User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Artificial sweeteners in processed foods tied to increased depression risk
new data from the Nurses Health Study II (NHS II) suggest.
Nurses who consumed more than eight servings daily had about a 50% higher risk of developing depression than nurses who consumed four or fewer servings daily.
However, in a secondary analysis, in which the researchers tried to tease out specific foods that may be associated with increased risk, only artificial sweeteners and artificially sweetened beverages were associated with an increased risk of depression.
“Animal studies have shown that artificial sweeteners may trigger the transmission of particular signaling molecules in the brain that are important for mood,” study investigator Andrew T. Chan, MD, MPH, of the clinical and translational epidemiology unit at Massachusetts General Hospital, Boston, said in an interview.
“Given this potential association between ultraprocessed food and multiple adverse health conditions, wherever possible individuals may wish to limit their intake of such foods. This may be a lifestyle change that could have important benefits, particularly for those who struggle with mental health,” Dr. Chan said.
The study was published online in JAMA Network Open.
Multiple potential mechanisms
The findings are based on 31,712 mostly non-Hispanic White women who were free of depression at baseline. The mean age of the patients at baseline was 52 years. As part of the NHS II, the women provided information on diet every 4 years using validated food frequency questionnaires.
Compared with women with low UPF intake, those with high UPF intake had greater body mass index (BMI). In addition, they were apt to smoke and have diabetes, hypertension, and dyslipidemia, and they were less apt to exercise regularly.
During the study period, there were 2,122 incident cases of depression, as determined using a strict definition that required self-reported clinician-diagnosed depression and regular antidepressant use. There were 4,840 incident cases, as determined using a broad definition that required clinical diagnosis and/or antidepressant use.
Compared with women in the lowest quintile of UPF consumption (fewer than four daily servings), those in the highest quintile (more than 8.8 daily servings) had an increased risk of depression.
This was noted for both the strict depression definition (hazard ratio, 1.49; 95% confidence interval, 1.26-1.76; P < .001) and the broad one (HR, 1.34; 95% CI, 1.20-1.50; P < .001).
“Models were not materially altered after inclusion of potential confounders. We did not observe differential associations in subgroups defined by age, BMI, physical activity, or smoking,” the researchers reported.
In secondary analyses, they classified UPF into their components, including ultraprocessed grain foods, sweet snacks, ready-to-eat meals, fats, sauces, ultraprocessed dairy products, savory snacks, processed meat, beverages, and artificial sweeteners.
Comparing the highest with the lowest quintiles, only high intake of artificially sweetened beverages (HR, 1.37; 95% CI, 1.19-1.57; P < .001) and artificial sweeteners (HR, 1.26; 95% CI, 1.10-1.43; P < .001) was associated with greater risk of depression and after multivariable regression.
In an exploratory analysis, women who reduced their UPF intake by at least three servings per day were at lower risk of depression (strict definition: HR, 0.84; 95% CI, 0.71-0.99), compared with those with relatively stable intake in each 4-year period.
“Ultraprocessed foods have been associated with several different health outcomes which may reflect an effect on common pathways that underlie chronic conditions,” said Dr. Chan.
For example, UPF intake has been associated with chronic inflammation, which in turns leads to multiple potential adverse health effects, including depression, he explained.
There is also a link between UPF and disruption of the gut microbiome.
“This is an important potential mechanism linking ultraprocessed food to depression since there is emerging evidence that microbes in the gut have been linked with mood through their role in metabolizing and producing proteins that have activity in the brain,” Dr. Chan said.
Association, not causation
Several experts weighed in on the study results in a statement from the U.K. nonprofit organization, Science Media Centre.
Gunter Kuhnle, PhD, professor of nutrition and food science, University of Reading (England), cautioned that the study only offers information on association – not causation.
“It is very possible that people with depression change their diet and might decide to consume foods that are easier to prepare – which would often be foods considered to be ultraprocessed,” Dr. Kuhnle said.
What’s most interesting is that the association between UPF intake and depression was driven by a single factor – artificial sweeteners.
“This supports one of the main criticisms of the UPF concept, that it combines a wide range of different foods and thereby makes it difficult to identify underlying causes,” Dr. Kuhnle added.
“There are currently no data that link artificial sweetener use to mental health, despite most of them having been available for some time. It is also important to note that there are a wide range of different artificial sweeteners that are metabolized very differently and that there might be reverse causality,” Dr. Kuhnle commented.
Paul Keedwell, MBChB, PhD, consultant psychiatrist and fellow of the Royal College of Psychiatrists, said this is an “interesting and important finding, but one that raises more questions. At this stage, we cannot say how big an effect diet has on depression risk compared to other risk factors, like family history of depression, stress levels, and having a supportive social network.”
Dr. Keedwell noted that the investigators carefully excluded the possibility that the effect is mediated by obesity or lack of exercise.
“However, an important consideration is that a diet based on ready meals and artificially sweetened drinks might indicate a hectic lifestyle or one with shift work. In other words, a fast-food diet could be an indirect marker of chronic stress. Prolonged stress probably remains the main risk factor for depression,” Dr. Keedwell said.
Keith Frayn, PhD, professor emeritus of human metabolism, University of Oxford (England), noted that the relationship between artificial sweeteners and depression “stands out clearly” even after adjusting for multiple confounding factors, including BMI, smoking, and exercise.
“This adds to growing concerns about artificial sweeteners and cardiometabolic health. The link with depression needs confirmation and further research to suggest how it might be brought about,” Dr. Frayn cautioned.
The NHS II was funded by a grant from the National Cancer Institute. Dr. Chan reported receiving grants from Bayer and Zoe and personal fees from Boehringer Ingelheim, Pfizer, and Freenome outside this work. Dr. Keedwell and Dr. Kuhnle disclosed no relevant financial relationships. Dr. Frayn is an author of books on nutrition and metabolism.
A version of this article first appeared on Medscape.com.
new data from the Nurses Health Study II (NHS II) suggest.
Nurses who consumed more than eight servings daily had about a 50% higher risk of developing depression than nurses who consumed four or fewer servings daily.
However, in a secondary analysis, in which the researchers tried to tease out specific foods that may be associated with increased risk, only artificial sweeteners and artificially sweetened beverages were associated with an increased risk of depression.
“Animal studies have shown that artificial sweeteners may trigger the transmission of particular signaling molecules in the brain that are important for mood,” study investigator Andrew T. Chan, MD, MPH, of the clinical and translational epidemiology unit at Massachusetts General Hospital, Boston, said in an interview.
“Given this potential association between ultraprocessed food and multiple adverse health conditions, wherever possible individuals may wish to limit their intake of such foods. This may be a lifestyle change that could have important benefits, particularly for those who struggle with mental health,” Dr. Chan said.
The study was published online in JAMA Network Open.
Multiple potential mechanisms
The findings are based on 31,712 mostly non-Hispanic White women who were free of depression at baseline. The mean age of the patients at baseline was 52 years. As part of the NHS II, the women provided information on diet every 4 years using validated food frequency questionnaires.
Compared with women with low UPF intake, those with high UPF intake had greater body mass index (BMI). In addition, they were apt to smoke and have diabetes, hypertension, and dyslipidemia, and they were less apt to exercise regularly.
During the study period, there were 2,122 incident cases of depression, as determined using a strict definition that required self-reported clinician-diagnosed depression and regular antidepressant use. There were 4,840 incident cases, as determined using a broad definition that required clinical diagnosis and/or antidepressant use.
Compared with women in the lowest quintile of UPF consumption (fewer than four daily servings), those in the highest quintile (more than 8.8 daily servings) had an increased risk of depression.
This was noted for both the strict depression definition (hazard ratio, 1.49; 95% confidence interval, 1.26-1.76; P < .001) and the broad one (HR, 1.34; 95% CI, 1.20-1.50; P < .001).
“Models were not materially altered after inclusion of potential confounders. We did not observe differential associations in subgroups defined by age, BMI, physical activity, or smoking,” the researchers reported.
In secondary analyses, they classified UPF into their components, including ultraprocessed grain foods, sweet snacks, ready-to-eat meals, fats, sauces, ultraprocessed dairy products, savory snacks, processed meat, beverages, and artificial sweeteners.
Comparing the highest with the lowest quintiles, only high intake of artificially sweetened beverages (HR, 1.37; 95% CI, 1.19-1.57; P < .001) and artificial sweeteners (HR, 1.26; 95% CI, 1.10-1.43; P < .001) was associated with greater risk of depression and after multivariable regression.
In an exploratory analysis, women who reduced their UPF intake by at least three servings per day were at lower risk of depression (strict definition: HR, 0.84; 95% CI, 0.71-0.99), compared with those with relatively stable intake in each 4-year period.
“Ultraprocessed foods have been associated with several different health outcomes which may reflect an effect on common pathways that underlie chronic conditions,” said Dr. Chan.
For example, UPF intake has been associated with chronic inflammation, which in turns leads to multiple potential adverse health effects, including depression, he explained.
There is also a link between UPF and disruption of the gut microbiome.
“This is an important potential mechanism linking ultraprocessed food to depression since there is emerging evidence that microbes in the gut have been linked with mood through their role in metabolizing and producing proteins that have activity in the brain,” Dr. Chan said.
Association, not causation
Several experts weighed in on the study results in a statement from the U.K. nonprofit organization, Science Media Centre.
Gunter Kuhnle, PhD, professor of nutrition and food science, University of Reading (England), cautioned that the study only offers information on association – not causation.
“It is very possible that people with depression change their diet and might decide to consume foods that are easier to prepare – which would often be foods considered to be ultraprocessed,” Dr. Kuhnle said.
What’s most interesting is that the association between UPF intake and depression was driven by a single factor – artificial sweeteners.
“This supports one of the main criticisms of the UPF concept, that it combines a wide range of different foods and thereby makes it difficult to identify underlying causes,” Dr. Kuhnle added.
“There are currently no data that link artificial sweetener use to mental health, despite most of them having been available for some time. It is also important to note that there are a wide range of different artificial sweeteners that are metabolized very differently and that there might be reverse causality,” Dr. Kuhnle commented.
Paul Keedwell, MBChB, PhD, consultant psychiatrist and fellow of the Royal College of Psychiatrists, said this is an “interesting and important finding, but one that raises more questions. At this stage, we cannot say how big an effect diet has on depression risk compared to other risk factors, like family history of depression, stress levels, and having a supportive social network.”
Dr. Keedwell noted that the investigators carefully excluded the possibility that the effect is mediated by obesity or lack of exercise.
“However, an important consideration is that a diet based on ready meals and artificially sweetened drinks might indicate a hectic lifestyle or one with shift work. In other words, a fast-food diet could be an indirect marker of chronic stress. Prolonged stress probably remains the main risk factor for depression,” Dr. Keedwell said.
Keith Frayn, PhD, professor emeritus of human metabolism, University of Oxford (England), noted that the relationship between artificial sweeteners and depression “stands out clearly” even after adjusting for multiple confounding factors, including BMI, smoking, and exercise.
“This adds to growing concerns about artificial sweeteners and cardiometabolic health. The link with depression needs confirmation and further research to suggest how it might be brought about,” Dr. Frayn cautioned.
The NHS II was funded by a grant from the National Cancer Institute. Dr. Chan reported receiving grants from Bayer and Zoe and personal fees from Boehringer Ingelheim, Pfizer, and Freenome outside this work. Dr. Keedwell and Dr. Kuhnle disclosed no relevant financial relationships. Dr. Frayn is an author of books on nutrition and metabolism.
A version of this article first appeared on Medscape.com.
new data from the Nurses Health Study II (NHS II) suggest.
Nurses who consumed more than eight servings daily had about a 50% higher risk of developing depression than nurses who consumed four or fewer servings daily.
However, in a secondary analysis, in which the researchers tried to tease out specific foods that may be associated with increased risk, only artificial sweeteners and artificially sweetened beverages were associated with an increased risk of depression.
“Animal studies have shown that artificial sweeteners may trigger the transmission of particular signaling molecules in the brain that are important for mood,” study investigator Andrew T. Chan, MD, MPH, of the clinical and translational epidemiology unit at Massachusetts General Hospital, Boston, said in an interview.
“Given this potential association between ultraprocessed food and multiple adverse health conditions, wherever possible individuals may wish to limit their intake of such foods. This may be a lifestyle change that could have important benefits, particularly for those who struggle with mental health,” Dr. Chan said.
The study was published online in JAMA Network Open.
Multiple potential mechanisms
The findings are based on 31,712 mostly non-Hispanic White women who were free of depression at baseline. The mean age of the patients at baseline was 52 years. As part of the NHS II, the women provided information on diet every 4 years using validated food frequency questionnaires.
Compared with women with low UPF intake, those with high UPF intake had greater body mass index (BMI). In addition, they were apt to smoke and have diabetes, hypertension, and dyslipidemia, and they were less apt to exercise regularly.
During the study period, there were 2,122 incident cases of depression, as determined using a strict definition that required self-reported clinician-diagnosed depression and regular antidepressant use. There were 4,840 incident cases, as determined using a broad definition that required clinical diagnosis and/or antidepressant use.
Compared with women in the lowest quintile of UPF consumption (fewer than four daily servings), those in the highest quintile (more than 8.8 daily servings) had an increased risk of depression.
This was noted for both the strict depression definition (hazard ratio, 1.49; 95% confidence interval, 1.26-1.76; P < .001) and the broad one (HR, 1.34; 95% CI, 1.20-1.50; P < .001).
“Models were not materially altered after inclusion of potential confounders. We did not observe differential associations in subgroups defined by age, BMI, physical activity, or smoking,” the researchers reported.
In secondary analyses, they classified UPF into their components, including ultraprocessed grain foods, sweet snacks, ready-to-eat meals, fats, sauces, ultraprocessed dairy products, savory snacks, processed meat, beverages, and artificial sweeteners.
Comparing the highest with the lowest quintiles, only high intake of artificially sweetened beverages (HR, 1.37; 95% CI, 1.19-1.57; P < .001) and artificial sweeteners (HR, 1.26; 95% CI, 1.10-1.43; P < .001) was associated with greater risk of depression and after multivariable regression.
In an exploratory analysis, women who reduced their UPF intake by at least three servings per day were at lower risk of depression (strict definition: HR, 0.84; 95% CI, 0.71-0.99), compared with those with relatively stable intake in each 4-year period.
“Ultraprocessed foods have been associated with several different health outcomes which may reflect an effect on common pathways that underlie chronic conditions,” said Dr. Chan.
For example, UPF intake has been associated with chronic inflammation, which in turns leads to multiple potential adverse health effects, including depression, he explained.
There is also a link between UPF and disruption of the gut microbiome.
“This is an important potential mechanism linking ultraprocessed food to depression since there is emerging evidence that microbes in the gut have been linked with mood through their role in metabolizing and producing proteins that have activity in the brain,” Dr. Chan said.
Association, not causation
Several experts weighed in on the study results in a statement from the U.K. nonprofit organization, Science Media Centre.
Gunter Kuhnle, PhD, professor of nutrition and food science, University of Reading (England), cautioned that the study only offers information on association – not causation.
“It is very possible that people with depression change their diet and might decide to consume foods that are easier to prepare – which would often be foods considered to be ultraprocessed,” Dr. Kuhnle said.
What’s most interesting is that the association between UPF intake and depression was driven by a single factor – artificial sweeteners.
“This supports one of the main criticisms of the UPF concept, that it combines a wide range of different foods and thereby makes it difficult to identify underlying causes,” Dr. Kuhnle added.
“There are currently no data that link artificial sweetener use to mental health, despite most of them having been available for some time. It is also important to note that there are a wide range of different artificial sweeteners that are metabolized very differently and that there might be reverse causality,” Dr. Kuhnle commented.
Paul Keedwell, MBChB, PhD, consultant psychiatrist and fellow of the Royal College of Psychiatrists, said this is an “interesting and important finding, but one that raises more questions. At this stage, we cannot say how big an effect diet has on depression risk compared to other risk factors, like family history of depression, stress levels, and having a supportive social network.”
Dr. Keedwell noted that the investigators carefully excluded the possibility that the effect is mediated by obesity or lack of exercise.
“However, an important consideration is that a diet based on ready meals and artificially sweetened drinks might indicate a hectic lifestyle or one with shift work. In other words, a fast-food diet could be an indirect marker of chronic stress. Prolonged stress probably remains the main risk factor for depression,” Dr. Keedwell said.
Keith Frayn, PhD, professor emeritus of human metabolism, University of Oxford (England), noted that the relationship between artificial sweeteners and depression “stands out clearly” even after adjusting for multiple confounding factors, including BMI, smoking, and exercise.
“This adds to growing concerns about artificial sweeteners and cardiometabolic health. The link with depression needs confirmation and further research to suggest how it might be brought about,” Dr. Frayn cautioned.
The NHS II was funded by a grant from the National Cancer Institute. Dr. Chan reported receiving grants from Bayer and Zoe and personal fees from Boehringer Ingelheim, Pfizer, and Freenome outside this work. Dr. Keedwell and Dr. Kuhnle disclosed no relevant financial relationships. Dr. Frayn is an author of books on nutrition and metabolism.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Do you agree with recent authors that patient satisfaction questionnaires should be modified to account for inherent societal biases, such as gender inequality and racism, to improve patient feedback?
[polldaddy:12782738]
[polldaddy:12782738]
[polldaddy:12782738]
Premenstrual disorders may be preview of early menopause
Women with premenstrual disorders may be more likely go through menopause before they are 45 years old, a new study suggests.
Women with premenstrual disorders, or PMDs, were also more likely to have moderate or severe night sweats or hot flashes during menopause, the researchers found.
Published in JAMA Network Open, the new findings stem from data from more than 3,600 nurses who contributed their health information to a database between 1991 and 2017. Women with PMDs were more than twice as likely as women without PMDs to have early menopause.
Most women have menopause between the ages of 45 and 55 years old, according to the World Health Organization.
There are numerous PMDs, including the well-known premenstrual syndrome, which is considered a mild disorder affecting up to 30% of women that causes symptoms like crankiness and bloating. A less common PMD is premenstrual dysphoric disorder, which can severely impact a woman’s life through psychological, gastrointestinal, skin, and neurological problems.
Previous research has linked PMDs during the reproductive years and postmenopausal issues like hot flashes and night sweats to increased risks of health problems like high blood pressure, heart conditions, and diabetes.
“It is important to identify women at risk for early menopause because of its link with poorer heart, brain, and bone health,” Stephanie Faubion, MD, MBA, a doctor at the Mayo Clinic and medical director of the North American Menopause Society, told CNN. Dr. Faubion was not involved in the study.
That said, it’s important to note that the study was observational – meaning researchers can’t say for certain that PMDs will cause early menopause. Rather, the study shows there may be a correlation between the two, Donghao Lu, MD, an associate professor in the department of medical epidemiology and biostatistics at the Karolinska Institute, told CNN.
A version of this article first appeared on Medscape.com.
Women with premenstrual disorders may be more likely go through menopause before they are 45 years old, a new study suggests.
