User login
News and Views that Matter to Pediatricians
The leading independent newspaper covering news and commentary in pediatrics.
‘Reassuring’ findings for second-generation antipsychotics during pregnancy
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.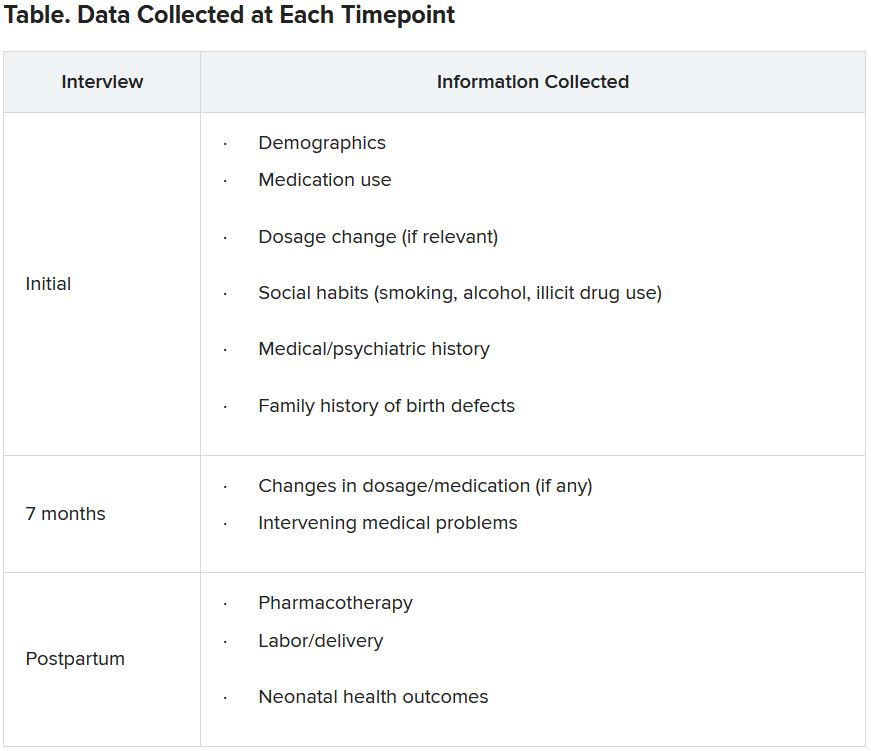
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.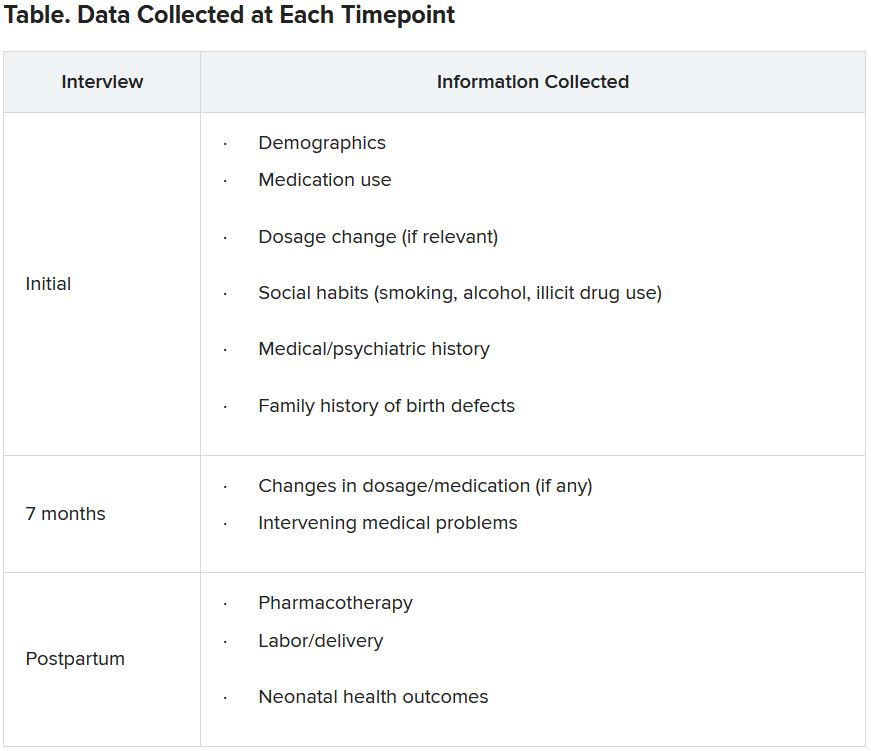
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.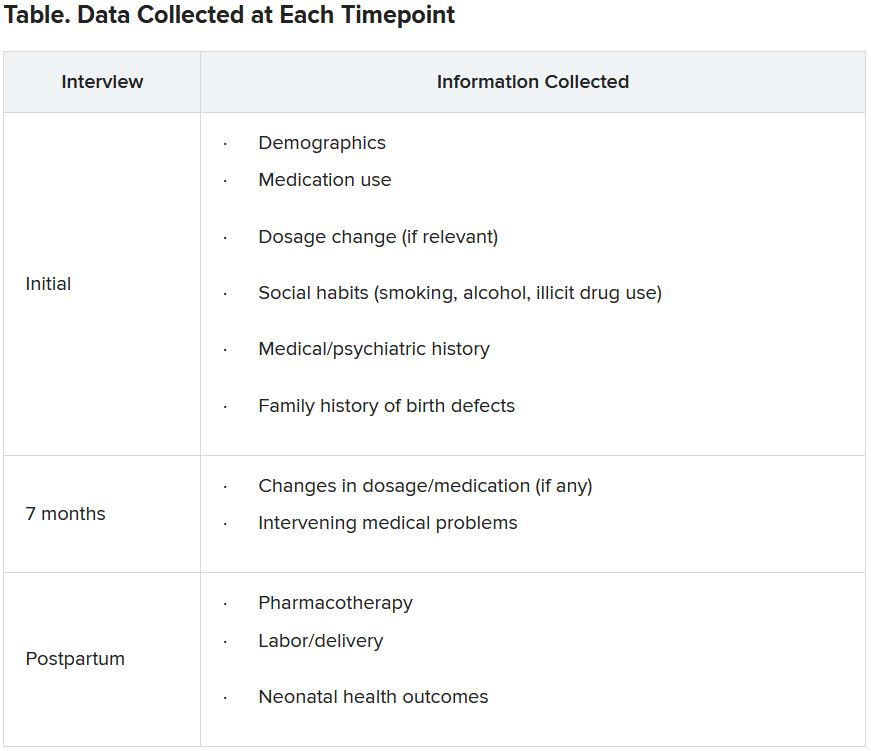
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AAP ‘silencing debate’ on gender dysphoria, says doctor group
The American Academy of Pediatrics (AAP) is at the center of a row with an international group of doctors who question whether hormone treatment is the most appropriate way to treat adolescents with gender dysphoria.
After initially accepting the application and payment from the Society for Evidence-Based Gender Medicine (SEGM) for the organization to have an information booth at the AAP annual meeting in October, the AAP did a U-turn earlier this month and canceled the registration, with no explanation as to why.
“Just days earlier,” says SEGM in a statement on its website, “over 80% of AAP members” had indicated they wanted more discussion on the topic of “addressing alternatives to the use of hormone therapies for gender dysphoric youth.”
“This rejection sends a strong signal that the AAP does not want to see any debate on what constitutes evidence-based care for gender-diverse youth,” they add.
Asked for an explanation as to why it accepted but later rescinded SEGM’s application for a booth, the AAP has given no response to date.
A Wall Street Journal article on the furor, published last week, has clocked up 785 comments to date.
There has been an exponential increase in the number of adolescents who identify as transgender – reporting discomfort with their birth sex – in Western countries, and the debate has been covered in detail, having intensified worldwide in the last 12 months, regarding how best to treat youth with gender dysphoria.
Although “affirmative” medical care, defined as treatment with puberty blockers and cross-sex hormones to transition to the opposite sex, is supported by the AAP and other medical organizations, there is growing concern among many doctors and other health care professionals as to whether this is, in fact, the best way to proceed, given that there are a number of irreversible changes associated with treatment. There is also a growing number of “detransitioners” – mostly young people who transitioned and then changed their minds, and “detransitioned” back to their birth sex.
“Because of the low quality of the available evidence and the marked change in the presentation of gender dysphoria in youth in the last several years (many more adolescents with recently emerging transgender identities and significant mental health comorbidities are presenting for care), what constitutes good health care for this patient group is far from clear,” notes SEGM.
“Quelling the debate will not help America’s pediatricians guide patients and their families based on best available evidence. The politicization of the field of gender medicine must end, if we care about gender-variant youth and their long-term health,” they conclude.
A version of this article first appeared on Medscape.com.
The American Academy of Pediatrics (AAP) is at the center of a row with an international group of doctors who question whether hormone treatment is the most appropriate way to treat adolescents with gender dysphoria.
After initially accepting the application and payment from the Society for Evidence-Based Gender Medicine (SEGM) for the organization to have an information booth at the AAP annual meeting in October, the AAP did a U-turn earlier this month and canceled the registration, with no explanation as to why.
“Just days earlier,” says SEGM in a statement on its website, “over 80% of AAP members” had indicated they wanted more discussion on the topic of “addressing alternatives to the use of hormone therapies for gender dysphoric youth.”
“This rejection sends a strong signal that the AAP does not want to see any debate on what constitutes evidence-based care for gender-diverse youth,” they add.
Asked for an explanation as to why it accepted but later rescinded SEGM’s application for a booth, the AAP has given no response to date.
A Wall Street Journal article on the furor, published last week, has clocked up 785 comments to date.
There has been an exponential increase in the number of adolescents who identify as transgender – reporting discomfort with their birth sex – in Western countries, and the debate has been covered in detail, having intensified worldwide in the last 12 months, regarding how best to treat youth with gender dysphoria.
Although “affirmative” medical care, defined as treatment with puberty blockers and cross-sex hormones to transition to the opposite sex, is supported by the AAP and other medical organizations, there is growing concern among many doctors and other health care professionals as to whether this is, in fact, the best way to proceed, given that there are a number of irreversible changes associated with treatment. There is also a growing number of “detransitioners” – mostly young people who transitioned and then changed their minds, and “detransitioned” back to their birth sex.
“Because of the low quality of the available evidence and the marked change in the presentation of gender dysphoria in youth in the last several years (many more adolescents with recently emerging transgender identities and significant mental health comorbidities are presenting for care), what constitutes good health care for this patient group is far from clear,” notes SEGM.
“Quelling the debate will not help America’s pediatricians guide patients and their families based on best available evidence. The politicization of the field of gender medicine must end, if we care about gender-variant youth and their long-term health,” they conclude.
A version of this article first appeared on Medscape.com.
The American Academy of Pediatrics (AAP) is at the center of a row with an international group of doctors who question whether hormone treatment is the most appropriate way to treat adolescents with gender dysphoria.
After initially accepting the application and payment from the Society for Evidence-Based Gender Medicine (SEGM) for the organization to have an information booth at the AAP annual meeting in October, the AAP did a U-turn earlier this month and canceled the registration, with no explanation as to why.
“Just days earlier,” says SEGM in a statement on its website, “over 80% of AAP members” had indicated they wanted more discussion on the topic of “addressing alternatives to the use of hormone therapies for gender dysphoric youth.”
“This rejection sends a strong signal that the AAP does not want to see any debate on what constitutes evidence-based care for gender-diverse youth,” they add.
Asked for an explanation as to why it accepted but later rescinded SEGM’s application for a booth, the AAP has given no response to date.
A Wall Street Journal article on the furor, published last week, has clocked up 785 comments to date.
There has been an exponential increase in the number of adolescents who identify as transgender – reporting discomfort with their birth sex – in Western countries, and the debate has been covered in detail, having intensified worldwide in the last 12 months, regarding how best to treat youth with gender dysphoria.
Although “affirmative” medical care, defined as treatment with puberty blockers and cross-sex hormones to transition to the opposite sex, is supported by the AAP and other medical organizations, there is growing concern among many doctors and other health care professionals as to whether this is, in fact, the best way to proceed, given that there are a number of irreversible changes associated with treatment. There is also a growing number of “detransitioners” – mostly young people who transitioned and then changed their minds, and “detransitioned” back to their birth sex.
“Because of the low quality of the available evidence and the marked change in the presentation of gender dysphoria in youth in the last several years (many more adolescents with recently emerging transgender identities and significant mental health comorbidities are presenting for care), what constitutes good health care for this patient group is far from clear,” notes SEGM.
“Quelling the debate will not help America’s pediatricians guide patients and their families based on best available evidence. The politicization of the field of gender medicine must end, if we care about gender-variant youth and their long-term health,” they conclude.
A version of this article first appeared on Medscape.com.
What’s under my toenail?
After the teledermatology consultation, an x-ray was recommended. The x-ray showed an elongated irregular radiopaque mass projecting from the anterior medial aspect of the midshaft of the distal phalanx of the great toe (Picture 3). With these findings, subungual exostosis was suspected, and she was referred to orthopedic surgery for excision of the lesion. Histopathology showed a stack of trabecular bone with a fibrocartilaginous cap, confirming the diagnosis of subungual exostosis.
Subungual exostosis is a benign osteocartilaginous tumor, first described by Dupuytren in 1874. These lesions are rare and are seen mainly in children and young adults. Females appear to be affected more often than males.1 In a systematic review by DaCambra and colleagues, 55% of the cases occur in patients aged younger than 18 years, and the hallux was the most commonly affected digit, though any finger or toe can be affected.2 There are reported case of congenital multiple exostosis delineated to translocation t(X;6)(q22;q13-14).3
The exact cause of these lesions is unknown, but there are multiple theories, which include a reactive process secondary to trauma, infection, or genetic causes. Pathologic examination of the lesions shows an osseous center covered by a fibrocartilaginous cap. There is proliferation of spindle cells that generate cartilage, which later forms trabecular bone.4
On physical examination, subungual exostosis appear like a firm, fixed nodule with a hyperkeratotic smooth surface at the distal end of the nail bed, that slowly grows and can distort and lift up the nail. Dermoscopy features of these lesions include vascular ectasia, hyperkeratosis, onycholysis, and ulceration.
The differential diagnosis of subungual growths includes osteochondromas, which can present in a similar way but are rarer. Pathologic examination is usually required to differentiate between both lesions.5 In exostoses, bone is formed directly from fibrous tissue, whereas in osteochondromas they derive from enchondral ossification.6 The cartilaginous cap of this lesion is what helps to differentiate it in histopathology. In subungual exostosis, the cap is composed of fibrocartilage, while in osteochondromas it is made of hyaline cartilage similar to what is seen in normal growing epiphysis.5 Subungual exostosis can be confused with pyogenic granulomas and verruca, and often are treated as such, which delays appropriate surgical management.
