User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Children and COVID: New cases fall again, ED rates rebound for some
The 7-day average percentage of ED visits with diagnosed COVID, which had reached a post-Omicron high of 3.5% in late July for those aged 12-15, began to fall and was down to 3.0% on Aug. 12. That trend reversed, however, and the rate was up to 3.6% on Aug. 19, the last date for which data are available from the Centers for Disease Control and Prevention.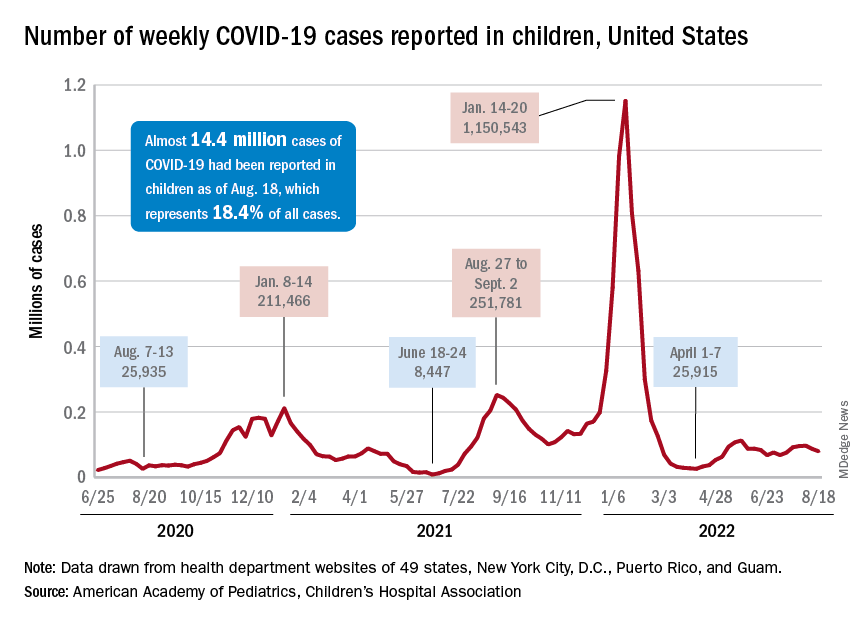
That change of COVID fortunes cannot yet be seen for all children. The 7-day average ED visit rate for those aged 0-11 years peaked at 6.8% during the last week of July and has continued to fall, dropping from 5.7% on Aug. 12 to 5.1% on Aug. 19. Children aged 16-17 years seem to be taking a middle path: Their ED-visit rate declined from late July into mid-August but held steady over the last week, according to the CDC’s COVID Data Tracker.
There is a hint of the same trend regarding new admissions among children aged 0-17 years. The national rate, which had declined in recent weeks, ticked up from 0.42 to 0.43 new admissions per 100,000 population over the last week of available data, the CDC said.
Weekly cases fall below 80,000
New cases in general were down by 8.5% from the previous week, dropping from 87,902 for the week of Aug. 5-11 to 79,525 for Aug. 12-18. That marked the second straight week with fewer cases after a 4-week period that saw weekly totals increase from almost 68,000 to nearly 97,000, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP and CHA put the cumulative number of child COVID-19 cases at just under 14.4 million since the pandemic began, which represents 18.4% of cases among all ages. The CDC estimates that there have been almost 14.7 million cases in children aged 0-17 years, as well as 1,750 deaths, of which 14 were reported in the last week (Aug. 16-22).
The CDC age subgroups indicate that children aged 0-4 years have experienced fewer cases (2.9 million) than children aged 5-11 years (5.6 million cases) and 12-15 (3.0 million cases) but more deaths: 548 so far, versus 432 for 5- to 11-year-olds and 437 for 12- to 15-year-olds, the COVID Data Tracker shows. Those aged 0-4 make up 6% of the total U.S. population, compared with 8.7% and 5.1%, respectively, for the older children.
Most younger children still not vaccinated
Although it may not qualify as a big push to vaccinate children before the start of the new school year, first-time vaccinations did rise somewhat in late July and August for children aged 5-17 years. Among children younger than 5 years, though, initial doses of the vaccine fell during the second full week of August, especially in 2- to 4-year-olds, based on the CDC data.
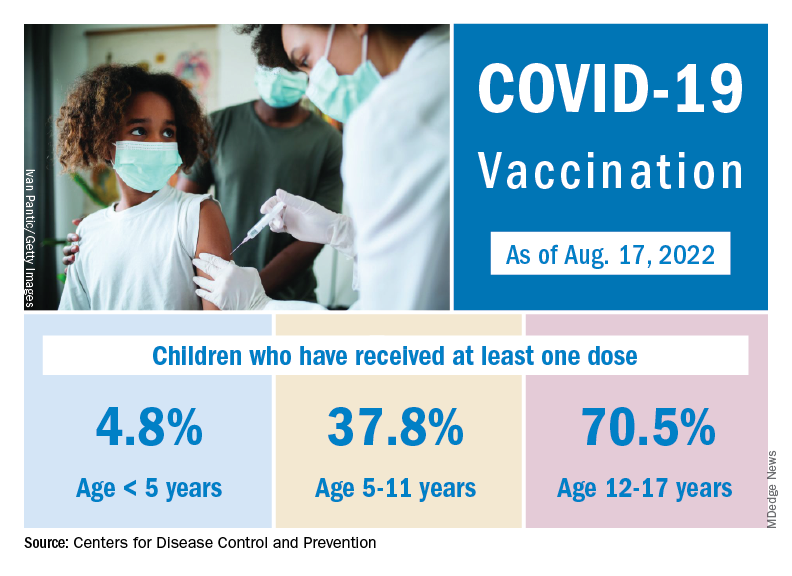
Through almost 2 months of vaccine eligibility, 4.8% of children under age 5 have received at least one dose and 0.9% are fully vaccinated as of Aug. 17. The current rates are 37.8% (one dose) and 30.4% (completed) for those aged 5-11 and 70.5% and 60.3% for 12- to 17-year-olds.
The 7-day average percentage of ED visits with diagnosed COVID, which had reached a post-Omicron high of 3.5% in late July for those aged 12-15, began to fall and was down to 3.0% on Aug. 12. That trend reversed, however, and the rate was up to 3.6% on Aug. 19, the last date for which data are available from the Centers for Disease Control and Prevention.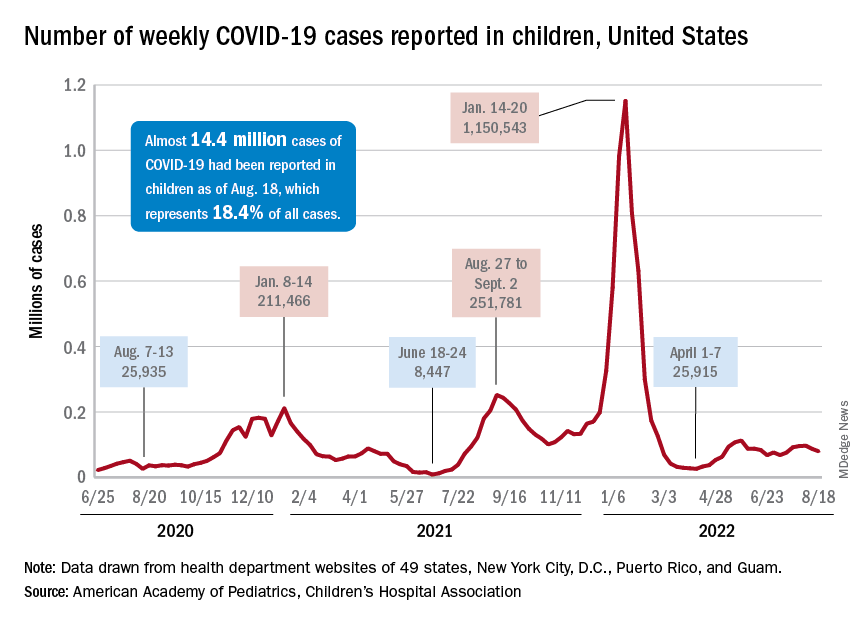
That change of COVID fortunes cannot yet be seen for all children. The 7-day average ED visit rate for those aged 0-11 years peaked at 6.8% during the last week of July and has continued to fall, dropping from 5.7% on Aug. 12 to 5.1% on Aug. 19. Children aged 16-17 years seem to be taking a middle path: Their ED-visit rate declined from late July into mid-August but held steady over the last week, according to the CDC’s COVID Data Tracker.
There is a hint of the same trend regarding new admissions among children aged 0-17 years. The national rate, which had declined in recent weeks, ticked up from 0.42 to 0.43 new admissions per 100,000 population over the last week of available data, the CDC said.
Weekly cases fall below 80,000
New cases in general were down by 8.5% from the previous week, dropping from 87,902 for the week of Aug. 5-11 to 79,525 for Aug. 12-18. That marked the second straight week with fewer cases after a 4-week period that saw weekly totals increase from almost 68,000 to nearly 97,000, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP and CHA put the cumulative number of child COVID-19 cases at just under 14.4 million since the pandemic began, which represents 18.4% of cases among all ages. The CDC estimates that there have been almost 14.7 million cases in children aged 0-17 years, as well as 1,750 deaths, of which 14 were reported in the last week (Aug. 16-22).
The CDC age subgroups indicate that children aged 0-4 years have experienced fewer cases (2.9 million) than children aged 5-11 years (5.6 million cases) and 12-15 (3.0 million cases) but more deaths: 548 so far, versus 432 for 5- to 11-year-olds and 437 for 12- to 15-year-olds, the COVID Data Tracker shows. Those aged 0-4 make up 6% of the total U.S. population, compared with 8.7% and 5.1%, respectively, for the older children.
Most younger children still not vaccinated
Although it may not qualify as a big push to vaccinate children before the start of the new school year, first-time vaccinations did rise somewhat in late July and August for children aged 5-17 years. Among children younger than 5 years, though, initial doses of the vaccine fell during the second full week of August, especially in 2- to 4-year-olds, based on the CDC data.
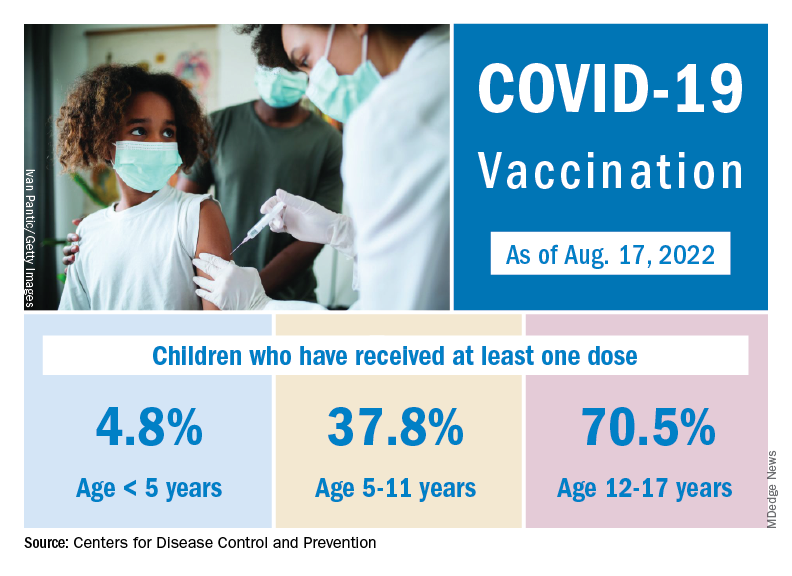
Through almost 2 months of vaccine eligibility, 4.8% of children under age 5 have received at least one dose and 0.9% are fully vaccinated as of Aug. 17. The current rates are 37.8% (one dose) and 30.4% (completed) for those aged 5-11 and 70.5% and 60.3% for 12- to 17-year-olds.
The 7-day average percentage of ED visits with diagnosed COVID, which had reached a post-Omicron high of 3.5% in late July for those aged 12-15, began to fall and was down to 3.0% on Aug. 12. That trend reversed, however, and the rate was up to 3.6% on Aug. 19, the last date for which data are available from the Centers for Disease Control and Prevention.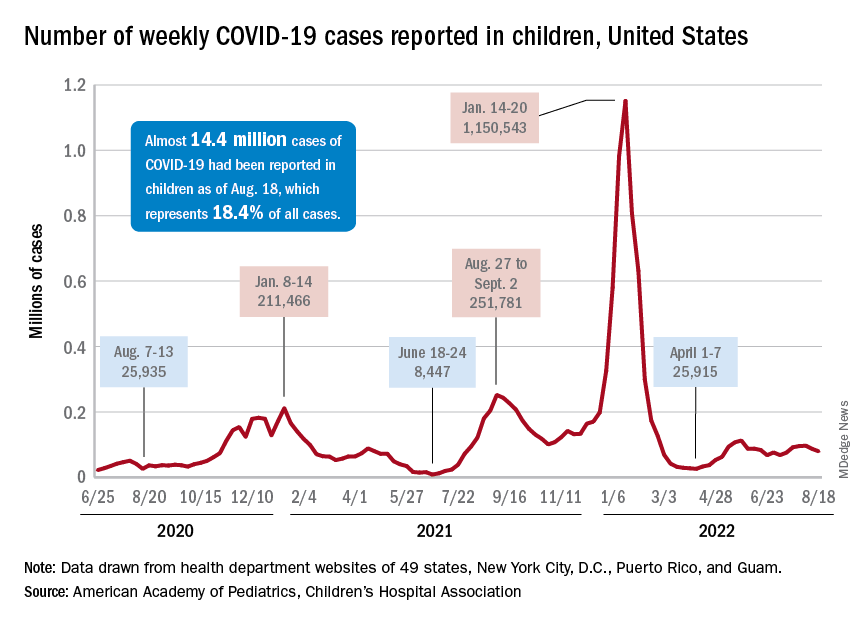
That change of COVID fortunes cannot yet be seen for all children. The 7-day average ED visit rate for those aged 0-11 years peaked at 6.8% during the last week of July and has continued to fall, dropping from 5.7% on Aug. 12 to 5.1% on Aug. 19. Children aged 16-17 years seem to be taking a middle path: Their ED-visit rate declined from late July into mid-August but held steady over the last week, according to the CDC’s COVID Data Tracker.
There is a hint of the same trend regarding new admissions among children aged 0-17 years. The national rate, which had declined in recent weeks, ticked up from 0.42 to 0.43 new admissions per 100,000 population over the last week of available data, the CDC said.
Weekly cases fall below 80,000
New cases in general were down by 8.5% from the previous week, dropping from 87,902 for the week of Aug. 5-11 to 79,525 for Aug. 12-18. That marked the second straight week with fewer cases after a 4-week period that saw weekly totals increase from almost 68,000 to nearly 97,000, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP and CHA put the cumulative number of child COVID-19 cases at just under 14.4 million since the pandemic began, which represents 18.4% of cases among all ages. The CDC estimates that there have been almost 14.7 million cases in children aged 0-17 years, as well as 1,750 deaths, of which 14 were reported in the last week (Aug. 16-22).
The CDC age subgroups indicate that children aged 0-4 years have experienced fewer cases (2.9 million) than children aged 5-11 years (5.6 million cases) and 12-15 (3.0 million cases) but more deaths: 548 so far, versus 432 for 5- to 11-year-olds and 437 for 12- to 15-year-olds, the COVID Data Tracker shows. Those aged 0-4 make up 6% of the total U.S. population, compared with 8.7% and 5.1%, respectively, for the older children.