Women with premenstrual disorders, or PMDs, were also more likely to have moderate or severe night sweats or hot flashes during menopause, the researchers found.
Published in JAMA Network Open, the new findings stem from data from more than 3,600 nurses who contributed their health information to a database between 1991 and 2017. Women with PMDs were more than twice as likely as women without PMDs to have early menopause.
Most women have menopause between the ages of 45 and 55 years old, according to the World Health Organization.
There are numerous PMDs, including the well-known premenstrual syndrome, which is considered a mild disorder affecting up to 30% of women that causes symptoms like crankiness and bloating. A less common PMD is premenstrual dysphoric disorder, which can severely impact a woman’s life through psychological, gastrointestinal, skin, and neurological problems.
Previous research has linked PMDs during the reproductive years and postmenopausal issues like hot flashes and night sweats to increased risks of health problems like high blood pressure, heart conditions, and diabetes.
“It is important to identify women at risk for early menopause because of its link with poorer heart, brain, and bone health,” Stephanie Faubion, MD, MBA, a doctor at the Mayo Clinic and medical director of the North American Menopause Society, told CNN. Dr. Faubion was not involved in the study.
That said, it’s important to note that the study was observational – meaning researchers can’t say for certain that PMDs will cause early menopause. Rather, the study shows there may be a correlation between the two, Donghao Lu, MD, an associate professor in the department of medical epidemiology and biostatistics at the Karolinska Institute, told CNN.
A version of this article first appeared on Medscape.com.
Women with premenstrual disorders may be more likely go through menopause before they are 45 years old, a new study suggests.
Women with premenstrual disorders, or PMDs, were also more likely to have moderate or severe night sweats or hot flashes during menopause, the researchers found.
Published in JAMA Network Open, the new findings stem from data from more than 3,600 nurses who contributed their health information to a database between 1991 and 2017. Women with PMDs were more than twice as likely as women without PMDs to have early menopause.
Most women have menopause between the ages of 45 and 55 years old, according to the World Health Organization.
There are numerous PMDs, including the well-known premenstrual syndrome, which is considered a mild disorder affecting up to 30% of women that causes symptoms like crankiness and bloating. A less common PMD is premenstrual dysphoric disorder, which can severely impact a woman’s life through psychological, gastrointestinal, skin, and neurological problems.
Previous research has linked PMDs during the reproductive years and postmenopausal issues like hot flashes and night sweats to increased risks of health problems like high blood pressure, heart conditions, and diabetes.
“It is important to identify women at risk for early menopause because of its link with poorer heart, brain, and bone health,” Stephanie Faubion, MD, MBA, a doctor at the Mayo Clinic and medical director of the North American Menopause Society, told CNN. Dr. Faubion was not involved in the study.
That said, it’s important to note that the study was observational – meaning researchers can’t say for certain that PMDs will cause early menopause. Rather, the study shows there may be a correlation between the two, Donghao Lu, MD, an associate professor in the department of medical epidemiology and biostatistics at the Karolinska Institute, told CNN.
A version of this article first appeared on Medscape.com.
Hypertensive disorders screening recommended for all pregnant women
Hypertensive disorders of pregnancy in the United States increased from approximately 500 cases per 10,000 deliveries to 1,021 cases per 10,000 deliveries from 1993 to 2016-2017, and remain a leading cause of maternal morbidity and mortality, wrote Task Force Chair Michael J. Barry, MD, of Massachusetts General Hospital, Boston, and colleagues in the final recommendation statement published in JAMA.
The USPSTF commissioned a systematic review to assess the risks and benefits of hypertensive screening for asymptomatic pregnant women. The resulting grade B recommendation indicates that screening for hypertensive disorders in pregnancy using blood pressure measurements yields a substantial net benefit.
The recommendation applies to “all pregnant women and pregnant persons of all genders without a known diagnosis of a hypertensive disorder of pregnancy or chronic hypertension,” the authors said.
The recommendation calls for the use of blood pressure measurements to evaluate hypertensive disorders, with measurements taken at each prenatal visit. A positive result for new-onset hypertension was defined as systolic blood pressure of 140 mm Hg or diastolic blood pressure 90 mm Hg in the absence of chronic hypertension, based on two measurements at least 4 hours apart. Regular review of blood pressure can help identify and manage potentially fatal conditions.
However, screening alone is insufficient to improve inequities in health outcomes associated with hypertensive disorders of pregnancy, the authors emphasized. Data from previous studies have shown that Black patients are at increased risk for hypertensive disorders of pregnancy and severe complications, and that Black and Hispanic patients have twice the risk of stroke with hypertensive disorders of pregnancy as White patients.
In the evidence report that supported the recommendation, Jillian T. Henderson, PhD, of Kaiser Permanente in Portland, Ore., and colleagues reviewed six studies including 10,165 individuals. The studies (five clinical trials and one nonrandomized study) compared changes in prenatal screening with usual care.
Overall, the review yielded no evidence that any other screening strategies were more useful than routine blood pressure measurement to identify hypertensive disorders of pregnancy in asymptomatic women.
The findings cited to support the recommendation were limited by several factors, including the lack of power to detect pregnancy health outcomes and potential harms of different screening programs, and the lack of power to evaluate outcomes for American Indian, Alaska Native, or Black individuals, who have disproportionately high rates of hypertensive disorders of pregnancy, the authors said.
More research is needed to identify which screening approaches may lead to improved disease detection and better health outcomes, but the results of the review support the grade B recommendation for hypertensive screening of all pregnant women, they concluded.
Early identification makes a difference
The new recommendation is important because it can help all moms and babies to be healthier, said Wanda Nicholson, MD, vice chair of the task force, in an interview.
“We are recommending that all pregnant persons have a blood pressure check at every visit throughout pregnancy,” said Dr. Nicholson, an ob.gyn. by training who also serves as professor of prevention and community health at George Washington University in Washington. “We know that there is a maternal health crisis in this country, and we know that hypertensive disorders of pregnancy are one of the key factors related to that,” she said.
Unfortunately, barriers to routine screening for hypertensive disorders of pregnancy persist, said Dr. Nicholson. The incidence of hypertensive disorders of pregnancy is higher in many of the same populations who also have challenges in accessing regular prenatal care, notably those who are Black, Native American, or Alaska Native, she noted.
The new recommendation also serves as an opportunity to call attention to the health care disparities for these populations, not only during pregnancy, but in general, she emphasized.
In clinical practice, the definition of hypertensive disorders of pregnancy involves three different diagnoses – gestational hypertension, preeclampsia, and eclampsia – that can be seen as points on a continuum, said Dr. Nicholson. The sooner patients are identified with hypertensive disorders of pregnancy, the sooner intervention and treatment can begin, she said. To that end, she added the clinical pearl of using a properly sized blood pressure cuff to obtain an accurate reading and avoid missed diagnoses.
The task force also outlined several key areas for additional research, said Dr. Nicholson. First, more research is needed on alternative screening strategies, such as at-home blood pressure monitoring for patients, as well as teleheath visits. Second, more studies are needed to address the disparities in prenatal care and include more diverse populations in clinical research. Third, future studies need to consider social determinants of health and other factors that might impact maternal health outcomes. “These steps will help achieve the larger goal of healthier mothers and babies,” Dr. Nicholson said.
Back to basics to improve women’s health
Some clinicians may be disappointed by the Evidence Report’s primary finding that no alternative screening strategies outperformed routine blood pressure measurement, wrote Anne E. Denoble, MD, and Christian M. Pettker, MD, both of Yale University, New Haven, Conn., in an accompanying editorial.
While potentially frustrating at first glance, the findings of the Evidence Report provide a foundation for improvement and reassurance that the best existing screening methods are basic and fundamental: regular prenatal visits with routine, in-office blood pressure measurements, and urine protein screening when clinically indicated, they said.
However, the USPSTF review also noted persistent research gaps that must be addressed to significantly improve maternal health outcomes, they said. Notable gaps include the disproportionately low numbers of Black patients in current studies, and the need for studies of alternate models of prenatal care, including the use of remote blood pressure monitoring, and the use of biomarkers to screen for and predict hypertensive disorders of pregnancy.
The most striking limitation may be the focus on prenatal care, with lack of attention to postpartum mortality risk, given that more than half of pregnancy-related deaths occur postpartum, the authors noted.
Although current screening tools may be used in practice “with skill and might,” more effort at multiple levels is needed to address the larger maternal health crisis in the United States, they said.
Expand screening, engage primary care for long-term benefits
Screening for hypertensive disorders of pregnancy “can and should be within the purview of internists,” wrote Srilakshmi Mitta, MD; Cary P. Gross, MD; Melissa A. Simon, MD, of Brown University, Yale University, and Northwestern University, respectively, in a separate editorial. The recommendation to extend screening beyond preeclampsia is timely, given the consistent increase in all hypertensive disorders of pregnancy since 1990, the authors said.
Pregnancy is not the only time for screening, counseling, and management of hypertensive disorders, they emphasized. “All persons who have reproductive capacity and/or are planning pregnancy, along with those who are post partum, should be screened for hypertensive disorders, aligning the USPSTF with guidelines from the American College of Obstetricians and Gynecologists, the American College of Cardiology, and the American Heart Association,” they said, and all clinicians should be on board to identify and treat hypertensive disorders of pregnancy, especially in underserved racial and ethnic minorities for whom primary care may be their only source of health care.
“Pregnancy is a window of opportunity to influence current and future life course, not just of the individual, but also of the fetus(es),other children, and family,” and timely intervention has the potential for great public health impact, they said.
Dr. Denoble disclosed grants from the HealthPartners Institute for Education and Research and from the Patient-Centered Outcomes Research Institute. Dr. Simon serves on the Advisory Committee for Research on Women’s Health for the National Institutes of Health Office of Research on Women’s Health and serves as a member of the Centers for Disease Control and Prevention Community Preventive Services Task Force; she was a member of the USPSTF from 2017 to 2020. Dr. Gross disclosed grants from Johnson and Johnson and the National Comprehensive Cancer Network (through a grant to the NCCN from AstraZeneca) and personal fees from Genentech.
Hypertensive disorders of pregnancy in the United States increased from approximately 500 cases per 10,000 deliveries to 1,021 cases per 10,000 deliveries from 1993 to 2016-2017, and remain a leading cause of maternal morbidity and mortality, wrote Task Force Chair Michael J. Barry, MD, of Massachusetts General Hospital, Boston, and colleagues in the final recommendation statement published in JAMA.
The USPSTF commissioned a systematic review to assess the risks and benefits of hypertensive screening for asymptomatic pregnant women. The resulting grade B recommendation indicates that screening for hypertensive disorders in pregnancy using blood pressure measurements yields a substantial net benefit.
The recommendation applies to “all pregnant women and pregnant persons of all genders without a known diagnosis of a hypertensive disorder of pregnancy or chronic hypertension,” the authors said.
The recommendation calls for the use of blood pressure measurements to evaluate hypertensive disorders, with measurements taken at each prenatal visit. A positive result for new-onset hypertension was defined as systolic blood pressure of 140 mm Hg or diastolic blood pressure 90 mm Hg in the absence of chronic hypertension, based on two measurements at least 4 hours apart. Regular review of blood pressure can help identify and manage potentially fatal conditions.
However, screening alone is insufficient to improve inequities in health outcomes associated with hypertensive disorders of pregnancy, the authors emphasized. Data from previous studies have shown that Black patients are at increased risk for hypertensive disorders of pregnancy and severe complications, and that Black and Hispanic patients have twice the risk of stroke with hypertensive disorders of pregnancy as White patients.
In the evidence report that supported the recommendation, Jillian T. Henderson, PhD, of Kaiser Permanente in Portland, Ore., and colleagues reviewed six studies including 10,165 individuals. The studies (five clinical trials and one nonrandomized study) compared changes in prenatal screening with usual care.
Overall, the review yielded no evidence that any other screening strategies were more useful than routine blood pressure measurement to identify hypertensive disorders of pregnancy in asymptomatic women.
The findings cited to support the recommendation were limited by several factors, including the lack of power to detect pregnancy health outcomes and potential harms of different screening programs, and the lack of power to evaluate outcomes for American Indian, Alaska Native, or Black individuals, who have disproportionately high rates of hypertensive disorders of pregnancy, the authors said.
More research is needed to identify which screening approaches may lead to improved disease detection and better health outcomes, but the results of the review support the grade B recommendation for hypertensive screening of all pregnant women, they concluded.
Early identification makes a difference
The new recommendation is important because it can help all moms and babies to be healthier, said Wanda Nicholson, MD, vice chair of the task force, in an interview.
“We are recommending that all pregnant persons have a blood pressure check at every visit throughout pregnancy,” said Dr. Nicholson, an ob.gyn. by training who also serves as professor of prevention and community health at George Washington University in Washington. “We know that there is a maternal health crisis in this country, and we know that hypertensive disorders of pregnancy are one of the key factors related to that,” she said.
Unfortunately, barriers to routine screening for hypertensive disorders of pregnancy persist, said Dr. Nicholson. The incidence of hypertensive disorders of pregnancy is higher in many of the same populations who also have challenges in accessing regular prenatal care, notably those who are Black, Native American, or Alaska Native, she noted.
The new recommendation also serves as an opportunity to call attention to the health care disparities for these populations, not only during pregnancy, but in general, she emphasized.
In clinical practice, the definition of hypertensive disorders of pregnancy involves three different diagnoses – gestational hypertension, preeclampsia, and eclampsia – that can be seen as points on a continuum, said Dr. Nicholson. The sooner patients are identified with hypertensive disorders of pregnancy, the sooner intervention and treatment can begin, she said. To that end, she added the clinical pearl of using a properly sized blood pressure cuff to obtain an accurate reading and avoid missed diagnoses.
The task force also outlined several key areas for additional research, said Dr. Nicholson. First, more research is needed on alternative screening strategies, such as at-home blood pressure monitoring for patients, as well as teleheath visits. Second, more studies are needed to address the disparities in prenatal care and include more diverse populations in clinical research. Third, future studies need to consider social determinants of health and other factors that might impact maternal health outcomes. “These steps will help achieve the larger goal of healthier mothers and babies,” Dr. Nicholson said.
Back to basics to improve women’s health
Some clinicians may be disappointed by the Evidence Report’s primary finding that no alternative screening strategies outperformed routine blood pressure measurement, wrote Anne E. Denoble, MD, and Christian M. Pettker, MD, both of Yale University, New Haven, Conn., in an accompanying editorial.
While potentially frustrating at first glance, the findings of the Evidence Report provide a foundation for improvement and reassurance that the best existing screening methods are basic and fundamental: regular prenatal visits with routine, in-office blood pressure measurements, and urine protein screening when clinically indicated, they said.
However, the USPSTF review also noted persistent research gaps that must be addressed to significantly improve maternal health outcomes, they said. Notable gaps include the disproportionately low numbers of Black patients in current studies, and the need for studies of alternate models of prenatal care, including the use of remote blood pressure monitoring, and the use of biomarkers to screen for and predict hypertensive disorders of pregnancy.
The most striking limitation may be the focus on prenatal care, with lack of attention to postpartum mortality risk, given that more than half of pregnancy-related deaths occur postpartum, the authors noted.
Although current screening tools may be used in practice “with skill and might,” more effort at multiple levels is needed to address the larger maternal health crisis in the United States, they said.
Expand screening, engage primary care for long-term benefits
Screening for hypertensive disorders of pregnancy “can and should be within the purview of internists,” wrote Srilakshmi Mitta, MD; Cary P. Gross, MD; Melissa A. Simon, MD, of Brown University, Yale University, and Northwestern University, respectively, in a separate editorial. The recommendation to extend screening beyond preeclampsia is timely, given the consistent increase in all hypertensive disorders of pregnancy since 1990, the authors said.
Pregnancy is not the only time for screening, counseling, and management of hypertensive disorders, they emphasized. “All persons who have reproductive capacity and/or are planning pregnancy, along with those who are post partum, should be screened for hypertensive disorders, aligning the USPSTF with guidelines from the American College of Obstetricians and Gynecologists, the American College of Cardiology, and the American Heart Association,” they said, and all clinicians should be on board to identify and treat hypertensive disorders of pregnancy, especially in underserved racial and ethnic minorities for whom primary care may be their only source of health care.
“Pregnancy is a window of opportunity to influence current and future life course, not just of the individual, but also of the fetus(es),other children, and family,” and timely intervention has the potential for great public health impact, they said.
Dr. Denoble disclosed grants from the HealthPartners Institute for Education and Research and from the Patient-Centered Outcomes Research Institute. Dr. Simon serves on the Advisory Committee for Research on Women’s Health for the National Institutes of Health Office of Research on Women’s Health and serves as a member of the Centers for Disease Control and Prevention Community Preventive Services Task Force; she was a member of the USPSTF from 2017 to 2020. Dr. Gross disclosed grants from Johnson and Johnson and the National Comprehensive Cancer Network (through a grant to the NCCN from AstraZeneca) and personal fees from Genentech.
Hypertensive disorders of pregnancy in the United States increased from approximately 500 cases per 10,000 deliveries to 1,021 cases per 10,000 deliveries from 1993 to 2016-2017, and remain a leading cause of maternal morbidity and mortality, wrote Task Force Chair Michael J. Barry, MD, of Massachusetts General Hospital, Boston, and colleagues in the final recommendation statement published in JAMA.
The USPSTF commissioned a systematic review to assess the risks and benefits of hypertensive screening for asymptomatic pregnant women. The resulting grade B recommendation indicates that screening for hypertensive disorders in pregnancy using blood pressure measurements yields a substantial net benefit.
The recommendation applies to “all pregnant women and pregnant persons of all genders without a known diagnosis of a hypertensive disorder of pregnancy or chronic hypertension,” the authors said.
The recommendation calls for the use of blood pressure measurements to evaluate hypertensive disorders, with measurements taken at each prenatal visit. A positive result for new-onset hypertension was defined as systolic blood pressure of 140 mm Hg or diastolic blood pressure 90 mm Hg in the absence of chronic hypertension, based on two measurements at least 4 hours apart. Regular review of blood pressure can help identify and manage potentially fatal conditions.
However, screening alone is insufficient to improve inequities in health outcomes associated with hypertensive disorders of pregnancy, the authors emphasized. Data from previous studies have shown that Black patients are at increased risk for hypertensive disorders of pregnancy and severe complications, and that Black and Hispanic patients have twice the risk of stroke with hypertensive disorders of pregnancy as White patients.
In the evidence report that supported the recommendation, Jillian T. Henderson, PhD, of Kaiser Permanente in Portland, Ore., and colleagues reviewed six studies including 10,165 individuals. The studies (five clinical trials and one nonrandomized study) compared changes in prenatal screening with usual care.
Overall, the review yielded no evidence that any other screening strategies were more useful than routine blood pressure measurement to identify hypertensive disorders of pregnancy in asymptomatic women.
The findings cited to support the recommendation were limited by several factors, including the lack of power to detect pregnancy health outcomes and potential harms of different screening programs, and the lack of power to evaluate outcomes for American Indian, Alaska Native, or Black individuals, who have disproportionately high rates of hypertensive disorders of pregnancy, the authors said.
