment for Insulin Resistance index ≥ 2.5) was present in 97 participants, 22 had prediabetes, and 3 had type 2 diabetes. Clinical data were collected retrospectively.
Among the boys aged 9-14 years, those with overweight and obesity had significantly lower testicular volume, compared with those of normal weight.
Those who were in Tanner Stage 1 were more likely to have overweight and obesity than those with normal weight, suggesting that “overweight and obese adolescents start puberty later than those of normal weight,” Dr. Cannarella said.
In the 14- to 16-year-old age group, those with insulin resistance had lower testicular volume, compared with those without insulin resistance (HOMA index < 2.5). The number of insulin-resistant adolescents was greater than that of controls in the Tanner stage 2 group.
In both the prepubertal (< 9 years) and pubertal (14-16 years) groups, hyperinsulinemia was associated with lower levels of testicular volume.
Hyperinsulinemia did not influence the timing of puberty onset.
No way to quantify the effect of obesity on fertility just yet
During a press briefing, Dr. Cannarella commented that obesity is likely just one of several factors influencing what appears to be an increase in male infertility over time. “It isn’t of course the only reason, but many factors in our environment have drastically changed, compared to 40 years ago, including the prevalence of heavy metals and endocrine disruptors, and of course, the change in habits and higher prevalence of metabolic disease. All of this has an impact on the proliferation of Sertoli cells in childhood and this may explain the trend toward the decline of sperm concentration and count.”
Longitudinal data are needed to establish cause and effect, she noted. “We need longitudinal studies that link the degrees of testicular volume with the degree of the sperm concentration and count starting from childhood and ending with the adult age. This is the missing link so far.”
Dr. Cannarella has reported no relevant financial relationships. Dr. Herati has reported being an advisor for Dadi, LiNA Medical, and Teleflex.
A version of this article first appeared on Medscape.com.
FROM ENDO 2022
Jury out on low-FODMAP diet for kids
There is scarce evidence to support the use of a FODMAP-lowering diet for children with irritable bowel syndrome (IBS), and there is no evidence to recommend its use for other gastrointestinal (GI) diseases and complaints in children, according to a position paper from the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN).
A low-FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) diet is increasingly being used to treat children with various GI complaints and disorders.
“Awareness of how and when to use the diet is crucial, as a restrictive diet may impact nutritional adequacy and/or promote distorted eating in vulnerable subjects,” the authors note.
Rut Anne Thomassen, department of pediatric medicine, Oslo University Hospital, and an international team of experts conducted a systematic literature review of the evidence on the safety and efficacy of the low-FODMAP diet in children.
The low-FODMAP diet has not been well studied in children, they report.
From 53 publications and registers that they screened, only seven studies (four randomized clinical trials and three interventions without control group or observational studies) were included in their assessment.
In the seven studies, only 111 children received the low-FODMAP diet, while 85 followed a control diet for comparison (a diet described as healthy, usual, or typical American diet for children).
All of the pediatric studies focused on functional abdominal pain disorders. None addressed nonceliac gluten sensitivity, small-intestinal bacterial overgrowth, or inflammatory bowel disease.
From their review, the authors conclude that, at present, there is “insufficient evidence” to routinely recommend the low-FODMAP diet for the treatment of functional GI disorders, nonceliac gluten sensitivity, inflammatory bowel diseases, or small-intestinal bacterial overgrowth in children.
When the low-FODMAP diet is considered for children, the authors recommend a thorough clinical history, physical examination, and assessment of nutritional status and GI symptoms by a multidisciplinary team.
“Ideally, a standardized questionnaire should be used before and following the start of the diet to assess objectively the effect of the low-FODMAP diet,” the authors advise.
A dietitian should assess the child’s diet to highlight any potential deficiencies, which could be exacerbated by the restrictions of the low-FODMAP diet.
To promote adherence to the diet, potential difficulties, such as how to provide a suitable lunch at school or what to do when the child is staying at a friend’s house, should be addressed.
The authors suggest providing parents with written information about sources of FODMAPs and suitable replacement foods. Offering meal plans can reduce the risk of diet mistakes as well as the risk of offering a diet insufficient in essential nutrients, they say.
‘Useful paper’
“This is a useful paper primarily to outline the paucity of data regarding dietary therapies in children and the importance of doing studies in this population,” Ashwin Ananthakrishnan, MD, MPH, a gastroenterologist with Massachusetts General Hospital and Harvard Medical School, both in Boston, who wasn’t involved in the research, told this news organization.
