User login
Digital Tools in the Management of IBS/ Functional GI Disorders
- Hasan SS et al. Neurogastroenterol Motil. 2023;35(4):e14554. doi:10.1111/nmo.14554
- Peters SL et al. Neurogastroenterol Motil. 2023;35(4):e14533. doi:10.1111/nmo.14533
- Zhou C et al. Neurogastroenterol Motil. 2019;31(2):e13461. doi:10.1111/nmo.13461
- Staudacher HM et al. Nat Rev Gastroenterol Hepatol. 2023;1-15. doi:10.1038/s41575-023-00794-z
- Qin HY et al. World J Gastroenterol. 2014;20(39):14126-14131. doi:10.3748/wjg.v20.i39.14126
- Varjú P et al. PLoS One. 2017;12(8):e0182942. doi:10.1371/journal.pone.0182942
- Saleh ZM et al. Am J Gastroenterol. 2023. doi:10.14309/ajg.0000000000002220
- Yu C et al. Clin Transl Gastroenterol. 2022;13(9):e00515. doi:10.14309/ctg.0000000000000515
- Jagannath B et al. Inflamm Bowel Dis. 2020;26(10):1533-1542. doi:10.1093/ibd/izaa191
- Zhang H et al. J Nutr. 2023;153(4):924-939. doi:10.1016/j.tjnut.2023.01.026
- Karakan T et al. Gut Microbes. 2022;14(1):2138672. doi:10.1080/19490976.2022.2138672
- Kordi M et al. Inform Med Unlocked. 2022;29:100891. doi:10.1016/j.imu.2022.100891
- Gubatan J et al. World J Gastroenterol. 2021;27(17):1920-1935. doi:10.3748/wjg.v27.i17.1920
- Boucher EM et al. Expert Rev Med Devices. 2021;18(suppl 1):37-49. doi:10.1080/17434440.2021.2013200
- Babel A et al. Front Digit Health. 2021;3:669869. doi:10.3389/fdgth.2021.669869
- Hasan SS et al. Neurogastroenterol Motil. 2023;35(4):e14554. doi:10.1111/nmo.14554
- Peters SL et al. Neurogastroenterol Motil. 2023;35(4):e14533. doi:10.1111/nmo.14533
- Zhou C et al. Neurogastroenterol Motil. 2019;31(2):e13461. doi:10.1111/nmo.13461
- Staudacher HM et al. Nat Rev Gastroenterol Hepatol. 2023;1-15. doi:10.1038/s41575-023-00794-z
- Qin HY et al. World J Gastroenterol. 2014;20(39):14126-14131. doi:10.3748/wjg.v20.i39.14126
- Varjú P et al. PLoS One. 2017;12(8):e0182942. doi:10.1371/journal.pone.0182942
- Saleh ZM et al. Am J Gastroenterol. 2023. doi:10.14309/ajg.0000000000002220
- Yu C et al. Clin Transl Gastroenterol. 2022;13(9):e00515. doi:10.14309/ctg.0000000000000515
- Jagannath B et al. Inflamm Bowel Dis. 2020;26(10):1533-1542. doi:10.1093/ibd/izaa191
- Zhang H et al. J Nutr. 2023;153(4):924-939. doi:10.1016/j.tjnut.2023.01.026
- Karakan T et al. Gut Microbes. 2022;14(1):2138672. doi:10.1080/19490976.2022.2138672
- Kordi M et al. Inform Med Unlocked. 2022;29:100891. doi:10.1016/j.imu.2022.100891
- Gubatan J et al. World J Gastroenterol. 2021;27(17):1920-1935. doi:10.3748/wjg.v27.i17.1920
- Boucher EM et al. Expert Rev Med Devices. 2021;18(suppl 1):37-49. doi:10.1080/17434440.2021.2013200
- Babel A et al. Front Digit Health. 2021;3:669869. doi:10.3389/fdgth.2021.669869
- Hasan SS et al. Neurogastroenterol Motil. 2023;35(4):e14554. doi:10.1111/nmo.14554
- Peters SL et al. Neurogastroenterol Motil. 2023;35(4):e14533. doi:10.1111/nmo.14533
- Zhou C et al. Neurogastroenterol Motil. 2019;31(2):e13461. doi:10.1111/nmo.13461
- Staudacher HM et al. Nat Rev Gastroenterol Hepatol. 2023;1-15. doi:10.1038/s41575-023-00794-z
- Qin HY et al. World J Gastroenterol. 2014;20(39):14126-14131. doi:10.3748/wjg.v20.i39.14126
- Varjú P et al. PLoS One. 2017;12(8):e0182942. doi:10.1371/journal.pone.0182942
- Saleh ZM et al. Am J Gastroenterol. 2023. doi:10.14309/ajg.0000000000002220
- Yu C et al. Clin Transl Gastroenterol. 2022;13(9):e00515. doi:10.14309/ctg.0000000000000515
- Jagannath B et al. Inflamm Bowel Dis. 2020;26(10):1533-1542. doi:10.1093/ibd/izaa191
- Zhang H et al. J Nutr. 2023;153(4):924-939. doi:10.1016/j.tjnut.2023.01.026
- Karakan T et al. Gut Microbes. 2022;14(1):2138672. doi:10.1080/19490976.2022.2138672
- Kordi M et al. Inform Med Unlocked. 2022;29:100891. doi:10.1016/j.imu.2022.100891
- Gubatan J et al. World J Gastroenterol. 2021;27(17):1920-1935. doi:10.3748/wjg.v27.i17.1920
- Boucher EM et al. Expert Rev Med Devices. 2021;18(suppl 1):37-49. doi:10.1080/17434440.2021.2013200
- Babel A et al. Front Digit Health. 2021;3:669869. doi:10.3389/fdgth.2021.669869
‘Old school’ laser resurfacing remains an effective option for rejuvenation
SAN DIEGO – , according to Arisa E. Ortiz, MD.
“Fractional resurfacing is great because there is less downtime, but the results are not as dramatic as with fully ablative resurfacing,” Dr. Ortiz, director of laser and cosmetic dermatology at the University of California, San Diego, said at the annual Masters of Aesthetics Symposium. In her practice, she said, “we do a combination,” which can include “fully ablative around the mouth and eyes and fractional everywhere else.”
Key drawbacks to fully ablative laser resurfacing include significant downtime and extensive wound care, “so it’s not for everybody,” she said. Prolonged erythema following treatment is expected, “so patients need to plan for this. It can last 3-4 months, and it will continue to fade and can be covered up with makeup, but it does last a while,” she noted. “One of the things that made ablative resurfacing fall out of favor was the delayed and permanent hypopigmentation where there’s a stark line of demarcation because you can’t treat the neck [with this modality], so patients have this pearly white looking face that appears 6 months after the treatment,” she added.
Preoperatively, Dr. Ortiz asks patients what other cosmetic procedures they have had in the past. For example, if they have had a facelift, they might have neck skin on their jawline, which will react differently to fully ablative resurfacing than facial skin. “I don’t perform fully ablative resurfacing on the neck or body, or in patients with darker skin types,” she said.
To optimize results, she recommends pretreatment of the area with a neuromodulator a week or 2 before the procedure, “so that they’re not actively contracting and recreating creases,” she said. Studies, she noted, have shown that this approach results in better outcomes. She also asks patients to apply a tripeptide serum daily a week or 2 prior to their procedure to stimulate wound healing and collagen remodeling.
For antibiotic and antiviral prophylaxis, Dr. Ortiz typically prescribes doxycycline 100 mg b.i.d. for 7 days and valacyclovir 500 mg b.i.d. for 7 days and asks patients to start the course the night before the procedure. “If they break through the antiviral, I increase to zoster dosing,” she said. “I make sure they have my cell phone number and call me right away if that happens. I don’t routinely prescribe an antifungal, but you can if you want to.”
For anesthesia, Dr. Ortiz applies lidocaine 23%/tetracaine 7% an hour before the procedure and performs nerve blocks at the mentalis, infraorbital, supraorbital, and nasalis muscles. “I also do local infiltration with a three-pronged Mesoram adapter,” she said. “That has changed the comfort level for these patients. I don’t offer any sedation in my practice but that is an option if you have it available. If you’re going to be resurfacing within the orbital rim you need to know how to place corneal shields. Only use injectable lidocaine in this area because if topical lidocaine gets into the eye, it can cause a chemical corneal abrasion. Nothing happens to their vision permanently, but it’s extremely painful for 24-48 hours.”
Dr. Ortiz described postoperative wound care as “the hardest part” of fully ablative laser resurfacing treatments. The treated area will look “bloody and crusty” for 1-2 weeks. She instructs patients to do vinegar soaks four times per day for 2-3 weeks, “depending on how quickly they heal,” she said. She also counsels patients to apply petrolatum ointment to the area and provides them with a bottle of hypochlorous acid spray, an antiseptic – which also helps with the itching they may experience. “They need to avoid the sun, so I recommend full face visors,” she added.
In her clinical experience, postoperative pain medications are not required. “If the patient calls you on day 3 with increased pain, that’s usually a sign of infection; don’t ignore that,” said Dr. Ortiz, who is also president-elect of the American Society for Laser Medicine and Surgery. In a case of suspected infection, she asks the patient to come in right away, and obtains a bacterial culture. “If they break through the doxycycline, it’s usually a gram-negative infection, so I’ll treat them prophylactically for that,” she said.
“Significant itching may be a sign of Candida infection,” she noted. “Because the epidermis has been disrupted, if they have systemic symptoms then you want to consider IV antibiotics because the infection can spread rapidly.”
Dr. Ortiz disclosed having financial relationships with several pharmaceutical and device companies. She is also cochair of the MOAS.
SAN DIEGO – , according to Arisa E. Ortiz, MD.
“Fractional resurfacing is great because there is less downtime, but the results are not as dramatic as with fully ablative resurfacing,” Dr. Ortiz, director of laser and cosmetic dermatology at the University of California, San Diego, said at the annual Masters of Aesthetics Symposium. In her practice, she said, “we do a combination,” which can include “fully ablative around the mouth and eyes and fractional everywhere else.”
Key drawbacks to fully ablative laser resurfacing include significant downtime and extensive wound care, “so it’s not for everybody,” she said. Prolonged erythema following treatment is expected, “so patients need to plan for this. It can last 3-4 months, and it will continue to fade and can be covered up with makeup, but it does last a while,” she noted. “One of the things that made ablative resurfacing fall out of favor was the delayed and permanent hypopigmentation where there’s a stark line of demarcation because you can’t treat the neck [with this modality], so patients have this pearly white looking face that appears 6 months after the treatment,” she added.
Preoperatively, Dr. Ortiz asks patients what other cosmetic procedures they have had in the past. For example, if they have had a facelift, they might have neck skin on their jawline, which will react differently to fully ablative resurfacing than facial skin. “I don’t perform fully ablative resurfacing on the neck or body, or in patients with darker skin types,” she said.
To optimize results, she recommends pretreatment of the area with a neuromodulator a week or 2 before the procedure, “so that they’re not actively contracting and recreating creases,” she said. Studies, she noted, have shown that this approach results in better outcomes. She also asks patients to apply a tripeptide serum daily a week or 2 prior to their procedure to stimulate wound healing and collagen remodeling.
For antibiotic and antiviral prophylaxis, Dr. Ortiz typically prescribes doxycycline 100 mg b.i.d. for 7 days and valacyclovir 500 mg b.i.d. for 7 days and asks patients to start the course the night before the procedure. “If they break through the antiviral, I increase to zoster dosing,” she said. “I make sure they have my cell phone number and call me right away if that happens. I don’t routinely prescribe an antifungal, but you can if you want to.”
