User login
A Pennsylvania Practice
More than 20 years before the term hospitalist was coined, the Brockie Medical Group, a strong internal medicine practice led by Benjamin Hoover, MD, relished its hospital work at York Hospital in York, Pa. Back then, the doctors didn’t call themselves hospitalists, but the time they spent on hospital duties made them the forebears of today’s hospitalists.
According to John McConville, MD, chairman of York Hospital’s department of medicine and a hospital fixture since 1976, some of Brockie Internal Medicine group’s physicians devoted 60% to 70% of their practice time to inpatient tasks. “That was the culture when I arrived on the scene,” he recounts. Shortly thereafter, the group grew stronger when The Brockie Internal Medicine Group’s main competition—a sizable family practice group—fell apart. Brockie absorbed its like-minded physicians.
York, pa.
The Brockie Internal Medical Group is firmly anchored in York, Pa., home to factories that produce barbells and Harley-Davidson motorcycles. York has a soft side, though—it produced the first Peppermint Pattie, a mint-chocolate candy. It is an affordable, rapidly growing suburb, a place where commuters to Philadelphia, Baltimore, and Washington, D.C., can have a comfortable lifestyle without big city housing prices and the hassles of urban life.
The medical community is close-knit, described by Jonathan Whitney, MD, a Brockie hospitalist leader, as “a collegial environment with a growing population and plenty of patients, so there’s not a sense of competition among physicians.” Dr. Whitney, along with William “Tex” Landis, MD, and Michael Lamanteer, MD, form the Brockie Hospitalist Group’s executive committee, elected decision makers who deal with WellSpan Health and York Hospital on behalf of their colleagues.
WellSpan’s Role
As York grew, so did the Brockie Internal Medical Group. Then came managed care in the 1980s and 1990s, and Brockie’s internists were not happy. “We saw the medical landscape changing everywhere, and we didn’t want managed care pushing us around,” explains Dr. Landis, a Lancaster, Pa., native and now the Brockie Hospitalist Group’s lead physician. “Analyzing how medicine was changing, we felt vulnerable as a single specialty group. We considered various scenarios for becoming a multi-specialty practice, but decided that wasn’t right for us.”
So, in 1995, five group partners decided to sell the practice to WellSpan Health, an integrated nonprofit healthcare system located in South Central Pennsylvania. Their expectation? That WellSpan’s administrative support and financial muscle would protect them against managed care’s encroachment.
Affiliating with WellSpan Health aligned Brockie with the medical services line of York Hospital, providing the administrative support they needed to grow and thrive. Working together, Brockie’s medical leaders and WellSpan administrators oversee the following areas: strategic planning; budgeting, compensation, benefits, and incentives; collections and coding; care management and performance improvement; recruiting and other personnel issues; and scheduling and coverage.
The Hospitalist Program
York Hospital and its surrounding community continued to grow, as did the need for more office-based and inpatient physician services. By 2001, York Hospital’s top executives recognized that a dedicated hospitalist group was the best solution for its overflowing emergency department (ED), booming admissions, and climbing average daily census. As specialists in internal medicine already heavily involved in inpatient care, the Brockie Internal Medical Group was York Hospital’s obvious choice to pioneer a hospital medicine program. Five Brockie physicians chose to join the newly minted inpatient hospital group (the Brockie Hospitalist Group), with four others continuing outpatient care. Over time, seven more hospitalists came on board, with more anticipated in late 2006 through mid-2007.
Part of the York Hospital mindset is that the demand for inpatient services would keep climbing as the community continued to attract newcomers. An unanticipated consequence of having a hospital medicine program was that outpatient practices quickly grew by 20% because they had offloaded their hospital work, in turn generating more hospital admissions. Brockie and York leaders, recognizing the possibility of stress and burnout on hospitalists as their volume of work grew, took steps to avert problems. “We’re in a sustained growth mode and we need the hospitalists to be satisfied with their compensation and schedules to be able to recruit new physicians,” says Dr. McConville. “Hospital administration underwrites the hospitalist program’s shortfall so that we can pay [the hospitalists] a salary commensurate with MGMA [Medical Group Management Association] guidelines plus productivity. It’s a substantial amount annually and well worth it,” he adds.
Unlike many hospitalist programs, York Hospital’s did not arise because physicians wanted to avoid driving to the hospital to make rounds. “Some groups are five minutes away and they gave us their inpatient work, while a group that’s 45 minutes away still does hospital rounds. What drives physicians here is their view of continuity of care,” says Dr. McConville.
Brockie is York’s only hospitalist group, although three other medical groups have hired two doctors to handle their inpatient work. “It’s not a problem for us. We don’t have a sense of competition,” says Dr. Whitney.
The Nuts and Bolts
Perhaps it’s Brockie’s long tenure as a medical group, its acquisition by WellSpan and the performance expectations that such an acquisition denotes, the thoroughness of its hospitalist leaders, or some combination of the above, but the hospitalists have their schedules and compensation calculations down pat.
Dr. Lamanteer spends much time and thought on the hospitalists’ compensation package. He studies national salary data and factors them into a sophisticated system of relative value units (RVUs) and case-based data to maintain a “competitive compensation package that provides incentives for both our physicians and the hospital to balance productivity with keeping length of stay in check,” he says. That’s not as easy as he makes it sound, because bumping up RVUs and volume has to be balanced with a length of stay that is both efficient and safe for patients.
Compensation begins with base salary—either Level I for 132 hours or Level II for 147 hours over three weeks. Productivity bonuses start with one point awarded for each admission, discharge, consult, and ED evaluation. Point values are then adjusted for average professional revenue generated per patient. The threshold for bonus pay is 806 points. Additionally, three clinical performance criteria, chosen annually, impact the bonus. For example, recent targets include ordering a tentative discharge time one or more days in advance (>65%), abiding by the “do not use” abbreviation list created by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) (>90%), and complying with diagnostic coding rules (>75% accuracy).
The hospitalists’ schedule is challenging, particularly for doctors way past residency, involving 8 a.m. to 10 p.m. shifts on a three-week cycle that starts on a Friday. Physicians work eight 14-hour days, followed by a weekend off, then five days on (Monday-Friday) and six days off (Saturday-Thursday). The hospitalists don’t routinely cover night call. A full-time nocturnist, who started in 1992, and moonlighters cover the 10 p.m. to 8 a.m. shift seven days a week, with hospitalists covering only for major emergencies.
Avoiding Burnout
York Hospital’s ED and a cap on residents’ hours keep the Brockie hospitalists busy. But, early in 2005, it looked as if the workload had reached a plateau. Although Dr. Whitney suspected that the breather wouldn’t last, the group had no evidence that the tempo would increase and voted to maintain the number of hospitalists. The tempo picked up.
“We had estimated an 11 percent growth in RVUs, which actually grew by 23 percent last year,” says Dr. Whitney. Then a large primary care group agreed to shift its inpatient work to Brockie in 2006. Dr. Whitney estimated that assuming that practice’s hospital patients would add 5,000 RVUs and 600 more admissions.
“We realized we could approach a point of stress and burnout with the increased workload, so we recruited two new hospitalists,” says Dr. Whitney.
Still, the hospitalists face a balancing act of census peaks and valleys. “The variations with census and admissions go well beyond the bell curve,” says Whitney, who prepares for crunches by finding volunteers among the hospitalists to cover unexpected peaks.
If Brockie sounds like a Harvard case study on hospitalist medicine, it should. Its long tenure, physician leadership, and administrative support have shaped the business practices that facilitated the program’s growth. For one, the sophisticated compensation/productivity scheme didn’t come about by accident. Dr. McConville, a representative of WellSpan’s medical service line, meets with three Brockie hospitalists to fine-tune the program’s metrics. QI measures that are newly written each year, regular individual feedback, and inclusion of evidence-based guidelines contribute to measures and practices that address many of hospital medicine’s problems.
A Big Step to Little Things
But Brockie isn’t perfect. The responsibility of 24/7 coverage and 14-hour days allows little things to fall through the cracks—things like finding the time to promote the hospitalist service on the Web site, getting new formulary updates out quickly, and immediately informing all of those concerned that a patient has died. Brockie has addressed those and other issues that are the mortar to the bricks of a hospitalist practice by hiring David Orskey, an ex-Navy corpsman, as its senior practice manager in July 2006.
Orskey, co-chair of the medical group’s process improvement committee, sees his work as finding efficiencies, working for better care, and increasing patient satisfaction, plus attending to the budget and human resources issues and networking with outpatient practices.
“Twenty-one years in Navy medicine prepared me for this job,” says Orskey. “I’m enjoying this community, which has everything from farmland to executive homes and an influx of Hispanic migrants.”
He’s able to focus on both the details and the big picture, such as making sure that everyone works toward implementing and using the electronic medical record and improving after-hours answering services, as well as refining credentialing and risk management.
LTAC Unit
Brockie’s hospitalists also serve Mechanicsburg, Pa.,-based Select Medical Corporation’s long-term acute care (LTAC) unit, a 30-bed unit within York Hospital that supports patients needing a bridge between an acute hospital and skilled nursing care. The patients run the gamut in their needs—some have pulmonary/ventilator issues; others present medically complex situations such as heart failure, multi-system organ impairment, and cancer; some are neurosurgical/post trauma; and others need specialized wound care.
Dr. Whitney explains that all Brockie hospitalists add the LTAC to their rounds, usually leaving them for the end of the day, when the physicians can better attend to their complex situations. “Many of these patients are older, have been in the ICU with complicated medical issues, and face weeks of care in the LTAC before they can go to a nursing home or another long-term care setting,” he says. “It’s a whole different LOS, and it’s good that we have the LTAC because it reduces the hospital’s burden of caring for them as acute patients, when they really need what the LTAC offers.”
Conclusion
Dr. Lamanteer keeps an eye on the Brockie hospitalists’ future. “It’s clear that we benefit patients, that we provide excellent care, and that we need a large subsidy to do it,” he says. And the big picture means keeping focused on the peaks and valleys of admissions and wondering how volume will grow in the next ten years. He’d like to limit the number of 14-hour shifts to help physicians avoid burnout and to limit weekend duty to one out of three (sustainable) or one out of four (heaven). TH
Marlene Piturro is based in New York.
More than 20 years before the term hospitalist was coined, the Brockie Medical Group, a strong internal medicine practice led by Benjamin Hoover, MD, relished its hospital work at York Hospital in York, Pa. Back then, the doctors didn’t call themselves hospitalists, but the time they spent on hospital duties made them the forebears of today’s hospitalists.
According to John McConville, MD, chairman of York Hospital’s department of medicine and a hospital fixture since 1976, some of Brockie Internal Medicine group’s physicians devoted 60% to 70% of their practice time to inpatient tasks. “That was the culture when I arrived on the scene,” he recounts. Shortly thereafter, the group grew stronger when The Brockie Internal Medicine Group’s main competition—a sizable family practice group—fell apart. Brockie absorbed its like-minded physicians.
York, pa.
The Brockie Internal Medical Group is firmly anchored in York, Pa., home to factories that produce barbells and Harley-Davidson motorcycles. York has a soft side, though—it produced the first Peppermint Pattie, a mint-chocolate candy. It is an affordable, rapidly growing suburb, a place where commuters to Philadelphia, Baltimore, and Washington, D.C., can have a comfortable lifestyle without big city housing prices and the hassles of urban life.
The medical community is close-knit, described by Jonathan Whitney, MD, a Brockie hospitalist leader, as “a collegial environment with a growing population and plenty of patients, so there’s not a sense of competition among physicians.” Dr. Whitney, along with William “Tex” Landis, MD, and Michael Lamanteer, MD, form the Brockie Hospitalist Group’s executive committee, elected decision makers who deal with WellSpan Health and York Hospital on behalf of their colleagues.
WellSpan’s Role
As York grew, so did the Brockie Internal Medical Group. Then came managed care in the 1980s and 1990s, and Brockie’s internists were not happy. “We saw the medical landscape changing everywhere, and we didn’t want managed care pushing us around,” explains Dr. Landis, a Lancaster, Pa., native and now the Brockie Hospitalist Group’s lead physician. “Analyzing how medicine was changing, we felt vulnerable as a single specialty group. We considered various scenarios for becoming a multi-specialty practice, but decided that wasn’t right for us.”
So, in 1995, five group partners decided to sell the practice to WellSpan Health, an integrated nonprofit healthcare system located in South Central Pennsylvania. Their expectation? That WellSpan’s administrative support and financial muscle would protect them against managed care’s encroachment.
Affiliating with WellSpan Health aligned Brockie with the medical services line of York Hospital, providing the administrative support they needed to grow and thrive. Working together, Brockie’s medical leaders and WellSpan administrators oversee the following areas: strategic planning; budgeting, compensation, benefits, and incentives; collections and coding; care management and performance improvement; recruiting and other personnel issues; and scheduling and coverage.
The Hospitalist Program
York Hospital and its surrounding community continued to grow, as did the need for more office-based and inpatient physician services. By 2001, York Hospital’s top executives recognized that a dedicated hospitalist group was the best solution for its overflowing emergency department (ED), booming admissions, and climbing average daily census. As specialists in internal medicine already heavily involved in inpatient care, the Brockie Internal Medical Group was York Hospital’s obvious choice to pioneer a hospital medicine program. Five Brockie physicians chose to join the newly minted inpatient hospital group (the Brockie Hospitalist Group), with four others continuing outpatient care. Over time, seven more hospitalists came on board, with more anticipated in late 2006 through mid-2007.
Part of the York Hospital mindset is that the demand for inpatient services would keep climbing as the community continued to attract newcomers. An unanticipated consequence of having a hospital medicine program was that outpatient practices quickly grew by 20% because they had offloaded their hospital work, in turn generating more hospital admissions. Brockie and York leaders, recognizing the possibility of stress and burnout on hospitalists as their volume of work grew, took steps to avert problems. “We’re in a sustained growth mode and we need the hospitalists to be satisfied with their compensation and schedules to be able to recruit new physicians,” says Dr. McConville. “Hospital administration underwrites the hospitalist program’s shortfall so that we can pay [the hospitalists] a salary commensurate with MGMA [Medical Group Management Association] guidelines plus productivity. It’s a substantial amount annually and well worth it,” he adds.
Unlike many hospitalist programs, York Hospital’s did not arise because physicians wanted to avoid driving to the hospital to make rounds. “Some groups are five minutes away and they gave us their inpatient work, while a group that’s 45 minutes away still does hospital rounds. What drives physicians here is their view of continuity of care,” says Dr. McConville.
Brockie is York’s only hospitalist group, although three other medical groups have hired two doctors to handle their inpatient work. “It’s not a problem for us. We don’t have a sense of competition,” says Dr. Whitney.
The Nuts and Bolts
Perhaps it’s Brockie’s long tenure as a medical group, its acquisition by WellSpan and the performance expectations that such an acquisition denotes, the thoroughness of its hospitalist leaders, or some combination of the above, but the hospitalists have their schedules and compensation calculations down pat.
Dr. Lamanteer spends much time and thought on the hospitalists’ compensation package. He studies national salary data and factors them into a sophisticated system of relative value units (RVUs) and case-based data to maintain a “competitive compensation package that provides incentives for both our physicians and the hospital to balance productivity with keeping length of stay in check,” he says. That’s not as easy as he makes it sound, because bumping up RVUs and volume has to be balanced with a length of stay that is both efficient and safe for patients.
Compensation begins with base salary—either Level I for 132 hours or Level II for 147 hours over three weeks. Productivity bonuses start with one point awarded for each admission, discharge, consult, and ED evaluation. Point values are then adjusted for average professional revenue generated per patient. The threshold for bonus pay is 806 points. Additionally, three clinical performance criteria, chosen annually, impact the bonus. For example, recent targets include ordering a tentative discharge time one or more days in advance (>65%), abiding by the “do not use” abbreviation list created by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) (>90%), and complying with diagnostic coding rules (>75% accuracy).
The hospitalists’ schedule is challenging, particularly for doctors way past residency, involving 8 a.m. to 10 p.m. shifts on a three-week cycle that starts on a Friday. Physicians work eight 14-hour days, followed by a weekend off, then five days on (Monday-Friday) and six days off (Saturday-Thursday). The hospitalists don’t routinely cover night call. A full-time nocturnist, who started in 1992, and moonlighters cover the 10 p.m. to 8 a.m. shift seven days a week, with hospitalists covering only for major emergencies.
Avoiding Burnout
York Hospital’s ED and a cap on residents’ hours keep the Brockie hospitalists busy. But, early in 2005, it looked as if the workload had reached a plateau. Although Dr. Whitney suspected that the breather wouldn’t last, the group had no evidence that the tempo would increase and voted to maintain the number of hospitalists. The tempo picked up.
“We had estimated an 11 percent growth in RVUs, which actually grew by 23 percent last year,” says Dr. Whitney. Then a large primary care group agreed to shift its inpatient work to Brockie in 2006. Dr. Whitney estimated that assuming that practice’s hospital patients would add 5,000 RVUs and 600 more admissions.
“We realized we could approach a point of stress and burnout with the increased workload, so we recruited two new hospitalists,” says Dr. Whitney.
Still, the hospitalists face a balancing act of census peaks and valleys. “The variations with census and admissions go well beyond the bell curve,” says Whitney, who prepares for crunches by finding volunteers among the hospitalists to cover unexpected peaks.
If Brockie sounds like a Harvard case study on hospitalist medicine, it should. Its long tenure, physician leadership, and administrative support have shaped the business practices that facilitated the program’s growth. For one, the sophisticated compensation/productivity scheme didn’t come about by accident. Dr. McConville, a representative of WellSpan’s medical service line, meets with three Brockie hospitalists to fine-tune the program’s metrics. QI measures that are newly written each year, regular individual feedback, and inclusion of evidence-based guidelines contribute to measures and practices that address many of hospital medicine’s problems.
A Big Step to Little Things
But Brockie isn’t perfect. The responsibility of 24/7 coverage and 14-hour days allows little things to fall through the cracks—things like finding the time to promote the hospitalist service on the Web site, getting new formulary updates out quickly, and immediately informing all of those concerned that a patient has died. Brockie has addressed those and other issues that are the mortar to the bricks of a hospitalist practice by hiring David Orskey, an ex-Navy corpsman, as its senior practice manager in July 2006.
Orskey, co-chair of the medical group’s process improvement committee, sees his work as finding efficiencies, working for better care, and increasing patient satisfaction, plus attending to the budget and human resources issues and networking with outpatient practices.
“Twenty-one years in Navy medicine prepared me for this job,” says Orskey. “I’m enjoying this community, which has everything from farmland to executive homes and an influx of Hispanic migrants.”
He’s able to focus on both the details and the big picture, such as making sure that everyone works toward implementing and using the electronic medical record and improving after-hours answering services, as well as refining credentialing and risk management.
LTAC Unit
Brockie’s hospitalists also serve Mechanicsburg, Pa.,-based Select Medical Corporation’s long-term acute care (LTAC) unit, a 30-bed unit within York Hospital that supports patients needing a bridge between an acute hospital and skilled nursing care. The patients run the gamut in their needs—some have pulmonary/ventilator issues; others present medically complex situations such as heart failure, multi-system organ impairment, and cancer; some are neurosurgical/post trauma; and others need specialized wound care.
Dr. Whitney explains that all Brockie hospitalists add the LTAC to their rounds, usually leaving them for the end of the day, when the physicians can better attend to their complex situations. “Many of these patients are older, have been in the ICU with complicated medical issues, and face weeks of care in the LTAC before they can go to a nursing home or another long-term care setting,” he says. “It’s a whole different LOS, and it’s good that we have the LTAC because it reduces the hospital’s burden of caring for them as acute patients, when they really need what the LTAC offers.”
Conclusion
Dr. Lamanteer keeps an eye on the Brockie hospitalists’ future. “It’s clear that we benefit patients, that we provide excellent care, and that we need a large subsidy to do it,” he says. And the big picture means keeping focused on the peaks and valleys of admissions and wondering how volume will grow in the next ten years. He’d like to limit the number of 14-hour shifts to help physicians avoid burnout and to limit weekend duty to one out of three (sustainable) or one out of four (heaven). TH
Marlene Piturro is based in New York.
More than 20 years before the term hospitalist was coined, the Brockie Medical Group, a strong internal medicine practice led by Benjamin Hoover, MD, relished its hospital work at York Hospital in York, Pa. Back then, the doctors didn’t call themselves hospitalists, but the time they spent on hospital duties made them the forebears of today’s hospitalists.
According to John McConville, MD, chairman of York Hospital’s department of medicine and a hospital fixture since 1976, some of Brockie Internal Medicine group’s physicians devoted 60% to 70% of their practice time to inpatient tasks. “That was the culture when I arrived on the scene,” he recounts. Shortly thereafter, the group grew stronger when The Brockie Internal Medicine Group’s main competition—a sizable family practice group—fell apart. Brockie absorbed its like-minded physicians.
York, pa.
The Brockie Internal Medical Group is firmly anchored in York, Pa., home to factories that produce barbells and Harley-Davidson motorcycles. York has a soft side, though—it produced the first Peppermint Pattie, a mint-chocolate candy. It is an affordable, rapidly growing suburb, a place where commuters to Philadelphia, Baltimore, and Washington, D.C., can have a comfortable lifestyle without big city housing prices and the hassles of urban life.
The medical community is close-knit, described by Jonathan Whitney, MD, a Brockie hospitalist leader, as “a collegial environment with a growing population and plenty of patients, so there’s not a sense of competition among physicians.” Dr. Whitney, along with William “Tex” Landis, MD, and Michael Lamanteer, MD, form the Brockie Hospitalist Group’s executive committee, elected decision makers who deal with WellSpan Health and York Hospital on behalf of their colleagues.
WellSpan’s Role
As York grew, so did the Brockie Internal Medical Group. Then came managed care in the 1980s and 1990s, and Brockie’s internists were not happy. “We saw the medical landscape changing everywhere, and we didn’t want managed care pushing us around,” explains Dr. Landis, a Lancaster, Pa., native and now the Brockie Hospitalist Group’s lead physician. “Analyzing how medicine was changing, we felt vulnerable as a single specialty group. We considered various scenarios for becoming a multi-specialty practice, but decided that wasn’t right for us.”
So, in 1995, five group partners decided to sell the practice to WellSpan Health, an integrated nonprofit healthcare system located in South Central Pennsylvania. Their expectation? That WellSpan’s administrative support and financial muscle would protect them against managed care’s encroachment.
Affiliating with WellSpan Health aligned Brockie with the medical services line of York Hospital, providing the administrative support they needed to grow and thrive. Working together, Brockie’s medical leaders and WellSpan administrators oversee the following areas: strategic planning; budgeting, compensation, benefits, and incentives; collections and coding; care management and performance improvement; recruiting and other personnel issues; and scheduling and coverage.
The Hospitalist Program
York Hospital and its surrounding community continued to grow, as did the need for more office-based and inpatient physician services. By 2001, York Hospital’s top executives recognized that a dedicated hospitalist group was the best solution for its overflowing emergency department (ED), booming admissions, and climbing average daily census. As specialists in internal medicine already heavily involved in inpatient care, the Brockie Internal Medical Group was York Hospital’s obvious choice to pioneer a hospital medicine program. Five Brockie physicians chose to join the newly minted inpatient hospital group (the Brockie Hospitalist Group), with four others continuing outpatient care. Over time, seven more hospitalists came on board, with more anticipated in late 2006 through mid-2007.
Part of the York Hospital mindset is that the demand for inpatient services would keep climbing as the community continued to attract newcomers. An unanticipated consequence of having a hospital medicine program was that outpatient practices quickly grew by 20% because they had offloaded their hospital work, in turn generating more hospital admissions. Brockie and York leaders, recognizing the possibility of stress and burnout on hospitalists as their volume of work grew, took steps to avert problems. “We’re in a sustained growth mode and we need the hospitalists to be satisfied with their compensation and schedules to be able to recruit new physicians,” says Dr. McConville. “Hospital administration underwrites the hospitalist program’s shortfall so that we can pay [the hospitalists] a salary commensurate with MGMA [Medical Group Management Association] guidelines plus productivity. It’s a substantial amount annually and well worth it,” he adds.
Unlike many hospitalist programs, York Hospital’s did not arise because physicians wanted to avoid driving to the hospital to make rounds. “Some groups are five minutes away and they gave us their inpatient work, while a group that’s 45 minutes away still does hospital rounds. What drives physicians here is their view of continuity of care,” says Dr. McConville.
Brockie is York’s only hospitalist group, although three other medical groups have hired two doctors to handle their inpatient work. “It’s not a problem for us. We don’t have a sense of competition,” says Dr. Whitney.
The Nuts and Bolts
Perhaps it’s Brockie’s long tenure as a medical group, its acquisition by WellSpan and the performance expectations that such an acquisition denotes, the thoroughness of its hospitalist leaders, or some combination of the above, but the hospitalists have their schedules and compensation calculations down pat.
Dr. Lamanteer spends much time and thought on the hospitalists’ compensation package. He studies national salary data and factors them into a sophisticated system of relative value units (RVUs) and case-based data to maintain a “competitive compensation package that provides incentives for both our physicians and the hospital to balance productivity with keeping length of stay in check,” he says. That’s not as easy as he makes it sound, because bumping up RVUs and volume has to be balanced with a length of stay that is both efficient and safe for patients.
Compensation begins with base salary—either Level I for 132 hours or Level II for 147 hours over three weeks. Productivity bonuses start with one point awarded for each admission, discharge, consult, and ED evaluation. Point values are then adjusted for average professional revenue generated per patient. The threshold for bonus pay is 806 points. Additionally, three clinical performance criteria, chosen annually, impact the bonus. For example, recent targets include ordering a tentative discharge time one or more days in advance (>65%), abiding by the “do not use” abbreviation list created by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) (>90%), and complying with diagnostic coding rules (>75% accuracy).
The hospitalists’ schedule is challenging, particularly for doctors way past residency, involving 8 a.m. to 10 p.m. shifts on a three-week cycle that starts on a Friday. Physicians work eight 14-hour days, followed by a weekend off, then five days on (Monday-Friday) and six days off (Saturday-Thursday). The hospitalists don’t routinely cover night call. A full-time nocturnist, who started in 1992, and moonlighters cover the 10 p.m. to 8 a.m. shift seven days a week, with hospitalists covering only for major emergencies.
Avoiding Burnout
York Hospital’s ED and a cap on residents’ hours keep the Brockie hospitalists busy. But, early in 2005, it looked as if the workload had reached a plateau. Although Dr. Whitney suspected that the breather wouldn’t last, the group had no evidence that the tempo would increase and voted to maintain the number of hospitalists. The tempo picked up.
“We had estimated an 11 percent growth in RVUs, which actually grew by 23 percent last year,” says Dr. Whitney. Then a large primary care group agreed to shift its inpatient work to Brockie in 2006. Dr. Whitney estimated that assuming that practice’s hospital patients would add 5,000 RVUs and 600 more admissions.
“We realized we could approach a point of stress and burnout with the increased workload, so we recruited two new hospitalists,” says Dr. Whitney.
Still, the hospitalists face a balancing act of census peaks and valleys. “The variations with census and admissions go well beyond the bell curve,” says Whitney, who prepares for crunches by finding volunteers among the hospitalists to cover unexpected peaks.
If Brockie sounds like a Harvard case study on hospitalist medicine, it should. Its long tenure, physician leadership, and administrative support have shaped the business practices that facilitated the program’s growth. For one, the sophisticated compensation/productivity scheme didn’t come about by accident. Dr. McConville, a representative of WellSpan’s medical service line, meets with three Brockie hospitalists to fine-tune the program’s metrics. QI measures that are newly written each year, regular individual feedback, and inclusion of evidence-based guidelines contribute to measures and practices that address many of hospital medicine’s problems.
A Big Step to Little Things
But Brockie isn’t perfect. The responsibility of 24/7 coverage and 14-hour days allows little things to fall through the cracks—things like finding the time to promote the hospitalist service on the Web site, getting new formulary updates out quickly, and immediately informing all of those concerned that a patient has died. Brockie has addressed those and other issues that are the mortar to the bricks of a hospitalist practice by hiring David Orskey, an ex-Navy corpsman, as its senior practice manager in July 2006.
Orskey, co-chair of the medical group’s process improvement committee, sees his work as finding efficiencies, working for better care, and increasing patient satisfaction, plus attending to the budget and human resources issues and networking with outpatient practices.
“Twenty-one years in Navy medicine prepared me for this job,” says Orskey. “I’m enjoying this community, which has everything from farmland to executive homes and an influx of Hispanic migrants.”
He’s able to focus on both the details and the big picture, such as making sure that everyone works toward implementing and using the electronic medical record and improving after-hours answering services, as well as refining credentialing and risk management.
LTAC Unit
Brockie’s hospitalists also serve Mechanicsburg, Pa.,-based Select Medical Corporation’s long-term acute care (LTAC) unit, a 30-bed unit within York Hospital that supports patients needing a bridge between an acute hospital and skilled nursing care. The patients run the gamut in their needs—some have pulmonary/ventilator issues; others present medically complex situations such as heart failure, multi-system organ impairment, and cancer; some are neurosurgical/post trauma; and others need specialized wound care.
