User login
Team Rapid
The origin of the RRT can be found in medical emergency teams (METs). METs began in Australia as a result of the realization that earlier intervention could lead to better outcomes.1 In December 2004, in response to persistent problems with patient safety, the Institute for Healthcare Improvement launched its “100,000 Lives Campaign.”2 The Institute’s key plan for saving some of these 100,000 lives was to create RRTs at every participating medical center. Participating facilities would also submit data on mortality.
Olive View-UCLA Medical Center (OV-UCLA) signed on to participate in the campaign, and part of that effort was the creation and implementation of an RRT. We joined a University Health Consortium “Commit to Action” team, which assisted us by providing support as we began the creation and implementation of the RRT. What follows is the story of how we created an RRT.
We chose team members from all disciplines that were to be part of the RRT response—both at and behind the scenes: RNs, nursing administrators, hospital administrators, ICU attendings, house staff, laboratory personnel, nursing educators, radiology technicians, and hospital operators. The group was further organized into specific teams to solve problems and present solutions. At this point we learned our first important lesson: We needed to meet individually with all inpatient department chairs to discuss the effect of RRTs.
Activation and Notification
How would the RRT call be activated—overhead or beeper? Who could call, and what would the indications be? The OV-UCLA activation and notification team decided that the RRT could be activated by any staff member. Criteria, including vital signs, mental status, or simply “concern about the patient,” were created and posted. A telephone line in the ICU (X4415) was dedicated for RRT calls, and all other activation was overhead due to the lack of an adequate beeper system. (Other than code pagers, our beeper system can’t be simultaneously activated, and ancillaries don’t have beepers.)
The primary nurse’s responsibilities included calling the primary team or cross-covering team and obtaining a fingerstick glucose on all patients while waiting for the team. In discussions the primary team, we learned our second important lesson: As we presented the RRT to the hospital staff, everyone was concerned about the primary team. Ensuring that a mechanism for notifying the primary team was in place and reassuring staff that the primary team would be involved emerged as essential tasks. It was also imperative to identify the chain of command.
With this need in mind, we decided the primary team would always be the captain and would, therefore, have the authority to dismiss whomever they wanted from the RRT. An ICU attending was assigned to RRT call as supervision for the ICU resident responder. At OV-UCLA, our attending is not in-house and, to date, has not been called.
Documentation
The OV-UCLA documentation team was called on to answer the following questions: How would the RRT call be documented? How would medication orders be sent to the pharmacy? How would quality indicators (QI) and data be collected on the calls?
The team’s solution involved creating a one-page, primarily check-based document. The ICU nurse who answered the X4415 telephone in the ICU would begin documentation, which included the time of the call and the chief complaint. When the RRT reached the patient, however, the documentation duties were transferred to the primary RN. All providers were to document on the same page—similar to a code sheet. The RRT nurse and the attending doctor were to check vitals and perform the physical exam, as all information was called out to the documenter.
Medications were to be verbally ordered by the doctor, then read back and verified by the nurses documenting and administering for the RRT. For the most part, medication orders were restricted to what was carried in the RRT bag. The document was eventually copied three times: The original was placed in the chart, one copy was sent to the pharmacy for a record of medication, and the other was saved for QI. The primary team was expected to write a note in the chart’s disposition and time of disposition were to be included in this message.
Equipment
The OV-UCLA equipment team had one important question to answer: What supplies did we need at the bedside?
Although equipment and medications are readily available outside the ICU, the team didn’t want to spend time looking for equipment during an RRT call. “I don’t want a quick RRT call to evolve into a three-hour scavenger hunt,” says one team member.
Because OV-UCLA does not have a 24-hour pharmacist, the group felt it essential to bring medications to the bedside to avoid delays. Our solution to this potential problem was simple. The medication box is prepared by the pharmacy and sealed with one expiration date. Once the box is opened, it is exchanged for a new sealed box. The team chose a rolling duffle to store and transport the supplies, which are compartmentalized into the following sections: infection control, medications, airway and respiratory, IV access and blood draw, and IV start. Medications include respiratory treatments, antibiotics, furosemide, nitroglycerin, metoprolol, heparin and low molecular weight heparin, naloxone, ephedrine, dopamine, glucose, glucagons, and so on. The bag is restocked upon its return to the ICU.
Because of the stress involved in maintaining emergency equipment, we opted to call the supplies a “convenience bag.” This label ensured that only the sealed medication box would require a mandatory check; the rest of the equipment would be monitored on a more informal basis. Because all equipment is available on every floor, and because any RRT call can be converted to a code blue, the team felt that this was reasonable. The committee also purchased a five-pound patient monitor that has a screen for a cardiac tracing, a pulse oximeter, a noninvasive blood pressure monitor, and a temperature probe. This monitor fits easily in a pocket of the duffle.
Education and Publicity
How would staff know to call the RRT? The OV-UCLA team, anticipating that the majority of RRT calls would be activated by the primary RNs, decided that educating all nursing staff was essential.
The hospital nursing education office trained all nurses on all shifts in a short period of time. All nursing staff were taught to use SBAR (situation, background, assessment, and recommendation) communication and to identify early warning signs.1 The importance of recognizing the early warning signs was stressed during the nursing and physician training sessions. Staff were reassured that they didn’t have to know what was wrong with the patient to know that something was wrong and that help was required.
Publicity was accomplished in a variety of ways. The facility purchased pencils in our official color—lime green—that said “Rapid Response Team X4415.” The duffle was wheeled to all nursing stations so that staff could see it. We also ordered custom green-and-white M&M candy (available at www.mms.com) labeled “RRT X4415” to give as a promotional gift when an RRT was called.
Staffing
One last question remained for our team members: Who would respond to the RRT?
The committee felt strongly that an ICU nurse, an ICU resident, and a respiratory therapist should respond. Many physicians on the team did not want a doctor to respond, mostly due to concerns over chain of command. Who would be responsible for decisions made by the RRT? What if an ICU R2 disagreed with a surgery R4? Could they write a “do not call RRT order?” Nursing, on the other hand, wanted physician response; they wanted to be able to stabilize the patient.
Standardized protocols were discussed, but the team felt that the they would unreasonably delay the start. Radiology, which has no code blue response, volunteered to respond to all calls and hand-deliver the film to a computerized viewing system. The lab volunteered to run all RRT labs—designated with a lime green sticker—as quickly as possible.
The medical staff wanted to pilot the RRT, but because we are a small facility (220 beds) and to avoid confusion we launched the RRT for all inpatients. We went live in October 2005. The original plan was to staff an ICU nurse/RRT position. This RRT RN would relieve ICU nurses for breaks to maintain staffing ratios and provide RRT coverage. Because of the omnipresent nursing shortage, however, the RRT position is often pulled and the charge nurse must cover calls. Nurses sign up for RRT overtime and get pulled for patient care duties.
Mock RRT Calls
We performed three RRT drills to determine problem areas. For the first call, we involved a physician who had been vocal about the need for an RRT. The call was for a patient with shortness of breath. Two problems occurred during this drill: The primary team was never called, and there was no overhead page. So a member of our team worked with the hospital operator on our committee and clarified our protocols.
At the second drill, the main problem was documentation. The ICU nurse was so busy documenting that he wasn’t involved with the patient. Because the expertise of the ICU nurse is essential (in fact, there are times when this RN is the most experienced person on the team) we restructured the response so that the primary nurse would document and the ICU nurse was free to provide the hands-on care required.
At the final mock RRT, the major problem was again communication; that is, everyone spoke at once. The team members were encouraged to direct all comments to the team leader and keep any other conversation to a minimum.
A Successful RRT
The following case example, which describes the successful use of our OV-UCLA’s RRT, provides an illuminating look at its effectiveness. In this case, the RRT comprised the ICU nurse, the ICU physician, and the respiratory therapist. The team carried the following equipment: a patient monitor, medications, an IV start, blood sampling tubes, a central line, oxygen masks, and suctioning equipment.
The case began when the primary nurse activated the call. The patient—a 36-year-old HIV-positive male with acute rectal bleeding—was found to have a systolic blood pressure (SBP) reading of 70 and a heart rate of 144. The patient was admitted for anal warts but was noted to have acute bright red blood per rectum. The primary physician team had been called, but had not yet arrived. The primary nurse used the bedside phone to call X4415, and the RRT arrived within three minutes.
Upon arrival, the RRT started a wide bore IV and a central line. The team then called for O-negative blood from the blood bank. The transfusion began seven minutes after the team’s arrival in the patient’s room. The patient was transferred to the ICU and was discharged to the floor the following day.
Results
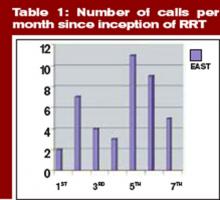
In four-and-a-half months, we have had 43 calls. The warning signs that precipitated the calls include:
- Respiratory distress: 14 (resulting in eight intubations);
- Cardiac problems: six;
- Altered mental status: four;
- Hypotension: four;
- Post-procedure oversedation: three;
- Vomiting: two;
- Bleeding: two;
- Gastrointestinal: one;
- Mouth bleeding: one;
- Hypoglycemia: one; and
- Unclear etiology: five. TH
Dr. Stein is the medical director, Intensive Care Unit/SDU, at Olive View UCLA Medical Center.
References
- Bellomo R, Goldsmith D, Uchino S, et al. A prospective before-and-after trial of a medical emergency team. Med J Aust. 2003 Sep 15:179(6):283-287
- The Institute for Healthcare Improvement’s 100,000 Lives Campaign. Available at: www.ihi.org. Last accessed July 10, 2006.
- Leonard MS, Graham S, Taggart B. The human factor: effective teamwork and communication in patient strategy. In: Leonard M, Frankel A, Simmonds T, eds. Achieving safe and reliable health care strategies and solutions. 1st ed. ACHE Management Series; 2004. p.37-65.
- Schein RM, Hazday N, Pena M, et al. Clinical antecedents to in-hospital cardiopulmonary arrests. Chest. 1990;98:1388-1392.
- Franklin C, Matthew J. Developing strategies to prevent-in hospital cardiac arrest: analyzing responses of physicians and nurses in the hours before the event. Crit Care Med. 1994;22(2):244-247.
The origin of the RRT can be found in medical emergency teams (METs). METs began in Australia as a result of the realization that earlier intervention could lead to better outcomes.1 In December 2004, in response to persistent problems with patient safety, the Institute for Healthcare Improvement launched its “100,000 Lives Campaign.”2 The Institute’s key plan for saving some of these 100,000 lives was to create RRTs at every participating medical center. Participating facilities would also submit data on mortality.
Olive View-UCLA Medical Center (OV-UCLA) signed on to participate in the campaign, and part of that effort was the creation and implementation of an RRT. We joined a University Health Consortium “Commit to Action” team, which assisted us by providing support as we began the creation and implementation of the RRT. What follows is the story of how we created an RRT.
We chose team members from all disciplines that were to be part of the RRT response—both at and behind the scenes: RNs, nursing administrators, hospital administrators, ICU attendings, house staff, laboratory personnel, nursing educators, radiology technicians, and hospital operators. The group was further organized into specific teams to solve problems and present solutions. At this point we learned our first important lesson: We needed to meet individually with all inpatient department chairs to discuss the effect of RRTs.
Activation and Notification
How would the RRT call be activated—overhead or beeper? Who could call, and what would the indications be? The OV-UCLA activation and notification team decided that the RRT could be activated by any staff member. Criteria, including vital signs, mental status, or simply “concern about the patient,” were created and posted. A telephone line in the ICU (X4415) was dedicated for RRT calls, and all other activation was overhead due to the lack of an adequate beeper system. (Other than code pagers, our beeper system can’t be simultaneously activated, and ancillaries don’t have beepers.)
The primary nurse’s responsibilities included calling the primary team or cross-covering team and obtaining a fingerstick glucose on all patients while waiting for the team. In discussions the primary team, we learned our second important lesson: As we presented the RRT to the hospital staff, everyone was concerned about the primary team. Ensuring that a mechanism for notifying the primary team was in place and reassuring staff that the primary team would be involved emerged as essential tasks. It was also imperative to identify the chain of command.
With this need in mind, we decided the primary team would always be the captain and would, therefore, have the authority to dismiss whomever they wanted from the RRT. An ICU attending was assigned to RRT call as supervision for the ICU resident responder. At OV-UCLA, our attending is not in-house and, to date, has not been called.
Documentation
The OV-UCLA documentation team was called on to answer the following questions: How would the RRT call be documented? How would medication orders be sent to the pharmacy? How would quality indicators (QI) and data be collected on the calls?
The team’s solution involved creating a one-page, primarily check-based document. The ICU nurse who answered the X4415 telephone in the ICU would begin documentation, which included the time of the call and the chief complaint. When the RRT reached the patient, however, the documentation duties were transferred to the primary RN. All providers were to document on the same page—similar to a code sheet. The RRT nurse and the attending doctor were to check vitals and perform the physical exam, as all information was called out to the documenter.
Medications were to be verbally ordered by the doctor, then read back and verified by the nurses documenting and administering for the RRT. For the most part, medication orders were restricted to what was carried in the RRT bag. The document was eventually copied three times: The original was placed in the chart, one copy was sent to the pharmacy for a record of medication, and the other was saved for QI. The primary team was expected to write a note in the chart’s disposition and time of disposition were to be included in this message.
Equipment
The OV-UCLA equipment team had one important question to answer: What supplies did we need at the bedside?
Although equipment and medications are readily available outside the ICU, the team didn’t want to spend time looking for equipment during an RRT call. “I don’t want a quick RRT call to evolve into a three-hour scavenger hunt,” says one team member.
Because OV-UCLA does not have a 24-hour pharmacist, the group felt it essential to bring medications to the bedside to avoid delays. Our solution to this potential problem was simple. The medication box is prepared by the pharmacy and sealed with one expiration date. Once the box is opened, it is exchanged for a new sealed box. The team chose a rolling duffle to store and transport the supplies, which are compartmentalized into the following sections: infection control, medications, airway and respiratory, IV access and blood draw, and IV start. Medications include respiratory treatments, antibiotics, furosemide, nitroglycerin, metoprolol, heparin and low molecular weight heparin, naloxone, ephedrine, dopamine, glucose, glucagons, and so on. The bag is restocked upon its return to the ICU.
Because of the stress involved in maintaining emergency equipment, we opted to call the supplies a “convenience bag.” This label ensured that only the sealed medication box would require a mandatory check; the rest of the equipment would be monitored on a more informal basis. Because all equipment is available on every floor, and because any RRT call can be converted to a code blue, the team felt that this was reasonable. The committee also purchased a five-pound patient monitor that has a screen for a cardiac tracing, a pulse oximeter, a noninvasive blood pressure monitor, and a temperature probe. This monitor fits easily in a pocket of the duffle.
Education and Publicity
How would staff know to call the RRT? The OV-UCLA team, anticipating that the majority of RRT calls would be activated by the primary RNs, decided that educating all nursing staff was essential.
The hospital nursing education office trained all nurses on all shifts in a short period of time. All nursing staff were taught to use SBAR (situation, background, assessment, and recommendation) communication and to identify early warning signs.1 The importance of recognizing the early warning signs was stressed during the nursing and physician training sessions. Staff were reassured that they didn’t have to know what was wrong with the patient to know that something was wrong and that help was required.
Publicity was accomplished in a variety of ways. The facility purchased pencils in our official color—lime green—that said “Rapid Response Team X4415.” The duffle was wheeled to all nursing stations so that staff could see it. We also ordered custom green-and-white M&M candy (available at www.mms.com) labeled “RRT X4415” to give as a promotional gift when an RRT was called.
Staffing
One last question remained for our team members: Who would respond to the RRT?
The committee felt strongly that an ICU nurse, an ICU resident, and a respiratory therapist should respond. Many physicians on the team did not want a doctor to respond, mostly due to concerns over chain of command. Who would be responsible for decisions made by the RRT? What if an ICU R2 disagreed with a surgery R4? Could they write a “do not call RRT order?” Nursing, on the other hand, wanted physician response; they wanted to be able to stabilize the patient.
Standardized protocols were discussed, but the team felt that the they would unreasonably delay the start. Radiology, which has no code blue response, volunteered to respond to all calls and hand-deliver the film to a computerized viewing system. The lab volunteered to run all RRT labs—designated with a lime green sticker—as quickly as possible.
The medical staff wanted to pilot the RRT, but because we are a small facility (220 beds) and to avoid confusion we launched the RRT for all inpatients. We went live in October 2005. The original plan was to staff an ICU nurse/RRT position. This RRT RN would relieve ICU nurses for breaks to maintain staffing ratios and provide RRT coverage. Because of the omnipresent nursing shortage, however, the RRT position is often pulled and the charge nurse must cover calls. Nurses sign up for RRT overtime and get pulled for patient care duties.
Mock RRT Calls
We performed three RRT drills to determine problem areas. For the first call, we involved a physician who had been vocal about the need for an RRT. The call was for a patient with shortness of breath. Two problems occurred during this drill: The primary team was never called, and there was no overhead page. So a member of our team worked with the hospital operator on our committee and clarified our protocols.
At the second drill, the main problem was documentation. The ICU nurse was so busy documenting that he wasn’t involved with the patient. Because the expertise of the ICU nurse is essential (in fact, there are times when this RN is the most experienced person on the team) we restructured the response so that the primary nurse would document and the ICU nurse was free to provide the hands-on care required.
At the final mock RRT, the major problem was again communication; that is, everyone spoke at once. The team members were encouraged to direct all comments to the team leader and keep any other conversation to a minimum.
A Successful RRT
The following case example, which describes the successful use of our OV-UCLA’s RRT, provides an illuminating look at its effectiveness. In this case, the RRT comprised the ICU nurse, the ICU physician, and the respiratory therapist. The team carried the following equipment: a patient monitor, medications, an IV start, blood sampling tubes, a central line, oxygen masks, and suctioning equipment.
The case began when the primary nurse activated the call. The patient—a 36-year-old HIV-positive male with acute rectal bleeding—was found to have a systolic blood pressure (SBP) reading of 70 and a heart rate of 144. The patient was admitted for anal warts but was noted to have acute bright red blood per rectum. The primary physician team had been called, but had not yet arrived. The primary nurse used the bedside phone to call X4415, and the RRT arrived within three minutes.
Upon arrival, the RRT started a wide bore IV and a central line. The team then called for O-negative blood from the blood bank. The transfusion began seven minutes after the team’s arrival in the patient’s room. The patient was transferred to the ICU and was discharged to the floor the following day.
Results
In four-and-a-half months, we have had 43 calls. The warning signs that precipitated the calls include:
- Respiratory distress: 14 (resulting in eight intubations);
- Cardiac problems: six;
- Altered mental status: four;
- Hypotension: four;
- Post-procedure oversedation: three;
- Vomiting: two;
- Bleeding: two;
- Gastrointestinal: one;
- Mouth bleeding: one;
- Hypoglycemia: one; and
- Unclear etiology: five. TH
Dr. Stein is the medical director, Intensive Care Unit/SDU, at Olive View UCLA Medical Center.
References
- Bellomo R, Goldsmith D, Uchino S, et al. A prospective before-and-after trial of a medical emergency team. Med J Aust. 2003 Sep 15:179(6):283-287
- The Institute for Healthcare Improvement’s 100,000 Lives Campaign. Available at: www.ihi.org. Last accessed July 10, 2006.
- Leonard MS, Graham S, Taggart B. The human factor: effective teamwork and communication in patient strategy. In: Leonard M, Frankel A, Simmonds T, eds. Achieving safe and reliable health care strategies and solutions. 1st ed. ACHE Management Series; 2004. p.37-65.
- Schein RM, Hazday N, Pena M, et al. Clinical antecedents to in-hospital cardiopulmonary arrests. Chest. 1990;98:1388-1392.
- Franklin C, Matthew J. Developing strategies to prevent-in hospital cardiac arrest: analyzing responses of physicians and nurses in the hours before the event. Crit Care Med. 1994;22(2):244-247.
The origin of the RRT can be found in medical emergency teams (METs). METs began in Australia as a result of the realization that earlier intervention could lead to better outcomes.1 In December 2004, in response to persistent problems with patient safety, the Institute for Healthcare Improvement launched its “100,000 Lives Campaign.”2 The Institute’s key plan for saving some of these 100,000 lives was to create RRTs at every participating medical center. Participating facilities would also submit data on mortality.
Olive View-UCLA Medical Center (OV-UCLA) signed on to participate in the campaign, and part of that effort was the creation and implementation of an RRT. We joined a University Health Consortium “Commit to Action” team, which assisted us by providing support as we began the creation and implementation of the RRT. What follows is the story of how we created an RRT.
We chose team members from all disciplines that were to be part of the RRT response—both at and behind the scenes: RNs, nursing administrators, hospital administrators, ICU attendings, house staff, laboratory personnel, nursing educators, radiology technicians, and hospital operators. The group was further organized into specific teams to solve problems and present solutions. At this point we learned our first important lesson: We needed to meet individually with all inpatient department chairs to discuss the effect of RRTs.
Activation and Notification
How would the RRT call be activated—overhead or beeper? Who could call, and what would the indications be? The OV-UCLA activation and notification team decided that the RRT could be activated by any staff member. Criteria, including vital signs, mental status, or simply “concern about the patient,” were created and posted. A telephone line in the ICU (X4415) was dedicated for RRT calls, and all other activation was overhead due to the lack of an adequate beeper system. (Other than code pagers, our beeper system can’t be simultaneously activated, and ancillaries don’t have beepers.)
The primary nurse’s responsibilities included calling the primary team or cross-covering team and obtaining a fingerstick glucose on all patients while waiting for the team. In discussions the primary team, we learned our second important lesson: As we presented the RRT to the hospital staff, everyone was concerned about the primary team. Ensuring that a mechanism for notifying the primary team was in place and reassuring staff that the primary team would be involved emerged as essential tasks. It was also imperative to identify the chain of command.
With this need in mind, we decided the primary team would always be the captain and would, therefore, have the authority to dismiss whomever they wanted from the RRT. An ICU attending was assigned to RRT call as supervision for the ICU resident responder. At OV-UCLA, our attending is not in-house and, to date, has not been called.
Documentation
The OV-UCLA documentation team was called on to answer the following questions: How would the RRT call be documented? How would medication orders be sent to the pharmacy? How would quality indicators (QI) and data be collected on the calls?
The team’s solution involved creating a one-page, primarily check-based document. The ICU nurse who answered the X4415 telephone in the ICU would begin documentation, which included the time of the call and the chief complaint. When the RRT reached the patient, however, the documentation duties were transferred to the primary RN. All providers were to document on the same page—similar to a code sheet. The RRT nurse and the attending doctor were to check vitals and perform the physical exam, as all information was called out to the documenter.
Medications were to be verbally ordered by the doctor, then read back and verified by the nurses documenting and administering for the RRT. For the most part, medication orders were restricted to what was carried in the RRT bag. The document was eventually copied three times: The original was placed in the chart, one copy was sent to the pharmacy for a record of medication, and the other was saved for QI. The primary team was expected to write a note in the chart’s disposition and time of disposition were to be included in this message.
Equipment
The OV-UCLA equipment team had one important question to answer: What supplies did we need at the bedside?
Although equipment and medications are readily available outside the ICU, the team didn’t want to spend time looking for equipment during an RRT call. “I don’t want a quick RRT call to evolve into a three-hour scavenger hunt,” says one team member.
Because OV-UCLA does not have a 24-hour pharmacist, the group felt it essential to bring medications to the bedside to avoid delays. Our solution to this potential problem was simple. The medication box is prepared by the pharmacy and sealed with one expiration date. Once the box is opened, it is exchanged for a new sealed box. The team chose a rolling duffle to store and transport the supplies, which are compartmentalized into the following sections: infection control, medications, airway and respiratory, IV access and blood draw, and IV start. Medications include respiratory treatments, antibiotics, furosemide, nitroglycerin, metoprolol, heparin and low molecular weight heparin, naloxone, ephedrine, dopamine, glucose, glucagons, and so on. The bag is restocked upon its return to the ICU.
Because of the stress involved in maintaining emergency equipment, we opted to call the supplies a “convenience bag.” This label ensured that only the sealed medication box would require a mandatory check; the rest of the equipment would be monitored on a more informal basis. Because all equipment is available on every floor, and because any RRT call can be converted to a code blue, the team felt that this was reasonable. The committee also purchased a five-pound patient monitor that has a screen for a cardiac tracing, a pulse oximeter, a noninvasive blood pressure monitor, and a temperature probe. This monitor fits easily in a pocket of the duffle.
Education and Publicity
How would staff know to call the RRT? The OV-UCLA team, anticipating that the majority of RRT calls would be activated by the primary RNs, decided that educating all nursing staff was essential.
The hospital nursing education office trained all nurses on all shifts in a short period of time. All nursing staff were taught to use SBAR (situation, background, assessment, and recommendation) communication and to identify early warning signs.1 The importance of recognizing the early warning signs was stressed during the nursing and physician training sessions. Staff were reassured that they didn’t have to know what was wrong with the patient to know that something was wrong and that help was required.
Publicity was accomplished in a variety of ways. The facility purchased pencils in our official color—lime green—that said “Rapid Response Team X4415.” The duffle was wheeled to all nursing stations so that staff could see it. We also ordered custom green-and-white M&M candy (available at www.mms.com) labeled “RRT X4415” to give as a promotional gift when an RRT was called.
Staffing
One last question remained for our team members: Who would respond to the RRT?
The committee felt strongly that an ICU nurse, an ICU resident, and a respiratory therapist should respond. Many physicians on the team did not want a doctor to respond, mostly due to concerns over chain of command. Who would be responsible for decisions made by the RRT? What if an ICU R2 disagreed with a surgery R4? Could they write a “do not call RRT order?” Nursing, on the other hand, wanted physician response; they wanted to be able to stabilize the patient.
Standardized protocols were discussed, but the team felt that the they would unreasonably delay the start. Radiology, which has no code blue response, volunteered to respond to all calls and hand-deliver the film to a computerized viewing system. The lab volunteered to run all RRT labs—designated with a lime green sticker—as quickly as possible.
The medical staff wanted to pilot the RRT, but because we are a small facility (220 beds) and to avoid confusion we launched the RRT for all inpatients. We went live in October 2005. The original plan was to staff an ICU nurse/RRT position. This RRT RN would relieve ICU nurses for breaks to maintain staffing ratios and provide RRT coverage. Because of the omnipresent nursing shortage, however, the RRT position is often pulled and the charge nurse must cover calls. Nurses sign up for RRT overtime and get pulled for patient care duties.
Mock RRT Calls
We performed three RRT drills to determine problem areas. For the first call, we involved a physician who had been vocal about the need for an RRT. The call was for a patient with shortness of breath. Two problems occurred during this drill: The primary team was never called, and there was no overhead page. So a member of our team worked with the hospital operator on our committee and clarified our protocols.
At the second drill, the main problem was documentation. The ICU nurse was so busy documenting that he wasn’t involved with the patient. Because the expertise of the ICU nurse is essential (in fact, there are times when this RN is the most experienced person on the team) we restructured the response so that the primary nurse would document and the ICU nurse was free to provide the hands-on care required.
At the final mock RRT, the major problem was again communication; that is, everyone spoke at once. The team members were encouraged to direct all comments to the team leader and keep any other conversation to a minimum.
A Successful RRT
The following case example, which describes the successful use of our OV-UCLA’s RRT, provides an illuminating look at its effectiveness. In this case, the RRT comprised the ICU nurse, the ICU physician, and the respiratory therapist. The team carried the following equipment: a patient monitor, medications, an IV start, blood sampling tubes, a central line, oxygen masks, and suctioning equipment.
The case began when the primary nurse activated the call. The patient—a 36-year-old HIV-positive male with acute rectal bleeding—was found to have a systolic blood pressure (SBP) reading of 70 and a heart rate of 144. The patient was admitted for anal warts but was noted to have acute bright red blood per rectum. The primary physician team had been called, but had not yet arrived. The primary nurse used the bedside phone to call X4415, and the RRT arrived within three minutes.
