User login
Triple Therapy Helped Type 1 Patients Improve Glycemia
NEW ORLEANS – The addition of dapagliflozin to insulin and liraglutide in patients with type 1 diabetes resulted in a significant improvement in glycemia, results from a single-center randomized trial showed.
“Because liraglutide suppresses glucagon and lowers free fatty acids while SGLT-2 inhibitors increase glucagon and risk of diabetic ketoacidosis, it’s possible that the combination of the two agents may neutralize the diabetic ketoacidosis risk,” Paresh Dandona, MD, said at the annual scientific sessions of the American Diabetes Association.
In a recent study Dr. Dandona, chief of endocrinology at the University of Buffalo (N.Y.), and his associates showed that the addition of liraglutide to insulin significantly improved glycemic control in patients with type 1 diabetes (Diabetes Care 2016 Jun; 39[6]:1027-35). The purpose of the current study was to investigate whether the addition of dapagliflozin, a sodium-glucose cotransporter–2 inhibitor, to the combination of insulin and liraglutide would further improve glycemic control.
A total of 30 type 1 diabetes patients on insulin and liraglutide therapy for a minimum of 6 months were randomized to receive either dapagliflozin 10 mg or placebo daily for 12 weeks. Dapagliflozin was initiated at 5 mg daily for 1 week and increased to 10 mg daily thereafter. All patients had type 1 diabetes for at least 1 year, were on insulin therapy, had no detectable C-peptide in plasma, and were on 1.8 mg of liraglutide for 7 months. These patients were evaluated every week for the first and last 2 weeks and then every 2 weeks for 12 weeks. Blood and 24-hour urine samples were collected before and after intervention.
At baseline, the mean age of patients was 54 years and both groups were similar in terms of mean hemoglobin A1c, glucose levels, and insulin dosages. After 12 weeks, the mean HbA1c did not change in the placebo group, but it dropped significantly in the triple-therapy group, by .66% (P less than .01). In addition, the average weekly glucose concentration fell in the triple-therapy group by 13 mg/dL (P = .35) and there was a reduction in standard deviations of glycemic excursions. The triple-therapy group also experienced a small reduction in the total insulin dose, compared with the placebo group (–3.5 vs. –.4 units, respectively; P = .29)
Dr. Dandona went on to note that the episodes of hypoglycemia did not increase after triple therapy but body weight fell by 1.9 kg after 12 weeks, while there was no real change in the placebo arm. Two patients had to withdraw from the study because they developed diabetic ketoacidosis within a day after increasing the dose of dapagliflozin to 10 mg. “One of these patients had euglycemic DKA with blood glucose concentrations of less than 160 mg/dL, while the other had marked hyperglycemia with unchanged insulin dose at 26 units,” Dr. Dandona said. “This patient had experienced a marked reduction in insulin dose during the time she was on liraglutide prior to starting on dapagliflozin.”
Dr. Dandona disclosed that he has received research support from AstraZeneca and Novo Nordisk.
NEW ORLEANS – The addition of dapagliflozin to insulin and liraglutide in patients with type 1 diabetes resulted in a significant improvement in glycemia, results from a single-center randomized trial showed.
“Because liraglutide suppresses glucagon and lowers free fatty acids while SGLT-2 inhibitors increase glucagon and risk of diabetic ketoacidosis, it’s possible that the combination of the two agents may neutralize the diabetic ketoacidosis risk,” Paresh Dandona, MD, said at the annual scientific sessions of the American Diabetes Association.
In a recent study Dr. Dandona, chief of endocrinology at the University of Buffalo (N.Y.), and his associates showed that the addition of liraglutide to insulin significantly improved glycemic control in patients with type 1 diabetes (Diabetes Care 2016 Jun; 39[6]:1027-35). The purpose of the current study was to investigate whether the addition of dapagliflozin, a sodium-glucose cotransporter–2 inhibitor, to the combination of insulin and liraglutide would further improve glycemic control.
A total of 30 type 1 diabetes patients on insulin and liraglutide therapy for a minimum of 6 months were randomized to receive either dapagliflozin 10 mg or placebo daily for 12 weeks. Dapagliflozin was initiated at 5 mg daily for 1 week and increased to 10 mg daily thereafter. All patients had type 1 diabetes for at least 1 year, were on insulin therapy, had no detectable C-peptide in plasma, and were on 1.8 mg of liraglutide for 7 months. These patients were evaluated every week for the first and last 2 weeks and then every 2 weeks for 12 weeks. Blood and 24-hour urine samples were collected before and after intervention.
At baseline, the mean age of patients was 54 years and both groups were similar in terms of mean hemoglobin A1c, glucose levels, and insulin dosages. After 12 weeks, the mean HbA1c did not change in the placebo group, but it dropped significantly in the triple-therapy group, by .66% (P less than .01). In addition, the average weekly glucose concentration fell in the triple-therapy group by 13 mg/dL (P = .35) and there was a reduction in standard deviations of glycemic excursions. The triple-therapy group also experienced a small reduction in the total insulin dose, compared with the placebo group (–3.5 vs. –.4 units, respectively; P = .29)
Dr. Dandona went on to note that the episodes of hypoglycemia did not increase after triple therapy but body weight fell by 1.9 kg after 12 weeks, while there was no real change in the placebo arm. Two patients had to withdraw from the study because they developed diabetic ketoacidosis within a day after increasing the dose of dapagliflozin to 10 mg. “One of these patients had euglycemic DKA with blood glucose concentrations of less than 160 mg/dL, while the other had marked hyperglycemia with unchanged insulin dose at 26 units,” Dr. Dandona said. “This patient had experienced a marked reduction in insulin dose during the time she was on liraglutide prior to starting on dapagliflozin.”
Dr. Dandona disclosed that he has received research support from AstraZeneca and Novo Nordisk.
NEW ORLEANS – The addition of dapagliflozin to insulin and liraglutide in patients with type 1 diabetes resulted in a significant improvement in glycemia, results from a single-center randomized trial showed.
“Because liraglutide suppresses glucagon and lowers free fatty acids while SGLT-2 inhibitors increase glucagon and risk of diabetic ketoacidosis, it’s possible that the combination of the two agents may neutralize the diabetic ketoacidosis risk,” Paresh Dandona, MD, said at the annual scientific sessions of the American Diabetes Association.
In a recent study Dr. Dandona, chief of endocrinology at the University of Buffalo (N.Y.), and his associates showed that the addition of liraglutide to insulin significantly improved glycemic control in patients with type 1 diabetes (Diabetes Care 2016 Jun; 39[6]:1027-35). The purpose of the current study was to investigate whether the addition of dapagliflozin, a sodium-glucose cotransporter–2 inhibitor, to the combination of insulin and liraglutide would further improve glycemic control.
A total of 30 type 1 diabetes patients on insulin and liraglutide therapy for a minimum of 6 months were randomized to receive either dapagliflozin 10 mg or placebo daily for 12 weeks. Dapagliflozin was initiated at 5 mg daily for 1 week and increased to 10 mg daily thereafter. All patients had type 1 diabetes for at least 1 year, were on insulin therapy, had no detectable C-peptide in plasma, and were on 1.8 mg of liraglutide for 7 months. These patients were evaluated every week for the first and last 2 weeks and then every 2 weeks for 12 weeks. Blood and 24-hour urine samples were collected before and after intervention.
At baseline, the mean age of patients was 54 years and both groups were similar in terms of mean hemoglobin A1c, glucose levels, and insulin dosages. After 12 weeks, the mean HbA1c did not change in the placebo group, but it dropped significantly in the triple-therapy group, by .66% (P less than .01). In addition, the average weekly glucose concentration fell in the triple-therapy group by 13 mg/dL (P = .35) and there was a reduction in standard deviations of glycemic excursions. The triple-therapy group also experienced a small reduction in the total insulin dose, compared with the placebo group (–3.5 vs. –.4 units, respectively; P = .29)
Dr. Dandona went on to note that the episodes of hypoglycemia did not increase after triple therapy but body weight fell by 1.9 kg after 12 weeks, while there was no real change in the placebo arm. Two patients had to withdraw from the study because they developed diabetic ketoacidosis within a day after increasing the dose of dapagliflozin to 10 mg. “One of these patients had euglycemic DKA with blood glucose concentrations of less than 160 mg/dL, while the other had marked hyperglycemia with unchanged insulin dose at 26 units,” Dr. Dandona said. “This patient had experienced a marked reduction in insulin dose during the time she was on liraglutide prior to starting on dapagliflozin.”
Dr. Dandona disclosed that he has received research support from AstraZeneca and Novo Nordisk.
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Triple therapy helped type 1 patients improve glycemia
NEW ORLEANS – The addition of dapagliflozin to insulin and liraglutide in patients with type 1 diabetes resulted in a significant improvement in glycemia, results from a single-center randomized trial showed.
“Because liraglutide suppresses glucagon and lowers free fatty acids while SGLT-2 inhibitors increase glucagon and risk of diabetic ketoacidosis, it’s possible that the combination of the two agents may neutralize the diabetic ketoacidosis risk,” Paresh Dandona, MD, said at the annual scientific sessions of the American Diabetes Association.
In a recent study Dr. Dandona, chief of endocrinology at the University of Buffalo (N.Y.), and his associates showed that the addition of liraglutide to insulin significantly improved glycemic control in patients with type 1 diabetes (Diabetes Care 2016 Jun; 39[6]:1027-35). The purpose of the current study was to investigate whether the addition of dapagliflozin, a sodium-glucose cotransporter–2 inhibitor, to the combination of insulin and liraglutide would further improve glycemic control.
A total of 30 type 1 diabetes patients on insulin and liraglutide therapy for a minimum of 6 months were randomized to receive either dapagliflozin 10 mg or placebo daily for 12 weeks. Dapagliflozin was initiated at 5 mg daily for 1 week and increased to 10 mg daily thereafter. All patients had type 1 diabetes for at least 1 year, were on insulin therapy, had no detectable C-peptide in plasma, and were on 1.8 mg of liraglutide for 7 months. These patients were evaluated every week for the first and last 2 weeks and then every 2 weeks for 12 weeks. Blood and 24-hour urine samples were collected before and after intervention.
At baseline, the mean age of patients was 54 years and both groups were similar in terms of mean hemoglobin A1c, glucose levels, and insulin dosages. After 12 weeks, the mean HbA1c did not change in the placebo group, but it dropped significantly in the triple-therapy group, by .66% (P less than .01). In addition, the average weekly glucose concentration fell in the triple-therapy group by 13 mg/dL (P = .35) and there was a reduction in standard deviations of glycemic excursions. The triple-therapy group also experienced a small reduction in the total insulin dose, compared with the placebo group (–3.5 vs. –.4 units, respectively; P = .29)
Dr. Dandona went on to note that the episodes of hypoglycemia did not increase after triple therapy but body weight fell by 1.9 kg after 12 weeks, while there was no real change in the placebo arm. Two patients had to withdraw from the study because they developed diabetic ketoacidosis within a day after increasing the dose of dapagliflozin to 10 mg. “One of these patients had euglycemic DKA with blood glucose concentrations of less than 160 mg/dL, while the other had marked hyperglycemia with unchanged insulin dose at 26 units,” Dr. Dandona said. “This patient had experienced a marked reduction in insulin dose during the time she was on liraglutide prior to starting on dapagliflozin.”
Dr. Dandona disclosed that he has received research support from AstraZeneca and Novo Nordisk.
NEW ORLEANS – The addition of dapagliflozin to insulin and liraglutide in patients with type 1 diabetes resulted in a significant improvement in glycemia, results from a single-center randomized trial showed.
“Because liraglutide suppresses glucagon and lowers free fatty acids while SGLT-2 inhibitors increase glucagon and risk of diabetic ketoacidosis, it’s possible that the combination of the two agents may neutralize the diabetic ketoacidosis risk,” Paresh Dandona, MD, said at the annual scientific sessions of the American Diabetes Association.
In a recent study Dr. Dandona, chief of endocrinology at the University of Buffalo (N.Y.), and his associates showed that the addition of liraglutide to insulin significantly improved glycemic control in patients with type 1 diabetes (Diabetes Care 2016 Jun; 39[6]:1027-35). The purpose of the current study was to investigate whether the addition of dapagliflozin, a sodium-glucose cotransporter–2 inhibitor, to the combination of insulin and liraglutide would further improve glycemic control.
A total of 30 type 1 diabetes patients on insulin and liraglutide therapy for a minimum of 6 months were randomized to receive either dapagliflozin 10 mg or placebo daily for 12 weeks. Dapagliflozin was initiated at 5 mg daily for 1 week and increased to 10 mg daily thereafter. All patients had type 1 diabetes for at least 1 year, were on insulin therapy, had no detectable C-peptide in plasma, and were on 1.8 mg of liraglutide for 7 months. These patients were evaluated every week for the first and last 2 weeks and then every 2 weeks for 12 weeks. Blood and 24-hour urine samples were collected before and after intervention.
At baseline, the mean age of patients was 54 years and both groups were similar in terms of mean hemoglobin A1c, glucose levels, and insulin dosages. After 12 weeks, the mean HbA1c did not change in the placebo group, but it dropped significantly in the triple-therapy group, by .66% (P less than .01). In addition, the average weekly glucose concentration fell in the triple-therapy group by 13 mg/dL (P = .35) and there was a reduction in standard deviations of glycemic excursions. The triple-therapy group also experienced a small reduction in the total insulin dose, compared with the placebo group (–3.5 vs. –.4 units, respectively; P = .29)
Dr. Dandona went on to note that the episodes of hypoglycemia did not increase after triple therapy but body weight fell by 1.9 kg after 12 weeks, while there was no real change in the placebo arm. Two patients had to withdraw from the study because they developed diabetic ketoacidosis within a day after increasing the dose of dapagliflozin to 10 mg. “One of these patients had euglycemic DKA with blood glucose concentrations of less than 160 mg/dL, while the other had marked hyperglycemia with unchanged insulin dose at 26 units,” Dr. Dandona said. “This patient had experienced a marked reduction in insulin dose during the time she was on liraglutide prior to starting on dapagliflozin.”
Dr. Dandona disclosed that he has received research support from AstraZeneca and Novo Nordisk.
NEW ORLEANS – The addition of dapagliflozin to insulin and liraglutide in patients with type 1 diabetes resulted in a significant improvement in glycemia, results from a single-center randomized trial showed.
“Because liraglutide suppresses glucagon and lowers free fatty acids while SGLT-2 inhibitors increase glucagon and risk of diabetic ketoacidosis, it’s possible that the combination of the two agents may neutralize the diabetic ketoacidosis risk,” Paresh Dandona, MD, said at the annual scientific sessions of the American Diabetes Association.
In a recent study Dr. Dandona, chief of endocrinology at the University of Buffalo (N.Y.), and his associates showed that the addition of liraglutide to insulin significantly improved glycemic control in patients with type 1 diabetes (Diabetes Care 2016 Jun; 39[6]:1027-35). The purpose of the current study was to investigate whether the addition of dapagliflozin, a sodium-glucose cotransporter–2 inhibitor, to the combination of insulin and liraglutide would further improve glycemic control.
A total of 30 type 1 diabetes patients on insulin and liraglutide therapy for a minimum of 6 months were randomized to receive either dapagliflozin 10 mg or placebo daily for 12 weeks. Dapagliflozin was initiated at 5 mg daily for 1 week and increased to 10 mg daily thereafter. All patients had type 1 diabetes for at least 1 year, were on insulin therapy, had no detectable C-peptide in plasma, and were on 1.8 mg of liraglutide for 7 months. These patients were evaluated every week for the first and last 2 weeks and then every 2 weeks for 12 weeks. Blood and 24-hour urine samples were collected before and after intervention.
At baseline, the mean age of patients was 54 years and both groups were similar in terms of mean hemoglobin A1c, glucose levels, and insulin dosages. After 12 weeks, the mean HbA1c did not change in the placebo group, but it dropped significantly in the triple-therapy group, by .66% (P less than .01). In addition, the average weekly glucose concentration fell in the triple-therapy group by 13 mg/dL (P = .35) and there was a reduction in standard deviations of glycemic excursions. The triple-therapy group also experienced a small reduction in the total insulin dose, compared with the placebo group (–3.5 vs. –.4 units, respectively; P = .29)
Dr. Dandona went on to note that the episodes of hypoglycemia did not increase after triple therapy but body weight fell by 1.9 kg after 12 weeks, while there was no real change in the placebo arm. Two patients had to withdraw from the study because they developed diabetic ketoacidosis within a day after increasing the dose of dapagliflozin to 10 mg. “One of these patients had euglycemic DKA with blood glucose concentrations of less than 160 mg/dL, while the other had marked hyperglycemia with unchanged insulin dose at 26 units,” Dr. Dandona said. “This patient had experienced a marked reduction in insulin dose during the time she was on liraglutide prior to starting on dapagliflozin.”
Dr. Dandona disclosed that he has received research support from AstraZeneca and Novo Nordisk.
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point: Adding dapagliflozin to insulin and liraglutide in patients with type 1 diabetes led to a significant improvement in glycemia.
Major finding: After 12 weeks, the mean HbA1c did not change in the placebo group, but it dropped in the triple-therapy group by 0.66% (P less than .01).
Data source: A single-center study in which 30 type 1 diabetes patients on insulin and liraglutide therapy for a minimum of 6 months were randomized to receive either dapagliflozin 10 mg or placebo daily for 12 weeks.
Disclosures: Dr. Dandona disclosed that he has received research support from AstraZeneca and Novo Nordisk.
New antibiotics targeting MDR pathogens are expensive, but not impressive
The U.S. Food and Drug Administration has approved a number of new antibiotics targeting multidrug-resistant bacteria in the past 5 years, but the new drugs have not led to a substantial improvement in patient outcomes when compared with existing antibiotics, according to a recent analysis in the Annals of Internal Medicine.
The eight new antibiotics approved by the FDA between January 2010 and December 2015 were ceftaroline, fidaxomicin, bedaquiline, dalbavancin, tedizolid, oritavancin, ceftolozane/tazobactam, and ceftazidime/avibactam. Of those eight drugs, only three showed in vitro activity against the so-called ESKAPE pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumonia, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species). Only one drug, fidaxomicin, demonstrated in vitro activity against an urgent-threat pathogen from the Centers for Disease Control and Prevention, Clostridium difficile. Bedaquiline was the only new antibiotic specifically indicated for a disease from a multidrug-resistant pathogen, although the investigators said most of the drugs demonstrated in vitro activity against gram-positive drug-resistant pathogens.
Importantly, the authors noted that in vitro activity does not necessarily reflect benefits on actual patient clinical outcomes, as exemplified by such drugs as tigecycline and doripenem.
The researchers found what they called “important deficiencies in the clinical trials leading to approval of these new antibiotic products.” Most pivotal trial designs were primarily noninferiority trials, and the antibiotics were not studied to evaluate whether they have substantial benefits in efficacy over what is currently available, they noted. Additionally, none of the trials evaluated direct patient outcomes as primary end points, and some drugs did not have confirmatory evidence from a second independent trial or did not have any confirmatory trials.
Researchers also examined the prices of a single dose of the new antibiotics. The prices ranged from $1,195 to $4,183 (4-14 days of ceftolozane/tazobactam for acute pyelonephritis and intra-abdominal infections) to $69,702 (24 weeks of bedaquiline) – quite a premium for antibiotics showing unclear evidence of additional benefit.
“As antibiotic innovation continues to move forward, greater attention needs to be paid to incentives for developing high-quality new products with demonstrated superiority to existing products on outcomes in patients with multidrug-resistant disease, replacing the current focus on quantity and presumed future benefits,” researchers concluded.
Read the full study in the Annals of Internal Medicine (doi: 10.7326/M16-0291).
The U.S. Food and Drug Administration has approved a number of new antibiotics targeting multidrug-resistant bacteria in the past 5 years, but the new drugs have not led to a substantial improvement in patient outcomes when compared with existing antibiotics, according to a recent analysis in the Annals of Internal Medicine.
The eight new antibiotics approved by the FDA between January 2010 and December 2015 were ceftaroline, fidaxomicin, bedaquiline, dalbavancin, tedizolid, oritavancin, ceftolozane/tazobactam, and ceftazidime/avibactam. Of those eight drugs, only three showed in vitro activity against the so-called ESKAPE pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumonia, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species). Only one drug, fidaxomicin, demonstrated in vitro activity against an urgent-threat pathogen from the Centers for Disease Control and Prevention, Clostridium difficile. Bedaquiline was the only new antibiotic specifically indicated for a disease from a multidrug-resistant pathogen, although the investigators said most of the drugs demonstrated in vitro activity against gram-positive drug-resistant pathogens.
Importantly, the authors noted that in vitro activity does not necessarily reflect benefits on actual patient clinical outcomes, as exemplified by such drugs as tigecycline and doripenem.
The researchers found what they called “important deficiencies in the clinical trials leading to approval of these new antibiotic products.” Most pivotal trial designs were primarily noninferiority trials, and the antibiotics were not studied to evaluate whether they have substantial benefits in efficacy over what is currently available, they noted. Additionally, none of the trials evaluated direct patient outcomes as primary end points, and some drugs did not have confirmatory evidence from a second independent trial or did not have any confirmatory trials.
Researchers also examined the prices of a single dose of the new antibiotics. The prices ranged from $1,195 to $4,183 (4-14 days of ceftolozane/tazobactam for acute pyelonephritis and intra-abdominal infections) to $69,702 (24 weeks of bedaquiline) – quite a premium for antibiotics showing unclear evidence of additional benefit.
“As antibiotic innovation continues to move forward, greater attention needs to be paid to incentives for developing high-quality new products with demonstrated superiority to existing products on outcomes in patients with multidrug-resistant disease, replacing the current focus on quantity and presumed future benefits,” researchers concluded.
Read the full study in the Annals of Internal Medicine (doi: 10.7326/M16-0291).
The U.S. Food and Drug Administration has approved a number of new antibiotics targeting multidrug-resistant bacteria in the past 5 years, but the new drugs have not led to a substantial improvement in patient outcomes when compared with existing antibiotics, according to a recent analysis in the Annals of Internal Medicine.
The eight new antibiotics approved by the FDA between January 2010 and December 2015 were ceftaroline, fidaxomicin, bedaquiline, dalbavancin, tedizolid, oritavancin, ceftolozane/tazobactam, and ceftazidime/avibactam. Of those eight drugs, only three showed in vitro activity against the so-called ESKAPE pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumonia, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species). Only one drug, fidaxomicin, demonstrated in vitro activity against an urgent-threat pathogen from the Centers for Disease Control and Prevention, Clostridium difficile. Bedaquiline was the only new antibiotic specifically indicated for a disease from a multidrug-resistant pathogen, although the investigators said most of the drugs demonstrated in vitro activity against gram-positive drug-resistant pathogens.
Importantly, the authors noted that in vitro activity does not necessarily reflect benefits on actual patient clinical outcomes, as exemplified by such drugs as tigecycline and doripenem.
The researchers found what they called “important deficiencies in the clinical trials leading to approval of these new antibiotic products.” Most pivotal trial designs were primarily noninferiority trials, and the antibiotics were not studied to evaluate whether they have substantial benefits in efficacy over what is currently available, they noted. Additionally, none of the trials evaluated direct patient outcomes as primary end points, and some drugs did not have confirmatory evidence from a second independent trial or did not have any confirmatory trials.
Researchers also examined the prices of a single dose of the new antibiotics. The prices ranged from $1,195 to $4,183 (4-14 days of ceftolozane/tazobactam for acute pyelonephritis and intra-abdominal infections) to $69,702 (24 weeks of bedaquiline) – quite a premium for antibiotics showing unclear evidence of additional benefit.
“As antibiotic innovation continues to move forward, greater attention needs to be paid to incentives for developing high-quality new products with demonstrated superiority to existing products on outcomes in patients with multidrug-resistant disease, replacing the current focus on quantity and presumed future benefits,” researchers concluded.
Read the full study in the Annals of Internal Medicine (doi: 10.7326/M16-0291).
FROM ANNALS OF INTERNAL MEDICINE
Study links adipocytes and myeloma progression

