User login
SSRI activation in children, adolescents often misdiagnosed as bipolar
SAN FRANCISCO – It’s not uncommon for children to arrive at the Western Psychiatric Institute and Clinic in Pittsburgh with selective serotonin reuptake inhibitor activation that was misdiagnosed as bipolar disorder, according to Boris Birmaher, MD.
“We get many kids into our clinic with a diagnosis of bipolar because of this, and they are not bipolar. You have to be careful,” he said during a talk about pediatric depression at a psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
SSRIs activate about 5%-10% of children. There might be sleep problems, fast speech, hyperactivity, agitation, aggression, and even suicidality, he said.
Younger children and those with autism or developmental disabilities are particularly at risk. Occasionally, a child might be a slow metabolizer so that even low SSRI doses cause problems. “Once in a blue moon,” Dr. Birmaher said he will screen for genetic cytochrome P450 deficiency, especially if a child doesn’t seem able to tolerate medications in general, not just psychiatric ones. He’s found a few slow metabolizers over the years.
Psychiatrists also have to be careful when children and adolescents are tagged as “treatment resistant.” It’s important to teach parents what treatment resistance would actually look like for their child, so they don’t jump to conclusions and misdirect therapy, he said.
For example, when a child has been prescribed an SSRI for anxiety, parents might come in and say it’s not helping, when in fact they’re concerned about homework not getting done and restlessness in class. “There’s no treatment resistance. You teach the parent how to measure improvement of anxiety” and tackle the ADHD if it’s truly a problem, said Dr. Birmaher, also professor of psychiatry at the University of Pittsburgh.
If there really is SSRI treatment resistance, he said he first ensures that a maximum dose of the drug has been tried, so long as it’s tolerated. If it doesn’t work after 4-6 weeks, he’ll switch to another SSRI or selective norepinephrine reuptake inhibitor, or combination treatment with, for instance, bupropion (Wellbutrin) or an atypical antipsychotic, which are particularly helpful for irritability, even in small doses. Atypicals seem to take the edge off, he said.
It’s trial and error, since there aren’t much data in children to guide treatment. “The only thing I highly recommend is to make one change at a time. Sometimes we see kids who’ve had two or three changes at the same time.” In those cases, he said, it’s impossible to know what to blame if there are side effects or what to credit if depression improves.
Dr. Birmaher said he had no pharmaceutical industry ties.
SAN FRANCISCO – It’s not uncommon for children to arrive at the Western Psychiatric Institute and Clinic in Pittsburgh with selective serotonin reuptake inhibitor activation that was misdiagnosed as bipolar disorder, according to Boris Birmaher, MD.
“We get many kids into our clinic with a diagnosis of bipolar because of this, and they are not bipolar. You have to be careful,” he said during a talk about pediatric depression at a psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
SSRIs activate about 5%-10% of children. There might be sleep problems, fast speech, hyperactivity, agitation, aggression, and even suicidality, he said.
Younger children and those with autism or developmental disabilities are particularly at risk. Occasionally, a child might be a slow metabolizer so that even low SSRI doses cause problems. “Once in a blue moon,” Dr. Birmaher said he will screen for genetic cytochrome P450 deficiency, especially if a child doesn’t seem able to tolerate medications in general, not just psychiatric ones. He’s found a few slow metabolizers over the years.
Psychiatrists also have to be careful when children and adolescents are tagged as “treatment resistant.” It’s important to teach parents what treatment resistance would actually look like for their child, so they don’t jump to conclusions and misdirect therapy, he said.
For example, when a child has been prescribed an SSRI for anxiety, parents might come in and say it’s not helping, when in fact they’re concerned about homework not getting done and restlessness in class. “There’s no treatment resistance. You teach the parent how to measure improvement of anxiety” and tackle the ADHD if it’s truly a problem, said Dr. Birmaher, also professor of psychiatry at the University of Pittsburgh.
If there really is SSRI treatment resistance, he said he first ensures that a maximum dose of the drug has been tried, so long as it’s tolerated. If it doesn’t work after 4-6 weeks, he’ll switch to another SSRI or selective norepinephrine reuptake inhibitor, or combination treatment with, for instance, bupropion (Wellbutrin) or an atypical antipsychotic, which are particularly helpful for irritability, even in small doses. Atypicals seem to take the edge off, he said.
It’s trial and error, since there aren’t much data in children to guide treatment. “The only thing I highly recommend is to make one change at a time. Sometimes we see kids who’ve had two or three changes at the same time.” In those cases, he said, it’s impossible to know what to blame if there are side effects or what to credit if depression improves.
Dr. Birmaher said he had no pharmaceutical industry ties.
SAN FRANCISCO – It’s not uncommon for children to arrive at the Western Psychiatric Institute and Clinic in Pittsburgh with selective serotonin reuptake inhibitor activation that was misdiagnosed as bipolar disorder, according to Boris Birmaher, MD.
“We get many kids into our clinic with a diagnosis of bipolar because of this, and they are not bipolar. You have to be careful,” he said during a talk about pediatric depression at a psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
SSRIs activate about 5%-10% of children. There might be sleep problems, fast speech, hyperactivity, agitation, aggression, and even suicidality, he said.
Younger children and those with autism or developmental disabilities are particularly at risk. Occasionally, a child might be a slow metabolizer so that even low SSRI doses cause problems. “Once in a blue moon,” Dr. Birmaher said he will screen for genetic cytochrome P450 deficiency, especially if a child doesn’t seem able to tolerate medications in general, not just psychiatric ones. He’s found a few slow metabolizers over the years.
Psychiatrists also have to be careful when children and adolescents are tagged as “treatment resistant.” It’s important to teach parents what treatment resistance would actually look like for their child, so they don’t jump to conclusions and misdirect therapy, he said.
For example, when a child has been prescribed an SSRI for anxiety, parents might come in and say it’s not helping, when in fact they’re concerned about homework not getting done and restlessness in class. “There’s no treatment resistance. You teach the parent how to measure improvement of anxiety” and tackle the ADHD if it’s truly a problem, said Dr. Birmaher, also professor of psychiatry at the University of Pittsburgh.
If there really is SSRI treatment resistance, he said he first ensures that a maximum dose of the drug has been tried, so long as it’s tolerated. If it doesn’t work after 4-6 weeks, he’ll switch to another SSRI or selective norepinephrine reuptake inhibitor, or combination treatment with, for instance, bupropion (Wellbutrin) or an atypical antipsychotic, which are particularly helpful for irritability, even in small doses. Atypicals seem to take the edge off, he said.
It’s trial and error, since there aren’t much data in children to guide treatment. “The only thing I highly recommend is to make one change at a time. Sometimes we see kids who’ve had two or three changes at the same time.” In those cases, he said, it’s impossible to know what to blame if there are side effects or what to credit if depression improves.
Dr. Birmaher said he had no pharmaceutical industry ties.
EXPERT ANALYSIS AT THE PSYCHOPHARMACOLOGY UPDATE INSTITUTE
Medical organizations respond to Trump’s immigration order
Organizations representing physicians and medical students have expressed their concern regarding President Trump’s executive order of Jan. 27 that curtails entry into the United States by travelers from seven Muslim-majority countries. The order also suspends for 120 days entry into the United States for all persons seeking refugee status, and it bars refugees from Syria indefinitely.
Following are direct excerpts from statements issued by medical organizations.
American Academy of Family Physicians
“We are deeply concerned that steps your Administration has taken will have a chilling effect on our nation’s physician workforce, biomedical research, and global health. It is often America’s physicians who answer the call to assist people around the world when a public health crisis occurs. Imagine a world where physicians fail to answer the call of the needy because they fear they may not be able to return to their home and families in the United States.
Many family physicians are international medical graduates (IMG), who have completed all or part of their education and training in the United States. They are professionals who dedicate their careers to the service of their patients in communities large and small, urban and rural. In fact, 20% of our membership and over 25% of family medicine residents [comprise] IMGs. The AAFP applauds and supports wholly the contributions of these individual family physicians to their patients and communities and we celebrate their diversity.
We recognize that one of your primary responsibilities as President is to ensure the safety and security of the country and its citizens. This is, without question, a daunting responsibility. But we strongly urge that the methods of doing so be examined carefully, so that the many people who can add so much to our country through immigration have the opportunity to do so, and those who are doing so already are treated with the respect and dignity they deserve.”
American Academy of Pediatrics
“The executive orders signed today are harmful to immigrant children and families throughout our country. Many of the children who will be most affected are the victims of unspeakable violence and have been exposed to trauma. Children do not immigrate, they flee. They are coming to the United States seeking safe haven in our country and they need our compassion and assistance. Broad scale expansion of family detention only exacerbates their suffering ... The AAP is non-partisan and pro-children. We urge President Trump and his administration to ensure that children and families who are fleeing violence and adversity can continue to seek refuge in our country. Immigrant children and families are an integral part of our communities and our nation, and they deserve to be cared for, treated with compassion, and celebrated. Most of all, they deserve to be healthy and safe. Pediatricians stand with the immigrant families we care for and will continue to advocate that their needs are met and prioritized.”
American Association of Medical Colleges
“The United States is facing a serious shortage of physicians. IMGs play an important role in U.S. health care, representing roughly 25% of the workforce. Current immigration pathways – including student, exchange-visitor, and employment visas – provide a balanced solution that improves health care access across the country through programs like the National Interest Waiver and the Conrad 30 J-1 Visa Waiver. In the last decade, Conrad 30 alone has directed nearly 10,000 physicians into rural and urban underserved communities. Impeding these U.S. immigration pathways jeopardizes critical access to high-quality physician care for our nation’s most vulnerable populations.
Our ability to attract top talent from around the world also enriches the research laboratories at medical schools and teaching hospitals that are working toward cures and has helped position the United States as a global leader in medical research, strengthening our economy and bolstering the public’s health. Because disease knows no geographic boundaries, it is essential to ensure that we continue to foster, rather than impede, scientific cooperation with physicians and researchers of all nationalities, as we strive to keep our country healthy.”
American College of Cardiology
“The ability to share ideas and knowledge necessary to address [the global epidemic of cardiovascular disease] is imperative. Policies that impede this free-flow of ideas will have a detrimental impact on scientific discovery, as well as the lives of patients around the world. If we are to realize a future where cardiovascular disease is no longer the number one killer of men and women worldwide we must ensure that our system of scientific exchange allows for health care professionals to learn from each other regardless of their nationality.
Additionally, IMGs, naturalized citizens, and legal residents make up a significant portion of the health care workforce in hospitals and practices across the country. More than 25% of current practicing physicians are IMGs, with cardiology ranking among the top when broken down by medical specialty. Policies that bring the immigration status of those already here into question, while also limiting the ability of others to legally train in the United States going forward, will only serve to exacerbate the already existing cardiovascular workforce shortage, especially in rural America. Such policies also threaten the care continuum of patients who rely on these providers for their medical care.”
American College of Physicians
“The executive order could deny entry or reentry to tens of thousands more persons, including medical students and physicians who are being trained in the United States and/or are delivering direct patient care. ... It also creates a precedent for barring entry of IMGs based on their religion and country of origin. ... Approximately 30% of ACP members are IMGs.”
American Gastroenterological Association
Science and illness ignore borders and political divides. That is why AGA is concerned that the recent U.S. executive order on immigration could limit scientific exchange, delay patient care and impair medical training.
AGA is committed to diversity, which we define as inclusive of race, ethnicity and national origin. Diversity within training programs and laboratories in the United States built today’s practice of gastroenterology. Scientists from around the world publish in our journals, work in our laboratories, train in our programs and present data at Digestive Disease Week. This exchange leads to better patient care, and very sick patients travel to the United States from around the world for the best digestive health care.
AGA adds our support to a growing number of medical institutions urging the administration to consider the devastating impact of the executive order on the health of the nation that will result from turning away patients, health professionals, and researchers. The recent immigration policy is clearly detrimental to America’s leadership role in advancing health care, and to the standing of the United States within the international community.
American Society of Clinical Oncology
ASCO is deeply concerned about the potential impact of the recent executive order on cancer research, patient care, and international scientific collaboration.
Our more than 40,000 members in 148 countries lead the charge to conquer cancer in all its forms and in every nation. Tens of thousands of people from more than 100 countries participate in our scientific meetings to exchange advances and ideas to improve patient care. Millions of cancer survivors are alive today because of the progress made possible by scientific collaboration. Progress against this disease will falter if the close-knit global community of cancer care providers is divided by policies that bar members of certain nationalities from entering the United States to conduct research, care for people with cancer, or participate in scientific and medical conferences.
American Society of Hematology
We express our deep concern about the Administration’s executive order that has denied U.S. entry to people who bring unique expertise to the practice of medicine and the conduct of cancer and biomedical research. Our nation depends on the contributions of the greatest minds from around the world to maintain the high quality of our biomedical research enterprise and health care services.
The benefits of scientific collaborations are amplified by our diversity. Limiting the exchange of ideas, practices, and data across cultures has the potential to significantly retard scientific progress and adversely affect public health. Any loss of researchers and physicians will render the United States less competitive over time, and our traditionally strong research institutions and the patients they serve will be negatively affected.
We remain deeply concerned that restricting travel will prohibit participation in scientific meetings, where cutting-edge science and treatment methods are often first introduced. These in-person meetings and other global exchanges are vitally important because they provide unparalleled opportunities for collaborations and information-sharing. Such scientific and medical meetings are absolutely essential to the conquest of cancer and blood diseases.
(Statement issued on behalf of ASH, American Association for Cancer Research, Association of American Cancer Institutes, American Society for Radiation Oncology, The American Society for Pediatric Hematology/Oncology, and LUNGevity Foundation.)
The text of the executive order can be found on the White House website.
Updated 2/2/17 to include the position of the American Gastroenterological Association.
[email protected]
On Twitter @denisefulton
Organizations representing physicians and medical students have expressed their concern regarding President Trump’s executive order of Jan. 27 that curtails entry into the United States by travelers from seven Muslim-majority countries. The order also suspends for 120 days entry into the United States for all persons seeking refugee status, and it bars refugees from Syria indefinitely.
Following are direct excerpts from statements issued by medical organizations.
American Academy of Family Physicians
“We are deeply concerned that steps your Administration has taken will have a chilling effect on our nation’s physician workforce, biomedical research, and global health. It is often America’s physicians who answer the call to assist people around the world when a public health crisis occurs. Imagine a world where physicians fail to answer the call of the needy because they fear they may not be able to return to their home and families in the United States.
Many family physicians are international medical graduates (IMG), who have completed all or part of their education and training in the United States. They are professionals who dedicate their careers to the service of their patients in communities large and small, urban and rural. In fact, 20% of our membership and over 25% of family medicine residents [comprise] IMGs. The AAFP applauds and supports wholly the contributions of these individual family physicians to their patients and communities and we celebrate their diversity.
We recognize that one of your primary responsibilities as President is to ensure the safety and security of the country and its citizens. This is, without question, a daunting responsibility. But we strongly urge that the methods of doing so be examined carefully, so that the many people who can add so much to our country through immigration have the opportunity to do so, and those who are doing so already are treated with the respect and dignity they deserve.”
American Academy of Pediatrics
“The executive orders signed today are harmful to immigrant children and families throughout our country. Many of the children who will be most affected are the victims of unspeakable violence and have been exposed to trauma. Children do not immigrate, they flee. They are coming to the United States seeking safe haven in our country and they need our compassion and assistance. Broad scale expansion of family detention only exacerbates their suffering ... The AAP is non-partisan and pro-children. We urge President Trump and his administration to ensure that children and families who are fleeing violence and adversity can continue to seek refuge in our country. Immigrant children and families are an integral part of our communities and our nation, and they deserve to be cared for, treated with compassion, and celebrated. Most of all, they deserve to be healthy and safe. Pediatricians stand with the immigrant families we care for and will continue to advocate that their needs are met and prioritized.”
American Association of Medical Colleges
“The United States is facing a serious shortage of physicians. IMGs play an important role in U.S. health care, representing roughly 25% of the workforce. Current immigration pathways – including student, exchange-visitor, and employment visas – provide a balanced solution that improves health care access across the country through programs like the National Interest Waiver and the Conrad 30 J-1 Visa Waiver. In the last decade, Conrad 30 alone has directed nearly 10,000 physicians into rural and urban underserved communities. Impeding these U.S. immigration pathways jeopardizes critical access to high-quality physician care for our nation’s most vulnerable populations.
Our ability to attract top talent from around the world also enriches the research laboratories at medical schools and teaching hospitals that are working toward cures and has helped position the United States as a global leader in medical research, strengthening our economy and bolstering the public’s health. Because disease knows no geographic boundaries, it is essential to ensure that we continue to foster, rather than impede, scientific cooperation with physicians and researchers of all nationalities, as we strive to keep our country healthy.”
American College of Cardiology
“The ability to share ideas and knowledge necessary to address [the global epidemic of cardiovascular disease] is imperative. Policies that impede this free-flow of ideas will have a detrimental impact on scientific discovery, as well as the lives of patients around the world. If we are to realize a future where cardiovascular disease is no longer the number one killer of men and women worldwide we must ensure that our system of scientific exchange allows for health care professionals to learn from each other regardless of their nationality.
Additionally, IMGs, naturalized citizens, and legal residents make up a significant portion of the health care workforce in hospitals and practices across the country. More than 25% of current practicing physicians are IMGs, with cardiology ranking among the top when broken down by medical specialty. Policies that bring the immigration status of those already here into question, while also limiting the ability of others to legally train in the United States going forward, will only serve to exacerbate the already existing cardiovascular workforce shortage, especially in rural America. Such policies also threaten the care continuum of patients who rely on these providers for their medical care.”
American College of Physicians
“The executive order could deny entry or reentry to tens of thousands more persons, including medical students and physicians who are being trained in the United States and/or are delivering direct patient care. ... It also creates a precedent for barring entry of IMGs based on their religion and country of origin. ... Approximately 30% of ACP members are IMGs.”
American Gastroenterological Association
Science and illness ignore borders and political divides. That is why AGA is concerned that the recent U.S. executive order on immigration could limit scientific exchange, delay patient care and impair medical training.
AGA is committed to diversity, which we define as inclusive of race, ethnicity and national origin. Diversity within training programs and laboratories in the United States built today’s practice of gastroenterology. Scientists from around the world publish in our journals, work in our laboratories, train in our programs and present data at Digestive Disease Week. This exchange leads to better patient care, and very sick patients travel to the United States from around the world for the best digestive health care.
AGA adds our support to a growing number of medical institutions urging the administration to consider the devastating impact of the executive order on the health of the nation that will result from turning away patients, health professionals, and researchers. The recent immigration policy is clearly detrimental to America’s leadership role in advancing health care, and to the standing of the United States within the international community.
American Society of Clinical Oncology
ASCO is deeply concerned about the potential impact of the recent executive order on cancer research, patient care, and international scientific collaboration.
Our more than 40,000 members in 148 countries lead the charge to conquer cancer in all its forms and in every nation. Tens of thousands of people from more than 100 countries participate in our scientific meetings to exchange advances and ideas to improve patient care. Millions of cancer survivors are alive today because of the progress made possible by scientific collaboration. Progress against this disease will falter if the close-knit global community of cancer care providers is divided by policies that bar members of certain nationalities from entering the United States to conduct research, care for people with cancer, or participate in scientific and medical conferences.
American Society of Hematology
We express our deep concern about the Administration’s executive order that has denied U.S. entry to people who bring unique expertise to the practice of medicine and the conduct of cancer and biomedical research. Our nation depends on the contributions of the greatest minds from around the world to maintain the high quality of our biomedical research enterprise and health care services.
The benefits of scientific collaborations are amplified by our diversity. Limiting the exchange of ideas, practices, and data across cultures has the potential to significantly retard scientific progress and adversely affect public health. Any loss of researchers and physicians will render the United States less competitive over time, and our traditionally strong research institutions and the patients they serve will be negatively affected.
We remain deeply concerned that restricting travel will prohibit participation in scientific meetings, where cutting-edge science and treatment methods are often first introduced. These in-person meetings and other global exchanges are vitally important because they provide unparalleled opportunities for collaborations and information-sharing. Such scientific and medical meetings are absolutely essential to the conquest of cancer and blood diseases.
(Statement issued on behalf of ASH, American Association for Cancer Research, Association of American Cancer Institutes, American Society for Radiation Oncology, The American Society for Pediatric Hematology/Oncology, and LUNGevity Foundation.)
The text of the executive order can be found on the White House website.
Updated 2/2/17 to include the position of the American Gastroenterological Association.
[email protected]
On Twitter @denisefulton
Organizations representing physicians and medical students have expressed their concern regarding President Trump’s executive order of Jan. 27 that curtails entry into the United States by travelers from seven Muslim-majority countries. The order also suspends for 120 days entry into the United States for all persons seeking refugee status, and it bars refugees from Syria indefinitely.
