User login
HM13 Session Analysis: Overdoses and Other Taxing Toxicology
I attended a presentation titled, “Overdoses and Other Taxing Toxicology,” presented by Kennon Heard, MD, of the University of Colorado Department of Emergency Medicine and the Rocky Mountain Poison and Drug Center. He updated HM13 attendees on current overdose management in a rapid-fire, question-and-answer format.
Here is a summary of Dr. Heard’s key points:
- Modest QTc prolongation can be common after many overdoses, but most do not require prolonged cardiac monitoring. The key is to optimize electrolytes, such as magnesium, phosphorus, and potassium, and to treat other effects caused by the overdose, such as central nervous depression.
- Bath salts are not truly bath salts or plant food, but are actually substituted amphetamines. Treatment is mainly supportive, similar to methamphetamine overdose. Most patients do not require treatment, but providers may need to treat for agitation, seizures or rhabdomyolysis.
Key Takeaways
- Physicians need to remember to treat the symptoms, not necessarily the poisons. First, you may not always be able to accurately identify the poison--there can be both false positives and false negatives on toxicology screens. Second, co-ingestions are common and again may not be easily identified. Toxidromes are specific, but not sensitive.
- Current acetaminophen overdose management is to treat based on clinical endpoints, rather than on a time-based protocol. Treat until all acetaminophen has been metabolized and markers of liver injury, such as liver enzymes and coagulation factors, are improving. TH
Dr. O’Callaghan is pediatric hospitalist and clinical assistant professor of pediatrics at Seattle Children’s Hospital and the University of Washington School of Medicine. He also is a Team Hospitalist member.
I attended a presentation titled, “Overdoses and Other Taxing Toxicology,” presented by Kennon Heard, MD, of the University of Colorado Department of Emergency Medicine and the Rocky Mountain Poison and Drug Center. He updated HM13 attendees on current overdose management in a rapid-fire, question-and-answer format.
Here is a summary of Dr. Heard’s key points:
- Modest QTc prolongation can be common after many overdoses, but most do not require prolonged cardiac monitoring. The key is to optimize electrolytes, such as magnesium, phosphorus, and potassium, and to treat other effects caused by the overdose, such as central nervous depression.
- Bath salts are not truly bath salts or plant food, but are actually substituted amphetamines. Treatment is mainly supportive, similar to methamphetamine overdose. Most patients do not require treatment, but providers may need to treat for agitation, seizures or rhabdomyolysis.
Key Takeaways
- Physicians need to remember to treat the symptoms, not necessarily the poisons. First, you may not always be able to accurately identify the poison--there can be both false positives and false negatives on toxicology screens. Second, co-ingestions are common and again may not be easily identified. Toxidromes are specific, but not sensitive.
- Current acetaminophen overdose management is to treat based on clinical endpoints, rather than on a time-based protocol. Treat until all acetaminophen has been metabolized and markers of liver injury, such as liver enzymes and coagulation factors, are improving. TH
Dr. O’Callaghan is pediatric hospitalist and clinical assistant professor of pediatrics at Seattle Children’s Hospital and the University of Washington School of Medicine. He also is a Team Hospitalist member.
I attended a presentation titled, “Overdoses and Other Taxing Toxicology,” presented by Kennon Heard, MD, of the University of Colorado Department of Emergency Medicine and the Rocky Mountain Poison and Drug Center. He updated HM13 attendees on current overdose management in a rapid-fire, question-and-answer format.
Here is a summary of Dr. Heard’s key points:
- Modest QTc prolongation can be common after many overdoses, but most do not require prolonged cardiac monitoring. The key is to optimize electrolytes, such as magnesium, phosphorus, and potassium, and to treat other effects caused by the overdose, such as central nervous depression.
- Bath salts are not truly bath salts or plant food, but are actually substituted amphetamines. Treatment is mainly supportive, similar to methamphetamine overdose. Most patients do not require treatment, but providers may need to treat for agitation, seizures or rhabdomyolysis.
Key Takeaways
- Physicians need to remember to treat the symptoms, not necessarily the poisons. First, you may not always be able to accurately identify the poison--there can be both false positives and false negatives on toxicology screens. Second, co-ingestions are common and again may not be easily identified. Toxidromes are specific, but not sensitive.
- Current acetaminophen overdose management is to treat based on clinical endpoints, rather than on a time-based protocol. Treat until all acetaminophen has been metabolized and markers of liver injury, such as liver enzymes and coagulation factors, are improving. TH
Dr. O’Callaghan is pediatric hospitalist and clinical assistant professor of pediatrics at Seattle Children’s Hospital and the University of Washington School of Medicine. He also is a Team Hospitalist member.
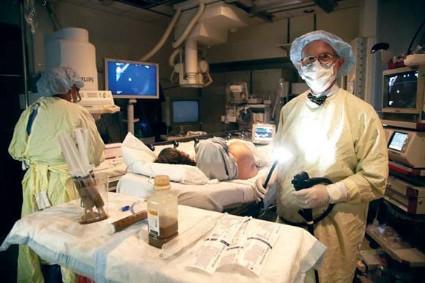
Fecal microbiota transplant designated a biologic, requiring IND status
BETHESDA, MD. – The Food and Drug Administration has designated stool for transplant as a biologic drug, necessitating that any gastroenterologist performing fecal microbiota transplants obtain an Investigational New Drug permit.
By designating stool for transplant as a biologic drug, anyone who performs fecal microbiota transplants (FMTs) – whether they perform a single transplant for one patient or recruit dozens for a study – needs to have an IND permit.
The announcement was made at a 2-day public workshop convened by the National Institutes of Health and the Food and Drug Administration to sift through some of the evidence surrounding FMTs.
The intent of the IND requirement, said Dr. Jay Slater, director of FDA’s Division of Bacterial, Parasitic, and Allergenic Products, is not to stamp out the care that patients can now receive, but to make sure it’s safe, effective, and data driven.
"This is a low-tech procedure that already has a CPT code. A ‘how-to’ guide recently appeared online, and it walks you right through how to do the procedure. There are a very large number of people doing this off the grid. What we need are long-term controlled trials on this that will enhance our understanding of its safety and efficacy."
Although neither the biologic designation nor the IND requirement is brand new, they have not been well publicized, according to one of the innovators of FMT, Dr. Lawrence Brandt, of Albert Einstein Medical Center in New York.
"I am struck by the fact that FDA wants these INDs and yet FDA has never publicly set forth any message on it. So from this moment on, all of us who continue to do this without an IND are violating FDA’s policy," he said at the meeting.
One of the primary concerns now, according to Dr. Brandt, is a burgeoning public interest in FMTs, even to the point of do-it-yourself treatments. With online instructions for self-treatment, and a procedure that is rife with variations, regulators can no longer tacitly ignore the issue.
There’s no standardization of how the stool is prepared and filtered – it could be blended in a kitchen blender or by hand with a tongue depressor, or strained through gauze or a coffee filter, he said. Dosing is all over the place, listed as spoonfuls, grams, and milliliters. Different institutions screen donors in different ways. Some patients get a bowel prep, which can be mild or aggressive, and some don’t get one at all. Should the stool be fresh, and if so, how fresh? Is frozen okay? These are all issues that need to be examined from a safety and efficacy perspective and standardized.
Even the method of delivery varies. The transplant can be administered via nasogastric tube or colonoscope, or by enema. There’s no standardization of data collection either. Some large institutions keep records of everything from the first workup to the last visit. Doctors who perform transplants occasionally may not be as conscientious. And no one knows anything about the do-it-yourselfers, at home with a family member’s donation and a squeeze enema.
Dr. Brandt – and a number of clinicians at the meeting – agreed that answers must be found for all these questions. And they agree that well-conducted clinical trials are the best way to go forward.
Dr. Colleen Kelly, one of the gastroenterologists launching one of 22 currently recruiting studies on FMT, started doing the procedure 5 years ago. Her first patient was a 26-year-old medical student with recurrent bouts of a Clostridium difficile infection.
"I’d heard of [FMT], but never, ever thought of doing one," said Dr. Kelly, of Brown University Medical Center, Providence, R.I. "I thought it was something at the far fringes of medicine."
At her patient’s insistence, Dr. Kelly contacted Dr. Brandt and learned about his process for performing FMT. The following year, she performed 10 FMTs. She is now undertaking a study with Dr. Brandt to recruit about 48 patients with relapsing C. difficile to be randomized to FMT or to a sham treatment with their own stool. Patients who have clinical failure in the sham group will be offered FMT; patients in the active arm who fail on initial FMT will get another FMT from a different donor.
While most trials are examining the utility of FMT in patients with recurrent C. difficile, a few are investigating FMT for use in patients with Crohn’s disease and inflammatory bowel disease. Some clinicians and individual patients are now using FMTs for this condition outside a clinical trial, with no understanding of how a compromised intestinal mucosa might react to transplanted stool.