Most younger children still not vaccinated
Although it may not qualify as a big push to vaccinate children before the start of the new school year, first-time vaccinations did rise somewhat in late July and August for children aged 5-17 years. Among children younger than 5 years, though, initial doses of the vaccine fell during the second full week of August, especially in 2- to 4-year-olds, based on the CDC data.
Through almost 2 months of vaccine eligibility, 4.8% of children under age 5 have received at least one dose and 0.9% are fully vaccinated as of Aug. 17. The current rates are 37.8% (one dose) and 30.4% (completed) for those aged 5-11 and 70.5% and 60.3% for 12- to 17-year-olds.
How does not getting enough sleep affect the developing brain?
Children who do not get enough sleep for one night can be cranky, groggy, or meltdown prone the next day.
Over time, though, insufficient sleep may impair neurodevelopment in ways that can be measured on brain scans and tests long term, a new study shows.
Research published in The Lancet Child & Adolescent Health found that 9- and 10-year-olds who do not get at least 9 hours of sleep most nights tend to have less gray matter and smaller areas of the brain responsible for attention, memory, and inhibition control, relative to children who do get enough sleep.
The researchers also found a relationship between insufficient sleep and disrupted connections between the basal ganglia and cortical regions of the brain. These disruptions appeared to be linked to depression, thought problems, and impairments in crystallized intelligence, a type of intelligence that depends on memory.
The overall patterns persisted 2 years later, even as those who got enough sleep at baseline gradually slept less over time, while those who were not getting enough sleep to begin with continued to sleep about the same amount, the researchers reported.
The results bolster the case for delaying school start times, as California recently did, according one researcher who was not involved in the study.
The ABCD Study
To examine how insufficient sleep affects children’s mental health, cognition, brain function, and brain structure over 2 years, Ze Wang, PhD, professor of diagnostic radiology and nuclear medicine at the University of Maryland, Baltimore, and colleagues analyzed data from the ongoing Adolescent Brain Cognitive Development (ABCD) Study. The ABCD Study is tracking the biologic and behavioral development of more than 11,000 children in the United States who were recruited for the study when they were 9 or 10 years old.
For their new analysis, Dr. Wang’s group focused on 6,042 participants: 3,021 children with insufficient sleep who were matched with an equal number of participants who were similar in many respects, including sex, socioeconomic status, and puberty status, except they got at least 9 hours of sleep. They also looked at outcomes 2 years later from 749 of the matched pairs who had results available.
The investigators determined sleep duration based on how parents answered the question: “How many hours of sleep does your child get on most nights in the past 6 months?” Possible answers included at least 9 hours, 8-9 hours, 7-8 hours, 5-7 hours, or less than 5 hours. They also looked at functional and structural MRI scans, test results, and responses to questionnaires.
Negative effects of inadequate sleep were spread over “several different domains including brain structure, function, cognition, behavior, and mental health,” Dr. Wang said.
The strength of the relationship between sleep duration and the various outcomes was “modest” and based on group averages, he said. So, a given child who does not sleep for 9 hours most nights won’t necessarily perform worse than a child who gets enough sleep.
Still, modest effects may accumulate and have lasting consequences, Dr. Wang said.
Crystallized intelligence
The researchers looked at 42 behavioral outcomes, 32 of which were significantly different between the groups. Four outcomes in particular – depression, thought problems, performance on a picture-vocabulary test, and crystallized intelligence – were areas where insufficient sleep seemed to have a larger negative effect.
Sleep duration’s relationship with crystallized intelligence was twice that for fluid intelligence, which does not depend on memory.
“Sleep affects memory,” Dr. Wang said. “Crystallized intelligence depends on learned skills and knowledge, which are memory. In this sense, sleep is related to crystallized intelligence.”
One limitation of the study is that some parents may not accurately report how much sleep their child gets, Dr. Wang acknowledged. Children may be awake when parents think they are asleep, for example.
And although the results show getting 9 hours of sleep may help neurocognitive development, it’s also possible that excessive amounts of sleep could be problematic, the study authors wrote.
Further experiments are needed to prove that insufficient sleep – and not some other, unaccounted for factor – causes the observed impairments in neurodevelopment.
To promote healthy sleep, parents should keep a strict routine for their children, such as a regular bedtime and no electronic devices in the bedroom, Dr. Wang suggested. More physical activity during the day also should help.
If children have high levels of stress and depression, “finding the source is critical,” he said. Likewise, clinicians should consider how mental health can affect their patients’ sleep.
More to healthy sleep than duration
“This study both aligns with and advances existing research on the importance of sufficient sleep for child well-being,” said Ariel A. Williamson, PhD, DBSM, a psychologist and pediatric sleep expert in the department of child and adolescent psychiatry and behavioral sciences at Children’s Hospital of Philadelphia and assistant professor of psychiatry and pediatrics at University of Pennsylvania, also in Philadelphia.
The researchers used rigorous propensity score matching, longitudinal data, and brain imaging, which are “innovative methods that provide more evidence on potential mechanisms linking insufficient sleep and child outcomes,” said Dr. Williamson, who was not involved in the study.
While the investigators focused on sleep duration, child sleep health is multidimensional and includes other elements like timing and perception of sleep quality, Dr. Williamson noted. “For example, some research shows that having a sleep schedule that varies night to night is linked to poor child outcomes.”
Dr. Williamson tells families and clinicians that “sleep is a pillar of health,” equal to diet and exercise. That said, sleep recommendations need to fit within a family’s life – taking into account after school activities and late-night homework sessions. But extending sleep by just “20-30 minutes can make a meaningful difference for daytime functioning,” Dr. Williamson said.
Start school later?
Researchers have only relatively recently begun to understand how insufficient sleep affects adolescent neurocognitive development long term, and this study provides “crucial evidence” about the consequences, Lydia Gabriela Speyer, PhD, said in an editorial published with the study. Dr. Speyer is affiliated with the department of psychology at the University of Cambridge (England).
“Given the novel finding that insufficient sleep is associated with changes in brain structure and connectivity that are long-lasting, early intervention is crucial because such neural changes are probably not reversible and might consequently affect adolescents’ development into adulthood,” Dr. Speyer wrote.
Delaying school start times could be one way to help kids get more sleep. The American Academy of Pediatrics and the American Academy of Sleep Medicine recommend that middle schools and high schools start no earlier than 8:30 a.m. to better align with students’ circadian rhythm, Dr. Speyer noted.
As it is in the United States, most schools start closer to 8 a.m. In California, though, a law that went into effect on July 1 prohibits high schools from starting before 8:30 a.m. Other states are weighing similar legislation.
The research was supported by the National Institutes of Health. Dr. Wang and his coauthors and Dr. Speyer had no conflict of interest disclosures. Dr. Williamson is a sleep expert for the Pediatric Sleep Council (www.babysleep.com), which provides free information about early childhood sleep, but she does not receive compensation for this role.
Children who do not get enough sleep for one night can be cranky, groggy, or meltdown prone the next day.
Over time, though, insufficient sleep may impair neurodevelopment in ways that can be measured on brain scans and tests long term, a new study shows.
Research published in The Lancet Child & Adolescent Health found that 9- and 10-year-olds who do not get at least 9 hours of sleep most nights tend to have less gray matter and smaller areas of the brain responsible for attention, memory, and inhibition control, relative to children who do get enough sleep.
The researchers also found a relationship between insufficient sleep and disrupted connections between the basal ganglia and cortical regions of the brain. These disruptions appeared to be linked to depression, thought problems, and impairments in crystallized intelligence, a type of intelligence that depends on memory.
The overall patterns persisted 2 years later, even as those who got enough sleep at baseline gradually slept less over time, while those who were not getting enough sleep to begin with continued to sleep about the same amount, the researchers reported.
The results bolster the case for delaying school start times, as California recently did, according one researcher who was not involved in the study.
The ABCD Study
To examine how insufficient sleep affects children’s mental health, cognition, brain function, and brain structure over 2 years, Ze Wang, PhD, professor of diagnostic radiology and nuclear medicine at the University of Maryland, Baltimore, and colleagues analyzed data from the ongoing Adolescent Brain Cognitive Development (ABCD) Study. The ABCD Study is tracking the biologic and behavioral development of more than 11,000 children in the United States who were recruited for the study when they were 9 or 10 years old.
For their new analysis, Dr. Wang’s group focused on 6,042 participants: 3,021 children with insufficient sleep who were matched with an equal number of participants who were similar in many respects, including sex, socioeconomic status, and puberty status, except they got at least 9 hours of sleep. They also looked at outcomes 2 years later from 749 of the matched pairs who had results available.
The investigators determined sleep duration based on how parents answered the question: “How many hours of sleep does your child get on most nights in the past 6 months?” Possible answers included at least 9 hours, 8-9 hours, 7-8 hours, 5-7 hours, or less than 5 hours. They also looked at functional and structural MRI scans, test results, and responses to questionnaires.
Negative effects of inadequate sleep were spread over “several different domains including brain structure, function, cognition, behavior, and mental health,” Dr. Wang said.
The strength of the relationship between sleep duration and the various outcomes was “modest” and based on group averages, he said. So, a given child who does not sleep for 9 hours most nights won’t necessarily perform worse than a child who gets enough sleep.
Still, modest effects may accumulate and have lasting consequences, Dr. Wang said.
Crystallized intelligence
The researchers looked at 42 behavioral outcomes, 32 of which were significantly different between the groups. Four outcomes in particular – depression, thought problems, performance on a picture-vocabulary test, and crystallized intelligence – were areas where insufficient sleep seemed to have a larger negative effect.
Sleep duration’s relationship with crystallized intelligence was twice that for fluid intelligence, which does not depend on memory.
“Sleep affects memory,” Dr. Wang said. “Crystallized intelligence depends on learned skills and knowledge, which are memory. In this sense, sleep is related to crystallized intelligence.”
One limitation of the study is that some parents may not accurately report how much sleep their child gets, Dr. Wang acknowledged. Children may be awake when parents think they are asleep, for example.
And although the results show getting 9 hours of sleep may help neurocognitive development, it’s also possible that excessive amounts of sleep could be problematic, the study authors wrote.
Further experiments are needed to prove that insufficient sleep – and not some other, unaccounted for factor – causes the observed impairments in neurodevelopment.
To promote healthy sleep, parents should keep a strict routine for their children, such as a regular bedtime and no electronic devices in the bedroom, Dr. Wang suggested. More physical activity during the day also should help.
If children have high levels of stress and depression, “finding the source is critical,” he said. Likewise, clinicians should consider how mental health can affect their patients’ sleep.
More to healthy sleep than duration
“This study both aligns with and advances existing research on the importance of sufficient sleep for child well-being,” said Ariel A. Williamson, PhD, DBSM, a psychologist and pediatric sleep expert in the department of child and adolescent psychiatry and behavioral sciences at Children’s Hospital of Philadelphia and assistant professor of psychiatry and pediatrics at University of Pennsylvania, also in Philadelphia.
The researchers used rigorous propensity score matching, longitudinal data, and brain imaging, which are “innovative methods that provide more evidence on potential mechanisms linking insufficient sleep and child outcomes,” said Dr. Williamson, who was not involved in the study.
While the investigators focused on sleep duration, child sleep health is multidimensional and includes other elements like timing and perception of sleep quality, Dr. Williamson noted. “For example, some research shows that having a sleep schedule that varies night to night is linked to poor child outcomes.”
Dr. Williamson tells families and clinicians that “sleep is a pillar of health,” equal to diet and exercise. That said, sleep recommendations need to fit within a family’s life – taking into account after school activities and late-night homework sessions. But extending sleep by just “20-30 minutes can make a meaningful difference for daytime functioning,” Dr. Williamson said.
Start school later?
Researchers have only relatively recently begun to understand how insufficient sleep affects adolescent neurocognitive development long term, and this study provides “crucial evidence” about the consequences, Lydia Gabriela Speyer, PhD, said in an editorial published with the study. Dr. Speyer is affiliated with the department of psychology at the University of Cambridge (England).
“Given the novel finding that insufficient sleep is associated with changes in brain structure and connectivity that are long-lasting, early intervention is crucial because such neural changes are probably not reversible and might consequently affect adolescents’ development into adulthood,” Dr. Speyer wrote.
Delaying school start times could be one way to help kids get more sleep. The American Academy of Pediatrics and the American Academy of Sleep Medicine recommend that middle schools and high schools start no earlier than 8:30 a.m. to better align with students’ circadian rhythm, Dr. Speyer noted.
As it is in the United States, most schools start closer to 8 a.m. In California, though, a law that went into effect on July 1 prohibits high schools from starting before 8:30 a.m. Other states are weighing similar legislation.
The research was supported by the National Institutes of Health. Dr. Wang and his coauthors and Dr. Speyer had no conflict of interest disclosures. Dr. Williamson is a sleep expert for the Pediatric Sleep Council (www.babysleep.com), which provides free information about early childhood sleep, but she does not receive compensation for this role.
Children who do not get enough sleep for one night can be cranky, groggy, or meltdown prone the next day.
Over time, though, insufficient sleep may impair neurodevelopment in ways that can be measured on brain scans and tests long term, a new study shows.
Research published in The Lancet Child & Adolescent Health found that 9- and 10-year-olds who do not get at least 9 hours of sleep most nights tend to have less gray matter and smaller areas of the brain responsible for attention, memory, and inhibition control, relative to children who do get enough sleep.
The researchers also found a relationship between insufficient sleep and disrupted connections between the basal ganglia and cortical regions of the brain. These disruptions appeared to be linked to depression, thought problems, and impairments in crystallized intelligence, a type of intelligence that depends on memory.
The overall patterns persisted 2 years later, even as those who got enough sleep at baseline gradually slept less over time, while those who were not getting enough sleep to begin with continued to sleep about the same amount, the researchers reported.
The results bolster the case for delaying school start times, as California recently did, according one researcher who was not involved in the study.
The ABCD Study
To examine how insufficient sleep affects children’s mental health, cognition, brain function, and brain structure over 2 years, Ze Wang, PhD, professor of diagnostic radiology and nuclear medicine at the University of Maryland, Baltimore, and colleagues analyzed data from the ongoing Adolescent Brain Cognitive Development (ABCD) Study. The ABCD Study is tracking the biologic and behavioral development of more than 11,000 children in the United States who were recruited for the study when they were 9 or 10 years old.
For their new analysis, Dr. Wang’s group focused on 6,042 participants: 3,021 children with insufficient sleep who were matched with an equal number of participants who were similar in many respects, including sex, socioeconomic status, and puberty status, except they got at least 9 hours of sleep. They also looked at outcomes 2 years later from 749 of the matched pairs who had results available.
The investigators determined sleep duration based on how parents answered the question: “How many hours of sleep does your child get on most nights in the past 6 months?” Possible answers included at least 9 hours, 8-9 hours, 7-8 hours, 5-7 hours, or less than 5 hours. They also looked at functional and structural MRI scans, test results, and responses to questionnaires.
Negative effects of inadequate sleep were spread over “several different domains including brain structure, function, cognition, behavior, and mental health,” Dr. Wang said.
The strength of the relationship between sleep duration and the various outcomes was “modest” and based on group averages, he said. So, a given child who does not sleep for 9 hours most nights won’t necessarily perform worse than a child who gets enough sleep.