For anesthesia, Dr. Ortiz applies lidocaine 23%/tetracaine 7% an hour before the procedure and performs nerve blocks at the mentalis, infraorbital, supraorbital, and nasalis muscles. “I also do local infiltration with a three-pronged Mesoram adapter,” she said. “That has changed the comfort level for these patients. I don’t offer any sedation in my practice but that is an option if you have it available. If you’re going to be resurfacing within the orbital rim you need to know how to place corneal shields. Only use injectable lidocaine in this area because if topical lidocaine gets into the eye, it can cause a chemical corneal abrasion. Nothing happens to their vision permanently, but it’s extremely painful for 24-48 hours.”
Dr. Ortiz described postoperative wound care as “the hardest part” of fully ablative laser resurfacing treatments. The treated area will look “bloody and crusty” for 1-2 weeks. She instructs patients to do vinegar soaks four times per day for 2-3 weeks, “depending on how quickly they heal,” she said. She also counsels patients to apply petrolatum ointment to the area and provides them with a bottle of hypochlorous acid spray, an antiseptic – which also helps with the itching they may experience. “They need to avoid the sun, so I recommend full face visors,” she added.
In her clinical experience, postoperative pain medications are not required. “If the patient calls you on day 3 with increased pain, that’s usually a sign of infection; don’t ignore that,” said Dr. Ortiz, who is also president-elect of the American Society for Laser Medicine and Surgery. In a case of suspected infection, she asks the patient to come in right away, and obtains a bacterial culture. “If they break through the doxycycline, it’s usually a gram-negative infection, so I’ll treat them prophylactically for that,” she said.
“Significant itching may be a sign of Candida infection,” she noted. “Because the epidermis has been disrupted, if they have systemic symptoms then you want to consider IV antibiotics because the infection can spread rapidly.”
Dr. Ortiz disclosed having financial relationships with several pharmaceutical and device companies. She is also cochair of the MOAS.
SAN DIEGO – , according to Arisa E. Ortiz, MD.
“Fractional resurfacing is great because there is less downtime, but the results are not as dramatic as with fully ablative resurfacing,” Dr. Ortiz, director of laser and cosmetic dermatology at the University of California, San Diego, said at the annual Masters of Aesthetics Symposium. In her practice, she said, “we do a combination,” which can include “fully ablative around the mouth and eyes and fractional everywhere else.”
Key drawbacks to fully ablative laser resurfacing include significant downtime and extensive wound care, “so it’s not for everybody,” she said. Prolonged erythema following treatment is expected, “so patients need to plan for this. It can last 3-4 months, and it will continue to fade and can be covered up with makeup, but it does last a while,” she noted. “One of the things that made ablative resurfacing fall out of favor was the delayed and permanent hypopigmentation where there’s a stark line of demarcation because you can’t treat the neck [with this modality], so patients have this pearly white looking face that appears 6 months after the treatment,” she added.
Preoperatively, Dr. Ortiz asks patients what other cosmetic procedures they have had in the past. For example, if they have had a facelift, they might have neck skin on their jawline, which will react differently to fully ablative resurfacing than facial skin. “I don’t perform fully ablative resurfacing on the neck or body, or in patients with darker skin types,” she said.
To optimize results, she recommends pretreatment of the area with a neuromodulator a week or 2 before the procedure, “so that they’re not actively contracting and recreating creases,” she said. Studies, she noted, have shown that this approach results in better outcomes. She also asks patients to apply a tripeptide serum daily a week or 2 prior to their procedure to stimulate wound healing and collagen remodeling.
For antibiotic and antiviral prophylaxis, Dr. Ortiz typically prescribes doxycycline 100 mg b.i.d. for 7 days and valacyclovir 500 mg b.i.d. for 7 days and asks patients to start the course the night before the procedure. “If they break through the antiviral, I increase to zoster dosing,” she said. “I make sure they have my cell phone number and call me right away if that happens. I don’t routinely prescribe an antifungal, but you can if you want to.”
For anesthesia, Dr. Ortiz applies lidocaine 23%/tetracaine 7% an hour before the procedure and performs nerve blocks at the mentalis, infraorbital, supraorbital, and nasalis muscles. “I also do local infiltration with a three-pronged Mesoram adapter,” she said. “That has changed the comfort level for these patients. I don’t offer any sedation in my practice but that is an option if you have it available. If you’re going to be resurfacing within the orbital rim you need to know how to place corneal shields. Only use injectable lidocaine in this area because if topical lidocaine gets into the eye, it can cause a chemical corneal abrasion. Nothing happens to their vision permanently, but it’s extremely painful for 24-48 hours.”
Dr. Ortiz described postoperative wound care as “the hardest part” of fully ablative laser resurfacing treatments. The treated area will look “bloody and crusty” for 1-2 weeks. She instructs patients to do vinegar soaks four times per day for 2-3 weeks, “depending on how quickly they heal,” she said. She also counsels patients to apply petrolatum ointment to the area and provides them with a bottle of hypochlorous acid spray, an antiseptic – which also helps with the itching they may experience. “They need to avoid the sun, so I recommend full face visors,” she added.
In her clinical experience, postoperative pain medications are not required. “If the patient calls you on day 3 with increased pain, that’s usually a sign of infection; don’t ignore that,” said Dr. Ortiz, who is also president-elect of the American Society for Laser Medicine and Surgery. In a case of suspected infection, she asks the patient to come in right away, and obtains a bacterial culture. “If they break through the doxycycline, it’s usually a gram-negative infection, so I’ll treat them prophylactically for that,” she said.
“Significant itching may be a sign of Candida infection,” she noted. “Because the epidermis has been disrupted, if they have systemic symptoms then you want to consider IV antibiotics because the infection can spread rapidly.”
Dr. Ortiz disclosed having financial relationships with several pharmaceutical and device companies. She is also cochair of the MOAS.
AT MOAS 2023
Anxiety and panic attacks
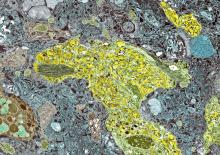
Given the patient's insidious cognitive decline, as well as increased agitation, irritability, anxiety, social isolation, inability to fully manage finances, loss of routine hygienic practices, and loss of interest in regular meals, this patient is diagnosed with probable Alzheimer's disease (AD) dementia and is referred to a specialist for further testing.
AD is one of the most common forms of dementia. More than 6 million people in the United States have clinical AD or mild cognitive impairment because of AD. By 2060, the incidence of AD is expected to grow to 15 million people. AD is classified into four stages: preclinical, mild, moderate, and severe. Patients with preclinical AD — a relatively new classification currently only used for research — do not yet show abnormal results on physical exam or mental status testing, but areas of the brain are undergoing pathologic changes. Mild AD signs and symptoms include memory loss, compromised judgment, trouble handling money and paying bills, mood and personality changes, and increased anxiety. People with moderate AD show increasing signs of memory loss and confusion, problems with recognizing family and friends, and difficulty with organizing thoughts and thinking logically, and they repeat themselves in conversation, among other symptoms. Severe AD is generally described as a complete loss of self, with the inability to recognize family and friends, inability to communicate effectively, and complete dependence on others for care.
Diagnosing AD currently relies on a clinical approach. A complete physical examination, with a detailed neurologic examination and a mental status examination, is used to evaluate disease stage and rule out comorbid conditions. Initial mental status testing should evaluate attention and concentration, recent and remote memory, language, praxis, executive function, and visuospatial function. Imaging studies may be performed to rule out other treatable causes of cognitive decline. In addition, volumetric studies of the hippocampus and 2-[18F]fluoro-2-deoxy-D-glucose PET with or without amyloid imaging can be used for early detection and differentiating dementia etiologies. Lumbar puncture as a diagnostic measure for levels of tau (which is often elevated in AD) and amyloid (which is often reduced in AD) is currently reserved for research settings.
Although the cause of AD is unknown, experts believe that environmental and genetic risk factors trigger a pathophysiologic cascade that, over decades, leads to Alzheimer's pathology and dementia. Universally accepted pathologic hallmarks of AD are beta-amyloid plaques and neurofibrillary tangles (NFTs). NFTs result from changes in the tau protein, a key chemical in neuronal support structures, and are associated with malfunctions in communication between neurons as well as cell death. Beta-amyloid plaques are dense, mostly insoluble deposits that develop around neurons in the hippocampus and other regions in the cerebral cortex used for decision-making, disrupting function and leading to brain atrophy. Risk factors for AD include advancing age, family history, APOE e4 genotype, insulin resistance, hypertension, depression, and traumatic brain injury.
After an AD diagnosis, physicians should encourage the involvement of family and friends who agree to become more involved in the patient's care as the disease progresses. These individuals need to understand the patient's wishes around care, especially for the future, when the patient is no longer able to make decisions. The patient may also consider establishing medical advance directives and durable power of attorney for medical and financial decision-making. Caregivers supporting the patient are encouraged to help balance the physical needs of the patient while maintaining respect for them as a competent adult to the extent allowed by the progression of their disease.
Currently, AD treatments are focused on symptomatic therapies that modulate neurotransmitters — either acetylcholine or glutamate. The standard medical treatment includes cholinesterase inhibitors and a partial N-methyl-D-aspartate antagonist. Two amyloid-directed antibodies (aducanumab, lecanemab) are currently available in the US for individuals with AD exhibiting mild cognitive impairment or mild dementia. A third agent currently in clinical trials (donanemab) has shown significantly slowed clinical progression after 1.5 years among clinical trial participants with early symptomatic AD and amyloid and tau pathology.
Jasvinder Chawla, MD, Professor of Neurology, Loyola University Medical Center, Maywood; Director, Clinical Neurophysiology Lab, Department of Neurology, Hines VA Hospital, Hines, IL.
Jasvinder Chawla, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Given the patient's insidious cognitive decline, as well as increased agitation, irritability, anxiety, social isolation, inability to fully manage finances, loss of routine hygienic practices, and loss of interest in regular meals, this patient is diagnosed with probable Alzheimer's disease (AD) dementia and is referred to a specialist for further testing.
AD is one of the most common forms of dementia. More than 6 million people in the United States have clinical AD or mild cognitive impairment because of AD. By 2060, the incidence of AD is expected to grow to 15 million people. AD is classified into four stages: preclinical, mild, moderate, and severe. Patients with preclinical AD — a relatively new classification currently only used for research — do not yet show abnormal results on physical exam or mental status testing, but areas of the brain are undergoing pathologic changes. Mild AD signs and symptoms include memory loss, compromised judgment, trouble handling money and paying bills, mood and personality changes, and increased anxiety. People with moderate AD show increasing signs of memory loss and confusion, problems with recognizing family and friends, and difficulty with organizing thoughts and thinking logically, and they repeat themselves in conversation, among other symptoms. Severe AD is generally described as a complete loss of self, with the inability to recognize family and friends, inability to communicate effectively, and complete dependence on others for care.
Diagnosing AD currently relies on a clinical approach. A complete physical examination, with a detailed neurologic examination and a mental status examination, is used to evaluate disease stage and rule out comorbid conditions. Initial mental status testing should evaluate attention and concentration, recent and remote memory, language, praxis, executive function, and visuospatial function. Imaging studies may be performed to rule out other treatable causes of cognitive decline. In addition, volumetric studies of the hippocampus and 2-[18F]fluoro-2-deoxy-D-glucose PET with or without amyloid imaging can be used for early detection and differentiating dementia etiologies. Lumbar puncture as a diagnostic measure for levels of tau (which is often elevated in AD) and amyloid (which is often reduced in AD) is currently reserved for research settings.
