User login
Report: Many cancer patients may be dying of VTE

chemotherapy
Photo by Rhoda Baer
Thousands of annual deaths among cancer patients in England and Wales may be caused by venous thromboembolism (VTE), according to a report from the All-Party Parliamentary Thrombosis Group (APPTG).
The report showed that, of the patients who died of cancer from 2012 through 2014, about 2.6% also had VTE listed on their death certificate as a cause of death.
This percentage corresponds to nearly 4000 deaths annually.
The report also indicated that many hospitals are not taking appropriate action to reduce the risk of VTE in cancer patients.
The APPTG conducted this research to determine awareness about VTE risk in cancer patients within the National Health Service (NHS). So the group requested data from 150 NHS hospitals in England and 7 in Wales.
The researchers received responses from 92 hospitals—28 in North England, 21 in South England, 25 in the Midlands and East England, 13 in London, and 5 in Wales. The responses included data spanning the period from 2012 through 2014.
On average, 7% of cancer patients in England and Wales were also diagnosed with VTE during the 3-year period.
The incidence of VTE in cancer patients varied by region. For example, it was 2% in the South of England and 3.6% in Wales.
The yearly incidences of cancer and VTE among all hospitals studied were as follows:
| Patients diagnosed with cancer and VTE in England and Wales | ||
| Year | Patients treated
for cancer |
Cancer patients
diagnosed with VTE |
| 2014 | 363,692 | 6301 (1.7%) |
| 2013 | 353,614 | 6506 (1.8%) |
| 2012 | 339,125 | 5716 (1.7%) |
Mortality rates among these patients were as follows:
| Mortality rates involving cancer and VTE in England and Wales | ||
| Year | Cancer deaths | Cancer deaths where VTE
was also listed as cause of death |
| 2014 | 159,187 | 4088 (2.6%) |
| 2013 | 157,848 | 4028 (2.6%) |
| 2012 | 157,293 | 3848 (2.5%) |
The researchers also found that only 41% of the hospitals studied have a dedicated policy or pathway for the management of suspected VTE in patients receiving chemotherapy.
Slightly less than half of the hospitals provide patients with both written and verbal information about the risk of developing VTE during chemotherapy, what symptoms to look out for, and what action patients should take if they suspect a VTE.
“It is a tragedy that, in today’s NHS, a patient can beat their cancer, only to then die of a clot,” said Andrew Gwynne, chair of the APPTG.
“We hope that by raising awareness of this overlooked issue, we can drive up patient safety and provide better outcomes for patients.” ![]()

chemotherapy
Photo by Rhoda Baer
Thousands of annual deaths among cancer patients in England and Wales may be caused by venous thromboembolism (VTE), according to a report from the All-Party Parliamentary Thrombosis Group (APPTG).
The report showed that, of the patients who died of cancer from 2012 through 2014, about 2.6% also had VTE listed on their death certificate as a cause of death.
This percentage corresponds to nearly 4000 deaths annually.
The report also indicated that many hospitals are not taking appropriate action to reduce the risk of VTE in cancer patients.
The APPTG conducted this research to determine awareness about VTE risk in cancer patients within the National Health Service (NHS). So the group requested data from 150 NHS hospitals in England and 7 in Wales.
The researchers received responses from 92 hospitals—28 in North England, 21 in South England, 25 in the Midlands and East England, 13 in London, and 5 in Wales. The responses included data spanning the period from 2012 through 2014.
On average, 7% of cancer patients in England and Wales were also diagnosed with VTE during the 3-year period.
The incidence of VTE in cancer patients varied by region. For example, it was 2% in the South of England and 3.6% in Wales.
The yearly incidences of cancer and VTE among all hospitals studied were as follows:
| Patients diagnosed with cancer and VTE in England and Wales | ||
| Year | Patients treated
for cancer |
Cancer patients
diagnosed with VTE |
| 2014 | 363,692 | 6301 (1.7%) |
| 2013 | 353,614 | 6506 (1.8%) |
| 2012 | 339,125 | 5716 (1.7%) |
Mortality rates among these patients were as follows:
| Mortality rates involving cancer and VTE in England and Wales | ||
| Year | Cancer deaths | Cancer deaths where VTE
was also listed as cause of death |
| 2014 | 159,187 | 4088 (2.6%) |
| 2013 | 157,848 | 4028 (2.6%) |
| 2012 | 157,293 | 3848 (2.5%) |
The researchers also found that only 41% of the hospitals studied have a dedicated policy or pathway for the management of suspected VTE in patients receiving chemotherapy.
Slightly less than half of the hospitals provide patients with both written and verbal information about the risk of developing VTE during chemotherapy, what symptoms to look out for, and what action patients should take if they suspect a VTE.
“It is a tragedy that, in today’s NHS, a patient can beat their cancer, only to then die of a clot,” said Andrew Gwynne, chair of the APPTG.
“We hope that by raising awareness of this overlooked issue, we can drive up patient safety and provide better outcomes for patients.” ![]()

chemotherapy
Photo by Rhoda Baer
Thousands of annual deaths among cancer patients in England and Wales may be caused by venous thromboembolism (VTE), according to a report from the All-Party Parliamentary Thrombosis Group (APPTG).
The report showed that, of the patients who died of cancer from 2012 through 2014, about 2.6% also had VTE listed on their death certificate as a cause of death.
This percentage corresponds to nearly 4000 deaths annually.
The report also indicated that many hospitals are not taking appropriate action to reduce the risk of VTE in cancer patients.
The APPTG conducted this research to determine awareness about VTE risk in cancer patients within the National Health Service (NHS). So the group requested data from 150 NHS hospitals in England and 7 in Wales.
The researchers received responses from 92 hospitals—28 in North England, 21 in South England, 25 in the Midlands and East England, 13 in London, and 5 in Wales. The responses included data spanning the period from 2012 through 2014.
On average, 7% of cancer patients in England and Wales were also diagnosed with VTE during the 3-year period.
The incidence of VTE in cancer patients varied by region. For example, it was 2% in the South of England and 3.6% in Wales.
The yearly incidences of cancer and VTE among all hospitals studied were as follows:
| Patients diagnosed with cancer and VTE in England and Wales | ||
| Year | Patients treated
for cancer |
Cancer patients
diagnosed with VTE |
| 2014 | 363,692 | 6301 (1.7%) |
| 2013 | 353,614 | 6506 (1.8%) |
| 2012 | 339,125 | 5716 (1.7%) |
Mortality rates among these patients were as follows:
| Mortality rates involving cancer and VTE in England and Wales | ||
| Year | Cancer deaths | Cancer deaths where VTE
was also listed as cause of death |
| 2014 | 159,187 | 4088 (2.6%) |
| 2013 | 157,848 | 4028 (2.6%) |
| 2012 | 157,293 | 3848 (2.5%) |
The researchers also found that only 41% of the hospitals studied have a dedicated policy or pathway for the management of suspected VTE in patients receiving chemotherapy.
Slightly less than half of the hospitals provide patients with both written and verbal information about the risk of developing VTE during chemotherapy, what symptoms to look out for, and what action patients should take if they suspect a VTE.
“It is a tragedy that, in today’s NHS, a patient can beat their cancer, only to then die of a clot,” said Andrew Gwynne, chair of the APPTG.
“We hope that by raising awareness of this overlooked issue, we can drive up patient safety and provide better outcomes for patients.” ![]()
Explaining treatment-related anemia

Research conducted in mice suggests that genomic screening might reveal cancer patients who are likely to develop treatment-related anemia.
The study showed that mice lacking Pten and Shp2—enzymes targeted by certain anticancer therapies—can’t produce and sustain enough red blood cells.
Investigators said this helps explain why anemia is a common side effect of anticancer drugs that target enzymes involved in tumor growth.
“Based on this unexpected finding, we might want to think about screening cancer patients’ genetic backgrounds for loss of Pten or Pten-regulated signals before prescribing anticancer drugs that might do more harm than good,” said Gen-Sheng Feng, PhD, of the University of California San Diego School of Medicine.
Dr Feng and his colleagues described their research in PNAS.
First, the team genetically engineered mice to lack Pten, Shp2, or both enzymes. The Pten-deficient mice had elevated white blood cells counts, consistent with myeloproliferative neoplasms (MPNs).
The Shp2-deficient mice experienced the opposite—lower white blood cell counts. And mice lacking both Pten and Shp2 had relatively normal white blood cell counts, suggesting that loss of Shp2 suppresses MPNs induced by Pten loss.
However, the investigators also discovered that mice lacking both enzymes had shorter lifespans than wild-type mice or mice lacking 1 of the enzymes.
This was because the combined deficiency of Shp2 and Pten induced lethal anemia. And this anemia was a result of 2 factors: red blood cells failed to develop properly and those that did form had a shortened lifespan.
To build upon these findings, the investigators treated Pten-deficient mice with the Shp2 inhibitor 11a-1 or with the MEK inhibitor trametinib. (MEK belongs to the same cellular communication network as Shp2.)
As with genetic deletion of Shp2, pharmacologic inhibition of Shp2 suppressed MPN induced by Pten loss and induced severe anemia in the mice.
Trametinib treatment had a similar effect, inducing anemia in Pten-deficient mice but not wild-type mice.
“What we’ve learned is that even if we know a lot about how individual molecules function in a cell, designing effective therapeutics that target them will require a more comprehensive understanding of the cross-talk between molecules in a particular cell type and in the context of disease,” Dr Feng concluded. ![]()

Research conducted in mice suggests that genomic screening might reveal cancer patients who are likely to develop treatment-related anemia.
The study showed that mice lacking Pten and Shp2—enzymes targeted by certain anticancer therapies—can’t produce and sustain enough red blood cells.
Investigators said this helps explain why anemia is a common side effect of anticancer drugs that target enzymes involved in tumor growth.
“Based on this unexpected finding, we might want to think about screening cancer patients’ genetic backgrounds for loss of Pten or Pten-regulated signals before prescribing anticancer drugs that might do more harm than good,” said Gen-Sheng Feng, PhD, of the University of California San Diego School of Medicine.
Dr Feng and his colleagues described their research in PNAS.
First, the team genetically engineered mice to lack Pten, Shp2, or both enzymes. The Pten-deficient mice had elevated white blood cells counts, consistent with myeloproliferative neoplasms (MPNs).
The Shp2-deficient mice experienced the opposite—lower white blood cell counts. And mice lacking both Pten and Shp2 had relatively normal white blood cell counts, suggesting that loss of Shp2 suppresses MPNs induced by Pten loss.
However, the investigators also discovered that mice lacking both enzymes had shorter lifespans than wild-type mice or mice lacking 1 of the enzymes.
This was because the combined deficiency of Shp2 and Pten induced lethal anemia. And this anemia was a result of 2 factors: red blood cells failed to develop properly and those that did form had a shortened lifespan.
To build upon these findings, the investigators treated Pten-deficient mice with the Shp2 inhibitor 11a-1 or with the MEK inhibitor trametinib. (MEK belongs to the same cellular communication network as Shp2.)
As with genetic deletion of Shp2, pharmacologic inhibition of Shp2 suppressed MPN induced by Pten loss and induced severe anemia in the mice.
Trametinib treatment had a similar effect, inducing anemia in Pten-deficient mice but not wild-type mice.
“What we’ve learned is that even if we know a lot about how individual molecules function in a cell, designing effective therapeutics that target them will require a more comprehensive understanding of the cross-talk between molecules in a particular cell type and in the context of disease,” Dr Feng concluded. ![]()

Research conducted in mice suggests that genomic screening might reveal cancer patients who are likely to develop treatment-related anemia.
The study showed that mice lacking Pten and Shp2—enzymes targeted by certain anticancer therapies—can’t produce and sustain enough red blood cells.
Investigators said this helps explain why anemia is a common side effect of anticancer drugs that target enzymes involved in tumor growth.
“Based on this unexpected finding, we might want to think about screening cancer patients’ genetic backgrounds for loss of Pten or Pten-regulated signals before prescribing anticancer drugs that might do more harm than good,” said Gen-Sheng Feng, PhD, of the University of California San Diego School of Medicine.
Dr Feng and his colleagues described their research in PNAS.
First, the team genetically engineered mice to lack Pten, Shp2, or both enzymes. The Pten-deficient mice had elevated white blood cells counts, consistent with myeloproliferative neoplasms (MPNs).
The Shp2-deficient mice experienced the opposite—lower white blood cell counts. And mice lacking both Pten and Shp2 had relatively normal white blood cell counts, suggesting that loss of Shp2 suppresses MPNs induced by Pten loss.
However, the investigators also discovered that mice lacking both enzymes had shorter lifespans than wild-type mice or mice lacking 1 of the enzymes.
This was because the combined deficiency of Shp2 and Pten induced lethal anemia. And this anemia was a result of 2 factors: red blood cells failed to develop properly and those that did form had a shortened lifespan.
To build upon these findings, the investigators treated Pten-deficient mice with the Shp2 inhibitor 11a-1 or with the MEK inhibitor trametinib. (MEK belongs to the same cellular communication network as Shp2.)
As with genetic deletion of Shp2, pharmacologic inhibition of Shp2 suppressed MPN induced by Pten loss and induced severe anemia in the mice.
Trametinib treatment had a similar effect, inducing anemia in Pten-deficient mice but not wild-type mice.
“What we’ve learned is that even if we know a lot about how individual molecules function in a cell, designing effective therapeutics that target them will require a more comprehensive understanding of the cross-talk between molecules in a particular cell type and in the context of disease,” Dr Feng concluded. ![]()
Anticoagulant granted fast track designation

Image by Kevin MacKenzie
The US Food and Drug Administration (FDA) has granted fast track designation to betrixaban as extended-duration venous thromboembolism (VTE) prophylaxis for acute medically ill patients.
This includes patients who are hospitalized for serious medical conditions such as heart failure, stroke, infection, and pulmonary disease.
Betrixaban is an investigational oral anticoagulant that directly inhibits the activity of factor Xa.
According to Portola Pharmaceuticals, the company developing betrixaban, the drug has distinct properties that may allow it to demonstrate clinical benefit without significantly increasing the risk of fatal bleeding and certain other serious side effects.
These benefits include a 19- to 25-hour half-life for once-daily dosing, a low peak-to-trough drug concentration ratio that minimizes anticoagulant variability, low renal clearance, and no significant CYP3A4 metabolism, which may reduce the risk of drug-drug interactions.
Betrixaban trials
In the phase 2 Explore-Xa trial, researchers compared betrixaban and warfarin in patients with atrial fibrillation. The team randomized 508 patients to 1 of 3 blinded doses of betrixaban (40 mg, 60 mg, or 80 mg once daily) or unblinded warfarin, adjusted to an international normalized ratio of 2.0-3.0.
The primary outcome was major or clinically relevant non-major bleeding. At a mean follow-up of 147 days, the primary outcome had been met by 1 patient in the 40 mg betrixaban arm, 5 each in the 60 mg and 80 mg betrixaban arms, and 7 in the warfarin arm.
One patient each in the 60 mg and 80 mg arms experienced an ischemic stroke. And there were 2 vascular deaths, 1 each in the 40 mg arm and the warfarin arm.
In the phase 2 EXPERT trial, researchers compared betrixaban and enoxaparin as VTE prophylaxis in patients who underwent total knee replacement.
The team enrolled 215 patients and assigned them to 1 of 3 post-operative prophylaxis regimens: betrixaban at 15 mg twice daily, betrixaban at 40 mg twice daily, or enoxaparin at 30 mg every 12 hours—all for 10 to 14 days.
The primary efficacy outcome was the incidence of VTE during the dosing period, and 175 patients were evaluable for this outcome. VTE occurred in 20% of patients in the 15 mg betrixaban arm (14/70), 15% in the 40 mg betrixaban arm (10/65), and 10% (4/40) in the enoxaparin arm.
Safety outcomes included major and clinically significant non-major bleeds through 48 hours after treatment. There were no bleeds in the 15 mg betrixaban arm, 2 (2.4%) clinically significant non-major bleeds in the 40 mg betrixaban arm, and 1 (2.3%) major bleed and 2 (4.6%) clinically significant non-major bleeds in the enoxaparin arm.
Betrixaban is currently being tested in the phase 3 APEX trial for the prevention of VTE in acute medically ill patients. Portola said it expects to complete enrollment in APEX by the end of this year and report top-line data in the first quarter of 2016.
If the trial is successful, the company plans to submit a new drug application to the FDA later in 2016 under the fast track designation.
About fast track designation
The FDA’s fast track program is designed to facilitate and expedite the development and review of new drugs intended to treat serious or life-threatening conditions and address unmet medical need.
Through the fast track program, a product may be eligible for priority review. In addition, the company developing the drug may be allowed to submit sections of the biologic license application or new drug application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings with the FDA to discuss the drug’s development plan and ensure collection of the appropriate data needed to support drug approval. And the designation allows for more frequent written communication from the FDA about things such as the design of proposed clinical trials and the use of biomarkers. ![]()

Image by Kevin MacKenzie
The US Food and Drug Administration (FDA) has granted fast track designation to betrixaban as extended-duration venous thromboembolism (VTE) prophylaxis for acute medically ill patients.
This includes patients who are hospitalized for serious medical conditions such as heart failure, stroke, infection, and pulmonary disease.
Betrixaban is an investigational oral anticoagulant that directly inhibits the activity of factor Xa.
According to Portola Pharmaceuticals, the company developing betrixaban, the drug has distinct properties that may allow it to demonstrate clinical benefit without significantly increasing the risk of fatal bleeding and certain other serious side effects.
These benefits include a 19- to 25-hour half-life for once-daily dosing, a low peak-to-trough drug concentration ratio that minimizes anticoagulant variability, low renal clearance, and no significant CYP3A4 metabolism, which may reduce the risk of drug-drug interactions.
Betrixaban trials
In the phase 2 Explore-Xa trial, researchers compared betrixaban and warfarin in patients with atrial fibrillation. The team randomized 508 patients to 1 of 3 blinded doses of betrixaban (40 mg, 60 mg, or 80 mg once daily) or unblinded warfarin, adjusted to an international normalized ratio of 2.0-3.0.
The primary outcome was major or clinically relevant non-major bleeding. At a mean follow-up of 147 days, the primary outcome had been met by 1 patient in the 40 mg betrixaban arm, 5 each in the 60 mg and 80 mg betrixaban arms, and 7 in the warfarin arm.
One patient each in the 60 mg and 80 mg arms experienced an ischemic stroke. And there were 2 vascular deaths, 1 each in the 40 mg arm and the warfarin arm.
In the phase 2 EXPERT trial, researchers compared betrixaban and enoxaparin as VTE prophylaxis in patients who underwent total knee replacement.
The team enrolled 215 patients and assigned them to 1 of 3 post-operative prophylaxis regimens: betrixaban at 15 mg twice daily, betrixaban at 40 mg twice daily, or enoxaparin at 30 mg every 12 hours—all for 10 to 14 days.
The primary efficacy outcome was the incidence of VTE during the dosing period, and 175 patients were evaluable for this outcome. VTE occurred in 20% of patients in the 15 mg betrixaban arm (14/70), 15% in the 40 mg betrixaban arm (10/65), and 10% (4/40) in the enoxaparin arm.
Safety outcomes included major and clinically significant non-major bleeds through 48 hours after treatment. There were no bleeds in the 15 mg betrixaban arm, 2 (2.4%) clinically significant non-major bleeds in the 40 mg betrixaban arm, and 1 (2.3%) major bleed and 2 (4.6%) clinically significant non-major bleeds in the enoxaparin arm.
Betrixaban is currently being tested in the phase 3 APEX trial for the prevention of VTE in acute medically ill patients. Portola said it expects to complete enrollment in APEX by the end of this year and report top-line data in the first quarter of 2016.
If the trial is successful, the company plans to submit a new drug application to the FDA later in 2016 under the fast track designation.
About fast track designation
The FDA’s fast track program is designed to facilitate and expedite the development and review of new drugs intended to treat serious or life-threatening conditions and address unmet medical need.
Through the fast track program, a product may be eligible for priority review. In addition, the company developing the drug may be allowed to submit sections of the biologic license application or new drug application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings with the FDA to discuss the drug’s development plan and ensure collection of the appropriate data needed to support drug approval. And the designation allows for more frequent written communication from the FDA about things such as the design of proposed clinical trials and the use of biomarkers. ![]()