Still, modest effects may accumulate and have lasting consequences, Dr. Wang said.
Crystallized intelligence
The researchers looked at 42 behavioral outcomes, 32 of which were significantly different between the groups. Four outcomes in particular – depression, thought problems, performance on a picture-vocabulary test, and crystallized intelligence – were areas where insufficient sleep seemed to have a larger negative effect.
Sleep duration’s relationship with crystallized intelligence was twice that for fluid intelligence, which does not depend on memory.
“Sleep affects memory,” Dr. Wang said. “Crystallized intelligence depends on learned skills and knowledge, which are memory. In this sense, sleep is related to crystallized intelligence.”
One limitation of the study is that some parents may not accurately report how much sleep their child gets, Dr. Wang acknowledged. Children may be awake when parents think they are asleep, for example.
And although the results show getting 9 hours of sleep may help neurocognitive development, it’s also possible that excessive amounts of sleep could be problematic, the study authors wrote.
Further experiments are needed to prove that insufficient sleep – and not some other, unaccounted for factor – causes the observed impairments in neurodevelopment.
To promote healthy sleep, parents should keep a strict routine for their children, such as a regular bedtime and no electronic devices in the bedroom, Dr. Wang suggested. More physical activity during the day also should help.
If children have high levels of stress and depression, “finding the source is critical,” he said. Likewise, clinicians should consider how mental health can affect their patients’ sleep.
More to healthy sleep than duration
“This study both aligns with and advances existing research on the importance of sufficient sleep for child well-being,” said Ariel A. Williamson, PhD, DBSM, a psychologist and pediatric sleep expert in the department of child and adolescent psychiatry and behavioral sciences at Children’s Hospital of Philadelphia and assistant professor of psychiatry and pediatrics at University of Pennsylvania, also in Philadelphia.
The researchers used rigorous propensity score matching, longitudinal data, and brain imaging, which are “innovative methods that provide more evidence on potential mechanisms linking insufficient sleep and child outcomes,” said Dr. Williamson, who was not involved in the study.
While the investigators focused on sleep duration, child sleep health is multidimensional and includes other elements like timing and perception of sleep quality, Dr. Williamson noted. “For example, some research shows that having a sleep schedule that varies night to night is linked to poor child outcomes.”
Dr. Williamson tells families and clinicians that “sleep is a pillar of health,” equal to diet and exercise. That said, sleep recommendations need to fit within a family’s life – taking into account after school activities and late-night homework sessions. But extending sleep by just “20-30 minutes can make a meaningful difference for daytime functioning,” Dr. Williamson said.
Start school later?
Researchers have only relatively recently begun to understand how insufficient sleep affects adolescent neurocognitive development long term, and this study provides “crucial evidence” about the consequences, Lydia Gabriela Speyer, PhD, said in an editorial published with the study. Dr. Speyer is affiliated with the department of psychology at the University of Cambridge (England).
“Given the novel finding that insufficient sleep is associated with changes in brain structure and connectivity that are long-lasting, early intervention is crucial because such neural changes are probably not reversible and might consequently affect adolescents’ development into adulthood,” Dr. Speyer wrote.
Delaying school start times could be one way to help kids get more sleep. The American Academy of Pediatrics and the American Academy of Sleep Medicine recommend that middle schools and high schools start no earlier than 8:30 a.m. to better align with students’ circadian rhythm, Dr. Speyer noted.
As it is in the United States, most schools start closer to 8 a.m. In California, though, a law that went into effect on July 1 prohibits high schools from starting before 8:30 a.m. Other states are weighing similar legislation.
The research was supported by the National Institutes of Health. Dr. Wang and his coauthors and Dr. Speyer had no conflict of interest disclosures. Dr. Williamson is a sleep expert for the Pediatric Sleep Council (www.babysleep.com), which provides free information about early childhood sleep, but she does not receive compensation for this role.
FROM THE LANCET CHILD & ADOLESCENT HEALTH
Consider essential oil allergy in patient with dermatitis
PORTLAND, ORE. – When patients present to Brandon L. Adler, MD, with dermatitis on the eyelid, face, or neck, he routinely asks them if they apply essential oils on their skin, or if they have an essential oil diffuser or nebulizer in their home.
“The answer is frequently ‘yes,’ ” Dr. Adler, clinical assistant professor of dermatology at the University of Southern California, Los Angeles, said at the annual meeting of the Pacific Dermatologic Association. “Essential oils are widely used throughout the wellness industry. They are contained in personal care products, beauty products, natural cleaning products, and they’re being diffused by our patients into the air. More than 75 essential oils are reported to cause allergic contact dermatitis.”
“Linalool is most classically associated with lavender, while limonene is associated with citrus, but they’re found in many different plants,” said Dr. Adler, who directs USC’s contact dermatitis clinic. “On their own, linalool and limonene are not particularly allergenic; they’re not a big deal in the patch test clinic. The problem comes when we add air to the mix, because they oxidize to hydroperoxides of linalool and limonene. These are quite potent allergens.”
According to the most recent North American Contact Dermatitis Group data, 8.9% of patients undergoing patch testing tested positive to linalool hydroperoxides and 2.6% were positive to limonene hydroperoxides.
Dr. Adler discussed the case of a female massage therapist who presented with refractory hand dermatitis and was on methotrexate and dupilumab at the time of consultation but was still symptomatic. She patch-tested positive to limonene and linalool hydroperoxides as well as multiple essential oils that she had been using with her clients, ranging from sacred frankincense oil to basil oil, and she was advised to massage using only coconut or vegetable oils.
Essential oil allergy may also be related to cannabis allergy. According to Dr. Adler, allergic contact dermatitis to cannabis has been rarely reported, but in an analysis of 103 commercial topical cannabinoid preparations that he published with Vincent DeLeo, MD, also with USC, 84% contained a NACDG allergen, frequently essential oils.
More recently, Dr. Adler and colleagues reported the case of a 40-year-old woman who was referred for patch testing for nummular dermatitis that wasn’t responding to treatment. The patient was found to be using topical cannabis and also grew cannabis at home. “She asked to be patch-tested to her homegrown cannabis and had a strong positive patch test to the cannabis, linalool and limonene hydroperoxides, and other essential oils,” Dr. Adler recalled. “We sent her cannabis sample for analysis at a commercial lab and found that it contained limonene and other allergenic terpene chemicals.
“We’re just starting to unravel what this means in terms of our patients and how to manage them, but many are using topical cannabis and topical CBD. I suspect this is a lot less rare than we realize.”
Another recent case from Europe reported allergic contact dermatitis to Cannabis sativa (hemp) seed oil following topical application, with positive patch testing.
Dr. Adler disclosed that he has received research grants from the American Contact Dermatitis Society. He is also an investigator for AbbVie and a consultant for the Skin Research Institute.
PORTLAND, ORE. – When patients present to Brandon L. Adler, MD, with dermatitis on the eyelid, face, or neck, he routinely asks them if they apply essential oils on their skin, or if they have an essential oil diffuser or nebulizer in their home.
“The answer is frequently ‘yes,’ ” Dr. Adler, clinical assistant professor of dermatology at the University of Southern California, Los Angeles, said at the annual meeting of the Pacific Dermatologic Association. “Essential oils are widely used throughout the wellness industry. They are contained in personal care products, beauty products, natural cleaning products, and they’re being diffused by our patients into the air. More than 75 essential oils are reported to cause allergic contact dermatitis.”
“Linalool is most classically associated with lavender, while limonene is associated with citrus, but they’re found in many different plants,” said Dr. Adler, who directs USC’s contact dermatitis clinic. “On their own, linalool and limonene are not particularly allergenic; they’re not a big deal in the patch test clinic. The problem comes when we add air to the mix, because they oxidize to hydroperoxides of linalool and limonene. These are quite potent allergens.”
According to the most recent North American Contact Dermatitis Group data, 8.9% of patients undergoing patch testing tested positive to linalool hydroperoxides and 2.6% were positive to limonene hydroperoxides.
Dr. Adler discussed the case of a female massage therapist who presented with refractory hand dermatitis and was on methotrexate and dupilumab at the time of consultation but was still symptomatic. She patch-tested positive to limonene and linalool hydroperoxides as well as multiple essential oils that she had been using with her clients, ranging from sacred frankincense oil to basil oil, and she was advised to massage using only coconut or vegetable oils.
Essential oil allergy may also be related to cannabis allergy. According to Dr. Adler, allergic contact dermatitis to cannabis has been rarely reported, but in an analysis of 103 commercial topical cannabinoid preparations that he published with Vincent DeLeo, MD, also with USC, 84% contained a NACDG allergen, frequently essential oils.
More recently, Dr. Adler and colleagues reported the case of a 40-year-old woman who was referred for patch testing for nummular dermatitis that wasn’t responding to treatment. The patient was found to be using topical cannabis and also grew cannabis at home. “She asked to be patch-tested to her homegrown cannabis and had a strong positive patch test to the cannabis, linalool and limonene hydroperoxides, and other essential oils,” Dr. Adler recalled. “We sent her cannabis sample for analysis at a commercial lab and found that it contained limonene and other allergenic terpene chemicals.
“We’re just starting to unravel what this means in terms of our patients and how to manage them, but many are using topical cannabis and topical CBD. I suspect this is a lot less rare than we realize.”
Another recent case from Europe reported allergic contact dermatitis to Cannabis sativa (hemp) seed oil following topical application, with positive patch testing.
Dr. Adler disclosed that he has received research grants from the American Contact Dermatitis Society. He is also an investigator for AbbVie and a consultant for the Skin Research Institute.
PORTLAND, ORE. – When patients present to Brandon L. Adler, MD, with dermatitis on the eyelid, face, or neck, he routinely asks them if they apply essential oils on their skin, or if they have an essential oil diffuser or nebulizer in their home.
“The answer is frequently ‘yes,’ ” Dr. Adler, clinical assistant professor of dermatology at the University of Southern California, Los Angeles, said at the annual meeting of the Pacific Dermatologic Association. “Essential oils are widely used throughout the wellness industry. They are contained in personal care products, beauty products, natural cleaning products, and they’re being diffused by our patients into the air. More than 75 essential oils are reported to cause allergic contact dermatitis.”
“Linalool is most classically associated with lavender, while limonene is associated with citrus, but they’re found in many different plants,” said Dr. Adler, who directs USC’s contact dermatitis clinic. “On their own, linalool and limonene are not particularly allergenic; they’re not a big deal in the patch test clinic. The problem comes when we add air to the mix, because they oxidize to hydroperoxides of linalool and limonene. These are quite potent allergens.”
According to the most recent North American Contact Dermatitis Group data, 8.9% of patients undergoing patch testing tested positive to linalool hydroperoxides and 2.6% were positive to limonene hydroperoxides.
Dr. Adler discussed the case of a female massage therapist who presented with refractory hand dermatitis and was on methotrexate and dupilumab at the time of consultation but was still symptomatic. She patch-tested positive to limonene and linalool hydroperoxides as well as multiple essential oils that she had been using with her clients, ranging from sacred frankincense oil to basil oil, and she was advised to massage using only coconut or vegetable oils.
Essential oil allergy may also be related to cannabis allergy. According to Dr. Adler, allergic contact dermatitis to cannabis has been rarely reported, but in an analysis of 103 commercial topical cannabinoid preparations that he published with Vincent DeLeo, MD, also with USC, 84% contained a NACDG allergen, frequently essential oils.
More recently, Dr. Adler and colleagues reported the case of a 40-year-old woman who was referred for patch testing for nummular dermatitis that wasn’t responding to treatment. The patient was found to be using topical cannabis and also grew cannabis at home. “She asked to be patch-tested to her homegrown cannabis and had a strong positive patch test to the cannabis, linalool and limonene hydroperoxides, and other essential oils,” Dr. Adler recalled. “We sent her cannabis sample for analysis at a commercial lab and found that it contained limonene and other allergenic terpene chemicals.
“We’re just starting to unravel what this means in terms of our patients and how to manage them, but many are using topical cannabis and topical CBD. I suspect this is a lot less rare than we realize.”
Another recent case from Europe reported allergic contact dermatitis to Cannabis sativa (hemp) seed oil following topical application, with positive patch testing.
Dr. Adler disclosed that he has received research grants from the American Contact Dermatitis Society. He is also an investigator for AbbVie and a consultant for the Skin Research Institute.
AT PDA 2022
Leukemia rates two to three times higher in children born near fracking
Children born near fracking and other “unconventional” drilling sites are at two to three times greater risk of developing childhood leukemia, according to new research.
The study, published in the journal Environmental Health Perspectives, compared proximity of homes to unconventional oil and gas development (UOGD) sites and risk of the most common form of childhood leukemia, acute lymphoblastic leukemia (ALL).
Researchers looked at 405 children aged 2-7 diagnosed with ALL in Pennsylvania from 2009 to 2017. These children were compared to a control group of 2,080 without the disease matched on the year of birth.
“Unconventional oil and gas development can both use and release chemicals that have been linked to cancer,” study coauthor Nicole Deziel, PhD, of the Yale School of Public Health, New Haven, Conn., said in a statement . She noted that the possibility that children living in close proximity to such sites are “exposed to these chemical carcinogens is a major public health concern.”
About 17 million Americans live within a half-mile of active oil and gas production, according to the Oil & Gas Threat Map, Common Dreams reports. That number includes 4 million children.
The Yale study also found that drinking water could be an important pathway of exposure to oil- and gas-related chemicals used in the UOGD methods of extraction.
Researchers used a new metric that measures exposure to contaminated drinking water and distance to a well. They were able to identify UOGD-affected wells that fell within watersheds where children and their families likely obtained their water.
“Previous health studies have found links between proximity to oil and gas drilling and various children’s health outcomes,” said Dr. Deziel. “This study is among the few to focus on drinking water specifically and the first to apply a novel metric designed to capture potential exposure through this pathway.”
A version of this article first appeared on WebMD.com.
Children born near fracking and other “unconventional” drilling sites are at two to three times greater risk of developing childhood leukemia, according to new research.
The study, published in the journal Environmental Health Perspectives, compared proximity of homes to unconventional oil and gas development (UOGD) sites and risk of the most common form of childhood leukemia, acute lymphoblastic leukemia (ALL).
Researchers looked at 405 children aged 2-7 diagnosed with ALL in Pennsylvania from 2009 to 2017. These children were compared to a control group of 2,080 without the disease matched on the year of birth.
“Unconventional oil and gas development can both use and release chemicals that have been linked to cancer,” study coauthor Nicole Deziel, PhD, of the Yale School of Public Health, New Haven, Conn., said in a statement . She noted that the possibility that children living in close proximity to such sites are “exposed to these chemical carcinogens is a major public health concern.”
About 17 million Americans live within a half-mile of active oil and gas production, according to the Oil & Gas Threat Map, Common Dreams reports. That number includes 4 million children.
The Yale study also found that drinking water could be an important pathway of exposure to oil- and gas-related chemicals used in the UOGD methods of extraction.
Researchers used a new metric that measures exposure to contaminated drinking water and distance to a well. They were able to identify UOGD-affected wells that fell within watersheds where children and their families likely obtained their water.
“Previous health studies have found links between proximity to oil and gas drilling and various children’s health outcomes,” said Dr. Deziel. “This study is among the few to focus on drinking water specifically and the first to apply a novel metric designed to capture potential exposure through this pathway.”
