User login
Cosmetic procedures in pregnancy
Cosmetic procedures in general should be postponed until after pregnancy. Factors to consider in a pregnant patient include the hormonal and physiologic changes of the patient during pregnancy, as well as the risk to the fetus.
Many dermatologic changes occur during a pregnancy. Pregnant women may develop hyperpigmentation, formation of vascular lesions and varicose veins, hirsutism, striae, acne, and increased skin growths. These changes may lead pregnant women to seek cosmetic treatments.
However, physiologic changes such as increased blood volume, decreased hematocrit, increased flushing, increased melanocyte stimulation, and decreased wound healing should prompt a delay of cosmetic procedures until 3-6 months after the postpartum period, when these factors return to normal and the risk of complications is reduced.
The safety of many cosmetic treatments during pregnancy remains unknown. This includes microdermabrasion, chemical peels, and laser treatments. Given the increased risk of postinflammatory hyperpigmentation, as well as poor wound healing and increased risk of hypertrophic and keloidal scarring in pregnancy, these procedures are often avoided.
The safety of injectable treatments during pregnancy, such as liquid sclerosants and fillers, has not been evaluated. However, the manufacturers list pregnancy and breastfeeding as contraindications to treatment. Neurotoxins are also avoided during pregnancy and breastfeeding, based on teratogenicity in animal studies. There have been no controlled trials in humans.
Though there have been incidental exposures of botulinum toxin in women who did not know they were pregnant, no documented reports of fetal anomaly during these incidental exposures has been reported. In addition, no studies have been conducted to evaluate whether the toxin is excreted in breast milk, or when it is safe to use neurotoxins, fillers, or liquid sclerosants prior to conception.
The 10 months of pregnancy and many months of nursing can be a long stretch to wait for women who get regular cosmetic treatments. The skin changes of pregnancy can be bothersome; however, the risks of complications to the mother and the fetus outweigh the transient benefits of cosmetic procedures. The hormonal and physiologic changes of pregnancy are widely different in each woman, and sometimes the long-term side effects and complications can be completely unpredictable. Thus, patience and thorough counseling are the best strategies for treating our pregnant and nursing moms.
References
Nussbaum, R. and Benedetto, A.V. Cosmetic aspects of pregnancy. Clinics in Dermatology 2006;24:133-41.
Morgan, J.C. et al. Botulinum Toxin and Pregnancy Skinmed 2006;5:308.
Monteiro, E. Botulinum toxin A during pregnancy: a survey of treating physicians. J. Neurol. Neurosurg. Psychiatry 2006;77:117-9.
Lee, K.C., et al. Safety of cosmetic dermatologic procedures during pregnancy. Dermatol. Surg. 2013;39:1573-86.
Goldberg, D. and Maloney, M. Dermatologic surgery and cosmetic procedures during pregnancy and the postpartum period. Dermatologic Therapy 2013;26:321-30.
Dr. Talakoub and Dr. Wesley are co-contributors to a monthly Aesthetic Dermatology column in Dermatology News. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub.
Cosmetic procedures in general should be postponed until after pregnancy. Factors to consider in a pregnant patient include the hormonal and physiologic changes of the patient during pregnancy, as well as the risk to the fetus.
Many dermatologic changes occur during a pregnancy. Pregnant women may develop hyperpigmentation, formation of vascular lesions and varicose veins, hirsutism, striae, acne, and increased skin growths. These changes may lead pregnant women to seek cosmetic treatments.
However, physiologic changes such as increased blood volume, decreased hematocrit, increased flushing, increased melanocyte stimulation, and decreased wound healing should prompt a delay of cosmetic procedures until 3-6 months after the postpartum period, when these factors return to normal and the risk of complications is reduced.
The safety of many cosmetic treatments during pregnancy remains unknown. This includes microdermabrasion, chemical peels, and laser treatments. Given the increased risk of postinflammatory hyperpigmentation, as well as poor wound healing and increased risk of hypertrophic and keloidal scarring in pregnancy, these procedures are often avoided.
The safety of injectable treatments during pregnancy, such as liquid sclerosants and fillers, has not been evaluated. However, the manufacturers list pregnancy and breastfeeding as contraindications to treatment. Neurotoxins are also avoided during pregnancy and breastfeeding, based on teratogenicity in animal studies. There have been no controlled trials in humans.
Though there have been incidental exposures of botulinum toxin in women who did not know they were pregnant, no documented reports of fetal anomaly during these incidental exposures has been reported. In addition, no studies have been conducted to evaluate whether the toxin is excreted in breast milk, or when it is safe to use neurotoxins, fillers, or liquid sclerosants prior to conception.
The 10 months of pregnancy and many months of nursing can be a long stretch to wait for women who get regular cosmetic treatments. The skin changes of pregnancy can be bothersome; however, the risks of complications to the mother and the fetus outweigh the transient benefits of cosmetic procedures. The hormonal and physiologic changes of pregnancy are widely different in each woman, and sometimes the long-term side effects and complications can be completely unpredictable. Thus, patience and thorough counseling are the best strategies for treating our pregnant and nursing moms.
References
Nussbaum, R. and Benedetto, A.V. Cosmetic aspects of pregnancy. Clinics in Dermatology 2006;24:133-41.
Morgan, J.C. et al. Botulinum Toxin and Pregnancy Skinmed 2006;5:308.
Monteiro, E. Botulinum toxin A during pregnancy: a survey of treating physicians. J. Neurol. Neurosurg. Psychiatry 2006;77:117-9.
Lee, K.C., et al. Safety of cosmetic dermatologic procedures during pregnancy. Dermatol. Surg. 2013;39:1573-86.
Goldberg, D. and Maloney, M. Dermatologic surgery and cosmetic procedures during pregnancy and the postpartum period. Dermatologic Therapy 2013;26:321-30.
Dr. Talakoub and Dr. Wesley are co-contributors to a monthly Aesthetic Dermatology column in Dermatology News. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub.
Cosmetic procedures in general should be postponed until after pregnancy. Factors to consider in a pregnant patient include the hormonal and physiologic changes of the patient during pregnancy, as well as the risk to the fetus.
Many dermatologic changes occur during a pregnancy. Pregnant women may develop hyperpigmentation, formation of vascular lesions and varicose veins, hirsutism, striae, acne, and increased skin growths. These changes may lead pregnant women to seek cosmetic treatments.
However, physiologic changes such as increased blood volume, decreased hematocrit, increased flushing, increased melanocyte stimulation, and decreased wound healing should prompt a delay of cosmetic procedures until 3-6 months after the postpartum period, when these factors return to normal and the risk of complications is reduced.
The safety of many cosmetic treatments during pregnancy remains unknown. This includes microdermabrasion, chemical peels, and laser treatments. Given the increased risk of postinflammatory hyperpigmentation, as well as poor wound healing and increased risk of hypertrophic and keloidal scarring in pregnancy, these procedures are often avoided.
The safety of injectable treatments during pregnancy, such as liquid sclerosants and fillers, has not been evaluated. However, the manufacturers list pregnancy and breastfeeding as contraindications to treatment. Neurotoxins are also avoided during pregnancy and breastfeeding, based on teratogenicity in animal studies. There have been no controlled trials in humans.
Though there have been incidental exposures of botulinum toxin in women who did not know they were pregnant, no documented reports of fetal anomaly during these incidental exposures has been reported. In addition, no studies have been conducted to evaluate whether the toxin is excreted in breast milk, or when it is safe to use neurotoxins, fillers, or liquid sclerosants prior to conception.
The 10 months of pregnancy and many months of nursing can be a long stretch to wait for women who get regular cosmetic treatments. The skin changes of pregnancy can be bothersome; however, the risks of complications to the mother and the fetus outweigh the transient benefits of cosmetic procedures. The hormonal and physiologic changes of pregnancy are widely different in each woman, and sometimes the long-term side effects and complications can be completely unpredictable. Thus, patience and thorough counseling are the best strategies for treating our pregnant and nursing moms.
References
Nussbaum, R. and Benedetto, A.V. Cosmetic aspects of pregnancy. Clinics in Dermatology 2006;24:133-41.
Morgan, J.C. et al. Botulinum Toxin and Pregnancy Skinmed 2006;5:308.
Monteiro, E. Botulinum toxin A during pregnancy: a survey of treating physicians. J. Neurol. Neurosurg. Psychiatry 2006;77:117-9.
Lee, K.C., et al. Safety of cosmetic dermatologic procedures during pregnancy. Dermatol. Surg. 2013;39:1573-86.
Goldberg, D. and Maloney, M. Dermatologic surgery and cosmetic procedures during pregnancy and the postpartum period. Dermatologic Therapy 2013;26:321-30.
Dr. Talakoub and Dr. Wesley are co-contributors to a monthly Aesthetic Dermatology column in Dermatology News. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub.
What Is Your Diagnosis? New World Cutaneous Leishmaniasis
A 40-year-old man presented with a nonhealing ulcer on the right hand of 2 months’ duration. The lesion had started as a pruritic papule while he was visiting Guyana 2 months prior. The area had slowly enlarged with progressive ulceration. He denied any systemic signs including fever, chills, or weight loss, and his medical history was unremarkable. Physical examination revealed a 4-cm fungating ulceration with heaped-up borders on the dorsal aspect of the right hand.
The Diagnosis: New World Cutaneous Leishmaniasis
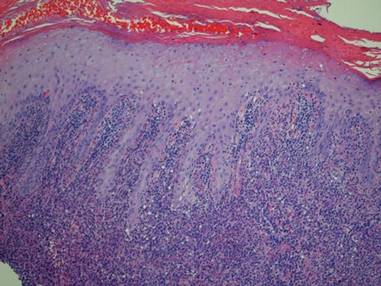
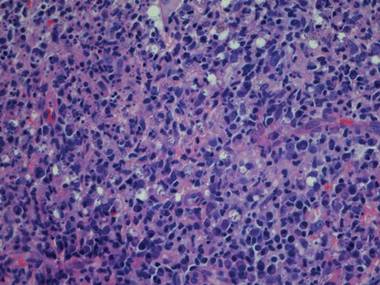
In addition to the ulceration on the right hand, a 2-cm ulcerated plaque also had developed on the right side of the chin a few days later (Figure 1). A biopsy was obtained from the lesion on the hand. Histopathologic examination revealed granulomatous inflammation with numerous histiocytes containing intracellular organisms (Figure 2). The microorganisms had pale pink nuclei with basophilic kinetoplasts (Figure 3). Tissue culture showed a mixed growth of gram-positive and gram-negative organisms but no predominant organism. Fungal and mycobacterial cultures were negative. A diagnosis of New World cutaneous leishmaniasis (CL) was made due to visualization of intracellular microorganisms containing basophilic kinetoplasts. Polymerase chain reaction on the tissue block confirmed the presence of Leishmania guyanensis.
|
Cutaneous leishmaniasis is caused by protozoa from the Leishmania species and is transmitted by the bite of the female sandfly. There are 2 classifications for the disease: Old World and New World. Old World CL is transmitted by the sandfly of the genus Phlebotomus, which is endemic in Asia, Africa, the Mediterranean, and the Middle East. New World CL is transmitted by the sandflies of the genus Lutzomyia, which are endemic in Mexico, Central America, and South America. There have been occasional cases of autochthonous transmission reported in Texas and Oklahoma,1 but there has been no known transmission of CL in Australia or the Pacific Islands.2 Human infection can be transmitted by 21 species of Leishmania and can be speciated by designated laboratories such as the US Centers for Disease Control and Prevention (CDC) and the Walter Reed Army Institute of Research (Silver Spring, Maryland) using tissue culture and polymerase chain reaction.1 The CDC can assist with the collection of specimens and supply of culture medium for cases occurring in the United States. Identification of the species is important because there are associated implications for treatment and prognosis.
There are 3 major forms of leishmaniasis: cutaneous, mucocutaneous, and visceral. Cutaneous leishmaniasis is the most common form. There are approximately 1.5 million new cases of CL each year worldwide,3 and more than 90% of these cases occur in Afghanistan, Algeria, Iran, Iraq, Saudi Arabia, Syria, Brazil, and Peru.1 New World CL is caused by 2 species complexes: Leishmania mexicana and Leishmania viannia, including the subspecies L guyanensis, which was seen in our patient.
Cutaneous leishmaniasis usually begins as a small, well-defined papule at the site of the insect bite that then enlarges and becomes a nodule or plaque. Next, the lesion becomes ulcerated with raised borders (Figure 1). The ulcer typically is painless unless there is secondary bacterial or fungal infection.3,4 The incubation period usually is 2 to 8 weeks and multiple lesions may be present, as seen in our patient.4
Old World CL can resolve without treatment, but New World CL is less likely to spontaneously resolve. Additionally, there is a greater risk for spread of the infection to mucous membranes or for systemic dissemination if New World CL is left untreated.2,5 Patients with multiple lesions (ie, ≥3); large lesions (ie, >2.5 cm); lesions on the face, hands, feet, or joints; and those who are immunocompromised should be treated promptly.2 Pentavalent antimonials (eg, meglumine antimoniate, sodium stibogluconate) are the treatment of choice for New World CL, except for infections caused by L guyanensis. The most common pentavalent antimonial agent used in the United States is sodium stibogluconate and is given at a standard intravenous dose of 20 mg antimony/kg daily for 20 days.2 The drug is only available through the CDC’s Drug Service under an Investigational New Drug protocol.1
Intramuscular pentamidine (3 mg/kg daily every other day for 4 doses) is the first-line treatment of CL caused by L guyanensis because systemic antimony usually is not effective.2,6,7 Intralesional injection with pentavalent antimonials usually is not recommended for treatment of New World CL because of the possibility of disseminated disease.2 Liposomal amphotericin B has mainly been used to treat visceral and mucosal leishmaniasis, but there have been some small studies and case reports that have showed it to be successful in treating CL.8-10 Larger controlled studies need to be performed. Oral antifungal drugs (eg, fluconazole, ketoconazole, itraconazole) also have been used to treat CL with variable results depending on the Leishmania species.11
There currently are no vaccines or drugs available to prevent against leishmaniasis. Preventive measures such as avoiding outdoor activities from dusk to dawn when sandflies are the most active, wearing protective clothing, and applying insect repellent that contains DEET (diethyltoluamide) can help reduce a traveler’s risk for becoming infected. Mosquito nets also should be treated with permethrin, which acts as an insect repellent, as sandflies are so small that they can penetrate mosquito nets.1,3,11
Acknowledgements—We would like to thank Francis Steurer, MS, and Barbara Herwaldt, MD, MPH, at the CDC in Atlanta, Georgia, for their help with the identification of the Leishmania species.
1. Herwaldt BL, Magill AJ. Infectious diseases related to travel: leishmaniasis, cutaneous. Centers for Disease Control and Prevention Web site. http://wwwnc.cdc.gov/travel/yellowbook/2010/chapter-5/cutaneous-leish maniasis.htm. Published August 1, 2013. Accessed March 5, 2015.
2. Mitropolos P, Konidas P, Durkin-Konidas M. New World cutaneous leishmaniasis: updated review of current and future diagnosis and treatment. J Am Acad Dermatol. 2010;63:309-322.
3. Hepburn NC. Cutaneous leishmaniasis: an overview. J Postgrad Med. 2003;49:50-54.
4. Markle WH, Makhoul K. Cutaneous leishmaniasis: recognition and treatment. Am Fam Physician. 2004;69:1455-1460.
5. Couppié P, Clyti E, Sainte Marie D, et al. Disseminated cutaneous leishmaniasis due to Leishmania guyanensis: case of a patient with 425 lesions. Am J Trop Med Hyg. 2004;71:558-560.
6. Nacher M, Carme B, Sainte Marie D, et al. Influence of clinical presentation on the efficacy of a short course of pentamidine in the treatment of cutaneous leishmaniasis in French Guiana. Ann Trop Med Parasitol. 2001;95:331-336.
7. Minodier P, Parola P. Cutaneous leishmaniasis treatment. Trav Med Inf Dis. 2007;5:150-158.
8. Solomon M, Baum S, Barzilai A, et al. Liposomal amphotericin B in comparison to sodium stibogluconate for cutaneous infection due to Leishmania braziliensis. J Am Acad Dermatol. 2007;56:612-616.
9. Konecny P, Stark DJ. An Australian case of New World cutaneous leishmaniasis. Med J Aust. 2007;186:315-317.
10. Brown M, Noursadeghi M, Boyle J, et al. Successful liposomal amphotericin B treatment of Leishmania braziliensis cutaneous leishmaniasis. Br J Dermatol. 2005;153:203-205.
11. Parasites: leishmaniasis. Centers for Disease Control and Prevention Web site. http://www.cdc.gov/parasites/leishmaniasis/index.html. Updated January 10, 2013. Accessed March 5, 2015.
A 40-year-old man presented with a nonhealing ulcer on the right hand of 2 months’ duration. The lesion had started as a pruritic papule while he was visiting Guyana 2 months prior. The area had slowly enlarged with progressive ulceration. He denied any systemic signs including fever, chills, or weight loss, and his medical history was unremarkable. Physical examination revealed a 4-cm fungating ulceration with heaped-up borders on the dorsal aspect of the right hand.
The Diagnosis: New World Cutaneous Leishmaniasis
In addition to the ulceration on the right hand, a 2-cm ulcerated plaque also had developed on the right side of the chin a few days later (Figure 1). A biopsy was obtained from the lesion on the hand. Histopathologic examination revealed granulomatous inflammation with numerous histiocytes containing intracellular organisms (Figure 2). The microorganisms had pale pink nuclei with basophilic kinetoplasts (Figure 3). Tissue culture showed a mixed growth of gram-positive and gram-negative organisms but no predominant organism. Fungal and mycobacterial cultures were negative. A diagnosis of New World cutaneous leishmaniasis (CL) was made due to visualization of intracellular microorganisms containing basophilic kinetoplasts. Polymerase chain reaction on the tissue block confirmed the presence of Leishmania guyanensis.
|
Cutaneous leishmaniasis is caused by protozoa from the Leishmania species and is transmitted by the bite of the female sandfly. There are 2 classifications for the disease: Old World and New World. Old World CL is transmitted by the sandfly of the genus Phlebotomus, which is endemic in Asia, Africa, the Mediterranean, and the Middle East. New World CL is transmitted by the sandflies of the genus Lutzomyia, which are endemic in Mexico, Central America, and South America. There have been occasional cases of autochthonous transmission reported in Texas and Oklahoma,1 but there has been no known transmission of CL in Australia or the Pacific Islands.2 Human infection can be transmitted by 21 species of Leishmania and can be speciated by designated laboratories such as the US Centers for Disease Control and Prevention (CDC) and the Walter Reed Army Institute of Research (Silver Spring, Maryland) using tissue culture and polymerase chain reaction.1 The CDC can assist with the collection of specimens and supply of culture medium for cases occurring in the United States. Identification of the species is important because there are associated implications for treatment and prognosis.
There are 3 major forms of leishmaniasis: cutaneous, mucocutaneous, and visceral. Cutaneous leishmaniasis is the most common form. There are approximately 1.5 million new cases of CL each year worldwide,3 and more than 90% of these cases occur in Afghanistan, Algeria, Iran, Iraq, Saudi Arabia, Syria, Brazil, and Peru.1 New World CL is caused by 2 species complexes: Leishmania mexicana and Leishmania viannia, including the subspecies L guyanensis, which was seen in our patient.
Cutaneous leishmaniasis usually begins as a small, well-defined papule at the site of the insect bite that then enlarges and becomes a nodule or plaque. Next, the lesion becomes ulcerated with raised borders (Figure 1). The ulcer typically is painless unless there is secondary bacterial or fungal infection.3,4 The incubation period usually is 2 to 8 weeks and multiple lesions may be present, as seen in our patient.4
Old World CL can resolve without treatment, but New World CL is less likely to spontaneously resolve. Additionally, there is a greater risk for spread of the infection to mucous membranes or for systemic dissemination if New World CL is left untreated.2,5 Patients with multiple lesions (ie, ≥3); large lesions (ie, >2.5 cm); lesions on the face, hands, feet, or joints; and those who are immunocompromised should be treated promptly.2 Pentavalent antimonials (eg, meglumine antimoniate, sodium stibogluconate) are the treatment of choice for New World CL, except for infections caused by L guyanensis. The most common pentavalent antimonial agent used in the United States is sodium stibogluconate and is given at a standard intravenous dose of 20 mg antimony/kg daily for 20 days.2 The drug is only available through the CDC’s Drug Service under an Investigational New Drug protocol.1
Intramuscular pentamidine (3 mg/kg daily every other day for 4 doses) is the first-line treatment of CL caused by L guyanensis because systemic antimony usually is not effective.2,6,7 Intralesional injection with pentavalent antimonials usually is not recommended for treatment of New World CL because of the possibility of disseminated disease.2 Liposomal amphotericin B has mainly been used to treat visceral and mucosal leishmaniasis, but there have been some small studies and case reports that have showed it to be successful in treating CL.8-10 Larger controlled studies need to be performed. Oral antifungal drugs (eg, fluconazole, ketoconazole, itraconazole) also have been used to treat CL with variable results depending on the Leishmania species.11
There currently are no vaccines or drugs available to prevent against leishmaniasis. Preventive measures such as avoiding outdoor activities from dusk to dawn when sandflies are the most active, wearing protective clothing, and applying insect repellent that contains DEET (diethyltoluamide) can help reduce a traveler’s risk for becoming infected. Mosquito nets also should be treated with permethrin, which acts as an insect repellent, as sandflies are so small that they can penetrate mosquito nets.1,3,11
Acknowledgements—We would like to thank Francis Steurer, MS, and Barbara Herwaldt, MD, MPH, at the CDC in Atlanta, Georgia, for their help with the identification of the Leishmania species.
A 40-year-old man presented with a nonhealing ulcer on the right hand of 2 months’ duration. The lesion had started as a pruritic papule while he was visiting Guyana 2 months prior. The area had slowly enlarged with progressive ulceration. He denied any systemic signs including fever, chills, or weight loss, and his medical history was unremarkable. Physical examination revealed a 4-cm fungating ulceration with heaped-up borders on the dorsal aspect of the right hand.
The Diagnosis: New World Cutaneous Leishmaniasis
In addition to the ulceration on the right hand, a 2-cm ulcerated plaque also had developed on the right side of the chin a few days later (Figure 1). A biopsy was obtained from the lesion on the hand. Histopathologic examination revealed granulomatous inflammation with numerous histiocytes containing intracellular organisms (Figure 2). The microorganisms had pale pink nuclei with basophilic kinetoplasts (Figure 3). Tissue culture showed a mixed growth of gram-positive and gram-negative organisms but no predominant organism. Fungal and mycobacterial cultures were negative. A diagnosis of New World cutaneous leishmaniasis (CL) was made due to visualization of intracellular microorganisms containing basophilic kinetoplasts. Polymerase chain reaction on the tissue block confirmed the presence of Leishmania guyanensis.
|
Cutaneous leishmaniasis is caused by protozoa from the Leishmania species and is transmitted by the bite of the female sandfly. There are 2 classifications for the disease: Old World and New World. Old World CL is transmitted by the sandfly of the genus Phlebotomus, which is endemic in Asia, Africa, the Mediterranean, and the Middle East. New World CL is transmitted by the sandflies of the genus Lutzomyia, which are endemic in Mexico, Central America, and South America. There have been occasional cases of autochthonous transmission reported in Texas and Oklahoma,1 but there has been no known transmission of CL in Australia or the Pacific Islands.2 Human infection can be transmitted by 21 species of Leishmania and can be speciated by designated laboratories such as the US Centers for Disease Control and Prevention (CDC) and the Walter Reed Army Institute of Research (Silver Spring, Maryland) using tissue culture and polymerase chain reaction.1 The CDC can assist with the collection of specimens and supply of culture medium for cases occurring in the United States. Identification of the species is important because there are associated implications for treatment and prognosis.
There are 3 major forms of leishmaniasis: cutaneous, mucocutaneous, and visceral. Cutaneous leishmaniasis is the most common form. There are approximately 1.5 million new cases of CL each year worldwide,3 and more than 90% of these cases occur in Afghanistan, Algeria, Iran, Iraq, Saudi Arabia, Syria, Brazil, and Peru.1 New World CL is caused by 2 species complexes: Leishmania mexicana and Leishmania viannia, including the subspecies L guyanensis, which was seen in our patient.
Cutaneous leishmaniasis usually begins as a small, well-defined papule at the site of the insect bite that then enlarges and becomes a nodule or plaque. Next, the lesion becomes ulcerated with raised borders (Figure 1). The ulcer typically is painless unless there is secondary bacterial or fungal infection.3,4 The incubation period usually is 2 to 8 weeks and multiple lesions may be present, as seen in our patient.4
Old World CL can resolve without treatment, but New World CL is less likely to spontaneously resolve. Additionally, there is a greater risk for spread of the infection to mucous membranes or for systemic dissemination if New World CL is left untreated.2,5 Patients with multiple lesions (ie, ≥3); large lesions (ie, >2.5 cm); lesions on the face, hands, feet, or joints; and those who are immunocompromised should be treated promptly.2 Pentavalent antimonials (eg, meglumine antimoniate, sodium stibogluconate) are the treatment of choice for New World CL, except for infections caused by L guyanensis. The most common pentavalent antimonial agent used in the United States is sodium stibogluconate and is given at a standard intravenous dose of 20 mg antimony/kg daily for 20 days.2 The drug is only available through the CDC’s Drug Service under an Investigational New Drug protocol.1
Intramuscular pentamidine (3 mg/kg daily every other day for 4 doses) is the first-line treatment of CL caused by L guyanensis because systemic antimony usually is not effective.2,6,7 Intralesional injection with pentavalent antimonials usually is not recommended for treatment of New World CL because of the possibility of disseminated disease.2 Liposomal amphotericin B has mainly been used to treat visceral and mucosal leishmaniasis, but there have been some small studies and case reports that have showed it to be successful in treating CL.8-10 Larger controlled studies need to be performed. Oral antifungal drugs (eg, fluconazole, ketoconazole, itraconazole) also have been used to treat CL with variable results depending on the Leishmania species.11
There currently are no vaccines or drugs available to prevent against leishmaniasis. Preventive measures such as avoiding outdoor activities from dusk to dawn when sandflies are the most active, wearing protective clothing, and applying insect repellent that contains DEET (diethyltoluamide) can help reduce a traveler’s risk for becoming infected. Mosquito nets also should be treated with permethrin, which acts as an insect repellent, as sandflies are so small that they can penetrate mosquito nets.1,3,11
Acknowledgements—We would like to thank Francis Steurer, MS, and Barbara Herwaldt, MD, MPH, at the CDC in Atlanta, Georgia, for their help with the identification of the Leishmania species.
1. Herwaldt BL, Magill AJ. Infectious diseases related to travel: leishmaniasis, cutaneous. Centers for Disease Control and Prevention Web site. http://wwwnc.cdc.gov/travel/yellowbook/2010/chapter-5/cutaneous-leish maniasis.htm. Published August 1, 2013. Accessed March 5, 2015.
2. Mitropolos P, Konidas P, Durkin-Konidas M. New World cutaneous leishmaniasis: updated review of current and future diagnosis and treatment. J Am Acad Dermatol. 2010;63:309-322.
3. Hepburn NC. Cutaneous leishmaniasis: an overview. J Postgrad Med. 2003;49:50-54.
4. Markle WH, Makhoul K. Cutaneous leishmaniasis: recognition and treatment. Am Fam Physician. 2004;69:1455-1460.
5. Couppié P, Clyti E, Sainte Marie D, et al. Disseminated cutaneous leishmaniasis due to Leishmania guyanensis: case of a patient with 425 lesions. Am J Trop Med Hyg. 2004;71:558-560.
6. Nacher M, Carme B, Sainte Marie D, et al. Influence of clinical presentation on the efficacy of a short course of pentamidine in the treatment of cutaneous leishmaniasis in French Guiana. Ann Trop Med Parasitol. 2001;95:331-336.
7. Minodier P, Parola P. Cutaneous leishmaniasis treatment. Trav Med Inf Dis. 2007;5:150-158.
8. Solomon M, Baum S, Barzilai A, et al. Liposomal amphotericin B in comparison to sodium stibogluconate for cutaneous infection due to Leishmania braziliensis. J Am Acad Dermatol. 2007;56:612-616.
9. Konecny P, Stark DJ. An Australian case of New World cutaneous leishmaniasis. Med J Aust. 2007;186:315-317.
10. Brown M, Noursadeghi M, Boyle J, et al. Successful liposomal amphotericin B treatment of Leishmania braziliensis cutaneous leishmaniasis. Br J Dermatol. 2005;153:203-205.
11. Parasites: leishmaniasis. Centers for Disease Control and Prevention Web site. http://www.cdc.gov/parasites/leishmaniasis/index.html. Updated January 10, 2013. Accessed March 5, 2015.
1. Herwaldt BL, Magill AJ. Infectious diseases related to travel: leishmaniasis, cutaneous. Centers for Disease Control and Prevention Web site. http://wwwnc.cdc.gov/travel/yellowbook/2010/chapter-5/cutaneous-leish maniasis.htm. Published August 1, 2013. Accessed March 5, 2015.
2. Mitropolos P, Konidas P, Durkin-Konidas M. New World cutaneous leishmaniasis: updated review of current and future diagnosis and treatment. J Am Acad Dermatol. 2010;63:309-322.
3. Hepburn NC. Cutaneous leishmaniasis: an overview. J Postgrad Med. 2003;49:50-54.
4. Markle WH, Makhoul K. Cutaneous leishmaniasis: recognition and treatment. Am Fam Physician. 2004;69:1455-1460.
5. Couppié P, Clyti E, Sainte Marie D, et al. Disseminated cutaneous leishmaniasis due to Leishmania guyanensis: case of a patient with 425 lesions. Am J Trop Med Hyg. 2004;71:558-560.
6. Nacher M, Carme B, Sainte Marie D, et al. Influence of clinical presentation on the efficacy of a short course of pentamidine in the treatment of cutaneous leishmaniasis in French Guiana. Ann Trop Med Parasitol. 2001;95:331-336.
7. Minodier P, Parola P. Cutaneous leishmaniasis treatment. Trav Med Inf Dis. 2007;5:150-158.
8. Solomon M, Baum S, Barzilai A, et al. Liposomal amphotericin B in comparison to sodium stibogluconate for cutaneous infection due to Leishmania braziliensis. J Am Acad Dermatol. 2007;56:612-616.
9. Konecny P, Stark DJ. An Australian case of New World cutaneous leishmaniasis. Med J Aust. 2007;186:315-317.
10. Brown M, Noursadeghi M, Boyle J, et al. Successful liposomal amphotericin B treatment of Leishmania braziliensis cutaneous leishmaniasis. Br J Dermatol. 2005;153:203-205.