A study published in Cancer Letters suggests that adipocytes contribute to the growth and progression of multiple myeloma (MM).
Researchers co-cultured MM cells with adipocytes derived from patients defined as normal weight, overweight, obese, or super obese.
This revealed a positive correlation between adipocytes and indicators of MM progression, which was most pronounced in cells from obese and super obese individuals.
“Once a person with cancer is out of the normal weight category, their BMI [body mass index] is contributing to multiple myeloma growth and progression,” said study author Katie DeCicco-Skinner, PhD, of American University in Washington, DC.
For this study, Dr DeCicco-Skinner and her colleagues obtained human adipose-derived stem cells from 29 patients who underwent liposuction and were defined as normal weight (BMI = 20–25 kg/m2), overweight (25–30 kg/m2), obese (30–35 kg/m2), or super obese (35–40 kg/m2).
Once the cells matured into adipocytes, they were co-cultured with the MM cell lines RPMI-8226 and NCI-H929.
The researchers found that adipocytes from overweight, obese, and super obese patients had increased levels of proteins linked to cancer, including PPAR-gamma, cytochrome C, interleukin-6, and leptin.
In addition, adipocyte-conditioned media from obese and super obese patients significantly increased MM cell adhesion.
And conditioned media from overweight, obese, and super obese patients increased angiogenic potential and expression of matrix metalloproteinase-2.
“We know multiple myeloma cells will anchor into bone marrow, and fat cells in the bone marrow will support the growth and spread of the cancer,” Dr DeCicco-Skinner said.
“In our study, as BMI increased, we started seeing an increase in the ability of multiple myeloma cells to adhere, which causes the cancer to better anchor. With angiogenesis, cancer cells cannot exist without their own blood supply. We also found the amount of blood vessels that developed was directly proportional to a patient’s BMI.”
Dr DeCicco-Skinner and her colleagues had assumed that cancer proliferation would benefit from a higher-than-normal BMI because of the epidemiological link between obesity and cancer. But the relationship between MM and the BMI of obese and super obese patients was drastic.
“We found that fat cells from obese or morbidly obese patients secreted a high amount of inflammatory proteins, which contributed to tumor progression,” Dr DeCicco-Skinner said.
These findings suggest a new approach for MM treatment, according to the researchers. They say physicians may want to consider tailoring drugs based on a patient’s BMI because a drug may not be as effective in obese or super obese patients.
“A patient may need to receive drugs to block inflammatory or other obesity-specific proteins, in addition to standard anticancer drugs they receive,” Dr DeCicco-Skinner said.
“Obesity increasingly plays a role in cancer cases, as the numbers of those who are obese rise. Improving our understanding of how fat cells and cancer cells communicate with each other, and how the communication changes during obesity, is critical.” ![]()