Following are direct excerpts from statements issued by medical organizations.
American Academy of Family Physicians
“We are deeply concerned that steps your Administration has taken will have a chilling effect on our nation’s physician workforce, biomedical research, and global health. It is often America’s physicians who answer the call to assist people around the world when a public health crisis occurs. Imagine a world where physicians fail to answer the call of the needy because they fear they may not be able to return to their home and families in the United States.
Many family physicians are international medical graduates (IMG), who have completed all or part of their education and training in the United States. They are professionals who dedicate their careers to the service of their patients in communities large and small, urban and rural. In fact, 20% of our membership and over 25% of family medicine residents [comprise] IMGs. The AAFP applauds and supports wholly the contributions of these individual family physicians to their patients and communities and we celebrate their diversity.
We recognize that one of your primary responsibilities as President is to ensure the safety and security of the country and its citizens. This is, without question, a daunting responsibility. But we strongly urge that the methods of doing so be examined carefully, so that the many people who can add so much to our country through immigration have the opportunity to do so, and those who are doing so already are treated with the respect and dignity they deserve.”
American Academy of Pediatrics
“The executive orders signed today are harmful to immigrant children and families throughout our country. Many of the children who will be most affected are the victims of unspeakable violence and have been exposed to trauma. Children do not immigrate, they flee. They are coming to the United States seeking safe haven in our country and they need our compassion and assistance. Broad scale expansion of family detention only exacerbates their suffering ... The AAP is non-partisan and pro-children. We urge President Trump and his administration to ensure that children and families who are fleeing violence and adversity can continue to seek refuge in our country. Immigrant children and families are an integral part of our communities and our nation, and they deserve to be cared for, treated with compassion, and celebrated. Most of all, they deserve to be healthy and safe. Pediatricians stand with the immigrant families we care for and will continue to advocate that their needs are met and prioritized.”
American Association of Medical Colleges
“The United States is facing a serious shortage of physicians. IMGs play an important role in U.S. health care, representing roughly 25% of the workforce. Current immigration pathways – including student, exchange-visitor, and employment visas – provide a balanced solution that improves health care access across the country through programs like the National Interest Waiver and the Conrad 30 J-1 Visa Waiver. In the last decade, Conrad 30 alone has directed nearly 10,000 physicians into rural and urban underserved communities. Impeding these U.S. immigration pathways jeopardizes critical access to high-quality physician care for our nation’s most vulnerable populations.
Our ability to attract top talent from around the world also enriches the research laboratories at medical schools and teaching hospitals that are working toward cures and has helped position the United States as a global leader in medical research, strengthening our economy and bolstering the public’s health. Because disease knows no geographic boundaries, it is essential to ensure that we continue to foster, rather than impede, scientific cooperation with physicians and researchers of all nationalities, as we strive to keep our country healthy.”
American College of Cardiology
“The ability to share ideas and knowledge necessary to address [the global epidemic of cardiovascular disease] is imperative. Policies that impede this free-flow of ideas will have a detrimental impact on scientific discovery, as well as the lives of patients around the world. If we are to realize a future where cardiovascular disease is no longer the number one killer of men and women worldwide we must ensure that our system of scientific exchange allows for health care professionals to learn from each other regardless of their nationality.
Additionally, IMGs, naturalized citizens, and legal residents make up a significant portion of the health care workforce in hospitals and practices across the country. More than 25% of current practicing physicians are IMGs, with cardiology ranking among the top when broken down by medical specialty. Policies that bring the immigration status of those already here into question, while also limiting the ability of others to legally train in the United States going forward, will only serve to exacerbate the already existing cardiovascular workforce shortage, especially in rural America. Such policies also threaten the care continuum of patients who rely on these providers for their medical care.”
American College of Physicians
“The executive order could deny entry or reentry to tens of thousands more persons, including medical students and physicians who are being trained in the United States and/or are delivering direct patient care. ... It also creates a precedent for barring entry of IMGs based on their religion and country of origin. ... Approximately 30% of ACP members are IMGs.”
American Gastroenterological Association
Science and illness ignore borders and political divides. That is why AGA is concerned that the recent U.S. executive order on immigration could limit scientific exchange, delay patient care and impair medical training.
AGA is committed to diversity, which we define as inclusive of race, ethnicity and national origin. Diversity within training programs and laboratories in the United States built today’s practice of gastroenterology. Scientists from around the world publish in our journals, work in our laboratories, train in our programs and present data at Digestive Disease Week. This exchange leads to better patient care, and very sick patients travel to the United States from around the world for the best digestive health care.
AGA adds our support to a growing number of medical institutions urging the administration to consider the devastating impact of the executive order on the health of the nation that will result from turning away patients, health professionals, and researchers. The recent immigration policy is clearly detrimental to America’s leadership role in advancing health care, and to the standing of the United States within the international community.
American Society of Clinical Oncology
ASCO is deeply concerned about the potential impact of the recent executive order on cancer research, patient care, and international scientific collaboration.
Our more than 40,000 members in 148 countries lead the charge to conquer cancer in all its forms and in every nation. Tens of thousands of people from more than 100 countries participate in our scientific meetings to exchange advances and ideas to improve patient care. Millions of cancer survivors are alive today because of the progress made possible by scientific collaboration. Progress against this disease will falter if the close-knit global community of cancer care providers is divided by policies that bar members of certain nationalities from entering the United States to conduct research, care for people with cancer, or participate in scientific and medical conferences.
American Society of Hematology
We express our deep concern about the Administration’s executive order that has denied U.S. entry to people who bring unique expertise to the practice of medicine and the conduct of cancer and biomedical research. Our nation depends on the contributions of the greatest minds from around the world to maintain the high quality of our biomedical research enterprise and health care services.
The benefits of scientific collaborations are amplified by our diversity. Limiting the exchange of ideas, practices, and data across cultures has the potential to significantly retard scientific progress and adversely affect public health. Any loss of researchers and physicians will render the United States less competitive over time, and our traditionally strong research institutions and the patients they serve will be negatively affected.
We remain deeply concerned that restricting travel will prohibit participation in scientific meetings, where cutting-edge science and treatment methods are often first introduced. These in-person meetings and other global exchanges are vitally important because they provide unparalleled opportunities for collaborations and information-sharing. Such scientific and medical meetings are absolutely essential to the conquest of cancer and blood diseases.
(Statement issued on behalf of ASH, American Association for Cancer Research, Association of American Cancer Institutes, American Society for Radiation Oncology, The American Society for Pediatric Hematology/Oncology, and LUNGevity Foundation.)
The text of the executive order can be found on the White House website.
Updated 2/2/17 to include the position of the American Gastroenterological Association.
[email protected]
On Twitter @denisefulton
February 2017 Quiz 2
Q2: Answer: B
Objective: Recognize the features of CVID-associated noninfectious gastrointestinal manifestations.
Explanation: This patient has gastrointestinal manifestations of common variable immune deficiency (CVID), which can present similarly to celiac disease or inflammatory bowel disease. Histologically, intestinal biopsies will reveal villous atrophy, crypt hyperplasia, and intraepithelial lymphocytosis similar to celiac disease. However, while plasma cells are increased in celiac disease, they are absent in CVID.
The initial treatment strategy for CVID typically includes oral corticosteroids, either prednisone or budesonide, with other immunosuppressants such as the thiopurines or anti–tumor necrosis factor agents reserved for steroid-dependent or refractory disease.
Gluten-free diet is ineffective for the treatment of CVID-associated enteropathy. Intravenous immunoglobulin therapy reduces the frequency of infections associated with CVID, but does not affect the noninfectious GI symptoms. While bacterial overgrowth can occur in CVID, it is typically the consequence of the luminal changes, not the cause.
Reference
1. Agarwal S., Mayer L. Gastrointestinal manifestations in primary immune disorders. Inflamm Bowel Dis. 2010;16:703-11.
Q2: Answer: B
Objective: Recognize the features of CVID-associated noninfectious gastrointestinal manifestations.
Explanation: This patient has gastrointestinal manifestations of common variable immune deficiency (CVID), which can present similarly to celiac disease or inflammatory bowel disease. Histologically, intestinal biopsies will reveal villous atrophy, crypt hyperplasia, and intraepithelial lymphocytosis similar to celiac disease. However, while plasma cells are increased in celiac disease, they are absent in CVID.
The initial treatment strategy for CVID typically includes oral corticosteroids, either prednisone or budesonide, with other immunosuppressants such as the thiopurines or anti–tumor necrosis factor agents reserved for steroid-dependent or refractory disease.
Gluten-free diet is ineffective for the treatment of CVID-associated enteropathy. Intravenous immunoglobulin therapy reduces the frequency of infections associated with CVID, but does not affect the noninfectious GI symptoms. While bacterial overgrowth can occur in CVID, it is typically the consequence of the luminal changes, not the cause.
Reference
1. Agarwal S., Mayer L. Gastrointestinal manifestations in primary immune disorders. Inflamm Bowel Dis. 2010;16:703-11.
Q2: Answer: B
Objective: Recognize the features of CVID-associated noninfectious gastrointestinal manifestations.
Explanation: This patient has gastrointestinal manifestations of common variable immune deficiency (CVID), which can present similarly to celiac disease or inflammatory bowel disease. Histologically, intestinal biopsies will reveal villous atrophy, crypt hyperplasia, and intraepithelial lymphocytosis similar to celiac disease. However, while plasma cells are increased in celiac disease, they are absent in CVID.
The initial treatment strategy for CVID typically includes oral corticosteroids, either prednisone or budesonide, with other immunosuppressants such as the thiopurines or anti–tumor necrosis factor agents reserved for steroid-dependent or refractory disease.
Gluten-free diet is ineffective for the treatment of CVID-associated enteropathy. Intravenous immunoglobulin therapy reduces the frequency of infections associated with CVID, but does not affect the noninfectious GI symptoms. While bacterial overgrowth can occur in CVID, it is typically the consequence of the luminal changes, not the cause.
Reference
1. Agarwal S., Mayer L. Gastrointestinal manifestations in primary immune disorders. Inflamm Bowel Dis. 2010;16:703-11.
Q2: A 34-year-old woman presents with a 3-year history of watery, nonbloody diarrhea with associated weight loss, and recurrent bacterial bronchitis and pneumonias. Laboratory studies show iron deficiency anemia, low 25-OH vitamin D, and a slightly elevated INR. Celiac serologies were negative, and small bowel biopsies revealed near total villous atrophy, increased intraepithelial lymphocytes, and crypt hyperplasia with absent plasma cells.
February 2017 Quiz 1
Q1: Answer: D
Current recommendations suggest H. pylori testing for patients with active or a documented history of peptic ulcer disease, gastric MALT lymphoma, or gastric carcinoma. The H. pylori test-and-treat strategy is also recommended for patients less than 55 years of age who present with dyspepsia symptoms without “alarm features.”
There is currently no recommendation for asymptomatic family members of patients diagnosed with H. pylori infection to be tested, unless there are known factors that may increase the patient’s risk for gastric malignancy (e.g., family history of gastric carcinoma, and ethnic background from areas with high prevalence of H. pylori and gastric cancer such as East Asia, Latin America, and Eastern Europe).
References
1. Chey W.D., Wong B.C. Practice Parameters Committee of the American College of Gastroenterology. American College of Gastroenterology guideline on the management of Helicobacter pylori infection. Am J Gastroenterol. 2007;102:1808-25.
2. Talley N.J., Vakil N.B., Moayyedi P. American Gastroenterological Association technical review on the evaluation of dyspepsia. Gastroenterology 2005;129:1756-80.
3. Suerbaum S., Michetti P. Helicobacter pylori infection. N Engl J Med. 2002;347:1175-86.
4. Everhart J.E., Kruszon-Moran D., Perez-Perez G.I., et al. Seroprevalence and ethnic differences in Helicobacter pylori infection among adults in the United States. J Infect Dis. 2000;181:1359-63.
Q1: Answer: D
Current recommendations suggest H. pylori testing for patients with active or a documented history of peptic ulcer disease, gastric MALT lymphoma, or gastric carcinoma. The H. pylori test-and-treat strategy is also recommended for patients less than 55 years of age who present with dyspepsia symptoms without “alarm features.”
There is currently no recommendation for asymptomatic family members of patients diagnosed with H. pylori infection to be tested, unless there are known factors that may increase the patient’s risk for gastric malignancy (e.g., family history of gastric carcinoma, and ethnic background from areas with high prevalence of H. pylori and gastric cancer such as East Asia, Latin America, and Eastern Europe).
References
1. Chey W.D., Wong B.C. Practice Parameters Committee of the American College of Gastroenterology. American College of Gastroenterology guideline on the management of Helicobacter pylori infection. Am J Gastroenterol. 2007;102:1808-25.
2. Talley N.J., Vakil N.B., Moayyedi P. American Gastroenterological Association technical review on the evaluation of dyspepsia. Gastroenterology 2005;129:1756-80.
3. Suerbaum S., Michetti P. Helicobacter pylori infection. N Engl J Med. 2002;347:1175-86.
4. Everhart J.E., Kruszon-Moran D., Perez-Perez G.I., et al. Seroprevalence and ethnic differences in Helicobacter pylori infection among adults in the United States. J Infect Dis. 2000;181:1359-63.
Q1: Answer: D
Current recommendations suggest H. pylori testing for patients with active or a documented history of peptic ulcer disease, gastric MALT lymphoma, or gastric carcinoma. The H. pylori test-and-treat strategy is also recommended for patients less than 55 years of age who present with dyspepsia symptoms without “alarm features.”
There is currently no recommendation for asymptomatic family members of patients diagnosed with H. pylori infection to be tested, unless there are known factors that may increase the patient’s risk for gastric malignancy (e.g., family history of gastric carcinoma, and ethnic background from areas with high prevalence of H. pylori and gastric cancer such as East Asia, Latin America, and Eastern Europe).
References
1. Chey W.D., Wong B.C. Practice Parameters Committee of the American College of Gastroenterology. American College of Gastroenterology guideline on the management of Helicobacter pylori infection. Am J Gastroenterol. 2007;102:1808-25.
2. Talley N.J., Vakil N.B., Moayyedi P. American Gastroenterological Association technical review on the evaluation of dyspepsia. Gastroenterology 2005;129:1756-80.
3. Suerbaum S., Michetti P. Helicobacter pylori infection. N Engl J Med. 2002;347:1175-86.
4. Everhart J.E., Kruszon-Moran D., Perez-Perez G.I., et al. Seroprevalence and ethnic differences in Helicobacter pylori infection among adults in the United States. J Infect Dis. 2000;181:1359-63.
A Primary Hospital Antimicrobial Stewardship Intervention on Pneumonia Treatment Duration
The safety and the efficacy of shorter durations of antibiotic therapy for uncomplicated pneumonia have been clearly established in the past decade.1,2 Guidelines from the Infectious Diseases Society of America (IDSA) and the American Thoracic Society have been available since 2007. These expert consensus statements recommend that uncomplicated community-acquired pneumonia (CAP) should be treated for 5 to 7 days, as long as the patient exhibits signs and symptoms of clinical stability.3 Similarly, recently updated guidelines for hospital-acquired and ventilator-associated pneumonias call for short-course therapy.4 Despite this guidance, pneumonia treatment duration is often discordant.5 Unnecessary antimicrobial use is associated with greater selection pressure on pathogens, increased risk of adverse events (AEs), and elevated treatment costs.6 The growing burden of antibiotic resistance coupled with limited availability of new antibiotics requires judicious use of these agents.
The IDSA guidelines for Clostridium difficile infection (CDI) note that exposure to antimicrobial agents is the most important modifiable risk factor for the development of CDI.7 Longer durations of antibiotics increase the risk of CDI compared with shorter durations.8,9 Antibiotics are a frequent cause of drug-associated AEs and likely are underestimated.10 To decrease the unwanted effects of excessive therapy, IDSA and CDC suggest that antimicrobial stewardship interventions should be implemented.11-13
Antimicrobial stewardship efforts in small community hospitals (also known as district, rural, general, and primary hospitals) are varied and can be challenging due to limited staff and resources.14,15 The World Health Organization defines a primary care facility as having few specialties, mainly internal medicine and general surgery with limited laboratory services for general (but not specialized) pathologic analysis, and bed size ranging from 30 to 200 beds.16 Although guidance is available for effective intervention strategies in smaller hospitals, there are limited data in the literature regarding successful outcomes.17-22
The purpose of this study was to establish the need and evaluate the impact of a pharmacy-initiated 3-part intervention targeting treatment duration in patients hospitalized with uncomplicated pneumonia in a primary hospital setting. The Veterans Health Care System of the Ozarks (VHSO) in Fayetteville, Arkansas, has 50 acute care beds, including 7 intensive care unit beds and excluding 15 mental health beds. The pharmacy is staffed 24 hours a day. Acute-care providers consist of 7 full-time hospitalists, not including nocturnists and contract physicians. The VHSO does not have an infectious disease physician on staff.
The antimicrobial stewardship committee consists of 3 clinical pharmacists, a pulmonologist, a pathologist, and 2 infection-control nurses. There is 1 full-time equivalent allotted for inpatient clinical pharmacy activities in the acute care areas, including enforcement of all antimicrobial stewardship policies, which are conducted by a single pharmacist.
Methods
This was a retrospective chart review of two 12-month periods using a before and after study design. Medical records were reviewed during October 2012 through September 2013 (before the stewardship implementation) and December 2014 through November 2015 (after implementation). Inclusion criteria consisted of a primary discharge diagnosis of pneumonia as documented by the provider (or secondary diagnosis if sepsis was primary), hospitalization for at least 48 hours, administration of antibiotics for a minimum of 24 hours, and survival to discharge.
Exclusion criteria consisted of direct transfer from another facility, inappropriate empiric therapy as evidenced by culture data (isolated pathogens not covered by prescribed antibiotics), pneumonia that developed 48 hours after admission, extrapulmonary sources of infection, hospitalization > 14 days, discharge without a known duration of outpatient antibiotics, discharge for pneumonia within 28 days prior to admission, documented infection caused by Pseudomonas aeruginosa or other nonlactose fermenting Gram-negative rod, and complicated pneumonias defined as lung abscess, empyema, or severe immunosuppression (eg, cancer with chemotherapy within the previous 30 days, transplant recipients, HIV infection, acquired or congenital immunodeficiency, or absolute neutrophil count 1,500 cell/mm3 within past 28 days).
Patients were designated with health care-associated pneumonia (HCAP) if they were hospitalized ≥ 2 days or resided in a skilled nursing or extended-care facility within the previous 90 days; on chronic dialysis; or had wound care, tracheostomy care, or ventilator care from a health care professional within the previous 28 days. Criteria for clinical stability were defined as ≤ 100.4º F temperature, ≤ 100 beats/min heart rate, ≤ 24 breaths/min respiratory rate, ≥ 90 mm Hg systolic blood pressure, ≥ 90% or PaO2 ≥ 60 mm Hg oxygen saturation on room air (or baseline oxygen requirements), and return to baseline mental status. To compare groups, researchers tabulated the pneumonia severity index on hospital day 1.
The intervention consisted of a 3-part process. First, hospitalists were educated on VHSO’s baseline treatment duration data, and these were compared with current IDSA recommendations. The education was followed by an open-discussion component to solicit feedback from providers on perceived barriers to following guidelines. Provider feedback was used to tailor an antimicrobial stewardship intervention to address perceived barriers to optimal antibiotic treatment duration.
After the education component, prospective intervention and feedback were provided for hospitalized patients by a single clinical pharmacist. This pharmacist interacted verbally and in writing with the patients’ providers, discussing antimicrobial appropriateness, de-escalation, duration of therapy, and intravenous to oral switching. Finally, a stewardship note for the Computerized Patient Record System (CPRS) was generated and included a template with reminders of clinical stability, duration of current therapy, and a request to discontinue therapy if the patient met criteria. For patients who remained hospitalized, this note was entered into CPRS on or about day 7 of antibiotic therapy; this required an electronic signature from the provider.
The VHSO Pharmacy and Therapeutics Committee approved both the provider education and the stewardship note in November 2014, and implementation of the stewardship intervention occurred immediately afterward. The pharmacy staff also was educated on the VHSO baseline data and stewardship efforts.
The primary outcome of the study was the change in days of total antibiotic treatment. Secondary outcomes included days of intravenous antibiotic therapy, days of inpatient oral therapy, mean length of stay (LOS), and number of outpatient antibiotic days once discharged. Incidence of CDI and 28-day readmissions were also evaluated. The VHSO Institutional Review Board approved these methods and the procedures that followed were in accord with the ethical standards of the VHSO Committee on Human Experimentation.
