User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Ob.gyns. reveal heavier suicide ideation burden than most specialists
Obstetricians and gynecologists are more likely than most specialists to have thoughts of suicide, and almost of quarter of physicians in general reported that they were depressed in a recent survey conducted by Medscape.
“Too much work with too little control is a recipe for depression in anyone,” Andrea Giedinghagen, MD, of Washington University, St. Louis, said in the Medscape Physician Suicide Report: Doctors’ Burden 2023. “Physicians are also still coping with a pandemic – the trauma from COVID-19 didn’t disappear just because the full ICUs did – and with a fractured health care system that virtually guarantees moral distress.”
About 23% of the almost 9,200 survey respondents said that they were depressed in 2022, compared with 21% the previous year. Suicide ideation was down in 2022, however, with 9% of all responding physicians reporting contemplation versus 13% in 2021, based on the results of the latest survey, which was conducted from June 28, 2022, to Oct. 2, 2022.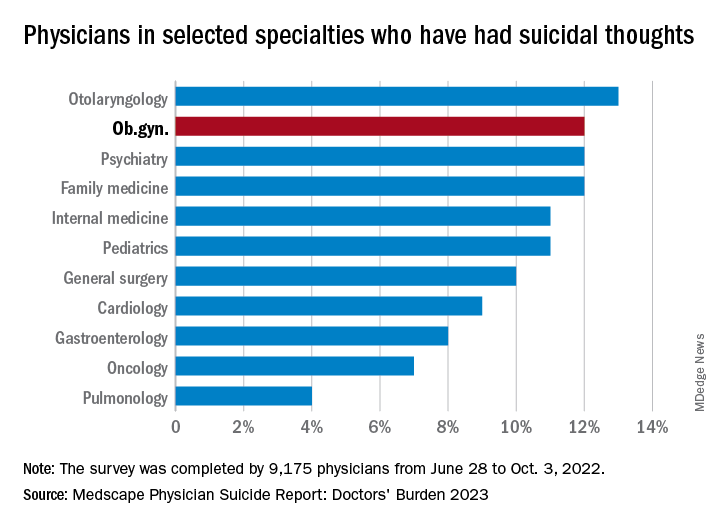
Ob.gyns. were above that average, with 12% reporting suicidal thoughts over the past year, equaling psychiatrists, family physicians, anesthesiologists, and emergency physicians and trailing only the otolaryngologists at 13%. The lowest rate among the 29 specialties included in the report was 4% for pulmonary medicine.
Differences between physicians, general population
Comparisons with the general U.S. population show that physicians are about twice as likely to report thoughts of suicide (9% vs. 4.9%) and to attempt it (1% vs. 0.5%). Among the overall population, however, “females are two to three times more likely to attempt suicide than males are,” noted Perry Lin, MD, national cochair of the American Association of Suicidology’s Physician Suicide Awareness Committee. That was not the case for survey respondents, as men and women both had an attempt rate of 1% and women were slightly ahead in ideation (11% to 9%).
There was a somewhat larger gap when age group was considered. Among physicians aged 57-75 years, 8% had thought about suicide, compared with 10% of those aged 42-56 years and 12% of respondents aged 27-41. This, again, runs counter to the general population, where older men typically deal with higher suicide rates, Michael F. Myers of the State University of New York, Brooklyn, said in the Medscape report.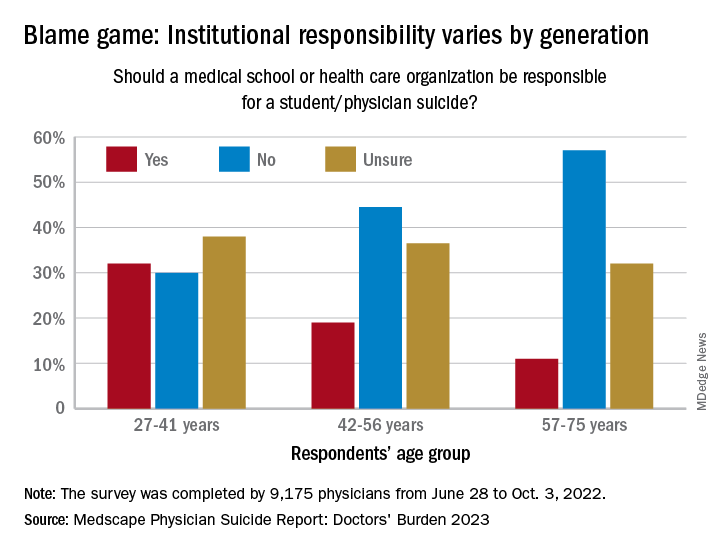
Age also was a factor when responsibility was brought into the equation. Over 30% of the youngest group of respondents (age 27-41) said that medical schools and health care organizations should be held responsible for an individual’s suicide, compared with 19% of those aged 42-56 and 11% of the 57- to 75-year-olds.
That trend was concerning to Dr. Myers: “Most suicides are multifactorial, many stressors coming together all at once in a person’s life, a so-called ‘perfect storm.’ ... But there are suicides each year involving medical students and physicians that have nothing to do with the medical school or place of work.”
Reasons to avoid professional help
Many of the survey respondents also were thinking about third parties when asked why they might not seek professional help for their suicidal thoughts. The most common response, cited by 52%, was that they didn’t need professional help, but 42% didn’t want to risk disclosure to a medical board, 33% were concerned about it being on their insurance record, and 25% were concerned about colleagues finding out.
“Doctors are willing and able to treat suicidal ideation among patients but appear fearful to seek such help themselves. We must do better,” Dr. Lin said in an interview.
Exact numbers of survey respondents were not given by specialty, but about 5% of the 9,175 total responses were completed by ob.gyns. The margin of error for the survey was ±1.02% at the 95% confidence interval.
Obstetricians and gynecologists are more likely than most specialists to have thoughts of suicide, and almost of quarter of physicians in general reported that they were depressed in a recent survey conducted by Medscape.
“Too much work with too little control is a recipe for depression in anyone,” Andrea Giedinghagen, MD, of Washington University, St. Louis, said in the Medscape Physician Suicide Report: Doctors’ Burden 2023. “Physicians are also still coping with a pandemic – the trauma from COVID-19 didn’t disappear just because the full ICUs did – and with a fractured health care system that virtually guarantees moral distress.”
About 23% of the almost 9,200 survey respondents said that they were depressed in 2022, compared with 21% the previous year. Suicide ideation was down in 2022, however, with 9% of all responding physicians reporting contemplation versus 13% in 2021, based on the results of the latest survey, which was conducted from June 28, 2022, to Oct. 2, 2022.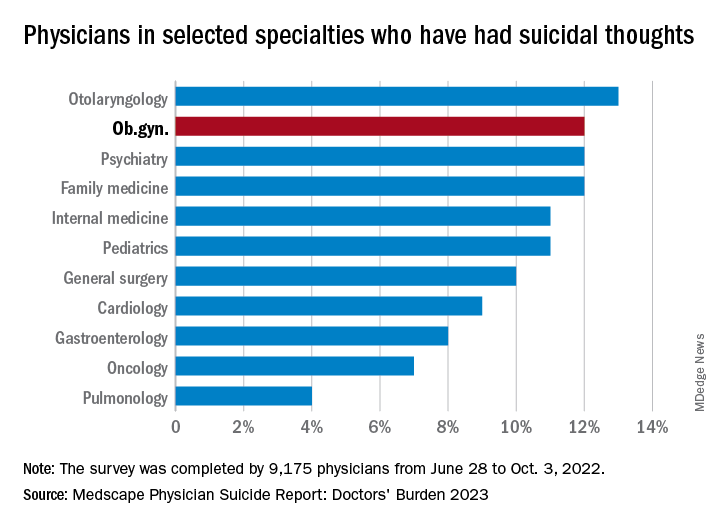
Ob.gyns. were above that average, with 12% reporting suicidal thoughts over the past year, equaling psychiatrists, family physicians, anesthesiologists, and emergency physicians and trailing only the otolaryngologists at 13%. The lowest rate among the 29 specialties included in the report was 4% for pulmonary medicine.
Differences between physicians, general population
Comparisons with the general U.S. population show that physicians are about twice as likely to report thoughts of suicide (9% vs. 4.9%) and to attempt it (1% vs. 0.5%). Among the overall population, however, “females are two to three times more likely to attempt suicide than males are,” noted Perry Lin, MD, national cochair of the American Association of Suicidology’s Physician Suicide Awareness Committee. That was not the case for survey respondents, as men and women both had an attempt rate of 1% and women were slightly ahead in ideation (11% to 9%).
There was a somewhat larger gap when age group was considered. Among physicians aged 57-75 years, 8% had thought about suicide, compared with 10% of those aged 42-56 years and 12% of respondents aged 27-41. This, again, runs counter to the general population, where older men typically deal with higher suicide rates, Michael F. Myers of the State University of New York, Brooklyn, said in the Medscape report.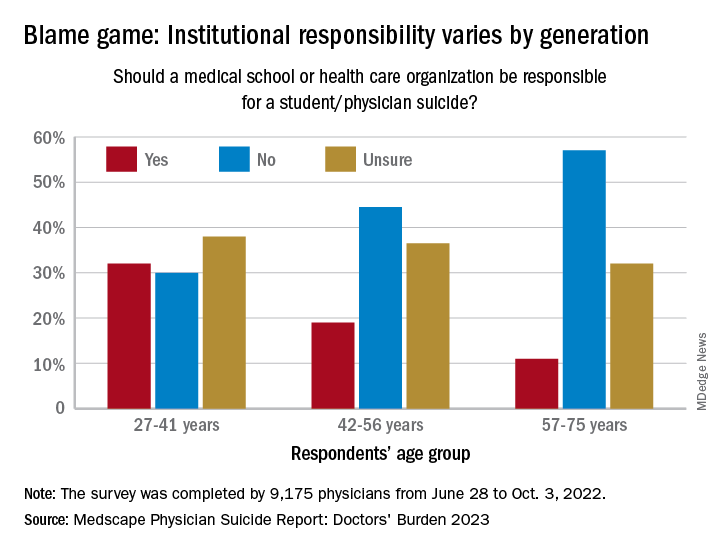
Age also was a factor when responsibility was brought into the equation. Over 30% of the youngest group of respondents (age 27-41) said that medical schools and health care organizations should be held responsible for an individual’s suicide, compared with 19% of those aged 42-56 and 11% of the 57- to 75-year-olds.
That trend was concerning to Dr. Myers: “Most suicides are multifactorial, many stressors coming together all at once in a person’s life, a so-called ‘perfect storm.’ ... But there are suicides each year involving medical students and physicians that have nothing to do with the medical school or place of work.”
Reasons to avoid professional help
Many of the survey respondents also were thinking about third parties when asked why they might not seek professional help for their suicidal thoughts. The most common response, cited by 52%, was that they didn’t need professional help, but 42% didn’t want to risk disclosure to a medical board, 33% were concerned about it being on their insurance record, and 25% were concerned about colleagues finding out.
“Doctors are willing and able to treat suicidal ideation among patients but appear fearful to seek such help themselves. We must do better,” Dr. Lin said in an interview.
Exact numbers of survey respondents were not given by specialty, but about 5% of the 9,175 total responses were completed by ob.gyns. The margin of error for the survey was ±1.02% at the 95% confidence interval.
Obstetricians and gynecologists are more likely than most specialists to have thoughts of suicide, and almost of quarter of physicians in general reported that they were depressed in a recent survey conducted by Medscape.
“Too much work with too little control is a recipe for depression in anyone,” Andrea Giedinghagen, MD, of Washington University, St. Louis, said in the Medscape Physician Suicide Report: Doctors’ Burden 2023. “Physicians are also still coping with a pandemic – the trauma from COVID-19 didn’t disappear just because the full ICUs did – and with a fractured health care system that virtually guarantees moral distress.”
About 23% of the almost 9,200 survey respondents said that they were depressed in 2022, compared with 21% the previous year. Suicide ideation was down in 2022, however, with 9% of all responding physicians reporting contemplation versus 13% in 2021, based on the results of the latest survey, which was conducted from June 28, 2022, to Oct. 2, 2022.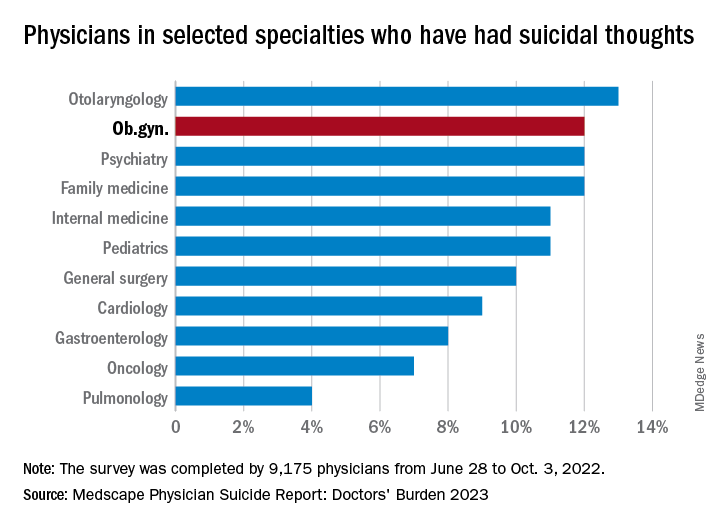
Ob.gyns. were above that average, with 12% reporting suicidal thoughts over the past year, equaling psychiatrists, family physicians, anesthesiologists, and emergency physicians and trailing only the otolaryngologists at 13%. The lowest rate among the 29 specialties included in the report was 4% for pulmonary medicine.
Differences between physicians, general population
Comparisons with the general U.S. population show that physicians are about twice as likely to report thoughts of suicide (9% vs. 4.9%) and to attempt it (1% vs. 0.5%). Among the overall population, however, “females are two to three times more likely to attempt suicide than males are,” noted Perry Lin, MD, national cochair of the American Association of Suicidology’s Physician Suicide Awareness Committee. That was not the case for survey respondents, as men and women both had an attempt rate of 1% and women were slightly ahead in ideation (11% to 9%).
There was a somewhat larger gap when age group was considered. Among physicians aged 57-75 years, 8% had thought about suicide, compared with 10% of those aged 42-56 years and 12% of respondents aged 27-41. This, again, runs counter to the general population, where older men typically deal with higher suicide rates, Michael F. Myers of the State University of New York, Brooklyn, said in the Medscape report.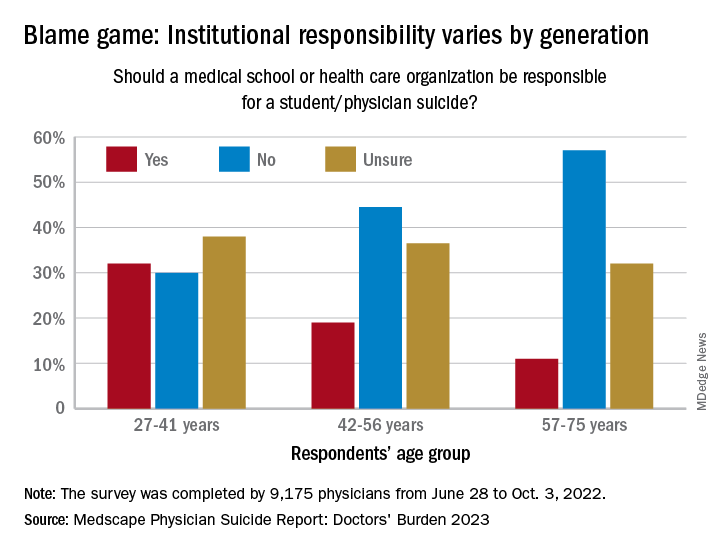
Age also was a factor when responsibility was brought into the equation. Over 30% of the youngest group of respondents (age 27-41) said that medical schools and health care organizations should be held responsible for an individual’s suicide, compared with 19% of those aged 42-56 and 11% of the 57- to 75-year-olds.
