User login
Major medical, insurance, health groups agree on pre-auth improvement areas
The prior authorization approval process required by health insurance companies for patients’ medical treatments, also called preapproval, eats up countless hours of time and costs, over $80,000 per year, per provider. The average provider deals with 35 of these prior authorization requests per day, and each request takes an average of 20 minutes. Physicians, pharmacists, hospitals, medical groups, and health insurance companies are working together to come up with a solution.
The American Hospital Association, America’s Health Insurance Plans, American Medical Association, American Pharmacists Association, Blue Cross Blue Shield Association, and Medical Group Management Association announced a consensus statement delineating where they agree the health care industry can improve the prior authorization process.
Most of the solutions outlined in the document are intuitive – they include reducing the number of health care professionals subject to prior authorization requirements based on their performance; adherence to evidence-based medical practices or participation in a value-based agreement with the health insurance provider; reviewing the services and medications that require prior authorization and eliminating requirements for therapies that no longer warrant them; improving communications between health insurance providers, health care professionals, and patients to provide clarity on prior authorization requirements and changes; protecting continuity of care for patients; improving formulary information and coverage restrictions at point-of-care; and adopting national electronic standards for prior authorization.
Jack Resneck Jr., MD, chair-elect of the AMA board of trustees, described the document as a “good initial step” toward reducing the difficulties imposed by prior authorizations.
Prior authorization requests are particularly burdensome for medications that are expensive, a headache that doctors working with patients who have rheumatoid arthritis or lupus know well.
As insurance and provider groups work to improve the prior authorization process “it will be vital that they consider the issue from the perspective of general practitioners as well as specialists, the latter of whom prescribe more of the specialty tier medications that are subject to more protocols before patients can access these often life-improving medications,” Stephen Marmaras, director of policy and advocacy at Global Healthy Living Foundation, said in an interview. “Ultimately, improved communication between both parties – the physician offices and the payers – will allow us to identify barriers existing in current appeals processes and work toward collectively building solutions that benefit patients, particularly those with chronic disease who rely on stable access to medications.”
Sean Fahey, MD, chair of the American College of Rheumatology’s insurance subcommittee, said that, while the consensus statement is “a step in the right direction, like a lot of things, the devil is in the details.
“There’s good concepts in the statement without a whole lot of specifics,” Dr. Fahey said. Most changes will be addressed at the state level, because the federal legislature is very hesitant to legislate decisions for nongovernment insurance.
“A lot of the ideas set forth in this consensus statement are wonderful,” said Dr. Fahey. “Unfortunately for our patients, many of their medications are ludicrously expensive. … Every time you write a prescription for one of these medications, after appropriate therapy, you have to do [a preauthorization] just to get the medicine that people want and need. It’s frustrating that the issue of drug cost is driving the whole process. For a $60,000 a year price you’re going to have to do a preauthorization every single time, as opposed to a drug that’s $100 a year.”
Still, the statement is “an important step” toward ultimately making vital medications “more accessible for patients,” Dr. Fahey said.
The prior authorization approval process required by health insurance companies for patients’ medical treatments, also called preapproval, eats up countless hours of time and costs, over $80,000 per year, per provider. The average provider deals with 35 of these prior authorization requests per day, and each request takes an average of 20 minutes. Physicians, pharmacists, hospitals, medical groups, and health insurance companies are working together to come up with a solution.
The American Hospital Association, America’s Health Insurance Plans, American Medical Association, American Pharmacists Association, Blue Cross Blue Shield Association, and Medical Group Management Association announced a consensus statement delineating where they agree the health care industry can improve the prior authorization process.
Most of the solutions outlined in the document are intuitive – they include reducing the number of health care professionals subject to prior authorization requirements based on their performance; adherence to evidence-based medical practices or participation in a value-based agreement with the health insurance provider; reviewing the services and medications that require prior authorization and eliminating requirements for therapies that no longer warrant them; improving communications between health insurance providers, health care professionals, and patients to provide clarity on prior authorization requirements and changes; protecting continuity of care for patients; improving formulary information and coverage restrictions at point-of-care; and adopting national electronic standards for prior authorization.
Jack Resneck Jr., MD, chair-elect of the AMA board of trustees, described the document as a “good initial step” toward reducing the difficulties imposed by prior authorizations.
Prior authorization requests are particularly burdensome for medications that are expensive, a headache that doctors working with patients who have rheumatoid arthritis or lupus know well.
As insurance and provider groups work to improve the prior authorization process “it will be vital that they consider the issue from the perspective of general practitioners as well as specialists, the latter of whom prescribe more of the specialty tier medications that are subject to more protocols before patients can access these often life-improving medications,” Stephen Marmaras, director of policy and advocacy at Global Healthy Living Foundation, said in an interview. “Ultimately, improved communication between both parties – the physician offices and the payers – will allow us to identify barriers existing in current appeals processes and work toward collectively building solutions that benefit patients, particularly those with chronic disease who rely on stable access to medications.”
Sean Fahey, MD, chair of the American College of Rheumatology’s insurance subcommittee, said that, while the consensus statement is “a step in the right direction, like a lot of things, the devil is in the details.
“There’s good concepts in the statement without a whole lot of specifics,” Dr. Fahey said. Most changes will be addressed at the state level, because the federal legislature is very hesitant to legislate decisions for nongovernment insurance.
“A lot of the ideas set forth in this consensus statement are wonderful,” said Dr. Fahey. “Unfortunately for our patients, many of their medications are ludicrously expensive. … Every time you write a prescription for one of these medications, after appropriate therapy, you have to do [a preauthorization] just to get the medicine that people want and need. It’s frustrating that the issue of drug cost is driving the whole process. For a $60,000 a year price you’re going to have to do a preauthorization every single time, as opposed to a drug that’s $100 a year.”
Still, the statement is “an important step” toward ultimately making vital medications “more accessible for patients,” Dr. Fahey said.
The prior authorization approval process required by health insurance companies for patients’ medical treatments, also called preapproval, eats up countless hours of time and costs, over $80,000 per year, per provider. The average provider deals with 35 of these prior authorization requests per day, and each request takes an average of 20 minutes. Physicians, pharmacists, hospitals, medical groups, and health insurance companies are working together to come up with a solution.
The American Hospital Association, America’s Health Insurance Plans, American Medical Association, American Pharmacists Association, Blue Cross Blue Shield Association, and Medical Group Management Association announced a consensus statement delineating where they agree the health care industry can improve the prior authorization process.
Most of the solutions outlined in the document are intuitive – they include reducing the number of health care professionals subject to prior authorization requirements based on their performance; adherence to evidence-based medical practices or participation in a value-based agreement with the health insurance provider; reviewing the services and medications that require prior authorization and eliminating requirements for therapies that no longer warrant them; improving communications between health insurance providers, health care professionals, and patients to provide clarity on prior authorization requirements and changes; protecting continuity of care for patients; improving formulary information and coverage restrictions at point-of-care; and adopting national electronic standards for prior authorization.
Jack Resneck Jr., MD, chair-elect of the AMA board of trustees, described the document as a “good initial step” toward reducing the difficulties imposed by prior authorizations.
Prior authorization requests are particularly burdensome for medications that are expensive, a headache that doctors working with patients who have rheumatoid arthritis or lupus know well.
As insurance and provider groups work to improve the prior authorization process “it will be vital that they consider the issue from the perspective of general practitioners as well as specialists, the latter of whom prescribe more of the specialty tier medications that are subject to more protocols before patients can access these often life-improving medications,” Stephen Marmaras, director of policy and advocacy at Global Healthy Living Foundation, said in an interview. “Ultimately, improved communication between both parties – the physician offices and the payers – will allow us to identify barriers existing in current appeals processes and work toward collectively building solutions that benefit patients, particularly those with chronic disease who rely on stable access to medications.”
Sean Fahey, MD, chair of the American College of Rheumatology’s insurance subcommittee, said that, while the consensus statement is “a step in the right direction, like a lot of things, the devil is in the details.
“There’s good concepts in the statement without a whole lot of specifics,” Dr. Fahey said. Most changes will be addressed at the state level, because the federal legislature is very hesitant to legislate decisions for nongovernment insurance.
“A lot of the ideas set forth in this consensus statement are wonderful,” said Dr. Fahey. “Unfortunately for our patients, many of their medications are ludicrously expensive. … Every time you write a prescription for one of these medications, after appropriate therapy, you have to do [a preauthorization] just to get the medicine that people want and need. It’s frustrating that the issue of drug cost is driving the whole process. For a $60,000 a year price you’re going to have to do a preauthorization every single time, as opposed to a drug that’s $100 a year.”
Still, the statement is “an important step” toward ultimately making vital medications “more accessible for patients,” Dr. Fahey said.
Yellow-Orange Hairless Plaque on the Scalp
The Diagnosis: Nevus Sebaceous
The patient presented with a typical solitary scalp lesion characteristic of nevus sebaceous (NS). The lesion was present at birth as a flat and smooth hairless plaque; however, over time it became more thickened and noticeable, which prompted the parents to seek medical advice.
Nevus sebaceous, also known as NS of Jadassohn, is a benign congenital hamartoma of the sebaceous gland that usually is present at birth and frequently involves the scalp and/or the face. The classic NS lesion is solitary and appears as a well-circumscribed, waxy, yellow-orange or tan, hairless plaque. Despite the presence of these lesions at birth, they may not be noted until early childhood or rarely until adulthood. Generally, the lesion tends to thicken and become more verrucous and velvety over time, particularly around the time of reaching puberty.1 Clinically, NS lesions vary in size from 1 cm to several centimeters. Lesions initially tend to grow proportionately with the child until puberty when they become notably thicker, greasier, and verrucous or nodular under hormonal influences. The yellow discoloration of the lesion is due to sebaceous gland secretion, and the characteristic color usually becomes less evident with age.
Nevus sebaceous occurs in approximately 0.3% of newborns and tends to be sporadic in nature; however, rare familial forms have been reported.2,3 Nevus sebaceous can present as multiple nevi that tend to be extensive and distributed along the Blaschko lines, and they usually are associated with neurologic, ocular, or skeletal defects. Involvement of the central nervous system frequently is associated with large sebaceous nevi located on the face or scalp. This association has been termed NS syndrome.4 Neurologic abnormalities associated with NS syndrome include seizures, mental retardation, and hemimegalencephaly.5 Ocular findings most communally associated with the syndrome are choristomas and colobomas.6-8
There are several benign and malignant epithelial neoplasms that may develop within sebaceous nevi. Benign tumors include trichoblastoma, syringocystadenoma papilliferum, trichilemmoma, sebaceoma, nodular hidradenoma, and hidrocystoma.1,8,9 Malignant neoplasms include basal cell carcinoma (BCC), apocrine carcinoma, sebaceous carcinoma, and squamous cell carcinoma. The lifetime risk of malignancy in NS is unknown. In an extensive literature review by Moody et al10 of 4923 cases of NS for the development of secondary benign and malignant neoplasms, 16% developed benign tumors while 8% developed malignant tumors such as BCC. However, subsequent studies suggested that the incidence of BCC may have been overestimated due to misinterpretation of trichoblastoma and may be less than 1%.11-13
Usually the diagnosis of NS is made clinically and rarely a biopsy for histopathologic confirmation may be needed when the diagnosis is uncertain. Typically, these histopathologic findings include immature hair follicles, hyperplastic immature sebaceous glands, dilated apocrine glands, and epidermal hyperplasia.9 For patients with suspected NS syndrome, additional neurologic and ophthalmologic evaluations should be performed including neuroimaging studies, skeletal radiography, and analysis of liver and renal function.14
The current standard of care in treating NS is full-thickness excision. However, the decision should be individualized based on patient age, extension and location of the lesion, concerns about the cosmetic appearance, and the risk for malignancy.
The 2 main reasons to excise NS include concern about malignancy and undesirable cosmetic appearance. Once a malignant lesion develops within NS, it generally is agreed that the tumor and the entire nevus should be removed; however, recommendations vary for excising NS prophylactically to decrease the risk for malignant growths. Because the risk for malignant transformation seems to be lower than previously thought, observation can be a reasonable choice for lesions that are not associated with cosmetic concern.12,13
Photodynamic therapy, CO2 laser resurfacing, and dermabrasion have been reported as alternative therapeutic approaches. However, there is a growing concern on how effective these treatment modalities are in completely removing the lesion and whether the risk for recurrence and potential for neoplasm development remains.1,9
This patient was healthy with normal development and growth and no signs of neurologic or ocular involvement. The parents were counseled about the risk for malignancy and the long-term cosmetic appearance of the lesion. They opted for surgical excision of the lesion at 18 months of age.
- Eisen DB, Michael DJ. Sebaceous lesions and their associated syndromes: part I. J Am Acad Dermatol. 2009;61:549-560; quiz 561-562.
- Happle R, König A. Familial naevus sebaceus may be explained by paradominant transmission. Br J Dermatol. 1999;141:377.
- Hughes SM, Wilkerson AE, Winfield HL, et al. Familial nevus sebaceus in dizygotic male twins. J Am Acad Dermatol. 2006;54(2 suppl):S47-S48.
- Sugarman JL. Epidermal nevus syndromes. Semin Cutan Med Surg. 2007;26:221-230.
- Davies D, Rogers M. Review of neurological manifestations in 196 patients with sebaceous naevi. Australas J Dermatol. 2002;43:20-23.
- Trivedi N, Nehete G. Complex limbal choristoma in linear nevus sebaceous syndrome managed with scleral grafting. Indian J Ophthalmol. 2016;64:692-694.
- Nema N, Singh K, Verma A. Complex limbal choristoma in nevus sebaceous syndrome [published online February 14, 2012]. Pediatr Dermatol. 2012;29:227-229.
- Park JM, Kim DS, Kim J, et al. Epibulbar complex choristoma and hemimegalencephaly in linear sebaceous naevus syndrome [published online July 2, 2009]. Clin Exp Dermatol. 2009;34:E686-E689.
- Simi CM, Rajalakshmi T, Correa M. Clinicopathologic analysis of 21 cases of nevus sebaceus: a retrospective study. Indian J Dermatol Venereol Leprol. 2008;74:625-627.
- Moody MN, Landau JM, Goldberg LH. Nevus sebaceous revisited. Pediatr Dermatol. 2012;29:15-23.
- Cribier B, Scrivener Y, Grosshans E. Tumors arising in nevus sebaceus: a study of 596 cases. J Am Acad Dermatol. 2000;42(2 pt 1):263-268.
- Santibanez-Gallerani A, Marshall D, Duarte AM, et al. Should nevus sebaceus of Jadassohn in children be excised? a study of 757 cases, and literature review. J Craniofac Surg. 2003;14:658-660.
- Rosen H, Schmidt B, Lam HP, et al. Management of nevus sebaceous and the risk of basal cell carcinoma: an 18-year review. Pediatr Dermatol. 2009;26:676-681.
- Brandling-Bennett HA, Morel KD. Epidermal nevi. Pediatr Clin North Am. 2010;57:1177-1198.
The Diagnosis: Nevus Sebaceous
The patient presented with a typical solitary scalp lesion characteristic of nevus sebaceous (NS). The lesion was present at birth as a flat and smooth hairless plaque; however, over time it became more thickened and noticeable, which prompted the parents to seek medical advice.
Nevus sebaceous, also known as NS of Jadassohn, is a benign congenital hamartoma of the sebaceous gland that usually is present at birth and frequently involves the scalp and/or the face. The classic NS lesion is solitary and appears as a well-circumscribed, waxy, yellow-orange or tan, hairless plaque. Despite the presence of these lesions at birth, they may not be noted until early childhood or rarely until adulthood. Generally, the lesion tends to thicken and become more verrucous and velvety over time, particularly around the time of reaching puberty.1 Clinically, NS lesions vary in size from 1 cm to several centimeters. Lesions initially tend to grow proportionately with the child until puberty when they become notably thicker, greasier, and verrucous or nodular under hormonal influences. The yellow discoloration of the lesion is due to sebaceous gland secretion, and the characteristic color usually becomes less evident with age.