A study published in Cancer Letters suggests that adipocytes contribute to the growth and progression of multiple myeloma (MM).
Researchers co-cultured MM cells with adipocytes derived from patients defined as normal weight, overweight, obese, or super obese.
This revealed a positive correlation between adipocytes and indicators of MM progression, which was most pronounced in cells from obese and super obese individuals.
“Once a person with cancer is out of the normal weight category, their BMI [body mass index] is contributing to multiple myeloma growth and progression,” said study author Katie DeCicco-Skinner, PhD, of American University in Washington, DC.
For this study, Dr DeCicco-Skinner and her colleagues obtained human adipose-derived stem cells from 29 patients who underwent liposuction and were defined as normal weight (BMI = 20–25 kg/m2), overweight (25–30 kg/m2), obese (30–35 kg/m2), or super obese (35–40 kg/m2).
Once the cells matured into adipocytes, they were co-cultured with the MM cell lines RPMI-8226 and NCI-H929.
The researchers found that adipocytes from overweight, obese, and super obese patients had increased levels of proteins linked to cancer, including PPAR-gamma, cytochrome C, interleukin-6, and leptin.
In addition, adipocyte-conditioned media from obese and super obese patients significantly increased MM cell adhesion.
And conditioned media from overweight, obese, and super obese patients increased angiogenic potential and expression of matrix metalloproteinase-2.
“We know multiple myeloma cells will anchor into bone marrow, and fat cells in the bone marrow will support the growth and spread of the cancer,” Dr DeCicco-Skinner said.
“In our study, as BMI increased, we started seeing an increase in the ability of multiple myeloma cells to adhere, which causes the cancer to better anchor. With angiogenesis, cancer cells cannot exist without their own blood supply. We also found the amount of blood vessels that developed was directly proportional to a patient’s BMI.”
Dr DeCicco-Skinner and her colleagues had assumed that cancer proliferation would benefit from a higher-than-normal BMI because of the epidemiological link between obesity and cancer. But the relationship between MM and the BMI of obese and super obese patients was drastic.
“We found that fat cells from obese or morbidly obese patients secreted a high amount of inflammatory proteins, which contributed to tumor progression,” Dr DeCicco-Skinner said.
These findings suggest a new approach for MM treatment, according to the researchers. They say physicians may want to consider tailoring drugs based on a patient’s BMI because a drug may not be as effective in obese or super obese patients.
“A patient may need to receive drugs to block inflammatory or other obesity-specific proteins, in addition to standard anticancer drugs they receive,” Dr DeCicco-Skinner said.
“Obesity increasingly plays a role in cancer cases, as the numbers of those who are obese rise. Improving our understanding of how fat cells and cancer cells communicate with each other, and how the communication changes during obesity, is critical.” ![]()

A study published in Cancer Letters suggests that adipocytes contribute to the growth and progression of multiple myeloma (MM).
Researchers co-cultured MM cells with adipocytes derived from patients defined as normal weight, overweight, obese, or super obese.
This revealed a positive correlation between adipocytes and indicators of MM progression, which was most pronounced in cells from obese and super obese individuals.
“Once a person with cancer is out of the normal weight category, their BMI [body mass index] is contributing to multiple myeloma growth and progression,” said study author Katie DeCicco-Skinner, PhD, of American University in Washington, DC.
For this study, Dr DeCicco-Skinner and her colleagues obtained human adipose-derived stem cells from 29 patients who underwent liposuction and were defined as normal weight (BMI = 20–25 kg/m2), overweight (25–30 kg/m2), obese (30–35 kg/m2), or super obese (35–40 kg/m2).
Once the cells matured into adipocytes, they were co-cultured with the MM cell lines RPMI-8226 and NCI-H929.
The researchers found that adipocytes from overweight, obese, and super obese patients had increased levels of proteins linked to cancer, including PPAR-gamma, cytochrome C, interleukin-6, and leptin.
In addition, adipocyte-conditioned media from obese and super obese patients significantly increased MM cell adhesion.
And conditioned media from overweight, obese, and super obese patients increased angiogenic potential and expression of matrix metalloproteinase-2.
“We know multiple myeloma cells will anchor into bone marrow, and fat cells in the bone marrow will support the growth and spread of the cancer,” Dr DeCicco-Skinner said.
“In our study, as BMI increased, we started seeing an increase in the ability of multiple myeloma cells to adhere, which causes the cancer to better anchor. With angiogenesis, cancer cells cannot exist without their own blood supply. We also found the amount of blood vessels that developed was directly proportional to a patient’s BMI.”
Dr DeCicco-Skinner and her colleagues had assumed that cancer proliferation would benefit from a higher-than-normal BMI because of the epidemiological link between obesity and cancer. But the relationship between MM and the BMI of obese and super obese patients was drastic.
“We found that fat cells from obese or morbidly obese patients secreted a high amount of inflammatory proteins, which contributed to tumor progression,” Dr DeCicco-Skinner said.
These findings suggest a new approach for MM treatment, according to the researchers. They say physicians may want to consider tailoring drugs based on a patient’s BMI because a drug may not be as effective in obese or super obese patients.
“A patient may need to receive drugs to block inflammatory or other obesity-specific proteins, in addition to standard anticancer drugs they receive,” Dr DeCicco-Skinner said.
“Obesity increasingly plays a role in cancer cases, as the numbers of those who are obese rise. Improving our understanding of how fat cells and cancer cells communicate with each other, and how the communication changes during obesity, is critical.” ![]()
INR monitoring systems to be pulled from market

The Alere INRatio® and INRatio®2 PT/INR Monitoring Systems are being withdrawn from the US market because they may provide inaccurate international normalized ratio (INR) results.
These handheld blood coagulation systems, which consist of a small monitor and disposable test strips, are used to monitor patients taking warfarin.
The manufacturer of these systems, Alere Inc., said it is working with the US Food and Drug Administration (FDA) to determine the most appropriate timing for product discontinuation.
The company also said it will provide guidance on transitioning patients using the INRatio systems to an alternate solution to allow them to continue anticoagulation monitoring in the least disruptive manner possible.
Background on the withdrawal
In December 2014, Alere initiated a voluntary correction to inform users of the INRatio® and INRatio®2 PT/INR Monitoring Systems that patients with certain medical conditions should not be tested with the systems.
The company found that, in certain cases, the systems provided an INR result that was clinically significantly lower than a result obtained using a reference INR system (laboratory method).
In fact, there has been speculation that this issue may have affected the results of the ROCKET AF trial, a comparison of rivaroxaban and warfarin in which INRs were measured with the INRatio systems.
The FDA is currently investigating this possibility, although the European Medicines Agency has said the study’s overall results were not affected by the issue.
After Alere reported the issue with the INRatio systems to the FDA, the company began conducting its own investigation.
Over the past 2 years, Alere invested in the research and development of software enhancements to address the potential of the INRatio systems to deliver results that differ from laboratory INR measurement.
Alere said it is confident the software enhancements it developed and submitted to the FDA at the end of 2015 effectively address this issue.
However, the FDA said the company’s studies do not adequately demonstrate the effectiveness of the software modification. The agency therefore advised Alere to submit a proposed plan to voluntarily remove the INRatio systems from the market.
The company decided to follow this recommendation and plans to provide a timeline to discontinue the product line. Alere said it will provide further information on patient transition to patients and healthcare providers.
For more information regarding this product discontinuation, visit http://www.inr-care.com. ![]()

The Alere INRatio® and INRatio®2 PT/INR Monitoring Systems are being withdrawn from the US market because they may provide inaccurate international normalized ratio (INR) results.
These handheld blood coagulation systems, which consist of a small monitor and disposable test strips, are used to monitor patients taking warfarin.
The manufacturer of these systems, Alere Inc., said it is working with the US Food and Drug Administration (FDA) to determine the most appropriate timing for product discontinuation.
The company also said it will provide guidance on transitioning patients using the INRatio systems to an alternate solution to allow them to continue anticoagulation monitoring in the least disruptive manner possible.
Background on the withdrawal
In December 2014, Alere initiated a voluntary correction to inform users of the INRatio® and INRatio®2 PT/INR Monitoring Systems that patients with certain medical conditions should not be tested with the systems.
The company found that, in certain cases, the systems provided an INR result that was clinically significantly lower than a result obtained using a reference INR system (laboratory method).
In fact, there has been speculation that this issue may have affected the results of the ROCKET AF trial, a comparison of rivaroxaban and warfarin in which INRs were measured with the INRatio systems.
The FDA is currently investigating this possibility, although the European Medicines Agency has said the study’s overall results were not affected by the issue.
After Alere reported the issue with the INRatio systems to the FDA, the company began conducting its own investigation.
Over the past 2 years, Alere invested in the research and development of software enhancements to address the potential of the INRatio systems to deliver results that differ from laboratory INR measurement.
Alere said it is confident the software enhancements it developed and submitted to the FDA at the end of 2015 effectively address this issue.
However, the FDA said the company’s studies do not adequately demonstrate the effectiveness of the software modification. The agency therefore advised Alere to submit a proposed plan to voluntarily remove the INRatio systems from the market.
The company decided to follow this recommendation and plans to provide a timeline to discontinue the product line. Alere said it will provide further information on patient transition to patients and healthcare providers.
For more information regarding this product discontinuation, visit http://www.inr-care.com. ![]()

The Alere INRatio® and INRatio®2 PT/INR Monitoring Systems are being withdrawn from the US market because they may provide inaccurate international normalized ratio (INR) results.
These handheld blood coagulation systems, which consist of a small monitor and disposable test strips, are used to monitor patients taking warfarin.
The manufacturer of these systems, Alere Inc., said it is working with the US Food and Drug Administration (FDA) to determine the most appropriate timing for product discontinuation.
The company also said it will provide guidance on transitioning patients using the INRatio systems to an alternate solution to allow them to continue anticoagulation monitoring in the least disruptive manner possible.
Background on the withdrawal
In December 2014, Alere initiated a voluntary correction to inform users of the INRatio® and INRatio®2 PT/INR Monitoring Systems that patients with certain medical conditions should not be tested with the systems.
The company found that, in certain cases, the systems provided an INR result that was clinically significantly lower than a result obtained using a reference INR system (laboratory method).
In fact, there has been speculation that this issue may have affected the results of the ROCKET AF trial, a comparison of rivaroxaban and warfarin in which INRs were measured with the INRatio systems.
The FDA is currently investigating this possibility, although the European Medicines Agency has said the study’s overall results were not affected by the issue.
After Alere reported the issue with the INRatio systems to the FDA, the company began conducting its own investigation.
Over the past 2 years, Alere invested in the research and development of software enhancements to address the potential of the INRatio systems to deliver results that differ from laboratory INR measurement.
Alere said it is confident the software enhancements it developed and submitted to the FDA at the end of 2015 effectively address this issue.
However, the FDA said the company’s studies do not adequately demonstrate the effectiveness of the software modification. The agency therefore advised Alere to submit a proposed plan to voluntarily remove the INRatio systems from the market.
The company decided to follow this recommendation and plans to provide a timeline to discontinue the product line. Alere said it will provide further information on patient transition to patients and healthcare providers.
For more information regarding this product discontinuation, visit http://www.inr-care.com. ![]()
COMP recommends orphan status for drug to treat PNH

