User login
Proposed PMR guidelines aim to standardize therapy
PARIS – New international guidelines for polymyalgia rheumatica will focus on standardizing treatment practice across specialties.
When adopted, the proposed guidelines will succeed those published by the British Society of Rheumatology in 2009, according to Dr. Bhaskar Dasgupta, a primary author of the new guidelines and leader of the study group.
"This is the first transatlantic EULAR-ACR [European League against Rheumatism-American College of Rheumatology] guideline in rheumatology," he said at the annual European Congress of Rheumatology. "It is very patient-centered and was developed with patient input."
There has been a great need for a document such as this, he said. Primary care physicians are almost always on the front line of diagnosing polymyalgia rheumatica and often [the first] to treat these patients – with variable success, said Dr. Dasgupta, head of the Southend Hospital rheumatology department, Essex, England.
"This disorder is as common as – or more common than – rheumatoid arthritis, with a very high prevalence and incidence," he said. "It’s often diagnosed by general practitioners, with patients referred to nonrheumatologists. Yet there is a very wide variation in practice and a lot of uncertainty in the diagnosis. We are concerned that we have handed this over to primary care physicians when it needs so much clinical acumen to tease this out from other conditions.
The guidelines were developed using GRADE (Grading of Recommendations Assessment, Development and Evaluation) methodology and involving appraisal of 445 relevant publications in polymyalgia rheumatica (PMR), published since 1970. The document was reviewed on several occasions by an international panel that included 51 investigators from the United States and represented countries in Western and Eastern Europe, as well as Australia, New Zealand, Brazil, South America, Japan, and India. All recommendations were adopted unanimously without the need to vote, according to Dr. Dasgupta.
According to the proposed document, most patients are diagnosed and treated in primary care settings, but there are no well-elucidated referral algorithms for referral to specialty care. This can contribute to variability in treatment.
For instance, "a proportion of PMR patients do not adequately respond to glucocorticoid therapy and suffer frequent relapses and dependency on long-term high doses," according to the guidelines. "Prolonged glucocorticoid therapy is associated with considerable side effects especially when high doses are employed." Dr. Dasgupta said the proposed guidelines address groups that are at especially high risk for these problems. "While effective, steroids have the potential to cause serious side effects," he said. "It is important to know how to use them [steroids] correctly in PMR. The subgroups that are vulnerable to side effects – such as patients with diabetes, hypertension, osteoporosis, and glaucoma, and high disease activity should be recognized – female sex and those with peripheral arthritis or high inflammatory markers."
The guidelines are structured as a treatment algorithm, which begins with accurate diagnosis and patient assessment. They recommend that most patients be started on oral prednisone at the equivalent of 12.5-25 mg/day, or if the patient is at high risk of steroid-related side effects, to begin with intramuscular glucocorticoids.
If there is inadequate response, the guidelines recommend an increase in glucocorticoid dose or methotrexate for those at high risk of side effects, relapse, or prolonged therapy.
If there is improvement within 4 weeks, consider a gradual tapering of steroids. If not, a confirmation of the diagnosis is in order, the guidelines note. Patients who respond well to the taper will likely go into remission and may continue the taper. Patients who relapse should have a diagnostic confirmation and/or specialist referral.
"Ultimately, in order to be accepted, the guidelines will require confirmation of their usefulness in clinical practice. PMR recommendations endorsed by both the ACR and EULAR would have a significant impact on clinical decision making, would reduce practice variation, and would stimulate further research in areas where there is currently lack of adequate evidence."
In addition, he said, the role for early methotrexate in treatment of the condition is now emerging and will be included in the guidelines for consideration in special subgroups.
The guidelines must still be ratified by both the ACR and EULAR. Once that happens, they will be simultaneously published in both associations’ journals – no later than mid-2015, Dr. Dasgupta said.
Dr. Dasgupta disclosed that he has helped design clinical trials for a number of drug companies and has received remuneration for educational symposia from others.
On Twitter @alz_gal
PARIS – New international guidelines for polymyalgia rheumatica will focus on standardizing treatment practice across specialties.
When adopted, the proposed guidelines will succeed those published by the British Society of Rheumatology in 2009, according to Dr. Bhaskar Dasgupta, a primary author of the new guidelines and leader of the study group.
"This is the first transatlantic EULAR-ACR [European League against Rheumatism-American College of Rheumatology] guideline in rheumatology," he said at the annual European Congress of Rheumatology. "It is very patient-centered and was developed with patient input."
There has been a great need for a document such as this, he said. Primary care physicians are almost always on the front line of diagnosing polymyalgia rheumatica and often [the first] to treat these patients – with variable success, said Dr. Dasgupta, head of the Southend Hospital rheumatology department, Essex, England.
"This disorder is as common as – or more common than – rheumatoid arthritis, with a very high prevalence and incidence," he said. "It’s often diagnosed by general practitioners, with patients referred to nonrheumatologists. Yet there is a very wide variation in practice and a lot of uncertainty in the diagnosis. We are concerned that we have handed this over to primary care physicians when it needs so much clinical acumen to tease this out from other conditions.
The guidelines were developed using GRADE (Grading of Recommendations Assessment, Development and Evaluation) methodology and involving appraisal of 445 relevant publications in polymyalgia rheumatica (PMR), published since 1970. The document was reviewed on several occasions by an international panel that included 51 investigators from the United States and represented countries in Western and Eastern Europe, as well as Australia, New Zealand, Brazil, South America, Japan, and India. All recommendations were adopted unanimously without the need to vote, according to Dr. Dasgupta.
According to the proposed document, most patients are diagnosed and treated in primary care settings, but there are no well-elucidated referral algorithms for referral to specialty care. This can contribute to variability in treatment.
For instance, "a proportion of PMR patients do not adequately respond to glucocorticoid therapy and suffer frequent relapses and dependency on long-term high doses," according to the guidelines. "Prolonged glucocorticoid therapy is associated with considerable side effects especially when high doses are employed." Dr. Dasgupta said the proposed guidelines address groups that are at especially high risk for these problems. "While effective, steroids have the potential to cause serious side effects," he said. "It is important to know how to use them [steroids] correctly in PMR. The subgroups that are vulnerable to side effects – such as patients with diabetes, hypertension, osteoporosis, and glaucoma, and high disease activity should be recognized – female sex and those with peripheral arthritis or high inflammatory markers."
The guidelines are structured as a treatment algorithm, which begins with accurate diagnosis and patient assessment. They recommend that most patients be started on oral prednisone at the equivalent of 12.5-25 mg/day, or if the patient is at high risk of steroid-related side effects, to begin with intramuscular glucocorticoids.
If there is inadequate response, the guidelines recommend an increase in glucocorticoid dose or methotrexate for those at high risk of side effects, relapse, or prolonged therapy.
If there is improvement within 4 weeks, consider a gradual tapering of steroids. If not, a confirmation of the diagnosis is in order, the guidelines note. Patients who respond well to the taper will likely go into remission and may continue the taper. Patients who relapse should have a diagnostic confirmation and/or specialist referral.
"Ultimately, in order to be accepted, the guidelines will require confirmation of their usefulness in clinical practice. PMR recommendations endorsed by both the ACR and EULAR would have a significant impact on clinical decision making, would reduce practice variation, and would stimulate further research in areas where there is currently lack of adequate evidence."
In addition, he said, the role for early methotrexate in treatment of the condition is now emerging and will be included in the guidelines for consideration in special subgroups.
The guidelines must still be ratified by both the ACR and EULAR. Once that happens, they will be simultaneously published in both associations’ journals – no later than mid-2015, Dr. Dasgupta said.
Dr. Dasgupta disclosed that he has helped design clinical trials for a number of drug companies and has received remuneration for educational symposia from others.
On Twitter @alz_gal
PARIS – New international guidelines for polymyalgia rheumatica will focus on standardizing treatment practice across specialties.
When adopted, the proposed guidelines will succeed those published by the British Society of Rheumatology in 2009, according to Dr. Bhaskar Dasgupta, a primary author of the new guidelines and leader of the study group.
"This is the first transatlantic EULAR-ACR [European League against Rheumatism-American College of Rheumatology] guideline in rheumatology," he said at the annual European Congress of Rheumatology. "It is very patient-centered and was developed with patient input."
There has been a great need for a document such as this, he said. Primary care physicians are almost always on the front line of diagnosing polymyalgia rheumatica and often [the first] to treat these patients – with variable success, said Dr. Dasgupta, head of the Southend Hospital rheumatology department, Essex, England.
"This disorder is as common as – or more common than – rheumatoid arthritis, with a very high prevalence and incidence," he said. "It’s often diagnosed by general practitioners, with patients referred to nonrheumatologists. Yet there is a very wide variation in practice and a lot of uncertainty in the diagnosis. We are concerned that we have handed this over to primary care physicians when it needs so much clinical acumen to tease this out from other conditions.
The guidelines were developed using GRADE (Grading of Recommendations Assessment, Development and Evaluation) methodology and involving appraisal of 445 relevant publications in polymyalgia rheumatica (PMR), published since 1970. The document was reviewed on several occasions by an international panel that included 51 investigators from the United States and represented countries in Western and Eastern Europe, as well as Australia, New Zealand, Brazil, South America, Japan, and India. All recommendations were adopted unanimously without the need to vote, according to Dr. Dasgupta.
According to the proposed document, most patients are diagnosed and treated in primary care settings, but there are no well-elucidated referral algorithms for referral to specialty care. This can contribute to variability in treatment.
For instance, "a proportion of PMR patients do not adequately respond to glucocorticoid therapy and suffer frequent relapses and dependency on long-term high doses," according to the guidelines. "Prolonged glucocorticoid therapy is associated with considerable side effects especially when high doses are employed." Dr. Dasgupta said the proposed guidelines address groups that are at especially high risk for these problems. "While effective, steroids have the potential to cause serious side effects," he said. "It is important to know how to use them [steroids] correctly in PMR. The subgroups that are vulnerable to side effects – such as patients with diabetes, hypertension, osteoporosis, and glaucoma, and high disease activity should be recognized – female sex and those with peripheral arthritis or high inflammatory markers."
The guidelines are structured as a treatment algorithm, which begins with accurate diagnosis and patient assessment. They recommend that most patients be started on oral prednisone at the equivalent of 12.5-25 mg/day, or if the patient is at high risk of steroid-related side effects, to begin with intramuscular glucocorticoids.
If there is inadequate response, the guidelines recommend an increase in glucocorticoid dose or methotrexate for those at high risk of side effects, relapse, or prolonged therapy.
If there is improvement within 4 weeks, consider a gradual tapering of steroids. If not, a confirmation of the diagnosis is in order, the guidelines note. Patients who respond well to the taper will likely go into remission and may continue the taper. Patients who relapse should have a diagnostic confirmation and/or specialist referral.
"Ultimately, in order to be accepted, the guidelines will require confirmation of their usefulness in clinical practice. PMR recommendations endorsed by both the ACR and EULAR would have a significant impact on clinical decision making, would reduce practice variation, and would stimulate further research in areas where there is currently lack of adequate evidence."
In addition, he said, the role for early methotrexate in treatment of the condition is now emerging and will be included in the guidelines for consideration in special subgroups.
The guidelines must still be ratified by both the ACR and EULAR. Once that happens, they will be simultaneously published in both associations’ journals – no later than mid-2015, Dr. Dasgupta said.
Dr. Dasgupta disclosed that he has helped design clinical trials for a number of drug companies and has received remuneration for educational symposia from others.
On Twitter @alz_gal
AT THE EULAR CONGRESS 2014
Mentorship: An essential key to growth and success
In 2011, an article titled "Building a Successful Career: Advice From Leaders in Thoracic Surgery" was published in Thoracic Surgical Clinics of North America.1 In developing this paper, Dr. Sean Grondin states, "I have been fortunate to have had mentors who have guided me through my surgical training and early years of practice," and he continues, "I realize how much I have learned from and been influenced by the experience and guidance of other surgeons."
Based on his experiences, Dr. Grondin selected a group of 20 outstanding leaders in thoracic surgery, and asked them to each write a short summary of what they deemed to be key elements for developing a successful thoracic surgical career. The inspiration for the paper was an appreciation for mentorship and a desire to further disseminate the influences of the greats in our field; it is both revealing and remarkably appropriate that, in their responses, the majority of the recognized leaders discussed the importance of cultivating strong mentorship relationships, with the word "mentor" mentioned 34 times in the article. The importance of having strong mentors to guide oneself in career development is highlighted over and over again.
In his comments, Dr. Douglas Mathisen states, "Residency training usually introduces you to the most important mentors in your life. They will be the ones who nurture you, educate you, and point you in the right direction. They are likely to bring out the desire in you to become an academic surgeon and educator."
Advice for success from Dr. Valerie Rusch included eight key points, one of which focused on mentorship: "Peer review and senior advice are frequently helpful, and most senior academic physicians are delighted to provide this. Mentors may be surgeons but are also often found in other specialties or even nonclinical settings." And, from the mentors’ perspective, Dr. F.G. Pearson remarks, "In a residency training program, the opportunity to act as a meaningful mentor is a gift and a rewarding opportunity."
For a cardiothoracic surgeon’s individual success, it is clear that having (and utilizing) the right mentors can make a significant impact. Further, when one considers the success of a group of individuals, it is equally important that mentorship relationships are present and strong. In the summer of 2011, the Senior Tour (a group of retired cardiothoracic surgeons committed to education and service for their profession) was asked by the Joint Council on Thoracic Surgery Education to visit 10 thoracic surgical training programs that were considered above average according to a poll taken of thoracic surgical residents in the fall of 2010 by the Thoracic Surgery Residents Association.2
As they summarized their findings, they noted that the top programs possessed many common features leading to superior training in cardiac and general thoracic surgery. The authors specifically noted seven key factors, and, among them, was "a significant emphasis on mentorship, with the program director playing the primary roles and with voluntary relationships between residents and other faculty and with mentorship also including involvement in job finding."
If mentorship is so important to success in this career path, exactly what opportunities exist for trainees seeking mentorship? A Google search for ["mentor" AND "thoracic surgery"] yields a number of results, with ultimate direction leading to essentially two organizations: the AATS and Women in Thoracic Surgery (WTS).
From the AATS website, there is a list of names and contact information for mentors who have been selected or self-nominated for prospective candidates for thoracic surgery residency. These mentors are available to offer guidance, recommendations, and research opportunities, as well as clinical rotations in cardiothoracic surgery (http://aats.org/TSR/contactsMentors.cgi).
A number of opportunities for mentorship are also available through WTS. There is a formal mentoring program, aiming to pair women interested in cardiothoracic surgical careers with established WTS members. Dr. Shanda Blackmon, the Mentoring Chair for the WTS, reflects on the program, stating, "Many surgeons think that mentorship has to be a formal relationship at the same institution. What we have learned at WTS is that mentorship relationships can be equally effective even when they are not formal and the mentor is not from the same institution." She continues, reporting that, "in the survey we conducted through WTS, we discovered that mentorship was one of the most important factors to young surgeons aspiring to start a career in thoracic surgery." It is for this reason that WTS places such emphasis on helping trainees find and sustain mentorship opportunities.
WTS specifically offers scholarships to the Society of Thoracic Surgeons meeting, the Scanlan/WTS Traveling Mentorship, the Carolyn Reed Award, a list of mentors online, and resident mentors. (Further details of all of these programs can be found at www.wtsnet.org.) WTS provides a number of opportunities for female trainees to connect with female mentors. But is it absolutely necessary to find mentors who are "like you"?
Dr. Jennifer Lawton, president of WTS, acknowledges that everyone needs mentoring, but urges that "mentoring of women and minorities is particularly important in order to take advantage of the vast array of benefits to be gained by ethnic, racial, and gender diversity in the workplace."
She continues: "If we don’t see others successful in a chosen field, we do not perceive the goal attainable for ourselves. I have seen this many times in cardiothoracic surgery and women. Women who are not exposed to female mentors have expressed concern that practice in the field is not possible for women (especially those who aspire to have a family)." And, further, she explains that "we are typically more comfortable in mentoring situations with others like ourselves (similar challenges, needs, concerns). Surveys demonstrate that medical students often choose fields of interest because of mentors. For these reasons, it is important for individuals to find mentors who are similar to themselves."
Additional formal mentoring programs exist, and include the Brooks Scholarship through the Southern Thoracic Surgical Association (STSA), the Society of Thoracic Surgeons Looking to the Future scholarship program, the AATS Member for a Day program, and more.
Exactly what should one hope to get out of a mentorship relationship? The truth is, it really depends on the stage of career and the specific needs of the mentee. Mentorship needs change over time, and even well-established mentoring relationships will evolve and adjust along with participants in the interaction.
Sarah Schubert is a fourth-year medical student at Penn State, who has matched into the I-6 program at the University of Virginia and is the current recipient of the Scanlan/WTS scholarship. This award provides trainees with an opportunity to gain exposure to women cardiothoracic surgeon mentors by visiting a WTS member for an elective period. Ms. Schubert reports that she applied for the scholarship because she "wanted to work with and learn from a highly successful female cardiac surgeon in hopes of initiating and developing a professional relationship with a woman in the field."
As a medical student, she has fairly basic mentorship needs. She tells us that "right now, I need mentors who can serve as good role models – in the OR, with patients, with colleagues and trainees, and in their personal lives outside the hospital. As I prepare to enter residency, I anticipate that I will need to further develop my patient care skills and operative techniques, as well as skills to manage time and obligations. Knowing and working with people who have already figured out how to juggle those different obligations will be immensely helpful." Other medical students may be looking for advice on interviewing and ranking residency programs, and, like Ms. Schubert, may be interested in tips on how to get a great start in internship.
For individuals deep in the throes of cardiothoracic training, the needs are clearly different. Dr. Ryan Shelstad, a first-year fellow at the University of Colorado, states: "In my mind, the primary objective of clinical fellowship is acquisition of technical skills and clinical decision making in CT surgery. Thus, mentorship at this stage follows this objective." He continues, "CT fellowship is a relatively short time to achieve this goal as well as position oneself to successfully transition to a faculty position or private practice, which is the second objective—and area for mentoring."
Dr. Shelstad acknowledges and explains the transition in his mentorship needs, "I think earlier in training, mentorship focused on career choice, research, and transition to a fellowship. Much was focused on getting to the next step. While that is still important, now is the time to focus on the clinical aspects of CT surgery that I will use the rest of my career." And, certainly, the specific mentoring needs will continue to change with time.
Dr. Lawton, who holds the rank of professor at Washington University, St. Louis, states that, "after reaching full professor, surgeons need mentoring and sponsoring to reach goals such as dean positions, leadership positions, national organization officer positions, etc. We also all continually need mosaic mentoring that evolves over time (someone to mentor for research career aspects, managing work-life balance issues, family issues, teaching issues, financial issues, etc.). As we progress in our careers, we have the opportunity to also be mentored in other areas by younger generations."
Wait, did she just say that progressing surgeons can be mentored by younger generations? Yes, she did. And not only can seasoned surgeons be mentored by younger surgeons, they also stand to gain considerably from their own mentees. Dr. Lawton further states, "There is always reciprocal gain in a mentoring relationship for the mentor. There is no better joy than to see a mentee succeed and be fulfilled and happy in her chosen field. For some, this provides a rich legacy of trainees and mentees to provide continued enrichment, excitement, and a source of tremendous pride in later years." In the previously mentioned article by Grondin, Dr. Gail Darling states, "Academic careers are usually measured in papers published, grants awarded, invited lectures, and academic standing. Equally important are the students we teach and motivate toward careers in surgery, residents and fellows we have taught and mentored who will provide care to patients and who will go out and teach new generations of surgeons who will in turn provide care."
Once mentorship bonds have been established, it is critical to cultivate these relationships and to gain the most possible from these interactions. When asked how he has achieved these ends, Dr. Shelstad replies, "You and your mentors have the same goal: mutual success. Work hard for your mentors, and they will work hard for you. I would encourage explicit discussion of goals and expectations to ensure you and a potential mentor are on the same page. Mentorship is essential to success in cardiothoracic surgery."