Dr. Whitney explains that all Brockie hospitalists add the LTAC to their rounds, usually leaving them for the end of the day, when the physicians can better attend to their complex situations. “Many of these patients are older, have been in the ICU with complicated medical issues, and face weeks of care in the LTAC before they can go to a nursing home or another long-term care setting,” he says. “It’s a whole different LOS, and it’s good that we have the LTAC because it reduces the hospital’s burden of caring for them as acute patients, when they really need what the LTAC offers.”
Conclusion
Dr. Lamanteer keeps an eye on the Brockie hospitalists’ future. “It’s clear that we benefit patients, that we provide excellent care, and that we need a large subsidy to do it,” he says. And the big picture means keeping focused on the peaks and valleys of admissions and wondering how volume will grow in the next ten years. He’d like to limit the number of 14-hour shifts to help physicians avoid burnout and to limit weekend duty to one out of three (sustainable) or one out of four (heaven). TH
Marlene Piturro is based in New York.
Brazil Blossoms
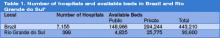
The establishment of a hospital medicine program in Brazil and the attempt to develop the specialty nationwide is both fascinating and challenging. Brazil has about 7,155 hospitals, with 443,210 beds available (including 2,727 public hospitals with 148,966 beds and 4,428 private facilities with 294,244 beds). 1 (See Table 1, p. 44.)
Historical problems in the public health system—also found in private sectors—have motivated physicians to address and improve inefficient management, insufficient financial support, the high number of frequent unnecessary admissions and re-admissions, extended length of stays, limited access to beds and medical services of high complexity, and overcrowded emergency departments.
SUS—Principles and Problems
The Brazilian public health system, called Sistema Único de Saúde, or SUS, is based on universal care and health as a right of citizenship and a state responsibility. Its main principles are universality, integrality, equity, decentralization, and social control.2 Less than half of the Brazilian population uses the SUS system exclusively. They use private health systems as a complement. This situation reflects the difficulties in the Brazilian public health system. The reasons for this duplicity highlight the challenges of our situation.
At the same time, physicians face serious problems. Most are employed by both the public and private sectors. Average salaries in the public system (by far the largest employer) are extremely low. Medical doctors are forced to work many extra hours, including numerous night shifts, creating a major barrier to the growth of physicians dedicated to horizontal inpatient care.
The government, in an attempt to improve medical—and hospital—assistance in the country with “a new kind of health assistance focused on high quality and efficient services,” has created the following projects: Humaniza SUS and QualiSUS.3,4 Theoretical support, operational contours, extent, and applicability are still not clear, however. For many medical doctors, these are merely abstract ideas. QualiSUS has renovated emergency departments in Brazil, but service quality has not improved enough. In our opinion, there are no public policies capable of providing good hospital services and efficient management in Brazilian hospitals, and—even if they existed—we would need to stop corruption in order to meet public commitments.
In Rio Grande do Sul, the Brazilian state where we work as medical doctors, the inadequate SUS reimbursement points to a calamitous future. Here, most hospital care is provided by philanthropic hospitals, which are more vulnerable in financial terms.5 (See Table 2, p. 44.) Despite being in a pioneer state in terms of hospital administration schools, with more than 2,000 graduates in recent years, these philanthropic hospitals have an estimated reimbursement deficit of more than 80%, an unattainable amount even for the best administrator.
Could Hospitalists Be Part of a Solution?
On top of these growing deficits, we have witnessed the closing of more than 2,000 available beds in the last four years, as well as the loss of 10,000 hospital positions and the complete closing of eight hospitals. Aiming to ensure the survival of this hospital system, physicians, health professionals, and organizations involved with hospitals have joined forces to find a solution. Their logo is best translated as “More Health for the Hospitals,” and our group supports their goals.6
Looking at the situation from a different perspective, we see many opportunities for Brazilian hospitalists. Their potential contribution to the quality and safety of medical care is an obvious advantage for hospital management and patients. We predict that this scenario can be accomplished—even in our state. It is possible to make a profit in public as well as in lucrative private institutions. In public institutions, a profit can be made as long as hospital administrators use adequate policy. We believe that in private institutions, though not in philanthropic ones, the key point is hospital administration cooperation and goodwill. Elucidation of hospitalists’ capabilities will open the necessary doors. We are ready to reduce the hospitalization fee and length of stay—among other costs. In this way, we can work with the administrator to develop tools for systems and quality improvements.
Hospital Medicine’s Emergence in Brazil
The implementation of hospital medicine, especially those aspects that involve more than just having a general medicine physician dealing with inpatient care, is brand new in Brazil. So far, the U.S. hospitalist model of care is unfamiliar to most Brazilian medical doctors and healthcare managers. Some institutions have hired hospitalists to be part of rapid response teams, neglecting the more specialized dimension of this new model of care; they are not aware of this title’s real meaning. There is a long way to go until the hospitalist is seen as a specialist, and we hope all our efforts will earn this new specialty official recognition in Brazil.
Our group is based in the Brazilian state of Rio Grande do Sul, mainly in Porto Alegre, its capital. Most of our time is dedicated to inpatient care, and we started our movement after studying the model of care delineated by Wachter and Lee.7-9 In 2005, we formed a local association called GEAMH (Grupo de Estudos e Atualização em Medicina Hospitalar) to promote the understanding and diffusion of hospitalist principles, integrated by the professors and former and current residents of a large local internal medicine residence program from the Internal Medicine Department of Nossa Senhora da Conceição Hospital (HNSC).
We have created a Web site (www.medicinahospitalar.com.br) where you can find history, news, and information about hospital medicine fellowships in the United States, as well as online hospital medicine continuing education. As you can see, we are spreading SHM’s ideas.
The third year of the HNSC Internal Medicine Residence Program (R3) focused on hospital medicine was developed in 2005. We believe this to be the first initiative of its kind in Brazil. HNSC is part of Conceição Hospital Group, which is composed of four hospital units and is one of the biggest public hospital networks in Brazil.
The Internal Medicine Residence Program started at HNSC in 1968. The department itself has more than 100 hospital beds. Medical residents’ activities all take place in the hospital, and there are nine professors: Eduardo Fernandes, Guilherme Barcellos, Janete Brauner, José Luiz F. Soares, Nelson Roessler, Paulo Almeida, Paulo Ricardo Cardoso, Sergio Dedavid, and Sergio Prezzi. We would like to make special mention of our colleagues Eduardo Fernandes, current head of HNSC Internal Medicine Medical Residence Program, and Sergio Prezzi, the R3 coordinator.
The HNSC Internal Medicine Service is well known for graduating internists skilled in hospital practices, mainly because the program is run by professors who specialize in that area. The R3 is a one-year training program. Our goal is to train physicians to provide outstanding and comprehensive inpatient care. Through supervised training, our residents are able to treat common hospital illnesses; we are also training them in consultative medicine and in the clinical management of surgical patients. Other areas of medical residents’ education include medical ethics, end-of-life care, inpatient nutritional support, risk management, rational use of drugs, and technology and evidence-based medicine.
Our third-year residents have the opportunity to try bone marrow biopsy, pleural biopsy, and thorax draining—all of which are usually handled by other medical specialists. In general, residents also have many opportunities to learn about and practice endotracheal intubations, ventilator management, central vein access, and many other procedures.
Based on HNSC experience, a formal stage in hospital medicine under the supervision of Luciano Bauer Grohs, MD, one of the founders of GEAMH, has also been integrated into internal medicine training at Nossa Senhora de Pompéia Hospital in the city of Caxias do Sul, located 125 kilometers from Porto Alegre.
Our group has developed medical education in the inpatient setting. Because there is no hospital medicine society in Brazil, we have tried to coordinate with the Brazilian Society of Internal Medicine, encouraging discussions about hospital care and promoting workshops about mechanical ventilation, central vein access, and early goal-directed therapy for sepsis. More recently, we have chosen to work independently, believing that hospital medicine is distinct from internal medicine.
When we organized the Brazilian Annual Congress of Medical Residents in 2006, we had the opportunity to bring together medical residents and professors from different medical areas. The Congress’ main focuses were rational use of drugs and technology and the relationship between the young physician and the pharmaceutical industry. The participation of Robert Goodman (of No Free Lunch fame) was an important part of the convention.10
Slow and Steady Growth
We understand that there is a long journey ahead, beyond educational and medical assistance. Our group is still far from promoting research. But hospital medicine specialization has launched in Brazil. Dr. Watcher has said to us, “In the United States, the hospitalist field is the fastest growing specialty in the country—and probably in the history of the country. Hospitalists are transforming the delivery of American hospital care and improving quality, patient safety, education, end-of-life care, and more. We are thrilled to partner with our Brazilian colleagues as, together, we try to improve the quality of care for hospitalized patients everywhere.” We are confident that his vision will become a reality in Brazil in the near future. TH
Note: We are in debt to the professors at the Hospital Conceição Internal Medicine Residency Program, without whom our initiatives would never have blossomed. Special thanks to Eduardo Fernandes, Sergio Prezzi, and Paulo Ricardo Cardoso.
Dr. Barcellos is a specialist in internal medicine, emergency medicine, and critical care. He is professor in Nossa Senhora da Conceição Hospital’s Hospital Medicine Residence Program and president of GEAMH, a local association designed to promote the understanding and diffusion of hospitalist principles.
Dr. Wajner is a specialist in internal medicine and emergency medicine and a Master of Science student at Universidade Federal do Rio Grande do Sul.
Dr. de Waldemar is a specialist in internal medicine and emergency medicine.
References
- Departamento de População e Indicadores Sociais. Estatísticas da saúde: assistência médico-sanitária 2005/IBGE. Departamento de População e Indicadores Sociais. 2006. Available at: www.ibge.gov.br/home/estatistica/populacao/condicaodevida/ams/2005/ams2005.pdf. Last accessed January 28, 2007.
- Agência Nacional de Vigilância Sanitária. Lei nº 8080. D.O.U. - Diário Oficial da União; Poder Executivo. September 20, 1990. Available at: http://e-legis.bvs.br/leisref/public/showAct.php?id=16619&word=. Last accessed January 28, 2007.
- Brazilian Ministry of Health Web site. Available at: http://portal.saude.gov.br/saude. Last accessed January 28, 2007.
- Deslandes SF. Análise do discurso oficial sobre a humanização da assistência hospitalar. Ciência e saúde coletiva. 2004;9:7-14. Available at: www.scielo.br/pdf/csc/v9n1/19819.pdf. Last ccessed January 28, 2007.
- Portela MC, Lima SML, Barbosa PR, et al. Caracterização assistencial de hospitais filantrópicos no Brasil. Rev Saúde Pública. 2004;38:811-818. Available at: www.scielo.br/pdf/rsp/v38n6/09.pdf. Last accessed January 28, 2007.
- Sindicato Médico do Rio Grande do Sul Web site. Available at: www.simers.org.br/entquerem.php. Last accessed January 28, 2007.
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996 Aug 15;335(7):514-517.
- Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002 Feb 16;287:487–494. Review.
- Wachter RM. An introduction to the hospitalist model. Ann Intern Med. 1999 Feb 16;130(4 Pt 2):338–342.
- No Free Lunch Web site. Available at: www.nofreelunch.org. Last accessed January 28, 2007.
The establishment of a hospital medicine program in Brazil and the attempt to develop the specialty nationwide is both fascinating and challenging. Brazil has about 7,155 hospitals, with 443,210 beds available (including 2,727 public hospitals with 148,966 beds and 4,428 private facilities with 294,244 beds). 1 (See Table 1, p. 44.)
Historical problems in the public health system—also found in private sectors—have motivated physicians to address and improve inefficient management, insufficient financial support, the high number of frequent unnecessary admissions and re-admissions, extended length of stays, limited access to beds and medical services of high complexity, and overcrowded emergency departments.
SUS—Principles and Problems
The Brazilian public health system, called Sistema Único de Saúde, or SUS, is based on universal care and health as a right of citizenship and a state responsibility. Its main principles are universality, integrality, equity, decentralization, and social control.2 Less than half of the Brazilian population uses the SUS system exclusively. They use private health systems as a complement. This situation reflects the difficulties in the Brazilian public health system. The reasons for this duplicity highlight the challenges of our situation.
At the same time, physicians face serious problems. Most are employed by both the public and private sectors. Average salaries in the public system (by far the largest employer) are extremely low. Medical doctors are forced to work many extra hours, including numerous night shifts, creating a major barrier to the growth of physicians dedicated to horizontal inpatient care.
The government, in an attempt to improve medical—and hospital—assistance in the country with “a new kind of health assistance focused on high quality and efficient services,” has created the following projects: Humaniza SUS and QualiSUS.3,4 Theoretical support, operational contours, extent, and applicability are still not clear, however. For many medical doctors, these are merely abstract ideas. QualiSUS has renovated emergency departments in Brazil, but service quality has not improved enough. In our opinion, there are no public policies capable of providing good hospital services and efficient management in Brazilian hospitals, and—even if they existed—we would need to stop corruption in order to meet public commitments.
In Rio Grande do Sul, the Brazilian state where we work as medical doctors, the inadequate SUS reimbursement points to a calamitous future. Here, most hospital care is provided by philanthropic hospitals, which are more vulnerable in financial terms.5 (See Table 2, p. 44.) Despite being in a pioneer state in terms of hospital administration schools, with more than 2,000 graduates in recent years, these philanthropic hospitals have an estimated reimbursement deficit of more than 80%, an unattainable amount even for the best administrator.
Could Hospitalists Be Part of a Solution?
On top of these growing deficits, we have witnessed the closing of more than 2,000 available beds in the last four years, as well as the loss of 10,000 hospital positions and the complete closing of eight hospitals. Aiming to ensure the survival of this hospital system, physicians, health professionals, and organizations involved with hospitals have joined forces to find a solution. Their logo is best translated as “More Health for the Hospitals,” and our group supports their goals.6
Looking at the situation from a different perspective, we see many opportunities for Brazilian hospitalists. Their potential contribution to the quality and safety of medical care is an obvious advantage for hospital management and patients. We predict that this scenario can be accomplished—even in our state. It is possible to make a profit in public as well as in lucrative private institutions. In public institutions, a profit can be made as long as hospital administrators use adequate policy. We believe that in private institutions, though not in philanthropic ones, the key point is hospital administration cooperation and goodwill. Elucidation of hospitalists’ capabilities will open the necessary doors. We are ready to reduce the hospitalization fee and length of stay—among other costs. In this way, we can work with the administrator to develop tools for systems and quality improvements.
Hospital Medicine’s Emergence in Brazil
The implementation of hospital medicine, especially those aspects that involve more than just having a general medicine physician dealing with inpatient care, is brand new in Brazil. So far, the U.S. hospitalist model of care is unfamiliar to most Brazilian medical doctors and healthcare managers. Some institutions have hired hospitalists to be part of rapid response teams, neglecting the more specialized dimension of this new model of care; they are not aware of this title’s real meaning. There is a long way to go until the hospitalist is seen as a specialist, and we hope all our efforts will earn this new specialty official recognition in Brazil.
Our group is based in the Brazilian state of Rio Grande do Sul, mainly in Porto Alegre, its capital. Most of our time is dedicated to inpatient care, and we started our movement after studying the model of care delineated by Wachter and Lee.7-9 In 2005, we formed a local association called GEAMH (Grupo de Estudos e Atualização em Medicina Hospitalar) to promote the understanding and diffusion of hospitalist principles, integrated by the professors and former and current residents of a large local internal medicine residence program from the Internal Medicine Department of Nossa Senhora da Conceição Hospital (HNSC).
We have created a Web site (www.medicinahospitalar.com.br) where you can find history, news, and information about hospital medicine fellowships in the United States, as well as online hospital medicine continuing education. As you can see, we are spreading SHM’s ideas.
The third year of the HNSC Internal Medicine Residence Program (R3) focused on hospital medicine was developed in 2005. We believe this to be the first initiative of its kind in Brazil. HNSC is part of Conceição Hospital Group, which is composed of four hospital units and is one of the biggest public hospital networks in Brazil.
The Internal Medicine Residence Program started at HNSC in 1968. The department itself has more than 100 hospital beds. Medical residents’ activities all take place in the hospital, and there are nine professors: Eduardo Fernandes, Guilherme Barcellos, Janete Brauner, José Luiz F. Soares, Nelson Roessler, Paulo Almeida, Paulo Ricardo Cardoso, Sergio Dedavid, and Sergio Prezzi. We would like to make special mention of our colleagues Eduardo Fernandes, current head of HNSC Internal Medicine Medical Residence Program, and Sergio Prezzi, the R3 coordinator.
The HNSC Internal Medicine Service is well known for graduating internists skilled in hospital practices, mainly because the program is run by professors who specialize in that area. The R3 is a one-year training program. Our goal is to train physicians to provide outstanding and comprehensive inpatient care. Through supervised training, our residents are able to treat common hospital illnesses; we are also training them in consultative medicine and in the clinical management of surgical patients. Other areas of medical residents’ education include medical ethics, end-of-life care, inpatient nutritional support, risk management, rational use of drugs, and technology and evidence-based medicine.
Our third-year residents have the opportunity to try bone marrow biopsy, pleural biopsy, and thorax draining—all of which are usually handled by other medical specialists. In general, residents also have many opportunities to learn about and practice endotracheal intubations, ventilator management, central vein access, and many other procedures.
Based on HNSC experience, a formal stage in hospital medicine under the supervision of Luciano Bauer Grohs, MD, one of the founders of GEAMH, has also been integrated into internal medicine training at Nossa Senhora de Pompéia Hospital in the city of Caxias do Sul, located 125 kilometers from Porto Alegre.
Our group has developed medical education in the inpatient setting. Because there is no hospital medicine society in Brazil, we have tried to coordinate with the Brazilian Society of Internal Medicine, encouraging discussions about hospital care and promoting workshops about mechanical ventilation, central vein access, and early goal-directed therapy for sepsis. More recently, we have chosen to work independently, believing that hospital medicine is distinct from internal medicine.
When we organized the Brazilian Annual Congress of Medical Residents in 2006, we had the opportunity to bring together medical residents and professors from different medical areas. The Congress’ main focuses were rational use of drugs and technology and the relationship between the young physician and the pharmaceutical industry. The participation of Robert Goodman (of No Free Lunch fame) was an important part of the convention.10
Slow and Steady Growth
We understand that there is a long journey ahead, beyond educational and medical assistance. Our group is still far from promoting research. But hospital medicine specialization has launched in Brazil. Dr. Watcher has said to us, “In the United States, the hospitalist field is the fastest growing specialty in the country—and probably in the history of the country. Hospitalists are transforming the delivery of American hospital care and improving quality, patient safety, education, end-of-life care, and more. We are thrilled to partner with our Brazilian colleagues as, together, we try to improve the quality of care for hospitalized patients everywhere.” We are confident that his vision will become a reality in Brazil in the near future. TH
Note: We are in debt to the professors at the Hospital Conceição Internal Medicine Residency Program, without whom our initiatives would never have blossomed. Special thanks to Eduardo Fernandes, Sergio Prezzi, and Paulo Ricardo Cardoso.
Dr. Barcellos is a specialist in internal medicine, emergency medicine, and critical care. He is professor in Nossa Senhora da Conceição Hospital’s Hospital Medicine Residence Program and president of GEAMH, a local association designed to promote the understanding and diffusion of hospitalist principles.
Dr. Wajner is a specialist in internal medicine and emergency medicine and a Master of Science student at Universidade Federal do Rio Grande do Sul.
Dr. de Waldemar is a specialist in internal medicine and emergency medicine.
References
- Departamento de População e Indicadores Sociais. Estatísticas da saúde: assistência médico-sanitária 2005/IBGE. Departamento de População e Indicadores Sociais. 2006. Available at: www.ibge.gov.br/home/estatistica/populacao/condicaodevida/ams/2005/ams2005.pdf. Last accessed January 28, 2007.
- Agência Nacional de Vigilância Sanitária. Lei nº 8080. D.O.U. - Diário Oficial da União; Poder Executivo. September 20, 1990. Available at: http://e-legis.bvs.br/leisref/public/showAct.php?id=16619&word=. Last accessed January 28, 2007.
- Brazilian Ministry of Health Web site. Available at: http://portal.saude.gov.br/saude. Last accessed January 28, 2007.
- Deslandes SF. Análise do discurso oficial sobre a humanização da assistência hospitalar. Ciência e saúde coletiva. 2004;9:7-14. Available at: www.scielo.br/pdf/csc/v9n1/19819.pdf. Last ccessed January 28, 2007.
- Portela MC, Lima SML, Barbosa PR, et al. Caracterização assistencial de hospitais filantrópicos no Brasil. Rev Saúde Pública. 2004;38:811-818. Available at: www.scielo.br/pdf/rsp/v38n6/09.pdf. Last accessed January 28, 2007.
- Sindicato Médico do Rio Grande do Sul Web site. Available at: www.simers.org.br/entquerem.php. Last accessed January 28, 2007.
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996 Aug 15;335(7):514-517.
- Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002 Feb 16;287:487–494. Review.
- Wachter RM. An introduction to the hospitalist model. Ann Intern Med. 1999 Feb 16;130(4 Pt 2):338–342.
- No Free Lunch Web site. Available at: www.nofreelunch.org. Last accessed January 28, 2007.
The establishment of a hospital medicine program in Brazil and the attempt to develop the specialty nationwide is both fascinating and challenging. Brazil has about 7,155 hospitals, with 443,210 beds available (including 2,727 public hospitals with 148,966 beds and 4,428 private facilities with 294,244 beds). 1 (See Table 1, p. 44.)
Historical problems in the public health system—also found in private sectors—have motivated physicians to address and improve inefficient management, insufficient financial support, the high number of frequent unnecessary admissions and re-admissions, extended length of stays, limited access to beds and medical services of high complexity, and overcrowded emergency departments.
SUS—Principles and Problems
The Brazilian public health system, called Sistema Único de Saúde, or SUS, is based on universal care and health as a right of citizenship and a state responsibility. Its main principles are universality, integrality, equity, decentralization, and social control.2 Less than half of the Brazilian population uses the SUS system exclusively. They use private health systems as a complement. This situation reflects the difficulties in the Brazilian public health system. The reasons for this duplicity highlight the challenges of our situation.
At the same time, physicians face serious problems. Most are employed by both the public and private sectors. Average salaries in the public system (by far the largest employer) are extremely low. Medical doctors are forced to work many extra hours, including numerous night shifts, creating a major barrier to the growth of physicians dedicated to horizontal inpatient care.
The government, in an attempt to improve medical—and hospital—assistance in the country with “a new kind of health assistance focused on high quality and efficient services,” has created the following projects: Humaniza SUS and QualiSUS.3,4 Theoretical support, operational contours, extent, and applicability are still not clear, however. For many medical doctors, these are merely abstract ideas. QualiSUS has renovated emergency departments in Brazil, but service quality has not improved enough. In our opinion, there are no public policies capable of providing good hospital services and efficient management in Brazilian hospitals, and—even if they existed—we would need to stop corruption in order to meet public commitments.
In Rio Grande do Sul, the Brazilian state where we work as medical doctors, the inadequate SUS reimbursement points to a calamitous future. Here, most hospital care is provided by philanthropic hospitals, which are more vulnerable in financial terms.5 (See Table 2, p. 44.) Despite being in a pioneer state in terms of hospital administration schools, with more than 2,000 graduates in recent years, these philanthropic hospitals have an estimated reimbursement deficit of more than 80%, an unattainable amount even for the best administrator.
Could Hospitalists Be Part of a Solution?
On top of these growing deficits, we have witnessed the closing of more than 2,000 available beds in the last four years, as well as the loss of 10,000 hospital positions and the complete closing of eight hospitals. Aiming to ensure the survival of this hospital system, physicians, health professionals, and organizations involved with hospitals have joined forces to find a solution. Their logo is best translated as “More Health for the Hospitals,” and our group supports their goals.6
Looking at the situation from a different perspective, we see many opportunities for Brazilian hospitalists. Their potential contribution to the quality and safety of medical care is an obvious advantage for hospital management and patients. We predict that this scenario can be accomplished—even in our state. It is possible to make a profit in public as well as in lucrative private institutions. In public institutions, a profit can be made as long as hospital administrators use adequate policy. We believe that in private institutions, though not in philanthropic ones, the key point is hospital administration cooperation and goodwill. Elucidation of hospitalists’ capabilities will open the necessary doors. We are ready to reduce the hospitalization fee and length of stay—among other costs. In this way, we can work with the administrator to develop tools for systems and quality improvements.
Hospital Medicine’s Emergence in Brazil
The implementation of hospital medicine, especially those aspects that involve more than just having a general medicine physician dealing with inpatient care, is brand new in Brazil. So far, the U.S. hospitalist model of care is unfamiliar to most Brazilian medical doctors and healthcare managers. Some institutions have hired hospitalists to be part of rapid response teams, neglecting the more specialized dimension of this new model of care; they are not aware of this title’s real meaning. There is a long way to go until the hospitalist is seen as a specialist, and we hope all our efforts will earn this new specialty official recognition in Brazil.
Our group is based in the Brazilian state of Rio Grande do Sul, mainly in Porto Alegre, its capital. Most of our time is dedicated to inpatient care, and we started our movement after studying the model of care delineated by Wachter and Lee.7-9 In 2005, we formed a local association called GEAMH (Grupo de Estudos e Atualização em Medicina Hospitalar) to promote the understanding and diffusion of hospitalist principles, integrated by the professors and former and current residents of a large local internal medicine residence program from the Internal Medicine Department of Nossa Senhora da Conceição Hospital (HNSC).
We have created a Web site (www.medicinahospitalar.com.br) where you can find history, news, and information about hospital medicine fellowships in the United States, as well as online hospital medicine continuing education. As you can see, we are spreading SHM’s ideas.
The third year of the HNSC Internal Medicine Residence Program (R3) focused on hospital medicine was developed in 2005. We believe this to be the first initiative of its kind in Brazil. HNSC is part of Conceição Hospital Group, which is composed of four hospital units and is one of the biggest public hospital networks in Brazil.
The Internal Medicine Residence Program started at HNSC in 1968. The department itself has more than 100 hospital beds. Medical residents’ activities all take place in the hospital, and there are nine professors: Eduardo Fernandes, Guilherme Barcellos, Janete Brauner, José Luiz F. Soares, Nelson Roessler, Paulo Almeida, Paulo Ricardo Cardoso, Sergio Dedavid, and Sergio Prezzi. We would like to make special mention of our colleagues Eduardo Fernandes, current head of HNSC Internal Medicine Medical Residence Program, and Sergio Prezzi, the R3 coordinator.
The HNSC Internal Medicine Service is well known for graduating internists skilled in hospital practices, mainly because the program is run by professors who specialize in that area. The R3 is a one-year training program. Our goal is to train physicians to provide outstanding and comprehensive inpatient care. Through supervised training, our residents are able to treat common hospital illnesses; we are also training them in consultative medicine and in the clinical management of surgical patients. Other areas of medical residents’ education include medical ethics, end-of-life care, inpatient nutritional support, risk management, rational use of drugs, and technology and evidence-based medicine.
Our third-year residents have the opportunity to try bone marrow biopsy, pleural biopsy, and thorax draining—all of which are usually handled by other medical specialists. In general, residents also have many opportunities to learn about and practice endotracheal intubations, ventilator management, central vein access, and many other procedures.
Based on HNSC experience, a formal stage in hospital medicine under the supervision of Luciano Bauer Grohs, MD, one of the founders of GEAMH, has also been integrated into internal medicine training at Nossa Senhora de Pompéia Hospital in the city of Caxias do Sul, located 125 kilometers from Porto Alegre.
Our group has developed medical education in the inpatient setting. Because there is no hospital medicine society in Brazil, we have tried to coordinate with the Brazilian Society of Internal Medicine, encouraging discussions about hospital care and promoting workshops about mechanical ventilation, central vein access, and early goal-directed therapy for sepsis. More recently, we have chosen to work independently, believing that hospital medicine is distinct from internal medicine.
When we organized the Brazilian Annual Congress of Medical Residents in 2006, we had the opportunity to bring together medical residents and professors from different medical areas. The Congress’ main focuses were rational use of drugs and technology and the relationship between the young physician and the pharmaceutical industry. The participation of Robert Goodman (of No Free Lunch fame) was an important part of the convention.10
Slow and Steady Growth
We understand that there is a long journey ahead, beyond educational and medical assistance. Our group is still far from promoting research. But hospital medicine specialization has launched in Brazil. Dr. Watcher has said to us, “In the United States, the hospitalist field is the fastest growing specialty in the country—and probably in the history of the country. Hospitalists are transforming the delivery of American hospital care and improving quality, patient safety, education, end-of-life care, and more. We are thrilled to partner with our Brazilian colleagues as, together, we try to improve the quality of care for hospitalized patients everywhere.” We are confident that his vision will become a reality in Brazil in the near future. TH
Note: We are in debt to the professors at the Hospital Conceição Internal Medicine Residency Program, without whom our initiatives would never have blossomed. Special thanks to Eduardo Fernandes, Sergio Prezzi, and Paulo Ricardo Cardoso.