11. Parasites: leishmaniasis. Centers for Disease Control and Prevention Web site. http://www.cdc.gov/parasites/leishmaniasis/index.html. Updated January 10, 2013. Accessed March 5, 2015.
Team discovers transmissible leukemia in clams

Photo by Michael J. Metzger
Results of a new study indicate that leukemia may be contagious—at least in clams.
Researchers found that outbreaks of leukemia in soft-shell clams along the east coast of North America can be explained by the spread of cancerous cells from one clam to another.
“The evidence indicates that the tumor cells themselves are contagious—that the cells can spread from one animal to another in the ocean,” said Stephen Goff, PhD, of Columbia University in New York, New York.
“We know this must be true because the genotypes of the tumor cells do not match those of the host animals that acquire the disease, but instead all derive from a single lineage of tumor cells.”
In other words, a leukemia that has killed many clams can be traced to one incidence of disease. The cancer originated in some unfortunate clam and has persisted ever since, as those cancerous cells divide, break free, and make their way to other clams.
Dr Goff and his colleagues described this discovery in Cell.
The researchers noted that only 2 other examples of transmissible cancer are known in the wild. These include the canine transmissible venereal tumor, transmitted by sexual contact, and the Tasmanian devil facial tumor disease, transmitted through biting.
In early studies of the leukemia in clams, Dr Goff and his colleagues found high levels of a particular sequence of DNA they named “Steamer.” While normal cells contain only 2 to 5 copies of Steamer, leukemic cells can have 150 copies. The researchers initially thought this difference was the result of a genetic amplification process occurring within each individual clam.
But when the team analyzed the genomes of leukemia cells collected in New York, Maine, and Prince Edward Island, they discovered something else entirely. The cancerous cells they had collected from clams living at different locations were nearly identical to one another at the genetic level.
“We were astonished to realize that the tumors did not arise from the cells of their diseased host animals, but rather from a rogue clonal cell line spreading over huge geographical distances,” Dr Goff said.
The results showed the cells can survive in seawater long enough to reach and sicken a new host. It is not yet known whether this leukemia can spread to other molluscs or whether there are mechanisms that recognize the malignant cells as foreign invaders and attack them.
Dr Goff said there is plenty the researchers don’t know about this leukemia, including when it first arose and how it spreads from one clam to another. They don’t know what role Steamer played in the cancer’s origin, if any. And they don’t know how often these sorts of cancers might arise in molluscs or other marine animals.
But the findings do suggest that transmissible cancers are more common than anyone suspected. ![]()

Photo by Michael J. Metzger
Results of a new study indicate that leukemia may be contagious—at least in clams.
Researchers found that outbreaks of leukemia in soft-shell clams along the east coast of North America can be explained by the spread of cancerous cells from one clam to another.
“The evidence indicates that the tumor cells themselves are contagious—that the cells can spread from one animal to another in the ocean,” said Stephen Goff, PhD, of Columbia University in New York, New York.
“We know this must be true because the genotypes of the tumor cells do not match those of the host animals that acquire the disease, but instead all derive from a single lineage of tumor cells.”
In other words, a leukemia that has killed many clams can be traced to one incidence of disease. The cancer originated in some unfortunate clam and has persisted ever since, as those cancerous cells divide, break free, and make their way to other clams.
Dr Goff and his colleagues described this discovery in Cell.
The researchers noted that only 2 other examples of transmissible cancer are known in the wild. These include the canine transmissible venereal tumor, transmitted by sexual contact, and the Tasmanian devil facial tumor disease, transmitted through biting.
In early studies of the leukemia in clams, Dr Goff and his colleagues found high levels of a particular sequence of DNA they named “Steamer.” While normal cells contain only 2 to 5 copies of Steamer, leukemic cells can have 150 copies. The researchers initially thought this difference was the result of a genetic amplification process occurring within each individual clam.
But when the team analyzed the genomes of leukemia cells collected in New York, Maine, and Prince Edward Island, they discovered something else entirely. The cancerous cells they had collected from clams living at different locations were nearly identical to one another at the genetic level.
“We were astonished to realize that the tumors did not arise from the cells of their diseased host animals, but rather from a rogue clonal cell line spreading over huge geographical distances,” Dr Goff said.
The results showed the cells can survive in seawater long enough to reach and sicken a new host. It is not yet known whether this leukemia can spread to other molluscs or whether there are mechanisms that recognize the malignant cells as foreign invaders and attack them.
Dr Goff said there is plenty the researchers don’t know about this leukemia, including when it first arose and how it spreads from one clam to another. They don’t know what role Steamer played in the cancer’s origin, if any. And they don’t know how often these sorts of cancers might arise in molluscs or other marine animals.
But the findings do suggest that transmissible cancers are more common than anyone suspected. ![]()

Photo by Michael J. Metzger
Results of a new study indicate that leukemia may be contagious—at least in clams.
Researchers found that outbreaks of leukemia in soft-shell clams along the east coast of North America can be explained by the spread of cancerous cells from one clam to another.
“The evidence indicates that the tumor cells themselves are contagious—that the cells can spread from one animal to another in the ocean,” said Stephen Goff, PhD, of Columbia University in New York, New York.
“We know this must be true because the genotypes of the tumor cells do not match those of the host animals that acquire the disease, but instead all derive from a single lineage of tumor cells.”
In other words, a leukemia that has killed many clams can be traced to one incidence of disease. The cancer originated in some unfortunate clam and has persisted ever since, as those cancerous cells divide, break free, and make their way to other clams.
Dr Goff and his colleagues described this discovery in Cell.
The researchers noted that only 2 other examples of transmissible cancer are known in the wild. These include the canine transmissible venereal tumor, transmitted by sexual contact, and the Tasmanian devil facial tumor disease, transmitted through biting.
In early studies of the leukemia in clams, Dr Goff and his colleagues found high levels of a particular sequence of DNA they named “Steamer.” While normal cells contain only 2 to 5 copies of Steamer, leukemic cells can have 150 copies. The researchers initially thought this difference was the result of a genetic amplification process occurring within each individual clam.
But when the team analyzed the genomes of leukemia cells collected in New York, Maine, and Prince Edward Island, they discovered something else entirely. The cancerous cells they had collected from clams living at different locations were nearly identical to one another at the genetic level.
“We were astonished to realize that the tumors did not arise from the cells of their diseased host animals, but rather from a rogue clonal cell line spreading over huge geographical distances,” Dr Goff said.
The results showed the cells can survive in seawater long enough to reach and sicken a new host. It is not yet known whether this leukemia can spread to other molluscs or whether there are mechanisms that recognize the malignant cells as foreign invaders and attack them.
Dr Goff said there is plenty the researchers don’t know about this leukemia, including when it first arose and how it spreads from one clam to another. They don’t know what role Steamer played in the cancer’s origin, if any. And they don’t know how often these sorts of cancers might arise in molluscs or other marine animals.
But the findings do suggest that transmissible cancers are more common than anyone suspected. ![]()
Regulatory monocytes can inhibit GVHD

Image courtesy of PLOS ONE
Researchers believe they have identified a population of monocytes that can protect against graft-vs-host disease (GVHD).
While analyzing peripheral blood stem cells from healthy donors, the team found CD34+ cells with the features of mature monocytes.
They said these cells are transcriptionally distinct from myeloid and monocytic precursors, but they are similar to mature monocytes and endowed with immunosuppressive properties.
Maud D’Aveni, MD, of INSERM in Paris, France, and colleagues described these cells and their abilities in Science Translational Medicine.
The researchers found that granulocyte colony-stimulating factor mobilized the monocytes, which strongly suppressed the activation of donor T cells.
In fact, patients who received peripheral blood stem cells containing high levels of the monocytes had lower rates of GVHD.
Experiments in mice revealed that the monocytes release nitric oxide, which triggers reactive T cells to self-destruct and activates a subset of T cells that suppress the immune system to produce immune tolerance.
The researchers said these results indicate that boosting this population of monocytes could help prevent GVHD in transplant recipients. ![]()

Image courtesy of PLOS ONE
Researchers believe they have identified a population of monocytes that can protect against graft-vs-host disease (GVHD).
While analyzing peripheral blood stem cells from healthy donors, the team found CD34+ cells with the features of mature monocytes.
They said these cells are transcriptionally distinct from myeloid and monocytic precursors, but they are similar to mature monocytes and endowed with immunosuppressive properties.
Maud D’Aveni, MD, of INSERM in Paris, France, and colleagues described these cells and their abilities in Science Translational Medicine.
The researchers found that granulocyte colony-stimulating factor mobilized the monocytes, which strongly suppressed the activation of donor T cells.
In fact, patients who received peripheral blood stem cells containing high levels of the monocytes had lower rates of GVHD.
Experiments in mice revealed that the monocytes release nitric oxide, which triggers reactive T cells to self-destruct and activates a subset of T cells that suppress the immune system to produce immune tolerance.
The researchers said these results indicate that boosting this population of monocytes could help prevent GVHD in transplant recipients. ![]()

Image courtesy of PLOS ONE
Researchers believe they have identified a population of monocytes that can protect against graft-vs-host disease (GVHD).
While analyzing peripheral blood stem cells from healthy donors, the team found CD34+ cells with the features of mature monocytes.
They said these cells are transcriptionally distinct from myeloid and monocytic precursors, but they are similar to mature monocytes and endowed with immunosuppressive properties.
Maud D’Aveni, MD, of INSERM in Paris, France, and colleagues described these cells and their abilities in Science Translational Medicine.
The researchers found that granulocyte colony-stimulating factor mobilized the monocytes, which strongly suppressed the activation of donor T cells.
In fact, patients who received peripheral blood stem cells containing high levels of the monocytes had lower rates of GVHD.
Experiments in mice revealed that the monocytes release nitric oxide, which triggers reactive T cells to self-destruct and activates a subset of T cells that suppress the immune system to produce immune tolerance.
The researchers said these results indicate that boosting this population of monocytes could help prevent GVHD in transplant recipients. ![]()
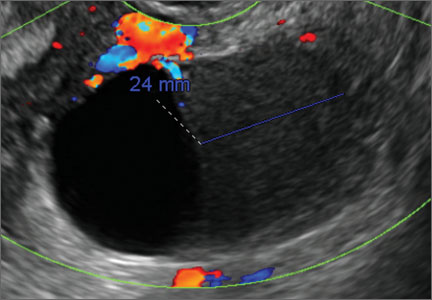
Imaging the endometrioma and mature cystic teratoma
The preferred imaging method to evaluate the majority of adnexal cysts is ultrasonography, which can help characterize the cyst type. Common benign adnexal cyst types include simple, hemorrhagic, endometrioma, and mature teratoma (dermoid cyst). In this part 2 of a 4-part series on cystic adnexal pathology, we focus on imaging signs for, and follow-up of, endometriomas and mature teratomas.
Endometriomas
Endometriomas are common, typically benign, cysts that produce homogenous, low-level internal echoes and a “ground glass” appearance on ultrasonography. No internal flow is apparent on color Doppler. The presence of tiny echogenic wall foci can distinguish an endometrioma from a hemorrhagic cyst.
Rarely, endometriomas may undergo malignant transformation. Usually this occurs with cysts greater than 9 cm and in patients aged 45 years or older. A malignancy often exhibits rapid growth or the development of a solid nodule with flow on color Doppler.
Management
Although surgery remains the first-line management for women with symptomatic or enlarging endometriomas, there appears to be a role for sonographic observation, with continuous progestational treatment, in women with small (< 5 cm) asymptomatic endometriomas.
The Society of Radiologists in Ultrasound 2010 Consensus Conference Statement recommended1:
- Short-interval follow-up (6 to 12 weeks) in reproductive-aged women to ensure acute hemorrhagic cysts are not mistaken for endometriomas
- If not removed surgically, sonographic follow-up is recommended, with frequency of follow up based on patient age and symptoms and cyst size and characteristics.
In FIGURES 1 through 11 (slides of image collections), we present several cases, including one of a 25-year-old patient presenting with pelvic pain and dyspareunia who was later found to have bilateral endometriomas.
Mature teratomas
Mature cystic teratomas display several telltale signs on imaging, including:
- hyperechoic lines/dots (“dermoid mesh”) corresponding to hair/skeletal components
- “Rokitanski nodule” – a peripherally placed mass of sebum, bones, and hair
- posterior acoustic shadowing
- cystic or floating spherical structures
- no internal flow on color Doppler
Rarely, dermoid cysts may undergo malignant transformation. Usually this occurs in cysts greater than 10 cm and in patients aged 50 years or older. Internal flow on color Doppler, branching, or invasion into adjacent structures can indicate malignancy.
Management
The traditional treatment for dermoid cysts is surgical. However, given the ability for accurate diagnosis with vaginal ultrasonography, there appears to be a role for sonographic observation in asymptomatic women with small dermoids.2
If the cyst is not surgically removed, the Society of Radiologists in Ultrasound 2010 Consensus Conference Statement recommended initial sonographic follow up at no more than 6 months to 1 year to ensure no change in size or internal architecture.1
In FIGURES 12 through 24 below (slides of image collections), we offer imaging from the case presentation and follow-up of a 19-year-old patient with pelvic pain who has a history of ovarian cystectomy for dermoid cyst, as well as 6 additional case illustrations.
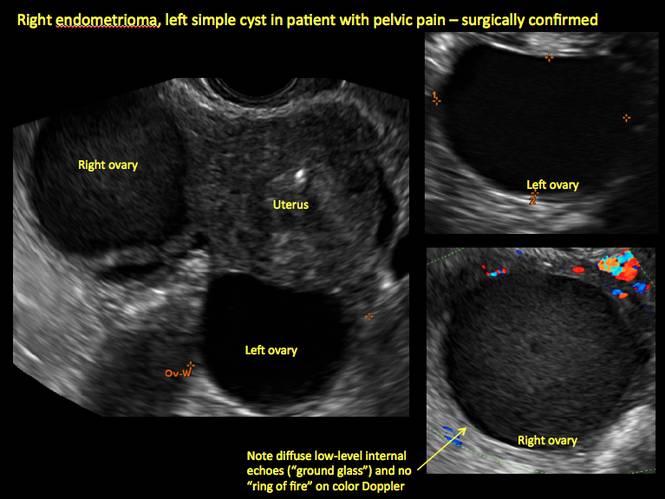
Figure 1
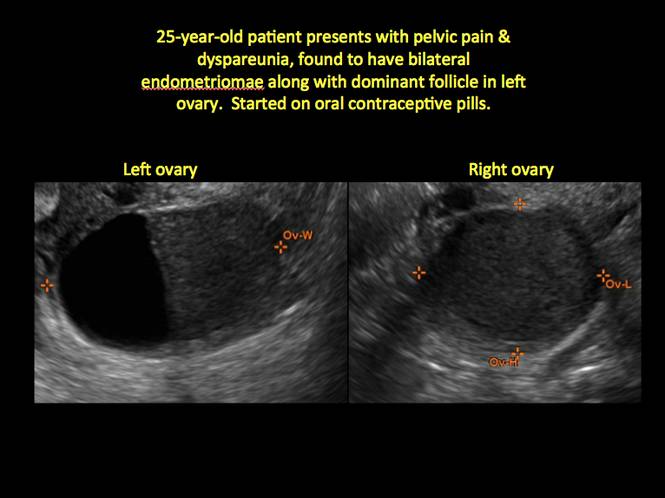
Figure 2
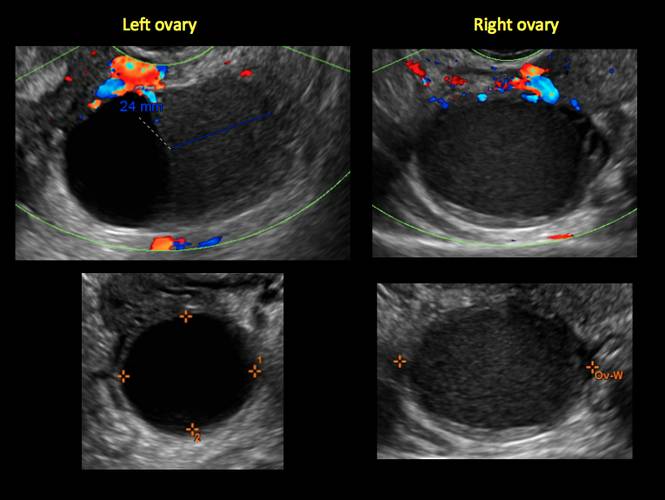
Figure 3
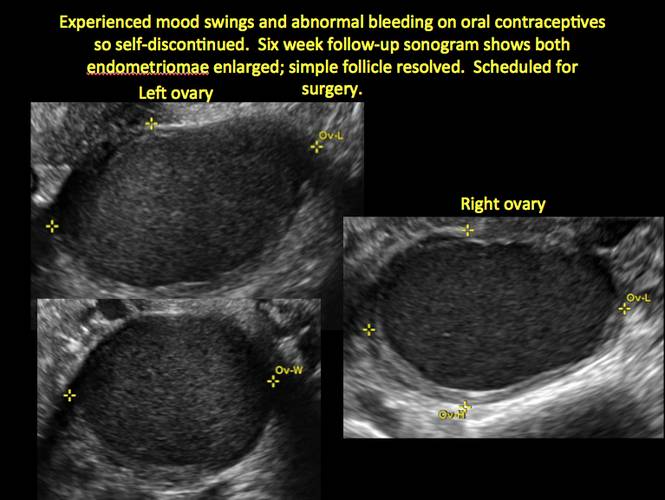
Figure 4
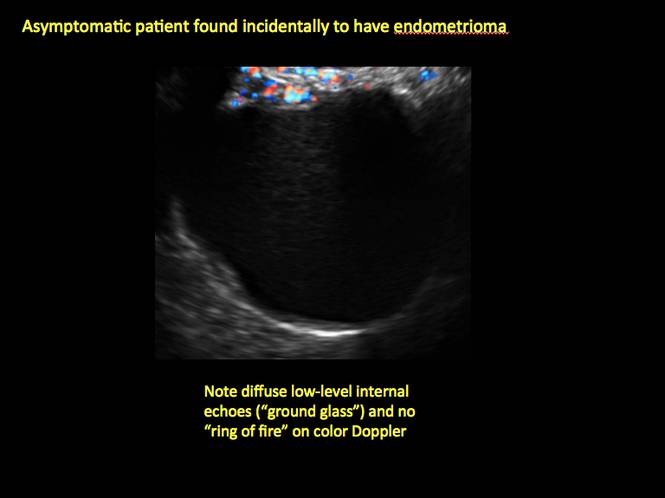
Figure 5
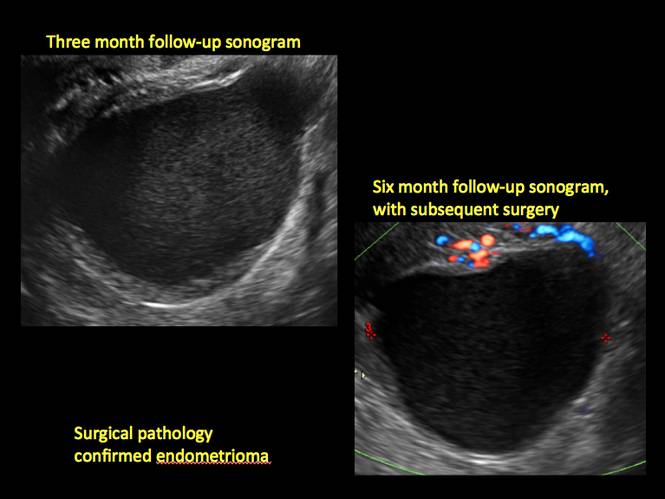
Figure 6
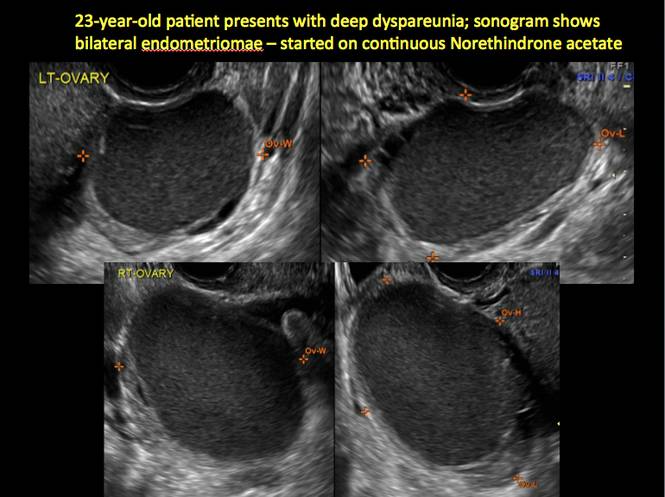
Figure 7
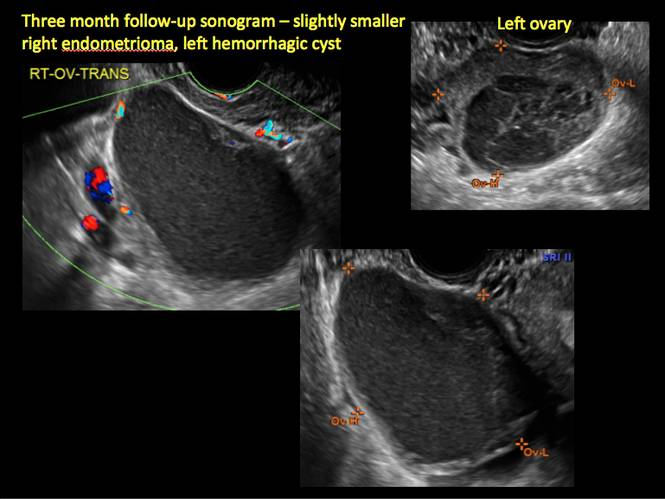
Figure 8
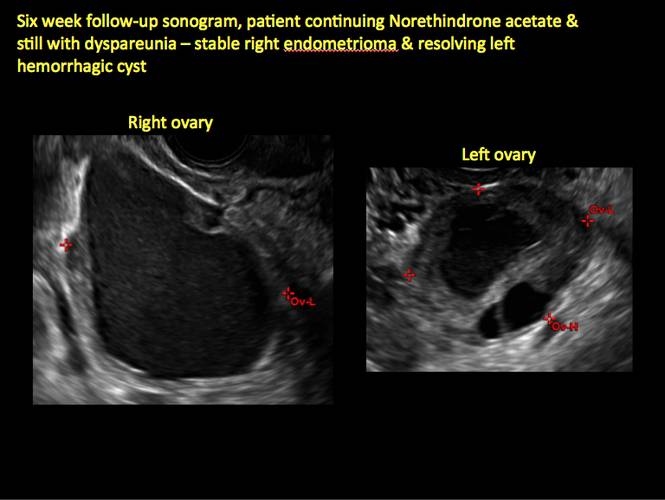
Figure 9
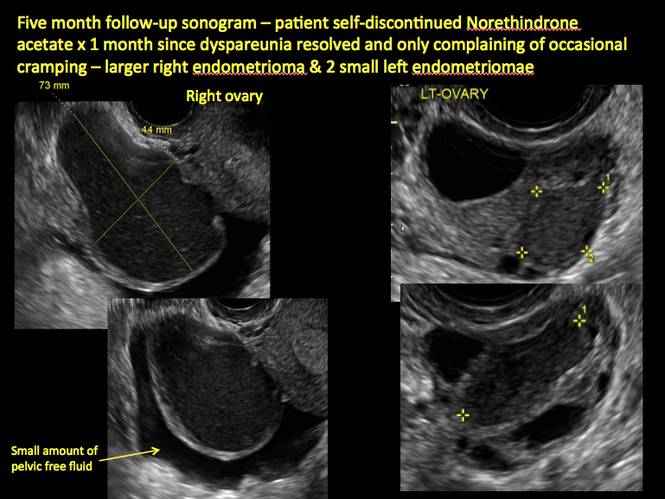
Figure 10
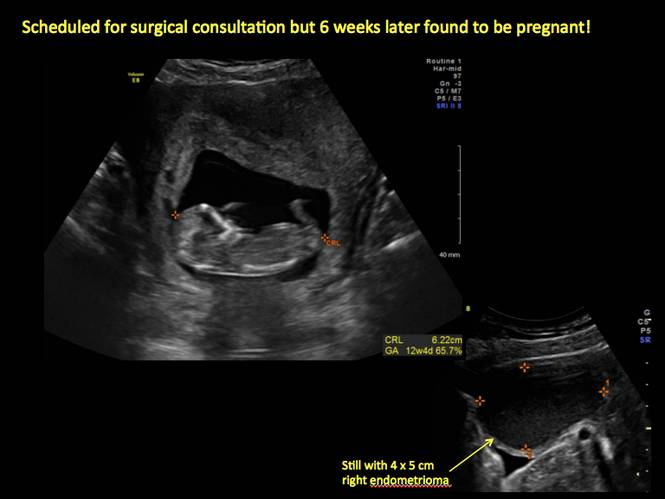
Figure 11
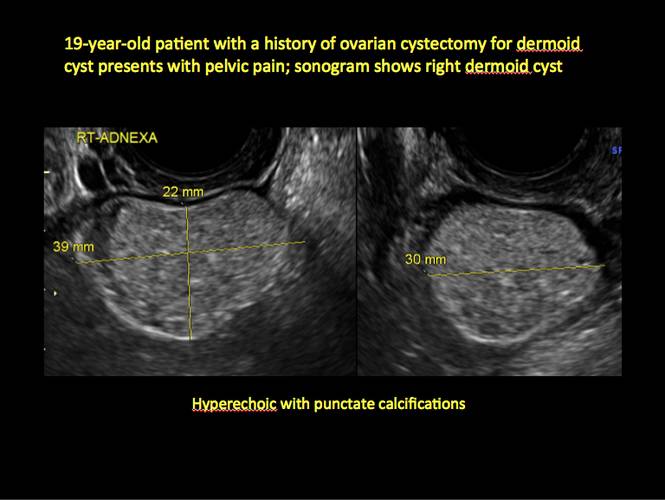
Figure 12

Figure 13
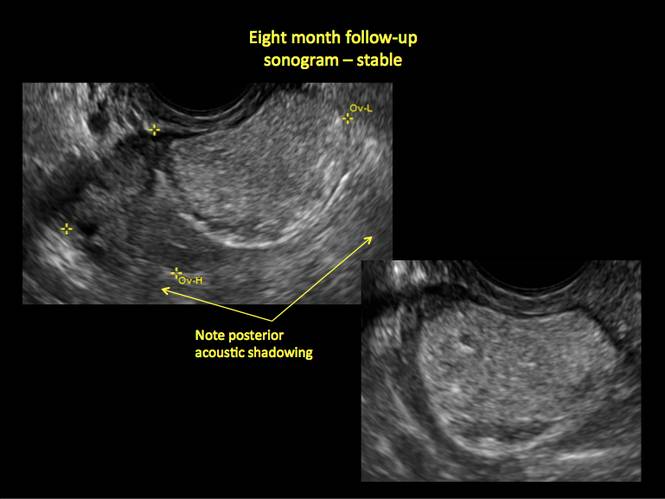
Figure 14
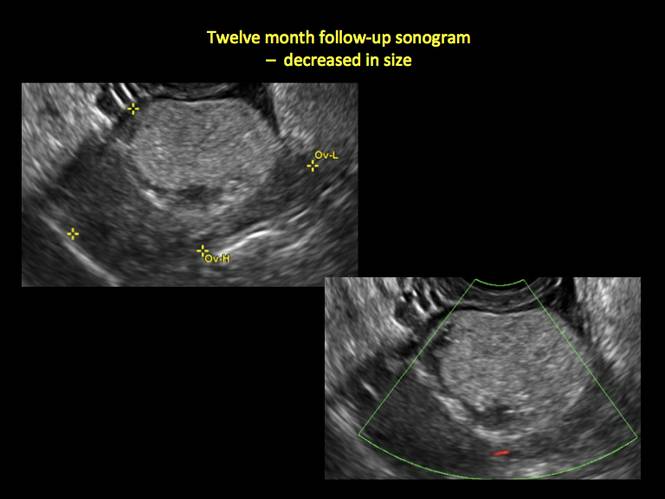
Figure 15
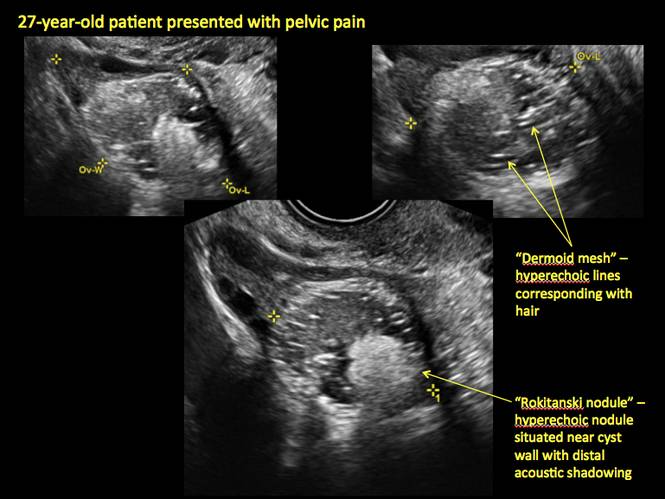
Figure 16
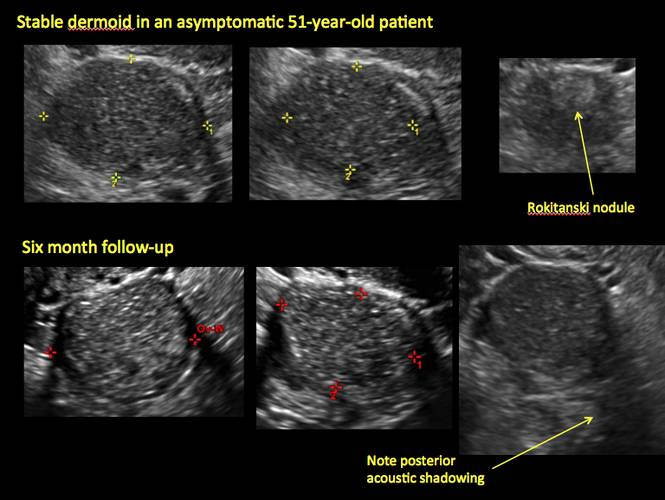
Figure 17
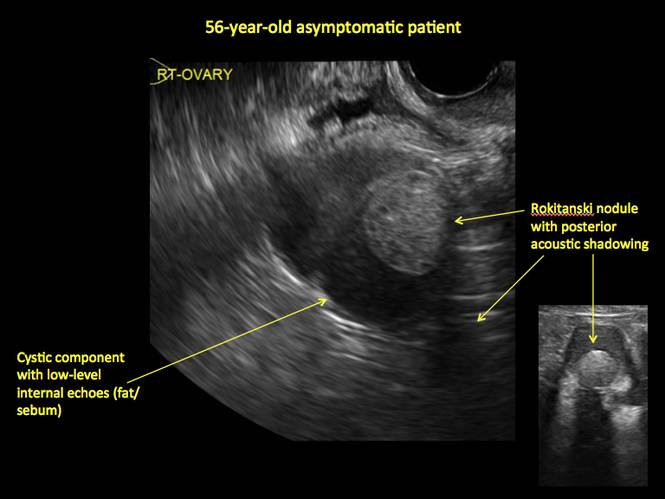
Figure 18
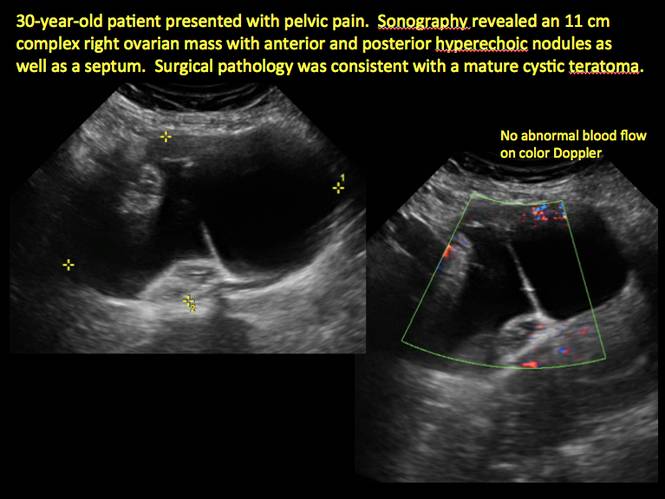
Figure 19
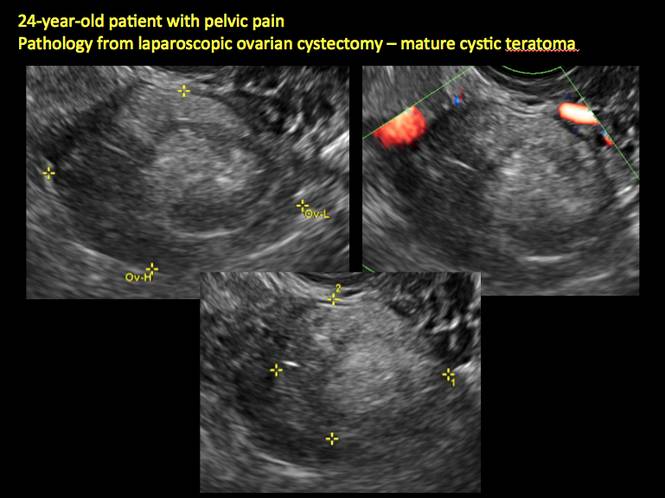
Figure 20
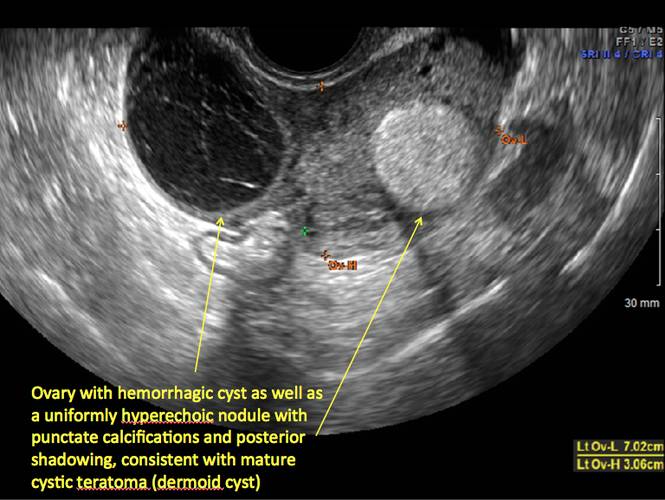
Figure 21
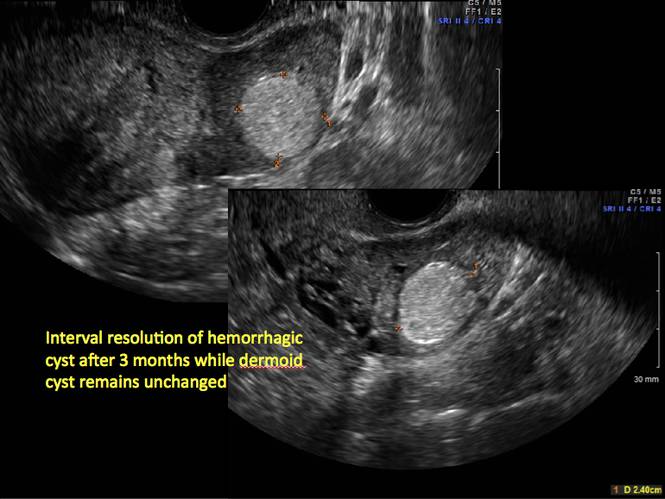
Figure 22
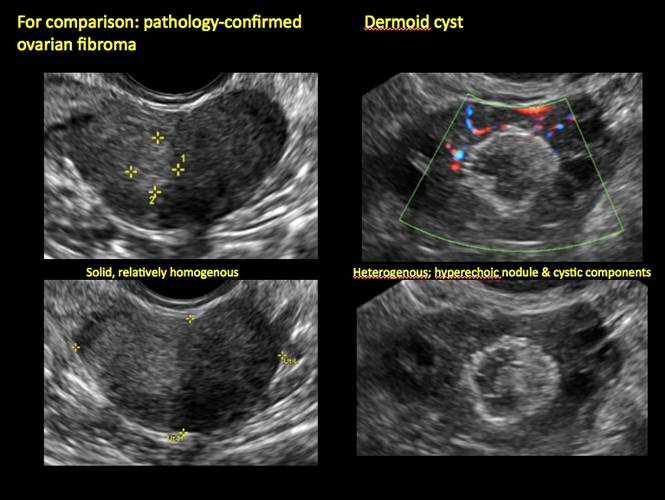
Figure 23
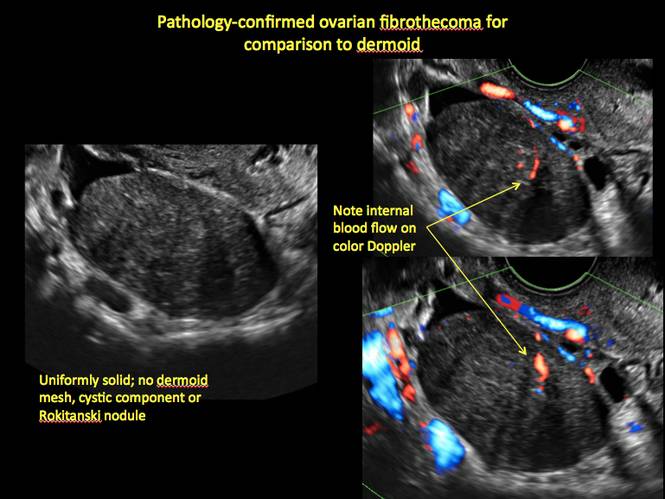
Figure 24
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Levine D, Brown DL, Andreotti RF, et al. Management of asymptomatic ovarian and other adnexal cysts imaged at US: Society of Radiologists in Ultrasound Consensus Conference Statement. Radiology. 2010;256(3):943–954.