Upon arrival, the RRT started a wide bore IV and a central line. The team then called for O-negative blood from the blood bank. The transfusion began seven minutes after the team’s arrival in the patient’s room. The patient was transferred to the ICU and was discharged to the floor the following day.
Results
In four-and-a-half months, we have had 43 calls. The warning signs that precipitated the calls include:
- Respiratory distress: 14 (resulting in eight intubations);
- Cardiac problems: six;
- Altered mental status: four;
- Hypotension: four;
- Post-procedure oversedation: three;
- Vomiting: two;
- Bleeding: two;
- Gastrointestinal: one;
- Mouth bleeding: one;
- Hypoglycemia: one; and
- Unclear etiology: five. TH
Dr. Stein is the medical director, Intensive Care Unit/SDU, at Olive View UCLA Medical Center.
References
- Bellomo R, Goldsmith D, Uchino S, et al. A prospective before-and-after trial of a medical emergency team. Med J Aust. 2003 Sep 15:179(6):283-287
- The Institute for Healthcare Improvement’s 100,000 Lives Campaign. Available at: www.ihi.org. Last accessed July 10, 2006.
- Leonard MS, Graham S, Taggart B. The human factor: effective teamwork and communication in patient strategy. In: Leonard M, Frankel A, Simmonds T, eds. Achieving safe and reliable health care strategies and solutions. 1st ed. ACHE Management Series; 2004. p.37-65.
- Schein RM, Hazday N, Pena M, et al. Clinical antecedents to in-hospital cardiopulmonary arrests. Chest. 1990;98:1388-1392.
- Franklin C, Matthew J. Developing strategies to prevent-in hospital cardiac arrest: analyzing responses of physicians and nurses in the hours before the event. Crit Care Med. 1994;22(2):244-247.
Doctors of the American Frontier
Discussions of the mid-19th century American physician often conjure up images of the surgeons of the Civil War who tirelessly plied their trade during battle: “During the rest of the night and early morning, he [amputated] arms below the elbow and legs below the knee in less than five minutes. The deep incision … the sweeping cut … pull back the soft parts to expose the bone … saw swiftly.”1
However, in the same period but some thousand miles west, frontier physicians faced similar battle wounds sustained in campaigns against American Indians, as well as a myriad of other duties. Some frontier physicians met these challenges with remarkable ingenuity, while others resorted to treatments later deemed quackery. They often practiced alone in the wilderness without a hospital or colleagues for support.
The first and most obvious task of a military physician on the frontier was to attend to soldiers wounded during battle. The first hurdle was reaching the soldier. In 1874, Surgeon George Miller Sternberg faced daunting challenges in aiding seriously wounded soldiers of General Oliver Otis Howard’s company after a melee with Chief Joseph’s Nez Percé tribe. As dark settled across Clearwater River, Idaho, “Surgeon George Miller Sternberg and an aide crawled out onto the battlefield looking for the wounded. They crept so close to the enemy that they could hear the Indians talking.”1 Dr. Sternberg worked tirelessly throughout the night ligating pulsing arteries and soothing the suffering soldiers with whatever means he had, from opium balls to whiskey. During the course of the evening, an American Indian sentinel spotted Dr. Sternberg’s lantern and shot it out, forcing Dr. Sternberg to continue his treatment in darkness.
In other conflicts, the frontier physician often found himself an active participant in a battle. In the Battle of the Lava Beds fought in Oregon in 1873, Dr. George Martin Kober received a gunshot wound in the arm during the course of the battle. Despite his wound he continued to “treat the wounded before he allowed Dr. Skinner to come to his relief.”1
In the Battle of Bates Creek, fought in the summer of 1874, Dr. Thomas Maghee “was the object of the direct fire of an Indian. Until, laying down his instruments for a moment, he took his carbine and killed the Indian and then returned quietly to his work.”1
When the battle concluded and the soldiers returned to camp, the physicians began to wage a fierce war with disease. Among the plagues that stalked the camps: cholera, scurvy, yellow fever, tuberculosis, and typhoid fever. On one occasion in 1874 cholera struck in the heat of the summer at Fort Riley in Kansas. The pestilence devastated the fort by swiftly taking the lives of dozens of soldiers and compelling a hundred more to desert the fort in fear. One ignorant physician attempted in vain to combat the disease by “burning barrels of pine tar beneath the open windows of the fort hospital.”1
Eventually, Dr. Sternberg conquered the outbreak by implementing a strict disinfection and isolation campaign. In the battle against scurvy, military physicians noted that the typical diet of “meat, white bread, soda biscuits, syrup, lard, and black coffee” was insufficient and often attempted to plant and harvest their own supply of vegetables to treat the vitamin C-deficient soldiers.1
The frontier physician’s duties often expanded outside of the realms of medicine because “by order of the Secretary of War they also studied weather, geography, plants, fauna, Indian customs, and antiquities.”1 In fulfilling these duties, physicians made remarkable contributions to the preservation of the history of the American West, such as Dr. James Kimball’s purchase of the autobiography of Sitting Bull. Indeed, life as a military physician on the American frontier tested the courage, durability, and ingenuity of the early American doctor. TH
John Bois is a second-year medical student at the Mayo Clinic College of Medicine, Rochester, Minn.
Reference
- Dunlop R. Doctors of the American Frontier. Garden City, New York: Doubleday & Company; 1965: 73.
Discussions of the mid-19th century American physician often conjure up images of the surgeons of the Civil War who tirelessly plied their trade during battle: “During the rest of the night and early morning, he [amputated] arms below the elbow and legs below the knee in less than five minutes. The deep incision … the sweeping cut … pull back the soft parts to expose the bone … saw swiftly.”1
However, in the same period but some thousand miles west, frontier physicians faced similar battle wounds sustained in campaigns against American Indians, as well as a myriad of other duties. Some frontier physicians met these challenges with remarkable ingenuity, while others resorted to treatments later deemed quackery. They often practiced alone in the wilderness without a hospital or colleagues for support.
The first and most obvious task of a military physician on the frontier was to attend to soldiers wounded during battle. The first hurdle was reaching the soldier. In 1874, Surgeon George Miller Sternberg faced daunting challenges in aiding seriously wounded soldiers of General Oliver Otis Howard’s company after a melee with Chief Joseph’s Nez Percé tribe. As dark settled across Clearwater River, Idaho, “Surgeon George Miller Sternberg and an aide crawled out onto the battlefield looking for the wounded. They crept so close to the enemy that they could hear the Indians talking.”1 Dr. Sternberg worked tirelessly throughout the night ligating pulsing arteries and soothing the suffering soldiers with whatever means he had, from opium balls to whiskey. During the course of the evening, an American Indian sentinel spotted Dr. Sternberg’s lantern and shot it out, forcing Dr. Sternberg to continue his treatment in darkness.
In other conflicts, the frontier physician often found himself an active participant in a battle. In the Battle of the Lava Beds fought in Oregon in 1873, Dr. George Martin Kober received a gunshot wound in the arm during the course of the battle. Despite his wound he continued to “treat the wounded before he allowed Dr. Skinner to come to his relief.”1
In the Battle of Bates Creek, fought in the summer of 1874, Dr. Thomas Maghee “was the object of the direct fire of an Indian. Until, laying down his instruments for a moment, he took his carbine and killed the Indian and then returned quietly to his work.”1
When the battle concluded and the soldiers returned to camp, the physicians began to wage a fierce war with disease. Among the plagues that stalked the camps: cholera, scurvy, yellow fever, tuberculosis, and typhoid fever. On one occasion in 1874 cholera struck in the heat of the summer at Fort Riley in Kansas. The pestilence devastated the fort by swiftly taking the lives of dozens of soldiers and compelling a hundred more to desert the fort in fear. One ignorant physician attempted in vain to combat the disease by “burning barrels of pine tar beneath the open windows of the fort hospital.”1
Eventually, Dr. Sternberg conquered the outbreak by implementing a strict disinfection and isolation campaign. In the battle against scurvy, military physicians noted that the typical diet of “meat, white bread, soda biscuits, syrup, lard, and black coffee” was insufficient and often attempted to plant and harvest their own supply of vegetables to treat the vitamin C-deficient soldiers.1
The frontier physician’s duties often expanded outside of the realms of medicine because “by order of the Secretary of War they also studied weather, geography, plants, fauna, Indian customs, and antiquities.”1 In fulfilling these duties, physicians made remarkable contributions to the preservation of the history of the American West, such as Dr. James Kimball’s purchase of the autobiography of Sitting Bull. Indeed, life as a military physician on the American frontier tested the courage, durability, and ingenuity of the early American doctor. TH
John Bois is a second-year medical student at the Mayo Clinic College of Medicine, Rochester, Minn.
Reference
- Dunlop R. Doctors of the American Frontier. Garden City, New York: Doubleday & Company; 1965: 73.
Discussions of the mid-19th century American physician often conjure up images of the surgeons of the Civil War who tirelessly plied their trade during battle: “During the rest of the night and early morning, he [amputated] arms below the elbow and legs below the knee in less than five minutes. The deep incision … the sweeping cut … pull back the soft parts to expose the bone … saw swiftly.”1
However, in the same period but some thousand miles west, frontier physicians faced similar battle wounds sustained in campaigns against American Indians, as well as a myriad of other duties. Some frontier physicians met these challenges with remarkable ingenuity, while others resorted to treatments later deemed quackery. They often practiced alone in the wilderness without a hospital or colleagues for support.
The first and most obvious task of a military physician on the frontier was to attend to soldiers wounded during battle. The first hurdle was reaching the soldier. In 1874, Surgeon George Miller Sternberg faced daunting challenges in aiding seriously wounded soldiers of General Oliver Otis Howard’s company after a melee with Chief Joseph’s Nez Percé tribe. As dark settled across Clearwater River, Idaho, “Surgeon George Miller Sternberg and an aide crawled out onto the battlefield looking for the wounded. They crept so close to the enemy that they could hear the Indians talking.”1 Dr. Sternberg worked tirelessly throughout the night ligating pulsing arteries and soothing the suffering soldiers with whatever means he had, from opium balls to whiskey. During the course of the evening, an American Indian sentinel spotted Dr. Sternberg’s lantern and shot it out, forcing Dr. Sternberg to continue his treatment in darkness.
In other conflicts, the frontier physician often found himself an active participant in a battle. In the Battle of the Lava Beds fought in Oregon in 1873, Dr. George Martin Kober received a gunshot wound in the arm during the course of the battle. Despite his wound he continued to “treat the wounded before he allowed Dr. Skinner to come to his relief.”1
In the Battle of Bates Creek, fought in the summer of 1874, Dr. Thomas Maghee “was the object of the direct fire of an Indian. Until, laying down his instruments for a moment, he took his carbine and killed the Indian and then returned quietly to his work.”1
When the battle concluded and the soldiers returned to camp, the physicians began to wage a fierce war with disease. Among the plagues that stalked the camps: cholera, scurvy, yellow fever, tuberculosis, and typhoid fever. On one occasion in 1874 cholera struck in the heat of the summer at Fort Riley in Kansas. The pestilence devastated the fort by swiftly taking the lives of dozens of soldiers and compelling a hundred more to desert the fort in fear. One ignorant physician attempted in vain to combat the disease by “burning barrels of pine tar beneath the open windows of the fort hospital.”1
Eventually, Dr. Sternberg conquered the outbreak by implementing a strict disinfection and isolation campaign. In the battle against scurvy, military physicians noted that the typical diet of “meat, white bread, soda biscuits, syrup, lard, and black coffee” was insufficient and often attempted to plant and harvest their own supply of vegetables to treat the vitamin C-deficient soldiers.1
The frontier physician’s duties often expanded outside of the realms of medicine because “by order of the Secretary of War they also studied weather, geography, plants, fauna, Indian customs, and antiquities.”1 In fulfilling these duties, physicians made remarkable contributions to the preservation of the history of the American West, such as Dr. James Kimball’s purchase of the autobiography of Sitting Bull. Indeed, life as a military physician on the American frontier tested the courage, durability, and ingenuity of the early American doctor. TH
John Bois is a second-year medical student at the Mayo Clinic College of Medicine, Rochester, Minn.
Reference
- Dunlop R. Doctors of the American Frontier. Garden City, New York: Doubleday & Company; 1965: 73.
The Yuk Factor
Despite modern wound treatment and broad-spectrum antibiotic treatment, patients with chronic wounds still exist. The appearance of antibiotic resistant bacteria, such as methicillin-resistant Staphylococcus aureus (MRSA) in the 1980s and ’90s, gave rise to a search for other remedies. One of the remedies that has been rediscovered and subsequently successfully reintroduced is maggot debridement therapy (MDT).1 The fact that more than 100 articles were published on the subject in the past two decades indicates that the use of maggots is making a strong comeback in medicine.2 In January 2004, the U.S. Food and Drug Administration (FDA) issued 510(k)#33391, allowing production and marketing of maggots as a medical device. In this article, we discuss the use of MDT in patients with a chronic wound.
A Long History of Maggot Therapy
MDT has been used in many cultures and has been known for centuries.3 Ambroise Parè is credited as the father of modern MDT. Unfortunately, no evidence can be found of Parè using maggots as a means to clean or heal wounds. The only reference is the often-cited case that occurred in 1557 at the battle of St. Quentin, when Parè observed soldiers whose wounds were covered by maggots. He mainly described the negative effects of the maggots, and, above all, believed they were spontaneously produced by the wound itself, not by the eggs of fly.4
Baron Larey (1766-1842) a famous surgeon in the army of Napoleon Bonaparte, wrote about soldiers who had larvae-infested wounds, but was frustrated that it was difficult to persuade his patients to leave the maggots in place, believing that “they promoted healing without leaving any damage.”5
The first surgeon to use MDT in patients in the hospital was the orthopedic surgeon William Baer. In the 1920s he was faced with a group of untreatable patients with severe osteomyelitis (antibiotics had not yet been discovered). He successfully treated many patients with maggots, and because of his success the therapy became regularly used in the United States.6
By 1934 more than 1,000 surgeons were using maggot therapy. Surgical Maggots were available commercially from Lederle Corporation.7 But with the introduction of antibiotics in the 1940s, the use of maggots dropped off. In the following years, case reports were published only occasionally.
The Negative Image of Maggots
A large problem of MDT is the difficulty of this type of therapy to gain acceptance in the medical community. Maggots are associated with rotting and decay. The image is of filthy, low-life creatures that are ugly and disgusting. Although a nice recent example for the general public is the scene in the movie Gladiator. The main character (played by Russell Crow) is advised to leave the maggots that spontaneously infested a wound on his shoulder in place so that the wound would heal. He leaves them in place and the wound heals without any problem, enabling Crow’s character to fight many battles.
In contrast, in an oral presentation we held recently at a Dutch scientific surgical meeting, a surgical professor in the audience said, “I will never allow those creatures in my ward.”8 This remark shows that widespread use and acceptance of MDT has not yet been reached. It seems there is still much work to do before MDT is generally accepted as a therapeutic method.
Fortunately, the negative image that seems to exist among nurses and physicians does not seem to bother patients.9 We have treated more than 100 patients in our clinic with MDT. All patients to whom we proposed MDT agreed to the therapy. All were allowed to discontinue the therapy whenever they wanted; none did. In a survey of the first 38 MDT-treated patients, 89% agreed to another session of MDT if the surgeon believed it would be beneficial, and 94% of the patients said that they would recommend it to others. This is despite the fact that the therapy was not successful in all patients (there was a below-knee of above the knee amputation-rate of 19% among patients who underwent MDT).10
Indications and Evidence
Indications and contra-indications for maggot therapy are not well defined. Some state that all kind of wounds that contain necrosis or slough can be good candidates for MDT. In our own study of 101 patients with 116 wounds treated with maggots, we had an overall success rate of 67%. (Seventy-eight out of 116 wounds had a beneficial outcome.) However, in 13 patients with septic arthritis, all wounds failed. Success rates where significantly reduced in cases of chronic limb ischemia, visible tendon or bone, and in cases of duration longer than three months before the start of MDT.11
Most physicians who start MDT use it mainly for worst-case scenarios. From our previous studies, it is clear that success rates in those patients are low. After witnessing a few failures, the physician is naturally reluctant to use it again.
What about evidence? Large randomized studies are lacking, although one containing 600 venous ulcer patients was initiated in 2004.12 There have been three randomized studies performed. Wayman, et al., have shown the cost-effectiveness of larval therapy in venous ulcers compared with hydrogel dressing.13 Contreras, et al., could not find a difference between MDT and curettage and topical silver sulfadiazine in patients with venous leg ulcers.14 At the 36th annual meeting of the European Association for the Study of Diabetes, Markevich, et al., reported on a randomized, multicenter, double-blind controlled clinical trial (n=140) for neuropathic diabetic foot lesions compared to conventional treatment. They found a significant higher percentage of granulation tissue after 10 days, compared with the hydrogel group.15 Results from large case-series indicate that MDT works and could even save limbs.2,16-18 The mechanism of action has not been unraveled yet.
Factors Influencing Effectiveness of MDT
Unfortunately, the statement made by Thomas, who said that maggot therapy works by “secreting proteolytic enzymes that break down dead tissue, turning it into a soup, which they then ingest,” still holds.19 It is known that there are mechanical effects, tissue growth effects, that direct killing of bacteria in the alimentary tract of the maggot takes place, and that maggots produce antibacterial factors.2,17,20-31
Although maggots are suitable agents for chronic wound treatment, it is likely that some wounds are more eligible than others for this type of treatment. In our opinion, all wounds that contain gangrenous or necrotic tissue with infection seem to be suited for MDT.32 Success rates of MDT reported in literature vary, but seem to be around 80% to 90%.16,17,33 In our own series, success rate is about 70%.
Patient-selection (case-mix) and method of outcome measurement play essential roles in these percentages. In our opinion, all wounds that contain necrotic tissue can be debrided effectively with MDT. However, if for example wound ischemia is the major etiologic factor, this should also be addressed. In our experience, diabetic foot, venous ulcers, traumatic ulcers, and infections after surgical procedures are all good candidates for MDT.
Absolute contraindications in our opinion are wounds close to large, uncovered blood vessels and wounds that need immediate surgical debridement (e.g., in the case of a septic patient). A relative contraindication is patients with natural of medically induced coagulopathies, but also patient preference could play a role.34 We have had very bad results with infected small joints of the foot; all wounds (n=13) eventually needed a small or large amputation.
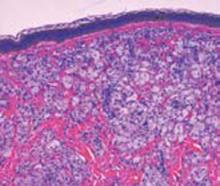
Even the technique of application has an effect on outcome. There are two different application techniques: the free-range and the contained technique. The free-range technique is more effective in vitro and in-vivo and has become our standard application technique—not only in the outpatient department, but also in the intra-mural setting.35,36 (Figure 1, p. 16, shows a patient with a necrotic wound on the leg after radiation therapy and a surgical excision for a malignant tumor was performed.) Earlier surgical debridement combined with split skin graft failed. After four applications of maggots, the wound was free of necrosis and could be subsequently closed. (See Figure 2, p. 16.)
The contained technique is used in patients with bleeding tendencies and wounds that do not have enough healthy skin surrounding the wound; in other words, where the covering “cage” needed in case of the free-range technique can’t be applied. (This problem is shown in Figure 3, p. 16: A patient with necrotizing fasciitis of the left upper leg was treated with the contained technique—BiologiQ, Apeldoorn, Netherlands—as there is no proximal skin border. Of course, patient preference plays a role as well in the choice of application technique.37
Wound Clinic
In the Netherlands maggots can be ordered easily and are delivered within 24 hours. We started a wound clinic in 2002. First it was for MDT alone, but now the scope is broader, and we treat chronic wounds with different kind of wound therapies. We have two nurses, one nurse practitioner, one resident-surgeon, and one vascular surgeon who apply the maggots.
Patients do not need to be admitted for MDT. Fifty-nine percent of our patients are treated in the outpatient department. We are able to treat as many as 10 or 15 patients in one session, but MDT-treated patients make up only two or three patients at a time.
We found that after fast, successful biological debridement with MDT we were left with a lot of patients with red, granulating wounds that needed our attention in order to prevent relapses. In our opinion, there are many different treatment methods after MDT. Plaster casting in case of diabetic feet, secondary closure, and split skin grafting are different methods. However, other therapies like VAC-therapy and recently OASIS are promising.
At this time, all patients are prospectively followed after MDT. We are especially interested in patient selection and are now also aiming to find the ideal wound therapy after MDT. TH
Dr. Steenvoorde is a resident surgeon at Rijnland Hospital Leiderdorp, the Netherlands. van Doorn is a nurse-practitioner at Rijnland Hospital Leiderdorp. Jacobi is a senior researcher in the Medical Decision Department at Leiden University Medical Center, in the Netherlands. Dr. Oskam is a vascular surgeon at Rijnland Hospital Leiderdorp.
References
- Beasley WD, Hirst G. Making a meal of MRSA-the role of biosurgery inhospital-acquired infection. J Hosp Infect. 2004;56(1):6-9.
- Jukema GN, Menon AG, Bernards AT. et al. Amputation-sparing treatment by nature: “surgical” maggots revisited. Clin Infect Dis. 2002 Dec 15;35(12):1566-1571.
- Church JC. The traditional use of maggots in wound healing, and the development of larva therapy (biosurgery) in modern medicine. J Altern Complement Med. 1996 Winter;2(4):525-527.
- Coppi C. I dressed your wounds, God healed you—a wounded person’s psychology according to Ambroise Parè. Ostomy Wound Manage. 2005;51:62-64.
- Goldstein HI. Maggots in the treatment of wound and bone infections. J Bone Joint Surg. 1931;13:476-478.
- Baer WS. The treatment of chronic osteomyelitis with the maggot (larva of the blow fly). J Bone Joint Surg. 1931;13:438-475.
- Puckner WA. New and nonofficial remedies, surgical maggots-Lederle. J Am Med Assoc. 1932;98(5):401.
- Steenvoorde P, Doorn Lv, Jacobi CE, et al. Maggot therapy: retrospective study comparing two different application-techniques. (Dutch). Nederlands Tijdschrift voor Heelkunde. 2006;15:86.
- Contreras RJ, Fuentes SA, Karam-Orantes M, et al. Larval debridement therapy in Mexico. Wound Care Canada. 2005;3:42-46.
- Steenvoorde P, Budding TJ, Engeland Av, et al. Maggot therapy and the “yuk factor”: an issue for the patient? Wound Repair Regen. 2005 May-Jun;13(3):350-352.
- Steenvoorde P, Jacobi CA, Doorn Lv, et al. Maggot debridement therapy of infected ulcers: patient and wound factors influencing outcome. Ann Royal Coll Surg Eng. 2006.
- Raynor P, Dumville J, Cullum N. A new clinical trial of the effect of larval therapy. J Tissue Viability. 2004 Jul;14(3):104-105.
- Wayman J, Nirojogi V, Walker A, et al. The cost effectiveness of larval therapy in venous ulcers. J Tissue Viability. 2001 Jan;11(1):51.
- Contreras RJ, Fuentes SA, Arroyo ES, et al. Larval debridement therapy and infection control in venous ulcers: a comparative study. Presented at: the Second World Union of Wound Healing Societies Meeting; July 8-13, 2004.
- Markevich YO, McLeod-Roberts J, Mousley M, et al. Maggot therapy for diabetic neuropathic foot wounds: a randomized study. Presented at: the 36th Annual Meeting of the EASD; September 17-21, 2000. Ref Type: Conference Proceeding.
- Wolff H, Hansson C. Larval therapy—an effective method for ulcer debridement. Clin Exp Dermatol. 2003;28:137.
- Mumcuoglu KY, Ingber A, Gilead L, et al. Maggot therapy for the treatment of intractable wounds. Int J Dermatol. 1999 Aug;38(8):623-627.
- Courtenay M. The use of larval therapy in wound management in the UK. J Wound Care. 1999 Apr;8 (4):177-179.
- Bonn D. Maggot therapy: an alternative for wound infection. Lancet. 2000 Sep 30;356 (9236):1174.
- Robinson W. Stimulation of healing in non-healing wounds. J Bone Joint Surgery. 1935;17:267-271.
- Robinson W. Ammonium bicarbonate secreted by surgical maggots stimulates healing in purulent wounds. Am J Surg. 1940;47:111-115.
- Mumcuoglu KY, Ingber A, Gilead L, et al. Maggot therapy for the treatment of diabetic foot ulcers. Diabetes Care. 1998 Nov;21(11):2030-2031.
- Simmons S. A bactericidal principle in excretions of surgical maggots which destroys important etiological agents of pyogenic infections. J Bacteriol. 1935;30:253-267.
- Simmons S. The bactericidal properties of excretions of the maggot of Lucilia sericata. Bull Entomol Res. 1935;26:559-563.
- Mumcuoglu KY. Clinical applications for maggots in wound care. Am J Clin Dermatol. 2001;2:219-227.
- Armstrong DG, Short B, Martin BR, et al. Maggot therapy in lower extremity hospice wound care. J Am Podiatr Med Assoc. 2005;95(3):254-257.
- Robinson W, Norwood VH. The role of surgical maggots in the disinfection of osteomyelitis and other infected wounds. J Bone Joint Surgery. 1933;15:409-412.
- Robinson W, Norwood VH. Destruction of pyogenic bacteria in the alimentary tract of surgical maggots implanted in infected wounds. J Lab Clin Med. 1933;19:581-585.
- Mumcuoglu KY, Miller J, Mumcuoglu M. et al. Destruction of bacteria in the digestive tract of the maggot of Lucilia sericata (Diptera: Calliphoridae). J Med Entomol. 2001 Mar;38(2):161-166.
- Sherman RA, Hall MJ, Thomas S. Medicinal maggots: an ancient remedy for some contemporary afflictions. Annu Rev Entomol. 2000;45:55-81.
- Prete PE. Growth effects of Phaenicia sericata larval extracts on fibroblasts: mechanism for wound healing by maggot therapy. Life Sci. 1997;60(8):505-510.
- Church JCT, Courtenay M. Maggot debridement therapy for chronic wounds. Int J Low Extrem Wounds. 2002 Jun;1(2):129-134.
- Courtenay M, Church JC, Ryan TJ. Larva therapy in wound management. J R Soc Med. 2000 Feb;93:72-74.
- 34. Steenvoorde P, Oskam J. Bleeding c omplications in patients treated with maggot debridement therapy (MDT). Letter to the editor. IJLEW. 2005;4:57-58.
- Thomas S, Wynn K, Fowler T, et al. The effect of containment on the properties of sterile maggots. Br J Nurs. 2002 Jun;11(12 Suppl):S21-S22, S24, S26 passim.
- Steenvoorde P, Jacobi CE, Oskam J. Maggot debridement therapy: free-range or contained? An in-vivo study. Adv Skin Wound Care. 2005;18:430-435.
- Steenvoorde P, Oskam J. Use of larval therapy to combat infection after breast-conserving surgery. J Wound Care. 2005 May;14(5):212-213.
Despite modern wound treatment and broad-spectrum antibiotic treatment, patients with chronic wounds still exist. The appearance of antibiotic resistant bacteria, such as methicillin-resistant Staphylococcus aureus (MRSA) in the 1980s and ’90s, gave rise to a search for other remedies. One of the remedies that has been rediscovered and subsequently successfully reintroduced is maggot debridement therapy (MDT).1 The fact that more than 100 articles were published on the subject in the past two decades indicates that the use of maggots is making a strong comeback in medicine.2 In January 2004, the U.S. Food and Drug Administration (FDA) issued 510(k)#33391, allowing production and marketing of maggots as a medical device. In this article, we discuss the use of MDT in patients with a chronic wound.