Firm, slow-growing tumors in the fingers or toes of children should raise suspicion for underlying bony lesions like subungual exostosis and osteochondromas. X-rays of the lesion should be performed in order to clarify the diagnosis. Referral to orthopedic surgery is needed for definitive surgical management.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
1. Zhang W et al. JAAD Case Rep. 2020 Jun 1;6(8):725-6.
2. DaCambra MP et al. Clin Orthop Relat Res. 2014 Apr;472(4):1251-9.
3. Torlazzi C et al. Int J Cancer. 2006;118:1972-6.
4. Calonje E et al. McKee’s pathology of the skin: With clinical correlations. (4th ed.) Philadelphia: Elsevier/Saunders, 2012.
5. Lee SK et al. Foot Ankle Int. 2007 May;28(5):595-601.
6. Mavrogenis A et al. Orthopedics. 2008 Oct;31(10).
After the teledermatology consultation, an x-ray was recommended. The x-ray showed an elongated irregular radiopaque mass projecting from the anterior medial aspect of the midshaft of the distal phalanx of the great toe (Picture 3). With these findings, subungual exostosis was suspected, and she was referred to orthopedic surgery for excision of the lesion. Histopathology showed a stack of trabecular bone with a fibrocartilaginous cap, confirming the diagnosis of subungual exostosis.
Subungual exostosis is a benign osteocartilaginous tumor, first described by Dupuytren in 1874. These lesions are rare and are seen mainly in children and young adults. Females appear to be affected more often than males.1 In a systematic review by DaCambra and colleagues, 55% of the cases occur in patients aged younger than 18 years, and the hallux was the most commonly affected digit, though any finger or toe can be affected.2 There are reported case of congenital multiple exostosis delineated to translocation t(X;6)(q22;q13-14).3
The exact cause of these lesions is unknown, but there are multiple theories, which include a reactive process secondary to trauma, infection, or genetic causes. Pathologic examination of the lesions shows an osseous center covered by a fibrocartilaginous cap. There is proliferation of spindle cells that generate cartilage, which later forms trabecular bone.4
On physical examination, subungual exostosis appear like a firm, fixed nodule with a hyperkeratotic smooth surface at the distal end of the nail bed, that slowly grows and can distort and lift up the nail. Dermoscopy features of these lesions include vascular ectasia, hyperkeratosis, onycholysis, and ulceration.
The differential diagnosis of subungual growths includes osteochondromas, which can present in a similar way but are rarer. Pathologic examination is usually required to differentiate between both lesions.5 In exostoses, bone is formed directly from fibrous tissue, whereas in osteochondromas they derive from enchondral ossification.6 The cartilaginous cap of this lesion is what helps to differentiate it in histopathology. In subungual exostosis, the cap is composed of fibrocartilage, while in osteochondromas it is made of hyaline cartilage similar to what is seen in normal growing epiphysis.5 Subungual exostosis can be confused with pyogenic granulomas and verruca, and often are treated as such, which delays appropriate surgical management.
Firm, slow-growing tumors in the fingers or toes of children should raise suspicion for underlying bony lesions like subungual exostosis and osteochondromas. X-rays of the lesion should be performed in order to clarify the diagnosis. Referral to orthopedic surgery is needed for definitive surgical management.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
1. Zhang W et al. JAAD Case Rep. 2020 Jun 1;6(8):725-6.
2. DaCambra MP et al. Clin Orthop Relat Res. 2014 Apr;472(4):1251-9.
3. Torlazzi C et al. Int J Cancer. 2006;118:1972-6.
4. Calonje E et al. McKee’s pathology of the skin: With clinical correlations. (4th ed.) Philadelphia: Elsevier/Saunders, 2012.
5. Lee SK et al. Foot Ankle Int. 2007 May;28(5):595-601.
6. Mavrogenis A et al. Orthopedics. 2008 Oct;31(10).
After the teledermatology consultation, an x-ray was recommended. The x-ray showed an elongated irregular radiopaque mass projecting from the anterior medial aspect of the midshaft of the distal phalanx of the great toe (Picture 3). With these findings, subungual exostosis was suspected, and she was referred to orthopedic surgery for excision of the lesion. Histopathology showed a stack of trabecular bone with a fibrocartilaginous cap, confirming the diagnosis of subungual exostosis.
Subungual exostosis is a benign osteocartilaginous tumor, first described by Dupuytren in 1874. These lesions are rare and are seen mainly in children and young adults. Females appear to be affected more often than males.1 In a systematic review by DaCambra and colleagues, 55% of the cases occur in patients aged younger than 18 years, and the hallux was the most commonly affected digit, though any finger or toe can be affected.2 There are reported case of congenital multiple exostosis delineated to translocation t(X;6)(q22;q13-14).3
The exact cause of these lesions is unknown, but there are multiple theories, which include a reactive process secondary to trauma, infection, or genetic causes. Pathologic examination of the lesions shows an osseous center covered by a fibrocartilaginous cap. There is proliferation of spindle cells that generate cartilage, which later forms trabecular bone.4
On physical examination, subungual exostosis appear like a firm, fixed nodule with a hyperkeratotic smooth surface at the distal end of the nail bed, that slowly grows and can distort and lift up the nail. Dermoscopy features of these lesions include vascular ectasia, hyperkeratosis, onycholysis, and ulceration.
The differential diagnosis of subungual growths includes osteochondromas, which can present in a similar way but are rarer. Pathologic examination is usually required to differentiate between both lesions.5 In exostoses, bone is formed directly from fibrous tissue, whereas in osteochondromas they derive from enchondral ossification.6 The cartilaginous cap of this lesion is what helps to differentiate it in histopathology. In subungual exostosis, the cap is composed of fibrocartilage, while in osteochondromas it is made of hyaline cartilage similar to what is seen in normal growing epiphysis.5 Subungual exostosis can be confused with pyogenic granulomas and verruca, and often are treated as such, which delays appropriate surgical management.
Firm, slow-growing tumors in the fingers or toes of children should raise suspicion for underlying bony lesions like subungual exostosis and osteochondromas. X-rays of the lesion should be performed in order to clarify the diagnosis. Referral to orthopedic surgery is needed for definitive surgical management.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
1. Zhang W et al. JAAD Case Rep. 2020 Jun 1;6(8):725-6.
2. DaCambra MP et al. Clin Orthop Relat Res. 2014 Apr;472(4):1251-9.
3. Torlazzi C et al. Int J Cancer. 2006;118:1972-6.
4. Calonje E et al. McKee’s pathology of the skin: With clinical correlations. (4th ed.) Philadelphia: Elsevier/Saunders, 2012.
5. Lee SK et al. Foot Ankle Int. 2007 May;28(5):595-601.
6. Mavrogenis A et al. Orthopedics. 2008 Oct;31(10).
A 13-year-old female was seen by her pediatrician for a lesion that had been on her right toe for about 6 months. She is unaware of any trauma to the area. The lesion has been growing slowly and recently it started lifting up the nail, became tender, and was bleeding, which is the reason why she sought care.
At the pediatrician's office, he noted a pink crusted papule under the nail. The nail was lifting up and was tender to the touch. She is a healthy girl who is not taking any medications and has no allergies. There is no family history of similar lesions.
The pediatrician took a picture of the lesion and he send it to our pediatric teledermatology service for consultation.
Children and COVID: New cases rise to winter levels
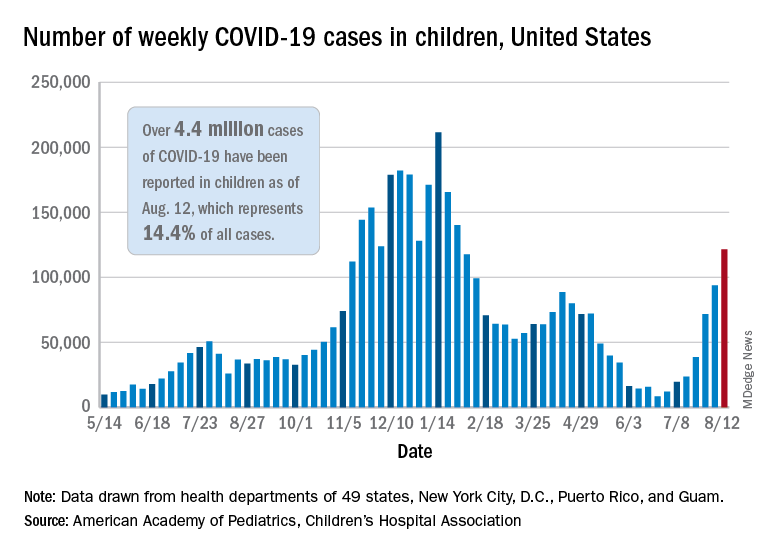
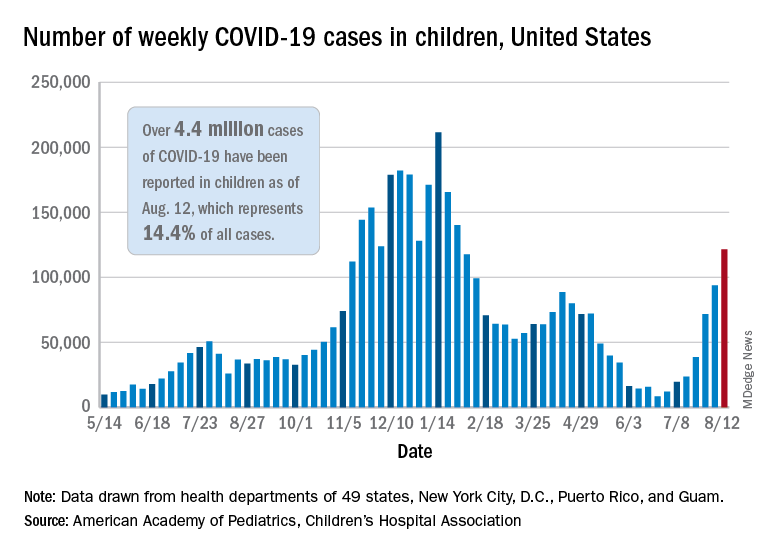
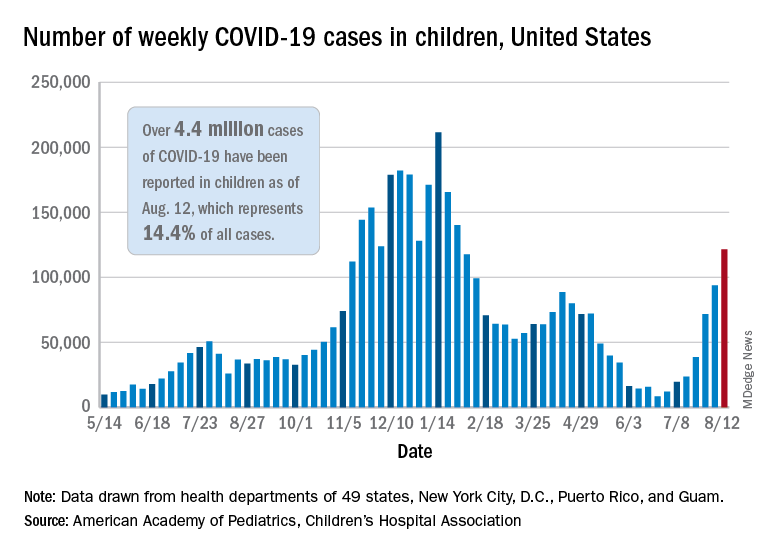
Weekly cases of COVID-19 in children topped 100,000 for the first time since early February, according to the American Academy of Pediatrics and the Children’s Hospital Association.
the AAP and CHA said in their weekly COVD-19 report. The recent surge in child COVID has also brought a record high in hospitalizations and shortages of pediatric ICU beds in some areas.
The 121,000 new cases represent an increase of almost 1,400% since June 18-24, when the weekly tally was just 8,447 and at its lowest point in over a year, the AAP/CHA data show.
On the vaccination front in the last week (Aug. 10-16), vaccine initiation for 12- to 17-year-olds was fairly robust but still down slightly, compared with the previous week. Just over 402,000 children aged 12-15 years received a first vaccination, which was down slightly from 411,000 the week before but still higher than any of the 6 weeks from June 22 to Aug. 2, based on data from the Centers for Disease Control and Prevention. Vaccinations were down by a similar margin for 15- to-17-year-olds.
Over 10.9 million children aged 12-17 have had at least one dose of COVID-19 vaccine administered, of whom 8.1 million are fully vaccinated. Among those aged 12-15 years, 44.5% have gotten at least one dose and 31.8% are fully vaccinated, with corresponding figures of 53.9% and 42.5% for 16- and 17-year-olds, according to the CDC’s COVID Data Tracker.
The number of COVID-19 cases reported in children since the start of the pandemic is up to 4.4 million, which makes up 14.4% of all cases in the United States, the AAP and CHA said. Other cumulative figures through Aug. 12 include almost 18,000 hospitalizations – reported by 23 states and New York City – and 378 deaths – reported by 43 states, New York City, Puerto Rico, and Guam.
In the latest edition of their ongoing report, compiled using state data since the summer of 2020, the two groups noted that, “in the summer of 2021, some states have revised cases counts previously reported, begun reporting less frequently, or dropped metrics previously reported.” Among those states are Nebraska, which shut down its online COVID dashboard in late June, and Alabama, which stopped reporting cumulative cases and deaths after July 29.
Weekly cases of COVID-19 in children topped 100,000 for the first time since early February, according to the American Academy of Pediatrics and the Children’s Hospital Association.
the AAP and CHA said in their weekly COVD-19 report. The recent surge in child COVID has also brought a record high in hospitalizations and shortages of pediatric ICU beds in some areas.
The 121,000 new cases represent an increase of almost 1,400% since June 18-24, when the weekly tally was just 8,447 and at its lowest point in over a year, the AAP/CHA data show.
On the vaccination front in the last week (Aug. 10-16), vaccine initiation for 12- to 17-year-olds was fairly robust but still down slightly, compared with the previous week. Just over 402,000 children aged 12-15 years received a first vaccination, which was down slightly from 411,000 the week before but still higher than any of the 6 weeks from June 22 to Aug. 2, based on data from the Centers for Disease Control and Prevention. Vaccinations were down by a similar margin for 15- to-17-year-olds.
Over 10.9 million children aged 12-17 have had at least one dose of COVID-19 vaccine administered, of whom 8.1 million are fully vaccinated. Among those aged 12-15 years, 44.5% have gotten at least one dose and 31.8% are fully vaccinated, with corresponding figures of 53.9% and 42.5% for 16- and 17-year-olds, according to the CDC’s COVID Data Tracker.
The number of COVID-19 cases reported in children since the start of the pandemic is up to 4.4 million, which makes up 14.4% of all cases in the United States, the AAP and CHA said. Other cumulative figures through Aug. 12 include almost 18,000 hospitalizations – reported by 23 states and New York City – and 378 deaths – reported by 43 states, New York City, Puerto Rico, and Guam.
In the latest edition of their ongoing report, compiled using state data since the summer of 2020, the two groups noted that, “in the summer of 2021, some states have revised cases counts previously reported, begun reporting less frequently, or dropped metrics previously reported.” Among those states are Nebraska, which shut down its online COVID dashboard in late June, and Alabama, which stopped reporting cumulative cases and deaths after July 29.