Image by Kevin MacKenzie
The US Food and Drug Administration (FDA) has granted fast track designation to betrixaban as extended-duration venous thromboembolism (VTE) prophylaxis for acute medically ill patients.
This includes patients who are hospitalized for serious medical conditions such as heart failure, stroke, infection, and pulmonary disease.
Betrixaban is an investigational oral anticoagulant that directly inhibits the activity of factor Xa.
According to Portola Pharmaceuticals, the company developing betrixaban, the drug has distinct properties that may allow it to demonstrate clinical benefit without significantly increasing the risk of fatal bleeding and certain other serious side effects.
These benefits include a 19- to 25-hour half-life for once-daily dosing, a low peak-to-trough drug concentration ratio that minimizes anticoagulant variability, low renal clearance, and no significant CYP3A4 metabolism, which may reduce the risk of drug-drug interactions.
Betrixaban trials
In the phase 2 Explore-Xa trial, researchers compared betrixaban and warfarin in patients with atrial fibrillation. The team randomized 508 patients to 1 of 3 blinded doses of betrixaban (40 mg, 60 mg, or 80 mg once daily) or unblinded warfarin, adjusted to an international normalized ratio of 2.0-3.0.
The primary outcome was major or clinically relevant non-major bleeding. At a mean follow-up of 147 days, the primary outcome had been met by 1 patient in the 40 mg betrixaban arm, 5 each in the 60 mg and 80 mg betrixaban arms, and 7 in the warfarin arm.
One patient each in the 60 mg and 80 mg arms experienced an ischemic stroke. And there were 2 vascular deaths, 1 each in the 40 mg arm and the warfarin arm.
In the phase 2 EXPERT trial, researchers compared betrixaban and enoxaparin as VTE prophylaxis in patients who underwent total knee replacement.
The team enrolled 215 patients and assigned them to 1 of 3 post-operative prophylaxis regimens: betrixaban at 15 mg twice daily, betrixaban at 40 mg twice daily, or enoxaparin at 30 mg every 12 hours—all for 10 to 14 days.
The primary efficacy outcome was the incidence of VTE during the dosing period, and 175 patients were evaluable for this outcome. VTE occurred in 20% of patients in the 15 mg betrixaban arm (14/70), 15% in the 40 mg betrixaban arm (10/65), and 10% (4/40) in the enoxaparin arm.
Safety outcomes included major and clinically significant non-major bleeds through 48 hours after treatment. There were no bleeds in the 15 mg betrixaban arm, 2 (2.4%) clinically significant non-major bleeds in the 40 mg betrixaban arm, and 1 (2.3%) major bleed and 2 (4.6%) clinically significant non-major bleeds in the enoxaparin arm.
Betrixaban is currently being tested in the phase 3 APEX trial for the prevention of VTE in acute medically ill patients. Portola said it expects to complete enrollment in APEX by the end of this year and report top-line data in the first quarter of 2016.
If the trial is successful, the company plans to submit a new drug application to the FDA later in 2016 under the fast track designation.
About fast track designation
The FDA’s fast track program is designed to facilitate and expedite the development and review of new drugs intended to treat serious or life-threatening conditions and address unmet medical need.
Through the fast track program, a product may be eligible for priority review. In addition, the company developing the drug may be allowed to submit sections of the biologic license application or new drug application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings with the FDA to discuss the drug’s development plan and ensure collection of the appropriate data needed to support drug approval. And the designation allows for more frequent written communication from the FDA about things such as the design of proposed clinical trials and the use of biomarkers. ![]()
Serum and Red Blood Cell Folate Testing
The Things We Do for No Reason (TWDFNR) series reviews practices which have become common parts of hospital care but which may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent black and white conclusions or clinical practice standards, but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion. https://www.choosingwisely.org/
CASE PRESENTATION
A 65‐year‐old man is admitted with pneumonia. Review of the medical record reveals a persistent macrocytic anemia (hematocrit 29%, hemoglobin 9.3 g/dL, mean corpuscular volume [MCV] 105 fL) with a low reticulocyte count and normal peripheral blood smear. The provider contemplates ordering a serum folate or red blood cell (RBC) folate test to workup the persistent macrocytic anemia.
BACKGROUND
Folate is a water‐soluble B vitamin essential for the synthesis of DNA and for converting homocysteine to methionine. Folate deficiency is causally linked with both neural tube defects and megaloblastic anemia. Low levels of folate are associated with cardiovascular disease, colon cancer, neuropathy, depression, hypercoagulability, and cognitive decline, though there is a paucity of evidence showing causation or risk reduction with folate supplementation.[1] In patients with inadequate folate intake, the earliest sign is a decline in serum folate levels, followed by a fall in RBC folate levels. Only weeks later do macrocytosis, megaloblastic bone marrow, and finally anemia occur.[2] Given that humans are unable to synthesize folate and are therefore dependent on dietary sources, those with inadequate intake or absorption are at risk of folate deficiency.
WHY FOLATE TESTING IS ORDERED
In hospitalized patients, the most common indication for folate testing is anemia, either with or without macrocytosis.[3, 4] Given that at least 10% to 15% of hospitalized patients are anemic,[5, 6] it is unsurprising that folate testing is frequently performed. Despite the link between folate deficiency and megaloblastic anemia, >85% of patients evaluated for folate deficiency have normocytic or microcytic anemia.[3, 4] In addition, a study found that 30% of all folate testing was performed not as part of an anemia workup but in the evaluation of other comorbidities (eg, dementia and altered mental status) that are not causally linked to folate deficiency.[7]
WHY THERE IS NO REASON TO ORDER FOLATE TESTING
There are 2 reasons why testing hospitalized patients for folate deficiency does not contribute value: (1) the poor characteristics of the tests used and (2) the low prevalence of folate deficiency in the postfortification era.
There is no accepted gold standard for the diagnosis of folate deficiency, though biological assays are considered more accurate than the now more commonly used protein binding assays.[8] The lack of a gold standard limits the ability to fully quantify the sensitivity and specificity of either serum or RBC folate testing, though falsely low and high serum folate results can be seen. Falsely low serum levels (false positives) are found with heavy alcohol use and with certain anticonvulsant or antineoplastic drug use.[9] The low levels in these patients indicate low serum folate but do not necessarily reflect tissue stores. Serum folate levels may fall rapidly within a few days of the start of low dietary folate intake, resulting in low serum folate levels that also do not represent true folate deficiency.[10] On the other hand, intake of folatethrough a meal or ingestion of an oral supplementdirectly preceding evaluation of serum folate can lead to falsely elevated levels (false negatives).[10]
Although RBC folate reflects body stores and is largely unaffected by diet, the available tests also lack sensitivity and specificity.[11] Furthermore, serum folate levels and RBC folate levels correlate well.[12] Because RBC folate testing is more expensive than serum folate testing, has results that correlate well with serum folate testing, and is without significantly better test characteristics, there is no added value to using RBC folate testing as compared to serum folate testing.
In addition to the issues with available diagnostic tests, numerous studies now indicate that the rate of folate deficiency in the United States is exceptionally low. This is largely driven by the United States Food and Drug Administration's mandate that all grain products be fortified with 0.14 mg of folic acid per gram of grains.[13] Fortification has been overwhelmingly successful at increasing folic acid intake[14, 15] and reducing the incidence of neural tube defects.[16] Although the serum and RBC folate tests are prone to inaccuracies for an individual patient, population trends postfortification, coupled with the data on intake and rates of neural tube defects, make a strong argument that the prevalence of deficiency has decreased dramatically.
Similar to these population‐based trends, studies of hospital‐based laboratories have shown a marked decrease in the rate of low serum and RBC folate levels, making for a very low pretest probability for folate deficiency (Table 1). Even before fortification had been fully implemented, a study of outpatients and inpatients cared for at 3 hospitals in Denver, Colorado in 1996 found that just 1.9% of patients had low serum folate levels and 4.4% had low RBC folate levels.[17] A retrospective study of 26,662 patients in 1998 showed a rate of serum deficiency (<2.7 ng/mL) of 0.3%.[18] The authors also found that despite a decline in rate of serum deficiency from 1.3% to 0.3% between 1994 and 1998, the total number of serum folate tests performed increased by 84%. A similar study found just 0.4% of 1007 patients with low serum folate levels (<3.0 ng/mL).[7] Parallel results have been seen in other countries after implementation of folate fortification with a cohort of 2154 Canadian patients reporting low serum folate (<6.8 nmol/L) and RBC folate (<417 nmol/L) levels in just 0.5% and 0.7% of patients, respectively.[19]
| Author, Study Year | Year of Testing | Country | Population | Serum Folate | Red Blood Cell Folate | ||||
|---|---|---|---|---|---|---|---|---|---|
| Patients (n) | Samples (n) | Low (%) | Patients (n) | Samples (n) | Low (%) | ||||
| Latif et al., [4] | 2001 | United States | Inpatient/outpatient | 4,315 | 4,689 | 1.6 | 1,215 | 1,335 | 1.2 |
| Shojania et al., 2010[19] | 2001 | Canada | Inpatient/outpatient | 2,154 | 0.5 | 560 | 0.7 | ||
| Ashraf et al., [7] | 2002 | United States | Inpatient/outpatient | 980 | 1,007 | 0.4 | |||
| Gudgeon et al., 2014[20] | 2010 | Canada | Inpatient | 2,563 | 0.2 | ||||
| Theisen‐Toupal et al., [3] | 2011 | United States | Inpatient/emergency department | 1,944 | 2,093 | 0.1 | |||
Few studies have looked exclusively at hospitalized and emergency room patients. In an evaluation of 2093 serum folate tests performed on hospitalized or emergency room patients (98.1% of whom were admitted) in 2011, only 2 (0.1%) deficient levels (<3 ng/mL) were identified, 1 of which was associated with a macrocytic anemia.[3] A similar study of RBC folate levels in 2562 patients at 3 Canadian hospitals found just 4 (0.16%) levels to be low (<254 nmol/L), only 1 of which was associated with macrocytic anemia.[20]
When examining only patients with macrocytic anemia, the rates of folate deficiency are only slightly higher than the general population. As noted above, each of the 2 studies of inpatients uncovered just 1 patient with macrocytic anemia and concomitant low serum or RBC folate levels.[3, 20] Other studies reveal rates of serum folate deficiency in patients with macrocytic anemia and macrocytosis of 2.8%[7] and 1%,[21] respectively, and RBC folate deficiency rates in patients with macrocytosis of 1.8%.[22] Patients with extreme macrocytosis (MCV >130) represent 1 subset of patients with a high pretest probability of low serum folate, with 1 study reporting low levels in 37% of patients.[23]
Despite the relatively inexpensive cost per serum and RBC folate test, expenses per test that result in an abnormally low level are significant. As the pretest probability for folate deficiency is extremely low, tests must be ordered on a large number of patients to find 1 patient with levels suggesting deficiency. For example, a study found that an institution charged $151 per serum folate test, which amounted to $158,000 per deficient result.[3] The institutional cost was <$2.00 per serum folate test and <$2093 per deficient result. Another study reported the institutional cost of RBC folate to be $12.54 per test and $8035 per deficient result.[20] The charges and costs are institution specific and will vary. However, in light of the low pretest probability of testing, any expense associated with these tests represents low value.
WHAT YOU SHOULD DO INSTEAD
The clinician in our case presentation is facing a common scenarioa patient with persistent anemia without a known etiology. The treatment of suspected or confirmed folate deficiency includes improving diet or adding a folic acid supplement, a low‐cost (as little $0.01 per tablet) intervention. Furthermore, other at‐risk patients (eg, those with sickle cell disease, alcoholism, or malabsorption) may be candidates for long‐term supplementation regardless of serum folate and/or RBC folate testing results.
Folate deficiency in patients living in the United States and Canada is exceedingly rare, making the pretest probability of testing low. Furthermore, even patients with typical hematologic characteristics for folate deficiency (anemia and macrocytosis) are unlikely to have folate deficiency. Importantly, there are no nonhematologic indications to test for folate deficiency, and testing those patients, just as in the general population, yields an extremely low rate of folate deficiency. The tests themselves are unreliable and inaccurate, and fortunately, treatment is cheap, easy to administer, and can be done empirically. In other words, testing for folate deficiency is a Thing We Do for No Reason.
RECOMMENDATIONS
In patients suspected of having folate deficiency or who are at high risk of folate deficiency (eg, diet poor in folate‐rich or folic acid fortified foods), treat with a diet containing folate or folic acid fortified foods and/or a supplement containing 400 to 1000 g of folic acid. Approximately 1 to 2 weeks following initiation of treatment, a complete blood count should be performed to evaluate for an appropriate increase in hematocrit/hemoglobin and decrease in MCV.[24] Once a full hematologic response is seen, treatment beyond this time is not required unless the cause (eg, malnutrition) persists.
Serum folate and RBC folate tests should not be routinely ordered. Even in those with macrocytic anemia, the pretest probability of folate deficiency remains low. Although testing may suggest a folate deficiency, it is still more likely there is another cause for the patient's anemia. This places providers at risk for premature closure. For patients such as the one presented in the case presentation, obtaining B12 levels is of greater importance, given the higher prevalence and the risks of untreated deficiency.
For patients in whom the pretest probability of folate deficiency is high (eg, those with an MCV >130), obtain fasting serum folate levels on samples taken before supplementation has begun or a diet administered.
Disclosures
Dr. Feldman is a consultant to Maven Medical, LLC. Maven Medical is a healthcare software startup.
Do you think this is a low‐value practice? Is this truly a Thing We Do for No Reason? Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and Liking It on Facebook. We invite you to propose ideas for other Things We Do for No Reason topics by emailing [email protected].
- Folic acid: nutritional biochemistry, molecular biology, and role in disease processes. Mol Genet Metab. 2000;71(1‐2):121–138.
- Experimental nutritional folate deficiency in man. Trans Assoc Am Physicians. 1962;75:307–320.
- , , Utility, charge, and cost of inpatient and emergency department serum folate testing. J Hosp Med. 2013;8(2):91–95.
- , , , Is there a role for folate determinations in current clinical practice in the USA? Clin Lab Haematol. 2004;26(6):379–383.
- , , , , Prevalence and impact of anemia in hospitalized patients. South Med J. 2013;106(3):202–206.
- Healthcare Cost and Utilization Project (HCUP). HCUP facts and figures: statistics on hospital‐based care in the United States, 2009. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
- , , Clinical utility of folic acid testing for patients with anemia or dementia. J Gen Intern Med. 2008;23(6):824–826.
- Utility of measuring serum or red blood cell folate in the era of folate fortification of flour. Clin Biochem. 2014;47(7‐8):533–538.
- Kelley's Textbook of Internal Medicine. Philadelphia, PA: Lippincott Williams 2000.
- Problems in the diagnosis and investigation of megaloblastic anemia. Can Med Assoc J. 1980;122(9):999–1004.
- Laboratory diagnosis of vitamin B12 and folate deficiency: a guide for the primary care physician. Arch Intern Med. 1999;159(12):1289–1298.
- , Erythrocyte folate levels: a clinical study. Am J Hematol. 1991;36(2):116–21.
- US Food and Drug Administration. Food standards: amendments of standards of identity for enriched grain products to require addition of folic acid. Fed Regist. 1996;61:8781–8797.
- , Effect of food fortification on folic acid intake in the United States. Am J Clin Nutr. 2003;77(1):221–225.
- , , , , , Folic acid intake from fortification in United States exceeds predictions. J Nutr. 2002;132(9):2792–2798.
- , , , , Impact of folic acid fortification of the US food supply on the occurrence of neural tube defects. JAMA. 2001;285(23):2981–2986.
- , Lack of clinical utility of folate levels in the evaluation of macrocytosis or anemia. Am J Med. 2001;110(2):88–90.
- , , , Trends in serum folate after food fortification. Lancet. 1999;354(9182):915–916.
- , Ordering folate assays is no longer justified for investigation of anemias, in folic acid fortified countries. BMC Res Notes. 2010;3:22.
- , Folate testing in hospital inpatients. Am J Med. 2015;128(1):56–59.
- , , , , Etiology and diagnostic evaluation of macrocytosis. Am J Med Sci. 2000;319(6):343–352.
- , , Diminished need for folate measurements among indigent populations in the post folic acid supplementation era. Arch Pathol Lab Med. 2007;131(3):477–480.
- , , , et al. Etiologies and diagnostic work‐up of extreme macrocytosis defined by an erythrocyte mean corpuscular volume over 130°fL: s study of 109 patients. Am J Hematol. 2014;89(6):665–666.
- , , , et al. Best practice in primary care pathology: review 1. J Clin Pathol. 2005;58(10):1016–1024.
The Things We Do for No Reason (TWDFNR) series reviews practices which have become common parts of hospital care but which may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent black and white conclusions or clinical practice standards, but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion. https://www.choosingwisely.org/
CASE PRESENTATION
A 65‐year‐old man is admitted with pneumonia. Review of the medical record reveals a persistent macrocytic anemia (hematocrit 29%, hemoglobin 9.3 g/dL, mean corpuscular volume [MCV] 105 fL) with a low reticulocyte count and normal peripheral blood smear. The provider contemplates ordering a serum folate or red blood cell (RBC) folate test to workup the persistent macrocytic anemia.
BACKGROUND
Folate is a water‐soluble B vitamin essential for the synthesis of DNA and for converting homocysteine to methionine. Folate deficiency is causally linked with both neural tube defects and megaloblastic anemia. Low levels of folate are associated with cardiovascular disease, colon cancer, neuropathy, depression, hypercoagulability, and cognitive decline, though there is a paucity of evidence showing causation or risk reduction with folate supplementation.[1] In patients with inadequate folate intake, the earliest sign is a decline in serum folate levels, followed by a fall in RBC folate levels. Only weeks later do macrocytosis, megaloblastic bone marrow, and finally anemia occur.[2] Given that humans are unable to synthesize folate and are therefore dependent on dietary sources, those with inadequate intake or absorption are at risk of folate deficiency.
WHY FOLATE TESTING IS ORDERED
In hospitalized patients, the most common indication for folate testing is anemia, either with or without macrocytosis.[3, 4] Given that at least 10% to 15% of hospitalized patients are anemic,[5, 6] it is unsurprising that folate testing is frequently performed. Despite the link between folate deficiency and megaloblastic anemia, >85% of patients evaluated for folate deficiency have normocytic or microcytic anemia.[3, 4] In addition, a study found that 30% of all folate testing was performed not as part of an anemia workup but in the evaluation of other comorbidities (eg, dementia and altered mental status) that are not causally linked to folate deficiency.[7]
WHY THERE IS NO REASON TO ORDER FOLATE TESTING
There are 2 reasons why testing hospitalized patients for folate deficiency does not contribute value: (1) the poor characteristics of the tests used and (2) the low prevalence of folate deficiency in the postfortification era.
There is no accepted gold standard for the diagnosis of folate deficiency, though biological assays are considered more accurate than the now more commonly used protein binding assays.[8] The lack of a gold standard limits the ability to fully quantify the sensitivity and specificity of either serum or RBC folate testing, though falsely low and high serum folate results can be seen. Falsely low serum levels (false positives) are found with heavy alcohol use and with certain anticonvulsant or antineoplastic drug use.[9] The low levels in these patients indicate low serum folate but do not necessarily reflect tissue stores. Serum folate levels may fall rapidly within a few days of the start of low dietary folate intake, resulting in low serum folate levels that also do not represent true folate deficiency.[10] On the other hand, intake of folatethrough a meal or ingestion of an oral supplementdirectly preceding evaluation of serum folate can lead to falsely elevated levels (false negatives).[10]
Although RBC folate reflects body stores and is largely unaffected by diet, the available tests also lack sensitivity and specificity.[11] Furthermore, serum folate levels and RBC folate levels correlate well.[12] Because RBC folate testing is more expensive than serum folate testing, has results that correlate well with serum folate testing, and is without significantly better test characteristics, there is no added value to using RBC folate testing as compared to serum folate testing.
In addition to the issues with available diagnostic tests, numerous studies now indicate that the rate of folate deficiency in the United States is exceptionally low. This is largely driven by the United States Food and Drug Administration's mandate that all grain products be fortified with 0.14 mg of folic acid per gram of grains.[13] Fortification has been overwhelmingly successful at increasing folic acid intake[14, 15] and reducing the incidence of neural tube defects.[16] Although the serum and RBC folate tests are prone to inaccuracies for an individual patient, population trends postfortification, coupled with the data on intake and rates of neural tube defects, make a strong argument that the prevalence of deficiency has decreased dramatically.
Similar to these population‐based trends, studies of hospital‐based laboratories have shown a marked decrease in the rate of low serum and RBC folate levels, making for a very low pretest probability for folate deficiency (Table 1). Even before fortification had been fully implemented, a study of outpatients and inpatients cared for at 3 hospitals in Denver, Colorado in 1996 found that just 1.9% of patients had low serum folate levels and 4.4% had low RBC folate levels.[17] A retrospective study of 26,662 patients in 1998 showed a rate of serum deficiency (<2.7 ng/mL) of 0.3%.[18] The authors also found that despite a decline in rate of serum deficiency from 1.3% to 0.3% between 1994 and 1998, the total number of serum folate tests performed increased by 84%. A similar study found just 0.4% of 1007 patients with low serum folate levels (<3.0 ng/mL).[7] Parallel results have been seen in other countries after implementation of folate fortification with a cohort of 2154 Canadian patients reporting low serum folate (<6.8 nmol/L) and RBC folate (<417 nmol/L) levels in just 0.5% and 0.7% of patients, respectively.[19]
| Author, Study Year | Year of Testing | Country | Population | Serum Folate | Red Blood Cell Folate | ||||
|---|---|---|---|---|---|---|---|---|---|
| Patients (n) | Samples (n) | Low (%) | Patients (n) | Samples (n) | Low (%) | ||||
| Latif et al., [4] | 2001 | United States | Inpatient/outpatient | 4,315 | 4,689 | 1.6 | 1,215 | 1,335 | 1.2 |
| Shojania et al., 2010[19] | 2001 | Canada | Inpatient/outpatient | 2,154 | 0.5 | 560 | 0.7 | ||
| Ashraf et al., [7] | 2002 | United States | Inpatient/outpatient | 980 | 1,007 | 0.4 | |||
| Gudgeon et al., 2014[20] | 2010 | Canada | Inpatient | 2,563 | 0.2 | ||||
| Theisen‐Toupal et al., [3] | 2011 | United States | Inpatient/emergency department | 1,944 | 2,093 | 0.1 | |||
Few studies have looked exclusively at hospitalized and emergency room patients. In an evaluation of 2093 serum folate tests performed on hospitalized or emergency room patients (98.1% of whom were admitted) in 2011, only 2 (0.1%) deficient levels (<3 ng/mL) were identified, 1 of which was associated with a macrocytic anemia.[3] A similar study of RBC folate levels in 2562 patients at 3 Canadian hospitals found just 4 (0.16%) levels to be low (<254 nmol/L), only 1 of which was associated with macrocytic anemia.[20]
When examining only patients with macrocytic anemia, the rates of folate deficiency are only slightly higher than the general population. As noted above, each of the 2 studies of inpatients uncovered just 1 patient with macrocytic anemia and concomitant low serum or RBC folate levels.[3, 20] Other studies reveal rates of serum folate deficiency in patients with macrocytic anemia and macrocytosis of 2.8%[7] and 1%,[21] respectively, and RBC folate deficiency rates in patients with macrocytosis of 1.8%.[22] Patients with extreme macrocytosis (MCV >130) represent 1 subset of patients with a high pretest probability of low serum folate, with 1 study reporting low levels in 37% of patients.[23]
Despite the relatively inexpensive cost per serum and RBC folate test, expenses per test that result in an abnormally low level are significant. As the pretest probability for folate deficiency is extremely low, tests must be ordered on a large number of patients to find 1 patient with levels suggesting deficiency. For example, a study found that an institution charged $151 per serum folate test, which amounted to $158,000 per deficient result.[3] The institutional cost was <$2.00 per serum folate test and <$2093 per deficient result. Another study reported the institutional cost of RBC folate to be $12.54 per test and $8035 per deficient result.[20] The charges and costs are institution specific and will vary. However, in light of the low pretest probability of testing, any expense associated with these tests represents low value.
WHAT YOU SHOULD DO INSTEAD
The clinician in our case presentation is facing a common scenarioa patient with persistent anemia without a known etiology. The treatment of suspected or confirmed folate deficiency includes improving diet or adding a folic acid supplement, a low‐cost (as little $0.01 per tablet) intervention. Furthermore, other at‐risk patients (eg, those with sickle cell disease, alcoholism, or malabsorption) may be candidates for long‐term supplementation regardless of serum folate and/or RBC folate testing results.
Folate deficiency in patients living in the United States and Canada is exceedingly rare, making the pretest probability of testing low. Furthermore, even patients with typical hematologic characteristics for folate deficiency (anemia and macrocytosis) are unlikely to have folate deficiency. Importantly, there are no nonhematologic indications to test for folate deficiency, and testing those patients, just as in the general population, yields an extremely low rate of folate deficiency. The tests themselves are unreliable and inaccurate, and fortunately, treatment is cheap, easy to administer, and can be done empirically. In other words, testing for folate deficiency is a Thing We Do for No Reason.
RECOMMENDATIONS
In patients suspected of having folate deficiency or who are at high risk of folate deficiency (eg, diet poor in folate‐rich or folic acid fortified foods), treat with a diet containing folate or folic acid fortified foods and/or a supplement containing 400 to 1000 g of folic acid. Approximately 1 to 2 weeks following initiation of treatment, a complete blood count should be performed to evaluate for an appropriate increase in hematocrit/hemoglobin and decrease in MCV.[24] Once a full hematologic response is seen, treatment beyond this time is not required unless the cause (eg, malnutrition) persists.
Serum folate and RBC folate tests should not be routinely ordered. Even in those with macrocytic anemia, the pretest probability of folate deficiency remains low. Although testing may suggest a folate deficiency, it is still more likely there is another cause for the patient's anemia. This places providers at risk for premature closure. For patients such as the one presented in the case presentation, obtaining B12 levels is of greater importance, given the higher prevalence and the risks of untreated deficiency.
For patients in whom the pretest probability of folate deficiency is high (eg, those with an MCV >130), obtain fasting serum folate levels on samples taken before supplementation has begun or a diet administered.
Disclosures
Dr. Feldman is a consultant to Maven Medical, LLC. Maven Medical is a healthcare software startup.
Do you think this is a low‐value practice? Is this truly a Thing We Do for No Reason? Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and Liking It on Facebook. We invite you to propose ideas for other Things We Do for No Reason topics by emailing [email protected].
The Things We Do for No Reason (TWDFNR) series reviews practices which have become common parts of hospital care but which may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent black and white conclusions or clinical practice standards, but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion. https://www.choosingwisely.org/
CASE PRESENTATION
A 65‐year‐old man is admitted with pneumonia. Review of the medical record reveals a persistent macrocytic anemia (hematocrit 29%, hemoglobin 9.3 g/dL, mean corpuscular volume [MCV] 105 fL) with a low reticulocyte count and normal peripheral blood smear. The provider contemplates ordering a serum folate or red blood cell (RBC) folate test to workup the persistent macrocytic anemia.
BACKGROUND