Nevus sebaceous occurs in approximately 0.3% of newborns and tends to be sporadic in nature; however, rare familial forms have been reported.2,3 Nevus sebaceous can present as multiple nevi that tend to be extensive and distributed along the Blaschko lines, and they usually are associated with neurologic, ocular, or skeletal defects. Involvement of the central nervous system frequently is associated with large sebaceous nevi located on the face or scalp. This association has been termed NS syndrome.4 Neurologic abnormalities associated with NS syndrome include seizures, mental retardation, and hemimegalencephaly.5 Ocular findings most communally associated with the syndrome are choristomas and colobomas.6-8
There are several benign and malignant epithelial neoplasms that may develop within sebaceous nevi. Benign tumors include trichoblastoma, syringocystadenoma papilliferum, trichilemmoma, sebaceoma, nodular hidradenoma, and hidrocystoma.1,8,9 Malignant neoplasms include basal cell carcinoma (BCC), apocrine carcinoma, sebaceous carcinoma, and squamous cell carcinoma. The lifetime risk of malignancy in NS is unknown. In an extensive literature review by Moody et al10 of 4923 cases of NS for the development of secondary benign and malignant neoplasms, 16% developed benign tumors while 8% developed malignant tumors such as BCC. However, subsequent studies suggested that the incidence of BCC may have been overestimated due to misinterpretation of trichoblastoma and may be less than 1%.11-13
Usually the diagnosis of NS is made clinically and rarely a biopsy for histopathologic confirmation may be needed when the diagnosis is uncertain. Typically, these histopathologic findings include immature hair follicles, hyperplastic immature sebaceous glands, dilated apocrine glands, and epidermal hyperplasia.9 For patients with suspected NS syndrome, additional neurologic and ophthalmologic evaluations should be performed including neuroimaging studies, skeletal radiography, and analysis of liver and renal function.14
The current standard of care in treating NS is full-thickness excision. However, the decision should be individualized based on patient age, extension and location of the lesion, concerns about the cosmetic appearance, and the risk for malignancy.
The 2 main reasons to excise NS include concern about malignancy and undesirable cosmetic appearance. Once a malignant lesion develops within NS, it generally is agreed that the tumor and the entire nevus should be removed; however, recommendations vary for excising NS prophylactically to decrease the risk for malignant growths. Because the risk for malignant transformation seems to be lower than previously thought, observation can be a reasonable choice for lesions that are not associated with cosmetic concern.12,13
Photodynamic therapy, CO2 laser resurfacing, and dermabrasion have been reported as alternative therapeutic approaches. However, there is a growing concern on how effective these treatment modalities are in completely removing the lesion and whether the risk for recurrence and potential for neoplasm development remains.1,9
This patient was healthy with normal development and growth and no signs of neurologic or ocular involvement. The parents were counseled about the risk for malignancy and the long-term cosmetic appearance of the lesion. They opted for surgical excision of the lesion at 18 months of age.
The Diagnosis: Nevus Sebaceous
The patient presented with a typical solitary scalp lesion characteristic of nevus sebaceous (NS). The lesion was present at birth as a flat and smooth hairless plaque; however, over time it became more thickened and noticeable, which prompted the parents to seek medical advice.
Nevus sebaceous, also known as NS of Jadassohn, is a benign congenital hamartoma of the sebaceous gland that usually is present at birth and frequently involves the scalp and/or the face. The classic NS lesion is solitary and appears as a well-circumscribed, waxy, yellow-orange or tan, hairless plaque. Despite the presence of these lesions at birth, they may not be noted until early childhood or rarely until adulthood. Generally, the lesion tends to thicken and become more verrucous and velvety over time, particularly around the time of reaching puberty.1 Clinically, NS lesions vary in size from 1 cm to several centimeters. Lesions initially tend to grow proportionately with the child until puberty when they become notably thicker, greasier, and verrucous or nodular under hormonal influences. The yellow discoloration of the lesion is due to sebaceous gland secretion, and the characteristic color usually becomes less evident with age.
Nevus sebaceous occurs in approximately 0.3% of newborns and tends to be sporadic in nature; however, rare familial forms have been reported.2,3 Nevus sebaceous can present as multiple nevi that tend to be extensive and distributed along the Blaschko lines, and they usually are associated with neurologic, ocular, or skeletal defects. Involvement of the central nervous system frequently is associated with large sebaceous nevi located on the face or scalp. This association has been termed NS syndrome.4 Neurologic abnormalities associated with NS syndrome include seizures, mental retardation, and hemimegalencephaly.5 Ocular findings most communally associated with the syndrome are choristomas and colobomas.6-8
There are several benign and malignant epithelial neoplasms that may develop within sebaceous nevi. Benign tumors include trichoblastoma, syringocystadenoma papilliferum, trichilemmoma, sebaceoma, nodular hidradenoma, and hidrocystoma.1,8,9 Malignant neoplasms include basal cell carcinoma (BCC), apocrine carcinoma, sebaceous carcinoma, and squamous cell carcinoma. The lifetime risk of malignancy in NS is unknown. In an extensive literature review by Moody et al10 of 4923 cases of NS for the development of secondary benign and malignant neoplasms, 16% developed benign tumors while 8% developed malignant tumors such as BCC. However, subsequent studies suggested that the incidence of BCC may have been overestimated due to misinterpretation of trichoblastoma and may be less than 1%.11-13
Usually the diagnosis of NS is made clinically and rarely a biopsy for histopathologic confirmation may be needed when the diagnosis is uncertain. Typically, these histopathologic findings include immature hair follicles, hyperplastic immature sebaceous glands, dilated apocrine glands, and epidermal hyperplasia.9 For patients with suspected NS syndrome, additional neurologic and ophthalmologic evaluations should be performed including neuroimaging studies, skeletal radiography, and analysis of liver and renal function.14
The current standard of care in treating NS is full-thickness excision. However, the decision should be individualized based on patient age, extension and location of the lesion, concerns about the cosmetic appearance, and the risk for malignancy.
The 2 main reasons to excise NS include concern about malignancy and undesirable cosmetic appearance. Once a malignant lesion develops within NS, it generally is agreed that the tumor and the entire nevus should be removed; however, recommendations vary for excising NS prophylactically to decrease the risk for malignant growths. Because the risk for malignant transformation seems to be lower than previously thought, observation can be a reasonable choice for lesions that are not associated with cosmetic concern.12,13
Photodynamic therapy, CO2 laser resurfacing, and dermabrasion have been reported as alternative therapeutic approaches. However, there is a growing concern on how effective these treatment modalities are in completely removing the lesion and whether the risk for recurrence and potential for neoplasm development remains.1,9
This patient was healthy with normal development and growth and no signs of neurologic or ocular involvement. The parents were counseled about the risk for malignancy and the long-term cosmetic appearance of the lesion. They opted for surgical excision of the lesion at 18 months of age.
- Eisen DB, Michael DJ. Sebaceous lesions and their associated syndromes: part I. J Am Acad Dermatol. 2009;61:549-560; quiz 561-562.
- Happle R, König A. Familial naevus sebaceus may be explained by paradominant transmission. Br J Dermatol. 1999;141:377.
- Hughes SM, Wilkerson AE, Winfield HL, et al. Familial nevus sebaceus in dizygotic male twins. J Am Acad Dermatol. 2006;54(2 suppl):S47-S48.
- Sugarman JL. Epidermal nevus syndromes. Semin Cutan Med Surg. 2007;26:221-230.
- Davies D, Rogers M. Review of neurological manifestations in 196 patients with sebaceous naevi. Australas J Dermatol. 2002;43:20-23.
- Trivedi N, Nehete G. Complex limbal choristoma in linear nevus sebaceous syndrome managed with scleral grafting. Indian J Ophthalmol. 2016;64:692-694.
- Nema N, Singh K, Verma A. Complex limbal choristoma in nevus sebaceous syndrome [published online February 14, 2012]. Pediatr Dermatol. 2012;29:227-229.
- Park JM, Kim DS, Kim J, et al. Epibulbar complex choristoma and hemimegalencephaly in linear sebaceous naevus syndrome [published online July 2, 2009]. Clin Exp Dermatol. 2009;34:E686-E689.
- Simi CM, Rajalakshmi T, Correa M. Clinicopathologic analysis of 21 cases of nevus sebaceus: a retrospective study. Indian J Dermatol Venereol Leprol. 2008;74:625-627.
- Moody MN, Landau JM, Goldberg LH. Nevus sebaceous revisited. Pediatr Dermatol. 2012;29:15-23.
- Cribier B, Scrivener Y, Grosshans E. Tumors arising in nevus sebaceus: a study of 596 cases. J Am Acad Dermatol. 2000;42(2 pt 1):263-268.
- Santibanez-Gallerani A, Marshall D, Duarte AM, et al. Should nevus sebaceus of Jadassohn in children be excised? a study of 757 cases, and literature review. J Craniofac Surg. 2003;14:658-660.
- Rosen H, Schmidt B, Lam HP, et al. Management of nevus sebaceous and the risk of basal cell carcinoma: an 18-year review. Pediatr Dermatol. 2009;26:676-681.
- Brandling-Bennett HA, Morel KD. Epidermal nevi. Pediatr Clin North Am. 2010;57:1177-1198.
- Eisen DB, Michael DJ. Sebaceous lesions and their associated syndromes: part I. J Am Acad Dermatol. 2009;61:549-560; quiz 561-562.
- Happle R, König A. Familial naevus sebaceus may be explained by paradominant transmission. Br J Dermatol. 1999;141:377.
- Hughes SM, Wilkerson AE, Winfield HL, et al. Familial nevus sebaceus in dizygotic male twins. J Am Acad Dermatol. 2006;54(2 suppl):S47-S48.
- Sugarman JL. Epidermal nevus syndromes. Semin Cutan Med Surg. 2007;26:221-230.
- Davies D, Rogers M. Review of neurological manifestations in 196 patients with sebaceous naevi. Australas J Dermatol. 2002;43:20-23.
- Trivedi N, Nehete G. Complex limbal choristoma in linear nevus sebaceous syndrome managed with scleral grafting. Indian J Ophthalmol. 2016;64:692-694.
- Nema N, Singh K, Verma A. Complex limbal choristoma in nevus sebaceous syndrome [published online February 14, 2012]. Pediatr Dermatol. 2012;29:227-229.
- Park JM, Kim DS, Kim J, et al. Epibulbar complex choristoma and hemimegalencephaly in linear sebaceous naevus syndrome [published online July 2, 2009]. Clin Exp Dermatol. 2009;34:E686-E689.
- Simi CM, Rajalakshmi T, Correa M. Clinicopathologic analysis of 21 cases of nevus sebaceus: a retrospective study. Indian J Dermatol Venereol Leprol. 2008;74:625-627.
- Moody MN, Landau JM, Goldberg LH. Nevus sebaceous revisited. Pediatr Dermatol. 2012;29:15-23.
- Cribier B, Scrivener Y, Grosshans E. Tumors arising in nevus sebaceus: a study of 596 cases. J Am Acad Dermatol. 2000;42(2 pt 1):263-268.
- Santibanez-Gallerani A, Marshall D, Duarte AM, et al. Should nevus sebaceus of Jadassohn in children be excised? a study of 757 cases, and literature review. J Craniofac Surg. 2003;14:658-660.
- Rosen H, Schmidt B, Lam HP, et al. Management of nevus sebaceous and the risk of basal cell carcinoma: an 18-year review. Pediatr Dermatol. 2009;26:676-681.
- Brandling-Bennett HA, Morel KD. Epidermal nevi. Pediatr Clin North Am. 2010;57:1177-1198.

An otherwise healthy 13-month-old boy presented with a well-circumscribed, 3×4-cm, yellow-orange plaque with a verrucous velvety surface on the right side of the posterior scalp. The patient was born at 33 weeks' gestation and had an uneventful perinatal course with a normal head ultrasound at 4 days of age. The lesion had been present since birth and initially was comprised of waxy, yellow-orange, hairless plaques that became more thickened and noticeable over time. The mother recalled that the surface of the plaque initially was flat and smooth but gradually became bumpier and greasier in consistency in the months prior to presentation. The patient was otherwise asymptomatic.
Surgical LAA occlusion tops anticoagulation for AF thromboprotection
Surgical left atrial appendage occlusion may be just as good as anticoagulation at preventing thromboembolic events in older people with atrial fibrillation, with less risk of bleeding into the brain, according to a database review of more than 10,000 patients.
Among elderly atrial fibrillation patients who underwent heart surgery with no oral follow-up oral anticoagulation, those who had the left atrial appendage surgically occluded were 74% less likely than were those who did not to be readmitted for a major thromboembolic event within 3 years, and 68% less likely to be readmitted for a hemorrhagic stroke, researchers at Duke University in Durham, N.C., found.
“The current study demonstrated that S-LAAO [surgical left atrial appendage occlusion] was associated with a significantly lower rate of thromboembolism among patients without oral anticoagulation. In the cohort of patients discharged with oral anticoagulation, S-LAAO was not associated with [reduced] thromboembolism but was associated with a lower risk for hemorrhagic stroke presumably related to eventual discontinuation of oral anticoagulation among S-LAAO patients,” reported Daniel Friedman, MD, and his coinvestigators. The study was published Jan. 23 in JAMA.
In short, the findings suggest that shutting down the left atrial appendage in older patients offers the same stroke protection as anticoagulation, but without the bleeding risk. Given the low rates of anticoagulant use, physicians have been considering that approach for a while. Even so, it’s only been a weak (IIb) recommendation so far in AF guidelines because of the lack of evidence.
That might change soon, but “additional randomized studies comparing S-LAAO without anticoagulation [versus] systemic anticoagulation alone will be needed to define the optimal use of S-LAAO,” said Dr. Friedman, a cardiothoracic surgeon at Duke, and his colleagues. Those studies are in the works.
The team found 10,524 older patients in the Society of Thoracic Surgeons Adult Cardiac Surgery Database during 2011-2012, and linked them to Medicare data so they could be followed for up to 3 years. About a third of the subjects had stand-alone coronary artery bypass grafting; the rest had mitral or aortic valve repairs with or without CABG.
The investigators compared outcomes among the 37% (3,892) who had S-LAAO with outcomes among those who did not. Participants were a median of 76 years of age, 61% were men, and they were all at high risk for AF stroke.
After a mean follow-up of 2.6 years, subjects who received S-LAAO without postoperative anticoagulation had a significantly lower risk of readmission for thromboembolism – stroke, transient ischemic attack, or systemic embolism – compared with those who received neither S-LAAO nor anticoagulation (unadjusted rate 4.2% versus 6.0%; adjusted subdistribution hazard ratio [sHR] 0.26, 95% CI, 0.17-0.40, P less than .001).
There was no extra embolic stroke protection from S-LAAO in patients who were discharged on anticoagulation (sHR 0.88, 95% CI, 0.56-1.39; P = .59), but the risk of returning with a hemorrhagic stroke was considerably less (sHR 0.32, 95% CI, 0.17-0.57, P less than .001).
The S-LAAO group more commonly had nonparoxysmal AF, a higher ejection fraction, a lower mortality risk score, and lower rates of common stroke risks, such as diabetes, hypertension, and prior stroke. The Duke team adjusted for those and a long list of other confounders, including smoking, age, preoperative warfarin, and academic hospital status.
There were important limitations. No one knows what surgeons did to close the LAA, or how well it worked, and most patients discharged on anticoagulation were sent home on warfarin, not the newer direct oral anticoagulants.
The investigators noted that “the strongest data to date for LAAO come from randomized trials comparing warfarin with percutaneous LAAO using the WATCHMAN device” from Boston Scientific.
The reduction in cardiovascular mortality in those trials appeared to be driven by a reduction in hemorrhagic stroke and occurred despite increased rates of ischemic stroke, they said.
The current study, however, showed that S-LAAO was associated with a significantly lower rate of thromboembolism in patients without oral anticoagulation, the authors said.
The work was funded, in part, by the Food and Drug Administration. Dr. Friedman reported grants from Boston Scientific and Abbott. Other authors reported financial relations with those and several other companies.
SOURCE: Friedman DJ, et. al. JAMA. 2018;319(4):365-74. doi: 10.1001/jama.2017.20125.
The implications of the study may have far-reaching consequences on the best treatment to reduce both thromboembolism and hemorrhage associated with AF treatment.