Statistical Analysis
All continuous variables are reported as mean ± standard deviation. Data analysis for significance was performed using a Student t test for continuous variables and a χ2 test (or Fisher exact test) for categorical variables in R Foundation for Statistical Computing version 3.1.0. All samples were 2-tailed. A P value < .05 was considered statistically significant. Using the smaller of the 2 study populations, the investigators calculated that the given sample size of 88 in each group would provide 99% power to detect a 2-day difference in the primary endpoint at a 2-sided significance level of 5%.
Results
During the baseline assessment (group 1), 192 cases were reviewed with 103 meeting the inclusion criteria. Group 1 consisted of 85 cases of CAP and 18 cases of HCAP (mean age, 70.7 years). During the follow-up assessment (group 2), 168 cases were reviewed with 88 meeting the inclusion criteria. Group 2 consisted of 68 cases of CAP and 20 cases of HCAP (mean age, 70.8 years).
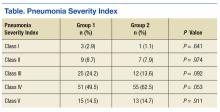
There was no difference in inpatient mortality rates between groups (3.1% vs 3.0%, P = .99). This mortality rate is consistent with published reports.23 Empiric antibiotic selection was appropriate because there were no exclusions for drug/pathogen mismatch. Pneumonia severity was similar in both groups (Table).
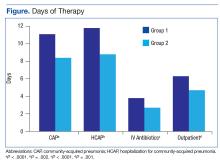
The total duration of antibiotic treatment decreased significantly for CAP and HCAP (Figure). The observed median treatment days for groups 1 and 2 were 11 days and 8 days, respectively. Outpatient antibiotic days also decreased. Mean LOS was shorter in the follow-up group (4.9 ± 2.6 days vs 4.0 ± 2.6 days, P = .02). Length of IV antibiotic duration decreased. Oral antibiotic days while inpatient were not statistically different (1.5 ± 1.8 days vs 1.1 ± 1.5 days, P = .15). During the follow-up period, 26 stewardship notes were entered into CPRS; antibiotics were stopped in 65% of cases.
There were no recorded cases of CDI in either group. There were eleven 28-day readmissions in group 1, only 3 of which were due to infectious causes. One patient had a primary diagnosis of necrotizing pneumonia, 1 had Pseudomonas pneumonia, and 1 patient had a new lung mass and was diagnosed with postobstructive pneumonia. Of eight 28-day readmissions in group 2, only 2 resulted from infectious causes. One readmission primary diagnosis was sinusitis and 1 was recurrent pneumonia (of note, this patient received a 10-day treatment course for pneumonia on initial admission). Two patients died within 28 days of discharge in each group.
Discussion
Other multifaceted single-center interventions have been shown to be effective in large, teaching hospitals,24,25 and it has been suggested that smaller, rural hospitals may be underserved in antimicrobial stewardship activities.26,27 In the global struggle with antimicrobial resistance, McGregor and colleagues highlighted the importance of evaluating successful stewardship methods in an array of clinical settings to help tailor an approach for a specific type of facility.28 To the authors knowledge, this is the first publication showing efficacy of such antimicrobial stewardship interventions specific to pneumonia therapy in a small, primary facility.
The intervention methods used at VHSO are supported by recent IDSA and Society for Healthcare Epidemiology of America guidelines for effective stewardship implementation.29 Prospective audit and feedback is considered a core recommendation, whereas didactic education is recommended only in conjunction with other stewardship activities. Additionally, the guidelines recommend evaluating specific infectious disease syndromes, in this case uncomplicated pneumonia, to focus on specific treatment guidelines. Last, the results of the 3-part intervention can be used to aid in demonstrating facility improvement and encourage continued success.
Of note, VHSO has had established inpatient and outpatient clinical pharmacy roles for several years. Stewardship interventions already in place included an intravenous-to-oral antibiotic switch policy, automatic antibiotic stop dates, as well as pharmacist-driven vancomycin and aminoglycoside dosing. Prior to this multifaceted intervention specific to pneumonia duration, prospective audit and feedback interventions (verbal and written) also were common. The number of interventions specific to this study outside of the stewardship note was not recorded. Using rapid diagnostic testing and biomarkers to aid in stewardship activities at VHSO have been considered, but these tools are not available due to a lab personnel shortage.
Soliciting feedback from providers on their preferred stewardship strategy and perceived barriers was a key component of the educational intervention. Of equal importance was presenting providers with their baseline prescribing data to provide objective evidence of a problem. While all were familiar with existing treatment guidelines, some feedback indicated that it can be difficult to determine accurate antibiotic duration in CPRS. Prescribers reported that identifying antibiotic duration was especially challenging when antibiotics as well as providers change during an admission. Also frequently overlooked were antibiotics given in the emergency department. This could be a key area for clinical pharmacists’ intervention given their familiarity with the CPRS medication sections.
Charani and colleagues suggest that recognizing barriers to implementing best practices and adapting to the local facility culture is paramount for changing prescribing behaviors and developing a successful stewardship intervention.30 At VHSO, the providers were presented with multiple stewardship options but agreed to the new note and template. This process gave providers a voice in selecting their own stewardship intervention. In a culture with no infectious disease physician to champion initiatives, the investigators felt that provider involvement in the intervention selection was unique and may have encouraged provider concurrence.
Although not directly targeted by the intervention strategies, average LOS was shorter in the follow-up group. According to investigators, frequent reminders of clinical stability in the stewardship notes may have influenced this. Even though the note was used only in patients who remained hospitalized for their entire treatment course, investigators felt that it still served as a reminder for prescribing habits as they were also able to show a decrease in outpatient prescription duration.
Limitations
Potential weaknesses of the study include changes in providers. During the transition between group 1 and group 2, 2 hospitalists left and 2 new hospitalists arrived. Given the small size of the staff, this could significantly impact prescribing trends. Another potential weakness is the high exclusion rate, although these rates were similar in both groups (46% group 1, 47% group 2). Furthermore, similar exclusion rates have been reported elsewhere.24,25,31 The most common reasons for exclusion were complicated pneumonias (36%) and immunocompromised patients (18%). These patient populations were not evaluated in the current study, and optimal treatment durations are unknown. Hospital-acquired and ventilator-associated pneumonias also were excluded. Therefore, limitations in applicability of the results should be noted.
The authors acknowledge that, prior to this publication, the IDSA guidelines have removed the designation of HCAP as a separate clinical entity.4 However, this should not affect the significance of the intervention for treatment duration.
The study facility experienced a hiring freeze resulting in a 9.3% decrease in overall admissions from fiscal year 2013 to fiscal year 2015. This is likely why there were fewer admissions for pneumonia in group 2. Regardless, power analysis revealed the study was of adequate sample size to detect its primary outcome. It is possible that patients in either group could have sought health care at other facilities, making the CDI and readmission endpoints less inclusive.
The study was not of a scale to detect changes in antimicrobial resistance pressure or clinical outcomes. Cost savings were not analyzed. However, this study adds to the growing body of evidence that a structured intervention can result in positive outcomes at the facility level. This study shows that interventions targeting pneumonia treatment duration could feasibly be added to the menu of stewardship options available to smaller facilities.
Like other stewardship studies in the literature, the follow-up treatment duration, while improved, still exceeded those recommended in the IDSA guidelines. The investigators noted that not all providers were equal regarding change in prescribing habits, perhaps making the average duration longer. Additionally, the request to discontinue antibiotic therapy through the stewardship note could have been entered earlier (eg, as early as day 5 of therapy) to target the shortest effective date as recommended in the recent stewardship guidelines.29 Future steps include continued feedback to providers on their progress in this area and encouragement to document day of antibiotic treatment in their daily progress notes.
Conclusion
This study showed a significant decrease in antibiotic duration for the treatment of uncomplicated pneumonia using a 3-part pharmacy intervention in a primary hospital setting. The investigators feel that each arm of the strategy was equally important and fewer interventions were not likely to be as effective.32 Although data collection for baseline prescribing and follow-up on outcomes may be a time-consuming task, it can be a valuable component of successful stewardship interventions.
1. Li JZ, Winston LG, Moore DH, Bent S. Efficacy of short-course antibiotic regimens for community-acquired pneumonia: a meta-analysis. Am J Med. 2007;120(9):783-790.
2. Dimopoulos G, Matthaiou DK, Karageorgopoulos DE, Grammatikos AP, Athanassa Z, Falagas ME. Short- versus long-course antibacterial therapy of community-acquired pneumonia: a meta-analysis. Drugs. 2008;68(13):1841-1854.
3. Mandell LA, Wunderink RG, Anzueto A, et al; Infectious Diseases Society of America; American Thoracic Society. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27-S72.
4. Kalil AC, Metersky ML, Klompas M, et al. Management of adults with hospital-acquired and ventilator associated pneumonia: 2016 clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;63(5):e61-e111.
5. Jenkins TC, Stella SA, Cervantes L, et al. Targets for antibiotic and healthcare resource stewardship in inpatient community-acquired pneumonia: a comparison of management practices with National Guideline Recommendations. Infection. 2013; 41(1):135-144.
6. Shlaes DM, Gerding DN, John JF Jr, et al. Society for Healthcare Epidemiology of America, and Infectious Diseases Society of America Joint Committee on the Prevention of Antimicrobial Resistance: guidelines for the prevention of antimicrobial resistance in hospitals. Clin Infect Dis. 1997;25(3):584-599.
7. Cohen SH, Gerding DN, Johnson S, et al; Society for Healthcare Epidemiology of America; Infectious Diseases Society of America. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hosp Epidemiol. 2010;31(5):431-455.
8. Brown E, Talbot GH, Axelrod P, Provencher M, Hoegg C. Risk factors for Clostridium-difficile toxin-associated diarrhea. Infect Control Hosp Epidemiol. 1990;11(6):283-290.
9. McFarland LV, Surawicz CM, Stamm WE. Risk factors for Clostridium-difficile carriage and C. difficile-associated diarrhea in a cohort of hospitalized patients. J Infect Dis. 1990;162(3):678-684.
10. Shehab N, Patel PR, Srinivasan A, Budnitz DS. Emergency department visits for antibiotic-associated adverse events. Clin Infect Dis. 2008;47(6):735-743.
11. Dellit TH, Owens RC, McGowan JE Jr, et al; Infectious Diseases Society of America; Society for Healthcare Epidemiology of America. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America Guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007;44(2):159-177.
12. Fridkin S, Baggs J, Fagan R, et al; Centers for Disease Control and Prevention (CDC). Vital signs: improving antibiotic use among hospitalized patients. MMWR Morb Mortal Wkly Rep. 2014;63(9):194-200.
13. Nussenblatt V, Avdic E, Cosgrove S. What is the role of antimicrobial stewardship in improving outcomes of patients with CAP? Infect Dis Clin North Am. 2013;27(1):211-228.
14. Septimus EJ, Owens RC Jr. Need and potential of antimicrobial stewardship in community hospitals. Clin Infect Dis. 2011;53(suppl 1):S8-S14.
15. Hensher M, Price M, Adomakoh S. Referral hospitals. In Jamison DT, Breman JG, Measham AR, eds, et al. Disease Control Priorities in Developing Countries. New York, NY: Oxford University Press; 2006:1230.
16. Mulligan J, Fox-Rushby JA, Adam T, Johns B, Mills A. Unit costs of health care inputs in low and middle income regions. 2003. Working Paper 9, Disease Control Priorities Project. Published September 2003. Revised June 2005.
17. Ohl CA, Dodds Ashley ES. Antimicrobial stewardship programs in community hospitals: the evidence base and case studies. Clin Infect Dis 2011;53(suppl 1):S23-S28.
18. Trevidi KK, Kuper K. Hospital antimicrobial stewardship in the nonuniversity setting. Infect Dis Clin North Am. 2014;28(2):281-289.
19. Yam P, Fales D, Jemison J, Gillum M, Bernstein M. Implementation of an antimicrobial stewardship program in a rural hospital. Am J Health Syst Pharm. 2012;69(13);1142-1148.
20. LaRocco A Jr. Concurrent antibiotic review programs—a role for infectious diseases specialists at small community hospitals. Clin Infect Dis. 2003;37(5):742-743.
21. Bartlett JM, Siola PL. Implementation and first-year results of an antimicrobial stewardship program at a community hospital. Am J Health Syst Pharm. 2014;71(11):943-949.
22. Storey DF, Pate PG, Nguyen AT, Chang F. Implementation of an antimicrobial stewardship program on the medical-surgical service of a 100-bed community hospital. Antimicrob Resist Infect Control. 2012;1(1):32.
23. Fine MJ, Smith MA, Carson CA, et al. Prognosis and outcomes of patients with community-acquired pneumonia. A meta-analysis. JAMA. 1996;275(2):134-141.
24. Advic E, Cushinotto LA, Hughes AH, et al. Impact of an antimicrobial stewardship intervention on shortening the duration of therapy for community-acquired pneumonia. Clin Infect Dis. 2012;54(11):1581-1587.
25. Carratallà J, Garcia-Vidal C, Ortega L, et al. Effect of a 3-step critical pathway to reduce duration of intravenous antibiotic therapy and length of stay in community-acquired pneumonia: a randomized controlled trial. Arch Intern Med. 2012;172(12):922-928.
26. Stevenson KB, Samore M, Barbera J, et al. Pharmacist involvement in antimicrobial use at rural community hospitals in four Western states. Am J Health Syst Pharm. 2004;61(8):787-792.
27. Reese SM, Gilmartin H, Rich KL, Price CS. Infection prevention needs assessment in Colorado hospitals: rural and urban settings. Am J Infect Control. 2014;42(6):597-601.
28. McGregor JC, Furuno JP. Optimizing research methods used for the evaluation of antimicrobial stewardship programs. Clin Infect Dis. 2014;59(suppl 3):S185-S192.
29. Barlam TF, Cosgrove SE, Abbo LM, et al. Implementing an antibiotic stewardship program: Guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis. 2016;62(10):e51-e77.
30. Charani E, Castro-Sánchez E, Holmes A. The role of behavior change in antimicrobial stewardship. Infect Dis Clin N Am. 2014;28(2):169-175.
31. Attridge RT, Frei CR, Restrepo MI, et al. Guideline-concordant therapy and outcomes in healthcare-associated pneumonia. Eur Respir J. 2011;38(4):878-887.
32. MacDougal C, Polk RE. Antimicrobial stewardship programs in health care systems. Clin Microbiol Rev. 2005;18(4):638-656.
The safety and the efficacy of shorter durations of antibiotic therapy for uncomplicated pneumonia have been clearly established in the past decade.1,2 Guidelines from the Infectious Diseases Society of America (IDSA) and the American Thoracic Society have been available since 2007. These expert consensus statements recommend that uncomplicated community-acquired pneumonia (CAP) should be treated for 5 to 7 days, as long as the patient exhibits signs and symptoms of clinical stability.3 Similarly, recently updated guidelines for hospital-acquired and ventilator-associated pneumonias call for short-course therapy.4 Despite this guidance, pneumonia treatment duration is often discordant.5 Unnecessary antimicrobial use is associated with greater selection pressure on pathogens, increased risk of adverse events (AEs), and elevated treatment costs.6 The growing burden of antibiotic resistance coupled with limited availability of new antibiotics requires judicious use of these agents.
The IDSA guidelines for Clostridium difficile infection (CDI) note that exposure to antimicrobial agents is the most important modifiable risk factor for the development of CDI.7 Longer durations of antibiotics increase the risk of CDI compared with shorter durations.8,9 Antibiotics are a frequent cause of drug-associated AEs and likely are underestimated.10 To decrease the unwanted effects of excessive therapy, IDSA and CDC suggest that antimicrobial stewardship interventions should be implemented.11-13
Antimicrobial stewardship efforts in small community hospitals (also known as district, rural, general, and primary hospitals) are varied and can be challenging due to limited staff and resources.14,15 The World Health Organization defines a primary care facility as having few specialties, mainly internal medicine and general surgery with limited laboratory services for general (but not specialized) pathologic analysis, and bed size ranging from 30 to 200 beds.16 Although guidance is available for effective intervention strategies in smaller hospitals, there are limited data in the literature regarding successful outcomes.17-22
The purpose of this study was to establish the need and evaluate the impact of a pharmacy-initiated 3-part intervention targeting treatment duration in patients hospitalized with uncomplicated pneumonia in a primary hospital setting. The Veterans Health Care System of the Ozarks (VHSO) in Fayetteville, Arkansas, has 50 acute care beds, including 7 intensive care unit beds and excluding 15 mental health beds. The pharmacy is staffed 24 hours a day. Acute-care providers consist of 7 full-time hospitalists, not including nocturnists and contract physicians. The VHSO does not have an infectious disease physician on staff.
The antimicrobial stewardship committee consists of 3 clinical pharmacists, a pulmonologist, a pathologist, and 2 infection-control nurses. There is 1 full-time equivalent allotted for inpatient clinical pharmacy activities in the acute care areas, including enforcement of all antimicrobial stewardship policies, which are conducted by a single pharmacist.
Methods
This was a retrospective chart review of two 12-month periods using a before and after study design. Medical records were reviewed during October 2012 through September 2013 (before the stewardship implementation) and December 2014 through November 2015 (after implementation). Inclusion criteria consisted of a primary discharge diagnosis of pneumonia as documented by the provider (or secondary diagnosis if sepsis was primary), hospitalization for at least 48 hours, administration of antibiotics for a minimum of 24 hours, and survival to discharge.
Exclusion criteria consisted of direct transfer from another facility, inappropriate empiric therapy as evidenced by culture data (isolated pathogens not covered by prescribed antibiotics), pneumonia that developed 48 hours after admission, extrapulmonary sources of infection, hospitalization > 14 days, discharge without a known duration of outpatient antibiotics, discharge for pneumonia within 28 days prior to admission, documented infection caused by Pseudomonas aeruginosa or other nonlactose fermenting Gram-negative rod, and complicated pneumonias defined as lung abscess, empyema, or severe immunosuppression (eg, cancer with chemotherapy within the previous 30 days, transplant recipients, HIV infection, acquired or congenital immunodeficiency, or absolute neutrophil count 1,500 cell/mm3 within past 28 days).
Patients were designated with health care-associated pneumonia (HCAP) if they were hospitalized ≥ 2 days or resided in a skilled nursing or extended-care facility within the previous 90 days; on chronic dialysis; or had wound care, tracheostomy care, or ventilator care from a health care professional within the previous 28 days. Criteria for clinical stability were defined as ≤ 100.4º F temperature, ≤ 100 beats/min heart rate, ≤ 24 breaths/min respiratory rate, ≥ 90 mm Hg systolic blood pressure, ≥ 90% or PaO2 ≥ 60 mm Hg oxygen saturation on room air (or baseline oxygen requirements), and return to baseline mental status. To compare groups, researchers tabulated the pneumonia severity index on hospital day 1.
The intervention consisted of a 3-part process. First, hospitalists were educated on VHSO’s baseline treatment duration data, and these were compared with current IDSA recommendations. The education was followed by an open-discussion component to solicit feedback from providers on perceived barriers to following guidelines. Provider feedback was used to tailor an antimicrobial stewardship intervention to address perceived barriers to optimal antibiotic treatment duration.
After the education component, prospective intervention and feedback were provided for hospitalized patients by a single clinical pharmacist. This pharmacist interacted verbally and in writing with the patients’ providers, discussing antimicrobial appropriateness, de-escalation, duration of therapy, and intravenous to oral switching. Finally, a stewardship note for the Computerized Patient Record System (CPRS) was generated and included a template with reminders of clinical stability, duration of current therapy, and a request to discontinue therapy if the patient met criteria. For patients who remained hospitalized, this note was entered into CPRS on or about day 7 of antibiotic therapy; this required an electronic signature from the provider.
The VHSO Pharmacy and Therapeutics Committee approved both the provider education and the stewardship note in November 2014, and implementation of the stewardship intervention occurred immediately afterward. The pharmacy staff also was educated on the VHSO baseline data and stewardship efforts.
The primary outcome of the study was the change in days of total antibiotic treatment. Secondary outcomes included days of intravenous antibiotic therapy, days of inpatient oral therapy, mean length of stay (LOS), and number of outpatient antibiotic days once discharged. Incidence of CDI and 28-day readmissions were also evaluated. The VHSO Institutional Review Board approved these methods and the procedures that followed were in accord with the ethical standards of the VHSO Committee on Human Experimentation.
Statistical Analysis
All continuous variables are reported as mean ± standard deviation. Data analysis for significance was performed using a Student t test for continuous variables and a χ2 test (or Fisher exact test) for categorical variables in R Foundation for Statistical Computing version 3.1.0. All samples were 2-tailed. A P value < .05 was considered statistically significant. Using the smaller of the 2 study populations, the investigators calculated that the given sample size of 88 in each group would provide 99% power to detect a 2-day difference in the primary endpoint at a 2-sided significance level of 5%.