A Long History of Maggot Therapy
MDT has been used in many cultures and has been known for centuries.3 Ambroise Parè is credited as the father of modern MDT. Unfortunately, no evidence can be found of Parè using maggots as a means to clean or heal wounds. The only reference is the often-cited case that occurred in 1557 at the battle of St. Quentin, when Parè observed soldiers whose wounds were covered by maggots. He mainly described the negative effects of the maggots, and, above all, believed they were spontaneously produced by the wound itself, not by the eggs of fly.4
Baron Larey (1766-1842) a famous surgeon in the army of Napoleon Bonaparte, wrote about soldiers who had larvae-infested wounds, but was frustrated that it was difficult to persuade his patients to leave the maggots in place, believing that “they promoted healing without leaving any damage.”5
The first surgeon to use MDT in patients in the hospital was the orthopedic surgeon William Baer. In the 1920s he was faced with a group of untreatable patients with severe osteomyelitis (antibiotics had not yet been discovered). He successfully treated many patients with maggots, and because of his success the therapy became regularly used in the United States.6
By 1934 more than 1,000 surgeons were using maggot therapy. Surgical Maggots were available commercially from Lederle Corporation.7 But with the introduction of antibiotics in the 1940s, the use of maggots dropped off. In the following years, case reports were published only occasionally.
The Negative Image of Maggots
A large problem of MDT is the difficulty of this type of therapy to gain acceptance in the medical community. Maggots are associated with rotting and decay. The image is of filthy, low-life creatures that are ugly and disgusting. Although a nice recent example for the general public is the scene in the movie Gladiator. The main character (played by Russell Crow) is advised to leave the maggots that spontaneously infested a wound on his shoulder in place so that the wound would heal. He leaves them in place and the wound heals without any problem, enabling Crow’s character to fight many battles.
In contrast, in an oral presentation we held recently at a Dutch scientific surgical meeting, a surgical professor in the audience said, “I will never allow those creatures in my ward.”8 This remark shows that widespread use and acceptance of MDT has not yet been reached. It seems there is still much work to do before MDT is generally accepted as a therapeutic method.
Fortunately, the negative image that seems to exist among nurses and physicians does not seem to bother patients.9 We have treated more than 100 patients in our clinic with MDT. All patients to whom we proposed MDT agreed to the therapy. All were allowed to discontinue the therapy whenever they wanted; none did. In a survey of the first 38 MDT-treated patients, 89% agreed to another session of MDT if the surgeon believed it would be beneficial, and 94% of the patients said that they would recommend it to others. This is despite the fact that the therapy was not successful in all patients (there was a below-knee of above the knee amputation-rate of 19% among patients who underwent MDT).10
Indications and Evidence
Indications and contra-indications for maggot therapy are not well defined. Some state that all kind of wounds that contain necrosis or slough can be good candidates for MDT. In our own study of 101 patients with 116 wounds treated with maggots, we had an overall success rate of 67%. (Seventy-eight out of 116 wounds had a beneficial outcome.) However, in 13 patients with septic arthritis, all wounds failed. Success rates where significantly reduced in cases of chronic limb ischemia, visible tendon or bone, and in cases of duration longer than three months before the start of MDT.11
Most physicians who start MDT use it mainly for worst-case scenarios. From our previous studies, it is clear that success rates in those patients are low. After witnessing a few failures, the physician is naturally reluctant to use it again.
What about evidence? Large randomized studies are lacking, although one containing 600 venous ulcer patients was initiated in 2004.12 There have been three randomized studies performed. Wayman, et al., have shown the cost-effectiveness of larval therapy in venous ulcers compared with hydrogel dressing.13 Contreras, et al., could not find a difference between MDT and curettage and topical silver sulfadiazine in patients with venous leg ulcers.14 At the 36th annual meeting of the European Association for the Study of Diabetes, Markevich, et al., reported on a randomized, multicenter, double-blind controlled clinical trial (n=140) for neuropathic diabetic foot lesions compared to conventional treatment. They found a significant higher percentage of granulation tissue after 10 days, compared with the hydrogel group.15 Results from large case-series indicate that MDT works and could even save limbs.2,16-18 The mechanism of action has not been unraveled yet.
Factors Influencing Effectiveness of MDT
Unfortunately, the statement made by Thomas, who said that maggot therapy works by “secreting proteolytic enzymes that break down dead tissue, turning it into a soup, which they then ingest,” still holds.19 It is known that there are mechanical effects, tissue growth effects, that direct killing of bacteria in the alimentary tract of the maggot takes place, and that maggots produce antibacterial factors.2,17,20-31
Although maggots are suitable agents for chronic wound treatment, it is likely that some wounds are more eligible than others for this type of treatment. In our opinion, all wounds that contain gangrenous or necrotic tissue with infection seem to be suited for MDT.32 Success rates of MDT reported in literature vary, but seem to be around 80% to 90%.16,17,33 In our own series, success rate is about 70%.
Patient-selection (case-mix) and method of outcome measurement play essential roles in these percentages. In our opinion, all wounds that contain necrotic tissue can be debrided effectively with MDT. However, if for example wound ischemia is the major etiologic factor, this should also be addressed. In our experience, diabetic foot, venous ulcers, traumatic ulcers, and infections after surgical procedures are all good candidates for MDT.
Absolute contraindications in our opinion are wounds close to large, uncovered blood vessels and wounds that need immediate surgical debridement (e.g., in the case of a septic patient). A relative contraindication is patients with natural of medically induced coagulopathies, but also patient preference could play a role.34 We have had very bad results with infected small joints of the foot; all wounds (n=13) eventually needed a small or large amputation.
Even the technique of application has an effect on outcome. There are two different application techniques: the free-range and the contained technique. The free-range technique is more effective in vitro and in-vivo and has become our standard application technique—not only in the outpatient department, but also in the intra-mural setting.35,36 (Figure 1, p. 16, shows a patient with a necrotic wound on the leg after radiation therapy and a surgical excision for a malignant tumor was performed.) Earlier surgical debridement combined with split skin graft failed. After four applications of maggots, the wound was free of necrosis and could be subsequently closed. (See Figure 2, p. 16.)
The contained technique is used in patients with bleeding tendencies and wounds that do not have enough healthy skin surrounding the wound; in other words, where the covering “cage” needed in case of the free-range technique can’t be applied. (This problem is shown in Figure 3, p. 16: A patient with necrotizing fasciitis of the left upper leg was treated with the contained technique—BiologiQ, Apeldoorn, Netherlands—as there is no proximal skin border. Of course, patient preference plays a role as well in the choice of application technique.37
Wound Clinic
In the Netherlands maggots can be ordered easily and are delivered within 24 hours. We started a wound clinic in 2002. First it was for MDT alone, but now the scope is broader, and we treat chronic wounds with different kind of wound therapies. We have two nurses, one nurse practitioner, one resident-surgeon, and one vascular surgeon who apply the maggots.
Patients do not need to be admitted for MDT. Fifty-nine percent of our patients are treated in the outpatient department. We are able to treat as many as 10 or 15 patients in one session, but MDT-treated patients make up only two or three patients at a time.
We found that after fast, successful biological debridement with MDT we were left with a lot of patients with red, granulating wounds that needed our attention in order to prevent relapses. In our opinion, there are many different treatment methods after MDT. Plaster casting in case of diabetic feet, secondary closure, and split skin grafting are different methods. However, other therapies like VAC-therapy and recently OASIS are promising.
At this time, all patients are prospectively followed after MDT. We are especially interested in patient selection and are now also aiming to find the ideal wound therapy after MDT. TH
Dr. Steenvoorde is a resident surgeon at Rijnland Hospital Leiderdorp, the Netherlands. van Doorn is a nurse-practitioner at Rijnland Hospital Leiderdorp. Jacobi is a senior researcher in the Medical Decision Department at Leiden University Medical Center, in the Netherlands. Dr. Oskam is a vascular surgeon at Rijnland Hospital Leiderdorp.
References
- Beasley WD, Hirst G. Making a meal of MRSA-the role of biosurgery inhospital-acquired infection. J Hosp Infect. 2004;56(1):6-9.
- Jukema GN, Menon AG, Bernards AT. et al. Amputation-sparing treatment by nature: “surgical” maggots revisited. Clin Infect Dis. 2002 Dec 15;35(12):1566-1571.
- Church JC. The traditional use of maggots in wound healing, and the development of larva therapy (biosurgery) in modern medicine. J Altern Complement Med. 1996 Winter;2(4):525-527.
- Coppi C. I dressed your wounds, God healed you—a wounded person’s psychology according to Ambroise Parè. Ostomy Wound Manage. 2005;51:62-64.
- Goldstein HI. Maggots in the treatment of wound and bone infections. J Bone Joint Surg. 1931;13:476-478.
- Baer WS. The treatment of chronic osteomyelitis with the maggot (larva of the blow fly). J Bone Joint Surg. 1931;13:438-475.
- Puckner WA. New and nonofficial remedies, surgical maggots-Lederle. J Am Med Assoc. 1932;98(5):401.
- Steenvoorde P, Doorn Lv, Jacobi CE, et al. Maggot therapy: retrospective study comparing two different application-techniques. (Dutch). Nederlands Tijdschrift voor Heelkunde. 2006;15:86.
- Contreras RJ, Fuentes SA, Karam-Orantes M, et al. Larval debridement therapy in Mexico. Wound Care Canada. 2005;3:42-46.
- Steenvoorde P, Budding TJ, Engeland Av, et al. Maggot therapy and the “yuk factor”: an issue for the patient? Wound Repair Regen. 2005 May-Jun;13(3):350-352.
- Steenvoorde P, Jacobi CA, Doorn Lv, et al. Maggot debridement therapy of infected ulcers: patient and wound factors influencing outcome. Ann Royal Coll Surg Eng. 2006.
- Raynor P, Dumville J, Cullum N. A new clinical trial of the effect of larval therapy. J Tissue Viability. 2004 Jul;14(3):104-105.
- Wayman J, Nirojogi V, Walker A, et al. The cost effectiveness of larval therapy in venous ulcers. J Tissue Viability. 2001 Jan;11(1):51.
- Contreras RJ, Fuentes SA, Arroyo ES, et al. Larval debridement therapy and infection control in venous ulcers: a comparative study. Presented at: the Second World Union of Wound Healing Societies Meeting; July 8-13, 2004.
- Markevich YO, McLeod-Roberts J, Mousley M, et al. Maggot therapy for diabetic neuropathic foot wounds: a randomized study. Presented at: the 36th Annual Meeting of the EASD; September 17-21, 2000. Ref Type: Conference Proceeding.
- Wolff H, Hansson C. Larval therapy—an effective method for ulcer debridement. Clin Exp Dermatol. 2003;28:137.
- Mumcuoglu KY, Ingber A, Gilead L, et al. Maggot therapy for the treatment of intractable wounds. Int J Dermatol. 1999 Aug;38(8):623-627.
- Courtenay M. The use of larval therapy in wound management in the UK. J Wound Care. 1999 Apr;8 (4):177-179.
- Bonn D. Maggot therapy: an alternative for wound infection. Lancet. 2000 Sep 30;356 (9236):1174.
- Robinson W. Stimulation of healing in non-healing wounds. J Bone Joint Surgery. 1935;17:267-271.
- Robinson W. Ammonium bicarbonate secreted by surgical maggots stimulates healing in purulent wounds. Am J Surg. 1940;47:111-115.
- Mumcuoglu KY, Ingber A, Gilead L, et al. Maggot therapy for the treatment of diabetic foot ulcers. Diabetes Care. 1998 Nov;21(11):2030-2031.
- Simmons S. A bactericidal principle in excretions of surgical maggots which destroys important etiological agents of pyogenic infections. J Bacteriol. 1935;30:253-267.
- Simmons S. The bactericidal properties of excretions of the maggot of Lucilia sericata. Bull Entomol Res. 1935;26:559-563.
- Mumcuoglu KY. Clinical applications for maggots in wound care. Am J Clin Dermatol. 2001;2:219-227.
- Armstrong DG, Short B, Martin BR, et al. Maggot therapy in lower extremity hospice wound care. J Am Podiatr Med Assoc. 2005;95(3):254-257.
- Robinson W, Norwood VH. The role of surgical maggots in the disinfection of osteomyelitis and other infected wounds. J Bone Joint Surgery. 1933;15:409-412.
- Robinson W, Norwood VH. Destruction of pyogenic bacteria in the alimentary tract of surgical maggots implanted in infected wounds. J Lab Clin Med. 1933;19:581-585.
- Mumcuoglu KY, Miller J, Mumcuoglu M. et al. Destruction of bacteria in the digestive tract of the maggot of Lucilia sericata (Diptera: Calliphoridae). J Med Entomol. 2001 Mar;38(2):161-166.
- Sherman RA, Hall MJ, Thomas S. Medicinal maggots: an ancient remedy for some contemporary afflictions. Annu Rev Entomol. 2000;45:55-81.
- Prete PE. Growth effects of Phaenicia sericata larval extracts on fibroblasts: mechanism for wound healing by maggot therapy. Life Sci. 1997;60(8):505-510.
- Church JCT, Courtenay M. Maggot debridement therapy for chronic wounds. Int J Low Extrem Wounds. 2002 Jun;1(2):129-134.
- Courtenay M, Church JC, Ryan TJ. Larva therapy in wound management. J R Soc Med. 2000 Feb;93:72-74.
- 34. Steenvoorde P, Oskam J. Bleeding c omplications in patients treated with maggot debridement therapy (MDT). Letter to the editor. IJLEW. 2005;4:57-58.
- Thomas S, Wynn K, Fowler T, et al. The effect of containment on the properties of sterile maggots. Br J Nurs. 2002 Jun;11(12 Suppl):S21-S22, S24, S26 passim.
- Steenvoorde P, Jacobi CE, Oskam J. Maggot debridement therapy: free-range or contained? An in-vivo study. Adv Skin Wound Care. 2005;18:430-435.
- Steenvoorde P, Oskam J. Use of larval therapy to combat infection after breast-conserving surgery. J Wound Care. 2005 May;14(5):212-213.
Despite modern wound treatment and broad-spectrum antibiotic treatment, patients with chronic wounds still exist. The appearance of antibiotic resistant bacteria, such as methicillin-resistant Staphylococcus aureus (MRSA) in the 1980s and ’90s, gave rise to a search for other remedies. One of the remedies that has been rediscovered and subsequently successfully reintroduced is maggot debridement therapy (MDT).1 The fact that more than 100 articles were published on the subject in the past two decades indicates that the use of maggots is making a strong comeback in medicine.2 In January 2004, the U.S. Food and Drug Administration (FDA) issued 510(k)#33391, allowing production and marketing of maggots as a medical device. In this article, we discuss the use of MDT in patients with a chronic wound.
A Long History of Maggot Therapy
MDT has been used in many cultures and has been known for centuries.3 Ambroise Parè is credited as the father of modern MDT. Unfortunately, no evidence can be found of Parè using maggots as a means to clean or heal wounds. The only reference is the often-cited case that occurred in 1557 at the battle of St. Quentin, when Parè observed soldiers whose wounds were covered by maggots. He mainly described the negative effects of the maggots, and, above all, believed they were spontaneously produced by the wound itself, not by the eggs of fly.4
Baron Larey (1766-1842) a famous surgeon in the army of Napoleon Bonaparte, wrote about soldiers who had larvae-infested wounds, but was frustrated that it was difficult to persuade his patients to leave the maggots in place, believing that “they promoted healing without leaving any damage.”5
The first surgeon to use MDT in patients in the hospital was the orthopedic surgeon William Baer. In the 1920s he was faced with a group of untreatable patients with severe osteomyelitis (antibiotics had not yet been discovered). He successfully treated many patients with maggots, and because of his success the therapy became regularly used in the United States.6
By 1934 more than 1,000 surgeons were using maggot therapy. Surgical Maggots were available commercially from Lederle Corporation.7 But with the introduction of antibiotics in the 1940s, the use of maggots dropped off. In the following years, case reports were published only occasionally.
The Negative Image of Maggots
A large problem of MDT is the difficulty of this type of therapy to gain acceptance in the medical community. Maggots are associated with rotting and decay. The image is of filthy, low-life creatures that are ugly and disgusting. Although a nice recent example for the general public is the scene in the movie Gladiator. The main character (played by Russell Crow) is advised to leave the maggots that spontaneously infested a wound on his shoulder in place so that the wound would heal. He leaves them in place and the wound heals without any problem, enabling Crow’s character to fight many battles.
In contrast, in an oral presentation we held recently at a Dutch scientific surgical meeting, a surgical professor in the audience said, “I will never allow those creatures in my ward.”8 This remark shows that widespread use and acceptance of MDT has not yet been reached. It seems there is still much work to do before MDT is generally accepted as a therapeutic method.
Fortunately, the negative image that seems to exist among nurses and physicians does not seem to bother patients.9 We have treated more than 100 patients in our clinic with MDT. All patients to whom we proposed MDT agreed to the therapy. All were allowed to discontinue the therapy whenever they wanted; none did. In a survey of the first 38 MDT-treated patients, 89% agreed to another session of MDT if the surgeon believed it would be beneficial, and 94% of the patients said that they would recommend it to others. This is despite the fact that the therapy was not successful in all patients (there was a below-knee of above the knee amputation-rate of 19% among patients who underwent MDT).10
Indications and Evidence
Indications and contra-indications for maggot therapy are not well defined. Some state that all kind of wounds that contain necrosis or slough can be good candidates for MDT. In our own study of 101 patients with 116 wounds treated with maggots, we had an overall success rate of 67%. (Seventy-eight out of 116 wounds had a beneficial outcome.) However, in 13 patients with septic arthritis, all wounds failed. Success rates where significantly reduced in cases of chronic limb ischemia, visible tendon or bone, and in cases of duration longer than three months before the start of MDT.11
Most physicians who start MDT use it mainly for worst-case scenarios. From our previous studies, it is clear that success rates in those patients are low. After witnessing a few failures, the physician is naturally reluctant to use it again.
What about evidence? Large randomized studies are lacking, although one containing 600 venous ulcer patients was initiated in 2004.12 There have been three randomized studies performed. Wayman, et al., have shown the cost-effectiveness of larval therapy in venous ulcers compared with hydrogel dressing.13 Contreras, et al., could not find a difference between MDT and curettage and topical silver sulfadiazine in patients with venous leg ulcers.14 At the 36th annual meeting of the European Association for the Study of Diabetes, Markevich, et al., reported on a randomized, multicenter, double-blind controlled clinical trial (n=140) for neuropathic diabetic foot lesions compared to conventional treatment. They found a significant higher percentage of granulation tissue after 10 days, compared with the hydrogel group.15 Results from large case-series indicate that MDT works and could even save limbs.2,16-18 The mechanism of action has not been unraveled yet.
Factors Influencing Effectiveness of MDT
Unfortunately, the statement made by Thomas, who said that maggot therapy works by “secreting proteolytic enzymes that break down dead tissue, turning it into a soup, which they then ingest,” still holds.19 It is known that there are mechanical effects, tissue growth effects, that direct killing of bacteria in the alimentary tract of the maggot takes place, and that maggots produce antibacterial factors.2,17,20-31
Although maggots are suitable agents for chronic wound treatment, it is likely that some wounds are more eligible than others for this type of treatment. In our opinion, all wounds that contain gangrenous or necrotic tissue with infection seem to be suited for MDT.32 Success rates of MDT reported in literature vary, but seem to be around 80% to 90%.16,17,33 In our own series, success rate is about 70%.
Patient-selection (case-mix) and method of outcome measurement play essential roles in these percentages. In our opinion, all wounds that contain necrotic tissue can be debrided effectively with MDT. However, if for example wound ischemia is the major etiologic factor, this should also be addressed. In our experience, diabetic foot, venous ulcers, traumatic ulcers, and infections after surgical procedures are all good candidates for MDT.
Absolute contraindications in our opinion are wounds close to large, uncovered blood vessels and wounds that need immediate surgical debridement (e.g., in the case of a septic patient). A relative contraindication is patients with natural of medically induced coagulopathies, but also patient preference could play a role.34 We have had very bad results with infected small joints of the foot; all wounds (n=13) eventually needed a small or large amputation.
Even the technique of application has an effect on outcome. There are two different application techniques: the free-range and the contained technique. The free-range technique is more effective in vitro and in-vivo and has become our standard application technique—not only in the outpatient department, but also in the intra-mural setting.35,36 (Figure 1, p. 16, shows a patient with a necrotic wound on the leg after radiation therapy and a surgical excision for a malignant tumor was performed.) Earlier surgical debridement combined with split skin graft failed. After four applications of maggots, the wound was free of necrosis and could be subsequently closed. (See Figure 2, p. 16.)
The contained technique is used in patients with bleeding tendencies and wounds that do not have enough healthy skin surrounding the wound; in other words, where the covering “cage” needed in case of the free-range technique can’t be applied. (This problem is shown in Figure 3, p. 16: A patient with necrotizing fasciitis of the left upper leg was treated with the contained technique—BiologiQ, Apeldoorn, Netherlands—as there is no proximal skin border. Of course, patient preference plays a role as well in the choice of application technique.37
Wound Clinic
In the Netherlands maggots can be ordered easily and are delivered within 24 hours. We started a wound clinic in 2002. First it was for MDT alone, but now the scope is broader, and we treat chronic wounds with different kind of wound therapies. We have two nurses, one nurse practitioner, one resident-surgeon, and one vascular surgeon who apply the maggots.
Patients do not need to be admitted for MDT. Fifty-nine percent of our patients are treated in the outpatient department. We are able to treat as many as 10 or 15 patients in one session, but MDT-treated patients make up only two or three patients at a time.
We found that after fast, successful biological debridement with MDT we were left with a lot of patients with red, granulating wounds that needed our attention in order to prevent relapses. In our opinion, there are many different treatment methods after MDT. Plaster casting in case of diabetic feet, secondary closure, and split skin grafting are different methods. However, other therapies like VAC-therapy and recently OASIS are promising.
At this time, all patients are prospectively followed after MDT. We are especially interested in patient selection and are now also aiming to find the ideal wound therapy after MDT. TH
Dr. Steenvoorde is a resident surgeon at Rijnland Hospital Leiderdorp, the Netherlands. van Doorn is a nurse-practitioner at Rijnland Hospital Leiderdorp. Jacobi is a senior researcher in the Medical Decision Department at Leiden University Medical Center, in the Netherlands. Dr. Oskam is a vascular surgeon at Rijnland Hospital Leiderdorp.
References
- Beasley WD, Hirst G. Making a meal of MRSA-the role of biosurgery inhospital-acquired infection. J Hosp Infect. 2004;56(1):6-9.
- Jukema GN, Menon AG, Bernards AT. et al. Amputation-sparing treatment by nature: “surgical” maggots revisited. Clin Infect Dis. 2002 Dec 15;35(12):1566-1571.
- Church JC. The traditional use of maggots in wound healing, and the development of larva therapy (biosurgery) in modern medicine. J Altern Complement Med. 1996 Winter;2(4):525-527.
- Coppi C. I dressed your wounds, God healed you—a wounded person’s psychology according to Ambroise Parè. Ostomy Wound Manage. 2005;51:62-64.
- Goldstein HI. Maggots in the treatment of wound and bone infections. J Bone Joint Surg. 1931;13:476-478.
- Baer WS. The treatment of chronic osteomyelitis with the maggot (larva of the blow fly). J Bone Joint Surg. 1931;13:438-475.
- Puckner WA. New and nonofficial remedies, surgical maggots-Lederle. J Am Med Assoc. 1932;98(5):401.
- Steenvoorde P, Doorn Lv, Jacobi CE, et al. Maggot therapy: retrospective study comparing two different application-techniques. (Dutch). Nederlands Tijdschrift voor Heelkunde. 2006;15:86.
- Contreras RJ, Fuentes SA, Karam-Orantes M, et al. Larval debridement therapy in Mexico. Wound Care Canada. 2005;3:42-46.
- Steenvoorde P, Budding TJ, Engeland Av, et al. Maggot therapy and the “yuk factor”: an issue for the patient? Wound Repair Regen. 2005 May-Jun;13(3):350-352.
- Steenvoorde P, Jacobi CA, Doorn Lv, et al. Maggot debridement therapy of infected ulcers: patient and wound factors influencing outcome. Ann Royal Coll Surg Eng. 2006.
- Raynor P, Dumville J, Cullum N. A new clinical trial of the effect of larval therapy. J Tissue Viability. 2004 Jul;14(3):104-105.
- Wayman J, Nirojogi V, Walker A, et al. The cost effectiveness of larval therapy in venous ulcers. J Tissue Viability. 2001 Jan;11(1):51.
- Contreras RJ, Fuentes SA, Arroyo ES, et al. Larval debridement therapy and infection control in venous ulcers: a comparative study. Presented at: the Second World Union of Wound Healing Societies Meeting; July 8-13, 2004.
- Markevich YO, McLeod-Roberts J, Mousley M, et al. Maggot therapy for diabetic neuropathic foot wounds: a randomized study. Presented at: the 36th Annual Meeting of the EASD; September 17-21, 2000. Ref Type: Conference Proceeding.
- Wolff H, Hansson C. Larval therapy—an effective method for ulcer debridement. Clin Exp Dermatol. 2003;28:137.
- Mumcuoglu KY, Ingber A, Gilead L, et al. Maggot therapy for the treatment of intractable wounds. Int J Dermatol. 1999 Aug;38(8):623-627.
- Courtenay M. The use of larval therapy in wound management in the UK. J Wound Care. 1999 Apr;8 (4):177-179.
- Bonn D. Maggot therapy: an alternative for wound infection. Lancet. 2000 Sep 30;356 (9236):1174.
- Robinson W. Stimulation of healing in non-healing wounds. J Bone Joint Surgery. 1935;17:267-271.
- Robinson W. Ammonium bicarbonate secreted by surgical maggots stimulates healing in purulent wounds. Am J Surg. 1940;47:111-115.
- Mumcuoglu KY, Ingber A, Gilead L, et al. Maggot therapy for the treatment of diabetic foot ulcers. Diabetes Care. 1998 Nov;21(11):2030-2031.
- Simmons S. A bactericidal principle in excretions of surgical maggots which destroys important etiological agents of pyogenic infections. J Bacteriol. 1935;30:253-267.
- Simmons S. The bactericidal properties of excretions of the maggot of Lucilia sericata. Bull Entomol Res. 1935;26:559-563.
- Mumcuoglu KY. Clinical applications for maggots in wound care. Am J Clin Dermatol. 2001;2:219-227.
- Armstrong DG, Short B, Martin BR, et al. Maggot therapy in lower extremity hospice wound care. J Am Podiatr Med Assoc. 2005;95(3):254-257.
- Robinson W, Norwood VH. The role of surgical maggots in the disinfection of osteomyelitis and other infected wounds. J Bone Joint Surgery. 1933;15:409-412.
- Robinson W, Norwood VH. Destruction of pyogenic bacteria in the alimentary tract of surgical maggots implanted in infected wounds. J Lab Clin Med. 1933;19:581-585.
- Mumcuoglu KY, Miller J, Mumcuoglu M. et al. Destruction of bacteria in the digestive tract of the maggot of Lucilia sericata (Diptera: Calliphoridae). J Med Entomol. 2001 Mar;38(2):161-166.
- Sherman RA, Hall MJ, Thomas S. Medicinal maggots: an ancient remedy for some contemporary afflictions. Annu Rev Entomol. 2000;45:55-81.
- Prete PE. Growth effects of Phaenicia sericata larval extracts on fibroblasts: mechanism for wound healing by maggot therapy. Life Sci. 1997;60(8):505-510.
- Church JCT, Courtenay M. Maggot debridement therapy for chronic wounds. Int J Low Extrem Wounds. 2002 Jun;1(2):129-134.
- Courtenay M, Church JC, Ryan TJ. Larva therapy in wound management. J R Soc Med. 2000 Feb;93:72-74.