A version of this article first appeared on WebMD.com.
Children born near fracking and other “unconventional” drilling sites are at two to three times greater risk of developing childhood leukemia, according to new research.
The study, published in the journal Environmental Health Perspectives, compared proximity of homes to unconventional oil and gas development (UOGD) sites and risk of the most common form of childhood leukemia, acute lymphoblastic leukemia (ALL).
Researchers looked at 405 children aged 2-7 diagnosed with ALL in Pennsylvania from 2009 to 2017. These children were compared to a control group of 2,080 without the disease matched on the year of birth.
“Unconventional oil and gas development can both use and release chemicals that have been linked to cancer,” study coauthor Nicole Deziel, PhD, of the Yale School of Public Health, New Haven, Conn., said in a statement . She noted that the possibility that children living in close proximity to such sites are “exposed to these chemical carcinogens is a major public health concern.”
About 17 million Americans live within a half-mile of active oil and gas production, according to the Oil & Gas Threat Map, Common Dreams reports. That number includes 4 million children.
The Yale study also found that drinking water could be an important pathway of exposure to oil- and gas-related chemicals used in the UOGD methods of extraction.
Researchers used a new metric that measures exposure to contaminated drinking water and distance to a well. They were able to identify UOGD-affected wells that fell within watersheds where children and their families likely obtained their water.
“Previous health studies have found links between proximity to oil and gas drilling and various children’s health outcomes,” said Dr. Deziel. “This study is among the few to focus on drinking water specifically and the first to apply a novel metric designed to capture potential exposure through this pathway.”
A version of this article first appeared on WebMD.com.
Watching TV, using computer have opposite ties to dementia risk
The relationship to dementia with these activities remained strong no matter how much physical activity a person did, the authors wrote in Proceedings of the National Academy of Sciences.
Both watching TV and using a computer have been linked to increased risk of chronic disease and mortality, while exercise and physical activity (PA) have shown benefit in reducing cognitive decline, structural brain atrophy, and dementia risk in older adults, the authors wrote.
The authors said they wanted to try to understand the effects of watching TV and using computers on dementia risk, because people in the United States and Europe have been engaging in both of these activities more often.
They concluded that it’s not the sitting part of sedentary behavior (SB) that potentially has the effect on dementia but what people are doing while sitting.
Some of the results were surprising, lead author David Raichlen, PhD, professor of Human and Evolutionary Biology at University of Southern California, Los Angeles, said in an interview.
Previous literature on sedentary behaviors have documented their negative effects on a wide range of health outcomes, rather than finding positive associations, he explained.
More than 140,000 included in study
The researchers conducted their prospective cohort study using data from the United Kingdom Biobank. After excluding people younger than 60, those with prevalent dementia at the start of follow-up, and those without complete data, 146,651 participants were included.
The participants were followed from their baseline visit until they received a dementia diagnosis, died, were lost to follow-up, or were last admitted to the hospital.
TV-watching time was linked with an increased risk of incident dementia (HR [95% confidence interval] = 1.31 [1.23-1.40]), and computer use was linked with a reduced risk of incident dementia HR [95% CI] = 0.80 [0.76-0.85]).
TV’s link with higher dementia risk increased in those who had the highest use, compared with those who had the lowest use (HR [95% CI] = 1.28 [1.18-1.39].
Similarly, the link with risk reduction for dementia with computer use increased with more use.
Both medium and high computer time were associated with reduced risk of incident dementia (HR [95% CI] = 0.70 [0.64-0.76] and HR [95% CI] = 0.76 [0.70-0.83] respectively).
Dr. Raichlen pointed out that the high use of TV in this study was 4 or more hours a day and computer use – which included leisure use, not work use – had benefits on dementia risk after just half an hour.
These results remained significant after researchers adjusted for demographic, health, and lifestyle variables, including time spent on physical activity, sleeping, obesity, alcohol consumption, smoking status, diet scores, education level, body mass index, and employment type.
Physical is still better than sedentary activity
One potential reason for the different effects on dementia risk in the two activities studied, the authors write, is that sitting down to watch TV is associated with “uniquely low levels of muscle activity and energy expenditure, compared with sitting to use a computer.”
Andrew Budson, MD, chief of Cognitive & Behavioral Neurology and Associate Chief of Staff for Education for the VA Boston Healthcare System, Mass., who was not part of the study, said he thinks a more likely explanation for the study findings lies in the active versus passive tasks required in the two kinds of viewing that the authors reference.
“When we’re doing cognitive activity involving using the computer, we’re using large parts of our cortex to carry out that activity, whereas when we’re watching TV, there are probably relatively small amounts of our brain that are actually active,” Dr. Budson, author of Seven Steps to Managing Your Memory, explained in an interview.
“This is one of the first times I’ve been convinced that even when the computer activity isn’t completely new and novel, it may be beneficial,” Dr. Budson said.
It would be much better to do physical activity, but if the choice is sedentary activity, active cognitive activities, such as computer use, are better than TV watching, he continued.
The results of the current study are consistent with previous work showing that the type of sedentary behavior matters, according to the authors.
“Several studies have shown that TV time is associated with mortality and poor cardiometabolic biomarkers, whereas computer time is not,” they wrote.
A limitation of the study is that sedentary behaviors were self-reported via questionnaires, and there may be errors in recall.
“The use of objective methods for measuring both SB and PA are needed in future studies,” they write.
The authors receive support from the National Institutes of Health, the State of Arizona, the Arizona Department of Health Services, and the McKnight Brain Research Foundation. Neither the authors nor Dr. Budson declared relevant financial relationships.
The relationship to dementia with these activities remained strong no matter how much physical activity a person did, the authors wrote in Proceedings of the National Academy of Sciences.
Both watching TV and using a computer have been linked to increased risk of chronic disease and mortality, while exercise and physical activity (PA) have shown benefit in reducing cognitive decline, structural brain atrophy, and dementia risk in older adults, the authors wrote.
The authors said they wanted to try to understand the effects of watching TV and using computers on dementia risk, because people in the United States and Europe have been engaging in both of these activities more often.
They concluded that it’s not the sitting part of sedentary behavior (SB) that potentially has the effect on dementia but what people are doing while sitting.
Some of the results were surprising, lead author David Raichlen, PhD, professor of Human and Evolutionary Biology at University of Southern California, Los Angeles, said in an interview.
Previous literature on sedentary behaviors have documented their negative effects on a wide range of health outcomes, rather than finding positive associations, he explained.
More than 140,000 included in study
The researchers conducted their prospective cohort study using data from the United Kingdom Biobank. After excluding people younger than 60, those with prevalent dementia at the start of follow-up, and those without complete data, 146,651 participants were included.
The participants were followed from their baseline visit until they received a dementia diagnosis, died, were lost to follow-up, or were last admitted to the hospital.
TV-watching time was linked with an increased risk of incident dementia (HR [95% confidence interval] = 1.31 [1.23-1.40]), and computer use was linked with a reduced risk of incident dementia HR [95% CI] = 0.80 [0.76-0.85]).
TV’s link with higher dementia risk increased in those who had the highest use, compared with those who had the lowest use (HR [95% CI] = 1.28 [1.18-1.39].
Similarly, the link with risk reduction for dementia with computer use increased with more use.
Both medium and high computer time were associated with reduced risk of incident dementia (HR [95% CI] = 0.70 [0.64-0.76] and HR [95% CI] = 0.76 [0.70-0.83] respectively).
Dr. Raichlen pointed out that the high use of TV in this study was 4 or more hours a day and computer use – which included leisure use, not work use – had benefits on dementia risk after just half an hour.
These results remained significant after researchers adjusted for demographic, health, and lifestyle variables, including time spent on physical activity, sleeping, obesity, alcohol consumption, smoking status, diet scores, education level, body mass index, and employment type.
Physical is still better than sedentary activity
One potential reason for the different effects on dementia risk in the two activities studied, the authors write, is that sitting down to watch TV is associated with “uniquely low levels of muscle activity and energy expenditure, compared with sitting to use a computer.”
Andrew Budson, MD, chief of Cognitive & Behavioral Neurology and Associate Chief of Staff for Education for the VA Boston Healthcare System, Mass., who was not part of the study, said he thinks a more likely explanation for the study findings lies in the active versus passive tasks required in the two kinds of viewing that the authors reference.
“When we’re doing cognitive activity involving using the computer, we’re using large parts of our cortex to carry out that activity, whereas when we’re watching TV, there are probably relatively small amounts of our brain that are actually active,” Dr. Budson, author of Seven Steps to Managing Your Memory, explained in an interview.
“This is one of the first times I’ve been convinced that even when the computer activity isn’t completely new and novel, it may be beneficial,” Dr. Budson said.
It would be much better to do physical activity, but if the choice is sedentary activity, active cognitive activities, such as computer use, are better than TV watching, he continued.
The results of the current study are consistent with previous work showing that the type of sedentary behavior matters, according to the authors.
“Several studies have shown that TV time is associated with mortality and poor cardiometabolic biomarkers, whereas computer time is not,” they wrote.
A limitation of the study is that sedentary behaviors were self-reported via questionnaires, and there may be errors in recall.
“The use of objective methods for measuring both SB and PA are needed in future studies,” they write.
The authors receive support from the National Institutes of Health, the State of Arizona, the Arizona Department of Health Services, and the McKnight Brain Research Foundation. Neither the authors nor Dr. Budson declared relevant financial relationships.
The relationship to dementia with these activities remained strong no matter how much physical activity a person did, the authors wrote in Proceedings of the National Academy of Sciences.
Both watching TV and using a computer have been linked to increased risk of chronic disease and mortality, while exercise and physical activity (PA) have shown benefit in reducing cognitive decline, structural brain atrophy, and dementia risk in older adults, the authors wrote.
The authors said they wanted to try to understand the effects of watching TV and using computers on dementia risk, because people in the United States and Europe have been engaging in both of these activities more often.
They concluded that it’s not the sitting part of sedentary behavior (SB) that potentially has the effect on dementia but what people are doing while sitting.
Some of the results were surprising, lead author David Raichlen, PhD, professor of Human and Evolutionary Biology at University of Southern California, Los Angeles, said in an interview.
Previous literature on sedentary behaviors have documented their negative effects on a wide range of health outcomes, rather than finding positive associations, he explained.
More than 140,000 included in study
The researchers conducted their prospective cohort study using data from the United Kingdom Biobank. After excluding people younger than 60, those with prevalent dementia at the start of follow-up, and those without complete data, 146,651 participants were included.
The participants were followed from their baseline visit until they received a dementia diagnosis, died, were lost to follow-up, or were last admitted to the hospital.
TV-watching time was linked with an increased risk of incident dementia (HR [95% confidence interval] = 1.31 [1.23-1.40]), and computer use was linked with a reduced risk of incident dementia HR [95% CI] = 0.80 [0.76-0.85]).
TV’s link with higher dementia risk increased in those who had the highest use, compared with those who had the lowest use (HR [95% CI] = 1.28 [1.18-1.39].
Similarly, the link with risk reduction for dementia with computer use increased with more use.
Both medium and high computer time were associated with reduced risk of incident dementia (HR [95% CI] = 0.70 [0.64-0.76] and HR [95% CI] = 0.76 [0.70-0.83] respectively).
Dr. Raichlen pointed out that the high use of TV in this study was 4 or more hours a day and computer use – which included leisure use, not work use – had benefits on dementia risk after just half an hour.
These results remained significant after researchers adjusted for demographic, health, and lifestyle variables, including time spent on physical activity, sleeping, obesity, alcohol consumption, smoking status, diet scores, education level, body mass index, and employment type.
Physical is still better than sedentary activity
One potential reason for the different effects on dementia risk in the two activities studied, the authors write, is that sitting down to watch TV is associated with “uniquely low levels of muscle activity and energy expenditure, compared with sitting to use a computer.”
Andrew Budson, MD, chief of Cognitive & Behavioral Neurology and Associate Chief of Staff for Education for the VA Boston Healthcare System, Mass., who was not part of the study, said he thinks a more likely explanation for the study findings lies in the active versus passive tasks required in the two kinds of viewing that the authors reference.
“When we’re doing cognitive activity involving using the computer, we’re using large parts of our cortex to carry out that activity, whereas when we’re watching TV, there are probably relatively small amounts of our brain that are actually active,” Dr. Budson, author of Seven Steps to Managing Your Memory, explained in an interview.
“This is one of the first times I’ve been convinced that even when the computer activity isn’t completely new and novel, it may be beneficial,” Dr. Budson said.
It would be much better to do physical activity, but if the choice is sedentary activity, active cognitive activities, such as computer use, are better than TV watching, he continued.
The results of the current study are consistent with previous work showing that the type of sedentary behavior matters, according to the authors.
“Several studies have shown that TV time is associated with mortality and poor cardiometabolic biomarkers, whereas computer time is not,” they wrote.
A limitation of the study is that sedentary behaviors were self-reported via questionnaires, and there may be errors in recall.
“The use of objective methods for measuring both SB and PA are needed in future studies,” they write.
The authors receive support from the National Institutes of Health, the State of Arizona, the Arizona Department of Health Services, and the McKnight Brain Research Foundation. Neither the authors nor Dr. Budson declared relevant financial relationships.
FROM PROCEEDINGS OF THE NATIONAL ACADEMY OF SCIENCES
Higher rates of group B strep disease found in Black and Asian newborns
Health charities called for action to address racial health disparities after population-wide analysis by the UK Health Security Agency found that Black and Asian neonates had a significantly higher risk of early-onset group B streptococcal disease (GBS), compared with White infants.
One support group said more research was now needed to identify the cause of the disparity, and called for pregnant women to be better informed about the disease and what it could mean for them and their baby.
The study, published in Pediatrics, used UKHSA data on laboratory-confirmed infant group B streptococcal (iGBS) disease cases between Jan. 1, 2016, and Dec. 31, 2020, and were linked to hospital ethnicity records.
Cases of iGBS were defined as isolation of Streptococcus agalactiae from a normally sterile site at 0-6 days of life for early-onset iGBS and 7-90 days for late-onset disease.
Hospital data and parent-reported ethnicity
Researchers found 2,512 iGBS cases in England during the study period, 65.3% were early onset and 34.8% late onset, equivalent to 0.52 and 0.28 cases per 1000 live births respectively.
Researchers were able to link 85.6% of those to ethnicity. Among those 2,149 cases, Black infants had a 48% higher risk, and Asian infants a 40% higher risk of early onset iGBS, compared with White infants. Among those from an Asian background, the risk was 87% higher for Bangladeshi and 38% higher for Pakistani neonates.
Rates of early onset iGBS per 1,000 live births were 0.43 for White infants, 0.63 for Black infants, and 0.60 for those of Asian ethnicity.
In contrast, Indian infants had an early-onset rate of 0.47 per 1,000 live births, which was similar to White infants.
Black infants had 57% higher rates of late-onset iGBS (0.37) than White infants (0.24), the researchers reported.
The study authors highlighted previous research which found higher prevalence of group B streptococcal colonization in mothers from Black and some Asian ethnic groups, but lower prevalence in mothers from the Indian subcontinent. More research was needed to establish causes, the researchers said, including whether higher preterm birth rates in minority ethnic groups led to increased iGBS risk in neonates, or whether maternal group B streptococcal disease led to higher preterm birth rates and subsequent neonatal iGBS.
