User login
Recent leaps in heart failure therapy spur ESC guideline–focused update
Two years is a long time in the world of heart failure (HF) management, enough to see publication of more than a dozen studies with insights that would supplant and expand key sections of a far-reaching European Society of Cardiology (ESC) clinical practice guideline on HF unveiled in 2021.
“Back in 2021, we had three and a half decades of data to consider,” but recent years have seen “an amazing amount of progress” that has necessitated some adjustments and key additions, including several Class I recommendations, observed Roy S. Gardner, MBChB, MD, Golden Jubilee National Hospital, Clydebank, United Kingdom.
, which Dr. Gardner helped unveil over several days at the annual congress of the European Society of Cardiology, held in Amsterdam.
The new document was also published in the European Heart Journal during the ESC sessions. Dr. Gardner is a co-author on both the 2021 and 2023 documents.
The task force that was charged with the focused update’s development “considered a large number of trials across the spectrum of acute chronic heart failure and the comorbidities associated with it,” Ultimately, it considered only those with “results that would lead to new or changed Class I or Class IIa recommendations,” noted Theresa A. McDonagh, MD, during the ESC sessions.
Dr. McDonagh, of King’s College Hospital, London, chaired the task force and led the document’s list of authors along with Marco Metra, MD, University of Brescia (Italy).
Chronic HF management
The 2021 document’s “beautiful algorithm” on managing HF with reduced ejection fraction, that is HF with an LVEF less than 40%, had helped enshrine the expeditious uptitration of the “four pillars” of drug therapy as a top management goal. That remains unchanged in the focused update, Dr. Gardner noted.
But the new document gives a boost to recommendations for HF with mildly reduced ejection fraction (HFmrEF), characterized by an LVEF greater than 40% to less than 50%. For that, the 2021 document recommended three of the four pillars of HF medical therapy: beta blockers, mineralocorticoid receptor antagonists (MRA), renin-angiotensin system (RAS) inhibitors.
The focused update, however, adds the fourth pillar – SGLT2 inhibitors – to core therapy for both HFmrEF and HF with preserved ejection fraction (HFpEF), the latter defined by an LVEF greater than 50%. Publication of trials supporting those new recommendations had narrowly missed availability for the 2021 document.
EMPEROR-Preserved, for example, was published during the same ESC 2021 sessions that introduced the 2021 guidelines. Its patients with HFpEF (which at the time included patients meeting the current definition of HFmrEF) assigned to the SGLT2 inhibitor empagliflozin (Jardiance) showed a 21% reduction in risk for a composite primary endpoint that was driven by the HF-hospitalization component.
“This wasn’t a fluke finding,” Dr. Gardner said, as the following year saw publication of the DELIVER trial, which resembled EMPEROR-Preserved in design and outcomes using the SGLT2 inhibitor dapagliflozin (Farxiga).
The two trials, backed up by meta-analyses that also included DAPA-HF and other studies, suggested as well that the two SGLT2 inhibitors “work across the spectrum of ejection fraction,” Dr. Gardner said.
The 2023 focused update indicates an SGLT2 inhibitor, either empagliflozin or dapagliflozin, for patients with either HFmrEF or HFpEF to reduce the risk of HF hospitalization or cardiovascular death. Both recommendations are of Class I, level of evidence A.
The new indications make SGLT2 inhibitors and diuretics (as needed for fluid retention) the only drugs for HFmrEF or HFpEF with a Class I recommendation. Previously established “rather weaker” Class IIb recommendation for RAS inhibitors, MRAs, and beta blockers that had been “based on subgroup analyses of neutral trials” remained unchanged in the focused update, Dr. McDonagh noted.
Patients hospitalized with HF
The 2021 guidelines had recommended that patients hospitalized with acute HF be started on evidence-based meds before discharge and that they return for evaluation 1 to 2 weeks after discharge. But the recommendation was unsupported by randomized trials.
That changed with the 2022 publication of STRONG-HF, in which a strategy of early and rapid uptitration of guideline-directed meds, initiated predischarge regardless of LVEF, led to a one-third reduced 6-month risk for death or HF readmission.
Based primarily on STRONG-HF, the focused update recommends “an intensive strategy of initiation and rapid up-titration of evidence-based treatment before discharge and during frequent and careful follow-up visits in the first 6 weeks after hospitalization” to reduce readmission and mortality: Class I, level of evidence B.
“There was a large consensus around this recommendation,” said STRONG-HF principal investigator Alexandre Mebazaa, MD, PhD, a co-author of both the 2021 and 2023 documents. Conducted before the advent of the four pillars of drug therapy, sometimes called quartet therapy, the trial’s requirement for evidence-based meds didn’t include SGLT2 inhibitors.
The new focused update considers the new status of those agents, especially with regard to their benefits independent of LVEF. So, it completed the quartet by adding empagliflozin or dapagliflozin to the agents that should be initiated predischarge, observed Dr. Mebazaa, University Hospitals Saint Louis‐Lariboisière, Paris, at the focused-update’s ESC 2023 sessions.
The new document also follows STRONG-HF with its emphasis on “frequent and careful follow-up” by recommending certain clinical and laboratory evaluations known to be prognostic in HF. They include congestion status, blood pressure, heart rate, natriuretic peptide (NT-proBNP) and potassium levels and estimated glomerular filtration rate.
Dr. Mebazaa stressed the importance of monitoring NT-proBNP after discharge. “What we saw in STRONG-HF is that sometimes the clinical signs do not necessarily tell you that the patient is still congested.”
After discharge, he said, NT-proBNP levels “should only go down.” So, knowing whether NT-proBNP levels “are stable or increasing” during the med optimization process can help guide diuretic dosing.
HF with comorbidities
The new document includes two new Class I recommendations for patients with HF and both type 2 diabetes and chronic kidney disease based on several recent randomized trials and meta-analyses.
The focused update recommends SGLT2 inhibitors as well as the selective, non-steroidal MRA finerenone (Kerendia) in HF patients with CKD and type-2 diabetes. Both Class I recommendations are supported by a level of evidence A.
The SGLT2 indication is based on DAPA-CKD and EMPA-KIDNEY plus meta-analyses that included those trials along with others. The recommendation for finerenone derives from the FIDELIO-DKD and FIGARO-DKD trials and a pooled analysis of the two studies.
The 2023 focused update also accounts for new clinical-trial insights for patients with HF and iron deficiency. The 2021 document featured recommendations for the diagnosis and iron-repletion therapy in such cases, but only as Class IIa or at lower low levels of evidence. The focused update considers more recent studies, especially IRONMAN and some meta-analyses.
The 2023 document indicates intravenous iron supplementation for symptomatic patients with iron deficiency and either HFrEF or HFmrEF to improve symptoms and quality of life (Class I, level of evidence A), and says it should be considered (Class IIa, level of evidence A) to reduce risk for HF hospitalization.
When the task force assembled to plan the 2023 focused update, Dr. Gardner observed, “the first thing we thought about was the nomenclature around the phenotyping of heart failure.”
Although the 2021 guidelines relied fundamentally on the distinctions between HFrEF, HFmrEF, and HFpEF, it had become apparent to some in the field that some meds, especially the SGLT2 inhibitors, were obscuring their LVEF-based boundaries, at least with respect to drug therapy.
The 2023 document’s developers, Dr. Gardner said, seriously considered changing the three categories to two, that is HFrEF and – to account for all other heart failure – HF with normal ejection fraction (HFnEF).
That didn’t happen, although the proposal was popular within the task force. Any changes to the 2021 document would require a 75% consensus on the matter, Dr. Gardner explained. When the task force took a vote on whether to change the nomenclature, he said, 71% favored the proposal.
Disclosures for members of the task force can be found in a supplement to the published 2023 Focused Update.
A version of this article first appeared on Medscape.com.
Two years is a long time in the world of heart failure (HF) management, enough to see publication of more than a dozen studies with insights that would supplant and expand key sections of a far-reaching European Society of Cardiology (ESC) clinical practice guideline on HF unveiled in 2021.
“Back in 2021, we had three and a half decades of data to consider,” but recent years have seen “an amazing amount of progress” that has necessitated some adjustments and key additions, including several Class I recommendations, observed Roy S. Gardner, MBChB, MD, Golden Jubilee National Hospital, Clydebank, United Kingdom.
, which Dr. Gardner helped unveil over several days at the annual congress of the European Society of Cardiology, held in Amsterdam.
The new document was also published in the European Heart Journal during the ESC sessions. Dr. Gardner is a co-author on both the 2021 and 2023 documents.
The task force that was charged with the focused update’s development “considered a large number of trials across the spectrum of acute chronic heart failure and the comorbidities associated with it,” Ultimately, it considered only those with “results that would lead to new or changed Class I or Class IIa recommendations,” noted Theresa A. McDonagh, MD, during the ESC sessions.
Dr. McDonagh, of King’s College Hospital, London, chaired the task force and led the document’s list of authors along with Marco Metra, MD, University of Brescia (Italy).
Chronic HF management
The 2021 document’s “beautiful algorithm” on managing HF with reduced ejection fraction, that is HF with an LVEF less than 40%, had helped enshrine the expeditious uptitration of the “four pillars” of drug therapy as a top management goal. That remains unchanged in the focused update, Dr. Gardner noted.
But the new document gives a boost to recommendations for HF with mildly reduced ejection fraction (HFmrEF), characterized by an LVEF greater than 40% to less than 50%. For that, the 2021 document recommended three of the four pillars of HF medical therapy: beta blockers, mineralocorticoid receptor antagonists (MRA), renin-angiotensin system (RAS) inhibitors.
The focused update, however, adds the fourth pillar – SGLT2 inhibitors – to core therapy for both HFmrEF and HF with preserved ejection fraction (HFpEF), the latter defined by an LVEF greater than 50%. Publication of trials supporting those new recommendations had narrowly missed availability for the 2021 document.
EMPEROR-Preserved, for example, was published during the same ESC 2021 sessions that introduced the 2021 guidelines. Its patients with HFpEF (which at the time included patients meeting the current definition of HFmrEF) assigned to the SGLT2 inhibitor empagliflozin (Jardiance) showed a 21% reduction in risk for a composite primary endpoint that was driven by the HF-hospitalization component.
“This wasn’t a fluke finding,” Dr. Gardner said, as the following year saw publication of the DELIVER trial, which resembled EMPEROR-Preserved in design and outcomes using the SGLT2 inhibitor dapagliflozin (Farxiga).
The two trials, backed up by meta-analyses that also included DAPA-HF and other studies, suggested as well that the two SGLT2 inhibitors “work across the spectrum of ejection fraction,” Dr. Gardner said.
The 2023 focused update indicates an SGLT2 inhibitor, either empagliflozin or dapagliflozin, for patients with either HFmrEF or HFpEF to reduce the risk of HF hospitalization or cardiovascular death. Both recommendations are of Class I, level of evidence A.
The new indications make SGLT2 inhibitors and diuretics (as needed for fluid retention) the only drugs for HFmrEF or HFpEF with a Class I recommendation. Previously established “rather weaker” Class IIb recommendation for RAS inhibitors, MRAs, and beta blockers that had been “based on subgroup analyses of neutral trials” remained unchanged in the focused update, Dr. McDonagh noted.
Patients hospitalized with HF
The 2021 guidelines had recommended that patients hospitalized with acute HF be started on evidence-based meds before discharge and that they return for evaluation 1 to 2 weeks after discharge. But the recommendation was unsupported by randomized trials.
That changed with the 2022 publication of STRONG-HF, in which a strategy of early and rapid uptitration of guideline-directed meds, initiated predischarge regardless of LVEF, led to a one-third reduced 6-month risk for death or HF readmission.
Based primarily on STRONG-HF, the focused update recommends “an intensive strategy of initiation and rapid up-titration of evidence-based treatment before discharge and during frequent and careful follow-up visits in the first 6 weeks after hospitalization” to reduce readmission and mortality: Class I, level of evidence B.
“There was a large consensus around this recommendation,” said STRONG-HF principal investigator Alexandre Mebazaa, MD, PhD, a co-author of both the 2021 and 2023 documents. Conducted before the advent of the four pillars of drug therapy, sometimes called quartet therapy, the trial’s requirement for evidence-based meds didn’t include SGLT2 inhibitors.
The new focused update considers the new status of those agents, especially with regard to their benefits independent of LVEF. So, it completed the quartet by adding empagliflozin or dapagliflozin to the agents that should be initiated predischarge, observed Dr. Mebazaa, University Hospitals Saint Louis‐Lariboisière, Paris, at the focused-update’s ESC 2023 sessions.
The new document also follows STRONG-HF with its emphasis on “frequent and careful follow-up” by recommending certain clinical and laboratory evaluations known to be prognostic in HF. They include congestion status, blood pressure, heart rate, natriuretic peptide (NT-proBNP) and potassium levels and estimated glomerular filtration rate.
Dr. Mebazaa stressed the importance of monitoring NT-proBNP after discharge. “What we saw in STRONG-HF is that sometimes the clinical signs do not necessarily tell you that the patient is still congested.”
After discharge, he said, NT-proBNP levels “should only go down.” So, knowing whether NT-proBNP levels “are stable or increasing” during the med optimization process can help guide diuretic dosing.
HF with comorbidities
The new document includes two new Class I recommendations for patients with HF and both type 2 diabetes and chronic kidney disease based on several recent randomized trials and meta-analyses.
The focused update recommends SGLT2 inhibitors as well as the selective, non-steroidal MRA finerenone (Kerendia) in HF patients with CKD and type-2 diabetes. Both Class I recommendations are supported by a level of evidence A.
The SGLT2 indication is based on DAPA-CKD and EMPA-KIDNEY plus meta-analyses that included those trials along with others. The recommendation for finerenone derives from the FIDELIO-DKD and FIGARO-DKD trials and a pooled analysis of the two studies.
The 2023 focused update also accounts for new clinical-trial insights for patients with HF and iron deficiency. The 2021 document featured recommendations for the diagnosis and iron-repletion therapy in such cases, but only as Class IIa or at lower low levels of evidence. The focused update considers more recent studies, especially IRONMAN and some meta-analyses.
The 2023 document indicates intravenous iron supplementation for symptomatic patients with iron deficiency and either HFrEF or HFmrEF to improve symptoms and quality of life (Class I, level of evidence A), and says it should be considered (Class IIa, level of evidence A) to reduce risk for HF hospitalization.
When the task force assembled to plan the 2023 focused update, Dr. Gardner observed, “the first thing we thought about was the nomenclature around the phenotyping of heart failure.”
Although the 2021 guidelines relied fundamentally on the distinctions between HFrEF, HFmrEF, and HFpEF, it had become apparent to some in the field that some meds, especially the SGLT2 inhibitors, were obscuring their LVEF-based boundaries, at least with respect to drug therapy.
The 2023 document’s developers, Dr. Gardner said, seriously considered changing the three categories to two, that is HFrEF and – to account for all other heart failure – HF with normal ejection fraction (HFnEF).
That didn’t happen, although the proposal was popular within the task force. Any changes to the 2021 document would require a 75% consensus on the matter, Dr. Gardner explained. When the task force took a vote on whether to change the nomenclature, he said, 71% favored the proposal.
Disclosures for members of the task force can be found in a supplement to the published 2023 Focused Update.
A version of this article first appeared on Medscape.com.
Two years is a long time in the world of heart failure (HF) management, enough to see publication of more than a dozen studies with insights that would supplant and expand key sections of a far-reaching European Society of Cardiology (ESC) clinical practice guideline on HF unveiled in 2021.
“Back in 2021, we had three and a half decades of data to consider,” but recent years have seen “an amazing amount of progress” that has necessitated some adjustments and key additions, including several Class I recommendations, observed Roy S. Gardner, MBChB, MD, Golden Jubilee National Hospital, Clydebank, United Kingdom.
, which Dr. Gardner helped unveil over several days at the annual congress of the European Society of Cardiology, held in Amsterdam.
The new document was also published in the European Heart Journal during the ESC sessions. Dr. Gardner is a co-author on both the 2021 and 2023 documents.
The task force that was charged with the focused update’s development “considered a large number of trials across the spectrum of acute chronic heart failure and the comorbidities associated with it,” Ultimately, it considered only those with “results that would lead to new or changed Class I or Class IIa recommendations,” noted Theresa A. McDonagh, MD, during the ESC sessions.
Dr. McDonagh, of King’s College Hospital, London, chaired the task force and led the document’s list of authors along with Marco Metra, MD, University of Brescia (Italy).
Chronic HF management
The 2021 document’s “beautiful algorithm” on managing HF with reduced ejection fraction, that is HF with an LVEF less than 40%, had helped enshrine the expeditious uptitration of the “four pillars” of drug therapy as a top management goal. That remains unchanged in the focused update, Dr. Gardner noted.
But the new document gives a boost to recommendations for HF with mildly reduced ejection fraction (HFmrEF), characterized by an LVEF greater than 40% to less than 50%. For that, the 2021 document recommended three of the four pillars of HF medical therapy: beta blockers, mineralocorticoid receptor antagonists (MRA), renin-angiotensin system (RAS) inhibitors.
The focused update, however, adds the fourth pillar – SGLT2 inhibitors – to core therapy for both HFmrEF and HF with preserved ejection fraction (HFpEF), the latter defined by an LVEF greater than 50%. Publication of trials supporting those new recommendations had narrowly missed availability for the 2021 document.
EMPEROR-Preserved, for example, was published during the same ESC 2021 sessions that introduced the 2021 guidelines. Its patients with HFpEF (which at the time included patients meeting the current definition of HFmrEF) assigned to the SGLT2 inhibitor empagliflozin (Jardiance) showed a 21% reduction in risk for a composite primary endpoint that was driven by the HF-hospitalization component.
“This wasn’t a fluke finding,” Dr. Gardner said, as the following year saw publication of the DELIVER trial, which resembled EMPEROR-Preserved in design and outcomes using the SGLT2 inhibitor dapagliflozin (Farxiga).
The two trials, backed up by meta-analyses that also included DAPA-HF and other studies, suggested as well that the two SGLT2 inhibitors “work across the spectrum of ejection fraction,” Dr. Gardner said.
The 2023 focused update indicates an SGLT2 inhibitor, either empagliflozin or dapagliflozin, for patients with either HFmrEF or HFpEF to reduce the risk of HF hospitalization or cardiovascular death. Both recommendations are of Class I, level of evidence A.
The new indications make SGLT2 inhibitors and diuretics (as needed for fluid retention) the only drugs for HFmrEF or HFpEF with a Class I recommendation. Previously established “rather weaker” Class IIb recommendation for RAS inhibitors, MRAs, and beta blockers that had been “based on subgroup analyses of neutral trials” remained unchanged in the focused update, Dr. McDonagh noted.
Patients hospitalized with HF
The 2021 guidelines had recommended that patients hospitalized with acute HF be started on evidence-based meds before discharge and that they return for evaluation 1 to 2 weeks after discharge. But the recommendation was unsupported by randomized trials.
That changed with the 2022 publication of STRONG-HF, in which a strategy of early and rapid uptitration of guideline-directed meds, initiated predischarge regardless of LVEF, led to a one-third reduced 6-month risk for death or HF readmission.
Based primarily on STRONG-HF, the focused update recommends “an intensive strategy of initiation and rapid up-titration of evidence-based treatment before discharge and during frequent and careful follow-up visits in the first 6 weeks after hospitalization” to reduce readmission and mortality: Class I, level of evidence B.
“There was a large consensus around this recommendation,” said STRONG-HF principal investigator Alexandre Mebazaa, MD, PhD, a co-author of both the 2021 and 2023 documents. Conducted before the advent of the four pillars of drug therapy, sometimes called quartet therapy, the trial’s requirement for evidence-based meds didn’t include SGLT2 inhibitors.
The new focused update considers the new status of those agents, especially with regard to their benefits independent of LVEF. So, it completed the quartet by adding empagliflozin or dapagliflozin to the agents that should be initiated predischarge, observed Dr. Mebazaa, University Hospitals Saint Louis‐Lariboisière, Paris, at the focused-update’s ESC 2023 sessions.
The new document also follows STRONG-HF with its emphasis on “frequent and careful follow-up” by recommending certain clinical and laboratory evaluations known to be prognostic in HF. They include congestion status, blood pressure, heart rate, natriuretic peptide (NT-proBNP) and potassium levels and estimated glomerular filtration rate.
Dr. Mebazaa stressed the importance of monitoring NT-proBNP after discharge. “What we saw in STRONG-HF is that sometimes the clinical signs do not necessarily tell you that the patient is still congested.”
After discharge, he said, NT-proBNP levels “should only go down.” So, knowing whether NT-proBNP levels “are stable or increasing” during the med optimization process can help guide diuretic dosing.
HF with comorbidities
The new document includes two new Class I recommendations for patients with HF and both type 2 diabetes and chronic kidney disease based on several recent randomized trials and meta-analyses.
The focused update recommends SGLT2 inhibitors as well as the selective, non-steroidal MRA finerenone (Kerendia) in HF patients with CKD and type-2 diabetes. Both Class I recommendations are supported by a level of evidence A.
The SGLT2 indication is based on DAPA-CKD and EMPA-KIDNEY plus meta-analyses that included those trials along with others. The recommendation for finerenone derives from the FIDELIO-DKD and FIGARO-DKD trials and a pooled analysis of the two studies.
The 2023 focused update also accounts for new clinical-trial insights for patients with HF and iron deficiency. The 2021 document featured recommendations for the diagnosis and iron-repletion therapy in such cases, but only as Class IIa or at lower low levels of evidence. The focused update considers more recent studies, especially IRONMAN and some meta-analyses.
The 2023 document indicates intravenous iron supplementation for symptomatic patients with iron deficiency and either HFrEF or HFmrEF to improve symptoms and quality of life (Class I, level of evidence A), and says it should be considered (Class IIa, level of evidence A) to reduce risk for HF hospitalization.
