User login
News and Views that Matter to Pediatricians
The leading independent newspaper covering news and commentary in pediatrics.
Air pollution may be causing eczema
The finding points scientists toward how to better treat the skin ailment. There are now more than three times as many eczema cases as there were in the 1970s, and it now affects as many as 20% of children and 10% of adults.
“I think these authors are spot-on in recognizing that the incidence of allergic conditions is increasing concurrently with how different pollutants are increasing in our environment,” said Denver-based pediatric allergist and immunologist Jessica Hui, MD, according to NBC News. “We’re finally understanding more about why people are getting eczema.”
Some people get eczema because of genetics, but the new research built on the previous understanding of how chemicals called diisocyanates can trigger the eczema symptoms of severe itching, skin redness, and oozing or painful rashes. An experiment on mice showed that exposure to a specific part of diisocyanates, called isocyanates, disrupted oil production that the skin needs to stay healthy.
Researchers at the National Institutes of Health “found that when bacteria that live on healthy skin are exposed to isocyanate, they must adapt to survive,” the agency summarized in a news release. “When they adapt, these bacteria shift their metabolism away from making the lipids, or oils, that skin needs to stay healthy. This finding suggests that eczema may be treatable by replacing the modified skin bacteria with healthy bacteria.”
The study was published in the journal Science Advances.
The chemicals also trigger a message to the brain that causes skin inflammation and itching, lead researcher Ian Myles, MD, told NBC News. Dr. Myles is also chief of the Epithelial Research Unit in the National Institute of Allergy and Infectious Diseases Laboratory of Clinical Immunology and Microbiology.
“So much of this is out of our control. I mean, you can’t shut the highways down,” he said of the environmental sources.
Previous research that explored attempting to restore healthy skin bacteria called Roseomonas mucosa to treat eczema symptoms had mixed results. The NIH says it has made the bacteria available “for commercial, nontherapeutic development ... as a potentially beneficial probiotic.”
A version of this article first appeared on WebMD.com.
The finding points scientists toward how to better treat the skin ailment. There are now more than three times as many eczema cases as there were in the 1970s, and it now affects as many as 20% of children and 10% of adults.
“I think these authors are spot-on in recognizing that the incidence of allergic conditions is increasing concurrently with how different pollutants are increasing in our environment,” said Denver-based pediatric allergist and immunologist Jessica Hui, MD, according to NBC News. “We’re finally understanding more about why people are getting eczema.”
Some people get eczema because of genetics, but the new research built on the previous understanding of how chemicals called diisocyanates can trigger the eczema symptoms of severe itching, skin redness, and oozing or painful rashes. An experiment on mice showed that exposure to a specific part of diisocyanates, called isocyanates, disrupted oil production that the skin needs to stay healthy.
Researchers at the National Institutes of Health “found that when bacteria that live on healthy skin are exposed to isocyanate, they must adapt to survive,” the agency summarized in a news release. “When they adapt, these bacteria shift their metabolism away from making the lipids, or oils, that skin needs to stay healthy. This finding suggests that eczema may be treatable by replacing the modified skin bacteria with healthy bacteria.”
The study was published in the journal Science Advances.
The chemicals also trigger a message to the brain that causes skin inflammation and itching, lead researcher Ian Myles, MD, told NBC News. Dr. Myles is also chief of the Epithelial Research Unit in the National Institute of Allergy and Infectious Diseases Laboratory of Clinical Immunology and Microbiology.
“So much of this is out of our control. I mean, you can’t shut the highways down,” he said of the environmental sources.
Previous research that explored attempting to restore healthy skin bacteria called Roseomonas mucosa to treat eczema symptoms had mixed results. The NIH says it has made the bacteria available “for commercial, nontherapeutic development ... as a potentially beneficial probiotic.”
A version of this article first appeared on WebMD.com.
The finding points scientists toward how to better treat the skin ailment. There are now more than three times as many eczema cases as there were in the 1970s, and it now affects as many as 20% of children and 10% of adults.
“I think these authors are spot-on in recognizing that the incidence of allergic conditions is increasing concurrently with how different pollutants are increasing in our environment,” said Denver-based pediatric allergist and immunologist Jessica Hui, MD, according to NBC News. “We’re finally understanding more about why people are getting eczema.”
Some people get eczema because of genetics, but the new research built on the previous understanding of how chemicals called diisocyanates can trigger the eczema symptoms of severe itching, skin redness, and oozing or painful rashes. An experiment on mice showed that exposure to a specific part of diisocyanates, called isocyanates, disrupted oil production that the skin needs to stay healthy.
Researchers at the National Institutes of Health “found that when bacteria that live on healthy skin are exposed to isocyanate, they must adapt to survive,” the agency summarized in a news release. “When they adapt, these bacteria shift their metabolism away from making the lipids, or oils, that skin needs to stay healthy. This finding suggests that eczema may be treatable by replacing the modified skin bacteria with healthy bacteria.”
The study was published in the journal Science Advances.
The chemicals also trigger a message to the brain that causes skin inflammation and itching, lead researcher Ian Myles, MD, told NBC News. Dr. Myles is also chief of the Epithelial Research Unit in the National Institute of Allergy and Infectious Diseases Laboratory of Clinical Immunology and Microbiology.
“So much of this is out of our control. I mean, you can’t shut the highways down,” he said of the environmental sources.
Previous research that explored attempting to restore healthy skin bacteria called Roseomonas mucosa to treat eczema symptoms had mixed results. The NIH says it has made the bacteria available “for commercial, nontherapeutic development ... as a potentially beneficial probiotic.”
A version of this article first appeared on WebMD.com.
FROM SCIENCE ADVANCES
COVID in pregnancy may affect boys’ neurodevelopment: Study
Boys born to mothers infected with SARS‐CoV‐2 during pregnancy may be more likely to receive a diagnosis of a neurodevelopmental disorder by age 12 months, according to new research.
Andrea G. Edlow, MD, MSc, with Massachusetts General Hospital and Harvard Medical School in Boston, and colleagues examined data from 18,355 births between March 1, 2020, and May 31, 2021, at eight hospitals across two health systems in Massachusetts.
Of these births, 883 (4.8%) were to individuals who tested positive for SARS‐CoV‐2 during pregnancy. Among the children exposed to SARS‐CoV‐2 in the womb, 26 (3%) received a neurodevelopmental diagnosis, including disorders of motor function, speech and language, and psychological development, by age 1 year. In the group unexposed to the virus, 1.8% received such a diagnosis.
After adjusting for factors such as race, insurance, maternal age, and preterm birth, Dr. Edlow’s group found that a positive test for SARS-CoV-2 during pregnancy was associated with an increased risk for neurodevelopmental diagnoses at 12 months among boys (adjusted odds ratio, 1.94; 95% confidence interval, 1.12-3.17; P = .01), but not among girls.
In a subset of children with data available at 18 months, the correlation among boys at that age was less pronounced and not statistically significant (aOR, 1.42; 95% CI, 0.92-2.11; P = .10).
The findings were published online in JAMA Network Open
Prior epidemiological research has suggested that maternal infection during pregnancy is associated with heightened risk for a range of neurodevelopmental disorders, including autism and schizophrenia, in offspring, the authors wrote.
“The neurodevelopmental risk associated with maternal SARS-CoV-2 infection was disproportionately high in male infants, consistent with the known increased vulnerability of males in the face of prenatal adverse exposures,” Dr. Edlow said in a news release about the findings.
Larger studies and longer follow‐up are needed to confirm and reliably estimate the risk, the researchers said.
“It is not clear that the changes we can detect at 12 and 18 months will be indicative of persistent risks for disorders such as autism spectrum disorder, intellectual disability, or schizophrenia,” they write.
New data published online by the Centers for Disease Control and Prevention show that in 11 communities in 2020, 1 in 36 (2.8%) 8-year-old children had been identified with autism spectrum disorder, an increase from 2.3% in 2018. The data also show that the early months of the pandemic may have disrupted autism detection efforts among 4-year-olds.
The investigators were supported by grants from the National Institutes of Health and the Simons Foundation Autism Research Initiative. Coauthors disclosed consulting for or receiving personal fees from biotechnology and pharmaceutical companies.
A version of this article first appeared on Medscape.com.
Boys born to mothers infected with SARS‐CoV‐2 during pregnancy may be more likely to receive a diagnosis of a neurodevelopmental disorder by age 12 months, according to new research.
Andrea G. Edlow, MD, MSc, with Massachusetts General Hospital and Harvard Medical School in Boston, and colleagues examined data from 18,355 births between March 1, 2020, and May 31, 2021, at eight hospitals across two health systems in Massachusetts.
Of these births, 883 (4.8%) were to individuals who tested positive for SARS‐CoV‐2 during pregnancy. Among the children exposed to SARS‐CoV‐2 in the womb, 26 (3%) received a neurodevelopmental diagnosis, including disorders of motor function, speech and language, and psychological development, by age 1 year. In the group unexposed to the virus, 1.8% received such a diagnosis.
After adjusting for factors such as race, insurance, maternal age, and preterm birth, Dr. Edlow’s group found that a positive test for SARS-CoV-2 during pregnancy was associated with an increased risk for neurodevelopmental diagnoses at 12 months among boys (adjusted odds ratio, 1.94; 95% confidence interval, 1.12-3.17; P = .01), but not among girls.
In a subset of children with data available at 18 months, the correlation among boys at that age was less pronounced and not statistically significant (aOR, 1.42; 95% CI, 0.92-2.11; P = .10).
The findings were published online in JAMA Network Open
Prior epidemiological research has suggested that maternal infection during pregnancy is associated with heightened risk for a range of neurodevelopmental disorders, including autism and schizophrenia, in offspring, the authors wrote.
“The neurodevelopmental risk associated with maternal SARS-CoV-2 infection was disproportionately high in male infants, consistent with the known increased vulnerability of males in the face of prenatal adverse exposures,” Dr. Edlow said in a news release about the findings.
Larger studies and longer follow‐up are needed to confirm and reliably estimate the risk, the researchers said.
“It is not clear that the changes we can detect at 12 and 18 months will be indicative of persistent risks for disorders such as autism spectrum disorder, intellectual disability, or schizophrenia,” they write.
New data published online by the Centers for Disease Control and Prevention show that in 11 communities in 2020, 1 in 36 (2.8%) 8-year-old children had been identified with autism spectrum disorder, an increase from 2.3% in 2018. The data also show that the early months of the pandemic may have disrupted autism detection efforts among 4-year-olds.
The investigators were supported by grants from the National Institutes of Health and the Simons Foundation Autism Research Initiative. Coauthors disclosed consulting for or receiving personal fees from biotechnology and pharmaceutical companies.
A version of this article first appeared on Medscape.com.
Boys born to mothers infected with SARS‐CoV‐2 during pregnancy may be more likely to receive a diagnosis of a neurodevelopmental disorder by age 12 months, according to new research.
Andrea G. Edlow, MD, MSc, with Massachusetts General Hospital and Harvard Medical School in Boston, and colleagues examined data from 18,355 births between March 1, 2020, and May 31, 2021, at eight hospitals across two health systems in Massachusetts.
Of these births, 883 (4.8%) were to individuals who tested positive for SARS‐CoV‐2 during pregnancy. Among the children exposed to SARS‐CoV‐2 in the womb, 26 (3%) received a neurodevelopmental diagnosis, including disorders of motor function, speech and language, and psychological development, by age 1 year. In the group unexposed to the virus, 1.8% received such a diagnosis.
After adjusting for factors such as race, insurance, maternal age, and preterm birth, Dr. Edlow’s group found that a positive test for SARS-CoV-2 during pregnancy was associated with an increased risk for neurodevelopmental diagnoses at 12 months among boys (adjusted odds ratio, 1.94; 95% confidence interval, 1.12-3.17; P = .01), but not among girls.
In a subset of children with data available at 18 months, the correlation among boys at that age was less pronounced and not statistically significant (aOR, 1.42; 95% CI, 0.92-2.11; P = .10).
The findings were published online in JAMA Network Open
Prior epidemiological research has suggested that maternal infection during pregnancy is associated with heightened risk for a range of neurodevelopmental disorders, including autism and schizophrenia, in offspring, the authors wrote.
“The neurodevelopmental risk associated with maternal SARS-CoV-2 infection was disproportionately high in male infants, consistent with the known increased vulnerability of males in the face of prenatal adverse exposures,” Dr. Edlow said in a news release about the findings.
Larger studies and longer follow‐up are needed to confirm and reliably estimate the risk, the researchers said.
“It is not clear that the changes we can detect at 12 and 18 months will be indicative of persistent risks for disorders such as autism spectrum disorder, intellectual disability, or schizophrenia,” they write.
New data published online by the Centers for Disease Control and Prevention show that in 11 communities in 2020, 1 in 36 (2.8%) 8-year-old children had been identified with autism spectrum disorder, an increase from 2.3% in 2018. The data also show that the early months of the pandemic may have disrupted autism detection efforts among 4-year-olds.
The investigators were supported by grants from the National Institutes of Health and the Simons Foundation Autism Research Initiative. Coauthors disclosed consulting for or receiving personal fees from biotechnology and pharmaceutical companies.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
eNose knows S. aureus in children with cystic fibrosis
An electronic nose effectively detected Staphylococcus aureus in children with cystic fibrosis, based on data from 100 individuals.
Staphylococcus aureus is the most common pathogen found in children with cystic fibrosis (CF), but current detection strategies are based on microbiology cultures, wrote Johann-Christoph Licht, a medical student at the University of Toronto, and colleagues.