Weekly cases of COVID-19 in children topped 100,000 for the first time since early February, according to the American Academy of Pediatrics and the Children’s Hospital Association.
the AAP and CHA said in their weekly COVD-19 report. The recent surge in child COVID has also brought a record high in hospitalizations and shortages of pediatric ICU beds in some areas.
The 121,000 new cases represent an increase of almost 1,400% since June 18-24, when the weekly tally was just 8,447 and at its lowest point in over a year, the AAP/CHA data show.
On the vaccination front in the last week (Aug. 10-16), vaccine initiation for 12- to 17-year-olds was fairly robust but still down slightly, compared with the previous week. Just over 402,000 children aged 12-15 years received a first vaccination, which was down slightly from 411,000 the week before but still higher than any of the 6 weeks from June 22 to Aug. 2, based on data from the Centers for Disease Control and Prevention. Vaccinations were down by a similar margin for 15- to-17-year-olds.
Over 10.9 million children aged 12-17 have had at least one dose of COVID-19 vaccine administered, of whom 8.1 million are fully vaccinated. Among those aged 12-15 years, 44.5% have gotten at least one dose and 31.8% are fully vaccinated, with corresponding figures of 53.9% and 42.5% for 16- and 17-year-olds, according to the CDC’s COVID Data Tracker.
The number of COVID-19 cases reported in children since the start of the pandemic is up to 4.4 million, which makes up 14.4% of all cases in the United States, the AAP and CHA said. Other cumulative figures through Aug. 12 include almost 18,000 hospitalizations – reported by 23 states and New York City – and 378 deaths – reported by 43 states, New York City, Puerto Rico, and Guam.
In the latest edition of their ongoing report, compiled using state data since the summer of 2020, the two groups noted that, “in the summer of 2021, some states have revised cases counts previously reported, begun reporting less frequently, or dropped metrics previously reported.” Among those states are Nebraska, which shut down its online COVID dashboard in late June, and Alabama, which stopped reporting cumulative cases and deaths after July 29.
U.S. pediatric hospitals in peril as Delta hits children
Over the course of the pandemic, COVID-19 has been a less serious illness for children than it has been for adults, and that continues to be true. But with the arrival of Delta, the risk for kids is rising, and that’s creating a perilous situation for hospitals across the United States that treat them.
Roughly 1,800 kids were hospitalized with COVID-19 in the United States last week, a 500% increase in the rate of COVID-19 hospitalizations for children since early July, according to data from the Centers for Disease Control and Prevention.
Emerging data from a large study in Canada suggest that children who test positive for COVID-19 during the Delta wave may be more than twice as likely to be hospitalized as they were when previous variants were dominating transmission. The new data support what many pediatric infectious disease experts say they’ve been seeing: Younger kids with more serious symptoms.
That may sound concerning, but keep in mind that the overall risk of hospitalization for kids who have COVID-19 is still very low – about one child for every hundred who test positive for the virus will end up needing hospital care for their symptoms, according to current statistics maintained by the American Academy of Pediatrics.
‘This is different’
At Le Bonheur Children’s Hospital in Memphis, they saw Delta coming.
Since last year, every kid that comes to the emergency department at the hospital gets a screening test for COVID-19.
In past waves, doctors usually found kids who were infected by accident – they tested positive after coming in for some other problem, a broken leg or appendicitis, said Nick Hysmith, MD, medical director of infection prevention at the hospital. But within the last few weeks, kids with fevers, sore throats, coughs, and runny noses started testing positive for COVID-19.
“We have seen our positive numbers go from, you know, close to about 8%-10% jump up to 20%, and then in recent weeks, we can get as high as 26% or 30%,” Dr. Hysmith said. “Then we started seeing kids sick enough to be admitted.”
“Over the last week, we’ve really seen an increase,” he said. As of August 16, the hospital had 24 children with COVID-19 admitted. Seven of the children were in the PICU, and two were on ventilators.
Arkansas Children’s Hospital had 23 young COVID-19 patients, 10 in intensive care, and five on ventilators, as of Friday, according to the Washington Post. At Children’s of Mississippi, the only hospital for kids in that state, 22 youth were hospitalized as of Monday, with three in intensive care as of August 16, according to the hospital. The nonprofit relief organization Samaritan’s Purse is setting up a second field hospital in the basement of Children’s to expand the hospital’s capacity.
“This is different,” Dr. Hysmith said. “What we’re seeing now is previously healthy kids coming in with symptomatic infection.”
This increased virulence is happening at a bad time. Schools around the United States are reopening for in-person classes, some for the first time in more than a year. Eight states have blocked districts from requiring masks, while many more have made them optional.
Children under 12 still have no access to a vaccine, so they are facing increased exposure to a germ that’s become more dangerous with little protection, especially in schools that have eschewed masks.
More than just COVID-19
Then there are the latent effects of the virus to contend with.
“We’re not only seeing more children now with acute SARS-CoV-2 in the hospital, we’re starting also to see an uptick of MISC – or Multisystem Inflammatory Syndrome in Children,” said Charlotte Hobbs, MD, a pediatric infectious disease specialist at Mississippi Children’s Hospital. “We are just beginning to [see] those cases, and we anticipate that’s going to get worse.”
Adding to COVID-19’s misery, another virus is also capitalizing on this increased mixing of kids back into the community. Respiratory syncytial virus (RSV) hospitalizes about 58,000 children under age 5 in the United States each year. The typical RSV season starts in the fall and peaks in February, along with influenza. This year, the RSV season is early, and it is ferocious.
The combination of the two infections is hitting children’s hospitals hard, and it’s layered on top of the indirect effects of the pandemic, such as the increased population of kids and teens who need mental health care in the wake of the crisis.
“It’s all these things happening at the same time,” said Mark Wietecha, CEO of the Children’s Hospital Association. “To have our hospitals this crowded in August is unusual.
And children’s hospitals are grappling with the same workforce shortages as hospitals that treat adults, while their pool of potential staff is much smaller.
“We can’t easily recruit physicians and nurses from adult hospitals in any practical way to staff a kids’ hospital,” Mr. Wietecha said.
Although pediatric doctors and nurses were trained to care for adults before they specialized, clinicians who primarily care for adults typically haven’t been taught how to care for kids.
Clinicians have fewer tools to fight COVID-19 infections in children than are available for adults.
“There have been many studies in terms of therapies and treatments for acute SARS-CoV-2 infection in adults. We have less data and information in children, and on top of that, some of these treatments aren’t even available under an EUA [emergency use authorization] to children: For example, the monoclonal antibodies,” Dr. Hobbs said.
Antibody treatments are being widely deployed to ease the pressure on hospitals that treat adults. But these therapies aren’t available for kids.
That means children’s hospitals could quickly become overwhelmed, especially in areas where community transmission is high, vaccination rates are low, and parents are screaming about masks.
“So we really have this constellation of events that really doesn’t favor children under the age of 12,” Dr. Hobbs said.
“Universal masking shouldn’t be a debate, because it’s the one thing, with adult vaccination, that can be done to protect this vulnerable population,” she said. “This isn’t a political issue. It’s a public health issue. Period.”
A version of this article first appeared on Medscape.com.
Over the course of the pandemic, COVID-19 has been a less serious illness for children than it has been for adults, and that continues to be true. But with the arrival of Delta, the risk for kids is rising, and that’s creating a perilous situation for hospitals across the United States that treat them.
Roughly 1,800 kids were hospitalized with COVID-19 in the United States last week, a 500% increase in the rate of COVID-19 hospitalizations for children since early July, according to data from the Centers for Disease Control and Prevention.
Emerging data from a large study in Canada suggest that children who test positive for COVID-19 during the Delta wave may be more than twice as likely to be hospitalized as they were when previous variants were dominating transmission. The new data support what many pediatric infectious disease experts say they’ve been seeing: Younger kids with more serious symptoms.
That may sound concerning, but keep in mind that the overall risk of hospitalization for kids who have COVID-19 is still very low – about one child for every hundred who test positive for the virus will end up needing hospital care for their symptoms, according to current statistics maintained by the American Academy of Pediatrics.
‘This is different’
At Le Bonheur Children’s Hospital in Memphis, they saw Delta coming.
Since last year, every kid that comes to the emergency department at the hospital gets a screening test for COVID-19.
In past waves, doctors usually found kids who were infected by accident – they tested positive after coming in for some other problem, a broken leg or appendicitis, said Nick Hysmith, MD, medical director of infection prevention at the hospital. But within the last few weeks, kids with fevers, sore throats, coughs, and runny noses started testing positive for COVID-19.
“We have seen our positive numbers go from, you know, close to about 8%-10% jump up to 20%, and then in recent weeks, we can get as high as 26% or 30%,” Dr. Hysmith said. “Then we started seeing kids sick enough to be admitted.”
“Over the last week, we’ve really seen an increase,” he said. As of August 16, the hospital had 24 children with COVID-19 admitted. Seven of the children were in the PICU, and two were on ventilators.
Arkansas Children’s Hospital had 23 young COVID-19 patients, 10 in intensive care, and five on ventilators, as of Friday, according to the Washington Post. At Children’s of Mississippi, the only hospital for kids in that state, 22 youth were hospitalized as of Monday, with three in intensive care as of August 16, according to the hospital. The nonprofit relief organization Samaritan’s Purse is setting up a second field hospital in the basement of Children’s to expand the hospital’s capacity.
“This is different,” Dr. Hysmith said. “What we’re seeing now is previously healthy kids coming in with symptomatic infection.”
This increased virulence is happening at a bad time. Schools around the United States are reopening for in-person classes, some for the first time in more than a year. Eight states have blocked districts from requiring masks, while many more have made them optional.
Children under 12 still have no access to a vaccine, so they are facing increased exposure to a germ that’s become more dangerous with little protection, especially in schools that have eschewed masks.
More than just COVID-19
Then there are the latent effects of the virus to contend with.
“We’re not only seeing more children now with acute SARS-CoV-2 in the hospital, we’re starting also to see an uptick of MISC – or Multisystem Inflammatory Syndrome in Children,” said Charlotte Hobbs, MD, a pediatric infectious disease specialist at Mississippi Children’s Hospital. “We are just beginning to [see] those cases, and we anticipate that’s going to get worse.”
Adding to COVID-19’s misery, another virus is also capitalizing on this increased mixing of kids back into the community. Respiratory syncytial virus (RSV) hospitalizes about 58,000 children under age 5 in the United States each year. The typical RSV season starts in the fall and peaks in February, along with influenza. This year, the RSV season is early, and it is ferocious.
The combination of the two infections is hitting children’s hospitals hard, and it’s layered on top of the indirect effects of the pandemic, such as the increased population of kids and teens who need mental health care in the wake of the crisis.
“It’s all these things happening at the same time,” said Mark Wietecha, CEO of the Children’s Hospital Association. “To have our hospitals this crowded in August is unusual.
And children’s hospitals are grappling with the same workforce shortages as hospitals that treat adults, while their pool of potential staff is much smaller.
“We can’t easily recruit physicians and nurses from adult hospitals in any practical way to staff a kids’ hospital,” Mr. Wietecha said.
Although pediatric doctors and nurses were trained to care for adults before they specialized, clinicians who primarily care for adults typically haven’t been taught how to care for kids.
Clinicians have fewer tools to fight COVID-19 infections in children than are available for adults.
“There have been many studies in terms of therapies and treatments for acute SARS-CoV-2 infection in adults. We have less data and information in children, and on top of that, some of these treatments aren’t even available under an EUA [emergency use authorization] to children: For example, the monoclonal antibodies,” Dr. Hobbs said.
Antibody treatments are being widely deployed to ease the pressure on hospitals that treat adults. But these therapies aren’t available for kids.
That means children’s hospitals could quickly become overwhelmed, especially in areas where community transmission is high, vaccination rates are low, and parents are screaming about masks.
“So we really have this constellation of events that really doesn’t favor children under the age of 12,” Dr. Hobbs said.
“Universal masking shouldn’t be a debate, because it’s the one thing, with adult vaccination, that can be done to protect this vulnerable population,” she said. “This isn’t a political issue. It’s a public health issue. Period.”
A version of this article first appeared on Medscape.com.
Over the course of the pandemic, COVID-19 has been a less serious illness for children than it has been for adults, and that continues to be true. But with the arrival of Delta, the risk for kids is rising, and that’s creating a perilous situation for hospitals across the United States that treat them.
Roughly 1,800 kids were hospitalized with COVID-19 in the United States last week, a 500% increase in the rate of COVID-19 hospitalizations for children since early July, according to data from the Centers for Disease Control and Prevention.
Emerging data from a large study in Canada suggest that children who test positive for COVID-19 during the Delta wave may be more than twice as likely to be hospitalized as they were when previous variants were dominating transmission. The new data support what many pediatric infectious disease experts say they’ve been seeing: Younger kids with more serious symptoms.
That may sound concerning, but keep in mind that the overall risk of hospitalization for kids who have COVID-19 is still very low – about one child for every hundred who test positive for the virus will end up needing hospital care for their symptoms, according to current statistics maintained by the American Academy of Pediatrics.
‘This is different’
At Le Bonheur Children’s Hospital in Memphis, they saw Delta coming.
Since last year, every kid that comes to the emergency department at the hospital gets a screening test for COVID-19.
In past waves, doctors usually found kids who were infected by accident – they tested positive after coming in for some other problem, a broken leg or appendicitis, said Nick Hysmith, MD, medical director of infection prevention at the hospital. But within the last few weeks, kids with fevers, sore throats, coughs, and runny noses started testing positive for COVID-19.
“We have seen our positive numbers go from, you know, close to about 8%-10% jump up to 20%, and then in recent weeks, we can get as high as 26% or 30%,” Dr. Hysmith said. “Then we started seeing kids sick enough to be admitted.”
“Over the last week, we’ve really seen an increase,” he said. As of August 16, the hospital had 24 children with COVID-19 admitted. Seven of the children were in the PICU, and two were on ventilators.
Arkansas Children’s Hospital had 23 young COVID-19 patients, 10 in intensive care, and five on ventilators, as of Friday, according to the Washington Post. At Children’s of Mississippi, the only hospital for kids in that state, 22 youth were hospitalized as of Monday, with three in intensive care as of August 16, according to the hospital. The nonprofit relief organization Samaritan’s Purse is setting up a second field hospital in the basement of Children’s to expand the hospital’s capacity.
“This is different,” Dr. Hysmith said. “What we’re seeing now is previously healthy kids coming in with symptomatic infection.”
This increased virulence is happening at a bad time. Schools around the United States are reopening for in-person classes, some for the first time in more than a year. Eight states have blocked districts from requiring masks, while many more have made them optional.
Children under 12 still have no access to a vaccine, so they are facing increased exposure to a germ that’s become more dangerous with little protection, especially in schools that have eschewed masks.
More than just COVID-19
Then there are the latent effects of the virus to contend with.
