User login
Implantable filter doesn’t cut rate of recurrent PE
Implanting a retrievable filter in the inferior vena cava did not reduce the rate of recurrent pulmonary embolism or mortality in high-risk patients, according to a report published online April 28 in JAMA.
In recent years, there has been a sharp increase in the use of these devices as an add-on to anticoagulant therapy among patients hospitalized for acute PE associated with lower-limb deep or superficial vein thrombosis. Several clinical guidelines advocate this strategy, though others do not, citing the paucity of reliable data concerning both risks and benefits.
The findings in this study “do not support the use of this type of filter in patients who can be treated with anticoagulation alone,” and clinical guidelines recommending this approach should be reexamined, Dr. Patrick Mismetti of the University Hospital of Saint-Etienne, France, and his associates said.
They performed a randomized, open-label clinical study at 17 French medical centers to compare anticoagulation alone against anticoagulation plus implanting a filter to be retrieved 3 months later.
The study participants were 399 adults enrolled during a 6-year period who were deemed at high risk for recurrent PE because of advanced age, active cancer, chronic cardiac or respiratory insufficiency, ischemic stroke with leg paralysis, DVT that was bilateral or affected the iliocaval segment, or signs of right ventricular dysfunction or myocardial injury.
The primary efficacy outcome, recurrent PE within 3 months of hospitalization, developed in 6 of 200 patients assigned to receive an implantable filter (3%) and 3 of the 199 assigned to the control group (1.5%). All but one of these episodes of recurrent PE were fatal. One additional PE developed in each study group between 3 and 6 months. There were no differences between patients who received an inferior vena cava filter and those who did not in the incidence of DVT, major bleeding, or death from any cause at 3 or 6 months, the investigators said (JAMA 2015 April 28 [doi:10.1001/jama.2015.3780]).
Besides failing to prevent recurrent PE, the filter implantation caused access site hematomas in five patients, and the filter itself caused thrombosis formation in three. One patient developed cardiac arrest during the procedure. In addition, retrieval of the device failed in 11 patients because of mechanical problems.
Implanting a retrievable filter in the inferior vena cava did not reduce the rate of recurrent pulmonary embolism or mortality in high-risk patients, according to a report published online April 28 in JAMA.
In recent years, there has been a sharp increase in the use of these devices as an add-on to anticoagulant therapy among patients hospitalized for acute PE associated with lower-limb deep or superficial vein thrombosis. Several clinical guidelines advocate this strategy, though others do not, citing the paucity of reliable data concerning both risks and benefits.
The findings in this study “do not support the use of this type of filter in patients who can be treated with anticoagulation alone,” and clinical guidelines recommending this approach should be reexamined, Dr. Patrick Mismetti of the University Hospital of Saint-Etienne, France, and his associates said.
They performed a randomized, open-label clinical study at 17 French medical centers to compare anticoagulation alone against anticoagulation plus implanting a filter to be retrieved 3 months later.
The study participants were 399 adults enrolled during a 6-year period who were deemed at high risk for recurrent PE because of advanced age, active cancer, chronic cardiac or respiratory insufficiency, ischemic stroke with leg paralysis, DVT that was bilateral or affected the iliocaval segment, or signs of right ventricular dysfunction or myocardial injury.
The primary efficacy outcome, recurrent PE within 3 months of hospitalization, developed in 6 of 200 patients assigned to receive an implantable filter (3%) and 3 of the 199 assigned to the control group (1.5%). All but one of these episodes of recurrent PE were fatal. One additional PE developed in each study group between 3 and 6 months. There were no differences between patients who received an inferior vena cava filter and those who did not in the incidence of DVT, major bleeding, or death from any cause at 3 or 6 months, the investigators said (JAMA 2015 April 28 [doi:10.1001/jama.2015.3780]).
Besides failing to prevent recurrent PE, the filter implantation caused access site hematomas in five patients, and the filter itself caused thrombosis formation in three. One patient developed cardiac arrest during the procedure. In addition, retrieval of the device failed in 11 patients because of mechanical problems.
Implanting a retrievable filter in the inferior vena cava did not reduce the rate of recurrent pulmonary embolism or mortality in high-risk patients, according to a report published online April 28 in JAMA.
In recent years, there has been a sharp increase in the use of these devices as an add-on to anticoagulant therapy among patients hospitalized for acute PE associated with lower-limb deep or superficial vein thrombosis. Several clinical guidelines advocate this strategy, though others do not, citing the paucity of reliable data concerning both risks and benefits.
The findings in this study “do not support the use of this type of filter in patients who can be treated with anticoagulation alone,” and clinical guidelines recommending this approach should be reexamined, Dr. Patrick Mismetti of the University Hospital of Saint-Etienne, France, and his associates said.
They performed a randomized, open-label clinical study at 17 French medical centers to compare anticoagulation alone against anticoagulation plus implanting a filter to be retrieved 3 months later.
The study participants were 399 adults enrolled during a 6-year period who were deemed at high risk for recurrent PE because of advanced age, active cancer, chronic cardiac or respiratory insufficiency, ischemic stroke with leg paralysis, DVT that was bilateral or affected the iliocaval segment, or signs of right ventricular dysfunction or myocardial injury.
The primary efficacy outcome, recurrent PE within 3 months of hospitalization, developed in 6 of 200 patients assigned to receive an implantable filter (3%) and 3 of the 199 assigned to the control group (1.5%). All but one of these episodes of recurrent PE were fatal. One additional PE developed in each study group between 3 and 6 months. There were no differences between patients who received an inferior vena cava filter and those who did not in the incidence of DVT, major bleeding, or death from any cause at 3 or 6 months, the investigators said (JAMA 2015 April 28 [doi:10.1001/jama.2015.3780]).
Besides failing to prevent recurrent PE, the filter implantation caused access site hematomas in five patients, and the filter itself caused thrombosis formation in three. One patient developed cardiac arrest during the procedure. In addition, retrieval of the device failed in 11 patients because of mechanical problems.
FROM JAMA
Key clinical point: Use of a retrievable filter implanted in the inferior vena cava did not reduce the rate of recurrent pulmonary embolism.
Major finding: The primary efficacy outcome, recurrent PE within 3 months of hospitalization, developed in 6 of 200 patients assigned to receive an implantable filter (3%) and 3 of 199 assigned to the control group (1.5%).
Data source: An open-label randomized trial involving 399 adults hospitalized in France for acute PE.
Disclosures: This study was sponsored by the University Hospital of Saint-Etienne and supported by the French Department of Health, Fondation de l’Avenir, and Fondation de France. Vena cava filters were provided free of charge by ALN Implants Chirurgicaux. Dr. Mismetti and his associates reported ties to numerous industry sources.
Imaging guides BCC laser ablation
KISSIMMEE, FLA. – Reflective confocal microscopic imaging successfully guided carbon dioxide laser ablation of basal cell carcinomas, and imaging results fully matched those from Mohs histology, a small study found.
“Our results suggest that reflective confocal microscopy can accurately guide carbon dioxide laser ablation of superficial and early nodular basal cell carcinomas,” said Dr. Brian Hibler of Memorial Sloan Kettering Cancer Center in New York. The technique provides a real-time, noninvasive way to delineate the tumor area before ablation and to check for residual tumor between passes with the laser, he said at the annual meeting of the American Society for Laser Medicine and surgery.
While conventional and Mohs microscopic surgeries remain the gold standard for removing basal carcinomas (BCC), surgery is not an option for some patients because of tumor location, comorbidities, or personal preferences, Dr. Hibler noted. Past studies have reported good clinical and cosmetic outcomes with laser ablation of BCCs, but use of the modality has been limited because there was no way to assess response without excision or biopsies. Reflective confocal microscopy (RCM) uses a low-powered laser system that provides cellular-level imaging and can distinguish BCCs, he said.
Dr. Hibler and his colleagues performed baseline RCM of eight BCCs (three on the trunk, three on the extremities, and two on the head and neck) from seven patients aged 29-83 years. Two patients were men and five were women. The patients then underwent carbon dioxide laser ablation with a wavelength of 10,600 nm, pulse duration of 750 microseconds, and fluence of 7.5 J/cm2, using a square pattern and density of 30%. If RCM revealed residual BCC, the researchers repeated the process up to two more times, for a maximum of three passes. They then removed the entire lesion using Mohs micrographic surgery, performing vertical histologic sectioning of the tissue.
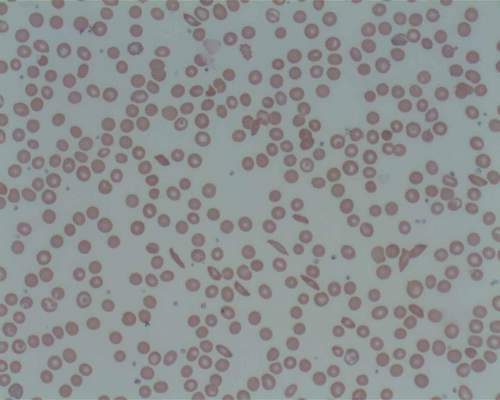
Reflective confocal microscopy generated reliable cellular-level images in real time on the tumor surface and up to 150 mcm deep, Dr. Hibler reported. Tissue from BCCs appears as dense nodular areas with adjacent spaces and red blood cell trafficking, he noted. Microscopy results were consistent with Mohs histology findings in all eight cases, including six in which the tumor was completely removed and two with residual tumor. One of these two cases was the only infiltrative BCC in the series, while the other might have been tissue artifact, Dr. Hibler said.
Patients experienced no adverse effects from the interventions, Dr. Hibler reported. “Future studies are planned are planned without Mohs, so we can use reflective confocal microscopy to longitudinally monitor for recurrence,” he added.
The study won an award at the meeting.
Dr. Hibler reported no funding sources and made no disclosures.
KISSIMMEE, FLA. – Reflective confocal microscopic imaging successfully guided carbon dioxide laser ablation of basal cell carcinomas, and imaging results fully matched those from Mohs histology, a small study found.
“Our results suggest that reflective confocal microscopy can accurately guide carbon dioxide laser ablation of superficial and early nodular basal cell carcinomas,” said Dr. Brian Hibler of Memorial Sloan Kettering Cancer Center in New York. The technique provides a real-time, noninvasive way to delineate the tumor area before ablation and to check for residual tumor between passes with the laser, he said at the annual meeting of the American Society for Laser Medicine and surgery.
While conventional and Mohs microscopic surgeries remain the gold standard for removing basal carcinomas (BCC), surgery is not an option for some patients because of tumor location, comorbidities, or personal preferences, Dr. Hibler noted. Past studies have reported good clinical and cosmetic outcomes with laser ablation of BCCs, but use of the modality has been limited because there was no way to assess response without excision or biopsies. Reflective confocal microscopy (RCM) uses a low-powered laser system that provides cellular-level imaging and can distinguish BCCs, he said.
Dr. Hibler and his colleagues performed baseline RCM of eight BCCs (three on the trunk, three on the extremities, and two on the head and neck) from seven patients aged 29-83 years. Two patients were men and five were women. The patients then underwent carbon dioxide laser ablation with a wavelength of 10,600 nm, pulse duration of 750 microseconds, and fluence of 7.5 J/cm2, using a square pattern and density of 30%. If RCM revealed residual BCC, the researchers repeated the process up to two more times, for a maximum of three passes. They then removed the entire lesion using Mohs micrographic surgery, performing vertical histologic sectioning of the tissue.
Reflective confocal microscopy generated reliable cellular-level images in real time on the tumor surface and up to 150 mcm deep, Dr. Hibler reported. Tissue from BCCs appears as dense nodular areas with adjacent spaces and red blood cell trafficking, he noted. Microscopy results were consistent with Mohs histology findings in all eight cases, including six in which the tumor was completely removed and two with residual tumor. One of these two cases was the only infiltrative BCC in the series, while the other might have been tissue artifact, Dr. Hibler said.
Patients experienced no adverse effects from the interventions, Dr. Hibler reported. “Future studies are planned are planned without Mohs, so we can use reflective confocal microscopy to longitudinally monitor for recurrence,” he added.
The study won an award at the meeting.
Dr. Hibler reported no funding sources and made no disclosures.
KISSIMMEE, FLA. – Reflective confocal microscopic imaging successfully guided carbon dioxide laser ablation of basal cell carcinomas, and imaging results fully matched those from Mohs histology, a small study found.
“Our results suggest that reflective confocal microscopy can accurately guide carbon dioxide laser ablation of superficial and early nodular basal cell carcinomas,” said Dr. Brian Hibler of Memorial Sloan Kettering Cancer Center in New York. The technique provides a real-time, noninvasive way to delineate the tumor area before ablation and to check for residual tumor between passes with the laser, he said at the annual meeting of the American Society for Laser Medicine and surgery.
While conventional and Mohs microscopic surgeries remain the gold standard for removing basal carcinomas (BCC), surgery is not an option for some patients because of tumor location, comorbidities, or personal preferences, Dr. Hibler noted. Past studies have reported good clinical and cosmetic outcomes with laser ablation of BCCs, but use of the modality has been limited because there was no way to assess response without excision or biopsies. Reflective confocal microscopy (RCM) uses a low-powered laser system that provides cellular-level imaging and can distinguish BCCs, he said.
Dr. Hibler and his colleagues performed baseline RCM of eight BCCs (three on the trunk, three on the extremities, and two on the head and neck) from seven patients aged 29-83 years. Two patients were men and five were women. The patients then underwent carbon dioxide laser ablation with a wavelength of 10,600 nm, pulse duration of 750 microseconds, and fluence of 7.5 J/cm2, using a square pattern and density of 30%. If RCM revealed residual BCC, the researchers repeated the process up to two more times, for a maximum of three passes. They then removed the entire lesion using Mohs micrographic surgery, performing vertical histologic sectioning of the tissue.
Reflective confocal microscopy generated reliable cellular-level images in real time on the tumor surface and up to 150 mcm deep, Dr. Hibler reported. Tissue from BCCs appears as dense nodular areas with adjacent spaces and red blood cell trafficking, he noted. Microscopy results were consistent with Mohs histology findings in all eight cases, including six in which the tumor was completely removed and two with residual tumor. One of these two cases was the only infiltrative BCC in the series, while the other might have been tissue artifact, Dr. Hibler said.
Patients experienced no adverse effects from the interventions, Dr. Hibler reported. “Future studies are planned are planned without Mohs, so we can use reflective confocal microscopy to longitudinally monitor for recurrence,” he added.
The study won an award at the meeting.
Dr. Hibler reported no funding sources and made no disclosures.
Key clinical point: Reflective confocal microscopy offers noninvasive, real-time imaging to guide laser ablation of basal cell carcinomas.
Major finding: Results from RCM matched those from Mohs histology in all patients.
Data source: Prospective study of eight BCCs in seven patients.
Disclosures: Dr. Hibler reported no funding sources and made no disclosures.
NASPAG: Hormonal add-back prevents GnRH-A–related bone loss in adolescents
ORLANDO – Hormonal add-back therapy using combination norethindrone acetate and conjugated equine estrogens was effective and better than norethindrone acetate plus placebo for preserving bone health and improving quality of life in adolescents receiving treatment with gonadotropin-releasing hormone agonists (GnRH-A) for endometriosis in a randomized, double-blind, placebo-controlled study.
Of 51 adolescents aged 15-22 years who were initiating GnRH-A therapy for endometriosis, 25 were randomized to receive add-back therapy with 5 mg daily oral norethindrone acetate (NA) plus 0.625 mg oral daily conjugated equine estrogens (CEE), and 26 were randomized to receive NA plus placebo; 18 and 16, respectively, completed the study.
Those in the combination-therapy group experienced significant increases over 12 months in both total body bone mineral content (BMC) and bone mineral density (BMD), compared with those who received NA plus placebo. BMC increased by nearly 40 g/unit scanned in the combination-therapy group, compared with about 12 g in the NA plus placebo group, and BMD increased more than 0.01 g/cm2, compared with no change in the NA plus placebo group, Dr. Amy D. DiVasta reported at the North American Society for Pediatric and Adolescent Gynecology annual meeting.