Noninvasive tools are needed to screen children with CF early for respiratory infections, the researchers said.
The electronic Nose (eNose) is a technology that detects volatile organic compounds (VOCs). Although exhaled breath can be used to create distinct profiles, the ability of eNose to identify S. aureus (SA) in the breath of children with CF remains unclear, they wrote.
In a study published in the Journal of Cystic Fibrosis, the researchers analyzed breath profiles data from 100 children with CF. The study population included children aged 5-18 years with clinically stable CF who were recruited from CF clinics during routine visits. Patients with a CF pulmonary exacerbation were excluded.
The children’s median predicted FEV1 was 91%. The researchers collected sputum from 67 patients and throat cultures for 33 patients. A group of 25 age-matched healthy controls served for comparison.
Eighty patients were positive for CF pathogens. Of these, 67 were positive for SA (44 with SA only and 23 with SA and at least one other pathogen).
Overall, patients with any CF pathogen on airway cultures were identified compared to airway cultures with no CF pathogens with an area under the curve accuracy of 79.0%.
Previous studies have shown a high rate of accuracy using eNose to detect Pseudomonas aeruginosa (PA). In the current study, the area under the curve accuracy for PA infection compared to no CF pathogens was 78%. Both SA-specific and PA-specific signatures were driven by different sensors in the eNose, which suggests pathogen-specific breath signatures, the researchers wrote.
The study findings were limited by several factors including the small number of patients with positive airway cultures for PA and the lack of data on variability of measures over time or treatment-induced changes, the researchers noted.
However, the results confirm the value of the eNose in real-time point-of-care detection of airway infection in children with CF, and this is the first study known to suggest the potential of an eNose to detect SA infection in particular in a routine clinical setting, the researchers wrote in their discussion.
Other points in favor of eNose compared to current practice include “low cost, ease of use and portability to the point-of-care,” they said. The eNose provides an opportunity for early detection of pathogens that challenges conventional microbiology testing, they concluded.
The study received no outside funding. Two coauthors disclosed fees and/or an interest in the company Breathomix BV.
An electronic nose effectively detected Staphylococcus aureus in children with cystic fibrosis, based on data from 100 individuals.
Staphylococcus aureus is the most common pathogen found in children with cystic fibrosis (CF), but current detection strategies are based on microbiology cultures, wrote Johann-Christoph Licht, a medical student at the University of Toronto, and colleagues.
Noninvasive tools are needed to screen children with CF early for respiratory infections, the researchers said.
The electronic Nose (eNose) is a technology that detects volatile organic compounds (VOCs). Although exhaled breath can be used to create distinct profiles, the ability of eNose to identify S. aureus (SA) in the breath of children with CF remains unclear, they wrote.
In a study published in the Journal of Cystic Fibrosis, the researchers analyzed breath profiles data from 100 children with CF. The study population included children aged 5-18 years with clinically stable CF who were recruited from CF clinics during routine visits. Patients with a CF pulmonary exacerbation were excluded.
The children’s median predicted FEV1 was 91%. The researchers collected sputum from 67 patients and throat cultures for 33 patients. A group of 25 age-matched healthy controls served for comparison.
Eighty patients were positive for CF pathogens. Of these, 67 were positive for SA (44 with SA only and 23 with SA and at least one other pathogen).
Overall, patients with any CF pathogen on airway cultures were identified compared to airway cultures with no CF pathogens with an area under the curve accuracy of 79.0%.
Previous studies have shown a high rate of accuracy using eNose to detect Pseudomonas aeruginosa (PA). In the current study, the area under the curve accuracy for PA infection compared to no CF pathogens was 78%. Both SA-specific and PA-specific signatures were driven by different sensors in the eNose, which suggests pathogen-specific breath signatures, the researchers wrote.
The study findings were limited by several factors including the small number of patients with positive airway cultures for PA and the lack of data on variability of measures over time or treatment-induced changes, the researchers noted.
However, the results confirm the value of the eNose in real-time point-of-care detection of airway infection in children with CF, and this is the first study known to suggest the potential of an eNose to detect SA infection in particular in a routine clinical setting, the researchers wrote in their discussion.
Other points in favor of eNose compared to current practice include “low cost, ease of use and portability to the point-of-care,” they said. The eNose provides an opportunity for early detection of pathogens that challenges conventional microbiology testing, they concluded.
The study received no outside funding. Two coauthors disclosed fees and/or an interest in the company Breathomix BV.
An electronic nose effectively detected Staphylococcus aureus in children with cystic fibrosis, based on data from 100 individuals.
Staphylococcus aureus is the most common pathogen found in children with cystic fibrosis (CF), but current detection strategies are based on microbiology cultures, wrote Johann-Christoph Licht, a medical student at the University of Toronto, and colleagues.
Noninvasive tools are needed to screen children with CF early for respiratory infections, the researchers said.
The electronic Nose (eNose) is a technology that detects volatile organic compounds (VOCs). Although exhaled breath can be used to create distinct profiles, the ability of eNose to identify S. aureus (SA) in the breath of children with CF remains unclear, they wrote.
In a study published in the Journal of Cystic Fibrosis, the researchers analyzed breath profiles data from 100 children with CF. The study population included children aged 5-18 years with clinically stable CF who were recruited from CF clinics during routine visits. Patients with a CF pulmonary exacerbation were excluded.
The children’s median predicted FEV1 was 91%. The researchers collected sputum from 67 patients and throat cultures for 33 patients. A group of 25 age-matched healthy controls served for comparison.
Eighty patients were positive for CF pathogens. Of these, 67 were positive for SA (44 with SA only and 23 with SA and at least one other pathogen).
Overall, patients with any CF pathogen on airway cultures were identified compared to airway cultures with no CF pathogens with an area under the curve accuracy of 79.0%.
Previous studies have shown a high rate of accuracy using eNose to detect Pseudomonas aeruginosa (PA). In the current study, the area under the curve accuracy for PA infection compared to no CF pathogens was 78%. Both SA-specific and PA-specific signatures were driven by different sensors in the eNose, which suggests pathogen-specific breath signatures, the researchers wrote.
The study findings were limited by several factors including the small number of patients with positive airway cultures for PA and the lack of data on variability of measures over time or treatment-induced changes, the researchers noted.
However, the results confirm the value of the eNose in real-time point-of-care detection of airway infection in children with CF, and this is the first study known to suggest the potential of an eNose to detect SA infection in particular in a routine clinical setting, the researchers wrote in their discussion.
Other points in favor of eNose compared to current practice include “low cost, ease of use and portability to the point-of-care,” they said. The eNose provides an opportunity for early detection of pathogens that challenges conventional microbiology testing, they concluded.
The study received no outside funding. Two coauthors disclosed fees and/or an interest in the company Breathomix BV.
FROM THE JOURNAL OF CYSTIC FIBROSIS
Hydroxyurea underused in youth with sickle cell anemia
Even after endorsement in updated guidelines, hydroxyurea is substantially underused in youth with sickle cell anemia (SCA), new research indicates.
SCA can lead to pain crises, stroke, and early death. Hydroxyurea, an oral disease-modifying medication, can reduce the complications.
In 2014, the National Heart, Lung, and Blood Institute published revised guidelines that hydroxyurea should be offered as the primary therapy to all patients who were at least 9 months old and living with SCA, regardless of disease severity.
Low uptake even after guideline revision
Yet, a research team led by Sarah L. Reeves, PhD, MPH, with the Child Health Evaluation and Research Center at University of Michigan, Ann Arbor, found in their study of use in two sample states – Michigan and New York – that hydroxyurea use was low in children and adolescents enrolled in Medicaid and increased only slightly in Michigan and not at all in New York after the guideline revision.
After the guidelines were updated, the researchers observed that, on average, children and adolescents were getting the medication less than a third of the days in a year (32% maximum in the year with the highest uptake). The data were gathered from a study population that included 4,302 youths aged 1-17 years with SCA.
Findings were published online in JAMA Network Open.
‘A national issue’
Russell Ware, MD, PhD, chair of hematology translational research at Cincinnati Children’s Hospital, who was not part of the research, says that though data were gathered from Michigan and New York, “this is a national issue.”
Dr. Ware says the main problem is the way the health system describes the importance of hydroxyurea.
“There needs to be a realization that hydroxyurea is the standard of care for children with sickle cell anemia. It’s not just something they should take when they’re sick,” Dr. Ware said.
He added, “If you have diabetes, should you only take insulin if you’re really sick and hospitalized with a diabetic coma? Of course not.”
He said often providers aren’t giving a clear and consistent message to families.
“They’re not all sure they want to recommend it. They might offer it,” Dr. Ware said, which jeopardizes uptake. “Providers need to be more committed to it. They need to know how to dose it.”
Bad rap from past indications
Dr. Ware says hydroxyurea also gets a bad rap from use decades ago as a chemotherapeutic agent for cancer and then as an anti-HIV medication.
Now it’s used in a completely different way with SCA, but the fear of the association lingers.
“This label as a chemotherapeutic agent has really dogged hydroxyurea,” he said. “It’s a completely different mechanism. It’s a different dose. It’s a different purpose.”
The message to families should be more direct, he says: “Your child has sickle cell anemia and needs to be on disease-modifying therapy because this is a life-threatening disease.”
The underuse of this drug is particularly ironic, he says, as each capsule, taken daily, “costs about fifty cents.”
Medicaid support critical
Authors conclude that multifaceted interventions may be necessary to increase the number of filled prescriptions and use. They also point out that the interventions rely on states’ Medicaid support regarding hydroxyurea use. From 70% to 90% of young people with SCA are covered by Medicaid at some point, the researchers write.
“Variation may exist across states, as well as within states, in the coverage of hydroxyurea, outpatient visits, and associated lab monitoring,” they note.
The authors point to interventions in clinical trials that have had some success in hydroxyurea use.
Creary et al., for example, found that electronic directly observed therapy was associated with high adherence. That involved sending daily texts to patients to take hydroxyurea and patients recording and sending daily videos that show they took the medication.
The authors add that incorporating clinical pharmacists into the care team to provide education and support for families has been shown to be associated with successful outcomes for other chronic conditions – this approach may be particularly well suited to hydroxyurea given that this medication requires significant dosage monitoring.
Dr. Ware, however, says that solutions should focus on the health system more clearly communicating that hydroxyurea is the standard of care for all kids with SCA.
“We need to dispel these myths and these labels that are unfairly attributed to it. Then we’d probably do a lot better,” he said.
He added that children with SCA, “are a marginalized, neglected population of patients historically,” and addressing social determinants of health is also important in getting better uptake.
“Our pharmacy, for example, ships the drug to the families if they’re just getting a refill rather than making them drive all the way in,” Dr. Ware says.
Dr. Ware said given the interruption in doctor/patient relationships in the pandemic, the poor uptake of hydroxyurea could be even worse now.
The work was funded by the Agency for Healthcare Research and Quality and National Heart, Lung, and Blood Institute. Coauthor Dr. Green was the principal investigator of an NIH-funded trial of hydroxyurea in Uganda with a study drug provided by Siklos. No other author disclosures were reported. In addition to receiving research funding from the National Institutes of Health, Dr. Ware receives research donations from Bristol Myers Squibb, Addmedica, and Hemex Health. He is a medical adviser for Nova Laboratories and Octapharma, and serves on Data Safety Monitoring Boards for Novartis and Editas.
Even after endorsement in updated guidelines, hydroxyurea is substantially underused in youth with sickle cell anemia (SCA), new research indicates.
SCA can lead to pain crises, stroke, and early death. Hydroxyurea, an oral disease-modifying medication, can reduce the complications.
In 2014, the National Heart, Lung, and Blood Institute published revised guidelines that hydroxyurea should be offered as the primary therapy to all patients who were at least 9 months old and living with SCA, regardless of disease severity.
Low uptake even after guideline revision
Yet, a research team led by Sarah L. Reeves, PhD, MPH, with the Child Health Evaluation and Research Center at University of Michigan, Ann Arbor, found in their study of use in two sample states – Michigan and New York – that hydroxyurea use was low in children and adolescents enrolled in Medicaid and increased only slightly in Michigan and not at all in New York after the guideline revision.
After the guidelines were updated, the researchers observed that, on average, children and adolescents were getting the medication less than a third of the days in a year (32% maximum in the year with the highest uptake). The data were gathered from a study population that included 4,302 youths aged 1-17 years with SCA.
Findings were published online in JAMA Network Open.
‘A national issue’
Russell Ware, MD, PhD, chair of hematology translational research at Cincinnati Children’s Hospital, who was not part of the research, says that though data were gathered from Michigan and New York, “this is a national issue.”
Dr. Ware says the main problem is the way the health system describes the importance of hydroxyurea.
“There needs to be a realization that hydroxyurea is the standard of care for children with sickle cell anemia. It’s not just something they should take when they’re sick,” Dr. Ware said.
He added, “If you have diabetes, should you only take insulin if you’re really sick and hospitalized with a diabetic coma? Of course not.”
He said often providers aren’t giving a clear and consistent message to families.
“They’re not all sure they want to recommend it. They might offer it,” Dr. Ware said, which jeopardizes uptake. “Providers need to be more committed to it. They need to know how to dose it.”
Bad rap from past indications
Dr. Ware says hydroxyurea also gets a bad rap from use decades ago as a chemotherapeutic agent for cancer and then as an anti-HIV medication.
