User login
Epicardial GP ablation of no benefit in advanced atrial fibrillation
San Francisco – Routine ganglionic plexus ablation increases risk and offers no clinical benefit in patients undergoing thoracoscopic surgery for advanced atrial fibrillation, according to a randomized Dutch trial.
“Most surgeons who do epicardial ablation do GP [ganglionic plexus] ablation because of the assumption that they are doing something good; that assumption is wrong. GP ablation should not be performed in patients with advanced AF [atrial fibrillation],” said lead investigator Dr. Joris de Groot, a cardiologist at the University of Amsterdam.
Following pulmonary vein isolation (PVI), 117 patients were randomized to GP ablation, and 123 to no GP ablation. GP ablation eliminated 100% of evoked vagal responses; vagal responses remained intact in nearly all of the control subjects.
At 1 year, 70.9% in the GP group compared with 68.4% in control arm were free of recurrence (P = .7); there were no statistically significant differences when the analysis was limited to the 59% of patients who went into the trial with persistent AF or limited to the rest of the patients with paroxysmal AF. Recurrences constituted significantly more atrial tachycardia in the GP group than in the control group. Even after the researchers controlled for a wide variety of demographic, anatomical, and clinical variables, “GP ablation made no difference in atrial fibrillation recurrence at 1 year,” Dr. de Groot said at the annual scientific sessions of the Hearth Rhythm Society.
Meanwhile, major perioperative bleeding occurred in nine patients, all in the GP group, and one required a sternotomy for hemostatic control. Clinically relevant sinus node dysfunction occurred in 12 of the GP group, but only four control patients; six GP patients – but no one in the control arm – required subsequent pacemakers, three while in the hospital after surgery and three during follow-up. Almost 30 patients in each arm required cardioversion during the 3-month blanking period, and about 20 in each arm afterwards.
“The largest randomized study in thoracoscopic surgery for advanced AF to date demonstrates that GP ablation is associated with significantly more periprocedural major bleeding, sinus node dysfunction, and pacemaker implantation, but not with improved rhythm outcome,” the investigators concluded.
Procedure time was 185 +/– 54 minutes in the GP arm, and 168 +/– 54 minutes in the control arm (P = .015). In the GP group, four major GPs and the ligament of Marshall were ablated.
Patients were 60 years old, on average, and three-quarters were men. AF duration was a median of 4 years. Four patients had died at 1 year, all in the GP arm, but none related to the procedure. All antiarrhythmic drugs were stopped after the blanking period; any atrial arrhythmia lasting 30 seconds or longer thereafter was considered a recurrence.
Dr. de Groot disclosed payments for services from AtriCure, Daiichi, and St. Jude Medical and research funding from AtriCure and St. Jude.
AF ablation is an evolving field, and we are constantly trying to think of new ways to improve our success rates. Some of the things we try turn out to be advantageous and others do not. Negative studies like this have a very important clinical impact; they help us figure out what road to take.

|
Dr. Thomas Deering |
Dr. Thomas Deering is chief of the Arrhythmia Center at the Piedmont Heart Institute in Atlanta, where he is also chairman of the Executive Council and the Clinical Centers for Excellence. He moderated Dr. de Groot’s presentation, and wasn’t involved in the work.
AF ablation is an evolving field, and we are constantly trying to think of new ways to improve our success rates. Some of the things we try turn out to be advantageous and others do not. Negative studies like this have a very important clinical impact; they help us figure out what road to take.

|
Dr. Thomas Deering |
Dr. Thomas Deering is chief of the Arrhythmia Center at the Piedmont Heart Institute in Atlanta, where he is also chairman of the Executive Council and the Clinical Centers for Excellence. He moderated Dr. de Groot’s presentation, and wasn’t involved in the work.
AF ablation is an evolving field, and we are constantly trying to think of new ways to improve our success rates. Some of the things we try turn out to be advantageous and others do not. Negative studies like this have a very important clinical impact; they help us figure out what road to take.

|
Dr. Thomas Deering |
Dr. Thomas Deering is chief of the Arrhythmia Center at the Piedmont Heart Institute in Atlanta, where he is also chairman of the Executive Council and the Clinical Centers for Excellence. He moderated Dr. de Groot’s presentation, and wasn’t involved in the work.
San Francisco – Routine ganglionic plexus ablation increases risk and offers no clinical benefit in patients undergoing thoracoscopic surgery for advanced atrial fibrillation, according to a randomized Dutch trial.
“Most surgeons who do epicardial ablation do GP [ganglionic plexus] ablation because of the assumption that they are doing something good; that assumption is wrong. GP ablation should not be performed in patients with advanced AF [atrial fibrillation],” said lead investigator Dr. Joris de Groot, a cardiologist at the University of Amsterdam.
Following pulmonary vein isolation (PVI), 117 patients were randomized to GP ablation, and 123 to no GP ablation. GP ablation eliminated 100% of evoked vagal responses; vagal responses remained intact in nearly all of the control subjects.
At 1 year, 70.9% in the GP group compared with 68.4% in control arm were free of recurrence (P = .7); there were no statistically significant differences when the analysis was limited to the 59% of patients who went into the trial with persistent AF or limited to the rest of the patients with paroxysmal AF. Recurrences constituted significantly more atrial tachycardia in the GP group than in the control group. Even after the researchers controlled for a wide variety of demographic, anatomical, and clinical variables, “GP ablation made no difference in atrial fibrillation recurrence at 1 year,” Dr. de Groot said at the annual scientific sessions of the Hearth Rhythm Society.
Meanwhile, major perioperative bleeding occurred in nine patients, all in the GP group, and one required a sternotomy for hemostatic control. Clinically relevant sinus node dysfunction occurred in 12 of the GP group, but only four control patients; six GP patients – but no one in the control arm – required subsequent pacemakers, three while in the hospital after surgery and three during follow-up. Almost 30 patients in each arm required cardioversion during the 3-month blanking period, and about 20 in each arm afterwards.
“The largest randomized study in thoracoscopic surgery for advanced AF to date demonstrates that GP ablation is associated with significantly more periprocedural major bleeding, sinus node dysfunction, and pacemaker implantation, but not with improved rhythm outcome,” the investigators concluded.
Procedure time was 185 +/– 54 minutes in the GP arm, and 168 +/– 54 minutes in the control arm (P = .015). In the GP group, four major GPs and the ligament of Marshall were ablated.
Patients were 60 years old, on average, and three-quarters were men. AF duration was a median of 4 years. Four patients had died at 1 year, all in the GP arm, but none related to the procedure. All antiarrhythmic drugs were stopped after the blanking period; any atrial arrhythmia lasting 30 seconds or longer thereafter was considered a recurrence.
Dr. de Groot disclosed payments for services from AtriCure, Daiichi, and St. Jude Medical and research funding from AtriCure and St. Jude.
San Francisco – Routine ganglionic plexus ablation increases risk and offers no clinical benefit in patients undergoing thoracoscopic surgery for advanced atrial fibrillation, according to a randomized Dutch trial.
“Most surgeons who do epicardial ablation do GP [ganglionic plexus] ablation because of the assumption that they are doing something good; that assumption is wrong. GP ablation should not be performed in patients with advanced AF [atrial fibrillation],” said lead investigator Dr. Joris de Groot, a cardiologist at the University of Amsterdam.
Following pulmonary vein isolation (PVI), 117 patients were randomized to GP ablation, and 123 to no GP ablation. GP ablation eliminated 100% of evoked vagal responses; vagal responses remained intact in nearly all of the control subjects.
At 1 year, 70.9% in the GP group compared with 68.4% in control arm were free of recurrence (P = .7); there were no statistically significant differences when the analysis was limited to the 59% of patients who went into the trial with persistent AF or limited to the rest of the patients with paroxysmal AF. Recurrences constituted significantly more atrial tachycardia in the GP group than in the control group. Even after the researchers controlled for a wide variety of demographic, anatomical, and clinical variables, “GP ablation made no difference in atrial fibrillation recurrence at 1 year,” Dr. de Groot said at the annual scientific sessions of the Hearth Rhythm Society.
Meanwhile, major perioperative bleeding occurred in nine patients, all in the GP group, and one required a sternotomy for hemostatic control. Clinically relevant sinus node dysfunction occurred in 12 of the GP group, but only four control patients; six GP patients – but no one in the control arm – required subsequent pacemakers, three while in the hospital after surgery and three during follow-up. Almost 30 patients in each arm required cardioversion during the 3-month blanking period, and about 20 in each arm afterwards.
“The largest randomized study in thoracoscopic surgery for advanced AF to date demonstrates that GP ablation is associated with significantly more periprocedural major bleeding, sinus node dysfunction, and pacemaker implantation, but not with improved rhythm outcome,” the investigators concluded.
Procedure time was 185 +/– 54 minutes in the GP arm, and 168 +/– 54 minutes in the control arm (P = .015). In the GP group, four major GPs and the ligament of Marshall were ablated.
Patients were 60 years old, on average, and three-quarters were men. AF duration was a median of 4 years. Four patients had died at 1 year, all in the GP arm, but none related to the procedure. All antiarrhythmic drugs were stopped after the blanking period; any atrial arrhythmia lasting 30 seconds or longer thereafter was considered a recurrence.
Dr. de Groot disclosed payments for services from AtriCure, Daiichi, and St. Jude Medical and research funding from AtriCure and St. Jude.
AT HEART RHYTHM 2016
Key clinical point: Routine ganglionic plexus ablation increases risk and offers no clinical benefit in patients undergoing thoracoscopic surgery for advanced atrial fibrillation.
Major finding: At 1 year, 70.9% in the GP ablation group, but 68.4% in the control arm, were free of recurrence (P = .7)
Data source: Randomized trial of 240 AF patients, almost two-thirds with persistent disease
Disclosures: The lead investigator disclosed payments for services from AtriCure, Daiichi, and St. Jude Medical, and research funding from AtriCure and St. Jude.
FDA publishes draft guidance for developing HCV antivirals
The U.S. Food and Drug Administration has issued revised draft guidance intended to foster the development of direct-acting antiviral drugs to treat chronic hepatitis C virus infection.
The guidance, developed by the FDA’s Center for Drug Evaluation and Research, delineates the drug development process from the preinvestigational new drug application through the new drug application and postmarketing stages.
According to the FDA, the draft guidance, when finalized, will represent the current thinking of the agency on development of direct-acting antivirals and clinical trial designs, but is not binding on the FDA or the public. It explicitly states that industry may use an alternative approach to drug development if it “satisfies the requirements of the applicable statutes and regulations.” For the purposes of drug development, the FDA defines direct-acting HCV antivirals as drugs that “interfere with specific steps in the HCV replication cycle through a direct interaction with the HCV genome, polyprotein, or its polyprotein cleavage products.”
The guidance does not address the development of drugs that target host functions necessary for viral replication or immune-based drugs for the treatment of HCV infection, including new interferon drugs or therapeutics “without antiviral mechanisms intended to mitigate or reverse clinical or pathophysiological outcomes” of chronic HCV infection, such as prevention of hepatocellular carcinoma or reversal of fibrosis.