More research is needed to identify which screening approaches may lead to improved disease detection and better health outcomes, but the results of the review support the grade B recommendation for hypertensive screening of all pregnant women, they concluded.
Early identification makes a difference
The new recommendation is important because it can help all moms and babies to be healthier, said Wanda Nicholson, MD, vice chair of the task force, in an interview.
“We are recommending that all pregnant persons have a blood pressure check at every visit throughout pregnancy,” said Dr. Nicholson, an ob.gyn. by training who also serves as professor of prevention and community health at George Washington University in Washington. “We know that there is a maternal health crisis in this country, and we know that hypertensive disorders of pregnancy are one of the key factors related to that,” she said.
Unfortunately, barriers to routine screening for hypertensive disorders of pregnancy persist, said Dr. Nicholson. The incidence of hypertensive disorders of pregnancy is higher in many of the same populations who also have challenges in accessing regular prenatal care, notably those who are Black, Native American, or Alaska Native, she noted.
The new recommendation also serves as an opportunity to call attention to the health care disparities for these populations, not only during pregnancy, but in general, she emphasized.
In clinical practice, the definition of hypertensive disorders of pregnancy involves three different diagnoses – gestational hypertension, preeclampsia, and eclampsia – that can be seen as points on a continuum, said Dr. Nicholson. The sooner patients are identified with hypertensive disorders of pregnancy, the sooner intervention and treatment can begin, she said. To that end, she added the clinical pearl of using a properly sized blood pressure cuff to obtain an accurate reading and avoid missed diagnoses.
The task force also outlined several key areas for additional research, said Dr. Nicholson. First, more research is needed on alternative screening strategies, such as at-home blood pressure monitoring for patients, as well as teleheath visits. Second, more studies are needed to address the disparities in prenatal care and include more diverse populations in clinical research. Third, future studies need to consider social determinants of health and other factors that might impact maternal health outcomes. “These steps will help achieve the larger goal of healthier mothers and babies,” Dr. Nicholson said.
Back to basics to improve women’s health
Some clinicians may be disappointed by the Evidence Report’s primary finding that no alternative screening strategies outperformed routine blood pressure measurement, wrote Anne E. Denoble, MD, and Christian M. Pettker, MD, both of Yale University, New Haven, Conn., in an accompanying editorial.
While potentially frustrating at first glance, the findings of the Evidence Report provide a foundation for improvement and reassurance that the best existing screening methods are basic and fundamental: regular prenatal visits with routine, in-office blood pressure measurements, and urine protein screening when clinically indicated, they said.
However, the USPSTF review also noted persistent research gaps that must be addressed to significantly improve maternal health outcomes, they said. Notable gaps include the disproportionately low numbers of Black patients in current studies, and the need for studies of alternate models of prenatal care, including the use of remote blood pressure monitoring, and the use of biomarkers to screen for and predict hypertensive disorders of pregnancy.
The most striking limitation may be the focus on prenatal care, with lack of attention to postpartum mortality risk, given that more than half of pregnancy-related deaths occur postpartum, the authors noted.
Although current screening tools may be used in practice “with skill and might,” more effort at multiple levels is needed to address the larger maternal health crisis in the United States, they said.
Expand screening, engage primary care for long-term benefits
Screening for hypertensive disorders of pregnancy “can and should be within the purview of internists,” wrote Srilakshmi Mitta, MD; Cary P. Gross, MD; Melissa A. Simon, MD, of Brown University, Yale University, and Northwestern University, respectively, in a separate editorial. The recommendation to extend screening beyond preeclampsia is timely, given the consistent increase in all hypertensive disorders of pregnancy since 1990, the authors said.
Pregnancy is not the only time for screening, counseling, and management of hypertensive disorders, they emphasized. “All persons who have reproductive capacity and/or are planning pregnancy, along with those who are post partum, should be screened for hypertensive disorders, aligning the USPSTF with guidelines from the American College of Obstetricians and Gynecologists, the American College of Cardiology, and the American Heart Association,” they said, and all clinicians should be on board to identify and treat hypertensive disorders of pregnancy, especially in underserved racial and ethnic minorities for whom primary care may be their only source of health care.
“Pregnancy is a window of opportunity to influence current and future life course, not just of the individual, but also of the fetus(es),other children, and family,” and timely intervention has the potential for great public health impact, they said.
Dr. Denoble disclosed grants from the HealthPartners Institute for Education and Research and from the Patient-Centered Outcomes Research Institute. Dr. Simon serves on the Advisory Committee for Research on Women’s Health for the National Institutes of Health Office of Research on Women’s Health and serves as a member of the Centers for Disease Control and Prevention Community Preventive Services Task Force; she was a member of the USPSTF from 2017 to 2020. Dr. Gross disclosed grants from Johnson and Johnson and the National Comprehensive Cancer Network (through a grant to the NCCN from AstraZeneca) and personal fees from Genentech.
FROM JAMA
CPT updates for 2024 include new RSV vaccines, Spanish translation
The American Medical Association recently released the Current Procedural Terminology (CPT) 2024 Code Set. The update included 349 editorial changes, including 230 additions, 49 deletions, and 70 revisions. With more than 11,100 codes in use, the CPT system continues “to grow and evolve with the rapid pace of innovation in medical science and health technology,” AMA said.
The AMA said the CPT update includes five new codes created to report product-specific RSV products (90380, 90381, 90683, 90679, and 90678) for better tracking, reporting and analysis that supports data-driven planning and allocation, AMA said.
There’s been a flurry of new U.S. vaccines and drugs to address RSV. The Food and Drug Administration in May granted the first U.S. approval of an RSV vaccine to Arexy, manufactured by GSK. The FDA cleared it for prevention of lower respiratory tract disease caused by RSV in adults age 60 years and older.
In June, Pfizer won FDA approval of Abrysvo, another vaccine meant to protect adults older than 60 years from RSV. The following month, the FDA approved nirsevimab (Beyfortus, AstraZeneca/Sanofi), for the prevention of RSV in neonates and infants entering their first RSV season, and in children up to 24 months of age who remain vulnerable to severe RSV disease through their second RSV season. (This is not a vaccine, but a monoclonal antibody used for prevention. There has been confusion on this issue in part because monoclonal antibodies are often used for treatment rather than prevention.)
The FDA also has approved Abrysvo for use in pregnant individuals.
In addition, new CPT codes aim to streamline COVID-19 immunizations reporting. A new code (90480) was approved for reporting the administration of any COVID-19 vaccine for any patient. New provisional codes (91318-91322) will identify monovalent vaccine products from Moderna and Pfizer for immunization against COVID-19.
These provisional codes will be effective for use when the monovalent vaccine products from Moderna and Pfizer receive FDA approval, AMA said.
More codes explained in Spanish
The 2024 update includes more code descriptions in Spanish. Many hospitals, health plans, and medical offices already incorporate CPT descriptors in English-language medical documents, insurance forms, price sheets, and patient portals. This expansion is intended to help patients who may not read English well or at all.
“Providing approximately 41 million Spanish-speaking individuals in the United States with an easy-to-understand description of medical procedures and services can help build a more inclusive health care environment, where language is no longer a barrier and patients can actively engage in their own care,” Lori Prestesater, AMA’s senior vice president of health solutions, said in a statement.
In addition, the 2024 update includes clarifications sought by the Centers for Medicare & Medicaid Services about the reporting of evaluation and management (E/M) services. The revisions include:
- Removal of time ranges from office or other outpatient visit codes (99202-99205, 99212-99215) and format alignment with other E/M codes.
- Definition of the “substantive portion” of a split/shared E/M visit in which a physician and a nonphysician practitioner work jointly to furnish all the work related to the visit.
- Instructions for reporting hospital inpatient or observation care services and admission and discharge services for the use of codes. 99234-99236 when the patient stay crosses over two calendar dates.
A version of this article appeared on Medscape.com.
The American Medical Association recently released the Current Procedural Terminology (CPT) 2024 Code Set. The update included 349 editorial changes, including 230 additions, 49 deletions, and 70 revisions. With more than 11,100 codes in use, the CPT system continues “to grow and evolve with the rapid pace of innovation in medical science and health technology,” AMA said.
The AMA said the CPT update includes five new codes created to report product-specific RSV products (90380, 90381, 90683, 90679, and 90678) for better tracking, reporting and analysis that supports data-driven planning and allocation, AMA said.
There’s been a flurry of new U.S. vaccines and drugs to address RSV. The Food and Drug Administration in May granted the first U.S. approval of an RSV vaccine to Arexy, manufactured by GSK. The FDA cleared it for prevention of lower respiratory tract disease caused by RSV in adults age 60 years and older.
In June, Pfizer won FDA approval of Abrysvo, another vaccine meant to protect adults older than 60 years from RSV. The following month, the FDA approved nirsevimab (Beyfortus, AstraZeneca/Sanofi), for the prevention of RSV in neonates and infants entering their first RSV season, and in children up to 24 months of age who remain vulnerable to severe RSV disease through their second RSV season. (This is not a vaccine, but a monoclonal antibody used for prevention. There has been confusion on this issue in part because monoclonal antibodies are often used for treatment rather than prevention.)
The FDA also has approved Abrysvo for use in pregnant individuals.
In addition, new CPT codes aim to streamline COVID-19 immunizations reporting. A new code (90480) was approved for reporting the administration of any COVID-19 vaccine for any patient. New provisional codes (91318-91322) will identify monovalent vaccine products from Moderna and Pfizer for immunization against COVID-19.
These provisional codes will be effective for use when the monovalent vaccine products from Moderna and Pfizer receive FDA approval, AMA said.
More codes explained in Spanish
The 2024 update includes more code descriptions in Spanish. Many hospitals, health plans, and medical offices already incorporate CPT descriptors in English-language medical documents, insurance forms, price sheets, and patient portals. This expansion is intended to help patients who may not read English well or at all.
“Providing approximately 41 million Spanish-speaking individuals in the United States with an easy-to-understand description of medical procedures and services can help build a more inclusive health care environment, where language is no longer a barrier and patients can actively engage in their own care,” Lori Prestesater, AMA’s senior vice president of health solutions, said in a statement.
In addition, the 2024 update includes clarifications sought by the Centers for Medicare & Medicaid Services about the reporting of evaluation and management (E/M) services. The revisions include:
- Removal of time ranges from office or other outpatient visit codes (99202-99205, 99212-99215) and format alignment with other E/M codes.
- Definition of the “substantive portion” of a split/shared E/M visit in which a physician and a nonphysician practitioner work jointly to furnish all the work related to the visit.
- Instructions for reporting hospital inpatient or observation care services and admission and discharge services for the use of codes. 99234-99236 when the patient stay crosses over two calendar dates.
A version of this article appeared on Medscape.com.
The American Medical Association recently released the Current Procedural Terminology (CPT) 2024 Code Set. The update included 349 editorial changes, including 230 additions, 49 deletions, and 70 revisions. With more than 11,100 codes in use, the CPT system continues “to grow and evolve with the rapid pace of innovation in medical science and health technology,” AMA said.
The AMA said the CPT update includes five new codes created to report product-specific RSV products (90380, 90381, 90683, 90679, and 90678) for better tracking, reporting and analysis that supports data-driven planning and allocation, AMA said.
There’s been a flurry of new U.S. vaccines and drugs to address RSV. The Food and Drug Administration in May granted the first U.S. approval of an RSV vaccine to Arexy, manufactured by GSK. The FDA cleared it for prevention of lower respiratory tract disease caused by RSV in adults age 60 years and older.
In June, Pfizer won FDA approval of Abrysvo, another vaccine meant to protect adults older than 60 years from RSV. The following month, the FDA approved nirsevimab (Beyfortus, AstraZeneca/Sanofi), for the prevention of RSV in neonates and infants entering their first RSV season, and in children up to 24 months of age who remain vulnerable to severe RSV disease through their second RSV season. (This is not a vaccine, but a monoclonal antibody used for prevention. There has been confusion on this issue in part because monoclonal antibodies are often used for treatment rather than prevention.)
The FDA also has approved Abrysvo for use in pregnant individuals.
In addition, new CPT codes aim to streamline COVID-19 immunizations reporting. A new code (90480) was approved for reporting the administration of any COVID-19 vaccine for any patient. New provisional codes (91318-91322) will identify monovalent vaccine products from Moderna and Pfizer for immunization against COVID-19.
These provisional codes will be effective for use when the monovalent vaccine products from Moderna and Pfizer receive FDA approval, AMA said.
More codes explained in Spanish
The 2024 update includes more code descriptions in Spanish. Many hospitals, health plans, and medical offices already incorporate CPT descriptors in English-language medical documents, insurance forms, price sheets, and patient portals. This expansion is intended to help patients who may not read English well or at all.
“Providing approximately 41 million Spanish-speaking individuals in the United States with an easy-to-understand description of medical procedures and services can help build a more inclusive health care environment, where language is no longer a barrier and patients can actively engage in their own care,” Lori Prestesater, AMA’s senior vice president of health solutions, said in a statement.
In addition, the 2024 update includes clarifications sought by the Centers for Medicare & Medicaid Services about the reporting of evaluation and management (E/M) services. The revisions include:
- Removal of time ranges from office or other outpatient visit codes (99202-99205, 99212-99215) and format alignment with other E/M codes.
- Definition of the “substantive portion” of a split/shared E/M visit in which a physician and a nonphysician practitioner work jointly to furnish all the work related to the visit.
- Instructions for reporting hospital inpatient or observation care services and admission and discharge services for the use of codes. 99234-99236 when the patient stay crosses over two calendar dates.
A version of this article appeared on Medscape.com.
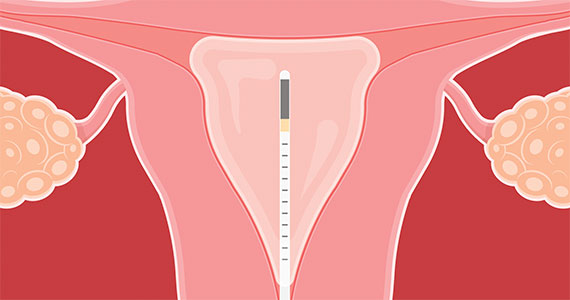
2023 Update on abnormal uterine bleeding
Endometrial ablation continues to be performed in significant numbers in the United States, with an estimated 500,000 cases annually. Several nonresectoscopic endometrial ablation devices have been approved for use, and some are now discontinued. The newest endometrial ablation therapy to gain US Food and Drug Administration (FDA) approval and to have published outcomes is the Cerene cryotherapy ablation device (Channel Medsystems, Inc). The results of 36-month outcomes from the CLARITY study were published last year, and we have chosen to review these long-term data in addition to that of a second study in which investigators assessed the ability to access the endometrial cavity postcryoablation. We believe this is important because of concerns about the inability to access the endometrial cavity after ablation, as well as the potential for delay in the diagnosis of endometrial cancer. It is interesting that 2 publications simultaneously reviewed the incidence of endometrial cancer after endometrial ablation within the past 12 months, and we therefore present those findings as they provide valuable information.
Our second focus in this year’s Update is to provide additional information about the burgeoning data on gonadotropin-releasing hormone (GnRH) antagonists. We review evidence on linzagolix from the PRIMROSE 1 and PRIMROSE 2 trials and longer-term data on relugolix combination therapy for symptomatic uterine fibroids.
Three-year follow-up after endometrial cryoablation with the Cerene device found high patient satisfaction, low hysterectomy rates
Curlin HL, Cintron LC, Anderson TL. A prospective, multicenter, clinical trial evaluating the safety and effectiveness of the Cerene device to treat heavy menstrual bleeding. J Minim Invasive Gynecol. 2021;28;899-908.
Curlin HL, Anderson TL. Endometrial cryoablation for the treatment of heavy menstrual bleeding: 36-month outcomes from the CLARITY study. Int J Womens Health. 2022;14:1083-1092.
The 12-month data on the clinical safety and effectiveness of the Cerene cryoablation device were published in 2021 in the CLARITY trial.1 The 36-month outcomes were published in 2022 and showed sustained clinical effects through month 36 with a low risk of adverse outcomes.2 The interesting aspect of this trial is that although the amenorrhea rate was relatively low at 12 months (6.5%), it continued to remain relatively low compared with rates found with other devices, but the amenorrhea rate increased at 36 months (14.4%). This was the percentage of patients who reported, “I no longer get my period.”
Patient satisfaction was high
Despite a relatively low amenorrhea rate, study participants had a high satisfaction rate and a low 3-year hysterectomy rate. Eighty-five percent of the participants were satisfied or very satisfied, and the cumulative hysterectomy rate was low at 5%.
The overall reintervention rate was 8.7%. Six patients were treated with medications, 2 patients underwent repeat endometrial ablation, 1 received a levonorgestrel-releasing intrauterine device, and 12 underwent hysterectomy.
At 36 months, 201 of the original 242 participants were available for assessment. Unfortunately, 5 pregnancies were reported through the 6-month posttreatment period, which emphasizes the importance of having reliable contraception. However, there were no reports of hematometra or postablation tubal sterilization syndrome (PATSS).
Effect on bleeding was long term
The main finding of the CLARITY study is that the Cerene cryoablation device appears to have a relatively stable effect on bleedingfor the first 3 years after therapy, with minimal risk of hematometra and PATSS. What we find interesting is that despite Cerene cryoablation having one of the lowest amenorrhea rates, it not only had a satisfaction rate in line with that of other devices but also had a low hysterectomy rate—only 5%—at 3 years.
The study authors pointed out that there is a lack of scarring within the endometrial cavity with the Cerene device. Some may find less endometrial scarring worth a low amenorrhea rate in the context of a favorable satisfaction rate. This begs the question, how well can the endometrial cavity be assessed? For answers, keep reading.
Can the endometrial cavity be reliably accessed after Cerene cryoablation?
Endometrial ablation has been associated with intracavitary scarring that results in hematometra, PATSS, and a concern for difficulty in performing an adequate endometrial assessment in patients who develop postablation abnormal uterine bleeding.
In a prospective study, 230 participants (of an initial 242) treated with Cerene cyroablation were studied with hysteroscopic evaluation of the endometrial cavity 12 months after surgery.3 The uterine cavity was accessible in 98.7% of participants. The cavity was not accessible in 3 participants due to pain or cervical stenosis.
Visualization of the uterine cavity was possible by hysteroscopy in 92.7% of study participants (204 of 220), with 1 or both tubal ostia identified in 89.2%. Both tubal ostia were visible in 78.4% and 1 ostium was visible in 10.8%. The cavity was not visualized in 16 of the 220 patients (7.2%) due to intrauterine adhesions, technical difficulties, or menstruation. Also of note, 97 of the 230 participants available at the 12-month follow-up had undergone tubal sterilization before cryoablation and none reported symptoms of PATSS or hematometra, which may be considered surrogate markers for adhesions.