2. Hoo WL, Yazbek WL, Holland T, Mavrelos D, Tong EN, Jurkovic D. Expectant management of ultrasonically diagnosed ovarian dermoid cysts: is it possible to predict outcome? Ultrasound Obstet Gynecol. 2010;36(2): 235–240.
The preferred imaging method to evaluate the majority of adnexal cysts is ultrasonography, which can help characterize the cyst type. Common benign adnexal cyst types include simple, hemorrhagic, endometrioma, and mature teratoma (dermoid cyst). In this part 2 of a 4-part series on cystic adnexal pathology, we focus on imaging signs for, and follow-up of, endometriomas and mature teratomas.
Endometriomas
Endometriomas are common, typically benign, cysts that produce homogenous, low-level internal echoes and a “ground glass” appearance on ultrasonography. No internal flow is apparent on color Doppler. The presence of tiny echogenic wall foci can distinguish an endometrioma from a hemorrhagic cyst.
Rarely, endometriomas may undergo malignant transformation. Usually this occurs with cysts greater than 9 cm and in patients aged 45 years or older. A malignancy often exhibits rapid growth or the development of a solid nodule with flow on color Doppler.
Management
Although surgery remains the first-line management for women with symptomatic or enlarging endometriomas, there appears to be a role for sonographic observation, with continuous progestational treatment, in women with small (< 5 cm) asymptomatic endometriomas.
The Society of Radiologists in Ultrasound 2010 Consensus Conference Statement recommended1:
- Short-interval follow-up (6 to 12 weeks) in reproductive-aged women to ensure acute hemorrhagic cysts are not mistaken for endometriomas
- If not removed surgically, sonographic follow-up is recommended, with frequency of follow up based on patient age and symptoms and cyst size and characteristics.
In FIGURES 1 through 11 (slides of image collections), we present several cases, including one of a 25-year-old patient presenting with pelvic pain and dyspareunia who was later found to have bilateral endometriomas.
Mature teratomas
Mature cystic teratomas display several telltale signs on imaging, including:
- hyperechoic lines/dots (“dermoid mesh”) corresponding to hair/skeletal components
- “Rokitanski nodule” – a peripherally placed mass of sebum, bones, and hair
- posterior acoustic shadowing
- cystic or floating spherical structures
- no internal flow on color Doppler
Rarely, dermoid cysts may undergo malignant transformation. Usually this occurs in cysts greater than 10 cm and in patients aged 50 years or older. Internal flow on color Doppler, branching, or invasion into adjacent structures can indicate malignancy.
Management
The traditional treatment for dermoid cysts is surgical. However, given the ability for accurate diagnosis with vaginal ultrasonography, there appears to be a role for sonographic observation in asymptomatic women with small dermoids.2
If the cyst is not surgically removed, the Society of Radiologists in Ultrasound 2010 Consensus Conference Statement recommended initial sonographic follow up at no more than 6 months to 1 year to ensure no change in size or internal architecture.1
In FIGURES 12 through 24 below (slides of image collections), we offer imaging from the case presentation and follow-up of a 19-year-old patient with pelvic pain who has a history of ovarian cystectomy for dermoid cyst, as well as 6 additional case illustrations.
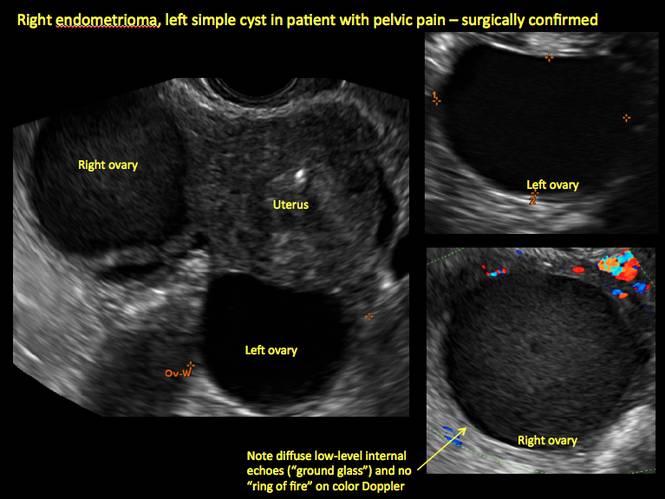
Figure 1
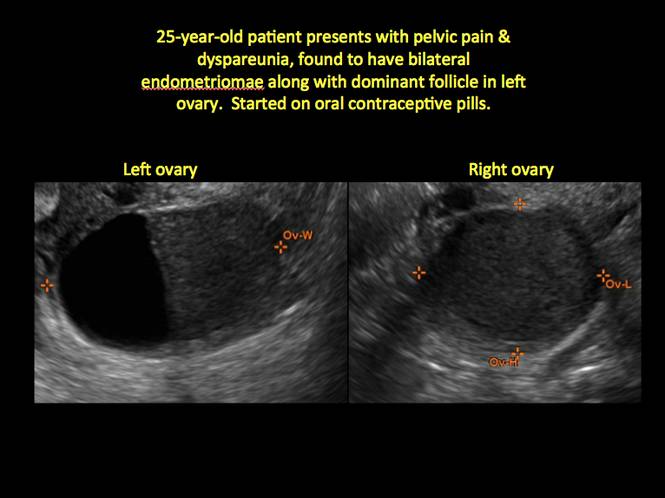
Figure 2
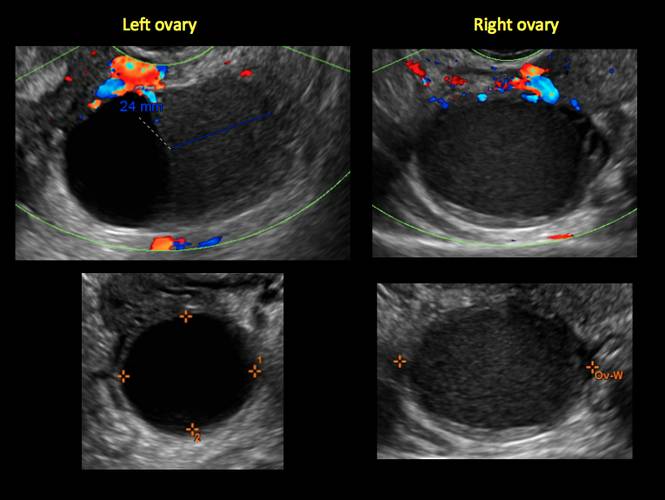
Figure 3
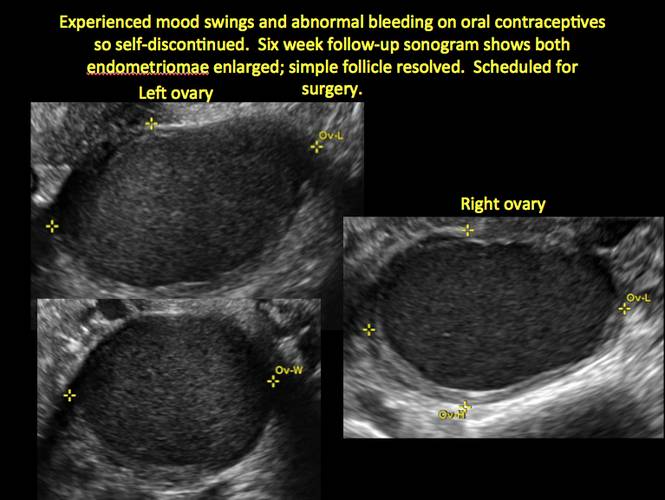
Figure 4
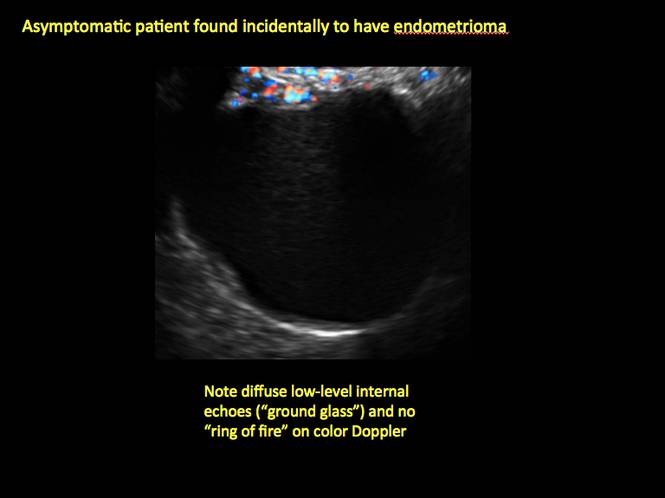
Figure 5
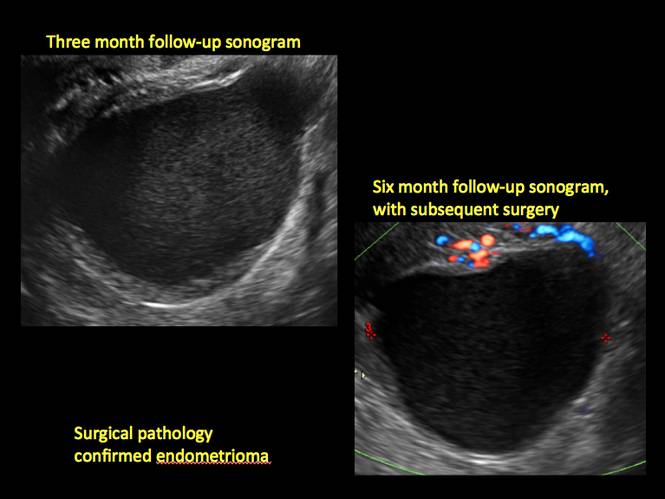
Figure 6
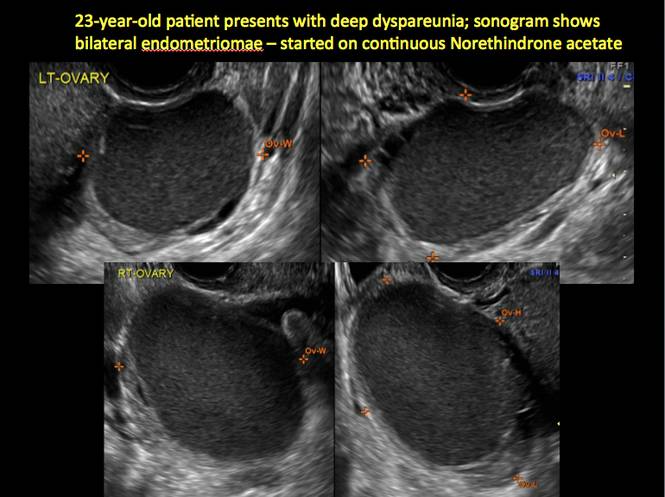
Figure 7
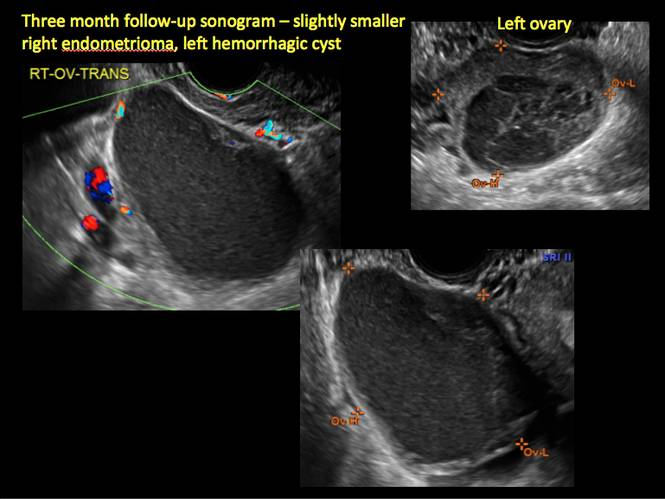
Figure 8
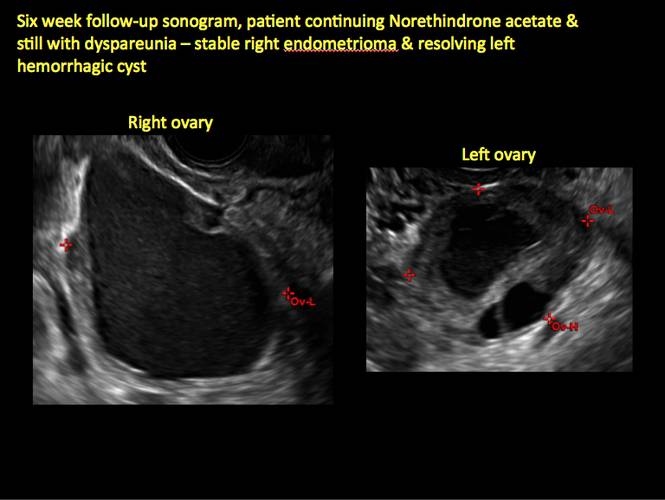
Figure 9
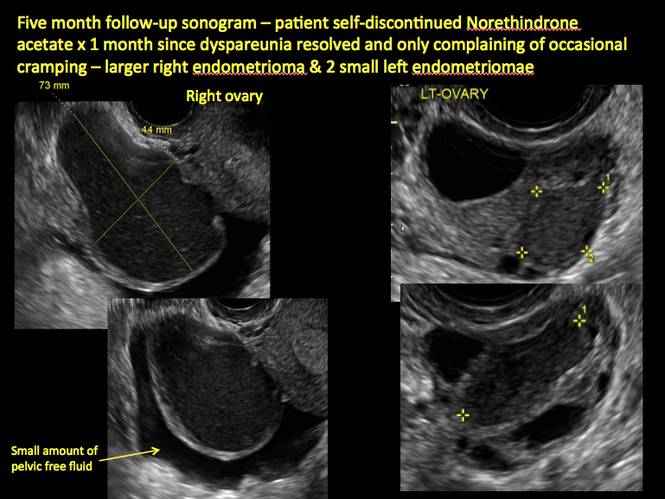
Figure 10
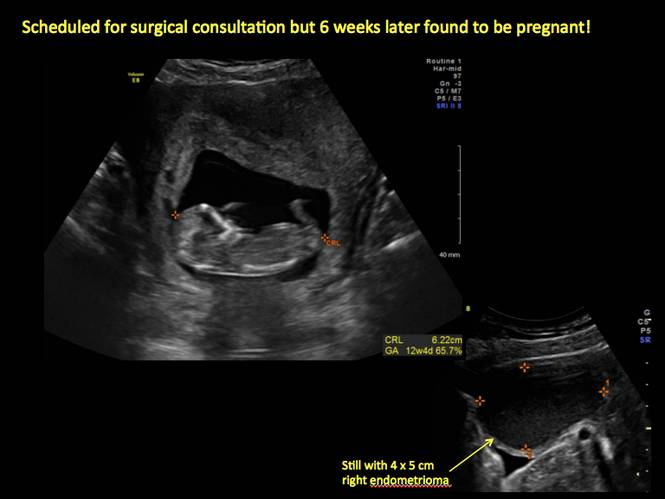
Figure 11
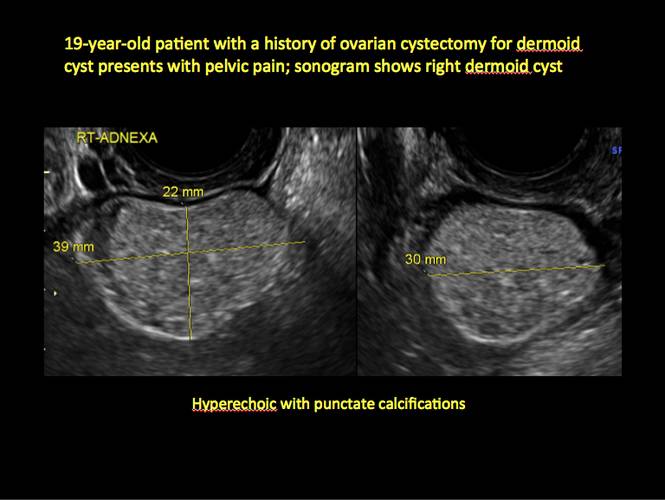
Figure 12

Figure 13
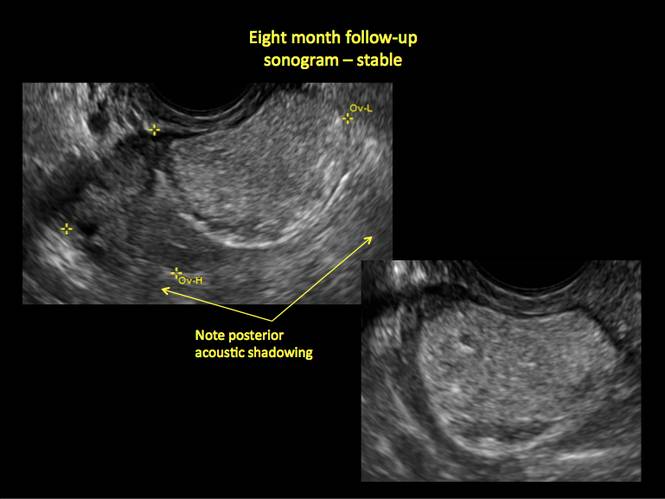
Figure 14
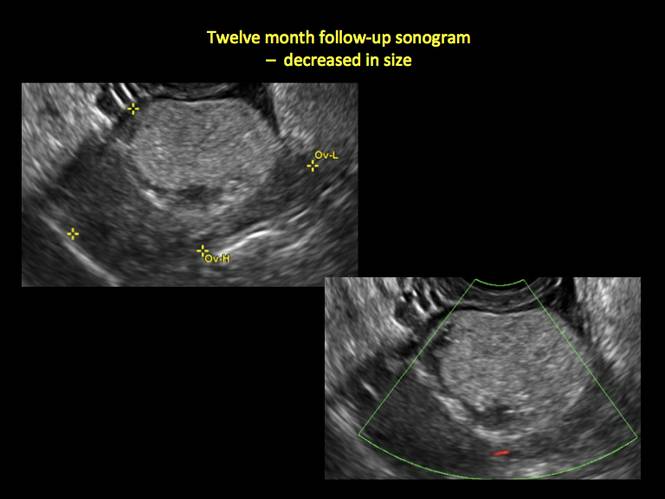
Figure 15
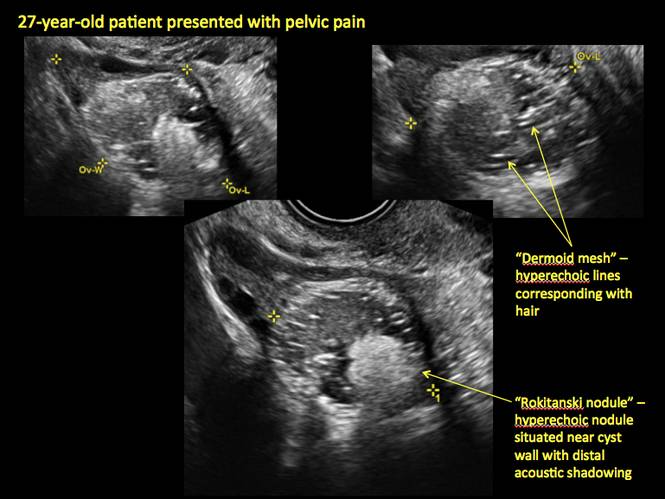
Figure 16
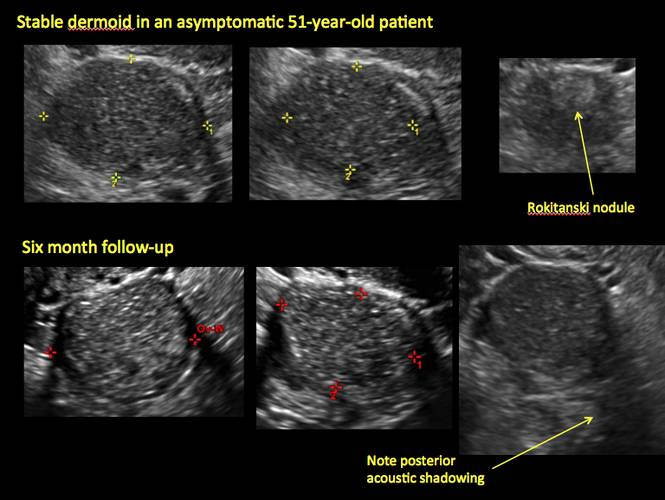
Figure 17
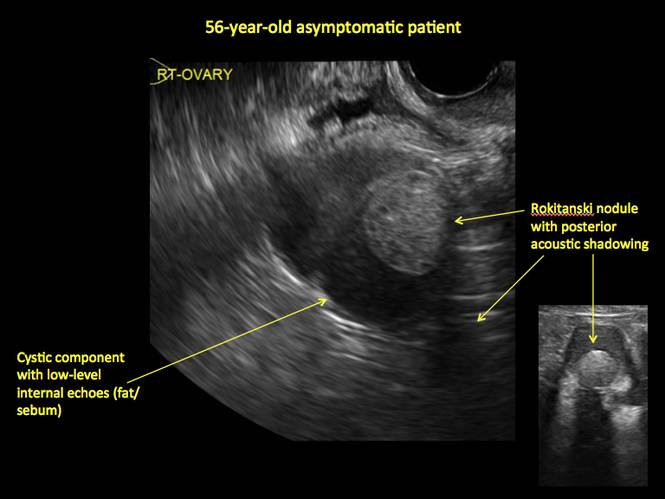
Figure 18
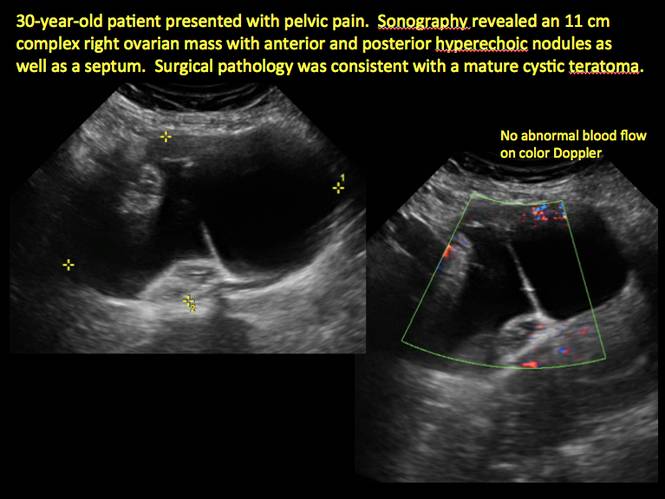
Figure 19
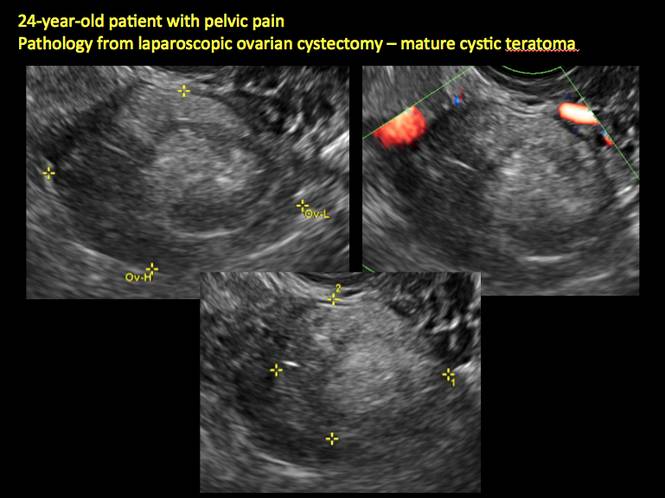
Figure 20
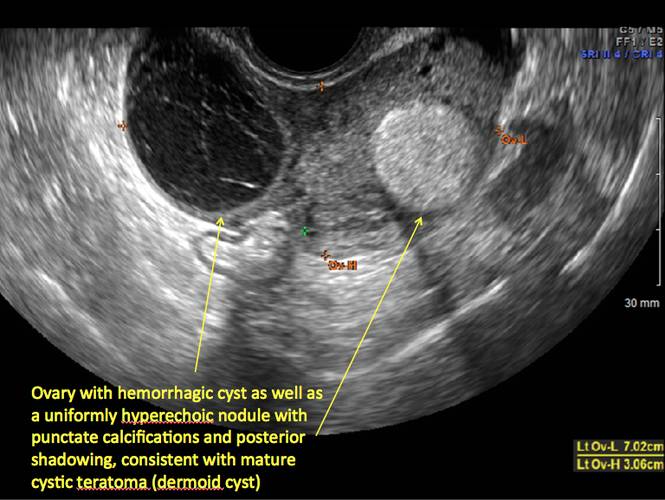
Figure 21
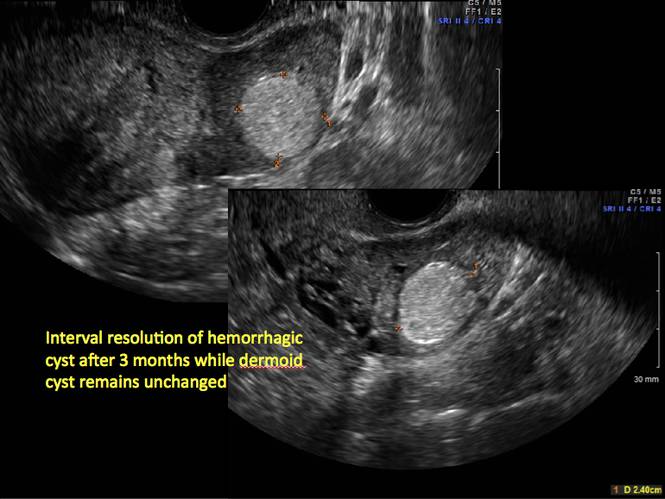
Figure 22
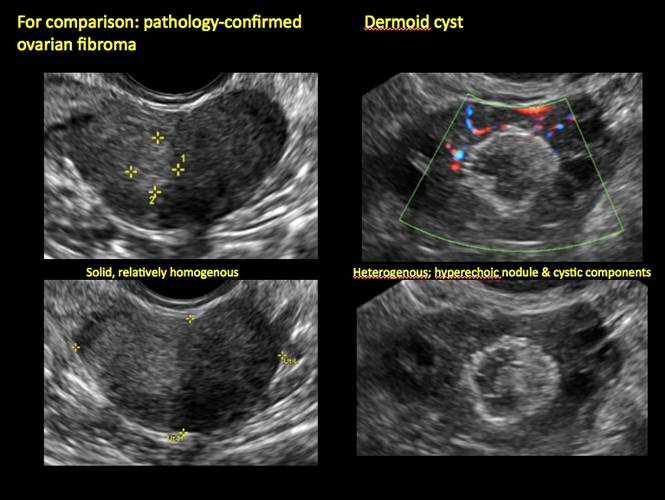
Figure 23
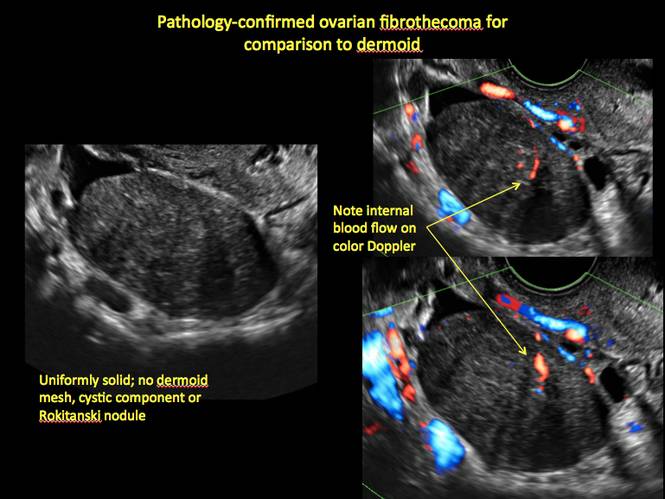
Figure 24
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The preferred imaging method to evaluate the majority of adnexal cysts is ultrasonography, which can help characterize the cyst type. Common benign adnexal cyst types include simple, hemorrhagic, endometrioma, and mature teratoma (dermoid cyst). In this part 2 of a 4-part series on cystic adnexal pathology, we focus on imaging signs for, and follow-up of, endometriomas and mature teratomas.