Once the draft guidance has been published in the Federal Register, the FDA will accept comments and suggestions at www.regulations.gov for 60 days.
On Twitter @richpizzi
The U.S. Food and Drug Administration has issued revised draft guidance intended to foster the development of direct-acting antiviral drugs to treat chronic hepatitis C virus infection.
The guidance, developed by the FDA’s Center for Drug Evaluation and Research, delineates the drug development process from the preinvestigational new drug application through the new drug application and postmarketing stages.
According to the FDA, the draft guidance, when finalized, will represent the current thinking of the agency on development of direct-acting antivirals and clinical trial designs, but is not binding on the FDA or the public. It explicitly states that industry may use an alternative approach to drug development if it “satisfies the requirements of the applicable statutes and regulations.” For the purposes of drug development, the FDA defines direct-acting HCV antivirals as drugs that “interfere with specific steps in the HCV replication cycle through a direct interaction with the HCV genome, polyprotein, or its polyprotein cleavage products.”
The guidance does not address the development of drugs that target host functions necessary for viral replication or immune-based drugs for the treatment of HCV infection, including new interferon drugs or therapeutics “without antiviral mechanisms intended to mitigate or reverse clinical or pathophysiological outcomes” of chronic HCV infection, such as prevention of hepatocellular carcinoma or reversal of fibrosis.
Once the draft guidance has been published in the Federal Register, the FDA will accept comments and suggestions at www.regulations.gov for 60 days.
On Twitter @richpizzi
The U.S. Food and Drug Administration has issued revised draft guidance intended to foster the development of direct-acting antiviral drugs to treat chronic hepatitis C virus infection.
The guidance, developed by the FDA’s Center for Drug Evaluation and Research, delineates the drug development process from the preinvestigational new drug application through the new drug application and postmarketing stages.
According to the FDA, the draft guidance, when finalized, will represent the current thinking of the agency on development of direct-acting antivirals and clinical trial designs, but is not binding on the FDA or the public. It explicitly states that industry may use an alternative approach to drug development if it “satisfies the requirements of the applicable statutes and regulations.” For the purposes of drug development, the FDA defines direct-acting HCV antivirals as drugs that “interfere with specific steps in the HCV replication cycle through a direct interaction with the HCV genome, polyprotein, or its polyprotein cleavage products.”
The guidance does not address the development of drugs that target host functions necessary for viral replication or immune-based drugs for the treatment of HCV infection, including new interferon drugs or therapeutics “without antiviral mechanisms intended to mitigate or reverse clinical or pathophysiological outcomes” of chronic HCV infection, such as prevention of hepatocellular carcinoma or reversal of fibrosis.
Once the draft guidance has been published in the Federal Register, the FDA will accept comments and suggestions at www.regulations.gov for 60 days.
On Twitter @richpizzi
Study: Number of MRSA cases in Japan may be underestimated
In Japan, sentinel disease surveillance systems may underestimate the actual number of patients with methicillin-resistant Staphylococcus aureus (MRSA) infection because they do not include information about patients who visit nonsentinel medical facilities, according to a study published in Epidemiology and Infection.
Dr. Shinichi Tanihara of the department of public health and preventive medicine in the School of Medicine at Fukuoka University and Dr. Satowa Suzuki of the department of bacteriology II at the National Institute of Infectious Diseases in Tokyo assessed and compared the incidences of MRSA patients based on health insurance claims data and data reported to the Japan Nosocomial Infections Surveillance system (Epidemiol Infect. 2016 April 8. doi: 10.1017/S0950268816000674).
The study results suggested that health insurance claims data for MRSA cases were more useful for determining the incidence of MRSA cases in Japan from 2011 to 2012. For example, of the 2,052 eligible hospitals with 200 or more beds in 2011, roughly one-quarter (495, 23.8%) participated in the Japan Nosocomial Infections Surveillance system. Data from this relatively low percentage of eligible facilities most likely underestimated the true number of MRSA patients in Japan, the authors said.
Based on their findings, the investigators noted three major advantages of using health insurance claims data for infection surveillance. Firstly, information from health insurance claims data is not affected by health care providers’ notifications to surveillance systems. Secondly, data on patients with MRSA can be collected at low cost because of Japan’s uniform and computerized health insurance system, and the data are easy to access. Lastly, health insurance claims data prevent the duplication of patient information, as insurers can determine if a patient was treated at multiple medical facilities for the same disease.
The only noted drawback involving the use of health insurance claims data for infection surveillance pertained to its timeliness, the researchers wrote. This issue arises because these data are submitted monthly rather than immediately, which may limit their use in surveillance systems.
According to Dr. Tanihara and Dr. Suzuki, strengths of the study include its evaluation of sentinel surveillance quality through the use of data that were not based on physician reports, as well as the calculation of MRSA incidence by use of a standardized definition in a specific population. Reported limitations included the assessment of anti-MRSA medicine use and patients’ age only, and the lack of information on the degree of drug resistance from health insurance claims data.
Funding was provided by the Ministry of Health, Labour, and Welfare of Japan, and by the Research Programme on Emerging and Re-emerging Infectious Diseases from the Japan Agency for Medical Research and Development. Neither author reported any conflicts of interest.
In Japan, sentinel disease surveillance systems may underestimate the actual number of patients with methicillin-resistant Staphylococcus aureus (MRSA) infection because they do not include information about patients who visit nonsentinel medical facilities, according to a study published in Epidemiology and Infection.
Dr. Shinichi Tanihara of the department of public health and preventive medicine in the School of Medicine at Fukuoka University and Dr. Satowa Suzuki of the department of bacteriology II at the National Institute of Infectious Diseases in Tokyo assessed and compared the incidences of MRSA patients based on health insurance claims data and data reported to the Japan Nosocomial Infections Surveillance system (Epidemiol Infect. 2016 April 8. doi: 10.1017/S0950268816000674).
The study results suggested that health insurance claims data for MRSA cases were more useful for determining the incidence of MRSA cases in Japan from 2011 to 2012. For example, of the 2,052 eligible hospitals with 200 or more beds in 2011, roughly one-quarter (495, 23.8%) participated in the Japan Nosocomial Infections Surveillance system. Data from this relatively low percentage of eligible facilities most likely underestimated the true number of MRSA patients in Japan, the authors said.
Based on their findings, the investigators noted three major advantages of using health insurance claims data for infection surveillance. Firstly, information from health insurance claims data is not affected by health care providers’ notifications to surveillance systems. Secondly, data on patients with MRSA can be collected at low cost because of Japan’s uniform and computerized health insurance system, and the data are easy to access. Lastly, health insurance claims data prevent the duplication of patient information, as insurers can determine if a patient was treated at multiple medical facilities for the same disease.
The only noted drawback involving the use of health insurance claims data for infection surveillance pertained to its timeliness, the researchers wrote. This issue arises because these data are submitted monthly rather than immediately, which may limit their use in surveillance systems.
According to Dr. Tanihara and Dr. Suzuki, strengths of the study include its evaluation of sentinel surveillance quality through the use of data that were not based on physician reports, as well as the calculation of MRSA incidence by use of a standardized definition in a specific population. Reported limitations included the assessment of anti-MRSA medicine use and patients’ age only, and the lack of information on the degree of drug resistance from health insurance claims data.
Funding was provided by the Ministry of Health, Labour, and Welfare of Japan, and by the Research Programme on Emerging and Re-emerging Infectious Diseases from the Japan Agency for Medical Research and Development. Neither author reported any conflicts of interest.
In Japan, sentinel disease surveillance systems may underestimate the actual number of patients with methicillin-resistant Staphylococcus aureus (MRSA) infection because they do not include information about patients who visit nonsentinel medical facilities, according to a study published in Epidemiology and Infection.
Dr. Shinichi Tanihara of the department of public health and preventive medicine in the School of Medicine at Fukuoka University and Dr. Satowa Suzuki of the department of bacteriology II at the National Institute of Infectious Diseases in Tokyo assessed and compared the incidences of MRSA patients based on health insurance claims data and data reported to the Japan Nosocomial Infections Surveillance system (Epidemiol Infect. 2016 April 8. doi: 10.1017/S0950268816000674).
The study results suggested that health insurance claims data for MRSA cases were more useful for determining the incidence of MRSA cases in Japan from 2011 to 2012. For example, of the 2,052 eligible hospitals with 200 or more beds in 2011, roughly one-quarter (495, 23.8%) participated in the Japan Nosocomial Infections Surveillance system. Data from this relatively low percentage of eligible facilities most likely underestimated the true number of MRSA patients in Japan, the authors said.
Based on their findings, the investigators noted three major advantages of using health insurance claims data for infection surveillance. Firstly, information from health insurance claims data is not affected by health care providers’ notifications to surveillance systems. Secondly, data on patients with MRSA can be collected at low cost because of Japan’s uniform and computerized health insurance system, and the data are easy to access. Lastly, health insurance claims data prevent the duplication of patient information, as insurers can determine if a patient was treated at multiple medical facilities for the same disease.
The only noted drawback involving the use of health insurance claims data for infection surveillance pertained to its timeliness, the researchers wrote. This issue arises because these data are submitted monthly rather than immediately, which may limit their use in surveillance systems.
According to Dr. Tanihara and Dr. Suzuki, strengths of the study include its evaluation of sentinel surveillance quality through the use of data that were not based on physician reports, as well as the calculation of MRSA incidence by use of a standardized definition in a specific population. Reported limitations included the assessment of anti-MRSA medicine use and patients’ age only, and the lack of information on the degree of drug resistance from health insurance claims data.
Funding was provided by the Ministry of Health, Labour, and Welfare of Japan, and by the Research Programme on Emerging and Re-emerging Infectious Diseases from the Japan Agency for Medical Research and Development. Neither author reported any conflicts of interest.
Key clinical point: Sentinel surveillance systems may substantially underestimate the number of methicillin-resistant Staphylococcus aureus cases in Japan.
Major finding: Direct notification to the Japan Nosocomial Infections Surveillance system regarding methicillin-resistant Staphylococcus aureus patients was not affected by patients’ age, and information from health insurance claims was useful for evaluation of the sentinel infection surveillance system.
Data sources: The Japan Nosocomial Infections Surveillance system and the National Health Insurance Organization.
Disclosures: Funding was provided by the Ministry of Health, Labour, and Welfare of Japan, and by the Research Programme on Emerging and Re-emerging Infectious Diseases from the Japan Agency for Medical Research and Development. Neither author reported any conflicts of interest.
Aesthetic Dermatology: Effects of climate change on skin
Global climate appears to be changing at an unprecedented rate. Climate change can be caused by many factors, including variations in solar radiation received by the earth, oceanic circulation, plate tectonics, as well as human-induced alterations of the natural world. Many human activities, such as the use of fossil fuel and the consequent accumulation of greenhouse gases in the atmosphere, land consumption, deforestation, industrial processes, as well as some agriculture practices, are contributing to global climate change. Many have reported on the current trend toward global warming (average surface temperature has augmented by 0.6°C over the past 100 years), decreased precipitation, atmospheric humidity changes, and the rise in global extreme climatic events. The magnitude and cause of these changes and their impact on human activity have become important matters of debate worldwide, representing climate change as one of the greatest challenges of the modern age.
