User login
ONLINE EXCLUSIVE: Hospitals Forced to Adapt Amid Shifting Slate of Quality Measures
With the arrival of value-based purchasing (VBP), many hospitals have faced hard decisions about where to allocate scarce resources to maximize their performance potential. In some cases, those decisions have been made even more difficult by a set of core measures still very much in flux. For hospitalists, that means the ability to quickly adapt and reprioritize will be in high demand as measures are added or subtracted from the value-based purchasing program.
In the proposed program rules released in mid-January, CMS initially selected 17 core clinical measures from a list of 28 eligible candidates included in the Hospital Inpatient Quality Reporting (IQR) Program (https://www.cms.gov/HospitalQualityInits/08_HospitalRHQDAPU.asp) and also listed on the public Hospital Compare website (www.hospitalcompare.hhs.gov/) for at least one year. CMS explained its decision to withhold some of the remaining core measures from the program by noting that they were “topped out” and thus provided a poor basis of comparison among hospitals. Others, according to the agency, were of little value or were encouraging bad behavior.
CMS used the latter reason in its explanation for why it was not including an eligible core measure on administering antibiotics to pneumonia patients within six hours of their arrival at a hospital. “We do not believe that this measure is appropriate for inclusion because it could lead to inappropriate antibiotic use,” the rules stated. For that measure and others not recommended for inclusion in the hospital VBP program, CMS added that it would propose retiring them “in the near future.”

—Laura M. Dietzel, program director for High-Tech Meaningful Use, PeaceHealth
Laura M. Dietzel, program director for High-Tech Meaningful Use at PeaceHealth, a faith-based healthcare system that operates eight hospitals in three Western states, says CMS’ short statement caught her health system off-guard and forced a rapid shift in its priorities. “We were really focusing on moving some numbers and making some technology changes for some core measures that now, based on what CMS has in the proposed value-based purchasing, will not be around even as of next year,” she says.
Dietzel says the move to high-tech tools like electronic medical records (EMRs) has further complicated how hospitals and healthcare systems like PeaceHealth are preparing for the VBP program. For two other measures that relate to pneumonia immunization, she says, some of PeaceHealth’s hospitals have “less than ideal” scores that could potentially create some financial risk.
An EMR system on tap for next year, she says, likely will help the hospitals significantly improve their scores. But what should they do between now and then: Reinvent the wheel to prop up their numbers, only to do it again in a year? Or should they take a temporary hit until the more comprehensive system is in place?
Similar questions are likely to confront more healthcare providers as the program expands and evolves. Even as it will likely retire some measures in fiscal year 2014, CMS will add more from a list of 20 related to hospital-acquired conditions and complications, patient safety indicators, inpatient quality indicators, and mortality rates.
With the arrival of value-based purchasing (VBP), many hospitals have faced hard decisions about where to allocate scarce resources to maximize their performance potential. In some cases, those decisions have been made even more difficult by a set of core measures still very much in flux. For hospitalists, that means the ability to quickly adapt and reprioritize will be in high demand as measures are added or subtracted from the value-based purchasing program.
In the proposed program rules released in mid-January, CMS initially selected 17 core clinical measures from a list of 28 eligible candidates included in the Hospital Inpatient Quality Reporting (IQR) Program (https://www.cms.gov/HospitalQualityInits/08_HospitalRHQDAPU.asp) and also listed on the public Hospital Compare website (www.hospitalcompare.hhs.gov/) for at least one year. CMS explained its decision to withhold some of the remaining core measures from the program by noting that they were “topped out” and thus provided a poor basis of comparison among hospitals. Others, according to the agency, were of little value or were encouraging bad behavior.
CMS used the latter reason in its explanation for why it was not including an eligible core measure on administering antibiotics to pneumonia patients within six hours of their arrival at a hospital. “We do not believe that this measure is appropriate for inclusion because it could lead to inappropriate antibiotic use,” the rules stated. For that measure and others not recommended for inclusion in the hospital VBP program, CMS added that it would propose retiring them “in the near future.”

—Laura M. Dietzel, program director for High-Tech Meaningful Use, PeaceHealth
Laura M. Dietzel, program director for High-Tech Meaningful Use at PeaceHealth, a faith-based healthcare system that operates eight hospitals in three Western states, says CMS’ short statement caught her health system off-guard and forced a rapid shift in its priorities. “We were really focusing on moving some numbers and making some technology changes for some core measures that now, based on what CMS has in the proposed value-based purchasing, will not be around even as of next year,” she says.
Dietzel says the move to high-tech tools like electronic medical records (EMRs) has further complicated how hospitals and healthcare systems like PeaceHealth are preparing for the VBP program. For two other measures that relate to pneumonia immunization, she says, some of PeaceHealth’s hospitals have “less than ideal” scores that could potentially create some financial risk.
An EMR system on tap for next year, she says, likely will help the hospitals significantly improve their scores. But what should they do between now and then: Reinvent the wheel to prop up their numbers, only to do it again in a year? Or should they take a temporary hit until the more comprehensive system is in place?
Similar questions are likely to confront more healthcare providers as the program expands and evolves. Even as it will likely retire some measures in fiscal year 2014, CMS will add more from a list of 20 related to hospital-acquired conditions and complications, patient safety indicators, inpatient quality indicators, and mortality rates.
With the arrival of value-based purchasing (VBP), many hospitals have faced hard decisions about where to allocate scarce resources to maximize their performance potential. In some cases, those decisions have been made even more difficult by a set of core measures still very much in flux. For hospitalists, that means the ability to quickly adapt and reprioritize will be in high demand as measures are added or subtracted from the value-based purchasing program.
In the proposed program rules released in mid-January, CMS initially selected 17 core clinical measures from a list of 28 eligible candidates included in the Hospital Inpatient Quality Reporting (IQR) Program (https://www.cms.gov/HospitalQualityInits/08_HospitalRHQDAPU.asp) and also listed on the public Hospital Compare website (www.hospitalcompare.hhs.gov/) for at least one year. CMS explained its decision to withhold some of the remaining core measures from the program by noting that they were “topped out” and thus provided a poor basis of comparison among hospitals. Others, according to the agency, were of little value or were encouraging bad behavior.
CMS used the latter reason in its explanation for why it was not including an eligible core measure on administering antibiotics to pneumonia patients within six hours of their arrival at a hospital. “We do not believe that this measure is appropriate for inclusion because it could lead to inappropriate antibiotic use,” the rules stated. For that measure and others not recommended for inclusion in the hospital VBP program, CMS added that it would propose retiring them “in the near future.”

—Laura M. Dietzel, program director for High-Tech Meaningful Use, PeaceHealth
Laura M. Dietzel, program director for High-Tech Meaningful Use at PeaceHealth, a faith-based healthcare system that operates eight hospitals in three Western states, says CMS’ short statement caught her health system off-guard and forced a rapid shift in its priorities. “We were really focusing on moving some numbers and making some technology changes for some core measures that now, based on what CMS has in the proposed value-based purchasing, will not be around even as of next year,” she says.
Dietzel says the move to high-tech tools like electronic medical records (EMRs) has further complicated how hospitals and healthcare systems like PeaceHealth are preparing for the VBP program. For two other measures that relate to pneumonia immunization, she says, some of PeaceHealth’s hospitals have “less than ideal” scores that could potentially create some financial risk.
An EMR system on tap for next year, she says, likely will help the hospitals significantly improve their scores. But what should they do between now and then: Reinvent the wheel to prop up their numbers, only to do it again in a year? Or should they take a temporary hit until the more comprehensive system is in place?
Similar questions are likely to confront more healthcare providers as the program expands and evolves. Even as it will likely retire some measures in fiscal year 2014, CMS will add more from a list of 20 related to hospital-acquired conditions and complications, patient safety indicators, inpatient quality indicators, and mortality rates.
ONLINE EXCLUSIVE: Experts explain how hospitalists can thrive in a new era of payment reform
ONLINE EXCLUSIVE: Listen to billing and coding consultants discuss the importance of provider buy-in
Click here to listen to Dr. Pinson
Click here to listen to Ms. Leong
Click here to listen to Dr. Pinson
Click here to listen to Ms. Leong
Click here to listen to Dr. Pinson
Click here to listen to Ms. Leong
ONLINE EXCLUSIVE: PEERist Program Provides Rural Nebraska Hospital 24/7 HM Coverage
Hospitalist programs take many shapes, and the organizational flowchart typically depends on the number and makeup of the physicians, the hospital, the patients, and the community. Adequately covering the needs of inpatient units can be especially frustrating in rural communities, some hospitalists say.
“There are only five physicians total in our town,” says Gary Ensz, MD, a partner in the Auburn Family Health Center in Auburn, Neb. “In addition to being family practitioners, we are our own hospitalists. Covering the emergency room, seeing patients in clinic, and following hospitalized patients is a big burden.”
To address these issues, Dr. Ensz and his partners developed the Physician Extender Emergency Room Hospitalist (PEERist) program. They utilize physician assistants (PAs) to serve many hospitalist functions under their supervision.
“We hired PAs to work in the hospital and the emergency room,” Dr. Ensz explains. “They do not work in the clinic and then take call. Their only responsibilities are to the hospital and ER.”

—Gary Ensz, MD, partner, Auburn (Neb.) Family Health Center
PEERists work under protocols addressing treatment concerns and give guidance on when physicians should be called. On-call doctors round in the morning with the PA. The physicians like this approach, Dr. Ensz says, because they see the PEERist when it is convenient for them; before, they would leave clinic patients to attend to concerns at the hospital.
Impact of ER Call
“For most of us practicing in rural situations, the demands of ER call force people to retire,” Dr. Ensz says. “Now we have someone at the hospital highly trained and, as they get more experience, actually do some work better simply because they are there all the time. At worst, you now have two sets of hands working on the patient.”
PAs work a rotating schedule of up to 72 hours with as many as nine days off in a row. PAs can be recruited from a much larger area; in fact, one commutes four hours each way. PEERists say the time off makes it easier to do things with their families or work another job.
Other Benefits
In addition to pluses associated with the practice, Dr. Ensz is seeing other benefits, such as closer working relationships with the nurses. He also stresses that his hospital now has 24/7 in-house coverage, something almost unheard of in small rural hospitals.
One of the more subtle improvements might have been in getting people to the hospital quicker. “It wasn’t unusual for someone to come to clinic with symptoms they had for a while,” Dr. Ensz says. “The PEERists being in-house all the time have done away with these concerns.”
Hospitalist programs take many shapes, and the organizational flowchart typically depends on the number and makeup of the physicians, the hospital, the patients, and the community. Adequately covering the needs of inpatient units can be especially frustrating in rural communities, some hospitalists say.
“There are only five physicians total in our town,” says Gary Ensz, MD, a partner in the Auburn Family Health Center in Auburn, Neb. “In addition to being family practitioners, we are our own hospitalists. Covering the emergency room, seeing patients in clinic, and following hospitalized patients is a big burden.”
To address these issues, Dr. Ensz and his partners developed the Physician Extender Emergency Room Hospitalist (PEERist) program. They utilize physician assistants (PAs) to serve many hospitalist functions under their supervision.
“We hired PAs to work in the hospital and the emergency room,” Dr. Ensz explains. “They do not work in the clinic and then take call. Their only responsibilities are to the hospital and ER.”

—Gary Ensz, MD, partner, Auburn (Neb.) Family Health Center
PEERists work under protocols addressing treatment concerns and give guidance on when physicians should be called. On-call doctors round in the morning with the PA. The physicians like this approach, Dr. Ensz says, because they see the PEERist when it is convenient for them; before, they would leave clinic patients to attend to concerns at the hospital.
Impact of ER Call
“For most of us practicing in rural situations, the demands of ER call force people to retire,” Dr. Ensz says. “Now we have someone at the hospital highly trained and, as they get more experience, actually do some work better simply because they are there all the time. At worst, you now have two sets of hands working on the patient.”
PAs work a rotating schedule of up to 72 hours with as many as nine days off in a row. PAs can be recruited from a much larger area; in fact, one commutes four hours each way. PEERists say the time off makes it easier to do things with their families or work another job.
Other Benefits
In addition to pluses associated with the practice, Dr. Ensz is seeing other benefits, such as closer working relationships with the nurses. He also stresses that his hospital now has 24/7 in-house coverage, something almost unheard of in small rural hospitals.
One of the more subtle improvements might have been in getting people to the hospital quicker. “It wasn’t unusual for someone to come to clinic with symptoms they had for a while,” Dr. Ensz says. “The PEERists being in-house all the time have done away with these concerns.”
Hospitalist programs take many shapes, and the organizational flowchart typically depends on the number and makeup of the physicians, the hospital, the patients, and the community. Adequately covering the needs of inpatient units can be especially frustrating in rural communities, some hospitalists say.