Endometriomas
Endometriomas are common, typically benign, cysts that produce homogenous, low-level internal echoes and a “ground glass” appearance on ultrasonography. No internal flow is apparent on color Doppler. The presence of tiny echogenic wall foci can distinguish an endometrioma from a hemorrhagic cyst.
Rarely, endometriomas may undergo malignant transformation. Usually this occurs with cysts greater than 9 cm and in patients aged 45 years or older. A malignancy often exhibits rapid growth or the development of a solid nodule with flow on color Doppler.
Management
Although surgery remains the first-line management for women with symptomatic or enlarging endometriomas, there appears to be a role for sonographic observation, with continuous progestational treatment, in women with small (< 5 cm) asymptomatic endometriomas.
The Society of Radiologists in Ultrasound 2010 Consensus Conference Statement recommended1:
- Short-interval follow-up (6 to 12 weeks) in reproductive-aged women to ensure acute hemorrhagic cysts are not mistaken for endometriomas
- If not removed surgically, sonographic follow-up is recommended, with frequency of follow up based on patient age and symptoms and cyst size and characteristics.
In FIGURES 1 through 11 (slides of image collections), we present several cases, including one of a 25-year-old patient presenting with pelvic pain and dyspareunia who was later found to have bilateral endometriomas.
Mature teratomas
Mature cystic teratomas display several telltale signs on imaging, including:
- hyperechoic lines/dots (“dermoid mesh”) corresponding to hair/skeletal components
- “Rokitanski nodule” – a peripherally placed mass of sebum, bones, and hair
- posterior acoustic shadowing
- cystic or floating spherical structures
- no internal flow on color Doppler
Rarely, dermoid cysts may undergo malignant transformation. Usually this occurs in cysts greater than 10 cm and in patients aged 50 years or older. Internal flow on color Doppler, branching, or invasion into adjacent structures can indicate malignancy.
Management
The traditional treatment for dermoid cysts is surgical. However, given the ability for accurate diagnosis with vaginal ultrasonography, there appears to be a role for sonographic observation in asymptomatic women with small dermoids.2
If the cyst is not surgically removed, the Society of Radiologists in Ultrasound 2010 Consensus Conference Statement recommended initial sonographic follow up at no more than 6 months to 1 year to ensure no change in size or internal architecture.1
In FIGURES 12 through 24 below (slides of image collections), we offer imaging from the case presentation and follow-up of a 19-year-old patient with pelvic pain who has a history of ovarian cystectomy for dermoid cyst, as well as 6 additional case illustrations.
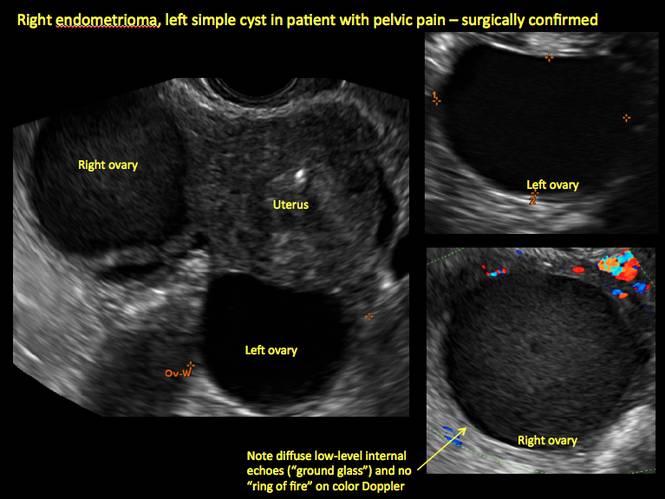
Figure 1
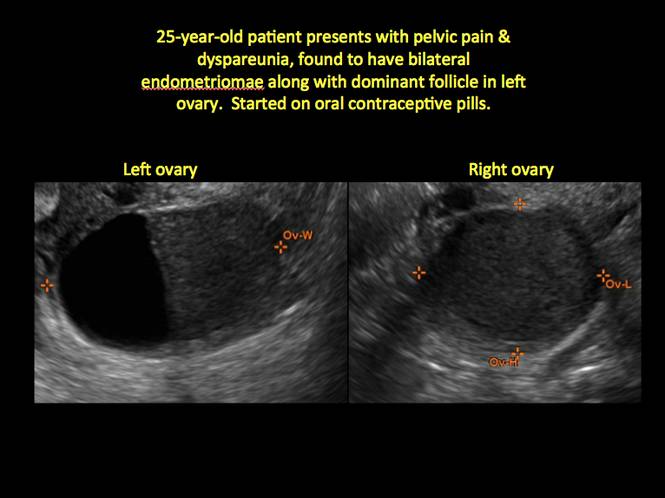
Figure 2
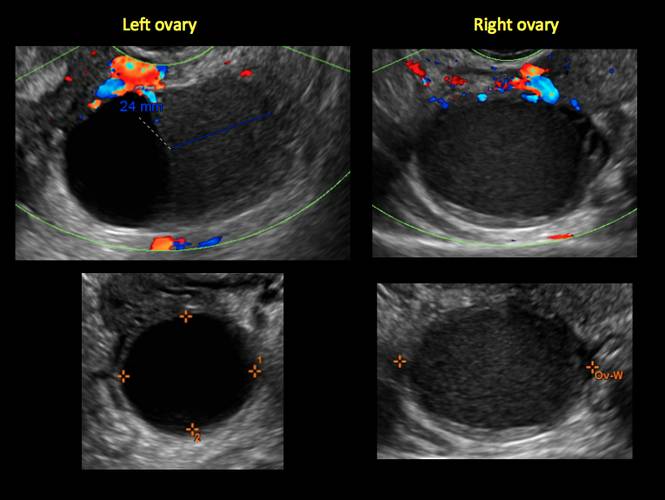
Figure 3
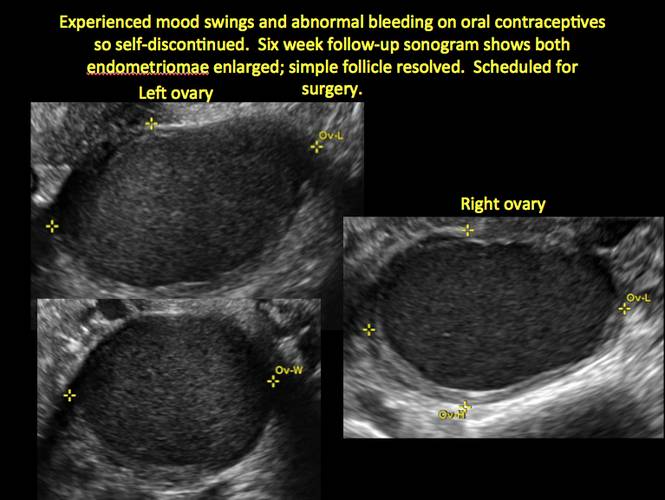
Figure 4
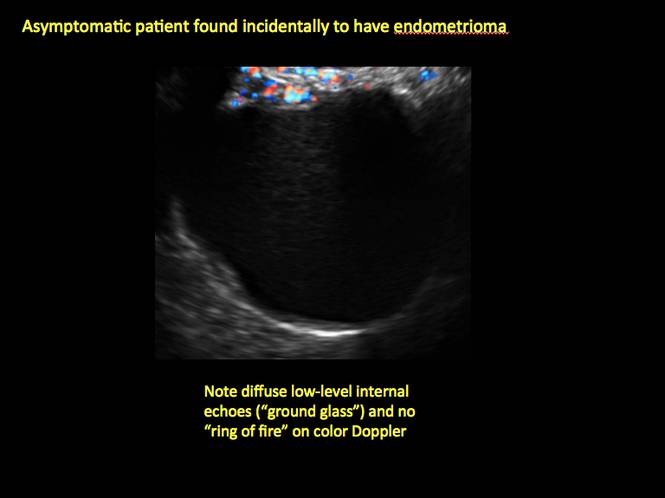
Figure 5
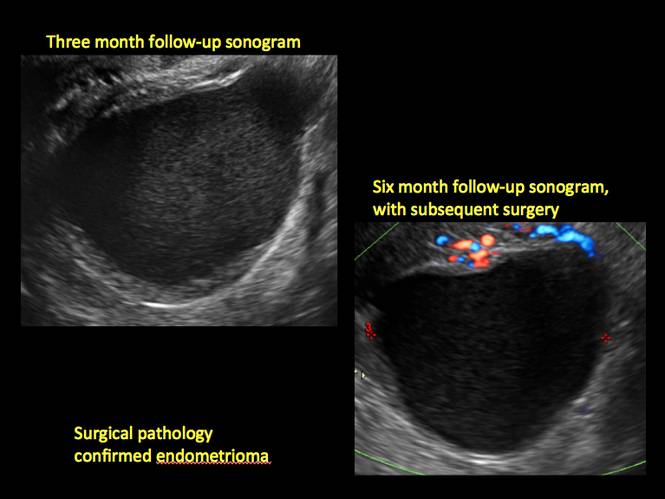
Figure 6
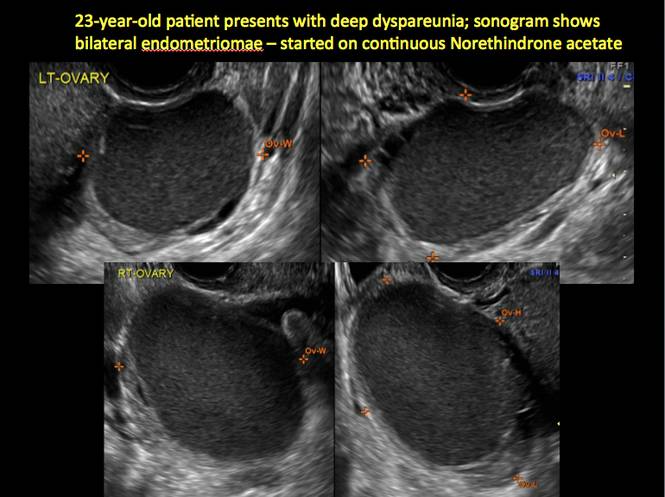
Figure 7
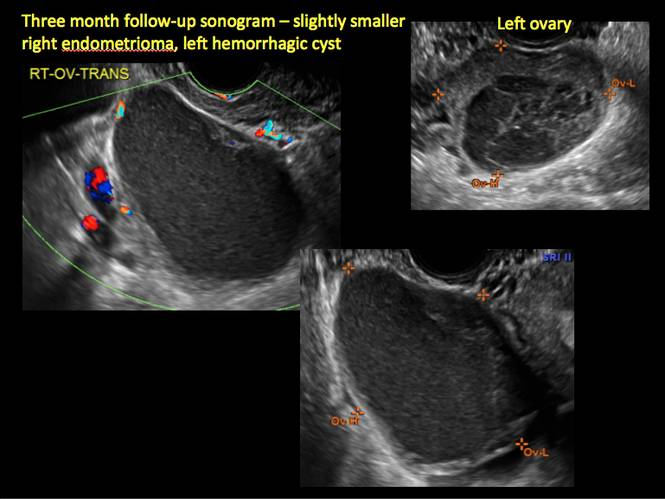
Figure 8
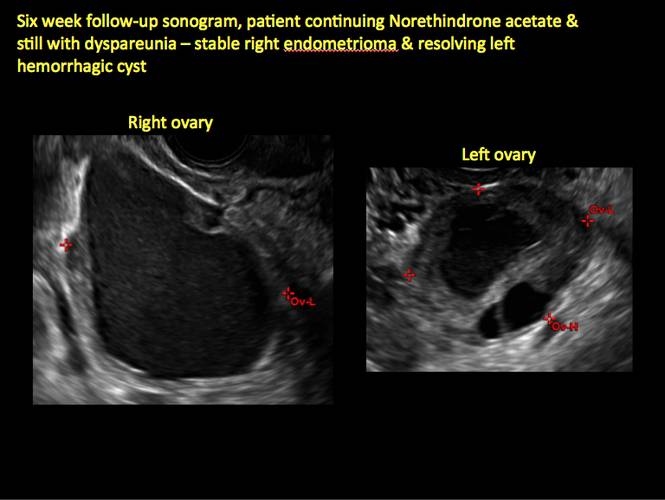
Figure 9
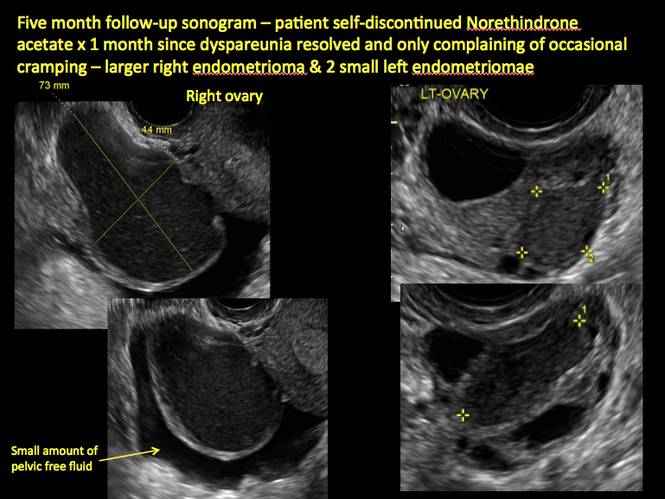
Figure 10
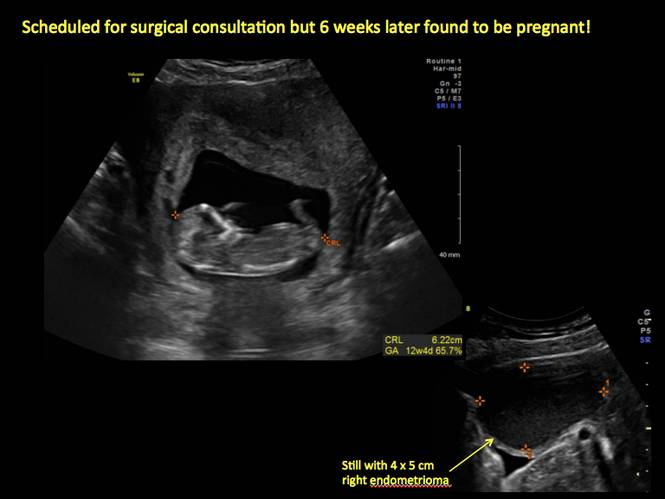
Figure 11
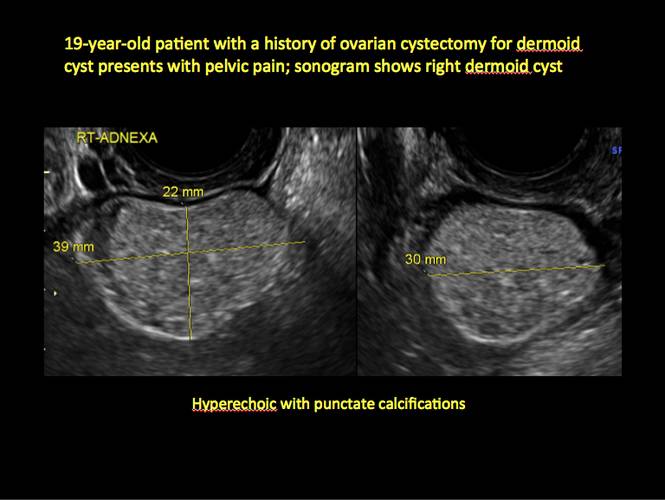
Figure 12

Figure 13
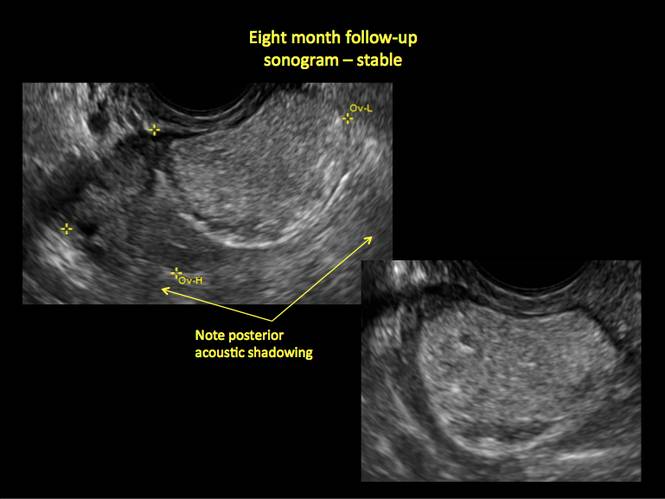
Figure 14
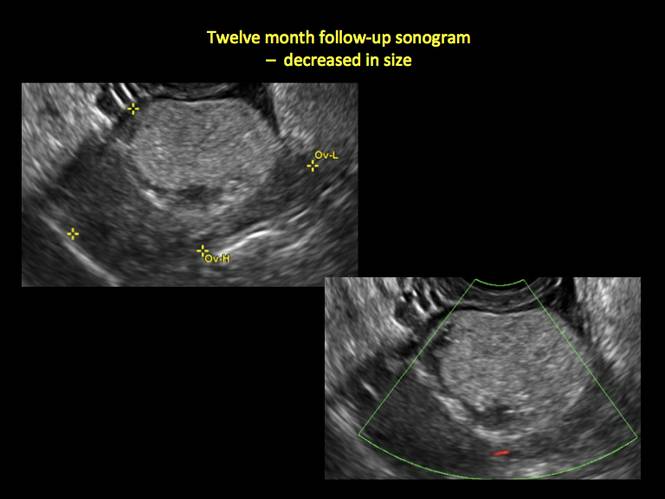
Figure 15
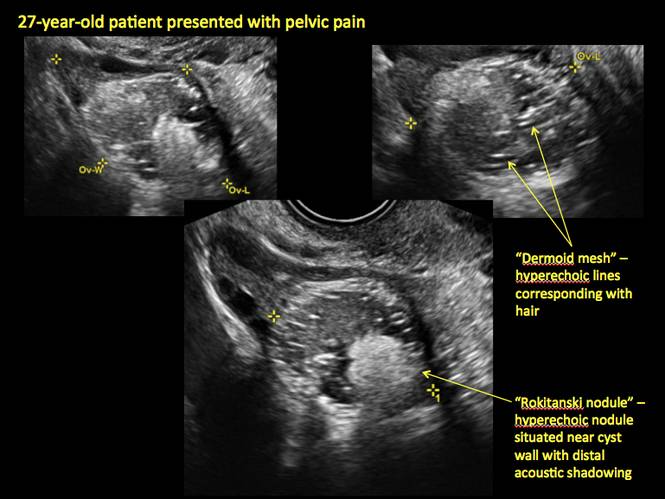
Figure 16
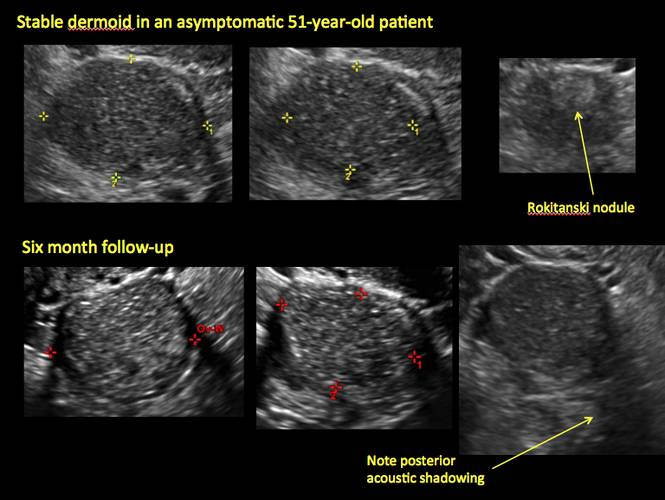
Figure 17
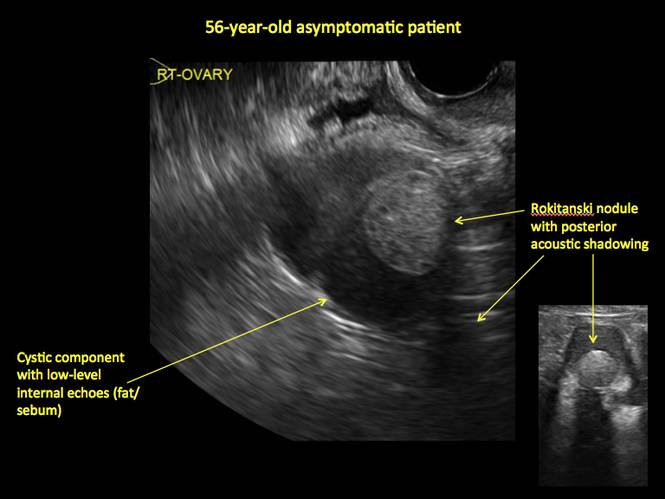
Figure 18
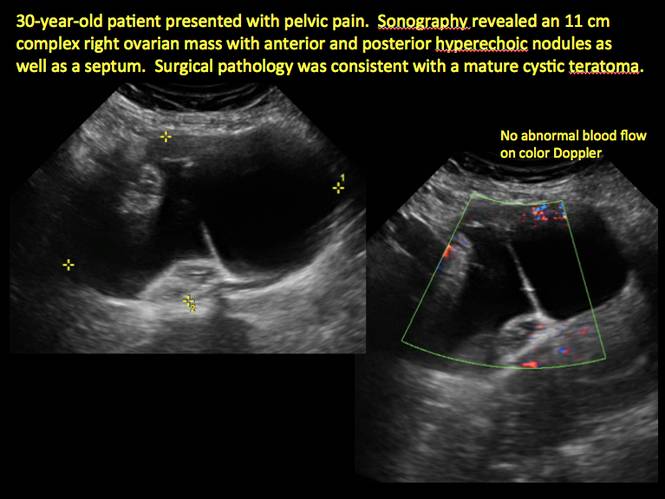
Figure 19
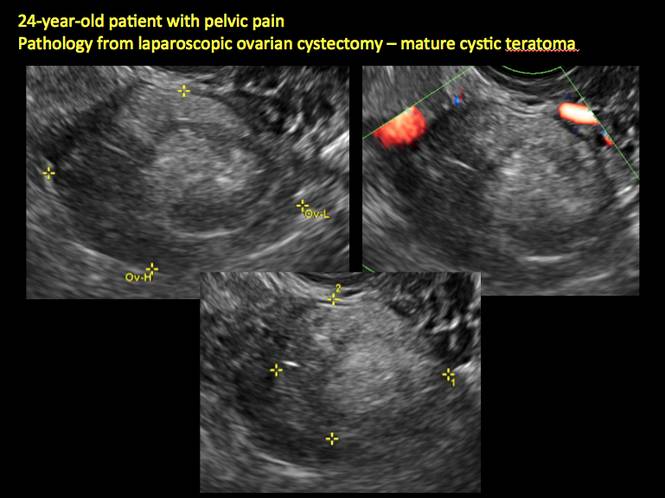
Figure 20
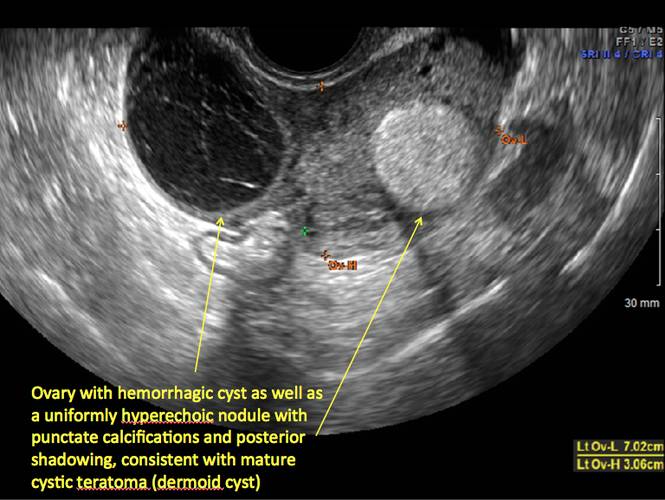
Figure 21
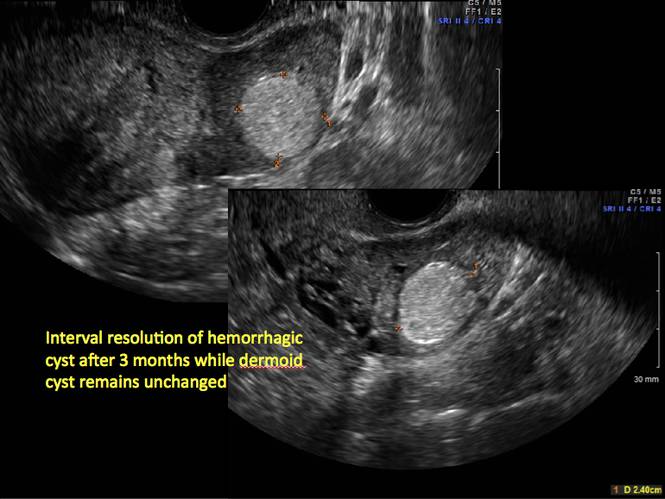
Figure 22
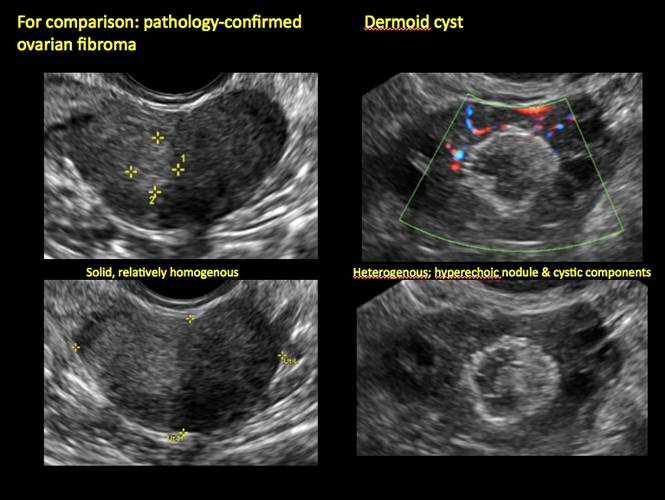
Figure 23
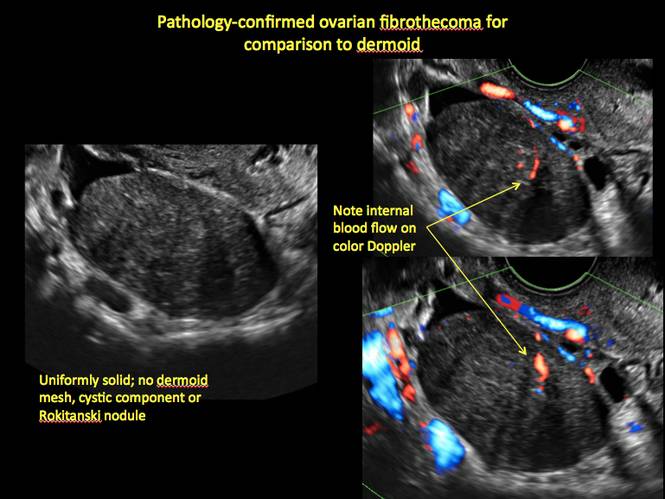
Figure 24
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Levine D, Brown DL, Andreotti RF, et al. Management of asymptomatic ovarian and other adnexal cysts imaged at US: Society of Radiologists in Ultrasound Consensus Conference Statement. Radiology. 2010;256(3):943–954.