Although many articles have been written based on observations and various predictive models of how climate change could affect social, economic, and health systems, only a few studies exist about the effects of this change on skin and skin disease. However, the skin is the most highly exposed organ to the environment; therefore, cutaneous conditions are inclined to respond to changes in climate.
Skin cancer
The World Health Organization predicts that the depletion of the ozone layer could lead to further increased rates of melanoma and nonmelanoma skin cancer. In humans, it has been speculated that a long-term rise of temperature by 2°C could increase the carcinogenic effectiveness of solar UV by 10%.
Strictly speaking, stratospheric ozone depletion is not part of “global climate change,” which occurs in the troposphere. There are, however, several recently described interactions between ozone depletion and greenhouse gas–induced warming. Stratospheric ozone absorbs much of the incoming solar ultraviolet radiation, especially the biologically more damaging, shorter-wavelength UVB wavelengths. We now know that various industrial halogenated chemicals such as the chlorofluorocarbons or CFCs (used in refrigeration, insulation, and spray-can propellants) and methyl bromide, while inert at ambient Earth-surface temperatures, react with ozone in the extremely cold polar stratosphere. This destruction of ozone occurs especially in late winter and early spring.
During the 1980s and 1990s at northern midlatitudes (such as Europe), the average year-round ozone concentration declined by around 4% per decade; over the southern regions of Australia, New Zealand, Argentina, and South Africa, the figure approximated 6%-7%. UV exposures at northern midlatitudes are likely to peak around 2020, with an estimated 10% increase in effective ultraviolet radiation relative to 1980s levels.
The modeling of future ozone levels and UV radiation (UVR) exposures has estimated that, in consequence, a ‘European’ population living at around 45 degrees North will experience, by 2050, an approximate 5% excess of total skin cancer incidence (assuming, conservatively, no change in age distribution). The equivalent estimation for the U.S. population is for a 10% increase in skin cancer incidence by around 2050.
In the mid-1980s, governments recognized the emerging hazard from ozone depletion. The Montreal Protocol of 1987 was adopted, and the phasing out of major ozone-destroying gases began. Some anticipate a slow but near-complete recovery of stratospheric ozone by the middle of the twenty-first century; the Environmental Protection Agency (EPA) estimates recovery by 2065 with strict adherence to protection protocols.
Increased exposure to UVR also leads to increased rates of lens opacification, cataracts, and whole-body immunosuppression. UVR-induced immunosuppression could influence patterns of infectious disease. It may also influence the occurrence and progression of various autoimmune diseases and, less certainly, vaccine efficacy.
Extreme weather events
The International Society of Dermatology Task Force on Climate Change reports that weather phenomena such as El Niño also result in changes to dermatologic conditions. The El Niño Southern Oscillation (ENSO) is a complex climate phenomenon occurring in the Pacific Ocean at intervals of 2-7 years. The term refers to fluctuations in ocean temperatures in the tropical eastern Pacific Ocean (El Niño, the warm phase of ENSO, and La Niña, the cool phase of ENSO) and in atmospheric pressure across the Pacific basin (Southern Oscillation). This weather pattern is attributed with causing climate change in certain parts of the world and is associated with disease outbreaks.
El Niño has been associated with increases in the occurrence of actinic keratosis, tinea, pityriasis versicolor, miliaria, folliculitis, rosacea, dermatitis caused by Paederus irritans and Paederus sabaeus, and certain vector-borne and waterborne diseases (such as dengue fever, leishmaniasis, Chagas disease, Barmah Forest virus, and leptospirosis), and with decreases in the occurrence of dermatitis, scabies, psoriasis, and papular urticaria. La Niña has been associated with increases in the occurrence of varicella; hand, foot, and mouth disease; and Ross River virus (in certain areas), and decreases in viral warts and leishmaniasis.
Separately, global warming is expected to affect the start, duration, and intensity of the pollen season, and secondarily the rate of asthma exacerbations due to air pollution, respiratory infections, and/or cold air inhalation, with probable increases in eczema and other atopy-related conditions as well.
Vector-borne diseases
In the past year, the largest Ebola virus outbreak in West Africa has resulted in importation of the virus to other countries and secondary local transmission. Autochthonous transmission of Chikungunya virus has occurred in nonendemic areas, including Europe, the Caribbean, and the Americas. Zika virus has re-emerged in the Pacific with local transmission from imported cases. Climate change, deforestation, and changes in precipitation have been linked to variations in the geographical distribution of vectors of some infectious diseases (leishmaniasis, Lyme disease, and now Zika virus) by changing their spread. A warm and humid environment from global warming can also encourage the colonization of the skin by bacteria and fungi.
Finally, there is a wider, ecological dimension to consider. UV radiation impairs the molecular chemistry of photosynthesis both on land (terrestrial plants) and at sea (phytoplankton). This could affect world food production, at least marginally, and thus contribute to nutritional and health problems in food-insecure populations.
Another reason of many, but from a dermatologist’s point of view, to be mindful of taking care of the planet and our environment.
References
1. World Health Organization (WHO).
2. Photochem Photobiol Sci. 2002 May;1(5):324-6.
3. G Ital Dermatol Venereol. 2013 Feb;148(1):135-46.
4. Int J Dermatol. 2012 Jun;51(6):656-61.
5. Int J Dermatol. 2015 Dec;54(12):1343-51.
6. Curr Opin Infect Dis. 2015 Apr;28(2):139-50.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Wesley. Write to them at [email protected].
Global climate appears to be changing at an unprecedented rate. Climate change can be caused by many factors, including variations in solar radiation received by the earth, oceanic circulation, plate tectonics, as well as human-induced alterations of the natural world. Many human activities, such as the use of fossil fuel and the consequent accumulation of greenhouse gases in the atmosphere, land consumption, deforestation, industrial processes, as well as some agriculture practices, are contributing to global climate change. Many have reported on the current trend toward global warming (average surface temperature has augmented by 0.6°C over the past 100 years), decreased precipitation, atmospheric humidity changes, and the rise in global extreme climatic events. The magnitude and cause of these changes and their impact on human activity have become important matters of debate worldwide, representing climate change as one of the greatest challenges of the modern age.
Although many articles have been written based on observations and various predictive models of how climate change could affect social, economic, and health systems, only a few studies exist about the effects of this change on skin and skin disease. However, the skin is the most highly exposed organ to the environment; therefore, cutaneous conditions are inclined to respond to changes in climate.
Skin cancer
The World Health Organization predicts that the depletion of the ozone layer could lead to further increased rates of melanoma and nonmelanoma skin cancer. In humans, it has been speculated that a long-term rise of temperature by 2°C could increase the carcinogenic effectiveness of solar UV by 10%.
Strictly speaking, stratospheric ozone depletion is not part of “global climate change,” which occurs in the troposphere. There are, however, several recently described interactions between ozone depletion and greenhouse gas–induced warming. Stratospheric ozone absorbs much of the incoming solar ultraviolet radiation, especially the biologically more damaging, shorter-wavelength UVB wavelengths. We now know that various industrial halogenated chemicals such as the chlorofluorocarbons or CFCs (used in refrigeration, insulation, and spray-can propellants) and methyl bromide, while inert at ambient Earth-surface temperatures, react with ozone in the extremely cold polar stratosphere. This destruction of ozone occurs especially in late winter and early spring.
During the 1980s and 1990s at northern midlatitudes (such as Europe), the average year-round ozone concentration declined by around 4% per decade; over the southern regions of Australia, New Zealand, Argentina, and South Africa, the figure approximated 6%-7%. UV exposures at northern midlatitudes are likely to peak around 2020, with an estimated 10% increase in effective ultraviolet radiation relative to 1980s levels.
The modeling of future ozone levels and UV radiation (UVR) exposures has estimated that, in consequence, a ‘European’ population living at around 45 degrees North will experience, by 2050, an approximate 5% excess of total skin cancer incidence (assuming, conservatively, no change in age distribution). The equivalent estimation for the U.S. population is for a 10% increase in skin cancer incidence by around 2050.
In the mid-1980s, governments recognized the emerging hazard from ozone depletion. The Montreal Protocol of 1987 was adopted, and the phasing out of major ozone-destroying gases began. Some anticipate a slow but near-complete recovery of stratospheric ozone by the middle of the twenty-first century; the Environmental Protection Agency (EPA) estimates recovery by 2065 with strict adherence to protection protocols.
Increased exposure to UVR also leads to increased rates of lens opacification, cataracts, and whole-body immunosuppression. UVR-induced immunosuppression could influence patterns of infectious disease. It may also influence the occurrence and progression of various autoimmune diseases and, less certainly, vaccine efficacy.
Extreme weather events
The International Society of Dermatology Task Force on Climate Change reports that weather phenomena such as El Niño also result in changes to dermatologic conditions. The El Niño Southern Oscillation (ENSO) is a complex climate phenomenon occurring in the Pacific Ocean at intervals of 2-7 years. The term refers to fluctuations in ocean temperatures in the tropical eastern Pacific Ocean (El Niño, the warm phase of ENSO, and La Niña, the cool phase of ENSO) and in atmospheric pressure across the Pacific basin (Southern Oscillation). This weather pattern is attributed with causing climate change in certain parts of the world and is associated with disease outbreaks.
El Niño has been associated with increases in the occurrence of actinic keratosis, tinea, pityriasis versicolor, miliaria, folliculitis, rosacea, dermatitis caused by Paederus irritans and Paederus sabaeus, and certain vector-borne and waterborne diseases (such as dengue fever, leishmaniasis, Chagas disease, Barmah Forest virus, and leptospirosis), and with decreases in the occurrence of dermatitis, scabies, psoriasis, and papular urticaria. La Niña has been associated with increases in the occurrence of varicella; hand, foot, and mouth disease; and Ross River virus (in certain areas), and decreases in viral warts and leishmaniasis.
Separately, global warming is expected to affect the start, duration, and intensity of the pollen season, and secondarily the rate of asthma exacerbations due to air pollution, respiratory infections, and/or cold air inhalation, with probable increases in eczema and other atopy-related conditions as well.
Vector-borne diseases
In the past year, the largest Ebola virus outbreak in West Africa has resulted in importation of the virus to other countries and secondary local transmission. Autochthonous transmission of Chikungunya virus has occurred in nonendemic areas, including Europe, the Caribbean, and the Americas. Zika virus has re-emerged in the Pacific with local transmission from imported cases. Climate change, deforestation, and changes in precipitation have been linked to variations in the geographical distribution of vectors of some infectious diseases (leishmaniasis, Lyme disease, and now Zika virus) by changing their spread. A warm and humid environment from global warming can also encourage the colonization of the skin by bacteria and fungi.
Finally, there is a wider, ecological dimension to consider. UV radiation impairs the molecular chemistry of photosynthesis both on land (terrestrial plants) and at sea (phytoplankton). This could affect world food production, at least marginally, and thus contribute to nutritional and health problems in food-insecure populations.
Another reason of many, but from a dermatologist’s point of view, to be mindful of taking care of the planet and our environment.