Now it’s used in a completely different way with SCA, but the fear of the association lingers.
“This label as a chemotherapeutic agent has really dogged hydroxyurea,” he said. “It’s a completely different mechanism. It’s a different dose. It’s a different purpose.”
The message to families should be more direct, he says: “Your child has sickle cell anemia and needs to be on disease-modifying therapy because this is a life-threatening disease.”
The underuse of this drug is particularly ironic, he says, as each capsule, taken daily, “costs about fifty cents.”
Medicaid support critical
Authors conclude that multifaceted interventions may be necessary to increase the number of filled prescriptions and use. They also point out that the interventions rely on states’ Medicaid support regarding hydroxyurea use. From 70% to 90% of young people with SCA are covered by Medicaid at some point, the researchers write.
“Variation may exist across states, as well as within states, in the coverage of hydroxyurea, outpatient visits, and associated lab monitoring,” they note.
The authors point to interventions in clinical trials that have had some success in hydroxyurea use.
Creary et al., for example, found that electronic directly observed therapy was associated with high adherence. That involved sending daily texts to patients to take hydroxyurea and patients recording and sending daily videos that show they took the medication.
The authors add that incorporating clinical pharmacists into the care team to provide education and support for families has been shown to be associated with successful outcomes for other chronic conditions – this approach may be particularly well suited to hydroxyurea given that this medication requires significant dosage monitoring.
Dr. Ware, however, says that solutions should focus on the health system more clearly communicating that hydroxyurea is the standard of care for all kids with SCA.
“We need to dispel these myths and these labels that are unfairly attributed to it. Then we’d probably do a lot better,” he said.
He added that children with SCA, “are a marginalized, neglected population of patients historically,” and addressing social determinants of health is also important in getting better uptake.
“Our pharmacy, for example, ships the drug to the families if they’re just getting a refill rather than making them drive all the way in,” Dr. Ware says.
Dr. Ware said given the interruption in doctor/patient relationships in the pandemic, the poor uptake of hydroxyurea could be even worse now.
The work was funded by the Agency for Healthcare Research and Quality and National Heart, Lung, and Blood Institute. Coauthor Dr. Green was the principal investigator of an NIH-funded trial of hydroxyurea in Uganda with a study drug provided by Siklos. No other author disclosures were reported. In addition to receiving research funding from the National Institutes of Health, Dr. Ware receives research donations from Bristol Myers Squibb, Addmedica, and Hemex Health. He is a medical adviser for Nova Laboratories and Octapharma, and serves on Data Safety Monitoring Boards for Novartis and Editas.
Even after endorsement in updated guidelines, hydroxyurea is substantially underused in youth with sickle cell anemia (SCA), new research indicates.
SCA can lead to pain crises, stroke, and early death. Hydroxyurea, an oral disease-modifying medication, can reduce the complications.
In 2014, the National Heart, Lung, and Blood Institute published revised guidelines that hydroxyurea should be offered as the primary therapy to all patients who were at least 9 months old and living with SCA, regardless of disease severity.
Low uptake even after guideline revision
Yet, a research team led by Sarah L. Reeves, PhD, MPH, with the Child Health Evaluation and Research Center at University of Michigan, Ann Arbor, found in their study of use in two sample states – Michigan and New York – that hydroxyurea use was low in children and adolescents enrolled in Medicaid and increased only slightly in Michigan and not at all in New York after the guideline revision.
After the guidelines were updated, the researchers observed that, on average, children and adolescents were getting the medication less than a third of the days in a year (32% maximum in the year with the highest uptake). The data were gathered from a study population that included 4,302 youths aged 1-17 years with SCA.
Findings were published online in JAMA Network Open.
‘A national issue’
Russell Ware, MD, PhD, chair of hematology translational research at Cincinnati Children’s Hospital, who was not part of the research, says that though data were gathered from Michigan and New York, “this is a national issue.”
Dr. Ware says the main problem is the way the health system describes the importance of hydroxyurea.
“There needs to be a realization that hydroxyurea is the standard of care for children with sickle cell anemia. It’s not just something they should take when they’re sick,” Dr. Ware said.
He added, “If you have diabetes, should you only take insulin if you’re really sick and hospitalized with a diabetic coma? Of course not.”
He said often providers aren’t giving a clear and consistent message to families.
“They’re not all sure they want to recommend it. They might offer it,” Dr. Ware said, which jeopardizes uptake. “Providers need to be more committed to it. They need to know how to dose it.”
Bad rap from past indications
Dr. Ware says hydroxyurea also gets a bad rap from use decades ago as a chemotherapeutic agent for cancer and then as an anti-HIV medication.
Now it’s used in a completely different way with SCA, but the fear of the association lingers.
“This label as a chemotherapeutic agent has really dogged hydroxyurea,” he said. “It’s a completely different mechanism. It’s a different dose. It’s a different purpose.”
The message to families should be more direct, he says: “Your child has sickle cell anemia and needs to be on disease-modifying therapy because this is a life-threatening disease.”
The underuse of this drug is particularly ironic, he says, as each capsule, taken daily, “costs about fifty cents.”
Medicaid support critical
Authors conclude that multifaceted interventions may be necessary to increase the number of filled prescriptions and use. They also point out that the interventions rely on states’ Medicaid support regarding hydroxyurea use. From 70% to 90% of young people with SCA are covered by Medicaid at some point, the researchers write.
“Variation may exist across states, as well as within states, in the coverage of hydroxyurea, outpatient visits, and associated lab monitoring,” they note.
The authors point to interventions in clinical trials that have had some success in hydroxyurea use.
Creary et al., for example, found that electronic directly observed therapy was associated with high adherence. That involved sending daily texts to patients to take hydroxyurea and patients recording and sending daily videos that show they took the medication.
The authors add that incorporating clinical pharmacists into the care team to provide education and support for families has been shown to be associated with successful outcomes for other chronic conditions – this approach may be particularly well suited to hydroxyurea given that this medication requires significant dosage monitoring.
Dr. Ware, however, says that solutions should focus on the health system more clearly communicating that hydroxyurea is the standard of care for all kids with SCA.
“We need to dispel these myths and these labels that are unfairly attributed to it. Then we’d probably do a lot better,” he said.
He added that children with SCA, “are a marginalized, neglected population of patients historically,” and addressing social determinants of health is also important in getting better uptake.
“Our pharmacy, for example, ships the drug to the families if they’re just getting a refill rather than making them drive all the way in,” Dr. Ware says.
Dr. Ware said given the interruption in doctor/patient relationships in the pandemic, the poor uptake of hydroxyurea could be even worse now.
The work was funded by the Agency for Healthcare Research and Quality and National Heart, Lung, and Blood Institute. Coauthor Dr. Green was the principal investigator of an NIH-funded trial of hydroxyurea in Uganda with a study drug provided by Siklos. No other author disclosures were reported. In addition to receiving research funding from the National Institutes of Health, Dr. Ware receives research donations from Bristol Myers Squibb, Addmedica, and Hemex Health. He is a medical adviser for Nova Laboratories and Octapharma, and serves on Data Safety Monitoring Boards for Novartis and Editas.
FROM JAMA NETWORK OPEN
Substance abuse disorders may share a common genetic signature
suggest new findings that researchers say could eventually lead to universal therapies to treat multiple and comorbid addictions.
“Genetics play a key role in determining health throughout our lives, but they are not destiny. Our hope with genomic studies is to further illuminate factors that may protect or predispose a person to substance use disorders – knowledge that can be used to expand preventative services and empower individuals to make informed decisions about drug use,” Nora Volkow, MD, director of the National Institute on Drug Abuse, said in news release.
“A better understanding of genetics also brings us one step closer to developing personalized interventions that are tailored to an individual’s unique biology, environment, and lived experience in order to provide the most benefits,” Dr. Volkow added.
The research was published online in Nature Mental Health.
Global research
Led by a team at the Washington University in St. Louis, the study included more than 150 collaborating investigators from around the world.
The risk of developing SUDs is influenced by a complex interplay between genetics and environmental factors. In a genomewide association study, the investigators looked for variations in the genome that were closely associated with SUDs in more than 1 million people of European ancestry and 92,630 people of African ancestry.
Among the European ancestry sample, they discovered 19 single-nucleotide polymorphisms that were significantly associated with general addiction risk and 47 genetic variants linked to specific SUDs – 9 for alcohol, 32 for tobacco, 5 for cannabis, and 1 for opioids.
The strongest gene signals consistent across the various SUDs mapped to areas in the genome involved in dopamine-signaling regulation, which reinforces the role of the dopamine system in addiction.
The genomic pattern also predicted higher risk of mental and physical illness, including psychiatric disorders, suicidal behavior, respiratory disease, heart disease, and chronic pain conditions. In children aged 9 or 10 years, presumably without any SUD, these genes correlated with parental substance use and externalizing behavior.
“Substance use disorders and mental disorders often co-occur, and we know that the most effective treatments help people address both issues at the same time. The shared genetic mechanisms between substance use and mental disorders revealed in this study underscore the importance of thinking about these disorders in tandem,” Joshua A. Gordon, MD, PhD, director of the National Institute of Mental Health, said in a news release.
Repurpose existing drugs for SUDs?
Separately, the genomic analysis of individuals of African ancestry showed only one genetic variation associated with general addiction risk and one substance-specific variation for risk of alcohol use disorder. The smaller sample size may be one reason for the more limited findings in this population.
“There is a tremendous need for treatments that target addiction generally, given patterns of the use of multiple substances, lifetime substance use, and severity seen in the clinic,” lead researcher Alexander Hatoum, PhD, at Washington University in St. Louis, said in a news release.
“Our study opens the door to identifying medications that may be leveraged to treat addiction broadly, which may be especially useful for treating more severe forms, including addiction to multiple substances,” Dr. Hatoum added.
As part of the study, the researchers compiled a list of approved and investigational pharmaceutical drugs that could potentially be repurposed to treat SUDs.
The list includes more than 100 drugs to investigate in future clinical trials, including those that can influence regulation of dopamine signaling.
This research was supported by NIDA, the National Institute on Alcohol Abuse and Alcoholism, NIMH, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, and the National Institute on Aging.
A version of this article first appeared on Medscape.com.
suggest new findings that researchers say could eventually lead to universal therapies to treat multiple and comorbid addictions.
“Genetics play a key role in determining health throughout our lives, but they are not destiny. Our hope with genomic studies is to further illuminate factors that may protect or predispose a person to substance use disorders – knowledge that can be used to expand preventative services and empower individuals to make informed decisions about drug use,” Nora Volkow, MD, director of the National Institute on Drug Abuse, said in news release.
“A better understanding of genetics also brings us one step closer to developing personalized interventions that are tailored to an individual’s unique biology, environment, and lived experience in order to provide the most benefits,” Dr. Volkow added.
The research was published online in Nature Mental Health.
Global research
Led by a team at the Washington University in St. Louis, the study included more than 150 collaborating investigators from around the world.
The risk of developing SUDs is influenced by a complex interplay between genetics and environmental factors. In a genomewide association study, the investigators looked for variations in the genome that were closely associated with SUDs in more than 1 million people of European ancestry and 92,630 people of African ancestry.
Among the European ancestry sample, they discovered 19 single-nucleotide polymorphisms that were significantly associated with general addiction risk and 47 genetic variants linked to specific SUDs – 9 for alcohol, 32 for tobacco, 5 for cannabis, and 1 for opioids.
The strongest gene signals consistent across the various SUDs mapped to areas in the genome involved in dopamine-signaling regulation, which reinforces the role of the dopamine system in addiction.
The genomic pattern also predicted higher risk of mental and physical illness, including psychiatric disorders, suicidal behavior, respiratory disease, heart disease, and chronic pain conditions. In children aged 9 or 10 years, presumably without any SUD, these genes correlated with parental substance use and externalizing behavior.
“Substance use disorders and mental disorders often co-occur, and we know that the most effective treatments help people address both issues at the same time. The shared genetic mechanisms between substance use and mental disorders revealed in this study underscore the importance of thinking about these disorders in tandem,” Joshua A. Gordon, MD, PhD, director of the National Institute of Mental Health, said in a news release.
Repurpose existing drugs for SUDs?
Separately, the genomic analysis of individuals of African ancestry showed only one genetic variation associated with general addiction risk and one substance-specific variation for risk of alcohol use disorder. The smaller sample size may be one reason for the more limited findings in this population.
“There is a tremendous need for treatments that target addiction generally, given patterns of the use of multiple substances, lifetime substance use, and severity seen in the clinic,” lead researcher Alexander Hatoum, PhD, at Washington University in St. Louis, said in a news release.
“Our study opens the door to identifying medications that may be leveraged to treat addiction broadly, which may be especially useful for treating more severe forms, including addiction to multiple substances,” Dr. Hatoum added.
As part of the study, the researchers compiled a list of approved and investigational pharmaceutical drugs that could potentially be repurposed to treat SUDs.
The list includes more than 100 drugs to investigate in future clinical trials, including those that can influence regulation of dopamine signaling.
This research was supported by NIDA, the National Institute on Alcohol Abuse and Alcoholism, NIMH, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, and the National Institute on Aging.
A version of this article first appeared on Medscape.com.
suggest new findings that researchers say could eventually lead to universal therapies to treat multiple and comorbid addictions.
“Genetics play a key role in determining health throughout our lives, but they are not destiny. Our hope with genomic studies is to further illuminate factors that may protect or predispose a person to substance use disorders – knowledge that can be used to expand preventative services and empower individuals to make informed decisions about drug use,” Nora Volkow, MD, director of the National Institute on Drug Abuse, said in news release.