No losses of total hip or lumbar spine BMC or BMD occurred, said Dr. DiVasta of Boston Children’s Hospital.
Further, lean mass increased in the combination-therapy group at 12 months – by about 1.4 kg, compared with no change in the placebo group. No differences were seen between the groups in change in fat mass.
As for quality of life measures, overall physical health scores at baseline were significantly below the U.S. mean in both groups, and overall mental health scores were above the U.S. mean in both groups. Both groups improved over time on both measures; the increase in the Physical Component Summary scale scores on the SF-36 (Short Form 36 Health Survey) was significantly greater with combination-therapy group (increase from about 40 to 50 out of 100 ), compared with NA plus placebo (increase from about 40 to 45), but the increases on the Mental Component Summary scale scores were not statistically significant in either group, or between the groups.
The study subjects, who were treated for 12 months between 2008 and 2012, were at least 2 years post menarche at baseline and had a surgical diagnosis of endometriosis. The two treatment groups were similar with respect to baseline characteristics, including age, BMD Z score, and disease severity. No significant side effects were observed in either the combination or NA plus placebo group, Dr. DiVasta said, noting that laboratory tests included liver function tests and lipid levels.
Areal BMD, BMC, and body composition were measured by dual-energy X-ray absorptiometry (DXA) at baseline, 6 months, and 12 months. Anthropometrics, quality of life measures, and laboratory studies were conducted at 1, 3, 6, and 12 months.
GnRH-A are commonly utilized for endometriosis patients who fail primary therapy, such as NSAIDs or combined oral contraceptives, but long-term use is associated with deleterious effects on bone mineralization; adults have been shown to lose 5%-8% of BMD after 3-6 months of treatment, Dr. DiVasta noted.
Hormonal add-back therapy is a promising adjunct to counteract these effects and could be an important tool for protecting adolescents, who are at the greatest risk for the deleterious effects of GnRH-A therapy, she said.
In the current study, hormonal add-back did successfully protect bone health and improve quality of life for adolescents with endometriosis who were treated with 12 months of GnRH-A. Combination therapy with NA and CEE appears to be more effective for increasing total body BMC and BMD, lean mass, and physical health-related quality of life, as compared with NA monotherapy, she said.
The findings are limited by the inclusion of only skeletally mature young women, as the results may not be generalizable to growing girls. Also, DXA measures provide two-dimensional measures of bone mineral density, and do not yield information regarding skeletal strength or bone microarchitecture, she noted.
“Given the prevalence of endometriosis, our data suggest norethindrone plus estrogens to be a useful adjunctive therapy to prevent bone loss in these young women while they receive appropriate medical treatment for their underlying disease,” she concluded, noting that future work will explore the effects of add-back on the peripheral skeleton and bone strength.
This study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the McCarthy Family Foundation, Thrasher Research Fund, and Boston Children’s Hospital department of medicine. Medications were provided by Abbott, Duramed Pharmaceuticals, and Wyeth Pharmaceuticals. Dr. DiVasta reported having no relevant financial disclosures.
ORLANDO – Hormonal add-back therapy using combination norethindrone acetate and conjugated equine estrogens was effective and better than norethindrone acetate plus placebo for preserving bone health and improving quality of life in adolescents receiving treatment with gonadotropin-releasing hormone agonists (GnRH-A) for endometriosis in a randomized, double-blind, placebo-controlled study.
Of 51 adolescents aged 15-22 years who were initiating GnRH-A therapy for endometriosis, 25 were randomized to receive add-back therapy with 5 mg daily oral norethindrone acetate (NA) plus 0.625 mg oral daily conjugated equine estrogens (CEE), and 26 were randomized to receive NA plus placebo; 18 and 16, respectively, completed the study.
Those in the combination-therapy group experienced significant increases over 12 months in both total body bone mineral content (BMC) and bone mineral density (BMD), compared with those who received NA plus placebo. BMC increased by nearly 40 g/unit scanned in the combination-therapy group, compared with about 12 g in the NA plus placebo group, and BMD increased more than 0.01 g/cm2, compared with no change in the NA plus placebo group, Dr. Amy D. DiVasta reported at the North American Society for Pediatric and Adolescent Gynecology annual meeting.
No losses of total hip or lumbar spine BMC or BMD occurred, said Dr. DiVasta of Boston Children’s Hospital.
Further, lean mass increased in the combination-therapy group at 12 months – by about 1.4 kg, compared with no change in the placebo group. No differences were seen between the groups in change in fat mass.
As for quality of life measures, overall physical health scores at baseline were significantly below the U.S. mean in both groups, and overall mental health scores were above the U.S. mean in both groups. Both groups improved over time on both measures; the increase in the Physical Component Summary scale scores on the SF-36 (Short Form 36 Health Survey) was significantly greater with combination-therapy group (increase from about 40 to 50 out of 100 ), compared with NA plus placebo (increase from about 40 to 45), but the increases on the Mental Component Summary scale scores were not statistically significant in either group, or between the groups.
The study subjects, who were treated for 12 months between 2008 and 2012, were at least 2 years post menarche at baseline and had a surgical diagnosis of endometriosis. The two treatment groups were similar with respect to baseline characteristics, including age, BMD Z score, and disease severity. No significant side effects were observed in either the combination or NA plus placebo group, Dr. DiVasta said, noting that laboratory tests included liver function tests and lipid levels.
Areal BMD, BMC, and body composition were measured by dual-energy X-ray absorptiometry (DXA) at baseline, 6 months, and 12 months. Anthropometrics, quality of life measures, and laboratory studies were conducted at 1, 3, 6, and 12 months.
GnRH-A are commonly utilized for endometriosis patients who fail primary therapy, such as NSAIDs or combined oral contraceptives, but long-term use is associated with deleterious effects on bone mineralization; adults have been shown to lose 5%-8% of BMD after 3-6 months of treatment, Dr. DiVasta noted.
Hormonal add-back therapy is a promising adjunct to counteract these effects and could be an important tool for protecting adolescents, who are at the greatest risk for the deleterious effects of GnRH-A therapy, she said.
In the current study, hormonal add-back did successfully protect bone health and improve quality of life for adolescents with endometriosis who were treated with 12 months of GnRH-A. Combination therapy with NA and CEE appears to be more effective for increasing total body BMC and BMD, lean mass, and physical health-related quality of life, as compared with NA monotherapy, she said.
The findings are limited by the inclusion of only skeletally mature young women, as the results may not be generalizable to growing girls. Also, DXA measures provide two-dimensional measures of bone mineral density, and do not yield information regarding skeletal strength or bone microarchitecture, she noted.
“Given the prevalence of endometriosis, our data suggest norethindrone plus estrogens to be a useful adjunctive therapy to prevent bone loss in these young women while they receive appropriate medical treatment for their underlying disease,” she concluded, noting that future work will explore the effects of add-back on the peripheral skeleton and bone strength.
This study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the McCarthy Family Foundation, Thrasher Research Fund, and Boston Children’s Hospital department of medicine. Medications were provided by Abbott, Duramed Pharmaceuticals, and Wyeth Pharmaceuticals. Dr. DiVasta reported having no relevant financial disclosures.
ORLANDO – Hormonal add-back therapy using combination norethindrone acetate and conjugated equine estrogens was effective and better than norethindrone acetate plus placebo for preserving bone health and improving quality of life in adolescents receiving treatment with gonadotropin-releasing hormone agonists (GnRH-A) for endometriosis in a randomized, double-blind, placebo-controlled study.
Of 51 adolescents aged 15-22 years who were initiating GnRH-A therapy for endometriosis, 25 were randomized to receive add-back therapy with 5 mg daily oral norethindrone acetate (NA) plus 0.625 mg oral daily conjugated equine estrogens (CEE), and 26 were randomized to receive NA plus placebo; 18 and 16, respectively, completed the study.
Those in the combination-therapy group experienced significant increases over 12 months in both total body bone mineral content (BMC) and bone mineral density (BMD), compared with those who received NA plus placebo. BMC increased by nearly 40 g/unit scanned in the combination-therapy group, compared with about 12 g in the NA plus placebo group, and BMD increased more than 0.01 g/cm2, compared with no change in the NA plus placebo group, Dr. Amy D. DiVasta reported at the North American Society for Pediatric and Adolescent Gynecology annual meeting.
No losses of total hip or lumbar spine BMC or BMD occurred, said Dr. DiVasta of Boston Children’s Hospital.
Further, lean mass increased in the combination-therapy group at 12 months – by about 1.4 kg, compared with no change in the placebo group. No differences were seen between the groups in change in fat mass.
As for quality of life measures, overall physical health scores at baseline were significantly below the U.S. mean in both groups, and overall mental health scores were above the U.S. mean in both groups. Both groups improved over time on both measures; the increase in the Physical Component Summary scale scores on the SF-36 (Short Form 36 Health Survey) was significantly greater with combination-therapy group (increase from about 40 to 50 out of 100 ), compared with NA plus placebo (increase from about 40 to 45), but the increases on the Mental Component Summary scale scores were not statistically significant in either group, or between the groups.
The study subjects, who were treated for 12 months between 2008 and 2012, were at least 2 years post menarche at baseline and had a surgical diagnosis of endometriosis. The two treatment groups were similar with respect to baseline characteristics, including age, BMD Z score, and disease severity. No significant side effects were observed in either the combination or NA plus placebo group, Dr. DiVasta said, noting that laboratory tests included liver function tests and lipid levels.
Areal BMD, BMC, and body composition were measured by dual-energy X-ray absorptiometry (DXA) at baseline, 6 months, and 12 months. Anthropometrics, quality of life measures, and laboratory studies were conducted at 1, 3, 6, and 12 months.
GnRH-A are commonly utilized for endometriosis patients who fail primary therapy, such as NSAIDs or combined oral contraceptives, but long-term use is associated with deleterious effects on bone mineralization; adults have been shown to lose 5%-8% of BMD after 3-6 months of treatment, Dr. DiVasta noted.
Hormonal add-back therapy is a promising adjunct to counteract these effects and could be an important tool for protecting adolescents, who are at the greatest risk for the deleterious effects of GnRH-A therapy, she said.
In the current study, hormonal add-back did successfully protect bone health and improve quality of life for adolescents with endometriosis who were treated with 12 months of GnRH-A. Combination therapy with NA and CEE appears to be more effective for increasing total body BMC and BMD, lean mass, and physical health-related quality of life, as compared with NA monotherapy, she said.
The findings are limited by the inclusion of only skeletally mature young women, as the results may not be generalizable to growing girls. Also, DXA measures provide two-dimensional measures of bone mineral density, and do not yield information regarding skeletal strength or bone microarchitecture, she noted.
“Given the prevalence of endometriosis, our data suggest norethindrone plus estrogens to be a useful adjunctive therapy to prevent bone loss in these young women while they receive appropriate medical treatment for their underlying disease,” she concluded, noting that future work will explore the effects of add-back on the peripheral skeleton and bone strength.
This study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the McCarthy Family Foundation, Thrasher Research Fund, and Boston Children’s Hospital department of medicine. Medications were provided by Abbott, Duramed Pharmaceuticals, and Wyeth Pharmaceuticals. Dr. DiVasta reported having no relevant financial disclosures.
AT THE NASPAG ANNUAL MEETING
Key clinical point: Add-back therapy could allow for safe long-term GnRH-A therapy in adolescents with endometriosis.
Major finding: Bone mineral content increased nearly 40 g/unit scanned in the combination therapy group vs. about 12 g in the norethindrone acetate plus placebo group.
Data source: A randomized, placebo-controlled study of 51 adolescents.
Disclosures: This study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the McCarthy Family Foundation, Thrasher Research Fund, and Boston Children’s Hospital department of medicine. Medications were provided by Abbott, Duramed Pharmaceuticals, and Wyeth Pharmaceuticals. Dr. DiVasta reported having no relevant financial disclosures.
Treating a Japanese patient with family pressures
Editors’ Note: This is the first installment of Curbside Consult, written by two Group for the Advancement of Psychiatry (GAP) committees – the Committee on Family Psychiatry and the Committee on Cultural Psychiatry.
Come back home
The patient is an unmarried Japanese man in his early 40s who presents with symptoms of social phobia. He was born and raised in Japan, and migrated to the United States to pursue a PhD. In Japan, he enjoyed middle-class status, but after immigrating to the United States, he has faced many financial difficulties. His language barriers have made him uncomfortable in front of his colleagues and supervisors and he has not been able to do well in his PhD program, ultimately leading to his expulsion. He does not want to go back to Japan, thinking he will not have a “good life” there. He believes that there is no respect for a person’s individuality in Japan. He is currently living in an urban location of New Jersey and works odd jobs. He states that his family does not understand his feelings about not returning to Japan, and instead they want him to support them. He has engaged in supportive psychotherapy and cognitive-behavioral therapy in the outpatient clinic along with psychopharmacological treatment.
Key questions
1. How is Japanese culture different from U.S. culture in terms of respecting a person’s individuality?
2. The expectations of the patient’s family are considered excessive by the patient. What is the role of Japanese culture in this situation?
3. In moving forward with treatment planning, what aspects of the patient’s culture should the clinician keep in mind?
Family perspective
This middle-aged Japanese man has had a challenging time since coming to the United States to study. He lives here alone. He has failed to achieve his goal of earning a PhD. He has had financial difficulties because of his job challenges. He has had the courage to seek mental health treatment, although the goals of his treatment are unclear. He is in contact with his family in Japan, who has asked that he come home, presumably to support his somewhat older parents. It is unclear who constitutes his “family.”
From a family perspective, it seems that the family/parents in Japan are expecting that family obligation will draw the man home while the patient is defying that expectation by seeking and building individuality in the United States. A family-oriented therapist would consider the patient’s relationship with his family and help him consider how to make his decision on where to live. The therapist also would support the patient in maintaining a connection with his family. The therapist would help the patient avoid both passively capitulating to his family and defiantly cutting off from them. This would entail discussing the role of family in the United States and Japan. It would be important to empower the patient to explore his reasons for wanting to stay in the United States, what he means by “a good life,” and what he senses as his obligation to his family.
The history of this man’s life in Japan, including recollections of his childhood and an understanding of the job history of other members of his family, will help the therapist understand this man and his experience of his family. The telling of the family narrative, from his perspective, may help the patient understand his wishes and his fears. Exploring his relationships with his mother and his father will help the therapist and the patient understand some of the problems he has had in the United States.
Given his current life circumstances, work, and social stresses, lack of social support, and problems functioning, he also should be clinically assessed for depression and any other significant mental health problems. Additional questions to explore include: Does he define himself as a “failure,” and what would it be like going back to Japan? Are there concerns about “losing face”? If his parents want him to support them, do they know about his financial situation? Would he be able to get a job in Japan, or would he end up living with his parents? Are their requests that he “come home” based on their need for support, or are they afraid that he really needs their help given his difficulties establishing a life here? As the patient explores these issues in more detail, he can begin the process of resolving his future.
Cultural psychiatry perspective
This case raises important cultural questions, which deserve further exploration in psychotherapy. Alternate approaches to evaluating culture in clinical settings have moved away from conceptualizing “U.S.” or “Japanese” cultures monolithically to understand how cultural dynamics matter to the individual.
Notably, clarifying what the patient means by the “individuality” that is “not respected in Japan” would be essential, as well as what he perceives as “excessive” in his family’s demands. Alan Roland, Ph.D., in his book “In Search of Self in India and Japan: Toward a Cross-Cultural Psychology” describes marked differences between traditional Japanese and U.S. expectations of family obligation and relationship: “dependence and interdependence with close emotional connectedness versus independence and autonomy; receptivity and deference to superiors in hierarchical relationships versus self-assertion and self-promotion in egalitarian-contractual relationships; communication on multiple levels and by innuendo versus verbal articulateness and forthrightness; maintaining and enhancing esteem at all costs versus forthright criticism and expressing the truth of the matter” (pp. 292-3).
Of course, these are intentionally polarized descriptions; yet many Japanese in the United States find themselves negotiating contrasting expectations about what it means to be a person in a family and a society, some finding value in at least parts of each tradition, some holding on to traditional Japanese values, and some adopting values related to the new environment.