Although the cause of AD is unknown, experts believe that environmental and genetic risk factors trigger a pathophysiologic cascade that, over decades, leads to Alzheimer's pathology and dementia. Universally accepted pathologic hallmarks of AD are beta-amyloid plaques and neurofibrillary tangles (NFTs). NFTs result from changes in the tau protein, a key chemical in neuronal support structures, and are associated with malfunctions in communication between neurons as well as cell death. Beta-amyloid plaques are dense, mostly insoluble deposits that develop around neurons in the hippocampus and other regions in the cerebral cortex used for decision-making, disrupting function and leading to brain atrophy. Risk factors for AD include advancing age, family history, APOE e4 genotype, insulin resistance, hypertension, depression, and traumatic brain injury.
After an AD diagnosis, physicians should encourage the involvement of family and friends who agree to become more involved in the patient's care as the disease progresses. These individuals need to understand the patient's wishes around care, especially for the future, when the patient is no longer able to make decisions. The patient may also consider establishing medical advance directives and durable power of attorney for medical and financial decision-making. Caregivers supporting the patient are encouraged to help balance the physical needs of the patient while maintaining respect for them as a competent adult to the extent allowed by the progression of their disease.
Currently, AD treatments are focused on symptomatic therapies that modulate neurotransmitters — either acetylcholine or glutamate. The standard medical treatment includes cholinesterase inhibitors and a partial N-methyl-D-aspartate antagonist. Two amyloid-directed antibodies (aducanumab, lecanemab) are currently available in the US for individuals with AD exhibiting mild cognitive impairment or mild dementia. A third agent currently in clinical trials (donanemab) has shown significantly slowed clinical progression after 1.5 years among clinical trial participants with early symptomatic AD and amyloid and tau pathology.
Jasvinder Chawla, MD, Professor of Neurology, Loyola University Medical Center, Maywood; Director, Clinical Neurophysiology Lab, Department of Neurology, Hines VA Hospital, Hines, IL.
Jasvinder Chawla, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Given the patient's insidious cognitive decline, as well as increased agitation, irritability, anxiety, social isolation, inability to fully manage finances, loss of routine hygienic practices, and loss of interest in regular meals, this patient is diagnosed with probable Alzheimer's disease (AD) dementia and is referred to a specialist for further testing.
AD is one of the most common forms of dementia. More than 6 million people in the United States have clinical AD or mild cognitive impairment because of AD. By 2060, the incidence of AD is expected to grow to 15 million people. AD is classified into four stages: preclinical, mild, moderate, and severe. Patients with preclinical AD — a relatively new classification currently only used for research — do not yet show abnormal results on physical exam or mental status testing, but areas of the brain are undergoing pathologic changes. Mild AD signs and symptoms include memory loss, compromised judgment, trouble handling money and paying bills, mood and personality changes, and increased anxiety. People with moderate AD show increasing signs of memory loss and confusion, problems with recognizing family and friends, and difficulty with organizing thoughts and thinking logically, and they repeat themselves in conversation, among other symptoms. Severe AD is generally described as a complete loss of self, with the inability to recognize family and friends, inability to communicate effectively, and complete dependence on others for care.
Diagnosing AD currently relies on a clinical approach. A complete physical examination, with a detailed neurologic examination and a mental status examination, is used to evaluate disease stage and rule out comorbid conditions. Initial mental status testing should evaluate attention and concentration, recent and remote memory, language, praxis, executive function, and visuospatial function. Imaging studies may be performed to rule out other treatable causes of cognitive decline. In addition, volumetric studies of the hippocampus and 2-[18F]fluoro-2-deoxy-D-glucose PET with or without amyloid imaging can be used for early detection and differentiating dementia etiologies. Lumbar puncture as a diagnostic measure for levels of tau (which is often elevated in AD) and amyloid (which is often reduced in AD) is currently reserved for research settings.
Although the cause of AD is unknown, experts believe that environmental and genetic risk factors trigger a pathophysiologic cascade that, over decades, leads to Alzheimer's pathology and dementia. Universally accepted pathologic hallmarks of AD are beta-amyloid plaques and neurofibrillary tangles (NFTs). NFTs result from changes in the tau protein, a key chemical in neuronal support structures, and are associated with malfunctions in communication between neurons as well as cell death. Beta-amyloid plaques are dense, mostly insoluble deposits that develop around neurons in the hippocampus and other regions in the cerebral cortex used for decision-making, disrupting function and leading to brain atrophy. Risk factors for AD include advancing age, family history, APOE e4 genotype, insulin resistance, hypertension, depression, and traumatic brain injury.
After an AD diagnosis, physicians should encourage the involvement of family and friends who agree to become more involved in the patient's care as the disease progresses. These individuals need to understand the patient's wishes around care, especially for the future, when the patient is no longer able to make decisions. The patient may also consider establishing medical advance directives and durable power of attorney for medical and financial decision-making. Caregivers supporting the patient are encouraged to help balance the physical needs of the patient while maintaining respect for them as a competent adult to the extent allowed by the progression of their disease.
Currently, AD treatments are focused on symptomatic therapies that modulate neurotransmitters — either acetylcholine or glutamate. The standard medical treatment includes cholinesterase inhibitors and a partial N-methyl-D-aspartate antagonist. Two amyloid-directed antibodies (aducanumab, lecanemab) are currently available in the US for individuals with AD exhibiting mild cognitive impairment or mild dementia. A third agent currently in clinical trials (donanemab) has shown significantly slowed clinical progression after 1.5 years among clinical trial participants with early symptomatic AD and amyloid and tau pathology.
Jasvinder Chawla, MD, Professor of Neurology, Loyola University Medical Center, Maywood; Director, Clinical Neurophysiology Lab, Department of Neurology, Hines VA Hospital, Hines, IL.
Jasvinder Chawla, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 73-year-old man who lives independently presents to his primary care physician (PCP) with irritability, anxiety, and panic attacks. Last year, he saw his PCP at the urging of his brother, who noticed that the patient was becoming more forgetful and agitated. At that time, the brother reported concerns that the patient, who normally enjoyed spending time with his extended family, was beginning to regularly forget to show up at family functions. When asked why he hadn't attended, the patient would become irate, saying it was his family who failed to invite him. The patient wouldn't have agreed to seeing the PCP except he was having issues with insomnia that he wanted to address. During last year's visit, the physician conducted a complete physical examination, as well as detailed neurologic and mental status examinations; all came back normal.
At today's visit, in addition to patient-reported mood fluctuations, the brother tells the physician that the patient has become reclusive, skipping nearly all family functions as well as daily walks with friends. His daily hygiene has suffered, and he has stopped eating regularly. The brother also mentions to the doctor that the patient has received some late-payment notices for utilities that he normally meticulously paid on time. The PCP orders another round of cognitive, behavioral, and functional assessments, which reveal a decline in all areas from last year's results, as well as a complete neurologic examination that reveals mild hyposmia.
MASLD/MASH and Weight Loss
- Younossi ZM et al. Gastroenterology. 2021;160(3):912-918. doi:10.1053/j.astro.2020.11.051
- Cusi K et al. Endocr Pract. 2022;28(5):528-562. doi:10.1016/j.eprac.2022.03.010
- Rinella ME et al. Hepatology. 2023;77(5):1797-1835. doi:10.1097/HEP.0000000000000323
- World obesity atlas 2023. World Obesity Day. Published March 2023. Accessed July 23, 2023. https://www.worldobesityday.org/assets/downloads/World_Obesity_Atlas_2023_Report.pdf
- Le MH et al. Clin Mol Hepatol. 2022;28(4):841-850. doi:10.3350/cmh.2022.0239
- Vilar-Gomez E et al. Gastroenterology. 2015;149(2):367-78.e5. doi:10.1053/j.gastro.2015.04.005
- Koutoukidis DA et al. Metabolism. 2021;115:154455. doi:10.1016/j.metabol.2020.154455
- Ma J et al. Gastroenterology. 2018;155(1):107-117. doi:10.1053/j.gastro.2018.03.038
- Ahern AL et al. Lancet. 2017;389(10085):2214-2225. doi:10.1016/S0140-6736(17)30647-5
- Newsome PN et al; NN9931-4296 Investigators. N Engl J Med. 2021;384(12):1113-1124. doi:10.1056/NEJMoa2028395
- Armstrong MJ et al. Lancet. 2016;387(10019):679-690. doi:10.1016/S0140-6736(15)00803-X
- Gastaldelli A et al. Lancet Diabetes Endocrinol. 2022;10(6):393-406. doi:10.1016/S2213-8587(22)00070-5
- Kahl S et al. Diabetes Care. 2020;43(2):298-305. doi:10.2337/dc19-0641
- Younossi ZM et al. Gastroenterology. 2021;160(3):912-918. doi:10.1053/j.astro.2020.11.051
- Cusi K et al. Endocr Pract. 2022;28(5):528-562. doi:10.1016/j.eprac.2022.03.010
- Rinella ME et al. Hepatology. 2023;77(5):1797-1835. doi:10.1097/HEP.0000000000000323
- World obesity atlas 2023. World Obesity Day. Published March 2023. Accessed July 23, 2023. https://www.worldobesityday.org/assets/downloads/World_Obesity_Atlas_2023_Report.pdf
- Le MH et al. Clin Mol Hepatol. 2022;28(4):841-850. doi:10.3350/cmh.2022.0239
- Vilar-Gomez E et al. Gastroenterology. 2015;149(2):367-78.e5. doi:10.1053/j.gastro.2015.04.005
- Koutoukidis DA et al. Metabolism. 2021;115:154455. doi:10.1016/j.metabol.2020.154455
- Ma J et al. Gastroenterology. 2018;155(1):107-117. doi:10.1053/j.gastro.2018.03.038
- Ahern AL et al. Lancet. 2017;389(10085):2214-2225. doi:10.1016/S0140-6736(17)30647-5
- Newsome PN et al; NN9931-4296 Investigators. N Engl J Med. 2021;384(12):1113-1124. doi:10.1056/NEJMoa2028395
- Armstrong MJ et al. Lancet. 2016;387(10019):679-690. doi:10.1016/S0140-6736(15)00803-X
- Gastaldelli A et al. Lancet Diabetes Endocrinol. 2022;10(6):393-406. doi:10.1016/S2213-8587(22)00070-5
- Kahl S et al. Diabetes Care. 2020;43(2):298-305. doi:10.2337/dc19-0641
