User login
Delivering Bad News in the Context of Culture: A Patient-Centered Approach
From the University of Virginia School of Medicine, Charlottesville, VA.
Abstract
- Objective: To describe the impact of culture on delivering bad news to patients and to describe a patient-centered approach physicians can use when delivering bad news.
- Methods: Descriptive report and discussion utilizing an illustrative case.
- Results: Physicians often find it challenging to deliver bad news in a culturally sensitive manner. Patients vary in their preferences for how they receive bad news, both within and across cultural groups. A strategy to address these preferences is presented that integrates the ethnographic Kleinman model and the SPIKES model.
- Conclusion: Delivering bad news is a challenging endeavor for many physicians. Strategies are available to guide clinicians through these conversations in a manner that is culturally sensitive and patient-centered.
A 52-year-old patient from Mexico is seeing his physician because he has been experiencing some fatigue and abdominal pain. The doctor asks the patient about his symptoms with the aid of an interpreter (in all the dialogues, a Spanish interpreter is present).
Doctor: How can I help you today?
Patient: I think it’s probably nothing, but my wife is worried and wanted me to see you. I don’t quite feel myself, just a little more tired than usual.
Doctor: Do you have any other symptoms?
Patient: Well, I have been having some pain in my stomach, just a little crampy feeling down low. My wife says I have lost some weight and she wanted me to see a doctor. I haven’t been eating as much as I usually do. I just don’t have much of an appetite, especially when I get the pain.
The doctor goes on to ask some additional questions and conducts a physical examination. He discovers the patient lost 20 pounds since his last visit 8 months ago. He is worried that the patient may have something serious going on, possibly colon cancer. He recommends some testing to the patient.
Doctor: I would like to do some tests to see what is going on.
Patient: What kind of tests?
Doctor: A few blood tests and a colonoscopy. Do you know what that is?
Patient: Yes, my brother had one a few years ago.
Doctor: Ok, my nurse will set that up and explain what you will need to do. We’ll schedule another appointment for you to come back to discuss the results. You mentioned your wife. Would you like her or anyone else to be with you at that appointment?
Patient: Yes, my wife and son. My son knows a lot more about medical things than I do, and I know he would want to come.
The Need for Culturally Sensitive Care
The concept of one’s culture encompasses a host of components including how an individual identifies oneself as well as the language, customs, beliefs, and value system one utilizes. Culture, in turn, profoundly affects patients’ belief systems regarding health and wellness, disease and illness, and the delivery of health care services, including the use of healers and alternative providers [1].In order to provide culturally sensitive and high-quality care to diverse patient populations, it is important for providers to gain an understanding and sensitivity to the influences of culture on patients’ beliefs and behaviors [2].
The ability to provide care to people of different cultures is more important than ever before. In 2011, the number of legal and unauthorized immigrants in the United States rose to 40.4 million (13% of the population) and between 2007 and 2011 alone, this number rose by 2.4 million [3].According to a 2010 census bureau report, in the last 30 years the number of individuals over the age of 5 who spoke a language other than English in their home more than doubled, an increase that was 4 times greater than the rate of population growth [4].In addition, in 2009 the United States resettled more refugees than any other nation (60,000+) and this number reached almost 70,000 in 2013 [5,6].Patient populations in the United States are becoming increasingly diverse, and providers must have the skills to communicate effectively with these groups. A one-size-fits-all approach is not sufficient for our changing population.
The Challenges of Delivering Bad News and the Impact of Culture
Perhaps one of the most challenging communication scenarios faced by physicians is the need to deliver bad news to a patient. “Bad news” can be described as any information that adversely alters one’s expectations for the future [7].Clinicians from nearly all specialties are confronted with the task of giving bad news [8],and this is particularly true regarding cancer care. Among oncologists, 60% reported the need to break bad news to patients between 5 to 20 times per month, with 14% reporting greater than 20 times per month [9].The concept of giving bad news is often viewed as stressful by clinicians [10], and clinicians must be able to balance a myriad of elements, including patients’ emotional responses, information needs, uncertainties of disease progression and treatments, patients’ preferred level of involvement in decision making, patient expectations, involvement of family members, and how to maintain hope, among others [9,11]. Indeed, it seems that clinicians find it difficult to take into account the full spectrum of patient needs [8]. While the descriptive literature indicates that patient satisfaction and psychological well-being is improved when a patient-centered approach is utilized that attends to the emotional needs of patients [12], clinicians often focus on biomedical information, with less focus on patients’ psychosocial needs and their level of understanding [13–15].
Further, the interaction of patient culture and context with the complexity of the “bad news” interaction can be daunting, and clinicians have noted their diminished level of comfort in adjusting to these cultural preferences [16].The ability of clinicians to “match” the patient’s preferred level of involvement in decision making is associated with higher patient satisfaction with decision making and lower depression after 3 months [11],yet clinicians often find it difficult to determine which patients want to be involved in the decision making to a greater or lesser extent [12].In addition, words have different meanings when used in medical settings or in lay contexts [8],not to mention the challenges of translation when dealing with non–English-speaking patients. Yet, the manner in which clinicians deliver bad news can affect patients’ understanding of their disease, treatment options, and patients’ adjustment to the diagnosis [8],as well as patients’ expected quality of life and intentions to adhere to recommendations [17].
Information Disclosure
One of the key areas impacted by culture relates to preferred disclosure of medical information. Walsh et al noted in their review that the majority of patients in English-speaking countries wanted relatively full disclosure regarding their illness in comparison to individuals from other countries [18].As a further distinction, Blackhall et al noted that African Americans and European Americans were more likely to believe that a patient should be told of a terminal diagnosis than Mexican and Korean Americans [19].In addition, Mexican and Korean Americans were more likely to believe that clinicians should not discuss death and dying with patients, as it could be harmful. Fujimori noted that Asians are less likely to prefer discussions of life expectancy in contrast to Westerners [20].In a survey of Albanian nationals, < 50% of patients wanted to know their true diagnosis; however, individuals who were male, urban, and educated demonstrated a significantly greater preference for disclosure [21].In the Middle East, the concept of disclosure is highly variable in terms of both provider and patient preferences [22].
Involvement of Family Members
A second important area relates to the involvement of family members. Fujimori noted high variability of patient preferences for having family members present when discussing bad news. Of Japanese patients, 78% preferred to be told with family members present, with the number decreasing for Portugal (61%), Australia (53%-57%), and Ireland (40%). Eighty-one percent of the US patients did not want anyone else present. However, almost all placed high value on physician expertise and honesty [20]. Blackhall noted that Mexican and Korean Americans were more likely to favor a family-centered approach to decision making [19]. In addition, Orona indicated that Mexican-American and Chinese-American families felt it was their duty to protect their relatives from a cancer diagnosis to keep the patient’s remaining time free of worry [23]. Haggerty found mixed evidence for patient preferences regarding disclosure of cancer prognosis to family members [24].
Given these variations and complexities, it is natural to try to develop a system for managing them, eg, a list of traits or attributes one can apply to certain groups. For example, patients of Asian origin prefer _______. However, there is an inherent danger in doing this, as it leads to stereotyping [25]. Cultural factors also may be given inappropriate meaning. Specifically, a well-meaning clinician might attribute certain characteristics to a patient when in fact it has little bearing on the patient’s perspective [25]. In addition, given the nature of communication, travel, and the fact that many individuals identify with more than one cultural group, it may be inappropriate to attribute a singular cultural identity to a group in contemporary society. As a result, Kleinman [25] proposed an ethnographic approach as opposed to a cultural approach. Specifically, this involves understanding a patient and his/her illness from an individual’s perspective as opposed to the cultural collective.
Communication Skills to Help Deliver Bad News
Set Up the Interview
Before meeting with the patient, it is important to review the medical data and have a plan in mind for delivering the bad news. Schedule adequate time for discussion and avoid interruptions. Meet in a quiet, private room that is large enough to accommodate family members or friends whom the patient may have brought. In our case example, the patient has brought his wife and son to the appointment.
Doctor: Hello, Mr. Ruiz. (Turning to the patient’s wife and son) I am Dr. Simon.
Patient: Hello, Doctor. This is my wife, Maria, and son, Alejandro.
Doctor: Please have a seat. Are you comfortable?
Patient: Yes. We are anxious to hear the results of the tests.
Son: My father doesn’t always understand medical terms and I wanted to be here to help. I am very worried about him.
Doctor: I understand your concern and I will explain everything to you.
Assess the Patient’s Perception of the Problem
Before telling the patient the diagnosis, it is important to get an idea of the patient’s understanding of the problem, including what he calls it, what he thinks caused it, and how severe he thinks it is.
Doctor: Before I tell you the results, I would like to get a sense first of what you think is going on.
Patient: Well, I really don’t know for sure, but I know the pain is getting worse and I have been feeling weaker. The pain started right after my son’s wedding. There was a lot of food and I ate more than usual. Maybe it was something bad that I ate?
Doctor: (Turning to the wife and son) Do you have any thoughts about the illness?
Wife: I can see he is in pain a lot, even though he tries to hide it from me. I want to know what’s wrong. I am worried it could be something bad.
Obtain the Patient’s Invitation to Disclose the Information
It is important to know if the patient wants to be told the information about his or her diagnosis. Ideally, physicians should discuss this in general terms as part of routine care, before any bad news needs to be delivered. For example,
Doctor: There may come a time when I will need to tell you something bad about your health. Hopefully, that time will never come, but I want to know your preferences so I can honor them if the time does arise. Would you want to be told about this, or would you want someone else, perhaps someone in your family, to be told?
Patient: I appreciate your asking, Doctor. I haven’t really thought about it, but I get kind of nervous and upset when I hear bad news. I would rather you tell me when my wife and son can be there too.
Give Knowledge and Information to the Patient
It is important to provide information that is at a level that the patient can understand. Avoid the use of medical jargon. When speaking through an interpreter, the clinician may need to have a conversation with the interpreter before meeting the patient to explain the situation and the need to be sensitive. For example, if the clinician does not use the word “cancer” after determining from the patient or family the preference for an alternative word, be sure to inform the interpreter not to use the word “cancer.” Provide the information in small chunks and check in frequently to make sure the patient understands. Avoid language that takes away hope. If there is a family member who speaks English, there is a tendency to speak to that person rather than the patient directly. Avoid doing this unless the patient explicitly requests that the clinician speak directly to that individual. This is often the case with older patients. The following might take place at a subsequent appointment:
Doctor: Mr. Ruiz, you told me previously that you would like me to tell you the results of your tests, along with you wife and son. Unfortunately, I have some bad news to tell you. (Pause) The colonoscopy showed that you have a tumor in the colon, also called the large intestine. It is located in the part that we call the ascending colon (draws a picture to show them where this is). We will need to do some other scans to make sure that the tumor is just in the colon and has not spread. I am hopeful, though, that we have caught it fairly early and it has not spread. That would be the best situation. (Pause) Do you understand what I have told you so far?
Address the Patient’s and Family’s Emotions
Every patient will express their reactions to bad news differently, and their reactions may be different from what the physician might experience in a similar situation. Thus, the clinician should be self-aware and be prepared to respond to a variety of responses. It is important to express empathy and validate the patient’s and family reactions and emotions. If the patient does not express any emotion, the clinician should explore this carefully. It may require more than one visit for the patient to open up with his feelings.
Doctor: I am so sorry. I know that this must be a big shock for you.
Patient: I kind of figured it might be something bad, but it is still a shock. Even so, I am a religious man and I believe that I will get through this with the help of my wife and family.
Doctor: It sounds as if you have a great support system and get strength from your faith. You are lucky to have such a wonderful family and that will be a big help as we move forward.
Strategize and Summarize
Ask the patient if he or she is ready to have a discussion about treatment, including his or her goals of treatment. Continue to explore the patient’s knowledge, expectations and hopes. Always allow the patient to express his fears and concerns. Most importantly, let the patient know that you will share the responsibility of decision making with the patient and be there to support him.
Doctor: This is never easy and it’s a lot to take in. Would you like to discuss the next steps and possible treatments at this time or should we make another appointment after your CAT scan?
Patient: My wife is pretty upset and I think it might be better if we stop here for now. Is that ok?
Son: We want to come back as soon as we can after the CAT scan. In the meantime, can you provide me with some information or a good website to check out?
Doctor: Yes, of course. That sounds like a good plan.
Conclusion
The task of giving bad news is a necessity for physicians of most specialties and is often viewed as challenging and even stressful to some. However, the manner in which information is discussed with patients can impact patients’ satisfaction, understanding of their illness, adjustment to the diagnosis, expected quality of life, and intentions to adhere to recommendations [8,17]. Providing bad news in a culturally sensitive manner adds an additional level of complexity to an already challenging encounter. While an individual’s culture can strongly influence patient belief systems and utilization of care, there is an inherent danger when clinicians make assumptions about individuals’ culture and the role it plays in their lives. Instead of focusing on creating a mental list of cultural attributes, we recommend a patient-centered approach where few assumptions about the patient are made and instead, the clinician gains an understanding of each individual patient through queries and adjusts his/her approach and language according to each individual’s needs.
Corresponding author: Lisa K. Rollins, PhD, Dept. of Family Medicine, Univ.of Virginia, PO Box 800729, Charlottesville,VA 22908-0729, [email protected].
Financial disclosures: None.
1. Cultural competency – clear communication. National Institutes of Health (NIH). Accessed at www.nih.gov/clearcommunication/culturalcompetency.htm on 15 Jul 2014.
2. Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O. Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Pub Health Rep 2003;118:293–302.
3. PEW research: Hispanic trends project, a nation of immigrants. Accessed at www.pewhispanic.org/2013/01/29/a-nation-of-immigrants/ on 31 Jul 2014.
4. U.S. Census Bureau. New census bureau report analyzes nation’s linguistic diversity. Accessed at www.census/gov/newsroom/releases/archives/american_community_survey_acs/cb10-cn58.html on 31 Jul 2014.
5. Immigration Policy Center. Refugees: a fact sheet. Accessed at www.immigrationpolicy.org on 28 May 2014.
6. U.S. Department of State. U.S. welcomes record number of refugees. Accessed at iipdigital.usembassy.gov/st/english/article/2013/10/20131023285033.html?CP.rss=true#axzz3GtyMkFSe on 28 May 2014.
7. Barclay JS, Blackhall L J, Tulsky JA. Communication strategies and cultural issues in the delivery of bad news. J Palliative Med 2007;10:958–77.
8. Fallowfield L, Jenkins V. Communicating sad, bad, and difficult news in medicine. Lancet 2004;363;312–9.
9. Baile WF, Buckman R, Lenzi R, et al. SPIKES—A six-step protocol for delivering bad news: application to the patient with cancer. Oncologist 2000;5:302–11.
10. Ptacek JT, McIntosh EG. Physician challenges in communicating bad news. J Behav Med 2009;32:380–7.
11. Vogel BA, Leonhart R, Helmes AW. Communication matters: the impact of communication and participation in decision making on breast cancer patients’ depression and quality of life. Patient Educ Couns 2009;77:391–7.
12. Hack TF, Degner LF, Parker PA. The communication goals and needs of cancer patients: a review. Psychooncology 2005;14:831–45.
13. Vail L, Sandhu H, Fisher J, et al. Hospital consultants breaking bad news with simulated patients: an analysis of communication using the roter interaction analysis system. Patient Educ Couns 2011;83:185–94.
14. Hack TF, Pickles T, Ruether JD, et al. Behind closed doors: systematic analysis of breast cancer consultation communication and predictors of satisfaction with communication.
Psychooncology 2010;19:626–36.
15. Cantwell BM, Ramirez A. Doctor-patient communication: a study of junior house officers. Med Educ 1997;31:17–21.
16. Rollins LK, Bradley EB, Hayden GF, et al. Responding to a changing nation: are faculty prepared for cross-cultural conversations and care? Fam Med 2013;45:736–9.
17. Burgers C, Beukeboom CJ, Sparks L. How the doc should (not) talk: when breaking bad news with negations influences patients’ immediate responses and medical adherence intentions. Patient Educ Couns 2012;89:267–73.
18. Walsh RA, Girgis A, Sanson-Fisher RW. Breaking bad news 2: what evidence is available to guide clinicians? Behav Med 1998;24:61–73.
19. Blackhall LJ, Murphy ST, Frank G, et al. Ethnicity and attitudes toward patient autonomy. JAMA 1995;274:820–5.
20. Fujimori M, Uchitomi Y. Preferences of cancer patients regarding communication of bad news: a systematic literature review. Jpn J Clin Oncol 2009;39:201–16.
21. Beqiri A, Toci E, Sallaku A, et al. Breaking bad news in a southeast european population: a survey among cancer patients in Albania. J Palliat Med 2012;15:1100–5.
22. Khalil RB. Attitudes, beliefs and perceptions regarding truth disclosure of cancer-related information in the Middle East: a review. Palliat Supp Care 2013;11:69–78.
23. Orona CJ, Koenig BA, Davis AJ. Cultural aspects of nondisclosure. Camb Q Healthc Ethics 1994;3:338–46.
24. Hagerty RG, Butow PN, Ellis PM, et al. Communicating prognosis in cancer care: a systematic review of the literature. Ann Oncol 2005;16:1005–53.
25. Kleinman A, Benson P. Anthropology in the clinic: the problem of cultural competency and how to fix it. PLoS Med 2006;3:1673–6.
From the University of Virginia School of Medicine, Charlottesville, VA.
Abstract
- Objective: To describe the impact of culture on delivering bad news to patients and to describe a patient-centered approach physicians can use when delivering bad news.
- Methods: Descriptive report and discussion utilizing an illustrative case.
- Results: Physicians often find it challenging to deliver bad news in a culturally sensitive manner. Patients vary in their preferences for how they receive bad news, both within and across cultural groups. A strategy to address these preferences is presented that integrates the ethnographic Kleinman model and the SPIKES model.
- Conclusion: Delivering bad news is a challenging endeavor for many physicians. Strategies are available to guide clinicians through these conversations in a manner that is culturally sensitive and patient-centered.
A 52-year-old patient from Mexico is seeing his physician because he has been experiencing some fatigue and abdominal pain. The doctor asks the patient about his symptoms with the aid of an interpreter (in all the dialogues, a Spanish interpreter is present).
Doctor: How can I help you today?
Patient: I think it’s probably nothing, but my wife is worried and wanted me to see you. I don’t quite feel myself, just a little more tired than usual.
Doctor: Do you have any other symptoms?
Patient: Well, I have been having some pain in my stomach, just a little crampy feeling down low. My wife says I have lost some weight and she wanted me to see a doctor. I haven’t been eating as much as I usually do. I just don’t have much of an appetite, especially when I get the pain.
The doctor goes on to ask some additional questions and conducts a physical examination. He discovers the patient lost 20 pounds since his last visit 8 months ago. He is worried that the patient may have something serious going on, possibly colon cancer. He recommends some testing to the patient.
Doctor: I would like to do some tests to see what is going on.
Patient: What kind of tests?
Doctor: A few blood tests and a colonoscopy. Do you know what that is?
Patient: Yes, my brother had one a few years ago.
Doctor: Ok, my nurse will set that up and explain what you will need to do. We’ll schedule another appointment for you to come back to discuss the results. You mentioned your wife. Would you like her or anyone else to be with you at that appointment?
Patient: Yes, my wife and son. My son knows a lot more about medical things than I do, and I know he would want to come.
The Need for Culturally Sensitive Care
The concept of one’s culture encompasses a host of components including how an individual identifies oneself as well as the language, customs, beliefs, and value system one utilizes. Culture, in turn, profoundly affects patients’ belief systems regarding health and wellness, disease and illness, and the delivery of health care services, including the use of healers and alternative providers [1].In order to provide culturally sensitive and high-quality care to diverse patient populations, it is important for providers to gain an understanding and sensitivity to the influences of culture on patients’ beliefs and behaviors [2].
The ability to provide care to people of different cultures is more important than ever before. In 2011, the number of legal and unauthorized immigrants in the United States rose to 40.4 million (13% of the population) and between 2007 and 2011 alone, this number rose by 2.4 million [3].According to a 2010 census bureau report, in the last 30 years the number of individuals over the age of 5 who spoke a language other than English in their home more than doubled, an increase that was 4 times greater than the rate of population growth [4].In addition, in 2009 the United States resettled more refugees than any other nation (60,000+) and this number reached almost 70,000 in 2013 [5,6].Patient populations in the United States are becoming increasingly diverse, and providers must have the skills to communicate effectively with these groups. A one-size-fits-all approach is not sufficient for our changing population.
The Challenges of Delivering Bad News and the Impact of Culture
Perhaps one of the most challenging communication scenarios faced by physicians is the need to deliver bad news to a patient. “Bad news” can be described as any information that adversely alters one’s expectations for the future [7].Clinicians from nearly all specialties are confronted with the task of giving bad news [8],and this is particularly true regarding cancer care. Among oncologists, 60% reported the need to break bad news to patients between 5 to 20 times per month, with 14% reporting greater than 20 times per month [9].The concept of giving bad news is often viewed as stressful by clinicians [10], and clinicians must be able to balance a myriad of elements, including patients’ emotional responses, information needs, uncertainties of disease progression and treatments, patients’ preferred level of involvement in decision making, patient expectations, involvement of family members, and how to maintain hope, among others [9,11]. Indeed, it seems that clinicians find it difficult to take into account the full spectrum of patient needs [8]. While the descriptive literature indicates that patient satisfaction and psychological well-being is improved when a patient-centered approach is utilized that attends to the emotional needs of patients [12], clinicians often focus on biomedical information, with less focus on patients’ psychosocial needs and their level of understanding [13–15].
Further, the interaction of patient culture and context with the complexity of the “bad news” interaction can be daunting, and clinicians have noted their diminished level of comfort in adjusting to these cultural preferences [16].The ability of clinicians to “match” the patient’s preferred level of involvement in decision making is associated with higher patient satisfaction with decision making and lower depression after 3 months [11],yet clinicians often find it difficult to determine which patients want to be involved in the decision making to a greater or lesser extent [12].In addition, words have different meanings when used in medical settings or in lay contexts [8],not to mention the challenges of translation when dealing with non–English-speaking patients. Yet, the manner in which clinicians deliver bad news can affect patients’ understanding of their disease, treatment options, and patients’ adjustment to the diagnosis [8],as well as patients’ expected quality of life and intentions to adhere to recommendations [17].
Information Disclosure
One of the key areas impacted by culture relates to preferred disclosure of medical information. Walsh et al noted in their review that the majority of patients in English-speaking countries wanted relatively full disclosure regarding their illness in comparison to individuals from other countries [18].As a further distinction, Blackhall et al noted that African Americans and European Americans were more likely to believe that a patient should be told of a terminal diagnosis than Mexican and Korean Americans [19].In addition, Mexican and Korean Americans were more likely to believe that clinicians should not discuss death and dying with patients, as it could be harmful. Fujimori noted that Asians are less likely to prefer discussions of life expectancy in contrast to Westerners [20].In a survey of Albanian nationals, < 50% of patients wanted to know their true diagnosis; however, individuals who were male, urban, and educated demonstrated a significantly greater preference for disclosure [21].In the Middle East, the concept of disclosure is highly variable in terms of both provider and patient preferences [22].
Involvement of Family Members
A second important area relates to the involvement of family members. Fujimori noted high variability of patient preferences for having family members present when discussing bad news. Of Japanese patients, 78% preferred to be told with family members present, with the number decreasing for Portugal (61%), Australia (53%-57%), and Ireland (40%). Eighty-one percent of the US patients did not want anyone else present. However, almost all placed high value on physician expertise and honesty [20]. Blackhall noted that Mexican and Korean Americans were more likely to favor a family-centered approach to decision making [19]. In addition, Orona indicated that Mexican-American and Chinese-American families felt it was their duty to protect their relatives from a cancer diagnosis to keep the patient’s remaining time free of worry [23]. Haggerty found mixed evidence for patient preferences regarding disclosure of cancer prognosis to family members [24].
Given these variations and complexities, it is natural to try to develop a system for managing them, eg, a list of traits or attributes one can apply to certain groups. For example, patients of Asian origin prefer _______. However, there is an inherent danger in doing this, as it leads to stereotyping [25]. Cultural factors also may be given inappropriate meaning. Specifically, a well-meaning clinician might attribute certain characteristics to a patient when in fact it has little bearing on the patient’s perspective [25]. In addition, given the nature of communication, travel, and the fact that many individuals identify with more than one cultural group, it may be inappropriate to attribute a singular cultural identity to a group in contemporary society. As a result, Kleinman [25] proposed an ethnographic approach as opposed to a cultural approach. Specifically, this involves understanding a patient and his/her illness from an individual’s perspective as opposed to the cultural collective.
Communication Skills to Help Deliver Bad News
Set Up the Interview
Before meeting with the patient, it is important to review the medical data and have a plan in mind for delivering the bad news. Schedule adequate time for discussion and avoid interruptions. Meet in a quiet, private room that is large enough to accommodate family members or friends whom the patient may have brought. In our case example, the patient has brought his wife and son to the appointment.
Doctor: Hello, Mr. Ruiz. (Turning to the patient’s wife and son) I am Dr. Simon.
Patient: Hello, Doctor. This is my wife, Maria, and son, Alejandro.
Doctor: Please have a seat. Are you comfortable?
Patient: Yes. We are anxious to hear the results of the tests.
Son: My father doesn’t always understand medical terms and I wanted to be here to help. I am very worried about him.
Doctor: I understand your concern and I will explain everything to you.
Assess the Patient’s Perception of the Problem
Before telling the patient the diagnosis, it is important to get an idea of the patient’s understanding of the problem, including what he calls it, what he thinks caused it, and how severe he thinks it is.
Doctor: Before I tell you the results, I would like to get a sense first of what you think is going on.
Patient: Well, I really don’t know for sure, but I know the pain is getting worse and I have been feeling weaker. The pain started right after my son’s wedding. There was a lot of food and I ate more than usual. Maybe it was something bad that I ate?
Doctor: (Turning to the wife and son) Do you have any thoughts about the illness?
Wife: I can see he is in pain a lot, even though he tries to hide it from me. I want to know what’s wrong. I am worried it could be something bad.