A key question in this case is what made the situation so difficult for this patient. Going forward, the clinician will want to characterize the biopsychosocial etiologies of his symptoms. Are the social phobia symptoms related to premorbid developmental issues hindering communication, planning, and sociability? Were they exacerbated by language difficulties and the acculturation challenges of finding himself in a new country and institution with potentially different expectations of fulfillment and success?
One wonders how he was accepted into this PhD program and why his performance led to expulsion so quickly. Are there additional symptoms and impairments beyond the breakdown in communication? For example, are there depressive symptoms? Does he have other somatic symptomatology as part of his idiom of distress that may be magnifying his impairment? Were academic supports in place that could have prevented his expulsion? Does he have other social supports and relationships? Is he struggling with intense isolation and, potentially, individuation issues triggered by his new setting?
The DSM-5 Cultural Formulation Interview (CFI), a standardized method for conducting a cultural assessment in mental health care, could help the clinician elicit the patient’s understandings of the problem, its causes and contextual stressors and supports, cultural identity, the cultural features of the relationship between the patient and the clinician, and options for self-coping and clinical care. This exploration of the patient’s lifeworld may clarify how to intervene. Selected supplementary modules to the CFI also may also be useful to ‘amplify’ the core CFI and to further explore the patient’s perception of the family’s role in his illness, including the Social Network Module and the Psychosocial Stressors Module.
Contributors
John Sargent, M.D. – Tufts University School of Medicine
Ellen Berman, M.D. – University of Pennsylvania, Perelman School of Medicine
Roberto Lewis-Fernández, M.D. – Columbia University and New York State Psychiatric Institute
Robert C. Like, M.D., M.S. – Rutgers University, Robert Wood Johnson Medical School
Resources
Lewis-Fernández R., Aggarwal N.K., Baarnhielm, S., et al. Culture and Psychiatric Evaluation: Operationalizing Cultural Formulation for DSM-5 (Psychiatry 2014;77:130-54).
Roland A. In Search of Self in India and Japan: Toward a Cross-Cultural Psychology (Princeton,
N.J.: Princeton University Press, 1988).
Shibusawa T. Japanese Families, in Ethnicity and Family Therapy, 3rd edition. Edited by McGoldrick M., Giordano J., and Garcia-Preto. (New York: Guilford Press, 2005, pp. 339-48).
Tseng W.S., Chang S.C., Nishizono M., eds. Asian Culture and Psychotherapy: Implications for East and West (Honolulu: University of Hawai’i Press).
To read about the goals of Curbside Consult, the guiding principles for assessment, and the guidelines for case submission, see “Considering patients’ family, culture,” Clinical Psychiatry News, January 2015, p. 12. To contribute a case, send it to [email protected]. The contributors have revised selected patient details to shield the identities of the patients/cases and to comply with HIPAA requirements. This column is meant to be educational and does not constitute medical advice. The opinions expressed are those of the contributors and do not represent those of the organizations they employed by or affiliated with or the Group for the Advancement of Psychiatry (GAP).
Editors’ Note: This is the first installment of Curbside Consult, written by two Group for the Advancement of Psychiatry (GAP) committees – the Committee on Family Psychiatry and the Committee on Cultural Psychiatry.
Come back home
The patient is an unmarried Japanese man in his early 40s who presents with symptoms of social phobia. He was born and raised in Japan, and migrated to the United States to pursue a PhD. In Japan, he enjoyed middle-class status, but after immigrating to the United States, he has faced many financial difficulties. His language barriers have made him uncomfortable in front of his colleagues and supervisors and he has not been able to do well in his PhD program, ultimately leading to his expulsion. He does not want to go back to Japan, thinking he will not have a “good life” there. He believes that there is no respect for a person’s individuality in Japan. He is currently living in an urban location of New Jersey and works odd jobs. He states that his family does not understand his feelings about not returning to Japan, and instead they want him to support them. He has engaged in supportive psychotherapy and cognitive-behavioral therapy in the outpatient clinic along with psychopharmacological treatment.
Key questions
1. How is Japanese culture different from U.S. culture in terms of respecting a person’s individuality?
2. The expectations of the patient’s family are considered excessive by the patient. What is the role of Japanese culture in this situation?
3. In moving forward with treatment planning, what aspects of the patient’s culture should the clinician keep in mind?
Family perspective
This middle-aged Japanese man has had a challenging time since coming to the United States to study. He lives here alone. He has failed to achieve his goal of earning a PhD. He has had financial difficulties because of his job challenges. He has had the courage to seek mental health treatment, although the goals of his treatment are unclear. He is in contact with his family in Japan, who has asked that he come home, presumably to support his somewhat older parents. It is unclear who constitutes his “family.”
From a family perspective, it seems that the family/parents in Japan are expecting that family obligation will draw the man home while the patient is defying that expectation by seeking and building individuality in the United States. A family-oriented therapist would consider the patient’s relationship with his family and help him consider how to make his decision on where to live. The therapist also would support the patient in maintaining a connection with his family. The therapist would help the patient avoid both passively capitulating to his family and defiantly cutting off from them. This would entail discussing the role of family in the United States and Japan. It would be important to empower the patient to explore his reasons for wanting to stay in the United States, what he means by “a good life,” and what he senses as his obligation to his family.
The history of this man’s life in Japan, including recollections of his childhood and an understanding of the job history of other members of his family, will help the therapist understand this man and his experience of his family. The telling of the family narrative, from his perspective, may help the patient understand his wishes and his fears. Exploring his relationships with his mother and his father will help the therapist and the patient understand some of the problems he has had in the United States.
Given his current life circumstances, work, and social stresses, lack of social support, and problems functioning, he also should be clinically assessed for depression and any other significant mental health problems. Additional questions to explore include: Does he define himself as a “failure,” and what would it be like going back to Japan? Are there concerns about “losing face”? If his parents want him to support them, do they know about his financial situation? Would he be able to get a job in Japan, or would he end up living with his parents? Are their requests that he “come home” based on their need for support, or are they afraid that he really needs their help given his difficulties establishing a life here? As the patient explores these issues in more detail, he can begin the process of resolving his future.
Cultural psychiatry perspective
This case raises important cultural questions, which deserve further exploration in psychotherapy. Alternate approaches to evaluating culture in clinical settings have moved away from conceptualizing “U.S.” or “Japanese” cultures monolithically to understand how cultural dynamics matter to the individual.
Notably, clarifying what the patient means by the “individuality” that is “not respected in Japan” would be essential, as well as what he perceives as “excessive” in his family’s demands. Alan Roland, Ph.D., in his book “In Search of Self in India and Japan: Toward a Cross-Cultural Psychology” describes marked differences between traditional Japanese and U.S. expectations of family obligation and relationship: “dependence and interdependence with close emotional connectedness versus independence and autonomy; receptivity and deference to superiors in hierarchical relationships versus self-assertion and self-promotion in egalitarian-contractual relationships; communication on multiple levels and by innuendo versus verbal articulateness and forthrightness; maintaining and enhancing esteem at all costs versus forthright criticism and expressing the truth of the matter” (pp. 292-3).
Of course, these are intentionally polarized descriptions; yet many Japanese in the United States find themselves negotiating contrasting expectations about what it means to be a person in a family and a society, some finding value in at least parts of each tradition, some holding on to traditional Japanese values, and some adopting values related to the new environment.
A key question in this case is what made the situation so difficult for this patient. Going forward, the clinician will want to characterize the biopsychosocial etiologies of his symptoms. Are the social phobia symptoms related to premorbid developmental issues hindering communication, planning, and sociability? Were they exacerbated by language difficulties and the acculturation challenges of finding himself in a new country and institution with potentially different expectations of fulfillment and success?
One wonders how he was accepted into this PhD program and why his performance led to expulsion so quickly. Are there additional symptoms and impairments beyond the breakdown in communication? For example, are there depressive symptoms? Does he have other somatic symptomatology as part of his idiom of distress that may be magnifying his impairment? Were academic supports in place that could have prevented his expulsion? Does he have other social supports and relationships? Is he struggling with intense isolation and, potentially, individuation issues triggered by his new setting?
The DSM-5 Cultural Formulation Interview (CFI), a standardized method for conducting a cultural assessment in mental health care, could help the clinician elicit the patient’s understandings of the problem, its causes and contextual stressors and supports, cultural identity, the cultural features of the relationship between the patient and the clinician, and options for self-coping and clinical care. This exploration of the patient’s lifeworld may clarify how to intervene. Selected supplementary modules to the CFI also may also be useful to ‘amplify’ the core CFI and to further explore the patient’s perception of the family’s role in his illness, including the Social Network Module and the Psychosocial Stressors Module.
Contributors
John Sargent, M.D. – Tufts University School of Medicine
Ellen Berman, M.D. – University of Pennsylvania, Perelman School of Medicine
Roberto Lewis-Fernández, M.D. – Columbia University and New York State Psychiatric Institute
Robert C. Like, M.D., M.S. – Rutgers University, Robert Wood Johnson Medical School
Resources
Lewis-Fernández R., Aggarwal N.K., Baarnhielm, S., et al. Culture and Psychiatric Evaluation: Operationalizing Cultural Formulation for DSM-5 (Psychiatry 2014;77:130-54).
Roland A. In Search of Self in India and Japan: Toward a Cross-Cultural Psychology (Princeton,
N.J.: Princeton University Press, 1988).
Shibusawa T. Japanese Families, in Ethnicity and Family Therapy, 3rd edition. Edited by McGoldrick M., Giordano J., and Garcia-Preto. (New York: Guilford Press, 2005, pp. 339-48).
Tseng W.S., Chang S.C., Nishizono M., eds. Asian Culture and Psychotherapy: Implications for East and West (Honolulu: University of Hawai’i Press).
To read about the goals of Curbside Consult, the guiding principles for assessment, and the guidelines for case submission, see “Considering patients’ family, culture,” Clinical Psychiatry News, January 2015, p. 12. To contribute a case, send it to [email protected]. The contributors have revised selected patient details to shield the identities of the patients/cases and to comply with HIPAA requirements. This column is meant to be educational and does not constitute medical advice. The opinions expressed are those of the contributors and do not represent those of the organizations they employed by or affiliated with or the Group for the Advancement of Psychiatry (GAP).
Editors’ Note: This is the first installment of Curbside Consult, written by two Group for the Advancement of Psychiatry (GAP) committees – the Committee on Family Psychiatry and the Committee on Cultural Psychiatry.
Come back home
The patient is an unmarried Japanese man in his early 40s who presents with symptoms of social phobia. He was born and raised in Japan, and migrated to the United States to pursue a PhD. In Japan, he enjoyed middle-class status, but after immigrating to the United States, he has faced many financial difficulties. His language barriers have made him uncomfortable in front of his colleagues and supervisors and he has not been able to do well in his PhD program, ultimately leading to his expulsion. He does not want to go back to Japan, thinking he will not have a “good life” there. He believes that there is no respect for a person’s individuality in Japan. He is currently living in an urban location of New Jersey and works odd jobs. He states that his family does not understand his feelings about not returning to Japan, and instead they want him to support them. He has engaged in supportive psychotherapy and cognitive-behavioral therapy in the outpatient clinic along with psychopharmacological treatment.
Key questions
1. How is Japanese culture different from U.S. culture in terms of respecting a person’s individuality?
2. The expectations of the patient’s family are considered excessive by the patient. What is the role of Japanese culture in this situation?
3. In moving forward with treatment planning, what aspects of the patient’s culture should the clinician keep in mind?
Family perspective
This middle-aged Japanese man has had a challenging time since coming to the United States to study. He lives here alone. He has failed to achieve his goal of earning a PhD. He has had financial difficulties because of his job challenges. He has had the courage to seek mental health treatment, although the goals of his treatment are unclear. He is in contact with his family in Japan, who has asked that he come home, presumably to support his somewhat older parents. It is unclear who constitutes his “family.”
From a family perspective, it seems that the family/parents in Japan are expecting that family obligation will draw the man home while the patient is defying that expectation by seeking and building individuality in the United States. A family-oriented therapist would consider the patient’s relationship with his family and help him consider how to make his decision on where to live. The therapist also would support the patient in maintaining a connection with his family. The therapist would help the patient avoid both passively capitulating to his family and defiantly cutting off from them. This would entail discussing the role of family in the United States and Japan. It would be important to empower the patient to explore his reasons for wanting to stay in the United States, what he means by “a good life,” and what he senses as his obligation to his family.
The history of this man’s life in Japan, including recollections of his childhood and an understanding of the job history of other members of his family, will help the therapist understand this man and his experience of his family. The telling of the family narrative, from his perspective, may help the patient understand his wishes and his fears. Exploring his relationships with his mother and his father will help the therapist and the patient understand some of the problems he has had in the United States.
Given his current life circumstances, work, and social stresses, lack of social support, and problems functioning, he also should be clinically assessed for depression and any other significant mental health problems. Additional questions to explore include: Does he define himself as a “failure,” and what would it be like going back to Japan? Are there concerns about “losing face”? If his parents want him to support them, do they know about his financial situation? Would he be able to get a job in Japan, or would he end up living with his parents? Are their requests that he “come home” based on their need for support, or are they afraid that he really needs their help given his difficulties establishing a life here? As the patient explores these issues in more detail, he can begin the process of resolving his future.
Cultural psychiatry perspective
This case raises important cultural questions, which deserve further exploration in psychotherapy. Alternate approaches to evaluating culture in clinical settings have moved away from conceptualizing “U.S.” or “Japanese” cultures monolithically to understand how cultural dynamics matter to the individual.
Notably, clarifying what the patient means by the “individuality” that is “not respected in Japan” would be essential, as well as what he perceives as “excessive” in his family’s demands. Alan Roland, Ph.D., in his book “In Search of Self in India and Japan: Toward a Cross-Cultural Psychology” describes marked differences between traditional Japanese and U.S. expectations of family obligation and relationship: “dependence and interdependence with close emotional connectedness versus independence and autonomy; receptivity and deference to superiors in hierarchical relationships versus self-assertion and self-promotion in egalitarian-contractual relationships; communication on multiple levels and by innuendo versus verbal articulateness and forthrightness; maintaining and enhancing esteem at all costs versus forthright criticism and expressing the truth of the matter” (pp. 292-3).
Of course, these are intentionally polarized descriptions; yet many Japanese in the United States find themselves negotiating contrasting expectations about what it means to be a person in a family and a society, some finding value in at least parts of each tradition, some holding on to traditional Japanese values, and some adopting values related to the new environment.
A key question in this case is what made the situation so difficult for this patient. Going forward, the clinician will want to characterize the biopsychosocial etiologies of his symptoms. Are the social phobia symptoms related to premorbid developmental issues hindering communication, planning, and sociability? Were they exacerbated by language difficulties and the acculturation challenges of finding himself in a new country and institution with potentially different expectations of fulfillment and success?
One wonders how he was accepted into this PhD program and why his performance led to expulsion so quickly. Are there additional symptoms and impairments beyond the breakdown in communication? For example, are there depressive symptoms? Does he have other somatic symptomatology as part of his idiom of distress that may be magnifying his impairment? Were academic supports in place that could have prevented his expulsion? Does he have other social supports and relationships? Is he struggling with intense isolation and, potentially, individuation issues triggered by his new setting?
The DSM-5 Cultural Formulation Interview (CFI), a standardized method for conducting a cultural assessment in mental health care, could help the clinician elicit the patient’s understandings of the problem, its causes and contextual stressors and supports, cultural identity, the cultural features of the relationship between the patient and the clinician, and options for self-coping and clinical care. This exploration of the patient’s lifeworld may clarify how to intervene. Selected supplementary modules to the CFI also may also be useful to ‘amplify’ the core CFI and to further explore the patient’s perception of the family’s role in his illness, including the Social Network Module and the Psychosocial Stressors Module.
Contributors
John Sargent, M.D. – Tufts University School of Medicine
Ellen Berman, M.D. – University of Pennsylvania, Perelman School of Medicine
Roberto Lewis-Fernández, M.D. – Columbia University and New York State Psychiatric Institute
Robert C. Like, M.D., M.S. – Rutgers University, Robert Wood Johnson Medical School
Resources
Lewis-Fernández R., Aggarwal N.K., Baarnhielm, S., et al. Culture and Psychiatric Evaluation: Operationalizing Cultural Formulation for DSM-5 (Psychiatry 2014;77:130-54).