“A better understanding of genetics also brings us one step closer to developing personalized interventions that are tailored to an individual’s unique biology, environment, and lived experience in order to provide the most benefits,” Dr. Volkow added.
The research was published online in Nature Mental Health.
Global research
Led by a team at the Washington University in St. Louis, the study included more than 150 collaborating investigators from around the world.
The risk of developing SUDs is influenced by a complex interplay between genetics and environmental factors. In a genomewide association study, the investigators looked for variations in the genome that were closely associated with SUDs in more than 1 million people of European ancestry and 92,630 people of African ancestry.
Among the European ancestry sample, they discovered 19 single-nucleotide polymorphisms that were significantly associated with general addiction risk and 47 genetic variants linked to specific SUDs – 9 for alcohol, 32 for tobacco, 5 for cannabis, and 1 for opioids.
The strongest gene signals consistent across the various SUDs mapped to areas in the genome involved in dopamine-signaling regulation, which reinforces the role of the dopamine system in addiction.
The genomic pattern also predicted higher risk of mental and physical illness, including psychiatric disorders, suicidal behavior, respiratory disease, heart disease, and chronic pain conditions. In children aged 9 or 10 years, presumably without any SUD, these genes correlated with parental substance use and externalizing behavior.
“Substance use disorders and mental disorders often co-occur, and we know that the most effective treatments help people address both issues at the same time. The shared genetic mechanisms between substance use and mental disorders revealed in this study underscore the importance of thinking about these disorders in tandem,” Joshua A. Gordon, MD, PhD, director of the National Institute of Mental Health, said in a news release.
Repurpose existing drugs for SUDs?
Separately, the genomic analysis of individuals of African ancestry showed only one genetic variation associated with general addiction risk and one substance-specific variation for risk of alcohol use disorder. The smaller sample size may be one reason for the more limited findings in this population.
“There is a tremendous need for treatments that target addiction generally, given patterns of the use of multiple substances, lifetime substance use, and severity seen in the clinic,” lead researcher Alexander Hatoum, PhD, at Washington University in St. Louis, said in a news release.
“Our study opens the door to identifying medications that may be leveraged to treat addiction broadly, which may be especially useful for treating more severe forms, including addiction to multiple substances,” Dr. Hatoum added.
As part of the study, the researchers compiled a list of approved and investigational pharmaceutical drugs that could potentially be repurposed to treat SUDs.
The list includes more than 100 drugs to investigate in future clinical trials, including those that can influence regulation of dopamine signaling.
This research was supported by NIDA, the National Institute on Alcohol Abuse and Alcoholism, NIMH, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, and the National Institute on Aging.
A version of this article first appeared on Medscape.com.
FROM NATURE MENTAL HEALTH
Celebrity death finally solved – with locks of hair
This transcript has been edited for clarity.
I’m going to open this week with a case.
A 56-year-old musician presents with diffuse abdominal pain, cramping, and jaundice. His medical history is notable for years of diffuse abdominal complaints, characterized by disabling bouts of diarrhea.
In addition to the jaundice, this acute illness was accompanied by fever as well as diffuse edema and ascites. The patient underwent several abdominal paracenteses to drain excess fluid. One consulting physician administered alcohol to relieve pain, to little avail.
The patient succumbed to his illness. An autopsy showed diffuse liver injury, as well as papillary necrosis of the kidneys. Notably, the nerves of his auditory canal were noted to be thickened, along with the bony part of the skull, consistent with Paget disease of the bone and explaining, potentially, why the talented musician had gone deaf at such a young age.
An interesting note on social history: The patient had apparently developed some feelings for the niece of that doctor who prescribed alcohol. Her name was Therese, perhaps mistranscribed as Elise, and it seems that he may have written this song for her.
We’re talking about this paper in Current Biology, by Tristan Begg and colleagues, which gives us a look into the very genome of what some would argue is the world’s greatest composer.
The ability to extract DNA from older specimens has transformed the fields of anthropology, archaeology, and history, and now, perhaps, musicology as well.
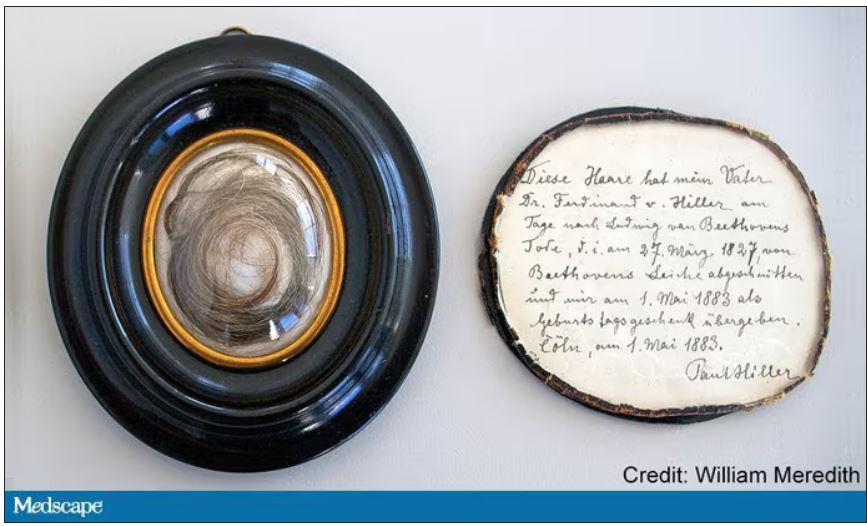
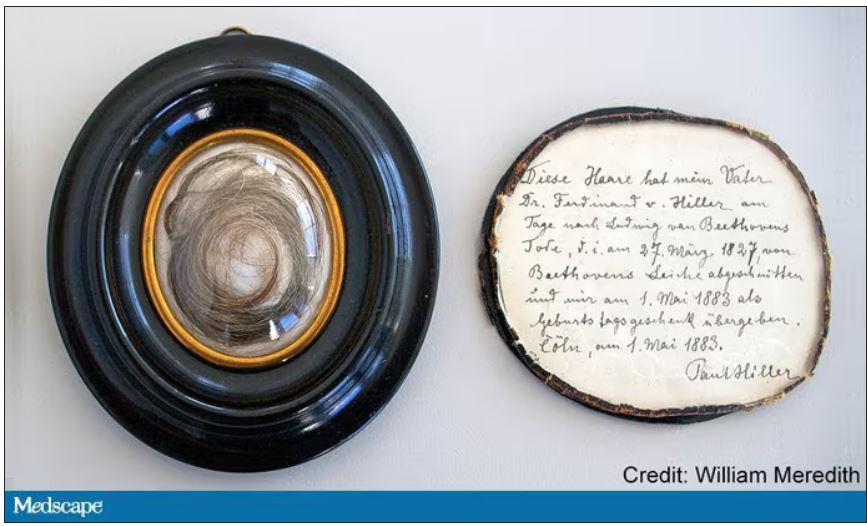
The researchers identified eight locks of hair in private and public collections, all attributed to the maestro.
Four of the samples had an intact chain of custody from the time the hair was cut. DNA sequencing on these four and an additional one of the eight locks came from the same individual, a male of European heritage.
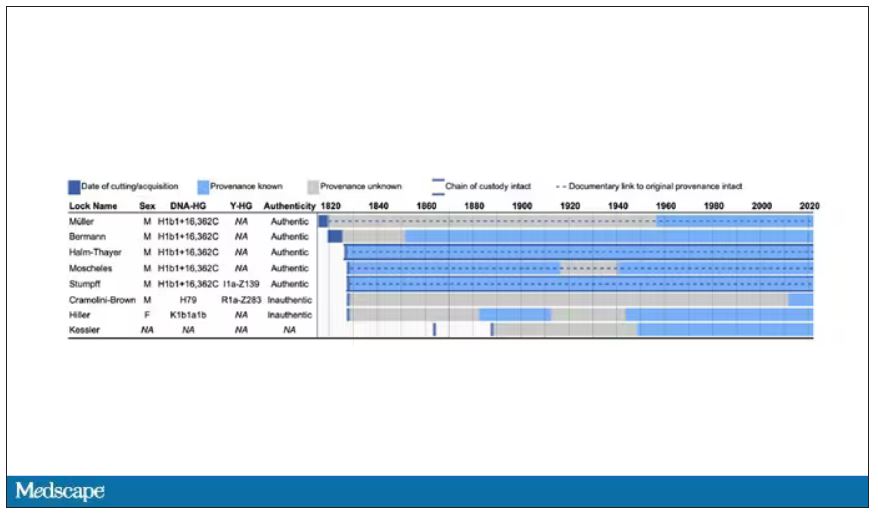
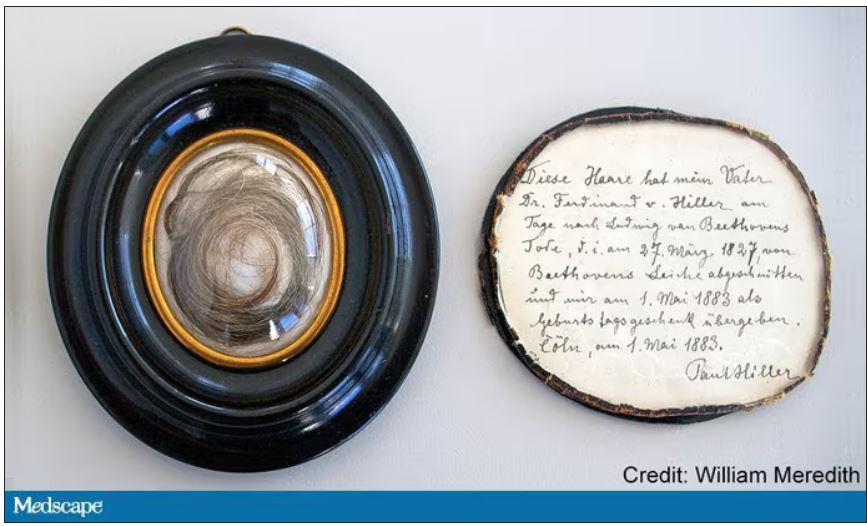
The three locks with less documentation came from three other unrelated individuals. Interestingly, analysis of one of those hair samples – the so-called Hiller Lock – had shown high levels of lead, leading historians to speculate that lead poisoning could account for some of Beethoven’s symptoms.
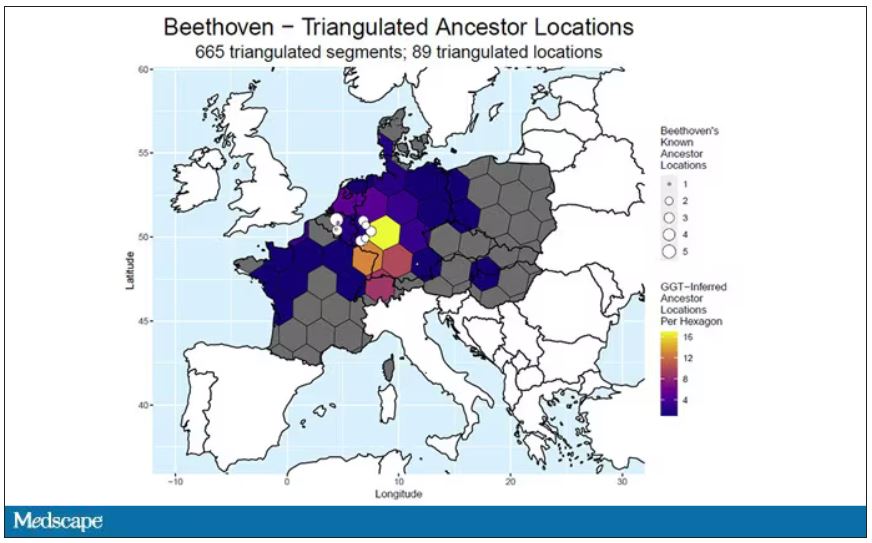
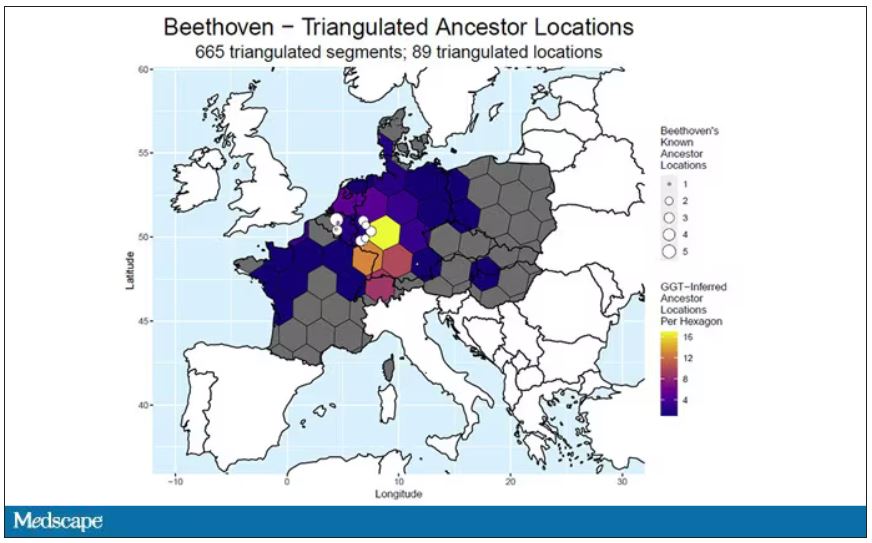
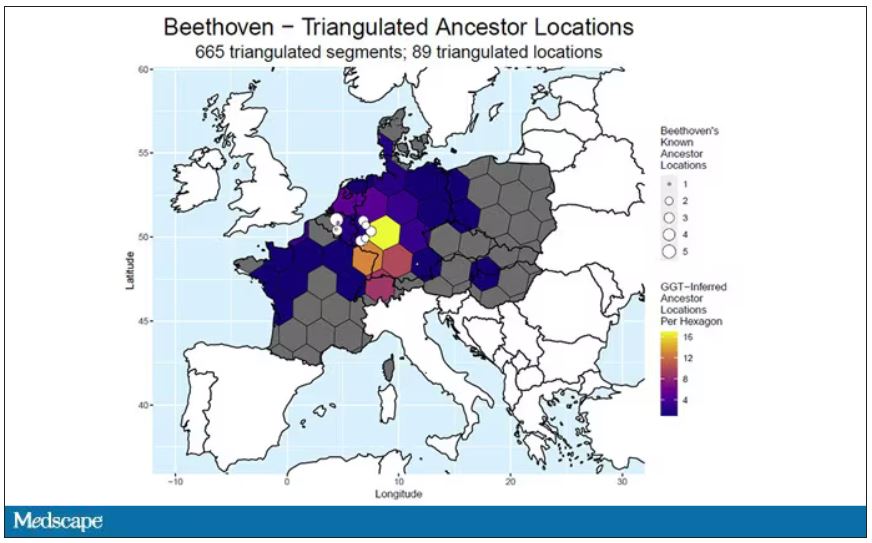
DNA analysis of that hair reveals it to have come from a woman likely of North African, Middle Eastern, or Jewish ancestry. We can no longer presume that plumbism was involved in Beethoven’s death. Beethoven’s ancestry turns out to be less exotic and maps quite well to ethnic German populations today.