That trend was concerning to Dr. Myers: “Most suicides are multifactorial, many stressors coming together all at once in a person’s life, a so-called ‘perfect storm.’ ... But there are suicides each year involving medical students and physicians that have nothing to do with the medical school or place of work.”
Reasons to avoid professional help
Many of the survey respondents also were thinking about third parties when asked why they might not seek professional help for their suicidal thoughts. The most common response, cited by 52%, was that they didn’t need professional help, but 42% didn’t want to risk disclosure to a medical board, 33% were concerned about it being on their insurance record, and 25% were concerned about colleagues finding out.
“Doctors are willing and able to treat suicidal ideation among patients but appear fearful to seek such help themselves. We must do better,” Dr. Lin said in an interview.
Exact numbers of survey respondents were not given by specialty, but about 5% of the 9,175 total responses were completed by ob.gyns. The margin of error for the survey was ±1.02% at the 95% confidence interval.
In utero exposure to asthma medication not tied to risks of neurodevelopmental disorders
The drugs included in the study were leukotriene-receptor antagonists (LTRAs), which are often used to treat allergic airway diseases, including asthma and allergic rhinitis.
“Over the years, the U.S. Food and Drug Administration has monitored post-marketing data about the potential harm of neuropsychiatric events (NEs) associated with montelukast, the first type of LTRAs, and issued boxed warnings about serious mental health side effects for montelukast in 2020,” said corresponding author Tsung-Chieh Yao, MD, of Chang Gung Memorial Hospital, Taiwan, in an interview.
However, evidence of a link between NEs and LTRA use has been inconsistent, according to Dr. Yao and colleagues.
“To date, it remains totally unknown whether the exposure to LTRAs during pregnancy is associated with the risk of neuropsychiatric events in offspring,” said Dr. Yao.
To address this question, the researchers used data from National Health Insurance Research Database in Taiwan to identify pregnant women and their offspring from 2009 to 2019. The initial study population included 576,157 mother-offspring pairs, including 1,995 LTRA-exposed and 574,162 nonexposed children.
The women had a diagnosis of asthma or allergic rhinitis; multiple births and children with congenital malformations were excluded. LTRA exposure was defined as any dispensed prescription for LTRAs during pregnancy. Approximately two-thirds of the mothers were aged 30-40 years at the time of delivery.
The findings were published in a research letter in JAMA Network Open.
In the study population at large, the incidence of the three neurodevelopmental disorders ADHD, autism spectrum disorder (ASD), and Tourette syndrome was not significantly different between those children exposed to LTRAs and those not exposed to LTRAs in utero (1.25% vs. 1.32%; 3.31% vs. 4.36%; and 0.45% vs. 0.83%, respectively).
After propensity score matching, the study population included 1,988 LTRA-exposed children and 19,863 nonexposed children. In this group, no significant associations appeared between prenatal LTRA exposure and the risk of attention-deficit/hyperactivity disorder (adjusted hazard ratio, 1.03), autism spectrum disorder (AHR, 1.01), and Tourette syndrome (AHR, 0.63).
Neither duration nor cumulative dose of LTRA use during pregnancy showed an association with ADHD, ASD, or Tourette syndrome in offspring. Duration of LTRA use was categorized as shorter or longer periods of 1-4 weeks vs. more than 4 weeks; cumulative dose was categorized as 1-170 mg vs. 170 mg or higher.
The findings were limited by the lack of randomization, inability to detect long-term risk, and potential lack of generalizability to non-Asian populations, and more research is needed to replicate the results, the researchers noted. However, the current findings were strengthened by the large study population, and suggest that LTRA use in pregnancy does not present a significant risk for NEs in children, which should be reassuring to clinicians and patients, they concluded.
The current study is the first to use the whole of Taiwan population data and extends previous studies by examining the association between LTRA use during pregnancy and risk of neuropsychiatric events in offspring, Dr. Yao said in an interview. “The possibly surprising, but reassuring, finding is that prenatal LTRA exposure did not increase risk of ADHD, ASD, and Tourette syndrome in offspring,” he said.
“Clinicians prescribing LTRAs such as montelukast (Singulair and generics) to pregnant women with asthma or allergic rhinitis may be reassured by our findings,” Dr. Yao added. The results offer real-world evidence to help inform decision-making about the use of LTRAs during pregnancy, although additional research is needed to replicate the study findings in other populations, he said.
The study was supported by the National Health Research Institutes, Taiwan, the Ministry of Science and Technology of Taiwan, the National Science and Technology Council of Taiwan, and the Chang Gung Medical Foundation. The researchers had no financial conflicts to disclose.
The drugs included in the study were leukotriene-receptor antagonists (LTRAs), which are often used to treat allergic airway diseases, including asthma and allergic rhinitis.
“Over the years, the U.S. Food and Drug Administration has monitored post-marketing data about the potential harm of neuropsychiatric events (NEs) associated with montelukast, the first type of LTRAs, and issued boxed warnings about serious mental health side effects for montelukast in 2020,” said corresponding author Tsung-Chieh Yao, MD, of Chang Gung Memorial Hospital, Taiwan, in an interview.
However, evidence of a link between NEs and LTRA use has been inconsistent, according to Dr. Yao and colleagues.
“To date, it remains totally unknown whether the exposure to LTRAs during pregnancy is associated with the risk of neuropsychiatric events in offspring,” said Dr. Yao.
To address this question, the researchers used data from National Health Insurance Research Database in Taiwan to identify pregnant women and their offspring from 2009 to 2019. The initial study population included 576,157 mother-offspring pairs, including 1,995 LTRA-exposed and 574,162 nonexposed children.
The women had a diagnosis of asthma or allergic rhinitis; multiple births and children with congenital malformations were excluded. LTRA exposure was defined as any dispensed prescription for LTRAs during pregnancy. Approximately two-thirds of the mothers were aged 30-40 years at the time of delivery.
The findings were published in a research letter in JAMA Network Open.
In the study population at large, the incidence of the three neurodevelopmental disorders ADHD, autism spectrum disorder (ASD), and Tourette syndrome was not significantly different between those children exposed to LTRAs and those not exposed to LTRAs in utero (1.25% vs. 1.32%; 3.31% vs. 4.36%; and 0.45% vs. 0.83%, respectively).
After propensity score matching, the study population included 1,988 LTRA-exposed children and 19,863 nonexposed children. In this group, no significant associations appeared between prenatal LTRA exposure and the risk of attention-deficit/hyperactivity disorder (adjusted hazard ratio, 1.03), autism spectrum disorder (AHR, 1.01), and Tourette syndrome (AHR, 0.63).
Neither duration nor cumulative dose of LTRA use during pregnancy showed an association with ADHD, ASD, or Tourette syndrome in offspring. Duration of LTRA use was categorized as shorter or longer periods of 1-4 weeks vs. more than 4 weeks; cumulative dose was categorized as 1-170 mg vs. 170 mg or higher.
The findings were limited by the lack of randomization, inability to detect long-term risk, and potential lack of generalizability to non-Asian populations, and more research is needed to replicate the results, the researchers noted. However, the current findings were strengthened by the large study population, and suggest that LTRA use in pregnancy does not present a significant risk for NEs in children, which should be reassuring to clinicians and patients, they concluded.
The current study is the first to use the whole of Taiwan population data and extends previous studies by examining the association between LTRA use during pregnancy and risk of neuropsychiatric events in offspring, Dr. Yao said in an interview. “The possibly surprising, but reassuring, finding is that prenatal LTRA exposure did not increase risk of ADHD, ASD, and Tourette syndrome in offspring,” he said.
“Clinicians prescribing LTRAs such as montelukast (Singulair and generics) to pregnant women with asthma or allergic rhinitis may be reassured by our findings,” Dr. Yao added. The results offer real-world evidence to help inform decision-making about the use of LTRAs during pregnancy, although additional research is needed to replicate the study findings in other populations, he said.
The study was supported by the National Health Research Institutes, Taiwan, the Ministry of Science and Technology of Taiwan, the National Science and Technology Council of Taiwan, and the Chang Gung Medical Foundation. The researchers had no financial conflicts to disclose.
The drugs included in the study were leukotriene-receptor antagonists (LTRAs), which are often used to treat allergic airway diseases, including asthma and allergic rhinitis.
“Over the years, the U.S. Food and Drug Administration has monitored post-marketing data about the potential harm of neuropsychiatric events (NEs) associated with montelukast, the first type of LTRAs, and issued boxed warnings about serious mental health side effects for montelukast in 2020,” said corresponding author Tsung-Chieh Yao, MD, of Chang Gung Memorial Hospital, Taiwan, in an interview.
However, evidence of a link between NEs and LTRA use has been inconsistent, according to Dr. Yao and colleagues.
“To date, it remains totally unknown whether the exposure to LTRAs during pregnancy is associated with the risk of neuropsychiatric events in offspring,” said Dr. Yao.
To address this question, the researchers used data from National Health Insurance Research Database in Taiwan to identify pregnant women and their offspring from 2009 to 2019. The initial study population included 576,157 mother-offspring pairs, including 1,995 LTRA-exposed and 574,162 nonexposed children.
The women had a diagnosis of asthma or allergic rhinitis; multiple births and children with congenital malformations were excluded. LTRA exposure was defined as any dispensed prescription for LTRAs during pregnancy. Approximately two-thirds of the mothers were aged 30-40 years at the time of delivery.
The findings were published in a research letter in JAMA Network Open.
In the study population at large, the incidence of the three neurodevelopmental disorders ADHD, autism spectrum disorder (ASD), and Tourette syndrome was not significantly different between those children exposed to LTRAs and those not exposed to LTRAs in utero (1.25% vs. 1.32%; 3.31% vs. 4.36%; and 0.45% vs. 0.83%, respectively).
After propensity score matching, the study population included 1,988 LTRA-exposed children and 19,863 nonexposed children. In this group, no significant associations appeared between prenatal LTRA exposure and the risk of attention-deficit/hyperactivity disorder (adjusted hazard ratio, 1.03), autism spectrum disorder (AHR, 1.01), and Tourette syndrome (AHR, 0.63).
Neither duration nor cumulative dose of LTRA use during pregnancy showed an association with ADHD, ASD, or Tourette syndrome in offspring. Duration of LTRA use was categorized as shorter or longer periods of 1-4 weeks vs. more than 4 weeks; cumulative dose was categorized as 1-170 mg vs. 170 mg or higher.
The findings were limited by the lack of randomization, inability to detect long-term risk, and potential lack of generalizability to non-Asian populations, and more research is needed to replicate the results, the researchers noted. However, the current findings were strengthened by the large study population, and suggest that LTRA use in pregnancy does not present a significant risk for NEs in children, which should be reassuring to clinicians and patients, they concluded.
The current study is the first to use the whole of Taiwan population data and extends previous studies by examining the association between LTRA use during pregnancy and risk of neuropsychiatric events in offspring, Dr. Yao said in an interview. “The possibly surprising, but reassuring, finding is that prenatal LTRA exposure did not increase risk of ADHD, ASD, and Tourette syndrome in offspring,” he said.
“Clinicians prescribing LTRAs such as montelukast (Singulair and generics) to pregnant women with asthma or allergic rhinitis may be reassured by our findings,” Dr. Yao added. The results offer real-world evidence to help inform decision-making about the use of LTRAs during pregnancy, although additional research is needed to replicate the study findings in other populations, he said.
The study was supported by the National Health Research Institutes, Taiwan, the Ministry of Science and Technology of Taiwan, the National Science and Technology Council of Taiwan, and the Chang Gung Medical Foundation. The researchers had no financial conflicts to disclose.
FROM JAMA NETWORK OPEN
Ob.gyn. loses PhD after committee finds he made up research
It was déjà vu last month when a university in Belgium stripped Egyptian physician Hatem Abu Hashim of his doctorate after he was found to have fabricated data in his thesis.
Just weeks earlier, another Egyptian doctor, Ahmed Badawy, lost the PhD degree he had earned at a Dutch university in 2008. Abu Hashim and Badawy are both professors in the department of obstetrics and gynecology at Mansoura University in Egypt.
According to an investigation by the Vrije Universeit Brussel (VUB), which awarded Abu Hashim his PhD in 2013, the researcher was in “serious violation of scientific integrity” based on “overwhelming evidence of fabrication of statistical outcomes” and “clear lack of statistical proficiency.”
Ben Mol of Monash University in Australia, a researcher turned data sleuth who alerted VUB and Utrecht University to problems with Abu Hashim and Badawy ‘s research in 2021 and 2020, respectively, told Retraction Watch by email, “The good news is obviously that there is a firm conclusion from both universities after a robust process independent of the complaint.”
Mol also laid out his concerns in a study published with then-PhD student Esmée Bordewijk and others in 2020, as Retraction Watch reported that year.
“Yes, it could have been a bit faster, but on the other hand we have this conversation because they took the right decision,” he added.
Abu Hashim’s PhD thesis is based on 11 randomized controlled trials, all of which have been published. Ostensibly, the studies were done at Mansoura University before Abu Hashim enrolled as an external PhD candidate at VUB.
A report from the Flemish Commission for Scientific Integrity, which gave a second opinion on the VUB findings following a request from Abu Hashim, offers a “credible” scenario for how the 11 papers came about, suggesting “that Abu Hashim had learned to write medical papers by reading others, that he made up all reported values and that he wrote more papers by adapting previous papers, copying results between articles and applying small alterations (+1 or -1 in some digits).”
The commission agreed with VUB that “complete (or virtually complete) fabrication is the only reasonable explanation for the findings.” It also noted that “strikingly,” the researcher did not address any of the allegations against him:
“To the contrary, his defence consists mainly of accusing those bringing forward the complaint of misconduct and questioning their work and methods.”
Neither Abu Hashim nor Mansoura University responded to requests for comment.
The school, however, has known about Abu Hashim’s fraudulent research for a decade. In an internal investigation from 2014, then-head of department Nasser El Lakany and five other professors found that one of the researcher’s trials had never been done; six trials included an impossibly large number of women with polycystic ovary syndrome; and two reported 366 ovarian-drilling procedures while records were found to exist only for 94. The latter two groups of studies formed part of Abu Hashim’s PhD thesis.
“There is no excuse for the researcher’ [sic] misconduct (fabricating imaginary data and studies not done at all, or studies with doubtful cases not in records),” the Mansoura professors wrote, according to an English translation of the original Arabic report.
In 2021, sleuth Nick Brown also began poring over the Egyptian researchers’ work after a Dutch journalist requested his opinion.
“People don’t read papers. They read the abstract. They say, congratulations, great paper. And then they go back to what they were doing the rest of their day because reading a paper is quite hard,” Brown told Retraction Watch. “I’m not very good at statistics, but I can read a table and things jump out at me.”
Brown quickly realized that Badawy and Abu Hashim’s publications were littered with “fatal flaws.” Virtually all of the P-values were wrong. In some cases, they exceeded 1 – a mathematical impossibility. In others, vastly different values were given for identical statistical tests that by definition should have yielded the same results.
“I assume the authors were just making up ‘likely-looking’ numbers in a hurry and didn’t realise that these needed to be identical,” Brown said in an email. “We often find that people who cheat are not very good at knowing what genuine numbers should look like.”
Brown, who himself has an external PhD from a Dutch university, noted that institutions receive the same amount of money from the government whether a PhD candidate is external or internal:
“So someone comes along with some papers already done. They need to write a top and tail of a thesis. They’re probably not going to need a whole lot of supervision. Exactly how many questions do you ask?”
A spokesperson for Utrecht University told Retraction Watch by email:
“We have asked ourselves the question how this could have happened. Why did the supervisor and the Doctoral Examination Committee not notice this? The articles that were the basis for the thesis, were published in peer reviewed journals. Only much later it came to light that the data underlying these articles had been compromised.”
She added that the rules for external PhD candidates have been tightened since 2008, when Badawy obtained his degree (the changes are described here).