Obtain the Patient’s Invitation to Disclose the Information
It is important to know if the patient wants to be told the information about his or her diagnosis. Ideally, physicians should discuss this in general terms as part of routine care, before any bad news needs to be delivered. For example,
Doctor: There may come a time when I will need to tell you something bad about your health. Hopefully, that time will never come, but I want to know your preferences so I can honor them if the time does arise. Would you want to be told about this, or would you want someone else, perhaps someone in your family, to be told?
Patient: I appreciate your asking, Doctor. I haven’t really thought about it, but I get kind of nervous and upset when I hear bad news. I would rather you tell me when my wife and son can be there too.
Give Knowledge and Information to the Patient
It is important to provide information that is at a level that the patient can understand. Avoid the use of medical jargon. When speaking through an interpreter, the clinician may need to have a conversation with the interpreter before meeting the patient to explain the situation and the need to be sensitive. For example, if the clinician does not use the word “cancer” after determining from the patient or family the preference for an alternative word, be sure to inform the interpreter not to use the word “cancer.” Provide the information in small chunks and check in frequently to make sure the patient understands. Avoid language that takes away hope. If there is a family member who speaks English, there is a tendency to speak to that person rather than the patient directly. Avoid doing this unless the patient explicitly requests that the clinician speak directly to that individual. This is often the case with older patients. The following might take place at a subsequent appointment:
Doctor: Mr. Ruiz, you told me previously that you would like me to tell you the results of your tests, along with you wife and son. Unfortunately, I have some bad news to tell you. (Pause) The colonoscopy showed that you have a tumor in the colon, also called the large intestine. It is located in the part that we call the ascending colon (draws a picture to show them where this is). We will need to do some other scans to make sure that the tumor is just in the colon and has not spread. I am hopeful, though, that we have caught it fairly early and it has not spread. That would be the best situation. (Pause) Do you understand what I have told you so far?
Address the Patient’s and Family’s Emotions
Every patient will express their reactions to bad news differently, and their reactions may be different from what the physician might experience in a similar situation. Thus, the clinician should be self-aware and be prepared to respond to a variety of responses. It is important to express empathy and validate the patient’s and family reactions and emotions. If the patient does not express any emotion, the clinician should explore this carefully. It may require more than one visit for the patient to open up with his feelings.
Doctor: I am so sorry. I know that this must be a big shock for you.
Patient: I kind of figured it might be something bad, but it is still a shock. Even so, I am a religious man and I believe that I will get through this with the help of my wife and family.
Doctor: It sounds as if you have a great support system and get strength from your faith. You are lucky to have such a wonderful family and that will be a big help as we move forward.
Strategize and Summarize
Ask the patient if he or she is ready to have a discussion about treatment, including his or her goals of treatment. Continue to explore the patient’s knowledge, expectations and hopes. Always allow the patient to express his fears and concerns. Most importantly, let the patient know that you will share the responsibility of decision making with the patient and be there to support him.
Doctor: This is never easy and it’s a lot to take in. Would you like to discuss the next steps and possible treatments at this time or should we make another appointment after your CAT scan?
Patient: My wife is pretty upset and I think it might be better if we stop here for now. Is that ok?
Son: We want to come back as soon as we can after the CAT scan. In the meantime, can you provide me with some information or a good website to check out?
Doctor: Yes, of course. That sounds like a good plan.
Conclusion
The task of giving bad news is a necessity for physicians of most specialties and is often viewed as challenging and even stressful to some. However, the manner in which information is discussed with patients can impact patients’ satisfaction, understanding of their illness, adjustment to the diagnosis, expected quality of life, and intentions to adhere to recommendations [8,17]. Providing bad news in a culturally sensitive manner adds an additional level of complexity to an already challenging encounter. While an individual’s culture can strongly influence patient belief systems and utilization of care, there is an inherent danger when clinicians make assumptions about individuals’ culture and the role it plays in their lives. Instead of focusing on creating a mental list of cultural attributes, we recommend a patient-centered approach where few assumptions about the patient are made and instead, the clinician gains an understanding of each individual patient through queries and adjusts his/her approach and language according to each individual’s needs.
Corresponding author: Lisa K. Rollins, PhD, Dept. of Family Medicine, Univ.of Virginia, PO Box 800729, Charlottesville,VA 22908-0729, [email protected].
Financial disclosures: None.
From the University of Virginia School of Medicine, Charlottesville, VA.
Abstract
- Objective: To describe the impact of culture on delivering bad news to patients and to describe a patient-centered approach physicians can use when delivering bad news.
- Methods: Descriptive report and discussion utilizing an illustrative case.
- Results: Physicians often find it challenging to deliver bad news in a culturally sensitive manner. Patients vary in their preferences for how they receive bad news, both within and across cultural groups. A strategy to address these preferences is presented that integrates the ethnographic Kleinman model and the SPIKES model.
- Conclusion: Delivering bad news is a challenging endeavor for many physicians. Strategies are available to guide clinicians through these conversations in a manner that is culturally sensitive and patient-centered.
A 52-year-old patient from Mexico is seeing his physician because he has been experiencing some fatigue and abdominal pain. The doctor asks the patient about his symptoms with the aid of an interpreter (in all the dialogues, a Spanish interpreter is present).
Doctor: How can I help you today?
Patient: I think it’s probably nothing, but my wife is worried and wanted me to see you. I don’t quite feel myself, just a little more tired than usual.
Doctor: Do you have any other symptoms?
Patient: Well, I have been having some pain in my stomach, just a little crampy feeling down low. My wife says I have lost some weight and she wanted me to see a doctor. I haven’t been eating as much as I usually do. I just don’t have much of an appetite, especially when I get the pain.
The doctor goes on to ask some additional questions and conducts a physical examination. He discovers the patient lost 20 pounds since his last visit 8 months ago. He is worried that the patient may have something serious going on, possibly colon cancer. He recommends some testing to the patient.
Doctor: I would like to do some tests to see what is going on.
Patient: What kind of tests?
Doctor: A few blood tests and a colonoscopy. Do you know what that is?
Patient: Yes, my brother had one a few years ago.
Doctor: Ok, my nurse will set that up and explain what you will need to do. We’ll schedule another appointment for you to come back to discuss the results. You mentioned your wife. Would you like her or anyone else to be with you at that appointment?
Patient: Yes, my wife and son. My son knows a lot more about medical things than I do, and I know he would want to come.
The Need for Culturally Sensitive Care
The concept of one’s culture encompasses a host of components including how an individual identifies oneself as well as the language, customs, beliefs, and value system one utilizes. Culture, in turn, profoundly affects patients’ belief systems regarding health and wellness, disease and illness, and the delivery of health care services, including the use of healers and alternative providers [1].In order to provide culturally sensitive and high-quality care to diverse patient populations, it is important for providers to gain an understanding and sensitivity to the influences of culture on patients’ beliefs and behaviors [2].
The ability to provide care to people of different cultures is more important than ever before. In 2011, the number of legal and unauthorized immigrants in the United States rose to 40.4 million (13% of the population) and between 2007 and 2011 alone, this number rose by 2.4 million [3].According to a 2010 census bureau report, in the last 30 years the number of individuals over the age of 5 who spoke a language other than English in their home more than doubled, an increase that was 4 times greater than the rate of population growth [4].In addition, in 2009 the United States resettled more refugees than any other nation (60,000+) and this number reached almost 70,000 in 2013 [5,6].Patient populations in the United States are becoming increasingly diverse, and providers must have the skills to communicate effectively with these groups. A one-size-fits-all approach is not sufficient for our changing population.
The Challenges of Delivering Bad News and the Impact of Culture
Perhaps one of the most challenging communication scenarios faced by physicians is the need to deliver bad news to a patient. “Bad news” can be described as any information that adversely alters one’s expectations for the future [7].Clinicians from nearly all specialties are confronted with the task of giving bad news [8],and this is particularly true regarding cancer care. Among oncologists, 60% reported the need to break bad news to patients between 5 to 20 times per month, with 14% reporting greater than 20 times per month [9].The concept of giving bad news is often viewed as stressful by clinicians [10], and clinicians must be able to balance a myriad of elements, including patients’ emotional responses, information needs, uncertainties of disease progression and treatments, patients’ preferred level of involvement in decision making, patient expectations, involvement of family members, and how to maintain hope, among others [9,11]. Indeed, it seems that clinicians find it difficult to take into account the full spectrum of patient needs [8]. While the descriptive literature indicates that patient satisfaction and psychological well-being is improved when a patient-centered approach is utilized that attends to the emotional needs of patients [12], clinicians often focus on biomedical information, with less focus on patients’ psychosocial needs and their level of understanding [13–15].
Further, the interaction of patient culture and context with the complexity of the “bad news” interaction can be daunting, and clinicians have noted their diminished level of comfort in adjusting to these cultural preferences [16].The ability of clinicians to “match” the patient’s preferred level of involvement in decision making is associated with higher patient satisfaction with decision making and lower depression after 3 months [11],yet clinicians often find it difficult to determine which patients want to be involved in the decision making to a greater or lesser extent [12].In addition, words have different meanings when used in medical settings or in lay contexts [8],not to mention the challenges of translation when dealing with non–English-speaking patients. Yet, the manner in which clinicians deliver bad news can affect patients’ understanding of their disease, treatment options, and patients’ adjustment to the diagnosis [8],as well as patients’ expected quality of life and intentions to adhere to recommendations [17].
Information Disclosure
One of the key areas impacted by culture relates to preferred disclosure of medical information. Walsh et al noted in their review that the majority of patients in English-speaking countries wanted relatively full disclosure regarding their illness in comparison to individuals from other countries [18].As a further distinction, Blackhall et al noted that African Americans and European Americans were more likely to believe that a patient should be told of a terminal diagnosis than Mexican and Korean Americans [19].In addition, Mexican and Korean Americans were more likely to believe that clinicians should not discuss death and dying with patients, as it could be harmful. Fujimori noted that Asians are less likely to prefer discussions of life expectancy in contrast to Westerners [20].In a survey of Albanian nationals, < 50% of patients wanted to know their true diagnosis; however, individuals who were male, urban, and educated demonstrated a significantly greater preference for disclosure [21].In the Middle East, the concept of disclosure is highly variable in terms of both provider and patient preferences [22].
Involvement of Family Members
A second important area relates to the involvement of family members. Fujimori noted high variability of patient preferences for having family members present when discussing bad news. Of Japanese patients, 78% preferred to be told with family members present, with the number decreasing for Portugal (61%), Australia (53%-57%), and Ireland (40%). Eighty-one percent of the US patients did not want anyone else present. However, almost all placed high value on physician expertise and honesty [20]. Blackhall noted that Mexican and Korean Americans were more likely to favor a family-centered approach to decision making [19]. In addition, Orona indicated that Mexican-American and Chinese-American families felt it was their duty to protect their relatives from a cancer diagnosis to keep the patient’s remaining time free of worry [23]. Haggerty found mixed evidence for patient preferences regarding disclosure of cancer prognosis to family members [24].
Given these variations and complexities, it is natural to try to develop a system for managing them, eg, a list of traits or attributes one can apply to certain groups. For example, patients of Asian origin prefer _______. However, there is an inherent danger in doing this, as it leads to stereotyping [25]. Cultural factors also may be given inappropriate meaning. Specifically, a well-meaning clinician might attribute certain characteristics to a patient when in fact it has little bearing on the patient’s perspective [25]. In addition, given the nature of communication, travel, and the fact that many individuals identify with more than one cultural group, it may be inappropriate to attribute a singular cultural identity to a group in contemporary society. As a result, Kleinman [25] proposed an ethnographic approach as opposed to a cultural approach. Specifically, this involves understanding a patient and his/her illness from an individual’s perspective as opposed to the cultural collective.
Communication Skills to Help Deliver Bad News
Set Up the Interview
Before meeting with the patient, it is important to review the medical data and have a plan in mind for delivering the bad news. Schedule adequate time for discussion and avoid interruptions. Meet in a quiet, private room that is large enough to accommodate family members or friends whom the patient may have brought. In our case example, the patient has brought his wife and son to the appointment.
Doctor: Hello, Mr. Ruiz. (Turning to the patient’s wife and son) I am Dr. Simon.
Patient: Hello, Doctor. This is my wife, Maria, and son, Alejandro.
Doctor: Please have a seat. Are you comfortable?
Patient: Yes. We are anxious to hear the results of the tests.
Son: My father doesn’t always understand medical terms and I wanted to be here to help. I am very worried about him.
Doctor: I understand your concern and I will explain everything to you.
Assess the Patient’s Perception of the Problem
Before telling the patient the diagnosis, it is important to get an idea of the patient’s understanding of the problem, including what he calls it, what he thinks caused it, and how severe he thinks it is.
Doctor: Before I tell you the results, I would like to get a sense first of what you think is going on.
Patient: Well, I really don’t know for sure, but I know the pain is getting worse and I have been feeling weaker. The pain started right after my son’s wedding. There was a lot of food and I ate more than usual. Maybe it was something bad that I ate?
Doctor: (Turning to the wife and son) Do you have any thoughts about the illness?
Wife: I can see he is in pain a lot, even though he tries to hide it from me. I want to know what’s wrong. I am worried it could be something bad.
Obtain the Patient’s Invitation to Disclose the Information
It is important to know if the patient wants to be told the information about his or her diagnosis. Ideally, physicians should discuss this in general terms as part of routine care, before any bad news needs to be delivered. For example,
Doctor: There may come a time when I will need to tell you something bad about your health. Hopefully, that time will never come, but I want to know your preferences so I can honor them if the time does arise. Would you want to be told about this, or would you want someone else, perhaps someone in your family, to be told?
Patient: I appreciate your asking, Doctor. I haven’t really thought about it, but I get kind of nervous and upset when I hear bad news. I would rather you tell me when my wife and son can be there too.
Give Knowledge and Information to the Patient
It is important to provide information that is at a level that the patient can understand. Avoid the use of medical jargon. When speaking through an interpreter, the clinician may need to have a conversation with the interpreter before meeting the patient to explain the situation and the need to be sensitive. For example, if the clinician does not use the word “cancer” after determining from the patient or family the preference for an alternative word, be sure to inform the interpreter not to use the word “cancer.” Provide the information in small chunks and check in frequently to make sure the patient understands. Avoid language that takes away hope. If there is a family member who speaks English, there is a tendency to speak to that person rather than the patient directly. Avoid doing this unless the patient explicitly requests that the clinician speak directly to that individual. This is often the case with older patients. The following might take place at a subsequent appointment:
Doctor: Mr. Ruiz, you told me previously that you would like me to tell you the results of your tests, along with you wife and son. Unfortunately, I have some bad news to tell you. (Pause) The colonoscopy showed that you have a tumor in the colon, also called the large intestine. It is located in the part that we call the ascending colon (draws a picture to show them where this is). We will need to do some other scans to make sure that the tumor is just in the colon and has not spread. I am hopeful, though, that we have caught it fairly early and it has not spread. That would be the best situation. (Pause) Do you understand what I have told you so far?
Address the Patient’s and Family’s Emotions
Every patient will express their reactions to bad news differently, and their reactions may be different from what the physician might experience in a similar situation. Thus, the clinician should be self-aware and be prepared to respond to a variety of responses. It is important to express empathy and validate the patient’s and family reactions and emotions. If the patient does not express any emotion, the clinician should explore this carefully. It may require more than one visit for the patient to open up with his feelings.
Doctor: I am so sorry. I know that this must be a big shock for you.
Patient: I kind of figured it might be something bad, but it is still a shock. Even so, I am a religious man and I believe that I will get through this with the help of my wife and family.
Doctor: It sounds as if you have a great support system and get strength from your faith. You are lucky to have such a wonderful family and that will be a big help as we move forward.
Strategize and Summarize
Ask the patient if he or she is ready to have a discussion about treatment, including his or her goals of treatment. Continue to explore the patient’s knowledge, expectations and hopes. Always allow the patient to express his fears and concerns. Most importantly, let the patient know that you will share the responsibility of decision making with the patient and be there to support him.
Doctor: This is never easy and it’s a lot to take in. Would you like to discuss the next steps and possible treatments at this time or should we make another appointment after your CAT scan?
Patient: My wife is pretty upset and I think it might be better if we stop here for now. Is that ok?
Son: We want to come back as soon as we can after the CAT scan. In the meantime, can you provide me with some information or a good website to check out?
Doctor: Yes, of course. That sounds like a good plan.
Conclusion
The task of giving bad news is a necessity for physicians of most specialties and is often viewed as challenging and even stressful to some. However, the manner in which information is discussed with patients can impact patients’ satisfaction, understanding of their illness, adjustment to the diagnosis, expected quality of life, and intentions to adhere to recommendations [8,17]. Providing bad news in a culturally sensitive manner adds an additional level of complexity to an already challenging encounter. While an individual’s culture can strongly influence patient belief systems and utilization of care, there is an inherent danger when clinicians make assumptions about individuals’ culture and the role it plays in their lives. Instead of focusing on creating a mental list of cultural attributes, we recommend a patient-centered approach where few assumptions about the patient are made and instead, the clinician gains an understanding of each individual patient through queries and adjusts his/her approach and language according to each individual’s needs.
Corresponding author: Lisa K. Rollins, PhD, Dept. of Family Medicine, Univ.of Virginia, PO Box 800729, Charlottesville,VA 22908-0729, [email protected].
Financial disclosures: None.
1. Cultural competency – clear communication. National Institutes of Health (NIH). Accessed at www.nih.gov/clearcommunication/culturalcompetency.htm on 15 Jul 2014.
2. Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O. Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Pub Health Rep 2003;118:293–302.
3. PEW research: Hispanic trends project, a nation of immigrants. Accessed at www.pewhispanic.org/2013/01/29/a-nation-of-immigrants/ on 31 Jul 2014.
4. U.S. Census Bureau. New census bureau report analyzes nation’s linguistic diversity. Accessed at www.census/gov/newsroom/releases/archives/american_community_survey_acs/cb10-cn58.html on 31 Jul 2014.
5. Immigration Policy Center. Refugees: a fact sheet. Accessed at www.immigrationpolicy.org on 28 May 2014.
6. U.S. Department of State. U.S. welcomes record number of refugees. Accessed at iipdigital.usembassy.gov/st/english/article/2013/10/20131023285033.html?CP.rss=true#axzz3GtyMkFSe on 28 May 2014.
7. Barclay JS, Blackhall L J, Tulsky JA. Communication strategies and cultural issues in the delivery of bad news. J Palliative Med 2007;10:958–77.
8. Fallowfield L, Jenkins V. Communicating sad, bad, and difficult news in medicine. Lancet 2004;363;312–9.
9. Baile WF, Buckman R, Lenzi R, et al. SPIKES—A six-step protocol for delivering bad news: application to the patient with cancer. Oncologist 2000;5:302–11.
10. Ptacek JT, McIntosh EG. Physician challenges in communicating bad news. J Behav Med 2009;32:380–7.
11. Vogel BA, Leonhart R, Helmes AW. Communication matters: the impact of communication and participation in decision making on breast cancer patients’ depression and quality of life. Patient Educ Couns 2009;77:391–7.
12. Hack TF, Degner LF, Parker PA. The communication goals and needs of cancer patients: a review. Psychooncology 2005;14:831–45.
13. Vail L, Sandhu H, Fisher J, et al. Hospital consultants breaking bad news with simulated patients: an analysis of communication using the roter interaction analysis system. Patient Educ Couns 2011;83:185–94.
14. Hack TF, Pickles T, Ruether JD, et al. Behind closed doors: systematic analysis of breast cancer consultation communication and predictors of satisfaction with communication.
Psychooncology 2010;19:626–36.
15. Cantwell BM, Ramirez A. Doctor-patient communication: a study of junior house officers. Med Educ 1997;31:17–21.
16. Rollins LK, Bradley EB, Hayden GF, et al. Responding to a changing nation: are faculty prepared for cross-cultural conversations and care? Fam Med 2013;45:736–9.
17. Burgers C, Beukeboom CJ, Sparks L. How the doc should (not) talk: when breaking bad news with negations influences patients’ immediate responses and medical adherence intentions. Patient Educ Couns 2012;89:267–73.
18. Walsh RA, Girgis A, Sanson-Fisher RW. Breaking bad news 2: what evidence is available to guide clinicians? Behav Med 1998;24:61–73.
19. Blackhall LJ, Murphy ST, Frank G, et al. Ethnicity and attitudes toward patient autonomy. JAMA 1995;274:820–5.
20. Fujimori M, Uchitomi Y. Preferences of cancer patients regarding communication of bad news: a systematic literature review. Jpn J Clin Oncol 2009;39:201–16.
21. Beqiri A, Toci E, Sallaku A, et al. Breaking bad news in a southeast european population: a survey among cancer patients in Albania. J Palliat Med 2012;15:1100–5.
22. Khalil RB. Attitudes, beliefs and perceptions regarding truth disclosure of cancer-related information in the Middle East: a review. Palliat Supp Care 2013;11:69–78.
23. Orona CJ, Koenig BA, Davis AJ. Cultural aspects of nondisclosure. Camb Q Healthc Ethics 1994;3:338–46.
24. Hagerty RG, Butow PN, Ellis PM, et al. Communicating prognosis in cancer care: a systematic review of the literature. Ann Oncol 2005;16:1005–53.
25. Kleinman A, Benson P. Anthropology in the clinic: the problem of cultural competency and how to fix it. PLoS Med 2006;3:1673–6.
1. Cultural competency – clear communication. National Institutes of Health (NIH). Accessed at www.nih.gov/clearcommunication/culturalcompetency.htm on 15 Jul 2014.
2. Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O. Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Pub Health Rep 2003;118:293–302.
3. PEW research: Hispanic trends project, a nation of immigrants. Accessed at www.pewhispanic.org/2013/01/29/a-nation-of-immigrants/ on 31 Jul 2014.
4. U.S. Census Bureau. New census bureau report analyzes nation’s linguistic diversity. Accessed at www.census/gov/newsroom/releases/archives/american_community_survey_acs/cb10-cn58.html on 31 Jul 2014.
5. Immigration Policy Center. Refugees: a fact sheet. Accessed at www.immigrationpolicy.org on 28 May 2014.
6. U.S. Department of State. U.S. welcomes record number of refugees. Accessed at iipdigital.usembassy.gov/st/english/article/2013/10/20131023285033.html?CP.rss=true#axzz3GtyMkFSe on 28 May 2014.
7. Barclay JS, Blackhall L J, Tulsky JA. Communication strategies and cultural issues in the delivery of bad news. J Palliative Med 2007;10:958–77.
8. Fallowfield L, Jenkins V. Communicating sad, bad, and difficult news in medicine. Lancet 2004;363;312–9.
9. Baile WF, Buckman R, Lenzi R, et al. SPIKES—A six-step protocol for delivering bad news: application to the patient with cancer. Oncologist 2000;5:302–11.
10. Ptacek JT, McIntosh EG. Physician challenges in communicating bad news. J Behav Med 2009;32:380–7.
11. Vogel BA, Leonhart R, Helmes AW. Communication matters: the impact of communication and participation in decision making on breast cancer patients’ depression and quality of life. Patient Educ Couns 2009;77:391–7.
12. Hack TF, Degner LF, Parker PA. The communication goals and needs of cancer patients: a review. Psychooncology 2005;14:831–45.
13. Vail L, Sandhu H, Fisher J, et al. Hospital consultants breaking bad news with simulated patients: an analysis of communication using the roter interaction analysis system. Patient Educ Couns 2011;83:185–94.
14. Hack TF, Pickles T, Ruether JD, et al. Behind closed doors: systematic analysis of breast cancer consultation communication and predictors of satisfaction with communication.
Psychooncology 2010;19:626–36.
15. Cantwell BM, Ramirez A. Doctor-patient communication: a study of junior house officers. Med Educ 1997;31:17–21.
16. Rollins LK, Bradley EB, Hayden GF, et al. Responding to a changing nation: are faculty prepared for cross-cultural conversations and care? Fam Med 2013;45:736–9.
17. Burgers C, Beukeboom CJ, Sparks L. How the doc should (not) talk: when breaking bad news with negations influences patients’ immediate responses and medical adherence intentions. Patient Educ Couns 2012;89:267–73.
18. Walsh RA, Girgis A, Sanson-Fisher RW. Breaking bad news 2: what evidence is available to guide clinicians? Behav Med 1998;24:61–73.
19. Blackhall LJ, Murphy ST, Frank G, et al. Ethnicity and attitudes toward patient autonomy. JAMA 1995;274:820–5.
20. Fujimori M, Uchitomi Y. Preferences of cancer patients regarding communication of bad news: a systematic literature review. Jpn J Clin Oncol 2009;39:201–16.
21. Beqiri A, Toci E, Sallaku A, et al. Breaking bad news in a southeast european population: a survey among cancer patients in Albania. J Palliat Med 2012;15:1100–5.
22. Khalil RB. Attitudes, beliefs and perceptions regarding truth disclosure of cancer-related information in the Middle East: a review. Palliat Supp Care 2013;11:69–78.
23. Orona CJ, Koenig BA, Davis AJ. Cultural aspects of nondisclosure. Camb Q Healthc Ethics 1994;3:338–46.
24. Hagerty RG, Butow PN, Ellis PM, et al. Communicating prognosis in cancer care: a systematic review of the literature. Ann Oncol 2005;16:1005–53.
25. Kleinman A, Benson P. Anthropology in the clinic: the problem of cultural competency and how to fix it. PLoS Med 2006;3:1673–6.
Emotional Distress, Barriers to Care, and Health-Related Quality of Life in Sickle Cell Disease
From the UCSF Benioff Children’s Hospital Oakland, Oakland, CA
Abstract
- Objective: Emotional distress may adversely affect the course and complicate treatment for individuals with sickle cell disease (SCD). We evaluated variables associated with physical and mental components of health-related quality of life (HRQL) in SCD in the context of a biobehavioral model.
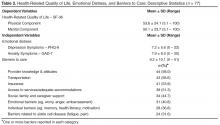
- Methods: We conducted a cross-sectional cohort study of 77 adults with SCD (18–69 years; 60% female; 73% Hgb SS) attending an urban, academic medical center. We measured emotional distress (Patient Health Questionnaire–9, Generalized Anxiety Disorder 7-item scale), clinical complications and utilization, barriers to health care, sociodemo-graphics and HRQL (SF-36 Health Survey). We developed models predictive of physical and mental HRQL by conducting stepwise regression analyses.