Dr. Barcellos is a specialist in internal medicine, emergency medicine, and critical care. He is professor in Nossa Senhora da Conceição Hospital’s Hospital Medicine Residence Program and president of GEAMH, a local association designed to promote the understanding and diffusion of hospitalist principles.
Dr. Wajner is a specialist in internal medicine and emergency medicine and a Master of Science student at Universidade Federal do Rio Grande do Sul.
Dr. de Waldemar is a specialist in internal medicine and emergency medicine.
References
- Departamento de População e Indicadores Sociais. Estatísticas da saúde: assistência médico-sanitária 2005/IBGE. Departamento de População e Indicadores Sociais. 2006. Available at: www.ibge.gov.br/home/estatistica/populacao/condicaodevida/ams/2005/ams2005.pdf. Last accessed January 28, 2007.
- Agência Nacional de Vigilância Sanitária. Lei nº 8080. D.O.U. - Diário Oficial da União; Poder Executivo. September 20, 1990. Available at: http://e-legis.bvs.br/leisref/public/showAct.php?id=16619&word=. Last accessed January 28, 2007.
- Brazilian Ministry of Health Web site. Available at: http://portal.saude.gov.br/saude. Last accessed January 28, 2007.
- Deslandes SF. Análise do discurso oficial sobre a humanização da assistência hospitalar. Ciência e saúde coletiva. 2004;9:7-14. Available at: www.scielo.br/pdf/csc/v9n1/19819.pdf. Last ccessed January 28, 2007.
- Portela MC, Lima SML, Barbosa PR, et al. Caracterização assistencial de hospitais filantrópicos no Brasil. Rev Saúde Pública. 2004;38:811-818. Available at: www.scielo.br/pdf/rsp/v38n6/09.pdf. Last accessed January 28, 2007.
- Sindicato Médico do Rio Grande do Sul Web site. Available at: www.simers.org.br/entquerem.php. Last accessed January 28, 2007.
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996 Aug 15;335(7):514-517.
- Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002 Feb 16;287:487–494. Review.
- Wachter RM. An introduction to the hospitalist model. Ann Intern Med. 1999 Feb 16;130(4 Pt 2):338–342.
- No Free Lunch Web site. Available at: www.nofreelunch.org. Last accessed January 28, 2007.
Perfect Pain Control
Skillful use of intravenous pain medications can be a powerful tool in the clinician’s pain management armamentarium. Yet many physicians are uncomfortable prescribing IV pain medications, especially opioids, even when their patients are experiencing severe pain—7-10 on the verbal analogue scale (VAS). This reticence, say the palliative care specialists interviewed for this article, may be due to a lack of training and knowledge, as well as misperceptions about proper use of IV opioids. The end result for patients can be inadequate pain control, which, according to researchers, continues to be a problem in U.S. hospitals.1
Even hospitalists not affiliated with a surgical service who do not treat perioperative patients are likely to encounter many different scenarios in which IV pain medications could appropriately address patients’ discomfort. David Ling, MD, a member of SHM’s Palliative Care Task Force, a hospitalist at Baystate Medical Center in Springfield, Mass., and assistant professor of medicine at Tufts University School of Medicine (Boston), says patients who need IV pain medicines range from those with acute abdominal pain, pancreatitis, or small bowel obstructions to patients with end-stage cancer, renal disease, or congestive heart failure.
“It’s probably a bigger number on the medical service than most people realize,” he says.
The Short List
When it comes to effective IV pain medications very few choices exist, according to recommendations from the National Comprehensive Cancer Network and other pain advocacy organizations. An informal poll of interview sources corroborates this revelation.
“Morphine is the gold standard in pain control,” says Thomas Bookwalter, PharmD, clinical pharmacist on the General Medicine Service at the University of California at San Francisco (UCSF) Medical Center, a Health Sciences associate clinical professor at the UCSF School of Pharmacy, and a member of SHM’s Palliative Care Task Force.
Preferences for morphine or other opioids vary by practitioner and institution. For instance, says Dr. Bookwalter, the pain service at UCSF has been using hydromorphone more frequently of late.
Nicole L. Artz, MD, director of the Adult Sickle Cell Disease Care Team at the University of Chicago Hospitals and instructor of medicine at the University of Chicago Medical School, also occasionally uses IV infusions of ketorolac—a powerful NSAID designed for short-term management of moderately severe pain in adults. But, like morphine, it is contraindicated in patients with renal insufficiency and can have GI side effects.
Common Missteps
That opioids remain the drugs of choice for controlling severe pain puts some physicians outside their comfort zone. Dr. Ling, who has extensive experience with IV opioids, has observed two common tendencies among physicians inexperienced with prescribing opioids. “There is a tendency, based on the traditional teaching, to prescribe a lower-than-necessary first dose and for those doses to not be frequent enough,” he says.
Dr. Artz, who has a special interest in pain management, lectures on effectively using opioids to house staff at the University of Chicago. She has observed a deficit in physician training in pain management and has seen physicians make many errors when writing orders for opioids, including mixing IV and short-acting oral opioids or two long-acting opioids, not distinguishing between patients who are opioid-naïve and opioid-tolerant in choosing a starting dose, failing to titrate short-acting opioids rapidly despite inadequate pain control, and giving orders for repeated doses of morphine in patients with renal insufficiency.
Dr. Bookwalter says the World Health Organization’s stepladder approach to treating pain (starting with oral NSAIDs and moving up to opioids) does not align with current scientific thinking on prescribing pain medication. For severe pain, a clinician should consider immediately starting an IV opioid, reassessing the patient every 15-30 minutes to see whether the dose is effectively decreasing the pain. National Comprehensive Cancer Network (NCCN) Guidelines for Adult Cancer Pain recommend rapid dose escalation to address the level of the patient’s pain.2
Skill Sets to Acquire
In addition to postgraduate and conference courses on pain control, another good first step in educating oneself about pain is to become familiar with equianalgesic doses of opioids. It is also mandatory to know not only how to convert between different opioids but between different routes of administration, Dr. Artz emphasizes. This step is crucial when patients have been stabilized and are ready for discharge. When conversions from IV opioids to equianalgesic doses of oral opioids are performed incorrectly, patients get the idea that the oral medication doesn’t work as well and that they need the IV pain medicine, “when, in reality, we didn’t give them an equivalent dose of oral pain medicine.”
Equianalgesic tables for use in converting 24-hour standing doses of an IV opioid to an oral formulation are readily available. Dr. Bookwalter offers a cautionary note about the use of conversion charts: “These charts are based on single-dose studies. The thing to remember is that these are ballpark numbers. Every place and every practitioner will use them in a slightly different way. The key thing is close monitoring to make sure the pain is relieved and that side effects are kept at a minimum.”
Familiarity with various pain intensity scales is also necessary. The Wong numerical rating scale—either written or verbal (0 = no pain and 10 = worst pain imaginable)—is the most commonly used. The Wong-Baker FACES Pain Rating Scale is helpful when assessing patients who are not English speakers or who have other impairments.3 Dr. Artz reminds hospitalists never to guess by just looking at their patients what their levels of pain are. Many patients have developed coping strategies to mask their pain.
Finally, Dr. Ling advises hospitalists to examine their own beliefs about using opioids for pain control. “Narcotics, in general, have a social stigma attached to them,” he points out. “I think most doctors, without additional experience and training [in prescribing IV opioids], will have a natural built-in response of, ‘Do I really want to give them that much?’ ”
Dr. Ling admits even he sometimes becomes a little uncomfortable with titrating to larger doses. “But some patients—especially those with a new diagnosis of metastatic cancer—or cancer that is invading an organ system, have appropriately high requirements for pain medication,” he stresses. Dr. Ling recalls one educational video made by the colleague of a patient who required a 400-mg dose of IV morphine daily. While the patient’s surgeon, anesthesiologist, and internist did not believe that the patient required that much morphine, her hospitalist finally convinced the treatment team by achieving adequate pain control using her own pain management skill.
“It’s not the dose so much as looking at the patient and talking with the patient” that should guide dosing decisions, says Eva Chittenden, MD, assistant director of the UCSF Palliative Care Service and chair of SHM’s Palliative Care Task Force. “You will know within 10 to 15 minutes if a dose is working.”
Adds Howard R. Epstein, MD, medical director of Care Management and Palliative Care at Regions Hospital in St. Paul, Minn., and also a member of SHM’s Palliative Care Task Force, “You have to assess your intervention: Was it effective? Did it relieve the patient’s pain? How long did it last?”
Dr. Bookwalter says hospitalists have an edge with pain patients. “The advantage that hospitalists have is that they can do more frequent monitoring,” he says. “The choice of drug is key, but frequent monitoring is even more key: You have to know if the patient is getting nauseated, or is still in pain, or how much the pain decreased with a certain dose.”
Special Considerations
Multiple variables influence a clinician’s decision to prescribe IV opioids for a patient—and at what dose and frequency. Basic principles of pain management dictate administering an initial IV bolus by a provider or by using patient-controlled analgesia (PCA) at lower doses if the patient is opioid-naïve, and at higher doses if a patient has already been taking oral narcotics. The NCCN recommends starting doses of 1-5 mg of IV morphine or equivalent for opioid-naïve patients, or a dose 10%-20% of a daily IV morphine equivalent for those already on opioids.2
The clinician should reassess the patient at 15 minutes to determine whether the pain score is unchanged, increased, or decreased. “If, after 15 minutes, that patient is still in severe pain, you want to be giving another dose,” emphasizes Dr. Chittenden. “You want to get the pain under control and then figure out what the standing dose should be.” The NCCN advises increasing the dose by 50%-100% if the pain score is unchanged or has increased after the initial dose.
IV opioids can also be indicated in elderly patients, unless they suffer from renal insufficiency. Palliative care specialists usually follow the maxim “start low and go slow” for elderly patients, and a 0.5 to 1-mg initial dose would be a reasonable place to begin treating an elderly patient in pain, says Dr. Chittenden. In addition to reassessing every 15 minutes for changes in the pain score, the hospitalist should also closely monitor the patient for sedation, respiratory rate, and other untoward side effects.
Hospitalists as Advocates
Hospitalists can play a vital role in advocating for better pain control for hospitalized patients. “Unfortunately,” notes Dr. Epstein, “pain management is not very well taught in most residency programs. But it’s an essential skill—not to mention a core competency—for hospitalists. If they don’t feel comfortable with their current fund of knowledge, there are plenty of resources out there to gain the skills or develop a higher comfort level and provide more competent pain management—to palliative as well as non-palliative patients.”
In actively dying patients, adequate pain control frees them from suffering. “If people have severe pain, they can’t talk with their families, and they can’t do the other things that might be important to them, whether they’re dying or not dying,” says Dr. Chittenden. “We should be trying to address pain in all patients in the hospital, not just those who are dying. Those in the ICU, those who have just had operations, those who have chronic pain—it’s not OK for them to come to the hospital and be having terrible pain.”
Dr. Artz agrees: “I cannot imagine that it is good for healing if a patient’s sympathetic nervous system is revved up because they’re in severe pain. I believe that adequate pain control is a really important piece of helping people get better.”
Dr. Ling urges colleagues to put themselves in the patient’s shoes, asking themselves, “If I were the patient, what would I need to control my pain?” Everyone’s pain threshold is different, he asserts, and physicians should listen to their patients’ reports. “Rather than asking why would we need to prescribe a large dose of narcotics, ask, ‘Why wouldn’t you want to control the pain?’ ” TH
Gretchen Henkel writes frequently for The Hospitalist.
References
- Gordon DB, Stevenson KK, Griffie J, et al. Opioid equianalgesic calculations. J Palliat Med. 1999 summer;2(2):209-218.
- National Comprehensive Cancer Network Practice Guidelines in Oncology. Adult cancer pain. Available at: www.nccn.org/professionals/physician_gls/PDF/pain.pdf. Last accessed January 28, 2007.
- Wong DL, Hockenberry-Eaton M, Wilson D, et al. Wong’s Essentials of Pediatric Nursing. 6th ed. St. Louis: Mosby;2001:1301.
Skillful use of intravenous pain medications can be a powerful tool in the clinician’s pain management armamentarium. Yet many physicians are uncomfortable prescribing IV pain medications, especially opioids, even when their patients are experiencing severe pain—7-10 on the verbal analogue scale (VAS). This reticence, say the palliative care specialists interviewed for this article, may be due to a lack of training and knowledge, as well as misperceptions about proper use of IV opioids. The end result for patients can be inadequate pain control, which, according to researchers, continues to be a problem in U.S. hospitals.1
Even hospitalists not affiliated with a surgical service who do not treat perioperative patients are likely to encounter many different scenarios in which IV pain medications could appropriately address patients’ discomfort. David Ling, MD, a member of SHM’s Palliative Care Task Force, a hospitalist at Baystate Medical Center in Springfield, Mass., and assistant professor of medicine at Tufts University School of Medicine (Boston), says patients who need IV pain medicines range from those with acute abdominal pain, pancreatitis, or small bowel obstructions to patients with end-stage cancer, renal disease, or congestive heart failure.
“It’s probably a bigger number on the medical service than most people realize,” he says.
The Short List
When it comes to effective IV pain medications very few choices exist, according to recommendations from the National Comprehensive Cancer Network and other pain advocacy organizations. An informal poll of interview sources corroborates this revelation.
“Morphine is the gold standard in pain control,” says Thomas Bookwalter, PharmD, clinical pharmacist on the General Medicine Service at the University of California at San Francisco (UCSF) Medical Center, a Health Sciences associate clinical professor at the UCSF School of Pharmacy, and a member of SHM’s Palliative Care Task Force.
Preferences for morphine or other opioids vary by practitioner and institution. For instance, says Dr. Bookwalter, the pain service at UCSF has been using hydromorphone more frequently of late.
Nicole L. Artz, MD, director of the Adult Sickle Cell Disease Care Team at the University of Chicago Hospitals and instructor of medicine at the University of Chicago Medical School, also occasionally uses IV infusions of ketorolac—a powerful NSAID designed for short-term management of moderately severe pain in adults. But, like morphine, it is contraindicated in patients with renal insufficiency and can have GI side effects.
Common Missteps
That opioids remain the drugs of choice for controlling severe pain puts some physicians outside their comfort zone. Dr. Ling, who has extensive experience with IV opioids, has observed two common tendencies among physicians inexperienced with prescribing opioids. “There is a tendency, based on the traditional teaching, to prescribe a lower-than-necessary first dose and for those doses to not be frequent enough,” he says.
Dr. Artz, who has a special interest in pain management, lectures on effectively using opioids to house staff at the University of Chicago. She has observed a deficit in physician training in pain management and has seen physicians make many errors when writing orders for opioids, including mixing IV and short-acting oral opioids or two long-acting opioids, not distinguishing between patients who are opioid-naïve and opioid-tolerant in choosing a starting dose, failing to titrate short-acting opioids rapidly despite inadequate pain control, and giving orders for repeated doses of morphine in patients with renal insufficiency.
Dr. Bookwalter says the World Health Organization’s stepladder approach to treating pain (starting with oral NSAIDs and moving up to opioids) does not align with current scientific thinking on prescribing pain medication. For severe pain, a clinician should consider immediately starting an IV opioid, reassessing the patient every 15-30 minutes to see whether the dose is effectively decreasing the pain. National Comprehensive Cancer Network (NCCN) Guidelines for Adult Cancer Pain recommend rapid dose escalation to address the level of the patient’s pain.2
Skill Sets to Acquire
In addition to postgraduate and conference courses on pain control, another good first step in educating oneself about pain is to become familiar with equianalgesic doses of opioids. It is also mandatory to know not only how to convert between different opioids but between different routes of administration, Dr. Artz emphasizes. This step is crucial when patients have been stabilized and are ready for discharge. When conversions from IV opioids to equianalgesic doses of oral opioids are performed incorrectly, patients get the idea that the oral medication doesn’t work as well and that they need the IV pain medicine, “when, in reality, we didn’t give them an equivalent dose of oral pain medicine.”
Equianalgesic tables for use in converting 24-hour standing doses of an IV opioid to an oral formulation are readily available. Dr. Bookwalter offers a cautionary note about the use of conversion charts: “These charts are based on single-dose studies. The thing to remember is that these are ballpark numbers. Every place and every practitioner will use them in a slightly different way. The key thing is close monitoring to make sure the pain is relieved and that side effects are kept at a minimum.”
Familiarity with various pain intensity scales is also necessary. The Wong numerical rating scale—either written or verbal (0 = no pain and 10 = worst pain imaginable)—is the most commonly used. The Wong-Baker FACES Pain Rating Scale is helpful when assessing patients who are not English speakers or who have other impairments.3 Dr. Artz reminds hospitalists never to guess by just looking at their patients what their levels of pain are. Many patients have developed coping strategies to mask their pain.
Finally, Dr. Ling advises hospitalists to examine their own beliefs about using opioids for pain control. “Narcotics, in general, have a social stigma attached to them,” he points out. “I think most doctors, without additional experience and training [in prescribing IV opioids], will have a natural built-in response of, ‘Do I really want to give them that much?’ ”
Dr. Ling admits even he sometimes becomes a little uncomfortable with titrating to larger doses. “But some patients—especially those with a new diagnosis of metastatic cancer—or cancer that is invading an organ system, have appropriately high requirements for pain medication,” he stresses. Dr. Ling recalls one educational video made by the colleague of a patient who required a 400-mg dose of IV morphine daily. While the patient’s surgeon, anesthesiologist, and internist did not believe that the patient required that much morphine, her hospitalist finally convinced the treatment team by achieving adequate pain control using her own pain management skill.
“It’s not the dose so much as looking at the patient and talking with the patient” that should guide dosing decisions, says Eva Chittenden, MD, assistant director of the UCSF Palliative Care Service and chair of SHM’s Palliative Care Task Force. “You will know within 10 to 15 minutes if a dose is working.”
Adds Howard R. Epstein, MD, medical director of Care Management and Palliative Care at Regions Hospital in St. Paul, Minn., and also a member of SHM’s Palliative Care Task Force, “You have to assess your intervention: Was it effective? Did it relieve the patient’s pain? How long did it last?”
Dr. Bookwalter says hospitalists have an edge with pain patients. “The advantage that hospitalists have is that they can do more frequent monitoring,” he says. “The choice of drug is key, but frequent monitoring is even more key: You have to know if the patient is getting nauseated, or is still in pain, or how much the pain decreased with a certain dose.”
Special Considerations
Multiple variables influence a clinician’s decision to prescribe IV opioids for a patient—and at what dose and frequency. Basic principles of pain management dictate administering an initial IV bolus by a provider or by using patient-controlled analgesia (PCA) at lower doses if the patient is opioid-naïve, and at higher doses if a patient has already been taking oral narcotics. The NCCN recommends starting doses of 1-5 mg of IV morphine or equivalent for opioid-naïve patients, or a dose 10%-20% of a daily IV morphine equivalent for those already on opioids.2
The clinician should reassess the patient at 15 minutes to determine whether the pain score is unchanged, increased, or decreased. “If, after 15 minutes, that patient is still in severe pain, you want to be giving another dose,” emphasizes Dr. Chittenden. “You want to get the pain under control and then figure out what the standing dose should be.” The NCCN advises increasing the dose by 50%-100% if the pain score is unchanged or has increased after the initial dose.
IV opioids can also be indicated in elderly patients, unless they suffer from renal insufficiency. Palliative care specialists usually follow the maxim “start low and go slow” for elderly patients, and a 0.5 to 1-mg initial dose would be a reasonable place to begin treating an elderly patient in pain, says Dr. Chittenden. In addition to reassessing every 15 minutes for changes in the pain score, the hospitalist should also closely monitor the patient for sedation, respiratory rate, and other untoward side effects.
Hospitalists as Advocates
Hospitalists can play a vital role in advocating for better pain control for hospitalized patients. “Unfortunately,” notes Dr. Epstein, “pain management is not very well taught in most residency programs. But it’s an essential skill—not to mention a core competency—for hospitalists. If they don’t feel comfortable with their current fund of knowledge, there are plenty of resources out there to gain the skills or develop a higher comfort level and provide more competent pain management—to palliative as well as non-palliative patients.”
In actively dying patients, adequate pain control frees them from suffering. “If people have severe pain, they can’t talk with their families, and they can’t do the other things that might be important to them, whether they’re dying or not dying,” says Dr. Chittenden. “We should be trying to address pain in all patients in the hospital, not just those who are dying. Those in the ICU, those who have just had operations, those who have chronic pain—it’s not OK for them to come to the hospital and be having terrible pain.”
Dr. Artz agrees: “I cannot imagine that it is good for healing if a patient’s sympathetic nervous system is revved up because they’re in severe pain. I believe that adequate pain control is a really important piece of helping people get better.”
Dr. Ling urges colleagues to put themselves in the patient’s shoes, asking themselves, “If I were the patient, what would I need to control my pain?” Everyone’s pain threshold is different, he asserts, and physicians should listen to their patients’ reports. “Rather than asking why would we need to prescribe a large dose of narcotics, ask, ‘Why wouldn’t you want to control the pain?’ ” TH
Gretchen Henkel writes frequently for The Hospitalist.
References
- Gordon DB, Stevenson KK, Griffie J, et al. Opioid equianalgesic calculations. J Palliat Med. 1999 summer;2(2):209-218.
- National Comprehensive Cancer Network Practice Guidelines in Oncology. Adult cancer pain. Available at: www.nccn.org/professionals/physician_gls/PDF/pain.pdf. Last accessed January 28, 2007.
- Wong DL, Hockenberry-Eaton M, Wilson D, et al. Wong’s Essentials of Pediatric Nursing. 6th ed. St. Louis: Mosby;2001:1301.
Skillful use of intravenous pain medications can be a powerful tool in the clinician’s pain management armamentarium. Yet many physicians are uncomfortable prescribing IV pain medications, especially opioids, even when their patients are experiencing severe pain—7-10 on the verbal analogue scale (VAS). This reticence, say the palliative care specialists interviewed for this article, may be due to a lack of training and knowledge, as well as misperceptions about proper use of IV opioids. The end result for patients can be inadequate pain control, which, according to researchers, continues to be a problem in U.S. hospitals.1
Even hospitalists not affiliated with a surgical service who do not treat perioperative patients are likely to encounter many different scenarios in which IV pain medications could appropriately address patients’ discomfort. David Ling, MD, a member of SHM’s Palliative Care Task Force, a hospitalist at Baystate Medical Center in Springfield, Mass., and assistant professor of medicine at Tufts University School of Medicine (Boston), says patients who need IV pain medicines range from those with acute abdominal pain, pancreatitis, or small bowel obstructions to patients with end-stage cancer, renal disease, or congestive heart failure.
“It’s probably a bigger number on the medical service than most people realize,” he says.
The Short List
When it comes to effective IV pain medications very few choices exist, according to recommendations from the National Comprehensive Cancer Network and other pain advocacy organizations. An informal poll of interview sources corroborates this revelation.
“Morphine is the gold standard in pain control,” says Thomas Bookwalter, PharmD, clinical pharmacist on the General Medicine Service at the University of California at San Francisco (UCSF) Medical Center, a Health Sciences associate clinical professor at the UCSF School of Pharmacy, and a member of SHM’s Palliative Care Task Force.
Preferences for morphine or other opioids vary by practitioner and institution. For instance, says Dr. Bookwalter, the pain service at UCSF has been using hydromorphone more frequently of late.
Nicole L. Artz, MD, director of the Adult Sickle Cell Disease Care Team at the University of Chicago Hospitals and instructor of medicine at the University of Chicago Medical School, also occasionally uses IV infusions of ketorolac—a powerful NSAID designed for short-term management of moderately severe pain in adults. But, like morphine, it is contraindicated in patients with renal insufficiency and can have GI side effects.
Common Missteps
That opioids remain the drugs of choice for controlling severe pain puts some physicians outside their comfort zone. Dr. Ling, who has extensive experience with IV opioids, has observed two common tendencies among physicians inexperienced with prescribing opioids. “There is a tendency, based on the traditional teaching, to prescribe a lower-than-necessary first dose and for those doses to not be frequent enough,” he says.
Dr. Artz, who has a special interest in pain management, lectures on effectively using opioids to house staff at the University of Chicago. She has observed a deficit in physician training in pain management and has seen physicians make many errors when writing orders for opioids, including mixing IV and short-acting oral opioids or two long-acting opioids, not distinguishing between patients who are opioid-naïve and opioid-tolerant in choosing a starting dose, failing to titrate short-acting opioids rapidly despite inadequate pain control, and giving orders for repeated doses of morphine in patients with renal insufficiency.
Dr. Bookwalter says the World Health Organization’s stepladder approach to treating pain (starting with oral NSAIDs and moving up to opioids) does not align with current scientific thinking on prescribing pain medication. For severe pain, a clinician should consider immediately starting an IV opioid, reassessing the patient every 15-30 minutes to see whether the dose is effectively decreasing the pain. National Comprehensive Cancer Network (NCCN) Guidelines for Adult Cancer Pain recommend rapid dose escalation to address the level of the patient’s pain.2
Skill Sets to Acquire
In addition to postgraduate and conference courses on pain control, another good first step in educating oneself about pain is to become familiar with equianalgesic doses of opioids. It is also mandatory to know not only how to convert between different opioids but between different routes of administration, Dr. Artz emphasizes. This step is crucial when patients have been stabilized and are ready for discharge. When conversions from IV opioids to equianalgesic doses of oral opioids are performed incorrectly, patients get the idea that the oral medication doesn’t work as well and that they need the IV pain medicine, “when, in reality, we didn’t give them an equivalent dose of oral pain medicine.”
Equianalgesic tables for use in converting 24-hour standing doses of an IV opioid to an oral formulation are readily available. Dr. Bookwalter offers a cautionary note about the use of conversion charts: “These charts are based on single-dose studies. The thing to remember is that these are ballpark numbers. Every place and every practitioner will use them in a slightly different way. The key thing is close monitoring to make sure the pain is relieved and that side effects are kept at a minimum.”
Familiarity with various pain intensity scales is also necessary. The Wong numerical rating scale—either written or verbal (0 = no pain and 10 = worst pain imaginable)—is the most commonly used. The Wong-Baker FACES Pain Rating Scale is helpful when assessing patients who are not English speakers or who have other impairments.3 Dr. Artz reminds hospitalists never to guess by just looking at their patients what their levels of pain are. Many patients have developed coping strategies to mask their pain.
Finally, Dr. Ling advises hospitalists to examine their own beliefs about using opioids for pain control. “Narcotics, in general, have a social stigma attached to them,” he points out. “I think most doctors, without additional experience and training [in prescribing IV opioids], will have a natural built-in response of, ‘Do I really want to give them that much?’ ”
Dr. Ling admits even he sometimes becomes a little uncomfortable with titrating to larger doses. “But some patients—especially those with a new diagnosis of metastatic cancer—or cancer that is invading an organ system, have appropriately high requirements for pain medication,” he stresses. Dr. Ling recalls one educational video made by the colleague of a patient who required a 400-mg dose of IV morphine daily. While the patient’s surgeon, anesthesiologist, and internist did not believe that the patient required that much morphine, her hospitalist finally convinced the treatment team by achieving adequate pain control using her own pain management skill.
“It’s not the dose so much as looking at the patient and talking with the patient” that should guide dosing decisions, says Eva Chittenden, MD, assistant director of the UCSF Palliative Care Service and chair of SHM’s Palliative Care Task Force. “You will know within 10 to 15 minutes if a dose is working.”
Adds Howard R. Epstein, MD, medical director of Care Management and Palliative Care at Regions Hospital in St. Paul, Minn., and also a member of SHM’s Palliative Care Task Force, “You have to assess your intervention: Was it effective? Did it relieve the patient’s pain? How long did it last?”
Dr. Bookwalter says hospitalists have an edge with pain patients. “The advantage that hospitalists have is that they can do more frequent monitoring,” he says. “The choice of drug is key, but frequent monitoring is even more key: You have to know if the patient is getting nauseated, or is still in pain, or how much the pain decreased with a certain dose.”
Special Considerations
Multiple variables influence a clinician’s decision to prescribe IV opioids for a patient—and at what dose and frequency. Basic principles of pain management dictate administering an initial IV bolus by a provider or by using patient-controlled analgesia (PCA) at lower doses if the patient is opioid-naïve, and at higher doses if a patient has already been taking oral narcotics. The NCCN recommends starting doses of 1-5 mg of IV morphine or equivalent for opioid-naïve patients, or a dose 10%-20% of a daily IV morphine equivalent for those already on opioids.2
The clinician should reassess the patient at 15 minutes to determine whether the pain score is unchanged, increased, or decreased. “If, after 15 minutes, that patient is still in severe pain, you want to be giving another dose,” emphasizes Dr. Chittenden. “You want to get the pain under control and then figure out what the standing dose should be.” The NCCN advises increasing the dose by 50%-100% if the pain score is unchanged or has increased after the initial dose.
IV opioids can also be indicated in elderly patients, unless they suffer from renal insufficiency. Palliative care specialists usually follow the maxim “start low and go slow” for elderly patients, and a 0.5 to 1-mg initial dose would be a reasonable place to begin treating an elderly patient in pain, says Dr. Chittenden. In addition to reassessing every 15 minutes for changes in the pain score, the hospitalist should also closely monitor the patient for sedation, respiratory rate, and other untoward side effects.