2. Hoo WL, Yazbek WL, Holland T, Mavrelos D, Tong EN, Jurkovic D. Expectant management of ultrasonically diagnosed ovarian dermoid cysts: is it possible to predict outcome? Ultrasound Obstet Gynecol. 2010;36(2): 235–240.
1. Levine D, Brown DL, Andreotti RF, et al. Management of asymptomatic ovarian and other adnexal cysts imaged at US: Society of Radiologists in Ultrasound Consensus Conference Statement. Radiology. 2010;256(3):943–954.
2. Hoo WL, Yazbek WL, Holland T, Mavrelos D, Tong EN, Jurkovic D. Expectant management of ultrasonically diagnosed ovarian dermoid cysts: is it possible to predict outcome? Ultrasound Obstet Gynecol. 2010;36(2): 235–240.
Try exposure therapy, SSRIs for PTSD
LAS VEGAS– There is no cure for posttraumatic stress disorder, but helping its sufferers reduce symptoms, improve resistance, and achieve a better quality of life is possible.
“We have no idea what the best treatments are for PTSD,” Dr. Charles B. Nemeroff, the Leonard M. Miller Professor, and chairman of the department of psychiatry and behavioral sciences at the University of Miami, told an audience at the annual psychopharmacology update held by the Nevada Psychiatric Association.
Whether to rely upon psychosocial or pharmacologic interventions, or a combination of the two, to help shift PTSD from a debilitating condition into a manageable, chronic one, it is important to understand PTSD as a brain disease. “To accurately treat PTSD, consider it within a neurobiological context,” Dr. Nemeroff said. “Ordinarily, the brain is evolved to deal with stress, but it can be compromised.”
In chronic PTSD, brain studies have shown a noted shrinkage in the hippocampus, contributing to memory impairment, similar to the reduced hippocampal volume in child-abuse victims. Additionally, cortical function in the brain is affected in PTSD, creating difficulty with exercising judgment and good decision making.
“One way to think about PTSD is that the cortex is unable to reign in the limbic system,” Dr. Nemeroff said. “The hippocampus is impaired, the amygdala is hyperactive, and there is a tremendous emotional drive, so the ‘thinking’ part of the brain can’t [overcome] the emotional, reptilian brain.”
The result is that a person remains stuck in a hyperaroused state. “We know that the neurobiological basis for PTSD involves a prolonged, vigilant response to stress [involving] a multitude of brain circuits ... and of course the sympathetic nervous system and the pituitary and adrenal systems,” Dr. Nemeroff said.
Beyond brain changes, a genetic predisposition to PTSD accounts for a third of all cases, while an additional one-third are attributable to additional biological risk factors, according to Dr. Nemeroff (Nature 2011;470:492-7).
Just as with all anxiety-related disorders, women are more PTSD susceptible than are men. One of the “few things everybody agrees on,” Dr. Nemeroff said, is that early-life trauma such as neglect or abuse is a definite risk factor for PTSD, in part because early-life stress is thought to permanently program the brain regions involved in stress- and anxiety-mediation. Add to that, any adult level trauma, and they two “synergize. The more adult trauma coupled with early childhood abuse or neglect, the higher the level of PTSD.”
Meanwhile, poor social support, especially after the occurrence of a traumatic event, is a traditional prognosticator of poor recovery from PTSD, as are a family history of mood disorders, lower I.Q. and education, and experiencing other stressors the year before or after a traumatic event.
Dr. Nemeroff said that although the goals of treatment are reduced core symptoms, improved quality of life and function, strength, and resilience against subsequent stress, “the sad fact of the matter is that we don’t have a clue what the best treatment is, because we have no predictors of treatment response for PTSD.”
The most common treatments for PTSD are selective serotonin reuptake inhibitors (SSRIs), although the best data available suggest that prolonged imaginal exposure therapy is the most effective, Dr. Nemeroff said. It can be provided either virtually or in person, and includes breathing techniques, psychoeducation, and cognitive therapy. The Institute of Medicine gives exposure therapy its highest rating for scientific evidence, said Dr. Nemeroff, who is a board member of the institute.
Pharmacologic treatments approved by the Food and Drug Administration for PTSD treatment include sertraline and paroxetine, although other antidepressants can be prescribed off-label to some effect.
With sertraline, there is a “pretty low bar” of efficacy, according to Dr. Nemeroff, since only a 30% improvement in symptoms was recorded in 60% of study participants for FDA approval. It’s important to remember the treatment-response in PTSD is much slower than in major depression, Dr. Nemeroff said. “It can take as much as 9 months, so don’t give up.”
Combining sertraline with prolonged exposure therapy is even more effective, he said (J. Trauma Stress 2006;19:625-38). Meanwhile, other data show what paroxetine alone performed better than placebo, but the data are mixed for the drug in combination with prolonged exposure therapy (Am. J. Psychiatry 2012;169:80-8), (J. Clin. Psychiatry 2008;69:400-5), (J. Clin. Neurosci. 2008;62:646-52), and (Am. J. Psychiatry 2001;158:1982-8).
Dr. Nemeroff said lately, he has been treating PTSD patients with venlafaxine 450 mg, which is much higher than the usual dose of about 220 mg, with “considerably good results” (Arch. Gen. Psychiatry 2006;63:1158-65).
Improvements in memory and hippocampal volume generally are found with SSRI treatments, as well as reductions in symptom severity, according to Dr. Nemeroff.
For PTSD patients who are struggling with insomnia and other sleep-related problems, Dr. Nemeroff said prazosin has been “phenomenal,” especially in reducing nightmares (Am. J. Psychiatry 2013;170:1003-10).
One drug class to avoid using with PTSD patients is benzodiazepines, he said. “Every study has shown that benzodiazepines in PTSD do not work, and they come with a high rate of substance abuse in this population.”
*Dr. Nemeroff disclosed that he receives research and grant support from the National Institutes of Health. He also serves as a consultant for several companies, including Xhale, Takeda, SK Pharma, Shire, Roche, Lilly, Allergan, Mitsubishi Tanabe Pharma Development America, Taisho Pharmaceutical, Lundbeck, Prismic Pharmaceuticals, and Clintara LLC. He is a stockholder in Xhale, Celgene, Seattle Genetics, Abbvie, Titan Pharmaceuticals, and OPKO Health.
In addition, he holds financial/proprietary interest in patents for method/devices for the transdermal delivery of lithium and for a method of assessing antidepressant drug therapy.
*Correction, 4/10/2015: An earlier version of this story misstated Dr. Nemeroff's disclosures.
On Twitter @whitneymcknight
LAS VEGAS– There is no cure for posttraumatic stress disorder, but helping its sufferers reduce symptoms, improve resistance, and achieve a better quality of life is possible.
“We have no idea what the best treatments are for PTSD,” Dr. Charles B. Nemeroff, the Leonard M. Miller Professor, and chairman of the department of psychiatry and behavioral sciences at the University of Miami, told an audience at the annual psychopharmacology update held by the Nevada Psychiatric Association.
Whether to rely upon psychosocial or pharmacologic interventions, or a combination of the two, to help shift PTSD from a debilitating condition into a manageable, chronic one, it is important to understand PTSD as a brain disease. “To accurately treat PTSD, consider it within a neurobiological context,” Dr. Nemeroff said. “Ordinarily, the brain is evolved to deal with stress, but it can be compromised.”
In chronic PTSD, brain studies have shown a noted shrinkage in the hippocampus, contributing to memory impairment, similar to the reduced hippocampal volume in child-abuse victims. Additionally, cortical function in the brain is affected in PTSD, creating difficulty with exercising judgment and good decision making.
“One way to think about PTSD is that the cortex is unable to reign in the limbic system,” Dr. Nemeroff said. “The hippocampus is impaired, the amygdala is hyperactive, and there is a tremendous emotional drive, so the ‘thinking’ part of the brain can’t [overcome] the emotional, reptilian brain.”
The result is that a person remains stuck in a hyperaroused state. “We know that the neurobiological basis for PTSD involves a prolonged, vigilant response to stress [involving] a multitude of brain circuits ... and of course the sympathetic nervous system and the pituitary and adrenal systems,” Dr. Nemeroff said.
Beyond brain changes, a genetic predisposition to PTSD accounts for a third of all cases, while an additional one-third are attributable to additional biological risk factors, according to Dr. Nemeroff (Nature 2011;470:492-7).
Just as with all anxiety-related disorders, women are more PTSD susceptible than are men. One of the “few things everybody agrees on,” Dr. Nemeroff said, is that early-life trauma such as neglect or abuse is a definite risk factor for PTSD, in part because early-life stress is thought to permanently program the brain regions involved in stress- and anxiety-mediation. Add to that, any adult level trauma, and they two “synergize. The more adult trauma coupled with early childhood abuse or neglect, the higher the level of PTSD.”
Meanwhile, poor social support, especially after the occurrence of a traumatic event, is a traditional prognosticator of poor recovery from PTSD, as are a family history of mood disorders, lower I.Q. and education, and experiencing other stressors the year before or after a traumatic event.
Dr. Nemeroff said that although the goals of treatment are reduced core symptoms, improved quality of life and function, strength, and resilience against subsequent stress, “the sad fact of the matter is that we don’t have a clue what the best treatment is, because we have no predictors of treatment response for PTSD.”
The most common treatments for PTSD are selective serotonin reuptake inhibitors (SSRIs), although the best data available suggest that prolonged imaginal exposure therapy is the most effective, Dr. Nemeroff said. It can be provided either virtually or in person, and includes breathing techniques, psychoeducation, and cognitive therapy. The Institute of Medicine gives exposure therapy its highest rating for scientific evidence, said Dr. Nemeroff, who is a board member of the institute.
Pharmacologic treatments approved by the Food and Drug Administration for PTSD treatment include sertraline and paroxetine, although other antidepressants can be prescribed off-label to some effect.
With sertraline, there is a “pretty low bar” of efficacy, according to Dr. Nemeroff, since only a 30% improvement in symptoms was recorded in 60% of study participants for FDA approval. It’s important to remember the treatment-response in PTSD is much slower than in major depression, Dr. Nemeroff said. “It can take as much as 9 months, so don’t give up.”
Combining sertraline with prolonged exposure therapy is even more effective, he said (J. Trauma Stress 2006;19:625-38). Meanwhile, other data show what paroxetine alone performed better than placebo, but the data are mixed for the drug in combination with prolonged exposure therapy (Am. J. Psychiatry 2012;169:80-8), (J. Clin. Psychiatry 2008;69:400-5), (J. Clin. Neurosci. 2008;62:646-52), and (Am. J. Psychiatry 2001;158:1982-8).
Dr. Nemeroff said lately, he has been treating PTSD patients with venlafaxine 450 mg, which is much higher than the usual dose of about 220 mg, with “considerably good results” (Arch. Gen. Psychiatry 2006;63:1158-65).
Improvements in memory and hippocampal volume generally are found with SSRI treatments, as well as reductions in symptom severity, according to Dr. Nemeroff.
For PTSD patients who are struggling with insomnia and other sleep-related problems, Dr. Nemeroff said prazosin has been “phenomenal,” especially in reducing nightmares (Am. J. Psychiatry 2013;170:1003-10).
One drug class to avoid using with PTSD patients is benzodiazepines, he said. “Every study has shown that benzodiazepines in PTSD do not work, and they come with a high rate of substance abuse in this population.”
*Dr. Nemeroff disclosed that he receives research and grant support from the National Institutes of Health. He also serves as a consultant for several companies, including Xhale, Takeda, SK Pharma, Shire, Roche, Lilly, Allergan, Mitsubishi Tanabe Pharma Development America, Taisho Pharmaceutical, Lundbeck, Prismic Pharmaceuticals, and Clintara LLC. He is a stockholder in Xhale, Celgene, Seattle Genetics, Abbvie, Titan Pharmaceuticals, and OPKO Health.
In addition, he holds financial/proprietary interest in patents for method/devices for the transdermal delivery of lithium and for a method of assessing antidepressant drug therapy.
*Correction, 4/10/2015: An earlier version of this story misstated Dr. Nemeroff's disclosures.
On Twitter @whitneymcknight
LAS VEGAS– There is no cure for posttraumatic stress disorder, but helping its sufferers reduce symptoms, improve resistance, and achieve a better quality of life is possible.
“We have no idea what the best treatments are for PTSD,” Dr. Charles B. Nemeroff, the Leonard M. Miller Professor, and chairman of the department of psychiatry and behavioral sciences at the University of Miami, told an audience at the annual psychopharmacology update held by the Nevada Psychiatric Association.
Whether to rely upon psychosocial or pharmacologic interventions, or a combination of the two, to help shift PTSD from a debilitating condition into a manageable, chronic one, it is important to understand PTSD as a brain disease. “To accurately treat PTSD, consider it within a neurobiological context,” Dr. Nemeroff said. “Ordinarily, the brain is evolved to deal with stress, but it can be compromised.”
In chronic PTSD, brain studies have shown a noted shrinkage in the hippocampus, contributing to memory impairment, similar to the reduced hippocampal volume in child-abuse victims. Additionally, cortical function in the brain is affected in PTSD, creating difficulty with exercising judgment and good decision making.
“One way to think about PTSD is that the cortex is unable to reign in the limbic system,” Dr. Nemeroff said. “The hippocampus is impaired, the amygdala is hyperactive, and there is a tremendous emotional drive, so the ‘thinking’ part of the brain can’t [overcome] the emotional, reptilian brain.”
The result is that a person remains stuck in a hyperaroused state. “We know that the neurobiological basis for PTSD involves a prolonged, vigilant response to stress [involving] a multitude of brain circuits ... and of course the sympathetic nervous system and the pituitary and adrenal systems,” Dr. Nemeroff said.
Beyond brain changes, a genetic predisposition to PTSD accounts for a third of all cases, while an additional one-third are attributable to additional biological risk factors, according to Dr. Nemeroff (Nature 2011;470:492-7).
Just as with all anxiety-related disorders, women are more PTSD susceptible than are men. One of the “few things everybody agrees on,” Dr. Nemeroff said, is that early-life trauma such as neglect or abuse is a definite risk factor for PTSD, in part because early-life stress is thought to permanently program the brain regions involved in stress- and anxiety-mediation. Add to that, any adult level trauma, and they two “synergize. The more adult trauma coupled with early childhood abuse or neglect, the higher the level of PTSD.”
Meanwhile, poor social support, especially after the occurrence of a traumatic event, is a traditional prognosticator of poor recovery from PTSD, as are a family history of mood disorders, lower I.Q. and education, and experiencing other stressors the year before or after a traumatic event.
Dr. Nemeroff said that although the goals of treatment are reduced core symptoms, improved quality of life and function, strength, and resilience against subsequent stress, “the sad fact of the matter is that we don’t have a clue what the best treatment is, because we have no predictors of treatment response for PTSD.”
The most common treatments for PTSD are selective serotonin reuptake inhibitors (SSRIs), although the best data available suggest that prolonged imaginal exposure therapy is the most effective, Dr. Nemeroff said. It can be provided either virtually or in person, and includes breathing techniques, psychoeducation, and cognitive therapy. The Institute of Medicine gives exposure therapy its highest rating for scientific evidence, said Dr. Nemeroff, who is a board member of the institute.
Pharmacologic treatments approved by the Food and Drug Administration for PTSD treatment include sertraline and paroxetine, although other antidepressants can be prescribed off-label to some effect.
With sertraline, there is a “pretty low bar” of efficacy, according to Dr. Nemeroff, since only a 30% improvement in symptoms was recorded in 60% of study participants for FDA approval. It’s important to remember the treatment-response in PTSD is much slower than in major depression, Dr. Nemeroff said. “It can take as much as 9 months, so don’t give up.”
Combining sertraline with prolonged exposure therapy is even more effective, he said (J. Trauma Stress 2006;19:625-38). Meanwhile, other data show what paroxetine alone performed better than placebo, but the data are mixed for the drug in combination with prolonged exposure therapy (Am. J. Psychiatry 2012;169:80-8), (J. Clin. Psychiatry 2008;69:400-5), (J. Clin. Neurosci. 2008;62:646-52), and (Am. J. Psychiatry 2001;158:1982-8).
Dr. Nemeroff said lately, he has been treating PTSD patients with venlafaxine 450 mg, which is much higher than the usual dose of about 220 mg, with “considerably good results” (Arch. Gen. Psychiatry 2006;63:1158-65).
Improvements in memory and hippocampal volume generally are found with SSRI treatments, as well as reductions in symptom severity, according to Dr. Nemeroff.
For PTSD patients who are struggling with insomnia and other sleep-related problems, Dr. Nemeroff said prazosin has been “phenomenal,” especially in reducing nightmares (Am. J. Psychiatry 2013;170:1003-10).
One drug class to avoid using with PTSD patients is benzodiazepines, he said. “Every study has shown that benzodiazepines in PTSD do not work, and they come with a high rate of substance abuse in this population.”
*Dr. Nemeroff disclosed that he receives research and grant support from the National Institutes of Health. He also serves as a consultant for several companies, including Xhale, Takeda, SK Pharma, Shire, Roche, Lilly, Allergan, Mitsubishi Tanabe Pharma Development America, Taisho Pharmaceutical, Lundbeck, Prismic Pharmaceuticals, and Clintara LLC. He is a stockholder in Xhale, Celgene, Seattle Genetics, Abbvie, Titan Pharmaceuticals, and OPKO Health.
In addition, he holds financial/proprietary interest in patents for method/devices for the transdermal delivery of lithium and for a method of assessing antidepressant drug therapy.
*Correction, 4/10/2015: An earlier version of this story misstated Dr. Nemeroff's disclosures.
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM THE NPA PSYCHOPHARMOCOLOGY UPDATE
Scalp Hyperkeratosis in Children With Skin of Color: Diagnostic and Therapeutic Considerations
Scalp hyperkeratosis (scaling or flaking) is a common symptom in childhood and is typified by fine to thick hyperkeratosis of the scalp with or without underlying erythema. The causes of scalp hyperkeratosis in childhood vary based on the demographics of the population. In a population where approximately half of the pediatric patients were white, scaling of the scalp was more common in patients with seborrheic dermatitis and/or atopic dermatitis (AD) who were aged 0 to 2 years, and tinea capitis was only noted in children who were black.1 In children with skin of color, scalp hyperkeratosis has been noted as a marker of tinea capitis, especially in patients aged 3 to 11 years,2,3 and the level of suspicion should consistently remain high for this age group. In another study of an all-black population of schoolchildren aged 5 to 13 years (N=224), 3% demonstrated signs and symptoms of tinea capitis and 14% were found to be asymptomatic carriers.4 Although generally benign in nature, scalp hyperkeratosis can be associated with systemic illnesses such as juvenile dermatomyositis and Langerhans cell histiocytosis.5 This article addresses the diagnosis and treatment of scalp hyperkeratosis in children with skin of color, focusing on differences in exposure to contagious cases, hairstyling practices, and biological factors that may impact the disease process.
CAUSES OF SCALP HYPERKERATOSIS IN CHILDHOOD
Scalp hyperkeratosis in childhood usually is caused by common benign conditions, but some level of suspicion should be maintained for more severe etiologic conditions such as Langerhans cell histiocytosis and collagen vascular diseases (eg, juvenile dermatomyositis).6 Langerhans cell histiocytosis of the scalp might be obscured by background pigmentation in black children.
Scalp scaling can be a minor criterion in the diagnosis of AD. Atopic dermatitis should be suspected in Asian children with scalp scaling. Although one study in Bangladesh revealed scalp involvement in only 5.2% of pediatric patients with AD,7 a study in China reported an incidence rate as high as 49.7% (with a similarly high incidence of eyelid dermatitis).8 Children with AD also may have dry hair.9 Atopic dermatitis of the scalp is typified by itching, fine hyperkeratosis, and notably eczematous scalp lesions ranging from excoriated or oozing erythematous plaques to lichenification with hair miniaturization, primarily from scratch-induced breakage.10 The latter finding often is noted in black adolescent girls with long-term moderate to severe AD (personal observation).
Seborrheic dermatitis is a hypersensitivity response to yeast colonization of the scalp with Malassezia species. The infantile form is extremely common (also known as cradle cap). Characteristically, greasy yellow hyperkeratosis in fine to thick sheets is noted on the scalp in children younger than 2 years, especially infants, often with involvement of skin folds. One study noted that seborrheic dermatitis occurs in 6% of school-aged children as opposed to 19% of children younger than 2 years.1 Severe seborrheic dermatitis in infancy may be a prelude to AD, with the incidence being 3 times higher in children with prior seborrheic dermatitis.11 In teenagers, seborrheic dermatitis often accompanies acne onset in the early pubertal years.12
Psoriasis is an autoimmune inflammatory dermatosis that most commonly affects white children. In childhood, pityriasis amiantacea, psoriasiform scalp hyperkeratosis, is more common than in adulthood, with thick, stuck-on scales bound to the hairs. This variant is uncommon in Hispanic and Asian children and is almost never seen in black children but has been reported in cohorts of Turkish children.13 In a series of 85 Egyptian children with pityriasis amiantacea, diagnosis of scalp psoriasis was made in 35.3%, eczematous dermatitis in 34.2%, and tinea capitis in 12.9%.14 Consequently, a high degree of suspicion for tinea capitis should be held if pityriasis amiantacea is found in children with skin of color.15,16
Tinea capitis is a dermatophyte infection of the scalp, hair, and surrounding skin. The presence of tinea capitis on the scalp is associated with environmental exposure to dermatophytes (eg, school, household).4,17 The infection is largely caused by Trichophyton tonsurans in the United States, which causes a seborrheic appearance and less commonly alopecia (black dot or thinning), plaques with scale, or kerion. The presence of cervical lymph nodes and/or alopecia increases the chances of tinea being the diagnosis. Potassium hydroxide preparation and fungal culture can be performed to corroborate the diagnosis.1-3 Other etiologies of scalp hyperkeratosis such as juvenile pityriasis rubra pilaris and lice are extremely uncommon in black children, but lice may be seen in Hispanic and Asian girls with long straight hair who attend school. Discoid lupus is more common in children with skin of color but is rare overall. When noted, accompanying mottled dyspigmentation and scarring alopecia are noted in addition to a high risk for developing systemic lupus erythematosus. Biopsy and screening for systemic lupus are necessary, as the risk for progression from discoid lupus to systemic disease is 26% over 3 years.18
THE BIOLOGY OF HAIR IN CHILDREN WITH SKIN OF COLOR
To some extent, the biology of hair impacts the occurrence, appearance, and treatment of scalp hyperkeratosis in children with skin of color. First, it is important to remember that follicular density is lower in black patients as compared to Asian patients with a consequently lower hair count overall, which results in the easy appearance of hair loss, particularly at the margins of the scalp.19,20 Second, the shape of the hair follicle differs among races and ethnicities. Asian patients have round hair shafts coming from straight follicles, which allows for greater natural hair hydration, resulting in somewhat less aggressive scalp disease. Hispanic patients may have similarly straight hair or may have elliptical or curled shafts, the latter being noted in black patients. Furthermore, a curled hair shaft results in poor flow of sebum across the hair, resulting in greater scalp xerosis, more susceptibility to traction alopecia, and ultimately a greater risk for infections.20-23 Finally, the scalp is continuous with the face and neck, and Asian patients have greater sensitivity to skin care products in these areas, resulting in difficulty of treatment in this patient population and the need for use of gentle products.
HAIR CARE PRACTICES IN CHILDREN WITH SKIN OF COLOR
Hair care in patients with skin of color can be costly, difficult, and potentially damaging, with 99% of black girls reporting pomade or oil usage. Costly and complex hair care practices begin in childhood for patients with skin of color. In a series of 201 surveyed black girls with a mean age of 9.8 years, 80% had used hot combs and 42% used relaxers.24 Traction styles were common with 81% using ponytails, 67% braids, and 49% cornrows in the last 12 months. These styles are thought to affect hair health, particularly through induction of traction-related damage, folliculitis, and alopecia. Furthermore, chemical relaxers, hot combs, blowouts, and hair setting may be introduced during childhood.24 These practices appear to disturb the integrity of the hair follicle, leaving it more susceptible to irritation and infection.
Hair care in the pediatric population often is complicated by the fact that multiple children are being styled in tandem, either at home or in a salon, resulting in shared equipment and fomite spread. Even just proximity to a case of tinea capitis in the household will increase risk for tinea capitis. Furthermore, it is quite commonplace for black patients to use pomades and shampoos that contain antifungals, especially selenium sulfide, which makes it difficult to obtain accurate culture results. In India, use of mustard oil also has been linked to increased risk for tinea capitis.25
Other issues related to hair care include frequent dry scalp in patients with skin of color due to poor sebum distribution along the hair shaft. As a result, frequent washing may exacerbate scalp xerosis and further irritate seborrheic dermatitis and/or AD.
DIAGNOSTIC CONSIDERATIONS FOR SCALP HYPERKERATOSIS IN CHILDHOOD
Dermatologists should have a greater level of suspicion for tinea capitis in black and Hispanic children compared to white children. The index of suspicion should be high given that antifungal shampoos and pomades may minimize the clinical appearance. Although trends in overall incidence in the United States suggest tinea capitis is becoming less common, there still is a stronger representation of the disease in black patients.26 A study of positive fungal cultures from one clinic in Mississippi (N=1220) showed that two-thirds of patients were children younger than 13 years; 87% of patients with positive cultures for dermatophytes were black.27 The endothrix type of tinea capitis caused by T tonsurans often presents with a seborrheic appearance, and fungal culture is warranted in all pediatric patients with skin of color who have scalp hyperkeratosis. Asian children can be regarded with a lower level of suspicion for tinea capitis, similar to white patients in the United States. Variation in incidence of tinea capitis does exist worldwide and the practitioner may need to address these issues in patients who travel or are recent immigrants.
When identifying tinea capitis infections in children with skin of color, physicians should consider the patient’s personal and family history, comorbid skin disorders, dermoscopy, microscopy and fungal staining, and fungal culture (Figure).
A paradigm for the diagnosis of scalp hyperkeratosis in children with skin of color.
Personal and Family History
The first diagnostic consideration is the patient’s personal and family history. A history of AD, asthma, or allergies will support but not confirm the diagnosis of AD. Prior tinea capitis infections and household contacts with tinea infections support the presence of tinea capitis.17 Recent implementation of anti–tumor necrosis factor a inhibitor therapy in a psoriatic child can flare scalp disease, mimicking tinea capitis.28 The patient’s guardians should be queried about potential infectious contacts, whether they themselves have signs of scalp disease or tinea corporis (ringworm) or whether they have a pet with problematic fur. Physicians also should query patients and their guardians about recent use of topical antifungal shampoos, pomades, creams (both over-the-counter [OTC] and prescription), and/or oral antifungals. When these agents are used, there is a possibility that fungal examinations may be negative in the presence of true infection with tinea capitis. Traction alopecia, often preceded by fine scale, is more likely to present in patients who wear their hair in cornrows, while seborrheic dermatitis may be associated with hair extensions, reduced frequency of washing (61% of black girls surveyed wash every 2 weeks), and/or reduced usage of hair oils in black girls.24 Knowledge of the patient’s personal hair care history, such as use of pomades; frequency and method of washing/drying hair; types of hair care products used daily to wash and style hair; use of chemical relaxers; or recent hairstyling with cornrows, braids, or hair extensions, also is essential to the diagnosis of tinea capitis. Usage of traction-related styling practices in patients with chemically relaxed hair can enhance the risk for traction alopecia.29
Comorbid Skin Disorders
The patient also should be examined for comorbid skin disorders, including tinea corporis, alopecia (particularly in the areas of hyperkeratosis), and the presence of nuchal lymphadenopathy. For each extra clinical finding, the chances of a final diagnosis of tinea capitis rises, allowing for empiric diagnosis to be made that can be confirmed by a variety of tests.1-3
Dermoscopy
Next, the patient should undergo dermoscopic evaluation. On dermoscopy, tinea capitis typically presents with broken hairs, black dots on the scalp, comma-shaped hairs, and short corkscrew hairs, all of which should clear with therapy.30-33 Dermoscopic findings of AD would reveal underlying xerosis and prominent vasculature due to inflammation, and alopecia areata would present with yellow dots at the orifices of the hair follicles, exclamation point hairs, and vellus hairs.34,35 Traction alopecia may be noted by retained hairs along the hairline, which is known as the fringe sign.36
Microscopy and Fungal Staining
Microscopic preparations can be performed to identify tinea capitis using fungal stains of slide-based specimens. Breakage of short hairs onto the slide and/or cotton swab is a soft sign corroborating endothrix infection of the hairs. Potassium hydroxide can enhance visualization of the hyperkeratotic scalp, but for most black patients, use of antifungal agents reduces fungal hyphae and spores in the areas of hyperkeratosis and may limit the utility of examining the skin microscopically. Assessment of the broken hairs obtained by gentle friction with one glass slide and catching the scales onto another glass slide may yield the best results in the evaluation of tinea capitis (a technique taught to me by Robin Hornung, MD, Everett, Washington). Hairs obtained in this manner often are fragile and break due to endothrix infection replacing and weakening the shaft of the hairs. In the United States, fungal samples usually are obtained with cotton swabs, but a recent study suggested that brushing is superior to scraping to obtain samples; the combination of sampling techniques may improve the yield of a culture.37 Because topical agents are unable to enter the hair cortex, the hair shaft is the most likely to show fungal spores under the microscope when antifungal shampoos or pomades are used. Other testing methods such as Swartz-Lamkins or calcofluor white staining can be used on similar scrapings. Biopsy and periodic acid–Schiff staining of thick scales or crust can help differentiate tinea capitis from pityriasis amiantacea when the crust is too thick to be softened via potassium hydroxide preparation.38
Fungal Culture
Fungal culture onto media that contains nutrients for dermatophyte growth can be used for 4 purposes in tinea capitis: (1) to confirm infection, (2) to identify species of infection, (3) to confirm mycological cure when difficulty in clearance of disease has been noted, and (4) to obtain a specimen for sensitivity screening regarding antifungals when necessary, an uncommon but occasionally useful test in individuals with disease that has failed treatment with 1 or more antifungals.27
THERAPY FOR SCALP HYPERKERATOSIS IN CHILDREN WITH SKIN OF COLOR
In patients with scalp hyperkeratosis, it is important to address the specific cause of the disease. Therapy for scalp hyperkeratosis in children with skin of color includes altered hair care practices, use of OTC and prescription agents, and containment of fomites in the case of infections. Biopsy of atypical scalp hyperkeratosis cases is needed to diagnose rare etiologies such as discoid lupus or Langerhans cell histiocytosis. For individuals with systemic disease including Langerhans cell histiocytosis, which is generally accompanied by nodes and plaques in the inguinal region or other intertriginous sites, immediate hematology and oncology workup is required.39 For collagen vascular diseases such as lupus or dermatomyositis, appropriate referral to rheumatology and systemic therapy is warranted.