Roland A. In Search of Self in India and Japan: Toward a Cross-Cultural Psychology (Princeton,
N.J.: Princeton University Press, 1988).
Shibusawa T. Japanese Families, in Ethnicity and Family Therapy, 3rd edition. Edited by McGoldrick M., Giordano J., and Garcia-Preto. (New York: Guilford Press, 2005, pp. 339-48).
Tseng W.S., Chang S.C., Nishizono M., eds. Asian Culture and Psychotherapy: Implications for East and West (Honolulu: University of Hawai’i Press).
To read about the goals of Curbside Consult, the guiding principles for assessment, and the guidelines for case submission, see “Considering patients’ family, culture,” Clinical Psychiatry News, January 2015, p. 12. To contribute a case, send it to [email protected]. The contributors have revised selected patient details to shield the identities of the patients/cases and to comply with HIPAA requirements. This column is meant to be educational and does not constitute medical advice. The opinions expressed are those of the contributors and do not represent those of the organizations they employed by or affiliated with or the Group for the Advancement of Psychiatry (GAP).
Are your patients vaccinated for travel?
Graduation season is rapidly approaching, with high school graduations, followed by summer vacations. While searching for that unique gift and /or summer experience, many of your patients may choose an international destination. Not to be forgotten are those who might travel to resource-limited areas to visit relatives, volunteer, or have extended stays because of parental job relocation. More U.S. high school graduates are participating in gap year programs, many of which involve extensive travel while providing the participant the opportunity to immerse and to actively participate in other cultures. For many, it may be their first experience in a country with poor hygiene. This week alone, I’ve helped prepare travelers, including adolescents and children, for a safari and one for 4 weeks of volunteerism in Tanzania. Another young traveler’s destinations were Rwanda, Uganda, and Kenya, and a fourth is planning to explore and trek regions in the high elevations of Bolivia and Peru. The question is, Will you be ready to help prepare young travelers to stay healthy and return home without any unwanted souvenirs?
For many, health concerns often are not the top priority when they are planning vacations. However, the primary care physician will most likely will be their initial call and resource once they realize their potential to be exposed to diseases and/or conditions not routinely encountered in the United States. Even if you receive the call late, there are still interventions you can provide.
To avoid that last-minute call, develop strategies to identify international travelers in your practice. Many practices send out reminders yearly for influenza and well visits, so consider developing one for international travel. Text-message reminders have been shown to improve influenza vaccine administration rates and are another form of communication that can be considered. Frequently remind families that if planning international travel, they should seek pretravel advice in a timely manner: Ideally advice should be obtained 4-6 weeks in advance, and definitely at least 2 weeks prior to departure. Remind them that adequate time is needed for the vaccine to become effective. In addition, depending on the patients’ destination, trip duration, and type of activity, two vaccines (rabies and Japanese encephalitis) may be recommended and are administered over a 28-day period. Yellow fever vaccine, which is recommended or required for entry into some countries, can be obtained only at centers designated by each state health department. It should be administered at least 10 days prior to travel.
Vaccine interventions are based on the potential risk for disease exposure/acquisition. Factors to consider include the age of the travelers, their health and immunization status, in addition to their destination, duration of stay, accommodations, activities, and reason for travel (such as business or visiting friends and relatives). If you have a child with a chronic disorder or who is immunocompromised, comparable medical care may not be available at all international destinations. In addition, not everyone may be a candidate to receive some recommended or required vaccines. Involvement with a health professional prior to booking the trip would be advisable.
Identify a travel health specialist in your area as a local resource who can provide the most up-to-date information and recommendations. Ensure that individual is willing to see children of all ages.
Make sure routine immunizations are up to date for age. Measles is the one exception. I know you have heard it before, but outbreaks persist, even in the United States. Travelers 6- to 11-months-old should receive one MMR dose prior to international travel. This dose will not count, so these children should receive two additional doses of vaccine once they are at least 1 year old. Many children travel with adults. All travelers at least 12 months of age and born after 1956 should have two documented doses of MMR prior to international travel unless they have serologic evidence of immunity. The second dose can be given as early as 4 weeks after the first. If two doses at least 4 weeks apart are administered when a child is at least 12 months of age, no additional doses are necessary.
In 2014, there were 668 cases of measles from 27 states in the United States. The United States is still experiencing a multistate outbreak of measles at press time, which began December 2014. As of April 24, 2015, 166 cases have been reported from 19 states. The Centers for Disease Control and Prevention analyzed the virus type (B3). It is identical to the one responsible for the outbreak in the Philippines in 2014, and it has now been identified in 14 other countries.
Most U.S. measles cases occur in unvaccinated travelers who become ill after their return and spread the disease to susceptible individuals. Do you have patients who are unimmunized? Another point to consider when speaking with these parents about travel is the potential loss of the herd immunity afforded their children while living in the United States. This benefit may not exist when they are visiting and/or relocating to countries with lower immunization rates. Measles outbreaks are occurring in multiple countries and are not limited to underdeveloped countries. For the most up-to-date travel health-related information from the CDC, click here.
Travelers’ diarrhea (TD) occurs in up to 70 % of travelers to developing countries. The World Health Organization defines it as passage of at least three loose stools in a 24-hour period. Most often it is self-limited, with symptoms lasting a median of 3-4 days. Although TD can be caused by bacteria, protozoa, and viruses, bacteria are usually the etiology, with enterotoxigenic Escherichia coli being the most common pathogens. Other bacterial etiologies include Shigella and Campylobacter species. Two antimicrobials are frequently prescribed to travelers for self-treatment of TD: ciprofloxacin and azithromycin. Most young children are prescribed the latter; however, in older children, ciprofloxacin may be prescribed off label, as its use in persons younger than 18 years is not approved by the Food and Drug Administration.
In December 2014, PulseNet, the national molecular subtyping network for food-borne disease, detected a multistate cluster of ciprofloxacin-resistant Shigella sonnei. Between May 2014 and February 2015, 157 cases including 37 children were detected in 32 states and Puerto Rico. Nine of the cases identified by PulseNet, and an additional 76 cases, were associated with an outbreak of ciprofloxacin-resistant S. sonnei in San Francisco. Antibiotic susceptibility was available for 126 isolates, of which 109 (87%) were not ciprofloxacin susceptible. Travel history was available for 75 patients not associated with the San Francisco outbreak, and slightly more than half (40) were associated with international travel. The island of Hispaniola (Dominican Republic = 22 cases and Haiti = 4 cases) was the most common destination, followed by India (8 cases) and Morocco (3 cases). The remaining destinations were Asia and Europe (MMWR 2015;64:318-20) Travel history was available and positive for 23 of the 37 children (62%).
Why such a concern? International travelers are at risk of becoming colonized with drug-resistant bacteria and have the potential to spread them domestically. It has already begun. In 2012, the National Antimicrobial Resistance Monitoring System (NARMS) revealed that isolates of S. sonnei had the following resistance pattern: trimethoprim/sulfamethoxazole, 42%; ampicillin, 18%; and ciprofloxacin, 2.1%. During this outbreak, 19 of the 126 isolates were tested by NARMS with the following resistance patterns noted: trimethoprim/sulfamethoxazole, 84%; ampicillin, 5%; and ciprofloxacin, 32%.
More judicious use of antibiotics is necessary. As pediatricians, we are not immune to this issue. The challenge is when, if at all, antibiotics should be prescribed for TD, and under what conditions should patients be instructed to use them. I’m rethinking my own practice. TD is one of the most common illnesses travelers acquire and is easily treated, but at what cost? The one expression I keep hearing myself say is, First do no harm.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She had no relevant financial disclosures.
Graduation season is rapidly approaching, with high school graduations, followed by summer vacations. While searching for that unique gift and /or summer experience, many of your patients may choose an international destination. Not to be forgotten are those who might travel to resource-limited areas to visit relatives, volunteer, or have extended stays because of parental job relocation. More U.S. high school graduates are participating in gap year programs, many of which involve extensive travel while providing the participant the opportunity to immerse and to actively participate in other cultures. For many, it may be their first experience in a country with poor hygiene. This week alone, I’ve helped prepare travelers, including adolescents and children, for a safari and one for 4 weeks of volunteerism in Tanzania. Another young traveler’s destinations were Rwanda, Uganda, and Kenya, and a fourth is planning to explore and trek regions in the high elevations of Bolivia and Peru. The question is, Will you be ready to help prepare young travelers to stay healthy and return home without any unwanted souvenirs?
For many, health concerns often are not the top priority when they are planning vacations. However, the primary care physician will most likely will be their initial call and resource once they realize their potential to be exposed to diseases and/or conditions not routinely encountered in the United States. Even if you receive the call late, there are still interventions you can provide.
To avoid that last-minute call, develop strategies to identify international travelers in your practice. Many practices send out reminders yearly for influenza and well visits, so consider developing one for international travel. Text-message reminders have been shown to improve influenza vaccine administration rates and are another form of communication that can be considered. Frequently remind families that if planning international travel, they should seek pretravel advice in a timely manner: Ideally advice should be obtained 4-6 weeks in advance, and definitely at least 2 weeks prior to departure. Remind them that adequate time is needed for the vaccine to become effective. In addition, depending on the patients’ destination, trip duration, and type of activity, two vaccines (rabies and Japanese encephalitis) may be recommended and are administered over a 28-day period. Yellow fever vaccine, which is recommended or required for entry into some countries, can be obtained only at centers designated by each state health department. It should be administered at least 10 days prior to travel.
Vaccine interventions are based on the potential risk for disease exposure/acquisition. Factors to consider include the age of the travelers, their health and immunization status, in addition to their destination, duration of stay, accommodations, activities, and reason for travel (such as business or visiting friends and relatives). If you have a child with a chronic disorder or who is immunocompromised, comparable medical care may not be available at all international destinations. In addition, not everyone may be a candidate to receive some recommended or required vaccines. Involvement with a health professional prior to booking the trip would be advisable.
Identify a travel health specialist in your area as a local resource who can provide the most up-to-date information and recommendations. Ensure that individual is willing to see children of all ages.
Make sure routine immunizations are up to date for age. Measles is the one exception. I know you have heard it before, but outbreaks persist, even in the United States. Travelers 6- to 11-months-old should receive one MMR dose prior to international travel. This dose will not count, so these children should receive two additional doses of vaccine once they are at least 1 year old. Many children travel with adults. All travelers at least 12 months of age and born after 1956 should have two documented doses of MMR prior to international travel unless they have serologic evidence of immunity. The second dose can be given as early as 4 weeks after the first. If two doses at least 4 weeks apart are administered when a child is at least 12 months of age, no additional doses are necessary.
In 2014, there were 668 cases of measles from 27 states in the United States. The United States is still experiencing a multistate outbreak of measles at press time, which began December 2014. As of April 24, 2015, 166 cases have been reported from 19 states. The Centers for Disease Control and Prevention analyzed the virus type (B3). It is identical to the one responsible for the outbreak in the Philippines in 2014, and it has now been identified in 14 other countries.
Most U.S. measles cases occur in unvaccinated travelers who become ill after their return and spread the disease to susceptible individuals. Do you have patients who are unimmunized? Another point to consider when speaking with these parents about travel is the potential loss of the herd immunity afforded their children while living in the United States. This benefit may not exist when they are visiting and/or relocating to countries with lower immunization rates. Measles outbreaks are occurring in multiple countries and are not limited to underdeveloped countries. For the most up-to-date travel health-related information from the CDC, click here.
Travelers’ diarrhea (TD) occurs in up to 70 % of travelers to developing countries. The World Health Organization defines it as passage of at least three loose stools in a 24-hour period. Most often it is self-limited, with symptoms lasting a median of 3-4 days. Although TD can be caused by bacteria, protozoa, and viruses, bacteria are usually the etiology, with enterotoxigenic Escherichia coli being the most common pathogens. Other bacterial etiologies include Shigella and Campylobacter species. Two antimicrobials are frequently prescribed to travelers for self-treatment of TD: ciprofloxacin and azithromycin. Most young children are prescribed the latter; however, in older children, ciprofloxacin may be prescribed off label, as its use in persons younger than 18 years is not approved by the Food and Drug Administration.
In December 2014, PulseNet, the national molecular subtyping network for food-borne disease, detected a multistate cluster of ciprofloxacin-resistant Shigella sonnei. Between May 2014 and February 2015, 157 cases including 37 children were detected in 32 states and Puerto Rico. Nine of the cases identified by PulseNet, and an additional 76 cases, were associated with an outbreak of ciprofloxacin-resistant S. sonnei in San Francisco. Antibiotic susceptibility was available for 126 isolates, of which 109 (87%) were not ciprofloxacin susceptible. Travel history was available for 75 patients not associated with the San Francisco outbreak, and slightly more than half (40) were associated with international travel. The island of Hispaniola (Dominican Republic = 22 cases and Haiti = 4 cases) was the most common destination, followed by India (8 cases) and Morocco (3 cases). The remaining destinations were Asia and Europe (MMWR 2015;64:318-20) Travel history was available and positive for 23 of the 37 children (62%).
Why such a concern? International travelers are at risk of becoming colonized with drug-resistant bacteria and have the potential to spread them domestically. It has already begun. In 2012, the National Antimicrobial Resistance Monitoring System (NARMS) revealed that isolates of S. sonnei had the following resistance pattern: trimethoprim/sulfamethoxazole, 42%; ampicillin, 18%; and ciprofloxacin, 2.1%. During this outbreak, 19 of the 126 isolates were tested by NARMS with the following resistance patterns noted: trimethoprim/sulfamethoxazole, 84%; ampicillin, 5%; and ciprofloxacin, 32%.
More judicious use of antibiotics is necessary. As pediatricians, we are not immune to this issue. The challenge is when, if at all, antibiotics should be prescribed for TD, and under what conditions should patients be instructed to use them. I’m rethinking my own practice. TD is one of the most common illnesses travelers acquire and is easily treated, but at what cost? The one expression I keep hearing myself say is, First do no harm.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She had no relevant financial disclosures.
Graduation season is rapidly approaching, with high school graduations, followed by summer vacations. While searching for that unique gift and /or summer experience, many of your patients may choose an international destination. Not to be forgotten are those who might travel to resource-limited areas to visit relatives, volunteer, or have extended stays because of parental job relocation. More U.S. high school graduates are participating in gap year programs, many of which involve extensive travel while providing the participant the opportunity to immerse and to actively participate in other cultures. For many, it may be their first experience in a country with poor hygiene. This week alone, I’ve helped prepare travelers, including adolescents and children, for a safari and one for 4 weeks of volunteerism in Tanzania. Another young traveler’s destinations were Rwanda, Uganda, and Kenya, and a fourth is planning to explore and trek regions in the high elevations of Bolivia and Peru. The question is, Will you be ready to help prepare young travelers to stay healthy and return home without any unwanted souvenirs?
For many, health concerns often are not the top priority when they are planning vacations. However, the primary care physician will most likely will be their initial call and resource once they realize their potential to be exposed to diseases and/or conditions not routinely encountered in the United States. Even if you receive the call late, there are still interventions you can provide.
To avoid that last-minute call, develop strategies to identify international travelers in your practice. Many practices send out reminders yearly for influenza and well visits, so consider developing one for international travel. Text-message reminders have been shown to improve influenza vaccine administration rates and are another form of communication that can be considered. Frequently remind families that if planning international travel, they should seek pretravel advice in a timely manner: Ideally advice should be obtained 4-6 weeks in advance, and definitely at least 2 weeks prior to departure. Remind them that adequate time is needed for the vaccine to become effective. In addition, depending on the patients’ destination, trip duration, and type of activity, two vaccines (rabies and Japanese encephalitis) may be recommended and are administered over a 28-day period. Yellow fever vaccine, which is recommended or required for entry into some countries, can be obtained only at centers designated by each state health department. It should be administered at least 10 days prior to travel.