The European Medicines Agency’s Committee for Orphan Medicinal Products (COMP) has issued a positive opinion recommending orphan designation for Coversin for the treatment of paroxysmal nocturnal hemoglobinuria (PNH).
Coversin is a second-generation complement inhibitor that acts on complement component-C5, preventing release of C5a and formation of C5b-9 (also known as the membrane attack complex).
Coversin is a recombinant small protein (16,740 Da) derived from a native protein found in the saliva of the Ornithodoros moubata tick.
The drug is being developed by Akari Therapeutics.
In vitro experiments have shown that Coversin inhibits red blood cell lysis in PNH, and the drug can achieve full complement inhibition in the blood of PNH patients who are resistant to the drug eculizumab.
In a phase 1a trial of healthy volunteers, Coversin completely inhibited complement C5 activity within 12 hours of administration.
Akari Therapeutics is currently conducting a phase 1b study of Coversin in healthy volunteers and is administering the drug to a patient with eculizumab-resistant PNH. Thus far, Coversin has prevented hemolytic episodes and improved disease symptoms in this patient. And the only drug-related adverse event has been occasional local and transient irritation at the injection site.
Coversin is also being studied in atypical hemolytic uremic syndrome and Guillain Barré syndrome.
About orphan designation
The COMP adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision.
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat a life-threatening or chronically debilitating condition affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity in the European Union if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure. ![]()

The European Medicines Agency’s Committee for Orphan Medicinal Products (COMP) has issued a positive opinion recommending orphan designation for Coversin for the treatment of paroxysmal nocturnal hemoglobinuria (PNH).
Coversin is a second-generation complement inhibitor that acts on complement component-C5, preventing release of C5a and formation of C5b-9 (also known as the membrane attack complex).
Coversin is a recombinant small protein (16,740 Da) derived from a native protein found in the saliva of the Ornithodoros moubata tick.
The drug is being developed by Akari Therapeutics.
In vitro experiments have shown that Coversin inhibits red blood cell lysis in PNH, and the drug can achieve full complement inhibition in the blood of PNH patients who are resistant to the drug eculizumab.
In a phase 1a trial of healthy volunteers, Coversin completely inhibited complement C5 activity within 12 hours of administration.
Akari Therapeutics is currently conducting a phase 1b study of Coversin in healthy volunteers and is administering the drug to a patient with eculizumab-resistant PNH. Thus far, Coversin has prevented hemolytic episodes and improved disease symptoms in this patient. And the only drug-related adverse event has been occasional local and transient irritation at the injection site.
Coversin is also being studied in atypical hemolytic uremic syndrome and Guillain Barré syndrome.
About orphan designation
The COMP adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision.
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat a life-threatening or chronically debilitating condition affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity in the European Union if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure. ![]()