“There are only five physicians total in our town,” says Gary Ensz, MD, a partner in the Auburn Family Health Center in Auburn, Neb. “In addition to being family practitioners, we are our own hospitalists. Covering the emergency room, seeing patients in clinic, and following hospitalized patients is a big burden.”
To address these issues, Dr. Ensz and his partners developed the Physician Extender Emergency Room Hospitalist (PEERist) program. They utilize physician assistants (PAs) to serve many hospitalist functions under their supervision.
“We hired PAs to work in the hospital and the emergency room,” Dr. Ensz explains. “They do not work in the clinic and then take call. Their only responsibilities are to the hospital and ER.”

—Gary Ensz, MD, partner, Auburn (Neb.) Family Health Center
PEERists work under protocols addressing treatment concerns and give guidance on when physicians should be called. On-call doctors round in the morning with the PA. The physicians like this approach, Dr. Ensz says, because they see the PEERist when it is convenient for them; before, they would leave clinic patients to attend to concerns at the hospital.
Impact of ER Call
“For most of us practicing in rural situations, the demands of ER call force people to retire,” Dr. Ensz says. “Now we have someone at the hospital highly trained and, as they get more experience, actually do some work better simply because they are there all the time. At worst, you now have two sets of hands working on the patient.”
PAs work a rotating schedule of up to 72 hours with as many as nine days off in a row. PAs can be recruited from a much larger area; in fact, one commutes four hours each way. PEERists say the time off makes it easier to do things with their families or work another job.
Other Benefits
In addition to pluses associated with the practice, Dr. Ensz is seeing other benefits, such as closer working relationships with the nurses. He also stresses that his hospital now has 24/7 in-house coverage, something almost unheard of in small rural hospitals.
One of the more subtle improvements might have been in getting people to the hospital quicker. “It wasn’t unusual for someone to come to clinic with symptoms they had for a while,” Dr. Ensz says. “The PEERists being in-house all the time have done away with these concerns.”
Nurse Practitioners, Physician Assistants to the Rescue
In 2004, the hospitalist group at the University of Michigan Health System in Ann Arbor faced a manpower problem: In a refrain common to hospitalist groups around the country, changes in duty-hour regulations were making it harder for medical residents to continue to provide inpatient coverage at the same levels as before.
Addressing the issue was difficult for the HM group and hospital administrators; they were going to need a significant number of new providers, and qualified physicians were in short supply. To address these issues, the HM group chose to add nonphysician providers (NPP) to their service.
“NPPs had worked at UM for a long time in other areas,” says Vikas Parekh, MD, SFHM, associate director of hospitalist management. “We had just created a new service that was hiring new people and thought NPPs would help in providing services.”
Hiring NPPs helped solve the University of Michigan’s problem, and the tactic has helped solve manpower issues at numerous HM groups around the country. But deciding whether your HM group should hire physicians, NPPs—usually nurse practitioners (NPs) and physician assistants (PAs)—or some combination of the two will not be easy. It is a complex decision, one that requires following state-level licensing and practice laws as well as local hospital bylaws and federal and private insurance payment rules. Such decisions also mean HM group directors need to keep in mind case mixes and the personalities of the physicians in the practice.
“There is no one-size-fits-all solution,” says Mitchell Wilson, MD, SFHM, corporate medical director for Eagle Hospital Physicians in Atlanta. “Not all environments are well-suited to NPP practice. Even when it is, you can’t just throw an NPP into the mix on their own with the expectation they will be successful.”
Whether it’s covering admissions, streamlining discharges, or working as an integral part of a care team, NPPs can be the solution expanding HM groups are looking for.

“Our physicians depend on NPPs to help them complete patient care in a more efficient manner and work to enhance continuity of care,” says Mary Whitehead, RN, APRN-BC, FNP, of Hospital Medicine Associates in Fort Worth, Texas. “We lower physician rounding time so patients are seen sooner and tests are requested sooner. In addition, the patients really appreciate the extra time we can spend with them.”
Trained, Licensed, Available
NPs must be registered nurses with clinical experience before they can enroll in an advanced degree program, which usually results in a master’s degree or doctorate. Generally, a state board of nursing, or a state board jointly with the state medical board, regulates NPs.
PAs are trained in more of a traditional medical model. They have a variable education level all the way up to a PhD, although more states are requiring at least a master’s degree. Practice and other legal parameters most often come under the authority of state medical boards.
NPPs can provide additional medical expertise to patients, says Ryan Genzink, PA, a physician assistant with Hospitalists of Western Michigan in Grand Rapids and the American Academy of Physician Assistants’ medical liaison to SHM. “One of the challenges faced by physicians is that they often have to be in two places at once,” he says. “There is a recognition that teams provide better care for complicated patients.”
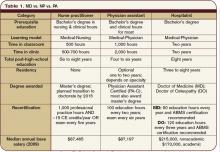
NPPs generally practice under the supervision of a physician hospitalist. Some states allow a greater degree of independence for NPs. However, most NPs and PAs are required to have a practice agreement outlining their responsibilities and the amount of oversight required (see Table 1, p. 39). There is no such thing as a “fire and forget” NPP.
“The practice needs to thoroughly understand the legal environment early in the process,” says John Nelson, MD, MHM, hospitalist director at Bellevue (Wash.) Medical Center, partner in Nelson Flores Hospital Medicine Consultants, and SHM cofounder. “NPPs are not a ‘hospitalist lite’ that can function entirely like a hospitalist.”
Hospital bylaws, which can vary greatly by city, county, or state, are another important consideration before you hire an NPP.
“In some areas, NPPs may not be able to practice in the ICU,” Dr. Wilson says. “In others, the physician may be required to see the patient instead of consulting with the NPP. The idiosyncrasies of the individual hospital’s bylaws may impact the efficiency of the NPP/MD team.”
Physician Characteristics
Environmental variables—namely, the personality of the physicians within the practice—should be considered before you head down the NPP path. It makes little practical or financial sense to spend the time and effort of hiring an NPP if the physicians still insist on doing all the work.
“[It’s] one of the most significant factors in successfully integrating an NPP program,” Dr. Wilson says. “Will [physicians] be able to tolerate some degree of uncertainty when letting others see their patients? Are they open to adapting to different practice styles? The thing we see most often in practices that use NPPs to their advantage is the recognition that there is an important role for the nonphysician at the bedside.”
Some physicians hesitate to work with NPPs, while others welcome the extra help and unique experience NPPs offer. Experts agree that forcing NPPs on a physician is not a good idea. They also agree that, especially when beginning a new program, group directors should let physicians who are interested in working with NPPs take the lead. As NPP use in the group matures, many of those who were at first unwilling can decide that there is a place for NPPs in their practice.
Case Mix Is Key
The types and kinds of patient seen might limit the use of NPPs in hospitalist practice. “Our experience is that acuity and complexity of the care, especially as it relates to diagnostic and therapeutic decision-making, makes it difficult for NPPs to function independently,” Dr. Parekh says.
Dr. Wilson agrees. “Depending on the specific attributes of the setting, a service with both high-complexity and high-acuity patients may be a more challenging environment to realize the efficiencies of NPPs,” he says. “There is a relationship between complexity, acuity, and physician involvement.”
Even so, a continuum of NPP use in HM practice is achievable. For example, as a patient improves, an NPP might be able to take on a larger role in treatment by participating in discharge planning. In more acute patients, the NPP can save valuable physician time by coordinating with consultants, staying on top of treatments, and consolidating clinically important data for the physician.
Many Models in Use
Historically, the widespread use of alternative providers began in 2004 as a result of the changes to resident duty-hours. The restrictions created a workforce gap, which led to a large number of new positions in hospitals nationwide. Many of HM’s early adopters essentially went with what they knew.
“We work in teams where the physician, NPP, and nurse see a group of patients similar in function to an attending, resident, and RN,” Genzink says. “We see ‘our’ patients in a collaborative fashion.”
There are other models that have proven successful in the correct setting. Some HM groups use specialist NPPs to cover specific clinical areas, such as orthopedics or oncology. This not only develops a cadre of providers with excellent understanding of their patients, but it also frees up physician time for more acute and complicated patients.
“Our physicians depend on us helping them get patient care completed more efficiently, so that length of stay is acceptable, and to enhance continuity of care,” says Whitehead, the American Academy of Nurse Practitioners’ liaison to SHM. “Having an NPP visit the patient daily, documenting progress, greatly enhances communications between physicians and consultants.”
Other groups have NPPs specialize by function—for example, they cover all admissions or work mainly with discharging a patient. Some groups have the physician see the patient on admission, work out a care plan, then turn over management to the NPP. Many agree that most NPPs are best utilized by having them cover specific shifts, such as overnight call or on a swing shift, to help during peak demand.
Monetary and Time Commitments
The financial impact of NPPs on a hospitalist practice depends on many factors. Groups will need to look not only at the salary and benefit costs associated with the position, but also how best to fit that person into the billing system.
Salary and benefit comparisons are fairly straightforward: The State of Hospital Medicine: 2010 Report Based on 2009 Data, produced by SHM and the Medical Group Management Association, shows median total compensation for adult hospitalists at $215,000 per year; NPP compensation is around $87,000.1
The general cost of benefits (health insurance, retirement, etc.) is fairly typical throughout a hospitalist practice, so there should be little difference between a new FTE hospitalist or NPP. Other considerations, including office space and support staff, would be roughly the same if the group hired a physician. The cost of continuing education and malpractice insurance likely will be less with an NPP, but it is best to check before making a new hire.
After the outgo has been established, the next step is to look at the differences in reimbursement for NPPs vs. physicians. Here, again, the math gets tricky. The Centers for Medicare & Medicaid Services (CMS) pay NPPs at 85% of the physician rate for a specific diagnosis. However, if there is direct physician involvement, the claim can be filed as “shared billing” and reimbursed at 100%.
For some hospitalist practices, adding NPPs is an easy decision to make. Dr. Parekh says his group already has policies in place that require a physician to see the patient every day. In that case, no extra physician time is necessary, so shared billing makes sense. Other hospitals’ bylaws might have similar requirements.
For practices in which the NPP is able to work with less oversight, it might be better to bill at 85% rather than use the physician time to meet shared-billing criteria. Even in practices with greater NPP autonomy, such variables as case mix and patient acuity might enter into the equation. If the patient is sick enough that the physician is involved for a significant amount of time, then shared billing probably is best.
Experts say group directors and hiring managers should look carefully at contracts with private insurers, too. There most likely will be considerable variation in how each plan handles NPP claims.
Managing performance expectations can have an impact on the successful use of NPPs in a hospitalist practice. Setting realistic goals and groupwide understanding of what the NPPs’ roles will be is crucial. The practice should look at the work that needs to be done and decide if that work provides a genuinely valuable role for an NPP.
Hire for Need, Not Desperation
“The mistake I see most often is hiring an NPP because a practice is desperate for help,” says Martin Buser, MPH, FACHE, a partner in Hospitalist Management Resources, LLC, in San Diego. “Smart practices are looking at NPPs, evaluating where they do the most good, and then setting out their role and expectations based on these needs and the practice environment.”
Hiring mistakes can be compounded if the NPP is not a good match to the job description or group expectations. If the practice hires an NPP fresh out of school, the group will need to establish training and have the new hire work more closely with physicians. If, on the other hand, an NP has 10 years of experience in an ICU, or a PA has worked in the ED for the past five years, a higher level of autonomy can be granted sooner. However, NPPs with established backgrounds are almost as rare as experienced hospitalists (see “Integrating NPPs Into HM Practice,” p. 38).
Inevitably, there will be changes in the interactions between patients and the hospitalists, as both physicians and NPPs become more comfortable with the other’s practice style, as well as each other’s strengths and weaknesses.
MD-to-NPP Ratio Varies
The practice structure and optimal mix of NPPs to MDs is something that will be specific to the hospitalist group. “We don’t really have good studies on this subject,” Buser says. “I usually get worried when we exceed two NPPs to one MD.”
Others disagree. Dr. Parekh, who works in an academic center, says his group has been successful having one MD work with as many as three NPPs. At the other end, Dr. Wilson says his 10 years of experience suggest 1:1 is the most efficient ratio.
However, all of them agree that having one NPP work with more than one physician is not sustainable. The NPP will be less familiar with each doctor’s practice style, what kind of information they need, and how things should be presented. If two or more hospitalists share an NPP, there can be internal friction over division of the NPP’s time, as well as extending the time before the MDs have a good feel for the NPP’s strengths and weaknesses.
In the final analysis, the HM group has to look at the amount and type of work available. In some cases, it will make financial and clinical sense to bring on an NPP. Under other circumstances, an FTE hospitalist is the best fit.