Without a doubt, participation in mentorship relationships is a key element of success at every stage of the career and development of a cardiothoracic surgeon. Outstanding programs already exist to support modern trainees, and further efforts will certainly be met with great enthusiasm. Also apparent is the need for ongoing, career-long mentorship – and the paucity of formal programs to support it. This need may be a great opportunity for the establishment of future programming.
On a personal note, when reflecting on mentorship, I think of a statement made by Benjamin Franklin: "Tell me and I forget, teach me and I may remember, involve me and I learn." To those incredible individuals who have taken the time, effort, and interest to truly involve me, I have immense gratitude. I will aim for the rest of my career to make it worth your while, with hopes to bring you pride and inspire others as you have inspired me. To all who have taken time to truly involve any student, resident, or junior colleague – you have motivated us and given strength to the ongoing legacy of our amazing field.
Citations
1. Grondin SC. Building a Successful Career: Advice From Leaders in Thoracic Surgery. Thorac. Surg. Clin. 2011;21(3):395-415.
2. J. Thorac. Cardiovasc. Surg. 2014;147(1):15-17.
In 2011, an article titled "Building a Successful Career: Advice From Leaders in Thoracic Surgery" was published in Thoracic Surgical Clinics of North America.1 In developing this paper, Dr. Sean Grondin states, "I have been fortunate to have had mentors who have guided me through my surgical training and early years of practice," and he continues, "I realize how much I have learned from and been influenced by the experience and guidance of other surgeons."
Based on his experiences, Dr. Grondin selected a group of 20 outstanding leaders in thoracic surgery, and asked them to each write a short summary of what they deemed to be key elements for developing a successful thoracic surgical career. The inspiration for the paper was an appreciation for mentorship and a desire to further disseminate the influences of the greats in our field; it is both revealing and remarkably appropriate that, in their responses, the majority of the recognized leaders discussed the importance of cultivating strong mentorship relationships, with the word "mentor" mentioned 34 times in the article. The importance of having strong mentors to guide oneself in career development is highlighted over and over again.
In his comments, Dr. Douglas Mathisen states, "Residency training usually introduces you to the most important mentors in your life. They will be the ones who nurture you, educate you, and point you in the right direction. They are likely to bring out the desire in you to become an academic surgeon and educator."
Advice for success from Dr. Valerie Rusch included eight key points, one of which focused on mentorship: "Peer review and senior advice are frequently helpful, and most senior academic physicians are delighted to provide this. Mentors may be surgeons but are also often found in other specialties or even nonclinical settings." And, from the mentors’ perspective, Dr. F.G. Pearson remarks, "In a residency training program, the opportunity to act as a meaningful mentor is a gift and a rewarding opportunity."
For a cardiothoracic surgeon’s individual success, it is clear that having (and utilizing) the right mentors can make a significant impact. Further, when one considers the success of a group of individuals, it is equally important that mentorship relationships are present and strong. In the summer of 2011, the Senior Tour (a group of retired cardiothoracic surgeons committed to education and service for their profession) was asked by the Joint Council on Thoracic Surgery Education to visit 10 thoracic surgical training programs that were considered above average according to a poll taken of thoracic surgical residents in the fall of 2010 by the Thoracic Surgery Residents Association.2
As they summarized their findings, they noted that the top programs possessed many common features leading to superior training in cardiac and general thoracic surgery. The authors specifically noted seven key factors, and, among them, was "a significant emphasis on mentorship, with the program director playing the primary roles and with voluntary relationships between residents and other faculty and with mentorship also including involvement in job finding."
If mentorship is so important to success in this career path, exactly what opportunities exist for trainees seeking mentorship? A Google search for ["mentor" AND "thoracic surgery"] yields a number of results, with ultimate direction leading to essentially two organizations: the AATS and Women in Thoracic Surgery (WTS).
From the AATS website, there is a list of names and contact information for mentors who have been selected or self-nominated for prospective candidates for thoracic surgery residency. These mentors are available to offer guidance, recommendations, and research opportunities, as well as clinical rotations in cardiothoracic surgery (http://aats.org/TSR/contactsMentors.cgi).
A number of opportunities for mentorship are also available through WTS. There is a formal mentoring program, aiming to pair women interested in cardiothoracic surgical careers with established WTS members. Dr. Shanda Blackmon, the Mentoring Chair for the WTS, reflects on the program, stating, "Many surgeons think that mentorship has to be a formal relationship at the same institution. What we have learned at WTS is that mentorship relationships can be equally effective even when they are not formal and the mentor is not from the same institution." She continues, reporting that, "in the survey we conducted through WTS, we discovered that mentorship was one of the most important factors to young surgeons aspiring to start a career in thoracic surgery." It is for this reason that WTS places such emphasis on helping trainees find and sustain mentorship opportunities.
WTS specifically offers scholarships to the Society of Thoracic Surgeons meeting, the Scanlan/WTS Traveling Mentorship, the Carolyn Reed Award, a list of mentors online, and resident mentors. (Further details of all of these programs can be found at www.wtsnet.org.) WTS provides a number of opportunities for female trainees to connect with female mentors. But is it absolutely necessary to find mentors who are "like you"?
Dr. Jennifer Lawton, president of WTS, acknowledges that everyone needs mentoring, but urges that "mentoring of women and minorities is particularly important in order to take advantage of the vast array of benefits to be gained by ethnic, racial, and gender diversity in the workplace."
She continues: "If we don’t see others successful in a chosen field, we do not perceive the goal attainable for ourselves. I have seen this many times in cardiothoracic surgery and women. Women who are not exposed to female mentors have expressed concern that practice in the field is not possible for women (especially those who aspire to have a family)." And, further, she explains that "we are typically more comfortable in mentoring situations with others like ourselves (similar challenges, needs, concerns). Surveys demonstrate that medical students often choose fields of interest because of mentors. For these reasons, it is important for individuals to find mentors who are similar to themselves."
Additional formal mentoring programs exist, and include the Brooks Scholarship through the Southern Thoracic Surgical Association (STSA), the Society of Thoracic Surgeons Looking to the Future scholarship program, the AATS Member for a Day program, and more.
Exactly what should one hope to get out of a mentorship relationship? The truth is, it really depends on the stage of career and the specific needs of the mentee. Mentorship needs change over time, and even well-established mentoring relationships will evolve and adjust along with participants in the interaction.
Sarah Schubert is a fourth-year medical student at Penn State, who has matched into the I-6 program at the University of Virginia and is the current recipient of the Scanlan/WTS scholarship. This award provides trainees with an opportunity to gain exposure to women cardiothoracic surgeon mentors by visiting a WTS member for an elective period. Ms. Schubert reports that she applied for the scholarship because she "wanted to work with and learn from a highly successful female cardiac surgeon in hopes of initiating and developing a professional relationship with a woman in the field."
As a medical student, she has fairly basic mentorship needs. She tells us that "right now, I need mentors who can serve as good role models – in the OR, with patients, with colleagues and trainees, and in their personal lives outside the hospital. As I prepare to enter residency, I anticipate that I will need to further develop my patient care skills and operative techniques, as well as skills to manage time and obligations. Knowing and working with people who have already figured out how to juggle those different obligations will be immensely helpful." Other medical students may be looking for advice on interviewing and ranking residency programs, and, like Ms. Schubert, may be interested in tips on how to get a great start in internship.
For individuals deep in the throes of cardiothoracic training, the needs are clearly different. Dr. Ryan Shelstad, a first-year fellow at the University of Colorado, states: "In my mind, the primary objective of clinical fellowship is acquisition of technical skills and clinical decision making in CT surgery. Thus, mentorship at this stage follows this objective." He continues, "CT fellowship is a relatively short time to achieve this goal as well as position oneself to successfully transition to a faculty position or private practice, which is the second objective—and area for mentoring."
Dr. Shelstad acknowledges and explains the transition in his mentorship needs, "I think earlier in training, mentorship focused on career choice, research, and transition to a fellowship. Much was focused on getting to the next step. While that is still important, now is the time to focus on the clinical aspects of CT surgery that I will use the rest of my career." And, certainly, the specific mentoring needs will continue to change with time.
Dr. Lawton, who holds the rank of professor at Washington University, St. Louis, states that, "after reaching full professor, surgeons need mentoring and sponsoring to reach goals such as dean positions, leadership positions, national organization officer positions, etc. We also all continually need mosaic mentoring that evolves over time (someone to mentor for research career aspects, managing work-life balance issues, family issues, teaching issues, financial issues, etc.). As we progress in our careers, we have the opportunity to also be mentored in other areas by younger generations."
Wait, did she just say that progressing surgeons can be mentored by younger generations? Yes, she did. And not only can seasoned surgeons be mentored by younger surgeons, they also stand to gain considerably from their own mentees. Dr. Lawton further states, "There is always reciprocal gain in a mentoring relationship for the mentor. There is no better joy than to see a mentee succeed and be fulfilled and happy in her chosen field. For some, this provides a rich legacy of trainees and mentees to provide continued enrichment, excitement, and a source of tremendous pride in later years." In the previously mentioned article by Grondin, Dr. Gail Darling states, "Academic careers are usually measured in papers published, grants awarded, invited lectures, and academic standing. Equally important are the students we teach and motivate toward careers in surgery, residents and fellows we have taught and mentored who will provide care to patients and who will go out and teach new generations of surgeons who will in turn provide care."
Once mentorship bonds have been established, it is critical to cultivate these relationships and to gain the most possible from these interactions. When asked how he has achieved these ends, Dr. Shelstad replies, "You and your mentors have the same goal: mutual success. Work hard for your mentors, and they will work hard for you. I would encourage explicit discussion of goals and expectations to ensure you and a potential mentor are on the same page. Mentorship is essential to success in cardiothoracic surgery."
Without a doubt, participation in mentorship relationships is a key element of success at every stage of the career and development of a cardiothoracic surgeon. Outstanding programs already exist to support modern trainees, and further efforts will certainly be met with great enthusiasm. Also apparent is the need for ongoing, career-long mentorship – and the paucity of formal programs to support it. This need may be a great opportunity for the establishment of future programming.
On a personal note, when reflecting on mentorship, I think of a statement made by Benjamin Franklin: "Tell me and I forget, teach me and I may remember, involve me and I learn." To those incredible individuals who have taken the time, effort, and interest to truly involve me, I have immense gratitude. I will aim for the rest of my career to make it worth your while, with hopes to bring you pride and inspire others as you have inspired me. To all who have taken time to truly involve any student, resident, or junior colleague – you have motivated us and given strength to the ongoing legacy of our amazing field.
Citations
1. Grondin SC. Building a Successful Career: Advice From Leaders in Thoracic Surgery. Thorac. Surg. Clin. 2011;21(3):395-415.
2. J. Thorac. Cardiovasc. Surg. 2014;147(1):15-17.
In 2011, an article titled "Building a Successful Career: Advice From Leaders in Thoracic Surgery" was published in Thoracic Surgical Clinics of North America.1 In developing this paper, Dr. Sean Grondin states, "I have been fortunate to have had mentors who have guided me through my surgical training and early years of practice," and he continues, "I realize how much I have learned from and been influenced by the experience and guidance of other surgeons."
Based on his experiences, Dr. Grondin selected a group of 20 outstanding leaders in thoracic surgery, and asked them to each write a short summary of what they deemed to be key elements for developing a successful thoracic surgical career. The inspiration for the paper was an appreciation for mentorship and a desire to further disseminate the influences of the greats in our field; it is both revealing and remarkably appropriate that, in their responses, the majority of the recognized leaders discussed the importance of cultivating strong mentorship relationships, with the word "mentor" mentioned 34 times in the article. The importance of having strong mentors to guide oneself in career development is highlighted over and over again.
In his comments, Dr. Douglas Mathisen states, "Residency training usually introduces you to the most important mentors in your life. They will be the ones who nurture you, educate you, and point you in the right direction. They are likely to bring out the desire in you to become an academic surgeon and educator."
Advice for success from Dr. Valerie Rusch included eight key points, one of which focused on mentorship: "Peer review and senior advice are frequently helpful, and most senior academic physicians are delighted to provide this. Mentors may be surgeons but are also often found in other specialties or even nonclinical settings." And, from the mentors’ perspective, Dr. F.G. Pearson remarks, "In a residency training program, the opportunity to act as a meaningful mentor is a gift and a rewarding opportunity."
For a cardiothoracic surgeon’s individual success, it is clear that having (and utilizing) the right mentors can make a significant impact. Further, when one considers the success of a group of individuals, it is equally important that mentorship relationships are present and strong. In the summer of 2011, the Senior Tour (a group of retired cardiothoracic surgeons committed to education and service for their profession) was asked by the Joint Council on Thoracic Surgery Education to visit 10 thoracic surgical training programs that were considered above average according to a poll taken of thoracic surgical residents in the fall of 2010 by the Thoracic Surgery Residents Association.2
As they summarized their findings, they noted that the top programs possessed many common features leading to superior training in cardiac and general thoracic surgery. The authors specifically noted seven key factors, and, among them, was "a significant emphasis on mentorship, with the program director playing the primary roles and with voluntary relationships between residents and other faculty and with mentorship also including involvement in job finding."
If mentorship is so important to success in this career path, exactly what opportunities exist for trainees seeking mentorship? A Google search for ["mentor" AND "thoracic surgery"] yields a number of results, with ultimate direction leading to essentially two organizations: the AATS and Women in Thoracic Surgery (WTS).
From the AATS website, there is a list of names and contact information for mentors who have been selected or self-nominated for prospective candidates for thoracic surgery residency. These mentors are available to offer guidance, recommendations, and research opportunities, as well as clinical rotations in cardiothoracic surgery (http://aats.org/TSR/contactsMentors.cgi).
A number of opportunities for mentorship are also available through WTS. There is a formal mentoring program, aiming to pair women interested in cardiothoracic surgical careers with established WTS members. Dr. Shanda Blackmon, the Mentoring Chair for the WTS, reflects on the program, stating, "Many surgeons think that mentorship has to be a formal relationship at the same institution. What we have learned at WTS is that mentorship relationships can be equally effective even when they are not formal and the mentor is not from the same institution." She continues, reporting that, "in the survey we conducted through WTS, we discovered that mentorship was one of the most important factors to young surgeons aspiring to start a career in thoracic surgery." It is for this reason that WTS places such emphasis on helping trainees find and sustain mentorship opportunities.
WTS specifically offers scholarships to the Society of Thoracic Surgeons meeting, the Scanlan/WTS Traveling Mentorship, the Carolyn Reed Award, a list of mentors online, and resident mentors. (Further details of all of these programs can be found at www.wtsnet.org.) WTS provides a number of opportunities for female trainees to connect with female mentors. But is it absolutely necessary to find mentors who are "like you"?
Dr. Jennifer Lawton, president of WTS, acknowledges that everyone needs mentoring, but urges that "mentoring of women and minorities is particularly important in order to take advantage of the vast array of benefits to be gained by ethnic, racial, and gender diversity in the workplace."
She continues: "If we don’t see others successful in a chosen field, we do not perceive the goal attainable for ourselves. I have seen this many times in cardiothoracic surgery and women. Women who are not exposed to female mentors have expressed concern that practice in the field is not possible for women (especially those who aspire to have a family)." And, further, she explains that "we are typically more comfortable in mentoring situations with others like ourselves (similar challenges, needs, concerns). Surveys demonstrate that medical students often choose fields of interest because of mentors. For these reasons, it is important for individuals to find mentors who are similar to themselves."
Additional formal mentoring programs exist, and include the Brooks Scholarship through the Southern Thoracic Surgical Association (STSA), the Society of Thoracic Surgeons Looking to the Future scholarship program, the AATS Member for a Day program, and more.
Exactly what should one hope to get out of a mentorship relationship? The truth is, it really depends on the stage of career and the specific needs of the mentee. Mentorship needs change over time, and even well-established mentoring relationships will evolve and adjust along with participants in the interaction.
Sarah Schubert is a fourth-year medical student at Penn State, who has matched into the I-6 program at the University of Virginia and is the current recipient of the Scanlan/WTS scholarship. This award provides trainees with an opportunity to gain exposure to women cardiothoracic surgeon mentors by visiting a WTS member for an elective period. Ms. Schubert reports that she applied for the scholarship because she "wanted to work with and learn from a highly successful female cardiac surgeon in hopes of initiating and developing a professional relationship with a woman in the field."
As a medical student, she has fairly basic mentorship needs. She tells us that "right now, I need mentors who can serve as good role models – in the OR, with patients, with colleagues and trainees, and in their personal lives outside the hospital. As I prepare to enter residency, I anticipate that I will need to further develop my patient care skills and operative techniques, as well as skills to manage time and obligations. Knowing and working with people who have already figured out how to juggle those different obligations will be immensely helpful." Other medical students may be looking for advice on interviewing and ranking residency programs, and, like Ms. Schubert, may be interested in tips on how to get a great start in internship.
For individuals deep in the throes of cardiothoracic training, the needs are clearly different. Dr. Ryan Shelstad, a first-year fellow at the University of Colorado, states: "In my mind, the primary objective of clinical fellowship is acquisition of technical skills and clinical decision making in CT surgery. Thus, mentorship at this stage follows this objective." He continues, "CT fellowship is a relatively short time to achieve this goal as well as position oneself to successfully transition to a faculty position or private practice, which is the second objective—and area for mentoring."
Dr. Shelstad acknowledges and explains the transition in his mentorship needs, "I think earlier in training, mentorship focused on career choice, research, and transition to a fellowship. Much was focused on getting to the next step. While that is still important, now is the time to focus on the clinical aspects of CT surgery that I will use the rest of my career." And, certainly, the specific mentoring needs will continue to change with time.
Dr. Lawton, who holds the rank of professor at Washington University, St. Louis, states that, "after reaching full professor, surgeons need mentoring and sponsoring to reach goals such as dean positions, leadership positions, national organization officer positions, etc. We also all continually need mosaic mentoring that evolves over time (someone to mentor for research career aspects, managing work-life balance issues, family issues, teaching issues, financial issues, etc.). As we progress in our careers, we have the opportunity to also be mentored in other areas by younger generations."
Wait, did she just say that progressing surgeons can be mentored by younger generations? Yes, she did. And not only can seasoned surgeons be mentored by younger surgeons, they also stand to gain considerably from their own mentees. Dr. Lawton further states, "There is always reciprocal gain in a mentoring relationship for the mentor. There is no better joy than to see a mentee succeed and be fulfilled and happy in her chosen field. For some, this provides a rich legacy of trainees and mentees to provide continued enrichment, excitement, and a source of tremendous pride in later years." In the previously mentioned article by Grondin, Dr. Gail Darling states, "Academic careers are usually measured in papers published, grants awarded, invited lectures, and academic standing. Equally important are the students we teach and motivate toward careers in surgery, residents and fellows we have taught and mentored who will provide care to patients and who will go out and teach new generations of surgeons who will in turn provide care."
Once mentorship bonds have been established, it is critical to cultivate these relationships and to gain the most possible from these interactions. When asked how he has achieved these ends, Dr. Shelstad replies, "You and your mentors have the same goal: mutual success. Work hard for your mentors, and they will work hard for you. I would encourage explicit discussion of goals and expectations to ensure you and a potential mentor are on the same page. Mentorship is essential to success in cardiothoracic surgery."
Without a doubt, participation in mentorship relationships is a key element of success at every stage of the career and development of a cardiothoracic surgeon. Outstanding programs already exist to support modern trainees, and further efforts will certainly be met with great enthusiasm. Also apparent is the need for ongoing, career-long mentorship – and the paucity of formal programs to support it. This need may be a great opportunity for the establishment of future programming.