Sam Jaspers, a VUB press officer, told us, “the Vrije Universiteit Brussel is updating its PhD regulations. External PhD students working with existing datasets created at a university other than the VUB and publications reviewed by scientific journals will soon (this spring) be fully audited by the VUB.”
Meanwhile, Mol, whose work on various cases recently featured in The Economist, worries about all the fake studies that have not yet been retracted, and the impact they might have on patient care.
“I cannot understand that ... three years after our publication of the Bordewijk study, still half of the Badawy and Abu Hashim studies are out there even without an expression of concern,” he said. “What ideally should happen is that there should be a mechanism that all the journals and publishers bundle their investigation.”
A version of this article first appeared on retractionwatch.com.
It was déjà vu last month when a university in Belgium stripped Egyptian physician Hatem Abu Hashim of his doctorate after he was found to have fabricated data in his thesis.
Just weeks earlier, another Egyptian doctor, Ahmed Badawy, lost the PhD degree he had earned at a Dutch university in 2008. Abu Hashim and Badawy are both professors in the department of obstetrics and gynecology at Mansoura University in Egypt.
According to an investigation by the Vrije Universeit Brussel (VUB), which awarded Abu Hashim his PhD in 2013, the researcher was in “serious violation of scientific integrity” based on “overwhelming evidence of fabrication of statistical outcomes” and “clear lack of statistical proficiency.”
Ben Mol of Monash University in Australia, a researcher turned data sleuth who alerted VUB and Utrecht University to problems with Abu Hashim and Badawy ‘s research in 2021 and 2020, respectively, told Retraction Watch by email, “The good news is obviously that there is a firm conclusion from both universities after a robust process independent of the complaint.”
Mol also laid out his concerns in a study published with then-PhD student Esmée Bordewijk and others in 2020, as Retraction Watch reported that year.
“Yes, it could have been a bit faster, but on the other hand we have this conversation because they took the right decision,” he added.
Abu Hashim’s PhD thesis is based on 11 randomized controlled trials, all of which have been published. Ostensibly, the studies were done at Mansoura University before Abu Hashim enrolled as an external PhD candidate at VUB.
A report from the Flemish Commission for Scientific Integrity, which gave a second opinion on the VUB findings following a request from Abu Hashim, offers a “credible” scenario for how the 11 papers came about, suggesting “that Abu Hashim had learned to write medical papers by reading others, that he made up all reported values and that he wrote more papers by adapting previous papers, copying results between articles and applying small alterations (+1 or -1 in some digits).”
The commission agreed with VUB that “complete (or virtually complete) fabrication is the only reasonable explanation for the findings.” It also noted that “strikingly,” the researcher did not address any of the allegations against him:
“To the contrary, his defence consists mainly of accusing those bringing forward the complaint of misconduct and questioning their work and methods.”
Neither Abu Hashim nor Mansoura University responded to requests for comment.
The school, however, has known about Abu Hashim’s fraudulent research for a decade. In an internal investigation from 2014, then-head of department Nasser El Lakany and five other professors found that one of the researcher’s trials had never been done; six trials included an impossibly large number of women with polycystic ovary syndrome; and two reported 366 ovarian-drilling procedures while records were found to exist only for 94. The latter two groups of studies formed part of Abu Hashim’s PhD thesis.
“There is no excuse for the researcher’ [sic] misconduct (fabricating imaginary data and studies not done at all, or studies with doubtful cases not in records),” the Mansoura professors wrote, according to an English translation of the original Arabic report.
In 2021, sleuth Nick Brown also began poring over the Egyptian researchers’ work after a Dutch journalist requested his opinion.
“People don’t read papers. They read the abstract. They say, congratulations, great paper. And then they go back to what they were doing the rest of their day because reading a paper is quite hard,” Brown told Retraction Watch. “I’m not very good at statistics, but I can read a table and things jump out at me.”
Brown quickly realized that Badawy and Abu Hashim’s publications were littered with “fatal flaws.” Virtually all of the P-values were wrong. In some cases, they exceeded 1 – a mathematical impossibility. In others, vastly different values were given for identical statistical tests that by definition should have yielded the same results.
“I assume the authors were just making up ‘likely-looking’ numbers in a hurry and didn’t realise that these needed to be identical,” Brown said in an email. “We often find that people who cheat are not very good at knowing what genuine numbers should look like.”
Brown, who himself has an external PhD from a Dutch university, noted that institutions receive the same amount of money from the government whether a PhD candidate is external or internal:
“So someone comes along with some papers already done. They need to write a top and tail of a thesis. They’re probably not going to need a whole lot of supervision. Exactly how many questions do you ask?”
A spokesperson for Utrecht University told Retraction Watch by email:
“We have asked ourselves the question how this could have happened. Why did the supervisor and the Doctoral Examination Committee not notice this? The articles that were the basis for the thesis, were published in peer reviewed journals. Only much later it came to light that the data underlying these articles had been compromised.”
She added that the rules for external PhD candidates have been tightened since 2008, when Badawy obtained his degree (the changes are described here).
Sam Jaspers, a VUB press officer, told us, “the Vrije Universiteit Brussel is updating its PhD regulations. External PhD students working with existing datasets created at a university other than the VUB and publications reviewed by scientific journals will soon (this spring) be fully audited by the VUB.”
Meanwhile, Mol, whose work on various cases recently featured in The Economist, worries about all the fake studies that have not yet been retracted, and the impact they might have on patient care.
“I cannot understand that ... three years after our publication of the Bordewijk study, still half of the Badawy and Abu Hashim studies are out there even without an expression of concern,” he said. “What ideally should happen is that there should be a mechanism that all the journals and publishers bundle their investigation.”
A version of this article first appeared on retractionwatch.com.
It was déjà vu last month when a university in Belgium stripped Egyptian physician Hatem Abu Hashim of his doctorate after he was found to have fabricated data in his thesis.
Just weeks earlier, another Egyptian doctor, Ahmed Badawy, lost the PhD degree he had earned at a Dutch university in 2008. Abu Hashim and Badawy are both professors in the department of obstetrics and gynecology at Mansoura University in Egypt.
According to an investigation by the Vrije Universeit Brussel (VUB), which awarded Abu Hashim his PhD in 2013, the researcher was in “serious violation of scientific integrity” based on “overwhelming evidence of fabrication of statistical outcomes” and “clear lack of statistical proficiency.”
Ben Mol of Monash University in Australia, a researcher turned data sleuth who alerted VUB and Utrecht University to problems with Abu Hashim and Badawy ‘s research in 2021 and 2020, respectively, told Retraction Watch by email, “The good news is obviously that there is a firm conclusion from both universities after a robust process independent of the complaint.”
Mol also laid out his concerns in a study published with then-PhD student Esmée Bordewijk and others in 2020, as Retraction Watch reported that year.
“Yes, it could have been a bit faster, but on the other hand we have this conversation because they took the right decision,” he added.
Abu Hashim’s PhD thesis is based on 11 randomized controlled trials, all of which have been published. Ostensibly, the studies were done at Mansoura University before Abu Hashim enrolled as an external PhD candidate at VUB.
A report from the Flemish Commission for Scientific Integrity, which gave a second opinion on the VUB findings following a request from Abu Hashim, offers a “credible” scenario for how the 11 papers came about, suggesting “that Abu Hashim had learned to write medical papers by reading others, that he made up all reported values and that he wrote more papers by adapting previous papers, copying results between articles and applying small alterations (+1 or -1 in some digits).”
The commission agreed with VUB that “complete (or virtually complete) fabrication is the only reasonable explanation for the findings.” It also noted that “strikingly,” the researcher did not address any of the allegations against him:
“To the contrary, his defence consists mainly of accusing those bringing forward the complaint of misconduct and questioning their work and methods.”
Neither Abu Hashim nor Mansoura University responded to requests for comment.
The school, however, has known about Abu Hashim’s fraudulent research for a decade. In an internal investigation from 2014, then-head of department Nasser El Lakany and five other professors found that one of the researcher’s trials had never been done; six trials included an impossibly large number of women with polycystic ovary syndrome; and two reported 366 ovarian-drilling procedures while records were found to exist only for 94. The latter two groups of studies formed part of Abu Hashim’s PhD thesis.
“There is no excuse for the researcher’ [sic] misconduct (fabricating imaginary data and studies not done at all, or studies with doubtful cases not in records),” the Mansoura professors wrote, according to an English translation of the original Arabic report.
In 2021, sleuth Nick Brown also began poring over the Egyptian researchers’ work after a Dutch journalist requested his opinion.
“People don’t read papers. They read the abstract. They say, congratulations, great paper. And then they go back to what they were doing the rest of their day because reading a paper is quite hard,” Brown told Retraction Watch. “I’m not very good at statistics, but I can read a table and things jump out at me.”
Brown quickly realized that Badawy and Abu Hashim’s publications were littered with “fatal flaws.” Virtually all of the P-values were wrong. In some cases, they exceeded 1 – a mathematical impossibility. In others, vastly different values were given for identical statistical tests that by definition should have yielded the same results.
“I assume the authors were just making up ‘likely-looking’ numbers in a hurry and didn’t realise that these needed to be identical,” Brown said in an email. “We often find that people who cheat are not very good at knowing what genuine numbers should look like.”
Brown, who himself has an external PhD from a Dutch university, noted that institutions receive the same amount of money from the government whether a PhD candidate is external or internal:
“So someone comes along with some papers already done. They need to write a top and tail of a thesis. They’re probably not going to need a whole lot of supervision. Exactly how many questions do you ask?”
A spokesperson for Utrecht University told Retraction Watch by email:
“We have asked ourselves the question how this could have happened. Why did the supervisor and the Doctoral Examination Committee not notice this? The articles that were the basis for the thesis, were published in peer reviewed journals. Only much later it came to light that the data underlying these articles had been compromised.”
She added that the rules for external PhD candidates have been tightened since 2008, when Badawy obtained his degree (the changes are described here).
Sam Jaspers, a VUB press officer, told us, “the Vrije Universiteit Brussel is updating its PhD regulations. External PhD students working with existing datasets created at a university other than the VUB and publications reviewed by scientific journals will soon (this spring) be fully audited by the VUB.”
Meanwhile, Mol, whose work on various cases recently featured in The Economist, worries about all the fake studies that have not yet been retracted, and the impact they might have on patient care.
“I cannot understand that ... three years after our publication of the Bordewijk study, still half of the Badawy and Abu Hashim studies are out there even without an expression of concern,” he said. “What ideally should happen is that there should be a mechanism that all the journals and publishers bundle their investigation.”
A version of this article first appeared on retractionwatch.com.
Telehealth doctor indicted on health care fraud, opioid distribution charges
Sangita Patel, MD, 50, practiced at Advance Medical Home Physicians in Troy.
According to court documents, between July 2020 and June 2022 Patel was responsible for submitting Medicare claims for improper telehealth visits she didn’t conduct herself.
Dr. Patel, who accepted patients who paid in cash as well as those with Medicare and Medicaid coverage, billed approximately $3.4 million to Medicare between 2018 and 2022, according to court documents. An unusual number of these visits were billed using complex codes, an indication of health care fraud. The investigation also found that on many days, Dr. Patel billed for more than 24 hours of services. During this period, according to the document, 76% of Dr. Patel’s Medicare reimbursements were for telehealth.
Prosecutors say that Dr. Patel prescribed Schedule II controlled substances to more than 90% of the patients in these telehealth visits. She delegated her prescription authority to an unlicensed medical assistant. Through undercover visits and cell site search warrant data, the investigation found that Dr. Patel directed patients to contact, via cell phone, this assistant, who then entered electronic prescriptions into the electronic medical records system. Dr. Patel then signed the prescriptions and sent them to the pharmacies without ever interacting with the patients. Prosecutors also used text messages, obtained by search warrant, between Dr. Patel and her assistant and between the assistant and undercover informers to build their case.
Dr. Patel is also accused of referring patients to other providers, who in turn billed Medicare for claims associated with those patients. Advance Medical received $143,000 from these providers, potentially in violation of anti-kickback laws, according to bank records obtained by subpoena.
If convicted, Dr. Patel could be sentenced to up to 10 years in federal prison.
A version of this article first appeared on Medscape.com.
Sangita Patel, MD, 50, practiced at Advance Medical Home Physicians in Troy.
According to court documents, between July 2020 and June 2022 Patel was responsible for submitting Medicare claims for improper telehealth visits she didn’t conduct herself.
Dr. Patel, who accepted patients who paid in cash as well as those with Medicare and Medicaid coverage, billed approximately $3.4 million to Medicare between 2018 and 2022, according to court documents. An unusual number of these visits were billed using complex codes, an indication of health care fraud. The investigation also found that on many days, Dr. Patel billed for more than 24 hours of services. During this period, according to the document, 76% of Dr. Patel’s Medicare reimbursements were for telehealth.
Prosecutors say that Dr. Patel prescribed Schedule II controlled substances to more than 90% of the patients in these telehealth visits. She delegated her prescription authority to an unlicensed medical assistant. Through undercover visits and cell site search warrant data, the investigation found that Dr. Patel directed patients to contact, via cell phone, this assistant, who then entered electronic prescriptions into the electronic medical records system. Dr. Patel then signed the prescriptions and sent them to the pharmacies without ever interacting with the patients. Prosecutors also used text messages, obtained by search warrant, between Dr. Patel and her assistant and between the assistant and undercover informers to build their case.
Dr. Patel is also accused of referring patients to other providers, who in turn billed Medicare for claims associated with those patients. Advance Medical received $143,000 from these providers, potentially in violation of anti-kickback laws, according to bank records obtained by subpoena.
If convicted, Dr. Patel could be sentenced to up to 10 years in federal prison.
A version of this article first appeared on Medscape.com.
Sangita Patel, MD, 50, practiced at Advance Medical Home Physicians in Troy.
According to court documents, between July 2020 and June 2022 Patel was responsible for submitting Medicare claims for improper telehealth visits she didn’t conduct herself.
Dr. Patel, who accepted patients who paid in cash as well as those with Medicare and Medicaid coverage, billed approximately $3.4 million to Medicare between 2018 and 2022, according to court documents. An unusual number of these visits were billed using complex codes, an indication of health care fraud. The investigation also found that on many days, Dr. Patel billed for more than 24 hours of services. During this period, according to the document, 76% of Dr. Patel’s Medicare reimbursements were for telehealth.
Prosecutors say that Dr. Patel prescribed Schedule II controlled substances to more than 90% of the patients in these telehealth visits. She delegated her prescription authority to an unlicensed medical assistant. Through undercover visits and cell site search warrant data, the investigation found that Dr. Patel directed patients to contact, via cell phone, this assistant, who then entered electronic prescriptions into the electronic medical records system. Dr. Patel then signed the prescriptions and sent them to the pharmacies without ever interacting with the patients. Prosecutors also used text messages, obtained by search warrant, between Dr. Patel and her assistant and between the assistant and undercover informers to build their case.
Dr. Patel is also accused of referring patients to other providers, who in turn billed Medicare for claims associated with those patients. Advance Medical received $143,000 from these providers, potentially in violation of anti-kickback laws, according to bank records obtained by subpoena.
If convicted, Dr. Patel could be sentenced to up to 10 years in federal prison.
A version of this article first appeared on Medscape.com.
Midwife-led care linked to positive outcomes across medical risk levels
Midwives provide safe primary care for pregnant women who are at various levels of medical risk in British Columbia, Canada, new data suggest.
In most cases, for midwifery clients, birth outcomes were similar to or were better than birth outcomes of patients who had physician-led or obstetrician-led care.
In addition, midwifery clients were less likely to experience preterm births or have low-birth-weight babies and to experience cesarean deliveries or births involving instruments.
“Based on previous research, we know that midwives provide safe care for healthy childbearing people or those with no or few risk factors that might complicate the pregnancy or birth,” lead author Kathrin Stoll, PhD, a research associate in the University of British Columbia’s department of family practice, told this news organization.