When the task force assembled to plan the 2023 focused update, Dr. Gardner observed, “the first thing we thought about was the nomenclature around the phenotyping of heart failure.”
Although the 2021 guidelines relied fundamentally on the distinctions between HFrEF, HFmrEF, and HFpEF, it had become apparent to some in the field that some meds, especially the SGLT2 inhibitors, were obscuring their LVEF-based boundaries, at least with respect to drug therapy.
The 2023 document’s developers, Dr. Gardner said, seriously considered changing the three categories to two, that is HFrEF and – to account for all other heart failure – HF with normal ejection fraction (HFnEF).
That didn’t happen, although the proposal was popular within the task force. Any changes to the 2021 document would require a 75% consensus on the matter, Dr. Gardner explained. When the task force took a vote on whether to change the nomenclature, he said, 71% favored the proposal.
Disclosures for members of the task force can be found in a supplement to the published 2023 Focused Update.
A version of this article first appeared on Medscape.com.
FROM THE ESC CONGRESS 2023
Metastatic Urothelial Carcinoma Presenting as Mediastinal Lymphadenopathy Without Appreciable Bladder Mass in a Patient With Chronic Lymphocytic Leukemia
INTRODUCTION
Lymphadenopathy in Chronic Lymphocytic Leukemia (CLL) is a very common feature. However, sudden increase in lymphadenopathy or other symptoms like weight loss should be evaluated for possible metastatic malignancy. We describe a CLL patient with diffuse mediastinal lymphadenopathy who was diagnosed with metastatic bladder cancer without a primary bladder tumor mass on imaging.
CASE DESCRIPTION
A 60-year-old man with a 60 pack-year smoking history, alcoholic cirrhosis, and a 5-year history of stage 1 CLL presented with 3 months of progressive shortness of breath; persistent cough; chills; hemoptysis; and a steady weight loss of 35 lbs. Notably, he had no bladder symptoms. Initial labs showed leukocytosis of 35.8k with a lymphocytic predominance. Screening low-dose chest CT was positive for diffuse mediastinal lymphadenopathy. Subsequent PET/CT revealed numerous hypermetabolic lymph nodes in the neck, mediastinum, left hilum, and right periaortic abdominal region. CT Chest, Abdomen, Pelvis revealed progressive lymphadenopathy as seen in prior imaging, stable pulmonary nodules up to 4 mm in size, and splenomegaly. No distant primary sites, including of the bladder, were identified. Mediastinal lymph node biopsy confirmed metastatic poorly differentiated carcinoma with immunohistochemical staining negative for p40, p63, CK20, TTF-1, Napsin A, CDX2, CA19- 9, Calretinin, and D2-40 and positive for CK7, GATA3, Ber-EP4, and Uroplakin, supporting bladder as primary origin. Urology deferred a cystoscopy given his lack of urinary symptoms and positive biopsy and was started on Carboplatin/Gemcitabine for his metastatic disease. He was ineligible for Cisplatin given his cirrhosis and hearing impairment.
DISCUSSION
In patients with CLL, new onset mediastinal lymphadenopathy is concerning for disease progression and possible transformation to a diffuse b-cell lymphoma. However, this symptom has a broad differential, including primary lung carcinomas, sarcomas, and metastatic disease. While our patient’s PET/CT and pan-CT failed to identify a distant primary site, maintaining a low clinical suspicion for metastatic disease and doing a thorough work-up was paramount. Only through immunohistochemical staining were we able to diagnosis this patient with urothelial carcinoma.
CONCLUSIONS
Biopsy with immunohistochemical staining and maintaining a low suspicion for worsening lymphadenopathy can identify unusually presenting urothelial carcinomas in CLL patients.
INTRODUCTION
Lymphadenopathy in Chronic Lymphocytic Leukemia (CLL) is a very common feature. However, sudden increase in lymphadenopathy or other symptoms like weight loss should be evaluated for possible metastatic malignancy. We describe a CLL patient with diffuse mediastinal lymphadenopathy who was diagnosed with metastatic bladder cancer without a primary bladder tumor mass on imaging.
CASE DESCRIPTION
A 60-year-old man with a 60 pack-year smoking history, alcoholic cirrhosis, and a 5-year history of stage 1 CLL presented with 3 months of progressive shortness of breath; persistent cough; chills; hemoptysis; and a steady weight loss of 35 lbs. Notably, he had no bladder symptoms. Initial labs showed leukocytosis of 35.8k with a lymphocytic predominance. Screening low-dose chest CT was positive for diffuse mediastinal lymphadenopathy. Subsequent PET/CT revealed numerous hypermetabolic lymph nodes in the neck, mediastinum, left hilum, and right periaortic abdominal region. CT Chest, Abdomen, Pelvis revealed progressive lymphadenopathy as seen in prior imaging, stable pulmonary nodules up to 4 mm in size, and splenomegaly. No distant primary sites, including of the bladder, were identified. Mediastinal lymph node biopsy confirmed metastatic poorly differentiated carcinoma with immunohistochemical staining negative for p40, p63, CK20, TTF-1, Napsin A, CDX2, CA19- 9, Calretinin, and D2-40 and positive for CK7, GATA3, Ber-EP4, and Uroplakin, supporting bladder as primary origin. Urology deferred a cystoscopy given his lack of urinary symptoms and positive biopsy and was started on Carboplatin/Gemcitabine for his metastatic disease. He was ineligible for Cisplatin given his cirrhosis and hearing impairment.
DISCUSSION
In patients with CLL, new onset mediastinal lymphadenopathy is concerning for disease progression and possible transformation to a diffuse b-cell lymphoma. However, this symptom has a broad differential, including primary lung carcinomas, sarcomas, and metastatic disease. While our patient’s PET/CT and pan-CT failed to identify a distant primary site, maintaining a low clinical suspicion for metastatic disease and doing a thorough work-up was paramount. Only through immunohistochemical staining were we able to diagnosis this patient with urothelial carcinoma.
CONCLUSIONS
Biopsy with immunohistochemical staining and maintaining a low suspicion for worsening lymphadenopathy can identify unusually presenting urothelial carcinomas in CLL patients.
INTRODUCTION
Lymphadenopathy in Chronic Lymphocytic Leukemia (CLL) is a very common feature. However, sudden increase in lymphadenopathy or other symptoms like weight loss should be evaluated for possible metastatic malignancy. We describe a CLL patient with diffuse mediastinal lymphadenopathy who was diagnosed with metastatic bladder cancer without a primary bladder tumor mass on imaging.
CASE DESCRIPTION
A 60-year-old man with a 60 pack-year smoking history, alcoholic cirrhosis, and a 5-year history of stage 1 CLL presented with 3 months of progressive shortness of breath; persistent cough; chills; hemoptysis; and a steady weight loss of 35 lbs. Notably, he had no bladder symptoms. Initial labs showed leukocytosis of 35.8k with a lymphocytic predominance. Screening low-dose chest CT was positive for diffuse mediastinal lymphadenopathy. Subsequent PET/CT revealed numerous hypermetabolic lymph nodes in the neck, mediastinum, left hilum, and right periaortic abdominal region. CT Chest, Abdomen, Pelvis revealed progressive lymphadenopathy as seen in prior imaging, stable pulmonary nodules up to 4 mm in size, and splenomegaly. No distant primary sites, including of the bladder, were identified. Mediastinal lymph node biopsy confirmed metastatic poorly differentiated carcinoma with immunohistochemical staining negative for p40, p63, CK20, TTF-1, Napsin A, CDX2, CA19- 9, Calretinin, and D2-40 and positive for CK7, GATA3, Ber-EP4, and Uroplakin, supporting bladder as primary origin. Urology deferred a cystoscopy given his lack of urinary symptoms and positive biopsy and was started on Carboplatin/Gemcitabine for his metastatic disease. He was ineligible for Cisplatin given his cirrhosis and hearing impairment.
DISCUSSION
In patients with CLL, new onset mediastinal lymphadenopathy is concerning for disease progression and possible transformation to a diffuse b-cell lymphoma. However, this symptom has a broad differential, including primary lung carcinomas, sarcomas, and metastatic disease. While our patient’s PET/CT and pan-CT failed to identify a distant primary site, maintaining a low clinical suspicion for metastatic disease and doing a thorough work-up was paramount. Only through immunohistochemical staining were we able to diagnosis this patient with urothelial carcinoma.
CONCLUSIONS
Biopsy with immunohistochemical staining and maintaining a low suspicion for worsening lymphadenopathy can identify unusually presenting urothelial carcinomas in CLL patients.
Freezing the biological clock: A 2023 update on preserving fertility
Throughout the 20th century, the management of ectopic pregnancy evolved from preserving the life of the mother to preserving fertility by utilizing the conservative treatment of methotrexate and/or tubal surgery. I make this, seemingly obscure, reference to managing ectopic pregnancy to consider an analogous shift over time in the management of patients with cancer. Over the next decade, the number of people who have lived 5 or more years after their cancer diagnosis is projected to increase approximately 30%, to 16.3 million. Due to the improved survival rates following a cancer diagnosis,1 revolutionary developments have been made in fertility preservation to obviate the impact of gonadotoxic therapy. We have evolved, however, from shielding and transposing ovaries to ovarian tissue cryopreservation,2 with rapid implementation.
While advances in reproductive cryopreservation have allowed for the delay, or even potential “prevention” of infertility, assisted reproductive technology (ART) cannot yet claim a “cure” in ensuring procreation. Nevertheless, fertility preservation is a burgeoning field that has transitioned from an experimental label to a standard of care in 2012, as designated by the American Society for Reproductive Medicine (ASRM).3 From the original intention of offering oocyte cryopreservation to women at risk of ovarian failure from impending gonadotoxic cancer treatment, fertility preservation has accelerated to include freezing for nonmedical reasons—eg, planned oocyte cryopreservation (POC), or “social” egg freezing, to ovarian tissue cryopreservation to accommodate the expediency needed for the treatment of certain cancer treatments. Additionally, across the United States, the number of donor egg banks, which allow women an easily accessible option, is rivaling enduring sperm banks. Due to the advanced methodology of vitrification and growing demand for the technology due to increasing IVF cycles, cryopreservation has become a specialized area of reproductive medicine, and a target of venture capital and private equity commercialization. This article will review the latest techniques, appropriate counseling, and cost/benefit ratio of fertility preservation, with an emphasis on POC.
CASE 1 Fertility preservation options for patient with breast cancer
A 37-year-old woman with newly diagnosed hormone receptor−positive breast cancer is referred for a fertility preservation consultation prior to initiating treatment. Her oncologist plans chemotherapy, followed by radiation and a minimum of 5 years of tamoxifen therapy.
What is the best consultation approach for this patient?
Consultation involves understanding several factors
The consultation approach to this patient involves ascertaining her medical, social, and family history, along with her reproductive plans.
Medical history. For the medical component, we must focus on her diagnosis, anticipated treatment with timeline, risks of gonadal toxicity with planned treatments, her current medical stability, and prognosis for expected survival.
Social history. Her age, relationship status, and desired family size address her social history.
Family history. Given that her cancer affects the breast, there is the risk of genetic susceptibility and potential for embryo testing for the BRCA gene.
Reproductive plans. These include her and her partner’s, if applicable, number of desired children and their risk factors for infertility.
Regarding the reproductive timeline, the antihormonal therapy that may be required for her treatment may improve overall survival, but it would delay the time to pregnancy. Consequently, the pursuit of fertility preservation prior to cancer treatment is a multidisciplinary approach that can involve medical oncology, radiation oncology, REI, medical genetics, and often, psychology. Fortunately, evidence continues to support fertility preservation, with or without hormonal ovarian stimulation, for patients with breast cancer. Data, with up to 5 years of follow-up, has indicated that it is safe.4
Continue to: Oncofertility...
Oncofertility
To address the need to maximize the reproductive potential of patients with newly diagnosed cancer, the field of oncofertility combines the specialties of oncology and reproductive medicine. The reproductive risk of cancer treatment is gonadotoxicity, with subsequent iatrogenic primary ovarian insufficiency (POI) and infertility. Alkylating agents (including cyclosphosphamide) have the highest risk for amenorrhea, while antimetabolites (including methotrexate, 5–fluorouracil) have the lowest risk.5 Treating bone marrow/stem cell transplantation using high-dose alkylating agents, with or without whole body irradiation, results in ≥80% amenorrhea. The minimum radiation dose to induce ovarian failure decreases with advancing age, from 18.4 Gy at age 10 years to 6 Gy at age 40 years, due to biologically diminishing ovarian reserve and an increase in the radiosensitivity of oocytes.6 An online tool—using varying factors including age, chemotherapy dose, prior treatment, smoking, and baseline diminished ovarian reserve—is available to help predict the chance of ovarian failure following chemotherapy.7
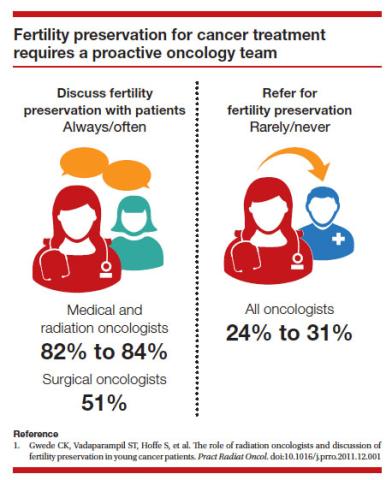
Since 2006, the American Society of Clinical Oncology recommended, as part of the consent prior to therapy, oncologists should address the possibility of infertility with patients “as early in treatment planning as possible” and “...Fertility preservation is an important, if not necessary, consideration when planning cancer treatment in reproductive-age patients.”
Reference
1. Lee SJ, Schover LR, Partridge AH, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006;24:2917-2931.
Cryopreservation to the rescue
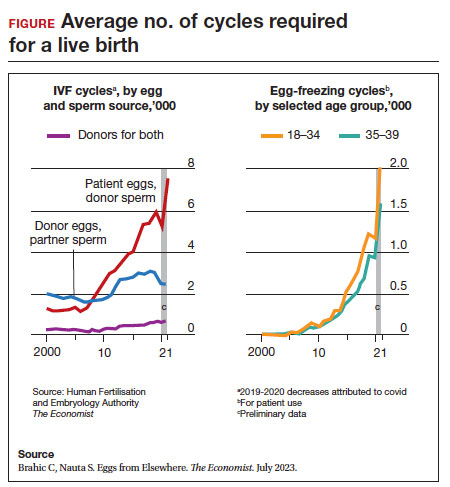
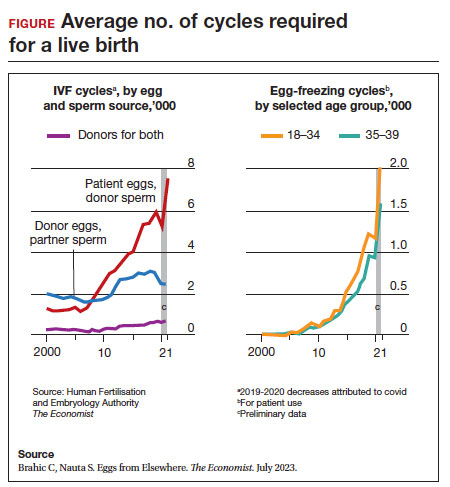
Since 2012, when ASRM removed the experimental designation on oocyte cryopreservation (OC), the number of cycles offered for fertility preservation has increased dramatically (FIGURE),8 initially being used for patients with cancer and now also including women desiring POC.
Ovarian and embryo cryopreservation. Ovarian stimulation and egg retrieval for OC can now occur within 2 weeks due to a random start protocol whereby women can begin ovarian stimulation any day in their cycle (ie, preovulation or postovulation).9
OC followed by thawing for subsequent fertilization and embryo transfer is employed as a matter of routine when patients with infertility utilize frozen eggs from a donor. While there remains debate over better live birth rates with frozen eggs versus fresh eggs, clinic experience may be a critical factor.10
Ovarian tissue cryopreservation. In addition to the fertility preservation procedures of oocytes and embryo cryopreservation, ovarian tissue cryopreservation became a standard option in 2019 when ASRM removed its experimental designation.11 Given the potential time constraints of urgent cancer treatment, ovarian tissue cryopreservation has the advantage of not requiring ovarian stimulation or sexual maturity and is able to be performed while patients are receiving chemotherapy. If successful, ovarian tissue cryopreservation followed by orthotopic transplantation has the potential to restore natural ovarian function and natural conceptions.12 However, despite first successfully being described in 2004, ovarian tissue cryopreservation, which does require subsequent thawing and tissue transplantation, remains less available to patients due to low usage rates, which have resulted in few clinics having adequate proficiency.13,14
Ovarian tissue cryopreservation involves obtaining ovarian cortical tissue, dissecting the tissue into small fragments, and cryopreserving it using either a slow-cool technique or vitrification. Orthotopic transplantation has been the most successful method for using ovarian tissue in humans. Live birth rates are modest.15 In all cancer survivors, particularly those with leukemia, autologous ovarian tissue transplantation may contain malignant cells that could lead to the reintroduction of cancer as the tissue is removed prior to treatment.16
Pregnancy outcomes using embryos created from ovaries recently exposed to chemotherapy in humans is not known, but animal studies suggest that there may be higher rates of miscarriage and birth defects given the severe DNA damage to oocytes of developing follicles.17 Hence, ovarian stimulation should be initiated and completed before the start of chemotherapy.
Continue to: Planned oocyte cryopreservation...
Planned oocyte cryopreservation
With advances in ART, POC offers patients the opportunity to preserve fertility until desired. However, despite its potential benefits, POC compels the discussion of various considerations in addition to oncofertility, such as ethical concerns and insurance coverage.
CASE 2 Woman plans for elective egg freezing
A 32-year-old single, professional woman is advancing in her career and wishes to delay childbearing. She is concerned about the potential for age-related fertility decline and wants to explore the option of elective egg freezing. Emily has no medical conditions that would impair her fertility, but she wants to ensure that she has the option of having biological children in the future. She is unsure about the potential financial burden of the procedure and whether her employer’s insurance covers such elective procedures.
How do you counsel her about her options?
Medical considerations
Approximately 25% of reproductive-aged women have considered POC.18 An analysis revealed POC was more cost-effective than delaying procreation and undergoing IVF with preimplantation genetic testing for aneuploidies at an advanced reproductive age.19
The process of planned oocyte cryopreservation. POC involves ovarian stimulation, usually with parenteral gonadotropins, to produce multiple mature oocytes for same-day cryopreservation following transvaginal retrieval, typically in an office-based surgery center as an outpatient procedure while the patient is under IV sedation. While the procedure has been proven effective, there are inherent risks and limitations. The success rates of subsequent fertility treatments using the cryopreserved eggs are influenced by the woman’s age at the time of freezing, the number of mature oocytes retrieved and vitrified, and the quality of the oocytes following thaw. A recent study reported a 70% live-birth rate in women aged less than 38 years who cryopreserved ≥ 20 mature eggs.20 To increase the number of cryopreserved oocytes, multiple egg retrievals or “batching” may be of benefit for women with diminished ovarian reserve.21
It is important for clinicians to thoroughly assess a patient’s medical history, ovarian reserve (by antral follicle count and levels of anti-müllerian hormone [AMH]), and reproductive goals before recommending proceeding with POC. Of note, AMH is a useful marker for ovarian reserve but has not been shown to predict natural fertility. Its value is in providing a guide to the dosage of ovarian stimulation and an estimation of the number of oocytes to be retrieved. Per ASRM, “Extremely low AMH values should not be used to refuse treatment in IVF.” AMH levels and antral follicle count have only a weak association with such qualitative outcomes as oocyte quality, clinical pregnancy rates, and live birth rates. Complications from egg retrieval, both short and long term, are rare. The inherent risk from POC is the lack of a guaranteed subsequent live birth.22
Ethical and social considerations
POC raises several ethical considerations, including concerns of perpetuating societal pressure on women to defer procreation to prioritize their careers over family planning.23 Despite controversies, POC appears as a chosen strategy against age-related infertility and may allow women to feel that they are more socially, psychologically, and financially stable before pursuing motherhood.24 Open and honest discussions between clinicians and patients are crucial to ensure informed decision making and address these ethical concerns.
Per an ACOG statement from February 2023 (https://www.acog.org/womens-health/faqs/having-a-baby-after-age-35-how-aging-affects-fertility-and-pregnancy) “...egg freezing is recommended mainly for patients having cancer treatment that will affect their future fertility. There is not enough research to recommend routine egg freezing for the sole purpose of delaying childbearing.”
A recent survey of patients who had elected egg freezing at some point included more than 80% who were aged 35 or older, and revealed that 93% of the survey participants had not yet returned to use their frozen oocytes.25 The most common reason cited in the survey for a delay in attempted procreation was lack of a partner. Another reason was undergoing oocyte cryopreservation after an optimal reproductive age, with participants concluding that they felt they had improved their reproductive future after undergoing oocyte cryopreservation and feeling empowered by the process. As part of counseling, women should be informed of the possibility of not utilizing their frozen eggs in the future, whether due to natural conception or other personal reasons.
Continue to: Employer insurance coverage...
Employer insurance coverage
Access to elective egg freezing is largely influenced by insurance coverage. Currently, employer-provided insurance coverage for this procedure varies widely. While some companies offer comprehensive coverage, others provide limited or no coverage at all. The cost of elective egg freezing can range from $10,000 to $15,000, excluding additional expenses such as medications and annual storage fees. The financial burden can create a gap between patients who desire POC and those with an ability to implement the process. The cost can be a significant barrier for many patients considering this option and perpetuates the lack of universal diversity, equity, and inclusion.
CASE 3 Gender dysphoria and fertility preservation
A 22-year-old transgender man is preparing to undergo gender-affirming hormone therapy and surgery. He is concerned about the potential impact of testosterone therapy on his oocytes and wishes to explore options for fertility preservation prior to oophorectomy.26
What are the patient’s options for fertility preservation?