Results
During the baseline assessment (group 1), 192 cases were reviewed with 103 meeting the inclusion criteria. Group 1 consisted of 85 cases of CAP and 18 cases of HCAP (mean age, 70.7 years). During the follow-up assessment (group 2), 168 cases were reviewed with 88 meeting the inclusion criteria. Group 2 consisted of 68 cases of CAP and 20 cases of HCAP (mean age, 70.8 years).
There was no difference in inpatient mortality rates between groups (3.1% vs 3.0%, P = .99). This mortality rate is consistent with published reports.23 Empiric antibiotic selection was appropriate because there were no exclusions for drug/pathogen mismatch. Pneumonia severity was similar in both groups (Table).
The total duration of antibiotic treatment decreased significantly for CAP and HCAP (Figure). The observed median treatment days for groups 1 and 2 were 11 days and 8 days, respectively. Outpatient antibiotic days also decreased. Mean LOS was shorter in the follow-up group (4.9 ± 2.6 days vs 4.0 ± 2.6 days, P = .02). Length of IV antibiotic duration decreased. Oral antibiotic days while inpatient were not statistically different (1.5 ± 1.8 days vs 1.1 ± 1.5 days, P = .15). During the follow-up period, 26 stewardship notes were entered into CPRS; antibiotics were stopped in 65% of cases.
There were no recorded cases of CDI in either group. There were eleven 28-day readmissions in group 1, only 3 of which were due to infectious causes. One patient had a primary diagnosis of necrotizing pneumonia, 1 had Pseudomonas pneumonia, and 1 patient had a new lung mass and was diagnosed with postobstructive pneumonia. Of eight 28-day readmissions in group 2, only 2 resulted from infectious causes. One readmission primary diagnosis was sinusitis and 1 was recurrent pneumonia (of note, this patient received a 10-day treatment course for pneumonia on initial admission). Two patients died within 28 days of discharge in each group.
Discussion
Other multifaceted single-center interventions have been shown to be effective in large, teaching hospitals,24,25 and it has been suggested that smaller, rural hospitals may be underserved in antimicrobial stewardship activities.26,27 In the global struggle with antimicrobial resistance, McGregor and colleagues highlighted the importance of evaluating successful stewardship methods in an array of clinical settings to help tailor an approach for a specific type of facility.28 To the authors knowledge, this is the first publication showing efficacy of such antimicrobial stewardship interventions specific to pneumonia therapy in a small, primary facility.
The intervention methods used at VHSO are supported by recent IDSA and Society for Healthcare Epidemiology of America guidelines for effective stewardship implementation.29 Prospective audit and feedback is considered a core recommendation, whereas didactic education is recommended only in conjunction with other stewardship activities. Additionally, the guidelines recommend evaluating specific infectious disease syndromes, in this case uncomplicated pneumonia, to focus on specific treatment guidelines. Last, the results of the 3-part intervention can be used to aid in demonstrating facility improvement and encourage continued success.
Of note, VHSO has had established inpatient and outpatient clinical pharmacy roles for several years. Stewardship interventions already in place included an intravenous-to-oral antibiotic switch policy, automatic antibiotic stop dates, as well as pharmacist-driven vancomycin and aminoglycoside dosing. Prior to this multifaceted intervention specific to pneumonia duration, prospective audit and feedback interventions (verbal and written) also were common. The number of interventions specific to this study outside of the stewardship note was not recorded. Using rapid diagnostic testing and biomarkers to aid in stewardship activities at VHSO have been considered, but these tools are not available due to a lab personnel shortage.
Soliciting feedback from providers on their preferred stewardship strategy and perceived barriers was a key component of the educational intervention. Of equal importance was presenting providers with their baseline prescribing data to provide objective evidence of a problem. While all were familiar with existing treatment guidelines, some feedback indicated that it can be difficult to determine accurate antibiotic duration in CPRS. Prescribers reported that identifying antibiotic duration was especially challenging when antibiotics as well as providers change during an admission. Also frequently overlooked were antibiotics given in the emergency department. This could be a key area for clinical pharmacists’ intervention given their familiarity with the CPRS medication sections.
Charani and colleagues suggest that recognizing barriers to implementing best practices and adapting to the local facility culture is paramount for changing prescribing behaviors and developing a successful stewardship intervention.30 At VHSO, the providers were presented with multiple stewardship options but agreed to the new note and template. This process gave providers a voice in selecting their own stewardship intervention. In a culture with no infectious disease physician to champion initiatives, the investigators felt that provider involvement in the intervention selection was unique and may have encouraged provider concurrence.
Although not directly targeted by the intervention strategies, average LOS was shorter in the follow-up group. According to investigators, frequent reminders of clinical stability in the stewardship notes may have influenced this. Even though the note was used only in patients who remained hospitalized for their entire treatment course, investigators felt that it still served as a reminder for prescribing habits as they were also able to show a decrease in outpatient prescription duration.
Limitations
Potential weaknesses of the study include changes in providers. During the transition between group 1 and group 2, 2 hospitalists left and 2 new hospitalists arrived. Given the small size of the staff, this could significantly impact prescribing trends. Another potential weakness is the high exclusion rate, although these rates were similar in both groups (46% group 1, 47% group 2). Furthermore, similar exclusion rates have been reported elsewhere.24,25,31 The most common reasons for exclusion were complicated pneumonias (36%) and immunocompromised patients (18%). These patient populations were not evaluated in the current study, and optimal treatment durations are unknown. Hospital-acquired and ventilator-associated pneumonias also were excluded. Therefore, limitations in applicability of the results should be noted.
The authors acknowledge that, prior to this publication, the IDSA guidelines have removed the designation of HCAP as a separate clinical entity.4 However, this should not affect the significance of the intervention for treatment duration.
The study facility experienced a hiring freeze resulting in a 9.3% decrease in overall admissions from fiscal year 2013 to fiscal year 2015. This is likely why there were fewer admissions for pneumonia in group 2. Regardless, power analysis revealed the study was of adequate sample size to detect its primary outcome. It is possible that patients in either group could have sought health care at other facilities, making the CDI and readmission endpoints less inclusive.
The study was not of a scale to detect changes in antimicrobial resistance pressure or clinical outcomes. Cost savings were not analyzed. However, this study adds to the growing body of evidence that a structured intervention can result in positive outcomes at the facility level. This study shows that interventions targeting pneumonia treatment duration could feasibly be added to the menu of stewardship options available to smaller facilities.
Like other stewardship studies in the literature, the follow-up treatment duration, while improved, still exceeded those recommended in the IDSA guidelines. The investigators noted that not all providers were equal regarding change in prescribing habits, perhaps making the average duration longer. Additionally, the request to discontinue antibiotic therapy through the stewardship note could have been entered earlier (eg, as early as day 5 of therapy) to target the shortest effective date as recommended in the recent stewardship guidelines.29 Future steps include continued feedback to providers on their progress in this area and encouragement to document day of antibiotic treatment in their daily progress notes.
Conclusion
This study showed a significant decrease in antibiotic duration for the treatment of uncomplicated pneumonia using a 3-part pharmacy intervention in a primary hospital setting. The investigators feel that each arm of the strategy was equally important and fewer interventions were not likely to be as effective.32 Although data collection for baseline prescribing and follow-up on outcomes may be a time-consuming task, it can be a valuable component of successful stewardship interventions.
The safety and the efficacy of shorter durations of antibiotic therapy for uncomplicated pneumonia have been clearly established in the past decade.1,2 Guidelines from the Infectious Diseases Society of America (IDSA) and the American Thoracic Society have been available since 2007. These expert consensus statements recommend that uncomplicated community-acquired pneumonia (CAP) should be treated for 5 to 7 days, as long as the patient exhibits signs and symptoms of clinical stability.3 Similarly, recently updated guidelines for hospital-acquired and ventilator-associated pneumonias call for short-course therapy.4 Despite this guidance, pneumonia treatment duration is often discordant.5 Unnecessary antimicrobial use is associated with greater selection pressure on pathogens, increased risk of adverse events (AEs), and elevated treatment costs.6 The growing burden of antibiotic resistance coupled with limited availability of new antibiotics requires judicious use of these agents.
The IDSA guidelines for Clostridium difficile infection (CDI) note that exposure to antimicrobial agents is the most important modifiable risk factor for the development of CDI.7 Longer durations of antibiotics increase the risk of CDI compared with shorter durations.8,9 Antibiotics are a frequent cause of drug-associated AEs and likely are underestimated.10 To decrease the unwanted effects of excessive therapy, IDSA and CDC suggest that antimicrobial stewardship interventions should be implemented.11-13
Antimicrobial stewardship efforts in small community hospitals (also known as district, rural, general, and primary hospitals) are varied and can be challenging due to limited staff and resources.14,15 The World Health Organization defines a primary care facility as having few specialties, mainly internal medicine and general surgery with limited laboratory services for general (but not specialized) pathologic analysis, and bed size ranging from 30 to 200 beds.16 Although guidance is available for effective intervention strategies in smaller hospitals, there are limited data in the literature regarding successful outcomes.17-22
The purpose of this study was to establish the need and evaluate the impact of a pharmacy-initiated 3-part intervention targeting treatment duration in patients hospitalized with uncomplicated pneumonia in a primary hospital setting. The Veterans Health Care System of the Ozarks (VHSO) in Fayetteville, Arkansas, has 50 acute care beds, including 7 intensive care unit beds and excluding 15 mental health beds. The pharmacy is staffed 24 hours a day. Acute-care providers consist of 7 full-time hospitalists, not including nocturnists and contract physicians. The VHSO does not have an infectious disease physician on staff.
The antimicrobial stewardship committee consists of 3 clinical pharmacists, a pulmonologist, a pathologist, and 2 infection-control nurses. There is 1 full-time equivalent allotted for inpatient clinical pharmacy activities in the acute care areas, including enforcement of all antimicrobial stewardship policies, which are conducted by a single pharmacist.
Methods
This was a retrospective chart review of two 12-month periods using a before and after study design. Medical records were reviewed during October 2012 through September 2013 (before the stewardship implementation) and December 2014 through November 2015 (after implementation). Inclusion criteria consisted of a primary discharge diagnosis of pneumonia as documented by the provider (or secondary diagnosis if sepsis was primary), hospitalization for at least 48 hours, administration of antibiotics for a minimum of 24 hours, and survival to discharge.
Exclusion criteria consisted of direct transfer from another facility, inappropriate empiric therapy as evidenced by culture data (isolated pathogens not covered by prescribed antibiotics), pneumonia that developed 48 hours after admission, extrapulmonary sources of infection, hospitalization > 14 days, discharge without a known duration of outpatient antibiotics, discharge for pneumonia within 28 days prior to admission, documented infection caused by Pseudomonas aeruginosa or other nonlactose fermenting Gram-negative rod, and complicated pneumonias defined as lung abscess, empyema, or severe immunosuppression (eg, cancer with chemotherapy within the previous 30 days, transplant recipients, HIV infection, acquired or congenital immunodeficiency, or absolute neutrophil count 1,500 cell/mm3 within past 28 days).
Patients were designated with health care-associated pneumonia (HCAP) if they were hospitalized ≥ 2 days or resided in a skilled nursing or extended-care facility within the previous 90 days; on chronic dialysis; or had wound care, tracheostomy care, or ventilator care from a health care professional within the previous 28 days. Criteria for clinical stability were defined as ≤ 100.4º F temperature, ≤ 100 beats/min heart rate, ≤ 24 breaths/min respiratory rate, ≥ 90 mm Hg systolic blood pressure, ≥ 90% or PaO2 ≥ 60 mm Hg oxygen saturation on room air (or baseline oxygen requirements), and return to baseline mental status. To compare groups, researchers tabulated the pneumonia severity index on hospital day 1.
The intervention consisted of a 3-part process. First, hospitalists were educated on VHSO’s baseline treatment duration data, and these were compared with current IDSA recommendations. The education was followed by an open-discussion component to solicit feedback from providers on perceived barriers to following guidelines. Provider feedback was used to tailor an antimicrobial stewardship intervention to address perceived barriers to optimal antibiotic treatment duration.
After the education component, prospective intervention and feedback were provided for hospitalized patients by a single clinical pharmacist. This pharmacist interacted verbally and in writing with the patients’ providers, discussing antimicrobial appropriateness, de-escalation, duration of therapy, and intravenous to oral switching. Finally, a stewardship note for the Computerized Patient Record System (CPRS) was generated and included a template with reminders of clinical stability, duration of current therapy, and a request to discontinue therapy if the patient met criteria. For patients who remained hospitalized, this note was entered into CPRS on or about day 7 of antibiotic therapy; this required an electronic signature from the provider.
The VHSO Pharmacy and Therapeutics Committee approved both the provider education and the stewardship note in November 2014, and implementation of the stewardship intervention occurred immediately afterward. The pharmacy staff also was educated on the VHSO baseline data and stewardship efforts.
The primary outcome of the study was the change in days of total antibiotic treatment. Secondary outcomes included days of intravenous antibiotic therapy, days of inpatient oral therapy, mean length of stay (LOS), and number of outpatient antibiotic days once discharged. Incidence of CDI and 28-day readmissions were also evaluated. The VHSO Institutional Review Board approved these methods and the procedures that followed were in accord with the ethical standards of the VHSO Committee on Human Experimentation.
Statistical Analysis
All continuous variables are reported as mean ± standard deviation. Data analysis for significance was performed using a Student t test for continuous variables and a χ2 test (or Fisher exact test) for categorical variables in R Foundation for Statistical Computing version 3.1.0. All samples were 2-tailed. A P value < .05 was considered statistically significant. Using the smaller of the 2 study populations, the investigators calculated that the given sample size of 88 in each group would provide 99% power to detect a 2-day difference in the primary endpoint at a 2-sided significance level of 5%.
Results
During the baseline assessment (group 1), 192 cases were reviewed with 103 meeting the inclusion criteria. Group 1 consisted of 85 cases of CAP and 18 cases of HCAP (mean age, 70.7 years). During the follow-up assessment (group 2), 168 cases were reviewed with 88 meeting the inclusion criteria. Group 2 consisted of 68 cases of CAP and 20 cases of HCAP (mean age, 70.8 years).
There was no difference in inpatient mortality rates between groups (3.1% vs 3.0%, P = .99). This mortality rate is consistent with published reports.23 Empiric antibiotic selection was appropriate because there were no exclusions for drug/pathogen mismatch. Pneumonia severity was similar in both groups (Table).
The total duration of antibiotic treatment decreased significantly for CAP and HCAP (Figure). The observed median treatment days for groups 1 and 2 were 11 days and 8 days, respectively. Outpatient antibiotic days also decreased. Mean LOS was shorter in the follow-up group (4.9 ± 2.6 days vs 4.0 ± 2.6 days, P = .02). Length of IV antibiotic duration decreased. Oral antibiotic days while inpatient were not statistically different (1.5 ± 1.8 days vs 1.1 ± 1.5 days, P = .15). During the follow-up period, 26 stewardship notes were entered into CPRS; antibiotics were stopped in 65% of cases.
There were no recorded cases of CDI in either group. There were eleven 28-day readmissions in group 1, only 3 of which were due to infectious causes. One patient had a primary diagnosis of necrotizing pneumonia, 1 had Pseudomonas pneumonia, and 1 patient had a new lung mass and was diagnosed with postobstructive pneumonia. Of eight 28-day readmissions in group 2, only 2 resulted from infectious causes. One readmission primary diagnosis was sinusitis and 1 was recurrent pneumonia (of note, this patient received a 10-day treatment course for pneumonia on initial admission). Two patients died within 28 days of discharge in each group.
Discussion
Other multifaceted single-center interventions have been shown to be effective in large, teaching hospitals,24,25 and it has been suggested that smaller, rural hospitals may be underserved in antimicrobial stewardship activities.26,27 In the global struggle with antimicrobial resistance, McGregor and colleagues highlighted the importance of evaluating successful stewardship methods in an array of clinical settings to help tailor an approach for a specific type of facility.28 To the authors knowledge, this is the first publication showing efficacy of such antimicrobial stewardship interventions specific to pneumonia therapy in a small, primary facility.
The intervention methods used at VHSO are supported by recent IDSA and Society for Healthcare Epidemiology of America guidelines for effective stewardship implementation.29 Prospective audit and feedback is considered a core recommendation, whereas didactic education is recommended only in conjunction with other stewardship activities. Additionally, the guidelines recommend evaluating specific infectious disease syndromes, in this case uncomplicated pneumonia, to focus on specific treatment guidelines. Last, the results of the 3-part intervention can be used to aid in demonstrating facility improvement and encourage continued success.
Of note, VHSO has had established inpatient and outpatient clinical pharmacy roles for several years. Stewardship interventions already in place included an intravenous-to-oral antibiotic switch policy, automatic antibiotic stop dates, as well as pharmacist-driven vancomycin and aminoglycoside dosing. Prior to this multifaceted intervention specific to pneumonia duration, prospective audit and feedback interventions (verbal and written) also were common. The number of interventions specific to this study outside of the stewardship note was not recorded. Using rapid diagnostic testing and biomarkers to aid in stewardship activities at VHSO have been considered, but these tools are not available due to a lab personnel shortage.
Soliciting feedback from providers on their preferred stewardship strategy and perceived barriers was a key component of the educational intervention. Of equal importance was presenting providers with their baseline prescribing data to provide objective evidence of a problem. While all were familiar with existing treatment guidelines, some feedback indicated that it can be difficult to determine accurate antibiotic duration in CPRS. Prescribers reported that identifying antibiotic duration was especially challenging when antibiotics as well as providers change during an admission. Also frequently overlooked were antibiotics given in the emergency department. This could be a key area for clinical pharmacists’ intervention given their familiarity with the CPRS medication sections.
Charani and colleagues suggest that recognizing barriers to implementing best practices and adapting to the local facility culture is paramount for changing prescribing behaviors and developing a successful stewardship intervention.30 At VHSO, the providers were presented with multiple stewardship options but agreed to the new note and template. This process gave providers a voice in selecting their own stewardship intervention. In a culture with no infectious disease physician to champion initiatives, the investigators felt that provider involvement in the intervention selection was unique and may have encouraged provider concurrence.
Although not directly targeted by the intervention strategies, average LOS was shorter in the follow-up group. According to investigators, frequent reminders of clinical stability in the stewardship notes may have influenced this. Even though the note was used only in patients who remained hospitalized for their entire treatment course, investigators felt that it still served as a reminder for prescribing habits as they were also able to show a decrease in outpatient prescription duration.
Limitations
Potential weaknesses of the study include changes in providers. During the transition between group 1 and group 2, 2 hospitalists left and 2 new hospitalists arrived. Given the small size of the staff, this could significantly impact prescribing trends. Another potential weakness is the high exclusion rate, although these rates were similar in both groups (46% group 1, 47% group 2). Furthermore, similar exclusion rates have been reported elsewhere.24,25,31 The most common reasons for exclusion were complicated pneumonias (36%) and immunocompromised patients (18%). These patient populations were not evaluated in the current study, and optimal treatment durations are unknown. Hospital-acquired and ventilator-associated pneumonias also were excluded. Therefore, limitations in applicability of the results should be noted.
The authors acknowledge that, prior to this publication, the IDSA guidelines have removed the designation of HCAP as a separate clinical entity.4 However, this should not affect the significance of the intervention for treatment duration.
The study facility experienced a hiring freeze resulting in a 9.3% decrease in overall admissions from fiscal year 2013 to fiscal year 2015. This is likely why there were fewer admissions for pneumonia in group 2. Regardless, power analysis revealed the study was of adequate sample size to detect its primary outcome. It is possible that patients in either group could have sought health care at other facilities, making the CDI and readmission endpoints less inclusive.
The study was not of a scale to detect changes in antimicrobial resistance pressure or clinical outcomes. Cost savings were not analyzed. However, this study adds to the growing body of evidence that a structured intervention can result in positive outcomes at the facility level. This study shows that interventions targeting pneumonia treatment duration could feasibly be added to the menu of stewardship options available to smaller facilities.
Like other stewardship studies in the literature, the follow-up treatment duration, while improved, still exceeded those recommended in the IDSA guidelines. The investigators noted that not all providers were equal regarding change in prescribing habits, perhaps making the average duration longer. Additionally, the request to discontinue antibiotic therapy through the stewardship note could have been entered earlier (eg, as early as day 5 of therapy) to target the shortest effective date as recommended in the recent stewardship guidelines.29 Future steps include continued feedback to providers on their progress in this area and encouragement to document day of antibiotic treatment in their daily progress notes.
Conclusion
This study showed a significant decrease in antibiotic duration for the treatment of uncomplicated pneumonia using a 3-part pharmacy intervention in a primary hospital setting. The investigators feel that each arm of the strategy was equally important and fewer interventions were not likely to be as effective.32 Although data collection for baseline prescribing and follow-up on outcomes may be a time-consuming task, it can be a valuable component of successful stewardship interventions.