“Sustainability, quality, and efficiency are the drivers for NPP/MD teams. Increasing pressure to offset program costs is not,” Dr. Wilson says. “You do it because it helps sustain the program, helps with recruiting, and effects your efficiency.” TH
Kurt Ullman is a freelance medical writer based in Indiana.
Reference
- Medical Group Management Association and the Society of Hospital Medicine. State of Hospital Medicine: 2010 Report Based on 2009 Data. 2010. Philadelphia and Englewood, Colo.
In 2004, the hospitalist group at the University of Michigan Health System in Ann Arbor faced a manpower problem: In a refrain common to hospitalist groups around the country, changes in duty-hour regulations were making it harder for medical residents to continue to provide inpatient coverage at the same levels as before.
Addressing the issue was difficult for the HM group and hospital administrators; they were going to need a significant number of new providers, and qualified physicians were in short supply. To address these issues, the HM group chose to add nonphysician providers (NPP) to their service.
“NPPs had worked at UM for a long time in other areas,” says Vikas Parekh, MD, SFHM, associate director of hospitalist management. “We had just created a new service that was hiring new people and thought NPPs would help in providing services.”
Hiring NPPs helped solve the University of Michigan’s problem, and the tactic has helped solve manpower issues at numerous HM groups around the country. But deciding whether your HM group should hire physicians, NPPs—usually nurse practitioners (NPs) and physician assistants (PAs)—or some combination of the two will not be easy. It is a complex decision, one that requires following state-level licensing and practice laws as well as local hospital bylaws and federal and private insurance payment rules. Such decisions also mean HM group directors need to keep in mind case mixes and the personalities of the physicians in the practice.
“There is no one-size-fits-all solution,” says Mitchell Wilson, MD, SFHM, corporate medical director for Eagle Hospital Physicians in Atlanta. “Not all environments are well-suited to NPP practice. Even when it is, you can’t just throw an NPP into the mix on their own with the expectation they will be successful.”
Whether it’s covering admissions, streamlining discharges, or working as an integral part of a care team, NPPs can be the solution expanding HM groups are looking for.

“Our physicians depend on NPPs to help them complete patient care in a more efficient manner and work to enhance continuity of care,” says Mary Whitehead, RN, APRN-BC, FNP, of Hospital Medicine Associates in Fort Worth, Texas. “We lower physician rounding time so patients are seen sooner and tests are requested sooner. In addition, the patients really appreciate the extra time we can spend with them.”
Trained, Licensed, Available
NPs must be registered nurses with clinical experience before they can enroll in an advanced degree program, which usually results in a master’s degree or doctorate. Generally, a state board of nursing, or a state board jointly with the state medical board, regulates NPs.
PAs are trained in more of a traditional medical model. They have a variable education level all the way up to a PhD, although more states are requiring at least a master’s degree. Practice and other legal parameters most often come under the authority of state medical boards.
NPPs can provide additional medical expertise to patients, says Ryan Genzink, PA, a physician assistant with Hospitalists of Western Michigan in Grand Rapids and the American Academy of Physician Assistants’ medical liaison to SHM. “One of the challenges faced by physicians is that they often have to be in two places at once,” he says. “There is a recognition that teams provide better care for complicated patients.”
NPPs generally practice under the supervision of a physician hospitalist. Some states allow a greater degree of independence for NPs. However, most NPs and PAs are required to have a practice agreement outlining their responsibilities and the amount of oversight required (see Table 1, p. 39). There is no such thing as a “fire and forget” NPP.
“The practice needs to thoroughly understand the legal environment early in the process,” says John Nelson, MD, MHM, hospitalist director at Bellevue (Wash.) Medical Center, partner in Nelson Flores Hospital Medicine Consultants, and SHM cofounder. “NPPs are not a ‘hospitalist lite’ that can function entirely like a hospitalist.”
Hospital bylaws, which can vary greatly by city, county, or state, are another important consideration before you hire an NPP.
“In some areas, NPPs may not be able to practice in the ICU,” Dr. Wilson says. “In others, the physician may be required to see the patient instead of consulting with the NPP. The idiosyncrasies of the individual hospital’s bylaws may impact the efficiency of the NPP/MD team.”
Physician Characteristics
Environmental variables—namely, the personality of the physicians within the practice—should be considered before you head down the NPP path. It makes little practical or financial sense to spend the time and effort of hiring an NPP if the physicians still insist on doing all the work.
“[It’s] one of the most significant factors in successfully integrating an NPP program,” Dr. Wilson says. “Will [physicians] be able to tolerate some degree of uncertainty when letting others see their patients? Are they open to adapting to different practice styles? The thing we see most often in practices that use NPPs to their advantage is the recognition that there is an important role for the nonphysician at the bedside.”
Some physicians hesitate to work with NPPs, while others welcome the extra help and unique experience NPPs offer. Experts agree that forcing NPPs on a physician is not a good idea. They also agree that, especially when beginning a new program, group directors should let physicians who are interested in working with NPPs take the lead. As NPP use in the group matures, many of those who were at first unwilling can decide that there is a place for NPPs in their practice.
Case Mix Is Key
The types and kinds of patient seen might limit the use of NPPs in hospitalist practice. “Our experience is that acuity and complexity of the care, especially as it relates to diagnostic and therapeutic decision-making, makes it difficult for NPPs to function independently,” Dr. Parekh says.
Dr. Wilson agrees. “Depending on the specific attributes of the setting, a service with both high-complexity and high-acuity patients may be a more challenging environment to realize the efficiencies of NPPs,” he says. “There is a relationship between complexity, acuity, and physician involvement.”
Even so, a continuum of NPP use in HM practice is achievable. For example, as a patient improves, an NPP might be able to take on a larger role in treatment by participating in discharge planning. In more acute patients, the NPP can save valuable physician time by coordinating with consultants, staying on top of treatments, and consolidating clinically important data for the physician.
Many Models in Use
Historically, the widespread use of alternative providers began in 2004 as a result of the changes to resident duty-hours. The restrictions created a workforce gap, which led to a large number of new positions in hospitals nationwide. Many of HM’s early adopters essentially went with what they knew.
“We work in teams where the physician, NPP, and nurse see a group of patients similar in function to an attending, resident, and RN,” Genzink says. “We see ‘our’ patients in a collaborative fashion.”
There are other models that have proven successful in the correct setting. Some HM groups use specialist NPPs to cover specific clinical areas, such as orthopedics or oncology. This not only develops a cadre of providers with excellent understanding of their patients, but it also frees up physician time for more acute and complicated patients.
“Our physicians depend on us helping them get patient care completed more efficiently, so that length of stay is acceptable, and to enhance continuity of care,” says Whitehead, the American Academy of Nurse Practitioners’ liaison to SHM. “Having an NPP visit the patient daily, documenting progress, greatly enhances communications between physicians and consultants.”
Other groups have NPPs specialize by function—for example, they cover all admissions or work mainly with discharging a patient. Some groups have the physician see the patient on admission, work out a care plan, then turn over management to the NPP. Many agree that most NPPs are best utilized by having them cover specific shifts, such as overnight call or on a swing shift, to help during peak demand.
Monetary and Time Commitments
The financial impact of NPPs on a hospitalist practice depends on many factors. Groups will need to look not only at the salary and benefit costs associated with the position, but also how best to fit that person into the billing system.
Salary and benefit comparisons are fairly straightforward: The State of Hospital Medicine: 2010 Report Based on 2009 Data, produced by SHM and the Medical Group Management Association, shows median total compensation for adult hospitalists at $215,000 per year; NPP compensation is around $87,000.1
The general cost of benefits (health insurance, retirement, etc.) is fairly typical throughout a hospitalist practice, so there should be little difference between a new FTE hospitalist or NPP. Other considerations, including office space and support staff, would be roughly the same if the group hired a physician. The cost of continuing education and malpractice insurance likely will be less with an NPP, but it is best to check before making a new hire.
After the outgo has been established, the next step is to look at the differences in reimbursement for NPPs vs. physicians. Here, again, the math gets tricky. The Centers for Medicare & Medicaid Services (CMS) pay NPPs at 85% of the physician rate for a specific diagnosis. However, if there is direct physician involvement, the claim can be filed as “shared billing” and reimbursed at 100%.
For some hospitalist practices, adding NPPs is an easy decision to make. Dr. Parekh says his group already has policies in place that require a physician to see the patient every day. In that case, no extra physician time is necessary, so shared billing makes sense. Other hospitals’ bylaws might have similar requirements.
For practices in which the NPP is able to work with less oversight, it might be better to bill at 85% rather than use the physician time to meet shared-billing criteria. Even in practices with greater NPP autonomy, such variables as case mix and patient acuity might enter into the equation. If the patient is sick enough that the physician is involved for a significant amount of time, then shared billing probably is best.
Experts say group directors and hiring managers should look carefully at contracts with private insurers, too. There most likely will be considerable variation in how each plan handles NPP claims.
Managing performance expectations can have an impact on the successful use of NPPs in a hospitalist practice. Setting realistic goals and groupwide understanding of what the NPPs’ roles will be is crucial. The practice should look at the work that needs to be done and decide if that work provides a genuinely valuable role for an NPP.
Hire for Need, Not Desperation
“The mistake I see most often is hiring an NPP because a practice is desperate for help,” says Martin Buser, MPH, FACHE, a partner in Hospitalist Management Resources, LLC, in San Diego. “Smart practices are looking at NPPs, evaluating where they do the most good, and then setting out their role and expectations based on these needs and the practice environment.”
Hiring mistakes can be compounded if the NPP is not a good match to the job description or group expectations. If the practice hires an NPP fresh out of school, the group will need to establish training and have the new hire work more closely with physicians. If, on the other hand, an NP has 10 years of experience in an ICU, or a PA has worked in the ED for the past five years, a higher level of autonomy can be granted sooner. However, NPPs with established backgrounds are almost as rare as experienced hospitalists (see “Integrating NPPs Into HM Practice,” p. 38).
Inevitably, there will be changes in the interactions between patients and the hospitalists, as both physicians and NPPs become more comfortable with the other’s practice style, as well as each other’s strengths and weaknesses.
MD-to-NPP Ratio Varies
The practice structure and optimal mix of NPPs to MDs is something that will be specific to the hospitalist group. “We don’t really have good studies on this subject,” Buser says. “I usually get worried when we exceed two NPPs to one MD.”
Others disagree. Dr. Parekh, who works in an academic center, says his group has been successful having one MD work with as many as three NPPs. At the other end, Dr. Wilson says his 10 years of experience suggest 1:1 is the most efficient ratio.
However, all of them agree that having one NPP work with more than one physician is not sustainable. The NPP will be less familiar with each doctor’s practice style, what kind of information they need, and how things should be presented. If two or more hospitalists share an NPP, there can be internal friction over division of the NPP’s time, as well as extending the time before the MDs have a good feel for the NPP’s strengths and weaknesses.
In the final analysis, the HM group has to look at the amount and type of work available. In some cases, it will make financial and clinical sense to bring on an NPP. Under other circumstances, an FTE hospitalist is the best fit.
“Sustainability, quality, and efficiency are the drivers for NPP/MD teams. Increasing pressure to offset program costs is not,” Dr. Wilson says. “You do it because it helps sustain the program, helps with recruiting, and effects your efficiency.” TH
Kurt Ullman is a freelance medical writer based in Indiana.
Reference
- Medical Group Management Association and the Society of Hospital Medicine. State of Hospital Medicine: 2010 Report Based on 2009 Data. 2010. Philadelphia and Englewood, Colo.
In 2004, the hospitalist group at the University of Michigan Health System in Ann Arbor faced a manpower problem: In a refrain common to hospitalist groups around the country, changes in duty-hour regulations were making it harder for medical residents to continue to provide inpatient coverage at the same levels as before.
Addressing the issue was difficult for the HM group and hospital administrators; they were going to need a significant number of new providers, and qualified physicians were in short supply. To address these issues, the HM group chose to add nonphysician providers (NPP) to their service.
“NPPs had worked at UM for a long time in other areas,” says Vikas Parekh, MD, SFHM, associate director of hospitalist management. “We had just created a new service that was hiring new people and thought NPPs would help in providing services.”
Hiring NPPs helped solve the University of Michigan’s problem, and the tactic has helped solve manpower issues at numerous HM groups around the country. But deciding whether your HM group should hire physicians, NPPs—usually nurse practitioners (NPs) and physician assistants (PAs)—or some combination of the two will not be easy. It is a complex decision, one that requires following state-level licensing and practice laws as well as local hospital bylaws and federal and private insurance payment rules. Such decisions also mean HM group directors need to keep in mind case mixes and the personalities of the physicians in the practice.