“What we didn’t know until now is whether midwives provide safe care to people with moderate and high medical risks and what proportion of B.C. [British Columbia] midwifery clients are low, moderate, and high risk,” she said. “This is important to know because of the misperception that midwives only look after low-risk people. This misperception is sometimes used against midwives to justify giving them fewer resources and supports.”
The study was published in the Canadian Medical Association Journal.
Increasing demand
Registered midwives have been part of the health care system in British Columbia since 1998, according to the study authors. The number of pregnant people who are attended by midwives during birth has steadily increased from 4.8% in 2004-2005 to 15.6% in 2019-2020.
The investigators analyzed 2008-2018 data from the British Columbia Perinatal Data Registry, which contains data for 99% of births, including home births. Their analysis included 425,056 births for which a family physician, an obstetrician, or a midwife was listed as the most responsible provider (MRP). The investigators assessed pregnancy risk status (low, moderate, or high), which was determined on the basis of an adapted perinatal risk scoring system used by the Alberta Perinatal Health Program. They estimated the differences in neonatal and maternal outcomes between MRP groups by calculating adjusted absolute and relative risks.
Among the 425,056 births, 63,151 (14.9%) had a midwife as the MRP, 189,679 (44.6%) had a family physician, and 172,226 (40.5%) had an obstetrician. The antenatal risk score ranged from 0 to 23 (median score, 2).
The proportion of births with midwife-led care increased from 9.2% to 19.8% from 2008-2018. In 2018, midwives were listed as the MRP for 24.3% of low-risk, 14.3% of moderate-risk, and 7.9% of high-risk births in the province. This represented an absolute increase of 9.1% for low-risk, 7.7% for moderate-risk, and 5.7% for high-risk births during the study period.
Among the 12,169 at-home births that took place during the study period, 9,776 (80.3%) were low-risk, 2,329 (19.1%) were moderate-risk, and 64 (0.5%) were high-risk births. As the risk score increased, so did the proportion of midwifery and family physician clients who were delivered by obstetricians. Across all risk strata, more family physician clients than midwifery clients underwent deliveries by obstetricians.
Overall, the risk of perinatal death for midwifery clients was similar to the risk for those under the care of family physicians across all risk levels. Low- and moderate-risk clients with midwife-led care were significantly less likely to experience a perinatal death, compared with those with obstetrician-led care, although the adjusted absolute risk differences were small. In the high-risk group, there was no significant difference in the rate of perinatal deaths between midwife-led and physician-led care.
In addition, clients with midwife-led care were significantly less likely to experience preterm birth and have a low-birth-weight baby regardless of medical risk level. The adjusted relative risk of an Apgar score of less than 7 at 5 minutes was significantly lower for midwife-led care than for physician-led care for nearly all comparisons.
The cesarean delivery rate among midwifery clients in the low-risk group was 7.2%, compared with 12.2% for family physicians and 42.3% for obstetrician clients. Cesarean delivery rates increased for midwifery clients as medical risk increased but were significantly lower than the physician rates across all medical risk levels.
Among low-risk clients, the absolute risk reduction for cesarean delivery was 34.4% with midwife-led care, compared with obstetrician-led care. The absolute risk difference increased to 55.3% for moderate-risk clients and to 42.2% for high-risk clients.
Labor induction varied
Although low-risk midwifery clients were significantly less likely to experience labor induction with oxytocin, high-risk midwifery clients were more than twice as likely to undergo induction with oxytocin than obstetrician clients (adjusted absolute difference, 11.3%).
For most risk levels, midwifery clients were less likely to have an assisted vaginal birth than physician clients, and they were significantly more likely to have a spontaneous vaginal birth. Low-risk clients who had a midwife as the MRP were nearly twice as likely to have a spontaneous vaginal birth than obstetricians’ clients, and moderate-risk clients were nearly four times as likely to have a spontaneous vaginal birth.
The rates of vaginal birth after cesarean delivery (VBAC) were significantly higher when a midwife was the MRP. In comparing midwifery clients with family physician clients, the relative and absolute differences were small, but they were larger when comparing midwifery clients with obstetrician clients. Among low-risk clients, the VBAC rate was 85.3% among midwifery clients, compared with 78.6% among family physician clients and 51.5% among obstetrician clients.
In general, the prevalence rates of adverse maternal outcomes (including blood transfusion, intensive care admissions, uterine rupture, and postpartum wound infection) were low for midwifery clients across all risk levels.
Breast- or chest-feeding at birth was significantly more common among midwifery clients across all risk levels as well.
Today, nearly 1 in 4 childbearing people in British Columbia receive care from a midwife at some point during pregnancy, birth, or the postpartum period, the study authors write. During the past 20 years, the profile of clients has evolved to include more moderate- and high-risk patients.
“Clients with more complex medical needs take more time and need more support,” said Dr. Stoll. “This means that midwives continue to stay on call, responding to pages and urgent medical concerns for their clients with no pay for being on call, no days off even for sick days, and unsafe working hours, often working more than 24 hours at a time. If we want to expand midwifery to communities where they are needed most, we need to provide an enabling environment.”
Additional studies are needed as to how different practice and remuneration models affect clinical outcomes, health care costs, and client and provider experiences, the study authors write. At the same time, there are several barriers to obtaining funding, conducting studies, and publishing research by and about midwives in Canada, Dr. Stoll said – barriers that she and her co-authors faced.
Seeking broader access
Alixandra Bacon, a registered midwife and president of the Canadian Association of Midwives, said, “These findings demonstrate that pregnant people at any level of medical risk can benefit from midwifery care. This is a testament both to the benefits of the Canadian midwifery model of care and to the seamless integration of midwifery into collaborative teams and the health system.” Ms. Bacon wasn’t involved with this study.
“If we can realize our goal of equitable access to midwifery care for all families in Canada, we can help to decrease rates of unnecessary medical intervention, preterm labor, and stillbirth,” she added.
“Midwifery is well established across most of Canada. This is yet one more piece of evidence that shows the clinical benefits of midwifery care,” Jasmin Tecson, a registered midwife and president of the Association of Ontario Midwives, said in an interview.
Ms. Tecson, who wasn’t involved with this study, noted the increasing number of clients with more complex health and social needs in Ontario. “It is time to think about how the skills and knowledge of midwives can be used with clients of different risk profiles and how the current scope of practice of midwives can be optimized and expanded,” she said. “For example, Ontario midwives are still required to prescribe medications from a limited list, despite the potential additional clinical risks and health system costs that this creates.”
The study received financial support from the University of British Columbia Stollery Fund and the University of British Columbia Work Learn Program. Dr. Stoll has an unpaid role with the Midwives Association Contract Negotiation Advisory Council. Ms. Bacon and Ms. Tecson disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Midwives provide safe primary care for pregnant women who are at various levels of medical risk in British Columbia, Canada, new data suggest.
In most cases, for midwifery clients, birth outcomes were similar to or were better than birth outcomes of patients who had physician-led or obstetrician-led care.
In addition, midwifery clients were less likely to experience preterm births or have low-birth-weight babies and to experience cesarean deliveries or births involving instruments.
“Based on previous research, we know that midwives provide safe care for healthy childbearing people or those with no or few risk factors that might complicate the pregnancy or birth,” lead author Kathrin Stoll, PhD, a research associate in the University of British Columbia’s department of family practice, told this news organization.
“What we didn’t know until now is whether midwives provide safe care to people with moderate and high medical risks and what proportion of B.C. [British Columbia] midwifery clients are low, moderate, and high risk,” she said. “This is important to know because of the misperception that midwives only look after low-risk people. This misperception is sometimes used against midwives to justify giving them fewer resources and supports.”
The study was published in the Canadian Medical Association Journal.
Increasing demand
Registered midwives have been part of the health care system in British Columbia since 1998, according to the study authors. The number of pregnant people who are attended by midwives during birth has steadily increased from 4.8% in 2004-2005 to 15.6% in 2019-2020.
The investigators analyzed 2008-2018 data from the British Columbia Perinatal Data Registry, which contains data for 99% of births, including home births. Their analysis included 425,056 births for which a family physician, an obstetrician, or a midwife was listed as the most responsible provider (MRP). The investigators assessed pregnancy risk status (low, moderate, or high), which was determined on the basis of an adapted perinatal risk scoring system used by the Alberta Perinatal Health Program. They estimated the differences in neonatal and maternal outcomes between MRP groups by calculating adjusted absolute and relative risks.
Among the 425,056 births, 63,151 (14.9%) had a midwife as the MRP, 189,679 (44.6%) had a family physician, and 172,226 (40.5%) had an obstetrician. The antenatal risk score ranged from 0 to 23 (median score, 2).
The proportion of births with midwife-led care increased from 9.2% to 19.8% from 2008-2018. In 2018, midwives were listed as the MRP for 24.3% of low-risk, 14.3% of moderate-risk, and 7.9% of high-risk births in the province. This represented an absolute increase of 9.1% for low-risk, 7.7% for moderate-risk, and 5.7% for high-risk births during the study period.
Among the 12,169 at-home births that took place during the study period, 9,776 (80.3%) were low-risk, 2,329 (19.1%) were moderate-risk, and 64 (0.5%) were high-risk births. As the risk score increased, so did the proportion of midwifery and family physician clients who were delivered by obstetricians. Across all risk strata, more family physician clients than midwifery clients underwent deliveries by obstetricians.
Overall, the risk of perinatal death for midwifery clients was similar to the risk for those under the care of family physicians across all risk levels. Low- and moderate-risk clients with midwife-led care were significantly less likely to experience a perinatal death, compared with those with obstetrician-led care, although the adjusted absolute risk differences were small. In the high-risk group, there was no significant difference in the rate of perinatal deaths between midwife-led and physician-led care.
In addition, clients with midwife-led care were significantly less likely to experience preterm birth and have a low-birth-weight baby regardless of medical risk level. The adjusted relative risk of an Apgar score of less than 7 at 5 minutes was significantly lower for midwife-led care than for physician-led care for nearly all comparisons.
The cesarean delivery rate among midwifery clients in the low-risk group was 7.2%, compared with 12.2% for family physicians and 42.3% for obstetrician clients. Cesarean delivery rates increased for midwifery clients as medical risk increased but were significantly lower than the physician rates across all medical risk levels.
Among low-risk clients, the absolute risk reduction for cesarean delivery was 34.4% with midwife-led care, compared with obstetrician-led care. The absolute risk difference increased to 55.3% for moderate-risk clients and to 42.2% for high-risk clients.
Labor induction varied
Although low-risk midwifery clients were significantly less likely to experience labor induction with oxytocin, high-risk midwifery clients were more than twice as likely to undergo induction with oxytocin than obstetrician clients (adjusted absolute difference, 11.3%).
For most risk levels, midwifery clients were less likely to have an assisted vaginal birth than physician clients, and they were significantly more likely to have a spontaneous vaginal birth. Low-risk clients who had a midwife as the MRP were nearly twice as likely to have a spontaneous vaginal birth than obstetricians’ clients, and moderate-risk clients were nearly four times as likely to have a spontaneous vaginal birth.
The rates of vaginal birth after cesarean delivery (VBAC) were significantly higher when a midwife was the MRP. In comparing midwifery clients with family physician clients, the relative and absolute differences were small, but they were larger when comparing midwifery clients with obstetrician clients. Among low-risk clients, the VBAC rate was 85.3% among midwifery clients, compared with 78.6% among family physician clients and 51.5% among obstetrician clients.
In general, the prevalence rates of adverse maternal outcomes (including blood transfusion, intensive care admissions, uterine rupture, and postpartum wound infection) were low for midwifery clients across all risk levels.
Breast- or chest-feeding at birth was significantly more common among midwifery clients across all risk levels as well.
Today, nearly 1 in 4 childbearing people in British Columbia receive care from a midwife at some point during pregnancy, birth, or the postpartum period, the study authors write. During the past 20 years, the profile of clients has evolved to include more moderate- and high-risk patients.
“Clients with more complex medical needs take more time and need more support,” said Dr. Stoll. “This means that midwives continue to stay on call, responding to pages and urgent medical concerns for their clients with no pay for being on call, no days off even for sick days, and unsafe working hours, often working more than 24 hours at a time. If we want to expand midwifery to communities where they are needed most, we need to provide an enabling environment.”
Additional studies are needed as to how different practice and remuneration models affect clinical outcomes, health care costs, and client and provider experiences, the study authors write. At the same time, there are several barriers to obtaining funding, conducting studies, and publishing research by and about midwives in Canada, Dr. Stoll said – barriers that she and her co-authors faced.
Seeking broader access
Alixandra Bacon, a registered midwife and president of the Canadian Association of Midwives, said, “These findings demonstrate that pregnant people at any level of medical risk can benefit from midwifery care. This is a testament both to the benefits of the Canadian midwifery model of care and to the seamless integration of midwifery into collaborative teams and the health system.” Ms. Bacon wasn’t involved with this study.
“If we can realize our goal of equitable access to midwifery care for all families in Canada, we can help to decrease rates of unnecessary medical intervention, preterm labor, and stillbirth,” she added.
“Midwifery is well established across most of Canada. This is yet one more piece of evidence that shows the clinical benefits of midwifery care,” Jasmin Tecson, a registered midwife and president of the Association of Ontario Midwives, said in an interview.
Ms. Tecson, who wasn’t involved with this study, noted the increasing number of clients with more complex health and social needs in Ontario. “It is time to think about how the skills and knowledge of midwives can be used with clients of different risk profiles and how the current scope of practice of midwives can be optimized and expanded,” she said. “For example, Ontario midwives are still required to prescribe medications from a limited list, despite the potential additional clinical risks and health system costs that this creates.”
The study received financial support from the University of British Columbia Stollery Fund and the University of British Columbia Work Learn Program. Dr. Stoll has an unpaid role with the Midwives Association Contract Negotiation Advisory Council. Ms. Bacon and Ms. Tecson disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Midwives provide safe primary care for pregnant women who are at various levels of medical risk in British Columbia, Canada, new data suggest.
In most cases, for midwifery clients, birth outcomes were similar to or were better than birth outcomes of patients who had physician-led or obstetrician-led care.
In addition, midwifery clients were less likely to experience preterm births or have low-birth-weight babies and to experience cesarean deliveries or births involving instruments.
“Based on previous research, we know that midwives provide safe care for healthy childbearing people or those with no or few risk factors that might complicate the pregnancy or birth,” lead author Kathrin Stoll, PhD, a research associate in the University of British Columbia’s department of family practice, told this news organization.
“What we didn’t know until now is whether midwives provide safe care to people with moderate and high medical risks and what proportion of B.C. [British Columbia] midwifery clients are low, moderate, and high risk,” she said. “This is important to know because of the misperception that midwives only look after low-risk people. This misperception is sometimes used against midwives to justify giving them fewer resources and supports.”
The study was published in the Canadian Medical Association Journal.
Increasing demand
Registered midwives have been part of the health care system in British Columbia since 1998, according to the study authors. The number of pregnant people who are attended by midwives during birth has steadily increased from 4.8% in 2004-2005 to 15.6% in 2019-2020.
The investigators analyzed 2008-2018 data from the British Columbia Perinatal Data Registry, which contains data for 99% of births, including home births. Their analysis included 425,056 births for which a family physician, an obstetrician, or a midwife was listed as the most responsible provider (MRP). The investigators assessed pregnancy risk status (low, moderate, or high), which was determined on the basis of an adapted perinatal risk scoring system used by the Alberta Perinatal Health Program. They estimated the differences in neonatal and maternal outcomes between MRP groups by calculating adjusted absolute and relative risks.
Among the 425,056 births, 63,151 (14.9%) had a midwife as the MRP, 189,679 (44.6%) had a family physician, and 172,226 (40.5%) had an obstetrician. The antenatal risk score ranged from 0 to 23 (median score, 2).
The proportion of births with midwife-led care increased from 9.2% to 19.8% from 2008-2018. In 2018, midwives were listed as the MRP for 24.3% of low-risk, 14.3% of moderate-risk, and 7.9% of high-risk births in the province. This represented an absolute increase of 9.1% for low-risk, 7.7% for moderate-risk, and 5.7% for high-risk births during the study period.