1. Li JZ, Winston LG, Moore DH, Bent S. Efficacy of short-course antibiotic regimens for community-acquired pneumonia: a meta-analysis. Am J Med. 2007;120(9):783-790.
2. Dimopoulos G, Matthaiou DK, Karageorgopoulos DE, Grammatikos AP, Athanassa Z, Falagas ME. Short- versus long-course antibacterial therapy of community-acquired pneumonia: a meta-analysis. Drugs. 2008;68(13):1841-1854.
3. Mandell LA, Wunderink RG, Anzueto A, et al; Infectious Diseases Society of America; American Thoracic Society. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27-S72.
4. Kalil AC, Metersky ML, Klompas M, et al. Management of adults with hospital-acquired and ventilator associated pneumonia: 2016 clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;63(5):e61-e111.
5. Jenkins TC, Stella SA, Cervantes L, et al. Targets for antibiotic and healthcare resource stewardship in inpatient community-acquired pneumonia: a comparison of management practices with National Guideline Recommendations. Infection. 2013; 41(1):135-144.
6. Shlaes DM, Gerding DN, John JF Jr, et al. Society for Healthcare Epidemiology of America, and Infectious Diseases Society of America Joint Committee on the Prevention of Antimicrobial Resistance: guidelines for the prevention of antimicrobial resistance in hospitals. Clin Infect Dis. 1997;25(3):584-599.
7. Cohen SH, Gerding DN, Johnson S, et al; Society for Healthcare Epidemiology of America; Infectious Diseases Society of America. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hosp Epidemiol. 2010;31(5):431-455.
8. Brown E, Talbot GH, Axelrod P, Provencher M, Hoegg C. Risk factors for Clostridium-difficile toxin-associated diarrhea. Infect Control Hosp Epidemiol. 1990;11(6):283-290.
9. McFarland LV, Surawicz CM, Stamm WE. Risk factors for Clostridium-difficile carriage and C. difficile-associated diarrhea in a cohort of hospitalized patients. J Infect Dis. 1990;162(3):678-684.
10. Shehab N, Patel PR, Srinivasan A, Budnitz DS. Emergency department visits for antibiotic-associated adverse events. Clin Infect Dis. 2008;47(6):735-743.
11. Dellit TH, Owens RC, McGowan JE Jr, et al; Infectious Diseases Society of America; Society for Healthcare Epidemiology of America. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America Guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007;44(2):159-177.
12. Fridkin S, Baggs J, Fagan R, et al; Centers for Disease Control and Prevention (CDC). Vital signs: improving antibiotic use among hospitalized patients. MMWR Morb Mortal Wkly Rep. 2014;63(9):194-200.
13. Nussenblatt V, Avdic E, Cosgrove S. What is the role of antimicrobial stewardship in improving outcomes of patients with CAP? Infect Dis Clin North Am. 2013;27(1):211-228.
14. Septimus EJ, Owens RC Jr. Need and potential of antimicrobial stewardship in community hospitals. Clin Infect Dis. 2011;53(suppl 1):S8-S14.
15. Hensher M, Price M, Adomakoh S. Referral hospitals. In Jamison DT, Breman JG, Measham AR, eds, et al. Disease Control Priorities in Developing Countries. New York, NY: Oxford University Press; 2006:1230.
16. Mulligan J, Fox-Rushby JA, Adam T, Johns B, Mills A. Unit costs of health care inputs in low and middle income regions. 2003. Working Paper 9, Disease Control Priorities Project. Published September 2003. Revised June 2005.
17. Ohl CA, Dodds Ashley ES. Antimicrobial stewardship programs in community hospitals: the evidence base and case studies. Clin Infect Dis 2011;53(suppl 1):S23-S28.
18. Trevidi KK, Kuper K. Hospital antimicrobial stewardship in the nonuniversity setting. Infect Dis Clin North Am. 2014;28(2):281-289.
19. Yam P, Fales D, Jemison J, Gillum M, Bernstein M. Implementation of an antimicrobial stewardship program in a rural hospital. Am J Health Syst Pharm. 2012;69(13);1142-1148.
20. LaRocco A Jr. Concurrent antibiotic review programs—a role for infectious diseases specialists at small community hospitals. Clin Infect Dis. 2003;37(5):742-743.
21. Bartlett JM, Siola PL. Implementation and first-year results of an antimicrobial stewardship program at a community hospital. Am J Health Syst Pharm. 2014;71(11):943-949.
22. Storey DF, Pate PG, Nguyen AT, Chang F. Implementation of an antimicrobial stewardship program on the medical-surgical service of a 100-bed community hospital. Antimicrob Resist Infect Control. 2012;1(1):32.
23. Fine MJ, Smith MA, Carson CA, et al. Prognosis and outcomes of patients with community-acquired pneumonia. A meta-analysis. JAMA. 1996;275(2):134-141.
24. Advic E, Cushinotto LA, Hughes AH, et al. Impact of an antimicrobial stewardship intervention on shortening the duration of therapy for community-acquired pneumonia. Clin Infect Dis. 2012;54(11):1581-1587.
25. Carratallà J, Garcia-Vidal C, Ortega L, et al. Effect of a 3-step critical pathway to reduce duration of intravenous antibiotic therapy and length of stay in community-acquired pneumonia: a randomized controlled trial. Arch Intern Med. 2012;172(12):922-928.
26. Stevenson KB, Samore M, Barbera J, et al. Pharmacist involvement in antimicrobial use at rural community hospitals in four Western states. Am J Health Syst Pharm. 2004;61(8):787-792.
27. Reese SM, Gilmartin H, Rich KL, Price CS. Infection prevention needs assessment in Colorado hospitals: rural and urban settings. Am J Infect Control. 2014;42(6):597-601.
28. McGregor JC, Furuno JP. Optimizing research methods used for the evaluation of antimicrobial stewardship programs. Clin Infect Dis. 2014;59(suppl 3):S185-S192.
29. Barlam TF, Cosgrove SE, Abbo LM, et al. Implementing an antibiotic stewardship program: Guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis. 2016;62(10):e51-e77.
30. Charani E, Castro-Sánchez E, Holmes A. The role of behavior change in antimicrobial stewardship. Infect Dis Clin N Am. 2014;28(2):169-175.
31. Attridge RT, Frei CR, Restrepo MI, et al. Guideline-concordant therapy and outcomes in healthcare-associated pneumonia. Eur Respir J. 2011;38(4):878-887.
32. MacDougal C, Polk RE. Antimicrobial stewardship programs in health care systems. Clin Microbiol Rev. 2005;18(4):638-656.
1. Li JZ, Winston LG, Moore DH, Bent S. Efficacy of short-course antibiotic regimens for community-acquired pneumonia: a meta-analysis. Am J Med. 2007;120(9):783-790.
2. Dimopoulos G, Matthaiou DK, Karageorgopoulos DE, Grammatikos AP, Athanassa Z, Falagas ME. Short- versus long-course antibacterial therapy of community-acquired pneumonia: a meta-analysis. Drugs. 2008;68(13):1841-1854.
3. Mandell LA, Wunderink RG, Anzueto A, et al; Infectious Diseases Society of America; American Thoracic Society. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27-S72.
4. Kalil AC, Metersky ML, Klompas M, et al. Management of adults with hospital-acquired and ventilator associated pneumonia: 2016 clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;63(5):e61-e111.
5. Jenkins TC, Stella SA, Cervantes L, et al. Targets for antibiotic and healthcare resource stewardship in inpatient community-acquired pneumonia: a comparison of management practices with National Guideline Recommendations. Infection. 2013; 41(1):135-144.
6. Shlaes DM, Gerding DN, John JF Jr, et al. Society for Healthcare Epidemiology of America, and Infectious Diseases Society of America Joint Committee on the Prevention of Antimicrobial Resistance: guidelines for the prevention of antimicrobial resistance in hospitals. Clin Infect Dis. 1997;25(3):584-599.
7. Cohen SH, Gerding DN, Johnson S, et al; Society for Healthcare Epidemiology of America; Infectious Diseases Society of America. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hosp Epidemiol. 2010;31(5):431-455.
8. Brown E, Talbot GH, Axelrod P, Provencher M, Hoegg C. Risk factors for Clostridium-difficile toxin-associated diarrhea. Infect Control Hosp Epidemiol. 1990;11(6):283-290.
9. McFarland LV, Surawicz CM, Stamm WE. Risk factors for Clostridium-difficile carriage and C. difficile-associated diarrhea in a cohort of hospitalized patients. J Infect Dis. 1990;162(3):678-684.
10. Shehab N, Patel PR, Srinivasan A, Budnitz DS. Emergency department visits for antibiotic-associated adverse events. Clin Infect Dis. 2008;47(6):735-743.
11. Dellit TH, Owens RC, McGowan JE Jr, et al; Infectious Diseases Society of America; Society for Healthcare Epidemiology of America. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America Guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007;44(2):159-177.
12. Fridkin S, Baggs J, Fagan R, et al; Centers for Disease Control and Prevention (CDC). Vital signs: improving antibiotic use among hospitalized patients. MMWR Morb Mortal Wkly Rep. 2014;63(9):194-200.
13. Nussenblatt V, Avdic E, Cosgrove S. What is the role of antimicrobial stewardship in improving outcomes of patients with CAP? Infect Dis Clin North Am. 2013;27(1):211-228.
14. Septimus EJ, Owens RC Jr. Need and potential of antimicrobial stewardship in community hospitals. Clin Infect Dis. 2011;53(suppl 1):S8-S14.
15. Hensher M, Price M, Adomakoh S. Referral hospitals. In Jamison DT, Breman JG, Measham AR, eds, et al. Disease Control Priorities in Developing Countries. New York, NY: Oxford University Press; 2006:1230.
16. Mulligan J, Fox-Rushby JA, Adam T, Johns B, Mills A. Unit costs of health care inputs in low and middle income regions. 2003. Working Paper 9, Disease Control Priorities Project. Published September 2003. Revised June 2005.
17. Ohl CA, Dodds Ashley ES. Antimicrobial stewardship programs in community hospitals: the evidence base and case studies. Clin Infect Dis 2011;53(suppl 1):S23-S28.
18. Trevidi KK, Kuper K. Hospital antimicrobial stewardship in the nonuniversity setting. Infect Dis Clin North Am. 2014;28(2):281-289.
19. Yam P, Fales D, Jemison J, Gillum M, Bernstein M. Implementation of an antimicrobial stewardship program in a rural hospital. Am J Health Syst Pharm. 2012;69(13);1142-1148.
20. LaRocco A Jr. Concurrent antibiotic review programs—a role for infectious diseases specialists at small community hospitals. Clin Infect Dis. 2003;37(5):742-743.
21. Bartlett JM, Siola PL. Implementation and first-year results of an antimicrobial stewardship program at a community hospital. Am J Health Syst Pharm. 2014;71(11):943-949.
22. Storey DF, Pate PG, Nguyen AT, Chang F. Implementation of an antimicrobial stewardship program on the medical-surgical service of a 100-bed community hospital. Antimicrob Resist Infect Control. 2012;1(1):32.
23. Fine MJ, Smith MA, Carson CA, et al. Prognosis and outcomes of patients with community-acquired pneumonia. A meta-analysis. JAMA. 1996;275(2):134-141.
24. Advic E, Cushinotto LA, Hughes AH, et al. Impact of an antimicrobial stewardship intervention on shortening the duration of therapy for community-acquired pneumonia. Clin Infect Dis. 2012;54(11):1581-1587.
25. Carratallà J, Garcia-Vidal C, Ortega L, et al. Effect of a 3-step critical pathway to reduce duration of intravenous antibiotic therapy and length of stay in community-acquired pneumonia: a randomized controlled trial. Arch Intern Med. 2012;172(12):922-928.
26. Stevenson KB, Samore M, Barbera J, et al. Pharmacist involvement in antimicrobial use at rural community hospitals in four Western states. Am J Health Syst Pharm. 2004;61(8):787-792.
27. Reese SM, Gilmartin H, Rich KL, Price CS. Infection prevention needs assessment in Colorado hospitals: rural and urban settings. Am J Infect Control. 2014;42(6):597-601.
28. McGregor JC, Furuno JP. Optimizing research methods used for the evaluation of antimicrobial stewardship programs. Clin Infect Dis. 2014;59(suppl 3):S185-S192.
29. Barlam TF, Cosgrove SE, Abbo LM, et al. Implementing an antibiotic stewardship program: Guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis. 2016;62(10):e51-e77.
30. Charani E, Castro-Sánchez E, Holmes A. The role of behavior change in antimicrobial stewardship. Infect Dis Clin N Am. 2014;28(2):169-175.
31. Attridge RT, Frei CR, Restrepo MI, et al. Guideline-concordant therapy and outcomes in healthcare-associated pneumonia. Eur Respir J. 2011;38(4):878-887.
32. MacDougal C, Polk RE. Antimicrobial stewardship programs in health care systems. Clin Microbiol Rev. 2005;18(4):638-656.
Positive experience reported for new AF ablation system
ORLANDO – A uniquely designed multielectrode radiofrequency ablation (RFA) balloon catheter system for the treatment of atrial fibrillation (AF) performed well in a first-in-man study.
The new ablation system is designed to provide the flexibility of conventional RFA devices in treating a broad array of AF triggers with the type of predictable energy delivery more closely associated with cryoballoon ablation, according to the principal investigator, Matthew G. Daly, MB, ChB, a cardiologist at Christchurch (New Zealand) Hospital.
The inflatable experimental device features 18 electrodes, a built-in camera, integrated mapping and pacing, and irrigation designed to reduce the risk of clot formation. On contact, the 12 electrodes situated on the equator of the spherical device, along with the six electrodes situated on the polar ends, are initially employed to select the ablation pattern. RFA can be delivered immediately through the same electrodes once proper contact is established using the built-in cameras for real-time visualization.
No significant adverse events were encountered during the procedure or over the course of follow-up, according to Dr. Daly. PV isolation was achieved in 65 of 68 (96%) of veins treated. The average number of ablations required per PV isolation was 3.1. On average, it took 12 minutes to isolate all veins per patient, according to Dr. Daly, who characterized this as “respectable,” given that this was a novel technology being performed in a clinical study for the first time. The average balloon time was 1 hour 39 minutes.
For the patients followed through 6 months, 80% remain free of AF and off all medications.
“The system allowed for quick ablation without excessive catheter manipulations,” said Dr. Daly, suggesting that the performance was consistent with the theoretical advantages of a multipoint, single-shot design. Overall, Dr. Daly suggested that this device appears to permit RFA to be delivered in a manner that has been more closely related to the efficiency of cryoballoon ablation.
“The disadvantage, or perhaps the advantage, is that this is a device that requires a knowledge of electrophysiology,” said Dr. Daly, who said that physicians need to be familiar with isolating pulmonary veins in order to deliver the energy appropriately.
One of the theoretical advantages of this device over conventional RFA ablation is that it will provide more consistent power and temperature as long as appropriate contact is achieved. He noted that the variability in energy delivery according to angle or contact force has been one of the weaknesses of conventional RFA devices.
“Contact is king. This has always been true, but with this device the manufacturer recommended that we only applied energy when we thought contact was perfect,” Dr. Daly said. He acknowledged that he deviated from this recommendation in some instances, “but it turns out that if you have good contact, you get signal elimination almost immediately or at least within a few seconds,” but less dependable results when contact is compromised, such as in those instances where blood is an obstacle.
Because of its ability to deliver energy in a single shot at multiple points, this device has the potential to permit successful ablation with a shorter procedure time than with conventional RFA. Dr. Daly said this device is “light on its feet” and required relatively little time to maneuver into place. However, he said that procedure times in this initial study were longer because of inexperience and the need for “checking and rechecking” settings and positions.
Dr. Daly reported no industry relationships relevant to this study.
ORLANDO – A uniquely designed multielectrode radiofrequency ablation (RFA) balloon catheter system for the treatment of atrial fibrillation (AF) performed well in a first-in-man study.
The new ablation system is designed to provide the flexibility of conventional RFA devices in treating a broad array of AF triggers with the type of predictable energy delivery more closely associated with cryoballoon ablation, according to the principal investigator, Matthew G. Daly, MB, ChB, a cardiologist at Christchurch (New Zealand) Hospital.
The inflatable experimental device features 18 electrodes, a built-in camera, integrated mapping and pacing, and irrigation designed to reduce the risk of clot formation. On contact, the 12 electrodes situated on the equator of the spherical device, along with the six electrodes situated on the polar ends, are initially employed to select the ablation pattern. RFA can be delivered immediately through the same electrodes once proper contact is established using the built-in cameras for real-time visualization.
No significant adverse events were encountered during the procedure or over the course of follow-up, according to Dr. Daly. PV isolation was achieved in 65 of 68 (96%) of veins treated. The average number of ablations required per PV isolation was 3.1. On average, it took 12 minutes to isolate all veins per patient, according to Dr. Daly, who characterized this as “respectable,” given that this was a novel technology being performed in a clinical study for the first time. The average balloon time was 1 hour 39 minutes.
For the patients followed through 6 months, 80% remain free of AF and off all medications.
“The system allowed for quick ablation without excessive catheter manipulations,” said Dr. Daly, suggesting that the performance was consistent with the theoretical advantages of a multipoint, single-shot design. Overall, Dr. Daly suggested that this device appears to permit RFA to be delivered in a manner that has been more closely related to the efficiency of cryoballoon ablation.
“The disadvantage, or perhaps the advantage, is that this is a device that requires a knowledge of electrophysiology,” said Dr. Daly, who said that physicians need to be familiar with isolating pulmonary veins in order to deliver the energy appropriately.
One of the theoretical advantages of this device over conventional RFA ablation is that it will provide more consistent power and temperature as long as appropriate contact is achieved. He noted that the variability in energy delivery according to angle or contact force has been one of the weaknesses of conventional RFA devices.
“Contact is king. This has always been true, but with this device the manufacturer recommended that we only applied energy when we thought contact was perfect,” Dr. Daly said. He acknowledged that he deviated from this recommendation in some instances, “but it turns out that if you have good contact, you get signal elimination almost immediately or at least within a few seconds,” but less dependable results when contact is compromised, such as in those instances where blood is an obstacle.
Because of its ability to deliver energy in a single shot at multiple points, this device has the potential to permit successful ablation with a shorter procedure time than with conventional RFA. Dr. Daly said this device is “light on its feet” and required relatively little time to maneuver into place. However, he said that procedure times in this initial study were longer because of inexperience and the need for “checking and rechecking” settings and positions.
Dr. Daly reported no industry relationships relevant to this study.
ORLANDO – A uniquely designed multielectrode radiofrequency ablation (RFA) balloon catheter system for the treatment of atrial fibrillation (AF) performed well in a first-in-man study.
The new ablation system is designed to provide the flexibility of conventional RFA devices in treating a broad array of AF triggers with the type of predictable energy delivery more closely associated with cryoballoon ablation, according to the principal investigator, Matthew G. Daly, MB, ChB, a cardiologist at Christchurch (New Zealand) Hospital.
The inflatable experimental device features 18 electrodes, a built-in camera, integrated mapping and pacing, and irrigation designed to reduce the risk of clot formation. On contact, the 12 electrodes situated on the equator of the spherical device, along with the six electrodes situated on the polar ends, are initially employed to select the ablation pattern. RFA can be delivered immediately through the same electrodes once proper contact is established using the built-in cameras for real-time visualization.
No significant adverse events were encountered during the procedure or over the course of follow-up, according to Dr. Daly. PV isolation was achieved in 65 of 68 (96%) of veins treated. The average number of ablations required per PV isolation was 3.1. On average, it took 12 minutes to isolate all veins per patient, according to Dr. Daly, who characterized this as “respectable,” given that this was a novel technology being performed in a clinical study for the first time. The average balloon time was 1 hour 39 minutes.
For the patients followed through 6 months, 80% remain free of AF and off all medications.
“The system allowed for quick ablation without excessive catheter manipulations,” said Dr. Daly, suggesting that the performance was consistent with the theoretical advantages of a multipoint, single-shot design. Overall, Dr. Daly suggested that this device appears to permit RFA to be delivered in a manner that has been more closely related to the efficiency of cryoballoon ablation.
“The disadvantage, or perhaps the advantage, is that this is a device that requires a knowledge of electrophysiology,” said Dr. Daly, who said that physicians need to be familiar with isolating pulmonary veins in order to deliver the energy appropriately.
One of the theoretical advantages of this device over conventional RFA ablation is that it will provide more consistent power and temperature as long as appropriate contact is achieved. He noted that the variability in energy delivery according to angle or contact force has been one of the weaknesses of conventional RFA devices.