- Younossi ZM et al. Gastroenterology. 2021;160(3):912-918. doi:10.1053/j.astro.2020.11.051
- Cusi K et al. Endocr Pract. 2022;28(5):528-562. doi:10.1016/j.eprac.2022.03.010
- Rinella ME et al. Hepatology. 2023;77(5):1797-1835. doi:10.1097/HEP.0000000000000323
- World obesity atlas 2023. World Obesity Day. Published March 2023. Accessed July 23, 2023. https://www.worldobesityday.org/assets/downloads/World_Obesity_Atlas_2023_Report.pdf
- Le MH et al. Clin Mol Hepatol. 2022;28(4):841-850. doi:10.3350/cmh.2022.0239
- Vilar-Gomez E et al. Gastroenterology. 2015;149(2):367-78.e5. doi:10.1053/j.gastro.2015.04.005
- Koutoukidis DA et al. Metabolism. 2021;115:154455. doi:10.1016/j.metabol.2020.154455
- Ma J et al. Gastroenterology. 2018;155(1):107-117. doi:10.1053/j.gastro.2018.03.038
- Ahern AL et al. Lancet. 2017;389(10085):2214-2225. doi:10.1016/S0140-6736(17)30647-5
- Newsome PN et al; NN9931-4296 Investigators. N Engl J Med. 2021;384(12):1113-1124. doi:10.1056/NEJMoa2028395
- Armstrong MJ et al. Lancet. 2016;387(10019):679-690. doi:10.1016/S0140-6736(15)00803-X
- Gastaldelli A et al. Lancet Diabetes Endocrinol. 2022;10(6):393-406. doi:10.1016/S2213-8587(22)00070-5
- Kahl S et al. Diabetes Care. 2020;43(2):298-305. doi:10.2337/dc19-0641
The Evolving Role of Surgery for IBD
- Gul F et al. Ann Med Surg (Lond). 2022;81:104476. doi:10.1016/j.amsu.2022.104476
- Kotze PG et al. Clin Colon Rectal Surg. 2021;34(3):172-180. doi:10.1055/s-0040-1718685
- Bemelman WA; S-ECCO collaborators. J Crohns Colitis. 2018;12(8):1005-1007. doi:10.1093/ecco-jcc/jjy056
- Ricci C et al. Dig Liver Dis. 2008;40(suppl 2):S285-S288. doi:10.1016/S1590-8658(08)60539-3
- Lin X et al. Therap Adv Gastroenterol. 2022;15:17562848221104951. doi:10.1177/17562848221104951
- Parigi TL et al. Dis Colon Rectum. 2022;65(suppl 1):S119-S128. doi:10.1097/DCR.0000000000002548
- Pilonis ND et al. Transl Gastroenterol Hepatol. 2022;7:7. doi:10.21037/tgh.2020.04.02
- Misawa M et al. Clin Endosc. 2021;54(4):455-463. doi:10.5946/ce.2021.165
- de Sousa HT et al. Curr Opin Gastroenterol. 2018;34(4):194-207. doi:10.1097/MOG.0000000000000440
- Whitehead A, Cataldo PA. Clin Colon Rectal Surg. 2017;30(3):162-171. doi:10.1055/s-0037-1598156
- Cannon LM. The use of enhanced recovery pathways in patients undergoing surgery for inflammatory bowel disease. In: Hyman N, Fleshner P, Strong S, eds Mastery of IBD Surgery. Chicago, IL: University of Chicago Press; 2019:29-38. doi:10.1007/978-3-030-16755-4_4
- Ljungqvist O et al. World J Surg. 2020;44(10):3197–3198. doi:10.1007/s00268-020-05734-5
- Gul F et al. Ann Med Surg (Lond). 2022;81:104476. doi:10.1016/j.amsu.2022.104476
- Kotze PG et al. Clin Colon Rectal Surg. 2021;34(3):172-180. doi:10.1055/s-0040-1718685
- Bemelman WA; S-ECCO collaborators. J Crohns Colitis. 2018;12(8):1005-1007. doi:10.1093/ecco-jcc/jjy056
- Ricci C et al. Dig Liver Dis. 2008;40(suppl 2):S285-S288. doi:10.1016/S1590-8658(08)60539-3
- Lin X et al. Therap Adv Gastroenterol. 2022;15:17562848221104951. doi:10.1177/17562848221104951
- Parigi TL et al. Dis Colon Rectum. 2022;65(suppl 1):S119-S128. doi:10.1097/DCR.0000000000002548
- Pilonis ND et al. Transl Gastroenterol Hepatol. 2022;7:7. doi:10.21037/tgh.2020.04.02
- Misawa M et al. Clin Endosc. 2021;54(4):455-463. doi:10.5946/ce.2021.165
- de Sousa HT et al. Curr Opin Gastroenterol. 2018;34(4):194-207. doi:10.1097/MOG.0000000000000440
- Whitehead A, Cataldo PA. Clin Colon Rectal Surg. 2017;30(3):162-171. doi:10.1055/s-0037-1598156
- Cannon LM. The use of enhanced recovery pathways in patients undergoing surgery for inflammatory bowel disease. In: Hyman N, Fleshner P, Strong S, eds Mastery of IBD Surgery. Chicago, IL: University of Chicago Press; 2019:29-38. doi:10.1007/978-3-030-16755-4_4
- Ljungqvist O et al. World J Surg. 2020;44(10):3197–3198. doi:10.1007/s00268-020-05734-5
- Gul F et al. Ann Med Surg (Lond). 2022;81:104476. doi:10.1016/j.amsu.2022.104476
- Kotze PG et al. Clin Colon Rectal Surg. 2021;34(3):172-180. doi:10.1055/s-0040-1718685
- Bemelman WA; S-ECCO collaborators. J Crohns Colitis. 2018;12(8):1005-1007. doi:10.1093/ecco-jcc/jjy056
- Ricci C et al. Dig Liver Dis. 2008;40(suppl 2):S285-S288. doi:10.1016/S1590-8658(08)60539-3
- Lin X et al. Therap Adv Gastroenterol. 2022;15:17562848221104951. doi:10.1177/17562848221104951
- Parigi TL et al. Dis Colon Rectum. 2022;65(suppl 1):S119-S128. doi:10.1097/DCR.0000000000002548
- Pilonis ND et al. Transl Gastroenterol Hepatol. 2022;7:7. doi:10.21037/tgh.2020.04.02
- Misawa M et al. Clin Endosc. 2021;54(4):455-463. doi:10.5946/ce.2021.165
- de Sousa HT et al. Curr Opin Gastroenterol. 2018;34(4):194-207. doi:10.1097/MOG.0000000000000440
- Whitehead A, Cataldo PA. Clin Colon Rectal Surg. 2017;30(3):162-171. doi:10.1055/s-0037-1598156
- Cannon LM. The use of enhanced recovery pathways in patients undergoing surgery for inflammatory bowel disease. In: Hyman N, Fleshner P, Strong S, eds Mastery of IBD Surgery. Chicago, IL: University of Chicago Press; 2019:29-38. doi:10.1007/978-3-030-16755-4_4
- Ljungqvist O et al. World J Surg. 2020;44(10):3197–3198. doi:10.1007/s00268-020-05734-5
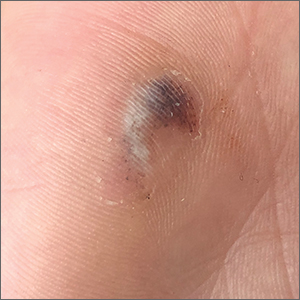
Hyperpigmented lesion on palm

This patient had a posttraumatic tache noir (also known as talon noir on the volar aspect of the feet); it is a subcorneal hematoma. The diagnosis is made clinically. Dermoscopic evaluation of tache/talon noir will reveal “pebbles on a ridge” or “satellite globules.” Confirmation of tache/talon noir can be made by paring the corneum with a #15 blade, which will reveal blood in the shavings and punctate lesions.1
This patient noted that the knob of his baseball bat rubbed the hypothenar eminence of his nondominant hand when he took a swing. The sheer force of the knob led to the subcorneal hematoma. Tache noir was high on the differential due to his physician’s clinical experience with similar cases. Tache noir occurs predominantly in people ages 12 to 24 years, without regard to gender.2 The condition is commonly found in athletes who participate in baseball, cricket, racquet sports, weightlifting, and rock climbing.2-4
Talon noir occurs most commonly in athletes who are frequently jumping, turning, and pivoting, as in football, basketball, tennis, and lacrosse.
Tache noir can be differentiated from other conditions by the presence of preserved architecture of the skin surface and punctate capillaries beneath the stratum corneum. The differential diagnosis includes verruca vulgaris, acral melanoma, and a traumatic tattoo.
Talon/tache noir are benign conditions that do not require treatment and do not affect sports performance. The lesion will usually self-resolve within a matter of weeks from onset or can even be gently scraped with a sterile needle or blade.
This patient was advised that the lesion would resolve on its own. His knee pain was determined to be a simple case of patellofemoral syndrome or “runner’s knee” and he opted to complete a home exercise program to obtain relief.
This case was adapted from: Warden D. Hyperpigmented lesion on left palm. J Fam Pract. 2021;70:459-460. Photos courtesy of Daniel Warden, MD
1. Googe AB, Schulmeier JS, Jackson AR, et al. Talon noir: paring can eliminate the need for biopsy. Postgrad Med J. 2014;90:730-731. doi: 10.1136/postgradmedj-2014-132996
2. Burkhart C, Nguyen N. Talon noire. Dermatology Advisor. Accessed October 19, 2021. www.dermatologyadvisor.com/home/decision-support-in-medicine/dermatology/talon-noire-black-heel-calcaneal-petechiae-runners-heel-basketball-heel-tennis-heel-hyperkeratosis-hemorrhagica-pseudochromhidrosis-plantaris-chromidrose-plantaire-eccrine-intracorne/
3. Talon noir. Primary Care Dermatology Society. Updated August 1, 2021. Accessed October 19, 2021. www.pcds.org.uk/clinical-guidance/talon-noir
4. Birrer RB, Griesemer BA, Cataletto MB, eds. Pediatric Sports Medicine for Primary Care. Lippincott Williams & Wilkins; 2002.

This patient had a posttraumatic tache noir (also known as talon noir on the volar aspect of the feet); it is a subcorneal hematoma. The diagnosis is made clinically. Dermoscopic evaluation of tache/talon noir will reveal “pebbles on a ridge” or “satellite globules.” Confirmation of tache/talon noir can be made by paring the corneum with a #15 blade, which will reveal blood in the shavings and punctate lesions.1
This patient noted that the knob of his baseball bat rubbed the hypothenar eminence of his nondominant hand when he took a swing. The sheer force of the knob led to the subcorneal hematoma. Tache noir was high on the differential due to his physician’s clinical experience with similar cases. Tache noir occurs predominantly in people ages 12 to 24 years, without regard to gender.2 The condition is commonly found in athletes who participate in baseball, cricket, racquet sports, weightlifting, and rock climbing.2-4
Talon noir occurs most commonly in athletes who are frequently jumping, turning, and pivoting, as in football, basketball, tennis, and lacrosse.
Tache noir can be differentiated from other conditions by the presence of preserved architecture of the skin surface and punctate capillaries beneath the stratum corneum. The differential diagnosis includes verruca vulgaris, acral melanoma, and a traumatic tattoo.
Talon/tache noir are benign conditions that do not require treatment and do not affect sports performance. The lesion will usually self-resolve within a matter of weeks from onset or can even be gently scraped with a sterile needle or blade.
This patient was advised that the lesion would resolve on its own. His knee pain was determined to be a simple case of patellofemoral syndrome or “runner’s knee” and he opted to complete a home exercise program to obtain relief.
This case was adapted from: Warden D. Hyperpigmented lesion on left palm. J Fam Pract. 2021;70:459-460. Photos courtesy of Daniel Warden, MD

This patient had a posttraumatic tache noir (also known as talon noir on the volar aspect of the feet); it is a subcorneal hematoma. The diagnosis is made clinically. Dermoscopic evaluation of tache/talon noir will reveal “pebbles on a ridge” or “satellite globules.” Confirmation of tache/talon noir can be made by paring the corneum with a #15 blade, which will reveal blood in the shavings and punctate lesions.1
This patient noted that the knob of his baseball bat rubbed the hypothenar eminence of his nondominant hand when he took a swing. The sheer force of the knob led to the subcorneal hematoma. Tache noir was high on the differential due to his physician’s clinical experience with similar cases. Tache noir occurs predominantly in people ages 12 to 24 years, without regard to gender.2 The condition is commonly found in athletes who participate in baseball, cricket, racquet sports, weightlifting, and rock climbing.2-4
Talon noir occurs most commonly in athletes who are frequently jumping, turning, and pivoting, as in football, basketball, tennis, and lacrosse.
Tache noir can be differentiated from other conditions by the presence of preserved architecture of the skin surface and punctate capillaries beneath the stratum corneum. The differential diagnosis includes verruca vulgaris, acral melanoma, and a traumatic tattoo.