It will take years to accumulate the data necessary to fully understand FMT and all its implications, Dr. Kelly said. In the interim, the IND requirement will likely shrink the already-small pool of gastroenterologists performing FMTs. "Some will be motivated to get an IND, but the average person in practice won’t," she predicted. "You need to put hours and hours of work into it, and then you’re still under FDA’s oversight because this is not an approved therapy. So that means you have to submit adverse events reports, keep records, and report annually on your program. And at any time, without any warning, [the FDA] can come and inspect your facility."
Dr. Brandt agreed. "It’s a huge amount of paperwork documentation, record-keeping, and follow-up that the average practitioner is simply not going to do." The requirement for an IND means there are simply going to be fewer and fewer physicians who do them, he said.
Admittedly, though, the risks of no regulation can endanger patients, Dr. Kelly said. "If things go on completely unregulated, stupid things will happen," including the spread of infectious diseases like hepatitis C and parasitic infestations.
Indeed, Dr. Alexander Khoruts of the University of Minnesota, Minneapolis, who spoke at the workshop, described the case of an FMT "do-it-yourselfer" who called for some advice on improving her outcomes. Specifically, she had mixed stool from a neighbor and her son’s mother-in-law and administered it to herself without results. "She wanted to know if maybe the chlorine in the water killed off everything. ... Six months later she called me back and said her C. diff was gone, but now she had parasites."
"There are already predatory practices out there [performing FMTs]," Dr. Khoruts said. "I got an e-mail from someone who couldn’t make the drive up to see me, but she found someone near her who would do it for $10,000."
Well-designed and well-executed studies would not only address these immediate safety questions, but would also examine the more nebulous concerns about the long-term effects of tampering with an individual’s unique ecosystem of gut microbes. In recent years, research has begun to document how the balance and proportion of microbial species in the gut can either protect from – or predispose to – metabolic syndrome, obesity, diabetes, cardiovascular disease, arthritis, and even cognitive disorders.
An engrafting microbial transplant could predispose the recipient to develop illnesses that would otherwise never have been destined to occur, Dr. Slater said. "All of the evidence we have suggests that manipulating the gut microbiome is a powerful act that may have long-reaching and subtle effects."
The move toward a standardized FMT product and process is inevitable, Dr. Brandt said. "We’re not going to be doing fecal transplants much longer. This is a temporary situation. We’re already developing compounds that will do the same thing."
Researchers at the University of Guelph, Ontario, have developed a machine that distills and cultures microbes from human feces, producing a kind of super-probiotic that can be used in place of fresh stool.
Also, the Canadian biotech company Rebiotix is working on a similar product, which it intends to test in a phase II randomized controlled trial.
But until those machine-made products are available, physicians and patients with have to stay with the man-made version. "We have access to a substance that is free and has a virtually unlimited supply," Dr. Kelly said. "We cannot deny this effective therapy to these patients who’ve failed all other available treatments."
None of the sources quoted in this article had any financial declarations.
BETHESDA, MD. – The Food and Drug Administration has designated stool for transplant as a biologic drug, necessitating that any gastroenterologist performing fecal microbiota transplants obtain an Investigational New Drug permit.
By designating stool for transplant as a biologic drug, anyone who performs fecal microbiota transplants (FMTs) – whether they perform a single transplant for one patient or recruit dozens for a study – needs to have an IND permit.
The announcement was made at a 2-day public workshop convened by the National Institutes of Health and the Food and Drug Administration to sift through some of the evidence surrounding FMTs.
The intent of the IND requirement, said Dr. Jay Slater, director of FDA’s Division of Bacterial, Parasitic, and Allergenic Products, is not to stamp out the care that patients can now receive, but to make sure it’s safe, effective, and data driven.
"This is a low-tech procedure that already has a CPT code. A ‘how-to’ guide recently appeared online, and it walks you right through how to do the procedure. There are a very large number of people doing this off the grid. What we need are long-term controlled trials on this that will enhance our understanding of its safety and efficacy."
Although neither the biologic designation nor the IND requirement is brand new, they have not been well publicized, according to one of the innovators of FMT, Dr. Lawrence Brandt, of Albert Einstein Medical Center in New York.
"I am struck by the fact that FDA wants these INDs and yet FDA has never publicly set forth any message on it. So from this moment on, all of us who continue to do this without an IND are violating FDA’s policy," he said at the meeting.
One of the primary concerns now, according to Dr. Brandt, is a burgeoning public interest in FMTs, even to the point of do-it-yourself treatments. With online instructions for self-treatment, and a procedure that is rife with variations, regulators can no longer tacitly ignore the issue.
There’s no standardization of how the stool is prepared and filtered – it could be blended in a kitchen blender or by hand with a tongue depressor, or strained through gauze or a coffee filter, he said. Dosing is all over the place, listed as spoonfuls, grams, and milliliters. Different institutions screen donors in different ways. Some patients get a bowel prep, which can be mild or aggressive, and some don’t get one at all. Should the stool be fresh, and if so, how fresh? Is frozen okay? These are all issues that need to be examined from a safety and efficacy perspective and standardized.
Even the method of delivery varies. The transplant can be administered via nasogastric tube or colonoscope, or by enema. There’s no standardization of data collection either. Some large institutions keep records of everything from the first workup to the last visit. Doctors who perform transplants occasionally may not be as conscientious. And no one knows anything about the do-it-yourselfers, at home with a family member’s donation and a squeeze enema.
Dr. Brandt – and a number of clinicians at the meeting – agreed that answers must be found for all these questions. And they agree that well-conducted clinical trials are the best way to go forward.
Dr. Colleen Kelly, one of the gastroenterologists launching one of 22 currently recruiting studies on FMT, started doing the procedure 5 years ago. Her first patient was a 26-year-old medical student with recurrent bouts of a Clostridium difficile infection.
"I’d heard of [FMT], but never, ever thought of doing one," said Dr. Kelly, of Brown University Medical Center, Providence, R.I. "I thought it was something at the far fringes of medicine."
At her patient’s insistence, Dr. Kelly contacted Dr. Brandt and learned about his process for performing FMT. The following year, she performed 10 FMTs. She is now undertaking a study with Dr. Brandt to recruit about 48 patients with relapsing C. difficile to be randomized to FMT or to a sham treatment with their own stool. Patients who have clinical failure in the sham group will be offered FMT; patients in the active arm who fail on initial FMT will get another FMT from a different donor.
While most trials are examining the utility of FMT in patients with recurrent C. difficile, a few are investigating FMT for use in patients with Crohn’s disease and inflammatory bowel disease. Some clinicians and individual patients are now using FMTs for this condition outside a clinical trial, with no understanding of how a compromised intestinal mucosa might react to transplanted stool.
It will take years to accumulate the data necessary to fully understand FMT and all its implications, Dr. Kelly said. In the interim, the IND requirement will likely shrink the already-small pool of gastroenterologists performing FMTs. "Some will be motivated to get an IND, but the average person in practice won’t," she predicted. "You need to put hours and hours of work into it, and then you’re still under FDA’s oversight because this is not an approved therapy. So that means you have to submit adverse events reports, keep records, and report annually on your program. And at any time, without any warning, [the FDA] can come and inspect your facility."
Dr. Brandt agreed. "It’s a huge amount of paperwork documentation, record-keeping, and follow-up that the average practitioner is simply not going to do." The requirement for an IND means there are simply going to be fewer and fewer physicians who do them, he said.
Admittedly, though, the risks of no regulation can endanger patients, Dr. Kelly said. "If things go on completely unregulated, stupid things will happen," including the spread of infectious diseases like hepatitis C and parasitic infestations.
Indeed, Dr. Alexander Khoruts of the University of Minnesota, Minneapolis, who spoke at the workshop, described the case of an FMT "do-it-yourselfer" who called for some advice on improving her outcomes. Specifically, she had mixed stool from a neighbor and her son’s mother-in-law and administered it to herself without results. "She wanted to know if maybe the chlorine in the water killed off everything. ... Six months later she called me back and said her C. diff was gone, but now she had parasites."
"There are already predatory practices out there [performing FMTs]," Dr. Khoruts said. "I got an e-mail from someone who couldn’t make the drive up to see me, but she found someone near her who would do it for $10,000."
Well-designed and well-executed studies would not only address these immediate safety questions, but would also examine the more nebulous concerns about the long-term effects of tampering with an individual’s unique ecosystem of gut microbes. In recent years, research has begun to document how the balance and proportion of microbial species in the gut can either protect from – or predispose to – metabolic syndrome, obesity, diabetes, cardiovascular disease, arthritis, and even cognitive disorders.
An engrafting microbial transplant could predispose the recipient to develop illnesses that would otherwise never have been destined to occur, Dr. Slater said. "All of the evidence we have suggests that manipulating the gut microbiome is a powerful act that may have long-reaching and subtle effects."