“We’re not only seeing more children now with acute SARS-CoV-2 in the hospital, we’re starting also to see an uptick of MISC – or Multisystem Inflammatory Syndrome in Children,” said Charlotte Hobbs, MD, a pediatric infectious disease specialist at Mississippi Children’s Hospital. “We are just beginning to [see] those cases, and we anticipate that’s going to get worse.”
Adding to COVID-19’s misery, another virus is also capitalizing on this increased mixing of kids back into the community. Respiratory syncytial virus (RSV) hospitalizes about 58,000 children under age 5 in the United States each year. The typical RSV season starts in the fall and peaks in February, along with influenza. This year, the RSV season is early, and it is ferocious.
The combination of the two infections is hitting children’s hospitals hard, and it’s layered on top of the indirect effects of the pandemic, such as the increased population of kids and teens who need mental health care in the wake of the crisis.
“It’s all these things happening at the same time,” said Mark Wietecha, CEO of the Children’s Hospital Association. “To have our hospitals this crowded in August is unusual.
And children’s hospitals are grappling with the same workforce shortages as hospitals that treat adults, while their pool of potential staff is much smaller.
“We can’t easily recruit physicians and nurses from adult hospitals in any practical way to staff a kids’ hospital,” Mr. Wietecha said.
Although pediatric doctors and nurses were trained to care for adults before they specialized, clinicians who primarily care for adults typically haven’t been taught how to care for kids.
Clinicians have fewer tools to fight COVID-19 infections in children than are available for adults.
“There have been many studies in terms of therapies and treatments for acute SARS-CoV-2 infection in adults. We have less data and information in children, and on top of that, some of these treatments aren’t even available under an EUA [emergency use authorization] to children: For example, the monoclonal antibodies,” Dr. Hobbs said.
Antibody treatments are being widely deployed to ease the pressure on hospitals that treat adults. But these therapies aren’t available for kids.
That means children’s hospitals could quickly become overwhelmed, especially in areas where community transmission is high, vaccination rates are low, and parents are screaming about masks.
“So we really have this constellation of events that really doesn’t favor children under the age of 12,” Dr. Hobbs said.
“Universal masking shouldn’t be a debate, because it’s the one thing, with adult vaccination, that can be done to protect this vulnerable population,” she said. “This isn’t a political issue. It’s a public health issue. Period.”
A version of this article first appeared on Medscape.com.
Youngest children more likely to spread SARS-CoV-2 to family: Study
Young children are more likely than are their older siblings to transmit SARS-CoV-2 in their households, according to an analysis of public health records in Ontario, Canada – a finding that upends the common belief that children play a minimal role in COVID-19 spread.
The study by researchers from Public Health Ontario, published online in JAMA Pediatrics, found that teenagers (14- to 17-year-olds) were more likely than were their younger siblings to bring the virus into the household, while infants and toddlers (up to age 3) were about 43% more likely than were the older teens to spread it to others in the home.
Children or teens were the source of SARS-CoV-2 in about 1 in 13 Ontario households between June and December 2020, the study shows. The researchers analyzed health records from 6,280 households with a pediatric COVID-19 case and a subset of 1,717 households in which a child up to age 17 was the source of transmission in a household.
When analyzing the data, the researchers controlled for gender differences, month of disease onset, testing delay, and mean family size.
The role of young children in transmission seemed logical to some experts who have been tracking the evolution of the pandemic. “I think what was more surprising was how long the narrative persisted that children weren’t transmitting SARS-CoV-2,” said Samuel Scarpino, PhD, managing director of pathogen surveillance at the Rockefeller Foundation.
Meanwhile, less mask-wearing, the return to school and activities, and the onslaught of the Delta variant have changed the dynamics of spread, said Andrew Pavia, MD, chief of the division of pediatric infectious diseases at the University of Utah.
“Adolescents and high-school-aged kids have had much, much higher rates of infection in the past,” he said. “Now when we look at the rates of school-aged kids, they are the same as high-school-aged kids, and we’re seeing more and more in the preschool age groups.”
Cases may be underestimated
If anything, the study may underestimate the role young children play in spreading COVID-19 in families, since it included only symptomatic cases as the initial source and young children are more likely to be asymptomatic, Dr. Pavia said.
The Delta variant heightens the concern; it is more than twice as infectious as previous strains and has spurred a rise in pediatric cases, including some coinfection with other circulating respiratory diseases, such as respiratory syncytial virus (RSV).
The Ontario study covers a period before vaccination and the spread of the Delta variant. “As the number of pediatric cases increases worldwide, the role of children in household transmission will continue to grow,” the authors concluded.
Following recommended respiratory hygiene is clearly more difficult with very young children. For example, parents, caregivers, and older siblings aren’t going to stay 6 feet away from a sick baby or toddler, Susan Coffin, MD, MPH, a pediatric infectious disease physician, and David Rubin, MD, a pediatrician and director of PolicyLab at Children’s Hospital of Philadelphia, noted in an accompanying commentary.
“Cuddling and touching are part and parcel of taking care of a sick young child, and that will obviously come with an increased risk of transmission to parents as well as to older siblings who may be helping to care for their sick brother or sister,” they wrote.
While parents may wash their hands more frequently when caring for a sick child, they aren’t likely to wear a mask, said William Schaffner, MD, an infectious disease specialist at Vanderbilt University, Nashville, Tenn.
“I imagine some moms even take a sick child into bed with them,” he said. “It’s probably just the extensive contact one has with a sick, very small child that augments their capacity to transmit this infection.”
What can be done
What can be done, then, to reduce the household spread of COVID-19? “The obvious solution to protect a household with a sick young infant or toddler is to make sure that all eligible members of the household are vaccinated,” Dr. Coffin and Dr. Rubin stated in their commentary.
The American Academy of Pediatrics recently wrote to Janet Woodcock, MD, acting commissioner of the Food and Drug Administration, asking for the agency to authorize use of SARS-CoV-2 vaccines for children under age 12 “as soon as possible,” noting that “the Delta variant has created a new and pressing risk to children and adolescents across this country, as it has also done for unvaccinated adults.”
The FDA reportedly asked vaccine makers Pfizer and Moderna to expand the clinical trials of children, which may delay authorization for younger age groups. Pfizer has said it plans to submit a request for emergency use authorization of its vaccine for 5- to 11-year-olds in September or October.
As with adult vaccination, hesitancy is likely to be a barrier. Less than half of parents said they are very or somewhat likely to have their children get a COVID-19 vaccine, according to a national survey conducted by researchers at the University of California, Los Angeles.
The Ontario study provides valuable evidence to support taking steps to protect children from transmission in schools, including mask requirements, frequent testing, and improved ventilation, said Dr. Scarpino.
“We’re not going to be able to control COVID without vaccinating younger individuals,” he said.
Dr. Pavia has consulted for GlaxoSmithKline on non–COVID-19–related issues. Sarah Buchan, PhD, study author and scientist at Public Health Ontario, reported grants from the Canadian Institutes of Health Research for research on influenza, RSV, and COVID-19, and grants from the Canadian Immunity Task Force for COVID-19 outside the submitted work. Dr. Coffin reported grants as a Centers for Disease Control and Prevention coinvestigator at a Vaccine and Treatment Evaluation Unit site conducting COVID-19 vaccine trials in children. Dr. Scarpino holds unexercised options in ILiAD Biotechnologies, which is focused on the prevention and treatment of pertussis. Dr. Schaffner is a consultant for VBI Vaccines.
A version of this article first appeared on Medscape.com.
Young children are more likely than are their older siblings to transmit SARS-CoV-2 in their households, according to an analysis of public health records in Ontario, Canada – a finding that upends the common belief that children play a minimal role in COVID-19 spread.
The study by researchers from Public Health Ontario, published online in JAMA Pediatrics, found that teenagers (14- to 17-year-olds) were more likely than were their younger siblings to bring the virus into the household, while infants and toddlers (up to age 3) were about 43% more likely than were the older teens to spread it to others in the home.
Children or teens were the source of SARS-CoV-2 in about 1 in 13 Ontario households between June and December 2020, the study shows. The researchers analyzed health records from 6,280 households with a pediatric COVID-19 case and a subset of 1,717 households in which a child up to age 17 was the source of transmission in a household.
When analyzing the data, the researchers controlled for gender differences, month of disease onset, testing delay, and mean family size.
The role of young children in transmission seemed logical to some experts who have been tracking the evolution of the pandemic. “I think what was more surprising was how long the narrative persisted that children weren’t transmitting SARS-CoV-2,” said Samuel Scarpino, PhD, managing director of pathogen surveillance at the Rockefeller Foundation.
Meanwhile, less mask-wearing, the return to school and activities, and the onslaught of the Delta variant have changed the dynamics of spread, said Andrew Pavia, MD, chief of the division of pediatric infectious diseases at the University of Utah.
“Adolescents and high-school-aged kids have had much, much higher rates of infection in the past,” he said. “Now when we look at the rates of school-aged kids, they are the same as high-school-aged kids, and we’re seeing more and more in the preschool age groups.”
Cases may be underestimated
If anything, the study may underestimate the role young children play in spreading COVID-19 in families, since it included only symptomatic cases as the initial source and young children are more likely to be asymptomatic, Dr. Pavia said.
The Delta variant heightens the concern; it is more than twice as infectious as previous strains and has spurred a rise in pediatric cases, including some coinfection with other circulating respiratory diseases, such as respiratory syncytial virus (RSV).
The Ontario study covers a period before vaccination and the spread of the Delta variant. “As the number of pediatric cases increases worldwide, the role of children in household transmission will continue to grow,” the authors concluded.
Following recommended respiratory hygiene is clearly more difficult with very young children. For example, parents, caregivers, and older siblings aren’t going to stay 6 feet away from a sick baby or toddler, Susan Coffin, MD, MPH, a pediatric infectious disease physician, and David Rubin, MD, a pediatrician and director of PolicyLab at Children’s Hospital of Philadelphia, noted in an accompanying commentary.
“Cuddling and touching are part and parcel of taking care of a sick young child, and that will obviously come with an increased risk of transmission to parents as well as to older siblings who may be helping to care for their sick brother or sister,” they wrote.
While parents may wash their hands more frequently when caring for a sick child, they aren’t likely to wear a mask, said William Schaffner, MD, an infectious disease specialist at Vanderbilt University, Nashville, Tenn.
“I imagine some moms even take a sick child into bed with them,” he said. “It’s probably just the extensive contact one has with a sick, very small child that augments their capacity to transmit this infection.”
What can be done
What can be done, then, to reduce the household spread of COVID-19? “The obvious solution to protect a household with a sick young infant or toddler is to make sure that all eligible members of the household are vaccinated,” Dr. Coffin and Dr. Rubin stated in their commentary.
The American Academy of Pediatrics recently wrote to Janet Woodcock, MD, acting commissioner of the Food and Drug Administration, asking for the agency to authorize use of SARS-CoV-2 vaccines for children under age 12 “as soon as possible,” noting that “the Delta variant has created a new and pressing risk to children and adolescents across this country, as it has also done for unvaccinated adults.”
The FDA reportedly asked vaccine makers Pfizer and Moderna to expand the clinical trials of children, which may delay authorization for younger age groups. Pfizer has said it plans to submit a request for emergency use authorization of its vaccine for 5- to 11-year-olds in September or October.
As with adult vaccination, hesitancy is likely to be a barrier. Less than half of parents said they are very or somewhat likely to have their children get a COVID-19 vaccine, according to a national survey conducted by researchers at the University of California, Los Angeles.
The Ontario study provides valuable evidence to support taking steps to protect children from transmission in schools, including mask requirements, frequent testing, and improved ventilation, said Dr. Scarpino.
“We’re not going to be able to control COVID without vaccinating younger individuals,” he said.
Dr. Pavia has consulted for GlaxoSmithKline on non–COVID-19–related issues. Sarah Buchan, PhD, study author and scientist at Public Health Ontario, reported grants from the Canadian Institutes of Health Research for research on influenza, RSV, and COVID-19, and grants from the Canadian Immunity Task Force for COVID-19 outside the submitted work. Dr. Coffin reported grants as a Centers for Disease Control and Prevention coinvestigator at a Vaccine and Treatment Evaluation Unit site conducting COVID-19 vaccine trials in children. Dr. Scarpino holds unexercised options in ILiAD Biotechnologies, which is focused on the prevention and treatment of pertussis. Dr. Schaffner is a consultant for VBI Vaccines.
A version of this article first appeared on Medscape.com.
Young children are more likely than are their older siblings to transmit SARS-CoV-2 in their households, according to an analysis of public health records in Ontario, Canada – a finding that upends the common belief that children play a minimal role in COVID-19 spread.
The study by researchers from Public Health Ontario, published online in JAMA Pediatrics, found that teenagers (14- to 17-year-olds) were more likely than were their younger siblings to bring the virus into the household, while infants and toddlers (up to age 3) were about 43% more likely than were the older teens to spread it to others in the home.
Children or teens were the source of SARS-CoV-2 in about 1 in 13 Ontario households between June and December 2020, the study shows. The researchers analyzed health records from 6,280 households with a pediatric COVID-19 case and a subset of 1,717 households in which a child up to age 17 was the source of transmission in a household.
When analyzing the data, the researchers controlled for gender differences, month of disease onset, testing delay, and mean family size.
The role of young children in transmission seemed logical to some experts who have been tracking the evolution of the pandemic. “I think what was more surprising was how long the narrative persisted that children weren’t transmitting SARS-CoV-2,” said Samuel Scarpino, PhD, managing director of pathogen surveillance at the Rockefeller Foundation.
Meanwhile, less mask-wearing, the return to school and activities, and the onslaught of the Delta variant have changed the dynamics of spread, said Andrew Pavia, MD, chief of the division of pediatric infectious diseases at the University of Utah.
“Adolescents and high-school-aged kids have had much, much higher rates of infection in the past,” he said. “Now when we look at the rates of school-aged kids, they are the same as high-school-aged kids, and we’re seeing more and more in the preschool age groups.”
Cases may be underestimated
If anything, the study may underestimate the role young children play in spreading COVID-19 in families, since it included only symptomatic cases as the initial source and young children are more likely to be asymptomatic, Dr. Pavia said.
The Delta variant heightens the concern; it is more than twice as infectious as previous strains and has spurred a rise in pediatric cases, including some coinfection with other circulating respiratory diseases, such as respiratory syncytial virus (RSV).
The Ontario study covers a period before vaccination and the spread of the Delta variant. “As the number of pediatric cases increases worldwide, the role of children in household transmission will continue to grow,” the authors concluded.
Following recommended respiratory hygiene is clearly more difficult with very young children. For example, parents, caregivers, and older siblings aren’t going to stay 6 feet away from a sick baby or toddler, Susan Coffin, MD, MPH, a pediatric infectious disease physician, and David Rubin, MD, a pediatrician and director of PolicyLab at Children’s Hospital of Philadelphia, noted in an accompanying commentary.
“Cuddling and touching are part and parcel of taking care of a sick young child, and that will obviously come with an increased risk of transmission to parents as well as to older siblings who may be helping to care for their sick brother or sister,” they wrote.