The researchers concluded: “Understanding the factors underpinning differences in rates of early-onset iGBS within south Asian groups in England may lead to new opportunities for prevention such as prioritized antenatal screening. Strategies to prevent neonatal iGBS must be tailored from high-quality quantitative and qualitative data to reach all women and protect all infants, irrespective of racial or ethnic background.”
‘Shocking but not surprising’
Commenting on the study, Edward Morris, president of the Royal College of Obstetricians and Gynaecologists, said: “This research is striking reading, and is yet another example of how far we have to go to tackle health inequalities within women’s health care.”
Philip Steer, professor emeritus at Imperial College London, said that the results were “consistent with previous reports of higher GBS carriage and higher maternal and neonatal mortality rates in minority groups” and “emphasize the importance of studying not just whether, but why, these differences exist.” He added: “We need to understand the reasons for the differences before we can design much-needed intervention to eliminate them.”
Jane Plumb, chief executive of Group B Strep Support, called the findings “shocking, but unfortunately not surprising” and said that they offered “another example of racial disparities in maternal and neonatal health.” She said: “We’re calling for all pregnant women and birthing people to be informed about GBS and its risks, so they can make empowered choices for themselves and their baby. It is also critical that trusts sign up to take part in the internationally significant [National Institute for Health and Care Research]–funded GBS3 clinical trial, designed to improve the prevention of GBS infection.”
Baroness Shaista Gohir, chief executive of the Muslim Women’s Network, said: “With significantly higher rates of group B Strep infection in Black and Asian babies, greater efforts must be made to improve awareness among pregnant women within these communities.”
A version of this article first appeared on Medscape UK.
Health charities called for action to address racial health disparities after population-wide analysis by the UK Health Security Agency found that Black and Asian neonates had a significantly higher risk of early-onset group B streptococcal disease (GBS), compared with White infants.
One support group said more research was now needed to identify the cause of the disparity, and called for pregnant women to be better informed about the disease and what it could mean for them and their baby.
The study, published in Pediatrics, used UKHSA data on laboratory-confirmed infant group B streptococcal (iGBS) disease cases between Jan. 1, 2016, and Dec. 31, 2020, and were linked to hospital ethnicity records.
Cases of iGBS were defined as isolation of Streptococcus agalactiae from a normally sterile site at 0-6 days of life for early-onset iGBS and 7-90 days for late-onset disease.
Hospital data and parent-reported ethnicity
Researchers found 2,512 iGBS cases in England during the study period, 65.3% were early onset and 34.8% late onset, equivalent to 0.52 and 0.28 cases per 1000 live births respectively.
Researchers were able to link 85.6% of those to ethnicity. Among those 2,149 cases, Black infants had a 48% higher risk, and Asian infants a 40% higher risk of early onset iGBS, compared with White infants. Among those from an Asian background, the risk was 87% higher for Bangladeshi and 38% higher for Pakistani neonates.
Rates of early onset iGBS per 1,000 live births were 0.43 for White infants, 0.63 for Black infants, and 0.60 for those of Asian ethnicity.
In contrast, Indian infants had an early-onset rate of 0.47 per 1,000 live births, which was similar to White infants.
Black infants had 57% higher rates of late-onset iGBS (0.37) than White infants (0.24), the researchers reported.
The study authors highlighted previous research which found higher prevalence of group B streptococcal colonization in mothers from Black and some Asian ethnic groups, but lower prevalence in mothers from the Indian subcontinent. More research was needed to establish causes, the researchers said, including whether higher preterm birth rates in minority ethnic groups led to increased iGBS risk in neonates, or whether maternal group B streptococcal disease led to higher preterm birth rates and subsequent neonatal iGBS.
The researchers concluded: “Understanding the factors underpinning differences in rates of early-onset iGBS within south Asian groups in England may lead to new opportunities for prevention such as prioritized antenatal screening. Strategies to prevent neonatal iGBS must be tailored from high-quality quantitative and qualitative data to reach all women and protect all infants, irrespective of racial or ethnic background.”
‘Shocking but not surprising’
Commenting on the study, Edward Morris, president of the Royal College of Obstetricians and Gynaecologists, said: “This research is striking reading, and is yet another example of how far we have to go to tackle health inequalities within women’s health care.”
Philip Steer, professor emeritus at Imperial College London, said that the results were “consistent with previous reports of higher GBS carriage and higher maternal and neonatal mortality rates in minority groups” and “emphasize the importance of studying not just whether, but why, these differences exist.” He added: “We need to understand the reasons for the differences before we can design much-needed intervention to eliminate them.”
Jane Plumb, chief executive of Group B Strep Support, called the findings “shocking, but unfortunately not surprising” and said that they offered “another example of racial disparities in maternal and neonatal health.” She said: “We’re calling for all pregnant women and birthing people to be informed about GBS and its risks, so they can make empowered choices for themselves and their baby. It is also critical that trusts sign up to take part in the internationally significant [National Institute for Health and Care Research]–funded GBS3 clinical trial, designed to improve the prevention of GBS infection.”
Baroness Shaista Gohir, chief executive of the Muslim Women’s Network, said: “With significantly higher rates of group B Strep infection in Black and Asian babies, greater efforts must be made to improve awareness among pregnant women within these communities.”
A version of this article first appeared on Medscape UK.
Health charities called for action to address racial health disparities after population-wide analysis by the UK Health Security Agency found that Black and Asian neonates had a significantly higher risk of early-onset group B streptococcal disease (GBS), compared with White infants.
One support group said more research was now needed to identify the cause of the disparity, and called for pregnant women to be better informed about the disease and what it could mean for them and their baby.
The study, published in Pediatrics, used UKHSA data on laboratory-confirmed infant group B streptococcal (iGBS) disease cases between Jan. 1, 2016, and Dec. 31, 2020, and were linked to hospital ethnicity records.
Cases of iGBS were defined as isolation of Streptococcus agalactiae from a normally sterile site at 0-6 days of life for early-onset iGBS and 7-90 days for late-onset disease.
Hospital data and parent-reported ethnicity
Researchers found 2,512 iGBS cases in England during the study period, 65.3% were early onset and 34.8% late onset, equivalent to 0.52 and 0.28 cases per 1000 live births respectively.
Researchers were able to link 85.6% of those to ethnicity. Among those 2,149 cases, Black infants had a 48% higher risk, and Asian infants a 40% higher risk of early onset iGBS, compared with White infants. Among those from an Asian background, the risk was 87% higher for Bangladeshi and 38% higher for Pakistani neonates.
Rates of early onset iGBS per 1,000 live births were 0.43 for White infants, 0.63 for Black infants, and 0.60 for those of Asian ethnicity.
In contrast, Indian infants had an early-onset rate of 0.47 per 1,000 live births, which was similar to White infants.
Black infants had 57% higher rates of late-onset iGBS (0.37) than White infants (0.24), the researchers reported.
The study authors highlighted previous research which found higher prevalence of group B streptococcal colonization in mothers from Black and some Asian ethnic groups, but lower prevalence in mothers from the Indian subcontinent. More research was needed to establish causes, the researchers said, including whether higher preterm birth rates in minority ethnic groups led to increased iGBS risk in neonates, or whether maternal group B streptococcal disease led to higher preterm birth rates and subsequent neonatal iGBS.
The researchers concluded: “Understanding the factors underpinning differences in rates of early-onset iGBS within south Asian groups in England may lead to new opportunities for prevention such as prioritized antenatal screening. Strategies to prevent neonatal iGBS must be tailored from high-quality quantitative and qualitative data to reach all women and protect all infants, irrespective of racial or ethnic background.”
‘Shocking but not surprising’
Commenting on the study, Edward Morris, president of the Royal College of Obstetricians and Gynaecologists, said: “This research is striking reading, and is yet another example of how far we have to go to tackle health inequalities within women’s health care.”
Philip Steer, professor emeritus at Imperial College London, said that the results were “consistent with previous reports of higher GBS carriage and higher maternal and neonatal mortality rates in minority groups” and “emphasize the importance of studying not just whether, but why, these differences exist.” He added: “We need to understand the reasons for the differences before we can design much-needed intervention to eliminate them.”
Jane Plumb, chief executive of Group B Strep Support, called the findings “shocking, but unfortunately not surprising” and said that they offered “another example of racial disparities in maternal and neonatal health.” She said: “We’re calling for all pregnant women and birthing people to be informed about GBS and its risks, so they can make empowered choices for themselves and their baby. It is also critical that trusts sign up to take part in the internationally significant [National Institute for Health and Care Research]–funded GBS3 clinical trial, designed to improve the prevention of GBS infection.”
Baroness Shaista Gohir, chief executive of the Muslim Women’s Network, said: “With significantly higher rates of group B Strep infection in Black and Asian babies, greater efforts must be made to improve awareness among pregnant women within these communities.”
A version of this article first appeared on Medscape UK.
FROM PEDIATRICS
Poor physician access linked with unplanned return ED visits
Difficulty in accessing a family physician is associated with a higher risk for unplanned return visits to the emergency department among patients aged 75 years and older, new data indicate.
In a prospective, observational study that included almost 2,000 patients in this age group, 16% of participants attempted to contact their family physicians before their ED visits. Of this group, more than half reported having difficulty seeing their physicians for urgent problems, more than 40% had difficulty speaking with their family physicians by telephone, and more than one-third had difficulty booking appointments for new health problems.
write study author Marc Afilalo, MD, director of the ED at Jewish General Hospital in Montreal, and colleagues. “Therefore, community-based programs that target patient education and improved access to primary care are necessary not only for reducing return visits to the ED, but also for continuity of care and patient satisfaction.”
The study was published in Canadian Family Physician.
Comorbidities increased risk
Researchers have estimated that half of Canadians aged 75 years or older use emergency services. Data indicate that the number of unplanned return visits to the ED is associated with increased functional decline and death. But the question of how patient access to primary care services affects unplanned ED return visits has received little attention, according to the investigators.
They conducted a multicenter study at three tertiary adult teaching hospitals in Montreal. From 2012 to 2014, they recruited patients aged 75 years and older who had visited the ED and who lived in their own homes or in an autonomous residence.
Investigators collected data through structured interviews, administrative databases, and medical chart reviews. They followed up with participants at 3 months by telephone. The study’s main outcome was return visit to the ED.
The researchers identified 4,577 patients and included 1,998 in their analysis. Of that total, 33% were 85 or older, 34% lived alone, and 91% had a family physician. Within 3 months, 562 patients (28%) had made 894 return visits to the ED.
Among patients aged 85 years or older (relative risk, 0.80), as well as those whose triage score was less severe (RR, 0.83) and those who were admitted during the index ED visit (RR, 0.76), rates of return ED visits were lower. Among patients who had trouble booking appointments with their family doctors to address new problems (RR, 1.19), as well as those who had made ED visits within the previous 6 months (RR, 1.47) or had a higher Charlson comorbidity index score (RR, 1.06 for every 1-unit increase), rates of return visits were higher.
Factors associated with a higher likelihood of return visits were visits to the ED in the previous 6 months (odds ratio, 2.11), increased Charlson comorbidity index score (OR, 1.41 for every 1-unit increase), and having received help from local community services (OR, 3.00).
Primary care access
The study suggests that improvements in primary care access are needed to decrease return visits to the ED, Samir Sinha, MD, DPhil, director of geriatrics at Mount Sinai and the University Health Network Hospitals in Toronto, told this news organization. Dr. Sinha was not involved in the study.
“It reminds us of the importance of having a strong primary care system,” he added. “Of this population, 91% had primary care providers. And what the paper demonstrates is that those who are having trouble accessing their primary care providers are more likely to be readmitted to an ED. We can only imagine how much worse the outcomes are for people who don’t have a primary care provider.”
Patients are frequently advised to visit the ED when they contact their primary care providers, said Mark Rosenberg, PhD, professor of geography and planning and the Canada Research Chair in Aging, Health, and Development at Queens University in Kingston, Ont., said in an interview. He noted that primary care is organized as an appointment-based system. Dr. Rosenberg did not participate in the study.
“If I were to call my primary care provider in the middle of the afternoon and say that I have got chest pains, they are going to simply tell me to go to emergency,” said Dr. Rosenberg. “It is not just older people. Many people end up in the ED because they are told to go to the ED.”
Associations with age
“The higher your Charlson comorbidity index, the more multiple, complex health issues you’re dealing with,” said Sinha. He added that the data suggest the frailty of the study population.
The association between age 85 years or older and a lower rate of a return ED visits might mean that the patient did not return to independent living after the ED visit, Dr. Rosenberg speculated. “If it’s a serious health problem, you’re more likely to end up going into long-term care at that stage, and you are not going back to living in the community in your home,” he said. “You’re likely going into some sort of transition care or alternative care.”
People aged 85 years or older who are hospitalized are more likely not to survive their index hospital admission, compared with patients who are aged 75-85 years. There would be no possibility that such patients would revisit the ED in the future, said Dr. Sinha.
Expanding primary care
The major solution to decreasing reliance on the ED lies in revamping primary health care so that it offers an expanded level of care and 24/7 access, said Dr. Rosenberg.
Providing continuity of care, identifying problems, and managing them in the community before they become urgent or require a hospitalization are priorities for primary care and will help shift away from return visits to the ED, which should be a last resort for patients, said Dr. Sinha.
Moreover, patients must be able to access primary care in various ways, be it a telephone consultation, a video consultation, or a face-to-face consultation, he added. Face-to-face consultations can take place in a provider’s office or even in a patient’s home when warranted, he said. “What we need to make sure of is that all three types of consultations are available, so that people can actually get the most appropriate care at the time they’re calling.”
The study had no external funding. Dr. Afilalo, Dr. Sinha, and Dr. Rosenberg have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Difficulty in accessing a family physician is associated with a higher risk for unplanned return visits to the emergency department among patients aged 75 years and older, new data indicate.
In a prospective, observational study that included almost 2,000 patients in this age group, 16% of participants attempted to contact their family physicians before their ED visits. Of this group, more than half reported having difficulty seeing their physicians for urgent problems, more than 40% had difficulty speaking with their family physicians by telephone, and more than one-third had difficulty booking appointments for new health problems.
write study author Marc Afilalo, MD, director of the ED at Jewish General Hospital in Montreal, and colleagues. “Therefore, community-based programs that target patient education and improved access to primary care are necessary not only for reducing return visits to the ED, but also for continuity of care and patient satisfaction.”
The study was published in Canadian Family Physician.
Comorbidities increased risk
Researchers have estimated that half of Canadians aged 75 years or older use emergency services. Data indicate that the number of unplanned return visits to the ED is associated with increased functional decline and death. But the question of how patient access to primary care services affects unplanned ED return visits has received little attention, according to the investigators.
They conducted a multicenter study at three tertiary adult teaching hospitals in Montreal. From 2012 to 2014, they recruited patients aged 75 years and older who had visited the ED and who lived in their own homes or in an autonomous residence.
Investigators collected data through structured interviews, administrative databases, and medical chart reviews. They followed up with participants at 3 months by telephone. The study’s main outcome was return visit to the ED.
The researchers identified 4,577 patients and included 1,998 in their analysis. Of that total, 33% were 85 or older, 34% lived alone, and 91% had a family physician. Within 3 months, 562 patients (28%) had made 894 return visits to the ED.