“There is no one-size-fits-all solution,” says Mitchell Wilson, MD, SFHM, corporate medical director for Eagle Hospital Physicians in Atlanta. “Not all environments are well-suited to NPP practice. Even when it is, you can’t just throw an NPP into the mix on their own with the expectation they will be successful.”
Whether it’s covering admissions, streamlining discharges, or working as an integral part of a care team, NPPs can be the solution expanding HM groups are looking for.

“Our physicians depend on NPPs to help them complete patient care in a more efficient manner and work to enhance continuity of care,” says Mary Whitehead, RN, APRN-BC, FNP, of Hospital Medicine Associates in Fort Worth, Texas. “We lower physician rounding time so patients are seen sooner and tests are requested sooner. In addition, the patients really appreciate the extra time we can spend with them.”
Trained, Licensed, Available
NPs must be registered nurses with clinical experience before they can enroll in an advanced degree program, which usually results in a master’s degree or doctorate. Generally, a state board of nursing, or a state board jointly with the state medical board, regulates NPs.
PAs are trained in more of a traditional medical model. They have a variable education level all the way up to a PhD, although more states are requiring at least a master’s degree. Practice and other legal parameters most often come under the authority of state medical boards.
NPPs can provide additional medical expertise to patients, says Ryan Genzink, PA, a physician assistant with Hospitalists of Western Michigan in Grand Rapids and the American Academy of Physician Assistants’ medical liaison to SHM. “One of the challenges faced by physicians is that they often have to be in two places at once,” he says. “There is a recognition that teams provide better care for complicated patients.”
NPPs generally practice under the supervision of a physician hospitalist. Some states allow a greater degree of independence for NPs. However, most NPs and PAs are required to have a practice agreement outlining their responsibilities and the amount of oversight required (see Table 1, p. 39). There is no such thing as a “fire and forget” NPP.
“The practice needs to thoroughly understand the legal environment early in the process,” says John Nelson, MD, MHM, hospitalist director at Bellevue (Wash.) Medical Center, partner in Nelson Flores Hospital Medicine Consultants, and SHM cofounder. “NPPs are not a ‘hospitalist lite’ that can function entirely like a hospitalist.”
Hospital bylaws, which can vary greatly by city, county, or state, are another important consideration before you hire an NPP.
“In some areas, NPPs may not be able to practice in the ICU,” Dr. Wilson says. “In others, the physician may be required to see the patient instead of consulting with the NPP. The idiosyncrasies of the individual hospital’s bylaws may impact the efficiency of the NPP/MD team.”
Physician Characteristics
Environmental variables—namely, the personality of the physicians within the practice—should be considered before you head down the NPP path. It makes little practical or financial sense to spend the time and effort of hiring an NPP if the physicians still insist on doing all the work.
“[It’s] one of the most significant factors in successfully integrating an NPP program,” Dr. Wilson says. “Will [physicians] be able to tolerate some degree of uncertainty when letting others see their patients? Are they open to adapting to different practice styles? The thing we see most often in practices that use NPPs to their advantage is the recognition that there is an important role for the nonphysician at the bedside.”
Some physicians hesitate to work with NPPs, while others welcome the extra help and unique experience NPPs offer. Experts agree that forcing NPPs on a physician is not a good idea. They also agree that, especially when beginning a new program, group directors should let physicians who are interested in working with NPPs take the lead. As NPP use in the group matures, many of those who were at first unwilling can decide that there is a place for NPPs in their practice.
Case Mix Is Key
The types and kinds of patient seen might limit the use of NPPs in hospitalist practice. “Our experience is that acuity and complexity of the care, especially as it relates to diagnostic and therapeutic decision-making, makes it difficult for NPPs to function independently,” Dr. Parekh says.
Dr. Wilson agrees. “Depending on the specific attributes of the setting, a service with both high-complexity and high-acuity patients may be a more challenging environment to realize the efficiencies of NPPs,” he says. “There is a relationship between complexity, acuity, and physician involvement.”
Even so, a continuum of NPP use in HM practice is achievable. For example, as a patient improves, an NPP might be able to take on a larger role in treatment by participating in discharge planning. In more acute patients, the NPP can save valuable physician time by coordinating with consultants, staying on top of treatments, and consolidating clinically important data for the physician.
Many Models in Use
Historically, the widespread use of alternative providers began in 2004 as a result of the changes to resident duty-hours. The restrictions created a workforce gap, which led to a large number of new positions in hospitals nationwide. Many of HM’s early adopters essentially went with what they knew.
“We work in teams where the physician, NPP, and nurse see a group of patients similar in function to an attending, resident, and RN,” Genzink says. “We see ‘our’ patients in a collaborative fashion.”
There are other models that have proven successful in the correct setting. Some HM groups use specialist NPPs to cover specific clinical areas, such as orthopedics or oncology. This not only develops a cadre of providers with excellent understanding of their patients, but it also frees up physician time for more acute and complicated patients.
“Our physicians depend on us helping them get patient care completed more efficiently, so that length of stay is acceptable, and to enhance continuity of care,” says Whitehead, the American Academy of Nurse Practitioners’ liaison to SHM. “Having an NPP visit the patient daily, documenting progress, greatly enhances communications between physicians and consultants.”
Other groups have NPPs specialize by function—for example, they cover all admissions or work mainly with discharging a patient. Some groups have the physician see the patient on admission, work out a care plan, then turn over management to the NPP. Many agree that most NPPs are best utilized by having them cover specific shifts, such as overnight call or on a swing shift, to help during peak demand.
Monetary and Time Commitments
The financial impact of NPPs on a hospitalist practice depends on many factors. Groups will need to look not only at the salary and benefit costs associated with the position, but also how best to fit that person into the billing system.
Salary and benefit comparisons are fairly straightforward: The State of Hospital Medicine: 2010 Report Based on 2009 Data, produced by SHM and the Medical Group Management Association, shows median total compensation for adult hospitalists at $215,000 per year; NPP compensation is around $87,000.1
The general cost of benefits (health insurance, retirement, etc.) is fairly typical throughout a hospitalist practice, so there should be little difference between a new FTE hospitalist or NPP. Other considerations, including office space and support staff, would be roughly the same if the group hired a physician. The cost of continuing education and malpractice insurance likely will be less with an NPP, but it is best to check before making a new hire.
After the outgo has been established, the next step is to look at the differences in reimbursement for NPPs vs. physicians. Here, again, the math gets tricky. The Centers for Medicare & Medicaid Services (CMS) pay NPPs at 85% of the physician rate for a specific diagnosis. However, if there is direct physician involvement, the claim can be filed as “shared billing” and reimbursed at 100%.
For some hospitalist practices, adding NPPs is an easy decision to make. Dr. Parekh says his group already has policies in place that require a physician to see the patient every day. In that case, no extra physician time is necessary, so shared billing makes sense. Other hospitals’ bylaws might have similar requirements.
For practices in which the NPP is able to work with less oversight, it might be better to bill at 85% rather than use the physician time to meet shared-billing criteria. Even in practices with greater NPP autonomy, such variables as case mix and patient acuity might enter into the equation. If the patient is sick enough that the physician is involved for a significant amount of time, then shared billing probably is best.
Experts say group directors and hiring managers should look carefully at contracts with private insurers, too. There most likely will be considerable variation in how each plan handles NPP claims.
Managing performance expectations can have an impact on the successful use of NPPs in a hospitalist practice. Setting realistic goals and groupwide understanding of what the NPPs’ roles will be is crucial. The practice should look at the work that needs to be done and decide if that work provides a genuinely valuable role for an NPP.
Hire for Need, Not Desperation
“The mistake I see most often is hiring an NPP because a practice is desperate for help,” says Martin Buser, MPH, FACHE, a partner in Hospitalist Management Resources, LLC, in San Diego. “Smart practices are looking at NPPs, evaluating where they do the most good, and then setting out their role and expectations based on these needs and the practice environment.”
Hiring mistakes can be compounded if the NPP is not a good match to the job description or group expectations. If the practice hires an NPP fresh out of school, the group will need to establish training and have the new hire work more closely with physicians. If, on the other hand, an NP has 10 years of experience in an ICU, or a PA has worked in the ED for the past five years, a higher level of autonomy can be granted sooner. However, NPPs with established backgrounds are almost as rare as experienced hospitalists (see “Integrating NPPs Into HM Practice,” p. 38).
Inevitably, there will be changes in the interactions between patients and the hospitalists, as both physicians and NPPs become more comfortable with the other’s practice style, as well as each other’s strengths and weaknesses.
MD-to-NPP Ratio Varies
The practice structure and optimal mix of NPPs to MDs is something that will be specific to the hospitalist group. “We don’t really have good studies on this subject,” Buser says. “I usually get worried when we exceed two NPPs to one MD.”
Others disagree. Dr. Parekh, who works in an academic center, says his group has been successful having one MD work with as many as three NPPs. At the other end, Dr. Wilson says his 10 years of experience suggest 1:1 is the most efficient ratio.
However, all of them agree that having one NPP work with more than one physician is not sustainable. The NPP will be less familiar with each doctor’s practice style, what kind of information they need, and how things should be presented. If two or more hospitalists share an NPP, there can be internal friction over division of the NPP’s time, as well as extending the time before the MDs have a good feel for the NPP’s strengths and weaknesses.
In the final analysis, the HM group has to look at the amount and type of work available. In some cases, it will make financial and clinical sense to bring on an NPP. Under other circumstances, an FTE hospitalist is the best fit.
“Sustainability, quality, and efficiency are the drivers for NPP/MD teams. Increasing pressure to offset program costs is not,” Dr. Wilson says. “You do it because it helps sustain the program, helps with recruiting, and effects your efficiency.” TH
Kurt Ullman is a freelance medical writer based in Indiana.
Reference
- Medical Group Management Association and the Society of Hospital Medicine. State of Hospital Medicine: 2010 Report Based on 2009 Data. 2010. Philadelphia and Englewood, Colo.
Hospitalists Are the Answer
Earlier this year, the Journal of the American Medical Association (JAMA) published the article “A Physician Management Infrastructure,” by Peter Pronovost and Jill Marsteller.1 Pronovost and Marsteller’s commentary gets to the very heart of the need for change in healthcare delivery and the major barriers to that change.
As they note, quality improvement (QI) continues to receive attention from every sector of the healthcare market, but systematic and widespread benefits—actual improvement in quality of care—are years away from reaching the patient. The major impediments to delivering performance changes at the front lines of healthcare are both attitudinal and structural.
However, such obstacles can be overcome, starting today.
The authors rightly cite the development of physician leadership as a significant factor in the long-term success of QI. For too long, healthcare leaders have taken a “learn as you go” approach to leadership development. This antiquated philosophy that the best physician leaders ascend naturally to leadership falsely assumes that today’s leaders are perfectly suited for their jobs.
Training Tomorrow’s Leaders Today
In order for meaningful QI to succeed, systematic leadership development in healthcare must be a priority. Those hospitals and healthcare systems that acknowledge this reality already are reaping the benefits. Across the country, more than 1,200 hospitalists have participated in SHM’s Leadership Academy, a rigorous multicourse program that trains physicians in the fundamentals of hospital-based leadership. Leadership Academy participants then go on to lead new programs, many of which are QI-related, in their hospitals. This year, SHM will announce a Certification for Leaders in Hospital Medicine, which will further raise the bar, and mentor, enable, and define the future leaders for our hospitals.
The collective experience of HM also indicates that formal mentorship programs are a critical element to systematic leadership development. The exponential growth of SHM’s mentor-based QI programs to reduce readmissions, prevent VTEs, and improve glycemic control in hospitals—now implemented in more than 300 hospital sites across the country—is a testament to the need for one-on-one mentorship and leadership development and the impact it can have on patient care.
SHM continues to provide broad training in performance improvement and patient safety in its one-day “Quality Improvement Skills” pre-course at the annual meeting (HM11, May 10-13, Grapevine, Texas, www. hospitalmedicine2011.org). In the coming months, SHM will debut a nine-part series of Web-based modules that are essential to any hospitalist now charged with taking an active role in improving performance at their hospital.
Teamwork Is Key
Looking at the evolved present-day hospital, but more to the future, SHM and hospitalists recognize that empowered and coordinated teams of health professionals will deliver the best care. SHM is working to promote the development of high-performing teams (HPTs) with the rest of the Hospital Care Collaborative (HCC), which includes national organizations for nurses, pharmacists, case managers, medical social workers, and respiratory therapists. SHM also has convened a senior group from C-suites, nursing executives, and the American Hospital Association; the plan is to publish a roadmap to promoting the growth and success of HPTs.
All the good intentions and teams and physician champions will still be hamstrung to affect real change in the current payment system, which still rewards healthcare in a transactional fashion, where we pay by the unit of the visit or the procedure. That is why SHM has taken our message to Washington and why we are supporting innovations that reward performance.