Results of the CLARITY study demonstrated the clinical safety and effectiveness of the Cerene cryoablation device at 12 months, with sustained clinical effects through 36 months and a low risk of adverse outcomes. Patient satisfaction rates were high, and the hysterectomy rate was low. In addition, in a prospective study of patients treated with Cerene cryoablation, hysteroscopic evaluation at 12 months found the uterine cavity accessible in more than 98% of participants, and uterine visualization also was high. Therefore, the Cerene cryoablation device may provide the advantage of an easier evaluation of patients who eventually develop abnormal bleeding after endometrial ablation.
Continue to: Tissue effects differ with ablation technique...
Tissue effects differ with ablation technique
The study authors suggested that different tissue effects occur with freezing compared with heating ablation techniques. With freezing, over weeks to months the chronic inflammatory tissue is eventually replaced by a fibrous scar of collagen, with some preservation of the collagen matrix during tissue repair. This may be different from the charring and boiling of heated tissue that results in architectural tissue loss and may interfere with wound repair and tissue remodeling. Although the incidence of postoperative adhesions after endometrial ablation is not well studied, it is encouraging that most patients who received cryoablation with the Cerene device were able to undergo an evaluation of the endometrium without general anesthesia.
Key takeaway
The main idea from this study is that the endometrium can be assessed by office hysteroscopy in most patients who undergo cryoablation with the Cerene device. This may have advantages in terms of reducing the risk of PATSS and hematometra, and it may allow easier evaluation of the endometrium for patients who have postablation abnormal uterine bleeding. This begs the question, does intrauterine scarring influence the detection of endometrial cancer? For answers, keep reading.
Does endometrial ablation place a patient at higher risk for a delay in the diagnosis of endometrial cancer?
Radestad AF, Dahm-Kahler P, Holmberg E, et al. Long-term incidence of endometrial cancer after endometrial resection and ablation: a population based Swedish gynecologic cancer group (SweGCG) study. Acta Obstet Gynecol Scand. 2022;101:923-930.
Oderkerk TJ, van de Kar MRD, Cornel KMC, et al. Endometrial cancer after endometrial ablation: a systematic review. Int J Gynecol Cancer. 2022;32:1555-1560.
The answer to this question appears to be no, based on 2 different types of studies. One study was a 20-year population database review from Sweden,4 and the other was a systematic review of 11 cohort studies.5
Population-based study findings
The data from the Swedish population database is interesting because since 1994 all Swedish citizens have been allocated a unique personal identification number at birth or immigration that enables official registries and research. In reviewing their data from 1997 through 2017, Radestad and colleagues compared transcervical resection of the endometrium (TCRE) and other forms of endometrial ablation against the Swedish National Patient Register data for endometrial cancer.4 They found no increase in the incidence of endometrial cancer after TCRE (0.3%) or after endometrial ablation (0.02%) and suggested a significantly lower incidence of endometrial cancer after endometrial ablation.
This study is beneficial because it is the largest study to explore the long-term incidence of endometrial cancer after TCRE and endometrial ablation. The investigators hypothesized that, as an explanation for the difference between rates, ablation may burn deeper into the myometrium and treat adenomyosis compared with TCRE. However, they also were cautious to note that although this was a 20-year study, the incidence of endometrial carcinoma likely will reach a peak in the next few years.
Systematic review conclusions
In the systematic review, out of 890 publications from the authors’ database search, 11 articles were eventually included for review.5 A total of 29,102 patients with endometrial ablation were followed for a period of up to 25 years, and the incidence of endometrial cancer after endometrial ablation varied from 0.0% to 1.6%. A total of 38 cases of endometrial cancer after endometrial ablation have been described in the literature. Of those cases, bleeding was the most common presenting symptom of the disease. Endometrial sampling was successful in 89% of cases, and in 90% of cases, histological exam showed an early-stage endometrial adenocarcinoma.
Based on their review, the authors concluded that the incidence of endometrial cancer was not increased in patients who received endometrial ablation, and more importantly, there was no apparent delay in the diagnosis of endometrial cancer after endometrial ablation. They further suggested that diagnostic management with endometrial sampling did not appear to be a barrier.
The main findings from these 2 studies by Radestad and colleagues and Oderkerk and associates are that endometrial cancer does not appear to be more common after endometrial ablation, and it appears to be diagnosed with endometrial sampling in most cases.4,5 There may be some protection against endometrial cancer with nonresectoscopic endometrial ablation, although this needs to be verified by additional studies. To juxtapose this information with the prior information about cryotherapy, it emphasizes that the scarring within the endometrium will likely reduce the incidence of PATSS and hematometra, which are relatively low-incidence occurrences at 5% to 7%, but it likely does not affect the detection of endometrial cancer.
Longer-term data for relugolix combination treatment of symptomatic uterine bleeding from fibroids shows sustained efficacy
Al-Hendy A, Lukes AS, Poindexter AN, et al. Long-term relugolix combination therapy for symptomatic uterine leiomyomas. Obstet Gynecol. 2022;140:920-930.
Relugolix combination therapy was previously reported to be effective for the treatment of fibroids based on the 24-week trials LIBERTY 1 and LIBERTY 2. We now have information about longer-term therapy for up to 52 weeks of treatment.6
Relugolix combination therapy is a once-daily single tablet for the treatment of heavy menstrual bleeding thought to be due to uterine fibroids in premenopausal women. It is comprised of relugolix 40 mg (a GnRH antagonist), estradiol 1.0 mg, and norethindrone acetate 0.5 mg.
Continue to: Extension study showed sustained efficacy...
Extension study showed sustained efficacy
The study by Al-Hendy and colleagues showed that the relugolix combination not only was well tolerated but also that there was sustained improvement in heavy bleeding, with the average patient having an approximately 90% decrease in menstrual bleeding from baseline.6 It was noted that 70.6% of patients achieved amenorrhea over the last 35 days of treatment.
Importantly, the treatment effect was independent of race, body mass index, baseline menstrual blood loss, and uterine fibroid volume. The bone mineral density (BMD) change trajectory was similar to what was observed in the pivotal study. No new safety concerns were identified, and BMD generally was preserved.
The extension study by Al-Hendy and colleagues demonstrated that that the reduced fibroid-associated bleeding treated with relugolix combination therapy is sustained throughout the 52-week period, with no new safety concerns.
Linzagolix is the newest GnRH antagonist to be studied in a randomized, placebo-controlled trial
Donnez J, Taylor HS, Stewart EA, et al. Linzagolix with and without hormonal add-back therapy for the treatment of symptomatic uterine fibroids: two randomised, placebo-controlled, phase 3 trials. Lancet. 2022;400:896-907.
At the time of this writing, linzagolix was not approved by the FDA. The results of the PRIMROSE 1 (P1) and PRIMROSE 2 (P2) trials were published last year as 2 identical 52-week randomized, parallel, double-blind, placebo-controlled, phase 3 trials.7 The difference between the development of linzagolix as a GnRH antagonist and other similar medications is the strategy of potential partial hypothalamic pituitary ovarian axis suppression at 100 mg versus complete suppression at 200 mg. In this trial by Donnez and colleagues, both linzagolix doses were evaluated with and without add-back hormonal therapy and also were compared with placebo in a 1:1:1:1:1 ratio.7
Study details and results
To be eligible for this study, participants had to have heavy menstrual bleeding, defined as more than 80 mL for at least 2 cycles, and have at least 1 fibroid that was 2 cm in diameter or multiple small fibroids with the calculated uterine volume of more than 200 cm3. No fibroid larger than 12 cm in diameter was included.
The primary end point was a menstrual blood loss of 80 mL or less and a 50% or more reduction in menstrual blood loss from baseline in the 28 days before week 24. Uterine fibroid volume reduction and a safety assessment, including BMD assessment, also were studied.
In the P1 trial, which was conducted in US sites, the response rate for the primary objective was 56.4% in the linzagolix 100-mg group, 66.4% in the 100-mg plus add-back therapy group, 71.4% in the 200-mg group, and 75.5% in the 200-mg plus add-back group, compared with 35.0% in the placebo group.
In the P2 trial, which included sites in both Europe and the United States, the response rates were 56.7% in the 100-mg group, 77.2% in the 100-mg plus add-back therapy group, 77.7% in the 200-mg group, and 93.9% in the 200-mg plus add-back therapy group, compared with 29.4% in the placebo group. Thus, in both trials a significantly higher proportion of menstrual reduction occurred in all linzagolix treatment groups compared with placebo.
As expected, the incidence of hot flushes was the highest in participants taking the linzagolix 200-mg dose without add-back hormonal therapy, with hot flushes occurring in 35% (P1) and 32% (P2) of patients, compared with all other groups, which was 3% to 14%. All treatment groups showed improvement in quality-of-life scores compared with placebo. Of note, to achieve reduction of fibroid volume in the 40% to 50% range, this was observed consistently only with the linzagolix 200-mg alone dose.
Linzagolix effect on bone
Decreases in BMD appeared to be dose dependent, as lumbar spine losses of up to 4% were noted with the linzgolix 200-mg dose, and a 2% loss was observed with the 100-mg dose at 24 weeks. However, these were improved with add-back therapy. There were continued BMD decreases at 52 weeks, with up to 2.4% with 100 mg of linzagolix and up to 1.5% with 100 mg plus add-back therapy, and up to 2% with 200 mg of linzagolix plus add-back therapy. ●
Results of the P1 and P2 trials suggest that there could be a potential niche for linzagolix in patients who need chronic use (> 6 months) without the need for concomitant add-back hormone therapy at lower doses. The non-add-back option may be a possibility for women who have both a contraindication to estrogen and an increased risk for hormone-related adverse events.
- Curlin HL, Cintron LC, Anderson TL. A prospective, multicenter, clinical trial evaluating the safety and effectiveness of the Cerene device to treat heavy menstrual bleeding. J Minim Invasive Gynecol. 2021;28;899-908.
- Curlin HL, Anderson TL. Endometrial cryoablation for the treatment of heavy menstrual bleeding: 36-month outcomes from the CLARITY study. Int J Womens Health. 2022;14:1083-1092.
- Curlin H, Cholkeri-Singh A, Leal JGG, et al. Hysteroscopic access and uterine cavity evaluation 12 months after endometrial ablation with the Cerene cryotherapy device. J Minim Invasive Gynecol. 2022;29:440-447.
- Radestad AF, Dahm-Kahler P, Holmberg E, et al. Longterm incidence of endometrial cancer after endometrial resection and ablation: a population based Swedish gynecologic cancer group (SweGCG) study. Acta Obstet Gynecol Scand. 2022;101:923-930.
- Oderkerk TJ, van de Kar MRD, Cornel KMC, et al. Endometrial cancer after endometrial ablation: a systematic review. Int J Gynecol Cancer. 2022;32:1555-1560.
- Al-Hendy A, Lukes AS, Poindexter AN, et al. Long-term relugolix combination therapy for symptomatic uterine leiomyomas. Obstet Gynecol. 2022;140:920-930.
- Donnez J, Taylor HS, Stewart EA, et al. Linzagolix with and without hormonal add-back therapy for the treatment of symptomatic uterine fibroids: two randomised, placebo- controlled, phase 3 trials. Lancet. 2022;400:896-907.
Endometrial ablation continues to be performed in significant numbers in the United States, with an estimated 500,000 cases annually. Several nonresectoscopic endometrial ablation devices have been approved for use, and some are now discontinued. The newest endometrial ablation therapy to gain US Food and Drug Administration (FDA) approval and to have published outcomes is the Cerene cryotherapy ablation device (Channel Medsystems, Inc). The results of 36-month outcomes from the CLARITY study were published last year, and we have chosen to review these long-term data in addition to that of a second study in which investigators assessed the ability to access the endometrial cavity postcryoablation. We believe this is important because of concerns about the inability to access the endometrial cavity after ablation, as well as the potential for delay in the diagnosis of endometrial cancer. It is interesting that 2 publications simultaneously reviewed the incidence of endometrial cancer after endometrial ablation within the past 12 months, and we therefore present those findings as they provide valuable information.
Our second focus in this year’s Update is to provide additional information about the burgeoning data on gonadotropin-releasing hormone (GnRH) antagonists. We review evidence on linzagolix from the PRIMROSE 1 and PRIMROSE 2 trials and longer-term data on relugolix combination therapy for symptomatic uterine fibroids.
Three-year follow-up after endometrial cryoablation with the Cerene device found high patient satisfaction, low hysterectomy rates
Curlin HL, Cintron LC, Anderson TL. A prospective, multicenter, clinical trial evaluating the safety and effectiveness of the Cerene device to treat heavy menstrual bleeding. J Minim Invasive Gynecol. 2021;28;899-908.
Curlin HL, Anderson TL. Endometrial cryoablation for the treatment of heavy menstrual bleeding: 36-month outcomes from the CLARITY study. Int J Womens Health. 2022;14:1083-1092.
The 12-month data on the clinical safety and effectiveness of the Cerene cryoablation device were published in 2021 in the CLARITY trial.1 The 36-month outcomes were published in 2022 and showed sustained clinical effects through month 36 with a low risk of adverse outcomes.2 The interesting aspect of this trial is that although the amenorrhea rate was relatively low at 12 months (6.5%), it continued to remain relatively low compared with rates found with other devices, but the amenorrhea rate increased at 36 months (14.4%). This was the percentage of patients who reported, “I no longer get my period.”
Patient satisfaction was high
Despite a relatively low amenorrhea rate, study participants had a high satisfaction rate and a low 3-year hysterectomy rate. Eighty-five percent of the participants were satisfied or very satisfied, and the cumulative hysterectomy rate was low at 5%.
The overall reintervention rate was 8.7%. Six patients were treated with medications, 2 patients underwent repeat endometrial ablation, 1 received a levonorgestrel-releasing intrauterine device, and 12 underwent hysterectomy.
At 36 months, 201 of the original 242 participants were available for assessment. Unfortunately, 5 pregnancies were reported through the 6-month posttreatment period, which emphasizes the importance of having reliable contraception. However, there were no reports of hematometra or postablation tubal sterilization syndrome (PATSS).
Effect on bleeding was long term
The main finding of the CLARITY study is that the Cerene cryoablation device appears to have a relatively stable effect on bleedingfor the first 3 years after therapy, with minimal risk of hematometra and PATSS. What we find interesting is that despite Cerene cryoablation having one of the lowest amenorrhea rates, it not only had a satisfaction rate in line with that of other devices but also had a low hysterectomy rate—only 5%—at 3 years.
The study authors pointed out that there is a lack of scarring within the endometrial cavity with the Cerene device. Some may find less endometrial scarring worth a low amenorrhea rate in the context of a favorable satisfaction rate. This begs the question, how well can the endometrial cavity be assessed? For answers, keep reading.
Can the endometrial cavity be reliably accessed after Cerene cryoablation?
Endometrial ablation has been associated with intracavitary scarring that results in hematometra, PATSS, and a concern for difficulty in performing an adequate endometrial assessment in patients who develop postablation abnormal uterine bleeding.
In a prospective study, 230 participants (of an initial 242) treated with Cerene cyroablation were studied with hysteroscopic evaluation of the endometrial cavity 12 months after surgery.3 The uterine cavity was accessible in 98.7% of participants. The cavity was not accessible in 3 participants due to pain or cervical stenosis.
Visualization of the uterine cavity was possible by hysteroscopy in 92.7% of study participants (204 of 220), with 1 or both tubal ostia identified in 89.2%. Both tubal ostia were visible in 78.4% and 1 ostium was visible in 10.8%. The cavity was not visualized in 16 of the 220 patients (7.2%) due to intrauterine adhesions, technical difficulties, or menstruation. Also of note, 97 of the 230 participants available at the 12-month follow-up had undergone tubal sterilization before cryoablation and none reported symptoms of PATSS or hematometra, which may be considered surrogate markers for adhesions.
Results of the CLARITY study demonstrated the clinical safety and effectiveness of the Cerene cryoablation device at 12 months, with sustained clinical effects through 36 months and a low risk of adverse outcomes. Patient satisfaction rates were high, and the hysterectomy rate was low. In addition, in a prospective study of patients treated with Cerene cryoablation, hysteroscopic evaluation at 12 months found the uterine cavity accessible in more than 98% of participants, and uterine visualization also was high. Therefore, the Cerene cryoablation device may provide the advantage of an easier evaluation of patients who eventually develop abnormal bleeding after endometrial ablation.
Continue to: Tissue effects differ with ablation technique...
Tissue effects differ with ablation technique
The study authors suggested that different tissue effects occur with freezing compared with heating ablation techniques. With freezing, over weeks to months the chronic inflammatory tissue is eventually replaced by a fibrous scar of collagen, with some preservation of the collagen matrix during tissue repair. This may be different from the charring and boiling of heated tissue that results in architectural tissue loss and may interfere with wound repair and tissue remodeling. Although the incidence of postoperative adhesions after endometrial ablation is not well studied, it is encouraging that most patients who received cryoablation with the Cerene device were able to undergo an evaluation of the endometrium without general anesthesia.
Key takeaway
The main idea from this study is that the endometrium can be assessed by office hysteroscopy in most patients who undergo cryoablation with the Cerene device. This may have advantages in terms of reducing the risk of PATSS and hematometra, and it may allow easier evaluation of the endometrium for patients who have postablation abnormal uterine bleeding. This begs the question, does intrauterine scarring influence the detection of endometrial cancer? For answers, keep reading.
Does endometrial ablation place a patient at higher risk for a delay in the diagnosis of endometrial cancer?
Radestad AF, Dahm-Kahler P, Holmberg E, et al. Long-term incidence of endometrial cancer after endometrial resection and ablation: a population based Swedish gynecologic cancer group (SweGCG) study. Acta Obstet Gynecol Scand. 2022;101:923-930.
Oderkerk TJ, van de Kar MRD, Cornel KMC, et al. Endometrial cancer after endometrial ablation: a systematic review. Int J Gynecol Cancer. 2022;32:1555-1560.
The answer to this question appears to be no, based on 2 different types of studies. One study was a 20-year population database review from Sweden,4 and the other was a systematic review of 11 cohort studies.5
Population-based study findings
The data from the Swedish population database is interesting because since 1994 all Swedish citizens have been allocated a unique personal identification number at birth or immigration that enables official registries and research. In reviewing their data from 1997 through 2017, Radestad and colleagues compared transcervical resection of the endometrium (TCRE) and other forms of endometrial ablation against the Swedish National Patient Register data for endometrial cancer.4 They found no increase in the incidence of endometrial cancer after TCRE (0.3%) or after endometrial ablation (0.02%) and suggested a significantly lower incidence of endometrial cancer after endometrial ablation.
This study is beneficial because it is the largest study to explore the long-term incidence of endometrial cancer after TCRE and endometrial ablation. The investigators hypothesized that, as an explanation for the difference between rates, ablation may burn deeper into the myometrium and treat adenomyosis compared with TCRE. However, they also were cautious to note that although this was a 20-year study, the incidence of endometrial carcinoma likely will reach a peak in the next few years.