The European Medicines Agency’s Committee for Orphan Medicinal Products (COMP) has issued a positive opinion recommending orphan designation for Coversin for the treatment of paroxysmal nocturnal hemoglobinuria (PNH).
Coversin is a second-generation complement inhibitor that acts on complement component-C5, preventing release of C5a and formation of C5b-9 (also known as the membrane attack complex).
Coversin is a recombinant small protein (16,740 Da) derived from a native protein found in the saliva of the Ornithodoros moubata tick.
The drug is being developed by Akari Therapeutics.
In vitro experiments have shown that Coversin inhibits red blood cell lysis in PNH, and the drug can achieve full complement inhibition in the blood of PNH patients who are resistant to the drug eculizumab.
In a phase 1a trial of healthy volunteers, Coversin completely inhibited complement C5 activity within 12 hours of administration.
Akari Therapeutics is currently conducting a phase 1b study of Coversin in healthy volunteers and is administering the drug to a patient with eculizumab-resistant PNH. Thus far, Coversin has prevented hemolytic episodes and improved disease symptoms in this patient. And the only drug-related adverse event has been occasional local and transient irritation at the injection site.
Coversin is also being studied in atypical hemolytic uremic syndrome and Guillain Barré syndrome.
About orphan designation
The COMP adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision.
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat a life-threatening or chronically debilitating condition affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity in the European Union if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure. ![]()
Drug could be disease-modifying for SCD, team says
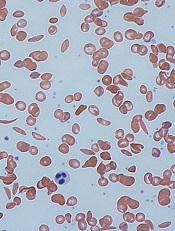
Image by Graham Beards
Researchers say the small molecule GBT440 could be a disease-modifying agent for patients with sickle cell disease (SCD).
Preclinical data showed that GBT440 can reduce sickling, extend the circulating half-life of red blood cells (RBCs), and decrease excessive erythropoiesis in SCD.
GBT440 binds specifically to hemoglobin and is designed to inhibit sickle hemoglobin (HbS) polymer formation.
“One promising strategy for preventing red blood cell sickling and subsequently modifying sickle cell disease over the long term involves inhibiting polymerization of HbS in red blood cells,” said David R. Archer, PhD, of Emory University School of Medicine in Atlanta, Georgia.
“This can be achieved by increasing the proportion of oxygenated HbS in those cells. We believe our preclinical results provide strong evidence that GBT440 inhibits HbS polymerization and red blood cell sickling, which is important because it addresses the underlying pathophysiology of sickle cell disease and has the potential to change its devastating clinical course.”
Dr Archer and his colleagues reported these results in the British Journal of Haematology. The research was supported by Global Blood Therapeutics, Inc., the company developing GBT440.
The researchers reported that, in vitro, GBT440 dose-dependently increased the affinity of HbS for oxygen, delayed polymerization of HbS, and reduced the number of sickled RBCs in whole blood from SCD patients.
In an animal model of SCD, GBT440 inhibited RBC sickling, prolonged the half-life of RBCs, and reduced reticulocyte counts.
The researchers said the drug also exhibited favorable pharmacokinetic properties in various animal species, suggesting the potential for once-daily oral dosing in SCD patients.
“Our preclinical work has developed a foundation of evidence that GBT440 is a potent inhibitor of the polymerization of HbS,” said Ted W. Love, MD, chief executive officer of Global Blood Therapeutics, Inc.
“We continue to build on these data with our ongoing phase 1/2 study, which has shown that GBT440 was well-tolerated over 90 days of dosing and that all SCD patients who received multiple doses of GBT440 exhibited improvements in one or more clinical markers of hemolysis and anemia. Our next step is to initiate a pivotal trial in adults with SCD later this year.” ![]()
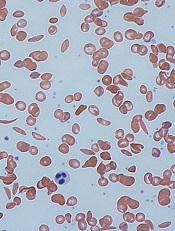
Image by Graham Beards
Researchers say the small molecule GBT440 could be a disease-modifying agent for patients with sickle cell disease (SCD).
Preclinical data showed that GBT440 can reduce sickling, extend the circulating half-life of red blood cells (RBCs), and decrease excessive erythropoiesis in SCD.
GBT440 binds specifically to hemoglobin and is designed to inhibit sickle hemoglobin (HbS) polymer formation.
“One promising strategy for preventing red blood cell sickling and subsequently modifying sickle cell disease over the long term involves inhibiting polymerization of HbS in red blood cells,” said David R. Archer, PhD, of Emory University School of Medicine in Atlanta, Georgia.
“This can be achieved by increasing the proportion of oxygenated HbS in those cells. We believe our preclinical results provide strong evidence that GBT440 inhibits HbS polymerization and red blood cell sickling, which is important because it addresses the underlying pathophysiology of sickle cell disease and has the potential to change its devastating clinical course.”
Dr Archer and his colleagues reported these results in the British Journal of Haematology. The research was supported by Global Blood Therapeutics, Inc., the company developing GBT440.
The researchers reported that, in vitro, GBT440 dose-dependently increased the affinity of HbS for oxygen, delayed polymerization of HbS, and reduced the number of sickled RBCs in whole blood from SCD patients.
In an animal model of SCD, GBT440 inhibited RBC sickling, prolonged the half-life of RBCs, and reduced reticulocyte counts.
The researchers said the drug also exhibited favorable pharmacokinetic properties in various animal species, suggesting the potential for once-daily oral dosing in SCD patients.
“Our preclinical work has developed a foundation of evidence that GBT440 is a potent inhibitor of the polymerization of HbS,” said Ted W. Love, MD, chief executive officer of Global Blood Therapeutics, Inc.
“We continue to build on these data with our ongoing phase 1/2 study, which has shown that GBT440 was well-tolerated over 90 days of dosing and that all SCD patients who received multiple doses of GBT440 exhibited improvements in one or more clinical markers of hemolysis and anemia. Our next step is to initiate a pivotal trial in adults with SCD later this year.” ![]()
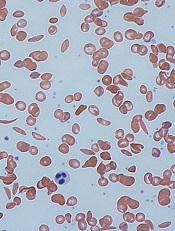
Image by Graham Beards
Researchers say the small molecule GBT440 could be a disease-modifying agent for patients with sickle cell disease (SCD).
Preclinical data showed that GBT440 can reduce sickling, extend the circulating half-life of red blood cells (RBCs), and decrease excessive erythropoiesis in SCD.
GBT440 binds specifically to hemoglobin and is designed to inhibit sickle hemoglobin (HbS) polymer formation.
“One promising strategy for preventing red blood cell sickling and subsequently modifying sickle cell disease over the long term involves inhibiting polymerization of HbS in red blood cells,” said David R. Archer, PhD, of Emory University School of Medicine in Atlanta, Georgia.
“This can be achieved by increasing the proportion of oxygenated HbS in those cells. We believe our preclinical results provide strong evidence that GBT440 inhibits HbS polymerization and red blood cell sickling, which is important because it addresses the underlying pathophysiology of sickle cell disease and has the potential to change its devastating clinical course.”
Dr Archer and his colleagues reported these results in the British Journal of Haematology. The research was supported by Global Blood Therapeutics, Inc., the company developing GBT440.
The researchers reported that, in vitro, GBT440 dose-dependently increased the affinity of HbS for oxygen, delayed polymerization of HbS, and reduced the number of sickled RBCs in whole blood from SCD patients.
In an animal model of SCD, GBT440 inhibited RBC sickling, prolonged the half-life of RBCs, and reduced reticulocyte counts.
The researchers said the drug also exhibited favorable pharmacokinetic properties in various animal species, suggesting the potential for once-daily oral dosing in SCD patients.
“Our preclinical work has developed a foundation of evidence that GBT440 is a potent inhibitor of the polymerization of HbS,” said Ted W. Love, MD, chief executive officer of Global Blood Therapeutics, Inc.
“We continue to build on these data with our ongoing phase 1/2 study, which has shown that GBT440 was well-tolerated over 90 days of dosing and that all SCD patients who received multiple doses of GBT440 exhibited improvements in one or more clinical markers of hemolysis and anemia. Our next step is to initiate a pivotal trial in adults with SCD later this year.” ![]()
NETWORKS
Airways Disorders
The asthma COPD overlap syndrome: hype or reality?
In 2014, the Global Initiative for Asthma (GINA) and the Global Initiative for Chronic Obstructive Lung Disease (GOLD) published a joint document on the asthma COPD overlap syndrome (ACOS). While the concept of ACOS is not new, it remains highly debated since its introduction in 1961. ACOS is characterized by persistent airflow limitation with features that are shared with both asthma and COPD. For example, younger asthmatics may develop persistent expiratory airflow limitation from airway remodeling or smoking. Alternatively, patients with COPD may have concurrent features of atopy. Prevalence of ACOS is estimated at 20% in those with obstructive airway disease (Gibson. Thorax. 2015;70[7]:683). Data from the COPDGene cohort suggest that patients with ACOS have more frequent and severe respiratory exacerbations, less emphysema, and greater airway wall thickness (Hardin. Eur Respir J. 2014;44[2]:341).
The mechanisms behind ACOS remain poorly understood. Gelb and colleagues recently reported their observations of loss of lung elastic recoil and presence of centrilobular emphysema in a subset of nonsmokers with chronic asthma and persistent expiratory airflow limitation (Chest. 2015; 148[2]:313; J Allergy Clin Immunol. 2015;136[3]:553). In two COPD cohorts, Christenson and colleagues found that asthma-associated gene signatures were associated with increased disease severity, eosinophil counts, bronchodilator reversibility, and ICS response (Am J Respir Crit Care Med. 2015;191[7]:758). Data presented recently from Spiromics COPD and SARP severe asthma cohorts suggest that subjects with ACOS share a phenotype that falls between COPD and asthma. Allele frequency of candidate genes associated with smoking behavior and allergy in ACOS was intermediate between COPD and asthma (Li et al. Am J Respir Crit Care Med. 2016;A6237).
As with asthma and COPD, there exists significant heterogeneity within ACOS. Despite its high prevalence, evidence on how to consistently identify and best manage this group of patients is lacking. This is in part due to large clinical studies excluding patients with asthma COPD overlap. Additional research will help better understand the different phenotypes and endotypes of ACOS. Real life pragmatic studies evaluating differences in response to therapy are needed to make ACOS more relevant to the practicing clinician.
Dr. Sandhya Khurana, FCCP
Vice-Chair
Clinical Research Network
Airway clearance therapies
Many acute and chronic respiratory conditions such as pneumonia and bronchiectasis, are not only associated with an increase in the quantity and viscosity of respiratory secretions but also with impaired ciliary function and cough, with the latter being very common during mechanical ventilation and after strokes or thoracic surgical procedures. Retention of these secretions are associated with poor patient outcomes, and airway clearance therapies (ACT) are key to improving these outcomes and optimizing recovery after acute illnesses (Kim et. al. Chest. 2011;140[3]:626).
But despite this knowledge, the study of simple ACTs has been largely overlooked for decades. Many of the treatments we currently use, such as positive expiratory pressure devices (for example, the Acapella device), percussive vests, and intrapulmonary percussive ventilation have few studies to support their efficacy, with the ones that exist having very small sample sizes and show no superiority to simple manual techniques (Flume et al. Respir Care. 2009; 54[4]:522). As I walk by a patient’s room and see a respiratory therapist clapping on a patient’s back, I reflect on the fact that research on ACTs has essentially been at a standstill, and we continue to rely on therapies that are no better than the ones used in the 1800s. Our institution has established an Airway Clearance Research Group and has already conducted several bench studies evaluating some of these airway clearance therapies, with goals to develop novel techniques and to start clinical trials, with collaboration from this research steering committee. We hope that furthering the study of ACTs, and determining which therapies are most effective under different clinical settings will not only improve clinical outcomes in chronic conditions such as bronchiectasis but also improve outcomes after pneumonia, strokes, thoracic surgeries, and during mechanical ventilation, where airway clearance is key. Something so simple has the potential to impact a wide population of patients.
Dr. Bravein Amalakuhan
Fellow-in-Training Member
Critical Care
Early mobilization of the critically ill patient
Deconditioning is a well known complication of prolonged ICU stays. It is a factor in long-term mechanical ventilation and contributes to an increased length of stay and comorbidities. The severity of illness, presence of invasive catheters, and the need for sedation in order to provide adequate ventilation are risk factors for immobility. Critically ill patients who are not mobilized experience a decreased quality of life (Needham. JAMA. 2008;300:1685). The changes seen have been shown to persist up to a year after discharge, with a mean loss of 18% body weight, a 5% loss of muscle strength, and a decreased 6-minute walk distance (Herridge et al. N Engl J Med. 2003;348[8]:683; Herridge. Crit Care Med. 2009;37:S457).
There are many safety concerns when mobilizing critically ill patients, but studies have shown that early mobilization is safe with less than 1% of patients having adverse events such as falling, tube removal, and blood pressure instability (Bailey et al. Crit Care Med. 2007;35[1]:139). Barriers to mobilization include ICU staffing, deep sedation, ICU culture, and resources. Adherence to therapy is improved with the use of protocols. These should include automated awakening trials and spontaneous breathing trials that allow for decreases in sedation and, therefore, improvement in mobilization performance (Drolet et al. Phys Ther. 2013;93[2]:197).
Early mobilization improves mortality and decreases morbidity. Safe protocols to implement early mobilization have been developed around the country. A decrease in ICU and hospital length of stay, time supported by mechanical ventilation, and cost reduction with mobilization has been shown in multiple studies. A multidisciplinary team approach and a change in ICU culture will help to accomplish this important initiative.
Dr. Mangala Narasimhan, FCCP
Steering Committee Member
Home-Based Mechanical Ventilation and Neuromuscular Disease
Caregivers and training for kids receiving chronic home invasive ventilation
Despite years of experience in discharging pediatric patients receiving chronic home invasive ventilation, their mortality rate remains high, ranging from 21% to 27.5% with unscheduled readmission at 40% (Boroughs et al. Home Health Nurse. 2012;30:103) to 21% (Edwards et al. J Pediatr. 2010;157[6]:955; Kun et al. Pediatr Pulmonol. 2012:47[4]:409). While there were major improvements in technology and newer ventilators, and better community resources, the one key component of our HMV program remains the same – the caregivers. It is a frightening experience for every family to hear that their child needs ventilator support: every discharge is a daunting task and a life-changing experience.
It seems logical to postulate that we might have improved mortality/readmission outcomes if we have competent caregivers. Recent ATS guidelines recommend that “an awake, trained caregiver should be present at all times, and at least two family caregivers should be trained specifically for the child’s care” (Am J Respir Crit Care Med. 2016;193[8]:e16).The need to shore up on emergency care in the home is further supported when we review studies examining pediatric emergency home ventilation practices for both families and licensed home health nurses (Kun et al. Pediatr Pulmonol. 2010;45[3]:270; Kun. Pediatr Pulmonol. 2015;50[7]:691). Understanding and responding to ventilator alarms remains a major challenge for caregivers and home health nurses. Future directions where we can help our caregivers and families improve home emergency care training include simulation video and using the technology of hand-held devices.
Sheila Kun, RN, BSN
Steering Committee Member
Interstitial and Diffuse Lung Disease
New clinic consortium offers help to patients with rare lung diseases
On the heels of the success of the LAM Foundation’s research and clinic networks, several patient advocacy groups for rare lung diseases approached the LAM Foundation about incorporating the care of other rare lung diseases into the same clinic network.
In 2015, the Rare Lung Diseases Consortium was established. It represents a unique collaboration of these patient advocacy groups, the National Institutes of Health, and clinical investigators. It hopes to utilize the Rare Lung Disease Clinic Network as a resource in understanding the clinical course of several rare lung diseases and as a vehicle to initiate funded clinical trials in patients under the care of clinical investigators working at those various sites.
There are currently 29 geographically distributed Rare Lung Disease Clinic Network clinics in the United States, and another 18 clinics distributed internationally. The clinic directors have held two organizational meetings, including the most recent one in May 2016. The initial three research projects are each noninterventional longitudinal disease observational studies. They include “National Pulmonary Alveolar Proteinosis Registry,” “A Longitudinal Study of Hermansky-Pudlak Syndrome,” and “Multicenter International Durability and Safety of Sirolimus in LAM Trial (MIDAS).”
The first Rare Lung Diseases Consortium Conference is scheduled for September 22-25, 2016, in Cincinnati. It will be a combined educational and research conference, with attendance from clinicians, scientists, patient advocacy organizations, and patients with their families. More information, including a list of the 22 diseases initially designated for care and study in the network and a map of all of the clinic network sites, is available at https://www.rarediseasesnetwork.org/cms/rld/.
Dr. Daniel F. Dilling, FCCP
Steering Committee Member
Airways Disorders
The asthma COPD overlap syndrome: hype or reality?
In 2014, the Global Initiative for Asthma (GINA) and the Global Initiative for Chronic Obstructive Lung Disease (GOLD) published a joint document on the asthma COPD overlap syndrome (ACOS). While the concept of ACOS is not new, it remains highly debated since its introduction in 1961. ACOS is characterized by persistent airflow limitation with features that are shared with both asthma and COPD. For example, younger asthmatics may develop persistent expiratory airflow limitation from airway remodeling or smoking. Alternatively, patients with COPD may have concurrent features of atopy. Prevalence of ACOS is estimated at 20% in those with obstructive airway disease (Gibson. Thorax. 2015;70[7]:683). Data from the COPDGene cohort suggest that patients with ACOS have more frequent and severe respiratory exacerbations, less emphysema, and greater airway wall thickness (Hardin. Eur Respir J. 2014;44[2]:341).
The mechanisms behind ACOS remain poorly understood. Gelb and colleagues recently reported their observations of loss of lung elastic recoil and presence of centrilobular emphysema in a subset of nonsmokers with chronic asthma and persistent expiratory airflow limitation (Chest. 2015; 148[2]:313; J Allergy Clin Immunol. 2015;136[3]:553). In two COPD cohorts, Christenson and colleagues found that asthma-associated gene signatures were associated with increased disease severity, eosinophil counts, bronchodilator reversibility, and ICS response (Am J Respir Crit Care Med. 2015;191[7]:758). Data presented recently from Spiromics COPD and SARP severe asthma cohorts suggest that subjects with ACOS share a phenotype that falls between COPD and asthma. Allele frequency of candidate genes associated with smoking behavior and allergy in ACOS was intermediate between COPD and asthma (Li et al. Am J Respir Crit Care Med. 2016;A6237).
As with asthma and COPD, there exists significant heterogeneity within ACOS. Despite its high prevalence, evidence on how to consistently identify and best manage this group of patients is lacking. This is in part due to large clinical studies excluding patients with asthma COPD overlap. Additional research will help better understand the different phenotypes and endotypes of ACOS. Real life pragmatic studies evaluating differences in response to therapy are needed to make ACOS more relevant to the practicing clinician.
Dr. Sandhya Khurana, FCCP
Vice-Chair
Clinical Research Network
Airway clearance therapies
Many acute and chronic respiratory conditions such as pneumonia and bronchiectasis, are not only associated with an increase in the quantity and viscosity of respiratory secretions but also with impaired ciliary function and cough, with the latter being very common during mechanical ventilation and after strokes or thoracic surgical procedures. Retention of these secretions are associated with poor patient outcomes, and airway clearance therapies (ACT) are key to improving these outcomes and optimizing recovery after acute illnesses (Kim et. al. Chest. 2011;140[3]:626).
But despite this knowledge, the study of simple ACTs has been largely overlooked for decades. Many of the treatments we currently use, such as positive expiratory pressure devices (for example, the Acapella device), percussive vests, and intrapulmonary percussive ventilation have few studies to support their efficacy, with the ones that exist having very small sample sizes and show no superiority to simple manual techniques (Flume et al. Respir Care. 2009; 54[4]:522). As I walk by a patient’s room and see a respiratory therapist clapping on a patient’s back, I reflect on the fact that research on ACTs has essentially been at a standstill, and we continue to rely on therapies that are no better than the ones used in the 1800s. Our institution has established an Airway Clearance Research Group and has already conducted several bench studies evaluating some of these airway clearance therapies, with goals to develop novel techniques and to start clinical trials, with collaboration from this research steering committee. We hope that furthering the study of ACTs, and determining which therapies are most effective under different clinical settings will not only improve clinical outcomes in chronic conditions such as bronchiectasis but also improve outcomes after pneumonia, strokes, thoracic surgeries, and during mechanical ventilation, where airway clearance is key. Something so simple has the potential to impact a wide population of patients.
Dr. Bravein Amalakuhan
Fellow-in-Training Member
Critical Care
Early mobilization of the critically ill patient
Deconditioning is a well known complication of prolonged ICU stays. It is a factor in long-term mechanical ventilation and contributes to an increased length of stay and comorbidities. The severity of illness, presence of invasive catheters, and the need for sedation in order to provide adequate ventilation are risk factors for immobility. Critically ill patients who are not mobilized experience a decreased quality of life (Needham. JAMA. 2008;300:1685). The changes seen have been shown to persist up to a year after discharge, with a mean loss of 18% body weight, a 5% loss of muscle strength, and a decreased 6-minute walk distance (Herridge et al. N Engl J Med. 2003;348[8]:683; Herridge. Crit Care Med. 2009;37:S457).
There are many safety concerns when mobilizing critically ill patients, but studies have shown that early mobilization is safe with less than 1% of patients having adverse events such as falling, tube removal, and blood pressure instability (Bailey et al. Crit Care Med. 2007;35[1]:139). Barriers to mobilization include ICU staffing, deep sedation, ICU culture, and resources. Adherence to therapy is improved with the use of protocols. These should include automated awakening trials and spontaneous breathing trials that allow for decreases in sedation and, therefore, improvement in mobilization performance (Drolet et al. Phys Ther. 2013;93[2]:197).
Early mobilization improves mortality and decreases morbidity. Safe protocols to implement early mobilization have been developed around the country. A decrease in ICU and hospital length of stay, time supported by mechanical ventilation, and cost reduction with mobilization has been shown in multiple studies. A multidisciplinary team approach and a change in ICU culture will help to accomplish this important initiative.
Dr. Mangala Narasimhan, FCCP
Steering Committee Member
Home-Based Mechanical Ventilation and Neuromuscular Disease
Caregivers and training for kids receiving chronic home invasive ventilation
Despite years of experience in discharging pediatric patients receiving chronic home invasive ventilation, their mortality rate remains high, ranging from 21% to 27.5% with unscheduled readmission at 40% (Boroughs et al. Home Health Nurse. 2012;30:103) to 21% (Edwards et al. J Pediatr. 2010;157[6]:955; Kun et al. Pediatr Pulmonol. 2012:47[4]:409). While there were major improvements in technology and newer ventilators, and better community resources, the one key component of our HMV program remains the same – the caregivers. It is a frightening experience for every family to hear that their child needs ventilator support: every discharge is a daunting task and a life-changing experience.
It seems logical to postulate that we might have improved mortality/readmission outcomes if we have competent caregivers. Recent ATS guidelines recommend that “an awake, trained caregiver should be present at all times, and at least two family caregivers should be trained specifically for the child’s care” (Am J Respir Crit Care Med. 2016;193[8]:e16).The need to shore up on emergency care in the home is further supported when we review studies examining pediatric emergency home ventilation practices for both families and licensed home health nurses (Kun et al. Pediatr Pulmonol. 2010;45[3]:270; Kun. Pediatr Pulmonol. 2015;50[7]:691). Understanding and responding to ventilator alarms remains a major challenge for caregivers and home health nurses. Future directions where we can help our caregivers and families improve home emergency care training include simulation video and using the technology of hand-held devices.
Sheila Kun, RN, BSN
Steering Committee Member
Interstitial and Diffuse Lung Disease
New clinic consortium offers help to patients with rare lung diseases
On the heels of the success of the LAM Foundation’s research and clinic networks, several patient advocacy groups for rare lung diseases approached the LAM Foundation about incorporating the care of other rare lung diseases into the same clinic network.
In 2015, the Rare Lung Diseases Consortium was established. It represents a unique collaboration of these patient advocacy groups, the National Institutes of Health, and clinical investigators. It hopes to utilize the Rare Lung Disease Clinic Network as a resource in understanding the clinical course of several rare lung diseases and as a vehicle to initiate funded clinical trials in patients under the care of clinical investigators working at those various sites.
There are currently 29 geographically distributed Rare Lung Disease Clinic Network clinics in the United States, and another 18 clinics distributed internationally. The clinic directors have held two organizational meetings, including the most recent one in May 2016. The initial three research projects are each noninterventional longitudinal disease observational studies. They include “National Pulmonary Alveolar Proteinosis Registry,” “A Longitudinal Study of Hermansky-Pudlak Syndrome,” and “Multicenter International Durability and Safety of Sirolimus in LAM Trial (MIDAS).”
The first Rare Lung Diseases Consortium Conference is scheduled for September 22-25, 2016, in Cincinnati. It will be a combined educational and research conference, with attendance from clinicians, scientists, patient advocacy organizations, and patients with their families. More information, including a list of the 22 diseases initially designated for care and study in the network and a map of all of the clinic network sites, is available at https://www.rarediseasesnetwork.org/cms/rld/.
Dr. Daniel F. Dilling, FCCP
Steering Committee Member
Airways Disorders
The asthma COPD overlap syndrome: hype or reality?
In 2014, the Global Initiative for Asthma (GINA) and the Global Initiative for Chronic Obstructive Lung Disease (GOLD) published a joint document on the asthma COPD overlap syndrome (ACOS). While the concept of ACOS is not new, it remains highly debated since its introduction in 1961. ACOS is characterized by persistent airflow limitation with features that are shared with both asthma and COPD. For example, younger asthmatics may develop persistent expiratory airflow limitation from airway remodeling or smoking. Alternatively, patients with COPD may have concurrent features of atopy. Prevalence of ACOS is estimated at 20% in those with obstructive airway disease (Gibson. Thorax. 2015;70[7]:683). Data from the COPDGene cohort suggest that patients with ACOS have more frequent and severe respiratory exacerbations, less emphysema, and greater airway wall thickness (Hardin. Eur Respir J. 2014;44[2]:341).
The mechanisms behind ACOS remain poorly understood. Gelb and colleagues recently reported their observations of loss of lung elastic recoil and presence of centrilobular emphysema in a subset of nonsmokers with chronic asthma and persistent expiratory airflow limitation (Chest. 2015; 148[2]:313; J Allergy Clin Immunol. 2015;136[3]:553). In two COPD cohorts, Christenson and colleagues found that asthma-associated gene signatures were associated with increased disease severity, eosinophil counts, bronchodilator reversibility, and ICS response (Am J Respir Crit Care Med. 2015;191[7]:758). Data presented recently from Spiromics COPD and SARP severe asthma cohorts suggest that subjects with ACOS share a phenotype that falls between COPD and asthma. Allele frequency of candidate genes associated with smoking behavior and allergy in ACOS was intermediate between COPD and asthma (Li et al. Am J Respir Crit Care Med. 2016;A6237).
As with asthma and COPD, there exists significant heterogeneity within ACOS. Despite its high prevalence, evidence on how to consistently identify and best manage this group of patients is lacking. This is in part due to large clinical studies excluding patients with asthma COPD overlap. Additional research will help better understand the different phenotypes and endotypes of ACOS. Real life pragmatic studies evaluating differences in response to therapy are needed to make ACOS more relevant to the practicing clinician.
Dr. Sandhya Khurana, FCCP
Vice-Chair
Clinical Research Network
Airway clearance therapies
Many acute and chronic respiratory conditions such as pneumonia and bronchiectasis, are not only associated with an increase in the quantity and viscosity of respiratory secretions but also with impaired ciliary function and cough, with the latter being very common during mechanical ventilation and after strokes or thoracic surgical procedures. Retention of these secretions are associated with poor patient outcomes, and airway clearance therapies (ACT) are key to improving these outcomes and optimizing recovery after acute illnesses (Kim et. al. Chest. 2011;140[3]:626).
But despite this knowledge, the study of simple ACTs has been largely overlooked for decades. Many of the treatments we currently use, such as positive expiratory pressure devices (for example, the Acapella device), percussive vests, and intrapulmonary percussive ventilation have few studies to support their efficacy, with the ones that exist having very small sample sizes and show no superiority to simple manual techniques (Flume et al. Respir Care. 2009; 54[4]:522). As I walk by a patient’s room and see a respiratory therapist clapping on a patient’s back, I reflect on the fact that research on ACTs has essentially been at a standstill, and we continue to rely on therapies that are no better than the ones used in the 1800s. Our institution has established an Airway Clearance Research Group and has already conducted several bench studies evaluating some of these airway clearance therapies, with goals to develop novel techniques and to start clinical trials, with collaboration from this research steering committee. We hope that furthering the study of ACTs, and determining which therapies are most effective under different clinical settings will not only improve clinical outcomes in chronic conditions such as bronchiectasis but also improve outcomes after pneumonia, strokes, thoracic surgeries, and during mechanical ventilation, where airway clearance is key. Something so simple has the potential to impact a wide population of patients.
Dr. Bravein Amalakuhan
Fellow-in-Training Member
Critical Care
Early mobilization of the critically ill patient
Deconditioning is a well known complication of prolonged ICU stays. It is a factor in long-term mechanical ventilation and contributes to an increased length of stay and comorbidities. The severity of illness, presence of invasive catheters, and the need for sedation in order to provide adequate ventilation are risk factors for immobility. Critically ill patients who are not mobilized experience a decreased quality of life (Needham. JAMA. 2008;300:1685). The changes seen have been shown to persist up to a year after discharge, with a mean loss of 18% body weight, a 5% loss of muscle strength, and a decreased 6-minute walk distance (Herridge et al. N Engl J Med. 2003;348[8]:683; Herridge. Crit Care Med. 2009;37:S457).
There are many safety concerns when mobilizing critically ill patients, but studies have shown that early mobilization is safe with less than 1% of patients having adverse events such as falling, tube removal, and blood pressure instability (Bailey et al. Crit Care Med. 2007;35[1]:139). Barriers to mobilization include ICU staffing, deep sedation, ICU culture, and resources. Adherence to therapy is improved with the use of protocols. These should include automated awakening trials and spontaneous breathing trials that allow for decreases in sedation and, therefore, improvement in mobilization performance (Drolet et al. Phys Ther. 2013;93[2]:197).
Early mobilization improves mortality and decreases morbidity. Safe protocols to implement early mobilization have been developed around the country. A decrease in ICU and hospital length of stay, time supported by mechanical ventilation, and cost reduction with mobilization has been shown in multiple studies. A multidisciplinary team approach and a change in ICU culture will help to accomplish this important initiative.
Dr. Mangala Narasimhan, FCCP
Steering Committee Member
Home-Based Mechanical Ventilation and Neuromuscular Disease
Caregivers and training for kids receiving chronic home invasive ventilation
Despite years of experience in discharging pediatric patients receiving chronic home invasive ventilation, their mortality rate remains high, ranging from 21% to 27.5% with unscheduled readmission at 40% (Boroughs et al. Home Health Nurse. 2012;30:103) to 21% (Edwards et al. J Pediatr. 2010;157[6]:955; Kun et al. Pediatr Pulmonol. 2012:47[4]:409). While there were major improvements in technology and newer ventilators, and better community resources, the one key component of our HMV program remains the same – the caregivers. It is a frightening experience for every family to hear that their child needs ventilator support: every discharge is a daunting task and a life-changing experience.
It seems logical to postulate that we might have improved mortality/readmission outcomes if we have competent caregivers. Recent ATS guidelines recommend that “an awake, trained caregiver should be present at all times, and at least two family caregivers should be trained specifically for the child’s care” (Am J Respir Crit Care Med. 2016;193[8]:e16).The need to shore up on emergency care in the home is further supported when we review studies examining pediatric emergency home ventilation practices for both families and licensed home health nurses (Kun et al. Pediatr Pulmonol. 2010;45[3]:270; Kun. Pediatr Pulmonol. 2015;50[7]:691). Understanding and responding to ventilator alarms remains a major challenge for caregivers and home health nurses. Future directions where we can help our caregivers and families improve home emergency care training include simulation video and using the technology of hand-held devices.
Sheila Kun, RN, BSN
Steering Committee Member
Interstitial and Diffuse Lung Disease
New clinic consortium offers help to patients with rare lung diseases
On the heels of the success of the LAM Foundation’s research and clinic networks, several patient advocacy groups for rare lung diseases approached the LAM Foundation about incorporating the care of other rare lung diseases into the same clinic network.
In 2015, the Rare Lung Diseases Consortium was established. It represents a unique collaboration of these patient advocacy groups, the National Institutes of Health, and clinical investigators. It hopes to utilize the Rare Lung Disease Clinic Network as a resource in understanding the clinical course of several rare lung diseases and as a vehicle to initiate funded clinical trials in patients under the care of clinical investigators working at those various sites.
There are currently 29 geographically distributed Rare Lung Disease Clinic Network clinics in the United States, and another 18 clinics distributed internationally. The clinic directors have held two organizational meetings, including the most recent one in May 2016. The initial three research projects are each noninterventional longitudinal disease observational studies. They include “National Pulmonary Alveolar Proteinosis Registry,” “A Longitudinal Study of Hermansky-Pudlak Syndrome,” and “Multicenter International Durability and Safety of Sirolimus in LAM Trial (MIDAS).”
The first Rare Lung Diseases Consortium Conference is scheduled for September 22-25, 2016, in Cincinnati. It will be a combined educational and research conference, with attendance from clinicians, scientists, patient advocacy organizations, and patients with their families. More information, including a list of the 22 diseases initially designated for care and study in the network and a map of all of the clinic network sites, is available at https://www.rarediseasesnetwork.org/cms/rld/.
Dr. Daniel F. Dilling, FCCP
Steering Committee Member
SLEEP STRATEGIES: The flexibility of STOP-Bang Questionnaire to screen for OSA: A practical approach
Obstructive sleep apnea (OSA) is a potentially serious sleep disorder in which breathing repeatedly stops and starts during sleep. OSA occurs when the throat muscles intermittently relax and block the airway during sleep. The condition is usually associated with several other chronic medical conditions leading to poor quality of life.
It is estimated that at least 25 million adults are affected by OSA in the United States. Further, the obesity epidemic has increased the prevalence of OSA in the last 2 decades. The prevalence of OSA can be higher in patients undergoing surgery. For example, 70% of the patients undergoing bariatric surgery have OSA, whereas 48% of patients undergoing cardiac surgery have moderate-severe OSA. Alarmingly, in 80% of patients with moderate-severe OSA, the disorder remains undiagnosed and untreated, threatening public health and safety.
Patients with OSA can experience multiple complications when receiving sedatives and opioids during anesthesia (Opperer. Anesthesia and Analgesia. 122[5]:1321). These drugs may diminish the protective arousal reflex triggered by bouts of hypoxia, thereby increasing the risk of prolonged periods of apnea and possibly respiratory arrest. Sedatives and narcotics can decrease pharyngeal muscle tone, which can worsen the existing OSA and increase upper airway resistance. Undiagnosed and untreated OSA may be a contributing factor in many of these complications. Effective screening/diagnosis and treatment of OSA are considered to be important steps to reduce health-care spending, improve chronic disease management, and reduce complications.
The STOP-Bang Questionnaire
The gold standard for the diagnosis of OSA is overnight polysomnography. However, it is time consuming, labor intensive, and costly. The STOP-Bang Questionnaire is considered to be the most validated screening tool for OSA for various populations (Nagappa et al. PLoS One. 2015;10[12]:e0143697).
The STOP-Bang Questionnaire includes four questions used in the STOP Questionnaire plus four additional demographic queries, a total of eight dichotomous (yes/no) questions related to the clinical features of sleep apnea (Snoring, Tiredness, Observed apnea, high blood Pressure, BMI, age, neck circumference, and male gender). For each question, answering “yes” scores 1, a “no” response scores 0, and the total score ranges from 0 to 8 (see www.stopbang.ca). The Questionnaire can be completed quickly and easily (usually within 1-2 minutes), and the overall response rates are typically high (90%-100%). Because of its ease of use, efficiency, and high sensitivity, the STOP-Bang Questionnaire has been widely adopted in various populations, such as sleep clinics and the surgical and general population.