The patient has the fertility preservation options of OC following ovarian stimulation or ovarian tissue cryopreservation at the time of oophorectomy. Preliminary evidence does not demonstrate impairment of ovarian stimulation and oocyte retrieval number with concurrent testosterone exposure. Ethical considerations, in this case, involve respecting the patient’s autonomy, addressing potential conflicts between gender-affirming care and fertility preservation (eg, a risk of dysphoria in transgender patients preserving biological gametes from a prior assigned gender), and ensuring access to fertility preservation services without discrimination. It is essential to provide the patient in this case with comprehensive information regarding the impact of hormone therapy on fertility, the available options, and the potential financial costs involved. Supportive counseling should also be offered to address any psychological or emotional aspects related to fertility preservation for all patients considering this option.
A call for diversity, equity, and inclusion
To improve access to POC, advocating for employer-offered insurance coverage is paramount. Women’s health providers can encourage dialogue between employers, insurers, and policymakers, which can lead to policy changes that prioritize coverage for fertilitypreservation options. This could include mandating coverage for POC as part of comprehensive health care plans or providing tax incentives to employers who offer coverage for these procedures. Furthermore, public awareness campaigns and advocacy efforts can help educate employers about the importance of including fertility preservation coverage in their employee benefits packages.
Conclusion
Just as physicians must recognize their responsibility to patients to distinguish unproven yet promising science from evidence-based and clinically established science, so too must they advise their patients to consider fertility preservation services in a way that is both clinically justified and ethically appropriate. Informed decisions must be made by appropriate counseling of evidence-based medicine to protect the interest of patients. POC provides patients with an opportunity to preserve their fertility and exercise reproductive autonomy. However, access to this procedure is often hindered by limited or nonexistent employer insurance coverage. By recognizing the medical, ethical, and social implications of POC and implementing strategies to improve coverage, collaborative efforts may increase accessibility and defray costs to provide patients with the option of deferring childbearing and preserving their reproductive potential. ●
1. Promptly offer fertility preservation treatment options with sensitivity and clarity.
2. Dedicate ample time and exercise patience during the consultation.
3. Provide education using multiple modalities to help patients assimilate information.
4. Encourage consultation with mental health professionals.
Special considerations for hematologic malignancies:
- Treatment can be associated with significant gonadal toxicity and premature ovarian failure.
- Patients are frequently ill at the time of presentation and ineligible for certain fertility preservation options.
References
1. Ethics Committee of the American Society for Reproductive Medicine. Fertility preservation and reproduction in patients facing gonadotoxic therapies: a committee opinion. Fertil Steril. 2018;110:380-386. doi:10.1016/j.fertnstert.2018.06.012
2. Kim SS, Klemp J, Fabian C. Breast cancer and fertility preservation. Fertil Steril. 2011;95:15351543. doi: 10.1016/j.fertnstert.2011.01.003
- American Cancer Society. Cancer Treatment & Survivorship Facts & Figures 2022-2024. Atlanta, Georgia: American Cancer Society; 2022.
- Oktay K, Karlikaya G. Ovarian function after autologous transplantation of frozen-banked human ovarian tissue. N Engl J Med. 2000;342:1919
- Practice Committees of the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology. Mature oocyte cryopreservation: a guideline. Fertil Steril. 2013;99:37-43. doi: 10.1016 /j.fertnstert.2012.09.028
- Marklund A, Lekberg T, Hedayati E, et al. Relapse rates and diseasespecific mortality following procedures for fertility preservation at time of breast cancer diagnosis. JAMA Oncol. 2022;8:1438-1446. doi:10.1001 /jamaoncol.2022.3677
- Zhao J, Liu J, Chen K, et al. What lies behind chemotherapy-induced amenorrhea for breast cancer patients: a meta-analysis. Breast Cancer Res Treat. 2014;145:113-128. https://doi.org/10.1007/s10549-014-2914-x
- Wallace WH, Thomson AB, Saran F, et al. Predicting age of ovarian failure after radiation to a field that includes the ovaries. Int J Radiat Oncol Biol Phys. 2005;62:738-744. http://doi.org10.1016/j.ijrobp.2004.11.038
- Chung EH, Acharya CR, Harris BS, et al. Development of a fertility risk calculator to predict individualized chance of hovarian failure after chemotherapy. J Assist Reprod Genetics. 2021;38:3047-3055. https://doi .org/10.1007/s10815-021-02311-0
- Brahic C, Nauta S. Eggs From Elsewhere. The Economist. July 2023.
- Cakmak H, Rosen MP. Random-start ovarian stimulation in patients with cancer. Curr Opin Obstet Gynecol. 2015;27:215-221. doi: 10.1097/ GCO.0000000000000180
- Eaton JL, Truong T, Li YJ, et al. Prevalence of a good perinatal outcome with cryopreserved compared with fresh donor oocytes. Obstet Gynecol. 2020;135:709-716. doi: 10.1097/AOG.0000000000003695
- Practice Committee of the American Society for Reproductive Medicine. Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: a committee opinion. Fertil Steril. 2019;112:1022-1033. doi: 10.1016/j.fertnstert.2019.09.013
- Oktay K, Marin L, Bedoschi G, et al. Ovarian transplantation with robotic surgery and a neovascularizing human extracellular matrix scaffold: a case series in comparison to meta-analytic data. Fertil Steril. 2021. doi:https ://doi.org/10.1016/j.fertnstert.2021.08.034
- Donnez J, Dolmans MM, Demylle D, et al. Livebirth after orthotopic transplantation of cryopreserved ovarian tissue. Lancet. 2004;364:1405-1410.
- Hoekman EJ, Louwe LA, Rooijers M, et al. Ovarian tissue cryopreservation: low usage rates and high live-birth rate after transplantation. Acta Obstet Gynecol Scand. 2020;99:213-221. doi: 10.1111/aogs.13735
- Donnez J, Dolmans MM, Diaz C, et al. Ovarian cortex transplantation: time to move on from experimental studies to open clinical application. Fertil Steril. 2015;104:1097-1098. doi: 10.1016/j.fertnstert.2015.08.005
- Rosendahl M, Greve T, Andersen CY. The safety of transplanting cryopreserved ovarian tissue in cancer patients: a review of the literature. J Assist Reprod Genet. 2013;30, 11-24. https://doi.org/10.1007/s10815-012-9912-x
- Soleimani R, Heytens E, Darzynkiewicz Z, et al. Mechanisms of chemotherapyinduced human ovarian aging: double strand DNA breaks and microvascular compromise. Aging (Albany NY). 2011;3:782-793.
- Milman LW, Senapati S, Sammel MD, et al. Assessing reproductive choices of women and the likelihood of oocyte cryopreservation in the era of elective oocyte freezing. Fertil Steril. 2017;107:1214-1222.e3. doi: 10.1016 /j.fertnstert.2017.03.010
- Bakkensen JB, Flannagan KSJ, Mumford SL, et al. A SART data cost-effectiveness analysis of planned oocyte cryopreservation versus in vitro fertilization with preimplantation genetic testing for aneuploidy considering ideal family size. Fertil Steril. 2022;118:875-884. https://doi.org/10.1016/j.fertnstert.2022.07.022
- Cascante SD, Blakemore JK, DeVore S. Fifteen years of autologous oocyte thaw outcomes from a large university-based fertility center. Fertil Steril. 2022;118:158-166. doi: 10.1016/j.fertnstert.2022.04.013
- Cobo A, Garrido N, Crespo J, et al. Accumulation of oocytes: a new strategy for managing low-responder patients. Reprod BioMedicine Online. 2018;37:669675. doi:10.1016/j.rbmo.2018.07.004
- Practice Committee of the American Society for Reproductive Medicine. Testing and interpreting measures of ovarian reserve: a committee opinion. Fertil Steril. 2020;114:1151-1157. doi: 10.1016/j.fertnstert.2020.09
- What you need to know about egg-freezing, the hot new perk at Google, Apple, and Facebook. Business Insider. September 17, 2017. Accessed August 9, 2023. https://www.businessinsider.com/egg-freezing-at-facebook-apple -google-hot-new-perk-2017-9
- Varlas VN, Bors RG, Albu D, et al. Social freezing: pressing pause on fertility. Int J Environ Res Public Health. 2021;18:8088. doi: 10.3390/ijerph18158088
- Hodes-Wertz B, Druckenmiller S, Smith M, et al. What do reproductive-age women who undergo oocyte cryopreservation think about the process as a means to preserve fertility? Fertil Steril. 2013;100:1343-1349. doi: 10.1016 /j.fertnstert.2013.07.201
- Moravek MB, Dixon M, Pena SM, et al. Management of testosterone around ovarian stimulation in transmasculine patients: challenging common practices to meet patient needs-2 case reports. Hum Reprod. 2023;38:482-488. doi: 10.1093/humrep/dead003
Throughout the 20th century, the management of ectopic pregnancy evolved from preserving the life of the mother to preserving fertility by utilizing the conservative treatment of methotrexate and/or tubal surgery. I make this, seemingly obscure, reference to managing ectopic pregnancy to consider an analogous shift over time in the management of patients with cancer. Over the next decade, the number of people who have lived 5 or more years after their cancer diagnosis is projected to increase approximately 30%, to 16.3 million. Due to the improved survival rates following a cancer diagnosis,1 revolutionary developments have been made in fertility preservation to obviate the impact of gonadotoxic therapy. We have evolved, however, from shielding and transposing ovaries to ovarian tissue cryopreservation,2 with rapid implementation.
While advances in reproductive cryopreservation have allowed for the delay, or even potential “prevention” of infertility, assisted reproductive technology (ART) cannot yet claim a “cure” in ensuring procreation. Nevertheless, fertility preservation is a burgeoning field that has transitioned from an experimental label to a standard of care in 2012, as designated by the American Society for Reproductive Medicine (ASRM).3 From the original intention of offering oocyte cryopreservation to women at risk of ovarian failure from impending gonadotoxic cancer treatment, fertility preservation has accelerated to include freezing for nonmedical reasons—eg, planned oocyte cryopreservation (POC), or “social” egg freezing, to ovarian tissue cryopreservation to accommodate the expediency needed for the treatment of certain cancer treatments. Additionally, across the United States, the number of donor egg banks, which allow women an easily accessible option, is rivaling enduring sperm banks. Due to the advanced methodology of vitrification and growing demand for the technology due to increasing IVF cycles, cryopreservation has become a specialized area of reproductive medicine, and a target of venture capital and private equity commercialization. This article will review the latest techniques, appropriate counseling, and cost/benefit ratio of fertility preservation, with an emphasis on POC.
CASE 1 Fertility preservation options for patient with breast cancer
A 37-year-old woman with newly diagnosed hormone receptor−positive breast cancer is referred for a fertility preservation consultation prior to initiating treatment. Her oncologist plans chemotherapy, followed by radiation and a minimum of 5 years of tamoxifen therapy.
What is the best consultation approach for this patient?
Consultation involves understanding several factors
The consultation approach to this patient involves ascertaining her medical, social, and family history, along with her reproductive plans.
Medical history. For the medical component, we must focus on her diagnosis, anticipated treatment with timeline, risks of gonadal toxicity with planned treatments, her current medical stability, and prognosis for expected survival.
Social history. Her age, relationship status, and desired family size address her social history.
Family history. Given that her cancer affects the breast, there is the risk of genetic susceptibility and potential for embryo testing for the BRCA gene.
Reproductive plans. These include her and her partner’s, if applicable, number of desired children and their risk factors for infertility.
Regarding the reproductive timeline, the antihormonal therapy that may be required for her treatment may improve overall survival, but it would delay the time to pregnancy. Consequently, the pursuit of fertility preservation prior to cancer treatment is a multidisciplinary approach that can involve medical oncology, radiation oncology, REI, medical genetics, and often, psychology. Fortunately, evidence continues to support fertility preservation, with or without hormonal ovarian stimulation, for patients with breast cancer. Data, with up to 5 years of follow-up, has indicated that it is safe.4
Continue to: Oncofertility...
Oncofertility
To address the need to maximize the reproductive potential of patients with newly diagnosed cancer, the field of oncofertility combines the specialties of oncology and reproductive medicine. The reproductive risk of cancer treatment is gonadotoxicity, with subsequent iatrogenic primary ovarian insufficiency (POI) and infertility. Alkylating agents (including cyclosphosphamide) have the highest risk for amenorrhea, while antimetabolites (including methotrexate, 5–fluorouracil) have the lowest risk.5 Treating bone marrow/stem cell transplantation using high-dose alkylating agents, with or without whole body irradiation, results in ≥80% amenorrhea. The minimum radiation dose to induce ovarian failure decreases with advancing age, from 18.4 Gy at age 10 years to 6 Gy at age 40 years, due to biologically diminishing ovarian reserve and an increase in the radiosensitivity of oocytes.6 An online tool—using varying factors including age, chemotherapy dose, prior treatment, smoking, and baseline diminished ovarian reserve—is available to help predict the chance of ovarian failure following chemotherapy.7
Since 2006, the American Society of Clinical Oncology recommended, as part of the consent prior to therapy, oncologists should address the possibility of infertility with patients “as early in treatment planning as possible” and “...Fertility preservation is an important, if not necessary, consideration when planning cancer treatment in reproductive-age patients.”
Reference
1. Lee SJ, Schover LR, Partridge AH, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006;24:2917-2931.
Cryopreservation to the rescue
Since 2012, when ASRM removed the experimental designation on oocyte cryopreservation (OC), the number of cycles offered for fertility preservation has increased dramatically (FIGURE),8 initially being used for patients with cancer and now also including women desiring POC.
Ovarian and embryo cryopreservation. Ovarian stimulation and egg retrieval for OC can now occur within 2 weeks due to a random start protocol whereby women can begin ovarian stimulation any day in their cycle (ie, preovulation or postovulation).9
OC followed by thawing for subsequent fertilization and embryo transfer is employed as a matter of routine when patients with infertility utilize frozen eggs from a donor. While there remains debate over better live birth rates with frozen eggs versus fresh eggs, clinic experience may be a critical factor.10
Ovarian tissue cryopreservation. In addition to the fertility preservation procedures of oocytes and embryo cryopreservation, ovarian tissue cryopreservation became a standard option in 2019 when ASRM removed its experimental designation.11 Given the potential time constraints of urgent cancer treatment, ovarian tissue cryopreservation has the advantage of not requiring ovarian stimulation or sexual maturity and is able to be performed while patients are receiving chemotherapy. If successful, ovarian tissue cryopreservation followed by orthotopic transplantation has the potential to restore natural ovarian function and natural conceptions.12 However, despite first successfully being described in 2004, ovarian tissue cryopreservation, which does require subsequent thawing and tissue transplantation, remains less available to patients due to low usage rates, which have resulted in few clinics having adequate proficiency.13,14
Ovarian tissue cryopreservation involves obtaining ovarian cortical tissue, dissecting the tissue into small fragments, and cryopreserving it using either a slow-cool technique or vitrification. Orthotopic transplantation has been the most successful method for using ovarian tissue in humans. Live birth rates are modest.15 In all cancer survivors, particularly those with leukemia, autologous ovarian tissue transplantation may contain malignant cells that could lead to the reintroduction of cancer as the tissue is removed prior to treatment.16
Pregnancy outcomes using embryos created from ovaries recently exposed to chemotherapy in humans is not known, but animal studies suggest that there may be higher rates of miscarriage and birth defects given the severe DNA damage to oocytes of developing follicles.17 Hence, ovarian stimulation should be initiated and completed before the start of chemotherapy.
Continue to: Planned oocyte cryopreservation...
Planned oocyte cryopreservation
With advances in ART, POC offers patients the opportunity to preserve fertility until desired. However, despite its potential benefits, POC compels the discussion of various considerations in addition to oncofertility, such as ethical concerns and insurance coverage.
CASE 2 Woman plans for elective egg freezing
A 32-year-old single, professional woman is advancing in her career and wishes to delay childbearing. She is concerned about the potential for age-related fertility decline and wants to explore the option of elective egg freezing. Emily has no medical conditions that would impair her fertility, but she wants to ensure that she has the option of having biological children in the future. She is unsure about the potential financial burden of the procedure and whether her employer’s insurance covers such elective procedures.
How do you counsel her about her options?
Medical considerations
Approximately 25% of reproductive-aged women have considered POC.18 An analysis revealed POC was more cost-effective than delaying procreation and undergoing IVF with preimplantation genetic testing for aneuploidies at an advanced reproductive age.19
The process of planned oocyte cryopreservation. POC involves ovarian stimulation, usually with parenteral gonadotropins, to produce multiple mature oocytes for same-day cryopreservation following transvaginal retrieval, typically in an office-based surgery center as an outpatient procedure while the patient is under IV sedation. While the procedure has been proven effective, there are inherent risks and limitations. The success rates of subsequent fertility treatments using the cryopreserved eggs are influenced by the woman’s age at the time of freezing, the number of mature oocytes retrieved and vitrified, and the quality of the oocytes following thaw. A recent study reported a 70% live-birth rate in women aged less than 38 years who cryopreserved ≥ 20 mature eggs.20 To increase the number of cryopreserved oocytes, multiple egg retrievals or “batching” may be of benefit for women with diminished ovarian reserve.21
It is important for clinicians to thoroughly assess a patient’s medical history, ovarian reserve (by antral follicle count and levels of anti-müllerian hormone [AMH]), and reproductive goals before recommending proceeding with POC. Of note, AMH is a useful marker for ovarian reserve but has not been shown to predict natural fertility. Its value is in providing a guide to the dosage of ovarian stimulation and an estimation of the number of oocytes to be retrieved. Per ASRM, “Extremely low AMH values should not be used to refuse treatment in IVF.” AMH levels and antral follicle count have only a weak association with such qualitative outcomes as oocyte quality, clinical pregnancy rates, and live birth rates. Complications from egg retrieval, both short and long term, are rare. The inherent risk from POC is the lack of a guaranteed subsequent live birth.22
Ethical and social considerations
POC raises several ethical considerations, including concerns of perpetuating societal pressure on women to defer procreation to prioritize their careers over family planning.23 Despite controversies, POC appears as a chosen strategy against age-related infertility and may allow women to feel that they are more socially, psychologically, and financially stable before pursuing motherhood.24 Open and honest discussions between clinicians and patients are crucial to ensure informed decision making and address these ethical concerns.
Per an ACOG statement from February 2023 (https://www.acog.org/womens-health/faqs/having-a-baby-after-age-35-how-aging-affects-fertility-and-pregnancy) “...egg freezing is recommended mainly for patients having cancer treatment that will affect their future fertility. There is not enough research to recommend routine egg freezing for the sole purpose of delaying childbearing.”
A recent survey of patients who had elected egg freezing at some point included more than 80% who were aged 35 or older, and revealed that 93% of the survey participants had not yet returned to use their frozen oocytes.25 The most common reason cited in the survey for a delay in attempted procreation was lack of a partner. Another reason was undergoing oocyte cryopreservation after an optimal reproductive age, with participants concluding that they felt they had improved their reproductive future after undergoing oocyte cryopreservation and feeling empowered by the process. As part of counseling, women should be informed of the possibility of not utilizing their frozen eggs in the future, whether due to natural conception or other personal reasons.
Continue to: Employer insurance coverage...
Employer insurance coverage
Access to elective egg freezing is largely influenced by insurance coverage. Currently, employer-provided insurance coverage for this procedure varies widely. While some companies offer comprehensive coverage, others provide limited or no coverage at all. The cost of elective egg freezing can range from $10,000 to $15,000, excluding additional expenses such as medications and annual storage fees. The financial burden can create a gap between patients who desire POC and those with an ability to implement the process. The cost can be a significant barrier for many patients considering this option and perpetuates the lack of universal diversity, equity, and inclusion.
CASE 3 Gender dysphoria and fertility preservation
A 22-year-old transgender man is preparing to undergo gender-affirming hormone therapy and surgery. He is concerned about the potential impact of testosterone therapy on his oocytes and wishes to explore options for fertility preservation prior to oophorectomy.26
What are the patient’s options for fertility preservation?
The patient has the fertility preservation options of OC following ovarian stimulation or ovarian tissue cryopreservation at the time of oophorectomy. Preliminary evidence does not demonstrate impairment of ovarian stimulation and oocyte retrieval number with concurrent testosterone exposure. Ethical considerations, in this case, involve respecting the patient’s autonomy, addressing potential conflicts between gender-affirming care and fertility preservation (eg, a risk of dysphoria in transgender patients preserving biological gametes from a prior assigned gender), and ensuring access to fertility preservation services without discrimination. It is essential to provide the patient in this case with comprehensive information regarding the impact of hormone therapy on fertility, the available options, and the potential financial costs involved. Supportive counseling should also be offered to address any psychological or emotional aspects related to fertility preservation for all patients considering this option.
A call for diversity, equity, and inclusion
To improve access to POC, advocating for employer-offered insurance coverage is paramount. Women’s health providers can encourage dialogue between employers, insurers, and policymakers, which can lead to policy changes that prioritize coverage for fertilitypreservation options. This could include mandating coverage for POC as part of comprehensive health care plans or providing tax incentives to employers who offer coverage for these procedures. Furthermore, public awareness campaigns and advocacy efforts can help educate employers about the importance of including fertility preservation coverage in their employee benefits packages.