- Results: Sample prevalence of moderate to severe depression and anxiety symptoms was 33% and 36%, respectively; prevalence of impaired physical and mental HRQL was 17% and 16%, respectively. Increased symptoms of depression, older age, and ≥ 3 emergency department visits in the previous 12 months were independently associated with lower ratings of physical HRQL, controlling for anxiety and sex. Increased symptoms of depression were independently associated with lower ratings of mental HRQL, controlling for barriers to care, insurance status, lifetime complications of SCD, and sex.
- Conclusion: Emotional distress is an important contributor to both physical and mental HRQL for adults with SCD, although sociodemographic variables and barriers to care must also be considered. Innovative approaches that integrate mental health interventions with SCD clinical care are needed.
Emotional distress, including symptoms of depression and anxiety, may adversely affect the course and complicate the treatment of chronic physical conditions [1]. For patients with sickle cell disease (SCD), a group of inherited red blood cell conditions, symptoms of depression and anxiety are more prevalent compared with rates found in the general population [2–8]. The most common symptom of SCD is acute pain events, and other complications range from mild to life-threatening, including anemia, increased risk of infection, acute chest syndrome, stroke, skin ulcers, and pulmonary hypertension [9]. Depression in adults with SCD has been associated with increased sickle cell vaso-occlusive pain events, poor pain control, multiple blood transfusions, and prescription of the disease-modifying therapy hydroxyurea [4]. Adults with SCD and comorbid depression and anxiety had more daily pain and greater distress and interference from pain compared with those who did not have comorbid depression or anxiety [10]. Patients have linked emotional distress and episodes of illness [11], and research has found a relation between pain episodes and depression [12]. In a diary study, negative mood was significantly higher on pain days compared with non-pain days [13].
Studies examining the consequences of emotional distress on health-related quality of life (HRQL) for patients with SCD are emerging. Depressed adults with SCD rated their quality of life on the SF-36 Health Survey [14] as significantly poorer in all areas compared with non-depressed adults with SCD [15]. In regression models, depression was a stronger predictor of SF-36 scores than demographics, hemoglobin type, and pain measures. In a multi-site study [16], 1046 adults with SCD completed the SF-36. Increasing age was associated with significantly lower scores on all subscales except mental health, while female sex additionally contributed to diminished physical function and vitality scale scores in multivariate models [16]. The presence of a mood disorder was associated with bodily pain, and diminished vitality, social functioning, emotional role, and the mental component of HRQL. Medical complications other than pain were not associated with impaired HRQL. Anie and colleagues [17,18] have highlighted the contributions of sickle cell–related pain to diminished mood and HRQL, both in the acute hospital phase and 1 week post discharge.
A comprehensive literature review of patient-reported outcomes for adults with SCD revealed broad categories of the impact of SCD and its treatment on the lives of adults [19]. Categories included pain and pain management, emotional distress, poor social role functioning, diminished overall quality of life, and poor quality of care. Follow-up individual and group interviews with adults with SCD (n = 122) as well as individual interviews with their providers (n = 15) revealed findings consistent with the literature review on the major effects of pain on the lives of adults with SCD, interwoven with emotional distress, poor quality of care, and stigmatization [19].
In the present study, our goal was to describe variables associated with physical and mental HRQL in SCD within the context of the recently published comprehensive conceptual model of broad clinical and life effects associated with SCD [19]. The present analysis uses an existing clinical database and evaluates the effects of the relations between clinical complications of SCD, emotional distress, health care utilization, and HRQL. Our model includes barriers to health care that might prevent vulnerable patients from accessing needed health care services. Sociodemographic variables including ethnic and racial minority status and lower socioeconomic status and educational attainment may create barriers to health care for patients with SCD, as they do for individuals with other chronic conditions [20–23]. Over 60% of patients with SCD are on public insurance [24] and can have difficulties with accessing quality health care [25]. Negative provider attitudes and stigmatization when patients are seeking care for acute pain episodes have been highlighted by patients as major barriers to seeking health care [19,26–28]. In a qualitative study, 45 youth with SCD reported that competing school or peer-group activities, “feeling good,” poor patient-provider relationships, adverse clinic experiences, and forgetting were barriers to clinic attendance [29]. Limited research suggests that barriers to accessing health care are associated with poorer HRQL [30,31]; however no studies were identified that directly evaluated the relation between barriers to care and HRQL for populations with SCD.
We hypothesized that clinical complications of SCD, including pain, and barriers to accessing health care would be independently associated with the physical component of HRQL for adult patients with SCD, controlling for demographic variables. Further, we hypothesized that emotional distress, clinical complications of SCD, and barriers to accessing health care would be independently associated with the mental component of HRQL for adult patients with SCD, controlling for demographic variables.
Methods
Patient Recruitment
Participants were 18 years and older and were a subgroup selected from a larger prospective cohort enrolled in the Sickle Cell Disease Treatment Demonstration Program (SCDTDP) funded by the Health Resources and Services Administration (HRSA). As 1 of 7 SCDTDP grantees, our network collected common demographic, disease-related, and HRQL data as the other grantees to examine sickle cell health and health care [32]. Enrollment at our site was n = 115 from birth through adult, with data collection occurring at baseline in 2010 and annually through 2014. Participants were eligible for enrollment if they had any confirmed diagnosis of SCD and if they were seen at any facility treating SCD in the San Francisco Bay Area region. Interpreter services were available where English was a second language; however, no participant requested those services. The data collection site was an urban comprehensive sickle cell center. Participants were recruited through mailings, posted flyers, or were introduced to the project by their clinical providers. The institutional review boards of the sponsoring hospitals approved all procedures. This report describes analyses from the baseline data collected in 2010 and excludes pediatric patients under the age of 18 years, as we developed our conceptual model based on the adult SCD literature.
Procedures
Patients directly contacted the project coordinator or were introduced by their health care provider. The project coordinator explained the study in more detail, and if the patient agreed to participate, the project coordinator obtained thier informed consent. Participants completed the study materials in a private space in the clinic immediately after or were scheduled for a separate visit at a convenient time and location. Participants with known or observed difficulties with reading completed the questionnaires as an interview. We allowed participants who were unable to complete the forms in one visit to take them home or schedule a follow-up visit to complete them. We asked participants who took the questionnaires home to return them within 2 business days and provided them with a stamped addressed envelope. Participants were compensated with gift cards for their involvement.
Measures
Demographics and Clinical Characteristics
Participants completed an Individual Utilization Questionnaire created for the SCDTDP grantees [32], either as an interview or in paper and pencil format. Participants indicated their age, race and ethnicity, education level, type of insurance, and annual household income. They indicated the type of SCD, number of hospital days and emergency department (ED) visits in the previous 12 months, disease-modifying therapies including hydroxyurea or transfusions, and lifetime incidence of sickle cell–related complications. Complications included pain, acute chest syndrome, fever, severe infection, stroke, kidney damage, gallbladder attack, spleen problems and priapism. Medical data was verified by reviewing medical records when possible; the clinical databases in the hematology/oncology department at the sponsoring hospital are maintained using Microsoft SQL Server, a relational database management system designed for the enterprise environment. However, not all of the participating institutions were linked via this common clinical database or by an electronic health record at the time the study was conducted.
Barriers to Care
We modified a checklist of barriers to accessing health care for patients with a range of chronic conditions [33] to create a SCD-specific checklist [34]. The final checklist consists of 53 items organized into 8 categories including insurance, transportation, accommodations and accessibility, provider knowledge and attitudes, social support, individual barriers such as forgetting or difficulties understanding instructions, emotional barriers such as fear or anger, and barriers posed by SCD itself (eg, pain, fatigue). Participants check off any applicable barrier, yielding a total score ranging from 0 to 53. The checklist overall has demonstrated face validity and test-retest reliability (Pearson r = 0.74, P < 0.05).
Depressive Symptoms
Adults with SCD completed the PHQ-9, the 9-item depression scale of the Patient Health Questionnaire [35]. The PHQ-9 is a tool for assisting primary care clinicians in assessing symptoms of depression, based on criteria from the Diagnostic and Statistical Manual 4th edition (DSM-IV [36]). The PHQ-9 asks about such symptoms as sleep disturbance and difficulty concentrating over the past 2 weeks with scores ranging from 0 (Not at all) to 3 (Every day). The total symptom count is based on the number of items in which the respondent answered as “more than half of days” or greater, and scores are categorized as reflecting no (< 10), mild (10–14), moderate (15–19) or severe (≥ 20) symptoms of depression. Respondents indicate how difficult the symptoms make it for them to engage in daily activities from 0 (Not difficult at all) to 3 (Extremely difficult). The sensitivity and diagnostic and criterion validity of the PHQ-9 have been established [37]. The internal consistency of the PHQ-9 is high, with α > 0.85 in several studies and 48-hour test-retest reliability of 0.84. The PHQ has been used widely, including with African-American and Hispanic populations, and with individuals with chronic conditions [38].
Symptoms of Anxiety
Participants completed the Generalized Anxiety Disorder 7-item (GAD-7) questionnaire for screening and measuring severity of generalized anxiety disorder [39]. The GAD-7 asks about such symptoms as feeling nervous, anxious, or on edge over the past two weeks. Scores from all 7 items are added to obtain a total score [40]. Cut-points of 5, 10, and 15 represent mild, moderate, and severe levels of anxiety symptoms. Respondents indicate how difficult the symptoms make it for them to engage in daily activities from 0 (Not difficult at all) to 3 (Extremely difficult). The internal consistency of the GAD-7 is excellent (α = 0.92). Test-retest reliability is also good (Pearson r = 0.83) as is procedural validity (intraclass correlation = 0.83). The GAD-7 has excellent sensitivity and specificity to identify generalized anxiety disorder [41].
Health-Related Quality of Life
Participants completed the SF-36, which asks about the patient’s health status in the past week [14]. Eight subscales include physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional and mental health. Two summary measures, the Physical Component Summary and the Mental Component Summary, are calculated from 4 scales each. Use of the summary measures has been shown to increase the reliability of scores and improve the validity of scores in discriminating between physical and psychosocial outcomes [14]. Higher scores represent better HRQL, with a mean score of 50 (SD = 50) for the general population. Internal consistency estimates for the component summary scores are α > 0.89, item discriminant validity estimates are greater than 92.5% and 2-week test-retest reliability was excellent. Scores on the SF-36 have been divided into categories of HRQL functioning [42,43]. Participants in the impaired to very impaired category have scores ≤ mean – 1 SD while participants with average to above average functioning have scores > mean – 1 SD.
The SF-36 has been used extensively in observational and randomized studies for a range of illness conditions. In SCD, some aspects of HRQL as measured by the SF-36 improved for adult patients who responded to hydroxyurea [44]. Participants in the Pain in Sickle Cell Epidemiology Study scored lower than national norms on all SF-36 subscales except psychosocial functioning [45]. HRQL decreased significantly as daily pain intensity increased [45]. Further, women reported worse bodily pain compared with men [46].
Data Analyses
All biostatistical analyses were conducted using Stata 13 [47]. Continuous variables were examined for normality with measures of skewness and peakedness. All variables satisfied the assumptions of normality with the exception of barriers to health care and ED utilization. The variable barriers to health care was transformed using a square root transformation, resulting in a more normally distributed variable. ED utilization was dichotomized as 0–2 versus 3 or more ED visits in the previous 12 months, based on the distribution of utilization in the sample. The cutpoint of ≥ 3 annual ED visits is consistent with other literature on SCD clinical severity [48].
Descriptive statistics were computed to include means, standard deviations and frequencies. Sociodemographic variables (age, sex, insurance status [public or private] and income) were examined as potential covariates using Pearson correlations and t tests. Associations among emotional distress (anxiety and depression symptoms), clinical complications and ED utilization, barriers to health care, and the outcomes of the Physical and Mental Component Summary scores from the SF-36 were examined using Pearson correlations. We conducted stepwise regression with forward selection to determine models predictive of physical and mental HRQL. We tested the addition of each chosen variable (anxiety symptoms, depression symptoms, clinical complications, ED utilization, barriers to health care, age, sex, insurance status, and income), adding the variables (if any) that were most correlated with the outcome, and repeated the process until the model was not improved. A significance level of 0.05 was used for all statistical tests.
Results
Demographic and Clinical Characteristics
The majority of patients (73%) were diagnosed with Hgb SS disease and the most common lifetime complication was pain, reported by almost all of participants (Table 1). The next most common complication was fever, followed by acute chest syndrome. Twenty-seven percent of participants were currently on the disease-modifying therapy hydroxyurea, while 61% had a lifetime history of transfusion therapy. These data were verified with information from the clinical database for 73 participants (95%).
The median number of ED visits in the previous year was 1 (range, 0–50), with 19 patients (25%) with zero visits. The median number of hospital days in the previous year was 13 (range, 0–81). Twenty-nine patients (38%) had no hospital days in the previous year. These data were verified with information from the clinical database for 53 participants (69%), since hospital and ED visits occurred at institutions not always linked with the clinical databases at the sponsoring hospitals.
Emotional Distress, Barriers to Care, and Health-Related Quality of Life
The mean score on the GAD-7 was 7.9 (SD = 6.0, α = 0.90, Table 2). The prevalence of moderate to severe symptoms of anxiety (scores ≥ 10) was 36.4% (n = 28). Fourteen patients with moderate to severe symptoms (50%) reported that anxiety symptoms created some difficulty in work, daily activities, or relationships. Twelve patients (43%) reported that symptoms created very much to extreme difficulty in work, daily activities, or relationships. Fifteen patients (29%) with moderate to severe symptoms of anxiety or depression exhibited comorbid anxiety and depression.
The mean Physical Component Summary score on the SF-36 was 53.6 (SD = 24.1, α = 0.94, Table 2). The prevalence of impaired to very impaired HRQL in the physical domain was 17% (n = 13). The mean Mental Component Summary score on the SF-36 for the sample was 50.1 (SD = 23.7, α = 0.93), with a prevalence of 16% (n = 12) in the impaired to very impaired range for HRQL in the mental domain.
The mean number of barriers from the barriers checklist was 9.2 (SD = 10.1) out of 53 possible. Sixty-five participants (86%) reported at least 1 barrier to accessing health care (Table 2). The most frequently cited barriers to care were provider knowledge and attitudes, followed by transportation, insurance, and access to services (eg, hours and location of services). Less frequently cited barriers to care were individual barriers, including memory, health literacy and motivation, as well as those related to SCD itself, ie, fatigue and pain.
Sociodemographic Variables, Emotional Distress, and Health-Related Quality of Life
Symptoms of anxiety and depression were highly correlated with one another, as would be expected (r = 0.75, P < 0.001). Physical and mental HRQL were significantly correlated with symptoms of depression (r = –0.67, P < 0.001 for physical HRQL component and r = –0.70 for mental HRQL component, P < 0.001), with impaired HRQL in both domains correlated with greater symptoms of depression. Physical and Mental Component Summary scores were significantly correlated with symptoms of anxiety (r = –0.58, P < 0.001 for the physical component and r = –0.62 for the mental component, P < 0.001), with impaired HRQL in both domains correlated with greater symptoms of anxiety. Ratings of difficulty with daily functioning from depressive symptoms were correlated with impaired HRQL in the physical (r = –0.46, P < 0.01) and mental domains (r = –0.52, P < 0.001). Ratings of difficulty with daily functioning from anxiety symptoms were also correlated with impaired HRQL in the physical (r = –0.58, P < 0.001) and mental domains (r = –0.63, P < 0.001). Reports of more barriers to health care were significantly correlated with reports of more depressive and anxiety symptoms (r = 0.53, P < 0.001 and r = 0.48, P < 0.001), with lower Mental Component Summary scores (r = –0.43, P < 0.05), and with more ED visits in the past year (r = 0.43, P < 0.05).
Relations Between Independent Variables and Outcomes
Discussion
Results of this study showed that as expected, symptoms of depression were independently associated with the mental component of HRQL, controlling for other variables. Symptoms of depression were also independently associated with the physical component of HRQL. The effect size for both models was moderate but comparable to effect sizes of other studies of predictive models of physical and mental HRQL in SCD [49]. Our findings were consistent with previous literature, with older age and increased ED utilization independently associated with lower ratings of physical HRQL, with sex and anxiety symptoms entering into the predictive model [15–18,44,45]. Contrary to our hypotheses, barriers to accessing health care were not independently associated with physical or mental HRQL but did contribute to the model for mental HRQL, as did clinical complications and private insurance status.
While our sample was similar to previous samples in mean age and percentage of women participants, our patients reported significantly higher physical HRQL scores, and a wider range of HRQL scores (eg, 53.6,
SD = 24.1 compared with 39.6, SD = 10.0 [16]). The mean Physical Component Summary score was in fact similar to the general population mean of 50. This may reflect improvements in quality of care and subsequent overall improved patient health and HRQL given that these data were collected in year 2 of the HRSA SCDTDP. As an SCDTDP grantee, we implemented goals to improve coordination of service delivery and to increase access to care. However, it should also be considered that there was a selection bias in our study, in favor of those with better HRQL. Nevertheless, as already noted, our findings are consistent with previous literature with regard to inter-relations between variables, ie, associations between lower physical HRQL ratings and symptoms of depression, older age, and increased ED utilization [15]. Future studies in SCD that directly evaluate reported access to a medical home in relation to HRQL are needed to assess the impact of access to care and care coordination on HRQL ratings.
Our use of a data collection tool that focused on lifetime rather than acute history of complications may have contributed to our failure to find a relation between clinical manifestations and physical HRQL. Further, we were not able to assess the effects of pain separately from other complications, since almost every participant reported a lifetime history of pain. However, our findings were consistent with those of researchers who have found psychosocial and sociodemographic factors, versus clinical manifestations, to be major influences on both physical and mental HRQL for individuals with SCD and other chronic and life-threatening conditions [15, 16, 50]. Our confidence is increased in this finding, given that we were able to verify self-reports of clinical manifestations with our clinical database. Our results contribute to the developing body of knowledge that emphasizes the importance of understanding the broad impact on the lives of adults of living with SCD, not just the physical symptomatology.
There has been limited research on barriers to accessing health care as associated with HRQL for SCD populations. Health care barriers have been identified for ethnic minorities, even within patient-centered medical homes, with minority status moderating the effect of barriers to care on HRQL [30]. Our findings that barriers to health care were correlated with depression and anxiety symptoms, mental HRQL, and greater ED utilization support the need to view SCD care within a biobehavioral framework. Health care provider negative attitudes and lack of knowledge were the most frequently cited barriers for adults in our study, particularly in the context of ED and inpatient care. These findings are similar to other studies that have highlighted the impact of these provider variables on quality of care [26,51]. We were not able to separate out effects of ethnic minority status, given that our patients were predominantly African American.
Contributors to poor HRQL that have been identified in SCD are poverty [42] and public insurance status [49]. While over half of our participants had family incomes of less than $30,000, despite a mean household size of 3 members, we did not find that income contributed to either of our models predicting physical or mental HRQL. Over half of our patients were well educated, which could have moderated the effect of their low incomes, but we did not measure other potential moderators such as active coping and supportive relationships [19]. These analyses were beyond the scope of our existing database, but future studies are needed on such resilience factors and processes. Our adults were predominantly on public insurance and we did find that private insurance status was positively associated with higher ratings of mental HRQL, consistent with other SCD research [49]. Taken together, our findings underscore the importance of considering the interplay between emotional distress, sociodemographic and clinical factors and quality of care in order to address risk factors for poor patient-reported outcomes [52,53].
There have not been previous reports of symptoms of emotional distress in SCD using the PHQ-9 and GAD-7, but both measures have been used widely for depression and anxiety screening, including with African-American populations. We selected these over other measures for their brevity, free availability, and psychometric properties. Our prevalence of moderate to severe depression and anxiety symptoms in the present study was similar to what has been found using other tools [2–8]. The PHQ-9 and GAD-7 also provide ratings of symptom interference on daily functioning, and we found that these ratings were associated with impaired physical and mental HRQL. Given that there generally are limited mental health resources in the communities where individuals with SCD reside and are treated, ratings of emotional distress and HRQL can be taken together to stratify those patients with the most immediate need for interventions. Further, screening can be used for early detection with the goal to intervene and prevent the progression of symptoms of emotional distress to long-term, disabling mental health disorders [54]. There is a need for innovative and cost-effective strategies for assessment and treatment of mental health symptoms and disorders for patients with SCD. One model for evidence-based practice in the management of emotional distress for patients with in SCD is the collaborative care model.
The collaborative care model integrates physical and mental health care in the patient-centered medical home and focuses on treating the whole person and family [55]. In this model, a care management staff (eg, nurse, social worker, psychologist) is integrated with the primary care team. The care management staff, in consultation with a psychiatrist, provides evidence-based care coordination, brief behavioral interventions, and support for other treatments, including medications. The effectiveness of collaborative care programs has been demonstrated for ethnic minority and safety net populations such as the SCD population, which is disproportionately low-income and on public insurance [56, 57]. Future research with SCD populations should investigate such interventions as the collaborative care model that addresses both emotional distress and barriers to care.
Limitations
Our results need to be interpreted with caution given the small sample size and the potential bias introduced by non-random sampling. In addition, as our patients are from an urban setting, findings might not generalize to rural populations. This study was cross sectional so no inferences can be made with regard to causality and temporal relations between anxiety symptoms, barriers to care, and HRQL. Our strategy for measuring total clinical complications and barriers to care conserved power but it was not possible to evaluate if specific complications or barriers may have exerted a greater impact on HRQL compared with others. Similarly, other studies have examined specific domains of HRQL, while we limited our analysis to the Physical and Mental Component Summary scores. The utilization questionnaire was designed to assess only lifetime complications, not complications more proximal to the HRQL ratings.
Patient-reported outcomes, now widely accepted as outcome measures, elicit patients’ descriptions of the impact of their condition on their day-to-day lives [34, 58–60]. However, measures of mental health symptoms and HRQL may be subject to recall bias, measurement error, and confounding [61,62]. Nevertheless, a range of studies support the idea that mental health symptoms and HRQL are distinct constructs, and that patients with physical and mental health symptoms are vulnerable to lower ratings of HRQL [63,64]. Disease-modifying therapies such as hydroxyurea can contribute to improved ratings of HRQL [44,65], but we were not able to evaluate the contribution of hydroxyurea to HRQL as it appears to have been underutilized in our sample.
Conclusion
We evaluated emotional distress and other variables in the context of a biobehavioral model of HRQL outcomes for adults with SCD. Integrating the patient's perspective of the impact of the disease and its treatment with assessment of clinical indications is critical to implementing and evaluating effective therapies [25]. However, there are conceptual challenges in determining what actually contributes to HRQL from the patient’s perspective in the context of genetic disorders such as SCD [50]. Our findings highlight the importance of incorporating comprehensive psychosocial screening in order to support optimal HRQL in SCD. Providers may be reluctant to include such screening if, as is often the case, mental health services are difficult to access. Models such as the collaborative care model, which include mental health interventions within the sickle cell center or primary care provider’s office, should be implented. Barriers to care and HRQL should also be routinely evaluated for patients with SCD. Use of disease-specific tools, such as the Adult Sickle Cell Quality of Life measurement system [66], may increase the specificity needed to detect differences within adults with SCD and improvements related to interventions, whether medical or psychosocial. Contributors to HRQL in SCD go beyond clinical manifestations to include psychological and social factors, as well as provider and health system variables. Research conducted within the framework of a comprehensive conceptual model of broad clinical and life effects associated with SCD can inform clinical applications that ultimately enhance HRQL for patients with SCD.
Acknowledgment: The authors wish to thank San Keller, PhD, for her helpful comments on a previous version of this manuscript.
Corresponding author: Marsha J. Treadwell, PhD, Hematology/Oncology Dept., UCSF Benioff Children’s Hospital Oakland, 747 52nd St., Oakland, CA 94609, [email protected].
Funding/support: This research was conducted as part of the National Initiative for Children’s Healthcare Quality (NICHQ) Working to Improve Sickle Cell Healthcare (WISCH) project. Further support came from a grant from the Health Resources and Services Administration (HRSA) Sickle Cell Disease Treatment Demonstration Project Grant No. U1EMC16492 and from the National Institutes of Health (NIH) Clinical and Translational Science Award UL1 RR024131. The views expressed in this publication do not necessarily reflect the views of WISCH, NICHQ, HRSA or NIH.
Financial disclosures: None.
Author contributions: conception and design, MJT; analysis and interpretation of data, MJT, GG; drafting of article, MJT, GG; critical revision of the article, MJT, KK, FB; statistical expertise, GG; obtaining of funding, MJT; administrative or technical support, KK, FB; collection and assembly of data, KK, FB.
From the UCSF Benioff Children’s Hospital Oakland, Oakland, CA
Abstract
- Objective: Emotional distress may adversely affect the course and complicate treatment for individuals with sickle cell disease (SCD). We evaluated variables associated with physical and mental components of health-related quality of life (HRQL) in SCD in the context of a biobehavioral model.
- Methods: We conducted a cross-sectional cohort study of 77 adults with SCD (18–69 years; 60% female; 73% Hgb SS) attending an urban, academic medical center. We measured emotional distress (Patient Health Questionnaire–9, Generalized Anxiety Disorder 7-item scale), clinical complications and utilization, barriers to health care, sociodemo-graphics and HRQL (SF-36 Health Survey). We developed models predictive of physical and mental HRQL by conducting stepwise regression analyses.
- Results: Sample prevalence of moderate to severe depression and anxiety symptoms was 33% and 36%, respectively; prevalence of impaired physical and mental HRQL was 17% and 16%, respectively. Increased symptoms of depression, older age, and ≥ 3 emergency department visits in the previous 12 months were independently associated with lower ratings of physical HRQL, controlling for anxiety and sex. Increased symptoms of depression were independently associated with lower ratings of mental HRQL, controlling for barriers to care, insurance status, lifetime complications of SCD, and sex.
- Conclusion: Emotional distress is an important contributor to both physical and mental HRQL for adults with SCD, although sociodemographic variables and barriers to care must also be considered. Innovative approaches that integrate mental health interventions with SCD clinical care are needed.