Hospitalists as Advocates
Hospitalists can play a vital role in advocating for better pain control for hospitalized patients. “Unfortunately,” notes Dr. Epstein, “pain management is not very well taught in most residency programs. But it’s an essential skill—not to mention a core competency—for hospitalists. If they don’t feel comfortable with their current fund of knowledge, there are plenty of resources out there to gain the skills or develop a higher comfort level and provide more competent pain management—to palliative as well as non-palliative patients.”
In actively dying patients, adequate pain control frees them from suffering. “If people have severe pain, they can’t talk with their families, and they can’t do the other things that might be important to them, whether they’re dying or not dying,” says Dr. Chittenden. “We should be trying to address pain in all patients in the hospital, not just those who are dying. Those in the ICU, those who have just had operations, those who have chronic pain—it’s not OK for them to come to the hospital and be having terrible pain.”
Dr. Artz agrees: “I cannot imagine that it is good for healing if a patient’s sympathetic nervous system is revved up because they’re in severe pain. I believe that adequate pain control is a really important piece of helping people get better.”
Dr. Ling urges colleagues to put themselves in the patient’s shoes, asking themselves, “If I were the patient, what would I need to control my pain?” Everyone’s pain threshold is different, he asserts, and physicians should listen to their patients’ reports. “Rather than asking why would we need to prescribe a large dose of narcotics, ask, ‘Why wouldn’t you want to control the pain?’ ” TH
Gretchen Henkel writes frequently for The Hospitalist.
References
- Gordon DB, Stevenson KK, Griffie J, et al. Opioid equianalgesic calculations. J Palliat Med. 1999 summer;2(2):209-218.
- National Comprehensive Cancer Network Practice Guidelines in Oncology. Adult cancer pain. Available at: www.nccn.org/professionals/physician_gls/PDF/pain.pdf. Last accessed January 28, 2007.
- Wong DL, Hockenberry-Eaton M, Wilson D, et al. Wong’s Essentials of Pediatric Nursing. 6th ed. St. Louis: Mosby;2001:1301.
Manage Sickle Cell Pain Crises
Standardized order sets reduce medication errors and create efficiency for physicians, nurses, and pharmacists.1 A less recognized benefit may be that standardized orders promote equity in care and may help to mitigate disparities that occur along racial and ethnic lines. Patients admitted with an acute pain crisis secondary to sickle cell disease (SCD) are often suspected of drug-seeking behavior and may be treated in a cursory manner because they are “frequent flyers” on the medical service. In view of these factors, this patient group may benefit more than others from a standardized treatment protocol. Over the past year, hospitalists and other clinicians at Novant Health in Charlotte, N.C., have composed an admission order set for SCD pain crisis in an effort to improve care for this underserved group.
Novant Health
Novant Health is a multi-hospital, non-profit system serving 3.5 million people from Virginia to South Carolina. Presbyterian Hospital, a 531-bed facility in Charlotte, N.C., is the flagship hospital for Novant’s Southern Piedmont Region (SPR). Presbyterian Inpatient Care Specialists (PICS) is a 44-provider group that offers hospitalist services for adult patients at Presbyterian Hospital, two community hospitals in Matthews and Huntersville, and Presbyterian Orthopedic Hospital.2 In 2005, 180 adult patients were discharged from the Novant-SPR hospitals with a principal diagnosis of SCD, and most of these patients were managed by PICS. This cohort of 180 patients accounted for more than 600 hospitalizations for SCD-related illness at the Novant-SPR facilities in 2005.
Process and Procedure
Standardized order sets have been in widespread use at the Novant-SPR facilities for a number of years. The process of order set development begins with patient needs as perceived by medical staff. Once a physician has drafted an order set, the draft is reviewed by the Order Set Subcommittee, a multidisciplinary team chaired by Susan Smith, RPh, PharmD, with nurses, physicians, and other support staff represented as needed. Once the subcommittee has approved the draft, it goes to the Pharmacy and Therapeutics Committee for final approval. In this fashion, more than 600 order sets have been developed and made available on the hospital’s intranet. The PICS team has helped to develop a number of disease management order sets and protocols, including the general medical admission orders. In addition, PICS has assisted in developing disease-specific orders for community-acquired pneumonia (CAP), CVA/TIA, and other common diseases admitted by the hospitalist service.
In the case of the adult SCD pain crisis order set, Stephen Wallenhaupt, MD, chief medical officer for Novant Health, recalls, “We recognize that SCD patients have unique needs in terms of pain management and that a standardized order set which incorporates aggressive pain management options is the best way to meet their needs.”
Fran Davis, RPh, PharmD, researched the pertinent literature and consulted the anesthesiologists on staff in an effort to tailor the pain management options for SCD patients. Using the recommendations of these specialists, the order set reflects the consensus that patients with a severe SCD pain crisis require parenteral opiate analgesia on admission.3
Because many patients admitted by PICS can be categorized as having severe pain, the order set contains choices for patient-controlled analgesia (PCA), in keeping with the recommendation for opiate administration at a fixed interval rather than on an as-needed basis.4 And because many hospitalists may not be familiar with ordering PCA, the SCD orders specify the dose ranges, as well as the lockout interval for morphine and hydromorphone PCA. With PCA options readily available, hospitalists need not delay therapy while awaiting a consultation from the pain management service. For all patients receiving opiates, the order set contains an automatic order for naloxone for respiratory depression manifested by a respiratory rate less than nine.
For patients with less severe pain, options for PRN (pro re nata, or as needed) bolus dose morphine and hydromorphone offer dose ranges that reflect the narcotic tolerance frequently observed in these patients. The order set includes options for non-opiate agents, including ketorolac and acetaminophen. Adjuvant therapies, including promethazine, zolpidem, and diphenhydramine, are also contained within the order set. Prompts for intravenous fluid replacement, oxygen therapy, and other supportive measures are incorporated into the orders as well.
The Novant-SPR hospitals have adopted a separate order set for the administration of pneumococcal vaccine. This order set allows for the automatic administration of pneumococcal vaccine, without a specific physician order, to every patient who meets criteria and who desires the vaccine. On admission, every patient is screened by a nurse regarding their need for pneumococcal vaccine; as a result, SCD patients who have not been immunized in the previous five years are offered the vaccine.
Day Hospital Model
In order to provide SCD patients with immediate and aggressive analgesic therapy and fluid replacement, some centers have adopted the Day Hospital (DH) model. The DH is a specific site at which patients with SCD pain crisis are treated by staff familiar with the patients and with their special analgesic needs.5 The DH model has been shown to provide rapid pain relief in an outpatient setting and to reduce the need for unnecessary hospitalizations. In addition, length of stay and cost per case are lower for DH patients admitted to the hospital than for patients not followed by DH staff. It has been suggested that the DH model is especially appropriate for centers with an emergency department too busy to begin treatment in a timely fashion.6
Novant Health has adopted the DH model in the urgent care setting. Patients with pain crises can be managed in one of Novant’s urgent care centers with a standard order set that includes options for IV hydration as well as parenteral morphine or hydromorphone. This outpatient order set parallels that designed for inpatients, because it prompts the physician to order aggressive analgesic therapy as well as adjuvant treatments for nausea and anxiety. Practitioners from Novant’s Sickle Cell Clinic often meet the patient at the urgent care center to assist with evaluation and management. In the past two years, approximately two-thirds of patients with SCD pain crisis have been discharged to home with good pain relief. The remaining one-third are referred to the hospital—usually to be admitted and managed by the PICS team.
Hope for the Future
It has been more than 50 years since the molecular defect in hemoglobin S was first described by Linus Pauling and 50 years since the genetic defect was first elucidated.7,8 Despite these and subsequent advances in understanding the pathogenesis of SCD at the cellular and molecular level, our treatment for SCD remains inadequate. It is akin to a “halfway technology” described by Lewis Thomas as, “the kinds of things that must be done … in order to compensate for the incapacitating effects of certain diseases whose course one is unable to do very much about. It is a technology designed to make up for disease, or to postpone death.”9
At present a number of agents designed to inhibit the sickling process are under investigation, including omega-3 fatty acids, Gardos channel blockers, and anti-adhesion therapies.10 In time, perhaps, one of these rational approaches to treatment will bridge the chasm in the halfway technology currently at our disposal. TH
Dr. Gardella is a board-certified internist and pulmonologist who currently serves as vice president for clinical improvement for Novant Health—Southern Piedmont Region.
Julie Swanger works with both pediatric and adult sickle cell populations through Presbyterian Community Care Services and Blume Pediatric Hematology and Oncology Clinic in Charlotte, N.C.
References
- Conlan M. Therapeutic interventions frequent among hospital pharmacists. Drug Top Hosp Pharmacist Rep. 2000;14(9):38-39.
- Piturro M. Top PICS: Presbyterian Inpatient Care Specialists bring high-quality hospitalist care to North Carolina. The Hospitalist. 2006;01(10):23-25.
- Elander J, Midence K. A review of evidence about factors affecting quality of pain management in sickle cell disease. Clin J Pain. 1996 Sep;12(3):180-193.
- Steinberg MH. Management of sickle cell disease. N Engl J Med. 1999;340:1021-1030.
- Sickle Cell Disease Association of America, Inc., Web site. Outpatient management issues in sickle cell disease. Available at: www.sicklecelldisease.org/research/scd_manage3.phtml. Last accessed January 26, 2007.
- Benjamin LJ, Swinson GI, Nagel RL. Sickle cell anemia day hospital: an approach for the management of uncomplicated painful crises. Blood. 2000 Feb;95(4):1130-1136.
- Pauling L, Itano HA, Singer SJ, et al. Sickle cell anemia a molecular disease. Science. 1949 Nov 25;110:543-548.
- Ingram VM. Gene mutations in human haemoglobin: the chemical difference between normal and sickle cell haemoglobin. Nature. 1957 Aug 17;180(4581):326-328.
- Thomas L. The technology of medicine. In: The Lives of a Cell. New York: Viking Press; 1974:31-36.
- Okpala IE. New therapies for sickle cell disease. Hematol Oncol Clin North Am. 2005 Oct;19(5):975-987.
Standardized order sets reduce medication errors and create efficiency for physicians, nurses, and pharmacists.1 A less recognized benefit may be that standardized orders promote equity in care and may help to mitigate disparities that occur along racial and ethnic lines. Patients admitted with an acute pain crisis secondary to sickle cell disease (SCD) are often suspected of drug-seeking behavior and may be treated in a cursory manner because they are “frequent flyers” on the medical service. In view of these factors, this patient group may benefit more than others from a standardized treatment protocol. Over the past year, hospitalists and other clinicians at Novant Health in Charlotte, N.C., have composed an admission order set for SCD pain crisis in an effort to improve care for this underserved group.
Novant Health
Novant Health is a multi-hospital, non-profit system serving 3.5 million people from Virginia to South Carolina. Presbyterian Hospital, a 531-bed facility in Charlotte, N.C., is the flagship hospital for Novant’s Southern Piedmont Region (SPR). Presbyterian Inpatient Care Specialists (PICS) is a 44-provider group that offers hospitalist services for adult patients at Presbyterian Hospital, two community hospitals in Matthews and Huntersville, and Presbyterian Orthopedic Hospital.2 In 2005, 180 adult patients were discharged from the Novant-SPR hospitals with a principal diagnosis of SCD, and most of these patients were managed by PICS. This cohort of 180 patients accounted for more than 600 hospitalizations for SCD-related illness at the Novant-SPR facilities in 2005.
Process and Procedure
Standardized order sets have been in widespread use at the Novant-SPR facilities for a number of years. The process of order set development begins with patient needs as perceived by medical staff. Once a physician has drafted an order set, the draft is reviewed by the Order Set Subcommittee, a multidisciplinary team chaired by Susan Smith, RPh, PharmD, with nurses, physicians, and other support staff represented as needed. Once the subcommittee has approved the draft, it goes to the Pharmacy and Therapeutics Committee for final approval. In this fashion, more than 600 order sets have been developed and made available on the hospital’s intranet. The PICS team has helped to develop a number of disease management order sets and protocols, including the general medical admission orders. In addition, PICS has assisted in developing disease-specific orders for community-acquired pneumonia (CAP), CVA/TIA, and other common diseases admitted by the hospitalist service.
In the case of the adult SCD pain crisis order set, Stephen Wallenhaupt, MD, chief medical officer for Novant Health, recalls, “We recognize that SCD patients have unique needs in terms of pain management and that a standardized order set which incorporates aggressive pain management options is the best way to meet their needs.”
Fran Davis, RPh, PharmD, researched the pertinent literature and consulted the anesthesiologists on staff in an effort to tailor the pain management options for SCD patients. Using the recommendations of these specialists, the order set reflects the consensus that patients with a severe SCD pain crisis require parenteral opiate analgesia on admission.3
Because many patients admitted by PICS can be categorized as having severe pain, the order set contains choices for patient-controlled analgesia (PCA), in keeping with the recommendation for opiate administration at a fixed interval rather than on an as-needed basis.4 And because many hospitalists may not be familiar with ordering PCA, the SCD orders specify the dose ranges, as well as the lockout interval for morphine and hydromorphone PCA. With PCA options readily available, hospitalists need not delay therapy while awaiting a consultation from the pain management service. For all patients receiving opiates, the order set contains an automatic order for naloxone for respiratory depression manifested by a respiratory rate less than nine.
For patients with less severe pain, options for PRN (pro re nata, or as needed) bolus dose morphine and hydromorphone offer dose ranges that reflect the narcotic tolerance frequently observed in these patients. The order set includes options for non-opiate agents, including ketorolac and acetaminophen. Adjuvant therapies, including promethazine, zolpidem, and diphenhydramine, are also contained within the order set. Prompts for intravenous fluid replacement, oxygen therapy, and other supportive measures are incorporated into the orders as well.
The Novant-SPR hospitals have adopted a separate order set for the administration of pneumococcal vaccine. This order set allows for the automatic administration of pneumococcal vaccine, without a specific physician order, to every patient who meets criteria and who desires the vaccine. On admission, every patient is screened by a nurse regarding their need for pneumococcal vaccine; as a result, SCD patients who have not been immunized in the previous five years are offered the vaccine.
Day Hospital Model
In order to provide SCD patients with immediate and aggressive analgesic therapy and fluid replacement, some centers have adopted the Day Hospital (DH) model. The DH is a specific site at which patients with SCD pain crisis are treated by staff familiar with the patients and with their special analgesic needs.5 The DH model has been shown to provide rapid pain relief in an outpatient setting and to reduce the need for unnecessary hospitalizations. In addition, length of stay and cost per case are lower for DH patients admitted to the hospital than for patients not followed by DH staff. It has been suggested that the DH model is especially appropriate for centers with an emergency department too busy to begin treatment in a timely fashion.6
Novant Health has adopted the DH model in the urgent care setting. Patients with pain crises can be managed in one of Novant’s urgent care centers with a standard order set that includes options for IV hydration as well as parenteral morphine or hydromorphone. This outpatient order set parallels that designed for inpatients, because it prompts the physician to order aggressive analgesic therapy as well as adjuvant treatments for nausea and anxiety. Practitioners from Novant’s Sickle Cell Clinic often meet the patient at the urgent care center to assist with evaluation and management. In the past two years, approximately two-thirds of patients with SCD pain crisis have been discharged to home with good pain relief. The remaining one-third are referred to the hospital—usually to be admitted and managed by the PICS team.
Hope for the Future
It has been more than 50 years since the molecular defect in hemoglobin S was first described by Linus Pauling and 50 years since the genetic defect was first elucidated.7,8 Despite these and subsequent advances in understanding the pathogenesis of SCD at the cellular and molecular level, our treatment for SCD remains inadequate. It is akin to a “halfway technology” described by Lewis Thomas as, “the kinds of things that must be done … in order to compensate for the incapacitating effects of certain diseases whose course one is unable to do very much about. It is a technology designed to make up for disease, or to postpone death.”9
At present a number of agents designed to inhibit the sickling process are under investigation, including omega-3 fatty acids, Gardos channel blockers, and anti-adhesion therapies.10 In time, perhaps, one of these rational approaches to treatment will bridge the chasm in the halfway technology currently at our disposal. TH
Dr. Gardella is a board-certified internist and pulmonologist who currently serves as vice president for clinical improvement for Novant Health—Southern Piedmont Region.
Julie Swanger works with both pediatric and adult sickle cell populations through Presbyterian Community Care Services and Blume Pediatric Hematology and Oncology Clinic in Charlotte, N.C.
References
- Conlan M. Therapeutic interventions frequent among hospital pharmacists. Drug Top Hosp Pharmacist Rep. 2000;14(9):38-39.
- Piturro M. Top PICS: Presbyterian Inpatient Care Specialists bring high-quality hospitalist care to North Carolina. The Hospitalist. 2006;01(10):23-25.
- Elander J, Midence K. A review of evidence about factors affecting quality of pain management in sickle cell disease. Clin J Pain. 1996 Sep;12(3):180-193.
- Steinberg MH. Management of sickle cell disease. N Engl J Med. 1999;340:1021-1030.
- Sickle Cell Disease Association of America, Inc., Web site. Outpatient management issues in sickle cell disease. Available at: www.sicklecelldisease.org/research/scd_manage3.phtml. Last accessed January 26, 2007.
- Benjamin LJ, Swinson GI, Nagel RL. Sickle cell anemia day hospital: an approach for the management of uncomplicated painful crises. Blood. 2000 Feb;95(4):1130-1136.
- Pauling L, Itano HA, Singer SJ, et al. Sickle cell anemia a molecular disease. Science. 1949 Nov 25;110:543-548.
- Ingram VM. Gene mutations in human haemoglobin: the chemical difference between normal and sickle cell haemoglobin. Nature. 1957 Aug 17;180(4581):326-328.
- Thomas L. The technology of medicine. In: The Lives of a Cell. New York: Viking Press; 1974:31-36.
- Okpala IE. New therapies for sickle cell disease. Hematol Oncol Clin North Am. 2005 Oct;19(5):975-987.
Standardized order sets reduce medication errors and create efficiency for physicians, nurses, and pharmacists.1 A less recognized benefit may be that standardized orders promote equity in care and may help to mitigate disparities that occur along racial and ethnic lines. Patients admitted with an acute pain crisis secondary to sickle cell disease (SCD) are often suspected of drug-seeking behavior and may be treated in a cursory manner because they are “frequent flyers” on the medical service. In view of these factors, this patient group may benefit more than others from a standardized treatment protocol. Over the past year, hospitalists and other clinicians at Novant Health in Charlotte, N.C., have composed an admission order set for SCD pain crisis in an effort to improve care for this underserved group.
Novant Health
Novant Health is a multi-hospital, non-profit system serving 3.5 million people from Virginia to South Carolina. Presbyterian Hospital, a 531-bed facility in Charlotte, N.C., is the flagship hospital for Novant’s Southern Piedmont Region (SPR). Presbyterian Inpatient Care Specialists (PICS) is a 44-provider group that offers hospitalist services for adult patients at Presbyterian Hospital, two community hospitals in Matthews and Huntersville, and Presbyterian Orthopedic Hospital.2 In 2005, 180 adult patients were discharged from the Novant-SPR hospitals with a principal diagnosis of SCD, and most of these patients were managed by PICS. This cohort of 180 patients accounted for more than 600 hospitalizations for SCD-related illness at the Novant-SPR facilities in 2005.
Process and Procedure
Standardized order sets have been in widespread use at the Novant-SPR facilities for a number of years. The process of order set development begins with patient needs as perceived by medical staff. Once a physician has drafted an order set, the draft is reviewed by the Order Set Subcommittee, a multidisciplinary team chaired by Susan Smith, RPh, PharmD, with nurses, physicians, and other support staff represented as needed. Once the subcommittee has approved the draft, it goes to the Pharmacy and Therapeutics Committee for final approval. In this fashion, more than 600 order sets have been developed and made available on the hospital’s intranet. The PICS team has helped to develop a number of disease management order sets and protocols, including the general medical admission orders. In addition, PICS has assisted in developing disease-specific orders for community-acquired pneumonia (CAP), CVA/TIA, and other common diseases admitted by the hospitalist service.
In the case of the adult SCD pain crisis order set, Stephen Wallenhaupt, MD, chief medical officer for Novant Health, recalls, “We recognize that SCD patients have unique needs in terms of pain management and that a standardized order set which incorporates aggressive pain management options is the best way to meet their needs.”
Fran Davis, RPh, PharmD, researched the pertinent literature and consulted the anesthesiologists on staff in an effort to tailor the pain management options for SCD patients. Using the recommendations of these specialists, the order set reflects the consensus that patients with a severe SCD pain crisis require parenteral opiate analgesia on admission.3
Because many patients admitted by PICS can be categorized as having severe pain, the order set contains choices for patient-controlled analgesia (PCA), in keeping with the recommendation for opiate administration at a fixed interval rather than on an as-needed basis.4 And because many hospitalists may not be familiar with ordering PCA, the SCD orders specify the dose ranges, as well as the lockout interval for morphine and hydromorphone PCA. With PCA options readily available, hospitalists need not delay therapy while awaiting a consultation from the pain management service. For all patients receiving opiates, the order set contains an automatic order for naloxone for respiratory depression manifested by a respiratory rate less than nine.
For patients with less severe pain, options for PRN (pro re nata, or as needed) bolus dose morphine and hydromorphone offer dose ranges that reflect the narcotic tolerance frequently observed in these patients. The order set includes options for non-opiate agents, including ketorolac and acetaminophen. Adjuvant therapies, including promethazine, zolpidem, and diphenhydramine, are also contained within the order set. Prompts for intravenous fluid replacement, oxygen therapy, and other supportive measures are incorporated into the orders as well.
The Novant-SPR hospitals have adopted a separate order set for the administration of pneumococcal vaccine. This order set allows for the automatic administration of pneumococcal vaccine, without a specific physician order, to every patient who meets criteria and who desires the vaccine. On admission, every patient is screened by a nurse regarding their need for pneumococcal vaccine; as a result, SCD patients who have not been immunized in the previous five years are offered the vaccine.
Day Hospital Model
In order to provide SCD patients with immediate and aggressive analgesic therapy and fluid replacement, some centers have adopted the Day Hospital (DH) model. The DH is a specific site at which patients with SCD pain crisis are treated by staff familiar with the patients and with their special analgesic needs.5 The DH model has been shown to provide rapid pain relief in an outpatient setting and to reduce the need for unnecessary hospitalizations. In addition, length of stay and cost per case are lower for DH patients admitted to the hospital than for patients not followed by DH staff. It has been suggested that the DH model is especially appropriate for centers with an emergency department too busy to begin treatment in a timely fashion.6
Novant Health has adopted the DH model in the urgent care setting. Patients with pain crises can be managed in one of Novant’s urgent care centers with a standard order set that includes options for IV hydration as well as parenteral morphine or hydromorphone. This outpatient order set parallels that designed for inpatients, because it prompts the physician to order aggressive analgesic therapy as well as adjuvant treatments for nausea and anxiety. Practitioners from Novant’s Sickle Cell Clinic often meet the patient at the urgent care center to assist with evaluation and management. In the past two years, approximately two-thirds of patients with SCD pain crisis have been discharged to home with good pain relief. The remaining one-third are referred to the hospital—usually to be admitted and managed by the PICS team.
Hope for the Future
It has been more than 50 years since the molecular defect in hemoglobin S was first described by Linus Pauling and 50 years since the genetic defect was first elucidated.7,8 Despite these and subsequent advances in understanding the pathogenesis of SCD at the cellular and molecular level, our treatment for SCD remains inadequate. It is akin to a “halfway technology” described by Lewis Thomas as, “the kinds of things that must be done … in order to compensate for the incapacitating effects of certain diseases whose course one is unable to do very much about. It is a technology designed to make up for disease, or to postpone death.”9
At present a number of agents designed to inhibit the sickling process are under investigation, including omega-3 fatty acids, Gardos channel blockers, and anti-adhesion therapies.10 In time, perhaps, one of these rational approaches to treatment will bridge the chasm in the halfway technology currently at our disposal. TH
Dr. Gardella is a board-certified internist and pulmonologist who currently serves as vice president for clinical improvement for Novant Health—Southern Piedmont Region.
Julie Swanger works with both pediatric and adult sickle cell populations through Presbyterian Community Care Services and Blume Pediatric Hematology and Oncology Clinic in Charlotte, N.C.
References
- Conlan M. Therapeutic interventions frequent among hospital pharmacists. Drug Top Hosp Pharmacist Rep. 2000;14(9):38-39.
- Piturro M. Top PICS: Presbyterian Inpatient Care Specialists bring high-quality hospitalist care to North Carolina. The Hospitalist. 2006;01(10):23-25.
- Elander J, Midence K. A review of evidence about factors affecting quality of pain management in sickle cell disease. Clin J Pain. 1996 Sep;12(3):180-193.
- Steinberg MH. Management of sickle cell disease. N Engl J Med. 1999;340:1021-1030.
- Sickle Cell Disease Association of America, Inc., Web site. Outpatient management issues in sickle cell disease. Available at: www.sicklecelldisease.org/research/scd_manage3.phtml. Last accessed January 26, 2007.
- Benjamin LJ, Swinson GI, Nagel RL. Sickle cell anemia day hospital: an approach for the management of uncomplicated painful crises. Blood. 2000 Feb;95(4):1130-1136.
- Pauling L, Itano HA, Singer SJ, et al. Sickle cell anemia a molecular disease. Science. 1949 Nov 25;110:543-548.
- Ingram VM. Gene mutations in human haemoglobin: the chemical difference between normal and sickle cell haemoglobin. Nature. 1957 Aug 17;180(4581):326-328.
- Thomas L. The technology of medicine. In: The Lives of a Cell. New York: Viking Press; 1974:31-36.
- Okpala IE. New therapies for sickle cell disease. Hematol Oncol Clin North Am. 2005 Oct;19(5):975-987.
Hospitalists & Handoffs
In the nearly 10 years since the word “hospitalist” entered our consciousness, it has been inspiring to witness the dramatic growth in the specialty and, accompanying it, the growth in the membership of SHM.1 Over this same period, the healthcare system has made progress toward ensuring that it provides the safest, highest quality healthcare possible.
In my mind, the two phenomena are related. SHM itself and—more generally—the hospitalist field have played a vital role in promoting the use of evidence-based care, improved teamwork, and health information technology. Each of these efforts has made a significant difference in the care patients receive in hospitals. Similarly, the mission of the Agency for Healthcare Research and Quality (AHRQ) is to improve the quality, safety, efficiency, and effectiveness of healthcare for all Americans. Both organizations are working to create positive change that will improve the health and healthcare of all patients.
As their numbers continue to grow, hospitalists are becoming integral members of the inpatient care team at many hospitals.
According to a recent survey conducted by SHM, a hospitalist averaged more than 2,300 inpatient encounters in 2005—a 7% increase over 2004.2 Today, hospital medicine groups practice not only in large metropolitan areas, but also in rural regions where one in three groups began operation during 2005.
In addition to their inpatient care responsibilities, the 15,000 hospitalists who practice today in the United States and Canada serve in key physician leadership roles that directly influence quality improvement and patient safety. Most hospitalists—86%—participate in quality improvement. More than half are involved in implementing information technology (54%) and teaching house staff (51%), and more than one-third—35%—are responsible for their organization’s rapid response team. The SHM survey found that nearly all hospital medicine groups provide round-the-clock patient care at their hospitals.
In this article I will emphasize two key areas relevant to improving patient safety for hospitalized patients: patient handoffs and communication.
Responsibility for Patient Handoffs
Hospitalists’ clinical and leadership roles are significant responsibilities for patient safety, including the critical period known as patient handoff or sign-out.
Patient handoffs refer to the interaction, communication, and planning required to achieve a seamless transition from one clinician to the next.3 When executed in a timely and thorough manner, patient handoffs can reduce the likelihood of medical errors and misinformation, prevent lost or missing clinical information, and maintain a high level of medical care.
Given today’s short hospital stays and the complex medical nature of the care necessary for many patients, timely and effective handoffs demand that hospitalists develop skills that extend beyond superior clinical care. They include:
- Communicating in an effective and efficient manner during patient sign-out;
- Demonstrating the use of “read-back” skills when communicating tasks;
- Developing oral and written patient summaries, including characteristics of the patient, provider, and time of the sign-out;
- Evaluating all medications for indication, dosing, and planned duration at the time of sign-out; and
- Anticipating what may go wrong with a patient after a transition in care occurs and clearly communicating this concern to the receiving clinician.
A Fumbled Handoff: A Case Study
A breakdown in communications—notably an error of omission in the patient handoff—contributed to a poor outcome for an elderly patient who was admitted to the hospital for an elective sigmoid resection.
The case, which was published in the AHRQ’s “Morbidity and Mortality Rounds on the Web” (developed by hospital medicine expert Robert Wachter, MD, and his team under contract to our agency), illustrates some of the challenges that face all clinicians in effectively transferring patient information and care responsibilities.4 It also underscores the need for close involvement by hospitalists in improving quality, teaching and supervising house staff, and implementing information systems.