The move toward a standardized FMT product and process is inevitable, Dr. Brandt said. "We’re not going to be doing fecal transplants much longer. This is a temporary situation. We’re already developing compounds that will do the same thing."
Researchers at the University of Guelph, Ontario, have developed a machine that distills and cultures microbes from human feces, producing a kind of super-probiotic that can be used in place of fresh stool.
Also, the Canadian biotech company Rebiotix is working on a similar product, which it intends to test in a phase II randomized controlled trial.
But until those machine-made products are available, physicians and patients with have to stay with the man-made version. "We have access to a substance that is free and has a virtually unlimited supply," Dr. Kelly said. "We cannot deny this effective therapy to these patients who’ve failed all other available treatments."
None of the sources quoted in this article had any financial declarations.
BETHESDA, MD. – The Food and Drug Administration has designated stool for transplant as a biologic drug, necessitating that any gastroenterologist performing fecal microbiota transplants obtain an Investigational New Drug permit.
By designating stool for transplant as a biologic drug, anyone who performs fecal microbiota transplants (FMTs) – whether they perform a single transplant for one patient or recruit dozens for a study – needs to have an IND permit.
The announcement was made at a 2-day public workshop convened by the National Institutes of Health and the Food and Drug Administration to sift through some of the evidence surrounding FMTs.
The intent of the IND requirement, said Dr. Jay Slater, director of FDA’s Division of Bacterial, Parasitic, and Allergenic Products, is not to stamp out the care that patients can now receive, but to make sure it’s safe, effective, and data driven.
"This is a low-tech procedure that already has a CPT code. A ‘how-to’ guide recently appeared online, and it walks you right through how to do the procedure. There are a very large number of people doing this off the grid. What we need are long-term controlled trials on this that will enhance our understanding of its safety and efficacy."
Although neither the biologic designation nor the IND requirement is brand new, they have not been well publicized, according to one of the innovators of FMT, Dr. Lawrence Brandt, of Albert Einstein Medical Center in New York.
"I am struck by the fact that FDA wants these INDs and yet FDA has never publicly set forth any message on it. So from this moment on, all of us who continue to do this without an IND are violating FDA’s policy," he said at the meeting.
One of the primary concerns now, according to Dr. Brandt, is a burgeoning public interest in FMTs, even to the point of do-it-yourself treatments. With online instructions for self-treatment, and a procedure that is rife with variations, regulators can no longer tacitly ignore the issue.
There’s no standardization of how the stool is prepared and filtered – it could be blended in a kitchen blender or by hand with a tongue depressor, or strained through gauze or a coffee filter, he said. Dosing is all over the place, listed as spoonfuls, grams, and milliliters. Different institutions screen donors in different ways. Some patients get a bowel prep, which can be mild or aggressive, and some don’t get one at all. Should the stool be fresh, and if so, how fresh? Is frozen okay? These are all issues that need to be examined from a safety and efficacy perspective and standardized.
Even the method of delivery varies. The transplant can be administered via nasogastric tube or colonoscope, or by enema. There’s no standardization of data collection either. Some large institutions keep records of everything from the first workup to the last visit. Doctors who perform transplants occasionally may not be as conscientious. And no one knows anything about the do-it-yourselfers, at home with a family member’s donation and a squeeze enema.
Dr. Brandt – and a number of clinicians at the meeting – agreed that answers must be found for all these questions. And they agree that well-conducted clinical trials are the best way to go forward.
Dr. Colleen Kelly, one of the gastroenterologists launching one of 22 currently recruiting studies on FMT, started doing the procedure 5 years ago. Her first patient was a 26-year-old medical student with recurrent bouts of a Clostridium difficile infection.
"I’d heard of [FMT], but never, ever thought of doing one," said Dr. Kelly, of Brown University Medical Center, Providence, R.I. "I thought it was something at the far fringes of medicine."
At her patient’s insistence, Dr. Kelly contacted Dr. Brandt and learned about his process for performing FMT. The following year, she performed 10 FMTs. She is now undertaking a study with Dr. Brandt to recruit about 48 patients with relapsing C. difficile to be randomized to FMT or to a sham treatment with their own stool. Patients who have clinical failure in the sham group will be offered FMT; patients in the active arm who fail on initial FMT will get another FMT from a different donor.
While most trials are examining the utility of FMT in patients with recurrent C. difficile, a few are investigating FMT for use in patients with Crohn’s disease and inflammatory bowel disease. Some clinicians and individual patients are now using FMTs for this condition outside a clinical trial, with no understanding of how a compromised intestinal mucosa might react to transplanted stool.
It will take years to accumulate the data necessary to fully understand FMT and all its implications, Dr. Kelly said. In the interim, the IND requirement will likely shrink the already-small pool of gastroenterologists performing FMTs. "Some will be motivated to get an IND, but the average person in practice won’t," she predicted. "You need to put hours and hours of work into it, and then you’re still under FDA’s oversight because this is not an approved therapy. So that means you have to submit adverse events reports, keep records, and report annually on your program. And at any time, without any warning, [the FDA] can come and inspect your facility."
Dr. Brandt agreed. "It’s a huge amount of paperwork documentation, record-keeping, and follow-up that the average practitioner is simply not going to do." The requirement for an IND means there are simply going to be fewer and fewer physicians who do them, he said.
Admittedly, though, the risks of no regulation can endanger patients, Dr. Kelly said. "If things go on completely unregulated, stupid things will happen," including the spread of infectious diseases like hepatitis C and parasitic infestations.
Indeed, Dr. Alexander Khoruts of the University of Minnesota, Minneapolis, who spoke at the workshop, described the case of an FMT "do-it-yourselfer" who called for some advice on improving her outcomes. Specifically, she had mixed stool from a neighbor and her son’s mother-in-law and administered it to herself without results. "She wanted to know if maybe the chlorine in the water killed off everything. ... Six months later she called me back and said her C. diff was gone, but now she had parasites."
"There are already predatory practices out there [performing FMTs]," Dr. Khoruts said. "I got an e-mail from someone who couldn’t make the drive up to see me, but she found someone near her who would do it for $10,000."
Well-designed and well-executed studies would not only address these immediate safety questions, but would also examine the more nebulous concerns about the long-term effects of tampering with an individual’s unique ecosystem of gut microbes. In recent years, research has begun to document how the balance and proportion of microbial species in the gut can either protect from – or predispose to – metabolic syndrome, obesity, diabetes, cardiovascular disease, arthritis, and even cognitive disorders.
An engrafting microbial transplant could predispose the recipient to develop illnesses that would otherwise never have been destined to occur, Dr. Slater said. "All of the evidence we have suggests that manipulating the gut microbiome is a powerful act that may have long-reaching and subtle effects."
The move toward a standardized FMT product and process is inevitable, Dr. Brandt said. "We’re not going to be doing fecal transplants much longer. This is a temporary situation. We’re already developing compounds that will do the same thing."
Researchers at the University of Guelph, Ontario, have developed a machine that distills and cultures microbes from human feces, producing a kind of super-probiotic that can be used in place of fresh stool.
Also, the Canadian biotech company Rebiotix is working on a similar product, which it intends to test in a phase II randomized controlled trial.
But until those machine-made products are available, physicians and patients with have to stay with the man-made version. "We have access to a substance that is free and has a virtually unlimited supply," Dr. Kelly said. "We cannot deny this effective therapy to these patients who’ve failed all other available treatments."
None of the sources quoted in this article had any financial declarations.
HM13 Session Analysis: The Business of Medicine
Denice Cora-Bramble, MD, of Children’s National Medical Center in Washington, D.C., presented “The Business of Medicine” breakout Friday at HM13.
Key Points
- Whether you are salaried, work for productivity, or have a combination of the two, it is important for hospitalists to understand the business side of medicine.
- Even if you are not a hospitalist group leader, there are several things that you should know about the finances of your hospitalist program. Dr. Cora-Bramble reviewed the basics of financial statements, hospital revenue reports, and expense reports. She also reviewed how the hospitalist division partners with the entire hospital.
- After understanding the basic finances of your program, there are ways to enhance your financial performance. These include noting any lack of payments, billing and patient trends, and looking at program losses.
Key Takeaways
- It is important to understand the general principles of financial statements, budgets and financial decision making.
- There are multiple strategies to improve your division’s financial performance.
- There are financial challenges inherent in leading an academic division.
Dr. Hale is a pediatric hospitalist at the Floating Hospital for Children at Tufts Medical Center in Boston, and a Team Hospitalist member.
Denice Cora-Bramble, MD, of Children’s National Medical Center in Washington, D.C., presented “The Business of Medicine” breakout Friday at HM13.
Key Points
- Whether you are salaried, work for productivity, or have a combination of the two, it is important for hospitalists to understand the business side of medicine.