The value-based purchasing initiatives that will move substantial dollars to those hospitals that show they can deliver better performance (we’re talking millions of dollars, even at the start) is a beginning of hopefully a sea change in how we think about paying for healthcare (see “Value-Based Purchasing Raises the Stakes,” p. 1). And SHM continues to actively promote having national hospitalist thought leaders be right in the middle of setting the new standards of healthcare at the National Quality Forum, the Joint Commission, and AMA’s Physician Consortium on Performance Improvement, along with other national organizations.
Dr. Pronovost sees the gaps and barriers in having a management structure at our nation’s hospitals that is staffed, financed, and trained to deliver high performance. He does specifically call out hospitalists as a new specialty that is better organized to potentially be part of the solution. SHM and our hospitalists want to move this from a possibility and a potential to affect real change, consistently, day after day, at as many hospitals as we can reach. That is the promise of hospital medicine, and that is the vision of SHM. TH
Dr. Wellikson is CEO of SHM.
Reference
- Pronovost PJ, Marstellar JA. A physician management infrastructure. JAMA. 2011;305(5):500-501.
Earlier this year, the Journal of the American Medical Association (JAMA) published the article “A Physician Management Infrastructure,” by Peter Pronovost and Jill Marsteller.1 Pronovost and Marsteller’s commentary gets to the very heart of the need for change in healthcare delivery and the major barriers to that change.
As they note, quality improvement (QI) continues to receive attention from every sector of the healthcare market, but systematic and widespread benefits—actual improvement in quality of care—are years away from reaching the patient. The major impediments to delivering performance changes at the front lines of healthcare are both attitudinal and structural.
However, such obstacles can be overcome, starting today.
The authors rightly cite the development of physician leadership as a significant factor in the long-term success of QI. For too long, healthcare leaders have taken a “learn as you go” approach to leadership development. This antiquated philosophy that the best physician leaders ascend naturally to leadership falsely assumes that today’s leaders are perfectly suited for their jobs.
Training Tomorrow’s Leaders Today
In order for meaningful QI to succeed, systematic leadership development in healthcare must be a priority. Those hospitals and healthcare systems that acknowledge this reality already are reaping the benefits. Across the country, more than 1,200 hospitalists have participated in SHM’s Leadership Academy, a rigorous multicourse program that trains physicians in the fundamentals of hospital-based leadership. Leadership Academy participants then go on to lead new programs, many of which are QI-related, in their hospitals. This year, SHM will announce a Certification for Leaders in Hospital Medicine, which will further raise the bar, and mentor, enable, and define the future leaders for our hospitals.
The collective experience of HM also indicates that formal mentorship programs are a critical element to systematic leadership development. The exponential growth of SHM’s mentor-based QI programs to reduce readmissions, prevent VTEs, and improve glycemic control in hospitals—now implemented in more than 300 hospital sites across the country—is a testament to the need for one-on-one mentorship and leadership development and the impact it can have on patient care.
SHM continues to provide broad training in performance improvement and patient safety in its one-day “Quality Improvement Skills” pre-course at the annual meeting (HM11, May 10-13, Grapevine, Texas, www. hospitalmedicine2011.org). In the coming months, SHM will debut a nine-part series of Web-based modules that are essential to any hospitalist now charged with taking an active role in improving performance at their hospital.
Teamwork Is Key
Looking at the evolved present-day hospital, but more to the future, SHM and hospitalists recognize that empowered and coordinated teams of health professionals will deliver the best care. SHM is working to promote the development of high-performing teams (HPTs) with the rest of the Hospital Care Collaborative (HCC), which includes national organizations for nurses, pharmacists, case managers, medical social workers, and respiratory therapists. SHM also has convened a senior group from C-suites, nursing executives, and the American Hospital Association; the plan is to publish a roadmap to promoting the growth and success of HPTs.
All the good intentions and teams and physician champions will still be hamstrung to affect real change in the current payment system, which still rewards healthcare in a transactional fashion, where we pay by the unit of the visit or the procedure. That is why SHM has taken our message to Washington and why we are supporting innovations that reward performance.
The value-based purchasing initiatives that will move substantial dollars to those hospitals that show they can deliver better performance (we’re talking millions of dollars, even at the start) is a beginning of hopefully a sea change in how we think about paying for healthcare (see “Value-Based Purchasing Raises the Stakes,” p. 1). And SHM continues to actively promote having national hospitalist thought leaders be right in the middle of setting the new standards of healthcare at the National Quality Forum, the Joint Commission, and AMA’s Physician Consortium on Performance Improvement, along with other national organizations.
Dr. Pronovost sees the gaps and barriers in having a management structure at our nation’s hospitals that is staffed, financed, and trained to deliver high performance. He does specifically call out hospitalists as a new specialty that is better organized to potentially be part of the solution. SHM and our hospitalists want to move this from a possibility and a potential to affect real change, consistently, day after day, at as many hospitals as we can reach. That is the promise of hospital medicine, and that is the vision of SHM. TH
Dr. Wellikson is CEO of SHM.
Reference
- Pronovost PJ, Marstellar JA. A physician management infrastructure. JAMA. 2011;305(5):500-501.
Earlier this year, the Journal of the American Medical Association (JAMA) published the article “A Physician Management Infrastructure,” by Peter Pronovost and Jill Marsteller.1 Pronovost and Marsteller’s commentary gets to the very heart of the need for change in healthcare delivery and the major barriers to that change.
As they note, quality improvement (QI) continues to receive attention from every sector of the healthcare market, but systematic and widespread benefits—actual improvement in quality of care—are years away from reaching the patient. The major impediments to delivering performance changes at the front lines of healthcare are both attitudinal and structural.
However, such obstacles can be overcome, starting today.
The authors rightly cite the development of physician leadership as a significant factor in the long-term success of QI. For too long, healthcare leaders have taken a “learn as you go” approach to leadership development. This antiquated philosophy that the best physician leaders ascend naturally to leadership falsely assumes that today’s leaders are perfectly suited for their jobs.
Training Tomorrow’s Leaders Today
In order for meaningful QI to succeed, systematic leadership development in healthcare must be a priority. Those hospitals and healthcare systems that acknowledge this reality already are reaping the benefits. Across the country, more than 1,200 hospitalists have participated in SHM’s Leadership Academy, a rigorous multicourse program that trains physicians in the fundamentals of hospital-based leadership. Leadership Academy participants then go on to lead new programs, many of which are QI-related, in their hospitals. This year, SHM will announce a Certification for Leaders in Hospital Medicine, which will further raise the bar, and mentor, enable, and define the future leaders for our hospitals.
The collective experience of HM also indicates that formal mentorship programs are a critical element to systematic leadership development. The exponential growth of SHM’s mentor-based QI programs to reduce readmissions, prevent VTEs, and improve glycemic control in hospitals—now implemented in more than 300 hospital sites across the country—is a testament to the need for one-on-one mentorship and leadership development and the impact it can have on patient care.
SHM continues to provide broad training in performance improvement and patient safety in its one-day “Quality Improvement Skills” pre-course at the annual meeting (HM11, May 10-13, Grapevine, Texas, www. hospitalmedicine2011.org). In the coming months, SHM will debut a nine-part series of Web-based modules that are essential to any hospitalist now charged with taking an active role in improving performance at their hospital.
Teamwork Is Key
Looking at the evolved present-day hospital, but more to the future, SHM and hospitalists recognize that empowered and coordinated teams of health professionals will deliver the best care. SHM is working to promote the development of high-performing teams (HPTs) with the rest of the Hospital Care Collaborative (HCC), which includes national organizations for nurses, pharmacists, case managers, medical social workers, and respiratory therapists. SHM also has convened a senior group from C-suites, nursing executives, and the American Hospital Association; the plan is to publish a roadmap to promoting the growth and success of HPTs.
All the good intentions and teams and physician champions will still be hamstrung to affect real change in the current payment system, which still rewards healthcare in a transactional fashion, where we pay by the unit of the visit or the procedure. That is why SHM has taken our message to Washington and why we are supporting innovations that reward performance.
The value-based purchasing initiatives that will move substantial dollars to those hospitals that show they can deliver better performance (we’re talking millions of dollars, even at the start) is a beginning of hopefully a sea change in how we think about paying for healthcare (see “Value-Based Purchasing Raises the Stakes,” p. 1). And SHM continues to actively promote having national hospitalist thought leaders be right in the middle of setting the new standards of healthcare at the National Quality Forum, the Joint Commission, and AMA’s Physician Consortium on Performance Improvement, along with other national organizations.
Dr. Pronovost sees the gaps and barriers in having a management structure at our nation’s hospitals that is staffed, financed, and trained to deliver high performance. He does specifically call out hospitalists as a new specialty that is better organized to potentially be part of the solution. SHM and our hospitalists want to move this from a possibility and a potential to affect real change, consistently, day after day, at as many hospitals as we can reach. That is the promise of hospital medicine, and that is the vision of SHM. TH
Dr. Wellikson is CEO of SHM.
Reference
- Pronovost PJ, Marstellar JA. A physician management infrastructure. JAMA. 2011;305(5):500-501.
Paid For Being Special
It’s official. I am a “recognized” hospitalist. I’m certified. I’m special.
Although I’ve always felt that HM was special, that it’s a field with its own defined body of knowledge, area of expertise, and dedicated providers, it is now official. It is special; I am special. I got the letter in the mail the other day to prove it.
The correspondence arrived in an important-looking white envelope, with a return address stamped with the “American Board of Internal Medicine” insignia. The letter itself congratulated me on becoming a member of the first class of internists to complete their Maintenance of Certification (MOC) with Recognition of Focused Practice in Hospital Medicine (FPHM). As you’ve no doubt heard, the ABIM developed this MOC process to recognize hospitalists who’ve been in practice for at least three years after their initial certification in internal medicine (IM).
This is the first ABIM certification program that recognizes physician expertise in a field that is not tied directly to either residency or specialty fellowship training. In other words, unlike the cardiology certification exam, which requires a physician to have completed a fellowship training program, the FPHM allows for clinical experience to substitute for fellowship training. While the FPHM does not confer true “specialty status” (like the cardiology certification exam does), it does, as the moniker implies, recognize that we have focused our practice.
Implicit within that is the understanding that this focus brings with it a level of expertise that distinguishes hospitalists from nonhospitalists. This is a massive step forward for HM, as it lends significant credibility to the work we do and helps the public better understand what a hospitalist is and does. Most important, it helps set apart that cadre of true hospitalists who are dedicating their careers to fundamentally improving the care and outcomes of hospitalized patients.
It is this last point that came to mind as I reviewed this month’s cover story on value-based purchasing (see “Value-Based Purchasing Raises the Stakes,” p. 1).
Sticky Yet Crucial Point
One of the sticking points that I’ve heard from some hospitalists is that the FPHM requires a three-year cycle of self-evaluation. For those new to this process, let’s clear up some of the nomenclature. When IM residents graduate, they are eligible to sit for the ABIM certification exam. Upon passage, they are board-certified internists and can choose to enter into the maintenance of certification process. This is a 10-year process whereby diplomates (ABIM-speak for those certified as a specialist, with a diploma in medicine; not to be confused with a diplomat—a person who conducts negotiations and maintains political rest through the tactful handling of delicate situations, something perhaps more appropriate to the bulk of patient situations we encounter) must complete self-evaluation of medical knowledge modules, self-evaluation of practice performance, and ultimately a secure exam. This is where the FPHM differs.
The 10-year cycle for MOC is maintained for FPHM, such that diplomates only recertify every 10 years. However, the self-evaluation must occur every three years to maintain one’s certification. In other words, fail to keep up with the self-evaluation process, and your FPHM is revoked. This is different than the MOC for IM, and it is why some hospitalists are choosing not to enroll in the FPHM. This is a mistake.
Unnecessary Burden?
For many hospitalists, this extra evaluation, especially the practice improvement, is seen as an undue burden. Why is it that hospitalists should have to do more frequent self-evaluation than other specialists? My answer is that this is an important part of what defines our hospitalist specialty—that is, our ability to go beyond the individual patient encounter to fundamentally improve outcomes for the patients under our care. This is not done through “good doctoring.” Hospitalists are not necessarily better doctors than nonhospitalists. Rather, we have embodied a commitment to process and quality improvement within the hospital. This is what our patients need from us. This is what makes us hospitalists. This is what makes us special.
And this brings me back to value-based purchasing.
The Next Phase: Purchasing Value
For those of you, like me, who struggle to comprehend what buying value actually means, take a few minutes to peruse Bryn Nelson’s cover story this month. Not only will it help you understand the healthcare reform bill, it will help you understand the future of our field. I’ve personally witnessed HM traverse three distinct phases.