While parents may wash their hands more frequently when caring for a sick child, they aren’t likely to wear a mask, said William Schaffner, MD, an infectious disease specialist at Vanderbilt University, Nashville, Tenn.
“I imagine some moms even take a sick child into bed with them,” he said. “It’s probably just the extensive contact one has with a sick, very small child that augments their capacity to transmit this infection.”
What can be done
What can be done, then, to reduce the household spread of COVID-19? “The obvious solution to protect a household with a sick young infant or toddler is to make sure that all eligible members of the household are vaccinated,” Dr. Coffin and Dr. Rubin stated in their commentary.
The American Academy of Pediatrics recently wrote to Janet Woodcock, MD, acting commissioner of the Food and Drug Administration, asking for the agency to authorize use of SARS-CoV-2 vaccines for children under age 12 “as soon as possible,” noting that “the Delta variant has created a new and pressing risk to children and adolescents across this country, as it has also done for unvaccinated adults.”
The FDA reportedly asked vaccine makers Pfizer and Moderna to expand the clinical trials of children, which may delay authorization for younger age groups. Pfizer has said it plans to submit a request for emergency use authorization of its vaccine for 5- to 11-year-olds in September or October.
As with adult vaccination, hesitancy is likely to be a barrier. Less than half of parents said they are very or somewhat likely to have their children get a COVID-19 vaccine, according to a national survey conducted by researchers at the University of California, Los Angeles.
The Ontario study provides valuable evidence to support taking steps to protect children from transmission in schools, including mask requirements, frequent testing, and improved ventilation, said Dr. Scarpino.
“We’re not going to be able to control COVID without vaccinating younger individuals,” he said.
Dr. Pavia has consulted for GlaxoSmithKline on non–COVID-19–related issues. Sarah Buchan, PhD, study author and scientist at Public Health Ontario, reported grants from the Canadian Institutes of Health Research for research on influenza, RSV, and COVID-19, and grants from the Canadian Immunity Task Force for COVID-19 outside the submitted work. Dr. Coffin reported grants as a Centers for Disease Control and Prevention coinvestigator at a Vaccine and Treatment Evaluation Unit site conducting COVID-19 vaccine trials in children. Dr. Scarpino holds unexercised options in ILiAD Biotechnologies, which is focused on the prevention and treatment of pertussis. Dr. Schaffner is a consultant for VBI Vaccines.
A version of this article first appeared on Medscape.com.
U.S. reports record COVID-19 hospitalizations of children
The number of children hospitalized with COVID-19 in the U.S. hit a record high on Aug. 14, with more than 1,900 in hospitals.
Hospitals across the South are running out of beds as the contagious Delta variant spreads, mostly among unvaccinated people. Children make up about 2.4% of the country’s COVID-19 hospitalizations, and those under 12 are particularly vulnerable since they’re not eligible to receive a vaccine.
“This is not last year’s COVID,” Sally Goza, MD, former president of the American Academy of Pediatrics, told CNN on Aug. 14.
“This one is worse, and our children are the ones that are going to be affected by it the most,” she said.
The number of newly hospitalized COVID-19 patients for ages 18-49 also hit record highs during the week of Aug. 9. A fifth of the nation’s hospitalizations are in Florida, where the number of COVID-19 patients hit a record high of 16,100 on Aug. 14. More than 90% of the state’s intensive care unit beds are filled.
More than 90% of the ICU beds in Texas are full as well. On Aug. 13, there were no pediatric ICU beds available in Dallas or the 19 surrounding counties, which means that young patients would be transported father away for care – even Oklahoma City.
“That means if your child’s in a car wreck, if your child has a congenital heart defect or something and needs an ICU bed, or more likely, if they have COVID and need an ICU bed, we don’t have one,” Clay Jenkins, a Dallas County judge, said on Aug. 13.
“Your child will wait for another child to die,” he said.
As children return to classes, educators are talking about the possibility of vaccine mandates. The National Education Association announced its support of mandatory vaccination for its members.
“Our students under 12 can’t get vaccinated,” Becky Pringle, president of the association, told CNN.
“It’s our responsibility to keep them safe,” she said. “Keeping them safe means that everyone who can be vaccinated should be vaccinated.”
The U.S. now has an average of about 129,000 new COVID-19 cases per day, Reuters reported, which has doubled in about 2 weeks. The number of hospitalized patients is at a 6-month high, and about 600 people are dying each day.
Arkansas, Florida, Louisiana, Mississippi, and Oregon have reported record numbers of COVID-19 hospitalizations.
In addition, eight states make up half of all the COVID-19 hospitalizations in the U.S. but only 24% of the nation’s population – Alabama, Arkansas, Florida, Georgia, Louisiana, Mississippi, Nevada, and Texas. These states have vaccination rates lower than the national average, and their COVID-19 patients account for at least 15% of their overall hospitalizations.
To address the surge in hospitalizations, Oregon Gov. Kate Brown has ordered the deployment of up to 1,500 Oregon National Guard members to help health care workers.
“I know this is not the summer many of us envisioned,” Gov. Brown said Aug. 13. “The harsh and frustrating reality is that the Delta variant has changed everything. Delta is highly contagious, and we must take action now.”
A version of this article first appeared on WebMD.com.
The number of children hospitalized with COVID-19 in the U.S. hit a record high on Aug. 14, with more than 1,900 in hospitals.
Hospitals across the South are running out of beds as the contagious Delta variant spreads, mostly among unvaccinated people. Children make up about 2.4% of the country’s COVID-19 hospitalizations, and those under 12 are particularly vulnerable since they’re not eligible to receive a vaccine.
“This is not last year’s COVID,” Sally Goza, MD, former president of the American Academy of Pediatrics, told CNN on Aug. 14.
“This one is worse, and our children are the ones that are going to be affected by it the most,” she said.
The number of newly hospitalized COVID-19 patients for ages 18-49 also hit record highs during the week of Aug. 9. A fifth of the nation’s hospitalizations are in Florida, where the number of COVID-19 patients hit a record high of 16,100 on Aug. 14. More than 90% of the state’s intensive care unit beds are filled.
More than 90% of the ICU beds in Texas are full as well. On Aug. 13, there were no pediatric ICU beds available in Dallas or the 19 surrounding counties, which means that young patients would be transported father away for care – even Oklahoma City.
“That means if your child’s in a car wreck, if your child has a congenital heart defect or something and needs an ICU bed, or more likely, if they have COVID and need an ICU bed, we don’t have one,” Clay Jenkins, a Dallas County judge, said on Aug. 13.
“Your child will wait for another child to die,” he said.
As children return to classes, educators are talking about the possibility of vaccine mandates. The National Education Association announced its support of mandatory vaccination for its members.
“Our students under 12 can’t get vaccinated,” Becky Pringle, president of the association, told CNN.
“It’s our responsibility to keep them safe,” she said. “Keeping them safe means that everyone who can be vaccinated should be vaccinated.”
The U.S. now has an average of about 129,000 new COVID-19 cases per day, Reuters reported, which has doubled in about 2 weeks. The number of hospitalized patients is at a 6-month high, and about 600 people are dying each day.
Arkansas, Florida, Louisiana, Mississippi, and Oregon have reported record numbers of COVID-19 hospitalizations.
In addition, eight states make up half of all the COVID-19 hospitalizations in the U.S. but only 24% of the nation’s population – Alabama, Arkansas, Florida, Georgia, Louisiana, Mississippi, Nevada, and Texas. These states have vaccination rates lower than the national average, and their COVID-19 patients account for at least 15% of their overall hospitalizations.
To address the surge in hospitalizations, Oregon Gov. Kate Brown has ordered the deployment of up to 1,500 Oregon National Guard members to help health care workers.
“I know this is not the summer many of us envisioned,” Gov. Brown said Aug. 13. “The harsh and frustrating reality is that the Delta variant has changed everything. Delta is highly contagious, and we must take action now.”
A version of this article first appeared on WebMD.com.
The number of children hospitalized with COVID-19 in the U.S. hit a record high on Aug. 14, with more than 1,900 in hospitals.
Hospitals across the South are running out of beds as the contagious Delta variant spreads, mostly among unvaccinated people. Children make up about 2.4% of the country’s COVID-19 hospitalizations, and those under 12 are particularly vulnerable since they’re not eligible to receive a vaccine.
“This is not last year’s COVID,” Sally Goza, MD, former president of the American Academy of Pediatrics, told CNN on Aug. 14.
“This one is worse, and our children are the ones that are going to be affected by it the most,” she said.
The number of newly hospitalized COVID-19 patients for ages 18-49 also hit record highs during the week of Aug. 9. A fifth of the nation’s hospitalizations are in Florida, where the number of COVID-19 patients hit a record high of 16,100 on Aug. 14. More than 90% of the state’s intensive care unit beds are filled.
More than 90% of the ICU beds in Texas are full as well. On Aug. 13, there were no pediatric ICU beds available in Dallas or the 19 surrounding counties, which means that young patients would be transported father away for care – even Oklahoma City.
“That means if your child’s in a car wreck, if your child has a congenital heart defect or something and needs an ICU bed, or more likely, if they have COVID and need an ICU bed, we don’t have one,” Clay Jenkins, a Dallas County judge, said on Aug. 13.
“Your child will wait for another child to die,” he said.
As children return to classes, educators are talking about the possibility of vaccine mandates. The National Education Association announced its support of mandatory vaccination for its members.
“Our students under 12 can’t get vaccinated,” Becky Pringle, president of the association, told CNN.
“It’s our responsibility to keep them safe,” she said. “Keeping them safe means that everyone who can be vaccinated should be vaccinated.”
The U.S. now has an average of about 129,000 new COVID-19 cases per day, Reuters reported, which has doubled in about 2 weeks. The number of hospitalized patients is at a 6-month high, and about 600 people are dying each day.
Arkansas, Florida, Louisiana, Mississippi, and Oregon have reported record numbers of COVID-19 hospitalizations.
In addition, eight states make up half of all the COVID-19 hospitalizations in the U.S. but only 24% of the nation’s population – Alabama, Arkansas, Florida, Georgia, Louisiana, Mississippi, Nevada, and Texas. These states have vaccination rates lower than the national average, and their COVID-19 patients account for at least 15% of their overall hospitalizations.
To address the surge in hospitalizations, Oregon Gov. Kate Brown has ordered the deployment of up to 1,500 Oregon National Guard members to help health care workers.
“I know this is not the summer many of us envisioned,” Gov. Brown said Aug. 13. “The harsh and frustrating reality is that the Delta variant has changed everything. Delta is highly contagious, and we must take action now.”
A version of this article first appeared on WebMD.com.
Shedding the super-doctor myth requires an honest look at systemic racism
An overwhelmingly loud and high-pitched screech rattles against your hip. You startle and groan into the pillow as your thoughts settle into conscious awareness. It is 3 a.m. You are a 2nd-year resident trudging through the night shift, alerted to the presence of a new patient awaiting an emergency assessment. You are the only in-house physician. Walking steadfastly toward the emergency unit, you enter and greet the patient. Immediately, you observe a look of surprise followed immediately by a scowl.
You extend a hand, but your greeting is abruptly cut short with: “I want to see a doctor!” You pace your breaths to quell annoyance and resume your introduction, asserting that you are a doctor and indeed the only doctor on duty. After moments of deep sighs and questions regarding your credentials, you persuade the patient to start the interview.
It is now 8 a.m. The frustration of the night starts to ease as you prepare to leave. While gathering your things, a visitor is overheard inquiring the whereabouts of a hospital unit. Volunteering as a guide, you walk the person toward the opposite end of the hospital. Bleary eyed, muscle laxed, and bone weary, you point out the entrance, then turn to leave. The steady rhythm of your steps suddenly halts as you hear from behind: “Thank you! You speak English really well!” Blankly, you stare. Your voice remains mute while your brain screams: “What is that supposed to mean?” But you do not utter a sound, because intuitively, you know the answer.
While reading this scenario, what did you feel? Pride in knowing that the physician was able to successfully navigate a busy night? Relief in the physician’s ability to maintain a professional demeanor despite belittling microaggressions? Are you angry? Would you replay those moments like reruns of a bad TV show? Can you imagine entering your home and collapsing onto the bed as your tears of fury pool over your rumpled sheets?
The emotional release of that morning is seared into my memory. Over the years, I questioned my reactions. Was I too passive? Should I have schooled them on their ignorance? Had I done so, would I have incurred reprimands? Would standing up for myself cause years of hard work to fall away? Moreover, had I defended myself, would I forever have been viewed as “The Angry Black Woman?”
This story is more than a vignette. For me, it is another reminder that, despite how far we have come, we have much further to go. As a Black woman in a professional sphere, I stand upon the shoulders of those who sacrificed for a dream, a greater purpose. My foremothers and forefathers fought bravely and tirelessly so that we could attain levels of success that were only once but a dream. Despite this progress, a grimace, carelessly spoken words, or a mindless gesture remind me that, no matter how much I toil and what levels of success I achieve, when I meet someone for the first time or encounter someone from my past, I find myself wondering whether I am remembered for me or because I am “The Black One.”
Honest look at medicine is imperative
It is important to consider multiple facets of the super-doctor myth. We are dedicated, fearless, authoritative, ambitious individuals. We do not yield to sickness, family obligations, or fatigue. Medicine is a calling, and the patient deserves the utmost respect and professional behavior. Impervious to ethnicity, race, nationality, or creed, we are unbiased and always in service of the greater good. Often, however, I wonder how the expectations of patient-focused, patient-centered care can prevail without an honest look at the vicissitudes facing medicine.
We find ourselves amid a tumultuous year overshadowed by a devastating pandemic that skews heavily toward Black and Brown communities, in addition to political turmoil and racial reckoning that sprang forth from fear, anger, and determination ignited by the murders of Breonna Taylor and George Floyd – communities united in outrage lamenting the cries of Black Lives Matter.
I remember the tears briskly falling upon my blouse as I watched Mr. Floyd’s life violently ripped from this Earth. Shortly thereafter, I remember the phone calls, emails, and texts from close friends, acquaintances, and colleagues offering support, listening ears, pledging to learn and endeavoring to understand the struggle for recognition and the fight for human rights. Even so, the deafening support was clouded by the preternatural silence of some medical organizations. Within the Black physician community, outrage was palpable. We reflected upon years of sacrifice and perseverance despite the challenge of bigotry, ignorance, and racism – not only from patients and their families – but also colleagues and administrators. Yet, in our time of horror and need, in those moments of vulnerability ... silence. Eventually, lengthy proclamations of support were expressed through various media. However, it felt too safe, too corporate, and too generic and inauthentic. As a result, an exodus of Black physicians from leadership positions and academic medicine took hold as the blatant continuation of rhetoric – coupled with ineffective outreach and support – finally took its toll.