On a personal note, when reflecting on mentorship, I think of a statement made by Benjamin Franklin: "Tell me and I forget, teach me and I may remember, involve me and I learn." To those incredible individuals who have taken the time, effort, and interest to truly involve me, I have immense gratitude. I will aim for the rest of my career to make it worth your while, with hopes to bring you pride and inspire others as you have inspired me. To all who have taken time to truly involve any student, resident, or junior colleague – you have motivated us and given strength to the ongoing legacy of our amazing field.
Citations
1. Grondin SC. Building a Successful Career: Advice From Leaders in Thoracic Surgery. Thorac. Surg. Clin. 2011;21(3):395-415.
2. J. Thorac. Cardiovasc. Surg. 2014;147(1):15-17.
Poor cardiovascular health predicted cognitive impairment
Adults in poor cardiovascular health were more likely to develop cognitive problems such as learning and memory impairment, compared with healthier peers, according to a large prospective study published online June 11 in the Journal of the American Heart Association.
But top scorers on the cardiovascular health (CVH) measure used in the study were not more protected against incident mental impairment than were intermediate scorers, reported Evan Thacker, Ph.D., of Brigham Young University in Provo, Utah, and his associates.
"This pattern suggests that even intermediate levels of CVH are preferable to low levels of CVH," the investigators said. "This is an encouraging message for population health promotion, because intermediate CVH is a more realistic target than ideal CVH for many individuals."
The investigators used the American Heart Association Life’s Simple 7 score to classify the cardiovascular health of 17,761 black and white adults in the United States aged 45 years and older (J. Am. Heart Assoc. 2014 June 11 [doi: 10.1161/JAHA.113.000635]). Individuals were participants in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study. The Six-Item Screener was used assess baseline global cognitive status; and a three-test measure of verbal learning, memory, and fluency was used to assess mental function at subsequent 2-year intervals. In all, 56% of individuals resided in "stroke belt" states, including Arkansas, Alabama, Louisiana, Georgia, Mississippi, North and South Carolina, and Tennessee, the investigators said. All study participants had normal cognitive function and no stroke history at the outset.
After adjustment for age, sex, race, and education, 4.6% of individuals with the worst CVH scores developed cognitive impairment after baseline (95% confidence interval, 4.0%-5.2%), compared with only 2.7% of those with intermediate scores (95% CI, 2.3%-3.1%) and 2.6% of those with the best scores (95% CI, 2.1%-3.1%), Dr. Thacker and his associates reported. Therefore, the odds of incident cognitive impairment were 35%-37% lower in the intermediate- and high-CVH groups than in the low-CVH group, the researchers added (odds ratios, 0.65 and 0.63; 95% CIs, 0.52-0.81 and 0.51-0.79, respectively).
"Rather than a dose-response pattern across the range of Life’s Simple 7 scores, we observed that associations with [incident clinical impairment] were the same for the highest tertile of Life’s Simple 7 score and the middle tertile, relative to the lowest tertile," the researchers wrote. "Based on these findings, we hypothesize that the AHA’s strategic efforts to improve CVH from poor to intermediate or higher levels could lead to reductions in cognitive decline, and we believe further research addressing this hypothesis is warranted."
The National Institute of Neurological Disorders and Stroke funded the study. The authors reported no conflicts of interest.
Adults in poor cardiovascular health were more likely to develop cognitive problems such as learning and memory impairment, compared with healthier peers, according to a large prospective study published online June 11 in the Journal of the American Heart Association.
But top scorers on the cardiovascular health (CVH) measure used in the study were not more protected against incident mental impairment than were intermediate scorers, reported Evan Thacker, Ph.D., of Brigham Young University in Provo, Utah, and his associates.
"This pattern suggests that even intermediate levels of CVH are preferable to low levels of CVH," the investigators said. "This is an encouraging message for population health promotion, because intermediate CVH is a more realistic target than ideal CVH for many individuals."
The investigators used the American Heart Association Life’s Simple 7 score to classify the cardiovascular health of 17,761 black and white adults in the United States aged 45 years and older (J. Am. Heart Assoc. 2014 June 11 [doi: 10.1161/JAHA.113.000635]). Individuals were participants in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study. The Six-Item Screener was used assess baseline global cognitive status; and a three-test measure of verbal learning, memory, and fluency was used to assess mental function at subsequent 2-year intervals. In all, 56% of individuals resided in "stroke belt" states, including Arkansas, Alabama, Louisiana, Georgia, Mississippi, North and South Carolina, and Tennessee, the investigators said. All study participants had normal cognitive function and no stroke history at the outset.
After adjustment for age, sex, race, and education, 4.6% of individuals with the worst CVH scores developed cognitive impairment after baseline (95% confidence interval, 4.0%-5.2%), compared with only 2.7% of those with intermediate scores (95% CI, 2.3%-3.1%) and 2.6% of those with the best scores (95% CI, 2.1%-3.1%), Dr. Thacker and his associates reported. Therefore, the odds of incident cognitive impairment were 35%-37% lower in the intermediate- and high-CVH groups than in the low-CVH group, the researchers added (odds ratios, 0.65 and 0.63; 95% CIs, 0.52-0.81 and 0.51-0.79, respectively).
"Rather than a dose-response pattern across the range of Life’s Simple 7 scores, we observed that associations with [incident clinical impairment] were the same for the highest tertile of Life’s Simple 7 score and the middle tertile, relative to the lowest tertile," the researchers wrote. "Based on these findings, we hypothesize that the AHA’s strategic efforts to improve CVH from poor to intermediate or higher levels could lead to reductions in cognitive decline, and we believe further research addressing this hypothesis is warranted."
The National Institute of Neurological Disorders and Stroke funded the study. The authors reported no conflicts of interest.
Adults in poor cardiovascular health were more likely to develop cognitive problems such as learning and memory impairment, compared with healthier peers, according to a large prospective study published online June 11 in the Journal of the American Heart Association.
But top scorers on the cardiovascular health (CVH) measure used in the study were not more protected against incident mental impairment than were intermediate scorers, reported Evan Thacker, Ph.D., of Brigham Young University in Provo, Utah, and his associates.
"This pattern suggests that even intermediate levels of CVH are preferable to low levels of CVH," the investigators said. "This is an encouraging message for population health promotion, because intermediate CVH is a more realistic target than ideal CVH for many individuals."
The investigators used the American Heart Association Life’s Simple 7 score to classify the cardiovascular health of 17,761 black and white adults in the United States aged 45 years and older (J. Am. Heart Assoc. 2014 June 11 [doi: 10.1161/JAHA.113.000635]). Individuals were participants in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study. The Six-Item Screener was used assess baseline global cognitive status; and a three-test measure of verbal learning, memory, and fluency was used to assess mental function at subsequent 2-year intervals. In all, 56% of individuals resided in "stroke belt" states, including Arkansas, Alabama, Louisiana, Georgia, Mississippi, North and South Carolina, and Tennessee, the investigators said. All study participants had normal cognitive function and no stroke history at the outset.
After adjustment for age, sex, race, and education, 4.6% of individuals with the worst CVH scores developed cognitive impairment after baseline (95% confidence interval, 4.0%-5.2%), compared with only 2.7% of those with intermediate scores (95% CI, 2.3%-3.1%) and 2.6% of those with the best scores (95% CI, 2.1%-3.1%), Dr. Thacker and his associates reported. Therefore, the odds of incident cognitive impairment were 35%-37% lower in the intermediate- and high-CVH groups than in the low-CVH group, the researchers added (odds ratios, 0.65 and 0.63; 95% CIs, 0.52-0.81 and 0.51-0.79, respectively).
"Rather than a dose-response pattern across the range of Life’s Simple 7 scores, we observed that associations with [incident clinical impairment] were the same for the highest tertile of Life’s Simple 7 score and the middle tertile, relative to the lowest tertile," the researchers wrote. "Based on these findings, we hypothesize that the AHA’s strategic efforts to improve CVH from poor to intermediate or higher levels could lead to reductions in cognitive decline, and we believe further research addressing this hypothesis is warranted."
The National Institute of Neurological Disorders and Stroke funded the study. The authors reported no conflicts of interest.
FROM THE JOURNAL OF THE AMERICAN HEART ASSOCIATION
Key clinical point: Intermediate or high cardiovascular health can lower the risk of cognitive impairment, compared with low CVH.
Major finding: The odds of incident cognitive impairment were 35%-37% lower in individuals with intermediate and high CVH scores than in individuals with the worst scores.
Data source: Prospective observational cohort study of 17,761 individuals aged 45 years and older with normal cognitive function and no stroke history at outset.
Disclosures: The National Institute of Neurological Disorders and Stroke funded the study. The authors reported no conflicts of interest.
Attendings in 'simultaneous' ORs
TORONTO – In academic medical centers, attending cardiothoracic surgeons often perform simultaneous procedures in different operating rooms as a means of increasing training opportunities for surgical fellows and to decrease hospital costs. However, the practice of running simultaneous operating rooms did not appear to affect perioperative timing or negatively affect patient outcomes, according to the results of a single institution review by Dr. Kenan W. Yount.
He and his colleagues at the University of Virginia, Charlottesville, wanted to examine their own data in guiding hospital policy as several major centers have recently proposed implementing a 1:1 ratio of attending surgeon-to-operating room.
In his presentation, Dr. Yount discussed the results of their review study, which categorized 1,377 cardiac and 1,682 general thoracic operations performed from July 2011 to July 2013 by attending, case type, and whether the attending was simultaneously supervising two surgeries. "Our institution adheres to a strict policy of attending surgeon oversight of and involvement in the critical and key portions of all operations," said Dr. Yount.
They compared operative duration, starting and closing times, postoperative complications, and 30-day mortality in each category. They also compared rates postoperative complications, hospital length of stay, and operative mortality in each category.
Interestingly, timing effects varied between the two overall types of surgery. Running two rooms had no effect on room start times, but thoracic rooms finished 16 minutes later than scheduled. Across six surgeons and 15 operation types, however, there were no differences in operative times.
"Furthermore, running two rooms was not associated with any differences in operative duration, morbidity, or mortality in our multivariate regression analyses, and there were no statistically significant differences in observed outcomes in any category," Dr. Yount said.
"In academic cardiothoracic surgical centers that rely on surgical support from fellowship training, the practice of running simultaneous operating rooms can be efficient and does not appear to negatively impact patient outcomes," said Dr. Yount. "In addition, the practice did not significantly increase operative duration or dramatically [affect] operating room starting or closing times," he concluded.
In discussing the implications of these results, he said, "Obviously, there are caveats: Attendings must be intimately involved in operations and scrubbed for every key and critical portion of the operation; also operations being scheduled in separate rooms must be done so with reasonable foresight."
As long as institutions are following these practices, he concluded, "It would appear that lens of current policy efforts is too narrow by focusing on perception. The debate should be refocused by challenging training programs to strengthen attending involvement and ensure the requisite competence of their trainees."
Dr. Yount reported no relevant disclosures.
TORONTO – In academic medical centers, attending cardiothoracic surgeons often perform simultaneous procedures in different operating rooms as a means of increasing training opportunities for surgical fellows and to decrease hospital costs. However, the practice of running simultaneous operating rooms did not appear to affect perioperative timing or negatively affect patient outcomes, according to the results of a single institution review by Dr. Kenan W. Yount.
He and his colleagues at the University of Virginia, Charlottesville, wanted to examine their own data in guiding hospital policy as several major centers have recently proposed implementing a 1:1 ratio of attending surgeon-to-operating room.
In his presentation, Dr. Yount discussed the results of their review study, which categorized 1,377 cardiac and 1,682 general thoracic operations performed from July 2011 to July 2013 by attending, case type, and whether the attending was simultaneously supervising two surgeries. "Our institution adheres to a strict policy of attending surgeon oversight of and involvement in the critical and key portions of all operations," said Dr. Yount.
They compared operative duration, starting and closing times, postoperative complications, and 30-day mortality in each category. They also compared rates postoperative complications, hospital length of stay, and operative mortality in each category.
Interestingly, timing effects varied between the two overall types of surgery. Running two rooms had no effect on room start times, but thoracic rooms finished 16 minutes later than scheduled. Across six surgeons and 15 operation types, however, there were no differences in operative times.
"Furthermore, running two rooms was not associated with any differences in operative duration, morbidity, or mortality in our multivariate regression analyses, and there were no statistically significant differences in observed outcomes in any category," Dr. Yount said.
"In academic cardiothoracic surgical centers that rely on surgical support from fellowship training, the practice of running simultaneous operating rooms can be efficient and does not appear to negatively impact patient outcomes," said Dr. Yount. "In addition, the practice did not significantly increase operative duration or dramatically [affect] operating room starting or closing times," he concluded.
In discussing the implications of these results, he said, "Obviously, there are caveats: Attendings must be intimately involved in operations and scrubbed for every key and critical portion of the operation; also operations being scheduled in separate rooms must be done so with reasonable foresight."
As long as institutions are following these practices, he concluded, "It would appear that lens of current policy efforts is too narrow by focusing on perception. The debate should be refocused by challenging training programs to strengthen attending involvement and ensure the requisite competence of their trainees."
Dr. Yount reported no relevant disclosures.
TORONTO – In academic medical centers, attending cardiothoracic surgeons often perform simultaneous procedures in different operating rooms as a means of increasing training opportunities for surgical fellows and to decrease hospital costs. However, the practice of running simultaneous operating rooms did not appear to affect perioperative timing or negatively affect patient outcomes, according to the results of a single institution review by Dr. Kenan W. Yount.
He and his colleagues at the University of Virginia, Charlottesville, wanted to examine their own data in guiding hospital policy as several major centers have recently proposed implementing a 1:1 ratio of attending surgeon-to-operating room.
In his presentation, Dr. Yount discussed the results of their review study, which categorized 1,377 cardiac and 1,682 general thoracic operations performed from July 2011 to July 2013 by attending, case type, and whether the attending was simultaneously supervising two surgeries. "Our institution adheres to a strict policy of attending surgeon oversight of and involvement in the critical and key portions of all operations," said Dr. Yount.
They compared operative duration, starting and closing times, postoperative complications, and 30-day mortality in each category. They also compared rates postoperative complications, hospital length of stay, and operative mortality in each category.
Interestingly, timing effects varied between the two overall types of surgery. Running two rooms had no effect on room start times, but thoracic rooms finished 16 minutes later than scheduled. Across six surgeons and 15 operation types, however, there were no differences in operative times.
"Furthermore, running two rooms was not associated with any differences in operative duration, morbidity, or mortality in our multivariate regression analyses, and there were no statistically significant differences in observed outcomes in any category," Dr. Yount said.
"In academic cardiothoracic surgical centers that rely on surgical support from fellowship training, the practice of running simultaneous operating rooms can be efficient and does not appear to negatively impact patient outcomes," said Dr. Yount. "In addition, the practice did not significantly increase operative duration or dramatically [affect] operating room starting or closing times," he concluded.
In discussing the implications of these results, he said, "Obviously, there are caveats: Attendings must be intimately involved in operations and scrubbed for every key and critical portion of the operation; also operations being scheduled in separate rooms must be done so with reasonable foresight."
As long as institutions are following these practices, he concluded, "It would appear that lens of current policy efforts is too narrow by focusing on perception. The debate should be refocused by challenging training programs to strengthen attending involvement and ensure the requisite competence of their trainees."
Dr. Yount reported no relevant disclosures.
Major finding: Running two rooms was not associated with any differences in operative duration, morbidity, or mortality in multivariate regression analyses, and there were no statistically significant differences in observed outcomes in any category.
Data source: The study reviewed 1,377 cardiac and 1682 general thoracic operations performed from July 2011 to July 2013 by attending, case type, and whether the attending was simultaneously supervising two surgeries.
Disclosures: Dr. Yount had no disclosures.
Oppositional behavior
Introduction
All children learn to say "no" and want to experiment with asserting their will, but children who frequently refuse to comply are extremely challenging, making oppositional behavior one of the most common presentations to pediatricians and child psychiatrists.
Case summary
A 4-and-a-half-year-old boy whose parents have been divorced for 2 years presents with a 2-year history of aggression toward other kids in day care, biting and kicking, and tantrums and defiance when he doesn’t want to do something, especially transition from one activity to another. These episodes are brief but have been increasing in frequency and severity, and recently, he has been hitting his mother when it is time to leave the playground. His parents have tried reasoning with him, providing warnings, time-outs, and counting to 3. "Nothing works." He argues constantly and gets irritable easily. He also has a high energy level and short attention span and sometimes gets anxious over small issues.
Discussion
Psychologists who systematically observe families that struggle with this kind of behavior often see a cycle of child refusal and parental frustration and desperate attempts to force the child to comply by finding the right punishment. Parents often repeat their instructions over and over without success, getting increasingly frustrated, sometimes yelling or hitting. When parents achieve success after yelling, they may end up thinking that it is only verbal, or even physical, aggression that will force the child to comply. Parents may also give up at other times, teaching the child that sometimes their refusals will help him to avoid a task. There can be gradual escalation in tantrums, yelling, or physical aggression on the part of both parents and the child over the years.
There are often underlying aspects of the child’s temperament and genetic make-up that contribute to this cycle. Aspects of temperament such as difficulties with transitions to new activities, quick negative emotional responses, and stubbornness contribute. Attention deficit/hyperactivity disorder (ADHD) and language difficulties are also common factors. Parents’ own personalities, emotional, and behavioral issues, and outside stressors affecting the family also increase the chance of entering this distressing cycle. In this case, the child’s behavior seemed to start or worsen after the stressor of the divorce, and he has some symptoms suggestive of ADHD as well as irritability and anxiety, which might be an adjustment response to the divorce, an aspect of his temperament, or a more clinical mood disorder.
When facing a complex picture such as this, it can be helpful to obtain general behavioral rating scales such as the Child Behavior Checklist (CBCL) or Behavior Assessment System for Children (BASC) from parents and teachers to assess how severe differing components of the presentation are in comparison to other children of the same age and sex. Developmental assessments including information from schools can help clarify cognitive and language issues that may play a role
In addition to addressing any underlying issues, the intervention best supported by evidence is training parents in behavioral skills to address the oppositional and impulsive behavior. Teaching parents specific skills to notice and reinforce good behaviors while decreasing reinforcement for bad behaviors improves the relationship and motivates children to behave better. The second part of this type of program involves replacing yelling and harsh punishments with mild consequences that are delivered calmly and very consistently.
These skills may sound simple but can be challenging to put in place. Specific programs that give parents abundant opportunities to practice and master the skills through practice with their child in session and role plays have repeatedly been demonstrated to improve compliance and relationships with the child. Specific, very-well-researched programs include Helping the Noncompliant Child, Parent Child Interaction Therapy, The Incredible Years, Triple P, Parent Management Training Oregon, Parent Management Training (Kazdin), and The Defiant Teen and The Defiant Child.
It can sometimes be difficult to find therapists experienced with these programs. It is worth inquiring about the specific programs therapists use or even encouraging therapists to get trained in a specific program. Manuals are readily available for Helping the Noncompliant Child, Parent Management Training (Kazdin), and The Defiant Child and The Defiant Teen among others. The Yale Parenting Center offers online or phone consultation. Information about training in all of the above programs is available online.
How we talk to parents about the complex factors that play into oppositional behavior sets the stage for treatment. Parents often feel overwhelmed, guilty, and defensive. I stress that the difficulties do not originate with the parent but are a mix of the stresses the family experiences, the child’s temperament and genetic make-up, and the parent’s own temperament, and parenting style. I emphasize how challenging children can be and that it is not obvious how to respond to these behaviors. And I stress that we want to address the issue in as many ways as we can and that parents are the most important people in their children’s lives. In the end, such programs often help parents feel empowered and closer to their children.
Dr. Hall is an assistant professor of psychiatry and pediatrics at the University of Vermont, Burlington. She provides periodic trainings in Helping the Noncompliant Child and the use of the manual Parent Management Training by Alan Kazdin but has no financial conflicts relevant to this article.