References
1. World Health Organization (WHO).
2. Photochem Photobiol Sci. 2002 May;1(5):324-6.
3. G Ital Dermatol Venereol. 2013 Feb;148(1):135-46.
4. Int J Dermatol. 2012 Jun;51(6):656-61.
5. Int J Dermatol. 2015 Dec;54(12):1343-51.
6. Curr Opin Infect Dis. 2015 Apr;28(2):139-50.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Wesley. Write to them at [email protected].
Global climate appears to be changing at an unprecedented rate. Climate change can be caused by many factors, including variations in solar radiation received by the earth, oceanic circulation, plate tectonics, as well as human-induced alterations of the natural world. Many human activities, such as the use of fossil fuel and the consequent accumulation of greenhouse gases in the atmosphere, land consumption, deforestation, industrial processes, as well as some agriculture practices, are contributing to global climate change. Many have reported on the current trend toward global warming (average surface temperature has augmented by 0.6°C over the past 100 years), decreased precipitation, atmospheric humidity changes, and the rise in global extreme climatic events. The magnitude and cause of these changes and their impact on human activity have become important matters of debate worldwide, representing climate change as one of the greatest challenges of the modern age.
Although many articles have been written based on observations and various predictive models of how climate change could affect social, economic, and health systems, only a few studies exist about the effects of this change on skin and skin disease. However, the skin is the most highly exposed organ to the environment; therefore, cutaneous conditions are inclined to respond to changes in climate.
Skin cancer
The World Health Organization predicts that the depletion of the ozone layer could lead to further increased rates of melanoma and nonmelanoma skin cancer. In humans, it has been speculated that a long-term rise of temperature by 2°C could increase the carcinogenic effectiveness of solar UV by 10%.
Strictly speaking, stratospheric ozone depletion is not part of “global climate change,” which occurs in the troposphere. There are, however, several recently described interactions between ozone depletion and greenhouse gas–induced warming. Stratospheric ozone absorbs much of the incoming solar ultraviolet radiation, especially the biologically more damaging, shorter-wavelength UVB wavelengths. We now know that various industrial halogenated chemicals such as the chlorofluorocarbons or CFCs (used in refrigeration, insulation, and spray-can propellants) and methyl bromide, while inert at ambient Earth-surface temperatures, react with ozone in the extremely cold polar stratosphere. This destruction of ozone occurs especially in late winter and early spring.
During the 1980s and 1990s at northern midlatitudes (such as Europe), the average year-round ozone concentration declined by around 4% per decade; over the southern regions of Australia, New Zealand, Argentina, and South Africa, the figure approximated 6%-7%. UV exposures at northern midlatitudes are likely to peak around 2020, with an estimated 10% increase in effective ultraviolet radiation relative to 1980s levels.
The modeling of future ozone levels and UV radiation (UVR) exposures has estimated that, in consequence, a ‘European’ population living at around 45 degrees North will experience, by 2050, an approximate 5% excess of total skin cancer incidence (assuming, conservatively, no change in age distribution). The equivalent estimation for the U.S. population is for a 10% increase in skin cancer incidence by around 2050.
In the mid-1980s, governments recognized the emerging hazard from ozone depletion. The Montreal Protocol of 1987 was adopted, and the phasing out of major ozone-destroying gases began. Some anticipate a slow but near-complete recovery of stratospheric ozone by the middle of the twenty-first century; the Environmental Protection Agency (EPA) estimates recovery by 2065 with strict adherence to protection protocols.
Increased exposure to UVR also leads to increased rates of lens opacification, cataracts, and whole-body immunosuppression. UVR-induced immunosuppression could influence patterns of infectious disease. It may also influence the occurrence and progression of various autoimmune diseases and, less certainly, vaccine efficacy.
Extreme weather events
The International Society of Dermatology Task Force on Climate Change reports that weather phenomena such as El Niño also result in changes to dermatologic conditions. The El Niño Southern Oscillation (ENSO) is a complex climate phenomenon occurring in the Pacific Ocean at intervals of 2-7 years. The term refers to fluctuations in ocean temperatures in the tropical eastern Pacific Ocean (El Niño, the warm phase of ENSO, and La Niña, the cool phase of ENSO) and in atmospheric pressure across the Pacific basin (Southern Oscillation). This weather pattern is attributed with causing climate change in certain parts of the world and is associated with disease outbreaks.
El Niño has been associated with increases in the occurrence of actinic keratosis, tinea, pityriasis versicolor, miliaria, folliculitis, rosacea, dermatitis caused by Paederus irritans and Paederus sabaeus, and certain vector-borne and waterborne diseases (such as dengue fever, leishmaniasis, Chagas disease, Barmah Forest virus, and leptospirosis), and with decreases in the occurrence of dermatitis, scabies, psoriasis, and papular urticaria. La Niña has been associated with increases in the occurrence of varicella; hand, foot, and mouth disease; and Ross River virus (in certain areas), and decreases in viral warts and leishmaniasis.
Separately, global warming is expected to affect the start, duration, and intensity of the pollen season, and secondarily the rate of asthma exacerbations due to air pollution, respiratory infections, and/or cold air inhalation, with probable increases in eczema and other atopy-related conditions as well.
Vector-borne diseases
In the past year, the largest Ebola virus outbreak in West Africa has resulted in importation of the virus to other countries and secondary local transmission. Autochthonous transmission of Chikungunya virus has occurred in nonendemic areas, including Europe, the Caribbean, and the Americas. Zika virus has re-emerged in the Pacific with local transmission from imported cases. Climate change, deforestation, and changes in precipitation have been linked to variations in the geographical distribution of vectors of some infectious diseases (leishmaniasis, Lyme disease, and now Zika virus) by changing their spread. A warm and humid environment from global warming can also encourage the colonization of the skin by bacteria and fungi.
Finally, there is a wider, ecological dimension to consider. UV radiation impairs the molecular chemistry of photosynthesis both on land (terrestrial plants) and at sea (phytoplankton). This could affect world food production, at least marginally, and thus contribute to nutritional and health problems in food-insecure populations.
Another reason of many, but from a dermatologist’s point of view, to be mindful of taking care of the planet and our environment.
References
1. World Health Organization (WHO).
2. Photochem Photobiol Sci. 2002 May;1(5):324-6.
3. G Ital Dermatol Venereol. 2013 Feb;148(1):135-46.
4. Int J Dermatol. 2012 Jun;51(6):656-61.
5. Int J Dermatol. 2015 Dec;54(12):1343-51.
6. Curr Opin Infect Dis. 2015 Apr;28(2):139-50.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Wesley. Write to them at [email protected].
RSS feeds
In my last column, I mentioned RSS news feeds as a useful, versatile online tool. As my editor later reminded me, however, it has been over a decade since I’ve discussed RSS feeds – so an update is certainly in order.
The sheer volume of information on the web makes quick and efficient searching an indispensable skill, but once you become quick and efficient at finding the information you need, a new problem arises: The information changes! All the good medical, news, and other information-based websites change and update their content on a regular but unpredictable basis. And checking each one for new information can be very tedious, if you can remember to do it at all.
Many sites offer an email service to notify you of new content, but multiple email subscriptions clutter your inbox and often can’t select out the information you’re really interested in. RSS feeds are a more efficient and increasingly popular method of staying current on all the subjects that interest you – medical and otherwise. RSS (which stands for Rich Site Summary or Really Simple Syndication, depending on whom you ask) is a file format that websites use (or a similar one called Atom) to produce a summary file, or “feed,” of new content, along with links to full versions of that content. When you subscribe to a given website’s feed, you’ll receive a summary of new content each time the website is updated.
Thousands of websites now offer RSS feeds, including most of the large medical information services, all the major news organizations, and many web logs.
To subscribe to feeds, you must download a program called a feed reader, which is basically just a browser specializing in RSS and Atom files. Dozens of readers (also known as aggregators) are available. Some can be accessed through browsers, others are integrated into email programs, and still others run as standalone applications. With the rise of cloud computing, some cloud-based services offer feed aggregation as part of their service.
Many readers are free, but those with the most advanced features usually come with a fee of some sort. (As always, I have no financial interest in any enterprise discussed in this column.) A comprehensive list of available readers can be found in the Wikipedia article “Comparison of Feed Aggregators.”
It’s not always easy to find out whether a particular website offers a feed, because there is no universally recognized method of indicating its existence. Look for a link to “RSS” or “Syndicate This,” or an orange rectangle with the letters “RSS” or “XML” (don’t ask). These links are not always on the home page. You may need to consult the site map to find a link to a page explaining available feeds and how to find them.
Some of the major sites have multiple feeds to choose from. For example, you can generate a feed of current stories related to the page that you are following on Google News by clicking the RSS link on any Google News page.
Once you know the URL of the RSS feed you want, you provide it to your reader program, which will monitor the feed for you. (Many RSS aggregators come preconfigured with a list of feed URLs for popular news websites.)
In addition to notifying you of important news headlines, changes to your favorite websites, and new developments in any medical (or other) field of interest to you, RSS feeds have many other uses. Some will notify you of new products in a store or catalog, new newsletter issues (including email newsletters), weather and other changing-condition alerts, and the addition of new items to a database – or new members to a group.
It can work the other way as well: If you want readers of your website, blog, or podcast to receive the latest news about your practice, such as new treatments and procedures you’re offering – or if you want to know immediately anytime your name pops up in news or gossip sites – you can create your own RSS feed. In my next column, I’ll explain exactly how to do that.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
In my last column, I mentioned RSS news feeds as a useful, versatile online tool. As my editor later reminded me, however, it has been over a decade since I’ve discussed RSS feeds – so an update is certainly in order.
The sheer volume of information on the web makes quick and efficient searching an indispensable skill, but once you become quick and efficient at finding the information you need, a new problem arises: The information changes! All the good medical, news, and other information-based websites change and update their content on a regular but unpredictable basis. And checking each one for new information can be very tedious, if you can remember to do it at all.
Many sites offer an email service to notify you of new content, but multiple email subscriptions clutter your inbox and often can’t select out the information you’re really interested in. RSS feeds are a more efficient and increasingly popular method of staying current on all the subjects that interest you – medical and otherwise. RSS (which stands for Rich Site Summary or Really Simple Syndication, depending on whom you ask) is a file format that websites use (or a similar one called Atom) to produce a summary file, or “feed,” of new content, along with links to full versions of that content. When you subscribe to a given website’s feed, you’ll receive a summary of new content each time the website is updated.
Thousands of websites now offer RSS feeds, including most of the large medical information services, all the major news organizations, and many web logs.
To subscribe to feeds, you must download a program called a feed reader, which is basically just a browser specializing in RSS and Atom files. Dozens of readers (also known as aggregators) are available. Some can be accessed through browsers, others are integrated into email programs, and still others run as standalone applications. With the rise of cloud computing, some cloud-based services offer feed aggregation as part of their service.
Many readers are free, but those with the most advanced features usually come with a fee of some sort. (As always, I have no financial interest in any enterprise discussed in this column.) A comprehensive list of available readers can be found in the Wikipedia article “Comparison of Feed Aggregators.”