According to the case study, a 73-year-old female patient with a history of hypertension, non-insulin dependent diabetes, and chronic renal insufficiency became tachycardic two days after surgery, despite receiving a low-dose beta-blocker. The same day, she informed her nurse that she had developed pain in her left leg.
Assuming the pain was related to the pre-operative epidural, the nurse contacted the anesthesia service, which responded by decreasing the epidural rate; the primary surgical team was not called. Late on the third day after surgery, the cross-covering intern was contacted about the patient’s left leg pain. No information about the intern’s findings was relayed to the primary team the following day.
On the fourth day, the patient complained to the nurse about mild chest discomfort, resulting in attention within 20 minutes by house staff and from the attending physician several hours later. The patient’s exam was unremarkable and a work-up was initiated.
Within an hour of the attending’s visit, the patient’s blood pressure dropped to 70/40, followed by a pulseless electrical activity arrest. The patient could not be resuscitated. A post-mortem examination revealed a pulmonary embolism.
Handoffs in an Era of Work-Hour Restrictions
Missing information about pain in the patient’s leg and a breakdown in communication between physicians contributed to the patient’s poor outcome. In this case, the breakdown may also have been influenced by the intern’s involvement on the third day. Like all medical residents this intern is subject to duty-hour restrictions.
Work-hour limits for all residents training in U.S. hospitals took effect in July 2003. Under these standards, created by the Accreditation Council for Graduate Medical Education (ACGME), residents are limited to a maximum of 30 consecutive work hours—known as the 30-hour rule, which includes time used for sign-out, teaching, and continuity of care. They are also prohibited from working more than 80 hours per week.
Despite the clear safety benefit of preventing fatigue-related mistakes, work-hour mandates have increased the number of patient handoffs and the potential for communication breakdowns.5 A survey of interns conducted at the hospital where this case study occurred identified a higher volume of sign-outs and the resulting potential for harm to patients as main concerns with the work-hour restrictions.6
Concerns about the quality and continuity of care that hospital patients receive are evident even among those medical residents whose work hours were restricted before the ACGME requirements took effect. (In New York state residents’ work hours have been restricted since 1998.)
A 2006 study of surgical residents at New York’s Beth Israel Hospital found that most believed that the quality of care patients received was either unchanged (63%) or worse (26%) since the work-hour restrictions took effect.7 Possible reasons for this perception include unresolved issues with continuity of care, miscommunication, and cross-coverage availability. The study concluded that interventions that target intern sign-out coverage constraints will be important for future efforts to improve the quality of care for hospital patients.
Written sign-outs appear to overcome some of the human errors that inevitably result from verbal patient summaries, such as disruptions and forgetfulness. Recent findings have, however, identified significant shortcomings in the quality and timeliness of written reports.
Critical information, such as code status and allergies, was missing in 80% of written sign-outs in one recent study.8 And in a 2006 study of the quality of discharge summaries, only 19% of hospital physicians with an outpatient practice reported being satisfied with the timeliness of discharge summaries. Only a third reported being satisfied with their quality of information. Most troubling, 41% believed that at least one of their patients hospitalized in the previous six months had experienced a preventable adverse event related to poor transfer of information at discharge.9
Use Redundancy and Simulation to Improve Safety
Given the clear challenges of providing quality and continuity of care in the inpatient setting, hospitalists are well positioned to identify strategies for safe and effective patient handoffs and advocate for a systems approach to their implementation.
Safety strategies that have been employed by industries outside of healthcare can provide a useful starting point. So-called “highly reliable” organizations use a variety of approaches to reduce the incidence of errors that occur during transitions in work staff. A recent review of transition methods used by NASA’s Johnson Space Center (Houston), Canadian nuclear power plants, and an ambulance dispatch center—organizations where lapses in transitions also have serious consequences—found that these entities used up to 21 handoff strategies.10 Techniques included verbal, face-to-face, and interactive questioning coordinated with written summaries just before a shift change.
Increasing redundancy is another technique used by highly reliable organizations to reduce the likelihood of missed, incomplete, or misinterpreted information. To create redundancy in clinical care, a physician would include more information at the outset of a procedure or medication order than is now typically provided. This additional information is then repeated and validated by other members of the care team throughout the process, reducing the likelihood of misinterpretation of an instruction or action based on incomplete information.
For example, if a physician always includes both the drug name and the condition for which it is prescribed, a medication order for “Celebrex, seizures,” instead of “Cerebyx, seizures,” would immediately indicate a mistake had occurred in ordering a pain medication instead of an anti-convulsant.11 Research has shown that increasing the amount of information about a medication order reduces the range of potentially valid clinical decisions.
Whether a hospital relies on verbal communication, written communication, computer-based communication, or a combination of all three, redundancy can be built into its sign-out processes. As PDAs become more widely used, structured sign-outs should incorporate redundancy into patient-specific checklists to include information on clinical status, recent and pending tests and study results, and similar, pertinent information.
Simulation-based training that incorporates redundancy and promotes read-back of patient information holds promise for error reduction, especially during patient handoffs.
AHRQ has recently funded research on simulation training projects that seek to:
- Reduce communication errors during patient handoffs in the emergency department by implementing a patient-specific checklist based on an electronic medical record and by testing the effect of companion simulation-based training; and
- Evaluate and improve safe communication and coordination between anesthesia providers and nurses during care transitions and during hand-offs between the operating room and the post-anesthesia care unit.12
The 24/7 role of hospital physicians brings unique experiences and insights to the challenges of patient safety that can test the feasibility of systems to reduce errors associated with care transitions. As their numbers and leadership roles expand, hospitalists are poised to make significant contributions to improving patient safety and outcomes.
We at AHRQ look forward to assisting hospitalists in making these contributions and to achieving these goals together. We also look forward to continuing our relationship with SHM and the hospitalist community as a whole. TH
Dr. Clancy is the director of the Agency for Healthcare Research and Quality.
References
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996 Aug 15;335(7):514-517.
- Impact of the nation’s hospitalists continues to grow new society of hospital medicine survey says [press release]. Society of Hospital Medicine. May 4, 2006.
- Society of Hospital Medicine. The core competencies in hospital medicine: a framework for curriculum development by the society of hospital medicine. J Hosp Med. 2006;1;S1. Available at: http://onlinelibrary.wiley.com/doi/10.1002/jhm.72/pdf. Last accessed January 17, 2007.
- Vidyarthi A [commentary]. Agency for Healthcare Research and Quality Web M&M: Morbidity and Mortality Rounds on the Web. Fumbled handoff. March 2004. Available at: www.webmm.ahrq.gov/case.aspx?caseID=55. Last accessed January 17, 2007.
- Wachter RM, Shojania KG. Internal Bleeding: The Truth Behind America’s Terrifying Epidemic of Medical Mistakes. New York: Rugged Land LLG; 2004.
- Vidyarthi A. Morbidity and Mortality Rounds on the Web, “Fumbled Handoff,” unpublished data, 2004.
- Biller CK, Antonacci AC, Pelletier S, et al. The 80-hour work guidelines and resident survey perceptions of quality. J Surg Res. 2006 Oct;135(2):275-281. Epub 2006 Aug 24.
- Lee LH, Levine JA, Schultz HJ. Utility of a standardized sign-out card for new medical interns. J Gen Intern Med. 1996;11(12):753-755.
- O’Leary KJ, Leibovitz DM, Feinglass J, et al. Outpatient physicians’ satisfaction with discharge summaries and perceived need for an electronic discharge summary. J Hosp Med. 2006;1:317-320. Published online Oct. 11, 2006.
- Reason JT. Managing the Risks of Organizational Accidents. Aldershot, England: Ashgate Publishing Company; 1997:135.
- Bar-Yam Y. System care: multiscale analysis of medical errors–eliminating errors and improving organizational capabilities. New England Complex Systems Institute: Technical Report; Sept 2004. Available at: http://necsi.org/projects/yaneer/NECSITechnicalReport2004-09.pdf. Last accessed January 17, 2007.
- Agency for Healthcare Research and Quality. Improving patient safety through simulation research. 2006 Simulation Projects. Available at: www.ahrq.gov/qual/simulproj.htm. Last accessed January 17, 2007.
In the nearly 10 years since the word “hospitalist” entered our consciousness, it has been inspiring to witness the dramatic growth in the specialty and, accompanying it, the growth in the membership of SHM.1 Over this same period, the healthcare system has made progress toward ensuring that it provides the safest, highest quality healthcare possible.
In my mind, the two phenomena are related. SHM itself and—more generally—the hospitalist field have played a vital role in promoting the use of evidence-based care, improved teamwork, and health information technology. Each of these efforts has made a significant difference in the care patients receive in hospitals. Similarly, the mission of the Agency for Healthcare Research and Quality (AHRQ) is to improve the quality, safety, efficiency, and effectiveness of healthcare for all Americans. Both organizations are working to create positive change that will improve the health and healthcare of all patients.
As their numbers continue to grow, hospitalists are becoming integral members of the inpatient care team at many hospitals.
According to a recent survey conducted by SHM, a hospitalist averaged more than 2,300 inpatient encounters in 2005—a 7% increase over 2004.2 Today, hospital medicine groups practice not only in large metropolitan areas, but also in rural regions where one in three groups began operation during 2005.
In addition to their inpatient care responsibilities, the 15,000 hospitalists who practice today in the United States and Canada serve in key physician leadership roles that directly influence quality improvement and patient safety. Most hospitalists—86%—participate in quality improvement. More than half are involved in implementing information technology (54%) and teaching house staff (51%), and more than one-third—35%—are responsible for their organization’s rapid response team. The SHM survey found that nearly all hospital medicine groups provide round-the-clock patient care at their hospitals.
In this article I will emphasize two key areas relevant to improving patient safety for hospitalized patients: patient handoffs and communication.
Responsibility for Patient Handoffs
Hospitalists’ clinical and leadership roles are significant responsibilities for patient safety, including the critical period known as patient handoff or sign-out.
Patient handoffs refer to the interaction, communication, and planning required to achieve a seamless transition from one clinician to the next.3 When executed in a timely and thorough manner, patient handoffs can reduce the likelihood of medical errors and misinformation, prevent lost or missing clinical information, and maintain a high level of medical care.
Given today’s short hospital stays and the complex medical nature of the care necessary for many patients, timely and effective handoffs demand that hospitalists develop skills that extend beyond superior clinical care. They include:
- Communicating in an effective and efficient manner during patient sign-out;
- Demonstrating the use of “read-back” skills when communicating tasks;
- Developing oral and written patient summaries, including characteristics of the patient, provider, and time of the sign-out;
- Evaluating all medications for indication, dosing, and planned duration at the time of sign-out; and
- Anticipating what may go wrong with a patient after a transition in care occurs and clearly communicating this concern to the receiving clinician.
A Fumbled Handoff: A Case Study
A breakdown in communications—notably an error of omission in the patient handoff—contributed to a poor outcome for an elderly patient who was admitted to the hospital for an elective sigmoid resection.
The case, which was published in the AHRQ’s “Morbidity and Mortality Rounds on the Web” (developed by hospital medicine expert Robert Wachter, MD, and his team under contract to our agency), illustrates some of the challenges that face all clinicians in effectively transferring patient information and care responsibilities.4 It also underscores the need for close involvement by hospitalists in improving quality, teaching and supervising house staff, and implementing information systems.
According to the case study, a 73-year-old female patient with a history of hypertension, non-insulin dependent diabetes, and chronic renal insufficiency became tachycardic two days after surgery, despite receiving a low-dose beta-blocker. The same day, she informed her nurse that she had developed pain in her left leg.
Assuming the pain was related to the pre-operative epidural, the nurse contacted the anesthesia service, which responded by decreasing the epidural rate; the primary surgical team was not called. Late on the third day after surgery, the cross-covering intern was contacted about the patient’s left leg pain. No information about the intern’s findings was relayed to the primary team the following day.
On the fourth day, the patient complained to the nurse about mild chest discomfort, resulting in attention within 20 minutes by house staff and from the attending physician several hours later. The patient’s exam was unremarkable and a work-up was initiated.
Within an hour of the attending’s visit, the patient’s blood pressure dropped to 70/40, followed by a pulseless electrical activity arrest. The patient could not be resuscitated. A post-mortem examination revealed a pulmonary embolism.
Handoffs in an Era of Work-Hour Restrictions
Missing information about pain in the patient’s leg and a breakdown in communication between physicians contributed to the patient’s poor outcome. In this case, the breakdown may also have been influenced by the intern’s involvement on the third day. Like all medical residents this intern is subject to duty-hour restrictions.
Work-hour limits for all residents training in U.S. hospitals took effect in July 2003. Under these standards, created by the Accreditation Council for Graduate Medical Education (ACGME), residents are limited to a maximum of 30 consecutive work hours—known as the 30-hour rule, which includes time used for sign-out, teaching, and continuity of care. They are also prohibited from working more than 80 hours per week.
Despite the clear safety benefit of preventing fatigue-related mistakes, work-hour mandates have increased the number of patient handoffs and the potential for communication breakdowns.5 A survey of interns conducted at the hospital where this case study occurred identified a higher volume of sign-outs and the resulting potential for harm to patients as main concerns with the work-hour restrictions.6
Concerns about the quality and continuity of care that hospital patients receive are evident even among those medical residents whose work hours were restricted before the ACGME requirements took effect. (In New York state residents’ work hours have been restricted since 1998.)
A 2006 study of surgical residents at New York’s Beth Israel Hospital found that most believed that the quality of care patients received was either unchanged (63%) or worse (26%) since the work-hour restrictions took effect.7 Possible reasons for this perception include unresolved issues with continuity of care, miscommunication, and cross-coverage availability. The study concluded that interventions that target intern sign-out coverage constraints will be important for future efforts to improve the quality of care for hospital patients.
Written sign-outs appear to overcome some of the human errors that inevitably result from verbal patient summaries, such as disruptions and forgetfulness. Recent findings have, however, identified significant shortcomings in the quality and timeliness of written reports.
Critical information, such as code status and allergies, was missing in 80% of written sign-outs in one recent study.8 And in a 2006 study of the quality of discharge summaries, only 19% of hospital physicians with an outpatient practice reported being satisfied with the timeliness of discharge summaries. Only a third reported being satisfied with their quality of information. Most troubling, 41% believed that at least one of their patients hospitalized in the previous six months had experienced a preventable adverse event related to poor transfer of information at discharge.9
Use Redundancy and Simulation to Improve Safety
Given the clear challenges of providing quality and continuity of care in the inpatient setting, hospitalists are well positioned to identify strategies for safe and effective patient handoffs and advocate for a systems approach to their implementation.
Safety strategies that have been employed by industries outside of healthcare can provide a useful starting point. So-called “highly reliable” organizations use a variety of approaches to reduce the incidence of errors that occur during transitions in work staff. A recent review of transition methods used by NASA’s Johnson Space Center (Houston), Canadian nuclear power plants, and an ambulance dispatch center—organizations where lapses in transitions also have serious consequences—found that these entities used up to 21 handoff strategies.10 Techniques included verbal, face-to-face, and interactive questioning coordinated with written summaries just before a shift change.
Increasing redundancy is another technique used by highly reliable organizations to reduce the likelihood of missed, incomplete, or misinterpreted information. To create redundancy in clinical care, a physician would include more information at the outset of a procedure or medication order than is now typically provided. This additional information is then repeated and validated by other members of the care team throughout the process, reducing the likelihood of misinterpretation of an instruction or action based on incomplete information.
For example, if a physician always includes both the drug name and the condition for which it is prescribed, a medication order for “Celebrex, seizures,” instead of “Cerebyx, seizures,” would immediately indicate a mistake had occurred in ordering a pain medication instead of an anti-convulsant.11 Research has shown that increasing the amount of information about a medication order reduces the range of potentially valid clinical decisions.
Whether a hospital relies on verbal communication, written communication, computer-based communication, or a combination of all three, redundancy can be built into its sign-out processes. As PDAs become more widely used, structured sign-outs should incorporate redundancy into patient-specific checklists to include information on clinical status, recent and pending tests and study results, and similar, pertinent information.
Simulation-based training that incorporates redundancy and promotes read-back of patient information holds promise for error reduction, especially during patient handoffs.
AHRQ has recently funded research on simulation training projects that seek to:
- Reduce communication errors during patient handoffs in the emergency department by implementing a patient-specific checklist based on an electronic medical record and by testing the effect of companion simulation-based training; and
- Evaluate and improve safe communication and coordination between anesthesia providers and nurses during care transitions and during hand-offs between the operating room and the post-anesthesia care unit.12
The 24/7 role of hospital physicians brings unique experiences and insights to the challenges of patient safety that can test the feasibility of systems to reduce errors associated with care transitions. As their numbers and leadership roles expand, hospitalists are poised to make significant contributions to improving patient safety and outcomes.
We at AHRQ look forward to assisting hospitalists in making these contributions and to achieving these goals together. We also look forward to continuing our relationship with SHM and the hospitalist community as a whole. TH
Dr. Clancy is the director of the Agency for Healthcare Research and Quality.
References
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996 Aug 15;335(7):514-517.
- Impact of the nation’s hospitalists continues to grow new society of hospital medicine survey says [press release]. Society of Hospital Medicine. May 4, 2006.
- Society of Hospital Medicine. The core competencies in hospital medicine: a framework for curriculum development by the society of hospital medicine. J Hosp Med. 2006;1;S1. Available at: http://onlinelibrary.wiley.com/doi/10.1002/jhm.72/pdf. Last accessed January 17, 2007.
- Vidyarthi A [commentary]. Agency for Healthcare Research and Quality Web M&M: Morbidity and Mortality Rounds on the Web. Fumbled handoff. March 2004. Available at: www.webmm.ahrq.gov/case.aspx?caseID=55. Last accessed January 17, 2007.
- Wachter RM, Shojania KG. Internal Bleeding: The Truth Behind America’s Terrifying Epidemic of Medical Mistakes. New York: Rugged Land LLG; 2004.
- Vidyarthi A. Morbidity and Mortality Rounds on the Web, “Fumbled Handoff,” unpublished data, 2004.
- Biller CK, Antonacci AC, Pelletier S, et al. The 80-hour work guidelines and resident survey perceptions of quality. J Surg Res. 2006 Oct;135(2):275-281. Epub 2006 Aug 24.
- Lee LH, Levine JA, Schultz HJ. Utility of a standardized sign-out card for new medical interns. J Gen Intern Med. 1996;11(12):753-755.
- O’Leary KJ, Leibovitz DM, Feinglass J, et al. Outpatient physicians’ satisfaction with discharge summaries and perceived need for an electronic discharge summary. J Hosp Med. 2006;1:317-320. Published online Oct. 11, 2006.
- Reason JT. Managing the Risks of Organizational Accidents. Aldershot, England: Ashgate Publishing Company; 1997:135.
- Bar-Yam Y. System care: multiscale analysis of medical errors–eliminating errors and improving organizational capabilities. New England Complex Systems Institute: Technical Report; Sept 2004. Available at: http://necsi.org/projects/yaneer/NECSITechnicalReport2004-09.pdf. Last accessed January 17, 2007.
- Agency for Healthcare Research and Quality. Improving patient safety through simulation research. 2006 Simulation Projects. Available at: www.ahrq.gov/qual/simulproj.htm. Last accessed January 17, 2007.
In the nearly 10 years since the word “hospitalist” entered our consciousness, it has been inspiring to witness the dramatic growth in the specialty and, accompanying it, the growth in the membership of SHM.1 Over this same period, the healthcare system has made progress toward ensuring that it provides the safest, highest quality healthcare possible.
In my mind, the two phenomena are related. SHM itself and—more generally—the hospitalist field have played a vital role in promoting the use of evidence-based care, improved teamwork, and health information technology. Each of these efforts has made a significant difference in the care patients receive in hospitals. Similarly, the mission of the Agency for Healthcare Research and Quality (AHRQ) is to improve the quality, safety, efficiency, and effectiveness of healthcare for all Americans. Both organizations are working to create positive change that will improve the health and healthcare of all patients.
As their numbers continue to grow, hospitalists are becoming integral members of the inpatient care team at many hospitals.
According to a recent survey conducted by SHM, a hospitalist averaged more than 2,300 inpatient encounters in 2005—a 7% increase over 2004.2 Today, hospital medicine groups practice not only in large metropolitan areas, but also in rural regions where one in three groups began operation during 2005.
In addition to their inpatient care responsibilities, the 15,000 hospitalists who practice today in the United States and Canada serve in key physician leadership roles that directly influence quality improvement and patient safety. Most hospitalists—86%—participate in quality improvement. More than half are involved in implementing information technology (54%) and teaching house staff (51%), and more than one-third—35%—are responsible for their organization’s rapid response team. The SHM survey found that nearly all hospital medicine groups provide round-the-clock patient care at their hospitals.
In this article I will emphasize two key areas relevant to improving patient safety for hospitalized patients: patient handoffs and communication.
Responsibility for Patient Handoffs
Hospitalists’ clinical and leadership roles are significant responsibilities for patient safety, including the critical period known as patient handoff or sign-out.
Patient handoffs refer to the interaction, communication, and planning required to achieve a seamless transition from one clinician to the next.3 When executed in a timely and thorough manner, patient handoffs can reduce the likelihood of medical errors and misinformation, prevent lost or missing clinical information, and maintain a high level of medical care.
Given today’s short hospital stays and the complex medical nature of the care necessary for many patients, timely and effective handoffs demand that hospitalists develop skills that extend beyond superior clinical care. They include:
- Communicating in an effective and efficient manner during patient sign-out;
- Demonstrating the use of “read-back” skills when communicating tasks;
- Developing oral and written patient summaries, including characteristics of the patient, provider, and time of the sign-out;
- Evaluating all medications for indication, dosing, and planned duration at the time of sign-out; and
- Anticipating what may go wrong with a patient after a transition in care occurs and clearly communicating this concern to the receiving clinician.
A Fumbled Handoff: A Case Study
A breakdown in communications—notably an error of omission in the patient handoff—contributed to a poor outcome for an elderly patient who was admitted to the hospital for an elective sigmoid resection.
The case, which was published in the AHRQ’s “Morbidity and Mortality Rounds on the Web” (developed by hospital medicine expert Robert Wachter, MD, and his team under contract to our agency), illustrates some of the challenges that face all clinicians in effectively transferring patient information and care responsibilities.4 It also underscores the need for close involvement by hospitalists in improving quality, teaching and supervising house staff, and implementing information systems.
According to the case study, a 73-year-old female patient with a history of hypertension, non-insulin dependent diabetes, and chronic renal insufficiency became tachycardic two days after surgery, despite receiving a low-dose beta-blocker. The same day, she informed her nurse that she had developed pain in her left leg.
Assuming the pain was related to the pre-operative epidural, the nurse contacted the anesthesia service, which responded by decreasing the epidural rate; the primary surgical team was not called. Late on the third day after surgery, the cross-covering intern was contacted about the patient’s left leg pain. No information about the intern’s findings was relayed to the primary team the following day.
On the fourth day, the patient complained to the nurse about mild chest discomfort, resulting in attention within 20 minutes by house staff and from the attending physician several hours later. The patient’s exam was unremarkable and a work-up was initiated.
Within an hour of the attending’s visit, the patient’s blood pressure dropped to 70/40, followed by a pulseless electrical activity arrest. The patient could not be resuscitated. A post-mortem examination revealed a pulmonary embolism.
Handoffs in an Era of Work-Hour Restrictions
Missing information about pain in the patient’s leg and a breakdown in communication between physicians contributed to the patient’s poor outcome. In this case, the breakdown may also have been influenced by the intern’s involvement on the third day. Like all medical residents this intern is subject to duty-hour restrictions.
Work-hour limits for all residents training in U.S. hospitals took effect in July 2003. Under these standards, created by the Accreditation Council for Graduate Medical Education (ACGME), residents are limited to a maximum of 30 consecutive work hours—known as the 30-hour rule, which includes time used for sign-out, teaching, and continuity of care. They are also prohibited from working more than 80 hours per week.
Despite the clear safety benefit of preventing fatigue-related mistakes, work-hour mandates have increased the number of patient handoffs and the potential for communication breakdowns.5 A survey of interns conducted at the hospital where this case study occurred identified a higher volume of sign-outs and the resulting potential for harm to patients as main concerns with the work-hour restrictions.6
Concerns about the quality and continuity of care that hospital patients receive are evident even among those medical residents whose work hours were restricted before the ACGME requirements took effect. (In New York state residents’ work hours have been restricted since 1998.)
A 2006 study of surgical residents at New York’s Beth Israel Hospital found that most believed that the quality of care patients received was either unchanged (63%) or worse (26%) since the work-hour restrictions took effect.7 Possible reasons for this perception include unresolved issues with continuity of care, miscommunication, and cross-coverage availability. The study concluded that interventions that target intern sign-out coverage constraints will be important for future efforts to improve the quality of care for hospital patients.
Written sign-outs appear to overcome some of the human errors that inevitably result from verbal patient summaries, such as disruptions and forgetfulness. Recent findings have, however, identified significant shortcomings in the quality and timeliness of written reports.
Critical information, such as code status and allergies, was missing in 80% of written sign-outs in one recent study.8 And in a 2006 study of the quality of discharge summaries, only 19% of hospital physicians with an outpatient practice reported being satisfied with the timeliness of discharge summaries. Only a third reported being satisfied with their quality of information. Most troubling, 41% believed that at least one of their patients hospitalized in the previous six months had experienced a preventable adverse event related to poor transfer of information at discharge.9
Use Redundancy and Simulation to Improve Safety
Given the clear challenges of providing quality and continuity of care in the inpatient setting, hospitalists are well positioned to identify strategies for safe and effective patient handoffs and advocate for a systems approach to their implementation.
Safety strategies that have been employed by industries outside of healthcare can provide a useful starting point. So-called “highly reliable” organizations use a variety of approaches to reduce the incidence of errors that occur during transitions in work staff. A recent review of transition methods used by NASA’s Johnson Space Center (Houston), Canadian nuclear power plants, and an ambulance dispatch center—organizations where lapses in transitions also have serious consequences—found that these entities used up to 21 handoff strategies.10 Techniques included verbal, face-to-face, and interactive questioning coordinated with written summaries just before a shift change.
Increasing redundancy is another technique used by highly reliable organizations to reduce the likelihood of missed, incomplete, or misinterpreted information. To create redundancy in clinical care, a physician would include more information at the outset of a procedure or medication order than is now typically provided. This additional information is then repeated and validated by other members of the care team throughout the process, reducing the likelihood of misinterpretation of an instruction or action based on incomplete information.
For example, if a physician always includes both the drug name and the condition for which it is prescribed, a medication order for “Celebrex, seizures,” instead of “Cerebyx, seizures,” would immediately indicate a mistake had occurred in ordering a pain medication instead of an anti-convulsant.11 Research has shown that increasing the amount of information about a medication order reduces the range of potentially valid clinical decisions.
Whether a hospital relies on verbal communication, written communication, computer-based communication, or a combination of all three, redundancy can be built into its sign-out processes. As PDAs become more widely used, structured sign-outs should incorporate redundancy into patient-specific checklists to include information on clinical status, recent and pending tests and study results, and similar, pertinent information.
Simulation-based training that incorporates redundancy and promotes read-back of patient information holds promise for error reduction, especially during patient handoffs.
AHRQ has recently funded research on simulation training projects that seek to:
- Reduce communication errors during patient handoffs in the emergency department by implementing a patient-specific checklist based on an electronic medical record and by testing the effect of companion simulation-based training; and
- Evaluate and improve safe communication and coordination between anesthesia providers and nurses during care transitions and during hand-offs between the operating room and the post-anesthesia care unit.12
The 24/7 role of hospital physicians brings unique experiences and insights to the challenges of patient safety that can test the feasibility of systems to reduce errors associated with care transitions. As their numbers and leadership roles expand, hospitalists are poised to make significant contributions to improving patient safety and outcomes.
We at AHRQ look forward to assisting hospitalists in making these contributions and to achieving these goals together. We also look forward to continuing our relationship with SHM and the hospitalist community as a whole. TH
Dr. Clancy is the director of the Agency for Healthcare Research and Quality.
References
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996 Aug 15;335(7):514-517.
- Impact of the nation’s hospitalists continues to grow new society of hospital medicine survey says [press release]. Society of Hospital Medicine. May 4, 2006.
- Society of Hospital Medicine. The core competencies in hospital medicine: a framework for curriculum development by the society of hospital medicine. J Hosp Med. 2006;1;S1. Available at: http://onlinelibrary.wiley.com/doi/10.1002/jhm.72/pdf. Last accessed January 17, 2007.
- Vidyarthi A [commentary]. Agency for Healthcare Research and Quality Web M&M: Morbidity and Mortality Rounds on the Web. Fumbled handoff. March 2004. Available at: www.webmm.ahrq.gov/case.aspx?caseID=55. Last accessed January 17, 2007.
- Wachter RM, Shojania KG. Internal Bleeding: The Truth Behind America’s Terrifying Epidemic of Medical Mistakes. New York: Rugged Land LLG; 2004.
- Vidyarthi A. Morbidity and Mortality Rounds on the Web, “Fumbled Handoff,” unpublished data, 2004.