Among patients aged 85 years or older (relative risk, 0.80), as well as those whose triage score was less severe (RR, 0.83) and those who were admitted during the index ED visit (RR, 0.76), rates of return ED visits were lower. Among patients who had trouble booking appointments with their family doctors to address new problems (RR, 1.19), as well as those who had made ED visits within the previous 6 months (RR, 1.47) or had a higher Charlson comorbidity index score (RR, 1.06 for every 1-unit increase), rates of return visits were higher.
Factors associated with a higher likelihood of return visits were visits to the ED in the previous 6 months (odds ratio, 2.11), increased Charlson comorbidity index score (OR, 1.41 for every 1-unit increase), and having received help from local community services (OR, 3.00).
Primary care access
The study suggests that improvements in primary care access are needed to decrease return visits to the ED, Samir Sinha, MD, DPhil, director of geriatrics at Mount Sinai and the University Health Network Hospitals in Toronto, told this news organization. Dr. Sinha was not involved in the study.
“It reminds us of the importance of having a strong primary care system,” he added. “Of this population, 91% had primary care providers. And what the paper demonstrates is that those who are having trouble accessing their primary care providers are more likely to be readmitted to an ED. We can only imagine how much worse the outcomes are for people who don’t have a primary care provider.”
Patients are frequently advised to visit the ED when they contact their primary care providers, said Mark Rosenberg, PhD, professor of geography and planning and the Canada Research Chair in Aging, Health, and Development at Queens University in Kingston, Ont., said in an interview. He noted that primary care is organized as an appointment-based system. Dr. Rosenberg did not participate in the study.
“If I were to call my primary care provider in the middle of the afternoon and say that I have got chest pains, they are going to simply tell me to go to emergency,” said Dr. Rosenberg. “It is not just older people. Many people end up in the ED because they are told to go to the ED.”
Associations with age
“The higher your Charlson comorbidity index, the more multiple, complex health issues you’re dealing with,” said Sinha. He added that the data suggest the frailty of the study population.
The association between age 85 years or older and a lower rate of a return ED visits might mean that the patient did not return to independent living after the ED visit, Dr. Rosenberg speculated. “If it’s a serious health problem, you’re more likely to end up going into long-term care at that stage, and you are not going back to living in the community in your home,” he said. “You’re likely going into some sort of transition care or alternative care.”
People aged 85 years or older who are hospitalized are more likely not to survive their index hospital admission, compared with patients who are aged 75-85 years. There would be no possibility that such patients would revisit the ED in the future, said Dr. Sinha.
Expanding primary care
The major solution to decreasing reliance on the ED lies in revamping primary health care so that it offers an expanded level of care and 24/7 access, said Dr. Rosenberg.
Providing continuity of care, identifying problems, and managing them in the community before they become urgent or require a hospitalization are priorities for primary care and will help shift away from return visits to the ED, which should be a last resort for patients, said Dr. Sinha.
Moreover, patients must be able to access primary care in various ways, be it a telephone consultation, a video consultation, or a face-to-face consultation, he added. Face-to-face consultations can take place in a provider’s office or even in a patient’s home when warranted, he said. “What we need to make sure of is that all three types of consultations are available, so that people can actually get the most appropriate care at the time they’re calling.”
The study had no external funding. Dr. Afilalo, Dr. Sinha, and Dr. Rosenberg have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Difficulty in accessing a family physician is associated with a higher risk for unplanned return visits to the emergency department among patients aged 75 years and older, new data indicate.
In a prospective, observational study that included almost 2,000 patients in this age group, 16% of participants attempted to contact their family physicians before their ED visits. Of this group, more than half reported having difficulty seeing their physicians for urgent problems, more than 40% had difficulty speaking with their family physicians by telephone, and more than one-third had difficulty booking appointments for new health problems.
write study author Marc Afilalo, MD, director of the ED at Jewish General Hospital in Montreal, and colleagues. “Therefore, community-based programs that target patient education and improved access to primary care are necessary not only for reducing return visits to the ED, but also for continuity of care and patient satisfaction.”
The study was published in Canadian Family Physician.
Comorbidities increased risk
Researchers have estimated that half of Canadians aged 75 years or older use emergency services. Data indicate that the number of unplanned return visits to the ED is associated with increased functional decline and death. But the question of how patient access to primary care services affects unplanned ED return visits has received little attention, according to the investigators.
They conducted a multicenter study at three tertiary adult teaching hospitals in Montreal. From 2012 to 2014, they recruited patients aged 75 years and older who had visited the ED and who lived in their own homes or in an autonomous residence.
Investigators collected data through structured interviews, administrative databases, and medical chart reviews. They followed up with participants at 3 months by telephone. The study’s main outcome was return visit to the ED.
The researchers identified 4,577 patients and included 1,998 in their analysis. Of that total, 33% were 85 or older, 34% lived alone, and 91% had a family physician. Within 3 months, 562 patients (28%) had made 894 return visits to the ED.
Among patients aged 85 years or older (relative risk, 0.80), as well as those whose triage score was less severe (RR, 0.83) and those who were admitted during the index ED visit (RR, 0.76), rates of return ED visits were lower. Among patients who had trouble booking appointments with their family doctors to address new problems (RR, 1.19), as well as those who had made ED visits within the previous 6 months (RR, 1.47) or had a higher Charlson comorbidity index score (RR, 1.06 for every 1-unit increase), rates of return visits were higher.
Factors associated with a higher likelihood of return visits were visits to the ED in the previous 6 months (odds ratio, 2.11), increased Charlson comorbidity index score (OR, 1.41 for every 1-unit increase), and having received help from local community services (OR, 3.00).
Primary care access
The study suggests that improvements in primary care access are needed to decrease return visits to the ED, Samir Sinha, MD, DPhil, director of geriatrics at Mount Sinai and the University Health Network Hospitals in Toronto, told this news organization. Dr. Sinha was not involved in the study.
“It reminds us of the importance of having a strong primary care system,” he added. “Of this population, 91% had primary care providers. And what the paper demonstrates is that those who are having trouble accessing their primary care providers are more likely to be readmitted to an ED. We can only imagine how much worse the outcomes are for people who don’t have a primary care provider.”
Patients are frequently advised to visit the ED when they contact their primary care providers, said Mark Rosenberg, PhD, professor of geography and planning and the Canada Research Chair in Aging, Health, and Development at Queens University in Kingston, Ont., said in an interview. He noted that primary care is organized as an appointment-based system. Dr. Rosenberg did not participate in the study.
“If I were to call my primary care provider in the middle of the afternoon and say that I have got chest pains, they are going to simply tell me to go to emergency,” said Dr. Rosenberg. “It is not just older people. Many people end up in the ED because they are told to go to the ED.”
Associations with age
“The higher your Charlson comorbidity index, the more multiple, complex health issues you’re dealing with,” said Sinha. He added that the data suggest the frailty of the study population.
The association between age 85 years or older and a lower rate of a return ED visits might mean that the patient did not return to independent living after the ED visit, Dr. Rosenberg speculated. “If it’s a serious health problem, you’re more likely to end up going into long-term care at that stage, and you are not going back to living in the community in your home,” he said. “You’re likely going into some sort of transition care or alternative care.”
People aged 85 years or older who are hospitalized are more likely not to survive their index hospital admission, compared with patients who are aged 75-85 years. There would be no possibility that such patients would revisit the ED in the future, said Dr. Sinha.
Expanding primary care
The major solution to decreasing reliance on the ED lies in revamping primary health care so that it offers an expanded level of care and 24/7 access, said Dr. Rosenberg.
Providing continuity of care, identifying problems, and managing them in the community before they become urgent or require a hospitalization are priorities for primary care and will help shift away from return visits to the ED, which should be a last resort for patients, said Dr. Sinha.
Moreover, patients must be able to access primary care in various ways, be it a telephone consultation, a video consultation, or a face-to-face consultation, he added. Face-to-face consultations can take place in a provider’s office or even in a patient’s home when warranted, he said. “What we need to make sure of is that all three types of consultations are available, so that people can actually get the most appropriate care at the time they’re calling.”
The study had no external funding. Dr. Afilalo, Dr. Sinha, and Dr. Rosenberg have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CANADIAN FAMILY PHYSICIAN
Is it COVID or long COVID? Your organs may know
There’s little doubt long COVID is real. The federal government recognizes long COVID as a condition and said in two reports issued in August that one in five adult COVID-19 survivors have a health condition related to their illness.
COVID-19 can damage multiple organs in the body. Sometimes this damage leads to long COVID; sometimes other reasons are at play. Doctors are beginning to sort it out.
“COVID itself can actually cause prolonged illness, and we don’t really call that long COVID,” said Nisha Viswanathan, MD, a doctor at UCLA Health in Los Angeles. But if symptoms extend beyond 12 weeks, that puts patients in the realm of long COVID.
Symptoms can range from mild to severe and can keep people from resuming their normal lives and jobs. Sometimes they last for months, according to the U.S. Department of Health & Human Services.
Multiorgan damage
Lung scarring and other lung problems are common after COVID, said Leora Horwitz, MD, an internal medicine specialist at New York University. Even after a mild case, people can have breathing issues for months, a team at Johns Hopkins Medicine, Baltimore, said in an online briefing. One study published in the journal Radiology found damage in people a full year after a COVID-19 diagnosis.
Some people have persistent heart, kidney, liver, and nervous system problems after COVID-19. A study published in 2020 in JAMA Cardiology found 60% of people who had COVID-19 had ongoing signs of heart inflammation. Nearly a third of people hospitalized for COVID-19 get kidney damage that can become chronic, and some end up needing dialysis or a transplant, said C. John Sperati, MD, a kidney specialist at Johns Hopkins Medicine.
This might be, in part, because SARS-CoV-2, the virus that causes COVID-19, directly infects the cells in many organs.
Nicole Bhave, MD, a cardiologist at University of Michigan Health, Ann Arbor is concerned that COVID-19 appears to increase the risk of heart problems in some people.
“Some of the uptick may just be recognition bias, in that people with symptoms are seeking care,” she said. “But there’s definitely a biological basis by which COVID could tip people over into a new diagnosis of heart failure.”
Inflammation
Inflammation is probably a key part of the long-term effects of COVID-19.
Some people have a serious immune reaction to COVID-19 called a cytokine storm, said Nitra Aggarwal Gilotra, MD, a cardiologist at Johns Hopkins Medicine. This release of inflammation-causing molecules called cytokines is meant to attack the invading virus. But it can be so severe that it wreaks havoc on healthy tissues and organs and causes lasting damage – if patients even survive it.
In some people, inflammation can affect the heart, causing myocarditis. Myocarditis symptoms include chest pain, breathlessness, and heart palpitations. Though rare, it can be serious and can raise the risk of other heart problems, including heart failure, down the line.
Long COVID may also trigger an autoimmune condition, said Eline Luning Prak, MD, PhD, a pathologist at the Hospital of the University of Pennsylvania, Philadelphia. Long COVID can share many hallmark symptoms with autoimmune diseases, including fatigue, widespread pain, memory problems, and mood disorders.
Blood clots
Studies have shown the overcharged inflammatory response to COVID-19 can cause blood clots. This sometimes overwhelming clotting was an early hallmark of COVID-19 infection, and when clots restrict blood flow in the brain, lungs, kidneys, or limbs, they can cause long-term damage. Some can be deadly. Researchers in Sweden found patients were at risk of deep vein thrombosis – a blood clot usually in the leg – up to 3 months after infection and at higher risk of a blood clot in the lung, called pulmonary embolism, for as long as 3 months.
Viral reservoirs
The virus itself may also linger in a patient’s body, causing continued symptoms and, potentially, new flare-ups. Zoe Swank, PhD, of Harvard Medical School, Boston, and colleagues reported in a preprint study that they found pieces of the SARS-CoV-2 virus in the blood of most patients with long COVID symptoms they tested – some as long as a year after infection. The study has not yet been peer reviewed.
Another team found evidence of the virus in stool up to 7 months later, which suggests the virus hides out in the gut. Other early studies have found bits of viral RNA in the appendix, breast tissue, heart, eyes, and brain.
Diabetes
Diabetes is a risk factor for getting severe COVID-19, and multiple studies have shown people can get diabetes both while battling infection and afterward. One study of veterans, published in The Lancet Diabetes and Endocrinology, found COVID-19 survivors were about 40% more likely to get diabetes over the next year.
There are a few ways this might happen. Insulin-producing cells in the pancreas have SARS-CoV-2 receptors – a type of molecular doorway the coronavirus can attach to. Damage to these cells could make the body less able to produce insulin, which in turn can lead to diabetes. The virus could also disrupt the balance in the body or cause inflammation that leads to insulin resistance, which can develop into diabetes, Ziad Al-Aly, MD, of the Veterans Affairs St. Louis Health Care System, and colleagues wrote.
Nervous system issues
People who get COVID-19 are also more vulnerable to postural orthostatic tachycardia syndrome (POTS). This affects what’s known as the autonomic nervous system, which regulates blood circulation, and includes those things that happen in your body without your having to think about them, like breathing, heartbeat, and digestion. POTS can cause common long COVID neurologic symptoms, including headaches, fatigue, brain fog, insomnia, and problems thinking and concentrating. “This was a known condition prior to COVID, but it was incredibly rare,” said Dr. Viswanathan. “After COVID, I’ve seen it with increasing frequency.”
Long-term outlook
Lasting issues after COVID-19 are much more likely after a moderate or severe infection. Still, plenty of people are battling them even after a mild illness. “As for why, that’s the billion-dollar question,” said Dr. Horwitz. “It’s well known that viral infections can cause long-term dysregulation. Why that is, we really just don’t know.”
Whether it’s virus hiding out in the body, long-term organ damage, or an autoimmune reaction likely differs from person to person. “I’m believing, increasingly, that it’s a combination of all of these, just based on how different patients are responding to different medications,” said Dr. Viswanathan. “One patient will respond to something beautifully, and another patient won’t at all.”
But it’s clear a significant number of people are facing long-term health struggles because of COVID-19, which has infected at least 580 million people globally and 92 million – likely many more – in the United States, according to Johns Hopkins University.
Even a small increased risk of conditions like heart disease or diabetes translates to a huge number of people, Dr. Horwitz said. “If even 1% of people getting COVID have long-term symptoms, that’s a major public health crisis, because that’s 1% of pretty much everybody in the country.”
A version of this article first appeared on WebMD.com.
There’s little doubt long COVID is real. The federal government recognizes long COVID as a condition and said in two reports issued in August that one in five adult COVID-19 survivors have a health condition related to their illness.
COVID-19 can damage multiple organs in the body. Sometimes this damage leads to long COVID; sometimes other reasons are at play. Doctors are beginning to sort it out.
“COVID itself can actually cause prolonged illness, and we don’t really call that long COVID,” said Nisha Viswanathan, MD, a doctor at UCLA Health in Los Angeles. But if symptoms extend beyond 12 weeks, that puts patients in the realm of long COVID.
Symptoms can range from mild to severe and can keep people from resuming their normal lives and jobs. Sometimes they last for months, according to the U.S. Department of Health & Human Services.
Multiorgan damage
Lung scarring and other lung problems are common after COVID, said Leora Horwitz, MD, an internal medicine specialist at New York University. Even after a mild case, people can have breathing issues for months, a team at Johns Hopkins Medicine, Baltimore, said in an online briefing. One study published in the journal Radiology found damage in people a full year after a COVID-19 diagnosis.