Samuel Nurko, MD, MPH, director of the Center for Motility and Functional Gastrointestinal Disorders at Boston Children’s Hospital, Massachusetts, noted that some studies have shown that a low-FODMAP diet can be effective in controlling symptoms for both adults and kids.
“The problem in kids is that the trials are very small, and there’s not a lot of them, so the evidence is limited,” said Dr. Nurko, who wasn’t involved in writing the position paper.
That’s not to say that it should not be tried in appropriate cases. “There’s no question that in some patients, taking away the FODMAPs gives them a big improvement in GI symptoms,” Dr. Nurko told this news organization.
“The problem with the low-FODMAP diet is, if you don’t do it right, then you get into trouble with nutritional deficiencies,” he cautioned.
“If you are going to try the low-FODMAP diet, it has to be short, no more than 4-6 weeks, and you need to do a top-down approach. Take FODMAPs out, and then start to reintroduce them. Either kids will respond to the diet, or they won’t. If they don’t, there is no reason to keep them on the diet. It’s a very hard diet to take,” Dr. Nurko said.
No source of funding for the study was disclosed. The authors, Dr. Ananthakrishnan, and Dr. Nurko have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
There is scarce evidence to support the use of a FODMAP-lowering diet for children with irritable bowel syndrome (IBS), and there is no evidence to recommend its use for other gastrointestinal (GI) diseases and complaints in children, according to a position paper from the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN).
A low-FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) diet is increasingly being used to treat children with various GI complaints and disorders.
“Awareness of how and when to use the diet is crucial, as a restrictive diet may impact nutritional adequacy and/or promote distorted eating in vulnerable subjects,” the authors note.
Rut Anne Thomassen, department of pediatric medicine, Oslo University Hospital, and an international team of experts conducted a systematic literature review of the evidence on the safety and efficacy of the low-FODMAP diet in children.
The low-FODMAP diet has not been well studied in children, they report.
From 53 publications and registers that they screened, only seven studies (four randomized clinical trials and three interventions without control group or observational studies) were included in their assessment.
In the seven studies, only 111 children received the low-FODMAP diet, while 85 followed a control diet for comparison (a diet described as healthy, usual, or typical American diet for children).
All of the pediatric studies focused on functional abdominal pain disorders. None addressed nonceliac gluten sensitivity, small-intestinal bacterial overgrowth, or inflammatory bowel disease.
From their review, the authors conclude that, at present, there is “insufficient evidence” to routinely recommend the low-FODMAP diet for the treatment of functional GI disorders, nonceliac gluten sensitivity, inflammatory bowel diseases, or small-intestinal bacterial overgrowth in children.
When the low-FODMAP diet is considered for children, the authors recommend a thorough clinical history, physical examination, and assessment of nutritional status and GI symptoms by a multidisciplinary team.
“Ideally, a standardized questionnaire should be used before and following the start of the diet to assess objectively the effect of the low-FODMAP diet,” the authors advise.
A dietitian should assess the child’s diet to highlight any potential deficiencies, which could be exacerbated by the restrictions of the low-FODMAP diet.
To promote adherence to the diet, potential difficulties, such as how to provide a suitable lunch at school or what to do when the child is staying at a friend’s house, should be addressed.
The authors suggest providing parents with written information about sources of FODMAPs and suitable replacement foods. Offering meal plans can reduce the risk of diet mistakes as well as the risk of offering a diet insufficient in essential nutrients, they say.
‘Useful paper’
“This is a useful paper primarily to outline the paucity of data regarding dietary therapies in children and the importance of doing studies in this population,” Ashwin Ananthakrishnan, MD, MPH, a gastroenterologist with Massachusetts General Hospital and Harvard Medical School, both in Boston, who wasn’t involved in the research, told this news organization.
Samuel Nurko, MD, MPH, director of the Center for Motility and Functional Gastrointestinal Disorders at Boston Children’s Hospital, Massachusetts, noted that some studies have shown that a low-FODMAP diet can be effective in controlling symptoms for both adults and kids.
“The problem in kids is that the trials are very small, and there’s not a lot of them, so the evidence is limited,” said Dr. Nurko, who wasn’t involved in writing the position paper.
That’s not to say that it should not be tried in appropriate cases. “There’s no question that in some patients, taking away the FODMAPs gives them a big improvement in GI symptoms,” Dr. Nurko told this news organization.
“The problem with the low-FODMAP diet is, if you don’t do it right, then you get into trouble with nutritional deficiencies,” he cautioned.