- Biller CK, Antonacci AC, Pelletier S, et al. The 80-hour work guidelines and resident survey perceptions of quality. J Surg Res. 2006 Oct;135(2):275-281. Epub 2006 Aug 24.
- Lee LH, Levine JA, Schultz HJ. Utility of a standardized sign-out card for new medical interns. J Gen Intern Med. 1996;11(12):753-755.
- O’Leary KJ, Leibovitz DM, Feinglass J, et al. Outpatient physicians’ satisfaction with discharge summaries and perceived need for an electronic discharge summary. J Hosp Med. 2006;1:317-320. Published online Oct. 11, 2006.
- Reason JT. Managing the Risks of Organizational Accidents. Aldershot, England: Ashgate Publishing Company; 1997:135.
- Bar-Yam Y. System care: multiscale analysis of medical errors–eliminating errors and improving organizational capabilities. New England Complex Systems Institute: Technical Report; Sept 2004. Available at: http://necsi.org/projects/yaneer/NECSITechnicalReport2004-09.pdf. Last accessed January 17, 2007.
- Agency for Healthcare Research and Quality. Improving patient safety through simulation research. 2006 Simulation Projects. Available at: www.ahrq.gov/qual/simulproj.htm. Last accessed January 17, 2007.
And the Band Played On...
On New Year’s Day while most men are engrossed in football, my 89-year-old father was sidelined by bilateral Achilles’ tendon ruptures—a rare complication of Levaquin therapy. Given my father’s age and his likely sedentary lifestyle, the orthopedist embarked upon conservative therapy. My father was disheartened to hear that he would need to have both ankles immobilized for many months, with only minimal weight bearing on one.
He thought that his life was over and became passive and dependent. He did what most people of his generation do in the hospital. He checked his independence at the door. He only did what the doctors or nurses told him to do, never asking to get up in the chair, never venturing outside his room, eating meals in bed unless nursing staff got him up.
A Musical Life
Until hospitalization, he had lived alone with his Brittany Spaniel in a two-story home with the full bath and bedroom on the second floor. He had even given music lessons in the basement. He had driven his car, bought groceries, walked his dog, and had been responsible for his own cooking, laundry, appointments, and medications, including warfarin.
Music, though, is the passion of his life. As a teenager in the 1930s, he learned to play the trombone by playing along with great players at night in the family car, which “had the best radio.” Later, he rode the train weekly from his home in Appleton, Wis., to Chicago to study with Jerry Chimera, a well-known master, and toured the Midwest with the region’s hottest bands while completing a Bachelor of Music degree at Lawrence University, Appleton, Wis.
At various times, he made a living as freelance trombonist in both New York City and Los Angeles. He was a studio musician with the NBC Orchestra and played lead with many great names, including Les Brown—and his Band of Renown!—and Doris Day during the Big Band Era, before embarking on an academic career. He completed his master’s degree at the University of Southern California (Los Angeles) and was a professor of music at universities in Montana and New York before settling in the Midwest to teach band to elementary and secondary students at public schools.
His personal life was filled with music. He was the principal trombonist with the Rochester (N.Y.) Symphony for 43 years, until macular degeneration made it impossible to continue. He also had an active schedule with a local jazz band, The Turkey River All-Stars, who have played a multitude of venues, both local and national. He has played with the Turkeys on the Delta Queen paddleboat, for four United States presidents, in Branson (Mo.), and at jazz festivals from here to New Orleans.
After “retirement” at age 70, he continued to give private music lessons for up to 42 students a week. At 89 he still gives private music lessons, though he now teaches on a less rigorous schedule with fewer students. When we ask him to tell us about his greatest source of satisfaction, he says, “The greatest achievement of my life was passing on my love of music to my sons. I am especially proud when they play together or Randy gets to play with the Rochester Orchestra.”
Dad’s Rehab
One of my first responsibilities after his hospitalization was to cancel his students’ lessons. One student, though, really needed some help with a piece for a competition. Because there was nothing wrong with Dad except his ankles, we wanted to help make that possible. We knew that Mayo hospitalists would support our goal of helping Dad to be as functional as possible. The staff needed to know—and Dad needed a reminder—that he wasn’t a typical 89-year-old.
My wife and I are both employed in healthcare professions. We knew of an outpatient examination room away from patient care areas that would provide good lighting and privacy. Isaac, a trombone student, brought his horn and his family for a visit. Dad left the floor for the most important hour of his therapy. He gave Isaac a lesson and then delighted us with his rendition of “Black Orpheus.”
After that lesson, he began to speak more positively of returning home. He is currently in a short-term rehabilitation facility for physical and occupational therapy. His goal is to return home after he learns to transfer safely and can navigate with a wheelchair.
Obviously, we have some work to do to prepare. We need to move his bedroom furniture and studio to the main floor. We need to acquire equipment and install grab bars. He may need assistance with dressing, housekeeping, bathing, transportation, and physical therapy for a few months. We are confident that a return home is on the horizon. Anything is possible with the right attitude. TH
Stroetz is a certified respiratory therapist at the Mayo Clinic. Lucinda Stroetz, PA, also contributed to this article.
On New Year’s Day while most men are engrossed in football, my 89-year-old father was sidelined by bilateral Achilles’ tendon ruptures—a rare complication of Levaquin therapy. Given my father’s age and his likely sedentary lifestyle, the orthopedist embarked upon conservative therapy. My father was disheartened to hear that he would need to have both ankles immobilized for many months, with only minimal weight bearing on one.
He thought that his life was over and became passive and dependent. He did what most people of his generation do in the hospital. He checked his independence at the door. He only did what the doctors or nurses told him to do, never asking to get up in the chair, never venturing outside his room, eating meals in bed unless nursing staff got him up.
A Musical Life
Until hospitalization, he had lived alone with his Brittany Spaniel in a two-story home with the full bath and bedroom on the second floor. He had even given music lessons in the basement. He had driven his car, bought groceries, walked his dog, and had been responsible for his own cooking, laundry, appointments, and medications, including warfarin.
Music, though, is the passion of his life. As a teenager in the 1930s, he learned to play the trombone by playing along with great players at night in the family car, which “had the best radio.” Later, he rode the train weekly from his home in Appleton, Wis., to Chicago to study with Jerry Chimera, a well-known master, and toured the Midwest with the region’s hottest bands while completing a Bachelor of Music degree at Lawrence University, Appleton, Wis.
At various times, he made a living as freelance trombonist in both New York City and Los Angeles. He was a studio musician with the NBC Orchestra and played lead with many great names, including Les Brown—and his Band of Renown!—and Doris Day during the Big Band Era, before embarking on an academic career. He completed his master’s degree at the University of Southern California (Los Angeles) and was a professor of music at universities in Montana and New York before settling in the Midwest to teach band to elementary and secondary students at public schools.
His personal life was filled with music. He was the principal trombonist with the Rochester (N.Y.) Symphony for 43 years, until macular degeneration made it impossible to continue. He also had an active schedule with a local jazz band, The Turkey River All-Stars, who have played a multitude of venues, both local and national. He has played with the Turkeys on the Delta Queen paddleboat, for four United States presidents, in Branson (Mo.), and at jazz festivals from here to New Orleans.
After “retirement” at age 70, he continued to give private music lessons for up to 42 students a week. At 89 he still gives private music lessons, though he now teaches on a less rigorous schedule with fewer students. When we ask him to tell us about his greatest source of satisfaction, he says, “The greatest achievement of my life was passing on my love of music to my sons. I am especially proud when they play together or Randy gets to play with the Rochester Orchestra.”
Dad’s Rehab
One of my first responsibilities after his hospitalization was to cancel his students’ lessons. One student, though, really needed some help with a piece for a competition. Because there was nothing wrong with Dad except his ankles, we wanted to help make that possible. We knew that Mayo hospitalists would support our goal of helping Dad to be as functional as possible. The staff needed to know—and Dad needed a reminder—that he wasn’t a typical 89-year-old.
My wife and I are both employed in healthcare professions. We knew of an outpatient examination room away from patient care areas that would provide good lighting and privacy. Isaac, a trombone student, brought his horn and his family for a visit. Dad left the floor for the most important hour of his therapy. He gave Isaac a lesson and then delighted us with his rendition of “Black Orpheus.”
After that lesson, he began to speak more positively of returning home. He is currently in a short-term rehabilitation facility for physical and occupational therapy. His goal is to return home after he learns to transfer safely and can navigate with a wheelchair.
Obviously, we have some work to do to prepare. We need to move his bedroom furniture and studio to the main floor. We need to acquire equipment and install grab bars. He may need assistance with dressing, housekeeping, bathing, transportation, and physical therapy for a few months. We are confident that a return home is on the horizon. Anything is possible with the right attitude. TH
Stroetz is a certified respiratory therapist at the Mayo Clinic. Lucinda Stroetz, PA, also contributed to this article.
On New Year’s Day while most men are engrossed in football, my 89-year-old father was sidelined by bilateral Achilles’ tendon ruptures—a rare complication of Levaquin therapy. Given my father’s age and his likely sedentary lifestyle, the orthopedist embarked upon conservative therapy. My father was disheartened to hear that he would need to have both ankles immobilized for many months, with only minimal weight bearing on one.
He thought that his life was over and became passive and dependent. He did what most people of his generation do in the hospital. He checked his independence at the door. He only did what the doctors or nurses told him to do, never asking to get up in the chair, never venturing outside his room, eating meals in bed unless nursing staff got him up.
A Musical Life
Until hospitalization, he had lived alone with his Brittany Spaniel in a two-story home with the full bath and bedroom on the second floor. He had even given music lessons in the basement. He had driven his car, bought groceries, walked his dog, and had been responsible for his own cooking, laundry, appointments, and medications, including warfarin.
Music, though, is the passion of his life. As a teenager in the 1930s, he learned to play the trombone by playing along with great players at night in the family car, which “had the best radio.” Later, he rode the train weekly from his home in Appleton, Wis., to Chicago to study with Jerry Chimera, a well-known master, and toured the Midwest with the region’s hottest bands while completing a Bachelor of Music degree at Lawrence University, Appleton, Wis.
At various times, he made a living as freelance trombonist in both New York City and Los Angeles. He was a studio musician with the NBC Orchestra and played lead with many great names, including Les Brown—and his Band of Renown!—and Doris Day during the Big Band Era, before embarking on an academic career. He completed his master’s degree at the University of Southern California (Los Angeles) and was a professor of music at universities in Montana and New York before settling in the Midwest to teach band to elementary and secondary students at public schools.
His personal life was filled with music. He was the principal trombonist with the Rochester (N.Y.) Symphony for 43 years, until macular degeneration made it impossible to continue. He also had an active schedule with a local jazz band, The Turkey River All-Stars, who have played a multitude of venues, both local and national. He has played with the Turkeys on the Delta Queen paddleboat, for four United States presidents, in Branson (Mo.), and at jazz festivals from here to New Orleans.
After “retirement” at age 70, he continued to give private music lessons for up to 42 students a week. At 89 he still gives private music lessons, though he now teaches on a less rigorous schedule with fewer students. When we ask him to tell us about his greatest source of satisfaction, he says, “The greatest achievement of my life was passing on my love of music to my sons. I am especially proud when they play together or Randy gets to play with the Rochester Orchestra.”
Dad’s Rehab
One of my first responsibilities after his hospitalization was to cancel his students’ lessons. One student, though, really needed some help with a piece for a competition. Because there was nothing wrong with Dad except his ankles, we wanted to help make that possible. We knew that Mayo hospitalists would support our goal of helping Dad to be as functional as possible. The staff needed to know—and Dad needed a reminder—that he wasn’t a typical 89-year-old.
My wife and I are both employed in healthcare professions. We knew of an outpatient examination room away from patient care areas that would provide good lighting and privacy. Isaac, a trombone student, brought his horn and his family for a visit. Dad left the floor for the most important hour of his therapy. He gave Isaac a lesson and then delighted us with his rendition of “Black Orpheus.”
After that lesson, he began to speak more positively of returning home. He is currently in a short-term rehabilitation facility for physical and occupational therapy. His goal is to return home after he learns to transfer safely and can navigate with a wheelchair.
Obviously, we have some work to do to prepare. We need to move his bedroom furniture and studio to the main floor. We need to acquire equipment and install grab bars. He may need assistance with dressing, housekeeping, bathing, transportation, and physical therapy for a few months. We are confident that a return home is on the horizon. Anything is possible with the right attitude. TH
Stroetz is a certified respiratory therapist at the Mayo Clinic. Lucinda Stroetz, PA, also contributed to this article.
Surgical Steroid Replacement
The subject of perioperative glucocorticoid replacement certainly needs no extensive preamble or introduction. Hospitalists are routinely required to exercise the art and science of estimating the steroid requirement for patients on steroids undergoing surgical procedures. What follows is a brief review of the literature for fellow internists.
History: Full Circle
It has been almost 60 years since corticosteroids were first recognized for their anti-inflammatory and immunosuppressive properties, initially in rheumatologic diseases. The beneficial effects of steroids in rheumatoid arthritis were described in 1949 by Philip S. Hench and colleagues, a discovery for which he received (together with Edward C. Kendall and Tadeus Reichstein) the Nobel Prize in medicine in 1950.1,2
Barely three years later, Fraser and coworkers reported the death of a 34-year-old man after routine orthopedic surgery due to shock, adrenal insufficiency, and circulatory collapse.3 The patient had been on corticosteroids for rheumatoid arthritis, but the treatment had been stopped prior to surgery. The potentially fatal consequences of steroid withdrawal prior to surgery were thrown into even greater prominence by a similar report, presented by Lewis and colleagues within a year of the first incident.4 This occurrence involved an even younger patient: a 24-year-old woman, who had been on steroids for rheumatoid arthritis and who died after her therapy was stopped a day prior to surgery.
The first recommendations for perioperative steroid replacement soon appeared.4 When loosely interpreted, routine steroid doses were often quadrupled prior to surgery—a practice that sometimes led to mammoth amounts of steroids administered during the surgical period.5 Not surprisingly, adverse clinical results were soon noted: decreased tissue repair and healing, infections, and hyperglycemia, to name a few.5 While mortality related to acute steroid withdrawal and circulatory collapse might have decreased, morbidity related to poor surgical wound healing and subsequent complications increased.
Finally, in 1994, the problem of perioperative glucocorticoid replacement was reassessed, and fresh guidelines were provided by Salem and colleagues.5 These guidelines recognized the need for steroid coverage but in more moderate doses than had previously been used, and this is where we stand today—replacement, but in moderation.
Why Perioperative Steroid Coverage?
Acute stress activates the hypothalamic-pituitary-adrenal (HPA) axis, resulting in increased plasma adrenocorticotropic hormone (ACTH) and cortisol levels.6 This increase is believed to be an adaptive mechanism meant to enhance the body’s ability to combat stress by increasing its sensitivity to catecholamines; its cardiac contractility and output; and its mobilization of energy sources with gluconeogenesis, proteolysis, and lipolysis.6 It follows that lack of increase in cortisol production during stress would cause the host to succumb to it. On the other hand, too much cortisol would be detrimental, causing increased tissue breakdown, poor wound healing, and immunosuppression.
Surgery is one of the most potent stressors that can cause activation of the HPA axis.6,7 The degree of activation depends on the type and duration of surgery and anesthesia, with many other variables adding to the picture, including analgesics, antihypertensive medications, infections, and age.5-9 The maximum stimulation of the HPA axis in uncomplicated surgery has been assessed to occur during reversal of anesthesia and in the immediate postoperative period.6,9,10 Normal daily cortisol production is about 15 to 20 mg/day.6 These levels can go up to as much as 75–100 mg/day with surgical stress.6,11,12
Given this background, it is clear that any patient who has inadequate cortisol production in response to surgical stress will fare poorly in such a situation. This patient will need to be recognized, and his acute steroid requirement will have to be estimated and supplemented; in addition, over- or under-dosing must be avoided in order to achieve a good post-surgical outcome.
Mechanisms of Adrenal Insufficiency in the Perioperative Period
Adrenal insufficiency can be primary, in which the adrenal gland itself does not function properly. It can also be secondary or central, in which the hypothalamic/pituitary axis is functioning at sub-par levels. It is, in fact, secondary adrenal insufficiency that is most commonly encountered in clinical practice; this condition is caused by HPA axis suppression due to negative feedback from exogenous administration of corticosteroids.
Who Needs Perioperative Steroid Replacement?
Following are situations in which perioperative steroid replacement should be considered:
- Any patient who has received more than 20 mg of prednisone daily (or an equivalent dose of other glucocorticoids) for more than five days in the previous year is at risk for HPA axis suppression;13,14
- Any patient who has clinical Cushing’s syndrome from any steroid dose should be considered to have a suppressed HPA axis;6 and
- Any steroid dose given at bedtime—even physiologic doses—is more likely to suppress the HPA axis than a similar dose given in the morning because, at nighttime, the negative feedback from steroids to ACTH and corticotropin-releasing hormone (CRH) is more prominent.6
Patients receiving doses equivalent to 5 mg of prednisone in the morning for any length of time are not associated with HPA axis suppression.13 If these patients are on steroid replacement for primary adrenal insufficiency, however, it is vital to realize that they do not have the capacity to compensate for increased stress, surgical or otherwise, and may need additional replacement depending upon the nature and duration of their stressors.14
Doses greater than physiologic range but less than 20 mg/day of prednisone can cause suppression of the HPA axis, but the demarcation of the time frame is not absolutely clear. It is said that doses closer to the physiologic range cause suppression after about one month, whereas doses closer to 20 mg/day can do so in five days or more.13, 14
For patients who cannot be clearly identified by these criteria, provocative testing is recommended, as discussed below.
Laboratory Testing for HPA Axis Function
The ACTH stimulation test is recommended to test for HPA axis adequacy in perioperative patients.5,13,14 It has been shown to correlate well with the insulin tolerance test. Exogenous corticosteroids have to be held for 24 hours prior to testing because they affect the measured cortisol level, with the exception of dexamethasone, which does not affect the results.13
The test involves the administration of 250 mcg of cosyntropin—synthetic ACTH—intramuscularly or intravenously, followed by measurement of peak cortisol levels after 30 minutes.5 Traditionally, a plasma cortisol level greater than 18–20 mcg/dl defines adequate adrenal function, as quoted from Salem and colleagues.5
Basal values and the calculation of delta max—the difference between basal and peak values—have not been shown to correlate with clinical outcome in routine surgical patients.13 Although these values have been demonstrated to be useful in the setting of septic shock, the subject is still under debate, and readers interested in this aspect of adrenal insufficiency may refer to articles by Annane, Hollenberg, Gonzalez and colleagues.15,16,17
Use of a 250-mcg dose of cosyntropin has often been criticized for being supraphysiologic, and use of a 1-mcg dose has been suggested instead. This test has not yet been characterized well enough, however.13,18 In addition, a standardized, commercial preparation of the 1-mcg dose is not available.13 Thus, the low-dose test is, as yet, not routinely advocated.
To Replace or Not to Replace?
It is interesting to note that biochemical evidence of HPA axis dysfunction does not necessarily translate into clinical problems with surgical stress.19 Additionally, patients on chronic steroid supplementation higher than 5 mg/day of prednisone—or equivalent—may not necessarily suffer inappropriate biochemical responses to stress.20 With these observations comes the following question: Even if HPA axis dysfunction exists, when does it matter clinically, or does it matter? The difficulty of this situation has been discussed in detail by Levy and Shaw.21,22
Shaw brings the topic to another level when he states that, given the evidence we have today, it is still prudent to consider perioperative steroid coverage.22 The benefit—avoiding life-threatening adrenal insufficiency—outweighs the risk of enhanced catabolism and immunosuppression, especially if the steroid coverage is physiologic and of a very short duration.
Perioperative Glucocorticoid Coverage
Current recommendations for steroid coverage take into account the normal physiologic response to routine surgery. The idea is to mimic the transient increase in cortisol levels during the surgical and postoperative period but not to exceed the levels or the duration of the physiologic response. Doses above the physiologic ranges offer no particular benefit in routine surgical stress.5
Most of the current recommendations stem from those proposed by Salem and colleagues in 1994.5
Conclusion
For almost 50 years after it was first recognized, the need for steroid replacement in surgical situations had been addressed with high doses that created new problems in the forms of poor tissue healing and immunosuppression, causing a major dilemma in the surgical world. Now, with a more conservative and physiologic approach, the adverse consequences of glucocorticoid supplementation can be minimized and perhaps even prevented. TH
References
- Hench PS, Kendall EC, Slocumb CH, et al. The effect of a hormone of the adrenal cortex (17-hydroxy-11-dehydrocorticosterone; compound E) and of pituitary adrenocorticotropic hormone on rheumatoid arthritis. Proc Staff Meet Mayo Clin. 1949;24:181-197.
- Hench PS, Slocumb CH, Polley HF, et al. Effect of cortisone and pituitary adrenocorticotropic hormone (ACTH) on rheumatic diseases. JAMA. 1950 Dec 16;144(16):1327-1335.
- Fraser CG, Preuss FS, Bigford WD. Adrenal atrophy and irreversible shock associated with cortisone therapy. JAMA. 1952;149:1542-1543.
- Lewis L, Robinson RF, Yee J, et al. Fatal adrenal cortical insufficiency precipitated by surgery during prolonged continuous cortisone treatment. Ann Intern Med. 1953; 39:116-126.
- Salem M, Tainsh RE Jr, Bromberg J, et al. Perioperative glucocorticoid coverage. A reassessment 42 years after emergence of a problem. Ann Surg. 1994 Apr;219(4):416-425.
- Jabbour SA. Steroids and the surgical patient. Med Clin North Am. 2001 Sep;85(5):1311-1317.
- Hume DM, Bell CC, Bartter F. Direct measurement of adrenal secretion during operative trauma and convalescence. Surgery. 1962 Jul;52:174-187.
- Chernow B, Alexander HR, Smallridge RC, et al. Hormonal responses to graded surgical stress. Arch Intern Med. 1987 Jul;147(4):1273-1278.
- Raff H, Norton AJ, Flemma RJ, et al. Inhibition of the adrenocorticotropin response to surgery in humans: interaction between dexamethasone and fentanyl. J Clin Endocrinol Metab. 1987 Aug;65(2):295-298.
- Udelsman R, Norton JA, Jelenich SE, et al. Responses of the hypothalamic-pituitary-adrenal and renin-angiotensin axes and the sympathetic system during controlled surgical and anesthetic stress. J Clin Endocrinol Metab. 1987 May;64(5):986-994.
- Kehlet H. A rational approach to dosage and preparation of parenteral glucocorticoid substitution therapy during surgical procedures. A short review. Acta Anaesthesiol Scand. 1975;19(4):260-264.
- Kehlet H. Clinical course and hypothalamic-pituitary-adrenocortical function in glucocorticoid-treated surgical patients. Copenhagen: FADL; 1976.
- Axelrod L. Perioperative management of patients treated with glucocorticoids. Endocrinol Metab Clin North Am. 2003;32:367-383.
- Connery LE, Coursin DB. Assessment and therapy of selected endocrine disorders. Anesthesiol Clin North America. 2004 Mar;22(1):93-123.
- Annane D, Sebille V, Troche G, et al. A 3-level prognostic classification in septic shock based on cortisol levels and cortisol response to corticotropin. JAMA. 2000 Feb 23;283(8):1038-1045.
- Hollenberg SM, Ahrens TS, Annane D, et al. Practice parameters for hemodynamic support of sepsis in adult patients: 2004 update. Crit Care Med. 2004 Sep;32(9):1928-1948.
- Gonzalez H, Nardi O, Annane D. Relative adrenal failure in the ICU: an identifiable problem requiring treatment. Crit Care Clin. 2006 Jan;22(1):105-118.
- Streeten DHP. Shortcomings in the low-dose (1 microg) ACTH test for the diagnosis of ACTH deficiency states. J Clin Endocrinol Metab. 1999 Mar;84(3):835-837.
- Bromberg JS, Alfrey EJ, Barker CF, et al. Adrenal suppression and steroid supplementation in renal transplant recipients. Transplantation. 1991 Feb;51(2):385-390.
- Friedman RJ, Schiff CF, Bromberg JS. Use of supplemental steroids in patients having orthopaedic operations. J Bone Joint Surg Am. 1995 Dec;77(12):1801-1806.
- Levy A. Perioperative steroid cover. Lancet. 1996 Mar;347(9005):846-847.
- Shaw M. When is perioperative ‘steroid coverage’ necessary? Available at: www.clevelandclinicmeded.com/ccjm/january2002/shaw.htm. Last accessed February 9, 2007.
The subject of perioperative glucocorticoid replacement certainly needs no extensive preamble or introduction. Hospitalists are routinely required to exercise the art and science of estimating the steroid requirement for patients on steroids undergoing surgical procedures. What follows is a brief review of the literature for fellow internists.
History: Full Circle
It has been almost 60 years since corticosteroids were first recognized for their anti-inflammatory and immunosuppressive properties, initially in rheumatologic diseases. The beneficial effects of steroids in rheumatoid arthritis were described in 1949 by Philip S. Hench and colleagues, a discovery for which he received (together with Edward C. Kendall and Tadeus Reichstein) the Nobel Prize in medicine in 1950.1,2
Barely three years later, Fraser and coworkers reported the death of a 34-year-old man after routine orthopedic surgery due to shock, adrenal insufficiency, and circulatory collapse.3 The patient had been on corticosteroids for rheumatoid arthritis, but the treatment had been stopped prior to surgery. The potentially fatal consequences of steroid withdrawal prior to surgery were thrown into even greater prominence by a similar report, presented by Lewis and colleagues within a year of the first incident.4 This occurrence involved an even younger patient: a 24-year-old woman, who had been on steroids for rheumatoid arthritis and who died after her therapy was stopped a day prior to surgery.
The first recommendations for perioperative steroid replacement soon appeared.4 When loosely interpreted, routine steroid doses were often quadrupled prior to surgery—a practice that sometimes led to mammoth amounts of steroids administered during the surgical period.5 Not surprisingly, adverse clinical results were soon noted: decreased tissue repair and healing, infections, and hyperglycemia, to name a few.5 While mortality related to acute steroid withdrawal and circulatory collapse might have decreased, morbidity related to poor surgical wound healing and subsequent complications increased.
Finally, in 1994, the problem of perioperative glucocorticoid replacement was reassessed, and fresh guidelines were provided by Salem and colleagues.5 These guidelines recognized the need for steroid coverage but in more moderate doses than had previously been used, and this is where we stand today—replacement, but in moderation.
Why Perioperative Steroid Coverage?
Acute stress activates the hypothalamic-pituitary-adrenal (HPA) axis, resulting in increased plasma adrenocorticotropic hormone (ACTH) and cortisol levels.6 This increase is believed to be an adaptive mechanism meant to enhance the body’s ability to combat stress by increasing its sensitivity to catecholamines; its cardiac contractility and output; and its mobilization of energy sources with gluconeogenesis, proteolysis, and lipolysis.6 It follows that lack of increase in cortisol production during stress would cause the host to succumb to it. On the other hand, too much cortisol would be detrimental, causing increased tissue breakdown, poor wound healing, and immunosuppression.
Surgery is one of the most potent stressors that can cause activation of the HPA axis.6,7 The degree of activation depends on the type and duration of surgery and anesthesia, with many other variables adding to the picture, including analgesics, antihypertensive medications, infections, and age.5-9 The maximum stimulation of the HPA axis in uncomplicated surgery has been assessed to occur during reversal of anesthesia and in the immediate postoperative period.6,9,10 Normal daily cortisol production is about 15 to 20 mg/day.6 These levels can go up to as much as 75–100 mg/day with surgical stress.6,11,12
Given this background, it is clear that any patient who has inadequate cortisol production in response to surgical stress will fare poorly in such a situation. This patient will need to be recognized, and his acute steroid requirement will have to be estimated and supplemented; in addition, over- or under-dosing must be avoided in order to achieve a good post-surgical outcome.
Mechanisms of Adrenal Insufficiency in the Perioperative Period
Adrenal insufficiency can be primary, in which the adrenal gland itself does not function properly. It can also be secondary or central, in which the hypothalamic/pituitary axis is functioning at sub-par levels. It is, in fact, secondary adrenal insufficiency that is most commonly encountered in clinical practice; this condition is caused by HPA axis suppression due to negative feedback from exogenous administration of corticosteroids.
Who Needs Perioperative Steroid Replacement?
Following are situations in which perioperative steroid replacement should be considered:
- Any patient who has received more than 20 mg of prednisone daily (or an equivalent dose of other glucocorticoids) for more than five days in the previous year is at risk for HPA axis suppression;13,14
- Any patient who has clinical Cushing’s syndrome from any steroid dose should be considered to have a suppressed HPA axis;6 and
- Any steroid dose given at bedtime—even physiologic doses—is more likely to suppress the HPA axis than a similar dose given in the morning because, at nighttime, the negative feedback from steroids to ACTH and corticotropin-releasing hormone (CRH) is more prominent.6
Patients receiving doses equivalent to 5 mg of prednisone in the morning for any length of time are not associated with HPA axis suppression.13 If these patients are on steroid replacement for primary adrenal insufficiency, however, it is vital to realize that they do not have the capacity to compensate for increased stress, surgical or otherwise, and may need additional replacement depending upon the nature and duration of their stressors.14
Doses greater than physiologic range but less than 20 mg/day of prednisone can cause suppression of the HPA axis, but the demarcation of the time frame is not absolutely clear. It is said that doses closer to the physiologic range cause suppression after about one month, whereas doses closer to 20 mg/day can do so in five days or more.13, 14
For patients who cannot be clearly identified by these criteria, provocative testing is recommended, as discussed below.
