User login
AGA issues CPU for CRC screening, postpolypectomy surveillance
Led by Rachel B. Issaka, MD, of Fred Hutchinson Cancer Center, Seattle, the Clinical Practice Update focuses primarily on time frames for surveillance based on known risk factors, plus a caution against widespread use of emerging risk-stratification tools that need more real-world evidence among diverse populations.
“Based on current evidence, risk stratification for initiating CRC screening or surveillance should be based on age, family history, predisposing hereditary CRC syndromes, prior screening, or other CRC predisposing conditions,” the authors wrote in Gastroenterology.
With these parameters in mind, Dr. Issaka and colleagues issued nine best practice advice statements, noting that systematic reviews were not conducted, so statements are not rated based on quality of evidence or strength of presented considerations.
To begin, the investigators characterized two risk strata for CRC. Individuals with a first-degree relative who was diagnosed with CRC have an increased risk of CRC, particularly if that relative was diagnosed before age 50. In contrast, people with no such family history, or a personal history of CRC, hereditary CRC syndromes, inflammatory bowel disease, or other predisposing conditions, have average risk for CRC.
Those with average risk should start CRC screening at age 45, while those with high risk should start screening at age 40, or 10 years before the age of diagnosis of their youngest affected relative, whichever is sooner.
“The age to initiate screening according to family history of CRC could be optimized based on the number of affected family members, age at diagnosis of the affected relatives, as well as the 10-year cumulative incidence of CRC according to age within a specific source population (e.g., country),” the investigators wrote. “However, in the absence of widely available risk calculators developed for such risk-adapted screenings, a simplified approach to consider is initiating screening approximately 10 years before the age of diagnosis of the youngest affected relative or at age 40 years.”
The decision to screen and conduct postpolypectomy surveillance beyond age 75 should factor in risks, benefits, screening history, and comorbidities.
According to Dr. Issaka and colleagues, individuals with average risk can choose between several options for screening based on preference and availability, including fecal immunochemical test, colonoscopy, flexible sigmoidoscopy plus fecal immunochemical test, multitarget stool DNA fecal immunochemical test, and computed tomography colonography. Those with high risk, however, should undergo colonoscopy.
The final best practice advice statement offers a word of caution against widespread use of new risk-stratification tools for CRC and postpolypectomy surveillance that have yet to demonstrate real-world effectiveness and cost-effectiveness in diverse populations.
“Validation within diverse racial and ethnic populations is critical for models that include genetic factors, because genetic discovery studies have focused largely on individuals with European ancestry, and because risk-relevant genetic factors may vary according to individual’s origin of genetic ancestry,” the investigators wrote. “Although many studies differentiate individuals by race and ethnicity, which may capture some information about the likely presence of certain genetic variants, ancestry is a better predictor and should be captured in validation studies.”
The update was commissioned and approved by the AGA, and supported by the National Cancer Institute of the National Institutes of Health. The investigators disclosed relationships with Geneoscopy, CellMax Life, Universal Diagnostics, and others.
Led by Rachel B. Issaka, MD, of Fred Hutchinson Cancer Center, Seattle, the Clinical Practice Update focuses primarily on time frames for surveillance based on known risk factors, plus a caution against widespread use of emerging risk-stratification tools that need more real-world evidence among diverse populations.
“Based on current evidence, risk stratification for initiating CRC screening or surveillance should be based on age, family history, predisposing hereditary CRC syndromes, prior screening, or other CRC predisposing conditions,” the authors wrote in Gastroenterology.
With these parameters in mind, Dr. Issaka and colleagues issued nine best practice advice statements, noting that systematic reviews were not conducted, so statements are not rated based on quality of evidence or strength of presented considerations.
To begin, the investigators characterized two risk strata for CRC. Individuals with a first-degree relative who was diagnosed with CRC have an increased risk of CRC, particularly if that relative was diagnosed before age 50. In contrast, people with no such family history, or a personal history of CRC, hereditary CRC syndromes, inflammatory bowel disease, or other predisposing conditions, have average risk for CRC.
Those with average risk should start CRC screening at age 45, while those with high risk should start screening at age 40, or 10 years before the age of diagnosis of their youngest affected relative, whichever is sooner.
“The age to initiate screening according to family history of CRC could be optimized based on the number of affected family members, age at diagnosis of the affected relatives, as well as the 10-year cumulative incidence of CRC according to age within a specific source population (e.g., country),” the investigators wrote. “However, in the absence of widely available risk calculators developed for such risk-adapted screenings, a simplified approach to consider is initiating screening approximately 10 years before the age of diagnosis of the youngest affected relative or at age 40 years.”
The decision to screen and conduct postpolypectomy surveillance beyond age 75 should factor in risks, benefits, screening history, and comorbidities.
According to Dr. Issaka and colleagues, individuals with average risk can choose between several options for screening based on preference and availability, including fecal immunochemical test, colonoscopy, flexible sigmoidoscopy plus fecal immunochemical test, multitarget stool DNA fecal immunochemical test, and computed tomography colonography. Those with high risk, however, should undergo colonoscopy.
The final best practice advice statement offers a word of caution against widespread use of new risk-stratification tools for CRC and postpolypectomy surveillance that have yet to demonstrate real-world effectiveness and cost-effectiveness in diverse populations.
“Validation within diverse racial and ethnic populations is critical for models that include genetic factors, because genetic discovery studies have focused largely on individuals with European ancestry, and because risk-relevant genetic factors may vary according to individual’s origin of genetic ancestry,” the investigators wrote. “Although many studies differentiate individuals by race and ethnicity, which may capture some information about the likely presence of certain genetic variants, ancestry is a better predictor and should be captured in validation studies.”
The update was commissioned and approved by the AGA, and supported by the National Cancer Institute of the National Institutes of Health. The investigators disclosed relationships with Geneoscopy, CellMax Life, Universal Diagnostics, and others.
Led by Rachel B. Issaka, MD, of Fred Hutchinson Cancer Center, Seattle, the Clinical Practice Update focuses primarily on time frames for surveillance based on known risk factors, plus a caution against widespread use of emerging risk-stratification tools that need more real-world evidence among diverse populations.
“Based on current evidence, risk stratification for initiating CRC screening or surveillance should be based on age, family history, predisposing hereditary CRC syndromes, prior screening, or other CRC predisposing conditions,” the authors wrote in Gastroenterology.
With these parameters in mind, Dr. Issaka and colleagues issued nine best practice advice statements, noting that systematic reviews were not conducted, so statements are not rated based on quality of evidence or strength of presented considerations.
To begin, the investigators characterized two risk strata for CRC. Individuals with a first-degree relative who was diagnosed with CRC have an increased risk of CRC, particularly if that relative was diagnosed before age 50. In contrast, people with no such family history, or a personal history of CRC, hereditary CRC syndromes, inflammatory bowel disease, or other predisposing conditions, have average risk for CRC.
Those with average risk should start CRC screening at age 45, while those with high risk should start screening at age 40, or 10 years before the age of diagnosis of their youngest affected relative, whichever is sooner.
“The age to initiate screening according to family history of CRC could be optimized based on the number of affected family members, age at diagnosis of the affected relatives, as well as the 10-year cumulative incidence of CRC according to age within a specific source population (e.g., country),” the investigators wrote. “However, in the absence of widely available risk calculators developed for such risk-adapted screenings, a simplified approach to consider is initiating screening approximately 10 years before the age of diagnosis of the youngest affected relative or at age 40 years.”
The decision to screen and conduct postpolypectomy surveillance beyond age 75 should factor in risks, benefits, screening history, and comorbidities.
According to Dr. Issaka and colleagues, individuals with average risk can choose between several options for screening based on preference and availability, including fecal immunochemical test, colonoscopy, flexible sigmoidoscopy plus fecal immunochemical test, multitarget stool DNA fecal immunochemical test, and computed tomography colonography. Those with high risk, however, should undergo colonoscopy.
The final best practice advice statement offers a word of caution against widespread use of new risk-stratification tools for CRC and postpolypectomy surveillance that have yet to demonstrate real-world effectiveness and cost-effectiveness in diverse populations.
“Validation within diverse racial and ethnic populations is critical for models that include genetic factors, because genetic discovery studies have focused largely on individuals with European ancestry, and because risk-relevant genetic factors may vary according to individual’s origin of genetic ancestry,” the investigators wrote. “Although many studies differentiate individuals by race and ethnicity, which may capture some information about the likely presence of certain genetic variants, ancestry is a better predictor and should be captured in validation studies.”
The update was commissioned and approved by the AGA, and supported by the National Cancer Institute of the National Institutes of Health. The investigators disclosed relationships with Geneoscopy, CellMax Life, Universal Diagnostics, and others.
FROM GASTROENTEROLOGY
Inadequate sleep & obesity: Breaking the vicious cycle
Sleep is fundamental to overall health and longevity, with the average person spending about one-third of their life sleeping.1 Adequate sleep is critical for optimal cognition, memory consolidation, mood regulation, metabolism, appetite regulation, and immune and hormone functioning. According to the American Academy of Sleep Medicine and the Sleep Research Society, adults should sleep at least 7 hours per night on a regular basis “to promote optimal health.”2 Yet, between 2013 and 2020, only about 65% of adults in the United States were meeting this amount.3 Insufficient sleep is associated with an increased risk for chronic health conditions, including obesity, diabetes, cardiovascular diseases, and even premature death.4

In a population-based longitudinal study of sleep disorders, short sleep duration was associated with increased body mass index (BMI), low blood levels of leptin, and high ghrelin levels.5 In addition to physical impairments, poor sleep can impair cognitive performance and lead to vehicular accidents and increased accidents at work.4 The potential economic impact that this may have is significant, and includes increased costs and loss of productivity in the workplace.6
Many factors may contribute to short sleep duration: environment, mental and physical condition, and social influences such as occupation, family responsibilities, travel, group activities, and personal care. Furthermore, the rapidly evolving and developing media, communication, and entertainment industries are already strongly implicated in poor sleep quality and quantity, both contributing to excessive daytime sleepiness.7 Poor sleep quality is most notable in modern societies, and it correlates with the increasing prevalence of obesity, likely due to sleep’s effect on food consumption and physical activity.8 Optimizing a person’s sleep will improve overall health and longevity by inhibiting the development of chronic disease.
How insufficient sleep raises the risk for obesity
Not only is sleep beneficial for brain health, memory, learning, and growth, its effect on food consumption and physical activity likely correlates with the increased prevalence of obesity in modern society. Yet the optimal amount of sleep is controversial, and current recommendations of 7 or more hours of sleep per night for adults are derived from expert panels only.2 The recommended sleep duration for children is longer, and it varies by age.9 The quality of sleep and its impact on neuroendocrine hormones, not just the quantity of sleep, needs to be factored into these recommendations.
Sleep restriction activates the orexigenic system via the hormones leptin and ghrelin. These hormones control the food reward system, essentially increasing hunger and food intake. Leptin, created by white adipose tissue, is responsible for satiety and decreased food consumption.10 Ghrelin, made by oxyntic glands in the stomach, is responsible for the sensation of hunger.
In a 2004 study by Spiegel et al,11 leptin and ghrelin levels were measured during 2 days of sleep restriction (4 hours in bed) and sleep extension (10 hours in bed). Sleep restriction was associated with a decrease in leptin levels and an increase in ghrelin levels. The researchers reported that participants experienced an increase in hunger and appetite—especially for calorie-dense foods with high carbohydrate content.
Although research design has limitations with predominantly self-reported sleep data, studies have shown that short sleep time leads to increased food intake by increasing hunger signals and craving of unhealthy foods, and by providing more opportunities to eat while awake. It also may lead to decreased physical activity, creating a sedentary lifestyle that further encourages obesity.8 Reduced sleep is even correlated to decreased efficacy of weight-loss treatments.12
Continue to: Other sleep characteristics weakly correlated with obesity
Other sleep characteristics weakly correlated with obesity are sleep variability, timing, efficiency, quality, and daytime napping.8 Sleep variability causes dysregulation of eating patterns, leading to increased food intake. A shift to later sleep and waking times often results in higher consumption of calories after 8
Poor sleep efficiency and quality decreases N3-stage (deep non-REM) sleep, affects the autonomic nervous system, and has been associated with increased abdominal obesity. Daytime napping, which can cause irregular circadian rhythms and sleep schedules, is associated with increased obesity.15 Thus, each component of sleep needs to be assessed to promote optimal regulation of the orexigenic system.
Another study showed that inadequate sleep not only promotes unhealthy lifestyle habits that can lead to obesity but also decreases the ability to lose weight.16 This small study with 10 overweight patients provided its subjects with a controlled caloric intake over 2 weeks. Patients spent two 14-day periods 3 months apart in the laboratory, divided into 2 time-in-bed arms of 8.5 and 5.5 hours per night. Neuroendocrine changes caused by decreased sleep were associated with a significant lean body mass loss while conserving energy-dense fat.16 This study highlights the importance of sleep hygiene counseling when developing a weight-management plan with patients.
Sleep, and its many components, play an integral role in the prevention and treatment of obesity.17 Poor sleep will increase the risk for obesity and hinder its treatment. Therefore, sleep quality and duration are vital components of obesity management.
The sleep–obesity link in children and the elderly
Childhood obesity is linked to several chronic diseases in adulthood, including type 2 diabetes, cardiovascular disease, nonalcoholic fatty liver disease, asthma, and obstructive sleep apnea (OSA).18 According to 2017-2018 NHANES (National Health and Nutrition Examination Surveys) data, obesity (BMI ≥ 95th percentile) prevalence among children and adolescents was reported at 19.3% and severe obesity (BMI ≥ 120% of the 95th percentile) at 6.1%. Pediatric overweight prevalence (≥ 85th percentile and < 95th percentile) was 16.1%.19
Continue to: Although poor sleep is associated...
Although poor sleep is associated with increased risk for obesity, there is no proven cause-effect relationship.20 Nutrition and physical activity have been identified as 2 critical factors in childhood obesity, but sleep health also needs to be investigated. Shorter sleep duration is strongly associated with the development of obesity. Furthermore, children with obesity are more likely to have shorter sleep duration.21 A short sleep duration alters plasma levels of insulin, low-density lipoprotein, and high-sensitivity C-reactive protein. It is associated with lower diet quality, an increased intake of nutrient-poor foods, and a lower intake of vegetables and fruits.22 Recent studies have shown that interventions to promote earlier bedtimes can improve sleep duration in children.
Older adults have many sleeping issues, including insomnia, circadian rhythm sleep-wake disorders, sleep-related movement disorders, and sleep-breathing disorders. Additionally, the older population has increased sleep latency, decreased sleep efficiency and total sleep time, decreased REM sleep, more frequent nighttime awakenings, and more daytime napping.23 The increased sleep disturbance with age is mainly related to higher risk factors for sleep disorders than the aging process itself. Sleeping 5 or fewer hours is associated with an increased risk for obesity and central abdominal fat compared with those who sleep 7 to 8 hours per night.24 Similar to children and youth, older adults also show a strong correlation between inadequate sleep and obesity.24
The consequence: A vicious cycle
Obesity in turn leads to shorter sleep duration and more disruptions. This negatively affects the orexigenic system, and the resulting hormonal derangement promotes worsening obesity. It is a cycle of poor sleep causing obesity and obesity causing poor sleep. Insomnia, in combination with shorter (and longer) sleep times, also has been linked with obesity.25 These patients experience more daytime sleepiness, fatigue, and nighttime sleep disturbances, all correlated with decreased quality of life and higher prevalence of medical comorbidities.8,26 Additional comorbidities secondary to obesity, including gastroesophageal reflux, depression, and asthma, also have been linked to sleep disturbances.8
OSA is a common sleep complication associated with obesity. With the increasing prevalence of obesity, the prevalence of OSA is rising.8,27 Factors that heighten the risk for OSA are male sex, age 40 to 70 years, postmenopausal status, elevated BMI, and craniofacial and upper airway abnormality.28 However, the US Preventive Services Task Force found insufficient evidence to screen for or treat OSA in asymptomatic adults.28 Signs and symptoms of OSA include nighttime awakenings with choking, loud snoring, and feeling unrefreshed after sleep.29
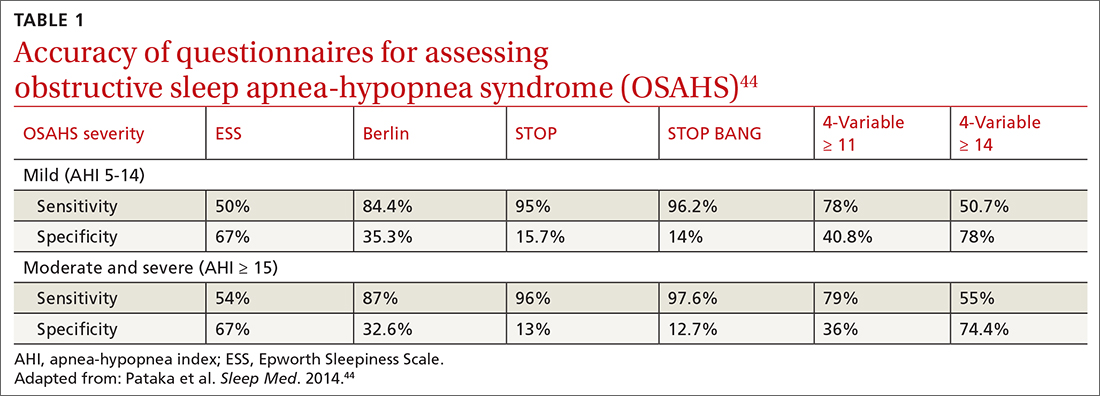
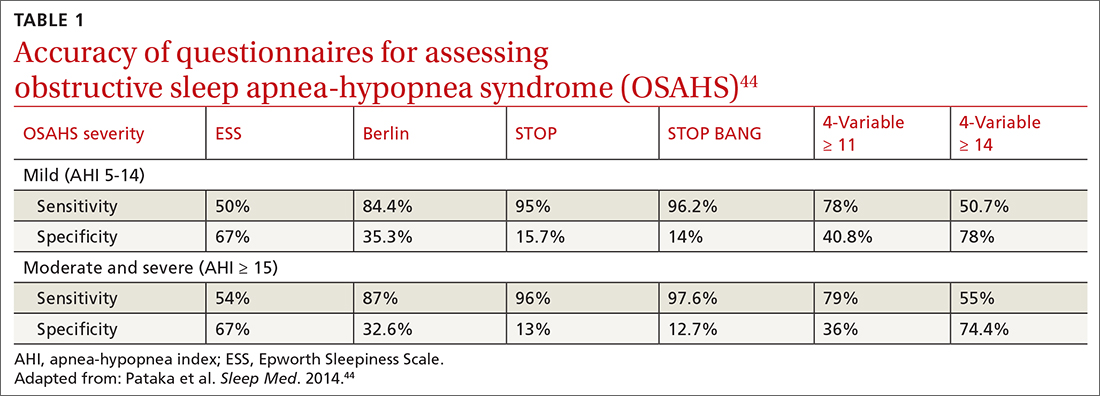
OSA is caused by the intermittent narrowing and obstruction of the pharyngeal airway due to anatomical and structural irregularities or neuromuscular impairments. Untreated OSA is associated with cardiovascular disease and cardiac arrhythmias such as atrial fibrillation. Even with this correlation between obesity and sleep, it is estimated that 80% of OSA remains undiagnosed.30 Approximately half of primary care clinicians do not screen at-risk patients for OSA, and 90% do not use validated OSA screening tools.31 Screening tools that have been validated are the STOP, STOP-BANG, Epworth Sleepiness Scale, and 4-Variable Screening Tool. However, the US Department of Veterans Affairs and the US Department of Defense have a more recent guideline recommending STOP as an easier-to-administer screen for OSA.32 A positive result with a screening tool should be confirmed with polysomnography.32
Continue to: Intervention for OSA
Intervention for OSA. The longest randomized controlled study to date, Sleep AHEAD, evaluated over a period of 10 years the effect of weight loss on OSA severity achieved with either an intensive lifestyle intervention (ILI) or with diabetes support and education (DSE).33 OSA severity is rated on an Apnea-Hypopnea Index (AHI), with scores reflecting the number of sleep apnea events per hour. This study demonstrated that weight loss was associated with decreased OSA severity. At 4-year follow-up, the greater the weight loss with ILI intervention, the lower the patients’ OSA severity scores. The study found an average decrease in AHI of 0.68 events per hour for every kilogram of weight loss in the ILI group (P < .0001).33,34 Over the follow-up visits, the ILI participants had 7.4 events per hour, a more significantly reduced AHI than the DSE participants (P < .0001).33,34
Additionally, a small cohort of study participants achieved OSA remission (ILI, 34.4%; DSE, 22.2%), indicated by a low AHI score (< 5 events per hour). At the conclusion of the study, OSA severity decreased to a greater degree with ILI intervention.33,34
Alcohol and drug use can negatively influence sleep patterns and obesity. Higher alcohol consumption is associated with poorer sleep quality and higher chances of developing short sleep duration and snoring.35 Alcohol, a muscle relaxant, causes upper airway narrowing and reduced tongue muscle tone, thereby increasing snoring and OSA as demonstrated by increased AHI on polysomnography after alcohol intake. Alcohol also changes sleep architecture by increasing slow-wave sleep, decreasing REM sleep duration, and increasing sleep arousal in the second half of the night.36 Disrupted circadian rhythm after alcohol consumption was correlated with increased adenosine neurotransmitters derived from ethanol metabolism.37 Alcohol dependence may be related to other psychiatric symptoms, and chronic alcohol use eventually alters sleep mechanisms leading to persistent insomnia, further perpetuating adverse outcomes such as suicidal ideation.36 There are positive associations between beer drinking and measures of abdominal adiposity in men, and “the combination of short sleep duration [and] disinhibited eating … is associated with greater alcohol intake and excess weight.”38
Therefore, counsel patients to avoid alcohol since it is a modifiable risk factor with pervasive adverse health effects.