Talon/tache noir are benign conditions that do not require treatment and do not affect sports performance. The lesion will usually self-resolve within a matter of weeks from onset or can even be gently scraped with a sterile needle or blade.
This patient was advised that the lesion would resolve on its own. His knee pain was determined to be a simple case of patellofemoral syndrome or “runner’s knee” and he opted to complete a home exercise program to obtain relief.
This case was adapted from: Warden D. Hyperpigmented lesion on left palm. J Fam Pract. 2021;70:459-460. Photos courtesy of Daniel Warden, MD
1. Googe AB, Schulmeier JS, Jackson AR, et al. Talon noir: paring can eliminate the need for biopsy. Postgrad Med J. 2014;90:730-731. doi: 10.1136/postgradmedj-2014-132996
2. Burkhart C, Nguyen N. Talon noire. Dermatology Advisor. Accessed October 19, 2021. www.dermatologyadvisor.com/home/decision-support-in-medicine/dermatology/talon-noire-black-heel-calcaneal-petechiae-runners-heel-basketball-heel-tennis-heel-hyperkeratosis-hemorrhagica-pseudochromhidrosis-plantaris-chromidrose-plantaire-eccrine-intracorne/
3. Talon noir. Primary Care Dermatology Society. Updated August 1, 2021. Accessed October 19, 2021. www.pcds.org.uk/clinical-guidance/talon-noir
4. Birrer RB, Griesemer BA, Cataletto MB, eds. Pediatric Sports Medicine for Primary Care. Lippincott Williams & Wilkins; 2002.
1. Googe AB, Schulmeier JS, Jackson AR, et al. Talon noir: paring can eliminate the need for biopsy. Postgrad Med J. 2014;90:730-731. doi: 10.1136/postgradmedj-2014-132996
2. Burkhart C, Nguyen N. Talon noire. Dermatology Advisor. Accessed October 19, 2021. www.dermatologyadvisor.com/home/decision-support-in-medicine/dermatology/talon-noire-black-heel-calcaneal-petechiae-runners-heel-basketball-heel-tennis-heel-hyperkeratosis-hemorrhagica-pseudochromhidrosis-plantaris-chromidrose-plantaire-eccrine-intracorne/
3. Talon noir. Primary Care Dermatology Society. Updated August 1, 2021. Accessed October 19, 2021. www.pcds.org.uk/clinical-guidance/talon-noir
4. Birrer RB, Griesemer BA, Cataletto MB, eds. Pediatric Sports Medicine for Primary Care. Lippincott Williams & Wilkins; 2002.
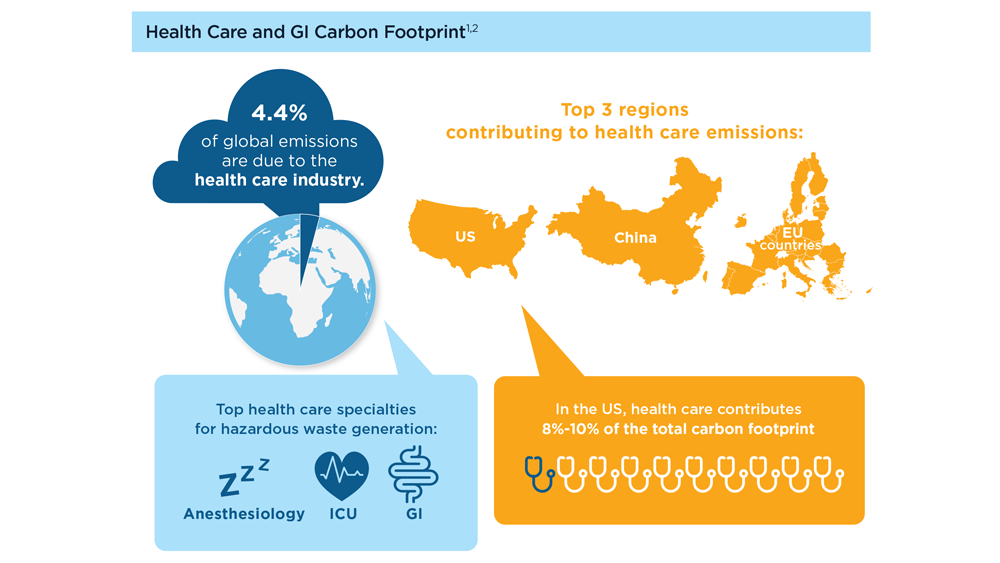
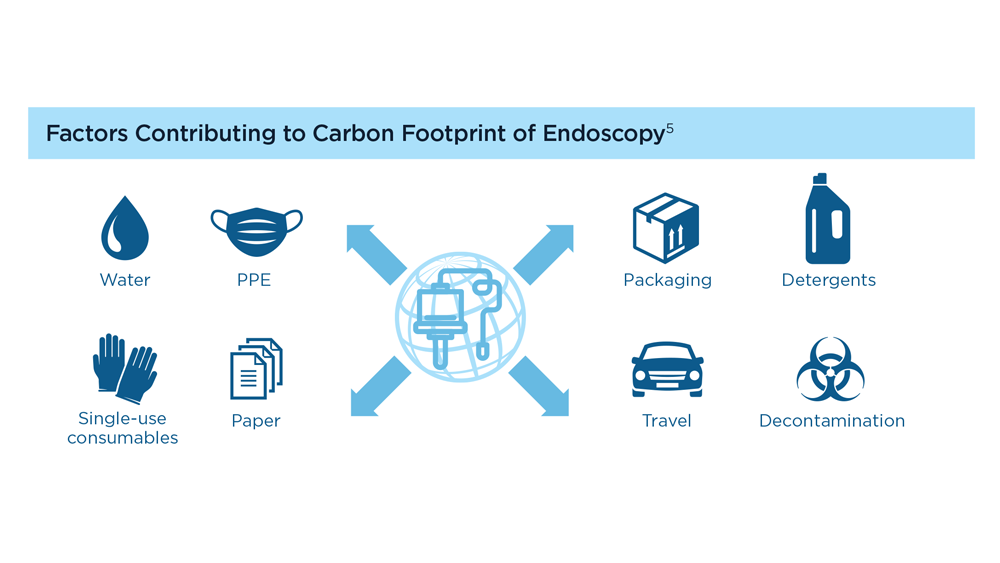
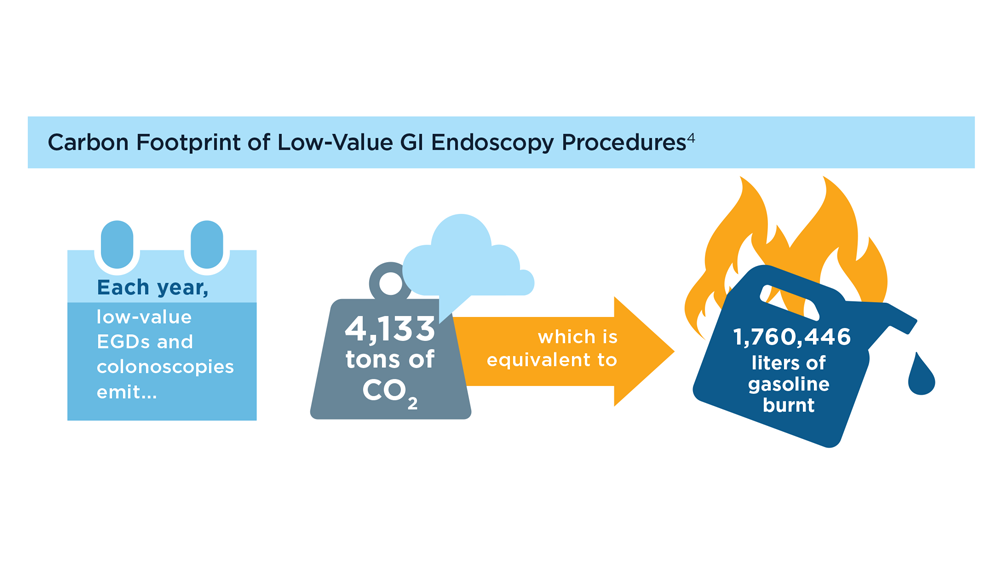
Gastroenterology and Climate Change: Assessing and Mitigating Impacts
- Karliner J et al. Eur J Public Health. 2020;30(suppl 5):v311. doi:10.1093/eurpub/ckaa165.843
- Vaccari M et al. Waste Manag Res. 2018;36(1):39-47. doi:10.1177/0734242X17739968
- Peery AF et al. Gastroenterology. 2019;156(1):254-272.e11. doi:10.1053/j.gastro.2018.08.063
- Sorge A et al. Endoscopy. 2023;55(suppl 2):S72-S73. https://www.esge.com/assets/downloads/pdfs/guidelines/ESGE_Days_2023.pdf
- Maurice JB et al. Lancet Gastroenterol Hepatol. 2020;5(7):636-638. doi:10.1016/S2468-1253(20)30157-6
- Gayam S. Am J Gastroenterol. 2020;115(12):1931-1932. doi:10.14309/ajg.0000000000001005
- Siau K et al. Tech Innov Gastrointest Endosc. 2021;23(4):344-352. doi:10.1016/j.tige.2021.06.005
- Namburar S et al. Gut. 2022;71(7):1326-1331. doi:10.1136/gutjnl-2021-324729
- Haddock R et al. Am J Gastroenterol. 2022;117(3):394-400. doi:10.14309/ajg.0000000000001604
- Donnelly MC et al. J Hepatol. 2022;76(5):995-1000. doi:10.1016/j.jhep.2022.02.01
- Leddin D, Macrae F. J Clin Gastroenterol. 2020;54(5):393-397. doi:10.1097/MCG.0000000000001336
- Pohl H et al. Hepatology. 2022;76(6):1836-1844. doi:10.1002/hep.32810
- Rodríguez de Santiago E et al. Endoscopy. 2022;54(8):797-826. doi:10.1055/a-1859-3726
- Sebastian S et al. Gut. 2023;72(1):12-26. doi:10.1136/gutjnl-2022-328460
- Cunha Neves JA et al. Gut. 2023;72(2):306-313. doi:10.1136/gutjnl-2022-327005
- Kaplan S et al. Issue Brief (Commonw Fund). 2012;29:1-14. PMID:23214181
- López-Muñoz P et al. Gut. 2023;gutjnl-2023-329544. doi:10.1136/gutjnl-2023-329544
- Karliner J et al. Eur J Public Health. 2020;30(suppl 5):v311. doi:10.1093/eurpub/ckaa165.843
- Vaccari M et al. Waste Manag Res. 2018;36(1):39-47. doi:10.1177/0734242X17739968
- Peery AF et al. Gastroenterology. 2019;156(1):254-272.e11. doi:10.1053/j.gastro.2018.08.063
- Sorge A et al. Endoscopy. 2023;55(suppl 2):S72-S73. https://www.esge.com/assets/downloads/pdfs/guidelines/ESGE_Days_2023.pdf
- Maurice JB et al. Lancet Gastroenterol Hepatol. 2020;5(7):636-638. doi:10.1016/S2468-1253(20)30157-6
- Gayam S. Am J Gastroenterol. 2020;115(12):1931-1932. doi:10.14309/ajg.0000000000001005
- Siau K et al. Tech Innov Gastrointest Endosc. 2021;23(4):344-352. doi:10.1016/j.tige.2021.06.005
- Namburar S et al. Gut. 2022;71(7):1326-1331. doi:10.1136/gutjnl-2021-324729
- Haddock R et al. Am J Gastroenterol. 2022;117(3):394-400. doi:10.14309/ajg.0000000000001604
- Donnelly MC et al. J Hepatol. 2022;76(5):995-1000. doi:10.1016/j.jhep.2022.02.01
- Leddin D, Macrae F. J Clin Gastroenterol. 2020;54(5):393-397. doi:10.1097/MCG.0000000000001336
- Pohl H et al. Hepatology. 2022;76(6):1836-1844. doi:10.1002/hep.32810
- Rodríguez de Santiago E et al. Endoscopy. 2022;54(8):797-826. doi:10.1055/a-1859-3726
- Sebastian S et al. Gut. 2023;72(1):12-26. doi:10.1136/gutjnl-2022-328460
- Cunha Neves JA et al. Gut. 2023;72(2):306-313. doi:10.1136/gutjnl-2022-327005
- Kaplan S et al. Issue Brief (Commonw Fund). 2012;29:1-14. PMID:23214181
- López-Muñoz P et al. Gut. 2023;gutjnl-2023-329544. doi:10.1136/gutjnl-2023-329544
- Karliner J et al. Eur J Public Health. 2020;30(suppl 5):v311. doi:10.1093/eurpub/ckaa165.843
- Vaccari M et al. Waste Manag Res. 2018;36(1):39-47. doi:10.1177/0734242X17739968
- Peery AF et al. Gastroenterology. 2019;156(1):254-272.e11. doi:10.1053/j.gastro.2018.08.063
- Sorge A et al. Endoscopy. 2023;55(suppl 2):S72-S73. https://www.esge.com/assets/downloads/pdfs/guidelines/ESGE_Days_2023.pdf
- Maurice JB et al. Lancet Gastroenterol Hepatol. 2020;5(7):636-638. doi:10.1016/S2468-1253(20)30157-6
- Gayam S. Am J Gastroenterol. 2020;115(12):1931-1932. doi:10.14309/ajg.0000000000001005
- Siau K et al. Tech Innov Gastrointest Endosc. 2021;23(4):344-352. doi:10.1016/j.tige.2021.06.005
- Namburar S et al. Gut. 2022;71(7):1326-1331. doi:10.1136/gutjnl-2021-324729
- Haddock R et al. Am J Gastroenterol. 2022;117(3):394-400. doi:10.14309/ajg.0000000000001604
- Donnelly MC et al. J Hepatol. 2022;76(5):995-1000. doi:10.1016/j.jhep.2022.02.01
- Leddin D, Macrae F. J Clin Gastroenterol. 2020;54(5):393-397. doi:10.1097/MCG.0000000000001336
- Pohl H et al. Hepatology. 2022;76(6):1836-1844. doi:10.1002/hep.32810
- Rodríguez de Santiago E et al. Endoscopy. 2022;54(8):797-826. doi:10.1055/a-1859-3726
- Sebastian S et al. Gut. 2023;72(1):12-26. doi:10.1136/gutjnl-2022-328460
- Cunha Neves JA et al. Gut. 2023;72(2):306-313. doi:10.1136/gutjnl-2022-327005
- Kaplan S et al. Issue Brief (Commonw Fund). 2012;29:1-14. PMID:23214181
- López-Muñoz P et al. Gut. 2023;gutjnl-2023-329544. doi:10.1136/gutjnl-2023-329544
Harnessing the Power of AI to Enhance Endoscopy: Promises and Pitfalls
- Jin Z et al. BioMed Eng OnLine. 2022;21(1):12. doi:10.1186/s12938-022-00979-
- Buendgens L, Cifci D, Ghaffari Laleh N, et al. Sci Rep. 2022;12(1):4829. doi:10.1038/s41598-022-08773-1