Conclusion
Just as physicians must recognize their responsibility to patients to distinguish unproven yet promising science from evidence-based and clinically established science, so too must they advise their patients to consider fertility preservation services in a way that is both clinically justified and ethically appropriate. Informed decisions must be made by appropriate counseling of evidence-based medicine to protect the interest of patients. POC provides patients with an opportunity to preserve their fertility and exercise reproductive autonomy. However, access to this procedure is often hindered by limited or nonexistent employer insurance coverage. By recognizing the medical, ethical, and social implications of POC and implementing strategies to improve coverage, collaborative efforts may increase accessibility and defray costs to provide patients with the option of deferring childbearing and preserving their reproductive potential. ●
1. Promptly offer fertility preservation treatment options with sensitivity and clarity.
2. Dedicate ample time and exercise patience during the consultation.
3. Provide education using multiple modalities to help patients assimilate information.
4. Encourage consultation with mental health professionals.
Special considerations for hematologic malignancies:
- Treatment can be associated with significant gonadal toxicity and premature ovarian failure.
- Patients are frequently ill at the time of presentation and ineligible for certain fertility preservation options.
References
1. Ethics Committee of the American Society for Reproductive Medicine. Fertility preservation and reproduction in patients facing gonadotoxic therapies: a committee opinion. Fertil Steril. 2018;110:380-386. doi:10.1016/j.fertnstert.2018.06.012
2. Kim SS, Klemp J, Fabian C. Breast cancer and fertility preservation. Fertil Steril. 2011;95:15351543. doi: 10.1016/j.fertnstert.2011.01.003
Throughout the 20th century, the management of ectopic pregnancy evolved from preserving the life of the mother to preserving fertility by utilizing the conservative treatment of methotrexate and/or tubal surgery. I make this, seemingly obscure, reference to managing ectopic pregnancy to consider an analogous shift over time in the management of patients with cancer. Over the next decade, the number of people who have lived 5 or more years after their cancer diagnosis is projected to increase approximately 30%, to 16.3 million. Due to the improved survival rates following a cancer diagnosis,1 revolutionary developments have been made in fertility preservation to obviate the impact of gonadotoxic therapy. We have evolved, however, from shielding and transposing ovaries to ovarian tissue cryopreservation,2 with rapid implementation.
While advances in reproductive cryopreservation have allowed for the delay, or even potential “prevention” of infertility, assisted reproductive technology (ART) cannot yet claim a “cure” in ensuring procreation. Nevertheless, fertility preservation is a burgeoning field that has transitioned from an experimental label to a standard of care in 2012, as designated by the American Society for Reproductive Medicine (ASRM).3 From the original intention of offering oocyte cryopreservation to women at risk of ovarian failure from impending gonadotoxic cancer treatment, fertility preservation has accelerated to include freezing for nonmedical reasons—eg, planned oocyte cryopreservation (POC), or “social” egg freezing, to ovarian tissue cryopreservation to accommodate the expediency needed for the treatment of certain cancer treatments. Additionally, across the United States, the number of donor egg banks, which allow women an easily accessible option, is rivaling enduring sperm banks. Due to the advanced methodology of vitrification and growing demand for the technology due to increasing IVF cycles, cryopreservation has become a specialized area of reproductive medicine, and a target of venture capital and private equity commercialization. This article will review the latest techniques, appropriate counseling, and cost/benefit ratio of fertility preservation, with an emphasis on POC.
CASE 1 Fertility preservation options for patient with breast cancer
A 37-year-old woman with newly diagnosed hormone receptor−positive breast cancer is referred for a fertility preservation consultation prior to initiating treatment. Her oncologist plans chemotherapy, followed by radiation and a minimum of 5 years of tamoxifen therapy.
What is the best consultation approach for this patient?
Consultation involves understanding several factors
The consultation approach to this patient involves ascertaining her medical, social, and family history, along with her reproductive plans.
Medical history. For the medical component, we must focus on her diagnosis, anticipated treatment with timeline, risks of gonadal toxicity with planned treatments, her current medical stability, and prognosis for expected survival.
Social history. Her age, relationship status, and desired family size address her social history.
Family history. Given that her cancer affects the breast, there is the risk of genetic susceptibility and potential for embryo testing for the BRCA gene.
Reproductive plans. These include her and her partner’s, if applicable, number of desired children and their risk factors for infertility.
Regarding the reproductive timeline, the antihormonal therapy that may be required for her treatment may improve overall survival, but it would delay the time to pregnancy. Consequently, the pursuit of fertility preservation prior to cancer treatment is a multidisciplinary approach that can involve medical oncology, radiation oncology, REI, medical genetics, and often, psychology. Fortunately, evidence continues to support fertility preservation, with or without hormonal ovarian stimulation, for patients with breast cancer. Data, with up to 5 years of follow-up, has indicated that it is safe.4
Continue to: Oncofertility...
Oncofertility
To address the need to maximize the reproductive potential of patients with newly diagnosed cancer, the field of oncofertility combines the specialties of oncology and reproductive medicine. The reproductive risk of cancer treatment is gonadotoxicity, with subsequent iatrogenic primary ovarian insufficiency (POI) and infertility. Alkylating agents (including cyclosphosphamide) have the highest risk for amenorrhea, while antimetabolites (including methotrexate, 5–fluorouracil) have the lowest risk.5 Treating bone marrow/stem cell transplantation using high-dose alkylating agents, with or without whole body irradiation, results in ≥80% amenorrhea. The minimum radiation dose to induce ovarian failure decreases with advancing age, from 18.4 Gy at age 10 years to 6 Gy at age 40 years, due to biologically diminishing ovarian reserve and an increase in the radiosensitivity of oocytes.6 An online tool—using varying factors including age, chemotherapy dose, prior treatment, smoking, and baseline diminished ovarian reserve—is available to help predict the chance of ovarian failure following chemotherapy.7
Since 2006, the American Society of Clinical Oncology recommended, as part of the consent prior to therapy, oncologists should address the possibility of infertility with patients “as early in treatment planning as possible” and “...Fertility preservation is an important, if not necessary, consideration when planning cancer treatment in reproductive-age patients.”
Reference
1. Lee SJ, Schover LR, Partridge AH, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006;24:2917-2931.
Cryopreservation to the rescue
Since 2012, when ASRM removed the experimental designation on oocyte cryopreservation (OC), the number of cycles offered for fertility preservation has increased dramatically (FIGURE),8 initially being used for patients with cancer and now also including women desiring POC.
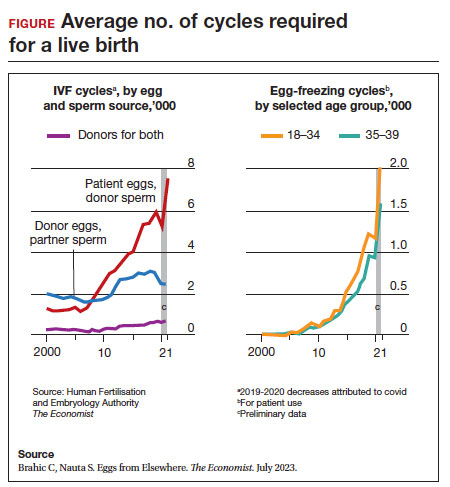
Ovarian and embryo cryopreservation. Ovarian stimulation and egg retrieval for OC can now occur within 2 weeks due to a random start protocol whereby women can begin ovarian stimulation any day in their cycle (ie, preovulation or postovulation).9
OC followed by thawing for subsequent fertilization and embryo transfer is employed as a matter of routine when patients with infertility utilize frozen eggs from a donor. While there remains debate over better live birth rates with frozen eggs versus fresh eggs, clinic experience may be a critical factor.10
Ovarian tissue cryopreservation. In addition to the fertility preservation procedures of oocytes and embryo cryopreservation, ovarian tissue cryopreservation became a standard option in 2019 when ASRM removed its experimental designation.11 Given the potential time constraints of urgent cancer treatment, ovarian tissue cryopreservation has the advantage of not requiring ovarian stimulation or sexual maturity and is able to be performed while patients are receiving chemotherapy. If successful, ovarian tissue cryopreservation followed by orthotopic transplantation has the potential to restore natural ovarian function and natural conceptions.12 However, despite first successfully being described in 2004, ovarian tissue cryopreservation, which does require subsequent thawing and tissue transplantation, remains less available to patients due to low usage rates, which have resulted in few clinics having adequate proficiency.13,14
Ovarian tissue cryopreservation involves obtaining ovarian cortical tissue, dissecting the tissue into small fragments, and cryopreserving it using either a slow-cool technique or vitrification. Orthotopic transplantation has been the most successful method for using ovarian tissue in humans. Live birth rates are modest.15 In all cancer survivors, particularly those with leukemia, autologous ovarian tissue transplantation may contain malignant cells that could lead to the reintroduction of cancer as the tissue is removed prior to treatment.16
Pregnancy outcomes using embryos created from ovaries recently exposed to chemotherapy in humans is not known, but animal studies suggest that there may be higher rates of miscarriage and birth defects given the severe DNA damage to oocytes of developing follicles.17 Hence, ovarian stimulation should be initiated and completed before the start of chemotherapy.
Continue to: Planned oocyte cryopreservation...
Planned oocyte cryopreservation
With advances in ART, POC offers patients the opportunity to preserve fertility until desired. However, despite its potential benefits, POC compels the discussion of various considerations in addition to oncofertility, such as ethical concerns and insurance coverage.
CASE 2 Woman plans for elective egg freezing
A 32-year-old single, professional woman is advancing in her career and wishes to delay childbearing. She is concerned about the potential for age-related fertility decline and wants to explore the option of elective egg freezing. Emily has no medical conditions that would impair her fertility, but she wants to ensure that she has the option of having biological children in the future. She is unsure about the potential financial burden of the procedure and whether her employer’s insurance covers such elective procedures.
How do you counsel her about her options?
Medical considerations
Approximately 25% of reproductive-aged women have considered POC.18 An analysis revealed POC was more cost-effective than delaying procreation and undergoing IVF with preimplantation genetic testing for aneuploidies at an advanced reproductive age.19
The process of planned oocyte cryopreservation. POC involves ovarian stimulation, usually with parenteral gonadotropins, to produce multiple mature oocytes for same-day cryopreservation following transvaginal retrieval, typically in an office-based surgery center as an outpatient procedure while the patient is under IV sedation. While the procedure has been proven effective, there are inherent risks and limitations. The success rates of subsequent fertility treatments using the cryopreserved eggs are influenced by the woman’s age at the time of freezing, the number of mature oocytes retrieved and vitrified, and the quality of the oocytes following thaw. A recent study reported a 70% live-birth rate in women aged less than 38 years who cryopreserved ≥ 20 mature eggs.20 To increase the number of cryopreserved oocytes, multiple egg retrievals or “batching” may be of benefit for women with diminished ovarian reserve.21
It is important for clinicians to thoroughly assess a patient’s medical history, ovarian reserve (by antral follicle count and levels of anti-müllerian hormone [AMH]), and reproductive goals before recommending proceeding with POC. Of note, AMH is a useful marker for ovarian reserve but has not been shown to predict natural fertility. Its value is in providing a guide to the dosage of ovarian stimulation and an estimation of the number of oocytes to be retrieved. Per ASRM, “Extremely low AMH values should not be used to refuse treatment in IVF.” AMH levels and antral follicle count have only a weak association with such qualitative outcomes as oocyte quality, clinical pregnancy rates, and live birth rates. Complications from egg retrieval, both short and long term, are rare. The inherent risk from POC is the lack of a guaranteed subsequent live birth.22
Ethical and social considerations
POC raises several ethical considerations, including concerns of perpetuating societal pressure on women to defer procreation to prioritize their careers over family planning.23 Despite controversies, POC appears as a chosen strategy against age-related infertility and may allow women to feel that they are more socially, psychologically, and financially stable before pursuing motherhood.24 Open and honest discussions between clinicians and patients are crucial to ensure informed decision making and address these ethical concerns.
Per an ACOG statement from February 2023 (https://www.acog.org/womens-health/faqs/having-a-baby-after-age-35-how-aging-affects-fertility-and-pregnancy) “...egg freezing is recommended mainly for patients having cancer treatment that will affect their future fertility. There is not enough research to recommend routine egg freezing for the sole purpose of delaying childbearing.”
A recent survey of patients who had elected egg freezing at some point included more than 80% who were aged 35 or older, and revealed that 93% of the survey participants had not yet returned to use their frozen oocytes.25 The most common reason cited in the survey for a delay in attempted procreation was lack of a partner. Another reason was undergoing oocyte cryopreservation after an optimal reproductive age, with participants concluding that they felt they had improved their reproductive future after undergoing oocyte cryopreservation and feeling empowered by the process. As part of counseling, women should be informed of the possibility of not utilizing their frozen eggs in the future, whether due to natural conception or other personal reasons.
Continue to: Employer insurance coverage...
Employer insurance coverage
Access to elective egg freezing is largely influenced by insurance coverage. Currently, employer-provided insurance coverage for this procedure varies widely. While some companies offer comprehensive coverage, others provide limited or no coverage at all. The cost of elective egg freezing can range from $10,000 to $15,000, excluding additional expenses such as medications and annual storage fees. The financial burden can create a gap between patients who desire POC and those with an ability to implement the process. The cost can be a significant barrier for many patients considering this option and perpetuates the lack of universal diversity, equity, and inclusion.
CASE 3 Gender dysphoria and fertility preservation
A 22-year-old transgender man is preparing to undergo gender-affirming hormone therapy and surgery. He is concerned about the potential impact of testosterone therapy on his oocytes and wishes to explore options for fertility preservation prior to oophorectomy.26
What are the patient’s options for fertility preservation?
The patient has the fertility preservation options of OC following ovarian stimulation or ovarian tissue cryopreservation at the time of oophorectomy. Preliminary evidence does not demonstrate impairment of ovarian stimulation and oocyte retrieval number with concurrent testosterone exposure. Ethical considerations, in this case, involve respecting the patient’s autonomy, addressing potential conflicts between gender-affirming care and fertility preservation (eg, a risk of dysphoria in transgender patients preserving biological gametes from a prior assigned gender), and ensuring access to fertility preservation services without discrimination. It is essential to provide the patient in this case with comprehensive information regarding the impact of hormone therapy on fertility, the available options, and the potential financial costs involved. Supportive counseling should also be offered to address any psychological or emotional aspects related to fertility preservation for all patients considering this option.
A call for diversity, equity, and inclusion
To improve access to POC, advocating for employer-offered insurance coverage is paramount. Women’s health providers can encourage dialogue between employers, insurers, and policymakers, which can lead to policy changes that prioritize coverage for fertilitypreservation options. This could include mandating coverage for POC as part of comprehensive health care plans or providing tax incentives to employers who offer coverage for these procedures. Furthermore, public awareness campaigns and advocacy efforts can help educate employers about the importance of including fertility preservation coverage in their employee benefits packages.
Conclusion
Just as physicians must recognize their responsibility to patients to distinguish unproven yet promising science from evidence-based and clinically established science, so too must they advise their patients to consider fertility preservation services in a way that is both clinically justified and ethically appropriate. Informed decisions must be made by appropriate counseling of evidence-based medicine to protect the interest of patients. POC provides patients with an opportunity to preserve their fertility and exercise reproductive autonomy. However, access to this procedure is often hindered by limited or nonexistent employer insurance coverage. By recognizing the medical, ethical, and social implications of POC and implementing strategies to improve coverage, collaborative efforts may increase accessibility and defray costs to provide patients with the option of deferring childbearing and preserving their reproductive potential. ●
1. Promptly offer fertility preservation treatment options with sensitivity and clarity.
2. Dedicate ample time and exercise patience during the consultation.
3. Provide education using multiple modalities to help patients assimilate information.
4. Encourage consultation with mental health professionals.
Special considerations for hematologic malignancies:
- Treatment can be associated with significant gonadal toxicity and premature ovarian failure.
- Patients are frequently ill at the time of presentation and ineligible for certain fertility preservation options.
References
1. Ethics Committee of the American Society for Reproductive Medicine. Fertility preservation and reproduction in patients facing gonadotoxic therapies: a committee opinion. Fertil Steril. 2018;110:380-386. doi:10.1016/j.fertnstert.2018.06.012
2. Kim SS, Klemp J, Fabian C. Breast cancer and fertility preservation. Fertil Steril. 2011;95:15351543. doi: 10.1016/j.fertnstert.2011.01.003
- American Cancer Society. Cancer Treatment & Survivorship Facts & Figures 2022-2024. Atlanta, Georgia: American Cancer Society; 2022.
- Oktay K, Karlikaya G. Ovarian function after autologous transplantation of frozen-banked human ovarian tissue. N Engl J Med. 2000;342:1919
- Practice Committees of the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology. Mature oocyte cryopreservation: a guideline. Fertil Steril. 2013;99:37-43. doi: 10.1016 /j.fertnstert.2012.09.028
- Marklund A, Lekberg T, Hedayati E, et al. Relapse rates and diseasespecific mortality following procedures for fertility preservation at time of breast cancer diagnosis. JAMA Oncol. 2022;8:1438-1446. doi:10.1001 /jamaoncol.2022.3677
- Zhao J, Liu J, Chen K, et al. What lies behind chemotherapy-induced amenorrhea for breast cancer patients: a meta-analysis. Breast Cancer Res Treat. 2014;145:113-128. https://doi.org/10.1007/s10549-014-2914-x
- Wallace WH, Thomson AB, Saran F, et al. Predicting age of ovarian failure after radiation to a field that includes the ovaries. Int J Radiat Oncol Biol Phys. 2005;62:738-744. http://doi.org10.1016/j.ijrobp.2004.11.038
- Chung EH, Acharya CR, Harris BS, et al. Development of a fertility risk calculator to predict individualized chance of hovarian failure after chemotherapy. J Assist Reprod Genetics. 2021;38:3047-3055. https://doi .org/10.1007/s10815-021-02311-0
- Brahic C, Nauta S. Eggs From Elsewhere. The Economist. July 2023.
- Cakmak H, Rosen MP. Random-start ovarian stimulation in patients with cancer. Curr Opin Obstet Gynecol. 2015;27:215-221. doi: 10.1097/ GCO.0000000000000180
- Eaton JL, Truong T, Li YJ, et al. Prevalence of a good perinatal outcome with cryopreserved compared with fresh donor oocytes. Obstet Gynecol. 2020;135:709-716. doi: 10.1097/AOG.0000000000003695
- Practice Committee of the American Society for Reproductive Medicine. Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: a committee opinion. Fertil Steril. 2019;112:1022-1033. doi: 10.1016/j.fertnstert.2019.09.013
- Oktay K, Marin L, Bedoschi G, et al. Ovarian transplantation with robotic surgery and a neovascularizing human extracellular matrix scaffold: a case series in comparison to meta-analytic data. Fertil Steril. 2021. doi:https ://doi.org/10.1016/j.fertnstert.2021.08.034
- Donnez J, Dolmans MM, Demylle D, et al. Livebirth after orthotopic transplantation of cryopreserved ovarian tissue. Lancet. 2004;364:1405-1410.
- Hoekman EJ, Louwe LA, Rooijers M, et al. Ovarian tissue cryopreservation: low usage rates and high live-birth rate after transplantation. Acta Obstet Gynecol Scand. 2020;99:213-221. doi: 10.1111/aogs.13735
- Donnez J, Dolmans MM, Diaz C, et al. Ovarian cortex transplantation: time to move on from experimental studies to open clinical application. Fertil Steril. 2015;104:1097-1098. doi: 10.1016/j.fertnstert.2015.08.005
- Rosendahl M, Greve T, Andersen CY. The safety of transplanting cryopreserved ovarian tissue in cancer patients: a review of the literature. J Assist Reprod Genet. 2013;30, 11-24. https://doi.org/10.1007/s10815-012-9912-x
- Soleimani R, Heytens E, Darzynkiewicz Z, et al. Mechanisms of chemotherapyinduced human ovarian aging: double strand DNA breaks and microvascular compromise. Aging (Albany NY). 2011;3:782-793.
- Milman LW, Senapati S, Sammel MD, et al. Assessing reproductive choices of women and the likelihood of oocyte cryopreservation in the era of elective oocyte freezing. Fertil Steril. 2017;107:1214-1222.e3. doi: 10.1016 /j.fertnstert.2017.03.010
- Bakkensen JB, Flannagan KSJ, Mumford SL, et al. A SART data cost-effectiveness analysis of planned oocyte cryopreservation versus in vitro fertilization with preimplantation genetic testing for aneuploidy considering ideal family size. Fertil Steril. 2022;118:875-884. https://doi.org/10.1016/j.fertnstert.2022.07.022
- Cascante SD, Blakemore JK, DeVore S. Fifteen years of autologous oocyte thaw outcomes from a large university-based fertility center. Fertil Steril. 2022;118:158-166. doi: 10.1016/j.fertnstert.2022.04.013
- Cobo A, Garrido N, Crespo J, et al. Accumulation of oocytes: a new strategy for managing low-responder patients. Reprod BioMedicine Online. 2018;37:669675. doi:10.1016/j.rbmo.2018.07.004
- Practice Committee of the American Society for Reproductive Medicine. Testing and interpreting measures of ovarian reserve: a committee opinion. Fertil Steril. 2020;114:1151-1157. doi: 10.1016/j.fertnstert.2020.09
- What you need to know about egg-freezing, the hot new perk at Google, Apple, and Facebook. Business Insider. September 17, 2017. Accessed August 9, 2023. https://www.businessinsider.com/egg-freezing-at-facebook-apple -google-hot-new-perk-2017-9
- Varlas VN, Bors RG, Albu D, et al. Social freezing: pressing pause on fertility. Int J Environ Res Public Health. 2021;18:8088. doi: 10.3390/ijerph18158088
- Hodes-Wertz B, Druckenmiller S, Smith M, et al. What do reproductive-age women who undergo oocyte cryopreservation think about the process as a means to preserve fertility? Fertil Steril. 2013;100:1343-1349. doi: 10.1016 /j.fertnstert.2013.07.201
- Moravek MB, Dixon M, Pena SM, et al. Management of testosterone around ovarian stimulation in transmasculine patients: challenging common practices to meet patient needs-2 case reports. Hum Reprod. 2023;38:482-488. doi: 10.1093/humrep/dead003
- American Cancer Society. Cancer Treatment & Survivorship Facts & Figures 2022-2024. Atlanta, Georgia: American Cancer Society; 2022.