- 34. Steenvoorde P, Oskam J. Bleeding c omplications in patients treated with maggot debridement therapy (MDT). Letter to the editor. IJLEW. 2005;4:57-58.
- Thomas S, Wynn K, Fowler T, et al. The effect of containment on the properties of sterile maggots. Br J Nurs. 2002 Jun;11(12 Suppl):S21-S22, S24, S26 passim.
- Steenvoorde P, Jacobi CE, Oskam J. Maggot debridement therapy: free-range or contained? An in-vivo study. Adv Skin Wound Care. 2005;18:430-435.
- Steenvoorde P, Oskam J. Use of larval therapy to combat infection after breast-conserving surgery. J Wound Care. 2005 May;14(5):212-213.
Pantilat Receives Endowed Chair
Increasingly, hospitals are making palliative care a priority; and more hospitalists are getting involved in providing these services and taking the lead on establishing and facilitating palliative care programs. Among the growing evidence that hospitalists are viewed as key players in the proliferation of hospital palliative care programs is the appointment of Steven Pantilat, MD, associate professor of clinical medicine, to the newly established Alan M. Kates and John M. Burnard Endowed Chair in Palliative Care at the University of California at San Francisco (UCSF).
The chair is the first palliative care chair in the University of California system and only the fifth nationwide. The endowment provides funding for salary support and efforts to build clinical, educational, research, and training components of the UCSF palliative care program. “This chair is important because hospitalists are often the main source of hospital palliative care services,” explains Dr. Pantilat. “Because I am a hospitalist, I understand the needs of these practitioners.”
Numerous Plans, Expectations
Dr. Pantilat has several expectations for what the chair will enable him to accomplish. “We hope to improve palliative care for patients, contribute to the field in terms of research and educational initiatives, and help UC advance in these areas,” he says. “Our main goal is to develop a world-class palliative care program that will advance the field in terms of education, research, and patient care and to provide the highest quality care to patients with life-threatening illness. This will provide seed money to develop educational and research programs that require some early investment when they are just ideas.”
There is a tremendous need for more and better palliative care in the hospital setting. “Patients have many needs, including management of symptoms such as shortness of breath, nausea, and fatigue,” he says. “There isn’t nearly enough research or information on these problems as compared to pain. We need more studies on the best way to treat symptoms.”
Additionally, Dr. Pantilat hopes to add to the body of literature on patient-physician communication, suggesting that hospitalists and other physicians need information about how to communicate sensitive issues such as bad news and how best to support patients and families throughout illnesses and fill their palliative care needs.
“We hope to develop and encourage more education and training on these topics,” he says. Stressing that there already are good educational programs about palliative care topics, Dr. Pantilat notes the need for more instruction specific to the unique needs of hospitalized patients and the hospitalists who care for them.
Create an Interdisciplinary System
“We need systems to provide palliative care. We also need to sensitize everyone who works in the hospital to comfort care issues,” says Dr. Pantilat, adding that there also is a need for programs and systems to ensure that patients and families will get the palliative care they need when they leave the hospital. “We need to work together to create a smooth transition from inpatient to outpatient palliative care. And we need to consider how we, as hospitalists, work with patients in the outpatient setting to ensure that someone is there to take care of them and their needs.”
Many of these needs require widespread education and training. “This grant will allow us to develop more robust and innovative educational efforts that engage ways to teach all team members about palliative care,” says Dr. Pantilat. “This will include projects such as using the Web to teach students.”
Expand the Definition
Dr. Pantilat also hopes to help expand the definition of palliative care and help people understand this as a broad concept of providing interdisciplinary care for people with terminal and chronic diseases. “An important point that we hope to emphasize is that palliative care is not just end-of-life care but something designed to improve life for people with illnesses—particularly chronic illnesses—either through the treatment of the diseases or the symptoms. It is an attempt to alleviate physical, emotional, and psychological suffering and promote the best possible quality of life,” he explains.
Helping people get “past the old limiting idea of palliative care” is another key goal. “A lot of palliative care can be provided while people are pursuing curative care,” explains Dr. Pantilat. “This is an important concept to promote.”
The Hospitalist’s Role
As a hospitalist, Dr. Pantilat also hopes to promote the growing recognition of the importance of hospitalists in palliative care programs: “The beautiful thing is that hospitalists are perfectly poised to handle palliative care programs, and with training they can become palliative care providers.”
The endowed chair reflects the importance of hospitalists in the palliative care field. “Hospitalists will be increasingly important in this area, and I hope to take a leadership role,” he says. While he is pleased and honored to have the chair at UCSF, he is confident that his work will have an impact well beyond his own university. “The chair will bring much recognition to our program but also to the field of palliative care in general and the role of hospitalists nationwide.” TH
Joanne Kaldy writes regularly for The Hospitalist.
Increasingly, hospitals are making palliative care a priority; and more hospitalists are getting involved in providing these services and taking the lead on establishing and facilitating palliative care programs. Among the growing evidence that hospitalists are viewed as key players in the proliferation of hospital palliative care programs is the appointment of Steven Pantilat, MD, associate professor of clinical medicine, to the newly established Alan M. Kates and John M. Burnard Endowed Chair in Palliative Care at the University of California at San Francisco (UCSF).
The chair is the first palliative care chair in the University of California system and only the fifth nationwide. The endowment provides funding for salary support and efforts to build clinical, educational, research, and training components of the UCSF palliative care program. “This chair is important because hospitalists are often the main source of hospital palliative care services,” explains Dr. Pantilat. “Because I am a hospitalist, I understand the needs of these practitioners.”
Numerous Plans, Expectations
Dr. Pantilat has several expectations for what the chair will enable him to accomplish. “We hope to improve palliative care for patients, contribute to the field in terms of research and educational initiatives, and help UC advance in these areas,” he says. “Our main goal is to develop a world-class palliative care program that will advance the field in terms of education, research, and patient care and to provide the highest quality care to patients with life-threatening illness. This will provide seed money to develop educational and research programs that require some early investment when they are just ideas.”
There is a tremendous need for more and better palliative care in the hospital setting. “Patients have many needs, including management of symptoms such as shortness of breath, nausea, and fatigue,” he says. “There isn’t nearly enough research or information on these problems as compared to pain. We need more studies on the best way to treat symptoms.”
Additionally, Dr. Pantilat hopes to add to the body of literature on patient-physician communication, suggesting that hospitalists and other physicians need information about how to communicate sensitive issues such as bad news and how best to support patients and families throughout illnesses and fill their palliative care needs.
“We hope to develop and encourage more education and training on these topics,” he says. Stressing that there already are good educational programs about palliative care topics, Dr. Pantilat notes the need for more instruction specific to the unique needs of hospitalized patients and the hospitalists who care for them.
Create an Interdisciplinary System
“We need systems to provide palliative care. We also need to sensitize everyone who works in the hospital to comfort care issues,” says Dr. Pantilat, adding that there also is a need for programs and systems to ensure that patients and families will get the palliative care they need when they leave the hospital. “We need to work together to create a smooth transition from inpatient to outpatient palliative care. And we need to consider how we, as hospitalists, work with patients in the outpatient setting to ensure that someone is there to take care of them and their needs.”
Many of these needs require widespread education and training. “This grant will allow us to develop more robust and innovative educational efforts that engage ways to teach all team members about palliative care,” says Dr. Pantilat. “This will include projects such as using the Web to teach students.”
Expand the Definition
Dr. Pantilat also hopes to help expand the definition of palliative care and help people understand this as a broad concept of providing interdisciplinary care for people with terminal and chronic diseases. “An important point that we hope to emphasize is that palliative care is not just end-of-life care but something designed to improve life for people with illnesses—particularly chronic illnesses—either through the treatment of the diseases or the symptoms. It is an attempt to alleviate physical, emotional, and psychological suffering and promote the best possible quality of life,” he explains.
Helping people get “past the old limiting idea of palliative care” is another key goal. “A lot of palliative care can be provided while people are pursuing curative care,” explains Dr. Pantilat. “This is an important concept to promote.”
The Hospitalist’s Role
As a hospitalist, Dr. Pantilat also hopes to promote the growing recognition of the importance of hospitalists in palliative care programs: “The beautiful thing is that hospitalists are perfectly poised to handle palliative care programs, and with training they can become palliative care providers.”
The endowed chair reflects the importance of hospitalists in the palliative care field. “Hospitalists will be increasingly important in this area, and I hope to take a leadership role,” he says. While he is pleased and honored to have the chair at UCSF, he is confident that his work will have an impact well beyond his own university. “The chair will bring much recognition to our program but also to the field of palliative care in general and the role of hospitalists nationwide.” TH
Joanne Kaldy writes regularly for The Hospitalist.
Increasingly, hospitals are making palliative care a priority; and more hospitalists are getting involved in providing these services and taking the lead on establishing and facilitating palliative care programs. Among the growing evidence that hospitalists are viewed as key players in the proliferation of hospital palliative care programs is the appointment of Steven Pantilat, MD, associate professor of clinical medicine, to the newly established Alan M. Kates and John M. Burnard Endowed Chair in Palliative Care at the University of California at San Francisco (UCSF).
The chair is the first palliative care chair in the University of California system and only the fifth nationwide. The endowment provides funding for salary support and efforts to build clinical, educational, research, and training components of the UCSF palliative care program. “This chair is important because hospitalists are often the main source of hospital palliative care services,” explains Dr. Pantilat. “Because I am a hospitalist, I understand the needs of these practitioners.”
Numerous Plans, Expectations
Dr. Pantilat has several expectations for what the chair will enable him to accomplish. “We hope to improve palliative care for patients, contribute to the field in terms of research and educational initiatives, and help UC advance in these areas,” he says. “Our main goal is to develop a world-class palliative care program that will advance the field in terms of education, research, and patient care and to provide the highest quality care to patients with life-threatening illness. This will provide seed money to develop educational and research programs that require some early investment when they are just ideas.”
There is a tremendous need for more and better palliative care in the hospital setting. “Patients have many needs, including management of symptoms such as shortness of breath, nausea, and fatigue,” he says. “There isn’t nearly enough research or information on these problems as compared to pain. We need more studies on the best way to treat symptoms.”
Additionally, Dr. Pantilat hopes to add to the body of literature on patient-physician communication, suggesting that hospitalists and other physicians need information about how to communicate sensitive issues such as bad news and how best to support patients and families throughout illnesses and fill their palliative care needs.
“We hope to develop and encourage more education and training on these topics,” he says. Stressing that there already are good educational programs about palliative care topics, Dr. Pantilat notes the need for more instruction specific to the unique needs of hospitalized patients and the hospitalists who care for them.
Create an Interdisciplinary System
“We need systems to provide palliative care. We also need to sensitize everyone who works in the hospital to comfort care issues,” says Dr. Pantilat, adding that there also is a need for programs and systems to ensure that patients and families will get the palliative care they need when they leave the hospital. “We need to work together to create a smooth transition from inpatient to outpatient palliative care. And we need to consider how we, as hospitalists, work with patients in the outpatient setting to ensure that someone is there to take care of them and their needs.”
Many of these needs require widespread education and training. “This grant will allow us to develop more robust and innovative educational efforts that engage ways to teach all team members about palliative care,” says Dr. Pantilat. “This will include projects such as using the Web to teach students.”
Expand the Definition
Dr. Pantilat also hopes to help expand the definition of palliative care and help people understand this as a broad concept of providing interdisciplinary care for people with terminal and chronic diseases. “An important point that we hope to emphasize is that palliative care is not just end-of-life care but something designed to improve life for people with illnesses—particularly chronic illnesses—either through the treatment of the diseases or the symptoms. It is an attempt to alleviate physical, emotional, and psychological suffering and promote the best possible quality of life,” he explains.
Helping people get “past the old limiting idea of palliative care” is another key goal. “A lot of palliative care can be provided while people are pursuing curative care,” explains Dr. Pantilat. “This is an important concept to promote.”
The Hospitalist’s Role
As a hospitalist, Dr. Pantilat also hopes to promote the growing recognition of the importance of hospitalists in palliative care programs: “The beautiful thing is that hospitalists are perfectly poised to handle palliative care programs, and with training they can become palliative care providers.”
The endowed chair reflects the importance of hospitalists in the palliative care field. “Hospitalists will be increasingly important in this area, and I hope to take a leadership role,” he says. While he is pleased and honored to have the chair at UCSF, he is confident that his work will have an impact well beyond his own university. “The chair will bring much recognition to our program but also to the field of palliative care in general and the role of hospitalists nationwide.” TH
Joanne Kaldy writes regularly for The Hospitalist.
Rash Judgement
A 38-year-old, healthy, incarcerated, African-American man presented with a one-and-a-half year history of an eruption in his axillae. The patient stated that the “rash” worsened with sweating but the lesions were otherwise asymptomatic.
Corticosteroid creams, antifungal creams, and oral antibiotics had not led to any improvement. The eruption progressed to involve his trunk, arms, and face. The skin exam showed hyperpigmented, firm plaques with erythematous papules in the axillae. The plaques were also present on the chest, back, and upper extremities. Verrucous papules were noted on the flexural areas of upper extremities as well as tan colored plaques at the lateral canthi of eyes. (See Figures 1-3 this page.)
CBC and serum electrolytes were normal. Lipid panel showed a cholesterol of 593 mg/dL, triglycerides 106 mg/dL, high density lipoprotein of 37 g/dL, low density lipoprotein of 535 mg/dL, and very low density lipoprotein of 21 mg/dL. A biopsy from the axilla and the umbilical area were sent for histologic examination. (See Figure 4 this page.)
What is this patient’s most likely diagnosis?
- Sarcoidosis
- Disseminated xanthomas
- Xanthoma disseminatum
- Erythema elevatum diutinum
- Necrobiosis lipoidica
Discussion
The answer is B: disseminated xanthomas. Punch biopsy from the axilla and shave biopsy from the periumbilical area both revealed localized infiltrates of lipid containing macrophages.
Xanthomas develop due to accumulation of lipid-filled macrophages and suggest an underlying disorder of lipid metabolism. Morbidity and mortality are primarily related to atherosclerosis (e.g., coronary artery disease) and pancreatitis, which occur secondarily to the increased lipid levels rather than the xanthoma itself.
In general, four clinical types of xanthomas exist: tendinous, planar, tuberous, and eruptive. A particular diagnosis cannot necessarily be made on the basis of clinical signs; however, certain types of xanthomas are more characteristic of specific hyperlipidemias. Eruptive xanthomas are found in the setting of primary or secondary hypertriglyeridemia. Tuberous xanthomas have both elevated serum cholesterol and triglycerides. This patient had plane xanthomas and xanthelasma and was especially notable for intertriginous plane xanthomas, which can be pathognomonic for homozygous familial hypercholesterolemia.
This patient’s histology from both the periumbilical area and the axilla depict the characteristic presence of vacuolated macrophages (foamy macrophages) to confirm the diagnosis as disseminated xanthoma.1-3 Sarcoidosis is a chronic idiopathic disorder characterized by noncaseating granulomas that can affect any organ system. Cutaneous sarcoidosis typically presents as asymptomatic, red-brown macules and papules affecting the face, periorbital areas, nasolabial folds, and/or extensor surfaces. Typical sarcoid lesions are characterized by the presence of circumscribed granulomas of epithelioid cells with little or no necrosis. The granulomas are characteristically referred to as “naked” due to the sparse lymphocytic infiltrate at the margins.
This patient’s histologic exam did not reveal any granulomas and localized infiltrates of lipid containing macrophages make the diagnosis of cutaneous sarcoidosis unlikely.4,5
Necrobiosis lipoidica (NL) is a cutaneous disorder that is often, but not always, associated with diabetes mellitus. NL is a disorder of collagen degeneration with a granulomatous response, thickening of blood vessel walls, and fat deposition. Patients usually present with asymptomatic shiny patches that slowly enlarge over months to years. The patient’s main complaint is the unsightly cosmetic appearance of the lesions.
Skin lesions of classic NL begin as 1- to 3-mm well-circumscribed papules or nodules that expand with an active border to become waxy, atrophic, round plaques centrally. Initially, these plaques are red-brown in color but progressively become more yellow and atrophic in appearance. Most cases of NL occur on the pretibial area, but cases have been reported on the face, scalp, trunk, and upper extremities where the diagnosis is more likely to be missed.
Although this patient’s mother had diabetes, his fasting blood glucose was well within normal limits (71 mg/dL). Histologically NL displays sclerotic collagen and obliteration of the bundle pattern, with interstitial and palisaded granulomas that involve the subcutaneous tissue and dermis. Fat containing foam cells are often present.
Although our patient’s biopsy showed fat containing foam cells, it did not have the interstitial granulomas or the sclerotic collagen. In addition, the lack of diabetes makes this diagnosis less likely.6,7
Erythema elevatum diutinum (EED) is a rare type of leukocytoclastic vasculitis characterized by red, purple, brown, or yellow papules, plaques, or nodules. These lesions are usually distributed on the extensor surfaces of the body. The lesions are usually asymptomatic but can be associated occasionally with joint pain. Clinical studies show a preference for the extensor surfaces of the hands, the wrists, the elbows, the ankles, the Achilles’ tendons, the fingers, and the toes. The buttocks, the face, and the ears as well as the palms, the soles, the legs, the forearms, and the genitals may be involved; however, the trunk is usually spared. EED is a type of necrotizing vasculitis.
In its early stages, there are no specific histologic findings that can be used to single out the diagnosis of EED from other leukocytoclastic diseases. Although the distribution and lack of symptomatology in EED is reminiscent of our patient, this patient’s lesions were more often found in the flexural areas rather than extensors. In addition, there was no necrotizing vasculitis on histology, which precludes this rare diagnosis of EED.8
Xanthoma disseminatum (XD) is a rare, benign, proliferative disorder in children and young adults characterized by xanthomatous lesions especially in the flexural folds and eyelids. Although it sounds like a disorder of lipid metabolism, it is actually a histiocytic disorder that is not associated with lipoprotein abnormalities and patients are normolipemic. Histologically, it shows mononuclear phagocyte proliferation with Touton giant cells and CD68 positivity on immunophenotyping. It is unlikely that this patient has XD despite the appropriate clinical presentation because histologically all that is found are foam cells. In addition, the patient had a definite lipoprotein abnormality while XD patients are normolipemic.9 TH
References
- Cruz PD, East C, Bergstresser P. Dermal, subcutaneous, and tendon xanthomas: diagnostic markers for specific lipoprotein disorders. J Am Acad Dermatol 1988 Jul;19(1 pt 1):95-111.
- Massengale WT, Nesbitt LT. Xanthomas. In: Bolognia JL, Jorrizo JL, Rapini RP, eds. Dermatology. Vol. 2. London: Mosby; 2003:1447-1454.
- Parker F. Xanthomas and hyperlipidemias. J Am Acad Dermatol. 1985 Jul;13 (1):1-30.
- Young RJ, 3rd, Gilson RT, Yanase D, et al. Cutaneous sarcoidosis. Int J Dermatol. 2001;40:249-253.
- English JC, Patel PJ, Greer KE. Sarcoidosis. J Am Acad Dermatol. 2001;44:725-743: quiz 744-746.
- Fitzpatrick TB, Johnson R, Wolff K, et al. Genetic, metabolic, endocrine and nutritional diseases. Color Atlas and Synopsis of Clinical Dermatology, Common and Serious Diseases. New York: McGraw-Hill; 2001:415-416.
- Lowitt MH, Dover JS. Necrobiosis lipoidica. J Am Acad Dermatol. 1991; 25:735-748.
- Yiannias JA, el-Azhary RA, Gibson LE. Erythema elevatum diutinum: a clinical and histopathologic study of 13 patients. J Am Acad Dermatol 1992 Jan;26(1):38-44.
- Alexander AS, Turner R, Uniate L, et al. Xanthoma disseminatum: a case report and literature review. Br J Radiol 2005 Feb;78(926):153-157.
A 38-year-old, healthy, incarcerated, African-American man presented with a one-and-a-half year history of an eruption in his axillae. The patient stated that the “rash” worsened with sweating but the lesions were otherwise asymptomatic.
Corticosteroid creams, antifungal creams, and oral antibiotics had not led to any improvement. The eruption progressed to involve his trunk, arms, and face. The skin exam showed hyperpigmented, firm plaques with erythematous papules in the axillae. The plaques were also present on the chest, back, and upper extremities. Verrucous papules were noted on the flexural areas of upper extremities as well as tan colored plaques at the lateral canthi of eyes. (See Figures 1-3 this page.)
CBC and serum electrolytes were normal. Lipid panel showed a cholesterol of 593 mg/dL, triglycerides 106 mg/dL, high density lipoprotein of 37 g/dL, low density lipoprotein of 535 mg/dL, and very low density lipoprotein of 21 mg/dL. A biopsy from the axilla and the umbilical area were sent for histologic examination. (See Figure 4 this page.)
What is this patient’s most likely diagnosis?
- Sarcoidosis
- Disseminated xanthomas
- Xanthoma disseminatum
- Erythema elevatum diutinum
- Necrobiosis lipoidica
Discussion
The answer is B: disseminated xanthomas. Punch biopsy from the axilla and shave biopsy from the periumbilical area both revealed localized infiltrates of lipid containing macrophages.
Xanthomas develop due to accumulation of lipid-filled macrophages and suggest an underlying disorder of lipid metabolism. Morbidity and mortality are primarily related to atherosclerosis (e.g., coronary artery disease) and pancreatitis, which occur secondarily to the increased lipid levels rather than the xanthoma itself.
In general, four clinical types of xanthomas exist: tendinous, planar, tuberous, and eruptive. A particular diagnosis cannot necessarily be made on the basis of clinical signs; however, certain types of xanthomas are more characteristic of specific hyperlipidemias. Eruptive xanthomas are found in the setting of primary or secondary hypertriglyeridemia. Tuberous xanthomas have both elevated serum cholesterol and triglycerides. This patient had plane xanthomas and xanthelasma and was especially notable for intertriginous plane xanthomas, which can be pathognomonic for homozygous familial hypercholesterolemia.
This patient’s histology from both the periumbilical area and the axilla depict the characteristic presence of vacuolated macrophages (foamy macrophages) to confirm the diagnosis as disseminated xanthoma.1-3 Sarcoidosis is a chronic idiopathic disorder characterized by noncaseating granulomas that can affect any organ system. Cutaneous sarcoidosis typically presents as asymptomatic, red-brown macules and papules affecting the face, periorbital areas, nasolabial folds, and/or extensor surfaces. Typical sarcoid lesions are characterized by the presence of circumscribed granulomas of epithelioid cells with little or no necrosis. The granulomas are characteristically referred to as “naked” due to the sparse lymphocytic infiltrate at the margins.
This patient’s histologic exam did not reveal any granulomas and localized infiltrates of lipid containing macrophages make the diagnosis of cutaneous sarcoidosis unlikely.4,5
Necrobiosis lipoidica (NL) is a cutaneous disorder that is often, but not always, associated with diabetes mellitus. NL is a disorder of collagen degeneration with a granulomatous response, thickening of blood vessel walls, and fat deposition. Patients usually present with asymptomatic shiny patches that slowly enlarge over months to years. The patient’s main complaint is the unsightly cosmetic appearance of the lesions.
Skin lesions of classic NL begin as 1- to 3-mm well-circumscribed papules or nodules that expand with an active border to become waxy, atrophic, round plaques centrally. Initially, these plaques are red-brown in color but progressively become more yellow and atrophic in appearance. Most cases of NL occur on the pretibial area, but cases have been reported on the face, scalp, trunk, and upper extremities where the diagnosis is more likely to be missed.
Although this patient’s mother had diabetes, his fasting blood glucose was well within normal limits (71 mg/dL). Histologically NL displays sclerotic collagen and obliteration of the bundle pattern, with interstitial and palisaded granulomas that involve the subcutaneous tissue and dermis. Fat containing foam cells are often present.
Although our patient’s biopsy showed fat containing foam cells, it did not have the interstitial granulomas or the sclerotic collagen. In addition, the lack of diabetes makes this diagnosis less likely.6,7
Erythema elevatum diutinum (EED) is a rare type of leukocytoclastic vasculitis characterized by red, purple, brown, or yellow papules, plaques, or nodules. These lesions are usually distributed on the extensor surfaces of the body. The lesions are usually asymptomatic but can be associated occasionally with joint pain. Clinical studies show a preference for the extensor surfaces of the hands, the wrists, the elbows, the ankles, the Achilles’ tendons, the fingers, and the toes. The buttocks, the face, and the ears as well as the palms, the soles, the legs, the forearms, and the genitals may be involved; however, the trunk is usually spared. EED is a type of necrotizing vasculitis.
In its early stages, there are no specific histologic findings that can be used to single out the diagnosis of EED from other leukocytoclastic diseases. Although the distribution and lack of symptomatology in EED is reminiscent of our patient, this patient’s lesions were more often found in the flexural areas rather than extensors. In addition, there was no necrotizing vasculitis on histology, which precludes this rare diagnosis of EED.8
Xanthoma disseminatum (XD) is a rare, benign, proliferative disorder in children and young adults characterized by xanthomatous lesions especially in the flexural folds and eyelids. Although it sounds like a disorder of lipid metabolism, it is actually a histiocytic disorder that is not associated with lipoprotein abnormalities and patients are normolipemic. Histologically, it shows mononuclear phagocyte proliferation with Touton giant cells and CD68 positivity on immunophenotyping. It is unlikely that this patient has XD despite the appropriate clinical presentation because histologically all that is found are foam cells. In addition, the patient had a definite lipoprotein abnormality while XD patients are normolipemic.9 TH
References
- Cruz PD, East C, Bergstresser P. Dermal, subcutaneous, and tendon xanthomas: diagnostic markers for specific lipoprotein disorders. J Am Acad Dermatol 1988 Jul;19(1 pt 1):95-111.
- Massengale WT, Nesbitt LT. Xanthomas. In: Bolognia JL, Jorrizo JL, Rapini RP, eds. Dermatology. Vol. 2. London: Mosby; 2003:1447-1454.
- Parker F. Xanthomas and hyperlipidemias. J Am Acad Dermatol. 1985 Jul;13 (1):1-30.
- Young RJ, 3rd, Gilson RT, Yanase D, et al. Cutaneous sarcoidosis. Int J Dermatol. 2001;40:249-253.
- English JC, Patel PJ, Greer KE. Sarcoidosis. J Am Acad Dermatol. 2001;44:725-743: quiz 744-746.
- Fitzpatrick TB, Johnson R, Wolff K, et al. Genetic, metabolic, endocrine and nutritional diseases. Color Atlas and Synopsis of Clinical Dermatology, Common and Serious Diseases. New York: McGraw-Hill; 2001:415-416.
- Lowitt MH, Dover JS. Necrobiosis lipoidica. J Am Acad Dermatol. 1991; 25:735-748.
- Yiannias JA, el-Azhary RA, Gibson LE. Erythema elevatum diutinum: a clinical and histopathologic study of 13 patients. J Am Acad Dermatol 1992 Jan;26(1):38-44.
- Alexander AS, Turner R, Uniate L, et al. Xanthoma disseminatum: a case report and literature review. Br J Radiol 2005 Feb;78(926):153-157.
A 38-year-old, healthy, incarcerated, African-American man presented with a one-and-a-half year history of an eruption in his axillae. The patient stated that the “rash” worsened with sweating but the lesions were otherwise asymptomatic.
Corticosteroid creams, antifungal creams, and oral antibiotics had not led to any improvement. The eruption progressed to involve his trunk, arms, and face. The skin exam showed hyperpigmented, firm plaques with erythematous papules in the axillae. The plaques were also present on the chest, back, and upper extremities. Verrucous papules were noted on the flexural areas of upper extremities as well as tan colored plaques at the lateral canthi of eyes. (See Figures 1-3 this page.)