Altered Hair Care Practices
The use of prophylactic ketoconazole 1% shampoo may not reduce the risk for recurrence of tinea capitis over standard good hygiene, removal of fomites, and adherence to prescribed therapy.40 Use of selenium sulfide has been shown to effectively reduce contagion risk.41
Fragrance- and dye-free shampoos can be helpful in providing gentle cleansing of the scalp, which is especially important in Asian patients who have greater facial and eyelid sensitivity. Free-and-clear shampoos can be used alternatively with shampoos containing selenium sulfide or sulfur to eliminate comorbid seborrhea. Black patients should be advised to shampoo and condition their hair once weekly, and Asian and Hispanic patients should shampoo and condition 2 to 3 times weekly to remove scale and potentially reduce risk for tinea acquisition.42 Children with straight hair should shampoo with increased frequency in the summer to manually remove sweat-induced macerated hyperkeratosis. Conditioners also should be used consistently after shampooing to enhance hair health.
Use of OTC and Prescription Agents
Atopic Dermatitis
Topical corticosteroid agents can be used in increasing strengths to treat AD of the scalp in children with skin of color, from OTC scalp products containing hydrocortisone 1% to prescription-based agents. Hydration of the hair also is needed to counteract reduced water content.43 Due to the innate xerosis of the scalp in black patients and atopic patients, the use of oil-based or lotion products may provide the most hydration for patients with scalp disease.44 Alcohol-based agents, either drops or foams, may enhance xerosis and should be used sparingly.
Seborrheic Dermatitis
Alternating treatment with medicated shampoos containing selenium sulfide and ketoconazole can aid in the removal of seborrhea. Pomades including borage seed oil–based agents can be massaged into the scalp,45 particularly for treatment of infantile seborrhea, and should not necessarily be washed off daily in dark-skinned patients. Additional focused application of topical corticosteroids to the scalp also is helpful. Due to innate scalp xerosis in black children, therapy should be similar to AD.
Psoriasis
In the setting of pityriasis amiantacea, albeit rare in children with skin of color, oil-based agents can soften hyperkeratosis for removal. Sterile mineral oil or commercially available scalp preparations of peanut oil with fluocinolone or mineral oil with glycerin can aid in the removal of scales without harming the hair, but usage must be age appropriate. The addition of focused application of age-appropriate topical corticosteroids for areas of severe hyperkeratosis can aid in clearance of the lesions.44 Recently, a stable combination of calcipo-triene 0.005%–betamethasone dipropionate 0.064% has been approved in the United States for the therapy of scalp psoriasis in adolescents.46
Tinea Capitis
Antifungal shampoos including selenium sulfide will reduce contagion risk when used by both the patient and his/her family members. Frequency of shampooing is similar to that described for AD. Between shampooing, pomades with selenium sulfide can be applied to the scalp to enhance overall clearance.
Oral antifungals are the basis of treatment and use of griseofulvin is the gold standard. Terbinafine has been approved by the US Food and Drug Administration for treatment of tinea capitis; for children weighing less than 25 kg the dosage is 125 mg daily, for 25 to 35 kg the dosage is 187.5 mg daily, and for more than 35 kg the dosage is 250 mg daily. Shorter therapeutic courses may be required, making it a good second-line agent. Laboratory screening in children prior to therapy is not always performed but should be done in cases where fatty liver might be suspected.47 Monitoring liver function tests is best when exceeding 3 months of usage or shifting from one antifungal to another.3
Containment of Fomites
There are several procedures that should be followed to contain scalp infection in children with skin of color. First, all objects that come into contact with the scalp (eg, hats, hoods, brushes, pillowcases) should be washed with hot water or replaced weekly. Sharing these objects with friends or family should be strongly discouraged. Patients and their family members also should be instructed to use medicated (eg, selenium sulfide) shampoos and conditioners. Finally, patients are advised to avoid use of shared classroom garments or mats for sleeping.
LONG-TERM SEQUELAE OF SCALP HYPERKERATOSIS
Long-term sequelae of scalp hyperkeratosis often are discounted in children, but the disease can have lasting and damaging effects on the scalp. Sequelae include discomfort from chronicity and psychological distress. In particular, years of scalp pruritus can promote lichenification of the scalp and miniaturization of the hair follicles. Furthermore, itching due to sweating can limit participation in sports. Finally, tinea capitis is thought to be a risk factor for central centrifugal cicatricial alopecia (or can occur comorbidly with central centrifugal cicatricial alopecia causing severe pruritus), a chronic scarring hair loss that is seen primarily in black adult females.48 Erythema nodosum also has been reported as an associated finding in the case of kerion.49 One study reported associated findings that included thyroid cancer in individuals irradiated for tinea capitis in the 1950s.50
Conclusion
Scalp hyperkeratosis in children with skin of color, especially black patients, is more likely to be associated with tinea capitis and is more challenging to treat due to innate scalp xerosis in black patients and increased sensitivity of facial skin in Asian children. Ultimately, institution of therapy when needed and good scalp and hair care may prevent long-term sequelae.
1. Williams JV, Eichenfield LF, Burke BL, et al. Prevalence of scalp scaling in prepubertal children. Pediatrics. 2005;115:e1-e6.
2. Coley MK, Bhanusali DG, Silverberg JI, et al. Scalp hyperkeratosis and alopecia in children of color. J Drugs Dermatol. 2011;10:511-516.
3. Bhanusali D, Coley M, Silverberg JI, et al. Treatment outcomes for tinea capitis in a skin of color population. J Drugs Dermatol. 2012;11:852-856.
4. Williams JV, Honig PJ, McGinley KJ, et al. Semiquantitative study of tinea capitis and the asymptomatic carrier state in inner-city school children. Pediatrics. 1995;96:265-267.
5. McDonald LL, Smith ML. Diagnostic dilemmas in pediatric/adolescent dermatology: scaly scalp. J Pediatr Health Care. 1998;12:80-84.
6. Peloro TM, Miller OF 3rd, Hahn TF, et al. Juvenile dermatomyositis: a retrospective review of a 30-year experience. J Am Acad Dermatol. 2001;45:28-34.
7. Wahab MA, Rahman MH, Khondker L, et al. Minor criteria for atopic dermatitis in children. Mymensingh Med J. 2011;20:419-424.
8. Shi M, Zhang H, Chen X, et al. Clinical features of atopic dermatitis in a hospital-based setting in China. J Eur Acad Dermatol Venereol [published online ahead of print January 9, 2011]. 2011;25:1206-1212.
9. Kim KS, Shin MK, Kim JH, et al. Effects of atopic dermatitis on the morphology and water content of scalp hair. Microsc Res Tech. 2012;75:620-625.
10. Sabin BR, Peters N, Peters AT. Chapter 20: atopic dermatitis. Allergy Asthma Proc. 2012;33:S67-S69.
11. Alexopoulos A, Kakourou T, Orfanou I, et al. Retrospective analysis of the relationship between infantile seborrheic dermatitis and atopic dermatitis [published online ahead of print November 13, 2013]. Pediatr Dermatol. 2014;31:125-130.
12. Elish D, Silverberg NB. Infantile seborrheic dermatitis. Cutis. 2006;77:297-300.
13. Sarifakioglu E, Yilmaz AE, Gorpelioglu C, et al. Prevalence of scalp disorders and hair loss in children. Cutis. 2012;90:225-229.
14. Abdel-Hamid IA, Agha SA, Moustafa YM, et al. Pityriasis amiantacea: a clinical and etiopathologic study of 85 patients. Int J Dermatol. 2003;42:260-264.
15. Oostveen AM, Jong EM, Evers AW, et al. Reliability, responsiveness and validity of Scalpdex in children with scalp psoriasis: the Dutch study. Acta Derm Venereol. 2014;94:198-202.
16. Silverberg NB. Atlas of Pediatric Cutaneous Biodiversity: Comparative Dermatologic Atlas of Pediatric Skin of All Colors. New York, NY: Springer; 2012.
17. Sharma V, Silverberg NB, Howard R, et al. Do hair care practices affect the acquisition of tinea capitis? a case-control study. Arch Pediatr Adolesc Med. 2001;155:818-821.
18. Moises-Alfaro C, Berrón-Pérez R, Carrasco-Daza D, et al. Discoid lupus erythematosus in children: clinical, histopathologic, and follow-up features in 27 cases. Pediatr Dermatol. 2003;20:103-107.
19. Ramos-e-Silva M. Ethnic hair and skin: what is the state of the science? Chicago, Illinois—September 29-30, 2001. Clin Dermatol. 2002;20:321-324.
20. Heath CR, McMichael AJ. Biology of hair follicle. In: Kelly AP, Taylor SC, eds. Dermatology for Skin of Color. New York, NY: McGraw Hill; 2009:105-109.
21. Khumalo NP. African hair morphology: macrostructure to ultrastructure. Int J Dermatol. 2005;44(suppl 1):10-12.
22. Thibaut S, Bernard BA. The biology of hair shape. Int J Dermatol. 2005;44(suppl 1):2-3.
23. Taylor SC. Skin of color: biology, structure, function, and implications for dermatologic disease. J Am Acad Dermatol. 2002;46(suppl 2):S41-S62.
24. Rucker Wright D, Gathers R, Kapke A, et al. Hair care practices and their association with scalp and hair disorders in African American girls. J Am Acad Dermatol. 2011;64:253-262.
25. Kumar V, Sharma RC, Chander R. Clinicomycological study of tinea capitis. Indian J Dermatol Venereol Leprol. 1996;62:207-209.
26. Mirmirani P, Tucker LY. Epidemiologic trends in pediatric tinea capitis: a population-based study from Kaiser Permanente Northern California [published online ahead of print October 2, 2013]. J Am Acad Dermatol. 2013;69:916-921.
27. Chapman JC, Daniel CR 3rd, Daniel JG, et al. Tinea capitis caused by dermatophytes: a 15-year retrospective study from a Mississippi Dermatology Clinic. Cutis. 2011;88:230-233.
28. Perman MJ, Lovell DJ, Denson LA, et al. Five cases of anti-tumor necrosis factor alpha-induced psoriasis presenting with severe scalp involvement in children. Pediatr Dermatol. 2012;29:454-459.
29. Khumalo NP, Jessop S, Gumedze F, et al. Determinants of marginal traction alopecia in African girls and women. J Am Acad Dermatol. 2008;59:432-438.
30. Vazquez-Lopez F, Palacios-Garcia L, Argenziano G. Dermoscopic corkscrew hairs dissolve after successful therapy of Trichophyton violaceum tinea capitis: a case report. Australas J Dermatol. 2012;53:118-119.
31. Pinheiro AM, Lobato LA, Varella TC. Dermoscopy findings in tinea capitis: case report and literature review. An Bras Dermatol. 2012;87:313-314.
32. Mapelli ET, Gualandri L, Cerri A, et al. Comma hairs in tinea capitis: a useful dermatoscopic sign for diagnosis of tinea capitis. Pediatr Dermatol. 2012;29:223-224.
33. Hughes R, Chiaverini C, Bahadoran P, et al. Corkscrew hair: a new dermoscopic sign for diagnosis of tinea capitis in black children. Arch Dermatol. 2011;147:355-356.
34. Ekiz O, Sen BB, Rifaiog˘lu EN, et al. Trichoscopy in paediatric patients with tinea capitis: a useful method to differentiate from alopecia areata [published online ahead of print August 24, 2013]. J Eur Acad Dermatol Venereol. 2014;28:1255-1258.
35. Lencastre A, Tosti A. Role of trichoscopy in children’s scalp and hair disorders [published online ahead of print Aug 13, 2013]. Pediatr Dermatol. 2013;30:674-682.
36. Samrao A, Price VH, Zedek D, et al. The “fringe sign”—a useful clinical finding in traction alopecia of the marginal hair line. Dermatol Online J. 2011;17:1.
37. Nasir S, Ralph N, O’Neill C, et al. Trends in tinea capitis in an Irish pediatric population and a comparison of scalp brushings versus scalp scrapings as methods of investigation [published online ahead of print February 22, 2013]. Pediatr Dermatol. 2014;31:622-623.
38. Alvarez MS, Silverberg NB. Tinea capitis. Cutis. 2006;78:189-196.
39. Simko SJ, Garmezy B, Abhyankar H, et al. Differentiating skin-limited and multisystem Langerhans cell histiocytosis. J Pediatr. 2014;165:990-996.
40. Bookstaver PB, Watson HJ, Winters SD, et al. Prophylactic ketoconazole shampoo for tinea capitis in a high-risk pediatric population. J Pediatr Pharmacol Ther. 2011;16:199-203.
41. Allen HB, Honig PJ, Leyden JJ, et al. Selenium sulfide: adjunctive therapy for tinea capitis. Pediatrics. 1982;69:81-83.
42. Crawford K, Hernandez C. A review of hair care products for black individuals. Cutis. 2014;93:289-293.
43. Kim KS, Shin MK, Kim JH, et al. Effects of atopic dermatitis on the morphology and water content of scalp hair [published online ahead of print November 7, 2011]. Microsc Res Tech. 2012;75:620-625.
44. Kapila S, Hong E, Fischer G. A comparative study of childhood psoriasis and atopic dermatitis and greater understanding of the overlapping condition, psoriasis-dermatitis. Australas J Dermatol. 2012;53:98-105.
45. Tollesson A, Frithz A. Borage oil, an effective new treatment for infantile seborrhoeic dermatitis. Br J Dermatol. 1993;129:95.
46. Gooderham M, Debarre JM, Keddy-Grant J, et al. Safety and efficacy of calcipotriol plus betamethasone dipropionate gel in the treatment of scalp psoriasis in adolescents 12-17 years of age [published online ahead of print October 22, 2014]. Br J Dermatol. 2014;171:1470-1477.
47. Singer C, Stancu P, Coşoveanu S, et al. Non-alcoholic fatty liver disease in children. Curr Health Sci J. 2014;40:170-176.
48. Chiang C, Price V, Mirmirani P. Central centrifugal cicatricial alopecia: superimposed tinea capitis as the etiology of chronic scalp pruritus. Dermatol Online J. 2008;14:3.
49. Morrone A, Calcaterra R, Valenzano M, et al. Erythema nodosum induced by kerion celsi of the scalp in a woman. Mycoses. 2011;54:e237-e239.
50. Boaventura P, Pereira D, Celestino R, et al. Genetic alterations in thyroid tumors from patients irradiated in childhood for tinea capitis treatment. Eur J Endocrinol. 2013;169:673-679.
Scalp hyperkeratosis (scaling or flaking) is a common symptom in childhood and is typified by fine to thick hyperkeratosis of the scalp with or without underlying erythema. The causes of scalp hyperkeratosis in childhood vary based on the demographics of the population. In a population where approximately half of the pediatric patients were white, scaling of the scalp was more common in patients with seborrheic dermatitis and/or atopic dermatitis (AD) who were aged 0 to 2 years, and tinea capitis was only noted in children who were black.1 In children with skin of color, scalp hyperkeratosis has been noted as a marker of tinea capitis, especially in patients aged 3 to 11 years,2,3 and the level of suspicion should consistently remain high for this age group. In another study of an all-black population of schoolchildren aged 5 to 13 years (N=224), 3% demonstrated signs and symptoms of tinea capitis and 14% were found to be asymptomatic carriers.4 Although generally benign in nature, scalp hyperkeratosis can be associated with systemic illnesses such as juvenile dermatomyositis and Langerhans cell histiocytosis.5 This article addresses the diagnosis and treatment of scalp hyperkeratosis in children with skin of color, focusing on differences in exposure to contagious cases, hairstyling practices, and biological factors that may impact the disease process.
CAUSES OF SCALP HYPERKERATOSIS IN CHILDHOOD
Scalp hyperkeratosis in childhood usually is caused by common benign conditions, but some level of suspicion should be maintained for more severe etiologic conditions such as Langerhans cell histiocytosis and collagen vascular diseases (eg, juvenile dermatomyositis).6 Langerhans cell histiocytosis of the scalp might be obscured by background pigmentation in black children.
Scalp scaling can be a minor criterion in the diagnosis of AD. Atopic dermatitis should be suspected in Asian children with scalp scaling. Although one study in Bangladesh revealed scalp involvement in only 5.2% of pediatric patients with AD,7 a study in China reported an incidence rate as high as 49.7% (with a similarly high incidence of eyelid dermatitis).8 Children with AD also may have dry hair.9 Atopic dermatitis of the scalp is typified by itching, fine hyperkeratosis, and notably eczematous scalp lesions ranging from excoriated or oozing erythematous plaques to lichenification with hair miniaturization, primarily from scratch-induced breakage.10 The latter finding often is noted in black adolescent girls with long-term moderate to severe AD (personal observation).
Seborrheic dermatitis is a hypersensitivity response to yeast colonization of the scalp with Malassezia species. The infantile form is extremely common (also known as cradle cap). Characteristically, greasy yellow hyperkeratosis in fine to thick sheets is noted on the scalp in children younger than 2 years, especially infants, often with involvement of skin folds. One study noted that seborrheic dermatitis occurs in 6% of school-aged children as opposed to 19% of children younger than 2 years.1 Severe seborrheic dermatitis in infancy may be a prelude to AD, with the incidence being 3 times higher in children with prior seborrheic dermatitis.11 In teenagers, seborrheic dermatitis often accompanies acne onset in the early pubertal years.12
Psoriasis is an autoimmune inflammatory dermatosis that most commonly affects white children. In childhood, pityriasis amiantacea, psoriasiform scalp hyperkeratosis, is more common than in adulthood, with thick, stuck-on scales bound to the hairs. This variant is uncommon in Hispanic and Asian children and is almost never seen in black children but has been reported in cohorts of Turkish children.13 In a series of 85 Egyptian children with pityriasis amiantacea, diagnosis of scalp psoriasis was made in 35.3%, eczematous dermatitis in 34.2%, and tinea capitis in 12.9%.14 Consequently, a high degree of suspicion for tinea capitis should be held if pityriasis amiantacea is found in children with skin of color.15,16
Tinea capitis is a dermatophyte infection of the scalp, hair, and surrounding skin. The presence of tinea capitis on the scalp is associated with environmental exposure to dermatophytes (eg, school, household).4,17 The infection is largely caused by Trichophyton tonsurans in the United States, which causes a seborrheic appearance and less commonly alopecia (black dot or thinning), plaques with scale, or kerion. The presence of cervical lymph nodes and/or alopecia increases the chances of tinea being the diagnosis. Potassium hydroxide preparation and fungal culture can be performed to corroborate the diagnosis.1-3 Other etiologies of scalp hyperkeratosis such as juvenile pityriasis rubra pilaris and lice are extremely uncommon in black children, but lice may be seen in Hispanic and Asian girls with long straight hair who attend school. Discoid lupus is more common in children with skin of color but is rare overall. When noted, accompanying mottled dyspigmentation and scarring alopecia are noted in addition to a high risk for developing systemic lupus erythematosus. Biopsy and screening for systemic lupus are necessary, as the risk for progression from discoid lupus to systemic disease is 26% over 3 years.18
THE BIOLOGY OF HAIR IN CHILDREN WITH SKIN OF COLOR
To some extent, the biology of hair impacts the occurrence, appearance, and treatment of scalp hyperkeratosis in children with skin of color. First, it is important to remember that follicular density is lower in black patients as compared to Asian patients with a consequently lower hair count overall, which results in the easy appearance of hair loss, particularly at the margins of the scalp.19,20 Second, the shape of the hair follicle differs among races and ethnicities. Asian patients have round hair shafts coming from straight follicles, which allows for greater natural hair hydration, resulting in somewhat less aggressive scalp disease. Hispanic patients may have similarly straight hair or may have elliptical or curled shafts, the latter being noted in black patients. Furthermore, a curled hair shaft results in poor flow of sebum across the hair, resulting in greater scalp xerosis, more susceptibility to traction alopecia, and ultimately a greater risk for infections.20-23 Finally, the scalp is continuous with the face and neck, and Asian patients have greater sensitivity to skin care products in these areas, resulting in difficulty of treatment in this patient population and the need for use of gentle products.
HAIR CARE PRACTICES IN CHILDREN WITH SKIN OF COLOR
Hair care in patients with skin of color can be costly, difficult, and potentially damaging, with 99% of black girls reporting pomade or oil usage. Costly and complex hair care practices begin in childhood for patients with skin of color. In a series of 201 surveyed black girls with a mean age of 9.8 years, 80% had used hot combs and 42% used relaxers.24 Traction styles were common with 81% using ponytails, 67% braids, and 49% cornrows in the last 12 months. These styles are thought to affect hair health, particularly through induction of traction-related damage, folliculitis, and alopecia. Furthermore, chemical relaxers, hot combs, blowouts, and hair setting may be introduced during childhood.24 These practices appear to disturb the integrity of the hair follicle, leaving it more susceptible to irritation and infection.
Hair care in the pediatric population often is complicated by the fact that multiple children are being styled in tandem, either at home or in a salon, resulting in shared equipment and fomite spread. Even just proximity to a case of tinea capitis in the household will increase risk for tinea capitis. Furthermore, it is quite commonplace for black patients to use pomades and shampoos that contain antifungals, especially selenium sulfide, which makes it difficult to obtain accurate culture results. In India, use of mustard oil also has been linked to increased risk for tinea capitis.25
Other issues related to hair care include frequent dry scalp in patients with skin of color due to poor sebum distribution along the hair shaft. As a result, frequent washing may exacerbate scalp xerosis and further irritate seborrheic dermatitis and/or AD.
DIAGNOSTIC CONSIDERATIONS FOR SCALP HYPERKERATOSIS IN CHILDHOOD
Dermatologists should have a greater level of suspicion for tinea capitis in black and Hispanic children compared to white children. The index of suspicion should be high given that antifungal shampoos and pomades may minimize the clinical appearance. Although trends in overall incidence in the United States suggest tinea capitis is becoming less common, there still is a stronger representation of the disease in black patients.26 A study of positive fungal cultures from one clinic in Mississippi (N=1220) showed that two-thirds of patients were children younger than 13 years; 87% of patients with positive cultures for dermatophytes were black.27 The endothrix type of tinea capitis caused by T tonsurans often presents with a seborrheic appearance, and fungal culture is warranted in all pediatric patients with skin of color who have scalp hyperkeratosis. Asian children can be regarded with a lower level of suspicion for tinea capitis, similar to white patients in the United States. Variation in incidence of tinea capitis does exist worldwide and the practitioner may need to address these issues in patients who travel or are recent immigrants.
When identifying tinea capitis infections in children with skin of color, physicians should consider the patient’s personal and family history, comorbid skin disorders, dermoscopy, microscopy and fungal staining, and fungal culture (Figure).
A paradigm for the diagnosis of scalp hyperkeratosis in children with skin of color.
Personal and Family History
The first diagnostic consideration is the patient’s personal and family history. A history of AD, asthma, or allergies will support but not confirm the diagnosis of AD. Prior tinea capitis infections and household contacts with tinea infections support the presence of tinea capitis.17 Recent implementation of anti–tumor necrosis factor a inhibitor therapy in a psoriatic child can flare scalp disease, mimicking tinea capitis.28 The patient’s guardians should be queried about potential infectious contacts, whether they themselves have signs of scalp disease or tinea corporis (ringworm) or whether they have a pet with problematic fur. Physicians also should query patients and their guardians about recent use of topical antifungal shampoos, pomades, creams (both over-the-counter [OTC] and prescription), and/or oral antifungals. When these agents are used, there is a possibility that fungal examinations may be negative in the presence of true infection with tinea capitis. Traction alopecia, often preceded by fine scale, is more likely to present in patients who wear their hair in cornrows, while seborrheic dermatitis may be associated with hair extensions, reduced frequency of washing (61% of black girls surveyed wash every 2 weeks), and/or reduced usage of hair oils in black girls.24 Knowledge of the patient’s personal hair care history, such as use of pomades; frequency and method of washing/drying hair; types of hair care products used daily to wash and style hair; use of chemical relaxers; or recent hairstyling with cornrows, braids, or hair extensions, also is essential to the diagnosis of tinea capitis. Usage of traction-related styling practices in patients with chemically relaxed hair can enhance the risk for traction alopecia.29
Comorbid Skin Disorders
The patient also should be examined for comorbid skin disorders, including tinea corporis, alopecia (particularly in the areas of hyperkeratosis), and the presence of nuchal lymphadenopathy. For each extra clinical finding, the chances of a final diagnosis of tinea capitis rises, allowing for empiric diagnosis to be made that can be confirmed by a variety of tests.1-3
Dermoscopy
Next, the patient should undergo dermoscopic evaluation. On dermoscopy, tinea capitis typically presents with broken hairs, black dots on the scalp, comma-shaped hairs, and short corkscrew hairs, all of which should clear with therapy.30-33 Dermoscopic findings of AD would reveal underlying xerosis and prominent vasculature due to inflammation, and alopecia areata would present with yellow dots at the orifices of the hair follicles, exclamation point hairs, and vellus hairs.34,35 Traction alopecia may be noted by retained hairs along the hairline, which is known as the fringe sign.36
Microscopy and Fungal Staining
Microscopic preparations can be performed to identify tinea capitis using fungal stains of slide-based specimens. Breakage of short hairs onto the slide and/or cotton swab is a soft sign corroborating endothrix infection of the hairs. Potassium hydroxide can enhance visualization of the hyperkeratotic scalp, but for most black patients, use of antifungal agents reduces fungal hyphae and spores in the areas of hyperkeratosis and may limit the utility of examining the skin microscopically. Assessment of the broken hairs obtained by gentle friction with one glass slide and catching the scales onto another glass slide may yield the best results in the evaluation of tinea capitis (a technique taught to me by Robin Hornung, MD, Everett, Washington). Hairs obtained in this manner often are fragile and break due to endothrix infection replacing and weakening the shaft of the hairs. In the United States, fungal samples usually are obtained with cotton swabs, but a recent study suggested that brushing is superior to scraping to obtain samples; the combination of sampling techniques may improve the yield of a culture.37 Because topical agents are unable to enter the hair cortex, the hair shaft is the most likely to show fungal spores under the microscope when antifungal shampoos or pomades are used. Other testing methods such as Swartz-Lamkins or calcofluor white staining can be used on similar scrapings. Biopsy and periodic acid–Schiff staining of thick scales or crust can help differentiate tinea capitis from pityriasis amiantacea when the crust is too thick to be softened via potassium hydroxide preparation.38
Fungal Culture
Fungal culture onto media that contains nutrients for dermatophyte growth can be used for 4 purposes in tinea capitis: (1) to confirm infection, (2) to identify species of infection, (3) to confirm mycological cure when difficulty in clearance of disease has been noted, and (4) to obtain a specimen for sensitivity screening regarding antifungals when necessary, an uncommon but occasionally useful test in individuals with disease that has failed treatment with 1 or more antifungals.27
THERAPY FOR SCALP HYPERKERATOSIS IN CHILDREN WITH SKIN OF COLOR
In patients with scalp hyperkeratosis, it is important to address the specific cause of the disease. Therapy for scalp hyperkeratosis in children with skin of color includes altered hair care practices, use of OTC and prescription agents, and containment of fomites in the case of infections. Biopsy of atypical scalp hyperkeratosis cases is needed to diagnose rare etiologies such as discoid lupus or Langerhans cell histiocytosis. For individuals with systemic disease including Langerhans cell histiocytosis, which is generally accompanied by nodes and plaques in the inguinal region or other intertriginous sites, immediate hematology and oncology workup is required.39 For collagen vascular diseases such as lupus or dermatomyositis, appropriate referral to rheumatology and systemic therapy is warranted.
Altered Hair Care Practices
The use of prophylactic ketoconazole 1% shampoo may not reduce the risk for recurrence of tinea capitis over standard good hygiene, removal of fomites, and adherence to prescribed therapy.40 Use of selenium sulfide has been shown to effectively reduce contagion risk.41
Fragrance- and dye-free shampoos can be helpful in providing gentle cleansing of the scalp, which is especially important in Asian patients who have greater facial and eyelid sensitivity. Free-and-clear shampoos can be used alternatively with shampoos containing selenium sulfide or sulfur to eliminate comorbid seborrhea. Black patients should be advised to shampoo and condition their hair once weekly, and Asian and Hispanic patients should shampoo and condition 2 to 3 times weekly to remove scale and potentially reduce risk for tinea acquisition.42 Children with straight hair should shampoo with increased frequency in the summer to manually remove sweat-induced macerated hyperkeratosis. Conditioners also should be used consistently after shampooing to enhance hair health.
Use of OTC and Prescription Agents
Atopic Dermatitis
Topical corticosteroid agents can be used in increasing strengths to treat AD of the scalp in children with skin of color, from OTC scalp products containing hydrocortisone 1% to prescription-based agents. Hydration of the hair also is needed to counteract reduced water content.43 Due to the innate xerosis of the scalp in black patients and atopic patients, the use of oil-based or lotion products may provide the most hydration for patients with scalp disease.44 Alcohol-based agents, either drops or foams, may enhance xerosis and should be used sparingly.
Seborrheic Dermatitis
Alternating treatment with medicated shampoos containing selenium sulfide and ketoconazole can aid in the removal of seborrhea. Pomades including borage seed oil–based agents can be massaged into the scalp,45 particularly for treatment of infantile seborrhea, and should not necessarily be washed off daily in dark-skinned patients. Additional focused application of topical corticosteroids to the scalp also is helpful. Due to innate scalp xerosis in black children, therapy should be similar to AD.