- Even if you are not a hospitalist group leader, there are several things that you should know about the finances of your hospitalist program. Dr. Cora-Bramble reviewed the basics of financial statements, hospital revenue reports, and expense reports. She also reviewed how the hospitalist division partners with the entire hospital.
- After understanding the basic finances of your program, there are ways to enhance your financial performance. These include noting any lack of payments, billing and patient trends, and looking at program losses.
Key Takeaways
- It is important to understand the general principles of financial statements, budgets and financial decision making.
- There are multiple strategies to improve your division’s financial performance.
- There are financial challenges inherent in leading an academic division.
Dr. Hale is a pediatric hospitalist at the Floating Hospital for Children at Tufts Medical Center in Boston, and a Team Hospitalist member.
Denice Cora-Bramble, MD, of Children’s National Medical Center in Washington, D.C., presented “The Business of Medicine” breakout Friday at HM13.
Key Points
- Whether you are salaried, work for productivity, or have a combination of the two, it is important for hospitalists to understand the business side of medicine.
- Even if you are not a hospitalist group leader, there are several things that you should know about the finances of your hospitalist program. Dr. Cora-Bramble reviewed the basics of financial statements, hospital revenue reports, and expense reports. She also reviewed how the hospitalist division partners with the entire hospital.
- After understanding the basic finances of your program, there are ways to enhance your financial performance. These include noting any lack of payments, billing and patient trends, and looking at program losses.
Key Takeaways
- It is important to understand the general principles of financial statements, budgets and financial decision making.
- There are multiple strategies to improve your division’s financial performance.
- There are financial challenges inherent in leading an academic division.
Dr. Hale is a pediatric hospitalist at the Floating Hospital for Children at Tufts Medical Center in Boston, and a Team Hospitalist member.
Medical Consultation and Co-Management in Perioperative Medicine
NATIONAL HARBOR, MD—Amir Jaffer, MD, and Steven Cohn, MD, chaired an excellent pre-course centered on common problems hospitalists encounter in managing medical problems in surgical patients. Topics covered were: the pre-operative evaluation and role of the consultant, cardiac risk assessment, pulmonary risk assessment, perioperative medication management, old and new antithrombotic therapy, diabetes management, co-management of the hip fracture, VTE prevention, and management of perioperative anemia.
Among other takeaway points, the physicians emphasized the importance of personal communication between surgeons and hospitalists. Frank Michota, MD, made an analogy using the patient as the plane, the surgeon as the pilot, the anesthesiologist as the co-pilot, and the hospitalist as the mechanic.
Check out The Hospitalist's Day One video from Hospital Medicine 2013
Others commented on cardiac management of the surgical patient, the risk assessment calculators available, and how noninvasive testing is rarely needed. Physicians also noted that partial functional dependence is the strongest predictor for patients needing recommendations regarding risk of postoperative respiratory failure. In reviewing patients’ medications in the perioperative phase, the speakers noted it is important to ask about herbal remedies and OTC drugs, as these may cause problems during and after surgery.
Additional topics addressed included: bridge therapy for anti coagulation, and the need to take into account the risk of bleeding among some, but not all, patients; how diabetic management should focus on a pre-meal glucose measurement of less than 140 mg/dl, and that all other glucose readings be under 180 mg/dl; how extended prophalyxis for VTE prevention is needed for elective hip surgery; and that hospitalists should be versed in the latest recommendations regarding restricted blood transfusion criteria. TH
NATIONAL HARBOR, MD—Amir Jaffer, MD, and Steven Cohn, MD, chaired an excellent pre-course centered on common problems hospitalists encounter in managing medical problems in surgical patients. Topics covered were: the pre-operative evaluation and role of the consultant, cardiac risk assessment, pulmonary risk assessment, perioperative medication management, old and new antithrombotic therapy, diabetes management, co-management of the hip fracture, VTE prevention, and management of perioperative anemia.
Among other takeaway points, the physicians emphasized the importance of personal communication between surgeons and hospitalists. Frank Michota, MD, made an analogy using the patient as the plane, the surgeon as the pilot, the anesthesiologist as the co-pilot, and the hospitalist as the mechanic.
Check out The Hospitalist's Day One video from Hospital Medicine 2013
Others commented on cardiac management of the surgical patient, the risk assessment calculators available, and how noninvasive testing is rarely needed. Physicians also noted that partial functional dependence is the strongest predictor for patients needing recommendations regarding risk of postoperative respiratory failure. In reviewing patients’ medications in the perioperative phase, the speakers noted it is important to ask about herbal remedies and OTC drugs, as these may cause problems during and after surgery.
Additional topics addressed included: bridge therapy for anti coagulation, and the need to take into account the risk of bleeding among some, but not all, patients; how diabetic management should focus on a pre-meal glucose measurement of less than 140 mg/dl, and that all other glucose readings be under 180 mg/dl; how extended prophalyxis for VTE prevention is needed for elective hip surgery; and that hospitalists should be versed in the latest recommendations regarding restricted blood transfusion criteria. TH
NATIONAL HARBOR, MD—Amir Jaffer, MD, and Steven Cohn, MD, chaired an excellent pre-course centered on common problems hospitalists encounter in managing medical problems in surgical patients. Topics covered were: the pre-operative evaluation and role of the consultant, cardiac risk assessment, pulmonary risk assessment, perioperative medication management, old and new antithrombotic therapy, diabetes management, co-management of the hip fracture, VTE prevention, and management of perioperative anemia.
Among other takeaway points, the physicians emphasized the importance of personal communication between surgeons and hospitalists. Frank Michota, MD, made an analogy using the patient as the plane, the surgeon as the pilot, the anesthesiologist as the co-pilot, and the hospitalist as the mechanic.
Check out The Hospitalist's Day One video from Hospital Medicine 2013
Others commented on cardiac management of the surgical patient, the risk assessment calculators available, and how noninvasive testing is rarely needed. Physicians also noted that partial functional dependence is the strongest predictor for patients needing recommendations regarding risk of postoperative respiratory failure. In reviewing patients’ medications in the perioperative phase, the speakers noted it is important to ask about herbal remedies and OTC drugs, as these may cause problems during and after surgery.
Additional topics addressed included: bridge therapy for anti coagulation, and the need to take into account the risk of bleeding among some, but not all, patients; how diabetic management should focus on a pre-meal glucose measurement of less than 140 mg/dl, and that all other glucose readings be under 180 mg/dl; how extended prophalyxis for VTE prevention is needed for elective hip surgery; and that hospitalists should be versed in the latest recommendations regarding restricted blood transfusion criteria. TH
Hands-On Training Helps Prepare Hospitalists for Procedures
Sally Wang MD, FHM, director of procedure education at Brigham and Women’s Hospital in Boston, and Brad Rosen, MD, MBA, FHM, medical director of the Inpatient Specialty Program (ISP) at Cedars-Sinai Hospital in Los Angeles, led another rapid-fire pre-course in ultrasound-guided procedures for the hospitalist at HM13.
Drs. Wang, Rosen, and a veteran group of faculty and trainers brought hands-on training in core bedside procedures, plus training in relatively new procedures to hospitalists such as intraosseous lines and skin biopsies. All attendees received close interaction with faculty and trainers, and participated in training exercises on tissue models, training models, and live models.
Additional discussion was focused on developing a proceduralist program. Experts explained the required commitment to proficiency and ongoing data collection, quality improvement, and “customer service” to stakeholders. But the basics of ongoing experiential learning are invaluable, they said, and often begin with simulation exercises.
Hospitalists thinking of becoming a proceduralist should start by making sure that they are proficient and experienced, and have invested the time necessary to maintain that experience. Beyond personal interest in procedures, administering an HM program that encourages and fosters procedural experience requires input from multiple stakeholders, as well as ongoing efforts to promote a climate of safety surrounding bedside procedures. TH
Dr. Chang is med-peds hospitalist at Univeristy of California San Diego, and a Team Hospitalist member.
Sally Wang MD, FHM, director of procedure education at Brigham and Women’s Hospital in Boston, and Brad Rosen, MD, MBA, FHM, medical director of the Inpatient Specialty Program (ISP) at Cedars-Sinai Hospital in Los Angeles, led another rapid-fire pre-course in ultrasound-guided procedures for the hospitalist at HM13.
Drs. Wang, Rosen, and a veteran group of faculty and trainers brought hands-on training in core bedside procedures, plus training in relatively new procedures to hospitalists such as intraosseous lines and skin biopsies. All attendees received close interaction with faculty and trainers, and participated in training exercises on tissue models, training models, and live models.
Additional discussion was focused on developing a proceduralist program. Experts explained the required commitment to proficiency and ongoing data collection, quality improvement, and “customer service” to stakeholders. But the basics of ongoing experiential learning are invaluable, they said, and often begin with simulation exercises.