In the late 1990s and early 2000s, HM growth was driven by the need to improve efficiency. In most ways, this was code for reducing costs. Hospital executives recognized that hospitalists could reduce the overall costs of a patient admission, thus turning the balance of the prospective payment into profit. In other words, the amount of money a hospital receives for a patient stay is most often fixed and determined up front (prospectively), such that more efficiently moving patients through the system equates to more profit (or less loss).
This growth phase was quickly supplanted by the volume phase—a phase that was driven by the relative departure of primary-care physicians and subspecialists from the hospital. Although some of these doctors still admit their own patients, most of them now take advantage of hospitalist programs to focus their own practice to the outpatient or procedural arenas. Effectively, many of the other doctors have left the house, and hospitalists have had to back-fill this patient volume. To a certain degree, we are all still filling this need.
Connect the Dots
However, it is clear that the next HM driver is going to be quality. And it is programs like VBP that will drive it. Essentially, VBP means that hospitals will be competing with each other to be the best. By best, I mean “most able” to achieve pre-determined quality, safety, and patient-satisfaction indicators. By competing, I mean the reimbursement pie is fixed and those who achieve will get more, and those who fall short will get less.
When you consider that as much as 2% of a hospital’s Medicare reimbursement will soon be at risk, we are talking about millions of dollars per hospital per year. To hospitals with a 1% to 2% profit margin, this is the difference between being in or out of business. It also is interestingly close to the amount of support most hospitals give their HM groups; the exact groups that touch the majority of the patients that will determine their VBP outcomes. Connect the dots, and you can see that your hospitalist group—indeed, your paycheck—is very much at risk.
Which brings me back to the FPHM. In a serendipitous turn of events, the FPHM not only recognizes hospitalists as “special,” but, more important, it also gives us the opportunity to simultaneously enhance both our patients’ outcomes and our compensation. If we get this right, the every-three-year improvement projects required to maintain your certification are exactly the type of work you’ll need to be doing to achieve the outcomes your hospital needs to maintain its Medicare payments. In turn, this will ensure your group maintains its hospital support, and you, your paycheck.
It’s the kind of work that will ensure the best possible outcomes for our patients. And in the end, that, more than an ABIM certificate, is what truly makes us special. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
It’s official. I am a “recognized” hospitalist. I’m certified. I’m special.
Although I’ve always felt that HM was special, that it’s a field with its own defined body of knowledge, area of expertise, and dedicated providers, it is now official. It is special; I am special. I got the letter in the mail the other day to prove it.
The correspondence arrived in an important-looking white envelope, with a return address stamped with the “American Board of Internal Medicine” insignia. The letter itself congratulated me on becoming a member of the first class of internists to complete their Maintenance of Certification (MOC) with Recognition of Focused Practice in Hospital Medicine (FPHM). As you’ve no doubt heard, the ABIM developed this MOC process to recognize hospitalists who’ve been in practice for at least three years after their initial certification in internal medicine (IM).
This is the first ABIM certification program that recognizes physician expertise in a field that is not tied directly to either residency or specialty fellowship training. In other words, unlike the cardiology certification exam, which requires a physician to have completed a fellowship training program, the FPHM allows for clinical experience to substitute for fellowship training. While the FPHM does not confer true “specialty status” (like the cardiology certification exam does), it does, as the moniker implies, recognize that we have focused our practice.
Implicit within that is the understanding that this focus brings with it a level of expertise that distinguishes hospitalists from nonhospitalists. This is a massive step forward for HM, as it lends significant credibility to the work we do and helps the public better understand what a hospitalist is and does. Most important, it helps set apart that cadre of true hospitalists who are dedicating their careers to fundamentally improving the care and outcomes of hospitalized patients.
It is this last point that came to mind as I reviewed this month’s cover story on value-based purchasing (see “Value-Based Purchasing Raises the Stakes,” p. 1).
Sticky Yet Crucial Point
One of the sticking points that I’ve heard from some hospitalists is that the FPHM requires a three-year cycle of self-evaluation. For those new to this process, let’s clear up some of the nomenclature. When IM residents graduate, they are eligible to sit for the ABIM certification exam. Upon passage, they are board-certified internists and can choose to enter into the maintenance of certification process. This is a 10-year process whereby diplomates (ABIM-speak for those certified as a specialist, with a diploma in medicine; not to be confused with a diplomat—a person who conducts negotiations and maintains political rest through the tactful handling of delicate situations, something perhaps more appropriate to the bulk of patient situations we encounter) must complete self-evaluation of medical knowledge modules, self-evaluation of practice performance, and ultimately a secure exam. This is where the FPHM differs.
The 10-year cycle for MOC is maintained for FPHM, such that diplomates only recertify every 10 years. However, the self-evaluation must occur every three years to maintain one’s certification. In other words, fail to keep up with the self-evaluation process, and your FPHM is revoked. This is different than the MOC for IM, and it is why some hospitalists are choosing not to enroll in the FPHM. This is a mistake.
Unnecessary Burden?
For many hospitalists, this extra evaluation, especially the practice improvement, is seen as an undue burden. Why is it that hospitalists should have to do more frequent self-evaluation than other specialists? My answer is that this is an important part of what defines our hospitalist specialty—that is, our ability to go beyond the individual patient encounter to fundamentally improve outcomes for the patients under our care. This is not done through “good doctoring.” Hospitalists are not necessarily better doctors than nonhospitalists. Rather, we have embodied a commitment to process and quality improvement within the hospital. This is what our patients need from us. This is what makes us hospitalists. This is what makes us special.
And this brings me back to value-based purchasing.
The Next Phase: Purchasing Value
For those of you, like me, who struggle to comprehend what buying value actually means, take a few minutes to peruse Bryn Nelson’s cover story this month. Not only will it help you understand the healthcare reform bill, it will help you understand the future of our field. I’ve personally witnessed HM traverse three distinct phases.
In the late 1990s and early 2000s, HM growth was driven by the need to improve efficiency. In most ways, this was code for reducing costs. Hospital executives recognized that hospitalists could reduce the overall costs of a patient admission, thus turning the balance of the prospective payment into profit. In other words, the amount of money a hospital receives for a patient stay is most often fixed and determined up front (prospectively), such that more efficiently moving patients through the system equates to more profit (or less loss).
This growth phase was quickly supplanted by the volume phase—a phase that was driven by the relative departure of primary-care physicians and subspecialists from the hospital. Although some of these doctors still admit their own patients, most of them now take advantage of hospitalist programs to focus their own practice to the outpatient or procedural arenas. Effectively, many of the other doctors have left the house, and hospitalists have had to back-fill this patient volume. To a certain degree, we are all still filling this need.
Connect the Dots
However, it is clear that the next HM driver is going to be quality. And it is programs like VBP that will drive it. Essentially, VBP means that hospitals will be competing with each other to be the best. By best, I mean “most able” to achieve pre-determined quality, safety, and patient-satisfaction indicators. By competing, I mean the reimbursement pie is fixed and those who achieve will get more, and those who fall short will get less.
When you consider that as much as 2% of a hospital’s Medicare reimbursement will soon be at risk, we are talking about millions of dollars per hospital per year. To hospitals with a 1% to 2% profit margin, this is the difference between being in or out of business. It also is interestingly close to the amount of support most hospitals give their HM groups; the exact groups that touch the majority of the patients that will determine their VBP outcomes. Connect the dots, and you can see that your hospitalist group—indeed, your paycheck—is very much at risk.
Which brings me back to the FPHM. In a serendipitous turn of events, the FPHM not only recognizes hospitalists as “special,” but, more important, it also gives us the opportunity to simultaneously enhance both our patients’ outcomes and our compensation. If we get this right, the every-three-year improvement projects required to maintain your certification are exactly the type of work you’ll need to be doing to achieve the outcomes your hospital needs to maintain its Medicare payments. In turn, this will ensure your group maintains its hospital support, and you, your paycheck.
It’s the kind of work that will ensure the best possible outcomes for our patients. And in the end, that, more than an ABIM certificate, is what truly makes us special. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
It’s official. I am a “recognized” hospitalist. I’m certified. I’m special.
Although I’ve always felt that HM was special, that it’s a field with its own defined body of knowledge, area of expertise, and dedicated providers, it is now official. It is special; I am special. I got the letter in the mail the other day to prove it.
The correspondence arrived in an important-looking white envelope, with a return address stamped with the “American Board of Internal Medicine” insignia. The letter itself congratulated me on becoming a member of the first class of internists to complete their Maintenance of Certification (MOC) with Recognition of Focused Practice in Hospital Medicine (FPHM). As you’ve no doubt heard, the ABIM developed this MOC process to recognize hospitalists who’ve been in practice for at least three years after their initial certification in internal medicine (IM).
This is the first ABIM certification program that recognizes physician expertise in a field that is not tied directly to either residency or specialty fellowship training. In other words, unlike the cardiology certification exam, which requires a physician to have completed a fellowship training program, the FPHM allows for clinical experience to substitute for fellowship training. While the FPHM does not confer true “specialty status” (like the cardiology certification exam does), it does, as the moniker implies, recognize that we have focused our practice.
Implicit within that is the understanding that this focus brings with it a level of expertise that distinguishes hospitalists from nonhospitalists. This is a massive step forward for HM, as it lends significant credibility to the work we do and helps the public better understand what a hospitalist is and does. Most important, it helps set apart that cadre of true hospitalists who are dedicating their careers to fundamentally improving the care and outcomes of hospitalized patients.
It is this last point that came to mind as I reviewed this month’s cover story on value-based purchasing (see “Value-Based Purchasing Raises the Stakes,” p. 1).
Sticky Yet Crucial Point
One of the sticking points that I’ve heard from some hospitalists is that the FPHM requires a three-year cycle of self-evaluation. For those new to this process, let’s clear up some of the nomenclature. When IM residents graduate, they are eligible to sit for the ABIM certification exam. Upon passage, they are board-certified internists and can choose to enter into the maintenance of certification process. This is a 10-year process whereby diplomates (ABIM-speak for those certified as a specialist, with a diploma in medicine; not to be confused with a diplomat—a person who conducts negotiations and maintains political rest through the tactful handling of delicate situations, something perhaps more appropriate to the bulk of patient situations we encounter) must complete self-evaluation of medical knowledge modules, self-evaluation of practice performance, and ultimately a secure exam. This is where the FPHM differs.
The 10-year cycle for MOC is maintained for FPHM, such that diplomates only recertify every 10 years. However, the self-evaluation must occur every three years to maintain one’s certification. In other words, fail to keep up with the self-evaluation process, and your FPHM is revoked. This is different than the MOC for IM, and it is why some hospitalists are choosing not to enroll in the FPHM. This is a mistake.
Unnecessary Burden?
For many hospitalists, this extra evaluation, especially the practice improvement, is seen as an undue burden. Why is it that hospitalists should have to do more frequent self-evaluation than other specialists? My answer is that this is an important part of what defines our hospitalist specialty—that is, our ability to go beyond the individual patient encounter to fundamentally improve outcomes for the patients under our care. This is not done through “good doctoring.” Hospitalists are not necessarily better doctors than nonhospitalists. Rather, we have embodied a commitment to process and quality improvement within the hospital. This is what our patients need from us. This is what makes us hospitalists. This is what makes us special.
And this brings me back to value-based purchasing.
The Next Phase: Purchasing Value
For those of you, like me, who struggle to comprehend what buying value actually means, take a few minutes to peruse Bryn Nelson’s cover story this month. Not only will it help you understand the healthcare reform bill, it will help you understand the future of our field. I’ve personally witnessed HM traverse three distinct phases.
In the late 1990s and early 2000s, HM growth was driven by the need to improve efficiency. In most ways, this was code for reducing costs. Hospital executives recognized that hospitalists could reduce the overall costs of a patient admission, thus turning the balance of the prospective payment into profit. In other words, the amount of money a hospital receives for a patient stay is most often fixed and determined up front (prospectively), such that more efficiently moving patients through the system equates to more profit (or less loss).
This growth phase was quickly supplanted by the volume phase—a phase that was driven by the relative departure of primary-care physicians and subspecialists from the hospital. Although some of these doctors still admit their own patients, most of them now take advantage of hospitalist programs to focus their own practice to the outpatient or procedural arenas. Effectively, many of the other doctors have left the house, and hospitalists have had to back-fill this patient volume. To a certain degree, we are all still filling this need.
Connect the Dots
However, it is clear that the next HM driver is going to be quality. And it is programs like VBP that will drive it. Essentially, VBP means that hospitals will be competing with each other to be the best. By best, I mean “most able” to achieve pre-determined quality, safety, and patient-satisfaction indicators. By competing, I mean the reimbursement pie is fixed and those who achieve will get more, and those who fall short will get less.