Introduction
All children learn to say "no" and want to experiment with asserting their will, but children who frequently refuse to comply are extremely challenging, making oppositional behavior one of the most common presentations to pediatricians and child psychiatrists.
Case summary
A 4-and-a-half-year-old boy whose parents have been divorced for 2 years presents with a 2-year history of aggression toward other kids in day care, biting and kicking, and tantrums and defiance when he doesn’t want to do something, especially transition from one activity to another. These episodes are brief but have been increasing in frequency and severity, and recently, he has been hitting his mother when it is time to leave the playground. His parents have tried reasoning with him, providing warnings, time-outs, and counting to 3. "Nothing works." He argues constantly and gets irritable easily. He also has a high energy level and short attention span and sometimes gets anxious over small issues.
Discussion
Psychologists who systematically observe families that struggle with this kind of behavior often see a cycle of child refusal and parental frustration and desperate attempts to force the child to comply by finding the right punishment. Parents often repeat their instructions over and over without success, getting increasingly frustrated, sometimes yelling or hitting. When parents achieve success after yelling, they may end up thinking that it is only verbal, or even physical, aggression that will force the child to comply. Parents may also give up at other times, teaching the child that sometimes their refusals will help him to avoid a task. There can be gradual escalation in tantrums, yelling, or physical aggression on the part of both parents and the child over the years.
There are often underlying aspects of the child’s temperament and genetic make-up that contribute to this cycle. Aspects of temperament such as difficulties with transitions to new activities, quick negative emotional responses, and stubbornness contribute. Attention deficit/hyperactivity disorder (ADHD) and language difficulties are also common factors. Parents’ own personalities, emotional, and behavioral issues, and outside stressors affecting the family also increase the chance of entering this distressing cycle. In this case, the child’s behavior seemed to start or worsen after the stressor of the divorce, and he has some symptoms suggestive of ADHD as well as irritability and anxiety, which might be an adjustment response to the divorce, an aspect of his temperament, or a more clinical mood disorder.
When facing a complex picture such as this, it can be helpful to obtain general behavioral rating scales such as the Child Behavior Checklist (CBCL) or Behavior Assessment System for Children (BASC) from parents and teachers to assess how severe differing components of the presentation are in comparison to other children of the same age and sex. Developmental assessments including information from schools can help clarify cognitive and language issues that may play a role
In addition to addressing any underlying issues, the intervention best supported by evidence is training parents in behavioral skills to address the oppositional and impulsive behavior. Teaching parents specific skills to notice and reinforce good behaviors while decreasing reinforcement for bad behaviors improves the relationship and motivates children to behave better. The second part of this type of program involves replacing yelling and harsh punishments with mild consequences that are delivered calmly and very consistently.
These skills may sound simple but can be challenging to put in place. Specific programs that give parents abundant opportunities to practice and master the skills through practice with their child in session and role plays have repeatedly been demonstrated to improve compliance and relationships with the child. Specific, very-well-researched programs include Helping the Noncompliant Child, Parent Child Interaction Therapy, The Incredible Years, Triple P, Parent Management Training Oregon, Parent Management Training (Kazdin), and The Defiant Teen and The Defiant Child.
It can sometimes be difficult to find therapists experienced with these programs. It is worth inquiring about the specific programs therapists use or even encouraging therapists to get trained in a specific program. Manuals are readily available for Helping the Noncompliant Child, Parent Management Training (Kazdin), and The Defiant Child and The Defiant Teen among others. The Yale Parenting Center offers online or phone consultation. Information about training in all of the above programs is available online.
How we talk to parents about the complex factors that play into oppositional behavior sets the stage for treatment. Parents often feel overwhelmed, guilty, and defensive. I stress that the difficulties do not originate with the parent but are a mix of the stresses the family experiences, the child’s temperament and genetic make-up, and the parent’s own temperament, and parenting style. I emphasize how challenging children can be and that it is not obvious how to respond to these behaviors. And I stress that we want to address the issue in as many ways as we can and that parents are the most important people in their children’s lives. In the end, such programs often help parents feel empowered and closer to their children.
Dr. Hall is an assistant professor of psychiatry and pediatrics at the University of Vermont, Burlington. She provides periodic trainings in Helping the Noncompliant Child and the use of the manual Parent Management Training by Alan Kazdin but has no financial conflicts relevant to this article.
Introduction
All children learn to say "no" and want to experiment with asserting their will, but children who frequently refuse to comply are extremely challenging, making oppositional behavior one of the most common presentations to pediatricians and child psychiatrists.
Case summary
A 4-and-a-half-year-old boy whose parents have been divorced for 2 years presents with a 2-year history of aggression toward other kids in day care, biting and kicking, and tantrums and defiance when he doesn’t want to do something, especially transition from one activity to another. These episodes are brief but have been increasing in frequency and severity, and recently, he has been hitting his mother when it is time to leave the playground. His parents have tried reasoning with him, providing warnings, time-outs, and counting to 3. "Nothing works." He argues constantly and gets irritable easily. He also has a high energy level and short attention span and sometimes gets anxious over small issues.
Discussion
Psychologists who systematically observe families that struggle with this kind of behavior often see a cycle of child refusal and parental frustration and desperate attempts to force the child to comply by finding the right punishment. Parents often repeat their instructions over and over without success, getting increasingly frustrated, sometimes yelling or hitting. When parents achieve success after yelling, they may end up thinking that it is only verbal, or even physical, aggression that will force the child to comply. Parents may also give up at other times, teaching the child that sometimes their refusals will help him to avoid a task. There can be gradual escalation in tantrums, yelling, or physical aggression on the part of both parents and the child over the years.
There are often underlying aspects of the child’s temperament and genetic make-up that contribute to this cycle. Aspects of temperament such as difficulties with transitions to new activities, quick negative emotional responses, and stubbornness contribute. Attention deficit/hyperactivity disorder (ADHD) and language difficulties are also common factors. Parents’ own personalities, emotional, and behavioral issues, and outside stressors affecting the family also increase the chance of entering this distressing cycle. In this case, the child’s behavior seemed to start or worsen after the stressor of the divorce, and he has some symptoms suggestive of ADHD as well as irritability and anxiety, which might be an adjustment response to the divorce, an aspect of his temperament, or a more clinical mood disorder.
When facing a complex picture such as this, it can be helpful to obtain general behavioral rating scales such as the Child Behavior Checklist (CBCL) or Behavior Assessment System for Children (BASC) from parents and teachers to assess how severe differing components of the presentation are in comparison to other children of the same age and sex. Developmental assessments including information from schools can help clarify cognitive and language issues that may play a role
In addition to addressing any underlying issues, the intervention best supported by evidence is training parents in behavioral skills to address the oppositional and impulsive behavior. Teaching parents specific skills to notice and reinforce good behaviors while decreasing reinforcement for bad behaviors improves the relationship and motivates children to behave better. The second part of this type of program involves replacing yelling and harsh punishments with mild consequences that are delivered calmly and very consistently.
These skills may sound simple but can be challenging to put in place. Specific programs that give parents abundant opportunities to practice and master the skills through practice with their child in session and role plays have repeatedly been demonstrated to improve compliance and relationships with the child. Specific, very-well-researched programs include Helping the Noncompliant Child, Parent Child Interaction Therapy, The Incredible Years, Triple P, Parent Management Training Oregon, Parent Management Training (Kazdin), and The Defiant Teen and The Defiant Child.
It can sometimes be difficult to find therapists experienced with these programs. It is worth inquiring about the specific programs therapists use or even encouraging therapists to get trained in a specific program. Manuals are readily available for Helping the Noncompliant Child, Parent Management Training (Kazdin), and The Defiant Child and The Defiant Teen among others. The Yale Parenting Center offers online or phone consultation. Information about training in all of the above programs is available online.
How we talk to parents about the complex factors that play into oppositional behavior sets the stage for treatment. Parents often feel overwhelmed, guilty, and defensive. I stress that the difficulties do not originate with the parent but are a mix of the stresses the family experiences, the child’s temperament and genetic make-up, and the parent’s own temperament, and parenting style. I emphasize how challenging children can be and that it is not obvious how to respond to these behaviors. And I stress that we want to address the issue in as many ways as we can and that parents are the most important people in their children’s lives. In the end, such programs often help parents feel empowered and closer to their children.
Dr. Hall is an assistant professor of psychiatry and pediatrics at the University of Vermont, Burlington. She provides periodic trainings in Helping the Noncompliant Child and the use of the manual Parent Management Training by Alan Kazdin but has no financial conflicts relevant to this article.
Novel agent shows promising activity in heavily pretreated NHL

©ASCO/Rodney White
CHICAGO—The novel, oral selective inhibitor of nuclear transport known as selinexor (KPT-330) can safely be given as monotherapy to patients with heavily pretreated non-Hodgkin lymphoma (NHL), according to a presentation at the 2014 ASCO Annual Meeting.
“Selinexor has favorable pharmacokinetic and pharmacodynamic characteristics,” said presenter Martin Gutierrez, MD, of the John Theurer Cancer Center at Hackensack University Medical Center in New Jersey.
Selinexor is a slowly reversible, selective inhibitor of nuclear transport that inhibits XPO1, which is elevated in NHL, chronic lymphocytic leukemia (CLL), and other malignances.
“It shows single-agent anti-tumor activity across all NHL types, with durable cancer control of more than 9 months [and] marked activity across germ cell B (GCB), non-germ cell B, and double-hit diffuse large B-cell lymphoma (DLBCL),” Dr Gutierrez said.
He provided an update of the ongoing phase 1 dose-escalation study at the meeting as abstract 8518.
The study now includes 51 patients, half of whom have NHL. Their median age is 60 years.
The patients received selinexor across 8 dose levels, ranging from 3 mg/m2 to 60 mg/m2. Dosing at 60 mg/m2 twice weekly is ongoing, and the maximum-tolerated dose has not been reached.
Among the 43 evaluable patients, the disease control rate was 74%, the overall response rate was 28%, and the complete response rate was 5%.
“All patients who had their disease controlled had a reduction in lymph nodes and some degree of activity across all dose levels,” Dr Gutierrez said. “GCB and non-GCB patients responded similarly.”
The length of response was up to 632 days in the DLBCL group.
Most adverse events were gastrointestinal in nature, and most of them were grade 1 or 2. The most common adverse events were nausea, anorexia, and fatigue.
The investigators found a higher incidence of side effects in the first treatment cycle. The dosing schedule was interrupted and reduced to maintain steady state levels.
“The results suggest that an intermittent dosing schedule optimally induces a steady state with maximal induction of XPO1 mRNA,” Dr Gutierrez said.
There were 3 dose-limiting toxicities, including 1 multiple myeloma patient with grade 4 thrombocytopenia, 1 follicular lymphoma patient with grade 4 thrombocytopenia, and 1 CLL patient with grade 2 fatigue.
ASCO discussant Owen O’Connor, MD, from Columbia University Medical Center in New York, commented, “These clinical data are interesting with a provocative target. I applaud the investigators for doing a trial across a diversity of B- and T-cell lymphomas . . . . The results suggest a potential effect in a rare subset of lymphoma patients that have little treatment options.”
Frontline trials of selinexor are planned, including patients with Richter transformation and follicular lymphoma.
Selinexor recently received orphan drug status from the US Food and Drug Administration for the treatment of DLBCL. ![]()

©ASCO/Rodney White
CHICAGO—The novel, oral selective inhibitor of nuclear transport known as selinexor (KPT-330) can safely be given as monotherapy to patients with heavily pretreated non-Hodgkin lymphoma (NHL), according to a presentation at the 2014 ASCO Annual Meeting.
“Selinexor has favorable pharmacokinetic and pharmacodynamic characteristics,” said presenter Martin Gutierrez, MD, of the John Theurer Cancer Center at Hackensack University Medical Center in New Jersey.
Selinexor is a slowly reversible, selective inhibitor of nuclear transport that inhibits XPO1, which is elevated in NHL, chronic lymphocytic leukemia (CLL), and other malignances.
“It shows single-agent anti-tumor activity across all NHL types, with durable cancer control of more than 9 months [and] marked activity across germ cell B (GCB), non-germ cell B, and double-hit diffuse large B-cell lymphoma (DLBCL),” Dr Gutierrez said.
He provided an update of the ongoing phase 1 dose-escalation study at the meeting as abstract 8518.
The study now includes 51 patients, half of whom have NHL. Their median age is 60 years.
The patients received selinexor across 8 dose levels, ranging from 3 mg/m2 to 60 mg/m2. Dosing at 60 mg/m2 twice weekly is ongoing, and the maximum-tolerated dose has not been reached.
Among the 43 evaluable patients, the disease control rate was 74%, the overall response rate was 28%, and the complete response rate was 5%.
“All patients who had their disease controlled had a reduction in lymph nodes and some degree of activity across all dose levels,” Dr Gutierrez said. “GCB and non-GCB patients responded similarly.”
The length of response was up to 632 days in the DLBCL group.
Most adverse events were gastrointestinal in nature, and most of them were grade 1 or 2. The most common adverse events were nausea, anorexia, and fatigue.
The investigators found a higher incidence of side effects in the first treatment cycle. The dosing schedule was interrupted and reduced to maintain steady state levels.
“The results suggest that an intermittent dosing schedule optimally induces a steady state with maximal induction of XPO1 mRNA,” Dr Gutierrez said.
There were 3 dose-limiting toxicities, including 1 multiple myeloma patient with grade 4 thrombocytopenia, 1 follicular lymphoma patient with grade 4 thrombocytopenia, and 1 CLL patient with grade 2 fatigue.
ASCO discussant Owen O’Connor, MD, from Columbia University Medical Center in New York, commented, “These clinical data are interesting with a provocative target. I applaud the investigators for doing a trial across a diversity of B- and T-cell lymphomas . . . . The results suggest a potential effect in a rare subset of lymphoma patients that have little treatment options.”
Frontline trials of selinexor are planned, including patients with Richter transformation and follicular lymphoma.
Selinexor recently received orphan drug status from the US Food and Drug Administration for the treatment of DLBCL. ![]()

©ASCO/Rodney White
CHICAGO—The novel, oral selective inhibitor of nuclear transport known as selinexor (KPT-330) can safely be given as monotherapy to patients with heavily pretreated non-Hodgkin lymphoma (NHL), according to a presentation at the 2014 ASCO Annual Meeting.
“Selinexor has favorable pharmacokinetic and pharmacodynamic characteristics,” said presenter Martin Gutierrez, MD, of the John Theurer Cancer Center at Hackensack University Medical Center in New Jersey.
Selinexor is a slowly reversible, selective inhibitor of nuclear transport that inhibits XPO1, which is elevated in NHL, chronic lymphocytic leukemia (CLL), and other malignances.
“It shows single-agent anti-tumor activity across all NHL types, with durable cancer control of more than 9 months [and] marked activity across germ cell B (GCB), non-germ cell B, and double-hit diffuse large B-cell lymphoma (DLBCL),” Dr Gutierrez said.
He provided an update of the ongoing phase 1 dose-escalation study at the meeting as abstract 8518.
The study now includes 51 patients, half of whom have NHL. Their median age is 60 years.
The patients received selinexor across 8 dose levels, ranging from 3 mg/m2 to 60 mg/m2. Dosing at 60 mg/m2 twice weekly is ongoing, and the maximum-tolerated dose has not been reached.
Among the 43 evaluable patients, the disease control rate was 74%, the overall response rate was 28%, and the complete response rate was 5%.
“All patients who had their disease controlled had a reduction in lymph nodes and some degree of activity across all dose levels,” Dr Gutierrez said. “GCB and non-GCB patients responded similarly.”
The length of response was up to 632 days in the DLBCL group.
Most adverse events were gastrointestinal in nature, and most of them were grade 1 or 2. The most common adverse events were nausea, anorexia, and fatigue.
The investigators found a higher incidence of side effects in the first treatment cycle. The dosing schedule was interrupted and reduced to maintain steady state levels.
“The results suggest that an intermittent dosing schedule optimally induces a steady state with maximal induction of XPO1 mRNA,” Dr Gutierrez said.
There were 3 dose-limiting toxicities, including 1 multiple myeloma patient with grade 4 thrombocytopenia, 1 follicular lymphoma patient with grade 4 thrombocytopenia, and 1 CLL patient with grade 2 fatigue.
ASCO discussant Owen O’Connor, MD, from Columbia University Medical Center in New York, commented, “These clinical data are interesting with a provocative target. I applaud the investigators for doing a trial across a diversity of B- and T-cell lymphomas . . . . The results suggest a potential effect in a rare subset of lymphoma patients that have little treatment options.”
Frontline trials of selinexor are planned, including patients with Richter transformation and follicular lymphoma.
Selinexor recently received orphan drug status from the US Food and Drug Administration for the treatment of DLBCL. ![]()
Method allows for high-resolution cell imaging

filaments (red), microtubules
(green), and nuclei (blue)
National Institutes of Health
A new technique allows scientists to view the cell cytoskeleton with “unprecedented resolution,” according to a paper published in Nature Methods.
A group of researchers exploited the properties of a fluorescent molecule they developed to generate 2 probes for imaging the cytoskeleton.
The team said these probes can easily enter live cells, are non-toxic, have long-lasting signals, and offer better image resolution than current imaging techniques.
This research began when Kai Johnsson, PhD, of École Polytechnique Fédérale de Lausanne in Switzerland, and his colleagues developed a fluorescent molecule called silicon-rhodamine (SiR).
The molecule switches “on” only when it binds to the charged surface of a protein like those found on the cytoskeleton. When SiR switches on, it emits light at far-red wavelengths.
The challenge was getting SiR to bind specifically to the cytoskeleton’s proteins, actin and tubulin. To achieve this, the researchers fused SiR molecules with compounds that bind tubulin or actin.
The resulting hybrid molecules consist of a SiR molecule, which provides the fluorescent signal, and a molecule of a natural compound that can bind the target protein.
One such compound was docetaxel, an anticancer drug that binds tubulin, and the other was jasplakinolide, which specifically binds the cytoskeletal form of actin. Both compounds, which are used here in very low, non-toxic concentrations, can easily pass through the cell’s membrane and into the cell itself.
The probes, called SiR-tubulin and SiR-actin, were used to visualize the dynamics of the cytoskeleton in human skin cells. Because the light signal of the probes is emitted in the far-red spectrum, it is easy to isolate from background noise, which generates images of unprecedented resolution when used with super-resolution microscopy.
An additional advantage of the probes, according to the researchers, is their practicality.
“You just add them directly into your cell culture, and they are taken up by the cells,” Dr Johnsson said.
The probes don’t require any washing or preparation of the cells before administration or any subsequent washing steps, which helps in maintaining the stability of their environment and their natural biological functions.
“Up to now, no probes were available that would allow you to get high-quality images of microtubules and microfilaments in living cells without some kind of genetic modification,” Dr Johnsson said.
“With this work, we provide the biological community with 2 high-performing, high-contrast fluorogenic probes that emit in the non-phototoxic part of the light spectrum, and can be even used in tissues like whole-blood samples.” ![]()

filaments (red), microtubules
(green), and nuclei (blue)
National Institutes of Health
A new technique allows scientists to view the cell cytoskeleton with “unprecedented resolution,” according to a paper published in Nature Methods.
A group of researchers exploited the properties of a fluorescent molecule they developed to generate 2 probes for imaging the cytoskeleton.
The team said these probes can easily enter live cells, are non-toxic, have long-lasting signals, and offer better image resolution than current imaging techniques.
This research began when Kai Johnsson, PhD, of École Polytechnique Fédérale de Lausanne in Switzerland, and his colleagues developed a fluorescent molecule called silicon-rhodamine (SiR).
The molecule switches “on” only when it binds to the charged surface of a protein like those found on the cytoskeleton. When SiR switches on, it emits light at far-red wavelengths.
The challenge was getting SiR to bind specifically to the cytoskeleton’s proteins, actin and tubulin. To achieve this, the researchers fused SiR molecules with compounds that bind tubulin or actin.