Some people have persistent heart, kidney, liver, and nervous system problems after COVID-19. A study published in 2020 in JAMA Cardiology found 60% of people who had COVID-19 had ongoing signs of heart inflammation. Nearly a third of people hospitalized for COVID-19 get kidney damage that can become chronic, and some end up needing dialysis or a transplant, said C. John Sperati, MD, a kidney specialist at Johns Hopkins Medicine.
This might be, in part, because SARS-CoV-2, the virus that causes COVID-19, directly infects the cells in many organs.
Nicole Bhave, MD, a cardiologist at University of Michigan Health, Ann Arbor is concerned that COVID-19 appears to increase the risk of heart problems in some people.
“Some of the uptick may just be recognition bias, in that people with symptoms are seeking care,” she said. “But there’s definitely a biological basis by which COVID could tip people over into a new diagnosis of heart failure.”
Inflammation
Inflammation is probably a key part of the long-term effects of COVID-19.
Some people have a serious immune reaction to COVID-19 called a cytokine storm, said Nitra Aggarwal Gilotra, MD, a cardiologist at Johns Hopkins Medicine. This release of inflammation-causing molecules called cytokines is meant to attack the invading virus. But it can be so severe that it wreaks havoc on healthy tissues and organs and causes lasting damage – if patients even survive it.
In some people, inflammation can affect the heart, causing myocarditis. Myocarditis symptoms include chest pain, breathlessness, and heart palpitations. Though rare, it can be serious and can raise the risk of other heart problems, including heart failure, down the line.
Long COVID may also trigger an autoimmune condition, said Eline Luning Prak, MD, PhD, a pathologist at the Hospital of the University of Pennsylvania, Philadelphia. Long COVID can share many hallmark symptoms with autoimmune diseases, including fatigue, widespread pain, memory problems, and mood disorders.
Blood clots
Studies have shown the overcharged inflammatory response to COVID-19 can cause blood clots. This sometimes overwhelming clotting was an early hallmark of COVID-19 infection, and when clots restrict blood flow in the brain, lungs, kidneys, or limbs, they can cause long-term damage. Some can be deadly. Researchers in Sweden found patients were at risk of deep vein thrombosis – a blood clot usually in the leg – up to 3 months after infection and at higher risk of a blood clot in the lung, called pulmonary embolism, for as long as 3 months.
Viral reservoirs
The virus itself may also linger in a patient’s body, causing continued symptoms and, potentially, new flare-ups. Zoe Swank, PhD, of Harvard Medical School, Boston, and colleagues reported in a preprint study that they found pieces of the SARS-CoV-2 virus in the blood of most patients with long COVID symptoms they tested – some as long as a year after infection. The study has not yet been peer reviewed.
Another team found evidence of the virus in stool up to 7 months later, which suggests the virus hides out in the gut. Other early studies have found bits of viral RNA in the appendix, breast tissue, heart, eyes, and brain.
Diabetes
Diabetes is a risk factor for getting severe COVID-19, and multiple studies have shown people can get diabetes both while battling infection and afterward. One study of veterans, published in The Lancet Diabetes and Endocrinology, found COVID-19 survivors were about 40% more likely to get diabetes over the next year.
There are a few ways this might happen. Insulin-producing cells in the pancreas have SARS-CoV-2 receptors – a type of molecular doorway the coronavirus can attach to. Damage to these cells could make the body less able to produce insulin, which in turn can lead to diabetes. The virus could also disrupt the balance in the body or cause inflammation that leads to insulin resistance, which can develop into diabetes, Ziad Al-Aly, MD, of the Veterans Affairs St. Louis Health Care System, and colleagues wrote.
Nervous system issues
People who get COVID-19 are also more vulnerable to postural orthostatic tachycardia syndrome (POTS). This affects what’s known as the autonomic nervous system, which regulates blood circulation, and includes those things that happen in your body without your having to think about them, like breathing, heartbeat, and digestion. POTS can cause common long COVID neurologic symptoms, including headaches, fatigue, brain fog, insomnia, and problems thinking and concentrating. “This was a known condition prior to COVID, but it was incredibly rare,” said Dr. Viswanathan. “After COVID, I’ve seen it with increasing frequency.”
Long-term outlook
Lasting issues after COVID-19 are much more likely after a moderate or severe infection. Still, plenty of people are battling them even after a mild illness. “As for why, that’s the billion-dollar question,” said Dr. Horwitz. “It’s well known that viral infections can cause long-term dysregulation. Why that is, we really just don’t know.”
Whether it’s virus hiding out in the body, long-term organ damage, or an autoimmune reaction likely differs from person to person. “I’m believing, increasingly, that it’s a combination of all of these, just based on how different patients are responding to different medications,” said Dr. Viswanathan. “One patient will respond to something beautifully, and another patient won’t at all.”
But it’s clear a significant number of people are facing long-term health struggles because of COVID-19, which has infected at least 580 million people globally and 92 million – likely many more – in the United States, according to Johns Hopkins University.
Even a small increased risk of conditions like heart disease or diabetes translates to a huge number of people, Dr. Horwitz said. “If even 1% of people getting COVID have long-term symptoms, that’s a major public health crisis, because that’s 1% of pretty much everybody in the country.”
A version of this article first appeared on WebMD.com.
There’s little doubt long COVID is real. The federal government recognizes long COVID as a condition and said in two reports issued in August that one in five adult COVID-19 survivors have a health condition related to their illness.
COVID-19 can damage multiple organs in the body. Sometimes this damage leads to long COVID; sometimes other reasons are at play. Doctors are beginning to sort it out.
“COVID itself can actually cause prolonged illness, and we don’t really call that long COVID,” said Nisha Viswanathan, MD, a doctor at UCLA Health in Los Angeles. But if symptoms extend beyond 12 weeks, that puts patients in the realm of long COVID.
Symptoms can range from mild to severe and can keep people from resuming their normal lives and jobs. Sometimes they last for months, according to the U.S. Department of Health & Human Services.
Multiorgan damage
Lung scarring and other lung problems are common after COVID, said Leora Horwitz, MD, an internal medicine specialist at New York University. Even after a mild case, people can have breathing issues for months, a team at Johns Hopkins Medicine, Baltimore, said in an online briefing. One study published in the journal Radiology found damage in people a full year after a COVID-19 diagnosis.
Some people have persistent heart, kidney, liver, and nervous system problems after COVID-19. A study published in 2020 in JAMA Cardiology found 60% of people who had COVID-19 had ongoing signs of heart inflammation. Nearly a third of people hospitalized for COVID-19 get kidney damage that can become chronic, and some end up needing dialysis or a transplant, said C. John Sperati, MD, a kidney specialist at Johns Hopkins Medicine.
This might be, in part, because SARS-CoV-2, the virus that causes COVID-19, directly infects the cells in many organs.
Nicole Bhave, MD, a cardiologist at University of Michigan Health, Ann Arbor is concerned that COVID-19 appears to increase the risk of heart problems in some people.
“Some of the uptick may just be recognition bias, in that people with symptoms are seeking care,” she said. “But there’s definitely a biological basis by which COVID could tip people over into a new diagnosis of heart failure.”
Inflammation
Inflammation is probably a key part of the long-term effects of COVID-19.
Some people have a serious immune reaction to COVID-19 called a cytokine storm, said Nitra Aggarwal Gilotra, MD, a cardiologist at Johns Hopkins Medicine. This release of inflammation-causing molecules called cytokines is meant to attack the invading virus. But it can be so severe that it wreaks havoc on healthy tissues and organs and causes lasting damage – if patients even survive it.
In some people, inflammation can affect the heart, causing myocarditis. Myocarditis symptoms include chest pain, breathlessness, and heart palpitations. Though rare, it can be serious and can raise the risk of other heart problems, including heart failure, down the line.
Long COVID may also trigger an autoimmune condition, said Eline Luning Prak, MD, PhD, a pathologist at the Hospital of the University of Pennsylvania, Philadelphia. Long COVID can share many hallmark symptoms with autoimmune diseases, including fatigue, widespread pain, memory problems, and mood disorders.
Blood clots
Studies have shown the overcharged inflammatory response to COVID-19 can cause blood clots. This sometimes overwhelming clotting was an early hallmark of COVID-19 infection, and when clots restrict blood flow in the brain, lungs, kidneys, or limbs, they can cause long-term damage. Some can be deadly. Researchers in Sweden found patients were at risk of deep vein thrombosis – a blood clot usually in the leg – up to 3 months after infection and at higher risk of a blood clot in the lung, called pulmonary embolism, for as long as 3 months.
Viral reservoirs
The virus itself may also linger in a patient’s body, causing continued symptoms and, potentially, new flare-ups. Zoe Swank, PhD, of Harvard Medical School, Boston, and colleagues reported in a preprint study that they found pieces of the SARS-CoV-2 virus in the blood of most patients with long COVID symptoms they tested – some as long as a year after infection. The study has not yet been peer reviewed.
Another team found evidence of the virus in stool up to 7 months later, which suggests the virus hides out in the gut. Other early studies have found bits of viral RNA in the appendix, breast tissue, heart, eyes, and brain.
Diabetes
Diabetes is a risk factor for getting severe COVID-19, and multiple studies have shown people can get diabetes both while battling infection and afterward. One study of veterans, published in The Lancet Diabetes and Endocrinology, found COVID-19 survivors were about 40% more likely to get diabetes over the next year.
There are a few ways this might happen. Insulin-producing cells in the pancreas have SARS-CoV-2 receptors – a type of molecular doorway the coronavirus can attach to. Damage to these cells could make the body less able to produce insulin, which in turn can lead to diabetes. The virus could also disrupt the balance in the body or cause inflammation that leads to insulin resistance, which can develop into diabetes, Ziad Al-Aly, MD, of the Veterans Affairs St. Louis Health Care System, and colleagues wrote.
Nervous system issues
People who get COVID-19 are also more vulnerable to postural orthostatic tachycardia syndrome (POTS). This affects what’s known as the autonomic nervous system, which regulates blood circulation, and includes those things that happen in your body without your having to think about them, like breathing, heartbeat, and digestion. POTS can cause common long COVID neurologic symptoms, including headaches, fatigue, brain fog, insomnia, and problems thinking and concentrating. “This was a known condition prior to COVID, but it was incredibly rare,” said Dr. Viswanathan. “After COVID, I’ve seen it with increasing frequency.”
Long-term outlook
Lasting issues after COVID-19 are much more likely after a moderate or severe infection. Still, plenty of people are battling them even after a mild illness. “As for why, that’s the billion-dollar question,” said Dr. Horwitz. “It’s well known that viral infections can cause long-term dysregulation. Why that is, we really just don’t know.”
Whether it’s virus hiding out in the body, long-term organ damage, or an autoimmune reaction likely differs from person to person. “I’m believing, increasingly, that it’s a combination of all of these, just based on how different patients are responding to different medications,” said Dr. Viswanathan. “One patient will respond to something beautifully, and another patient won’t at all.”
But it’s clear a significant number of people are facing long-term health struggles because of COVID-19, which has infected at least 580 million people globally and 92 million – likely many more – in the United States, according to Johns Hopkins University.
Even a small increased risk of conditions like heart disease or diabetes translates to a huge number of people, Dr. Horwitz said. “If even 1% of people getting COVID have long-term symptoms, that’s a major public health crisis, because that’s 1% of pretty much everybody in the country.”
A version of this article first appeared on WebMD.com.
Most people with Omicron don’t know they’re infected
Most people with Omicron likely don’t know it.
That’s according to a study in JAMA Network Open, which says 56% of people who have the Omicron variant of the coronavirus are unaware of their infection.
And it has an upside and a downside, depending on how you look at it, according to Time magazine.
“It’s good news, in some ways, since ) in vaccinated people,” Time says. “The downside is that many people are likely spreading the virus unintentionally.”
The study looked at 210 hospital patients and employees in the Los Angeles area. More than half who tested positive didn’t know it – because they had no symptoms, or they assumed they merely had a cold or allergies.
“The findings support early data from around the world suggesting that throughout the pandemic, anywhere from 25% to 40% of SARS-CoV-2 infections have been asymptomatic, which presents challenges for public health officials trying to control the spread of the virus,” Time reports.
The study found that awareness of infection rose after at-home tests became available this year. About three-quarters of people in January and February didn’t know their status, for example.
“Findings of this study suggest that low rates of Omicron variant infection awareness may be a key contributor to rapid transmission of the virus within communities,” the authors wrote. “Given that unawareness of active infection precludes self-initiated interventions, such as testing and self-isolation, even modest levels of undiagnosed infection can contribute to substantial population-level transmission.”
A version of this article first appeared on WebMD.com.
Most people with Omicron likely don’t know it.
That’s according to a study in JAMA Network Open, which says 56% of people who have the Omicron variant of the coronavirus are unaware of their infection.
And it has an upside and a downside, depending on how you look at it, according to Time magazine.
“It’s good news, in some ways, since ) in vaccinated people,” Time says. “The downside is that many people are likely spreading the virus unintentionally.”
The study looked at 210 hospital patients and employees in the Los Angeles area. More than half who tested positive didn’t know it – because they had no symptoms, or they assumed they merely had a cold or allergies.
“The findings support early data from around the world suggesting that throughout the pandemic, anywhere from 25% to 40% of SARS-CoV-2 infections have been asymptomatic, which presents challenges for public health officials trying to control the spread of the virus,” Time reports.
The study found that awareness of infection rose after at-home tests became available this year. About three-quarters of people in January and February didn’t know their status, for example.
“Findings of this study suggest that low rates of Omicron variant infection awareness may be a key contributor to rapid transmission of the virus within communities,” the authors wrote. “Given that unawareness of active infection precludes self-initiated interventions, such as testing and self-isolation, even modest levels of undiagnosed infection can contribute to substantial population-level transmission.”
A version of this article first appeared on WebMD.com.
Most people with Omicron likely don’t know it.
That’s according to a study in JAMA Network Open, which says 56% of people who have the Omicron variant of the coronavirus are unaware of their infection.
And it has an upside and a downside, depending on how you look at it, according to Time magazine.
“It’s good news, in some ways, since ) in vaccinated people,” Time says. “The downside is that many people are likely spreading the virus unintentionally.”
The study looked at 210 hospital patients and employees in the Los Angeles area. More than half who tested positive didn’t know it – because they had no symptoms, or they assumed they merely had a cold or allergies.
“The findings support early data from around the world suggesting that throughout the pandemic, anywhere from 25% to 40% of SARS-CoV-2 infections have been asymptomatic, which presents challenges for public health officials trying to control the spread of the virus,” Time reports.
The study found that awareness of infection rose after at-home tests became available this year. About three-quarters of people in January and February didn’t know their status, for example.
“Findings of this study suggest that low rates of Omicron variant infection awareness may be a key contributor to rapid transmission of the virus within communities,” the authors wrote. “Given that unawareness of active infection precludes self-initiated interventions, such as testing and self-isolation, even modest levels of undiagnosed infection can contribute to substantial population-level transmission.”
A version of this article first appeared on WebMD.com.
FROM JAMA NETWORK OPEN
Words, now actions: How medical associations try to fulfill pledges to combat racism in health care
– from health care outcomes, from the level and quality of patient treatment, from their own memberships. How have those pronouncements translated into programs that could have, or even have had, positive impacts?
For this article, this news organization asked several associations about tangible actions behind their vows to combat racism in health care. Meanwhile, a recent Medscape report focused on the degree to which physicians prioritize racial disparities as a leading social issue.