CBC and serum electrolytes were normal. Lipid panel showed a cholesterol of 593 mg/dL, triglycerides 106 mg/dL, high density lipoprotein of 37 g/dL, low density lipoprotein of 535 mg/dL, and very low density lipoprotein of 21 mg/dL. A biopsy from the axilla and the umbilical area were sent for histologic examination. (See Figure 4 this page.)
What is this patient’s most likely diagnosis?
- Sarcoidosis
- Disseminated xanthomas
- Xanthoma disseminatum
- Erythema elevatum diutinum
- Necrobiosis lipoidica
Discussion
The answer is B: disseminated xanthomas. Punch biopsy from the axilla and shave biopsy from the periumbilical area both revealed localized infiltrates of lipid containing macrophages.
Xanthomas develop due to accumulation of lipid-filled macrophages and suggest an underlying disorder of lipid metabolism. Morbidity and mortality are primarily related to atherosclerosis (e.g., coronary artery disease) and pancreatitis, which occur secondarily to the increased lipid levels rather than the xanthoma itself.
In general, four clinical types of xanthomas exist: tendinous, planar, tuberous, and eruptive. A particular diagnosis cannot necessarily be made on the basis of clinical signs; however, certain types of xanthomas are more characteristic of specific hyperlipidemias. Eruptive xanthomas are found in the setting of primary or secondary hypertriglyeridemia. Tuberous xanthomas have both elevated serum cholesterol and triglycerides. This patient had plane xanthomas and xanthelasma and was especially notable for intertriginous plane xanthomas, which can be pathognomonic for homozygous familial hypercholesterolemia.
This patient’s histology from both the periumbilical area and the axilla depict the characteristic presence of vacuolated macrophages (foamy macrophages) to confirm the diagnosis as disseminated xanthoma.1-3 Sarcoidosis is a chronic idiopathic disorder characterized by noncaseating granulomas that can affect any organ system. Cutaneous sarcoidosis typically presents as asymptomatic, red-brown macules and papules affecting the face, periorbital areas, nasolabial folds, and/or extensor surfaces. Typical sarcoid lesions are characterized by the presence of circumscribed granulomas of epithelioid cells with little or no necrosis. The granulomas are characteristically referred to as “naked” due to the sparse lymphocytic infiltrate at the margins.
This patient’s histologic exam did not reveal any granulomas and localized infiltrates of lipid containing macrophages make the diagnosis of cutaneous sarcoidosis unlikely.4,5
Necrobiosis lipoidica (NL) is a cutaneous disorder that is often, but not always, associated with diabetes mellitus. NL is a disorder of collagen degeneration with a granulomatous response, thickening of blood vessel walls, and fat deposition. Patients usually present with asymptomatic shiny patches that slowly enlarge over months to years. The patient’s main complaint is the unsightly cosmetic appearance of the lesions.
Skin lesions of classic NL begin as 1- to 3-mm well-circumscribed papules or nodules that expand with an active border to become waxy, atrophic, round plaques centrally. Initially, these plaques are red-brown in color but progressively become more yellow and atrophic in appearance. Most cases of NL occur on the pretibial area, but cases have been reported on the face, scalp, trunk, and upper extremities where the diagnosis is more likely to be missed.
Although this patient’s mother had diabetes, his fasting blood glucose was well within normal limits (71 mg/dL). Histologically NL displays sclerotic collagen and obliteration of the bundle pattern, with interstitial and palisaded granulomas that involve the subcutaneous tissue and dermis. Fat containing foam cells are often present.
Although our patient’s biopsy showed fat containing foam cells, it did not have the interstitial granulomas or the sclerotic collagen. In addition, the lack of diabetes makes this diagnosis less likely.6,7
Erythema elevatum diutinum (EED) is a rare type of leukocytoclastic vasculitis characterized by red, purple, brown, or yellow papules, plaques, or nodules. These lesions are usually distributed on the extensor surfaces of the body. The lesions are usually asymptomatic but can be associated occasionally with joint pain. Clinical studies show a preference for the extensor surfaces of the hands, the wrists, the elbows, the ankles, the Achilles’ tendons, the fingers, and the toes. The buttocks, the face, and the ears as well as the palms, the soles, the legs, the forearms, and the genitals may be involved; however, the trunk is usually spared. EED is a type of necrotizing vasculitis.
In its early stages, there are no specific histologic findings that can be used to single out the diagnosis of EED from other leukocytoclastic diseases. Although the distribution and lack of symptomatology in EED is reminiscent of our patient, this patient’s lesions were more often found in the flexural areas rather than extensors. In addition, there was no necrotizing vasculitis on histology, which precludes this rare diagnosis of EED.8
Xanthoma disseminatum (XD) is a rare, benign, proliferative disorder in children and young adults characterized by xanthomatous lesions especially in the flexural folds and eyelids. Although it sounds like a disorder of lipid metabolism, it is actually a histiocytic disorder that is not associated with lipoprotein abnormalities and patients are normolipemic. Histologically, it shows mononuclear phagocyte proliferation with Touton giant cells and CD68 positivity on immunophenotyping. It is unlikely that this patient has XD despite the appropriate clinical presentation because histologically all that is found are foam cells. In addition, the patient had a definite lipoprotein abnormality while XD patients are normolipemic.9 TH
References
- Cruz PD, East C, Bergstresser P. Dermal, subcutaneous, and tendon xanthomas: diagnostic markers for specific lipoprotein disorders. J Am Acad Dermatol 1988 Jul;19(1 pt 1):95-111.
- Massengale WT, Nesbitt LT. Xanthomas. In: Bolognia JL, Jorrizo JL, Rapini RP, eds. Dermatology. Vol. 2. London: Mosby; 2003:1447-1454.
- Parker F. Xanthomas and hyperlipidemias. J Am Acad Dermatol. 1985 Jul;13 (1):1-30.
- Young RJ, 3rd, Gilson RT, Yanase D, et al. Cutaneous sarcoidosis. Int J Dermatol. 2001;40:249-253.
- English JC, Patel PJ, Greer KE. Sarcoidosis. J Am Acad Dermatol. 2001;44:725-743: quiz 744-746.
- Fitzpatrick TB, Johnson R, Wolff K, et al. Genetic, metabolic, endocrine and nutritional diseases. Color Atlas and Synopsis of Clinical Dermatology, Common and Serious Diseases. New York: McGraw-Hill; 2001:415-416.
- Lowitt MH, Dover JS. Necrobiosis lipoidica. J Am Acad Dermatol. 1991; 25:735-748.
- Yiannias JA, el-Azhary RA, Gibson LE. Erythema elevatum diutinum: a clinical and histopathologic study of 13 patients. J Am Acad Dermatol 1992 Jan;26(1):38-44.
- Alexander AS, Turner R, Uniate L, et al. Xanthoma disseminatum: a case report and literature review. Br J Radiol 2005 Feb;78(926):153-157.
Shift Perspectives
The shifts worked by a hospital medicine group can reflect its values or simply ensure adequate coverage. Either way, the shifts your group assigns can play a significant role in recruiting new hospitalists and retaining those you have. And there may be more scheduling options than you have considered.
The Most Attractive Shift Debunked
Many new hospitalists seek as much time off as possible, and there are plenty of groups catering to that desire. “Most physicians prefer time off, and seven on, seven off is attractive in recruiting new people to your practice—but it strikes me as a poisonous way to work,” says John Nelson, MD, co-founder of SHM, medical director of the hospitalist practice at Overlake Hospital in Bellevue, Wash., and author of the “Practice Management” column in The Hospitalist. Dr. Nelson acts as a consultant to hospitalist practices around the country and has written articles and given presentations on the topic of scheduling for hospital medicine groups.
Dr. Nelson understands the attractions of working seven on, seven off—particularly for young physicians. “Even seven on is not as bad as being an intern; it’s easier than they were used to in their residency,” he says. “But I worry this schedule might increase burnout and resentment of work. It’s asystole/diastole lifestyle and may not be a healthy way to organize your life or your career.”
An Alternative Scheduling Idea
Dr. Nelson has his own unique ideas of how a group’s shift assignments should work to ensure better coverage and keep hospitalists happy. His ideas are not just theories—his own group lives and works by a flexible arrangement.
Their schedule is partly dictated by a desire to keep the physicians happy and healthy. “I believe a constant mix of work and the rest of your life is best,” says Dr. Nelson. “You shouldn’t have to put the rest of your life into the seven days that you’re off.”
So Dr. Nelson’s practice allows considerable flexibility to each physician, but ensures that any given workday is shorter than 12 hours. “I think it’s better not to have a rigidly repeating schedule,” he explains.
Dr. Nelson’s group uses pagers to ensure a hospitalist is always available during coverage hours, but they don’t adhere to a strict schedule. “So many groups work specified shifts, whether it’s 10 or 12 hours, and I think there’s a better idea,” he says. “If everyone has to punch a clock, it interferes with flexibility. I would not tell doctors when to start or stop.”
Of course, as a group, someone has to be available for emergencies all the time, and physicians may need to start daily rounds to write most discharge orders by a certain time. “I have a pager on by 7 a.m., but nothing says I have to be in the hospital by 7 a.m.,” says Dr. Nelson. “It’s often in my interest to start rounding earlier than 7 a.m. so that I can finish earlier or have time for a break later in the day.”
Greater Flexibility = Better Coverage
Another benefit to moving to shorter, more flexible days is ensuring adequate coverage. “Rigidly defined shifts almost never precisely match the day’s workload,” points out Dr. Nelson. Therefore, his practice boosts staffing to cover busy periods. “My recommendation is to intentionally overstaff for the average day’s workload. When it’s busy, everyone can pitch in and work an extra one or two hours.”
If it’s not busy, one or more doctors may leave early. “This is nimble and responsive to the day-to-day workload,” says Dr. Nelson.
To move from a seven on, seven off schedule to this model, Dr. Nelson recommends that every doctor in the practice work 30 to 40 more days annually. A seven on, seven off schedule would have a physician work 182.5 days per year; if you decrease the hours per day and boost the number of working days to 220 a year, your physicians will be working the same number of hours, but in shorter days—even if the practice workload stays the same and each individual doctor’s annual productivity stays the same.
“It’s more realistic to work more days when they’re not so grueling,” says Dr. Nelson. “Plus, you have a built-in capacity to meet a sudden increase in workload. Imagine an eight-man group, where four doctors each work 12-hour shifts. Now imagine that instead of four, you get a fifth doctor to show up every day. [You can get this fifth doctor without adding staff if each doctor works more days annually.] When a day is unpredictably busy, the physicians won’t be absolutely overwhelmed. If it’s not busy, you can send someone home early. You get a lot more flexibility.”
For a hospital medicine group, implementing a flexible schedule such as this generally requires payment for production, which ties individual physicians into the economic health of their group. Compensation matches workload, allowing individual physicians to work to their values—more money or more free time.
“I think it’s better to pay on production,” says Dr. Nelson. “That way each person has the opportunity to choose. If one values money, he can volunteer to stay and work more and make more money. Each works to their own sweet spot, whereas a seven on, seven off schedule with rigidly defined shifts forces everyone to do the same thing.”
Physicians working on a flexible schedule still need to get their work finished each day, but they have more autonomy in how and when they get it done. “Doctors who work fast can go home early; physicians can decide for themselves the right balance for spending time each patient,” says Dr. Nelson. “As long as they understand there are economic consequences … and act with reasonableness. In our group, we get the work done. There’s no official start or stop time. Each of us chooses an individual work style. There are boundaries; the work needs to be done. There are costs as well, but I believe this system is healthy and liberating.” TH
Jane Jerrard regularly writes “Career Development.”
The shifts worked by a hospital medicine group can reflect its values or simply ensure adequate coverage. Either way, the shifts your group assigns can play a significant role in recruiting new hospitalists and retaining those you have. And there may be more scheduling options than you have considered.
The Most Attractive Shift Debunked
Many new hospitalists seek as much time off as possible, and there are plenty of groups catering to that desire. “Most physicians prefer time off, and seven on, seven off is attractive in recruiting new people to your practice—but it strikes me as a poisonous way to work,” says John Nelson, MD, co-founder of SHM, medical director of the hospitalist practice at Overlake Hospital in Bellevue, Wash., and author of the “Practice Management” column in The Hospitalist. Dr. Nelson acts as a consultant to hospitalist practices around the country and has written articles and given presentations on the topic of scheduling for hospital medicine groups.
Dr. Nelson understands the attractions of working seven on, seven off—particularly for young physicians. “Even seven on is not as bad as being an intern; it’s easier than they were used to in their residency,” he says. “But I worry this schedule might increase burnout and resentment of work. It’s asystole/diastole lifestyle and may not be a healthy way to organize your life or your career.”
An Alternative Scheduling Idea
Dr. Nelson has his own unique ideas of how a group’s shift assignments should work to ensure better coverage and keep hospitalists happy. His ideas are not just theories—his own group lives and works by a flexible arrangement.
Their schedule is partly dictated by a desire to keep the physicians happy and healthy. “I believe a constant mix of work and the rest of your life is best,” says Dr. Nelson. “You shouldn’t have to put the rest of your life into the seven days that you’re off.”
So Dr. Nelson’s practice allows considerable flexibility to each physician, but ensures that any given workday is shorter than 12 hours. “I think it’s better not to have a rigidly repeating schedule,” he explains.
Dr. Nelson’s group uses pagers to ensure a hospitalist is always available during coverage hours, but they don’t adhere to a strict schedule. “So many groups work specified shifts, whether it’s 10 or 12 hours, and I think there’s a better idea,” he says. “If everyone has to punch a clock, it interferes with flexibility. I would not tell doctors when to start or stop.”
Of course, as a group, someone has to be available for emergencies all the time, and physicians may need to start daily rounds to write most discharge orders by a certain time. “I have a pager on by 7 a.m., but nothing says I have to be in the hospital by 7 a.m.,” says Dr. Nelson. “It’s often in my interest to start rounding earlier than 7 a.m. so that I can finish earlier or have time for a break later in the day.”
Greater Flexibility = Better Coverage
Another benefit to moving to shorter, more flexible days is ensuring adequate coverage. “Rigidly defined shifts almost never precisely match the day’s workload,” points out Dr. Nelson. Therefore, his practice boosts staffing to cover busy periods. “My recommendation is to intentionally overstaff for the average day’s workload. When it’s busy, everyone can pitch in and work an extra one or two hours.”
If it’s not busy, one or more doctors may leave early. “This is nimble and responsive to the day-to-day workload,” says Dr. Nelson.
To move from a seven on, seven off schedule to this model, Dr. Nelson recommends that every doctor in the practice work 30 to 40 more days annually. A seven on, seven off schedule would have a physician work 182.5 days per year; if you decrease the hours per day and boost the number of working days to 220 a year, your physicians will be working the same number of hours, but in shorter days—even if the practice workload stays the same and each individual doctor’s annual productivity stays the same.
“It’s more realistic to work more days when they’re not so grueling,” says Dr. Nelson. “Plus, you have a built-in capacity to meet a sudden increase in workload. Imagine an eight-man group, where four doctors each work 12-hour shifts. Now imagine that instead of four, you get a fifth doctor to show up every day. [You can get this fifth doctor without adding staff if each doctor works more days annually.] When a day is unpredictably busy, the physicians won’t be absolutely overwhelmed. If it’s not busy, you can send someone home early. You get a lot more flexibility.”
For a hospital medicine group, implementing a flexible schedule such as this generally requires payment for production, which ties individual physicians into the economic health of their group. Compensation matches workload, allowing individual physicians to work to their values—more money or more free time.
“I think it’s better to pay on production,” says Dr. Nelson. “That way each person has the opportunity to choose. If one values money, he can volunteer to stay and work more and make more money. Each works to their own sweet spot, whereas a seven on, seven off schedule with rigidly defined shifts forces everyone to do the same thing.”
Physicians working on a flexible schedule still need to get their work finished each day, but they have more autonomy in how and when they get it done. “Doctors who work fast can go home early; physicians can decide for themselves the right balance for spending time each patient,” says Dr. Nelson. “As long as they understand there are economic consequences … and act with reasonableness. In our group, we get the work done. There’s no official start or stop time. Each of us chooses an individual work style. There are boundaries; the work needs to be done. There are costs as well, but I believe this system is healthy and liberating.” TH
Jane Jerrard regularly writes “Career Development.”
The shifts worked by a hospital medicine group can reflect its values or simply ensure adequate coverage. Either way, the shifts your group assigns can play a significant role in recruiting new hospitalists and retaining those you have. And there may be more scheduling options than you have considered.
The Most Attractive Shift Debunked
Many new hospitalists seek as much time off as possible, and there are plenty of groups catering to that desire. “Most physicians prefer time off, and seven on, seven off is attractive in recruiting new people to your practice—but it strikes me as a poisonous way to work,” says John Nelson, MD, co-founder of SHM, medical director of the hospitalist practice at Overlake Hospital in Bellevue, Wash., and author of the “Practice Management” column in The Hospitalist. Dr. Nelson acts as a consultant to hospitalist practices around the country and has written articles and given presentations on the topic of scheduling for hospital medicine groups.
Dr. Nelson understands the attractions of working seven on, seven off—particularly for young physicians. “Even seven on is not as bad as being an intern; it’s easier than they were used to in their residency,” he says. “But I worry this schedule might increase burnout and resentment of work. It’s asystole/diastole lifestyle and may not be a healthy way to organize your life or your career.”
An Alternative Scheduling Idea
Dr. Nelson has his own unique ideas of how a group’s shift assignments should work to ensure better coverage and keep hospitalists happy. His ideas are not just theories—his own group lives and works by a flexible arrangement.
Their schedule is partly dictated by a desire to keep the physicians happy and healthy. “I believe a constant mix of work and the rest of your life is best,” says Dr. Nelson. “You shouldn’t have to put the rest of your life into the seven days that you’re off.”
So Dr. Nelson’s practice allows considerable flexibility to each physician, but ensures that any given workday is shorter than 12 hours. “I think it’s better not to have a rigidly repeating schedule,” he explains.
Dr. Nelson’s group uses pagers to ensure a hospitalist is always available during coverage hours, but they don’t adhere to a strict schedule. “So many groups work specified shifts, whether it’s 10 or 12 hours, and I think there’s a better idea,” he says. “If everyone has to punch a clock, it interferes with flexibility. I would not tell doctors when to start or stop.”
Of course, as a group, someone has to be available for emergencies all the time, and physicians may need to start daily rounds to write most discharge orders by a certain time. “I have a pager on by 7 a.m., but nothing says I have to be in the hospital by 7 a.m.,” says Dr. Nelson. “It’s often in my interest to start rounding earlier than 7 a.m. so that I can finish earlier or have time for a break later in the day.”
Greater Flexibility = Better Coverage
Another benefit to moving to shorter, more flexible days is ensuring adequate coverage. “Rigidly defined shifts almost never precisely match the day’s workload,” points out Dr. Nelson. Therefore, his practice boosts staffing to cover busy periods. “My recommendation is to intentionally overstaff for the average day’s workload. When it’s busy, everyone can pitch in and work an extra one or two hours.”
If it’s not busy, one or more doctors may leave early. “This is nimble and responsive to the day-to-day workload,” says Dr. Nelson.
To move from a seven on, seven off schedule to this model, Dr. Nelson recommends that every doctor in the practice work 30 to 40 more days annually. A seven on, seven off schedule would have a physician work 182.5 days per year; if you decrease the hours per day and boost the number of working days to 220 a year, your physicians will be working the same number of hours, but in shorter days—even if the practice workload stays the same and each individual doctor’s annual productivity stays the same.
“It’s more realistic to work more days when they’re not so grueling,” says Dr. Nelson. “Plus, you have a built-in capacity to meet a sudden increase in workload. Imagine an eight-man group, where four doctors each work 12-hour shifts. Now imagine that instead of four, you get a fifth doctor to show up every day. [You can get this fifth doctor without adding staff if each doctor works more days annually.] When a day is unpredictably busy, the physicians won’t be absolutely overwhelmed. If it’s not busy, you can send someone home early. You get a lot more flexibility.”
For a hospital medicine group, implementing a flexible schedule such as this generally requires payment for production, which ties individual physicians into the economic health of their group. Compensation matches workload, allowing individual physicians to work to their values—more money or more free time.
“I think it’s better to pay on production,” says Dr. Nelson. “That way each person has the opportunity to choose. If one values money, he can volunteer to stay and work more and make more money. Each works to their own sweet spot, whereas a seven on, seven off schedule with rigidly defined shifts forces everyone to do the same thing.”
Physicians working on a flexible schedule still need to get their work finished each day, but they have more autonomy in how and when they get it done. “Doctors who work fast can go home early; physicians can decide for themselves the right balance for spending time each patient,” says Dr. Nelson. “As long as they understand there are economic consequences … and act with reasonableness. In our group, we get the work done. There’s no official start or stop time. Each of us chooses an individual work style. There are boundaries; the work needs to be done. There are costs as well, but I believe this system is healthy and liberating.” TH
Jane Jerrard regularly writes “Career Development.”
SHM Surveys Revisited
The Benchmarks Committee has had a busy 2006 so far. Many thanks to the 400-plus hospital medicine groups that completed the 2005-06 SHM survey, “The Authoritative Source on the State of Hospital Medicine,” as well as those of you who participated in the follow-up survey to clarify questions around additional revenue or supplements to program income.
We had some behind-the-scenes work on the survey. After the first pass of data analysis, it became clear that there was something amiss with the responses pertaining to the supplemental income questions. Only 47% of programs reported that they received additional income from hospitals or other sources. This seemed incompatible with what we know about current payment rates for fee-for-service work. A quick discussion took place among the committee and we decided to resurvey the group with more precise questions on exactly how finances flow into a program. As you have seen, the additional results bore out our suspicions. With the revised survey tool, 97% of the programs (when re-queried) reported receiving income above and beyond fees from direct patient care.
It was a Herculean task of digesting and formatting the data into usable form. SHM Senior Vice President Joe Miller deserves many thanks for poring through the data and creating something that all of you can use to better your programs.
Now, a few words about the recent annual meeting in Washington, DC: The work of the Benchmarks Committee was highlighted by SHM CEO Larry Wellikson, MD, in a plenary session on the first day of the meeting. An insightful panel discussion followed in which panel members Bob Wachter, MD (representing academic hospital medicine), Mary Jo Gorman, MD (corporate hospital medicine), and John Nelson, MD (community hospital medicine) gave some insightful commentary on the results of the survey and then fielded questions from the audience.
In between sessions at the conference, the committee held its annual face-to-face meeting and discussed plans for the year.
Under the guidance and editorial excellence of committee member Leslie Flores, the Benchmarks Committee continues to make strong progress with the dashboard project. As you may recall, this project will document and describe 10 commonly used dashboard metrics, including sample reports. There are plans for this material to be published as a supplement to The Hospitalist later this year.
The committee discussed the type of surveys conducted by SHM. A recommendation came out of our meeting to change from large-scale, all-encompassing, biannual surveys to smaller annual surveys. The annual survey would alternate its focus every other year between evaluating individuals’ productivity and compensation, and the characteristics of hospital medicine groups. Each survey would also have the flexibility to address specific timely questions that might focus on a specific research or hot topic of the day. The goal is to get our first trial survey out by the end of 2006, which would focus on group characteristics.
Lastly, a big thank you to our outgoing chairperson, Teresa Jones. Her hard work and organizational skills are going to be a tough act to follow.
Dr. Kealey is chair of SHM’s Benchmarks Committee
Advocacy Day Educates Lawmakers about Hospital Medicine
By Eric Siegal, MD
As reported in the SHM Meeting Reporter (see July The Hospitalist, supplement 1), SHM’s first Legislative Advocacy Day was an overwhelming success. More than 70 members from 29 states visited Capitol Hill on May 3 to educate lawmakers and their staffs about hospital medicine and SHM’s proposals to improve the quality of care in our nation’s hospitals.
Advocacy Day participants attended a morning briefing that covered procedural tips on how to have a successful meeting and the health issues currently before Congress—and SHM’s positions—before leaving for previously scheduled appointments on Capitol Hill.
Once there, hospitalists took time to educate legislators and their staff members about the fastest growing medical specialty in the United States, and then turned to SHM’s recommendations for improving the quality, safety, and cost-effectiveness of inpatient medical care.
Among the issues discussed with lawmakers: the need for more funding for the Agency for Healthcare Research and Quality (AHRQ); SHM support for federal initiatives to measure resource use and improve quality, including a CMS demonstration project to assess the contributions of hospital medicine programs to improve patient care and more efficient management of hospital resources; and the importance of gainsharing demonstration projects that focus on inpatient medical services such as those provided by hospital medicine programs.
More than 130 appointments were scheduled with House and Senate offices, many with members of Congress who sit on the key health committees with jurisdiction over Medicare as well as on committees responsible for determining funding levels for the National Institutes of Health, the CDC, and the Agency for Healthcare Research and Quality.
SHM encourages those of you who participated in Advocacy Day to thank the lawmakers and staff with whom you visited (view the sample thank-you letter and instructions online at www.hospitalmedicine.org under “Advocacy & Policy”).
Advocacy Day opened doors to congressional offices; follow-up from SHM members will keep hospital medicine’s issues before lawmakers as they vote on legislation of importance to our specialty. The more SHM members interact with members of Congress and their staff, the louder our voices and the more effective our messages. Advocacy Day is just the beginning of regular contact by hospitalists with their elected representatives in Washington.
A New Way to Get Everything SHM
SHM has launched the SHM Store, a new Internet-based marketplace that will redefine the way SHM educational products and apparel are distributed. The online store will be a convenient option for hectic lifestyles because it will be open 24 hours a day and can be accessed from anywhere there is an Internet connection.
The SHM Store is user-friendly and allows you to easily and quickly purchase the quality products and apparel that you have come to expect from SHM. Apparel and accessories include men’s and women’s wind jackets, golf shirts, scrub tops, baseball caps, and lapel pins—all with the SHM logo.
You’ll also find the most up-to-date educational materials from SHM. The 2005-2006 results of the SHM survey, “The Authoritative Source on the State of Hospital Medicine,” can be ordered in CD and print format. The Practice Management Course CD with binder is also available. This combination package includes all of the materials distributed at an onsite presentation of the course. And, last but not least, get your very own copy or additional copies of The Core Competencies in Hospital Medicine: A Framework For Curriculum Development.
The ordering process is simple. Access the SHM Store at www.hospitalmedicine.org/shmstore or navigate from www.hospitalmedicine.org and click on SHM Store. The store allows you to browse available products and descriptions. When you see something you want, select the quantity you’d like to purchase and add the items to your shopping cart. Once you have completed your shopping trip, click “Check Out.” A confirmation of your transaction will be sent to your e-mail inbox and your products will be shipped to your attention.
It’s that easy. Make sure you go online to browse the new SHM Store. If you have any questions or would like to learn more about the SHM Store, contact SHM at CustomerService@hospitalmedicine. org.
SHM, Health Groups Urge House to Boost Discretionary Funding
SHM joined more than 800 health, education, and labor organizations in writing a May 8 letter to the House leadership. Organized by the Coalition for Health Funding and the Committee on Education Funding, the letter calls on Congress to add $7 billion to the budget in discretionary funding for health, education, and labor programs. It asks lawmakers to ensure that the final allocation for the House and Senate Labor, Health and Human Services, Education Appropriations Subcommittees reflects a $7 billion increase above the President’s request for these critically important programs in FY 2007.
“While our organizations represent a wide array of domestic priorities,” the letter states, “we are united in our effort to advance the bipartisan goal of adding $7 billion in discretionary funding for health, education, labor enforcement, job training, and social services programs as the budget process moves forward. On behalf of our millions of constituents, we strongly urge you to provide at least $7 billion in additional federal support to restore funding levels to FY 2005. This is essential to sustain the well-being and prosperity of our nation.”
Agencies whose funding could be boosted by the additional spending called for in the coalition letter include the Agency for Healthcare Research and Quality, the National Institutes of Health, and the Centers for Disease Control and Prevention.