There is a strong signal that S-LAAO may be equivalent to anticoagulation prophylaxis to avoid thromboembolism in certain patients. This possibility is intriguing because it suggests that S-LAAO may be as effective as anticoagulation and could potentially avoid the bleeding risks associated with anticoagulation. A reasonable hypothesis based on the authors’ findings is that ablation procedures that occlude the left atrial appendage are adequate treatments to avoid thromboembolism and to minimize postoperative anticoagulation-related hemorrhage. This somewhat novel hypothesis, if true, could avoid a significant morbidity associated with anticoagulation while providing adequate treatment for thromboembolic complications of AF.
Importantly, the results suggest that failure to perform an S-LAAO at the time of cardiac operation in patients with nonvalvular AF is associated with significantly increased intermediate-term thromboembolic risk.
Victor M. Ferraris , MD, PhD, a cardiothoracic surgeon at the University of Kentucky, Lexington, made his comments in an accompanying editorial. He had no conflicts of interest.
The implications of the study may have far-reaching consequences on the best treatment to reduce both thromboembolism and hemorrhage associated with AF treatment.
There is a strong signal that S-LAAO may be equivalent to anticoagulation prophylaxis to avoid thromboembolism in certain patients. This possibility is intriguing because it suggests that S-LAAO may be as effective as anticoagulation and could potentially avoid the bleeding risks associated with anticoagulation. A reasonable hypothesis based on the authors’ findings is that ablation procedures that occlude the left atrial appendage are adequate treatments to avoid thromboembolism and to minimize postoperative anticoagulation-related hemorrhage. This somewhat novel hypothesis, if true, could avoid a significant morbidity associated with anticoagulation while providing adequate treatment for thromboembolic complications of AF.
Importantly, the results suggest that failure to perform an S-LAAO at the time of cardiac operation in patients with nonvalvular AF is associated with significantly increased intermediate-term thromboembolic risk.
Victor M. Ferraris , MD, PhD, a cardiothoracic surgeon at the University of Kentucky, Lexington, made his comments in an accompanying editorial. He had no conflicts of interest.
The implications of the study may have far-reaching consequences on the best treatment to reduce both thromboembolism and hemorrhage associated with AF treatment.
There is a strong signal that S-LAAO may be equivalent to anticoagulation prophylaxis to avoid thromboembolism in certain patients. This possibility is intriguing because it suggests that S-LAAO may be as effective as anticoagulation and could potentially avoid the bleeding risks associated with anticoagulation. A reasonable hypothesis based on the authors’ findings is that ablation procedures that occlude the left atrial appendage are adequate treatments to avoid thromboembolism and to minimize postoperative anticoagulation-related hemorrhage. This somewhat novel hypothesis, if true, could avoid a significant morbidity associated with anticoagulation while providing adequate treatment for thromboembolic complications of AF.
Importantly, the results suggest that failure to perform an S-LAAO at the time of cardiac operation in patients with nonvalvular AF is associated with significantly increased intermediate-term thromboembolic risk.
Victor M. Ferraris , MD, PhD, a cardiothoracic surgeon at the University of Kentucky, Lexington, made his comments in an accompanying editorial. He had no conflicts of interest.
Surgical left atrial appendage occlusion may be just as good as anticoagulation at preventing thromboembolic events in older people with atrial fibrillation, with less risk of bleeding into the brain, according to a database review of more than 10,000 patients.
Among elderly atrial fibrillation patients who underwent heart surgery with no oral follow-up oral anticoagulation, those who had the left atrial appendage surgically occluded were 74% less likely than were those who did not to be readmitted for a major thromboembolic event within 3 years, and 68% less likely to be readmitted for a hemorrhagic stroke, researchers at Duke University in Durham, N.C., found.
“The current study demonstrated that S-LAAO [surgical left atrial appendage occlusion] was associated with a significantly lower rate of thromboembolism among patients without oral anticoagulation. In the cohort of patients discharged with oral anticoagulation, S-LAAO was not associated with [reduced] thromboembolism but was associated with a lower risk for hemorrhagic stroke presumably related to eventual discontinuation of oral anticoagulation among S-LAAO patients,” reported Daniel Friedman, MD, and his coinvestigators. The study was published Jan. 23 in JAMA.
In short, the findings suggest that shutting down the left atrial appendage in older patients offers the same stroke protection as anticoagulation, but without the bleeding risk. Given the low rates of anticoagulant use, physicians have been considering that approach for a while. Even so, it’s only been a weak (IIb) recommendation so far in AF guidelines because of the lack of evidence.
That might change soon, but “additional randomized studies comparing S-LAAO without anticoagulation [versus] systemic anticoagulation alone will be needed to define the optimal use of S-LAAO,” said Dr. Friedman, a cardiothoracic surgeon at Duke, and his colleagues. Those studies are in the works.
The team found 10,524 older patients in the Society of Thoracic Surgeons Adult Cardiac Surgery Database during 2011-2012, and linked them to Medicare data so they could be followed for up to 3 years. About a third of the subjects had stand-alone coronary artery bypass grafting; the rest had mitral or aortic valve repairs with or without CABG.
The investigators compared outcomes among the 37% (3,892) who had S-LAAO with outcomes among those who did not. Participants were a median of 76 years of age, 61% were men, and they were all at high risk for AF stroke.
After a mean follow-up of 2.6 years, subjects who received S-LAAO without postoperative anticoagulation had a significantly lower risk of readmission for thromboembolism – stroke, transient ischemic attack, or systemic embolism – compared with those who received neither S-LAAO nor anticoagulation (unadjusted rate 4.2% versus 6.0%; adjusted subdistribution hazard ratio [sHR] 0.26, 95% CI, 0.17-0.40, P less than .001).
There was no extra embolic stroke protection from S-LAAO in patients who were discharged on anticoagulation (sHR 0.88, 95% CI, 0.56-1.39; P = .59), but the risk of returning with a hemorrhagic stroke was considerably less (sHR 0.32, 95% CI, 0.17-0.57, P less than .001).
The S-LAAO group more commonly had nonparoxysmal AF, a higher ejection fraction, a lower mortality risk score, and lower rates of common stroke risks, such as diabetes, hypertension, and prior stroke. The Duke team adjusted for those and a long list of other confounders, including smoking, age, preoperative warfarin, and academic hospital status.
There were important limitations. No one knows what surgeons did to close the LAA, or how well it worked, and most patients discharged on anticoagulation were sent home on warfarin, not the newer direct oral anticoagulants.
The investigators noted that “the strongest data to date for LAAO come from randomized trials comparing warfarin with percutaneous LAAO using the WATCHMAN device” from Boston Scientific.
The reduction in cardiovascular mortality in those trials appeared to be driven by a reduction in hemorrhagic stroke and occurred despite increased rates of ischemic stroke, they said.
The current study, however, showed that S-LAAO was associated with a significantly lower rate of thromboembolism in patients without oral anticoagulation, the authors said.
The work was funded, in part, by the Food and Drug Administration. Dr. Friedman reported grants from Boston Scientific and Abbott. Other authors reported financial relations with those and several other companies.
SOURCE: Friedman DJ, et. al. JAMA. 2018;319(4):365-74. doi: 10.1001/jama.2017.20125.
Surgical left atrial appendage occlusion may be just as good as anticoagulation at preventing thromboembolic events in older people with atrial fibrillation, with less risk of bleeding into the brain, according to a database review of more than 10,000 patients.
Among elderly atrial fibrillation patients who underwent heart surgery with no oral follow-up oral anticoagulation, those who had the left atrial appendage surgically occluded were 74% less likely than were those who did not to be readmitted for a major thromboembolic event within 3 years, and 68% less likely to be readmitted for a hemorrhagic stroke, researchers at Duke University in Durham, N.C., found.
“The current study demonstrated that S-LAAO [surgical left atrial appendage occlusion] was associated with a significantly lower rate of thromboembolism among patients without oral anticoagulation. In the cohort of patients discharged with oral anticoagulation, S-LAAO was not associated with [reduced] thromboembolism but was associated with a lower risk for hemorrhagic stroke presumably related to eventual discontinuation of oral anticoagulation among S-LAAO patients,” reported Daniel Friedman, MD, and his coinvestigators. The study was published Jan. 23 in JAMA.
In short, the findings suggest that shutting down the left atrial appendage in older patients offers the same stroke protection as anticoagulation, but without the bleeding risk. Given the low rates of anticoagulant use, physicians have been considering that approach for a while. Even so, it’s only been a weak (IIb) recommendation so far in AF guidelines because of the lack of evidence.
That might change soon, but “additional randomized studies comparing S-LAAO without anticoagulation [versus] systemic anticoagulation alone will be needed to define the optimal use of S-LAAO,” said Dr. Friedman, a cardiothoracic surgeon at Duke, and his colleagues. Those studies are in the works.
The team found 10,524 older patients in the Society of Thoracic Surgeons Adult Cardiac Surgery Database during 2011-2012, and linked them to Medicare data so they could be followed for up to 3 years. About a third of the subjects had stand-alone coronary artery bypass grafting; the rest had mitral or aortic valve repairs with or without CABG.
The investigators compared outcomes among the 37% (3,892) who had S-LAAO with outcomes among those who did not. Participants were a median of 76 years of age, 61% were men, and they were all at high risk for AF stroke.
After a mean follow-up of 2.6 years, subjects who received S-LAAO without postoperative anticoagulation had a significantly lower risk of readmission for thromboembolism – stroke, transient ischemic attack, or systemic embolism – compared with those who received neither S-LAAO nor anticoagulation (unadjusted rate 4.2% versus 6.0%; adjusted subdistribution hazard ratio [sHR] 0.26, 95% CI, 0.17-0.40, P less than .001).
There was no extra embolic stroke protection from S-LAAO in patients who were discharged on anticoagulation (sHR 0.88, 95% CI, 0.56-1.39; P = .59), but the risk of returning with a hemorrhagic stroke was considerably less (sHR 0.32, 95% CI, 0.17-0.57, P less than .001).
The S-LAAO group more commonly had nonparoxysmal AF, a higher ejection fraction, a lower mortality risk score, and lower rates of common stroke risks, such as diabetes, hypertension, and prior stroke. The Duke team adjusted for those and a long list of other confounders, including smoking, age, preoperative warfarin, and academic hospital status.
There were important limitations. No one knows what surgeons did to close the LAA, or how well it worked, and most patients discharged on anticoagulation were sent home on warfarin, not the newer direct oral anticoagulants.
The investigators noted that “the strongest data to date for LAAO come from randomized trials comparing warfarin with percutaneous LAAO using the WATCHMAN device” from Boston Scientific.
The reduction in cardiovascular mortality in those trials appeared to be driven by a reduction in hemorrhagic stroke and occurred despite increased rates of ischemic stroke, they said.
The current study, however, showed that S-LAAO was associated with a significantly lower rate of thromboembolism in patients without oral anticoagulation, the authors said.
The work was funded, in part, by the Food and Drug Administration. Dr. Friedman reported grants from Boston Scientific and Abbott. Other authors reported financial relations with those and several other companies.
SOURCE: Friedman DJ, et. al. JAMA. 2018;319(4):365-74. doi: 10.1001/jama.2017.20125.
FROM JAMA
Key clinical point: Surgical left atrial appendage occlusion (S-LAAO) is probably just as good as anticoagulation at preventing thromboembolic events in older people with atrial fibrillation, with less risk of bleeding into the brain.
Major finding: within 3 years, and 68% less likely to be readmitted for a hemorrhagic stroke.
Study details: Database review of more than 10,000 elderly AF patients followed for up to 3 years after cardiac surgery.
Disclosures: The work was funded, in part, by the Food and Drug Administration. The authors had financial ties to Boston Scientific, Abbott, and several other companies.
Source: Friedman DJ, et. al. JAMA. 2018;319(4):365-74. doi: 10.1001/jama.2017.20125
Differentiating Trigeminal Motor Neuropathy and Progressive Hemifacial Atrophy
To the Editor:
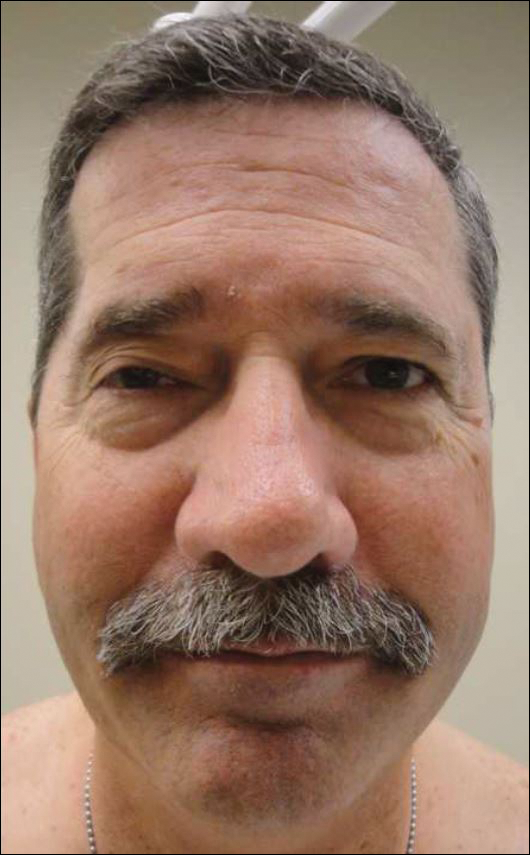
Trigeminal motor neuropathy is a rare condition presenting with muscle weakness and atrophy in the distribution of the trigeminal nerve without sensory changes. We present a challenging case with clinical features that mimic progressive hemifacial atrophy (PHA), a disease characterized by slowly progressive, unilateral facial atrophy that can be accompanied by inflammation and sclerosis as early features.