In fact, there are van Beethovens alive as we speak, primarily in Belgium. Genealogic records suggest that these van Beethovens share a common ancestor with the virtuoso composer, a man by the name of Aert van Beethoven.
But the DNA reveals a scandal.
The Y-chromosome that Beethoven inherited was not Aert van Beethoven’s. Questions of Beethoven’s paternity have been raised before, but this evidence strongly suggests an extramarital paternity event, at least in the generations preceding his birth. That’s right – Beethoven may not have been a Beethoven.
With five locks now essentially certain to have come from Beethoven himself, the authors could use DNA analysis to try to explain three significant health problems he experienced throughout his life and death: his hearing loss, his terrible gastrointestinal issues, and his liver failure.
Let’s start with the most disappointing results, explanations for his hearing loss. No genetic cause was forthcoming, though the authors note that they have little to go on in regard to the genetic risk for otosclerosis, to which his hearing loss has often been attributed. Lead poisoning is, of course, possible here, though this report focuses only on genetics – there was no testing for lead – and as I mentioned, the lock that was strongly lead-positive in prior studies is almost certainly inauthentic.
What about his lifelong GI complaints? Some have suggested celiac disease or lactose intolerance as explanations. These can essentially be ruled out by the genetic analysis, which shows no risk alleles for celiac disease and the presence of the lactase-persistence gene which confers the ability to metabolize lactose throughout one’s life. IBS is harder to assess genetically, but for what it’s worth, he scored quite low on a polygenic risk score for the condition, in just the 9th percentile of risk. We should probably be looking elsewhere to explain the GI distress.
The genetic information bore much more fruit in regard to his liver disease. Remember that Beethoven’s autopsy showed cirrhosis. His polygenic risk score for liver cirrhosis puts him in the 96th percentile of risk. He was also heterozygous for two variants that can cause hereditary hemochromatosis. The risk for cirrhosis among those with these variants is increased by the use of alcohol. And historical accounts are quite clear that Beethoven consumed more than his share.
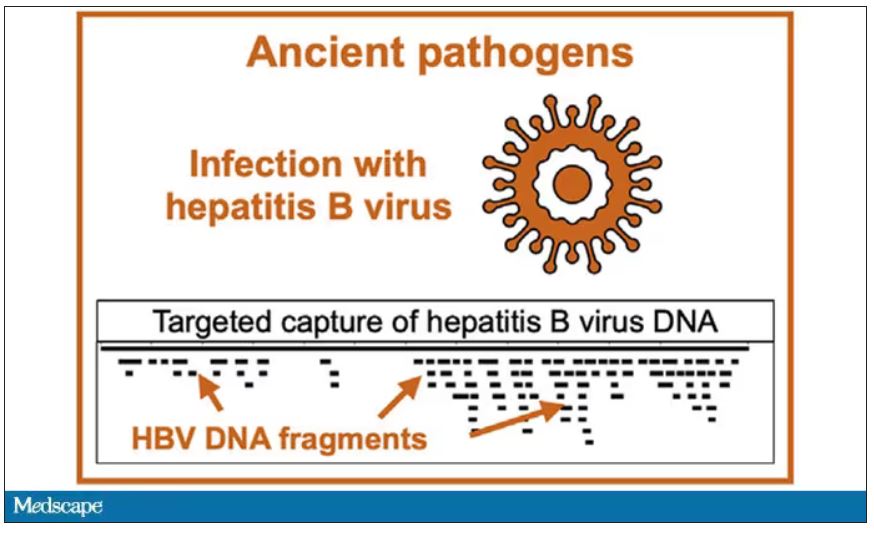
But it wasn’t just Beethoven’s DNA in these hair follicles. Analysis of a follicle from later in his life revealed the unmistakable presence of hepatitis B virus. Endemic in Europe at the time, this was a common cause of liver failure and is likely to have contributed to, if not directly caused, Beethoven’s demise.
It’s hard to read these results and not marvel at the fact that, two centuries after his death, our fascination with Beethoven has led us to probe every corner of his life – his letters, his writings, his medical records, and now his very DNA. What are we actually looking for? Is it relevant to us today what caused his hearing loss? His stomach troubles? Even his death? Will it help any patients in the future? I propose that what we are actually trying to understand is something ineffable: Genius of magnitude that is rarely seen in one or many lifetimes. And our scientific tools, as sharp as they may have become, are still far too blunt to probe the depths of that transcendence.
In any case, friends, no more of these sounds. Let us sing more cheerful songs, more full of joy.
For Medscape, I’m Perry Wilson.
Dr. Wilson is associate professor, department of medicine, and director, Clinical and Translational Research Accelerator, at Yale University, New Haven, Conn. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I’m going to open this week with a case.
A 56-year-old musician presents with diffuse abdominal pain, cramping, and jaundice. His medical history is notable for years of diffuse abdominal complaints, characterized by disabling bouts of diarrhea.
In addition to the jaundice, this acute illness was accompanied by fever as well as diffuse edema and ascites. The patient underwent several abdominal paracenteses to drain excess fluid. One consulting physician administered alcohol to relieve pain, to little avail.
The patient succumbed to his illness. An autopsy showed diffuse liver injury, as well as papillary necrosis of the kidneys. Notably, the nerves of his auditory canal were noted to be thickened, along with the bony part of the skull, consistent with Paget disease of the bone and explaining, potentially, why the talented musician had gone deaf at such a young age.
An interesting note on social history: The patient had apparently developed some feelings for the niece of that doctor who prescribed alcohol. Her name was Therese, perhaps mistranscribed as Elise, and it seems that he may have written this song for her.
We’re talking about this paper in Current Biology, by Tristan Begg and colleagues, which gives us a look into the very genome of what some would argue is the world’s greatest composer.
The ability to extract DNA from older specimens has transformed the fields of anthropology, archaeology, and history, and now, perhaps, musicology as well.
The researchers identified eight locks of hair in private and public collections, all attributed to the maestro.
Four of the samples had an intact chain of custody from the time the hair was cut. DNA sequencing on these four and an additional one of the eight locks came from the same individual, a male of European heritage.
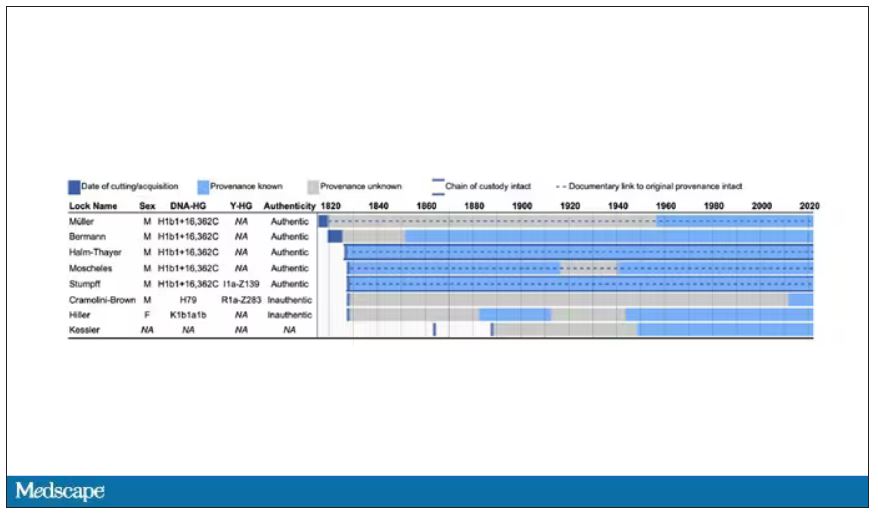
The three locks with less documentation came from three other unrelated individuals. Interestingly, analysis of one of those hair samples – the so-called Hiller Lock – had shown high levels of lead, leading historians to speculate that lead poisoning could account for some of Beethoven’s symptoms.
DNA analysis of that hair reveals it to have come from a woman likely of North African, Middle Eastern, or Jewish ancestry. We can no longer presume that plumbism was involved in Beethoven’s death. Beethoven’s ancestry turns out to be less exotic and maps quite well to ethnic German populations today.
In fact, there are van Beethovens alive as we speak, primarily in Belgium. Genealogic records suggest that these van Beethovens share a common ancestor with the virtuoso composer, a man by the name of Aert van Beethoven.
But the DNA reveals a scandal.
The Y-chromosome that Beethoven inherited was not Aert van Beethoven’s. Questions of Beethoven’s paternity have been raised before, but this evidence strongly suggests an extramarital paternity event, at least in the generations preceding his birth. That’s right – Beethoven may not have been a Beethoven.
With five locks now essentially certain to have come from Beethoven himself, the authors could use DNA analysis to try to explain three significant health problems he experienced throughout his life and death: his hearing loss, his terrible gastrointestinal issues, and his liver failure.
Let’s start with the most disappointing results, explanations for his hearing loss. No genetic cause was forthcoming, though the authors note that they have little to go on in regard to the genetic risk for otosclerosis, to which his hearing loss has often been attributed. Lead poisoning is, of course, possible here, though this report focuses only on genetics – there was no testing for lead – and as I mentioned, the lock that was strongly lead-positive in prior studies is almost certainly inauthentic.
What about his lifelong GI complaints? Some have suggested celiac disease or lactose intolerance as explanations. These can essentially be ruled out by the genetic analysis, which shows no risk alleles for celiac disease and the presence of the lactase-persistence gene which confers the ability to metabolize lactose throughout one’s life. IBS is harder to assess genetically, but for what it’s worth, he scored quite low on a polygenic risk score for the condition, in just the 9th percentile of risk. We should probably be looking elsewhere to explain the GI distress.
The genetic information bore much more fruit in regard to his liver disease. Remember that Beethoven’s autopsy showed cirrhosis. His polygenic risk score for liver cirrhosis puts him in the 96th percentile of risk. He was also heterozygous for two variants that can cause hereditary hemochromatosis. The risk for cirrhosis among those with these variants is increased by the use of alcohol. And historical accounts are quite clear that Beethoven consumed more than his share.
But it wasn’t just Beethoven’s DNA in these hair follicles. Analysis of a follicle from later in his life revealed the unmistakable presence of hepatitis B virus. Endemic in Europe at the time, this was a common cause of liver failure and is likely to have contributed to, if not directly caused, Beethoven’s demise.
It’s hard to read these results and not marvel at the fact that, two centuries after his death, our fascination with Beethoven has led us to probe every corner of his life – his letters, his writings, his medical records, and now his very DNA. What are we actually looking for? Is it relevant to us today what caused his hearing loss? His stomach troubles? Even his death? Will it help any patients in the future? I propose that what we are actually trying to understand is something ineffable: Genius of magnitude that is rarely seen in one or many lifetimes. And our scientific tools, as sharp as they may have become, are still far too blunt to probe the depths of that transcendence.
In any case, friends, no more of these sounds. Let us sing more cheerful songs, more full of joy.
For Medscape, I’m Perry Wilson.
Dr. Wilson is associate professor, department of medicine, and director, Clinical and Translational Research Accelerator, at Yale University, New Haven, Conn. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I’m going to open this week with a case.
A 56-year-old musician presents with diffuse abdominal pain, cramping, and jaundice. His medical history is notable for years of diffuse abdominal complaints, characterized by disabling bouts of diarrhea.
In addition to the jaundice, this acute illness was accompanied by fever as well as diffuse edema and ascites. The patient underwent several abdominal paracenteses to drain excess fluid. One consulting physician administered alcohol to relieve pain, to little avail.