Laboratory Testing for HPA Axis Function
The ACTH stimulation test is recommended to test for HPA axis adequacy in perioperative patients.5,13,14 It has been shown to correlate well with the insulin tolerance test. Exogenous corticosteroids have to be held for 24 hours prior to testing because they affect the measured cortisol level, with the exception of dexamethasone, which does not affect the results.13
The test involves the administration of 250 mcg of cosyntropin—synthetic ACTH—intramuscularly or intravenously, followed by measurement of peak cortisol levels after 30 minutes.5 Traditionally, a plasma cortisol level greater than 18–20 mcg/dl defines adequate adrenal function, as quoted from Salem and colleagues.5
Basal values and the calculation of delta max—the difference between basal and peak values—have not been shown to correlate with clinical outcome in routine surgical patients.13 Although these values have been demonstrated to be useful in the setting of septic shock, the subject is still under debate, and readers interested in this aspect of adrenal insufficiency may refer to articles by Annane, Hollenberg, Gonzalez and colleagues.15,16,17
Use of a 250-mcg dose of cosyntropin has often been criticized for being supraphysiologic, and use of a 1-mcg dose has been suggested instead. This test has not yet been characterized well enough, however.13,18 In addition, a standardized, commercial preparation of the 1-mcg dose is not available.13 Thus, the low-dose test is, as yet, not routinely advocated.
To Replace or Not to Replace?
It is interesting to note that biochemical evidence of HPA axis dysfunction does not necessarily translate into clinical problems with surgical stress.19 Additionally, patients on chronic steroid supplementation higher than 5 mg/day of prednisone—or equivalent—may not necessarily suffer inappropriate biochemical responses to stress.20 With these observations comes the following question: Even if HPA axis dysfunction exists, when does it matter clinically, or does it matter? The difficulty of this situation has been discussed in detail by Levy and Shaw.21,22
Shaw brings the topic to another level when he states that, given the evidence we have today, it is still prudent to consider perioperative steroid coverage.22 The benefit—avoiding life-threatening adrenal insufficiency—outweighs the risk of enhanced catabolism and immunosuppression, especially if the steroid coverage is physiologic and of a very short duration.
Perioperative Glucocorticoid Coverage
Current recommendations for steroid coverage take into account the normal physiologic response to routine surgery. The idea is to mimic the transient increase in cortisol levels during the surgical and postoperative period but not to exceed the levels or the duration of the physiologic response. Doses above the physiologic ranges offer no particular benefit in routine surgical stress.5
Most of the current recommendations stem from those proposed by Salem and colleagues in 1994.5
Conclusion
For almost 50 years after it was first recognized, the need for steroid replacement in surgical situations had been addressed with high doses that created new problems in the forms of poor tissue healing and immunosuppression, causing a major dilemma in the surgical world. Now, with a more conservative and physiologic approach, the adverse consequences of glucocorticoid supplementation can be minimized and perhaps even prevented. TH
References
- Hench PS, Kendall EC, Slocumb CH, et al. The effect of a hormone of the adrenal cortex (17-hydroxy-11-dehydrocorticosterone; compound E) and of pituitary adrenocorticotropic hormone on rheumatoid arthritis. Proc Staff Meet Mayo Clin. 1949;24:181-197.
- Hench PS, Slocumb CH, Polley HF, et al. Effect of cortisone and pituitary adrenocorticotropic hormone (ACTH) on rheumatic diseases. JAMA. 1950 Dec 16;144(16):1327-1335.
- Fraser CG, Preuss FS, Bigford WD. Adrenal atrophy and irreversible shock associated with cortisone therapy. JAMA. 1952;149:1542-1543.
- Lewis L, Robinson RF, Yee J, et al. Fatal adrenal cortical insufficiency precipitated by surgery during prolonged continuous cortisone treatment. Ann Intern Med. 1953; 39:116-126.
- Salem M, Tainsh RE Jr, Bromberg J, et al. Perioperative glucocorticoid coverage. A reassessment 42 years after emergence of a problem. Ann Surg. 1994 Apr;219(4):416-425.
- Jabbour SA. Steroids and the surgical patient. Med Clin North Am. 2001 Sep;85(5):1311-1317.
- Hume DM, Bell CC, Bartter F. Direct measurement of adrenal secretion during operative trauma and convalescence. Surgery. 1962 Jul;52:174-187.
- Chernow B, Alexander HR, Smallridge RC, et al. Hormonal responses to graded surgical stress. Arch Intern Med. 1987 Jul;147(4):1273-1278.
- Raff H, Norton AJ, Flemma RJ, et al. Inhibition of the adrenocorticotropin response to surgery in humans: interaction between dexamethasone and fentanyl. J Clin Endocrinol Metab. 1987 Aug;65(2):295-298.
- Udelsman R, Norton JA, Jelenich SE, et al. Responses of the hypothalamic-pituitary-adrenal and renin-angiotensin axes and the sympathetic system during controlled surgical and anesthetic stress. J Clin Endocrinol Metab. 1987 May;64(5):986-994.
- Kehlet H. A rational approach to dosage and preparation of parenteral glucocorticoid substitution therapy during surgical procedures. A short review. Acta Anaesthesiol Scand. 1975;19(4):260-264.
- Kehlet H. Clinical course and hypothalamic-pituitary-adrenocortical function in glucocorticoid-treated surgical patients. Copenhagen: FADL; 1976.
- Axelrod L. Perioperative management of patients treated with glucocorticoids. Endocrinol Metab Clin North Am. 2003;32:367-383.
- Connery LE, Coursin DB. Assessment and therapy of selected endocrine disorders. Anesthesiol Clin North America. 2004 Mar;22(1):93-123.
- Annane D, Sebille V, Troche G, et al. A 3-level prognostic classification in septic shock based on cortisol levels and cortisol response to corticotropin. JAMA. 2000 Feb 23;283(8):1038-1045.
- Hollenberg SM, Ahrens TS, Annane D, et al. Practice parameters for hemodynamic support of sepsis in adult patients: 2004 update. Crit Care Med. 2004 Sep;32(9):1928-1948.
- Gonzalez H, Nardi O, Annane D. Relative adrenal failure in the ICU: an identifiable problem requiring treatment. Crit Care Clin. 2006 Jan;22(1):105-118.
- Streeten DHP. Shortcomings in the low-dose (1 microg) ACTH test for the diagnosis of ACTH deficiency states. J Clin Endocrinol Metab. 1999 Mar;84(3):835-837.
- Bromberg JS, Alfrey EJ, Barker CF, et al. Adrenal suppression and steroid supplementation in renal transplant recipients. Transplantation. 1991 Feb;51(2):385-390.
- Friedman RJ, Schiff CF, Bromberg JS. Use of supplemental steroids in patients having orthopaedic operations. J Bone Joint Surg Am. 1995 Dec;77(12):1801-1806.
- Levy A. Perioperative steroid cover. Lancet. 1996 Mar;347(9005):846-847.
- Shaw M. When is perioperative ‘steroid coverage’ necessary? Available at: www.clevelandclinicmeded.com/ccjm/january2002/shaw.htm. Last accessed February 9, 2007.
The subject of perioperative glucocorticoid replacement certainly needs no extensive preamble or introduction. Hospitalists are routinely required to exercise the art and science of estimating the steroid requirement for patients on steroids undergoing surgical procedures. What follows is a brief review of the literature for fellow internists.
History: Full Circle
It has been almost 60 years since corticosteroids were first recognized for their anti-inflammatory and immunosuppressive properties, initially in rheumatologic diseases. The beneficial effects of steroids in rheumatoid arthritis were described in 1949 by Philip S. Hench and colleagues, a discovery for which he received (together with Edward C. Kendall and Tadeus Reichstein) the Nobel Prize in medicine in 1950.1,2
Barely three years later, Fraser and coworkers reported the death of a 34-year-old man after routine orthopedic surgery due to shock, adrenal insufficiency, and circulatory collapse.3 The patient had been on corticosteroids for rheumatoid arthritis, but the treatment had been stopped prior to surgery. The potentially fatal consequences of steroid withdrawal prior to surgery were thrown into even greater prominence by a similar report, presented by Lewis and colleagues within a year of the first incident.4 This occurrence involved an even younger patient: a 24-year-old woman, who had been on steroids for rheumatoid arthritis and who died after her therapy was stopped a day prior to surgery.
The first recommendations for perioperative steroid replacement soon appeared.4 When loosely interpreted, routine steroid doses were often quadrupled prior to surgery—a practice that sometimes led to mammoth amounts of steroids administered during the surgical period.5 Not surprisingly, adverse clinical results were soon noted: decreased tissue repair and healing, infections, and hyperglycemia, to name a few.5 While mortality related to acute steroid withdrawal and circulatory collapse might have decreased, morbidity related to poor surgical wound healing and subsequent complications increased.
Finally, in 1994, the problem of perioperative glucocorticoid replacement was reassessed, and fresh guidelines were provided by Salem and colleagues.5 These guidelines recognized the need for steroid coverage but in more moderate doses than had previously been used, and this is where we stand today—replacement, but in moderation.
Why Perioperative Steroid Coverage?
Acute stress activates the hypothalamic-pituitary-adrenal (HPA) axis, resulting in increased plasma adrenocorticotropic hormone (ACTH) and cortisol levels.6 This increase is believed to be an adaptive mechanism meant to enhance the body’s ability to combat stress by increasing its sensitivity to catecholamines; its cardiac contractility and output; and its mobilization of energy sources with gluconeogenesis, proteolysis, and lipolysis.6 It follows that lack of increase in cortisol production during stress would cause the host to succumb to it. On the other hand, too much cortisol would be detrimental, causing increased tissue breakdown, poor wound healing, and immunosuppression.
Surgery is one of the most potent stressors that can cause activation of the HPA axis.6,7 The degree of activation depends on the type and duration of surgery and anesthesia, with many other variables adding to the picture, including analgesics, antihypertensive medications, infections, and age.5-9 The maximum stimulation of the HPA axis in uncomplicated surgery has been assessed to occur during reversal of anesthesia and in the immediate postoperative period.6,9,10 Normal daily cortisol production is about 15 to 20 mg/day.6 These levels can go up to as much as 75–100 mg/day with surgical stress.6,11,12
Given this background, it is clear that any patient who has inadequate cortisol production in response to surgical stress will fare poorly in such a situation. This patient will need to be recognized, and his acute steroid requirement will have to be estimated and supplemented; in addition, over- or under-dosing must be avoided in order to achieve a good post-surgical outcome.
Mechanisms of Adrenal Insufficiency in the Perioperative Period
Adrenal insufficiency can be primary, in which the adrenal gland itself does not function properly. It can also be secondary or central, in which the hypothalamic/pituitary axis is functioning at sub-par levels. It is, in fact, secondary adrenal insufficiency that is most commonly encountered in clinical practice; this condition is caused by HPA axis suppression due to negative feedback from exogenous administration of corticosteroids.
Who Needs Perioperative Steroid Replacement?
Following are situations in which perioperative steroid replacement should be considered:
- Any patient who has received more than 20 mg of prednisone daily (or an equivalent dose of other glucocorticoids) for more than five days in the previous year is at risk for HPA axis suppression;13,14
- Any patient who has clinical Cushing’s syndrome from any steroid dose should be considered to have a suppressed HPA axis;6 and
- Any steroid dose given at bedtime—even physiologic doses—is more likely to suppress the HPA axis than a similar dose given in the morning because, at nighttime, the negative feedback from steroids to ACTH and corticotropin-releasing hormone (CRH) is more prominent.6
Patients receiving doses equivalent to 5 mg of prednisone in the morning for any length of time are not associated with HPA axis suppression.13 If these patients are on steroid replacement for primary adrenal insufficiency, however, it is vital to realize that they do not have the capacity to compensate for increased stress, surgical or otherwise, and may need additional replacement depending upon the nature and duration of their stressors.14
Doses greater than physiologic range but less than 20 mg/day of prednisone can cause suppression of the HPA axis, but the demarcation of the time frame is not absolutely clear. It is said that doses closer to the physiologic range cause suppression after about one month, whereas doses closer to 20 mg/day can do so in five days or more.13, 14
For patients who cannot be clearly identified by these criteria, provocative testing is recommended, as discussed below.
Laboratory Testing for HPA Axis Function
The ACTH stimulation test is recommended to test for HPA axis adequacy in perioperative patients.5,13,14 It has been shown to correlate well with the insulin tolerance test. Exogenous corticosteroids have to be held for 24 hours prior to testing because they affect the measured cortisol level, with the exception of dexamethasone, which does not affect the results.13
The test involves the administration of 250 mcg of cosyntropin—synthetic ACTH—intramuscularly or intravenously, followed by measurement of peak cortisol levels after 30 minutes.5 Traditionally, a plasma cortisol level greater than 18–20 mcg/dl defines adequate adrenal function, as quoted from Salem and colleagues.5
Basal values and the calculation of delta max—the difference between basal and peak values—have not been shown to correlate with clinical outcome in routine surgical patients.13 Although these values have been demonstrated to be useful in the setting of septic shock, the subject is still under debate, and readers interested in this aspect of adrenal insufficiency may refer to articles by Annane, Hollenberg, Gonzalez and colleagues.15,16,17
Use of a 250-mcg dose of cosyntropin has often been criticized for being supraphysiologic, and use of a 1-mcg dose has been suggested instead. This test has not yet been characterized well enough, however.13,18 In addition, a standardized, commercial preparation of the 1-mcg dose is not available.13 Thus, the low-dose test is, as yet, not routinely advocated.
To Replace or Not to Replace?
It is interesting to note that biochemical evidence of HPA axis dysfunction does not necessarily translate into clinical problems with surgical stress.19 Additionally, patients on chronic steroid supplementation higher than 5 mg/day of prednisone—or equivalent—may not necessarily suffer inappropriate biochemical responses to stress.20 With these observations comes the following question: Even if HPA axis dysfunction exists, when does it matter clinically, or does it matter? The difficulty of this situation has been discussed in detail by Levy and Shaw.21,22
Shaw brings the topic to another level when he states that, given the evidence we have today, it is still prudent to consider perioperative steroid coverage.22 The benefit—avoiding life-threatening adrenal insufficiency—outweighs the risk of enhanced catabolism and immunosuppression, especially if the steroid coverage is physiologic and of a very short duration.
Perioperative Glucocorticoid Coverage
Current recommendations for steroid coverage take into account the normal physiologic response to routine surgery. The idea is to mimic the transient increase in cortisol levels during the surgical and postoperative period but not to exceed the levels or the duration of the physiologic response. Doses above the physiologic ranges offer no particular benefit in routine surgical stress.5
Most of the current recommendations stem from those proposed by Salem and colleagues in 1994.5
Conclusion
For almost 50 years after it was first recognized, the need for steroid replacement in surgical situations had been addressed with high doses that created new problems in the forms of poor tissue healing and immunosuppression, causing a major dilemma in the surgical world. Now, with a more conservative and physiologic approach, the adverse consequences of glucocorticoid supplementation can be minimized and perhaps even prevented. TH
References
- Hench PS, Kendall EC, Slocumb CH, et al. The effect of a hormone of the adrenal cortex (17-hydroxy-11-dehydrocorticosterone; compound E) and of pituitary adrenocorticotropic hormone on rheumatoid arthritis. Proc Staff Meet Mayo Clin. 1949;24:181-197.
- Hench PS, Slocumb CH, Polley HF, et al. Effect of cortisone and pituitary adrenocorticotropic hormone (ACTH) on rheumatic diseases. JAMA. 1950 Dec 16;144(16):1327-1335.
- Fraser CG, Preuss FS, Bigford WD. Adrenal atrophy and irreversible shock associated with cortisone therapy. JAMA. 1952;149:1542-1543.
- Lewis L, Robinson RF, Yee J, et al. Fatal adrenal cortical insufficiency precipitated by surgery during prolonged continuous cortisone treatment. Ann Intern Med. 1953; 39:116-126.
- Salem M, Tainsh RE Jr, Bromberg J, et al. Perioperative glucocorticoid coverage. A reassessment 42 years after emergence of a problem. Ann Surg. 1994 Apr;219(4):416-425.
- Jabbour SA. Steroids and the surgical patient. Med Clin North Am. 2001 Sep;85(5):1311-1317.
- Hume DM, Bell CC, Bartter F. Direct measurement of adrenal secretion during operative trauma and convalescence. Surgery. 1962 Jul;52:174-187.
- Chernow B, Alexander HR, Smallridge RC, et al. Hormonal responses to graded surgical stress. Arch Intern Med. 1987 Jul;147(4):1273-1278.
- Raff H, Norton AJ, Flemma RJ, et al. Inhibition of the adrenocorticotropin response to surgery in humans: interaction between dexamethasone and fentanyl. J Clin Endocrinol Metab. 1987 Aug;65(2):295-298.
- Udelsman R, Norton JA, Jelenich SE, et al. Responses of the hypothalamic-pituitary-adrenal and renin-angiotensin axes and the sympathetic system during controlled surgical and anesthetic stress. J Clin Endocrinol Metab. 1987 May;64(5):986-994.
- Kehlet H. A rational approach to dosage and preparation of parenteral glucocorticoid substitution therapy during surgical procedures. A short review. Acta Anaesthesiol Scand. 1975;19(4):260-264.
- Kehlet H. Clinical course and hypothalamic-pituitary-adrenocortical function in glucocorticoid-treated surgical patients. Copenhagen: FADL; 1976.
- Axelrod L. Perioperative management of patients treated with glucocorticoids. Endocrinol Metab Clin North Am. 2003;32:367-383.
- Connery LE, Coursin DB. Assessment and therapy of selected endocrine disorders. Anesthesiol Clin North America. 2004 Mar;22(1):93-123.
- Annane D, Sebille V, Troche G, et al. A 3-level prognostic classification in septic shock based on cortisol levels and cortisol response to corticotropin. JAMA. 2000 Feb 23;283(8):1038-1045.
- Hollenberg SM, Ahrens TS, Annane D, et al. Practice parameters for hemodynamic support of sepsis in adult patients: 2004 update. Crit Care Med. 2004 Sep;32(9):1928-1948.
- Gonzalez H, Nardi O, Annane D. Relative adrenal failure in the ICU: an identifiable problem requiring treatment. Crit Care Clin. 2006 Jan;22(1):105-118.
- Streeten DHP. Shortcomings in the low-dose (1 microg) ACTH test for the diagnosis of ACTH deficiency states. J Clin Endocrinol Metab. 1999 Mar;84(3):835-837.
- Bromberg JS, Alfrey EJ, Barker CF, et al. Adrenal suppression and steroid supplementation in renal transplant recipients. Transplantation. 1991 Feb;51(2):385-390.
- Friedman RJ, Schiff CF, Bromberg JS. Use of supplemental steroids in patients having orthopaedic operations. J Bone Joint Surg Am. 1995 Dec;77(12):1801-1806.
- Levy A. Perioperative steroid cover. Lancet. 1996 Mar;347(9005):846-847.
- Shaw M. When is perioperative ‘steroid coverage’ necessary? Available at: www.clevelandclinicmeded.com/ccjm/january2002/shaw.htm. Last accessed February 9, 2007.
Dysphagia, Dizziness, and Dysarthria
Brief history: A 32-year-old female presents with dysphagia, dizziness, and dysarthria.
Salient findings: Chest X-ray demonstrates many embolization coils within both lungs. Photographs demonstrate superficial telangiectasias of the tongue and distal phalanx. These findings indicate the patient’s diagnosis: hereditary hemorrhagic telangiectasia (HHT), previously known as Osler-Weber-Rendu syndrome.
Patient population/natural history of disease: HHT is an autosomal dominant trait, so family members should be counseled on the implications of having a relative with the disease. HHT patients have abnormal vessels prone to bleeding and often develop arteriovenous malformations (AVMs). Diagnosis is made with 75% of the following symptoms:
- Epistaxis;
- Mucocutaneous telangiectasias;
- GI, pulmonary, or hepatic AVMs; and/or
- A first-degree relative with HHT.
Patients often present with dyspnea and hemoptysis. With pulmonary AVMs, the oxygenation and filtration functions of the lungs are bypassed, placing the patient at risk for hypoxia, polycythemia, paradoxical strokes, and brain abscesses.
Management: AVMs can be diagnosed and treated with angiography and embolization. In this patient the coils had been placed elsewhere. The use of coils larger than 3 mm in AVMs should be treated because they are associated with significantly increased morbidity and mortality. Steel coils are covered with thrombogenic fibers that induce clotting and sealing of the AVM; blood is no longer shunted through the right-to-left shunt. Unfortunately, a long-term complication of pulmonary AVMs treated by embolization therapy is the development of new pulmonary AVMs.
The patient in this case had many metallic coils visible on chest X-ray and because she had required multiple pulmonary angiograms and embolizations over the years.
It’s important to administer an ECG to all HHT patients prior to treatment; those with a left bundle branch block must have pacing mechanisms in place or at hand because catheter placement and manipulation within the right heart can induce right heart blockage. Take care to avoid air emboli in all lines due to right-to-left shunting in these patients.
Take-Home Points:
- Untreated pulmonary AVMs are associated with paradoxical strokes, brain abscesses, and hypoxia;
- HHT is associated with pulmonary AVMs;
- Coil embolization of pulmonary AVMs has been shown to improve dyspnea and oxygen saturation while decreasing right-to-left shunt fraction in HHT patients.
- Complications of embolization therapy may include development of new pulmonary AVMs; and
- All patients should undergo ECG prior to pulmonary angiography to screen for left bundle branch block. TH
Helena Summers is a radiology resident and Erik Summers is a hospitalist at the Mayo Clinic College of Medicine, Rochester, Minn.
References
- Swanson KL, Prakash UB, Stanson AW. Pulmonary arteriovenous fistulas: Mayo Clinic experience, 1982-1997. Mayo Clin Proc. 1999 Jul;74(7):671-680.
- Cottin V, Plauchu H, Bayle JY, et al. Pulmonary arteriovenous malformations in patients with hereditary hemorrhagic telangiectasia. Am J Respir Crit Care Med. 2004 May 1;169(9):994-1000. Epub 2004 Jan 23.
Brief history: A 32-year-old female presents with dysphagia, dizziness, and dysarthria.
Salient findings: Chest X-ray demonstrates many embolization coils within both lungs. Photographs demonstrate superficial telangiectasias of the tongue and distal phalanx. These findings indicate the patient’s diagnosis: hereditary hemorrhagic telangiectasia (HHT), previously known as Osler-Weber-Rendu syndrome.
Patient population/natural history of disease: HHT is an autosomal dominant trait, so family members should be counseled on the implications of having a relative with the disease. HHT patients have abnormal vessels prone to bleeding and often develop arteriovenous malformations (AVMs). Diagnosis is made with 75% of the following symptoms:
- Epistaxis;
- Mucocutaneous telangiectasias;
- GI, pulmonary, or hepatic AVMs; and/or
- A first-degree relative with HHT.
Patients often present with dyspnea and hemoptysis. With pulmonary AVMs, the oxygenation and filtration functions of the lungs are bypassed, placing the patient at risk for hypoxia, polycythemia, paradoxical strokes, and brain abscesses.
Management: AVMs can be diagnosed and treated with angiography and embolization. In this patient the coils had been placed elsewhere. The use of coils larger than 3 mm in AVMs should be treated because they are associated with significantly increased morbidity and mortality. Steel coils are covered with thrombogenic fibers that induce clotting and sealing of the AVM; blood is no longer shunted through the right-to-left shunt. Unfortunately, a long-term complication of pulmonary AVMs treated by embolization therapy is the development of new pulmonary AVMs.
The patient in this case had many metallic coils visible on chest X-ray and because she had required multiple pulmonary angiograms and embolizations over the years.
It’s important to administer an ECG to all HHT patients prior to treatment; those with a left bundle branch block must have pacing mechanisms in place or at hand because catheter placement and manipulation within the right heart can induce right heart blockage. Take care to avoid air emboli in all lines due to right-to-left shunting in these patients.
Take-Home Points:
- Untreated pulmonary AVMs are associated with paradoxical strokes, brain abscesses, and hypoxia;
- HHT is associated with pulmonary AVMs;
- Coil embolization of pulmonary AVMs has been shown to improve dyspnea and oxygen saturation while decreasing right-to-left shunt fraction in HHT patients.
- Complications of embolization therapy may include development of new pulmonary AVMs; and
- All patients should undergo ECG prior to pulmonary angiography to screen for left bundle branch block. TH
Helena Summers is a radiology resident and Erik Summers is a hospitalist at the Mayo Clinic College of Medicine, Rochester, Minn.
References
- Swanson KL, Prakash UB, Stanson AW. Pulmonary arteriovenous fistulas: Mayo Clinic experience, 1982-1997. Mayo Clin Proc. 1999 Jul;74(7):671-680.
- Cottin V, Plauchu H, Bayle JY, et al. Pulmonary arteriovenous malformations in patients with hereditary hemorrhagic telangiectasia. Am J Respir Crit Care Med. 2004 May 1;169(9):994-1000. Epub 2004 Jan 23.
Brief history: A 32-year-old female presents with dysphagia, dizziness, and dysarthria.
Salient findings: Chest X-ray demonstrates many embolization coils within both lungs. Photographs demonstrate superficial telangiectasias of the tongue and distal phalanx. These findings indicate the patient’s diagnosis: hereditary hemorrhagic telangiectasia (HHT), previously known as Osler-Weber-Rendu syndrome.
Patient population/natural history of disease: HHT is an autosomal dominant trait, so family members should be counseled on the implications of having a relative with the disease. HHT patients have abnormal vessels prone to bleeding and often develop arteriovenous malformations (AVMs). Diagnosis is made with 75% of the following symptoms:
- Epistaxis;
- Mucocutaneous telangiectasias;
- GI, pulmonary, or hepatic AVMs; and/or
- A first-degree relative with HHT.
Patients often present with dyspnea and hemoptysis. With pulmonary AVMs, the oxygenation and filtration functions of the lungs are bypassed, placing the patient at risk for hypoxia, polycythemia, paradoxical strokes, and brain abscesses.
Management: AVMs can be diagnosed and treated with angiography and embolization. In this patient the coils had been placed elsewhere. The use of coils larger than 3 mm in AVMs should be treated because they are associated with significantly increased morbidity and mortality. Steel coils are covered with thrombogenic fibers that induce clotting and sealing of the AVM; blood is no longer shunted through the right-to-left shunt. Unfortunately, a long-term complication of pulmonary AVMs treated by embolization therapy is the development of new pulmonary AVMs.
The patient in this case had many metallic coils visible on chest X-ray and because she had required multiple pulmonary angiograms and embolizations over the years.
It’s important to administer an ECG to all HHT patients prior to treatment; those with a left bundle branch block must have pacing mechanisms in place or at hand because catheter placement and manipulation within the right heart can induce right heart blockage. Take care to avoid air emboli in all lines due to right-to-left shunting in these patients.
Take-Home Points:
- Untreated pulmonary AVMs are associated with paradoxical strokes, brain abscesses, and hypoxia;
- HHT is associated with pulmonary AVMs;
- Coil embolization of pulmonary AVMs has been shown to improve dyspnea and oxygen saturation while decreasing right-to-left shunt fraction in HHT patients.
- Complications of embolization therapy may include development of new pulmonary AVMs; and
- All patients should undergo ECG prior to pulmonary angiography to screen for left bundle branch block. TH
Helena Summers is a radiology resident and Erik Summers is a hospitalist at the Mayo Clinic College of Medicine, Rochester, Minn.
References
- Swanson KL, Prakash UB, Stanson AW. Pulmonary arteriovenous fistulas: Mayo Clinic experience, 1982-1997. Mayo Clin Proc. 1999 Jul;74(7):671-680.
- Cottin V, Plauchu H, Bayle JY, et al. Pulmonary arteriovenous malformations in patients with hereditary hemorrhagic telangiectasia. Am J Respir Crit Care Med. 2004 May 1;169(9):994-1000. Epub 2004 Jan 23.
Constructive Criticism, Part 2
This is the second in a two-part series on providing constructive criticism to your hospitalist peers. Part 1 appeared in the March issue on p. 12.
Have concerns about a colleague’s work performance? Then you have two main options: You can bring it up in a formal peer review (if it’s a clinical issue) or you can approach the individual yourself.
“Medicine is an art and a science. Many problems relate to the art side—communications and relationships, primarily,” says Richard Rohr, MD, director, Hospitalist Service, Milford Hospital, Conn. “You may need to talk to a colleague about how they approach family members or how they communicate with patients. In this instance, you’d offer more of a coaching comment.”
While you may hesitate to point out another hospitalist’s problem areas, keep in mind that it is constructive criticism.