The resulting hybrid molecules consist of a SiR molecule, which provides the fluorescent signal, and a molecule of a natural compound that can bind the target protein.
One such compound was docetaxel, an anticancer drug that binds tubulin, and the other was jasplakinolide, which specifically binds the cytoskeletal form of actin. Both compounds, which are used here in very low, non-toxic concentrations, can easily pass through the cell’s membrane and into the cell itself.
The probes, called SiR-tubulin and SiR-actin, were used to visualize the dynamics of the cytoskeleton in human skin cells. Because the light signal of the probes is emitted in the far-red spectrum, it is easy to isolate from background noise, which generates images of unprecedented resolution when used with super-resolution microscopy.
An additional advantage of the probes, according to the researchers, is their practicality.
“You just add them directly into your cell culture, and they are taken up by the cells,” Dr Johnsson said.
The probes don’t require any washing or preparation of the cells before administration or any subsequent washing steps, which helps in maintaining the stability of their environment and their natural biological functions.
“Up to now, no probes were available that would allow you to get high-quality images of microtubules and microfilaments in living cells without some kind of genetic modification,” Dr Johnsson said.
“With this work, we provide the biological community with 2 high-performing, high-contrast fluorogenic probes that emit in the non-phototoxic part of the light spectrum, and can be even used in tissues like whole-blood samples.” ![]()

filaments (red), microtubules
(green), and nuclei (blue)
National Institutes of Health
A new technique allows scientists to view the cell cytoskeleton with “unprecedented resolution,” according to a paper published in Nature Methods.
A group of researchers exploited the properties of a fluorescent molecule they developed to generate 2 probes for imaging the cytoskeleton.
The team said these probes can easily enter live cells, are non-toxic, have long-lasting signals, and offer better image resolution than current imaging techniques.
This research began when Kai Johnsson, PhD, of École Polytechnique Fédérale de Lausanne in Switzerland, and his colleagues developed a fluorescent molecule called silicon-rhodamine (SiR).
The molecule switches “on” only when it binds to the charged surface of a protein like those found on the cytoskeleton. When SiR switches on, it emits light at far-red wavelengths.
The challenge was getting SiR to bind specifically to the cytoskeleton’s proteins, actin and tubulin. To achieve this, the researchers fused SiR molecules with compounds that bind tubulin or actin.
The resulting hybrid molecules consist of a SiR molecule, which provides the fluorescent signal, and a molecule of a natural compound that can bind the target protein.
One such compound was docetaxel, an anticancer drug that binds tubulin, and the other was jasplakinolide, which specifically binds the cytoskeletal form of actin. Both compounds, which are used here in very low, non-toxic concentrations, can easily pass through the cell’s membrane and into the cell itself.
The probes, called SiR-tubulin and SiR-actin, were used to visualize the dynamics of the cytoskeleton in human skin cells. Because the light signal of the probes is emitted in the far-red spectrum, it is easy to isolate from background noise, which generates images of unprecedented resolution when used with super-resolution microscopy.
An additional advantage of the probes, according to the researchers, is their practicality.
“You just add them directly into your cell culture, and they are taken up by the cells,” Dr Johnsson said.
The probes don’t require any washing or preparation of the cells before administration or any subsequent washing steps, which helps in maintaining the stability of their environment and their natural biological functions.
“Up to now, no probes were available that would allow you to get high-quality images of microtubules and microfilaments in living cells without some kind of genetic modification,” Dr Johnsson said.
“With this work, we provide the biological community with 2 high-performing, high-contrast fluorogenic probes that emit in the non-phototoxic part of the light spectrum, and can be even used in tissues like whole-blood samples.” ![]()
A3 to Improve STAT
STAT is an abbreviation of the Latin word statim, meaning immediately,[1] and has been a part of healthcare's lexicon for almost as long as there have been hospitals. STAT conveys a sense of urgency, compelling those who hear STAT to act quickly. Unfortunately, given the lack of a consistent understanding of STAT, the term in reality often has an alternate use: to hurry up or to complete sooner than routine, and is sometimes used to circumvent a system that is perceived to be too slow to accomplish a routine task in a timely manner.
As part of a larger systems redesign effort to improve patient safety and quality of care, an institutional review board (IRB)‐approved qualitative study was conducted on 2 medical‐surgical units in a US Department of Veterans Affairs (VA) hospital to explore communication patterns between physicians and nurses.[2] The study revealed wide variation in understanding between physicians and nurses on the ordering and administration of STAT medication. Physicians were unaware that when they placed a STAT order into the computerized patient record system (CPRS), nurses were not automatically alerted about the order. At this facility, nurses did not carry pagers. Although each unit had a supply of wireless telephones, they were often unreliable and therefore not used consistently. Nurses were required by policy to check the CPRS for new orders every 2 hours. This was an inefficient and possibly dangerous process,[3] because if a nurse was not expecting a STAT order, 2 hours could elapse before she or he saw the order in the CPRS and began to look for the medication. A follow‐up survey completed by physicians, nurses, pharmacists, and pharmacy technicians demonstrated stark differences on the definition of STAT and overlap with similar terms such as NOW and ASAP. Interviews with ordering providers indicated that 36% of the time a STAT was ordered it was not clinically urgent, but instead ordered STAT to speed up the process.
The STAT medication process was clearly in need of improvement, but previous quality improvement projects in our organization had varying degrees of success. For example, we used Lean methodology in an attempt to improve our discharge process. We conducted a modified rapid process discharge improvement workshop[4] structured in phases over 4 weeks. During the workshops, a strong emphasis remained on the solutions to the problem, and we were unable to help the team move from a mindset of fix it to create it. This limited the buy‐in of team members, the creativity of their ideas for improvement, and ultimately the momentum to improve the process.
In this article we describe our adaptation of A3 Thinking,[5, 6] a structure for guiding quality improvement based in Lean methodology, to improve the STAT medication process. We chose A3 Thinking for several reasons. A3 Thinking focuses on process improvement and thus aligned well with our interest in improving the STAT medication process. A3 Thinking also reveals otherwise hidden nonvalue‐added activities that should be eliminated.[7] Finally A3 Thinking reinforces a deeper understanding of the way the work is currently being done, providing critical information needed before making a change. This provides a tremendous opportunity to look at work differently and see opportunities for improvement.[8] Given these strengths as well as the lack of congruence between what the STAT process should consist of and how the STAT process was actually being used in our organization, A3 Thinking offered the best fit between an improvement process and the problem to be solved.
METHODS
A search of healthcare literature yielded very few studies on the STAT process.[9, 10] Only 1 intervention to improve the process was found, and this focused on a specific procedure.[10] An informal survey of local VA and non‐VA hospitals regarding their experiences with the STAT medication process revealed insufficient information to aid our efforts. We next searched the business and manufacturing literature and found examples of how the Lean methodology was successfully applied to other problems in healthcare, including improving pediatric surgery workflow and decreasing ventilator‐associated pneumonia.[11, 12]
Therefore, the STAT project was structured to adapt a problem‐solving process commonly used in Lean organizationsA3 Thinkingwhich challenges team members to work through a discovery phase to develop a shared understanding of the process, an envisioning phase to conceptualize an ideal process experience, and finally an experimentation phase to identify and trial possible solutions through prioritization, iterative testing, structured reflection, and adjustment on resulting changes. Our application of the term experimentation in this context is distinct from that of controlled experimentation in clinical research; the term is intended to convey iterative learning as changes are tested, evaluated, and modified during this quality improvement project. Figure 1 displays a conceptual model of our adaptation of A3 Thinking. As this was a quality‐improvement project, it was exempt from IRB review.
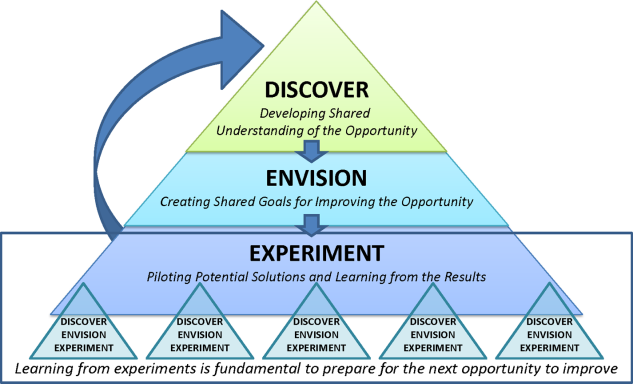
DISCOVERY
To begin the discovery phase, a workgroup consisting of representatives of all groups that had a role in the STAT process (ie, physician, pharmacist, nurse, pharmacy technician, clerk) gathered to identify the opportunity we are looking to address and learn from each other's individual experiences with the STAT medication process. The group was facilitated by an industrial engineer familiar with the A3 Thinking process. The team completed a mapping exercise to lay out, step‐by‐step, the current STAT medication process. This activity allowed the team to build shared empathy with others' experiences and to appreciate the challenges experienced by others through their individual responsibilities in the process. The current process was found to consist of 4 overarching components: a provider entered the STAT order into the CPRS; the order was verified by a pharmacist; a pharmacy technician delivered the medication to the unit (or a nurse retrieved the medication from the Omnicell (Omnicell Inc., Mountain View, CA), a proprietary automated medication dispensing system); and finally the nurse administered the medication to a patient.
A large, color‐coded flow map of the STAT medication process was constructed over several meetings to capture all perspectives and allow team members to gather feedback from their peers. To further our understanding of the current process, the team participated in a modified Go to the Gemba (ie, go to where the work is done)[13] on a real‐time STAT order. Once all workgroup members were satisfied that the flow map represented the current state of the STAT medication process, we came to a consensus on the goals needed to meet our main objective.
We agreed that our main objective was that STAT medication orders should be recognized, verified, and administered to patients in a timely and appropriate manner to ensure quality care. We identified 3 goals to meet this objective: (1) STAT should be consistently defined and understood by everyone; (2) an easy, intuitive STAT process should be available for all stakeholders; and (3) the STAT process should be transparent and ideally visual so that everyone involved can understand at which point in the process a specific STAT order is currently situated. We also identified additional information we would need to reach the goals.
Shortly after the process‐mapping sessions, 2 workgroup members conducted real‐time STAT order time studies to track medications from order to administration. Three time periods in the STAT process were identified for observation and measurement: the time from physician order entry in the CPRS to the time a pharmacist verified the medication, the time from verification to when the medication arrived on the nursing unit, and the time from arrival on the nursing unit to when that medication was administered. Using a data‐collection template, each time period was recorded, and 28 time studies were collected over 1 month. To monitor the progress of our initiatives, the time study was repeated 3 months into the project.
ENVISIONING
Following the discovery phase, the team was better equipped to identify the specific changes needed to achieve an improved process. The envisioning phase allowed the team freedom to imagine an ideal process barring any preconceived notion of constraints within the current process.
In 2 meetings we brainstormed as many improvement ideas as possible. To prioritize and focus our ideas, we developed a matrix (see Supporting Information, Appendix A, in the online version of this article), placing our ideas in 1 of 4 quadrants based on the anticipated effort to implement the change (x‐axis) and impact of making the change (y‐axis). The matrix helped us see that some ideas would be relatively simple to implement (eg, color‐coded bags for STAT medication delivery), whereas others would require more sophisticated efforts and involvement of other people (eg, monthly education sessions to resident physicians).
EXPERIMENTING
Experiments were conducted to meet each of the 3 goals identified above. The team used the outcomes of the prioritization exercise to identify initial experiments to test. To build momentum by showing progress and improvement with a few quick wins, the team began with low‐effort/high‐impact opportunities. Each experiment followed a standard Plan‐Do‐Study‐Act (PDSA) cycle to encourage reflection, learning, adaptation, and adjustment as a result of the experiential learning process.[5]
Goal 1: STAT Should Be Consistently Defined and Understood by Everyone
To address the first goal, a subgroup collected policies and procedures related to the STAT medication administration process. The policy defined a STAT medication as a medication that has the potential to significantly and negatively impact a patient's clinical condition if not given within 30 minutes. The group found that the policy requiring a 30‐minute time to administration was clinically appropriate, reinforcing our goals to create a practice congruent with the policy.
A subgroup led by the pharmacy department collected data related to STAT medications on the 3 medical‐surgical units. Within 1 month, 550 STAT medications were ordered, consisting of medications ranging from furosemide to nicotine lozenges, the latter being a medication clearly outside of the policy definition of STAT. The workgroup reviewed the information and realized education would be required to align practice with policy. According to our matrix, education was a high‐impact/high‐effort activity, so efforts were focused on the high‐impact/low‐effort activities initially. We addressed educational opportunities in later PDSA cycles.
Goal 2: An Easy, Intuitive STAT Process for All Stakeholders
The CPRS contains prefabricated templates that conform to regulatory requirements and ensure completeness. However, the CPRS does not intuitively enable ordering providers to choose the time for the first dose of a new routine medication. This often creates a situation where a provider orders the medication STAT, so that the medication can be given earlier than the CPRS would otherwise allow. Although there is a check box, Give additional dose now, it was not being used because it was visually obscure in the interface. The CPRS restricted our ability to change the template for ordering medications to include a specific time for first‐dose administration before defaulting to the routine order; thus, complementary countermeasures were trialed first. These are outlined in Table 1.
| Countermeasure | Intended Outcome |
|---|---|
| Remove duplicate dosing frequencies from medication order template | Reduce list of dosing frequencies to sort through to find desired selection |
| Develop 1‐page job aid for ordering providers to utilize | Assist in the correct methods of ordering STAT, NOW, and routine medications |
| Added STAT ONCE as a dosing frequency selection | Clarify the medication, if ordered STAT, will only be a 1‐time administration to avoid the recurrence of a STAT order should the orders be transferred to a new unit with the patient |
| Modify existing policies to add STAT ONCE option | Ensure documentation is congruent with new expectations |
| Educate interns and residents with the job aid and a hands‐on how to ordering exercise | Inform ordering physicians on the available references for ordering and educate according to desired practice |
| Provide interns and residents with a visual job aid at their workstation and a hands‐on how to ordering exercise | In addition to providing information and educating according to desired practice, provide a just‐in‐time reference resource |
Goal 3: The STAT Process Should Be Transparent and Ideally Visual
During the time studies, the time period from when the medication arrived on the unit to the time it was administered to the patient averaged 34 minutes. Of 28 STAT orders followed through the entire process, 5 pharmacy technicians (26%) were not informed of 19 STAT medication orders requiring delivery, and 12 nurses (63%) were not notified of the delivery of those 19 medications. The remaining 9 STAT medications were stocked in the Omnicell. Informal interviews with nurses and pharmacy technicians, as well as input from the nurses and pharmacy technicians in our workgroup, revealed several explanations for these findings.
First, the delivering technicians could not always find the patient's nurse, and because the delivery procedure was not standardized, there was no consistency between technicians in where medications were delivered. Second, each unit had a different medication inventory stored in the Omnicell, and the inventory was frequently changed (eg, due to unit‐specific needs, backorders), which made it difficult for nurses to keep track of what was available in Omnicell at any given time. Finally, the STAT medication was not consistently labeled with a visual STAT notation, so even if a nurse saw that new medications had been delivered, he or she would not be able to easily identify which was STAT. The team made several low‐tech process changes to improve the visibility of a STAT medication and ensure reliable communication upon delivery. A subgroup of pharmacists, technicians, and nurses developed and implemented the countermeasures described in Table 2.
| Countermeasure | Intended Outcome |
|---|---|
| Designate delivery preferences with the patient's nurse as the first preference and a set location in the med room as the only alternative preference | Attempt to deliver medications directly to the patient's nurse as frequently as possible to eliminate any unnecessary delays and avoid miscommunication |
| Identify a location in each unit's med room to place a red bin to deliver the STAT medications that are unable to be delivered to the patient's nurse directly | Provide 1 alternate location to retrieve STAT medications if the technician is unable to locate the patient's nurse to deliver the medication directly |
| Utilize a plastic bag with a red STAT indication for transportation of STAT medications to the units | Provide a visual to assist in pharmacy technicians prioritizing their deliveries to the inpatient units |
| Utilize red STAT magnets on the patient's door frame to signal nurses a medication had been delivered to the med room | Provide a visual to assist in timely recognition of a STAT medication delivery given the technician was unable to find the nurse to hand it off directly |
RESULTS
At the start of our project, the average time from STAT order to medication administration was 1 hour and 7 minutes (range, 6 minutes 2 hours and 22 minutes). As a result of the 2 sets of countermeasures outlined in Tables 1 and 2, the average total time from STAT order entry to administration decreased by 21% to an average of 53 minutes. The total time from medication delivery to administration decreased by 26% from 34 minutes to 25 minutes postimplementation. On average, 391 STAT medications were ordered per month during the project period, which represents a decrease of 9.5% from the 432 orders per month for the same time period the previous year. After implementing the countermeasures in Table 2, we followed another 26 STAT medications through the process to evaluate our efforts. Of 15 STAT medications requiring delivery, only 1 nurse (7%) was not notified of the delivery of a STAT medication, and 1 pharmacy technician (7%) was not informed the medication was STAT. The 151% increase in notification of nurses to delivery of a STAT medication suggests that use of the STAT bags, STAT magnets on patient doors, and whenever possible direct delivery of STAT medications to the nurse has improved communication between the technicians and nurses. Similarly, the 27% increase in technician awareness of a STAT designation suggests STAT is being better communicated to them. The improvement in awareness and notification of a STAT medication is summarized in Figure 2.
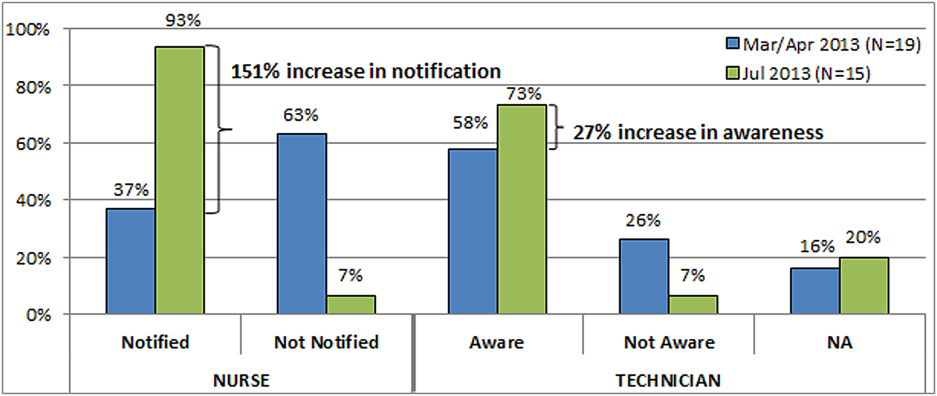
Due to time and financial constraints, the following limitations may have affected our findings. First, resident physicians were not directly represented in our discussions. Attending medicine hospitalists provided the physician perspective, which provides a biased view given their intimate knowledge of the CPRS and additional years of experience. Similarly, nurse perspectives were limited to staff and clinical nurse leaders. Last, our low‐cost approach was mandated by limited resources; a more resource‐rich environment may have devised alternative approaches.
CONCLUSIONS
Adapting A3 Thinking for process improvement was a low‐cost/low‐tech option for a VA facility. Having buy‐in from all levels was crucial to the success of the project. The size and diversity of the group was also very important, as different opinions and aspects of the process were represented. Cross‐discipline relationships and respect were formed, which will be valuable for collaboration in future projects. Although we focused on the STAT medication process, other quality‐improvement projects could also benefit from A3 Thinking. Moreover, there were enough people to serve as ambassadors, taking the project back to their work areas to share with their peers, gather consensus, and elicit additional feedback. The collaboration led to comprehensive understanding of the process, the nature of the problems within the process, and the complexity of solving the problem. For example, although the number of STAT orders did not decrease dramatically, we have learned from these experiments that we may need to change how we approach structuring additional experiments. Future work will focus on increasing communication between physicians and nurses when placing STAT medication orders, enhancing resident education to ensure appropriate use of the STAT designation, and continuing our efforts to improve the delivery process of STAT medications.