“If you are going to try the low-FODMAP diet, it has to be short, no more than 4-6 weeks, and you need to do a top-down approach. Take FODMAPs out, and then start to reintroduce them. Either kids will respond to the diet, or they won’t. If they don’t, there is no reason to keep them on the diet. It’s a very hard diet to take,” Dr. Nurko said.
No source of funding for the study was disclosed. The authors, Dr. Ananthakrishnan, and Dr. Nurko have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
There is scarce evidence to support the use of a FODMAP-lowering diet for children with irritable bowel syndrome (IBS), and there is no evidence to recommend its use for other gastrointestinal (GI) diseases and complaints in children, according to a position paper from the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN).
A low-FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) diet is increasingly being used to treat children with various GI complaints and disorders.
“Awareness of how and when to use the diet is crucial, as a restrictive diet may impact nutritional adequacy and/or promote distorted eating in vulnerable subjects,” the authors note.
Rut Anne Thomassen, department of pediatric medicine, Oslo University Hospital, and an international team of experts conducted a systematic literature review of the evidence on the safety and efficacy of the low-FODMAP diet in children.
The low-FODMAP diet has not been well studied in children, they report.
From 53 publications and registers that they screened, only seven studies (four randomized clinical trials and three interventions without control group or observational studies) were included in their assessment.
In the seven studies, only 111 children received the low-FODMAP diet, while 85 followed a control diet for comparison (a diet described as healthy, usual, or typical American diet for children).
All of the pediatric studies focused on functional abdominal pain disorders. None addressed nonceliac gluten sensitivity, small-intestinal bacterial overgrowth, or inflammatory bowel disease.
From their review, the authors conclude that, at present, there is “insufficient evidence” to routinely recommend the low-FODMAP diet for the treatment of functional GI disorders, nonceliac gluten sensitivity, inflammatory bowel diseases, or small-intestinal bacterial overgrowth in children.
When the low-FODMAP diet is considered for children, the authors recommend a thorough clinical history, physical examination, and assessment of nutritional status and GI symptoms by a multidisciplinary team.
“Ideally, a standardized questionnaire should be used before and following the start of the diet to assess objectively the effect of the low-FODMAP diet,” the authors advise.
A dietitian should assess the child’s diet to highlight any potential deficiencies, which could be exacerbated by the restrictions of the low-FODMAP diet.
To promote adherence to the diet, potential difficulties, such as how to provide a suitable lunch at school or what to do when the child is staying at a friend’s house, should be addressed.
The authors suggest providing parents with written information about sources of FODMAPs and suitable replacement foods. Offering meal plans can reduce the risk of diet mistakes as well as the risk of offering a diet insufficient in essential nutrients, they say.
‘Useful paper’
“This is a useful paper primarily to outline the paucity of data regarding dietary therapies in children and the importance of doing studies in this population,” Ashwin Ananthakrishnan, MD, MPH, a gastroenterologist with Massachusetts General Hospital and Harvard Medical School, both in Boston, who wasn’t involved in the research, told this news organization.
Samuel Nurko, MD, MPH, director of the Center for Motility and Functional Gastrointestinal Disorders at Boston Children’s Hospital, Massachusetts, noted that some studies have shown that a low-FODMAP diet can be effective in controlling symptoms for both adults and kids.
“The problem in kids is that the trials are very small, and there’s not a lot of them, so the evidence is limited,” said Dr. Nurko, who wasn’t involved in writing the position paper.
That’s not to say that it should not be tried in appropriate cases. “There’s no question that in some patients, taking away the FODMAPs gives them a big improvement in GI symptoms,” Dr. Nurko told this news organization.
“The problem with the low-FODMAP diet is, if you don’t do it right, then you get into trouble with nutritional deficiencies,” he cautioned.
“If you are going to try the low-FODMAP diet, it has to be short, no more than 4-6 weeks, and you need to do a top-down approach. Take FODMAPs out, and then start to reintroduce them. Either kids will respond to the diet, or they won’t. If they don’t, there is no reason to keep them on the diet. It’s a very hard diet to take,” Dr. Nurko said.
No source of funding for the study was disclosed. The authors, Dr. Ananthakrishnan, and Dr. Nurko have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
American Academy of Pediatrics recommends adolescent suicide screening
With suicide rates among young people rising in recent years, the American Academy of Pediatrics is now recommending adolescents 12 and up be screened for suicide risk as a part of regular preventive care.
The group recently added the recommendation on screening for suicide risk to its depression screening guidelines. Health care providers are urged to ask their young patients a set of questions to identify thoughts and plans for suicide, WDEF.com reported.