Systematic review conclusions
In the systematic review, out of 890 publications from the authors’ database search, 11 articles were eventually included for review.5 A total of 29,102 patients with endometrial ablation were followed for a period of up to 25 years, and the incidence of endometrial cancer after endometrial ablation varied from 0.0% to 1.6%. A total of 38 cases of endometrial cancer after endometrial ablation have been described in the literature. Of those cases, bleeding was the most common presenting symptom of the disease. Endometrial sampling was successful in 89% of cases, and in 90% of cases, histological exam showed an early-stage endometrial adenocarcinoma.
Based on their review, the authors concluded that the incidence of endometrial cancer was not increased in patients who received endometrial ablation, and more importantly, there was no apparent delay in the diagnosis of endometrial cancer after endometrial ablation. They further suggested that diagnostic management with endometrial sampling did not appear to be a barrier.
The main findings from these 2 studies by Radestad and colleagues and Oderkerk and associates are that endometrial cancer does not appear to be more common after endometrial ablation, and it appears to be diagnosed with endometrial sampling in most cases.4,5 There may be some protection against endometrial cancer with nonresectoscopic endometrial ablation, although this needs to be verified by additional studies. To juxtapose this information with the prior information about cryotherapy, it emphasizes that the scarring within the endometrium will likely reduce the incidence of PATSS and hematometra, which are relatively low-incidence occurrences at 5% to 7%, but it likely does not affect the detection of endometrial cancer.
Longer-term data for relugolix combination treatment of symptomatic uterine bleeding from fibroids shows sustained efficacy
Al-Hendy A, Lukes AS, Poindexter AN, et al. Long-term relugolix combination therapy for symptomatic uterine leiomyomas. Obstet Gynecol. 2022;140:920-930.
Relugolix combination therapy was previously reported to be effective for the treatment of fibroids based on the 24-week trials LIBERTY 1 and LIBERTY 2. We now have information about longer-term therapy for up to 52 weeks of treatment.6
Relugolix combination therapy is a once-daily single tablet for the treatment of heavy menstrual bleeding thought to be due to uterine fibroids in premenopausal women. It is comprised of relugolix 40 mg (a GnRH antagonist), estradiol 1.0 mg, and norethindrone acetate 0.5 mg.
Continue to: Extension study showed sustained efficacy...
Extension study showed sustained efficacy
The study by Al-Hendy and colleagues showed that the relugolix combination not only was well tolerated but also that there was sustained improvement in heavy bleeding, with the average patient having an approximately 90% decrease in menstrual bleeding from baseline.6 It was noted that 70.6% of patients achieved amenorrhea over the last 35 days of treatment.
Importantly, the treatment effect was independent of race, body mass index, baseline menstrual blood loss, and uterine fibroid volume. The bone mineral density (BMD) change trajectory was similar to what was observed in the pivotal study. No new safety concerns were identified, and BMD generally was preserved.
The extension study by Al-Hendy and colleagues demonstrated that that the reduced fibroid-associated bleeding treated with relugolix combination therapy is sustained throughout the 52-week period, with no new safety concerns.
Linzagolix is the newest GnRH antagonist to be studied in a randomized, placebo-controlled trial
Donnez J, Taylor HS, Stewart EA, et al. Linzagolix with and without hormonal add-back therapy for the treatment of symptomatic uterine fibroids: two randomised, placebo-controlled, phase 3 trials. Lancet. 2022;400:896-907.
At the time of this writing, linzagolix was not approved by the FDA. The results of the PRIMROSE 1 (P1) and PRIMROSE 2 (P2) trials were published last year as 2 identical 52-week randomized, parallel, double-blind, placebo-controlled, phase 3 trials.7 The difference between the development of linzagolix as a GnRH antagonist and other similar medications is the strategy of potential partial hypothalamic pituitary ovarian axis suppression at 100 mg versus complete suppression at 200 mg. In this trial by Donnez and colleagues, both linzagolix doses were evaluated with and without add-back hormonal therapy and also were compared with placebo in a 1:1:1:1:1 ratio.7
Study details and results
To be eligible for this study, participants had to have heavy menstrual bleeding, defined as more than 80 mL for at least 2 cycles, and have at least 1 fibroid that was 2 cm in diameter or multiple small fibroids with the calculated uterine volume of more than 200 cm3. No fibroid larger than 12 cm in diameter was included.
The primary end point was a menstrual blood loss of 80 mL or less and a 50% or more reduction in menstrual blood loss from baseline in the 28 days before week 24. Uterine fibroid volume reduction and a safety assessment, including BMD assessment, also were studied.
In the P1 trial, which was conducted in US sites, the response rate for the primary objective was 56.4% in the linzagolix 100-mg group, 66.4% in the 100-mg plus add-back therapy group, 71.4% in the 200-mg group, and 75.5% in the 200-mg plus add-back group, compared with 35.0% in the placebo group.
In the P2 trial, which included sites in both Europe and the United States, the response rates were 56.7% in the 100-mg group, 77.2% in the 100-mg plus add-back therapy group, 77.7% in the 200-mg group, and 93.9% in the 200-mg plus add-back therapy group, compared with 29.4% in the placebo group. Thus, in both trials a significantly higher proportion of menstrual reduction occurred in all linzagolix treatment groups compared with placebo.
As expected, the incidence of hot flushes was the highest in participants taking the linzagolix 200-mg dose without add-back hormonal therapy, with hot flushes occurring in 35% (P1) and 32% (P2) of patients, compared with all other groups, which was 3% to 14%. All treatment groups showed improvement in quality-of-life scores compared with placebo. Of note, to achieve reduction of fibroid volume in the 40% to 50% range, this was observed consistently only with the linzagolix 200-mg alone dose.
Linzagolix effect on bone
Decreases in BMD appeared to be dose dependent, as lumbar spine losses of up to 4% were noted with the linzgolix 200-mg dose, and a 2% loss was observed with the 100-mg dose at 24 weeks. However, these were improved with add-back therapy. There were continued BMD decreases at 52 weeks, with up to 2.4% with 100 mg of linzagolix and up to 1.5% with 100 mg plus add-back therapy, and up to 2% with 200 mg of linzagolix plus add-back therapy. ●
Results of the P1 and P2 trials suggest that there could be a potential niche for linzagolix in patients who need chronic use (> 6 months) without the need for concomitant add-back hormone therapy at lower doses. The non-add-back option may be a possibility for women who have both a contraindication to estrogen and an increased risk for hormone-related adverse events.
Endometrial ablation continues to be performed in significant numbers in the United States, with an estimated 500,000 cases annually. Several nonresectoscopic endometrial ablation devices have been approved for use, and some are now discontinued. The newest endometrial ablation therapy to gain US Food and Drug Administration (FDA) approval and to have published outcomes is the Cerene cryotherapy ablation device (Channel Medsystems, Inc). The results of 36-month outcomes from the CLARITY study were published last year, and we have chosen to review these long-term data in addition to that of a second study in which investigators assessed the ability to access the endometrial cavity postcryoablation. We believe this is important because of concerns about the inability to access the endometrial cavity after ablation, as well as the potential for delay in the diagnosis of endometrial cancer. It is interesting that 2 publications simultaneously reviewed the incidence of endometrial cancer after endometrial ablation within the past 12 months, and we therefore present those findings as they provide valuable information.
Our second focus in this year’s Update is to provide additional information about the burgeoning data on gonadotropin-releasing hormone (GnRH) antagonists. We review evidence on linzagolix from the PRIMROSE 1 and PRIMROSE 2 trials and longer-term data on relugolix combination therapy for symptomatic uterine fibroids.
Three-year follow-up after endometrial cryoablation with the Cerene device found high patient satisfaction, low hysterectomy rates
Curlin HL, Cintron LC, Anderson TL. A prospective, multicenter, clinical trial evaluating the safety and effectiveness of the Cerene device to treat heavy menstrual bleeding. J Minim Invasive Gynecol. 2021;28;899-908.
Curlin HL, Anderson TL. Endometrial cryoablation for the treatment of heavy menstrual bleeding: 36-month outcomes from the CLARITY study. Int J Womens Health. 2022;14:1083-1092.
The 12-month data on the clinical safety and effectiveness of the Cerene cryoablation device were published in 2021 in the CLARITY trial.1 The 36-month outcomes were published in 2022 and showed sustained clinical effects through month 36 with a low risk of adverse outcomes.2 The interesting aspect of this trial is that although the amenorrhea rate was relatively low at 12 months (6.5%), it continued to remain relatively low compared with rates found with other devices, but the amenorrhea rate increased at 36 months (14.4%). This was the percentage of patients who reported, “I no longer get my period.”
Patient satisfaction was high
Despite a relatively low amenorrhea rate, study participants had a high satisfaction rate and a low 3-year hysterectomy rate. Eighty-five percent of the participants were satisfied or very satisfied, and the cumulative hysterectomy rate was low at 5%.
The overall reintervention rate was 8.7%. Six patients were treated with medications, 2 patients underwent repeat endometrial ablation, 1 received a levonorgestrel-releasing intrauterine device, and 12 underwent hysterectomy.
At 36 months, 201 of the original 242 participants were available for assessment. Unfortunately, 5 pregnancies were reported through the 6-month posttreatment period, which emphasizes the importance of having reliable contraception. However, there were no reports of hematometra or postablation tubal sterilization syndrome (PATSS).
Effect on bleeding was long term
The main finding of the CLARITY study is that the Cerene cryoablation device appears to have a relatively stable effect on bleedingfor the first 3 years after therapy, with minimal risk of hematometra and PATSS. What we find interesting is that despite Cerene cryoablation having one of the lowest amenorrhea rates, it not only had a satisfaction rate in line with that of other devices but also had a low hysterectomy rate—only 5%—at 3 years.
The study authors pointed out that there is a lack of scarring within the endometrial cavity with the Cerene device. Some may find less endometrial scarring worth a low amenorrhea rate in the context of a favorable satisfaction rate. This begs the question, how well can the endometrial cavity be assessed? For answers, keep reading.
Can the endometrial cavity be reliably accessed after Cerene cryoablation?
Endometrial ablation has been associated with intracavitary scarring that results in hematometra, PATSS, and a concern for difficulty in performing an adequate endometrial assessment in patients who develop postablation abnormal uterine bleeding.
In a prospective study, 230 participants (of an initial 242) treated with Cerene cyroablation were studied with hysteroscopic evaluation of the endometrial cavity 12 months after surgery.3 The uterine cavity was accessible in 98.7% of participants. The cavity was not accessible in 3 participants due to pain or cervical stenosis.
Visualization of the uterine cavity was possible by hysteroscopy in 92.7% of study participants (204 of 220), with 1 or both tubal ostia identified in 89.2%. Both tubal ostia were visible in 78.4% and 1 ostium was visible in 10.8%. The cavity was not visualized in 16 of the 220 patients (7.2%) due to intrauterine adhesions, technical difficulties, or menstruation. Also of note, 97 of the 230 participants available at the 12-month follow-up had undergone tubal sterilization before cryoablation and none reported symptoms of PATSS or hematometra, which may be considered surrogate markers for adhesions.
Results of the CLARITY study demonstrated the clinical safety and effectiveness of the Cerene cryoablation device at 12 months, with sustained clinical effects through 36 months and a low risk of adverse outcomes. Patient satisfaction rates were high, and the hysterectomy rate was low. In addition, in a prospective study of patients treated with Cerene cryoablation, hysteroscopic evaluation at 12 months found the uterine cavity accessible in more than 98% of participants, and uterine visualization also was high. Therefore, the Cerene cryoablation device may provide the advantage of an easier evaluation of patients who eventually develop abnormal bleeding after endometrial ablation.
Continue to: Tissue effects differ with ablation technique...
Tissue effects differ with ablation technique
The study authors suggested that different tissue effects occur with freezing compared with heating ablation techniques. With freezing, over weeks to months the chronic inflammatory tissue is eventually replaced by a fibrous scar of collagen, with some preservation of the collagen matrix during tissue repair. This may be different from the charring and boiling of heated tissue that results in architectural tissue loss and may interfere with wound repair and tissue remodeling. Although the incidence of postoperative adhesions after endometrial ablation is not well studied, it is encouraging that most patients who received cryoablation with the Cerene device were able to undergo an evaluation of the endometrium without general anesthesia.
Key takeaway
The main idea from this study is that the endometrium can be assessed by office hysteroscopy in most patients who undergo cryoablation with the Cerene device. This may have advantages in terms of reducing the risk of PATSS and hematometra, and it may allow easier evaluation of the endometrium for patients who have postablation abnormal uterine bleeding. This begs the question, does intrauterine scarring influence the detection of endometrial cancer? For answers, keep reading.
Does endometrial ablation place a patient at higher risk for a delay in the diagnosis of endometrial cancer?
Radestad AF, Dahm-Kahler P, Holmberg E, et al. Long-term incidence of endometrial cancer after endometrial resection and ablation: a population based Swedish gynecologic cancer group (SweGCG) study. Acta Obstet Gynecol Scand. 2022;101:923-930.
Oderkerk TJ, van de Kar MRD, Cornel KMC, et al. Endometrial cancer after endometrial ablation: a systematic review. Int J Gynecol Cancer. 2022;32:1555-1560.
The answer to this question appears to be no, based on 2 different types of studies. One study was a 20-year population database review from Sweden,4 and the other was a systematic review of 11 cohort studies.5
Population-based study findings
The data from the Swedish population database is interesting because since 1994 all Swedish citizens have been allocated a unique personal identification number at birth or immigration that enables official registries and research. In reviewing their data from 1997 through 2017, Radestad and colleagues compared transcervical resection of the endometrium (TCRE) and other forms of endometrial ablation against the Swedish National Patient Register data for endometrial cancer.4 They found no increase in the incidence of endometrial cancer after TCRE (0.3%) or after endometrial ablation (0.02%) and suggested a significantly lower incidence of endometrial cancer after endometrial ablation.
This study is beneficial because it is the largest study to explore the long-term incidence of endometrial cancer after TCRE and endometrial ablation. The investigators hypothesized that, as an explanation for the difference between rates, ablation may burn deeper into the myometrium and treat adenomyosis compared with TCRE. However, they also were cautious to note that although this was a 20-year study, the incidence of endometrial carcinoma likely will reach a peak in the next few years.
Systematic review conclusions
In the systematic review, out of 890 publications from the authors’ database search, 11 articles were eventually included for review.5 A total of 29,102 patients with endometrial ablation were followed for a period of up to 25 years, and the incidence of endometrial cancer after endometrial ablation varied from 0.0% to 1.6%. A total of 38 cases of endometrial cancer after endometrial ablation have been described in the literature. Of those cases, bleeding was the most common presenting symptom of the disease. Endometrial sampling was successful in 89% of cases, and in 90% of cases, histological exam showed an early-stage endometrial adenocarcinoma.
Based on their review, the authors concluded that the incidence of endometrial cancer was not increased in patients who received endometrial ablation, and more importantly, there was no apparent delay in the diagnosis of endometrial cancer after endometrial ablation. They further suggested that diagnostic management with endometrial sampling did not appear to be a barrier.
The main findings from these 2 studies by Radestad and colleagues and Oderkerk and associates are that endometrial cancer does not appear to be more common after endometrial ablation, and it appears to be diagnosed with endometrial sampling in most cases.4,5 There may be some protection against endometrial cancer with nonresectoscopic endometrial ablation, although this needs to be verified by additional studies. To juxtapose this information with the prior information about cryotherapy, it emphasizes that the scarring within the endometrium will likely reduce the incidence of PATSS and hematometra, which are relatively low-incidence occurrences at 5% to 7%, but it likely does not affect the detection of endometrial cancer.
Longer-term data for relugolix combination treatment of symptomatic uterine bleeding from fibroids shows sustained efficacy
Al-Hendy A, Lukes AS, Poindexter AN, et al. Long-term relugolix combination therapy for symptomatic uterine leiomyomas. Obstet Gynecol. 2022;140:920-930.
Relugolix combination therapy was previously reported to be effective for the treatment of fibroids based on the 24-week trials LIBERTY 1 and LIBERTY 2. We now have information about longer-term therapy for up to 52 weeks of treatment.6
Relugolix combination therapy is a once-daily single tablet for the treatment of heavy menstrual bleeding thought to be due to uterine fibroids in premenopausal women. It is comprised of relugolix 40 mg (a GnRH antagonist), estradiol 1.0 mg, and norethindrone acetate 0.5 mg.
Continue to: Extension study showed sustained efficacy...
Extension study showed sustained efficacy
The study by Al-Hendy and colleagues showed that the relugolix combination not only was well tolerated but also that there was sustained improvement in heavy bleeding, with the average patient having an approximately 90% decrease in menstrual bleeding from baseline.6 It was noted that 70.6% of patients achieved amenorrhea over the last 35 days of treatment.
Importantly, the treatment effect was independent of race, body mass index, baseline menstrual blood loss, and uterine fibroid volume. The bone mineral density (BMD) change trajectory was similar to what was observed in the pivotal study. No new safety concerns were identified, and BMD generally was preserved.
The extension study by Al-Hendy and colleagues demonstrated that that the reduced fibroid-associated bleeding treated with relugolix combination therapy is sustained throughout the 52-week period, with no new safety concerns.
Linzagolix is the newest GnRH antagonist to be studied in a randomized, placebo-controlled trial
Donnez J, Taylor HS, Stewart EA, et al. Linzagolix with and without hormonal add-back therapy for the treatment of symptomatic uterine fibroids: two randomised, placebo-controlled, phase 3 trials. Lancet. 2022;400:896-907.
At the time of this writing, linzagolix was not approved by the FDA. The results of the PRIMROSE 1 (P1) and PRIMROSE 2 (P2) trials were published last year as 2 identical 52-week randomized, parallel, double-blind, placebo-controlled, phase 3 trials.7 The difference between the development of linzagolix as a GnRH antagonist and other similar medications is the strategy of potential partial hypothalamic pituitary ovarian axis suppression at 100 mg versus complete suppression at 200 mg. In this trial by Donnez and colleagues, both linzagolix doses were evaluated with and without add-back hormonal therapy and also were compared with placebo in a 1:1:1:1:1 ratio.7
Study details and results
To be eligible for this study, participants had to have heavy menstrual bleeding, defined as more than 80 mL for at least 2 cycles, and have at least 1 fibroid that was 2 cm in diameter or multiple small fibroids with the calculated uterine volume of more than 200 cm3. No fibroid larger than 12 cm in diameter was included.
The primary end point was a menstrual blood loss of 80 mL or less and a 50% or more reduction in menstrual blood loss from baseline in the 28 days before week 24. Uterine fibroid volume reduction and a safety assessment, including BMD assessment, also were studied.
In the P1 trial, which was conducted in US sites, the response rate for the primary objective was 56.4% in the linzagolix 100-mg group, 66.4% in the 100-mg plus add-back therapy group, 71.4% in the 200-mg group, and 75.5% in the 200-mg plus add-back group, compared with 35.0% in the placebo group.
In the P2 trial, which included sites in both Europe and the United States, the response rates were 56.7% in the 100-mg group, 77.2% in the 100-mg plus add-back therapy group, 77.7% in the 200-mg group, and 93.9% in the 200-mg plus add-back therapy group, compared with 29.4% in the placebo group. Thus, in both trials a significantly higher proportion of menstrual reduction occurred in all linzagolix treatment groups compared with placebo.