Frequently, I question how the obstacles of medical school, residency, and beyond are expected to be traversed while living in a world that consistently affords additional challenges to those who look, act, or speak in a manner that varies from the perceived standard. In a culture where the myth of the super doctor reigns, how do we reconcile attainment of a false and detrimental narrative while the overarching pressure acutely felt by Black physicians magnifies in the setting of stereotypes, sociopolitical turbulence, bigotry, and racism? How can one sacrifice for an entity that is unwilling to acknowledge the psychological implications of that sacrifice?
For instance, while in medical school, I transitioned my hair to its natural state but was counseled against doing so because of the risk of losing residency opportunities as a direct result of my “unprofessional” appearance. Throughout residency, multiple incidents come to mind, including frequent demands to see my hospital badge despite the same not being of asked of my White cohorts; denial of entry into physician entrance within the residency building because, despite my professional attire, I was presumed to be a member of the custodial staff; and patients being confused and asking for a doctor despite my long white coat and clear introductions.
Furthermore, the fluency of my speech and the absence of regional dialect or vernacular are quite often lauded by patients. Inquiries to touch my hair as well as hypotheses regarding my nationality or degree of “blackness” with respect to the shape of my nose, eyes, and lips are openly questioned. Unfortunately, those uncomfortable incidents have not been limited to patient encounters.
In one instance, while presenting a patient in the presence of my attending and a 3rd-year medical student, I was sternly admonished for disclosing the race of the patient. I sat still and resolute as this doctor spoke on increased risk of bias in diagnosis and treatment when race is identified. Outwardly, I projected patience but inside, I seethed. In that moment, I realized that I would never have the luxury of ignorance or denial. Although I desire to be valued for my prowess in medicine, the mythical status was not created with my skin color in mind. For is avoidance not but a reflection of denial?
In these chaotic and uncertain times, how can we continue to promote a pathological ideal when the roads traveled are so fundamentally skewed? If a White physician faces a belligerent and argumentative patient, there is opportunity for debriefing both individually and among a larger cohort via classes, conferences, and supervisions. Conversely, when a Black physician is derided with racist sentiment, will they have the same opportunity for reflection and support? Despite identical expectations of professionalism and growth, how can one be successful in a system that either directly or indirectly encourages the opposite?
As we try to shed the super-doctor myth, we must recognize that this unattainable and detrimental persona hinders progress. This myth undermines our ability to understand our fragility, the limitations of our capabilities, and the strength of our vulnerability. We must take an honest look at the manner in which our individual biases and the deeply ingrained (and potentially unconscious) systemic biases are counterintuitive to the success and support of physicians of color.
Dr. Thomas is a board-certified adult psychiatrist with an interest in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. She has no conflicts of interest.
An overwhelmingly loud and high-pitched screech rattles against your hip. You startle and groan into the pillow as your thoughts settle into conscious awareness. It is 3 a.m. You are a 2nd-year resident trudging through the night shift, alerted to the presence of a new patient awaiting an emergency assessment. You are the only in-house physician. Walking steadfastly toward the emergency unit, you enter and greet the patient. Immediately, you observe a look of surprise followed immediately by a scowl.
You extend a hand, but your greeting is abruptly cut short with: “I want to see a doctor!” You pace your breaths to quell annoyance and resume your introduction, asserting that you are a doctor and indeed the only doctor on duty. After moments of deep sighs and questions regarding your credentials, you persuade the patient to start the interview.
It is now 8 a.m. The frustration of the night starts to ease as you prepare to leave. While gathering your things, a visitor is overheard inquiring the whereabouts of a hospital unit. Volunteering as a guide, you walk the person toward the opposite end of the hospital. Bleary eyed, muscle laxed, and bone weary, you point out the entrance, then turn to leave. The steady rhythm of your steps suddenly halts as you hear from behind: “Thank you! You speak English really well!” Blankly, you stare. Your voice remains mute while your brain screams: “What is that supposed to mean?” But you do not utter a sound, because intuitively, you know the answer.
While reading this scenario, what did you feel? Pride in knowing that the physician was able to successfully navigate a busy night? Relief in the physician’s ability to maintain a professional demeanor despite belittling microaggressions? Are you angry? Would you replay those moments like reruns of a bad TV show? Can you imagine entering your home and collapsing onto the bed as your tears of fury pool over your rumpled sheets?
The emotional release of that morning is seared into my memory. Over the years, I questioned my reactions. Was I too passive? Should I have schooled them on their ignorance? Had I done so, would I have incurred reprimands? Would standing up for myself cause years of hard work to fall away? Moreover, had I defended myself, would I forever have been viewed as “The Angry Black Woman?”
This story is more than a vignette. For me, it is another reminder that, despite how far we have come, we have much further to go. As a Black woman in a professional sphere, I stand upon the shoulders of those who sacrificed for a dream, a greater purpose. My foremothers and forefathers fought bravely and tirelessly so that we could attain levels of success that were only once but a dream. Despite this progress, a grimace, carelessly spoken words, or a mindless gesture remind me that, no matter how much I toil and what levels of success I achieve, when I meet someone for the first time or encounter someone from my past, I find myself wondering whether I am remembered for me or because I am “The Black One.”
Honest look at medicine is imperative
It is important to consider multiple facets of the super-doctor myth. We are dedicated, fearless, authoritative, ambitious individuals. We do not yield to sickness, family obligations, or fatigue. Medicine is a calling, and the patient deserves the utmost respect and professional behavior. Impervious to ethnicity, race, nationality, or creed, we are unbiased and always in service of the greater good. Often, however, I wonder how the expectations of patient-focused, patient-centered care can prevail without an honest look at the vicissitudes facing medicine.
We find ourselves amid a tumultuous year overshadowed by a devastating pandemic that skews heavily toward Black and Brown communities, in addition to political turmoil and racial reckoning that sprang forth from fear, anger, and determination ignited by the murders of Breonna Taylor and George Floyd – communities united in outrage lamenting the cries of Black Lives Matter.
I remember the tears briskly falling upon my blouse as I watched Mr. Floyd’s life violently ripped from this Earth. Shortly thereafter, I remember the phone calls, emails, and texts from close friends, acquaintances, and colleagues offering support, listening ears, pledging to learn and endeavoring to understand the struggle for recognition and the fight for human rights. Even so, the deafening support was clouded by the preternatural silence of some medical organizations. Within the Black physician community, outrage was palpable. We reflected upon years of sacrifice and perseverance despite the challenge of bigotry, ignorance, and racism – not only from patients and their families – but also colleagues and administrators. Yet, in our time of horror and need, in those moments of vulnerability ... silence. Eventually, lengthy proclamations of support were expressed through various media. However, it felt too safe, too corporate, and too generic and inauthentic. As a result, an exodus of Black physicians from leadership positions and academic medicine took hold as the blatant continuation of rhetoric – coupled with ineffective outreach and support – finally took its toll.
Frequently, I question how the obstacles of medical school, residency, and beyond are expected to be traversed while living in a world that consistently affords additional challenges to those who look, act, or speak in a manner that varies from the perceived standard. In a culture where the myth of the super doctor reigns, how do we reconcile attainment of a false and detrimental narrative while the overarching pressure acutely felt by Black physicians magnifies in the setting of stereotypes, sociopolitical turbulence, bigotry, and racism? How can one sacrifice for an entity that is unwilling to acknowledge the psychological implications of that sacrifice?
For instance, while in medical school, I transitioned my hair to its natural state but was counseled against doing so because of the risk of losing residency opportunities as a direct result of my “unprofessional” appearance. Throughout residency, multiple incidents come to mind, including frequent demands to see my hospital badge despite the same not being of asked of my White cohorts; denial of entry into physician entrance within the residency building because, despite my professional attire, I was presumed to be a member of the custodial staff; and patients being confused and asking for a doctor despite my long white coat and clear introductions.
Furthermore, the fluency of my speech and the absence of regional dialect or vernacular are quite often lauded by patients. Inquiries to touch my hair as well as hypotheses regarding my nationality or degree of “blackness” with respect to the shape of my nose, eyes, and lips are openly questioned. Unfortunately, those uncomfortable incidents have not been limited to patient encounters.
In one instance, while presenting a patient in the presence of my attending and a 3rd-year medical student, I was sternly admonished for disclosing the race of the patient. I sat still and resolute as this doctor spoke on increased risk of bias in diagnosis and treatment when race is identified. Outwardly, I projected patience but inside, I seethed. In that moment, I realized that I would never have the luxury of ignorance or denial. Although I desire to be valued for my prowess in medicine, the mythical status was not created with my skin color in mind. For is avoidance not but a reflection of denial?
In these chaotic and uncertain times, how can we continue to promote a pathological ideal when the roads traveled are so fundamentally skewed? If a White physician faces a belligerent and argumentative patient, there is opportunity for debriefing both individually and among a larger cohort via classes, conferences, and supervisions. Conversely, when a Black physician is derided with racist sentiment, will they have the same opportunity for reflection and support? Despite identical expectations of professionalism and growth, how can one be successful in a system that either directly or indirectly encourages the opposite?
As we try to shed the super-doctor myth, we must recognize that this unattainable and detrimental persona hinders progress. This myth undermines our ability to understand our fragility, the limitations of our capabilities, and the strength of our vulnerability. We must take an honest look at the manner in which our individual biases and the deeply ingrained (and potentially unconscious) systemic biases are counterintuitive to the success and support of physicians of color.
Dr. Thomas is a board-certified adult psychiatrist with an interest in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. She has no conflicts of interest.
An overwhelmingly loud and high-pitched screech rattles against your hip. You startle and groan into the pillow as your thoughts settle into conscious awareness. It is 3 a.m. You are a 2nd-year resident trudging through the night shift, alerted to the presence of a new patient awaiting an emergency assessment. You are the only in-house physician. Walking steadfastly toward the emergency unit, you enter and greet the patient. Immediately, you observe a look of surprise followed immediately by a scowl.
You extend a hand, but your greeting is abruptly cut short with: “I want to see a doctor!” You pace your breaths to quell annoyance and resume your introduction, asserting that you are a doctor and indeed the only doctor on duty. After moments of deep sighs and questions regarding your credentials, you persuade the patient to start the interview.
It is now 8 a.m. The frustration of the night starts to ease as you prepare to leave. While gathering your things, a visitor is overheard inquiring the whereabouts of a hospital unit. Volunteering as a guide, you walk the person toward the opposite end of the hospital. Bleary eyed, muscle laxed, and bone weary, you point out the entrance, then turn to leave. The steady rhythm of your steps suddenly halts as you hear from behind: “Thank you! You speak English really well!” Blankly, you stare. Your voice remains mute while your brain screams: “What is that supposed to mean?” But you do not utter a sound, because intuitively, you know the answer.
While reading this scenario, what did you feel? Pride in knowing that the physician was able to successfully navigate a busy night? Relief in the physician’s ability to maintain a professional demeanor despite belittling microaggressions? Are you angry? Would you replay those moments like reruns of a bad TV show? Can you imagine entering your home and collapsing onto the bed as your tears of fury pool over your rumpled sheets?
The emotional release of that morning is seared into my memory. Over the years, I questioned my reactions. Was I too passive? Should I have schooled them on their ignorance? Had I done so, would I have incurred reprimands? Would standing up for myself cause years of hard work to fall away? Moreover, had I defended myself, would I forever have been viewed as “The Angry Black Woman?”
This story is more than a vignette. For me, it is another reminder that, despite how far we have come, we have much further to go. As a Black woman in a professional sphere, I stand upon the shoulders of those who sacrificed for a dream, a greater purpose. My foremothers and forefathers fought bravely and tirelessly so that we could attain levels of success that were only once but a dream. Despite this progress, a grimace, carelessly spoken words, or a mindless gesture remind me that, no matter how much I toil and what levels of success I achieve, when I meet someone for the first time or encounter someone from my past, I find myself wondering whether I am remembered for me or because I am “The Black One.”
Honest look at medicine is imperative
It is important to consider multiple facets of the super-doctor myth. We are dedicated, fearless, authoritative, ambitious individuals. We do not yield to sickness, family obligations, or fatigue. Medicine is a calling, and the patient deserves the utmost respect and professional behavior. Impervious to ethnicity, race, nationality, or creed, we are unbiased and always in service of the greater good. Often, however, I wonder how the expectations of patient-focused, patient-centered care can prevail without an honest look at the vicissitudes facing medicine.
We find ourselves amid a tumultuous year overshadowed by a devastating pandemic that skews heavily toward Black and Brown communities, in addition to political turmoil and racial reckoning that sprang forth from fear, anger, and determination ignited by the murders of Breonna Taylor and George Floyd – communities united in outrage lamenting the cries of Black Lives Matter.
I remember the tears briskly falling upon my blouse as I watched Mr. Floyd’s life violently ripped from this Earth. Shortly thereafter, I remember the phone calls, emails, and texts from close friends, acquaintances, and colleagues offering support, listening ears, pledging to learn and endeavoring to understand the struggle for recognition and the fight for human rights. Even so, the deafening support was clouded by the preternatural silence of some medical organizations. Within the Black physician community, outrage was palpable. We reflected upon years of sacrifice and perseverance despite the challenge of bigotry, ignorance, and racism – not only from patients and their families – but also colleagues and administrators. Yet, in our time of horror and need, in those moments of vulnerability ... silence. Eventually, lengthy proclamations of support were expressed through various media. However, it felt too safe, too corporate, and too generic and inauthentic. As a result, an exodus of Black physicians from leadership positions and academic medicine took hold as the blatant continuation of rhetoric – coupled with ineffective outreach and support – finally took its toll.
Frequently, I question how the obstacles of medical school, residency, and beyond are expected to be traversed while living in a world that consistently affords additional challenges to those who look, act, or speak in a manner that varies from the perceived standard. In a culture where the myth of the super doctor reigns, how do we reconcile attainment of a false and detrimental narrative while the overarching pressure acutely felt by Black physicians magnifies in the setting of stereotypes, sociopolitical turbulence, bigotry, and racism? How can one sacrifice for an entity that is unwilling to acknowledge the psychological implications of that sacrifice?
For instance, while in medical school, I transitioned my hair to its natural state but was counseled against doing so because of the risk of losing residency opportunities as a direct result of my “unprofessional” appearance. Throughout residency, multiple incidents come to mind, including frequent demands to see my hospital badge despite the same not being of asked of my White cohorts; denial of entry into physician entrance within the residency building because, despite my professional attire, I was presumed to be a member of the custodial staff; and patients being confused and asking for a doctor despite my long white coat and clear introductions.
Furthermore, the fluency of my speech and the absence of regional dialect or vernacular are quite often lauded by patients. Inquiries to touch my hair as well as hypotheses regarding my nationality or degree of “blackness” with respect to the shape of my nose, eyes, and lips are openly questioned. Unfortunately, those uncomfortable incidents have not been limited to patient encounters.
In one instance, while presenting a patient in the presence of my attending and a 3rd-year medical student, I was sternly admonished for disclosing the race of the patient. I sat still and resolute as this doctor spoke on increased risk of bias in diagnosis and treatment when race is identified. Outwardly, I projected patience but inside, I seethed. In that moment, I realized that I would never have the luxury of ignorance or denial. Although I desire to be valued for my prowess in medicine, the mythical status was not created with my skin color in mind. For is avoidance not but a reflection of denial?