Many drugs have a profound effect on sleep patterns. Illicit drug use in particular can affect the brain’s neurotransmitter serotonin system. For example, ecstasy users have an increased risk for OSA.39 People with cocaine and heroin use disorder tend to have more sleep-maintenance insomnia.40
Continue to: In contrast, those with alcohol...
In contrast, those with alcohol or cannabis use disorder tend to have more sleep-onset insomnia.40 Not only do illicit drugs interrupt sleep, but daily tobacco use also has been correlated with increased insomnia and shorter sleep duration since nicotine is a stimulant.41
Insomnia is commonly treated with sedative antidepressants and hypnotics—eg, mirtazapine and olanzapine—that contribute to weight gain.42 In addition, other common pharmaceuticals used for sleep disorders, such as diphenhydramine, have sedative properties and tend to lead to weight gain.43 Because so many medications affect sleep and weight, carefully review patients’ medication lists and switch offending agents to weight-neutral drugs if possible.
Treatment and tools to improve sleep in patients with obesity
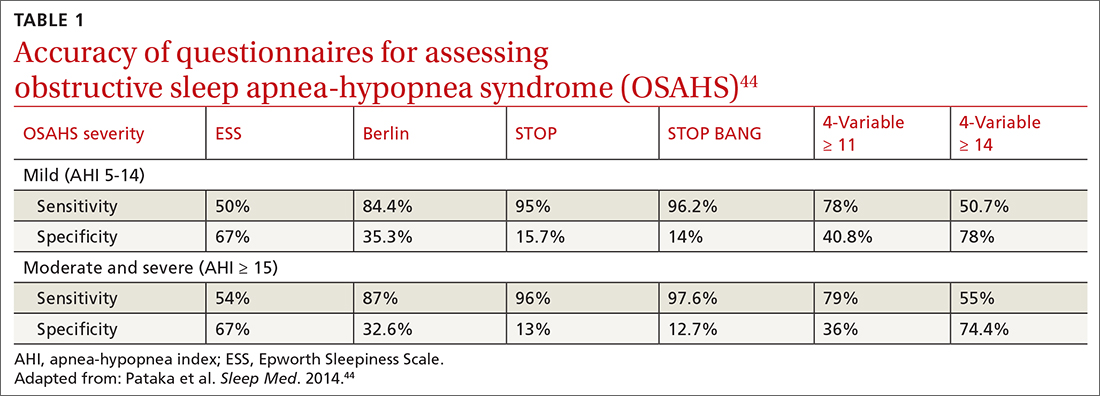
Given the strong correlation between obesity and sleep disorders, validated screening tools should be used to assess sleep quality, including onset and potential symptoms associated with poor sleep (TABLE 144). For weight management to succeed in patients with obesity, it is crucial to address sleep in addition to nutrition and physical activity.17,45
Physical activity has many benefits to overall health, especially for chronic diseases such as type 2 diabetes and hypertension. The Centers for Disease Control and Prevention recommends at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic exercise per week in addition to muscle-strengthening activities 2 or more days per week.46 However, approximately 300 minutes of moderate-
Physical activity and diet in combination are vital, but diet restriction has a more substantial effect on weight loss than physical activity alone.48 Still, physical activity is essential in helping maintain and prevent weight regain.
Continue to: Nonpharmacologic interventions
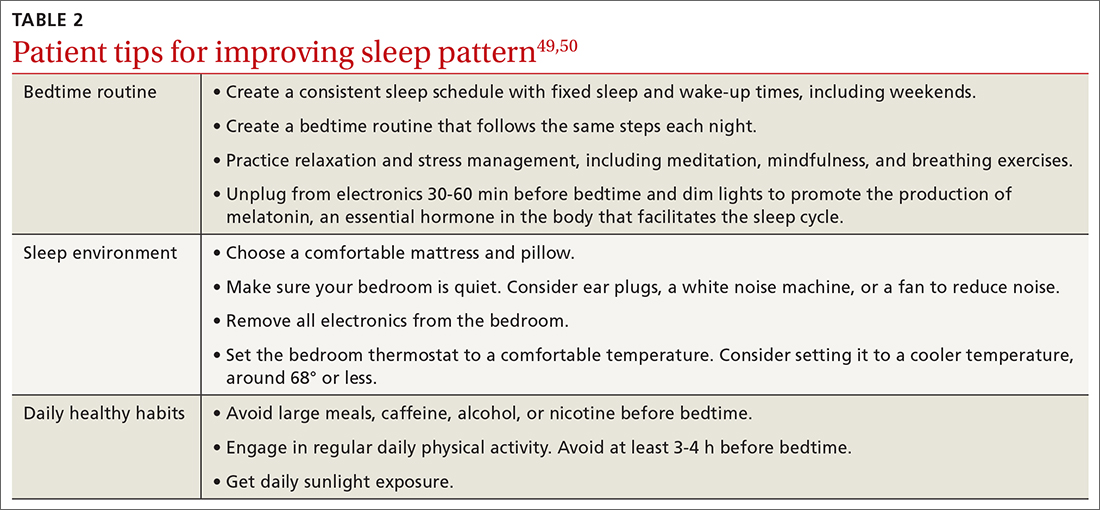
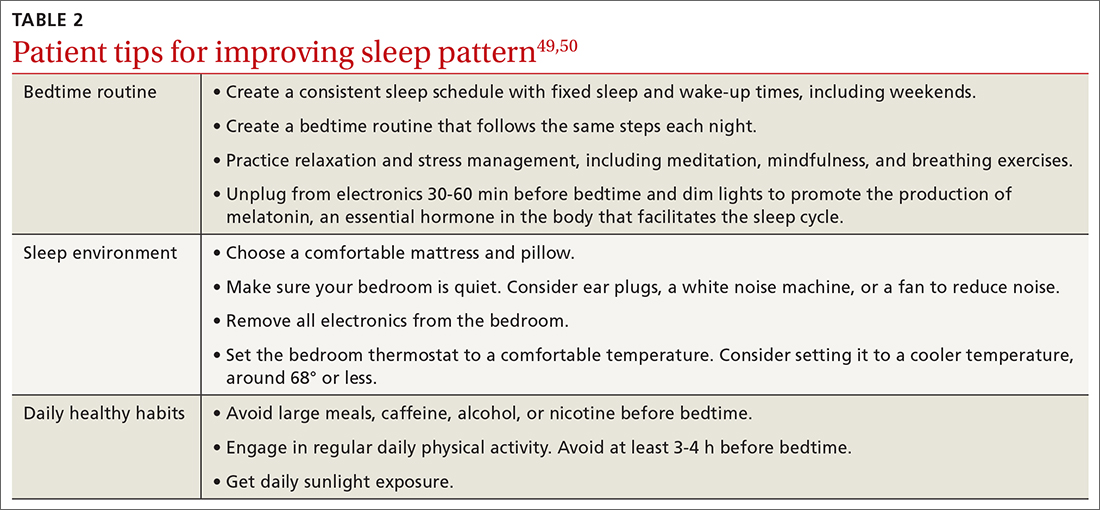
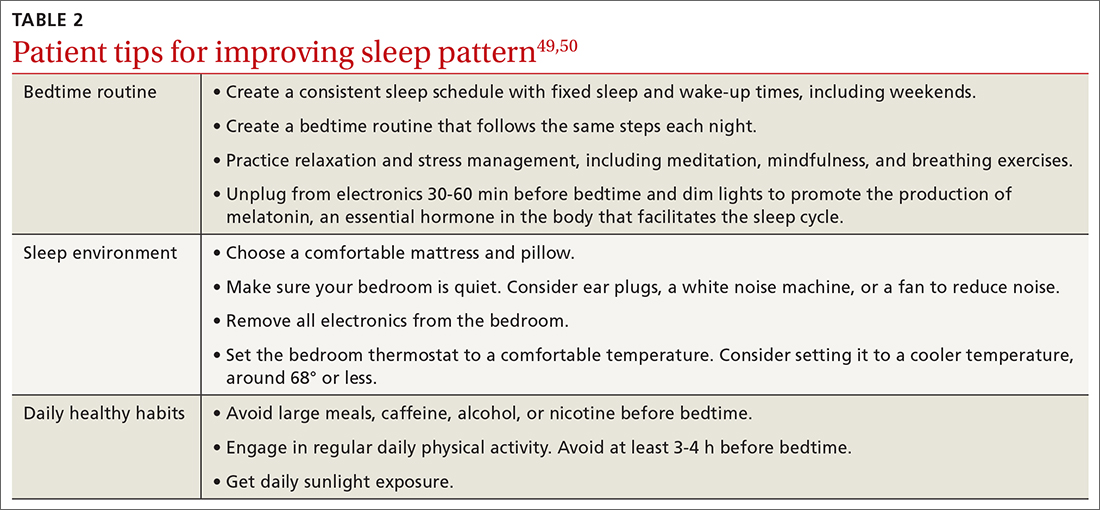
Nonpharmacologic interventions include promoting greater sleep quality and quantity by emphasizing good sleep hygiene practices. Developing a practical and effective bedtime routine, creating a quiet sleep environment, and practicing healthy daily habits are essential components to sleep hygiene (TABLE 249,50). Relaxation techniques and cognitive behavioral therapy (CBT) also can help. CBT for insomnia (CBT-I) is the first-line intervention for chronic insomnia.51 Sleep restriction is a type of CBT used to treat insomnia, encouraging short-term sleep loss in the hopes of improving insomnia. A trial by Logue et al showed that patients with overweight and obesity randomized to undergo CBT with better sleep hygiene (nonpharmacologic) interventions had a greater mean weight loss percentage (5% vs 2%; P = .04) than did those who received CBT alone.52
Eastern medicine including herbal interventions lack evidence of efficacy and safety. Further studies need to be done on the effects that chamomile, kava, valerian root (Valeriana officinalis), tryptophan, and Wu Ling (from mycelia Xylaria nigripes) might have on sleep.53
Proceed cautiously with medication. The American College of Physicians recommends a shared decision-making approach when considering pharmacologic therapy for chronic insomnia and the American Academy of Sleep Medicine (AASM) offers guidance on options.51,54 However, the evidence behind AASM sleep pharmacologic recommendations is weak, implying a lesser degree of confidence in the outcome and, therefore, in its appropriateness. Thus, it falls upon the clinician and patient to weigh the benefits and burdens of the pharmacologic treatments of insomnia. If indicated, medications suggested to treat sleep onset and sleep maintenance insomnia are eszopiclone, zolpidem, and temazepam. Zaleplon, triazolam, and ramelteon may improve sleep initiation. Suvorexant and doxepin are used for sleep-maintenance insomnia.54 Exploring patient preferences, cost of treatment, health care options, and available resources should all be considered.
CORRESPONDENCE
Ecler Ercole Jaqua, MD, MBA, FAAFP, AGSF, FACLM, DipABOM, Loma Linda University Health, 25455 Barton Road, Suite 206A, Loma Linda, CA 92354; [email protected]
1. Aminoff MJ, Boller F, Swaab DF. We spend about one-third of our life either sleeping or attempting to do so. Handb Clin Neurol. 2011;98:vii. doi: 10.1016/B978-0-444-52006-7.00047-2
2. Watson NF, Badr MS, Belenky G, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38:843-844. doi: 10.5665/sleep.4716
3. CDC. Sleep and sleep disorders, adults. Accessed September 21, 2023. www.cdc.gov/sleep/data-and-statistics/adults.html
4. Chattu VK, Manzar MD, Kumary S. The global problem of insufficient sleep and its serious public health implications. Healthcare (Basel). 2019;7:1. doi: 10.3390/healthcare7010001
5. Taheri S, Lin L, Austin D, et al. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:e62. doi: 10.1371/journal.pmed.0010062
6. Hafner M, Stepanek M, Taylor J, et al. Why sleep matters—the economic costs of insufficient sleep. Rand Health Q. 2017;6:11.
7. Hisler G, Twenge JM, Krizan Z. Associations between screen time and short sleep duration among adolescents varies by media type: evidence from a cohort study. Sleep Med. 2020;66:92-102. doi: 10.1016/j.sleep.2019.08.007
8. Ogilvie RP, Patel SR. The epidemiology of sleep and obesity. Sleep Health. 2017;3:383-388. doi: 10.1016/j.sleh.2017.07.013
9. CDC. Sleep and sleep disorders: How much sleep do I need? Accessed September 21, 2023. www.cdc.gov/sleep/about_sleep/how_much_sleep.html
10. van Egmond LT, Meth EMS, Engström J, et al. Effects of acute sleep loss on leptin, ghrelin, and adiponectin in adults with healthy weight and obesity: a laboratory study. Obesity (Silver Spring). 2023;31:635-641. doi: 10.1002/oby.23616
11. Spiegel K, Tasali E, Penev P, et al. Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141:846-850. doi: 10.7326/0003-4819-141-11-200412070-00008
12. Antza C, Kostopoulos G, Mostafa S, et al. The links between sleep duration, obesity and type 2 diabetes mellitus. J Endocrinol. 2021;252:125-141. doi: 10.1530/JOE-21-0155
13. Baron KG, Reid KJ, Kern AS, et al. Role of sleep timing in caloric intake and BMI. Obesity (Silver Spring). 2011;19:1374-1381. doi: 10.1038/oby.2011.100
14. Liu XY, Zheng CL, Xu C, et al. Nighttime snacking is associated with risk of obesity and hyperglycemia in adults: a cross-sectional survey from Chinese adult teachers J Biomed Res. 2017;31:541-547. doi: 10.7555/JBR.31.20160083
15. Cai Z, Yang Y, Zhang J, et al. The relationship between daytime napping and obesity: a systematic review and meta-analysis. Sci Rep. 2023.13:12124. doi: 10.1038/s41598-023-37883-7
16. Nedeltcheva AV, Kilkus JM, Imperial J, et al. Insufficient sleep undermines dietary efforts to reduce adiposity. Ann Intern Med. 2010;153:435-441. doi: 10.7326/0003-4819-153-7-201010050-00006
17. Chaput JP, Tremblay A. Adequate sleep to improve the treatment of obesity. CMAJ. 2012;184:1975-1976. doi: 10.1503/cmaj.120876
18. Kelsey MM, Zaepfel A, Bjornstad P, et al. Age-related consequences of childhood obesity. Gerontology. 2014;60:222-228. doi: 10.1159/000356023
19. Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2-19 years: United States, 1963-1965 through 2017-2018. National Center for Health Statistics Health E-Stats. Updated January 29, 2021. Accessed September 21, 2021. www.cdc.gov/nchs/data/hestat/obesity-child-17-18/overweight-obesity-child-H.pdf
20. Fatima Y, Doi SAR, Mamun AA. Sleep quality and obesity in young subjects: a meta-analysis. Obes Rev. 2016;17:1154-1166. doi: 10.1111/obr.12444
21. Gohil A, Hannon TS. Poor sleep and obesity: concurrent epidemics in adolescent youth. Front Endocrinol. 2018;9:364. doi: 10.3389/fendo.2018.00364
22. Golley RK, Maher CA, Matricciani L, et al. Sleep duration or bedtime? Exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. Int J Obes (Lond). 2013;37:546-551. doi: 10.1038/ijo.2012.212
23. Alessi CA. Sleep issues. In: Harper GM, Lyons WL, Potter JF, eds. Geriatrics Review Syllabus (GRS 10). Updated January 2021. Accessed August 29, 2023. http://geriatricscareonline.org
24. Patel SR, Blackwell T, Redline S, et al. The association between sleep duration and obesity in older adults. Int J Obes (Lond). 2008;32:1825-1834. doi: 10.1038/ijo.2008.198
25. Cai GH, Theorell-Haglöw J, Janson C, et al. Insomnia symptoms and sleep duration and their combined effects in relation to associations with obesity and central obesity. Sleep Med. 2018;46:81-87. doi: 10.1016/j.sleep.2018.03.009
26. Beccuti G, Pannain S. Sleep and obesity. Curr Opin Clin Nutr Metab Care. 2011;14:402-412. doi: 10.1097/MCO.0b013 e3283479109
27. Franklin KA, Lindberg E. Obstructive sleep apnea is a common disorder in the population–a review on the epidemiology of sleep apnea. J Thorac Dis. 2015;7:1311-1322. doi: 10.3978/j.issn.2072-1439.2015.06.11
28. USPSTF. Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Screening for obstructive sleep apnea in adults: US Preventive Services Task Force recommendation statement. JAMA. 2017;317:407-414. doi: 10.1001/jama.2016.20325
29. Goyal M, Johnson J. Obstructive sleep apnea diagnosis and management. Mo Med. 2017;114:120-124.
30. American Academy of Sleep Medicine. Hidden health crisis costing America billions: underdiagnosing and undertreating obstructive sleep apnea draining healthcare system. 2016. Accessed September 25, 2023. https://aasm.org/wp-content/uploads/2017/10/sleep-apnea-economic-crisis.pdf
31. Devaraj, NK. Knowledge, attitude, and practice regarding obstructive sleep apnea among primary care physicians. Sleep Breath. 2020;24:1581-1590. doi: 10.1007/s11325-020-02040-1
32. Mysliwiec V, Martin JL, Ulmer CS, et al. The management of chronic insomnia disorder and obstructive sleep apnea: synopsis of the 2019 U.S. Department of Veterans Affairs and U.S. Department of Defense Clinical Practice Guidelines. Ann Intern Med. 2020;172:325-336. doi: 10.7326/M19-3575
33. Kuna ST, Reboussin DM, Strotmeyer ES, et al. Effects of weight loss on obstructive sleep apnea severity. Ten-year results of the Sleep AHEAD study. Am J Respir Crit Care Med. 2021;203:221-229. doi: 10.1164/rccm.201912-2511OC
34. St-Onge MP, Tasali E. Weight loss is integral to obstructive sleep apnea management. Ten-year follow-up in Sleep AHEAD. Am J Respir Crit Care Med. 2021;203:161-162. doi: 10.1164/rccm.202007-2906ED
35. Zheng D, Yuan X, Ma C, et al. Alcohol consumption and sleep quality: a community-based study. Public Health Nutr. 2021;24:4851-4858. doi: 10.1017/S1368980020004553
36. Chakravorty S, Chaudhary NS, Brower KJ. Alcohol dependence and its relationship with insomnia and other sleep disorders. Alcohol Clin Exp Res. 2016;40:2271-2282. doi: 10.1111/acer.13217
37. Elmenhorst EM, Elmenhorst D, Benderoth S, et al. Cognitive impairments by alcohol and sleep deprivation indicate trait characteristics and a potential role for adenosine A1 receptors. Proc Natl Acad Sci U S A. 2018;115:8009-8014. doi: 10.1073/pnas.1803770115
38. Traversy G, Chaput JP. Alcohol consumption and obesity: an update. Curr Obes Rep. 2015;4:122-130. doi: 10.1007/s13679-014-0129-4
39. McCann UD, Sgambati FP, Schwartz AR, et al. Sleep apnea in young abstinent recreational MDMA (“ecstasy”) consumers. Neurology. 2009;73:2011-2017. doi: 10.1212/WNL.0b013e3181c51a62
40. Grau-López L, Grau-López L, Daigre C, et al. Insomnia symptoms in patients with substance use disorders during detoxification and associated clinical features. Front Psychiatry. 2020;11:540022. doi: 10.3389/fpsyt.2020.540022
41. Boehm MA, Lei QM, Lloyd RM, et al. Depression, anxiety, and tobacco use: overlapping impediments to sleep in a national sample of college students. J Am Coll Health. 2016;64:565-574. doi: 10.1080/07448481.2016.1205073
42. Gracious BL, Meyer AE. Psychotropic-induced weight gain and potential pharmacologic treatment strategies. Psychiatry (Edgmont). 2005;2:36-42.