Emotional distress, including symptoms of depression and anxiety, may adversely affect the course and complicate the treatment of chronic physical conditions [1]. For patients with sickle cell disease (SCD), a group of inherited red blood cell conditions, symptoms of depression and anxiety are more prevalent compared with rates found in the general population [2–8]. The most common symptom of SCD is acute pain events, and other complications range from mild to life-threatening, including anemia, increased risk of infection, acute chest syndrome, stroke, skin ulcers, and pulmonary hypertension [9]. Depression in adults with SCD has been associated with increased sickle cell vaso-occlusive pain events, poor pain control, multiple blood transfusions, and prescription of the disease-modifying therapy hydroxyurea [4]. Adults with SCD and comorbid depression and anxiety had more daily pain and greater distress and interference from pain compared with those who did not have comorbid depression or anxiety [10]. Patients have linked emotional distress and episodes of illness [11], and research has found a relation between pain episodes and depression [12]. In a diary study, negative mood was significantly higher on pain days compared with non-pain days [13].
Studies examining the consequences of emotional distress on health-related quality of life (HRQL) for patients with SCD are emerging. Depressed adults with SCD rated their quality of life on the SF-36 Health Survey [14] as significantly poorer in all areas compared with non-depressed adults with SCD [15]. In regression models, depression was a stronger predictor of SF-36 scores than demographics, hemoglobin type, and pain measures. In a multi-site study [16], 1046 adults with SCD completed the SF-36. Increasing age was associated with significantly lower scores on all subscales except mental health, while female sex additionally contributed to diminished physical function and vitality scale scores in multivariate models [16]. The presence of a mood disorder was associated with bodily pain, and diminished vitality, social functioning, emotional role, and the mental component of HRQL. Medical complications other than pain were not associated with impaired HRQL. Anie and colleagues [17,18] have highlighted the contributions of sickle cell–related pain to diminished mood and HRQL, both in the acute hospital phase and 1 week post discharge.
A comprehensive literature review of patient-reported outcomes for adults with SCD revealed broad categories of the impact of SCD and its treatment on the lives of adults [19]. Categories included pain and pain management, emotional distress, poor social role functioning, diminished overall quality of life, and poor quality of care. Follow-up individual and group interviews with adults with SCD (n = 122) as well as individual interviews with their providers (n = 15) revealed findings consistent with the literature review on the major effects of pain on the lives of adults with SCD, interwoven with emotional distress, poor quality of care, and stigmatization [19].
In the present study, our goal was to describe variables associated with physical and mental HRQL in SCD within the context of the recently published comprehensive conceptual model of broad clinical and life effects associated with SCD [19]. The present analysis uses an existing clinical database and evaluates the effects of the relations between clinical complications of SCD, emotional distress, health care utilization, and HRQL. Our model includes barriers to health care that might prevent vulnerable patients from accessing needed health care services. Sociodemographic variables including ethnic and racial minority status and lower socioeconomic status and educational attainment may create barriers to health care for patients with SCD, as they do for individuals with other chronic conditions [20–23]. Over 60% of patients with SCD are on public insurance [24] and can have difficulties with accessing quality health care [25]. Negative provider attitudes and stigmatization when patients are seeking care for acute pain episodes have been highlighted by patients as major barriers to seeking health care [19,26–28]. In a qualitative study, 45 youth with SCD reported that competing school or peer-group activities, “feeling good,” poor patient-provider relationships, adverse clinic experiences, and forgetting were barriers to clinic attendance [29]. Limited research suggests that barriers to accessing health care are associated with poorer HRQL [30,31]; however no studies were identified that directly evaluated the relation between barriers to care and HRQL for populations with SCD.
We hypothesized that clinical complications of SCD, including pain, and barriers to accessing health care would be independently associated with the physical component of HRQL for adult patients with SCD, controlling for demographic variables. Further, we hypothesized that emotional distress, clinical complications of SCD, and barriers to accessing health care would be independently associated with the mental component of HRQL for adult patients with SCD, controlling for demographic variables.
Methods
Patient Recruitment
Participants were 18 years and older and were a subgroup selected from a larger prospective cohort enrolled in the Sickle Cell Disease Treatment Demonstration Program (SCDTDP) funded by the Health Resources and Services Administration (HRSA). As 1 of 7 SCDTDP grantees, our network collected common demographic, disease-related, and HRQL data as the other grantees to examine sickle cell health and health care [32]. Enrollment at our site was n = 115 from birth through adult, with data collection occurring at baseline in 2010 and annually through 2014. Participants were eligible for enrollment if they had any confirmed diagnosis of SCD and if they were seen at any facility treating SCD in the San Francisco Bay Area region. Interpreter services were available where English was a second language; however, no participant requested those services. The data collection site was an urban comprehensive sickle cell center. Participants were recruited through mailings, posted flyers, or were introduced to the project by their clinical providers. The institutional review boards of the sponsoring hospitals approved all procedures. This report describes analyses from the baseline data collected in 2010 and excludes pediatric patients under the age of 18 years, as we developed our conceptual model based on the adult SCD literature.
Procedures
Patients directly contacted the project coordinator or were introduced by their health care provider. The project coordinator explained the study in more detail, and if the patient agreed to participate, the project coordinator obtained thier informed consent. Participants completed the study materials in a private space in the clinic immediately after or were scheduled for a separate visit at a convenient time and location. Participants with known or observed difficulties with reading completed the questionnaires as an interview. We allowed participants who were unable to complete the forms in one visit to take them home or schedule a follow-up visit to complete them. We asked participants who took the questionnaires home to return them within 2 business days and provided them with a stamped addressed envelope. Participants were compensated with gift cards for their involvement.
Measures
Demographics and Clinical Characteristics
Participants completed an Individual Utilization Questionnaire created for the SCDTDP grantees [32], either as an interview or in paper and pencil format. Participants indicated their age, race and ethnicity, education level, type of insurance, and annual household income. They indicated the type of SCD, number of hospital days and emergency department (ED) visits in the previous 12 months, disease-modifying therapies including hydroxyurea or transfusions, and lifetime incidence of sickle cell–related complications. Complications included pain, acute chest syndrome, fever, severe infection, stroke, kidney damage, gallbladder attack, spleen problems and priapism. Medical data was verified by reviewing medical records when possible; the clinical databases in the hematology/oncology department at the sponsoring hospital are maintained using Microsoft SQL Server, a relational database management system designed for the enterprise environment. However, not all of the participating institutions were linked via this common clinical database or by an electronic health record at the time the study was conducted.
Barriers to Care
We modified a checklist of barriers to accessing health care for patients with a range of chronic conditions [33] to create a SCD-specific checklist [34]. The final checklist consists of 53 items organized into 8 categories including insurance, transportation, accommodations and accessibility, provider knowledge and attitudes, social support, individual barriers such as forgetting or difficulties understanding instructions, emotional barriers such as fear or anger, and barriers posed by SCD itself (eg, pain, fatigue). Participants check off any applicable barrier, yielding a total score ranging from 0 to 53. The checklist overall has demonstrated face validity and test-retest reliability (Pearson r = 0.74, P < 0.05).
Depressive Symptoms
Adults with SCD completed the PHQ-9, the 9-item depression scale of the Patient Health Questionnaire [35]. The PHQ-9 is a tool for assisting primary care clinicians in assessing symptoms of depression, based on criteria from the Diagnostic and Statistical Manual 4th edition (DSM-IV [36]). The PHQ-9 asks about such symptoms as sleep disturbance and difficulty concentrating over the past 2 weeks with scores ranging from 0 (Not at all) to 3 (Every day). The total symptom count is based on the number of items in which the respondent answered as “more than half of days” or greater, and scores are categorized as reflecting no (< 10), mild (10–14), moderate (15–19) or severe (≥ 20) symptoms of depression. Respondents indicate how difficult the symptoms make it for them to engage in daily activities from 0 (Not difficult at all) to 3 (Extremely difficult). The sensitivity and diagnostic and criterion validity of the PHQ-9 have been established [37]. The internal consistency of the PHQ-9 is high, with α > 0.85 in several studies and 48-hour test-retest reliability of 0.84. The PHQ has been used widely, including with African-American and Hispanic populations, and with individuals with chronic conditions [38].
Symptoms of Anxiety
Participants completed the Generalized Anxiety Disorder 7-item (GAD-7) questionnaire for screening and measuring severity of generalized anxiety disorder [39]. The GAD-7 asks about such symptoms as feeling nervous, anxious, or on edge over the past two weeks. Scores from all 7 items are added to obtain a total score [40]. Cut-points of 5, 10, and 15 represent mild, moderate, and severe levels of anxiety symptoms. Respondents indicate how difficult the symptoms make it for them to engage in daily activities from 0 (Not difficult at all) to 3 (Extremely difficult). The internal consistency of the GAD-7 is excellent (α = 0.92). Test-retest reliability is also good (Pearson r = 0.83) as is procedural validity (intraclass correlation = 0.83). The GAD-7 has excellent sensitivity and specificity to identify generalized anxiety disorder [41].
Health-Related Quality of Life
Participants completed the SF-36, which asks about the patient’s health status in the past week [14]. Eight subscales include physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional and mental health. Two summary measures, the Physical Component Summary and the Mental Component Summary, are calculated from 4 scales each. Use of the summary measures has been shown to increase the reliability of scores and improve the validity of scores in discriminating between physical and psychosocial outcomes [14]. Higher scores represent better HRQL, with a mean score of 50 (SD = 50) for the general population. Internal consistency estimates for the component summary scores are α > 0.89, item discriminant validity estimates are greater than 92.5% and 2-week test-retest reliability was excellent. Scores on the SF-36 have been divided into categories of HRQL functioning [42,43]. Participants in the impaired to very impaired category have scores ≤ mean – 1 SD while participants with average to above average functioning have scores > mean – 1 SD.
The SF-36 has been used extensively in observational and randomized studies for a range of illness conditions. In SCD, some aspects of HRQL as measured by the SF-36 improved for adult patients who responded to hydroxyurea [44]. Participants in the Pain in Sickle Cell Epidemiology Study scored lower than national norms on all SF-36 subscales except psychosocial functioning [45]. HRQL decreased significantly as daily pain intensity increased [45]. Further, women reported worse bodily pain compared with men [46].
Data Analyses
All biostatistical analyses were conducted using Stata 13 [47]. Continuous variables were examined for normality with measures of skewness and peakedness. All variables satisfied the assumptions of normality with the exception of barriers to health care and ED utilization. The variable barriers to health care was transformed using a square root transformation, resulting in a more normally distributed variable. ED utilization was dichotomized as 0–2 versus 3 or more ED visits in the previous 12 months, based on the distribution of utilization in the sample. The cutpoint of ≥ 3 annual ED visits is consistent with other literature on SCD clinical severity [48].
Descriptive statistics were computed to include means, standard deviations and frequencies. Sociodemographic variables (age, sex, insurance status [public or private] and income) were examined as potential covariates using Pearson correlations and t tests. Associations among emotional distress (anxiety and depression symptoms), clinical complications and ED utilization, barriers to health care, and the outcomes of the Physical and Mental Component Summary scores from the SF-36 were examined using Pearson correlations. We conducted stepwise regression with forward selection to determine models predictive of physical and mental HRQL. We tested the addition of each chosen variable (anxiety symptoms, depression symptoms, clinical complications, ED utilization, barriers to health care, age, sex, insurance status, and income), adding the variables (if any) that were most correlated with the outcome, and repeated the process until the model was not improved. A significance level of 0.05 was used for all statistical tests.
Results
Demographic and Clinical Characteristics
The majority of patients (73%) were diagnosed with Hgb SS disease and the most common lifetime complication was pain, reported by almost all of participants (Table 1). The next most common complication was fever, followed by acute chest syndrome. Twenty-seven percent of participants were currently on the disease-modifying therapy hydroxyurea, while 61% had a lifetime history of transfusion therapy. These data were verified with information from the clinical database for 73 participants (95%).
The median number of ED visits in the previous year was 1 (range, 0–50), with 19 patients (25%) with zero visits. The median number of hospital days in the previous year was 13 (range, 0–81). Twenty-nine patients (38%) had no hospital days in the previous year. These data were verified with information from the clinical database for 53 participants (69%), since hospital and ED visits occurred at institutions not always linked with the clinical databases at the sponsoring hospitals.
Emotional Distress, Barriers to Care, and Health-Related Quality of Life
The mean score on the GAD-7 was 7.9 (SD = 6.0, α = 0.90, Table 2). The prevalence of moderate to severe symptoms of anxiety (scores ≥ 10) was 36.4% (n = 28). Fourteen patients with moderate to severe symptoms (50%) reported that anxiety symptoms created some difficulty in work, daily activities, or relationships. Twelve patients (43%) reported that symptoms created very much to extreme difficulty in work, daily activities, or relationships. Fifteen patients (29%) with moderate to severe symptoms of anxiety or depression exhibited comorbid anxiety and depression.
The mean Physical Component Summary score on the SF-36 was 53.6 (SD = 24.1, α = 0.94, Table 2). The prevalence of impaired to very impaired HRQL in the physical domain was 17% (n = 13). The mean Mental Component Summary score on the SF-36 for the sample was 50.1 (SD = 23.7, α = 0.93), with a prevalence of 16% (n = 12) in the impaired to very impaired range for HRQL in the mental domain.
The mean number of barriers from the barriers checklist was 9.2 (SD = 10.1) out of 53 possible. Sixty-five participants (86%) reported at least 1 barrier to accessing health care (Table 2). The most frequently cited barriers to care were provider knowledge and attitudes, followed by transportation, insurance, and access to services (eg, hours and location of services). Less frequently cited barriers to care were individual barriers, including memory, health literacy and motivation, as well as those related to SCD itself, ie, fatigue and pain.
Sociodemographic Variables, Emotional Distress, and Health-Related Quality of Life
Symptoms of anxiety and depression were highly correlated with one another, as would be expected (r = 0.75, P < 0.001). Physical and mental HRQL were significantly correlated with symptoms of depression (r = –0.67, P < 0.001 for physical HRQL component and r = –0.70 for mental HRQL component, P < 0.001), with impaired HRQL in both domains correlated with greater symptoms of depression. Physical and Mental Component Summary scores were significantly correlated with symptoms of anxiety (r = –0.58, P < 0.001 for the physical component and r = –0.62 for the mental component, P < 0.001), with impaired HRQL in both domains correlated with greater symptoms of anxiety. Ratings of difficulty with daily functioning from depressive symptoms were correlated with impaired HRQL in the physical (r = –0.46, P < 0.01) and mental domains (r = –0.52, P < 0.001). Ratings of difficulty with daily functioning from anxiety symptoms were also correlated with impaired HRQL in the physical (r = –0.58, P < 0.001) and mental domains (r = –0.63, P < 0.001). Reports of more barriers to health care were significantly correlated with reports of more depressive and anxiety symptoms (r = 0.53, P < 0.001 and r = 0.48, P < 0.001), with lower Mental Component Summary scores (r = –0.43, P < 0.05), and with more ED visits in the past year (r = 0.43, P < 0.05).
Relations Between Independent Variables and Outcomes
Discussion
Results of this study showed that as expected, symptoms of depression were independently associated with the mental component of HRQL, controlling for other variables. Symptoms of depression were also independently associated with the physical component of HRQL. The effect size for both models was moderate but comparable to effect sizes of other studies of predictive models of physical and mental HRQL in SCD [49]. Our findings were consistent with previous literature, with older age and increased ED utilization independently associated with lower ratings of physical HRQL, with sex and anxiety symptoms entering into the predictive model [15–18,44,45]. Contrary to our hypotheses, barriers to accessing health care were not independently associated with physical or mental HRQL but did contribute to the model for mental HRQL, as did clinical complications and private insurance status.
While our sample was similar to previous samples in mean age and percentage of women participants, our patients reported significantly higher physical HRQL scores, and a wider range of HRQL scores (eg, 53.6,
SD = 24.1 compared with 39.6, SD = 10.0 [16]). The mean Physical Component Summary score was in fact similar to the general population mean of 50. This may reflect improvements in quality of care and subsequent overall improved patient health and HRQL given that these data were collected in year 2 of the HRSA SCDTDP. As an SCDTDP grantee, we implemented goals to improve coordination of service delivery and to increase access to care. However, it should also be considered that there was a selection bias in our study, in favor of those with better HRQL. Nevertheless, as already noted, our findings are consistent with previous literature with regard to inter-relations between variables, ie, associations between lower physical HRQL ratings and symptoms of depression, older age, and increased ED utilization [15]. Future studies in SCD that directly evaluate reported access to a medical home in relation to HRQL are needed to assess the impact of access to care and care coordination on HRQL ratings.
Our use of a data collection tool that focused on lifetime rather than acute history of complications may have contributed to our failure to find a relation between clinical manifestations and physical HRQL. Further, we were not able to assess the effects of pain separately from other complications, since almost every participant reported a lifetime history of pain. However, our findings were consistent with those of researchers who have found psychosocial and sociodemographic factors, versus clinical manifestations, to be major influences on both physical and mental HRQL for individuals with SCD and other chronic and life-threatening conditions [15, 16, 50]. Our confidence is increased in this finding, given that we were able to verify self-reports of clinical manifestations with our clinical database. Our results contribute to the developing body of knowledge that emphasizes the importance of understanding the broad impact on the lives of adults of living with SCD, not just the physical symptomatology.
There has been limited research on barriers to accessing health care as associated with HRQL for SCD populations. Health care barriers have been identified for ethnic minorities, even within patient-centered medical homes, with minority status moderating the effect of barriers to care on HRQL [30]. Our findings that barriers to health care were correlated with depression and anxiety symptoms, mental HRQL, and greater ED utilization support the need to view SCD care within a biobehavioral framework. Health care provider negative attitudes and lack of knowledge were the most frequently cited barriers for adults in our study, particularly in the context of ED and inpatient care. These findings are similar to other studies that have highlighted the impact of these provider variables on quality of care [26,51]. We were not able to separate out effects of ethnic minority status, given that our patients were predominantly African American.
Contributors to poor HRQL that have been identified in SCD are poverty [42] and public insurance status [49]. While over half of our participants had family incomes of less than $30,000, despite a mean household size of 3 members, we did not find that income contributed to either of our models predicting physical or mental HRQL. Over half of our patients were well educated, which could have moderated the effect of their low incomes, but we did not measure other potential moderators such as active coping and supportive relationships [19]. These analyses were beyond the scope of our existing database, but future studies are needed on such resilience factors and processes. Our adults were predominantly on public insurance and we did find that private insurance status was positively associated with higher ratings of mental HRQL, consistent with other SCD research [49]. Taken together, our findings underscore the importance of considering the interplay between emotional distress, sociodemographic and clinical factors and quality of care in order to address risk factors for poor patient-reported outcomes [52,53].
There have not been previous reports of symptoms of emotional distress in SCD using the PHQ-9 and GAD-7, but both measures have been used widely for depression and anxiety screening, including with African-American populations. We selected these over other measures for their brevity, free availability, and psychometric properties. Our prevalence of moderate to severe depression and anxiety symptoms in the present study was similar to what has been found using other tools [2–8]. The PHQ-9 and GAD-7 also provide ratings of symptom interference on daily functioning, and we found that these ratings were associated with impaired physical and mental HRQL. Given that there generally are limited mental health resources in the communities where individuals with SCD reside and are treated, ratings of emotional distress and HRQL can be taken together to stratify those patients with the most immediate need for interventions. Further, screening can be used for early detection with the goal to intervene and prevent the progression of symptoms of emotional distress to long-term, disabling mental health disorders [54]. There is a need for innovative and cost-effective strategies for assessment and treatment of mental health symptoms and disorders for patients with SCD. One model for evidence-based practice in the management of emotional distress for patients with in SCD is the collaborative care model.
The collaborative care model integrates physical and mental health care in the patient-centered medical home and focuses on treating the whole person and family [55]. In this model, a care management staff (eg, nurse, social worker, psychologist) is integrated with the primary care team. The care management staff, in consultation with a psychiatrist, provides evidence-based care coordination, brief behavioral interventions, and support for other treatments, including medications. The effectiveness of collaborative care programs has been demonstrated for ethnic minority and safety net populations such as the SCD population, which is disproportionately low-income and on public insurance [56, 57]. Future research with SCD populations should investigate such interventions as the collaborative care model that addresses both emotional distress and barriers to care.
Limitations
Our results need to be interpreted with caution given the small sample size and the potential bias introduced by non-random sampling. In addition, as our patients are from an urban setting, findings might not generalize to rural populations. This study was cross sectional so no inferences can be made with regard to causality and temporal relations between anxiety symptoms, barriers to care, and HRQL. Our strategy for measuring total clinical complications and barriers to care conserved power but it was not possible to evaluate if specific complications or barriers may have exerted a greater impact on HRQL compared with others. Similarly, other studies have examined specific domains of HRQL, while we limited our analysis to the Physical and Mental Component Summary scores. The utilization questionnaire was designed to assess only lifetime complications, not complications more proximal to the HRQL ratings.
Patient-reported outcomes, now widely accepted as outcome measures, elicit patients’ descriptions of the impact of their condition on their day-to-day lives [34, 58–60]. However, measures of mental health symptoms and HRQL may be subject to recall bias, measurement error, and confounding [61,62]. Nevertheless, a range of studies support the idea that mental health symptoms and HRQL are distinct constructs, and that patients with physical and mental health symptoms are vulnerable to lower ratings of HRQL [63,64]. Disease-modifying therapies such as hydroxyurea can contribute to improved ratings of HRQL [44,65], but we were not able to evaluate the contribution of hydroxyurea to HRQL as it appears to have been underutilized in our sample.
Conclusion
We evaluated emotional distress and other variables in the context of a biobehavioral model of HRQL outcomes for adults with SCD. Integrating the patient's perspective of the impact of the disease and its treatment with assessment of clinical indications is critical to implementing and evaluating effective therapies [25]. However, there are conceptual challenges in determining what actually contributes to HRQL from the patient’s perspective in the context of genetic disorders such as SCD [50]. Our findings highlight the importance of incorporating comprehensive psychosocial screening in order to support optimal HRQL in SCD. Providers may be reluctant to include such screening if, as is often the case, mental health services are difficult to access. Models such as the collaborative care model, which include mental health interventions within the sickle cell center or primary care provider’s office, should be implented. Barriers to care and HRQL should also be routinely evaluated for patients with SCD. Use of disease-specific tools, such as the Adult Sickle Cell Quality of Life measurement system [66], may increase the specificity needed to detect differences within adults with SCD and improvements related to interventions, whether medical or psychosocial. Contributors to HRQL in SCD go beyond clinical manifestations to include psychological and social factors, as well as provider and health system variables. Research conducted within the framework of a comprehensive conceptual model of broad clinical and life effects associated with SCD can inform clinical applications that ultimately enhance HRQL for patients with SCD.
Acknowledgment: The authors wish to thank San Keller, PhD, for her helpful comments on a previous version of this manuscript.
Corresponding author: Marsha J. Treadwell, PhD, Hematology/Oncology Dept., UCSF Benioff Children’s Hospital Oakland, 747 52nd St., Oakland, CA 94609, [email protected].
Funding/support: This research was conducted as part of the National Initiative for Children’s Healthcare Quality (NICHQ) Working to Improve Sickle Cell Healthcare (WISCH) project. Further support came from a grant from the Health Resources and Services Administration (HRSA) Sickle Cell Disease Treatment Demonstration Project Grant No. U1EMC16492 and from the National Institutes of Health (NIH) Clinical and Translational Science Award UL1 RR024131. The views expressed in this publication do not necessarily reflect the views of WISCH, NICHQ, HRSA or NIH.
Financial disclosures: None.
Author contributions: conception and design, MJT; analysis and interpretation of data, MJT, GG; drafting of article, MJT, GG; critical revision of the article, MJT, KK, FB; statistical expertise, GG; obtaining of funding, MJT; administrative or technical support, KK, FB; collection and assembly of data, KK, FB.
From the UCSF Benioff Children’s Hospital Oakland, Oakland, CA
Abstract
- Objective: Emotional distress may adversely affect the course and complicate treatment for individuals with sickle cell disease (SCD). We evaluated variables associated with physical and mental components of health-related quality of life (HRQL) in SCD in the context of a biobehavioral model.
- Methods: We conducted a cross-sectional cohort study of 77 adults with SCD (18–69 years; 60% female; 73% Hgb SS) attending an urban, academic medical center. We measured emotional distress (Patient Health Questionnaire–9, Generalized Anxiety Disorder 7-item scale), clinical complications and utilization, barriers to health care, sociodemo-graphics and HRQL (SF-36 Health Survey). We developed models predictive of physical and mental HRQL by conducting stepwise regression analyses.
- Results: Sample prevalence of moderate to severe depression and anxiety symptoms was 33% and 36%, respectively; prevalence of impaired physical and mental HRQL was 17% and 16%, respectively. Increased symptoms of depression, older age, and ≥ 3 emergency department visits in the previous 12 months were independently associated with lower ratings of physical HRQL, controlling for anxiety and sex. Increased symptoms of depression were independently associated with lower ratings of mental HRQL, controlling for barriers to care, insurance status, lifetime complications of SCD, and sex.
- Conclusion: Emotional distress is an important contributor to both physical and mental HRQL for adults with SCD, although sociodemographic variables and barriers to care must also be considered. Innovative approaches that integrate mental health interventions with SCD clinical care are needed.
Emotional distress, including symptoms of depression and anxiety, may adversely affect the course and complicate the treatment of chronic physical conditions [1]. For patients with sickle cell disease (SCD), a group of inherited red blood cell conditions, symptoms of depression and anxiety are more prevalent compared with rates found in the general population [2–8]. The most common symptom of SCD is acute pain events, and other complications range from mild to life-threatening, including anemia, increased risk of infection, acute chest syndrome, stroke, skin ulcers, and pulmonary hypertension [9]. Depression in adults with SCD has been associated with increased sickle cell vaso-occlusive pain events, poor pain control, multiple blood transfusions, and prescription of the disease-modifying therapy hydroxyurea [4]. Adults with SCD and comorbid depression and anxiety had more daily pain and greater distress and interference from pain compared with those who did not have comorbid depression or anxiety [10]. Patients have linked emotional distress and episodes of illness [11], and research has found a relation between pain episodes and depression [12]. In a diary study, negative mood was significantly higher on pain days compared with non-pain days [13].