Folate is a water‐soluble B vitamin essential for the synthesis of DNA and for converting homocysteine to methionine. Folate deficiency is causally linked with both neural tube defects and megaloblastic anemia. Low levels of folate are associated with cardiovascular disease, colon cancer, neuropathy, depression, hypercoagulability, and cognitive decline, though there is a paucity of evidence showing causation or risk reduction with folate supplementation.[1] In patients with inadequate folate intake, the earliest sign is a decline in serum folate levels, followed by a fall in RBC folate levels. Only weeks later do macrocytosis, megaloblastic bone marrow, and finally anemia occur.[2] Given that humans are unable to synthesize folate and are therefore dependent on dietary sources, those with inadequate intake or absorption are at risk of folate deficiency.
WHY FOLATE TESTING IS ORDERED
In hospitalized patients, the most common indication for folate testing is anemia, either with or without macrocytosis.[3, 4] Given that at least 10% to 15% of hospitalized patients are anemic,[5, 6] it is unsurprising that folate testing is frequently performed. Despite the link between folate deficiency and megaloblastic anemia, >85% of patients evaluated for folate deficiency have normocytic or microcytic anemia.[3, 4] In addition, a study found that 30% of all folate testing was performed not as part of an anemia workup but in the evaluation of other comorbidities (eg, dementia and altered mental status) that are not causally linked to folate deficiency.[7]
WHY THERE IS NO REASON TO ORDER FOLATE TESTING
There are 2 reasons why testing hospitalized patients for folate deficiency does not contribute value: (1) the poor characteristics of the tests used and (2) the low prevalence of folate deficiency in the postfortification era.
There is no accepted gold standard for the diagnosis of folate deficiency, though biological assays are considered more accurate than the now more commonly used protein binding assays.[8] The lack of a gold standard limits the ability to fully quantify the sensitivity and specificity of either serum or RBC folate testing, though falsely low and high serum folate results can be seen. Falsely low serum levels (false positives) are found with heavy alcohol use and with certain anticonvulsant or antineoplastic drug use.[9] The low levels in these patients indicate low serum folate but do not necessarily reflect tissue stores. Serum folate levels may fall rapidly within a few days of the start of low dietary folate intake, resulting in low serum folate levels that also do not represent true folate deficiency.[10] On the other hand, intake of folatethrough a meal or ingestion of an oral supplementdirectly preceding evaluation of serum folate can lead to falsely elevated levels (false negatives).[10]
Although RBC folate reflects body stores and is largely unaffected by diet, the available tests also lack sensitivity and specificity.[11] Furthermore, serum folate levels and RBC folate levels correlate well.[12] Because RBC folate testing is more expensive than serum folate testing, has results that correlate well with serum folate testing, and is without significantly better test characteristics, there is no added value to using RBC folate testing as compared to serum folate testing.
In addition to the issues with available diagnostic tests, numerous studies now indicate that the rate of folate deficiency in the United States is exceptionally low. This is largely driven by the United States Food and Drug Administration's mandate that all grain products be fortified with 0.14 mg of folic acid per gram of grains.[13] Fortification has been overwhelmingly successful at increasing folic acid intake[14, 15] and reducing the incidence of neural tube defects.[16] Although the serum and RBC folate tests are prone to inaccuracies for an individual patient, population trends postfortification, coupled with the data on intake and rates of neural tube defects, make a strong argument that the prevalence of deficiency has decreased dramatically.
Similar to these population‐based trends, studies of hospital‐based laboratories have shown a marked decrease in the rate of low serum and RBC folate levels, making for a very low pretest probability for folate deficiency (Table 1). Even before fortification had been fully implemented, a study of outpatients and inpatients cared for at 3 hospitals in Denver, Colorado in 1996 found that just 1.9% of patients had low serum folate levels and 4.4% had low RBC folate levels.[17] A retrospective study of 26,662 patients in 1998 showed a rate of serum deficiency (<2.7 ng/mL) of 0.3%.[18] The authors also found that despite a decline in rate of serum deficiency from 1.3% to 0.3% between 1994 and 1998, the total number of serum folate tests performed increased by 84%. A similar study found just 0.4% of 1007 patients with low serum folate levels (<3.0 ng/mL).[7] Parallel results have been seen in other countries after implementation of folate fortification with a cohort of 2154 Canadian patients reporting low serum folate (<6.8 nmol/L) and RBC folate (<417 nmol/L) levels in just 0.5% and 0.7% of patients, respectively.[19]
| Author, Study Year | Year of Testing | Country | Population | Serum Folate | Red Blood Cell Folate | ||||
|---|---|---|---|---|---|---|---|---|---|
| Patients (n) | Samples (n) | Low (%) | Patients (n) | Samples (n) | Low (%) | ||||
| Latif et al., [4] | 2001 | United States | Inpatient/outpatient | 4,315 | 4,689 | 1.6 | 1,215 | 1,335 | 1.2 |
| Shojania et al., 2010[19] | 2001 | Canada | Inpatient/outpatient | 2,154 | 0.5 | 560 | 0.7 | ||
| Ashraf et al., [7] | 2002 | United States | Inpatient/outpatient | 980 | 1,007 | 0.4 | |||
| Gudgeon et al., 2014[20] | 2010 | Canada | Inpatient | 2,563 | 0.2 | ||||
| Theisen‐Toupal et al., [3] | 2011 | United States | Inpatient/emergency department | 1,944 | 2,093 | 0.1 | |||
Few studies have looked exclusively at hospitalized and emergency room patients. In an evaluation of 2093 serum folate tests performed on hospitalized or emergency room patients (98.1% of whom were admitted) in 2011, only 2 (0.1%) deficient levels (<3 ng/mL) were identified, 1 of which was associated with a macrocytic anemia.[3] A similar study of RBC folate levels in 2562 patients at 3 Canadian hospitals found just 4 (0.16%) levels to be low (<254 nmol/L), only 1 of which was associated with macrocytic anemia.[20]
When examining only patients with macrocytic anemia, the rates of folate deficiency are only slightly higher than the general population. As noted above, each of the 2 studies of inpatients uncovered just 1 patient with macrocytic anemia and concomitant low serum or RBC folate levels.[3, 20] Other studies reveal rates of serum folate deficiency in patients with macrocytic anemia and macrocytosis of 2.8%[7] and 1%,[21] respectively, and RBC folate deficiency rates in patients with macrocytosis of 1.8%.[22] Patients with extreme macrocytosis (MCV >130) represent 1 subset of patients with a high pretest probability of low serum folate, with 1 study reporting low levels in 37% of patients.[23]
Despite the relatively inexpensive cost per serum and RBC folate test, expenses per test that result in an abnormally low level are significant. As the pretest probability for folate deficiency is extremely low, tests must be ordered on a large number of patients to find 1 patient with levels suggesting deficiency. For example, a study found that an institution charged $151 per serum folate test, which amounted to $158,000 per deficient result.[3] The institutional cost was <$2.00 per serum folate test and <$2093 per deficient result. Another study reported the institutional cost of RBC folate to be $12.54 per test and $8035 per deficient result.[20] The charges and costs are institution specific and will vary. However, in light of the low pretest probability of testing, any expense associated with these tests represents low value.
WHAT YOU SHOULD DO INSTEAD
The clinician in our case presentation is facing a common scenarioa patient with persistent anemia without a known etiology. The treatment of suspected or confirmed folate deficiency includes improving diet or adding a folic acid supplement, a low‐cost (as little $0.01 per tablet) intervention. Furthermore, other at‐risk patients (eg, those with sickle cell disease, alcoholism, or malabsorption) may be candidates for long‐term supplementation regardless of serum folate and/or RBC folate testing results.
Folate deficiency in patients living in the United States and Canada is exceedingly rare, making the pretest probability of testing low. Furthermore, even patients with typical hematologic characteristics for folate deficiency (anemia and macrocytosis) are unlikely to have folate deficiency. Importantly, there are no nonhematologic indications to test for folate deficiency, and testing those patients, just as in the general population, yields an extremely low rate of folate deficiency. The tests themselves are unreliable and inaccurate, and fortunately, treatment is cheap, easy to administer, and can be done empirically. In other words, testing for folate deficiency is a Thing We Do for No Reason.
RECOMMENDATIONS
In patients suspected of having folate deficiency or who are at high risk of folate deficiency (eg, diet poor in folate‐rich or folic acid fortified foods), treat with a diet containing folate or folic acid fortified foods and/or a supplement containing 400 to 1000 g of folic acid. Approximately 1 to 2 weeks following initiation of treatment, a complete blood count should be performed to evaluate for an appropriate increase in hematocrit/hemoglobin and decrease in MCV.[24] Once a full hematologic response is seen, treatment beyond this time is not required unless the cause (eg, malnutrition) persists.
Serum folate and RBC folate tests should not be routinely ordered. Even in those with macrocytic anemia, the pretest probability of folate deficiency remains low. Although testing may suggest a folate deficiency, it is still more likely there is another cause for the patient's anemia. This places providers at risk for premature closure. For patients such as the one presented in the case presentation, obtaining B12 levels is of greater importance, given the higher prevalence and the risks of untreated deficiency.
For patients in whom the pretest probability of folate deficiency is high (eg, those with an MCV >130), obtain fasting serum folate levels on samples taken before supplementation has begun or a diet administered.
Disclosures
Dr. Feldman is a consultant to Maven Medical, LLC. Maven Medical is a healthcare software startup.
Do you think this is a low‐value practice? Is this truly a Thing We Do for No Reason? Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and Liking It on Facebook. We invite you to propose ideas for other Things We Do for No Reason topics by emailing [email protected].
- Folic acid: nutritional biochemistry, molecular biology, and role in disease processes. Mol Genet Metab. 2000;71(1‐2):121–138.
- Experimental nutritional folate deficiency in man. Trans Assoc Am Physicians. 1962;75:307–320.
- , , Utility, charge, and cost of inpatient and emergency department serum folate testing. J Hosp Med. 2013;8(2):91–95.
- , , , Is there a role for folate determinations in current clinical practice in the USA? Clin Lab Haematol. 2004;26(6):379–383.
- , , , , Prevalence and impact of anemia in hospitalized patients. South Med J. 2013;106(3):202–206.
- Healthcare Cost and Utilization Project (HCUP). HCUP facts and figures: statistics on hospital‐based care in the United States, 2009. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
- , , Clinical utility of folic acid testing for patients with anemia or dementia. J Gen Intern Med. 2008;23(6):824–826.
- Utility of measuring serum or red blood cell folate in the era of folate fortification of flour. Clin Biochem. 2014;47(7‐8):533–538.
- Kelley's Textbook of Internal Medicine. Philadelphia, PA: Lippincott Williams 2000.
- Problems in the diagnosis and investigation of megaloblastic anemia. Can Med Assoc J. 1980;122(9):999–1004.
- Laboratory diagnosis of vitamin B12 and folate deficiency: a guide for the primary care physician. Arch Intern Med. 1999;159(12):1289–1298.
- , Erythrocyte folate levels: a clinical study. Am J Hematol. 1991;36(2):116–21.
- US Food and Drug Administration. Food standards: amendments of standards of identity for enriched grain products to require addition of folic acid. Fed Regist. 1996;61:8781–8797.
- , Effect of food fortification on folic acid intake in the United States. Am J Clin Nutr. 2003;77(1):221–225.
- , , , , , Folic acid intake from fortification in United States exceeds predictions. J Nutr. 2002;132(9):2792–2798.
- , , , , Impact of folic acid fortification of the US food supply on the occurrence of neural tube defects. JAMA. 2001;285(23):2981–2986.
- , Lack of clinical utility of folate levels in the evaluation of macrocytosis or anemia. Am J Med. 2001;110(2):88–90.
- , , , Trends in serum folate after food fortification. Lancet. 1999;354(9182):915–916.
- , Ordering folate assays is no longer justified for investigation of anemias, in folic acid fortified countries. BMC Res Notes. 2010;3:22.
- , Folate testing in hospital inpatients. Am J Med. 2015;128(1):56–59.
- , , , , Etiology and diagnostic evaluation of macrocytosis. Am J Med Sci. 2000;319(6):343–352.
- , , Diminished need for folate measurements among indigent populations in the post folic acid supplementation era. Arch Pathol Lab Med. 2007;131(3):477–480.
- , , , et al. Etiologies and diagnostic work‐up of extreme macrocytosis defined by an erythrocyte mean corpuscular volume over 130°fL: s study of 109 patients. Am J Hematol. 2014;89(6):665–666.
- , , , et al. Best practice in primary care pathology: review 1. J Clin Pathol. 2005;58(10):1016–1024.
- Folic acid: nutritional biochemistry, molecular biology, and role in disease processes. Mol Genet Metab. 2000;71(1‐2):121–138.
- Experimental nutritional folate deficiency in man. Trans Assoc Am Physicians. 1962;75:307–320.
- , , Utility, charge, and cost of inpatient and emergency department serum folate testing. J Hosp Med. 2013;8(2):91–95.
- , , , Is there a role for folate determinations in current clinical practice in the USA? Clin Lab Haematol. 2004;26(6):379–383.
- , , , , Prevalence and impact of anemia in hospitalized patients. South Med J. 2013;106(3):202–206.
- Healthcare Cost and Utilization Project (HCUP). HCUP facts and figures: statistics on hospital‐based care in the United States, 2009. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
- , , Clinical utility of folic acid testing for patients with anemia or dementia. J Gen Intern Med. 2008;23(6):824–826.
- Utility of measuring serum or red blood cell folate in the era of folate fortification of flour. Clin Biochem. 2014;47(7‐8):533–538.
- Kelley's Textbook of Internal Medicine. Philadelphia, PA: Lippincott Williams 2000.
- Problems in the diagnosis and investigation of megaloblastic anemia. Can Med Assoc J. 1980;122(9):999–1004.
- Laboratory diagnosis of vitamin B12 and folate deficiency: a guide for the primary care physician. Arch Intern Med. 1999;159(12):1289–1298.
- , Erythrocyte folate levels: a clinical study. Am J Hematol. 1991;36(2):116–21.
- US Food and Drug Administration. Food standards: amendments of standards of identity for enriched grain products to require addition of folic acid. Fed Regist. 1996;61:8781–8797.
- , Effect of food fortification on folic acid intake in the United States. Am J Clin Nutr. 2003;77(1):221–225.
- , , , , , Folic acid intake from fortification in United States exceeds predictions. J Nutr. 2002;132(9):2792–2798.
- , , , , Impact of folic acid fortification of the US food supply on the occurrence of neural tube defects. JAMA. 2001;285(23):2981–2986.
- , Lack of clinical utility of folate levels in the evaluation of macrocytosis or anemia. Am J Med. 2001;110(2):88–90.
- , , , Trends in serum folate after food fortification. Lancet. 1999;354(9182):915–916.
- , Ordering folate assays is no longer justified for investigation of anemias, in folic acid fortified countries. BMC Res Notes. 2010;3:22.
- , Folate testing in hospital inpatients. Am J Med. 2015;128(1):56–59.
- , , , , Etiology and diagnostic evaluation of macrocytosis. Am J Med Sci. 2000;319(6):343–352.
- , , Diminished need for folate measurements among indigent populations in the post folic acid supplementation era. Arch Pathol Lab Med. 2007;131(3):477–480.
- , , , et al. Etiologies and diagnostic work‐up of extreme macrocytosis defined by an erythrocyte mean corpuscular volume over 130°fL: s study of 109 patients. Am J Hematol. 2014;89(6):665–666.
- , , , et al. Best practice in primary care pathology: review 1. J Clin Pathol. 2005;58(10):1016–1024.
© 2015 Society of Hospital Medicine
Essure reoperation risk 10 times higher than tubal ligation
The risk of reoperation is more than 10 times greater after hysteroscopic sterilization with the Essure device than after laparoscopic bilateral tubal ligation, according to an observational cohort study published online Oct. 13 in the BMJ.
The finding raises “a serious safety concern” about Essure, a sterilization coil approved in 2002 for hysteroscopic placement into the fallopian tube, and the subject of a recent Food and Drug Administration safety hearing following more than 5,000 adverse event reports.
“While reoperation following sterilization procedure can be related to unintended pregnancy, the similar risk of unintended pregnancy for both procedures in our study indicated that additional surgeries were performed to alleviate complications such as device migration or incompatibility after surgery,” wrote Dr. Art Sedrakyan and his colleagues from Cornell University, New York (BMJ 2015;351:h5162. doi: 10.1136/bmj.h5162).
The Cornell study is believed to be the first to pit Essure against laparoscopic tubal ligation. The investigators compared outcomes of 8,048 patients who underwent hysteroscopic sterilization using the Essure device with 44,278 laparoscopic tubal ligation patients between 2005 and 2013, using a New York state database that captures hospital discharges, outpatient services, ambulatory surgeries, and emergency department records statewide.
Overall, 2.4% of Essure patients, but 0.2% of tubal ligation patients, required reoperation within a year, yielding an odds ratio for Essure of 10.16 (95% C.I., 7.47-13.81), which translates to about 21 additional reoperations per 1,000 Essure patients. Essure patients were eight times more likely to undergo reoperation within 2 years of placement, and six times more likely within 3 years.
Meanwhile, the rate of unintended pregnancy was not statistically different in the two groups, at 1.2% for Essure and 1.1% for tubal ligation within the first year. Essure was also associated with a lower risk of iatrogenic complications within 30 days after surgery, compared with laparoscopic tubal ligation (odds ratio, 0.35).
The use of Essure skyrocketed during the study, from 0.6% of sterilization procedures in 2005 to 25.9% in 2013, with a corresponding drop in tubal ligations. Essure was more likely to be used in women over 40 years old, Medicaid patients, and women with histories of pelvic inflammatory disease, abdominal surgery, and cesarean section. The analysis adjusted for such differences.
Median charges were higher for Essure than for tubal ligation – $7,832 versus $5,068 – despite shorter procedure times, fewer immediate postoperative complications, and less frequent use of general anesthesia.
Although general anesthesia was used less often with Essure, it was still used in about half of patients. “This finding is remarkable in light of the marketing and proposed benefits of avoiding general anesthesia associated with the Essure device,” the investigators wrote.
Tara DiFlumeri, a spokeswoman for Bayer, which manufacturers Essure, said the Cornell study supports the high efficacy rate of Essure. But she also noted that “detection bias” in the study could account for the high reoperation rate identified.
“A required Essure confirmation test is administered 3 months after the procedure to determine whether or not a woman’s fallopian tubes are blocked and she can rely on Essure for birth control. This follow-up test may detect unsatisfactory device placement, resulting in the need for ‘reoperation’ to remove the device and/or complete a tubal ligation if sterilization is still desired. Because there is no confirmation test that could identify potential failure of a laparoscopic tubal ligation procedure, it stands to reason that the comparative reoperation rate would be lower,” she said.
The investigators reported having no financial disclosures. The work was funded in part by the National Institutes of Health and the Food and Drug Administration.
The risk of reoperation is more than 10 times greater after hysteroscopic sterilization with the Essure device than after laparoscopic bilateral tubal ligation, according to an observational cohort study published online Oct. 13 in the BMJ.
The finding raises “a serious safety concern” about Essure, a sterilization coil approved in 2002 for hysteroscopic placement into the fallopian tube, and the subject of a recent Food and Drug Administration safety hearing following more than 5,000 adverse event reports.
“While reoperation following sterilization procedure can be related to unintended pregnancy, the similar risk of unintended pregnancy for both procedures in our study indicated that additional surgeries were performed to alleviate complications such as device migration or incompatibility after surgery,” wrote Dr. Art Sedrakyan and his colleagues from Cornell University, New York (BMJ 2015;351:h5162. doi: 10.1136/bmj.h5162).
The Cornell study is believed to be the first to pit Essure against laparoscopic tubal ligation. The investigators compared outcomes of 8,048 patients who underwent hysteroscopic sterilization using the Essure device with 44,278 laparoscopic tubal ligation patients between 2005 and 2013, using a New York state database that captures hospital discharges, outpatient services, ambulatory surgeries, and emergency department records statewide.
Overall, 2.4% of Essure patients, but 0.2% of tubal ligation patients, required reoperation within a year, yielding an odds ratio for Essure of 10.16 (95% C.I., 7.47-13.81), which translates to about 21 additional reoperations per 1,000 Essure patients. Essure patients were eight times more likely to undergo reoperation within 2 years of placement, and six times more likely within 3 years.
Meanwhile, the rate of unintended pregnancy was not statistically different in the two groups, at 1.2% for Essure and 1.1% for tubal ligation within the first year. Essure was also associated with a lower risk of iatrogenic complications within 30 days after surgery, compared with laparoscopic tubal ligation (odds ratio, 0.35).
The use of Essure skyrocketed during the study, from 0.6% of sterilization procedures in 2005 to 25.9% in 2013, with a corresponding drop in tubal ligations. Essure was more likely to be used in women over 40 years old, Medicaid patients, and women with histories of pelvic inflammatory disease, abdominal surgery, and cesarean section. The analysis adjusted for such differences.
Median charges were higher for Essure than for tubal ligation – $7,832 versus $5,068 – despite shorter procedure times, fewer immediate postoperative complications, and less frequent use of general anesthesia.
Although general anesthesia was used less often with Essure, it was still used in about half of patients. “This finding is remarkable in light of the marketing and proposed benefits of avoiding general anesthesia associated with the Essure device,” the investigators wrote.
Tara DiFlumeri, a spokeswoman for Bayer, which manufacturers Essure, said the Cornell study supports the high efficacy rate of Essure. But she also noted that “detection bias” in the study could account for the high reoperation rate identified.
“A required Essure confirmation test is administered 3 months after the procedure to determine whether or not a woman’s fallopian tubes are blocked and she can rely on Essure for birth control. This follow-up test may detect unsatisfactory device placement, resulting in the need for ‘reoperation’ to remove the device and/or complete a tubal ligation if sterilization is still desired. Because there is no confirmation test that could identify potential failure of a laparoscopic tubal ligation procedure, it stands to reason that the comparative reoperation rate would be lower,” she said.
The investigators reported having no financial disclosures. The work was funded in part by the National Institutes of Health and the Food and Drug Administration.
The risk of reoperation is more than 10 times greater after hysteroscopic sterilization with the Essure device than after laparoscopic bilateral tubal ligation, according to an observational cohort study published online Oct. 13 in the BMJ.
The finding raises “a serious safety concern” about Essure, a sterilization coil approved in 2002 for hysteroscopic placement into the fallopian tube, and the subject of a recent Food and Drug Administration safety hearing following more than 5,000 adverse event reports.
“While reoperation following sterilization procedure can be related to unintended pregnancy, the similar risk of unintended pregnancy for both procedures in our study indicated that additional surgeries were performed to alleviate complications such as device migration or incompatibility after surgery,” wrote Dr. Art Sedrakyan and his colleagues from Cornell University, New York (BMJ 2015;351:h5162. doi: 10.1136/bmj.h5162).
The Cornell study is believed to be the first to pit Essure against laparoscopic tubal ligation. The investigators compared outcomes of 8,048 patients who underwent hysteroscopic sterilization using the Essure device with 44,278 laparoscopic tubal ligation patients between 2005 and 2013, using a New York state database that captures hospital discharges, outpatient services, ambulatory surgeries, and emergency department records statewide.
Overall, 2.4% of Essure patients, but 0.2% of tubal ligation patients, required reoperation within a year, yielding an odds ratio for Essure of 10.16 (95% C.I., 7.47-13.81), which translates to about 21 additional reoperations per 1,000 Essure patients. Essure patients were eight times more likely to undergo reoperation within 2 years of placement, and six times more likely within 3 years.
Meanwhile, the rate of unintended pregnancy was not statistically different in the two groups, at 1.2% for Essure and 1.1% for tubal ligation within the first year. Essure was also associated with a lower risk of iatrogenic complications within 30 days after surgery, compared with laparoscopic tubal ligation (odds ratio, 0.35).
The use of Essure skyrocketed during the study, from 0.6% of sterilization procedures in 2005 to 25.9% in 2013, with a corresponding drop in tubal ligations. Essure was more likely to be used in women over 40 years old, Medicaid patients, and women with histories of pelvic inflammatory disease, abdominal surgery, and cesarean section. The analysis adjusted for such differences.
Median charges were higher for Essure than for tubal ligation – $7,832 versus $5,068 – despite shorter procedure times, fewer immediate postoperative complications, and less frequent use of general anesthesia.
Although general anesthesia was used less often with Essure, it was still used in about half of patients. “This finding is remarkable in light of the marketing and proposed benefits of avoiding general anesthesia associated with the Essure device,” the investigators wrote.
Tara DiFlumeri, a spokeswoman for Bayer, which manufacturers Essure, said the Cornell study supports the high efficacy rate of Essure. But she also noted that “detection bias” in the study could account for the high reoperation rate identified.
“A required Essure confirmation test is administered 3 months after the procedure to determine whether or not a woman’s fallopian tubes are blocked and she can rely on Essure for birth control. This follow-up test may detect unsatisfactory device placement, resulting in the need for ‘reoperation’ to remove the device and/or complete a tubal ligation if sterilization is still desired. Because there is no confirmation test that could identify potential failure of a laparoscopic tubal ligation procedure, it stands to reason that the comparative reoperation rate would be lower,” she said.
The investigators reported having no financial disclosures. The work was funded in part by the National Institutes of Health and the Food and Drug Administration.
FROM BMJ
Key clinical point: Laparoscopic tubal ligation is as effective as Essure at preventing pregnancy, with fewer reoperations and a lower price tag.
Major finding: Overall, 2.4% of Essure patients, but 0.2% of tubal ligation patients, required reoperation within a year (odds ratio, 10.16), translating to 21 additional reoperations per 1,000 patients.
Data source: Observational cohort study of 8,048 Essure and 44,278 tubal ligation patients between 2005 and 2013.
Disclosures: The investigators reported having no financial disclosures. The work was funded in part by the National Institutes of Health and the Food and Drug Administration.
A Novel Method of Skin Closure for Aging or Fragile Skin
Patients who have been on steroids, aspirin, or anticoagulants or who are elderly may have a fragile outer skin layer that is similar to parchment paper, which may be challenging for surgeons. In these patients, the epidermal layer is thin and translucent; when a surgeon cuts through this thin layer, the tissue beneath shows minimal dermis and poor-quality fat with weakened tissue support. When undergoing excisional surgery, there is no strong tissue to help the closure sutures remain intact. Surgeons may struggle with skin tears around the sutures and dehiscence on suture removal.
This article describes a novel approach to skin closure in patients with aging or thin skin using a polyethylene film with an acrylate adhesive in the excision area to aid in maintaining skin integrity throughout the healing process following surgery.
Closure Technique
First, the skin area is cleansed with a sterilizing soap preparation. A sterile marking pen then is used to outline the excision area. A 10×12-cm layer of polyethylene film is then attached to the excision site. Excision of the tumor is performed by cutting through the film in the marked area (Figure 1A), and closure is performed by suturing the wound edges through the polyethylene film while the area is still covered with the film (Figure 1B). The sutures can be left in for 2 weeks or longer if necessary. The patient should be instructed not to remove the film or perform any extensive cleansing of the treatment area. Antibiotics should be administered, as the polyethylene film maintains its sterile integrity for 7 days only. Because sutures are on the surface of the film, they are easily accessed for removal. Figure 1C shows the excision site after removal of the sutures and polyethylene film on the left tibia of a 95-year-old woman. Adhesive butterfly closures can be applied to strengthen the excision area after suture removal and prevent dehiscence.