It’s not always easy to find out whether a particular website offers a feed, because there is no universally recognized method of indicating its existence. Look for a link to “RSS” or “Syndicate This,” or an orange rectangle with the letters “RSS” or “XML” (don’t ask). These links are not always on the home page. You may need to consult the site map to find a link to a page explaining available feeds and how to find them.
Some of the major sites have multiple feeds to choose from. For example, you can generate a feed of current stories related to the page that you are following on Google News by clicking the RSS link on any Google News page.
Once you know the URL of the RSS feed you want, you provide it to your reader program, which will monitor the feed for you. (Many RSS aggregators come preconfigured with a list of feed URLs for popular news websites.)
In addition to notifying you of important news headlines, changes to your favorite websites, and new developments in any medical (or other) field of interest to you, RSS feeds have many other uses. Some will notify you of new products in a store or catalog, new newsletter issues (including email newsletters), weather and other changing-condition alerts, and the addition of new items to a database – or new members to a group.
It can work the other way as well: If you want readers of your website, blog, or podcast to receive the latest news about your practice, such as new treatments and procedures you’re offering – or if you want to know immediately anytime your name pops up in news or gossip sites – you can create your own RSS feed. In my next column, I’ll explain exactly how to do that.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
In my last column, I mentioned RSS news feeds as a useful, versatile online tool. As my editor later reminded me, however, it has been over a decade since I’ve discussed RSS feeds – so an update is certainly in order.
The sheer volume of information on the web makes quick and efficient searching an indispensable skill, but once you become quick and efficient at finding the information you need, a new problem arises: The information changes! All the good medical, news, and other information-based websites change and update their content on a regular but unpredictable basis. And checking each one for new information can be very tedious, if you can remember to do it at all.
Many sites offer an email service to notify you of new content, but multiple email subscriptions clutter your inbox and often can’t select out the information you’re really interested in. RSS feeds are a more efficient and increasingly popular method of staying current on all the subjects that interest you – medical and otherwise. RSS (which stands for Rich Site Summary or Really Simple Syndication, depending on whom you ask) is a file format that websites use (or a similar one called Atom) to produce a summary file, or “feed,” of new content, along with links to full versions of that content. When you subscribe to a given website’s feed, you’ll receive a summary of new content each time the website is updated.
Thousands of websites now offer RSS feeds, including most of the large medical information services, all the major news organizations, and many web logs.
To subscribe to feeds, you must download a program called a feed reader, which is basically just a browser specializing in RSS and Atom files. Dozens of readers (also known as aggregators) are available. Some can be accessed through browsers, others are integrated into email programs, and still others run as standalone applications. With the rise of cloud computing, some cloud-based services offer feed aggregation as part of their service.
Many readers are free, but those with the most advanced features usually come with a fee of some sort. (As always, I have no financial interest in any enterprise discussed in this column.) A comprehensive list of available readers can be found in the Wikipedia article “Comparison of Feed Aggregators.”
It’s not always easy to find out whether a particular website offers a feed, because there is no universally recognized method of indicating its existence. Look for a link to “RSS” or “Syndicate This,” or an orange rectangle with the letters “RSS” or “XML” (don’t ask). These links are not always on the home page. You may need to consult the site map to find a link to a page explaining available feeds and how to find them.
Some of the major sites have multiple feeds to choose from. For example, you can generate a feed of current stories related to the page that you are following on Google News by clicking the RSS link on any Google News page.
Once you know the URL of the RSS feed you want, you provide it to your reader program, which will monitor the feed for you. (Many RSS aggregators come preconfigured with a list of feed URLs for popular news websites.)
In addition to notifying you of important news headlines, changes to your favorite websites, and new developments in any medical (or other) field of interest to you, RSS feeds have many other uses. Some will notify you of new products in a store or catalog, new newsletter issues (including email newsletters), weather and other changing-condition alerts, and the addition of new items to a database – or new members to a group.
It can work the other way as well: If you want readers of your website, blog, or podcast to receive the latest news about your practice, such as new treatments and procedures you’re offering – or if you want to know immediately anytime your name pops up in news or gossip sites – you can create your own RSS feed. In my next column, I’ll explain exactly how to do that.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
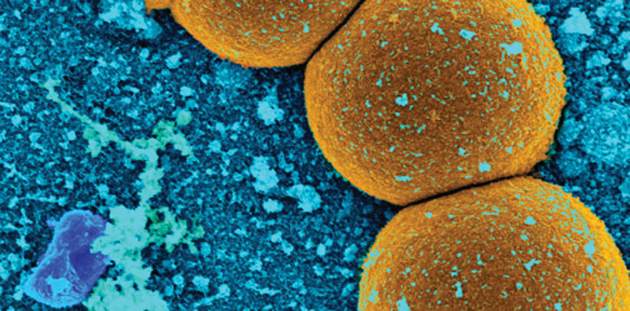
VIDEO: Del Nido cardioplegic solution receives high grade
BALTIMORE – A cardioplegic solution developed by a noted cardiac surgeon has been deemed a “simple and safe” cardio protective strategy in a study presented at the annual meeting of the American Association for Thoracic Surgery.
In an interview at the event, Pedro J. del Nido, MD, chief of cardiac surgery at Boston Children’s Hospital, and inventor of the long-acting Del Nido solution, explained how and why he and his colleagues developed the new cardioplegic solution. He praised the study as uniquely important, given that there have been few prospective, randomized, and controlled comparative studies of cardioplegia targeted at pediatric patients.
“Baby hearts have a slightly different metabolism than adult hearts,” Dr. del Nido said. “Typically in pediatric procedures we not only cool the heart but we lower the whole body temperature... In the adult world we don’t drop the temperature so much.” He also said the method and flow rate of cardioplegia delivery was unique for pediatric patients, given the fragility of the endothelial cells lining their blood vessels.
The study compared the Del Nido solution with the St. Thomas cardioplegia solution. The investigators praised the Del Nido solution’s performance for “better cardiac index profile, lesser troponin-I release, and decreased morbidity.”
Dr. del Nido developed the Del Nido cardioplegic solution, but reported no other relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – A cardioplegic solution developed by a noted cardiac surgeon has been deemed a “simple and safe” cardio protective strategy in a study presented at the annual meeting of the American Association for Thoracic Surgery.
In an interview at the event, Pedro J. del Nido, MD, chief of cardiac surgery at Boston Children’s Hospital, and inventor of the long-acting Del Nido solution, explained how and why he and his colleagues developed the new cardioplegic solution. He praised the study as uniquely important, given that there have been few prospective, randomized, and controlled comparative studies of cardioplegia targeted at pediatric patients.
“Baby hearts have a slightly different metabolism than adult hearts,” Dr. del Nido said. “Typically in pediatric procedures we not only cool the heart but we lower the whole body temperature... In the adult world we don’t drop the temperature so much.” He also said the method and flow rate of cardioplegia delivery was unique for pediatric patients, given the fragility of the endothelial cells lining their blood vessels.
The study compared the Del Nido solution with the St. Thomas cardioplegia solution. The investigators praised the Del Nido solution’s performance for “better cardiac index profile, lesser troponin-I release, and decreased morbidity.”
Dr. del Nido developed the Del Nido cardioplegic solution, but reported no other relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – A cardioplegic solution developed by a noted cardiac surgeon has been deemed a “simple and safe” cardio protective strategy in a study presented at the annual meeting of the American Association for Thoracic Surgery.
In an interview at the event, Pedro J. del Nido, MD, chief of cardiac surgery at Boston Children’s Hospital, and inventor of the long-acting Del Nido solution, explained how and why he and his colleagues developed the new cardioplegic solution. He praised the study as uniquely important, given that there have been few prospective, randomized, and controlled comparative studies of cardioplegia targeted at pediatric patients.
“Baby hearts have a slightly different metabolism than adult hearts,” Dr. del Nido said. “Typically in pediatric procedures we not only cool the heart but we lower the whole body temperature... In the adult world we don’t drop the temperature so much.” He also said the method and flow rate of cardioplegia delivery was unique for pediatric patients, given the fragility of the endothelial cells lining their blood vessels.
The study compared the Del Nido solution with the St. Thomas cardioplegia solution. The investigators praised the Del Nido solution’s performance for “better cardiac index profile, lesser troponin-I release, and decreased morbidity.”
Dr. del Nido developed the Del Nido cardioplegic solution, but reported no other relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
AT THE AATS ANNUAL MEETING
Primary small cell cancer of the anus rare, but devastating
LOS ANGELES – Primary small cell cancer of the anus is a rare but devastating condition and overall survival may not be improved with surgical treatment.
Those are key findings from what is believed to be the largest analysis of its kind to date.
“There are very limited data for patients with anal small cell cancers who need preoperative counseling and risk stratification,” study author Dr. Cornelius A. Thiels said in an interview at the annual meeting of the American Society of Colon and Rectal Surgeons. “There are also no data to guide treatment, so, until now, management was based on the treatment of small cell of the lung, and other anal cancers.”
Cancers of the anal canal are estimated to represent about 2.5% of all gastrointestinal neoplasms, while primary small cell cancer of the anus is believed to account for less than 1% of all anal neoplasms, according to Dr. Thiels, who is a third-year general surgery resident in the department of surgery and a surgical outcomes fellow in the Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery at the Mayo Clinic, Rochester, Minn.
In an effort to evaluate the outcomes of patients with primary small cell cancer of the anus, the researchers reviewed their own institutional experience in treating nine patients with this condition between from 1994-2014, as well as National Cancer Data Base (NCDB) records of 174 patients from 1998-2014. The NCDB is maintained by collecting data prospectively from more than 1,500 facilities across the United States and is estimated to capture approximately 70% of all newly diagnosed cases of cancer annually. Institutional data allowed the researchers to identify details, including how these patients presented and what type of chemotherapy they received. However, analysis of a national database was necessary given the rarity of the diagnosis.
In the analysis of NCDB records, the mean patient age was 59 years and 74% were female. Most of the tumors (95%) were high grade and the majority of patients presented with advanced disease (50 with stage IV disease, 49 with stage III disease, 29 with stage II disease, 25 with stage I disease, and 21 with unknown stage). Overall survival was 66% at 12 months and 29% at 36 months. Among patients with stage I-III disease, survival was 72% at 12 months and 39% at 36 months.
Of the 103 patients with stage I-III disease, 95% received medical therapy, 70% underwent medical management alone, while 30% underwent surgery with curative intent. Patients who did not undergo surgery tended to have a higher stage of disease, compared with those who did (57% vs. 26%: P = .005). Overall survival at 36 months was similar between the two groups (33.9% in the surgery group vs. 35.8% in the no surgery group; P = .87).
“Unfortunately, it seems from our own experience and from national data that additional research is needed to determine how best to treat these patients and that surgery may not prolong survival in many of these patients,” Dr. Thiels said. “Although additional research is needed to optimize outcomes for these patients, harnessing the power of a national cancer database like the NCDB allows us to improve our understanding of these otherwise extremely rare, and difficult to study, tumors.”
Dr. Thiels reported having no financial disclosures.