“Number one we need to screen for depression and the presence of depression, and those people will usually have a feeling of depressed mood, hopelessness, helplessness, and/or basically a lack of interest in pleasure or anticipation of happiness,” Timothy Fuller, DO, medical director of behavioral health and pediatrics for the American Academy of Pediatrics, told WDEF.
It’s a myth that talking about suicide makes it more likely a person will attempt suicide, he said.
“One of the biggest things you can do, as well, if you do have a child or teenager that has suicidality or that have depression with serious, significant suicide risk, is to just ask them how they’re doing every day,” Dr. Fuller said, according to WDEF.
The recommendation comes about 6 months after U.S. Surgeon General Vivek Murthy, MD, urged more attention be paid to youth mental health.
“Mental health challenges in children, adolescents, and young adults are real and widespread. Even before the pandemic, an alarming number of young people struggled with feelings of helplessness, depression, and thoughts of suicide – and rates have increased over the past decade,” Dr. Murthy said, according to a news release from the U.S. Department of Health & Human Services.
Between 2007 and 2018, suicide rates among people ages 10-24 in the United States went up by 57%, the department said. Estimates showed over 6,600 suicides among this age group in 2020, it said.
A version of this article first appeared on WebMD.com.
With suicide rates among young people rising in recent years, the American Academy of Pediatrics is now recommending adolescents 12 and up be screened for suicide risk as a part of regular preventive care.
The group recently added the recommendation on screening for suicide risk to its depression screening guidelines. Health care providers are urged to ask their young patients a set of questions to identify thoughts and plans for suicide, WDEF.com reported.
“Number one we need to screen for depression and the presence of depression, and those people will usually have a feeling of depressed mood, hopelessness, helplessness, and/or basically a lack of interest in pleasure or anticipation of happiness,” Timothy Fuller, DO, medical director of behavioral health and pediatrics for the American Academy of Pediatrics, told WDEF.
It’s a myth that talking about suicide makes it more likely a person will attempt suicide, he said.
“One of the biggest things you can do, as well, if you do have a child or teenager that has suicidality or that have depression with serious, significant suicide risk, is to just ask them how they’re doing every day,” Dr. Fuller said, according to WDEF.
The recommendation comes about 6 months after U.S. Surgeon General Vivek Murthy, MD, urged more attention be paid to youth mental health.
“Mental health challenges in children, adolescents, and young adults are real and widespread. Even before the pandemic, an alarming number of young people struggled with feelings of helplessness, depression, and thoughts of suicide – and rates have increased over the past decade,” Dr. Murthy said, according to a news release from the U.S. Department of Health & Human Services.
Between 2007 and 2018, suicide rates among people ages 10-24 in the United States went up by 57%, the department said. Estimates showed over 6,600 suicides among this age group in 2020, it said.
A version of this article first appeared on WebMD.com.
With suicide rates among young people rising in recent years, the American Academy of Pediatrics is now recommending adolescents 12 and up be screened for suicide risk as a part of regular preventive care.
The group recently added the recommendation on screening for suicide risk to its depression screening guidelines. Health care providers are urged to ask their young patients a set of questions to identify thoughts and plans for suicide, WDEF.com reported.
“Number one we need to screen for depression and the presence of depression, and those people will usually have a feeling of depressed mood, hopelessness, helplessness, and/or basically a lack of interest in pleasure or anticipation of happiness,” Timothy Fuller, DO, medical director of behavioral health and pediatrics for the American Academy of Pediatrics, told WDEF.
It’s a myth that talking about suicide makes it more likely a person will attempt suicide, he said.
“One of the biggest things you can do, as well, if you do have a child or teenager that has suicidality or that have depression with serious, significant suicide risk, is to just ask them how they’re doing every day,” Dr. Fuller said, according to WDEF.
The recommendation comes about 6 months after U.S. Surgeon General Vivek Murthy, MD, urged more attention be paid to youth mental health.
“Mental health challenges in children, adolescents, and young adults are real and widespread. Even before the pandemic, an alarming number of young people struggled with feelings of helplessness, depression, and thoughts of suicide – and rates have increased over the past decade,” Dr. Murthy said, according to a news release from the U.S. Department of Health & Human Services.
Between 2007 and 2018, suicide rates among people ages 10-24 in the United States went up by 57%, the department said. Estimates showed over 6,600 suicides among this age group in 2020, it said.
A version of this article first appeared on WebMD.com.