- Uche-Anya EN, Berzin TM. Artificial intelligence applications in colonoscopy. GI & Hepatology News. January 24, 2023. https://www.mdedge.com/gihepnews/article/260769/mixed-topics/artificial-intelligence-applications-colonoscopy
- Rondonotti E et al. Endoscopy. 2023;55(1):14-22. doi:10.1055/a-1852-0330
- Antonelli G et al. Ann Gastroenterol. 2023;36(2):114-122. doi:10.20524/aog.2023.0781
- van der Zander QEW et al. Endoscopy. 2021;53(12):1219-1226. doi:10.1055/a-1343-159
- Areia PM et al. Lancet Digital Health. 2022;4(6):e436-e444. doi:10.1016/S2589-7500(22)00042-5
- Sumiyama K et al. Dig Endosc. 2021;33(2):218-230. doi:10.1111/den.13837
- Berzin TM et al. Gastrointest Endosc. 2020;92(4):951-959. doi:10.1016/j.gie.2020.06.035
- Mori Y et al. Dig Endosc. 2023;35(4):422-429. doi:10.1111/den.14531
- Uche-Anya E et al. Gut. 2022;71(9):1909-1915. doi:10.1136/gutjnl-2021-326271
- Moor M et al. Nature. 2023;616(7956):259-265. 10.1038/s41586-023-05881-4
- Kather JN et al. NPJ Digit Med. 2022;5(1):90. doi:10.1038/s41746-022-00634-5
- Jin Z et al. BioMed Eng OnLine. 2022;21(1):12. doi:10.1186/s12938-022-00979-
- Buendgens L, Cifci D, Ghaffari Laleh N, et al. Sci Rep. 2022;12(1):4829. doi:10.1038/s41598-022-08773-1
- Uche-Anya EN, Berzin TM. Artificial intelligence applications in colonoscopy. GI & Hepatology News. January 24, 2023. https://www.mdedge.com/gihepnews/article/260769/mixed-topics/artificial-intelligence-applications-colonoscopy
- Rondonotti E et al. Endoscopy. 2023;55(1):14-22. doi:10.1055/a-1852-0330
- Antonelli G et al. Ann Gastroenterol. 2023;36(2):114-122. doi:10.20524/aog.2023.0781
- van der Zander QEW et al. Endoscopy. 2021;53(12):1219-1226. doi:10.1055/a-1343-159
- Areia PM et al. Lancet Digital Health. 2022;4(6):e436-e444. doi:10.1016/S2589-7500(22)00042-5
- Sumiyama K et al. Dig Endosc. 2021;33(2):218-230. doi:10.1111/den.13837
- Berzin TM et al. Gastrointest Endosc. 2020;92(4):951-959. doi:10.1016/j.gie.2020.06.035
- Mori Y et al. Dig Endosc. 2023;35(4):422-429. doi:10.1111/den.14531
- Uche-Anya E et al. Gut. 2022;71(9):1909-1915. doi:10.1136/gutjnl-2021-326271
- Moor M et al. Nature. 2023;616(7956):259-265. 10.1038/s41586-023-05881-4
- Kather JN et al. NPJ Digit Med. 2022;5(1):90. doi:10.1038/s41746-022-00634-5
- Jin Z et al. BioMed Eng OnLine. 2022;21(1):12. doi:10.1186/s12938-022-00979-
- Buendgens L, Cifci D, Ghaffari Laleh N, et al. Sci Rep. 2022;12(1):4829. doi:10.1038/s41598-022-08773-1
- Uche-Anya EN, Berzin TM. Artificial intelligence applications in colonoscopy. GI & Hepatology News. January 24, 2023. https://www.mdedge.com/gihepnews/article/260769/mixed-topics/artificial-intelligence-applications-colonoscopy
- Rondonotti E et al. Endoscopy. 2023;55(1):14-22. doi:10.1055/a-1852-0330
- Antonelli G et al. Ann Gastroenterol. 2023;36(2):114-122. doi:10.20524/aog.2023.0781
- van der Zander QEW et al. Endoscopy. 2021;53(12):1219-1226. doi:10.1055/a-1343-159
- Areia PM et al. Lancet Digital Health. 2022;4(6):e436-e444. doi:10.1016/S2589-7500(22)00042-5
- Sumiyama K et al. Dig Endosc. 2021;33(2):218-230. doi:10.1111/den.13837
- Berzin TM et al. Gastrointest Endosc. 2020;92(4):951-959. doi:10.1016/j.gie.2020.06.035
- Mori Y et al. Dig Endosc. 2023;35(4):422-429. doi:10.1111/den.14531
- Uche-Anya E et al. Gut. 2022;71(9):1909-1915. doi:10.1136/gutjnl-2021-326271
- Moor M et al. Nature. 2023;616(7956):259-265. 10.1038/s41586-023-05881-4
- Kather JN et al. NPJ Digit Med. 2022;5(1):90. doi:10.1038/s41746-022-00634-5
EASD 2023: A deeper dive into type 1 and type 2 diabetes
Noteworthy at the meeting, taking place Oct. 3-6, in Hamburg, Germany, will be final detailed data from the SURMOUNT-4 trial of the “twincretin” tirzepatide (Mounjaro, Lilly) on obesity. The top-line results, announced by the company in July, showed an average 21.1% weight loss at 36 weeks with tirzepatide injections once weekly among adults with overweight or obesity. The drug is approved in the United States and Europe for treating type 2 diabetes, and approval for obesity is expected in the United States later this year.
In addition, a symposium will present a new EASD/American Diabetes Association (ADA) consensus report, Hyperglycaemic Crisis in Adult Patients with Diabetes, scheduled to be simultaneously published in Diabetologia and Diabetes Care on Oct. 6.
Aside from those, much of the EASD meeting content will feature smaller studies on both type 2 and type 1 diabetes, along with award lectures, symposia, debates, and lots of discussion on hot topics in diabetes and clinical challenges including complications. In essence, it will provide a forum for in-depth follow-up to the jam-packed clinical trial–filled agenda at the ADA meeting in June, said EASD Honorary Secretary Tina Vilsbøll, MD, clinical professor and head of clinic at the Steno Diabetes Center, Copenhagen.
“There were so many large trials at ADA that we just took them in without really having a chance to discuss them. ... There’s so much to discuss with all these new treatments, how do we place them in obesity and diabetes? ... All the data that we have from ADA will make good discussions at EASD,” Dr. Vilsbøll said in an interview.
Indeed, said EASD President Chantal Mathieu, MD, PhD, chair of endocrinology at University Hospital Gasthuisberg Leuven, Belgium, “We always come after ADA. That puts us in a position where we can take deeper dives into the data. ... EASD is a calmer meeting where you can really look at the details.”
Type 2 diabetes: Disease modifying in many ways
Dr. Mathieu told this news organization that a unifying theme for much of the EASD meeting’s content is “We are now entering the era of disease-modifying and disease-disrupting therapies” in both diabetes types.
In type 2, this means “getting to the root, which is obesity, so you’ll see a lot of presentations on the incretin system, but you also don’t get type 2 diabetes if you have an iron-clad beta cell. ... So, we also gave a lot of attention to basic translational research that helps us to understand the role of the beta cell in type 2 diabetes.”
In addition to SURMOUNT-4, there will be oral abstract sessions with follow-up data from the SURPASS series of studies of tirzepatide in type 2 diabetes, other abstract sessions, symposia about incretins and obesity, and an oral abstract session on beta cell function in both diabetes types.
Three debates will address controversial questions in the type 2 diabetes arena. In one, speakers will take opposite sides on “Initial combined therapy for type 2 diabetes: Should diabetes follow hypertension?”
In another, speakers will argue over “Is lasting remission of type 2 diabetes feasible in the real-world setting?” That’s an important question, Dr. Vilsbøll said.
“A person might be able to have a remission but go back if they regain the weight. Do we really have remission? How do we define it? Now, suddenly, we have tools to help people go in the right direction. Now we’re in a place where we can actually help our patients with their cravings and their body weight and all that. It’s more fun to discuss when we have the tools.”