LOS ANGELES – Primary small cell cancer of the anus is a rare but devastating condition and overall survival may not be improved with surgical treatment.
Those are key findings from what is believed to be the largest analysis of its kind to date.
“There are very limited data for patients with anal small cell cancers who need preoperative counseling and risk stratification,” study author Dr. Cornelius A. Thiels said in an interview at the annual meeting of the American Society of Colon and Rectal Surgeons. “There are also no data to guide treatment, so, until now, management was based on the treatment of small cell of the lung, and other anal cancers.”
Cancers of the anal canal are estimated to represent about 2.5% of all gastrointestinal neoplasms, while primary small cell cancer of the anus is believed to account for less than 1% of all anal neoplasms, according to Dr. Thiels, who is a third-year general surgery resident in the department of surgery and a surgical outcomes fellow in the Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery at the Mayo Clinic, Rochester, Minn.
In an effort to evaluate the outcomes of patients with primary small cell cancer of the anus, the researchers reviewed their own institutional experience in treating nine patients with this condition between from 1994-2014, as well as National Cancer Data Base (NCDB) records of 174 patients from 1998-2014. The NCDB is maintained by collecting data prospectively from more than 1,500 facilities across the United States and is estimated to capture approximately 70% of all newly diagnosed cases of cancer annually. Institutional data allowed the researchers to identify details, including how these patients presented and what type of chemotherapy they received. However, analysis of a national database was necessary given the rarity of the diagnosis.
In the analysis of NCDB records, the mean patient age was 59 years and 74% were female. Most of the tumors (95%) were high grade and the majority of patients presented with advanced disease (50 with stage IV disease, 49 with stage III disease, 29 with stage II disease, 25 with stage I disease, and 21 with unknown stage). Overall survival was 66% at 12 months and 29% at 36 months. Among patients with stage I-III disease, survival was 72% at 12 months and 39% at 36 months.
Of the 103 patients with stage I-III disease, 95% received medical therapy, 70% underwent medical management alone, while 30% underwent surgery with curative intent. Patients who did not undergo surgery tended to have a higher stage of disease, compared with those who did (57% vs. 26%: P = .005). Overall survival at 36 months was similar between the two groups (33.9% in the surgery group vs. 35.8% in the no surgery group; P = .87).
“Unfortunately, it seems from our own experience and from national data that additional research is needed to determine how best to treat these patients and that surgery may not prolong survival in many of these patients,” Dr. Thiels said. “Although additional research is needed to optimize outcomes for these patients, harnessing the power of a national cancer database like the NCDB allows us to improve our understanding of these otherwise extremely rare, and difficult to study, tumors.”
Dr. Thiels reported having no financial disclosures.
LOS ANGELES – Primary small cell cancer of the anus is a rare but devastating condition and overall survival may not be improved with surgical treatment.
Those are key findings from what is believed to be the largest analysis of its kind to date.
“There are very limited data for patients with anal small cell cancers who need preoperative counseling and risk stratification,” study author Dr. Cornelius A. Thiels said in an interview at the annual meeting of the American Society of Colon and Rectal Surgeons. “There are also no data to guide treatment, so, until now, management was based on the treatment of small cell of the lung, and other anal cancers.”
Cancers of the anal canal are estimated to represent about 2.5% of all gastrointestinal neoplasms, while primary small cell cancer of the anus is believed to account for less than 1% of all anal neoplasms, according to Dr. Thiels, who is a third-year general surgery resident in the department of surgery and a surgical outcomes fellow in the Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery at the Mayo Clinic, Rochester, Minn.
In an effort to evaluate the outcomes of patients with primary small cell cancer of the anus, the researchers reviewed their own institutional experience in treating nine patients with this condition between from 1994-2014, as well as National Cancer Data Base (NCDB) records of 174 patients from 1998-2014. The NCDB is maintained by collecting data prospectively from more than 1,500 facilities across the United States and is estimated to capture approximately 70% of all newly diagnosed cases of cancer annually. Institutional data allowed the researchers to identify details, including how these patients presented and what type of chemotherapy they received. However, analysis of a national database was necessary given the rarity of the diagnosis.
In the analysis of NCDB records, the mean patient age was 59 years and 74% were female. Most of the tumors (95%) were high grade and the majority of patients presented with advanced disease (50 with stage IV disease, 49 with stage III disease, 29 with stage II disease, 25 with stage I disease, and 21 with unknown stage). Overall survival was 66% at 12 months and 29% at 36 months. Among patients with stage I-III disease, survival was 72% at 12 months and 39% at 36 months.
Of the 103 patients with stage I-III disease, 95% received medical therapy, 70% underwent medical management alone, while 30% underwent surgery with curative intent. Patients who did not undergo surgery tended to have a higher stage of disease, compared with those who did (57% vs. 26%: P = .005). Overall survival at 36 months was similar between the two groups (33.9% in the surgery group vs. 35.8% in the no surgery group; P = .87).
“Unfortunately, it seems from our own experience and from national data that additional research is needed to determine how best to treat these patients and that surgery may not prolong survival in many of these patients,” Dr. Thiels said. “Although additional research is needed to optimize outcomes for these patients, harnessing the power of a national cancer database like the NCDB allows us to improve our understanding of these otherwise extremely rare, and difficult to study, tumors.”
Dr. Thiels reported having no financial disclosures.
AT THE ASCRS ANNUAL MEETING
Key clinical point: Among patients with primary small cell cancer of the anus, survival was 29% at 36 months.
Major finding: Overall survival among patients with primary small cell cancer of the anus was 66% at 12 months and 29% at 36 months.
Data source: A review of National Cancer Data Base records from 174 patients with primary cell cancer of the anus who were treated from 1998-2014.
Disclosures: Dr. Thiels reported having no financial disclosures.
Serious infections are increasing among psoriasis inpatients
SCOTTSDALE, ARIZ. – From enterocolitis to MRSA, serious infections are on the rise among inpatients with psoriasis, and psoriasis is an independent risk factor for serious infections, according to findings from large retrospective studies from the United States and the United Kingdom.
Inpatients with psoriasis in the United States also were at greater risk of serious infections, compared with nonpsoriatic inpatients at every time point studied, and serious infections were associated with increased hospital costs, length of stay, and risk of mortality, reported Derek Hsu, a medical student at Northwestern University, Chicago, and his associates. “Research is needed to determine how to reduce the risk of serious infections in patients with psoriasis,” the investigators emphasized.
Psoriasis affects some 7 million adults in the United States. Biologics, which are transforming the treatment landscape for moderate-to-severe psoriasis, “should reduce inherent infectious risk by controlling the inflammatory process and reducing disease severity, [but] these effects may be immunosuppressing and increase the risk of infection in other ways,” according to Mr. Hsu and his associates. For their study, they analyzed data for 2002-2012 from the Nationwide Inpatient Sample, which covers 20% of hospitalizations in the United States. They extracted validated ICD-9 codes for psoriasis and serious infections, and calculated costs of care after adjusting for 2014 inflation, based on the United States Consumer Price Index.
Overall rates of serious infection and rates of pneumonia, MRSA, septicemia, diverticulitis, enterocolitis, encephalitis, and any viral or fungal infection rose significantly among inpatients with psoriasis between 2002 and 2012 (all P-values less than .05). Predictors of serious infections among inpatients with psoriasis included diabetes mellitus, obesity, and being of non-Caucasian race or ethnicity, female, older than 60 years, and on Medicare or Medicaid, the researchers reported at the annual meeting of the Society for Investigative Dermatology.
Furthermore, after controlling for age, sex, and race, psoriasis was a significant risk factor for many different types of serious infections. Among these were cellulitis, herpes simplex virus, infectious arthritis, osteomyelitis, meningitis, influenza, encephalitis, septicemia, enterocolitis, MRSA, methicillin-sensitive Staphylococcus aureus infections, and Clostridium difficile. Further, inpatients with psoriasis were more prone to urinary tract infection, peritonitis or intestinal abscess, appendicitis, tuberculosis, and viral and fungal infections (all P-values less than .05). The average cost of hospital stay for inpatients with psoriasis was more than $2,200 greater when they were diagnosed with one or more serious infections than otherwise, and their average length of hospital stay was 2 days longer.
The study in the United Kingdom included nearly 200,000 patients with psoriasis and almost 1 million patients without psoriasis from The Health Improvement Network electronic medical record database. Between 2002 and 2013, patients without psoriasis developed an estimated 78.5 serious infections per 100,000 person-years, compared with 88.9, 85.7, and 145.7 serious infections per 100,000 person-years, respectively, for all psoriasis patients, patients with mild disease, and patients with severe disease requiring systemic or phototherapy, said Dr. Junko Takeshita and her colleagues at the University of Pennsylvania in Philadelphia. After controlling for many potential demographic and clinical confounders, psoriasis increased the risk of serious infection by about 21% (hazard ratio, 1.21; 95% confidence interval, 1.18-1.23). Patients with severe psoriasis had a 63% greater risk of infection than patients without psoriasis, compared with an 18% increase for patients with mild psoriasis.
The findings show “serious infection, particularly respiratory and skin or soft tissue infections, to be an important and common cause of morbidity among patients with psoriasis, especially those with more severe disease,” Dr. Takeshita and her associates said. Notably, the link between psoriasis and risk of serious infection persisted after excluding patients on immunosuppressive therapies, suggesting “that the greater infection risk is at least partially attributable to more severe psoriasis, itself,” they added.
The analysis of Nationwide Inpatient Sample data was funded by the Agency for Healthcare Research and Quality and by the Dermatology Foundation. The analysis of Health Improvement Network data was funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases, which is part of the National Institutes of Health, and by the Dermatology Foundation. None of the investigators reported conflicts of interest.
SCOTTSDALE, ARIZ. – From enterocolitis to MRSA, serious infections are on the rise among inpatients with psoriasis, and psoriasis is an independent risk factor for serious infections, according to findings from large retrospective studies from the United States and the United Kingdom.
Inpatients with psoriasis in the United States also were at greater risk of serious infections, compared with nonpsoriatic inpatients at every time point studied, and serious infections were associated with increased hospital costs, length of stay, and risk of mortality, reported Derek Hsu, a medical student at Northwestern University, Chicago, and his associates. “Research is needed to determine how to reduce the risk of serious infections in patients with psoriasis,” the investigators emphasized.
Psoriasis affects some 7 million adults in the United States. Biologics, which are transforming the treatment landscape for moderate-to-severe psoriasis, “should reduce inherent infectious risk by controlling the inflammatory process and reducing disease severity, [but] these effects may be immunosuppressing and increase the risk of infection in other ways,” according to Mr. Hsu and his associates. For their study, they analyzed data for 2002-2012 from the Nationwide Inpatient Sample, which covers 20% of hospitalizations in the United States. They extracted validated ICD-9 codes for psoriasis and serious infections, and calculated costs of care after adjusting for 2014 inflation, based on the United States Consumer Price Index.