43. Ratliff JC, Barber JA, Palmese LB, et al. Association of prescription H1 antihistamine use with obesity: results from the National Health and Nutrition Examination Survey. Obesity (Silver Spring). 2010;18:2398-2400. doi: 10.1038/oby.2010.176
44. Pataka A, Daskalopoulou E, Kalamaras G, et al. Evaluation of five different questionnaires for assessing sleep apnea syndrome in a sleep clinic. Sleep Med. 2014;15:776-781. doi: 10.1016/j.sleep.2014.03.012
45. Kline CE, Chasens ER, Bizhanova Z, et al. The association between sleep health and weight change during a 12-month behavioral weight loss intervention. Int J Obes (Lond). 2021;45:639-649. doi: 10.1038/s41366-020-00728-8
46. CDC. How much physical activity do adults need? Accessed August 23, 2023. www.cdc.gov/physicalactivity/basics/adults/index.htm
47. Flack KD, Hays HM, Moreland J, et al. Exercise for weight loss: further evaluating energy compensation with exercise. Med Sci Sports Exerc. 2020;52:2466-2475. doi: 10.1249/MSS.0000000000002376
48. Swift DL, Johannsen NM, Lavie CJ, et al. The role of exercise and physical activity in weight loss and maintenance. Prog Cardiovasc Dis. 2014;56:441-447. doi: 10.1016/j.pcad.2013.09.012
49. Irish LA, Kline CE, Gunn HE, et al. The role of sleep hygiene in promoting public health: a review of empirical evidence. Sleep Med Rev. 2015;22:23-36. doi: 10.1016/j.smrv.2014.10.001
50. CDC. Tips for better sleep. 2022. Accessed August 4, 2023. www.cdc.gov/sleep/about_sleep/sleep_hygiene.html
51. Qaseem A, Kansagara D, Forciea MA, et al. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165:125-133. doi: 10.7326/M15-2175
52. Logue EE, Bourguet CC, Palmieri PA, et al. The better weight-better sleep study: a pilot intervention in primary care. Am J Health Behav. 2012;36:319-334. doi: 10.5993/AJHB.36.3.4
53. Leach MJ, Page AT. Herbal medicine for insomnia: a systematic review and meta-analysis. Sleep Med Rev. 2015;24:1-12. doi: 10.1016/j.smrv.2014.12.003
54. Sateia MJ, Buysse DJ, Krystal AD, et al. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13:307-349. doi: 10.5664/jcsm.6470
Sleep is fundamental to overall health and longevity, with the average person spending about one-third of their life sleeping.1 Adequate sleep is critical for optimal cognition, memory consolidation, mood regulation, metabolism, appetite regulation, and immune and hormone functioning. According to the American Academy of Sleep Medicine and the Sleep Research Society, adults should sleep at least 7 hours per night on a regular basis “to promote optimal health.”2 Yet, between 2013 and 2020, only about 65% of adults in the United States were meeting this amount.3 Insufficient sleep is associated with an increased risk for chronic health conditions, including obesity, diabetes, cardiovascular diseases, and even premature death.4

In a population-based longitudinal study of sleep disorders, short sleep duration was associated with increased body mass index (BMI), low blood levels of leptin, and high ghrelin levels.5 In addition to physical impairments, poor sleep can impair cognitive performance and lead to vehicular accidents and increased accidents at work.4 The potential economic impact that this may have is significant, and includes increased costs and loss of productivity in the workplace.6
Many factors may contribute to short sleep duration: environment, mental and physical condition, and social influences such as occupation, family responsibilities, travel, group activities, and personal care. Furthermore, the rapidly evolving and developing media, communication, and entertainment industries are already strongly implicated in poor sleep quality and quantity, both contributing to excessive daytime sleepiness.7 Poor sleep quality is most notable in modern societies, and it correlates with the increasing prevalence of obesity, likely due to sleep’s effect on food consumption and physical activity.8 Optimizing a person’s sleep will improve overall health and longevity by inhibiting the development of chronic disease.
How insufficient sleep raises the risk for obesity
Not only is sleep beneficial for brain health, memory, learning, and growth, its effect on food consumption and physical activity likely correlates with the increased prevalence of obesity in modern society. Yet the optimal amount of sleep is controversial, and current recommendations of 7 or more hours of sleep per night for adults are derived from expert panels only.2 The recommended sleep duration for children is longer, and it varies by age.9 The quality of sleep and its impact on neuroendocrine hormones, not just the quantity of sleep, needs to be factored into these recommendations.
Sleep restriction activates the orexigenic system via the hormones leptin and ghrelin. These hormones control the food reward system, essentially increasing hunger and food intake. Leptin, created by white adipose tissue, is responsible for satiety and decreased food consumption.10 Ghrelin, made by oxyntic glands in the stomach, is responsible for the sensation of hunger.
In a 2004 study by Spiegel et al,11 leptin and ghrelin levels were measured during 2 days of sleep restriction (4 hours in bed) and sleep extension (10 hours in bed). Sleep restriction was associated with a decrease in leptin levels and an increase in ghrelin levels. The researchers reported that participants experienced an increase in hunger and appetite—especially for calorie-dense foods with high carbohydrate content.
Although research design has limitations with predominantly self-reported sleep data, studies have shown that short sleep time leads to increased food intake by increasing hunger signals and craving of unhealthy foods, and by providing more opportunities to eat while awake. It also may lead to decreased physical activity, creating a sedentary lifestyle that further encourages obesity.8 Reduced sleep is even correlated to decreased efficacy of weight-loss treatments.12
Continue to: Other sleep characteristics weakly correlated with obesity
Other sleep characteristics weakly correlated with obesity are sleep variability, timing, efficiency, quality, and daytime napping.8 Sleep variability causes dysregulation of eating patterns, leading to increased food intake. A shift to later sleep and waking times often results in higher consumption of calories after 8
Poor sleep efficiency and quality decreases N3-stage (deep non-REM) sleep, affects the autonomic nervous system, and has been associated with increased abdominal obesity. Daytime napping, which can cause irregular circadian rhythms and sleep schedules, is associated with increased obesity.15 Thus, each component of sleep needs to be assessed to promote optimal regulation of the orexigenic system.
Another study showed that inadequate sleep not only promotes unhealthy lifestyle habits that can lead to obesity but also decreases the ability to lose weight.16 This small study with 10 overweight patients provided its subjects with a controlled caloric intake over 2 weeks. Patients spent two 14-day periods 3 months apart in the laboratory, divided into 2 time-in-bed arms of 8.5 and 5.5 hours per night. Neuroendocrine changes caused by decreased sleep were associated with a significant lean body mass loss while conserving energy-dense fat.16 This study highlights the importance of sleep hygiene counseling when developing a weight-management plan with patients.
Sleep, and its many components, play an integral role in the prevention and treatment of obesity.17 Poor sleep will increase the risk for obesity and hinder its treatment. Therefore, sleep quality and duration are vital components of obesity management.
The sleep–obesity link in children and the elderly
Childhood obesity is linked to several chronic diseases in adulthood, including type 2 diabetes, cardiovascular disease, nonalcoholic fatty liver disease, asthma, and obstructive sleep apnea (OSA).18 According to 2017-2018 NHANES (National Health and Nutrition Examination Surveys) data, obesity (BMI ≥ 95th percentile) prevalence among children and adolescents was reported at 19.3% and severe obesity (BMI ≥ 120% of the 95th percentile) at 6.1%. Pediatric overweight prevalence (≥ 85th percentile and < 95th percentile) was 16.1%.19
Continue to: Although poor sleep is associated...
Although poor sleep is associated with increased risk for obesity, there is no proven cause-effect relationship.20 Nutrition and physical activity have been identified as 2 critical factors in childhood obesity, but sleep health also needs to be investigated. Shorter sleep duration is strongly associated with the development of obesity. Furthermore, children with obesity are more likely to have shorter sleep duration.21 A short sleep duration alters plasma levels of insulin, low-density lipoprotein, and high-sensitivity C-reactive protein. It is associated with lower diet quality, an increased intake of nutrient-poor foods, and a lower intake of vegetables and fruits.22 Recent studies have shown that interventions to promote earlier bedtimes can improve sleep duration in children.
Older adults have many sleeping issues, including insomnia, circadian rhythm sleep-wake disorders, sleep-related movement disorders, and sleep-breathing disorders. Additionally, the older population has increased sleep latency, decreased sleep efficiency and total sleep time, decreased REM sleep, more frequent nighttime awakenings, and more daytime napping.23 The increased sleep disturbance with age is mainly related to higher risk factors for sleep disorders than the aging process itself. Sleeping 5 or fewer hours is associated with an increased risk for obesity and central abdominal fat compared with those who sleep 7 to 8 hours per night.24 Similar to children and youth, older adults also show a strong correlation between inadequate sleep and obesity.24
The consequence: A vicious cycle
Obesity in turn leads to shorter sleep duration and more disruptions. This negatively affects the orexigenic system, and the resulting hormonal derangement promotes worsening obesity. It is a cycle of poor sleep causing obesity and obesity causing poor sleep. Insomnia, in combination with shorter (and longer) sleep times, also has been linked with obesity.25 These patients experience more daytime sleepiness, fatigue, and nighttime sleep disturbances, all correlated with decreased quality of life and higher prevalence of medical comorbidities.8,26 Additional comorbidities secondary to obesity, including gastroesophageal reflux, depression, and asthma, also have been linked to sleep disturbances.8
OSA is a common sleep complication associated with obesity. With the increasing prevalence of obesity, the prevalence of OSA is rising.8,27 Factors that heighten the risk for OSA are male sex, age 40 to 70 years, postmenopausal status, elevated BMI, and craniofacial and upper airway abnormality.28 However, the US Preventive Services Task Force found insufficient evidence to screen for or treat OSA in asymptomatic adults.28 Signs and symptoms of OSA include nighttime awakenings with choking, loud snoring, and feeling unrefreshed after sleep.29
OSA is caused by the intermittent narrowing and obstruction of the pharyngeal airway due to anatomical and structural irregularities or neuromuscular impairments. Untreated OSA is associated with cardiovascular disease and cardiac arrhythmias such as atrial fibrillation. Even with this correlation between obesity and sleep, it is estimated that 80% of OSA remains undiagnosed.30 Approximately half of primary care clinicians do not screen at-risk patients for OSA, and 90% do not use validated OSA screening tools.31 Screening tools that have been validated are the STOP, STOP-BANG, Epworth Sleepiness Scale, and 4-Variable Screening Tool. However, the US Department of Veterans Affairs and the US Department of Defense have a more recent guideline recommending STOP as an easier-to-administer screen for OSA.32 A positive result with a screening tool should be confirmed with polysomnography.32
Continue to: Intervention for OSA
Intervention for OSA. The longest randomized controlled study to date, Sleep AHEAD, evaluated over a period of 10 years the effect of weight loss on OSA severity achieved with either an intensive lifestyle intervention (ILI) or with diabetes support and education (DSE).33 OSA severity is rated on an Apnea-Hypopnea Index (AHI), with scores reflecting the number of sleep apnea events per hour. This study demonstrated that weight loss was associated with decreased OSA severity. At 4-year follow-up, the greater the weight loss with ILI intervention, the lower the patients’ OSA severity scores. The study found an average decrease in AHI of 0.68 events per hour for every kilogram of weight loss in the ILI group (P < .0001).33,34 Over the follow-up visits, the ILI participants had 7.4 events per hour, a more significantly reduced AHI than the DSE participants (P < .0001).33,34
Additionally, a small cohort of study participants achieved OSA remission (ILI, 34.4%; DSE, 22.2%), indicated by a low AHI score (< 5 events per hour). At the conclusion of the study, OSA severity decreased to a greater degree with ILI intervention.33,34
Alcohol and drug use can negatively influence sleep patterns and obesity. Higher alcohol consumption is associated with poorer sleep quality and higher chances of developing short sleep duration and snoring.35 Alcohol, a muscle relaxant, causes upper airway narrowing and reduced tongue muscle tone, thereby increasing snoring and OSA as demonstrated by increased AHI on polysomnography after alcohol intake. Alcohol also changes sleep architecture by increasing slow-wave sleep, decreasing REM sleep duration, and increasing sleep arousal in the second half of the night.36 Disrupted circadian rhythm after alcohol consumption was correlated with increased adenosine neurotransmitters derived from ethanol metabolism.37 Alcohol dependence may be related to other psychiatric symptoms, and chronic alcohol use eventually alters sleep mechanisms leading to persistent insomnia, further perpetuating adverse outcomes such as suicidal ideation.36 There are positive associations between beer drinking and measures of abdominal adiposity in men, and “the combination of short sleep duration [and] disinhibited eating … is associated with greater alcohol intake and excess weight.”38
Therefore, counsel patients to avoid alcohol since it is a modifiable risk factor with pervasive adverse health effects.
Many drugs have a profound effect on sleep patterns. Illicit drug use in particular can affect the brain’s neurotransmitter serotonin system. For example, ecstasy users have an increased risk for OSA.39 People with cocaine and heroin use disorder tend to have more sleep-maintenance insomnia.40
Continue to: In contrast, those with alcohol...
In contrast, those with alcohol or cannabis use disorder tend to have more sleep-onset insomnia.40 Not only do illicit drugs interrupt sleep, but daily tobacco use also has been correlated with increased insomnia and shorter sleep duration since nicotine is a stimulant.41
Insomnia is commonly treated with sedative antidepressants and hypnotics—eg, mirtazapine and olanzapine—that contribute to weight gain.42 In addition, other common pharmaceuticals used for sleep disorders, such as diphenhydramine, have sedative properties and tend to lead to weight gain.43 Because so many medications affect sleep and weight, carefully review patients’ medication lists and switch offending agents to weight-neutral drugs if possible.
Treatment and tools to improve sleep in patients with obesity
Given the strong correlation between obesity and sleep disorders, validated screening tools should be used to assess sleep quality, including onset and potential symptoms associated with poor sleep (TABLE 144). For weight management to succeed in patients with obesity, it is crucial to address sleep in addition to nutrition and physical activity.17,45
Physical activity has many benefits to overall health, especially for chronic diseases such as type 2 diabetes and hypertension. The Centers for Disease Control and Prevention recommends at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic exercise per week in addition to muscle-strengthening activities 2 or more days per week.46 However, approximately 300 minutes of moderate-
Physical activity and diet in combination are vital, but diet restriction has a more substantial effect on weight loss than physical activity alone.48 Still, physical activity is essential in helping maintain and prevent weight regain.
Continue to: Nonpharmacologic interventions
Nonpharmacologic interventions include promoting greater sleep quality and quantity by emphasizing good sleep hygiene practices. Developing a practical and effective bedtime routine, creating a quiet sleep environment, and practicing healthy daily habits are essential components to sleep hygiene (TABLE 249,50). Relaxation techniques and cognitive behavioral therapy (CBT) also can help. CBT for insomnia (CBT-I) is the first-line intervention for chronic insomnia.51 Sleep restriction is a type of CBT used to treat insomnia, encouraging short-term sleep loss in the hopes of improving insomnia. A trial by Logue et al showed that patients with overweight and obesity randomized to undergo CBT with better sleep hygiene (nonpharmacologic) interventions had a greater mean weight loss percentage (5% vs 2%; P = .04) than did those who received CBT alone.52
Eastern medicine including herbal interventions lack evidence of efficacy and safety. Further studies need to be done on the effects that chamomile, kava, valerian root (Valeriana officinalis), tryptophan, and Wu Ling (from mycelia Xylaria nigripes) might have on sleep.53
Proceed cautiously with medication. The American College of Physicians recommends a shared decision-making approach when considering pharmacologic therapy for chronic insomnia and the American Academy of Sleep Medicine (AASM) offers guidance on options.51,54 However, the evidence behind AASM sleep pharmacologic recommendations is weak, implying a lesser degree of confidence in the outcome and, therefore, in its appropriateness. Thus, it falls upon the clinician and patient to weigh the benefits and burdens of the pharmacologic treatments of insomnia. If indicated, medications suggested to treat sleep onset and sleep maintenance insomnia are eszopiclone, zolpidem, and temazepam. Zaleplon, triazolam, and ramelteon may improve sleep initiation. Suvorexant and doxepin are used for sleep-maintenance insomnia.54 Exploring patient preferences, cost of treatment, health care options, and available resources should all be considered.
CORRESPONDENCE
Ecler Ercole Jaqua, MD, MBA, FAAFP, AGSF, FACLM, DipABOM, Loma Linda University Health, 25455 Barton Road, Suite 206A, Loma Linda, CA 92354; [email protected]
Sleep is fundamental to overall health and longevity, with the average person spending about one-third of their life sleeping.1 Adequate sleep is critical for optimal cognition, memory consolidation, mood regulation, metabolism, appetite regulation, and immune and hormone functioning. According to the American Academy of Sleep Medicine and the Sleep Research Society, adults should sleep at least 7 hours per night on a regular basis “to promote optimal health.”2 Yet, between 2013 and 2020, only about 65% of adults in the United States were meeting this amount.3 Insufficient sleep is associated with an increased risk for chronic health conditions, including obesity, diabetes, cardiovascular diseases, and even premature death.4

In a population-based longitudinal study of sleep disorders, short sleep duration was associated with increased body mass index (BMI), low blood levels of leptin, and high ghrelin levels.5 In addition to physical impairments, poor sleep can impair cognitive performance and lead to vehicular accidents and increased accidents at work.4 The potential economic impact that this may have is significant, and includes increased costs and loss of productivity in the workplace.6
Many factors may contribute to short sleep duration: environment, mental and physical condition, and social influences such as occupation, family responsibilities, travel, group activities, and personal care. Furthermore, the rapidly evolving and developing media, communication, and entertainment industries are already strongly implicated in poor sleep quality and quantity, both contributing to excessive daytime sleepiness.7 Poor sleep quality is most notable in modern societies, and it correlates with the increasing prevalence of obesity, likely due to sleep’s effect on food consumption and physical activity.8 Optimizing a person’s sleep will improve overall health and longevity by inhibiting the development of chronic disease.
How insufficient sleep raises the risk for obesity
Not only is sleep beneficial for brain health, memory, learning, and growth, its effect on food consumption and physical activity likely correlates with the increased prevalence of obesity in modern society. Yet the optimal amount of sleep is controversial, and current recommendations of 7 or more hours of sleep per night for adults are derived from expert panels only.2 The recommended sleep duration for children is longer, and it varies by age.9 The quality of sleep and its impact on neuroendocrine hormones, not just the quantity of sleep, needs to be factored into these recommendations.
Sleep restriction activates the orexigenic system via the hormones leptin and ghrelin. These hormones control the food reward system, essentially increasing hunger and food intake. Leptin, created by white adipose tissue, is responsible for satiety and decreased food consumption.10 Ghrelin, made by oxyntic glands in the stomach, is responsible for the sensation of hunger.
In a 2004 study by Spiegel et al,11 leptin and ghrelin levels were measured during 2 days of sleep restriction (4 hours in bed) and sleep extension (10 hours in bed). Sleep restriction was associated with a decrease in leptin levels and an increase in ghrelin levels. The researchers reported that participants experienced an increase in hunger and appetite—especially for calorie-dense foods with high carbohydrate content.