In these chaotic and uncertain times, how can we continue to promote a pathological ideal when the roads traveled are so fundamentally skewed? If a White physician faces a belligerent and argumentative patient, there is opportunity for debriefing both individually and among a larger cohort via classes, conferences, and supervisions. Conversely, when a Black physician is derided with racist sentiment, will they have the same opportunity for reflection and support? Despite identical expectations of professionalism and growth, how can one be successful in a system that either directly or indirectly encourages the opposite?
As we try to shed the super-doctor myth, we must recognize that this unattainable and detrimental persona hinders progress. This myth undermines our ability to understand our fragility, the limitations of our capabilities, and the strength of our vulnerability. We must take an honest look at the manner in which our individual biases and the deeply ingrained (and potentially unconscious) systemic biases are counterintuitive to the success and support of physicians of color.
Dr. Thomas is a board-certified adult psychiatrist with an interest in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. She has no conflicts of interest.
‘No justification’ for suicide warning on all antiseizure meds
, new research shows. “There appears to be no justification for the FDA to label every new antiseizure medication with a warning that it may increase risk of suicidality,” said study investigator Michael R. Sperling, MD, professor of neurology, Thomas Jefferson University, Philadelphia.
“How many patients are afraid of their medication and do not take it because of the warning – and are consequently at risk because of that? We do not know, but have anecdotal experience that this is certainly an issue,” Dr. Sperling, who is director of the Jefferson Comprehensive Epilepsy Center, added.
The study was published online August 2 in JAMA Neurology.
Blanket warning
In 2008, the FDA issued an alert stating that antiseizure medications increase suicidality. The alert was based on pooled data from placebo-controlled clinical trials that included 11 antiseizure medications – carbamazepine, felbamate, gabapentin, lamotrigine, levetiracetam, oxcarbazepine, pregabalin, tiagabine, topiramate, valproate, and zonisamide.
The meta-analytic review showed that, compared with placebo, antiseizure medications nearly doubled suicide risk among patients treated for epilepsy, psychiatric disorders, and other diseases. As a result of the FDA study, all antiseizure medications that have been approved since 2008 carry a warning for suicidality.
However, subsequent analyses did not show the same results, Dr. Sperling and colleagues noted.
“Pivotal” antiseizure medication epilepsy trials since 2008 have evaluated suicidality prospectively. Since 2011, trials have included the validated Columbia Suicidality Severity Rating Scale, they noted.
Meta analysis showed no increased risk
Dr. Sperling and colleagues conducted a meta-analysis of 17 randomized placebo-controlled epilepsy trials of five antiseizure medications approved since 2008. These antiseizure medications were eslicarbazepine, perampanel, brivaracetam, cannabidiol, and cenobamate. The trials involved 5,996 patients, including 4,000 who were treated with antiseizure medications and 1,996 who were treated with placebo.
Confining the analysis to epilepsy trials avoids potential confounders, such as possible differences in suicidality risks between different diseases, the researchers noted.
They found no evidence of increased risk for suicidal ideation (overall risk ratio, antiseizure medications vs. placebo: 0.75; 95% confidence interval: 0.35-1.60) or suicide attempt (risk ratio, 0.75; 95% CI: 0.30-1.87) overall or for any individual antiseizure medication.
Suicidal ideation occurred in 12 of 4,000 patients treated with antiseizure medications (0.30%), versus 7 of 1,996 patients treated with placebo (0.35%) (P = .74). Three patients who were treated with antiseizure medications attempted suicide; no patients who were treated with placebo attempted suicide (P = .22). There were no completed suicides.
“There is no current evidence that the five antiseizure medications evaluated in this study increase suicidality in epilepsy and merit a suicidality class warning,” the investigators wrote. When prescribed for epilepsy, “evidence does not support the FDA’s labeling practice of a blanket assumption of increased suicidality,” said Dr. Sperling.
“Our findings indicate the nonspecific suicide warning for all epilepsy drugs is simply not justifiable,” he said. “The results are not surprising. Different drugs affect cells in different ways. So there’s no reason to expect that every drug would increase suicide risk for every patient,” Dr. Sperling said in a statement.
“It’s important to recognize that epilepsy has many causes – perinatal injury, stroke, tumor, head trauma, developmental malformations, genetic causes, and others – and these underlying etiologies may well contribute to the presence of depression and suicidality in this population,” he said in an interview. “Psychodynamic influences also may occur as a consequence of having seizures. This is a complicated area, and drugs are simply one piece of the puzzle,” he added.
Dr. Sperling said the FDA has accomplished “one useful thing with its warning – it highlighted that physicians and other health care providers must pay attention to their patients’ psychological state, ask questions, and treat accordingly.”
The study had no specific funding. Dr. Sperling has received grants from Eisai, Medtronic, Neurelis, SK Life Science, Sunovion, Takeda, Xenon, Cerevel Therapeutics, UCB Pharma, and Engage Pharma; personal fees from Neurelis, Medscape, Neurology Live, International Medical Press, UCB Pharma, Eisai, Oxford University Press, and Projects in Knowledge. He has also consulted for Medtronic outside the submitted work; payments went to Thomas Jefferson University. A complete list of authors’ disclosures is available with the original article.
A version of this article first appeared on Medscape.com.
, new research shows. “There appears to be no justification for the FDA to label every new antiseizure medication with a warning that it may increase risk of suicidality,” said study investigator Michael R. Sperling, MD, professor of neurology, Thomas Jefferson University, Philadelphia.
“How many patients are afraid of their medication and do not take it because of the warning – and are consequently at risk because of that? We do not know, but have anecdotal experience that this is certainly an issue,” Dr. Sperling, who is director of the Jefferson Comprehensive Epilepsy Center, added.
The study was published online August 2 in JAMA Neurology.
Blanket warning
In 2008, the FDA issued an alert stating that antiseizure medications increase suicidality. The alert was based on pooled data from placebo-controlled clinical trials that included 11 antiseizure medications – carbamazepine, felbamate, gabapentin, lamotrigine, levetiracetam, oxcarbazepine, pregabalin, tiagabine, topiramate, valproate, and zonisamide.
The meta-analytic review showed that, compared with placebo, antiseizure medications nearly doubled suicide risk among patients treated for epilepsy, psychiatric disorders, and other diseases. As a result of the FDA study, all antiseizure medications that have been approved since 2008 carry a warning for suicidality.
However, subsequent analyses did not show the same results, Dr. Sperling and colleagues noted.
“Pivotal” antiseizure medication epilepsy trials since 2008 have evaluated suicidality prospectively. Since 2011, trials have included the validated Columbia Suicidality Severity Rating Scale, they noted.
Meta analysis showed no increased risk
Dr. Sperling and colleagues conducted a meta-analysis of 17 randomized placebo-controlled epilepsy trials of five antiseizure medications approved since 2008. These antiseizure medications were eslicarbazepine, perampanel, brivaracetam, cannabidiol, and cenobamate. The trials involved 5,996 patients, including 4,000 who were treated with antiseizure medications and 1,996 who were treated with placebo.
Confining the analysis to epilepsy trials avoids potential confounders, such as possible differences in suicidality risks between different diseases, the researchers noted.
They found no evidence of increased risk for suicidal ideation (overall risk ratio, antiseizure medications vs. placebo: 0.75; 95% confidence interval: 0.35-1.60) or suicide attempt (risk ratio, 0.75; 95% CI: 0.30-1.87) overall or for any individual antiseizure medication.
Suicidal ideation occurred in 12 of 4,000 patients treated with antiseizure medications (0.30%), versus 7 of 1,996 patients treated with placebo (0.35%) (P = .74). Three patients who were treated with antiseizure medications attempted suicide; no patients who were treated with placebo attempted suicide (P = .22). There were no completed suicides.
“There is no current evidence that the five antiseizure medications evaluated in this study increase suicidality in epilepsy and merit a suicidality class warning,” the investigators wrote. When prescribed for epilepsy, “evidence does not support the FDA’s labeling practice of a blanket assumption of increased suicidality,” said Dr. Sperling.
“Our findings indicate the nonspecific suicide warning for all epilepsy drugs is simply not justifiable,” he said. “The results are not surprising. Different drugs affect cells in different ways. So there’s no reason to expect that every drug would increase suicide risk for every patient,” Dr. Sperling said in a statement.
“It’s important to recognize that epilepsy has many causes – perinatal injury, stroke, tumor, head trauma, developmental malformations, genetic causes, and others – and these underlying etiologies may well contribute to the presence of depression and suicidality in this population,” he said in an interview. “Psychodynamic influences also may occur as a consequence of having seizures. This is a complicated area, and drugs are simply one piece of the puzzle,” he added.
Dr. Sperling said the FDA has accomplished “one useful thing with its warning – it highlighted that physicians and other health care providers must pay attention to their patients’ psychological state, ask questions, and treat accordingly.”
The study had no specific funding. Dr. Sperling has received grants from Eisai, Medtronic, Neurelis, SK Life Science, Sunovion, Takeda, Xenon, Cerevel Therapeutics, UCB Pharma, and Engage Pharma; personal fees from Neurelis, Medscape, Neurology Live, International Medical Press, UCB Pharma, Eisai, Oxford University Press, and Projects in Knowledge. He has also consulted for Medtronic outside the submitted work; payments went to Thomas Jefferson University. A complete list of authors’ disclosures is available with the original article.
A version of this article first appeared on Medscape.com.
, new research shows. “There appears to be no justification for the FDA to label every new antiseizure medication with a warning that it may increase risk of suicidality,” said study investigator Michael R. Sperling, MD, professor of neurology, Thomas Jefferson University, Philadelphia.
“How many patients are afraid of their medication and do not take it because of the warning – and are consequently at risk because of that? We do not know, but have anecdotal experience that this is certainly an issue,” Dr. Sperling, who is director of the Jefferson Comprehensive Epilepsy Center, added.
The study was published online August 2 in JAMA Neurology.
Blanket warning
In 2008, the FDA issued an alert stating that antiseizure medications increase suicidality. The alert was based on pooled data from placebo-controlled clinical trials that included 11 antiseizure medications – carbamazepine, felbamate, gabapentin, lamotrigine, levetiracetam, oxcarbazepine, pregabalin, tiagabine, topiramate, valproate, and zonisamide.
The meta-analytic review showed that, compared with placebo, antiseizure medications nearly doubled suicide risk among patients treated for epilepsy, psychiatric disorders, and other diseases. As a result of the FDA study, all antiseizure medications that have been approved since 2008 carry a warning for suicidality.
However, subsequent analyses did not show the same results, Dr. Sperling and colleagues noted.
“Pivotal” antiseizure medication epilepsy trials since 2008 have evaluated suicidality prospectively. Since 2011, trials have included the validated Columbia Suicidality Severity Rating Scale, they noted.
Meta analysis showed no increased risk
Dr. Sperling and colleagues conducted a meta-analysis of 17 randomized placebo-controlled epilepsy trials of five antiseizure medications approved since 2008. These antiseizure medications were eslicarbazepine, perampanel, brivaracetam, cannabidiol, and cenobamate. The trials involved 5,996 patients, including 4,000 who were treated with antiseizure medications and 1,996 who were treated with placebo.
Confining the analysis to epilepsy trials avoids potential confounders, such as possible differences in suicidality risks between different diseases, the researchers noted.
They found no evidence of increased risk for suicidal ideation (overall risk ratio, antiseizure medications vs. placebo: 0.75; 95% confidence interval: 0.35-1.60) or suicide attempt (risk ratio, 0.75; 95% CI: 0.30-1.87) overall or for any individual antiseizure medication.
Suicidal ideation occurred in 12 of 4,000 patients treated with antiseizure medications (0.30%), versus 7 of 1,996 patients treated with placebo (0.35%) (P = .74). Three patients who were treated with antiseizure medications attempted suicide; no patients who were treated with placebo attempted suicide (P = .22). There were no completed suicides.
“There is no current evidence that the five antiseizure medications evaluated in this study increase suicidality in epilepsy and merit a suicidality class warning,” the investigators wrote. When prescribed for epilepsy, “evidence does not support the FDA’s labeling practice of a blanket assumption of increased suicidality,” said Dr. Sperling.
“Our findings indicate the nonspecific suicide warning for all epilepsy drugs is simply not justifiable,” he said. “The results are not surprising. Different drugs affect cells in different ways. So there’s no reason to expect that every drug would increase suicide risk for every patient,” Dr. Sperling said in a statement.
“It’s important to recognize that epilepsy has many causes – perinatal injury, stroke, tumor, head trauma, developmental malformations, genetic causes, and others – and these underlying etiologies may well contribute to the presence of depression and suicidality in this population,” he said in an interview. “Psychodynamic influences also may occur as a consequence of having seizures. This is a complicated area, and drugs are simply one piece of the puzzle,” he added.
Dr. Sperling said the FDA has accomplished “one useful thing with its warning – it highlighted that physicians and other health care providers must pay attention to their patients’ psychological state, ask questions, and treat accordingly.”
The study had no specific funding. Dr. Sperling has received grants from Eisai, Medtronic, Neurelis, SK Life Science, Sunovion, Takeda, Xenon, Cerevel Therapeutics, UCB Pharma, and Engage Pharma; personal fees from Neurelis, Medscape, Neurology Live, International Medical Press, UCB Pharma, Eisai, Oxford University Press, and Projects in Knowledge. He has also consulted for Medtronic outside the submitted work; payments went to Thomas Jefferson University. A complete list of authors’ disclosures is available with the original article.
A version of this article first appeared on Medscape.com.
FROM JAMA NEUROLOGY
Universal masking is the key to safe school attendance
“I want my child to go back to school,” the mother said to me. “I just want you to tell me it will be safe.”
As the summer break winds down for children across the United States, pediatric COVID-19 cases are rising. According to the American Academy of Pediatrics, nearly 94,000 cases were reported for the week ending Aug. 5, more than double the case count from 2 weeks earlier.1
Anecdotally, some children’s hospitals are reporting an increase in pediatric COVID-19 admissions. In the hospital in which I practice, we are seeing numbers similar to those we saw in December and January: a typical daily census of 10 kids admitted with COVID-19, with 4 of them in the intensive care unit. It is a stark contrast to June when, most days, we had no patients with COVID-19 in the hospital. About half of our hospitalized patients are too young to be vaccinated against COVID-19, while the rest are unvaccinated children 12 years and older.
Vaccination of eligible children and teachers is an essential strategy for preventing the spread of COVID-19 in schools, but as children head back to school, immunization rates of educators are largely unknown and are suboptimal among students in most states. As of Aug. 11, 10.7 million U.S. children had received at least one dose of COVID-19 vaccine, representing 43% of 12- to 15-year-olds and 53% of 16- to 17-year-olds.2 Rates vary substantially by state, with more than 70% of kids in Vermont receiving at least one dose of vaccine, compared with less than 25% in Wyoming and Alabama.
Still, in the absence of robust immunization rates, we have data that schools can still reopen successfully. We need to follow the science and implement universal masking, a safe, effective, and practical mitigation strategy.