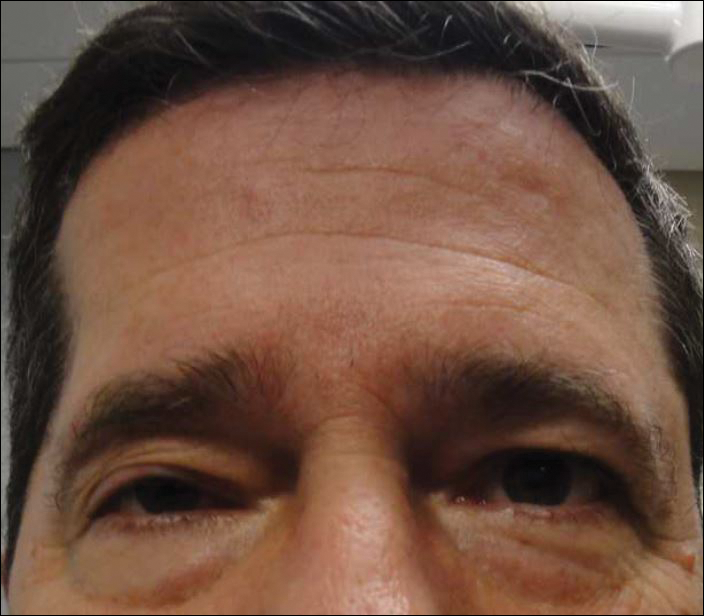
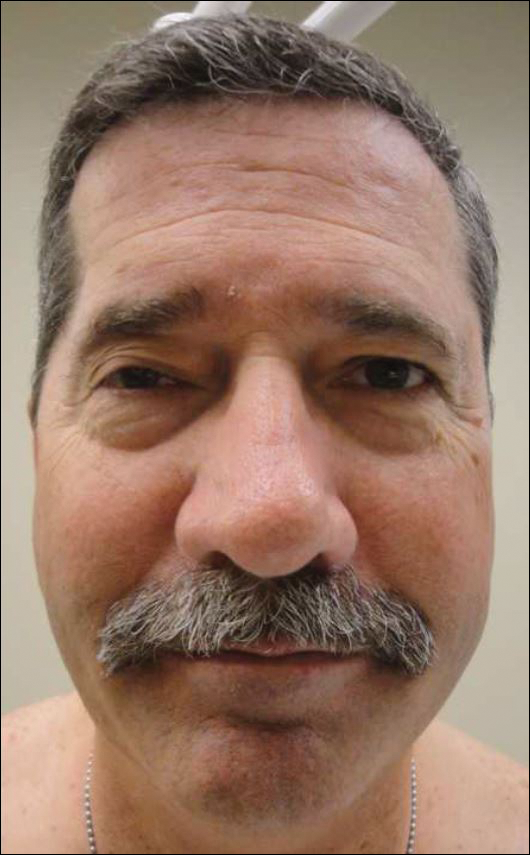
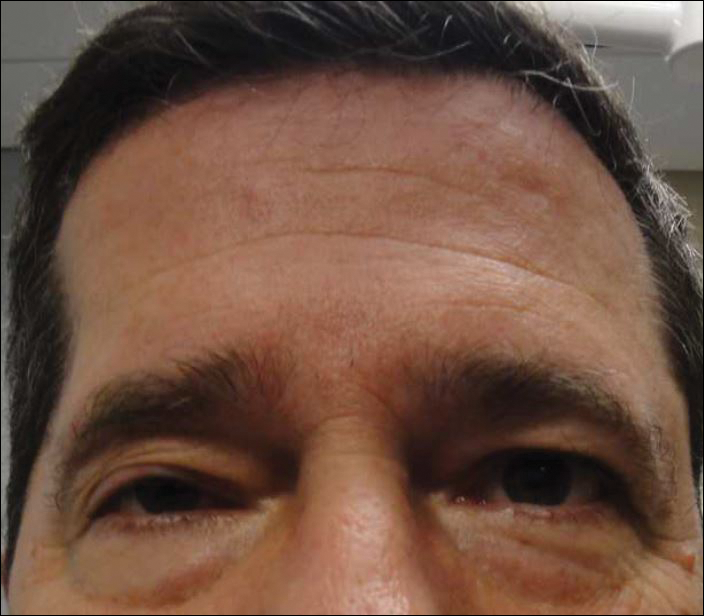
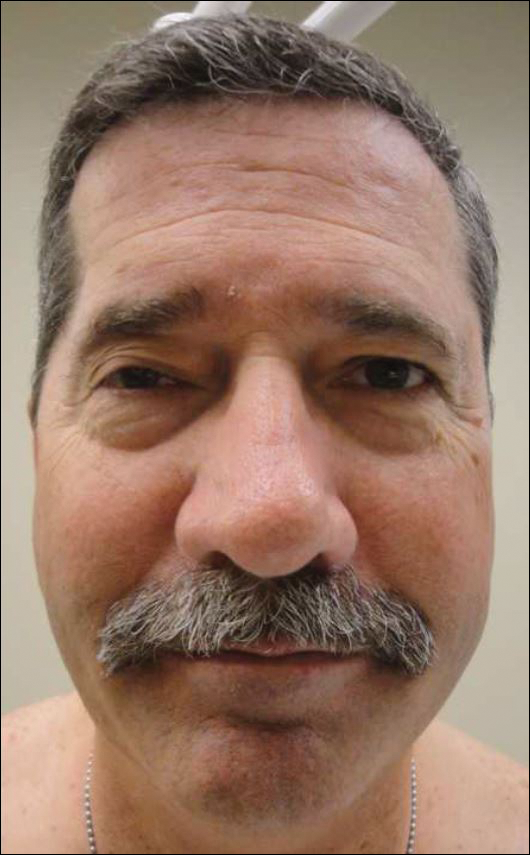
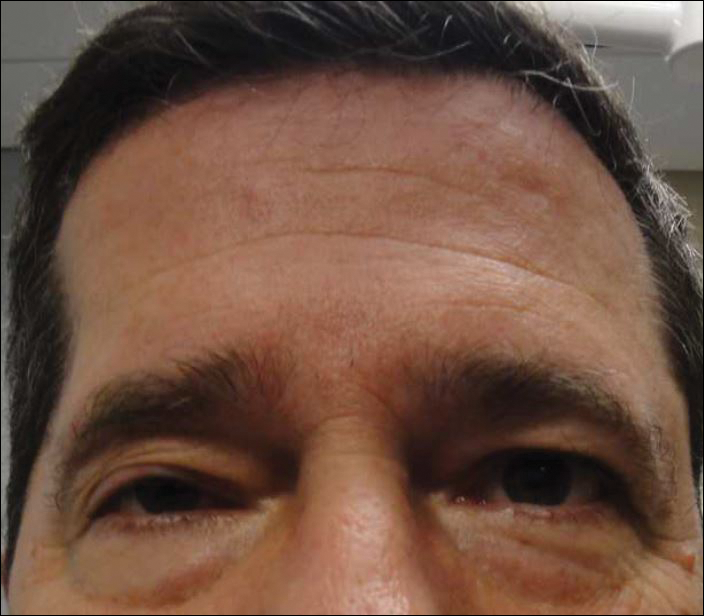
A 55-year-old man presented with right-sided ptosis and progressive right-sided facial atrophy of 4 years’ duration. A clinical diagnosis of PHA was made by the rheumatology department, and the patient was referred to the dermatology department for further evaluation. Examination at presentation revealed right-sided subcutaneous atrophy of the cheek, temple, and forehead extending to the scalp with absence of sclerosis, pigmentary alteration, or typical linear morphea lesions (Figures 1 and 2). The patient had no sensory changes in the affected area.
Workup by the dermatology department included magnetic resonance imaging (MRI) of the face and scalp, which demonstrated denervation muscle atrophy exclusively in the distribution of the third branch of the right trigeminal nerve, including severe atrophy of the right temporalis and masseter muscles and moderate atrophy of the pterygoid muscles. No signs of inflammation, fibrosis, or atrophy of the skin or subcutaneous fat were found, ruling out a diagnosis of PHA.
The patient was referred to the neurology department where he was found to have a normal neurologic examination with the exception of right-sided ptosis and temporalis and masseter muscle atrophy. Notably, the patient had normal sensation in the distribution of the trigeminal nerve and normal strength of the masseter and temporalis muscles.
An extensive workup by the neurology department was completed, including magnetic resonance angiography, eyeblink testing, and testing for causes of neuropathies (eg, infectious, autoimmune, vitamin deficiencies, toxin related). Of note, magnetic resonance angiography showed no abnormalities within the cavernous sinus or trigeminal cave but showed potential vascular compression of the trigeminal nerve, which was believed to be an incidental finding. The remainder of the workup was unremarkable. Based on muscle denervation atrophy in the distribution of the third branch of the trigeminal nerve in the absence of sensory symptoms or deficits, the patient’s presentation was consistent with trigeminal motor neuropathy.
In reported cases, the pathogenesis of trigeminal motor neuropathy is attributed to tumors, trauma, stroke, viral infection, and autoimmune reaction.1-6 In other reported cases the cause is unknown,6-8 as was the case in our patient. Magnetic resonance angiography revealed potential vascular compression of the trigeminal nerve, which has been previously reported to cause trigeminal neuropathy.9 However, patients with trigeminal neuropathy presented with sensory changes in the distribution of the trigeminal nerve as opposed to motor symptoms and muscle atrophy.
We present a case of trigeminal motor neuropathy presenting as PHA. Progressive hemifacial atrophy is a rare, slowly progressive disease characterized by unilateral atrophy of the skin, subcutis, muscle, and bony structures of the face. Onset usually is during childhood, though later onset has been reported.10 The pathogenesis of PHA is not well understood, though trauma, infection, immune-mediated causes, sympathetic dysfunction, and metabolic dysfunction have been proposed.11 Diagnosis of PHA typically is based on clinical presentation, but histology and imaging are useful. In contrast to trigeminal motor neuropathy, MRI findings in PHA demonstrate involvement of the skin.12
Differentiation between PHA and trigeminal motor neuropathy is important because treatment differs. Treatment of trigeminal motor neuropathy depends on the etiology and may include removal of underlying neoplasms, while treatment of PHA depends on disease activity. The initial goal when treating PHA is to improve symptoms and slow disease progression; immunosuppressants may be considered. Facial reconstruction is an option when PHA is stable.
In this case, the features differentiating trigeminal motor neuropathy from PHA include age of onset and MRI as well as clinical findings of muscle atrophy limited to the distribution of the third branch of the trigeminal nerve. Although PHA is a rare disorder, this case demonstrates the importance of including trigeminal motor neuropathy in the differential diagnosis.
- Beydoun SR. Unilateral trigeminal motor neuropathy as a presenting feature of neurofibromatosis type 2 (NF2). Muscle Nerve. 1993;16:1136-1137.
- Kang YK, Lee EH, Hwang M. Pure trigeminal motor neuropathy: a case report. Arch Phys Med Rehabil. 2000;81:995-998.
- Kim DH, Kim JK, Kang JY. Pure motor trigeminal neuropathy in a woman with tegmental pontine infarction. J Clin Neurosci. 2013;20:1792-1794.
- Ko KF, Chan KL. A case of isolated pure trigeminal motor neuropathy. Clin Neurol Neurosurg. 1995;97:199-200.
- Park KS, Chung JM, Jeon BS, et al. Unilateral trigeminal mandibular motor neuropathy caused by tumor in the foramen ovale. J Clin Neurol. 2006;2:194-197.
- Chia LG. Pure trigeminal motor neuropathy. Br Med J (Clin Res Ed). 1988;296:609-610.
- Braun JS, Hahn K, Bauknecht HC, et al. Progressive facial asymmetry due to trigeminal motor neuropathy. Eur Neurol. 2006;55:96-98.
- Chiba M, Echigo S. Unilateral atrophy of the masticatory muscles and mandibular ramus due to pure trigeminal motor neuropathy: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:E30-E34.
- Jannetta PJ, Robbins LJ. Trigeminal neuropathy—new observations. Neurosurgery. 1980;7:347-351.
- Stone J. Parry-Romberg syndrome: a global survey of 205 patients using the Internet. Neurology. 2003;61:674-676.
- El-Kehdy J, Abbas O, Rubeiz N. A review of Parry-Romberg syndrome. J Am Acad Dermatol. 2012;67:769-784.
- Taylor HM, Robinson R, Cox T. Progressive facial hemiatrophy: MRI appearances. Dev Med Child Neurol. 1997;39:484-486.
To the Editor:
Trigeminal motor neuropathy is a rare condition presenting with muscle weakness and atrophy in the distribution of the trigeminal nerve without sensory changes. We present a challenging case with clinical features that mimic progressive hemifacial atrophy (PHA), a disease characterized by slowly progressive, unilateral facial atrophy that can be accompanied by inflammation and sclerosis as early features.
A 55-year-old man presented with right-sided ptosis and progressive right-sided facial atrophy of 4 years’ duration. A clinical diagnosis of PHA was made by the rheumatology department, and the patient was referred to the dermatology department for further evaluation. Examination at presentation revealed right-sided subcutaneous atrophy of the cheek, temple, and forehead extending to the scalp with absence of sclerosis, pigmentary alteration, or typical linear morphea lesions (Figures 1 and 2). The patient had no sensory changes in the affected area.
Workup by the dermatology department included magnetic resonance imaging (MRI) of the face and scalp, which demonstrated denervation muscle atrophy exclusively in the distribution of the third branch of the right trigeminal nerve, including severe atrophy of the right temporalis and masseter muscles and moderate atrophy of the pterygoid muscles. No signs of inflammation, fibrosis, or atrophy of the skin or subcutaneous fat were found, ruling out a diagnosis of PHA.
The patient was referred to the neurology department where he was found to have a normal neurologic examination with the exception of right-sided ptosis and temporalis and masseter muscle atrophy. Notably, the patient had normal sensation in the distribution of the trigeminal nerve and normal strength of the masseter and temporalis muscles.
An extensive workup by the neurology department was completed, including magnetic resonance angiography, eyeblink testing, and testing for causes of neuropathies (eg, infectious, autoimmune, vitamin deficiencies, toxin related). Of note, magnetic resonance angiography showed no abnormalities within the cavernous sinus or trigeminal cave but showed potential vascular compression of the trigeminal nerve, which was believed to be an incidental finding. The remainder of the workup was unremarkable. Based on muscle denervation atrophy in the distribution of the third branch of the trigeminal nerve in the absence of sensory symptoms or deficits, the patient’s presentation was consistent with trigeminal motor neuropathy.
In reported cases, the pathogenesis of trigeminal motor neuropathy is attributed to tumors, trauma, stroke, viral infection, and autoimmune reaction.1-6 In other reported cases the cause is unknown,6-8 as was the case in our patient. Magnetic resonance angiography revealed potential vascular compression of the trigeminal nerve, which has been previously reported to cause trigeminal neuropathy.9 However, patients with trigeminal neuropathy presented with sensory changes in the distribution of the trigeminal nerve as opposed to motor symptoms and muscle atrophy.
We present a case of trigeminal motor neuropathy presenting as PHA. Progressive hemifacial atrophy is a rare, slowly progressive disease characterized by unilateral atrophy of the skin, subcutis, muscle, and bony structures of the face. Onset usually is during childhood, though later onset has been reported.10 The pathogenesis of PHA is not well understood, though trauma, infection, immune-mediated causes, sympathetic dysfunction, and metabolic dysfunction have been proposed.11 Diagnosis of PHA typically is based on clinical presentation, but histology and imaging are useful. In contrast to trigeminal motor neuropathy, MRI findings in PHA demonstrate involvement of the skin.12
Differentiation between PHA and trigeminal motor neuropathy is important because treatment differs. Treatment of trigeminal motor neuropathy depends on the etiology and may include removal of underlying neoplasms, while treatment of PHA depends on disease activity. The initial goal when treating PHA is to improve symptoms and slow disease progression; immunosuppressants may be considered. Facial reconstruction is an option when PHA is stable.
In this case, the features differentiating trigeminal motor neuropathy from PHA include age of onset and MRI as well as clinical findings of muscle atrophy limited to the distribution of the third branch of the trigeminal nerve. Although PHA is a rare disorder, this case demonstrates the importance of including trigeminal motor neuropathy in the differential diagnosis.
To the Editor:
Trigeminal motor neuropathy is a rare condition presenting with muscle weakness and atrophy in the distribution of the trigeminal nerve without sensory changes. We present a challenging case with clinical features that mimic progressive hemifacial atrophy (PHA), a disease characterized by slowly progressive, unilateral facial atrophy that can be accompanied by inflammation and sclerosis as early features.
A 55-year-old man presented with right-sided ptosis and progressive right-sided facial atrophy of 4 years’ duration. A clinical diagnosis of PHA was made by the rheumatology department, and the patient was referred to the dermatology department for further evaluation. Examination at presentation revealed right-sided subcutaneous atrophy of the cheek, temple, and forehead extending to the scalp with absence of sclerosis, pigmentary alteration, or typical linear morphea lesions (Figures 1 and 2). The patient had no sensory changes in the affected area.
Workup by the dermatology department included magnetic resonance imaging (MRI) of the face and scalp, which demonstrated denervation muscle atrophy exclusively in the distribution of the third branch of the right trigeminal nerve, including severe atrophy of the right temporalis and masseter muscles and moderate atrophy of the pterygoid muscles. No signs of inflammation, fibrosis, or atrophy of the skin or subcutaneous fat were found, ruling out a diagnosis of PHA.
The patient was referred to the neurology department where he was found to have a normal neurologic examination with the exception of right-sided ptosis and temporalis and masseter muscle atrophy. Notably, the patient had normal sensation in the distribution of the trigeminal nerve and normal strength of the masseter and temporalis muscles.
An extensive workup by the neurology department was completed, including magnetic resonance angiography, eyeblink testing, and testing for causes of neuropathies (eg, infectious, autoimmune, vitamin deficiencies, toxin related). Of note, magnetic resonance angiography showed no abnormalities within the cavernous sinus or trigeminal cave but showed potential vascular compression of the trigeminal nerve, which was believed to be an incidental finding. The remainder of the workup was unremarkable. Based on muscle denervation atrophy in the distribution of the third branch of the trigeminal nerve in the absence of sensory symptoms or deficits, the patient’s presentation was consistent with trigeminal motor neuropathy.
In reported cases, the pathogenesis of trigeminal motor neuropathy is attributed to tumors, trauma, stroke, viral infection, and autoimmune reaction.1-6 In other reported cases the cause is unknown,6-8 as was the case in our patient. Magnetic resonance angiography revealed potential vascular compression of the trigeminal nerve, which has been previously reported to cause trigeminal neuropathy.9 However, patients with trigeminal neuropathy presented with sensory changes in the distribution of the trigeminal nerve as opposed to motor symptoms and muscle atrophy.