Although research design has limitations with predominantly self-reported sleep data, studies have shown that short sleep time leads to increased food intake by increasing hunger signals and craving of unhealthy foods, and by providing more opportunities to eat while awake. It also may lead to decreased physical activity, creating a sedentary lifestyle that further encourages obesity.8 Reduced sleep is even correlated to decreased efficacy of weight-loss treatments.12
Continue to: Other sleep characteristics weakly correlated with obesity
Other sleep characteristics weakly correlated with obesity are sleep variability, timing, efficiency, quality, and daytime napping.8 Sleep variability causes dysregulation of eating patterns, leading to increased food intake. A shift to later sleep and waking times often results in higher consumption of calories after 8
Poor sleep efficiency and quality decreases N3-stage (deep non-REM) sleep, affects the autonomic nervous system, and has been associated with increased abdominal obesity. Daytime napping, which can cause irregular circadian rhythms and sleep schedules, is associated with increased obesity.15 Thus, each component of sleep needs to be assessed to promote optimal regulation of the orexigenic system.
Another study showed that inadequate sleep not only promotes unhealthy lifestyle habits that can lead to obesity but also decreases the ability to lose weight.16 This small study with 10 overweight patients provided its subjects with a controlled caloric intake over 2 weeks. Patients spent two 14-day periods 3 months apart in the laboratory, divided into 2 time-in-bed arms of 8.5 and 5.5 hours per night. Neuroendocrine changes caused by decreased sleep were associated with a significant lean body mass loss while conserving energy-dense fat.16 This study highlights the importance of sleep hygiene counseling when developing a weight-management plan with patients.
Sleep, and its many components, play an integral role in the prevention and treatment of obesity.17 Poor sleep will increase the risk for obesity and hinder its treatment. Therefore, sleep quality and duration are vital components of obesity management.
The sleep–obesity link in children and the elderly
Childhood obesity is linked to several chronic diseases in adulthood, including type 2 diabetes, cardiovascular disease, nonalcoholic fatty liver disease, asthma, and obstructive sleep apnea (OSA).18 According to 2017-2018 NHANES (National Health and Nutrition Examination Surveys) data, obesity (BMI ≥ 95th percentile) prevalence among children and adolescents was reported at 19.3% and severe obesity (BMI ≥ 120% of the 95th percentile) at 6.1%. Pediatric overweight prevalence (≥ 85th percentile and < 95th percentile) was 16.1%.19
Continue to: Although poor sleep is associated...
Although poor sleep is associated with increased risk for obesity, there is no proven cause-effect relationship.20 Nutrition and physical activity have been identified as 2 critical factors in childhood obesity, but sleep health also needs to be investigated. Shorter sleep duration is strongly associated with the development of obesity. Furthermore, children with obesity are more likely to have shorter sleep duration.21 A short sleep duration alters plasma levels of insulin, low-density lipoprotein, and high-sensitivity C-reactive protein. It is associated with lower diet quality, an increased intake of nutrient-poor foods, and a lower intake of vegetables and fruits.22 Recent studies have shown that interventions to promote earlier bedtimes can improve sleep duration in children.
Older adults have many sleeping issues, including insomnia, circadian rhythm sleep-wake disorders, sleep-related movement disorders, and sleep-breathing disorders. Additionally, the older population has increased sleep latency, decreased sleep efficiency and total sleep time, decreased REM sleep, more frequent nighttime awakenings, and more daytime napping.23 The increased sleep disturbance with age is mainly related to higher risk factors for sleep disorders than the aging process itself. Sleeping 5 or fewer hours is associated with an increased risk for obesity and central abdominal fat compared with those who sleep 7 to 8 hours per night.24 Similar to children and youth, older adults also show a strong correlation between inadequate sleep and obesity.24
The consequence: A vicious cycle
Obesity in turn leads to shorter sleep duration and more disruptions. This negatively affects the orexigenic system, and the resulting hormonal derangement promotes worsening obesity. It is a cycle of poor sleep causing obesity and obesity causing poor sleep. Insomnia, in combination with shorter (and longer) sleep times, also has been linked with obesity.25 These patients experience more daytime sleepiness, fatigue, and nighttime sleep disturbances, all correlated with decreased quality of life and higher prevalence of medical comorbidities.8,26 Additional comorbidities secondary to obesity, including gastroesophageal reflux, depression, and asthma, also have been linked to sleep disturbances.8
OSA is a common sleep complication associated with obesity. With the increasing prevalence of obesity, the prevalence of OSA is rising.8,27 Factors that heighten the risk for OSA are male sex, age 40 to 70 years, postmenopausal status, elevated BMI, and craniofacial and upper airway abnormality.28 However, the US Preventive Services Task Force found insufficient evidence to screen for or treat OSA in asymptomatic adults.28 Signs and symptoms of OSA include nighttime awakenings with choking, loud snoring, and feeling unrefreshed after sleep.29
OSA is caused by the intermittent narrowing and obstruction of the pharyngeal airway due to anatomical and structural irregularities or neuromuscular impairments. Untreated OSA is associated with cardiovascular disease and cardiac arrhythmias such as atrial fibrillation. Even with this correlation between obesity and sleep, it is estimated that 80% of OSA remains undiagnosed.30 Approximately half of primary care clinicians do not screen at-risk patients for OSA, and 90% do not use validated OSA screening tools.31 Screening tools that have been validated are the STOP, STOP-BANG, Epworth Sleepiness Scale, and 4-Variable Screening Tool. However, the US Department of Veterans Affairs and the US Department of Defense have a more recent guideline recommending STOP as an easier-to-administer screen for OSA.32 A positive result with a screening tool should be confirmed with polysomnography.32
Continue to: Intervention for OSA
Intervention for OSA. The longest randomized controlled study to date, Sleep AHEAD, evaluated over a period of 10 years the effect of weight loss on OSA severity achieved with either an intensive lifestyle intervention (ILI) or with diabetes support and education (DSE).33 OSA severity is rated on an Apnea-Hypopnea Index (AHI), with scores reflecting the number of sleep apnea events per hour. This study demonstrated that weight loss was associated with decreased OSA severity. At 4-year follow-up, the greater the weight loss with ILI intervention, the lower the patients’ OSA severity scores. The study found an average decrease in AHI of 0.68 events per hour for every kilogram of weight loss in the ILI group (P < .0001).33,34 Over the follow-up visits, the ILI participants had 7.4 events per hour, a more significantly reduced AHI than the DSE participants (P < .0001).33,34
Additionally, a small cohort of study participants achieved OSA remission (ILI, 34.4%; DSE, 22.2%), indicated by a low AHI score (< 5 events per hour). At the conclusion of the study, OSA severity decreased to a greater degree with ILI intervention.33,34
Alcohol and drug use can negatively influence sleep patterns and obesity. Higher alcohol consumption is associated with poorer sleep quality and higher chances of developing short sleep duration and snoring.35 Alcohol, a muscle relaxant, causes upper airway narrowing and reduced tongue muscle tone, thereby increasing snoring and OSA as demonstrated by increased AHI on polysomnography after alcohol intake. Alcohol also changes sleep architecture by increasing slow-wave sleep, decreasing REM sleep duration, and increasing sleep arousal in the second half of the night.36 Disrupted circadian rhythm after alcohol consumption was correlated with increased adenosine neurotransmitters derived from ethanol metabolism.37 Alcohol dependence may be related to other psychiatric symptoms, and chronic alcohol use eventually alters sleep mechanisms leading to persistent insomnia, further perpetuating adverse outcomes such as suicidal ideation.36 There are positive associations between beer drinking and measures of abdominal adiposity in men, and “the combination of short sleep duration [and] disinhibited eating … is associated with greater alcohol intake and excess weight.”38
Therefore, counsel patients to avoid alcohol since it is a modifiable risk factor with pervasive adverse health effects.
Many drugs have a profound effect on sleep patterns. Illicit drug use in particular can affect the brain’s neurotransmitter serotonin system. For example, ecstasy users have an increased risk for OSA.39 People with cocaine and heroin use disorder tend to have more sleep-maintenance insomnia.40
Continue to: In contrast, those with alcohol...
In contrast, those with alcohol or cannabis use disorder tend to have more sleep-onset insomnia.40 Not only do illicit drugs interrupt sleep, but daily tobacco use also has been correlated with increased insomnia and shorter sleep duration since nicotine is a stimulant.41
Insomnia is commonly treated with sedative antidepressants and hypnotics—eg, mirtazapine and olanzapine—that contribute to weight gain.42 In addition, other common pharmaceuticals used for sleep disorders, such as diphenhydramine, have sedative properties and tend to lead to weight gain.43 Because so many medications affect sleep and weight, carefully review patients’ medication lists and switch offending agents to weight-neutral drugs if possible.
Treatment and tools to improve sleep in patients with obesity
Given the strong correlation between obesity and sleep disorders, validated screening tools should be used to assess sleep quality, including onset and potential symptoms associated with poor sleep (TABLE 144). For weight management to succeed in patients with obesity, it is crucial to address sleep in addition to nutrition and physical activity.17,45
Physical activity has many benefits to overall health, especially for chronic diseases such as type 2 diabetes and hypertension. The Centers for Disease Control and Prevention recommends at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic exercise per week in addition to muscle-strengthening activities 2 or more days per week.46 However, approximately 300 minutes of moderate-
Physical activity and diet in combination are vital, but diet restriction has a more substantial effect on weight loss than physical activity alone.48 Still, physical activity is essential in helping maintain and prevent weight regain.
Continue to: Nonpharmacologic interventions
Nonpharmacologic interventions include promoting greater sleep quality and quantity by emphasizing good sleep hygiene practices. Developing a practical and effective bedtime routine, creating a quiet sleep environment, and practicing healthy daily habits are essential components to sleep hygiene (TABLE 249,50). Relaxation techniques and cognitive behavioral therapy (CBT) also can help. CBT for insomnia (CBT-I) is the first-line intervention for chronic insomnia.51 Sleep restriction is a type of CBT used to treat insomnia, encouraging short-term sleep loss in the hopes of improving insomnia. A trial by Logue et al showed that patients with overweight and obesity randomized to undergo CBT with better sleep hygiene (nonpharmacologic) interventions had a greater mean weight loss percentage (5% vs 2%; P = .04) than did those who received CBT alone.52
Eastern medicine including herbal interventions lack evidence of efficacy and safety. Further studies need to be done on the effects that chamomile, kava, valerian root (Valeriana officinalis), tryptophan, and Wu Ling (from mycelia Xylaria nigripes) might have on sleep.53
Proceed cautiously with medication. The American College of Physicians recommends a shared decision-making approach when considering pharmacologic therapy for chronic insomnia and the American Academy of Sleep Medicine (AASM) offers guidance on options.51,54 However, the evidence behind AASM sleep pharmacologic recommendations is weak, implying a lesser degree of confidence in the outcome and, therefore, in its appropriateness. Thus, it falls upon the clinician and patient to weigh the benefits and burdens of the pharmacologic treatments of insomnia. If indicated, medications suggested to treat sleep onset and sleep maintenance insomnia are eszopiclone, zolpidem, and temazepam. Zaleplon, triazolam, and ramelteon may improve sleep initiation. Suvorexant and doxepin are used for sleep-maintenance insomnia.54 Exploring patient preferences, cost of treatment, health care options, and available resources should all be considered.
CORRESPONDENCE
Ecler Ercole Jaqua, MD, MBA, FAAFP, AGSF, FACLM, DipABOM, Loma Linda University Health, 25455 Barton Road, Suite 206A, Loma Linda, CA 92354; [email protected]
1. Aminoff MJ, Boller F, Swaab DF. We spend about one-third of our life either sleeping or attempting to do so. Handb Clin Neurol. 2011;98:vii. doi: 10.1016/B978-0-444-52006-7.00047-2
2. Watson NF, Badr MS, Belenky G, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38:843-844. doi: 10.5665/sleep.4716
3. CDC. Sleep and sleep disorders, adults. Accessed September 21, 2023. www.cdc.gov/sleep/data-and-statistics/adults.html
4. Chattu VK, Manzar MD, Kumary S. The global problem of insufficient sleep and its serious public health implications. Healthcare (Basel). 2019;7:1. doi: 10.3390/healthcare7010001
5. Taheri S, Lin L, Austin D, et al. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:e62. doi: 10.1371/journal.pmed.0010062
6. Hafner M, Stepanek M, Taylor J, et al. Why sleep matters—the economic costs of insufficient sleep. Rand Health Q. 2017;6:11.
7. Hisler G, Twenge JM, Krizan Z. Associations between screen time and short sleep duration among adolescents varies by media type: evidence from a cohort study. Sleep Med. 2020;66:92-102. doi: 10.1016/j.sleep.2019.08.007
8. Ogilvie RP, Patel SR. The epidemiology of sleep and obesity. Sleep Health. 2017;3:383-388. doi: 10.1016/j.sleh.2017.07.013
9. CDC. Sleep and sleep disorders: How much sleep do I need? Accessed September 21, 2023. www.cdc.gov/sleep/about_sleep/how_much_sleep.html
10. van Egmond LT, Meth EMS, Engström J, et al. Effects of acute sleep loss on leptin, ghrelin, and adiponectin in adults with healthy weight and obesity: a laboratory study. Obesity (Silver Spring). 2023;31:635-641. doi: 10.1002/oby.23616
11. Spiegel K, Tasali E, Penev P, et al. Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141:846-850. doi: 10.7326/0003-4819-141-11-200412070-00008
12. Antza C, Kostopoulos G, Mostafa S, et al. The links between sleep duration, obesity and type 2 diabetes mellitus. J Endocrinol. 2021;252:125-141. doi: 10.1530/JOE-21-0155
13. Baron KG, Reid KJ, Kern AS, et al. Role of sleep timing in caloric intake and BMI. Obesity (Silver Spring). 2011;19:1374-1381. doi: 10.1038/oby.2011.100
14. Liu XY, Zheng CL, Xu C, et al. Nighttime snacking is associated with risk of obesity and hyperglycemia in adults: a cross-sectional survey from Chinese adult teachers J Biomed Res. 2017;31:541-547. doi: 10.7555/JBR.31.20160083
15. Cai Z, Yang Y, Zhang J, et al. The relationship between daytime napping and obesity: a systematic review and meta-analysis. Sci Rep. 2023.13:12124. doi: 10.1038/s41598-023-37883-7
16. Nedeltcheva AV, Kilkus JM, Imperial J, et al. Insufficient sleep undermines dietary efforts to reduce adiposity. Ann Intern Med. 2010;153:435-441. doi: 10.7326/0003-4819-153-7-201010050-00006
17. Chaput JP, Tremblay A. Adequate sleep to improve the treatment of obesity. CMAJ. 2012;184:1975-1976. doi: 10.1503/cmaj.120876
18. Kelsey MM, Zaepfel A, Bjornstad P, et al. Age-related consequences of childhood obesity. Gerontology. 2014;60:222-228. doi: 10.1159/000356023
19. Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2-19 years: United States, 1963-1965 through 2017-2018. National Center for Health Statistics Health E-Stats. Updated January 29, 2021. Accessed September 21, 2021. www.cdc.gov/nchs/data/hestat/obesity-child-17-18/overweight-obesity-child-H.pdf
20. Fatima Y, Doi SAR, Mamun AA. Sleep quality and obesity in young subjects: a meta-analysis. Obes Rev. 2016;17:1154-1166. doi: 10.1111/obr.12444
21. Gohil A, Hannon TS. Poor sleep and obesity: concurrent epidemics in adolescent youth. Front Endocrinol. 2018;9:364. doi: 10.3389/fendo.2018.00364
22. Golley RK, Maher CA, Matricciani L, et al. Sleep duration or bedtime? Exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. Int J Obes (Lond). 2013;37:546-551. doi: 10.1038/ijo.2012.212
23. Alessi CA. Sleep issues. In: Harper GM, Lyons WL, Potter JF, eds. Geriatrics Review Syllabus (GRS 10). Updated January 2021. Accessed August 29, 2023. http://geriatricscareonline.org
24. Patel SR, Blackwell T, Redline S, et al. The association between sleep duration and obesity in older adults. Int J Obes (Lond). 2008;32:1825-1834. doi: 10.1038/ijo.2008.198
25. Cai GH, Theorell-Haglöw J, Janson C, et al. Insomnia symptoms and sleep duration and their combined effects in relation to associations with obesity and central obesity. Sleep Med. 2018;46:81-87. doi: 10.1016/j.sleep.2018.03.009
26. Beccuti G, Pannain S. Sleep and obesity. Curr Opin Clin Nutr Metab Care. 2011;14:402-412. doi: 10.1097/MCO.0b013 e3283479109
27. Franklin KA, Lindberg E. Obstructive sleep apnea is a common disorder in the population–a review on the epidemiology of sleep apnea. J Thorac Dis. 2015;7:1311-1322. doi: 10.3978/j.issn.2072-1439.2015.06.11
28. USPSTF. Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Screening for obstructive sleep apnea in adults: US Preventive Services Task Force recommendation statement. JAMA. 2017;317:407-414. doi: 10.1001/jama.2016.20325
29. Goyal M, Johnson J. Obstructive sleep apnea diagnosis and management. Mo Med. 2017;114:120-124.
30. American Academy of Sleep Medicine. Hidden health crisis costing America billions: underdiagnosing and undertreating obstructive sleep apnea draining healthcare system. 2016. Accessed September 25, 2023. https://aasm.org/wp-content/uploads/2017/10/sleep-apnea-economic-crisis.pdf
31. Devaraj, NK. Knowledge, attitude, and practice regarding obstructive sleep apnea among primary care physicians. Sleep Breath. 2020;24:1581-1590. doi: 10.1007/s11325-020-02040-1
32. Mysliwiec V, Martin JL, Ulmer CS, et al. The management of chronic insomnia disorder and obstructive sleep apnea: synopsis of the 2019 U.S. Department of Veterans Affairs and U.S. Department of Defense Clinical Practice Guidelines. Ann Intern Med. 2020;172:325-336. doi: 10.7326/M19-3575
33. Kuna ST, Reboussin DM, Strotmeyer ES, et al. Effects of weight loss on obstructive sleep apnea severity. Ten-year results of the Sleep AHEAD study. Am J Respir Crit Care Med. 2021;203:221-229. doi: 10.1164/rccm.201912-2511OC
34. St-Onge MP, Tasali E. Weight loss is integral to obstructive sleep apnea management. Ten-year follow-up in Sleep AHEAD. Am J Respir Crit Care Med. 2021;203:161-162. doi: 10.1164/rccm.202007-2906ED
35. Zheng D, Yuan X, Ma C, et al. Alcohol consumption and sleep quality: a community-based study. Public Health Nutr. 2021;24:4851-4858. doi: 10.1017/S1368980020004553
36. Chakravorty S, Chaudhary NS, Brower KJ. Alcohol dependence and its relationship with insomnia and other sleep disorders. Alcohol Clin Exp Res. 2016;40:2271-2282. doi: 10.1111/acer.13217
37. Elmenhorst EM, Elmenhorst D, Benderoth S, et al. Cognitive impairments by alcohol and sleep deprivation indicate trait characteristics and a potential role for adenosine A1 receptors. Proc Natl Acad Sci U S A. 2018;115:8009-8014. doi: 10.1073/pnas.1803770115
38. Traversy G, Chaput JP. Alcohol consumption and obesity: an update. Curr Obes Rep. 2015;4:122-130. doi: 10.1007/s13679-014-0129-4
39. McCann UD, Sgambati FP, Schwartz AR, et al. Sleep apnea in young abstinent recreational MDMA (“ecstasy”) consumers. Neurology. 2009;73:2011-2017. doi: 10.1212/WNL.0b013e3181c51a62
40. Grau-López L, Grau-López L, Daigre C, et al. Insomnia symptoms in patients with substance use disorders during detoxification and associated clinical features. Front Psychiatry. 2020;11:540022. doi: 10.3389/fpsyt.2020.540022
41. Boehm MA, Lei QM, Lloyd RM, et al. Depression, anxiety, and tobacco use: overlapping impediments to sleep in a national sample of college students. J Am Coll Health. 2016;64:565-574. doi: 10.1080/07448481.2016.1205073
42. Gracious BL, Meyer AE. Psychotropic-induced weight gain and potential pharmacologic treatment strategies. Psychiatry (Edgmont). 2005;2:36-42.