The patient succumbed to his illness. An autopsy showed diffuse liver injury, as well as papillary necrosis of the kidneys. Notably, the nerves of his auditory canal were noted to be thickened, along with the bony part of the skull, consistent with Paget disease of the bone and explaining, potentially, why the talented musician had gone deaf at such a young age.
An interesting note on social history: The patient had apparently developed some feelings for the niece of that doctor who prescribed alcohol. Her name was Therese, perhaps mistranscribed as Elise, and it seems that he may have written this song for her.
We’re talking about this paper in Current Biology, by Tristan Begg and colleagues, which gives us a look into the very genome of what some would argue is the world’s greatest composer.
The ability to extract DNA from older specimens has transformed the fields of anthropology, archaeology, and history, and now, perhaps, musicology as well.
The researchers identified eight locks of hair in private and public collections, all attributed to the maestro.
Four of the samples had an intact chain of custody from the time the hair was cut. DNA sequencing on these four and an additional one of the eight locks came from the same individual, a male of European heritage.
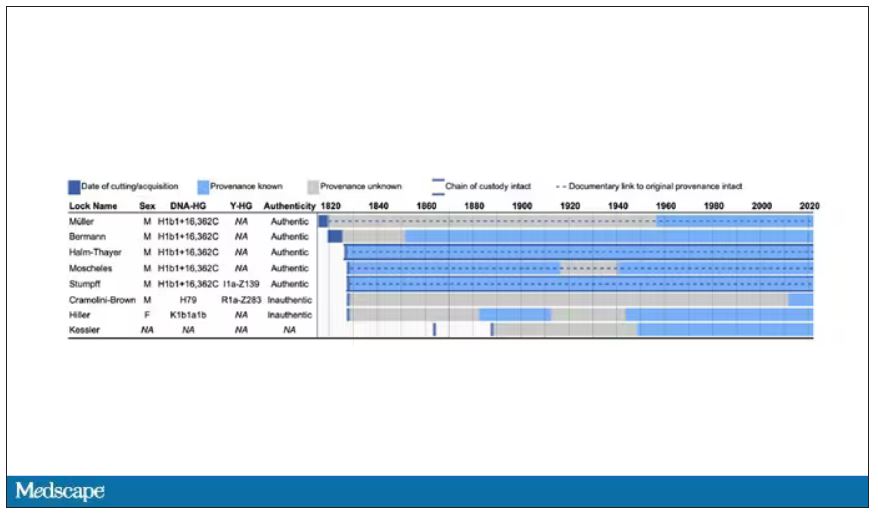
The three locks with less documentation came from three other unrelated individuals. Interestingly, analysis of one of those hair samples – the so-called Hiller Lock – had shown high levels of lead, leading historians to speculate that lead poisoning could account for some of Beethoven’s symptoms.
DNA analysis of that hair reveals it to have come from a woman likely of North African, Middle Eastern, or Jewish ancestry. We can no longer presume that plumbism was involved in Beethoven’s death. Beethoven’s ancestry turns out to be less exotic and maps quite well to ethnic German populations today.
In fact, there are van Beethovens alive as we speak, primarily in Belgium. Genealogic records suggest that these van Beethovens share a common ancestor with the virtuoso composer, a man by the name of Aert van Beethoven.
But the DNA reveals a scandal.
The Y-chromosome that Beethoven inherited was not Aert van Beethoven’s. Questions of Beethoven’s paternity have been raised before, but this evidence strongly suggests an extramarital paternity event, at least in the generations preceding his birth. That’s right – Beethoven may not have been a Beethoven.
With five locks now essentially certain to have come from Beethoven himself, the authors could use DNA analysis to try to explain three significant health problems he experienced throughout his life and death: his hearing loss, his terrible gastrointestinal issues, and his liver failure.
Let’s start with the most disappointing results, explanations for his hearing loss. No genetic cause was forthcoming, though the authors note that they have little to go on in regard to the genetic risk for otosclerosis, to which his hearing loss has often been attributed. Lead poisoning is, of course, possible here, though this report focuses only on genetics – there was no testing for lead – and as I mentioned, the lock that was strongly lead-positive in prior studies is almost certainly inauthentic.
What about his lifelong GI complaints? Some have suggested celiac disease or lactose intolerance as explanations. These can essentially be ruled out by the genetic analysis, which shows no risk alleles for celiac disease and the presence of the lactase-persistence gene which confers the ability to metabolize lactose throughout one’s life. IBS is harder to assess genetically, but for what it’s worth, he scored quite low on a polygenic risk score for the condition, in just the 9th percentile of risk. We should probably be looking elsewhere to explain the GI distress.
The genetic information bore much more fruit in regard to his liver disease. Remember that Beethoven’s autopsy showed cirrhosis. His polygenic risk score for liver cirrhosis puts him in the 96th percentile of risk. He was also heterozygous for two variants that can cause hereditary hemochromatosis. The risk for cirrhosis among those with these variants is increased by the use of alcohol. And historical accounts are quite clear that Beethoven consumed more than his share.
But it wasn’t just Beethoven’s DNA in these hair follicles. Analysis of a follicle from later in his life revealed the unmistakable presence of hepatitis B virus. Endemic in Europe at the time, this was a common cause of liver failure and is likely to have contributed to, if not directly caused, Beethoven’s demise.
It’s hard to read these results and not marvel at the fact that, two centuries after his death, our fascination with Beethoven has led us to probe every corner of his life – his letters, his writings, his medical records, and now his very DNA. What are we actually looking for? Is it relevant to us today what caused his hearing loss? His stomach troubles? Even his death? Will it help any patients in the future? I propose that what we are actually trying to understand is something ineffable: Genius of magnitude that is rarely seen in one or many lifetimes. And our scientific tools, as sharp as they may have become, are still far too blunt to probe the depths of that transcendence.
In any case, friends, no more of these sounds. Let us sing more cheerful songs, more full of joy.
For Medscape, I’m Perry Wilson.
Dr. Wilson is associate professor, department of medicine, and director, Clinical and Translational Research Accelerator, at Yale University, New Haven, Conn. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Nurse makes millions selling her licensing exam study sheets
Ms. Beggs, 28, sells one-page study sheets or bundles of sheets, sometimes with colorful drawings, conversation bubbles and underlining, that boil down concepts for particular conditions into easy-to-understand language.
The biggest seller on Ms. Beggs’ online marketplace Etsy site, RNExplained, is a bundle of study guides covering eight core nursing classes. The notes range in price from $2 to $150. More than 70,000 customers have bought the $60 bundle, according to the website.
Ms. Beggs’ business developed in a “very unintentional” way when COVID hit with just months left in her nursing program at Mount Saint Mary’s University, Los Angeles, she told this news organization.
Classes had switched to Zoom, and she had no one to study with as she prepared to take her board exams.
“The best way I know how to study is to teach things out loud. But because I had nobody to teach out loud to, I would literally teach them to the wall,” Ms. Beggs said. “I would record myself so I could play it back and teach myself these topics that were hard for me to understand.”
Just for fun, she says, she posted them on TikTok and the responses started flowing in, with followers asking where she was selling the sheets. She now has more than 660,000 TikTok followers and 9 million likes.
Ms. Beggs said that every sheet highlights a condition, and she has made 308 of them.
Traditional classroom lessons typically teach one medical condition in 5-6 pages, Ms. Beggs said. “I go straight to the point.”
One reviewer on Ms. Beggs’ Etsy site appreciated the handwritten notes, calling them “simplified and concise.” Another commented: “Definitely helped me pass my last exam.”
Ms. Beggs says that her notes may seem simple, but each page represents comprehensive research.
“I have to go through not just one source of information to make sure my information is factual,” Ms. Beggs says. “What you teach in California might be a little different than what you teach in Florida. It’s very meticulous. The lab values will be a little different everywhere you go.”
She acknowledges her competition, noting that there are many other study guides for the NCLEX and nursing courses.
Nursing groups weigh in
Dawn Kappel, spokesperson for the National Council of State Boards of Nursing, which oversees NCLEX, said in an interview that “NCSBN has no issue with the current content of Stephanee Beggs’ business venture.”
For many students, the study guides will be helpful, especially for visual learners, said Carole Kenner, PhD, RN, dean and professor in the School of Nursing and Health Sciences at The College of New Jersey.
But for students “who are less confident in their knowledge, I would want to see a lot more in-depth explanation and rationale,” Dr. Kenner said.
“Since the NCLEX is moving to more cased-based scenarios, the next-gen unfolding cases, you really have to understand a lot of the rationale.”
The notes remind Dr. Kenner of traditional flash cards. “I don’t think it will work for all students, but even the fanciest of onsite review courses are useful to everyone,” she said.
‘Not cutting corners’
As an emergency nurse, Ms. Beggs said, “I have the experience as a nurse to show people that what you are learning will be seen in real life.”
“The way I teach my brand is not to take shortcuts. I love to teach to understand rather than teaching to memorize for an exam.”
She said she sees her guides as a supplement to learning, not a replacement.
“It’s not cutting corners,” she says. “I condense a medical condition that could take a very long time to understand and break it into layman’s terms.”
Ms. Beggs said when people hear about the $2 million, they often ask her whether she plans to give up her shifts in the emergency department for the more lucrative venture.
The answer is no, at least not yet.
“Aside from teaching, I genuinely love being at the bedside,” Ms. Beggs said. “I don’t foresee myself leaving that for good for as long as I can handle both.” She acknowledged, though, that her business now takes up most of her time.
“I love everything about both aspects, so it’s hard for me to choose.”
A version of this article first appeared on Medscape.com.
Ms. Beggs, 28, sells one-page study sheets or bundles of sheets, sometimes with colorful drawings, conversation bubbles and underlining, that boil down concepts for particular conditions into easy-to-understand language.
The biggest seller on Ms. Beggs’ online marketplace Etsy site, RNExplained, is a bundle of study guides covering eight core nursing classes. The notes range in price from $2 to $150. More than 70,000 customers have bought the $60 bundle, according to the website.
Ms. Beggs’ business developed in a “very unintentional” way when COVID hit with just months left in her nursing program at Mount Saint Mary’s University, Los Angeles, she told this news organization.
Classes had switched to Zoom, and she had no one to study with as she prepared to take her board exams.
“The best way I know how to study is to teach things out loud. But because I had nobody to teach out loud to, I would literally teach them to the wall,” Ms. Beggs said. “I would record myself so I could play it back and teach myself these topics that were hard for me to understand.”
Just for fun, she says, she posted them on TikTok and the responses started flowing in, with followers asking where she was selling the sheets. She now has more than 660,000 TikTok followers and 9 million likes.
Ms. Beggs said that every sheet highlights a condition, and she has made 308 of them.
Traditional classroom lessons typically teach one medical condition in 5-6 pages, Ms. Beggs said. “I go straight to the point.”
One reviewer on Ms. Beggs’ Etsy site appreciated the handwritten notes, calling them “simplified and concise.” Another commented: “Definitely helped me pass my last exam.”
Ms. Beggs says that her notes may seem simple, but each page represents comprehensive research.
“I have to go through not just one source of information to make sure my information is factual,” Ms. Beggs says. “What you teach in California might be a little different than what you teach in Florida. It’s very meticulous. The lab values will be a little different everywhere you go.”
She acknowledges her competition, noting that there are many other study guides for the NCLEX and nursing courses.
Nursing groups weigh in
Dawn Kappel, spokesperson for the National Council of State Boards of Nursing, which oversees NCLEX, said in an interview that “NCSBN has no issue with the current content of Stephanee Beggs’ business venture.”
For many students, the study guides will be helpful, especially for visual learners, said Carole Kenner, PhD, RN, dean and professor in the School of Nursing and Health Sciences at The College of New Jersey.
But for students “who are less confident in their knowledge, I would want to see a lot more in-depth explanation and rationale,” Dr. Kenner said.
“Since the NCLEX is moving to more cased-based scenarios, the next-gen unfolding cases, you really have to understand a lot of the rationale.”
The notes remind Dr. Kenner of traditional flash cards. “I don’t think it will work for all students, but even the fanciest of onsite review courses are useful to everyone,” she said.
‘Not cutting corners’
As an emergency nurse, Ms. Beggs said, “I have the experience as a nurse to show people that what you are learning will be seen in real life.”
“The way I teach my brand is not to take shortcuts. I love to teach to understand rather than teaching to memorize for an exam.”
She said she sees her guides as a supplement to learning, not a replacement.
“It’s not cutting corners,” she says. “I condense a medical condition that could take a very long time to understand and break it into layman’s terms.”
Ms. Beggs said when people hear about the $2 million, they often ask her whether she plans to give up her shifts in the emergency department for the more lucrative venture.
The answer is no, at least not yet.
“Aside from teaching, I genuinely love being at the bedside,” Ms. Beggs said. “I don’t foresee myself leaving that for good for as long as I can handle both.” She acknowledged, though, that her business now takes up most of her time.
“I love everything about both aspects, so it’s hard for me to choose.”
A version of this article first appeared on Medscape.com.
Ms. Beggs, 28, sells one-page study sheets or bundles of sheets, sometimes with colorful drawings, conversation bubbles and underlining, that boil down concepts for particular conditions into easy-to-understand language.
The biggest seller on Ms. Beggs’ online marketplace Etsy site, RNExplained, is a bundle of study guides covering eight core nursing classes. The notes range in price from $2 to $150. More than 70,000 customers have bought the $60 bundle, according to the website.
Ms. Beggs’ business developed in a “very unintentional” way when COVID hit with just months left in her nursing program at Mount Saint Mary’s University, Los Angeles, she told this news organization.