“Contact is king. This has always been true, but with this device the manufacturer recommended that we only applied energy when we thought contact was perfect,” Dr. Daly said. He acknowledged that he deviated from this recommendation in some instances, “but it turns out that if you have good contact, you get signal elimination almost immediately or at least within a few seconds,” but less dependable results when contact is compromised, such as in those instances where blood is an obstacle.
Because of its ability to deliver energy in a single shot at multiple points, this device has the potential to permit successful ablation with a shorter procedure time than with conventional RFA. Dr. Daly said this device is “light on its feet” and required relatively little time to maneuver into place. However, he said that procedure times in this initial study were longer because of inexperience and the need for “checking and rechecking” settings and positions.
Dr. Daly reported no industry relationships relevant to this study.
AT AF SYMPOSIUM 2017
Key clinical point: A novel ablation catheter system for atrial fibrillation appears to minimize the disadvantages of existing strategies in initial study.
Major finding: A first-in-man study documents safety with 98% technical success rate.
Data source: A prospective, multicenter study.
Disclosures: Dr. Daly reported no industry relationships relevant to this study.
Hot-button issue: physician burnout
Some 15 years ago, when Daniel Roberts, MD, FHM, decided at the end of his medical residency that his career path was going to be that of a hospitalist, he heard the same thing. A lot.
“Geesh, don’t you think you’re going to burn out?”
The reasons for such a response are well known in HM circles: the 7-on, 7-off shift structure; the constant rounding; the push-pull between clinical, administrative, and – what many would term – clerical work.
“The truth is somewhere between,” Dr. Roberts said.
Burnout is a hot topic among hospitalists and all of health care these days, as the increasing burdens of a system in seemingly constant change have fostered pressures inside and out of hospitals. Increasingly, researchers are studying and publishing about how to recognize burnout, ways to deal with, or even proactively address the issues. Some MDs – experts in physician burnout – make a living by touring the country and talking about the issue.
But what causes burnout, specifically and exactly?
“The simplistic answer is that burnout is what happens when resources do not meet demand,” said Colin West, MD, PhD, FACP, of the departments of internal medicine and health sciences research at the Mayo Clinic in Rochester, Minn., and a leading researcher on the topic of burnout. “The more complicated answer, which, at this point, is fairly solidly evidence based actually, is that there are five broad categories of drivers of physician distress and burnout.”
Dr. West’s hierarchy of stressors encompasses:
• Work effort.
• Work efficiency.
• Work-home interference.
• A sense of meaning.
• “Flexibility, control, and autonomy.”
Basically, the five drivers lead to this: Physicians who work too much and too inefficiently, with too little control and sense of purpose, end up flaming out more so than do doctors who work fewer hours, with fewer obstacles – all the while feeling satisfied with their autonomy and value.
Academic hospitalist John Yoon, MD, assistant professor of medicine at the University of Chicago, says that health care has to work harder to promote its benefits as being more important than a highly paid profession. Instead, health care should focus on giving meaning to its practitioners.
“I think it is time for leaders of HM groups to honestly discuss the intrinsic meaning and essential ‘calling’ of what it means to be a good hospitalist,” Dr. Yoon wrote in an email interview with The Hospitalist. “What can we do to make the hospitalist vocation a meaningful, long-term career, so that they do not feel like simply revenue-generating ‘pawns’ in a medical-bureaucratic system?”
A ‘meaningful’ career
The modern discussion of burnout as a phenomenon traces back to the Maslach Burnout Inventory, a three-pronged test that measures emotional exhaustion, depersonalization, and personal accomplishment.1 But why does burnout hit physicians – hospitalists, in particular – so intensely? In part, it’s because – like their predecessors in emergency medicine – hospitalists are responsible for managing the care of patients other specialties consult with, operate on, or for whom they run tests.
“Once the patients come up from the emergency room or get admitted to the hospital from the outside, the hospitalist is the one who is largely running that show,” said Dr. West, whose researchshows that HM doctors suffer burnout more than the average across medical specialties.2 “So they’re the front line of inpatient medicine.”
Another factor contributing to burnout’s impact on hospitalists is that the specialty’s rank and file (by definition) work within the walls of institutions that have a lot of contentious and complicated issues that – while outside the purview of HM – can directly or indirectly affect the field. Dr. West calls it the hassle factor.
“You want to get a test in the hospital and, even though you’re the attending on the service, you end up going through three layers of bureaucracy with an insurance company to be able to finally get what you know that patient needs,” he said. “Anything like that contributes to the burnout problem because it pulls the physician away from what they want to be doing, what is purposeful, what is meaningful for them.”
For Dr. Yoon, the exhaustion and cynicism borne out by the work of Maslach and Dr. West’s team are measures indicative of a field where physicians struggle more and more to “make sense of why their practice is worthwhile.
“In the contemporary medical literature, we have been encouraged to adopt the concepts and practices of industrial engineering and quality improvement,” Dr. Yoon added. “In other words, it seems that to the extent physicians’ aspirations to practice good medicine are confined to the narrow and unimaginative constraints of mere scientific technique (more data, higher ‘quality,’ better outcomes) physicians will struggle to recognize and respond to their practice as meaningful. There is no intrinsic meaning to simply being a ‘cog’ in a medical-industrial process or an ‘independent variable’ in an economic equation.”
Finding meaning in one’s job, of course, is less empirical an endpoint than using a reversal agent for a GI bleed. Therein lies the challenge of battling burnout, whose causes and interventions can be as varied as the people who suffer the syndrome.
Local, customized solutions
Once a group leader identifies the symptoms of burnout, the obvious question is how to address it.
Dr. West and his colleagues have identified two broad categories of interventions: individual-focused approaches and organizational solutions. Physician-centered efforts include such tacks as mindfulness, stress reduction, resilience training and small-group communication. Institutional-level changes are, typically, much harder to implement and make successful.
“It doesn’t make sense to ... simply send physicians to stress-management training so that they’re better equipped to deal with a system that is not working to improve itself,” Dr. West said. “The system and the leadership in that system needs to take responsibility from an organizational standpoint.”
Health care as a whole has worked to address the systems-level issue. Duty-hour regulations have been reined in for trainees to be proactive in addressing both fatigue and its inevitable endpoint: burnout.
In a report, “Controlled Interventions to Reduce Burnout in Physicians: A Systematic Review and Meta-Analysis,”3 published online Dec. 5 in JAMA Internal Medicine, researchers concluded that interventions associated with small benefits “may be boosted by adoption of organization-directed approaches.
“This finding provides support for the view that burnout is a problem of the whole health care organization, rather than individuals,” they wrote.
But the issue typically remains a local one, as group leaders need to realize that what could cause or contribute to burnout in one employee might be enjoyable to another.
“The prospect of doing that was daunting,” Dr. Roberts recalled. “I didn’t know much about EHRs and it was going to be a lot of meetings ... and [it] was going to take me away from patient care. It really ended up being rewarding, despite all the time and frustration, because I got to help represent the interests of my hospitalist colleagues, the physician assistants, and nurses that I work with in trying to avoid some real problems that could have arisen in the EHR.”
Doing that work appealed to Dr. Roberts, so he embraced it. That approach is one championed by Thom Mayer, MD, FACEP, FAAP, executive vice president of EmCare, founder and CEO of BestPractices Inc., medical director for the NFL Players Association, and clinical professor of emergency medicine at George Washington University, Washington, and University of Virginia, Charlottesville. Dr. Mayer travels the country talking about burnout and suggests a three-pronged approach.
First, find what you like about your job and maximize those duties.
Second, label those tasks that are tolerable and don’t allow them to become issues leading to burnout.
Third, and perhaps most difficult, “take the things [you] hate and eliminate them to the best extent possible from [your] job.”
“I’ll give you an example,” he said. “What I hear from emergency physicians and hospitalists is: ‘What do I hate? Well, I hate chronic pain patients.’ Well, does that mean you’re going to be able to eliminate the fact that there are chronic pain patients? No. But, what you can do is ... really drill down on it, and say ‘Why do you hate that?’ The answer is, “Well, I don’t have a strategy for it.” No one likes doing things when they don’t know what they’re doing.
“Now you take the chronic pain patient and the problem is, most of us just haven’t really thought that out. Most of us haven’t sat down with our colleagues and said, “What are you doing that’s working? How are you handling these people? What are the scripts that I can use, the evidence-based language that I can use? What alternatives can I give them?” Instead of just assuming that the only answer to the problem of chronic pain is opioids.”
The silent epidemic
So if there are measurements for burnout, and even best practices on how to address it, why is the issue one that Dr. Mayer calls a silent epidemic? One word: stigma.
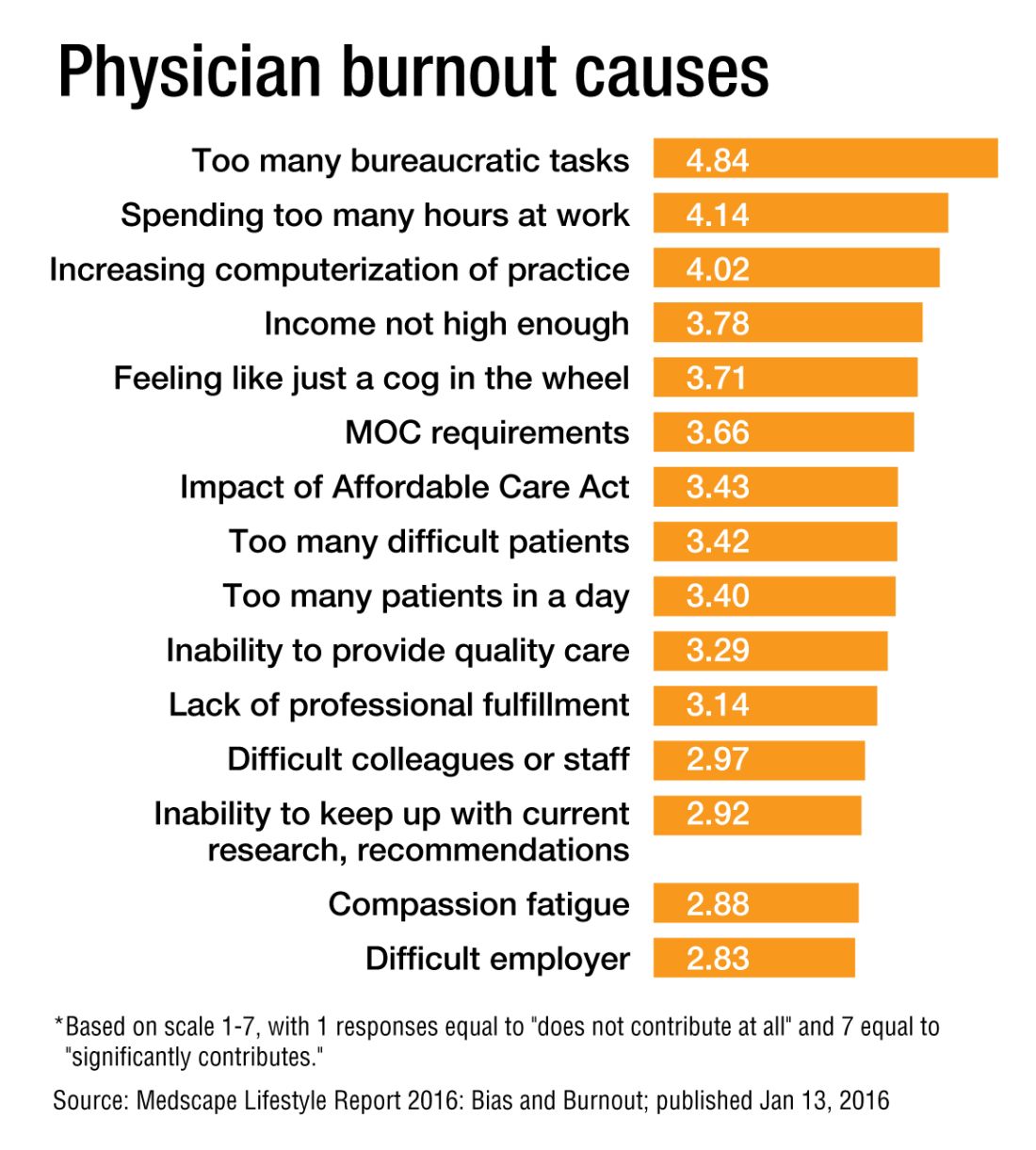
“We as physicians can’t afford to propagate that stigma any further,” Dr. Roberts said. “People who have even tougher jobs than we have, involving combat and hostage negotiation and things like that, have found a way to have honest conversations about the impact of their work on their lives. There is no reason physicians shouldn’t be able to slowly change the culture of medicine to be able to do that, so that there isn’t a stigma around saying, ‘I need some time away before this begins to impact the safety of our patients.’ ”
Dr. West said that when data show that as many as half of all physicians show symptoms of burnout, there is no need to stigmatize a group that large.
Dike Drummond, MD, a family physician, coach, and consultant on burnout prevention, said that the No. 1 mistake physicians and leaders make about burnout is labeling it a “problem.”
“Burnout does not have a single solution because it is not a problem to begin with,” he added. “Burnout is a classic dilemma – a never-ending balancing act. Think of the balancing act of burnout as a teeter-totter, like the one you see in a children’s playground. On one side is the energy you put into your practice and larger life … and on the other side your ability to recharge your energy levels.
“To prevent burnout you must keep your energy expenditure and your recharge activities in balance to keep this teeter-totter in a relatively horizontal position. And the way you address the dilemma is with a strategy: three to five individual tools you use to lower your stress levels or recharge your energy balance.”
And a strategy is a long-term approach to a long-term problem, he said.
“Burnout is not necessarily a terminal condition,” Dr. Roberts said. “If we can structure their work and the balance in their life in such a way that they don’t experience it, or that when they do experience it, they can recognize it and make the changes they need to avoid it getting worse, I think we’d be better off as a profession.”
Richard Quinn is a freelance writer in New Jersey.
References
1. Maslach C, Jackson S. The measurement of experienced burnout. J Occup Behavior. 1981;2:99-113
2. Roberts DL, Shanafelt TD, Dyrbye LN, West CP. A national comparison of burnout and work-life balance among internal medicine hospitalists and outpatient general internists. J Hosp Med. 2014;9(3):176-81.
3. Panagioti M, Panagopoulou E, Brower P. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis [published online Dec. 5, 2016 ahead of print]. JAMA Intern Med. doi: 10.1001/jamainternmed.2016.7674.
Some 15 years ago, when Daniel Roberts, MD, FHM, decided at the end of his medical residency that his career path was going to be that of a hospitalist, he heard the same thing. A lot.
“Geesh, don’t you think you’re going to burn out?”
The reasons for such a response are well known in HM circles: the 7-on, 7-off shift structure; the constant rounding; the push-pull between clinical, administrative, and – what many would term – clerical work.
“The truth is somewhere between,” Dr. Roberts said.
Burnout is a hot topic among hospitalists and all of health care these days, as the increasing burdens of a system in seemingly constant change have fostered pressures inside and out of hospitals. Increasingly, researchers are studying and publishing about how to recognize burnout, ways to deal with, or even proactively address the issues. Some MDs – experts in physician burnout – make a living by touring the country and talking about the issue.
But what causes burnout, specifically and exactly?
“The simplistic answer is that burnout is what happens when resources do not meet demand,” said Colin West, MD, PhD, FACP, of the departments of internal medicine and health sciences research at the Mayo Clinic in Rochester, Minn., and a leading researcher on the topic of burnout. “The more complicated answer, which, at this point, is fairly solidly evidence based actually, is that there are five broad categories of drivers of physician distress and burnout.”
Dr. West’s hierarchy of stressors encompasses:
• Work effort.
• Work efficiency.
• Work-home interference.
• A sense of meaning.
• “Flexibility, control, and autonomy.”
Basically, the five drivers lead to this: Physicians who work too much and too inefficiently, with too little control and sense of purpose, end up flaming out more so than do doctors who work fewer hours, with fewer obstacles – all the while feeling satisfied with their autonomy and value.
Academic hospitalist John Yoon, MD, assistant professor of medicine at the University of Chicago, says that health care has to work harder to promote its benefits as being more important than a highly paid profession. Instead, health care should focus on giving meaning to its practitioners.
“I think it is time for leaders of HM groups to honestly discuss the intrinsic meaning and essential ‘calling’ of what it means to be a good hospitalist,” Dr. Yoon wrote in an email interview with The Hospitalist. “What can we do to make the hospitalist vocation a meaningful, long-term career, so that they do not feel like simply revenue-generating ‘pawns’ in a medical-bureaucratic system?”
A ‘meaningful’ career
The modern discussion of burnout as a phenomenon traces back to the Maslach Burnout Inventory, a three-pronged test that measures emotional exhaustion, depersonalization, and personal accomplishment.1 But why does burnout hit physicians – hospitalists, in particular – so intensely? In part, it’s because – like their predecessors in emergency medicine – hospitalists are responsible for managing the care of patients other specialties consult with, operate on, or for whom they run tests.
“Once the patients come up from the emergency room or get admitted to the hospital from the outside, the hospitalist is the one who is largely running that show,” said Dr. West, whose researchshows that HM doctors suffer burnout more than the average across medical specialties.2 “So they’re the front line of inpatient medicine.”
Another factor contributing to burnout’s impact on hospitalists is that the specialty’s rank and file (by definition) work within the walls of institutions that have a lot of contentious and complicated issues that – while outside the purview of HM – can directly or indirectly affect the field. Dr. West calls it the hassle factor.
“You want to get a test in the hospital and, even though you’re the attending on the service, you end up going through three layers of bureaucracy with an insurance company to be able to finally get what you know that patient needs,” he said. “Anything like that contributes to the burnout problem because it pulls the physician away from what they want to be doing, what is purposeful, what is meaningful for them.”
For Dr. Yoon, the exhaustion and cynicism borne out by the work of Maslach and Dr. West’s team are measures indicative of a field where physicians struggle more and more to “make sense of why their practice is worthwhile.
“In the contemporary medical literature, we have been encouraged to adopt the concepts and practices of industrial engineering and quality improvement,” Dr. Yoon added. “In other words, it seems that to the extent physicians’ aspirations to practice good medicine are confined to the narrow and unimaginative constraints of mere scientific technique (more data, higher ‘quality,’ better outcomes) physicians will struggle to recognize and respond to their practice as meaningful. There is no intrinsic meaning to simply being a ‘cog’ in a medical-industrial process or an ‘independent variable’ in an economic equation.”
Finding meaning in one’s job, of course, is less empirical an endpoint than using a reversal agent for a GI bleed. Therein lies the challenge of battling burnout, whose causes and interventions can be as varied as the people who suffer the syndrome.
Local, customized solutions
Once a group leader identifies the symptoms of burnout, the obvious question is how to address it.
Dr. West and his colleagues have identified two broad categories of interventions: individual-focused approaches and organizational solutions. Physician-centered efforts include such tacks as mindfulness, stress reduction, resilience training and small-group communication. Institutional-level changes are, typically, much harder to implement and make successful.
“It doesn’t make sense to ... simply send physicians to stress-management training so that they’re better equipped to deal with a system that is not working to improve itself,” Dr. West said. “The system and the leadership in that system needs to take responsibility from an organizational standpoint.”
Health care as a whole has worked to address the systems-level issue. Duty-hour regulations have been reined in for trainees to be proactive in addressing both fatigue and its inevitable endpoint: burnout.
In a report, “Controlled Interventions to Reduce Burnout in Physicians: A Systematic Review and Meta-Analysis,”3 published online Dec. 5 in JAMA Internal Medicine, researchers concluded that interventions associated with small benefits “may be boosted by adoption of organization-directed approaches.
“This finding provides support for the view that burnout is a problem of the whole health care organization, rather than individuals,” they wrote.
But the issue typically remains a local one, as group leaders need to realize that what could cause or contribute to burnout in one employee might be enjoyable to another.
“The prospect of doing that was daunting,” Dr. Roberts recalled. “I didn’t know much about EHRs and it was going to be a lot of meetings ... and [it] was going to take me away from patient care. It really ended up being rewarding, despite all the time and frustration, because I got to help represent the interests of my hospitalist colleagues, the physician assistants, and nurses that I work with in trying to avoid some real problems that could have arisen in the EHR.”
Doing that work appealed to Dr. Roberts, so he embraced it. That approach is one championed by Thom Mayer, MD, FACEP, FAAP, executive vice president of EmCare, founder and CEO of BestPractices Inc., medical director for the NFL Players Association, and clinical professor of emergency medicine at George Washington University, Washington, and University of Virginia, Charlottesville. Dr. Mayer travels the country talking about burnout and suggests a three-pronged approach.
First, find what you like about your job and maximize those duties.
Second, label those tasks that are tolerable and don’t allow them to become issues leading to burnout.
Third, and perhaps most difficult, “take the things [you] hate and eliminate them to the best extent possible from [your] job.”