Overall rates of serious infection and rates of pneumonia, MRSA, septicemia, diverticulitis, enterocolitis, encephalitis, and any viral or fungal infection rose significantly among inpatients with psoriasis between 2002 and 2012 (all P-values less than .05). Predictors of serious infections among inpatients with psoriasis included diabetes mellitus, obesity, and being of non-Caucasian race or ethnicity, female, older than 60 years, and on Medicare or Medicaid, the researchers reported at the annual meeting of the Society for Investigative Dermatology.
Furthermore, after controlling for age, sex, and race, psoriasis was a significant risk factor for many different types of serious infections. Among these were cellulitis, herpes simplex virus, infectious arthritis, osteomyelitis, meningitis, influenza, encephalitis, septicemia, enterocolitis, MRSA, methicillin-sensitive Staphylococcus aureus infections, and Clostridium difficile. Further, inpatients with psoriasis were more prone to urinary tract infection, peritonitis or intestinal abscess, appendicitis, tuberculosis, and viral and fungal infections (all P-values less than .05). The average cost of hospital stay for inpatients with psoriasis was more than $2,200 greater when they were diagnosed with one or more serious infections than otherwise, and their average length of hospital stay was 2 days longer.
The study in the United Kingdom included nearly 200,000 patients with psoriasis and almost 1 million patients without psoriasis from The Health Improvement Network electronic medical record database. Between 2002 and 2013, patients without psoriasis developed an estimated 78.5 serious infections per 100,000 person-years, compared with 88.9, 85.7, and 145.7 serious infections per 100,000 person-years, respectively, for all psoriasis patients, patients with mild disease, and patients with severe disease requiring systemic or phototherapy, said Dr. Junko Takeshita and her colleagues at the University of Pennsylvania in Philadelphia. After controlling for many potential demographic and clinical confounders, psoriasis increased the risk of serious infection by about 21% (hazard ratio, 1.21; 95% confidence interval, 1.18-1.23). Patients with severe psoriasis had a 63% greater risk of infection than patients without psoriasis, compared with an 18% increase for patients with mild psoriasis.
The findings show “serious infection, particularly respiratory and skin or soft tissue infections, to be an important and common cause of morbidity among patients with psoriasis, especially those with more severe disease,” Dr. Takeshita and her associates said. Notably, the link between psoriasis and risk of serious infection persisted after excluding patients on immunosuppressive therapies, suggesting “that the greater infection risk is at least partially attributable to more severe psoriasis, itself,” they added.
The analysis of Nationwide Inpatient Sample data was funded by the Agency for Healthcare Research and Quality and by the Dermatology Foundation. The analysis of Health Improvement Network data was funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases, which is part of the National Institutes of Health, and by the Dermatology Foundation. None of the investigators reported conflicts of interest.
SCOTTSDALE, ARIZ. – From enterocolitis to MRSA, serious infections are on the rise among inpatients with psoriasis, and psoriasis is an independent risk factor for serious infections, according to findings from large retrospective studies from the United States and the United Kingdom.
Inpatients with psoriasis in the United States also were at greater risk of serious infections, compared with nonpsoriatic inpatients at every time point studied, and serious infections were associated with increased hospital costs, length of stay, and risk of mortality, reported Derek Hsu, a medical student at Northwestern University, Chicago, and his associates. “Research is needed to determine how to reduce the risk of serious infections in patients with psoriasis,” the investigators emphasized.
Psoriasis affects some 7 million adults in the United States. Biologics, which are transforming the treatment landscape for moderate-to-severe psoriasis, “should reduce inherent infectious risk by controlling the inflammatory process and reducing disease severity, [but] these effects may be immunosuppressing and increase the risk of infection in other ways,” according to Mr. Hsu and his associates. For their study, they analyzed data for 2002-2012 from the Nationwide Inpatient Sample, which covers 20% of hospitalizations in the United States. They extracted validated ICD-9 codes for psoriasis and serious infections, and calculated costs of care after adjusting for 2014 inflation, based on the United States Consumer Price Index.
Overall rates of serious infection and rates of pneumonia, MRSA, septicemia, diverticulitis, enterocolitis, encephalitis, and any viral or fungal infection rose significantly among inpatients with psoriasis between 2002 and 2012 (all P-values less than .05). Predictors of serious infections among inpatients with psoriasis included diabetes mellitus, obesity, and being of non-Caucasian race or ethnicity, female, older than 60 years, and on Medicare or Medicaid, the researchers reported at the annual meeting of the Society for Investigative Dermatology.
Furthermore, after controlling for age, sex, and race, psoriasis was a significant risk factor for many different types of serious infections. Among these were cellulitis, herpes simplex virus, infectious arthritis, osteomyelitis, meningitis, influenza, encephalitis, septicemia, enterocolitis, MRSA, methicillin-sensitive Staphylococcus aureus infections, and Clostridium difficile. Further, inpatients with psoriasis were more prone to urinary tract infection, peritonitis or intestinal abscess, appendicitis, tuberculosis, and viral and fungal infections (all P-values less than .05). The average cost of hospital stay for inpatients with psoriasis was more than $2,200 greater when they were diagnosed with one or more serious infections than otherwise, and their average length of hospital stay was 2 days longer.
The study in the United Kingdom included nearly 200,000 patients with psoriasis and almost 1 million patients without psoriasis from The Health Improvement Network electronic medical record database. Between 2002 and 2013, patients without psoriasis developed an estimated 78.5 serious infections per 100,000 person-years, compared with 88.9, 85.7, and 145.7 serious infections per 100,000 person-years, respectively, for all psoriasis patients, patients with mild disease, and patients with severe disease requiring systemic or phototherapy, said Dr. Junko Takeshita and her colleagues at the University of Pennsylvania in Philadelphia. After controlling for many potential demographic and clinical confounders, psoriasis increased the risk of serious infection by about 21% (hazard ratio, 1.21; 95% confidence interval, 1.18-1.23). Patients with severe psoriasis had a 63% greater risk of infection than patients without psoriasis, compared with an 18% increase for patients with mild psoriasis.
The findings show “serious infection, particularly respiratory and skin or soft tissue infections, to be an important and common cause of morbidity among patients with psoriasis, especially those with more severe disease,” Dr. Takeshita and her associates said. Notably, the link between psoriasis and risk of serious infection persisted after excluding patients on immunosuppressive therapies, suggesting “that the greater infection risk is at least partially attributable to more severe psoriasis, itself,” they added.
The analysis of Nationwide Inpatient Sample data was funded by the Agency for Healthcare Research and Quality and by the Dermatology Foundation. The analysis of Health Improvement Network data was funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases, which is part of the National Institutes of Health, and by the Dermatology Foundation. None of the investigators reported conflicts of interest.
AT THE 2016 SID ANNUAL MEETING
Key clinical point: Psoriasis is an independent risk factor for serious infections, and serious infections are increasing among inpatients with psoriasis.
Major finding: Overall rates of serious infection and rates of pneumonia, MRSA, septicemia, diverticulitis, enterocolitis, encephalitis, and any viral or fungal infection rose significantly among inpatients in the United States with psoriasis between 2002 and 2012 (all P-values less than .05). In the United Kingdom during the same time period, patients with severe psoriasis had a 63% greater risk of serious infection than patients without psoriasis.
Data source: Analyses of data from the Nationwide Inpatient Sample for 2002 through 2012, and from The Health Improvement Network for 2003 through 2012.
Disclosures: The Nationwide Inpatient Sample analysis was funded by the Agency for Healthcare Research and Quality and the Dermatology Foundation. The analysis of The Health Improvement Network was funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases, which is part of the National Institutes of Health, and by the Dermatology Foundation. None of the investigators reported conflicts of interest.
CDC announces availability of funds to fight Zika

Photo courtesy of
Muhammad Mahdi Karim
The US Centers for Disease Control and Prevention (CDC) has announced that US states and territories can now apply for funds to fight Zika locally.
The agency said more than $85 million in redirected funds identified by the Department of Health and Human Services is being made available to support efforts to protect Americans from Zika infection and associated adverse health outcomes.
“These funds will allow states and territories to continue implementation of their Zika preparedness plans but are not enough to support a comprehensive Zika response and can only temporarily address what is needed,” said Stephen C. Redd, MD, director of the CDC’s Office of Public Health Preparedness and Response.
“Without the full amount of requested emergency supplemental funding, many activities that need to start now are being delayed or may have to be stopped within months.”
The more than $85 million in funds includes the more $60 million reported earlier this year (Funding opportunity number CDC-RFA-CK14-1401CONTPPHF16) as well as another $25 million that was just announced (Funding opportunity number CDC-RFA-TP16-1602).
Earlier this year, states and cities participating in the Epidemiology and Lab Capacity program became eligible for more than $60 million in funds to:
- Build laboratory capacity
- Enhance epidemiological surveillance and investigation
- Improve mosquito control and monitoring
- Keep blood supplies safe
- Contribute data to the US Zika Pregnancy registry.
Applications for these funds are due May 27, 2016, and will be disbursed during the summer.
Under the latest announcement, $25 million in FY 2016 preparedness and response funding will go to 53 states, cities, and territories at risk for outbreaks of Zika virus infection.
Recipients will receive funds based on the geographic locations of the two mosquitoes known to transmit Zika virus (Aedes aegypti and Aedes albopictus), history of mosquito-borne disease outbreaks, and size of population.
The funds are intended to strengthen incident management and emergency operations coordination, information management and sharing, and community recovery and resilience.
State, local, and territorial health officials can use the funds to identify and investigate a possible outbreak of Zika virus disease in their communities, coordinate a comprehensive response across all levels of government and non-governmental partners (including the healthcare sector), and identify and connect to community services families affected by Zika virus disease.
Applications for the funds are due June 13, 2016. Funds will be disbursed during the summer and remain available through July 2017.
Zika virus disease is caused by the Zika virus, which is spread to people primarily through the bite of infected Aedes aegypti and Aedes albopictus mosquitoes, though Aedes aegypti are more likely to spread Zika. Sexual transmission and transmission via blood transfusion have been documented as well.
There is currently no vaccine or treatment for Zika. The most common symptoms of Zika are fever, rash, joint pain, and conjunctivitis. In previous outbreaks, the illness has typically been mild, with symptoms lasting for several days to a week after a person is bitten by an infected mosquito.
Zika virus infection in pregnant women is a cause of microcephaly and other severe fetal brain defects. Zika has also been linked to Guillain-Barré syndrome. ![]()

Photo courtesy of
Muhammad Mahdi Karim
The US Centers for Disease Control and Prevention (CDC) has announced that US states and territories can now apply for funds to fight Zika locally.
The agency said more than $85 million in redirected funds identified by the Department of Health and Human Services is being made available to support efforts to protect Americans from Zika infection and associated adverse health outcomes.
“These funds will allow states and territories to continue implementation of their Zika preparedness plans but are not enough to support a comprehensive Zika response and can only temporarily address what is needed,” said Stephen C. Redd, MD, director of the CDC’s Office of Public Health Preparedness and Response.
“Without the full amount of requested emergency supplemental funding, many activities that need to start now are being delayed or may have to be stopped within months.”
The more than $85 million in funds includes the more $60 million reported earlier this year (Funding opportunity number CDC-RFA-CK14-1401CONTPPHF16) as well as another $25 million that was just announced (Funding opportunity number CDC-RFA-TP16-1602).