Psoriasis
In the setting of pityriasis amiantacea, albeit rare in children with skin of color, oil-based agents can soften hyperkeratosis for removal. Sterile mineral oil or commercially available scalp preparations of peanut oil with fluocinolone or mineral oil with glycerin can aid in the removal of scales without harming the hair, but usage must be age appropriate. The addition of focused application of age-appropriate topical corticosteroids for areas of severe hyperkeratosis can aid in clearance of the lesions.44 Recently, a stable combination of calcipo-triene 0.005%–betamethasone dipropionate 0.064% has been approved in the United States for the therapy of scalp psoriasis in adolescents.46
Tinea Capitis
Antifungal shampoos including selenium sulfide will reduce contagion risk when used by both the patient and his/her family members. Frequency of shampooing is similar to that described for AD. Between shampooing, pomades with selenium sulfide can be applied to the scalp to enhance overall clearance.
Oral antifungals are the basis of treatment and use of griseofulvin is the gold standard. Terbinafine has been approved by the US Food and Drug Administration for treatment of tinea capitis; for children weighing less than 25 kg the dosage is 125 mg daily, for 25 to 35 kg the dosage is 187.5 mg daily, and for more than 35 kg the dosage is 250 mg daily. Shorter therapeutic courses may be required, making it a good second-line agent. Laboratory screening in children prior to therapy is not always performed but should be done in cases where fatty liver might be suspected.47 Monitoring liver function tests is best when exceeding 3 months of usage or shifting from one antifungal to another.3
Containment of Fomites
There are several procedures that should be followed to contain scalp infection in children with skin of color. First, all objects that come into contact with the scalp (eg, hats, hoods, brushes, pillowcases) should be washed with hot water or replaced weekly. Sharing these objects with friends or family should be strongly discouraged. Patients and their family members also should be instructed to use medicated (eg, selenium sulfide) shampoos and conditioners. Finally, patients are advised to avoid use of shared classroom garments or mats for sleeping.
LONG-TERM SEQUELAE OF SCALP HYPERKERATOSIS
Long-term sequelae of scalp hyperkeratosis often are discounted in children, but the disease can have lasting and damaging effects on the scalp. Sequelae include discomfort from chronicity and psychological distress. In particular, years of scalp pruritus can promote lichenification of the scalp and miniaturization of the hair follicles. Furthermore, itching due to sweating can limit participation in sports. Finally, tinea capitis is thought to be a risk factor for central centrifugal cicatricial alopecia (or can occur comorbidly with central centrifugal cicatricial alopecia causing severe pruritus), a chronic scarring hair loss that is seen primarily in black adult females.48 Erythema nodosum also has been reported as an associated finding in the case of kerion.49 One study reported associated findings that included thyroid cancer in individuals irradiated for tinea capitis in the 1950s.50
Conclusion
Scalp hyperkeratosis in children with skin of color, especially black patients, is more likely to be associated with tinea capitis and is more challenging to treat due to innate scalp xerosis in black patients and increased sensitivity of facial skin in Asian children. Ultimately, institution of therapy when needed and good scalp and hair care may prevent long-term sequelae.
Scalp hyperkeratosis (scaling or flaking) is a common symptom in childhood and is typified by fine to thick hyperkeratosis of the scalp with or without underlying erythema. The causes of scalp hyperkeratosis in childhood vary based on the demographics of the population. In a population where approximately half of the pediatric patients were white, scaling of the scalp was more common in patients with seborrheic dermatitis and/or atopic dermatitis (AD) who were aged 0 to 2 years, and tinea capitis was only noted in children who were black.1 In children with skin of color, scalp hyperkeratosis has been noted as a marker of tinea capitis, especially in patients aged 3 to 11 years,2,3 and the level of suspicion should consistently remain high for this age group. In another study of an all-black population of schoolchildren aged 5 to 13 years (N=224), 3% demonstrated signs and symptoms of tinea capitis and 14% were found to be asymptomatic carriers.4 Although generally benign in nature, scalp hyperkeratosis can be associated with systemic illnesses such as juvenile dermatomyositis and Langerhans cell histiocytosis.5 This article addresses the diagnosis and treatment of scalp hyperkeratosis in children with skin of color, focusing on differences in exposure to contagious cases, hairstyling practices, and biological factors that may impact the disease process.
CAUSES OF SCALP HYPERKERATOSIS IN CHILDHOOD
Scalp hyperkeratosis in childhood usually is caused by common benign conditions, but some level of suspicion should be maintained for more severe etiologic conditions such as Langerhans cell histiocytosis and collagen vascular diseases (eg, juvenile dermatomyositis).6 Langerhans cell histiocytosis of the scalp might be obscured by background pigmentation in black children.
Scalp scaling can be a minor criterion in the diagnosis of AD. Atopic dermatitis should be suspected in Asian children with scalp scaling. Although one study in Bangladesh revealed scalp involvement in only 5.2% of pediatric patients with AD,7 a study in China reported an incidence rate as high as 49.7% (with a similarly high incidence of eyelid dermatitis).8 Children with AD also may have dry hair.9 Atopic dermatitis of the scalp is typified by itching, fine hyperkeratosis, and notably eczematous scalp lesions ranging from excoriated or oozing erythematous plaques to lichenification with hair miniaturization, primarily from scratch-induced breakage.10 The latter finding often is noted in black adolescent girls with long-term moderate to severe AD (personal observation).
Seborrheic dermatitis is a hypersensitivity response to yeast colonization of the scalp with Malassezia species. The infantile form is extremely common (also known as cradle cap). Characteristically, greasy yellow hyperkeratosis in fine to thick sheets is noted on the scalp in children younger than 2 years, especially infants, often with involvement of skin folds. One study noted that seborrheic dermatitis occurs in 6% of school-aged children as opposed to 19% of children younger than 2 years.1 Severe seborrheic dermatitis in infancy may be a prelude to AD, with the incidence being 3 times higher in children with prior seborrheic dermatitis.11 In teenagers, seborrheic dermatitis often accompanies acne onset in the early pubertal years.12
Psoriasis is an autoimmune inflammatory dermatosis that most commonly affects white children. In childhood, pityriasis amiantacea, psoriasiform scalp hyperkeratosis, is more common than in adulthood, with thick, stuck-on scales bound to the hairs. This variant is uncommon in Hispanic and Asian children and is almost never seen in black children but has been reported in cohorts of Turkish children.13 In a series of 85 Egyptian children with pityriasis amiantacea, diagnosis of scalp psoriasis was made in 35.3%, eczematous dermatitis in 34.2%, and tinea capitis in 12.9%.14 Consequently, a high degree of suspicion for tinea capitis should be held if pityriasis amiantacea is found in children with skin of color.15,16
Tinea capitis is a dermatophyte infection of the scalp, hair, and surrounding skin. The presence of tinea capitis on the scalp is associated with environmental exposure to dermatophytes (eg, school, household).4,17 The infection is largely caused by Trichophyton tonsurans in the United States, which causes a seborrheic appearance and less commonly alopecia (black dot or thinning), plaques with scale, or kerion. The presence of cervical lymph nodes and/or alopecia increases the chances of tinea being the diagnosis. Potassium hydroxide preparation and fungal culture can be performed to corroborate the diagnosis.1-3 Other etiologies of scalp hyperkeratosis such as juvenile pityriasis rubra pilaris and lice are extremely uncommon in black children, but lice may be seen in Hispanic and Asian girls with long straight hair who attend school. Discoid lupus is more common in children with skin of color but is rare overall. When noted, accompanying mottled dyspigmentation and scarring alopecia are noted in addition to a high risk for developing systemic lupus erythematosus. Biopsy and screening for systemic lupus are necessary, as the risk for progression from discoid lupus to systemic disease is 26% over 3 years.18
THE BIOLOGY OF HAIR IN CHILDREN WITH SKIN OF COLOR
To some extent, the biology of hair impacts the occurrence, appearance, and treatment of scalp hyperkeratosis in children with skin of color. First, it is important to remember that follicular density is lower in black patients as compared to Asian patients with a consequently lower hair count overall, which results in the easy appearance of hair loss, particularly at the margins of the scalp.19,20 Second, the shape of the hair follicle differs among races and ethnicities. Asian patients have round hair shafts coming from straight follicles, which allows for greater natural hair hydration, resulting in somewhat less aggressive scalp disease. Hispanic patients may have similarly straight hair or may have elliptical or curled shafts, the latter being noted in black patients. Furthermore, a curled hair shaft results in poor flow of sebum across the hair, resulting in greater scalp xerosis, more susceptibility to traction alopecia, and ultimately a greater risk for infections.20-23 Finally, the scalp is continuous with the face and neck, and Asian patients have greater sensitivity to skin care products in these areas, resulting in difficulty of treatment in this patient population and the need for use of gentle products.
HAIR CARE PRACTICES IN CHILDREN WITH SKIN OF COLOR
Hair care in patients with skin of color can be costly, difficult, and potentially damaging, with 99% of black girls reporting pomade or oil usage. Costly and complex hair care practices begin in childhood for patients with skin of color. In a series of 201 surveyed black girls with a mean age of 9.8 years, 80% had used hot combs and 42% used relaxers.24 Traction styles were common with 81% using ponytails, 67% braids, and 49% cornrows in the last 12 months. These styles are thought to affect hair health, particularly through induction of traction-related damage, folliculitis, and alopecia. Furthermore, chemical relaxers, hot combs, blowouts, and hair setting may be introduced during childhood.24 These practices appear to disturb the integrity of the hair follicle, leaving it more susceptible to irritation and infection.
Hair care in the pediatric population often is complicated by the fact that multiple children are being styled in tandem, either at home or in a salon, resulting in shared equipment and fomite spread. Even just proximity to a case of tinea capitis in the household will increase risk for tinea capitis. Furthermore, it is quite commonplace for black patients to use pomades and shampoos that contain antifungals, especially selenium sulfide, which makes it difficult to obtain accurate culture results. In India, use of mustard oil also has been linked to increased risk for tinea capitis.25
Other issues related to hair care include frequent dry scalp in patients with skin of color due to poor sebum distribution along the hair shaft. As a result, frequent washing may exacerbate scalp xerosis and further irritate seborrheic dermatitis and/or AD.
DIAGNOSTIC CONSIDERATIONS FOR SCALP HYPERKERATOSIS IN CHILDHOOD
Dermatologists should have a greater level of suspicion for tinea capitis in black and Hispanic children compared to white children. The index of suspicion should be high given that antifungal shampoos and pomades may minimize the clinical appearance. Although trends in overall incidence in the United States suggest tinea capitis is becoming less common, there still is a stronger representation of the disease in black patients.26 A study of positive fungal cultures from one clinic in Mississippi (N=1220) showed that two-thirds of patients were children younger than 13 years; 87% of patients with positive cultures for dermatophytes were black.27 The endothrix type of tinea capitis caused by T tonsurans often presents with a seborrheic appearance, and fungal culture is warranted in all pediatric patients with skin of color who have scalp hyperkeratosis. Asian children can be regarded with a lower level of suspicion for tinea capitis, similar to white patients in the United States. Variation in incidence of tinea capitis does exist worldwide and the practitioner may need to address these issues in patients who travel or are recent immigrants.
When identifying tinea capitis infections in children with skin of color, physicians should consider the patient’s personal and family history, comorbid skin disorders, dermoscopy, microscopy and fungal staining, and fungal culture (Figure).
A paradigm for the diagnosis of scalp hyperkeratosis in children with skin of color.
Personal and Family History
The first diagnostic consideration is the patient’s personal and family history. A history of AD, asthma, or allergies will support but not confirm the diagnosis of AD. Prior tinea capitis infections and household contacts with tinea infections support the presence of tinea capitis.17 Recent implementation of anti–tumor necrosis factor a inhibitor therapy in a psoriatic child can flare scalp disease, mimicking tinea capitis.28 The patient’s guardians should be queried about potential infectious contacts, whether they themselves have signs of scalp disease or tinea corporis (ringworm) or whether they have a pet with problematic fur. Physicians also should query patients and their guardians about recent use of topical antifungal shampoos, pomades, creams (both over-the-counter [OTC] and prescription), and/or oral antifungals. When these agents are used, there is a possibility that fungal examinations may be negative in the presence of true infection with tinea capitis. Traction alopecia, often preceded by fine scale, is more likely to present in patients who wear their hair in cornrows, while seborrheic dermatitis may be associated with hair extensions, reduced frequency of washing (61% of black girls surveyed wash every 2 weeks), and/or reduced usage of hair oils in black girls.24 Knowledge of the patient’s personal hair care history, such as use of pomades; frequency and method of washing/drying hair; types of hair care products used daily to wash and style hair; use of chemical relaxers; or recent hairstyling with cornrows, braids, or hair extensions, also is essential to the diagnosis of tinea capitis. Usage of traction-related styling practices in patients with chemically relaxed hair can enhance the risk for traction alopecia.29
Comorbid Skin Disorders
The patient also should be examined for comorbid skin disorders, including tinea corporis, alopecia (particularly in the areas of hyperkeratosis), and the presence of nuchal lymphadenopathy. For each extra clinical finding, the chances of a final diagnosis of tinea capitis rises, allowing for empiric diagnosis to be made that can be confirmed by a variety of tests.1-3
Dermoscopy
Next, the patient should undergo dermoscopic evaluation. On dermoscopy, tinea capitis typically presents with broken hairs, black dots on the scalp, comma-shaped hairs, and short corkscrew hairs, all of which should clear with therapy.30-33 Dermoscopic findings of AD would reveal underlying xerosis and prominent vasculature due to inflammation, and alopecia areata would present with yellow dots at the orifices of the hair follicles, exclamation point hairs, and vellus hairs.34,35 Traction alopecia may be noted by retained hairs along the hairline, which is known as the fringe sign.36
Microscopy and Fungal Staining
Microscopic preparations can be performed to identify tinea capitis using fungal stains of slide-based specimens. Breakage of short hairs onto the slide and/or cotton swab is a soft sign corroborating endothrix infection of the hairs. Potassium hydroxide can enhance visualization of the hyperkeratotic scalp, but for most black patients, use of antifungal agents reduces fungal hyphae and spores in the areas of hyperkeratosis and may limit the utility of examining the skin microscopically. Assessment of the broken hairs obtained by gentle friction with one glass slide and catching the scales onto another glass slide may yield the best results in the evaluation of tinea capitis (a technique taught to me by Robin Hornung, MD, Everett, Washington). Hairs obtained in this manner often are fragile and break due to endothrix infection replacing and weakening the shaft of the hairs. In the United States, fungal samples usually are obtained with cotton swabs, but a recent study suggested that brushing is superior to scraping to obtain samples; the combination of sampling techniques may improve the yield of a culture.37 Because topical agents are unable to enter the hair cortex, the hair shaft is the most likely to show fungal spores under the microscope when antifungal shampoos or pomades are used. Other testing methods such as Swartz-Lamkins or calcofluor white staining can be used on similar scrapings. Biopsy and periodic acid–Schiff staining of thick scales or crust can help differentiate tinea capitis from pityriasis amiantacea when the crust is too thick to be softened via potassium hydroxide preparation.38
Fungal Culture
Fungal culture onto media that contains nutrients for dermatophyte growth can be used for 4 purposes in tinea capitis: (1) to confirm infection, (2) to identify species of infection, (3) to confirm mycological cure when difficulty in clearance of disease has been noted, and (4) to obtain a specimen for sensitivity screening regarding antifungals when necessary, an uncommon but occasionally useful test in individuals with disease that has failed treatment with 1 or more antifungals.27
THERAPY FOR SCALP HYPERKERATOSIS IN CHILDREN WITH SKIN OF COLOR
In patients with scalp hyperkeratosis, it is important to address the specific cause of the disease. Therapy for scalp hyperkeratosis in children with skin of color includes altered hair care practices, use of OTC and prescription agents, and containment of fomites in the case of infections. Biopsy of atypical scalp hyperkeratosis cases is needed to diagnose rare etiologies such as discoid lupus or Langerhans cell histiocytosis. For individuals with systemic disease including Langerhans cell histiocytosis, which is generally accompanied by nodes and plaques in the inguinal region or other intertriginous sites, immediate hematology and oncology workup is required.39 For collagen vascular diseases such as lupus or dermatomyositis, appropriate referral to rheumatology and systemic therapy is warranted.
Altered Hair Care Practices
The use of prophylactic ketoconazole 1% shampoo may not reduce the risk for recurrence of tinea capitis over standard good hygiene, removal of fomites, and adherence to prescribed therapy.40 Use of selenium sulfide has been shown to effectively reduce contagion risk.41
Fragrance- and dye-free shampoos can be helpful in providing gentle cleansing of the scalp, which is especially important in Asian patients who have greater facial and eyelid sensitivity. Free-and-clear shampoos can be used alternatively with shampoos containing selenium sulfide or sulfur to eliminate comorbid seborrhea. Black patients should be advised to shampoo and condition their hair once weekly, and Asian and Hispanic patients should shampoo and condition 2 to 3 times weekly to remove scale and potentially reduce risk for tinea acquisition.42 Children with straight hair should shampoo with increased frequency in the summer to manually remove sweat-induced macerated hyperkeratosis. Conditioners also should be used consistently after shampooing to enhance hair health.
Use of OTC and Prescription Agents
Atopic Dermatitis
Topical corticosteroid agents can be used in increasing strengths to treat AD of the scalp in children with skin of color, from OTC scalp products containing hydrocortisone 1% to prescription-based agents. Hydration of the hair also is needed to counteract reduced water content.43 Due to the innate xerosis of the scalp in black patients and atopic patients, the use of oil-based or lotion products may provide the most hydration for patients with scalp disease.44 Alcohol-based agents, either drops or foams, may enhance xerosis and should be used sparingly.
Seborrheic Dermatitis
Alternating treatment with medicated shampoos containing selenium sulfide and ketoconazole can aid in the removal of seborrhea. Pomades including borage seed oil–based agents can be massaged into the scalp,45 particularly for treatment of infantile seborrhea, and should not necessarily be washed off daily in dark-skinned patients. Additional focused application of topical corticosteroids to the scalp also is helpful. Due to innate scalp xerosis in black children, therapy should be similar to AD.
Psoriasis
In the setting of pityriasis amiantacea, albeit rare in children with skin of color, oil-based agents can soften hyperkeratosis for removal. Sterile mineral oil or commercially available scalp preparations of peanut oil with fluocinolone or mineral oil with glycerin can aid in the removal of scales without harming the hair, but usage must be age appropriate. The addition of focused application of age-appropriate topical corticosteroids for areas of severe hyperkeratosis can aid in clearance of the lesions.44 Recently, a stable combination of calcipo-triene 0.005%–betamethasone dipropionate 0.064% has been approved in the United States for the therapy of scalp psoriasis in adolescents.46
Tinea Capitis
Antifungal shampoos including selenium sulfide will reduce contagion risk when used by both the patient and his/her family members. Frequency of shampooing is similar to that described for AD. Between shampooing, pomades with selenium sulfide can be applied to the scalp to enhance overall clearance.
Oral antifungals are the basis of treatment and use of griseofulvin is the gold standard. Terbinafine has been approved by the US Food and Drug Administration for treatment of tinea capitis; for children weighing less than 25 kg the dosage is 125 mg daily, for 25 to 35 kg the dosage is 187.5 mg daily, and for more than 35 kg the dosage is 250 mg daily. Shorter therapeutic courses may be required, making it a good second-line agent. Laboratory screening in children prior to therapy is not always performed but should be done in cases where fatty liver might be suspected.47 Monitoring liver function tests is best when exceeding 3 months of usage or shifting from one antifungal to another.3
Containment of Fomites
There are several procedures that should be followed to contain scalp infection in children with skin of color. First, all objects that come into contact with the scalp (eg, hats, hoods, brushes, pillowcases) should be washed with hot water or replaced weekly. Sharing these objects with friends or family should be strongly discouraged. Patients and their family members also should be instructed to use medicated (eg, selenium sulfide) shampoos and conditioners. Finally, patients are advised to avoid use of shared classroom garments or mats for sleeping.
LONG-TERM SEQUELAE OF SCALP HYPERKERATOSIS
Long-term sequelae of scalp hyperkeratosis often are discounted in children, but the disease can have lasting and damaging effects on the scalp. Sequelae include discomfort from chronicity and psychological distress. In particular, years of scalp pruritus can promote lichenification of the scalp and miniaturization of the hair follicles. Furthermore, itching due to sweating can limit participation in sports. Finally, tinea capitis is thought to be a risk factor for central centrifugal cicatricial alopecia (or can occur comorbidly with central centrifugal cicatricial alopecia causing severe pruritus), a chronic scarring hair loss that is seen primarily in black adult females.48 Erythema nodosum also has been reported as an associated finding in the case of kerion.49 One study reported associated findings that included thyroid cancer in individuals irradiated for tinea capitis in the 1950s.50
Conclusion
Scalp hyperkeratosis in children with skin of color, especially black patients, is more likely to be associated with tinea capitis and is more challenging to treat due to innate scalp xerosis in black patients and increased sensitivity of facial skin in Asian children. Ultimately, institution of therapy when needed and good scalp and hair care may prevent long-term sequelae.
1. Williams JV, Eichenfield LF, Burke BL, et al. Prevalence of scalp scaling in prepubertal children. Pediatrics. 2005;115:e1-e6.
2. Coley MK, Bhanusali DG, Silverberg JI, et al. Scalp hyperkeratosis and alopecia in children of color. J Drugs Dermatol. 2011;10:511-516.
3. Bhanusali D, Coley M, Silverberg JI, et al. Treatment outcomes for tinea capitis in a skin of color population. J Drugs Dermatol. 2012;11:852-856.
4. Williams JV, Honig PJ, McGinley KJ, et al. Semiquantitative study of tinea capitis and the asymptomatic carrier state in inner-city school children. Pediatrics. 1995;96:265-267.
5. McDonald LL, Smith ML. Diagnostic dilemmas in pediatric/adolescent dermatology: scaly scalp. J Pediatr Health Care. 1998;12:80-84.
6. Peloro TM, Miller OF 3rd, Hahn TF, et al. Juvenile dermatomyositis: a retrospective review of a 30-year experience. J Am Acad Dermatol. 2001;45:28-34.
7. Wahab MA, Rahman MH, Khondker L, et al. Minor criteria for atopic dermatitis in children. Mymensingh Med J. 2011;20:419-424.
8. Shi M, Zhang H, Chen X, et al. Clinical features of atopic dermatitis in a hospital-based setting in China. J Eur Acad Dermatol Venereol [published online ahead of print January 9, 2011]. 2011;25:1206-1212.
9. Kim KS, Shin MK, Kim JH, et al. Effects of atopic dermatitis on the morphology and water content of scalp hair. Microsc Res Tech. 2012;75:620-625.
10. Sabin BR, Peters N, Peters AT. Chapter 20: atopic dermatitis. Allergy Asthma Proc. 2012;33:S67-S69.
11. Alexopoulos A, Kakourou T, Orfanou I, et al. Retrospective analysis of the relationship between infantile seborrheic dermatitis and atopic dermatitis [published online ahead of print November 13, 2013]. Pediatr Dermatol. 2014;31:125-130.
12. Elish D, Silverberg NB. Infantile seborrheic dermatitis. Cutis. 2006;77:297-300.
13. Sarifakioglu E, Yilmaz AE, Gorpelioglu C, et al. Prevalence of scalp disorders and hair loss in children. Cutis. 2012;90:225-229.
14. Abdel-Hamid IA, Agha SA, Moustafa YM, et al. Pityriasis amiantacea: a clinical and etiopathologic study of 85 patients. Int J Dermatol. 2003;42:260-264.
15. Oostveen AM, Jong EM, Evers AW, et al. Reliability, responsiveness and validity of Scalpdex in children with scalp psoriasis: the Dutch study. Acta Derm Venereol. 2014;94:198-202.
16. Silverberg NB. Atlas of Pediatric Cutaneous Biodiversity: Comparative Dermatologic Atlas of Pediatric Skin of All Colors. New York, NY: Springer; 2012.
17. Sharma V, Silverberg NB, Howard R, et al. Do hair care practices affect the acquisition of tinea capitis? a case-control study. Arch Pediatr Adolesc Med. 2001;155:818-821.
18. Moises-Alfaro C, Berrón-Pérez R, Carrasco-Daza D, et al. Discoid lupus erythematosus in children: clinical, histopathologic, and follow-up features in 27 cases. Pediatr Dermatol. 2003;20:103-107.
19. Ramos-e-Silva M. Ethnic hair and skin: what is the state of the science? Chicago, Illinois—September 29-30, 2001. Clin Dermatol. 2002;20:321-324.
20. Heath CR, McMichael AJ. Biology of hair follicle. In: Kelly AP, Taylor SC, eds. Dermatology for Skin of Color. New York, NY: McGraw Hill; 2009:105-109.
21. Khumalo NP. African hair morphology: macrostructure to ultrastructure. Int J Dermatol. 2005;44(suppl 1):10-12.
22. Thibaut S, Bernard BA. The biology of hair shape. Int J Dermatol. 2005;44(suppl 1):2-3.
23. Taylor SC. Skin of color: biology, structure, function, and implications for dermatologic disease. J Am Acad Dermatol. 2002;46(suppl 2):S41-S62.
24. Rucker Wright D, Gathers R, Kapke A, et al. Hair care practices and their association with scalp and hair disorders in African American girls. J Am Acad Dermatol. 2011;64:253-262.
25. Kumar V, Sharma RC, Chander R. Clinicomycological study of tinea capitis. Indian J Dermatol Venereol Leprol. 1996;62:207-209.
26. Mirmirani P, Tucker LY. Epidemiologic trends in pediatric tinea capitis: a population-based study from Kaiser Permanente Northern California [published online ahead of print October 2, 2013]. J Am Acad Dermatol. 2013;69:916-921.
27. Chapman JC, Daniel CR 3rd, Daniel JG, et al. Tinea capitis caused by dermatophytes: a 15-year retrospective study from a Mississippi Dermatology Clinic. Cutis. 2011;88:230-233.
28. Perman MJ, Lovell DJ, Denson LA, et al. Five cases of anti-tumor necrosis factor alpha-induced psoriasis presenting with severe scalp involvement in children. Pediatr Dermatol. 2012;29:454-459.
29. Khumalo NP, Jessop S, Gumedze F, et al. Determinants of marginal traction alopecia in African girls and women. J Am Acad Dermatol. 2008;59:432-438.
30. Vazquez-Lopez F, Palacios-Garcia L, Argenziano G. Dermoscopic corkscrew hairs dissolve after successful therapy of Trichophyton violaceum tinea capitis: a case report. Australas J Dermatol. 2012;53:118-119.
31. Pinheiro AM, Lobato LA, Varella TC. Dermoscopy findings in tinea capitis: case report and literature review. An Bras Dermatol. 2012;87:313-314.
32. Mapelli ET, Gualandri L, Cerri A, et al. Comma hairs in tinea capitis: a useful dermatoscopic sign for diagnosis of tinea capitis. Pediatr Dermatol. 2012;29:223-224.
33. Hughes R, Chiaverini C, Bahadoran P, et al. Corkscrew hair: a new dermoscopic sign for diagnosis of tinea capitis in black children. Arch Dermatol. 2011;147:355-356.
34. Ekiz O, Sen BB, Rifaiog˘lu EN, et al. Trichoscopy in paediatric patients with tinea capitis: a useful method to differentiate from alopecia areata [published online ahead of print August 24, 2013]. J Eur Acad Dermatol Venereol. 2014;28:1255-1258.
35. Lencastre A, Tosti A. Role of trichoscopy in children’s scalp and hair disorders [published online ahead of print Aug 13, 2013]. Pediatr Dermatol. 2013;30:674-682.
36. Samrao A, Price VH, Zedek D, et al. The “fringe sign”—a useful clinical finding in traction alopecia of the marginal hair line. Dermatol Online J. 2011;17:1.
37. Nasir S, Ralph N, O’Neill C, et al. Trends in tinea capitis in an Irish pediatric population and a comparison of scalp brushings versus scalp scrapings as methods of investigation [published online ahead of print February 22, 2013]. Pediatr Dermatol. 2014;31:622-623.
38. Alvarez MS, Silverberg NB. Tinea capitis. Cutis. 2006;78:189-196.
39. Simko SJ, Garmezy B, Abhyankar H, et al. Differentiating skin-limited and multisystem Langerhans cell histiocytosis. J Pediatr. 2014;165:990-996.
40. Bookstaver PB, Watson HJ, Winters SD, et al. Prophylactic ketoconazole shampoo for tinea capitis in a high-risk pediatric population. J Pediatr Pharmacol Ther. 2011;16:199-203.
41. Allen HB, Honig PJ, Leyden JJ, et al. Selenium sulfide: adjunctive therapy for tinea capitis. Pediatrics. 1982;69:81-83.
42. Crawford K, Hernandez C. A review of hair care products for black individuals. Cutis. 2014;93:289-293.
43. Kim KS, Shin MK, Kim JH, et al. Effects of atopic dermatitis on the morphology and water content of scalp hair [published online ahead of print November 7, 2011]. Microsc Res Tech. 2012;75:620-625.
44. Kapila S, Hong E, Fischer G. A comparative study of childhood psoriasis and atopic dermatitis and greater understanding of the overlapping condition, psoriasis-dermatitis. Australas J Dermatol. 2012;53:98-105.
45. Tollesson A, Frithz A. Borage oil, an effective new treatment for infantile seborrhoeic dermatitis. Br J Dermatol. 1993;129:95.
46. Gooderham M, Debarre JM, Keddy-Grant J, et al. Safety and efficacy of calcipotriol plus betamethasone dipropionate gel in the treatment of scalp psoriasis in adolescents 12-17 years of age [published online ahead of print October 22, 2014]. Br J Dermatol. 2014;171:1470-1477.
47. Singer C, Stancu P, Coşoveanu S, et al. Non-alcoholic fatty liver disease in children. Curr Health Sci J. 2014;40:170-176.
48. Chiang C, Price V, Mirmirani P. Central centrifugal cicatricial alopecia: superimposed tinea capitis as the etiology of chronic scalp pruritus. Dermatol Online J. 2008;14:3.
49. Morrone A, Calcaterra R, Valenzano M, et al. Erythema nodosum induced by kerion celsi of the scalp in a woman. Mycoses. 2011;54:e237-e239.
50. Boaventura P, Pereira D, Celestino R, et al. Genetic alterations in thyroid tumors from patients irradiated in childhood for tinea capitis treatment. Eur J Endocrinol. 2013;169:673-679.
1. Williams JV, Eichenfield LF, Burke BL, et al. Prevalence of scalp scaling in prepubertal children. Pediatrics. 2005;115:e1-e6.
2. Coley MK, Bhanusali DG, Silverberg JI, et al. Scalp hyperkeratosis and alopecia in children of color. J Drugs Dermatol. 2011;10:511-516.
3. Bhanusali D, Coley M, Silverberg JI, et al. Treatment outcomes for tinea capitis in a skin of color population. J Drugs Dermatol. 2012;11:852-856.