The STOP-Bang Questionnaire has demonstrated a high sensitivity using a cutoff score of greater than or equal to 3: 84% in detecting any sleep apnea (apnea-hypopnea index greater than 5 events/h), 93% in detecting moderate to severe sleep apnea (AHI greater than 15 events/h), and almost 100% in detecting severe sleep apnea (AHI greater than 30 events/h). The corresponding specificities were 56.4%, 43%, and 37% (Chung et al. Anesthesiology. 2008;108[5]:812). If patients score 0-2 on the STOP-Bang Questionnaire, they are considered to be at low risk of OSA, and the possibility of moderate to severe sleep apnea can be ruled out.
The modest specificity of the STOP-Bang Questionnaire may yield moderately high false-positive cases. This may lead to unwanted sleep study referrals and increased health care expenditure. There are several ways by which the specificity can be improved, thereby decreasing false-positive rates.
Setting a threshold for the STOP-Bang scores in different population
The main advantage of the STOP-Bang scores is its flexibility to use different scores for different populations. For example, in a bariatric population, a STOP-Bang score of greater than or equal to 4 can be used. On the other hand, in an ENT population, where we would like to identify a majority of patients with moderate-severe OSA, a STOP-Bang score of greater than or equal to 5 can be used. In the sleep clinic population, as the STOP-Bang score cut-off increased from 3 to 8, the specificity increased from 52% to 100%, and the PPV increased continuously from 93% to 100% for any OSA (AHI greater than or equal to 5). A similar pattern was seen in the surgical population, as the STOP-Bang score cutoff increased from 3 to greater than or equal to 7, the specificity increased from 40% to 98%, and the PPV increased from 75% to 82% for any OSA (AHI greater than or equal to 5) (Nagappa et al. PLoS One. 2015;10[12]:e0143697).
Regional practices should decide the appropriate threshold of screening tests, after considering the implications for missed diagnoses and cost of care. There is a trade-off between sensitivity and specificity. At lower thresholds, there is improved sensitivity with potentially increased resource utilization, whereas increasing the threshold will result in loss of sensitivity and increased false-negative rates but improved resource utilization. A higher threshold should be adopted in the population with a lower prevalence of OSA.
STOP-Bang score and probability of OSA
In both sleep clinic patients (Fig 1; Panel A) and surgical patients (Fig 1; Panel B), the probability of moderate-to-severe OSA or severe OSA increased a s the STOP-Bang score increased from 3 to 7/8. With higher scores, there is a more profound increase in the probability of severe OSA, compared with moderate OSA (Chung et al. Br J Anaesth. 2012;108[5]:768).
Alternative models for scoring the STOP-Bang Questionnaire
The individual items on the Questionnaire do not share an equal predictive weight for OSA. In the “Bang” components, body mass index greater than 35 kg/m2, neck circumference greater than 40 cm, and male gender are more predictive than age greater than 50 years. The predictive performance of the specific combinations of items has been explored. Compared with the specificity of 31% for detecting moderate to severe OSA, specific combinations significantly improve the specificity to detect any OSA (AHI greater than 5), moderate to severe OSA (AHI greater than 15), and severe OSA (AHI greater than 30) at the expense of sensitivity. The specificity to detect moderate to severe OSA increases to 85% for a STOP score greater than or equal to 2 + BMI greater than 35 kg/m2; to 79% for a STOP score greater than or equal to 2 + neck circumference > greater than 40 cm (16 in); and to 77% for a STOP score greater than or equal to 2 + male, respectively. These combinations can assist in accurately identifying more patients with moderate to severe OSA (Chung et al. J Clin Sleep Med. 2014;10[9]:951).
The STOP-Bang Questionnaire and serum bicarbonate
Serum bicarbonate (HCO3–) is significantly correlated to AHI, and the addition of serum HCO3– greater than or equal to 28 mmol/L to a STOP-Bang score greater than or equal to 3 improves the specificity to predict moderate-severe OSA but decreases its sensitivity (Chung et al. Chest. 2013;143[5]:1284). For a STOP-Bang score of greater than or equal to 3 + HCO3– greater than or equal to 28 mmol/L), the specificity for detecting moderate to severe OSA increases from 30% to 82%, and from 28% to 80% for detecting severe OSA, respectively.
A two-step strategy for using STOP-Bang Questionnaire
A two-step algorithm using the STOP-Bang Questionnaire identifies patients effectively with a high probability of moderate to severe sleep apnea (Fig 2) (Chung et al. Chest. 2016;149[3]:631). The first step is to check the STOP-Bang score. If a patient scores 0-2 on the STOP-Bang Questionnaire, he or she is unlikely to have moderate to severe OSA. Conversely, a patient with a STOP-Bang score of 5-8 has a high probability of moderate to severe OSA.