Other quality‐improvement methodologies we could have used include: total quality management (TQM), continuous quality improvement (CQI), business process redesign, Lean, Six Sigma, and others.[14] Differences between these can be broadly classified as putting an emphasis on people (eg, inclusion of front line staff in CQI or leadership in TQM) or on process (eg, understanding process function to reduce waste in Lean or statistical process control in Six Sigma).[14] Using A3 Thinking methodology was more useful than these others for the STAT medication process for some very important reasons. The A3 process not only led to a better understanding of the meaning of STAT across disciplines, increasing the intuitive nature, transparency and visual aspects of the whole process, but also promoted a collaborative, multidisciplinary, integrative culture, in which other hospital‐wide problems may be addressed in the future.
Acknowledgements
This work could not have been done without the contribution of all members of the STAT Improvement Workgroup, including Charles Alday; Allison Brenner, PharmD; Paula Carroll; Garry Davis; Michele Delaney, RN, MSN, CWCN; Mary East, MD; Stacy Frick, MSN, RN, CNL; Corry Gessner, CPhT; Kenya Harbin, MSN, RN, CNL; Crystal Heath, MS, RN‐BC; Tom Kerr, MPH; Diane Klemer, RPh; Diane Kohmescher, PharmD, BCPS; Sara Oberdick; Antanita Pickett; Ana Preda, CPhT; Joseph Pugh, RPh, MS; Gloria Salazar, CPhT; Samar Sheth, MD; Andrea Starnes, RN; Christine Wagner, PharmD; Leo Wallace; Roderick Williams; and Marilyn Woodruff.
Disclosures: This work was funded by a US Department of Veterans Affairs, Office of Systems Redesign Improvement Capability Grant and the Veterans in Partnership (VISN11) Healthcare Network. The findings and conclusions in this report are those of the authors and do not necessarily represent the position or policy of the US Department of Veterans Affairs. The authors have no other disclosures or conflicts to report.
- The American Heritage Medical Dictionary of the English Language website. 2011. Available at: http://ahdictionary.com/word/search.html?q=STAT. Accessed December 22, 2013.
- , , , , , . The use of multiple qualitative methods to characterize communication events between physicians and nurses [published online ahead of print January 31, 2014]. Health Commun. doi: 10.1080/10410236.2013.835894.
- , , . Fifteen best practice recommendations for bar‐code medication administration in the Veterans Health Administration. Jt Comm J Qual Saf. 2004;30(7):355–365.
- , , , , . Going lean in health care. Cambridge, MA: Institute for Healthcare Improvement; 2005. Available at: http://www.ihi.org. Accessed March 19, 2014.
- , . Understanding A3 Thinking: A Critical Component of Toyota's PDCA Management System. New York, NY: Productivity Press, Taylor 2008.
- . Managing to Learn: Using the A3 Management Process to Solve Problems, Gain Agreement, Mentor and Lead. Cambridge, MA: Lean Enterprise Institute; 2008.
- , , . Basics of quality improvement in health care. Mayo Clin Proc. 2007;82(6):735–739.
- , . A3 problem solving: unique features of the A3 problem solving method. Available at: http://leanhealthcarewest.com/Page/A3‐Problem‐Solving. Accessed March 27, 2014.
- , , . Evaluation of stat orders in a teaching hospital: a chart review. Clin Drug Investig. 2011;31(4):231–235.
- . Using STAT properly. Radiol Manage. 2006;28(1):26–30; quiz 31–33.
- , . The promise of Lean in health care. Mayo Clin Proc. 2013;88(1):74–82.
- , , , . Lean health care: what can hospitals learn from a world‐class automaker? J Hosp Med. 2006;1(3):191–199.
- . Gemba Kaizen: A Commonsense Approach to a Continuous Improvement Strategy. 2nd ed. New York, NY: McGraw‐Hill; 2012.
- . Pseudoinnovation: the development and spread of healthcare quality improvement methodologies. Int J Qual Health Care. 2009;21(3):153–159.
STAT is an abbreviation of the Latin word statim, meaning immediately,[1] and has been a part of healthcare's lexicon for almost as long as there have been hospitals. STAT conveys a sense of urgency, compelling those who hear STAT to act quickly. Unfortunately, given the lack of a consistent understanding of STAT, the term in reality often has an alternate use: to hurry up or to complete sooner than routine, and is sometimes used to circumvent a system that is perceived to be too slow to accomplish a routine task in a timely manner.
As part of a larger systems redesign effort to improve patient safety and quality of care, an institutional review board (IRB)‐approved qualitative study was conducted on 2 medical‐surgical units in a US Department of Veterans Affairs (VA) hospital to explore communication patterns between physicians and nurses.[2] The study revealed wide variation in understanding between physicians and nurses on the ordering and administration of STAT medication. Physicians were unaware that when they placed a STAT order into the computerized patient record system (CPRS), nurses were not automatically alerted about the order. At this facility, nurses did not carry pagers. Although each unit had a supply of wireless telephones, they were often unreliable and therefore not used consistently. Nurses were required by policy to check the CPRS for new orders every 2 hours. This was an inefficient and possibly dangerous process,[3] because if a nurse was not expecting a STAT order, 2 hours could elapse before she or he saw the order in the CPRS and began to look for the medication. A follow‐up survey completed by physicians, nurses, pharmacists, and pharmacy technicians demonstrated stark differences on the definition of STAT and overlap with similar terms such as NOW and ASAP. Interviews with ordering providers indicated that 36% of the time a STAT was ordered it was not clinically urgent, but instead ordered STAT to speed up the process.
The STAT medication process was clearly in need of improvement, but previous quality improvement projects in our organization had varying degrees of success. For example, we used Lean methodology in an attempt to improve our discharge process. We conducted a modified rapid process discharge improvement workshop[4] structured in phases over 4 weeks. During the workshops, a strong emphasis remained on the solutions to the problem, and we were unable to help the team move from a mindset of fix it to create it. This limited the buy‐in of team members, the creativity of their ideas for improvement, and ultimately the momentum to improve the process.
In this article we describe our adaptation of A3 Thinking,[5, 6] a structure for guiding quality improvement based in Lean methodology, to improve the STAT medication process. We chose A3 Thinking for several reasons. A3 Thinking focuses on process improvement and thus aligned well with our interest in improving the STAT medication process. A3 Thinking also reveals otherwise hidden nonvalue‐added activities that should be eliminated.[7] Finally A3 Thinking reinforces a deeper understanding of the way the work is currently being done, providing critical information needed before making a change. This provides a tremendous opportunity to look at work differently and see opportunities for improvement.[8] Given these strengths as well as the lack of congruence between what the STAT process should consist of and how the STAT process was actually being used in our organization, A3 Thinking offered the best fit between an improvement process and the problem to be solved.
METHODS
A search of healthcare literature yielded very few studies on the STAT process.[9, 10] Only 1 intervention to improve the process was found, and this focused on a specific procedure.[10] An informal survey of local VA and non‐VA hospitals regarding their experiences with the STAT medication process revealed insufficient information to aid our efforts. We next searched the business and manufacturing literature and found examples of how the Lean methodology was successfully applied to other problems in healthcare, including improving pediatric surgery workflow and decreasing ventilator‐associated pneumonia.[11, 12]
Therefore, the STAT project was structured to adapt a problem‐solving process commonly used in Lean organizationsA3 Thinkingwhich challenges team members to work through a discovery phase to develop a shared understanding of the process, an envisioning phase to conceptualize an ideal process experience, and finally an experimentation phase to identify and trial possible solutions through prioritization, iterative testing, structured reflection, and adjustment on resulting changes. Our application of the term experimentation in this context is distinct from that of controlled experimentation in clinical research; the term is intended to convey iterative learning as changes are tested, evaluated, and modified during this quality improvement project. Figure 1 displays a conceptual model of our adaptation of A3 Thinking. As this was a quality‐improvement project, it was exempt from IRB review.
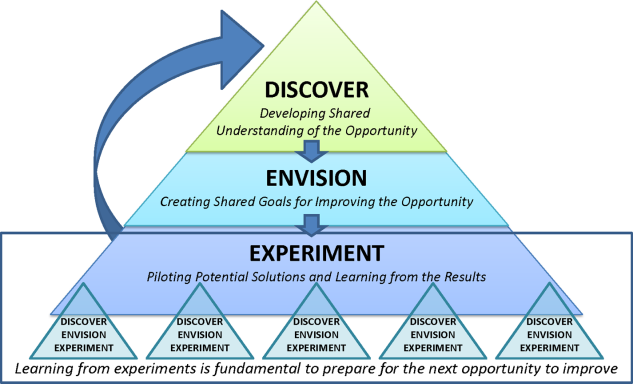
DISCOVERY
To begin the discovery phase, a workgroup consisting of representatives of all groups that had a role in the STAT process (ie, physician, pharmacist, nurse, pharmacy technician, clerk) gathered to identify the opportunity we are looking to address and learn from each other's individual experiences with the STAT medication process. The group was facilitated by an industrial engineer familiar with the A3 Thinking process. The team completed a mapping exercise to lay out, step‐by‐step, the current STAT medication process. This activity allowed the team to build shared empathy with others' experiences and to appreciate the challenges experienced by others through their individual responsibilities in the process. The current process was found to consist of 4 overarching components: a provider entered the STAT order into the CPRS; the order was verified by a pharmacist; a pharmacy technician delivered the medication to the unit (or a nurse retrieved the medication from the Omnicell (Omnicell Inc., Mountain View, CA), a proprietary automated medication dispensing system); and finally the nurse administered the medication to a patient.
A large, color‐coded flow map of the STAT medication process was constructed over several meetings to capture all perspectives and allow team members to gather feedback from their peers. To further our understanding of the current process, the team participated in a modified Go to the Gemba (ie, go to where the work is done)[13] on a real‐time STAT order. Once all workgroup members were satisfied that the flow map represented the current state of the STAT medication process, we came to a consensus on the goals needed to meet our main objective.
We agreed that our main objective was that STAT medication orders should be recognized, verified, and administered to patients in a timely and appropriate manner to ensure quality care. We identified 3 goals to meet this objective: (1) STAT should be consistently defined and understood by everyone; (2) an easy, intuitive STAT process should be available for all stakeholders; and (3) the STAT process should be transparent and ideally visual so that everyone involved can understand at which point in the process a specific STAT order is currently situated. We also identified additional information we would need to reach the goals.
Shortly after the process‐mapping sessions, 2 workgroup members conducted real‐time STAT order time studies to track medications from order to administration. Three time periods in the STAT process were identified for observation and measurement: the time from physician order entry in the CPRS to the time a pharmacist verified the medication, the time from verification to when the medication arrived on the nursing unit, and the time from arrival on the nursing unit to when that medication was administered. Using a data‐collection template, each time period was recorded, and 28 time studies were collected over 1 month. To monitor the progress of our initiatives, the time study was repeated 3 months into the project.
ENVISIONING
Following the discovery phase, the team was better equipped to identify the specific changes needed to achieve an improved process. The envisioning phase allowed the team freedom to imagine an ideal process barring any preconceived notion of constraints within the current process.
In 2 meetings we brainstormed as many improvement ideas as possible. To prioritize and focus our ideas, we developed a matrix (see Supporting Information, Appendix A, in the online version of this article), placing our ideas in 1 of 4 quadrants based on the anticipated effort to implement the change (x‐axis) and impact of making the change (y‐axis). The matrix helped us see that some ideas would be relatively simple to implement (eg, color‐coded bags for STAT medication delivery), whereas others would require more sophisticated efforts and involvement of other people (eg, monthly education sessions to resident physicians).
EXPERIMENTING
Experiments were conducted to meet each of the 3 goals identified above. The team used the outcomes of the prioritization exercise to identify initial experiments to test. To build momentum by showing progress and improvement with a few quick wins, the team began with low‐effort/high‐impact opportunities. Each experiment followed a standard Plan‐Do‐Study‐Act (PDSA) cycle to encourage reflection, learning, adaptation, and adjustment as a result of the experiential learning process.[5]
Goal 1: STAT Should Be Consistently Defined and Understood by Everyone
To address the first goal, a subgroup collected policies and procedures related to the STAT medication administration process. The policy defined a STAT medication as a medication that has the potential to significantly and negatively impact a patient's clinical condition if not given within 30 minutes. The group found that the policy requiring a 30‐minute time to administration was clinically appropriate, reinforcing our goals to create a practice congruent with the policy.
A subgroup led by the pharmacy department collected data related to STAT medications on the 3 medical‐surgical units. Within 1 month, 550 STAT medications were ordered, consisting of medications ranging from furosemide to nicotine lozenges, the latter being a medication clearly outside of the policy definition of STAT. The workgroup reviewed the information and realized education would be required to align practice with policy. According to our matrix, education was a high‐impact/high‐effort activity, so efforts were focused on the high‐impact/low‐effort activities initially. We addressed educational opportunities in later PDSA cycles.
Goal 2: An Easy, Intuitive STAT Process for All Stakeholders
The CPRS contains prefabricated templates that conform to regulatory requirements and ensure completeness. However, the CPRS does not intuitively enable ordering providers to choose the time for the first dose of a new routine medication. This often creates a situation where a provider orders the medication STAT, so that the medication can be given earlier than the CPRS would otherwise allow. Although there is a check box, Give additional dose now, it was not being used because it was visually obscure in the interface. The CPRS restricted our ability to change the template for ordering medications to include a specific time for first‐dose administration before defaulting to the routine order; thus, complementary countermeasures were trialed first. These are outlined in Table 1.
| Countermeasure | Intended Outcome |
|---|---|
| Remove duplicate dosing frequencies from medication order template | Reduce list of dosing frequencies to sort through to find desired selection |
| Develop 1‐page job aid for ordering providers to utilize | Assist in the correct methods of ordering STAT, NOW, and routine medications |
| Added STAT ONCE as a dosing frequency selection | Clarify the medication, if ordered STAT, will only be a 1‐time administration to avoid the recurrence of a STAT order should the orders be transferred to a new unit with the patient |
| Modify existing policies to add STAT ONCE option | Ensure documentation is congruent with new expectations |
| Educate interns and residents with the job aid and a hands‐on how to ordering exercise | Inform ordering physicians on the available references for ordering and educate according to desired practice |
| Provide interns and residents with a visual job aid at their workstation and a hands‐on how to ordering exercise | In addition to providing information and educating according to desired practice, provide a just‐in‐time reference resource |
Goal 3: The STAT Process Should Be Transparent and Ideally Visual
During the time studies, the time period from when the medication arrived on the unit to the time it was administered to the patient averaged 34 minutes. Of 28 STAT orders followed through the entire process, 5 pharmacy technicians (26%) were not informed of 19 STAT medication orders requiring delivery, and 12 nurses (63%) were not notified of the delivery of those 19 medications. The remaining 9 STAT medications were stocked in the Omnicell. Informal interviews with nurses and pharmacy technicians, as well as input from the nurses and pharmacy technicians in our workgroup, revealed several explanations for these findings.
First, the delivering technicians could not always find the patient's nurse, and because the delivery procedure was not standardized, there was no consistency between technicians in where medications were delivered. Second, each unit had a different medication inventory stored in the Omnicell, and the inventory was frequently changed (eg, due to unit‐specific needs, backorders), which made it difficult for nurses to keep track of what was available in Omnicell at any given time. Finally, the STAT medication was not consistently labeled with a visual STAT notation, so even if a nurse saw that new medications had been delivered, he or she would not be able to easily identify which was STAT. The team made several low‐tech process changes to improve the visibility of a STAT medication and ensure reliable communication upon delivery. A subgroup of pharmacists, technicians, and nurses developed and implemented the countermeasures described in Table 2.
| Countermeasure | Intended Outcome |
|---|---|
| Designate delivery preferences with the patient's nurse as the first preference and a set location in the med room as the only alternative preference | Attempt to deliver medications directly to the patient's nurse as frequently as possible to eliminate any unnecessary delays and avoid miscommunication |
| Identify a location in each unit's med room to place a red bin to deliver the STAT medications that are unable to be delivered to the patient's nurse directly | Provide 1 alternate location to retrieve STAT medications if the technician is unable to locate the patient's nurse to deliver the medication directly |
| Utilize a plastic bag with a red STAT indication for transportation of STAT medications to the units | Provide a visual to assist in pharmacy technicians prioritizing their deliveries to the inpatient units |
| Utilize red STAT magnets on the patient's door frame to signal nurses a medication had been delivered to the med room | Provide a visual to assist in timely recognition of a STAT medication delivery given the technician was unable to find the nurse to hand it off directly |
RESULTS
At the start of our project, the average time from STAT order to medication administration was 1 hour and 7 minutes (range, 6 minutes 2 hours and 22 minutes). As a result of the 2 sets of countermeasures outlined in Tables 1 and 2, the average total time from STAT order entry to administration decreased by 21% to an average of 53 minutes. The total time from medication delivery to administration decreased by 26% from 34 minutes to 25 minutes postimplementation. On average, 391 STAT medications were ordered per month during the project period, which represents a decrease of 9.5% from the 432 orders per month for the same time period the previous year. After implementing the countermeasures in Table 2, we followed another 26 STAT medications through the process to evaluate our efforts. Of 15 STAT medications requiring delivery, only 1 nurse (7%) was not notified of the delivery of a STAT medication, and 1 pharmacy technician (7%) was not informed the medication was STAT. The 151% increase in notification of nurses to delivery of a STAT medication suggests that use of the STAT bags, STAT magnets on patient doors, and whenever possible direct delivery of STAT medications to the nurse has improved communication between the technicians and nurses. Similarly, the 27% increase in technician awareness of a STAT designation suggests STAT is being better communicated to them. The improvement in awareness and notification of a STAT medication is summarized in Figure 2.
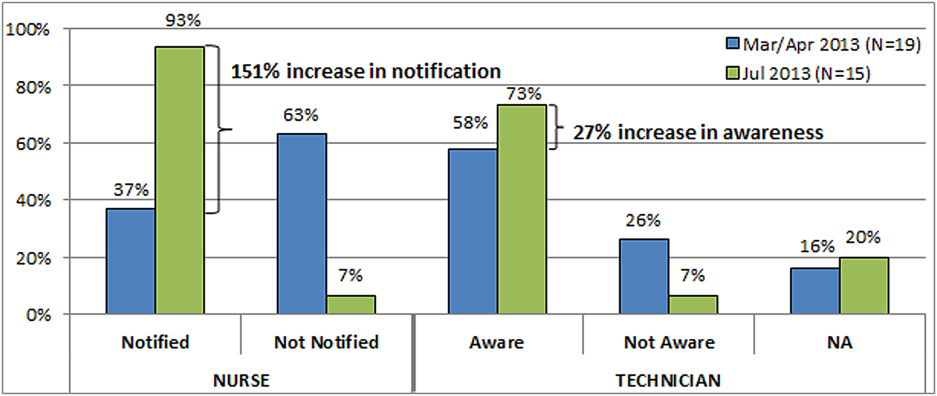
Due to time and financial constraints, the following limitations may have affected our findings. First, resident physicians were not directly represented in our discussions. Attending medicine hospitalists provided the physician perspective, which provides a biased view given their intimate knowledge of the CPRS and additional years of experience. Similarly, nurse perspectives were limited to staff and clinical nurse leaders. Last, our low‐cost approach was mandated by limited resources; a more resource‐rich environment may have devised alternative approaches.