4. Williams JV, Honig PJ, McGinley KJ, et al. Semiquantitative study of tinea capitis and the asymptomatic carrier state in inner-city school children. Pediatrics. 1995;96:265-267.
5. McDonald LL, Smith ML. Diagnostic dilemmas in pediatric/adolescent dermatology: scaly scalp. J Pediatr Health Care. 1998;12:80-84.
6. Peloro TM, Miller OF 3rd, Hahn TF, et al. Juvenile dermatomyositis: a retrospective review of a 30-year experience. J Am Acad Dermatol. 2001;45:28-34.
7. Wahab MA, Rahman MH, Khondker L, et al. Minor criteria for atopic dermatitis in children. Mymensingh Med J. 2011;20:419-424.
8. Shi M, Zhang H, Chen X, et al. Clinical features of atopic dermatitis in a hospital-based setting in China. J Eur Acad Dermatol Venereol [published online ahead of print January 9, 2011]. 2011;25:1206-1212.
9. Kim KS, Shin MK, Kim JH, et al. Effects of atopic dermatitis on the morphology and water content of scalp hair. Microsc Res Tech. 2012;75:620-625.
10. Sabin BR, Peters N, Peters AT. Chapter 20: atopic dermatitis. Allergy Asthma Proc. 2012;33:S67-S69.
11. Alexopoulos A, Kakourou T, Orfanou I, et al. Retrospective analysis of the relationship between infantile seborrheic dermatitis and atopic dermatitis [published online ahead of print November 13, 2013]. Pediatr Dermatol. 2014;31:125-130.
12. Elish D, Silverberg NB. Infantile seborrheic dermatitis. Cutis. 2006;77:297-300.
13. Sarifakioglu E, Yilmaz AE, Gorpelioglu C, et al. Prevalence of scalp disorders and hair loss in children. Cutis. 2012;90:225-229.
14. Abdel-Hamid IA, Agha SA, Moustafa YM, et al. Pityriasis amiantacea: a clinical and etiopathologic study of 85 patients. Int J Dermatol. 2003;42:260-264.
15. Oostveen AM, Jong EM, Evers AW, et al. Reliability, responsiveness and validity of Scalpdex in children with scalp psoriasis: the Dutch study. Acta Derm Venereol. 2014;94:198-202.
16. Silverberg NB. Atlas of Pediatric Cutaneous Biodiversity: Comparative Dermatologic Atlas of Pediatric Skin of All Colors. New York, NY: Springer; 2012.
17. Sharma V, Silverberg NB, Howard R, et al. Do hair care practices affect the acquisition of tinea capitis? a case-control study. Arch Pediatr Adolesc Med. 2001;155:818-821.
18. Moises-Alfaro C, Berrón-Pérez R, Carrasco-Daza D, et al. Discoid lupus erythematosus in children: clinical, histopathologic, and follow-up features in 27 cases. Pediatr Dermatol. 2003;20:103-107.
19. Ramos-e-Silva M. Ethnic hair and skin: what is the state of the science? Chicago, Illinois—September 29-30, 2001. Clin Dermatol. 2002;20:321-324.
20. Heath CR, McMichael AJ. Biology of hair follicle. In: Kelly AP, Taylor SC, eds. Dermatology for Skin of Color. New York, NY: McGraw Hill; 2009:105-109.
21. Khumalo NP. African hair morphology: macrostructure to ultrastructure. Int J Dermatol. 2005;44(suppl 1):10-12.
22. Thibaut S, Bernard BA. The biology of hair shape. Int J Dermatol. 2005;44(suppl 1):2-3.
23. Taylor SC. Skin of color: biology, structure, function, and implications for dermatologic disease. J Am Acad Dermatol. 2002;46(suppl 2):S41-S62.
24. Rucker Wright D, Gathers R, Kapke A, et al. Hair care practices and their association with scalp and hair disorders in African American girls. J Am Acad Dermatol. 2011;64:253-262.
25. Kumar V, Sharma RC, Chander R. Clinicomycological study of tinea capitis. Indian J Dermatol Venereol Leprol. 1996;62:207-209.
26. Mirmirani P, Tucker LY. Epidemiologic trends in pediatric tinea capitis: a population-based study from Kaiser Permanente Northern California [published online ahead of print October 2, 2013]. J Am Acad Dermatol. 2013;69:916-921.
27. Chapman JC, Daniel CR 3rd, Daniel JG, et al. Tinea capitis caused by dermatophytes: a 15-year retrospective study from a Mississippi Dermatology Clinic. Cutis. 2011;88:230-233.
28. Perman MJ, Lovell DJ, Denson LA, et al. Five cases of anti-tumor necrosis factor alpha-induced psoriasis presenting with severe scalp involvement in children. Pediatr Dermatol. 2012;29:454-459.
29. Khumalo NP, Jessop S, Gumedze F, et al. Determinants of marginal traction alopecia in African girls and women. J Am Acad Dermatol. 2008;59:432-438.
30. Vazquez-Lopez F, Palacios-Garcia L, Argenziano G. Dermoscopic corkscrew hairs dissolve after successful therapy of Trichophyton violaceum tinea capitis: a case report. Australas J Dermatol. 2012;53:118-119.
31. Pinheiro AM, Lobato LA, Varella TC. Dermoscopy findings in tinea capitis: case report and literature review. An Bras Dermatol. 2012;87:313-314.
32. Mapelli ET, Gualandri L, Cerri A, et al. Comma hairs in tinea capitis: a useful dermatoscopic sign for diagnosis of tinea capitis. Pediatr Dermatol. 2012;29:223-224.
33. Hughes R, Chiaverini C, Bahadoran P, et al. Corkscrew hair: a new dermoscopic sign for diagnosis of tinea capitis in black children. Arch Dermatol. 2011;147:355-356.
34. Ekiz O, Sen BB, Rifaiog˘lu EN, et al. Trichoscopy in paediatric patients with tinea capitis: a useful method to differentiate from alopecia areata [published online ahead of print August 24, 2013]. J Eur Acad Dermatol Venereol. 2014;28:1255-1258.
35. Lencastre A, Tosti A. Role of trichoscopy in children’s scalp and hair disorders [published online ahead of print Aug 13, 2013]. Pediatr Dermatol. 2013;30:674-682.
36. Samrao A, Price VH, Zedek D, et al. The “fringe sign”—a useful clinical finding in traction alopecia of the marginal hair line. Dermatol Online J. 2011;17:1.
37. Nasir S, Ralph N, O’Neill C, et al. Trends in tinea capitis in an Irish pediatric population and a comparison of scalp brushings versus scalp scrapings as methods of investigation [published online ahead of print February 22, 2013]. Pediatr Dermatol. 2014;31:622-623.
38. Alvarez MS, Silverberg NB. Tinea capitis. Cutis. 2006;78:189-196.
39. Simko SJ, Garmezy B, Abhyankar H, et al. Differentiating skin-limited and multisystem Langerhans cell histiocytosis. J Pediatr. 2014;165:990-996.
40. Bookstaver PB, Watson HJ, Winters SD, et al. Prophylactic ketoconazole shampoo for tinea capitis in a high-risk pediatric population. J Pediatr Pharmacol Ther. 2011;16:199-203.
41. Allen HB, Honig PJ, Leyden JJ, et al. Selenium sulfide: adjunctive therapy for tinea capitis. Pediatrics. 1982;69:81-83.
42. Crawford K, Hernandez C. A review of hair care products for black individuals. Cutis. 2014;93:289-293.
43. Kim KS, Shin MK, Kim JH, et al. Effects of atopic dermatitis on the morphology and water content of scalp hair [published online ahead of print November 7, 2011]. Microsc Res Tech. 2012;75:620-625.
44. Kapila S, Hong E, Fischer G. A comparative study of childhood psoriasis and atopic dermatitis and greater understanding of the overlapping condition, psoriasis-dermatitis. Australas J Dermatol. 2012;53:98-105.
45. Tollesson A, Frithz A. Borage oil, an effective new treatment for infantile seborrhoeic dermatitis. Br J Dermatol. 1993;129:95.
46. Gooderham M, Debarre JM, Keddy-Grant J, et al. Safety and efficacy of calcipotriol plus betamethasone dipropionate gel in the treatment of scalp psoriasis in adolescents 12-17 years of age [published online ahead of print October 22, 2014]. Br J Dermatol. 2014;171:1470-1477.
47. Singer C, Stancu P, Coşoveanu S, et al. Non-alcoholic fatty liver disease in children. Curr Health Sci J. 2014;40:170-176.
48. Chiang C, Price V, Mirmirani P. Central centrifugal cicatricial alopecia: superimposed tinea capitis as the etiology of chronic scalp pruritus. Dermatol Online J. 2008;14:3.
49. Morrone A, Calcaterra R, Valenzano M, et al. Erythema nodosum induced by kerion celsi of the scalp in a woman. Mycoses. 2011;54:e237-e239.
50. Boaventura P, Pereira D, Celestino R, et al. Genetic alterations in thyroid tumors from patients irradiated in childhood for tinea capitis treatment. Eur J Endocrinol. 2013;169:673-679.
Practice Points
- Scalp hyperkeratosis is a common finding in children, especially those with skin of color.
- Fungal culture may be helpful in the diagnosis of scalp hyperkeratosis in children of any age but should be performed in patients aged 3 to 11 years with skin of color.
- Therapy of scalp disease in children with skin of color should be adjusted based on hair type and disease features.
HM15 Session Analysis: The Physician-Administrator Management Dyad
Hm15 Presenters: Chuck Ainsworth, MD, MCC,; Dan Virnich, MD, MBA; Roberta Himebaugh, MBA, SFHM; Robert Hickling, MHA; Sendil Krishnan, MD
Summation: The presenters, a group of physicians and administrators for hospital medicine groups, explored three dyad models. These three models were:
- Office of the Executive, where there is one senior executive and a junior executive;
- Coordinated Co-Leadership, where each of the two co-leaders has separate direct reports; and
- Integrated Co-Leadership, where there are two co-leaders and the staff report to the co-leader team.
The discussion ensued to outline the benefit of a dyad leadership model, which can lead to growth and success in advancing the commitment to patient care. The group also emphasized the importance of providing leadership training and education to optimize the dyad leadership model. Bringing together physician and administrator dyads enables an organization to have complimentary expertise to advance hospital medicine programs into the next era.
Hm15 Presenters: Chuck Ainsworth, MD, MCC,; Dan Virnich, MD, MBA; Roberta Himebaugh, MBA, SFHM; Robert Hickling, MHA; Sendil Krishnan, MD
Summation: The presenters, a group of physicians and administrators for hospital medicine groups, explored three dyad models. These three models were:
- Office of the Executive, where there is one senior executive and a junior executive;
- Coordinated Co-Leadership, where each of the two co-leaders has separate direct reports; and
- Integrated Co-Leadership, where there are two co-leaders and the staff report to the co-leader team.
The discussion ensued to outline the benefit of a dyad leadership model, which can lead to growth and success in advancing the commitment to patient care. The group also emphasized the importance of providing leadership training and education to optimize the dyad leadership model. Bringing together physician and administrator dyads enables an organization to have complimentary expertise to advance hospital medicine programs into the next era.
Hm15 Presenters: Chuck Ainsworth, MD, MCC,; Dan Virnich, MD, MBA; Roberta Himebaugh, MBA, SFHM; Robert Hickling, MHA; Sendil Krishnan, MD
Summation: The presenters, a group of physicians and administrators for hospital medicine groups, explored three dyad models. These three models were:
- Office of the Executive, where there is one senior executive and a junior executive;
- Coordinated Co-Leadership, where each of the two co-leaders has separate direct reports; and
- Integrated Co-Leadership, where there are two co-leaders and the staff report to the co-leader team.
The discussion ensued to outline the benefit of a dyad leadership model, which can lead to growth and success in advancing the commitment to patient care. The group also emphasized the importance of providing leadership training and education to optimize the dyad leadership model. Bringing together physician and administrator dyads enables an organization to have complimentary expertise to advance hospital medicine programs into the next era.
HM15 Session Analysis: Innovative Hospitalist Staffing Models
HM15 Presenters: John Nelson, MD, MHM; Daniel Hanson, MD, FHM; Darren Thomas, MD
Summation: The presenters, from three entirely different geographic regions across the U.S., walked the audience through several different innovative hospitalist staffing models, from staffing in a multi-hospital system to integrating of advanced practice clinicians to deploying staggered staffing techniques to match the patient demand and enhance continuity of care.
Many multi-hospital systems are challenged to consider creative solutions on how to meet individual hospital staffing needs, while also creating staffing efficiencies across the system, such as cross coverage at night and back-up staffing solutions for increased patient volumes and unexpected staffing vacancies.
Examples to enhance patient continuity were presented throughout, such as pairing together a hospitalist from one week to a hospitalist from an alternate week to care for the same patients.
Similarly, the experts provided a compelling case to consider pairing hospitalist providers with patients, and referring physicians longitudinally across multiple admissions.
Key Takeaways:
1. Patients Come First - consider patient alignment, or continuity, in determing provider scheduling options.
2. Multi-hospital Systems - establish the onboarding parameters needed for providers to be successful in covering more than one hospital and how to build into your scheduling model.
3. Integrate the Care Team - ensure the roles of the integrated provider team (e.g., physicians and advanced practice clinicians) are clearly understood when developing the schedule.
4. Know Your Numbers - clearly understand the workload demands to properly balance the scheduling needs before establishing the schedule.
5. Regular Review - regularly review all of these areas and revise your schedule based on the changing landscape of demands on your hospital medicine group.
HM15 Presenters: John Nelson, MD, MHM; Daniel Hanson, MD, FHM; Darren Thomas, MD
Summation: The presenters, from three entirely different geographic regions across the U.S., walked the audience through several different innovative hospitalist staffing models, from staffing in a multi-hospital system to integrating of advanced practice clinicians to deploying staggered staffing techniques to match the patient demand and enhance continuity of care.
Many multi-hospital systems are challenged to consider creative solutions on how to meet individual hospital staffing needs, while also creating staffing efficiencies across the system, such as cross coverage at night and back-up staffing solutions for increased patient volumes and unexpected staffing vacancies.
Examples to enhance patient continuity were presented throughout, such as pairing together a hospitalist from one week to a hospitalist from an alternate week to care for the same patients.
Similarly, the experts provided a compelling case to consider pairing hospitalist providers with patients, and referring physicians longitudinally across multiple admissions.
Key Takeaways:
1. Patients Come First - consider patient alignment, or continuity, in determing provider scheduling options.
2. Multi-hospital Systems - establish the onboarding parameters needed for providers to be successful in covering more than one hospital and how to build into your scheduling model.
3. Integrate the Care Team - ensure the roles of the integrated provider team (e.g., physicians and advanced practice clinicians) are clearly understood when developing the schedule.
4. Know Your Numbers - clearly understand the workload demands to properly balance the scheduling needs before establishing the schedule.
5. Regular Review - regularly review all of these areas and revise your schedule based on the changing landscape of demands on your hospital medicine group.
HM15 Presenters: John Nelson, MD, MHM; Daniel Hanson, MD, FHM; Darren Thomas, MD
Summation: The presenters, from three entirely different geographic regions across the U.S., walked the audience through several different innovative hospitalist staffing models, from staffing in a multi-hospital system to integrating of advanced practice clinicians to deploying staggered staffing techniques to match the patient demand and enhance continuity of care.
Many multi-hospital systems are challenged to consider creative solutions on how to meet individual hospital staffing needs, while also creating staffing efficiencies across the system, such as cross coverage at night and back-up staffing solutions for increased patient volumes and unexpected staffing vacancies.
Examples to enhance patient continuity were presented throughout, such as pairing together a hospitalist from one week to a hospitalist from an alternate week to care for the same patients.
Similarly, the experts provided a compelling case to consider pairing hospitalist providers with patients, and referring physicians longitudinally across multiple admissions.
Key Takeaways:
1. Patients Come First - consider patient alignment, or continuity, in determing provider scheduling options.
2. Multi-hospital Systems - establish the onboarding parameters needed for providers to be successful in covering more than one hospital and how to build into your scheduling model.
3. Integrate the Care Team - ensure the roles of the integrated provider team (e.g., physicians and advanced practice clinicians) are clearly understood when developing the schedule.
4. Know Your Numbers - clearly understand the workload demands to properly balance the scheduling needs before establishing the schedule.
5. Regular Review - regularly review all of these areas and revise your schedule based on the changing landscape of demands on your hospital medicine group.
A look at top upcoming clinical trials in electrophysiology
SAN DIEGO – How to prevent sudden arrhythmic death in vulnerable but currently unprotected populations is being addressed by ongoing studies that variously evaluate a pharmacologic, an implanted device-based, or a wearable solution, according to Dr. Bruce D. Lindsay.
Dr. Lindsay, head of the cardiac electrophysiology and pacing section at the Cleveland Clinic, presented an overview of selected major ongoing clinical trials in electrophysiology at the annual meeting of the American College of Cardiology. He focused on five hot topics: prevention of sudden death, atrial fibrillation (AF) ablation, prevention of implantable device-related infections, device-based treatment of heart failure, and leadless pacing systems.
Preventing sudden death
Ongoing phase III trials are evaluating the safety, tolerability, and efficacy of an oral Gilead drug known for now as GS-6615. The drug, a selective late sodium current inhibitor, is designed to shorten the corrected QTc interval in patients with several forms of long QT syndrome.
A different approach is being studied in REFINE-ICD (Risk Estimation Following Infarction Noninvasive Evaluation – ICD Efficacy), a 1,400-subject trial recruiting patients who’ve had an acute MI within the previous year, have abnormal findings on 24-hour Holter monitoring, and have moderate left ventricular dysfunction as defined by an ejection fraction of 35%-50%. The trial will assess whether prophylactic placement of an implantable cardioverter-defibrillator (ICD) guided by noninvasive risk assessment based on heart rate turbulence and T-wave alternans analysis will reduce mortality in MI survivors.
“This is a group that’s at lower risk than current ICD recipients, but because it’s such a large group they account for a lot of sudden deaths,” the cardiologist said.
Another phase III trial currently recruiting participants is a 1,900-patient postmarketing study aimed at defining which patients benefit from using the LifeVest wearable defibrillator during the first 3 months following an acute MI resulting in ventricular dysfunction.
AF ablation
The most important ongoing study in this field, in Dr. Lindsay’s view, is CABANA (Catheter Ablation Versus Anti-Arrhythmic Drug Therapy for Atrial Fibrillation Trial). This National Institutes of Health–sponsored study is aimed at showing whether ablation is superior to rate or rhythm control drug therapy in terms of all-cause mortality, disabling stroke, serious bleeding, and/or cardiac arrest. Secondary endpoints include cost, quality of life, hospitalization rates, and the relationship of left atrial size to progression of AF and its contribution to morbidity and mortality.
A promising, innovative ablation strategy known as focal impulse and rotor ablation for paroxysmal AF is under evaluation in the German REAFFIRM (Randomized Evaluation of Atrial Fibrillation Treatment With Focal Impulse and Rotor Modulation Guided Procedures). A similar U.S. study known as FIRMAT-PAF (Focal Impulse and Rotor Modulation Ablation Trial for Treatment of Paroxysmal Atrial Fibrillation) had to be abandoned, however, because of its inability to recruit patients.
New ablation technologies are also being introduced. Three pivotal trials totaling roughly 1,500 patients are evaluating the Biosense Webster nMARQ multielectrode irrigated catheter for paroxysmal AF in the reMARQable trial; a Medtronic phased radiofrequency ablation catheter for persistent AF in the VICTORY AF study; and a CardioFocus endoscopic ablation catheter for paroxysmal AF.
Preventing cardiac implantable device infections
WRAP-IT (the World-Wide Randomized Antibiotic Envelope Infection Trial) is currently enrolling 7,000 patients at 225 sites. This is a Merck-sponsored randomized, prospective, single-blind postmarketing study examining the ability of a proprietary mesh envelope to reduce major infections and costs in the 12 months following device generator replacement, upgrade, or revision, or new implantation of a cardiac resynchronization device. The Tyrx mesh envelope releases minocycline and rifampin for at least 7 days, then eventually becomes fully absorbed.
“Device infection is a huge problem in our field,” Dr. Lindsay noted. “This envelope may have important implications at large, or it may prove to be especially useful in people at high risk for infection.”
Heart failure
Vagal nerve stimulation via an implantable system is one of the hottest areas in the field of heart failure, the electrophysiologist said. Two major trials are ongoing: the Sorin-sponsored VANGUARD (Vagal Nerve Stimulation: Safeguarding Heart Failure Patients) trial, and INNOVATE HF (Increase of Vagal Tone in CHF), sponsored by Biocontrol Medical.
Leadless pacing
St. Jude’s Nanostim and Medtronic’s Micra are very small leadless devices implanted in the right ventricular apex via minimally invasive techniques. Both devices are investigational in the United States, although the Nanostim is approved in Europe. Clinical interest is enormous because lead-related problems have always been the Achilles’ heel of pacemaker therapy. While the Nanostim and Micra can be utilized only for single right ventricular pacing in VVI or VVIR mode, Dr. Lindsay said further advances, including leadless dual-chamber sensing and pacing and biventricular pacing, are likely.
He reported serving as a consultant to Biosense Webster, Boston Scientific, and Medtronic.
SAN DIEGO – How to prevent sudden arrhythmic death in vulnerable but currently unprotected populations is being addressed by ongoing studies that variously evaluate a pharmacologic, an implanted device-based, or a wearable solution, according to Dr. Bruce D. Lindsay.
Dr. Lindsay, head of the cardiac electrophysiology and pacing section at the Cleveland Clinic, presented an overview of selected major ongoing clinical trials in electrophysiology at the annual meeting of the American College of Cardiology. He focused on five hot topics: prevention of sudden death, atrial fibrillation (AF) ablation, prevention of implantable device-related infections, device-based treatment of heart failure, and leadless pacing systems.
Preventing sudden death
Ongoing phase III trials are evaluating the safety, tolerability, and efficacy of an oral Gilead drug known for now as GS-6615. The drug, a selective late sodium current inhibitor, is designed to shorten the corrected QTc interval in patients with several forms of long QT syndrome.
A different approach is being studied in REFINE-ICD (Risk Estimation Following Infarction Noninvasive Evaluation – ICD Efficacy), a 1,400-subject trial recruiting patients who’ve had an acute MI within the previous year, have abnormal findings on 24-hour Holter monitoring, and have moderate left ventricular dysfunction as defined by an ejection fraction of 35%-50%. The trial will assess whether prophylactic placement of an implantable cardioverter-defibrillator (ICD) guided by noninvasive risk assessment based on heart rate turbulence and T-wave alternans analysis will reduce mortality in MI survivors.
“This is a group that’s at lower risk than current ICD recipients, but because it’s such a large group they account for a lot of sudden deaths,” the cardiologist said.
Another phase III trial currently recruiting participants is a 1,900-patient postmarketing study aimed at defining which patients benefit from using the LifeVest wearable defibrillator during the first 3 months following an acute MI resulting in ventricular dysfunction.
AF ablation
The most important ongoing study in this field, in Dr. Lindsay’s view, is CABANA (Catheter Ablation Versus Anti-Arrhythmic Drug Therapy for Atrial Fibrillation Trial). This National Institutes of Health–sponsored study is aimed at showing whether ablation is superior to rate or rhythm control drug therapy in terms of all-cause mortality, disabling stroke, serious bleeding, and/or cardiac arrest. Secondary endpoints include cost, quality of life, hospitalization rates, and the relationship of left atrial size to progression of AF and its contribution to morbidity and mortality.
A promising, innovative ablation strategy known as focal impulse and rotor ablation for paroxysmal AF is under evaluation in the German REAFFIRM (Randomized Evaluation of Atrial Fibrillation Treatment With Focal Impulse and Rotor Modulation Guided Procedures). A similar U.S. study known as FIRMAT-PAF (Focal Impulse and Rotor Modulation Ablation Trial for Treatment of Paroxysmal Atrial Fibrillation) had to be abandoned, however, because of its inability to recruit patients.
New ablation technologies are also being introduced. Three pivotal trials totaling roughly 1,500 patients are evaluating the Biosense Webster nMARQ multielectrode irrigated catheter for paroxysmal AF in the reMARQable trial; a Medtronic phased radiofrequency ablation catheter for persistent AF in the VICTORY AF study; and a CardioFocus endoscopic ablation catheter for paroxysmal AF.
Preventing cardiac implantable device infections
WRAP-IT (the World-Wide Randomized Antibiotic Envelope Infection Trial) is currently enrolling 7,000 patients at 225 sites. This is a Merck-sponsored randomized, prospective, single-blind postmarketing study examining the ability of a proprietary mesh envelope to reduce major infections and costs in the 12 months following device generator replacement, upgrade, or revision, or new implantation of a cardiac resynchronization device. The Tyrx mesh envelope releases minocycline and rifampin for at least 7 days, then eventually becomes fully absorbed.
“Device infection is a huge problem in our field,” Dr. Lindsay noted. “This envelope may have important implications at large, or it may prove to be especially useful in people at high risk for infection.”
Heart failure
Vagal nerve stimulation via an implantable system is one of the hottest areas in the field of heart failure, the electrophysiologist said. Two major trials are ongoing: the Sorin-sponsored VANGUARD (Vagal Nerve Stimulation: Safeguarding Heart Failure Patients) trial, and INNOVATE HF (Increase of Vagal Tone in CHF), sponsored by Biocontrol Medical.
Leadless pacing
St. Jude’s Nanostim and Medtronic’s Micra are very small leadless devices implanted in the right ventricular apex via minimally invasive techniques. Both devices are investigational in the United States, although the Nanostim is approved in Europe. Clinical interest is enormous because lead-related problems have always been the Achilles’ heel of pacemaker therapy. While the Nanostim and Micra can be utilized only for single right ventricular pacing in VVI or VVIR mode, Dr. Lindsay said further advances, including leadless dual-chamber sensing and pacing and biventricular pacing, are likely.
He reported serving as a consultant to Biosense Webster, Boston Scientific, and Medtronic.
SAN DIEGO – How to prevent sudden arrhythmic death in vulnerable but currently unprotected populations is being addressed by ongoing studies that variously evaluate a pharmacologic, an implanted device-based, or a wearable solution, according to Dr. Bruce D. Lindsay.
Dr. Lindsay, head of the cardiac electrophysiology and pacing section at the Cleveland Clinic, presented an overview of selected major ongoing clinical trials in electrophysiology at the annual meeting of the American College of Cardiology. He focused on five hot topics: prevention of sudden death, atrial fibrillation (AF) ablation, prevention of implantable device-related infections, device-based treatment of heart failure, and leadless pacing systems.
Preventing sudden death
Ongoing phase III trials are evaluating the safety, tolerability, and efficacy of an oral Gilead drug known for now as GS-6615. The drug, a selective late sodium current inhibitor, is designed to shorten the corrected QTc interval in patients with several forms of long QT syndrome.
A different approach is being studied in REFINE-ICD (Risk Estimation Following Infarction Noninvasive Evaluation – ICD Efficacy), a 1,400-subject trial recruiting patients who’ve had an acute MI within the previous year, have abnormal findings on 24-hour Holter monitoring, and have moderate left ventricular dysfunction as defined by an ejection fraction of 35%-50%. The trial will assess whether prophylactic placement of an implantable cardioverter-defibrillator (ICD) guided by noninvasive risk assessment based on heart rate turbulence and T-wave alternans analysis will reduce mortality in MI survivors.
“This is a group that’s at lower risk than current ICD recipients, but because it’s such a large group they account for a lot of sudden deaths,” the cardiologist said.
Another phase III trial currently recruiting participants is a 1,900-patient postmarketing study aimed at defining which patients benefit from using the LifeVest wearable defibrillator during the first 3 months following an acute MI resulting in ventricular dysfunction.
AF ablation
The most important ongoing study in this field, in Dr. Lindsay’s view, is CABANA (Catheter Ablation Versus Anti-Arrhythmic Drug Therapy for Atrial Fibrillation Trial). This National Institutes of Health–sponsored study is aimed at showing whether ablation is superior to rate or rhythm control drug therapy in terms of all-cause mortality, disabling stroke, serious bleeding, and/or cardiac arrest. Secondary endpoints include cost, quality of life, hospitalization rates, and the relationship of left atrial size to progression of AF and its contribution to morbidity and mortality.
A promising, innovative ablation strategy known as focal impulse and rotor ablation for paroxysmal AF is under evaluation in the German REAFFIRM (Randomized Evaluation of Atrial Fibrillation Treatment With Focal Impulse and Rotor Modulation Guided Procedures). A similar U.S. study known as FIRMAT-PAF (Focal Impulse and Rotor Modulation Ablation Trial for Treatment of Paroxysmal Atrial Fibrillation) had to be abandoned, however, because of its inability to recruit patients.
New ablation technologies are also being introduced. Three pivotal trials totaling roughly 1,500 patients are evaluating the Biosense Webster nMARQ multielectrode irrigated catheter for paroxysmal AF in the reMARQable trial; a Medtronic phased radiofrequency ablation catheter for persistent AF in the VICTORY AF study; and a CardioFocus endoscopic ablation catheter for paroxysmal AF.
Preventing cardiac implantable device infections
WRAP-IT (the World-Wide Randomized Antibiotic Envelope Infection Trial) is currently enrolling 7,000 patients at 225 sites. This is a Merck-sponsored randomized, prospective, single-blind postmarketing study examining the ability of a proprietary mesh envelope to reduce major infections and costs in the 12 months following device generator replacement, upgrade, or revision, or new implantation of a cardiac resynchronization device. The Tyrx mesh envelope releases minocycline and rifampin for at least 7 days, then eventually becomes fully absorbed.
“Device infection is a huge problem in our field,” Dr. Lindsay noted. “This envelope may have important implications at large, or it may prove to be especially useful in people at high risk for infection.”
Heart failure
Vagal nerve stimulation via an implantable system is one of the hottest areas in the field of heart failure, the electrophysiologist said. Two major trials are ongoing: the Sorin-sponsored VANGUARD (Vagal Nerve Stimulation: Safeguarding Heart Failure Patients) trial, and INNOVATE HF (Increase of Vagal Tone in CHF), sponsored by Biocontrol Medical.
Leadless pacing
St. Jude’s Nanostim and Medtronic’s Micra are very small leadless devices implanted in the right ventricular apex via minimally invasive techniques. Both devices are investigational in the United States, although the Nanostim is approved in Europe. Clinical interest is enormous because lead-related problems have always been the Achilles’ heel of pacemaker therapy. While the Nanostim and Micra can be utilized only for single right ventricular pacing in VVI or VVIR mode, Dr. Lindsay said further advances, including leadless dual-chamber sensing and pacing and biventricular pacing, are likely.
He reported serving as a consultant to Biosense Webster, Boston Scientific, and Medtronic.
EXPERT ANALYSIS FROM ACC 15