|
Figure 1. The excision site was marked after polyethylene adhesive film was applied to a squamous cell carcinoma on the left tibia of 95-year-old woman (A). Closure was performed by suturing the wound edges through the polyethylene film (B). The excision site appeared to have no dehiscence or signs of infection after removal of the sutures and polyethylene film (C). |
Case Reports
Twelve procedures for skin cancer excision were conducted in 10 patients using polyethylene adhesive film as a surgical aid due to extremely poor quality of the epidermis. The tumors were all squamous cell carcinomas and were located on the arms and legs. Patients were aged 73 to 95 years. Figure 2 demonstrates an example of excision of a squamous cell carcinoma on the left tibia of an 82-year-old man with prior dehiscence and infection after leg surgeries. Good results were achieved using the closure technique described here, along with prophylactic antibiotics.


|
Figure 2. A squamous cell carcinoma excision site on the left tibia of an 82-year-old man that had been covered with polyethylene adhesive film prior to excision (A) and 17 days following removal of the sutures and film (B). |
One patient had complications from a Staphylococcus infection because antibiotics were not administered. The patient had prior infections with other surgeries. Antibiotics were given 4 days after surgery. The infection was cleared and the polyethylene film was retained for a total of 12 days.
Sutures were removed after 14 days for excision sites on the arms and 17 days for excision sites on the legs. All excision sites healed without dehiscence with a cosmetically acceptable scar. Figure 3A shows a completed excision on the left hand of a 92-year-old man, and Figure 3B is the result 5 weeks after excision.


|
Figure 3. A squamous cell carcinoma excision site on the left thumb of a 92-year-old man that had been covered with polyethylene adhesive film prior to exci- sion (A). No visible scarring or dehiscence was noted 5 weeks after excision, following removal of the sutures and film (B). |
None of the patients reported discomfort from the polyethylene film remaining on the skin following surgery, though postoperative care required extra caution when dressing so as not to disturb or compromise the film. Patients were advised about postoperative care and were instructed not to remove the dressing. They were all given antibiotics as a necessary adjunct to maintain a lessened bacteria burden imposed by an impervious layer of acrylate adhesive. Complications resulted from failure to immediately provide antibiotics to 1 patient. The polyethylene film did not hinder healing or postoperative results.
Comment
Various techniques for handling fragile skin during surgery have been described in the literature. Fomon et al1 discussed aging skin as it relates to plastic surgery. Foster and Chan2 described a skin support technique for closing elliptical incisions in patients with fragile skin. Mazzurco and Krach3 discussed the use of a hydrocolloid dressing to aid in the closure of surgical wounds in patients with fragile skin.
The closure method described here was found to be particularly helpful when used as an adjunct to surgery in patients with fragile skin that lacked a suitable dermis. The polyethylene adhesive film helped to hold the sutures more securely. This method is cost-effective and is associated with a high level of patient satisfaction. For the surgeon, this technique may aid in dealing with difficult surgical situations and helps prevent wound complications in elderly patients or those with fragile skin.
1. Fomon S, Bell JW, Schattner A. Aging skin, a surgical challenge. AMA Arch Otolaryngol. 1955;61:554-562.
2. Foster RS, Chan J. The Fixomull skin support method for wound closure in patients with fragile skin. Australas J Dermatol. 2011;52:209-211.
3. Mazzurco JD, Krach KJ. Use of a hydrocolloid dressing to aid in the closure of surgical wounds in patients with fragile skin. J Am Acad Dermatol. 2012;66:335-336.
Patients who have been on steroids, aspirin, or anticoagulants or who are elderly may have a fragile outer skin layer that is similar to parchment paper, which may be challenging for surgeons. In these patients, the epidermal layer is thin and translucent; when a surgeon cuts through this thin layer, the tissue beneath shows minimal dermis and poor-quality fat with weakened tissue support. When undergoing excisional surgery, there is no strong tissue to help the closure sutures remain intact. Surgeons may struggle with skin tears around the sutures and dehiscence on suture removal.
This article describes a novel approach to skin closure in patients with aging or thin skin using a polyethylene film with an acrylate adhesive in the excision area to aid in maintaining skin integrity throughout the healing process following surgery.
Closure Technique
First, the skin area is cleansed with a sterilizing soap preparation. A sterile marking pen then is used to outline the excision area. A 10×12-cm layer of polyethylene film is then attached to the excision site. Excision of the tumor is performed by cutting through the film in the marked area (Figure 1A), and closure is performed by suturing the wound edges through the polyethylene film while the area is still covered with the film (Figure 1B). The sutures can be left in for 2 weeks or longer if necessary. The patient should be instructed not to remove the film or perform any extensive cleansing of the treatment area. Antibiotics should be administered, as the polyethylene film maintains its sterile integrity for 7 days only. Because sutures are on the surface of the film, they are easily accessed for removal. Figure 1C shows the excision site after removal of the sutures and polyethylene film on the left tibia of a 95-year-old woman. Adhesive butterfly closures can be applied to strengthen the excision area after suture removal and prevent dehiscence.



|
Figure 1. The excision site was marked after polyethylene adhesive film was applied to a squamous cell carcinoma on the left tibia of 95-year-old woman (A). Closure was performed by suturing the wound edges through the polyethylene film (B). The excision site appeared to have no dehiscence or signs of infection after removal of the sutures and polyethylene film (C). |
Case Reports
Twelve procedures for skin cancer excision were conducted in 10 patients using polyethylene adhesive film as a surgical aid due to extremely poor quality of the epidermis. The tumors were all squamous cell carcinomas and were located on the arms and legs. Patients were aged 73 to 95 years. Figure 2 demonstrates an example of excision of a squamous cell carcinoma on the left tibia of an 82-year-old man with prior dehiscence and infection after leg surgeries. Good results were achieved using the closure technique described here, along with prophylactic antibiotics.


|
Figure 2. A squamous cell carcinoma excision site on the left tibia of an 82-year-old man that had been covered with polyethylene adhesive film prior to excision (A) and 17 days following removal of the sutures and film (B). |
One patient had complications from a Staphylococcus infection because antibiotics were not administered. The patient had prior infections with other surgeries. Antibiotics were given 4 days after surgery. The infection was cleared and the polyethylene film was retained for a total of 12 days.
Sutures were removed after 14 days for excision sites on the arms and 17 days for excision sites on the legs. All excision sites healed without dehiscence with a cosmetically acceptable scar. Figure 3A shows a completed excision on the left hand of a 92-year-old man, and Figure 3B is the result 5 weeks after excision.


|
Figure 3. A squamous cell carcinoma excision site on the left thumb of a 92-year-old man that had been covered with polyethylene adhesive film prior to exci- sion (A). No visible scarring or dehiscence was noted 5 weeks after excision, following removal of the sutures and film (B). |
None of the patients reported discomfort from the polyethylene film remaining on the skin following surgery, though postoperative care required extra caution when dressing so as not to disturb or compromise the film. Patients were advised about postoperative care and were instructed not to remove the dressing. They were all given antibiotics as a necessary adjunct to maintain a lessened bacteria burden imposed by an impervious layer of acrylate adhesive. Complications resulted from failure to immediately provide antibiotics to 1 patient. The polyethylene film did not hinder healing or postoperative results.
Comment
Various techniques for handling fragile skin during surgery have been described in the literature. Fomon et al1 discussed aging skin as it relates to plastic surgery. Foster and Chan2 described a skin support technique for closing elliptical incisions in patients with fragile skin. Mazzurco and Krach3 discussed the use of a hydrocolloid dressing to aid in the closure of surgical wounds in patients with fragile skin.
The closure method described here was found to be particularly helpful when used as an adjunct to surgery in patients with fragile skin that lacked a suitable dermis. The polyethylene adhesive film helped to hold the sutures more securely. This method is cost-effective and is associated with a high level of patient satisfaction. For the surgeon, this technique may aid in dealing with difficult surgical situations and helps prevent wound complications in elderly patients or those with fragile skin.
Patients who have been on steroids, aspirin, or anticoagulants or who are elderly may have a fragile outer skin layer that is similar to parchment paper, which may be challenging for surgeons. In these patients, the epidermal layer is thin and translucent; when a surgeon cuts through this thin layer, the tissue beneath shows minimal dermis and poor-quality fat with weakened tissue support. When undergoing excisional surgery, there is no strong tissue to help the closure sutures remain intact. Surgeons may struggle with skin tears around the sutures and dehiscence on suture removal.
This article describes a novel approach to skin closure in patients with aging or thin skin using a polyethylene film with an acrylate adhesive in the excision area to aid in maintaining skin integrity throughout the healing process following surgery.
Closure Technique
First, the skin area is cleansed with a sterilizing soap preparation. A sterile marking pen then is used to outline the excision area. A 10×12-cm layer of polyethylene film is then attached to the excision site. Excision of the tumor is performed by cutting through the film in the marked area (Figure 1A), and closure is performed by suturing the wound edges through the polyethylene film while the area is still covered with the film (Figure 1B). The sutures can be left in for 2 weeks or longer if necessary. The patient should be instructed not to remove the film or perform any extensive cleansing of the treatment area. Antibiotics should be administered, as the polyethylene film maintains its sterile integrity for 7 days only. Because sutures are on the surface of the film, they are easily accessed for removal. Figure 1C shows the excision site after removal of the sutures and polyethylene film on the left tibia of a 95-year-old woman. Adhesive butterfly closures can be applied to strengthen the excision area after suture removal and prevent dehiscence.



|
Figure 1. The excision site was marked after polyethylene adhesive film was applied to a squamous cell carcinoma on the left tibia of 95-year-old woman (A). Closure was performed by suturing the wound edges through the polyethylene film (B). The excision site appeared to have no dehiscence or signs of infection after removal of the sutures and polyethylene film (C). |
Case Reports
Twelve procedures for skin cancer excision were conducted in 10 patients using polyethylene adhesive film as a surgical aid due to extremely poor quality of the epidermis. The tumors were all squamous cell carcinomas and were located on the arms and legs. Patients were aged 73 to 95 years. Figure 2 demonstrates an example of excision of a squamous cell carcinoma on the left tibia of an 82-year-old man with prior dehiscence and infection after leg surgeries. Good results were achieved using the closure technique described here, along with prophylactic antibiotics.


|
Figure 2. A squamous cell carcinoma excision site on the left tibia of an 82-year-old man that had been covered with polyethylene adhesive film prior to excision (A) and 17 days following removal of the sutures and film (B). |
One patient had complications from a Staphylococcus infection because antibiotics were not administered. The patient had prior infections with other surgeries. Antibiotics were given 4 days after surgery. The infection was cleared and the polyethylene film was retained for a total of 12 days.
Sutures were removed after 14 days for excision sites on the arms and 17 days for excision sites on the legs. All excision sites healed without dehiscence with a cosmetically acceptable scar. Figure 3A shows a completed excision on the left hand of a 92-year-old man, and Figure 3B is the result 5 weeks after excision.