American Academy of Family Physicians
The American Academy of Family Physicians’ approach is to integrate diversity, equity, and inclusion (DEI) efforts into all existing and new projects rather than tackle racial disparities as a discrete problem.
“Our policies, our advocacy efforts, everything our commissions and staff do ... is through a lens of diversity, equity, and inclusiveness,” said AAFP Board Chair Ada D. Stewart, MD, FAAP.
That lens is ground by a DEI center the AAFP created in 2017. Run by AAFP staff, members, and chapters, the center focuses on five areas: policy, education and training, practice, diversifying the workplace, and strategic partnerships.
The center has established a special project called EveryONE to provide AAFP members with relevant research, policy templates, and other resources to address patient needs. One example is the Neighborhood Navigator, an online tool that shows food, housing, transportation, and other needs in a patient’s neighborhood.
Meanwhile, the DEI center has created training programs for AAFP members on topics like unconscious and implicit racial biases. And the AAFP has implemented several relevant governing policies regarding pushes to improve childbirth conditions and limit race-based treatment, among other areas.
In January, the AAFP established a new DEI commission for family medicine to set the academy’s agenda on racial issues moving forward. “We only had 10 physician positions available on the commission, and over 100 individuals applied, which gave us comfort that we were going in the right direction,” Dr. Stewart said.
Association of American Medical Colleges
The Association of American Medical Colleges, which represents nearly 600 U.S. and Canadian medical schools and teaching hospitals, has a “longstanding” focus on racial equity, said Philip Alberti, founder of the AAMC Center for Health Justice. However, in 2020 that focus became more detailed and layered.
Those layers include:
- Encouraging self-reflection by members on how personal racial biases and stereotypes can lead to systemic racism in health care.
- Working on the AAMC organizational structure. Priorities range from hiring a consultant to help guide antiracism efforts, to establishing a DEI council and advisors, to regularly seeking input from staff. In 2021, the AAMC launched a Center for Health Justice to work more closely with communities.
- Ramping up collaboration with national and local academic medicine organizations and partners. As one example, the AAMC and American Medical Association released a guide for physicians and health care professionals on language that could be interpreted as racist or disrespectful.
- Continuing to be outspoken about racial disparities in health care in society generally.
Meanwhile, the AAMC is supporting more specific, localized health equity efforts in cities such as Cincinnati and Boston.
Cincinnati Children’s Hospital research has found that children in poor neighborhoods are five times more likely to need hospital stays. AAMC members have helped identify “hot spots” for social needs among children and focused specifically on two neighborhoods in the city. The initiative has roped in partnerships with community and social service organizations as well as health care providers, and proponents say the number of child hospital stays in those neighborhoods has dropped by 20%.
Boston Medical Center researchers learned that Black and Latino patients experiencing problems with heart failure were less likely to be referred to a cardiologist. AAMC members assisted with a program to encourage physicians to make medically necessary referrals more often.
National Health Council
The National Health Council, an umbrella association of health organizations, similarly has made a “commitment, not just around policy work but anytime and anything the NHC is doing, to build around trying to identify and solve issues of health equity,” CEO Randall Rutta said.
The NHC has identified four strategic policy areas including race and in 2021 issued a statement signed by 45 other health care organizations vowing to take on systemic racism and advance equity, through public policy and law.
In relation to policy, Mr. Rutta said his organization is lobbying Congress and federal agencies to diversify clinical trials.
“We want to make sure that clinical trials are inclusive of people from different racial and ethnic groups, in order to understand how [they are] affected by a particular condition,” he said. “As you would imagine, some conditions hit certain groups harder than others for genetic or other reasons, or it may just be a reflection of other disparities that occur across health care.”
The organization has issued suggestions for policy change in the Food and Drug Administration’s clinical trial policy and separately targeted telemedicine policy to promote equity and greater patient access. For example, one initiative aims to ensure patients’ privacy and civil rights as telemedicine’s popularity grows after the COVID-19 pandemic. The NHC presented the initiative in a congressional briefing last year.
American Public Health Association
The American Public Health Association says it started focusing on racial disparities in health care in 2015, following a series of racially fueled violent acts. The APHA started with a four-part webinar series on racism in health (more than 10,000 live participants and 40,000 replays to date).
Shortly afterward, then-APHA President Camara Jones, MD, MPH, PhD, launched a national campaign encouraging APHA members, affiliates, and partners to name and address racism as a determinant of health.
More recently in 2021, the APHA adopted a “Truth, Racial Healing & Transformation” guiding framework and “Healing Through Policy” initiative that offer local leaders policy templates and best practices.
“We have identified a suite of policies that have actually been implemented successfully and are advancing racial equity,” said Regina Davis Moss, APHA’s associate executive director of health policy and practice. “You can’t advance health without having a policy that supports it.”
Montgomery County, Md., is one community that has used the framework (for racial equity training of county employees). Leaders in Evanston, Ill., also used it in crafting a resolution to end structural racism in the city.
A version of this article first appeared on Medscape.com.
– from health care outcomes, from the level and quality of patient treatment, from their own memberships. How have those pronouncements translated into programs that could have, or even have had, positive impacts?
For this article, this news organization asked several associations about tangible actions behind their vows to combat racism in health care. Meanwhile, a recent Medscape report focused on the degree to which physicians prioritize racial disparities as a leading social issue.
American Academy of Family Physicians
The American Academy of Family Physicians’ approach is to integrate diversity, equity, and inclusion (DEI) efforts into all existing and new projects rather than tackle racial disparities as a discrete problem.
“Our policies, our advocacy efforts, everything our commissions and staff do ... is through a lens of diversity, equity, and inclusiveness,” said AAFP Board Chair Ada D. Stewart, MD, FAAP.
That lens is ground by a DEI center the AAFP created in 2017. Run by AAFP staff, members, and chapters, the center focuses on five areas: policy, education and training, practice, diversifying the workplace, and strategic partnerships.
The center has established a special project called EveryONE to provide AAFP members with relevant research, policy templates, and other resources to address patient needs. One example is the Neighborhood Navigator, an online tool that shows food, housing, transportation, and other needs in a patient’s neighborhood.
Meanwhile, the DEI center has created training programs for AAFP members on topics like unconscious and implicit racial biases. And the AAFP has implemented several relevant governing policies regarding pushes to improve childbirth conditions and limit race-based treatment, among other areas.
In January, the AAFP established a new DEI commission for family medicine to set the academy’s agenda on racial issues moving forward. “We only had 10 physician positions available on the commission, and over 100 individuals applied, which gave us comfort that we were going in the right direction,” Dr. Stewart said.
Association of American Medical Colleges
The Association of American Medical Colleges, which represents nearly 600 U.S. and Canadian medical schools and teaching hospitals, has a “longstanding” focus on racial equity, said Philip Alberti, founder of the AAMC Center for Health Justice. However, in 2020 that focus became more detailed and layered.
Those layers include:
- Encouraging self-reflection by members on how personal racial biases and stereotypes can lead to systemic racism in health care.
- Working on the AAMC organizational structure. Priorities range from hiring a consultant to help guide antiracism efforts, to establishing a DEI council and advisors, to regularly seeking input from staff. In 2021, the AAMC launched a Center for Health Justice to work more closely with communities.
- Ramping up collaboration with national and local academic medicine organizations and partners. As one example, the AAMC and American Medical Association released a guide for physicians and health care professionals on language that could be interpreted as racist or disrespectful.
- Continuing to be outspoken about racial disparities in health care in society generally.
Meanwhile, the AAMC is supporting more specific, localized health equity efforts in cities such as Cincinnati and Boston.
Cincinnati Children’s Hospital research has found that children in poor neighborhoods are five times more likely to need hospital stays. AAMC members have helped identify “hot spots” for social needs among children and focused specifically on two neighborhoods in the city. The initiative has roped in partnerships with community and social service organizations as well as health care providers, and proponents say the number of child hospital stays in those neighborhoods has dropped by 20%.
Boston Medical Center researchers learned that Black and Latino patients experiencing problems with heart failure were less likely to be referred to a cardiologist. AAMC members assisted with a program to encourage physicians to make medically necessary referrals more often.
National Health Council
The National Health Council, an umbrella association of health organizations, similarly has made a “commitment, not just around policy work but anytime and anything the NHC is doing, to build around trying to identify and solve issues of health equity,” CEO Randall Rutta said.
The NHC has identified four strategic policy areas including race and in 2021 issued a statement signed by 45 other health care organizations vowing to take on systemic racism and advance equity, through public policy and law.
In relation to policy, Mr. Rutta said his organization is lobbying Congress and federal agencies to diversify clinical trials.
“We want to make sure that clinical trials are inclusive of people from different racial and ethnic groups, in order to understand how [they are] affected by a particular condition,” he said. “As you would imagine, some conditions hit certain groups harder than others for genetic or other reasons, or it may just be a reflection of other disparities that occur across health care.”
The organization has issued suggestions for policy change in the Food and Drug Administration’s clinical trial policy and separately targeted telemedicine policy to promote equity and greater patient access. For example, one initiative aims to ensure patients’ privacy and civil rights as telemedicine’s popularity grows after the COVID-19 pandemic. The NHC presented the initiative in a congressional briefing last year.
American Public Health Association
The American Public Health Association says it started focusing on racial disparities in health care in 2015, following a series of racially fueled violent acts. The APHA started with a four-part webinar series on racism in health (more than 10,000 live participants and 40,000 replays to date).
Shortly afterward, then-APHA President Camara Jones, MD, MPH, PhD, launched a national campaign encouraging APHA members, affiliates, and partners to name and address racism as a determinant of health.
More recently in 2021, the APHA adopted a “Truth, Racial Healing & Transformation” guiding framework and “Healing Through Policy” initiative that offer local leaders policy templates and best practices.
“We have identified a suite of policies that have actually been implemented successfully and are advancing racial equity,” said Regina Davis Moss, APHA’s associate executive director of health policy and practice. “You can’t advance health without having a policy that supports it.”
Montgomery County, Md., is one community that has used the framework (for racial equity training of county employees). Leaders in Evanston, Ill., also used it in crafting a resolution to end structural racism in the city.
A version of this article first appeared on Medscape.com.
– from health care outcomes, from the level and quality of patient treatment, from their own memberships. How have those pronouncements translated into programs that could have, or even have had, positive impacts?
For this article, this news organization asked several associations about tangible actions behind their vows to combat racism in health care. Meanwhile, a recent Medscape report focused on the degree to which physicians prioritize racial disparities as a leading social issue.
American Academy of Family Physicians
The American Academy of Family Physicians’ approach is to integrate diversity, equity, and inclusion (DEI) efforts into all existing and new projects rather than tackle racial disparities as a discrete problem.
“Our policies, our advocacy efforts, everything our commissions and staff do ... is through a lens of diversity, equity, and inclusiveness,” said AAFP Board Chair Ada D. Stewart, MD, FAAP.
That lens is ground by a DEI center the AAFP created in 2017. Run by AAFP staff, members, and chapters, the center focuses on five areas: policy, education and training, practice, diversifying the workplace, and strategic partnerships.
The center has established a special project called EveryONE to provide AAFP members with relevant research, policy templates, and other resources to address patient needs. One example is the Neighborhood Navigator, an online tool that shows food, housing, transportation, and other needs in a patient’s neighborhood.
Meanwhile, the DEI center has created training programs for AAFP members on topics like unconscious and implicit racial biases. And the AAFP has implemented several relevant governing policies regarding pushes to improve childbirth conditions and limit race-based treatment, among other areas.
In January, the AAFP established a new DEI commission for family medicine to set the academy’s agenda on racial issues moving forward. “We only had 10 physician positions available on the commission, and over 100 individuals applied, which gave us comfort that we were going in the right direction,” Dr. Stewart said.
Association of American Medical Colleges
The Association of American Medical Colleges, which represents nearly 600 U.S. and Canadian medical schools and teaching hospitals, has a “longstanding” focus on racial equity, said Philip Alberti, founder of the AAMC Center for Health Justice. However, in 2020 that focus became more detailed and layered.
Those layers include:
- Encouraging self-reflection by members on how personal racial biases and stereotypes can lead to systemic racism in health care.
- Working on the AAMC organizational structure. Priorities range from hiring a consultant to help guide antiracism efforts, to establishing a DEI council and advisors, to regularly seeking input from staff. In 2021, the AAMC launched a Center for Health Justice to work more closely with communities.
- Ramping up collaboration with national and local academic medicine organizations and partners. As one example, the AAMC and American Medical Association released a guide for physicians and health care professionals on language that could be interpreted as racist or disrespectful.
- Continuing to be outspoken about racial disparities in health care in society generally.
Meanwhile, the AAMC is supporting more specific, localized health equity efforts in cities such as Cincinnati and Boston.
Cincinnati Children’s Hospital research has found that children in poor neighborhoods are five times more likely to need hospital stays. AAMC members have helped identify “hot spots” for social needs among children and focused specifically on two neighborhoods in the city. The initiative has roped in partnerships with community and social service organizations as well as health care providers, and proponents say the number of child hospital stays in those neighborhoods has dropped by 20%.
Boston Medical Center researchers learned that Black and Latino patients experiencing problems with heart failure were less likely to be referred to a cardiologist. AAMC members assisted with a program to encourage physicians to make medically necessary referrals more often.
National Health Council
The National Health Council, an umbrella association of health organizations, similarly has made a “commitment, not just around policy work but anytime and anything the NHC is doing, to build around trying to identify and solve issues of health equity,” CEO Randall Rutta said.
The NHC has identified four strategic policy areas including race and in 2021 issued a statement signed by 45 other health care organizations vowing to take on systemic racism and advance equity, through public policy and law.
In relation to policy, Mr. Rutta said his organization is lobbying Congress and federal agencies to diversify clinical trials.
“We want to make sure that clinical trials are inclusive of people from different racial and ethnic groups, in order to understand how [they are] affected by a particular condition,” he said. “As you would imagine, some conditions hit certain groups harder than others for genetic or other reasons, or it may just be a reflection of other disparities that occur across health care.”
The organization has issued suggestions for policy change in the Food and Drug Administration’s clinical trial policy and separately targeted telemedicine policy to promote equity and greater patient access. For example, one initiative aims to ensure patients’ privacy and civil rights as telemedicine’s popularity grows after the COVID-19 pandemic. The NHC presented the initiative in a congressional briefing last year.
American Public Health Association
The American Public Health Association says it started focusing on racial disparities in health care in 2015, following a series of racially fueled violent acts. The APHA started with a four-part webinar series on racism in health (more than 10,000 live participants and 40,000 replays to date).
Shortly afterward, then-APHA President Camara Jones, MD, MPH, PhD, launched a national campaign encouraging APHA members, affiliates, and partners to name and address racism as a determinant of health.
More recently in 2021, the APHA adopted a “Truth, Racial Healing & Transformation” guiding framework and “Healing Through Policy” initiative that offer local leaders policy templates and best practices.
“We have identified a suite of policies that have actually been implemented successfully and are advancing racial equity,” said Regina Davis Moss, APHA’s associate executive director of health policy and practice. “You can’t advance health without having a policy that supports it.”
Montgomery County, Md., is one community that has used the framework (for racial equity training of county employees). Leaders in Evanston, Ill., also used it in crafting a resolution to end structural racism in the city.
A version of this article first appeared on Medscape.com.