It worked in Wisconsin. Seventeen K-12 schools in rural Wisconsin opened last fall for in-person instruction.3 Reported compliance with masking was high, ranging from 92.1% to 97.4%, and in-school transmission of COVID-19 was low, with seven cases among 4,876 students.
It worked in Salt Lake City.4 In 20 elementary schools open for in-person instruction Dec. 3, 2020, to Jan. 31, 2021, compliance with mask-wearing was high and in-school transmission was very low, despite a high community incidence of COVID-19. Notably, students’ classroom seats were less than 6 feet apart, suggesting that consistent mask-wearing works even when physical distancing is challenging.
One of the best examples of successful school reopening happened in North Carolina, where pediatricians, pediatric infectious disease specialists, and other experts affiliated with Duke University formed the ABC Science Collaborative to support school districts that requested scientific input to help guide return-to-school policies during the COVID-19 pandemic. From Oct. 26, 2020, to Feb. 28, 2021, the ABC Science Collaborative worked with 13 school districts that were open for in-person instruction using basic mitigation strategies, including universal masking.5 During this time period, there were 4,969 community-acquired SARS-CoV-2 infections in the more than 100,000 students and staff present in schools. Transmission to school contacts was identified in only 209 individuals for a secondary attack rate of less than 1%.
Duke investigator Kanecia Zimmerman, MD, told Duke Today, “We know that, if our goal is to reduce transmission of COVID-19 in schools, there are two effective ways to do that: 1. vaccination, 2. masking. In the setting of schools ... the science suggests masking can be extremely effective, particularly for those who can’t get vaccinated while COVID-19 is still circulating.”
Both the AAP6 and the Pediatric Infectious Diseases Society7 have emphasized the importance of in-person instruction and endorsed universal masking in school. Mask-optional policies or “mask-if-you-are-unvaccinated” policies don’t work, as we have seen in society at large. They are likely to be especially challenging in school settings. Given an option, many, if not most kids, will take off their masks. Kids who leave them on run the risk of stigmatization or bullying.
On Aug. 4, the Centers for Disease Control and Prevention updated its guidance to recommend universal indoor masking for all students, staff, teachers, and visitors to K-12 schools, regardless of vaccination status. Now we’ll have to wait and see if school districts, elected officials, and parents will get on board with masks. ... and we’ll be left to count the number of rising COVID-19 cases that occur until they do.
Case in point: Kids in Greater Clark County, Ind., headed back to school on July 28. Masks were not required on school property, although unvaccinated students and teachers were “strongly encouraged” to wear them.8
Over the first 8 days of in-person instruction, schools in Greater Clark County identified 70 cases of COVID-19 in students and quarantined more than 1,100 of the district’s 10,300 students. Only the unvaccinated were required to quarantine. The district began requiring masks in all school buildings on Aug. 9.9
The worried mother had one last question for me. “What’s the best mask for a child to wear?” For most kids, a simple, well-fitting cloth mask is fine. The best mask is ultimately the mask a child will wear. A toolkit with practical tips for helping children successfully wear a mask is available on the ABC Science Collaborative website.
Dr. Bryant, president of the Pediatric Infectious Diseases Society, is a pediatrician at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at [email protected].
References
1. American Academy of Pediatrics. “Children and COVID-19: State-level data report.”
2. American Academy of Pediatrics. “Children and COVID-19 vaccination trends.”
3. Falk A et al. MMWR Morb Mortal Wkly Rep. 2021;70:136-40.
4. Hershow RB et al. MMWR Morb Mortal Wkly Rep 2021;70:442-8.
5. Zimmerman KO et al. Pediatrics. 2021 Jul;e2021052686. doi: 10.1542/peds.2021-052686.
6. American Academy of Pediatrics. “American Academy of Pediatrics updates recommendations for opening schools in fall 2021.”
7. Pediatric Infectious Diseases Society. “PIDS supports universal masking for students, school staff.”
8. Courtney Hayden. WHAS11. “Greater Clark County Schools return to class July 28.”
9. Dustin Vogt. WAVE3 News. “Greater Clark Country Schools to require masks amid 70 positive cases.”
“I want my child to go back to school,” the mother said to me. “I just want you to tell me it will be safe.”
As the summer break winds down for children across the United States, pediatric COVID-19 cases are rising. According to the American Academy of Pediatrics, nearly 94,000 cases were reported for the week ending Aug. 5, more than double the case count from 2 weeks earlier.1
Anecdotally, some children’s hospitals are reporting an increase in pediatric COVID-19 admissions. In the hospital in which I practice, we are seeing numbers similar to those we saw in December and January: a typical daily census of 10 kids admitted with COVID-19, with 4 of them in the intensive care unit. It is a stark contrast to June when, most days, we had no patients with COVID-19 in the hospital. About half of our hospitalized patients are too young to be vaccinated against COVID-19, while the rest are unvaccinated children 12 years and older.
Vaccination of eligible children and teachers is an essential strategy for preventing the spread of COVID-19 in schools, but as children head back to school, immunization rates of educators are largely unknown and are suboptimal among students in most states. As of Aug. 11, 10.7 million U.S. children had received at least one dose of COVID-19 vaccine, representing 43% of 12- to 15-year-olds and 53% of 16- to 17-year-olds.2 Rates vary substantially by state, with more than 70% of kids in Vermont receiving at least one dose of vaccine, compared with less than 25% in Wyoming and Alabama.
Still, in the absence of robust immunization rates, we have data that schools can still reopen successfully. We need to follow the science and implement universal masking, a safe, effective, and practical mitigation strategy.
It worked in Wisconsin. Seventeen K-12 schools in rural Wisconsin opened last fall for in-person instruction.3 Reported compliance with masking was high, ranging from 92.1% to 97.4%, and in-school transmission of COVID-19 was low, with seven cases among 4,876 students.
It worked in Salt Lake City.4 In 20 elementary schools open for in-person instruction Dec. 3, 2020, to Jan. 31, 2021, compliance with mask-wearing was high and in-school transmission was very low, despite a high community incidence of COVID-19. Notably, students’ classroom seats were less than 6 feet apart, suggesting that consistent mask-wearing works even when physical distancing is challenging.
One of the best examples of successful school reopening happened in North Carolina, where pediatricians, pediatric infectious disease specialists, and other experts affiliated with Duke University formed the ABC Science Collaborative to support school districts that requested scientific input to help guide return-to-school policies during the COVID-19 pandemic. From Oct. 26, 2020, to Feb. 28, 2021, the ABC Science Collaborative worked with 13 school districts that were open for in-person instruction using basic mitigation strategies, including universal masking.5 During this time period, there were 4,969 community-acquired SARS-CoV-2 infections in the more than 100,000 students and staff present in schools. Transmission to school contacts was identified in only 209 individuals for a secondary attack rate of less than 1%.
Duke investigator Kanecia Zimmerman, MD, told Duke Today, “We know that, if our goal is to reduce transmission of COVID-19 in schools, there are two effective ways to do that: 1. vaccination, 2. masking. In the setting of schools ... the science suggests masking can be extremely effective, particularly for those who can’t get vaccinated while COVID-19 is still circulating.”
Both the AAP6 and the Pediatric Infectious Diseases Society7 have emphasized the importance of in-person instruction and endorsed universal masking in school. Mask-optional policies or “mask-if-you-are-unvaccinated” policies don’t work, as we have seen in society at large. They are likely to be especially challenging in school settings. Given an option, many, if not most kids, will take off their masks. Kids who leave them on run the risk of stigmatization or bullying.
On Aug. 4, the Centers for Disease Control and Prevention updated its guidance to recommend universal indoor masking for all students, staff, teachers, and visitors to K-12 schools, regardless of vaccination status. Now we’ll have to wait and see if school districts, elected officials, and parents will get on board with masks. ... and we’ll be left to count the number of rising COVID-19 cases that occur until they do.
Case in point: Kids in Greater Clark County, Ind., headed back to school on July 28. Masks were not required on school property, although unvaccinated students and teachers were “strongly encouraged” to wear them.8
Over the first 8 days of in-person instruction, schools in Greater Clark County identified 70 cases of COVID-19 in students and quarantined more than 1,100 of the district’s 10,300 students. Only the unvaccinated were required to quarantine. The district began requiring masks in all school buildings on Aug. 9.9
The worried mother had one last question for me. “What’s the best mask for a child to wear?” For most kids, a simple, well-fitting cloth mask is fine. The best mask is ultimately the mask a child will wear. A toolkit with practical tips for helping children successfully wear a mask is available on the ABC Science Collaborative website.
Dr. Bryant, president of the Pediatric Infectious Diseases Society, is a pediatrician at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at [email protected].
References
1. American Academy of Pediatrics. “Children and COVID-19: State-level data report.”
2. American Academy of Pediatrics. “Children and COVID-19 vaccination trends.”
3. Falk A et al. MMWR Morb Mortal Wkly Rep. 2021;70:136-40.
4. Hershow RB et al. MMWR Morb Mortal Wkly Rep 2021;70:442-8.
5. Zimmerman KO et al. Pediatrics. 2021 Jul;e2021052686. doi: 10.1542/peds.2021-052686.
6. American Academy of Pediatrics. “American Academy of Pediatrics updates recommendations for opening schools in fall 2021.”
7. Pediatric Infectious Diseases Society. “PIDS supports universal masking for students, school staff.”
8. Courtney Hayden. WHAS11. “Greater Clark County Schools return to class July 28.”
9. Dustin Vogt. WAVE3 News. “Greater Clark Country Schools to require masks amid 70 positive cases.”
“I want my child to go back to school,” the mother said to me. “I just want you to tell me it will be safe.”
As the summer break winds down for children across the United States, pediatric COVID-19 cases are rising. According to the American Academy of Pediatrics, nearly 94,000 cases were reported for the week ending Aug. 5, more than double the case count from 2 weeks earlier.1
Anecdotally, some children’s hospitals are reporting an increase in pediatric COVID-19 admissions. In the hospital in which I practice, we are seeing numbers similar to those we saw in December and January: a typical daily census of 10 kids admitted with COVID-19, with 4 of them in the intensive care unit. It is a stark contrast to June when, most days, we had no patients with COVID-19 in the hospital. About half of our hospitalized patients are too young to be vaccinated against COVID-19, while the rest are unvaccinated children 12 years and older.
Vaccination of eligible children and teachers is an essential strategy for preventing the spread of COVID-19 in schools, but as children head back to school, immunization rates of educators are largely unknown and are suboptimal among students in most states. As of Aug. 11, 10.7 million U.S. children had received at least one dose of COVID-19 vaccine, representing 43% of 12- to 15-year-olds and 53% of 16- to 17-year-olds.2 Rates vary substantially by state, with more than 70% of kids in Vermont receiving at least one dose of vaccine, compared with less than 25% in Wyoming and Alabama.
Still, in the absence of robust immunization rates, we have data that schools can still reopen successfully. We need to follow the science and implement universal masking, a safe, effective, and practical mitigation strategy.
It worked in Wisconsin. Seventeen K-12 schools in rural Wisconsin opened last fall for in-person instruction.3 Reported compliance with masking was high, ranging from 92.1% to 97.4%, and in-school transmission of COVID-19 was low, with seven cases among 4,876 students.
It worked in Salt Lake City.4 In 20 elementary schools open for in-person instruction Dec. 3, 2020, to Jan. 31, 2021, compliance with mask-wearing was high and in-school transmission was very low, despite a high community incidence of COVID-19. Notably, students’ classroom seats were less than 6 feet apart, suggesting that consistent mask-wearing works even when physical distancing is challenging.
One of the best examples of successful school reopening happened in North Carolina, where pediatricians, pediatric infectious disease specialists, and other experts affiliated with Duke University formed the ABC Science Collaborative to support school districts that requested scientific input to help guide return-to-school policies during the COVID-19 pandemic. From Oct. 26, 2020, to Feb. 28, 2021, the ABC Science Collaborative worked with 13 school districts that were open for in-person instruction using basic mitigation strategies, including universal masking.5 During this time period, there were 4,969 community-acquired SARS-CoV-2 infections in the more than 100,000 students and staff present in schools. Transmission to school contacts was identified in only 209 individuals for a secondary attack rate of less than 1%.
Duke investigator Kanecia Zimmerman, MD, told Duke Today, “We know that, if our goal is to reduce transmission of COVID-19 in schools, there are two effective ways to do that: 1. vaccination, 2. masking. In the setting of schools ... the science suggests masking can be extremely effective, particularly for those who can’t get vaccinated while COVID-19 is still circulating.”
Both the AAP6 and the Pediatric Infectious Diseases Society7 have emphasized the importance of in-person instruction and endorsed universal masking in school. Mask-optional policies or “mask-if-you-are-unvaccinated” policies don’t work, as we have seen in society at large. They are likely to be especially challenging in school settings. Given an option, many, if not most kids, will take off their masks. Kids who leave them on run the risk of stigmatization or bullying.
On Aug. 4, the Centers for Disease Control and Prevention updated its guidance to recommend universal indoor masking for all students, staff, teachers, and visitors to K-12 schools, regardless of vaccination status. Now we’ll have to wait and see if school districts, elected officials, and parents will get on board with masks. ... and we’ll be left to count the number of rising COVID-19 cases that occur until they do.
Case in point: Kids in Greater Clark County, Ind., headed back to school on July 28. Masks were not required on school property, although unvaccinated students and teachers were “strongly encouraged” to wear them.8
Over the first 8 days of in-person instruction, schools in Greater Clark County identified 70 cases of COVID-19 in students and quarantined more than 1,100 of the district’s 10,300 students. Only the unvaccinated were required to quarantine. The district began requiring masks in all school buildings on Aug. 9.9
The worried mother had one last question for me. “What’s the best mask for a child to wear?” For most kids, a simple, well-fitting cloth mask is fine. The best mask is ultimately the mask a child will wear. A toolkit with practical tips for helping children successfully wear a mask is available on the ABC Science Collaborative website.
Dr. Bryant, president of the Pediatric Infectious Diseases Society, is a pediatrician at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at [email protected].
References
1. American Academy of Pediatrics. “Children and COVID-19: State-level data report.”
2. American Academy of Pediatrics. “Children and COVID-19 vaccination trends.”
3. Falk A et al. MMWR Morb Mortal Wkly Rep. 2021;70:136-40.
4. Hershow RB et al. MMWR Morb Mortal Wkly Rep 2021;70:442-8.
5. Zimmerman KO et al. Pediatrics. 2021 Jul;e2021052686. doi: 10.1542/peds.2021-052686.
6. American Academy of Pediatrics. “American Academy of Pediatrics updates recommendations for opening schools in fall 2021.”
7. Pediatric Infectious Diseases Society. “PIDS supports universal masking for students, school staff.”
8. Courtney Hayden. WHAS11. “Greater Clark County Schools return to class July 28.”
9. Dustin Vogt. WAVE3 News. “Greater Clark Country Schools to require masks amid 70 positive cases.”