Hospitalists thinking of becoming a proceduralist should start by making sure that they are proficient and experienced, and have invested the time necessary to maintain that experience. Beyond personal interest in procedures, administering an HM program that encourages and fosters procedural experience requires input from multiple stakeholders, as well as ongoing efforts to promote a climate of safety surrounding bedside procedures. TH
Dr. Chang is med-peds hospitalist at Univeristy of California San Diego, and a Team Hospitalist member.
Sally Wang MD, FHM, director of procedure education at Brigham and Women’s Hospital in Boston, and Brad Rosen, MD, MBA, FHM, medical director of the Inpatient Specialty Program (ISP) at Cedars-Sinai Hospital in Los Angeles, led another rapid-fire pre-course in ultrasound-guided procedures for the hospitalist at HM13.
Drs. Wang, Rosen, and a veteran group of faculty and trainers brought hands-on training in core bedside procedures, plus training in relatively new procedures to hospitalists such as intraosseous lines and skin biopsies. All attendees received close interaction with faculty and trainers, and participated in training exercises on tissue models, training models, and live models.
Additional discussion was focused on developing a proceduralist program. Experts explained the required commitment to proficiency and ongoing data collection, quality improvement, and “customer service” to stakeholders. But the basics of ongoing experiential learning are invaluable, they said, and often begin with simulation exercises.
Hospitalists thinking of becoming a proceduralist should start by making sure that they are proficient and experienced, and have invested the time necessary to maintain that experience. Beyond personal interest in procedures, administering an HM program that encourages and fosters procedural experience requires input from multiple stakeholders, as well as ongoing efforts to promote a climate of safety surrounding bedside procedures. TH
Dr. Chang is med-peds hospitalist at Univeristy of California San Diego, and a Team Hospitalist member.
Bugs, Drugs, and You: HM13 Pre-Course Reviews Infectious Disease Essentials for the Hospitalist
This ID focused pre-course was a jam-packed, practical, and high-yield review of relevant ID topics encountered by practicing hospitalists. Here are some of the key takeaways:
HIV and the Hospitalist in 2013
John Flaherty, MD, prof. of medicine at Northwestern University Feinberg School of Medicine
• Lower the threshold for HIV testing; don’t limit to “high-risk” behaviors, 20% of those living with HIV/AID are unaware—so TEST!
• Recognize clinical clues to HIV infection: acute mono-like syndrome, unexplained chronic illness, comm.-acquired pneumonia.
Thomas Fraser, MD, FACP, FSHEA, vice chairman, Dept. of Infectious Disease, Medical Director for Infection Prevention, Cleveland Clinic
• Risk Factors for CDI: disease severity (sicker patients=higher risk), antibiotics, PPI use, NG tubes and tube feeds, stool softeners and enemas, GI surgery, increasing age.
• Treatment: stop abx if possible, no antiperistaltics, metronidazole 500mg po tid x 10d- 1st line, alt. vancomycin 125-150mg po qid x 10d, vancomycin preferred rx for seriously ill (wbc>20k, ARF, abd.distention, hemodynamic instability).
• Do not treat asymptomatic patient with stool sample + for C. diff.
Emerging Antimicrobial Resistance Issues
COL Glenn Wortmann, MD Chief of integrated Infectious Diseases Services Walter Reed army Medical Center and Bethesda Naval National Naval Center, Program Director of National Capital Consortium Infectious Diseases Fellowship Program, Assoc. Prof. of Medicine Uniformed Services University of the Health Sciences
• Global trends in rising antimicrobial resistance suggest that the antibiotic era may be ending.
• Emphasis shifting from infection treatment to prevention.
• Maximize hand washing: Wash in, wash out and lead by example.
• Consider chlorhexidine washes in high-risk patients as well as environmental decontamination devices.
• Judicious Use of Antimicrobial Agents: use narrow spectrum agents for shortest duration of therapy feasible, formulary restriction, mandatory ID or pharmacy consultation.
How to be a Leader in Antimicrobial Stewardship in Your Hospital
Arjun Srinivasan, MD FSHEA Assoc. Dir. for Healthcare Associated Infection Prevention Programs in the Div. of Healthcare Quality Promotion at the Centers for Disease Control and Prevention (CDC)
• Hospitalists have the greatest influence over how abx are used in hospitals.
• Hospitalists have the background, experience and strong interest in QI work to affect change; know that up to 50% of all antibiotic use is inappropriate.
• Hospitalists can help tackle issues of abx misuse with signouts, handoffs, and care transitions.
•
ID Emergencies: Diagnoses you can’t afford to miss
James Pile, MD FACP SFHM practicing hospitalist and ID specialist at Cleveland Clinic
• Acute Bacterial Meningitis: LP and Brain Imaging, subset of low-risk patients appears not to require imaging prior to LP, even pts with mild mass effects can probably be safely tapped, herniation may occur even with normal CT-if clinical evidence suggests increasing icp, consider deferring lp or using small gauge needle
• Rx: all adults-cover pneumococcus and meningococcus, empiric coverage of resistant S. pneumoniae is standard of care; cover for listeria for age >50, immunocompromised, alcoholic, pregnant, diabetic; recent head trauma or neurosurgery cover S. aureus and GNB (including pseudomonas).
• Steroids are recommended for suspected BM give dexamethasone with or before antibiotics.
• Spinal Epidural Abscess: It’s easy to miss!
• Necrotizing Fasciitis/Necrotizing Soft Tissue Infections (NSTI): Pain out of proportion to physical findings, systemic findings (delirium, fever, diaphoresis, tachycardia) out of proportion to physical findings; consider Dx to make Dx, easy to miss or delay diagnosis→worsening outcomes. Have low threshold for surgical consultation and/or CT in patients with what appears to be severe cellulitis; include clindamycin (with other abx) for empiric coverage
ID Pearls Every Hospitalist Should Know
John Flaherty, MD
• Re: Perioperative Abx, “Better late than never” does NOT apply. Ensure appropriate timing of peri-op abx.
• Fever ≠ Infection, No Fever ≠ No Infection.
• Sepsis and Hypotension: start broad-spectrum abx NOW.
• Persistent pna despite empiric rx and neg cx, think TB and blastomycoses.
• Fatigue, low-grade fever, and anemia- r/o infective endocarditis.
• Single+blood cx is not always a contaminant; is IS a source of prolonged hospitalization and further testing, so choose wisely when ordering blood cx.
Implementing Socio-Adaptive Change: The role of leaders, followers and bundles in preventing infection
Sanjay Saint, MD MPH Prof. of Int. Medicine University of Michigan, Dir. of the VA/Univeristy of Michigan Patient Safety Enhancement Program, Assoc. Chief of Medicine Ann Arbor VAMC
• Successful implementation of change requires recognition of both the technical and socio-adaptive barriers.
• The key to good leadership is good followership—very little written on subject of followership.
Infective Endocarditis and Intravascular Device Infections
Thomas Fraser, MD FACP FSHEA
• Management Highlights: If patient is sick, pull the line out. If patient has a bad bug, pull the line out. Most people with lines are health care experienced—start broad-spectrum abx and tailor rx once cx available. If you do not pull the line, follow very closely, have low threshold to call ID consult, S. aureus is in a class all its own.
• When can line be replaced? Timing depends on clinical need ultimately, clinically well with resolving syndrome, receiving effective rx, blood cx neg for 72 hrs; maybe longer for Candida species.
• Who should get a TEE for HCA S. aureus bacteremia? Patients with prolonged bacteremia; >4 days; presence of an intracardiac device (valve, icd, ppm); metastatic complication; vertebral or other osteomyelitis, etc. TH
Dr. Lindsey is a COO at Strategist Synergy Surgicalists, lead consultant at Asynd Consulting, and a Team Hospitalist member.
This ID focused pre-course was a jam-packed, practical, and high-yield review of relevant ID topics encountered by practicing hospitalists. Here are some of the key takeaways:
HIV and the Hospitalist in 2013
John Flaherty, MD, prof. of medicine at Northwestern University Feinberg School of Medicine
• Lower the threshold for HIV testing; don’t limit to “high-risk” behaviors, 20% of those living with HIV/AID are unaware—so TEST!
• Recognize clinical clues to HIV infection: acute mono-like syndrome, unexplained chronic illness, comm.-acquired pneumonia.
Thomas Fraser, MD, FACP, FSHEA, vice chairman, Dept. of Infectious Disease, Medical Director for Infection Prevention, Cleveland Clinic
• Risk Factors for CDI: disease severity (sicker patients=higher risk), antibiotics, PPI use, NG tubes and tube feeds, stool softeners and enemas, GI surgery, increasing age.
• Treatment: stop abx if possible, no antiperistaltics, metronidazole 500mg po tid x 10d- 1st line, alt. vancomycin 125-150mg po qid x 10d, vancomycin preferred rx for seriously ill (wbc>20k, ARF, abd.distention, hemodynamic instability).