43. Ratliff JC, Barber JA, Palmese LB, et al. Association of prescription H1 antihistamine use with obesity: results from the National Health and Nutrition Examination Survey. Obesity (Silver Spring). 2010;18:2398-2400. doi: 10.1038/oby.2010.176
44. Pataka A, Daskalopoulou E, Kalamaras G, et al. Evaluation of five different questionnaires for assessing sleep apnea syndrome in a sleep clinic. Sleep Med. 2014;15:776-781. doi: 10.1016/j.sleep.2014.03.012
45. Kline CE, Chasens ER, Bizhanova Z, et al. The association between sleep health and weight change during a 12-month behavioral weight loss intervention. Int J Obes (Lond). 2021;45:639-649. doi: 10.1038/s41366-020-00728-8
46. CDC. How much physical activity do adults need? Accessed August 23, 2023. www.cdc.gov/physicalactivity/basics/adults/index.htm
47. Flack KD, Hays HM, Moreland J, et al. Exercise for weight loss: further evaluating energy compensation with exercise. Med Sci Sports Exerc. 2020;52:2466-2475. doi: 10.1249/MSS.0000000000002376
48. Swift DL, Johannsen NM, Lavie CJ, et al. The role of exercise and physical activity in weight loss and maintenance. Prog Cardiovasc Dis. 2014;56:441-447. doi: 10.1016/j.pcad.2013.09.012
49. Irish LA, Kline CE, Gunn HE, et al. The role of sleep hygiene in promoting public health: a review of empirical evidence. Sleep Med Rev. 2015;22:23-36. doi: 10.1016/j.smrv.2014.10.001
50. CDC. Tips for better sleep. 2022. Accessed August 4, 2023. www.cdc.gov/sleep/about_sleep/sleep_hygiene.html
51. Qaseem A, Kansagara D, Forciea MA, et al. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165:125-133. doi: 10.7326/M15-2175
52. Logue EE, Bourguet CC, Palmieri PA, et al. The better weight-better sleep study: a pilot intervention in primary care. Am J Health Behav. 2012;36:319-334. doi: 10.5993/AJHB.36.3.4
53. Leach MJ, Page AT. Herbal medicine for insomnia: a systematic review and meta-analysis. Sleep Med Rev. 2015;24:1-12. doi: 10.1016/j.smrv.2014.12.003
54. Sateia MJ, Buysse DJ, Krystal AD, et al. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13:307-349. doi: 10.5664/jcsm.6470
1. Aminoff MJ, Boller F, Swaab DF. We spend about one-third of our life either sleeping or attempting to do so. Handb Clin Neurol. 2011;98:vii. doi: 10.1016/B978-0-444-52006-7.00047-2
2. Watson NF, Badr MS, Belenky G, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38:843-844. doi: 10.5665/sleep.4716
3. CDC. Sleep and sleep disorders, adults. Accessed September 21, 2023. www.cdc.gov/sleep/data-and-statistics/adults.html
4. Chattu VK, Manzar MD, Kumary S. The global problem of insufficient sleep and its serious public health implications. Healthcare (Basel). 2019;7:1. doi: 10.3390/healthcare7010001
5. Taheri S, Lin L, Austin D, et al. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:e62. doi: 10.1371/journal.pmed.0010062
6. Hafner M, Stepanek M, Taylor J, et al. Why sleep matters—the economic costs of insufficient sleep. Rand Health Q. 2017;6:11.
7. Hisler G, Twenge JM, Krizan Z. Associations between screen time and short sleep duration among adolescents varies by media type: evidence from a cohort study. Sleep Med. 2020;66:92-102. doi: 10.1016/j.sleep.2019.08.007
8. Ogilvie RP, Patel SR. The epidemiology of sleep and obesity. Sleep Health. 2017;3:383-388. doi: 10.1016/j.sleh.2017.07.013
9. CDC. Sleep and sleep disorders: How much sleep do I need? Accessed September 21, 2023. www.cdc.gov/sleep/about_sleep/how_much_sleep.html
10. van Egmond LT, Meth EMS, Engström J, et al. Effects of acute sleep loss on leptin, ghrelin, and adiponectin in adults with healthy weight and obesity: a laboratory study. Obesity (Silver Spring). 2023;31:635-641. doi: 10.1002/oby.23616
11. Spiegel K, Tasali E, Penev P, et al. Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141:846-850. doi: 10.7326/0003-4819-141-11-200412070-00008
12. Antza C, Kostopoulos G, Mostafa S, et al. The links between sleep duration, obesity and type 2 diabetes mellitus. J Endocrinol. 2021;252:125-141. doi: 10.1530/JOE-21-0155
13. Baron KG, Reid KJ, Kern AS, et al. Role of sleep timing in caloric intake and BMI. Obesity (Silver Spring). 2011;19:1374-1381. doi: 10.1038/oby.2011.100
14. Liu XY, Zheng CL, Xu C, et al. Nighttime snacking is associated with risk of obesity and hyperglycemia in adults: a cross-sectional survey from Chinese adult teachers J Biomed Res. 2017;31:541-547. doi: 10.7555/JBR.31.20160083
15. Cai Z, Yang Y, Zhang J, et al. The relationship between daytime napping and obesity: a systematic review and meta-analysis. Sci Rep. 2023.13:12124. doi: 10.1038/s41598-023-37883-7
16. Nedeltcheva AV, Kilkus JM, Imperial J, et al. Insufficient sleep undermines dietary efforts to reduce adiposity. Ann Intern Med. 2010;153:435-441. doi: 10.7326/0003-4819-153-7-201010050-00006
17. Chaput JP, Tremblay A. Adequate sleep to improve the treatment of obesity. CMAJ. 2012;184:1975-1976. doi: 10.1503/cmaj.120876
18. Kelsey MM, Zaepfel A, Bjornstad P, et al. Age-related consequences of childhood obesity. Gerontology. 2014;60:222-228. doi: 10.1159/000356023
19. Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2-19 years: United States, 1963-1965 through 2017-2018. National Center for Health Statistics Health E-Stats. Updated January 29, 2021. Accessed September 21, 2021. www.cdc.gov/nchs/data/hestat/obesity-child-17-18/overweight-obesity-child-H.pdf
20. Fatima Y, Doi SAR, Mamun AA. Sleep quality and obesity in young subjects: a meta-analysis. Obes Rev. 2016;17:1154-1166. doi: 10.1111/obr.12444
21. Gohil A, Hannon TS. Poor sleep and obesity: concurrent epidemics in adolescent youth. Front Endocrinol. 2018;9:364. doi: 10.3389/fendo.2018.00364
22. Golley RK, Maher CA, Matricciani L, et al. Sleep duration or bedtime? Exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. Int J Obes (Lond). 2013;37:546-551. doi: 10.1038/ijo.2012.212
23. Alessi CA. Sleep issues. In: Harper GM, Lyons WL, Potter JF, eds. Geriatrics Review Syllabus (GRS 10). Updated January 2021. Accessed August 29, 2023. http://geriatricscareonline.org
24. Patel SR, Blackwell T, Redline S, et al. The association between sleep duration and obesity in older adults. Int J Obes (Lond). 2008;32:1825-1834. doi: 10.1038/ijo.2008.198
25. Cai GH, Theorell-Haglöw J, Janson C, et al. Insomnia symptoms and sleep duration and their combined effects in relation to associations with obesity and central obesity. Sleep Med. 2018;46:81-87. doi: 10.1016/j.sleep.2018.03.009
26. Beccuti G, Pannain S. Sleep and obesity. Curr Opin Clin Nutr Metab Care. 2011;14:402-412. doi: 10.1097/MCO.0b013 e3283479109
27. Franklin KA, Lindberg E. Obstructive sleep apnea is a common disorder in the population–a review on the epidemiology of sleep apnea. J Thorac Dis. 2015;7:1311-1322. doi: 10.3978/j.issn.2072-1439.2015.06.11
28. USPSTF. Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Screening for obstructive sleep apnea in adults: US Preventive Services Task Force recommendation statement. JAMA. 2017;317:407-414. doi: 10.1001/jama.2016.20325
29. Goyal M, Johnson J. Obstructive sleep apnea diagnosis and management. Mo Med. 2017;114:120-124.
30. American Academy of Sleep Medicine. Hidden health crisis costing America billions: underdiagnosing and undertreating obstructive sleep apnea draining healthcare system. 2016. Accessed September 25, 2023. https://aasm.org/wp-content/uploads/2017/10/sleep-apnea-economic-crisis.pdf
31. Devaraj, NK. Knowledge, attitude, and practice regarding obstructive sleep apnea among primary care physicians. Sleep Breath. 2020;24:1581-1590. doi: 10.1007/s11325-020-02040-1
32. Mysliwiec V, Martin JL, Ulmer CS, et al. The management of chronic insomnia disorder and obstructive sleep apnea: synopsis of the 2019 U.S. Department of Veterans Affairs and U.S. Department of Defense Clinical Practice Guidelines. Ann Intern Med. 2020;172:325-336. doi: 10.7326/M19-3575
33. Kuna ST, Reboussin DM, Strotmeyer ES, et al. Effects of weight loss on obstructive sleep apnea severity. Ten-year results of the Sleep AHEAD study. Am J Respir Crit Care Med. 2021;203:221-229. doi: 10.1164/rccm.201912-2511OC
34. St-Onge MP, Tasali E. Weight loss is integral to obstructive sleep apnea management. Ten-year follow-up in Sleep AHEAD. Am J Respir Crit Care Med. 2021;203:161-162. doi: 10.1164/rccm.202007-2906ED
35. Zheng D, Yuan X, Ma C, et al. Alcohol consumption and sleep quality: a community-based study. Public Health Nutr. 2021;24:4851-4858. doi: 10.1017/S1368980020004553
36. Chakravorty S, Chaudhary NS, Brower KJ. Alcohol dependence and its relationship with insomnia and other sleep disorders. Alcohol Clin Exp Res. 2016;40:2271-2282. doi: 10.1111/acer.13217
37. Elmenhorst EM, Elmenhorst D, Benderoth S, et al. Cognitive impairments by alcohol and sleep deprivation indicate trait characteristics and a potential role for adenosine A1 receptors. Proc Natl Acad Sci U S A. 2018;115:8009-8014. doi: 10.1073/pnas.1803770115
38. Traversy G, Chaput JP. Alcohol consumption and obesity: an update. Curr Obes Rep. 2015;4:122-130. doi: 10.1007/s13679-014-0129-4
39. McCann UD, Sgambati FP, Schwartz AR, et al. Sleep apnea in young abstinent recreational MDMA (“ecstasy”) consumers. Neurology. 2009;73:2011-2017. doi: 10.1212/WNL.0b013e3181c51a62
40. Grau-López L, Grau-López L, Daigre C, et al. Insomnia symptoms in patients with substance use disorders during detoxification and associated clinical features. Front Psychiatry. 2020;11:540022. doi: 10.3389/fpsyt.2020.540022
41. Boehm MA, Lei QM, Lloyd RM, et al. Depression, anxiety, and tobacco use: overlapping impediments to sleep in a national sample of college students. J Am Coll Health. 2016;64:565-574. doi: 10.1080/07448481.2016.1205073
42. Gracious BL, Meyer AE. Psychotropic-induced weight gain and potential pharmacologic treatment strategies. Psychiatry (Edgmont). 2005;2:36-42.
43. Ratliff JC, Barber JA, Palmese LB, et al. Association of prescription H1 antihistamine use with obesity: results from the National Health and Nutrition Examination Survey. Obesity (Silver Spring). 2010;18:2398-2400. doi: 10.1038/oby.2010.176
44. Pataka A, Daskalopoulou E, Kalamaras G, et al. Evaluation of five different questionnaires for assessing sleep apnea syndrome in a sleep clinic. Sleep Med. 2014;15:776-781. doi: 10.1016/j.sleep.2014.03.012
45. Kline CE, Chasens ER, Bizhanova Z, et al. The association between sleep health and weight change during a 12-month behavioral weight loss intervention. Int J Obes (Lond). 2021;45:639-649. doi: 10.1038/s41366-020-00728-8
46. CDC. How much physical activity do adults need? Accessed August 23, 2023. www.cdc.gov/physicalactivity/basics/adults/index.htm
47. Flack KD, Hays HM, Moreland J, et al. Exercise for weight loss: further evaluating energy compensation with exercise. Med Sci Sports Exerc. 2020;52:2466-2475. doi: 10.1249/MSS.0000000000002376
48. Swift DL, Johannsen NM, Lavie CJ, et al. The role of exercise and physical activity in weight loss and maintenance. Prog Cardiovasc Dis. 2014;56:441-447. doi: 10.1016/j.pcad.2013.09.012
49. Irish LA, Kline CE, Gunn HE, et al. The role of sleep hygiene in promoting public health: a review of empirical evidence. Sleep Med Rev. 2015;22:23-36. doi: 10.1016/j.smrv.2014.10.001
50. CDC. Tips for better sleep. 2022. Accessed August 4, 2023. www.cdc.gov/sleep/about_sleep/sleep_hygiene.html
51. Qaseem A, Kansagara D, Forciea MA, et al. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165:125-133. doi: 10.7326/M15-2175
52. Logue EE, Bourguet CC, Palmieri PA, et al. The better weight-better sleep study: a pilot intervention in primary care. Am J Health Behav. 2012;36:319-334. doi: 10.5993/AJHB.36.3.4
53. Leach MJ, Page AT. Herbal medicine for insomnia: a systematic review and meta-analysis. Sleep Med Rev. 2015;24:1-12. doi: 10.1016/j.smrv.2014.12.003
54. Sateia MJ, Buysse DJ, Krystal AD, et al. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13:307-349. doi: 10.5664/jcsm.6470
PRACTICE RECOMMENDATIONS
› Consider cognitive behaviorial therapy for insomnia (CBT-I) first-line treatment for insomnia. A
› Carefully review patients’ medication lists, as many pharmaceuticals can affect weight and sleep. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Biologics linked to fewer hospitalizations after asthma exacerbation
In a real-world study of asthma patients,
The data fill a gap, according to Sushan Gupta, MD, who presented the results at the annual meeting of the American College of Chest Physicians. “There’s some ample real-world data that shows that biologics reduce the incidence of asthma exacerbation, but the data regarding what happens after an exacerbation is still lacking, especially real-world data,” said Dr. Gupta, who is a resident at Carle Foundation Hospital in Champaign, Ill.
The findings were encouraging. “Patients with severe asthma on biologics fare well even after an exacerbation event, which includes a reduced incidence of hospitalization, ICU admission, and need for mechanical ventilation. We did not have any patient in the biologic group that required intubation, so that is pretty significant as compared to other patients who did not receive biologics,” said Dr. Gupta.
The results weren’t surprising, but underscore the benefits of biologics, according to Brittany Duchene, MD, who moderated the session where the results were presented. “I think it reinforced that they’re really good drugs,” said Dr. Duchene, who is a pulmonary critical care physician at Northeastern Vermont Regional Hospital, St. Johnsbury.
Although the study was retrospective, it suggests that the threshold for initiating biologics could potentially be lowered for patients with uncontrolled asthma despite adequate use of inhalers, according to Dr. Gupta. “Should that threshold be lower, and would that improve the overall morbidity and eventually the health care cost of utilization? Our study does not prove any of those data, but moving forward that data will also come out.”
Dr. Duchene noted that the accumulating scientific and clinical data for biologics is “really, really strong.” She also speculated that biologics could be used increasingly in the acute setting, which she admitted is a controversial topic. “I think there’s going to be a lot more push to early initiation, and you can see from the [new] study that it decreased a lot of hospitalizations.”
Dr. Gupta emphasized the need for prospective studies, and Dr. Duchene agreed that any such change would need to be patient centric, considering the diversity of available biologics. “It depends what their true issue is. The broader the biologic [mechanism of action], probably the more success you’ll have. I’ve found there’s not a pure allergic or a pure eosinophilic asthma patient. They’re usually more a combination.”
Some key questions remain about biologics treatment, especially in the long term. These include when a patient should be switched from one biologic to another, and whether biologic treatment should be continued over the patient’s lifetime and potential long-term side effects. “I think that data is still evolving and will come to us with time,” said Dr. Gupta.
The researchers analyzed retrospective data from 316 asthma patients treated with biologics and 9,645 treated with nonbiologic therapy between February 2018 and February 2023 at a tertiary care teaching hospital in the Midwest. There was a higher proportion of females in the biologics (69.7%) and nonbiologics groups (63.8%, P = .032), but there was no significant difference in the proportion of Whites in the biologics and nonbiologics groups (78.2% vs. 74.3%, P = .103).
The lack of a difference in racial groups was a surprise, according to Dr. Duchene, especially since other studies have noted disparities in biologic therapy among asthma patients.
Among the biologics group, 0.9% were hospitalized during the study period, compared with 6.5% of the nonbiologics group (P = .00006). They also had fewer ICU visits (0.3% vs. 1.8%; P = .04).
Dr. Gupta’s team attempted to subdivide the data by individual biologic, but there was no statistical significance in outcomes between biologics, perhaps because of the relatively small sample size.
Dr. Gupta noted that his group’s results are generally similar to other studies, including a U.S. study that found a decrease in exacerbation rates after staring or switching biologics and a slightly higher prevalence of biologics use among White patients (77% of biologic users versus 71% of nonbiologics users). A study in southwestern England found fewer ED visits and hospitalizations among patients on biologics.
Dr. Gupta and Dr. Duchene have no relevant financial disclosures.
In a real-world study of asthma patients,
The data fill a gap, according to Sushan Gupta, MD, who presented the results at the annual meeting of the American College of Chest Physicians. “There’s some ample real-world data that shows that biologics reduce the incidence of asthma exacerbation, but the data regarding what happens after an exacerbation is still lacking, especially real-world data,” said Dr. Gupta, who is a resident at Carle Foundation Hospital in Champaign, Ill.
The findings were encouraging. “Patients with severe asthma on biologics fare well even after an exacerbation event, which includes a reduced incidence of hospitalization, ICU admission, and need for mechanical ventilation. We did not have any patient in the biologic group that required intubation, so that is pretty significant as compared to other patients who did not receive biologics,” said Dr. Gupta.
The results weren’t surprising, but underscore the benefits of biologics, according to Brittany Duchene, MD, who moderated the session where the results were presented. “I think it reinforced that they’re really good drugs,” said Dr. Duchene, who is a pulmonary critical care physician at Northeastern Vermont Regional Hospital, St. Johnsbury.
Although the study was retrospective, it suggests that the threshold for initiating biologics could potentially be lowered for patients with uncontrolled asthma despite adequate use of inhalers, according to Dr. Gupta. “Should that threshold be lower, and would that improve the overall morbidity and eventually the health care cost of utilization? Our study does not prove any of those data, but moving forward that data will also come out.”
Dr. Duchene noted that the accumulating scientific and clinical data for biologics is “really, really strong.” She also speculated that biologics could be used increasingly in the acute setting, which she admitted is a controversial topic. “I think there’s going to be a lot more push to early initiation, and you can see from the [new] study that it decreased a lot of hospitalizations.”
Dr. Gupta emphasized the need for prospective studies, and Dr. Duchene agreed that any such change would need to be patient centric, considering the diversity of available biologics. “It depends what their true issue is. The broader the biologic [mechanism of action], probably the more success you’ll have. I’ve found there’s not a pure allergic or a pure eosinophilic asthma patient. They’re usually more a combination.”
Some key questions remain about biologics treatment, especially in the long term. These include when a patient should be switched from one biologic to another, and whether biologic treatment should be continued over the patient’s lifetime and potential long-term side effects. “I think that data is still evolving and will come to us with time,” said Dr. Gupta.
The researchers analyzed retrospective data from 316 asthma patients treated with biologics and 9,645 treated with nonbiologic therapy between February 2018 and February 2023 at a tertiary care teaching hospital in the Midwest. There was a higher proportion of females in the biologics (69.7%) and nonbiologics groups (63.8%, P = .032), but there was no significant difference in the proportion of Whites in the biologics and nonbiologics groups (78.2% vs. 74.3%, P = .103).
The lack of a difference in racial groups was a surprise, according to Dr. Duchene, especially since other studies have noted disparities in biologic therapy among asthma patients.