The second step is for the patients with STOP-Bang scores of 3 or 4. These patients can be further classified as having a higher risk for moderate to severe OSA if one of the following conditions is met: (1) a STOP score greater than or equal to 2 + BMI greater than 35 kg/m2; (2) a STOP score greater than or equal to 2 + male gender; (3) a STOP score greater than or equal to 2 + neck circumference greater than 40 cm (16 in); or (4) a STOP-Bang score greater than or equal to 3 + serum HCO3– greater than or equal to 28 mmol/L.
The STOP-Bang Questionnaire and perioperative complications
The STOP-Bang Questionnaire not only identifies the high-risk patients with OSA but also may have a strong association toward predicting perioperative complications (Vasu et al. Arch Otolaryngol Head Neck Surg. 2010;136[10]:1020). The important step of screening patients with OSA using the STOP-Bang Questionnaire may create an awareness among the perioperative team resulting in decreased complications (Veenstra et al. Crit Care Nurs Clin N Am. 2014;26[4]:499).
The Joint Commission’s Division of Healthcare Improvement has raised strong concerns regarding the lack of training for health-care professionals to recognize OSA. A recent guideline published by the Society of Anesthesia and Sleep Medicine recommends using a screening tool to identify high-risk patients with OSA (Chung et al. Anesthesia Analgesia. 2016;June 1: Epub ahead of print).
There is preliminary evidence that patients with diagnosed OSA and a CPAP prescription had significantly reduced postoperative cardiovascular complications (cardiac arrest and shock) by more than 50% vs patients with undiagnosed OSA (Mutter et al. Anesthesiology. 2014;121[4]:707).
Conclusion
The STOP-Bang Questionnaire is a simple, practical, and flexible screening tool to identify the high-risk OSA patients. More information is available at www.stopbang.ca.
Dr. Chung is with the department of anesthesia, Toronto Western Hospital – University Health Network, University of Toronto, ON, Canada; Dr. Nagappa is with the department of anesthesia & perioperative medicine, London Health Sciences Centre and St. Joseph Health Care London, Western University, London, ON, Canada.
Obstructive sleep apnea (OSA) is a potentially serious sleep disorder in which breathing repeatedly stops and starts during sleep. OSA occurs when the throat muscles intermittently relax and block the airway during sleep. The condition is usually associated with several other chronic medical conditions leading to poor quality of life.
It is estimated that at least 25 million adults are affected by OSA in the United States. Further, the obesity epidemic has increased the prevalence of OSA in the last 2 decades. The prevalence of OSA can be higher in patients undergoing surgery. For example, 70% of the patients undergoing bariatric surgery have OSA, whereas 48% of patients undergoing cardiac surgery have moderate-severe OSA. Alarmingly, in 80% of patients with moderate-severe OSA, the disorder remains undiagnosed and untreated, threatening public health and safety.
Patients with OSA can experience multiple complications when receiving sedatives and opioids during anesthesia (Opperer. Anesthesia and Analgesia. 122[5]:1321). These drugs may diminish the protective arousal reflex triggered by bouts of hypoxia, thereby increasing the risk of prolonged periods of apnea and possibly respiratory arrest. Sedatives and narcotics can decrease pharyngeal muscle tone, which can worsen the existing OSA and increase upper airway resistance. Undiagnosed and untreated OSA may be a contributing factor in many of these complications. Effective screening/diagnosis and treatment of OSA are considered to be important steps to reduce health-care spending, improve chronic disease management, and reduce complications.
The STOP-Bang Questionnaire
The gold standard for the diagnosis of OSA is overnight polysomnography. However, it is time consuming, labor intensive, and costly. The STOP-Bang Questionnaire is considered to be the most validated screening tool for OSA for various populations (Nagappa et al. PLoS One. 2015;10[12]:e0143697).
The STOP-Bang Questionnaire includes four questions used in the STOP Questionnaire plus four additional demographic queries, a total of eight dichotomous (yes/no) questions related to the clinical features of sleep apnea (Snoring, Tiredness, Observed apnea, high blood Pressure, BMI, age, neck circumference, and male gender). For each question, answering “yes” scores 1, a “no” response scores 0, and the total score ranges from 0 to 8 (see www.stopbang.ca). The Questionnaire can be completed quickly and easily (usually within 1-2 minutes), and the overall response rates are typically high (90%-100%). Because of its ease of use, efficiency, and high sensitivity, the STOP-Bang Questionnaire has been widely adopted in various populations, such as sleep clinics and the surgical and general population.

The STOP-Bang Questionnaire has demonstrated a high sensitivity using a cutoff score of greater than or equal to 3: 84% in detecting any sleep apnea (apnea-hypopnea index greater than 5 events/h), 93% in detecting moderate to severe sleep apnea (AHI greater than 15 events/h), and almost 100% in detecting severe sleep apnea (AHI greater than 30 events/h). The corresponding specificities were 56.4%, 43%, and 37% (Chung et al. Anesthesiology. 2008;108[5]:812). If patients score 0-2 on the STOP-Bang Questionnaire, they are considered to be at low risk of OSA, and the possibility of moderate to severe sleep apnea can be ruled out.
The modest specificity of the STOP-Bang Questionnaire may yield moderately high false-positive cases. This may lead to unwanted sleep study referrals and increased health care expenditure. There are several ways by which the specificity can be improved, thereby decreasing false-positive rates.
Setting a threshold for the STOP-Bang scores in different population
The main advantage of the STOP-Bang scores is its flexibility to use different scores for different populations. For example, in a bariatric population, a STOP-Bang score of greater than or equal to 4 can be used. On the other hand, in an ENT population, where we would like to identify a majority of patients with moderate-severe OSA, a STOP-Bang score of greater than or equal to 5 can be used. In the sleep clinic population, as the STOP-Bang score cut-off increased from 3 to 8, the specificity increased from 52% to 100%, and the PPV increased continuously from 93% to 100% for any OSA (AHI greater than or equal to 5). A similar pattern was seen in the surgical population, as the STOP-Bang score cutoff increased from 3 to greater than or equal to 7, the specificity increased from 40% to 98%, and the PPV increased from 75% to 82% for any OSA (AHI greater than or equal to 5) (Nagappa et al. PLoS One. 2015;10[12]:e0143697).
Regional practices should decide the appropriate threshold of screening tests, after considering the implications for missed diagnoses and cost of care. There is a trade-off between sensitivity and specificity. At lower thresholds, there is improved sensitivity with potentially increased resource utilization, whereas increasing the threshold will result in loss of sensitivity and increased false-negative rates but improved resource utilization. A higher threshold should be adopted in the population with a lower prevalence of OSA.
STOP-Bang score and probability of OSA
In both sleep clinic patients (Fig 1; Panel A) and surgical patients (Fig 1; Panel B), the probability of moderate-to-severe OSA or severe OSA increased a s the STOP-Bang score increased from 3 to 7/8. With higher scores, there is a more profound increase in the probability of severe OSA, compared with moderate OSA (Chung et al. Br J Anaesth. 2012;108[5]:768).
Alternative models for scoring the STOP-Bang Questionnaire
The individual items on the Questionnaire do not share an equal predictive weight for OSA. In the “Bang” components, body mass index greater than 35 kg/m2, neck circumference greater than 40 cm, and male gender are more predictive than age greater than 50 years. The predictive performance of the specific combinations of items has been explored. Compared with the specificity of 31% for detecting moderate to severe OSA, specific combinations significantly improve the specificity to detect any OSA (AHI greater than 5), moderate to severe OSA (AHI greater than 15), and severe OSA (AHI greater than 30) at the expense of sensitivity. The specificity to detect moderate to severe OSA increases to 85% for a STOP score greater than or equal to 2 + BMI greater than 35 kg/m2; to 79% for a STOP score greater than or equal to 2 + neck circumference > greater than 40 cm (16 in); and to 77% for a STOP score greater than or equal to 2 + male, respectively. These combinations can assist in accurately identifying more patients with moderate to severe OSA (Chung et al. J Clin Sleep Med. 2014;10[9]:951).
The STOP-Bang Questionnaire and serum bicarbonate
Serum bicarbonate (HCO3–) is significantly correlated to AHI, and the addition of serum HCO3– greater than or equal to 28 mmol/L to a STOP-Bang score greater than or equal to 3 improves the specificity to predict moderate-severe OSA but decreases its sensitivity (Chung et al. Chest. 2013;143[5]:1284). For a STOP-Bang score of greater than or equal to 3 + HCO3– greater than or equal to 28 mmol/L), the specificity for detecting moderate to severe OSA increases from 30% to 82%, and from 28% to 80% for detecting severe OSA, respectively.
A two-step strategy for using STOP-Bang Questionnaire
A two-step algorithm using the STOP-Bang Questionnaire identifies patients effectively with a high probability of moderate to severe sleep apnea (Fig 2) (Chung et al. Chest. 2016;149[3]:631). The first step is to check the STOP-Bang score. If a patient scores 0-2 on the STOP-Bang Questionnaire, he or she is unlikely to have moderate to severe OSA. Conversely, a patient with a STOP-Bang score of 5-8 has a high probability of moderate to severe OSA.