For full coverage of May 2006 advocacy and policy news, visit www.hospitalmedicine.org. TH
Dr. Siegal is chair of SHM’s Public Policy Committee.
The Benchmarks Committee has had a busy 2006 so far. Many thanks to the 400-plus hospital medicine groups that completed the 2005-06 SHM survey, “The Authoritative Source on the State of Hospital Medicine,” as well as those of you who participated in the follow-up survey to clarify questions around additional revenue or supplements to program income.
We had some behind-the-scenes work on the survey. After the first pass of data analysis, it became clear that there was something amiss with the responses pertaining to the supplemental income questions. Only 47% of programs reported that they received additional income from hospitals or other sources. This seemed incompatible with what we know about current payment rates for fee-for-service work. A quick discussion took place among the committee and we decided to resurvey the group with more precise questions on exactly how finances flow into a program. As you have seen, the additional results bore out our suspicions. With the revised survey tool, 97% of the programs (when re-queried) reported receiving income above and beyond fees from direct patient care.
It was a Herculean task of digesting and formatting the data into usable form. SHM Senior Vice President Joe Miller deserves many thanks for poring through the data and creating something that all of you can use to better your programs.
Now, a few words about the recent annual meeting in Washington, DC: The work of the Benchmarks Committee was highlighted by SHM CEO Larry Wellikson, MD, in a plenary session on the first day of the meeting. An insightful panel discussion followed in which panel members Bob Wachter, MD (representing academic hospital medicine), Mary Jo Gorman, MD (corporate hospital medicine), and John Nelson, MD (community hospital medicine) gave some insightful commentary on the results of the survey and then fielded questions from the audience.
In between sessions at the conference, the committee held its annual face-to-face meeting and discussed plans for the year.
Under the guidance and editorial excellence of committee member Leslie Flores, the Benchmarks Committee continues to make strong progress with the dashboard project. As you may recall, this project will document and describe 10 commonly used dashboard metrics, including sample reports. There are plans for this material to be published as a supplement to The Hospitalist later this year.
The committee discussed the type of surveys conducted by SHM. A recommendation came out of our meeting to change from large-scale, all-encompassing, biannual surveys to smaller annual surveys. The annual survey would alternate its focus every other year between evaluating individuals’ productivity and compensation, and the characteristics of hospital medicine groups. Each survey would also have the flexibility to address specific timely questions that might focus on a specific research or hot topic of the day. The goal is to get our first trial survey out by the end of 2006, which would focus on group characteristics.
Lastly, a big thank you to our outgoing chairperson, Teresa Jones. Her hard work and organizational skills are going to be a tough act to follow.
Dr. Kealey is chair of SHM’s Benchmarks Committee
Advocacy Day Educates Lawmakers about Hospital Medicine
By Eric Siegal, MD
As reported in the SHM Meeting Reporter (see July The Hospitalist, supplement 1), SHM’s first Legislative Advocacy Day was an overwhelming success. More than 70 members from 29 states visited Capitol Hill on May 3 to educate lawmakers and their staffs about hospital medicine and SHM’s proposals to improve the quality of care in our nation’s hospitals.
Advocacy Day participants attended a morning briefing that covered procedural tips on how to have a successful meeting and the health issues currently before Congress—and SHM’s positions—before leaving for previously scheduled appointments on Capitol Hill.
Once there, hospitalists took time to educate legislators and their staff members about the fastest growing medical specialty in the United States, and then turned to SHM’s recommendations for improving the quality, safety, and cost-effectiveness of inpatient medical care.
Among the issues discussed with lawmakers: the need for more funding for the Agency for Healthcare Research and Quality (AHRQ); SHM support for federal initiatives to measure resource use and improve quality, including a CMS demonstration project to assess the contributions of hospital medicine programs to improve patient care and more efficient management of hospital resources; and the importance of gainsharing demonstration projects that focus on inpatient medical services such as those provided by hospital medicine programs.
More than 130 appointments were scheduled with House and Senate offices, many with members of Congress who sit on the key health committees with jurisdiction over Medicare as well as on committees responsible for determining funding levels for the National Institutes of Health, the CDC, and the Agency for Healthcare Research and Quality.
SHM encourages those of you who participated in Advocacy Day to thank the lawmakers and staff with whom you visited (view the sample thank-you letter and instructions online at www.hospitalmedicine.org under “Advocacy & Policy”).
Advocacy Day opened doors to congressional offices; follow-up from SHM members will keep hospital medicine’s issues before lawmakers as they vote on legislation of importance to our specialty. The more SHM members interact with members of Congress and their staff, the louder our voices and the more effective our messages. Advocacy Day is just the beginning of regular contact by hospitalists with their elected representatives in Washington.
A New Way to Get Everything SHM
SHM has launched the SHM Store, a new Internet-based marketplace that will redefine the way SHM educational products and apparel are distributed. The online store will be a convenient option for hectic lifestyles because it will be open 24 hours a day and can be accessed from anywhere there is an Internet connection.
The SHM Store is user-friendly and allows you to easily and quickly purchase the quality products and apparel that you have come to expect from SHM. Apparel and accessories include men’s and women’s wind jackets, golf shirts, scrub tops, baseball caps, and lapel pins—all with the SHM logo.
You’ll also find the most up-to-date educational materials from SHM. The 2005-2006 results of the SHM survey, “The Authoritative Source on the State of Hospital Medicine,” can be ordered in CD and print format. The Practice Management Course CD with binder is also available. This combination package includes all of the materials distributed at an onsite presentation of the course. And, last but not least, get your very own copy or additional copies of The Core Competencies in Hospital Medicine: A Framework For Curriculum Development.
The ordering process is simple. Access the SHM Store at www.hospitalmedicine.org/shmstore or navigate from www.hospitalmedicine.org and click on SHM Store. The store allows you to browse available products and descriptions. When you see something you want, select the quantity you’d like to purchase and add the items to your shopping cart. Once you have completed your shopping trip, click “Check Out.” A confirmation of your transaction will be sent to your e-mail inbox and your products will be shipped to your attention.
It’s that easy. Make sure you go online to browse the new SHM Store. If you have any questions or would like to learn more about the SHM Store, contact SHM at CustomerService@hospitalmedicine. org.
SHM, Health Groups Urge House to Boost Discretionary Funding
SHM joined more than 800 health, education, and labor organizations in writing a May 8 letter to the House leadership. Organized by the Coalition for Health Funding and the Committee on Education Funding, the letter calls on Congress to add $7 billion to the budget in discretionary funding for health, education, and labor programs. It asks lawmakers to ensure that the final allocation for the House and Senate Labor, Health and Human Services, Education Appropriations Subcommittees reflects a $7 billion increase above the President’s request for these critically important programs in FY 2007.
“While our organizations represent a wide array of domestic priorities,” the letter states, “we are united in our effort to advance the bipartisan goal of adding $7 billion in discretionary funding for health, education, labor enforcement, job training, and social services programs as the budget process moves forward. On behalf of our millions of constituents, we strongly urge you to provide at least $7 billion in additional federal support to restore funding levels to FY 2005. This is essential to sustain the well-being and prosperity of our nation.”
Agencies whose funding could be boosted by the additional spending called for in the coalition letter include the Agency for Healthcare Research and Quality, the National Institutes of Health, and the Centers for Disease Control and Prevention.
For full coverage of May 2006 advocacy and policy news, visit www.hospitalmedicine.org. TH
Dr. Siegal is chair of SHM’s Public Policy Committee.
The Benchmarks Committee has had a busy 2006 so far. Many thanks to the 400-plus hospital medicine groups that completed the 2005-06 SHM survey, “The Authoritative Source on the State of Hospital Medicine,” as well as those of you who participated in the follow-up survey to clarify questions around additional revenue or supplements to program income.
We had some behind-the-scenes work on the survey. After the first pass of data analysis, it became clear that there was something amiss with the responses pertaining to the supplemental income questions. Only 47% of programs reported that they received additional income from hospitals or other sources. This seemed incompatible with what we know about current payment rates for fee-for-service work. A quick discussion took place among the committee and we decided to resurvey the group with more precise questions on exactly how finances flow into a program. As you have seen, the additional results bore out our suspicions. With the revised survey tool, 97% of the programs (when re-queried) reported receiving income above and beyond fees from direct patient care.
It was a Herculean task of digesting and formatting the data into usable form. SHM Senior Vice President Joe Miller deserves many thanks for poring through the data and creating something that all of you can use to better your programs.
Now, a few words about the recent annual meeting in Washington, DC: The work of the Benchmarks Committee was highlighted by SHM CEO Larry Wellikson, MD, in a plenary session on the first day of the meeting. An insightful panel discussion followed in which panel members Bob Wachter, MD (representing academic hospital medicine), Mary Jo Gorman, MD (corporate hospital medicine), and John Nelson, MD (community hospital medicine) gave some insightful commentary on the results of the survey and then fielded questions from the audience.
In between sessions at the conference, the committee held its annual face-to-face meeting and discussed plans for the year.
Under the guidance and editorial excellence of committee member Leslie Flores, the Benchmarks Committee continues to make strong progress with the dashboard project. As you may recall, this project will document and describe 10 commonly used dashboard metrics, including sample reports. There are plans for this material to be published as a supplement to The Hospitalist later this year.
The committee discussed the type of surveys conducted by SHM. A recommendation came out of our meeting to change from large-scale, all-encompassing, biannual surveys to smaller annual surveys. The annual survey would alternate its focus every other year between evaluating individuals’ productivity and compensation, and the characteristics of hospital medicine groups. Each survey would also have the flexibility to address specific timely questions that might focus on a specific research or hot topic of the day. The goal is to get our first trial survey out by the end of 2006, which would focus on group characteristics.
Lastly, a big thank you to our outgoing chairperson, Teresa Jones. Her hard work and organizational skills are going to be a tough act to follow.
Dr. Kealey is chair of SHM’s Benchmarks Committee
Advocacy Day Educates Lawmakers about Hospital Medicine
By Eric Siegal, MD
As reported in the SHM Meeting Reporter (see July The Hospitalist, supplement 1), SHM’s first Legislative Advocacy Day was an overwhelming success. More than 70 members from 29 states visited Capitol Hill on May 3 to educate lawmakers and their staffs about hospital medicine and SHM’s proposals to improve the quality of care in our nation’s hospitals.
Advocacy Day participants attended a morning briefing that covered procedural tips on how to have a successful meeting and the health issues currently before Congress—and SHM’s positions—before leaving for previously scheduled appointments on Capitol Hill.
Once there, hospitalists took time to educate legislators and their staff members about the fastest growing medical specialty in the United States, and then turned to SHM’s recommendations for improving the quality, safety, and cost-effectiveness of inpatient medical care.
Among the issues discussed with lawmakers: the need for more funding for the Agency for Healthcare Research and Quality (AHRQ); SHM support for federal initiatives to measure resource use and improve quality, including a CMS demonstration project to assess the contributions of hospital medicine programs to improve patient care and more efficient management of hospital resources; and the importance of gainsharing demonstration projects that focus on inpatient medical services such as those provided by hospital medicine programs.
More than 130 appointments were scheduled with House and Senate offices, many with members of Congress who sit on the key health committees with jurisdiction over Medicare as well as on committees responsible for determining funding levels for the National Institutes of Health, the CDC, and the Agency for Healthcare Research and Quality.
SHM encourages those of you who participated in Advocacy Day to thank the lawmakers and staff with whom you visited (view the sample thank-you letter and instructions online at www.hospitalmedicine.org under “Advocacy & Policy”).
Advocacy Day opened doors to congressional offices; follow-up from SHM members will keep hospital medicine’s issues before lawmakers as they vote on legislation of importance to our specialty. The more SHM members interact with members of Congress and their staff, the louder our voices and the more effective our messages. Advocacy Day is just the beginning of regular contact by hospitalists with their elected representatives in Washington.
A New Way to Get Everything SHM
SHM has launched the SHM Store, a new Internet-based marketplace that will redefine the way SHM educational products and apparel are distributed. The online store will be a convenient option for hectic lifestyles because it will be open 24 hours a day and can be accessed from anywhere there is an Internet connection.
The SHM Store is user-friendly and allows you to easily and quickly purchase the quality products and apparel that you have come to expect from SHM. Apparel and accessories include men’s and women’s wind jackets, golf shirts, scrub tops, baseball caps, and lapel pins—all with the SHM logo.
You’ll also find the most up-to-date educational materials from SHM. The 2005-2006 results of the SHM survey, “The Authoritative Source on the State of Hospital Medicine,” can be ordered in CD and print format. The Practice Management Course CD with binder is also available. This combination package includes all of the materials distributed at an onsite presentation of the course. And, last but not least, get your very own copy or additional copies of The Core Competencies in Hospital Medicine: A Framework For Curriculum Development.
The ordering process is simple. Access the SHM Store at www.hospitalmedicine.org/shmstore or navigate from www.hospitalmedicine.org and click on SHM Store. The store allows you to browse available products and descriptions. When you see something you want, select the quantity you’d like to purchase and add the items to your shopping cart. Once you have completed your shopping trip, click “Check Out.” A confirmation of your transaction will be sent to your e-mail inbox and your products will be shipped to your attention.
It’s that easy. Make sure you go online to browse the new SHM Store. If you have any questions or would like to learn more about the SHM Store, contact SHM at CustomerService@hospitalmedicine. org.
SHM, Health Groups Urge House to Boost Discretionary Funding
SHM joined more than 800 health, education, and labor organizations in writing a May 8 letter to the House leadership. Organized by the Coalition for Health Funding and the Committee on Education Funding, the letter calls on Congress to add $7 billion to the budget in discretionary funding for health, education, and labor programs. It asks lawmakers to ensure that the final allocation for the House and Senate Labor, Health and Human Services, Education Appropriations Subcommittees reflects a $7 billion increase above the President’s request for these critically important programs in FY 2007.
“While our organizations represent a wide array of domestic priorities,” the letter states, “we are united in our effort to advance the bipartisan goal of adding $7 billion in discretionary funding for health, education, labor enforcement, job training, and social services programs as the budget process moves forward. On behalf of our millions of constituents, we strongly urge you to provide at least $7 billion in additional federal support to restore funding levels to FY 2005. This is essential to sustain the well-being and prosperity of our nation.”
Agencies whose funding could be boosted by the additional spending called for in the coalition letter include the Agency for Healthcare Research and Quality, the National Institutes of Health, and the Centers for Disease Control and Prevention.
For full coverage of May 2006 advocacy and policy news, visit www.hospitalmedicine.org. TH
Dr. Siegal is chair of SHM’s Public Policy Committee.
Virus Alerts
CDC Urges Awareness of Measles in Americans Returning from Germany
By Alfred Valles, resident, internal medicine, Mayo Clinic College of Medicine
The Centers for Disease Control and Prevention (CDC) has issued an alert urging American travelers to remain aware of the possibility of measles exposure. Many Americans have traveled to and from Germany for the World Cup soccer championship games. Three of the twelve hosting cities—Cologne, Dortmund, and Gelsenkirchen—are of particular concern, given the recent measles outbreaks that have been reported in those cities and their surrounding areas.
Since January 1 of this year, some 1,200 cases have been identified in or near these cities. American travelers were undoubtedly among the large crowds of people gathered to pay homage to their favorite sport, and many others will visit Germany on vacation or business, making transmission of this respiratory droplet-born pathogen a very real threat.
The CDC recommends the following precautions:
- Travelers who plan to go to Germany should check their immunization records and visit their doctors if they are not immune to measles or are not sure they are.
- People returning from Germany, especially those who went to see the World Cup, should see a healthcare provider if they develop the symptoms of measles, including a fever, a raised rash that begins on the face and spreads to the arms and legs, a cough, red eyes, or a runny nose.
- People with these symptoms should limit their contact with others.
- Clinicians seeing patients with these symptoms should inquire about travel history and immunization status.
This warning is not to be taken lightly. Approximately two of every 1,000 patients infected with measles will die of the disease. Complications such as encephalitis are of particular concern for those who are malnourished or immunosuppressed.
Remember, live virus measles vaccine given within 72 hours of exposure may prevent the disease, while immune globulin given up to six days after exposure may prevent complications of measles in those who are at risk, including pregnant women, people with weak immune systems, and children.
The World cup can be dangerous, even for non-players. For more information about the measles outbreak and travel precautions, visit www.cdc.gov.
Lymphocytic Choriomeningitis Virus: Facts and Prevention
By the Special Pathogens Branch, CDC
In May 2005, the CDC investigated a cluster of lymphocytic choriomeningitis virus (LCMV) illnesses in four solid organ transplant recipients from a common donor, three of whom died. The source of the LCMV was traced to a hamster that had recently been acquired by a member of the donor’s household. It was subsequently determined that several LCMV-infected pet rodents had originated from a single distributor, who may have distributed other infected rodents to pet stores in the northeastern and midwestern United States.1 However, the risk of contracting LCMV from rodent exposure is not limited only to this outbreak, nor is the danger confined only to patients undergoing organ transplant.
Clinicians need to be familiar with LCMV because of its potential to cause meningitis, its teratogenicity, and the risk that it may bring about serious disease in immunocompromised individuals.
LCMV is normally carried by wild house mice, but can be transmitted to laboratory and pet rodents at breeding facilities, in pet stores, and in homes. Humans become infected in one of the following ways:
- Through direct contact with the secretions or excretions of infected rodents;
- By inhalation of dust or droplets containing LCMV from rodents;
- As a result of transplacental spread from an infected pregnant woman to her fetus; and
- By receipt of an organ transplant from an infected donor.2
Among those tested, about 5% have shown serologic evidence of previous infection with LCMV.3,4 In healthy adults, LCMV is typically a nonspecific viral syndrome sometimes followed by aseptic meningitis or other neurologic signs. Patients with weakened immune systems can suffer severe, possibly fatal systemic illness.2,5 Maternal infection with LCMV during pregnancy can result in spontaneous abortion or early neonatal death, as well as in defects similar to those of other congenital infections such as toxoplasmosis and cytomegalovirus (“TORCH” infections).6-10 The proportion of developmental defects caused by LCMV is not known.
Clinicians should consider LCMV in the differential diagnosis of patients with aseptic meningitis; in cases of fetal demise or congenital defects, including congenital hydrocephalus, chorioretinitis, blindness, or mental retardation; or in recent transplant recipients who present with signs of post-transplant infection. A detailed rodent exposure history should be taken. Contact your state health department or Special Pathogens Branch, CDC (404-639-1510), for information about testing for LCMV.
Currently, there is no specific treatment for LCMV infection other than supportive care. Ribavirin inhibits LCMV multiplication in laboratory experiments but has not been tested in clinical trials.
Clinicians should counsel their patients about the risks of contracting LCMV from laboratory, pet, and wild rodents. Wild mice in the home should be controlled and removed promptly. Immunocompromised individuals and women who are pregnant or planning to become pregnant should avoid any contact with wild or pet rodents, their excretions, and their nesting materials. While a woman is pregnant, pet rodents should be housed outside the home or in a separate part of the home where other individuals can care for the pets and clean their cages. Counseling a woman already exposed to rodents during pregnancy can be challenging; for assistance, contact your state health department.
Further information about LCMV infection and its prevention, including management and prevention of rodent infestation in the home, is available from Special Pathogens Branch, CDC, at www.cdc.gov/ncidod/dvrd/spb/mnpages/dispages/lcmv.htm. For more information about diseases commonly carried by rodents, please visit www.cdc.gov/rodents. TH
References
- Centers for Disease Control and Prevention. Update: interim guidance for minimizing risk for human lymphocytic choriomeningitis virus infection associated with pet rodents. MMWR. Aug 19, 2005;54(32):799-801.
- Fischer SA, Graham MB, Kuehnert MJ, et al. Transmission of lymphocytic choriomeningitis virus by organ transplantation. N Engl J Med. 2006;354(21):2235-2249.
- Childs JE, Glass GE, Ksiazek TG, et al. Human-rodent contact and infection with lymphocytic choriomeningitis and Seoul viruses in an inner-city population. Am J Trop Med Hyg. 1991 Feb;44(2):117–121.
- Park JY, Peters CJ, Rollin PE, et al. Age distribution of lymphocytic choriomeningitis virus serum antibody in Birmingham, Alabama: evidence of a decreased risk of infection. Am J Trop Med Hyg. 1997 Jul;57(1):37–41.
- Horton J, Hotchin JE, Olson KB, et al. The effects of MP virus infection in lymphoma. Cancer Res. 1971 Aug;31(8):1066–1068.
- Barton LL, Mets MB. Congenital lymphocytic choriomeningitis virus infection: decade of rediscovery. Clin Infect Dis. 2001 Aug 1;33(3):370–374.
- Barton LL, Mets MB, Beauchamp CL. Lymphocytic choriomeningitis virus: emerging fetal teratogen. Am J Obstet Gynecol. 2002 Dec ;187(6):1715–1716.
- Wright R, Johnson D, Neumann M, et al. Congenital lymphocytic choriomeningitis virus syndrome: a disease that mimics congenital toxoplasmosis or cytomegalovirus infection. Pediatrics. 1997 Jul;100(1):E9.
- Ford-Jones EL, Ryan G . Implications for the fetus of maternal infections in pregnancy. In: Cohen J, Powderly WG, eds. Infectious Diseases, 2nd ed. New York, NY: Mosby; 2004: 709–723.
- Greenhow TL, Weintrub PS. Your diagnosis, please. Neonate with hydrocephalus. Pediatr Infect Dis J. 2003 Dec;22(12):1099, 1111–1112.
CDC Urges Awareness of Measles in Americans Returning from Germany
By Alfred Valles, resident, internal medicine, Mayo Clinic College of Medicine
The Centers for Disease Control and Prevention (CDC) has issued an alert urging American travelers to remain aware of the possibility of measles exposure. Many Americans have traveled to and from Germany for the World Cup soccer championship games. Three of the twelve hosting cities—Cologne, Dortmund, and Gelsenkirchen—are of particular concern, given the recent measles outbreaks that have been reported in those cities and their surrounding areas.
Since January 1 of this year, some 1,200 cases have been identified in or near these cities. American travelers were undoubtedly among the large crowds of people gathered to pay homage to their favorite sport, and many others will visit Germany on vacation or business, making transmission of this respiratory droplet-born pathogen a very real threat.
The CDC recommends the following precautions:
- Travelers who plan to go to Germany should check their immunization records and visit their doctors if they are not immune to measles or are not sure they are.
- People returning from Germany, especially those who went to see the World Cup, should see a healthcare provider if they develop the symptoms of measles, including a fever, a raised rash that begins on the face and spreads to the arms and legs, a cough, red eyes, or a runny nose.
- People with these symptoms should limit their contact with others.
- Clinicians seeing patients with these symptoms should inquire about travel history and immunization status.
This warning is not to be taken lightly. Approximately two of every 1,000 patients infected with measles will die of the disease. Complications such as encephalitis are of particular concern for those who are malnourished or immunosuppressed.
Remember, live virus measles vaccine given within 72 hours of exposure may prevent the disease, while immune globulin given up to six days after exposure may prevent complications of measles in those who are at risk, including pregnant women, people with weak immune systems, and children.
The World cup can be dangerous, even for non-players. For more information about the measles outbreak and travel precautions, visit www.cdc.gov.
Lymphocytic Choriomeningitis Virus: Facts and Prevention
By the Special Pathogens Branch, CDC
In May 2005, the CDC investigated a cluster of lymphocytic choriomeningitis virus (LCMV) illnesses in four solid organ transplant recipients from a common donor, three of whom died. The source of the LCMV was traced to a hamster that had recently been acquired by a member of the donor’s household. It was subsequently determined that several LCMV-infected pet rodents had originated from a single distributor, who may have distributed other infected rodents to pet stores in the northeastern and midwestern United States.1 However, the risk of contracting LCMV from rodent exposure is not limited only to this outbreak, nor is the danger confined only to patients undergoing organ transplant.
Clinicians need to be familiar with LCMV because of its potential to cause meningitis, its teratogenicity, and the risk that it may bring about serious disease in immunocompromised individuals.
LCMV is normally carried by wild house mice, but can be transmitted to laboratory and pet rodents at breeding facilities, in pet stores, and in homes. Humans become infected in one of the following ways:
- Through direct contact with the secretions or excretions of infected rodents;
- By inhalation of dust or droplets containing LCMV from rodents;
- As a result of transplacental spread from an infected pregnant woman to her fetus; and
- By receipt of an organ transplant from an infected donor.2
Among those tested, about 5% have shown serologic evidence of previous infection with LCMV.3,4 In healthy adults, LCMV is typically a nonspecific viral syndrome sometimes followed by aseptic meningitis or other neurologic signs. Patients with weakened immune systems can suffer severe, possibly fatal systemic illness.2,5 Maternal infection with LCMV during pregnancy can result in spontaneous abortion or early neonatal death, as well as in defects similar to those of other congenital infections such as toxoplasmosis and cytomegalovirus (“TORCH” infections).6-10 The proportion of developmental defects caused by LCMV is not known.
Clinicians should consider LCMV in the differential diagnosis of patients with aseptic meningitis; in cases of fetal demise or congenital defects, including congenital hydrocephalus, chorioretinitis, blindness, or mental retardation; or in recent transplant recipients who present with signs of post-transplant infection. A detailed rodent exposure history should be taken. Contact your state health department or Special Pathogens Branch, CDC (404-639-1510), for information about testing for LCMV.
Currently, there is no specific treatment for LCMV infection other than supportive care. Ribavirin inhibits LCMV multiplication in laboratory experiments but has not been tested in clinical trials.
Clinicians should counsel their patients about the risks of contracting LCMV from laboratory, pet, and wild rodents. Wild mice in the home should be controlled and removed promptly. Immunocompromised individuals and women who are pregnant or planning to become pregnant should avoid any contact with wild or pet rodents, their excretions, and their nesting materials. While a woman is pregnant, pet rodents should be housed outside the home or in a separate part of the home where other individuals can care for the pets and clean their cages. Counseling a woman already exposed to rodents during pregnancy can be challenging; for assistance, contact your state health department.
Further information about LCMV infection and its prevention, including management and prevention of rodent infestation in the home, is available from Special Pathogens Branch, CDC, at www.cdc.gov/ncidod/dvrd/spb/mnpages/dispages/lcmv.htm. For more information about diseases commonly carried by rodents, please visit www.cdc.gov/rodents. TH
References
- Centers for Disease Control and Prevention. Update: interim guidance for minimizing risk for human lymphocytic choriomeningitis virus infection associated with pet rodents. MMWR. Aug 19, 2005;54(32):799-801.
- Fischer SA, Graham MB, Kuehnert MJ, et al. Transmission of lymphocytic choriomeningitis virus by organ transplantation. N Engl J Med. 2006;354(21):2235-2249.
- Childs JE, Glass GE, Ksiazek TG, et al. Human-rodent contact and infection with lymphocytic choriomeningitis and Seoul viruses in an inner-city population. Am J Trop Med Hyg. 1991 Feb;44(2):117–121.
- Park JY, Peters CJ, Rollin PE, et al. Age distribution of lymphocytic choriomeningitis virus serum antibody in Birmingham, Alabama: evidence of a decreased risk of infection. Am J Trop Med Hyg. 1997 Jul;57(1):37–41.
- Horton J, Hotchin JE, Olson KB, et al. The effects of MP virus infection in lymphoma. Cancer Res. 1971 Aug;31(8):1066–1068.
- Barton LL, Mets MB. Congenital lymphocytic choriomeningitis virus infection: decade of rediscovery. Clin Infect Dis. 2001 Aug 1;33(3):370–374.
- Barton LL, Mets MB, Beauchamp CL. Lymphocytic choriomeningitis virus: emerging fetal teratogen. Am J Obstet Gynecol. 2002 Dec ;187(6):1715–1716.
- Wright R, Johnson D, Neumann M, et al. Congenital lymphocytic choriomeningitis virus syndrome: a disease that mimics congenital toxoplasmosis or cytomegalovirus infection. Pediatrics. 1997 Jul;100(1):E9.