Among the biologics group, 0.9% were hospitalized during the study period, compared with 6.5% of the nonbiologics group (P = .00006). They also had fewer ICU visits (0.3% vs. 1.8%; P = .04).
Dr. Gupta’s team attempted to subdivide the data by individual biologic, but there was no statistical significance in outcomes between biologics, perhaps because of the relatively small sample size.
Dr. Gupta noted that his group’s results are generally similar to other studies, including a U.S. study that found a decrease in exacerbation rates after staring or switching biologics and a slightly higher prevalence of biologics use among White patients (77% of biologic users versus 71% of nonbiologics users). A study in southwestern England found fewer ED visits and hospitalizations among patients on biologics.
Dr. Gupta and Dr. Duchene have no relevant financial disclosures.
In a real-world study of asthma patients,
The data fill a gap, according to Sushan Gupta, MD, who presented the results at the annual meeting of the American College of Chest Physicians. “There’s some ample real-world data that shows that biologics reduce the incidence of asthma exacerbation, but the data regarding what happens after an exacerbation is still lacking, especially real-world data,” said Dr. Gupta, who is a resident at Carle Foundation Hospital in Champaign, Ill.
The findings were encouraging. “Patients with severe asthma on biologics fare well even after an exacerbation event, which includes a reduced incidence of hospitalization, ICU admission, and need for mechanical ventilation. We did not have any patient in the biologic group that required intubation, so that is pretty significant as compared to other patients who did not receive biologics,” said Dr. Gupta.
The results weren’t surprising, but underscore the benefits of biologics, according to Brittany Duchene, MD, who moderated the session where the results were presented. “I think it reinforced that they’re really good drugs,” said Dr. Duchene, who is a pulmonary critical care physician at Northeastern Vermont Regional Hospital, St. Johnsbury.
Although the study was retrospective, it suggests that the threshold for initiating biologics could potentially be lowered for patients with uncontrolled asthma despite adequate use of inhalers, according to Dr. Gupta. “Should that threshold be lower, and would that improve the overall morbidity and eventually the health care cost of utilization? Our study does not prove any of those data, but moving forward that data will also come out.”
Dr. Duchene noted that the accumulating scientific and clinical data for biologics is “really, really strong.” She also speculated that biologics could be used increasingly in the acute setting, which she admitted is a controversial topic. “I think there’s going to be a lot more push to early initiation, and you can see from the [new] study that it decreased a lot of hospitalizations.”
Dr. Gupta emphasized the need for prospective studies, and Dr. Duchene agreed that any such change would need to be patient centric, considering the diversity of available biologics. “It depends what their true issue is. The broader the biologic [mechanism of action], probably the more success you’ll have. I’ve found there’s not a pure allergic or a pure eosinophilic asthma patient. They’re usually more a combination.”
Some key questions remain about biologics treatment, especially in the long term. These include when a patient should be switched from one biologic to another, and whether biologic treatment should be continued over the patient’s lifetime and potential long-term side effects. “I think that data is still evolving and will come to us with time,” said Dr. Gupta.
The researchers analyzed retrospective data from 316 asthma patients treated with biologics and 9,645 treated with nonbiologic therapy between February 2018 and February 2023 at a tertiary care teaching hospital in the Midwest. There was a higher proportion of females in the biologics (69.7%) and nonbiologics groups (63.8%, P = .032), but there was no significant difference in the proportion of Whites in the biologics and nonbiologics groups (78.2% vs. 74.3%, P = .103).
The lack of a difference in racial groups was a surprise, according to Dr. Duchene, especially since other studies have noted disparities in biologic therapy among asthma patients.
Among the biologics group, 0.9% were hospitalized during the study period, compared with 6.5% of the nonbiologics group (P = .00006). They also had fewer ICU visits (0.3% vs. 1.8%; P = .04).
Dr. Gupta’s team attempted to subdivide the data by individual biologic, but there was no statistical significance in outcomes between biologics, perhaps because of the relatively small sample size.
Dr. Gupta noted that his group’s results are generally similar to other studies, including a U.S. study that found a decrease in exacerbation rates after staring or switching biologics and a slightly higher prevalence of biologics use among White patients (77% of biologic users versus 71% of nonbiologics users). A study in southwestern England found fewer ED visits and hospitalizations among patients on biologics.
Dr. Gupta and Dr. Duchene have no relevant financial disclosures.
FROM CHEST 2023
Talking to your patients: Colorectal cancer screening starts at age 45
Your patients may be confused by conflicting guidance about when to start getting screened for colorectal cancer (CRC). AGA stands firmly behind our Multi-Society Task Force on CRC recommendations, and those of the U.S. Preventive Services Taskforce, the American Cancer Society, and other national medical societies and advocacy organizations, that colorectal cancer screening for average risk individuals should start at age 45.
But
View the talking points below to help your patients understand screening guidelines and why they need to get screened for colorectal cancer.
One outlier medical group says colorectal cancer screening can wait until age 50, but the consensus of the government and multiple expert groups, including the American Gastroenterological Association, is that getting screened starting at age 45 could save your life.
Colorectal cancer will be the leading cause of cancer-related death among 20- to 49-year-olds by 2030. Putting off screening until age 50 is a grave mistake.
Screening for colorectal cancer can help find polyps in your colon and rectum early, sometimes even before they become cancer. A polyp is a mushroom-like or flat growth on the inside wall of your colon or rectum. Polyps grow slowly over many years and not all turn into cancer. I can remove these growths, which might mean that I can help stop the cancer before it starts, remove tissue that shows cancer, or let us start treatment early if cancer has already started.
There are several tests for colorectal cancer screening, including colonoscopy, but there are also tests that are noninvasive, meaning they don’t need tools that enter your body. Let’s talk about each test and which one you feel most comfortable using.
For more resources to share with your patients, visit the AGA GI Patient Center.
Your patients may be confused by conflicting guidance about when to start getting screened for colorectal cancer (CRC). AGA stands firmly behind our Multi-Society Task Force on CRC recommendations, and those of the U.S. Preventive Services Taskforce, the American Cancer Society, and other national medical societies and advocacy organizations, that colorectal cancer screening for average risk individuals should start at age 45.
But
View the talking points below to help your patients understand screening guidelines and why they need to get screened for colorectal cancer.
One outlier medical group says colorectal cancer screening can wait until age 50, but the consensus of the government and multiple expert groups, including the American Gastroenterological Association, is that getting screened starting at age 45 could save your life.
Colorectal cancer will be the leading cause of cancer-related death among 20- to 49-year-olds by 2030. Putting off screening until age 50 is a grave mistake.
Screening for colorectal cancer can help find polyps in your colon and rectum early, sometimes even before they become cancer. A polyp is a mushroom-like or flat growth on the inside wall of your colon or rectum. Polyps grow slowly over many years and not all turn into cancer. I can remove these growths, which might mean that I can help stop the cancer before it starts, remove tissue that shows cancer, or let us start treatment early if cancer has already started.
There are several tests for colorectal cancer screening, including colonoscopy, but there are also tests that are noninvasive, meaning they don’t need tools that enter your body. Let’s talk about each test and which one you feel most comfortable using.
For more resources to share with your patients, visit the AGA GI Patient Center.
Your patients may be confused by conflicting guidance about when to start getting screened for colorectal cancer (CRC). AGA stands firmly behind our Multi-Society Task Force on CRC recommendations, and those of the U.S. Preventive Services Taskforce, the American Cancer Society, and other national medical societies and advocacy organizations, that colorectal cancer screening for average risk individuals should start at age 45.
But
View the talking points below to help your patients understand screening guidelines and why they need to get screened for colorectal cancer.
One outlier medical group says colorectal cancer screening can wait until age 50, but the consensus of the government and multiple expert groups, including the American Gastroenterological Association, is that getting screened starting at age 45 could save your life.
Colorectal cancer will be the leading cause of cancer-related death among 20- to 49-year-olds by 2030. Putting off screening until age 50 is a grave mistake.
Screening for colorectal cancer can help find polyps in your colon and rectum early, sometimes even before they become cancer. A polyp is a mushroom-like or flat growth on the inside wall of your colon or rectum. Polyps grow slowly over many years and not all turn into cancer. I can remove these growths, which might mean that I can help stop the cancer before it starts, remove tissue that shows cancer, or let us start treatment early if cancer has already started.
There are several tests for colorectal cancer screening, including colonoscopy, but there are also tests that are noninvasive, meaning they don’t need tools that enter your body. Let’s talk about each test and which one you feel most comfortable using.
For more resources to share with your patients, visit the AGA GI Patient Center.
Running vs. meds for depression: Is there a clear winner?
BARCELONA – However, running provides greater physical health benefits while adherence is greater with drug treatment.
“Both interventions helped with the depression to around the same extent,” study presenter Brenda W.J.H. Penninx, PhD, professor of psychiatric epidemiology at the VU University Medical Center in Amsterdam said in a release.
However, medication “generally had worse impact on body weight, heart rate variability, and blood pressure, whereas running therapy led to improved effect on general fitness and heart rate,” Dr. Penninx added.
The findings were presented at the annual congress of the European College of Neuropsychopharmacology and recently published in the Journal of Affective Disorders.
Research gap
Previous research suggests exercise interventions can have a therapeutic effect equivalent to antidepressants, but their impact on physical health has been “poorly examined in a psychiatric population, the investigators note.
The authors note that depressive and anxiety disorders “cause immense suffering by compromising both mental and physical health,” and the need for effective treatments is “pressing.”
Although antidepressant medication is considered a “standard first-line treatment” alongside psychotherapy, the drugs are “not effective for all and [are] often associated with side effects.”
The Mood Treatment with Antidepressant or Running (MOTAR) study was a partially randomized pragmatic trial in adults with depression and/or anxiety disorder, as determined using the DSM-IV algorithms with the Composite International Diagnostic Interview (CIDI).
The 16-week intervention study included 141 patients with depression and/or anxiety. The mean age was 38.2 years and 58% were women. Participants were offered a choice of treatment: 16 weeks of treatment with the selective serotonin reuptake inhibitor (SSRI) escitalopram (Lexapro) or a 16-week group-based running therapy.
Patients without a strong preference for treatment allocation were randomly assigned to either antidepressant medication or running therapy, while those unwilling to be randomized were allocated to their preferred intervention.
A total of 22 patients were randomly assigned to receive antidepressant treatment and 13 to running therapy. A total of 36 participants chose antidepressant treatment, while 83 chose the running therapy.
Running therapy involved 16 weeks of supervised 45-minute outdoor running sessions to a target of two to three sessions per week, in line with U.S. Centers for Disease Control and Prevention/American College of Sports Medicine recommendations.
Physical health benefits
Treatment adherence in the antidepressant group, defined as still using treatment at the posttreatment assessment, was 82.2% vs. 52.1% among running therapy participants, where adherence was specified as completing more than 22 sessions.
Remission was defined as no longer meeting the criteria of a current depressive or anxiety disorder via CIDI at week 16.
On intention-to-treat analysis, this requirement was met by 44.8% of patients taking antidepressants and 43.3% of those in the running therapy group (P = .88).
However, running therapy patients showed significant improvements in weight (P = .001), waist circumference (P = .011), systolic and diastolic blood pressure (P = .011 and P = .002, respectively), heart rate (P = .033), and heart rate variability (P = .006).
The investigators note the more favorable physical health changes in the running therapy group were attributable to “larger improvements in the running therapy group but also due to larger deterioration in the antidepressant group.”
Antidepressants are generally safe and effective and work for most people, said Dr. Penninx. She also noted that untreated depression leads to worse outcomes, so “antidepressants are generally a good choice.”
Nevertheless, she said, “we need to extend our treatment arsenal as not all patients respond to antidepressants or are willing to take them.”
The study’s results, she added, suggest that “implementing exercise therapy is something we should take much more seriously, as it could be a good, and maybe even better, choice for some of our patients.”
Francesca Cirulli, PhD, senior researcher and group leader at the National Institute of Health, Rome, said in an interview that the study is notable because it is one of the first to prospectively measure the effects of antidepressants and running on physical health.
Dr. Cirulli suggested that running therapy could be tried ahead of treatment with antidepressants if patients prefer physical exercise and can adhere to it. However, she said, the findings also suggest that an increase in physical activity should accompany treatment with antidepressant medications.
Overall, Dr. Cirulli said “the message should not be that everyone can be helped by running and antidepressants are bad,” but rather “these are both helpful, but not excellent, interventions against depression.”
‘Important limitations’
In a comment, Eduard Vieta, MD, PhD, chair of the department of psychiatry and psychology at the University of Barcelona Hospital Clinic, noted the study has “very important limitations.”
Among the limitations: the inclusion of nonrandomized patients who received the treatment of their choice, causing obvious bias and the “lack of binding and power issues” over the number of patients enrolled.
Dr. Vieta also said that the results “seem obvious, because it is known that exercise improves physical health.”
The trial therefore shows, “if you can find people who are able to do exercise while depressed and adhere to it, those would benefit from that practice,” he noted.
Also commenting on the research, Eric Ruhe, MD, PhD, Radboud University Medical Center, Nijmegen, the Netherlands, said the results are confirmatory and “again show physical health can influence mental health.”
However, Dr. Ruhe underlined, while it is “common practice” to allow patients to follow their treatment preference and is “understandable from a pragmatic point of view,” the group comparison may be “biased,” compared with a “truly randomized study.”
“For example, patients in the antidepressant group were more depressed, which might be associated with less chance of persisting engagement in the exercises,” he said. “So, we have to be careful not to overinterpret the comparisons between groups, which the authors acknowledge properly.”
Turning to the difference in adherence between the two interventions, Dr. Ruhe said the results show adopting, and adhering to, a lifestyle habit is more difficult than taking a pill.
“This is not exclusively found in psychiatry, indicating that we also have to focus on how to improve compliance to healthy behavior. This could have tremendous impact on health care more generally, but also on psychiatric diseases,” Dr. Ruhe said.
The MOTAR study was funded by a NWO-VICI grant. Funding for the inflammatory markers was provided by ZonMw: The Netherlands Organization for Health Research and Development. The study authors and clinicians interviewed for this story declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BARCELONA – However, running provides greater physical health benefits while adherence is greater with drug treatment.
“Both interventions helped with the depression to around the same extent,” study presenter Brenda W.J.H. Penninx, PhD, professor of psychiatric epidemiology at the VU University Medical Center in Amsterdam said in a release.
However, medication “generally had worse impact on body weight, heart rate variability, and blood pressure, whereas running therapy led to improved effect on general fitness and heart rate,” Dr. Penninx added.
The findings were presented at the annual congress of the European College of Neuropsychopharmacology and recently published in the Journal of Affective Disorders.
Research gap
Previous research suggests exercise interventions can have a therapeutic effect equivalent to antidepressants, but their impact on physical health has been “poorly examined in a psychiatric population, the investigators note.
The authors note that depressive and anxiety disorders “cause immense suffering by compromising both mental and physical health,” and the need for effective treatments is “pressing.”
Although antidepressant medication is considered a “standard first-line treatment” alongside psychotherapy, the drugs are “not effective for all and [are] often associated with side effects.”
The Mood Treatment with Antidepressant or Running (MOTAR) study was a partially randomized pragmatic trial in adults with depression and/or anxiety disorder, as determined using the DSM-IV algorithms with the Composite International Diagnostic Interview (CIDI).
The 16-week intervention study included 141 patients with depression and/or anxiety. The mean age was 38.2 years and 58% were women. Participants were offered a choice of treatment: 16 weeks of treatment with the selective serotonin reuptake inhibitor (SSRI) escitalopram (Lexapro) or a 16-week group-based running therapy.
Patients without a strong preference for treatment allocation were randomly assigned to either antidepressant medication or running therapy, while those unwilling to be randomized were allocated to their preferred intervention.
A total of 22 patients were randomly assigned to receive antidepressant treatment and 13 to running therapy. A total of 36 participants chose antidepressant treatment, while 83 chose the running therapy.
Running therapy involved 16 weeks of supervised 45-minute outdoor running sessions to a target of two to three sessions per week, in line with U.S. Centers for Disease Control and Prevention/American College of Sports Medicine recommendations.
Physical health benefits
Treatment adherence in the antidepressant group, defined as still using treatment at the posttreatment assessment, was 82.2% vs. 52.1% among running therapy participants, where adherence was specified as completing more than 22 sessions.
Remission was defined as no longer meeting the criteria of a current depressive or anxiety disorder via CIDI at week 16.
On intention-to-treat analysis, this requirement was met by 44.8% of patients taking antidepressants and 43.3% of those in the running therapy group (P = .88).
However, running therapy patients showed significant improvements in weight (P = .001), waist circumference (P = .011), systolic and diastolic blood pressure (P = .011 and P = .002, respectively), heart rate (P = .033), and heart rate variability (P = .006).
The investigators note the more favorable physical health changes in the running therapy group were attributable to “larger improvements in the running therapy group but also due to larger deterioration in the antidepressant group.”
Antidepressants are generally safe and effective and work for most people, said Dr. Penninx. She also noted that untreated depression leads to worse outcomes, so “antidepressants are generally a good choice.”
Nevertheless, she said, “we need to extend our treatment arsenal as not all patients respond to antidepressants or are willing to take them.”
The study’s results, she added, suggest that “implementing exercise therapy is something we should take much more seriously, as it could be a good, and maybe even better, choice for some of our patients.”
Francesca Cirulli, PhD, senior researcher and group leader at the National Institute of Health, Rome, said in an interview that the study is notable because it is one of the first to prospectively measure the effects of antidepressants and running on physical health.
Dr. Cirulli suggested that running therapy could be tried ahead of treatment with antidepressants if patients prefer physical exercise and can adhere to it. However, she said, the findings also suggest that an increase in physical activity should accompany treatment with antidepressant medications.
Overall, Dr. Cirulli said “the message should not be that everyone can be helped by running and antidepressants are bad,” but rather “these are both helpful, but not excellent, interventions against depression.”
‘Important limitations’
In a comment, Eduard Vieta, MD, PhD, chair of the department of psychiatry and psychology at the University of Barcelona Hospital Clinic, noted the study has “very important limitations.”
Among the limitations: the inclusion of nonrandomized patients who received the treatment of their choice, causing obvious bias and the “lack of binding and power issues” over the number of patients enrolled.
Dr. Vieta also said that the results “seem obvious, because it is known that exercise improves physical health.”
The trial therefore shows, “if you can find people who are able to do exercise while depressed and adhere to it, those would benefit from that practice,” he noted.
Also commenting on the research, Eric Ruhe, MD, PhD, Radboud University Medical Center, Nijmegen, the Netherlands, said the results are confirmatory and “again show physical health can influence mental health.”
However, Dr. Ruhe underlined, while it is “common practice” to allow patients to follow their treatment preference and is “understandable from a pragmatic point of view,” the group comparison may be “biased,” compared with a “truly randomized study.”
“For example, patients in the antidepressant group were more depressed, which might be associated with less chance of persisting engagement in the exercises,” he said. “So, we have to be careful not to overinterpret the comparisons between groups, which the authors acknowledge properly.”
Turning to the difference in adherence between the two interventions, Dr. Ruhe said the results show adopting, and adhering to, a lifestyle habit is more difficult than taking a pill.
“This is not exclusively found in psychiatry, indicating that we also have to focus on how to improve compliance to healthy behavior. This could have tremendous impact on health care more generally, but also on psychiatric diseases,” Dr. Ruhe said.
The MOTAR study was funded by a NWO-VICI grant. Funding for the inflammatory markers was provided by ZonMw: The Netherlands Organization for Health Research and Development. The study authors and clinicians interviewed for this story declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BARCELONA – However, running provides greater physical health benefits while adherence is greater with drug treatment.
“Both interventions helped with the depression to around the same extent,” study presenter Brenda W.J.H. Penninx, PhD, professor of psychiatric epidemiology at the VU University Medical Center in Amsterdam said in a release.
However, medication “generally had worse impact on body weight, heart rate variability, and blood pressure, whereas running therapy led to improved effect on general fitness and heart rate,” Dr. Penninx added.
The findings were presented at the annual congress of the European College of Neuropsychopharmacology and recently published in the Journal of Affective Disorders.
Research gap
Previous research suggests exercise interventions can have a therapeutic effect equivalent to antidepressants, but their impact on physical health has been “poorly examined in a psychiatric population, the investigators note.