Classes had switched to Zoom, and she had no one to study with as she prepared to take her board exams.
“The best way I know how to study is to teach things out loud. But because I had nobody to teach out loud to, I would literally teach them to the wall,” Ms. Beggs said. “I would record myself so I could play it back and teach myself these topics that were hard for me to understand.”
Just for fun, she says, she posted them on TikTok and the responses started flowing in, with followers asking where she was selling the sheets. She now has more than 660,000 TikTok followers and 9 million likes.
Ms. Beggs said that every sheet highlights a condition, and she has made 308 of them.
Traditional classroom lessons typically teach one medical condition in 5-6 pages, Ms. Beggs said. “I go straight to the point.”
One reviewer on Ms. Beggs’ Etsy site appreciated the handwritten notes, calling them “simplified and concise.” Another commented: “Definitely helped me pass my last exam.”
Ms. Beggs says that her notes may seem simple, but each page represents comprehensive research.
“I have to go through not just one source of information to make sure my information is factual,” Ms. Beggs says. “What you teach in California might be a little different than what you teach in Florida. It’s very meticulous. The lab values will be a little different everywhere you go.”
She acknowledges her competition, noting that there are many other study guides for the NCLEX and nursing courses.
Nursing groups weigh in
Dawn Kappel, spokesperson for the National Council of State Boards of Nursing, which oversees NCLEX, said in an interview that “NCSBN has no issue with the current content of Stephanee Beggs’ business venture.”
For many students, the study guides will be helpful, especially for visual learners, said Carole Kenner, PhD, RN, dean and professor in the School of Nursing and Health Sciences at The College of New Jersey.
But for students “who are less confident in their knowledge, I would want to see a lot more in-depth explanation and rationale,” Dr. Kenner said.
“Since the NCLEX is moving to more cased-based scenarios, the next-gen unfolding cases, you really have to understand a lot of the rationale.”
The notes remind Dr. Kenner of traditional flash cards. “I don’t think it will work for all students, but even the fanciest of onsite review courses are useful to everyone,” she said.
‘Not cutting corners’
As an emergency nurse, Ms. Beggs said, “I have the experience as a nurse to show people that what you are learning will be seen in real life.”
“The way I teach my brand is not to take shortcuts. I love to teach to understand rather than teaching to memorize for an exam.”
She said she sees her guides as a supplement to learning, not a replacement.
“It’s not cutting corners,” she says. “I condense a medical condition that could take a very long time to understand and break it into layman’s terms.”
Ms. Beggs said when people hear about the $2 million, they often ask her whether she plans to give up her shifts in the emergency department for the more lucrative venture.
The answer is no, at least not yet.
“Aside from teaching, I genuinely love being at the bedside,” Ms. Beggs said. “I don’t foresee myself leaving that for good for as long as I can handle both.” She acknowledged, though, that her business now takes up most of her time.
“I love everything about both aspects, so it’s hard for me to choose.”
A version of this article first appeared on Medscape.com.
FDA expands evinacumab approval to younger kids with HoFH
The U.S. Food and Drug Administration has expanded the indicated age range for evinacumab-dgnb (Evkeeza, Regeneron Pharmaceuticals), which was approved 2 years ago as an adjunct to other lipid-lowering therapies for homozygous familial hypercholesterolemia (HoFH) in patients aged 12 and older.
The antibody-based agent’s indication now also covers patients aged 5-11 years with the rare genetic disorder, Regeneron announced. It blocks angiopoietin-like 3 (ANGPTL3), inhibiting lipoprotein lipase and endothelial lipase, thereby cutting LDL-cholesterol levels by mechanisms not directly involving the LDL receptor.
The expanded indication is based on a study that saw a 48% drop in LDL-cholesterol levels over 24 weeks, the primary endpoint, across 20 HoFH patients aged 5-11 years who received evinacumab-dgnb on top of maximally tolerated standard lipid-modifying therapy, the company reports.
Levels of apolipoprotein B, non-HDL cholesterol, and total cholesterol also fell significantly in the trial, which was completed in January.
The drug’s efficacy and safety resembled those of a previously reported larger study of patients with HoFH aged 12 years and older (mean age about 40 years) that led to its initial approval.
“The safety and effectiveness of Evkeeza have not been established in patients with other causes of hypercholesterolemia, including those with heterozygous familial hypercholesterolemia,” the company states. Nor is it known whether the drug affects clinical outcomes.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has expanded the indicated age range for evinacumab-dgnb (Evkeeza, Regeneron Pharmaceuticals), which was approved 2 years ago as an adjunct to other lipid-lowering therapies for homozygous familial hypercholesterolemia (HoFH) in patients aged 12 and older.
The antibody-based agent’s indication now also covers patients aged 5-11 years with the rare genetic disorder, Regeneron announced. It blocks angiopoietin-like 3 (ANGPTL3), inhibiting lipoprotein lipase and endothelial lipase, thereby cutting LDL-cholesterol levels by mechanisms not directly involving the LDL receptor.
The expanded indication is based on a study that saw a 48% drop in LDL-cholesterol levels over 24 weeks, the primary endpoint, across 20 HoFH patients aged 5-11 years who received evinacumab-dgnb on top of maximally tolerated standard lipid-modifying therapy, the company reports.
Levels of apolipoprotein B, non-HDL cholesterol, and total cholesterol also fell significantly in the trial, which was completed in January.
The drug’s efficacy and safety resembled those of a previously reported larger study of patients with HoFH aged 12 years and older (mean age about 40 years) that led to its initial approval.
“The safety and effectiveness of Evkeeza have not been established in patients with other causes of hypercholesterolemia, including those with heterozygous familial hypercholesterolemia,” the company states. Nor is it known whether the drug affects clinical outcomes.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has expanded the indicated age range for evinacumab-dgnb (Evkeeza, Regeneron Pharmaceuticals), which was approved 2 years ago as an adjunct to other lipid-lowering therapies for homozygous familial hypercholesterolemia (HoFH) in patients aged 12 and older.
The antibody-based agent’s indication now also covers patients aged 5-11 years with the rare genetic disorder, Regeneron announced. It blocks angiopoietin-like 3 (ANGPTL3), inhibiting lipoprotein lipase and endothelial lipase, thereby cutting LDL-cholesterol levels by mechanisms not directly involving the LDL receptor.
The expanded indication is based on a study that saw a 48% drop in LDL-cholesterol levels over 24 weeks, the primary endpoint, across 20 HoFH patients aged 5-11 years who received evinacumab-dgnb on top of maximally tolerated standard lipid-modifying therapy, the company reports.
Levels of apolipoprotein B, non-HDL cholesterol, and total cholesterol also fell significantly in the trial, which was completed in January.
The drug’s efficacy and safety resembled those of a previously reported larger study of patients with HoFH aged 12 years and older (mean age about 40 years) that led to its initial approval.
“The safety and effectiveness of Evkeeza have not been established in patients with other causes of hypercholesterolemia, including those with heterozygous familial hypercholesterolemia,” the company states. Nor is it known whether the drug affects clinical outcomes.
A version of this article first appeared on Medscape.com.
The air up there: Oxygen could be a bit overrated
Into thin, but healthy, air
Human civilization has essentially been built on proximity to water. Ancient civilizations in Mesopotamia, Egypt, Greece, China, and India were all intimately connected to either rivers or the ocean. Even today, with all our technology, about a third of Earth’s 8 billion people live within 100 vertical meters of sea level, and the median person lives at an elevation of just 200 meters.
All things considered, one might imagine life is pretty tough for the 2 million people living at an elevation of 4,500 meters (nearly 15,000 feet). Not too many Wal-Marts or McDonalds up there. Oh, and not much air either. And for most of us not named Spongebob, air is good.
Or is it? That’s the question posed by a new study. After all, the researchers said, people living at high altitudes, where the air has only 11% effective oxygen instead of the 21% we have at low altitude, have significantly lower rates of metabolic disorders such as diabetes and heart diseases. Maybe breathing isn’t all it’s cracked up to be.
To find out, the researchers placed a group of mice in environments with either 11% oxygen or 8% oxygen. This netted them a bunch of very tired mice. Hey, sudden altitude gain doesn’t go too well for us either, but after 3 weeks, all the mice in the hypoxic environments had regained their normal movement and were behaving as any mouse would.
While the critters seemed normal on the outside, a closer examination found the truth. Their metabolism had been permanently altered, and their blood sugar and weight went down and never bounced back up. Further examination through PET scans showed that the hypoxic mice’s organs showed an increase in glucose metabolism and that brown fat and skeletal muscles reduced the amount of sugar they used.
This goes against the prevailing assumption about hypoxic conditions, the researchers said, since it was previously theorized that the body simply burned more glucose in response to having less oxygen. And while that’s true, our organs also conspicuously use less glucose. Currently, many athletes use hypoxic environments to train, but these new data suggest that people with metabolic disorders also would see benefits from living in low-oxygen environments.
Do you know what this means? All we have to do to stop diabetes is take civilization and push it somewhere else. This can’t possibly end badly.
Sleep survey: The restless majority
Newsflash! This just in: Nobody is sleeping well.
When we go to bed, our goal is to get rest, right? Sorry America, but you’re falling short. In a recent survey conducted by OnePoll for Purple Mattress, almost two-thirds of the 2,011 participants considered themselves restless sleepers.
Not surprised. So what’s keeping us up?
Snoring partners (20%) and anxiety (26%) made the list, but the award for top complaint goes to body pain. Back pain was most prevalent, reported by 36% of respondents, followed by neck pain (33%) and shoulder pain (24%). No wonder, then, that only 10% of the group reported feeling well rested when they woke up.
Do you ever blame your tiredness on sleeping funny? Well, we all kind of sleep funny, and yet we’re still not sleeping well.
The largest proportion of people like to sleep on their side (48%), compared with 18% on their back and 17% on their stomach. The main reasons to choose certain positions were to ease soreness or sleep better, both at 28%. The largest share of participants (47%) reported sleeping in a “yearner” position, while 40% lay on their stomachs in the “free faller” position, and 39% reported using the “soldier” position.
Regardless of the method people use to get to sleep or the position they’re in, the goal is always the same. We’re all just trying to figure out what’s the right one for us.
Seen a UFO recently? Don’t blame COVID
First of all, because we know you’re going to be thinking it in a minute, no, we did not make this up. With COVID-19 still hanging around, there’s no need for fabrication on our part.
The pandemic, clearly, has caused humans to do some strange things over the last 3 years, but what about some of the more, shall we say … eccentric behavior that people were already exhibiting before COVID found its way into our lives?
If, like R. Chase Cockrell, PhD, of the University of Vermont and associates at the Center for UFO Studies, you were wondering if the pandemic affected UFO reporting, then wonder no more. After all, with all that extra time being spent outdoors back in 2020 and all the additional anxiety, surely somebody must have seen something.
The investigators started with the basics by analyzing data from the National UFO Reporting Center and the Mutual UFO Network. Sightings did increase by about 600 in each database during 2020, compared with 2018 and 2019, but not because of the pandemic.
That’s right, we can’t pin this one on our good friend SARS-CoV-2. Further analysis showed that the launches of SpaceX Starlink satellites – sometimes as many as 60 at a time – probably caused the increase in UFO sightings, which means that our favorite billionaire, Elon Musk, is to blame. Yup, the genial Mr. Muskellunge did something that even a global pandemic couldn’t, and yet we vaccinate for COVID.
Next week on tenuous connections: A new study links the 2020 presidential election to increased emergency department visits for external hemorrhoids.
See? That’s fabrication. We made that up.
This article was updated 5/15/23.
Into thin, but healthy, air
Human civilization has essentially been built on proximity to water. Ancient civilizations in Mesopotamia, Egypt, Greece, China, and India were all intimately connected to either rivers or the ocean. Even today, with all our technology, about a third of Earth’s 8 billion people live within 100 vertical meters of sea level, and the median person lives at an elevation of just 200 meters.
All things considered, one might imagine life is pretty tough for the 2 million people living at an elevation of 4,500 meters (nearly 15,000 feet). Not too many Wal-Marts or McDonalds up there. Oh, and not much air either. And for most of us not named Spongebob, air is good.
Or is it? That’s the question posed by a new study. After all, the researchers said, people living at high altitudes, where the air has only 11% effective oxygen instead of the 21% we have at low altitude, have significantly lower rates of metabolic disorders such as diabetes and heart diseases. Maybe breathing isn’t all it’s cracked up to be.
To find out, the researchers placed a group of mice in environments with either 11% oxygen or 8% oxygen. This netted them a bunch of very tired mice. Hey, sudden altitude gain doesn’t go too well for us either, but after 3 weeks, all the mice in the hypoxic environments had regained their normal movement and were behaving as any mouse would.
While the critters seemed normal on the outside, a closer examination found the truth. Their metabolism had been permanently altered, and their blood sugar and weight went down and never bounced back up. Further examination through PET scans showed that the hypoxic mice’s organs showed an increase in glucose metabolism and that brown fat and skeletal muscles reduced the amount of sugar they used.
This goes against the prevailing assumption about hypoxic conditions, the researchers said, since it was previously theorized that the body simply burned more glucose in response to having less oxygen. And while that’s true, our organs also conspicuously use less glucose. Currently, many athletes use hypoxic environments to train, but these new data suggest that people with metabolic disorders also would see benefits from living in low-oxygen environments.
Do you know what this means? All we have to do to stop diabetes is take civilization and push it somewhere else. This can’t possibly end badly.