As expected, the incidence of hot flushes was the highest in participants taking the linzagolix 200-mg dose without add-back hormonal therapy, with hot flushes occurring in 35% (P1) and 32% (P2) of patients, compared with all other groups, which was 3% to 14%. All treatment groups showed improvement in quality-of-life scores compared with placebo. Of note, to achieve reduction of fibroid volume in the 40% to 50% range, this was observed consistently only with the linzagolix 200-mg alone dose.
Linzagolix effect on bone
Decreases in BMD appeared to be dose dependent, as lumbar spine losses of up to 4% were noted with the linzgolix 200-mg dose, and a 2% loss was observed with the 100-mg dose at 24 weeks. However, these were improved with add-back therapy. There were continued BMD decreases at 52 weeks, with up to 2.4% with 100 mg of linzagolix and up to 1.5% with 100 mg plus add-back therapy, and up to 2% with 200 mg of linzagolix plus add-back therapy. ●
Results of the P1 and P2 trials suggest that there could be a potential niche for linzagolix in patients who need chronic use (> 6 months) without the need for concomitant add-back hormone therapy at lower doses. The non-add-back option may be a possibility for women who have both a contraindication to estrogen and an increased risk for hormone-related adverse events.
- Curlin HL, Cintron LC, Anderson TL. A prospective, multicenter, clinical trial evaluating the safety and effectiveness of the Cerene device to treat heavy menstrual bleeding. J Minim Invasive Gynecol. 2021;28;899-908.
- Curlin HL, Anderson TL. Endometrial cryoablation for the treatment of heavy menstrual bleeding: 36-month outcomes from the CLARITY study. Int J Womens Health. 2022;14:1083-1092.
- Curlin H, Cholkeri-Singh A, Leal JGG, et al. Hysteroscopic access and uterine cavity evaluation 12 months after endometrial ablation with the Cerene cryotherapy device. J Minim Invasive Gynecol. 2022;29:440-447.
- Radestad AF, Dahm-Kahler P, Holmberg E, et al. Longterm incidence of endometrial cancer after endometrial resection and ablation: a population based Swedish gynecologic cancer group (SweGCG) study. Acta Obstet Gynecol Scand. 2022;101:923-930.
- Oderkerk TJ, van de Kar MRD, Cornel KMC, et al. Endometrial cancer after endometrial ablation: a systematic review. Int J Gynecol Cancer. 2022;32:1555-1560.
- Al-Hendy A, Lukes AS, Poindexter AN, et al. Long-term relugolix combination therapy for symptomatic uterine leiomyomas. Obstet Gynecol. 2022;140:920-930.
- Donnez J, Taylor HS, Stewart EA, et al. Linzagolix with and without hormonal add-back therapy for the treatment of symptomatic uterine fibroids: two randomised, placebo- controlled, phase 3 trials. Lancet. 2022;400:896-907.
- Curlin HL, Cintron LC, Anderson TL. A prospective, multicenter, clinical trial evaluating the safety and effectiveness of the Cerene device to treat heavy menstrual bleeding. J Minim Invasive Gynecol. 2021;28;899-908.
- Curlin HL, Anderson TL. Endometrial cryoablation for the treatment of heavy menstrual bleeding: 36-month outcomes from the CLARITY study. Int J Womens Health. 2022;14:1083-1092.
- Curlin H, Cholkeri-Singh A, Leal JGG, et al. Hysteroscopic access and uterine cavity evaluation 12 months after endometrial ablation with the Cerene cryotherapy device. J Minim Invasive Gynecol. 2022;29:440-447.
- Radestad AF, Dahm-Kahler P, Holmberg E, et al. Longterm incidence of endometrial cancer after endometrial resection and ablation: a population based Swedish gynecologic cancer group (SweGCG) study. Acta Obstet Gynecol Scand. 2022;101:923-930.
- Oderkerk TJ, van de Kar MRD, Cornel KMC, et al. Endometrial cancer after endometrial ablation: a systematic review. Int J Gynecol Cancer. 2022;32:1555-1560.
- Al-Hendy A, Lukes AS, Poindexter AN, et al. Long-term relugolix combination therapy for symptomatic uterine leiomyomas. Obstet Gynecol. 2022;140:920-930.
- Donnez J, Taylor HS, Stewart EA, et al. Linzagolix with and without hormonal add-back therapy for the treatment of symptomatic uterine fibroids: two randomised, placebo- controlled, phase 3 trials. Lancet. 2022;400:896-907.
News & Perspectives from Ob.Gyn. News
COMMENTARY
Answering the protein question when prescribing plant-based diets
Science supports the use of a whole food, predominantly plant-based dietary pattern for optimal health, including reduced risk for chronic disease, and best practice in treatment of leading chronic disease.
But clinicians who prescribe such eating patterns encounter a common concern from patients whose health may benefit.
“Where will I get my protein?”
We’ve all heard it, and it’s understandable
To ensure that patients have all the facts when making dietary decisions, clinicians need to be prepared to respond to concerns about protein adequacy and quality with evidence-based information. A good starting point for these conversations is to assess how much protein patients are already consuming. A review of the 2015-2016 National Health and Nutrition Examination Survey found that women normally consume an average of 69 g and men an average of 97 g of protein daily.
As a general point of reference, the recommended dietary allowance for protein is about 0.8 g/kg of bodyweight (or 0.36 g/lb), which equates to about 52 g of protein per day for a 145-lb woman and 65 g for a 180-lb man. But for many patients, it may be best to get a more precise recommendation based upon age, gender and physical activity level by using a handy Department of Agriculture tool for health care professionals to calculate daily protein and other nutrient needs. Patients can also use one of countless apps to track their protein and other nutrient intake. By using the tool and a tracking app, both clinician and patients can be fully informed whether protein needs are being met.
LATEST NEWS
Continuous glucose monitors for pregnant patients?
Patients with pregestational diabetes may benefit from use of a continuous subcutaneous insulin infusion pump paired with a continuous glucose monitor. Use of the tools has been associated with a reduction in maternal and neonatal morbidity, a recent study found.
“We were seeing an unacceptable burden of both maternal and fetal disease in our diabetic population,” said Neil Hamill, MD, a maternal-fetal medicine specialist at Methodist Women’s Hospital, Omaha, Neb., and an author of the study. “We thought the success with this technology in the nonpregnant population would and should translate into the pregnant population.”
Dr. Hamill and his colleagues analyzed data from 55 pregnant patients who received care at the Women’s Hospital Perinatal Center at the Nebraska Methodist Health System between October 2019 and October 2022. Everyone in the cohort had pregestational diabetes and required insulin prior to week 20 of pregnancy. They used CGMs for more than 2 weeks. The study set blood glucose levels of less than 140 mg/dL as a healthy benchmark.
Participants who had severe preeclampsia, who had delivered preterm, who had delivered a neonate with respiratory distress syndrome, and/or who had given birth to a larger-than-expected infant spent less time in the safe zone — having a blood glucose level below 140 mg/dL—than women who did not have those risk factors.
“When blood sugar control is better, maternal and fetal outcomes are improved,” Dr. Hamill said.
Neetu Sodhi, MD, an ob.gyn. at Providence Cedars-Sinai Tarzana Medical Center, Los Angeles, expressed optimism that use of blood glucose monitors and insulin pumps can improve outcomes for pregnant patients with pregestational diabetes.
“This is just another case for why it’s so important for patients to have access to these types of devices that really, really improve their outcomes and their health, and now it’s proven in the case of pregnancy outcomes too – or at least suggested strongly with this data,” Dr. Sodhi said.
Continue to: It may be time to pay attention to COVID again...
It may be time to pay attention to COVID again
More than 3 years into the COVID-19 era, most Americans have settled back into their prepandemic lifestyles. But a new dominant variant and rising hospitalization numbers may give way to another summer surge.
Since April, a new COVID variant has cropped up. According to recent Centers for Disease Control and Prevention data, EG.5—from the Omicron family—now makes up 17% of all cases in the United States, up from 7.5% in the first week of July.
A summary from the Center for Infectious Disease Research and Policy at the University of Minnesota says that EG.5, nicknamed “Eris” by health trackers, is nearly the same as its parent strain, XBB.1.9.2, but has one extra spike mutation.
Along with the news of EG.5’s growing prevalence, COVID-related hospitalization rates have increased by 12.5% during the week ending on July 29—the most significant uptick since December. Still, no connection has been made between the new variant and rising hospital admissions. And so far, experts have found no difference in the severity of illness or symptoms between Eris and the strains that came before it.
Cause for concern?
The COVID virus has a great tendency to mutate, said William Schaffner, MD, a professor of infectious diseases at Vanderbilt University, Nashville, Tenn.
“Fortunately, these are relatively minor mutations.” Even so, SARS-CoV-2, the virus that causes COVID-19, continues to be highly contagious. “There isn’t any doubt that it’s spreading—but it’s not more serious.”
So, Dr. Schaffner doesn’t think it’s time to panic. He prefers calling it an “uptick” in cases instead of a “surge,” because a surge “sounds too big.”
While the numbers are still low, compared with 2022’s summer surge, experts still urge people to stay aware of changes in the virus. “I do not think that there is any cause for alarm,” agreed Bernard Camins, MD, an infectious disease specialist at Mount Sinai Hospital, New York.
So why the higher number of cases? “There has been an increase in COVID cases this summer, probably related to travel, socializing, and dwindling masking,” said Anne Liu, MD, an allergy, immunology, and infectious disease specialist at Stanford (Calif.) University. Even so, “because of an existing level of immunity from vaccination and prior infections, it has been limited and case severity has been lower than in prior surges.” ●
COMMENTARY
Answering the protein question when prescribing plant-based diets
Science supports the use of a whole food, predominantly plant-based dietary pattern for optimal health, including reduced risk for chronic disease, and best practice in treatment of leading chronic disease.
But clinicians who prescribe such eating patterns encounter a common concern from patients whose health may benefit.
“Where will I get my protein?”
We’ve all heard it, and it’s understandable
To ensure that patients have all the facts when making dietary decisions, clinicians need to be prepared to respond to concerns about protein adequacy and quality with evidence-based information. A good starting point for these conversations is to assess how much protein patients are already consuming. A review of the 2015-2016 National Health and Nutrition Examination Survey found that women normally consume an average of 69 g and men an average of 97 g of protein daily.
As a general point of reference, the recommended dietary allowance for protein is about 0.8 g/kg of bodyweight (or 0.36 g/lb), which equates to about 52 g of protein per day for a 145-lb woman and 65 g for a 180-lb man. But for many patients, it may be best to get a more precise recommendation based upon age, gender and physical activity level by using a handy Department of Agriculture tool for health care professionals to calculate daily protein and other nutrient needs. Patients can also use one of countless apps to track their protein and other nutrient intake. By using the tool and a tracking app, both clinician and patients can be fully informed whether protein needs are being met.
LATEST NEWS
Continuous glucose monitors for pregnant patients?
Patients with pregestational diabetes may benefit from use of a continuous subcutaneous insulin infusion pump paired with a continuous glucose monitor. Use of the tools has been associated with a reduction in maternal and neonatal morbidity, a recent study found.
“We were seeing an unacceptable burden of both maternal and fetal disease in our diabetic population,” said Neil Hamill, MD, a maternal-fetal medicine specialist at Methodist Women’s Hospital, Omaha, Neb., and an author of the study. “We thought the success with this technology in the nonpregnant population would and should translate into the pregnant population.”
Dr. Hamill and his colleagues analyzed data from 55 pregnant patients who received care at the Women’s Hospital Perinatal Center at the Nebraska Methodist Health System between October 2019 and October 2022. Everyone in the cohort had pregestational diabetes and required insulin prior to week 20 of pregnancy. They used CGMs for more than 2 weeks. The study set blood glucose levels of less than 140 mg/dL as a healthy benchmark.
Participants who had severe preeclampsia, who had delivered preterm, who had delivered a neonate with respiratory distress syndrome, and/or who had given birth to a larger-than-expected infant spent less time in the safe zone — having a blood glucose level below 140 mg/dL—than women who did not have those risk factors.
“When blood sugar control is better, maternal and fetal outcomes are improved,” Dr. Hamill said.
Neetu Sodhi, MD, an ob.gyn. at Providence Cedars-Sinai Tarzana Medical Center, Los Angeles, expressed optimism that use of blood glucose monitors and insulin pumps can improve outcomes for pregnant patients with pregestational diabetes.
“This is just another case for why it’s so important for patients to have access to these types of devices that really, really improve their outcomes and their health, and now it’s proven in the case of pregnancy outcomes too – or at least suggested strongly with this data,” Dr. Sodhi said.
Continue to: It may be time to pay attention to COVID again...
It may be time to pay attention to COVID again
More than 3 years into the COVID-19 era, most Americans have settled back into their prepandemic lifestyles. But a new dominant variant and rising hospitalization numbers may give way to another summer surge.
Since April, a new COVID variant has cropped up. According to recent Centers for Disease Control and Prevention data, EG.5—from the Omicron family—now makes up 17% of all cases in the United States, up from 7.5% in the first week of July.
A summary from the Center for Infectious Disease Research and Policy at the University of Minnesota says that EG.5, nicknamed “Eris” by health trackers, is nearly the same as its parent strain, XBB.1.9.2, but has one extra spike mutation.
Along with the news of EG.5’s growing prevalence, COVID-related hospitalization rates have increased by 12.5% during the week ending on July 29—the most significant uptick since December. Still, no connection has been made between the new variant and rising hospital admissions. And so far, experts have found no difference in the severity of illness or symptoms between Eris and the strains that came before it.
Cause for concern?
The COVID virus has a great tendency to mutate, said William Schaffner, MD, a professor of infectious diseases at Vanderbilt University, Nashville, Tenn.
“Fortunately, these are relatively minor mutations.” Even so, SARS-CoV-2, the virus that causes COVID-19, continues to be highly contagious. “There isn’t any doubt that it’s spreading—but it’s not more serious.”
So, Dr. Schaffner doesn’t think it’s time to panic. He prefers calling it an “uptick” in cases instead of a “surge,” because a surge “sounds too big.”
While the numbers are still low, compared with 2022’s summer surge, experts still urge people to stay aware of changes in the virus. “I do not think that there is any cause for alarm,” agreed Bernard Camins, MD, an infectious disease specialist at Mount Sinai Hospital, New York.
So why the higher number of cases? “There has been an increase in COVID cases this summer, probably related to travel, socializing, and dwindling masking,” said Anne Liu, MD, an allergy, immunology, and infectious disease specialist at Stanford (Calif.) University. Even so, “because of an existing level of immunity from vaccination and prior infections, it has been limited and case severity has been lower than in prior surges.” ●
COMMENTARY
Answering the protein question when prescribing plant-based diets
Science supports the use of a whole food, predominantly plant-based dietary pattern for optimal health, including reduced risk for chronic disease, and best practice in treatment of leading chronic disease.
But clinicians who prescribe such eating patterns encounter a common concern from patients whose health may benefit.
“Where will I get my protein?”
We’ve all heard it, and it’s understandable
To ensure that patients have all the facts when making dietary decisions, clinicians need to be prepared to respond to concerns about protein adequacy and quality with evidence-based information. A good starting point for these conversations is to assess how much protein patients are already consuming. A review of the 2015-2016 National Health and Nutrition Examination Survey found that women normally consume an average of 69 g and men an average of 97 g of protein daily.
As a general point of reference, the recommended dietary allowance for protein is about 0.8 g/kg of bodyweight (or 0.36 g/lb), which equates to about 52 g of protein per day for a 145-lb woman and 65 g for a 180-lb man. But for many patients, it may be best to get a more precise recommendation based upon age, gender and physical activity level by using a handy Department of Agriculture tool for health care professionals to calculate daily protein and other nutrient needs. Patients can also use one of countless apps to track their protein and other nutrient intake. By using the tool and a tracking app, both clinician and patients can be fully informed whether protein needs are being met.
LATEST NEWS
Continuous glucose monitors for pregnant patients?
Patients with pregestational diabetes may benefit from use of a continuous subcutaneous insulin infusion pump paired with a continuous glucose monitor. Use of the tools has been associated with a reduction in maternal and neonatal morbidity, a recent study found.
“We were seeing an unacceptable burden of both maternal and fetal disease in our diabetic population,” said Neil Hamill, MD, a maternal-fetal medicine specialist at Methodist Women’s Hospital, Omaha, Neb., and an author of the study. “We thought the success with this technology in the nonpregnant population would and should translate into the pregnant population.”
Dr. Hamill and his colleagues analyzed data from 55 pregnant patients who received care at the Women’s Hospital Perinatal Center at the Nebraska Methodist Health System between October 2019 and October 2022. Everyone in the cohort had pregestational diabetes and required insulin prior to week 20 of pregnancy. They used CGMs for more than 2 weeks. The study set blood glucose levels of less than 140 mg/dL as a healthy benchmark.
Participants who had severe preeclampsia, who had delivered preterm, who had delivered a neonate with respiratory distress syndrome, and/or who had given birth to a larger-than-expected infant spent less time in the safe zone — having a blood glucose level below 140 mg/dL—than women who did not have those risk factors.
“When blood sugar control is better, maternal and fetal outcomes are improved,” Dr. Hamill said.
Neetu Sodhi, MD, an ob.gyn. at Providence Cedars-Sinai Tarzana Medical Center, Los Angeles, expressed optimism that use of blood glucose monitors and insulin pumps can improve outcomes for pregnant patients with pregestational diabetes.
“This is just another case for why it’s so important for patients to have access to these types of devices that really, really improve their outcomes and their health, and now it’s proven in the case of pregnancy outcomes too – or at least suggested strongly with this data,” Dr. Sodhi said.
Continue to: It may be time to pay attention to COVID again...
It may be time to pay attention to COVID again
More than 3 years into the COVID-19 era, most Americans have settled back into their prepandemic lifestyles. But a new dominant variant and rising hospitalization numbers may give way to another summer surge.
Since April, a new COVID variant has cropped up. According to recent Centers for Disease Control and Prevention data, EG.5—from the Omicron family—now makes up 17% of all cases in the United States, up from 7.5% in the first week of July.
A summary from the Center for Infectious Disease Research and Policy at the University of Minnesota says that EG.5, nicknamed “Eris” by health trackers, is nearly the same as its parent strain, XBB.1.9.2, but has one extra spike mutation.
Along with the news of EG.5’s growing prevalence, COVID-related hospitalization rates have increased by 12.5% during the week ending on July 29—the most significant uptick since December. Still, no connection has been made between the new variant and rising hospital admissions. And so far, experts have found no difference in the severity of illness or symptoms between Eris and the strains that came before it.
Cause for concern?
The COVID virus has a great tendency to mutate, said William Schaffner, MD, a professor of infectious diseases at Vanderbilt University, Nashville, Tenn.