Studies examining the consequences of emotional distress on health-related quality of life (HRQL) for patients with SCD are emerging. Depressed adults with SCD rated their quality of life on the SF-36 Health Survey [14] as significantly poorer in all areas compared with non-depressed adults with SCD [15]. In regression models, depression was a stronger predictor of SF-36 scores than demographics, hemoglobin type, and pain measures. In a multi-site study [16], 1046 adults with SCD completed the SF-36. Increasing age was associated with significantly lower scores on all subscales except mental health, while female sex additionally contributed to diminished physical function and vitality scale scores in multivariate models [16]. The presence of a mood disorder was associated with bodily pain, and diminished vitality, social functioning, emotional role, and the mental component of HRQL. Medical complications other than pain were not associated with impaired HRQL. Anie and colleagues [17,18] have highlighted the contributions of sickle cell–related pain to diminished mood and HRQL, both in the acute hospital phase and 1 week post discharge.
A comprehensive literature review of patient-reported outcomes for adults with SCD revealed broad categories of the impact of SCD and its treatment on the lives of adults [19]. Categories included pain and pain management, emotional distress, poor social role functioning, diminished overall quality of life, and poor quality of care. Follow-up individual and group interviews with adults with SCD (n = 122) as well as individual interviews with their providers (n = 15) revealed findings consistent with the literature review on the major effects of pain on the lives of adults with SCD, interwoven with emotional distress, poor quality of care, and stigmatization [19].
In the present study, our goal was to describe variables associated with physical and mental HRQL in SCD within the context of the recently published comprehensive conceptual model of broad clinical and life effects associated with SCD [19]. The present analysis uses an existing clinical database and evaluates the effects of the relations between clinical complications of SCD, emotional distress, health care utilization, and HRQL. Our model includes barriers to health care that might prevent vulnerable patients from accessing needed health care services. Sociodemographic variables including ethnic and racial minority status and lower socioeconomic status and educational attainment may create barriers to health care for patients with SCD, as they do for individuals with other chronic conditions [20–23]. Over 60% of patients with SCD are on public insurance [24] and can have difficulties with accessing quality health care [25]. Negative provider attitudes and stigmatization when patients are seeking care for acute pain episodes have been highlighted by patients as major barriers to seeking health care [19,26–28]. In a qualitative study, 45 youth with SCD reported that competing school or peer-group activities, “feeling good,” poor patient-provider relationships, adverse clinic experiences, and forgetting were barriers to clinic attendance [29]. Limited research suggests that barriers to accessing health care are associated with poorer HRQL [30,31]; however no studies were identified that directly evaluated the relation between barriers to care and HRQL for populations with SCD.
We hypothesized that clinical complications of SCD, including pain, and barriers to accessing health care would be independently associated with the physical component of HRQL for adult patients with SCD, controlling for demographic variables. Further, we hypothesized that emotional distress, clinical complications of SCD, and barriers to accessing health care would be independently associated with the mental component of HRQL for adult patients with SCD, controlling for demographic variables.
Methods
Patient Recruitment
Participants were 18 years and older and were a subgroup selected from a larger prospective cohort enrolled in the Sickle Cell Disease Treatment Demonstration Program (SCDTDP) funded by the Health Resources and Services Administration (HRSA). As 1 of 7 SCDTDP grantees, our network collected common demographic, disease-related, and HRQL data as the other grantees to examine sickle cell health and health care [32]. Enrollment at our site was n = 115 from birth through adult, with data collection occurring at baseline in 2010 and annually through 2014. Participants were eligible for enrollment if they had any confirmed diagnosis of SCD and if they were seen at any facility treating SCD in the San Francisco Bay Area region. Interpreter services were available where English was a second language; however, no participant requested those services. The data collection site was an urban comprehensive sickle cell center. Participants were recruited through mailings, posted flyers, or were introduced to the project by their clinical providers. The institutional review boards of the sponsoring hospitals approved all procedures. This report describes analyses from the baseline data collected in 2010 and excludes pediatric patients under the age of 18 years, as we developed our conceptual model based on the adult SCD literature.
Procedures
Patients directly contacted the project coordinator or were introduced by their health care provider. The project coordinator explained the study in more detail, and if the patient agreed to participate, the project coordinator obtained thier informed consent. Participants completed the study materials in a private space in the clinic immediately after or were scheduled for a separate visit at a convenient time and location. Participants with known or observed difficulties with reading completed the questionnaires as an interview. We allowed participants who were unable to complete the forms in one visit to take them home or schedule a follow-up visit to complete them. We asked participants who took the questionnaires home to return them within 2 business days and provided them with a stamped addressed envelope. Participants were compensated with gift cards for their involvement.
Measures
Demographics and Clinical Characteristics
Participants completed an Individual Utilization Questionnaire created for the SCDTDP grantees [32], either as an interview or in paper and pencil format. Participants indicated their age, race and ethnicity, education level, type of insurance, and annual household income. They indicated the type of SCD, number of hospital days and emergency department (ED) visits in the previous 12 months, disease-modifying therapies including hydroxyurea or transfusions, and lifetime incidence of sickle cell–related complications. Complications included pain, acute chest syndrome, fever, severe infection, stroke, kidney damage, gallbladder attack, spleen problems and priapism. Medical data was verified by reviewing medical records when possible; the clinical databases in the hematology/oncology department at the sponsoring hospital are maintained using Microsoft SQL Server, a relational database management system designed for the enterprise environment. However, not all of the participating institutions were linked via this common clinical database or by an electronic health record at the time the study was conducted.
Barriers to Care
We modified a checklist of barriers to accessing health care for patients with a range of chronic conditions [33] to create a SCD-specific checklist [34]. The final checklist consists of 53 items organized into 8 categories including insurance, transportation, accommodations and accessibility, provider knowledge and attitudes, social support, individual barriers such as forgetting or difficulties understanding instructions, emotional barriers such as fear or anger, and barriers posed by SCD itself (eg, pain, fatigue). Participants check off any applicable barrier, yielding a total score ranging from 0 to 53. The checklist overall has demonstrated face validity and test-retest reliability (Pearson r = 0.74, P < 0.05).
Depressive Symptoms
Adults with SCD completed the PHQ-9, the 9-item depression scale of the Patient Health Questionnaire [35]. The PHQ-9 is a tool for assisting primary care clinicians in assessing symptoms of depression, based on criteria from the Diagnostic and Statistical Manual 4th edition (DSM-IV [36]). The PHQ-9 asks about such symptoms as sleep disturbance and difficulty concentrating over the past 2 weeks with scores ranging from 0 (Not at all) to 3 (Every day). The total symptom count is based on the number of items in which the respondent answered as “more than half of days” or greater, and scores are categorized as reflecting no (< 10), mild (10–14), moderate (15–19) or severe (≥ 20) symptoms of depression. Respondents indicate how difficult the symptoms make it for them to engage in daily activities from 0 (Not difficult at all) to 3 (Extremely difficult). The sensitivity and diagnostic and criterion validity of the PHQ-9 have been established [37]. The internal consistency of the PHQ-9 is high, with α > 0.85 in several studies and 48-hour test-retest reliability of 0.84. The PHQ has been used widely, including with African-American and Hispanic populations, and with individuals with chronic conditions [38].
Symptoms of Anxiety
Participants completed the Generalized Anxiety Disorder 7-item (GAD-7) questionnaire for screening and measuring severity of generalized anxiety disorder [39]. The GAD-7 asks about such symptoms as feeling nervous, anxious, or on edge over the past two weeks. Scores from all 7 items are added to obtain a total score [40]. Cut-points of 5, 10, and 15 represent mild, moderate, and severe levels of anxiety symptoms. Respondents indicate how difficult the symptoms make it for them to engage in daily activities from 0 (Not difficult at all) to 3 (Extremely difficult). The internal consistency of the GAD-7 is excellent (α = 0.92). Test-retest reliability is also good (Pearson r = 0.83) as is procedural validity (intraclass correlation = 0.83). The GAD-7 has excellent sensitivity and specificity to identify generalized anxiety disorder [41].
Health-Related Quality of Life
Participants completed the SF-36, which asks about the patient’s health status in the past week [14]. Eight subscales include physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional and mental health. Two summary measures, the Physical Component Summary and the Mental Component Summary, are calculated from 4 scales each. Use of the summary measures has been shown to increase the reliability of scores and improve the validity of scores in discriminating between physical and psychosocial outcomes [14]. Higher scores represent better HRQL, with a mean score of 50 (SD = 50) for the general population. Internal consistency estimates for the component summary scores are α > 0.89, item discriminant validity estimates are greater than 92.5% and 2-week test-retest reliability was excellent. Scores on the SF-36 have been divided into categories of HRQL functioning [42,43]. Participants in the impaired to very impaired category have scores ≤ mean – 1 SD while participants with average to above average functioning have scores > mean – 1 SD.
The SF-36 has been used extensively in observational and randomized studies for a range of illness conditions. In SCD, some aspects of HRQL as measured by the SF-36 improved for adult patients who responded to hydroxyurea [44]. Participants in the Pain in Sickle Cell Epidemiology Study scored lower than national norms on all SF-36 subscales except psychosocial functioning [45]. HRQL decreased significantly as daily pain intensity increased [45]. Further, women reported worse bodily pain compared with men [46].
Data Analyses
All biostatistical analyses were conducted using Stata 13 [47]. Continuous variables were examined for normality with measures of skewness and peakedness. All variables satisfied the assumptions of normality with the exception of barriers to health care and ED utilization. The variable barriers to health care was transformed using a square root transformation, resulting in a more normally distributed variable. ED utilization was dichotomized as 0–2 versus 3 or more ED visits in the previous 12 months, based on the distribution of utilization in the sample. The cutpoint of ≥ 3 annual ED visits is consistent with other literature on SCD clinical severity [48].
Descriptive statistics were computed to include means, standard deviations and frequencies. Sociodemographic variables (age, sex, insurance status [public or private] and income) were examined as potential covariates using Pearson correlations and t tests. Associations among emotional distress (anxiety and depression symptoms), clinical complications and ED utilization, barriers to health care, and the outcomes of the Physical and Mental Component Summary scores from the SF-36 were examined using Pearson correlations. We conducted stepwise regression with forward selection to determine models predictive of physical and mental HRQL. We tested the addition of each chosen variable (anxiety symptoms, depression symptoms, clinical complications, ED utilization, barriers to health care, age, sex, insurance status, and income), adding the variables (if any) that were most correlated with the outcome, and repeated the process until the model was not improved. A significance level of 0.05 was used for all statistical tests.
Results
Demographic and Clinical Characteristics
The majority of patients (73%) were diagnosed with Hgb SS disease and the most common lifetime complication was pain, reported by almost all of participants (Table 1). The next most common complication was fever, followed by acute chest syndrome. Twenty-seven percent of participants were currently on the disease-modifying therapy hydroxyurea, while 61% had a lifetime history of transfusion therapy. These data were verified with information from the clinical database for 73 participants (95%).
The median number of ED visits in the previous year was 1 (range, 0–50), with 19 patients (25%) with zero visits. The median number of hospital days in the previous year was 13 (range, 0–81). Twenty-nine patients (38%) had no hospital days in the previous year. These data were verified with information from the clinical database for 53 participants (69%), since hospital and ED visits occurred at institutions not always linked with the clinical databases at the sponsoring hospitals.
Emotional Distress, Barriers to Care, and Health-Related Quality of Life
The mean score on the GAD-7 was 7.9 (SD = 6.0, α = 0.90, Table 2). The prevalence of moderate to severe symptoms of anxiety (scores ≥ 10) was 36.4% (n = 28). Fourteen patients with moderate to severe symptoms (50%) reported that anxiety symptoms created some difficulty in work, daily activities, or relationships. Twelve patients (43%) reported that symptoms created very much to extreme difficulty in work, daily activities, or relationships. Fifteen patients (29%) with moderate to severe symptoms of anxiety or depression exhibited comorbid anxiety and depression.
The mean Physical Component Summary score on the SF-36 was 53.6 (SD = 24.1, α = 0.94, Table 2). The prevalence of impaired to very impaired HRQL in the physical domain was 17% (n = 13). The mean Mental Component Summary score on the SF-36 for the sample was 50.1 (SD = 23.7, α = 0.93), with a prevalence of 16% (n = 12) in the impaired to very impaired range for HRQL in the mental domain.
The mean number of barriers from the barriers checklist was 9.2 (SD = 10.1) out of 53 possible. Sixty-five participants (86%) reported at least 1 barrier to accessing health care (Table 2). The most frequently cited barriers to care were provider knowledge and attitudes, followed by transportation, insurance, and access to services (eg, hours and location of services). Less frequently cited barriers to care were individual barriers, including memory, health literacy and motivation, as well as those related to SCD itself, ie, fatigue and pain.
Sociodemographic Variables, Emotional Distress, and Health-Related Quality of Life
Symptoms of anxiety and depression were highly correlated with one another, as would be expected (r = 0.75, P < 0.001). Physical and mental HRQL were significantly correlated with symptoms of depression (r = –0.67, P < 0.001 for physical HRQL component and r = –0.70 for mental HRQL component, P < 0.001), with impaired HRQL in both domains correlated with greater symptoms of depression. Physical and Mental Component Summary scores were significantly correlated with symptoms of anxiety (r = –0.58, P < 0.001 for the physical component and r = –0.62 for the mental component, P < 0.001), with impaired HRQL in both domains correlated with greater symptoms of anxiety. Ratings of difficulty with daily functioning from depressive symptoms were correlated with impaired HRQL in the physical (r = –0.46, P < 0.01) and mental domains (r = –0.52, P < 0.001). Ratings of difficulty with daily functioning from anxiety symptoms were also correlated with impaired HRQL in the physical (r = –0.58, P < 0.001) and mental domains (r = –0.63, P < 0.001). Reports of more barriers to health care were significantly correlated with reports of more depressive and anxiety symptoms (r = 0.53, P < 0.001 and r = 0.48, P < 0.001), with lower Mental Component Summary scores (r = –0.43, P < 0.05), and with more ED visits in the past year (r = 0.43, P < 0.05).
Relations Between Independent Variables and Outcomes
Discussion
Results of this study showed that as expected, symptoms of depression were independently associated with the mental component of HRQL, controlling for other variables. Symptoms of depression were also independently associated with the physical component of HRQL. The effect size for both models was moderate but comparable to effect sizes of other studies of predictive models of physical and mental HRQL in SCD [49]. Our findings were consistent with previous literature, with older age and increased ED utilization independently associated with lower ratings of physical HRQL, with sex and anxiety symptoms entering into the predictive model [15–18,44,45]. Contrary to our hypotheses, barriers to accessing health care were not independently associated with physical or mental HRQL but did contribute to the model for mental HRQL, as did clinical complications and private insurance status.
While our sample was similar to previous samples in mean age and percentage of women participants, our patients reported significantly higher physical HRQL scores, and a wider range of HRQL scores (eg, 53.6,
SD = 24.1 compared with 39.6, SD = 10.0 [16]). The mean Physical Component Summary score was in fact similar to the general population mean of 50. This may reflect improvements in quality of care and subsequent overall improved patient health and HRQL given that these data were collected in year 2 of the HRSA SCDTDP. As an SCDTDP grantee, we implemented goals to improve coordination of service delivery and to increase access to care. However, it should also be considered that there was a selection bias in our study, in favor of those with better HRQL. Nevertheless, as already noted, our findings are consistent with previous literature with regard to inter-relations between variables, ie, associations between lower physical HRQL ratings and symptoms of depression, older age, and increased ED utilization [15]. Future studies in SCD that directly evaluate reported access to a medical home in relation to HRQL are needed to assess the impact of access to care and care coordination on HRQL ratings.
Our use of a data collection tool that focused on lifetime rather than acute history of complications may have contributed to our failure to find a relation between clinical manifestations and physical HRQL. Further, we were not able to assess the effects of pain separately from other complications, since almost every participant reported a lifetime history of pain. However, our findings were consistent with those of researchers who have found psychosocial and sociodemographic factors, versus clinical manifestations, to be major influences on both physical and mental HRQL for individuals with SCD and other chronic and life-threatening conditions [15, 16, 50]. Our confidence is increased in this finding, given that we were able to verify self-reports of clinical manifestations with our clinical database. Our results contribute to the developing body of knowledge that emphasizes the importance of understanding the broad impact on the lives of adults of living with SCD, not just the physical symptomatology.
There has been limited research on barriers to accessing health care as associated with HRQL for SCD populations. Health care barriers have been identified for ethnic minorities, even within patient-centered medical homes, with minority status moderating the effect of barriers to care on HRQL [30]. Our findings that barriers to health care were correlated with depression and anxiety symptoms, mental HRQL, and greater ED utilization support the need to view SCD care within a biobehavioral framework. Health care provider negative attitudes and lack of knowledge were the most frequently cited barriers for adults in our study, particularly in the context of ED and inpatient care. These findings are similar to other studies that have highlighted the impact of these provider variables on quality of care [26,51]. We were not able to separate out effects of ethnic minority status, given that our patients were predominantly African American.
Contributors to poor HRQL that have been identified in SCD are poverty [42] and public insurance status [49]. While over half of our participants had family incomes of less than $30,000, despite a mean household size of 3 members, we did not find that income contributed to either of our models predicting physical or mental HRQL. Over half of our patients were well educated, which could have moderated the effect of their low incomes, but we did not measure other potential moderators such as active coping and supportive relationships [19]. These analyses were beyond the scope of our existing database, but future studies are needed on such resilience factors and processes. Our adults were predominantly on public insurance and we did find that private insurance status was positively associated with higher ratings of mental HRQL, consistent with other SCD research [49]. Taken together, our findings underscore the importance of considering the interplay between emotional distress, sociodemographic and clinical factors and quality of care in order to address risk factors for poor patient-reported outcomes [52,53].
There have not been previous reports of symptoms of emotional distress in SCD using the PHQ-9 and GAD-7, but both measures have been used widely for depression and anxiety screening, including with African-American populations. We selected these over other measures for their brevity, free availability, and psychometric properties. Our prevalence of moderate to severe depression and anxiety symptoms in the present study was similar to what has been found using other tools [2–8]. The PHQ-9 and GAD-7 also provide ratings of symptom interference on daily functioning, and we found that these ratings were associated with impaired physical and mental HRQL. Given that there generally are limited mental health resources in the communities where individuals with SCD reside and are treated, ratings of emotional distress and HRQL can be taken together to stratify those patients with the most immediate need for interventions. Further, screening can be used for early detection with the goal to intervene and prevent the progression of symptoms of emotional distress to long-term, disabling mental health disorders [54]. There is a need for innovative and cost-effective strategies for assessment and treatment of mental health symptoms and disorders for patients with SCD. One model for evidence-based practice in the management of emotional distress for patients with in SCD is the collaborative care model.
The collaborative care model integrates physical and mental health care in the patient-centered medical home and focuses on treating the whole person and family [55]. In this model, a care management staff (eg, nurse, social worker, psychologist) is integrated with the primary care team. The care management staff, in consultation with a psychiatrist, provides evidence-based care coordination, brief behavioral interventions, and support for other treatments, including medications. The effectiveness of collaborative care programs has been demonstrated for ethnic minority and safety net populations such as the SCD population, which is disproportionately low-income and on public insurance [56, 57]. Future research with SCD populations should investigate such interventions as the collaborative care model that addresses both emotional distress and barriers to care.
Limitations
Our results need to be interpreted with caution given the small sample size and the potential bias introduced by non-random sampling. In addition, as our patients are from an urban setting, findings might not generalize to rural populations. This study was cross sectional so no inferences can be made with regard to causality and temporal relations between anxiety symptoms, barriers to care, and HRQL. Our strategy for measuring total clinical complications and barriers to care conserved power but it was not possible to evaluate if specific complications or barriers may have exerted a greater impact on HRQL compared with others. Similarly, other studies have examined specific domains of HRQL, while we limited our analysis to the Physical and Mental Component Summary scores. The utilization questionnaire was designed to assess only lifetime complications, not complications more proximal to the HRQL ratings.
Patient-reported outcomes, now widely accepted as outcome measures, elicit patients’ descriptions of the impact of their condition on their day-to-day lives [34, 58–60]. However, measures of mental health symptoms and HRQL may be subject to recall bias, measurement error, and confounding [61,62]. Nevertheless, a range of studies support the idea that mental health symptoms and HRQL are distinct constructs, and that patients with physical and mental health symptoms are vulnerable to lower ratings of HRQL [63,64]. Disease-modifying therapies such as hydroxyurea can contribute to improved ratings of HRQL [44,65], but we were not able to evaluate the contribution of hydroxyurea to HRQL as it appears to have been underutilized in our sample.
Conclusion
We evaluated emotional distress and other variables in the context of a biobehavioral model of HRQL outcomes for adults with SCD. Integrating the patient's perspective of the impact of the disease and its treatment with assessment of clinical indications is critical to implementing and evaluating effective therapies [25]. However, there are conceptual challenges in determining what actually contributes to HRQL from the patient’s perspective in the context of genetic disorders such as SCD [50]. Our findings highlight the importance of incorporating comprehensive psychosocial screening in order to support optimal HRQL in SCD. Providers may be reluctant to include such screening if, as is often the case, mental health services are difficult to access. Models such as the collaborative care model, which include mental health interventions within the sickle cell center or primary care provider’s office, should be implented. Barriers to care and HRQL should also be routinely evaluated for patients with SCD. Use of disease-specific tools, such as the Adult Sickle Cell Quality of Life measurement system [66], may increase the specificity needed to detect differences within adults with SCD and improvements related to interventions, whether medical or psychosocial. Contributors to HRQL in SCD go beyond clinical manifestations to include psychological and social factors, as well as provider and health system variables. Research conducted within the framework of a comprehensive conceptual model of broad clinical and life effects associated with SCD can inform clinical applications that ultimately enhance HRQL for patients with SCD.
Acknowledgment: The authors wish to thank San Keller, PhD, for her helpful comments on a previous version of this manuscript.
Corresponding author: Marsha J. Treadwell, PhD, Hematology/Oncology Dept., UCSF Benioff Children’s Hospital Oakland, 747 52nd St., Oakland, CA 94609, [email protected].
Funding/support: This research was conducted as part of the National Initiative for Children’s Healthcare Quality (NICHQ) Working to Improve Sickle Cell Healthcare (WISCH) project. Further support came from a grant from the Health Resources and Services Administration (HRSA) Sickle Cell Disease Treatment Demonstration Project Grant No. U1EMC16492 and from the National Institutes of Health (NIH) Clinical and Translational Science Award UL1 RR024131. The views expressed in this publication do not necessarily reflect the views of WISCH, NICHQ, HRSA or NIH.
Financial disclosures: None.
Author contributions: conception and design, MJT; analysis and interpretation of data, MJT, GG; drafting of article, MJT, GG; critical revision of the article, MJT, KK, FB; statistical expertise, GG; obtaining of funding, MJT; administrative or technical support, KK, FB; collection and assembly of data, KK, FB.
Label changes report new side effects for hematology drugs

Credit: CDC
Several hematology drugs approved by the US Food and Drug Administration (FDA) have recently undergone label changes to reflect newly reported adverse events.
Changes have been made to the labels for the JAK1/2 inhibitor ruxolitinib (Jakafi), the anti-CD20 monoclonal antibody obinutuzumab (Gazyva), the factor Xa inhibitor rivaroxaban (Xarelto), and the hematopoietic stem cell mobilizer plerixafor (Mozobil).
Plerixafor
Plerixafor is FDA-approved for use in combination with granulocyte-colony stimulating factor to mobilize hematopoietic stem cells to the peripheral blood for collection and subsequent autologous transplantation in patients with non-Hodgkin lymphoma and multiple myeloma.
The product’s label was changed to include a new entry under the “Adverse Reactions” heading. Postmarketing experience suggested the drug may cause abnormal dreams and nightmares.
Rivaroxaban
Rivaroxaban is a factor Xa inhibitor that’s FDA-approved to reduce the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation, for the treatment of deep vein thrombosis (DVT) and pulmonary embolism (PE), to reduce the risk of recurrent DVT and PE, and to prevent DVT, which may lead to PE, in patients undergoing knee or hip replacement surgery.
Postmarketing experience has led to two changes to the “Adverse Reactions” section of rivaroxaban’s label. Thrombocytopenia has been added as an adverse reaction, and the term “cytolytic hepatitis” has been replaced with “hepatitis (including hepatocellular injury).”
Obinutuzumab
Obinutuzumab is a CD20-directed cytolytic antibody that is FDA-approved in combination with chlorambucil to treat patients with previously untreated chronic lymphocytic leukemia.
The “Warnings and Precautions” section of obinutuzumab’s label has been changed to reflect that fatal infections have been reported in patients who received the drug.
The label has also been changed to coincide with changes in trial data. The label now states that obinutuzumab caused grade 3 or 4 neutropenia in 33% of patients and grade 3 or 4 thrombocytopenia in 10% of patients.
Ruxolitinib
Ruxolitinib is a JAK1/JAK2 inhibitor that’s FDA-approved to treat patients with polycythemia vera (PV) who cannot tolerate or don’t respond to hydroxyurea, as well as patients with intermediate or high-risk myelofibrosis.
Ruxolitinib’s label now includes a warning that symptoms of myeloproliferative neoplasms may return about a week after discontinuing treatment. The label also advises healthcare professionals to discourage patients form interrupting or discontinuing ruxolitinib without consulting their physician.
In addition, a warning about the risk of non-melanoma skin cancer associated with ruxolitinib, as well as advice for informing patients of this risk, have been added to ruxolitinib’s label.
The label has undergone significant changes in sections 6.1, “Clinical Trials Experience in Myelofibrosis” and 6.2 “Clinical Trial Experience in Polycythemia Vera.” It now includes additional information on the risk of thrombocytopenia, anemia, and neutropenia.