Among the 12,169 at-home births that took place during the study period, 9,776 (80.3%) were low-risk, 2,329 (19.1%) were moderate-risk, and 64 (0.5%) were high-risk births. As the risk score increased, so did the proportion of midwifery and family physician clients who were delivered by obstetricians. Across all risk strata, more family physician clients than midwifery clients underwent deliveries by obstetricians.
Overall, the risk of perinatal death for midwifery clients was similar to the risk for those under the care of family physicians across all risk levels. Low- and moderate-risk clients with midwife-led care were significantly less likely to experience a perinatal death, compared with those with obstetrician-led care, although the adjusted absolute risk differences were small. In the high-risk group, there was no significant difference in the rate of perinatal deaths between midwife-led and physician-led care.
In addition, clients with midwife-led care were significantly less likely to experience preterm birth and have a low-birth-weight baby regardless of medical risk level. The adjusted relative risk of an Apgar score of less than 7 at 5 minutes was significantly lower for midwife-led care than for physician-led care for nearly all comparisons.
The cesarean delivery rate among midwifery clients in the low-risk group was 7.2%, compared with 12.2% for family physicians and 42.3% for obstetrician clients. Cesarean delivery rates increased for midwifery clients as medical risk increased but were significantly lower than the physician rates across all medical risk levels.
Among low-risk clients, the absolute risk reduction for cesarean delivery was 34.4% with midwife-led care, compared with obstetrician-led care. The absolute risk difference increased to 55.3% for moderate-risk clients and to 42.2% for high-risk clients.
Labor induction varied
Although low-risk midwifery clients were significantly less likely to experience labor induction with oxytocin, high-risk midwifery clients were more than twice as likely to undergo induction with oxytocin than obstetrician clients (adjusted absolute difference, 11.3%).
For most risk levels, midwifery clients were less likely to have an assisted vaginal birth than physician clients, and they were significantly more likely to have a spontaneous vaginal birth. Low-risk clients who had a midwife as the MRP were nearly twice as likely to have a spontaneous vaginal birth than obstetricians’ clients, and moderate-risk clients were nearly four times as likely to have a spontaneous vaginal birth.
The rates of vaginal birth after cesarean delivery (VBAC) were significantly higher when a midwife was the MRP. In comparing midwifery clients with family physician clients, the relative and absolute differences were small, but they were larger when comparing midwifery clients with obstetrician clients. Among low-risk clients, the VBAC rate was 85.3% among midwifery clients, compared with 78.6% among family physician clients and 51.5% among obstetrician clients.
In general, the prevalence rates of adverse maternal outcomes (including blood transfusion, intensive care admissions, uterine rupture, and postpartum wound infection) were low for midwifery clients across all risk levels.
Breast- or chest-feeding at birth was significantly more common among midwifery clients across all risk levels as well.
Today, nearly 1 in 4 childbearing people in British Columbia receive care from a midwife at some point during pregnancy, birth, or the postpartum period, the study authors write. During the past 20 years, the profile of clients has evolved to include more moderate- and high-risk patients.
“Clients with more complex medical needs take more time and need more support,” said Dr. Stoll. “This means that midwives continue to stay on call, responding to pages and urgent medical concerns for their clients with no pay for being on call, no days off even for sick days, and unsafe working hours, often working more than 24 hours at a time. If we want to expand midwifery to communities where they are needed most, we need to provide an enabling environment.”
Additional studies are needed as to how different practice and remuneration models affect clinical outcomes, health care costs, and client and provider experiences, the study authors write. At the same time, there are several barriers to obtaining funding, conducting studies, and publishing research by and about midwives in Canada, Dr. Stoll said – barriers that she and her co-authors faced.
Seeking broader access
Alixandra Bacon, a registered midwife and president of the Canadian Association of Midwives, said, “These findings demonstrate that pregnant people at any level of medical risk can benefit from midwifery care. This is a testament both to the benefits of the Canadian midwifery model of care and to the seamless integration of midwifery into collaborative teams and the health system.” Ms. Bacon wasn’t involved with this study.
“If we can realize our goal of equitable access to midwifery care for all families in Canada, we can help to decrease rates of unnecessary medical intervention, preterm labor, and stillbirth,” she added.
“Midwifery is well established across most of Canada. This is yet one more piece of evidence that shows the clinical benefits of midwifery care,” Jasmin Tecson, a registered midwife and president of the Association of Ontario Midwives, said in an interview.
Ms. Tecson, who wasn’t involved with this study, noted the increasing number of clients with more complex health and social needs in Ontario. “It is time to think about how the skills and knowledge of midwives can be used with clients of different risk profiles and how the current scope of practice of midwives can be optimized and expanded,” she said. “For example, Ontario midwives are still required to prescribe medications from a limited list, despite the potential additional clinical risks and health system costs that this creates.”
The study received financial support from the University of British Columbia Stollery Fund and the University of British Columbia Work Learn Program. Dr. Stoll has an unpaid role with the Midwives Association Contract Negotiation Advisory Council. Ms. Bacon and Ms. Tecson disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
We have seen the future of healthy muffins, and its name is Roselle
Get ‘em while they’re hot … for your health
Today on the Eating Channel, it’s a very special episode of “Much Ado About Muffin.”
The muffin. For some of us, it’s a good way to pretend we’re not having dessert for breakfast. A bran muffin can be loaded with calcium and fiber, and our beloved blueberry is full of yummy antioxidants and vitamins. Definitely not dessert.
Well, the muffin denial can stop there because there’s a new flavor on the scene, and research suggests it may actually be healthy. (Disclaimer: Muffin may not be considered healthy in Norway.) This new muffin has a name, Roselle, that comes from the calyx extract used in it, which is found in the Hibiscus sabdariffa plant of the same name.
Now, when it comes to new foods, especially ones that are supposed to be healthy, the No. 1 criteria is the same: It has to taste good. Researchers at the Norwegian University of Science and Technology and Amity University in India agreed, but they also set out to make it nutritionally valuable and give it a long shelf life without the addition of preservatives.
Sounds like a tall order, but they figured it out.
Not only is it tasty, but the properties of it could rival your morning multivitamin. Hibiscus extract has huge amounts of antioxidants, like phenolics, which are believed to help prevent cell membrane damage. Foods like vegetables, flax seed, and whole grains also have these antioxidants, but why not just have a Roselle muffin instead? You also get a dose of ascorbic acid without the glass of OJ in the morning.
The ascorbic acid, however, is not there just to help you. It also helps to check the researcher’s third box, shelf life. These naturally rosy-colored pastries will stay mold-free for 6 days without refrigeration at room temperature and without added preservatives.
Our guess, though, is they won’t be on the kitchen counter long enough to find out.
A sobering proposition
If Hollywood is to be believed, there’s no amount of drunkenness that can’t be cured with a cup of coffee or a stern slap in the face. Unfortunately, here in the real world the only thing that can make you less drunk is time. Maybe next time you’ll stop after that seventh Manhattan.
But what if we could beat time? What if there’s an actual sobriety drug out there?
Say hello to fibroblast growth factor 21. Although the liver already does good work filtering out what is essentially poison, it then goes the extra mile and produces fibroblast growth factor 21 (or, as her friends call her, FGF21), a hormone that suppresses the desire to drink, makes you desire water, and protects the liver all at the same time.
Now, FGF21 in its current role is great, but if you’ve ever seen or been a drunk person before, you’ve experienced the lack of interest in listening to reason, especially when it comes from within our own bodies. Who are you to tell us what to do, body? You’re not the boss of us! So a group of scientists decided to push the limits of FGF21. Could it do more than it already does?
First off, they genetically altered a group of mice so that they didn’t produce FGF21 on their own. Then they got them drunk. We’re going to assume they built a scale model of the bar from Cheers and had the mice filter in through the front door as they served their subjects beer out of tiny little glasses.
Once the mice were nice and liquored up, some were given a treatment of FGF21 while others were given a placebo. Lo and behold, the mice given FGF21 recovered about 50% faster than those that received the control treatment. Not exactly instant, but 50% is nothing to sniff at.
Before you bring your FGF21 supplement to the bar, though, this research only applies to mice. We don’t know if it works in people. And make sure you stick to booze. If your choice of intoxication is a bit more exotic, FGF21 isn’t going to do anything for you. Yes, the scientists tried. Yes, those mice are living a very interesting life. And yes, we are jealous of drugged-up lab mice.
Supersize your imagination, shrink your snacks
Have you ever heard of the meal-recall effect? Did you know that, in England, a biscuit is really a cookie? Did you also know that the magazine Bon Appétit is not the same as the peer-reviewed journal Appetite? We do … now.
The meal-recall effect is the subsequent reduction in snacking that comes from remembering a recent meal. It was used to great effect in a recent study conducted at the University of Cambridge, which is in England, where they feed their experimental humans cookies but, for some reason, call them biscuits.
For the first part of the study, the participants were invited to dine at Che Laboratory, where they “were given a microwave ready meal of rice and sauce and a cup of water,” according to a statement from the university. As our Uncle Ernie would say, “Gourmet all the way.”
The test subjects were instructed not to eat anything for 3 hours and “then invited back to the lab to perform imagination tasks.” Those who did come back were randomly divided into five different groups, each with a different task:
- Imagine moving their recent lunch at the lab around a plate.
- Recall eating their recent lunch in detail.
- Imagine that the lunch was twice as big and filling as it really was.
- Look at a photograph of spaghetti hoops in tomato sauce and write a description of it before imagining moving the food around a plate.
- Look at a photo of paper clips and rubber bands and imagine moving them around.
Now, at last, we get to the biscuits/cookies, which were the subject of a taste test that “was simply a rouse for covertly assessing snacking,” the investigators explained. As part of that test, participants were told they could eat as many biscuits as they wanted.
When the tables were cleared and the leftovers examined, the group that imagined spaghetti hoops had eaten the most biscuits (75.9 g), followed by the group that imagined paper clips (75.5 g), the moving-their-lunch-around-the-plate group (72.0 g), and the group that relived eating their lunch (70.0 g).
In a victory for the meal-recall effect, the people who imagined their meal being twice as big ate the fewest biscuits (51.1 g). “Your mind can be more powerful than your stomach in dictating how much you eat,” lead author Joanna Szypula, PhD, said in the university statement.
Oh! One more thing. The study appeared in Appetite, which is a peer-reviewed journal, not in Bon Appétit, which is not a peer-reviewed journal. Thanks to the fine folks at both publications for pointing that out to us.
Get ‘em while they’re hot … for your health
Today on the Eating Channel, it’s a very special episode of “Much Ado About Muffin.”
The muffin. For some of us, it’s a good way to pretend we’re not having dessert for breakfast. A bran muffin can be loaded with calcium and fiber, and our beloved blueberry is full of yummy antioxidants and vitamins. Definitely not dessert.
Well, the muffin denial can stop there because there’s a new flavor on the scene, and research suggests it may actually be healthy. (Disclaimer: Muffin may not be considered healthy in Norway.) This new muffin has a name, Roselle, that comes from the calyx extract used in it, which is found in the Hibiscus sabdariffa plant of the same name.
Now, when it comes to new foods, especially ones that are supposed to be healthy, the No. 1 criteria is the same: It has to taste good. Researchers at the Norwegian University of Science and Technology and Amity University in India agreed, but they also set out to make it nutritionally valuable and give it a long shelf life without the addition of preservatives.
Sounds like a tall order, but they figured it out.
Not only is it tasty, but the properties of it could rival your morning multivitamin. Hibiscus extract has huge amounts of antioxidants, like phenolics, which are believed to help prevent cell membrane damage. Foods like vegetables, flax seed, and whole grains also have these antioxidants, but why not just have a Roselle muffin instead? You also get a dose of ascorbic acid without the glass of OJ in the morning.
The ascorbic acid, however, is not there just to help you. It also helps to check the researcher’s third box, shelf life. These naturally rosy-colored pastries will stay mold-free for 6 days without refrigeration at room temperature and without added preservatives.
Our guess, though, is they won’t be on the kitchen counter long enough to find out.
A sobering proposition
If Hollywood is to be believed, there’s no amount of drunkenness that can’t be cured with a cup of coffee or a stern slap in the face. Unfortunately, here in the real world the only thing that can make you less drunk is time. Maybe next time you’ll stop after that seventh Manhattan.
But what if we could beat time? What if there’s an actual sobriety drug out there?
Say hello to fibroblast growth factor 21. Although the liver already does good work filtering out what is essentially poison, it then goes the extra mile and produces fibroblast growth factor 21 (or, as her friends call her, FGF21), a hormone that suppresses the desire to drink, makes you desire water, and protects the liver all at the same time.
Now, FGF21 in its current role is great, but if you’ve ever seen or been a drunk person before, you’ve experienced the lack of interest in listening to reason, especially when it comes from within our own bodies. Who are you to tell us what to do, body? You’re not the boss of us! So a group of scientists decided to push the limits of FGF21. Could it do more than it already does?
First off, they genetically altered a group of mice so that they didn’t produce FGF21 on their own. Then they got them drunk. We’re going to assume they built a scale model of the bar from Cheers and had the mice filter in through the front door as they served their subjects beer out of tiny little glasses.
Once the mice were nice and liquored up, some were given a treatment of FGF21 while others were given a placebo. Lo and behold, the mice given FGF21 recovered about 50% faster than those that received the control treatment. Not exactly instant, but 50% is nothing to sniff at.
Before you bring your FGF21 supplement to the bar, though, this research only applies to mice. We don’t know if it works in people. And make sure you stick to booze. If your choice of intoxication is a bit more exotic, FGF21 isn’t going to do anything for you. Yes, the scientists tried. Yes, those mice are living a very interesting life. And yes, we are jealous of drugged-up lab mice.
Supersize your imagination, shrink your snacks
Have you ever heard of the meal-recall effect? Did you know that, in England, a biscuit is really a cookie? Did you also know that the magazine Bon Appétit is not the same as the peer-reviewed journal Appetite? We do … now.
The meal-recall effect is the subsequent reduction in snacking that comes from remembering a recent meal. It was used to great effect in a recent study conducted at the University of Cambridge, which is in England, where they feed their experimental humans cookies but, for some reason, call them biscuits.
For the first part of the study, the participants were invited to dine at Che Laboratory, where they “were given a microwave ready meal of rice and sauce and a cup of water,” according to a statement from the university. As our Uncle Ernie would say, “Gourmet all the way.”
The test subjects were instructed not to eat anything for 3 hours and “then invited back to the lab to perform imagination tasks.” Those who did come back were randomly divided into five different groups, each with a different task:
- Imagine moving their recent lunch at the lab around a plate.
- Recall eating their recent lunch in detail.
- Imagine that the lunch was twice as big and filling as it really was.
- Look at a photograph of spaghetti hoops in tomato sauce and write a description of it before imagining moving the food around a plate.
- Look at a photo of paper clips and rubber bands and imagine moving them around.
Now, at last, we get to the biscuits/cookies, which were the subject of a taste test that “was simply a rouse for covertly assessing snacking,” the investigators explained. As part of that test, participants were told they could eat as many biscuits as they wanted.
When the tables were cleared and the leftovers examined, the group that imagined spaghetti hoops had eaten the most biscuits (75.9 g), followed by the group that imagined paper clips (75.5 g), the moving-their-lunch-around-the-plate group (72.0 g), and the group that relived eating their lunch (70.0 g).
In a victory for the meal-recall effect, the people who imagined their meal being twice as big ate the fewest biscuits (51.1 g). “Your mind can be more powerful than your stomach in dictating how much you eat,” lead author Joanna Szypula, PhD, said in the university statement.
Oh! One more thing. The study appeared in Appetite, which is a peer-reviewed journal, not in Bon Appétit, which is not a peer-reviewed journal. Thanks to the fine folks at both publications for pointing that out to us.
Get ‘em while they’re hot … for your health
Today on the Eating Channel, it’s a very special episode of “Much Ado About Muffin.”