A third debate will tackle the question of whether all people with type 2 diabetes and chronic kidney disease should be on [sodium-glucose co-transporter 2] (SGLT2) inhibitors “by default.”
The Minkowski Prize Lecture will address the regulation of energy and glucose metabolism by the dual incretin receptor agonists, while the EASD-Lilly Anniversary Prize Lecture will be about the role of ectopic lipid in insulin resistance and cardiometabolic disease.
Type 1 diabetes: Both disease modifying and disruptive
For type 1 diabetes, “disease-modifying” and “disruptive” approaches on the meeting agenda include new data on immune modulation for people in early stages in order to prevent or delay insulin dependence, islet transplantation including the use of stem cell–derived beta cells, and the latest in technology including automated insulin delivery systems, also known colloquially as the “artificial pancreas.”
Prize lectures about type 1 diabetes will include the Claude Bernard Lecture, on etiologies of autoimmune diabetes, the Albert Renold Lecture, on “disrupted RNA editing as a path to type 1 diabetes,” and the EASD/Novo Nordisk Foundation Diabetes Prize for Excellence Lecture on automated insulin delivery.
Focus on complications: The known and the emerging
The meeting also will focus a great deal on complications of diabetes, including the well-studied cardiovascular disease, neuropathy, nephropathy, retinopathy, and fatty liver disease as well as others that typically receive less attention, such as gastrointestinal problems and cardiomyopathy.
Another debate will address the question “Is it time to reclassify diabetes complications because microvascular and macrovascular classification is no longer sufficient?” And, the Camillo Golgi Lecture will cover “Diabetes Complications: From Classical to Emerging.”
As always, there’s much more on the agenda including pregnancy and diabetes, cystic fibrosis–derived diabetes, mental health in diabetes, COVID-19 and diabetes, hypoglycemia, and hypoglycemia unawareness.
According to Dr. Vilsbøll, “Clinicians should come and enjoy all the great science we have, interact, and be inspired.”
Dr. Vilsbøll has served on scientific advisory panels, been part of speaker bureaus, and served as a consultant to and/or received research support from Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Gilead, GSK, Mundipharma, Novo Nordisk, Sanofi, and Sun Pharmaceuticals. Dr. Mathieu serves or has served on the advisory panel for Novo Nordisk, Sanofi, Merck Sharp and Dohme Ltd., Eli Lilly and Company, Novartis, AstraZeneca, Boehringer Ingelheim, Roche, Medtronic, ActoBio Therapeutics, Pfizer, Imcyse, Insulet, Zealand Pharma, Avotres, Mannkind, Sandoz, and Vertex. She has served on the speakers bureau for Novo Nordisk, Sanofi, Eli Lilly and Company, Boehringer Ingelheim, AstraZeneca, and Novartis. Financial compensation for these activities has been received by KU Leuven.
A version of this article appeared on Medscape.com.
Noteworthy at the meeting, taking place Oct. 3-6, in Hamburg, Germany, will be final detailed data from the SURMOUNT-4 trial of the “twincretin” tirzepatide (Mounjaro, Lilly) on obesity. The top-line results, announced by the company in July, showed an average 21.1% weight loss at 36 weeks with tirzepatide injections once weekly among adults with overweight or obesity. The drug is approved in the United States and Europe for treating type 2 diabetes, and approval for obesity is expected in the United States later this year.
In addition, a symposium will present a new EASD/American Diabetes Association (ADA) consensus report, Hyperglycaemic Crisis in Adult Patients with Diabetes, scheduled to be simultaneously published in Diabetologia and Diabetes Care on Oct. 6.
Aside from those, much of the EASD meeting content will feature smaller studies on both type 2 and type 1 diabetes, along with award lectures, symposia, debates, and lots of discussion on hot topics in diabetes and clinical challenges including complications. In essence, it will provide a forum for in-depth follow-up to the jam-packed clinical trial–filled agenda at the ADA meeting in June, said EASD Honorary Secretary Tina Vilsbøll, MD, clinical professor and head of clinic at the Steno Diabetes Center, Copenhagen.
“There were so many large trials at ADA that we just took them in without really having a chance to discuss them. ... There’s so much to discuss with all these new treatments, how do we place them in obesity and diabetes? ... All the data that we have from ADA will make good discussions at EASD,” Dr. Vilsbøll said in an interview.
Indeed, said EASD President Chantal Mathieu, MD, PhD, chair of endocrinology at University Hospital Gasthuisberg Leuven, Belgium, “We always come after ADA. That puts us in a position where we can take deeper dives into the data. ... EASD is a calmer meeting where you can really look at the details.”
Type 2 diabetes: Disease modifying in many ways
Dr. Mathieu told this news organization that a unifying theme for much of the EASD meeting’s content is “We are now entering the era of disease-modifying and disease-disrupting therapies” in both diabetes types.
In type 2, this means “getting to the root, which is obesity, so you’ll see a lot of presentations on the incretin system, but you also don’t get type 2 diabetes if you have an iron-clad beta cell. ... So, we also gave a lot of attention to basic translational research that helps us to understand the role of the beta cell in type 2 diabetes.”
In addition to SURMOUNT-4, there will be oral abstract sessions with follow-up data from the SURPASS series of studies of tirzepatide in type 2 diabetes, other abstract sessions, symposia about incretins and obesity, and an oral abstract session on beta cell function in both diabetes types.
Three debates will address controversial questions in the type 2 diabetes arena. In one, speakers will take opposite sides on “Initial combined therapy for type 2 diabetes: Should diabetes follow hypertension?”
In another, speakers will argue over “Is lasting remission of type 2 diabetes feasible in the real-world setting?” That’s an important question, Dr. Vilsbøll said.
“A person might be able to have a remission but go back if they regain the weight. Do we really have remission? How do we define it? Now, suddenly, we have tools to help people go in the right direction. Now we’re in a place where we can actually help our patients with their cravings and their body weight and all that. It’s more fun to discuss when we have the tools.”
A third debate will tackle the question of whether all people with type 2 diabetes and chronic kidney disease should be on [sodium-glucose co-transporter 2] (SGLT2) inhibitors “by default.”
The Minkowski Prize Lecture will address the regulation of energy and glucose metabolism by the dual incretin receptor agonists, while the EASD-Lilly Anniversary Prize Lecture will be about the role of ectopic lipid in insulin resistance and cardiometabolic disease.
Type 1 diabetes: Both disease modifying and disruptive
For type 1 diabetes, “disease-modifying” and “disruptive” approaches on the meeting agenda include new data on immune modulation for people in early stages in order to prevent or delay insulin dependence, islet transplantation including the use of stem cell–derived beta cells, and the latest in technology including automated insulin delivery systems, also known colloquially as the “artificial pancreas.”
Prize lectures about type 1 diabetes will include the Claude Bernard Lecture, on etiologies of autoimmune diabetes, the Albert Renold Lecture, on “disrupted RNA editing as a path to type 1 diabetes,” and the EASD/Novo Nordisk Foundation Diabetes Prize for Excellence Lecture on automated insulin delivery.
Focus on complications: The known and the emerging
The meeting also will focus a great deal on complications of diabetes, including the well-studied cardiovascular disease, neuropathy, nephropathy, retinopathy, and fatty liver disease as well as others that typically receive less attention, such as gastrointestinal problems and cardiomyopathy.
Another debate will address the question “Is it time to reclassify diabetes complications because microvascular and macrovascular classification is no longer sufficient?” And, the Camillo Golgi Lecture will cover “Diabetes Complications: From Classical to Emerging.”
As always, there’s much more on the agenda including pregnancy and diabetes, cystic fibrosis–derived diabetes, mental health in diabetes, COVID-19 and diabetes, hypoglycemia, and hypoglycemia unawareness.
According to Dr. Vilsbøll, “Clinicians should come and enjoy all the great science we have, interact, and be inspired.”
Dr. Vilsbøll has served on scientific advisory panels, been part of speaker bureaus, and served as a consultant to and/or received research support from Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Gilead, GSK, Mundipharma, Novo Nordisk, Sanofi, and Sun Pharmaceuticals. Dr. Mathieu serves or has served on the advisory panel for Novo Nordisk, Sanofi, Merck Sharp and Dohme Ltd., Eli Lilly and Company, Novartis, AstraZeneca, Boehringer Ingelheim, Roche, Medtronic, ActoBio Therapeutics, Pfizer, Imcyse, Insulet, Zealand Pharma, Avotres, Mannkind, Sandoz, and Vertex. She has served on the speakers bureau for Novo Nordisk, Sanofi, Eli Lilly and Company, Boehringer Ingelheim, AstraZeneca, and Novartis. Financial compensation for these activities has been received by KU Leuven.
A version of this article appeared on Medscape.com.
Noteworthy at the meeting, taking place Oct. 3-6, in Hamburg, Germany, will be final detailed data from the SURMOUNT-4 trial of the “twincretin” tirzepatide (Mounjaro, Lilly) on obesity. The top-line results, announced by the company in July, showed an average 21.1% weight loss at 36 weeks with tirzepatide injections once weekly among adults with overweight or obesity. The drug is approved in the United States and Europe for treating type 2 diabetes, and approval for obesity is expected in the United States later this year.
In addition, a symposium will present a new EASD/American Diabetes Association (ADA) consensus report, Hyperglycaemic Crisis in Adult Patients with Diabetes, scheduled to be simultaneously published in Diabetologia and Diabetes Care on Oct. 6.
Aside from those, much of the EASD meeting content will feature smaller studies on both type 2 and type 1 diabetes, along with award lectures, symposia, debates, and lots of discussion on hot topics in diabetes and clinical challenges including complications. In essence, it will provide a forum for in-depth follow-up to the jam-packed clinical trial–filled agenda at the ADA meeting in June, said EASD Honorary Secretary Tina Vilsbøll, MD, clinical professor and head of clinic at the Steno Diabetes Center, Copenhagen.
“There were so many large trials at ADA that we just took them in without really having a chance to discuss them. ... There’s so much to discuss with all these new treatments, how do we place them in obesity and diabetes? ... All the data that we have from ADA will make good discussions at EASD,” Dr. Vilsbøll said in an interview.
Indeed, said EASD President Chantal Mathieu, MD, PhD, chair of endocrinology at University Hospital Gasthuisberg Leuven, Belgium, “We always come after ADA. That puts us in a position where we can take deeper dives into the data. ... EASD is a calmer meeting where you can really look at the details.”
Type 2 diabetes: Disease modifying in many ways
Dr. Mathieu told this news organization that a unifying theme for much of the EASD meeting’s content is “We are now entering the era of disease-modifying and disease-disrupting therapies” in both diabetes types.
In type 2, this means “getting to the root, which is obesity, so you’ll see a lot of presentations on the incretin system, but you also don’t get type 2 diabetes if you have an iron-clad beta cell. ... So, we also gave a lot of attention to basic translational research that helps us to understand the role of the beta cell in type 2 diabetes.”
In addition to SURMOUNT-4, there will be oral abstract sessions with follow-up data from the SURPASS series of studies of tirzepatide in type 2 diabetes, other abstract sessions, symposia about incretins and obesity, and an oral abstract session on beta cell function in both diabetes types.
Three debates will address controversial questions in the type 2 diabetes arena. In one, speakers will take opposite sides on “Initial combined therapy for type 2 diabetes: Should diabetes follow hypertension?”
In another, speakers will argue over “Is lasting remission of type 2 diabetes feasible in the real-world setting?” That’s an important question, Dr. Vilsbøll said.
“A person might be able to have a remission but go back if they regain the weight. Do we really have remission? How do we define it? Now, suddenly, we have tools to help people go in the right direction. Now we’re in a place where we can actually help our patients with their cravings and their body weight and all that. It’s more fun to discuss when we have the tools.”