Under the “Special Populations” heading, recommendations were added to reduce the drug’s dose in patients with PV and moderate or severe renal impairment, as well as PV patients with hepatic impairment. ![]()

Credit: CDC
Several hematology drugs approved by the US Food and Drug Administration (FDA) have recently undergone label changes to reflect newly reported adverse events.
Changes have been made to the labels for the JAK1/2 inhibitor ruxolitinib (Jakafi), the anti-CD20 monoclonal antibody obinutuzumab (Gazyva), the factor Xa inhibitor rivaroxaban (Xarelto), and the hematopoietic stem cell mobilizer plerixafor (Mozobil).
Plerixafor
Plerixafor is FDA-approved for use in combination with granulocyte-colony stimulating factor to mobilize hematopoietic stem cells to the peripheral blood for collection and subsequent autologous transplantation in patients with non-Hodgkin lymphoma and multiple myeloma.
The product’s label was changed to include a new entry under the “Adverse Reactions” heading. Postmarketing experience suggested the drug may cause abnormal dreams and nightmares.
Rivaroxaban
Rivaroxaban is a factor Xa inhibitor that’s FDA-approved to reduce the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation, for the treatment of deep vein thrombosis (DVT) and pulmonary embolism (PE), to reduce the risk of recurrent DVT and PE, and to prevent DVT, which may lead to PE, in patients undergoing knee or hip replacement surgery.
Postmarketing experience has led to two changes to the “Adverse Reactions” section of rivaroxaban’s label. Thrombocytopenia has been added as an adverse reaction, and the term “cytolytic hepatitis” has been replaced with “hepatitis (including hepatocellular injury).”
Obinutuzumab
Obinutuzumab is a CD20-directed cytolytic antibody that is FDA-approved in combination with chlorambucil to treat patients with previously untreated chronic lymphocytic leukemia.
The “Warnings and Precautions” section of obinutuzumab’s label has been changed to reflect that fatal infections have been reported in patients who received the drug.
The label has also been changed to coincide with changes in trial data. The label now states that obinutuzumab caused grade 3 or 4 neutropenia in 33% of patients and grade 3 or 4 thrombocytopenia in 10% of patients.
Ruxolitinib
Ruxolitinib is a JAK1/JAK2 inhibitor that’s FDA-approved to treat patients with polycythemia vera (PV) who cannot tolerate or don’t respond to hydroxyurea, as well as patients with intermediate or high-risk myelofibrosis.
Ruxolitinib’s label now includes a warning that symptoms of myeloproliferative neoplasms may return about a week after discontinuing treatment. The label also advises healthcare professionals to discourage patients form interrupting or discontinuing ruxolitinib without consulting their physician.
In addition, a warning about the risk of non-melanoma skin cancer associated with ruxolitinib, as well as advice for informing patients of this risk, have been added to ruxolitinib’s label.
The label has undergone significant changes in sections 6.1, “Clinical Trials Experience in Myelofibrosis” and 6.2 “Clinical Trial Experience in Polycythemia Vera.” It now includes additional information on the risk of thrombocytopenia, anemia, and neutropenia.
Under the “Special Populations” heading, recommendations were added to reduce the drug’s dose in patients with PV and moderate or severe renal impairment, as well as PV patients with hepatic impairment. ![]()

Credit: CDC
Several hematology drugs approved by the US Food and Drug Administration (FDA) have recently undergone label changes to reflect newly reported adverse events.
Changes have been made to the labels for the JAK1/2 inhibitor ruxolitinib (Jakafi), the anti-CD20 monoclonal antibody obinutuzumab (Gazyva), the factor Xa inhibitor rivaroxaban (Xarelto), and the hematopoietic stem cell mobilizer plerixafor (Mozobil).
Plerixafor
Plerixafor is FDA-approved for use in combination with granulocyte-colony stimulating factor to mobilize hematopoietic stem cells to the peripheral blood for collection and subsequent autologous transplantation in patients with non-Hodgkin lymphoma and multiple myeloma.
The product’s label was changed to include a new entry under the “Adverse Reactions” heading. Postmarketing experience suggested the drug may cause abnormal dreams and nightmares.
Rivaroxaban
Rivaroxaban is a factor Xa inhibitor that’s FDA-approved to reduce the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation, for the treatment of deep vein thrombosis (DVT) and pulmonary embolism (PE), to reduce the risk of recurrent DVT and PE, and to prevent DVT, which may lead to PE, in patients undergoing knee or hip replacement surgery.
Postmarketing experience has led to two changes to the “Adverse Reactions” section of rivaroxaban’s label. Thrombocytopenia has been added as an adverse reaction, and the term “cytolytic hepatitis” has been replaced with “hepatitis (including hepatocellular injury).”
Obinutuzumab
Obinutuzumab is a CD20-directed cytolytic antibody that is FDA-approved in combination with chlorambucil to treat patients with previously untreated chronic lymphocytic leukemia.
The “Warnings and Precautions” section of obinutuzumab’s label has been changed to reflect that fatal infections have been reported in patients who received the drug.
The label has also been changed to coincide with changes in trial data. The label now states that obinutuzumab caused grade 3 or 4 neutropenia in 33% of patients and grade 3 or 4 thrombocytopenia in 10% of patients.
Ruxolitinib
Ruxolitinib is a JAK1/JAK2 inhibitor that’s FDA-approved to treat patients with polycythemia vera (PV) who cannot tolerate or don’t respond to hydroxyurea, as well as patients with intermediate or high-risk myelofibrosis.
Ruxolitinib’s label now includes a warning that symptoms of myeloproliferative neoplasms may return about a week after discontinuing treatment. The label also advises healthcare professionals to discourage patients form interrupting or discontinuing ruxolitinib without consulting their physician.
In addition, a warning about the risk of non-melanoma skin cancer associated with ruxolitinib, as well as advice for informing patients of this risk, have been added to ruxolitinib’s label.
The label has undergone significant changes in sections 6.1, “Clinical Trials Experience in Myelofibrosis” and 6.2 “Clinical Trial Experience in Polycythemia Vera.” It now includes additional information on the risk of thrombocytopenia, anemia, and neutropenia.
Under the “Special Populations” heading, recommendations were added to reduce the drug’s dose in patients with PV and moderate or severe renal impairment, as well as PV patients with hepatic impairment. ![]()
Psoriasis treatment recommendations address four clinical scenarios
New guidelines on nail psoriasis address four clinical manifestations of the disease. The recommendations by the Medical Board of the National Psoriasis Foundation appeared as a consensus statement in the January issue of JAMA Dermatology.
Limitations in clinical trial data make comparing treatments difficult, noted lead author Dr. Jeffrey J. Crowley of Bakersfield (Calif.) Dermatology and his associates. “There are limited data to evaluate or support the use of combination therapy in nail psoriasis. Thus, treatment options recommended in this review are monotherapy,” the guidelines authors added (JAMA Dermatol. 2015;151:87-94).
To develop the guidelines, the research team searched PubMed for articles on nail psoriasis dating from Jan. 1, 1947 through May 11, 2014. They evaluated these studies for level of evidence based on recommendations for writing guidelines from Dr. Paul G. Shekelle of the VA West Los Angeles Medical Center and his associates (BMJ 1999;318:593-6).
They also polled the Medical Board of the National Psoriasis Foundation regarding their treatment approach for four clinical presentations of nail psoriasis:
• For treatment-naive patients with psoriasis of the nails only (affecting at least 3 of 10 fingernails), the board recommended initial treatment with high-potency topical corticosteroids (with or without calcipotriol), with intralesional corticosteroids as a secondary option. Intralesional corticosteroids have been used for decades, but clinical data supporting their use are “extremely limited,” the guidelines state.
• For extensive nail psoriasis (affecting at least five fingernails and causing moderate to severe pain) that has failed topical treatment, the board recommended adalimumab most enthusiastically, followed by etanercept, intralesional corticosteroids, ustekinumab, methotrexate sodium, and acitretin in decreasing order.
• For concurrent skin and nail disease without joint involvement (defined as skin disease on at least 8% of the body surface and moderately to severely painful dystrophy of at least 5 of 10 nails), the board strongly recommended adalimumab, etanercept, and ustekinumab, and also recommended methotrexate, acitretin, infliximab, and apremilast.
• For concurrent nail, skin, and joint involvement (defined as skin disease on 8% of the body surface, a history of dactylitis and morning stiffness (psoriatic arthritis), and severe, painful involvement of at least 5 of 10 nails), the board most strongly recommended adalimumab, followed by etanercept, ustekinumab, infliximab, methotrexate, apremilast, and golimumab.
Because nails grow slowly, psoriatic joint and skin disease often improve before nail psoriasis does, the authors noted. “Few studies show any significant improvement before 12 weeks, and several studies with etanercept, infliximab, and ustekinumab demonstrate continued improvement beyond 6 months,” they wrote.
About half of patients with psoriasis have some amount of nail involvement, and about 70% of patients with psoriatic arthritis have nail disease, according to the literature review. Dermatophyte infections can further complicate treatment of nail psoriasis, and immunosuppressive therapies can lead to onychomycosis in patients whose psoriasis includes the toenails, the authors added.
Dr. Crowley reported speaker and consulting honoraria from AbbVie, Abbott, and Amgen, and research funding from Abbott, AbbVie, Amgen, AstraZeneca, Celgene, Eli Lilly, Janssen Pharmaceutica, Merck, Pfizer, and Regeneron Pharmaceuticals. Four coauthors reported advisory, consulting, or financial relationships with Amgen, Abbott, Janssen Biotech Inc., Celgene, Novartis International AG, Abbvie, Merck, Celgene, Leo Pharma, Eli Lilly, Pfizer, and the National Psoriasis Foundation.
New guidelines on nail psoriasis address four clinical manifestations of the disease. The recommendations by the Medical Board of the National Psoriasis Foundation appeared as a consensus statement in the January issue of JAMA Dermatology.
Limitations in clinical trial data make comparing treatments difficult, noted lead author Dr. Jeffrey J. Crowley of Bakersfield (Calif.) Dermatology and his associates. “There are limited data to evaluate or support the use of combination therapy in nail psoriasis. Thus, treatment options recommended in this review are monotherapy,” the guidelines authors added (JAMA Dermatol. 2015;151:87-94).
To develop the guidelines, the research team searched PubMed for articles on nail psoriasis dating from Jan. 1, 1947 through May 11, 2014. They evaluated these studies for level of evidence based on recommendations for writing guidelines from Dr. Paul G. Shekelle of the VA West Los Angeles Medical Center and his associates (BMJ 1999;318:593-6).
They also polled the Medical Board of the National Psoriasis Foundation regarding their treatment approach for four clinical presentations of nail psoriasis:
• For treatment-naive patients with psoriasis of the nails only (affecting at least 3 of 10 fingernails), the board recommended initial treatment with high-potency topical corticosteroids (with or without calcipotriol), with intralesional corticosteroids as a secondary option. Intralesional corticosteroids have been used for decades, but clinical data supporting their use are “extremely limited,” the guidelines state.
• For extensive nail psoriasis (affecting at least five fingernails and causing moderate to severe pain) that has failed topical treatment, the board recommended adalimumab most enthusiastically, followed by etanercept, intralesional corticosteroids, ustekinumab, methotrexate sodium, and acitretin in decreasing order.
• For concurrent skin and nail disease without joint involvement (defined as skin disease on at least 8% of the body surface and moderately to severely painful dystrophy of at least 5 of 10 nails), the board strongly recommended adalimumab, etanercept, and ustekinumab, and also recommended methotrexate, acitretin, infliximab, and apremilast.
• For concurrent nail, skin, and joint involvement (defined as skin disease on 8% of the body surface, a history of dactylitis and morning stiffness (psoriatic arthritis), and severe, painful involvement of at least 5 of 10 nails), the board most strongly recommended adalimumab, followed by etanercept, ustekinumab, infliximab, methotrexate, apremilast, and golimumab.
Because nails grow slowly, psoriatic joint and skin disease often improve before nail psoriasis does, the authors noted. “Few studies show any significant improvement before 12 weeks, and several studies with etanercept, infliximab, and ustekinumab demonstrate continued improvement beyond 6 months,” they wrote.
About half of patients with psoriasis have some amount of nail involvement, and about 70% of patients with psoriatic arthritis have nail disease, according to the literature review. Dermatophyte infections can further complicate treatment of nail psoriasis, and immunosuppressive therapies can lead to onychomycosis in patients whose psoriasis includes the toenails, the authors added.
Dr. Crowley reported speaker and consulting honoraria from AbbVie, Abbott, and Amgen, and research funding from Abbott, AbbVie, Amgen, AstraZeneca, Celgene, Eli Lilly, Janssen Pharmaceutica, Merck, Pfizer, and Regeneron Pharmaceuticals. Four coauthors reported advisory, consulting, or financial relationships with Amgen, Abbott, Janssen Biotech Inc., Celgene, Novartis International AG, Abbvie, Merck, Celgene, Leo Pharma, Eli Lilly, Pfizer, and the National Psoriasis Foundation.
New guidelines on nail psoriasis address four clinical manifestations of the disease. The recommendations by the Medical Board of the National Psoriasis Foundation appeared as a consensus statement in the January issue of JAMA Dermatology.
Limitations in clinical trial data make comparing treatments difficult, noted lead author Dr. Jeffrey J. Crowley of Bakersfield (Calif.) Dermatology and his associates. “There are limited data to evaluate or support the use of combination therapy in nail psoriasis. Thus, treatment options recommended in this review are monotherapy,” the guidelines authors added (JAMA Dermatol. 2015;151:87-94).
To develop the guidelines, the research team searched PubMed for articles on nail psoriasis dating from Jan. 1, 1947 through May 11, 2014. They evaluated these studies for level of evidence based on recommendations for writing guidelines from Dr. Paul G. Shekelle of the VA West Los Angeles Medical Center and his associates (BMJ 1999;318:593-6).
They also polled the Medical Board of the National Psoriasis Foundation regarding their treatment approach for four clinical presentations of nail psoriasis:
• For treatment-naive patients with psoriasis of the nails only (affecting at least 3 of 10 fingernails), the board recommended initial treatment with high-potency topical corticosteroids (with or without calcipotriol), with intralesional corticosteroids as a secondary option. Intralesional corticosteroids have been used for decades, but clinical data supporting their use are “extremely limited,” the guidelines state.
• For extensive nail psoriasis (affecting at least five fingernails and causing moderate to severe pain) that has failed topical treatment, the board recommended adalimumab most enthusiastically, followed by etanercept, intralesional corticosteroids, ustekinumab, methotrexate sodium, and acitretin in decreasing order.
• For concurrent skin and nail disease without joint involvement (defined as skin disease on at least 8% of the body surface and moderately to severely painful dystrophy of at least 5 of 10 nails), the board strongly recommended adalimumab, etanercept, and ustekinumab, and also recommended methotrexate, acitretin, infliximab, and apremilast.
• For concurrent nail, skin, and joint involvement (defined as skin disease on 8% of the body surface, a history of dactylitis and morning stiffness (psoriatic arthritis), and severe, painful involvement of at least 5 of 10 nails), the board most strongly recommended adalimumab, followed by etanercept, ustekinumab, infliximab, methotrexate, apremilast, and golimumab.
Because nails grow slowly, psoriatic joint and skin disease often improve before nail psoriasis does, the authors noted. “Few studies show any significant improvement before 12 weeks, and several studies with etanercept, infliximab, and ustekinumab demonstrate continued improvement beyond 6 months,” they wrote.
About half of patients with psoriasis have some amount of nail involvement, and about 70% of patients with psoriatic arthritis have nail disease, according to the literature review. Dermatophyte infections can further complicate treatment of nail psoriasis, and immunosuppressive therapies can lead to onychomycosis in patients whose psoriasis includes the toenails, the authors added.
Dr. Crowley reported speaker and consulting honoraria from AbbVie, Abbott, and Amgen, and research funding from Abbott, AbbVie, Amgen, AstraZeneca, Celgene, Eli Lilly, Janssen Pharmaceutica, Merck, Pfizer, and Regeneron Pharmaceuticals. Four coauthors reported advisory, consulting, or financial relationships with Amgen, Abbott, Janssen Biotech Inc., Celgene, Novartis International AG, Abbvie, Merck, Celgene, Leo Pharma, Eli Lilly, Pfizer, and the National Psoriasis Foundation.
FROM JAMA DERMATOLOGY
Promising new therapy for critical limb ischemia
CHICAGO – A single set of intramuscular injections of stromal cell–derived factor-1 in patients with critical limb ischemia showed safety as well as evidence of efficacy through 12 months of follow-up in the STOP-CLI trial.
“Patients treated with JVS-100 demonstrated dose-dependent improvement across multiple patient-centered outcomes, including pain, quality of life, and wound healing, with less change in macrovascular objective measures in this small study,” Dr. Melina R. Kibbe reported at the American Heart Association scientific sessions. JVS-100 is a nonviral plasmid encoding human stromal cell–derived factor-1 (SDF-1), a natural chemokine protein that promotes angiogenesis by recruiting endothelial progenitor cells from the bone marrow to ischemic sites, explained Dr. Kibbe, professor and vice chair of surgical research and deputy director of the Simpson Querrey Institute for BioNanotechnology at Northwestern University, Chicago.
STOP-CLI was an exploratory, phase IIa, double-blind, first-in-humans study involving 48 patients with Rutherford classification 4 or 5 critical climb ischemia (CLI). All had an ankle-brachial index of 0.4 or lower, an ankle systolic blood pressure of 70 mm Hg or less or a toe systolic blood pressure of 50 or less, and were poor candidates for surgical revascularization. None had Buerger’s disease.
Participants were randomized to one of four study arms, and within each study arm further randomized 3:1 to stromal cell–derived factor-1 (SDF-1) or placebo injections. The patients received either 8 or 16 injections, each containing either 0.5 or 1.0 mg of SDF-1 or placebo. The injections, given in a single session, were placed at least 0.5 cm apart throughout the ischemic area of the affected limb.
By chance, most patients randomized to the placebo group were Rutherford 4, a category of CLI defined by rest pain, while the majority in the active treatment arms were Rutherford 5, a more severe disease manifestation characterized by ulcers. As a consequence, the SDF-1 recipients also had far larger nonhealing wounds, with an average area of 6.4 cm2, compared with 1.5 cm2, in controls.
The SDF-1 injections proved safe and were well tolerated, with no treatment-related serious adverse events and no safety signals evident in the laboratory results.
Turning to efficacy endpoints, Dr. Kibbe said self-rated visual analog scale pain scores showed clear, dose-dependent improvement over time in the SDF-1 treatment cohorts and no change in controls.
Similarly, the active treatment groups showed improved quality of life scores on all domains of the Short Form-36: physical functioning, bodily pain, general health, social functioning, energy/fatigue, emotional well-being, and overall physical and mental health, the surgeon continued.
Wound area decreased significantly in the SDF-1-treated groups, with the biggest reduction – more than 8 cm2 – being noted in the three patients who received eight 1-mg injections. That was also the group with the largest wounds at baseline, with an average area of 11.4 cm2.
Of note, the major limb amputation rate was “remarkably low” for patients with such severe CLI, according to Dr. Kibbe. The rate was less than 10% over the course of 12 months, with one patient in each of the four active treatment arms having a major amputation at time intervals of 58-112 days post injection. No major limb amputations occurred in the control group.
There was a hint of improvement with SDF-1 therapy over placebo in ankle-brachial index and transcutaneous oxygen pressure, but the between-group differences were too narrow in this study to allow for any conclusions. That must await planned much larger phase III trials, according to Dr. Kibbe.
Audience members, citing the numerous failures of once-promising stem cell therapies for CLI at phase III testing over the last 10-15 years, wondered why Dr. Kibbe thinks SDF-1 will fare any better.
“This is much debated and discussed among all the people involved in these kinds of trials,” she replied. “I’d say, briefly, that a lot of it has to do with patient selection. I think when you have a mixed bag of patients in a trial, including patients with Buerger’s disease, treated in multiple different countries, using different definitions of when to amputate, all those things come into play and could account for why those phase III trials were not successful.”
“Having been involved in lots of the different gene- and cell-based therapy trials, I think one of the unique benefits of this therapy is that it kind of bridges between the two. SDF-1 basically homes your endothelial progenitor cells to the site of ischemic injury for enhanced vasculogenesis. But SDF-1 also has direct effects on endothelial cells, including stimulating proliferation and preventing apoptosis,” she added.
JVS-100 has also successfully completed a phase II clinical trial for the treatment of heart failure. In addition, the agent is being developed as a treatment for acute MI, chronic angina, and for muscle regeneration.
The STOP-CLI study was sponsored by Juventas Therapeutics. Dr. Kibbe reported serving as a consultant to Johnson & Johnson/Cordis and Pluristem.
CHICAGO – A single set of intramuscular injections of stromal cell–derived factor-1 in patients with critical limb ischemia showed safety as well as evidence of efficacy through 12 months of follow-up in the STOP-CLI trial.
“Patients treated with JVS-100 demonstrated dose-dependent improvement across multiple patient-centered outcomes, including pain, quality of life, and wound healing, with less change in macrovascular objective measures in this small study,” Dr. Melina R. Kibbe reported at the American Heart Association scientific sessions. JVS-100 is a nonviral plasmid encoding human stromal cell–derived factor-1 (SDF-1), a natural chemokine protein that promotes angiogenesis by recruiting endothelial progenitor cells from the bone marrow to ischemic sites, explained Dr. Kibbe, professor and vice chair of surgical research and deputy director of the Simpson Querrey Institute for BioNanotechnology at Northwestern University, Chicago.
STOP-CLI was an exploratory, phase IIa, double-blind, first-in-humans study involving 48 patients with Rutherford classification 4 or 5 critical climb ischemia (CLI). All had an ankle-brachial index of 0.4 or lower, an ankle systolic blood pressure of 70 mm Hg or less or a toe systolic blood pressure of 50 or less, and were poor candidates for surgical revascularization. None had Buerger’s disease.
Participants were randomized to one of four study arms, and within each study arm further randomized 3:1 to stromal cell–derived factor-1 (SDF-1) or placebo injections. The patients received either 8 or 16 injections, each containing either 0.5 or 1.0 mg of SDF-1 or placebo. The injections, given in a single session, were placed at least 0.5 cm apart throughout the ischemic area of the affected limb.
By chance, most patients randomized to the placebo group were Rutherford 4, a category of CLI defined by rest pain, while the majority in the active treatment arms were Rutherford 5, a more severe disease manifestation characterized by ulcers. As a consequence, the SDF-1 recipients also had far larger nonhealing wounds, with an average area of 6.4 cm2, compared with 1.5 cm2, in controls.
The SDF-1 injections proved safe and were well tolerated, with no treatment-related serious adverse events and no safety signals evident in the laboratory results.
Turning to efficacy endpoints, Dr. Kibbe said self-rated visual analog scale pain scores showed clear, dose-dependent improvement over time in the SDF-1 treatment cohorts and no change in controls.
Similarly, the active treatment groups showed improved quality of life scores on all domains of the Short Form-36: physical functioning, bodily pain, general health, social functioning, energy/fatigue, emotional well-being, and overall physical and mental health, the surgeon continued.
Wound area decreased significantly in the SDF-1-treated groups, with the biggest reduction – more than 8 cm2 – being noted in the three patients who received eight 1-mg injections. That was also the group with the largest wounds at baseline, with an average area of 11.4 cm2.
Of note, the major limb amputation rate was “remarkably low” for patients with such severe CLI, according to Dr. Kibbe. The rate was less than 10% over the course of 12 months, with one patient in each of the four active treatment arms having a major amputation at time intervals of 58-112 days post injection. No major limb amputations occurred in the control group.
There was a hint of improvement with SDF-1 therapy over placebo in ankle-brachial index and transcutaneous oxygen pressure, but the between-group differences were too narrow in this study to allow for any conclusions. That must await planned much larger phase III trials, according to Dr. Kibbe.
Audience members, citing the numerous failures of once-promising stem cell therapies for CLI at phase III testing over the last 10-15 years, wondered why Dr. Kibbe thinks SDF-1 will fare any better.
“This is much debated and discussed among all the people involved in these kinds of trials,” she replied. “I’d say, briefly, that a lot of it has to do with patient selection. I think when you have a mixed bag of patients in a trial, including patients with Buerger’s disease, treated in multiple different countries, using different definitions of when to amputate, all those things come into play and could account for why those phase III trials were not successful.”
“Having been involved in lots of the different gene- and cell-based therapy trials, I think one of the unique benefits of this therapy is that it kind of bridges between the two. SDF-1 basically homes your endothelial progenitor cells to the site of ischemic injury for enhanced vasculogenesis. But SDF-1 also has direct effects on endothelial cells, including stimulating proliferation and preventing apoptosis,” she added.
JVS-100 has also successfully completed a phase II clinical trial for the treatment of heart failure. In addition, the agent is being developed as a treatment for acute MI, chronic angina, and for muscle regeneration.
The STOP-CLI study was sponsored by Juventas Therapeutics. Dr. Kibbe reported serving as a consultant to Johnson & Johnson/Cordis and Pluristem.
CHICAGO – A single set of intramuscular injections of stromal cell–derived factor-1 in patients with critical limb ischemia showed safety as well as evidence of efficacy through 12 months of follow-up in the STOP-CLI trial.
“Patients treated with JVS-100 demonstrated dose-dependent improvement across multiple patient-centered outcomes, including pain, quality of life, and wound healing, with less change in macrovascular objective measures in this small study,” Dr. Melina R. Kibbe reported at the American Heart Association scientific sessions. JVS-100 is a nonviral plasmid encoding human stromal cell–derived factor-1 (SDF-1), a natural chemokine protein that promotes angiogenesis by recruiting endothelial progenitor cells from the bone marrow to ischemic sites, explained Dr. Kibbe, professor and vice chair of surgical research and deputy director of the Simpson Querrey Institute for BioNanotechnology at Northwestern University, Chicago.
STOP-CLI was an exploratory, phase IIa, double-blind, first-in-humans study involving 48 patients with Rutherford classification 4 or 5 critical climb ischemia (CLI). All had an ankle-brachial index of 0.4 or lower, an ankle systolic blood pressure of 70 mm Hg or less or a toe systolic blood pressure of 50 or less, and were poor candidates for surgical revascularization. None had Buerger’s disease.