We present a case of trigeminal motor neuropathy presenting as PHA. Progressive hemifacial atrophy is a rare, slowly progressive disease characterized by unilateral atrophy of the skin, subcutis, muscle, and bony structures of the face. Onset usually is during childhood, though later onset has been reported.10 The pathogenesis of PHA is not well understood, though trauma, infection, immune-mediated causes, sympathetic dysfunction, and metabolic dysfunction have been proposed.11 Diagnosis of PHA typically is based on clinical presentation, but histology and imaging are useful. In contrast to trigeminal motor neuropathy, MRI findings in PHA demonstrate involvement of the skin.12
Differentiation between PHA and trigeminal motor neuropathy is important because treatment differs. Treatment of trigeminal motor neuropathy depends on the etiology and may include removal of underlying neoplasms, while treatment of PHA depends on disease activity. The initial goal when treating PHA is to improve symptoms and slow disease progression; immunosuppressants may be considered. Facial reconstruction is an option when PHA is stable.
In this case, the features differentiating trigeminal motor neuropathy from PHA include age of onset and MRI as well as clinical findings of muscle atrophy limited to the distribution of the third branch of the trigeminal nerve. Although PHA is a rare disorder, this case demonstrates the importance of including trigeminal motor neuropathy in the differential diagnosis.
- Beydoun SR. Unilateral trigeminal motor neuropathy as a presenting feature of neurofibromatosis type 2 (NF2). Muscle Nerve. 1993;16:1136-1137.
- Kang YK, Lee EH, Hwang M. Pure trigeminal motor neuropathy: a case report. Arch Phys Med Rehabil. 2000;81:995-998.
- Kim DH, Kim JK, Kang JY. Pure motor trigeminal neuropathy in a woman with tegmental pontine infarction. J Clin Neurosci. 2013;20:1792-1794.
- Ko KF, Chan KL. A case of isolated pure trigeminal motor neuropathy. Clin Neurol Neurosurg. 1995;97:199-200.
- Park KS, Chung JM, Jeon BS, et al. Unilateral trigeminal mandibular motor neuropathy caused by tumor in the foramen ovale. J Clin Neurol. 2006;2:194-197.
- Chia LG. Pure trigeminal motor neuropathy. Br Med J (Clin Res Ed). 1988;296:609-610.
- Braun JS, Hahn K, Bauknecht HC, et al. Progressive facial asymmetry due to trigeminal motor neuropathy. Eur Neurol. 2006;55:96-98.
- Chiba M, Echigo S. Unilateral atrophy of the masticatory muscles and mandibular ramus due to pure trigeminal motor neuropathy: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:E30-E34.
- Jannetta PJ, Robbins LJ. Trigeminal neuropathy—new observations. Neurosurgery. 1980;7:347-351.
- Stone J. Parry-Romberg syndrome: a global survey of 205 patients using the Internet. Neurology. 2003;61:674-676.
- El-Kehdy J, Abbas O, Rubeiz N. A review of Parry-Romberg syndrome. J Am Acad Dermatol. 2012;67:769-784.
- Taylor HM, Robinson R, Cox T. Progressive facial hemiatrophy: MRI appearances. Dev Med Child Neurol. 1997;39:484-486.
- Beydoun SR. Unilateral trigeminal motor neuropathy as a presenting feature of neurofibromatosis type 2 (NF2). Muscle Nerve. 1993;16:1136-1137.
- Kang YK, Lee EH, Hwang M. Pure trigeminal motor neuropathy: a case report. Arch Phys Med Rehabil. 2000;81:995-998.
- Kim DH, Kim JK, Kang JY. Pure motor trigeminal neuropathy in a woman with tegmental pontine infarction. J Clin Neurosci. 2013;20:1792-1794.
- Ko KF, Chan KL. A case of isolated pure trigeminal motor neuropathy. Clin Neurol Neurosurg. 1995;97:199-200.
- Park KS, Chung JM, Jeon BS, et al. Unilateral trigeminal mandibular motor neuropathy caused by tumor in the foramen ovale. J Clin Neurol. 2006;2:194-197.
- Chia LG. Pure trigeminal motor neuropathy. Br Med J (Clin Res Ed). 1988;296:609-610.
- Braun JS, Hahn K, Bauknecht HC, et al. Progressive facial asymmetry due to trigeminal motor neuropathy. Eur Neurol. 2006;55:96-98.
- Chiba M, Echigo S. Unilateral atrophy of the masticatory muscles and mandibular ramus due to pure trigeminal motor neuropathy: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:E30-E34.
- Jannetta PJ, Robbins LJ. Trigeminal neuropathy—new observations. Neurosurgery. 1980;7:347-351.
- Stone J. Parry-Romberg syndrome: a global survey of 205 patients using the Internet. Neurology. 2003;61:674-676.
- El-Kehdy J, Abbas O, Rubeiz N. A review of Parry-Romberg syndrome. J Am Acad Dermatol. 2012;67:769-784.
- Taylor HM, Robinson R, Cox T. Progressive facial hemiatrophy: MRI appearances. Dev Med Child Neurol. 1997;39:484-486.
Practice Points
- The differential diagnosis of progressive hemifacial atrophy includes disorders of the trigeminal nerve.
- Trigeminal motor neuropathy presents with muscle weakness and atrophy without involvement of the skin, subcutis, or bone.
Study probes predictors of response to vedolizumab
LAS VEGAS – , a small, single-center study showed.
“Right now there are a variety of medications to treat Crohn’s disease, but there isn’t a set criteria [for] what [drug] works for which kind of patient,” Adam A. Dhedhi, MD, said in an interview at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association. “We’re trying to figure out if we can find a predictor of response to vedolizumab.” Manufactured by Millennium Pharmaceuticals, vedolizumab is a gut-selective monoclonal antibody to alpha4beta7 integrin that prevents transportation of leukocytes into gastrointestinal mucosa.
He and his associates reported that a low CRP value at time of initiation (a mean of 6.6 mg/L) was found to be a positive predictor of both response and remission (odds ratio, 0.3045; P = .001), while the mean CRP value for nonresponders was 29.9 mg/L. In addition, any smoking history was a predictor of poor response to vedolizumab (OR, 0.0008; P = .009). “That was surprising and useful information to carry forward,” Dr. Dhedhi said. “If you’re making a decision between an anti-TNF [tumor necrosis factor] agent and vedolizumab, [and] if the patient is a smoker or has a higher active disease state, that may help tip the scales one way or the other.” In their abstract, the researchers noted that cigarette smoke “has been found to be involved in beta-2 integrin activation and neutrophil migration in lung tissue and may play a similar role in the gut” (Respiratory Research 2011;12[1]:75). Dr. Dhedhi and his associates also found that more than half of patients who had previously used two or more anti-TNF therapies (58%) achieved remission, compared with 47% who had used one prior anti-TNF drug and 43% who were anti-TNF naive.
He acknowledged certain limitations of the study, including its retrospective design and small sample size. Dr. Dhedhi reported having no financial disclosures.
*This story was updated on 3/26.
SOURCE: Dhedhi AA et al. Crohn’s & Colitis Congress, Poster 207.
LAS VEGAS – , a small, single-center study showed.
“Right now there are a variety of medications to treat Crohn’s disease, but there isn’t a set criteria [for] what [drug] works for which kind of patient,” Adam A. Dhedhi, MD, said in an interview at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association. “We’re trying to figure out if we can find a predictor of response to vedolizumab.” Manufactured by Millennium Pharmaceuticals, vedolizumab is a gut-selective monoclonal antibody to alpha4beta7 integrin that prevents transportation of leukocytes into gastrointestinal mucosa.
He and his associates reported that a low CRP value at time of initiation (a mean of 6.6 mg/L) was found to be a positive predictor of both response and remission (odds ratio, 0.3045; P = .001), while the mean CRP value for nonresponders was 29.9 mg/L. In addition, any smoking history was a predictor of poor response to vedolizumab (OR, 0.0008; P = .009). “That was surprising and useful information to carry forward,” Dr. Dhedhi said. “If you’re making a decision between an anti-TNF [tumor necrosis factor] agent and vedolizumab, [and] if the patient is a smoker or has a higher active disease state, that may help tip the scales one way or the other.” In their abstract, the researchers noted that cigarette smoke “has been found to be involved in beta-2 integrin activation and neutrophil migration in lung tissue and may play a similar role in the gut” (Respiratory Research 2011;12[1]:75). Dr. Dhedhi and his associates also found that more than half of patients who had previously used two or more anti-TNF therapies (58%) achieved remission, compared with 47% who had used one prior anti-TNF drug and 43% who were anti-TNF naive.
He acknowledged certain limitations of the study, including its retrospective design and small sample size. Dr. Dhedhi reported having no financial disclosures.
*This story was updated on 3/26.
SOURCE: Dhedhi AA et al. Crohn’s & Colitis Congress, Poster 207.
LAS VEGAS – , a small, single-center study showed.
“Right now there are a variety of medications to treat Crohn’s disease, but there isn’t a set criteria [for] what [drug] works for which kind of patient,” Adam A. Dhedhi, MD, said in an interview at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association. “We’re trying to figure out if we can find a predictor of response to vedolizumab.” Manufactured by Millennium Pharmaceuticals, vedolizumab is a gut-selective monoclonal antibody to alpha4beta7 integrin that prevents transportation of leukocytes into gastrointestinal mucosa.
He and his associates reported that a low CRP value at time of initiation (a mean of 6.6 mg/L) was found to be a positive predictor of both response and remission (odds ratio, 0.3045; P = .001), while the mean CRP value for nonresponders was 29.9 mg/L. In addition, any smoking history was a predictor of poor response to vedolizumab (OR, 0.0008; P = .009). “That was surprising and useful information to carry forward,” Dr. Dhedhi said. “If you’re making a decision between an anti-TNF [tumor necrosis factor] agent and vedolizumab, [and] if the patient is a smoker or has a higher active disease state, that may help tip the scales one way or the other.” In their abstract, the researchers noted that cigarette smoke “has been found to be involved in beta-2 integrin activation and neutrophil migration in lung tissue and may play a similar role in the gut” (Respiratory Research 2011;12[1]:75). Dr. Dhedhi and his associates also found that more than half of patients who had previously used two or more anti-TNF therapies (58%) achieved remission, compared with 47% who had used one prior anti-TNF drug and 43% who were anti-TNF naive.
He acknowledged certain limitations of the study, including its retrospective design and small sample size. Dr. Dhedhi reported having no financial disclosures.
*This story was updated on 3/26.
SOURCE: Dhedhi AA et al. Crohn’s & Colitis Congress, Poster 207.
REPORTING FROM THE CROHN’S & COLITIS CONGRESS
Key clinical point: More aggressive Crohn’s disease or highly active disease is less likely to respond to vedolizumab therapy.
Major finding: A low baseline CRP level significantly predicted response and remission with vedolizumab (P = .001), while a history of smoking was a negative predictor of response and remission (P = .009).
Study details: A single-center, retrospective analysis of 45 Crohn’s patients treated with vedolizumab between 2014 and 2017.
Disclosures: Dr. Dhedhi reported having no financial disclosures.
Source: Dhedhi AA et al. Crohn’s & Colitis Congress, Poster 207.
Hungry or what?
“She will eat when she is hungry.” That in so many words is the mantra of grandparents blessed with experience and common sense and of most pediatricians when consulting parents challenged with a picky eater. From birth, children understand the simple equation that to survive they must eat. With rare exception, the motivating power of hunger can be leveraged for success even with infants who have spent their first months relying on enteral feedings. I have written an entire book based solely on the premise that if you present a young child food she will eat it ... eventually (“Coping With a Picky Eater: A Guide for the Perplexed Parent” New York: Simon and Schuster, 1998).
But if we reverse the words to read, “When she is eating, she is hungry,” do we have an equally valid observation? I think we have ample evidence that it is not.
The result was a year-long odyssey of pumping that included consultations with five different lactation consultants in the first frustrating month and a half. She eventually received some comforting advice from a pediatrician who reassured her that there was little research to guide her and to “just feed him; trust your instincts.”
While it is unfortunately true that there is very little good science we can fall back on when counseling women who are struggling with breastfeeding, I wonder about the wisdom of telling this mother to trust her instincts. I guess my hesitancy is based on 40 years of primary care pediatrics in which I could generally count on the instincts of young children, but their parents’ not so much. While maternal intuition is generally superior to the paternal version, I am hesitant to rely totally on either when facing a clinical dilemma such as defining hunger.
What about the fussy baby who is comforted by just a pacifier? What is the difference? There are several explanations, but it will require introducing the concept of nutrition deficiency.
Most babies who are satisfied with just a nipple, be it silicone or flesh, simply find sucking a comfort measure. A few, and I am sure you have seen some of them, are overly patient. They seem to be saying, “I need the calories, but you’re a good mom and I enjoy sucking. I can wait. Some day, you may make more milk or give me a bottle.” In the worst-case scenarios, their patience leaves these babies so nutritionally deficient that they can slip into apathy and die.
There are no easy answers. As pediatricians, our job is to sort out those fussy “hungry” babies whose behavior means they are overtired from those who are nutritionally deficient, from those with a dysfunctional satiety center. Making the differentiation is difficult but much easier than helping parents ignore one of their instincts.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
“She will eat when she is hungry.” That in so many words is the mantra of grandparents blessed with experience and common sense and of most pediatricians when consulting parents challenged with a picky eater. From birth, children understand the simple equation that to survive they must eat. With rare exception, the motivating power of hunger can be leveraged for success even with infants who have spent their first months relying on enteral feedings. I have written an entire book based solely on the premise that if you present a young child food she will eat it ... eventually (“Coping With a Picky Eater: A Guide for the Perplexed Parent” New York: Simon and Schuster, 1998).
But if we reverse the words to read, “When she is eating, she is hungry,” do we have an equally valid observation? I think we have ample evidence that it is not.
The result was a year-long odyssey of pumping that included consultations with five different lactation consultants in the first frustrating month and a half. She eventually received some comforting advice from a pediatrician who reassured her that there was little research to guide her and to “just feed him; trust your instincts.”
While it is unfortunately true that there is very little good science we can fall back on when counseling women who are struggling with breastfeeding, I wonder about the wisdom of telling this mother to trust her instincts. I guess my hesitancy is based on 40 years of primary care pediatrics in which I could generally count on the instincts of young children, but their parents’ not so much. While maternal intuition is generally superior to the paternal version, I am hesitant to rely totally on either when facing a clinical dilemma such as defining hunger.
What about the fussy baby who is comforted by just a pacifier? What is the difference? There are several explanations, but it will require introducing the concept of nutrition deficiency.
Most babies who are satisfied with just a nipple, be it silicone or flesh, simply find sucking a comfort measure. A few, and I am sure you have seen some of them, are overly patient. They seem to be saying, “I need the calories, but you’re a good mom and I enjoy sucking. I can wait. Some day, you may make more milk or give me a bottle.” In the worst-case scenarios, their patience leaves these babies so nutritionally deficient that they can slip into apathy and die.
There are no easy answers. As pediatricians, our job is to sort out those fussy “hungry” babies whose behavior means they are overtired from those who are nutritionally deficient, from those with a dysfunctional satiety center. Making the differentiation is difficult but much easier than helping parents ignore one of their instincts.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
“She will eat when she is hungry.” That in so many words is the mantra of grandparents blessed with experience and common sense and of most pediatricians when consulting parents challenged with a picky eater. From birth, children understand the simple equation that to survive they must eat. With rare exception, the motivating power of hunger can be leveraged for success even with infants who have spent their first months relying on enteral feedings. I have written an entire book based solely on the premise that if you present a young child food she will eat it ... eventually (“Coping With a Picky Eater: A Guide for the Perplexed Parent” New York: Simon and Schuster, 1998).
But if we reverse the words to read, “When she is eating, she is hungry,” do we have an equally valid observation? I think we have ample evidence that it is not.
The result was a year-long odyssey of pumping that included consultations with five different lactation consultants in the first frustrating month and a half. She eventually received some comforting advice from a pediatrician who reassured her that there was little research to guide her and to “just feed him; trust your instincts.”
While it is unfortunately true that there is very little good science we can fall back on when counseling women who are struggling with breastfeeding, I wonder about the wisdom of telling this mother to trust her instincts. I guess my hesitancy is based on 40 years of primary care pediatrics in which I could generally count on the instincts of young children, but their parents’ not so much. While maternal intuition is generally superior to the paternal version, I am hesitant to rely totally on either when facing a clinical dilemma such as defining hunger.
What about the fussy baby who is comforted by just a pacifier? What is the difference? There are several explanations, but it will require introducing the concept of nutrition deficiency.