The muffin. For some of us, it’s a good way to pretend we’re not having dessert for breakfast. A bran muffin can be loaded with calcium and fiber, and our beloved blueberry is full of yummy antioxidants and vitamins. Definitely not dessert.
Well, the muffin denial can stop there because there’s a new flavor on the scene, and research suggests it may actually be healthy. (Disclaimer: Muffin may not be considered healthy in Norway.) This new muffin has a name, Roselle, that comes from the calyx extract used in it, which is found in the Hibiscus sabdariffa plant of the same name.
Now, when it comes to new foods, especially ones that are supposed to be healthy, the No. 1 criteria is the same: It has to taste good. Researchers at the Norwegian University of Science and Technology and Amity University in India agreed, but they also set out to make it nutritionally valuable and give it a long shelf life without the addition of preservatives.
Sounds like a tall order, but they figured it out.
Not only is it tasty, but the properties of it could rival your morning multivitamin. Hibiscus extract has huge amounts of antioxidants, like phenolics, which are believed to help prevent cell membrane damage. Foods like vegetables, flax seed, and whole grains also have these antioxidants, but why not just have a Roselle muffin instead? You also get a dose of ascorbic acid without the glass of OJ in the morning.
The ascorbic acid, however, is not there just to help you. It also helps to check the researcher’s third box, shelf life. These naturally rosy-colored pastries will stay mold-free for 6 days without refrigeration at room temperature and without added preservatives.
Our guess, though, is they won’t be on the kitchen counter long enough to find out.
A sobering proposition
If Hollywood is to be believed, there’s no amount of drunkenness that can’t be cured with a cup of coffee or a stern slap in the face. Unfortunately, here in the real world the only thing that can make you less drunk is time. Maybe next time you’ll stop after that seventh Manhattan.
But what if we could beat time? What if there’s an actual sobriety drug out there?
Say hello to fibroblast growth factor 21. Although the liver already does good work filtering out what is essentially poison, it then goes the extra mile and produces fibroblast growth factor 21 (or, as her friends call her, FGF21), a hormone that suppresses the desire to drink, makes you desire water, and protects the liver all at the same time.
Now, FGF21 in its current role is great, but if you’ve ever seen or been a drunk person before, you’ve experienced the lack of interest in listening to reason, especially when it comes from within our own bodies. Who are you to tell us what to do, body? You’re not the boss of us! So a group of scientists decided to push the limits of FGF21. Could it do more than it already does?
First off, they genetically altered a group of mice so that they didn’t produce FGF21 on their own. Then they got them drunk. We’re going to assume they built a scale model of the bar from Cheers and had the mice filter in through the front door as they served their subjects beer out of tiny little glasses.
Once the mice were nice and liquored up, some were given a treatment of FGF21 while others were given a placebo. Lo and behold, the mice given FGF21 recovered about 50% faster than those that received the control treatment. Not exactly instant, but 50% is nothing to sniff at.
Before you bring your FGF21 supplement to the bar, though, this research only applies to mice. We don’t know if it works in people. And make sure you stick to booze. If your choice of intoxication is a bit more exotic, FGF21 isn’t going to do anything for you. Yes, the scientists tried. Yes, those mice are living a very interesting life. And yes, we are jealous of drugged-up lab mice.
Supersize your imagination, shrink your snacks
Have you ever heard of the meal-recall effect? Did you know that, in England, a biscuit is really a cookie? Did you also know that the magazine Bon Appétit is not the same as the peer-reviewed journal Appetite? We do … now.
The meal-recall effect is the subsequent reduction in snacking that comes from remembering a recent meal. It was used to great effect in a recent study conducted at the University of Cambridge, which is in England, where they feed their experimental humans cookies but, for some reason, call them biscuits.
For the first part of the study, the participants were invited to dine at Che Laboratory, where they “were given a microwave ready meal of rice and sauce and a cup of water,” according to a statement from the university. As our Uncle Ernie would say, “Gourmet all the way.”
The test subjects were instructed not to eat anything for 3 hours and “then invited back to the lab to perform imagination tasks.” Those who did come back were randomly divided into five different groups, each with a different task:
- Imagine moving their recent lunch at the lab around a plate.
- Recall eating their recent lunch in detail.
- Imagine that the lunch was twice as big and filling as it really was.
- Look at a photograph of spaghetti hoops in tomato sauce and write a description of it before imagining moving the food around a plate.
- Look at a photo of paper clips and rubber bands and imagine moving them around.
Now, at last, we get to the biscuits/cookies, which were the subject of a taste test that “was simply a rouse for covertly assessing snacking,” the investigators explained. As part of that test, participants were told they could eat as many biscuits as they wanted.
When the tables were cleared and the leftovers examined, the group that imagined spaghetti hoops had eaten the most biscuits (75.9 g), followed by the group that imagined paper clips (75.5 g), the moving-their-lunch-around-the-plate group (72.0 g), and the group that relived eating their lunch (70.0 g).
In a victory for the meal-recall effect, the people who imagined their meal being twice as big ate the fewest biscuits (51.1 g). “Your mind can be more powerful than your stomach in dictating how much you eat,” lead author Joanna Szypula, PhD, said in the university statement.
Oh! One more thing. The study appeared in Appetite, which is a peer-reviewed journal, not in Bon Appétit, which is not a peer-reviewed journal. Thanks to the fine folks at both publications for pointing that out to us.
Black women have higher state-level rates of TNBC
New national data on the occurrence of triple-negative breast cancer (TNBC) among different racial groups confirms that the disease is more common among Black women nationwide. A state-by-state analysis in the study, published online in JAMA Oncology, shows that these trends persist at the state level.
The analysis revealed that incidence rate ratios of TNBC were significantly higher among Black women, compared with White women, in all states with data on this population. Rates ranged from a low of 1.38 in Colorado to a high of 2.32 in Delaware.
The state-level disparities highlight gaps in physicians’ understanding of how social factors contribute to disparities in TNBC risk and the need “to develop effective preventative measures,” the study authors explain.
“We’ve realized for a long time that Black women have a higher incidence of TNBC. This is related to the genetic signature of the cancer. So that is not at all surprising,” said Arnold M. Baskies, MD, past chairman of the national board of directors of the American Cancer Society, Atlanta, who was not involved in the research. However, “the variance of TNBC among women from state to state is somewhat surprising.”
Existing research shows that TNBC is diagnosed more frequently among non-Hispanic Black women than among other populations in the United States, but it’s unclear whether these racial and ethnic disparities differ at the state level.
The authors identified 133,579 women with TNBC from the U.S. Cancer Statistics Public Use Research Database whose conditions were diagnosed from January 2015 through the end of December 2019. Most patients (64.5%) were White, 21.5% were Black, nearly 10% were Hispanic, 3.7% were Asian or Pacific Islander, and 0.6% were American Indian or Alaska Native. States with fewer than 30 cases were excluded, as was Nevada, owing to concerns regarding data quality. That left eight states for American Indian or Alaska Natives, 22 for Asian or Pacific Islanders, 35 for Hispanic women, 38 for Black women, and 50 for White women.
Overall, the incidence ratios of TNBC were highest among Black women (IR, 25.2 per 100,000), followed by White women (IR, 12.9 per 100,000), American Indian or Alaska Native women (IR, 11.2 per 100,000), Hispanic women (IR, 11.1 per 100,000 women), and Asian or Pacific Islander (IR, 9.0 per 100,000) women.
The authors also uncovered significant state-by-state variations in TNBC incidence by racial and ethnic groups. The lowest IR rates occurred among Asian or Pacific Islander women in Oregon and Pennsylvania – fewer than 7 per 100,000 women – and the highest occurred among Black women in Delaware, Missouri, Louisiana, and Mississippi – more than 29 per 100,000 women.
In the 38 states for which data on Black women were available, IR rates were significantly higher among Black women in all 38, compared with White women. The IR rates ranged from a low of 1.38 (IR, 17.4 per 100 000 women) in Colorado to a high of 2.32 (IR, 32.0 per 100 000 women) in Delaware.
While genetics play a role in TNBC risk, “the substantial geographic variation we found within each racial and ethnic group is highly suggestive that there are structural, environmental, and social factors at play in determining women’s risk of TNBC,” said lead study author Hyuna Sung, PhD, senior principal scientist and cancer epidemiologist at the American Cancer Society, Atlanta.
Existing evidence indicates that Black and White women living in socioeconomically disadvantaged neighborhoods are at higher risk of developing more aggressive subtypes of breast cancer, Dr. Sung said. Another factor, Dr. Sung and co-authors note, is breastfeeding. Across races, women who breastfeed have lower rates of TNBC.
Getting more definitive answers as to what causes differences in TNBC rates across states and what strategies can help reduce these disparities will be difficult and requires more research. “We really need to do a better job at researching and treating TNBC to improve health care equality for all women,” Dr. Baskies said. “The mortality rates from this cancer are high, and we rely heavily on surgery and toxic chemotherapy to treat it.”
Dr. Sung agreed, noting that “the observed state variation in TNBC rates merits further studies with risk factor data at multiple levels to better understand the associations of social exposures with the risk of TNBC.”
In states such as Louisiana and Mississippi, which are known to have a disproportionately higher burden of many types of cancers, “addressing barriers to access to preventive care and empowering public health efforts to promote a healthy living environment are the best policy prescription that could be deduced from our results,” Dr. Sung concluded.
Dr. Baskies is on the board of directors of Anixa Biosciences, which is currently conducting a clinical trial of a TNBC vaccine at the Cleveland Clinic. Dr. Sung has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New national data on the occurrence of triple-negative breast cancer (TNBC) among different racial groups confirms that the disease is more common among Black women nationwide. A state-by-state analysis in the study, published online in JAMA Oncology, shows that these trends persist at the state level.
The analysis revealed that incidence rate ratios of TNBC were significantly higher among Black women, compared with White women, in all states with data on this population. Rates ranged from a low of 1.38 in Colorado to a high of 2.32 in Delaware.
The state-level disparities highlight gaps in physicians’ understanding of how social factors contribute to disparities in TNBC risk and the need “to develop effective preventative measures,” the study authors explain.
“We’ve realized for a long time that Black women have a higher incidence of TNBC. This is related to the genetic signature of the cancer. So that is not at all surprising,” said Arnold M. Baskies, MD, past chairman of the national board of directors of the American Cancer Society, Atlanta, who was not involved in the research. However, “the variance of TNBC among women from state to state is somewhat surprising.”
Existing research shows that TNBC is diagnosed more frequently among non-Hispanic Black women than among other populations in the United States, but it’s unclear whether these racial and ethnic disparities differ at the state level.
The authors identified 133,579 women with TNBC from the U.S. Cancer Statistics Public Use Research Database whose conditions were diagnosed from January 2015 through the end of December 2019. Most patients (64.5%) were White, 21.5% were Black, nearly 10% were Hispanic, 3.7% were Asian or Pacific Islander, and 0.6% were American Indian or Alaska Native. States with fewer than 30 cases were excluded, as was Nevada, owing to concerns regarding data quality. That left eight states for American Indian or Alaska Natives, 22 for Asian or Pacific Islanders, 35 for Hispanic women, 38 for Black women, and 50 for White women.
Overall, the incidence ratios of TNBC were highest among Black women (IR, 25.2 per 100,000), followed by White women (IR, 12.9 per 100,000), American Indian or Alaska Native women (IR, 11.2 per 100,000), Hispanic women (IR, 11.1 per 100,000 women), and Asian or Pacific Islander (IR, 9.0 per 100,000) women.
The authors also uncovered significant state-by-state variations in TNBC incidence by racial and ethnic groups. The lowest IR rates occurred among Asian or Pacific Islander women in Oregon and Pennsylvania – fewer than 7 per 100,000 women – and the highest occurred among Black women in Delaware, Missouri, Louisiana, and Mississippi – more than 29 per 100,000 women.
In the 38 states for which data on Black women were available, IR rates were significantly higher among Black women in all 38, compared with White women. The IR rates ranged from a low of 1.38 (IR, 17.4 per 100 000 women) in Colorado to a high of 2.32 (IR, 32.0 per 100 000 women) in Delaware.
While genetics play a role in TNBC risk, “the substantial geographic variation we found within each racial and ethnic group is highly suggestive that there are structural, environmental, and social factors at play in determining women’s risk of TNBC,” said lead study author Hyuna Sung, PhD, senior principal scientist and cancer epidemiologist at the American Cancer Society, Atlanta.
Existing evidence indicates that Black and White women living in socioeconomically disadvantaged neighborhoods are at higher risk of developing more aggressive subtypes of breast cancer, Dr. Sung said. Another factor, Dr. Sung and co-authors note, is breastfeeding. Across races, women who breastfeed have lower rates of TNBC.
Getting more definitive answers as to what causes differences in TNBC rates across states and what strategies can help reduce these disparities will be difficult and requires more research. “We really need to do a better job at researching and treating TNBC to improve health care equality for all women,” Dr. Baskies said. “The mortality rates from this cancer are high, and we rely heavily on surgery and toxic chemotherapy to treat it.”
Dr. Sung agreed, noting that “the observed state variation in TNBC rates merits further studies with risk factor data at multiple levels to better understand the associations of social exposures with the risk of TNBC.”
In states such as Louisiana and Mississippi, which are known to have a disproportionately higher burden of many types of cancers, “addressing barriers to access to preventive care and empowering public health efforts to promote a healthy living environment are the best policy prescription that could be deduced from our results,” Dr. Sung concluded.
Dr. Baskies is on the board of directors of Anixa Biosciences, which is currently conducting a clinical trial of a TNBC vaccine at the Cleveland Clinic. Dr. Sung has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New national data on the occurrence of triple-negative breast cancer (TNBC) among different racial groups confirms that the disease is more common among Black women nationwide. A state-by-state analysis in the study, published online in JAMA Oncology, shows that these trends persist at the state level.
The analysis revealed that incidence rate ratios of TNBC were significantly higher among Black women, compared with White women, in all states with data on this population. Rates ranged from a low of 1.38 in Colorado to a high of 2.32 in Delaware.
The state-level disparities highlight gaps in physicians’ understanding of how social factors contribute to disparities in TNBC risk and the need “to develop effective preventative measures,” the study authors explain.
“We’ve realized for a long time that Black women have a higher incidence of TNBC. This is related to the genetic signature of the cancer. So that is not at all surprising,” said Arnold M. Baskies, MD, past chairman of the national board of directors of the American Cancer Society, Atlanta, who was not involved in the research. However, “the variance of TNBC among women from state to state is somewhat surprising.”
Existing research shows that TNBC is diagnosed more frequently among non-Hispanic Black women than among other populations in the United States, but it’s unclear whether these racial and ethnic disparities differ at the state level.
The authors identified 133,579 women with TNBC from the U.S. Cancer Statistics Public Use Research Database whose conditions were diagnosed from January 2015 through the end of December 2019. Most patients (64.5%) were White, 21.5% were Black, nearly 10% were Hispanic, 3.7% were Asian or Pacific Islander, and 0.6% were American Indian or Alaska Native. States with fewer than 30 cases were excluded, as was Nevada, owing to concerns regarding data quality. That left eight states for American Indian or Alaska Natives, 22 for Asian or Pacific Islanders, 35 for Hispanic women, 38 for Black women, and 50 for White women.
Overall, the incidence ratios of TNBC were highest among Black women (IR, 25.2 per 100,000), followed by White women (IR, 12.9 per 100,000), American Indian or Alaska Native women (IR, 11.2 per 100,000), Hispanic women (IR, 11.1 per 100,000 women), and Asian or Pacific Islander (IR, 9.0 per 100,000) women.
The authors also uncovered significant state-by-state variations in TNBC incidence by racial and ethnic groups. The lowest IR rates occurred among Asian or Pacific Islander women in Oregon and Pennsylvania – fewer than 7 per 100,000 women – and the highest occurred among Black women in Delaware, Missouri, Louisiana, and Mississippi – more than 29 per 100,000 women.