“I’ll give you an example,” he said. “What I hear from emergency physicians and hospitalists is: ‘What do I hate? Well, I hate chronic pain patients.’ Well, does that mean you’re going to be able to eliminate the fact that there are chronic pain patients? No. But, what you can do is ... really drill down on it, and say ‘Why do you hate that?’ The answer is, “Well, I don’t have a strategy for it.” No one likes doing things when they don’t know what they’re doing.
“Now you take the chronic pain patient and the problem is, most of us just haven’t really thought that out. Most of us haven’t sat down with our colleagues and said, “What are you doing that’s working? How are you handling these people? What are the scripts that I can use, the evidence-based language that I can use? What alternatives can I give them?” Instead of just assuming that the only answer to the problem of chronic pain is opioids.”
The silent epidemic
So if there are measurements for burnout, and even best practices on how to address it, why is the issue one that Dr. Mayer calls a silent epidemic? One word: stigma.
“We as physicians can’t afford to propagate that stigma any further,” Dr. Roberts said. “People who have even tougher jobs than we have, involving combat and hostage negotiation and things like that, have found a way to have honest conversations about the impact of their work on their lives. There is no reason physicians shouldn’t be able to slowly change the culture of medicine to be able to do that, so that there isn’t a stigma around saying, ‘I need some time away before this begins to impact the safety of our patients.’ ”
Dr. West said that when data show that as many as half of all physicians show symptoms of burnout, there is no need to stigmatize a group that large.
Dike Drummond, MD, a family physician, coach, and consultant on burnout prevention, said that the No. 1 mistake physicians and leaders make about burnout is labeling it a “problem.”
“Burnout does not have a single solution because it is not a problem to begin with,” he added. “Burnout is a classic dilemma – a never-ending balancing act. Think of the balancing act of burnout as a teeter-totter, like the one you see in a children’s playground. On one side is the energy you put into your practice and larger life … and on the other side your ability to recharge your energy levels.
“To prevent burnout you must keep your energy expenditure and your recharge activities in balance to keep this teeter-totter in a relatively horizontal position. And the way you address the dilemma is with a strategy: three to five individual tools you use to lower your stress levels or recharge your energy balance.”
And a strategy is a long-term approach to a long-term problem, he said.
“Burnout is not necessarily a terminal condition,” Dr. Roberts said. “If we can structure their work and the balance in their life in such a way that they don’t experience it, or that when they do experience it, they can recognize it and make the changes they need to avoid it getting worse, I think we’d be better off as a profession.”
Richard Quinn is a freelance writer in New Jersey.
References
1. Maslach C, Jackson S. The measurement of experienced burnout. J Occup Behavior. 1981;2:99-113
2. Roberts DL, Shanafelt TD, Dyrbye LN, West CP. A national comparison of burnout and work-life balance among internal medicine hospitalists and outpatient general internists. J Hosp Med. 2014;9(3):176-81.
3. Panagioti M, Panagopoulou E, Brower P. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis [published online Dec. 5, 2016 ahead of print]. JAMA Intern Med. doi: 10.1001/jamainternmed.2016.7674.
Some 15 years ago, when Daniel Roberts, MD, FHM, decided at the end of his medical residency that his career path was going to be that of a hospitalist, he heard the same thing. A lot.
“Geesh, don’t you think you’re going to burn out?”
The reasons for such a response are well known in HM circles: the 7-on, 7-off shift structure; the constant rounding; the push-pull between clinical, administrative, and – what many would term – clerical work.
“The truth is somewhere between,” Dr. Roberts said.
Burnout is a hot topic among hospitalists and all of health care these days, as the increasing burdens of a system in seemingly constant change have fostered pressures inside and out of hospitals. Increasingly, researchers are studying and publishing about how to recognize burnout, ways to deal with, or even proactively address the issues. Some MDs – experts in physician burnout – make a living by touring the country and talking about the issue.
But what causes burnout, specifically and exactly?
“The simplistic answer is that burnout is what happens when resources do not meet demand,” said Colin West, MD, PhD, FACP, of the departments of internal medicine and health sciences research at the Mayo Clinic in Rochester, Minn., and a leading researcher on the topic of burnout. “The more complicated answer, which, at this point, is fairly solidly evidence based actually, is that there are five broad categories of drivers of physician distress and burnout.”
Dr. West’s hierarchy of stressors encompasses:
• Work effort.
• Work efficiency.
• Work-home interference.
• A sense of meaning.
• “Flexibility, control, and autonomy.”
Basically, the five drivers lead to this: Physicians who work too much and too inefficiently, with too little control and sense of purpose, end up flaming out more so than do doctors who work fewer hours, with fewer obstacles – all the while feeling satisfied with their autonomy and value.
Academic hospitalist John Yoon, MD, assistant professor of medicine at the University of Chicago, says that health care has to work harder to promote its benefits as being more important than a highly paid profession. Instead, health care should focus on giving meaning to its practitioners.
“I think it is time for leaders of HM groups to honestly discuss the intrinsic meaning and essential ‘calling’ of what it means to be a good hospitalist,” Dr. Yoon wrote in an email interview with The Hospitalist. “What can we do to make the hospitalist vocation a meaningful, long-term career, so that they do not feel like simply revenue-generating ‘pawns’ in a medical-bureaucratic system?”
A ‘meaningful’ career
The modern discussion of burnout as a phenomenon traces back to the Maslach Burnout Inventory, a three-pronged test that measures emotional exhaustion, depersonalization, and personal accomplishment.1 But why does burnout hit physicians – hospitalists, in particular – so intensely? In part, it’s because – like their predecessors in emergency medicine – hospitalists are responsible for managing the care of patients other specialties consult with, operate on, or for whom they run tests.
“Once the patients come up from the emergency room or get admitted to the hospital from the outside, the hospitalist is the one who is largely running that show,” said Dr. West, whose researchshows that HM doctors suffer burnout more than the average across medical specialties.2 “So they’re the front line of inpatient medicine.”
Another factor contributing to burnout’s impact on hospitalists is that the specialty’s rank and file (by definition) work within the walls of institutions that have a lot of contentious and complicated issues that – while outside the purview of HM – can directly or indirectly affect the field. Dr. West calls it the hassle factor.
“You want to get a test in the hospital and, even though you’re the attending on the service, you end up going through three layers of bureaucracy with an insurance company to be able to finally get what you know that patient needs,” he said. “Anything like that contributes to the burnout problem because it pulls the physician away from what they want to be doing, what is purposeful, what is meaningful for them.”
For Dr. Yoon, the exhaustion and cynicism borne out by the work of Maslach and Dr. West’s team are measures indicative of a field where physicians struggle more and more to “make sense of why their practice is worthwhile.
“In the contemporary medical literature, we have been encouraged to adopt the concepts and practices of industrial engineering and quality improvement,” Dr. Yoon added. “In other words, it seems that to the extent physicians’ aspirations to practice good medicine are confined to the narrow and unimaginative constraints of mere scientific technique (more data, higher ‘quality,’ better outcomes) physicians will struggle to recognize and respond to their practice as meaningful. There is no intrinsic meaning to simply being a ‘cog’ in a medical-industrial process or an ‘independent variable’ in an economic equation.”
Finding meaning in one’s job, of course, is less empirical an endpoint than using a reversal agent for a GI bleed. Therein lies the challenge of battling burnout, whose causes and interventions can be as varied as the people who suffer the syndrome.
Local, customized solutions
Once a group leader identifies the symptoms of burnout, the obvious question is how to address it.
Dr. West and his colleagues have identified two broad categories of interventions: individual-focused approaches and organizational solutions. Physician-centered efforts include such tacks as mindfulness, stress reduction, resilience training and small-group communication. Institutional-level changes are, typically, much harder to implement and make successful.
“It doesn’t make sense to ... simply send physicians to stress-management training so that they’re better equipped to deal with a system that is not working to improve itself,” Dr. West said. “The system and the leadership in that system needs to take responsibility from an organizational standpoint.”
Health care as a whole has worked to address the systems-level issue. Duty-hour regulations have been reined in for trainees to be proactive in addressing both fatigue and its inevitable endpoint: burnout.
In a report, “Controlled Interventions to Reduce Burnout in Physicians: A Systematic Review and Meta-Analysis,”3 published online Dec. 5 in JAMA Internal Medicine, researchers concluded that interventions associated with small benefits “may be boosted by adoption of organization-directed approaches.
“This finding provides support for the view that burnout is a problem of the whole health care organization, rather than individuals,” they wrote.
But the issue typically remains a local one, as group leaders need to realize that what could cause or contribute to burnout in one employee might be enjoyable to another.
“The prospect of doing that was daunting,” Dr. Roberts recalled. “I didn’t know much about EHRs and it was going to be a lot of meetings ... and [it] was going to take me away from patient care. It really ended up being rewarding, despite all the time and frustration, because I got to help represent the interests of my hospitalist colleagues, the physician assistants, and nurses that I work with in trying to avoid some real problems that could have arisen in the EHR.”
Doing that work appealed to Dr. Roberts, so he embraced it. That approach is one championed by Thom Mayer, MD, FACEP, FAAP, executive vice president of EmCare, founder and CEO of BestPractices Inc., medical director for the NFL Players Association, and clinical professor of emergency medicine at George Washington University, Washington, and University of Virginia, Charlottesville. Dr. Mayer travels the country talking about burnout and suggests a three-pronged approach.
First, find what you like about your job and maximize those duties.
Second, label those tasks that are tolerable and don’t allow them to become issues leading to burnout.
Third, and perhaps most difficult, “take the things [you] hate and eliminate them to the best extent possible from [your] job.”
“I’ll give you an example,” he said. “What I hear from emergency physicians and hospitalists is: ‘What do I hate? Well, I hate chronic pain patients.’ Well, does that mean you’re going to be able to eliminate the fact that there are chronic pain patients? No. But, what you can do is ... really drill down on it, and say ‘Why do you hate that?’ The answer is, “Well, I don’t have a strategy for it.” No one likes doing things when they don’t know what they’re doing.
“Now you take the chronic pain patient and the problem is, most of us just haven’t really thought that out. Most of us haven’t sat down with our colleagues and said, “What are you doing that’s working? How are you handling these people? What are the scripts that I can use, the evidence-based language that I can use? What alternatives can I give them?” Instead of just assuming that the only answer to the problem of chronic pain is opioids.”
The silent epidemic
So if there are measurements for burnout, and even best practices on how to address it, why is the issue one that Dr. Mayer calls a silent epidemic? One word: stigma.
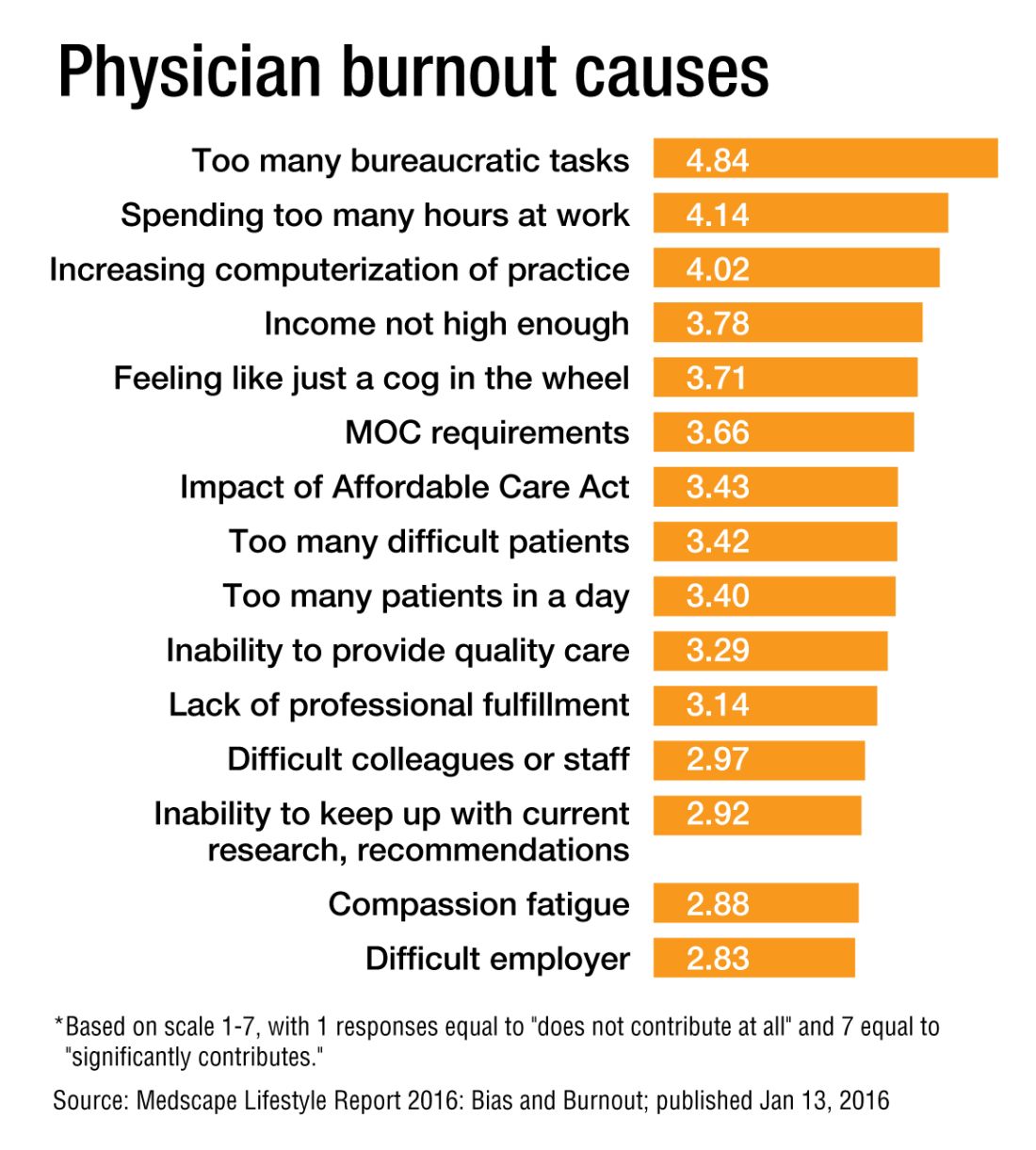
“We as physicians can’t afford to propagate that stigma any further,” Dr. Roberts said. “People who have even tougher jobs than we have, involving combat and hostage negotiation and things like that, have found a way to have honest conversations about the impact of their work on their lives. There is no reason physicians shouldn’t be able to slowly change the culture of medicine to be able to do that, so that there isn’t a stigma around saying, ‘I need some time away before this begins to impact the safety of our patients.’ ”
Dr. West said that when data show that as many as half of all physicians show symptoms of burnout, there is no need to stigmatize a group that large.
Dike Drummond, MD, a family physician, coach, and consultant on burnout prevention, said that the No. 1 mistake physicians and leaders make about burnout is labeling it a “problem.”
“Burnout does not have a single solution because it is not a problem to begin with,” he added. “Burnout is a classic dilemma – a never-ending balancing act. Think of the balancing act of burnout as a teeter-totter, like the one you see in a children’s playground. On one side is the energy you put into your practice and larger life … and on the other side your ability to recharge your energy levels.
“To prevent burnout you must keep your energy expenditure and your recharge activities in balance to keep this teeter-totter in a relatively horizontal position. And the way you address the dilemma is with a strategy: three to five individual tools you use to lower your stress levels or recharge your energy balance.”
And a strategy is a long-term approach to a long-term problem, he said.
“Burnout is not necessarily a terminal condition,” Dr. Roberts said. “If we can structure their work and the balance in their life in such a way that they don’t experience it, or that when they do experience it, they can recognize it and make the changes they need to avoid it getting worse, I think we’d be better off as a profession.”
Richard Quinn is a freelance writer in New Jersey.
References
1. Maslach C, Jackson S. The measurement of experienced burnout. J Occup Behavior. 1981;2:99-113
2. Roberts DL, Shanafelt TD, Dyrbye LN, West CP. A national comparison of burnout and work-life balance among internal medicine hospitalists and outpatient general internists. J Hosp Med. 2014;9(3):176-81.
3. Panagioti M, Panagopoulou E, Brower P. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis [published online Dec. 5, 2016 ahead of print]. JAMA Intern Med. doi: 10.1001/jamainternmed.2016.7674.
The Pill: A pediatric perspective
Arguably, the introduction of the birth control pill has transformed female health more than any other drug in modern medicine. Although many of us practicing now do not know life without it, its history is not that long.
“The Pill” – as it is often referred to – was introduced in May of 1950.1 At that time, prevention of pregnancy was not listed as an indication, and promoting birth control was politically, socially, and legally unacceptable. In fact, the Comstock Law prohibited public discussion and research about contraception.1 Therefore, when the birth control pill was introduced, it was for cycle control and for married women only. It was not indicated for use as contraception in the United States until 1960.
Since that time, the birth control pill has evolved dramatically, not only in its formulation but in its indications as well. As pediatricians, we do not always find it easy to discuss with parents hormonal regulation and starting a patient on the birth control pill, particularly when it will not be used for contraception. There are many fears about using hormonal control, but there are many useful indications that improve the health and well-being of the pediatric patient.
Menorrhagia and dysmenorrhea are likely the most common reasons that hormonal therapy is started in adolescence. Beginning with the lowest estrogen dose to reduce side effects is prudent, adjusting accordingly if side effects should occur. Breakthrough bleeding is a common side effect that usually improves over time. Patients should continue treatment for at least 3 months before deciding if treatment is effective or not. If breakthrough bleeding continues, increasing the estrogen component or changing to a triphasic pill might reduce bleeding.
For a child with mental or significant physical disabilities, suppression of ovulation to prevent a menstrual cycle is very useful. Extended regimens can help to completely suppress ovulation, thereby avoiding withdrawal bleeding. There is anxiety about extended regimens, but there is no greater risk with using hormonal therapy continuously vs. intermittently.2 In fact, using it continuously reduces many of the unwanted side effects associated with the use of oral contraceptive pills (OCPs), for example, heavy bleeding, headaches, and nausea. Complete suppression is difficult, but the odds are better with continuous treatment. Using monophasic OCPs for 42-63 days on and 4-7 days off can be tried. The benefit of using monophasic pills is if a dose is missed, it is easy to make it up by just taking an extra pill. Companies have come out with extended-regimen packs, for example, Seasonale, Seasonique, Quartette, and Lybrel. There now is a chewable pill known as Femcon Fe, which would be useful in those patients who are not able to swallow pills.
Another indication for OCPs in the adolescent patient is acne. Although the exact mechanism is not completely understood, estrogen does decrease sebum by reducing the size of the gland4, and, therefore, all OCPs can reduce acne. Norgestimate combinations have the highest androgen to progesterone binding ratio, so they are more effective than OCPs that do not. A newer progestin, drospirenone, is a 17 alpha-spironolactone derivative that produces antiandrogenic activity.5 When used in a combination OCP, acne control appears to be even greater. Hormonal therapy should be considered whenever there has been limited improvement with topical treatment or if acne breakouts are associated with the onset of menses.
Another consideration is to add spironolactone 100 mg by mouth daily to the regimen. Studies have shown it can be safely used in women to reduce acne.6 Patients should be monitored frequently for hyperkalemia, and it should not be used in patients who are already pregnant.4 Lab work should be done to rule out other causes of hyperandrogenism; lab tests would include serum testosterone, androstenedione, dehydroepiandrosterone, sex hormone–binding globulin, and prolactin.4
Premenstrual syndrome (PMS) or premenstrual dysphoric disorder (PMDD) – which is the onset of depression, irritability, or anxiety in the second half of the menstrual cycle and remits with the onset of the menstrual cycle – also can be treated with hormonal therapy. This can be particularly helpful in teens with depression, as well as in those who are on treatment without significant resolution. PMS/PMDD appears to be best regulated with OCPs containing drospirenone,7 and using either a shortened course of the placebo phase or a continuous regimen appears to be the most beneficial.
Regardless of the indication for hormonal therapy, the initiation and management are essentially the same. Initiation can be on the first day of the menstrual cycle, on the Sunday after, or at the time of the visit. Initiation midcycle may result in breakthrough bleeding, but that will likely resolve over the next 3 months. No lab tests are required to start hormonal therapy, except for an HCG to rule out pregnancy. Weight and blood pressure should be documented so they can be monitored on follow-up visits. A detailed verbal explanation along with a handout should be provided on proper administration and side effects. Contraindications for the use of OCPs can be found on the Centers for Disease Control and Prevention’s website under medical criteria for the use of contraceptives.
Educating families and patients on their options for hormonal therapy can be life changing. Detailed questions about the menstrual cycle should be asked at every visit, and understanding the wide variety of indications for hormonal therapy can maximize treatment for a better outcome.