- Ford-Jones EL, Ryan G . Implications for the fetus of maternal infections in pregnancy. In: Cohen J, Powderly WG, eds. Infectious Diseases, 2nd ed. New York, NY: Mosby; 2004: 709–723.
- Greenhow TL, Weintrub PS. Your diagnosis, please. Neonate with hydrocephalus. Pediatr Infect Dis J. 2003 Dec;22(12):1099, 1111–1112.
CDC Urges Awareness of Measles in Americans Returning from Germany
By Alfred Valles, resident, internal medicine, Mayo Clinic College of Medicine
The Centers for Disease Control and Prevention (CDC) has issued an alert urging American travelers to remain aware of the possibility of measles exposure. Many Americans have traveled to and from Germany for the World Cup soccer championship games. Three of the twelve hosting cities—Cologne, Dortmund, and Gelsenkirchen—are of particular concern, given the recent measles outbreaks that have been reported in those cities and their surrounding areas.
Since January 1 of this year, some 1,200 cases have been identified in or near these cities. American travelers were undoubtedly among the large crowds of people gathered to pay homage to their favorite sport, and many others will visit Germany on vacation or business, making transmission of this respiratory droplet-born pathogen a very real threat.
The CDC recommends the following precautions:
- Travelers who plan to go to Germany should check their immunization records and visit their doctors if they are not immune to measles or are not sure they are.
- People returning from Germany, especially those who went to see the World Cup, should see a healthcare provider if they develop the symptoms of measles, including a fever, a raised rash that begins on the face and spreads to the arms and legs, a cough, red eyes, or a runny nose.
- People with these symptoms should limit their contact with others.
- Clinicians seeing patients with these symptoms should inquire about travel history and immunization status.
This warning is not to be taken lightly. Approximately two of every 1,000 patients infected with measles will die of the disease. Complications such as encephalitis are of particular concern for those who are malnourished or immunosuppressed.
Remember, live virus measles vaccine given within 72 hours of exposure may prevent the disease, while immune globulin given up to six days after exposure may prevent complications of measles in those who are at risk, including pregnant women, people with weak immune systems, and children.
The World cup can be dangerous, even for non-players. For more information about the measles outbreak and travel precautions, visit www.cdc.gov.
Lymphocytic Choriomeningitis Virus: Facts and Prevention
By the Special Pathogens Branch, CDC
In May 2005, the CDC investigated a cluster of lymphocytic choriomeningitis virus (LCMV) illnesses in four solid organ transplant recipients from a common donor, three of whom died. The source of the LCMV was traced to a hamster that had recently been acquired by a member of the donor’s household. It was subsequently determined that several LCMV-infected pet rodents had originated from a single distributor, who may have distributed other infected rodents to pet stores in the northeastern and midwestern United States.1 However, the risk of contracting LCMV from rodent exposure is not limited only to this outbreak, nor is the danger confined only to patients undergoing organ transplant.
Clinicians need to be familiar with LCMV because of its potential to cause meningitis, its teratogenicity, and the risk that it may bring about serious disease in immunocompromised individuals.
LCMV is normally carried by wild house mice, but can be transmitted to laboratory and pet rodents at breeding facilities, in pet stores, and in homes. Humans become infected in one of the following ways:
- Through direct contact with the secretions or excretions of infected rodents;
- By inhalation of dust or droplets containing LCMV from rodents;
- As a result of transplacental spread from an infected pregnant woman to her fetus; and
- By receipt of an organ transplant from an infected donor.2
Among those tested, about 5% have shown serologic evidence of previous infection with LCMV.3,4 In healthy adults, LCMV is typically a nonspecific viral syndrome sometimes followed by aseptic meningitis or other neurologic signs. Patients with weakened immune systems can suffer severe, possibly fatal systemic illness.2,5 Maternal infection with LCMV during pregnancy can result in spontaneous abortion or early neonatal death, as well as in defects similar to those of other congenital infections such as toxoplasmosis and cytomegalovirus (“TORCH” infections).6-10 The proportion of developmental defects caused by LCMV is not known.
Clinicians should consider LCMV in the differential diagnosis of patients with aseptic meningitis; in cases of fetal demise or congenital defects, including congenital hydrocephalus, chorioretinitis, blindness, or mental retardation; or in recent transplant recipients who present with signs of post-transplant infection. A detailed rodent exposure history should be taken. Contact your state health department or Special Pathogens Branch, CDC (404-639-1510), for information about testing for LCMV.
Currently, there is no specific treatment for LCMV infection other than supportive care. Ribavirin inhibits LCMV multiplication in laboratory experiments but has not been tested in clinical trials.
Clinicians should counsel their patients about the risks of contracting LCMV from laboratory, pet, and wild rodents. Wild mice in the home should be controlled and removed promptly. Immunocompromised individuals and women who are pregnant or planning to become pregnant should avoid any contact with wild or pet rodents, their excretions, and their nesting materials. While a woman is pregnant, pet rodents should be housed outside the home or in a separate part of the home where other individuals can care for the pets and clean their cages. Counseling a woman already exposed to rodents during pregnancy can be challenging; for assistance, contact your state health department.
Further information about LCMV infection and its prevention, including management and prevention of rodent infestation in the home, is available from Special Pathogens Branch, CDC, at www.cdc.gov/ncidod/dvrd/spb/mnpages/dispages/lcmv.htm. For more information about diseases commonly carried by rodents, please visit www.cdc.gov/rodents. TH
References
- Centers for Disease Control and Prevention. Update: interim guidance for minimizing risk for human lymphocytic choriomeningitis virus infection associated with pet rodents. MMWR. Aug 19, 2005;54(32):799-801.
- Fischer SA, Graham MB, Kuehnert MJ, et al. Transmission of lymphocytic choriomeningitis virus by organ transplantation. N Engl J Med. 2006;354(21):2235-2249.
- Childs JE, Glass GE, Ksiazek TG, et al. Human-rodent contact and infection with lymphocytic choriomeningitis and Seoul viruses in an inner-city population. Am J Trop Med Hyg. 1991 Feb;44(2):117–121.
- Park JY, Peters CJ, Rollin PE, et al. Age distribution of lymphocytic choriomeningitis virus serum antibody in Birmingham, Alabama: evidence of a decreased risk of infection. Am J Trop Med Hyg. 1997 Jul;57(1):37–41.
- Horton J, Hotchin JE, Olson KB, et al. The effects of MP virus infection in lymphoma. Cancer Res. 1971 Aug;31(8):1066–1068.
- Barton LL, Mets MB. Congenital lymphocytic choriomeningitis virus infection: decade of rediscovery. Clin Infect Dis. 2001 Aug 1;33(3):370–374.
- Barton LL, Mets MB, Beauchamp CL. Lymphocytic choriomeningitis virus: emerging fetal teratogen. Am J Obstet Gynecol. 2002 Dec ;187(6):1715–1716.
- Wright R, Johnson D, Neumann M, et al. Congenital lymphocytic choriomeningitis virus syndrome: a disease that mimics congenital toxoplasmosis or cytomegalovirus infection. Pediatrics. 1997 Jul;100(1):E9.
- Ford-Jones EL, Ryan G . Implications for the fetus of maternal infections in pregnancy. In: Cohen J, Powderly WG, eds. Infectious Diseases, 2nd ed. New York, NY: Mosby; 2004: 709–723.
- Greenhow TL, Weintrub PS. Your diagnosis, please. Neonate with hydrocephalus. Pediatr Infect Dis J. 2003 Dec;22(12):1099, 1111–1112.
The Reality of Today
SHM has been working with JCAHO on its Hospital of the Future Roundtable. JCAHO has brought together an interesting international group made up of leaders representing hospital administrators, architects, social behaviorists, nurses, pharmacists, physicians, economists, government, technology experts, and others with a stake in the evolution of the hospital as an institution.
At our recent meeting in Chicago we discussed some aspects of the economics of hospitals that I thought would be worth sharing with the hospital medicine audience.
Right now many hospitals are actually in a good economic position. For the past 12 months hospitals have had an operating margin of 3.6% with a total margin of more than 6%. A number of factors have favored the hospital’s bottom line in recent years. There has been hospital consolidation with the closing of some hospitals. Managed care’s tightening of revenue forced hospitals in the 1990s to examine their operations and many hospitals became more efficient. This reduced hospital size and forced changes in staffing and other parts of the expense equation. Now that managed care has loosened its grip on the fees paid to hospitals, revenues have risen faster than costs, especially on the commercial side. There has actually been an increase of 8.6% in revenue to hospitals in the past year.
The dark side of this equation is that while many hospitals have benefited, some hospitals continue to run in the red because of geography (inner city, rural), and patient mix. This gap between haves and have-nots is increasing. The specter of more Americans without insurance coverage (or undercovered) also raises the burden of undercompensated care on hospitals in general.
Competition and Transparency
Recently, some people have been talking about trying to make true competition work in healthcare. One step in creating a marketplace is to have price and cost transparency. The thought is if the users of healthcare (patients) and the buyers of healthcare (businesses and government) could see each hospital’s charges, then people would make their decisions armed with information like they have when buying a car or a house.
Unfortunately that is not how the healthcare marketplace (if you can call it that) operates. The reality is that the government (as Medicare and Medicaid) sets price levels fairly arbitrarily and very often below the actual cost of delivering the services. You also have to throw into the mix all the care hospitals provide to patients without any insurance coverage or means to pay for their care. This leads to cost shifting to the tune that hospitals now expect private insurers to pay 122% of costs just to balance the CMS shortfall. Price transparency makes it more difficult to cost shift because a hospital would set its “price,” but would that be the price for Medicare, for Medicaid, for the “Blues” (Blue Cross/Blue Shield) as well?
Now that employers are cost shifting to their employees with larger co-pays and basically offering a fixed benefit and asking the workers to pick up more of the health tab, it is even harder for hospitals to cost shift to the private commercial side (i.e., people under 65 with insurance).
Hospital Disaggregation
The good old Marcus Welby, MD-era hospital as the total community resource that takes the profitable and the needy is eroding. Specialty hospitals have sprung up to siphon some of the best revenue sources and help physicians get on the facility side of the equation. Many of the most lucrative outpatient modalities (e.g., surgicenters, imaging) have moved off campus and out of the hospital’s domain. And there sits the full-service hospital left with many of the responsibilities and a disproportionate share of expense, but with less of the high-ticket revenue.
Populations Demographics
Our population is getting older, but aging baby boomers will account for only about a 10% increase in healthcare spending. The bigger problem is that as the population ages a greater proportion of healthcare spending shifts from private to public (i.e., from the Blues to Medicare). There is already a problem in cost shifting as I mentioned above with Medicare and Medicaid paying <95% of healthcare costs. You can’t make up those losses with volume. It’s predicted that more than 65% of hospital funding will come from the government by 2025. How can a hospital survive with those dynamics?
There are only three options. Faced with decreasing revenues, hospitals can further reduce expenses. With much of the fat already trimmed this is a daunting proposition. Second, the hospital can cost shift and ask a greater percentage from the private insurer. This will be difficult with price transparency and a greater portion of the bill being paid by the patient. Third, we can all pray that the government will increase its reimbursement; unlikely, when it’s such a fight just to not be cut each year.
Need to Add Capacity
With the aging population and the increasing acuity of hospitalized patients, changes need to occur in the hospital’s physical plant. Recent surveys have shown that more than 85% of hospitals plan to add or change their capacity. While this is significant in Florida, Arizona, Nevada, and other places faced with population migrations, in other places this is driven by the need to expand the emergency department, add telemetry beds, and expand the ICU.
This is further complicated by the movement of well-heeled (and well-insured) populations to the suburbs with the hospitals following them and leaving disturbing realities for the older inner city in their wake.
Technology Is Your Friend
New advances are more than gadgetry gone wild. When best deployed these 21st-century advances can lead to better outcomes, safer hospitals, and actually make economic sense. The problem: Where can hospitals go to find out just which technology to use? At many hospitals these decisions are made by committees with less than perfect knowledge in a rapidly evolving market. Once the technology is chosen, the implementation can be disruptive more than helpful, especially in the short run, and the processes of care can be thrown off course. Sometimes this can have convulsive results such as in the failed implementation of CPOE at Cedars Sinai Hospital in Los Angeles.
And whether it is new technology or the adding of capacity, just where will the hospitals get the capital to pay for all this investment in the future? Not from Medicare and Medicaid, not from big business, and not from the out-of-pocket dollars of their patients.
This is the reality of today flavored with best guesses for the future. From this vantage point will arise the ideas of how to shape the hospital of the future. This is the world tomorrow’s hospitalists will inhabit. We need to understand how this will shape resource availability, hospital design, the commitment to quality improvement and accountability, and the environment in which hospitalists will work and our patients will receive care.
Once we understand what will shape the hospital of the future, hospitalists can be better prepared to be active partners in the shaping the new reality. TH
Dr. Wellikson has been CEO of SHM since 2000.
SHM has been working with JCAHO on its Hospital of the Future Roundtable. JCAHO has brought together an interesting international group made up of leaders representing hospital administrators, architects, social behaviorists, nurses, pharmacists, physicians, economists, government, technology experts, and others with a stake in the evolution of the hospital as an institution.
At our recent meeting in Chicago we discussed some aspects of the economics of hospitals that I thought would be worth sharing with the hospital medicine audience.
Right now many hospitals are actually in a good economic position. For the past 12 months hospitals have had an operating margin of 3.6% with a total margin of more than 6%. A number of factors have favored the hospital’s bottom line in recent years. There has been hospital consolidation with the closing of some hospitals. Managed care’s tightening of revenue forced hospitals in the 1990s to examine their operations and many hospitals became more efficient. This reduced hospital size and forced changes in staffing and other parts of the expense equation. Now that managed care has loosened its grip on the fees paid to hospitals, revenues have risen faster than costs, especially on the commercial side. There has actually been an increase of 8.6% in revenue to hospitals in the past year.
The dark side of this equation is that while many hospitals have benefited, some hospitals continue to run in the red because of geography (inner city, rural), and patient mix. This gap between haves and have-nots is increasing. The specter of more Americans without insurance coverage (or undercovered) also raises the burden of undercompensated care on hospitals in general.
Competition and Transparency
Recently, some people have been talking about trying to make true competition work in healthcare. One step in creating a marketplace is to have price and cost transparency. The thought is if the users of healthcare (patients) and the buyers of healthcare (businesses and government) could see each hospital’s charges, then people would make their decisions armed with information like they have when buying a car or a house.
Unfortunately that is not how the healthcare marketplace (if you can call it that) operates. The reality is that the government (as Medicare and Medicaid) sets price levels fairly arbitrarily and very often below the actual cost of delivering the services. You also have to throw into the mix all the care hospitals provide to patients without any insurance coverage or means to pay for their care. This leads to cost shifting to the tune that hospitals now expect private insurers to pay 122% of costs just to balance the CMS shortfall. Price transparency makes it more difficult to cost shift because a hospital would set its “price,” but would that be the price for Medicare, for Medicaid, for the “Blues” (Blue Cross/Blue Shield) as well?
Now that employers are cost shifting to their employees with larger co-pays and basically offering a fixed benefit and asking the workers to pick up more of the health tab, it is even harder for hospitals to cost shift to the private commercial side (i.e., people under 65 with insurance).
Hospital Disaggregation
The good old Marcus Welby, MD-era hospital as the total community resource that takes the profitable and the needy is eroding. Specialty hospitals have sprung up to siphon some of the best revenue sources and help physicians get on the facility side of the equation. Many of the most lucrative outpatient modalities (e.g., surgicenters, imaging) have moved off campus and out of the hospital’s domain. And there sits the full-service hospital left with many of the responsibilities and a disproportionate share of expense, but with less of the high-ticket revenue.
Populations Demographics
Our population is getting older, but aging baby boomers will account for only about a 10% increase in healthcare spending. The bigger problem is that as the population ages a greater proportion of healthcare spending shifts from private to public (i.e., from the Blues to Medicare). There is already a problem in cost shifting as I mentioned above with Medicare and Medicaid paying <95% of healthcare costs. You can’t make up those losses with volume. It’s predicted that more than 65% of hospital funding will come from the government by 2025. How can a hospital survive with those dynamics?
There are only three options. Faced with decreasing revenues, hospitals can further reduce expenses. With much of the fat already trimmed this is a daunting proposition. Second, the hospital can cost shift and ask a greater percentage from the private insurer. This will be difficult with price transparency and a greater portion of the bill being paid by the patient. Third, we can all pray that the government will increase its reimbursement; unlikely, when it’s such a fight just to not be cut each year.
Need to Add Capacity
With the aging population and the increasing acuity of hospitalized patients, changes need to occur in the hospital’s physical plant. Recent surveys have shown that more than 85% of hospitals plan to add or change their capacity. While this is significant in Florida, Arizona, Nevada, and other places faced with population migrations, in other places this is driven by the need to expand the emergency department, add telemetry beds, and expand the ICU.
This is further complicated by the movement of well-heeled (and well-insured) populations to the suburbs with the hospitals following them and leaving disturbing realities for the older inner city in their wake.
Technology Is Your Friend
New advances are more than gadgetry gone wild. When best deployed these 21st-century advances can lead to better outcomes, safer hospitals, and actually make economic sense. The problem: Where can hospitals go to find out just which technology to use? At many hospitals these decisions are made by committees with less than perfect knowledge in a rapidly evolving market. Once the technology is chosen, the implementation can be disruptive more than helpful, especially in the short run, and the processes of care can be thrown off course. Sometimes this can have convulsive results such as in the failed implementation of CPOE at Cedars Sinai Hospital in Los Angeles.
And whether it is new technology or the adding of capacity, just where will the hospitals get the capital to pay for all this investment in the future? Not from Medicare and Medicaid, not from big business, and not from the out-of-pocket dollars of their patients.
This is the reality of today flavored with best guesses for the future. From this vantage point will arise the ideas of how to shape the hospital of the future. This is the world tomorrow’s hospitalists will inhabit. We need to understand how this will shape resource availability, hospital design, the commitment to quality improvement and accountability, and the environment in which hospitalists will work and our patients will receive care.
Once we understand what will shape the hospital of the future, hospitalists can be better prepared to be active partners in the shaping the new reality. TH
Dr. Wellikson has been CEO of SHM since 2000.
SHM has been working with JCAHO on its Hospital of the Future Roundtable. JCAHO has brought together an interesting international group made up of leaders representing hospital administrators, architects, social behaviorists, nurses, pharmacists, physicians, economists, government, technology experts, and others with a stake in the evolution of the hospital as an institution.
At our recent meeting in Chicago we discussed some aspects of the economics of hospitals that I thought would be worth sharing with the hospital medicine audience.
Right now many hospitals are actually in a good economic position. For the past 12 months hospitals have had an operating margin of 3.6% with a total margin of more than 6%. A number of factors have favored the hospital’s bottom line in recent years. There has been hospital consolidation with the closing of some hospitals. Managed care’s tightening of revenue forced hospitals in the 1990s to examine their operations and many hospitals became more efficient. This reduced hospital size and forced changes in staffing and other parts of the expense equation. Now that managed care has loosened its grip on the fees paid to hospitals, revenues have risen faster than costs, especially on the commercial side. There has actually been an increase of 8.6% in revenue to hospitals in the past year.
The dark side of this equation is that while many hospitals have benefited, some hospitals continue to run in the red because of geography (inner city, rural), and patient mix. This gap between haves and have-nots is increasing. The specter of more Americans without insurance coverage (or undercovered) also raises the burden of undercompensated care on hospitals in general.
Competition and Transparency
Recently, some people have been talking about trying to make true competition work in healthcare. One step in creating a marketplace is to have price and cost transparency. The thought is if the users of healthcare (patients) and the buyers of healthcare (businesses and government) could see each hospital’s charges, then people would make their decisions armed with information like they have when buying a car or a house.
Unfortunately that is not how the healthcare marketplace (if you can call it that) operates. The reality is that the government (as Medicare and Medicaid) sets price levels fairly arbitrarily and very often below the actual cost of delivering the services. You also have to throw into the mix all the care hospitals provide to patients without any insurance coverage or means to pay for their care. This leads to cost shifting to the tune that hospitals now expect private insurers to pay 122% of costs just to balance the CMS shortfall. Price transparency makes it more difficult to cost shift because a hospital would set its “price,” but would that be the price for Medicare, for Medicaid, for the “Blues” (Blue Cross/Blue Shield) as well?
Now that employers are cost shifting to their employees with larger co-pays and basically offering a fixed benefit and asking the workers to pick up more of the health tab, it is even harder for hospitals to cost shift to the private commercial side (i.e., people under 65 with insurance).
Hospital Disaggregation
The good old Marcus Welby, MD-era hospital as the total community resource that takes the profitable and the needy is eroding. Specialty hospitals have sprung up to siphon some of the best revenue sources and help physicians get on the facility side of the equation. Many of the most lucrative outpatient modalities (e.g., surgicenters, imaging) have moved off campus and out of the hospital’s domain. And there sits the full-service hospital left with many of the responsibilities and a disproportionate share of expense, but with less of the high-ticket revenue.
Populations Demographics
Our population is getting older, but aging baby boomers will account for only about a 10% increase in healthcare spending. The bigger problem is that as the population ages a greater proportion of healthcare spending shifts from private to public (i.e., from the Blues to Medicare). There is already a problem in cost shifting as I mentioned above with Medicare and Medicaid paying <95% of healthcare costs. You can’t make up those losses with volume. It’s predicted that more than 65% of hospital funding will come from the government by 2025. How can a hospital survive with those dynamics?
There are only three options. Faced with decreasing revenues, hospitals can further reduce expenses. With much of the fat already trimmed this is a daunting proposition. Second, the hospital can cost shift and ask a greater percentage from the private insurer. This will be difficult with price transparency and a greater portion of the bill being paid by the patient. Third, we can all pray that the government will increase its reimbursement; unlikely, when it’s such a fight just to not be cut each year.
Need to Add Capacity
With the aging population and the increasing acuity of hospitalized patients, changes need to occur in the hospital’s physical plant. Recent surveys have shown that more than 85% of hospitals plan to add or change their capacity. While this is significant in Florida, Arizona, Nevada, and other places faced with population migrations, in other places this is driven by the need to expand the emergency department, add telemetry beds, and expand the ICU.
This is further complicated by the movement of well-heeled (and well-insured) populations to the suburbs with the hospitals following them and leaving disturbing realities for the older inner city in their wake.
Technology Is Your Friend
New advances are more than gadgetry gone wild. When best deployed these 21st-century advances can lead to better outcomes, safer hospitals, and actually make economic sense. The problem: Where can hospitals go to find out just which technology to use? At many hospitals these decisions are made by committees with less than perfect knowledge in a rapidly evolving market. Once the technology is chosen, the implementation can be disruptive more than helpful, especially in the short run, and the processes of care can be thrown off course. Sometimes this can have convulsive results such as in the failed implementation of CPOE at Cedars Sinai Hospital in Los Angeles.
And whether it is new technology or the adding of capacity, just where will the hospitals get the capital to pay for all this investment in the future? Not from Medicare and Medicaid, not from big business, and not from the out-of-pocket dollars of their patients.
This is the reality of today flavored with best guesses for the future. From this vantage point will arise the ideas of how to shape the hospital of the future. This is the world tomorrow’s hospitalists will inhabit. We need to understand how this will shape resource availability, hospital design, the commitment to quality improvement and accountability, and the environment in which hospitalists will work and our patients will receive care.
Once we understand what will shape the hospital of the future, hospitalists can be better prepared to be active partners in the shaping the new reality. TH
Dr. Wellikson has been CEO of SHM since 2000.
Tough Negotiations Avert B.C. Hospitalist Walkout
Two weeks of intense talks between hospitalists and government officials resulted in an 11th-hour compromise on June 29th in British Columbia, one day before hospitalists’ contracts were set to expire. Throughout the month of June, the B.C. hospitalists had threatened to move back to community practice if the Ministry of Health (MOH) did not offer a contract that recognized the value of their work. The hospitalists contended that low payment schedules and staffing levels were seriously undermining staff retention and recruiting—as well as patient safety. During the dispute, MOH officials had been equally adamant about their position. The province’s Minister of Health, George Abbott, said that the salaries were fair, and that the government would not be “held for ransom on this issue.”
Hospitalists believed that failure to reach agreement would have left many hospitals scrambling to provide coverage for hospitalized patients.
Wayne DeMott, MD, is a hospitalist at Royal Jubilee Hospital in Victoria, B.C., and chief negotiator for the British Columbia Medical Association’s Section of Hospitalist Medicine.
Hospitalists in B.C., he says, “are in a position to … severely compromise many functions of most major hospitals in this province. If an agreement had not been reached, we were quite prepared to stand up and take our leave.”
The June 29 compromise established a one-year period to re-examine workload issues and clarify funding models. If hospitalists are not satisfied at the six-month mark with the provisions to address ongoing funding, workload, recruitment and retention issues, they can give six months’ notice.
Roots of the Dispute
The majority of primary care in British Columbia has traditionally been provided by general practitioners. According to David Wilton, MD, one of the directors of the Vancouver Hospitalist Society, a nonprofit society that contracts with Vancouver General Hospital and the University of British Columbia Hospital (overseen by the Vancouver Coastal Health Authority), and a core negotiator for B.C. hospitalists at the talks, “the economic model for hospital care faltered through the late ’80s and early ’90s, and general practitioners started giving up their hospital privileges and focusing on their community-based practices.”
To fill the gap, many hospitals in the more populated urban areas started hospitalist programs, which evolved through the late ’90s and grew quickly after the year 2000. One of the largest health authorities in the province—the Fraser Health Authority—serves approximately 1.3 million people on the B.C. mainland, runs 12 hospitals, and now has 110 hospitalists working for that health authority alone. Most (85%-90%) Canadian hospitalists are trained in family practice medicine, as opposed to internal medicine.
In some ways, B.C. hospitalists have been victims of their own success. As programs grew and as house staff became aware of hospitalists’ skill sets and expertise, many shifted their work burdens to the hospitalist services, says Dr. Wilton. The workload climbed exponentially, but appreciation of hospitalists’ value-added services on the part of MOH officials did not keep pace with the workload. The result, explains Dr. Wilton, was a kind of disconnect between the intense nature of hospitalists’ services and their compensation and staffing structures.
“In British Columbia the local hospital administrators saw the efficiencies that we were bringing to the system,” explains Dr. Wilton. “They saw the improved quality of care and the fact that we were able to step in, be flexible, and help specialists in various areas and fill the gaps of care. But we hadn’t yet broken through to the higher levels of the provincial Ministry of Health. They didn’t fully recognize the value that we were bringing to the healthcare system and the fact that hospitalists are the cornerstone of the acute care system now.”
Mike Morris, MD, president of the Section of Hospital Medicine, agrees with this characterization. A hospitalist at Nanaimo Regional General Hospital (part of the Vancouver Island Health Authority), Dr. Morris believes that most of the health authorities, which administer the region’s hospitals, appreciate hospitalists’ value. “They know how much we help the patient flow and problems in the emergency room,” he says. Emergency department crowding has been a huge problem in British Columbia, due to lack of hospital beds and a dearth of long-term-care beds. “Hospitalists are able to come in and safely discharge people on a timely basis, and help the flow through the emergency department. That’s one of our biggest values to the hospital. We think that the family physicians coming into the hospital are platinum doctors because they’re keeping up with the rapid changes in hospital medicine. And we feel that they are being highly undervalued.”
On average, hospitalists were making $111 an hour (Canadian dollars, equating to about $98 U.S. dollars at the July 12 exchange rate). According to Dr. Wilton, the hospitalists contended that their earning potential was at least equivalent to that of a lower-intensity Monday-Friday community-based general practice. At the negotiations, they valued their services at $135/hour. If the government was unwilling to value hospitalists’ compensation appropriately, they warned they could easily return to a community-based practice model.