- Oktay K, Karlikaya G. Ovarian function after autologous transplantation of frozen-banked human ovarian tissue. N Engl J Med. 2000;342:1919
- Practice Committees of the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology. Mature oocyte cryopreservation: a guideline. Fertil Steril. 2013;99:37-43. doi: 10.1016 /j.fertnstert.2012.09.028
- Marklund A, Lekberg T, Hedayati E, et al. Relapse rates and diseasespecific mortality following procedures for fertility preservation at time of breast cancer diagnosis. JAMA Oncol. 2022;8:1438-1446. doi:10.1001 /jamaoncol.2022.3677
- Zhao J, Liu J, Chen K, et al. What lies behind chemotherapy-induced amenorrhea for breast cancer patients: a meta-analysis. Breast Cancer Res Treat. 2014;145:113-128. https://doi.org/10.1007/s10549-014-2914-x
- Wallace WH, Thomson AB, Saran F, et al. Predicting age of ovarian failure after radiation to a field that includes the ovaries. Int J Radiat Oncol Biol Phys. 2005;62:738-744. http://doi.org10.1016/j.ijrobp.2004.11.038
- Chung EH, Acharya CR, Harris BS, et al. Development of a fertility risk calculator to predict individualized chance of hovarian failure after chemotherapy. J Assist Reprod Genetics. 2021;38:3047-3055. https://doi .org/10.1007/s10815-021-02311-0
- Brahic C, Nauta S. Eggs From Elsewhere. The Economist. July 2023.
- Cakmak H, Rosen MP. Random-start ovarian stimulation in patients with cancer. Curr Opin Obstet Gynecol. 2015;27:215-221. doi: 10.1097/ GCO.0000000000000180
- Eaton JL, Truong T, Li YJ, et al. Prevalence of a good perinatal outcome with cryopreserved compared with fresh donor oocytes. Obstet Gynecol. 2020;135:709-716. doi: 10.1097/AOG.0000000000003695
- Practice Committee of the American Society for Reproductive Medicine. Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: a committee opinion. Fertil Steril. 2019;112:1022-1033. doi: 10.1016/j.fertnstert.2019.09.013
- Oktay K, Marin L, Bedoschi G, et al. Ovarian transplantation with robotic surgery and a neovascularizing human extracellular matrix scaffold: a case series in comparison to meta-analytic data. Fertil Steril. 2021. doi:https ://doi.org/10.1016/j.fertnstert.2021.08.034
- Donnez J, Dolmans MM, Demylle D, et al. Livebirth after orthotopic transplantation of cryopreserved ovarian tissue. Lancet. 2004;364:1405-1410.
- Hoekman EJ, Louwe LA, Rooijers M, et al. Ovarian tissue cryopreservation: low usage rates and high live-birth rate after transplantation. Acta Obstet Gynecol Scand. 2020;99:213-221. doi: 10.1111/aogs.13735
- Donnez J, Dolmans MM, Diaz C, et al. Ovarian cortex transplantation: time to move on from experimental studies to open clinical application. Fertil Steril. 2015;104:1097-1098. doi: 10.1016/j.fertnstert.2015.08.005
- Rosendahl M, Greve T, Andersen CY. The safety of transplanting cryopreserved ovarian tissue in cancer patients: a review of the literature. J Assist Reprod Genet. 2013;30, 11-24. https://doi.org/10.1007/s10815-012-9912-x
- Soleimani R, Heytens E, Darzynkiewicz Z, et al. Mechanisms of chemotherapyinduced human ovarian aging: double strand DNA breaks and microvascular compromise. Aging (Albany NY). 2011;3:782-793.
- Milman LW, Senapati S, Sammel MD, et al. Assessing reproductive choices of women and the likelihood of oocyte cryopreservation in the era of elective oocyte freezing. Fertil Steril. 2017;107:1214-1222.e3. doi: 10.1016 /j.fertnstert.2017.03.010
- Bakkensen JB, Flannagan KSJ, Mumford SL, et al. A SART data cost-effectiveness analysis of planned oocyte cryopreservation versus in vitro fertilization with preimplantation genetic testing for aneuploidy considering ideal family size. Fertil Steril. 2022;118:875-884. https://doi.org/10.1016/j.fertnstert.2022.07.022
- Cascante SD, Blakemore JK, DeVore S. Fifteen years of autologous oocyte thaw outcomes from a large university-based fertility center. Fertil Steril. 2022;118:158-166. doi: 10.1016/j.fertnstert.2022.04.013
- Cobo A, Garrido N, Crespo J, et al. Accumulation of oocytes: a new strategy for managing low-responder patients. Reprod BioMedicine Online. 2018;37:669675. doi:10.1016/j.rbmo.2018.07.004
- Practice Committee of the American Society for Reproductive Medicine. Testing and interpreting measures of ovarian reserve: a committee opinion. Fertil Steril. 2020;114:1151-1157. doi: 10.1016/j.fertnstert.2020.09
- What you need to know about egg-freezing, the hot new perk at Google, Apple, and Facebook. Business Insider. September 17, 2017. Accessed August 9, 2023. https://www.businessinsider.com/egg-freezing-at-facebook-apple -google-hot-new-perk-2017-9
- Varlas VN, Bors RG, Albu D, et al. Social freezing: pressing pause on fertility. Int J Environ Res Public Health. 2021;18:8088. doi: 10.3390/ijerph18158088
- Hodes-Wertz B, Druckenmiller S, Smith M, et al. What do reproductive-age women who undergo oocyte cryopreservation think about the process as a means to preserve fertility? Fertil Steril. 2013;100:1343-1349. doi: 10.1016 /j.fertnstert.2013.07.201
- Moravek MB, Dixon M, Pena SM, et al. Management of testosterone around ovarian stimulation in transmasculine patients: challenging common practices to meet patient needs-2 case reports. Hum Reprod. 2023;38:482-488. doi: 10.1093/humrep/dead003
Safely skip PET2 after brentuximab in Hodgkin lymphoma?
FROM SOHO 2023
Data from four recent studies indicate that adding frontline brentuximab vedotin to AVD chemotherapy (doxorubicin, vinblastine, dacarbazine) improves outcomes for patients, regardless of PET2 scan results, according to lead investigator Ravand Samaeekia, MD, MSc, from Loma Linda (Calif.) University Medical Center.
These studies, including one conducted by Dr. Samaeekia’s team, provide “evidence for the safe omission of PET2 in treatment regimens that contain brentuximab vedotin,” Dr. Samaeekia, who presented the data, concluded.
Performing an interim PET-CT scan after two cycles of chemotherapy can help oncologists adapt treatment protocols for patients with Hodgkin lymphoma and has become the standard of care for these patients.
However, “there are obviously challenges associated with implementing a PET-guided approach,” said Dr. Samaeekia. Additional PET-CT scans can be costly, time consuming, and increase patients’ risk for toxicities when treatment is escalated based on the scan results.
Given these caveats, Dr. Samaeekia reviewed data exploring whether PET2 has predictive value for patients who receive the anti-CD30 antibody-drug conjugate, brentuximab vedotin, as part of first-line treatment alongside AVD chemotherapy.
Dr. Samaeekia’s team analyzed findings from three trials – ECHELON-1, AHOD1331, and BREACH – which assessed frontline standard of care chemotherapy with or without brentuximab. The team found that incorporating brentuximab into frontline treatment resulted in superior efficacy, and PET2 scans results generally did not change how patients were managed.
In ECHELON-1, 6-year overall survival favored patients with advanced Hodgkin lymphoma who received brentuximab and were PET2 negative (94.9% vs. 90.6%; hazard ratio for death, 0.54) as well as those who were PET2 positive (95% vs. 77%; HR, 0.16). Overall, just over 2% of patients who received the brentuximab regimen switched to an alternative chemotherapy and even fewer did so based on PET2 results.
In AHOD1331, 3-year event-free survival was significantly higher among adolescents and children with Hodgkin lymphoma who received brentuximab – 90.7% for those who had slow-responding lesions and 92.3% for those with rapid-responding lesions. Based on these results, the authors concluded that adding brentuximab “eliminated the predictive value of the interim PET assessment.” The BREACH trial echoed the findings from ECHELON-1 and AHOD1331.
Finally, in a retrospective study of 40 patients treated at Loma Linda with brentuximab vedotin plus AVD, Dr. Samaeekia and colleagues found that 24 were PET2 negative and 12 were PET2 positive. All patients who were PET2 negative remained negative on the end-of-treatment PET, indicating no cancer progression. Of the 12 PET2-positive patients, four (33%) remained PET positive at the end of treatment. Only one patient overall changed regimens following PET2.
Dr. Samaeekia’s team concluded that PET2 scan results “did not have any meaningful impact” on patient management or outcomes.
During the Q&A, Martin Hutchings, MD, PhD, challenged the idea that PET2 can be omitted. Dr. Hutchings, from the Rigshospitalet in Copenhagen, pointed out that 4 of the 12 PET2-positive patients treated at Loma Linda were still PET positive at the end of treatment.
Even so, Dr. Samaeekia explained, PET2 findings did not alter treatment for most patients, noting that doing a PET2 scan may make “us feel better,” but it ultimately doesn’t “make any difference in our management.”
In the AHOD1331 study, “the findings on the interim PET scan were not helpful in the ultimate outcome, whether it was either positive or negative,” added session comoderator Jonathan W. Friedberg, MD, MMSc, director of the James P. Wilmot Cancer Institute at the University of Rochester (N.Y.) Medical Center.
The study by Dr. Samaeekia and colleagues was internally funded. Dr. Samaeekia reports no relevant financial relationships. Dr. Hutchings has previously reported consultancy and research funding from numerous companies. Dr. Friedberg reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM SOHO 2023
Data from four recent studies indicate that adding frontline brentuximab vedotin to AVD chemotherapy (doxorubicin, vinblastine, dacarbazine) improves outcomes for patients, regardless of PET2 scan results, according to lead investigator Ravand Samaeekia, MD, MSc, from Loma Linda (Calif.) University Medical Center.
These studies, including one conducted by Dr. Samaeekia’s team, provide “evidence for the safe omission of PET2 in treatment regimens that contain brentuximab vedotin,” Dr. Samaeekia, who presented the data, concluded.
Performing an interim PET-CT scan after two cycles of chemotherapy can help oncologists adapt treatment protocols for patients with Hodgkin lymphoma and has become the standard of care for these patients.
However, “there are obviously challenges associated with implementing a PET-guided approach,” said Dr. Samaeekia. Additional PET-CT scans can be costly, time consuming, and increase patients’ risk for toxicities when treatment is escalated based on the scan results.
Given these caveats, Dr. Samaeekia reviewed data exploring whether PET2 has predictive value for patients who receive the anti-CD30 antibody-drug conjugate, brentuximab vedotin, as part of first-line treatment alongside AVD chemotherapy.
Dr. Samaeekia’s team analyzed findings from three trials – ECHELON-1, AHOD1331, and BREACH – which assessed frontline standard of care chemotherapy with or without brentuximab. The team found that incorporating brentuximab into frontline treatment resulted in superior efficacy, and PET2 scans results generally did not change how patients were managed.
In ECHELON-1, 6-year overall survival favored patients with advanced Hodgkin lymphoma who received brentuximab and were PET2 negative (94.9% vs. 90.6%; hazard ratio for death, 0.54) as well as those who were PET2 positive (95% vs. 77%; HR, 0.16). Overall, just over 2% of patients who received the brentuximab regimen switched to an alternative chemotherapy and even fewer did so based on PET2 results.
In AHOD1331, 3-year event-free survival was significantly higher among adolescents and children with Hodgkin lymphoma who received brentuximab – 90.7% for those who had slow-responding lesions and 92.3% for those with rapid-responding lesions. Based on these results, the authors concluded that adding brentuximab “eliminated the predictive value of the interim PET assessment.” The BREACH trial echoed the findings from ECHELON-1 and AHOD1331.
Finally, in a retrospective study of 40 patients treated at Loma Linda with brentuximab vedotin plus AVD, Dr. Samaeekia and colleagues found that 24 were PET2 negative and 12 were PET2 positive. All patients who were PET2 negative remained negative on the end-of-treatment PET, indicating no cancer progression. Of the 12 PET2-positive patients, four (33%) remained PET positive at the end of treatment. Only one patient overall changed regimens following PET2.
Dr. Samaeekia’s team concluded that PET2 scan results “did not have any meaningful impact” on patient management or outcomes.
During the Q&A, Martin Hutchings, MD, PhD, challenged the idea that PET2 can be omitted. Dr. Hutchings, from the Rigshospitalet in Copenhagen, pointed out that 4 of the 12 PET2-positive patients treated at Loma Linda were still PET positive at the end of treatment.
Even so, Dr. Samaeekia explained, PET2 findings did not alter treatment for most patients, noting that doing a PET2 scan may make “us feel better,” but it ultimately doesn’t “make any difference in our management.”
In the AHOD1331 study, “the findings on the interim PET scan were not helpful in the ultimate outcome, whether it was either positive or negative,” added session comoderator Jonathan W. Friedberg, MD, MMSc, director of the James P. Wilmot Cancer Institute at the University of Rochester (N.Y.) Medical Center.
The study by Dr. Samaeekia and colleagues was internally funded. Dr. Samaeekia reports no relevant financial relationships. Dr. Hutchings has previously reported consultancy and research funding from numerous companies. Dr. Friedberg reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM SOHO 2023
Data from four recent studies indicate that adding frontline brentuximab vedotin to AVD chemotherapy (doxorubicin, vinblastine, dacarbazine) improves outcomes for patients, regardless of PET2 scan results, according to lead investigator Ravand Samaeekia, MD, MSc, from Loma Linda (Calif.) University Medical Center.
These studies, including one conducted by Dr. Samaeekia’s team, provide “evidence for the safe omission of PET2 in treatment regimens that contain brentuximab vedotin,” Dr. Samaeekia, who presented the data, concluded.
Performing an interim PET-CT scan after two cycles of chemotherapy can help oncologists adapt treatment protocols for patients with Hodgkin lymphoma and has become the standard of care for these patients.
However, “there are obviously challenges associated with implementing a PET-guided approach,” said Dr. Samaeekia. Additional PET-CT scans can be costly, time consuming, and increase patients’ risk for toxicities when treatment is escalated based on the scan results.
Given these caveats, Dr. Samaeekia reviewed data exploring whether PET2 has predictive value for patients who receive the anti-CD30 antibody-drug conjugate, brentuximab vedotin, as part of first-line treatment alongside AVD chemotherapy.
Dr. Samaeekia’s team analyzed findings from three trials – ECHELON-1, AHOD1331, and BREACH – which assessed frontline standard of care chemotherapy with or without brentuximab. The team found that incorporating brentuximab into frontline treatment resulted in superior efficacy, and PET2 scans results generally did not change how patients were managed.
In ECHELON-1, 6-year overall survival favored patients with advanced Hodgkin lymphoma who received brentuximab and were PET2 negative (94.9% vs. 90.6%; hazard ratio for death, 0.54) as well as those who were PET2 positive (95% vs. 77%; HR, 0.16). Overall, just over 2% of patients who received the brentuximab regimen switched to an alternative chemotherapy and even fewer did so based on PET2 results.
In AHOD1331, 3-year event-free survival was significantly higher among adolescents and children with Hodgkin lymphoma who received brentuximab – 90.7% for those who had slow-responding lesions and 92.3% for those with rapid-responding lesions. Based on these results, the authors concluded that adding brentuximab “eliminated the predictive value of the interim PET assessment.” The BREACH trial echoed the findings from ECHELON-1 and AHOD1331.
Finally, in a retrospective study of 40 patients treated at Loma Linda with brentuximab vedotin plus AVD, Dr. Samaeekia and colleagues found that 24 were PET2 negative and 12 were PET2 positive. All patients who were PET2 negative remained negative on the end-of-treatment PET, indicating no cancer progression. Of the 12 PET2-positive patients, four (33%) remained PET positive at the end of treatment. Only one patient overall changed regimens following PET2.
Dr. Samaeekia’s team concluded that PET2 scan results “did not have any meaningful impact” on patient management or outcomes.
During the Q&A, Martin Hutchings, MD, PhD, challenged the idea that PET2 can be omitted. Dr. Hutchings, from the Rigshospitalet in Copenhagen, pointed out that 4 of the 12 PET2-positive patients treated at Loma Linda were still PET positive at the end of treatment.
Even so, Dr. Samaeekia explained, PET2 findings did not alter treatment for most patients, noting that doing a PET2 scan may make “us feel better,” but it ultimately doesn’t “make any difference in our management.”
In the AHOD1331 study, “the findings on the interim PET scan were not helpful in the ultimate outcome, whether it was either positive or negative,” added session comoderator Jonathan W. Friedberg, MD, MMSc, director of the James P. Wilmot Cancer Institute at the University of Rochester (N.Y.) Medical Center.
The study by Dr. Samaeekia and colleagues was internally funded. Dr. Samaeekia reports no relevant financial relationships. Dr. Hutchings has previously reported consultancy and research funding from numerous companies. Dr. Friedberg reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
High rate of subsequent cancers in MCC
.
In a cohort of 6,146 patients with a first primary MCC, a total of 725 (11.8%) developed subsequent primary cancers. For solid tumors, the risk was highest for cutaneous melanoma and papillary thyroid carcinoma, while for hematologic cancers, the risk was increased for non-Hodgkin lymphoma.
“Our study does confirm that patients with MCC are at higher risk for developing other cancers,” study author Lisa C. Zaba, MD, PhD, associate professor of dermatology and director of the Merkel cell carcinoma multidisciplinary clinic, Stanford (Calif.) Cancer Center, said in an interview. “MCC is a highly malignant cancer with a 40% recurrence risk.”
Because of this high risk, Dr. Zaba noted that patients with MCC get frequent surveillance with both imaging studies (PET-CT and CT) as well as frequent visits in clinic with MCC experts. “Specifically, a patient with MCC is imaged and seen in clinic every 3-6 months for the first 3 years after diagnosis, and every 6-12 months thereafter for up to 5 years,” she said. “Interestingly, this high level of surveillance may be one reason that we find so many cancers in patients who have been diagnosed with MCC, compared to the general population.”
The study was published online in JAMA Dermatology.
With the death of “Margaritaville” singer Jimmy Buffett, who recently died of MCC 4 years after his diagnosis, this rare, aggressive skin cancer has been put in the spotlight. Survival has been increasing, primarily because of the advent of immunotherapy, and the authors note that it is therefore imperative to better understand the risk of subsequent primary tumors to inform screening and treatment recommendations.
In this cohort study, Dr. Zaba and colleagues identified 6,146 patients from 17 registries of the Surveillance, Epidemiology, and End Results (SEER) Program who had been diagnosed with a first primary cutaneous MCC between 2000 and 2018.
Endpoints were the ratio of observed to expected number of cases of subsequent cancer (Standardized incidence ratio, or SIR) and the excess risk.
Overall, there was an elevated risk of developing a subsequent primary cancer after being diagnosed with MCC (SIR, 1.28; excess risk, 57.25 per 10,000 person-years). This included the risk for all solid tumors including liver (SIR, 1.92; excess risk, 2.77 per 10,000 person-years), pancreas (SIR, 1.65; excess risk, 4.55 per 10,000 person-years), cutaneous melanoma (SIR, 2.36; excess risk, 15.27 per 10,000 person-years), and kidney (SIR, 1.64; excess risk, 3.83 per 10,000 person-years).
There was also a higher risk of developing papillary thyroid carcinoma (PTC) (SIR, 5.26; excess risk, 6.16 per 10,000 person-years).
The risk of developing hematological cancers after MCC was also increased, especially for non-Hodgkin lymphoma (SIR, 2.62; excess risk, 15.48 per 10,000 person-years) and myelodysplastic syndrome (SIR, 2.17; excess risk, 2.73 per 10,000 person-years).
The risk for developing subsequent tumors, including melanoma and non-Hodgkin lymphoma, remained significant for up to 10 years, while the risk for developing PTC and kidney cancers remained for up to 5 years.
“After 3-5 years, when a MCC patient’s risk of MCC recurrence drops below 2%, we do not currently have guidelines in place for additional cancer screening,” Dr. Zaba said. “Regarding patient education, patients with MCC are educated to let us know if they experience any symptoms of cancer between visits, including unintentional weight loss, night sweats, headaches that increasingly worsen, or growing lumps or bumps. These symptoms may occur in a multitude of cancers and not just MCC.”
Weighing in on the study, Jeffrey M. Farma, MD, interim chair, department of surgical oncology at Fox Chase Cancer Center, Philadelphia, noted that MCC is considered to be high risk because of its chances of recurring after surgical resection or spreading to lymph nodes or other areas of the body. “There are approximately 3,000 new cases of melanoma a year in the U.S., and it is 40 times rarer than melanoma,” he said. “Patients are usually diagnosed with Merkel cell carcinoma later in life, and the tumors have been associated with sun exposure and immunosuppression and have also been associated with the polyomavirus.”
That said, however, he emphasized that great strides have been made in treatment. “These tumors are very sensitive to radiation, and we generally treat earlier-stage MCC with a combination of surgery and radiation therapy,” said Dr. Farma. “More recently we have had a lot of success with the use of immunotherapy to treat more advanced MCC.”
Dr. Zaba reported receiving grants from the Kuni Foundation outside the submitted work. No other disclosures were reported. Author Eleni Linos, MD, DrPH, MPH, is supported by grant K24AR075060 from the National Institutes of Health. No other outside funding was reported. Dr. Farma had no disclosures.
.