In the 38 states for which data on Black women were available, IR rates were significantly higher among Black women in all 38, compared with White women. The IR rates ranged from a low of 1.38 (IR, 17.4 per 100 000 women) in Colorado to a high of 2.32 (IR, 32.0 per 100 000 women) in Delaware.
While genetics play a role in TNBC risk, “the substantial geographic variation we found within each racial and ethnic group is highly suggestive that there are structural, environmental, and social factors at play in determining women’s risk of TNBC,” said lead study author Hyuna Sung, PhD, senior principal scientist and cancer epidemiologist at the American Cancer Society, Atlanta.
Existing evidence indicates that Black and White women living in socioeconomically disadvantaged neighborhoods are at higher risk of developing more aggressive subtypes of breast cancer, Dr. Sung said. Another factor, Dr. Sung and co-authors note, is breastfeeding. Across races, women who breastfeed have lower rates of TNBC.
Getting more definitive answers as to what causes differences in TNBC rates across states and what strategies can help reduce these disparities will be difficult and requires more research. “We really need to do a better job at researching and treating TNBC to improve health care equality for all women,” Dr. Baskies said. “The mortality rates from this cancer are high, and we rely heavily on surgery and toxic chemotherapy to treat it.”
Dr. Sung agreed, noting that “the observed state variation in TNBC rates merits further studies with risk factor data at multiple levels to better understand the associations of social exposures with the risk of TNBC.”
In states such as Louisiana and Mississippi, which are known to have a disproportionately higher burden of many types of cancers, “addressing barriers to access to preventive care and empowering public health efforts to promote a healthy living environment are the best policy prescription that could be deduced from our results,” Dr. Sung concluded.
Dr. Baskies is on the board of directors of Anixa Biosciences, which is currently conducting a clinical trial of a TNBC vaccine at the Cleveland Clinic. Dr. Sung has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Specialty and age may contribute to suicidal thoughts among physicians
A physician’s specialty can make a difference when it comes to having suicidal thoughts. Doctors who specialize in family medicine, obstetrics-gynecology, and psychiatry reported double the rates of suicidal thoughts than doctors in oncology, rheumatology, and pulmonary medicine, according to Doctors’ Burden: Medscape Physician Suicide Report 2023.
“The specialties with the highest reporting of physician suicidal thoughts are also those with the greatest physician shortages, based on the number of job openings posted by recruiting sites,” said Peter Yellowlees, MD, professor of psychiatry and chief wellness officer at UC Davis Health.
Doctors in those specialties are overworked, which can lead to burnout, he said.
There’s also a generational divide among physicians who reported suicidal thoughts. Millennials (age 27-41) and Gen-X physicians (age 42-56) were more likely to report these thoughts than were Baby Boomers (age 57-75) and the Silent Generation (age 76-95).
“Younger physicians are more burned out – they may have less control over their lives and less meaning than some older doctors who can do what they want,” said Dr. Yellowlees.
One millennial respondent commented that being on call and being required to chart detailed notes in the EHR has contributed to her burnout. “I’m more impatient and make less time and effort to see my friends and family.”
One Silent Generation respondent commented, “I am semi-retired, I take no call, I work no weekends, I provide anesthesia care in my area of special expertise, I work clinically about 46 days a year. Life is good, particularly compared to my younger colleagues who are working 60-plus hours a week with evening work, weekend work, and call. I feel really sorry for them.”
When young people enter medical school, they’re quite healthy, with low rates of depression and burnout, said Dr. Yellowlees. Yet, studies have shown that rates of burnout and suicidal thoughts increased within 2 years. “That reflects what happens when a group of idealistic young people hit a horrible system,” he said.
Who’s responsible?
Millennials were three times as likely as baby boomers to say that a medical school or health care organization should be responsible when a student or physician commits suicide.
“Young physicians may expect more of their employers than my generation did, which we see in residency programs that have unionized,” said Dr. Yellowlees, a Baby Boomer.
“As more young doctors are employed by health care organizations, they also may expect more resources to be available to them, such as wellness programs,” he added.
Younger doctors also focus more on work-life balance than older doctors, including time off and having hobbies, he said. “They are much more rational in terms of their overall beliefs and expectations than the older generation.”
Whom doctors confide in
Nearly 60% of physician-respondents with suicidal thoughts said they confided in a professional or someone they knew. Men were just as likely as women to reach out to a therapist (38%), whereas men were slightly more likely to confide in a family member and women were slightly more likely to confide in a colleague.
“It’s interesting that women are more active in seeking support at work – they often have developed a network of colleagues to support each other’s careers and whom they can confide in,” said Dr. Yellowlees.
He emphasized that 40% of physicians said they didn’t confide in anyone when they had suicidal thoughts. Of those, just over half said they could cope without professional help.
One respondent commented, “It’s just a thought; nothing I would actually do.” Another commented, “Mental health professionals can’t fix the underlying reason for the problem.”
Many doctors were concerned about risking disclosure to their medical boards (42%); that it would show up on their insurance records (33%); and that their colleagues would find out (25%), according to the report.
One respondent commented, “I don’t trust doctors to keep it to themselves.”
Another barrier doctors mentioned was a lack of time to seek help. One commented, “Time. I have none, when am I supposed to find an hour for counseling?”
A version of this article originally appeared on Medscape.com.
A physician’s specialty can make a difference when it comes to having suicidal thoughts. Doctors who specialize in family medicine, obstetrics-gynecology, and psychiatry reported double the rates of suicidal thoughts than doctors in oncology, rheumatology, and pulmonary medicine, according to Doctors’ Burden: Medscape Physician Suicide Report 2023.
“The specialties with the highest reporting of physician suicidal thoughts are also those with the greatest physician shortages, based on the number of job openings posted by recruiting sites,” said Peter Yellowlees, MD, professor of psychiatry and chief wellness officer at UC Davis Health.
Doctors in those specialties are overworked, which can lead to burnout, he said.
There’s also a generational divide among physicians who reported suicidal thoughts. Millennials (age 27-41) and Gen-X physicians (age 42-56) were more likely to report these thoughts than were Baby Boomers (age 57-75) and the Silent Generation (age 76-95).
“Younger physicians are more burned out – they may have less control over their lives and less meaning than some older doctors who can do what they want,” said Dr. Yellowlees.
One millennial respondent commented that being on call and being required to chart detailed notes in the EHR has contributed to her burnout. “I’m more impatient and make less time and effort to see my friends and family.”
One Silent Generation respondent commented, “I am semi-retired, I take no call, I work no weekends, I provide anesthesia care in my area of special expertise, I work clinically about 46 days a year. Life is good, particularly compared to my younger colleagues who are working 60-plus hours a week with evening work, weekend work, and call. I feel really sorry for them.”
When young people enter medical school, they’re quite healthy, with low rates of depression and burnout, said Dr. Yellowlees. Yet, studies have shown that rates of burnout and suicidal thoughts increased within 2 years. “That reflects what happens when a group of idealistic young people hit a horrible system,” he said.
Who’s responsible?
Millennials were three times as likely as baby boomers to say that a medical school or health care organization should be responsible when a student or physician commits suicide.
“Young physicians may expect more of their employers than my generation did, which we see in residency programs that have unionized,” said Dr. Yellowlees, a Baby Boomer.
“As more young doctors are employed by health care organizations, they also may expect more resources to be available to them, such as wellness programs,” he added.
Younger doctors also focus more on work-life balance than older doctors, including time off and having hobbies, he said. “They are much more rational in terms of their overall beliefs and expectations than the older generation.”
Whom doctors confide in
Nearly 60% of physician-respondents with suicidal thoughts said they confided in a professional or someone they knew. Men were just as likely as women to reach out to a therapist (38%), whereas men were slightly more likely to confide in a family member and women were slightly more likely to confide in a colleague.
“It’s interesting that women are more active in seeking support at work – they often have developed a network of colleagues to support each other’s careers and whom they can confide in,” said Dr. Yellowlees.
He emphasized that 40% of physicians said they didn’t confide in anyone when they had suicidal thoughts. Of those, just over half said they could cope without professional help.
One respondent commented, “It’s just a thought; nothing I would actually do.” Another commented, “Mental health professionals can’t fix the underlying reason for the problem.”
Many doctors were concerned about risking disclosure to their medical boards (42%); that it would show up on their insurance records (33%); and that their colleagues would find out (25%), according to the report.
One respondent commented, “I don’t trust doctors to keep it to themselves.”
Another barrier doctors mentioned was a lack of time to seek help. One commented, “Time. I have none, when am I supposed to find an hour for counseling?”
A version of this article originally appeared on Medscape.com.
A physician’s specialty can make a difference when it comes to having suicidal thoughts. Doctors who specialize in family medicine, obstetrics-gynecology, and psychiatry reported double the rates of suicidal thoughts than doctors in oncology, rheumatology, and pulmonary medicine, according to Doctors’ Burden: Medscape Physician Suicide Report 2023.
“The specialties with the highest reporting of physician suicidal thoughts are also those with the greatest physician shortages, based on the number of job openings posted by recruiting sites,” said Peter Yellowlees, MD, professor of psychiatry and chief wellness officer at UC Davis Health.
Doctors in those specialties are overworked, which can lead to burnout, he said.
There’s also a generational divide among physicians who reported suicidal thoughts. Millennials (age 27-41) and Gen-X physicians (age 42-56) were more likely to report these thoughts than were Baby Boomers (age 57-75) and the Silent Generation (age 76-95).
“Younger physicians are more burned out – they may have less control over their lives and less meaning than some older doctors who can do what they want,” said Dr. Yellowlees.
One millennial respondent commented that being on call and being required to chart detailed notes in the EHR has contributed to her burnout. “I’m more impatient and make less time and effort to see my friends and family.”
One Silent Generation respondent commented, “I am semi-retired, I take no call, I work no weekends, I provide anesthesia care in my area of special expertise, I work clinically about 46 days a year. Life is good, particularly compared to my younger colleagues who are working 60-plus hours a week with evening work, weekend work, and call. I feel really sorry for them.”
When young people enter medical school, they’re quite healthy, with low rates of depression and burnout, said Dr. Yellowlees. Yet, studies have shown that rates of burnout and suicidal thoughts increased within 2 years. “That reflects what happens when a group of idealistic young people hit a horrible system,” he said.
Who’s responsible?
Millennials were three times as likely as baby boomers to say that a medical school or health care organization should be responsible when a student or physician commits suicide.
“Young physicians may expect more of their employers than my generation did, which we see in residency programs that have unionized,” said Dr. Yellowlees, a Baby Boomer.
“As more young doctors are employed by health care organizations, they also may expect more resources to be available to them, such as wellness programs,” he added.
Younger doctors also focus more on work-life balance than older doctors, including time off and having hobbies, he said. “They are much more rational in terms of their overall beliefs and expectations than the older generation.”
Whom doctors confide in
Nearly 60% of physician-respondents with suicidal thoughts said they confided in a professional or someone they knew. Men were just as likely as women to reach out to a therapist (38%), whereas men were slightly more likely to confide in a family member and women were slightly more likely to confide in a colleague.
“It’s interesting that women are more active in seeking support at work – they often have developed a network of colleagues to support each other’s careers and whom they can confide in,” said Dr. Yellowlees.
He emphasized that 40% of physicians said they didn’t confide in anyone when they had suicidal thoughts. Of those, just over half said they could cope without professional help.
One respondent commented, “It’s just a thought; nothing I would actually do.” Another commented, “Mental health professionals can’t fix the underlying reason for the problem.”
Many doctors were concerned about risking disclosure to their medical boards (42%); that it would show up on their insurance records (33%); and that their colleagues would find out (25%), according to the report.
One respondent commented, “I don’t trust doctors to keep it to themselves.”
Another barrier doctors mentioned was a lack of time to seek help. One commented, “Time. I have none, when am I supposed to find an hour for counseling?”
A version of this article originally appeared on Medscape.com.
For young people on Medicare, a hysterectomy sometimes is more affordable than birth control
Sam Chavarría said her doctor was clear about the birth defects her medication could cause if she became pregnant but agreed to keep her on it as long as she had an IUD.
As she was waiting to get her contraceptive intrauterine device replaced at her local clinic, however, the billing nurse told her that her insurance wouldn’t cover the removal – or a new IUD. Chavarría didn’t understand why not.
“Then she said very delicately, ‘Well, people on this insurance typically tend to be older,’ ” Chavarría recalled.
Although Chavarría is 34, she is enrolled in Medicare, the government insurance program designed for those 65 and older. Chavarría, who lives in Houston, is disabled by fibromyalgia, rheumatoid arthritis, and mental health issues. Medicare automatically enrolls anyone who has received Social Security disability benefits for two years and this was her first time getting an IUD while in the government program.
Without insurance, just removing her expired IUD would cost Chavarría $350 out of pocket; exchanging it for a new one would be $2,000. She left the clinic in tears.
Chavarría’s experience is not rare. Medicare was originally intended for people of retirement age. Over the years, the program has evolved to include new populations, such as those who have disabilities or are critically ill, said Jennifer Lea Huer, a public health expert at Yale University, New Haven, Conn. In 2020, 1.7 million people ages 18-44 were enrolled in Medicare.
An estimated 70% of childbearing-age women on Medicare are also eligible for Medicaid, a state and federal program for those with low incomes, which should fill the gap for contraception. It’s not clear how many transgender or nonbinary people – who also might need contraception – are on Medicare or are eligible for Medicaid.
Medicaid, like the plans offered via the federal Affordable Care Act, mandates coverage of birth control. But those who aren’t eligible for Medicaid are left in the lurch – Medicare’s origins mean it does not require access to birth control.
Traditional Medicare includes two parts: Part A covers hospital costs, while Part B covers physicians’ care and certain other services, such as ambulance rides. Neither ordinarily includes contraception.
People can get contraception through a Medicare Advantage plan or Part D of Medicare, which covers prescription drugs, but those come at a cost. And even people who pay for Part D often aren’t covered for some types of birth control, such as IUDs.
“So, if you are disabled, if you are locked outside of the labor market, if you do not have the means or any other way to financially support yourself, you were likely still on traditional Medicare, which is Part A and Part B,” Huer said. “In which case, your access to contraception is incredibly difficult.”
Contraception for those with traditional Medicare is given on a case-by-case basis, Huer said. It can be covered only if a doctor can make a credible case that the patient needs it for medical reasons – because their body cannot sustain a pregnancy – as opposed to merely wanting to avoid one.
“You have to have a champion physician who’s willing to partner with you and make those arguments,” Huer said.
That’s what Chavarría’s doctor tried to do. Before she left the clinic, staffers there told her they would try to make the case she needed the IUD for medical reasons. The IUD exchange was scheduled almost 10 weeks later, but during those weeks, she got pregnant. Her body couldn’t sustain a pregnancy, so she and her partner rushed to get an abortion just before Texas tightened its rules Sept. 1, 2021.
“If Medicare had just covered the IUD removal or exchange to begin with, none of this would have happened,” Chavarría said. “It would have saved me having to make a really tough decision that I never thought I’d have to make.”
Women with disabilities often face a stigma from health care practitioners, especially when it comes to birth control, said Willi Horner-Johnson, a public health researcher specializing in disabilities at Oregon Health & Science University, Portland. In her research, women with disabilities have described being treated like children or having to go to multiple doctors to find someone with whom they felt comfortable.
“We don’t want to acknowledge that disabled people have sex,” said Miriam Garber, a 36-year-old sex worker who lives in Rhode Island and is also on Medicare because of her disabilities. Garber got an IUD from Planned Parenthood because her insurance wouldn’t cover it.
Even those who pay for Part D to have their prescription drugs covered and have a “champion physician” face difficulties. Liz Moore, a nonbinary person in their 30s who lives in the Washington, D.C., area, could not get Medicare to pay for the Mirena IUD their doctor prescribed for their polycystic ovary syndrome. Moore is disabled with fibromyalgia and dysautonomia, a condition of the autonomic nervous system, which regulates breathing, heart rate, and more.