|
Figure 3. A squamous cell carcinoma excision site on the left thumb of a 92-year-old man that had been covered with polyethylene adhesive film prior to exci- sion (A). No visible scarring or dehiscence was noted 5 weeks after excision, following removal of the sutures and film (B). |
None of the patients reported discomfort from the polyethylene film remaining on the skin following surgery, though postoperative care required extra caution when dressing so as not to disturb or compromise the film. Patients were advised about postoperative care and were instructed not to remove the dressing. They were all given antibiotics as a necessary adjunct to maintain a lessened bacteria burden imposed by an impervious layer of acrylate adhesive. Complications resulted from failure to immediately provide antibiotics to 1 patient. The polyethylene film did not hinder healing or postoperative results.
Comment
Various techniques for handling fragile skin during surgery have been described in the literature. Fomon et al1 discussed aging skin as it relates to plastic surgery. Foster and Chan2 described a skin support technique for closing elliptical incisions in patients with fragile skin. Mazzurco and Krach3 discussed the use of a hydrocolloid dressing to aid in the closure of surgical wounds in patients with fragile skin.
The closure method described here was found to be particularly helpful when used as an adjunct to surgery in patients with fragile skin that lacked a suitable dermis. The polyethylene adhesive film helped to hold the sutures more securely. This method is cost-effective and is associated with a high level of patient satisfaction. For the surgeon, this technique may aid in dealing with difficult surgical situations and helps prevent wound complications in elderly patients or those with fragile skin.
1. Fomon S, Bell JW, Schattner A. Aging skin, a surgical challenge. AMA Arch Otolaryngol. 1955;61:554-562.
2. Foster RS, Chan J. The Fixomull skin support method for wound closure in patients with fragile skin. Australas J Dermatol. 2011;52:209-211.
3. Mazzurco JD, Krach KJ. Use of a hydrocolloid dressing to aid in the closure of surgical wounds in patients with fragile skin. J Am Acad Dermatol. 2012;66:335-336.
1. Fomon S, Bell JW, Schattner A. Aging skin, a surgical challenge. AMA Arch Otolaryngol. 1955;61:554-562.
2. Foster RS, Chan J. The Fixomull skin support method for wound closure in patients with fragile skin. Australas J Dermatol. 2011;52:209-211.
3. Mazzurco JD, Krach KJ. Use of a hydrocolloid dressing to aid in the closure of surgical wounds in patients with fragile skin. J Am Acad Dermatol. 2012;66:335-336.
Practice Points
- A novel method of skin closure using a polyethylene film with an acrylate adhesive can aid in strengthening suture integrity and preventing skin tears.
- Dehiscence of excision sites in patients with aging or fragile skin can be prevented.
- This closure technique promotes healing and efficient scar formation.
VIDEO: Flu shot lowered hospitalization risk for influenza pneumonia
Getting a flu shot may be a highly effective method to prevent hospitalization for influenza-associated pneumonia.
That’s according to researchers who found that patients hospitalized with influenza-associated pneumonia were more likely to not have been vaccinated than patients whose pneumonia was due to other causes.
In video interviews, Dr. Kathryn M. Edwards and Dr. Carlos G. Grijalva of Vanderbilt University, Nashville, discussed their study of patients admitted through the emergency department for pneumonia and the benefits of flu vaccination in preventing hospitalization for influenza pneumonia.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Getting a flu shot may be a highly effective method to prevent hospitalization for influenza-associated pneumonia.
That’s according to researchers who found that patients hospitalized with influenza-associated pneumonia were more likely to not have been vaccinated than patients whose pneumonia was due to other causes.
In video interviews, Dr. Kathryn M. Edwards and Dr. Carlos G. Grijalva of Vanderbilt University, Nashville, discussed their study of patients admitted through the emergency department for pneumonia and the benefits of flu vaccination in preventing hospitalization for influenza pneumonia.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Getting a flu shot may be a highly effective method to prevent hospitalization for influenza-associated pneumonia.
That’s according to researchers who found that patients hospitalized with influenza-associated pneumonia were more likely to not have been vaccinated than patients whose pneumonia was due to other causes.
In video interviews, Dr. Kathryn M. Edwards and Dr. Carlos G. Grijalva of Vanderbilt University, Nashville, discussed their study of patients admitted through the emergency department for pneumonia and the benefits of flu vaccination in preventing hospitalization for influenza pneumonia.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
FROM JAMA
Concussionlike symptoms prevalent in uninjured teen athletes
Ensuring a high school athlete has returned to an asymptomatic state after a concussion can be challenging, according to the authors of a study that found a significant proportion of uninjured adolescent athletes report at least one symptom of concussion.
A cross-sectional observational study of 31,958 high school athletes, none of whom had experienced a concussion in the prior 6 months, showed 19% of boys and 28% of girls reported a symptom burden resembling an ICD-10 diagnosis of mild postconcussional syndrome, according to a paper published online Oct. 12 in JAMA Pediatrics.
Concussion symptoms were particularly prevalent among students with preexisting conditions such as psychiatric problems, learning disorders, migraine, attention deficit/hyperactivity disorder, or substance abuse. Students who had experienced a concussion previously were the least likely to show concussion symptoms (JAMA Pediatrics. 2015 Oct. 12 [doi: 10.1001/jamapediatrics.2015.2374]).
Boys most commonly reported symptoms such as fatigue, sleep troubles, and difficult concentration, while girls were more likely to report fatigue, sleep troubles, headaches, sadness, feeling emotional, and difficulty concentrating.
“When managing a student athlete with a concussion, it has been widely noted that the athlete should be ‘asymptomatic’ at rest and with exercise before returning to sports, and sometimes athletes are kept out of school for prolonged periods while they wait for symptoms to resolve, which could have negative consequences for their academic, social, and emotional functioning and contribute to symptom reporting,” wrote Grant L. Iverson, Ph.D., from Harvard Medical School, Boston, and his coauthors.
“These results reinforce that ‘asymptomatic’ status after concussion can be difficult to define,” they added.
The study was supported by the Goldfarb Center for Public Policy and Civic Engagement/Colby College, the Bill and Joan Alfond Foundation, the Harvard Integrated Program to Protect and Improve the Health of National Football League Players Association Members, and the Mooney-Reed Charitable Foundation. The lead author declared speakers fees from private industry, but there were no other conflicts of interest declared.
Ensuring a high school athlete has returned to an asymptomatic state after a concussion can be challenging, according to the authors of a study that found a significant proportion of uninjured adolescent athletes report at least one symptom of concussion.
A cross-sectional observational study of 31,958 high school athletes, none of whom had experienced a concussion in the prior 6 months, showed 19% of boys and 28% of girls reported a symptom burden resembling an ICD-10 diagnosis of mild postconcussional syndrome, according to a paper published online Oct. 12 in JAMA Pediatrics.
Concussion symptoms were particularly prevalent among students with preexisting conditions such as psychiatric problems, learning disorders, migraine, attention deficit/hyperactivity disorder, or substance abuse. Students who had experienced a concussion previously were the least likely to show concussion symptoms (JAMA Pediatrics. 2015 Oct. 12 [doi: 10.1001/jamapediatrics.2015.2374]).
Boys most commonly reported symptoms such as fatigue, sleep troubles, and difficult concentration, while girls were more likely to report fatigue, sleep troubles, headaches, sadness, feeling emotional, and difficulty concentrating.
“When managing a student athlete with a concussion, it has been widely noted that the athlete should be ‘asymptomatic’ at rest and with exercise before returning to sports, and sometimes athletes are kept out of school for prolonged periods while they wait for symptoms to resolve, which could have negative consequences for their academic, social, and emotional functioning and contribute to symptom reporting,” wrote Grant L. Iverson, Ph.D., from Harvard Medical School, Boston, and his coauthors.
“These results reinforce that ‘asymptomatic’ status after concussion can be difficult to define,” they added.
The study was supported by the Goldfarb Center for Public Policy and Civic Engagement/Colby College, the Bill and Joan Alfond Foundation, the Harvard Integrated Program to Protect and Improve the Health of National Football League Players Association Members, and the Mooney-Reed Charitable Foundation. The lead author declared speakers fees from private industry, but there were no other conflicts of interest declared.
Ensuring a high school athlete has returned to an asymptomatic state after a concussion can be challenging, according to the authors of a study that found a significant proportion of uninjured adolescent athletes report at least one symptom of concussion.
A cross-sectional observational study of 31,958 high school athletes, none of whom had experienced a concussion in the prior 6 months, showed 19% of boys and 28% of girls reported a symptom burden resembling an ICD-10 diagnosis of mild postconcussional syndrome, according to a paper published online Oct. 12 in JAMA Pediatrics.
Concussion symptoms were particularly prevalent among students with preexisting conditions such as psychiatric problems, learning disorders, migraine, attention deficit/hyperactivity disorder, or substance abuse. Students who had experienced a concussion previously were the least likely to show concussion symptoms (JAMA Pediatrics. 2015 Oct. 12 [doi: 10.1001/jamapediatrics.2015.2374]).
Boys most commonly reported symptoms such as fatigue, sleep troubles, and difficult concentration, while girls were more likely to report fatigue, sleep troubles, headaches, sadness, feeling emotional, and difficulty concentrating.
“When managing a student athlete with a concussion, it has been widely noted that the athlete should be ‘asymptomatic’ at rest and with exercise before returning to sports, and sometimes athletes are kept out of school for prolonged periods while they wait for symptoms to resolve, which could have negative consequences for their academic, social, and emotional functioning and contribute to symptom reporting,” wrote Grant L. Iverson, Ph.D., from Harvard Medical School, Boston, and his coauthors.
“These results reinforce that ‘asymptomatic’ status after concussion can be difficult to define,” they added.
The study was supported by the Goldfarb Center for Public Policy and Civic Engagement/Colby College, the Bill and Joan Alfond Foundation, the Harvard Integrated Program to Protect and Improve the Health of National Football League Players Association Members, and the Mooney-Reed Charitable Foundation. The lead author declared speakers fees from private industry, but there were no other conflicts of interest declared.
FROM JAMA PEDIATRICS
Key clinical point: A significant proportion of uninjured high school athletes reported at least one symptom of concussion.
Major finding: About one in five male high school athletes and one in four female high school athletes reported a symptom burden resembling an ICD-10 diagnosis of mild postconcussional syndrome.
Data source: A cross-sectional observational study of 31,958 high school athletes who had not experienced a concussion in the previous 6 months.
Disclosures: The study was supported by the Goldfarb Center for Public Policy and Civic Engagement/Colby College, the Bill and Joan Alfond Foundation, the Harvard Integrated Program to Protect and Improve the Health of National Football League Players Association Members, and the Mooney-Reed Charitable Foundation. The lead author declared speakers fees from private industry, but there were no other conflicts of interest declared.
Tolerance of Fragranced and Fragrance-Free Facial Cleansers in Adults With Clinically Sensitive Skin
For thousands of years, humans have used fragrances to change or affect their mood and enhance an “aura of beauty.”1 Fragrance is a primary driver in consumer choice and purchasing decisions, especially when considering personal care products.2 In addition to fragrance, consumers choose cleanser products based on compatibility with skin, cleansing properties, and sensory attributes such as viscosity and foaming.3,4 However, fragrance sensitivity is among the most common causes of allergic contact dermatitis from cosmetics and personal care products,5 and estimates of the prevalence of fragrance sensitivity range from 1.8% to 4.2%.6
A panel of 26 fragrance ingredients that frequently induce contact dermatitis in sensitive individuals has been identified.7 Since 2003, regulatory authorities in the European Union require these compounds to be listed on the labels of consumer products to protect presensitized consumers.7,8 However, manufacturers of cosmetics are not required to specify allergenic fragrance ingredients outside the European Union, and therefore it is difficult for consumers in the United States to avoid fragrance allergens.
Creation of a fragranced product for fragrance-sensitive individuals begins with careful selection of ingredients and extensive formulation testing and evaluation. This process usually is followed by testing in normal individuals to confirm that the fragranced product is well accepted and then evaluation is done in clinically confirmed fragrance-sensitive patients and those with a compromised skin barrier from atopic dermatitis, rosacea, or eczema.
Sensitive skin may be due to increased immune responsiveness, altered neurosensory input, and/or decreased skin barrier function, and presents a complex challenge for dermatologists.9 Subjective perceptions of sensitive skin include stinging, burning, pruritus, and tightness following product application. Clinically sensitive skin is defined by the presence of erythema, stratum corneum desquamation, papules, pustules, wheals, vesicles, bullae, and/or erosions.9 Although some of these symptoms may be observed immediately, others may be delayed by minutes, hours, or days following the use of an irritating product. Patients who present with subjective symptoms of sensitive skin may or may not show objective symptoms.
Gentle skin cleansing is particularly important for patients with compromised skin barrier integrity, such as those with acne, atopic dermatitis, eczema, or rosacea. Standard alkaline surfactants in skin cleansers help to remove dirt and oily soil and produce lather but can impair the skin barrier function and facilitate development of irritation.10-13 The tolerability of a cleanser is influenced by its pH, the type and amount of surfactant ingredients, the presence of moisturizing agents, and the amount of residue left on the skin after washing.11,12 Mild cleansers have been developed for patients with sensitive skin conditions and are expected to provide cleansing benefits without negatively affecting the hydration and viscoelastic properties of skin.11 Mild cleansers interact minimally with skin proteins and lipids because they usually contain nonionic synthetic surfactant mixtures; they also have a pH value close to the slightly acidic pH of normal skin, contain moisturizing agents,11,14,15 and usually produce less foam.10,16 In patients with sensitive skin, mild and fragrance-free cleansers often are recommended.17,18 Because fragrances often affect consumers’ perception of product performance19 and enhance the cleaning experience of the user, consumer compliance with clinical recommendations to use fragrance-free cleansers often is poor.
Low–molecular-weight, water-soluble, hydrophobically modified polymers (HMPs) have been used to create gentle foaming cleansers with reduced impact on the skin barrier.12,16,20 In the presence of HMPs, surfactants assemble into larger, more stable polymer-surfactant structures that are less likely to penetrate the skin.16 Hydrophobically modified polymers can potentially reduce skin irritation by lowering the concentration of free micelles in solution. Additionally, both HMPs and HMP-surfactant complexes stabilize newly formed air-water interfaces, leading to thicker, denser, and longer-lasting foams.16 A gentle, fragrance-free, foaming liquid facial test cleanser with HMPs has been shown to be well tolerated in women with sensitive skin.20
This report describes 2 studies of a new mild, HMP-containing, foaming facial cleanser with a fragrance that was free of common allergens and irritating essential oils in patients with sensitive skin. Study 1 was designed to evaluate the tolerance and acceptability of 2 variations of the HMP-containing cleanser—one fragrance free and the other with fragrance—in a small sample of healthy adults with clinically diagnosed fragrance-sensitive skin. Study 2 was a large, 2-center study of the tolerability and effectiveness of the fragranced HMP-containing cleanser compared with a benchmark dermatologist-recommended, gentle, fragrance-free, nonfoaming cleanser in women with clinically diagnosed sensitive skin.
Methods
Study 1 Design
The primary objective of this prospective, randomized, single-center, crossover study was to evaluate the tolerability of fragranced versus fragrance-free formulations of a mild, HMP-containing liquid facial cleanser in healthy male and female adults with Fitzpatrick skin types I to IV who were clinically diagnosed as having fragrance sensitivity. Fragrance sensitivity was defined as a history of positive reactions to a fragrance mixture of 8 components (fragrance mixture I) and/or a fragrance mixture of 14 fragrances (fragrance mixture II) that included balsam of Peru (Myroxylonpereirae), geraniol, jasmine oil, and oakmoss.5 All participants provided written informed consent prior to enrolling in the study, and both the study protocol and informed consent agreement were approved by an institutional review board.
Participants were instructed to wash their face twice daily, noting the time of cleansing and providing commentary about their cleansing experience in a diary. The liquid facial test cleansers contained the HMP potassium acrylates copolymer, glycerin, and a surfactant system primarily containing cocamidopropyl betaine and lauryl glucoside prepared without added fragrance (as previously described20) or with a fragrance free of common allergens and irritating essential oils.
Half of the participants used the fragranced test cleanser and half used the fragrance-free test cleanser for a 3-week treatment period (weeks 1–3). Each treatment group subsequently switched to the other test cleanser for a second 3-week treatment period (weeks 4–6). Clinicians assessed global disease severity (an overall assessment of skin condition that was independent of other evaluation criteria), itching/burning, visible irritation, erythema, and desquamation at weekly time points throughout the study and graded each clinical tolerance attribute on a 5-point scale (0=none; 1=minimal; 2=mild; 3=moderate; 4=severe). Ordinal scores at baseline and at weeks 1 and 3 were used to calculate change from baseline.
A 7-item questionnaire also was administered to participants at each visit to assess skin condition, smoothness, softness, cleanliness, radiance, satisfaction with cleansing experience, and lathering. Each item was scored on a 5-point ordinal scale (0=none; 1=minimal; 2=good; 3=excellent; 4=superior). The scores for all parameters were statistically compared with baseline values using a paired t test with a significance level of P≤.05.
Study 2 Design
This prospective, 3-week, double-blind, randomized, comparative, 2-center study to evaluate the tolerability of the fragranced, HMP-containing test cleanser from study 1 versus a benchmark gentle, fragrance-free, nonfoaming cleanser in a large population of otherwise healthy females who had been clinically diagnosed with sensitive skin (not limited to fragrance sensitivity). The study sponsor provided blinded test materials, and neither the examiner nor the recorder knew which investigational product was administered to which participants. Additionally, personnel who dispensed the test cleansers to participants or supervised their use did not participate in the evaluation to minimize potential bias. All participants provided written informed consent prior to enrolling in the study, and the study protocol and informed consent agreement were approved by an institutional review board.
Participants included women aged 18 to 65 years with mild to moderate clinical symptoms of atopic dermatitis, eczema, acne, or rosacea within the 90 days prior to the study period. They were randomized into 2 balanced treatment groups: group 1 received the mild, fragranced, HMP-containing liquid facial cleanser from study 1 and group 2 received a leading, dermatologist-recommended, gentle, fragrance-free, nonfoaming cleanser. Each treatment group used the test cleansers at least once daily for 3 weeks.
Clinicians evaluated facial skin for softness and smoothness, global disease severity (rated visually by the investigator as an overall assessment of skin condition that was independent of other evaluation criteria [as previously described20]), itching, irritation, erythema, and desquamation at baseline and at weeks 1 and 3. The effectiveness of each product to remove facial dirt, cosmetics, and sebum also was assessed; clinical grading was performed as described for study 1 using the same grading scale as in study 1 and percentage change from baseline (improvement) was calculated.
The study also included a self-assessment of skin irritation in which participants responded yes or no to the following question: Have you experienced irritation using this product? Participants also completed a questionnaire in which they were asked to select the most appropriate answer—agree strongly, agree somewhat, neither, disagree somewhat, and disagree strongly— to the following statements: the cleanser leaves no residue; cleanses deep to remove dirt, oil, and makeup; the cleanser effectively removes makeup; the cleanser leaves my skin smooth; the cleanser leaves my skin soft; the cleanser rinses completely clean; cleanser does not over dry my skin; and my skin is completely clean.
The statistical analysis was performed using a nonparametric, 2-tailed, paired Mann-Whitney U test, and statistical significance was set at P≤.05.
Results
Study 1 Assessment
Eight female participants aged 22 to 60 years with clinically diagnosed fragrance sensitivity were enrolled in the study. After 3 weeks of use, clinician assessment showed that both the fragranced and fragrance-free test cleansers with HMPs improved several skin tolerance attributes, including global disease severity, irritation, and erythema (Figure 1). No notable differences in skin tolerance attributes were reported in the fragranced versus the fragrance-free formulations.
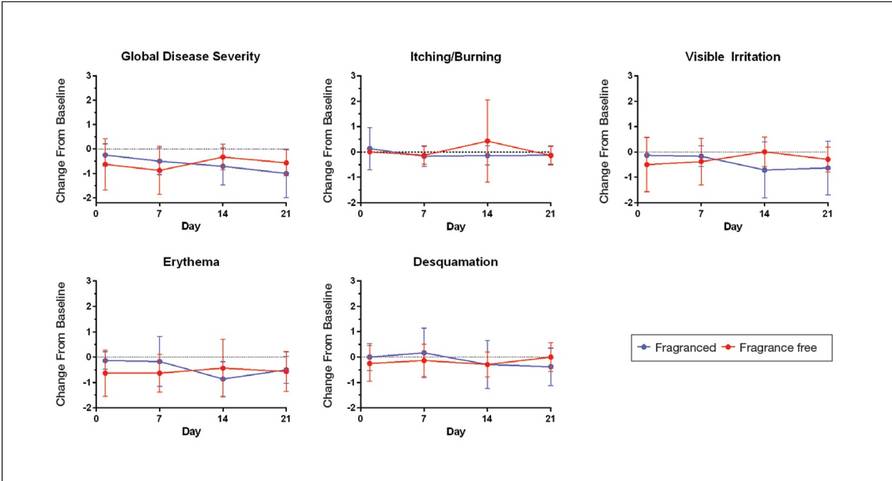
There were no reported differences in participant-reported cleanser effectiveness for the fragranced versus the fragrance-free cleanser either at baseline or weeks 1 or 3 (data not shown).
Study 2 Assessment
A total of 153 women aged 25 to 54 years with sensitive skin were enrolled in the study. Seventy-three participants were randomized to receive the fragranced test cleanser and 80 were randomized to receive the benchmark fragrance-free cleanser.
At week 3, there were no differences between the fragranced test cleanser and the benchmark cleanser in any of the clinician-assessed skin parameters (Figure 2). Of the parameters assessed, itching, irritation, and desquamation were the most improved from baseline in both treatment groups. Similar results were observed at week 1 (data not shown).
There were no apparent differences in subjective self-assessment of skin irritation between the test and benchmark cleansers at week 1 (15.7% vs 13.0%) or week 3 (24.3% vs 12.3%). When asked to respond to a series of 8 statements related to cleanser effectiveness, most participants either agreed strongly or agreed somewhat with the statements (Figure 3). There were no statistically significant differences between treatment groups, and responses to all statements indicated that participants were as satisfied with the test cleanser as they were with the benchmark cleanser.
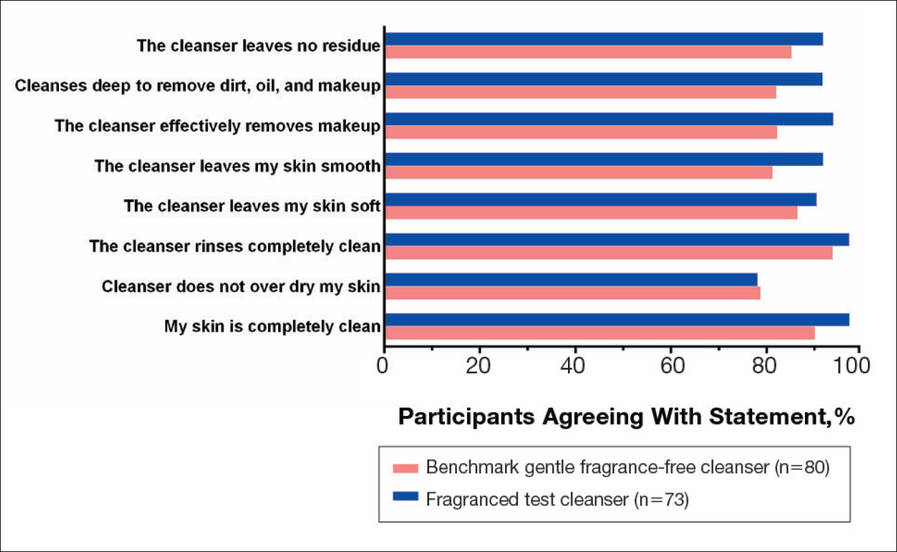
Comment
Consumers value cleansing, fragrance, viscosity, and foaming attributes in skin care products very highly.3,4,10 Fragrances are added to personal care products to positively affect consumers’ perception of product performance and to add emotional benefits by implying social or economic prestige to the use of a product.19 In one study, shampoo formulations that varied only in the added fragrance received different consumer evaluations for cleansing effectiveness and foaming.4
Although mild nonfoaming cleansers can be effective, adult consumers generally use cleansers that foam10,16 and often judge the performance of a cleansing product based on its foaming properties.3,10 Mild cleansers with HMPs maintain the ability to foam while also reducing the likelihood of skin irritation.16 One study showed that a mild, fragrance-free, foaming cleanser containing HMPs was as effective, well tolerated, and nonirritating in patients with sensitive skin as a benchmark nonfoaming gentle cleanser.20
Results from study 1 presented here show that fragranced and fragrance-free formulations of a mild, HMP-containing cleanser are equally efficacious and well tolerated in a small sample of participants with clinically diagnosed fragrance sensitivity. Skin tolerance attributes improved with both cleansers over a 3-week period, particularly global disease severity, irritation, and erythema. These results suggest that a fragrance free of common allergens and irritating essential oils could be introduced into a mild foaming cleanser containing HMPs without causing adverse reactions, even in patients who are fragrance sensitive.