Vaccine interventions are based on the potential risk for disease exposure/acquisition. Factors to consider include the age of the travelers, their health and immunization status, in addition to their destination, duration of stay, accommodations, activities, and reason for travel (such as business or visiting friends and relatives). If you have a child with a chronic disorder or who is immunocompromised, comparable medical care may not be available at all international destinations. In addition, not everyone may be a candidate to receive some recommended or required vaccines. Involvement with a health professional prior to booking the trip would be advisable.
Identify a travel health specialist in your area as a local resource who can provide the most up-to-date information and recommendations. Ensure that individual is willing to see children of all ages.
Make sure routine immunizations are up to date for age. Measles is the one exception. I know you have heard it before, but outbreaks persist, even in the United States. Travelers 6- to 11-months-old should receive one MMR dose prior to international travel. This dose will not count, so these children should receive two additional doses of vaccine once they are at least 1 year old. Many children travel with adults. All travelers at least 12 months of age and born after 1956 should have two documented doses of MMR prior to international travel unless they have serologic evidence of immunity. The second dose can be given as early as 4 weeks after the first. If two doses at least 4 weeks apart are administered when a child is at least 12 months of age, no additional doses are necessary.
In 2014, there were 668 cases of measles from 27 states in the United States. The United States is still experiencing a multistate outbreak of measles at press time, which began December 2014. As of April 24, 2015, 166 cases have been reported from 19 states. The Centers for Disease Control and Prevention analyzed the virus type (B3). It is identical to the one responsible for the outbreak in the Philippines in 2014, and it has now been identified in 14 other countries.
Most U.S. measles cases occur in unvaccinated travelers who become ill after their return and spread the disease to susceptible individuals. Do you have patients who are unimmunized? Another point to consider when speaking with these parents about travel is the potential loss of the herd immunity afforded their children while living in the United States. This benefit may not exist when they are visiting and/or relocating to countries with lower immunization rates. Measles outbreaks are occurring in multiple countries and are not limited to underdeveloped countries. For the most up-to-date travel health-related information from the CDC, click here.
Travelers’ diarrhea (TD) occurs in up to 70 % of travelers to developing countries. The World Health Organization defines it as passage of at least three loose stools in a 24-hour period. Most often it is self-limited, with symptoms lasting a median of 3-4 days. Although TD can be caused by bacteria, protozoa, and viruses, bacteria are usually the etiology, with enterotoxigenic Escherichia coli being the most common pathogens. Other bacterial etiologies include Shigella and Campylobacter species. Two antimicrobials are frequently prescribed to travelers for self-treatment of TD: ciprofloxacin and azithromycin. Most young children are prescribed the latter; however, in older children, ciprofloxacin may be prescribed off label, as its use in persons younger than 18 years is not approved by the Food and Drug Administration.
In December 2014, PulseNet, the national molecular subtyping network for food-borne disease, detected a multistate cluster of ciprofloxacin-resistant Shigella sonnei. Between May 2014 and February 2015, 157 cases including 37 children were detected in 32 states and Puerto Rico. Nine of the cases identified by PulseNet, and an additional 76 cases, were associated with an outbreak of ciprofloxacin-resistant S. sonnei in San Francisco. Antibiotic susceptibility was available for 126 isolates, of which 109 (87%) were not ciprofloxacin susceptible. Travel history was available for 75 patients not associated with the San Francisco outbreak, and slightly more than half (40) were associated with international travel. The island of Hispaniola (Dominican Republic = 22 cases and Haiti = 4 cases) was the most common destination, followed by India (8 cases) and Morocco (3 cases). The remaining destinations were Asia and Europe (MMWR 2015;64:318-20) Travel history was available and positive for 23 of the 37 children (62%).
Why such a concern? International travelers are at risk of becoming colonized with drug-resistant bacteria and have the potential to spread them domestically. It has already begun. In 2012, the National Antimicrobial Resistance Monitoring System (NARMS) revealed that isolates of S. sonnei had the following resistance pattern: trimethoprim/sulfamethoxazole, 42%; ampicillin, 18%; and ciprofloxacin, 2.1%. During this outbreak, 19 of the 126 isolates were tested by NARMS with the following resistance patterns noted: trimethoprim/sulfamethoxazole, 84%; ampicillin, 5%; and ciprofloxacin, 32%.
More judicious use of antibiotics is necessary. As pediatricians, we are not immune to this issue. The challenge is when, if at all, antibiotics should be prescribed for TD, and under what conditions should patients be instructed to use them. I’m rethinking my own practice. TD is one of the most common illnesses travelers acquire and is easily treated, but at what cost? The one expression I keep hearing myself say is, First do no harm.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She had no relevant financial disclosures.
Families in Psychiatry: Parental alienation and shared delusional disorders
Disturbances in family emotional involvement are best understood at the extremes. At one end, there is extreme cutoff in the controversial diagnosis of parental alienation. At the other end is the extreme enmeshment in shared delusional disorders. What are the mechanisms that allow these conditions to develop? Helping families understand these mechanisms can help them change the trajectory of the family, by moving toward the middle, toward appropriate family emotional involvement.
How does enmeshment begin?
Good parents want to instill good morals, values, and behaviors in their children. Good parents want to teach their children to be good citizens, have good manners, and to treat others with respect. However, sometimes parents desire something more from their children; they want their children to continue a family business, be part of their religious organization, or to be “just like us.” Parental influence is easier when communities are isolated. When shared family beliefs are pervasive and impede the individuation of thoughts, feelings, and behaviors, these families are considered enmeshed and undifferentiated. Enmeshed families are more susceptible to indoctrination. Indoctrination is easier when there is a high level of emotional involvement, meaning that children are kept close, and differentiation and individuation are discouraged.
Using a child for one’s own needs is exploitative;however, many parents might not understand how their own unconscious psychological needs affect their children. This is seen clearly when children are rejected because they are “different.” For example, some parents have stated that a lesbian, gay, bisexual, and transgender sexual orientation is “against their religion,” and demand that their child conform to the family beliefs and norms. In these cases, the adolescent or young adult has to decide whether to leave the family, conform to its beliefs, or hide his or her identity.
Enmeshment
Emotional overinvolvement in undifferentiated enmeshed families is central to the diagnosis of shared delusional disorder. One example of a shared delusion is delusional parasitosis. This is a rare delusional disorder where the patient is convinced of being infested with worms, insects, parasites, or bacteria while no objective evidence exists to support this belief. Somatic delusions are shared with one or more members of a family in 5%-15% of cases (J. Behav. Health 2014;3:200-2).
Salvador Minuchin, Ph.D., and his colleagues outlined the impact of enmeshment in families where a child has an eating disorder. They described children so overprotected that there was a virtual moat around the family system, blocking out the world. Interpersonal differentiation in an enmeshed family system was poor, with identity fusion between parent and child. In this dynamic, the child is unable to establish a clear identity apart from the parent. Orthorexia, a term coined in 1997 by Dr. Steven Bratman, is defined as an obsession with “healthy or righteous eating.” The obsession with healthy foods can be structured within family habits. When enmeshment and family isolation are present, orthorexia can show up as a folie à famille (Heru, personal experience).
More exotic examples are known by the French terms folie à deux and folie à famille. Dr. Ernest-Charles Lasegue (Ann. Med. Psychol. 1877;18:321) was the first person to describe folie à deux. He stated that the inducer created the delusions from his/her psychosis and imposed them upon a “passive” individual; the induced subject was not truly psychotic but instead “absurdly credulous.” Several varieties are described. Folie imposée is the one we typically think of, where the naive individual has a resolution of symptoms when removed from the dominant person. Folie simultanée is where simultaneous and identical psychoses occur in two predisposed people who have had a long and intimate association with each other. There is usually no dominant partner, and separation does not alleviate the symptomatology. Folie communiquée involves the transfer of psychotic delusions after a long period of resistance by the passive partner. The recipient of the delusions subsequently develops his own delusions, independent of the primary subject’s, and these persist following separation.
Folie induite, a variant of folie communiquée, is diagnosed when new delusions are added to old ones under the influence of another deluded patient. The secondary person enriches the newly acquired delusions. Another method of classification is based on the number of individuals involved: folie à trois (three), folie à quatre (four), folie à cinq (five), and, as mentioned earlier, folie àfamille.
What is the mechanism for enmeshment? Several predisposing factors can occur: social isolation, the presence of a naive or “absurdly credulous” person, and in the case of relatives, a shared genetic predisposition. It is most common for the dominant person to drive the belief that is then accepted by dependent family members. In the case of children, there is also identification with a parent and a lack of drive for separation.
Role of alienation
At the opposite end of the spectrum is alienation, most publicly described in the disputed diagnosis of parental alienation syndrome (PAS) (The Parental Alienation Syndrome, 2nd ed., Cresskill, N.J.:Creative Therapeutics Inc., 1998). PAS sometimes arises in the context of child-custody disputes. The primary manifestation is the child’s unjustified denigration of one parent. According to Dr. William Bernet and Amy J.L. Baker, Ph.D., PAS features “abnormal, maladaptive behavior (refusal to have a relationship with a loving parent) that is driven by an abnormal mental state (the false belief that the rejected parent is evil, dangerous, or unworthy of love)” (J. Am. Acad. Psychiatry Law 2013;41:98-104). There is considered to be brainwashing of the child by one parent against the other parent in order to gain leverage in a court of law.
What is the mechanism in alienation? Enmeshment and overidentification of the child with the favored custodial parent is common. The child depends on this adult for his survival. The process of divorce can increase enmeshment with the custodial parent. The parent might reinforce the enmeshment by instilling fear of the “other” parent. The belief that the “other parent” is “bad” is transmitted through conscious and unconscious mechanisms.
The conscious mechanism is direct expression of anger toward the alienated parent. The anger might be motivated by rejection or as revenge for rejection with a desire to punish. The unconscious mechanisms include projective identification. In this situation, anger is seen as being embodied within the “other.” The projecting parent who continues to “hate” keeps the children tied to her out of projected fear of the “other.” The parent who uses projection is likely to have a primitive character structure. The child of the narcissistic custodial parent then acts out the shame and rage at the failure of the marriage.
These domestic tragedies have been around since the beginning of time. In Greek mythology, Medea, having been abandoned by Jason, took her revenge by murdering her two children. “Hell hath no fury like a woman scorned” is a paraphrase from William Congreve’s The Mourning Bride (1697).
What does the DSM-5 say?
Are these disorders and syndromes “real” psychiatric illnesses? The DSM-5 no longer separates delusional disorder from shared delusional disorder. If criteria are met for delusional disorder, that diagnosis is made. If the diagnosis cannot be made but shared beliefs are present, the diagnosis “other specified schizophrenia spectrum and other psychotic disorder” is used.
Those who advocated for inclusion of PAS cited the benefits that follow from a legitimate diagnosis such as legitimatizing problems that family therapists and psychotherapists encounter, allowing insurance coverage, and stimulating research. However, PAS was rejected as not having a good enough scientific basis.
Managing affective involvement
How does the psychiatrist manage families where emotional involvement is extreme? Psychiatrists first need to decide whether the family is capable of making changes and is willing to work on structural change within the family. If not, we can help patients remove themselves from destructive family situations. If the patient in your office wants to leave the family system or minimize the impact of the family system, individual psychotherapy that identifies the impact of family dysfunction, such as cognitive-behavioral therapy, can be used as a type of deprogramming. Exit strategies also can be discussed.
Al-Anon, for example, clarifies the influence of the family system on family members’ well-being by asking several questions, including:
Do you tell lies to cover up for someone else’s drinking?
Do you feel that if they cared about you, they would stop drinking to please you?
Do you make threats, such as, “If you don’t stop drinking, I’ll leave you?”
Are you afraid to upset someone for fear it will set off a drinking bout?
Have you considered calling the police for help in fear of abuse?
Do you feel like a failure because you can’t control the drinking?
Do you think that if they stopped drinking, your other problems would be solved?
If you think there is capacity for family change, the following strategies are helpful:
1. Education about appropriate differentiation
According to Dr. Murray Bowen, one of the main tasks of individuation is finding the right level of differentiation from parents. At one end of the differentiation spectrum is emotional fusion, and at the other end is emotional cutoff (disconnection between family members or refusal to engage with certain family members) (see “Family Evaluation,” New York: W.W. Norton & Co., 1988).
When family enmeshment is present, we can educate the family about individuation. In this way, the family develops a greater intellectual understanding of how they function, compared to their cultural norm. The family may benefit from creating a genogram that clarifies patterns of emotional involvement in their family of origin. Look for intergenerational patterns, and discuss how emotional differentiation occurred in prior generations. Teach the family about the emotional tasks of differentiation.
2. If there is alienation, parse out the reasons
Clarify conscious mechanisms that force the child to reject the other parent. Help the parent understand the consequences for the child in having no access to the other parent. Again, using a genogram helps identify intergenerational patterns, such as emotional cutoffs. Explore the reason for prior family emotional cutoffs. Identify typical patterns in the family for managing anger and conflicts.
In cases of divorce of the custodial parent, look at how anger is managed and stages of grief. Look for the presence of narcissistic injury. Discuss what a good divorce is and the healthiest way for the child to grow up. Help the parent manage and process her own affect without contaminating the child. It is not the role of the child to be the parental caregiver.
Help the child see that there was a loving relationship in the past and that new family goals can be created. The child also might experience anger and grief, and it is important to educate the child about how to manage those feelings appropriately rather than using blame and alienation. Help the child be empowered by positive ideals rather than negative emotions.
Psychiatrists often avoid working with these families, and perceive them as stuck and unable to change. This might be true for some families but certainly not all. Many families find themselves in situations that they do not understand and with problems they need help resolving. Educating and working with families who are stuck and who ask for and want change can change the life trajectory of many people.
Dr. Heru is with the department of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013).
Disturbances in family emotional involvement are best understood at the extremes. At one end, there is extreme cutoff in the controversial diagnosis of parental alienation. At the other end is the extreme enmeshment in shared delusional disorders. What are the mechanisms that allow these conditions to develop? Helping families understand these mechanisms can help them change the trajectory of the family, by moving toward the middle, toward appropriate family emotional involvement.
How does enmeshment begin?
Good parents want to instill good morals, values, and behaviors in their children. Good parents want to teach their children to be good citizens, have good manners, and to treat others with respect. However, sometimes parents desire something more from their children; they want their children to continue a family business, be part of their religious organization, or to be “just like us.” Parental influence is easier when communities are isolated. When shared family beliefs are pervasive and impede the individuation of thoughts, feelings, and behaviors, these families are considered enmeshed and undifferentiated. Enmeshed families are more susceptible to indoctrination. Indoctrination is easier when there is a high level of emotional involvement, meaning that children are kept close, and differentiation and individuation are discouraged.
Using a child for one’s own needs is exploitative;however, many parents might not understand how their own unconscious psychological needs affect their children. This is seen clearly when children are rejected because they are “different.” For example, some parents have stated that a lesbian, gay, bisexual, and transgender sexual orientation is “against their religion,” and demand that their child conform to the family beliefs and norms. In these cases, the adolescent or young adult has to decide whether to leave the family, conform to its beliefs, or hide his or her identity.
Enmeshment
Emotional overinvolvement in undifferentiated enmeshed families is central to the diagnosis of shared delusional disorder. One example of a shared delusion is delusional parasitosis. This is a rare delusional disorder where the patient is convinced of being infested with worms, insects, parasites, or bacteria while no objective evidence exists to support this belief. Somatic delusions are shared with one or more members of a family in 5%-15% of cases (J. Behav. Health 2014;3:200-2).
Salvador Minuchin, Ph.D., and his colleagues outlined the impact of enmeshment in families where a child has an eating disorder. They described children so overprotected that there was a virtual moat around the family system, blocking out the world. Interpersonal differentiation in an enmeshed family system was poor, with identity fusion between parent and child. In this dynamic, the child is unable to establish a clear identity apart from the parent. Orthorexia, a term coined in 1997 by Dr. Steven Bratman, is defined as an obsession with “healthy or righteous eating.” The obsession with healthy foods can be structured within family habits. When enmeshment and family isolation are present, orthorexia can show up as a folie à famille (Heru, personal experience).