• Do not treat asymptomatic patient with stool sample + for C. diff.
Emerging Antimicrobial Resistance Issues
COL Glenn Wortmann, MD Chief of integrated Infectious Diseases Services Walter Reed army Medical Center and Bethesda Naval National Naval Center, Program Director of National Capital Consortium Infectious Diseases Fellowship Program, Assoc. Prof. of Medicine Uniformed Services University of the Health Sciences
• Global trends in rising antimicrobial resistance suggest that the antibiotic era may be ending.
• Emphasis shifting from infection treatment to prevention.
• Maximize hand washing: Wash in, wash out and lead by example.
• Consider chlorhexidine washes in high-risk patients as well as environmental decontamination devices.
• Judicious Use of Antimicrobial Agents: use narrow spectrum agents for shortest duration of therapy feasible, formulary restriction, mandatory ID or pharmacy consultation.
How to be a Leader in Antimicrobial Stewardship in Your Hospital
Arjun Srinivasan, MD FSHEA Assoc. Dir. for Healthcare Associated Infection Prevention Programs in the Div. of Healthcare Quality Promotion at the Centers for Disease Control and Prevention (CDC)
• Hospitalists have the greatest influence over how abx are used in hospitals.
• Hospitalists have the background, experience and strong interest in QI work to affect change; know that up to 50% of all antibiotic use is inappropriate.
• Hospitalists can help tackle issues of abx misuse with signouts, handoffs, and care transitions.
•
ID Emergencies: Diagnoses you can’t afford to miss
James Pile, MD FACP SFHM practicing hospitalist and ID specialist at Cleveland Clinic
• Acute Bacterial Meningitis: LP and Brain Imaging, subset of low-risk patients appears not to require imaging prior to LP, even pts with mild mass effects can probably be safely tapped, herniation may occur even with normal CT-if clinical evidence suggests increasing icp, consider deferring lp or using small gauge needle
• Rx: all adults-cover pneumococcus and meningococcus, empiric coverage of resistant S. pneumoniae is standard of care; cover for listeria for age >50, immunocompromised, alcoholic, pregnant, diabetic; recent head trauma or neurosurgery cover S. aureus and GNB (including pseudomonas).
• Steroids are recommended for suspected BM give dexamethasone with or before antibiotics.
• Spinal Epidural Abscess: It’s easy to miss!
• Necrotizing Fasciitis/Necrotizing Soft Tissue Infections (NSTI): Pain out of proportion to physical findings, systemic findings (delirium, fever, diaphoresis, tachycardia) out of proportion to physical findings; consider Dx to make Dx, easy to miss or delay diagnosis→worsening outcomes. Have low threshold for surgical consultation and/or CT in patients with what appears to be severe cellulitis; include clindamycin (with other abx) for empiric coverage
ID Pearls Every Hospitalist Should Know
John Flaherty, MD
• Re: Perioperative Abx, “Better late than never” does NOT apply. Ensure appropriate timing of peri-op abx.
• Fever ≠ Infection, No Fever ≠ No Infection.
• Sepsis and Hypotension: start broad-spectrum abx NOW.
• Persistent pna despite empiric rx and neg cx, think TB and blastomycoses.
• Fatigue, low-grade fever, and anemia- r/o infective endocarditis.
• Single+blood cx is not always a contaminant; is IS a source of prolonged hospitalization and further testing, so choose wisely when ordering blood cx.
Implementing Socio-Adaptive Change: The role of leaders, followers and bundles in preventing infection
Sanjay Saint, MD MPH Prof. of Int. Medicine University of Michigan, Dir. of the VA/Univeristy of Michigan Patient Safety Enhancement Program, Assoc. Chief of Medicine Ann Arbor VAMC
• Successful implementation of change requires recognition of both the technical and socio-adaptive barriers.
• The key to good leadership is good followership—very little written on subject of followership.
Infective Endocarditis and Intravascular Device Infections
Thomas Fraser, MD FACP FSHEA
• Management Highlights: If patient is sick, pull the line out. If patient has a bad bug, pull the line out. Most people with lines are health care experienced—start broad-spectrum abx and tailor rx once cx available. If you do not pull the line, follow very closely, have low threshold to call ID consult, S. aureus is in a class all its own.
• When can line be replaced? Timing depends on clinical need ultimately, clinically well with resolving syndrome, receiving effective rx, blood cx neg for 72 hrs; maybe longer for Candida species.
• Who should get a TEE for HCA S. aureus bacteremia? Patients with prolonged bacteremia; >4 days; presence of an intracardiac device (valve, icd, ppm); metastatic complication; vertebral or other osteomyelitis, etc. TH
Dr. Lindsey is a COO at Strategist Synergy Surgicalists, lead consultant at Asynd Consulting, and a Team Hospitalist member.
This ID focused pre-course was a jam-packed, practical, and high-yield review of relevant ID topics encountered by practicing hospitalists. Here are some of the key takeaways:
HIV and the Hospitalist in 2013
John Flaherty, MD, prof. of medicine at Northwestern University Feinberg School of Medicine
• Lower the threshold for HIV testing; don’t limit to “high-risk” behaviors, 20% of those living with HIV/AID are unaware—so TEST!
• Recognize clinical clues to HIV infection: acute mono-like syndrome, unexplained chronic illness, comm.-acquired pneumonia.
Thomas Fraser, MD, FACP, FSHEA, vice chairman, Dept. of Infectious Disease, Medical Director for Infection Prevention, Cleveland Clinic
• Risk Factors for CDI: disease severity (sicker patients=higher risk), antibiotics, PPI use, NG tubes and tube feeds, stool softeners and enemas, GI surgery, increasing age.
• Treatment: stop abx if possible, no antiperistaltics, metronidazole 500mg po tid x 10d- 1st line, alt. vancomycin 125-150mg po qid x 10d, vancomycin preferred rx for seriously ill (wbc>20k, ARF, abd.distention, hemodynamic instability).
• Do not treat asymptomatic patient with stool sample + for C. diff.
Emerging Antimicrobial Resistance Issues
COL Glenn Wortmann, MD Chief of integrated Infectious Diseases Services Walter Reed army Medical Center and Bethesda Naval National Naval Center, Program Director of National Capital Consortium Infectious Diseases Fellowship Program, Assoc. Prof. of Medicine Uniformed Services University of the Health Sciences
• Global trends in rising antimicrobial resistance suggest that the antibiotic era may be ending.
• Emphasis shifting from infection treatment to prevention.
• Maximize hand washing: Wash in, wash out and lead by example.
• Consider chlorhexidine washes in high-risk patients as well as environmental decontamination devices.
• Judicious Use of Antimicrobial Agents: use narrow spectrum agents for shortest duration of therapy feasible, formulary restriction, mandatory ID or pharmacy consultation.
How to be a Leader in Antimicrobial Stewardship in Your Hospital
Arjun Srinivasan, MD FSHEA Assoc. Dir. for Healthcare Associated Infection Prevention Programs in the Div. of Healthcare Quality Promotion at the Centers for Disease Control and Prevention (CDC)
• Hospitalists have the greatest influence over how abx are used in hospitals.
• Hospitalists have the background, experience and strong interest in QI work to affect change; know that up to 50% of all antibiotic use is inappropriate.
• Hospitalists can help tackle issues of abx misuse with signouts, handoffs, and care transitions.
•
ID Emergencies: Diagnoses you can’t afford to miss
James Pile, MD FACP SFHM practicing hospitalist and ID specialist at Cleveland Clinic
• Acute Bacterial Meningitis: LP and Brain Imaging, subset of low-risk patients appears not to require imaging prior to LP, even pts with mild mass effects can probably be safely tapped, herniation may occur even with normal CT-if clinical evidence suggests increasing icp, consider deferring lp or using small gauge needle
• Rx: all adults-cover pneumococcus and meningococcus, empiric coverage of resistant S. pneumoniae is standard of care; cover for listeria for age >50, immunocompromised, alcoholic, pregnant, diabetic; recent head trauma or neurosurgery cover S. aureus and GNB (including pseudomonas).
• Steroids are recommended for suspected BM give dexamethasone with or before antibiotics.
• Spinal Epidural Abscess: It’s easy to miss!
• Necrotizing Fasciitis/Necrotizing Soft Tissue Infections (NSTI): Pain out of proportion to physical findings, systemic findings (delirium, fever, diaphoresis, tachycardia) out of proportion to physical findings; consider Dx to make Dx, easy to miss or delay diagnosis→worsening outcomes. Have low threshold for surgical consultation and/or CT in patients with what appears to be severe cellulitis; include clindamycin (with other abx) for empiric coverage
ID Pearls Every Hospitalist Should Know
John Flaherty, MD
• Re: Perioperative Abx, “Better late than never” does NOT apply. Ensure appropriate timing of peri-op abx.