Although the populations of studies 1 and 2 both included female participants with sensitive skin, they were not identical. While study 1 assessed a limited number of participants with clinically diagnosed fragrance sensitivity, study 2 was larger and included a broader range of participants with clinically diagnosed skin sensitivity, which could include fragrance sensitivity. The well-chosen fragrance of the test cleanser containing HMPs was well tolerated; however, this does not imply that any other fragrances added to this cleanser formulation would be as well tolerated.
Conclusion
The current studies indicate that a gentle fragranced foaming cleanser with HMPs was well tolerated in a small population of participants with clinically diagnosed fragrance sensitivity. In a larger population of female participants with sensitive skin, the gentle fragranced foaming cleanser with HMPs was as effective as a leading dermatologist-recommended, fragrance-free, gentle, nonfoaming cleanser. The gentle, HMP-containing, foaming cleanser with a fragrance that does not contain common allergens and irritating essential oils offers a new cleansing option for adults with sensitive skin who may prefer to use a fragranced and foaming product.
Acknowledgments—The authors are grateful to the patients and clinicians who participated in these studies. Editorial and medical writing support was provided by Tove Anderson, PhD, and Alex Loeb, PhD, both from Evidence Scientific Solutions, Inc, Philadelphia, Pennsylvania, and was funded by Johnson & Johnson Consumer Inc.
- Draelos ZD. To smell or not to smell? that is the question! J Cosmet Dermatol. 2013;12:1-2.
- Milotic D. The impact of fragrance on consumer choice. J Consumer Behaviour. 2003;3:179-191.
- Klein K. Evaluating shampoo foam. Cosmetics & Toiletries. 2004;119:32-36.
- Herman S. Skin care: the importance of feel. GCI Magazine. December 2007:70-74.
- Larsen WG. How to test for fragrance allergy. Cutis. 2000;65:39-41.
- Schnuch A, Uter W, Geier J, et al. Epidemiology of contact allergy: an estimation of morbidity employing the clinical epidemiology and drug-utilization research (CE-DUR) approach. Contact Dermatitis. 2002;47:32-39.
- Directive 2003/15/EC of the European Parliament and of the Council of 27 February 2003 amending Council Directive 76/768/EEC on the approximation of the laws of the Member States relating to cosmetic products. Official Journal of the European Communities. 2003;L66:26-35.
- Guidance note: labelling of ingredients in Cosmetics Directive 76/768/EEC. European Commission Web site. http: //ec.europa.eu/consumers/sectors/cosmetics/files/doc/guide _labelling200802_en.pdf. Updated February 2008. Accessed September 2, 2015.
- Draelos ZD. Sensitive skin: perceptions, evaluation, and treatment. Am J Contact Dermatitis. 1997;8:67-78.
- Abbas S, Goldberg JW, Massaro M. Personal cleanser technology and clinical performance. Dermatol Ther. 2004;17(suppl 1):35-42.
- Ananthapadmanabhan KP, Moore DJ, Subramanyan K, et al. Cleansing without compromise: the impact of cleansers on the skin barrier and the technology of mild cleansing. Dermatol Ther. 2004;17(suppl 1):16-25.
- Walters RM, Mao G, Gunn ET, et al. Cleansing formulations that respect skin barrier integrity. Dermatol Res Pract. 2012;2012:495917.
- Saad P, Flach CR, Walters RM, et al. Infrared spectroscopic studies of sodium dodecyl sulphate permeation and interaction with stratum corneum lipids in skin. Int J Cosmet Sci. 2012;34:36-43.
- Bikowski J. The use of cleansers as therapeutic concomitants in various dermatologic disorders. Cutis. 2001;68(suppl 5):12-19.
- Walters RM, Fevola MJ, LiBrizzi JJ, et al. Designing cleansers for the unique needs of baby skin. Cosmetics & Toiletries. 2008;123:53-60.
- Fevola MJ, Walters RM, LiBrizzi JJ. A new approach to formulating mild cleansers: hydrophobically-modified polymers for irritation mitigation. In: Morgan SE, Lochhead RY, eds. Polymeric Delivery of Therapeutics. Vol 1053. Washington, DC: American Chemical Society; 2011:221-242.
- Nelson SA, Yiannias JA. Relevance and avoidance of skin-care product allergens: pearls and pitfalls. Dermatol Clin. 2009;27:329-336.
- Arribas MP, Soro P, Silvestre JF. Allergic contact dermatitis to fragrances: part 2. Actas Dermosifiliogr. 2013;104:29-37.
- Schroeder W. Understanding fragrance in personal care. Cosmetics & Toiletries. 2009;124:36-44.
- Draelos Z, Hornby S, Walters RM, et al. Hydrophobically-modified polymers can minimize skin irritation potential caused by surfactant-based cleansers. J Cosmet Dermatol. 2013;12:314-321.
For thousands of years, humans have used fragrances to change or affect their mood and enhance an “aura of beauty.”1 Fragrance is a primary driver in consumer choice and purchasing decisions, especially when considering personal care products.2 In addition to fragrance, consumers choose cleanser products based on compatibility with skin, cleansing properties, and sensory attributes such as viscosity and foaming.3,4 However, fragrance sensitivity is among the most common causes of allergic contact dermatitis from cosmetics and personal care products,5 and estimates of the prevalence of fragrance sensitivity range from 1.8% to 4.2%.6
A panel of 26 fragrance ingredients that frequently induce contact dermatitis in sensitive individuals has been identified.7 Since 2003, regulatory authorities in the European Union require these compounds to be listed on the labels of consumer products to protect presensitized consumers.7,8 However, manufacturers of cosmetics are not required to specify allergenic fragrance ingredients outside the European Union, and therefore it is difficult for consumers in the United States to avoid fragrance allergens.
Creation of a fragranced product for fragrance-sensitive individuals begins with careful selection of ingredients and extensive formulation testing and evaluation. This process usually is followed by testing in normal individuals to confirm that the fragranced product is well accepted and then evaluation is done in clinically confirmed fragrance-sensitive patients and those with a compromised skin barrier from atopic dermatitis, rosacea, or eczema.
Sensitive skin may be due to increased immune responsiveness, altered neurosensory input, and/or decreased skin barrier function, and presents a complex challenge for dermatologists.9 Subjective perceptions of sensitive skin include stinging, burning, pruritus, and tightness following product application. Clinically sensitive skin is defined by the presence of erythema, stratum corneum desquamation, papules, pustules, wheals, vesicles, bullae, and/or erosions.9 Although some of these symptoms may be observed immediately, others may be delayed by minutes, hours, or days following the use of an irritating product. Patients who present with subjective symptoms of sensitive skin may or may not show objective symptoms.
Gentle skin cleansing is particularly important for patients with compromised skin barrier integrity, such as those with acne, atopic dermatitis, eczema, or rosacea. Standard alkaline surfactants in skin cleansers help to remove dirt and oily soil and produce lather but can impair the skin barrier function and facilitate development of irritation.10-13 The tolerability of a cleanser is influenced by its pH, the type and amount of surfactant ingredients, the presence of moisturizing agents, and the amount of residue left on the skin after washing.11,12 Mild cleansers have been developed for patients with sensitive skin conditions and are expected to provide cleansing benefits without negatively affecting the hydration and viscoelastic properties of skin.11 Mild cleansers interact minimally with skin proteins and lipids because they usually contain nonionic synthetic surfactant mixtures; they also have a pH value close to the slightly acidic pH of normal skin, contain moisturizing agents,11,14,15 and usually produce less foam.10,16 In patients with sensitive skin, mild and fragrance-free cleansers often are recommended.17,18 Because fragrances often affect consumers’ perception of product performance19 and enhance the cleaning experience of the user, consumer compliance with clinical recommendations to use fragrance-free cleansers often is poor.
Low–molecular-weight, water-soluble, hydrophobically modified polymers (HMPs) have been used to create gentle foaming cleansers with reduced impact on the skin barrier.12,16,20 In the presence of HMPs, surfactants assemble into larger, more stable polymer-surfactant structures that are less likely to penetrate the skin.16 Hydrophobically modified polymers can potentially reduce skin irritation by lowering the concentration of free micelles in solution. Additionally, both HMPs and HMP-surfactant complexes stabilize newly formed air-water interfaces, leading to thicker, denser, and longer-lasting foams.16 A gentle, fragrance-free, foaming liquid facial test cleanser with HMPs has been shown to be well tolerated in women with sensitive skin.20
This report describes 2 studies of a new mild, HMP-containing, foaming facial cleanser with a fragrance that was free of common allergens and irritating essential oils in patients with sensitive skin. Study 1 was designed to evaluate the tolerance and acceptability of 2 variations of the HMP-containing cleanser—one fragrance free and the other with fragrance—in a small sample of healthy adults with clinically diagnosed fragrance-sensitive skin. Study 2 was a large, 2-center study of the tolerability and effectiveness of the fragranced HMP-containing cleanser compared with a benchmark dermatologist-recommended, gentle, fragrance-free, nonfoaming cleanser in women with clinically diagnosed sensitive skin.
Methods
Study 1 Design
The primary objective of this prospective, randomized, single-center, crossover study was to evaluate the tolerability of fragranced versus fragrance-free formulations of a mild, HMP-containing liquid facial cleanser in healthy male and female adults with Fitzpatrick skin types I to IV who were clinically diagnosed as having fragrance sensitivity. Fragrance sensitivity was defined as a history of positive reactions to a fragrance mixture of 8 components (fragrance mixture I) and/or a fragrance mixture of 14 fragrances (fragrance mixture II) that included balsam of Peru (Myroxylonpereirae), geraniol, jasmine oil, and oakmoss.5 All participants provided written informed consent prior to enrolling in the study, and both the study protocol and informed consent agreement were approved by an institutional review board.
Participants were instructed to wash their face twice daily, noting the time of cleansing and providing commentary about their cleansing experience in a diary. The liquid facial test cleansers contained the HMP potassium acrylates copolymer, glycerin, and a surfactant system primarily containing cocamidopropyl betaine and lauryl glucoside prepared without added fragrance (as previously described20) or with a fragrance free of common allergens and irritating essential oils.
Half of the participants used the fragranced test cleanser and half used the fragrance-free test cleanser for a 3-week treatment period (weeks 1–3). Each treatment group subsequently switched to the other test cleanser for a second 3-week treatment period (weeks 4–6). Clinicians assessed global disease severity (an overall assessment of skin condition that was independent of other evaluation criteria), itching/burning, visible irritation, erythema, and desquamation at weekly time points throughout the study and graded each clinical tolerance attribute on a 5-point scale (0=none; 1=minimal; 2=mild; 3=moderate; 4=severe). Ordinal scores at baseline and at weeks 1 and 3 were used to calculate change from baseline.
A 7-item questionnaire also was administered to participants at each visit to assess skin condition, smoothness, softness, cleanliness, radiance, satisfaction with cleansing experience, and lathering. Each item was scored on a 5-point ordinal scale (0=none; 1=minimal; 2=good; 3=excellent; 4=superior). The scores for all parameters were statistically compared with baseline values using a paired t test with a significance level of P≤.05.
Study 2 Design
This prospective, 3-week, double-blind, randomized, comparative, 2-center study to evaluate the tolerability of the fragranced, HMP-containing test cleanser from study 1 versus a benchmark gentle, fragrance-free, nonfoaming cleanser in a large population of otherwise healthy females who had been clinically diagnosed with sensitive skin (not limited to fragrance sensitivity). The study sponsor provided blinded test materials, and neither the examiner nor the recorder knew which investigational product was administered to which participants. Additionally, personnel who dispensed the test cleansers to participants or supervised their use did not participate in the evaluation to minimize potential bias. All participants provided written informed consent prior to enrolling in the study, and the study protocol and informed consent agreement were approved by an institutional review board.
Participants included women aged 18 to 65 years with mild to moderate clinical symptoms of atopic dermatitis, eczema, acne, or rosacea within the 90 days prior to the study period. They were randomized into 2 balanced treatment groups: group 1 received the mild, fragranced, HMP-containing liquid facial cleanser from study 1 and group 2 received a leading, dermatologist-recommended, gentle, fragrance-free, nonfoaming cleanser. Each treatment group used the test cleansers at least once daily for 3 weeks.
Clinicians evaluated facial skin for softness and smoothness, global disease severity (rated visually by the investigator as an overall assessment of skin condition that was independent of other evaluation criteria [as previously described20]), itching, irritation, erythema, and desquamation at baseline and at weeks 1 and 3. The effectiveness of each product to remove facial dirt, cosmetics, and sebum also was assessed; clinical grading was performed as described for study 1 using the same grading scale as in study 1 and percentage change from baseline (improvement) was calculated.
The study also included a self-assessment of skin irritation in which participants responded yes or no to the following question: Have you experienced irritation using this product? Participants also completed a questionnaire in which they were asked to select the most appropriate answer—agree strongly, agree somewhat, neither, disagree somewhat, and disagree strongly— to the following statements: the cleanser leaves no residue; cleanses deep to remove dirt, oil, and makeup; the cleanser effectively removes makeup; the cleanser leaves my skin smooth; the cleanser leaves my skin soft; the cleanser rinses completely clean; cleanser does not over dry my skin; and my skin is completely clean.
The statistical analysis was performed using a nonparametric, 2-tailed, paired Mann-Whitney U test, and statistical significance was set at P≤.05.
Results
Study 1 Assessment
Eight female participants aged 22 to 60 years with clinically diagnosed fragrance sensitivity were enrolled in the study. After 3 weeks of use, clinician assessment showed that both the fragranced and fragrance-free test cleansers with HMPs improved several skin tolerance attributes, including global disease severity, irritation, and erythema (Figure 1). No notable differences in skin tolerance attributes were reported in the fragranced versus the fragrance-free formulations.
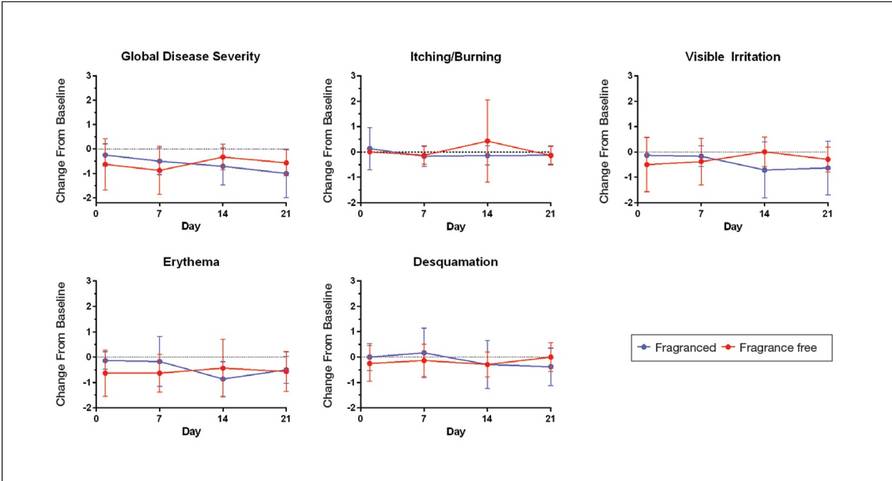
There were no reported differences in participant-reported cleanser effectiveness for the fragranced versus the fragrance-free cleanser either at baseline or weeks 1 or 3 (data not shown).
Study 2 Assessment
A total of 153 women aged 25 to 54 years with sensitive skin were enrolled in the study. Seventy-three participants were randomized to receive the fragranced test cleanser and 80 were randomized to receive the benchmark fragrance-free cleanser.
At week 3, there were no differences between the fragranced test cleanser and the benchmark cleanser in any of the clinician-assessed skin parameters (Figure 2). Of the parameters assessed, itching, irritation, and desquamation were the most improved from baseline in both treatment groups. Similar results were observed at week 1 (data not shown).
There were no apparent differences in subjective self-assessment of skin irritation between the test and benchmark cleansers at week 1 (15.7% vs 13.0%) or week 3 (24.3% vs 12.3%). When asked to respond to a series of 8 statements related to cleanser effectiveness, most participants either agreed strongly or agreed somewhat with the statements (Figure 3). There were no statistically significant differences between treatment groups, and responses to all statements indicated that participants were as satisfied with the test cleanser as they were with the benchmark cleanser.
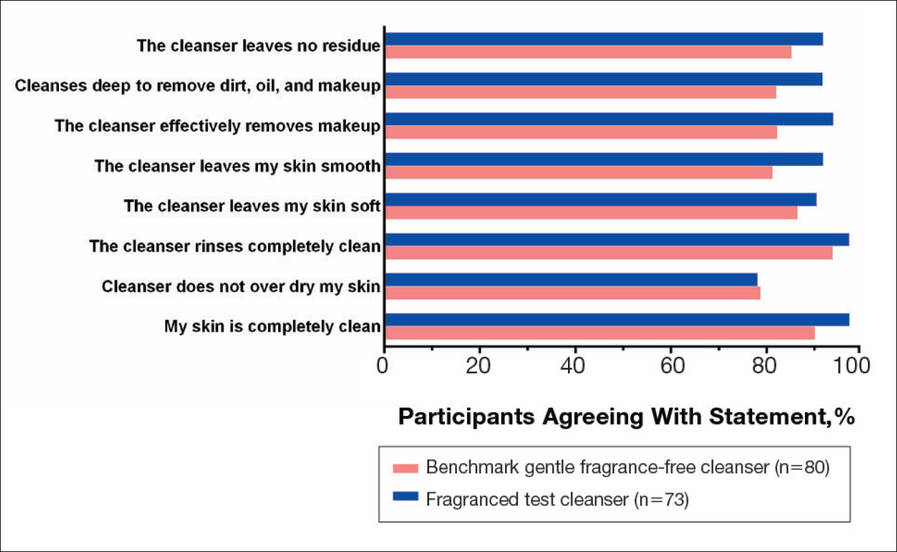
Comment
Consumers value cleansing, fragrance, viscosity, and foaming attributes in skin care products very highly.3,4,10 Fragrances are added to personal care products to positively affect consumers’ perception of product performance and to add emotional benefits by implying social or economic prestige to the use of a product.19 In one study, shampoo formulations that varied only in the added fragrance received different consumer evaluations for cleansing effectiveness and foaming.4
Although mild nonfoaming cleansers can be effective, adult consumers generally use cleansers that foam10,16 and often judge the performance of a cleansing product based on its foaming properties.3,10 Mild cleansers with HMPs maintain the ability to foam while also reducing the likelihood of skin irritation.16 One study showed that a mild, fragrance-free, foaming cleanser containing HMPs was as effective, well tolerated, and nonirritating in patients with sensitive skin as a benchmark nonfoaming gentle cleanser.20
Results from study 1 presented here show that fragranced and fragrance-free formulations of a mild, HMP-containing cleanser are equally efficacious and well tolerated in a small sample of participants with clinically diagnosed fragrance sensitivity. Skin tolerance attributes improved with both cleansers over a 3-week period, particularly global disease severity, irritation, and erythema. These results suggest that a fragrance free of common allergens and irritating essential oils could be introduced into a mild foaming cleanser containing HMPs without causing adverse reactions, even in patients who are fragrance sensitive.
Although the populations of studies 1 and 2 both included female participants with sensitive skin, they were not identical. While study 1 assessed a limited number of participants with clinically diagnosed fragrance sensitivity, study 2 was larger and included a broader range of participants with clinically diagnosed skin sensitivity, which could include fragrance sensitivity. The well-chosen fragrance of the test cleanser containing HMPs was well tolerated; however, this does not imply that any other fragrances added to this cleanser formulation would be as well tolerated.
Conclusion
The current studies indicate that a gentle fragranced foaming cleanser with HMPs was well tolerated in a small population of participants with clinically diagnosed fragrance sensitivity. In a larger population of female participants with sensitive skin, the gentle fragranced foaming cleanser with HMPs was as effective as a leading dermatologist-recommended, fragrance-free, gentle, nonfoaming cleanser. The gentle, HMP-containing, foaming cleanser with a fragrance that does not contain common allergens and irritating essential oils offers a new cleansing option for adults with sensitive skin who may prefer to use a fragranced and foaming product.
Acknowledgments—The authors are grateful to the patients and clinicians who participated in these studies. Editorial and medical writing support was provided by Tove Anderson, PhD, and Alex Loeb, PhD, both from Evidence Scientific Solutions, Inc, Philadelphia, Pennsylvania, and was funded by Johnson & Johnson Consumer Inc.
For thousands of years, humans have used fragrances to change or affect their mood and enhance an “aura of beauty.”1 Fragrance is a primary driver in consumer choice and purchasing decisions, especially when considering personal care products.2 In addition to fragrance, consumers choose cleanser products based on compatibility with skin, cleansing properties, and sensory attributes such as viscosity and foaming.3,4 However, fragrance sensitivity is among the most common causes of allergic contact dermatitis from cosmetics and personal care products,5 and estimates of the prevalence of fragrance sensitivity range from 1.8% to 4.2%.6
A panel of 26 fragrance ingredients that frequently induce contact dermatitis in sensitive individuals has been identified.7 Since 2003, regulatory authorities in the European Union require these compounds to be listed on the labels of consumer products to protect presensitized consumers.7,8 However, manufacturers of cosmetics are not required to specify allergenic fragrance ingredients outside the European Union, and therefore it is difficult for consumers in the United States to avoid fragrance allergens.
Creation of a fragranced product for fragrance-sensitive individuals begins with careful selection of ingredients and extensive formulation testing and evaluation. This process usually is followed by testing in normal individuals to confirm that the fragranced product is well accepted and then evaluation is done in clinically confirmed fragrance-sensitive patients and those with a compromised skin barrier from atopic dermatitis, rosacea, or eczema.
Sensitive skin may be due to increased immune responsiveness, altered neurosensory input, and/or decreased skin barrier function, and presents a complex challenge for dermatologists.9 Subjective perceptions of sensitive skin include stinging, burning, pruritus, and tightness following product application. Clinically sensitive skin is defined by the presence of erythema, stratum corneum desquamation, papules, pustules, wheals, vesicles, bullae, and/or erosions.9 Although some of these symptoms may be observed immediately, others may be delayed by minutes, hours, or days following the use of an irritating product. Patients who present with subjective symptoms of sensitive skin may or may not show objective symptoms.
Gentle skin cleansing is particularly important for patients with compromised skin barrier integrity, such as those with acne, atopic dermatitis, eczema, or rosacea. Standard alkaline surfactants in skin cleansers help to remove dirt and oily soil and produce lather but can impair the skin barrier function and facilitate development of irritation.10-13 The tolerability of a cleanser is influenced by its pH, the type and amount of surfactant ingredients, the presence of moisturizing agents, and the amount of residue left on the skin after washing.11,12 Mild cleansers have been developed for patients with sensitive skin conditions and are expected to provide cleansing benefits without negatively affecting the hydration and viscoelastic properties of skin.11 Mild cleansers interact minimally with skin proteins and lipids because they usually contain nonionic synthetic surfactant mixtures; they also have a pH value close to the slightly acidic pH of normal skin, contain moisturizing agents,11,14,15 and usually produce less foam.10,16 In patients with sensitive skin, mild and fragrance-free cleansers often are recommended.17,18 Because fragrances often affect consumers’ perception of product performance19 and enhance the cleaning experience of the user, consumer compliance with clinical recommendations to use fragrance-free cleansers often is poor.
Low–molecular-weight, water-soluble, hydrophobically modified polymers (HMPs) have been used to create gentle foaming cleansers with reduced impact on the skin barrier.12,16,20 In the presence of HMPs, surfactants assemble into larger, more stable polymer-surfactant structures that are less likely to penetrate the skin.16 Hydrophobically modified polymers can potentially reduce skin irritation by lowering the concentration of free micelles in solution. Additionally, both HMPs and HMP-surfactant complexes stabilize newly formed air-water interfaces, leading to thicker, denser, and longer-lasting foams.16 A gentle, fragrance-free, foaming liquid facial test cleanser with HMPs has been shown to be well tolerated in women with sensitive skin.20
This report describes 2 studies of a new mild, HMP-containing, foaming facial cleanser with a fragrance that was free of common allergens and irritating essential oils in patients with sensitive skin. Study 1 was designed to evaluate the tolerance and acceptability of 2 variations of the HMP-containing cleanser—one fragrance free and the other with fragrance—in a small sample of healthy adults with clinically diagnosed fragrance-sensitive skin. Study 2 was a large, 2-center study of the tolerability and effectiveness of the fragranced HMP-containing cleanser compared with a benchmark dermatologist-recommended, gentle, fragrance-free, nonfoaming cleanser in women with clinically diagnosed sensitive skin.
Methods
Study 1 Design
The primary objective of this prospective, randomized, single-center, crossover study was to evaluate the tolerability of fragranced versus fragrance-free formulations of a mild, HMP-containing liquid facial cleanser in healthy male and female adults with Fitzpatrick skin types I to IV who were clinically diagnosed as having fragrance sensitivity. Fragrance sensitivity was defined as a history of positive reactions to a fragrance mixture of 8 components (fragrance mixture I) and/or a fragrance mixture of 14 fragrances (fragrance mixture II) that included balsam of Peru (Myroxylonpereirae), geraniol, jasmine oil, and oakmoss.5 All participants provided written informed consent prior to enrolling in the study, and both the study protocol and informed consent agreement were approved by an institutional review board.
Participants were instructed to wash their face twice daily, noting the time of cleansing and providing commentary about their cleansing experience in a diary. The liquid facial test cleansers contained the HMP potassium acrylates copolymer, glycerin, and a surfactant system primarily containing cocamidopropyl betaine and lauryl glucoside prepared without added fragrance (as previously described20) or with a fragrance free of common allergens and irritating essential oils.
Half of the participants used the fragranced test cleanser and half used the fragrance-free test cleanser for a 3-week treatment period (weeks 1–3). Each treatment group subsequently switched to the other test cleanser for a second 3-week treatment period (weeks 4–6). Clinicians assessed global disease severity (an overall assessment of skin condition that was independent of other evaluation criteria), itching/burning, visible irritation, erythema, and desquamation at weekly time points throughout the study and graded each clinical tolerance attribute on a 5-point scale (0=none; 1=minimal; 2=mild; 3=moderate; 4=severe). Ordinal scores at baseline and at weeks 1 and 3 were used to calculate change from baseline.