Most babies who are satisfied with just a nipple, be it silicone or flesh, simply find sucking a comfort measure. A few, and I am sure you have seen some of them, are overly patient. They seem to be saying, “I need the calories, but you’re a good mom and I enjoy sucking. I can wait. Some day, you may make more milk or give me a bottle.” In the worst-case scenarios, their patience leaves these babies so nutritionally deficient that they can slip into apathy and die.
There are no easy answers. As pediatricians, our job is to sort out those fussy “hungry” babies whose behavior means they are overtired from those who are nutritionally deficient, from those with a dysfunctional satiety center. Making the differentiation is difficult but much easier than helping parents ignore one of their instincts.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Beware the COPD exacerbation
A 70-year-old man with chronic obstructive pulmonary disease (COPD) is admitted with increased shortness of breath. His O2 saturation levels are usually 90%, but they’re now running 84%-88%. He has had increasing symptoms for the past 3 days.

What would be your next step?
A) Begin a 5-day course of corticosteroids.
B) Begin a 14-day course of corticosteroids.
C) Begin azithromycin.
D) Start BiPAP.
E) Obtain D-dimer.
This is a situation we face frequently. COPD exacerbations are a clinical diagnosis that is often jumped to as the diagnosis in patients with COPD who have increasing dyspnea. This diagnosis is frequently correct – but not always.
Patients with COPD also may be at risk for or have heart failure, which can present with identical symptoms, including widespread wheezing. We are currently in a severe influenza epidemic, and influenza can mimic a COPD exacerbation or be the trigger.
About 20 years ago, I was out of the country when one of my patients with COPD was admitted to the hospital with a COPD exacerbation. I saw him in follow-up a week after his hospitalization. He was very dyspneic and had a room air oxygen saturation of 75%. He told me his dyspnea started a few days after he had injured his leg on a wood pile in his yard.
On exam, his right leg had 3+ edema; left leg, no edema. He reported to me that he was treated for 5 days with steroids and nebulizers, with minimal change in his dyspnea. I reviewed the chart, and five physicians had seen him while he was in the hospital. Starting with the emergency department, the diagnosis was COPD exacerbation, with no differential diagnosis in any note.
The patient had multiple pulmonary emboli, and he eventually improved with anticoagulation.
In 2009, Jacques Rizkallah, MD, and his colleagues published a systematic review and meta-analysis of articles looking at the prevalence of pulmonary emboli (PE) in patients diagnosed/treated for a COPD exacerbation.1 They found five articles comprising a total of 550 patients who met inclusion criteria. The prevalence was 19.9% (P = .014). The prevalence was much higher (24.7%) for hospitalized patients than it was for outpatients (3.3%). A very important finding in this study: There was no difference in symptoms between patients who did and did not have a pulmonary embolus.
Evrim Eylem Akpinar, MD, and colleagues studied all admissions for acute exacerbations of COPD at one hospital in Turkey over a 2-year period.2 A total of 172 patients admitted for COPD exacerbations were studied. The prevalence of pulmonary embolus was 29%.
In this study, patients who were obese or immobile were more likely to have pulmonary emboli. Pleuritic chest pain and lower-limb asymmetry were signs and symptoms more commonly found in patients who had PE. Obesity was the highest independent predictor (odds ratio, 4.97) for pulmonary embolus.
Floor Aleva, MD, and colleagues recently completed a systematic review and meta-analysis on prevalence and localization of pulmonary embolus in patients with acute exacerbations of COPD.3 They found similar numbers to the previous meta-analysis (16.1%) in a total of 880 patients. They also looked at location in the lungs of the emboli and found that two-thirds of the patients had pulmonary emboli in locations that had clear indication for anticoagulation treatment.
This is important, because criticisms of earlier studies were that clinically insignificant pulmonary emboli might be being found in the studies and that they had little to do with the patients’ symptoms.
In the case presented, I think that getting a D-dimer test would be the next best step. Acute exacerbation of COPD still is the most likely diagnosis, but PE is a plausible diagnosis that should be evaluated. If the D-dimer is normal, workup for PE would be complete. If elevated, then given the 20% prevalence of PE, a CT angiography would be warranted.
Key pearl: Among patients hospitalized for COPD exacerbations, 16%-24% have pulmonary embolism.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. Chest. 2009 Mar;135(3):786-93.
2. J Bras Pneumol. 2014 Jan-Feb;40(1):38-45.
3. Chest. 2017 Mar;151(3):544-54.
A 70-year-old man with chronic obstructive pulmonary disease (COPD) is admitted with increased shortness of breath. His O2 saturation levels are usually 90%, but they’re now running 84%-88%. He has had increasing symptoms for the past 3 days.

What would be your next step?
A) Begin a 5-day course of corticosteroids.
B) Begin a 14-day course of corticosteroids.
C) Begin azithromycin.
D) Start BiPAP.
E) Obtain D-dimer.
This is a situation we face frequently. COPD exacerbations are a clinical diagnosis that is often jumped to as the diagnosis in patients with COPD who have increasing dyspnea. This diagnosis is frequently correct – but not always.
Patients with COPD also may be at risk for or have heart failure, which can present with identical symptoms, including widespread wheezing. We are currently in a severe influenza epidemic, and influenza can mimic a COPD exacerbation or be the trigger.
About 20 years ago, I was out of the country when one of my patients with COPD was admitted to the hospital with a COPD exacerbation. I saw him in follow-up a week after his hospitalization. He was very dyspneic and had a room air oxygen saturation of 75%. He told me his dyspnea started a few days after he had injured his leg on a wood pile in his yard.
On exam, his right leg had 3+ edema; left leg, no edema. He reported to me that he was treated for 5 days with steroids and nebulizers, with minimal change in his dyspnea. I reviewed the chart, and five physicians had seen him while he was in the hospital. Starting with the emergency department, the diagnosis was COPD exacerbation, with no differential diagnosis in any note.
The patient had multiple pulmonary emboli, and he eventually improved with anticoagulation.
In 2009, Jacques Rizkallah, MD, and his colleagues published a systematic review and meta-analysis of articles looking at the prevalence of pulmonary emboli (PE) in patients diagnosed/treated for a COPD exacerbation.1 They found five articles comprising a total of 550 patients who met inclusion criteria. The prevalence was 19.9% (P = .014). The prevalence was much higher (24.7%) for hospitalized patients than it was for outpatients (3.3%). A very important finding in this study: There was no difference in symptoms between patients who did and did not have a pulmonary embolus.
Evrim Eylem Akpinar, MD, and colleagues studied all admissions for acute exacerbations of COPD at one hospital in Turkey over a 2-year period.2 A total of 172 patients admitted for COPD exacerbations were studied. The prevalence of pulmonary embolus was 29%.
In this study, patients who were obese or immobile were more likely to have pulmonary emboli. Pleuritic chest pain and lower-limb asymmetry were signs and symptoms more commonly found in patients who had PE. Obesity was the highest independent predictor (odds ratio, 4.97) for pulmonary embolus.
Floor Aleva, MD, and colleagues recently completed a systematic review and meta-analysis on prevalence and localization of pulmonary embolus in patients with acute exacerbations of COPD.3 They found similar numbers to the previous meta-analysis (16.1%) in a total of 880 patients. They also looked at location in the lungs of the emboli and found that two-thirds of the patients had pulmonary emboli in locations that had clear indication for anticoagulation treatment.
This is important, because criticisms of earlier studies were that clinically insignificant pulmonary emboli might be being found in the studies and that they had little to do with the patients’ symptoms.
In the case presented, I think that getting a D-dimer test would be the next best step. Acute exacerbation of COPD still is the most likely diagnosis, but PE is a plausible diagnosis that should be evaluated. If the D-dimer is normal, workup for PE would be complete. If elevated, then given the 20% prevalence of PE, a CT angiography would be warranted.
Key pearl: Among patients hospitalized for COPD exacerbations, 16%-24% have pulmonary embolism.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. Chest. 2009 Mar;135(3):786-93.
2. J Bras Pneumol. 2014 Jan-Feb;40(1):38-45.
3. Chest. 2017 Mar;151(3):544-54.
A 70-year-old man with chronic obstructive pulmonary disease (COPD) is admitted with increased shortness of breath. His O2 saturation levels are usually 90%, but they’re now running 84%-88%. He has had increasing symptoms for the past 3 days.

What would be your next step?
A) Begin a 5-day course of corticosteroids.
B) Begin a 14-day course of corticosteroids.
C) Begin azithromycin.
D) Start BiPAP.
E) Obtain D-dimer.
This is a situation we face frequently. COPD exacerbations are a clinical diagnosis that is often jumped to as the diagnosis in patients with COPD who have increasing dyspnea. This diagnosis is frequently correct – but not always.
Patients with COPD also may be at risk for or have heart failure, which can present with identical symptoms, including widespread wheezing. We are currently in a severe influenza epidemic, and influenza can mimic a COPD exacerbation or be the trigger.
About 20 years ago, I was out of the country when one of my patients with COPD was admitted to the hospital with a COPD exacerbation. I saw him in follow-up a week after his hospitalization. He was very dyspneic and had a room air oxygen saturation of 75%. He told me his dyspnea started a few days after he had injured his leg on a wood pile in his yard.
On exam, his right leg had 3+ edema; left leg, no edema. He reported to me that he was treated for 5 days with steroids and nebulizers, with minimal change in his dyspnea. I reviewed the chart, and five physicians had seen him while he was in the hospital. Starting with the emergency department, the diagnosis was COPD exacerbation, with no differential diagnosis in any note.
The patient had multiple pulmonary emboli, and he eventually improved with anticoagulation.
In 2009, Jacques Rizkallah, MD, and his colleagues published a systematic review and meta-analysis of articles looking at the prevalence of pulmonary emboli (PE) in patients diagnosed/treated for a COPD exacerbation.1 They found five articles comprising a total of 550 patients who met inclusion criteria. The prevalence was 19.9% (P = .014). The prevalence was much higher (24.7%) for hospitalized patients than it was for outpatients (3.3%). A very important finding in this study: There was no difference in symptoms between patients who did and did not have a pulmonary embolus.
Evrim Eylem Akpinar, MD, and colleagues studied all admissions for acute exacerbations of COPD at one hospital in Turkey over a 2-year period.2 A total of 172 patients admitted for COPD exacerbations were studied. The prevalence of pulmonary embolus was 29%.
In this study, patients who were obese or immobile were more likely to have pulmonary emboli. Pleuritic chest pain and lower-limb asymmetry were signs and symptoms more commonly found in patients who had PE. Obesity was the highest independent predictor (odds ratio, 4.97) for pulmonary embolus.
Floor Aleva, MD, and colleagues recently completed a systematic review and meta-analysis on prevalence and localization of pulmonary embolus in patients with acute exacerbations of COPD.3 They found similar numbers to the previous meta-analysis (16.1%) in a total of 880 patients. They also looked at location in the lungs of the emboli and found that two-thirds of the patients had pulmonary emboli in locations that had clear indication for anticoagulation treatment.
This is important, because criticisms of earlier studies were that clinically insignificant pulmonary emboli might be being found in the studies and that they had little to do with the patients’ symptoms.
In the case presented, I think that getting a D-dimer test would be the next best step. Acute exacerbation of COPD still is the most likely diagnosis, but PE is a plausible diagnosis that should be evaluated. If the D-dimer is normal, workup for PE would be complete. If elevated, then given the 20% prevalence of PE, a CT angiography would be warranted.
Key pearl: Among patients hospitalized for COPD exacerbations, 16%-24% have pulmonary embolism.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. Chest. 2009 Mar;135(3):786-93.
2. J Bras Pneumol. 2014 Jan-Feb;40(1):38-45.
3. Chest. 2017 Mar;151(3):544-54.
Cesarean delivery reduces some risks, raises others
Cesarean deliveries may reduce a woman’s risk for urinary incontinence and pelvic organ prolapse but may raise her risk of complications with future pregnancies, based on data from a literature review including nearly 30,000,000 women.
Rates of cesarean delivery in 2016, often without medical indication, were approximately 25%, 32%, and 41% in Western Europe, North America, and South America, respectively, wrote Oonagh E. Keag, MD, of the Royal Infirmary of Edinburgh and colleagues in a study published in PLOS Medicine.
The researchers reviewed data from 79 observational studies and 1 randomized, controlled trial for a study population of 29,928,274 individuals.
Overall, women who had cesarean deliveries had a significantly lower risk of urinary incontinence (odds ratio, 0.56) and pelvic organ prolapse (OR, 0.29), compared with women who had vaginal deliveries.
No significant association appeared between type of delivery and risk of perinatal death, but women with a history of cesarean delivery were significantly more likely to experience miscarriage or stillbirth on a subsequent pregnancy, as well as placenta previa, placenta accreta, and placental abruption.
In addition, children born via cesarean delivery were significantly more likely than those born via vaginal delivery to have asthma at age 12 years (OR, 1.21) and to be obese up to age 5 years (OR, 1.59).
The findings were limited by the observational nature of most of the data, which does not imply causation, the researchers said. In addition, the study was not designed for subanalysis of elective vs. emergency cesarean delivery.
Although women will attach varying degrees of significance to the risks and benefits associated with cesarean delivery, “it is imperative that clinicians take care to ensure that women are made aware of any risk that they are likely to attach significance to,” the researchers said. “Women and clinicians thus should be aware of both the short- and long-term risks and benefits of cesarean delivery and discuss these when deciding on mode of delivery,” they noted.
The researchers had no financial conflicts to disclose.
SOURCE: Keag OE et al. PLoS Med. 2018 Jan 23. 15(1):e1002494.
As health care practitioners, ob.gyns. must continually evaluate potential consequences of a management strategy to our patients’ health and well-being. This is especially true when determining the best method of delivery – vaginal or cesarean section – because our approach can affect not only the mother but also the baby.
It is well known that vaginal deliveries can be associated with long-term complications for women, including pelvic floor disorders (that is, prolapse), pelvic injury, and incontinence. For women who have undergone a cesarean section, the uterine scars caused by the surgery can lead to increased risk for placenta previa or, more seriously, placenta accreta, as well as possible miscarriage or stillbirth.
Because the best possible care must also be informed care, every ob.gyn. should conduct periodic reviews of the scientific literature. Research continually advances our knowledge and our practice. For example, the recent work on the use of statins to prevent preeclampsia is an area of intense interest. Although we’ve known about hypertensive disorders of pregnancy for many years, management and prevention strategies are adequate at best. This new and exciting line of research has the potential to solve a conundrum we’ve grappled with for centuries.
The study by Keag et al. analyzes the findings from observational studies on the risks and benefits of cesarean versus vaginal delivery, within certain limitations. The study authors found that cesarean deliveries are associated with lower risk of urinary incontinence and pelvic prolapse, but higher risk of placenta previa, miscarriage, and stillbirth. Additionally, the authors reported that babies delivered by cesarean section had a higher risk of developing asthma and obesity.
Although the results of the study are not surprising, the findings reinforce the idea that ob.gyns must make decisions on a case-by-case basis and on obstetrical indications. We cannot use a set of possible complications as a reason to choose one delivery route over another. Every patient is unique. Every circumstance is unique. Every delivery requires us to make an informed decision to achieve the best possible outcome. Otherwise, we run the great risk of doing a disservice to our patients and their families.
E. Albert Reece, MD , PhD, MBA, specializes in maternal-fetal medicine and is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He has no relevant financial disclosures.
As health care practitioners, ob.gyns. must continually evaluate potential consequences of a management strategy to our patients’ health and well-being. This is especially true when determining the best method of delivery – vaginal or cesarean section – because our approach can affect not only the mother but also the baby.
It is well known that vaginal deliveries can be associated with long-term complications for women, including pelvic floor disorders (that is, prolapse), pelvic injury, and incontinence. For women who have undergone a cesarean section, the uterine scars caused by the surgery can lead to increased risk for placenta previa or, more seriously, placenta accreta, as well as possible miscarriage or stillbirth.
Because the best possible care must also be informed care, every ob.gyn. should conduct periodic reviews of the scientific literature. Research continually advances our knowledge and our practice. For example, the recent work on the use of statins to prevent preeclampsia is an area of intense interest. Although we’ve known about hypertensive disorders of pregnancy for many years, management and prevention strategies are adequate at best. This new and exciting line of research has the potential to solve a conundrum we’ve grappled with for centuries.