CONCLUSIONS
Adapting A3 Thinking for process improvement was a low‐cost/low‐tech option for a VA facility. Having buy‐in from all levels was crucial to the success of the project. The size and diversity of the group was also very important, as different opinions and aspects of the process were represented. Cross‐discipline relationships and respect were formed, which will be valuable for collaboration in future projects. Although we focused on the STAT medication process, other quality‐improvement projects could also benefit from A3 Thinking. Moreover, there were enough people to serve as ambassadors, taking the project back to their work areas to share with their peers, gather consensus, and elicit additional feedback. The collaboration led to comprehensive understanding of the process, the nature of the problems within the process, and the complexity of solving the problem. For example, although the number of STAT orders did not decrease dramatically, we have learned from these experiments that we may need to change how we approach structuring additional experiments. Future work will focus on increasing communication between physicians and nurses when placing STAT medication orders, enhancing resident education to ensure appropriate use of the STAT designation, and continuing our efforts to improve the delivery process of STAT medications.
Other quality‐improvement methodologies we could have used include: total quality management (TQM), continuous quality improvement (CQI), business process redesign, Lean, Six Sigma, and others.[14] Differences between these can be broadly classified as putting an emphasis on people (eg, inclusion of front line staff in CQI or leadership in TQM) or on process (eg, understanding process function to reduce waste in Lean or statistical process control in Six Sigma).[14] Using A3 Thinking methodology was more useful than these others for the STAT medication process for some very important reasons. The A3 process not only led to a better understanding of the meaning of STAT across disciplines, increasing the intuitive nature, transparency and visual aspects of the whole process, but also promoted a collaborative, multidisciplinary, integrative culture, in which other hospital‐wide problems may be addressed in the future.
Acknowledgements
This work could not have been done without the contribution of all members of the STAT Improvement Workgroup, including Charles Alday; Allison Brenner, PharmD; Paula Carroll; Garry Davis; Michele Delaney, RN, MSN, CWCN; Mary East, MD; Stacy Frick, MSN, RN, CNL; Corry Gessner, CPhT; Kenya Harbin, MSN, RN, CNL; Crystal Heath, MS, RN‐BC; Tom Kerr, MPH; Diane Klemer, RPh; Diane Kohmescher, PharmD, BCPS; Sara Oberdick; Antanita Pickett; Ana Preda, CPhT; Joseph Pugh, RPh, MS; Gloria Salazar, CPhT; Samar Sheth, MD; Andrea Starnes, RN; Christine Wagner, PharmD; Leo Wallace; Roderick Williams; and Marilyn Woodruff.
Disclosures: This work was funded by a US Department of Veterans Affairs, Office of Systems Redesign Improvement Capability Grant and the Veterans in Partnership (VISN11) Healthcare Network. The findings and conclusions in this report are those of the authors and do not necessarily represent the position or policy of the US Department of Veterans Affairs. The authors have no other disclosures or conflicts to report.
STAT is an abbreviation of the Latin word statim, meaning immediately,[1] and has been a part of healthcare's lexicon for almost as long as there have been hospitals. STAT conveys a sense of urgency, compelling those who hear STAT to act quickly. Unfortunately, given the lack of a consistent understanding of STAT, the term in reality often has an alternate use: to hurry up or to complete sooner than routine, and is sometimes used to circumvent a system that is perceived to be too slow to accomplish a routine task in a timely manner.
As part of a larger systems redesign effort to improve patient safety and quality of care, an institutional review board (IRB)‐approved qualitative study was conducted on 2 medical‐surgical units in a US Department of Veterans Affairs (VA) hospital to explore communication patterns between physicians and nurses.[2] The study revealed wide variation in understanding between physicians and nurses on the ordering and administration of STAT medication. Physicians were unaware that when they placed a STAT order into the computerized patient record system (CPRS), nurses were not automatically alerted about the order. At this facility, nurses did not carry pagers. Although each unit had a supply of wireless telephones, they were often unreliable and therefore not used consistently. Nurses were required by policy to check the CPRS for new orders every 2 hours. This was an inefficient and possibly dangerous process,[3] because if a nurse was not expecting a STAT order, 2 hours could elapse before she or he saw the order in the CPRS and began to look for the medication. A follow‐up survey completed by physicians, nurses, pharmacists, and pharmacy technicians demonstrated stark differences on the definition of STAT and overlap with similar terms such as NOW and ASAP. Interviews with ordering providers indicated that 36% of the time a STAT was ordered it was not clinically urgent, but instead ordered STAT to speed up the process.
The STAT medication process was clearly in need of improvement, but previous quality improvement projects in our organization had varying degrees of success. For example, we used Lean methodology in an attempt to improve our discharge process. We conducted a modified rapid process discharge improvement workshop[4] structured in phases over 4 weeks. During the workshops, a strong emphasis remained on the solutions to the problem, and we were unable to help the team move from a mindset of fix it to create it. This limited the buy‐in of team members, the creativity of their ideas for improvement, and ultimately the momentum to improve the process.
In this article we describe our adaptation of A3 Thinking,[5, 6] a structure for guiding quality improvement based in Lean methodology, to improve the STAT medication process. We chose A3 Thinking for several reasons. A3 Thinking focuses on process improvement and thus aligned well with our interest in improving the STAT medication process. A3 Thinking also reveals otherwise hidden nonvalue‐added activities that should be eliminated.[7] Finally A3 Thinking reinforces a deeper understanding of the way the work is currently being done, providing critical information needed before making a change. This provides a tremendous opportunity to look at work differently and see opportunities for improvement.[8] Given these strengths as well as the lack of congruence between what the STAT process should consist of and how the STAT process was actually being used in our organization, A3 Thinking offered the best fit between an improvement process and the problem to be solved.
METHODS
A search of healthcare literature yielded very few studies on the STAT process.[9, 10] Only 1 intervention to improve the process was found, and this focused on a specific procedure.[10] An informal survey of local VA and non‐VA hospitals regarding their experiences with the STAT medication process revealed insufficient information to aid our efforts. We next searched the business and manufacturing literature and found examples of how the Lean methodology was successfully applied to other problems in healthcare, including improving pediatric surgery workflow and decreasing ventilator‐associated pneumonia.[11, 12]
Therefore, the STAT project was structured to adapt a problem‐solving process commonly used in Lean organizationsA3 Thinkingwhich challenges team members to work through a discovery phase to develop a shared understanding of the process, an envisioning phase to conceptualize an ideal process experience, and finally an experimentation phase to identify and trial possible solutions through prioritization, iterative testing, structured reflection, and adjustment on resulting changes. Our application of the term experimentation in this context is distinct from that of controlled experimentation in clinical research; the term is intended to convey iterative learning as changes are tested, evaluated, and modified during this quality improvement project. Figure 1 displays a conceptual model of our adaptation of A3 Thinking. As this was a quality‐improvement project, it was exempt from IRB review.
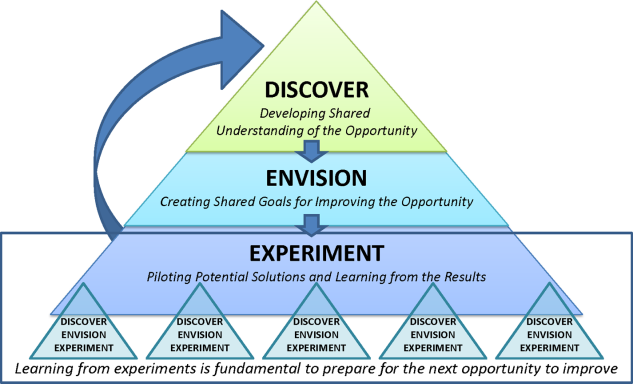
DISCOVERY
To begin the discovery phase, a workgroup consisting of representatives of all groups that had a role in the STAT process (ie, physician, pharmacist, nurse, pharmacy technician, clerk) gathered to identify the opportunity we are looking to address and learn from each other's individual experiences with the STAT medication process. The group was facilitated by an industrial engineer familiar with the A3 Thinking process. The team completed a mapping exercise to lay out, step‐by‐step, the current STAT medication process. This activity allowed the team to build shared empathy with others' experiences and to appreciate the challenges experienced by others through their individual responsibilities in the process. The current process was found to consist of 4 overarching components: a provider entered the STAT order into the CPRS; the order was verified by a pharmacist; a pharmacy technician delivered the medication to the unit (or a nurse retrieved the medication from the Omnicell (Omnicell Inc., Mountain View, CA), a proprietary automated medication dispensing system); and finally the nurse administered the medication to a patient.
A large, color‐coded flow map of the STAT medication process was constructed over several meetings to capture all perspectives and allow team members to gather feedback from their peers. To further our understanding of the current process, the team participated in a modified Go to the Gemba (ie, go to where the work is done)[13] on a real‐time STAT order. Once all workgroup members were satisfied that the flow map represented the current state of the STAT medication process, we came to a consensus on the goals needed to meet our main objective.
We agreed that our main objective was that STAT medication orders should be recognized, verified, and administered to patients in a timely and appropriate manner to ensure quality care. We identified 3 goals to meet this objective: (1) STAT should be consistently defined and understood by everyone; (2) an easy, intuitive STAT process should be available for all stakeholders; and (3) the STAT process should be transparent and ideally visual so that everyone involved can understand at which point in the process a specific STAT order is currently situated. We also identified additional information we would need to reach the goals.
Shortly after the process‐mapping sessions, 2 workgroup members conducted real‐time STAT order time studies to track medications from order to administration. Three time periods in the STAT process were identified for observation and measurement: the time from physician order entry in the CPRS to the time a pharmacist verified the medication, the time from verification to when the medication arrived on the nursing unit, and the time from arrival on the nursing unit to when that medication was administered. Using a data‐collection template, each time period was recorded, and 28 time studies were collected over 1 month. To monitor the progress of our initiatives, the time study was repeated 3 months into the project.
ENVISIONING
Following the discovery phase, the team was better equipped to identify the specific changes needed to achieve an improved process. The envisioning phase allowed the team freedom to imagine an ideal process barring any preconceived notion of constraints within the current process.
In 2 meetings we brainstormed as many improvement ideas as possible. To prioritize and focus our ideas, we developed a matrix (see Supporting Information, Appendix A, in the online version of this article), placing our ideas in 1 of 4 quadrants based on the anticipated effort to implement the change (x‐axis) and impact of making the change (y‐axis). The matrix helped us see that some ideas would be relatively simple to implement (eg, color‐coded bags for STAT medication delivery), whereas others would require more sophisticated efforts and involvement of other people (eg, monthly education sessions to resident physicians).
EXPERIMENTING
Experiments were conducted to meet each of the 3 goals identified above. The team used the outcomes of the prioritization exercise to identify initial experiments to test. To build momentum by showing progress and improvement with a few quick wins, the team began with low‐effort/high‐impact opportunities. Each experiment followed a standard Plan‐Do‐Study‐Act (PDSA) cycle to encourage reflection, learning, adaptation, and adjustment as a result of the experiential learning process.[5]
Goal 1: STAT Should Be Consistently Defined and Understood by Everyone
To address the first goal, a subgroup collected policies and procedures related to the STAT medication administration process. The policy defined a STAT medication as a medication that has the potential to significantly and negatively impact a patient's clinical condition if not given within 30 minutes. The group found that the policy requiring a 30‐minute time to administration was clinically appropriate, reinforcing our goals to create a practice congruent with the policy.
A subgroup led by the pharmacy department collected data related to STAT medications on the 3 medical‐surgical units. Within 1 month, 550 STAT medications were ordered, consisting of medications ranging from furosemide to nicotine lozenges, the latter being a medication clearly outside of the policy definition of STAT. The workgroup reviewed the information and realized education would be required to align practice with policy. According to our matrix, education was a high‐impact/high‐effort activity, so efforts were focused on the high‐impact/low‐effort activities initially. We addressed educational opportunities in later PDSA cycles.
Goal 2: An Easy, Intuitive STAT Process for All Stakeholders
The CPRS contains prefabricated templates that conform to regulatory requirements and ensure completeness. However, the CPRS does not intuitively enable ordering providers to choose the time for the first dose of a new routine medication. This often creates a situation where a provider orders the medication STAT, so that the medication can be given earlier than the CPRS would otherwise allow. Although there is a check box, Give additional dose now, it was not being used because it was visually obscure in the interface. The CPRS restricted our ability to change the template for ordering medications to include a specific time for first‐dose administration before defaulting to the routine order; thus, complementary countermeasures were trialed first. These are outlined in Table 1.
| Countermeasure | Intended Outcome |
|---|---|
| Remove duplicate dosing frequencies from medication order template | Reduce list of dosing frequencies to sort through to find desired selection |
| Develop 1‐page job aid for ordering providers to utilize | Assist in the correct methods of ordering STAT, NOW, and routine medications |
| Added STAT ONCE as a dosing frequency selection | Clarify the medication, if ordered STAT, will only be a 1‐time administration to avoid the recurrence of a STAT order should the orders be transferred to a new unit with the patient |
| Modify existing policies to add STAT ONCE option | Ensure documentation is congruent with new expectations |
| Educate interns and residents with the job aid and a hands‐on how to ordering exercise | Inform ordering physicians on the available references for ordering and educate according to desired practice |
| Provide interns and residents with a visual job aid at their workstation and a hands‐on how to ordering exercise | In addition to providing information and educating according to desired practice, provide a just‐in‐time reference resource |
Goal 3: The STAT Process Should Be Transparent and Ideally Visual
During the time studies, the time period from when the medication arrived on the unit to the time it was administered to the patient averaged 34 minutes. Of 28 STAT orders followed through the entire process, 5 pharmacy technicians (26%) were not informed of 19 STAT medication orders requiring delivery, and 12 nurses (63%) were not notified of the delivery of those 19 medications. The remaining 9 STAT medications were stocked in the Omnicell. Informal interviews with nurses and pharmacy technicians, as well as input from the nurses and pharmacy technicians in our workgroup, revealed several explanations for these findings.
First, the delivering technicians could not always find the patient's nurse, and because the delivery procedure was not standardized, there was no consistency between technicians in where medications were delivered. Second, each unit had a different medication inventory stored in the Omnicell, and the inventory was frequently changed (eg, due to unit‐specific needs, backorders), which made it difficult for nurses to keep track of what was available in Omnicell at any given time. Finally, the STAT medication was not consistently labeled with a visual STAT notation, so even if a nurse saw that new medications had been delivered, he or she would not be able to easily identify which was STAT. The team made several low‐tech process changes to improve the visibility of a STAT medication and ensure reliable communication upon delivery. A subgroup of pharmacists, technicians, and nurses developed and implemented the countermeasures described in Table 2.
| Countermeasure | Intended Outcome |
|---|---|
| Designate delivery preferences with the patient's nurse as the first preference and a set location in the med room as the only alternative preference | Attempt to deliver medications directly to the patient's nurse as frequently as possible to eliminate any unnecessary delays and avoid miscommunication |
| Identify a location in each unit's med room to place a red bin to deliver the STAT medications that are unable to be delivered to the patient's nurse directly | Provide 1 alternate location to retrieve STAT medications if the technician is unable to locate the patient's nurse to deliver the medication directly |
| Utilize a plastic bag with a red STAT indication for transportation of STAT medications to the units | Provide a visual to assist in pharmacy technicians prioritizing their deliveries to the inpatient units |
| Utilize red STAT magnets on the patient's door frame to signal nurses a medication had been delivered to the med room | Provide a visual to assist in timely recognition of a STAT medication delivery given the technician was unable to find the nurse to hand it off directly |
RESULTS
At the start of our project, the average time from STAT order to medication administration was 1 hour and 7 minutes (range, 6 minutes 2 hours and 22 minutes). As a result of the 2 sets of countermeasures outlined in Tables 1 and 2, the average total time from STAT order entry to administration decreased by 21% to an average of 53 minutes. The total time from medication delivery to administration decreased by 26% from 34 minutes to 25 minutes postimplementation. On average, 391 STAT medications were ordered per month during the project period, which represents a decrease of 9.5% from the 432 orders per month for the same time period the previous year. After implementing the countermeasures in Table 2, we followed another 26 STAT medications through the process to evaluate our efforts. Of 15 STAT medications requiring delivery, only 1 nurse (7%) was not notified of the delivery of a STAT medication, and 1 pharmacy technician (7%) was not informed the medication was STAT. The 151% increase in notification of nurses to delivery of a STAT medication suggests that use of the STAT bags, STAT magnets on patient doors, and whenever possible direct delivery of STAT medications to the nurse has improved communication between the technicians and nurses. Similarly, the 27% increase in technician awareness of a STAT designation suggests STAT is being better communicated to them. The improvement in awareness and notification of a STAT medication is summarized in Figure 2.
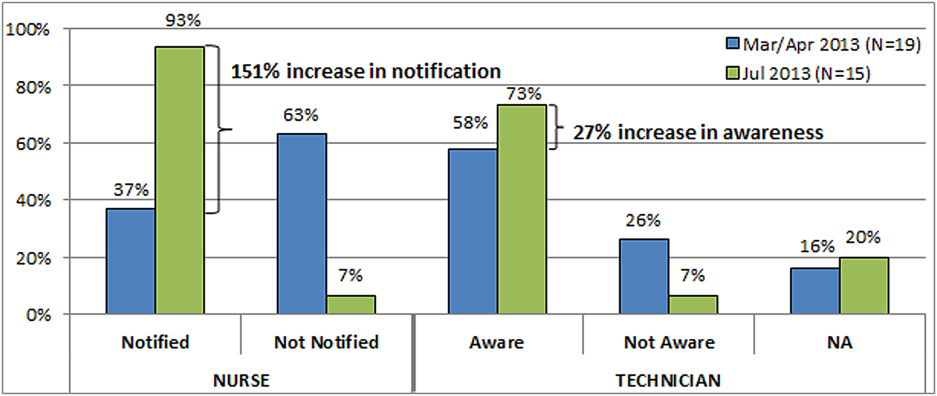
Due to time and financial constraints, the following limitations may have affected our findings. First, resident physicians were not directly represented in our discussions. Attending medicine hospitalists provided the physician perspective, which provides a biased view given their intimate knowledge of the CPRS and additional years of experience. Similarly, nurse perspectives were limited to staff and clinical nurse leaders. Last, our low‐cost approach was mandated by limited resources; a more resource‐rich environment may have devised alternative approaches.
CONCLUSIONS
Adapting A3 Thinking for process improvement was a low‐cost/low‐tech option for a VA facility. Having buy‐in from all levels was crucial to the success of the project. The size and diversity of the group was also very important, as different opinions and aspects of the process were represented. Cross‐discipline relationships and respect were formed, which will be valuable for collaboration in future projects. Although we focused on the STAT medication process, other quality‐improvement projects could also benefit from A3 Thinking. Moreover, there were enough people to serve as ambassadors, taking the project back to their work areas to share with their peers, gather consensus, and elicit additional feedback. The collaboration led to comprehensive understanding of the process, the nature of the problems within the process, and the complexity of solving the problem. For example, although the number of STAT orders did not decrease dramatically, we have learned from these experiments that we may need to change how we approach structuring additional experiments. Future work will focus on increasing communication between physicians and nurses when placing STAT medication orders, enhancing resident education to ensure appropriate use of the STAT designation, and continuing our efforts to improve the delivery process of STAT medications.
Other quality‐improvement methodologies we could have used include: total quality management (TQM), continuous quality improvement (CQI), business process redesign, Lean, Six Sigma, and others.[14] Differences between these can be broadly classified as putting an emphasis on people (eg, inclusion of front line staff in CQI or leadership in TQM) or on process (eg, understanding process function to reduce waste in Lean or statistical process control in Six Sigma).[14] Using A3 Thinking methodology was more useful than these others for the STAT medication process for some very important reasons. The A3 process not only led to a better understanding of the meaning of STAT across disciplines, increasing the intuitive nature, transparency and visual aspects of the whole process, but also promoted a collaborative, multidisciplinary, integrative culture, in which other hospital‐wide problems may be addressed in the future.