Participants were randomized to one of four study arms, and within each study arm further randomized 3:1 to stromal cell–derived factor-1 (SDF-1) or placebo injections. The patients received either 8 or 16 injections, each containing either 0.5 or 1.0 mg of SDF-1 or placebo. The injections, given in a single session, were placed at least 0.5 cm apart throughout the ischemic area of the affected limb.
By chance, most patients randomized to the placebo group were Rutherford 4, a category of CLI defined by rest pain, while the majority in the active treatment arms were Rutherford 5, a more severe disease manifestation characterized by ulcers. As a consequence, the SDF-1 recipients also had far larger nonhealing wounds, with an average area of 6.4 cm2, compared with 1.5 cm2, in controls.
The SDF-1 injections proved safe and were well tolerated, with no treatment-related serious adverse events and no safety signals evident in the laboratory results.
Turning to efficacy endpoints, Dr. Kibbe said self-rated visual analog scale pain scores showed clear, dose-dependent improvement over time in the SDF-1 treatment cohorts and no change in controls.
Similarly, the active treatment groups showed improved quality of life scores on all domains of the Short Form-36: physical functioning, bodily pain, general health, social functioning, energy/fatigue, emotional well-being, and overall physical and mental health, the surgeon continued.
Wound area decreased significantly in the SDF-1-treated groups, with the biggest reduction – more than 8 cm2 – being noted in the three patients who received eight 1-mg injections. That was also the group with the largest wounds at baseline, with an average area of 11.4 cm2.
Of note, the major limb amputation rate was “remarkably low” for patients with such severe CLI, according to Dr. Kibbe. The rate was less than 10% over the course of 12 months, with one patient in each of the four active treatment arms having a major amputation at time intervals of 58-112 days post injection. No major limb amputations occurred in the control group.
There was a hint of improvement with SDF-1 therapy over placebo in ankle-brachial index and transcutaneous oxygen pressure, but the between-group differences were too narrow in this study to allow for any conclusions. That must await planned much larger phase III trials, according to Dr. Kibbe.
Audience members, citing the numerous failures of once-promising stem cell therapies for CLI at phase III testing over the last 10-15 years, wondered why Dr. Kibbe thinks SDF-1 will fare any better.
“This is much debated and discussed among all the people involved in these kinds of trials,” she replied. “I’d say, briefly, that a lot of it has to do with patient selection. I think when you have a mixed bag of patients in a trial, including patients with Buerger’s disease, treated in multiple different countries, using different definitions of when to amputate, all those things come into play and could account for why those phase III trials were not successful.”
“Having been involved in lots of the different gene- and cell-based therapy trials, I think one of the unique benefits of this therapy is that it kind of bridges between the two. SDF-1 basically homes your endothelial progenitor cells to the site of ischemic injury for enhanced vasculogenesis. But SDF-1 also has direct effects on endothelial cells, including stimulating proliferation and preventing apoptosis,” she added.
JVS-100 has also successfully completed a phase II clinical trial for the treatment of heart failure. In addition, the agent is being developed as a treatment for acute MI, chronic angina, and for muscle regeneration.
The STOP-CLI study was sponsored by Juventas Therapeutics. Dr. Kibbe reported serving as a consultant to Johnson & Johnson/Cordis and Pluristem.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Intramuscular injections of stromal cell–derived factor-1 in patients with critical limb ischemia demonstrated safety and efficacy; the therapy is moving forward to phase III testing.
Major finding: The major limb amputation rate was less than 10% during 12 months of follow-up after a single dose of the novel therapy.
Data source: The STOP-CLI trial was a phase IIa, 12-month, randomized, double-blind, placebo-controlled, six-center trial including 48 patients with critical limb ischemia.
Disclosures: The STOP-CLI trial was sponsored by Juventas Therapeutics. The presenter reported serving as a consultant to Johnson & Johnson/Cordis and Pluristem.
CHA2DS2-VASc score of 1 linked to lower stroke risk than previously reported
Patients with atrial fibrillation who had CHA2DS2-VASc scores of 1 were at lower risk of ischemic stroke than previously reported, according to a retrospective analysis of hospital registry data. The research appeared online January 19 in the Journal of American College of Cardiology.
Depending on the definition of stroke used, risk was 0.1% to 0.2% in women and 0.5% to 0.7% in men – so low that oral anticoagulants (OACs) would not be expected to benefit patients of either sex, said Dr. Leif Friberg at the Karolinska Institute in Stockholm and his associates. Past studies had potentially overestimated the risk of stroke in this population, which “may have led to unnecessary, and potentially harmful, OAC treatment of low-risk patients,” they said.
European and U.S. guidelines both recommend using the CHA2DS2-VASc (heart failure, hypertension, age ≥75, diabetes mellitus, prior stroke or transient ischemic attack, vascular disease, age 65-74 years, female) scoring system to assess stroke risk in patients with atrial fibrillation (AF). But past studies have reported a threefold variation (ranging from 0.6% to greater than 2.0%) in stroke risk among AF patients with CHA2DS2-VASc scores of 1 who were not receiving OAC, the researchers noted. Anticoagulation therapy is likely to benefit AF patients whose annual risk of stroke exceeds 1%, but not patients whose risk is only 0.6%, they added.
Their study, which included 140,420 patients in Sweden with nonvalvular AF, assessed the effect of varying definitions of stroke on estimates of stroke risk. Using a broad definition that included ischemic stroke, transient ischemic attack (TIA), and pulmonary embolism led to a 44% greater annual risk of stroke than if only ischemic strokes were considered, the investigators reported. They disagreed with classifying pulmonary embolism events and TIAs as strokes, as some past studies have done. “Primary prevention of pulmonary embolism among patients with AF has, to the best of our knowledge, not been studied and is not an approved indication for OAC treatment,” they said. “We also did not find it relevant to count TIA as an endpoint in studies that describe stroke risk. As a diagnosis, TIA is difficult to validate.”
Several Swedish foundations supported the study. Dr. Friberg reported no relevant financial conflicts of interest.
Given the current state of knowledge, patients with atrial fibrillation who are younger than 65 years but have a CHA2DS2-VASc score of 1 are unlikely to benefit from anticoagulation therapy.
Dr. Friberg and his colleagues make two important observations regarding risk score thresholds for oral anticoagulant therapy. First, they highlight the wide cohort-to-cohort variation in reported CHA2DS2-VASc–stratified rates of stroke for atrial fibrillation patients who are not anticoagulated. Second, they reveal how sensitive estimates of stroke rates are to variations in interrogating administrative databases, which are used repeatedly as sources of “real world” rates of stroke. They conclude that the true stroke rate for patients with a CHA2DS2-VASc score of 1 is less than 0.7% per year, too low for oral anticoagulant therapy to benefit patients with AF.
Going forward, guideline writers should be aware of the drawbacks of the CHA2DS2-VASc score. They should focus on the absolute rates of stroke corresponding to risk prediction point scores and be alert to potential biases in studies reporting these rates. Investigators should work to harmonize methods for analyzing large AF databases. If variation in reported rates cannot be reconciled, then recommendations should reflect this uncertainty.
Dr. Daniel E. Singer is at Harvard Medical School in Boston, and Dr. Michael D. Ezekowitz is at Sidney Kimmel Medical College at Thomas Jefferson University in Philadelphia. Dr. Singer has been a consultant to, advised, and or received research funding from Boehringer Ingelheim, Bristol-Myers Squibb, Johnson & Johnson, Merck, and St. Jude Medical, and Medtronic. Dr. Ezekowitz reported having been a consultant and advisory board member for all those companies and several others. These remarks were taken from their editorial accompanying Dr. Friberg’s report (J. Am. Coll. Cardiol. 2015 Jan. 19 [doi:10.1016/j.jacc.2014.11.013]).
Given the current state of knowledge, patients with atrial fibrillation who are younger than 65 years but have a CHA2DS2-VASc score of 1 are unlikely to benefit from anticoagulation therapy.
Dr. Friberg and his colleagues make two important observations regarding risk score thresholds for oral anticoagulant therapy. First, they highlight the wide cohort-to-cohort variation in reported CHA2DS2-VASc–stratified rates of stroke for atrial fibrillation patients who are not anticoagulated. Second, they reveal how sensitive estimates of stroke rates are to variations in interrogating administrative databases, which are used repeatedly as sources of “real world” rates of stroke. They conclude that the true stroke rate for patients with a CHA2DS2-VASc score of 1 is less than 0.7% per year, too low for oral anticoagulant therapy to benefit patients with AF.
Going forward, guideline writers should be aware of the drawbacks of the CHA2DS2-VASc score. They should focus on the absolute rates of stroke corresponding to risk prediction point scores and be alert to potential biases in studies reporting these rates. Investigators should work to harmonize methods for analyzing large AF databases. If variation in reported rates cannot be reconciled, then recommendations should reflect this uncertainty.
Dr. Daniel E. Singer is at Harvard Medical School in Boston, and Dr. Michael D. Ezekowitz is at Sidney Kimmel Medical College at Thomas Jefferson University in Philadelphia. Dr. Singer has been a consultant to, advised, and or received research funding from Boehringer Ingelheim, Bristol-Myers Squibb, Johnson & Johnson, Merck, and St. Jude Medical, and Medtronic. Dr. Ezekowitz reported having been a consultant and advisory board member for all those companies and several others. These remarks were taken from their editorial accompanying Dr. Friberg’s report (J. Am. Coll. Cardiol. 2015 Jan. 19 [doi:10.1016/j.jacc.2014.11.013]).
Given the current state of knowledge, patients with atrial fibrillation who are younger than 65 years but have a CHA2DS2-VASc score of 1 are unlikely to benefit from anticoagulation therapy.
Dr. Friberg and his colleagues make two important observations regarding risk score thresholds for oral anticoagulant therapy. First, they highlight the wide cohort-to-cohort variation in reported CHA2DS2-VASc–stratified rates of stroke for atrial fibrillation patients who are not anticoagulated. Second, they reveal how sensitive estimates of stroke rates are to variations in interrogating administrative databases, which are used repeatedly as sources of “real world” rates of stroke. They conclude that the true stroke rate for patients with a CHA2DS2-VASc score of 1 is less than 0.7% per year, too low for oral anticoagulant therapy to benefit patients with AF.
Going forward, guideline writers should be aware of the drawbacks of the CHA2DS2-VASc score. They should focus on the absolute rates of stroke corresponding to risk prediction point scores and be alert to potential biases in studies reporting these rates. Investigators should work to harmonize methods for analyzing large AF databases. If variation in reported rates cannot be reconciled, then recommendations should reflect this uncertainty.
Dr. Daniel E. Singer is at Harvard Medical School in Boston, and Dr. Michael D. Ezekowitz is at Sidney Kimmel Medical College at Thomas Jefferson University in Philadelphia. Dr. Singer has been a consultant to, advised, and or received research funding from Boehringer Ingelheim, Bristol-Myers Squibb, Johnson & Johnson, Merck, and St. Jude Medical, and Medtronic. Dr. Ezekowitz reported having been a consultant and advisory board member for all those companies and several others. These remarks were taken from their editorial accompanying Dr. Friberg’s report (J. Am. Coll. Cardiol. 2015 Jan. 19 [doi:10.1016/j.jacc.2014.11.013]).
Patients with atrial fibrillation who had CHA2DS2-VASc scores of 1 were at lower risk of ischemic stroke than previously reported, according to a retrospective analysis of hospital registry data. The research appeared online January 19 in the Journal of American College of Cardiology.
Depending on the definition of stroke used, risk was 0.1% to 0.2% in women and 0.5% to 0.7% in men – so low that oral anticoagulants (OACs) would not be expected to benefit patients of either sex, said Dr. Leif Friberg at the Karolinska Institute in Stockholm and his associates. Past studies had potentially overestimated the risk of stroke in this population, which “may have led to unnecessary, and potentially harmful, OAC treatment of low-risk patients,” they said.
European and U.S. guidelines both recommend using the CHA2DS2-VASc (heart failure, hypertension, age ≥75, diabetes mellitus, prior stroke or transient ischemic attack, vascular disease, age 65-74 years, female) scoring system to assess stroke risk in patients with atrial fibrillation (AF). But past studies have reported a threefold variation (ranging from 0.6% to greater than 2.0%) in stroke risk among AF patients with CHA2DS2-VASc scores of 1 who were not receiving OAC, the researchers noted. Anticoagulation therapy is likely to benefit AF patients whose annual risk of stroke exceeds 1%, but not patients whose risk is only 0.6%, they added.
Their study, which included 140,420 patients in Sweden with nonvalvular AF, assessed the effect of varying definitions of stroke on estimates of stroke risk. Using a broad definition that included ischemic stroke, transient ischemic attack (TIA), and pulmonary embolism led to a 44% greater annual risk of stroke than if only ischemic strokes were considered, the investigators reported. They disagreed with classifying pulmonary embolism events and TIAs as strokes, as some past studies have done. “Primary prevention of pulmonary embolism among patients with AF has, to the best of our knowledge, not been studied and is not an approved indication for OAC treatment,” they said. “We also did not find it relevant to count TIA as an endpoint in studies that describe stroke risk. As a diagnosis, TIA is difficult to validate.”
Several Swedish foundations supported the study. Dr. Friberg reported no relevant financial conflicts of interest.
Patients with atrial fibrillation who had CHA2DS2-VASc scores of 1 were at lower risk of ischemic stroke than previously reported, according to a retrospective analysis of hospital registry data. The research appeared online January 19 in the Journal of American College of Cardiology.
Depending on the definition of stroke used, risk was 0.1% to 0.2% in women and 0.5% to 0.7% in men – so low that oral anticoagulants (OACs) would not be expected to benefit patients of either sex, said Dr. Leif Friberg at the Karolinska Institute in Stockholm and his associates. Past studies had potentially overestimated the risk of stroke in this population, which “may have led to unnecessary, and potentially harmful, OAC treatment of low-risk patients,” they said.
European and U.S. guidelines both recommend using the CHA2DS2-VASc (heart failure, hypertension, age ≥75, diabetes mellitus, prior stroke or transient ischemic attack, vascular disease, age 65-74 years, female) scoring system to assess stroke risk in patients with atrial fibrillation (AF). But past studies have reported a threefold variation (ranging from 0.6% to greater than 2.0%) in stroke risk among AF patients with CHA2DS2-VASc scores of 1 who were not receiving OAC, the researchers noted. Anticoagulation therapy is likely to benefit AF patients whose annual risk of stroke exceeds 1%, but not patients whose risk is only 0.6%, they added.
Their study, which included 140,420 patients in Sweden with nonvalvular AF, assessed the effect of varying definitions of stroke on estimates of stroke risk. Using a broad definition that included ischemic stroke, transient ischemic attack (TIA), and pulmonary embolism led to a 44% greater annual risk of stroke than if only ischemic strokes were considered, the investigators reported. They disagreed with classifying pulmonary embolism events and TIAs as strokes, as some past studies have done. “Primary prevention of pulmonary embolism among patients with AF has, to the best of our knowledge, not been studied and is not an approved indication for OAC treatment,” they said. “We also did not find it relevant to count TIA as an endpoint in studies that describe stroke risk. As a diagnosis, TIA is difficult to validate.”
Several Swedish foundations supported the study. Dr. Friberg reported no relevant financial conflicts of interest.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Key clinical point: Stroke risk was low in patients with atrial fibrillation and a CHA2DS2-VASc score of 1.
Major finding: Risk of stroke was 0.1% to 0.2% in women and 0.5% to 0.7% in men.
Data source: Retrospective study of 140,420 patients with nonvalvular AF.
Disclosures: Several Swedish foundations supported the study. Dr. Friberg reported no relevant financial conflicts of interest.
Promising new therapy for critical limb ischemia
CHICAGO– A single set of intramuscular injections of stromal cell–derived factor-1 in patients with critical limb ischemia showed safety as well as evidence of efficacy through 12 months of follow-up in the STOP-CLI trial.
“Patients treated with JVS-100 demonstrated dose-dependent improvement across multiple patient-centered outcomes, including pain, quality of life, and wound healing, with less change in macrovascular objective measures in this small study,” Dr. Melina R. Kibbe reported at the American Heart Association scientific sessions. JVS-100 is a nonviral plasmid encoding human stromal cell–derived factor-1 (SDF-1), a natural chemokine protein that promotes angiogenesis by recruiting endothelial progenitor cells from the bone marrow to ischemic sites, explained Dr. Kibbe, professor and vice chair of surgical research and deputy director of the Simpson Querrey Institute for BioNanotechnology at Northwestern University, Chicago.
STOP-CLI was an exploratory, phase IIa, double-blind, first-in-humans study involving 48 patients with Rutherford classification 4 or 5 critical climb ischemia (CLI). All had an ankle-brachial index of 0.4 or lower, an ankle systolic blood pressure of 70 mm Hg or less or a toe systolic blood pressure of 50 or less, and were poor candidates for surgical revascularization. None had Buerger’s disease.
Participants were randomized to one of four study arms, and within each study arm further randomized 3:1 to stromal cell–derived factor-1 (SDF-1) or placebo injections. The patients received either 8 or 16 injections, each containing either 0.5 or 1.0 mg of SDF-1 or placebo. The injections, given in a single session, were placed at least 0.5 cm apart throughout the ischemic area of the affected limb.
By chance, most patients randomized to the placebo group were Rutherford 4, a category of CLI defined by rest pain, while the majority in the active treatment arms were Rutherford 5, a more severe disease manifestation characterized by ulcers. As a consequence, the SDF-1 recipients also had far larger nonhealing wounds, with an average area of 6.4 cm2, compared with 1.5 cm2, in controls.
The SDF-1 injections proved safe and were well tolerated, with no treatment-related serious adverse events and no safety signals evident in the laboratory results.
Turning to efficacy endpoints, Dr. Kibbe said self-rated visual analog scale pain scores showed clear, dose-dependent improvement over time in the SDF-1 treatment cohorts and no change in controls.
Similarly, the active treatment groups showed improved quality of life scores on all domains of the Short Form-36: physical functioning, bodily pain, general health, social functioning, energy/fatigue, emotional well-being, and overall physical and mental health, the surgeon continued.
Wound area decreased significantly in the SDF-1-treated groups, with the biggest reduction – more than 8 cm2 – being noted in the three patients who received eight 1-mg injections. That was also the group with the largest wounds at baseline, with an average area of 11.4 cm2.
Of note, the major limb amputation rate was “remarkably low” for patients with such severe CLI, according to Dr. Kibbe. The rate was less than 10% over the course of 12 months, with one patient in each of the four active treatment arms having a major amputation at time intervals of 58-112 days post injection. No major limb amputations occurred in the control group.
There was a hint of improvement with SDF-1 therapy over placebo in ankle-brachial index and transcutaneous oxygen pressure, but the between-group differences were too narrow in this study to allow for any conclusions. That must await planned much larger phase III trials, according to Dr. Kibbe.
Audience members, citing the numerous failures of once-promising stem cell therapies for CLI at phase III testing over the last 10-15 years, wondered why Dr. Kibbe thinks SDF-1 will fare any better.
“This is much debated and discussed among all the people involved in these kinds of trials,” she replied. “I’d say, briefly, that a lot of it has to do with patient selection. I think when you have a mixed bag of patients in a trial, including patients with Buerger’s disease, treated in multiple different countries, using different definitions of when to amputate, all those things come into play and could account for why those phase III trials were not successful.”
“Having been involved in lots of the different gene- and cell-based therapy trials, I think one of the unique benefits of this therapy is that it kind of bridges between the two. SDF-1 basically homes your endothelial progenitor cells to the site of ischemic injury for enhanced vasculogenesis. But SDF-1 also has direct effects on endothelial cells, including stimulating proliferation and preventing apoptosis,” she added.
JVS-100 has also successfully completed a phase II clinical trial for the treatment of heart failure. In addition, the agent is being developed as a treatment for acute MI, chronic angina, and for muscle regeneration.
The STOP-CLI study was sponsored by Juventas Therapeutics. Dr. Kibbe reported serving as a consultant to Johnson & Johnson/Cordis and Pluristem.
CHICAGO– A single set of intramuscular injections of stromal cell–derived factor-1 in patients with critical limb ischemia showed safety as well as evidence of efficacy through 12 months of follow-up in the STOP-CLI trial.
“Patients treated with JVS-100 demonstrated dose-dependent improvement across multiple patient-centered outcomes, including pain, quality of life, and wound healing, with less change in macrovascular objective measures in this small study,” Dr. Melina R. Kibbe reported at the American Heart Association scientific sessions. JVS-100 is a nonviral plasmid encoding human stromal cell–derived factor-1 (SDF-1), a natural chemokine protein that promotes angiogenesis by recruiting endothelial progenitor cells from the bone marrow to ischemic sites, explained Dr. Kibbe, professor and vice chair of surgical research and deputy director of the Simpson Querrey Institute for BioNanotechnology at Northwestern University, Chicago.
STOP-CLI was an exploratory, phase IIa, double-blind, first-in-humans study involving 48 patients with Rutherford classification 4 or 5 critical climb ischemia (CLI). All had an ankle-brachial index of 0.4 or lower, an ankle systolic blood pressure of 70 mm Hg or less or a toe systolic blood pressure of 50 or less, and were poor candidates for surgical revascularization. None had Buerger’s disease.
Participants were randomized to one of four study arms, and within each study arm further randomized 3:1 to stromal cell–derived factor-1 (SDF-1) or placebo injections. The patients received either 8 or 16 injections, each containing either 0.5 or 1.0 mg of SDF-1 or placebo. The injections, given in a single session, were placed at least 0.5 cm apart throughout the ischemic area of the affected limb.
By chance, most patients randomized to the placebo group were Rutherford 4, a category of CLI defined by rest pain, while the majority in the active treatment arms were Rutherford 5, a more severe disease manifestation characterized by ulcers. As a consequence, the SDF-1 recipients also had far larger nonhealing wounds, with an average area of 6.4 cm2, compared with 1.5 cm2, in controls.
The SDF-1 injections proved safe and were well tolerated, with no treatment-related serious adverse events and no safety signals evident in the laboratory results.
Turning to efficacy endpoints, Dr. Kibbe said self-rated visual analog scale pain scores showed clear, dose-dependent improvement over time in the SDF-1 treatment cohorts and no change in controls.
Similarly, the active treatment groups showed improved quality of life scores on all domains of the Short Form-36: physical functioning, bodily pain, general health, social functioning, energy/fatigue, emotional well-being, and overall physical and mental health, the surgeon continued.
Wound area decreased significantly in the SDF-1-treated groups, with the biggest reduction – more than 8 cm2 – being noted in the three patients who received eight 1-mg injections. That was also the group with the largest wounds at baseline, with an average area of 11.4 cm2.
Of note, the major limb amputation rate was “remarkably low” for patients with such severe CLI, according to Dr. Kibbe. The rate was less than 10% over the course of 12 months, with one patient in each of the four active treatment arms having a major amputation at time intervals of 58-112 days post injection. No major limb amputations occurred in the control group.
There was a hint of improvement with SDF-1 therapy over placebo in ankle-brachial index and transcutaneous oxygen pressure, but the between-group differences were too narrow in this study to allow for any conclusions. That must await planned much larger phase III trials, according to Dr. Kibbe.
Audience members, citing the numerous failures of once-promising stem cell therapies for CLI at phase III testing over the last 10-15 years, wondered why Dr. Kibbe thinks SDF-1 will fare any better.
“This is much debated and discussed among all the people involved in these kinds of trials,” she replied. “I’d say, briefly, that a lot of it has to do with patient selection. I think when you have a mixed bag of patients in a trial, including patients with Buerger’s disease, treated in multiple different countries, using different definitions of when to amputate, all those things come into play and could account for why those phase III trials were not successful.”
“Having been involved in lots of the different gene- and cell-based therapy trials, I think one of the unique benefits of this therapy is that it kind of bridges between the two. SDF-1 basically homes your endothelial progenitor cells to the site of ischemic injury for enhanced vasculogenesis. But SDF-1 also has direct effects on endothelial cells, including stimulating proliferation and preventing apoptosis,” she added.
JVS-100 has also successfully completed a phase II clinical trial for the treatment of heart failure. In addition, the agent is being developed as a treatment for acute MI, chronic angina, and for muscle regeneration.
The STOP-CLI study was sponsored by Juventas Therapeutics. Dr. Kibbe reported serving as a consultant to Johnson & Johnson/Cordis and Pluristem.
CHICAGO– A single set of intramuscular injections of stromal cell–derived factor-1 in patients with critical limb ischemia showed safety as well as evidence of efficacy through 12 months of follow-up in the STOP-CLI trial.
“Patients treated with JVS-100 demonstrated dose-dependent improvement across multiple patient-centered outcomes, including pain, quality of life, and wound healing, with less change in macrovascular objective measures in this small study,” Dr. Melina R. Kibbe reported at the American Heart Association scientific sessions. JVS-100 is a nonviral plasmid encoding human stromal cell–derived factor-1 (SDF-1), a natural chemokine protein that promotes angiogenesis by recruiting endothelial progenitor cells from the bone marrow to ischemic sites, explained Dr. Kibbe, professor and vice chair of surgical research and deputy director of the Simpson Querrey Institute for BioNanotechnology at Northwestern University, Chicago.
STOP-CLI was an exploratory, phase IIa, double-blind, first-in-humans study involving 48 patients with Rutherford classification 4 or 5 critical climb ischemia (CLI). All had an ankle-brachial index of 0.4 or lower, an ankle systolic blood pressure of 70 mm Hg or less or a toe systolic blood pressure of 50 or less, and were poor candidates for surgical revascularization. None had Buerger’s disease.
Participants were randomized to one of four study arms, and within each study arm further randomized 3:1 to stromal cell–derived factor-1 (SDF-1) or placebo injections. The patients received either 8 or 16 injections, each containing either 0.5 or 1.0 mg of SDF-1 or placebo. The injections, given in a single session, were placed at least 0.5 cm apart throughout the ischemic area of the affected limb.