More exotic examples are known by the French terms folie à deux and folie à famille. Dr. Ernest-Charles Lasegue (Ann. Med. Psychol. 1877;18:321) was the first person to describe folie à deux. He stated that the inducer created the delusions from his/her psychosis and imposed them upon a “passive” individual; the induced subject was not truly psychotic but instead “absurdly credulous.” Several varieties are described. Folie imposée is the one we typically think of, where the naive individual has a resolution of symptoms when removed from the dominant person. Folie simultanée is where simultaneous and identical psychoses occur in two predisposed people who have had a long and intimate association with each other. There is usually no dominant partner, and separation does not alleviate the symptomatology. Folie communiquée involves the transfer of psychotic delusions after a long period of resistance by the passive partner. The recipient of the delusions subsequently develops his own delusions, independent of the primary subject’s, and these persist following separation.
Folie induite, a variant of folie communiquée, is diagnosed when new delusions are added to old ones under the influence of another deluded patient. The secondary person enriches the newly acquired delusions. Another method of classification is based on the number of individuals involved: folie à trois (three), folie à quatre (four), folie à cinq (five), and, as mentioned earlier, folie àfamille.
What is the mechanism for enmeshment? Several predisposing factors can occur: social isolation, the presence of a naive or “absurdly credulous” person, and in the case of relatives, a shared genetic predisposition. It is most common for the dominant person to drive the belief that is then accepted by dependent family members. In the case of children, there is also identification with a parent and a lack of drive for separation.
Role of alienation
At the opposite end of the spectrum is alienation, most publicly described in the disputed diagnosis of parental alienation syndrome (PAS) (The Parental Alienation Syndrome, 2nd ed., Cresskill, N.J.:Creative Therapeutics Inc., 1998). PAS sometimes arises in the context of child-custody disputes. The primary manifestation is the child’s unjustified denigration of one parent. According to Dr. William Bernet and Amy J.L. Baker, Ph.D., PAS features “abnormal, maladaptive behavior (refusal to have a relationship with a loving parent) that is driven by an abnormal mental state (the false belief that the rejected parent is evil, dangerous, or unworthy of love)” (J. Am. Acad. Psychiatry Law 2013;41:98-104). There is considered to be brainwashing of the child by one parent against the other parent in order to gain leverage in a court of law.
What is the mechanism in alienation? Enmeshment and overidentification of the child with the favored custodial parent is common. The child depends on this adult for his survival. The process of divorce can increase enmeshment with the custodial parent. The parent might reinforce the enmeshment by instilling fear of the “other” parent. The belief that the “other parent” is “bad” is transmitted through conscious and unconscious mechanisms.
The conscious mechanism is direct expression of anger toward the alienated parent. The anger might be motivated by rejection or as revenge for rejection with a desire to punish. The unconscious mechanisms include projective identification. In this situation, anger is seen as being embodied within the “other.” The projecting parent who continues to “hate” keeps the children tied to her out of projected fear of the “other.” The parent who uses projection is likely to have a primitive character structure. The child of the narcissistic custodial parent then acts out the shame and rage at the failure of the marriage.
These domestic tragedies have been around since the beginning of time. In Greek mythology, Medea, having been abandoned by Jason, took her revenge by murdering her two children. “Hell hath no fury like a woman scorned” is a paraphrase from William Congreve’s The Mourning Bride (1697).
What does the DSM-5 say?
Are these disorders and syndromes “real” psychiatric illnesses? The DSM-5 no longer separates delusional disorder from shared delusional disorder. If criteria are met for delusional disorder, that diagnosis is made. If the diagnosis cannot be made but shared beliefs are present, the diagnosis “other specified schizophrenia spectrum and other psychotic disorder” is used.
Those who advocated for inclusion of PAS cited the benefits that follow from a legitimate diagnosis such as legitimatizing problems that family therapists and psychotherapists encounter, allowing insurance coverage, and stimulating research. However, PAS was rejected as not having a good enough scientific basis.
Managing affective involvement
How does the psychiatrist manage families where emotional involvement is extreme? Psychiatrists first need to decide whether the family is capable of making changes and is willing to work on structural change within the family. If not, we can help patients remove themselves from destructive family situations. If the patient in your office wants to leave the family system or minimize the impact of the family system, individual psychotherapy that identifies the impact of family dysfunction, such as cognitive-behavioral therapy, can be used as a type of deprogramming. Exit strategies also can be discussed.
Al-Anon, for example, clarifies the influence of the family system on family members’ well-being by asking several questions, including:
Do you tell lies to cover up for someone else’s drinking?
Do you feel that if they cared about you, they would stop drinking to please you?
Do you make threats, such as, “If you don’t stop drinking, I’ll leave you?”
Are you afraid to upset someone for fear it will set off a drinking bout?
Have you considered calling the police for help in fear of abuse?
Do you feel like a failure because you can’t control the drinking?
Do you think that if they stopped drinking, your other problems would be solved?
If you think there is capacity for family change, the following strategies are helpful:
1. Education about appropriate differentiation
According to Dr. Murray Bowen, one of the main tasks of individuation is finding the right level of differentiation from parents. At one end of the differentiation spectrum is emotional fusion, and at the other end is emotional cutoff (disconnection between family members or refusal to engage with certain family members) (see “Family Evaluation,” New York: W.W. Norton & Co., 1988).
When family enmeshment is present, we can educate the family about individuation. In this way, the family develops a greater intellectual understanding of how they function, compared to their cultural norm. The family may benefit from creating a genogram that clarifies patterns of emotional involvement in their family of origin. Look for intergenerational patterns, and discuss how emotional differentiation occurred in prior generations. Teach the family about the emotional tasks of differentiation.
2. If there is alienation, parse out the reasons
Clarify conscious mechanisms that force the child to reject the other parent. Help the parent understand the consequences for the child in having no access to the other parent. Again, using a genogram helps identify intergenerational patterns, such as emotional cutoffs. Explore the reason for prior family emotional cutoffs. Identify typical patterns in the family for managing anger and conflicts.
In cases of divorce of the custodial parent, look at how anger is managed and stages of grief. Look for the presence of narcissistic injury. Discuss what a good divorce is and the healthiest way for the child to grow up. Help the parent manage and process her own affect without contaminating the child. It is not the role of the child to be the parental caregiver.
Help the child see that there was a loving relationship in the past and that new family goals can be created. The child also might experience anger and grief, and it is important to educate the child about how to manage those feelings appropriately rather than using blame and alienation. Help the child be empowered by positive ideals rather than negative emotions.
Psychiatrists often avoid working with these families, and perceive them as stuck and unable to change. This might be true for some families but certainly not all. Many families find themselves in situations that they do not understand and with problems they need help resolving. Educating and working with families who are stuck and who ask for and want change can change the life trajectory of many people.
Dr. Heru is with the department of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013).
Disturbances in family emotional involvement are best understood at the extremes. At one end, there is extreme cutoff in the controversial diagnosis of parental alienation. At the other end is the extreme enmeshment in shared delusional disorders. What are the mechanisms that allow these conditions to develop? Helping families understand these mechanisms can help them change the trajectory of the family, by moving toward the middle, toward appropriate family emotional involvement.
How does enmeshment begin?
Good parents want to instill good morals, values, and behaviors in their children. Good parents want to teach their children to be good citizens, have good manners, and to treat others with respect. However, sometimes parents desire something more from their children; they want their children to continue a family business, be part of their religious organization, or to be “just like us.” Parental influence is easier when communities are isolated. When shared family beliefs are pervasive and impede the individuation of thoughts, feelings, and behaviors, these families are considered enmeshed and undifferentiated. Enmeshed families are more susceptible to indoctrination. Indoctrination is easier when there is a high level of emotional involvement, meaning that children are kept close, and differentiation and individuation are discouraged.
Using a child for one’s own needs is exploitative;however, many parents might not understand how their own unconscious psychological needs affect their children. This is seen clearly when children are rejected because they are “different.” For example, some parents have stated that a lesbian, gay, bisexual, and transgender sexual orientation is “against their religion,” and demand that their child conform to the family beliefs and norms. In these cases, the adolescent or young adult has to decide whether to leave the family, conform to its beliefs, or hide his or her identity.
Enmeshment
Emotional overinvolvement in undifferentiated enmeshed families is central to the diagnosis of shared delusional disorder. One example of a shared delusion is delusional parasitosis. This is a rare delusional disorder where the patient is convinced of being infested with worms, insects, parasites, or bacteria while no objective evidence exists to support this belief. Somatic delusions are shared with one or more members of a family in 5%-15% of cases (J. Behav. Health 2014;3:200-2).
Salvador Minuchin, Ph.D., and his colleagues outlined the impact of enmeshment in families where a child has an eating disorder. They described children so overprotected that there was a virtual moat around the family system, blocking out the world. Interpersonal differentiation in an enmeshed family system was poor, with identity fusion between parent and child. In this dynamic, the child is unable to establish a clear identity apart from the parent. Orthorexia, a term coined in 1997 by Dr. Steven Bratman, is defined as an obsession with “healthy or righteous eating.” The obsession with healthy foods can be structured within family habits. When enmeshment and family isolation are present, orthorexia can show up as a folie à famille (Heru, personal experience).
More exotic examples are known by the French terms folie à deux and folie à famille. Dr. Ernest-Charles Lasegue (Ann. Med. Psychol. 1877;18:321) was the first person to describe folie à deux. He stated that the inducer created the delusions from his/her psychosis and imposed them upon a “passive” individual; the induced subject was not truly psychotic but instead “absurdly credulous.” Several varieties are described. Folie imposée is the one we typically think of, where the naive individual has a resolution of symptoms when removed from the dominant person. Folie simultanée is where simultaneous and identical psychoses occur in two predisposed people who have had a long and intimate association with each other. There is usually no dominant partner, and separation does not alleviate the symptomatology. Folie communiquée involves the transfer of psychotic delusions after a long period of resistance by the passive partner. The recipient of the delusions subsequently develops his own delusions, independent of the primary subject’s, and these persist following separation.
Folie induite, a variant of folie communiquée, is diagnosed when new delusions are added to old ones under the influence of another deluded patient. The secondary person enriches the newly acquired delusions. Another method of classification is based on the number of individuals involved: folie à trois (three), folie à quatre (four), folie à cinq (five), and, as mentioned earlier, folie àfamille.
What is the mechanism for enmeshment? Several predisposing factors can occur: social isolation, the presence of a naive or “absurdly credulous” person, and in the case of relatives, a shared genetic predisposition. It is most common for the dominant person to drive the belief that is then accepted by dependent family members. In the case of children, there is also identification with a parent and a lack of drive for separation.
Role of alienation
At the opposite end of the spectrum is alienation, most publicly described in the disputed diagnosis of parental alienation syndrome (PAS) (The Parental Alienation Syndrome, 2nd ed., Cresskill, N.J.:Creative Therapeutics Inc., 1998). PAS sometimes arises in the context of child-custody disputes. The primary manifestation is the child’s unjustified denigration of one parent. According to Dr. William Bernet and Amy J.L. Baker, Ph.D., PAS features “abnormal, maladaptive behavior (refusal to have a relationship with a loving parent) that is driven by an abnormal mental state (the false belief that the rejected parent is evil, dangerous, or unworthy of love)” (J. Am. Acad. Psychiatry Law 2013;41:98-104). There is considered to be brainwashing of the child by one parent against the other parent in order to gain leverage in a court of law.
What is the mechanism in alienation? Enmeshment and overidentification of the child with the favored custodial parent is common. The child depends on this adult for his survival. The process of divorce can increase enmeshment with the custodial parent. The parent might reinforce the enmeshment by instilling fear of the “other” parent. The belief that the “other parent” is “bad” is transmitted through conscious and unconscious mechanisms.
The conscious mechanism is direct expression of anger toward the alienated parent. The anger might be motivated by rejection or as revenge for rejection with a desire to punish. The unconscious mechanisms include projective identification. In this situation, anger is seen as being embodied within the “other.” The projecting parent who continues to “hate” keeps the children tied to her out of projected fear of the “other.” The parent who uses projection is likely to have a primitive character structure. The child of the narcissistic custodial parent then acts out the shame and rage at the failure of the marriage.
These domestic tragedies have been around since the beginning of time. In Greek mythology, Medea, having been abandoned by Jason, took her revenge by murdering her two children. “Hell hath no fury like a woman scorned” is a paraphrase from William Congreve’s The Mourning Bride (1697).
What does the DSM-5 say?
Are these disorders and syndromes “real” psychiatric illnesses? The DSM-5 no longer separates delusional disorder from shared delusional disorder. If criteria are met for delusional disorder, that diagnosis is made. If the diagnosis cannot be made but shared beliefs are present, the diagnosis “other specified schizophrenia spectrum and other psychotic disorder” is used.
Those who advocated for inclusion of PAS cited the benefits that follow from a legitimate diagnosis such as legitimatizing problems that family therapists and psychotherapists encounter, allowing insurance coverage, and stimulating research. However, PAS was rejected as not having a good enough scientific basis.
Managing affective involvement
How does the psychiatrist manage families where emotional involvement is extreme? Psychiatrists first need to decide whether the family is capable of making changes and is willing to work on structural change within the family. If not, we can help patients remove themselves from destructive family situations. If the patient in your office wants to leave the family system or minimize the impact of the family system, individual psychotherapy that identifies the impact of family dysfunction, such as cognitive-behavioral therapy, can be used as a type of deprogramming. Exit strategies also can be discussed.
Al-Anon, for example, clarifies the influence of the family system on family members’ well-being by asking several questions, including:
Do you tell lies to cover up for someone else’s drinking?
Do you feel that if they cared about you, they would stop drinking to please you?
Do you make threats, such as, “If you don’t stop drinking, I’ll leave you?”
Are you afraid to upset someone for fear it will set off a drinking bout?
Have you considered calling the police for help in fear of abuse?
Do you feel like a failure because you can’t control the drinking?
Do you think that if they stopped drinking, your other problems would be solved?
If you think there is capacity for family change, the following strategies are helpful:
1. Education about appropriate differentiation
According to Dr. Murray Bowen, one of the main tasks of individuation is finding the right level of differentiation from parents. At one end of the differentiation spectrum is emotional fusion, and at the other end is emotional cutoff (disconnection between family members or refusal to engage with certain family members) (see “Family Evaluation,” New York: W.W. Norton & Co., 1988).
When family enmeshment is present, we can educate the family about individuation. In this way, the family develops a greater intellectual understanding of how they function, compared to their cultural norm. The family may benefit from creating a genogram that clarifies patterns of emotional involvement in their family of origin. Look for intergenerational patterns, and discuss how emotional differentiation occurred in prior generations. Teach the family about the emotional tasks of differentiation.
2. If there is alienation, parse out the reasons
Clarify conscious mechanisms that force the child to reject the other parent. Help the parent understand the consequences for the child in having no access to the other parent. Again, using a genogram helps identify intergenerational patterns, such as emotional cutoffs. Explore the reason for prior family emotional cutoffs. Identify typical patterns in the family for managing anger and conflicts.
In cases of divorce of the custodial parent, look at how anger is managed and stages of grief. Look for the presence of narcissistic injury. Discuss what a good divorce is and the healthiest way for the child to grow up. Help the parent manage and process her own affect without contaminating the child. It is not the role of the child to be the parental caregiver.
Help the child see that there was a loving relationship in the past and that new family goals can be created. The child also might experience anger and grief, and it is important to educate the child about how to manage those feelings appropriately rather than using blame and alienation. Help the child be empowered by positive ideals rather than negative emotions.
Psychiatrists often avoid working with these families, and perceive them as stuck and unable to change. This might be true for some families but certainly not all. Many families find themselves in situations that they do not understand and with problems they need help resolving. Educating and working with families who are stuck and who ask for and want change can change the life trajectory of many people.
Dr. Heru is with the department of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013).
More than 75% with sickle cell crises don’t get hydroxyurea
More than 75% of adults with sickle cell anemia who have frequent pain crises fail to receive hydroxyurea therapy as strongly recommended in National Heart, Lung, and Blood Institute clinical guidelines, according to a Research Letter to the Editor published online April 28 in JAMA.