• Fever ≠ Infection, No Fever ≠ No Infection.
• Sepsis and Hypotension: start broad-spectrum abx NOW.
• Persistent pna despite empiric rx and neg cx, think TB and blastomycoses.
• Fatigue, low-grade fever, and anemia- r/o infective endocarditis.
• Single+blood cx is not always a contaminant; is IS a source of prolonged hospitalization and further testing, so choose wisely when ordering blood cx.
Implementing Socio-Adaptive Change: The role of leaders, followers and bundles in preventing infection
Sanjay Saint, MD MPH Prof. of Int. Medicine University of Michigan, Dir. of the VA/Univeristy of Michigan Patient Safety Enhancement Program, Assoc. Chief of Medicine Ann Arbor VAMC
• Successful implementation of change requires recognition of both the technical and socio-adaptive barriers.
• The key to good leadership is good followership—very little written on subject of followership.
Infective Endocarditis and Intravascular Device Infections
Thomas Fraser, MD FACP FSHEA
• Management Highlights: If patient is sick, pull the line out. If patient has a bad bug, pull the line out. Most people with lines are health care experienced—start broad-spectrum abx and tailor rx once cx available. If you do not pull the line, follow very closely, have low threshold to call ID consult, S. aureus is in a class all its own.
• When can line be replaced? Timing depends on clinical need ultimately, clinically well with resolving syndrome, receiving effective rx, blood cx neg for 72 hrs; maybe longer for Candida species.
• Who should get a TEE for HCA S. aureus bacteremia? Patients with prolonged bacteremia; >4 days; presence of an intracardiac device (valve, icd, ppm); metastatic complication; vertebral or other osteomyelitis, etc. TH
Dr. Lindsey is a COO at Strategist Synergy Surgicalists, lead consultant at Asynd Consulting, and a Team Hospitalist member.
CME, Procedures, and Advocacy Highlight Hospital Medicine 2013 Kickoff
Top 10 Strategies to Improve Patient Safety
Clinical question
What are the most effective strategies in improving patient safety?
Bottom line
This group of experts, commissioned by the Agency for Healthcare Research and Quality (AHRQ), outlined the top 10 strategies for improved patient safety. These strategies, which are "strongly encouraged" for adoption in all health care systems, consist primarily of interventions that help prevent health care-associated infections and avoid medical errors. LOE = 5
Reference
Study design
Systematic review
Funding source
Government
Allocation
Uncertain
Setting
Various (guideline)
Synopsis
Previous publications by the Institute of Medicine and the AHRQ have highlighted the importance of patient safety practices. A group of researchers, supported by the AHRQ, evaluated the data on current strategies to improve patient safety. The group assessed the quality of existing systematic reviews on these topics and performed new literature searches when needed. The focus was on data that reported on implementation and adoption of these strategies, as well as on the context in which they have been used. Individual studies on safety interventions were examined for quality and risk of bias. The authors rated the strength of evidence of the effectiveness of each intervention, reported evidence on possible harmful consequences, assessed difficulty in implementation, and estimated costs. Of the 41 safety strategies that were evaluated, the following 10 were chosen as strategies that are "strongly encouraged" for adoption now: 1. Preoperative and anesthesia checklists to prevent perioperative events 2. Bundles that include checklists to prevent central line-associated bloodstream infections 3. Interventions to reduce urinary catheter use, including catheter reminders, stop orders , or nurse-initiated removal protocols 4. Bundles that include head-of-bed elevation, sedation vacations, oral care with chlorhexidine, and subglottic suctioning endotracheal tubes to prevent ventilator-associated pneumonia 5. Hand hygiene 6. The do-not-use list for hazardous abbreviations 7. Multicomponent interventions to reduce pressure ulcers 8. Barrier precautions to prevent health care-associated infections 9. Use of real-time ultrasonography for central line placement 10. Interventions to improve prophylaxis for venous thromboembolism.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question
What are the most effective strategies in improving patient safety?
Bottom line
This group of experts, commissioned by the Agency for Healthcare Research and Quality (AHRQ), outlined the top 10 strategies for improved patient safety. These strategies, which are "strongly encouraged" for adoption in all health care systems, consist primarily of interventions that help prevent health care-associated infections and avoid medical errors. LOE = 5
Reference
Study design
Systematic review
Funding source
Government
Allocation
Uncertain
Setting
Various (guideline)
Synopsis
Previous publications by the Institute of Medicine and the AHRQ have highlighted the importance of patient safety practices. A group of researchers, supported by the AHRQ, evaluated the data on current strategies to improve patient safety. The group assessed the quality of existing systematic reviews on these topics and performed new literature searches when needed. The focus was on data that reported on implementation and adoption of these strategies, as well as on the context in which they have been used. Individual studies on safety interventions were examined for quality and risk of bias. The authors rated the strength of evidence of the effectiveness of each intervention, reported evidence on possible harmful consequences, assessed difficulty in implementation, and estimated costs. Of the 41 safety strategies that were evaluated, the following 10 were chosen as strategies that are "strongly encouraged" for adoption now: 1. Preoperative and anesthesia checklists to prevent perioperative events 2. Bundles that include checklists to prevent central line-associated bloodstream infections 3. Interventions to reduce urinary catheter use, including catheter reminders, stop orders , or nurse-initiated removal protocols 4. Bundles that include head-of-bed elevation, sedation vacations, oral care with chlorhexidine, and subglottic suctioning endotracheal tubes to prevent ventilator-associated pneumonia 5. Hand hygiene 6. The do-not-use list for hazardous abbreviations 7. Multicomponent interventions to reduce pressure ulcers 8. Barrier precautions to prevent health care-associated infections 9. Use of real-time ultrasonography for central line placement 10. Interventions to improve prophylaxis for venous thromboembolism.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question
What are the most effective strategies in improving patient safety?
Bottom line
This group of experts, commissioned by the Agency for Healthcare Research and Quality (AHRQ), outlined the top 10 strategies for improved patient safety. These strategies, which are "strongly encouraged" for adoption in all health care systems, consist primarily of interventions that help prevent health care-associated infections and avoid medical errors. LOE = 5
Reference
Study design
Systematic review
Funding source
Government
Allocation
Uncertain
Setting
Various (guideline)
Synopsis
Previous publications by the Institute of Medicine and the AHRQ have highlighted the importance of patient safety practices. A group of researchers, supported by the AHRQ, evaluated the data on current strategies to improve patient safety. The group assessed the quality of existing systematic reviews on these topics and performed new literature searches when needed. The focus was on data that reported on implementation and adoption of these strategies, as well as on the context in which they have been used. Individual studies on safety interventions were examined for quality and risk of bias. The authors rated the strength of evidence of the effectiveness of each intervention, reported evidence on possible harmful consequences, assessed difficulty in implementation, and estimated costs. Of the 41 safety strategies that were evaluated, the following 10 were chosen as strategies that are "strongly encouraged" for adoption now: 1. Preoperative and anesthesia checklists to prevent perioperative events 2. Bundles that include checklists to prevent central line-associated bloodstream infections 3. Interventions to reduce urinary catheter use, including catheter reminders, stop orders , or nurse-initiated removal protocols 4. Bundles that include head-of-bed elevation, sedation vacations, oral care with chlorhexidine, and subglottic suctioning endotracheal tubes to prevent ventilator-associated pneumonia 5. Hand hygiene 6. The do-not-use list for hazardous abbreviations 7. Multicomponent interventions to reduce pressure ulcers 8. Barrier precautions to prevent health care-associated infections 9. Use of real-time ultrasonography for central line placement 10. Interventions to improve prophylaxis for venous thromboembolism.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
No Reduction in Mortality or Readmission with Addition of Aliskiren for HF Patients (ASTRONAUT)
Clinical question
Does the addition of aliskiren, a direct renin inhibitor, to standard therapy decrease mortality and readmission in patients hospitalized for worsening heart failure?
Bottom line
The addition of aliskiren to standard therapy in patients hospitalized with heart failure (HF) does not reduce cardiovascular mortality or HF readmission rates. LOE = 1b
Reference
Study design
Randomized controlled trial (double-blinded)
Funding source
Industry
Allocation
Uncertain
Setting
Inpatient (any location) with outpatient follow-up
Synopsis
Despite current standard therapy, postdischarge mortality and rehospitalizations remain high for patients hospitalized for HF. To study the effect of direct renin inhibitors on these outcomes, investigators enrolled adults hospitalized for worsening HF with a left ventricular ejection fraction (LVEF) of 40% or less. Once these patients were clinically and hemodynamically stable, they were randomized to receive aliskiren 150 mg daily or placebo. Study patients were followed up at regular intervals and the aliskiren dose was increased to 300 mg daily as long as the initial dose was tolerated. Aliskiren, either 150 mg or 300 mg, was then continued up to a maximum follow-up time of 12 months. All patients also received standard HF therapy at the discretion of their treating physicians. The 2 groups had similar baseline characteristics. The patients' mean age was 65 years, mean LVEF was 28%, and the majority were New York Heart Association Class III-IV at randomization. For the primary end point of either cardiovascular death or HF rehospitalization at 6 months, there was no significant difference between the aliskiren and placebo groups. Events rates between the 2 groups were also similar at 12 months. The aliskiren group was more likely to experience hyperkalemia, hypotension, and renal impairment or renal failure. Additionally, a subgroup analysis showed that patients with diabetes fared worse with aliskiren, with a greater risk of all-cause mortality at 12 months, than those who took placebo.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question
Does the addition of aliskiren, a direct renin inhibitor, to standard therapy decrease mortality and readmission in patients hospitalized for worsening heart failure?