The study by Keag et al. analyzes the findings from observational studies on the risks and benefits of cesarean versus vaginal delivery, within certain limitations. The study authors found that cesarean deliveries are associated with lower risk of urinary incontinence and pelvic prolapse, but higher risk of placenta previa, miscarriage, and stillbirth. Additionally, the authors reported that babies delivered by cesarean section had a higher risk of developing asthma and obesity.
Although the results of the study are not surprising, the findings reinforce the idea that ob.gyns must make decisions on a case-by-case basis and on obstetrical indications. We cannot use a set of possible complications as a reason to choose one delivery route over another. Every patient is unique. Every circumstance is unique. Every delivery requires us to make an informed decision to achieve the best possible outcome. Otherwise, we run the great risk of doing a disservice to our patients and their families.
E. Albert Reece, MD , PhD, MBA, specializes in maternal-fetal medicine and is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He has no relevant financial disclosures.
As health care practitioners, ob.gyns. must continually evaluate potential consequences of a management strategy to our patients’ health and well-being. This is especially true when determining the best method of delivery – vaginal or cesarean section – because our approach can affect not only the mother but also the baby.
It is well known that vaginal deliveries can be associated with long-term complications for women, including pelvic floor disorders (that is, prolapse), pelvic injury, and incontinence. For women who have undergone a cesarean section, the uterine scars caused by the surgery can lead to increased risk for placenta previa or, more seriously, placenta accreta, as well as possible miscarriage or stillbirth.
Because the best possible care must also be informed care, every ob.gyn. should conduct periodic reviews of the scientific literature. Research continually advances our knowledge and our practice. For example, the recent work on the use of statins to prevent preeclampsia is an area of intense interest. Although we’ve known about hypertensive disorders of pregnancy for many years, management and prevention strategies are adequate at best. This new and exciting line of research has the potential to solve a conundrum we’ve grappled with for centuries.
The study by Keag et al. analyzes the findings from observational studies on the risks and benefits of cesarean versus vaginal delivery, within certain limitations. The study authors found that cesarean deliveries are associated with lower risk of urinary incontinence and pelvic prolapse, but higher risk of placenta previa, miscarriage, and stillbirth. Additionally, the authors reported that babies delivered by cesarean section had a higher risk of developing asthma and obesity.
Although the results of the study are not surprising, the findings reinforce the idea that ob.gyns must make decisions on a case-by-case basis and on obstetrical indications. We cannot use a set of possible complications as a reason to choose one delivery route over another. Every patient is unique. Every circumstance is unique. Every delivery requires us to make an informed decision to achieve the best possible outcome. Otherwise, we run the great risk of doing a disservice to our patients and their families.
E. Albert Reece, MD , PhD, MBA, specializes in maternal-fetal medicine and is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He has no relevant financial disclosures.
Cesarean deliveries may reduce a woman’s risk for urinary incontinence and pelvic organ prolapse but may raise her risk of complications with future pregnancies, based on data from a literature review including nearly 30,000,000 women.
Rates of cesarean delivery in 2016, often without medical indication, were approximately 25%, 32%, and 41% in Western Europe, North America, and South America, respectively, wrote Oonagh E. Keag, MD, of the Royal Infirmary of Edinburgh and colleagues in a study published in PLOS Medicine.
The researchers reviewed data from 79 observational studies and 1 randomized, controlled trial for a study population of 29,928,274 individuals.
Overall, women who had cesarean deliveries had a significantly lower risk of urinary incontinence (odds ratio, 0.56) and pelvic organ prolapse (OR, 0.29), compared with women who had vaginal deliveries.
No significant association appeared between type of delivery and risk of perinatal death, but women with a history of cesarean delivery were significantly more likely to experience miscarriage or stillbirth on a subsequent pregnancy, as well as placenta previa, placenta accreta, and placental abruption.
In addition, children born via cesarean delivery were significantly more likely than those born via vaginal delivery to have asthma at age 12 years (OR, 1.21) and to be obese up to age 5 years (OR, 1.59).
The findings were limited by the observational nature of most of the data, which does not imply causation, the researchers said. In addition, the study was not designed for subanalysis of elective vs. emergency cesarean delivery.
Although women will attach varying degrees of significance to the risks and benefits associated with cesarean delivery, “it is imperative that clinicians take care to ensure that women are made aware of any risk that they are likely to attach significance to,” the researchers said. “Women and clinicians thus should be aware of both the short- and long-term risks and benefits of cesarean delivery and discuss these when deciding on mode of delivery,” they noted.
The researchers had no financial conflicts to disclose.
SOURCE: Keag OE et al. PLoS Med. 2018 Jan 23. 15(1):e1002494.
Cesarean deliveries may reduce a woman’s risk for urinary incontinence and pelvic organ prolapse but may raise her risk of complications with future pregnancies, based on data from a literature review including nearly 30,000,000 women.
Rates of cesarean delivery in 2016, often without medical indication, were approximately 25%, 32%, and 41% in Western Europe, North America, and South America, respectively, wrote Oonagh E. Keag, MD, of the Royal Infirmary of Edinburgh and colleagues in a study published in PLOS Medicine.
The researchers reviewed data from 79 observational studies and 1 randomized, controlled trial for a study population of 29,928,274 individuals.
Overall, women who had cesarean deliveries had a significantly lower risk of urinary incontinence (odds ratio, 0.56) and pelvic organ prolapse (OR, 0.29), compared with women who had vaginal deliveries.
No significant association appeared between type of delivery and risk of perinatal death, but women with a history of cesarean delivery were significantly more likely to experience miscarriage or stillbirth on a subsequent pregnancy, as well as placenta previa, placenta accreta, and placental abruption.
In addition, children born via cesarean delivery were significantly more likely than those born via vaginal delivery to have asthma at age 12 years (OR, 1.21) and to be obese up to age 5 years (OR, 1.59).
The findings were limited by the observational nature of most of the data, which does not imply causation, the researchers said. In addition, the study was not designed for subanalysis of elective vs. emergency cesarean delivery.
Although women will attach varying degrees of significance to the risks and benefits associated with cesarean delivery, “it is imperative that clinicians take care to ensure that women are made aware of any risk that they are likely to attach significance to,” the researchers said. “Women and clinicians thus should be aware of both the short- and long-term risks and benefits of cesarean delivery and discuss these when deciding on mode of delivery,” they noted.
The researchers had no financial conflicts to disclose.
SOURCE: Keag OE et al. PLoS Med. 2018 Jan 23. 15(1):e1002494.
FROM PLOS MEDICINE
Key clinical point: Cesarean delivery was associated with a reduced risk for incontinence and prolapse.
Major finding: Urinary incontinence and pelvic organ prolapse were less likely after cesarean vs. vaginal deliveries (OR, 0.56 and 0.29, respectively).
Study details: The data come from a review of 80 studies.
Disclosures: The researchers had no financial conflicts to disclose.
Source: Keag OE et al. PLoS Med. 2018 Jan 23. 15(1):e1002494.
Protocols to reduce opioid use and shorten length of stay
While originally pioneered by European anesthesiologists and surgeons in Europe in the 1990s, enhanced recovery after surgery (ERAS) programs, also known as enhanced recovery protocols or fast-track surgery, have now gained popularity across the surgical spectrum within the United States. The goal of these programs is to utilize multidisciplinary and multimodal interventions to minimize the physiologic changes associated with surgery and thereby enhance the perioperative experience – reduced morbidity and mortality, shorter length of stay, less postoperative opioid use, and faster resumption to normal activity, at a decreased cost of care.
1. Enhanced patient education, including managing expectations.
2. Decreased perioperative fasting periods.
3. Blood volume and temperature maintenance intraoperatively.
4. Postoperative mobilization early and often.
5. Multimodal pain relief and nausea/vomiting prophylaxis.
6. Use of postoperative drains and catheters only as long as required.
Today, I have asked Kirsten Sasaki, MD, to discuss some of these ERAS concepts. I have asked Dr. Sasaki to especially focus on decreasing opioid utilization. For a thorough discussion on ERAS recommendations using an evidence-based approach, one can review two excellent papers by Nelson et al. (Gynecol Oncol. 2016 Feb;140[2]:313-22; Gynecol Oncol. 2016 Feb;140[2]:323-32).
Dr. Sasaki completed her internship and residency at Tufts Medical Center, Boston. Dr. Sasaki then went on to become our second fellow at the Fellowship in Minimally Invasive Gynecologic Surgery in affiliation with AAGL and Society of Reproductive Surgeons at Advocate Lutheran General Hospital, Park Ridge, Ill. As a Fellow, Dr. Sasaki was recognized for her excellent teaching and research capabilities. Ultimately, however, it was her tremendous surgical skills and surgical sense that led me to invite her to join my practice in 2014.
Dr. Miller is a clinical associate professor at the University of Illinois in Chicago and past president of the AAGL. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in metropolitan Chicago and the director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill. He has no disclosures relevant to this Master Class.
While originally pioneered by European anesthesiologists and surgeons in Europe in the 1990s, enhanced recovery after surgery (ERAS) programs, also known as enhanced recovery protocols or fast-track surgery, have now gained popularity across the surgical spectrum within the United States. The goal of these programs is to utilize multidisciplinary and multimodal interventions to minimize the physiologic changes associated with surgery and thereby enhance the perioperative experience – reduced morbidity and mortality, shorter length of stay, less postoperative opioid use, and faster resumption to normal activity, at a decreased cost of care.
1. Enhanced patient education, including managing expectations.
2. Decreased perioperative fasting periods.
3. Blood volume and temperature maintenance intraoperatively.
4. Postoperative mobilization early and often.
5. Multimodal pain relief and nausea/vomiting prophylaxis.
6. Use of postoperative drains and catheters only as long as required.
Today, I have asked Kirsten Sasaki, MD, to discuss some of these ERAS concepts. I have asked Dr. Sasaki to especially focus on decreasing opioid utilization. For a thorough discussion on ERAS recommendations using an evidence-based approach, one can review two excellent papers by Nelson et al. (Gynecol Oncol. 2016 Feb;140[2]:313-22; Gynecol Oncol. 2016 Feb;140[2]:323-32).
Dr. Sasaki completed her internship and residency at Tufts Medical Center, Boston. Dr. Sasaki then went on to become our second fellow at the Fellowship in Minimally Invasive Gynecologic Surgery in affiliation with AAGL and Society of Reproductive Surgeons at Advocate Lutheran General Hospital, Park Ridge, Ill. As a Fellow, Dr. Sasaki was recognized for her excellent teaching and research capabilities. Ultimately, however, it was her tremendous surgical skills and surgical sense that led me to invite her to join my practice in 2014.
Dr. Miller is a clinical associate professor at the University of Illinois in Chicago and past president of the AAGL. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in metropolitan Chicago and the director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill. He has no disclosures relevant to this Master Class.
While originally pioneered by European anesthesiologists and surgeons in Europe in the 1990s, enhanced recovery after surgery (ERAS) programs, also known as enhanced recovery protocols or fast-track surgery, have now gained popularity across the surgical spectrum within the United States. The goal of these programs is to utilize multidisciplinary and multimodal interventions to minimize the physiologic changes associated with surgery and thereby enhance the perioperative experience – reduced morbidity and mortality, shorter length of stay, less postoperative opioid use, and faster resumption to normal activity, at a decreased cost of care.
1. Enhanced patient education, including managing expectations.
2. Decreased perioperative fasting periods.
3. Blood volume and temperature maintenance intraoperatively.
4. Postoperative mobilization early and often.
5. Multimodal pain relief and nausea/vomiting prophylaxis.
6. Use of postoperative drains and catheters only as long as required.
Today, I have asked Kirsten Sasaki, MD, to discuss some of these ERAS concepts. I have asked Dr. Sasaki to especially focus on decreasing opioid utilization. For a thorough discussion on ERAS recommendations using an evidence-based approach, one can review two excellent papers by Nelson et al. (Gynecol Oncol. 2016 Feb;140[2]:313-22; Gynecol Oncol. 2016 Feb;140[2]:323-32).
Dr. Sasaki completed her internship and residency at Tufts Medical Center, Boston. Dr. Sasaki then went on to become our second fellow at the Fellowship in Minimally Invasive Gynecologic Surgery in affiliation with AAGL and Society of Reproductive Surgeons at Advocate Lutheran General Hospital, Park Ridge, Ill. As a Fellow, Dr. Sasaki was recognized for her excellent teaching and research capabilities. Ultimately, however, it was her tremendous surgical skills and surgical sense that led me to invite her to join my practice in 2014.
Dr. Miller is a clinical associate professor at the University of Illinois in Chicago and past president of the AAGL. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in metropolitan Chicago and the director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill. He has no disclosures relevant to this Master Class.
Supportive oncodermatology: Cancer advances spawn new subspecialty
Not too long ago at the Dana-Farber/Brigham and Women’s Cancer Center in Boston, a woman with widely metastatic melanoma, who had been planning her own funeral, was surprised when she had a phenomenal response to immunotherapy.
She was shocked to learn that her cancer was almost completely gone after 12 weeks, but she was stunned when she developed a rash that made her oncologist think she needed to stop treatment.
With traditional cytotoxic chemotherapies, there were a few well-defined skin side effects that oncologists were comfortable managing on their own with steroids or by reducing or stopping treatment for a bit.
But over the last decade, new cancer options have become available, most notably immunotherapies and targeted biologics, which are keeping some people alive longer but also causing cutaneous side effects that have never been seen before in oncology and are being reported frequently.
An urgent need
Currently in the United States, there’s only a handful of dedicated supportive oncodermatology services, which can be found at major academic cancer centers such as Dana-Farber/Brigham and Women’s, but the residents and fellows being trained at these centers are starting to fan out across the country and set up new services.
One day, it’s likely that every major cancer institution will have “a toxicities team with expert dermatologists,” said Dr. LeBoeuf, who launched the supportive oncodermatology program at Dana-Farber in 2014 and who now runs it with a team of dermatologists and clinics every week. Dr. LeBoeuf is a leader in the field, like the other dermatologists interviewed for this story.
With all the new treatments and with even more on the way, “there’s an urgent need for dermatologists to be involved in care of cancer patients,” Dr. LeBoeuf said.
The problem
Immunotherapies like the PD-1 blocking agents pembrolizumab (Keytruda) and nivolumab (Opdivo) – both used for an ever-expanding list of tumors – amp up the immune system to fight cancer, but they also tend to cause adverse events that mimic autoimmune diseases such as lupus, psoriasis, lichen planus, and vitiligo. Dermatologists are familiar with those problems and how to manage them, but oncologists generally are not.
Meanwhile, the many targeted therapies approved over the past decade interfere with specific molecules needed for tumor growth, but they also are associated with a wide range of skin, hair, and nail side effects that include skin growths, itching, paronychia, and more.
Agents that target vascular endothelial growth factors, such as sorafenib (Nexavar) and bevacizumab (Avastin), can trigger a painful hand-foot skin reaction that’s different from the hand-foot syndrome reported with older cytotoxic agents.
Epidermal growth factor receptor (EGFR) inhibitors, such as erlotinib (Tarceva) or gefitinib (Iressa), often cause miserable acne-like eruptions, but that can mean the drug is working.
It’s hard for oncologists to know what’s life-threatening and what isn’t; that’s where dermatologists come in.
A solution
When problems come up, oncologists and patients need answers right away, she said. There’s no time to wait a month or two for a dermatology appointment to find out whether, for instance, a new mouth ulcer is a minor inconvenience or the first sign of Stevens-Johnson syndrome, and the last thing an exhausted cancer patient needs is to be told to go to yet another clinic for a dermatology consult.
For supportive oncodermatology, that means being where the patients are: in the cancer centers. “Our clinic is situated on the same cancer floor as all the other oncology clinics,” which means easy access for both patients and oncologists, Dr. Choi said. “They just come down the hall.”
Build it, and they will come
The Stanford (Calif.) Cancer Center is a good example of what happens once a supportive oncodermatology service is up and running.
The program there was the brainchild of dermatologist Bernice Kwong, MD, who helped launch it in 2012 with 2 half-day outpatient clinics per week.
“Once people knew we were there seeing patients, we needed to expand it to 3 half days, and within 6 months, we knew we had to be” in the cancer center daily, she said. “The oncologists felt we were helping them keep their patients on treatment longer; they didn’t have to stop therapy to sort out a rash.”