A 7-item questionnaire also was administered to participants at each visit to assess skin condition, smoothness, softness, cleanliness, radiance, satisfaction with cleansing experience, and lathering. Each item was scored on a 5-point ordinal scale (0=none; 1=minimal; 2=good; 3=excellent; 4=superior). The scores for all parameters were statistically compared with baseline values using a paired t test with a significance level of P≤.05.
Study 2 Design
This prospective, 3-week, double-blind, randomized, comparative, 2-center study to evaluate the tolerability of the fragranced, HMP-containing test cleanser from study 1 versus a benchmark gentle, fragrance-free, nonfoaming cleanser in a large population of otherwise healthy females who had been clinically diagnosed with sensitive skin (not limited to fragrance sensitivity). The study sponsor provided blinded test materials, and neither the examiner nor the recorder knew which investigational product was administered to which participants. Additionally, personnel who dispensed the test cleansers to participants or supervised their use did not participate in the evaluation to minimize potential bias. All participants provided written informed consent prior to enrolling in the study, and the study protocol and informed consent agreement were approved by an institutional review board.
Participants included women aged 18 to 65 years with mild to moderate clinical symptoms of atopic dermatitis, eczema, acne, or rosacea within the 90 days prior to the study period. They were randomized into 2 balanced treatment groups: group 1 received the mild, fragranced, HMP-containing liquid facial cleanser from study 1 and group 2 received a leading, dermatologist-recommended, gentle, fragrance-free, nonfoaming cleanser. Each treatment group used the test cleansers at least once daily for 3 weeks.
Clinicians evaluated facial skin for softness and smoothness, global disease severity (rated visually by the investigator as an overall assessment of skin condition that was independent of other evaluation criteria [as previously described20]), itching, irritation, erythema, and desquamation at baseline and at weeks 1 and 3. The effectiveness of each product to remove facial dirt, cosmetics, and sebum also was assessed; clinical grading was performed as described for study 1 using the same grading scale as in study 1 and percentage change from baseline (improvement) was calculated.
The study also included a self-assessment of skin irritation in which participants responded yes or no to the following question: Have you experienced irritation using this product? Participants also completed a questionnaire in which they were asked to select the most appropriate answer—agree strongly, agree somewhat, neither, disagree somewhat, and disagree strongly— to the following statements: the cleanser leaves no residue; cleanses deep to remove dirt, oil, and makeup; the cleanser effectively removes makeup; the cleanser leaves my skin smooth; the cleanser leaves my skin soft; the cleanser rinses completely clean; cleanser does not over dry my skin; and my skin is completely clean.
The statistical analysis was performed using a nonparametric, 2-tailed, paired Mann-Whitney U test, and statistical significance was set at P≤.05.
Results
Study 1 Assessment
Eight female participants aged 22 to 60 years with clinically diagnosed fragrance sensitivity were enrolled in the study. After 3 weeks of use, clinician assessment showed that both the fragranced and fragrance-free test cleansers with HMPs improved several skin tolerance attributes, including global disease severity, irritation, and erythema (Figure 1). No notable differences in skin tolerance attributes were reported in the fragranced versus the fragrance-free formulations.
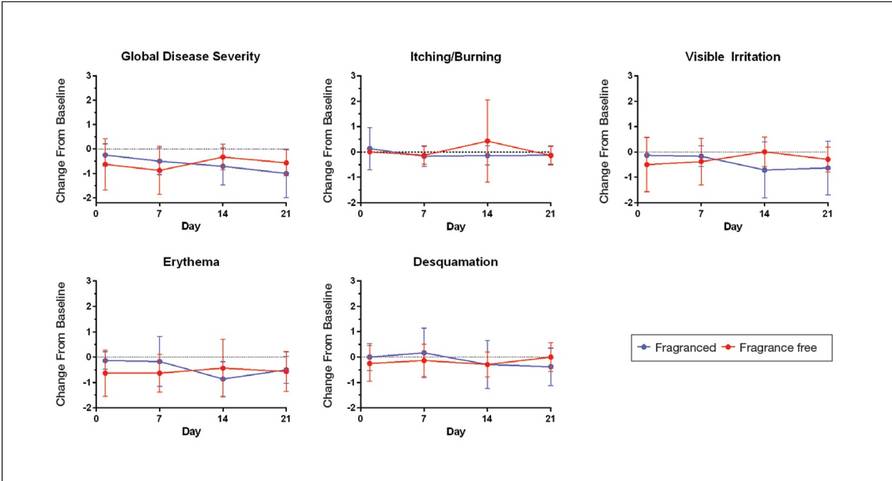
There were no reported differences in participant-reported cleanser effectiveness for the fragranced versus the fragrance-free cleanser either at baseline or weeks 1 or 3 (data not shown).
Study 2 Assessment
A total of 153 women aged 25 to 54 years with sensitive skin were enrolled in the study. Seventy-three participants were randomized to receive the fragranced test cleanser and 80 were randomized to receive the benchmark fragrance-free cleanser.
At week 3, there were no differences between the fragranced test cleanser and the benchmark cleanser in any of the clinician-assessed skin parameters (Figure 2). Of the parameters assessed, itching, irritation, and desquamation were the most improved from baseline in both treatment groups. Similar results were observed at week 1 (data not shown).
There were no apparent differences in subjective self-assessment of skin irritation between the test and benchmark cleansers at week 1 (15.7% vs 13.0%) or week 3 (24.3% vs 12.3%). When asked to respond to a series of 8 statements related to cleanser effectiveness, most participants either agreed strongly or agreed somewhat with the statements (Figure 3). There were no statistically significant differences between treatment groups, and responses to all statements indicated that participants were as satisfied with the test cleanser as they were with the benchmark cleanser.
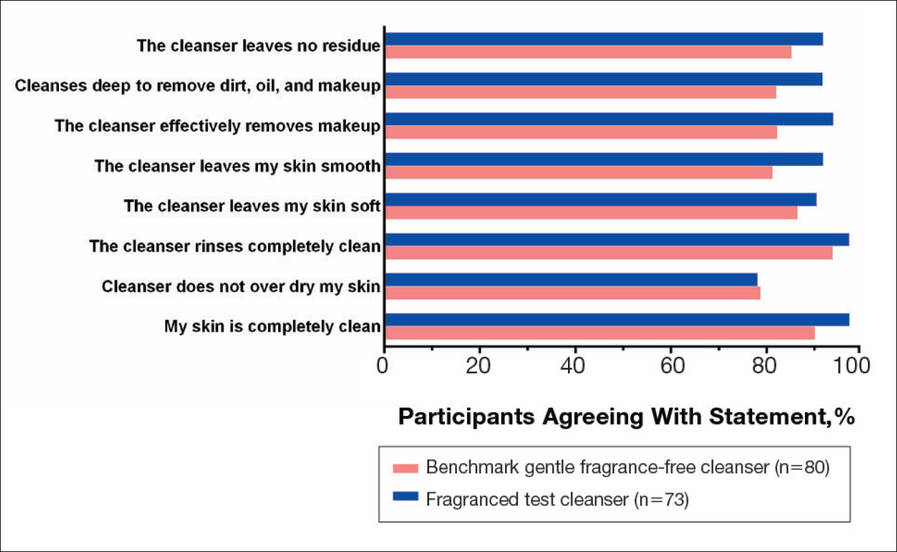
Comment
Consumers value cleansing, fragrance, viscosity, and foaming attributes in skin care products very highly.3,4,10 Fragrances are added to personal care products to positively affect consumers’ perception of product performance and to add emotional benefits by implying social or economic prestige to the use of a product.19 In one study, shampoo formulations that varied only in the added fragrance received different consumer evaluations for cleansing effectiveness and foaming.4
Although mild nonfoaming cleansers can be effective, adult consumers generally use cleansers that foam10,16 and often judge the performance of a cleansing product based on its foaming properties.3,10 Mild cleansers with HMPs maintain the ability to foam while also reducing the likelihood of skin irritation.16 One study showed that a mild, fragrance-free, foaming cleanser containing HMPs was as effective, well tolerated, and nonirritating in patients with sensitive skin as a benchmark nonfoaming gentle cleanser.20
Results from study 1 presented here show that fragranced and fragrance-free formulations of a mild, HMP-containing cleanser are equally efficacious and well tolerated in a small sample of participants with clinically diagnosed fragrance sensitivity. Skin tolerance attributes improved with both cleansers over a 3-week period, particularly global disease severity, irritation, and erythema. These results suggest that a fragrance free of common allergens and irritating essential oils could be introduced into a mild foaming cleanser containing HMPs without causing adverse reactions, even in patients who are fragrance sensitive.
Although the populations of studies 1 and 2 both included female participants with sensitive skin, they were not identical. While study 1 assessed a limited number of participants with clinically diagnosed fragrance sensitivity, study 2 was larger and included a broader range of participants with clinically diagnosed skin sensitivity, which could include fragrance sensitivity. The well-chosen fragrance of the test cleanser containing HMPs was well tolerated; however, this does not imply that any other fragrances added to this cleanser formulation would be as well tolerated.
Conclusion
The current studies indicate that a gentle fragranced foaming cleanser with HMPs was well tolerated in a small population of participants with clinically diagnosed fragrance sensitivity. In a larger population of female participants with sensitive skin, the gentle fragranced foaming cleanser with HMPs was as effective as a leading dermatologist-recommended, fragrance-free, gentle, nonfoaming cleanser. The gentle, HMP-containing, foaming cleanser with a fragrance that does not contain common allergens and irritating essential oils offers a new cleansing option for adults with sensitive skin who may prefer to use a fragranced and foaming product.
Acknowledgments—The authors are grateful to the patients and clinicians who participated in these studies. Editorial and medical writing support was provided by Tove Anderson, PhD, and Alex Loeb, PhD, both from Evidence Scientific Solutions, Inc, Philadelphia, Pennsylvania, and was funded by Johnson & Johnson Consumer Inc.
- Draelos ZD. To smell or not to smell? that is the question! J Cosmet Dermatol. 2013;12:1-2.
- Milotic D. The impact of fragrance on consumer choice. J Consumer Behaviour. 2003;3:179-191.
- Klein K. Evaluating shampoo foam. Cosmetics & Toiletries. 2004;119:32-36.
- Herman S. Skin care: the importance of feel. GCI Magazine. December 2007:70-74.
- Larsen WG. How to test for fragrance allergy. Cutis. 2000;65:39-41.
- Schnuch A, Uter W, Geier J, et al. Epidemiology of contact allergy: an estimation of morbidity employing the clinical epidemiology and drug-utilization research (CE-DUR) approach. Contact Dermatitis. 2002;47:32-39.
- Directive 2003/15/EC of the European Parliament and of the Council of 27 February 2003 amending Council Directive 76/768/EEC on the approximation of the laws of the Member States relating to cosmetic products. Official Journal of the European Communities. 2003;L66:26-35.
- Guidance note: labelling of ingredients in Cosmetics Directive 76/768/EEC. European Commission Web site. http: //ec.europa.eu/consumers/sectors/cosmetics/files/doc/guide _labelling200802_en.pdf. Updated February 2008. Accessed September 2, 2015.
- Draelos ZD. Sensitive skin: perceptions, evaluation, and treatment. Am J Contact Dermatitis. 1997;8:67-78.
- Abbas S, Goldberg JW, Massaro M. Personal cleanser technology and clinical performance. Dermatol Ther. 2004;17(suppl 1):35-42.
- Ananthapadmanabhan KP, Moore DJ, Subramanyan K, et al. Cleansing without compromise: the impact of cleansers on the skin barrier and the technology of mild cleansing. Dermatol Ther. 2004;17(suppl 1):16-25.
- Walters RM, Mao G, Gunn ET, et al. Cleansing formulations that respect skin barrier integrity. Dermatol Res Pract. 2012;2012:495917.
- Saad P, Flach CR, Walters RM, et al. Infrared spectroscopic studies of sodium dodecyl sulphate permeation and interaction with stratum corneum lipids in skin. Int J Cosmet Sci. 2012;34:36-43.
- Bikowski J. The use of cleansers as therapeutic concomitants in various dermatologic disorders. Cutis. 2001;68(suppl 5):12-19.
- Walters RM, Fevola MJ, LiBrizzi JJ, et al. Designing cleansers for the unique needs of baby skin. Cosmetics & Toiletries. 2008;123:53-60.
- Fevola MJ, Walters RM, LiBrizzi JJ. A new approach to formulating mild cleansers: hydrophobically-modified polymers for irritation mitigation. In: Morgan SE, Lochhead RY, eds. Polymeric Delivery of Therapeutics. Vol 1053. Washington, DC: American Chemical Society; 2011:221-242.
- Nelson SA, Yiannias JA. Relevance and avoidance of skin-care product allergens: pearls and pitfalls. Dermatol Clin. 2009;27:329-336.
- Arribas MP, Soro P, Silvestre JF. Allergic contact dermatitis to fragrances: part 2. Actas Dermosifiliogr. 2013;104:29-37.
- Schroeder W. Understanding fragrance in personal care. Cosmetics & Toiletries. 2009;124:36-44.
- Draelos Z, Hornby S, Walters RM, et al. Hydrophobically-modified polymers can minimize skin irritation potential caused by surfactant-based cleansers. J Cosmet Dermatol. 2013;12:314-321.
- Draelos ZD. To smell or not to smell? that is the question! J Cosmet Dermatol. 2013;12:1-2.
- Milotic D. The impact of fragrance on consumer choice. J Consumer Behaviour. 2003;3:179-191.
- Klein K. Evaluating shampoo foam. Cosmetics & Toiletries. 2004;119:32-36.
- Herman S. Skin care: the importance of feel. GCI Magazine. December 2007:70-74.
- Larsen WG. How to test for fragrance allergy. Cutis. 2000;65:39-41.
- Schnuch A, Uter W, Geier J, et al. Epidemiology of contact allergy: an estimation of morbidity employing the clinical epidemiology and drug-utilization research (CE-DUR) approach. Contact Dermatitis. 2002;47:32-39.
- Directive 2003/15/EC of the European Parliament and of the Council of 27 February 2003 amending Council Directive 76/768/EEC on the approximation of the laws of the Member States relating to cosmetic products. Official Journal of the European Communities. 2003;L66:26-35.
- Guidance note: labelling of ingredients in Cosmetics Directive 76/768/EEC. European Commission Web site. http: //ec.europa.eu/consumers/sectors/cosmetics/files/doc/guide _labelling200802_en.pdf. Updated February 2008. Accessed September 2, 2015.
- Draelos ZD. Sensitive skin: perceptions, evaluation, and treatment. Am J Contact Dermatitis. 1997;8:67-78.
- Abbas S, Goldberg JW, Massaro M. Personal cleanser technology and clinical performance. Dermatol Ther. 2004;17(suppl 1):35-42.
- Ananthapadmanabhan KP, Moore DJ, Subramanyan K, et al. Cleansing without compromise: the impact of cleansers on the skin barrier and the technology of mild cleansing. Dermatol Ther. 2004;17(suppl 1):16-25.
- Walters RM, Mao G, Gunn ET, et al. Cleansing formulations that respect skin barrier integrity. Dermatol Res Pract. 2012;2012:495917.
- Saad P, Flach CR, Walters RM, et al. Infrared spectroscopic studies of sodium dodecyl sulphate permeation and interaction with stratum corneum lipids in skin. Int J Cosmet Sci. 2012;34:36-43.
- Bikowski J. The use of cleansers as therapeutic concomitants in various dermatologic disorders. Cutis. 2001;68(suppl 5):12-19.
- Walters RM, Fevola MJ, LiBrizzi JJ, et al. Designing cleansers for the unique needs of baby skin. Cosmetics & Toiletries. 2008;123:53-60.
- Fevola MJ, Walters RM, LiBrizzi JJ. A new approach to formulating mild cleansers: hydrophobically-modified polymers for irritation mitigation. In: Morgan SE, Lochhead RY, eds. Polymeric Delivery of Therapeutics. Vol 1053. Washington, DC: American Chemical Society; 2011:221-242.
- Nelson SA, Yiannias JA. Relevance and avoidance of skin-care product allergens: pearls and pitfalls. Dermatol Clin. 2009;27:329-336.
- Arribas MP, Soro P, Silvestre JF. Allergic contact dermatitis to fragrances: part 2. Actas Dermosifiliogr. 2013;104:29-37.
- Schroeder W. Understanding fragrance in personal care. Cosmetics & Toiletries. 2009;124:36-44.
- Draelos Z, Hornby S, Walters RM, et al. Hydrophobically-modified polymers can minimize skin irritation potential caused by surfactant-based cleansers. J Cosmet Dermatol. 2013;12:314-321.
Practice Points
- Fragranced and fragrance-free versions of a gentle foaming cleanser with hydrophobically modified polymers (HMPs) were similarly well tolerated in participants with clinically diagnosed fragrance sensitivity.
- In a large population of female participants with sensitive skin, the fragranced gentle foaming cleanser with HMPs was as effective as a leading dermatologist-recommended, fragrance-free, gentle, nonfoaming cleanser.
- The gentle, HMP-containing, foaming cleanser with a fragrance offers a new cleansing option for adults with sensitive skin who may prefer to use a fragranced and foaming product.
Bullous Henoch-Schönlein Purpura in Children
Henoch-Schönlein purpura (HSP) is a systemic, small vessel vasculitis affecting the skin, joints, gastrointestinal tract, and kidneys. It usually is self-limited, but relapses can be seen in one-third of cases.1 The classic cutaneous presentation includes palpable purpura localized to the legs and buttocks. Painful hemorrhagic bullae are uncommonly observed in childhood HSP and often could lead to a diagnostic dilemma. We report the case of a patient who presented with atypical features of painful hemorrhagic bullae and provide a review of the literature.
Case Report
An otherwise healthy 14-year-old adolescent girl presented to the hospital with painful ulcerative lesions covering the arms, legs, lower abdomen, and buttocks of 3 weeks’ duration. The rash first appeared on the ankles and spread in an ascending fashion, starting with bullous formation that was accompanied by joint pain, especially in the ankles and elbows. No abdominal pain was reported. The patient attributed the lesions to prolonged cold exposure followed by a hot bath. She had tried naproxen without any improvement of pain. She was afebrile with normal blood pressure.
On physical examination, numerous petechiae, palpable purpura, hemorrhagic bullae, and ulcers with surrounding erythematous to violaceous induration as well as central necrosis were noted on the arms, legs (Figure 1), abdomen, and buttocks. The palms, soles, trunk, and face were spared.
Laboratory values on admission revealed leukocytosis (17,500/μL [reference range, 4500–11,000/μL]), elevated erythrocyte sedimentation rate (42 mm/h [reference range, 0–20 mm/h]), elevated C-reactive protein (15.59 mg/L [reference range, 0.08–3.1 mg/L]), elevated C3 (174 mg/dL [reference range, 75–135 mg/dL]), normal C4 (32 mg/dL [reference range, 3–75 mg/dL]), normal blood urea nitrogen (13 mg/dL [reference range, 8–23 mg/dL]), and normal creatinine (0.72 mg/dL [reference range, 0.6–1.2 mg/dL]). Urinalysis showed microscopic hematuria and trace proteinuria. Platelet count was normal.
Diagnostic considerations included HSP, drug-induced leukocytoclastic vasculitis, and bullous pyoderma gangrenosum. The patient was started on oral prednisone 80 mg once daily. Additionally, oral doxycycline 100 mg twice daily was added for prevention of secondary bacterial infections and for anti-inflammatory effects. All nonsteroidal anti-inflammatory drugs were avoided. A commercial ointment containing 8-hydroxyquinoline sulfate 0.3% and triamcinolone acetonide ointment 0.1% were used to minimize skin irritation. Morphine, oxycodone-acetaminophen, and pregabalin followed by gabapentin were used for pain control. Hydrotherapy also was used for the treatment of skin lesions.
Two skin punch biopsies were performed at different stages. Biopsy of an early palpable purpuric lesion showed small vessel leukocytoclastic vasculitis with perivascular IgA on direct immunofluorescence. A second biopsy from a more hemorrhagic lesion performed 96 hours after admission to the hospital showed subepidermal vesicles with partial epidermal necrosis, confluent neutrophilic infiltrate in the papillary dermis, and small vessel vasculitis (Figures 2 and 3). Gram, periodic acid–Schiff, and acid-fast bacilli staining and cultures were negative. With continued treatment for 7 days, the clinical appearance of the lesions improved. On the tenth day of hospitalization, oral dapsone 25 mg once daily was initiated with the goal of weaning the patient off the prednisone as tolerated. She was discharged on prednisone (60 mg once daily) after 14 days of hospitalization. Dapsone also was continued.
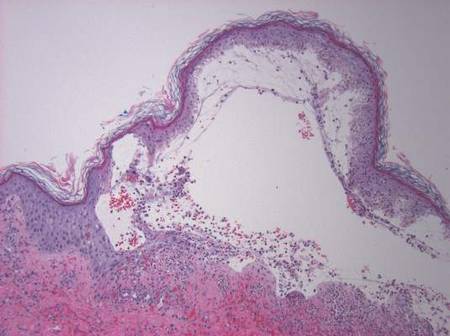
| 
| |
Figure 2. Biopsy of a subepidermal bulla revealed neutrophilic inflammation within bullous space and evidence of dermal hemorrhage (H&E, original magnification ×100). | Figure 3. Leukocytoclastic vasculitis on biopsy (H&E, original magnification ×400). |
At 4-week follow-up, the lesions showed healing with mild residual pigmentation. The patient’s blood pressure and serum urea and creatinine levels were normal but the proteinuria was persistent, so the patient was started on oral lisinopril 5 mg once daily. Tapering of steroids over several months was initiated and the dose of dapsone was increased to 50 mg daily. Follow-up with a nephrologist was arranged to monitor renal function. She continued on lisinopril 5 mg once daily for treatment of nonnephrotic-range proteinuria, which was detected at 6 months following discharge.
Comment
The presence of atypical symptoms such as bullae and painful lesions in patients with suspected HSP can complicate the diagnosis. Initially, one of the top diagnostic considerations in our patient was bullous pyoderma gangrenosum, a neutrophilic dermatosis that typically presents with painful ulcerative lesions and inflammatory bullae. Other causes of bullae in children include erythema multiforme, toxic epidermal necrolysis, epidermolysis bullosa, bullous mastocytosis, pemphigus, bullous pemphigoid, dermatitis herpetiformis, linear IgA dermatosis, bullous impetigo, gangrenous cellulitis, and Vibrio vulnificus infection. However, the clinical symptoms of joint pain and hematuria/proteinuria in our patient as well as the punch biopsy findings pointed toward HSP as the most likely diagnosis.
Although bullous lesions are relatively common in adult-onset HSP (16%–60% of patients), they are very rare in pediatric patients (2% of patients).2-4 We performed a PubMed search of articles indexed for MEDLINE for bullous Henoch-Schönlein purpura in childhood using the search term Henoch-Schönlein purpura and bullous. The Table provides a summary of our search results from the English-language literature.5-22
Bullae often develop on several parts of the body but are more commonly observed on the legs.17 Pathergy and edema have been implicated in the pathogenesis, as these findings have been observed in sites such as malleoli and legs, respectively.12 Matrix metalloproteinases secreted in polymorphonuclear neutrophils have been found to be elevated in blister fluid and can cause bullae formation via degrading collagen in the basement membrane.9 Corticosteroids, by virtue of their inhibition of proinflammatory transcription factors (eg, nuclear factor κβ, intranuclear activator protein 1) and decreasing metalloproteinase levels, may be efficacious in bullous HSP. Although there is no consensus, corticosteroid therapy seems to be efficacious in treating the bullae, according to several reports.17-22
The use of glucocorticoids in bullous HSP in childhood remains controversial. Studies report shortening of the duration of abdominal pain, reducing risk of intussusception, decreasing recurrence risk, and reducing the risk of renal involvement with use of steroids in HSP.23-25 The use of systemic steroids has been described in children with bullous HSP to reduce the severity of HSP-related bullae and its associated painful ulcers and necrosis.16,21,25,26 The duration of steroid use ranged from a short burst to a prolonged course of weaning over weeks. Azathioprine also has been used in conjunction with methylprednisolone, prednisone, and dexamethasone.17,22 Because of its anti-IgA antioxidant antineutrophil effects, dapsone has been shown to be effective in the treatment of cutaneous HSP.27 In our patient, we used dapsone to help in weaning the patient off the prednisone. Based on our review of the literature, few cases of bullous HSP in children have reported remission without drug therapy. IgA was not found in all the reported cases in which a skin biopsy was done. As shown by the comparison of the 2 biopsies in our patient, biopsying an early lesion within 48 hours of appearance is essential to make a diagnosis because the biopsy of the older lesion could not rule out bullous pyoderma gangrenosum. Immunoreactants (IgA, C3) are destroyed within 48 hours and might lead to false-negative results on immunofluorescence in old and necrotic lesions.28,29 Most reported cases of bullous HSP showed resolution, but few resulted in scarring and/or pigmentation.10,17,18 Henoch-Schönlein purpura usually is self-limited but relapses can be seen in one-third of cases.1 One of the reported cases of bullous HSP showed recurrence of lesions.15 One of the cases showed persistent hematuria.8 Our patient also was started on lisinopril for persistent proteinuria.
1. Saulsbury FT. Henoch-Schönlein purpura in children. report of 100 patients and the review of literature. Medicine. 1999;78:395-409.
2. Cream JJ, Gumpel JM, Peachey RD. Schönlein-Henoch purpura in the adult. a study of 77 adults with anaphylactoid or Schönlein-Henoch purpura. Q J Med. 1970;39:461-484.
3. Tancrede-Bohin E, Ochonisky S, Vignon-Pennamen MD, et al. Schönlein-Henoch purpura in adult patients. predictive factors for IgA glomerulonephritis in a retrospective study of 57 cases. Arch Dermatol. 1997;133:438-442.
4. Abdel-Al YK, Hejazi Z, Majeed HA. Henoch Schönlein purpura in Arab children. analysis of 52 cases. Trop Geogr Med. 1990;42:52-57.
5. Garland JS, Chusid MJ. Henoch-Schöenlein purpura: association with unusual vesicular lesions. Wis Med J. 1985;84:21-23.
6. Crosby DL, Feldman SD. A pruritic vesicular eruption. Henoch-Schönlein purpura. Arch Dermatol. 1990;126:1497-1498.
7. Wananukul S, Pongprasit P, Korkij W. Henoch-Schönlein purpura presenting as hemorrhagic vesicles and bullae: case report and literature review. Pediatr Dermatol. 1995;12:314-317.
8. Saulsbury FT. Hemorrhagic bullous lesions in Henoch-Schönlein purpura. Pediatr Dermatol. 1998;15:357-359.
9. Kobayashi T, Sakuraoka K, Iwamoto M, et al. A case of anaphylactoid purpura with multiple blister formation: possible pathophysiological role of gelatinase (MMP-9). Dermatology. 1998;197:62-64.
10. Liu PM, Bong CN, Chen HH, et al. Henoch-Schönlein purpura with hemorrhagic bullae in children: report of two cases. J Microbiol Immunol Infect. 2004;37:375-378.
11. Ishii Y, Takizawa T, Arakawa H, et al. Hemorrhagic bullous lesions in Henoch-Schönlein purpura. Pediatr Int. 2005;47:694-697.
12. Leung AK, Robson WL. Hemorrhagic bullous lesions in a child with Henoch-Schönlein purpura. Pediatr Dermatol. 2006;23:139-141.
13. Chan K, Han N, Tang W, et al. Lesions in Henoch-Schönlein purpura. Pediatr Dermatol. 2007;24: 325-326.
14. Kausar S, Yalamanchili A. Management of haemorrhagic bullous lesions in Henoch-Schonlein purpura: is there any consensus? J Dermatolog Treat. 2009;20:88-90.
15. Maguiness S, Balma-Mena A, Pope E, et al. Bullous Henoch-Schönlein purpura in children: a report of 6 cases and review of the literature. Clin Pediatr. 2010;49: 1033-1037.
16. den Boer SL, Pasmans SG, Wulffraat NM, et al. Bullous lesions in Henoch-Schönlein purpura as indication to start systemic prednisone. Acta Paediatr. 2010;99:781-783.
17. Trapani S, Mariotti P, Resti M, et al. Severe hemorrhagic bullous lesions in Henoch Schönlein purpura: three pediatric cases and review of the literature. Rheumatol Int. 2010;30:1355-1359.
18. Park SE, Lee JH. Haemorrhagic bullous lesions in a 3-year-old girl with Henoch-Schönlein purpura. Acta Paediatr. 2011;100:e283-e284.
19. Parikh K. 14-year-old boy with bullous lesions. Pediatr Ann. 2012;41:275-277.
20. Raymond M, Spinks J. Bullous Henoch Schönlein purpura. Arch Dis Child. 2012;97:617.
21. Kocaoglu C, Ozturk R, Unlu Y, et al. Successful treatment of hemorrhagic bullous Henoch-Schönlein purpura with oral corticosteroid: a case report [published online ahead of print April 16, 2013]. Case Rep Pediatr. 2013;2013:680208.
22. Mehra S, Suri D, Dogra S, et al. Hemorrhagic bullous lesions in a girl with Henoch Schönlein purpura. Indian J Pediatr. 2014;81:210-211.