In a cohort of 6,146 patients with a first primary MCC, a total of 725 (11.8%) developed subsequent primary cancers. For solid tumors, the risk was highest for cutaneous melanoma and papillary thyroid carcinoma, while for hematologic cancers, the risk was increased for non-Hodgkin lymphoma.
“Our study does confirm that patients with MCC are at higher risk for developing other cancers,” study author Lisa C. Zaba, MD, PhD, associate professor of dermatology and director of the Merkel cell carcinoma multidisciplinary clinic, Stanford (Calif.) Cancer Center, said in an interview. “MCC is a highly malignant cancer with a 40% recurrence risk.”
Because of this high risk, Dr. Zaba noted that patients with MCC get frequent surveillance with both imaging studies (PET-CT and CT) as well as frequent visits in clinic with MCC experts. “Specifically, a patient with MCC is imaged and seen in clinic every 3-6 months for the first 3 years after diagnosis, and every 6-12 months thereafter for up to 5 years,” she said. “Interestingly, this high level of surveillance may be one reason that we find so many cancers in patients who have been diagnosed with MCC, compared to the general population.”
The study was published online in JAMA Dermatology.
With the death of “Margaritaville” singer Jimmy Buffett, who recently died of MCC 4 years after his diagnosis, this rare, aggressive skin cancer has been put in the spotlight. Survival has been increasing, primarily because of the advent of immunotherapy, and the authors note that it is therefore imperative to better understand the risk of subsequent primary tumors to inform screening and treatment recommendations.
In this cohort study, Dr. Zaba and colleagues identified 6,146 patients from 17 registries of the Surveillance, Epidemiology, and End Results (SEER) Program who had been diagnosed with a first primary cutaneous MCC between 2000 and 2018.
Endpoints were the ratio of observed to expected number of cases of subsequent cancer (Standardized incidence ratio, or SIR) and the excess risk.
Overall, there was an elevated risk of developing a subsequent primary cancer after being diagnosed with MCC (SIR, 1.28; excess risk, 57.25 per 10,000 person-years). This included the risk for all solid tumors including liver (SIR, 1.92; excess risk, 2.77 per 10,000 person-years), pancreas (SIR, 1.65; excess risk, 4.55 per 10,000 person-years), cutaneous melanoma (SIR, 2.36; excess risk, 15.27 per 10,000 person-years), and kidney (SIR, 1.64; excess risk, 3.83 per 10,000 person-years).
There was also a higher risk of developing papillary thyroid carcinoma (PTC) (SIR, 5.26; excess risk, 6.16 per 10,000 person-years).
The risk of developing hematological cancers after MCC was also increased, especially for non-Hodgkin lymphoma (SIR, 2.62; excess risk, 15.48 per 10,000 person-years) and myelodysplastic syndrome (SIR, 2.17; excess risk, 2.73 per 10,000 person-years).
The risk for developing subsequent tumors, including melanoma and non-Hodgkin lymphoma, remained significant for up to 10 years, while the risk for developing PTC and kidney cancers remained for up to 5 years.
“After 3-5 years, when a MCC patient’s risk of MCC recurrence drops below 2%, we do not currently have guidelines in place for additional cancer screening,” Dr. Zaba said. “Regarding patient education, patients with MCC are educated to let us know if they experience any symptoms of cancer between visits, including unintentional weight loss, night sweats, headaches that increasingly worsen, or growing lumps or bumps. These symptoms may occur in a multitude of cancers and not just MCC.”
Weighing in on the study, Jeffrey M. Farma, MD, interim chair, department of surgical oncology at Fox Chase Cancer Center, Philadelphia, noted that MCC is considered to be high risk because of its chances of recurring after surgical resection or spreading to lymph nodes or other areas of the body. “There are approximately 3,000 new cases of melanoma a year in the U.S., and it is 40 times rarer than melanoma,” he said. “Patients are usually diagnosed with Merkel cell carcinoma later in life, and the tumors have been associated with sun exposure and immunosuppression and have also been associated with the polyomavirus.”
That said, however, he emphasized that great strides have been made in treatment. “These tumors are very sensitive to radiation, and we generally treat earlier-stage MCC with a combination of surgery and radiation therapy,” said Dr. Farma. “More recently we have had a lot of success with the use of immunotherapy to treat more advanced MCC.”
Dr. Zaba reported receiving grants from the Kuni Foundation outside the submitted work. No other disclosures were reported. Author Eleni Linos, MD, DrPH, MPH, is supported by grant K24AR075060 from the National Institutes of Health. No other outside funding was reported. Dr. Farma had no disclosures.
.
In a cohort of 6,146 patients with a first primary MCC, a total of 725 (11.8%) developed subsequent primary cancers. For solid tumors, the risk was highest for cutaneous melanoma and papillary thyroid carcinoma, while for hematologic cancers, the risk was increased for non-Hodgkin lymphoma.
“Our study does confirm that patients with MCC are at higher risk for developing other cancers,” study author Lisa C. Zaba, MD, PhD, associate professor of dermatology and director of the Merkel cell carcinoma multidisciplinary clinic, Stanford (Calif.) Cancer Center, said in an interview. “MCC is a highly malignant cancer with a 40% recurrence risk.”
Because of this high risk, Dr. Zaba noted that patients with MCC get frequent surveillance with both imaging studies (PET-CT and CT) as well as frequent visits in clinic with MCC experts. “Specifically, a patient with MCC is imaged and seen in clinic every 3-6 months for the first 3 years after diagnosis, and every 6-12 months thereafter for up to 5 years,” she said. “Interestingly, this high level of surveillance may be one reason that we find so many cancers in patients who have been diagnosed with MCC, compared to the general population.”
The study was published online in JAMA Dermatology.
With the death of “Margaritaville” singer Jimmy Buffett, who recently died of MCC 4 years after his diagnosis, this rare, aggressive skin cancer has been put in the spotlight. Survival has been increasing, primarily because of the advent of immunotherapy, and the authors note that it is therefore imperative to better understand the risk of subsequent primary tumors to inform screening and treatment recommendations.
In this cohort study, Dr. Zaba and colleagues identified 6,146 patients from 17 registries of the Surveillance, Epidemiology, and End Results (SEER) Program who had been diagnosed with a first primary cutaneous MCC between 2000 and 2018.
Endpoints were the ratio of observed to expected number of cases of subsequent cancer (Standardized incidence ratio, or SIR) and the excess risk.
Overall, there was an elevated risk of developing a subsequent primary cancer after being diagnosed with MCC (SIR, 1.28; excess risk, 57.25 per 10,000 person-years). This included the risk for all solid tumors including liver (SIR, 1.92; excess risk, 2.77 per 10,000 person-years), pancreas (SIR, 1.65; excess risk, 4.55 per 10,000 person-years), cutaneous melanoma (SIR, 2.36; excess risk, 15.27 per 10,000 person-years), and kidney (SIR, 1.64; excess risk, 3.83 per 10,000 person-years).
There was also a higher risk of developing papillary thyroid carcinoma (PTC) (SIR, 5.26; excess risk, 6.16 per 10,000 person-years).
The risk of developing hematological cancers after MCC was also increased, especially for non-Hodgkin lymphoma (SIR, 2.62; excess risk, 15.48 per 10,000 person-years) and myelodysplastic syndrome (SIR, 2.17; excess risk, 2.73 per 10,000 person-years).
The risk for developing subsequent tumors, including melanoma and non-Hodgkin lymphoma, remained significant for up to 10 years, while the risk for developing PTC and kidney cancers remained for up to 5 years.
“After 3-5 years, when a MCC patient’s risk of MCC recurrence drops below 2%, we do not currently have guidelines in place for additional cancer screening,” Dr. Zaba said. “Regarding patient education, patients with MCC are educated to let us know if they experience any symptoms of cancer between visits, including unintentional weight loss, night sweats, headaches that increasingly worsen, or growing lumps or bumps. These symptoms may occur in a multitude of cancers and not just MCC.”
Weighing in on the study, Jeffrey M. Farma, MD, interim chair, department of surgical oncology at Fox Chase Cancer Center, Philadelphia, noted that MCC is considered to be high risk because of its chances of recurring after surgical resection or spreading to lymph nodes or other areas of the body. “There are approximately 3,000 new cases of melanoma a year in the U.S., and it is 40 times rarer than melanoma,” he said. “Patients are usually diagnosed with Merkel cell carcinoma later in life, and the tumors have been associated with sun exposure and immunosuppression and have also been associated with the polyomavirus.”
That said, however, he emphasized that great strides have been made in treatment. “These tumors are very sensitive to radiation, and we generally treat earlier-stage MCC with a combination of surgery and radiation therapy,” said Dr. Farma. “More recently we have had a lot of success with the use of immunotherapy to treat more advanced MCC.”
Dr. Zaba reported receiving grants from the Kuni Foundation outside the submitted work. No other disclosures were reported. Author Eleni Linos, MD, DrPH, MPH, is supported by grant K24AR075060 from the National Institutes of Health. No other outside funding was reported. Dr. Farma had no disclosures.
FROM JAMA DERMATOLOGY
Lead exposure still a global health burden
TOPLINE:
Globally, lead exposure is linked to more than 5.5 million adult cardiovascular deaths in 2019, as well as loss of 765 million intelligence quotient (IQ) points in children younger than 5 years, which cost U.S. $6 trillion in lost productivity, new research suggests.
METHODOLOGY:
- Global lead exposure has declined substantially since leaded gasoline was phased out, but several sources of lead remain, resulting in adverse health and economic effects, particularly in low- and middle-income countries (LMICs).
- Estimates of cardiovascular disease (CVD) deaths from lead exposure have been limited to effects of increased blood pressure, but studies show that lead exposure has cardiovascular impacts through mechanisms other than hypertension.
- Drawing from various sources and studies, researchers estimated global blood lead levels and the impact of lead exposure on CVD mortality in 2019 among adults aged 25 years or older, IQ loss in children younger than 5 years, and the related economic costs.
TAKEAWAY:
- Researchers estimated that there were 5,545,000 (95% confidence interval, 2,305,000-8,271,000) cardiovascular deaths in adults from lead exposure in 2019, with as many as 90.2% of these deaths in LMICs; however, this estimate may be incomplete because it does not include the effect of lead exposure on CVD mortality mediated through hypertension.
- The estimated global IQ loss in children younger than 5 years due to lead exposure was 765 million (95% CI, 443 million-1,098 million) IQ points in 2019, 95.3% of which occurred in LMICs.
- These estimates place lead exposure on a par with ambient particulate matter and household air pollution combined, and ahead of unsafe household drinking water, sanitation, and handwashing, as an environmental risk factor.
- The estimated global cost of lead exposure from CVD mortality and IQ loss combined is U.S. $6.0 trillion (range, $2.6 trillion-9.0 trillion) in 2019, equivalent to 6.9% of the 2019 global gross domestic product.
IN PRACTICE:
Given the magnitude of the estimated health effects of lead exposure, particularly in LMICs, “it is imperative that nationally representative periodic blood lead level measurements be institutionalized,” write the authors, adding that these measurements could be incorporated into existing household surveys.
STUDY DETAILS:
The study was conducted by Bjorn Larsen, PhD, environmental economist and consultant to the World Bank, and Ernesto Sánchez-Triana. It was published online in The Lancet Planetary Health.
LIMITATIONS:
- Global blood lead level estimates may be inaccurate, given that measurements are absent for many countries.
- Certain income projections and income losses are uncertain.
- Because the study does not capture the detrimental effects of lead exposure other than IQ loss and CVD mortality, the estimates of global costs are conservative.
DISCLOSURES:
The study received support from the Korea Green Growth Trust Fund and the World Bank’s Pollution Management and Environmental Health Program. The authors have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
Globally, lead exposure is linked to more than 5.5 million adult cardiovascular deaths in 2019, as well as loss of 765 million intelligence quotient (IQ) points in children younger than 5 years, which cost U.S. $6 trillion in lost productivity, new research suggests.
METHODOLOGY:
- Global lead exposure has declined substantially since leaded gasoline was phased out, but several sources of lead remain, resulting in adverse health and economic effects, particularly in low- and middle-income countries (LMICs).
- Estimates of cardiovascular disease (CVD) deaths from lead exposure have been limited to effects of increased blood pressure, but studies show that lead exposure has cardiovascular impacts through mechanisms other than hypertension.
- Drawing from various sources and studies, researchers estimated global blood lead levels and the impact of lead exposure on CVD mortality in 2019 among adults aged 25 years or older, IQ loss in children younger than 5 years, and the related economic costs.
TAKEAWAY:
- Researchers estimated that there were 5,545,000 (95% confidence interval, 2,305,000-8,271,000) cardiovascular deaths in adults from lead exposure in 2019, with as many as 90.2% of these deaths in LMICs; however, this estimate may be incomplete because it does not include the effect of lead exposure on CVD mortality mediated through hypertension.
- The estimated global IQ loss in children younger than 5 years due to lead exposure was 765 million (95% CI, 443 million-1,098 million) IQ points in 2019, 95.3% of which occurred in LMICs.
- These estimates place lead exposure on a par with ambient particulate matter and household air pollution combined, and ahead of unsafe household drinking water, sanitation, and handwashing, as an environmental risk factor.
- The estimated global cost of lead exposure from CVD mortality and IQ loss combined is U.S. $6.0 trillion (range, $2.6 trillion-9.0 trillion) in 2019, equivalent to 6.9% of the 2019 global gross domestic product.
IN PRACTICE:
Given the magnitude of the estimated health effects of lead exposure, particularly in LMICs, “it is imperative that nationally representative periodic blood lead level measurements be institutionalized,” write the authors, adding that these measurements could be incorporated into existing household surveys.
STUDY DETAILS:
The study was conducted by Bjorn Larsen, PhD, environmental economist and consultant to the World Bank, and Ernesto Sánchez-Triana. It was published online in The Lancet Planetary Health.
LIMITATIONS:
- Global blood lead level estimates may be inaccurate, given that measurements are absent for many countries.
- Certain income projections and income losses are uncertain.
- Because the study does not capture the detrimental effects of lead exposure other than IQ loss and CVD mortality, the estimates of global costs are conservative.
DISCLOSURES:
The study received support from the Korea Green Growth Trust Fund and the World Bank’s Pollution Management and Environmental Health Program. The authors have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
Globally, lead exposure is linked to more than 5.5 million adult cardiovascular deaths in 2019, as well as loss of 765 million intelligence quotient (IQ) points in children younger than 5 years, which cost U.S. $6 trillion in lost productivity, new research suggests.
METHODOLOGY:
- Global lead exposure has declined substantially since leaded gasoline was phased out, but several sources of lead remain, resulting in adverse health and economic effects, particularly in low- and middle-income countries (LMICs).
- Estimates of cardiovascular disease (CVD) deaths from lead exposure have been limited to effects of increased blood pressure, but studies show that lead exposure has cardiovascular impacts through mechanisms other than hypertension.
- Drawing from various sources and studies, researchers estimated global blood lead levels and the impact of lead exposure on CVD mortality in 2019 among adults aged 25 years or older, IQ loss in children younger than 5 years, and the related economic costs.
TAKEAWAY:
- Researchers estimated that there were 5,545,000 (95% confidence interval, 2,305,000-8,271,000) cardiovascular deaths in adults from lead exposure in 2019, with as many as 90.2% of these deaths in LMICs; however, this estimate may be incomplete because it does not include the effect of lead exposure on CVD mortality mediated through hypertension.
- The estimated global IQ loss in children younger than 5 years due to lead exposure was 765 million (95% CI, 443 million-1,098 million) IQ points in 2019, 95.3% of which occurred in LMICs.
- These estimates place lead exposure on a par with ambient particulate matter and household air pollution combined, and ahead of unsafe household drinking water, sanitation, and handwashing, as an environmental risk factor.
- The estimated global cost of lead exposure from CVD mortality and IQ loss combined is U.S. $6.0 trillion (range, $2.6 trillion-9.0 trillion) in 2019, equivalent to 6.9% of the 2019 global gross domestic product.
IN PRACTICE:
Given the magnitude of the estimated health effects of lead exposure, particularly in LMICs, “it is imperative that nationally representative periodic blood lead level measurements be institutionalized,” write the authors, adding that these measurements could be incorporated into existing household surveys.
STUDY DETAILS:
The study was conducted by Bjorn Larsen, PhD, environmental economist and consultant to the World Bank, and Ernesto Sánchez-Triana. It was published online in The Lancet Planetary Health.
LIMITATIONS:
- Global blood lead level estimates may be inaccurate, given that measurements are absent for many countries.
- Certain income projections and income losses are uncertain.
- Because the study does not capture the detrimental effects of lead exposure other than IQ loss and CVD mortality, the estimates of global costs are conservative.
DISCLOSURES:
The study received support from the Korea Green Growth Trust Fund and the World Bank’s Pollution Management and Environmental Health Program. The authors have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Your workplace is toxic: Can you make it better?
A physician in your office is hot-tempered, critical, and upsets both the physicians and staff. Two of your partners are arguing over a software vendor and refuse to compromise. One doctor’s spouse is the office manager and snipes at everyone; the lead partner micromanages and second-guesses other doctors’ treatment plans, and no one will stand up to her.
If your practice has similar scenarios, you’re likely dealing with your own anger, irritation, and dread at work. You’re struggling with a toxic practice atmosphere, and you must make changes – fast.
However, this isn’t easy, given that what goes on in a doctor’s office is “high consequence,” says Leonard J. Marcus, PhD, founding director of the program for health care negotiation and conflict resolution at the Harvard School of Public Health in Boston.
The two things that tend to plague medical practices most: A culture of fear and someone who is letting ego run the day-to-day, he says.
“Fear overwhelms any chance for good morale among colleagues,” says Dr. Marcus, who is also the coauthor of “Renegotiating Health Care: Resolving Conflict to Build Collaboration.” “In a work environment where the fear is overwhelming, the ego can take over, and someone at the practice becomes overly concerned about getting credit, taking control, ordering other people around, and deciding who is on top and who is on the bottom.”
Tension, stress, back-biting, and rudeness are also symptoms of a more significant problem, says Jes Montgomery, MD, a psychiatrist and medical director of APN Dallas, a mental health–focused practice.
“If you don’t get toxicity under control, it will blow the office apart,” Dr. Montgomery says.
1. Recognize the signs
Part of the problem with a toxic medical practice is that, culturally, we don’t treat mental health and burnout as real illnesses. “A physician who is depressed is not going to be melancholy or bursting into tears with patients,” Dr. Montgomery says. “They’ll get behind on paperwork, skip meals, or find that it’s difficult to sleep at night. Next, they’ll yell at the partners and staff, always be in a foul mood, and gripe about inconsequential things. Their behavior affects everyone.”
Dr. Montgomery says that physicians aren’t taught to ask for help, making it difficult to see what’s really going on when someone displays toxic behavior in the practice. If it’s a partner, take time to ask what’s going on. If it’s yourself, step back and see if you can ask someone for the help you need.
2. Have difficult conversations
This is tough for most of us, says Jeremy Pollack, PhD, CEO and founder of Pollack Peacebuilding Systems, a conflict resolution consulting firm. If a team member is hot-tempered, disrespectful, or talking to patients in an unproductive manner, see if you can have an effective conversation with that person. The tricky part is critiquing in a way that doesn’t make them feel defensive – and wanting to push back.
For a micromanaging office manager, for example, you could say something like,”You’re doing a great job with the inventory, but I need you to let the staff have some autonomy and not hover over every supply they use in the break room, so that people won’t feel resentful toward us.” Make it clear you’re a team, and this is a team challenge. “However, if a doctor feels like they’ve tried to communicate to that colleague and are still walking on eggshells, it’s time to try to get help from someone – perhaps a practice management organization,” says Dr. Pollack.
3. Open lines of communication
It’s critical to create a comfortable space to speak with your colleagues, says Marisa Garshick, MD, a dermatologist in private practice in New York. “Creating an environment where there is an open line of communication, whether it’s directly to somebody in charge or having a system where you can give feedback more privately or anonymously, is important so that tension doesn’t build.”
“Being a doctor is a social enterprise,” Dr. Marcus says. “The science of medicine is critically important, but patients and the other health care workers on your team are also critically important. In the long run, the most successful physicians pay attention to both. It’s a full package.”
4. Emphasize the positive
Instead of discussing things only when they go wrong, try optimism, Dr. Garshick said. When positive things happen, whether it’s an excellent patient encounter or the office did something really well together, highlight it so everyone has a sense of accomplishment. If a patient compliments a medical assistant or raves about a nurse, share those compliments with the employees so that not every encounter you have calls out problems and staff missteps.
Suppose partners have a conflict with one another or are arguing over something. In that case, you may need to mediate or invest in a meaningful intervention so people can reflect on the narrative they’re contributing to the culture.
5. Practice self-care
Finally, the work of a physician is exhausting, so it’s crucial to practice personal TLC. That may mean taking micro breaks, getting adequate sleep, maintaining a healthy diet, and exercising well and managing stress to maintain energy levels and patience.
“Sometimes, when I’m fed up with the office, I need to get away,” Dr. Montgomery says. “I’ll take a day to go fishing, golfing, and not think about the office.” Just a small break can shift the lens that you see through when you return to the office and put problems in perspective.
A version of this article first appeared on Medscape.com.
A physician in your office is hot-tempered, critical, and upsets both the physicians and staff. Two of your partners are arguing over a software vendor and refuse to compromise. One doctor’s spouse is the office manager and snipes at everyone; the lead partner micromanages and second-guesses other doctors’ treatment plans, and no one will stand up to her.
If your practice has similar scenarios, you’re likely dealing with your own anger, irritation, and dread at work. You’re struggling with a toxic practice atmosphere, and you must make changes – fast.
However, this isn’t easy, given that what goes on in a doctor’s office is “high consequence,” says Leonard J. Marcus, PhD, founding director of the program for health care negotiation and conflict resolution at the Harvard School of Public Health in Boston.