When you consider that as much as 2% of a hospital’s Medicare reimbursement will soon be at risk, we are talking about millions of dollars per hospital per year. To hospitals with a 1% to 2% profit margin, this is the difference between being in or out of business. It also is interestingly close to the amount of support most hospitals give their HM groups; the exact groups that touch the majority of the patients that will determine their VBP outcomes. Connect the dots, and you can see that your hospitalist group—indeed, your paycheck—is very much at risk.
Which brings me back to the FPHM. In a serendipitous turn of events, the FPHM not only recognizes hospitalists as “special,” but, more important, it also gives us the opportunity to simultaneously enhance both our patients’ outcomes and our compensation. If we get this right, the every-three-year improvement projects required to maintain your certification are exactly the type of work you’ll need to be doing to achieve the outcomes your hospital needs to maintain its Medicare payments. In turn, this will ensure your group maintains its hospital support, and you, your paycheck.
It’s the kind of work that will ensure the best possible outcomes for our patients. And in the end, that, more than an ABIM certificate, is what truly makes us special. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
The To-Don’t List, Part 2
A couple of additions to the list that I started last month, in which I mentioned the problems associated with fixed-duration day shifts, a contractual vacation provision, tenure-based salary increases, poor roles for NPs and PAs, and blinded performance reporting. I think most practices would be better off without those things, and this month I’ll add a few more to the list.
I readily admit that there are some relatively rare situations in which the following things might be a good idea. But most hospitalist practices should think about alternatives.
Extra shifts. I think every hospitalist should have, within reason, a chance to work more or less than others in an HM group. And, of course, compensation should match the amount of work. So those who want to work more than the normal, or contractually required, number of shifts should have at it. But I think it is best to avoid categorizing the work into “normal” shifts and “extra” shifts. Essentially, all shifts should be thought of as “normal.”
What is the problem with having an “extra” shift category? It pretty reliably leads to confusion.
This confusion is easiest to illustrate with an example. Consider Dr. Krause, a hospitalist working in a practice with a seven-on/seven-off schedule. However, the first week in July, she works only six days, but she plans to “pay that back” and more when she works a 10-day stretch two months hence. So far, this sounds easy. By the end of September, Dr. Krause will have worked two extra shifts.
But when another hospitalist in Dr. Krause’s group is out sick in August, several hospitalists in the group rearrange their schedules to fill in. In September, Dr. Krause works the two days that she originally was scheduled to be off and trades away three of the consecutive days she was to work in September.
While it will be clear to Dr. Krause that she will be “even” in the number of shifts worked at the end of September, it probably isn’t clear to anyone else. The person who determines payroll will probably have a really hard time figuring out whether Dr. Krause is to be paid extra for “extra” shifts during any two-week pay period.
The most reliable way to figure out if a doctor worked extra shifts is to add up all worked shifts at the end of the year. But that would mean waiting until the end of the year to compensate the doctor for any extra shifts worked. And most docs would find that really unattractive.
It would be easy enough to just add up the shifts worked every pay period (usually two weeks) and compensate for any above the number expected, but that would then require lowering the salary for any pay period in which the doctor works fewer than the expected number. Although it might not be popular, I see this as the best arrangement. That is, just pay per shift so that there is no need to keep track of whether any particular shift is “normal” or “extra.”
Even if this illustration doesn’t convince you how messy it can be to keep track of extra vs. normal shifts, trust me on this one. It causes lots of problems for lots of physician practices. If your practice is among the few that has a clear-cut system that doesn’t confuse those in payroll, then stick with it.
Shift duration symmetry. Rarely is there a reason to keep every shift the same duration.
Let’s consider a common scenario. A small hospitalist group has a schedule that consists of a 12-hour day shift followed by a 12-hour night shift. As patient volume grows, the day-shift doctor(s) often have to stay after their shift to finish the initial care of new referrals, or the night doctor typically starts their shift with several patients in the ED awaiting admission. So the practice makes a good decision and creates an evening shift, which often is referred to as a “swing shift.” And because all existing shifts are 12 hours, the evening shift will be 12 hours, right?
Not so fast.
Why should the evening shift be the same duration as the day shift? Shouldn’t it be however long is necessary? Practices of no more than about 15 FTEs typically require an evening shift of only about four to six hours. It should start an hour or so before the last day doctor should be finishing work; it should continue until the night doctor has resolved the backlog of patients. As the practice volume grows, it will probably be necessary to lengthen the evening shift until it eventually reaches the same length as other shifts. But there is almost never a real workload or patient-care reason that the shift length needs to be the same duration as other shifts when it is first put into place.
While an evening shift should have a clearly defined start time, it will work best if the end of shift time is left loose and is based on just how busy that night it. For example, it might be reasonable to have the evening doctor accept their last new referral no later than a specified time (10 p.m. is the deadline in my hospitalist group). The swing shift can leave after completing the care of that patient and addressing any other issues that came up during the shift. Some nights, that will mean the evening doctor can leave at 10 p.m.; other nights, it might be 11 p.m. or midnight.
While we’re talking about it, there is no clear reason day and night shifts need to be the same length, either. It is fine to make both 12 hours long, but that isn’t the only reasonable option.
Of course, your compensation formula might influence what can be reasonably done with shift lengths. But if a practice compensates the doctors in a way that requires that all shifts be identical in duration, then the compensation method needs another look. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
A couple of additions to the list that I started last month, in which I mentioned the problems associated with fixed-duration day shifts, a contractual vacation provision, tenure-based salary increases, poor roles for NPs and PAs, and blinded performance reporting. I think most practices would be better off without those things, and this month I’ll add a few more to the list.
I readily admit that there are some relatively rare situations in which the following things might be a good idea. But most hospitalist practices should think about alternatives.
Extra shifts. I think every hospitalist should have, within reason, a chance to work more or less than others in an HM group. And, of course, compensation should match the amount of work. So those who want to work more than the normal, or contractually required, number of shifts should have at it. But I think it is best to avoid categorizing the work into “normal” shifts and “extra” shifts. Essentially, all shifts should be thought of as “normal.”
What is the problem with having an “extra” shift category? It pretty reliably leads to confusion.
This confusion is easiest to illustrate with an example. Consider Dr. Krause, a hospitalist working in a practice with a seven-on/seven-off schedule. However, the first week in July, she works only six days, but she plans to “pay that back” and more when she works a 10-day stretch two months hence. So far, this sounds easy. By the end of September, Dr. Krause will have worked two extra shifts.
But when another hospitalist in Dr. Krause’s group is out sick in August, several hospitalists in the group rearrange their schedules to fill in. In September, Dr. Krause works the two days that she originally was scheduled to be off and trades away three of the consecutive days she was to work in September.
While it will be clear to Dr. Krause that she will be “even” in the number of shifts worked at the end of September, it probably isn’t clear to anyone else. The person who determines payroll will probably have a really hard time figuring out whether Dr. Krause is to be paid extra for “extra” shifts during any two-week pay period.
The most reliable way to figure out if a doctor worked extra shifts is to add up all worked shifts at the end of the year. But that would mean waiting until the end of the year to compensate the doctor for any extra shifts worked. And most docs would find that really unattractive.
It would be easy enough to just add up the shifts worked every pay period (usually two weeks) and compensate for any above the number expected, but that would then require lowering the salary for any pay period in which the doctor works fewer than the expected number. Although it might not be popular, I see this as the best arrangement. That is, just pay per shift so that there is no need to keep track of whether any particular shift is “normal” or “extra.”
Even if this illustration doesn’t convince you how messy it can be to keep track of extra vs. normal shifts, trust me on this one. It causes lots of problems for lots of physician practices. If your practice is among the few that has a clear-cut system that doesn’t confuse those in payroll, then stick with it.
Shift duration symmetry. Rarely is there a reason to keep every shift the same duration.
Let’s consider a common scenario. A small hospitalist group has a schedule that consists of a 12-hour day shift followed by a 12-hour night shift. As patient volume grows, the day-shift doctor(s) often have to stay after their shift to finish the initial care of new referrals, or the night doctor typically starts their shift with several patients in the ED awaiting admission. So the practice makes a good decision and creates an evening shift, which often is referred to as a “swing shift.” And because all existing shifts are 12 hours, the evening shift will be 12 hours, right?
Not so fast.
Why should the evening shift be the same duration as the day shift? Shouldn’t it be however long is necessary? Practices of no more than about 15 FTEs typically require an evening shift of only about four to six hours. It should start an hour or so before the last day doctor should be finishing work; it should continue until the night doctor has resolved the backlog of patients. As the practice volume grows, it will probably be necessary to lengthen the evening shift until it eventually reaches the same length as other shifts. But there is almost never a real workload or patient-care reason that the shift length needs to be the same duration as other shifts when it is first put into place.
While an evening shift should have a clearly defined start time, it will work best if the end of shift time is left loose and is based on just how busy that night it. For example, it might be reasonable to have the evening doctor accept their last new referral no later than a specified time (10 p.m. is the deadline in my hospitalist group). The swing shift can leave after completing the care of that patient and addressing any other issues that came up during the shift. Some nights, that will mean the evening doctor can leave at 10 p.m.; other nights, it might be 11 p.m. or midnight.
While we’re talking about it, there is no clear reason day and night shifts need to be the same length, either. It is fine to make both 12 hours long, but that isn’t the only reasonable option.
Of course, your compensation formula might influence what can be reasonably done with shift lengths. But if a practice compensates the doctors in a way that requires that all shifts be identical in duration, then the compensation method needs another look. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
A couple of additions to the list that I started last month, in which I mentioned the problems associated with fixed-duration day shifts, a contractual vacation provision, tenure-based salary increases, poor roles for NPs and PAs, and blinded performance reporting. I think most practices would be better off without those things, and this month I’ll add a few more to the list.
I readily admit that there are some relatively rare situations in which the following things might be a good idea. But most hospitalist practices should think about alternatives.
Extra shifts. I think every hospitalist should have, within reason, a chance to work more or less than others in an HM group. And, of course, compensation should match the amount of work. So those who want to work more than the normal, or contractually required, number of shifts should have at it. But I think it is best to avoid categorizing the work into “normal” shifts and “extra” shifts. Essentially, all shifts should be thought of as “normal.”
What is the problem with having an “extra” shift category? It pretty reliably leads to confusion.
This confusion is easiest to illustrate with an example. Consider Dr. Krause, a hospitalist working in a practice with a seven-on/seven-off schedule. However, the first week in July, she works only six days, but she plans to “pay that back” and more when she works a 10-day stretch two months hence. So far, this sounds easy. By the end of September, Dr. Krause will have worked two extra shifts.
But when another hospitalist in Dr. Krause’s group is out sick in August, several hospitalists in the group rearrange their schedules to fill in. In September, Dr. Krause works the two days that she originally was scheduled to be off and trades away three of the consecutive days she was to work in September.
While it will be clear to Dr. Krause that she will be “even” in the number of shifts worked at the end of September, it probably isn’t clear to anyone else. The person who determines payroll will probably have a really hard time figuring out whether Dr. Krause is to be paid extra for “extra” shifts during any two-week pay period.
The most reliable way to figure out if a doctor worked extra shifts is to add up all worked shifts at the end of the year. But that would mean waiting until the end of the year to compensate the doctor for any extra shifts worked. And most docs would find that really unattractive.
It would be easy enough to just add up the shifts worked every pay period (usually two weeks) and compensate for any above the number expected, but that would then require lowering the salary for any pay period in which the doctor works fewer than the expected number. Although it might not be popular, I see this as the best arrangement. That is, just pay per shift so that there is no need to keep track of whether any particular shift is “normal” or “extra.”
Even if this illustration doesn’t convince you how messy it can be to keep track of extra vs. normal shifts, trust me on this one. It causes lots of problems for lots of physician practices. If your practice is among the few that has a clear-cut system that doesn’t confuse those in payroll, then stick with it.
Shift duration symmetry. Rarely is there a reason to keep every shift the same duration.
Let’s consider a common scenario. A small hospitalist group has a schedule that consists of a 12-hour day shift followed by a 12-hour night shift. As patient volume grows, the day-shift doctor(s) often have to stay after their shift to finish the initial care of new referrals, or the night doctor typically starts their shift with several patients in the ED awaiting admission. So the practice makes a good decision and creates an evening shift, which often is referred to as a “swing shift.” And because all existing shifts are 12 hours, the evening shift will be 12 hours, right?
Not so fast.
Why should the evening shift be the same duration as the day shift? Shouldn’t it be however long is necessary? Practices of no more than about 15 FTEs typically require an evening shift of only about four to six hours. It should start an hour or so before the last day doctor should be finishing work; it should continue until the night doctor has resolved the backlog of patients. As the practice volume grows, it will probably be necessary to lengthen the evening shift until it eventually reaches the same length as other shifts. But there is almost never a real workload or patient-care reason that the shift length needs to be the same duration as other shifts when it is first put into place.