By chance, most patients randomized to the placebo group were Rutherford 4, a category of CLI defined by rest pain, while the majority in the active treatment arms were Rutherford 5, a more severe disease manifestation characterized by ulcers. As a consequence, the SDF-1 recipients also had far larger nonhealing wounds, with an average area of 6.4 cm2, compared with 1.5 cm2, in controls.
The SDF-1 injections proved safe and were well tolerated, with no treatment-related serious adverse events and no safety signals evident in the laboratory results.
Turning to efficacy endpoints, Dr. Kibbe said self-rated visual analog scale pain scores showed clear, dose-dependent improvement over time in the SDF-1 treatment cohorts and no change in controls.
Similarly, the active treatment groups showed improved quality of life scores on all domains of the Short Form-36: physical functioning, bodily pain, general health, social functioning, energy/fatigue, emotional well-being, and overall physical and mental health, the surgeon continued.
Wound area decreased significantly in the SDF-1-treated groups, with the biggest reduction – more than 8 cm2 – being noted in the three patients who received eight 1-mg injections. That was also the group with the largest wounds at baseline, with an average area of 11.4 cm2.
Of note, the major limb amputation rate was “remarkably low” for patients with such severe CLI, according to Dr. Kibbe. The rate was less than 10% over the course of 12 months, with one patient in each of the four active treatment arms having a major amputation at time intervals of 58-112 days post injection. No major limb amputations occurred in the control group.
There was a hint of improvement with SDF-1 therapy over placebo in ankle-brachial index and transcutaneous oxygen pressure, but the between-group differences were too narrow in this study to allow for any conclusions. That must await planned much larger phase III trials, according to Dr. Kibbe.
Audience members, citing the numerous failures of once-promising stem cell therapies for CLI at phase III testing over the last 10-15 years, wondered why Dr. Kibbe thinks SDF-1 will fare any better.
“This is much debated and discussed among all the people involved in these kinds of trials,” she replied. “I’d say, briefly, that a lot of it has to do with patient selection. I think when you have a mixed bag of patients in a trial, including patients with Buerger’s disease, treated in multiple different countries, using different definitions of when to amputate, all those things come into play and could account for why those phase III trials were not successful.”
“Having been involved in lots of the different gene- and cell-based therapy trials, I think one of the unique benefits of this therapy is that it kind of bridges between the two. SDF-1 basically homes your endothelial progenitor cells to the site of ischemic injury for enhanced vasculogenesis. But SDF-1 also has direct effects on endothelial cells, including stimulating proliferation and preventing apoptosis,” she added.
JVS-100 has also successfully completed a phase II clinical trial for the treatment of heart failure. In addition, the agent is being developed as a treatment for acute MI, chronic angina, and for muscle regeneration.
The STOP-CLI study was sponsored by Juventas Therapeutics. Dr. Kibbe reported serving as a consultant to Johnson & Johnson/Cordis and Pluristem.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Intramuscular injections of stromal cell–derived factor-1 in patients with critical limb ischemia demonstrated safety and efficacy; the therapy is moving forward to phase III testing.
Major finding: The major limb amputation rate was less than 10% during 12 months of follow-up after a single dose of the novel therapy.
Data source: The STOP-CLI trial was a phase IIa, 12-month, randomized, double-blind, placebo-controlled, six-center trial including 48 patients with critical limb ischemia.
Disclosures: The STOP-CLI trial was sponsored by Juventas Therapeutics. The presenter reported serving as a consultant to Johnson & Johnson/Cordis and Pluristem.
Handheld device illuminates possible routes of melanoma metastases
Investigators using a handheld dermoscopy device that allows visualization of colors, structures, and patterns in skin lesions not evident to the naked eye were able to visualize nonblanching blue and red lines in a branched pattern in two patients with in-transit cutaneous melanoma metastases.
Dr. Michael A. Marchetti and his associates at Memorial Sloan Kettering Cancer Center, New York, reported the “intriguing” visualization of dissemination for cutaneous melanoma metastases in a letter to JAMA Dermatology.
In-transit cutaneous melanoma metastases are those located more than 2 cm from the primary melanoma, but not beyond the regional nodal basin.
The first patient had wide local excision of a primary cutaneous melanoma on the forehead, and a year later, received localized irradiation for satellite skin metastases. A year after that, skin examination revealed six blue macules on the scalp more than 2 cm from the excision scar. Dermoscopy revealed nonblanching bluish lines in a branched pattern. Histopathologic examination of a skin biopsy confirmed in-transit metastatic melanoma with atypical melanocytes present in superficial dermal lymphatics, Dr. Marchetti and his associates reported (JAMA Dermatology 2015;103-5)
The second patient had a history of multiple primary melanomas, the most recent being one on the chest treated with wide local excision. At a follow-up visit 5 years later, skin examination revealed eight blue-gray macules on the chest, all more than 2 cm from the excision scar. Dermoscopy revealed nonblanching, red-bluish, fuzzy, branching lines. Histopathologic examination of a skin biopsy confirmed in-transit metastatic melanoma with atypical melanocytes present in superficial dermal blood vessels, the investigators wrote.
Typical dermoscopic features of cutaneous melanoma metastases include peripheral gray spots, atypical vessels, and a blue nevus-like pattern. The histopathologic findings in these two cases suggest that the dermoscopic color differences correspond to unique microanatomic routes of melanoma dissemination, with blue and red-blue lines corresponding to lymphatic and hematogenous dissemination of tumors, respectively, they said.
“While the factors driving lymphatic vs. hematogenous in-transit dissemination of melanoma remain unknown, as do any differences in their biologic significance, our finding is an intriguing clinical/dermoscopic/histopathologic observation,” the investigators concluded.
On Twitter @nikolaideslaura
Investigators using a handheld dermoscopy device that allows visualization of colors, structures, and patterns in skin lesions not evident to the naked eye were able to visualize nonblanching blue and red lines in a branched pattern in two patients with in-transit cutaneous melanoma metastases.
Dr. Michael A. Marchetti and his associates at Memorial Sloan Kettering Cancer Center, New York, reported the “intriguing” visualization of dissemination for cutaneous melanoma metastases in a letter to JAMA Dermatology.
In-transit cutaneous melanoma metastases are those located more than 2 cm from the primary melanoma, but not beyond the regional nodal basin.
The first patient had wide local excision of a primary cutaneous melanoma on the forehead, and a year later, received localized irradiation for satellite skin metastases. A year after that, skin examination revealed six blue macules on the scalp more than 2 cm from the excision scar. Dermoscopy revealed nonblanching bluish lines in a branched pattern. Histopathologic examination of a skin biopsy confirmed in-transit metastatic melanoma with atypical melanocytes present in superficial dermal lymphatics, Dr. Marchetti and his associates reported (JAMA Dermatology 2015;103-5)
The second patient had a history of multiple primary melanomas, the most recent being one on the chest treated with wide local excision. At a follow-up visit 5 years later, skin examination revealed eight blue-gray macules on the chest, all more than 2 cm from the excision scar. Dermoscopy revealed nonblanching, red-bluish, fuzzy, branching lines. Histopathologic examination of a skin biopsy confirmed in-transit metastatic melanoma with atypical melanocytes present in superficial dermal blood vessels, the investigators wrote.
Typical dermoscopic features of cutaneous melanoma metastases include peripheral gray spots, atypical vessels, and a blue nevus-like pattern. The histopathologic findings in these two cases suggest that the dermoscopic color differences correspond to unique microanatomic routes of melanoma dissemination, with blue and red-blue lines corresponding to lymphatic and hematogenous dissemination of tumors, respectively, they said.
“While the factors driving lymphatic vs. hematogenous in-transit dissemination of melanoma remain unknown, as do any differences in their biologic significance, our finding is an intriguing clinical/dermoscopic/histopathologic observation,” the investigators concluded.
On Twitter @nikolaideslaura
Investigators using a handheld dermoscopy device that allows visualization of colors, structures, and patterns in skin lesions not evident to the naked eye were able to visualize nonblanching blue and red lines in a branched pattern in two patients with in-transit cutaneous melanoma metastases.
Dr. Michael A. Marchetti and his associates at Memorial Sloan Kettering Cancer Center, New York, reported the “intriguing” visualization of dissemination for cutaneous melanoma metastases in a letter to JAMA Dermatology.
In-transit cutaneous melanoma metastases are those located more than 2 cm from the primary melanoma, but not beyond the regional nodal basin.
The first patient had wide local excision of a primary cutaneous melanoma on the forehead, and a year later, received localized irradiation for satellite skin metastases. A year after that, skin examination revealed six blue macules on the scalp more than 2 cm from the excision scar. Dermoscopy revealed nonblanching bluish lines in a branched pattern. Histopathologic examination of a skin biopsy confirmed in-transit metastatic melanoma with atypical melanocytes present in superficial dermal lymphatics, Dr. Marchetti and his associates reported (JAMA Dermatology 2015;103-5)
The second patient had a history of multiple primary melanomas, the most recent being one on the chest treated with wide local excision. At a follow-up visit 5 years later, skin examination revealed eight blue-gray macules on the chest, all more than 2 cm from the excision scar. Dermoscopy revealed nonblanching, red-bluish, fuzzy, branching lines. Histopathologic examination of a skin biopsy confirmed in-transit metastatic melanoma with atypical melanocytes present in superficial dermal blood vessels, the investigators wrote.
Typical dermoscopic features of cutaneous melanoma metastases include peripheral gray spots, atypical vessels, and a blue nevus-like pattern. The histopathologic findings in these two cases suggest that the dermoscopic color differences correspond to unique microanatomic routes of melanoma dissemination, with blue and red-blue lines corresponding to lymphatic and hematogenous dissemination of tumors, respectively, they said.
“While the factors driving lymphatic vs. hematogenous in-transit dissemination of melanoma remain unknown, as do any differences in their biologic significance, our finding is an intriguing clinical/dermoscopic/histopathologic observation,” the investigators concluded.
On Twitter @nikolaideslaura
FROM JAMA DERMATOLOGY
System can detect Candida better, faster than blood culture

Credit: Jeremy L. Grisham
A diagnostic system can detect sepsis pathogens with high sensitivity and specificity in 3 to 5 hours, eliminating the need for blood culture, according to a study published in Clinical Infectious Diseases.
The system consists of the T2Candida Panel and the T2Dx Instrument, and it provides direct detection of 5 yeast pathogens—Candida albicans, Candida tropicalis, Candida parapsilosis, Candida glabrata, and Candida krusei—in whole blood samples.
T2Candida and T2Dx were cleared for use by the US Food and Drug Administration in September. They are the first diagnostic products powered by T2MR, a magnetic resonance-based diagnostic technology platform that does not require blood culture and sample purification or preparation.
“The ability to determine the presence or absence of Candida within hours—compared to days [with blood culture]—is paradigm-changing for patients at risk for these infections,” said study author Eleftherios Mylonakis, MD, PhD, of Rhode Island Hospital and The Miriam Hospital in Providence.
“It will allow us to move from a ‘best-guess’ approach in treating high-risk patients, such as cancer and transplant patients and patients in the intensive care unit, to a more informed approach where we can quickly direct the best course of therapy, potentially improving patient outcomes and saving lives.”
Study findings
For this multicenter study, Dr Mylonakis and his colleagues collected blood specimens from 1801 hospitalized patients between the ages of 18 and 95 who had a blood culture ordered as part of routine care.
T2Candida and T2Dx demonstrated an overall specificity of 99.4% per assay and 98.1% per patient. The system yielded a specificity of 98.9% for C albicans/C tropicalis, 99.3% for C parapsilosis, and 99.9% for C krusei/C glabrata.
The system had an overall sensitivity of 91.1% per assay and 91.0% per patient. It yielded a sensitivity of 92.3% for C albicans/C tropicalis, 94.2% for C parapsilosis, and 88.1% for C krusei/C glabrata.
The mean time to a positive result for T2Candida and T2Dx was 4.4 hours, compared to 129 hours for blood culture and species identification. The mean time to negative result for T2Candida and T2Dx was 4.2 hours, compared to at least 120 hours for blood culture.
In one case described in the paper, T2Candida and T2Dx detected a Candida infection that blood culture missed in 12 successive tests.
Seven days after the T2Candida result was obtained, physicians performed an invasive procedure to obtain a tissue culture, which proved that the T2Candida result accurately identified a case of intra-abdominal candidiasis.
“Blood culture, the current standard of care for the diagnosis of Candida infections, is known to have poor sensitivity overall and has 38% sensitivity in proven and probable cases of invasive candidiasis,” said study author Cornelius J. Clancy, MD, of the University of Pittsburgh in Pennsylvania.
“In our case, the T2Candida Panel has shown that it can rapidly identify intra-abdominal candidiasis where 12 serial blood culture results were negative. In many patients at risk for candidiasis, the collection of tissue samples for diagnosis is not possible due to their underlying medical conditions. Achieving the level of sensitivity demonstrated in this case, without requiring an intra-abdominal sample, has the potential to positively impact the practice of medicine for these patients.” ![]()

Credit: Jeremy L. Grisham
A diagnostic system can detect sepsis pathogens with high sensitivity and specificity in 3 to 5 hours, eliminating the need for blood culture, according to a study published in Clinical Infectious Diseases.
The system consists of the T2Candida Panel and the T2Dx Instrument, and it provides direct detection of 5 yeast pathogens—Candida albicans, Candida tropicalis, Candida parapsilosis, Candida glabrata, and Candida krusei—in whole blood samples.
T2Candida and T2Dx were cleared for use by the US Food and Drug Administration in September. They are the first diagnostic products powered by T2MR, a magnetic resonance-based diagnostic technology platform that does not require blood culture and sample purification or preparation.
“The ability to determine the presence or absence of Candida within hours—compared to days [with blood culture]—is paradigm-changing for patients at risk for these infections,” said study author Eleftherios Mylonakis, MD, PhD, of Rhode Island Hospital and The Miriam Hospital in Providence.
“It will allow us to move from a ‘best-guess’ approach in treating high-risk patients, such as cancer and transplant patients and patients in the intensive care unit, to a more informed approach where we can quickly direct the best course of therapy, potentially improving patient outcomes and saving lives.”
Study findings
For this multicenter study, Dr Mylonakis and his colleagues collected blood specimens from 1801 hospitalized patients between the ages of 18 and 95 who had a blood culture ordered as part of routine care.
T2Candida and T2Dx demonstrated an overall specificity of 99.4% per assay and 98.1% per patient. The system yielded a specificity of 98.9% for C albicans/C tropicalis, 99.3% for C parapsilosis, and 99.9% for C krusei/C glabrata.
The system had an overall sensitivity of 91.1% per assay and 91.0% per patient. It yielded a sensitivity of 92.3% for C albicans/C tropicalis, 94.2% for C parapsilosis, and 88.1% for C krusei/C glabrata.
The mean time to a positive result for T2Candida and T2Dx was 4.4 hours, compared to 129 hours for blood culture and species identification. The mean time to negative result for T2Candida and T2Dx was 4.2 hours, compared to at least 120 hours for blood culture.
In one case described in the paper, T2Candida and T2Dx detected a Candida infection that blood culture missed in 12 successive tests.
Seven days after the T2Candida result was obtained, physicians performed an invasive procedure to obtain a tissue culture, which proved that the T2Candida result accurately identified a case of intra-abdominal candidiasis.
“Blood culture, the current standard of care for the diagnosis of Candida infections, is known to have poor sensitivity overall and has 38% sensitivity in proven and probable cases of invasive candidiasis,” said study author Cornelius J. Clancy, MD, of the University of Pittsburgh in Pennsylvania.
“In our case, the T2Candida Panel has shown that it can rapidly identify intra-abdominal candidiasis where 12 serial blood culture results were negative. In many patients at risk for candidiasis, the collection of tissue samples for diagnosis is not possible due to their underlying medical conditions. Achieving the level of sensitivity demonstrated in this case, without requiring an intra-abdominal sample, has the potential to positively impact the practice of medicine for these patients.” ![]()

Credit: Jeremy L. Grisham
A diagnostic system can detect sepsis pathogens with high sensitivity and specificity in 3 to 5 hours, eliminating the need for blood culture, according to a study published in Clinical Infectious Diseases.
The system consists of the T2Candida Panel and the T2Dx Instrument, and it provides direct detection of 5 yeast pathogens—Candida albicans, Candida tropicalis, Candida parapsilosis, Candida glabrata, and Candida krusei—in whole blood samples.
T2Candida and T2Dx were cleared for use by the US Food and Drug Administration in September. They are the first diagnostic products powered by T2MR, a magnetic resonance-based diagnostic technology platform that does not require blood culture and sample purification or preparation.
“The ability to determine the presence or absence of Candida within hours—compared to days [with blood culture]—is paradigm-changing for patients at risk for these infections,” said study author Eleftherios Mylonakis, MD, PhD, of Rhode Island Hospital and The Miriam Hospital in Providence.
“It will allow us to move from a ‘best-guess’ approach in treating high-risk patients, such as cancer and transplant patients and patients in the intensive care unit, to a more informed approach where we can quickly direct the best course of therapy, potentially improving patient outcomes and saving lives.”
Study findings
For this multicenter study, Dr Mylonakis and his colleagues collected blood specimens from 1801 hospitalized patients between the ages of 18 and 95 who had a blood culture ordered as part of routine care.
T2Candida and T2Dx demonstrated an overall specificity of 99.4% per assay and 98.1% per patient. The system yielded a specificity of 98.9% for C albicans/C tropicalis, 99.3% for C parapsilosis, and 99.9% for C krusei/C glabrata.
The system had an overall sensitivity of 91.1% per assay and 91.0% per patient. It yielded a sensitivity of 92.3% for C albicans/C tropicalis, 94.2% for C parapsilosis, and 88.1% for C krusei/C glabrata.
The mean time to a positive result for T2Candida and T2Dx was 4.4 hours, compared to 129 hours for blood culture and species identification. The mean time to negative result for T2Candida and T2Dx was 4.2 hours, compared to at least 120 hours for blood culture.
In one case described in the paper, T2Candida and T2Dx detected a Candida infection that blood culture missed in 12 successive tests.
Seven days after the T2Candida result was obtained, physicians performed an invasive procedure to obtain a tissue culture, which proved that the T2Candida result accurately identified a case of intra-abdominal candidiasis.
“Blood culture, the current standard of care for the diagnosis of Candida infections, is known to have poor sensitivity overall and has 38% sensitivity in proven and probable cases of invasive candidiasis,” said study author Cornelius J. Clancy, MD, of the University of Pittsburgh in Pennsylvania.
“In our case, the T2Candida Panel has shown that it can rapidly identify intra-abdominal candidiasis where 12 serial blood culture results were negative. In many patients at risk for candidiasis, the collection of tissue samples for diagnosis is not possible due to their underlying medical conditions. Achieving the level of sensitivity demonstrated in this case, without requiring an intra-abdominal sample, has the potential to positively impact the practice of medicine for these patients.” ![]()
Study offers explanation for gender gaps in academia

Credit: Rhoda Baer
New research offers an explanation for the lack of women in certain academic fields.
It isn’t that women don’t want to work long hours or can’t compete in highly selective fields, and it isn’t that they are less analytical than men, the researchers reported.
Instead, it appears that women are underrepresented in academic fields whose practitioners put a lot of emphasis on the importance of being brilliant—a quality some people assume women lack.
Sarah-Jane Leslie, PhD, of Princeton University in New Jersey, and her colleagues reported these findings in Science.
The researchers focused on a broad swath of academic disciplines, including those in the sciences, the humanities, social sciences, and math.
They focused on the culture of different fields, reasoning that stereotypes of women’s inferior intellectual abilities might help explain why women are underrepresented in fields—such as physics or philosophy—that idolize geniuses.
The team surveyed more than 1800 graduate students, post-doctoral researchers, and faculty members in 30 academic disciplines and, among other things, asked them what qualities were required for success in their fields.
Across the board, in the sciences, technology, engineering, and math (STEM) fields, as well as in the humanities and social sciences, women were found to be underrepresented in those disciplines whose practitioners put a premium on brilliance.
“We’re not saying brilliance—or valuing brilliance—is a bad thing,” said study author Andrei Cimpian, PhD, of the University of Illinois at Urbana-Champaign.
“And we’re not saying women are not brilliant or that being brilliant isn’t helpful to one’s academic career. Our data don’t address that. What they suggest is that conveying to your students a belief that brilliance is required for success may have a differential effect on males and females that are looking to pursue careers in your field.”
The team also tested 3 other hypotheses that might help explain women’s underrepresentation in some fields: that women avoid careers that require them to work long hours, that women are less able than men to get into highly selective fields, and that women are outnumbered by men in fields that require analytical, systematical reasoning.
“We found that none of these 3 alternative hypotheses was able to predict women’s representation across the academic spectrum,” Dr Leslie said. “A strong emphasis on brilliance among practitioners of particular fields was the best predictor of women’s underrepresentation in those fields.”
The researchers are still investigating whether women are actively avoiding fields that focus on cultivating brilliant individuals, or if practitioners in those fields are discriminating against women based on their beliefs about women’s aptitudes. A combination of the two is certainly plausible, according to Dr Cimpian.
“There is no convincing evidence in the literature that men and women differ intellectually in ways that would be relevant to their success across the entire range of fields we surveyed,” Dr Cimpian said. “So it is most likely that female underrepresentation is not the result of actual differences in intellectual ability but rather the result of perceived or presumed differences between women and men.” ![]()

Credit: Rhoda Baer
New research offers an explanation for the lack of women in certain academic fields.
It isn’t that women don’t want to work long hours or can’t compete in highly selective fields, and it isn’t that they are less analytical than men, the researchers reported.
Instead, it appears that women are underrepresented in academic fields whose practitioners put a lot of emphasis on the importance of being brilliant—a quality some people assume women lack.
Sarah-Jane Leslie, PhD, of Princeton University in New Jersey, and her colleagues reported these findings in Science.
The researchers focused on a broad swath of academic disciplines, including those in the sciences, the humanities, social sciences, and math.
They focused on the culture of different fields, reasoning that stereotypes of women’s inferior intellectual abilities might help explain why women are underrepresented in fields—such as physics or philosophy—that idolize geniuses.
The team surveyed more than 1800 graduate students, post-doctoral researchers, and faculty members in 30 academic disciplines and, among other things, asked them what qualities were required for success in their fields.
Across the board, in the sciences, technology, engineering, and math (STEM) fields, as well as in the humanities and social sciences, women were found to be underrepresented in those disciplines whose practitioners put a premium on brilliance.
“We’re not saying brilliance—or valuing brilliance—is a bad thing,” said study author Andrei Cimpian, PhD, of the University of Illinois at Urbana-Champaign.
“And we’re not saying women are not brilliant or that being brilliant isn’t helpful to one’s academic career. Our data don’t address that. What they suggest is that conveying to your students a belief that brilliance is required for success may have a differential effect on males and females that are looking to pursue careers in your field.”
The team also tested 3 other hypotheses that might help explain women’s underrepresentation in some fields: that women avoid careers that require them to work long hours, that women are less able than men to get into highly selective fields, and that women are outnumbered by men in fields that require analytical, systematical reasoning.
“We found that none of these 3 alternative hypotheses was able to predict women’s representation across the academic spectrum,” Dr Leslie said. “A strong emphasis on brilliance among practitioners of particular fields was the best predictor of women’s underrepresentation in those fields.”
The researchers are still investigating whether women are actively avoiding fields that focus on cultivating brilliant individuals, or if practitioners in those fields are discriminating against women based on their beliefs about women’s aptitudes. A combination of the two is certainly plausible, according to Dr Cimpian.
“There is no convincing evidence in the literature that men and women differ intellectually in ways that would be relevant to their success across the entire range of fields we surveyed,” Dr Cimpian said. “So it is most likely that female underrepresentation is not the result of actual differences in intellectual ability but rather the result of perceived or presumed differences between women and men.” ![]()

Credit: Rhoda Baer
New research offers an explanation for the lack of women in certain academic fields.
It isn’t that women don’t want to work long hours or can’t compete in highly selective fields, and it isn’t that they are less analytical than men, the researchers reported.
Instead, it appears that women are underrepresented in academic fields whose practitioners put a lot of emphasis on the importance of being brilliant—a quality some people assume women lack.
Sarah-Jane Leslie, PhD, of Princeton University in New Jersey, and her colleagues reported these findings in Science.
The researchers focused on a broad swath of academic disciplines, including those in the sciences, the humanities, social sciences, and math.
They focused on the culture of different fields, reasoning that stereotypes of women’s inferior intellectual abilities might help explain why women are underrepresented in fields—such as physics or philosophy—that idolize geniuses.
The team surveyed more than 1800 graduate students, post-doctoral researchers, and faculty members in 30 academic disciplines and, among other things, asked them what qualities were required for success in their fields.
Across the board, in the sciences, technology, engineering, and math (STEM) fields, as well as in the humanities and social sciences, women were found to be underrepresented in those disciplines whose practitioners put a premium on brilliance.
“We’re not saying brilliance—or valuing brilliance—is a bad thing,” said study author Andrei Cimpian, PhD, of the University of Illinois at Urbana-Champaign.
“And we’re not saying women are not brilliant or that being brilliant isn’t helpful to one’s academic career. Our data don’t address that. What they suggest is that conveying to your students a belief that brilliance is required for success may have a differential effect on males and females that are looking to pursue careers in your field.”
The team also tested 3 other hypotheses that might help explain women’s underrepresentation in some fields: that women avoid careers that require them to work long hours, that women are less able than men to get into highly selective fields, and that women are outnumbered by men in fields that require analytical, systematical reasoning.
“We found that none of these 3 alternative hypotheses was able to predict women’s representation across the academic spectrum,” Dr Leslie said. “A strong emphasis on brilliance among practitioners of particular fields was the best predictor of women’s underrepresentation in those fields.”
The researchers are still investigating whether women are actively avoiding fields that focus on cultivating brilliant individuals, or if practitioners in those fields are discriminating against women based on their beliefs about women’s aptitudes. A combination of the two is certainly plausible, according to Dr Cimpian.
“There is no convincing evidence in the literature that men and women differ intellectually in ways that would be relevant to their success across the entire range of fields we surveyed,” Dr Cimpian said. “So it is most likely that female underrepresentation is not the result of actual differences in intellectual ability but rather the result of perceived or presumed differences between women and men.” ![]()