“Fortunately, these are relatively minor mutations.” Even so, SARS-CoV-2, the virus that causes COVID-19, continues to be highly contagious. “There isn’t any doubt that it’s spreading—but it’s not more serious.”
So, Dr. Schaffner doesn’t think it’s time to panic. He prefers calling it an “uptick” in cases instead of a “surge,” because a surge “sounds too big.”
While the numbers are still low, compared with 2022’s summer surge, experts still urge people to stay aware of changes in the virus. “I do not think that there is any cause for alarm,” agreed Bernard Camins, MD, an infectious disease specialist at Mount Sinai Hospital, New York.
So why the higher number of cases? “There has been an increase in COVID cases this summer, probably related to travel, socializing, and dwindling masking,” said Anne Liu, MD, an allergy, immunology, and infectious disease specialist at Stanford (Calif.) University. Even so, “because of an existing level of immunity from vaccination and prior infections, it has been limited and case severity has been lower than in prior surges.” ●
Two landmark papers change treatment paradigm for advanced endometrial cancer
I wanted to very briefly highlight a truly extraordinary event in my professional experience as a clinical investigator for almost 40 years in the area of the gynecologic malignancies:
In my career, of course, I’ve treated endometrial cancer, but the paradigm, the algorithms, and the strategies we’ve used have, for the most part, simply followed what we’ve done for ovarian cancer. If platinums worked in ovarian cancer, they probably worked in endometrial cancer, and that was true. If paclitaxel worked and had activity in ovarian cancer, it probably would in endometrial cancer, and that was true. It took some time, but basically, we use the same frontline chemotherapy in advanced or recurrent endometrial cancer as we’ve used in ovarian cancer, and on and on.
That world has changed, very much for the positive. Not only have pharmaceutical companies, academic investigators, and individual investigators in the community setting seen endometrial cancer as a major priority, but we have exciting new developments, and very specifically, of course, the immunotherapeutic agents known as checkpoint inhibitors.
One of these two papers was titled “Pembrolizumab Plus Chemotherapy in Advanced Endometrial Cancer” and the second one was titled “Dostarlimab for Primary Advanced or Recurrent Endometrial Cancer.” Obviously, these were separate studies, but both used checkpoint inhibitor plus the chemotherapeutic agents carboplatin-paclitaxel, compared with chemotherapy alone as frontline therapy for advanced or recurrent ovarian cancer and demonstrated a statistically significant, and in my opinion, highly clinically meaningful improvement, in progression-free survival in favor of the regimen that included the checkpoint inhibitors.
Clearly, we will need longer follow-up to see both the overall magnitude of the effect of these therapies on overall survival and the duration of the effect – the shape of the curve. Do we cure many more people? Do we delay time to progression and death? That remains to be seen.
But the outcomes we have now are remarkably positive for patients and have absolutely changed the standard of care in the management of recurrent or advanced endometrial cancer.
I should note that this includes both patients who have evidence of mismatch repair deficiency and those patients who do not have evidence of deficiency, which is a large patient population. These studies demonstrated the benefit to the entire population of patients.
However, on the basis of the data that we have – not only in endometrial cancer, but in other tumor types – the greatest impact was seen in patients with evidence of mismatch repair deficiency, where the immunotherapy agent has been shown to be most relevant; not exclusively, but most relevant.
These are very important papers. If you have an interest in endometrial cancer or immunotherapy, I would encourage you to read these papers. They change the paradigm of management for advanced endometrial cancer, and they clearly point out directions for future research in the management of this class of gynecologic cancers.
Dr. Markman is a professor in the department of medical oncology and therapeutics research at City of Hope in Duarte, Calif., and the president of Medicine & Science at City of Hope Atlanta, Chicago, and Phoenix. He reported conflicts of interest with AstraZeneca and GlaxoSmithKline.
This transcript has been edited for clarity. A version of this article first appeared on Medscape.com.
I wanted to very briefly highlight a truly extraordinary event in my professional experience as a clinical investigator for almost 40 years in the area of the gynecologic malignancies:
In my career, of course, I’ve treated endometrial cancer, but the paradigm, the algorithms, and the strategies we’ve used have, for the most part, simply followed what we’ve done for ovarian cancer. If platinums worked in ovarian cancer, they probably worked in endometrial cancer, and that was true. If paclitaxel worked and had activity in ovarian cancer, it probably would in endometrial cancer, and that was true. It took some time, but basically, we use the same frontline chemotherapy in advanced or recurrent endometrial cancer as we’ve used in ovarian cancer, and on and on.
That world has changed, very much for the positive. Not only have pharmaceutical companies, academic investigators, and individual investigators in the community setting seen endometrial cancer as a major priority, but we have exciting new developments, and very specifically, of course, the immunotherapeutic agents known as checkpoint inhibitors.
One of these two papers was titled “Pembrolizumab Plus Chemotherapy in Advanced Endometrial Cancer” and the second one was titled “Dostarlimab for Primary Advanced or Recurrent Endometrial Cancer.” Obviously, these were separate studies, but both used checkpoint inhibitor plus the chemotherapeutic agents carboplatin-paclitaxel, compared with chemotherapy alone as frontline therapy for advanced or recurrent ovarian cancer and demonstrated a statistically significant, and in my opinion, highly clinically meaningful improvement, in progression-free survival in favor of the regimen that included the checkpoint inhibitors.
Clearly, we will need longer follow-up to see both the overall magnitude of the effect of these therapies on overall survival and the duration of the effect – the shape of the curve. Do we cure many more people? Do we delay time to progression and death? That remains to be seen.
But the outcomes we have now are remarkably positive for patients and have absolutely changed the standard of care in the management of recurrent or advanced endometrial cancer.
I should note that this includes both patients who have evidence of mismatch repair deficiency and those patients who do not have evidence of deficiency, which is a large patient population. These studies demonstrated the benefit to the entire population of patients.
However, on the basis of the data that we have – not only in endometrial cancer, but in other tumor types – the greatest impact was seen in patients with evidence of mismatch repair deficiency, where the immunotherapy agent has been shown to be most relevant; not exclusively, but most relevant.
These are very important papers. If you have an interest in endometrial cancer or immunotherapy, I would encourage you to read these papers. They change the paradigm of management for advanced endometrial cancer, and they clearly point out directions for future research in the management of this class of gynecologic cancers.
Dr. Markman is a professor in the department of medical oncology and therapeutics research at City of Hope in Duarte, Calif., and the president of Medicine & Science at City of Hope Atlanta, Chicago, and Phoenix. He reported conflicts of interest with AstraZeneca and GlaxoSmithKline.
This transcript has been edited for clarity. A version of this article first appeared on Medscape.com.
I wanted to very briefly highlight a truly extraordinary event in my professional experience as a clinical investigator for almost 40 years in the area of the gynecologic malignancies:
In my career, of course, I’ve treated endometrial cancer, but the paradigm, the algorithms, and the strategies we’ve used have, for the most part, simply followed what we’ve done for ovarian cancer. If platinums worked in ovarian cancer, they probably worked in endometrial cancer, and that was true. If paclitaxel worked and had activity in ovarian cancer, it probably would in endometrial cancer, and that was true. It took some time, but basically, we use the same frontline chemotherapy in advanced or recurrent endometrial cancer as we’ve used in ovarian cancer, and on and on.
That world has changed, very much for the positive. Not only have pharmaceutical companies, academic investigators, and individual investigators in the community setting seen endometrial cancer as a major priority, but we have exciting new developments, and very specifically, of course, the immunotherapeutic agents known as checkpoint inhibitors.
One of these two papers was titled “Pembrolizumab Plus Chemotherapy in Advanced Endometrial Cancer” and the second one was titled “Dostarlimab for Primary Advanced or Recurrent Endometrial Cancer.” Obviously, these were separate studies, but both used checkpoint inhibitor plus the chemotherapeutic agents carboplatin-paclitaxel, compared with chemotherapy alone as frontline therapy for advanced or recurrent ovarian cancer and demonstrated a statistically significant, and in my opinion, highly clinically meaningful improvement, in progression-free survival in favor of the regimen that included the checkpoint inhibitors.
Clearly, we will need longer follow-up to see both the overall magnitude of the effect of these therapies on overall survival and the duration of the effect – the shape of the curve. Do we cure many more people? Do we delay time to progression and death? That remains to be seen.
But the outcomes we have now are remarkably positive for patients and have absolutely changed the standard of care in the management of recurrent or advanced endometrial cancer.
I should note that this includes both patients who have evidence of mismatch repair deficiency and those patients who do not have evidence of deficiency, which is a large patient population. These studies demonstrated the benefit to the entire population of patients.
However, on the basis of the data that we have – not only in endometrial cancer, but in other tumor types – the greatest impact was seen in patients with evidence of mismatch repair deficiency, where the immunotherapy agent has been shown to be most relevant; not exclusively, but most relevant.
These are very important papers. If you have an interest in endometrial cancer or immunotherapy, I would encourage you to read these papers. They change the paradigm of management for advanced endometrial cancer, and they clearly point out directions for future research in the management of this class of gynecologic cancers.
Dr. Markman is a professor in the department of medical oncology and therapeutics research at City of Hope in Duarte, Calif., and the president of Medicine & Science at City of Hope Atlanta, Chicago, and Phoenix. He reported conflicts of interest with AstraZeneca and GlaxoSmithKline.
This transcript has been edited for clarity. A version of this article first appeared on Medscape.com.
New risk factors for cardiovascular disease in women emerging
Multiple emerging risk factors for cardiovascular disease in women must be recognized and assessed to provide timely diagnosis and treatment, according to Dipti N. Itchhaporia, MD, an interventional cardiologist in southern California. These risk factors include pregnancy complications, autoimmune diseases, depression, breast cancer, and breast arterial calcification.
During the session titled “Cardiac Care in Women: Emerging Risk Factors” at CardioAcademic 2023, the former president of the American College of Cardiology emphasized that gender equity in care for cardiovascular disease will be achieved only when risk factors are evaluated from a gender-dependent perspective and when assessments are broadened to include novel and unrecognized risk factors, not just traditional risk factors.
Dr. Itchhaporia also remarked that
“Cardiovascular disease remains the leading cause of death in women, at least in the United States, and globally the outlook is similar,” she explained. “That’s why we need to provide our patients with guidance and carefully investigate when they experience chest pain. We need to remember that smoking and obesity pose a higher risk for cardiovascular disease in women than in men. Taking these risk factors into account will really make a difference by allowing us to provide more timely and targeted care.”
In her presentation, Dr. Itchhaporia noted that cardiovascular disease accounts for 35% of deaths in women worldwide. She reminded her audience that, according to The Lancet Women and Cardiovascular Disease Commission, heart diseases in this population remain “understudied, underrecognized, underdiagnosed, and undertreated. Furthermore, women are underrepresented in cardiovascular [clinical practice].”
She mentioned this because, despite U.S. legislation enacted between 1980 and 1990 that mandated the inclusion of women in clinical trials, women accounted for less than 39% of participants in cardiovascular clinical trials between 2010 and 2017. According to Dr. Itchhaporia, this situation limits the potential for developing tailored strategies and recommendations to treat the cardiovascular diseases affecting women.
Emerging risk factors
Dr. Itchhaporia pointed out that traditional risk factors have been known for many years. For example, 80% of women aged 75 years or younger have arterial hypertension. Only 29% receive adequate blood pressure control, those living with diabetes have a 45% greater risk of suffering ischemic heart disease, and obesity confers a 64% higher risk of developing ischemic heart disease in women versus 46% in men.
In addition to these factors, she noted that emerging factors must be assessed carefully. For example, women who experience pregnancy complications like gestational diabetes have a higher risk for ischemic heart disease and type 2 diabetes. Women with hypertension and preeclampsia are at a threefold higher risk of developing ischemic heart disease.
“Pregnancy can really be a major stress test for the heart, and I believe that, as health care professionals, we should all be asking women if they have had pregnancy-related complications. I don’t think that’s something we’ve been doing on a regular basis. Statistically, we know that 10%-20% of pregnant women report complications during pregnancy, and strong associations have been shown between gestational hypertension [and] preeclampsia.”
Dr. Itchhaporia explained that depression, a condition that globally affects women twice as much as men, is another emerging factor (though it has received some increased recognition). She explained that, in women, depression is a significant risk factor for developing a major adverse cardiovascular event or a combined event of cardiac death and myocardial infarction related to the target lesion and revascularization of the target lesion because of ischemia. Furthermore, women who have experienced a cardiac-related event are more likely to have depression than men.
“If we look into it in more detail, depression leads to changes in behavioral habits and physiological mechanisms,” she said. “Women living with depression are at higher risk of smoking, not exercising as much, are perhaps less careful with their hygiene, are not likely to adhere to their medications, and don’t sleep as well. All this moves them in the direction of heart disease.”
Added to these factors are autoimmune diseases like rheumatoid arthritis and systemic lupus erythematosus, where the female-to-male ratio for rheumatoid arthritis is 2½:1 and for lupus it’s 9:1. Dr. Itchhaporia explained that patients with rheumatoid arthritis are at two- to threefold greater risk for myocardial infarction and have a 50% higher risk for stroke. In the case of systemic lupus, the risk of myocardial infarction is 7-50 times greater than in the general population. She noted that cardiovascular risk calculators underestimate the burden of risk in patients with these diseases.
Lastly, she brought up breast cancer and breast arterial calcification as additional emerging risk factors. She explained that women with breast cancer are more likely to develop hypertension and diabetes, compared with women without this diagnosis. Women with hypertension or diabetes before developing breast cancer have twice the risk for heart problems after cancer.
She added that 12.7% of women screened for breast cancer have some degree of breast calcification. She explained that this occurs when calcium accumulates in the middle layer of artery walls in the breast, which is linked to aging, type 2 diabetes, or arterial hypertension and may be a marker of arterial stiffening, which is a cardiovascular disease.
“It’s extremely important to take into consideration data suggesting a strong association between breast calcifications and cardiovascular disease, independent of other known risk factors of cardiovascular disease. We need to improve our tests for detecting cardiovascular disease in women and we need to ask specific questions and not overlook these emerging factors,” she noted.
Improving health outcomes
Panelist María Guadalupe Parra Machuca, MD, a cardiologist in Guadalajara, Mexico, specializing in women’s heart disease, agreed that it is high time that clinical practice reflect public health policies, so that efforts to diagnose and treat cardiovascular diseases in women more effectively can transition from theory to reality.
“As physicians, we cannot allow public policy to remain outside of the reality we face,” she stressed. “We need to let it impact the decisions we make. Everything we see day to day, the things we learn at these conferences – let’s put it into practice. Otherwise, all our discussions and all the steps taken to improve care, from primary to highly specialized care and to detect and treat cardiovascular disease in women, will be nothing but rhetoric.”
Clinical cardiology specialist Victor Leal, MD, noted that, according to preliminary results from the national survey of cardiovascular risk factors in Mexican women, Mexico is no exception to these emerging risk factors for cardiovascular disease in women. More than 50% of women in Mexico have traditional risk factors, most notably hypertension, obesity, and diabetes, while hypertensive disorders of pregnancy top the list of other sex-specific risk factors.
“Not only are these factors increasing, but also having them increases the risk of a worse prognosis, leaving us with a very challenging scenario,” said Dr. Leal. “Not only do we need to educate patients about the traditional risk factors, but also about factors that might not be on our radar. We need to get women to link these factors to cardiovascular disease and to the possibility of developing much more adverse outcomes. This will reinforce our diagnosis and treatment.”
In an interview, Dr. Itchhaporia emphasized the changing face of cardiovascular disease for women, who have worse short- and long-term outcomes than men because they are not asked sex-specific questions during initial encounters and they experience greater prehospital delays.
She noted that, while experts need to raise awareness of the emerging risk factors among health care professionals, they also need to use information campaigns to make women aware of what the risks are. Then, if they experience any of the emerging risk factors, they can discuss it with their treating physicians.
“We need to assess both the traditional risk factors and the novel ones, those that are underrecognized. We need to include the history of pregnancy and complications during this period and we need to educate women about symptoms of heart disease like chest pain, difficulty breathing, and increasing fatigue,” she emphasized. “We must also provide guidance as to lifestyle, diet, and levels of physical activity and be aware of stress and symptoms of depression. Only then will we bring greater awareness to the fact that cardiovascular disease is the leading cause of death among women, and then we can reverse these trends.”
Dr. Itchhaporia, Dr. Parra, and Dr. Leal reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Multiple emerging risk factors for cardiovascular disease in women must be recognized and assessed to provide timely diagnosis and treatment, according to Dipti N. Itchhaporia, MD, an interventional cardiologist in southern California. These risk factors include pregnancy complications, autoimmune diseases, depression, breast cancer, and breast arterial calcification.
During the session titled “Cardiac Care in Women: Emerging Risk Factors” at CardioAcademic 2023, the former president of the American College of Cardiology emphasized that gender equity in care for cardiovascular disease will be achieved only when risk factors are evaluated from a gender-dependent perspective and when assessments are broadened to include novel and unrecognized risk factors, not just traditional risk factors.
Dr. Itchhaporia also remarked that
“Cardiovascular disease remains the leading cause of death in women, at least in the United States, and globally the outlook is similar,” she explained. “That’s why we need to provide our patients with guidance and carefully investigate when they experience chest pain. We need to remember that smoking and obesity pose a higher risk for cardiovascular disease in women than in men. Taking these risk factors into account will really make a difference by allowing us to provide more timely and targeted care.”
In her presentation, Dr. Itchhaporia noted that cardiovascular disease accounts for 35% of deaths in women worldwide. She reminded her audience that, according to The Lancet Women and Cardiovascular Disease Commission, heart diseases in this population remain “understudied, underrecognized, underdiagnosed, and undertreated. Furthermore, women are underrepresented in cardiovascular [clinical practice].”
She mentioned this because, despite U.S. legislation enacted between 1980 and 1990 that mandated the inclusion of women in clinical trials, women accounted for less than 39% of participants in cardiovascular clinical trials between 2010 and 2017. According to Dr. Itchhaporia, this situation limits the potential for developing tailored strategies and recommendations to treat the cardiovascular diseases affecting women.
Emerging risk factors
Dr. Itchhaporia pointed out that traditional risk factors have been known for many years. For example, 80% of women aged 75 years or younger have arterial hypertension. Only 29% receive adequate blood pressure control, those living with diabetes have a 45% greater risk of suffering ischemic heart disease, and obesity confers a 64% higher risk of developing ischemic heart disease in women versus 46% in men.
In addition to these factors, she noted that emerging factors must be assessed carefully. For example, women who experience pregnancy complications like gestational diabetes have a higher risk for ischemic heart disease and type 2 diabetes. Women with hypertension and preeclampsia are at a threefold higher risk of developing ischemic heart disease.
“Pregnancy can really be a major stress test for the heart, and I believe that, as health care professionals, we should all be asking women if they have had pregnancy-related complications. I don’t think that’s something we’ve been doing on a regular basis. Statistically, we know that 10%-20% of pregnant women report complications during pregnancy, and strong associations have been shown between gestational hypertension [and] preeclampsia.”