Payment Not the Only Issue
The province of British Columbia is divided into six health authorities, five of which have active hospitalist programs. Overarching compensation frameworks for all physicians are established through negotiations between the British Columbia Medical Association (BCMA) and the MOH. Individual health authorities then negotiate specific terms of compensation and workload expectations with physicians. There is considerable variation between health authorities (and indeed throughout each of the Canadian provinces) regarding hospitalists’ workload models, such as the number of expected patient encounters per shift and compensation packages.
The BCMA had recently completed contract renewal negotiations involving the entire physician body in British Columbia and the government on April 1, resulting in a new six-year Letter of Agreement that hospitalists maintained did not address their needs.
“The way we saw [the Letter of Agreement] being interpreted,” says Dr. Wilton, “was that the base rate for calculating our advances going forward was going to be between 10% and 25% less than what we were currently earning. Part of our goal was to get a wage that is consistent with the complexity and intensity of our work. I think that, in the eyes of the government, they were seeing our work and our value more in the range of the less-intense community-based general practice work. We wanted to shift that focus more towards the intensity of the acute care setting, where we think we’re more comparable to emergency medicine and internal medicine specialists.”
Dr. DeMott adds, “The workload model is a very important aspect of what we do. It isn’t only what you are paid, it is what you are being asked to do for what you’re being paid. Workload expectations have tremendous implications for the health of this career path in the future, the ability to recruit into this career path, and the ability to retain people, so that they do not become burnt out or personally destroyed.”
Views of the Dispute
B.C. hospitalists decided to hire their own attorney (the Vancouver firm of Tevlin Gleadle) and a press relations person to take their dispute public. Margaret MacDiarmid, MD, is president of the BCMA and has her own family practice in the Kootenays region eight hours east/southeast of Vancouver on the British Columbian mainland. “We [the BCMA] were very keen to assist, if we could, in the resolution of the conflict, and we were calling them about that,” she explains. “But we felt we had to operate within the Letter of Agreement that we had just signed, which I think is reasonable. So we did not play any active role in the final resolution.”
Assistant Deputy Minister for Medical Services Stephen Brown, PhD, the MOH official who oversees physician compensation, admits that the issue of the threatened walkout was “a bit of a surprise” to him because the government had just signed the Letter of Agreement with the BCMA. He became engaged with the health authorities and the hospitalists, “trying to understand how we got to where we were when we had just signed an agreement.”
Although hospitalists felt the Letter of Agreement did not address their concerns, Brown did not characterize the talks with the various stakeholders as negotiations. “I acknowledged that we were trying to understand the issues they were presenting and how we could address those issues within the context of the BCMA-government negotiated agreement,” he said during a telephone interview.
“Over the period of a couple weeks of dialogue, we got to a tentative agreement—which hopefully will now translate into contracts over the next week—that is within the framework of the Agreement.”
Goals Accomplished
Key figures involved in the talks expressed satisfaction with some of the goals achieved. Dr. Wilton reflects that the dispute has resulted in more public awareness of the presence of hospitalists and more awareness of hospitalists’ value within the BCMA. Most importantly, he says, “we sat across the table from some of the senior administrators in the Ministry of Health and were able to educate them about the values that hospitalists can bring to the system. We’re hoping that by having the opportunity to educate them, they will take a more proactive and organized approach to supporting the hospitalist model of care and utilizing it to its full potential.”
“I wasn’t thrilled that we were in this situation,” says Brown. “But the positive that’s come out of it is that I think we’ve got a platform, we’ve got a dialogue, and we have committed to work with them over the next six months to look at workload and see if we can get some level of consistency on that.”
Brown indicated that he had acquired more understanding of how hospitalists’ roles have evolved in the province and the difficulties they encounter to provide quality care. “The reality of what we found was that regions had developed hospitalist services in slightly different ways, with slightly different compensation arrangements,” he noted. “I hope what we have just done is we have now created the same platform for all the hospitalists across the province. They’re going to have a contract that looks similar and dialogue is now underway with the HAs [health authorities] about the range of services that hospitalists will provide. So I think that’s an opportunity as well, over the next six months now, to clean that up.”
While hospitalists gained some traction on the development of new workload standards, they did not fully accomplish their financial goals, the two key negotiators said. According to Dr. DeMott, “We became lost in a complex political and economic struggle that involved all of the doctors in the province. The doctors had recently ratified an agreement that left us completely out in the cold. In the end, we had to comply with the essential terms of that [BCMA-negotiated Letter of Agreement].”
To have insisted on the hospitalists’ financial goals, he says, would have injured too many programs, and—if they had walked off the job—ultimately would have compromised patient care. “In the end,” says Dr. DeMott, “we acquiesced and came up with a compromise that should work for the short term.”
Parallels with the United States?
Many of those interviewed for this article observed that hospitalist programs in British Columbia are still evolving, and that U.S. hospitalist programs are probably five years ahead in terms of established program models. Dr. DeMott praises the pioneering work done by SHM: “We look to you for guidance, and we really do appreciate the SHM advancement that is moving the hospitalist profession along.”
As negotiators for the Section of Hospital Medicine during the talks, Dr. DeMott says that his team used the surveys and studies that SHM has pioneered about the value-added contributions of hospitalists to increase awareness with the MOH, the government of British Columbia, and the BCMA about hospitalists’ roles. Dr. Morris notes that B.C. hospitalists, taking the lead from SHM, are now developing their core competencies.
William D. Atchley, Jr., MD, FACP, medical director of Peninsula Inpatient Care Specialists at Sentara Careplex Hospital in Hampton, Va., is a long-time member of the SHM board of directors. He has followed the growth of hospitalists in Canada, and applauds the efforts of those like Echo-Marie Enns, MD, who served as a National Association of Inpatient Physicians (NAIP) Canadian chapter president in Calgary. He has also conducted surveys of Canadian hospitalists. He doubts that a parallel strike situation could develop here in the United States.
“Their situation is unique to Canada,” he says. “From SHM’s perspective, we have always acted as an advocate for hospitalists in Canada and offered whatever we have learned here in the United States to help facilitate their movement. They are still in the process of explaining what a hospitalist is, and explaining to their national medical societies about what hospitalists can do. Their ability to get the message across is just going to take some time.”
Summing up their accomplishments thus far, Dr. DeMott says, “We considered this disagreement a defining moment for hospitalists in this province and quite possibly for [Canada]. We’re not there yet, but we put ourselves on the map. There will likely be another battle on the horizon for us, but hopefully one colored by a much greater appreciation of the expertise we bring to the acute care arena.” TH
Gretchen Henkel writes regularly for The Hospitalist.
Two weeks of intense talks between hospitalists and government officials resulted in an 11th-hour compromise on June 29th in British Columbia, one day before hospitalists’ contracts were set to expire. Throughout the month of June, the B.C. hospitalists had threatened to move back to community practice if the Ministry of Health (MOH) did not offer a contract that recognized the value of their work. The hospitalists contended that low payment schedules and staffing levels were seriously undermining staff retention and recruiting—as well as patient safety. During the dispute, MOH officials had been equally adamant about their position. The province’s Minister of Health, George Abbott, said that the salaries were fair, and that the government would not be “held for ransom on this issue.”
Hospitalists believed that failure to reach agreement would have left many hospitals scrambling to provide coverage for hospitalized patients.
Wayne DeMott, MD, is a hospitalist at Royal Jubilee Hospital in Victoria, B.C., and chief negotiator for the British Columbia Medical Association’s Section of Hospitalist Medicine.
Hospitalists in B.C., he says, “are in a position to … severely compromise many functions of most major hospitals in this province. If an agreement had not been reached, we were quite prepared to stand up and take our leave.”
The June 29 compromise established a one-year period to re-examine workload issues and clarify funding models. If hospitalists are not satisfied at the six-month mark with the provisions to address ongoing funding, workload, recruitment and retention issues, they can give six months’ notice.
Roots of the Dispute
The majority of primary care in British Columbia has traditionally been provided by general practitioners. According to David Wilton, MD, one of the directors of the Vancouver Hospitalist Society, a nonprofit society that contracts with Vancouver General Hospital and the University of British Columbia Hospital (overseen by the Vancouver Coastal Health Authority), and a core negotiator for B.C. hospitalists at the talks, “the economic model for hospital care faltered through the late ’80s and early ’90s, and general practitioners started giving up their hospital privileges and focusing on their community-based practices.”
To fill the gap, many hospitals in the more populated urban areas started hospitalist programs, which evolved through the late ’90s and grew quickly after the year 2000. One of the largest health authorities in the province—the Fraser Health Authority—serves approximately 1.3 million people on the B.C. mainland, runs 12 hospitals, and now has 110 hospitalists working for that health authority alone. Most (85%-90%) Canadian hospitalists are trained in family practice medicine, as opposed to internal medicine.
In some ways, B.C. hospitalists have been victims of their own success. As programs grew and as house staff became aware of hospitalists’ skill sets and expertise, many shifted their work burdens to the hospitalist services, says Dr. Wilton. The workload climbed exponentially, but appreciation of hospitalists’ value-added services on the part of MOH officials did not keep pace with the workload. The result, explains Dr. Wilton, was a kind of disconnect between the intense nature of hospitalists’ services and their compensation and staffing structures.
“In British Columbia the local hospital administrators saw the efficiencies that we were bringing to the system,” explains Dr. Wilton. “They saw the improved quality of care and the fact that we were able to step in, be flexible, and help specialists in various areas and fill the gaps of care. But we hadn’t yet broken through to the higher levels of the provincial Ministry of Health. They didn’t fully recognize the value that we were bringing to the healthcare system and the fact that hospitalists are the cornerstone of the acute care system now.”
Mike Morris, MD, president of the Section of Hospital Medicine, agrees with this characterization. A hospitalist at Nanaimo Regional General Hospital (part of the Vancouver Island Health Authority), Dr. Morris believes that most of the health authorities, which administer the region’s hospitals, appreciate hospitalists’ value. “They know how much we help the patient flow and problems in the emergency room,” he says. Emergency department crowding has been a huge problem in British Columbia, due to lack of hospital beds and a dearth of long-term-care beds. “Hospitalists are able to come in and safely discharge people on a timely basis, and help the flow through the emergency department. That’s one of our biggest values to the hospital. We think that the family physicians coming into the hospital are platinum doctors because they’re keeping up with the rapid changes in hospital medicine. And we feel that they are being highly undervalued.”
On average, hospitalists were making $111 an hour (Canadian dollars, equating to about $98 U.S. dollars at the July 12 exchange rate). According to Dr. Wilton, the hospitalists contended that their earning potential was at least equivalent to that of a lower-intensity Monday-Friday community-based general practice. At the negotiations, they valued their services at $135/hour. If the government was unwilling to value hospitalists’ compensation appropriately, they warned they could easily return to a community-based practice model.
Payment Not the Only Issue
The province of British Columbia is divided into six health authorities, five of which have active hospitalist programs. Overarching compensation frameworks for all physicians are established through negotiations between the British Columbia Medical Association (BCMA) and the MOH. Individual health authorities then negotiate specific terms of compensation and workload expectations with physicians. There is considerable variation between health authorities (and indeed throughout each of the Canadian provinces) regarding hospitalists’ workload models, such as the number of expected patient encounters per shift and compensation packages.
The BCMA had recently completed contract renewal negotiations involving the entire physician body in British Columbia and the government on April 1, resulting in a new six-year Letter of Agreement that hospitalists maintained did not address their needs.
“The way we saw [the Letter of Agreement] being interpreted,” says Dr. Wilton, “was that the base rate for calculating our advances going forward was going to be between 10% and 25% less than what we were currently earning. Part of our goal was to get a wage that is consistent with the complexity and intensity of our work. I think that, in the eyes of the government, they were seeing our work and our value more in the range of the less-intense community-based general practice work. We wanted to shift that focus more towards the intensity of the acute care setting, where we think we’re more comparable to emergency medicine and internal medicine specialists.”
Dr. DeMott adds, “The workload model is a very important aspect of what we do. It isn’t only what you are paid, it is what you are being asked to do for what you’re being paid. Workload expectations have tremendous implications for the health of this career path in the future, the ability to recruit into this career path, and the ability to retain people, so that they do not become burnt out or personally destroyed.”
Views of the Dispute
B.C. hospitalists decided to hire their own attorney (the Vancouver firm of Tevlin Gleadle) and a press relations person to take their dispute public. Margaret MacDiarmid, MD, is president of the BCMA and has her own family practice in the Kootenays region eight hours east/southeast of Vancouver on the British Columbian mainland. “We [the BCMA] were very keen to assist, if we could, in the resolution of the conflict, and we were calling them about that,” she explains. “But we felt we had to operate within the Letter of Agreement that we had just signed, which I think is reasonable. So we did not play any active role in the final resolution.”
Assistant Deputy Minister for Medical Services Stephen Brown, PhD, the MOH official who oversees physician compensation, admits that the issue of the threatened walkout was “a bit of a surprise” to him because the government had just signed the Letter of Agreement with the BCMA. He became engaged with the health authorities and the hospitalists, “trying to understand how we got to where we were when we had just signed an agreement.”
Although hospitalists felt the Letter of Agreement did not address their concerns, Brown did not characterize the talks with the various stakeholders as negotiations. “I acknowledged that we were trying to understand the issues they were presenting and how we could address those issues within the context of the BCMA-government negotiated agreement,” he said during a telephone interview.
“Over the period of a couple weeks of dialogue, we got to a tentative agreement—which hopefully will now translate into contracts over the next week—that is within the framework of the Agreement.”
Goals Accomplished
Key figures involved in the talks expressed satisfaction with some of the goals achieved. Dr. Wilton reflects that the dispute has resulted in more public awareness of the presence of hospitalists and more awareness of hospitalists’ value within the BCMA. Most importantly, he says, “we sat across the table from some of the senior administrators in the Ministry of Health and were able to educate them about the values that hospitalists can bring to the system. We’re hoping that by having the opportunity to educate them, they will take a more proactive and organized approach to supporting the hospitalist model of care and utilizing it to its full potential.”
“I wasn’t thrilled that we were in this situation,” says Brown. “But the positive that’s come out of it is that I think we’ve got a platform, we’ve got a dialogue, and we have committed to work with them over the next six months to look at workload and see if we can get some level of consistency on that.”
Brown indicated that he had acquired more understanding of how hospitalists’ roles have evolved in the province and the difficulties they encounter to provide quality care. “The reality of what we found was that regions had developed hospitalist services in slightly different ways, with slightly different compensation arrangements,” he noted. “I hope what we have just done is we have now created the same platform for all the hospitalists across the province. They’re going to have a contract that looks similar and dialogue is now underway with the HAs [health authorities] about the range of services that hospitalists will provide. So I think that’s an opportunity as well, over the next six months now, to clean that up.”
While hospitalists gained some traction on the development of new workload standards, they did not fully accomplish their financial goals, the two key negotiators said. According to Dr. DeMott, “We became lost in a complex political and economic struggle that involved all of the doctors in the province. The doctors had recently ratified an agreement that left us completely out in the cold. In the end, we had to comply with the essential terms of that [BCMA-negotiated Letter of Agreement].”
To have insisted on the hospitalists’ financial goals, he says, would have injured too many programs, and—if they had walked off the job—ultimately would have compromised patient care. “In the end,” says Dr. DeMott, “we acquiesced and came up with a compromise that should work for the short term.”
Parallels with the United States?
Many of those interviewed for this article observed that hospitalist programs in British Columbia are still evolving, and that U.S. hospitalist programs are probably five years ahead in terms of established program models. Dr. DeMott praises the pioneering work done by SHM: “We look to you for guidance, and we really do appreciate the SHM advancement that is moving the hospitalist profession along.”
As negotiators for the Section of Hospital Medicine during the talks, Dr. DeMott says that his team used the surveys and studies that SHM has pioneered about the value-added contributions of hospitalists to increase awareness with the MOH, the government of British Columbia, and the BCMA about hospitalists’ roles. Dr. Morris notes that B.C. hospitalists, taking the lead from SHM, are now developing their core competencies.
William D. Atchley, Jr., MD, FACP, medical director of Peninsula Inpatient Care Specialists at Sentara Careplex Hospital in Hampton, Va., is a long-time member of the SHM board of directors. He has followed the growth of hospitalists in Canada, and applauds the efforts of those like Echo-Marie Enns, MD, who served as a National Association of Inpatient Physicians (NAIP) Canadian chapter president in Calgary. He has also conducted surveys of Canadian hospitalists. He doubts that a parallel strike situation could develop here in the United States.
“Their situation is unique to Canada,” he says. “From SHM’s perspective, we have always acted as an advocate for hospitalists in Canada and offered whatever we have learned here in the United States to help facilitate their movement. They are still in the process of explaining what a hospitalist is, and explaining to their national medical societies about what hospitalists can do. Their ability to get the message across is just going to take some time.”
Summing up their accomplishments thus far, Dr. DeMott says, “We considered this disagreement a defining moment for hospitalists in this province and quite possibly for [Canada]. We’re not there yet, but we put ourselves on the map. There will likely be another battle on the horizon for us, but hopefully one colored by a much greater appreciation of the expertise we bring to the acute care arena.” TH
Gretchen Henkel writes regularly for The Hospitalist.
Two weeks of intense talks between hospitalists and government officials resulted in an 11th-hour compromise on June 29th in British Columbia, one day before hospitalists’ contracts were set to expire. Throughout the month of June, the B.C. hospitalists had threatened to move back to community practice if the Ministry of Health (MOH) did not offer a contract that recognized the value of their work. The hospitalists contended that low payment schedules and staffing levels were seriously undermining staff retention and recruiting—as well as patient safety. During the dispute, MOH officials had been equally adamant about their position. The province’s Minister of Health, George Abbott, said that the salaries were fair, and that the government would not be “held for ransom on this issue.”
Hospitalists believed that failure to reach agreement would have left many hospitals scrambling to provide coverage for hospitalized patients.
Wayne DeMott, MD, is a hospitalist at Royal Jubilee Hospital in Victoria, B.C., and chief negotiator for the British Columbia Medical Association’s Section of Hospitalist Medicine.
Hospitalists in B.C., he says, “are in a position to … severely compromise many functions of most major hospitals in this province. If an agreement had not been reached, we were quite prepared to stand up and take our leave.”
The June 29 compromise established a one-year period to re-examine workload issues and clarify funding models. If hospitalists are not satisfied at the six-month mark with the provisions to address ongoing funding, workload, recruitment and retention issues, they can give six months’ notice.
Roots of the Dispute
The majority of primary care in British Columbia has traditionally been provided by general practitioners. According to David Wilton, MD, one of the directors of the Vancouver Hospitalist Society, a nonprofit society that contracts with Vancouver General Hospital and the University of British Columbia Hospital (overseen by the Vancouver Coastal Health Authority), and a core negotiator for B.C. hospitalists at the talks, “the economic model for hospital care faltered through the late ’80s and early ’90s, and general practitioners started giving up their hospital privileges and focusing on their community-based practices.”
To fill the gap, many hospitals in the more populated urban areas started hospitalist programs, which evolved through the late ’90s and grew quickly after the year 2000. One of the largest health authorities in the province—the Fraser Health Authority—serves approximately 1.3 million people on the B.C. mainland, runs 12 hospitals, and now has 110 hospitalists working for that health authority alone. Most (85%-90%) Canadian hospitalists are trained in family practice medicine, as opposed to internal medicine.
In some ways, B.C. hospitalists have been victims of their own success. As programs grew and as house staff became aware of hospitalists’ skill sets and expertise, many shifted their work burdens to the hospitalist services, says Dr. Wilton. The workload climbed exponentially, but appreciation of hospitalists’ value-added services on the part of MOH officials did not keep pace with the workload. The result, explains Dr. Wilton, was a kind of disconnect between the intense nature of hospitalists’ services and their compensation and staffing structures.
“In British Columbia the local hospital administrators saw the efficiencies that we were bringing to the system,” explains Dr. Wilton. “They saw the improved quality of care and the fact that we were able to step in, be flexible, and help specialists in various areas and fill the gaps of care. But we hadn’t yet broken through to the higher levels of the provincial Ministry of Health. They didn’t fully recognize the value that we were bringing to the healthcare system and the fact that hospitalists are the cornerstone of the acute care system now.”
Mike Morris, MD, president of the Section of Hospital Medicine, agrees with this characterization. A hospitalist at Nanaimo Regional General Hospital (part of the Vancouver Island Health Authority), Dr. Morris believes that most of the health authorities, which administer the region’s hospitals, appreciate hospitalists’ value. “They know how much we help the patient flow and problems in the emergency room,” he says. Emergency department crowding has been a huge problem in British Columbia, due to lack of hospital beds and a dearth of long-term-care beds. “Hospitalists are able to come in and safely discharge people on a timely basis, and help the flow through the emergency department. That’s one of our biggest values to the hospital. We think that the family physicians coming into the hospital are platinum doctors because they’re keeping up with the rapid changes in hospital medicine. And we feel that they are being highly undervalued.”
On average, hospitalists were making $111 an hour (Canadian dollars, equating to about $98 U.S. dollars at the July 12 exchange rate). According to Dr. Wilton, the hospitalists contended that their earning potential was at least equivalent to that of a lower-intensity Monday-Friday community-based general practice. At the negotiations, they valued their services at $135/hour. If the government was unwilling to value hospitalists’ compensation appropriately, they warned they could easily return to a community-based practice model.
Payment Not the Only Issue
The province of British Columbia is divided into six health authorities, five of which have active hospitalist programs. Overarching compensation frameworks for all physicians are established through negotiations between the British Columbia Medical Association (BCMA) and the MOH. Individual health authorities then negotiate specific terms of compensation and workload expectations with physicians. There is considerable variation between health authorities (and indeed throughout each of the Canadian provinces) regarding hospitalists’ workload models, such as the number of expected patient encounters per shift and compensation packages.
The BCMA had recently completed contract renewal negotiations involving the entire physician body in British Columbia and the government on April 1, resulting in a new six-year Letter of Agreement that hospitalists maintained did not address their needs.
“The way we saw [the Letter of Agreement] being interpreted,” says Dr. Wilton, “was that the base rate for calculating our advances going forward was going to be between 10% and 25% less than what we were currently earning. Part of our goal was to get a wage that is consistent with the complexity and intensity of our work. I think that, in the eyes of the government, they were seeing our work and our value more in the range of the less-intense community-based general practice work. We wanted to shift that focus more towards the intensity of the acute care setting, where we think we’re more comparable to emergency medicine and internal medicine specialists.”
Dr. DeMott adds, “The workload model is a very important aspect of what we do. It isn’t only what you are paid, it is what you are being asked to do for what you’re being paid. Workload expectations have tremendous implications for the health of this career path in the future, the ability to recruit into this career path, and the ability to retain people, so that they do not become burnt out or personally destroyed.”
Views of the Dispute
B.C. hospitalists decided to hire their own attorney (the Vancouver firm of Tevlin Gleadle) and a press relations person to take their dispute public. Margaret MacDiarmid, MD, is president of the BCMA and has her own family practice in the Kootenays region eight hours east/southeast of Vancouver on the British Columbian mainland. “We [the BCMA] were very keen to assist, if we could, in the resolution of the conflict, and we were calling them about that,” she explains. “But we felt we had to operate within the Letter of Agreement that we had just signed, which I think is reasonable. So we did not play any active role in the final resolution.”
Assistant Deputy Minister for Medical Services Stephen Brown, PhD, the MOH official who oversees physician compensation, admits that the issue of the threatened walkout was “a bit of a surprise” to him because the government had just signed the Letter of Agreement with the BCMA. He became engaged with the health authorities and the hospitalists, “trying to understand how we got to where we were when we had just signed an agreement.”
Although hospitalists felt the Letter of Agreement did not address their concerns, Brown did not characterize the talks with the various stakeholders as negotiations. “I acknowledged that we were trying to understand the issues they were presenting and how we could address those issues within the context of the BCMA-government negotiated agreement,” he said during a telephone interview.
“Over the period of a couple weeks of dialogue, we got to a tentative agreement—which hopefully will now translate into contracts over the next week—that is within the framework of the Agreement.”
Goals Accomplished
Key figures involved in the talks expressed satisfaction with some of the goals achieved. Dr. Wilton reflects that the dispute has resulted in more public awareness of the presence of hospitalists and more awareness of hospitalists’ value within the BCMA. Most importantly, he says, “we sat across the table from some of the senior administrators in the Ministry of Health and were able to educate them about the values that hospitalists can bring to the system. We’re hoping that by having the opportunity to educate them, they will take a more proactive and organized approach to supporting the hospitalist model of care and utilizing it to its full potential.”
“I wasn’t thrilled that we were in this situation,” says Brown. “But the positive that’s come out of it is that I think we’ve got a platform, we’ve got a dialogue, and we have committed to work with them over the next six months to look at workload and see if we can get some level of consistency on that.”
Brown indicated that he had acquired more understanding of how hospitalists’ roles have evolved in the province and the difficulties they encounter to provide quality care. “The reality of what we found was that regions had developed hospitalist services in slightly different ways, with slightly different compensation arrangements,” he noted. “I hope what we have just done is we have now created the same platform for all the hospitalists across the province. They’re going to have a contract that looks similar and dialogue is now underway with the HAs [health authorities] about the range of services that hospitalists will provide. So I think that’s an opportunity as well, over the next six months now, to clean that up.”
While hospitalists gained some traction on the development of new workload standards, they did not fully accomplish their financial goals, the two key negotiators said. According to Dr. DeMott, “We became lost in a complex political and economic struggle that involved all of the doctors in the province. The doctors had recently ratified an agreement that left us completely out in the cold. In the end, we had to comply with the essential terms of that [BCMA-negotiated Letter of Agreement].”
To have insisted on the hospitalists’ financial goals, he says, would have injured too many programs, and—if they had walked off the job—ultimately would have compromised patient care. “In the end,” says Dr. DeMott, “we acquiesced and came up with a compromise that should work for the short term.”
Parallels with the United States?
Many of those interviewed for this article observed that hospitalist programs in British Columbia are still evolving, and that U.S. hospitalist programs are probably five years ahead in terms of established program models. Dr. DeMott praises the pioneering work done by SHM: “We look to you for guidance, and we really do appreciate the SHM advancement that is moving the hospitalist profession along.”
As negotiators for the Section of Hospital Medicine during the talks, Dr. DeMott says that his team used the surveys and studies that SHM has pioneered about the value-added contributions of hospitalists to increase awareness with the MOH, the government of British Columbia, and the BCMA about hospitalists’ roles. Dr. Morris notes that B.C. hospitalists, taking the lead from SHM, are now developing their core competencies.
William D. Atchley, Jr., MD, FACP, medical director of Peninsula Inpatient Care Specialists at Sentara Careplex Hospital in Hampton, Va., is a long-time member of the SHM board of directors. He has followed the growth of hospitalists in Canada, and applauds the efforts of those like Echo-Marie Enns, MD, who served as a National Association of Inpatient Physicians (NAIP) Canadian chapter president in Calgary. He has also conducted surveys of Canadian hospitalists. He doubts that a parallel strike situation could develop here in the United States.
“Their situation is unique to Canada,” he says. “From SHM’s perspective, we have always acted as an advocate for hospitalists in Canada and offered whatever we have learned here in the United States to help facilitate their movement. They are still in the process of explaining what a hospitalist is, and explaining to their national medical societies about what hospitalists can do. Their ability to get the message across is just going to take some time.”
Summing up their accomplishments thus far, Dr. DeMott says, “We considered this disagreement a defining moment for hospitalists in this province and quite possibly for [Canada]. We’re not there yet, but we put ourselves on the map. There will likely be another battle on the horizon for us, but hopefully one colored by a much greater appreciation of the expertise we bring to the acute care arena.” TH
Gretchen Henkel writes regularly for The Hospitalist.