“Physicians love to run things past colleagues,” says Kenneth G. Simone, DO, founder and president of Hospitalist and Practice Solutions, Veazie, Maine, and a consultant to hospital medicine groups. “Informal feedback can provide an unbiased and objective perspective, as opposed to [a formal peer review].”
When to Offer Constructive Criticism
In some practices, or for some individuals, sharing constructive criticism with peers is part of the job. “Informal peer discussions should take place every day,” advises Dr. Rohr. “While handoffs pose a risk for losing vital information, they are also an opportunity to consider alternatives for diagnosis and treatment that may benefit patients greatly.”
If this seems like a natural thing to do within your hospital medicine group, follow Dr. Rohr’s advice: “These discussions should be frank but nonjudgmental. If someone has a problem discussing cases in this manner, then the group leader needs to get involved. If a life-threatening error is exposed, then the formal peer review system needs to be activated.”
Providing Peer Feedback
When there is no personal conflict, you may still consider offering constructive criticism if you feel it’s warranted. “I think [peer feedback] is extremely important—if it’s done correctly,” says Dr. Simone. “It provides a safe haven for discussion and can contribute to professional growth.”
According to Dr. Simone, appropriate topics to discuss regarding a colleague’s performance include logistical problems within the practice, such as a doctor who is chronically late for morning rounds; continuity issues, such as a physician who fails to provide detailed information when handing off patients; communication breakdowns, such as forgetting to check out the labs pending on a newly admitted unit-patient with chest pain; behavioral issues, such as a physician who’s verbally abusive to the nurses or disruptive at morning rounds; problems with work ethic, responsiveness, or availability, such as the doctor who never responds to his/her beeper (necessitating a call from nursing to an accommodating provider who’s always willing and available to help); and general team play.
If you believe you need to address one of these topics regarding a colleague’s performance, plan the logistics of the discussion. “This is a conversation best held one on one—in private,” stresses Dr. Simone. “Don’t discuss these issues in front of colleagues, nurses, patients, families … and don’t do it at the end of a long, difficult day.
“Ideally, do it after hours and out of the workplace, though that can be difficult. Remove the person from the hospital floor or the office, and the emotions and adrenaline associated with work,” continues Dr. Simone. “If the environment is stressful, it will raise their defenses, making them more likely to be resistant and argumentative.”
Talking Points
When you offer constructive criticism, approach the topic carefully. “Take a non-confrontational approach,” says Dr. Simone. “Don’t raise your voice, and don’t take the discussion to a personal level. Use objective data as much as possible. Avoid saying ‘I feel that you’re …’ and instead use ‘Coming in 15 minutes late throws everyone’s schedule off.’ ”
Keep the conversation as casual and as light as possible. “This is not a peer review meeting,” Dr. Simone stresses. “Use a soft approach, and you might have greater success. Stay away from power words such as ‘you shouldn’t’ or ‘don’t.’ ”
Some phrases you might use include:
- “I find it helpful if I … ”
- “This has worked for me.”
- “Have you considered … ?”
Even if you use careful wording, don’t be surprised if the other hospitalist doesn’t react well—at least initially. “Unless you’re seasoned at doing this, the individual may get defensive,” warns Dr. Simone. “If you’re consistent throughout the conversation, show support, and are astute enough to break down their defenses, you should be effective.”
Also, keep your cool: “Don’t respond to defensiveness in like [manner],” says Dr. Simone. Throughout the conversation, show your support. “Convey that your intent is to help the individual—not harm them. Ask if you can be of help, and offer to be a resource” to help them improve.
Also remember that your colleague is part of the conversation. “Allow responses,” adds Dr. Simone. “Give them a chance to express themselves.”
End the conversation with an offer to follow up or suggest a next step. “Offer your personal help or suggest a resource such as the employee assistance program,” advises Dr. Simone. “You can check in with them from time to time, but if you have an unwilling party this may be construed as meddlesome. You must consider the personality involved and if you think they’d be amenable to continued conversations.”
Even without a formal follow-up, be sure to voice your approval if you see their negative behavior change. “If you take the time to provide criticism, you should also offer positive feedback if warranted,” says Dr. Simone. “Tell them they’re doing a great job.”
One final piece of advice regarding informal peer feedback: “Avoid writing anything down,” says Dr. Simone. “This may make it discoverable in a court of law, and it’s not your place to put the discussion in writing. If the issue is that serious, take it to the powers that be.” TH
Jane Jerrard has written for The Hospitalist since 2005.
This is the second in a two-part series on providing constructive criticism to your hospitalist peers. Part 1 appeared in the March issue on p. 12.
Have concerns about a colleague’s work performance? Then you have two main options: You can bring it up in a formal peer review (if it’s a clinical issue) or you can approach the individual yourself.
“Medicine is an art and a science. Many problems relate to the art side—communications and relationships, primarily,” says Richard Rohr, MD, director, Hospitalist Service, Milford Hospital, Conn. “You may need to talk to a colleague about how they approach family members or how they communicate with patients. In this instance, you’d offer more of a coaching comment.”
While you may hesitate to point out another hospitalist’s problem areas, keep in mind that it is constructive criticism.
“Physicians love to run things past colleagues,” says Kenneth G. Simone, DO, founder and president of Hospitalist and Practice Solutions, Veazie, Maine, and a consultant to hospital medicine groups. “Informal feedback can provide an unbiased and objective perspective, as opposed to [a formal peer review].”
When to Offer Constructive Criticism
In some practices, or for some individuals, sharing constructive criticism with peers is part of the job. “Informal peer discussions should take place every day,” advises Dr. Rohr. “While handoffs pose a risk for losing vital information, they are also an opportunity to consider alternatives for diagnosis and treatment that may benefit patients greatly.”
If this seems like a natural thing to do within your hospital medicine group, follow Dr. Rohr’s advice: “These discussions should be frank but nonjudgmental. If someone has a problem discussing cases in this manner, then the group leader needs to get involved. If a life-threatening error is exposed, then the formal peer review system needs to be activated.”
Providing Peer Feedback
When there is no personal conflict, you may still consider offering constructive criticism if you feel it’s warranted. “I think [peer feedback] is extremely important—if it’s done correctly,” says Dr. Simone. “It provides a safe haven for discussion and can contribute to professional growth.”
According to Dr. Simone, appropriate topics to discuss regarding a colleague’s performance include logistical problems within the practice, such as a doctor who is chronically late for morning rounds; continuity issues, such as a physician who fails to provide detailed information when handing off patients; communication breakdowns, such as forgetting to check out the labs pending on a newly admitted unit-patient with chest pain; behavioral issues, such as a physician who’s verbally abusive to the nurses or disruptive at morning rounds; problems with work ethic, responsiveness, or availability, such as the doctor who never responds to his/her beeper (necessitating a call from nursing to an accommodating provider who’s always willing and available to help); and general team play.
If you believe you need to address one of these topics regarding a colleague’s performance, plan the logistics of the discussion. “This is a conversation best held one on one—in private,” stresses Dr. Simone. “Don’t discuss these issues in front of colleagues, nurses, patients, families … and don’t do it at the end of a long, difficult day.
“Ideally, do it after hours and out of the workplace, though that can be difficult. Remove the person from the hospital floor or the office, and the emotions and adrenaline associated with work,” continues Dr. Simone. “If the environment is stressful, it will raise their defenses, making them more likely to be resistant and argumentative.”
Talking Points
When you offer constructive criticism, approach the topic carefully. “Take a non-confrontational approach,” says Dr. Simone. “Don’t raise your voice, and don’t take the discussion to a personal level. Use objective data as much as possible. Avoid saying ‘I feel that you’re …’ and instead use ‘Coming in 15 minutes late throws everyone’s schedule off.’ ”
Keep the conversation as casual and as light as possible. “This is not a peer review meeting,” Dr. Simone stresses. “Use a soft approach, and you might have greater success. Stay away from power words such as ‘you shouldn’t’ or ‘don’t.’ ”
Some phrases you might use include:
- “I find it helpful if I … ”
- “This has worked for me.”
- “Have you considered … ?”
Even if you use careful wording, don’t be surprised if the other hospitalist doesn’t react well—at least initially. “Unless you’re seasoned at doing this, the individual may get defensive,” warns Dr. Simone. “If you’re consistent throughout the conversation, show support, and are astute enough to break down their defenses, you should be effective.”
Also, keep your cool: “Don’t respond to defensiveness in like [manner],” says Dr. Simone. Throughout the conversation, show your support. “Convey that your intent is to help the individual—not harm them. Ask if you can be of help, and offer to be a resource” to help them improve.
Also remember that your colleague is part of the conversation. “Allow responses,” adds Dr. Simone. “Give them a chance to express themselves.”
End the conversation with an offer to follow up or suggest a next step. “Offer your personal help or suggest a resource such as the employee assistance program,” advises Dr. Simone. “You can check in with them from time to time, but if you have an unwilling party this may be construed as meddlesome. You must consider the personality involved and if you think they’d be amenable to continued conversations.”
Even without a formal follow-up, be sure to voice your approval if you see their negative behavior change. “If you take the time to provide criticism, you should also offer positive feedback if warranted,” says Dr. Simone. “Tell them they’re doing a great job.”
One final piece of advice regarding informal peer feedback: “Avoid writing anything down,” says Dr. Simone. “This may make it discoverable in a court of law, and it’s not your place to put the discussion in writing. If the issue is that serious, take it to the powers that be.” TH
Jane Jerrard has written for The Hospitalist since 2005.
This is the second in a two-part series on providing constructive criticism to your hospitalist peers. Part 1 appeared in the March issue on p. 12.
Have concerns about a colleague’s work performance? Then you have two main options: You can bring it up in a formal peer review (if it’s a clinical issue) or you can approach the individual yourself.
“Medicine is an art and a science. Many problems relate to the art side—communications and relationships, primarily,” says Richard Rohr, MD, director, Hospitalist Service, Milford Hospital, Conn. “You may need to talk to a colleague about how they approach family members or how they communicate with patients. In this instance, you’d offer more of a coaching comment.”
While you may hesitate to point out another hospitalist’s problem areas, keep in mind that it is constructive criticism.
“Physicians love to run things past colleagues,” says Kenneth G. Simone, DO, founder and president of Hospitalist and Practice Solutions, Veazie, Maine, and a consultant to hospital medicine groups. “Informal feedback can provide an unbiased and objective perspective, as opposed to [a formal peer review].”
When to Offer Constructive Criticism
In some practices, or for some individuals, sharing constructive criticism with peers is part of the job. “Informal peer discussions should take place every day,” advises Dr. Rohr. “While handoffs pose a risk for losing vital information, they are also an opportunity to consider alternatives for diagnosis and treatment that may benefit patients greatly.”
If this seems like a natural thing to do within your hospital medicine group, follow Dr. Rohr’s advice: “These discussions should be frank but nonjudgmental. If someone has a problem discussing cases in this manner, then the group leader needs to get involved. If a life-threatening error is exposed, then the formal peer review system needs to be activated.”
Providing Peer Feedback
When there is no personal conflict, you may still consider offering constructive criticism if you feel it’s warranted. “I think [peer feedback] is extremely important—if it’s done correctly,” says Dr. Simone. “It provides a safe haven for discussion and can contribute to professional growth.”
According to Dr. Simone, appropriate topics to discuss regarding a colleague’s performance include logistical problems within the practice, such as a doctor who is chronically late for morning rounds; continuity issues, such as a physician who fails to provide detailed information when handing off patients; communication breakdowns, such as forgetting to check out the labs pending on a newly admitted unit-patient with chest pain; behavioral issues, such as a physician who’s verbally abusive to the nurses or disruptive at morning rounds; problems with work ethic, responsiveness, or availability, such as the doctor who never responds to his/her beeper (necessitating a call from nursing to an accommodating provider who’s always willing and available to help); and general team play.
If you believe you need to address one of these topics regarding a colleague’s performance, plan the logistics of the discussion. “This is a conversation best held one on one—in private,” stresses Dr. Simone. “Don’t discuss these issues in front of colleagues, nurses, patients, families … and don’t do it at the end of a long, difficult day.
“Ideally, do it after hours and out of the workplace, though that can be difficult. Remove the person from the hospital floor or the office, and the emotions and adrenaline associated with work,” continues Dr. Simone. “If the environment is stressful, it will raise their defenses, making them more likely to be resistant and argumentative.”
Talking Points
When you offer constructive criticism, approach the topic carefully. “Take a non-confrontational approach,” says Dr. Simone. “Don’t raise your voice, and don’t take the discussion to a personal level. Use objective data as much as possible. Avoid saying ‘I feel that you’re …’ and instead use ‘Coming in 15 minutes late throws everyone’s schedule off.’ ”
Keep the conversation as casual and as light as possible. “This is not a peer review meeting,” Dr. Simone stresses. “Use a soft approach, and you might have greater success. Stay away from power words such as ‘you shouldn’t’ or ‘don’t.’ ”
Some phrases you might use include:
- “I find it helpful if I … ”
- “This has worked for me.”
- “Have you considered … ?”
Even if you use careful wording, don’t be surprised if the other hospitalist doesn’t react well—at least initially. “Unless you’re seasoned at doing this, the individual may get defensive,” warns Dr. Simone. “If you’re consistent throughout the conversation, show support, and are astute enough to break down their defenses, you should be effective.”
Also, keep your cool: “Don’t respond to defensiveness in like [manner],” says Dr. Simone. Throughout the conversation, show your support. “Convey that your intent is to help the individual—not harm them. Ask if you can be of help, and offer to be a resource” to help them improve.
Also remember that your colleague is part of the conversation. “Allow responses,” adds Dr. Simone. “Give them a chance to express themselves.”
End the conversation with an offer to follow up or suggest a next step. “Offer your personal help or suggest a resource such as the employee assistance program,” advises Dr. Simone. “You can check in with them from time to time, but if you have an unwilling party this may be construed as meddlesome. You must consider the personality involved and if you think they’d be amenable to continued conversations.”
Even without a formal follow-up, be sure to voice your approval if you see their negative behavior change. “If you take the time to provide criticism, you should also offer positive feedback if warranted,” says Dr. Simone. “Tell them they’re doing a great job.”
One final piece of advice regarding informal peer feedback: “Avoid writing anything down,” says Dr. Simone. “This may make it discoverable in a court of law, and it’s not your place to put the discussion in writing. If the issue is that serious, take it to the powers that be.” TH
Jane Jerrard has written for The Hospitalist since 2005.
Medicare Prepares to “Pay for Performance”
This year, interested physicians will participate in Medicare’s first ever pay-for-performance program. Legislation passed in late 2006 calls for a voluntary Medicare quality reporting program that financially rewards physicians reporting on specific quality measures. Those physicians may receive a bonus of 1.5% of their total Medicare payments during the reporting period. This adds a pay-for-performance component to the current Physician Voluntary Reporting Program (PVRP) that the Centers for Medicare and Medicaid Services (CMS) established in January 2006.
“Medicare is really serious about improving quality of care for beneficiaries, and they’re committed to pay for performance as the way to go about it,” says Patrick Torcson, MD, MMM, FACP, medical director, Hospital Medicine, St. Tammany Parish Hospital, Covington, La.
Performance Measures in the Works
The pay-for-performance quality reporting program will use the 66 unique clinical measures CMS announced in December 2006, with additional modifications to be made through April 2007 using a consensus process.
“From looking at the proposed list of 66 performance measures, we’ve identified seven that are going to be available to hospitalists to report,” says Dr. Torcson. “The seven involve stroke and [myocardial infarction] care.”
Most of the internal medicine-related measures of the 16 included in the original PVRP were designed for an outpatient, office-based practice, and that seems true of the expanded list as well.
The current 66 measures are slightly more relevant to the hospital setting and can potentially be reported by hospitalists, as Dr. Torcson specified. Specifically, quality measures have been added for giving beta-blockers upon admission (quality measure #29) and for stroke and stroke rehabilitation (quality measures #31-#36).
Other measures are expected to be added before the July implementation date, and some may be reportable by hospitalists. These include creation of an advance care plan (#47) and measures for emergency medicine services (#54-#59).
“Medicare plans to have specific performance measures for each of the 39 specialties that they recognize,” explains Dr. Torcson. “Hospital medicine is not yet a CMS-recognized specialty; we’re typically lumped under general internal medicine.”
You can view all the measures at www.cms.hhs.gov/PVRP/01_overview.asp.
How the Program Will Work
The initial reporting period set by the legislation is July 1 through December 31, 2007, and there will be an enrollment period before that for physicians who wish to participate. When a physician enrolls in the program, she will identify which measures apply to her. At that point, CMS will determine if a measure applies.
If less than three quality measures apply for a physician, then 80% reporting on those applicable measures is required to be eligible for the bonus. If four or more measures apply, the physician must report on at least three in order to be eligible.
Bonuses for voluntary reporting would be in a lump sum and won’t be paid until the first quarter of 2008. The method of payment may be subject to certain limits—and it may not offset the physicians’ administrative costs for reporting. Hospital medicine programs will have to consider whether the costs of reporting are worth the bonus.
SHM Involvement
SHM’s Public Policy Committee (PPC) and its Performance and Standards Task Force (PSTF) have been actively involved in getting measures included on the PRVP list that are applicable to hospitalists.
“SHM is a member of the AMA’s Physician Consortium for Performance Improvement (PCPI) and has representatives on work groups that have developed performance measures and will be revising and maintaining measures over time,” says Dr. Torcson. “We hope to eventually include measures that are specific to hospitalized patients.”
In addition to the PCPI, SHM is represented and has influence in the National Quality Forum and the Ambulatory Care Quality Alliance.
“SHM leadership—CEO Larry Wellikson, Eric Siegal, Public Policy chair, and Lakshmi Halasyamani, chair of the Hospital Quality and Patient Safety (HQPS) Committee—have been proactive in positioning SHM to be very involved in the national quality improvement agenda,” says Dr. Torcson. “It’s really a work in progress, but SHM is part of the work groups that are driving this process.”
The Effect on Hospitalists
As they can with the original PVRP, hospitalists can find a few applicable performance measures to report on, so they are eligible to participate—and SHM encourages them to do so.
“The amount of money will be small and the number of [applicable] measures will be limited and not truly representative of a hospitalist’s practice,” says Dr. Torcson, “but performance reporting should be something that every physician, including hospitalists, has as a skill set as their practice moves into the future.”
Moving Ahead
Details on the new program still need to be clarified by CMS in the first half of 2007. Regardless of the details still to be determined for this first major foray into Medicare pay for performance, one thing is clear: CMS is dedicated to the idea of tying financial reward to quality care. And they aren’t the only ones.
“Medicare is not as far along as private insurers,” says Dr. Torcson. “Commercial insurers are much more aggressive about pursuing physician-level performance and efficiency—I think we’ll see more impactful pay-for-performance plans from them first. However, the CMS model will affect 70 million patients, and commercial insurers have tended to use the CMS model for physician reimbursement.”
Dr. Torcson believes this program is simply a first step on that road. “We’re in the infancy of pay-for-performance models for physician reimbursement,” he says. “I think the ultimate model for physician-level value-based purchasing is going to look a lot different than the proposed CMS payment for reporting and payment for performance.”
In the immediate future, the PPC and PSTF will continue to participate in formulating the final quality measures for the CMS voluntary reporting program. Watch the SHM Web site for updates on the status of the program. TH
Jane Jerrard writes “Public Policy” for The Hospitalist.
This year, interested physicians will participate in Medicare’s first ever pay-for-performance program. Legislation passed in late 2006 calls for a voluntary Medicare quality reporting program that financially rewards physicians reporting on specific quality measures. Those physicians may receive a bonus of 1.5% of their total Medicare payments during the reporting period. This adds a pay-for-performance component to the current Physician Voluntary Reporting Program (PVRP) that the Centers for Medicare and Medicaid Services (CMS) established in January 2006.
“Medicare is really serious about improving quality of care for beneficiaries, and they’re committed to pay for performance as the way to go about it,” says Patrick Torcson, MD, MMM, FACP, medical director, Hospital Medicine, St. Tammany Parish Hospital, Covington, La.
Performance Measures in the Works
The pay-for-performance quality reporting program will use the 66 unique clinical measures CMS announced in December 2006, with additional modifications to be made through April 2007 using a consensus process.
“From looking at the proposed list of 66 performance measures, we’ve identified seven that are going to be available to hospitalists to report,” says Dr. Torcson. “The seven involve stroke and [myocardial infarction] care.”
Most of the internal medicine-related measures of the 16 included in the original PVRP were designed for an outpatient, office-based practice, and that seems true of the expanded list as well.
The current 66 measures are slightly more relevant to the hospital setting and can potentially be reported by hospitalists, as Dr. Torcson specified. Specifically, quality measures have been added for giving beta-blockers upon admission (quality measure #29) and for stroke and stroke rehabilitation (quality measures #31-#36).
Other measures are expected to be added before the July implementation date, and some may be reportable by hospitalists. These include creation of an advance care plan (#47) and measures for emergency medicine services (#54-#59).
“Medicare plans to have specific performance measures for each of the 39 specialties that they recognize,” explains Dr. Torcson. “Hospital medicine is not yet a CMS-recognized specialty; we’re typically lumped under general internal medicine.”
You can view all the measures at www.cms.hhs.gov/PVRP/01_overview.asp.
How the Program Will Work
The initial reporting period set by the legislation is July 1 through December 31, 2007, and there will be an enrollment period before that for physicians who wish to participate. When a physician enrolls in the program, she will identify which measures apply to her. At that point, CMS will determine if a measure applies.
If less than three quality measures apply for a physician, then 80% reporting on those applicable measures is required to be eligible for the bonus. If four or more measures apply, the physician must report on at least three in order to be eligible.
Bonuses for voluntary reporting would be in a lump sum and won’t be paid until the first quarter of 2008. The method of payment may be subject to certain limits—and it may not offset the physicians’ administrative costs for reporting. Hospital medicine programs will have to consider whether the costs of reporting are worth the bonus.
SHM Involvement
SHM’s Public Policy Committee (PPC) and its Performance and Standards Task Force (PSTF) have been actively involved in getting measures included on the PRVP list that are applicable to hospitalists.
“SHM is a member of the AMA’s Physician Consortium for Performance Improvement (PCPI) and has representatives on work groups that have developed performance measures and will be revising and maintaining measures over time,” says Dr. Torcson. “We hope to eventually include measures that are specific to hospitalized patients.”
In addition to the PCPI, SHM is represented and has influence in the National Quality Forum and the Ambulatory Care Quality Alliance.
“SHM leadership—CEO Larry Wellikson, Eric Siegal, Public Policy chair, and Lakshmi Halasyamani, chair of the Hospital Quality and Patient Safety (HQPS) Committee—have been proactive in positioning SHM to be very involved in the national quality improvement agenda,” says Dr. Torcson. “It’s really a work in progress, but SHM is part of the work groups that are driving this process.”
The Effect on Hospitalists
As they can with the original PVRP, hospitalists can find a few applicable performance measures to report on, so they are eligible to participate—and SHM encourages them to do so.
“The amount of money will be small and the number of [applicable] measures will be limited and not truly representative of a hospitalist’s practice,” says Dr. Torcson, “but performance reporting should be something that every physician, including hospitalists, has as a skill set as their practice moves into the future.”
Moving Ahead
Details on the new program still need to be clarified by CMS in the first half of 2007. Regardless of the details still to be determined for this first major foray into Medicare pay for performance, one thing is clear: CMS is dedicated to the idea of tying financial reward to quality care. And they aren’t the only ones.
“Medicare is not as far along as private insurers,” says Dr. Torcson. “Commercial insurers are much more aggressive about pursuing physician-level performance and efficiency—I think we’ll see more impactful pay-for-performance plans from them first. However, the CMS model will affect 70 million patients, and commercial insurers have tended to use the CMS model for physician reimbursement.”
Dr. Torcson believes this program is simply a first step on that road. “We’re in the infancy of pay-for-performance models for physician reimbursement,” he says. “I think the ultimate model for physician-level value-based purchasing is going to look a lot different than the proposed CMS payment for reporting and payment for performance.”
In the immediate future, the PPC and PSTF will continue to participate in formulating the final quality measures for the CMS voluntary reporting program. Watch the SHM Web site for updates on the status of the program. TH
Jane Jerrard writes “Public Policy” for The Hospitalist.
This year, interested physicians will participate in Medicare’s first ever pay-for-performance program. Legislation passed in late 2006 calls for a voluntary Medicare quality reporting program that financially rewards physicians reporting on specific quality measures. Those physicians may receive a bonus of 1.5% of their total Medicare payments during the reporting period. This adds a pay-for-performance component to the current Physician Voluntary Reporting Program (PVRP) that the Centers for Medicare and Medicaid Services (CMS) established in January 2006.
“Medicare is really serious about improving quality of care for beneficiaries, and they’re committed to pay for performance as the way to go about it,” says Patrick Torcson, MD, MMM, FACP, medical director, Hospital Medicine, St. Tammany Parish Hospital, Covington, La.
Performance Measures in the Works
The pay-for-performance quality reporting program will use the 66 unique clinical measures CMS announced in December 2006, with additional modifications to be made through April 2007 using a consensus process.
“From looking at the proposed list of 66 performance measures, we’ve identified seven that are going to be available to hospitalists to report,” says Dr. Torcson. “The seven involve stroke and [myocardial infarction] care.”
Most of the internal medicine-related measures of the 16 included in the original PVRP were designed for an outpatient, office-based practice, and that seems true of the expanded list as well.
The current 66 measures are slightly more relevant to the hospital setting and can potentially be reported by hospitalists, as Dr. Torcson specified. Specifically, quality measures have been added for giving beta-blockers upon admission (quality measure #29) and for stroke and stroke rehabilitation (quality measures #31-#36).
Other measures are expected to be added before the July implementation date, and some may be reportable by hospitalists. These include creation of an advance care plan (#47) and measures for emergency medicine services (#54-#59).
“Medicare plans to have specific performance measures for each of the 39 specialties that they recognize,” explains Dr. Torcson. “Hospital medicine is not yet a CMS-recognized specialty; we’re typically lumped under general internal medicine.”
You can view all the measures at www.cms.hhs.gov/PVRP/01_overview.asp.
How the Program Will Work
The initial reporting period set by the legislation is July 1 through December 31, 2007, and there will be an enrollment period before that for physicians who wish to participate. When a physician enrolls in the program, she will identify which measures apply to her. At that point, CMS will determine if a measure applies.
If less than three quality measures apply for a physician, then 80% reporting on those applicable measures is required to be eligible for the bonus. If four or more measures apply, the physician must report on at least three in order to be eligible.
Bonuses for voluntary reporting would be in a lump sum and won’t be paid until the first quarter of 2008. The method of payment may be subject to certain limits—and it may not offset the physicians’ administrative costs for reporting. Hospital medicine programs will have to consider whether the costs of reporting are worth the bonus.
SHM Involvement
SHM’s Public Policy Committee (PPC) and its Performance and Standards Task Force (PSTF) have been actively involved in getting measures included on the PRVP list that are applicable to hospitalists.
“SHM is a member of the AMA’s Physician Consortium for Performance Improvement (PCPI) and has representatives on work groups that have developed performance measures and will be revising and maintaining measures over time,” says Dr. Torcson. “We hope to eventually include measures that are specific to hospitalized patients.”
In addition to the PCPI, SHM is represented and has influence in the National Quality Forum and the Ambulatory Care Quality Alliance.
“SHM leadership—CEO Larry Wellikson, Eric Siegal, Public Policy chair, and Lakshmi Halasyamani, chair of the Hospital Quality and Patient Safety (HQPS) Committee—have been proactive in positioning SHM to be very involved in the national quality improvement agenda,” says Dr. Torcson. “It’s really a work in progress, but SHM is part of the work groups that are driving this process.”
The Effect on Hospitalists
As they can with the original PVRP, hospitalists can find a few applicable performance measures to report on, so they are eligible to participate—and SHM encourages them to do so.
“The amount of money will be small and the number of [applicable] measures will be limited and not truly representative of a hospitalist’s practice,” says Dr. Torcson, “but performance reporting should be something that every physician, including hospitalists, has as a skill set as their practice moves into the future.”
Moving Ahead
Details on the new program still need to be clarified by CMS in the first half of 2007. Regardless of the details still to be determined for this first major foray into Medicare pay for performance, one thing is clear: CMS is dedicated to the idea of tying financial reward to quality care. And they aren’t the only ones.
“Medicare is not as far along as private insurers,” says Dr. Torcson. “Commercial insurers are much more aggressive about pursuing physician-level performance and efficiency—I think we’ll see more impactful pay-for-performance plans from them first. However, the CMS model will affect 70 million patients, and commercial insurers have tended to use the CMS model for physician reimbursement.”
Dr. Torcson believes this program is simply a first step on that road. “We’re in the infancy of pay-for-performance models for physician reimbursement,” he says. “I think the ultimate model for physician-level value-based purchasing is going to look a lot different than the proposed CMS payment for reporting and payment for performance.”
In the immediate future, the PPC and PSTF will continue to participate in formulating the final quality measures for the CMS voluntary reporting program. Watch the SHM Web site for updates on the status of the program. TH
Jane Jerrard writes “Public Policy” for The Hospitalist.