The two things that tend to plague medical practices most: A culture of fear and someone who is letting ego run the day-to-day, he says.
“Fear overwhelms any chance for good morale among colleagues,” says Dr. Marcus, who is also the coauthor of “Renegotiating Health Care: Resolving Conflict to Build Collaboration.” “In a work environment where the fear is overwhelming, the ego can take over, and someone at the practice becomes overly concerned about getting credit, taking control, ordering other people around, and deciding who is on top and who is on the bottom.”
Tension, stress, back-biting, and rudeness are also symptoms of a more significant problem, says Jes Montgomery, MD, a psychiatrist and medical director of APN Dallas, a mental health–focused practice.
“If you don’t get toxicity under control, it will blow the office apart,” Dr. Montgomery says.
1. Recognize the signs
Part of the problem with a toxic medical practice is that, culturally, we don’t treat mental health and burnout as real illnesses. “A physician who is depressed is not going to be melancholy or bursting into tears with patients,” Dr. Montgomery says. “They’ll get behind on paperwork, skip meals, or find that it’s difficult to sleep at night. Next, they’ll yell at the partners and staff, always be in a foul mood, and gripe about inconsequential things. Their behavior affects everyone.”
Dr. Montgomery says that physicians aren’t taught to ask for help, making it difficult to see what’s really going on when someone displays toxic behavior in the practice. If it’s a partner, take time to ask what’s going on. If it’s yourself, step back and see if you can ask someone for the help you need.
2. Have difficult conversations
This is tough for most of us, says Jeremy Pollack, PhD, CEO and founder of Pollack Peacebuilding Systems, a conflict resolution consulting firm. If a team member is hot-tempered, disrespectful, or talking to patients in an unproductive manner, see if you can have an effective conversation with that person. The tricky part is critiquing in a way that doesn’t make them feel defensive – and wanting to push back.
For a micromanaging office manager, for example, you could say something like,”You’re doing a great job with the inventory, but I need you to let the staff have some autonomy and not hover over every supply they use in the break room, so that people won’t feel resentful toward us.” Make it clear you’re a team, and this is a team challenge. “However, if a doctor feels like they’ve tried to communicate to that colleague and are still walking on eggshells, it’s time to try to get help from someone – perhaps a practice management organization,” says Dr. Pollack.
3. Open lines of communication
It’s critical to create a comfortable space to speak with your colleagues, says Marisa Garshick, MD, a dermatologist in private practice in New York. “Creating an environment where there is an open line of communication, whether it’s directly to somebody in charge or having a system where you can give feedback more privately or anonymously, is important so that tension doesn’t build.”
“Being a doctor is a social enterprise,” Dr. Marcus says. “The science of medicine is critically important, but patients and the other health care workers on your team are also critically important. In the long run, the most successful physicians pay attention to both. It’s a full package.”
4. Emphasize the positive
Instead of discussing things only when they go wrong, try optimism, Dr. Garshick said. When positive things happen, whether it’s an excellent patient encounter or the office did something really well together, highlight it so everyone has a sense of accomplishment. If a patient compliments a medical assistant or raves about a nurse, share those compliments with the employees so that not every encounter you have calls out problems and staff missteps.
Suppose partners have a conflict with one another or are arguing over something. In that case, you may need to mediate or invest in a meaningful intervention so people can reflect on the narrative they’re contributing to the culture.
5. Practice self-care
Finally, the work of a physician is exhausting, so it’s crucial to practice personal TLC. That may mean taking micro breaks, getting adequate sleep, maintaining a healthy diet, and exercising well and managing stress to maintain energy levels and patience.
“Sometimes, when I’m fed up with the office, I need to get away,” Dr. Montgomery says. “I’ll take a day to go fishing, golfing, and not think about the office.” Just a small break can shift the lens that you see through when you return to the office and put problems in perspective.
A version of this article first appeared on Medscape.com.
A physician in your office is hot-tempered, critical, and upsets both the physicians and staff. Two of your partners are arguing over a software vendor and refuse to compromise. One doctor’s spouse is the office manager and snipes at everyone; the lead partner micromanages and second-guesses other doctors’ treatment plans, and no one will stand up to her.
If your practice has similar scenarios, you’re likely dealing with your own anger, irritation, and dread at work. You’re struggling with a toxic practice atmosphere, and you must make changes – fast.
However, this isn’t easy, given that what goes on in a doctor’s office is “high consequence,” says Leonard J. Marcus, PhD, founding director of the program for health care negotiation and conflict resolution at the Harvard School of Public Health in Boston.
The two things that tend to plague medical practices most: A culture of fear and someone who is letting ego run the day-to-day, he says.
“Fear overwhelms any chance for good morale among colleagues,” says Dr. Marcus, who is also the coauthor of “Renegotiating Health Care: Resolving Conflict to Build Collaboration.” “In a work environment where the fear is overwhelming, the ego can take over, and someone at the practice becomes overly concerned about getting credit, taking control, ordering other people around, and deciding who is on top and who is on the bottom.”
Tension, stress, back-biting, and rudeness are also symptoms of a more significant problem, says Jes Montgomery, MD, a psychiatrist and medical director of APN Dallas, a mental health–focused practice.
“If you don’t get toxicity under control, it will blow the office apart,” Dr. Montgomery says.
1. Recognize the signs
Part of the problem with a toxic medical practice is that, culturally, we don’t treat mental health and burnout as real illnesses. “A physician who is depressed is not going to be melancholy or bursting into tears with patients,” Dr. Montgomery says. “They’ll get behind on paperwork, skip meals, or find that it’s difficult to sleep at night. Next, they’ll yell at the partners and staff, always be in a foul mood, and gripe about inconsequential things. Their behavior affects everyone.”
Dr. Montgomery says that physicians aren’t taught to ask for help, making it difficult to see what’s really going on when someone displays toxic behavior in the practice. If it’s a partner, take time to ask what’s going on. If it’s yourself, step back and see if you can ask someone for the help you need.
2. Have difficult conversations
This is tough for most of us, says Jeremy Pollack, PhD, CEO and founder of Pollack Peacebuilding Systems, a conflict resolution consulting firm. If a team member is hot-tempered, disrespectful, or talking to patients in an unproductive manner, see if you can have an effective conversation with that person. The tricky part is critiquing in a way that doesn’t make them feel defensive – and wanting to push back.
For a micromanaging office manager, for example, you could say something like,”You’re doing a great job with the inventory, but I need you to let the staff have some autonomy and not hover over every supply they use in the break room, so that people won’t feel resentful toward us.” Make it clear you’re a team, and this is a team challenge. “However, if a doctor feels like they’ve tried to communicate to that colleague and are still walking on eggshells, it’s time to try to get help from someone – perhaps a practice management organization,” says Dr. Pollack.
3. Open lines of communication
It’s critical to create a comfortable space to speak with your colleagues, says Marisa Garshick, MD, a dermatologist in private practice in New York. “Creating an environment where there is an open line of communication, whether it’s directly to somebody in charge or having a system where you can give feedback more privately or anonymously, is important so that tension doesn’t build.”
“Being a doctor is a social enterprise,” Dr. Marcus says. “The science of medicine is critically important, but patients and the other health care workers on your team are also critically important. In the long run, the most successful physicians pay attention to both. It’s a full package.”
4. Emphasize the positive
Instead of discussing things only when they go wrong, try optimism, Dr. Garshick said. When positive things happen, whether it’s an excellent patient encounter or the office did something really well together, highlight it so everyone has a sense of accomplishment. If a patient compliments a medical assistant or raves about a nurse, share those compliments with the employees so that not every encounter you have calls out problems and staff missteps.
Suppose partners have a conflict with one another or are arguing over something. In that case, you may need to mediate or invest in a meaningful intervention so people can reflect on the narrative they’re contributing to the culture.
5. Practice self-care
Finally, the work of a physician is exhausting, so it’s crucial to practice personal TLC. That may mean taking micro breaks, getting adequate sleep, maintaining a healthy diet, and exercising well and managing stress to maintain energy levels and patience.
“Sometimes, when I’m fed up with the office, I need to get away,” Dr. Montgomery says. “I’ll take a day to go fishing, golfing, and not think about the office.” Just a small break can shift the lens that you see through when you return to the office and put problems in perspective.
A version of this article first appeared on Medscape.com.
Can skin bleaching lead to cancer?
SINGAPORE –
This question was posed by Ousmane Faye, MD, PhD, director general of Mali’s Bamako Dermatology Hospital, at the World Congress of Dermatology.
Dr. Faye explored the issue during a hot topics session at the meeting, prefacing that it was an important question to ask because “in West Africa, skin bleaching is very common.”
“There are many local names” for skin bleaching, he said. “For example, in Senegal, it’s called xessal; in Mali and Ivory Coast, its name is caco; in South Africa, there are many names, like ukutsheyisa.”
Skin bleaching refers to the cosmetic misuse of topical agents to change one’s natural skin color. It’s a centuries-old practice that people, mainly women, adopt “to increase attractiveness and self-esteem,” explained Dr. Faye.
To demonstrate how pervasive skin bleaching is on the continent, he presented a slide that summarized figures from six studies spanning the past 2 decades. Prevalence ranged from 25% in Mali (based on a 1993 survey of 210 women) to a high of 79.25% in Benin (from a sample size of 511 women in 2019). In other studies of women in Burkina Faso and Togo, the figures were 44.3% and 58.9%, respectively. The most recently conducted study, which involved 2,689 Senegalese women and was published in 2022, found that nearly 6 in 10 (59.2%) respondents used skin-lightening products.
But skin bleaching isn’t just limited to Africa, said session moderator Omar Lupi, MD, PhD, associate professor of dermatology at the Federal University of the State of Rio de Janeiro, when approached for an independent comment. “It’s a traditional practice around the world. Maybe not in the developed countries, but it’s quite common in Africa, in South America, and in Asia.”
His sentiments are echoed in a meta-analysis that was published in the International Journal of Dermatology in 2019. The work examined 68 studies involving more than 67,000 people across Africa, Asia, Europe, the Middle East, and North America. It found that the pooled lifetime prevalence of skin bleaching was 27.7% (95% confidence interval, 19.6-37.5; P < .01).
“This is an important and interesting topic because our world is shrinking,” Dr. Lupi told this news organization. “Even in countries that don’t have bleaching as a common situation, we now have patients who are migrating from one part [of the world] to another, so bleaching is something that can knock on your door and you need to be prepared.”
Misuse leads to complications
The issue is pertinent to dermatologists because skin bleaching is associated with a wide range of complications. Take, for example, topical steroids, which are the most common products used for bleaching, said Dr. Faye in his talk.
“Clobetasol can suppress the hypothalamic-pituitary-adrenal (HPA) function,” he said, referring to the body’s main stress response system. “It can also foster skin infection, including bacterial, fungal, viral, and parasitic infection.”
In addition, topical steroids that are misused as skin lighteners have been reported to cause stretch marks, skin atrophy, inflammatory acne, and even metabolic disorders such as diabetes and hypertension, said Dr. Faye.
To further his point, he cited a 2021 prospective case-control study conducted across five sub-Saharan countries, which found that the use of “voluntary cosmetic depigmentation” significantly increased a person’s risk for necrotizing fasciitis of the lower limbs (odds ratio, 2.29; 95% CI, 1.19-3.73; P = .0226).
Similarly, mercury, another substance found in products commonly used to bleach skin, has been associated with problems ranging from rashes to renal toxicity. And because it’s so incredibly harmful, mercury is also known to cause neurologic abnormalities.
Apart from causing certain conditions, prolonged use of skin-lightening products can change the way existing diseases present themselves as well as their severity, added Dr. Faye.
An increased risk
But what about skin bleaching’s link with cancer? “Skin cancer on Black skin is uncommon, yet it occurs in skin-bleaching women,” said Dr. Faye.
“Since 2000, we have had some cases of skin cancer associated with skin bleaching,” he continued, adding that squamous cell carcinoma (SCC) is the most frequent type of cancer observed.
If you look at what’s been published on the topic so far, you’ll see that “all the cases of skin cancer are located over the neck or some exposed area when skin bleaching products are used for more than 10 years,” said Dr. Faye. “And most of the time, the age of the patient ranges from 30 to 60 years.”
The first known case in Africa was reported in a 58-year-old woman from Ghana, who had been using skin bleaching products for close to 30 years. The patient presented with tumors on her face, neck, and arms.
Dr. Faye then proceeded to share more than 10 such carcinoma cases. “These previous reports strongly suggest a relationship between skin bleaching and skin cancers,” said Dr. Faye.
Indeed, there have been reports and publications in the literature that support his observation, including one last year, which found that use of the tyrosinase inhibitor hydroquinone was associated with approximately a threefold increased risk for skin cancer.
For some, including Brazil’s Dr. Lupi, Dr. Faye’s talk was enlightening: “I didn’t know about this relationship [of bleaching] with skin cancer, it was something new for me.”
But the prevalence of SCC is very low, compared with that of skin bleaching, Dr. Faye acknowledged. Moreover, the cancer observed in the cases reported could have resulted from a number of reasons, including exposure to harmful ultraviolet rays from the sun and genetic predisposition in addition to the use of bleaching products such as hydroquinone. “Other causes of skin cancer are not excluded,” he said.
To further explore the link between skin bleaching and cancer, “we need case-control studies to provide more evidence,” he added. Until then, dermatologists “should keep on promoting messages” to prevent SCC from occurring. This includes encouraging the use of proper sun protection in addition to discouraging the practice of skin bleaching, which still persists despite more than 10 African nations banning the use of toxic skin-lightening products.
Dr. Faye and Dr. Lupi report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SINGAPORE –
This question was posed by Ousmane Faye, MD, PhD, director general of Mali’s Bamako Dermatology Hospital, at the World Congress of Dermatology.
Dr. Faye explored the issue during a hot topics session at the meeting, prefacing that it was an important question to ask because “in West Africa, skin bleaching is very common.”
“There are many local names” for skin bleaching, he said. “For example, in Senegal, it’s called xessal; in Mali and Ivory Coast, its name is caco; in South Africa, there are many names, like ukutsheyisa.”
Skin bleaching refers to the cosmetic misuse of topical agents to change one’s natural skin color. It’s a centuries-old practice that people, mainly women, adopt “to increase attractiveness and self-esteem,” explained Dr. Faye.
To demonstrate how pervasive skin bleaching is on the continent, he presented a slide that summarized figures from six studies spanning the past 2 decades. Prevalence ranged from 25% in Mali (based on a 1993 survey of 210 women) to a high of 79.25% in Benin (from a sample size of 511 women in 2019). In other studies of women in Burkina Faso and Togo, the figures were 44.3% and 58.9%, respectively. The most recently conducted study, which involved 2,689 Senegalese women and was published in 2022, found that nearly 6 in 10 (59.2%) respondents used skin-lightening products.
But skin bleaching isn’t just limited to Africa, said session moderator Omar Lupi, MD, PhD, associate professor of dermatology at the Federal University of the State of Rio de Janeiro, when approached for an independent comment. “It’s a traditional practice around the world. Maybe not in the developed countries, but it’s quite common in Africa, in South America, and in Asia.”
His sentiments are echoed in a meta-analysis that was published in the International Journal of Dermatology in 2019. The work examined 68 studies involving more than 67,000 people across Africa, Asia, Europe, the Middle East, and North America. It found that the pooled lifetime prevalence of skin bleaching was 27.7% (95% confidence interval, 19.6-37.5; P < .01).
“This is an important and interesting topic because our world is shrinking,” Dr. Lupi told this news organization. “Even in countries that don’t have bleaching as a common situation, we now have patients who are migrating from one part [of the world] to another, so bleaching is something that can knock on your door and you need to be prepared.”
Misuse leads to complications
The issue is pertinent to dermatologists because skin bleaching is associated with a wide range of complications. Take, for example, topical steroids, which are the most common products used for bleaching, said Dr. Faye in his talk.
“Clobetasol can suppress the hypothalamic-pituitary-adrenal (HPA) function,” he said, referring to the body’s main stress response system. “It can also foster skin infection, including bacterial, fungal, viral, and parasitic infection.”
In addition, topical steroids that are misused as skin lighteners have been reported to cause stretch marks, skin atrophy, inflammatory acne, and even metabolic disorders such as diabetes and hypertension, said Dr. Faye.
To further his point, he cited a 2021 prospective case-control study conducted across five sub-Saharan countries, which found that the use of “voluntary cosmetic depigmentation” significantly increased a person’s risk for necrotizing fasciitis of the lower limbs (odds ratio, 2.29; 95% CI, 1.19-3.73; P = .0226).
Similarly, mercury, another substance found in products commonly used to bleach skin, has been associated with problems ranging from rashes to renal toxicity. And because it’s so incredibly harmful, mercury is also known to cause neurologic abnormalities.
Apart from causing certain conditions, prolonged use of skin-lightening products can change the way existing diseases present themselves as well as their severity, added Dr. Faye.
An increased risk
But what about skin bleaching’s link with cancer? “Skin cancer on Black skin is uncommon, yet it occurs in skin-bleaching women,” said Dr. Faye.
“Since 2000, we have had some cases of skin cancer associated with skin bleaching,” he continued, adding that squamous cell carcinoma (SCC) is the most frequent type of cancer observed.
If you look at what’s been published on the topic so far, you’ll see that “all the cases of skin cancer are located over the neck or some exposed area when skin bleaching products are used for more than 10 years,” said Dr. Faye. “And most of the time, the age of the patient ranges from 30 to 60 years.”
The first known case in Africa was reported in a 58-year-old woman from Ghana, who had been using skin bleaching products for close to 30 years. The patient presented with tumors on her face, neck, and arms.
Dr. Faye then proceeded to share more than 10 such carcinoma cases. “These previous reports strongly suggest a relationship between skin bleaching and skin cancers,” said Dr. Faye.
Indeed, there have been reports and publications in the literature that support his observation, including one last year, which found that use of the tyrosinase inhibitor hydroquinone was associated with approximately a threefold increased risk for skin cancer.
For some, including Brazil’s Dr. Lupi, Dr. Faye’s talk was enlightening: “I didn’t know about this relationship [of bleaching] with skin cancer, it was something new for me.”
But the prevalence of SCC is very low, compared with that of skin bleaching, Dr. Faye acknowledged. Moreover, the cancer observed in the cases reported could have resulted from a number of reasons, including exposure to harmful ultraviolet rays from the sun and genetic predisposition in addition to the use of bleaching products such as hydroquinone. “Other causes of skin cancer are not excluded,” he said.
To further explore the link between skin bleaching and cancer, “we need case-control studies to provide more evidence,” he added. Until then, dermatologists “should keep on promoting messages” to prevent SCC from occurring. This includes encouraging the use of proper sun protection in addition to discouraging the practice of skin bleaching, which still persists despite more than 10 African nations banning the use of toxic skin-lightening products.
Dr. Faye and Dr. Lupi report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SINGAPORE –
This question was posed by Ousmane Faye, MD, PhD, director general of Mali’s Bamako Dermatology Hospital, at the World Congress of Dermatology.
Dr. Faye explored the issue during a hot topics session at the meeting, prefacing that it was an important question to ask because “in West Africa, skin bleaching is very common.”
“There are many local names” for skin bleaching, he said. “For example, in Senegal, it’s called xessal; in Mali and Ivory Coast, its name is caco; in South Africa, there are many names, like ukutsheyisa.”
Skin bleaching refers to the cosmetic misuse of topical agents to change one’s natural skin color. It’s a centuries-old practice that people, mainly women, adopt “to increase attractiveness and self-esteem,” explained Dr. Faye.
To demonstrate how pervasive skin bleaching is on the continent, he presented a slide that summarized figures from six studies spanning the past 2 decades. Prevalence ranged from 25% in Mali (based on a 1993 survey of 210 women) to a high of 79.25% in Benin (from a sample size of 511 women in 2019). In other studies of women in Burkina Faso and Togo, the figures were 44.3% and 58.9%, respectively. The most recently conducted study, which involved 2,689 Senegalese women and was published in 2022, found that nearly 6 in 10 (59.2%) respondents used skin-lightening products.
But skin bleaching isn’t just limited to Africa, said session moderator Omar Lupi, MD, PhD, associate professor of dermatology at the Federal University of the State of Rio de Janeiro, when approached for an independent comment. “It’s a traditional practice around the world. Maybe not in the developed countries, but it’s quite common in Africa, in South America, and in Asia.”
His sentiments are echoed in a meta-analysis that was published in the International Journal of Dermatology in 2019. The work examined 68 studies involving more than 67,000 people across Africa, Asia, Europe, the Middle East, and North America. It found that the pooled lifetime prevalence of skin bleaching was 27.7% (95% confidence interval, 19.6-37.5; P < .01).
“This is an important and interesting topic because our world is shrinking,” Dr. Lupi told this news organization. “Even in countries that don’t have bleaching as a common situation, we now have patients who are migrating from one part [of the world] to another, so bleaching is something that can knock on your door and you need to be prepared.”
Misuse leads to complications
The issue is pertinent to dermatologists because skin bleaching is associated with a wide range of complications. Take, for example, topical steroids, which are the most common products used for bleaching, said Dr. Faye in his talk.
“Clobetasol can suppress the hypothalamic-pituitary-adrenal (HPA) function,” he said, referring to the body’s main stress response system. “It can also foster skin infection, including bacterial, fungal, viral, and parasitic infection.”
In addition, topical steroids that are misused as skin lighteners have been reported to cause stretch marks, skin atrophy, inflammatory acne, and even metabolic disorders such as diabetes and hypertension, said Dr. Faye.
To further his point, he cited a 2021 prospective case-control study conducted across five sub-Saharan countries, which found that the use of “voluntary cosmetic depigmentation” significantly increased a person’s risk for necrotizing fasciitis of the lower limbs (odds ratio, 2.29; 95% CI, 1.19-3.73; P = .0226).