The second step is for the patients with STOP-Bang scores of 3 or 4. These patients can be further classified as having a higher risk for moderate to severe OSA if one of the following conditions is met: (1) a STOP score greater than or equal to 2 + BMI greater than 35 kg/m2; (2) a STOP score greater than or equal to 2 + male gender; (3) a STOP score greater than or equal to 2 + neck circumference greater than 40 cm (16 in); or (4) a STOP-Bang score greater than or equal to 3 + serum HCO3– greater than or equal to 28 mmol/L.
The STOP-Bang Questionnaire and perioperative complications
The STOP-Bang Questionnaire not only identifies the high-risk patients with OSA but also may have a strong association toward predicting perioperative complications (Vasu et al. Arch Otolaryngol Head Neck Surg. 2010;136[10]:1020). The important step of screening patients with OSA using the STOP-Bang Questionnaire may create an awareness among the perioperative team resulting in decreased complications (Veenstra et al. Crit Care Nurs Clin N Am. 2014;26[4]:499).
The Joint Commission’s Division of Healthcare Improvement has raised strong concerns regarding the lack of training for health-care professionals to recognize OSA. A recent guideline published by the Society of Anesthesia and Sleep Medicine recommends using a screening tool to identify high-risk patients with OSA (Chung et al. Anesthesia Analgesia. 2016;June 1: Epub ahead of print).
There is preliminary evidence that patients with diagnosed OSA and a CPAP prescription had significantly reduced postoperative cardiovascular complications (cardiac arrest and shock) by more than 50% vs patients with undiagnosed OSA (Mutter et al. Anesthesiology. 2014;121[4]:707).
Conclusion
The STOP-Bang Questionnaire is a simple, practical, and flexible screening tool to identify the high-risk OSA patients. More information is available at www.stopbang.ca.
Dr. Chung is with the department of anesthesia, Toronto Western Hospital – University Health Network, University of Toronto, ON, Canada; Dr. Nagappa is with the department of anesthesia & perioperative medicine, London Health Sciences Centre and St. Joseph Health Care London, Western University, London, ON, Canada.
Obstructive sleep apnea (OSA) is a potentially serious sleep disorder in which breathing repeatedly stops and starts during sleep. OSA occurs when the throat muscles intermittently relax and block the airway during sleep. The condition is usually associated with several other chronic medical conditions leading to poor quality of life.
It is estimated that at least 25 million adults are affected by OSA in the United States. Further, the obesity epidemic has increased the prevalence of OSA in the last 2 decades. The prevalence of OSA can be higher in patients undergoing surgery. For example, 70% of the patients undergoing bariatric surgery have OSA, whereas 48% of patients undergoing cardiac surgery have moderate-severe OSA. Alarmingly, in 80% of patients with moderate-severe OSA, the disorder remains undiagnosed and untreated, threatening public health and safety.
Patients with OSA can experience multiple complications when receiving sedatives and opioids during anesthesia (Opperer. Anesthesia and Analgesia. 122[5]:1321). These drugs may diminish the protective arousal reflex triggered by bouts of hypoxia, thereby increasing the risk of prolonged periods of apnea and possibly respiratory arrest. Sedatives and narcotics can decrease pharyngeal muscle tone, which can worsen the existing OSA and increase upper airway resistance. Undiagnosed and untreated OSA may be a contributing factor in many of these complications. Effective screening/diagnosis and treatment of OSA are considered to be important steps to reduce health-care spending, improve chronic disease management, and reduce complications.
The STOP-Bang Questionnaire
The gold standard for the diagnosis of OSA is overnight polysomnography. However, it is time consuming, labor intensive, and costly. The STOP-Bang Questionnaire is considered to be the most validated screening tool for OSA for various populations (Nagappa et al. PLoS One. 2015;10[12]:e0143697).
The STOP-Bang Questionnaire includes four questions used in the STOP Questionnaire plus four additional demographic queries, a total of eight dichotomous (yes/no) questions related to the clinical features of sleep apnea (Snoring, Tiredness, Observed apnea, high blood Pressure, BMI, age, neck circumference, and male gender). For each question, answering “yes” scores 1, a “no” response scores 0, and the total score ranges from 0 to 8 (see www.stopbang.ca). The Questionnaire can be completed quickly and easily (usually within 1-2 minutes), and the overall response rates are typically high (90%-100%). Because of its ease of use, efficiency, and high sensitivity, the STOP-Bang Questionnaire has been widely adopted in various populations, such as sleep clinics and the surgical and general population.

The STOP-Bang Questionnaire has demonstrated a high sensitivity using a cutoff score of greater than or equal to 3: 84% in detecting any sleep apnea (apnea-hypopnea index greater than 5 events/h), 93% in detecting moderate to severe sleep apnea (AHI greater than 15 events/h), and almost 100% in detecting severe sleep apnea (AHI greater than 30 events/h). The corresponding specificities were 56.4%, 43%, and 37% (Chung et al. Anesthesiology. 2008;108[5]:812). If patients score 0-2 on the STOP-Bang Questionnaire, they are considered to be at low risk of OSA, and the possibility of moderate to severe sleep apnea can be ruled out.
The modest specificity of the STOP-Bang Questionnaire may yield moderately high false-positive cases. This may lead to unwanted sleep study referrals and increased health care expenditure. There are several ways by which the specificity can be improved, thereby decreasing false-positive rates.
Setting a threshold for the STOP-Bang scores in different population
The main advantage of the STOP-Bang scores is its flexibility to use different scores for different populations. For example, in a bariatric population, a STOP-Bang score of greater than or equal to 4 can be used. On the other hand, in an ENT population, where we would like to identify a majority of patients with moderate-severe OSA, a STOP-Bang score of greater than or equal to 5 can be used. In the sleep clinic population, as the STOP-Bang score cut-off increased from 3 to 8, the specificity increased from 52% to 100%, and the PPV increased continuously from 93% to 100% for any OSA (AHI greater than or equal to 5). A similar pattern was seen in the surgical population, as the STOP-Bang score cutoff increased from 3 to greater than or equal to 7, the specificity increased from 40% to 98%, and the PPV increased from 75% to 82% for any OSA (AHI greater than or equal to 5) (Nagappa et al. PLoS One. 2015;10[12]:e0143697).
Regional practices should decide the appropriate threshold of screening tests, after considering the implications for missed diagnoses and cost of care. There is a trade-off between sensitivity and specificity. At lower thresholds, there is improved sensitivity with potentially increased resource utilization, whereas increasing the threshold will result in loss of sensitivity and increased false-negative rates but improved resource utilization. A higher threshold should be adopted in the population with a lower prevalence of OSA.
STOP-Bang score and probability of OSA
In both sleep clinic patients (Fig 1; Panel A) and surgical patients (Fig 1; Panel B), the probability of moderate-to-severe OSA or severe OSA increased a s the STOP-Bang score increased from 3 to 7/8. With higher scores, there is a more profound increase in the probability of severe OSA, compared with moderate OSA (Chung et al. Br J Anaesth. 2012;108[5]:768).
Alternative models for scoring the STOP-Bang Questionnaire
The individual items on the Questionnaire do not share an equal predictive weight for OSA. In the “Bang” components, body mass index greater than 35 kg/m2, neck circumference greater than 40 cm, and male gender are more predictive than age greater than 50 years. The predictive performance of the specific combinations of items has been explored. Compared with the specificity of 31% for detecting moderate to severe OSA, specific combinations significantly improve the specificity to detect any OSA (AHI greater than 5), moderate to severe OSA (AHI greater than 15), and severe OSA (AHI greater than 30) at the expense of sensitivity. The specificity to detect moderate to severe OSA increases to 85% for a STOP score greater than or equal to 2 + BMI greater than 35 kg/m2; to 79% for a STOP score greater than or equal to 2 + neck circumference > greater than 40 cm (16 in); and to 77% for a STOP score greater than or equal to 2 + male, respectively. These combinations can assist in accurately identifying more patients with moderate to severe OSA (Chung et al. J Clin Sleep Med. 2014;10[9]:951).
The STOP-Bang Questionnaire and serum bicarbonate
Serum bicarbonate (HCO3–) is significantly correlated to AHI, and the addition of serum HCO3– greater than or equal to 28 mmol/L to a STOP-Bang score greater than or equal to 3 improves the specificity to predict moderate-severe OSA but decreases its sensitivity (Chung et al. Chest. 2013;143[5]:1284). For a STOP-Bang score of greater than or equal to 3 + HCO3– greater than or equal to 28 mmol/L), the specificity for detecting moderate to severe OSA increases from 30% to 82%, and from 28% to 80% for detecting severe OSA, respectively.
A two-step strategy for using STOP-Bang Questionnaire
A two-step algorithm using the STOP-Bang Questionnaire identifies patients effectively with a high probability of moderate to severe sleep apnea (Fig 2) (Chung et al. Chest. 2016;149[3]:631). The first step is to check the STOP-Bang score. If a patient scores 0-2 on the STOP-Bang Questionnaire, he or she is unlikely to have moderate to severe OSA. Conversely, a patient with a STOP-Bang score of 5-8 has a high probability of moderate to severe OSA.

The second step is for the patients with STOP-Bang scores of 3 or 4. These patients can be further classified as having a higher risk for moderate to severe OSA if one of the following conditions is met: (1) a STOP score greater than or equal to 2 + BMI greater than 35 kg/m2; (2) a STOP score greater than or equal to 2 + male gender; (3) a STOP score greater than or equal to 2 + neck circumference greater than 40 cm (16 in); or (4) a STOP-Bang score greater than or equal to 3 + serum HCO3– greater than or equal to 28 mmol/L.
The STOP-Bang Questionnaire and perioperative complications
The STOP-Bang Questionnaire not only identifies the high-risk patients with OSA but also may have a strong association toward predicting perioperative complications (Vasu et al. Arch Otolaryngol Head Neck Surg. 2010;136[10]:1020). The important step of screening patients with OSA using the STOP-Bang Questionnaire may create an awareness among the perioperative team resulting in decreased complications (Veenstra et al. Crit Care Nurs Clin N Am. 2014;26[4]:499).
The Joint Commission’s Division of Healthcare Improvement has raised strong concerns regarding the lack of training for health-care professionals to recognize OSA. A recent guideline published by the Society of Anesthesia and Sleep Medicine recommends using a screening tool to identify high-risk patients with OSA (Chung et al. Anesthesia Analgesia. 2016;June 1: Epub ahead of print).
There is preliminary evidence that patients with diagnosed OSA and a CPAP prescription had significantly reduced postoperative cardiovascular complications (cardiac arrest and shock) by more than 50% vs patients with undiagnosed OSA (Mutter et al. Anesthesiology. 2014;121[4]:707).
Conclusion
The STOP-Bang Questionnaire is a simple, practical, and flexible screening tool to identify the high-risk OSA patients. More information is available at www.stopbang.ca.
Dr. Chung is with the department of anesthesia, Toronto Western Hospital – University Health Network, University of Toronto, ON, Canada; Dr. Nagappa is with the department of anesthesia & perioperative medicine, London Health Sciences Centre and St. Joseph Health Care London, Western University, London, ON, Canada.
Announcements of the deaths of CHEST members
CHEST has been informed of the following members’ deaths and extends sincere condolences.
Vincent C. Manganiello, MD, PhD, died January 2016.
Lawrence H. Cohn, MD, FCCP – Past President, died January 9, 2016.
Suzanne K. Wedel, MD, FCCP, died March 2016.
CHEST has been informed of the following members’ deaths and extends sincere condolences.
Vincent C. Manganiello, MD, PhD, died January 2016.
Lawrence H. Cohn, MD, FCCP – Past President, died January 9, 2016.
Suzanne K. Wedel, MD, FCCP, died March 2016.
CHEST has been informed of the following members’ deaths and extends sincere condolences.
Vincent C. Manganiello, MD, PhD, died January 2016.
Lawrence H. Cohn, MD, FCCP – Past President, died January 9, 2016.
Suzanne K. Wedel, MD, FCCP, died March 2016.