Despite proven benefits in decreasing pain crises, hospitalizations, blood transfusions, and possibly mortality, hydroxyurea, a “safe and inexpensive drug,” is thought to be underused. To document the actual use of the drug when indicated, investigators analyzed information in a nationwide insurance claims database covering nearly 27 million patients per year. They focused on the records of 570 adults hospitalized or treated in an emergency department for a sickle cell pain crisis at least three times during a 1-year period, said Dr. Nicolas Stettler of the Lewin Group, a health care consulting firm in Falls Church, Va., and his associates.
Only 15.1% of these patients received hydroxyurea within 3 months of their third crisis, only 18.2% received the agent within 6 months, and only 22.7% received it within 12 months. These figures likely represent a conservative estimate of the hydroxyurea treatment gap, since the study didn’t include the large uninsured and publicly insured populations who have more limited access to health care, Dr. Stettler and his associates noted (JAMA 2015;313:1671-2).
Several barriers to this treatment have been identified in previous research, including fear of adverse events, lack of clinician training, and failure to use shared decision making. “To address this gap, it may be necessary to enhance patient outreach and clinician training and develop health care quality measures aimed at increasing the use of hydroxyurea for all patients who would benefit,” they added.
More than 75% of adults with sickle cell anemia who have frequent pain crises fail to receive hydroxyurea therapy as strongly recommended in National Heart, Lung, and Blood Institute clinical guidelines, according to a Research Letter to the Editor published online April 28 in JAMA.
Despite proven benefits in decreasing pain crises, hospitalizations, blood transfusions, and possibly mortality, hydroxyurea, a “safe and inexpensive drug,” is thought to be underused. To document the actual use of the drug when indicated, investigators analyzed information in a nationwide insurance claims database covering nearly 27 million patients per year. They focused on the records of 570 adults hospitalized or treated in an emergency department for a sickle cell pain crisis at least three times during a 1-year period, said Dr. Nicolas Stettler of the Lewin Group, a health care consulting firm in Falls Church, Va., and his associates.
Only 15.1% of these patients received hydroxyurea within 3 months of their third crisis, only 18.2% received the agent within 6 months, and only 22.7% received it within 12 months. These figures likely represent a conservative estimate of the hydroxyurea treatment gap, since the study didn’t include the large uninsured and publicly insured populations who have more limited access to health care, Dr. Stettler and his associates noted (JAMA 2015;313:1671-2).
Several barriers to this treatment have been identified in previous research, including fear of adverse events, lack of clinician training, and failure to use shared decision making. “To address this gap, it may be necessary to enhance patient outreach and clinician training and develop health care quality measures aimed at increasing the use of hydroxyurea for all patients who would benefit,” they added.
More than 75% of adults with sickle cell anemia who have frequent pain crises fail to receive hydroxyurea therapy as strongly recommended in National Heart, Lung, and Blood Institute clinical guidelines, according to a Research Letter to the Editor published online April 28 in JAMA.
Despite proven benefits in decreasing pain crises, hospitalizations, blood transfusions, and possibly mortality, hydroxyurea, a “safe and inexpensive drug,” is thought to be underused. To document the actual use of the drug when indicated, investigators analyzed information in a nationwide insurance claims database covering nearly 27 million patients per year. They focused on the records of 570 adults hospitalized or treated in an emergency department for a sickle cell pain crisis at least three times during a 1-year period, said Dr. Nicolas Stettler of the Lewin Group, a health care consulting firm in Falls Church, Va., and his associates.
Only 15.1% of these patients received hydroxyurea within 3 months of their third crisis, only 18.2% received the agent within 6 months, and only 22.7% received it within 12 months. These figures likely represent a conservative estimate of the hydroxyurea treatment gap, since the study didn’t include the large uninsured and publicly insured populations who have more limited access to health care, Dr. Stettler and his associates noted (JAMA 2015;313:1671-2).
Several barriers to this treatment have been identified in previous research, including fear of adverse events, lack of clinician training, and failure to use shared decision making. “To address this gap, it may be necessary to enhance patient outreach and clinician training and develop health care quality measures aimed at increasing the use of hydroxyurea for all patients who would benefit,” they added.
FROM JAMA
Key clinical point: More than 75% of adults with sickle cell anemia who have frequent pain crises fail to get hydroxyurea therapy as recommended.
Major finding: Only 15.1% of adults with sickle cell anemia received hydroxyurea within 3 months of their third pain crisis, only 18.2% received the agent within 6 months, and only 22.7% received it within 12 months.
Data source: An analysis of information in a large nationwide insurance claims database involving 570 adults with frequent hospitalizations for sickle cell pain crises.
Disclosures: This study was funded by the Lewin Group, a health care consulting firm. Dr. Stettler and his associates reported having no relevant financial disclosures.
Phone Counseling Bolsters Recovery and Reduces Pain Following Spinal Surgery
Participating in a short series of phone conversations with trained counselors can substantially boost recovery and reduce pain in patients after spinal surgery, according to a study published online ahead of print March 28 in Archives of Physical Medicine and Rehabilitation.
The phone calls were designed to enhance standard pre- and post-operative care by reinforcing the value of continuing with physical therapy and back-strengthening exercise regimens.
“Phone counseling appears to be an easy, low-cost strategy that yields meaningful results by improving patient engagement in physical therapy and at-home exercise programs that are so vital for their recovery,” said lead study author Richard Skolasky Jr., ScD, Associate Professor of Orthopedic Surgery at the Johns Hopkins University School of Medicine in Baltimore.
The study included 122 patients ages 46 to 72, who underwent surgery at Johns Hopkins University between 2009 and 2012 to correct spinal stenosis. Each patient was assigned either home exercise programs or physical therapy to help accelerate their recovery time. About half of the patients also received a series of phone counseling sessions from a trained spinal surgery counselor to discuss the importance of exercise in their recovery. The first and most detailed phone session took place a few weeks before the patients had their surgeries. Two follow-up sessions occurred at 6 weeks and at 3 months after the operation was performed.
The study found that patients who received phone calls participated in physical therapy and home exercise at higher rates, and had less pain and less disability 6 months after their surgery, compared with the standard-approach group. Six months after surgery, 74% of patients who received phone counseling experienced significant improvements on standard measures of physical functioning and self-reported measures of pain, compared with 41% of people who did not receive phone calls.
“Modern orthopedic science has made great strides in surgical techniques to correct spinal deformities and achieved significant progress in developing physical therapies that boost the benefits of surgery, but we have not been all that good at motivating and engaging patients to partake in such post-surgical recovery programs,” said co-investigator Stephen Wegener, PhD, Associate Professor of Physical Medicine and Rehabilitation at Johns Hopkins University.
“The findings of our research suggest we may have found a way to add that missing ingredient that draws patients to be more active participants in their physical rehabilitation and recovery,” stated Dr. Wegener.
Suggested Reading
Skolasky RL, Maggard AM, Li D, et al. Health behavior change counseling in surgery for degenerative lumbar spinal stenosis. part I: improvement in rehabilitation engagement and functional outcomes. Arch Phys Med Rehabil. 2015 Mar 28 [Epub ahead of print].
Participating in a short series of phone conversations with trained counselors can substantially boost recovery and reduce pain in patients after spinal surgery, according to a study published online ahead of print March 28 in Archives of Physical Medicine and Rehabilitation.
The phone calls were designed to enhance standard pre- and post-operative care by reinforcing the value of continuing with physical therapy and back-strengthening exercise regimens.
“Phone counseling appears to be an easy, low-cost strategy that yields meaningful results by improving patient engagement in physical therapy and at-home exercise programs that are so vital for their recovery,” said lead study author Richard Skolasky Jr., ScD, Associate Professor of Orthopedic Surgery at the Johns Hopkins University School of Medicine in Baltimore.
The study included 122 patients ages 46 to 72, who underwent surgery at Johns Hopkins University between 2009 and 2012 to correct spinal stenosis. Each patient was assigned either home exercise programs or physical therapy to help accelerate their recovery time. About half of the patients also received a series of phone counseling sessions from a trained spinal surgery counselor to discuss the importance of exercise in their recovery. The first and most detailed phone session took place a few weeks before the patients had their surgeries. Two follow-up sessions occurred at 6 weeks and at 3 months after the operation was performed.
The study found that patients who received phone calls participated in physical therapy and home exercise at higher rates, and had less pain and less disability 6 months after their surgery, compared with the standard-approach group. Six months after surgery, 74% of patients who received phone counseling experienced significant improvements on standard measures of physical functioning and self-reported measures of pain, compared with 41% of people who did not receive phone calls.
“Modern orthopedic science has made great strides in surgical techniques to correct spinal deformities and achieved significant progress in developing physical therapies that boost the benefits of surgery, but we have not been all that good at motivating and engaging patients to partake in such post-surgical recovery programs,” said co-investigator Stephen Wegener, PhD, Associate Professor of Physical Medicine and Rehabilitation at Johns Hopkins University.
“The findings of our research suggest we may have found a way to add that missing ingredient that draws patients to be more active participants in their physical rehabilitation and recovery,” stated Dr. Wegener.
Participating in a short series of phone conversations with trained counselors can substantially boost recovery and reduce pain in patients after spinal surgery, according to a study published online ahead of print March 28 in Archives of Physical Medicine and Rehabilitation.
The phone calls were designed to enhance standard pre- and post-operative care by reinforcing the value of continuing with physical therapy and back-strengthening exercise regimens.
“Phone counseling appears to be an easy, low-cost strategy that yields meaningful results by improving patient engagement in physical therapy and at-home exercise programs that are so vital for their recovery,” said lead study author Richard Skolasky Jr., ScD, Associate Professor of Orthopedic Surgery at the Johns Hopkins University School of Medicine in Baltimore.
The study included 122 patients ages 46 to 72, who underwent surgery at Johns Hopkins University between 2009 and 2012 to correct spinal stenosis. Each patient was assigned either home exercise programs or physical therapy to help accelerate their recovery time. About half of the patients also received a series of phone counseling sessions from a trained spinal surgery counselor to discuss the importance of exercise in their recovery. The first and most detailed phone session took place a few weeks before the patients had their surgeries. Two follow-up sessions occurred at 6 weeks and at 3 months after the operation was performed.
The study found that patients who received phone calls participated in physical therapy and home exercise at higher rates, and had less pain and less disability 6 months after their surgery, compared with the standard-approach group. Six months after surgery, 74% of patients who received phone counseling experienced significant improvements on standard measures of physical functioning and self-reported measures of pain, compared with 41% of people who did not receive phone calls.
“Modern orthopedic science has made great strides in surgical techniques to correct spinal deformities and achieved significant progress in developing physical therapies that boost the benefits of surgery, but we have not been all that good at motivating and engaging patients to partake in such post-surgical recovery programs,” said co-investigator Stephen Wegener, PhD, Associate Professor of Physical Medicine and Rehabilitation at Johns Hopkins University.
“The findings of our research suggest we may have found a way to add that missing ingredient that draws patients to be more active participants in their physical rehabilitation and recovery,” stated Dr. Wegener.
Suggested Reading
Skolasky RL, Maggard AM, Li D, et al. Health behavior change counseling in surgery for degenerative lumbar spinal stenosis. part I: improvement in rehabilitation engagement and functional outcomes. Arch Phys Med Rehabil. 2015 Mar 28 [Epub ahead of print].
Suggested Reading
Skolasky RL, Maggard AM, Li D, et al. Health behavior change counseling in surgery for degenerative lumbar spinal stenosis. part I: improvement in rehabilitation engagement and functional outcomes. Arch Phys Med Rehabil. 2015 Mar 28 [Epub ahead of print].
Molecule increases TRAIL expression to fight NHL

Convention Center, site of the
AACR Annual Meeting 2015
PHILADELPHIA—When current treatment approaches failed to save a young patient with non-Hodgkin lymphoma (NHL), a researcher from The Children’s Hospital of Philadelphia was driven to investigate new therapeutic options.
The investigation led the researcher, Mala Talekar, MBBS, to ONC201 (formerly TIC10), a small molecule that induces apoptosis by increasing surface expression of tumor necrosis factor-related apoptosis-inducing ligand (TRAIL).
Preclinical experiments showed that ONC201 is active against NHL as a single agent, and it synergizes with chemotherapeutic drugs that are already used to treat NHL.
Dr Talekar and her colleagues described these experiments in a poster presented at the AACR Annual Meeting 2015 (abstract 5387). Some of the investigators involved in this research are employed by Oncoceutics, Inc., the company developing ONC201.
A researcher’s inspiration
“When I was doing my fellowship training, I had a teenage boy who had a rare form of non-Hodgkin’s lymphoma,” Dr Talekar explained. “He did not survive, despite receiving multiple treatments that are available for pediatric non-Hodgkin’s lymphoma.”
The boy’s death inspired Dr Talekar to seek new and better approaches to treat NHL. A search of the medical literature unearthed several articles detailing a TRAIL-based approach to treating lymphoma. So she decided to further investigate the effects of TRAIL in NHL.
“I first tried TRAIL in one lymphoma cell line,” she said. “And even though it did kill the cancer cells, it did not really give a satisfactory response.”
So Dr Talekar turned to the TRAIL agonist antibodies lexatumumab and mapatumumab, introducing each of them to human lymphoma cells. Although the antibodies caused more cell death than TRAIL itself, the response was still not satisfactory, she said.
“Fortunately for me, while I was working in the lab, one of the postdocs, Joshua Allen, discovered a new molecule called TRAIL-inducing compound 10, or TIC10,” Dr Talekar said. “So I tried TIC10—it is now called ONC201—and it gave a beautiful dose-response curve, causing complete cell death of the lymphoma cells.”
Dr Talekar was “very inspired” by this result and decided to test ONC201 in 8 different NHL cell lines—4 Burkitt lymphoma (Daudi, Raji, Ramos, and BJAB), 1 anaplastic large-cell lymphoma (Karpas299), and 3 mantle cell lymphoma (UPN2, Granta, and NCEB) cell lines.
“I found a beautiful dose-response curve,” Dr Talekar said, “suggesting that this molecule works in micromolar concentrations across all of the lymphoma cell lines.”
Elucidating the mechanism
Dr Talekar then set out to determine exactly how ONC201 causes cell death in NHL. Flow cytometry revealed that, as the dose of ONC201 increases, cell death increases, as does sub-G1 DNA content. This suggests the drug is causing cell death by apoptosis.
Next, Dr Talekar introduced ONC201 to NHL cell lines along with a pan-caspase inhibitor. She found the inhibitor blocked ONC201-induced apoptosis, which suggests ONC201 works via the caspase-mediated apoptotic pathway.
“The initial mechanism of action proposed for ONC201 was dual inactivation of two kinases, Akt and ERK,” Dr Talekar noted. “The dual inactivation causes dephosphorylation of Foxo3a. This causes its translocation to the nucleus and downstream upregulation of TRAIL, and, therefore, increased surface TRAIL expression. And we know increases in surface TRAIL cause cell death by apoptosis.”
With this in mind, Dr Talekar looked for increases in surface TRIAL after she incubated lymphoma cells with ONC201. She observed a dose-dependent increase in surface TRAIL and a linear correlation between the increase in TRAIL and apoptosis.
Then, she introduced ONC201 and a TRAIL-sequestering antibody, RIK-2, to lymphoma cells. RIK-2 inhibited apoptosis, which suggests ONC201 works as an anti-apoptotic agent via the TRAIL pathway.
Further testing
As a final step, Dr Talekar tested ONC201 in combination with chemotherapy drugs that are already used to treat pediatric NHL. She observed at least an additive effect, and sometimes a synergistic effect, between the drugs. The best responses occurred when she combined ONC201 with cytarabine, bortezomib, or doxorubicin.
Now, Dr Talekar is working on testing ONC201 in combination with cytarabine in a xenograft model of Burkitt lymphoma.
She noted that other in vivo research has suggested ONC201 has a “very benign safety profile.” In another poster presented at AACR 2015 (abstract 4479), researchers reported results indicating that ONC201 is safe.
“They have tested it in mice and dogs and found that, at 10-fold the therapeutic dose, you don’t see much toxicity at all,” Dr Talekar said.