Similarly, mercury, another substance found in products commonly used to bleach skin, has been associated with problems ranging from rashes to renal toxicity. And because it’s so incredibly harmful, mercury is also known to cause neurologic abnormalities.
Apart from causing certain conditions, prolonged use of skin-lightening products can change the way existing diseases present themselves as well as their severity, added Dr. Faye.
An increased risk
But what about skin bleaching’s link with cancer? “Skin cancer on Black skin is uncommon, yet it occurs in skin-bleaching women,” said Dr. Faye.
“Since 2000, we have had some cases of skin cancer associated with skin bleaching,” he continued, adding that squamous cell carcinoma (SCC) is the most frequent type of cancer observed.
If you look at what’s been published on the topic so far, you’ll see that “all the cases of skin cancer are located over the neck or some exposed area when skin bleaching products are used for more than 10 years,” said Dr. Faye. “And most of the time, the age of the patient ranges from 30 to 60 years.”
The first known case in Africa was reported in a 58-year-old woman from Ghana, who had been using skin bleaching products for close to 30 years. The patient presented with tumors on her face, neck, and arms.
Dr. Faye then proceeded to share more than 10 such carcinoma cases. “These previous reports strongly suggest a relationship between skin bleaching and skin cancers,” said Dr. Faye.
Indeed, there have been reports and publications in the literature that support his observation, including one last year, which found that use of the tyrosinase inhibitor hydroquinone was associated with approximately a threefold increased risk for skin cancer.
For some, including Brazil’s Dr. Lupi, Dr. Faye’s talk was enlightening: “I didn’t know about this relationship [of bleaching] with skin cancer, it was something new for me.”
But the prevalence of SCC is very low, compared with that of skin bleaching, Dr. Faye acknowledged. Moreover, the cancer observed in the cases reported could have resulted from a number of reasons, including exposure to harmful ultraviolet rays from the sun and genetic predisposition in addition to the use of bleaching products such as hydroquinone. “Other causes of skin cancer are not excluded,” he said.
To further explore the link between skin bleaching and cancer, “we need case-control studies to provide more evidence,” he added. Until then, dermatologists “should keep on promoting messages” to prevent SCC from occurring. This includes encouraging the use of proper sun protection in addition to discouraging the practice of skin bleaching, which still persists despite more than 10 African nations banning the use of toxic skin-lightening products.
Dr. Faye and Dr. Lupi report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT WCD 2023
Remodeling broken systems
In the wake of the COVID-19 pandemic, the American Academy of Child and Adolescent Psychiatry, American Academy of Pediatrics, and Children’s Hospital Association declared a national emergency in child and adolescent mental health. Additionally, the U.S. Surgeon General issued an advisory highlighting increased prevalence of mental health challenges in youth, impacts of the COVID-19 pandemic, and recommendations to address this crisis.
The pandemic required youth to isolate from peers and community supports, navigate remote learning environments, and cope with grief and loss; some 140,000 children in the United States experienced the death of a caregiver due to COVID-19.1 Virtually every system that supports children was affected. Whereas schools have historically been a main provider of child and adolescent mental health services, delivery of many school-based mental health programs was disrupted by school closures and staffing challenges. Subgroups of children (for example, those with intellectual and developmental disabilities) were particularly affected by these disruptions to daily life, and their use of emergency services increased.2 Surges in psychiatric emergency department visits among children led to increased boarding, reflecting unleveraged opportunities for early intervention. Families faced changes in child care, economic uncertainty, educational responsibilities, and increased rates of domestic violence.3 Communities of color were disproportionately affected in every way, from disease mortality to learning loss and increased school dropout rates.
To address gaps in the system, we must leverage school-based mental health programs, bolster access to and support of primary care providers, and embrace new, innovative models.
School-based mental health programs
Schools may be an ideal setting for universal mental health screening and opportunities for training, leadership, and whole school interventions. There is promising evidence that school-based interventions can decrease the incidence of suicide attempts and increase help-seeking behavior in students.4 There has long been interest in mental health screening in schools, though it has not been widely implemented given the significant resources required to both facilitate screening and effectively serve students who need additional support. Mobile apps may be one solution to scalability of both screening and interventions, but these initiatives should only be implemented within a stakeholder-engaged, family-centered multi-tiered model of behavioral support.
Other school-based initiatives include providing advice and training to teachers and school counselors and increasing access to specialized mental health professionals, including school psychologists, social workers, nurses, and behavior support workers, as well as community-based mental health providers. The 2021 American Rescue Plan Act included $170 billion for school funding, which many schools used to hire mental health workers. The Student Mental Health Helpline Act, if passed, will create helplines to support teachers as they help students address mental health issues.5 Educators can be trained to identify mental health needs, addressing mild symptoms themselves and referring students requiring more specialized services. Specific training programs for educators include Classroom Well-Being Information and Strategies for Educators (WISE), Youth Mental Health First Aid, and other resources funded by the U.S. Department of Health and Human Services. In addition to educators, other non–mental health professions interfacing with youth, including other youth, parents, clergy, coaches, and other community members, can be empowered with additional behavioral health knowledge and skills.
Increasing capacity in primary care
A number of programs are designed to improve knowledge and skills in children’s mental health among primary care providers, such as pediatricians. In Project ECHO, a “hub” of specialists, typically at an academic medical center, provides didactic lectures and case presentations for primary care “spokes” using teleconferencing.6 The REACH Institute uses interactive group learning followed by ongoing coaching and case-based training.
Collaborative care models known as Child Psychiatry Access Programs (CPAPs) engage child and adolescent psychiatrists to support primary care management of psychiatric disorders. Consultations may be direct or indirect, and involve technology or in-person care. Available in most states, these models increase access to mental health care, expand the capacity of the existing workforce, and decrease stigma and inconvenience for patients. Collaborative care models have been shown to lead to improved patient and family satisfaction, reduced utilization of emergency room and inpatient hospitalizations, and improved clinical outcomes. Off-site integrated care models may additionally serve larger and more geographically dispersed populations, minimize changes to existing infrastructure, reduce travel costs for clinicians, and decrease isolation of specialists. These programs are feasible, desirable, and sustainable. There is currently no cost to patients for their primary care providers’ participation in these models, as they are supported by the state, local, or insurance payer sources in addition to federal funding. Financially sustainable models are essential to ensure equitable access to these services in the future.
New service models
For adolescents and young adults, integrated youth service hubs such as those that have emerged in Australia, the United Kingdom, Canada, and more recently in the United States may be particularly appealing. These hubs emphasize rapid access to care and early intervention, youth and family engagement, youth-friendly settings and services, evidence-informed approaches, and partnerships and collaboration.7 In addition to mental health, these “one-stop shops” offer physical health, vocational supports, and case management to support basic needs. They address a particular system gap by providing services for transition-age youth rather than cutting off at age 18, as many children’s mental health services do.
Emerging solutions to the high utilization of emergency departments for pediatric mental health needs include utilization of pediatric Crisis Stabilization Units (CSUs). CSUs are community-based, short-term outpatient units that provide immediate care to children and families experiencing a mental health crisis. The goal of CSUs is to quickly stabilize the individual – often within 72 hours – and refer that individual to available community resources. This model may also reduce police involvement in mental health crises, which may be particularly important for racialized populations.
Conclusion
The thoughtful implementation and stable funding of evidence-based models can help schools, the health care system, and communities more effectively support children’s mental health in the post–COVID-19 pandemic era. Only with sufficient investments in the mental health system and other systems designed to support children and families, as well as careful consideration of unintended consequences on equity-deserving populations, will we see an end to this crisis.
Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences; program director of the child and adolescent psychiatry fellowship; and associate medical director of the perinatal program at the University of California, Los Angeles, Semel Institute for Neuroscience and Human Behavior.
References
1. Hillis SD et al. COVID-19–Associated orphanhood and caregiver death in the United States. Pediatrics. 2021;148:e2021053760.
2. Edgcomb JB et al. Mental health‐related emergency department visits among children during the early COVID‐19 pandemic. Psychiatr Res Clin Pract. 2022;4:4-11.
3. Pereda N, Díaz-Faes DA. Family violence against children in the wake of COVID-19 pandemic: A review of current perspectives and risk factors. Child and Adolescent Psychiatry and Mental Health. 2020;4:40.
4. Gijzen MWM et al. Effectiveness of school-based preventive programs in suicidal thoughts and behaviors: A meta-analysis. Journal of Affective Disorders. 2022;298:408-420.
5. Newman M: H.R.5235 – 117th Congress (2021-2022): Student Mental Health Helpline Act of 2021 [Internet] 2021; [cited 2023 Jan 11] Available from: http://www.congress.gov.
6. Raney L et al. Digitally driven integrated primary care and behavioral health: How technology can expand access to effective treatment. Curr Psychiatry Rep. 2017;19:86.
7. Settipani CA et al. Key attributes of integrated community-based youth service hubs for mental health: A scoping review. Int J Ment Health Syst. 2019;13:52.
In the wake of the COVID-19 pandemic, the American Academy of Child and Adolescent Psychiatry, American Academy of Pediatrics, and Children’s Hospital Association declared a national emergency in child and adolescent mental health. Additionally, the U.S. Surgeon General issued an advisory highlighting increased prevalence of mental health challenges in youth, impacts of the COVID-19 pandemic, and recommendations to address this crisis.
The pandemic required youth to isolate from peers and community supports, navigate remote learning environments, and cope with grief and loss; some 140,000 children in the United States experienced the death of a caregiver due to COVID-19.1 Virtually every system that supports children was affected. Whereas schools have historically been a main provider of child and adolescent mental health services, delivery of many school-based mental health programs was disrupted by school closures and staffing challenges. Subgroups of children (for example, those with intellectual and developmental disabilities) were particularly affected by these disruptions to daily life, and their use of emergency services increased.2 Surges in psychiatric emergency department visits among children led to increased boarding, reflecting unleveraged opportunities for early intervention. Families faced changes in child care, economic uncertainty, educational responsibilities, and increased rates of domestic violence.3 Communities of color were disproportionately affected in every way, from disease mortality to learning loss and increased school dropout rates.
To address gaps in the system, we must leverage school-based mental health programs, bolster access to and support of primary care providers, and embrace new, innovative models.
School-based mental health programs
Schools may be an ideal setting for universal mental health screening and opportunities for training, leadership, and whole school interventions. There is promising evidence that school-based interventions can decrease the incidence of suicide attempts and increase help-seeking behavior in students.4 There has long been interest in mental health screening in schools, though it has not been widely implemented given the significant resources required to both facilitate screening and effectively serve students who need additional support. Mobile apps may be one solution to scalability of both screening and interventions, but these initiatives should only be implemented within a stakeholder-engaged, family-centered multi-tiered model of behavioral support.
Other school-based initiatives include providing advice and training to teachers and school counselors and increasing access to specialized mental health professionals, including school psychologists, social workers, nurses, and behavior support workers, as well as community-based mental health providers. The 2021 American Rescue Plan Act included $170 billion for school funding, which many schools used to hire mental health workers. The Student Mental Health Helpline Act, if passed, will create helplines to support teachers as they help students address mental health issues.5 Educators can be trained to identify mental health needs, addressing mild symptoms themselves and referring students requiring more specialized services. Specific training programs for educators include Classroom Well-Being Information and Strategies for Educators (WISE), Youth Mental Health First Aid, and other resources funded by the U.S. Department of Health and Human Services. In addition to educators, other non–mental health professions interfacing with youth, including other youth, parents, clergy, coaches, and other community members, can be empowered with additional behavioral health knowledge and skills.
Increasing capacity in primary care
A number of programs are designed to improve knowledge and skills in children’s mental health among primary care providers, such as pediatricians. In Project ECHO, a “hub” of specialists, typically at an academic medical center, provides didactic lectures and case presentations for primary care “spokes” using teleconferencing.6 The REACH Institute uses interactive group learning followed by ongoing coaching and case-based training.
Collaborative care models known as Child Psychiatry Access Programs (CPAPs) engage child and adolescent psychiatrists to support primary care management of psychiatric disorders. Consultations may be direct or indirect, and involve technology or in-person care. Available in most states, these models increase access to mental health care, expand the capacity of the existing workforce, and decrease stigma and inconvenience for patients. Collaborative care models have been shown to lead to improved patient and family satisfaction, reduced utilization of emergency room and inpatient hospitalizations, and improved clinical outcomes. Off-site integrated care models may additionally serve larger and more geographically dispersed populations, minimize changes to existing infrastructure, reduce travel costs for clinicians, and decrease isolation of specialists. These programs are feasible, desirable, and sustainable. There is currently no cost to patients for their primary care providers’ participation in these models, as they are supported by the state, local, or insurance payer sources in addition to federal funding. Financially sustainable models are essential to ensure equitable access to these services in the future.
New service models
For adolescents and young adults, integrated youth service hubs such as those that have emerged in Australia, the United Kingdom, Canada, and more recently in the United States may be particularly appealing. These hubs emphasize rapid access to care and early intervention, youth and family engagement, youth-friendly settings and services, evidence-informed approaches, and partnerships and collaboration.7 In addition to mental health, these “one-stop shops” offer physical health, vocational supports, and case management to support basic needs. They address a particular system gap by providing services for transition-age youth rather than cutting off at age 18, as many children’s mental health services do.
Emerging solutions to the high utilization of emergency departments for pediatric mental health needs include utilization of pediatric Crisis Stabilization Units (CSUs). CSUs are community-based, short-term outpatient units that provide immediate care to children and families experiencing a mental health crisis. The goal of CSUs is to quickly stabilize the individual – often within 72 hours – and refer that individual to available community resources. This model may also reduce police involvement in mental health crises, which may be particularly important for racialized populations.
Conclusion
The thoughtful implementation and stable funding of evidence-based models can help schools, the health care system, and communities more effectively support children’s mental health in the post–COVID-19 pandemic era. Only with sufficient investments in the mental health system and other systems designed to support children and families, as well as careful consideration of unintended consequences on equity-deserving populations, will we see an end to this crisis.
Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences; program director of the child and adolescent psychiatry fellowship; and associate medical director of the perinatal program at the University of California, Los Angeles, Semel Institute for Neuroscience and Human Behavior.
References
1. Hillis SD et al. COVID-19–Associated orphanhood and caregiver death in the United States. Pediatrics. 2021;148:e2021053760.
2. Edgcomb JB et al. Mental health‐related emergency department visits among children during the early COVID‐19 pandemic. Psychiatr Res Clin Pract. 2022;4:4-11.
3. Pereda N, Díaz-Faes DA. Family violence against children in the wake of COVID-19 pandemic: A review of current perspectives and risk factors. Child and Adolescent Psychiatry and Mental Health. 2020;4:40.
4. Gijzen MWM et al. Effectiveness of school-based preventive programs in suicidal thoughts and behaviors: A meta-analysis. Journal of Affective Disorders. 2022;298:408-420.
5. Newman M: H.R.5235 – 117th Congress (2021-2022): Student Mental Health Helpline Act of 2021 [Internet] 2021; [cited 2023 Jan 11] Available from: http://www.congress.gov.
6. Raney L et al. Digitally driven integrated primary care and behavioral health: How technology can expand access to effective treatment. Curr Psychiatry Rep. 2017;19:86.
7. Settipani CA et al. Key attributes of integrated community-based youth service hubs for mental health: A scoping review. Int J Ment Health Syst. 2019;13:52.
In the wake of the COVID-19 pandemic, the American Academy of Child and Adolescent Psychiatry, American Academy of Pediatrics, and Children’s Hospital Association declared a national emergency in child and adolescent mental health. Additionally, the U.S. Surgeon General issued an advisory highlighting increased prevalence of mental health challenges in youth, impacts of the COVID-19 pandemic, and recommendations to address this crisis.
The pandemic required youth to isolate from peers and community supports, navigate remote learning environments, and cope with grief and loss; some 140,000 children in the United States experienced the death of a caregiver due to COVID-19.1 Virtually every system that supports children was affected. Whereas schools have historically been a main provider of child and adolescent mental health services, delivery of many school-based mental health programs was disrupted by school closures and staffing challenges. Subgroups of children (for example, those with intellectual and developmental disabilities) were particularly affected by these disruptions to daily life, and their use of emergency services increased.2 Surges in psychiatric emergency department visits among children led to increased boarding, reflecting unleveraged opportunities for early intervention. Families faced changes in child care, economic uncertainty, educational responsibilities, and increased rates of domestic violence.3 Communities of color were disproportionately affected in every way, from disease mortality to learning loss and increased school dropout rates.
To address gaps in the system, we must leverage school-based mental health programs, bolster access to and support of primary care providers, and embrace new, innovative models.
School-based mental health programs
Schools may be an ideal setting for universal mental health screening and opportunities for training, leadership, and whole school interventions. There is promising evidence that school-based interventions can decrease the incidence of suicide attempts and increase help-seeking behavior in students.4 There has long been interest in mental health screening in schools, though it has not been widely implemented given the significant resources required to both facilitate screening and effectively serve students who need additional support. Mobile apps may be one solution to scalability of both screening and interventions, but these initiatives should only be implemented within a stakeholder-engaged, family-centered multi-tiered model of behavioral support.
Other school-based initiatives include providing advice and training to teachers and school counselors and increasing access to specialized mental health professionals, including school psychologists, social workers, nurses, and behavior support workers, as well as community-based mental health providers. The 2021 American Rescue Plan Act included $170 billion for school funding, which many schools used to hire mental health workers. The Student Mental Health Helpline Act, if passed, will create helplines to support teachers as they help students address mental health issues.5 Educators can be trained to identify mental health needs, addressing mild symptoms themselves and referring students requiring more specialized services. Specific training programs for educators include Classroom Well-Being Information and Strategies for Educators (WISE), Youth Mental Health First Aid, and other resources funded by the U.S. Department of Health and Human Services. In addition to educators, other non–mental health professions interfacing with youth, including other youth, parents, clergy, coaches, and other community members, can be empowered with additional behavioral health knowledge and skills.
Increasing capacity in primary care
A number of programs are designed to improve knowledge and skills in children’s mental health among primary care providers, such as pediatricians. In Project ECHO, a “hub” of specialists, typically at an academic medical center, provides didactic lectures and case presentations for primary care “spokes” using teleconferencing.6 The REACH Institute uses interactive group learning followed by ongoing coaching and case-based training.
Collaborative care models known as Child Psychiatry Access Programs (CPAPs) engage child and adolescent psychiatrists to support primary care management of psychiatric disorders. Consultations may be direct or indirect, and involve technology or in-person care. Available in most states, these models increase access to mental health care, expand the capacity of the existing workforce, and decrease stigma and inconvenience for patients. Collaborative care models have been shown to lead to improved patient and family satisfaction, reduced utilization of emergency room and inpatient hospitalizations, and improved clinical outcomes. Off-site integrated care models may additionally serve larger and more geographically dispersed populations, minimize changes to existing infrastructure, reduce travel costs for clinicians, and decrease isolation of specialists. These programs are feasible, desirable, and sustainable. There is currently no cost to patients for their primary care providers’ participation in these models, as they are supported by the state, local, or insurance payer sources in addition to federal funding. Financially sustainable models are essential to ensure equitable access to these services in the future.
New service models
For adolescents and young adults, integrated youth service hubs such as those that have emerged in Australia, the United Kingdom, Canada, and more recently in the United States may be particularly appealing. These hubs emphasize rapid access to care and early intervention, youth and family engagement, youth-friendly settings and services, evidence-informed approaches, and partnerships and collaboration.7 In addition to mental health, these “one-stop shops” offer physical health, vocational supports, and case management to support basic needs. They address a particular system gap by providing services for transition-age youth rather than cutting off at age 18, as many children’s mental health services do.
Emerging solutions to the high utilization of emergency departments for pediatric mental health needs include utilization of pediatric Crisis Stabilization Units (CSUs). CSUs are community-based, short-term outpatient units that provide immediate care to children and families experiencing a mental health crisis. The goal of CSUs is to quickly stabilize the individual – often within 72 hours – and refer that individual to available community resources. This model may also reduce police involvement in mental health crises, which may be particularly important for racialized populations.
Conclusion
The thoughtful implementation and stable funding of evidence-based models can help schools, the health care system, and communities more effectively support children’s mental health in the post–COVID-19 pandemic era. Only with sufficient investments in the mental health system and other systems designed to support children and families, as well as careful consideration of unintended consequences on equity-deserving populations, will we see an end to this crisis.
Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences; program director of the child and adolescent psychiatry fellowship; and associate medical director of the perinatal program at the University of California, Los Angeles, Semel Institute for Neuroscience and Human Behavior.
References
1. Hillis SD et al. COVID-19–Associated orphanhood and caregiver death in the United States. Pediatrics. 2021;148:e2021053760.
2. Edgcomb JB et al. Mental health‐related emergency department visits among children during the early COVID‐19 pandemic. Psychiatr Res Clin Pract. 2022;4:4-11.
3. Pereda N, Díaz-Faes DA. Family violence against children in the wake of COVID-19 pandemic: A review of current perspectives and risk factors. Child and Adolescent Psychiatry and Mental Health. 2020;4:40.
4. Gijzen MWM et al. Effectiveness of school-based preventive programs in suicidal thoughts and behaviors: A meta-analysis. Journal of Affective Disorders. 2022;298:408-420.
5. Newman M: H.R.5235 – 117th Congress (2021-2022): Student Mental Health Helpline Act of 2021 [Internet] 2021; [cited 2023 Jan 11] Available from: http://www.congress.gov.
6. Raney L et al. Digitally driven integrated primary care and behavioral health: How technology can expand access to effective treatment. Curr Psychiatry Rep. 2017;19:86.
7. Settipani CA et al. Key attributes of integrated community-based youth service hubs for mental health: A scoping review. Int J Ment Health Syst. 2019;13:52.