Sleep survey: The restless majority
Newsflash! This just in: Nobody is sleeping well.
When we go to bed, our goal is to get rest, right? Sorry America, but you’re falling short. In a recent survey conducted by OnePoll for Purple Mattress, almost two-thirds of the 2,011 participants considered themselves restless sleepers.
Not surprised. So what’s keeping us up?
Snoring partners (20%) and anxiety (26%) made the list, but the award for top complaint goes to body pain. Back pain was most prevalent, reported by 36% of respondents, followed by neck pain (33%) and shoulder pain (24%). No wonder, then, that only 10% of the group reported feeling well rested when they woke up.
Do you ever blame your tiredness on sleeping funny? Well, we all kind of sleep funny, and yet we’re still not sleeping well.
The largest proportion of people like to sleep on their side (48%), compared with 18% on their back and 17% on their stomach. The main reasons to choose certain positions were to ease soreness or sleep better, both at 28%. The largest share of participants (47%) reported sleeping in a “yearner” position, while 40% lay on their stomachs in the “free faller” position, and 39% reported using the “soldier” position.
Regardless of the method people use to get to sleep or the position they’re in, the goal is always the same. We’re all just trying to figure out what’s the right one for us.
Seen a UFO recently? Don’t blame COVID
First of all, because we know you’re going to be thinking it in a minute, no, we did not make this up. With COVID-19 still hanging around, there’s no need for fabrication on our part.
The pandemic, clearly, has caused humans to do some strange things over the last 3 years, but what about some of the more, shall we say … eccentric behavior that people were already exhibiting before COVID found its way into our lives?
If, like R. Chase Cockrell, PhD, of the University of Vermont and associates at the Center for UFO Studies, you were wondering if the pandemic affected UFO reporting, then wonder no more. After all, with all that extra time being spent outdoors back in 2020 and all the additional anxiety, surely somebody must have seen something.
The investigators started with the basics by analyzing data from the National UFO Reporting Center and the Mutual UFO Network. Sightings did increase by about 600 in each database during 2020, compared with 2018 and 2019, but not because of the pandemic.
That’s right, we can’t pin this one on our good friend SARS-CoV-2. Further analysis showed that the launches of SpaceX Starlink satellites – sometimes as many as 60 at a time – probably caused the increase in UFO sightings, which means that our favorite billionaire, Elon Musk, is to blame. Yup, the genial Mr. Muskellunge did something that even a global pandemic couldn’t, and yet we vaccinate for COVID.
Next week on tenuous connections: A new study links the 2020 presidential election to increased emergency department visits for external hemorrhoids.
See? That’s fabrication. We made that up.
This article was updated 5/15/23.
Into thin, but healthy, air
Human civilization has essentially been built on proximity to water. Ancient civilizations in Mesopotamia, Egypt, Greece, China, and India were all intimately connected to either rivers or the ocean. Even today, with all our technology, about a third of Earth’s 8 billion people live within 100 vertical meters of sea level, and the median person lives at an elevation of just 200 meters.
All things considered, one might imagine life is pretty tough for the 2 million people living at an elevation of 4,500 meters (nearly 15,000 feet). Not too many Wal-Marts or McDonalds up there. Oh, and not much air either. And for most of us not named Spongebob, air is good.
Or is it? That’s the question posed by a new study. After all, the researchers said, people living at high altitudes, where the air has only 11% effective oxygen instead of the 21% we have at low altitude, have significantly lower rates of metabolic disorders such as diabetes and heart diseases. Maybe breathing isn’t all it’s cracked up to be.
To find out, the researchers placed a group of mice in environments with either 11% oxygen or 8% oxygen. This netted them a bunch of very tired mice. Hey, sudden altitude gain doesn’t go too well for us either, but after 3 weeks, all the mice in the hypoxic environments had regained their normal movement and were behaving as any mouse would.
While the critters seemed normal on the outside, a closer examination found the truth. Their metabolism had been permanently altered, and their blood sugar and weight went down and never bounced back up. Further examination through PET scans showed that the hypoxic mice’s organs showed an increase in glucose metabolism and that brown fat and skeletal muscles reduced the amount of sugar they used.
This goes against the prevailing assumption about hypoxic conditions, the researchers said, since it was previously theorized that the body simply burned more glucose in response to having less oxygen. And while that’s true, our organs also conspicuously use less glucose. Currently, many athletes use hypoxic environments to train, but these new data suggest that people with metabolic disorders also would see benefits from living in low-oxygen environments.
Do you know what this means? All we have to do to stop diabetes is take civilization and push it somewhere else. This can’t possibly end badly.
Sleep survey: The restless majority
Newsflash! This just in: Nobody is sleeping well.
When we go to bed, our goal is to get rest, right? Sorry America, but you’re falling short. In a recent survey conducted by OnePoll for Purple Mattress, almost two-thirds of the 2,011 participants considered themselves restless sleepers.
Not surprised. So what’s keeping us up?
Snoring partners (20%) and anxiety (26%) made the list, but the award for top complaint goes to body pain. Back pain was most prevalent, reported by 36% of respondents, followed by neck pain (33%) and shoulder pain (24%). No wonder, then, that only 10% of the group reported feeling well rested when they woke up.
Do you ever blame your tiredness on sleeping funny? Well, we all kind of sleep funny, and yet we’re still not sleeping well.
The largest proportion of people like to sleep on their side (48%), compared with 18% on their back and 17% on their stomach. The main reasons to choose certain positions were to ease soreness or sleep better, both at 28%. The largest share of participants (47%) reported sleeping in a “yearner” position, while 40% lay on their stomachs in the “free faller” position, and 39% reported using the “soldier” position.
Regardless of the method people use to get to sleep or the position they’re in, the goal is always the same. We’re all just trying to figure out what’s the right one for us.
Seen a UFO recently? Don’t blame COVID
First of all, because we know you’re going to be thinking it in a minute, no, we did not make this up. With COVID-19 still hanging around, there’s no need for fabrication on our part.
The pandemic, clearly, has caused humans to do some strange things over the last 3 years, but what about some of the more, shall we say … eccentric behavior that people were already exhibiting before COVID found its way into our lives?
If, like R. Chase Cockrell, PhD, of the University of Vermont and associates at the Center for UFO Studies, you were wondering if the pandemic affected UFO reporting, then wonder no more. After all, with all that extra time being spent outdoors back in 2020 and all the additional anxiety, surely somebody must have seen something.
The investigators started with the basics by analyzing data from the National UFO Reporting Center and the Mutual UFO Network. Sightings did increase by about 600 in each database during 2020, compared with 2018 and 2019, but not because of the pandemic.
That’s right, we can’t pin this one on our good friend SARS-CoV-2. Further analysis showed that the launches of SpaceX Starlink satellites – sometimes as many as 60 at a time – probably caused the increase in UFO sightings, which means that our favorite billionaire, Elon Musk, is to blame. Yup, the genial Mr. Muskellunge did something that even a global pandemic couldn’t, and yet we vaccinate for COVID.
Next week on tenuous connections: A new study links the 2020 presidential election to increased emergency department visits for external hemorrhoids.
See? That’s fabrication. We made that up.
This article was updated 5/15/23.
Cases of potentially deadly fungus jump 200%: CDC
prompting the Centers for Disease Control and Prevention to issue a warning to health care facilities about the rising threat.
C. auris is a yeast that spreads easily from touching it on a surface like a countertop. It can also spread from person to person. It isn’t a threat to healthy people, but people in hospitals and nursing homes are at a heightened risk because they might have weakened immune systems or be using invasive medical devices that can introduce the fungus inside their bodies. When C. auris progresses to causing an infection that reaches the brain, blood, or lungs, more than one in three people die.
The worrying increase was detailed in the journal Annals of Internal Medicine. In 2021, cases reached a count of 3,270 with an active infection, and 7,413 cases showed the fungus was present but hadn’t caused an infection. Infection counts were up 95% over the previous year, and the fungus showed up on screenings three times as often. The number of cases resistant to medication also tripled.
The CDC called the figures “alarming,” noting that the fungus was only detected in the United States in 2016.
“The timing of this increase and findings from public health investigations suggest C. auris spread may have worsened due to strain on health care and public health systems during the COVID-19 pandemic,” the CDC explained in a news release.
Another potential reason for the jump could be that screening for C. auris has simply increased and it’s being found more often because it’s being looked for more often. But researchers believe that, even with the increase in testing, the reported counts are underestimated. That’s because even though screening has increased, health care providers still aren’t looking for the presence of the fungus as often as the CDC would like.
“The rapid rise and geographic spread of cases is concerning and emphasizes the need for continued surveillance, expanded lab capacity, quicker diagnostic tests, and adherence to proven infection prevention and control,” said study author Meghan Lyman, MD, a CDC epidemiologist in Atlanta, in a statement.
Cases of C. auris continued to rise in 2022, the CDC said. A map on the agency’s website of reported cases from 2022 shows it was found in more than half of U.S. states, with the highest counts occurring in California, Florida, Illinois, Nevada, New York, and Texas. The fungus is a problem worldwide and is listed among the most threatening treatment-resistant fungi by the World Health Organization.
The study authors concluded that screening capacity for the fungus needs to be expanded nationwide so that when C. auris is detected, measures can be taken to prevent its spread.
A version of this article originally appeared on WebMD.com.
prompting the Centers for Disease Control and Prevention to issue a warning to health care facilities about the rising threat.
C. auris is a yeast that spreads easily from touching it on a surface like a countertop. It can also spread from person to person. It isn’t a threat to healthy people, but people in hospitals and nursing homes are at a heightened risk because they might have weakened immune systems or be using invasive medical devices that can introduce the fungus inside their bodies. When C. auris progresses to causing an infection that reaches the brain, blood, or lungs, more than one in three people die.
The worrying increase was detailed in the journal Annals of Internal Medicine. In 2021, cases reached a count of 3,270 with an active infection, and 7,413 cases showed the fungus was present but hadn’t caused an infection. Infection counts were up 95% over the previous year, and the fungus showed up on screenings three times as often. The number of cases resistant to medication also tripled.
The CDC called the figures “alarming,” noting that the fungus was only detected in the United States in 2016.
“The timing of this increase and findings from public health investigations suggest C. auris spread may have worsened due to strain on health care and public health systems during the COVID-19 pandemic,” the CDC explained in a news release.
Another potential reason for the jump could be that screening for C. auris has simply increased and it’s being found more often because it’s being looked for more often. But researchers believe that, even with the increase in testing, the reported counts are underestimated. That’s because even though screening has increased, health care providers still aren’t looking for the presence of the fungus as often as the CDC would like.
“The rapid rise and geographic spread of cases is concerning and emphasizes the need for continued surveillance, expanded lab capacity, quicker diagnostic tests, and adherence to proven infection prevention and control,” said study author Meghan Lyman, MD, a CDC epidemiologist in Atlanta, in a statement.
Cases of C. auris continued to rise in 2022, the CDC said. A map on the agency’s website of reported cases from 2022 shows it was found in more than half of U.S. states, with the highest counts occurring in California, Florida, Illinois, Nevada, New York, and Texas. The fungus is a problem worldwide and is listed among the most threatening treatment-resistant fungi by the World Health Organization.
The study authors concluded that screening capacity for the fungus needs to be expanded nationwide so that when C. auris is detected, measures can be taken to prevent its spread.
A version of this article originally appeared on WebMD.com.
prompting the Centers for Disease Control and Prevention to issue a warning to health care facilities about the rising threat.
C. auris is a yeast that spreads easily from touching it on a surface like a countertop. It can also spread from person to person. It isn’t a threat to healthy people, but people in hospitals and nursing homes are at a heightened risk because they might have weakened immune systems or be using invasive medical devices that can introduce the fungus inside their bodies. When C. auris progresses to causing an infection that reaches the brain, blood, or lungs, more than one in three people die.
The worrying increase was detailed in the journal Annals of Internal Medicine. In 2021, cases reached a count of 3,270 with an active infection, and 7,413 cases showed the fungus was present but hadn’t caused an infection. Infection counts were up 95% over the previous year, and the fungus showed up on screenings three times as often. The number of cases resistant to medication also tripled.
The CDC called the figures “alarming,” noting that the fungus was only detected in the United States in 2016.
“The timing of this increase and findings from public health investigations suggest C. auris spread may have worsened due to strain on health care and public health systems during the COVID-19 pandemic,” the CDC explained in a news release.
Another potential reason for the jump could be that screening for C. auris has simply increased and it’s being found more often because it’s being looked for more often. But researchers believe that, even with the increase in testing, the reported counts are underestimated. That’s because even though screening has increased, health care providers still aren’t looking for the presence of the fungus as often as the CDC would like.
“The rapid rise and geographic spread of cases is concerning and emphasizes the need for continued surveillance, expanded lab capacity, quicker diagnostic tests, and adherence to proven infection prevention and control,” said study author Meghan Lyman, MD, a CDC epidemiologist in Atlanta, in a statement.
Cases of C. auris continued to rise in 2022, the CDC said. A map on the agency’s website of reported cases from 2022 shows it was found in more than half of U.S. states, with the highest counts occurring in California, Florida, Illinois, Nevada, New York, and Texas. The fungus is a problem worldwide and is listed among the most threatening treatment-resistant fungi by the World Health Organization.
The study authors concluded that screening capacity for the fungus needs to be expanded nationwide so that when C. auris is detected, measures can be taken to prevent its spread.
A version of this article originally appeared on WebMD.com.