Earlier this year, states and cities participating in the Epidemiology and Lab Capacity program became eligible for more than $60 million in funds to:
- Build laboratory capacity
- Enhance epidemiological surveillance and investigation
- Improve mosquito control and monitoring
- Keep blood supplies safe
- Contribute data to the US Zika Pregnancy registry.
Applications for these funds are due May 27, 2016, and will be disbursed during the summer.
Under the latest announcement, $25 million in FY 2016 preparedness and response funding will go to 53 states, cities, and territories at risk for outbreaks of Zika virus infection.
Recipients will receive funds based on the geographic locations of the two mosquitoes known to transmit Zika virus (Aedes aegypti and Aedes albopictus), history of mosquito-borne disease outbreaks, and size of population.
The funds are intended to strengthen incident management and emergency operations coordination, information management and sharing, and community recovery and resilience.
State, local, and territorial health officials can use the funds to identify and investigate a possible outbreak of Zika virus disease in their communities, coordinate a comprehensive response across all levels of government and non-governmental partners (including the healthcare sector), and identify and connect to community services families affected by Zika virus disease.
Applications for the funds are due June 13, 2016. Funds will be disbursed during the summer and remain available through July 2017.
Zika virus disease is caused by the Zika virus, which is spread to people primarily through the bite of infected Aedes aegypti and Aedes albopictus mosquitoes, though Aedes aegypti are more likely to spread Zika. Sexual transmission and transmission via blood transfusion have been documented as well.
There is currently no vaccine or treatment for Zika. The most common symptoms of Zika are fever, rash, joint pain, and conjunctivitis. In previous outbreaks, the illness has typically been mild, with symptoms lasting for several days to a week after a person is bitten by an infected mosquito.
Zika virus infection in pregnant women is a cause of microcephaly and other severe fetal brain defects. Zika has also been linked to Guillain-Barré syndrome. ![]()

Photo courtesy of
Muhammad Mahdi Karim
The US Centers for Disease Control and Prevention (CDC) has announced that US states and territories can now apply for funds to fight Zika locally.
The agency said more than $85 million in redirected funds identified by the Department of Health and Human Services is being made available to support efforts to protect Americans from Zika infection and associated adverse health outcomes.
“These funds will allow states and territories to continue implementation of their Zika preparedness plans but are not enough to support a comprehensive Zika response and can only temporarily address what is needed,” said Stephen C. Redd, MD, director of the CDC’s Office of Public Health Preparedness and Response.
“Without the full amount of requested emergency supplemental funding, many activities that need to start now are being delayed or may have to be stopped within months.”
The more than $85 million in funds includes the more $60 million reported earlier this year (Funding opportunity number CDC-RFA-CK14-1401CONTPPHF16) as well as another $25 million that was just announced (Funding opportunity number CDC-RFA-TP16-1602).
Earlier this year, states and cities participating in the Epidemiology and Lab Capacity program became eligible for more than $60 million in funds to:
- Build laboratory capacity
- Enhance epidemiological surveillance and investigation
- Improve mosquito control and monitoring
- Keep blood supplies safe
- Contribute data to the US Zika Pregnancy registry.
Applications for these funds are due May 27, 2016, and will be disbursed during the summer.
Under the latest announcement, $25 million in FY 2016 preparedness and response funding will go to 53 states, cities, and territories at risk for outbreaks of Zika virus infection.
Recipients will receive funds based on the geographic locations of the two mosquitoes known to transmit Zika virus (Aedes aegypti and Aedes albopictus), history of mosquito-borne disease outbreaks, and size of population.
The funds are intended to strengthen incident management and emergency operations coordination, information management and sharing, and community recovery and resilience.
State, local, and territorial health officials can use the funds to identify and investigate a possible outbreak of Zika virus disease in their communities, coordinate a comprehensive response across all levels of government and non-governmental partners (including the healthcare sector), and identify and connect to community services families affected by Zika virus disease.
Applications for the funds are due June 13, 2016. Funds will be disbursed during the summer and remain available through July 2017.
Zika virus disease is caused by the Zika virus, which is spread to people primarily through the bite of infected Aedes aegypti and Aedes albopictus mosquitoes, though Aedes aegypti are more likely to spread Zika. Sexual transmission and transmission via blood transfusion have been documented as well.
There is currently no vaccine or treatment for Zika. The most common symptoms of Zika are fever, rash, joint pain, and conjunctivitis. In previous outbreaks, the illness has typically been mild, with symptoms lasting for several days to a week after a person is bitten by an infected mosquito.
Zika virus infection in pregnant women is a cause of microcephaly and other severe fetal brain defects. Zika has also been linked to Guillain-Barré syndrome. ![]()
PRAC: Products may not increase risk of inhibitors

Results of a meta-analysis suggest a pair of recombinant factor VIII (FVIII) products may not increase the risk of FVIII inhibitors in previously untreated patients with severe hemophilia A.
The European Medicines Agency’s Pharmacovigilance Risk Assessment Committee (PRAC) analyzed data from 3 observational studies and found that patients who received Kogenate or Helixate had a higher incidence of inhibitors than patients who received other recombinant FVIII products.
However, the difference was not significant, and the PRAC concluded that, overall, the evidence does not confirm an increased risk of inhibitors with Kogenate or Helixate.
This conclusion is consistent with the PRAC’s previous conclusions from a review carried out in 2013.
For the current analysis, the PRAC reviewed data from 3 studies, which were conducted by the RODIN study group, the UK Haemophilia Centre Doctors’ Organisation (UKHCDO), and the FranceCoag Network.
The analysis included 1102 previously untreated patients—481 in the RODIN study, 293 in the FranceCoag study, and 328 in the UKHCDO study—who received octocog alfa (Advate, Helixate, or Kogenate), moroctocog alfa (Refacto or Refacto AF), or other recombinant FVIII products.
Results suggested a trend toward an increase of high-titer inhibitor development and all inhibitor development with Kogenate or Helixate compared to Advate.
Overall, 37% of patients treated with Kogenate or Helixate (147/400) developed inhibitory antibodies, 22% of whom (n=88) had high-titer inhibitors. Twenty-six percent of patients who received Advate (100/385) developed inhibitors, 15% of whom (n=57) had high-titer inhibitors.
The PRAC said a similar trend was observed for other recombinant FVIII products, but the results were less pronounced due to sample size constraints.
The committee pointed out that there were several limitations with this meta-analysis, including the possibility of residual confounding. The group also said a number of parameters may have had an impact on the incidence of inhibitors in these previously untreated patients, and adjusting for all of these factors may not be possible.
In addition, the PRAC noted that there has been no signal for a similar trend of increases in inhibitor development with Kogenate in previously treated patients in other studies.
Finally, the committee recommended that companies marketing recombinant FVIII products monitor published studies on inhibitor development with the aim of keeping the product information up to date. ![]()

Results of a meta-analysis suggest a pair of recombinant factor VIII (FVIII) products may not increase the risk of FVIII inhibitors in previously untreated patients with severe hemophilia A.
The European Medicines Agency’s Pharmacovigilance Risk Assessment Committee (PRAC) analyzed data from 3 observational studies and found that patients who received Kogenate or Helixate had a higher incidence of inhibitors than patients who received other recombinant FVIII products.
However, the difference was not significant, and the PRAC concluded that, overall, the evidence does not confirm an increased risk of inhibitors with Kogenate or Helixate.
This conclusion is consistent with the PRAC’s previous conclusions from a review carried out in 2013.
For the current analysis, the PRAC reviewed data from 3 studies, which were conducted by the RODIN study group, the UK Haemophilia Centre Doctors’ Organisation (UKHCDO), and the FranceCoag Network.
The analysis included 1102 previously untreated patients—481 in the RODIN study, 293 in the FranceCoag study, and 328 in the UKHCDO study—who received octocog alfa (Advate, Helixate, or Kogenate), moroctocog alfa (Refacto or Refacto AF), or other recombinant FVIII products.
Results suggested a trend toward an increase of high-titer inhibitor development and all inhibitor development with Kogenate or Helixate compared to Advate.
Overall, 37% of patients treated with Kogenate or Helixate (147/400) developed inhibitory antibodies, 22% of whom (n=88) had high-titer inhibitors. Twenty-six percent of patients who received Advate (100/385) developed inhibitors, 15% of whom (n=57) had high-titer inhibitors.
The PRAC said a similar trend was observed for other recombinant FVIII products, but the results were less pronounced due to sample size constraints.
The committee pointed out that there were several limitations with this meta-analysis, including the possibility of residual confounding. The group also said a number of parameters may have had an impact on the incidence of inhibitors in these previously untreated patients, and adjusting for all of these factors may not be possible.
In addition, the PRAC noted that there has been no signal for a similar trend of increases in inhibitor development with Kogenate in previously treated patients in other studies.
Finally, the committee recommended that companies marketing recombinant FVIII products monitor published studies on inhibitor development with the aim of keeping the product information up to date. ![]()

Results of a meta-analysis suggest a pair of recombinant factor VIII (FVIII) products may not increase the risk of FVIII inhibitors in previously untreated patients with severe hemophilia A.
The European Medicines Agency’s Pharmacovigilance Risk Assessment Committee (PRAC) analyzed data from 3 observational studies and found that patients who received Kogenate or Helixate had a higher incidence of inhibitors than patients who received other recombinant FVIII products.
However, the difference was not significant, and the PRAC concluded that, overall, the evidence does not confirm an increased risk of inhibitors with Kogenate or Helixate.
This conclusion is consistent with the PRAC’s previous conclusions from a review carried out in 2013.
For the current analysis, the PRAC reviewed data from 3 studies, which were conducted by the RODIN study group, the UK Haemophilia Centre Doctors’ Organisation (UKHCDO), and the FranceCoag Network.
The analysis included 1102 previously untreated patients—481 in the RODIN study, 293 in the FranceCoag study, and 328 in the UKHCDO study—who received octocog alfa (Advate, Helixate, or Kogenate), moroctocog alfa (Refacto or Refacto AF), or other recombinant FVIII products.
Results suggested a trend toward an increase of high-titer inhibitor development and all inhibitor development with Kogenate or Helixate compared to Advate.
Overall, 37% of patients treated with Kogenate or Helixate (147/400) developed inhibitory antibodies, 22% of whom (n=88) had high-titer inhibitors. Twenty-six percent of patients who received Advate (100/385) developed inhibitors, 15% of whom (n=57) had high-titer inhibitors.
The PRAC said a similar trend was observed for other recombinant FVIII products, but the results were less pronounced due to sample size constraints.
The committee pointed out that there were several limitations with this meta-analysis, including the possibility of residual confounding. The group also said a number of parameters may have had an impact on the incidence of inhibitors in these previously untreated patients, and adjusting for all of these factors may not be possible.
In addition, the PRAC noted that there has been no signal for a similar trend of increases in inhibitor development with Kogenate in previously treated patients in other studies.
Finally, the committee recommended that companies marketing recombinant FVIII products monitor published studies on inhibitor development with the aim of keeping the product information up to date. ![]()