“After literally months of phone calls, it seemed like my Medicare Part D and original Medicare could not agree on who should pay for my IUD,” they wrote in a direct message. “Was it a prescription or durable medical equipment?”
When Moore finally learned it would cost $800 upfront, they said, they decided to get a hysterectomy – which Medicare would pay for – instead.
Chavarría’s doctor told her a tubal ligation also was more likely to be approved by Medicare than an IUD, because older people have that procedure more often. Like all surgeries, both come with risks of complications and recovery.
Even for those on both Medicare and Medicaid, getting contraception also isn’t always easy, as in Katie Elizabeth Walsh’s case.
Walsh, 34, who lives in northeastern Connecticut, is disabled by a traumatic brain injury, depression, and chronic fatigue syndrome. She got an IUD at an ob.gyn. clinic and was told there her insurance would cover it.
Then she got a bill for nearly $2,000.
Medicaid should cover contraceptive devices for dual-eligibility people, according to Centers for Medicare & Medicaid Services policy guidance, but when Walsh tried to get her bill covered, Medicare and Medicaid could not agree on which of them should pay.
“Every single time I have called one of the insurance offices, they are like, ‘Oh, no, you have to talk to the other one, and we don’t really talk to each other,’ ” Walsh said.
Walsh said the hassle to get her contraception covered feels like a kick in the stomach: “Like truly you do not have a place in this world, and your insurance is telling you that.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Sam Chavarría said her doctor was clear about the birth defects her medication could cause if she became pregnant but agreed to keep her on it as long as she had an IUD.
As she was waiting to get her contraceptive intrauterine device replaced at her local clinic, however, the billing nurse told her that her insurance wouldn’t cover the removal – or a new IUD. Chavarría didn’t understand why not.
“Then she said very delicately, ‘Well, people on this insurance typically tend to be older,’ ” Chavarría recalled.
Although Chavarría is 34, she is enrolled in Medicare, the government insurance program designed for those 65 and older. Chavarría, who lives in Houston, is disabled by fibromyalgia, rheumatoid arthritis, and mental health issues. Medicare automatically enrolls anyone who has received Social Security disability benefits for two years and this was her first time getting an IUD while in the government program.
Without insurance, just removing her expired IUD would cost Chavarría $350 out of pocket; exchanging it for a new one would be $2,000. She left the clinic in tears.
Chavarría’s experience is not rare. Medicare was originally intended for people of retirement age. Over the years, the program has evolved to include new populations, such as those who have disabilities or are critically ill, said Jennifer Lea Huer, a public health expert at Yale University, New Haven, Conn. In 2020, 1.7 million people ages 18-44 were enrolled in Medicare.
An estimated 70% of childbearing-age women on Medicare are also eligible for Medicaid, a state and federal program for those with low incomes, which should fill the gap for contraception. It’s not clear how many transgender or nonbinary people – who also might need contraception – are on Medicare or are eligible for Medicaid.
Medicaid, like the plans offered via the federal Affordable Care Act, mandates coverage of birth control. But those who aren’t eligible for Medicaid are left in the lurch – Medicare’s origins mean it does not require access to birth control.
Traditional Medicare includes two parts: Part A covers hospital costs, while Part B covers physicians’ care and certain other services, such as ambulance rides. Neither ordinarily includes contraception.
People can get contraception through a Medicare Advantage plan or Part D of Medicare, which covers prescription drugs, but those come at a cost. And even people who pay for Part D often aren’t covered for some types of birth control, such as IUDs.
“So, if you are disabled, if you are locked outside of the labor market, if you do not have the means or any other way to financially support yourself, you were likely still on traditional Medicare, which is Part A and Part B,” Huer said. “In which case, your access to contraception is incredibly difficult.”
Contraception for those with traditional Medicare is given on a case-by-case basis, Huer said. It can be covered only if a doctor can make a credible case that the patient needs it for medical reasons – because their body cannot sustain a pregnancy – as opposed to merely wanting to avoid one.
“You have to have a champion physician who’s willing to partner with you and make those arguments,” Huer said.
That’s what Chavarría’s doctor tried to do. Before she left the clinic, staffers there told her they would try to make the case she needed the IUD for medical reasons. The IUD exchange was scheduled almost 10 weeks later, but during those weeks, she got pregnant. Her body couldn’t sustain a pregnancy, so she and her partner rushed to get an abortion just before Texas tightened its rules Sept. 1, 2021.
“If Medicare had just covered the IUD removal or exchange to begin with, none of this would have happened,” Chavarría said. “It would have saved me having to make a really tough decision that I never thought I’d have to make.”
Women with disabilities often face a stigma from health care practitioners, especially when it comes to birth control, said Willi Horner-Johnson, a public health researcher specializing in disabilities at Oregon Health & Science University, Portland. In her research, women with disabilities have described being treated like children or having to go to multiple doctors to find someone with whom they felt comfortable.
“We don’t want to acknowledge that disabled people have sex,” said Miriam Garber, a 36-year-old sex worker who lives in Rhode Island and is also on Medicare because of her disabilities. Garber got an IUD from Planned Parenthood because her insurance wouldn’t cover it.
Even those who pay for Part D to have their prescription drugs covered and have a “champion physician” face difficulties. Liz Moore, a nonbinary person in their 30s who lives in the Washington, D.C., area, could not get Medicare to pay for the Mirena IUD their doctor prescribed for their polycystic ovary syndrome. Moore is disabled with fibromyalgia and dysautonomia, a condition of the autonomic nervous system, which regulates breathing, heart rate, and more.
“After literally months of phone calls, it seemed like my Medicare Part D and original Medicare could not agree on who should pay for my IUD,” they wrote in a direct message. “Was it a prescription or durable medical equipment?”
When Moore finally learned it would cost $800 upfront, they said, they decided to get a hysterectomy – which Medicare would pay for – instead.
Chavarría’s doctor told her a tubal ligation also was more likely to be approved by Medicare than an IUD, because older people have that procedure more often. Like all surgeries, both come with risks of complications and recovery.
Even for those on both Medicare and Medicaid, getting contraception also isn’t always easy, as in Katie Elizabeth Walsh’s case.
Walsh, 34, who lives in northeastern Connecticut, is disabled by a traumatic brain injury, depression, and chronic fatigue syndrome. She got an IUD at an ob.gyn. clinic and was told there her insurance would cover it.
Then she got a bill for nearly $2,000.
Medicaid should cover contraceptive devices for dual-eligibility people, according to Centers for Medicare & Medicaid Services policy guidance, but when Walsh tried to get her bill covered, Medicare and Medicaid could not agree on which of them should pay.
“Every single time I have called one of the insurance offices, they are like, ‘Oh, no, you have to talk to the other one, and we don’t really talk to each other,’ ” Walsh said.
Walsh said the hassle to get her contraception covered feels like a kick in the stomach: “Like truly you do not have a place in this world, and your insurance is telling you that.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Sam Chavarría said her doctor was clear about the birth defects her medication could cause if she became pregnant but agreed to keep her on it as long as she had an IUD.
As she was waiting to get her contraceptive intrauterine device replaced at her local clinic, however, the billing nurse told her that her insurance wouldn’t cover the removal – or a new IUD. Chavarría didn’t understand why not.
“Then she said very delicately, ‘Well, people on this insurance typically tend to be older,’ ” Chavarría recalled.
Although Chavarría is 34, she is enrolled in Medicare, the government insurance program designed for those 65 and older. Chavarría, who lives in Houston, is disabled by fibromyalgia, rheumatoid arthritis, and mental health issues. Medicare automatically enrolls anyone who has received Social Security disability benefits for two years and this was her first time getting an IUD while in the government program.
Without insurance, just removing her expired IUD would cost Chavarría $350 out of pocket; exchanging it for a new one would be $2,000. She left the clinic in tears.
Chavarría’s experience is not rare. Medicare was originally intended for people of retirement age. Over the years, the program has evolved to include new populations, such as those who have disabilities or are critically ill, said Jennifer Lea Huer, a public health expert at Yale University, New Haven, Conn. In 2020, 1.7 million people ages 18-44 were enrolled in Medicare.
An estimated 70% of childbearing-age women on Medicare are also eligible for Medicaid, a state and federal program for those with low incomes, which should fill the gap for contraception. It’s not clear how many transgender or nonbinary people – who also might need contraception – are on Medicare or are eligible for Medicaid.
Medicaid, like the plans offered via the federal Affordable Care Act, mandates coverage of birth control. But those who aren’t eligible for Medicaid are left in the lurch – Medicare’s origins mean it does not require access to birth control.
Traditional Medicare includes two parts: Part A covers hospital costs, while Part B covers physicians’ care and certain other services, such as ambulance rides. Neither ordinarily includes contraception.
People can get contraception through a Medicare Advantage plan or Part D of Medicare, which covers prescription drugs, but those come at a cost. And even people who pay for Part D often aren’t covered for some types of birth control, such as IUDs.
“So, if you are disabled, if you are locked outside of the labor market, if you do not have the means or any other way to financially support yourself, you were likely still on traditional Medicare, which is Part A and Part B,” Huer said. “In which case, your access to contraception is incredibly difficult.”
Contraception for those with traditional Medicare is given on a case-by-case basis, Huer said. It can be covered only if a doctor can make a credible case that the patient needs it for medical reasons – because their body cannot sustain a pregnancy – as opposed to merely wanting to avoid one.
“You have to have a champion physician who’s willing to partner with you and make those arguments,” Huer said.
That’s what Chavarría’s doctor tried to do. Before she left the clinic, staffers there told her they would try to make the case she needed the IUD for medical reasons. The IUD exchange was scheduled almost 10 weeks later, but during those weeks, she got pregnant. Her body couldn’t sustain a pregnancy, so she and her partner rushed to get an abortion just before Texas tightened its rules Sept. 1, 2021.
“If Medicare had just covered the IUD removal or exchange to begin with, none of this would have happened,” Chavarría said. “It would have saved me having to make a really tough decision that I never thought I’d have to make.”
Women with disabilities often face a stigma from health care practitioners, especially when it comes to birth control, said Willi Horner-Johnson, a public health researcher specializing in disabilities at Oregon Health & Science University, Portland. In her research, women with disabilities have described being treated like children or having to go to multiple doctors to find someone with whom they felt comfortable.
“We don’t want to acknowledge that disabled people have sex,” said Miriam Garber, a 36-year-old sex worker who lives in Rhode Island and is also on Medicare because of her disabilities. Garber got an IUD from Planned Parenthood because her insurance wouldn’t cover it.
Even those who pay for Part D to have their prescription drugs covered and have a “champion physician” face difficulties. Liz Moore, a nonbinary person in their 30s who lives in the Washington, D.C., area, could not get Medicare to pay for the Mirena IUD their doctor prescribed for their polycystic ovary syndrome. Moore is disabled with fibromyalgia and dysautonomia, a condition of the autonomic nervous system, which regulates breathing, heart rate, and more.
“After literally months of phone calls, it seemed like my Medicare Part D and original Medicare could not agree on who should pay for my IUD,” they wrote in a direct message. “Was it a prescription or durable medical equipment?”
When Moore finally learned it would cost $800 upfront, they said, they decided to get a hysterectomy – which Medicare would pay for – instead.
Chavarría’s doctor told her a tubal ligation also was more likely to be approved by Medicare than an IUD, because older people have that procedure more often. Like all surgeries, both come with risks of complications and recovery.
Even for those on both Medicare and Medicaid, getting contraception also isn’t always easy, as in Katie Elizabeth Walsh’s case.
Walsh, 34, who lives in northeastern Connecticut, is disabled by a traumatic brain injury, depression, and chronic fatigue syndrome. She got an IUD at an ob.gyn. clinic and was told there her insurance would cover it.
Then she got a bill for nearly $2,000.
Medicaid should cover contraceptive devices for dual-eligibility people, according to Centers for Medicare & Medicaid Services policy guidance, but when Walsh tried to get her bill covered, Medicare and Medicaid could not agree on which of them should pay.
“Every single time I have called one of the insurance offices, they are like, ‘Oh, no, you have to talk to the other one, and we don’t really talk to each other,’ ” Walsh said.
Walsh said the hassle to get her contraception covered feels like a kick in the stomach: “Like truly you do not have a place in this world, and your insurance is telling you that.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Popular book by USC oncologist pulled because of plagiarism
The Los Angeles Times reported earlier this week that it identified at least 95 instances of plagiarism by author David B. Agus, MD, in “The Book of Animal Secrets: Nature’s Lessons for a Long and Happy Life.”
According to the LA Times, Dr. Agus copied passages from numerous sources, including The New York Times, National Geographic, Wikipedia, and smaller niche sites. Some instances involved a sentence or two; others involved multiparagraph, word-for-word copying without attribution.
The book by Dr. Agus – who interviews celebrities for a health-related miniseries on Paramount Plus – had reached the top spot on Amazon’s list of best-selling books about animals a week before its planned March 7 release.
Publisher Simon & Schuster released a statement announcing a recall of the book at Dr. Agus’ expense “until a fully revised and corrected edition can be released.”
Dr. Agus included his own statement apologizing “to the scientists and writers whose work or words were used or not fully attributed,” and said he will “rewrite the passages in question with new language, will provide proper and full attribution, and when ready will announce a new publication date.”
“Writers should always be credited for their work, and I deeply regret these mistakes and the lack of rigor in finalizing the book,” he stated, adding that “[t]his book contains important lessons, messages, and guidance about health that I wanted to convey to the readers. I do not want these mistakes to interfere with that effort.”
A version of this article first appeared on Medscape.com.
The Los Angeles Times reported earlier this week that it identified at least 95 instances of plagiarism by author David B. Agus, MD, in “The Book of Animal Secrets: Nature’s Lessons for a Long and Happy Life.”
According to the LA Times, Dr. Agus copied passages from numerous sources, including The New York Times, National Geographic, Wikipedia, and smaller niche sites. Some instances involved a sentence or two; others involved multiparagraph, word-for-word copying without attribution.
The book by Dr. Agus – who interviews celebrities for a health-related miniseries on Paramount Plus – had reached the top spot on Amazon’s list of best-selling books about animals a week before its planned March 7 release.
Publisher Simon & Schuster released a statement announcing a recall of the book at Dr. Agus’ expense “until a fully revised and corrected edition can be released.”
Dr. Agus included his own statement apologizing “to the scientists and writers whose work or words were used or not fully attributed,” and said he will “rewrite the passages in question with new language, will provide proper and full attribution, and when ready will announce a new publication date.”
“Writers should always be credited for their work, and I deeply regret these mistakes and the lack of rigor in finalizing the book,” he stated, adding that “[t]his book contains important lessons, messages, and guidance about health that I wanted to convey to the readers. I do not want these mistakes to interfere with that effort.”
A version of this article first appeared on Medscape.com.
The Los Angeles Times reported earlier this week that it identified at least 95 instances of plagiarism by author David B. Agus, MD, in “The Book of Animal Secrets: Nature’s Lessons for a Long and Happy Life.”
According to the LA Times, Dr. Agus copied passages from numerous sources, including The New York Times, National Geographic, Wikipedia, and smaller niche sites. Some instances involved a sentence or two; others involved multiparagraph, word-for-word copying without attribution.
The book by Dr. Agus – who interviews celebrities for a health-related miniseries on Paramount Plus – had reached the top spot on Amazon’s list of best-selling books about animals a week before its planned March 7 release.
Publisher Simon & Schuster released a statement announcing a recall of the book at Dr. Agus’ expense “until a fully revised and corrected edition can be released.”
Dr. Agus included his own statement apologizing “to the scientists and writers whose work or words were used or not fully attributed,” and said he will “rewrite the passages in question with new language, will provide proper and full attribution, and when ready will announce a new publication date.”
“Writers should always be credited for their work, and I deeply regret these mistakes and the lack of rigor in finalizing the book,” he stated, adding that “[t]his book contains important lessons, messages, and guidance about health that I wanted to convey to the readers. I do not want these mistakes to interfere with that effort.”
A version of this article first appeared on Medscape.com.