Acknowledgements
This work could not have been done without the contribution of all members of the STAT Improvement Workgroup, including Charles Alday; Allison Brenner, PharmD; Paula Carroll; Garry Davis; Michele Delaney, RN, MSN, CWCN; Mary East, MD; Stacy Frick, MSN, RN, CNL; Corry Gessner, CPhT; Kenya Harbin, MSN, RN, CNL; Crystal Heath, MS, RN‐BC; Tom Kerr, MPH; Diane Klemer, RPh; Diane Kohmescher, PharmD, BCPS; Sara Oberdick; Antanita Pickett; Ana Preda, CPhT; Joseph Pugh, RPh, MS; Gloria Salazar, CPhT; Samar Sheth, MD; Andrea Starnes, RN; Christine Wagner, PharmD; Leo Wallace; Roderick Williams; and Marilyn Woodruff.
Disclosures: This work was funded by a US Department of Veterans Affairs, Office of Systems Redesign Improvement Capability Grant and the Veterans in Partnership (VISN11) Healthcare Network. The findings and conclusions in this report are those of the authors and do not necessarily represent the position or policy of the US Department of Veterans Affairs. The authors have no other disclosures or conflicts to report.
- The American Heritage Medical Dictionary of the English Language website. 2011. Available at: http://ahdictionary.com/word/search.html?q=STAT. Accessed December 22, 2013.
- , , , , , . The use of multiple qualitative methods to characterize communication events between physicians and nurses [published online ahead of print January 31, 2014]. Health Commun. doi: 10.1080/10410236.2013.835894.
- , , . Fifteen best practice recommendations for bar‐code medication administration in the Veterans Health Administration. Jt Comm J Qual Saf. 2004;30(7):355–365.
- , , , , . Going lean in health care. Cambridge, MA: Institute for Healthcare Improvement; 2005. Available at: http://www.ihi.org. Accessed March 19, 2014.
- , . Understanding A3 Thinking: A Critical Component of Toyota's PDCA Management System. New York, NY: Productivity Press, Taylor 2008.
- . Managing to Learn: Using the A3 Management Process to Solve Problems, Gain Agreement, Mentor and Lead. Cambridge, MA: Lean Enterprise Institute; 2008.
- , , . Basics of quality improvement in health care. Mayo Clin Proc. 2007;82(6):735–739.
- , . A3 problem solving: unique features of the A3 problem solving method. Available at: http://leanhealthcarewest.com/Page/A3‐Problem‐Solving. Accessed March 27, 2014.
- , , . Evaluation of stat orders in a teaching hospital: a chart review. Clin Drug Investig. 2011;31(4):231–235.
- . Using STAT properly. Radiol Manage. 2006;28(1):26–30; quiz 31–33.
- , . The promise of Lean in health care. Mayo Clin Proc. 2013;88(1):74–82.
- , , , . Lean health care: what can hospitals learn from a world‐class automaker? J Hosp Med. 2006;1(3):191–199.
- . Gemba Kaizen: A Commonsense Approach to a Continuous Improvement Strategy. 2nd ed. New York, NY: McGraw‐Hill; 2012.
- . Pseudoinnovation: the development and spread of healthcare quality improvement methodologies. Int J Qual Health Care. 2009;21(3):153–159.
- The American Heritage Medical Dictionary of the English Language website. 2011. Available at: http://ahdictionary.com/word/search.html?q=STAT. Accessed December 22, 2013.
- , , , , , . The use of multiple qualitative methods to characterize communication events between physicians and nurses [published online ahead of print January 31, 2014]. Health Commun. doi: 10.1080/10410236.2013.835894.
- , , . Fifteen best practice recommendations for bar‐code medication administration in the Veterans Health Administration. Jt Comm J Qual Saf. 2004;30(7):355–365.
- , , , , . Going lean in health care. Cambridge, MA: Institute for Healthcare Improvement; 2005. Available at: http://www.ihi.org. Accessed March 19, 2014.
- , . Understanding A3 Thinking: A Critical Component of Toyota's PDCA Management System. New York, NY: Productivity Press, Taylor 2008.
- . Managing to Learn: Using the A3 Management Process to Solve Problems, Gain Agreement, Mentor and Lead. Cambridge, MA: Lean Enterprise Institute; 2008.
- , , . Basics of quality improvement in health care. Mayo Clin Proc. 2007;82(6):735–739.
- , . A3 problem solving: unique features of the A3 problem solving method. Available at: http://leanhealthcarewest.com/Page/A3‐Problem‐Solving. Accessed March 27, 2014.
- , , . Evaluation of stat orders in a teaching hospital: a chart review. Clin Drug Investig. 2011;31(4):231–235.
- . Using STAT properly. Radiol Manage. 2006;28(1):26–30; quiz 31–33.
- , . The promise of Lean in health care. Mayo Clin Proc. 2013;88(1):74–82.
- , , , . Lean health care: what can hospitals learn from a world‐class automaker? J Hosp Med. 2006;1(3):191–199.
- . Gemba Kaizen: A Commonsense Approach to a Continuous Improvement Strategy. 2nd ed. New York, NY: McGraw‐Hill; 2012.
- . Pseudoinnovation: the development and spread of healthcare quality improvement methodologies. Int J Qual Health Care. 2009;21(3):153–159.
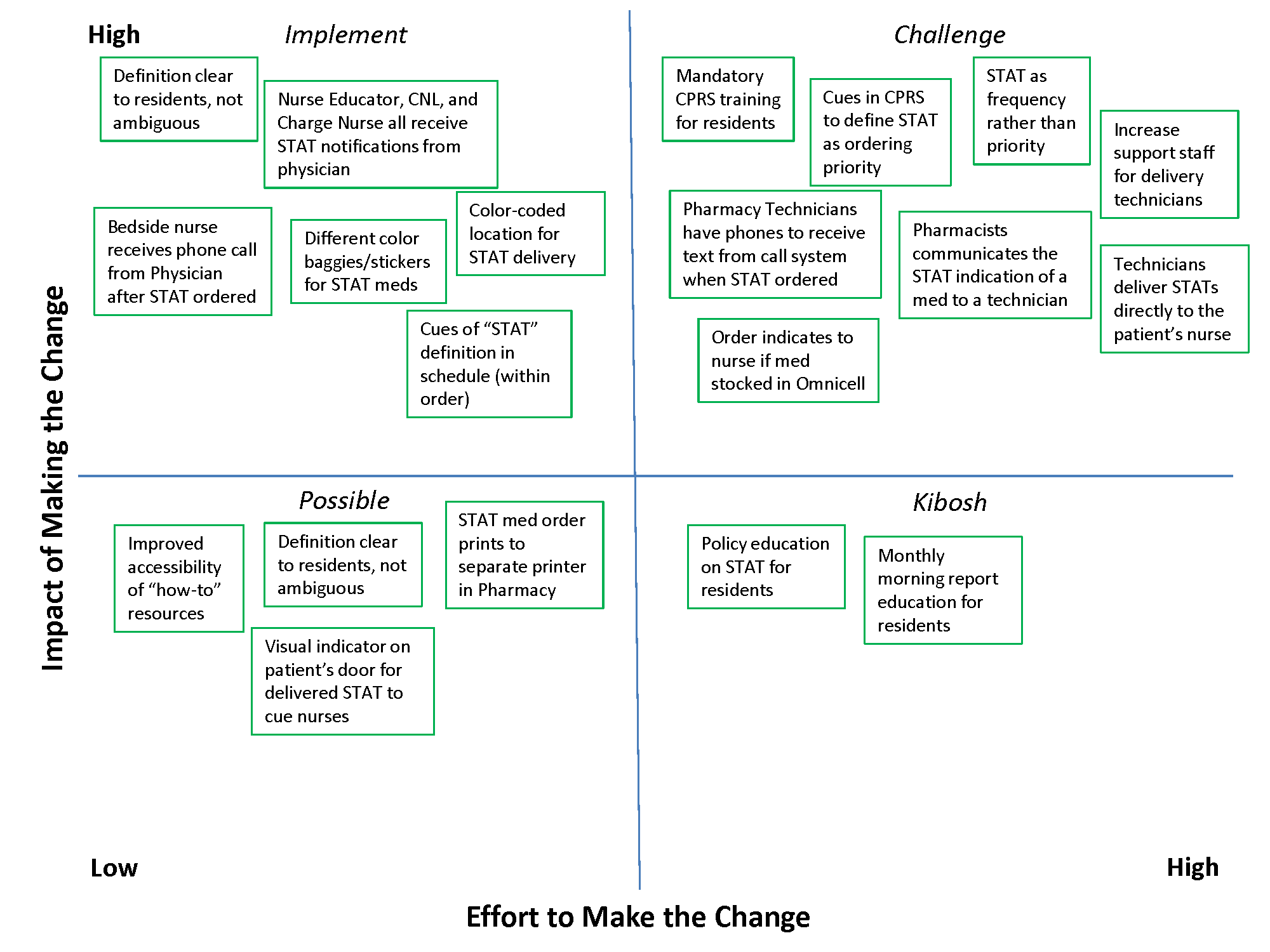
VIDEO EXCLUSIVE: Baystate Medical Center's Unit-Based, Multidisciplinary Rounding Enhances Inpatient Care
Click on the 5-minute video below...
)Click on the 5-minute video below...
)Click on the 5-minute video below...
)Uterine adenomyosis: Noninvasive diagnosis
INTRODUCTION
Steven R. Goldstein, MD, CCD, NCMP
Professor, Department of Obstetrics and Gynecology, New York University School of Medicine; Director, Gynecologic Ultrasound; and Co-Director, Bone Densitometry, New York University Medical Center, New York
In this month’s installment of Images in GYN Ultrasound, Drs. Stalnaker and Kaunitz have done an excellent job of describing what adenomyosis will look like on transvaginal ultrasound
In my first book, entitled Endovaginal Ultrasound,1 I coined the phrase “sonomicoscopy.” I maintain that we are seeing things with transvaginal ultrasound that you could not see with your naked eye if you could hold the structure at arms length and squint at it.
Adenomyosis is defined as endometrial glands and stroma embedded within the myometrium. Literature has shown that if you do three sections on a routine hysterectomy specimen the incidence of adenomyosis is 31%; with six sections the incidence is 61%! In other words, it is a very prevalent occurrence.
There is no question that adenomyosis CAN be a source of uterine enlargement, pain, and bleeding. But it is such a prevalent finding that the real question is: What percent of women, especially parous women, will have sonographic evidence of adenomyosis but be totally asymptomatic? Such women represent the denominator while the symptomatic ones represent the numerator. I worry about labeling asymptomatic patients with this entity—when they become perimenopausal and oligo-ovulatory, and may have irregular bleeding—their symptoms can be judged to be FROM adenomyosis and surgical correction is offered.
An important part of successful ultrasound use is being sure that we redefine what is “normal” as we examine patients with this “low power microscope.” So, while transvaginal ultrasound CAN identify glands and stroma within the myometrium, we must be careful not to automatically label this finding as a “disease.”
Reference
1. Goldstein SR. Endovaginal Ultrasound. 2nd ed. John Wiley & Sons, Inc: Hoboken, NJ; January 1991.
Uterine adenomyosis: Noninvasive diagnosis
Michelle L. Stalnaker, MD
Assistant Professor and Associate Program Director, Obstetrics and Gynecology Residency, Department of Obstetrics and Gynecology at the University of Florida College of Medicine–Jacksonville
Andrew M. Kaunitz, MD
University of Florida Research Foundation Professor and Associate Chairman, Department of Obstetrics and Gynecology at the University of Florida College of Medicine–Jacksonville. Dr. Kaunitz is a member of the OBG Management Board of Editors.
Uterine adenomyosis is a pathologic condition in which endometrial glands and stroma are present in the uterine myometrium. Uterine adenomyosis is common, and may coexist with leiomyomata or endometriosis. When present, it may cause dysmenorrhea and heavy menses.
Until recently, the best way to establish a diagnosis of uterine adenomyosis was through histologic examination of a hysterectomy specimen. However, transvaginal ultrasound and pelvic magnetic resonance imaging have been shown to be accurate for noninvasive diagnosis.
Signs on imaging include:
- Globular/bulky uterus
- Asymmetric thickening of myometrium
- Loss of clarity of endo-myometrial interface
- Diffuse heterogenous myometrial echogenicity
- Myometrial cysts
| Click to enlarge image |
1. Champaneria R, Abedin P, Daniels J, Balogun M, Khan KS. Ultrasound scan and magnetic resonance imaging for the diagnosis of adenomyosis: systematic review comparing test accuracy. Acta Obstetricia et Gynecologica. 2010;89(11):1374-1384.
2. Meredith SM, Sanchez-Ramos L, Kaunitz AM. Diagnostic accuracy of transvaginal sonography for the diagnosis of adenomyosis: systematic review and meta-analysis. Am J Obstet Gynecol. 2009;201(1):107.e1-e6.
3. Munro MG. Update: abnormal uterine bleeding. OBG Manag. 2014;26(3):27-32.
INTRODUCTION
Steven R. Goldstein, MD, CCD, NCMP
Professor, Department of Obstetrics and Gynecology, New York University School of Medicine; Director, Gynecologic Ultrasound; and Co-Director, Bone Densitometry, New York University Medical Center, New York
In this month’s installment of Images in GYN Ultrasound, Drs. Stalnaker and Kaunitz have done an excellent job of describing what adenomyosis will look like on transvaginal ultrasound
In my first book, entitled Endovaginal Ultrasound,1 I coined the phrase “sonomicoscopy.” I maintain that we are seeing things with transvaginal ultrasound that you could not see with your naked eye if you could hold the structure at arms length and squint at it.
Adenomyosis is defined as endometrial glands and stroma embedded within the myometrium. Literature has shown that if you do three sections on a routine hysterectomy specimen the incidence of adenomyosis is 31%; with six sections the incidence is 61%! In other words, it is a very prevalent occurrence.
There is no question that adenomyosis CAN be a source of uterine enlargement, pain, and bleeding. But it is such a prevalent finding that the real question is: What percent of women, especially parous women, will have sonographic evidence of adenomyosis but be totally asymptomatic? Such women represent the denominator while the symptomatic ones represent the numerator. I worry about labeling asymptomatic patients with this entity—when they become perimenopausal and oligo-ovulatory, and may have irregular bleeding—their symptoms can be judged to be FROM adenomyosis and surgical correction is offered.
An important part of successful ultrasound use is being sure that we redefine what is “normal” as we examine patients with this “low power microscope.” So, while transvaginal ultrasound CAN identify glands and stroma within the myometrium, we must be careful not to automatically label this finding as a “disease.”
Reference
1. Goldstein SR. Endovaginal Ultrasound. 2nd ed. John Wiley & Sons, Inc: Hoboken, NJ; January 1991.
Uterine adenomyosis: Noninvasive diagnosis
Michelle L. Stalnaker, MD
Assistant Professor and Associate Program Director, Obstetrics and Gynecology Residency, Department of Obstetrics and Gynecology at the University of Florida College of Medicine–Jacksonville
Andrew M. Kaunitz, MD
University of Florida Research Foundation Professor and Associate Chairman, Department of Obstetrics and Gynecology at the University of Florida College of Medicine–Jacksonville. Dr. Kaunitz is a member of the OBG Management Board of Editors.
Uterine adenomyosis is a pathologic condition in which endometrial glands and stroma are present in the uterine myometrium. Uterine adenomyosis is common, and may coexist with leiomyomata or endometriosis. When present, it may cause dysmenorrhea and heavy menses.
Until recently, the best way to establish a diagnosis of uterine adenomyosis was through histologic examination of a hysterectomy specimen. However, transvaginal ultrasound and pelvic magnetic resonance imaging have been shown to be accurate for noninvasive diagnosis.
Signs on imaging include:
- Globular/bulky uterus
- Asymmetric thickening of myometrium
- Loss of clarity of endo-myometrial interface
- Diffuse heterogenous myometrial echogenicity
- Myometrial cysts
| Click to enlarge image |
INTRODUCTION
Steven R. Goldstein, MD, CCD, NCMP
Professor, Department of Obstetrics and Gynecology, New York University School of Medicine; Director, Gynecologic Ultrasound; and Co-Director, Bone Densitometry, New York University Medical Center, New York
In this month’s installment of Images in GYN Ultrasound, Drs. Stalnaker and Kaunitz have done an excellent job of describing what adenomyosis will look like on transvaginal ultrasound
In my first book, entitled Endovaginal Ultrasound,1 I coined the phrase “sonomicoscopy.” I maintain that we are seeing things with transvaginal ultrasound that you could not see with your naked eye if you could hold the structure at arms length and squint at it.
Adenomyosis is defined as endometrial glands and stroma embedded within the myometrium. Literature has shown that if you do three sections on a routine hysterectomy specimen the incidence of adenomyosis is 31%; with six sections the incidence is 61%! In other words, it is a very prevalent occurrence.
There is no question that adenomyosis CAN be a source of uterine enlargement, pain, and bleeding. But it is such a prevalent finding that the real question is: What percent of women, especially parous women, will have sonographic evidence of adenomyosis but be totally asymptomatic? Such women represent the denominator while the symptomatic ones represent the numerator. I worry about labeling asymptomatic patients with this entity—when they become perimenopausal and oligo-ovulatory, and may have irregular bleeding—their symptoms can be judged to be FROM adenomyosis and surgical correction is offered.
An important part of successful ultrasound use is being sure that we redefine what is “normal” as we examine patients with this “low power microscope.” So, while transvaginal ultrasound CAN identify glands and stroma within the myometrium, we must be careful not to automatically label this finding as a “disease.”
Reference
1. Goldstein SR. Endovaginal Ultrasound. 2nd ed. John Wiley & Sons, Inc: Hoboken, NJ; January 1991.
Uterine adenomyosis: Noninvasive diagnosis
Michelle L. Stalnaker, MD
Assistant Professor and Associate Program Director, Obstetrics and Gynecology Residency, Department of Obstetrics and Gynecology at the University of Florida College of Medicine–Jacksonville
Andrew M. Kaunitz, MD
University of Florida Research Foundation Professor and Associate Chairman, Department of Obstetrics and Gynecology at the University of Florida College of Medicine–Jacksonville. Dr. Kaunitz is a member of the OBG Management Board of Editors.
Uterine adenomyosis is a pathologic condition in which endometrial glands and stroma are present in the uterine myometrium. Uterine adenomyosis is common, and may coexist with leiomyomata or endometriosis. When present, it may cause dysmenorrhea and heavy menses.
Until recently, the best way to establish a diagnosis of uterine adenomyosis was through histologic examination of a hysterectomy specimen. However, transvaginal ultrasound and pelvic magnetic resonance imaging have been shown to be accurate for noninvasive diagnosis.
Signs on imaging include:
- Globular/bulky uterus
- Asymmetric thickening of myometrium
- Loss of clarity of endo-myometrial interface
- Diffuse heterogenous myometrial echogenicity
- Myometrial cysts
| Click to enlarge image |
1. Champaneria R, Abedin P, Daniels J, Balogun M, Khan KS. Ultrasound scan and magnetic resonance imaging for the diagnosis of adenomyosis: systematic review comparing test accuracy. Acta Obstetricia et Gynecologica. 2010;89(11):1374-1384.
2. Meredith SM, Sanchez-Ramos L, Kaunitz AM. Diagnostic accuracy of transvaginal sonography for the diagnosis of adenomyosis: systematic review and meta-analysis. Am J Obstet Gynecol. 2009;201(1):107.e1-e6.
3. Munro MG. Update: abnormal uterine bleeding. OBG Manag. 2014;26(3):27-32.
1. Champaneria R, Abedin P, Daniels J, Balogun M, Khan KS. Ultrasound scan and magnetic resonance imaging for the diagnosis of adenomyosis: systematic review comparing test accuracy. Acta Obstetricia et Gynecologica. 2010;89(11):1374-1384.
2. Meredith SM, Sanchez-Ramos L, Kaunitz AM. Diagnostic accuracy of transvaginal sonography for the diagnosis of adenomyosis: systematic review and meta-analysis. Am J Obstet Gynecol. 2009;201(1):107.e1-e6.
3. Munro MG. Update: abnormal uterine bleeding. OBG Manag. 2014;26(3):27-32.