Bottom line
The addition of aliskiren to standard therapy in patients hospitalized with heart failure (HF) does not reduce cardiovascular mortality or HF readmission rates. LOE = 1b
Reference
Study design
Randomized controlled trial (double-blinded)
Funding source
Industry
Allocation
Uncertain
Setting
Inpatient (any location) with outpatient follow-up
Synopsis
Despite current standard therapy, postdischarge mortality and rehospitalizations remain high for patients hospitalized for HF. To study the effect of direct renin inhibitors on these outcomes, investigators enrolled adults hospitalized for worsening HF with a left ventricular ejection fraction (LVEF) of 40% or less. Once these patients were clinically and hemodynamically stable, they were randomized to receive aliskiren 150 mg daily or placebo. Study patients were followed up at regular intervals and the aliskiren dose was increased to 300 mg daily as long as the initial dose was tolerated. Aliskiren, either 150 mg or 300 mg, was then continued up to a maximum follow-up time of 12 months. All patients also received standard HF therapy at the discretion of their treating physicians. The 2 groups had similar baseline characteristics. The patients' mean age was 65 years, mean LVEF was 28%, and the majority were New York Heart Association Class III-IV at randomization. For the primary end point of either cardiovascular death or HF rehospitalization at 6 months, there was no significant difference between the aliskiren and placebo groups. Events rates between the 2 groups were also similar at 12 months. The aliskiren group was more likely to experience hyperkalemia, hypotension, and renal impairment or renal failure. Additionally, a subgroup analysis showed that patients with diabetes fared worse with aliskiren, with a greater risk of all-cause mortality at 12 months, than those who took placebo.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question
Does the addition of aliskiren, a direct renin inhibitor, to standard therapy decrease mortality and readmission in patients hospitalized for worsening heart failure?
Bottom line
The addition of aliskiren to standard therapy in patients hospitalized with heart failure (HF) does not reduce cardiovascular mortality or HF readmission rates. LOE = 1b
Reference
Study design
Randomized controlled trial (double-blinded)
Funding source
Industry
Allocation
Uncertain
Setting
Inpatient (any location) with outpatient follow-up
Synopsis
Despite current standard therapy, postdischarge mortality and rehospitalizations remain high for patients hospitalized for HF. To study the effect of direct renin inhibitors on these outcomes, investigators enrolled adults hospitalized for worsening HF with a left ventricular ejection fraction (LVEF) of 40% or less. Once these patients were clinically and hemodynamically stable, they were randomized to receive aliskiren 150 mg daily or placebo. Study patients were followed up at regular intervals and the aliskiren dose was increased to 300 mg daily as long as the initial dose was tolerated. Aliskiren, either 150 mg or 300 mg, was then continued up to a maximum follow-up time of 12 months. All patients also received standard HF therapy at the discretion of their treating physicians. The 2 groups had similar baseline characteristics. The patients' mean age was 65 years, mean LVEF was 28%, and the majority were New York Heart Association Class III-IV at randomization. For the primary end point of either cardiovascular death or HF rehospitalization at 6 months, there was no significant difference between the aliskiren and placebo groups. Events rates between the 2 groups were also similar at 12 months. The aliskiren group was more likely to experience hyperkalemia, hypotension, and renal impairment or renal failure. Additionally, a subgroup analysis showed that patients with diabetes fared worse with aliskiren, with a greater risk of all-cause mortality at 12 months, than those who took placebo.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Golimumab indication expanded to include ulcerative colitis
The approval of the biologic drug golimumab has been expanded to include the treatment of adults with moderate to severe ulcerative colitis that is refractory to prior treatment or requires continuous steroid therapy, the Food and Drug Administration announced on May 15.
Golimumab (Simponi), a tumor necrosis factor–blocker, was approved in 2009 for treatment of moderate to severe active rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis, all in adults. Simponi is marketed by Janssen Ortho Biotech.
The approval for ulcerative colitis was based on two studies of patients with moderate to severe ulcerative colitis, according to the FDA statement announcing the approval. In one study, which enrolled 513 patients who could not tolerate or had not responded to other treatments, "a greater proportion of Simponi-treated patients achieved clinical response, clinical remission and, as seen during endoscopy, had improved appearance of the colon after 6 weeks," compared with those on placebo, the statement said.
In a study of 310 patients who had responded to golimumab and were then randomized to continue treatment with golimumab or were switched to placebo, "a greater proportion of Simponi-treated patients maintained clinical response through week 54, had clinical remission at both weeks 30 and 54 and, as seen during endoscopy, had improved appearance of the colon at both weeks 30 and 54 compared with the placebo group," the FDA said. The most common adverse effects associated with golimumab are upper respiratory infection and redness at the injection site.
The risks of serious infections, invasive fungal infections, reactivation of hepatitis B infection, lymphoma, heart failure, nervous system disorders, and allergic reactions are increased with treatment.
Serious adverse events associated with golimumab should be reported to the FDA at 800-332-1088 or www.fda.gov/medwatch/.
The approval of the biologic drug golimumab has been expanded to include the treatment of adults with moderate to severe ulcerative colitis that is refractory to prior treatment or requires continuous steroid therapy, the Food and Drug Administration announced on May 15.
Golimumab (Simponi), a tumor necrosis factor–blocker, was approved in 2009 for treatment of moderate to severe active rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis, all in adults. Simponi is marketed by Janssen Ortho Biotech.
The approval for ulcerative colitis was based on two studies of patients with moderate to severe ulcerative colitis, according to the FDA statement announcing the approval. In one study, which enrolled 513 patients who could not tolerate or had not responded to other treatments, "a greater proportion of Simponi-treated patients achieved clinical response, clinical remission and, as seen during endoscopy, had improved appearance of the colon after 6 weeks," compared with those on placebo, the statement said.
In a study of 310 patients who had responded to golimumab and were then randomized to continue treatment with golimumab or were switched to placebo, "a greater proportion of Simponi-treated patients maintained clinical response through week 54, had clinical remission at both weeks 30 and 54 and, as seen during endoscopy, had improved appearance of the colon at both weeks 30 and 54 compared with the placebo group," the FDA said. The most common adverse effects associated with golimumab are upper respiratory infection and redness at the injection site.
The risks of serious infections, invasive fungal infections, reactivation of hepatitis B infection, lymphoma, heart failure, nervous system disorders, and allergic reactions are increased with treatment.
Serious adverse events associated with golimumab should be reported to the FDA at 800-332-1088 or www.fda.gov/medwatch/.
The approval of the biologic drug golimumab has been expanded to include the treatment of adults with moderate to severe ulcerative colitis that is refractory to prior treatment or requires continuous steroid therapy, the Food and Drug Administration announced on May 15.
Golimumab (Simponi), a tumor necrosis factor–blocker, was approved in 2009 for treatment of moderate to severe active rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis, all in adults. Simponi is marketed by Janssen Ortho Biotech.
The approval for ulcerative colitis was based on two studies of patients with moderate to severe ulcerative colitis, according to the FDA statement announcing the approval. In one study, which enrolled 513 patients who could not tolerate or had not responded to other treatments, "a greater proportion of Simponi-treated patients achieved clinical response, clinical remission and, as seen during endoscopy, had improved appearance of the colon after 6 weeks," compared with those on placebo, the statement said.
In a study of 310 patients who had responded to golimumab and were then randomized to continue treatment with golimumab or were switched to placebo, "a greater proportion of Simponi-treated patients maintained clinical response through week 54, had clinical remission at both weeks 30 and 54 and, as seen during endoscopy, had improved appearance of the colon at both weeks 30 and 54 compared with the placebo group," the FDA said. The most common adverse effects associated with golimumab are upper respiratory infection and redness at the injection site.
The risks of serious infections, invasive fungal infections, reactivation of hepatitis B infection, lymphoma, heart failure, nervous system disorders, and allergic reactions are increased with treatment.
Serious adverse events associated with golimumab should be reported to the FDA at 800-332-1088 or www.fda.gov/medwatch/.