The authors note that depressive and anxiety disorders “cause immense suffering by compromising both mental and physical health,” and the need for effective treatments is “pressing.”
Although antidepressant medication is considered a “standard first-line treatment” alongside psychotherapy, the drugs are “not effective for all and [are] often associated with side effects.”
The Mood Treatment with Antidepressant or Running (MOTAR) study was a partially randomized pragmatic trial in adults with depression and/or anxiety disorder, as determined using the DSM-IV algorithms with the Composite International Diagnostic Interview (CIDI).
The 16-week intervention study included 141 patients with depression and/or anxiety. The mean age was 38.2 years and 58% were women. Participants were offered a choice of treatment: 16 weeks of treatment with the selective serotonin reuptake inhibitor (SSRI) escitalopram (Lexapro) or a 16-week group-based running therapy.
Patients without a strong preference for treatment allocation were randomly assigned to either antidepressant medication or running therapy, while those unwilling to be randomized were allocated to their preferred intervention.
A total of 22 patients were randomly assigned to receive antidepressant treatment and 13 to running therapy. A total of 36 participants chose antidepressant treatment, while 83 chose the running therapy.
Running therapy involved 16 weeks of supervised 45-minute outdoor running sessions to a target of two to three sessions per week, in line with U.S. Centers for Disease Control and Prevention/American College of Sports Medicine recommendations.
Physical health benefits
Treatment adherence in the antidepressant group, defined as still using treatment at the posttreatment assessment, was 82.2% vs. 52.1% among running therapy participants, where adherence was specified as completing more than 22 sessions.
Remission was defined as no longer meeting the criteria of a current depressive or anxiety disorder via CIDI at week 16.
On intention-to-treat analysis, this requirement was met by 44.8% of patients taking antidepressants and 43.3% of those in the running therapy group (P = .88).
However, running therapy patients showed significant improvements in weight (P = .001), waist circumference (P = .011), systolic and diastolic blood pressure (P = .011 and P = .002, respectively), heart rate (P = .033), and heart rate variability (P = .006).
The investigators note the more favorable physical health changes in the running therapy group were attributable to “larger improvements in the running therapy group but also due to larger deterioration in the antidepressant group.”
Antidepressants are generally safe and effective and work for most people, said Dr. Penninx. She also noted that untreated depression leads to worse outcomes, so “antidepressants are generally a good choice.”
Nevertheless, she said, “we need to extend our treatment arsenal as not all patients respond to antidepressants or are willing to take them.”
The study’s results, she added, suggest that “implementing exercise therapy is something we should take much more seriously, as it could be a good, and maybe even better, choice for some of our patients.”
Francesca Cirulli, PhD, senior researcher and group leader at the National Institute of Health, Rome, said in an interview that the study is notable because it is one of the first to prospectively measure the effects of antidepressants and running on physical health.
Dr. Cirulli suggested that running therapy could be tried ahead of treatment with antidepressants if patients prefer physical exercise and can adhere to it. However, she said, the findings also suggest that an increase in physical activity should accompany treatment with antidepressant medications.
Overall, Dr. Cirulli said “the message should not be that everyone can be helped by running and antidepressants are bad,” but rather “these are both helpful, but not excellent, interventions against depression.”
‘Important limitations’
In a comment, Eduard Vieta, MD, PhD, chair of the department of psychiatry and psychology at the University of Barcelona Hospital Clinic, noted the study has “very important limitations.”
Among the limitations: the inclusion of nonrandomized patients who received the treatment of their choice, causing obvious bias and the “lack of binding and power issues” over the number of patients enrolled.
Dr. Vieta also said that the results “seem obvious, because it is known that exercise improves physical health.”
The trial therefore shows, “if you can find people who are able to do exercise while depressed and adhere to it, those would benefit from that practice,” he noted.
Also commenting on the research, Eric Ruhe, MD, PhD, Radboud University Medical Center, Nijmegen, the Netherlands, said the results are confirmatory and “again show physical health can influence mental health.”
However, Dr. Ruhe underlined, while it is “common practice” to allow patients to follow their treatment preference and is “understandable from a pragmatic point of view,” the group comparison may be “biased,” compared with a “truly randomized study.”
“For example, patients in the antidepressant group were more depressed, which might be associated with less chance of persisting engagement in the exercises,” he said. “So, we have to be careful not to overinterpret the comparisons between groups, which the authors acknowledge properly.”
Turning to the difference in adherence between the two interventions, Dr. Ruhe said the results show adopting, and adhering to, a lifestyle habit is more difficult than taking a pill.
“This is not exclusively found in psychiatry, indicating that we also have to focus on how to improve compliance to healthy behavior. This could have tremendous impact on health care more generally, but also on psychiatric diseases,” Dr. Ruhe said.
The MOTAR study was funded by a NWO-VICI grant. Funding for the inflammatory markers was provided by ZonMw: The Netherlands Organization for Health Research and Development. The study authors and clinicians interviewed for this story declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ECNP 2023
Breast reconstruction post mastectomy: What matters most to women?
TOPLINE:
, a new survey suggests.
METHODOLOGY:
- As many as 40% of women feel dissatisfied after breast reconstruction because of unexpected outcomes that are poorly aligned with their personal preferences. Identifying what women value when considering breast reconstruction surgery could improve shared decision-making.
- Researchers used an adaptive choice-based conjoint analysis, a survey-based method used in marketing research, to identify attributes of breast reconstruction that are most important to women considering it.
- A total of 406 women completed the survey, which assessed the relative importance of breast appearance (flap or implant), abdominal morbidity, recovery time, additional operations, and complications of breast reconstruction.
- The survey included 105 women from Duke University, Durham, N.C., who had a new diagnosis of, or genetic predisposition to, breast cancer and were considering mastectomy with reconstruction. The survey also included another 301 women, identified through the Love Research Army registry, who had a history of breast cancer or a genetic predisposition.
TAKEAWAY:
- Overall, the risk for abdominal morbidity was most important to patients (mean relative importance, 28%); women also rated the chance for major complications (RI, 25%), the number of additional surgeries (RI, 23%), breast appearance (RI, 13%), and recovery time (RI, 11%) as important factors.
- Most women preferred implant-based reconstruction (85%), and these women cared most about abdominal morbidity (RI, 30%), risk for complications (RI, 26%), and added operations (RI, 21%).
- Women who preferred flap reconstruction cared most about additional operations (RI, 31%), followed by breast appearance (RI, 27%) and risk of complications (RI, 18%), which suggests that the appearance of the reconstruction procedure was particularly important, the authors noted.
- Participants who preferred the flap appearance were willing to accept an increased risk for abdominal morbidity and a slightly higher risk for complications; among the participants who preferred the implant option, one-third actually preferred the flap appearance.
IN PRACTICE:
“This study provides information on how women value different aspects of their care when making decisions for breast reconstruction,” the authors conclude, adding that “developing decision aids that elicit individual-level preferences and align patient values with treatment may provide an avenue to improve patient-centered care.”
SOURCE:
The study, led by first author Ronnie Shammas, MD, of Duke University, Durham, N.C., was published online in JAMA Surgery.
LIMITATIONS:
The attributes included in the survey may not represent all factors that women consider during the decision-making process. The cohort was composed of predominately upper-middle class and White women, which may reflect an increased preference toward implant, compared with flap reconstruction, as suggested in previous studies.
DISCLOSURES:
Funding for the research was provided by a grant from the National Endowment for Plastic Surgery awarded by the Plastic Surgery Foundation. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
, a new survey suggests.
METHODOLOGY:
- As many as 40% of women feel dissatisfied after breast reconstruction because of unexpected outcomes that are poorly aligned with their personal preferences. Identifying what women value when considering breast reconstruction surgery could improve shared decision-making.
- Researchers used an adaptive choice-based conjoint analysis, a survey-based method used in marketing research, to identify attributes of breast reconstruction that are most important to women considering it.
- A total of 406 women completed the survey, which assessed the relative importance of breast appearance (flap or implant), abdominal morbidity, recovery time, additional operations, and complications of breast reconstruction.
- The survey included 105 women from Duke University, Durham, N.C., who had a new diagnosis of, or genetic predisposition to, breast cancer and were considering mastectomy with reconstruction. The survey also included another 301 women, identified through the Love Research Army registry, who had a history of breast cancer or a genetic predisposition.
TAKEAWAY:
- Overall, the risk for abdominal morbidity was most important to patients (mean relative importance, 28%); women also rated the chance for major complications (RI, 25%), the number of additional surgeries (RI, 23%), breast appearance (RI, 13%), and recovery time (RI, 11%) as important factors.
- Most women preferred implant-based reconstruction (85%), and these women cared most about abdominal morbidity (RI, 30%), risk for complications (RI, 26%), and added operations (RI, 21%).
- Women who preferred flap reconstruction cared most about additional operations (RI, 31%), followed by breast appearance (RI, 27%) and risk of complications (RI, 18%), which suggests that the appearance of the reconstruction procedure was particularly important, the authors noted.
- Participants who preferred the flap appearance were willing to accept an increased risk for abdominal morbidity and a slightly higher risk for complications; among the participants who preferred the implant option, one-third actually preferred the flap appearance.
IN PRACTICE:
“This study provides information on how women value different aspects of their care when making decisions for breast reconstruction,” the authors conclude, adding that “developing decision aids that elicit individual-level preferences and align patient values with treatment may provide an avenue to improve patient-centered care.”
SOURCE:
The study, led by first author Ronnie Shammas, MD, of Duke University, Durham, N.C., was published online in JAMA Surgery.
LIMITATIONS:
The attributes included in the survey may not represent all factors that women consider during the decision-making process. The cohort was composed of predominately upper-middle class and White women, which may reflect an increased preference toward implant, compared with flap reconstruction, as suggested in previous studies.
DISCLOSURES:
Funding for the research was provided by a grant from the National Endowment for Plastic Surgery awarded by the Plastic Surgery Foundation. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
, a new survey suggests.
METHODOLOGY:
- As many as 40% of women feel dissatisfied after breast reconstruction because of unexpected outcomes that are poorly aligned with their personal preferences. Identifying what women value when considering breast reconstruction surgery could improve shared decision-making.
- Researchers used an adaptive choice-based conjoint analysis, a survey-based method used in marketing research, to identify attributes of breast reconstruction that are most important to women considering it.
- A total of 406 women completed the survey, which assessed the relative importance of breast appearance (flap or implant), abdominal morbidity, recovery time, additional operations, and complications of breast reconstruction.
- The survey included 105 women from Duke University, Durham, N.C., who had a new diagnosis of, or genetic predisposition to, breast cancer and were considering mastectomy with reconstruction. The survey also included another 301 women, identified through the Love Research Army registry, who had a history of breast cancer or a genetic predisposition.
TAKEAWAY:
- Overall, the risk for abdominal morbidity was most important to patients (mean relative importance, 28%); women also rated the chance for major complications (RI, 25%), the number of additional surgeries (RI, 23%), breast appearance (RI, 13%), and recovery time (RI, 11%) as important factors.
- Most women preferred implant-based reconstruction (85%), and these women cared most about abdominal morbidity (RI, 30%), risk for complications (RI, 26%), and added operations (RI, 21%).
- Women who preferred flap reconstruction cared most about additional operations (RI, 31%), followed by breast appearance (RI, 27%) and risk of complications (RI, 18%), which suggests that the appearance of the reconstruction procedure was particularly important, the authors noted.
- Participants who preferred the flap appearance were willing to accept an increased risk for abdominal morbidity and a slightly higher risk for complications; among the participants who preferred the implant option, one-third actually preferred the flap appearance.
IN PRACTICE:
“This study provides information on how women value different aspects of their care when making decisions for breast reconstruction,” the authors conclude, adding that “developing decision aids that elicit individual-level preferences and align patient values with treatment may provide an avenue to improve patient-centered care.”
SOURCE:
The study, led by first author Ronnie Shammas, MD, of Duke University, Durham, N.C., was published online in JAMA Surgery.
LIMITATIONS:
The attributes included in the survey may not represent all factors that women consider during the decision-making process. The cohort was composed of predominately upper-middle class and White women, which may reflect an increased preference toward implant, compared with flap reconstruction, as suggested in previous studies.
DISCLOSURES:
Funding for the research was provided by a grant from the National Endowment for Plastic Surgery awarded by the Plastic Surgery Foundation. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AGA patient and physician advocates visit Capitol Hill to push for prior authorization reform

In our first in-person Advocacy Day on Capitol Hill since 2019, AGA leaders and patient advocates from 22 total states met with House and Senate offices to educate members of Congress and their staff about policies affecting GI patient care such as prior authorization and step therapy. Federal research funding and Medicare reimbursement were also on the agenda.
In the meetings, the patient shared their stories of living with various gastrointestinal diseases, including ulcerative colitis and Crohn’s disease, and the struggles they’ve gone through to get treatments approved by their insurers. AGA physicians shared the provider perspective of how policies like prior authorization negatively impact practices. According to a 2023 AGA member survey, 95% of respondents say that prior authorization restrictions have impacted patient access to clinically appropriate treatments and patient clinical outcomes and 84% described that the burden associated with prior authorization policies have increased “significantly” or “somewhat” over the last 5 years. AGA’s advocacy day came not long after UnitedHealthcare’s announcement of a new “Gold Card” prior authorization policy to be implemented in 2024, which will impact most colonoscopies and endoscopies for its 27 million commercial beneficiaries. The group expressed serious concerns about the proposed policy to lawmakers.

“It was a wonderful and empowering experience to share my personal story with my Representative/Senator and know that they were really listening to my concerns about insurer overreach,” said Aaron Blocker, a Crohn’s disease patient and advocate. “I hope Congress acts swiftly on passing prior authorization reform, so no more patients are forced to live in pain while they wait for treatments to be approved.” As gastroenterologists, too much administrative time is spent submitting onerous prior authorization requests on a near daily basis. We hope Congress takes our concerns seriously and comes together to rein in prior authorization.
AGA thanks the patient and physician advocates who participated in this year’s Advocacy Day and looks forward to continuing our work to ensure timely access to care.

In our first in-person Advocacy Day on Capitol Hill since 2019, AGA leaders and patient advocates from 22 total states met with House and Senate offices to educate members of Congress and their staff about policies affecting GI patient care such as prior authorization and step therapy. Federal research funding and Medicare reimbursement were also on the agenda.
In the meetings, the patient shared their stories of living with various gastrointestinal diseases, including ulcerative colitis and Crohn’s disease, and the struggles they’ve gone through to get treatments approved by their insurers. AGA physicians shared the provider perspective of how policies like prior authorization negatively impact practices. According to a 2023 AGA member survey, 95% of respondents say that prior authorization restrictions have impacted patient access to clinically appropriate treatments and patient clinical outcomes and 84% described that the burden associated with prior authorization policies have increased “significantly” or “somewhat” over the last 5 years. AGA’s advocacy day came not long after UnitedHealthcare’s announcement of a new “Gold Card” prior authorization policy to be implemented in 2024, which will impact most colonoscopies and endoscopies for its 27 million commercial beneficiaries. The group expressed serious concerns about the proposed policy to lawmakers.

“It was a wonderful and empowering experience to share my personal story with my Representative/Senator and know that they were really listening to my concerns about insurer overreach,” said Aaron Blocker, a Crohn’s disease patient and advocate. “I hope Congress acts swiftly on passing prior authorization reform, so no more patients are forced to live in pain while they wait for treatments to be approved.” As gastroenterologists, too much administrative time is spent submitting onerous prior authorization requests on a near daily basis. We hope Congress takes our concerns seriously and comes together to rein in prior authorization.
AGA thanks the patient and physician advocates who participated in this year’s Advocacy Day and looks forward to continuing our work to ensure timely access to care.

In our first in-person Advocacy Day on Capitol Hill since 2019, AGA leaders and patient advocates from 22 total states met with House and Senate offices to educate members of Congress and their staff about policies affecting GI patient care such as prior authorization and step therapy. Federal research funding and Medicare reimbursement were also on the agenda.
In the meetings, the patient shared their stories of living with various gastrointestinal diseases, including ulcerative colitis and Crohn’s disease, and the struggles they’ve gone through to get treatments approved by their insurers. AGA physicians shared the provider perspective of how policies like prior authorization negatively impact practices. According to a 2023 AGA member survey, 95% of respondents say that prior authorization restrictions have impacted patient access to clinically appropriate treatments and patient clinical outcomes and 84% described that the burden associated with prior authorization policies have increased “significantly” or “somewhat” over the last 5 years. AGA’s advocacy day came not long after UnitedHealthcare’s announcement of a new “Gold Card” prior authorization policy to be implemented in 2024, which will impact most colonoscopies and endoscopies for its 27 million commercial beneficiaries. The group expressed serious concerns about the proposed policy to lawmakers.

“It was a wonderful and empowering experience to share my personal story with my Representative/Senator and know that they were really listening to my concerns about insurer overreach,” said Aaron Blocker, a Crohn’s disease patient and advocate. “I hope Congress acts swiftly on passing prior authorization reform, so no more patients are forced to live in pain while they wait for treatments to be approved.” As gastroenterologists, too much administrative time is spent submitting onerous prior authorization requests on a near daily basis. We hope Congress takes our concerns seriously and comes together to rein in prior authorization.
AGA thanks the patient and physician advocates who participated in this year’s Advocacy Day and looks forward to continuing our work to ensure timely access to care.
Proton pump inhibitors linked to increased dementia risk
TOPLINE:
and was highest among those diagnosed before age 70 years regardless of when PPI treatment was initiated.
METHODOLOGY:
- Researchers used four Danish registries to collect data on dementia diagnoses and prescription PPI use among 1,983,785 individuals aged 60-75 years between 2000 and 2018.
- The median follow-up time was 10.3 years.
TAKEAWAY:
- There were 99,384 (5.0%) cases of all-cause dementia during follow-up, with a median age of diagnosis of 79 years.
- Twenty-one-point-two percent of dementia cases and 18.9% of controls reported a history of PPI use.
- Risk for all-cause dementia before age 90 years was 36% higher with PPI use in people aged 60-69 years at baseline (adjusted incidence rate ratio, 1.36; 95% confidence interval, 1.29-1.43) and 6% higher in those who were age 80-89 years at baseline (aIRR, 1.06; 95% CI, 1.03-1.09).
- Investigators found significant increased dementia risk before age 90 years with PPI use regardless of when PPI treatment began and found no link between PPI use and dementia diagnoses after age 90 years.
IN PRACTICE:
“The association between PPI use and dementia was unambiguously largest among the youngest cases of dementia, potentially suggestive of a critical window of exposure where midlife PPI use affects dementia risk to a larger degree compared to late-life use,” the authors wrote. “Further, the finding could signify a declining impact of individual risk factors with advancing age owing to lengthy ongoing neuropathological processes.”
SOURCE:
Lead author of the study was Nelsan Pourhadi, MD, Danish Dementia Research Centre, department of neurology, Copenhagen University Hospital–Rigshospitalet. It was published online in Alzheimer’s and Dementia.
LIMITATIONS:
The study did not include data on PPI prescriptions before 1995, over-the-counter PPI use, and in-hospital intravenous use of PPI during the study period.
DISCLOSURES:
The study was funded by the Danish Ministry of Health. The authors reported no relevant conflicts.
A version of this article first appeared on Medscape.com.
TOPLINE:
and was highest among those diagnosed before age 70 years regardless of when PPI treatment was initiated.
METHODOLOGY:
- Researchers used four Danish registries to collect data on dementia diagnoses and prescription PPI use among 1,983,785 individuals aged 60-75 years between 2000 and 2018.
- The median follow-up time was 10.3 years.
TAKEAWAY:
- There were 99,384 (5.0%) cases of all-cause dementia during follow-up, with a median age of diagnosis of 79 years.
- Twenty-one-point-two percent of dementia cases and 18.9% of controls reported a history of PPI use.
- Risk for all-cause dementia before age 90 years was 36% higher with PPI use in people aged 60-69 years at baseline (adjusted incidence rate ratio, 1.36; 95% confidence interval, 1.29-1.43) and 6% higher in those who were age 80-89 years at baseline (aIRR, 1.06; 95% CI, 1.03-1.09).
- Investigators found significant increased dementia risk before age 90 years with PPI use regardless of when PPI treatment began and found no link between PPI use and dementia diagnoses after age 90 years.