23. Ronkainen J, Koskimies O, Ala-Houhala M, et al. Early prednisone therapy in Henoch-Schönlein purpura: a randomized, double-blind, placebo-controlled trial. J Pediatr. 2006;149:241-247.
24. Weiss PF, Klink AJ, Localio R, et al. Corticosteroids may improve clinical outcomes during hospitalization for Henoch-Schönlein purpura. Pediatrics. 2010;126:674-681.
25. Rosato L, Chehade H, Cachat F. Re: steroids in haemorrhagic bullous Henoch-Schönlein purpura. Acta Paediatr. 2011;100:319-320.
26. Park SJ, Kim JH, Ha TS, et al. The role of corticosteroid in hemorrhagic bullous Henoch Schönlein purpura. Acta Paediatr. 2011;100:e3-e4.
27. Iqbal H, Evans A. Dapsone therapy for Henoch-Schönlein purpura: a case series. Arch Dis Child. 2005;90:985-986.
28. Davin JC, Weening JJ. Diagnosis of Henoch-Schönlein purpura: renal or skin biopsy? Pediatr Nephrol. 2003;18:1201-1203.
29. González LM, Janniger CK, Schwartz RA. Pediatric Henoch-Schönlein purpura. Int J Dermatol. 2009;48: 1157-1165.
Henoch-Schönlein purpura (HSP) is a systemic, small vessel vasculitis affecting the skin, joints, gastrointestinal tract, and kidneys. It usually is self-limited, but relapses can be seen in one-third of cases.1 The classic cutaneous presentation includes palpable purpura localized to the legs and buttocks. Painful hemorrhagic bullae are uncommonly observed in childhood HSP and often could lead to a diagnostic dilemma. We report the case of a patient who presented with atypical features of painful hemorrhagic bullae and provide a review of the literature.
Case Report
An otherwise healthy 14-year-old adolescent girl presented to the hospital with painful ulcerative lesions covering the arms, legs, lower abdomen, and buttocks of 3 weeks’ duration. The rash first appeared on the ankles and spread in an ascending fashion, starting with bullous formation that was accompanied by joint pain, especially in the ankles and elbows. No abdominal pain was reported. The patient attributed the lesions to prolonged cold exposure followed by a hot bath. She had tried naproxen without any improvement of pain. She was afebrile with normal blood pressure.
On physical examination, numerous petechiae, palpable purpura, hemorrhagic bullae, and ulcers with surrounding erythematous to violaceous induration as well as central necrosis were noted on the arms, legs (Figure 1), abdomen, and buttocks. The palms, soles, trunk, and face were spared.
Laboratory values on admission revealed leukocytosis (17,500/μL [reference range, 4500–11,000/μL]), elevated erythrocyte sedimentation rate (42 mm/h [reference range, 0–20 mm/h]), elevated C-reactive protein (15.59 mg/L [reference range, 0.08–3.1 mg/L]), elevated C3 (174 mg/dL [reference range, 75–135 mg/dL]), normal C4 (32 mg/dL [reference range, 3–75 mg/dL]), normal blood urea nitrogen (13 mg/dL [reference range, 8–23 mg/dL]), and normal creatinine (0.72 mg/dL [reference range, 0.6–1.2 mg/dL]). Urinalysis showed microscopic hematuria and trace proteinuria. Platelet count was normal.
Diagnostic considerations included HSP, drug-induced leukocytoclastic vasculitis, and bullous pyoderma gangrenosum. The patient was started on oral prednisone 80 mg once daily. Additionally, oral doxycycline 100 mg twice daily was added for prevention of secondary bacterial infections and for anti-inflammatory effects. All nonsteroidal anti-inflammatory drugs were avoided. A commercial ointment containing 8-hydroxyquinoline sulfate 0.3% and triamcinolone acetonide ointment 0.1% were used to minimize skin irritation. Morphine, oxycodone-acetaminophen, and pregabalin followed by gabapentin were used for pain control. Hydrotherapy also was used for the treatment of skin lesions.
Two skin punch biopsies were performed at different stages. Biopsy of an early palpable purpuric lesion showed small vessel leukocytoclastic vasculitis with perivascular IgA on direct immunofluorescence. A second biopsy from a more hemorrhagic lesion performed 96 hours after admission to the hospital showed subepidermal vesicles with partial epidermal necrosis, confluent neutrophilic infiltrate in the papillary dermis, and small vessel vasculitis (Figures 2 and 3). Gram, periodic acid–Schiff, and acid-fast bacilli staining and cultures were negative. With continued treatment for 7 days, the clinical appearance of the lesions improved. On the tenth day of hospitalization, oral dapsone 25 mg once daily was initiated with the goal of weaning the patient off the prednisone as tolerated. She was discharged on prednisone (60 mg once daily) after 14 days of hospitalization. Dapsone also was continued.
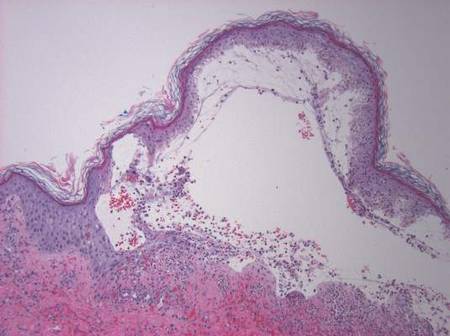
| 
| |
Figure 2. Biopsy of a subepidermal bulla revealed neutrophilic inflammation within bullous space and evidence of dermal hemorrhage (H&E, original magnification ×100). | Figure 3. Leukocytoclastic vasculitis on biopsy (H&E, original magnification ×400). |
At 4-week follow-up, the lesions showed healing with mild residual pigmentation. The patient’s blood pressure and serum urea and creatinine levels were normal but the proteinuria was persistent, so the patient was started on oral lisinopril 5 mg once daily. Tapering of steroids over several months was initiated and the dose of dapsone was increased to 50 mg daily. Follow-up with a nephrologist was arranged to monitor renal function. She continued on lisinopril 5 mg once daily for treatment of nonnephrotic-range proteinuria, which was detected at 6 months following discharge.
Comment
The presence of atypical symptoms such as bullae and painful lesions in patients with suspected HSP can complicate the diagnosis. Initially, one of the top diagnostic considerations in our patient was bullous pyoderma gangrenosum, a neutrophilic dermatosis that typically presents with painful ulcerative lesions and inflammatory bullae. Other causes of bullae in children include erythema multiforme, toxic epidermal necrolysis, epidermolysis bullosa, bullous mastocytosis, pemphigus, bullous pemphigoid, dermatitis herpetiformis, linear IgA dermatosis, bullous impetigo, gangrenous cellulitis, and Vibrio vulnificus infection. However, the clinical symptoms of joint pain and hematuria/proteinuria in our patient as well as the punch biopsy findings pointed toward HSP as the most likely diagnosis.
Although bullous lesions are relatively common in adult-onset HSP (16%–60% of patients), they are very rare in pediatric patients (2% of patients).2-4 We performed a PubMed search of articles indexed for MEDLINE for bullous Henoch-Schönlein purpura in childhood using the search term Henoch-Schönlein purpura and bullous. The Table provides a summary of our search results from the English-language literature.5-22
Bullae often develop on several parts of the body but are more commonly observed on the legs.17 Pathergy and edema have been implicated in the pathogenesis, as these findings have been observed in sites such as malleoli and legs, respectively.12 Matrix metalloproteinases secreted in polymorphonuclear neutrophils have been found to be elevated in blister fluid and can cause bullae formation via degrading collagen in the basement membrane.9 Corticosteroids, by virtue of their inhibition of proinflammatory transcription factors (eg, nuclear factor κβ, intranuclear activator protein 1) and decreasing metalloproteinase levels, may be efficacious in bullous HSP. Although there is no consensus, corticosteroid therapy seems to be efficacious in treating the bullae, according to several reports.17-22
The use of glucocorticoids in bullous HSP in childhood remains controversial. Studies report shortening of the duration of abdominal pain, reducing risk of intussusception, decreasing recurrence risk, and reducing the risk of renal involvement with use of steroids in HSP.23-25 The use of systemic steroids has been described in children with bullous HSP to reduce the severity of HSP-related bullae and its associated painful ulcers and necrosis.16,21,25,26 The duration of steroid use ranged from a short burst to a prolonged course of weaning over weeks. Azathioprine also has been used in conjunction with methylprednisolone, prednisone, and dexamethasone.17,22 Because of its anti-IgA antioxidant antineutrophil effects, dapsone has been shown to be effective in the treatment of cutaneous HSP.27 In our patient, we used dapsone to help in weaning the patient off the prednisone. Based on our review of the literature, few cases of bullous HSP in children have reported remission without drug therapy. IgA was not found in all the reported cases in which a skin biopsy was done. As shown by the comparison of the 2 biopsies in our patient, biopsying an early lesion within 48 hours of appearance is essential to make a diagnosis because the biopsy of the older lesion could not rule out bullous pyoderma gangrenosum. Immunoreactants (IgA, C3) are destroyed within 48 hours and might lead to false-negative results on immunofluorescence in old and necrotic lesions.28,29 Most reported cases of bullous HSP showed resolution, but few resulted in scarring and/or pigmentation.10,17,18 Henoch-Schönlein purpura usually is self-limited but relapses can be seen in one-third of cases.1 One of the reported cases of bullous HSP showed recurrence of lesions.15 One of the cases showed persistent hematuria.8 Our patient also was started on lisinopril for persistent proteinuria.
Henoch-Schönlein purpura (HSP) is a systemic, small vessel vasculitis affecting the skin, joints, gastrointestinal tract, and kidneys. It usually is self-limited, but relapses can be seen in one-third of cases.1 The classic cutaneous presentation includes palpable purpura localized to the legs and buttocks. Painful hemorrhagic bullae are uncommonly observed in childhood HSP and often could lead to a diagnostic dilemma. We report the case of a patient who presented with atypical features of painful hemorrhagic bullae and provide a review of the literature.
Case Report
An otherwise healthy 14-year-old adolescent girl presented to the hospital with painful ulcerative lesions covering the arms, legs, lower abdomen, and buttocks of 3 weeks’ duration. The rash first appeared on the ankles and spread in an ascending fashion, starting with bullous formation that was accompanied by joint pain, especially in the ankles and elbows. No abdominal pain was reported. The patient attributed the lesions to prolonged cold exposure followed by a hot bath. She had tried naproxen without any improvement of pain. She was afebrile with normal blood pressure.
On physical examination, numerous petechiae, palpable purpura, hemorrhagic bullae, and ulcers with surrounding erythematous to violaceous induration as well as central necrosis were noted on the arms, legs (Figure 1), abdomen, and buttocks. The palms, soles, trunk, and face were spared.
Laboratory values on admission revealed leukocytosis (17,500/μL [reference range, 4500–11,000/μL]), elevated erythrocyte sedimentation rate (42 mm/h [reference range, 0–20 mm/h]), elevated C-reactive protein (15.59 mg/L [reference range, 0.08–3.1 mg/L]), elevated C3 (174 mg/dL [reference range, 75–135 mg/dL]), normal C4 (32 mg/dL [reference range, 3–75 mg/dL]), normal blood urea nitrogen (13 mg/dL [reference range, 8–23 mg/dL]), and normal creatinine (0.72 mg/dL [reference range, 0.6–1.2 mg/dL]). Urinalysis showed microscopic hematuria and trace proteinuria. Platelet count was normal.
Diagnostic considerations included HSP, drug-induced leukocytoclastic vasculitis, and bullous pyoderma gangrenosum. The patient was started on oral prednisone 80 mg once daily. Additionally, oral doxycycline 100 mg twice daily was added for prevention of secondary bacterial infections and for anti-inflammatory effects. All nonsteroidal anti-inflammatory drugs were avoided. A commercial ointment containing 8-hydroxyquinoline sulfate 0.3% and triamcinolone acetonide ointment 0.1% were used to minimize skin irritation. Morphine, oxycodone-acetaminophen, and pregabalin followed by gabapentin were used for pain control. Hydrotherapy also was used for the treatment of skin lesions.
Two skin punch biopsies were performed at different stages. Biopsy of an early palpable purpuric lesion showed small vessel leukocytoclastic vasculitis with perivascular IgA on direct immunofluorescence. A second biopsy from a more hemorrhagic lesion performed 96 hours after admission to the hospital showed subepidermal vesicles with partial epidermal necrosis, confluent neutrophilic infiltrate in the papillary dermis, and small vessel vasculitis (Figures 2 and 3). Gram, periodic acid–Schiff, and acid-fast bacilli staining and cultures were negative. With continued treatment for 7 days, the clinical appearance of the lesions improved. On the tenth day of hospitalization, oral dapsone 25 mg once daily was initiated with the goal of weaning the patient off the prednisone as tolerated. She was discharged on prednisone (60 mg once daily) after 14 days of hospitalization. Dapsone also was continued.
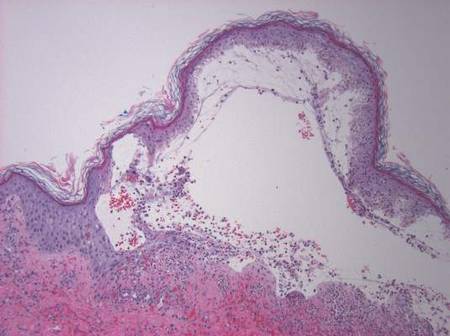
| 
| |
Figure 2. Biopsy of a subepidermal bulla revealed neutrophilic inflammation within bullous space and evidence of dermal hemorrhage (H&E, original magnification ×100). | Figure 3. Leukocytoclastic vasculitis on biopsy (H&E, original magnification ×400). |
At 4-week follow-up, the lesions showed healing with mild residual pigmentation. The patient’s blood pressure and serum urea and creatinine levels were normal but the proteinuria was persistent, so the patient was started on oral lisinopril 5 mg once daily. Tapering of steroids over several months was initiated and the dose of dapsone was increased to 50 mg daily. Follow-up with a nephrologist was arranged to monitor renal function. She continued on lisinopril 5 mg once daily for treatment of nonnephrotic-range proteinuria, which was detected at 6 months following discharge.
Comment
The presence of atypical symptoms such as bullae and painful lesions in patients with suspected HSP can complicate the diagnosis. Initially, one of the top diagnostic considerations in our patient was bullous pyoderma gangrenosum, a neutrophilic dermatosis that typically presents with painful ulcerative lesions and inflammatory bullae. Other causes of bullae in children include erythema multiforme, toxic epidermal necrolysis, epidermolysis bullosa, bullous mastocytosis, pemphigus, bullous pemphigoid, dermatitis herpetiformis, linear IgA dermatosis, bullous impetigo, gangrenous cellulitis, and Vibrio vulnificus infection. However, the clinical symptoms of joint pain and hematuria/proteinuria in our patient as well as the punch biopsy findings pointed toward HSP as the most likely diagnosis.
Although bullous lesions are relatively common in adult-onset HSP (16%–60% of patients), they are very rare in pediatric patients (2% of patients).2-4 We performed a PubMed search of articles indexed for MEDLINE for bullous Henoch-Schönlein purpura in childhood using the search term Henoch-Schönlein purpura and bullous. The Table provides a summary of our search results from the English-language literature.5-22
Bullae often develop on several parts of the body but are more commonly observed on the legs.17 Pathergy and edema have been implicated in the pathogenesis, as these findings have been observed in sites such as malleoli and legs, respectively.12 Matrix metalloproteinases secreted in polymorphonuclear neutrophils have been found to be elevated in blister fluid and can cause bullae formation via degrading collagen in the basement membrane.9 Corticosteroids, by virtue of their inhibition of proinflammatory transcription factors (eg, nuclear factor κβ, intranuclear activator protein 1) and decreasing metalloproteinase levels, may be efficacious in bullous HSP. Although there is no consensus, corticosteroid therapy seems to be efficacious in treating the bullae, according to several reports.17-22
The use of glucocorticoids in bullous HSP in childhood remains controversial. Studies report shortening of the duration of abdominal pain, reducing risk of intussusception, decreasing recurrence risk, and reducing the risk of renal involvement with use of steroids in HSP.23-25 The use of systemic steroids has been described in children with bullous HSP to reduce the severity of HSP-related bullae and its associated painful ulcers and necrosis.16,21,25,26 The duration of steroid use ranged from a short burst to a prolonged course of weaning over weeks. Azathioprine also has been used in conjunction with methylprednisolone, prednisone, and dexamethasone.17,22 Because of its anti-IgA antioxidant antineutrophil effects, dapsone has been shown to be effective in the treatment of cutaneous HSP.27 In our patient, we used dapsone to help in weaning the patient off the prednisone. Based on our review of the literature, few cases of bullous HSP in children have reported remission without drug therapy. IgA was not found in all the reported cases in which a skin biopsy was done. As shown by the comparison of the 2 biopsies in our patient, biopsying an early lesion within 48 hours of appearance is essential to make a diagnosis because the biopsy of the older lesion could not rule out bullous pyoderma gangrenosum. Immunoreactants (IgA, C3) are destroyed within 48 hours and might lead to false-negative results on immunofluorescence in old and necrotic lesions.28,29 Most reported cases of bullous HSP showed resolution, but few resulted in scarring and/or pigmentation.10,17,18 Henoch-Schönlein purpura usually is self-limited but relapses can be seen in one-third of cases.1 One of the reported cases of bullous HSP showed recurrence of lesions.15 One of the cases showed persistent hematuria.8 Our patient also was started on lisinopril for persistent proteinuria.
1. Saulsbury FT. Henoch-Schönlein purpura in children. report of 100 patients and the review of literature. Medicine. 1999;78:395-409.
2. Cream JJ, Gumpel JM, Peachey RD. Schönlein-Henoch purpura in the adult. a study of 77 adults with anaphylactoid or Schönlein-Henoch purpura. Q J Med. 1970;39:461-484.
3. Tancrede-Bohin E, Ochonisky S, Vignon-Pennamen MD, et al. Schönlein-Henoch purpura in adult patients. predictive factors for IgA glomerulonephritis in a retrospective study of 57 cases. Arch Dermatol. 1997;133:438-442.
4. Abdel-Al YK, Hejazi Z, Majeed HA. Henoch Schönlein purpura in Arab children. analysis of 52 cases. Trop Geogr Med. 1990;42:52-57.
5. Garland JS, Chusid MJ. Henoch-Schöenlein purpura: association with unusual vesicular lesions. Wis Med J. 1985;84:21-23.
6. Crosby DL, Feldman SD. A pruritic vesicular eruption. Henoch-Schönlein purpura. Arch Dermatol. 1990;126:1497-1498.
7. Wananukul S, Pongprasit P, Korkij W. Henoch-Schönlein purpura presenting as hemorrhagic vesicles and bullae: case report and literature review. Pediatr Dermatol. 1995;12:314-317.
8. Saulsbury FT. Hemorrhagic bullous lesions in Henoch-Schönlein purpura. Pediatr Dermatol. 1998;15:357-359.
9. Kobayashi T, Sakuraoka K, Iwamoto M, et al. A case of anaphylactoid purpura with multiple blister formation: possible pathophysiological role of gelatinase (MMP-9). Dermatology. 1998;197:62-64.
10. Liu PM, Bong CN, Chen HH, et al. Henoch-Schönlein purpura with hemorrhagic bullae in children: report of two cases. J Microbiol Immunol Infect. 2004;37:375-378.
11. Ishii Y, Takizawa T, Arakawa H, et al. Hemorrhagic bullous lesions in Henoch-Schönlein purpura. Pediatr Int. 2005;47:694-697.
12. Leung AK, Robson WL. Hemorrhagic bullous lesions in a child with Henoch-Schönlein purpura. Pediatr Dermatol. 2006;23:139-141.
13. Chan K, Han N, Tang W, et al. Lesions in Henoch-Schönlein purpura. Pediatr Dermatol. 2007;24: 325-326.
14. Kausar S, Yalamanchili A. Management of haemorrhagic bullous lesions in Henoch-Schonlein purpura: is there any consensus? J Dermatolog Treat. 2009;20:88-90.
15. Maguiness S, Balma-Mena A, Pope E, et al. Bullous Henoch-Schönlein purpura in children: a report of 6 cases and review of the literature. Clin Pediatr. 2010;49: 1033-1037.
16. den Boer SL, Pasmans SG, Wulffraat NM, et al. Bullous lesions in Henoch-Schönlein purpura as indication to start systemic prednisone. Acta Paediatr. 2010;99:781-783.
17. Trapani S, Mariotti P, Resti M, et al. Severe hemorrhagic bullous lesions in Henoch Schönlein purpura: three pediatric cases and review of the literature. Rheumatol Int. 2010;30:1355-1359.
18. Park SE, Lee JH. Haemorrhagic bullous lesions in a 3-year-old girl with Henoch-Schönlein purpura. Acta Paediatr. 2011;100:e283-e284.
19. Parikh K. 14-year-old boy with bullous lesions. Pediatr Ann. 2012;41:275-277.
20. Raymond M, Spinks J. Bullous Henoch Schönlein purpura. Arch Dis Child. 2012;97:617.
21. Kocaoglu C, Ozturk R, Unlu Y, et al. Successful treatment of hemorrhagic bullous Henoch-Schönlein purpura with oral corticosteroid: a case report [published online ahead of print April 16, 2013]. Case Rep Pediatr. 2013;2013:680208.
22. Mehra S, Suri D, Dogra S, et al. Hemorrhagic bullous lesions in a girl with Henoch Schönlein purpura. Indian J Pediatr. 2014;81:210-211.
23. Ronkainen J, Koskimies O, Ala-Houhala M, et al. Early prednisone therapy in Henoch-Schönlein purpura: a randomized, double-blind, placebo-controlled trial. J Pediatr. 2006;149:241-247.
24. Weiss PF, Klink AJ, Localio R, et al. Corticosteroids may improve clinical outcomes during hospitalization for Henoch-Schönlein purpura. Pediatrics. 2010;126:674-681.
25. Rosato L, Chehade H, Cachat F. Re: steroids in haemorrhagic bullous Henoch-Schönlein purpura. Acta Paediatr. 2011;100:319-320.
26. Park SJ, Kim JH, Ha TS, et al. The role of corticosteroid in hemorrhagic bullous Henoch Schönlein purpura. Acta Paediatr. 2011;100:e3-e4.
27. Iqbal H, Evans A. Dapsone therapy for Henoch-Schönlein purpura: a case series. Arch Dis Child. 2005;90:985-986.
28. Davin JC, Weening JJ. Diagnosis of Henoch-Schönlein purpura: renal or skin biopsy? Pediatr Nephrol. 2003;18:1201-1203.
29. González LM, Janniger CK, Schwartz RA. Pediatric Henoch-Schönlein purpura. Int J Dermatol. 2009;48: 1157-1165.
1. Saulsbury FT. Henoch-Schönlein purpura in children. report of 100 patients and the review of literature. Medicine. 1999;78:395-409.
2. Cream JJ, Gumpel JM, Peachey RD. Schönlein-Henoch purpura in the adult. a study of 77 adults with anaphylactoid or Schönlein-Henoch purpura. Q J Med. 1970;39:461-484.
3. Tancrede-Bohin E, Ochonisky S, Vignon-Pennamen MD, et al. Schönlein-Henoch purpura in adult patients. predictive factors for IgA glomerulonephritis in a retrospective study of 57 cases. Arch Dermatol. 1997;133:438-442.
4. Abdel-Al YK, Hejazi Z, Majeed HA. Henoch Schönlein purpura in Arab children. analysis of 52 cases. Trop Geogr Med. 1990;42:52-57.
5. Garland JS, Chusid MJ. Henoch-Schöenlein purpura: association with unusual vesicular lesions. Wis Med J. 1985;84:21-23.
6. Crosby DL, Feldman SD. A pruritic vesicular eruption. Henoch-Schönlein purpura. Arch Dermatol. 1990;126:1497-1498.
7. Wananukul S, Pongprasit P, Korkij W. Henoch-Schönlein purpura presenting as hemorrhagic vesicles and bullae: case report and literature review. Pediatr Dermatol. 1995;12:314-317.
8. Saulsbury FT. Hemorrhagic bullous lesions in Henoch-Schönlein purpura. Pediatr Dermatol. 1998;15:357-359.
9. Kobayashi T, Sakuraoka K, Iwamoto M, et al. A case of anaphylactoid purpura with multiple blister formation: possible pathophysiological role of gelatinase (MMP-9). Dermatology. 1998;197:62-64.
10. Liu PM, Bong CN, Chen HH, et al. Henoch-Schönlein purpura with hemorrhagic bullae in children: report of two cases. J Microbiol Immunol Infect. 2004;37:375-378.
11. Ishii Y, Takizawa T, Arakawa H, et al. Hemorrhagic bullous lesions in Henoch-Schönlein purpura. Pediatr Int. 2005;47:694-697.
12. Leung AK, Robson WL. Hemorrhagic bullous lesions in a child with Henoch-Schönlein purpura. Pediatr Dermatol. 2006;23:139-141.
13. Chan K, Han N, Tang W, et al. Lesions in Henoch-Schönlein purpura. Pediatr Dermatol. 2007;24: 325-326.
14. Kausar S, Yalamanchili A. Management of haemorrhagic bullous lesions in Henoch-Schonlein purpura: is there any consensus? J Dermatolog Treat. 2009;20:88-90.
15. Maguiness S, Balma-Mena A, Pope E, et al. Bullous Henoch-Schönlein purpura in children: a report of 6 cases and review of the literature. Clin Pediatr. 2010;49: 1033-1037.
16. den Boer SL, Pasmans SG, Wulffraat NM, et al. Bullous lesions in Henoch-Schönlein purpura as indication to start systemic prednisone. Acta Paediatr. 2010;99:781-783.
17. Trapani S, Mariotti P, Resti M, et al. Severe hemorrhagic bullous lesions in Henoch Schönlein purpura: three pediatric cases and review of the literature. Rheumatol Int. 2010;30:1355-1359.
18. Park SE, Lee JH. Haemorrhagic bullous lesions in a 3-year-old girl with Henoch-Schönlein purpura. Acta Paediatr. 2011;100:e283-e284.
19. Parikh K. 14-year-old boy with bullous lesions. Pediatr Ann. 2012;41:275-277.
20. Raymond M, Spinks J. Bullous Henoch Schönlein purpura. Arch Dis Child. 2012;97:617.
21. Kocaoglu C, Ozturk R, Unlu Y, et al. Successful treatment of hemorrhagic bullous Henoch-Schönlein purpura with oral corticosteroid: a case report [published online ahead of print April 16, 2013]. Case Rep Pediatr. 2013;2013:680208.
22. Mehra S, Suri D, Dogra S, et al. Hemorrhagic bullous lesions in a girl with Henoch Schönlein purpura. Indian J Pediatr. 2014;81:210-211.
23. Ronkainen J, Koskimies O, Ala-Houhala M, et al. Early prednisone therapy in Henoch-Schönlein purpura: a randomized, double-blind, placebo-controlled trial. J Pediatr. 2006;149:241-247.
24. Weiss PF, Klink AJ, Localio R, et al. Corticosteroids may improve clinical outcomes during hospitalization for Henoch-Schönlein purpura. Pediatrics. 2010;126:674-681.
25. Rosato L, Chehade H, Cachat F. Re: steroids in haemorrhagic bullous Henoch-Schönlein purpura. Acta Paediatr. 2011;100:319-320.
26. Park SJ, Kim JH, Ha TS, et al. The role of corticosteroid in hemorrhagic bullous Henoch Schönlein purpura. Acta Paediatr. 2011;100:e3-e4.
27. Iqbal H, Evans A. Dapsone therapy for Henoch-Schönlein purpura: a case series. Arch Dis Child. 2005;90:985-986.
28. Davin JC, Weening JJ. Diagnosis of Henoch-Schönlein purpura: renal or skin biopsy? Pediatr Nephrol. 2003;18:1201-1203.
29. González LM, Janniger CK, Schwartz RA. Pediatric Henoch-Schönlein purpura. Int J Dermatol. 2009;48: 1157-1165.
Practice Points
- The presence of painful hemorrhagic bullae is an uncommon presentation in pediatric patients with Henoch-Schönlein purpura (HSP) and can be a diagnostic challenge.
- Presence of joint pain, abdominal pain, or nephritis could corroborate the diagnosis.
- Early biopsy of the lesion within 48 hours of appearance is important for diagnosis. Presence of IgA deposits on immunofluorescence may aid in diagnosis.
- This finding of bullae in HSP does not seem to have any prognostic significance. Because of the rarity of incidence, there is no consensus on management. Supportive therapy and/or corticosteroids might be effective.