A third debate will tackle the question of whether all people with type 2 diabetes and chronic kidney disease should be on [sodium-glucose co-transporter 2] (SGLT2) inhibitors “by default.”
The Minkowski Prize Lecture will address the regulation of energy and glucose metabolism by the dual incretin receptor agonists, while the EASD-Lilly Anniversary Prize Lecture will be about the role of ectopic lipid in insulin resistance and cardiometabolic disease.
Type 1 diabetes: Both disease modifying and disruptive
For type 1 diabetes, “disease-modifying” and “disruptive” approaches on the meeting agenda include new data on immune modulation for people in early stages in order to prevent or delay insulin dependence, islet transplantation including the use of stem cell–derived beta cells, and the latest in technology including automated insulin delivery systems, also known colloquially as the “artificial pancreas.”
Prize lectures about type 1 diabetes will include the Claude Bernard Lecture, on etiologies of autoimmune diabetes, the Albert Renold Lecture, on “disrupted RNA editing as a path to type 1 diabetes,” and the EASD/Novo Nordisk Foundation Diabetes Prize for Excellence Lecture on automated insulin delivery.
Focus on complications: The known and the emerging
The meeting also will focus a great deal on complications of diabetes, including the well-studied cardiovascular disease, neuropathy, nephropathy, retinopathy, and fatty liver disease as well as others that typically receive less attention, such as gastrointestinal problems and cardiomyopathy.
Another debate will address the question “Is it time to reclassify diabetes complications because microvascular and macrovascular classification is no longer sufficient?” And, the Camillo Golgi Lecture will cover “Diabetes Complications: From Classical to Emerging.”
As always, there’s much more on the agenda including pregnancy and diabetes, cystic fibrosis–derived diabetes, mental health in diabetes, COVID-19 and diabetes, hypoglycemia, and hypoglycemia unawareness.
According to Dr. Vilsbøll, “Clinicians should come and enjoy all the great science we have, interact, and be inspired.”
Dr. Vilsbøll has served on scientific advisory panels, been part of speaker bureaus, and served as a consultant to and/or received research support from Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Gilead, GSK, Mundipharma, Novo Nordisk, Sanofi, and Sun Pharmaceuticals. Dr. Mathieu serves or has served on the advisory panel for Novo Nordisk, Sanofi, Merck Sharp and Dohme Ltd., Eli Lilly and Company, Novartis, AstraZeneca, Boehringer Ingelheim, Roche, Medtronic, ActoBio Therapeutics, Pfizer, Imcyse, Insulet, Zealand Pharma, Avotres, Mannkind, Sandoz, and Vertex. She has served on the speakers bureau for Novo Nordisk, Sanofi, Eli Lilly and Company, Boehringer Ingelheim, AstraZeneca, and Novartis. Financial compensation for these activities has been received by KU Leuven.
A version of this article appeared on Medscape.com.
FROM EASD 2023
Older women who get mammograms risk overdiagnosis
TOPLINE:
Women who continue breast cancer screening after age 70 face a considerable risk for overdiagnosis.
METHODOLOGY:
- Overdiagnosis – the risk of detecting and treating cancers that would never have caused issues in a person’s lifetime – is increasingly recognized as a harm of breast cancer screening; however, the scope of the problem among older women remains uncertain.
- To get an idea, investigators linked Medicare claims data with Surveillance, Epidemiology, and End Results (SEER) data for 54,635 women 70 years or older to compare the incidence of breast cancer and breast cancer–specific death among women who continued screening mammography with those who did not.
- The women all had undergone recent screening mammograms and had no history of breast cancer at study entry. Those who had a subsequent mammogram within 3 years were classified as undergoing continued screening while those who did not were classified as not undergoing continued screening.
- Overdiagnosis was defined as the difference in cumulative incidence of breast cancer between screened and unscreened women divided by the cumulative incidence among screened women.
- Results were adjusted for potential confounders, including age, race, and ethnicity.
TAKEAWAY:
- Over 80% of women 70-84 years old and more than 60% of women 85 years or older continued screening.
- Among women 70-74 years old, the adjusted cumulative incidence of breast cancer was 6.1 cases per 100 screened women vs. 4.2 cases per 100 unscreened women; for women aged 75-84 years old, the cumulative incidence was 4.9 per 100 screened women vs. 2.6 per 100 unscreened women, and for women 85 years and older, the cumulative incidence was 2.8 vs. 1.3 per 100, respectively.
- Estimates of overdiagnosis ranged from 31% of breast cancer cases among screened women in the 70-74 age group to 54% of cases in the 85 and older group.
- The researchers found no statistically significant reduction in breast cancer–specific death associated with screening in any age or life-expectancy group. Overdiagnosis appeared to be driven by in situ and localized invasive breast cancer, not advanced breast cancer.
IN PRACTICE:
The proportion of older women who continue to receive screening mammograms and may experience breast cancer overdiagnosis is “considerable” and “increases with advancing age and with decreasing life expectancy,” the authors conclude. Given potential benefits and harms of screening in this population, “patient preferences, including risk tolerance, comfort with uncertainty, and willingness to undergo treatment, are important for informing screening decisions.”
SOURCE:
The study was led by Ilana Richman, MD, MHS, of the Yale School of Medicine, New Haven, Connecticut, and published in the Annals of Internal Medicine.
LIMITATIONS:
The definition of screening mammography in the study may have misclassified some diagnostic mammograms as screening. Using a more conservative definition of screening mammogram, which largely accounted for this misclassification, estimates for overdiagnosis were smaller, ranging from 15% of cases in the 70-74 age group to 44% of cases in the 85 and older group. Results could not be adjusted for breast density, family history, and other breast cancer risk factors not captured by the data.
DISCLOSURES:
The work was funded by the National Cancer Institute. One author reported funding from Genentech and Johnson & Johnson.
A version of this article first appeared on Medscape.com.
TOPLINE:
Women who continue breast cancer screening after age 70 face a considerable risk for overdiagnosis.
METHODOLOGY:
- Overdiagnosis – the risk of detecting and treating cancers that would never have caused issues in a person’s lifetime – is increasingly recognized as a harm of breast cancer screening; however, the scope of the problem among older women remains uncertain.
- To get an idea, investigators linked Medicare claims data with Surveillance, Epidemiology, and End Results (SEER) data for 54,635 women 70 years or older to compare the incidence of breast cancer and breast cancer–specific death among women who continued screening mammography with those who did not.
- The women all had undergone recent screening mammograms and had no history of breast cancer at study entry. Those who had a subsequent mammogram within 3 years were classified as undergoing continued screening while those who did not were classified as not undergoing continued screening.
- Overdiagnosis was defined as the difference in cumulative incidence of breast cancer between screened and unscreened women divided by the cumulative incidence among screened women.
- Results were adjusted for potential confounders, including age, race, and ethnicity.
TAKEAWAY:
- Over 80% of women 70-84 years old and more than 60% of women 85 years or older continued screening.
- Among women 70-74 years old, the adjusted cumulative incidence of breast cancer was 6.1 cases per 100 screened women vs. 4.2 cases per 100 unscreened women; for women aged 75-84 years old, the cumulative incidence was 4.9 per 100 screened women vs. 2.6 per 100 unscreened women, and for women 85 years and older, the cumulative incidence was 2.8 vs. 1.3 per 100, respectively.
- Estimates of overdiagnosis ranged from 31% of breast cancer cases among screened women in the 70-74 age group to 54% of cases in the 85 and older group.
- The researchers found no statistically significant reduction in breast cancer–specific death associated with screening in any age or life-expectancy group. Overdiagnosis appeared to be driven by in situ and localized invasive breast cancer, not advanced breast cancer.
IN PRACTICE:
The proportion of older women who continue to receive screening mammograms and may experience breast cancer overdiagnosis is “considerable” and “increases with advancing age and with decreasing life expectancy,” the authors conclude. Given potential benefits and harms of screening in this population, “patient preferences, including risk tolerance, comfort with uncertainty, and willingness to undergo treatment, are important for informing screening decisions.”
SOURCE:
The study was led by Ilana Richman, MD, MHS, of the Yale School of Medicine, New Haven, Connecticut, and published in the Annals of Internal Medicine.
LIMITATIONS:
The definition of screening mammography in the study may have misclassified some diagnostic mammograms as screening. Using a more conservative definition of screening mammogram, which largely accounted for this misclassification, estimates for overdiagnosis were smaller, ranging from 15% of cases in the 70-74 age group to 44% of cases in the 85 and older group. Results could not be adjusted for breast density, family history, and other breast cancer risk factors not captured by the data.
DISCLOSURES:
The work was funded by the National Cancer Institute. One author reported funding from Genentech and Johnson & Johnson.
A version of this article first appeared on Medscape.com.
TOPLINE:
Women who continue breast cancer screening after age 70 face a considerable risk for overdiagnosis.
METHODOLOGY:
- Overdiagnosis – the risk of detecting and treating cancers that would never have caused issues in a person’s lifetime – is increasingly recognized as a harm of breast cancer screening; however, the scope of the problem among older women remains uncertain.
- To get an idea, investigators linked Medicare claims data with Surveillance, Epidemiology, and End Results (SEER) data for 54,635 women 70 years or older to compare the incidence of breast cancer and breast cancer–specific death among women who continued screening mammography with those who did not.
- The women all had undergone recent screening mammograms and had no history of breast cancer at study entry. Those who had a subsequent mammogram within 3 years were classified as undergoing continued screening while those who did not were classified as not undergoing continued screening.
- Overdiagnosis was defined as the difference in cumulative incidence of breast cancer between screened and unscreened women divided by the cumulative incidence among screened women.
- Results were adjusted for potential confounders, including age, race, and ethnicity.
TAKEAWAY:
- Over 80% of women 70-84 years old and more than 60% of women 85 years or older continued screening.
- Among women 70-74 years old, the adjusted cumulative incidence of breast cancer was 6.1 cases per 100 screened women vs. 4.2 cases per 100 unscreened women; for women aged 75-84 years old, the cumulative incidence was 4.9 per 100 screened women vs. 2.6 per 100 unscreened women, and for women 85 years and older, the cumulative incidence was 2.8 vs. 1.3 per 100, respectively.
- Estimates of overdiagnosis ranged from 31% of breast cancer cases among screened women in the 70-74 age group to 54% of cases in the 85 and older group.
- The researchers found no statistically significant reduction in breast cancer–specific death associated with screening in any age or life-expectancy group. Overdiagnosis appeared to be driven by in situ and localized invasive breast cancer, not advanced breast cancer.
IN PRACTICE:
The proportion of older women who continue to receive screening mammograms and may experience breast cancer overdiagnosis is “considerable” and “increases with advancing age and with decreasing life expectancy,” the authors conclude. Given potential benefits and harms of screening in this population, “patient preferences, including risk tolerance, comfort with uncertainty, and willingness to undergo treatment, are important for informing screening decisions.”
SOURCE:
The study was led by Ilana Richman, MD, MHS, of the Yale School of Medicine, New Haven, Connecticut, and published in the Annals of Internal Medicine.
LIMITATIONS:
The definition of screening mammography in the study may have misclassified some diagnostic mammograms as screening. Using a more conservative definition of screening mammogram, which largely accounted for this misclassification, estimates for overdiagnosis were smaller, ranging from 15% of cases in the 70-74 age group to 44% of cases in the 85 and older group. Results could not be adjusted for breast density, family history, and other breast cancer risk factors not captured by the data.
DISCLOSURES:
The work was funded by the National Cancer Institute. One author reported funding from Genentech and Johnson & Johnson.
A version of this article first appeared on Medscape.com.