Currently, the clinic sees about 15 to 20 patients a day, but “we have more need than that,” said Dr. Kwong, who is trying to recruit more dermatologists to help.
“The need is huge. There’s so much room for growth,” she noted, but first, “you need the oncologists to be on board.”
Dermatologist Adam Friedman, MD, director of supportive oncodermatology at the George Washington University Cancer Center, Washington, says his program is on the other end of the growth curve since it was only launched in the spring of 2017. Only about 80 patients have been treated so far, and there’s one dedicated clinic day a month, although he is on call for urgent cases, as is the case for many of the other dermatologists interviewed for this story.
Dr. Friedman expects business will pick up soon once word gets out, just like at Dana-Farber/Brigham and Women’s, Stanford, and elsewhere. “The places with the greatest need are going to have these services first, and then you’ll see them pop up elsewhere. I think we are going to see more,” he said.
The birth of supportive oncodermatology
Dermatologist Mario Lacouture, MD, director of the oncodermatology program at Memorial Sloan Kettering Cancer Center, New York, is considered by many oncodermatologists to be the father of the field.
He started the very first program in 2005 at Northwestern University, Chicago, followed by the program at Sloan Kettering a few years later. He has helped train many of the leaders in the field and coined the phrase “supportive oncodermatology” as the senior author in the field’s seminal paper, published in 2011 (J Am Acad Dermatol. 2011 Sep;65[3]:624-35). That article, in turn, inspired at least a few young dermatologists to make supportive oncodermatology their career choice. Dr. Lacouture speaks regularly at oncology and dermatology meetings to raise awareness about how dermatologists can improve cancer care.
Cancer survivors were also a concern. “Cancer treatment has improved so much that people are living longer, but the majority of survivors have either temporary or permanent cutaneous problems that would benefit from dermatologic care. However, the oncology community and patients are usually not aware that there are things we can do to help,” Dr. Lacouture said.
The message seems to have gotten out, however, among the hundreds of oncologists affiliated with Sloan Kettering. Dr. Lacouture needs a team of supportive oncodermatologists to meet the demand, with walk-in clinics every day and round-the-clock call.
He anticipates a day when visiting a supportive oncodermatologist will be routine, even before the start of cancer treatment, just as people visit a dentist before bone marrow transplants or radiation treatment to the head and neck. The idea would be to prevent cutaneous toxicity, something Dr. Lacouture and his team are already doing at Sloan Kettering. In time, supportive oncodermatology “is something that is going to be instituted early on” in treatment, he said.
“It’s important for dermatologists to reach out to their local oncologists; they will see there are many, many cancer patients and survivors who would benefit immensely from their care,” he said.
Dr. Lacouture is a consultant for Galderma, Janssen, and Johnson & Johnson. The other dermatologists interviewed for this story had no relevant industry disclosures. La Roche-Posay, a subsidiary of L’Oreal, is helping fund the supportive oncodermatology program at George Washington University. The company is interested in using cosmetics to camouflage cancer treatment skin lesions, Dr. Friedman said. Dr. Friedman is a member of the Dermatology News advisory board.
[email protected]
Not too long ago at the Dana-Farber/Brigham and Women’s Cancer Center in Boston, a woman with widely metastatic melanoma, who had been planning her own funeral, was surprised when she had a phenomenal response to immunotherapy.
She was shocked to learn that her cancer was almost completely gone after 12 weeks, but she was stunned when she developed a rash that made her oncologist think she needed to stop treatment.
With traditional cytotoxic chemotherapies, there were a few well-defined skin side effects that oncologists were comfortable managing on their own with steroids or by reducing or stopping treatment for a bit.
But over the last decade, new cancer options have become available, most notably immunotherapies and targeted biologics, which are keeping some people alive longer but also causing cutaneous side effects that have never been seen before in oncology and are being reported frequently.
An urgent need
Currently in the United States, there’s only a handful of dedicated supportive oncodermatology services, which can be found at major academic cancer centers such as Dana-Farber/Brigham and Women’s, but the residents and fellows being trained at these centers are starting to fan out across the country and set up new services.
One day, it’s likely that every major cancer institution will have “a toxicities team with expert dermatologists,” said Dr. LeBoeuf, who launched the supportive oncodermatology program at Dana-Farber in 2014 and who now runs it with a team of dermatologists and clinics every week. Dr. LeBoeuf is a leader in the field, like the other dermatologists interviewed for this story.
With all the new treatments and with even more on the way, “there’s an urgent need for dermatologists to be involved in care of cancer patients,” Dr. LeBoeuf said.
The problem
Immunotherapies like the PD-1 blocking agents pembrolizumab (Keytruda) and nivolumab (Opdivo) – both used for an ever-expanding list of tumors – amp up the immune system to fight cancer, but they also tend to cause adverse events that mimic autoimmune diseases such as lupus, psoriasis, lichen planus, and vitiligo. Dermatologists are familiar with those problems and how to manage them, but oncologists generally are not.
Meanwhile, the many targeted therapies approved over the past decade interfere with specific molecules needed for tumor growth, but they also are associated with a wide range of skin, hair, and nail side effects that include skin growths, itching, paronychia, and more.
Agents that target vascular endothelial growth factors, such as sorafenib (Nexavar) and bevacizumab (Avastin), can trigger a painful hand-foot skin reaction that’s different from the hand-foot syndrome reported with older cytotoxic agents.
Epidermal growth factor receptor (EGFR) inhibitors, such as erlotinib (Tarceva) or gefitinib (Iressa), often cause miserable acne-like eruptions, but that can mean the drug is working.
It’s hard for oncologists to know what’s life-threatening and what isn’t; that’s where dermatologists come in.
A solution
When problems come up, oncologists and patients need answers right away, she said. There’s no time to wait a month or two for a dermatology appointment to find out whether, for instance, a new mouth ulcer is a minor inconvenience or the first sign of Stevens-Johnson syndrome, and the last thing an exhausted cancer patient needs is to be told to go to yet another clinic for a dermatology consult.
For supportive oncodermatology, that means being where the patients are: in the cancer centers. “Our clinic is situated on the same cancer floor as all the other oncology clinics,” which means easy access for both patients and oncologists, Dr. Choi said. “They just come down the hall.”
Build it, and they will come
The Stanford (Calif.) Cancer Center is a good example of what happens once a supportive oncodermatology service is up and running.
The program there was the brainchild of dermatologist Bernice Kwong, MD, who helped launch it in 2012 with 2 half-day outpatient clinics per week.
“Once people knew we were there seeing patients, we needed to expand it to 3 half days, and within 6 months, we knew we had to be” in the cancer center daily, she said. “The oncologists felt we were helping them keep their patients on treatment longer; they didn’t have to stop therapy to sort out a rash.”
Currently, the clinic sees about 15 to 20 patients a day, but “we have more need than that,” said Dr. Kwong, who is trying to recruit more dermatologists to help.
“The need is huge. There’s so much room for growth,” she noted, but first, “you need the oncologists to be on board.”
Dermatologist Adam Friedman, MD, director of supportive oncodermatology at the George Washington University Cancer Center, Washington, says his program is on the other end of the growth curve since it was only launched in the spring of 2017. Only about 80 patients have been treated so far, and there’s one dedicated clinic day a month, although he is on call for urgent cases, as is the case for many of the other dermatologists interviewed for this story.
Dr. Friedman expects business will pick up soon once word gets out, just like at Dana-Farber/Brigham and Women’s, Stanford, and elsewhere. “The places with the greatest need are going to have these services first, and then you’ll see them pop up elsewhere. I think we are going to see more,” he said.
The birth of supportive oncodermatology
Dermatologist Mario Lacouture, MD, director of the oncodermatology program at Memorial Sloan Kettering Cancer Center, New York, is considered by many oncodermatologists to be the father of the field.
He started the very first program in 2005 at Northwestern University, Chicago, followed by the program at Sloan Kettering a few years later. He has helped train many of the leaders in the field and coined the phrase “supportive oncodermatology” as the senior author in the field’s seminal paper, published in 2011 (J Am Acad Dermatol. 2011 Sep;65[3]:624-35). That article, in turn, inspired at least a few young dermatologists to make supportive oncodermatology their career choice. Dr. Lacouture speaks regularly at oncology and dermatology meetings to raise awareness about how dermatologists can improve cancer care.
Cancer survivors were also a concern. “Cancer treatment has improved so much that people are living longer, but the majority of survivors have either temporary or permanent cutaneous problems that would benefit from dermatologic care. However, the oncology community and patients are usually not aware that there are things we can do to help,” Dr. Lacouture said.
The message seems to have gotten out, however, among the hundreds of oncologists affiliated with Sloan Kettering. Dr. Lacouture needs a team of supportive oncodermatologists to meet the demand, with walk-in clinics every day and round-the-clock call.
He anticipates a day when visiting a supportive oncodermatologist will be routine, even before the start of cancer treatment, just as people visit a dentist before bone marrow transplants or radiation treatment to the head and neck. The idea would be to prevent cutaneous toxicity, something Dr. Lacouture and his team are already doing at Sloan Kettering. In time, supportive oncodermatology “is something that is going to be instituted early on” in treatment, he said.
“It’s important for dermatologists to reach out to their local oncologists; they will see there are many, many cancer patients and survivors who would benefit immensely from their care,” he said.
Dr. Lacouture is a consultant for Galderma, Janssen, and Johnson & Johnson. The other dermatologists interviewed for this story had no relevant industry disclosures. La Roche-Posay, a subsidiary of L’Oreal, is helping fund the supportive oncodermatology program at George Washington University. The company is interested in using cosmetics to camouflage cancer treatment skin lesions, Dr. Friedman said. Dr. Friedman is a member of the Dermatology News advisory board.
[email protected]
Not too long ago at the Dana-Farber/Brigham and Women’s Cancer Center in Boston, a woman with widely metastatic melanoma, who had been planning her own funeral, was surprised when she had a phenomenal response to immunotherapy.
She was shocked to learn that her cancer was almost completely gone after 12 weeks, but she was stunned when she developed a rash that made her oncologist think she needed to stop treatment.
With traditional cytotoxic chemotherapies, there were a few well-defined skin side effects that oncologists were comfortable managing on their own with steroids or by reducing or stopping treatment for a bit.
But over the last decade, new cancer options have become available, most notably immunotherapies and targeted biologics, which are keeping some people alive longer but also causing cutaneous side effects that have never been seen before in oncology and are being reported frequently.
An urgent need
Currently in the United States, there’s only a handful of dedicated supportive oncodermatology services, which can be found at major academic cancer centers such as Dana-Farber/Brigham and Women’s, but the residents and fellows being trained at these centers are starting to fan out across the country and set up new services.
One day, it’s likely that every major cancer institution will have “a toxicities team with expert dermatologists,” said Dr. LeBoeuf, who launched the supportive oncodermatology program at Dana-Farber in 2014 and who now runs it with a team of dermatologists and clinics every week. Dr. LeBoeuf is a leader in the field, like the other dermatologists interviewed for this story.
With all the new treatments and with even more on the way, “there’s an urgent need for dermatologists to be involved in care of cancer patients,” Dr. LeBoeuf said.
The problem
Immunotherapies like the PD-1 blocking agents pembrolizumab (Keytruda) and nivolumab (Opdivo) – both used for an ever-expanding list of tumors – amp up the immune system to fight cancer, but they also tend to cause adverse events that mimic autoimmune diseases such as lupus, psoriasis, lichen planus, and vitiligo. Dermatologists are familiar with those problems and how to manage them, but oncologists generally are not.
Meanwhile, the many targeted therapies approved over the past decade interfere with specific molecules needed for tumor growth, but they also are associated with a wide range of skin, hair, and nail side effects that include skin growths, itching, paronychia, and more.
Agents that target vascular endothelial growth factors, such as sorafenib (Nexavar) and bevacizumab (Avastin), can trigger a painful hand-foot skin reaction that’s different from the hand-foot syndrome reported with older cytotoxic agents.
Epidermal growth factor receptor (EGFR) inhibitors, such as erlotinib (Tarceva) or gefitinib (Iressa), often cause miserable acne-like eruptions, but that can mean the drug is working.
It’s hard for oncologists to know what’s life-threatening and what isn’t; that’s where dermatologists come in.
A solution
When problems come up, oncologists and patients need answers right away, she said. There’s no time to wait a month or two for a dermatology appointment to find out whether, for instance, a new mouth ulcer is a minor inconvenience or the first sign of Stevens-Johnson syndrome, and the last thing an exhausted cancer patient needs is to be told to go to yet another clinic for a dermatology consult.
For supportive oncodermatology, that means being where the patients are: in the cancer centers. “Our clinic is situated on the same cancer floor as all the other oncology clinics,” which means easy access for both patients and oncologists, Dr. Choi said. “They just come down the hall.”
Build it, and they will come
The Stanford (Calif.) Cancer Center is a good example of what happens once a supportive oncodermatology service is up and running.
The program there was the brainchild of dermatologist Bernice Kwong, MD, who helped launch it in 2012 with 2 half-day outpatient clinics per week.
“Once people knew we were there seeing patients, we needed to expand it to 3 half days, and within 6 months, we knew we had to be” in the cancer center daily, she said. “The oncologists felt we were helping them keep their patients on treatment longer; they didn’t have to stop therapy to sort out a rash.”
Currently, the clinic sees about 15 to 20 patients a day, but “we have more need than that,” said Dr. Kwong, who is trying to recruit more dermatologists to help.
“The need is huge. There’s so much room for growth,” she noted, but first, “you need the oncologists to be on board.”
Dermatologist Adam Friedman, MD, director of supportive oncodermatology at the George Washington University Cancer Center, Washington, says his program is on the other end of the growth curve since it was only launched in the spring of 2017. Only about 80 patients have been treated so far, and there’s one dedicated clinic day a month, although he is on call for urgent cases, as is the case for many of the other dermatologists interviewed for this story.
Dr. Friedman expects business will pick up soon once word gets out, just like at Dana-Farber/Brigham and Women’s, Stanford, and elsewhere. “The places with the greatest need are going to have these services first, and then you’ll see them pop up elsewhere. I think we are going to see more,” he said.
The birth of supportive oncodermatology
Dermatologist Mario Lacouture, MD, director of the oncodermatology program at Memorial Sloan Kettering Cancer Center, New York, is considered by many oncodermatologists to be the father of the field.
He started the very first program in 2005 at Northwestern University, Chicago, followed by the program at Sloan Kettering a few years later. He has helped train many of the leaders in the field and coined the phrase “supportive oncodermatology” as the senior author in the field’s seminal paper, published in 2011 (J Am Acad Dermatol. 2011 Sep;65[3]:624-35). That article, in turn, inspired at least a few young dermatologists to make supportive oncodermatology their career choice. Dr. Lacouture speaks regularly at oncology and dermatology meetings to raise awareness about how dermatologists can improve cancer care.
Cancer survivors were also a concern. “Cancer treatment has improved so much that people are living longer, but the majority of survivors have either temporary or permanent cutaneous problems that would benefit from dermatologic care. However, the oncology community and patients are usually not aware that there are things we can do to help,” Dr. Lacouture said.
The message seems to have gotten out, however, among the hundreds of oncologists affiliated with Sloan Kettering. Dr. Lacouture needs a team of supportive oncodermatologists to meet the demand, with walk-in clinics every day and round-the-clock call.
He anticipates a day when visiting a supportive oncodermatologist will be routine, even before the start of cancer treatment, just as people visit a dentist before bone marrow transplants or radiation treatment to the head and neck. The idea would be to prevent cutaneous toxicity, something Dr. Lacouture and his team are already doing at Sloan Kettering. In time, supportive oncodermatology “is something that is going to be instituted early on” in treatment, he said.
“It’s important for dermatologists to reach out to their local oncologists; they will see there are many, many cancer patients and survivors who would benefit immensely from their care,” he said.
Dr. Lacouture is a consultant for Galderma, Janssen, and Johnson & Johnson. The other dermatologists interviewed for this story had no relevant industry disclosures. La Roche-Posay, a subsidiary of L’Oreal, is helping fund the supportive oncodermatology program at George Washington University. The company is interested in using cosmetics to camouflage cancer treatment skin lesions, Dr. Friedman said. Dr. Friedman is a member of the Dermatology News advisory board.
[email protected]