Dr. Itchhaporia explained that depression, a condition that globally affects women twice as much as men, is another emerging factor (though it has received some increased recognition). She explained that, in women, depression is a significant risk factor for developing a major adverse cardiovascular event or a combined event of cardiac death and myocardial infarction related to the target lesion and revascularization of the target lesion because of ischemia. Furthermore, women who have experienced a cardiac-related event are more likely to have depression than men.
“If we look into it in more detail, depression leads to changes in behavioral habits and physiological mechanisms,” she said. “Women living with depression are at higher risk of smoking, not exercising as much, are perhaps less careful with their hygiene, are not likely to adhere to their medications, and don’t sleep as well. All this moves them in the direction of heart disease.”
Added to these factors are autoimmune diseases like rheumatoid arthritis and systemic lupus erythematosus, where the female-to-male ratio for rheumatoid arthritis is 2½:1 and for lupus it’s 9:1. Dr. Itchhaporia explained that patients with rheumatoid arthritis are at two- to threefold greater risk for myocardial infarction and have a 50% higher risk for stroke. In the case of systemic lupus, the risk of myocardial infarction is 7-50 times greater than in the general population. She noted that cardiovascular risk calculators underestimate the burden of risk in patients with these diseases.
Lastly, she brought up breast cancer and breast arterial calcification as additional emerging risk factors. She explained that women with breast cancer are more likely to develop hypertension and diabetes, compared with women without this diagnosis. Women with hypertension or diabetes before developing breast cancer have twice the risk for heart problems after cancer.
She added that 12.7% of women screened for breast cancer have some degree of breast calcification. She explained that this occurs when calcium accumulates in the middle layer of artery walls in the breast, which is linked to aging, type 2 diabetes, or arterial hypertension and may be a marker of arterial stiffening, which is a cardiovascular disease.
“It’s extremely important to take into consideration data suggesting a strong association between breast calcifications and cardiovascular disease, independent of other known risk factors of cardiovascular disease. We need to improve our tests for detecting cardiovascular disease in women and we need to ask specific questions and not overlook these emerging factors,” she noted.
Improving health outcomes
Panelist María Guadalupe Parra Machuca, MD, a cardiologist in Guadalajara, Mexico, specializing in women’s heart disease, agreed that it is high time that clinical practice reflect public health policies, so that efforts to diagnose and treat cardiovascular diseases in women more effectively can transition from theory to reality.
“As physicians, we cannot allow public policy to remain outside of the reality we face,” she stressed. “We need to let it impact the decisions we make. Everything we see day to day, the things we learn at these conferences – let’s put it into practice. Otherwise, all our discussions and all the steps taken to improve care, from primary to highly specialized care and to detect and treat cardiovascular disease in women, will be nothing but rhetoric.”
Clinical cardiology specialist Victor Leal, MD, noted that, according to preliminary results from the national survey of cardiovascular risk factors in Mexican women, Mexico is no exception to these emerging risk factors for cardiovascular disease in women. More than 50% of women in Mexico have traditional risk factors, most notably hypertension, obesity, and diabetes, while hypertensive disorders of pregnancy top the list of other sex-specific risk factors.
“Not only are these factors increasing, but also having them increases the risk of a worse prognosis, leaving us with a very challenging scenario,” said Dr. Leal. “Not only do we need to educate patients about the traditional risk factors, but also about factors that might not be on our radar. We need to get women to link these factors to cardiovascular disease and to the possibility of developing much more adverse outcomes. This will reinforce our diagnosis and treatment.”
In an interview, Dr. Itchhaporia emphasized the changing face of cardiovascular disease for women, who have worse short- and long-term outcomes than men because they are not asked sex-specific questions during initial encounters and they experience greater prehospital delays.
She noted that, while experts need to raise awareness of the emerging risk factors among health care professionals, they also need to use information campaigns to make women aware of what the risks are. Then, if they experience any of the emerging risk factors, they can discuss it with their treating physicians.
“We need to assess both the traditional risk factors and the novel ones, those that are underrecognized. We need to include the history of pregnancy and complications during this period and we need to educate women about symptoms of heart disease like chest pain, difficulty breathing, and increasing fatigue,” she emphasized. “We must also provide guidance as to lifestyle, diet, and levels of physical activity and be aware of stress and symptoms of depression. Only then will we bring greater awareness to the fact that cardiovascular disease is the leading cause of death among women, and then we can reverse these trends.”
Dr. Itchhaporia, Dr. Parra, and Dr. Leal reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Multiple emerging risk factors for cardiovascular disease in women must be recognized and assessed to provide timely diagnosis and treatment, according to Dipti N. Itchhaporia, MD, an interventional cardiologist in southern California. These risk factors include pregnancy complications, autoimmune diseases, depression, breast cancer, and breast arterial calcification.
During the session titled “Cardiac Care in Women: Emerging Risk Factors” at CardioAcademic 2023, the former president of the American College of Cardiology emphasized that gender equity in care for cardiovascular disease will be achieved only when risk factors are evaluated from a gender-dependent perspective and when assessments are broadened to include novel and unrecognized risk factors, not just traditional risk factors.
Dr. Itchhaporia also remarked that
“Cardiovascular disease remains the leading cause of death in women, at least in the United States, and globally the outlook is similar,” she explained. “That’s why we need to provide our patients with guidance and carefully investigate when they experience chest pain. We need to remember that smoking and obesity pose a higher risk for cardiovascular disease in women than in men. Taking these risk factors into account will really make a difference by allowing us to provide more timely and targeted care.”
In her presentation, Dr. Itchhaporia noted that cardiovascular disease accounts for 35% of deaths in women worldwide. She reminded her audience that, according to The Lancet Women and Cardiovascular Disease Commission, heart diseases in this population remain “understudied, underrecognized, underdiagnosed, and undertreated. Furthermore, women are underrepresented in cardiovascular [clinical practice].”
She mentioned this because, despite U.S. legislation enacted between 1980 and 1990 that mandated the inclusion of women in clinical trials, women accounted for less than 39% of participants in cardiovascular clinical trials between 2010 and 2017. According to Dr. Itchhaporia, this situation limits the potential for developing tailored strategies and recommendations to treat the cardiovascular diseases affecting women.
Emerging risk factors
Dr. Itchhaporia pointed out that traditional risk factors have been known for many years. For example, 80% of women aged 75 years or younger have arterial hypertension. Only 29% receive adequate blood pressure control, those living with diabetes have a 45% greater risk of suffering ischemic heart disease, and obesity confers a 64% higher risk of developing ischemic heart disease in women versus 46% in men.
In addition to these factors, she noted that emerging factors must be assessed carefully. For example, women who experience pregnancy complications like gestational diabetes have a higher risk for ischemic heart disease and type 2 diabetes. Women with hypertension and preeclampsia are at a threefold higher risk of developing ischemic heart disease.
“Pregnancy can really be a major stress test for the heart, and I believe that, as health care professionals, we should all be asking women if they have had pregnancy-related complications. I don’t think that’s something we’ve been doing on a regular basis. Statistically, we know that 10%-20% of pregnant women report complications during pregnancy, and strong associations have been shown between gestational hypertension [and] preeclampsia.”
Dr. Itchhaporia explained that depression, a condition that globally affects women twice as much as men, is another emerging factor (though it has received some increased recognition). She explained that, in women, depression is a significant risk factor for developing a major adverse cardiovascular event or a combined event of cardiac death and myocardial infarction related to the target lesion and revascularization of the target lesion because of ischemia. Furthermore, women who have experienced a cardiac-related event are more likely to have depression than men.
“If we look into it in more detail, depression leads to changes in behavioral habits and physiological mechanisms,” she said. “Women living with depression are at higher risk of smoking, not exercising as much, are perhaps less careful with their hygiene, are not likely to adhere to their medications, and don’t sleep as well. All this moves them in the direction of heart disease.”
Added to these factors are autoimmune diseases like rheumatoid arthritis and systemic lupus erythematosus, where the female-to-male ratio for rheumatoid arthritis is 2½:1 and for lupus it’s 9:1. Dr. Itchhaporia explained that patients with rheumatoid arthritis are at two- to threefold greater risk for myocardial infarction and have a 50% higher risk for stroke. In the case of systemic lupus, the risk of myocardial infarction is 7-50 times greater than in the general population. She noted that cardiovascular risk calculators underestimate the burden of risk in patients with these diseases.
Lastly, she brought up breast cancer and breast arterial calcification as additional emerging risk factors. She explained that women with breast cancer are more likely to develop hypertension and diabetes, compared with women without this diagnosis. Women with hypertension or diabetes before developing breast cancer have twice the risk for heart problems after cancer.
She added that 12.7% of women screened for breast cancer have some degree of breast calcification. She explained that this occurs when calcium accumulates in the middle layer of artery walls in the breast, which is linked to aging, type 2 diabetes, or arterial hypertension and may be a marker of arterial stiffening, which is a cardiovascular disease.
“It’s extremely important to take into consideration data suggesting a strong association between breast calcifications and cardiovascular disease, independent of other known risk factors of cardiovascular disease. We need to improve our tests for detecting cardiovascular disease in women and we need to ask specific questions and not overlook these emerging factors,” she noted.
Improving health outcomes
Panelist María Guadalupe Parra Machuca, MD, a cardiologist in Guadalajara, Mexico, specializing in women’s heart disease, agreed that it is high time that clinical practice reflect public health policies, so that efforts to diagnose and treat cardiovascular diseases in women more effectively can transition from theory to reality.
“As physicians, we cannot allow public policy to remain outside of the reality we face,” she stressed. “We need to let it impact the decisions we make. Everything we see day to day, the things we learn at these conferences – let’s put it into practice. Otherwise, all our discussions and all the steps taken to improve care, from primary to highly specialized care and to detect and treat cardiovascular disease in women, will be nothing but rhetoric.”
Clinical cardiology specialist Victor Leal, MD, noted that, according to preliminary results from the national survey of cardiovascular risk factors in Mexican women, Mexico is no exception to these emerging risk factors for cardiovascular disease in women. More than 50% of women in Mexico have traditional risk factors, most notably hypertension, obesity, and diabetes, while hypertensive disorders of pregnancy top the list of other sex-specific risk factors.
“Not only are these factors increasing, but also having them increases the risk of a worse prognosis, leaving us with a very challenging scenario,” said Dr. Leal. “Not only do we need to educate patients about the traditional risk factors, but also about factors that might not be on our radar. We need to get women to link these factors to cardiovascular disease and to the possibility of developing much more adverse outcomes. This will reinforce our diagnosis and treatment.”
In an interview, Dr. Itchhaporia emphasized the changing face of cardiovascular disease for women, who have worse short- and long-term outcomes than men because they are not asked sex-specific questions during initial encounters and they experience greater prehospital delays.
She noted that, while experts need to raise awareness of the emerging risk factors among health care professionals, they also need to use information campaigns to make women aware of what the risks are. Then, if they experience any of the emerging risk factors, they can discuss it with their treating physicians.
“We need to assess both the traditional risk factors and the novel ones, those that are underrecognized. We need to include the history of pregnancy and complications during this period and we need to educate women about symptoms of heart disease like chest pain, difficulty breathing, and increasing fatigue,” she emphasized. “We must also provide guidance as to lifestyle, diet, and levels of physical activity and be aware of stress and symptoms of depression. Only then will we bring greater awareness to the fact that cardiovascular disease is the leading cause of death among women, and then we can reverse these trends.”
Dr. Itchhaporia, Dr. Parra, and Dr. Leal reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CARDIOACADEMIC 2023
Surgery approach may improve survival in advanced ovarian cancer
TOPLINE:
Neoadjuvant chemotherapy followed by interval cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (HIPEC) significantly improves progression-free survival (PFS) and overall survival, compared with interval cytoreductive surgery alone, in patients with advanced ovarian cancer, new research shows.
METHODOLOGY:
- Several randomized controlled trials have shown survival benefits with HIPEC followed by interval cytoreductive surgery in advanced ovarian cancer. Despite the data, the use of HIPEC in clinical practice remains limited.
- Potential downsides of HIPEC include longer operative time and treatment-related complications.
- This prospective, multicenter, comparative effectiveness study evaluated the safety and effectiveness of interval cytoreductive surgery with HIPEC versus the surgery alone.
- The study, conducted at seven Korean Gynecologic Oncology Group institutions, included 196 patients (mean age, 58 years) with stage III or IV ovarian cancer who had received at least three cycles of neoadjuvant chemotherapy followed by interval cytoreductive surgery with HIPEC (n = 109) or without HIPEC (n = 87).
- The researchers reported progression-free survival as well as overall survival and treatment-related toxic effects.
TAKEAWAY:
- During a median follow-up of 28.2 months, 128 patients (65%) had a recurrence and 30 died (15.3%) – 8.3% in the HIPEC group and 24.1% in the non-HIPEC group.
- Compared with no HIPEC, interval cytoreductive surgery with HIPEC led to a significant improvement in median PFS (22.9 months vs. 14.2 months; P = .005) and median overall survival (not reached vs. 53 months; P = .002).
- The frequency of grade 3 or 4 postoperative complications was similar in both groups: 2.8% with HIPEC versus 3.4% without HIPEC.
- Among patients with recurrence, the frequency of peritoneal recurrence was significantly lower among those who received HIPEC (32.8% vs. 64.1% without HIPEC; P = .001).
IN PRACTICE:
“We observed a significantly superior survival benefit associated with [interval cytoreductive surgery] with HIPEC, without higher rates of postoperative complications,” the authors concluded, adding that “the survival benefit remained consistent, irrespective of maintenance therapy.”
SOURCE:
The study, led by Jung-Yun Lee, MD, PhD, Yonsei University College of Medicine, Seoul, Korea, was published online in JAMA Surgery.
LIMITATIONS:
The patients were not randomly assigned and the decision to give HIPEC was at the clinician’s discretion, introducing the possibility of selection and treatment bias. The different types of drugs used in HIPEC could result in bias in data interpretation.
DISCLOSURES:
The authors reported no conflicts of interest. The study had no specific funding.
A version of this article first appeared on Medscape.com.
TOPLINE:
Neoadjuvant chemotherapy followed by interval cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (HIPEC) significantly improves progression-free survival (PFS) and overall survival, compared with interval cytoreductive surgery alone, in patients with advanced ovarian cancer, new research shows.
METHODOLOGY:
- Several randomized controlled trials have shown survival benefits with HIPEC followed by interval cytoreductive surgery in advanced ovarian cancer. Despite the data, the use of HIPEC in clinical practice remains limited.
- Potential downsides of HIPEC include longer operative time and treatment-related complications.
- This prospective, multicenter, comparative effectiveness study evaluated the safety and effectiveness of interval cytoreductive surgery with HIPEC versus the surgery alone.
- The study, conducted at seven Korean Gynecologic Oncology Group institutions, included 196 patients (mean age, 58 years) with stage III or IV ovarian cancer who had received at least three cycles of neoadjuvant chemotherapy followed by interval cytoreductive surgery with HIPEC (n = 109) or without HIPEC (n = 87).
- The researchers reported progression-free survival as well as overall survival and treatment-related toxic effects.
TAKEAWAY:
- During a median follow-up of 28.2 months, 128 patients (65%) had a recurrence and 30 died (15.3%) – 8.3% in the HIPEC group and 24.1% in the non-HIPEC group.
- Compared with no HIPEC, interval cytoreductive surgery with HIPEC led to a significant improvement in median PFS (22.9 months vs. 14.2 months; P = .005) and median overall survival (not reached vs. 53 months; P = .002).
- The frequency of grade 3 or 4 postoperative complications was similar in both groups: 2.8% with HIPEC versus 3.4% without HIPEC.
- Among patients with recurrence, the frequency of peritoneal recurrence was significantly lower among those who received HIPEC (32.8% vs. 64.1% without HIPEC; P = .001).
IN PRACTICE:
“We observed a significantly superior survival benefit associated with [interval cytoreductive surgery] with HIPEC, without higher rates of postoperative complications,” the authors concluded, adding that “the survival benefit remained consistent, irrespective of maintenance therapy.”
SOURCE:
The study, led by Jung-Yun Lee, MD, PhD, Yonsei University College of Medicine, Seoul, Korea, was published online in JAMA Surgery.
LIMITATIONS:
The patients were not randomly assigned and the decision to give HIPEC was at the clinician’s discretion, introducing the possibility of selection and treatment bias. The different types of drugs used in HIPEC could result in bias in data interpretation.
DISCLOSURES:
The authors reported no conflicts of interest. The study had no specific funding.
A version of this article first appeared on Medscape.com.
TOPLINE:
Neoadjuvant chemotherapy followed by interval cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (HIPEC) significantly improves progression-free survival (PFS) and overall survival, compared with interval cytoreductive surgery alone, in patients with advanced ovarian cancer, new research shows.
METHODOLOGY:
- Several randomized controlled trials have shown survival benefits with HIPEC followed by interval cytoreductive surgery in advanced ovarian cancer. Despite the data, the use of HIPEC in clinical practice remains limited.
- Potential downsides of HIPEC include longer operative time and treatment-related complications.
- This prospective, multicenter, comparative effectiveness study evaluated the safety and effectiveness of interval cytoreductive surgery with HIPEC versus the surgery alone.
- The study, conducted at seven Korean Gynecologic Oncology Group institutions, included 196 patients (mean age, 58 years) with stage III or IV ovarian cancer who had received at least three cycles of neoadjuvant chemotherapy followed by interval cytoreductive surgery with HIPEC (n = 109) or without HIPEC (n = 87).
- The researchers reported progression-free survival as well as overall survival and treatment-related toxic effects.
TAKEAWAY:
- During a median follow-up of 28.2 months, 128 patients (65%) had a recurrence and 30 died (15.3%) – 8.3% in the HIPEC group and 24.1% in the non-HIPEC group.
- Compared with no HIPEC, interval cytoreductive surgery with HIPEC led to a significant improvement in median PFS (22.9 months vs. 14.2 months; P = .005) and median overall survival (not reached vs. 53 months; P = .002).
- The frequency of grade 3 or 4 postoperative complications was similar in both groups: 2.8% with HIPEC versus 3.4% without HIPEC.
- Among patients with recurrence, the frequency of peritoneal recurrence was significantly lower among those who received HIPEC (32.8% vs. 64.1% without HIPEC; P = .001).
IN PRACTICE:
“We observed a significantly superior survival benefit associated with [interval cytoreductive surgery] with HIPEC, without higher rates of postoperative complications,” the authors concluded, adding that “the survival benefit remained consistent, irrespective of maintenance therapy.”
SOURCE:
The study, led by Jung-Yun Lee, MD, PhD, Yonsei University College of Medicine, Seoul, Korea, was published online in JAMA Surgery.
LIMITATIONS:
The patients were not randomly assigned and the decision to give HIPEC was at the clinician’s discretion, introducing the possibility of selection and treatment bias. The different types of drugs used in HIPEC could result in bias in data interpretation.
DISCLOSURES:
The authors reported no conflicts of interest. The study had no specific funding.
A version of this article first appeared on Medscape.com.
FROM JAMA SURGERY