ONC201 is also being tested in a phase 1 study of adults with advanced solid tumors. Phase 1 studies of the drug in relapsed or refractory NHL and relapsed or refractory acute leukemias and high-risk myelodysplastic syndromes are not yet recruiting patients. ![]()

Convention Center, site of the
AACR Annual Meeting 2015
PHILADELPHIA—When current treatment approaches failed to save a young patient with non-Hodgkin lymphoma (NHL), a researcher from The Children’s Hospital of Philadelphia was driven to investigate new therapeutic options.
The investigation led the researcher, Mala Talekar, MBBS, to ONC201 (formerly TIC10), a small molecule that induces apoptosis by increasing surface expression of tumor necrosis factor-related apoptosis-inducing ligand (TRAIL).
Preclinical experiments showed that ONC201 is active against NHL as a single agent, and it synergizes with chemotherapeutic drugs that are already used to treat NHL.
Dr Talekar and her colleagues described these experiments in a poster presented at the AACR Annual Meeting 2015 (abstract 5387). Some of the investigators involved in this research are employed by Oncoceutics, Inc., the company developing ONC201.
A researcher’s inspiration
“When I was doing my fellowship training, I had a teenage boy who had a rare form of non-Hodgkin’s lymphoma,” Dr Talekar explained. “He did not survive, despite receiving multiple treatments that are available for pediatric non-Hodgkin’s lymphoma.”
The boy’s death inspired Dr Talekar to seek new and better approaches to treat NHL. A search of the medical literature unearthed several articles detailing a TRAIL-based approach to treating lymphoma. So she decided to further investigate the effects of TRAIL in NHL.
“I first tried TRAIL in one lymphoma cell line,” she said. “And even though it did kill the cancer cells, it did not really give a satisfactory response.”
So Dr Talekar turned to the TRAIL agonist antibodies lexatumumab and mapatumumab, introducing each of them to human lymphoma cells. Although the antibodies caused more cell death than TRAIL itself, the response was still not satisfactory, she said.
“Fortunately for me, while I was working in the lab, one of the postdocs, Joshua Allen, discovered a new molecule called TRAIL-inducing compound 10, or TIC10,” Dr Talekar said. “So I tried TIC10—it is now called ONC201—and it gave a beautiful dose-response curve, causing complete cell death of the lymphoma cells.”
Dr Talekar was “very inspired” by this result and decided to test ONC201 in 8 different NHL cell lines—4 Burkitt lymphoma (Daudi, Raji, Ramos, and BJAB), 1 anaplastic large-cell lymphoma (Karpas299), and 3 mantle cell lymphoma (UPN2, Granta, and NCEB) cell lines.
“I found a beautiful dose-response curve,” Dr Talekar said, “suggesting that this molecule works in micromolar concentrations across all of the lymphoma cell lines.”
Elucidating the mechanism
Dr Talekar then set out to determine exactly how ONC201 causes cell death in NHL. Flow cytometry revealed that, as the dose of ONC201 increases, cell death increases, as does sub-G1 DNA content. This suggests the drug is causing cell death by apoptosis.
Next, Dr Talekar introduced ONC201 to NHL cell lines along with a pan-caspase inhibitor. She found the inhibitor blocked ONC201-induced apoptosis, which suggests ONC201 works via the caspase-mediated apoptotic pathway.
“The initial mechanism of action proposed for ONC201 was dual inactivation of two kinases, Akt and ERK,” Dr Talekar noted. “The dual inactivation causes dephosphorylation of Foxo3a. This causes its translocation to the nucleus and downstream upregulation of TRAIL, and, therefore, increased surface TRAIL expression. And we know increases in surface TRAIL cause cell death by apoptosis.”
With this in mind, Dr Talekar looked for increases in surface TRIAL after she incubated lymphoma cells with ONC201. She observed a dose-dependent increase in surface TRAIL and a linear correlation between the increase in TRAIL and apoptosis.
Then, she introduced ONC201 and a TRAIL-sequestering antibody, RIK-2, to lymphoma cells. RIK-2 inhibited apoptosis, which suggests ONC201 works as an anti-apoptotic agent via the TRAIL pathway.
Further testing
As a final step, Dr Talekar tested ONC201 in combination with chemotherapy drugs that are already used to treat pediatric NHL. She observed at least an additive effect, and sometimes a synergistic effect, between the drugs. The best responses occurred when she combined ONC201 with cytarabine, bortezomib, or doxorubicin.
Now, Dr Talekar is working on testing ONC201 in combination with cytarabine in a xenograft model of Burkitt lymphoma.
She noted that other in vivo research has suggested ONC201 has a “very benign safety profile.” In another poster presented at AACR 2015 (abstract 4479), researchers reported results indicating that ONC201 is safe.
“They have tested it in mice and dogs and found that, at 10-fold the therapeutic dose, you don’t see much toxicity at all,” Dr Talekar said.
ONC201 is also being tested in a phase 1 study of adults with advanced solid tumors. Phase 1 studies of the drug in relapsed or refractory NHL and relapsed or refractory acute leukemias and high-risk myelodysplastic syndromes are not yet recruiting patients. ![]()

Convention Center, site of the
AACR Annual Meeting 2015
PHILADELPHIA—When current treatment approaches failed to save a young patient with non-Hodgkin lymphoma (NHL), a researcher from The Children’s Hospital of Philadelphia was driven to investigate new therapeutic options.
The investigation led the researcher, Mala Talekar, MBBS, to ONC201 (formerly TIC10), a small molecule that induces apoptosis by increasing surface expression of tumor necrosis factor-related apoptosis-inducing ligand (TRAIL).
Preclinical experiments showed that ONC201 is active against NHL as a single agent, and it synergizes with chemotherapeutic drugs that are already used to treat NHL.
Dr Talekar and her colleagues described these experiments in a poster presented at the AACR Annual Meeting 2015 (abstract 5387). Some of the investigators involved in this research are employed by Oncoceutics, Inc., the company developing ONC201.
A researcher’s inspiration
“When I was doing my fellowship training, I had a teenage boy who had a rare form of non-Hodgkin’s lymphoma,” Dr Talekar explained. “He did not survive, despite receiving multiple treatments that are available for pediatric non-Hodgkin’s lymphoma.”
The boy’s death inspired Dr Talekar to seek new and better approaches to treat NHL. A search of the medical literature unearthed several articles detailing a TRAIL-based approach to treating lymphoma. So she decided to further investigate the effects of TRAIL in NHL.
“I first tried TRAIL in one lymphoma cell line,” she said. “And even though it did kill the cancer cells, it did not really give a satisfactory response.”
So Dr Talekar turned to the TRAIL agonist antibodies lexatumumab and mapatumumab, introducing each of them to human lymphoma cells. Although the antibodies caused more cell death than TRAIL itself, the response was still not satisfactory, she said.
“Fortunately for me, while I was working in the lab, one of the postdocs, Joshua Allen, discovered a new molecule called TRAIL-inducing compound 10, or TIC10,” Dr Talekar said. “So I tried TIC10—it is now called ONC201—and it gave a beautiful dose-response curve, causing complete cell death of the lymphoma cells.”
Dr Talekar was “very inspired” by this result and decided to test ONC201 in 8 different NHL cell lines—4 Burkitt lymphoma (Daudi, Raji, Ramos, and BJAB), 1 anaplastic large-cell lymphoma (Karpas299), and 3 mantle cell lymphoma (UPN2, Granta, and NCEB) cell lines.
“I found a beautiful dose-response curve,” Dr Talekar said, “suggesting that this molecule works in micromolar concentrations across all of the lymphoma cell lines.”
Elucidating the mechanism
Dr Talekar then set out to determine exactly how ONC201 causes cell death in NHL. Flow cytometry revealed that, as the dose of ONC201 increases, cell death increases, as does sub-G1 DNA content. This suggests the drug is causing cell death by apoptosis.
Next, Dr Talekar introduced ONC201 to NHL cell lines along with a pan-caspase inhibitor. She found the inhibitor blocked ONC201-induced apoptosis, which suggests ONC201 works via the caspase-mediated apoptotic pathway.
“The initial mechanism of action proposed for ONC201 was dual inactivation of two kinases, Akt and ERK,” Dr Talekar noted. “The dual inactivation causes dephosphorylation of Foxo3a. This causes its translocation to the nucleus and downstream upregulation of TRAIL, and, therefore, increased surface TRAIL expression. And we know increases in surface TRAIL cause cell death by apoptosis.”
With this in mind, Dr Talekar looked for increases in surface TRIAL after she incubated lymphoma cells with ONC201. She observed a dose-dependent increase in surface TRAIL and a linear correlation between the increase in TRAIL and apoptosis.
Then, she introduced ONC201 and a TRAIL-sequestering antibody, RIK-2, to lymphoma cells. RIK-2 inhibited apoptosis, which suggests ONC201 works as an anti-apoptotic agent via the TRAIL pathway.
Further testing
As a final step, Dr Talekar tested ONC201 in combination with chemotherapy drugs that are already used to treat pediatric NHL. She observed at least an additive effect, and sometimes a synergistic effect, between the drugs. The best responses occurred when she combined ONC201 with cytarabine, bortezomib, or doxorubicin.
Now, Dr Talekar is working on testing ONC201 in combination with cytarabine in a xenograft model of Burkitt lymphoma.
She noted that other in vivo research has suggested ONC201 has a “very benign safety profile.” In another poster presented at AACR 2015 (abstract 4479), researchers reported results indicating that ONC201 is safe.
“They have tested it in mice and dogs and found that, at 10-fold the therapeutic dose, you don’t see much toxicity at all,” Dr Talekar said.
ONC201 is also being tested in a phase 1 study of adults with advanced solid tumors. Phase 1 studies of the drug in relapsed or refractory NHL and relapsed or refractory acute leukemias and high-risk myelodysplastic syndromes are not yet recruiting patients. ![]()
Study sheds new light on decitabine

Image by Christoph Bock
A new study helps explain how the anticancer drug decitabine reverses cell damage and has revealed a potential biomarker that could indicate a
patient’s cancer stage and response to treatment.
Investigators found that decitabine combats some of cancer’s effects by taking the place of the nucleotide cytosine at specific locations on a replicating DNA strand.
In mimicking cytosine, the drug helps “tame” cancerous cells by turning on tumor suppressors and turning off oncogenes.
The investigators also found that decitabine causes an unexpected boost in the amount of a molecule known as 5-hydroxymethylcytosine (5hmC). Because many types of cancer cause 5hmC levels to plummet, an uptick in 5hmC could be a sign that cancer treatments are working.
“We think that the expression of 5hmC could be used as a biomarker to define the stage or the aggressiveness of cancer and to possibly indicate the effectiveness of cancer treatment,” said Joseph Irudayaraj, PhD, of Purdue University in West Lafayette, Indiana. “This could help us monitor the clinical success of patients receiving decitabine.”
Dr Irudayaraj and his colleagues reported these findings in Nature Scientific Reports.
Decitabine, one of the first epigenetic drugs, helps reverse the altered methylation patterns in cancerous cells, but its precise mode of action has not been clear.
Using a combination of models, Dr Irudayaraj and his colleagues showed that decitabine is taking the place of cytosine at strategic positions on replicating strands of DNA in cancer cells.
When an enzyme tries to add a methyl group to silence decitabine, the drug traps it in place, preventing methylation. This triggers another group of enzymes to transform a methylated cytosine on the parent DNA strand into 5hmC, a molecule whose biological function is not yet known.
The investigators confirmed the increase in 5hmC levels in decitabine-treated leukemia cells.
To better explain the team’s findings, Basudev Chowdhury, PhD, also of Purdue University, likened decitabine to a text editor that restores meaning to a garbled sentence and compared conventional chemotherapy to a delete button.
“Think of nucleotides as the alphabet with which our cells compose messages,” he said. “Epigenetics helps translate those messages into actions such as the production of proteins. But cancer can jumble the messages, making them nonsensical. Decitabine helps revise the messages so they can be understood.” ![]()

Image by Christoph Bock
A new study helps explain how the anticancer drug decitabine reverses cell damage and has revealed a potential biomarker that could indicate a
patient’s cancer stage and response to treatment.
Investigators found that decitabine combats some of cancer’s effects by taking the place of the nucleotide cytosine at specific locations on a replicating DNA strand.
In mimicking cytosine, the drug helps “tame” cancerous cells by turning on tumor suppressors and turning off oncogenes.
The investigators also found that decitabine causes an unexpected boost in the amount of a molecule known as 5-hydroxymethylcytosine (5hmC). Because many types of cancer cause 5hmC levels to plummet, an uptick in 5hmC could be a sign that cancer treatments are working.
“We think that the expression of 5hmC could be used as a biomarker to define the stage or the aggressiveness of cancer and to possibly indicate the effectiveness of cancer treatment,” said Joseph Irudayaraj, PhD, of Purdue University in West Lafayette, Indiana. “This could help us monitor the clinical success of patients receiving decitabine.”
Dr Irudayaraj and his colleagues reported these findings in Nature Scientific Reports.
Decitabine, one of the first epigenetic drugs, helps reverse the altered methylation patterns in cancerous cells, but its precise mode of action has not been clear.
Using a combination of models, Dr Irudayaraj and his colleagues showed that decitabine is taking the place of cytosine at strategic positions on replicating strands of DNA in cancer cells.
When an enzyme tries to add a methyl group to silence decitabine, the drug traps it in place, preventing methylation. This triggers another group of enzymes to transform a methylated cytosine on the parent DNA strand into 5hmC, a molecule whose biological function is not yet known.
The investigators confirmed the increase in 5hmC levels in decitabine-treated leukemia cells.
To better explain the team’s findings, Basudev Chowdhury, PhD, also of Purdue University, likened decitabine to a text editor that restores meaning to a garbled sentence and compared conventional chemotherapy to a delete button.
“Think of nucleotides as the alphabet with which our cells compose messages,” he said. “Epigenetics helps translate those messages into actions such as the production of proteins. But cancer can jumble the messages, making them nonsensical. Decitabine helps revise the messages so they can be understood.” ![]()

Image by Christoph Bock
A new study helps explain how the anticancer drug decitabine reverses cell damage and has revealed a potential biomarker that could indicate a
patient’s cancer stage and response to treatment.
Investigators found that decitabine combats some of cancer’s effects by taking the place of the nucleotide cytosine at specific locations on a replicating DNA strand.
In mimicking cytosine, the drug helps “tame” cancerous cells by turning on tumor suppressors and turning off oncogenes.
The investigators also found that decitabine causes an unexpected boost in the amount of a molecule known as 5-hydroxymethylcytosine (5hmC). Because many types of cancer cause 5hmC levels to plummet, an uptick in 5hmC could be a sign that cancer treatments are working.
“We think that the expression of 5hmC could be used as a biomarker to define the stage or the aggressiveness of cancer and to possibly indicate the effectiveness of cancer treatment,” said Joseph Irudayaraj, PhD, of Purdue University in West Lafayette, Indiana. “This could help us monitor the clinical success of patients receiving decitabine.”
Dr Irudayaraj and his colleagues reported these findings in Nature Scientific Reports.
Decitabine, one of the first epigenetic drugs, helps reverse the altered methylation patterns in cancerous cells, but its precise mode of action has not been clear.
Using a combination of models, Dr Irudayaraj and his colleagues showed that decitabine is taking the place of cytosine at strategic positions on replicating strands of DNA in cancer cells.
When an enzyme tries to add a methyl group to silence decitabine, the drug traps it in place, preventing methylation. This triggers another group of enzymes to transform a methylated cytosine on the parent DNA strand into 5hmC, a molecule whose biological function is not yet known.
The investigators confirmed the increase in 5hmC levels in decitabine-treated leukemia cells.
To better explain the team’s findings, Basudev Chowdhury, PhD, also of Purdue University, likened decitabine to a text editor that restores meaning to a garbled sentence and compared conventional chemotherapy to a delete button.
“Think of nucleotides as the alphabet with which our cells compose messages,” he said. “Epigenetics helps translate those messages into actions such as the production of proteins. But cancer can jumble the messages, making them nonsensical. Decitabine helps revise the messages so they can be understood.” ![]()