While an evening shift should have a clearly defined start time, it will work best if the end of shift time is left loose and is based on just how busy that night it. For example, it might be reasonable to have the evening doctor accept their last new referral no later than a specified time (10 p.m. is the deadline in my hospitalist group). The swing shift can leave after completing the care of that patient and addressing any other issues that came up during the shift. Some nights, that will mean the evening doctor can leave at 10 p.m.; other nights, it might be 11 p.m. or midnight.
While we’re talking about it, there is no clear reason day and night shifts need to be the same length, either. It is fine to make both 12 hours long, but that isn’t the only reasonable option.
Of course, your compensation formula might influence what can be reasonably done with shift lengths. But if a practice compensates the doctors in a way that requires that all shifts be identical in duration, then the compensation method needs another look. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
CMS Requires “In-Person Encounter” to Initiate Home Health Services
I’ve been told by home health agencies that I have to fill out some additional paperwork to get my patients outpatient services. Can you explain to me what these new rules are all about?
Alicia Farrouk, MD
Evansville, Ind.
Dr. Hospitalist responds: In June 2010, the Affordable Care Act changed the rules regarding physician orders for durable medical equipment and for certifying or recertifying the need for home health services. Last November, the Center for Medicare & Medicaid Services (CMS) published the final rules in the Federal Register.
The new law went into effect Jan. 1, and I suspect that is why you have been asked to adjust the way you fill out your paperwork. The upshot of the change in the law is that providers can no longer use the discharge plan or transfer form as evidence of “certification” of need for home health services. The ordering provider, as a condition for payment for services, must document an in-person encounter within the 90 days prior or 30 days after the initiation of home health services. The documentation must detail the clinical findings supporting the need for home health services.
If you are a hospitalist and discharging the patient from the hospital but will not be following the patient as an outpatient, you must document the name of the primary-care physician (PCP) who will follow the patient’s need for home health services and initiate the order and plan of care. The PCP will then sign the home health certification and document that they reviewed your note and plan for home health services and agree with the plan.
If you are a hospitalist working in a teaching hospital, the resident can fill out the form, but it must list your name (as attending physician) and your NPI number. This new rule applies only to home health services and durable medical equipment (things that can be used over and over again for medical purposes, such as crutches, walkers, wheelchairs, etc.) but does not include drugs or supplemental oxygen.
HM Model Spreads to Surgical Specialists
I have a friend who told me there is a neurologist in the hospital where he works who I understand is calling himself a hospitalist. What gives? I thought hospitalists were all internists or family physicians.
Bill Mulley, MD
Flagstaff, Ariz.
Dr. Hospitalist responds: The vast majority of hospitalists in the U.S. are general internists. There are smaller numbers of family physicians, pediatricians, and medical subspecialists who also work as hospitalists. Although this is the face of HM in America, we are seeing other fields of medicine adopting this model of care.
I know of surgical hospitalists, OB-GYN hospitalists, and yes, even neurohospitalists (see “Generation Next,” October 2010, p. 1). It is hard for some people to get their heads around the notion of a surgeon as a hospitalist because when one thinks of a surgeon, you are thinking of a physician who works in the operating room. But the traditional surgeon also has a clinic where they provide pre- and post-operative care.
Herein lies the difference between traditional surgeons and surgical hospitalists: The surgical hospitalist is, for the most part, only doing work in the hospital—sound familiar? (Think traditional internist vs. internist working as hospitalist.) The traditional general surgeon performs scheduled elective surgeries and typically only does emergency surgeries when they are on call for the hospital. As I understand it, the life of a surgical hospitalist is spending a shift in the hospital waiting for a patient to show up needing emergency surgery.
The hospital CEO today has increasing challenges convincing physicians to take hospital call. Some find themselves paying sizable sums of money for surgeons to take call from home. Some have decided their money is better spent paying for surgical hospitalists to spend nights in the hospital waiting for their pager to go off.
From a patient’s perspective, this seems to be a no-brainer. Having a surgeon in the hospital increases their chances of more timely care. You have to believe the providers in the ED and the medical hospitalist also love having a surgeon in-house, available to provide consults when requested.
I am a bit surprised that we don’t already have a large number of surgical hospitalists in the country. Then again, I have no idea of how many surgeons are working as surgical hospitalists. I am not sure anybody knows that answer.
There is a belief that we are going to see the continued growth of “specialty hospitalists” in the U.S. I believe we are going to see neurohospitalists managing inpatients with stroke and other neurosurgical issues, working side by side with medical hospitalists. I share in the excitement that was pervasive in the early days of the hospitalist movement, even though I’m not sure what we are going to see next.
I never imagined that we would have more than 30,000 hospitalists, as we do today. But while the HM model can help improve care, I will always feel strongly that no system will improve care without the dedication of motivated and compassionate healthcare providers driving the system. TH
I’ve been told by home health agencies that I have to fill out some additional paperwork to get my patients outpatient services. Can you explain to me what these new rules are all about?
Alicia Farrouk, MD
Evansville, Ind.
Dr. Hospitalist responds: In June 2010, the Affordable Care Act changed the rules regarding physician orders for durable medical equipment and for certifying or recertifying the need for home health services. Last November, the Center for Medicare & Medicaid Services (CMS) published the final rules in the Federal Register.
The new law went into effect Jan. 1, and I suspect that is why you have been asked to adjust the way you fill out your paperwork. The upshot of the change in the law is that providers can no longer use the discharge plan or transfer form as evidence of “certification” of need for home health services. The ordering provider, as a condition for payment for services, must document an in-person encounter within the 90 days prior or 30 days after the initiation of home health services. The documentation must detail the clinical findings supporting the need for home health services.
If you are a hospitalist and discharging the patient from the hospital but will not be following the patient as an outpatient, you must document the name of the primary-care physician (PCP) who will follow the patient’s need for home health services and initiate the order and plan of care. The PCP will then sign the home health certification and document that they reviewed your note and plan for home health services and agree with the plan.
If you are a hospitalist working in a teaching hospital, the resident can fill out the form, but it must list your name (as attending physician) and your NPI number. This new rule applies only to home health services and durable medical equipment (things that can be used over and over again for medical purposes, such as crutches, walkers, wheelchairs, etc.) but does not include drugs or supplemental oxygen.
HM Model Spreads to Surgical Specialists
I have a friend who told me there is a neurologist in the hospital where he works who I understand is calling himself a hospitalist. What gives? I thought hospitalists were all internists or family physicians.
Bill Mulley, MD
Flagstaff, Ariz.
Dr. Hospitalist responds: The vast majority of hospitalists in the U.S. are general internists. There are smaller numbers of family physicians, pediatricians, and medical subspecialists who also work as hospitalists. Although this is the face of HM in America, we are seeing other fields of medicine adopting this model of care.
I know of surgical hospitalists, OB-GYN hospitalists, and yes, even neurohospitalists (see “Generation Next,” October 2010, p. 1). It is hard for some people to get their heads around the notion of a surgeon as a hospitalist because when one thinks of a surgeon, you are thinking of a physician who works in the operating room. But the traditional surgeon also has a clinic where they provide pre- and post-operative care.
Herein lies the difference between traditional surgeons and surgical hospitalists: The surgical hospitalist is, for the most part, only doing work in the hospital—sound familiar? (Think traditional internist vs. internist working as hospitalist.) The traditional general surgeon performs scheduled elective surgeries and typically only does emergency surgeries when they are on call for the hospital. As I understand it, the life of a surgical hospitalist is spending a shift in the hospital waiting for a patient to show up needing emergency surgery.
The hospital CEO today has increasing challenges convincing physicians to take hospital call. Some find themselves paying sizable sums of money for surgeons to take call from home. Some have decided their money is better spent paying for surgical hospitalists to spend nights in the hospital waiting for their pager to go off.
From a patient’s perspective, this seems to be a no-brainer. Having a surgeon in the hospital increases their chances of more timely care. You have to believe the providers in the ED and the medical hospitalist also love having a surgeon in-house, available to provide consults when requested.
I am a bit surprised that we don’t already have a large number of surgical hospitalists in the country. Then again, I have no idea of how many surgeons are working as surgical hospitalists. I am not sure anybody knows that answer.
There is a belief that we are going to see the continued growth of “specialty hospitalists” in the U.S. I believe we are going to see neurohospitalists managing inpatients with stroke and other neurosurgical issues, working side by side with medical hospitalists. I share in the excitement that was pervasive in the early days of the hospitalist movement, even though I’m not sure what we are going to see next.
I never imagined that we would have more than 30,000 hospitalists, as we do today. But while the HM model can help improve care, I will always feel strongly that no system will improve care without the dedication of motivated and compassionate healthcare providers driving the system. TH
I’ve been told by home health agencies that I have to fill out some additional paperwork to get my patients outpatient services. Can you explain to me what these new rules are all about?
Alicia Farrouk, MD
Evansville, Ind.
Dr. Hospitalist responds: In June 2010, the Affordable Care Act changed the rules regarding physician orders for durable medical equipment and for certifying or recertifying the need for home health services. Last November, the Center for Medicare & Medicaid Services (CMS) published the final rules in the Federal Register.
The new law went into effect Jan. 1, and I suspect that is why you have been asked to adjust the way you fill out your paperwork. The upshot of the change in the law is that providers can no longer use the discharge plan or transfer form as evidence of “certification” of need for home health services. The ordering provider, as a condition for payment for services, must document an in-person encounter within the 90 days prior or 30 days after the initiation of home health services. The documentation must detail the clinical findings supporting the need for home health services.
If you are a hospitalist and discharging the patient from the hospital but will not be following the patient as an outpatient, you must document the name of the primary-care physician (PCP) who will follow the patient’s need for home health services and initiate the order and plan of care. The PCP will then sign the home health certification and document that they reviewed your note and plan for home health services and agree with the plan.
If you are a hospitalist working in a teaching hospital, the resident can fill out the form, but it must list your name (as attending physician) and your NPI number. This new rule applies only to home health services and durable medical equipment (things that can be used over and over again for medical purposes, such as crutches, walkers, wheelchairs, etc.) but does not include drugs or supplemental oxygen.
HM Model Spreads to Surgical Specialists
I have a friend who told me there is a neurologist in the hospital where he works who I understand is calling himself a hospitalist. What gives? I thought hospitalists were all internists or family physicians.
Bill Mulley, MD
Flagstaff, Ariz.
Dr. Hospitalist responds: The vast majority of hospitalists in the U.S. are general internists. There are smaller numbers of family physicians, pediatricians, and medical subspecialists who also work as hospitalists. Although this is the face of HM in America, we are seeing other fields of medicine adopting this model of care.
I know of surgical hospitalists, OB-GYN hospitalists, and yes, even neurohospitalists (see “Generation Next,” October 2010, p. 1). It is hard for some people to get their heads around the notion of a surgeon as a hospitalist because when one thinks of a surgeon, you are thinking of a physician who works in the operating room. But the traditional surgeon also has a clinic where they provide pre- and post-operative care.
Herein lies the difference between traditional surgeons and surgical hospitalists: The surgical hospitalist is, for the most part, only doing work in the hospital—sound familiar? (Think traditional internist vs. internist working as hospitalist.) The traditional general surgeon performs scheduled elective surgeries and typically only does emergency surgeries when they are on call for the hospital. As I understand it, the life of a surgical hospitalist is spending a shift in the hospital waiting for a patient to show up needing emergency surgery.
The hospital CEO today has increasing challenges convincing physicians to take hospital call. Some find themselves paying sizable sums of money for surgeons to take call from home. Some have decided their money is better spent paying for surgical hospitalists to spend nights in the hospital waiting for their pager to go off.
From a patient’s perspective, this seems to be a no-brainer. Having a surgeon in the hospital increases their chances of more timely care. You have to believe the providers in the ED and the medical hospitalist also love having a surgeon in-house, available to provide consults when requested.
I am a bit surprised that we don’t already have a large number of surgical hospitalists in the country. Then again, I have no idea of how many surgeons are working as surgical hospitalists. I am not sure anybody knows that answer.
There is a belief that we are going to see the continued growth of “specialty hospitalists” in the U.S. I believe we are going to see neurohospitalists managing inpatients with stroke and other neurosurgical issues, working side by side with medical hospitalists. I share in the excitement that was pervasive in the early days of the hospitalist movement, even though I’m not sure what we are going to see next.
I never imagined that we would have more than 30,000 hospitalists, as we do today. But while the HM model can help improve care, I will always feel strongly that no system will improve care without the dedication of motivated and compassionate healthcare providers driving the system. TH