IN PRACTICE:
“The association between PPI use and dementia was unambiguously largest among the youngest cases of dementia, potentially suggestive of a critical window of exposure where midlife PPI use affects dementia risk to a larger degree compared to late-life use,” the authors wrote. “Further, the finding could signify a declining impact of individual risk factors with advancing age owing to lengthy ongoing neuropathological processes.”
SOURCE:
Lead author of the study was Nelsan Pourhadi, MD, Danish Dementia Research Centre, department of neurology, Copenhagen University Hospital–Rigshospitalet. It was published online in Alzheimer’s and Dementia.
LIMITATIONS:
The study did not include data on PPI prescriptions before 1995, over-the-counter PPI use, and in-hospital intravenous use of PPI during the study period.
DISCLOSURES:
The study was funded by the Danish Ministry of Health. The authors reported no relevant conflicts.
A version of this article first appeared on Medscape.com.
TOPLINE:
and was highest among those diagnosed before age 70 years regardless of when PPI treatment was initiated.
METHODOLOGY:
- Researchers used four Danish registries to collect data on dementia diagnoses and prescription PPI use among 1,983,785 individuals aged 60-75 years between 2000 and 2018.
- The median follow-up time was 10.3 years.
TAKEAWAY:
- There were 99,384 (5.0%) cases of all-cause dementia during follow-up, with a median age of diagnosis of 79 years.
- Twenty-one-point-two percent of dementia cases and 18.9% of controls reported a history of PPI use.
- Risk for all-cause dementia before age 90 years was 36% higher with PPI use in people aged 60-69 years at baseline (adjusted incidence rate ratio, 1.36; 95% confidence interval, 1.29-1.43) and 6% higher in those who were age 80-89 years at baseline (aIRR, 1.06; 95% CI, 1.03-1.09).
- Investigators found significant increased dementia risk before age 90 years with PPI use regardless of when PPI treatment began and found no link between PPI use and dementia diagnoses after age 90 years.
IN PRACTICE:
“The association between PPI use and dementia was unambiguously largest among the youngest cases of dementia, potentially suggestive of a critical window of exposure where midlife PPI use affects dementia risk to a larger degree compared to late-life use,” the authors wrote. “Further, the finding could signify a declining impact of individual risk factors with advancing age owing to lengthy ongoing neuropathological processes.”
SOURCE:
Lead author of the study was Nelsan Pourhadi, MD, Danish Dementia Research Centre, department of neurology, Copenhagen University Hospital–Rigshospitalet. It was published online in Alzheimer’s and Dementia.
LIMITATIONS:
The study did not include data on PPI prescriptions before 1995, over-the-counter PPI use, and in-hospital intravenous use of PPI during the study period.
DISCLOSURES:
The study was funded by the Danish Ministry of Health. The authors reported no relevant conflicts.
A version of this article first appeared on Medscape.com.
ADHD rates holding steady in U.S. children
TOPLINE:
While the prevalence of attention-deficit/hyperactivity disorder in U.S. children increased from the late 1990s to 2016,
METHODOLOGY:
- Based on prior data, the prevalence of ADHD in children rose from 6.1% in 1997-1998 to 10.2% in 2015-2016, with a 42.0% increase from 2003 to 2011. The new report provides updated prevalence data for 2017-2022.
- The cross-sectional analysis used data from the National Health Interview Survey (NHIS) from 2017 to 2022 for more than 37,609 U.S. children and adolescents 4-17 years old (52% male, 53% non-Hispanic White, 24% Hispanic, 11% non-Hispanic Black, and 12% non-Hispanic other race).
- Information on health care provider–diagnosed ADHD was reported by a parent or guardian.
TAKEAWAY:
- A total of 4,098 children and adolescents (10.9%) were reported to have an ADHD diagnosis during the study period.
- The weighted prevalence of ADHD ranged from 10.08% to 10.47% from 2017 to 2022, which is similar to the prevalence in 2015-2016 (10.20%).
- There was no significant change on an annual basis or in all subgroups evaluated. Notably, the estimated prevalence of ADHD among U.S. children and adolescents was higher than worldwide estimates (5.3%) in earlier years (1978-2005).
- The prevalence of ADHD in U.S. children differed significantly by age, sex, race/ethnicity, and family income, in line with previous findings, with higher rates in those 12-17 years (vs. 4-11 years), males, non-Hispanic populations, and those with higher family income.
IN PRACTICE:
The estimated ADHD prevalence remains “high” and “further investigation is warranted to assess potentially modifiable risk factors and provide adequate resources for treatment of individuals with ADHD in the future,” the authors write.
SOURCE:
The study, with first author Yanmei Li, Guangdong Pharmaceutical University, Guangzhou, China, was published online in JAMA Network Open.
LIMITATIONS:
Information on ADHD relied on parent-reported diagnosis, which may lead to misreporting and recall bias. The NHIS underwent a major redesign in 2019, which may affect comparability with prior years, and the COVID-19 pandemic affected collection in 2020.
DISCLOSURES:
The study had no specific funding. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
While the prevalence of attention-deficit/hyperactivity disorder in U.S. children increased from the late 1990s to 2016,
METHODOLOGY:
- Based on prior data, the prevalence of ADHD in children rose from 6.1% in 1997-1998 to 10.2% in 2015-2016, with a 42.0% increase from 2003 to 2011. The new report provides updated prevalence data for 2017-2022.
- The cross-sectional analysis used data from the National Health Interview Survey (NHIS) from 2017 to 2022 for more than 37,609 U.S. children and adolescents 4-17 years old (52% male, 53% non-Hispanic White, 24% Hispanic, 11% non-Hispanic Black, and 12% non-Hispanic other race).
- Information on health care provider–diagnosed ADHD was reported by a parent or guardian.
TAKEAWAY:
- A total of 4,098 children and adolescents (10.9%) were reported to have an ADHD diagnosis during the study period.
- The weighted prevalence of ADHD ranged from 10.08% to 10.47% from 2017 to 2022, which is similar to the prevalence in 2015-2016 (10.20%).
- There was no significant change on an annual basis or in all subgroups evaluated. Notably, the estimated prevalence of ADHD among U.S. children and adolescents was higher than worldwide estimates (5.3%) in earlier years (1978-2005).
- The prevalence of ADHD in U.S. children differed significantly by age, sex, race/ethnicity, and family income, in line with previous findings, with higher rates in those 12-17 years (vs. 4-11 years), males, non-Hispanic populations, and those with higher family income.
IN PRACTICE:
The estimated ADHD prevalence remains “high” and “further investigation is warranted to assess potentially modifiable risk factors and provide adequate resources for treatment of individuals with ADHD in the future,” the authors write.
SOURCE:
The study, with first author Yanmei Li, Guangdong Pharmaceutical University, Guangzhou, China, was published online in JAMA Network Open.
LIMITATIONS:
Information on ADHD relied on parent-reported diagnosis, which may lead to misreporting and recall bias. The NHIS underwent a major redesign in 2019, which may affect comparability with prior years, and the COVID-19 pandemic affected collection in 2020.
DISCLOSURES:
The study had no specific funding. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
While the prevalence of attention-deficit/hyperactivity disorder in U.S. children increased from the late 1990s to 2016,
METHODOLOGY:
- Based on prior data, the prevalence of ADHD in children rose from 6.1% in 1997-1998 to 10.2% in 2015-2016, with a 42.0% increase from 2003 to 2011. The new report provides updated prevalence data for 2017-2022.
- The cross-sectional analysis used data from the National Health Interview Survey (NHIS) from 2017 to 2022 for more than 37,609 U.S. children and adolescents 4-17 years old (52% male, 53% non-Hispanic White, 24% Hispanic, 11% non-Hispanic Black, and 12% non-Hispanic other race).
- Information on health care provider–diagnosed ADHD was reported by a parent or guardian.
TAKEAWAY:
- A total of 4,098 children and adolescents (10.9%) were reported to have an ADHD diagnosis during the study period.
- The weighted prevalence of ADHD ranged from 10.08% to 10.47% from 2017 to 2022, which is similar to the prevalence in 2015-2016 (10.20%).
- There was no significant change on an annual basis or in all subgroups evaluated. Notably, the estimated prevalence of ADHD among U.S. children and adolescents was higher than worldwide estimates (5.3%) in earlier years (1978-2005).
- The prevalence of ADHD in U.S. children differed significantly by age, sex, race/ethnicity, and family income, in line with previous findings, with higher rates in those 12-17 years (vs. 4-11 years), males, non-Hispanic populations, and those with higher family income.
IN PRACTICE:
The estimated ADHD prevalence remains “high” and “further investigation is warranted to assess potentially modifiable risk factors and provide adequate resources for treatment of individuals with ADHD in the future,” the authors write.
SOURCE:
The study, with first author Yanmei Li, Guangdong Pharmaceutical University, Guangzhou, China, was published online in JAMA Network Open.
LIMITATIONS:
Information on ADHD relied on parent-reported diagnosis, which may lead to misreporting and recall bias. The NHIS underwent a major redesign in 2019, which may affect comparability with prior years, and the COVID-19 pandemic affected collection in 2020.
DISCLOSURES:
The study had no specific funding. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Nintedanib dose reductions in IPF may do no harm
HONOLULU – nintedanib (Ofev) for patients with idiopathic pulmonary fibrosis (IPF) who can’t tolerate the full 150-mg twice-daily dose.
An analysis of data from a large administrative claims database showed that there were no significant differences in either all-cause mortality or hospitalization rates between patients with IPF treated at the full 150-mg twice-daily dose and those treated with a reduced twice-daily dose of 100 mg nintedanib.
Although the results need to be confirmed by additional prospective and registry studies, they suggest that patients with IPF can still fare just as well with a reduced-dose nintedanib regimen, ideally with fewer gastrointestinal side effects such as diarrhea, reported Andrew Limper, MD, of the Mayo Clinic in Rochester, Minn.
“At least on this preliminary data you could ... rest assured,” Dr. Limper told his colleagues in an oral abstract session at the American College of Chest Physicians (CHEST) 2023 annual meeting.
“This is not definitive proof, I’m not making more out of this than it is, but we all put people on 100 mg twice daily because their guts don’t tolerate it; they live in the bathroom and they don’t want to live that way,” Dr. Limper said.
Hard to take
Nintedanib is approved in the United States for the treatment of IPF, chronic fibrosing interstitial lung diseases (ILD) with a progressive phenotype, and systemic sclerosis-associated ILD. For IPF, the standard dose established in randomized clinical trials is 150 mg twice daily.
However, nintedanib is associated with a number of side effects, including hepatic and other gastrointestinal toxicities, arterial thromboembolic events, and proteinuria within the nephrotic range. As a result, clinicians often reduce the dose to 100 mg twice daily, but there is a lack of data to indicate whether it’s safe to do so or if efficacy will be compromised.
To see whether dose reductions might result in poorer outcomes for patients with IPF, Dr. Limper and colleagues analyzed data from the OptumLabs Data Warehouse, a large administrative claims database, to compare outcomes for patients treated with IPF at either the 150-mg or 100-mg twice-daily doses.
They used propensity-score matching to account for differences among individuals according to age, sex, race/ethnicity, residence, insurance type, additional medication use, oxygen use, smoking status, health care use, and comorbidities. The final cohort included 346 patients in each dosing group.
There was no difference between the dosing groups for the primary outcome of all-cause mortality at 18 months, with a nonsignificant hazard ratio of 0.65 (P = .313), and no significant difference over 24 months in risk of hospitalization, with a hazard ratio of 0.98 (P = .899).
“This is not randomized controlled data; I doubt that [nintedanib maker Boehringer Ingelheim] is ever going to do a 150 vs. 100 milligram head-to-head trial, but it does give us some ground to start to look at this,” Dr. Limper said.
Not so sure
Session comoderator Misbah Baqir, MBBS, also from the Mayo Clinic, told this news organization that she would need to see more data from prospective studies using endpoints other than mortality before she could be convinced that nintedanib dose reductions do not adversely affect efficacy. She was not involved in the study.
“I feel that the endpoint should be different, either it should be forced vital capacity change, quality of life, or something else. The problem with a database study is that you don’t have everything in it. You have to play with what you have, and you don’t have forced vital capacity. You have to go into the charts to get it,” she said.
It would be more helpful to objectively compare, for example, diarrhea episodes or other adverse events to see whether they were significantly reduced with the 100-mg dose, she added.
In an interview, Dr. Limper said that he and his colleagues plan to gather additional observational data including the newly available Medicare fee-for-service data set, registry data, and other sources.
“If we get all of that, and it really still looks compelling – and that’s an if – then I think that would be the foothold to go back to the manufacturer and say, ‘Hey, maybe you ought to think about doing a prospective trial to prove it with lung function and other endpoints such as 6-minute walks,’ ” he said.
The study was supported by a grant from Three Lakes Foundation. Dr. Limper and Dr. Baqir have disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
HONOLULU – nintedanib (Ofev) for patients with idiopathic pulmonary fibrosis (IPF) who can’t tolerate the full 150-mg twice-daily dose.
An analysis of data from a large administrative claims database showed that there were no significant differences in either all-cause mortality or hospitalization rates between patients with IPF treated at the full 150-mg twice-daily dose and those treated with a reduced twice-daily dose of 100 mg nintedanib.
Although the results need to be confirmed by additional prospective and registry studies, they suggest that patients with IPF can still fare just as well with a reduced-dose nintedanib regimen, ideally with fewer gastrointestinal side effects such as diarrhea, reported Andrew Limper, MD, of the Mayo Clinic in Rochester, Minn.
“At least on this preliminary data you could ... rest assured,” Dr. Limper told his colleagues in an oral abstract session at the American College of Chest Physicians (CHEST) 2023 annual meeting.
“This is not definitive proof, I’m not making more out of this than it is, but we all put people on 100 mg twice daily because their guts don’t tolerate it; they live in the bathroom and they don’t want to live that way,” Dr. Limper said.
Hard to take
Nintedanib is approved in the United States for the treatment of IPF, chronic fibrosing interstitial lung diseases (ILD) with a progressive phenotype, and systemic sclerosis-associated ILD. For IPF, the standard dose established in randomized clinical trials is 150 mg twice daily.
However, nintedanib is associated with a number of side effects, including hepatic and other gastrointestinal toxicities, arterial thromboembolic events, and proteinuria within the nephrotic range. As a result, clinicians often reduce the dose to 100 mg twice daily, but there is a lack of data to indicate whether it’s safe to do so or if efficacy will be compromised.
To see whether dose reductions might result in poorer outcomes for patients with IPF, Dr. Limper and colleagues analyzed data from the OptumLabs Data Warehouse, a large administrative claims database, to compare outcomes for patients treated with IPF at either the 150-mg or 100-mg twice-daily doses.
They used propensity-score matching to account for differences among individuals according to age, sex, race/ethnicity, residence, insurance type, additional medication use, oxygen use, smoking status, health care use, and comorbidities. The final cohort included 346 patients in each dosing group.
There was no difference between the dosing groups for the primary outcome of all-cause mortality at 18 months, with a nonsignificant hazard ratio of 0.65 (P = .313), and no significant difference over 24 months in risk of hospitalization, with a hazard ratio of 0.98 (P = .899).
“This is not randomized controlled data; I doubt that [nintedanib maker Boehringer Ingelheim] is ever going to do a 150 vs. 100 milligram head-to-head trial, but it does give us some ground to start to look at this,” Dr. Limper said.
Not so sure
Session comoderator Misbah Baqir, MBBS, also from the Mayo Clinic, told this news organization that she would need to see more data from prospective studies using endpoints other than mortality before she could be convinced that nintedanib dose reductions do not adversely affect efficacy. She was not involved in the study.
“I feel that the endpoint should be different, either it should be forced vital capacity change, quality of life, or something else. The problem with a database study is that you don’t have everything in it. You have to play with what you have, and you don’t have forced vital capacity. You have to go into the charts to get it,” she said.
It would be more helpful to objectively compare, for example, diarrhea episodes or other adverse events to see whether they were significantly reduced with the 100-mg dose, she added.
In an interview, Dr. Limper said that he and his colleagues plan to gather additional observational data including the newly available Medicare fee-for-service data set, registry data, and other sources.
“If we get all of that, and it really still looks compelling – and that’s an if – then I think that would be the foothold to go back to the manufacturer and say, ‘Hey, maybe you ought to think about doing a prospective trial to prove it with lung function and other endpoints such as 6-minute walks,’ ” he said.
The study was supported by a grant from Three Lakes Foundation. Dr. Limper and Dr. Baqir have disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
HONOLULU – nintedanib (Ofev) for patients with idiopathic pulmonary fibrosis (IPF) who can’t tolerate the full 150-mg twice-daily dose.
An analysis of data from a large administrative claims database showed that there were no significant differences in either all-cause mortality or hospitalization rates between patients with IPF treated at the full 150-mg twice-daily dose and those treated with a reduced twice-daily dose of 100 mg nintedanib.
Although the results need to be confirmed by additional prospective and registry studies, they suggest that patients with IPF can still fare just as well with a reduced-dose nintedanib regimen, ideally with fewer gastrointestinal side effects such as diarrhea, reported Andrew Limper, MD, of the Mayo Clinic in Rochester, Minn.
“At least on this preliminary data you could ... rest assured,” Dr. Limper told his colleagues in an oral abstract session at the American College of Chest Physicians (CHEST) 2023 annual meeting.
“This is not definitive proof, I’m not making more out of this than it is, but we all put people on 100 mg twice daily because their guts don’t tolerate it; they live in the bathroom and they don’t want to live that way,” Dr. Limper said.
Hard to take
Nintedanib is approved in the United States for the treatment of IPF, chronic fibrosing interstitial lung diseases (ILD) with a progressive phenotype, and systemic sclerosis-associated ILD. For IPF, the standard dose established in randomized clinical trials is 150 mg twice daily.
However, nintedanib is associated with a number of side effects, including hepatic and other gastrointestinal toxicities, arterial thromboembolic events, and proteinuria within the nephrotic range. As a result, clinicians often reduce the dose to 100 mg twice daily, but there is a lack of data to indicate whether it’s safe to do so or if efficacy will be compromised.
To see whether dose reductions might result in poorer outcomes for patients with IPF, Dr. Limper and colleagues analyzed data from the OptumLabs Data Warehouse, a large administrative claims database, to compare outcomes for patients treated with IPF at either the 150-mg or 100-mg twice-daily doses.
They used propensity-score matching to account for differences among individuals according to age, sex, race/ethnicity, residence, insurance type, additional medication use, oxygen use, smoking status, health care use, and comorbidities. The final cohort included 346 patients in each dosing group.
There was no difference between the dosing groups for the primary outcome of all-cause mortality at 18 months, with a nonsignificant hazard ratio of 0.65 (P = .313), and no significant difference over 24 months in risk of hospitalization, with a hazard ratio of 0.98 (P = .899).
“This is not randomized controlled data; I doubt that [nintedanib maker Boehringer Ingelheim] is ever going to do a 150 vs. 100 milligram head-to-head trial, but it does give us some ground to start to look at this,” Dr. Limper said.
Not so sure
Session comoderator Misbah Baqir, MBBS, also from the Mayo Clinic, told this news organization that she would need to see more data from prospective studies using endpoints other than mortality before she could be convinced that nintedanib dose reductions do not adversely affect efficacy. She was not involved in the study.
“I feel that the endpoint should be different, either it should be forced vital capacity change, quality of life, or something else. The problem with a database study is that you don’t have everything in it. You have to play with what you have, and you don’t have forced vital capacity. You have to go into the charts to get it,” she said.
It would be more helpful to objectively compare, for example, diarrhea episodes or other adverse events to see whether they were significantly reduced with the 100-mg dose, she added.
In an interview, Dr. Limper said that he and his colleagues plan to gather additional observational data including the newly available Medicare fee-for-service data set, registry data, and other sources.
“If we get all of that, and it really still looks compelling – and that’s an if – then I think that would be the foothold to go back to the manufacturer and say, ‘Hey, maybe you ought to think about doing a prospective trial to prove it with lung function and other endpoints such as 6-minute walks,’ ” he said.
The study was supported by a grant from Three Lakes Foundation. Dr. Limper and Dr. Baqir have disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
AT CHEST 2023