References
1. Can Fam Physician. 2012 Dec;58(12):e757–60.
2. J Midwifery Womens Health. 2012 Nov-Dec;57(6):585-92.
3. Obstet Gynecol. 2009;114:1428-31.
4. Semin Cutan Med Surg. 2008 Sep;27(3):188-96.
5. Pediatr Rev. 2008;29(11);386-97.
6. J Eur Acad Dermatol Venereol. 2005 Mar;19(2):163-6.
7. Obstet Gynecol. 2005 Sep;106(3):492-501.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures.
Arguably, the introduction of the birth control pill has transformed female health more than any other drug in modern medicine. Although many of us practicing now do not know life without it, its history is not that long.
“The Pill” – as it is often referred to – was introduced in May of 1950.1 At that time, prevention of pregnancy was not listed as an indication, and promoting birth control was politically, socially, and legally unacceptable. In fact, the Comstock Law prohibited public discussion and research about contraception.1 Therefore, when the birth control pill was introduced, it was for cycle control and for married women only. It was not indicated for use as contraception in the United States until 1960.
Since that time, the birth control pill has evolved dramatically, not only in its formulation but in its indications as well. As pediatricians, we do not always find it easy to discuss with parents hormonal regulation and starting a patient on the birth control pill, particularly when it will not be used for contraception. There are many fears about using hormonal control, but there are many useful indications that improve the health and well-being of the pediatric patient.
Menorrhagia and dysmenorrhea are likely the most common reasons that hormonal therapy is started in adolescence. Beginning with the lowest estrogen dose to reduce side effects is prudent, adjusting accordingly if side effects should occur. Breakthrough bleeding is a common side effect that usually improves over time. Patients should continue treatment for at least 3 months before deciding if treatment is effective or not. If breakthrough bleeding continues, increasing the estrogen component or changing to a triphasic pill might reduce bleeding.
For a child with mental or significant physical disabilities, suppression of ovulation to prevent a menstrual cycle is very useful. Extended regimens can help to completely suppress ovulation, thereby avoiding withdrawal bleeding. There is anxiety about extended regimens, but there is no greater risk with using hormonal therapy continuously vs. intermittently.2 In fact, using it continuously reduces many of the unwanted side effects associated with the use of oral contraceptive pills (OCPs), for example, heavy bleeding, headaches, and nausea. Complete suppression is difficult, but the odds are better with continuous treatment. Using monophasic OCPs for 42-63 days on and 4-7 days off can be tried. The benefit of using monophasic pills is if a dose is missed, it is easy to make it up by just taking an extra pill. Companies have come out with extended-regimen packs, for example, Seasonale, Seasonique, Quartette, and Lybrel. There now is a chewable pill known as Femcon Fe, which would be useful in those patients who are not able to swallow pills.
Another indication for OCPs in the adolescent patient is acne. Although the exact mechanism is not completely understood, estrogen does decrease sebum by reducing the size of the gland4, and, therefore, all OCPs can reduce acne. Norgestimate combinations have the highest androgen to progesterone binding ratio, so they are more effective than OCPs that do not. A newer progestin, drospirenone, is a 17 alpha-spironolactone derivative that produces antiandrogenic activity.5 When used in a combination OCP, acne control appears to be even greater. Hormonal therapy should be considered whenever there has been limited improvement with topical treatment or if acne breakouts are associated with the onset of menses.
Another consideration is to add spironolactone 100 mg by mouth daily to the regimen. Studies have shown it can be safely used in women to reduce acne.6 Patients should be monitored frequently for hyperkalemia, and it should not be used in patients who are already pregnant.4 Lab work should be done to rule out other causes of hyperandrogenism; lab tests would include serum testosterone, androstenedione, dehydroepiandrosterone, sex hormone–binding globulin, and prolactin.4
Premenstrual syndrome (PMS) or premenstrual dysphoric disorder (PMDD) – which is the onset of depression, irritability, or anxiety in the second half of the menstrual cycle and remits with the onset of the menstrual cycle – also can be treated with hormonal therapy. This can be particularly helpful in teens with depression, as well as in those who are on treatment without significant resolution. PMS/PMDD appears to be best regulated with OCPs containing drospirenone,7 and using either a shortened course of the placebo phase or a continuous regimen appears to be the most beneficial.
Regardless of the indication for hormonal therapy, the initiation and management are essentially the same. Initiation can be on the first day of the menstrual cycle, on the Sunday after, or at the time of the visit. Initiation midcycle may result in breakthrough bleeding, but that will likely resolve over the next 3 months. No lab tests are required to start hormonal therapy, except for an HCG to rule out pregnancy. Weight and blood pressure should be documented so they can be monitored on follow-up visits. A detailed verbal explanation along with a handout should be provided on proper administration and side effects. Contraindications for the use of OCPs can be found on the Centers for Disease Control and Prevention’s website under medical criteria for the use of contraceptives.
Educating families and patients on their options for hormonal therapy can be life changing. Detailed questions about the menstrual cycle should be asked at every visit, and understanding the wide variety of indications for hormonal therapy can maximize treatment for a better outcome.
References
1. Can Fam Physician. 2012 Dec;58(12):e757–60.
2. J Midwifery Womens Health. 2012 Nov-Dec;57(6):585-92.
3. Obstet Gynecol. 2009;114:1428-31.
4. Semin Cutan Med Surg. 2008 Sep;27(3):188-96.
5. Pediatr Rev. 2008;29(11);386-97.
6. J Eur Acad Dermatol Venereol. 2005 Mar;19(2):163-6.
7. Obstet Gynecol. 2005 Sep;106(3):492-501.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures.
Arguably, the introduction of the birth control pill has transformed female health more than any other drug in modern medicine. Although many of us practicing now do not know life without it, its history is not that long.
“The Pill” – as it is often referred to – was introduced in May of 1950.1 At that time, prevention of pregnancy was not listed as an indication, and promoting birth control was politically, socially, and legally unacceptable. In fact, the Comstock Law prohibited public discussion and research about contraception.1 Therefore, when the birth control pill was introduced, it was for cycle control and for married women only. It was not indicated for use as contraception in the United States until 1960.
Since that time, the birth control pill has evolved dramatically, not only in its formulation but in its indications as well. As pediatricians, we do not always find it easy to discuss with parents hormonal regulation and starting a patient on the birth control pill, particularly when it will not be used for contraception. There are many fears about using hormonal control, but there are many useful indications that improve the health and well-being of the pediatric patient.
Menorrhagia and dysmenorrhea are likely the most common reasons that hormonal therapy is started in adolescence. Beginning with the lowest estrogen dose to reduce side effects is prudent, adjusting accordingly if side effects should occur. Breakthrough bleeding is a common side effect that usually improves over time. Patients should continue treatment for at least 3 months before deciding if treatment is effective or not. If breakthrough bleeding continues, increasing the estrogen component or changing to a triphasic pill might reduce bleeding.
For a child with mental or significant physical disabilities, suppression of ovulation to prevent a menstrual cycle is very useful. Extended regimens can help to completely suppress ovulation, thereby avoiding withdrawal bleeding. There is anxiety about extended regimens, but there is no greater risk with using hormonal therapy continuously vs. intermittently.2 In fact, using it continuously reduces many of the unwanted side effects associated with the use of oral contraceptive pills (OCPs), for example, heavy bleeding, headaches, and nausea. Complete suppression is difficult, but the odds are better with continuous treatment. Using monophasic OCPs for 42-63 days on and 4-7 days off can be tried. The benefit of using monophasic pills is if a dose is missed, it is easy to make it up by just taking an extra pill. Companies have come out with extended-regimen packs, for example, Seasonale, Seasonique, Quartette, and Lybrel. There now is a chewable pill known as Femcon Fe, which would be useful in those patients who are not able to swallow pills.
Another indication for OCPs in the adolescent patient is acne. Although the exact mechanism is not completely understood, estrogen does decrease sebum by reducing the size of the gland4, and, therefore, all OCPs can reduce acne. Norgestimate combinations have the highest androgen to progesterone binding ratio, so they are more effective than OCPs that do not. A newer progestin, drospirenone, is a 17 alpha-spironolactone derivative that produces antiandrogenic activity.5 When used in a combination OCP, acne control appears to be even greater. Hormonal therapy should be considered whenever there has been limited improvement with topical treatment or if acne breakouts are associated with the onset of menses.
Another consideration is to add spironolactone 100 mg by mouth daily to the regimen. Studies have shown it can be safely used in women to reduce acne.6 Patients should be monitored frequently for hyperkalemia, and it should not be used in patients who are already pregnant.4 Lab work should be done to rule out other causes of hyperandrogenism; lab tests would include serum testosterone, androstenedione, dehydroepiandrosterone, sex hormone–binding globulin, and prolactin.4
Premenstrual syndrome (PMS) or premenstrual dysphoric disorder (PMDD) – which is the onset of depression, irritability, or anxiety in the second half of the menstrual cycle and remits with the onset of the menstrual cycle – also can be treated with hormonal therapy. This can be particularly helpful in teens with depression, as well as in those who are on treatment without significant resolution. PMS/PMDD appears to be best regulated with OCPs containing drospirenone,7 and using either a shortened course of the placebo phase or a continuous regimen appears to be the most beneficial.
Regardless of the indication for hormonal therapy, the initiation and management are essentially the same. Initiation can be on the first day of the menstrual cycle, on the Sunday after, or at the time of the visit. Initiation midcycle may result in breakthrough bleeding, but that will likely resolve over the next 3 months. No lab tests are required to start hormonal therapy, except for an HCG to rule out pregnancy. Weight and blood pressure should be documented so they can be monitored on follow-up visits. A detailed verbal explanation along with a handout should be provided on proper administration and side effects. Contraindications for the use of OCPs can be found on the Centers for Disease Control and Prevention’s website under medical criteria for the use of contraceptives.
Educating families and patients on their options for hormonal therapy can be life changing. Detailed questions about the menstrual cycle should be asked at every visit, and understanding the wide variety of indications for hormonal therapy can maximize treatment for a better outcome.
References
1. Can Fam Physician. 2012 Dec;58(12):e757–60.
2. J Midwifery Womens Health. 2012 Nov-Dec;57(6):585-92.
3. Obstet Gynecol. 2009;114:1428-31.
4. Semin Cutan Med Surg. 2008 Sep;27(3):188-96.
5. Pediatr Rev. 2008;29(11);386-97.
6. J Eur Acad Dermatol Venereol. 2005 Mar;19(2):163-6.
7. Obstet Gynecol. 2005 Sep;106(3):492-501.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures.
VQI confirms improvements in vascular practice
CHICAGO – Five years after the Society for Vascular Surgery launched the Vascular Quality Initiative, participating centers are more likely to use chlorhexidine and have also cut their surgery times and reduced their transfusion rates, according to results presented at a symposium on vascular surgery sponsored by Northwestern University.
But more drastic have been the improvements once low-performing centers have made in these measures and others, Larry Kraiss, MD, of the University of Utah, Salt Lake City, said in reporting an update on VQI. “If you look at centers that had a big change in not using chlorhexidine to using chlorhexidine, the reduction of surgical site infections [SSI] in that subgroup was actually pretty significant,” said Dr. Kraiss, chair of the governing council of the SVS Patient Safety Organization, which oversees VQI.
These pivotal improvements came about after the VQI distributed what it calls COPI reports – for Center Opportunity Profile for Improvement – to participating centers. Currently, 379 centers in 46 states and Ontario participate in VQI, feeding data into 12 different vascular procedure registries ranging from peripheral vascular interventions to lower-extremity amputations. As of Nov. 1, 2016, 330,400 procedures had been submitted to VQI.
Dr. Kraiss called the COPI report the “workhorse” of the VQI. “It can give participating centers insight into what they can do to improve outcomes,” he said. It is one of three types of reports VQI provides. The others are benchmarking reports that show the masked ratings for all participating centers but confidentially highlight the rating of the individual center receiving the report; and reports for individual providers.
The most recent readout of the SSI COPI report compared measures in two periods: 2011-2012 and 2013-2014. In those periods, overall use of chlorhexidine rose from 66.6% to 81.2%; transfusion rates of more than 2 units fell from 14.4% to 11.5%; the share of procedures lasting 220 minutes or more fell from 50.2% to 47.7%; and SSI rate overall fell from 3.4% to 3.1%. While the change in SSI was not statistically significant, Dr. Kraiss said the 17 centers that had a large increase in chlorhexidine use did see statistically significant declines in SSI.
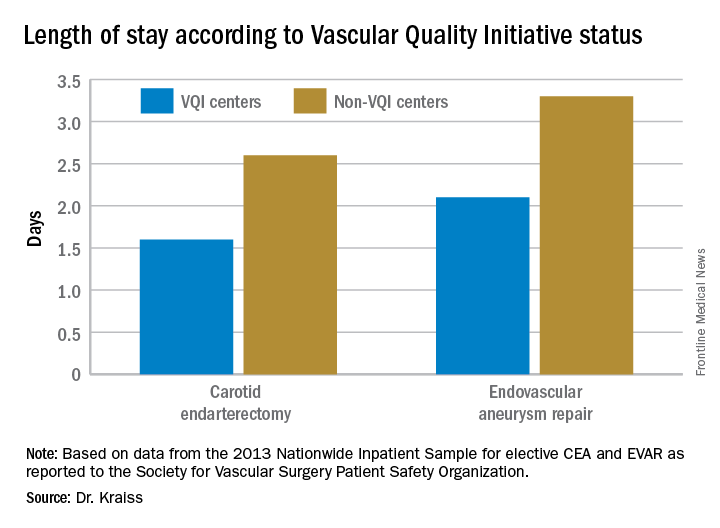
VQI also showed a 5-year survival rate of 79% of patients discharged with both statin and aspirin therapy vs. 61% for patients discharged without (J Vasc Surg. 2015;61[4]:1010-9). “This represents an opportunity to inform individual providers about how often they discharge patients on an aspirin and statin,” Dr. Kraiss said. Provider-targeted reports show how individual physicians rate in their region and nationwide.
VQI is more than a registry, Dr. Kraiss said; it’s also organized into 17 regional quality groups that provide surgeons a safe place to discuss VQI data and how to use that to encourage best practices. “There’s no risk of compromising or making the information identifiable,” he said. “It’s a matter of just getting together and trying to share best practices in a relatively informal environment, and hopefully through that drive quality improvement.
Other benefits of participating in VQI are that it can help surgeons comply with requirements for Medicare’s Merit-based Incentive Payment System (MIPS). VQI also offers opportunities to enroll in industry-sponsored clinical trials, which can help defray the cost of VQI participation, he said.
Dr. Kraiss had no relevant financial relationships to disclose.
CHICAGO – Five years after the Society for Vascular Surgery launched the Vascular Quality Initiative, participating centers are more likely to use chlorhexidine and have also cut their surgery times and reduced their transfusion rates, according to results presented at a symposium on vascular surgery sponsored by Northwestern University.
But more drastic have been the improvements once low-performing centers have made in these measures and others, Larry Kraiss, MD, of the University of Utah, Salt Lake City, said in reporting an update on VQI. “If you look at centers that had a big change in not using chlorhexidine to using chlorhexidine, the reduction of surgical site infections [SSI] in that subgroup was actually pretty significant,” said Dr. Kraiss, chair of the governing council of the SVS Patient Safety Organization, which oversees VQI.
These pivotal improvements came about after the VQI distributed what it calls COPI reports – for Center Opportunity Profile for Improvement – to participating centers. Currently, 379 centers in 46 states and Ontario participate in VQI, feeding data into 12 different vascular procedure registries ranging from peripheral vascular interventions to lower-extremity amputations. As of Nov. 1, 2016, 330,400 procedures had been submitted to VQI.
Dr. Kraiss called the COPI report the “workhorse” of the VQI. “It can give participating centers insight into what they can do to improve outcomes,” he said. It is one of three types of reports VQI provides. The others are benchmarking reports that show the masked ratings for all participating centers but confidentially highlight the rating of the individual center receiving the report; and reports for individual providers.
The most recent readout of the SSI COPI report compared measures in two periods: 2011-2012 and 2013-2014. In those periods, overall use of chlorhexidine rose from 66.6% to 81.2%; transfusion rates of more than 2 units fell from 14.4% to 11.5%; the share of procedures lasting 220 minutes or more fell from 50.2% to 47.7%; and SSI rate overall fell from 3.4% to 3.1%. While the change in SSI was not statistically significant, Dr. Kraiss said the 17 centers that had a large increase in chlorhexidine use did see statistically significant declines in SSI.
VQI also showed a 5-year survival rate of 79% of patients discharged with both statin and aspirin therapy vs. 61% for patients discharged without (J Vasc Surg. 2015;61[4]:1010-9). “This represents an opportunity to inform individual providers about how often they discharge patients on an aspirin and statin,” Dr. Kraiss said. Provider-targeted reports show how individual physicians rate in their region and nationwide.
VQI is more than a registry, Dr. Kraiss said; it’s also organized into 17 regional quality groups that provide surgeons a safe place to discuss VQI data and how to use that to encourage best practices. “There’s no risk of compromising or making the information identifiable,” he said. “It’s a matter of just getting together and trying to share best practices in a relatively informal environment, and hopefully through that drive quality improvement.
Other benefits of participating in VQI are that it can help surgeons comply with requirements for Medicare’s Merit-based Incentive Payment System (MIPS). VQI also offers opportunities to enroll in industry-sponsored clinical trials, which can help defray the cost of VQI participation, he said.
Dr. Kraiss had no relevant financial relationships to disclose.
CHICAGO – Five years after the Society for Vascular Surgery launched the Vascular Quality Initiative, participating centers are more likely to use chlorhexidine and have also cut their surgery times and reduced their transfusion rates, according to results presented at a symposium on vascular surgery sponsored by Northwestern University.
But more drastic have been the improvements once low-performing centers have made in these measures and others, Larry Kraiss, MD, of the University of Utah, Salt Lake City, said in reporting an update on VQI. “If you look at centers that had a big change in not using chlorhexidine to using chlorhexidine, the reduction of surgical site infections [SSI] in that subgroup was actually pretty significant,” said Dr. Kraiss, chair of the governing council of the SVS Patient Safety Organization, which oversees VQI.
These pivotal improvements came about after the VQI distributed what it calls COPI reports – for Center Opportunity Profile for Improvement – to participating centers. Currently, 379 centers in 46 states and Ontario participate in VQI, feeding data into 12 different vascular procedure registries ranging from peripheral vascular interventions to lower-extremity amputations. As of Nov. 1, 2016, 330,400 procedures had been submitted to VQI.
Dr. Kraiss called the COPI report the “workhorse” of the VQI. “It can give participating centers insight into what they can do to improve outcomes,” he said. It is one of three types of reports VQI provides. The others are benchmarking reports that show the masked ratings for all participating centers but confidentially highlight the rating of the individual center receiving the report; and reports for individual providers.
The most recent readout of the SSI COPI report compared measures in two periods: 2011-2012 and 2013-2014. In those periods, overall use of chlorhexidine rose from 66.6% to 81.2%; transfusion rates of more than 2 units fell from 14.4% to 11.5%; the share of procedures lasting 220 minutes or more fell from 50.2% to 47.7%; and SSI rate overall fell from 3.4% to 3.1%. While the change in SSI was not statistically significant, Dr. Kraiss said the 17 centers that had a large increase in chlorhexidine use did see statistically significant declines in SSI.
VQI also showed a 5-year survival rate of 79% of patients discharged with both statin and aspirin therapy vs. 61% for patients discharged without (J Vasc Surg. 2015;61[4]:1010-9). “This represents an opportunity to inform individual providers about how often they discharge patients on an aspirin and statin,” Dr. Kraiss said. Provider-targeted reports show how individual physicians rate in their region and nationwide.
VQI is more than a registry, Dr. Kraiss said; it’s also organized into 17 regional quality groups that provide surgeons a safe place to discuss VQI data and how to use that to encourage best practices. “There’s no risk of compromising or making the information identifiable,” he said. “It’s a matter of just getting together and trying to share best practices in a relatively informal environment, and hopefully through that drive quality improvement.
Other benefits of participating in VQI are that it can help surgeons comply with requirements for Medicare’s Merit-based Incentive Payment System (MIPS). VQI also offers opportunities to enroll in industry-sponsored clinical trials, which can help defray the cost of VQI participation, he said.
Dr. Kraiss had no relevant financial relationships to disclose.
AT THE NORTHWESTERN VASCULAR SYMPOSIUM
Key clinical point: The Vascular Quality Initiative (VQI) provides comparative outcomes data that centers and surgeons can use to improve quality.
Major finding: Hospital length of stay for carotid endarterectomy averages 1.6 days for VQI centers vs. 2.6 days for nonparticipating centers.
Data source: VQI database.
Disclosures: Dr. Kraiss reported having no financial disclosures.